We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs


Chapter 7: 10 Real Cases on Transient Ischemic Attack and Stroke: Diagnosis, Management, and Follow-Up
Jeirym Miranda; Fareeha S. Alavi; Muhammad Saad
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Case review, case discussion, clinical symptoms.
- Radiologic Findings
- Full Chapter
- Supplementary Content
Case 1: Management of Acute Thrombotic Cerebrovascular Accident Post Recombinant Tissue Plasminogen Activator Therapy
A 59-year-old Hispanic man presented with right upper and lower extremity weakness, associated with facial drop and slurred speech starting 2 hours before the presentation. He denied visual disturbance, headache, chest pain, palpitations, dyspnea, dysphagia, fever, dizziness, loss of consciousness, bowel or urinary incontinence, or trauma. His medical history was significant for uncontrolled type 2 diabetes mellitus, hypertension, hyperlipidemia, and benign prostatic hypertrophy. Social history included cigarette smoking (1 pack per day for 20 years) and alcohol intake of 3 to 4 beers daily. Family history was not significant, and he did not remember his medications. In the emergency department, his vital signs were stable. His physical examination was remarkable for right-sided facial droop, dysarthria, and right-sided hemiplegia. The rest of the examination findings were insignificant. His National Institutes of Health Stroke Scale (NIHSS) score was calculated as 7. Initial CT angiogram of head and neck reported no acute intracranial findings. The neurology team was consulted, and intravenous recombinant tissue plasminogen activator (t-PA) was administered along with high-intensity statin therapy. The patient was admitted to the intensive care unit where his hemodynamics were monitored for 24 hours and later transferred to the telemetry unit. MRI of the head revealed an acute 1.7-cm infarct of the left periventricular white matter and posterior left basal ganglia. How would you manage this case?
This case scenario presents a patient with acute ischemic cerebrovascular accident (CVA) requiring intravenous t-PA. Diagnosis was based on clinical neurologic symptoms and an NIHSS score of 7 and was later confirmed by neuroimaging. He had multiple comorbidities, including hypertension, diabetes, dyslipidemia, and smoking history, which put him at a higher risk for developing cardiovascular disease. Because his symptoms started within 4.5 hours of presentation, he was deemed to be a candidate for thrombolytics. The eligibility time line is estimated either by self-report or last witness of baseline status.
Ischemic strokes are caused by an obstruction of a blood vessel, which irrigates the brain mainly secondary to the development of atherosclerotic changes, leading to cerebral thrombosis and embolism. Diagnosis is made based on presenting symptoms and CT/MRI of the head, and the treatment is focused on cerebral reperfusion based on eligibility criteria and timing of presentation.
Symptoms include alteration of sensorium, numbness, decreased motor strength, facial drop, dysarthria, ataxia, visual disturbance, dizziness, and headache.
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
Case Presentation
Statement of ethics, conflict of interest statement, funding sources, author contributions, ischemic stroke in a 29-year-old patient with covid-19: a case report.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Christian Avvantaggiato , Loredana Amoruso , Maria Pia Lo Muzio , Maria Assunta Mimmo , Michelina Delli Bergoli , Nicoletta Cinone , Luigi Santoro , Lucia Stuppiello , Antonio Turitto , Chiara Ciritella , Pietro Fiore , Andrea Santamato; Ischemic Stroke in a 29-Year-Old Patient with COVID-19: A Case Report. Case Rep Neurol 2 September 2021; 13 (2): 334–340. https://doi.org/10.1159/000515457
Download citation file:
- Ris (Zotero)
- Reference Manager
Increasing evidence reports a greater incidence of stroke among patients with Coronavirus disease 2019 (COVID-19) than the non-COVID-19 population and suggests that SARS-CoV-2 infection represents a risk factor for thromboembolic and acute ischemic stroke. Elderly people have higher risk factors associated with acute ischemic stroke or embolization vascular events, and advanced age is strongly associated with severe COVID-19 and death. We reported, instead, a case of an ischemic stroke in a young woman during her hospitalization for COVID-19-related pneumonia. A 29-year-old woman presented to the emergency department of our institution with progressive respiratory distress associated with a 2-day history of fever, nausea, and vomiting. The patient was transferred to the intensive care unit (ICU) where she underwent a tracheostomy for mechanical ventilation due to her severe clinical condition and her very low arterial partial pressure of oxygen. The nasopharyngeal swab test confirmed SARS-CoV-2 infection. Laboratory tests showed neutrophilic leucocytosis, a prolonged prothrombin time, and elevated D-dimer and fibrinogen levels. After 18 days, during her stay in the ICU after suspension of the medications used for sedation, left hemiplegia was reported. Central facial palsy on the left side, dysarthria, and facial drop were present, with complete paralysis of the ipsilateral upper and lower limbs. Computed tomography (CT) of the head and magnetic resonance imaging of the brain confirmed the presence of lesions in the right hemisphere affecting the territories of the anterior and middle cerebral arteries, consistent with ischemic stroke. Pulmonary and splenic infarcts were also found after CT of the chest. The age of the patient and the absence of serious concomitant cardiovascular diseases place the emphasis on the capacity of SARS-CoV-2 infection to be an independent cerebrovascular risk factor. Increased levels of D-dimer and positivity to β2-glycoprotein antibodies could confirm the theory of endothelial activation and hypercoagulability, but other mechanisms – still under discussion – should not be excluded.
Coronavirus disease 2019 (COVID-19), caused by the novel coronavirus SARS-CoV-2, is characterized by a wide range of symptoms, most of which cause acute respiratory distress syndrome [1, 2], associated with intensive care unit (ICU) admission and high mortality [3]. On March 11, 2020, the large global outbreak of the disease led the World Health Organization (WHO) to declare COVID-19 a pandemic, with 11,874,226 confirmed cases and 545,481 deaths worldwide (July 9, 2020) [4]. In many cases, the clinical manifestations of COVID-19 are characteristic of a mild disease that may, however, worsen to a critical lower respiratory infection [2]. At the onset of the disease, the most frequent symptoms are fever, dry cough, fatigue, and shortness of breath as the infection progresses may appear signs and symptoms of respiratory failure that require ICU admission [5, 6]. Although acute respiratory distress syndrome is the most important cause of ICU admission for COVID-19 patients, several studies have underlined the presence of neurological symptoms such as confusion, dizziness, impaired consciousness, ataxia, seizure, anosmia, ageusia, vision impairment, and stroke [7, 8]. In particular, the state of hypercoagulability in patients affected by COVID-19 favors the formation of small and/or large blood clots in multiple organs, including the brain, potentially leading to cerebrovascular disease (ischemic stroke but also intracranial hemorrhage) [9, 10 ].
We found an interesting case of stroke following a SARS-CoV-2 infection in a young patient. A 29-year-old woman, during her ICU hospitalization for COVID-19-related pneumonia, was diagnosed with ischemic stroke of the right hemisphere, without other cardiac/cerebrovascular risk factors except hypertension. The young age of the patient and the absence of higher cerebrovascular risk factors make the present case very interesting as it can help demonstrate that COVID-19 is an independent risk factor for acute ischemic stroke. In a case series of 214 patients with COVID-19 (mean [SD] age, 52.7 [15.5] years), neurologic symptoms were more common in patients with severe infection who were older than the others [ 11 ]. New-onset CVD was more common in COVID-19 patients who had underlying cerebrovascular risk factors, such as older age (>65 years) [ 12 ], and very few cases of stroke in patients younger than 50 years have been reported [ 12, 13 ]. Our case seems to be the only one younger than 30 years.
On the night between March 19 and 20, 2020, a 29-year-old woman was referred to our hospital “Policlinico Riuniti di Foggia” due to a progressive respiratory distress associated with a 2-day history of fever, nausea, and vomiting. At presentation, the heart rate was 128 bpm, the blood oxygen saturation measured by means of the pulse oximeter was 27%, the respiratory rate was 27 breaths per minute, and the blood pressure was 116/77 mm Hg. The arterial blood gas test showed a pH of 7.52, pO 2 20 mm Hg, and pCO 2 34 mm Hg. The patient was immediately transferred to the ICU where she underwent tracheostomy and endotracheal intubation for mechanical ventilation due to her severe clinical condition and deteriorated pulmonary gas exchange. The diagnosis of COVID-19 was confirmed by PCR on a nasopharyngeal swab.
The family medical history was normal, and the only known pre-existing medical conditions were polycystic ovary syndrome (diagnosed 3 years earlier), conversion disorder, and hypertension (both diagnosed 2 years earlier). Ramipril and nebivolol were prescribed for the high blood pressure treatment, and sertraline was prescribed for the conversion disorder treatment. Drug therapy adherence was inconstant. The patient had no history of diabetes, cardiac pathologies, strokes, transient ischemic attacks, thromboembolic, or other vascular pathologies.
Laboratory tests showed neutrophilic leukocytosis (white blood cell count 14.79 × 10 3 , neutrophil percentage 89.8%, and neutrophil count 13.29 × 10 3 ), a prolonged prothrombin time (15.3 s) with a slightly elevated international normalized ratio (1.38), and elevated D-dimer (6,912 ng/mL) and fibrinogen levels (766 mg/dL). Other findings are shown in Table 1 .
Laboratory test

This pharmacological therapy was set as follows: enoxaparin 6,000 U.I. once a day, piperacillin 4 g/tazobactam 0.5 g twice a day; Kaletra, a combination of lopinavir and ritonavir indicated for human immunodeficiency virus (HIV) infection treatment, 2 tablets twice a day; hydroxychloroquine 200 mg once a day; and furosemide 250 mg, calcium gluconate, and aminophylline 240 mg 3 times a day. No adverse events were reported.
On April 7, 2020, during her stay in the ICU and after suspension of the medications used for sedation, left hemiplegia was reported. The same day, the patient underwent a computed tomography examination of the head, which showed areas of hypodensity in the right hemisphere due to recent cerebral ischemia.
On April 16, 2020, the patient was oriented to time, place, and person. Central facial palsy on the left side, dysarthria, and facial drop were present, with complete paralysis of the ipsilateral upper and lower limbs. The power of all the muscles of the left limbs was grade 0 according to the Medical Research Council (MRC) scale. Deep tendon reflexes were reduced on the left upper limb but hyperactive on the ipsilateral lower limb, with a slight increase in the muscle tonus. The senses of touch, vibration, and pain were reduced on the left side of the face and body.
On the same day, the patient underwent magnetic resonance imaging (MRI) of the brain (Fig. 1 a), showing lesions on the right hemisphere affecting the territories of the anterior and middle cerebral arteries. On May 5, 2020, magnetic resonance angiography showed an early duplication of the sphenoidal segment of the right middle cerebral artery, the branches of which are irregular with rosary bead-like aspects (Fig. 1 d, e); on the same day, the second MRI (Fig. 1 b) confirmed the lesions. Computed tomography of the chest (Fig. 1 c) and abdomen (Fig. 1 f), performed 5 days after the MRI of the brain, showed not only multifocal bilateral ground-glass opacities but also a basal subpleural area of increased density within the left lung (4 × 4 × 3 cm), consistent with a pulmonary infarction. In addition, a vascular lesion, consistent with a splenic infarct, was found in the inferior pole of the spleen. Doppler echocardiography of the hearth showed regular right chambers and left atrium and a slightly hypertrophic left ventricle with normal size and kinetics (ejection fraction: 55%). The age of the patient and the absence of serious concomitant cardiovascular diseases place the emphasis on the capacity of SARS-CoV-2 infection to be an independent cerebrovascular risk factor.

Imaging. a April 16, 2020; MRI of the brain: lesions in the right hemisphere affecting the territories of the anterior and the middle cerebral arteries. b May 5, 2020; MRI of the brain: same lesions in the right hemisphere shown in the previous image. d , e May 5, 2020; MRA showed an early duplication of the sphenoidal segment of the right middle cerebral artery, the branches of which are irregular with rosary bead-like aspect and reduction of blood flow in the middle cerebral artery. c April 20, 2020; CT of the abdomen: vascular lesion, consistent with a splenic infarct, found in the inferior pole of the spleen. f April 20, 2020; CT of the chest: basal subpleural area of increased density within the left lung (4 × 4 × 3 cm), consistent with a pulmonary infarction. MRA, magnetic resonance angiography; CT, computed tomography; MRI, magnetic resonance imaging.
The pandemic outbreak of novel SARS-CoV-2 infection has caused great concern among the services and authorities responsible for public health due to not only the mortality rate but also the danger of filling up hospital capacities in terms of ICU beds and acute non-ICU beds. In this regard, the nonrespiratory complications of COVID-19 should also be taken into great consideration, especially those that threaten patients’ lives and extend hospitalization times. Stroke is one of these complications, since a greater incidence of stroke among patients with COVID-19 than the non-COVID-19 population has been reported, and a preliminary case-control study demonstrated that SARS-CoV-2 infection represents a risk factor for acute ischemic stroke [ 14 ].
We found that the reported case is extremely interesting, since the woman is only 29 years old and considering how stroke in a young patient without other known risk factors is uncommon. Not only elderly people have higher risk factors associated with acute ischemic stroke or embolization vascular events [ 15 ], but it is also true that advanced age is strongly associated with severe COVID-19 and death. The severity of the disease is directly linked to immune dysregulation, cytokine storm, and acute inflammation state, which in turn are more common in patients who present immunosenescence [6].
Inflammation plays an important role in the occurrence of cardiovascular and cerebrovascular diseases since it favors atherosclerosis and affects plaque stability [ 16 ]. The ischemic stroke of the 29-year-old woman does not appear to be imputable to emboli originating a pre-existing atheromatous plaque, both for the age of the patient and for the absence of plaques at the Doppler ultrasound study of the supra-aortic trunks.
Most likely, COVID-19-associated hypercoagulability and endothelial dysfunction are the causes of ischemic stroke, as suggested by other studies and case reports [ 10, 13, 17 ]. Although the mechanisms by which SARS-CoV-2 infection leads to hypercoagulability are still being studied, current knowledge suggests that cross talk between inflammation and thrombosis has a crucial role [ 18 ]. The release of inflammatory cytokines leads to the activation of epithelial cells, monocytes, and macrophages. Direct infection of endothelial cells through the ACE2 receptor also leads to endothelial activation and dysfunction, expression of tissue factor, and platelet activation and increased levels of VWF and FVIII, all of which contribute to thrombin generation and fibrin clot formation [ 17 ]. The 29-year-old patient showed an increased level of D-dimer, which is a degradation product of cross-linked fibrin, indicating a global activation of hemostasis and fibrinolysis and conforming to the hypothesis of COVID-19-associated hypercoagulability. Endothelial activation and hypercoagulability are also confirmed by positivity to β2 glycoprotein antibodies. Anticardiolipin antibody and/or β2 glycoprotein antibody positivity has been reported in a few studies [ 17, 19, 20 ]. In addition, widespread thrombosis in SARS-CoV-2 infection could also be caused by neutrophil extracellular traps (NETs). Neutrophilia [ 21 ] and an elevated neutrophil-lymphocyte ratio [ 22 ] have been reported by numerous studies as predictive of worse disease outcomes, and recently, the contribution of NETs in the pathophysiology of COVID-19 was reported [ 23 ]. Thrombogenic involvement of NETs has been described in various settings of thrombosis, including stroke, myocardial infarction, and deep vein thrombosis [ 24 ]. The high neutrophil count found in our case does not exclude the hypothesis that NETs are involved in the pathogenesis of ischemic stroke.
Ischemic stroke in young patients without pre-existing cerebrovascular risk factors is very unusual. In this regard, our case of an ischemic stroke, reported in a 29-year-old woman, is very interesting. Although it is not possible to determine precisely when the thromboembolic event occurred, our case of stroke during COVID-19-related pneumonia seems to confirm that COVID-19 is an independent risk factor for acute ischemic stroke. The mechanisms by which coronavirus disease leads to stroke are still under study, but it is clear that hypercoagulability and endothelial activation play a key role. Testing for SARS-CoV-2 infection should be considered for patients who develop neurologic symptoms, but it is equally important to monitor COVID-19 patients during their hospitalization to find any neurological sign or symptom in a timely manner. Our case suggests that discovering neurological deficits in sedated patients promptly can be very difficult; for this reason, sedation in mechanically ventilated patients has to be considered only if strictly necessary. Performing serial laboratory testing and waking up the patient as soon as clinical conditions allow are strategies that should be taken into account.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editor-in-chief of this journal.
The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
No funding was received for the publication of this case report.
All authors agree with the contents of the manuscript and were fully involved in the study and preparation of the manuscript. All authors read and approved the final version of the manuscript. M.A. Mimmo, M.P. Lo Muzio, M. Delli Bergoli, and L. Amoruso collected the data. C. Avvantaggiato wrote the manuscript with support of N. Cinone, L. Santoro, and C. Ciritella. C. Avvantaggiato, A. Turitto, and L. Stuppiello researched and discussed the neurophysiological principles of this study. P. Fiore and A. Santamato supervised the project.

Email alerts
Citing articles via, suggested reading.
- Online ISSN 1662-680X
INFORMATION
- Contact & Support
- Information & Downloads
- Rights & Permissions
- Terms & Conditions
- Catalogue & Pricing
- Policies & Information
- People & Organization
- Stay Up-to-Date
- Regional Offices
- Community Voice
SERVICES FOR
- Researchers
- Healthcare Professionals
- Patients & Supporters
- Health Sciences Industry
- Medical Societies
- Agents & Booksellers
Karger International
- S. Karger AG
- P.O Box, CH-4009 Basel (Switzerland)
- Allschwilerstrasse 10, CH-4055 Basel
- Tel: +41 61 306 11 11
- Fax: +41 61 306 12 34
- Contact: Front Office
- Experience Blog
- Privacy Policy
- Terms of Use
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Amani Baidwan, Kendyl Egizi and Alysha Payne
Darrell Jackson, 81 year old male, came to the Emergency Department at Los Robles Hospital by ambulance after he collapsed in a coffee shop. Upon arrival he presented with left sided weakness, facial drooping, and aphasia. He was diagnosed with an ischemic stroke, right humerus head fracture, and right wrist fracture. The priority of care upon initial presentation to the Emergency Department included a CT scan, frequent monitoring of vital signs, starting a peripheral IV, drawing labs, assessing blood glucose, and an EKG. The nurse in the Emergency Department continuously monitored Mr. Jackson’s neurological status, changes in level of consciousness and signs and symptoms of complications.
After much discussion with the family, consent was given for tissue plasminogen activator (tPA). After tPA was given, Mr. Jackson converted to a hemorrhagic stroke, which is one of many risks associated with administration of tPA. He was His computed tomographic scans (CT) revealed intraparenchymal hematoma in both cerebral hemispheres and a large hemorrhage in the left parietal lobe. In the Intensive care Unit, Mr. Jackson was on a ventilator, had a RASS score of -5 and was only responsive to noxious stimuli. Priority in plan of care included airway management and a CPAP trial to begin weaning protocols. The CPAP trial failed, and a tracheostomy was placed. Mr.Jackson was then transferred to the Progressive Care Unit to continue treatment where the NG tube was removed and a PEG tube was inserted. Mr. Jackson has no known allergies and has a history of hypertension, dementia, Parkinson’s disease, stroke, diabetes, GERD, BPH, hypophosphatemia and anemia.
Collaborative interventions are necessary from all healthcare providers, such as physicians, nurses, physical therapy, occupational therapy, speech therapy, case management and social work, to adequate;y care for Mr. Jackson. Case management has been working closely with the family to provide necessary resources to continue care for Mr. Jackson after discharge from the hospital. Mr. Jackson was discharged home with home health after 3 weeks in the hospital. His condition prior to discharge was as follows: A/O x 3 with mild cognitive deficits, speech impairment and left sided weakness.
Discussion Questions
- What is the difference between an ischemic stroke and hemorrhagic stroke?
- What are some of the risk associated with tissue plasminogen activator (tPA) that the nurse would need to assess for and educate the patient about?
- What are some of the psychological needs the nurse should anticipate for a patient who has experienced a stroke?
Nursing Case Studies by and for Student Nurses Copyright © by jaimehannans is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book
Explore prestigious scientific journals and award and funding opportunities to advance your research.
Access practice-improvement tools, including guidelines, measures, Axon Registry, and practice management resources.
Learn to effectively advocate on behalf of neurologists and their patients, and access AAN position and policy statements.
Loading... please wait
We’re experiencing unusually high levels of traffic. Thank you for your patience.
Inpatient Stroke Case Studies
Inpatient e/m case studies.
Case study of a stroke patient at varying visit levels to better understand code selection for inpatient encounters under the revised guidelines for 2024.
67-year-old Female with Stroke
Total time* for Inpatient E/M in 2023
Refer to the following tables for correct code selection when billing based on time for inpatient E/M Services:
*Total time includes non face-to-face time on the date of service
Day 1: Critical Care (99291)
A 67-year-old woman with hypertension and diabetes presents to the emergency department with abrupt onset of left hemiparesis 45 minutes ago.
Pre-evaluation : Discussed presentation and vital signs with ED provider (3 mins).
Face-to-face evaluation : Performed medically appropriate history and exam. She has a dense left hemiparesis and an NIH Stroke Scale score of 8. Thrombolysis safety criteria reviewed (7 mins).
Post-evaluation : Non-contrast head CT, CTA of head and neck, and lab results reviewed in the ED. Case discussed with ED provider and thrombolysis recommended. Consultation documented in the ED (25 mins).
Total time : 35 minutes.
Critical Care Coding
According to the 2024 CPT code set, a provider may bill for critical care when the following requirements are met:
- A critical condition: one that acutely impairs a vital organ system with a high probability of imminent or life-threatening deterioration. This includes, for example, central nervous system failure.
- Direct delivery of critical care: high complexity decision-making to assess, manipulate, and support vital systems to treat organ system failure or prevent further life-threatening deterioration.
- At least 30 minutes of time spent solely in the care of the patient. It does not need to be continuous, and it includes both time at the bedside and time spent on the same floor or unit engaged in work directly related to the patient’s care (e.g., documenting critical care, reviewing test results, discussing care with other providers, obtaining history, or discussing treatments or treatment limitations with surrogates when the patient lacks the capacity to do so).
Specific critical care credentials are not required to bill critical care. Critical care is usually provided in a critical care area such as an intensive care unit or emergency department, but this is not always the case (for example, critical care provided to a deteriorating patient in a non-critical care unit).
Other examples of critical care might include:
- Evaluating a patient with status epilepticus and prescribing anti-epileptic drugs or sedative infusions,
- Evaluating a patient with acute respiratory failure from neuromuscular disease and prescribing plasmapheresis,
- Evaluating a patient with coma after cardiac arrest and discussing prognosis, treatment, and goals of care with surrogates (documenting the patient’s lack of capacity to participate)
Critical care, 30-74 minutes CPT 99291 is justified based on the above documentation, although E&M codes (e.g., 99223) associated with fewer wRVUs and lower reimbursement could be used as well.
Day 2: Subsequent Hospital Inpatient Care
Pre-rounds : Reviewed vitals, labs, and studies (LDL, Hemoglobin A1c, EKG, TTE). Review and document independent interpretation of MRI (8 mins).
On Rounds : Performed medically appropriate history and exam. The patient’s symptoms and findings improved somewhat overnight. Patient counseled about stroke evaluation and secondary prevention (10 mins).
Post-rounds : Order atorvastatin, order diabetes consult for management of diabetes. Document discussion with case management possible need for acute inpatient rehabilitation. Documentation completed (10 mins).
Total time : 28 minutes
In this situation, billing according to MDM would be associated with higher reimbursement.
Day 3: Discharge Day Management (By Primary Service)
Pre-rounds : Reviewed vitals, daily CBC and BMP, nursing notes and PT/OT notes (5 mins).
On Rounds : Performed medically appropriate history and exam. The patient reports continued slight improvement in symptoms and requests counseling on how complementary and alternative medicine might help manage her chronic conditions (15 mins).
Post-rounds : Prescribe antiplatelet agent, antidiabetic medications, and antihypertensives. Prepare discharge paperwork and document discharge summary (15 mins).
Total time : 35 minutes
Discharge Day Management Coding (Inpatient or Observation)
Discharge CPTs are selected based on total (face-to-face and non-face-to-face) time, not MDM:
- 99238: 30 minutes or less
- 99239: 31 minutes or more
Discharge CPTs would be used by the primary attending service (e.g., a Neurohospitalist service). Consulting services would continue to choose Subsequent Day codes based on time or MDM.
Discharge Day Management, 31 minutes or more CPT 99239
Disclaimer: The billing and coding information provided by the American Academy of Neurology and its affiliates (collectively, “Academy”) are assessments of clinical information provided as an educational service. The information (1) is not clinical advice; (2) does not account for how private payers cover and reimburse procedures or services*; (3) is not continually updated and may not reflect the most current clinical information (new clinical information may emerge between the time information is developed and when it is published or read); and (4) is not a substitute for the independent professional judgment of the treating provider, who is responsible for correctly coding procedures and services.
Using this information is voluntary. The Academy is providing the information on an “as is” basis and makes no warranty, expressed or implied, regarding the information. The Academy specifically disclaims any warranties of merchantability or fitness for a particular use or purpose. The Academy assumes no responsibility for any injury or damage to persons or property arising out of or related to any use of this information or for any errors or omissions.
*The Academy recommends always checking private payer policies before rendering procedures or services
This presents an analysis of a case of Ischemic stroke in terms of possible etiology, pathophysiology, drug analysis and nursing care
New? Questions? Start Here!
- Information Hub
- Important Notices
- Need Access to Evidence
- Communities & Collections
- Publication Date
- Posting Date
- Subject(CINAHL)
- Item Format
- Level of Evidence
- Research Approach
- Sigma Chapters
- Author Affiliations
- Review Type
Ischemic stroke: A case study
View file(s).
Author Information
- Martinez, Rudolf Cymorr Kirby P. ;
- Sigma Affiliation
Item Information
Item link - use this link for citations and online mentions..
Clinical Focus: Adult Medical/Surgical
Repository Posting Date
Type information, category information, original publication info, conference information, rights holder.
All rights reserved by the author(s) and/or publisher(s) listed in this item record unless relinquished in whole or part by a rights notation or a Creative Commons License present in this item record.
All permission requests should be directed accordingly and not to the Sigma Repository.
All submitting authors or publishers have affirmed that when using material in their work where they do not own copyright, they have obtained permission of the copyright holder prior to submission and the rights holder has been acknowledged as necessary.
Stroke Case Study (45 min)
Watch More! Unlock the full videos with a FREE trial
Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
Mrs. Blossom is a 57-year-old female who presented to the Emergency Room with new onset Atrial Fibrillation with Rapid Ventricular Response (RVR). She is admitted to the cardiac telemetry unit after being converted to normal sinus rhythm with a calcium channel blocker (diltiazem). When you enter the room to assess Mrs. Blossom, her daughter looks at you concerned and says “mom’s acting kinda funny.”
What nursing assessments should be completed at this time?
- Full set of vital signs (Temp, HR, BP, RR, SpO2)
- Should probably get a 12-lead EKG
- Assess symptoms using PQRST or OLDCARTS
You assess Mrs. Blossom to find she has a left sided facial droop, slurred speech, and is unable to hold her left arm up for more than 3 seconds.
What is/are your priority nursing action(s) at this time?
- Call a Code Stroke (or whatever the equivalent is at your facility) to initiate response of the neurologist or Stroke team.
- Notify the charge nurse to help you obtain emergency equipment if you don’t already have it at the bedside to be prepared in case of emergency
What may be occurring in Mrs. Blossom?
- She may be having a stroke
You call a Code Stroke and notify the charge nurse for help. You obtain suction to have at bedside just in case. The neurologist arrives at bedside within 7 minutes to assess Mrs. Blossom. He notes her NIH Stroke Scale score is 32. He orders a STAT CT scan, which shows there is no obvious bleed in the brain.
What are the possible interventions for Mrs. Blossom at this time?
- Since there is no bleed evident on scan, Mrs. Blossom would qualify for a thrombolytic like tPA (alteplase) or for surgical intervention, as long as there are no contraindications
What are the contraindications for thrombolytics like tPA (alteplase)?
- Recent surgery, current or recent GI bleed within the last 3 months, excessive hypertension, evidence of cerebral hemorrhage
You administer tPA per protocol, initiate q15min vital signs and neuro checks. You stay with the patient to continue to monitor her symptoms.
What are possible complications of tPA administration? What should you monitor for?
- Bleeding, especially into the brain or a GI bleed
- She may bruise easily or bleed from IV sites or her gums
- Monitor for s/s bleeding or worsening stroke symptoms, which may indicate a hemorrhagic stroke has developed.
After 2 hours, Mrs. Blossom is showing signs of improvement. She is able to speak more clearly, though with a slight slur. She is still slightly weak on the left side, but is able to hold her arm up for 10 seconds now. Her NIHSS is now 6. Mrs. Blossom’s daughter asks you why this happened.
What would you explain has happened to Mrs. Blossom physiologically?
- Because of her new onset atrial fibrillation, the blood was likely pooling in her atria because they were just quivering and not contracting. When blood pools, it clots. When she was converted back into a normal rhythm and her atria began contracting again, that likely dislodged a clot, which went to her brain.
- The clot in her brain caused brain tissue to die → ischemic stroke.
Two days later, Mrs. Blossom has recovered fully. She will be discharged today on Clopidogrel and Aspirin, plus a calcium channel blocker, with a follow up appointment in 1 week to see the neurologist.
What education topics should be included in the discharge teaching for Mrs. Blossom and her family?
- Anticoagulant therapy is imperative to prevent further clots from forming within Mrs. Blossom’s atria if she stays in Atrial Fibrillation.
- They should be taught the signs of a stroke (FAST) and call 911 if they notice them.
- They should be taught signs of Atrial Fibrillation with RVR and be sure to go to the hospital if this occurs – the patient is at higher risk for stroke.
- Medication instructions for calcium channel blockers and anticoagulants.
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
Nursing Case Studies

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions
Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions
Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.

Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Global health
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 13, Issue 8
- Clinical course of a 66-year-old man with an acute ischaemic stroke in the setting of a COVID-19 infection
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-7441-6952 Saajan Basi 1 , 2 ,
- Mohammad Hamdan 1 and
- Shuja Punekar 1
- 1 Department of Stroke and Acute Medicine , King's Mill Hospital , Sutton-in-Ashfield , UK
- 2 Department of Acute Medicine , University Hospitals of Derby and Burton , Derby , UK
- Correspondence to Dr Saajan Basi; saajan.basi{at}nhs.net
A 66-year-old man was admitted to hospital with a right frontal cerebral infarct producing left-sided weakness and a deterioration in his speech pattern. The cerebral infarct was confirmed with CT imaging. The only evidence of respiratory symptoms on admission was a 2 L oxygen requirement, maintaining oxygen saturations between 88% and 92%. In a matter of hours this patient developed a greater oxygen requirement, alongside reduced levels of consciousness. A positive COVID-19 throat swab, in addition to bilateral pneumonia on chest X-ray and lymphopaenia in his blood tests, confirmed a diagnosis of COVID-19 pneumonia. A proactive decision was made involving the patients’ family, ward and intensive care healthcare staff, to not escalate care above a ward-based ceiling of care. The patient died 5 days following admission under the palliative care provided by the medical team.
- respiratory medicine
- infectious diseases
- global health
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bcr-2020-235920
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) is a new strain of coronavirus that is thought to have originated in December 2019 in Wuhan, China. In a matter of months, it has erupted from non-existence to perhaps the greatest challenge to healthcare in modern times, grinding most societies globally to a sudden halt. Consequently, the study and research into SARS-CoV-2 is invaluable. Although coronaviruses are common, SARS-CoV-2 appears to be considerably more contagious. The WHO figures into the 2003 SARS-CoV-1 outbreak, from November 2002 to July 2003, indicate a total of 8439 confirmed cases globally. 1 In comparison, during a period of 4 months from December 2019 to July 2020, the number of global cases of COVID-19 reached 10 357 662, increasing exponentially, illustrating how much more contagious SARS-CoV-2 has been. 2
Previous literature has indicated infections, and influenza-like illness have been associated with an overall increase in the odds of stroke development. 3 There appears to be a growing correlation between COVID-19 positive patients presenting to hospital with ischaemic stroke; however, studies investigating this are in progress, with new data emerging daily. This patient report comments on and further characterises the link between COVID-19 pneumonia and the development of ischaemic stroke. At the time of this patients’ admission, there were 95 positive cases from 604 COVID-19 tests conducted in the local community, with a predicted population of 108 000. 4 Only 4 days later, when this patient died, the figure increased to 172 positive cases (81% increase), illustrating the rapid escalation towards the peak of the pandemic, and widespread transmission within the local community ( figure 1 ). As more cases of ischaemic stroke in COVID-19 pneumonia patients arise, the recognition and understanding of its presentation and aetiology can be deciphered. Considering the virulence of SARS-CoV-2 it is crucial as a global healthcare community, we develop this understanding, in order to intervene and reduce significant morbidity and mortality in stroke patients.
- Download figure
- Open in new tab
- Download powerpoint
A graph showing the number of patients with COVID-19 in the hospital and in the community over time.
Case presentation
A 66-year-old man presented to the hospital with signs of left-sided weakness. The patient had a background of chronic obstructive pulmonary disease (COPD), atrial fibrillation and had one previous ischaemic stroke, producing left-sided haemiparesis, which had completely resolved. He was a non-smoker and lived in a house. The patient was found slumped over on the sofa at home on 1 April 2020, by a relative at approximately 01:00, having been seen to have no acute medical illness at 22:00. The patients’ relative initially described disorientation and agitation with weakness noted in the left upper limb and dysarthria. At the time of presentation, neither the patient nor his relative identified any history of fever, cough, shortness of breath, loss of taste, smell or any other symptoms; however, the patient did have a prior admission 9 days earlier with shortness of breath.
The vague nature of symptoms, entwined with considerable concern over approaching the hospital, due to the risk of contracting COVID-19, created a delay in the patients’ attendance to the accident and emergency department. His primary survey conducted at 09:20 on 1 April 2020 demonstrated a patent airway, with spontaneous breathing and good perfusion. His Glasgow Coma Scale (GCS) score was 15 (a score of 15 is the highest level of consciousness), his blood glucose was 7.2, and he did not exhibit any signs of trauma. His abbreviated mental test score was 7 out of 10, indicating a degree of altered cognition. An ECG demonstrated atrial fibrillation with a normal heart rate. His admission weight measured 107 kg. At 09:57 the patient required 2 L of nasal cannula oxygen to maintain his oxygen saturations between 88% and 92%. He started to develop agitation associated with an increased respiratory rate at 36 breaths per minute. On auscultation of his chest, he demonstrated widespread coarse crepitation and bilateral wheeze. Throughout he was haemodynamically stable, with a systolic blood pressure between 143 mm Hg and 144 mm Hg and heart rate between 86 beats/min and 95 beats/min. From a neurological standpoint, he had a mild left facial droop, 2/5 power in both lower limbs, 2/5 power in his left upper limb and 5/5 power in his right upper limb. Tone in his left upper limb had increased. This patient was suspected of having COVID-19 pneumonia alongside an ischaemic stroke.
Investigations
A CT of his brain conducted at 11:38 on 1 April 2020 ( figure 2 ) illustrated an ill-defined hypodensity in the right frontal lobe medially, with sulcal effacement and loss of grey-white matter. This was highly likely to represent acute anterior cerebral artery territory infarction. Furthermore an oval low-density area in the right cerebellar hemisphere, that was also suspicious of an acute infarction. These vascular territories did not entirely correlate with his clinical picture, as limb weakness is not as prominent in anterior cerebral artery territory ischaemia. Therefore this left-sided weakness may have been an amalgamation of residual weakness from his previous stroke, in addition to his acute cerebral infarction. An erect AP chest X-ray with portable equipment ( figure 3 ) conducted on the same day demonstrated patchy peripheral consolidation bilaterally, with no evidence of significant pleural effusion. The pattern of lung involvement raised suspicion of COVID-19 infection, which at this stage was thought to have provoked the acute cerebral infarct. Clinically significant blood results from 1 April 2020 demonstrated a raised C-reactive protein (CRP) at 215 mg/L (normal 0–5 mg/L) and lymphopaenia at 0.5×10 9 (normal 1×10 9 to 3×10 9 ). Other routine blood results are provided in table 1 .
CT imaging of this patients’ brain demonstrating a wedge-shaped infarction of the anterior cerebral artery territory.
Chest X-ray demonstrating the bilateral COVID-19 pneumonia of this patient on admission.
- View inline
Clinical biochemistry and haematology blood results of the patient
Interestingly the patient, in this case, was clinically assessed in the accident and emergency department on 23 March 2020, 9 days prior to admission, with symptoms of shortness of breath. His blood results from this day showed a CRP of 22 mg/L and a greater lymphopaenia at 0.3×10 9 . He had a chest X-ray ( figure 4 ), which indicated mild radiopacification in the left mid zone. He was initially treated with intravenous co-amoxiclav and ciprofloxacin. The following day he had minimal symptoms (CURB 65 score 1 for being over 65 years). Given improving blood results (declining CRP), he was discharged home with a course of oral amoxicillin and clarithromycin. As national governmental restrictions due to COVID-19 had not been formally announced until 23 March 2020, and inconsistencies regarding personal protective equipment training and usage existed during the earlier stages of this rapidly evolving pandemic, it is possible that this patient contracted COVID-19 within the local community, or during his prior hospital admission. It could be argued that the patient had early COVID-19 signs and symptoms, having presented with shortness of breath, lymphopaenia, and having had subtle infective chest X-ray changes. The patient explained he developed a stagnant productive cough, which began 5 days prior to his attendance to hospital on 23 March 2020. He responded to antibiotics, making a full recovery following 7 days of treatment. This information does not assimilate with the typical features of a COVID-19 infection. A diagnosis of community-acquired pneumonia or infective exacerbation of COPD seem more likely. However, given the high incidence of COVID-19 infections during this patients’ illness, an exposure and early COVID-19 illness, prior to the 23 March 2020, cannot be completely ruled out.
Chest X-ray conducted on prior admission illustrating mild radiopacification in the left mid zone.
On the current admission, this patient was managed with nasal cannula oxygen at 2 L. By the end of the day, this had progressed to a venturi mask, requiring 8 L of oxygen to maintain oxygen saturation. He had also become increasingly drowsy and confused, his GCS declined from 15 to 12. However, the patient was still haemodynamically stable, as he had been in the morning. An arterial blood gas demonstrated a respiratory alkalosis (pH 7.55, pCO 2 3.1, pO 2 6.7 and HCO 3 24.9, lactate 1.8, base excess 0.5). He was commenced on intravenous co-amoxiclav and ciprofloxacin, to treat a potential exacerbation of COPD. This patient had a COVID-19 throat swab on 1 April 2020. Before the result of this swab, an early discussion was held with the intensive care unit staff, who decided at 17:00 on 1 April 2020 that given the patients presentation, rapid deterioration, comorbidities and likely COVID-19 diagnosis he would not be for escalation to the intensive care unit, and if he were to deteriorate further the end of life pathway would be most appropriate. The discussion was reiterated to the patients’ family, who were in agreement with this. Although he had evidence of an ischaemic stroke on CT of his brain, it was agreed by all clinicians that intervention for this was not as much of a priority as providing optimal palliative care, therefore, a minimally invasive method of treatment was advocated by the stroke team. The patient was given 300 mg of aspirin and was not a candidate for fibrinolysis.
Outcome and follow-up
The following day, before the throat swab result, had appeared the patient deteriorated further, requiring 15 L of oxygen through a non-rebreather face mask at 60% FiO 2 to maintain his oxygen saturation, at a maximum of 88% overnight. At this point, he was unresponsive to voice, with a GCS of 5. Although, he was still haemodynamically stable, with a blood pressure of 126/74 mm Hg and a heart rate of 98 beats/min. His respiratory rate was 30 breaths/min. His worsening respiratory condition, combined with his declining level of consciousness made it impossible to clinically assess progression of the neurological deficit generated by his cerebral infarction. Moreover, the patient was declining sharply while receiving the maximal ward-based treatment available. The senior respiratory physician overseeing the patients’ care decided that a palliative approach was in this his best interest, which was agreed on by all parties. The respiratory team completed the ‘recognising dying’ documentation, which signified that priorities of care had shifted from curative treatment to palliative care. Although the palliative team was not formally involved in the care of the patient, the patient received comfort measures without further attempts at supporting oxygenation, or conduction of regular clinical observations. The COVID-19 throat swab confirmed a positive result on 2 April 2020. The patient was treated by the medical team under jurisdiction of the hospital palliative care team. This included the prescribing of anticipatory medications and a syringe driver, which was established on 3 April 2020. His antibiotic treatment, non-essential medication and intravenous fluid treatment were discontinued. His comatose condition persisted throughout the admission. Once the patients’ GCS was 5, it did not improve. The patient was pronounced dead by doctors at 08:40 on 5 April 2020.
SARS-CoV-2 is a type of coronavirus that was first reported to have caused pneumonia-like infection in humans on 3 December 2019. 5 As a group, coronaviruses are a common cause of upper and lower respiratory tract infections (especially in children) and have been researched extensively since they were first characterised in the 1960s. 6 To date, there are seven coronaviruses that are known to cause infection in humans, including SARS-CoV-1, the first known zoonotic coronavirus outbreak in November 2002. 7 Coronavirus infections pass through communities during the winter months, causing small outbreaks in local communities, that do not cause significant mortality or morbidity.
SARS-CoV-2 strain of coronavirus is classed as a zoonotic coronavirus, meaning the virus pathogen is transmitted from non-humans to cause disease in humans. However the rapid spread of SARS-CoV-2 indicates human to human transmission is present. From previous research on the transmission of coronaviruses and that of SARS-CoV-2 it can be inferred that SARS-CoV-2 spreads via respiratory droplets, either from direct inhalation, or indirectly touching surfaces with the virus and exposing the eyes, nose or mouth. 8 Common signs and symptoms of the COVID-19 infection identified in patients include high fevers, severe fatigue, dry cough, acute breathing difficulties, bilateral pneumonia on radiological imaging and lymphopaenia. 9 Most of these features were identified in this case study. The significance of COVID-19 is illustrated by the speed of its global spread and the potential to cause severe clinical presentations, which as of April 2020 can only be treated symptomatically. In Italy, as of mid-March 2020, it was reported that 12% of the entire COVID-19 positive population and 16% of all hospitalised patients had an admission to the intensive care unit. 10
The patient, in this case, illustrates the clinical relevance of understanding COVID-19, as he presented with an ischaemic stroke underlined by minimal respiratory symptoms, which progressed expeditiously, resulting in acute respiratory distress syndrome and subsequent death.
Our case is an example of a new and ever-evolving clinical correlation, between patients who present with a radiological confirmed ischaemic stroke and severe COVID-19 pneumonia. As of April 2020, no comprehensive data of the relationship between ischaemic stroke and COVID-19 has been published, however early retrospective case series from three hospitals in Wuhan, China have indicated that up to 36% of COVID-19 patients had neurological manifestations, including stroke. 11 These studies have not yet undergone peer review, but they tell us a great deal about the relationship between COVID-19 and ischaemic stroke, and have been used to influence the American Heart Associations ‘Temporary Emergency Guidance to US Stroke Centres During the COVID-19 Pandemic’. 12
The relationship between similar coronaviruses and other viruses, such as influenza in the development of ischaemic stroke has previously been researched and provide a basis for further investigation, into the prominence of COVID-19 and its relation to ischaemic stroke. 3 Studies of SARS-CoV-2 indicate its receptor-binding region for entry into the host cell is the same as ACE2, which is present on endothelial cells throughout the body. It may be the case that SARS-CoV-2 alters the conventional ability of ACE2 to protect endothelial function in blood vessels, promoting atherosclerotic plaque displacement by producing an inflammatory response, thus increasing the risk of ischaemic stroke development. 13
Other hypothesised reasons for stroke development in COVID-19 patients are the development of hypercoagulability, as a result of critical illness or new onset of arrhythmias, caused by severe infection. Some case studies in Wuhan described immense inflammatory responses to COVID-19, including elevated acute phase reactants, such as CRP and D-dimer. Raised D-dimers are a non-specific marker of a prothrombotic state and have been associated with greater morbidity and mortality relating to stroke and other neurological features. 14
Arrhythmias such as atrial fibrillation had been identified in 17% of 138 COVID-19 patients, in a study conducted in Wuhan, China. 15 In this report, the patient was known to have atrial fibrillation and was treated with rivaroxaban. The acute inflammatory state COVID-19 is known to produce had the potential to create a prothrombotic environment, culminating in an ischaemic stroke.
Some early case studies produced in Wuhan describe patients in the sixth decade of life that had not been previously noted to have antiphospholipid antibodies, contain the antibodies in blood results. They are antibodies signify antiphospholipid syndrome; a prothrombotic condition. 16 This raises the hypothesis concerning the ability of COVID-19 to evoke the creation of these antibodies and potentiate thrombotic events, such as ischaemic stroke.
No peer-reviewed studies on the effects of COVID-19 and mechanism of stroke are published as of April 2020; therefore, it is difficult to evidence a specific reason as to why COVID-19 patients are developing neurological signs. It is suspected that a mixture of the factors mentioned above influence the development of ischaemic stroke.
If we delve further into this patients’ comorbid state exclusive to COVID-19 infection, it can be argued that this patient was already at a relatively higher risk of stroke development compared with the general population. The fact this patient had previously had an ischaemic stroke illustrates a prior susceptibility. This patient had a known background of hypertension and atrial fibrillation, which as mentioned previously, can influence blood clot or plaque propagation in the development of an acute ischaemic event. 15 Although the patient was prescribed rivaroxaban as an anticoagulant, true consistent compliance to rivaroxaban or other medications such as amlodipine, clopidogrel, candesartan and atorvastatin cannot be confirmed; all of which can contribute to the reduction of influential factors in the development of ischaemic stroke. Furthermore, the fear of contracting COVID-19, in addition to his vague symptoms, unlike his prior ischaemic stroke, which demonstrated dense left-sided haemiparesis, led to a delay in presentation to hospital. This made treatment options like fibrinolysis unachievable, although it can be argued that if he was already infected with COVID-19, he would have still developed life-threatening COVID-19 pneumonia, regardless of whether he underwent fibrinolysis. It is therefore important to consider that if this patient did not contract COVID-19 pneumonia, he still had many risk factors that made him prone to ischaemic stroke formation. Thus, we must consider whether similar patients would suffer from ischaemic stroke, regardless of COVID-19 infection and whether COVID-19 impacts on the severity of the stroke as an entity.
Having said this, the management of these patients is dependent on the likelihood of a positive outcome from the COVID-19 infection. Establishing the ceiling of care is crucial, as it prevents incredibly unwell or unfit patients’ from going through futile treatments, ensuring respect and dignity in death, if this is the likely outcome. It also allows for the provision of limited or intensive resources, such as intensive care beds or endotracheal intubation during the COVID-19 pandemic, to those who are assessed by the multidisciplinary team to benefit the most from their use. The way to establish this ceiling of care is through an early multidisciplinary discussion. In this case, the patient did not convey his wishes regarding his care to the medical team or his family; therefore it was decided among intensive care specialists, respiratory physicians, stroke physicians and the patients’ relatives. The patient was discussed with the intensive care team, who decided that as the patient sustained two acute life-threatening illnesses simultaneously and had rapidly deteriorated, ward-based care with a view to palliate if the further deterioration was in the patients’ best interests. These decisions were not easy to make, especially as it was on the first day of presentation. This decision was made in the context of the patients’ comorbidities, including COPD, the patients’ age, and the availability of intensive care beds during the steep rise in intensive care admissions, in the midst of the COVID-19 pandemic ( figure 1 ). Furthermore, the patients’ rapid and permanent decline in GCS, entwined with the severe stroke on CT imaging of the brain made it more unlikely that significant and permanent recovery could be achieved from mechanical intubation, especially as the damage caused by the stroke could not be significantly reversed. As hospitals manage patients with COVID-19 in many parts of the world, there may be tension between the need to provide higher levels of care for an individual patient and the need to preserve finite resources to maximise the benefits for most patients. This patient presented during a steep rise in intensive care admissions, which may have influenced the early decision not to treat the patient in an intensive care setting. Retrospective studies from Wuhan investigating mortality in patients with multiple organ failure, in the setting of COVID-19, requiring intubation have demonstrated mortality can be up to 61.5%. 17 The mortality risk is even higher in those over 65 years of age with respiratory comorbidities, indicating why this patient was unlikely to survive an admission to the intensive care unit. 18
Regularly updating the patients’ family ensured cooperation, empathy and sympathy. The patients’ stroke was not seen as a priority given the severity of his COVID-19 pneumonia, therefore the least invasive, but most appropriate treatment was provided for his stroke. The British Association of Stroke Physicians advocate this approach and also request the notification to their organisation of COVID-19-related stroke cases, in the UK. 19
Learning points
SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) is one of seven known coronaviruses that commonly cause upper and lower respiratory tract infections. It is the cause of the 2019–2020 global coronavirus pandemic.
The significance of COVID-19 is illustrated by the rapid speed of its spread globally and the potential to cause severe clinical presentations, such as ischaemic stroke.
Early retrospective data has indicated that up to 36% of COVID-19 patients had neurological manifestations, including stroke.
Potential mechanisms behind stroke in COVID-19 patients include a plethora of hypercoagulability secondary to critical illness and systemic inflammation, the development of arrhythmia, alteration to the vascular endothelium resulting in atherosclerotic plaque displacement and dehydration.
It is vital that effective, open communication between the multidisciplinary team, patient and patients relatives is conducted early in order to firmly establish the most appropriate ceiling of care for the patient.
- Cannine M , et al
- Wunderink RG
- van Doremalen N ,
- Bushmaker T ,
- Morris DH , et al
- Wang X-G , et al
- Grasselli G ,
- Pesenti A ,
- Wang M , et al
- American Stroke Assocation, 2020
- Zhang Y-H ,
- Zhang Y-huan ,
- Dong X-F , et al
- Li X , et al
- Hu C , et al
- Zhang S , et al
- Jiang B , et al
- Xu J , et al
- British Association of Stroke Physicians
Contributors SB was involved in the collecting of information for the case, the initial written draft of the case and researching existing data on acute stroke and COVID-19. He also edited drafts of the report. MH was involved in reviewing and editing drafts of the report and contributing new data. SP oversaw the conduction of the project and contributed addition research papers.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Next of kin consent obtained.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Patient Education

Image courtesy of https://www.acls.net/acls-suspected-stroke-algorithm.htm

- Open access
- Published: 01 May 2024
Triglyceride-glucose index as a potential predictor for in-hospital mortality in critically ill patients with intracerebral hemorrhage: a multicenter, case–control study
- Yang Yang 1 na1 ,
- Shengru Liang 2 na1 ,
- Jiangdong Liu 1 na1 ,
- Minghao Man 3 ,
- Dengfeng Jia 1 ,
- Jianwei Li 1 ,
- Xiaoxi Tian 1 na2 &
- Lihong Li 1 na2
BMC Geriatrics volume 24 , Article number: 385 ( 2024 ) Cite this article
229 Accesses
Metrics details
The correlation between the triglyceride-glucose index (TyG) and the prognosis of ischemic stroke has been well established. This study aims to assess the influence of the TyG index on the clinical outcomes of critically ill individuals suffering from intracerebral hemorrhage (ICH).
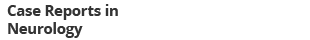
Patients diagnosed with ICH were retrospectively retrieved from the Medical Information Mart for Intensive Care (MIMIC-IV) and the eICU Collaborative Research Database (eICU-CRD). Various statistical methods, including restricted cubic spline (RCS) regression, multivariable logistic regression, subgroup analysis, and sensitivity analysis, were employed to examine the relationship between the TyG index and the primary outcomes of ICH.
A total of 791 patients from MIMIC-IV and 1,113 ones from eICU-CRD were analyzed. In MIMIC-IV, the in-hospital and ICU mortality rates were 14% and 10%, respectively, while in eICU-CRD, they were 16% and 8%. Results of the RCS regression revealed a consistent linear relationship between the TyG index and the risk of in-hospital and ICU mortality across the entire study population of both databases. Logistic regression analysis revealed a significant positive association between the TyG index and the likelihood of in-hospital and ICU death among ICH patients in both databases. Subgroup and sensitivity analysis further revealed an interaction between patients' age and the TyG index in relation to in-hospital and ICU mortality among ICH patients. Notably, for patients over 60 years old, the association between the TyG index and the risk of in-hospital and ICU mortality was more pronounced compared to the overall study population in both MIMIC-IV and eICU-CRD databases, suggesting a synergistic effect between old age (over 60 years) and the TyG index on the in-hospital and ICU mortality of patients with ICH.
Conclusions
This study established a positive correlation between the TyG index and the risk of in-hospital and ICU mortality in patients over 60 years who diagnosed with ICH, suggesting that the TyG index holds promise as an indicator for risk stratification in this patient population.
Peer Review reports
Introduction
Spontaneous, nontraumatic, intracerebral hemorrhage (ICH) is a catastrophic disease making up approximately 10–20% of all types of stroke [ 1 ]. Epidemiological data indicate that 30% of ICH patients requiring intensive care unit (ICU) management and 40% of them die within 30 days [ 2 ]. Despite ongoing research and advancements in this medical field, effective therapeutic options for improving the prognosis of patients with ICH are still lacking [ 3 ]. Consequently, there is an urgent need to identify remediable factors that may impact the outcomes of ICH, as this information could potentially lead to the development of new therapeutic targets.
Insulin resistance (IR), a pathological condition where tissue does not respond normally to insulin stimulation, plays a crucial role in the development of metabolic disorders [ 4 ]. More importantly, studies have revealed that compared with peripheral tissue, IR appears earlier in the central nervous system, indicating that brain is more vulnerable to IR, especially under various pathological states such as ICH and ischemic stroke (IS) [ 5 ]. Therefore, the indicators associated with IR may be closely related to the initiation of ICH and its prognosis.
The triglyceride-glucose (TyG) index, consisting of fasting triglyceride (FTG) and fasting blood glucose (FBG), is a valuable tool for analyzing lipid and glucose metabolism [ 6 , 7 ]. It is also recognized as an accurate indicator of IR [ 8 , 9 ]. Some researchers have observed a positive correlation between the TyG index and the incidence and mortality rates of progressed coronary artery disease [ 10 , 11 ]. Additional studies have indicated that the TyG index may have the potential to forecast negative cardiovascular events in individuals with coronary artery disease [ 12 ]. Moreover, multiple studies have demonstrated the predictive ability of the TyG index for the onset and mortality of IS [ 13 , 14 ]. These findings collectively highlight the association of the TyG index with cardiovascular and cerebrovascular diseases. However, the relationship between ICH and the TyG index, as well as the prognostic role of the TyG index in this condition, remains unexplored.
Therefore, the objective of this study is to evaluate the impact of the TyG index on the prognosis of critically ill patients with ICH, which may establish its potential utility as a risk stratification tool in ICH cases.
Data sources
Data used in this study were extracted from the Medical Information Mart for Intensive Care (MIMIC-IV version 2.2) and the eICU Collaborative Research Database (eICU-CRD) [ 15 , 16 ]. MIMIC-IV consists of medical records between 2008 and 2019 from over 190,000 patients who were treated in various types of ICU of the Beth Israel Deaconess Medical Center. The eICU-CRD included medical records of over 200,000 patients receiving clinical management in ICUs from over 200 medical centers between 2014 and 2015. Since data in these two databases are de-identified to hide patients’ information, the informed consent and ethics approval are not essential.
Data extraction
Structure query language (SQL), executed on the PostgresSQL (version 13.7.2), was utilized for data extraction from MIMIC-IV and eICU-CRD. One researcher (Yang Yang) with authorization to access both databases (Record ID: 48,776,647) conducted the data extraction. Inclusive criteria encompassed patients who were (1) aged 18 years and above; (2) diagnosed with ICH in accordance with International Classification of Diseases, 9th and 10th Revision (ICD9 and ICD10). Exclusion criteria included: (1) patients with multiple hospitalization entries, only data from the initial hospitalization due to ICH were considered; (2) patients lacking data of FTG and FBG on the first day of ICU admittance were omitted; (3) individuals who expired or were released within 24 h of ICU admission were excluded due to their significant missing data for key variables used in the regression analysis. Therefore, excluding this group of patients was necessary to ensure the reliability of the results of the regression analysis.
The following information was extracted for the final study cohort: (1) patients’ age and gender; (2) comorbidities identified by ICD-9 and ICD-10 codes; (3) initial FBG and FTG results within 24 h post-ICU admission; (4) average values of laboratory parameters within 24 h of ICU admittance; (5) minimum Glasgow Coma Scale (GCS) score on the first day of ICU admittance; (6) maximum Acute Physiology Score III (APSIII) and Sequential Organ Failure Assessment (SOFA) scores on the first day of ICU management; (7) treatment-related data that may impact the prognosis of ICH patients were extracted, which includes invasive mechanical ventilation, the use of anticoagulants, and the use of antiplatelet agents during hospitalization.
Assessment of the TyG index
The TyG index is calculated using the formula: TyG index = ln [FTG (mg/dl) × FBG (mg/dl)/2], where FTG and FBG represent the first recorded values of FBG and FTG since ICU admission [ 17 , 18 ]. In the subsequent statistical analysis, the TyG index was considered both as a continuous and categorical variable. When treated as a categorical variable, it was divided into four groups based on quartiles. The data extraction process is illustrated in Fig. 1 .
The flow chart for extracting data from the MIMIC-IV and eICU databases
Primary outcomes
The primary outcomes of interest were all-cause in-hospital mortality and ICU mortality, which were defined as deaths occurring during hospitalization and ICU staying, respectively.
Statistical analysis
Continuous variables were expressed as median (interquartile ranges) and categorical variables were described as number (percentages). Comparisons between groups were performed by Mann–Whitney U or Kruskal–Wallis test for continuous variables, and chi-squared or Fisher’s exact test for categorical ones.
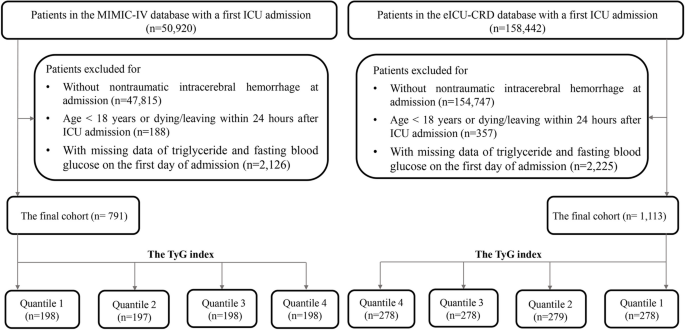
In order to investigate the relationship between the TyG index and the primary outcomes, an initial analysis utilizing restricted cubic splines (RCS) with four knots was carried out to assess any potential non-linear associations between the TyG index and the risk of in-hospital and ICU mortality. If a non-linear relationship was not detected, logistic regression analysis were performed using three different models: model 1 included only the TyG index, model 2 adjusted for age and gender, and model 3 further adjusted for various potential confounders relevant to the clinical outcomes of ICH, including GCS, hypertension, congestive heart failure, white blood cell count (WBC), serum urea nitrogen (BUN), serum creatinine, red cell distribution width (RDW), serum bilirubin, serum aspartate aminotransferase (AST), prothrombin time (PT), use of anticoagulants, and use of antiplatelet agents. Additionally, to check for multicollinearity in the logistic regression analysis, a Spearman rank correlation test was carried out and the square root of the variance inflation factor (VIF) was calculated.
To explore potential variations within specific populations, subgroup analysis was conducted by stratifying patients according to gender, age (> 60 vs. ≤ 60 years), diabetes, hypertension, use of anticoagulants, and use of antiplatelet agents. The interaction between the TyG index and the other variables utilized for stratification in subgroup analysis was evaluated through likelihood ratio test. Finally, a sensitivity analysis was performed by using Cox proportional hazard regression to verify the relationship between the TyG index and in-hospital and ICU mortality. The follow-up period was measured from the date of hospital or ICU admission to the date of death during the hospitalization or ICU stay. The Cox regression model was adjusted for possible confounders as outlined in the fully adjusted model (model 3) of logistic regression mentioned above.
All statistical analysis were performed using R software (version 4.3.1). The“VIM”package was used to visualize the distribution of missing values, from which we can see that all variables had missing ratio less than 20% (Additional file 1 : Figure S1). The “mice” package was adopted to address missing values by multiple imputation to obtain 5 imputation datasets in the process of logistic regression. Besides, the “corrplot” package was used to visualize the associations between continuous variables. The“plotRCS” package was used to perform RCS. The“forestploter” package was adopted to visualized the results of subgroup analysis. The “survminer” package was used to conduct Cox regression analysis. Statistically significant was set as a two tailed P < 0.05 .
Baseline characteristics
A total of 791 patients from MIMIC-IV and 1,113 from eICU-CRD were included in the final analysis. Among them, 418 (53%) individuals in MIMIC-IV and 627 (56%) in eICU-CRD were male. The in-hospital mortality rates were 14% in MIMIC-IV and 16% in eICU-CRD, with ICU mortality rates of 10% and 8% respectively. The median age was 72.25 (60.63, 82.59) years in MIMIC-IV and 66 (55, 77) years in eICU-CRD. Besides, the average value of TyG index was 8.72 (8.38, 9.17) in MIMIC-IV and 8.76 (8.33, 9.21) in eICU-CRD.
When dividing participants into groups based on the quartiles of the TyG index, patients in the upper quartiles had significantly higher APSIII scores, and higher proportion of invasive ventilation than those in the lower quartiles ( P < 0.001 for all ). Furthermore, hospital stay time, ICU stay time, in-hospital mortality, and ICU mortality all exhibited a gradual increase from the first to the fourth quartile of the TyG index. However, there was no significant difference in the mean hospital and ICU survival time of patients who died in the hospital or ICU across the quartiles of the TyG index. (Table 1 and Additional file 2 : Table S1).
Baseline data of participants divided by the hospital and ICU outcomes are presented in Table 2 and Additional file 3 : Table S2, respectively. Compared to in-hospital and ICU survivors, non-survivors in both the MIMIC-IV and eICU-CRD databases showed significantly higher APSIII and SOFA scores, shorter hospital stays, and a higher proportion of invasive ventilation. However, compared to in-hospital and ICU survivors, ICU stay time was shorter in non-survivors from eICU-CRD and longer in non-survivors from MIMIC-IV. Furthermore, GCS scores were lower in in-hospital and ICU non-survivors compared to survivors in eICU-CRD, but there was no significant difference in GCS scores between in-hospital and ICU survivors and non-survivors in MIMIC-IV. Interestingly, despite the potential risk of secondary hemorrhage associated with antiplatelet agents, their usage was more common among in-hospital and ICU non-survivors than survivors in MIMIC-IV. Moreover, the TyG index was notably higher in the in-hospital non-survivors compared to survivors (MIMIC-IV: 8.94 (8.51–9.48) vs. 8.70 (8.36–9.09); P < 0.001 . eICU-CRD: 8.98 (8.51–9.49) vs. 8.70 (8.31–9.16); P < 0.001 ). Similarly, the TyG index was significantly elevated in ICU non-survivors in contrast to ICU survivors (MIMIC-IV: 9.00 (8.51–9.48) vs. 8.70 (8.36–9.10); P < 0.001. eICU-CRD: 9.09 (8.76–9.65) vs. 8.71 (8.31–9.17); P < 0.001) (Additional file 4 : Figure S2).
Association between the TyG index and the primary outcomes
We initially conducted a nonlinear correlation analysis between the TyG index and the primary outcomes using RCS. Findings suggested no significant nonlinear correlation between the TyG indicator and the likelihood of either in-hospital or ICU mortality (In-hospital mortality: P for nonlinear = 0.751 in MIMIC-IV , P for nonlinear = 0.562 in eICU-CRD. ICU mortality: P for nonlinear = 0.986 in MIMIC-IV , P for nonlinear = 0.431 in eICU-CRD) (Fig. 2 ). Subsequently, logistic regression analysis was conducted to assess the linear relationship between the TyG index and the primary outcomes. In the fully adjusted model (model 3) that adjusted for various potential confounders related to the clinical outcomes of ICH, a positive correlation was found between the TyG index and the risk of in-hospital mortality (MIMIC-IV: OR 1.75 [95%CI 1.20–2.52], P = 0.003 . eICU-CRD: OR 1.37 [95%CI 1.05–1.80], P < 0.001 ) and ICU mortality (MIMIC-IV: OR 2.15 [95%CI 1.45–3.17], P < 0.001. eICU-CRD: OR 1.61 [95%CI 1.13–2.27], P < 0.001 ). Moreover, compared to the first quartile (Q1) of the TyG index, the results of model 3 indicated that the fourth quartile (Q4) was linked to a higher risk of in-hospital mortality (MIMIC-IV: OR 2.31 [95%CI 1.18–4.67], P = 0.017 . eICU-CRD: 1.73 [95%CI 1.02–3.06], P = 0.036 ) and ICU mortality (MIMIC-IV: OR 3.24 [95%CI 1.54–7.11], P = 0.002 . eICU-CRD: 2.30 [95%CI 1.09–5.16], P = 0.034 ) (Table 3 , Additional file 5 : Table S3).
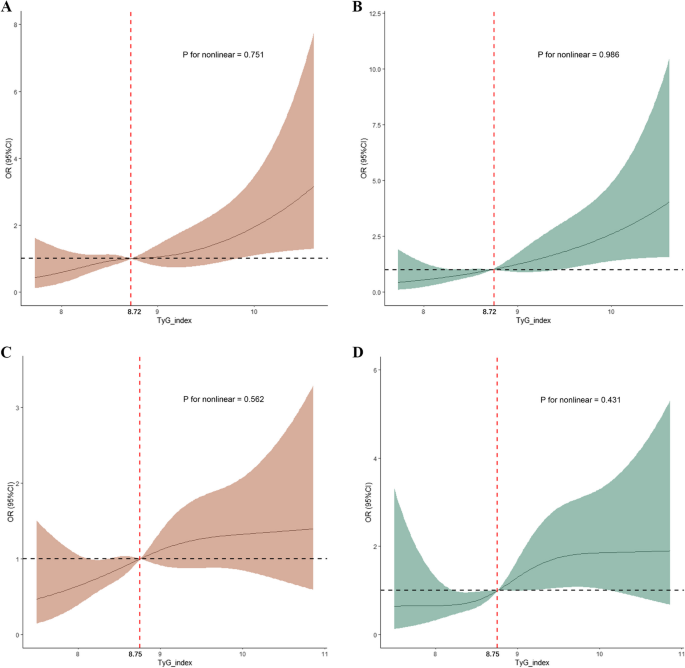
Restricted cubic spline analysis for the nonlinear association between the TyG index and the risk of, A in-hospital mortality of ICH patients from MIMIC-IV; B ICU mortality of ICH patients from MIMIC-IV; C in-hospital mortality of ICH patients from eICU-CRD; D ICU mortality of ICH patients from eICU-CRD
To assess multicollinearity in the logistic regression model, the Spearman rank correlation coefficient and VIF were calculated, respectively. Findings revealed that there was no linear correlation between the TyG index and the other continuous variables incorporated in model 3 (Additional file 6 : Figure S3). Additionally, none of the variables in model 3 exhibited a square root of VIF ≥ 2 (data not shown). Taken together, these results suggest that there is no multicollinearity present in the logistic regression model, indicating the reliability of the results.
Subgroup analysis
To investigate potential variations within specific populations, logistic regression analysis was conducted across various subgroups, including gender, age, diabetes, hypertension, use of anticoagulant agents, and use of antiplatelet agents. The forest plot revealed a significant positive correlation between the TyG index and in-hospital mortality among participants over 60 years (MIMIC-IV: OR 2.58 [95%CI 1.92–4.27], P = 0.005 . eICU-CRD: OR 1.56 [95%CI 1.10–2.22], P = 0.019 ), those without diabetes (MIMIC-IV: OR 2.20 [95%CI 1.34–3.57], P = 0.002 . eICU-CRD: OR 1.69 [95%CI 1.18–2.41], P = 0.004 ), and those with hypertension (MIMIC-IV: OR 1.97 [95%CI 1.28–3.01], P = 0.002 . eICU-CRD: OR 1.84 [95%CI 1.28–2.99], P = 0.014 ). Similarly, there was a positive association for ICU mortality in patients over 60 years (MIMIC-IV: OR 3.86 [95%CI 1.31–6.99], P < 0.001 . eICU-CRD: OR 1.70 [95%CI 1.23–2.90], P = 0.036 ), those without diabetes (MIMIC-IV: OR 2.62 [95%CI 1.56–4.40], P < 0.001 . eICU-CRD: OR 2.10 [95%CI 1.34–3.32], P = 0.001 ), and those with hypertension (MIMIC-IV: OR 2.44 [95%CI 1.54–3.84], P < 0.001 . eICU-CRD: OR 1.83 [95%CI 1.13–2.97], P = 0.013 ). Furthermore, in both MIMIC-IV and eICU-CRD, significant interactions were found between the TyG index and patients' age, diabetic status, and history of hypertension concerning in-hospital and ICU outcomes of individuals with ICH ( P for interaction < 0.05 for all) (Figs. 3 and 4 ).
Subgroup analysis for the correlation between the TyG index and the risk of in-hospital mortality in patients with ICH from MIMIC-IV and eICU-CRD databases
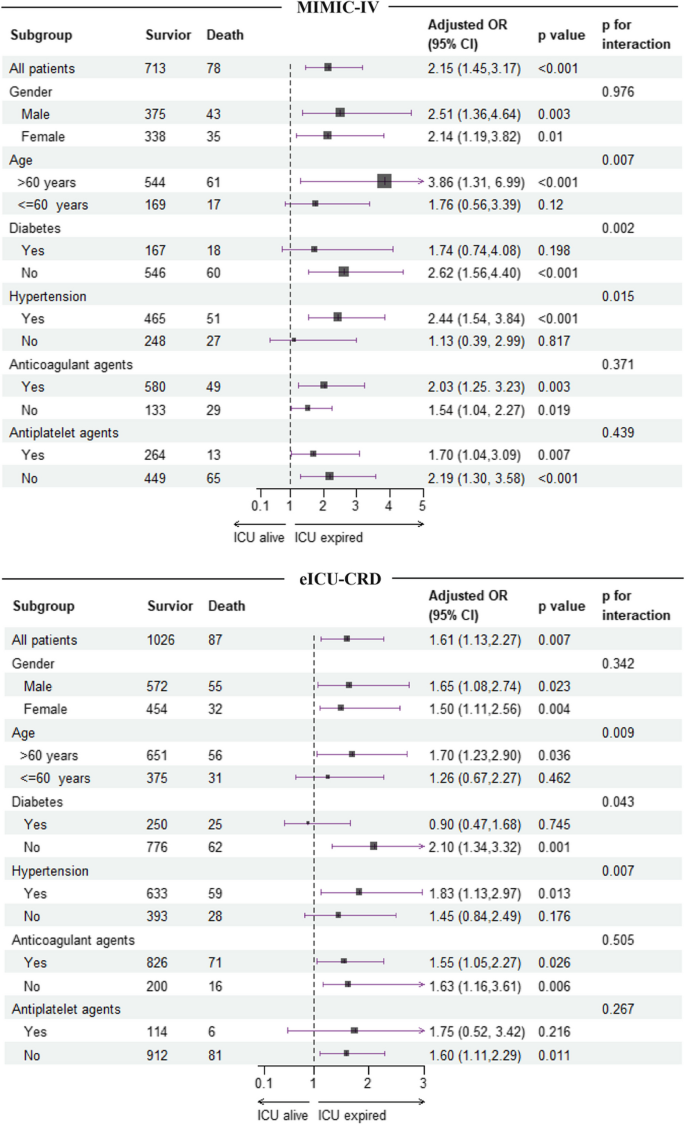
Subgroup analysis for the correlation between the TyG index and the risk of ICU mortality in patients with ICH from MIMIC-IV and eICU-CRD databases
Sensitivity analysis
To further verify the association between the TyG index and in-hospital and ICU mortality, as well as the significant interactions between the TyG index and patients' age regarding in-hospital and ICU outcomes, a sensitivity analysis was performed using Cox proportional hazard regression. Following fully adjusted, a positive correlation was observed between the TyG index and the risk of in-hospital mortality in ICH patients from both MIMI-IV and eICU-CRD datasets. The positive association between the TyG index and in-hospital and ICU mortality was also present in patients over 60 years old, those without diabetes, and those with hypertension in both databases. Importantly, significant interactions were only found between patients' age and the TyG index concerning in-hospital and ICU outcomes of ICH patients in both MIMIC-IV and eICU-CRD datasets (Table 4 and Additional file 7 : Table S4). These findings collectively suggest that the TyG index has the potential to serve as a prognostic indicator for ICH in patients over 60 years of age.
In this retrospective multicenter study, the impact of the TyG index on the prognosis of critically ill patients with ICH was evaluated, uncovering two important findings. Firstly, a positive correlation was found between the TyG index and the risk of in-hospital and ICU all-cause mortality in ICH patients. Secondly, this correlation was notably stronger in patients over 60 years old, especially in those with hypertension or lacking diabetes.
The association between the TyG index and the course of IS has been extensively studied. Wang et al. reported that individuals in the highest quartile of the TyG index face a 1.45 times greater risk of developing IS compared to those in the lowest quartile [ 19 ]. Results from a 9-year prospective study showed that keeping TyG index elevated was strongly related to an increased morbidity of IS, suggesting that monitoring and regulating the TyG index at an appropriate level could be beneficial in preventing IS [ 20 ]. Additionally, various studies have explored the capability of the TyG index in predicting the outcome of IS. Lee and colleagues found that the TyG index could forecast an adverse functional outcome three months post-reperfusion in IS patients [ 21 ]. Yang et al. noted a correlation between higher TyG index and elevated rates of both recurrence and mortality within one year following an IS event [ 22 ]. In critically ill patients, Cai W et al. found that the TyG index may assist in identifying IS patients at high risk of all-cause mortality [ 14 ]. Despite these findings highlight the significant relationship between the TyG index and IS as well as its prognosis, research on the association between the TyG index and ICH remains scarce.
To address this gap in knowledge, we conducted this study and found a positive correlation between the TyG index and the likelihood of either in-hospital or ICU mortality in individuals with ICH. The positive correlation persisted even after adjusting for potential confounders, suggesting that the TyG index could serve as an independent predictor of hospitalization outcomes in patients with ICH, potentially aiding clinicians in their decision-making process. More importantly, subgroup analysis revealed that there is a synergistic effect of old age (over 60 years), hypertension, and non-diabetic status on the TyG index’s impact on hospitalization outcomes in patients with ICH. Sensitivity analysis using Cox regression model further confirmed the synergistic effect between old age (over 60 years) and the TyG index on the in-hospital and ICU mortality of ICH patients in both MIMIC-IV and eICU-CRD databases. These results underscored the population-specific influence of the TyG index on ICH prognosis, highlighting the importance of focusing on elderly patients with ICH.
The exact mechanisms connecting the TyG index with the poor prognosis of ICH are still unclear, but evidence supports a key role of IR in this process. Patients with IR are more susceptible to hyperglycemia. A study has found that hyperglycemia could inhibit the expression of Aquaporin-4, resulting in the aggravation of vasogenic brain edema and blood–brain barrier (BBB) destruction [ 23 ]. Autophagy is a vital cellular process for maintaining homeostasis, but hyperglycemia can decrease autophagic activity in the brain during ICH, leading to the accumulation of macromolecular debris and damaged cells, ultimately causing neuronal injury [ 24 ]. In stoke rat treated with type plasminogen activator, hyperglycemia could enhance superoxide production in brain tissue and blood vessels, increasing BBB permeability in the peri-ischemic area and leading to a 3- to fivefold rise in the volume of secondary hemorrhage after thrombolysis [ 25 ]. This finding establishes a link between hyperglycemia-induced superoxide production and the increased risk of hematoma expansion in IS. The generation of reactive oxygen species has been demonstrated during ICH [ 26 , 27 ]. Moreover, studies have shown that an increase in blood glucose can exacerbate hematoma expansion in a rat model of ICH [ 28 ]. Therefore, it is plausible to infer that IR related hyperglycemia may result in poor outcomes of ICH by promoting superoxide production, thereby increasing the risk of hematoma expansion.
Adequate cerebral perfusion is crucial for determining the prognosis of patients with ICH. The automatic regulation ability of cerebral blood vessels plays a significant role in maintaining appropriate cerebral perfusion during cerebral hemorrhage. Studies have indicated that elevated intracranial pressure in patients with acute ICH can impair cerebrovascular autoregulation within a two-week period [ 29 ]. The myogenic response, which refers to the ability of smooth muscle cells to react to changes in blood pressure, is essential for preserving cerebrovascular autoregulation [ 30 ]. Animal studies have proved that IR can heighten the tension of cerebrovascular myogenic response, leading to a reduction in the diameter of the cerebrovascular lumen, subsequently causing brain tissue ischemia and nerve cell injury [ 31 ]. In addition, the smooth muscle activity of distal cerebral arteries is notably higher than that of proximal ones, making them more vulnerable to IR and resulting in impaired cerebral circulation function [ 30 ].
Chronic inflammatory response is one pathogenesis of IR, and IR in turn can reflect the level of systemic inflammation in the body [ 32 ]. Interestingly, our study revealed a gradual increase in WBC across quartile intervals of the TyG index, with values exceeding the upper limit of the reference range in the fourth quartile, suggesting an escalation of systemic inflammation during the course of ICH in patients with IR. Furthermore, the integrity of BBB was compromised during ICH, allowing the infiltration of peripheral immune cells and pro-inflammatory cytokines into the central nervous system. This heightened inflammatory response in the brain can further compromise the BBB, creating a detrimental cycle [ 33 ]. In addition, study has shown that dysregulation of the insulin signaling pathway can activate NF-κB, leading to the transcription and expression of inflammatory factors in the brain, thereby exacerbating neuroinflammation [ 34 ].
Intriguingly, although the evidence presented supports the significant role of IR in linking the TyG index to the unfavorable prognosis of intracerebral hemorrhage (ICH), our study found no correlation between the TyG index and either in-hospital or ICU mortality in ICH patients with a history of diabetes, a group known to have a higher risk of IR compared to non-diabetic individuals. Explaining the cause of this paradox is challenging. One potential reason could be reverse causality [ 14 , 35 ], where patients diagnosed with diabetes may be more likely to accept appropriate treatment or adopt healthy lifestyle habits. This could lead to their analytical parameters being similar to or even lower than those of non-diabetic counterparts. Consistent to this theory, in our study, no significant differences were observed in FBG, FTC, and TyG indexes between diabetic and non-diabetic individuals in both the MIMC-IV and eICU-CRD study cohorts (TyG index: 8.71 (8.38, 9.17) vs 8.77 (8.39, 9.14), P = 0.673 for MIMIC-IV. 8.75 (8.34, 9.22) vs 8.78 (8.3, 9.17), P = 0.925 for eICU-CRD). Additionally, as diabetic patients may have adopted a healthier lifestyle than their non-diabetic counterparts, their prognosis might be improved in subgroup analyses stratified by diabetes status.
The hyper-insulinemic-euglycemic clamp is considered the most accurate method for detecting IR, but its practicality is limited due to high costs, time-consuming procedures, and invasiveness. The homeostasis model assessment index for IR (HOMA-IR) is commonly used in clinical settings to assess beta-cell function and detect IR [ 36 ]. Nevertheless, its applicability is restricted in patients undergoing insulin therapy or those with ineffective beta cells [ 37 ]. Besides, HOMA-IR relies on measuring insulin levels, which are not routinely checked in clinical practice. Therefore, researchers have introduced the TyG index as a potentially reliable and cost-effective alternative marker for IR. Using hyper-insulin-normoglycemia clamp technique as the gold standard, a study showed excellent predictive efficiency of the TyG index for IR, with sensitive and specificity of 96.5% and 85.0%, respectively [ 8 ]. David and colleagues also demonstrated that the TyG index outperforms FBG and FTG in diagnosing type 2 diabetes and monitoring its progression [ 38 ]. Given that FBG and FTG measurements are available in most healthcare facilities, the TyG index has the potential to be widely utilized in blood glucose management and could serve as a valuable tool for risk assessment in patients with ICH.
The study has several limitations. First, the location and volume of hemorrhage, which are crucial factors influencing the prognosis of ICH, could not be extracted from the databases. Therefore, future research should incorporate these indicators to further validate the current findings. Secondly, specific population such as the Chinese or African are scarce in the study cohort. Consequently, the conclusions derived from this study should be cautiously interpreted in these population. Thirdly, the impact of dynamic changes in the TyG index on the prognosis of ICH patients was not assessed in this study. Given that variability in the TyG index has been linked to the incidence of IS [ 20 ], further studies are needed to investigate the cumulative effect of the TyG index on the incidence and outcome of ICH. Fourthly, exclusion of patients without FTG and FBG data on the first day of ICU admission may introduce bias if the missing data pattern is not completely random. Last but not the least, the utilization of propofol, fibrate, and glucose, along with insulin infusion prior to hospitalization, could have a notable effect on FTG and FBG levels. Nevertheless, neither MIMIC-IV nor eICU-CRD databases contains information on pre-hospitalization medications. Therefore, further investigation is required to confirm the current findings by incorporating these treatment-related information before ICU admission.
This study identified a positive correlation between the TyG index and in-hospital as well as ICU all-cause mortality in patients with ICH, particularly among individuals aged over 60 years with a history of hypertension. The findings indicate that the TyG index may be a useful tool for risk stratification in elderly patients with ICH, assisting clinicians in identifying high-risk individuals and providing timely intervention.
Availability of data and materials
The available data for MIMIC-IV can be accessed from the website https://mimic.physionet.org/ . The available data for eICU-CRD can be accessed from the website https://eicu-crd.mit.edu/ . The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Acute Physiology Score III
Serum aspartate aminotransferase
Blood–brain barrier
Serum urea nitrogen
The eICU Collaborative Research Database
Fasting blood glucose
Fasting triglyceride
Glasgow coma scale
The homeostasis model assessment index for IR
International Classification of Diseases
- Intensive care unit
- Intracerebral hemorrhage
Insulin resistance
Ischemic stroke
The Medical Information Mart for Intensive Care
Odds ratios
Prothrombin time
Restricted cubic spline
Red cell distribution width
Sequential Organ Failure Assessment
Structure Query Language
Triglyceride glucose index
Variance inflation factor
Qureshi A, Mendelow A, Hanley D. Intracerebral haemorrhage. Lancet (London, England). 2009;373(9675):1632–44.
Article PubMed Google Scholar
van Asch C, Luitse M, Rinkel G, van der Tweel I, Algra A, Klijn C. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. The Lancet Neurology. 2010;9(2):167–76.
Keep R, Hua Y, Xi G. Intracerebral haemorrhage: mechanisms of injury and therapeutic targets. The Lancet Neurology. 2012;11(8):720–31.
Article CAS PubMed Google Scholar
Lee S, Park S, Choi C. Insulin Resistance: From Mechanisms to Therapeutic Strategies. Diabetes Metab J. 2022;46(1):15–37.
Scherer T, Sakamoto K, Buettner C. Brain insulin signalling in metabolic homeostasis and disease. Nat Rev Endocrinol. 2021;17(8):468–83.
Gui J, Li Y, Liu H, et al. Obesity- and lipid-related indices as a predictor of obesity metabolic syndrome in a national cohort study. Front Public Health. 2023;11:1073824.
Article PubMed PubMed Central Google Scholar
Kim J, Kim J, Roh E, et al. Triglyceride and glucose index and the risk of gestational diabetes mellitus: A nationwide population-based cohort study. Diabetes Res Clin Pract. 2021;171:108533.
Guerrero-Romero F, Simental-Mendía L, González-Ortiz M, et al. The product of triglycerides and glucose, a simple measure of insulin sensitivity Comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocrinol Metabol. 2010;95(7):3347–51.
Article CAS Google Scholar
Irace C, Carallo C, Scavelli F, et al. Markers of insulin resistance and carotid atherosclerosis. A comparison of the homeostasis model assessment and triglyceride glucose index. Int J Clin Prac. 2013;67(7):665–72.
Li J, Ren L, Chang C, Luo L. Triglyceride-Glukose Index Predicts Adverse Events in Patients with Acute Coronary Syndrome: A Meta-Analysis of Cohort Studies. Horm Metabol Res. 2021;53(9):594–601.
Ding X, Wang X, Wu J, Zhang M, Cui M. Triglyceride-glucose index and the incidence of atherosclerotic cardiovascular diseases: a meta-analysis of cohort studies. Cardiovasc Diabetol. 2021;20(1):76.
Article CAS PubMed PubMed Central Google Scholar
Jin J, Cao Y, Wu L, et al. Triglyceride glucose index for predicting cardiovascular outcomes in patients with coronary artery disease. J Thorac Dis. 2018;10(11):6137–46.
Liu D, Yang K, Gu H, Li Z, Wang Y, Wang Y. Predictive effect of triglyceride-glucose index on clinical events in patients with acute ischemic stroke and type 2 diabetes mellitus. Cardiovasc Diabetol. 2022;21(1):280.
Cai W, Xu J, Wu X, et al. Association between triglyceride-glucose index and all-cause mortality in critically ill patients with ischemic stroke: analysis of the MIMIC-IV database. Cardiovasc Diabetol. 2023;22(1):138.
Pollard T, Johnson A, Raffa J, Celi L, Mark R, Badawi O. The eICU Collaborative Research Database, a freely available multi-center database for critical care research. Scientific data. 2018;5:180178.
Johnson A, Bulgarelli L, Shen L, et al. MIMIC-IV, a freely accessible electronic health record dataset. Scientific data. 2023;10(1):1.
Liao Y, Zhang R, Shi S, et al. Triglyceride-glucose index linked to all-cause mortality in critically ill patients: a cohort of 3026 patients. Cardiovasc Diabetol. 2022;21(1):128.
Zhang R, Shi S, Chen W, et al. Independent effects of the triglyceride-glucose index on all-cause mortality in critically ill patients with coronary heart disease: analysis of the MIMIC-III database. Cardiovasc Diabetol. 2023;22(1):10.
Wang A, Wang G, Liu Q, et al. Triglyceride-glucose index and the risk of stroke and its subtypes in the general population: an 11-year follow-up. Cardiovasc Diabetol. 2021;20(1):46.
Wang X, Feng B, Huang Z, et al. Relationship of cumulative exposure to the triglyceride-glucose index with ischemic stroke: a 9-year prospective study in the Kailuan cohort. Cardiovasc Diabetol. 2022;21(1):66.
Lee M, Kim C, Kim Y, et al. High Triglyceride Glucose Index Is Associated with Poor Outcomes in Ischemic Stroke Patients after Reperfusion Therapy. Cerebrovasc Dis. 2021;50(6):691–9.
Yang X, Wang G, Jing J, et al. Association of triglyceride-glucose index and stroke recurrence among nondiabetic patients with acute ischemic stroke. BMC Neurol. 2022;22(1):79.
Chiu C, Chen C, Shen C, et al. Hyperglycemia exacerbates intracerebral hemorrhage via the downregulation of aquaporin-4: temporal assessment with magnetic resonance imaging. Stroke. 2013;44(6):1682–9.
Liu R, Wang J, Qiu X, Wu J. Acute hyperglycemia together with hematoma of high-glucose blood exacerbates neurological injury in a rat model of intracerebral hemorrhage. Neurosci Bull. 2014;30(1):90–8.
Won S, Tang X, Suh S, Yenari M, Swanson R. Hyperglycemia promotes tissue plasminogen activator-induced hemorrhage by Increasing superoxide production. Ann Neurol. 2011;70(4):583–90.
Zhu F, Zi L, Yang P, et al. Efficient Iron and ROS Nanoscavengers for Brain Protection after Intracerebral Hemorrhage. ACS Appl Mater Interfaces. 2021;13(8):9729–38.
Ding R, Chen Y, Yang S, et al. Blood-brain barrier disruption induced by hemoglobin in vivo: Involvement of up-regulation of nitric oxide synthase and peroxynitrite formation. Brain Res. 2014;1571:25–38.
Liu J, Gao B, Clermont A, et al. Hyperglycemia-induced cerebral hematoma expansion is mediated by plasma kallikrein. Nat Med. 2011;17(2):206–10.
Ma H, Guo Z, Liu J, Xing Y, Zhao R, Yang Y. Temporal Course of Dynamic Cerebral Autoregulation in Patients With Intracerebral Hemorrhage. Stroke. 2016;47(3):674–81.
Coucha M, Abdelsaid M, Ward R, Abdul Y, Ergul A. Impact of Metabolic Diseases on Cerebral Circulation: Structural and Functional Consequences. Compr Physiol. 2018;8(2):773–99.
Butcher J, Goodwill A, Stanley S, Frisbee J. Differential impact of dilator stimuli on increased myogenic activation of cerebral and skeletal muscle resistance arterioles in obese zucker rats. Microcirculation. 2013;20(7):579–89.
Glass C, Olefsky J. Inflammation and lipid signaling in the etiology of insulin resistance. Cell Metab. 2012;15(5):635–45.
de la Monte S. Insulin Resistance and Neurodegeneration: Progress Towards the Development of New Therapeutics for Alzheimer’s Disease. Drugs. 2017;77(1):47–65.
Akhtar A, Sah S. Insulin signaling pathway and related molecules: Role in neurodegeneration and Alzheimer’s disease. Neurochem Int. 2020;135:104707.
Laura S, David N, Alejandro F, et al. The TyG index may predict the development of cardiovascular events. Eur J Clin Invest. 2015;46:189–97.
Google Scholar
Matthews D, Hosker J, Rudenski A, Naylor B, Treacher D, Turner R. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9.
Minh H, Tien H, Sinh C, et al. Assessment of preferred methods to measure insulin resistance in Asian patients with hypertension. J Clin Hypertens (Greenwich). 2021;23(3):529–37.
Navarro-González D, Sánchez-Íñigo L, Pastrana-Delgado J, Fernández-Montero A, Martinez J. Triglyceride-glucose index (TyG index) in comparison with fasting plasma glucose improved diabetes prediction in patients with normal fasting glucose: The Vascular-Metabolic CUN cohort. Prev Med. 2016;86:99–105.
Download references
Acknowledgements
The present study utilized data from the MIMIC-IV and eICU database. We express our gratitude to all the staff and patients who contributed to the development of the MIMIC-IV and eICU database.
This research was supported by Innovation Science Fund of Tangdu hospital, China (No. 2023BTDQN001), Shaanxi Province Key Research and Development Plan Project (2024SF-YBXM-210), and Air Force Medical University Clinical Research Program (2023LC2319).
Author information
Yang Yang, Shengru Liang and Jiangdong Liu contribute equally to this work and are co-first authors.
Lihong Li and Xiaoxi Tian contributed equally to this work and are co-corresponding authors.
Authors and Affiliations
Department of Emergency, Tangdu Hospital, Fourth Military Medical University, Xi’an, 710038, China
Yang Yang, Jiangdong Liu, Yue Si, Dengfeng Jia, Jianwei Li, Xiaoxi Tian & Lihong Li
Department of Endocrinology, Tangdu Hospital, Fourth Military Medical University, Xi’an, 710038, China
Shengru Liang
Department of Neurosurgery, Tangdu Hospital, Fourth Military Medical University, Xi’an, 710038, China
Minghao Man
You can also search for this author in PubMed Google Scholar
Contributions
YY extracted data from MIMIC-IV and eICU-database, analyzed the data, and wrote the original draft. SL conducted literature review, analyzed the data, and wrote the original draft. JDL conducted literature review, and operated software. MM and DJ organized the data and checked the integrity of the data. YS and JWL assisted in statistical analysis. XT designed the study, and checked the final results. LL designed the study, conceptualized the research aims, and revised the paper. All authors have made an intellectual contribution to the manuscript and approved the final submission.
Corresponding author
Correspondence to Lihong Li .
Ethics declarations
Ethics approval and consent to participate.
The study was conducted in accordance with the guidelines of the Helsinki Declaration. As the MIMIC-IV and the eICU-CRD database are publicly available and all data are de-identified to remove patients’ information, the requirement for informed consent of patients is not essential.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: figure s1..
The proportion and distribution of missing data for variables in (A) MIMIC-IV database and (B) eICU-CRD database.
Additional file 2.
Additional file 3., additional file 4: figure s2..
The boxplot of the TyG index stratified by the in-hospital and ICU outcomes. (A) The level of the TyG index in hospital survivors and non-survivors from the MIMIC-IV database. (B) The level of the TyG index in hospital survivors and non-survivors from the eICU-CRD database. (C) The level of the TyG index in ICU survivors and non-survivors from the MIMIC-IV database. (D) The level of the TyG index in ICU survivors and non-survivors from the eICU-CRD database.
Additional file 5.
Additional file 6: figure s3..
The correlation between continuous variables in the cohort derived from (A) MIMIC-IV and (B) eICU-CRD.
Additional file 7.
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Yang, Y., Liang, S., Liu, J. et al. Triglyceride-glucose index as a potential predictor for in-hospital mortality in critically ill patients with intracerebral hemorrhage: a multicenter, case–control study. BMC Geriatr 24 , 385 (2024). https://doi.org/10.1186/s12877-024-05002-4
Download citation
Received : 07 March 2024
Accepted : 22 April 2024
Published : 01 May 2024
DOI : https://doi.org/10.1186/s12877-024-05002-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Triglyceride-glucose index
- All-cause mortality
BMC Geriatrics
ISSN: 1471-2318
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Share full article
Advertisement
Supported by
Study Suggests Genetics as a Cause, Not Just a Risk, for Some Alzheimer’s
People with two copies of the gene variant APOE4 are almost certain to get Alzheimer’s, say researchers, who proposed a framework under which such patients could be diagnosed years before symptoms.

By Pam Belluck
Scientists are proposing a new way of understanding the genetics of Alzheimer’s that would mean that up to a fifth of patients would be considered to have a genetically caused form of the disease.
Currently, the vast majority of Alzheimer’s cases do not have a clearly identified cause. The new designation, proposed in a study published Monday, could broaden the scope of efforts to develop treatments, including gene therapy, and affect the design of clinical trials.
It could also mean that hundreds of thousands of people in the United States alone could, if they chose, receive a diagnosis of Alzheimer’s before developing any symptoms of cognitive decline, although there currently are no treatments for people at that stage.
The new classification would make this type of Alzheimer’s one of the most common genetic disorders in the world, medical experts said.
“This reconceptualization that we’re proposing affects not a small minority of people,” said Dr. Juan Fortea, an author of the study and the director of the Sant Pau Memory Unit in Barcelona, Spain. “Sometimes we say that we don’t know the cause of Alzheimer’s disease,” but, he said, this would mean that about 15 to 20 percent of cases “can be tracked back to a cause, and the cause is in the genes.”
The idea involves a gene variant called APOE4. Scientists have long known that inheriting one copy of the variant increases the risk of developing Alzheimer’s, and that people with two copies, inherited from each parent, have vastly increased risk.
The new study , published in the journal Nature Medicine, analyzed data from over 500 people with two copies of APOE4, a significantly larger pool than in previous studies. The researchers found that almost all of those patients developed the biological pathology of Alzheimer’s, and the authors say that two copies of APOE4 should now be considered a cause of Alzheimer’s — not simply a risk factor.
The patients also developed Alzheimer’s pathology relatively young, the study found. By age 55, over 95 percent had biological markers associated with the disease. By 65, almost all had abnormal levels of a protein called amyloid that forms plaques in the brain, a hallmark of Alzheimer’s. And many started developing symptoms of cognitive decline at age 65, younger than most people without the APOE4 variant.
“The critical thing is that these individuals are often symptomatic 10 years earlier than other forms of Alzheimer’s disease,” said Dr. Reisa Sperling, a neurologist at Mass General Brigham in Boston and an author of the study.
She added, “By the time they are picked up and clinically diagnosed, because they’re often younger, they have more pathology.”
People with two copies, known as APOE4 homozygotes, make up 2 to 3 percent of the general population, but are an estimated 15 to 20 percent of people with Alzheimer’s dementia, experts said. People with one copy make up about 15 to 25 percent of the general population, and about 50 percent of Alzheimer’s dementia patients.
The most common variant is called APOE3, which seems to have a neutral effect on Alzheimer’s risk. About 75 percent of the general population has one copy of APOE3, and more than half of the general population has two copies.
Alzheimer’s experts not involved in the study said classifying the two-copy condition as genetically determined Alzheimer’s could have significant implications, including encouraging drug development beyond the field’s recent major focus on treatments that target and reduce amyloid.
Dr. Samuel Gandy, an Alzheimer’s researcher at Mount Sinai in New York, who was not involved in the study, said that patients with two copies of APOE4 faced much higher safety risks from anti-amyloid drugs.
When the Food and Drug Administration approved the anti-amyloid drug Leqembi last year, it required a black-box warning on the label saying that the medication can cause “serious and life-threatening events” such as swelling and bleeding in the brain, especially for people with two copies of APOE4. Some treatment centers decided not to offer Leqembi, an intravenous infusion, to such patients.
Dr. Gandy and other experts said that classifying these patients as having a distinct genetic form of Alzheimer’s would galvanize interest in developing drugs that are safe and effective for them and add urgency to current efforts to prevent cognitive decline in people who do not yet have symptoms.
“Rather than say we have nothing for you, let’s look for a trial,” Dr. Gandy said, adding that such patients should be included in trials at younger ages, given how early their pathology starts.
Besides trying to develop drugs, some researchers are exploring gene editing to transform APOE4 into a variant called APOE2, which appears to protect against Alzheimer’s. Another gene-therapy approach being studied involves injecting APOE2 into patients’ brains.
The new study had some limitations, including a lack of diversity that might make the findings less generalizable. Most patients in the study had European ancestry. While two copies of APOE4 also greatly increase Alzheimer’s risk in other ethnicities, the risk levels differ, said Dr. Michael Greicius, a neurologist at Stanford University School of Medicine who was not involved in the research.
“One important argument against their interpretation is that the risk of Alzheimer’s disease in APOE4 homozygotes varies substantially across different genetic ancestries,” said Dr. Greicius, who cowrote a study that found that white people with two copies of APOE4 had 13 times the risk of white people with two copies of APOE3, while Black people with two copies of APOE4 had 6.5 times the risk of Black people with two copies of APOE3.
“This has critical implications when counseling patients about their ancestry-informed genetic risk for Alzheimer’s disease,” he said, “and it also speaks to some yet-to-be-discovered genetics and biology that presumably drive this massive difference in risk.”
Under the current genetic understanding of Alzheimer’s, less than 2 percent of cases are considered genetically caused. Some of those patients inherited a mutation in one of three genes and can develop symptoms as early as their 30s or 40s. Others are people with Down syndrome, who have three copies of a chromosome containing a protein that often leads to what is called Down syndrome-associated Alzheimer’s disease .
Dr. Sperling said the genetic alterations in those cases are believed to fuel buildup of amyloid, while APOE4 is believed to interfere with clearing amyloid buildup.
Under the researchers’ proposal, having one copy of APOE4 would continue to be considered a risk factor, not enough to cause Alzheimer’s, Dr. Fortea said. It is unusual for diseases to follow that genetic pattern, called “semidominance,” with two copies of a variant causing the disease, but one copy only increasing risk, experts said.
The new recommendation will prompt questions about whether people should get tested to determine if they have the APOE4 variant.
Dr. Greicius said that until there were treatments for people with two copies of APOE4 or trials of therapies to prevent them from developing dementia, “My recommendation is if you don’t have symptoms, you should definitely not figure out your APOE status.”
He added, “It will only cause grief at this point.”
Finding ways to help these patients cannot come soon enough, Dr. Sperling said, adding, “These individuals are desperate, they’ve seen it in both of their parents often and really need therapies.”
Pam Belluck is a health and science reporter, covering a range of subjects, including reproductive health, long Covid, brain science, neurological disorders, mental health and genetics. More about Pam Belluck
The Fight Against Alzheimer’s Disease
Alzheimer’s is the most common form of dementia, but much remains unknown about this daunting disease..
How is Alzheimer’s diagnosed? What causes Alzheimer’s? We answered some common questions .
A study suggests that genetics can be a cause of Alzheimer’s , not just a risk, raising the prospect of diagnosis years before symptoms appear.
Determining whether someone has Alzheimer’s usually requires an extended diagnostic process . But new criteria could lead to a diagnosis on the basis of a simple blood test .
The F.D.A. has given full approval to the Alzheimer’s drug Leqembi. Here is what to know about i t.
Alzheimer’s can make communicating difficult. We asked experts for tips on how to talk to someone with the disease .

IMAGES
VIDEO
COMMENTS
CASE 1. A 20 year old man with no past medical history presented to a primary stroke center with sudden left sided weakness and imbalance followed by decreased level of consciousness. Head CT showed no hemorrhage, no acute ischemic changes, and a hyper-dense basilar artery. CT angiography showed a mid-basilar occlusion.
Michael is a 61 year old Senior Partner in a Law Firm. While eating breakfast Michael experienced sudden onset slurring of speech, had facial droop on his left hand side with weakness in left side upper and lower limbs. Michael's wife Mary spotted these sudden onset of symptoms and immediately called for an ambulance, which arrived within 15 mins.
Other hypothesised reasons for stroke development in COVID-19 patients are the development of hypercoagulability, as a result of critical illness or new onset of arrhythmias, caused by severe infection. Some case studies in Wuhan described immense inflammatory responses to COVID-19, including elevated acute phase reactants, such as CRP and D-dimer.
Read chapter 7 of Patient Management in the Telemetry/Cardiac Step-Down Unit: A Case-Based Approach online now, exclusively on AccessMedicine. AccessMedicine is a subscription-based resource from McGraw Hill that features trusted medical content from the best minds in medicine.
Patient Case Presentation. Image courtesy of uofmhealthblogs.org. D.B. is a 72 year old African American female who presented to the ED with complaints of headache, altered mental status as evidenced by confusion and lethargy, slurred speech, right sided weakness, and a facial droop. Symptoms were first noted when patient woke up from a nap ...
Nurse Laura started an 18 gauge IV in Randall's left AC and started him on a bolus of 500 mL of NS. A blood sample was collected and quickly sent to the lab. Nurse Laura called the Emergency Department Tech to obtain a 12 lead EKG. Pertinent Lab Results for Randall. The physician and the nurse review the labs: WBC 7.3 x 10^9/L. RBC 4.6 x 10^12/L.
Dr. Lee H. Schwamm: This patient with acute stroke benefited from an integrated system of care, 2 which was implemented at a state-certified stroke center 3 and followed stroke-specific dispatch ...
Abstract. Increasing evidence reports a greater incidence of stroke among patients with Coronavirus disease 2019 (COVID-19) than the non-COVID-19 population and suggests that SARS-CoV-2 infection represents a risk factor for thromboembolic and acute ischemic stroke. Elderly people have higher risk factors associated with acute ischemic stroke or embolization vascular events, and advanced age ...
Amani Baidwan, Kendyl Egizi and Alysha Payne. Darrell Jackson, 81 year old male, came to the Emergency Department at Los Robles Hospital by ambulance after he collapsed in a coffee shop. Upon arrival he presented with left sided weakness, facial drooping, and aphasia. He was diagnosed with an ischemic stroke, right humerus head fracture, and ...
A PFO has been demonstrated in 10%-26% of healthy adults. 14 In young patients who have had a cryptogenic stroke, however, the prevalence is thought to be much higher, for example, 40% in one study. 15 It is thought that a PFO allows microemboli to pass into the systemic circulation leading to a stroke.
Go to Case Rubric. Kanika is a 38-year-old right-handed woman who was working as a social media coordinator for an international organization when she had a stroke in early June. Prior to the stroke, Kanika lived alone and frequently saw her sister and nieces, who lived in a nearby state. Her apartment is on the second floor, and there is no ...
MC study case Abnormal blood results recommendations • For major bleeding (e.g. intracerebral) within 48 h of administration of R-tpa we recommend: • All patients should be discussed with haematology team urgently • Stop infusion of fibrinolytic drugs and other antithrombotic drugs . • Administer FFP 12 ml/kg. • Administer intravenous tranexamic acid 1 g tds .
Day 1: Critical Care (99291) A 67-year-old woman with hypertension and diabetes presents to the emergency department with abrupt onset of left hemiparesis 45 minutes ago. Pre-evaluation: Discussed presentation and vital signs with ED provider (3 mins). Face-to-face evaluation: Performed medically appropriate history and exam.
Abstract. This presents an analysis of a case of Ischemic stroke in terms of possible etiology, pathophysiology, drug analysis and nursing care.
View Answer. You call a Code Stroke and notify the charge nurse for help. You obtain suction to have at bedside just in case. The neurologist arrives at bedside within 7 minutes to assess Mrs. Blossom. He notes her NIH Stroke Scale score is 32. He orders a STAT CT scan, which shows there is no obvious bleed in the brain. Critical Thinking Check.
This case study focuses on the comprehensive physiotherapy management of Ram Sagar, a 59-year-old patient who experienced a stroke. The study outlines the assessment, treatment plan, and interventions employed to aid Ram's functional recovery following a cerebrovascular accident (CVA). The case study highlights the
The phase three trial has completed subject enrollment but study results are pending collection of final patient follow-up assessments. A thrombolytic therapy to address IVH has been studied in the "Clot lysis evaluating accelerated resolution," or CLEAR. This study administered 1 mg of tPA through a ventricular drain every eight hours.
A 66-year-old man was admitted to hospital with a right frontal cerebral infarct producing left-sided weakness and a deterioration in his speech pattern. The cerebral infarct was confirmed with CT imaging. The only evidence of respiratory symptoms on admission was a 2 L oxygen requirement, maintaining oxygen saturations between 88% and 92%. In a matter of hours this patient developed a greater ...
Social work report: Background. Mrs Beryl Brown (01/11/33) is an 85 year old woman who was admitted to the Hume Hospital by ambulance after being found by her youngest daughter lying in front of her toilet. Her daughter estimates that she may have been on the ground overnight. On admission, Mrs Brown was diagnosed with a right sided stroke ...
Our reason for choosing this disorder. Stroke is the leading cause of disability in the United States. As advanced practice nurses, we anticipate caring for those impacted by strokes in many healthcare settings including emergency rooms, acute care, rehab settings, extended care facilities, and in primary care. Early diagnosis and treatment are ...
The content of this site is published by the site owner(s) and is not a statement of advice, opinion, or information pertaining to The Ohio State University.
In the case of stroke patients, communication between trained professionals and patients promotes shared decision making and prevents ethical conflicts . ... In the current study, the sample size was determined following the proposal by Turner-Bowker et al . These authors reported that 99.3% of concepts, ...
The correlation between the triglyceride-glucose index (TyG) and the prognosis of ischemic stroke has been well established. This study aims to assess the influence of the TyG index on the clinical outcomes of critically ill individuals suffering from intracerebral hemorrhage (ICH). Patients diagnosed with ICH were retrospectively retrieved from the Medical Information Mart for Intensive Care ...
Most patients in the study had European ancestry. While two copies of APOE4 also greatly increase Alzheimer's risk in other ethnicities, the risk levels differ, said Dr. Michael Greicius, a ...