How did COVID-19 affect Americans’ well-being and mental health?
Subscribe to global connection, emily dobson , emily dobson ph.d. student - university of maryland carol graham , carol graham senior fellow - economic studies @cgbrookings tim hua , and tim hua student - middlebury college, former intern - global economy and development sergio pinto sergio pinto doctoral student, university of maryland.
April 8, 2022
COVID-19 has justifiably raised widespread public concern about mental health worldwide. In the U.S., the pandemic was an unprecedented shock to society at a time when the nation was already coping with a crisis of despair and related deaths from suicides, overdoses, and alcohol poisoning. Meanwhile, COVID-19’s impact was inequitable: Deaths were concentrated among the elderly and minorities working in essential jobs, groups who up to the pandemic had been reporting better mental health. We still do not fully understand how the shock has affected society’s well-being and mental health.
In a recent paper in which we compared trends in 2019-2020 using several nationally representative datasets, we found a variety of contrasting stories. While data from the 2019 National Health Interview Survey (NHIS) and the 2020 Household Pulse Survey (HPS) containing the same mental health screening questions for depression and anxiety show that both increased significantly, especially among young and low-income Americans in 2020, we found no such changes when analyzing alternative depression questions that are also asked in a consistent manner in the 2019-2020 Behavioral Risk Factor Surveillance System (BRFSS) and the 2019-2020 NHIS. Despite the differences in trends, the basic determinants of mental health were similar in three data sets in the same two years.
Our findings raise questions about the robustness of the many studies claiming unprecedented increases in depression and anxiety among the young compared to older cohorts. Many of them, due to the urgency created by COVID-19 and a paucity of good, consistent data, matched datasets and used different questions therein in their attempt to identify changes in the trends between the two years. The inconsistency in the outcome changes over time across datasets points to the need for caution in drawing conclusions, as well as in relying too heavily on a single study; results generated from different data may differ considerably.
Given the paucity of comparable data and the usual one-year lag in the release of the final mortality data from the Centers for Disease Control and Prevention (CDC), we also tried to get a handle on changes in patterns in mental health by examining emergency medical services (EMS) data calls related to behavior, overdoses, suicide attempts, and gun violence. The EMS data has the advantage of using the same methods and samples over the two-year period. We found an increase in gun violence and opioid overdose calls in 2020 after lockdowns, but surprisingly, a sharp decrease in behavioral health calls and no change in suicide-related EMS activations. The latter trend is a puzzle, but possible explanations include opioid overdose deaths increasing markedly and possibly substituting for suicide deaths. Alternatively, many older men—who are the demographic groups with the most suicide deaths—died of COVID-19 in that same period; another tragic “substitution” effect.
Finally, we looked at whether over the long run there is a relationship between poor mental health and later deaths of despair in micropolitan and metropolitan statistical areas (MMSAs). We found modest support for that possibility. Based on mental health reports in the BRFSS and CDC mortality data, we find that two-to-three-year-lagged bad mental health days (at the individual level) are associated with higher rates of deaths of despair (at the MMSA level), and that the two-to-four-year-lagged rates of deaths of despair are associated with a higher number of bad mental health days in later years. We cannot establish a direction of causality, but it is possible that there are vicious circles at play with individual trends in mental health contributing to broader community distress, and communities with more despair-related deaths likely to have more mental health problems later as a result.
Our analysis, based on many different datasets and indicators of despair, does not contradict other studies in that despair is an ongoing problem in the U.S., as reflected by both mental health reports and trends in EMS activations. However, we do find that the effects of the COVID-19 pandemic are mixed, and that while some trends, such as opioid overdose deaths, worsened in 2020 compared to 2019, others, such as in some mental health reports and in suicide rates, improved slightly. Our work does not speak to the longer-term mental health consequences of the pandemic, but it does suggest that there were deep pockets of both despair and resilience throughout it. It also suggests that caution is necessary in drawing policy implications from any one study.
Related Content
Emily Dobson, Carol Graham, Tim Hua, Sergio Pinto
April 4, 2022
Carol Graham, Fred Dews
January 28, 2022
Related Books
Carol Graham
March 28, 2017
August 8, 2012
Global Economy and Development
Isabel V. Sawhill, Kai Smith
May 29, 2024
Harris A. Eyre, Carol Graham
January 3, 2022
- COVID-19 and your mental health
Worries and anxiety about COVID-19 can be overwhelming. Learn ways to cope as COVID-19 spreads.
At the start of the COVID-19 pandemic, life for many people changed very quickly. Worry and concern were natural partners of all that change — getting used to new routines, loneliness and financial pressure, among other issues. Information overload, rumor and misinformation didn't help.
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020.
Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19. And you're not alone if you've coped with the stress in less than healthy ways, such as substance use.
But healthier self-care choices can help you cope with COVID-19 or any other challenge you may face.
And knowing when to get help can be the most essential self-care action of all.

Recognize what's typical and what's not
Stress and worry are common during a crisis. But something like the COVID-19 pandemic can push people beyond their ability to cope.
In surveys, the most common symptoms reported were trouble sleeping and feeling anxiety or nervous. The number of people noting those symptoms went up and down in surveys given over time. Depression and loneliness were less common than nervousness or sleep problems, but more consistent across surveys given over time. Among adults, use of drugs, alcohol and other intoxicating substances has increased over time as well.
The first step is to notice how often you feel helpless, sad, angry, irritable, hopeless, anxious or afraid. Some people may feel numb.
Keep track of how often you have trouble focusing on daily tasks or doing routine chores. Are there things that you used to enjoy doing that you stopped doing because of how you feel? Note any big changes in appetite, any substance use, body aches and pains, and problems with sleep.
These feelings may come and go over time. But if these feelings don't go away or make it hard to do your daily tasks, it's time to ask for help.
Get help when you need it
If you're feeling suicidal or thinking of hurting yourself, seek help.
- Contact your healthcare professional or a mental health professional.
- Contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline , available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential.
If you are worried about yourself or someone else, contact your healthcare professional or mental health professional. Some may be able to see you in person or talk over the phone or online.
You also can reach out to a friend or loved one. Someone in your faith community also could help.
And you may be able to get counseling or a mental health appointment through an employer's employee assistance program.
Another option is information and treatment options from groups such as:
- National Alliance on Mental Illness (NAMI).
- Substance Abuse and Mental Health Services Administration (SAMHSA).
- Anxiety and Depression Association of America.
Self-care tips
Some people may use unhealthy ways to cope with anxiety around COVID-19. These unhealthy choices may include things such as misuse of medicines or legal drugs and use of illegal drugs. Unhealthy coping choices also can be things such as sleeping too much or too little, or overeating. It also can include avoiding other people and focusing on only one soothing thing, such as work, television or gaming.
Unhealthy coping methods can worsen mental and physical health. And that is particularly true if you're trying to manage or recover from COVID-19.
Self-care actions can help you restore a healthy balance in your life. They can lessen everyday stress or significant anxiety linked to events such as the COVID-19 pandemic. Self-care actions give your body and mind a chance to heal from the problems long-term stress can cause.
Take care of your body
Healthy self-care tips start with the basics. Give your body what it needs and avoid what it doesn't need. Some tips are:
- Get the right amount of sleep for you. A regular sleep schedule, when you go to bed and get up at similar times each day, can help avoid sleep problems.
- Move your body. Regular physical activity and exercise can help reduce anxiety and improve mood. Any activity you can do regularly is a good choice. That may be a scheduled workout, a walk or even dancing to your favorite music.
- Choose healthy food and drinks. Foods that are high in nutrients, such as protein, vitamins and minerals are healthy choices. Avoid food or drink with added sugar, fat or salt.
- Avoid tobacco, alcohol and drugs. If you smoke tobacco or if you vape, you're already at higher risk of lung disease. Because COVID-19 affects the lungs, your risk increases even more. Using alcohol to manage how you feel can make matters worse and reduce your coping skills. Avoid taking illegal drugs or misusing prescriptions to manage your feelings.
Take care of your mind
Healthy coping actions for your brain start with deciding how much news and social media is right for you. Staying informed, especially during a pandemic, helps you make the best choices but do it carefully.
Set aside a specific amount of time to find information in the news or on social media, stay limited to that time, and choose reliable sources. For example, give yourself up to 20 or 30 minutes a day of news and social media. That amount keeps people informed but not overwhelmed.
For COVID-19, consider reliable health sources. Examples are the U.S. Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
Other healthy self-care tips are:
- Relax and recharge. Many people benefit from relaxation exercises such as mindfulness, deep breathing, meditation and yoga. Find an activity that helps you relax and try to do it every day at least for a short time. Fitting time in for hobbies or activities you enjoy can help manage feelings of stress too.
- Stick to your health routine. If you see a healthcare professional for mental health services, keep up with your appointments. And stay up to date with all your wellness tests and screenings.
- Stay in touch and connect with others. Family, friends and your community are part of a healthy mental outlook. Together, you form a healthy support network for concerns or challenges. Social interactions, over time, are linked to a healthier and longer life.
Avoid stigma and discrimination
Stigma can make people feel isolated and even abandoned. They may feel sad, hurt and angry when people in their community avoid them for fear of getting COVID-19. People who have experienced stigma related to COVID-19 include people of Asian descent, health care workers and people with COVID-19.
Treating people differently because of their medical condition, called medical discrimination, isn't new to the COVID-19 pandemic. Stigma has long been a problem for people with various conditions such as Hansen's disease (leprosy), HIV, diabetes and many mental illnesses.
People who experience stigma may be left out or shunned, treated differently, or denied job and school options. They also may be targets of verbal, emotional and physical abuse.
Communication can help end stigma or discrimination. You can address stigma when you:
- Get to know people as more than just an illness. Using respectful language can go a long way toward making people comfortable talking about a health issue.
- Get the facts about COVID-19 or other medical issues from reputable sources such as the CDC and WHO.
- Speak up if you hear or see myths about an illness or people with an illness.
COVID-19 and health
The virus that causes COVID-19 is still a concern for many people. By recognizing when to get help and taking time for your health, life challenges such as COVID-19 can be managed.
- Mental health during the COVID-19 pandemic. National Institutes of Health. https://covid19.nih.gov/covid-19-topics/mental-health. Accessed March 12, 2024.
- Mental Health and COVID-19: Early evidence of the pandemic's impact: Scientific brief, 2 March 2022. World Health Organization. https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1. Accessed March 12, 2024.
- Mental health and the pandemic: What U.S. surveys have found. Pew Research Center. https://www.pewresearch.org/short-reads/2023/03/02/mental-health-and-the-pandemic-what-u-s-surveys-have-found/. Accessed March 12, 2024.
- Taking care of your emotional health. Centers for Disease Control and Prevention. https://emergency.cdc.gov/coping/selfcare.asp. Accessed March 12, 2024.
- #HealthyAtHome—Mental health. World Health Organization. www.who.int/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome---mental-health. Accessed March 12, 2024.
- Coping with stress. Centers for Disease Control and Prevention. www.cdc.gov/mentalhealth/stress-coping/cope-with-stress/. Accessed March 12, 2024.
- Manage stress. U.S. Department of Health and Human Services. https://health.gov/myhealthfinder/topics/health-conditions/heart-health/manage-stress. Accessed March 20, 2020.
- COVID-19 and substance abuse. National Institute on Drug Abuse. https://nida.nih.gov/research-topics/covid-19-substance-use#health-outcomes. Accessed March 12, 2024.
- COVID-19 resource and information guide. National Alliance on Mental Illness. https://www.nami.org/Support-Education/NAMI-HelpLine/COVID-19-Information-and-Resources/COVID-19-Resource-and-Information-Guide. Accessed March 15, 2024.
- Negative coping and PTSD. U.S. Department of Veterans Affairs. https://www.ptsd.va.gov/gethelp/negative_coping.asp. Accessed March 15, 2024.
- Health effects of cigarette smoking. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/index.htm#respiratory. Accessed March 15, 2024.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed March 15, 2024.
- Your healthiest self: Emotional wellness toolkit. National Institutes of Health. https://www.nih.gov/health-information/emotional-wellness-toolkit. Accessed March 15, 2024.
- World leprosy day: Bust the myths, learn the facts. Centers for Disease Control and Prevention. https://www.cdc.gov/leprosy/world-leprosy-day/. Accessed March 15, 2024.
- HIV stigma and discrimination. Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/basics/hiv-stigma/. Accessed March 15, 2024.
- Diabetes stigma: Learn about it, recognize it, reduce it. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/features/diabetes_stigma.html. Accessed March 15, 2024.
- Phelan SM, et al. Patient and health care professional perspectives on stigma in integrated behavioral health: Barriers and recommendations. Annals of Family Medicine. 2023; doi:10.1370/afm.2924.
- Stigma reduction. Centers for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/od2a/case-studies/stigma-reduction.html. Accessed March 15, 2024.
- Nyblade L, et al. Stigma in health facilities: Why it matters and how we can change it. BMC Medicine. 2019; doi:10.1186/s12916-019-1256-2.
- Combating bias and stigma related to COVID-19. American Psychological Association. https://www.apa.org/topics/covid-19-bias. Accessed March 15, 2024.
- Yashadhana A, et al. Pandemic-related racial discrimination and its health impact among non-Indigenous racially minoritized peoples in high-income contexts: A systematic review. Health Promotion International. 2021; doi:10.1093/heapro/daab144.
- Sawchuk CN (expert opinion). Mayo Clinic. March 25, 2024.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and respiratory illness
- COVID-19 and pets
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- Long-term effects of COVID-19
- COVID-19 tests
- COVID-19 drugs: Are there any that work?
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 travel advice
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to measure your respiratory rate
- How to take your pulse
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
Related information
- Mental health: What's normal, what's not - Related information Mental health: What's normal, what's not
- Mental illness - Related information Mental illness
Your gift holds great power – donate today!
Make your tax-deductible gift and be part of the cutting-edge research and care that's changing medicine.
- Open access
- Published: 11 April 2023
Effects of the COVID-19 pandemic on mental health, anxiety, and depression
- Ida Kupcova 1 ,
- Lubos Danisovic 1 ,
- Martin Klein 2 &
- Stefan Harsanyi 1
BMC Psychology volume 11 , Article number: 108 ( 2023 ) Cite this article
10k Accesses
21 Citations
46 Altmetric
Metrics details
The COVID-19 pandemic affected everyone around the globe. Depending on the country, there have been different restrictive epidemiologic measures and also different long-term repercussions. Morbidity and mortality of COVID-19 affected the mental state of every human being. However, social separation and isolation due to the restrictive measures considerably increased this impact. According to the World Health Organization (WHO), anxiety and depression prevalence increased by 25% globally. In this study, we aimed to examine the lasting effects of the COVID-19 pandemic on the general population.
A cross-sectional study using an anonymous online-based 45-question online survey was conducted at Comenius University in Bratislava. The questionnaire comprised five general questions and two assessment tools the Zung Self-Rating Anxiety Scale (SAS) and the Zung Self-Rating Depression Scale (SDS). The results of the Self-Rating Scales were statistically examined in association with sex, age, and level of education.
A total of 205 anonymous subjects participated in this study, and no responses were excluded. In the study group, 78 (38.05%) participants were male, and 127 (61.69%) were female. A higher tendency to anxiety was exhibited by female participants (p = 0.012) and the age group under 30 years of age (p = 0.042). The level of education has been identified as a significant factor for changes in mental state, as participants with higher levels of education tended to be in a worse mental state (p = 0.006).
Conclusions
Summarizing two years of the COVID-19 pandemic, the mental state of people with higher levels of education tended to feel worse, while females and younger adults felt more anxiety.
Peer Review reports
Introduction
The first mention of the novel coronavirus came in 2019, when this variant was discovered in the city of Wuhan, China, and became the first ever documented coronavirus pandemic [ 1 , 2 , 3 ]. At this time there was only a sliver of fear rising all over the globe. However, in March 2020, after the declaration of a global pandemic by the World Health Organization (WHO), the situation changed dramatically [ 4 ]. Answering this, yet an unknown threat thrust many countries into a psycho-socio-economic whirlwind [ 5 , 6 ]. Various measures taken by governments to control the spread of the virus presented the worldwide population with a series of new challenges to which it had to adjust [ 7 , 8 ]. Lockdowns, closed schools, losing employment or businesses, and rising deaths not only in nursing homes came to be a new reality [ 9 , 10 , 11 ]. Lack of scientific information on the novel coronavirus and its effects on the human body, its fast spread, the absence of effective causal treatment, and the restrictions which harmed people´s social life, financial situation and other areas of everyday life lead to long-term living conditions with increased stress levels and low predictability over which people had little control [ 12 ].
Risks of changes in the mental state of the population came mainly from external risk factors, including prolonged lockdowns, social isolation, inadequate or misinterpreted information, loss of income, and acute relationship with the rising death toll. According to the World Health Organization (WHO), since the outbreak of the COVID-19 pandemic, anxiety and depression prevalence increased by 25% globally [ 13 ]. Unemployment specifically has been proven to be also a predictor of suicidal behavior [ 14 , 15 , 16 , 17 , 18 ]. These risk factors then interact with individual psychological factors leading to psychopathologies such as threat appraisal, attentional bias to threat stimuli over neutral stimuli, avoidance, fear learning, impaired safety learning, impaired fear extinction due to habituation, intolerance of uncertainty, and psychological inflexibility. The threat responses are mediated by the limbic system and insula and mitigated by the pre-frontal cortex, which has also been reported in neuroimaging studies, with reduced insula thickness corresponding to more severe anxiety and amygdala volume correlated to anhedonia as a symptom of depression [ 19 , 20 , 21 , 22 , 23 ]. Speaking in psychological terms, the pandemic disturbed our core belief, that we are safe in our communities, cities, countries, or even the world. The lost sense of agency and confidence regarding our future diminished the sense of worth, identity, and meaningfulness of our lives and eroded security-enhancing relationships [ 24 ].
Slovakia introduced harsh public health measures in the first wave of the pandemic, but relaxed these measures during the summer, accompanied by a failure to develop effective find, test, trace, isolate and support systems. Due to this, the country experienced a steep growth in new COVID-19 cases in September 2020, which lead to the erosion of public´s trust in the government´s management of the situation [ 25 ]. As a means to control the second wave of the pandemic, the Slovak government decided to perform nationwide antigen testing over two weekends in November 2020, which was internationally perceived as a very controversial step, moreover, it failed to prevent further lockdowns [ 26 ]. In addition, there was a sharp rise in the unemployment rate since 2020, which continued until July 2020, when it gradually eased [ 27 ]. Pre-pandemic, every 9th citizen of Slovakia suffered from a mental health disorder, according to National Statistics Office in 2017, the majority being affective and anxiety disorders. A group of authors created a web questionnaire aimed at psychiatrists, psychologists, and their patients after the first wave of the COVID-19 pandemic in Slovakia. The results showed that 86.6% of respondents perceived the pathological effect of the pandemic on their mental status, 54.1% of whom were already treated for affective or anxiety disorders [ 28 ].
In this study, we aimed to examine the lasting effects of the COVID-19 pandemic on the general population. This study aimed to assess the symptoms of anxiety and depression in the general public of Slovakia. After the end of epidemiologic restrictive measures (from March to May 2022), we introduced an anonymous online questionnaire using adapted versions of Zung Self-Rating Anxiety Scale (SAS) and Zung Self-Rating Depression Scale (SDS) [ 29 , 30 ]. We focused on the general public because only a portion of people who experience psychological distress seek professional help. We sought to establish, whether during the pandemic the population showed a tendency to adapt to the situation or whether the anxiety and depression symptoms tended to be present even after months of better epidemiologic situation, vaccine availability, and studies putting its effects under review [ 31 , 32 , 33 , 34 ].
Materials and Methods
This study utilized a voluntary and anonymous online self-administered questionnaire, where the collected data cannot be linked to a specific respondent. This study did not process any personal data. The questionnaire consisted of 45 questions. The first three were open-ended questions about participants’ sex, age (date of birth was not recorded), and education. Followed by 2 questions aimed at mental health and changes in the will to live. Further 20 and 20 questions consisted of the Zung SAS and Zung SDS, respectively. Every question in SAS and SDS is scored from 1 to 4 points on a Likert-style scale. The scoring system is introduced in Fig. 1 . Questions were presented in the Slovak language, with emphasis on maintaining test integrity, so, if possible, literal translations were made from English to Slovak. The questionnaire was created and designed in Google Forms®. Data collection was carried out from March 2022 to May 2022. The study was aimed at the general population of Slovakia in times of difficult epidemiologic and social situations due to the high prevalence and incidence of COVID-19 cases during lockdowns and social distancing measures. Because of the character of this web-based study, the optimal distribution of respondents could not be achieved.
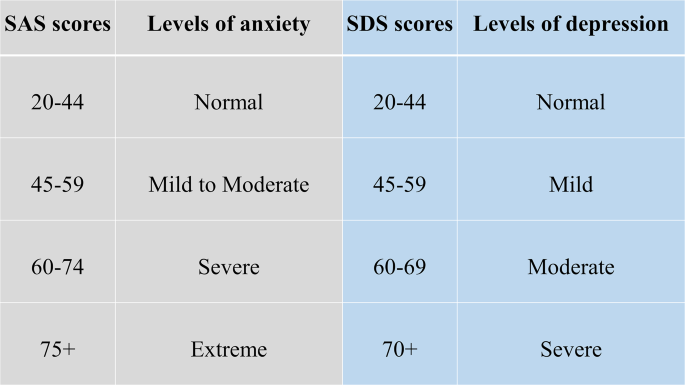
Categories of Zung SAS and SDS scores with clinical interpretation
During the course of this study, 205 respondents answered the anonymous questionnaire in full and were included in the study. All respondents were over 18 years of age. The data was later exported from Google Forms® as an Excel spreadsheet. Coding and analysis were carried out using IBM SPSS Statistics version 26 (IBM SPSS Statistics for Windows, Version 26.0, Armonk, NY, USA). Subject groups were created based on sex, age, and education level. First, sex due to differences in emotional expression. Second, age was a risk factor due to perceived stress and fear of the disease. Last, education due to different approaches to information. In these groups four factors were studied: (1) changes in mental state; (2) affected will to live, or frequent thoughts about death; (3) result of SAS; (4) result of SDS. For SAS, no subject in the study group scored anxiety levels of “severe” or “extreme”. Similarly for SDS, no subject depression levels reached “moderate” or “severe”. Pearson’s chi-squared test(χ2) was used to analyze the association between the subject groups and studied factors. The results were considered significant if the p-value was less than 0.05.
Ethical permission was obtained from the local ethics committee (Reference number: ULBGaKG-02/2022). This study was performed in line with the principles of the Declaration of Helsinki. All methods were carried out following the institutional guidelines. Due to the anonymous design of the study and by the institutional requirements, written informed consent for participation was not required for this study.
In the study, out of 205 subjects in the study group, 127 (62%) were female and 78 (38%) were male. The average age in the study group was 35.78 years of age (range 19–71 years), with a median of 34 years. In the age group under 30 years of age were 34 (16.6%) subjects, while 162 (79%) were in the range from 31 to 49 and 9 (0.4%) were over 50 years old. 48 (23.4%) participants achieved an education level of lower or higher secondary and 157 (76.6%) finished university or higher. All answers of study participants were included in the study, nothing was excluded.
In Tables 1 and 2 , we can see the distribution of changes in mental state and will to live as stated in the questionnaire. In Table 1 we can see a disproportion in education level and mental state, where participants with higher education tended to feel worse much more than those with lower levels of education. Changes based on sex and age did not show any statistically significant results.
In Table 2 . we can see, that decreased will to live and frequent thoughts about death were only marginally present in the study group, which suggests that coping mechanisms play a huge role in adaptation to such events (e.g. the global pandemic). There is also a possibility that living in times of better epidemiologic situations makes people more likely to forget about the bad past.
Anxiety and depression levels as seen in Tables 3 and 4 were different, where female participants and the age group under 30 years of age tended to feel more anxiety than other groups. No significant changes in depression levels based on sex, age, and education were found.
Compared to the estimated global prevalence of depression in 2017 (3.44%), in 2021 it was approximately 7 times higher (25%) [ 14 ]. Our study did not prove an increase in depression, while anxiety levels and changes in the mental state did prove elevated. No significant changes in depression levels go in hand with the unaffected will to live and infrequent thoughts about death, which were important findings, that did not supplement our primary hypothesis that the fear of death caused by COVID-19 or accompanying infections would enhance personal distress and depression, leading to decreases in studied factors. These results are drawn from our limited sample size and uneven demographic distribution. Suicide ideations rose from 5% pre-pandemic to 10.81% during the pandemic [ 35 ]. In our study, 9.3% of participants experienced thoughts about death and since we did not specifically ask if they thought about suicide, our results only partially correlate with suicidal ideations. However, as these subjects exhibited only moderate levels of anxiety and mild levels of depression, the rise of suicide ideations seems unlikely. The rise in suicidal ideations seemed to be especially true for the general population with no pre-existing psychiatric conditions in the first months of the pandemic [ 36 ]. The policies implemented by countries to contain the pandemic also took a toll on the population´s mental health, as it was reported, that more stringent policies, mainly the social distancing and perceived government´s handling of the pandemic, were related to worse psychological outcomes [ 37 ]. The effects of lockdowns are far-fetched and the increases in mental health challenges, well-being, and quality of life will require a long time to be understood, as Onyeaka et al. conclude [ 10 ]. These effects are not unforeseen, as the global population suffered from life-altering changes in the structure and accessibility of education or healthcare, fluctuations in prices and food insecurity, as well as the inevitable depression of the global economy [ 38 ].
The loneliness associated with enforced social distancing leads to an increase in depression, anxiety, and posttraumatic stress in children in adolescents, with possible long-term sequelae [ 39 ]. The increase in adolescent self-injury was 27.6% during the pandemic [ 40 ]. Similar findings were described in the middle-aged and elderly population, in which both depression and anxiety prevalence rose at the beginning of the pandemic, during the pandemic, with depression persisting later in the pandemic, while the anxiety-related disorders tended to subside [ 41 ]. Medical professionals represented another specific at-risk group, with reported anxiety and depression rates of 24.94% and 24.83% respectively [ 42 ]. The dynamic of psychopathology related to the COVID-19 pandemic is not clear, with studies reporting a return to normal later in 2020, while others describe increased distress later in the pandemic [ 20 , 43 ].
Concerning the general population, authors from Spain reported that lockdowns and COVID-19 were associated with depression and anxiety [ 44 ]. In January 2022 Zhao et al., reported an elevation in hoarding behavior due to fear of COVID-19, while this process was moderated by education and income levels, however, less in the general population if compared to students [ 45 ]. Higher education levels and better access to information could improve persons’ fear of the unknown, however, this fact was not consistent with our expectations in this study, as participants with university education tended to feel worse than participants with lower education. A study on adolescents and their perceived stress in the Czech Republic concluded that girls are more affected by lockdowns. The strongest predictor was loneliness, while having someone to talk to, scored the lowest [ 46 ]. Garbóczy et al. reported elevated perceived stress levels and health anxiety in 1289 Hungarian and international students, also affected by disengagement from home and inadequate coping strategies [ 47 ]. Wathelet et al. conducted a study on French University students confined during the pandemic with alarming results of a high prevalence of mental health issues in the study group [ 48 ]. Our study indicated similar results, as participants in the age group under 30 years of age tended to feel more anxious than others.
In conclusion, we can say that this pandemic changed the lives of many. Many of us, our family members, friends, and colleagues, experienced life-altering events and complicated situations unseen for decades. Our decisions and actions fueled the progress in medicine, while they also continue to impact society on all levels. The long-term effects on adolescents are yet to be seen, while effects of pain, fear, and isolation on the general population are already presenting themselves.
The limitations of this study were numerous and as this was a web-based study, the optimal distribution of respondents could not be achieved, due to the snowball sampling strategy. The main limitation was the small sample size and uneven demographic distribution of respondents, which could impact the representativeness of the studied population and increase the margin of error. Similarly, the limited number of older participants could significantly impact the reported results, as age was an important risk factor and thus an important stressor. The questionnaire omitted the presence of COVID-19-unrelated life-changing events or stressors, and also did not account for any preexisting condition or risk factor that may have affected the outcome of the used assessment scales.
Data Availability
The datasets generated and analyzed during the current study are not publicly available due to compliance with institutional guidelines but they are available from the corresponding author (SH) on a reasonable request.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506.
Article PubMed PubMed Central Google Scholar
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727–33.
Liu Y-C, Kuo R-L, Shih S-R. COVID-19: the first documented coronavirus pandemic in history. Biomed J. 2020;43:328–33.
Advice for the public on COVID-19 – World Health Organization. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public . Accessed 13 Nov 2022.
Osterrieder A, Cuman G, Pan-Ngum W, Cheah PK, Cheah P-K, Peerawaranun P, et al. Economic and social impacts of COVID-19 and public health measures: results from an anonymous online survey in Thailand, Malaysia, the UK, Italy and Slovenia. BMJ Open. 2021;11:e046863.
Article PubMed Google Scholar
Mofijur M, Fattah IMR, Alam MA, Islam ABMS, Ong HC, Rahman SMA, et al. Impact of COVID-19 on the social, economic, environmental and energy domains: Lessons learnt from a global pandemic. Sustainable Prod Consum. 2021;26:343–59.
Article Google Scholar
Vlachos J, Hertegård E, Svaleryd B. The effects of school closures on SARS-CoV-2 among parents and teachers. Proc Natl Acad Sci U S A. 2021;118:e2020834118.
Ludvigsson JF, Engerström L, Nordenhäll C, Larsson E, Open Schools. Covid-19, and child and teacher morbidity in Sweden. N Engl J Med. 2021;384:669–71.
Miralles O, Sanchez-Rodriguez D, Marco E, Annweiler C, Baztan A, Betancor É, et al. Unmet needs, health policies, and actions during the COVID-19 pandemic: a report from six european countries. Eur Geriatr Med. 2021;12:193–204.
Onyeaka H, Anumudu CK, Al-Sharify ZT, Egele-Godswill E, Mbaegbu P. COVID-19 pandemic: a review of the global lockdown and its far-reaching effects. Sci Prog. 2021;104:368504211019854.
The Lancet null. India under COVID-19 lockdown. Lancet. 2020;395:1315.
Lo Coco G, Gentile A, Bosnar K, Milovanović I, Bianco A, Drid P, et al. A cross-country examination on the fear of COVID-19 and the sense of loneliness during the First Wave of COVID-19 outbreak. Int J Environ Res Public Health. 2021;18:2586.
COVID-19 pandemic. triggers 25% increase in prevalence of anxiety and depression worldwide. https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide . Accessed 14 Nov 2022.
Bueno-Notivol J, Gracia-García P, Olaya B, Lasheras I, López-Antón R, Santabárbara J. Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. Int J Clin Health Psychol. 2021;21:100196.
Hajek A, Sabat I, Neumann-Böhme S, Schreyögg J, Barros PP, Stargardt T, et al. Prevalence and determinants of probable depression and anxiety during the COVID-19 pandemic in seven countries: longitudinal evidence from the european COvid Survey (ECOS). J Affect Disord. 2022;299:517–24.
Piumatti G, Levati S, Amati R, Crivelli L, Albanese E. Trajectories of depression, anxiety and stress among adults during the COVID-19 pandemic in Southern Switzerland: the Corona Immunitas Ticino cohort study. Public Health. 2022;206:63–9.
Korkmaz H, Güloğlu B. The role of uncertainty tolerance and meaning in life on depression and anxiety throughout Covid-19 pandemic. Pers Indiv Differ. 2021;179:110952.
McIntyre RS, Lee Y. Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Res. 2020;290:113104.
Funkhouser CJ, Klemballa DM, Shankman SA. Using what we know about threat reactivity models to understand mental health during the COVID-19 pandemic. Behav Res Ther. 2022;153:104082.
Landi G, Pakenham KI, Crocetti E, Tossani E, Grandi S. The trajectories of anxiety and depression during the COVID-19 pandemic and the protective role of psychological flexibility: a four-wave longitudinal study. J Affect Disord. 2022;307:69–78.
Holt-Gosselin B, Tozzi L, Ramirez CA, Gotlib IH, Williams LM. Coping strategies, neural structure, and depression and anxiety during the COVID-19 pandemic: a longitudinal study in a naturalistic sample spanning clinical diagnoses and subclinical symptoms. Biol Psychiatry Global Open Sci. 2021;1:261–71.
McCracken LM, Badinlou F, Buhrman M, Brocki KC. The role of psychological flexibility in the context of COVID-19: Associations with depression, anxiety, and insomnia. J Context Behav Sci. 2021;19:28–35.
Talkovsky AM, Norton PJ. Negative affect and intolerance of uncertainty as potential mediators of change in comorbid depression in transdiagnostic CBT for anxiety. J Affect Disord. 2018;236:259–65.
Milman E, Lee SA, Neimeyer RA, Mathis AA, Jobe MC. Modeling pandemic depression and anxiety: the mediational role of core beliefs and meaning making. J Affect Disorders Rep. 2020;2:100023.
Sagan A, Bryndova L, Kowalska-Bobko I, Smatana M, Spranger A, Szerencses V, et al. A reversal of fortune: comparison of health system responses to COVID-19 in the Visegrad group during the early phases of the pandemic. Health Policy. 2022;126:446–55.
Holt E. COVID-19 testing in Slovakia. Lancet Infect Dis. 2021;21:32.
Stalmachova K, Strenitzerova M. Impact of the COVID-19 pandemic on employment in transport and telecommunications sectors. Transp Res Procedia. 2021;55:87–94.
Izakova L, Breznoscakova D, Jandova K, Valkucakova V, Bezakova G, Suvada J. What mental health experts in Slovakia are learning from COVID-19 pandemic? Indian J Psychiatry. 2020;62(Suppl 3):459–66.
Rabinčák M, Tkáčová Ľ, VYUŽÍVANIE PSYCHOMETRICKÝCH KONŠTRUKTOV PRE, HODNOTENIE PORÚCH NÁLADY V OŠETROVATEĽSKEJ PRAXI. Zdravotnícke Listy. 2019;7:7.
Google Scholar
Sekot M, Gürlich R, Maruna P, Páv M, Uhlíková P. Hodnocení úzkosti a deprese u pacientů se zhoubnými nádory trávicího traktu. Čes a slov Psychiat. 2005;101:252–7.
Lipsitch M, Krammer F, Regev-Yochay G, Lustig Y, Balicer RD. SARS-CoV-2 breakthrough infections in vaccinated individuals: measurement, causes and impact. Nat Rev Immunol. 2022;22:57–65.
Accorsi EK, Britton A, Fleming-Dutra KE, Smith ZR, Shang N, Derado G, et al. Association between 3 doses of mRNA COVID-19 vaccine and symptomatic infection caused by the SARS-CoV-2 Omicron and Delta Variants. JAMA. 2022;327:639–51.
Barda N, Dagan N, Cohen C, Hernán MA, Lipsitch M, Kohane IS, et al. Effectiveness of a third dose of the BNT162b2 mRNA COVID-19 vaccine for preventing severe outcomes in Israel: an observational study. Lancet. 2021;398:2093–100.
Magen O, Waxman JG, Makov-Assif M, Vered R, Dicker D, Hernán MA, et al. Fourth dose of BNT162b2 mRNA Covid-19 vaccine in a nationwide setting. N Engl J Med. 2022;386:1603–14.
Dubé JP, Smith MM, Sherry SB, Hewitt PL, Stewart SH. Suicide behaviors during the COVID-19 pandemic: a meta-analysis of 54 studies. Psychiatry Res. 2021;301:113998.
Kok AAL, Pan K-Y, Rius-Ottenheim N, Jörg F, Eikelenboom M, Horsfall M, et al. Mental health and perceived impact during the first Covid-19 pandemic year: a longitudinal study in dutch case-control cohorts of persons with and without depressive, anxiety, and obsessive-compulsive disorders. J Affect Disord. 2022;305:85–93.
Aknin LB, Andretti B, Goldszmidt R, Helliwell JF, Petherick A, De Neve J-E, et al. Policy stringency and mental health during the COVID-19 pandemic: a longitudinal analysis of data from 15 countries. The Lancet Public Health. 2022;7:e417–26.
Prochazka J, Scheel T, Pirozek P, Kratochvil T, Civilotti C, Bollo M, et al. Data on work-related consequences of COVID-19 pandemic for employees across Europe. Data Brief. 2020;32:106174.
Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid systematic review: the impact of social isolation and loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59:1218–1239e3.
Zetterqvist M, Jonsson LS, Landberg Ã, Svedin CG. A potential increase in adolescent nonsuicidal self-injury during covid-19: a comparison of data from three different time points during 2011–2021. Psychiatry Res. 2021;305:114208.
Mooldijk SS, Dommershuijsen LJ, de Feijter M, Luik AI. Trajectories of depression and anxiety during the COVID-19 pandemic in a population-based sample of middle-aged and older adults. J Psychiatr Res. 2022;149:274–80.
Sahebi A, Nejati-Zarnaqi B, Moayedi S, Yousefi K, Torres M, Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Prog Neuropsychopharmacol Biol Psychiatry. 2021;107:110247.
Stephenson E, O’Neill B, Kalia S, Ji C, Crampton N, Butt DA, et al. Effects of COVID-19 pandemic on anxiety and depression in primary care: a retrospective cohort study. J Affect Disord. 2022;303:216–22.
Goldberg X, Castaño-Vinyals G, Espinosa A, Carreras A, Liutsko L, Sicuri E et al. Mental health and COVID-19 in a general population cohort in Spain (COVICAT study).Soc Psychiatry Psychiatr Epidemiol. 2022;:1–12.
Zhao Y, Yu Y, Zhao R, Cai Y, Gao S, Liu Y, et al. Association between fear of COVID-19 and hoarding behavior during the outbreak of the COVID-19 pandemic: the mediating role of mental health status. Front Psychol. 2022;13:996486.
Furstova J, Kascakova N, Sigmundova D, Zidkova R, Tavel P, Badura P. Perceived stress of adolescents during the COVID-19 lockdown: bayesian multilevel modeling of the Czech HBSC lockdown survey. Front Psychol. 2022;13:964313.
Garbóczy S, Szemán-Nagy A, Ahmad MS, Harsányi S, Ocsenás D, Rekenyi V, et al. Health anxiety, perceived stress, and coping styles in the shadow of the COVID-19. BMC Psychol. 2021;9:53.
Wathelet M, Duhem S, Vaiva G, Baubet T, Habran E, Veerapa E, et al. Factors Associated with Mental Health Disorders among University students in France Confined during the COVID-19 pandemic. JAMA Netw Open. 2020;3:e2025591.
Download references
Acknowledgements
We would like to provide our appreciation and thanks to all the respondents in this study.
This research project received no external funding.
Author information
Authors and affiliations.
Institute of Medical Biology, Genetics and Clinical Genetics, Faculty of Medicine, Comenius University in Bratislava, Sasinkova 4, Bratislava, 811 08, Slovakia
Ida Kupcova, Lubos Danisovic & Stefan Harsanyi
Institute of Histology and Embryology, Faculty of Medicine, Comenius University in Bratislava, Sasinkova 4, Bratislava, 811 08, Slovakia
Martin Klein
You can also search for this author in PubMed Google Scholar
Contributions
IK and SH have produced the study design. All authors contributed to the manuscript writing, revising, and editing. LD and MK have done data management and extraction, SH did the data analysis. Drafting and interpretation of the manuscript were made by all authors. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Stefan Harsanyi .
Ethics declarations
Ethics approval and consent to participate.
Ethical permission was obtained from the Ethics Committee of the Institute of Medical Biology, Genetics and Clinical Genetics, Faculty of Medicine, Comenius University in Bratislava (Reference number: ULBGaKG-02/2022). The need for informed consent was waived by the Ethics Committee of the Institute of Medical Biology, Genetics and Clinical Genetics, Faculty of Medicine, Comenius University in Bratislava due to the anonymous design of the study. This study did not process any personal data and the dataset does not contain any direct or indirect identifiers of participants. This study was performed in line with the principles of the Declaration of Helsinki. All methods were carried out following the institutional guidelines.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kupcova, I., Danisovic, L., Klein, M. et al. Effects of the COVID-19 pandemic on mental health, anxiety, and depression. BMC Psychol 11 , 108 (2023). https://doi.org/10.1186/s40359-023-01130-5
Download citation
Received : 14 November 2022
Accepted : 20 March 2023
Published : 11 April 2023
DOI : https://doi.org/10.1186/s40359-023-01130-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]

Mental Health
On This Page: -->
Mental Health During the COVID-19 Pandemic
Frequently asked questions, mental health resources.

NIH has compiled a library of resources related to COVID-19 and mental illnesses and disorders, including condition-specific and population-specific resources.

An Urgent Issue
Both SARS-CoV-2 and the COVID-19 pandemic have significantly affected the mental health of adults and children. In a 2021 study, nearly half of Americans surveyed reported recent symptoms of an anxiety or depressive disorder, and 10% of respondents felt their mental health needs were not being met. Rates of anxiety, depression, and substance use disorder have increased since the beginning of the pandemic. And people who have mental illnesses or disorders and then get COVID-19 are more likely to die than those who don’t have mental illnesses or disorders.
Mental health is a focus of NIH research during the COVID-19 pandemic. Researchers at NIH and supported by NIH are creating and studying tools and strategies to understand, diagnose, and prevent mental illnesses or disorders and improve mental health care for those in need.
How COVID-19 Can Impact Mental Health
If you get COVID-19, you may experience a number of symptoms related to brain and mental health, including:
Cognitive and attention deficits (brain fog)
Anxiety and depression
Suicidal behavior
Data suggest that people are more likely to develop mental illnesses or disorders in the months following infection, including symptoms of post-traumatic stress disorder (PTSD). People with Long COVID may experience many symptoms related to brain function and mental health.
How the Pandemic Affects Developing Brains
The impact of the COVID-19 pandemic on the mental health of children is not yet fully understood. NIH-supported research is investigating factors that may influence the cognitive, social, and emotional development of children during the pandemic, including:
Changes to routine
Virtual schooling
Mask wearing
Caregiver absence or loss
Financial instability
Not Everyone Is Affected Equally
While the COVID-19 pandemic can affect the mental health of anyone, some people are more likely to be affected than others. People who are more likely to experience symptoms of mental illnesses or disorders during the COVID-19 pandemic include:
People from racial and ethnic minority groups
Mothers and pregnant people
People with financial or housing insecurity
People with disabilities
People with preexisting mental illnesses or substance use problems
Health care workers
People who belong to more than one of these groups may be at an even greater risk for mental illness.
Telehealth’s Potential to Help
The pandemic has prevented many people from visiting health care professionals in person, and as a result, telehealth has been more widely adopted during this time. Telehealth visits for mental health and substance use disorders increased significantly from 2020 to 2021 and now make up nearly half of all total visits for behavioral health.
Widespread adoption of telehealth services may help people who otherwise would not be able to access mental health support, such as people in rural areas or places with few providers.

I have a preexisting mental illness. Is COVID-19 more dangerous to me?
COVID-19 can be worse for people with mental illnesses. Data suggest that people who reported symptoms of anxiety or depression had a greater chance of being hospitalized after a COVID-19 diagnosis than people without those symptoms.
The Centers for Disease Control and Prevention (CDC) reports that having mood disorders and schizophrenia spectrum disorders can increase a person’s chances of having severe COVID-19. People with mental illnesses who belong to minority groups are also more likely to get COVID-19. And people with schizophrenia are significantly more likely to get COVID-19 and more likely to die from it.
Despite these risks, effective treatments are available. If you have a preexisting mental illness and get COVID-19, talk to your health care professional to determine the treatment plan that’s appropriate for you.
I’m experiencing symptoms of a mental illness or disorder. What should I do?
If you are experiencing symptoms of anxiety, depression, or any other mental illness or disorder, there are ways you can get help. For immediate help:
Call or text the 988 Suicide & Crisis Lifeline at 988 (para ayuda en español, llame al 988)
Call or text the Disaster Distress Helpline , 1-800-985-5990 (press 2 for Spanish)
The Substance Abuse and Mental Health Services Administration can help you find mental health or substance use specialists.
Talk to your health care professional or mental health care professional. Together, you can work on a plan to manage or reduce your symptoms.
What research is NIH doing on the mental health impacts of COVID-19?
The National Institute of Mental Health (NIMH) and other NIH Institutes have created research initiatives to address mental health for people in general and for the most vulnerable people specifically. Examples of this research include:
NIH's Researching COVID to Enhance Recovery (RECOVER) Initiative has launched RECOVER-NEURO , a clinical trial that will test interventions to combat cognitive problems caused by Long COVID, including brain fog, memory problems, difficulty with attention, thinking clearly, and problem solving.
NIMH launched a five-year research study called RECOUP-NY to promote the mental health of New Yorkers from communities hard-hit by COVID-19. The study will test the use of a new care model called Problem Management Plus (PM+) that can be used by non-specialists.
A study funded by NIMH is examining the use of mobile apps to address mental health disparities .
The Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) is funding research to understand the effects of mask usage for children , including any impacts on their emotional and brain development.
NIMH is funding research on the impacts of the pandemic on underserved and vulnerable populations and on the cognitive, social, and emotional development of children .
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) is funding research on how COVID-19 and SARS-CoV-2 affect the causes and consequences of alcohol misuse .
A collaborative study supported by NIMH and the National Center for Complementary and Integrative Health (NCCIH) enrolled more than 3,600 people from all 50 U.S. states to understand the stressors affecting people during the pandemic.
Mental Health Resources by Topic
A library of resources related to COVID-19 and mental illnesses and disorders
Page last updated: September 28, 2023
- High Contrast
- Increase Font
- Decrease Font
- Default Font
- Turn Off Animations
Last updated 27/06/24: Online ordering is currently unavailable due to technical issues. We apologise for any delays responding to customers while we resolve this. For further updates please visit our website: https://www.cambridge.org/news-and-insights/technical-incident
We use cookies to distinguish you from other users and to provide you with a better experience on our websites. Close this message to accept cookies or find out how to manage your cookie settings .
Login Alert

- > Journals
- > Irish Journal of Psychological Medicine
- > Volume 37 Issue 4: Themed Issue: COVID-19 and Ment...
- > Mental health and the COVID-19 pandemic: looking back...

Article contents
Introduction, mental health effects of covid-19, research priorities, financial support, conflict of interest, ethical standards, mental health and the covid-19 pandemic: looking back and moving forward.
Published online by Cambridge University Press: 16 December 2020
COVID-19 continues to exert unprecedented challenges for society and it is now well recognised that mental health is a key healthcare issue related to the pandemic. The current edition of the Irish Journal of Psychological Medicine focusses on the impact of COVID-19 on mental illness by combining historical review papers, current perspectives and original research. It is important that psychiatrists leading mental health services in Ireland continue to advocate for mental health supports for healthcare workers and their patients, while aiming to deliver services flexibly. As the pandemic evolves, it remains to be seen whether the necessary funding to deliver effective mental healthcare will be allocated to psychiatric services. Ongoing service evaluation and research is needed as the myriad impacts of the pandemic continue to evolve. In a time of severe budgetary constraints, ensuring optimum use of scare resources becomes an imperative.
The COVID-19 pandemic continues to present the greatest global health challenge in modern history. While emerging data is improving our understanding of the virus and its impact on health, societal cohesion and world economies, the situation globally continues to evolve. As such, findings and learnings that emerge at one point of the pandemic can appear to have relatively limited utility at another point. Arguably, never in living memory has there been a global phenomenon impacting population mental health in such a dynamic fashion. The challenge for mental health science is to capture and report these dynamic trends in a timely manner to inform and support psychiatrists implementing evidence-based care in this uniquely challenging environment. A parallel requirement is that such services are adequately resourced to meet the needs of both service user and provider.
This COVID-19-themed issue of the Irish Journal of Psychological Medicine aims to provide a more nuanced understanding of the multifaceted mental health impact of the pandemic to date. In so doing, we sincerely hope that this issue will provide colleagues with a timely and useful resource in these uncertain times.
A number of commentators in the popular media have noted that one potential silver-lining of this pandemic has been a mainstreaming of mental health within the broader considerations of the health impact of the pandemic. It is has been noted that mental health needs have never been as central to public discourse as during recent media discussions about the impact of the various restrictions implemented due to the pandemic. The assumption that this increased consideration of mental health will indeed represent a true and meaningful shift in public policy towards psychiatric services and, by extension, increased funding, is yet to be borne out. Indeed, there remains a very real risk that this discourse will merely serve to enhance the already considerable societal focus on psychological well-being and continue to marginalise the moderate to severe end of the mental illness spectrum. It is particularly noteworthy that certain high-risk groups with pre-existing mental illness might remain most vulnerable to the potentially deleterious psychological impact of the pandemic, notwithstanding that many patients within these groups may display significant resilience. An ambiguous focus on mental health , which fails to take account of the urgent needs of overextended and under-resourced psychiatric services, represents a clear and pressing concern. Within this exceptional set of circumstances, the compelling need for effective advocacy emanating from psychiatrists to constructively inform and shape public discourse has been brought sharply into focus.
As predicted at the outset of the first wave of the pandemic, psychiatric morbidity is peaking later than the physical health consequences of the pandemic (Gunnell et al. Reference Gunnell, Appleby, Arensman, Hawton, John and Kapur 2020 ), and current trends suggest that this peak will indeed endure for longer than the impact on physical health. Emerging data from services nationwide indicates increasing referrals to psychiatric services following the initial pandemic lockdown, and ongoing evaluation of referrals to psychiatric services is now needed.
A further strategy which can help to determine the effects of the current pandemic is a reflection on historical events and the retrospective lessons that may be learned from them. Two historical papers in this issue focus on previous pandemics and other global events to evaluate how mental illness was impacted at the time. The multifaceted impact of COVID-19 on population mental health may not be realised for some time and it is important to start planning now for ongoing consequences such as the potential severe economic consequences in the months and years ahead.
Another somewhat double-edged silver-lining of the pandemic is the increased acknowledgement of the psychological burden associated with frontline healthcare service provision (Behrman et al. Reference Behrman, Baruch and Stegen 2020 ; Faderani et al. Reference Faderani, Monks, Peprah, Colori, Allen, Amphlett and Edwards 2020 ). Pre-pandemic data indicated a high-level of stress and burnout among doctors in Ireland (McNicholas et al. Reference McNicholas, Sharma, Oconnor and Barrett 2020 ; Humphries et al. Reference Humphries, McDermott, Creese, Matthews, Conway and Byrne 2020 ). Calls have been consistently made since the outset of the pandemic to enshrine the well-being of healthcare staff as a central tenet of the overall model of healthcare service response (Unadkat and Farquhar, Reference Unadkat and Farquhar 2020 ). This pro-active approach was advocated not only because protecting staff was recognised as the right thing to do but also to buffer against the predictable psychological consequences of providing healthcare within extremely challenging and rapidly-changing circumstances (Maunder et al. Reference Maunder, Leszcz, Savage, Adam, Peladeau and Romano 2008 ).
This Special Issue highlights some of the array of tools which have been proposed as helpful to clinicians to off-set stress and enhance resilience. To this end, there are considerations of mindfulness and story-telling which are proffered as possible means to pause and reflect and indeed the somewhat unique (for this journal) inclusion of poetry and prose represents an attempt to support and highlight the importance of enacting such strategies. Undoubtedly, however, research into what are described as psychological preparedness tools for healthcare workers is at a nascent stage and considerable further research is required prior to widespread implementation.
It is unsurprising, therefore, that while comprehensive Pandemic Preparedness Tools (Adelaja et al. Reference Adelaja, Sayma, Walton, McLachlan, de Boisanger and Bartlett-Pestell 2020 ) all incorporate specific elements designed to support the psychological well-being of healthcare staff, it appears reasonable to assert that additional support structures or tools have not been the experience of clinicians working throughout the pandemic. Indeed, a recent survey by the British Medical Association reported that 40% of the 6650 respondents indicated a worsening in their mental health status compared to pre-pandemic (Rimmer, Reference Rimmer 2020 ), with 10% describing their mental health as much worse . This is broadly in keeping with data from previous pandemics which suggest that, of those who experience negative psychological sequelae, the majority of healthcare staff will experience transient psychological distress rather than diagnosable moderate–severe conditions (Greenberg et al. Reference Greenberg, Docherty, Gnanapragasam and Wessely 2020 ; Maunder et al. Reference Maunder, Hunter, Vincent, Bennett, Peladeau and Leszcz 2003 , Reference Maunder, Lancee, Balderson, Bennett, Borgundvaag and Evans 2006 , Reference Maunder, Leszcz, Savage, Adam, Peladeau and Romano 2008 ).
These figures remain concerning however, and while Irish data does not exist, if the medical population in Ireland experiences similar trends to our international colleagues, the overall prevalence rates and service need for doctors as psychiatric patients will rise significantly. As psychiatrists, we have a particular duty to highlight these risks; effective advocacy within this context is paramount. Moreover, this underscores a recognised pressing but under-considered need to develop doctor specific psychiatry services within the psychiatric service framework in Ireland. This model, already piloted in England and extended in the context of the pandemic, has seen an exponential rise in referrals over the latter stages of the pandemic (Conference Proceedings for Occupational Health and Burnout among Healthcare Workers: https://www.ucd.ie/medicine/capsych/summerschool2020/ ).
As outlined above, the constantly evolving nature of the pandemic presents an unprecedented challenge to researchers aiming to identify strategies for addressing the mental health issues arising in the current pandemic. Risk factors for mental illness may coalesce in different ways at different time points of the pandemic waves. By extension, the particulars of service need and delivery will also shift against this backdrop and it is important that psychiatric services remain flexible in service delivery at this time. Despite these challenges, it is crucial to prioritise an integrated approach to psychiatric translational research in Ireland which can inform service innovation and development. The efforts of colleagues to continue to innovate and examine outcomes despite the aforementioned complexities and myriad pressures is indeed laudable and worthwhile as our efforts to transform and remodel services can have real impact for our service users.
As with the first edition dedicated to COVID-19, we sincerely hope that this themed issue provides a useful resource to colleagues as we continue to grapple with unprecedented demands. There is currently no road map to inform how the situation will evolve and what will be the ultimate extent of service need. Once again, we are most grateful to all contributors who, despite unparalleled service pressures, have taken the time to reflect and share perspectives on their experiences, innovations and clinical practice. This issue highlights the extraordinary demands on psychiatric services and the likely enduring nature of this need in the years to come as longer-term impacts of the pandemic, particularly potential economic contraction, exert their toll on population mental illness. Effective advocacy for our patients, ourselves and our colleagues remains paramount.
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Authors have no conflict of interest to disclore.
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committee on human experimentation with the Helsinki Declaration of 1975, as revised in 2008.

This article has been cited by the following publications. This list is generated based on data provided by Crossref .
- Google Scholar
View all Google Scholar citations for this article.
Save article to Kindle
To save this article to your Kindle, first ensure [email protected] is added to your Approved Personal Document E-mail List under your Personal Document Settings on the Manage Your Content and Devices page of your Amazon account. Then enter the ‘name’ part of your Kindle email address below. Find out more about saving to your Kindle .
Note you can select to save to either the @free.kindle.com or @kindle.com variations. ‘@free.kindle.com’ emails are free but can only be saved to your device when it is connected to wi-fi. ‘@kindle.com’ emails can be delivered even when you are not connected to wi-fi, but note that service fees apply.
Find out more about the Kindle Personal Document Service.
- Volume 37, Issue 4
- B. Gavin (a1) , J. Lyne (a2) (a3) and F. McNicholas (a4) (a5)
- DOI: https://doi.org/10.1017/ipm.2020.128
Save article to Dropbox
To save this article to your Dropbox account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Dropbox account. Find out more about saving content to Dropbox .
Save article to Google Drive
To save this article to your Google Drive account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Google Drive account. Find out more about saving content to Google Drive .
Reply to: Submit a response
- No HTML tags allowed - Web page URLs will display as text only - Lines and paragraphs break automatically - Attachments, images or tables are not permitted
Your details
Your email address will be used in order to notify you when your comment has been reviewed by the moderator and in case the author(s) of the article or the moderator need to contact you directly.
You have entered the maximum number of contributors
Conflicting interests.
Please list any fees and grants from, employment by, consultancy for, shared ownership in or any close relationship with, at any time over the preceding 36 months, any organisation whose interests may be affected by the publication of the response. Please also list any non-financial associations or interests (personal, professional, political, institutional, religious or other) that a reasonable reader would want to know about in relation to the submitted work. This pertains to all the authors of the piece, their spouses or partners.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 09 July 2021
Public mental health problems during COVID-19 pandemic: a large-scale meta-analysis of the evidence
- Xuerong Liu ORCID: orcid.org/0000-0002-9236-5773 1 ,
- Mengyin Zhu ORCID: orcid.org/0000-0001-5561-9570 1 ,
- Rong Zhang ORCID: orcid.org/0000-0003-4516-4116 2 ,
- Jingxuan Zhang ORCID: orcid.org/0000-0002-8979-5107 1 ,
- Chenyan Zhang ORCID: orcid.org/0000-0002-2945-6584 3 ,
- Peiwei Liu ORCID: orcid.org/0000-0003-2660-1106 4 ,
- Zhengzhi Feng ORCID: orcid.org/0000-0001-6144-5044 1 &
- Zhiyi Chen ORCID: orcid.org/0000-0003-1744-4647 1 , 2
Translational Psychiatry volume 11 , Article number: 384 ( 2021 ) Cite this article
19k Accesses
103 Citations
46 Altmetric
Metrics details
- Psychiatric disorders
- Scientific community
The coronavirus disease 2019 (COVID-19) pandemic has exposed humans to the highest physical and mental risks. Thus, it is becoming a priority to probe the mental health problems experienced during the pandemic in different populations. We performed a meta-analysis to clarify the prevalence of postpandemic mental health problems. Seventy-one published papers ( n = 146,139) from China, the United States, Japan, India, and Turkey were eligible to be included in the data pool. These papers reported results for Chinese, Japanese, Italian, American, Turkish, Indian, Spanish, Greek, and Singaporean populations. The results demonstrated a total prevalence of anxiety symptoms of 32.60% (95% confidence interval (CI): 29.10–36.30) during the COVID-19 pandemic. For depression, a prevalence of 27.60% (95% CI: 24.00–31.60) was found. Further, insomnia was found to have a prevalence of 30.30% (95% CI: 24.60–36.60). Of the total study population, 16.70% (95% CI: 8.90–29.20) experienced post-traumatic stress disorder (PTSD) symptoms during the COVID-19 pandemic. Subgroup analysis revealed the highest prevalence of anxiety (63.90%) and depression (55.40%) in confirmed and suspected patients compared with other cohorts. Notably, the prevalence of each symptom in other countries was higher than that in China. Finally, the prevalence of each mental problem differed depending on the measurement tools used. In conclusion, this study revealed the prevalence of mental problems during the COVID-19 pandemic by using a fairly large-scale sample and further clarified that the heterogeneous results for these mental health problems may be due to the nonstandardized use of psychometric tools.
Similar content being viewed by others
Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis

Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: a meta-analysis and systematic review
Mental disorders following COVID-19 and other epidemics: a systematic review and meta-analysis
Introduction.
Since the end of 2019, the coronavirus disease 2019 (COVID-19) outbreak has continued to spread worldwide. Researchers rapidly identified the cause of COVID-19 to be the transmission of serious acute respiratory syndrome by a novel coronavirus (SARS-CoV-2) [ 1 ]. Unfortunately, due to the lack of effective cures and vaccines, the ability of public medical systems to guard against COVID-19 is deteriorating rapidly. Although approved vaccines are now available, their safety is still a concern [ 2 , 3 ]. Further, because of reports regarding the potential to be reinfected with COVID-19, public panic is still spreading even though COVID-19 transmission has been contained substantially [ 4 ]. To date, projections regarding the end of the COVID-19 pandemic around the world are still far from optimistic. There were more than 158.95 million confirmed cases and 3.30 million deaths by May 11, 2021 (supported by Johns Hopkins University), a situation that has led to unprecedented losses and stress.
COVID-19 not only threatens physical health but has also led to mental health sequelae (i.e., loss of family, job loss, social constraints and uncertainty, and fear about the future) [ 5 , 6 , 7 ]. In general, mental health problems, including depression and anxiety, have had major negative impacts on the public during the COVID-19 pandemic [ 8 , 9 ]. Previous studies showed that mental health problems, such as depression, anxiety, insomnia, and post-traumatic stress disorder (PTSD), suddenly increased after the COVID-19 outbreak: 53.8% of respondents rated the psychological impact of the outbreak as moderate or severe; 16.5% of participants reported moderate to severe depressive symptoms; 28.8% of participants reported moderate to severe anxiety symptoms; and 24.5% of participants showed psychological stress [ 10 ]. Moreover, such mental health problems were worse in confirmed patients and healthcare workers. As a typical example, one early study revealed acute anxiety symptoms in 98.84% of confirmed patients and depression symptoms in 79.07% of confirmed cases [ 11 ]. In addition, an early investigation concerning the mental health status of 400 public health workers found that 31% of public health workers had anxiety symptoms, and 24.5% of them had depressive symptoms [ 12 ]. In this vein, it seems that the mental health sequelae of the COVID-19 pandemic warrant more attention. In addition, with the development of the epidemic situation, long-term isolation due to the increasing number of confirmed and suspected patients has caused losses to life and property, which has not only caused considerable psychological stress in the population but has also had physiological effects, such as insomnia and PTSD.
In brief, the COVID-19 pandemic has exposed public health to dramatic risks and resulted in unacceptable mental and physiological stresses. Despite considerable research, two critical concerns regarding mental health problems during the COVID-19 pandemic remain. One concern in previous studies is that the conclusions regarding the prevalence of these mental health problems are highly heterogeneous, irrespective of whether they are derived from original investigations or meta-analyses [ 13 , 14 ]. Another is that early investigations were almost all done during the peak of the COVID-19 pandemic and thus may overestimate the scale of mental health problems. Thus, the main purpose of this study is to provide comprehensive statistical results regarding the impact of COVID-19 on individual mental health through a large-scale meta-analysis of the existing research in this field and to provide an evidence-based reference for the prevention and control of psychological crises during this pandemic. It is noteworthy that this study employs a larger data pool than any of the existing meta-analyses to date. Further, much effort has been made to perform an in-depth investigation of the patterns of mental health problems triggered by the COVID-19 pandemic, including population-, region-, and measurement-specific patterns.
Materials and methods
To improve reproducibility and standardization, all the pipelines and protocols were in line with the Cochrane Handbook and were double-checked by using the PRISMA checklist [ 15 ]. This meta-analysis has been preregistered on OSF for open access ( https://doi.org/10.17605/OSF.IO/A5VMK ).
Search strategy and selection criteria
A systematic search was conducted for studies published from January 1, 2020 to July 1, 2020 (the period from the commencement of the outbreak to its initial control in China) in PubMed, EMBASE, the Cochrane Library, EBSCO, Web of Science, CNKI (Chinese database), WANGFANG DATA, the Chinese Biomedical Literature Service System, and public information release platforms (WeChat Subscription or microblogs). According to the indices of the various databases, keywords, including “2019 novel coronavirus,” “COVID-19,” “novel coronavirus pneumonia,” “NPC,” “2019-nCoV,” “mental health,” “anxiety,” “depression,” “psychological health,” “sleep,” “insomnia,” “Posttraumatic stress disorder,” and “PTSD,” were adopted to retrieve published surveys of psychological status during the COVID-19 epidemic from January 1, 2020 to July 1, 2020. In addition to identifying any target studies that may have been missed, we checked the reference list of each selected paper. The population was divided into three categories according to the probable psychological stress intensity experienced: public health workers, confirmed patients, and the general population (see Fig. 1 , Supplemental information, and Table S1 ).
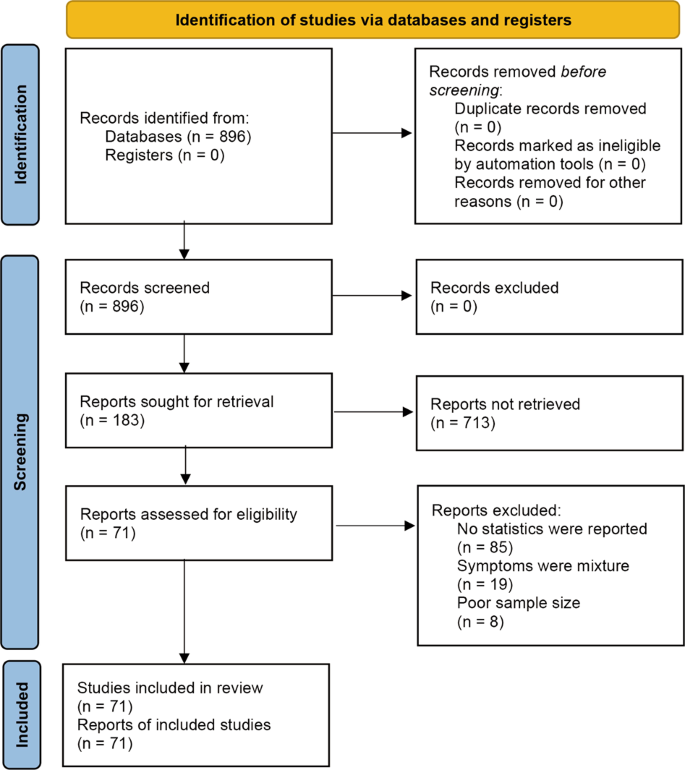
This flowchart is coincide with the broad-certified 2020 PRISMAstatement. Small sample size was predefined as < 30 participants.
Data extraction and quality assessment
The following data were extracted from each article by two researchers independently: study type; total number of participants; participation rate; region; percentage of physicians, nurses, and other healthcare workers screened in the survey; number of male and female participants; assessment methods used and their cutoffs; and the total number and percentage of participants who screened positive for depression, anxiety, insomnia or PTSD. If any of this information was not reported, the necessary calculations (e.g., transforming the percentage of healthcare workers to the number of healthcare workers) were performed. The accuracy of the extracted or calculated data was confirmed by comparing the collection forms of the two investigators.
In addition, two authors independently evaluated the risk of bias of the included cross-sectional studies using a modified form of the Newcastle-Ottawa scale. Potential disagreements were resolved by a third author. Specifically, the quality assessment criteria were as follows: sample representativeness and size; comparability between respondents and nonrespondents; ascertainment of depression, anxiety, and insomnia; and adequacy of the descriptive statistics. The total quality scores ranged between 0 and 5; studies scoring ≥3 points were regarded as having a low risk of bias, while studies scoring <3 points were regarded as having a high risk of bias (see Table S1 ).
Encoding and statistical analysis
The two investigators (XL and MZ), who performed the literature search, also extracted the data from the included studies independently. Disagreements were resolved with the third investigator (ZC) or by consensus. Then, the following variables were extracted: author, date of publication, age, gender, region, sample size, method, number of positive cases, and positivity rate. All these analytical procedures were performed with the CMA software (V3). In particular, given the heterogeneity within and between studies, random-effects models were used to estimate the average effect and its precision, which would give a more conservative estimate of the 95% confidence intervals (CIs). The I 2 statistic and Cochran’s Q test were conducted to assess statistical heterogeneity.
Prior researchers held that the fixed-effects model is ideally suited to the meta-analysis of a nonheterogeneous data pool ( I 2 < 50%, P value ≥0.1) [ 16 ]. Conversely, the random-effects model should be used when there is heterogeneity between the studies ( I 2 > 50%). According to the factors that may affect the heterogeneity between studies, moderation analysis was further carried out for distinct cohorts (i.e., health workers, confirmed and suspected patients, the general population) and distinct sample sources (China, other countries). A funnel chart was created for visual inspection to determine whether the included studies showed publication bias; Egger’s test and Kendall’s test for the quantitative analysis of publication bias were also used, with p > 0.05 indicating no publication bias.
In the current study, 896 Chinese and English studies were initially retrieved. According to the inclusion and exclusion criteria, 71 papers were eligible for inclusion in the data pool for the meta-analysis, and the total number of respondents reached 146,139 (see Table 1 and Table S2 ).
Heterogeneity test
The results of the heterogeneity test on the prevalence of mental problems in patients with COVID-19 showed that the heterogeneity across studies was large ( I 2 > 98%, P < 0.05), which suggested that the random-effects model was needed to analyze the total effect. Importantly, to increase the robustness of the results and reduce the heterogeneity between studies, population, nationality, and subgroup were analyzed as possible moderators.
Prevalence of mental problems
Four symptoms related to stress were selected as the mental problems, and the related symptoms and symptom groups were analyzed according to the definitions given in each study. The prevalence of anxiety was 32.6% (95% CI: 29.1–36.3; N = 86,035, see Fig. 2 ). In addition, the prevalence of depression was 27.60% (95% CI: 24.0–31.6; N = 90,156, see Fig. 3 ). Likewise, insomnia prevalence during the COVID-19 pandemic was 30.30% (95% CI: 24.6–36.6; N = 62,202, see Fig. 4A ). Finally, 16.70% of participants were found to meet the criteria for PTSD during the COVID-19 pandemic in this meta-analysis (95% CI: 8.9–29.2; N = 17,169, see Fig. 4B ).
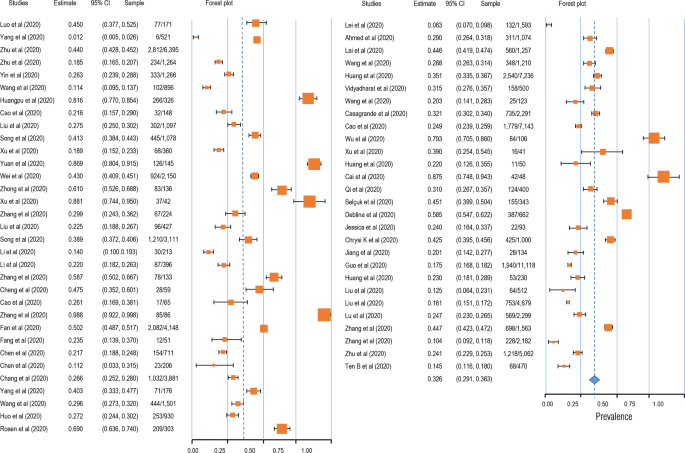
The squares colored by orange represent the point estimation foreffect towards corresponding study, with the large square size for high effect size. The orange diamond represent meta-analytic effect size.
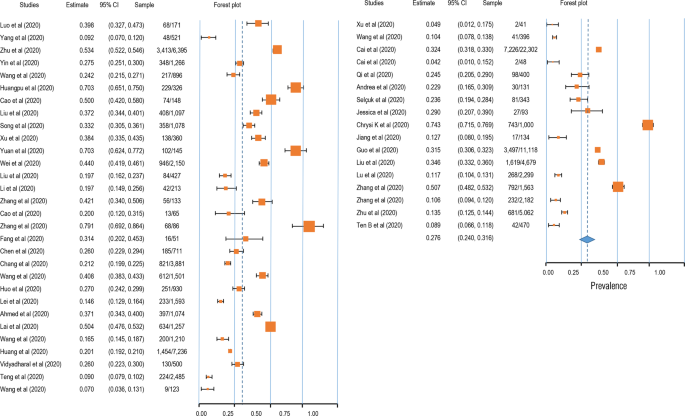
The squares colored by orange represent the point estimation for effect towards corresponding study, with the large square size for high effect size. The orange diamond represent meta-analytic effect size.
Moderation analysis
Given the high heterogeneity, we assumed that there were some potential moderators, including the cohort (confirmed patients, healthcare workers, and the general population), region (China and other countries), and measurement tool. The results demonstrated a significantly higher prevalence of mental health problems in confirmed patients than in others (see Table S3 ). Further, the prevalence of mental health problems was found to be lower in China than in other countries. In addition, these findings derived from the moderation analysis revealed the moderating role of the measurement tool, with the results varying significantly across different scales (see Table S3 and Figs. S1–3).
Publication bias assessment
A funnel plot was first used for qualitative analysis of the publication bias. As shown in Figure S4 , a symmetrical distribution was found for the four psychological symptoms. In addition, Begg’s rank test was performed to quantitatively analyze the publication bias. The results showed that there was no publication bias in the studies regarding anxiety (Kendall’s tau = 0.044, p = 0.614), depression (Kendall’s tau = −0.046, p = 0.647), insomnia (Kendall’s tau = −0.096, p = 0.592), or PTSD (Kendall’s tau = −0.145, p = 0.533).
In this study, a meta-analysis was performed to clarify the mental health situation in the population during the COVID-19 pandemic with respect to anxiety, depression, sleep problems, and PTSD. The results showed that the detection rate of anxiety symptoms in a total of 86,035 cases was 32.6% (95% CI: 29.1–363); the detection rate of depression symptoms in a total of 90,156 cases was 27.6% (95% CI: 24.0–31.6); the detection rate of insomnia symptoms in a total of 62,202 cases was 30.3% (95% CI: 24.6–36.6); and the detection rate of PTSD symptoms was 16.7% in a total of 17,169 cases (95% CI: 8.9–29.2). Furthermore, the moderator analysis showed that mental health problems (i.e., anxiety and depression) had the highest prevalence in COVID-19 patients, and fewer anxiety, depression, and sleep problems were observed in healthcare workers than in the general population. Overall, this study provided solid evidence of the mental health situation during the COVID-19 pandemic and indicated the potential heterogeneity across cohorts, regions, and measurement tools.
Furthermore, regarding anxiety symptoms, health workers accounted for 32.7% (95% CI: 27.9–38.2) of the detection rate; the general population accounted for 29.5% (95% CI: 25.2–34.3). A total of 25.8% (95% CI: 20.4–31.0), and 25.3% (95% CI: 20.4–32.0) of depressive symptoms were found in health workers and the general population, respectively. The highest detection rate of insomnia, which was 37.3% (95% CI: 32.1–42.8%), was found in health workers, and the general population represented 26.1% of cases (95% CI: 18.2–36.1). The detection rate of PTSD was 30.6% (95% CI: 9.1–65.9) in health workers and just 9.3% (95% CI: 4–19.8) in the general population. Moving beyond previous studies, this meta-analysis covered the latest COVID-19-related articles and examined more publications than its predecessors. In contrast to the existing research conclusions, this study found that the mental health problems of healthcare workers are the same as those of the general population, suggesting that the existing research may overestimate the mental health problems of healthcare workers (i.e., one study showed that 50.4% of healthcare workers reported symptoms of depression, 44.6% symptoms of anxiety, and 34.0% insomnia) [ 17 ]. This may be because in the early stage of COVID-19, the pressures experienced by healthcare workers were considerable due to the sudden workload and lack of adequate understanding of the COVID-19 pandemic. However, in later stages, as an understanding of COVID-19 improved, healthcare workers became familiar with the situation and gained a more comprehensive understanding of the disease. This led to higher self-regulation ability under the circumstance of the epidemic even though the stress level of the first-line workers was high. Therefore, a very important conclusion of this study is that the mental health problems of healthcare workers are not as serious as previously thought, and lagging research conclusions may lead to label effects, which in turn worsen the mental health status of healthcare workers. In addition, we found that the detection rate of mental health problems in infected patients is higher in the COVID-19 pandemic than it was during the SARS outbreak [ 18 ]. For example, during SARS, the detection rate of anxiety symptoms was 35.7% (95% CI: 27.6–44.2), and that of depressed mood was 32.6% (95% CI: 24.7–40.9); in contrast, we found anxiety and depression rates of 63.9% (95% CI: 29.6–88.2) and 55.4% (95% CI: 32.8–76.0), respectively, in the COVID-19 context. During the outbreak of SARS in 2003, information dissemination was less developed than at present, and the public understanding of the virus was based on official information, which made the spread of rumors and concomitant psychological distress less likely. This shows that we should pay attention not only to the spread of the virus but also to the spread of false/fake information about the virus.
The second core finding of this study is that the detection rates of anxiety, depression, insomnia, and PTSD in other countries are higher than those in China. Existing study demonstrated the higher anxiety and depression symptoms in overseas Chinese lived in Italy than do of overseas Chinese lived in mainland China [ 19 ]. This may be because China was the first country to have an outbreak of the diseases and has taken a series of effective measures. Civil society organizations took responsibility for isolating residents in every community and helped solve practical life difficulties. At the individual level, home isolation, social distancing, and the wearing of personal protective equipment such as face masks were implemented to prevent community transmission nationwide. Due to the development of advanced technology, residents have had easy access to reliable information and medical guidance, which can reduce misinformation and the impact of rumors. The public was well educated on the seriousness of COVID-19 complied cooperatively with the national approach of hand washing, mask wearing, social distancing, and universal temperature monitoring. All citizens were keenly aware of their roles in preventing the virus from spreading. To strike a balance between epidemic control and normal social and economic operations, industrial activities have gradually resumed in phases and batches since February 8, 2020 [ 20 ]. The supply of daily necessities was kept stable in every stage of the outbreak to ensure the smooth operation of society. The WHO-China Joint Mission report said that China has rolled out perhaps the most ambitious, agile, and aggressive disease containment efforts in history [ 21 ]. By striking contrast, the number of confirmed cases outside China is quickly climbing following an exponential growth trend. The total number of COVID-19 cases outside China has reached 333,706,43, including 999,603 deaths as of September 29, 2020. Furthermore, we also conjecture that the reason why fewer pandemic impacts were seen in mainland China is that the well-established psychological rescue system strongly guards against the potential panic arising from the COVID-19 pandemic. Specifically, Chinese governmental intervention agencies provide professional psychological intervention services for patients with confirmed diseases or mental disorders, front-line medical staff, and other key groups in special places such as designated hospitals and isolated hospitals. In addition, public psychological rescue organizations offer free 24/7 on-call professional psychological advice to the public. Ultimately, massive open online courses were released to enrich the Chinese public’s understanding of the COVID-19 pandemic, which has significantly strengthened belief in the ability to control this disaster [ 22 ]. In addition, the comparative analysis of the results obtained with different measurement tools showed heterogeneity and poor consistency across the tools. Therefore, it is suggested that reliable measurement tools should be established in future research to avoid deviation in research results caused by measurement tools.
This study adjusted the prevalence of mental health problems reported in previous studies by analyzing more recent studies and thus provided a more accurate picture of the mental health status of the population. Previous studies have provided very timely and important evidence to prove that the COVID-19 pandemic is a threat to individual mental health. However, most of the surveys were performed in the early and peak periods and may overestimate the prevalence of these problems. Moreover, for the sake of timeliness in sharing research findings, low-quality articles were published in some journals. Therefore, this study also adopts the method of quality control evaluation to exclude articles with lower quality and obtain more accurate and unbiased conclusions. In general, the detection rate of mental health problems found in this study was lower than that in previous studies. There may be two reasons for this. First, stricter quality control was adopted in this study, making the analysis results more accurate and unbiased. Second, more new studies were included in this study; that is, the investigation time extended from the initial stage to the peak of the pandemic and then to the later stage of COVID-19 pandemic in the present study. Therefore, the results of this study may reflect that, with better control and understanding of the epidemic situation, people’s mental health status has improved, which is a good sign.
This study has several limitations. First, the sample sizes were not matched well, with the number of healthcare workers being smaller than the number of people from the general population. Second, the international sample was insufficient, and the research on Chinese people significantly exceeded than that on people from other countries. Third, the impact of specific epidemic status was not taken into account. In future studies, covariates can be added to the meta-analysis to control the epidemic situation of samples in different regions.
In conclusion, our systematic review and meta-analysis provide a timely and comprehensive synthesis of existing evidence, confirming the presence of mental health problems in patients (including suspected patients) as well as insomnia and PTSD in medical staff. The findings help to quantify staff support in the context of a pandemic when stratified and customized interventions are needed to enhance resilience and reduce vulnerability. With the continuous emergence of new evidence, we can further update the meta-analysis and perform follow-ups to analyze the factors related to the epidemic situation to facilitate national-level planning, improve the hierarchical intervention of the mental health security system, and address similar public health events in the future.
Data and code availability
Study protocols and hypotheses were preregistered on the Open Science Framework (OSF) ( https://osf.io/a5vmk/ ). Raw data, protocols, and analysis scripts are available openly at the OSF ( https://osf.io/a5vmk/ ).
Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus:implications for virus origins and receptor binding. Lancet. 2020;395:565–74.
Article CAS PubMed PubMed Central Google Scholar
Hotez PJ, Corry BD, Bottazzi ME. COVID-19 vaccine design: the Janus face of immune enhancement. Nat Rev Immun. 2020;20:347–8. https://doi.org/10.1038/s41577-020-0323-4 .
Article CAS Google Scholar
Lurie N, Sharfstein JM, Goodman JL. The development of COVID-19 vaccines: safeguards needed. JAMA. 2020;324:439–40. https://doi.org/10.1001/jama.2020.12461 .
Article CAS PubMed Google Scholar
Deng W, et al. Primary exposure to SARS-CoV-2 protects against reinfection in rhesus macaques. Science. 2020;369:818–23. https://doi.org/10.1126/science.abc5343 .
Berg-Weger M, Morley JE. Editorial: loneliness and social isolation in older adults during the COVID-19 pandemic: implications for gerontological social work. J Nutr Health Aging. 2020;24:456–8. https://doi.org/10.1007/s12603-020-1366-8 .
Usher K, Bhullar N, Durkin J, Gyamfi N, Jackson D. Family violence and COVID-19: increased vulnerability and reduced options for support. Int J Ment Health Nurs. 2020;29:549–52. https://doi.org/10.1111/inm.12735 .
Article PubMed Google Scholar
Dubey S, Biswas P, Ghosh R, Chatterjee S, Dubey MJ, Chatterjee S, et al. Psychosocial impact of COVID-19. Diabetes & metabolic syndrome, 2020;14,779–88. https://doi.org/10.1016/j.dsx.2020.05.035 .
Choi EPH, Hui BPH, Wan EYF. Depression and anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health. 2020;17:10. https://doi.org/10.3390/ijerph17103740.
Article Google Scholar
Yang Y, Li W, Zhang Q, Zhang L, Cheung T, Xiang YT. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e19. https://doi.org/10.1016/S2215-0366(20)30079-1 .
Article PubMed PubMed Central Google Scholar
Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate Psychological Responses and Associated Factors during theInitial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health. 2020; 17:1729. https://doi.org/10.3390/ijerph17051729 .
Jinglong Z, Rong S, Juan Y. Anxiety and depression in elderly patients during epidemic of coronavirus disease 2019 and its influencing factors. J Clin Med Pract. 2020;04:246–50.
Google Scholar
Jing Q, et al. The evaluation of sleep disturbances for chinese frontline medical workers under the outbreak of COVID-19. Sleep Med. 2020;72:1–4.
Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–7. https://doi.org/10.1016/j.bbi.2020.05.026 .
Wei L, Caidi Z, Jin JL, Huijuan Z, Hui W, Bixi Y, et al. Meta analysis of mental state of different groups of people during the outbreak of new coronavirus pneumonia. J Tongji Univ. 2020;02:147–54. https://doi.org/10.16118/j.1008-0392.2020.02.002 .
Page MJ. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71 .
Hedges LV, Vevea JL. Fixed- and random-effects models in meta-analysis. Psychol Methods. 1998;3:486–504.
Lai J, et al. Factors associated with mental health outcomes among health care workers exposed to Coronavirus Disease 2019. JAMA Network Open. 2020;3:e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976 .
Jonathan PR, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7:7.
Chen W, Zhan H, Hong YLJY. COVID-19 epidemic survey of mental state of overseas Chinese in Italy abstract. Psychol Mon. 2020;17:46–47+50. 10.19738/j.cnki. psy.2020.17.014.
The State Council of the People’s Republic of China. The notice on orderly resuming production and resuming production in enterprises. 2020. http://www.gov.cn/xinwen/2020-02/09/content_5476550.htm (in Chinese). Accessed 7 Mar 2020.
WHO. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). 2020. https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-fifinal-report.pdf . Accessed 7 Mar 2020.
Chen LL, Du MJ. Research on the improvement of psychological counseling mechanism for major public emergencies in Hubei Province during the 14th Five Year Plan period. Soc Sci Trends. 2020;8:110–8.
Qianyi L, et al. Investigation of mental health status of frontline medical staff in COVID-19 treatment hospital in Guangdong Province. Guangdong Med. 2020;41:984–90. https://doi.org/10.13820/j.cnki.gdyx.20200920 .
Yang L, Zhang Y, Xu Y, Zheng J, Lin CQ. investigation on psychological stress in fighting against corona virus disease 2019 among community residents. Nurs Res. 2020;34:1140–5.
Xiaolin Z, et al. Psychological status of school students and employees during the COVID-19 epidemic. Chin J Ment Health. 2020;34:549–54.
Kaiheng Z, et al. Anxiety symptom and its associates among primary school students in Hubei province during 2019 novel coronavirus diseases epidemic. Chin Public Health. 2020;36:673–6.
Jiao Y, et al. Psychological investigation and analysis on mental care personnel in designated hospitals of coronavirus disease 2019. Med Philos. 2020;41:38–42+67.
Wang Z, Chen L, Li L, Zhang X, Wang YM, Xu X. Influence of COVID-2019 on mental health of medical students. J Changchun Univ Tradit Chin Med. 2020;36:1015–8. https://doi.org/10.13463/j.cnki.cczyy.2020.05.051 .
Huangfu M, Fu X, Wang LH. Investigation on psychological stress of frontline nurses in novel coronavirus pneumonia prevention. Chongqing Med. 2020;19:3172–6.
Cao J, Wen M, Shi Y, Wu Y, He Q. Prevalence and factors associated with anxiety and depression in patients with Coronavirus disease 2019 (COVID-19). J Nurs. 2020;35:15–17.
Xiaolei L, et al. Psychological state of nursing staff in a large scale of general hospital during COVID-19 epidemic. Chin J Hosp Infect. 2020;30:1641–6.
Song F, Wang X, Ju Z, Liu A, Junjie L, Wang T. Mental health status and related influencing factors during the epidemic of coronavirus disease 2019(COVID-19). Public Health Prev Med. 2020;31:23–27.
Xu Y, Zhao M, Tang X, Zhu X, Chen J. Correlation study between mental health and coping style of medical staff during COVID-19 epidemic. Anhui Med. 2020;41:368–71.
Yuan J, Du Y, Xu W, Chen Y. Study on the anxiety and depression levels and influencing factors in patients with suspected corona virus disease 2019 in isolation. Chongqing Med. 2020;19:3156–60.
Wei L, Shi L, Cao J. Psychological status of primary care workers during the COVID-19 epidemic in Shanghai. J Tongji Univ. 2020;41:155–60. https://doi.org/10.16118/j.1008-0392.2020.02.003 .
Zhong Y, Song X, Li J, Luo X, Chen W. Survey on the mental health of medical staffs in Emergency Department and Fever Clinic in Guiyang City under the Epidemic Situation of COVID-19. J Guizhou Univ Tradit Chin Med. 2020;42:16–22. https://doi.org/10.16588/j.cnki.issn1002-1108.2020.02.004 .
Xu Y. Investigation and analysis of the psychological status of the first batch of military nurses in “aiding Hubei to fight epidemic disease” and protection suggestions. Mil Med. 2020;04:313–5.
Zhang Y, Zhang X, Peng J, Fang P. A survey on mental of medical staff fighting 2019 Novel Coronavirus Disease in Wuhan. J Trop Med. 2020;10:1371–4.
Liu H, Liu Q, Li J. Investigation on the participation of mental health workers fighting against COVID-19 pandemic. Int J Psychiatry. 2020;02:201–4+209. https://doi.org/10.13479/j.cnki.jip.2020.02.003 .
Sun M, Li S, Yue HY, Li X, Li W, Xu S. analysis of Internet users’ anxiety and its influencing factors during the period of new crown pneumonia in China. World Sci Technol Modernization Chin Med. 2020;03:686–91.
Li X. novel coronavirus pneumonia isolation ward hope level, mental health and influencing factors. Gen Nurs. 2020;10:1203–6.
Li S, Wang Y, Yang Y, Lei X, Yang Y. Investigation on the influencing factors for anxiety related emotional disorders of children and adolescents with home quarantine during the prevalence of coronavirus disease 2019. China J Child Health. 2020;28:407–10.
Zhang X, et al. Survey of psychological status of front-line nurses staff during the period of epidemic and intervention measures. Nurs Pract Res. 2020;17:11–14.
Cheng J, Tan X, Zhang L, Zhu S, Yao H, Liu B. Research on the psychological status and influence factor of novel coronavirus pneumonia patients and people under medical observation. J Nurs Manag. 2020;20:247–51.
Cao X, Tang X, Xue JY. Knowledge Investigation,prevention and psychological analysis of patients with suspected coronavirus disease 2019. J Med Univ Chongqing. 2020. https://doi.org/10.13406/j.cnki.cyxb.002460 .
Fan Y, Wang J, Jia X, Liu X, Song YL, Zhang L. The role of mental problem evaluation and intervention in the university or college students kept at the home due to serious Corona Virus Disease-2019 epidemic during high education. Pharm Serv Res. 2020;20:81–85+91.
Fang X, et al. The mental health status of the close contacts of the new coronavirus pneumonia during the epidemic period. Chin J Crit Care Med. 2020;31:60–62.
Chen Y, Sun J, Hu J, Chen PL, Chen S. Analysis of mental health status of residents during COVID-19 epidemic. Clin Educ Gen Pract. 2020;18:237–9+244. https://doi.org/10.13558/j.cnki.issn1672-3686.2020.003.013 .
Chen J, Yin X, Luo J, Chen F, Ren J, Gong W. investigation and analysis of psychological anxiety status of medical staff in Qingbaijiang District of Chengdu city under new epidemic situation of coronavirus pneumonia. Shandong Med. 2020;60:70–72.
Chang J, Yuan Y, Wang D. Mental health status and its influencing factors among college students during the epidemic of COVID-19. J South Med Univ. 2020;40:171–6.
Yang Y, Qi Ling Z, Zhang H. The anxiety and social support of the spouses of front-line medical staff in Suining under the new coronavirus pneumonia situation. Gen Nurs. 2020;18:940–4.
Wang M, Liu X, Guo H, Fan HZ, Jiang R, Tan S. Mental health of middle-aged and elderly population during outbreak of coronavirus disease 2019. J Chin Geriatr Multi Organ Dis. 2020;19:241–5.
Fang P, et al. Analysis on psychological characteristics of the public in the epidemic of COVID-19. Infect Dis Inf. 2020;33:30–35.
Li C, et al. Investigation and analysis of post-traumatic stress disorder in front-line nursing staff of new coronavirus. Nurse’s Continuing Educ J. 2020;35:615–8. https://doi.org/10.16821/j.cnki.hsjx.2020.25.003 .
Mei J, et al. Analysis of psychological and sleep state of medical staff with novel coronavirus pneumonia. Med. Guidance. 2020;39:345–9.
Huo M, Yin Y, Jiang L, Duan X. Survey on the mental status of inhabitants living in Wuhan, Huanggang, Kunming and Yuxi epidemic outbreak stage of COVID-19. Int J Psychiatry. 2020;47:197–200.
Lei L. et al. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 eEpidemic in Southwestern China. Med Sci Monit. 2020;26:e924609. https://doi.org/10.12659/MSM.924609 .
Ahmed MZ, Ahmed O, Aibao Z, Hanbin S, Siyu L, Ahmad A. Epidemic of COVID-19 in China and associated psychological problems. Asian J Psychiatry. 2020;51:102092. https://doi.org/10.1016/j.ajp.2020.102092 .
Huang, Y, Zhao, N. Mental health burden for the public affected by the COVID-19 outbreak in China: Who will be the high-risk group?. Psychol Health Med. 2020;1–12. https://doi.org/10.1080/13548506.2020.1754438 .
Vidyadhara S, Chakravarthy A, Pramod Kumar A, Sri Harsha C, Rahul R. Mental health status among the South Indian Pharmacy students during Covid-19 pandemic’s quarantine period: a cross-sectional study. MedRxiv. May 12, 2020. https://doi.org/10.1101/2020.05.08.20093708 .
Tang W, et al. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J Affect Disord. 2020;274:1–7. https://doi.org/10.1016/j.jad.2020.05.009 .
Wang S, Xie L, Xu Y, Yu S, Yao B, Xiang D. Sleep disturbances among medical workers during the outbreak of COVID-2019. Occup Med. 2020;70:364–9. https://doi.org/10.1093/occmed/kqaa074 .
Casagrande M, Favieri F, Tambelli R, Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020;75:12–20. https://doi.org/10.1016/j.sleep.2020.05.011 .
Cao W. et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. https://doi.org/10.1016/j.psychres.2020.112934 .
Wu J, et al. Sleep quality survey and its influencing factors of clinical nurses in the first class of new coronavirus pneumonia. Chin Nurs Res. 2020;34:558–62.
Xu M, Zhang Y. Psychological survey of the first line supporting nurses who fight the new coronavirus pneumonia. Clin Nurs Res. 2020;34:368–70.
Kuang Z, Guo K, Liu Y, Li J, Kuang YF. investigation on cognition and psychological status of new university coronavirus pneumonia in Wuhan. J. Trop Med. 2020;03:283–5+288.
Wang Y, Yang Y, Li S, Lei X, Yang Y. Investigation on the status and influencing factors for depression symptom of children and adolescents with home quarantine during the prevalence of novel coronavirus pneumonia. Chin J Child Health. 2020;28:277–80.
Cai H, et al. Novel coronavirus pneumonia epidemic-related knowledge, behaviors and psychology status among college students and their family members and. China Public Health. 2020;36:152–5.
Tian Y, Zhang Y, Qian ZL. Investigation on the emotional status of villagers in a rural area of Hangzhou after the implementation of closure measures during the prevention and control of 2019–nCoV infection. Health Res. 2020;40:16–18+21.
Huang X, Ke P. Effect of standardized training novel coronavirus pneumonia on the anxiety level of the central sterile supply center. Gen Nurs. 2020;8:548–50.
Cai F, Yuan Q. The psychological status of the first line medical staff in combating new coronavirus pneumonia and intervention measures. Gen Nurs. 2020;18:827–8.
Amerio A, et al. Covid-19 pandemic impact on mental health: a web-based cross-sectional survey on a sample of Italian general practitioners. Acta Bio Med. 2020;91:83–88. https://doi.org/10.23750/abm.v91i2.9619 .
Özdin S, Bayrak Özdin Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int J Soc Psychiatry. 2020;66:504–11. https://doi.org/10.1177/0020764020927051 .
Roy D, Tripathy S, Kar SK, Sharma N, Verma SK, Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatry. 2020;51:102083. https://doi.org/10.1016/j.ajp.2020.102083 .
Goodman-Casanova JM, Dura-Perez E, Guzman-Parra J, Cuesta-Vargas A, Mayoral-Cleries F. Telehealth home support during COVID-19 confinement for community-dwelling older adults with mild cognitive impairment or mild dementia: survey study. J Med Internet Res. 2020;22:e19434. https://doi.org/10.2196/19434 .
Kaparounaki CK, Patsali ME, Mousa DV, Papadopoulou E, Papadopoulou K, Fountoulakis KN. University students’ mental health amidst the COVID-19 quarantine in Greece. Psychiatry Res. 2020;290:113111. https://doi.org/10.1016/j.psychres.2020.113111 .
Zohn R, Weinberger-Litman SL, Cheskie R, Rosmarin DH, Leib L. Anxiety and distress among the first community quarantined in the U.S due to COVID-19: Psychological implications for the unfolding crisis. 2020. https://doi.org/10.31234/osf.io/7eq8c .
Du J, et al. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen Hosp Psychiatry. 2020;20. https://doi.org/10.1016/j.genhosppsych.2020.03.011 .
Guo J, Liao L, Wang B, Li X, Guo L, Tong Z, et al. Psychological effects of covid-19 on hospital staff: a national cross-sectional survey in mainland China. Vasc Invest Ther. 2021;4:6–11.
Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. Mental health survey of novel coronavirus pneumonia patients receiving medical treatment in hospitals. Chin J Ind Hyg Occup Dis. 2020;38:192–5. https://doi.org/10.3760/cma.j.cn121094-20200219-00063 .
Liu C, Yang Y, Zhang XM, Xu X, Dou QL, Zhang WW. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiology and infection, 2020;148:e98. https://doi.org/10.1017/S0950268820001107 .
Liu Z, et al. Mental health status of doctors and nurses during COVID-19 epidemic in China. SSRN Electron J. 2020. https://doi.org/10.2139/ssrn.3551329 .
Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288:112936.
Qi J, Xu J, Li BZ, Huang JS, Yang Y, Zhang ZT, et al. The evaluation of sleep disturbances for Chinese frontline medical workers under the outbreak of COVID-19. Sleep medicine, 2020;72:1–4. https://doi.org/10.1016/j.sleep.2020.05.023 .
Zhang C, et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 Novel Coronavirus Disease outbreak. Front Psychiatry. 2020;11:306.
Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M, et al. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychotherapy and psychosomatics. 2020;89:242–50. https://doi.org/10.1159/000507639 .
Zhu Z, Xu S, Wang H, Liu Z, Wu J, Li G, et al. COVID-19 in Wuhan: Sociodemographic characteristics and hospital support measures associated with the immediate psychological impact on healthcare workers. EClinicalMedicine, 2020;24:100443. https://doi.org/10.1016/j.eclinm.2020.100443 .
Tan BYQ, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020. https://doi.org/10.7326/M20-1083 .
Download references
Acknowledgements
Special appreciations to Dr. Yancheng Tang (Peking University, Beijing, China; School of Business and Management, Shanghai International Studies University, Shanghai, China) for his comments on scientific contexts. Many thanks to Xi Luo and Ke Xu (Army Medical University, Chongqing, China) for their contributions to English writing. This study was supported by the People’s Liberation Army of China (PLA) Key Researches Foundation (CWS20J007).
Author information
Authors and affiliations.
Department of Medical Psychology, Army Medical University, Chongqing, China
Xuerong Liu, Mengyin Zhu, Jingxuan Zhang, Zhengzhi Feng & Zhiyi Chen
School of Psychology, Southwest University, Chongqing, China
Rong Zhang & Zhiyi Chen
Cognitive Psychology Unit, The Institute of Psychology, Faculty of Social and Behavioural Sciences, Leiden University, Leiden, Netherlands
Chenyan Zhang
Department of Psychology, University of Florida, Gainesville, FL, USA
You can also search for this author in PubMed Google Scholar
Contributions
XL and ZC: conceptualization, methodology, software, writing—original draft and visualization; MZ, JZ, and RZ: writing—review and editing, methodology, or validation; PL and CZ: writing—revision; RZ and XL: replication analysis and validation; ZC: formal analysis and validation; ZC and ZF: conceptualization, supervision, project administration, and funding acquisition.
Corresponding authors
Correspondence to Zhengzhi Feng or Zhiyi Chen .
Ethics declarations
Competing interests.
The authors declare no competing interests
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplemental material, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Liu, X., Zhu, M., Zhang, R. et al. Public mental health problems during COVID-19 pandemic: a large-scale meta-analysis of the evidence. Transl Psychiatry 11 , 384 (2021). https://doi.org/10.1038/s41398-021-01501-9
Download citation
Received : 09 October 2020
Revised : 07 June 2021
Accepted : 21 June 2021
Published : 09 July 2021
DOI : https://doi.org/10.1038/s41398-021-01501-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Work-related problems and the psychosocial characteristics of individuals with irritable bowel syndrome: an updated literature review.
- Nagisa Sugaya
BioPsychoSocial Medicine (2024)
An in-person survey of the influence of the COVID-19 pandemic on physical function, functional capacity, cognitive function, and mental health among community-dwelling older adults in Japan from 2016 to 2022
- Yuko Fukase
- Naoto Kamide
- Hirokuni Tagaya
BMC Geriatrics (2024)
A 2-year longitudinal study examining the change in psychosocial factors under the COVID-19 pandemic in Japan
- Tetsuya Yamamoto
- Chigusa Uchiumi
Scientific Data (2024)

Measuring various aspects of coronavirus anxiety: a psychometric evaluation of Pandemic anxiety and Coronophobia scales from the latent and network perspective
- Lenka Vargová
- Pavol Kačmár
- Gabriel Baník
Current Psychology (2024)
Symptoms and risk factors of depression and PTSD in the prolonged COVID-19 pandemic: a longitudinal survey conducted from 2020 to 2022 in Japan
- Kanako Ichikura
BMC Psychiatry (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Greater Good Science Center • Magazine • In Action • In Education
Seven Ways the Pandemic Is Affecting Our Mental Health
Epidemiologists and virologists around the world are scrambling to understand and prevent the spread of the novel coronavirus. There is another group of researchers who are concerned about a slightly different foe: the mental health pandemic.
Facing an infectious disease, we have been forced to maintain distance from each other, all while going through levels of fear, uncertainty, job loss, and grief that are unprecedented for many people.
“In an ironic twist, many of the strategies that are critical to ensuring our collective public health during this pandemic may put people at greater risk for . . . mental health issues,” write Frederick Buttell and Regardt J. Ferreira at Tulane University in a recent, special issue of the journal Psychological Trauma .
In brand-new studies coming out of China, Spain, the United States, and other countries, researchers are discovering in real time how we are collectively coping with this worldwide event. The results are not uplifting, but they aren’t surprising either. We are suffering, some of us worse than others. You don’t have to have lost a job or a loved one to be affected. Humans are complex, and so are emotional responses to the pandemic.
When this all started, we learned how viruses spread and how to wash our hands like pros. Now we have lessons to learn about what happens to mental health in a crisis like this, so we can find ways to address it.
1. We’re anxious, depressed, and traumatized
As COVID-19 spread through China in January and February, researchers were already sending out questionnaires to citizens locked down in their homes. In half a dozen studies with over 10,000 respondents, they found that people were experiencing worse mental health problems than before the pandemic—high symptoms of stress, anxiety, depression, and post-traumatic stress disorder (PTSD). Up to half showed serious signs of depression (depending on the study), while up to 35 percent showed serious anxiety .
One survey followed over 1,700 people in 190 Chinese cities from late January to late February. During the height of the pandemic, their stress, anxiety, and depression didn’t change. Their symptoms of PTSD declined slightly—but they were still high enough to be worrisome. People weren’t getting worse, but they also didn’t seem to be getting used to pandemic life.
The results look no better in other countries. In late March, nearly 3,500 people were surveyed in Spain, when the country ranked second in the world in COVID-19 deaths. Many people met the criteria for clinical mental health problems: 19 percent for depression, almost a quarter for anxiety, and 16 percent for PTSD. Within a week after Slovenia declared an epidemic, over half of the thousands of people surveyed had high stress levels. In April, 14 percent of Americans were experiencing serious psychological distress, more than triple the rate in 2018.
And studies find that this stress and anxiety fuels poor sleep , creating a vicious cycle. The more we lay awake at night during the pandemic, rehashing worries we have no control over, the worse our mental health becomes.
2. Some of us are lonely, but not all
Stay-at-home orders and social distancing have left many people isolated, so it makes sense that we would be feeling lonely. And, indeed, nearly 1 in 7 U.S. adults said they were often or always lonely in April 2020, up over 25 percent from 2018. But another study in the U.S., Canada, and the U.K. found that people’s feelings of connection to others didn’t change much from before to during the pandemic. When one group of researchers surveyed over 1,500 people in the U.S. from January to April, they were surprised to find “remarkable resilience.” Not only did people not become lonelier over time, but they actually gained a greater sense of support from others.
All the phone calls and video chats with family and friends may be helping, write Martina Luchetti and her coauthors from Florida State University, as well as a new sense of togetherness. “Many people have felt part of community-wide efforts to slow the spread of the virus. The feeling of . . . being in this together may increase resilience.”

Greater Good’s Guide to Well-Being During Coronavirus
Practices, resources, and articles for individuals, parents, and educators facing COVID-19
However, this hasn’t been true for everyone. People who are younger or living alone, or who have a chronic health condition, are lonelier than other groups. In fact, one study in the U.S. in April and May (before any restrictions were lifted) found that almost two thirds of people under 30 had high levels of loneliness, and 37 percent felt they had low support from their family.
“Feeling cut off from social groups may lead one to feel vulnerable and pessimistic about one’s circumstances,” write Cindy H. Liu and her coauthors.
3. Domestic violence has increased
In early April, the United Nations called for immediate global action to combat the increasing violence against women and girls during the pandemic.
According to news reports, domestic violence is increasing worldwide. At one police station just over 100 miles from Wuhan, China, for example, reports were three times higher in February 2020 compared to February 2019. In New Orleans, domestic aggravated assaults jumped 37 percent from January to April. Similar trends have been reported in Spain, Italy, Germany, and Brazil. As people are stuck at home, calls to helplines are surging.
Scientific surveys are only just beginning, but some preliminary results confirm these trends. Among people who were already experiencing domestic violence, the violence has gotten worse in nearly 60 percent of cases, report Buttell and Ferreira.
In their view, this comes down to a variety of factors: people spending more time at home with abusive partners, unemployment and other financial stressors causing conflict, shelters shutting their doors, and police being discouraged from making arrests.
Needless to say, the threat of abuse is compounding the stress, anxiety, and fear that many people are already experiencing during the pandemic.
4. The effects depend on your personality, lifestyle, and demographics
While older people have greater health risks from COVID-19, it seems to be younger people who are struggling emotionally. According to studies from Spain , China , and Slovenia , younger people tend to be more depressed, anxious, stressed, and traumatized in the era of COVID-19. The same is true for women , who may also be more lonely .
There’s no clear explanation for why this might be true, but researchers have some speculations. Women tend to have worse mental health in general, and certain stressors right now—like the added burden of caregiving and the risk of losing jobs—may fall more heavily on women.
For younger people, it could be the disruptions to their routines that are to blame, particularly for college students who have had to adjust to online schooling. In studies across both China and the United States , the more the pandemic was affecting people’s daily lives, the more anxious they felt.
Personality also influences how we fare in tough times. Two related traits that seem to matter during the pandemic are our ability to tolerate uncertainty and our ability to tolerate distress. While it’s hard for anyone to struggle or face the unknown, some people are less comfortable with it than others. And right now, it’s those people who seem to be ruminating more, feeling more afraid , and experiencing more depression, anxiety, and PTSD .
5. It’s worse for disadvantaged groups
In studies across the world, researchers investigated what else might make people vulnerable to mental health problems during the pandemic. They found a few key factors that put people at risk.
For one, people with poor health or chronic diseases tend to have higher symptoms of stress, anxiety, depression , and PTSD , several studies found . Of course, this might be because these are also the people with greater health risks from COVID-19.
Your income and education matter, too. The less stable your income and the less educated you are , studies suggest, the more anxiety, depression, and stress you will experience. The pandemic is threatening the economy, affecting everyone’s financial future, but the situation is worse for people who were already struggling. In a very real sense, we’re not all in the same boat.
“It is an inescapable fact that people lower on the socioeconomic ladder are struggling more”
A Pew survey of nearly 5,000 Americans in April found that the lowest-income people were most afraid of getting COVID-19, too. “[While] Americans may be struggling with the emotional challenges of the pandemic, it is an inescapable fact that people lower on the socioeconomic ladder are struggling more,” says psychologist David Sbarra.
6. The effects are compounded by racism
Those unequal effects extend all the way to who lives and who dies.
In fact, Black people are more likely to be infected, less likely to be tested and treated, and less likely to survive if they get COVID-19. According to Andrea King Collier in an article for Greater Good , a history of racism means the Black community is confronting the pandemic with worse health, less access to care, and more distrust of the medical system.
That means they have more reason to be fearful for their own lives, and they are more likely to experience loss. In fact, Pew research suggests that more than a quarter of Black Americans know someone who was hospitalized or died from COVID-19, compared to 1 in 10 white Americans.
These hardships worsened after the police killing of George Floyd, a Black man in Minnesota. His death catalyzed nationwide protests for racial justice—but at the same time, many observers say, it made the pandemic even harder for many Black Americans.
“Black people have been hit on all sides with the threat of loss of life,” says Riana Anderson, assistant professor at the University of Michigan’s School of Public Health. “It is exhausting. Depleting. Depressing. And absolutely an additional stressor.” She argues that family and community support is a strength of the Black community, but physical distancing restrictions have made it more difficult to access that power.
Other people of color are suffering disproportionally under the pandemic, too. Nearly one-fifth of Latino adults were experiencing serious psychological distress in April 2020; the CDC estimates that Latinos make up over half of the U.S. agricultural workforce, a group of essential workers whose jobs put them at greater risk of infection. Discrimination against Asians has risen since the pandemic started in Wuhan, China.

Anti-Racist Resources from Greater Good
Stories, tips, and tools to reduce prejudice in society and in ourselves.
All of these inequities create mental health problems that are even more aggravated by reduced and unequal access to mental health services .
7. Your work situation matters
One of the biggest disruptions to our daily lives today is how the pandemic has affected our work.
Doctors, nurses, and paramedics are taking on the urgent task of caring for COVID-19 patients, while other essential workers are putting themselves at risk to sell food, deliver mail, and pick up trash. Many office jobs have transitioned to remote work, asking employees to isolate at home, with many precariously juggling work and care for children or elders.
Other people have been unable to continue work during the pandemic, waiting for the time when they’ll be called back, while some have been laid off entirely. Unemployment in the U.S. more than quadrupled from February to April, leveling off in July at 10 percent.
A Chinese survey in mid-February examined some of these work situations, though not all. What was clear is that people who are unable to work temporarily—even if they don’t get laid off—have worse mental health. And while working in an office might seem risky, it was the people working from home who were actually more distressed and less satisfied with their lives.
Caring for yourself and others
There’s a lot we don’t have control over in this situation, which is stressful in and of itself. You may have some of the risk factors mentioned above, and there’s nothing you can do about it.
But what can you control? That’s the first question to ask.
For example, research from 28 countries conducted in mid-March found that the more people used social media, the more fearful they were. Frequent social media users in China were more likely to feel both depressed and anxious at the same time. Part of the reason may be because, particularly when the pandemic was ramping up, it was the main topic of discussion online. If being on Facebook doesn’t feel good, consider putting limits on social media time.
Does that mean ignorance is bliss? No. Finding the right sources of information is key. In fact, Chinese people who were highly satisfied with the health information they got about COVID-19 tended to have lower stress, anxiety, depression , and PTSD . Being informed helps reduce uncertainty and anxiety—but overloading ourselves with information can also be unsettling . Online or offline, reading news or imagining worst-case scenarios with family, the people who spent three or more hours a day focusing on COVID-19 were more anxious .
Besides taking breaks from news and social media, practicing basic safety and hygiene could go a long way for your mental health. In Chinese studies in January and February, people who engaged in proper hand washing, wore masks , and avoided sharing utensils tended to experience less depression, anxiety, stress, and PTSD.
Since March, Greater Good has been sharing tips for well-being during COVID-19 . For the most part, these are nothing new. In normal life and in a pandemic, we fare better when we try to stay connected in our relationships , cope with stress in healthy ways , and find a sense of agency .
But we can’t self-improve our way out of the pain and difficulty. What we’re going through right now is a trauma , or at least a major stressor on a global scale. This is one of those times when life really is harder by a little bit or a lot, depending on your situation. Feeling bad is part of being human—and right now, that’s something many of us need to face, even as we work to feel better, stay connected, and help others.
About the Author
Kira M. Newman
Kira M. Newman is the managing editor of Greater Good . Her work has been published in outlets including the Washington Post , Mindful magazine, Social Media Monthly , and Tech.co, and she is the co-editor of The Gratitude Project . Follow her on Twitter!
You May Also Enjoy

A Psychiatrist’s Tips for Calming Your Pandemic Stress

Three Tips from a Therapist for Calming Your Coronavirus Anxiety
Four Things to Do Every Day for Your Mental Health

Why Is COVID-19 Killing So Many Black Americans?

Seven Ways to Cope with Uncertainty

When Coronavirus Anxiety Is Useful and When It Isn’t
- Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- HIV and AIDS
- Hypertension
- Mental disorders
- Top 10 causes of death
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- Data collection tools
- Global Health Observatory
- Insights and visualizations
- COVID excess deaths
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Feature stories /
The impact of COVID-19 on mental health cannot be made light of

One of the biggest global crises in generations, the COVID-19 pandemic has had severe and far-reaching repercussions for health systems, economies and societies. Countless people have died, or lost their livelihoods. Families and communities have been strained and separated. Children and young people have missed out on learning and socializing. Businesses have gone bankrupt. Millions people have fallen below the poverty line.
As people grapple with these health, social and economic impacts, mental health has been widely affected. Plenty of us became more anxious; but for some COVID-19 has sparked or amplified much more serious mental health problems. A great number of people have reported psychological distress and symptoms of depression, anxiety or post-traumatic stress. And there have been worrying signs of more widespread suicidal thoughts and behaviours, including among health care workers.
Some groups of people have been affected much more than others. Faced with extended school and university closures young people have been left vulnerable to social isolation and disconnectedness which can fuel feelings of anxiety, uncertainty and loneliness and lead to affective and behavioural problems. For some children and adolescents being made to stay at home may have increased the risk of family stress or abuse, which are risk factors for mental health problems. Women have similarly faced greater stress in homes, with one rapid assessment reporting that 45% of women had experienced some form of violence, either directly or indirectly during the first year of the pandemic.
While mental health needs have risen, mental health services have been severely disrupted. This was especially true early on in the pandemic when staff and infrastructure were often redeployed to COVID-19 relief. Social measures also prevented people from accessing care at that time. And in many cases, poor knowledge and misinformation about the virus fuelled fears and worries that stopped people from seeking help.
Fear factor
Esenam Abra Drah lives with bipolar disorder in Ghana, where fear of the virus has been an unprecedented stressor to the mental health of many individuals. “I have many friends who had relapses in their mental health because of the increased levels of fear and panic,” says Esenam. “It was almost as if fear was contagious.”
Esenam explains that most people are afraid to seek help because they think that if they visit the hospital, they might end up getting infected with COVID-19. “I myself did not go to the clinic for therapy for an entire year partly because of this fear,” she says.
At that time Esenam, like so many others, was unemployed and did not have the funds for treatment. Even before the pandemic, cost of care was known to be a major barrier to people with mental health conditions seeking help.
“I have been privileged to have a good system of support,” says Esenam. “My pensioner parents managed to make sure my medications were always refilled.”
“But it is not the same for others,” she adds. “Some people could not afford treatment. It was and still is a very difficult time for a lot of people.”
Recommendations for response
Since the start of the pandemic, mental health service providers have tried to mitigate service disruptions, for example by delivering care via alternative routes when public health and social measures were in place. Community-based initiatives were often faster to adapt, finding innovative ways to provide psychosocial support, including through digital technologies and informal supports. And international organizations have also provided guidance, tools and resources to help responders, public health planners and the general public.
WHO recommends integrating Mental Health and Psychosocial Support (MHPSS) within all aspects of preparedness and response for all public health emergencies. To minimize the mental health consequences of the COVID-19 pandemic, WHO also recommends that countries:
- Apply a whole of society approach to promote, protect and care for mental health, including through social and financial protection to safeguard people from domestic violence or impoverishment, and by communicating widely about COVID-19 to counter misinformation and promote mental health.
- Ensure widespread availability of mental health and psychosocial support, including by scaling up access to self-help and supporting community initiatives.
- Support recovery from COVID-19 by building mental health services for the future.
The COVID-19 pandemic, like other ongoing crises, has made strengthening mental health systems more urgent all over the world. “The impact of COVID-19 on mental health cannot be underestimated. It cannot be made light of,” says Esenam. Change is possible.

Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
Mental health and the pandemic: What U.S. surveys have found
The coronavirus pandemic has been associated with worsening mental health among people in the United States and around the world . In the U.S, the COVID-19 outbreak in early 2020 caused widespread lockdowns and disruptions in daily life while triggering a short but severe economic recession that resulted in widespread unemployment. Three years later, Americans have largely returned to normal activities, but challenges with mental health remain.
Here’s a look at what surveys by Pew Research Center and other organizations have found about Americans’ mental health during the pandemic. These findings reflect a snapshot in time, and it’s possible that attitudes and experiences may have changed since these surveys were fielded. It’s also important to note that concerns about mental health were common in the U.S. long before the arrival of COVID-19 .
Three years into the COVID-19 outbreak in the United States , Pew Research Center published this collection of survey findings about Americans’ challenges with mental health during the pandemic. All findings are previously published. Methodological information about each survey cited here, including the sample sizes and field dates, can be found by following the links in the text.
The research behind the first item in this analysis, examining Americans’ experiences with psychological distress, benefited from the advice and counsel of the COVID-19 and mental health measurement group at Johns Hopkins Bloomberg School of Public Health.
At least four-in-ten U.S. adults (41%) have experienced high levels of psychological distress at some point during the pandemic, according to four Pew Research Center surveys conducted between March 2020 and September 2022.
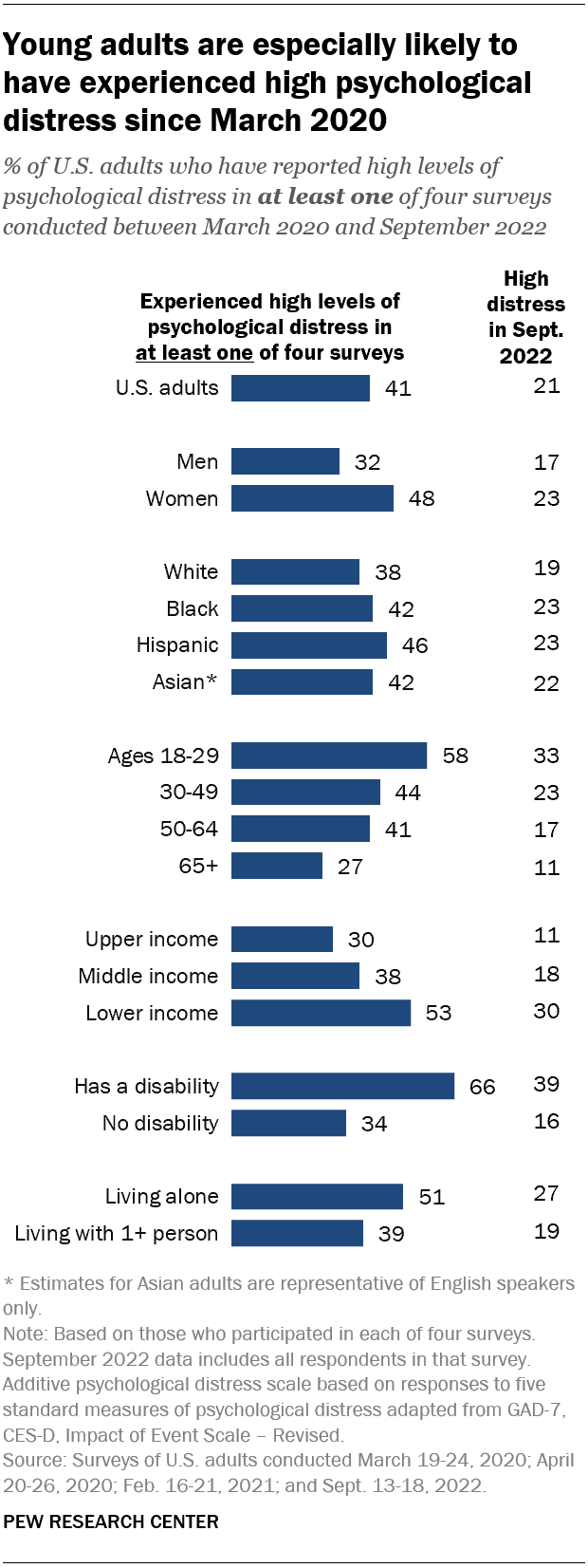
Young adults are especially likely to have faced high levels of psychological distress since the COVID-19 outbreak began: 58% of Americans ages 18 to 29 fall into this category, based on their answers in at least one of these four surveys.
Women are much more likely than men to have experienced high psychological distress (48% vs. 32%), as are people in lower-income households (53%) when compared with those in middle-income (38%) or upper-income (30%) households.
In addition, roughly two-thirds (66%) of adults who have a disability or health condition that prevents them from participating fully in work, school, housework or other activities have experienced a high level of distress during the pandemic.
The Center measured Americans’ psychological distress by asking them a series of five questions on subjects including loneliness, anxiety and trouble sleeping in the past week. The questions are not a clinical measure, nor a diagnostic tool. Instead, they describe people’s emotional experiences during the week before being surveyed.
While these questions did not ask specifically about the pandemic, a sixth question did, inquiring whether respondents had “had physical reactions, such as sweating, trouble breathing, nausea, or a pounding heart” when thinking about their experience with the coronavirus outbreak. In September 2022, the most recent time this question was asked, 14% of Americans said they’d experienced this at least some or a little of the time in the past seven days.
More than a third of high school students have reported mental health challenges during the pandemic. In a survey conducted by the Centers for Disease Control and Prevention from January to June 2021, 37% of students at public and private high schools said their mental health was not good most or all of the time during the pandemic. That included roughly half of girls (49%) and about a quarter of boys (24%).
In the same survey, an even larger share of high school students (44%) said that at some point during the previous 12 months, they had felt sad or hopeless almost every day for two or more weeks in a row – to the point where they had stopped doing some usual activities. Roughly six-in-ten high school girls (57%) said this, as did 31% of boys.
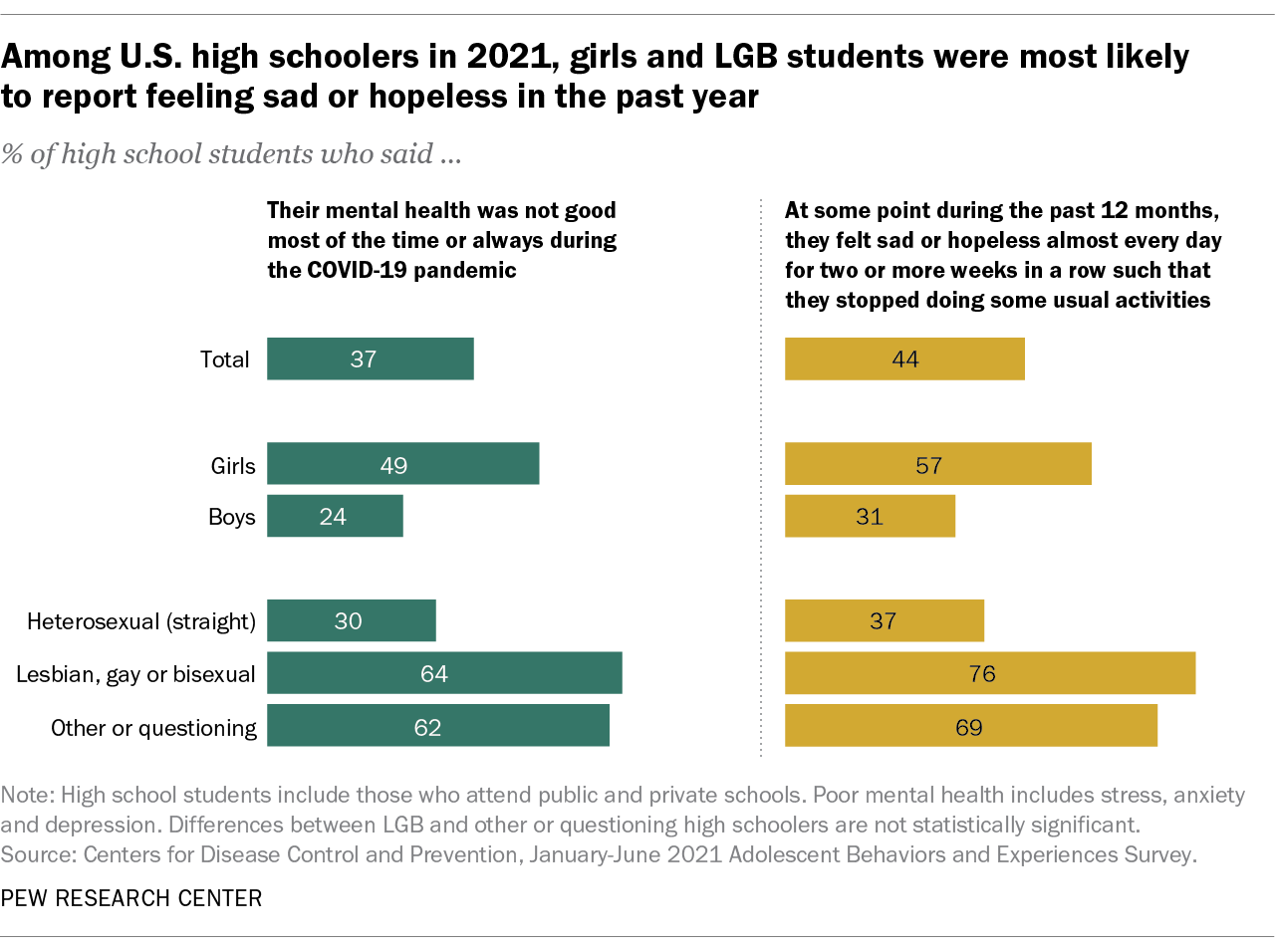
On both questions, high school students who identify as lesbian, gay, bisexual, other or questioning were far more likely than heterosexual students to report negative experiences related to their mental health.
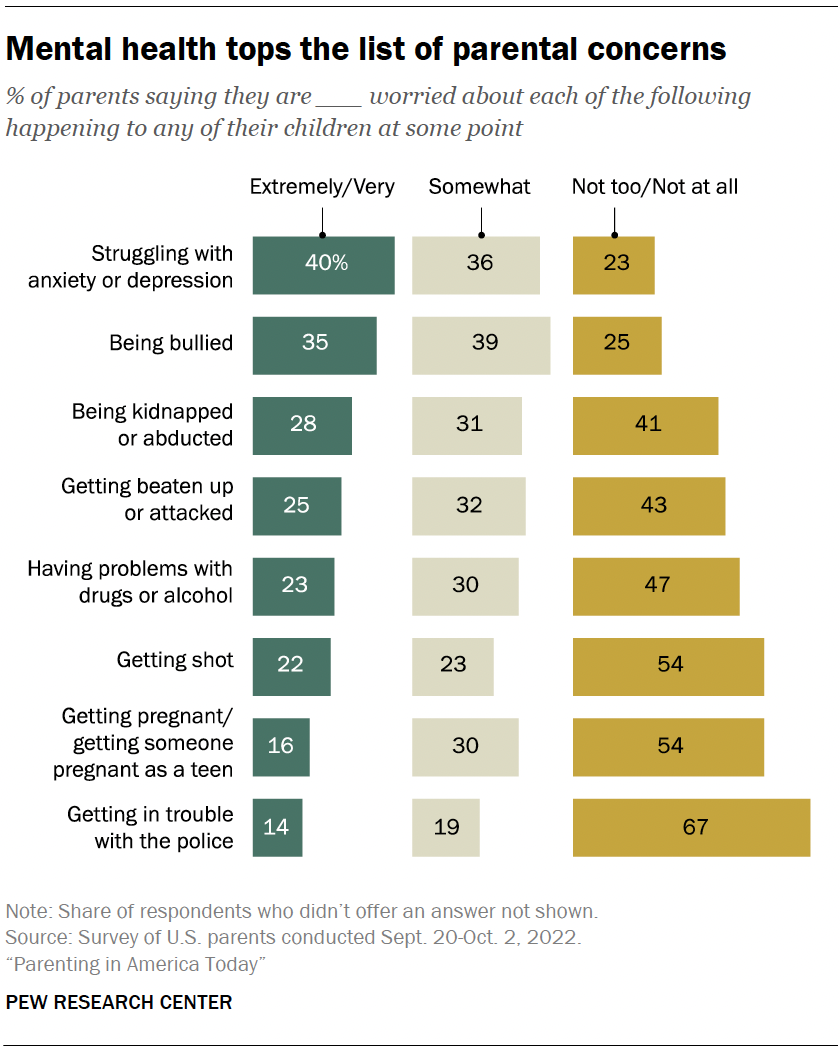
Mental health tops the list of worries that U.S. parents express about their kids’ well-being, according to a fall 2022 Pew Research Center survey of parents with children younger than 18. In that survey, four-in-ten U.S. parents said they’re extremely or very worried about their children struggling with anxiety or depression. That was greater than the share of parents who expressed high levels of concern over seven other dangers asked about.
While the fall 2022 survey was fielded amid the coronavirus outbreak, it did not ask about parental worries in the specific context of the pandemic. It’s also important to note that parental concerns about their kids struggling with anxiety and depression were common long before the pandemic, too . (Due to changes in question wording, the results from the fall 2022 survey of parents are not directly comparable with those from an earlier Center survey of parents, conducted in 2015.)
Among parents of teenagers, roughly three-in-ten (28%) are extremely or very worried that their teen’s use of social media could lead to problems with anxiety or depression, according to a spring 2022 survey of parents with children ages 13 to 17 . Parents of teen girls were more likely than parents of teen boys to be extremely or very worried on this front (32% vs. 24%). And Hispanic parents (37%) were more likely than those who are Black or White (26% each) to express a great deal of concern about this. (There were not enough Asian American parents in the sample to analyze separately. This survey also did not ask about parental concerns specifically in the context of the pandemic.)
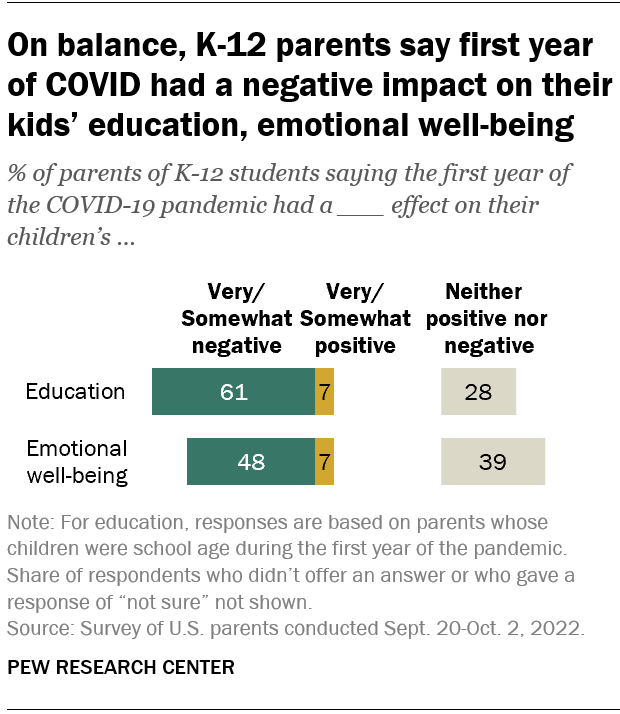
Looking back, many K-12 parents say the first year of the coronavirus pandemic had a negative effect on their children’s emotional health. In a fall 2022 survey of parents with K-12 children , 48% said the first year of the pandemic had a very or somewhat negative impact on their children’s emotional well-being, while 39% said it had neither a positive nor negative effect. A small share of parents (7%) said the first year of the pandemic had a very or somewhat positive effect in this regard.
White parents and those from upper-income households were especially likely to say the first year of the pandemic had a negative emotional impact on their K-12 children.
While around half of K-12 parents said the first year of the pandemic had a negative emotional impact on their kids, a larger share (61%) said it had a negative effect on their children’s education.
- Coronavirus (COVID-19)
- Happiness & Life Satisfaction
- Medicine & Health
- Teens & Youth

John Gramlich is an associate director at Pew Research Center .
How Americans View the Coronavirus, COVID-19 Vaccines Amid Declining Levels of Concern
Online religious services appeal to many americans, but going in person remains more popular, about a third of u.s. workers who can work from home now do so all the time, how the pandemic has affected attendance at u.s. religious services, economy remains the public’s top policy priority; covid-19 concerns decline again, most popular.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
© 2024 Pew Research Center
- News and Features
- Conferences
- Clinical Tools
- Special Collections
Position Paper: The Impact of COVID-19 on Mental Health

In a position paper published in The Lancet Psychiatry , a group of mental health experts and other individuals from around the world came together to discuss the influence coronavirus disease 2019 (COVID-19) poses to mental health care. The study authors noted that the pandemic reveals both system failings and opportunities for improving mental health delivery.
Potential Consequences of COVID-19
The COVID-19 public health crisis has led to a spike in known risk factors for mental health conditions, including everything from social isolation to unemployment to overall feelings of insecurity and instability. In light of these risk factors, as well as potential long-term mental health impacts, the researchers advocate for both short-term and ongoing responses.
Most general public surveys link COVID-19 to increased symptoms of depression, anxiety, and stress. Panic buying, binge-watching TV, and other unhealthy behaviors have been reported. Increased social media use, which is also reported, ups the odds of anxiety (odds ratio 1.72 [95% CI, 1.31–2.26]) and combined depression with anxiety (1.91 [1.52–2.41]). Quarantine can contribute to stress and anger and may also prompt behaviors such as online gambling.
People with COVID-19 face post-traumatic symptoms, psychological instability, depression, and anxiety. “The possibility that SARS-CoV-2 is neurotropic emphasizes the need for evaluation of potential short-term and long-term effects on the nervous system,” the study authors stated
People with pre-existing mental health conditions generally have an increased risk of infections, including SARS-CoV-2. Not only are older adults at a higher risk of severe COVID-19 illness, they also face a heightened risk of mental health issues due to possible cognitive decline. People with pre-existing mental health conditions and disorders are also especially sensitive to quarantine, physical distancing, food availability, and general disruption of their routine.
Mental Health Service Responses
The authors of the study suggest rethinking conventional mental health approaches in order to improve the cost and scale of treatment. The public health response to COVID-19 should include clear, up-to-date information about infection rates and distancing measures (to reduce uncertainty), as well as information on education, self-care, family support, and collaboration across agencies. Study authors also identified and supported steps already being taken to control infection and to promote wellness among special populations, such as healthcare workers.
Mental Health Care Adaptations
The study authors recommend an ethics- and rights-driven approach to care. They acknowledge potential discrimination “in adjudicating access to insufficiently available health interventions and applying and weighing the added risk of SARS-CoV-2 exposure in decisions about involuntary institutionalization.” Potential future service cuts, disproportionate additional illness burden, reduced service access, inadequate financial support, exacerbation of inequalities in access to health care, and the need for greater family and caregiver support are also valid concerns.
With access to care often limited, and in-person contact either limited or unavailable, patients and caregivers need to feel empowered to take ownership of their care to ensure the best outcomes, the study authors stated. Relative risks and benefits of treatment changes should be considered, especially with patients receiving clozapine, injectable medications, or electroconvulsive therapy.
“Treatment plans might need to be rapidly renegotiated, and should be based on best practices,” the researchers stated. “There is thus a need to enhance and create robust resources to support shared decision making.”
The benefit of person-centered care is noted and should not be ignored when there’s a need for rapid decision-making. Care design and delivery can be strengthened by “increased peer worker involvement in the co-design of adapted services and by increasing the number of peer workers, especially in countries with limited resources,” researchers stated.
Long-Term Needs
Moving forward, the study authors suggest community monitoring and mental health screening to mitigate the potential long-term mental health effects of COVID-19. Digital health and digital phenotyping are 2 possibilities. With local needs clarified, community stakeholder groups can design interventions.
Community support services can help people experiencing acute distress, as well as those who don’t trust mainstream mental health care. Healthcare systems should thereby anticipate an increase in “unmet mental health needs” among vulnerable groups and prepare for them. Telemedicine is one way to fill gaps in care during the COVID-19 pandemic.
Provision of Mental Health Care
The authors of the study list the following indicators that should be assessed regularly during and after the pandemic, and compared with pre-pandemic data, to determine changes in delivery:
- The proportion of all mental health services provided in inpatient, emergency, institutional (eg, prisons), outpatient, community, and home-based settings
- Rates of face-to-face, video, and telephone contact with different types of mental health providers
- Rates of prescription and use of psychiatric medication
- Access to, and use of, different mental health services both by people with pre-existing mental health disorders and those with new incident cases of mental illness, and the sociodemographic characteristics of these users
- Quality of care of different mental health services (including acceptability and satisfaction with healthcare providers), with a focus on user expectations and satisfaction and on functional, vocational, and clinical outcomes (including the views of families or caregivers)
- Disparities in mental health care, with socioeconomic, race, and ethnicity data linked to quality measures
- Integration of mental health services with general health services, social welfare, and other institutions (eg, schools, prisons), and community associations
- Governmental and non-governmental financial support for mental health and social care services, and healthcare leaders should regularly monitor the use and effectiveness of mental health care. Certain indicators should be assessed regularly during and after the pandemic, and then compared with pre-pandemic data to determine changes in delivery.
“There is an opportunity to replace the old way of managing the gap between the supply of and demand for mental health care (ie, rationing) with a system that prioritizes high-quality and equitable care rather than focusing only on how much work is done,” the study authors concluded.
Several study authors declared affiliations with the pharmaceutical industry. Please see the original reference for a full list of authors’ disclosures.
Moreno C, Wykes T, Galderisi S, et al. How mental health care should change as a consequence of the COVID-19 pandemic . Lancet Psychiatry . 2020;7(9):813-824.

Spotlight Course
Want to read more.
Please login or register first to view this content.
Login Register
Post-Pandemic Depression, Anxiety, and Stress: A Look at the Mental Health of Nursing and Administrative Staff
14 Pages Posted: 25 Jun 2024
Pacheco-Flores Laura Iraís
Universidad de las Americas Puebla
Pineda-Téllez Magno
affiliation not provided to SSRN
Erika Ramos-Tovar
Some research has shown how mental health was affected during the COVID-19 pandemic in hospital staff worldwide. However, there is little evidence of the physiological status of healthcare and administrative workers at the first level of medical care. Therefore, it is necessary to identify mental health problems among hospital staff once this pandemic has passed. This study aims to determine the prevalence of depression, anxiety, and post-pandemic stress in personnel in the medical and administrative workers.This research is an observational and cross-sectional study of the medical and administrative workers of the clinic who participated voluntarily through the application of the DASS-21 questionnaire to determine the prevalence and severity of depression, anxiety, and stress. The 190 participants had a mean age of 49 ± 11 years. The prevalence of depression was 20% with a predominantly moderate severity index (38.46%), 33% of anxiety with a predominant extremely severe index (36.51%), and 30% of stress with a predominantly moderate severity index (36.84%), related to the healthcare personnel and particularly in the nursing staff and administrative area. In conclusion, it was identified that post-pandemic depression, anxiety, and stress in the population studied, nursing staff showed an intensity of extremely severe anxiety, the administrative area had depression with severe stress, and workers with different responsibilities but focused on the operation of the hospital. However, additional studies are required to evaluate appropriate management strategies to diagnose, treat, and prevent mental health disorders among hospital staff.
Note: Funding Information: None declared. Declaration of Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Ethics Approval Statement: This study did not represent a bioethical risk and was carried out with the approval of the unit authorities after evaluation and ruling by the Research and Research Ethics Committee of the ISSSTE Puebla Regional Hospital, with registration number 490.2023. Written informed consent was obtained.
Keywords: Depression, anxiety, stress, medical area, administrative area, nursing staff
Suggested Citation: Suggested Citation
Universidad de las Americas Puebla ( email )
Affiliation not provided to ssrn ( email ).
No Address Available
Erika Ramos-Tovar (Contact Author)
Do you have a job opening that you would like to promote on ssrn, paper statistics, related ejournals, psychiatry ejournal.
Subscribe to this fee journal for more curated articles on this topic
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
The mental and behavioral health crisis in youth: Strategic solutions post COVID-19 pandemic: An American Academy of Nuring consensus paper
Affiliations.
- 1 Psychiatric, Mental Health, and Substance Use Expert Panel. Electronic address: [email protected].
- 2 Psychiatric, Mental Health, and Substance Use Expert Panel; Health Equity Expert Panel.
- 3 Child, Adolescent, and Family Expert Panel.
- 4 Psychiatric, Mental Health, and Substance Use Expert Panel.
- 5 Trauma and Violence Expert Panel.
- PMID: 38901064
- DOI: 10.1016/j.outlook.2024.102177
The COVID-19 pandemic wrought significant negative impacts on youth well-being, particularly among Black, Hispanic, American Indian, Alaska Native, and LGBTQ+ (Lesbian, gay, bisexual, transgender, queer or questioning) youth. The pandemic disrupted connections to family, school, and community, which are essential supports for youth mental health. Lessons learned from the pandemic suggest the role of stress and windows of opportunity to build resiliency. Drawing from a policy dialog on the youth mental health crisis conducted by 4 American Academy of Nursing Expert Panels, we present approaches to the current increase in youth mental health problems. Included is emerging literature on building youth resilience, particularly via re-establishing school and community connections. The role of families, schools, and community support is emphasized, particularly by creating a healing school environment and the pivotal role of school nurses. Recommendations include increased support for families, engaging the school nurse role, and developing school-based innovative programs to build connections and youth wellness.
Keywords: Adolescent; Behavioral health; Child; Mental health; Resiliency; School nursing.
Copyright © 2024 Elsevier Inc. All rights reserved.
PubMed Disclaimer
Conflict of interest statement
Declaration of Competing Interest The authors declare no conflicts of interest.
Similar articles
- Latinx LGBTQ Youth, COVID-19, and Psychological Well-Being: A Systematic Review. Abreu RL, Barrita AM, Martin JA, Sostre J, Gonzalez KA. Abreu RL, et al. J Clin Child Adolesc Psychol. 2024 Jan-Feb;53(1):98-113. doi: 10.1080/15374416.2022.2158839. Epub 2023 Jan 23. J Clin Child Adolesc Psychol. 2024. PMID: 36689641
- The Role of School and Community Involvement in the Psychosocial Health Outcomes of Black and Latinx LGBTQ Youth. Heath RD, Keene L. Heath RD, et al. J Adolesc Health. 2023 May;72(5):650-657. doi: 10.1016/j.jadohealth.2022.11.010. Epub 2023 Jan 3. J Adolesc Health. 2023. PMID: 36599760
- Teen, Queer, and Asian: Lesbian, Gay, Bisexual, Transgender, Queer, Plus Asian American Students' Experiences in Schools. Gorse MM, Bacolores JP, Cheung J, De Pedro KT. Gorse MM, et al. J Sch Health. 2021 Nov;91(11):906-914. doi: 10.1111/josh.13077. Epub 2021 Sep 5. J Sch Health. 2021. PMID: 34486117
- A National Analysis of State Policies on Lesbian, Gay, Bisexual, Transgender, and Questioning/Queer Inclusive Sex Education. Garg N, Volerman A. Garg N, et al. J Sch Health. 2021 Feb;91(2):164-175. doi: 10.1111/josh.12987. Epub 2020 Dec 13. J Sch Health. 2021. PMID: 33314223 Review.
- Strengthening Our Schools to Promote Resilience and Health Among LGBTQ Youth: Emerging Evidence and Research Priorities from The State of LGBTQ Youth Health and Wellbeing Symposium. Johns MM, Poteat VP, Horn SS, Kosciw J. Johns MM, et al. LGBT Health. 2019 May/Jun;6(4):146-155. doi: 10.1089/lgbt.2018.0109. Epub 2019 Apr 8. LGBT Health. 2019. PMID: 30958731 Free PMC article. Review.
Related information
Linkout - more resources, full text sources.
- Elsevier Science
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- DOI: 10.1007/s10615-024-00943-0
- Corpus ID: 270578443
The Role of Resilience in Social Services During the COVID-19 Pandemic
- I. Jindra , Darci M. Graves
- Published in Clinical social work journal 17 June 2024
34 References
Social service providers under covid-19 duress: adaptation, burnout, and resilience, psychological adjustment during the global outbreak of covid-19: a resilience perspective., resilience and stress in frontline social workers during the covid‐19 pandemic in singapore, exploring shared trauma in the time of covid: a simulation-based survey study of mental health clinicians, relationship between perceptions of risk of contracting covid-19 and resilience: a cross-sectional community survey of social service providers in canada, how resilient is your team exploring healthcare providers’ well-being during the covid-19 pandemic, psychological resilience, coping behaviours and social support among health care workers during the covid‐19 pandemic: a systematic review of quantitative studies, covid‐19 anxiety among front‐line nurses: predictive role of organisational support, personal resilience and social support, the perceived job performance of child welfare workers during the covid-19 pandemic, modelling resilience in adolescence and adversity: a novel framework to inform research and practice, related papers.
Showing 1 through 3 of 0 Related Papers

How is the loneliness epidemic affecting society?
Gen Z faces severe loneliness, worsened by social media and the pandemic. What are the solutions to this growing mental health crisis?
The loneliness epidemic profoundly affects Gen Z.
Despite being hyperconnected through social media, they experience high levels of isolation, worsened by the pandemic.
The consequences are severe, leading to mental health crises, increased rates of depression and anxiety, and a sense of disconnection from community and purpose.
A study by Cigna found Gen Z (ages 18-22) is the loneliest generation, with nearly half feeling lonely. What can be done to address this growing mental health crisis?
Presenter: Anelise Borges
Guests: Annie Ji – Sociocultural YouTuber Esther Fernandez – Copywriter Simone Heng – Human connection specialist
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Mental health during the COVID-19 pandemic: Effects of stay-at-home policies, social distancing behavior, and social resources
Brett marroquín.
a Department of Psychology, Loyola Marymount University, 1 LMU Drive, Suite 4700, Los Angeles, CA 90045, United States
b Department of Psychiatry, University of Pittsburgh, Pittsburgh, PA, United States
Reed Morgan
Associated data.
Social distancing is the most visible public health response to the COVID-19 pandemic, but its implications for mental health are unknown. In a nationwide online sample of 435 U.S. adults, conducted in March 2020 as the pandemic accelerated and states implemented stay-at-home orders, we examined whether stay-at-home orders and individuals’ personal distancing behavior were associated with symptoms of depression, generalized anxiety disorder (GAD), intrusive thoughts, insomnia, and acute stress. Stay-at-home order status and personal distancing were independently associated with higher symptoms, beyond protective effects of available social resources (social support and social network size). A subsample of 118 participants who had completed symptom measures earlier in the outbreak (February 2020) showed increases in depression and GAD between February and March, and personal distancing behavior was associated with these increases. Findings suggest that there are negative mental health correlates of social distancing, which should be addressed in research, policy, and clinical approaches to the COVID-19 pandemic.
1. Introduction
COVID-19, the disease caused by the coronavirus SARS-CoV-2, emerged in December 2019 in China and quickly became a global pandemic. Since then, as of late August 2020, over 22.5 million people have contracted COVID-19, with over 800,000 deaths; these include over 5.6 million cases and 170,000 deaths in the United States, with more expected as the pandemic continues ( CDC, 2020 ; World Health Organization, 2020 ). Beyond this enormous global threat to physical health and life, researchers and clinicians have voiced concern over its impact on mental health ( Cao et al., 2020 ; Gruber et al., 2020 ; Pfefferbaum and North, 2020 ; Van Bavel et al., 2020 ). As a highly contagious viral disease, COVID-19 is an inherently social phenomenon, and the success of containment depends on effectively limiting social contact. Public health responses emphasizing social distancing, including stay-at-home orders and individual behavior change, appear to have slowed the trajectory of COVID-19 when implemented. Although essential for containing the virus, these social interventions may deleteriously affect mental health, as observed following earlier epidemics, like the 2003 SARS outbreak ( Cava et al., 2005 ; Hawryluck et al., 2004 ; Mak et al., 2009 ) and 2009 H1N1 outbreak ( Pfefferbaum et al., 2012 ).
The interventions most essential for pandemics necessarily disrupt the very social processes that facilitate mental health, including social support availability, day-to-day interaction, and social influences on coping ( Marroquín et al., 2017 ). Research on true quarantine (i.e., complete isolation to contain an illness) shows substantial effects on emotional distress and mental health including depression, generalized anxiety, insomnia, and post-traumatic stress ( Brooks et al., 2020 ). There is therefore an urgent need to examine the mental health consequences of current social distancing measures. Recent studies in China showed that COVID-19-related disruption (e.g., stopping work) was associated with more anxiety and psychological distress ( Cao et al., 2020 ; Zhang et al., 2020 ). In the U.S., stay-at-home orders have been associated with concurrent health anxiety, financial worry, and loneliness ( Tull et al., 2020 ). Still, it remains to be confirmed whether mental health symptoms are increasing over time as COVID-19 unfolds, as presumed ( Gruber et al., 2020 ; Van Bavel et al., 2020 ). It also remains to be seen whether prospective symptom increases, not only cross-sectional symptom severities, are associated with social distancing. Answering these questions would have implications for clinical and public health measures that aim to ameliorate the mental health burden of COVID-19 andrelated policies.
We propose two additional considerations in order to understand the effects of social distancing more comprehensively. First, the umbrella term “social distancing” comprises interventions spanning both public and private levels that may have different implications. At the public level, government-imposed “stay-at-home” (colloquially “quarantine” or “lockdown”) policies, while varying by region, tend to prohibit travel outside the home for activities other than those deemed necessary (e.g., procuring food, obtaining medical care, completing “essential” or “front-line” work). But even before such public measures were enacted for COVID-19, people were encouraged by authorities, media, and peers to voluntarily adopt “personal distancing” behaviors to reduce virus transmission (e.g., avoiding physical contact or close proximity with non-household members; reducing use of shared public spaces). Both forms of social distancing have caused wide-ranging social disruption, but their potentially independent effects on mental health are unknown, given that existing studies have so far focused on government-imposed stay-at-home status only ( Cao et al., 2020 ; Tull et al., 2020 ; Zhang et al., 2020 ). Second, effects of social distancing on mental health do not occur in a vacuum. People's adaptation to stressors depends in part on social resources. Social support – receiving advice, assistance, or caring, or perceiving that such support is available – is positively associated with mental health ( Cohen and Wills, 1985 ; Thoits, 2011 ), as are larger and more diverse social networks ( Cohen, 2004 ; Uchino, 2009 ). Individuals “bring with them” such protective resources to psychological challenges like COVID-19, but whether these resources mitigate the potential negative effects of social distancing is an open question.
1.1. Current investigation
This study examines relationships among social distancing (stay-at-home status and personal distancing behavior), social resources (perceived social support and social network size), and mental health during the early course of the COVID-19 pandemic (mid-February to late March 2020). We focused on depression, generealized anxiety disorder, intrusive thoughts, insomnia, and acute stress, all of which are sensitive to social influences and are known outcomes of exposure to negative events, including disasters and epidemics ( Mak et al., 2009 ; Pfefferbaum et al., 2012 ). Depression and generalized anxiety disorder (GAD) are consistently associated with exposure to stressful life events ( Kendler and Gardner, 2016 ; Kendler et al., 2003 ). Intrusive thoughts , anxious thoughts that are unwanted, recurrent, and often come out of the blue, are stressful in and of themselves, and are also associated with several stress-related disorders (e.g., obsessive-compulsive disorder, Pascual-Vera et al., 2019 ; posttraumatic stress disorder, Falsetti et al., 2002 ). Insomnia , which contributes to a wide array of mental health and quality of life impairments, is often prompted by negative life events ( Sinha, 2016 ). Lastly, acute stress is not only a broadly applicable non-clinical index of mental health in the context of negative events, but also a major transdiagnostic precipitant of psychological disorders ( Harkness and Hayden, 2020 ) .
We made three specific predictions. First, social distancing would be associated cross-sectionally with more mental health symptoms in late March 2020, above and beyond expected protective effects of individuals’ social resources. This finding would elaborate previous cross-sectional findings on psychological distress during COVID-19 ( Cao et al., 2020 ; Tull et al., 2020 ; Zhang et al., 2020 ) and extend them to a broader set of mental health symptoms. Second, we predicted that March levels of prospectively measured symptoms would represent an increase over mid-February levels. Third, we expected the magnitudes of these prospective symptom increases to be positively associated with the extent of social distancing, independently of social resources.
2.1. Procedure
This article reports on 2 time points from an ongoing multi-wave study in a national online sample of adults. A COVID-focused battery of measures was collected online during a 3-day period (the “March 2020” wave), March 26 to March 28, 2020, which yielded a sample of 435 participants, as described below. Of these participants, 118 also had prospective mental health symptom data available from a previous study on emotion regulation and psychopathology (the “February 2020” wave), collected from February 18 to March 1, 2020, before COVID-19 had disrupted daily life on a widespread scale in the U.S.
Participants were recruited initially via Amazon's Mechanical Turk (MTurk) platform and directed to the survey in Qualtrics. After providing informed consent, participants completed a section of questionnaires, including those described below. The study was approved by an Institutional Review Board and followed APA ethical standards; participants were debriefed and provided with local mental health resources.
2.2. COVID-19 context
2.2.1. february 2020.
By the end of February data collection (i.e., by March 1, 2020), there were only 75 reported cases of COVID-19 in the United States, with the first death announced on February 29 ( Worldometer, 2020 ). At that time, no stay-at-home orders had been issued by any local, state, or federal government.
2.2.2. March 2020
Between the two waves of data collection, the World Health Organization declared COVID-19 a pandemic (on March 11) and the U.S. President declared a national emergency (March 13). The first local stay-at-home order in the U.S. went into effect (March 17, in the San Francisco Bay Area), followed quickly by the first statewide order (March 19, in California). By the beginning of March data collection (initiated March 26), 21 states had issued stay-at-home or similar orders, weekly unemployment filings reached a then-record 3 million, and the Dow Jones Industrial Average was 23.7% down from its February peak. By this time there were 86,379 cases of COVID-19 in the U.S. and 1,614 deaths ( Worldometer, 2020 ). During the 3 days of data collection, cases rose to 124,788, deaths to 2,754, and 6 additional states enacted stay-at-home orders, for a total of 27 states.
2.3. Participants
2.3.1. inclusion criteria and quality control.
Recruitment was limited to adults in the U.S. Following recommendations for maximizing valid data in MTurk samples (e.g., Paolacci and Chandler, 2014 ; Peer et al., 2014 ), participants were required to have an approval rate for past MTurk tasks of 99% or above, and to have completed at least 500 previously approved tasks. Initial data collected from 499 individuals were inspected for quality, and 29 were removed for failing 3 or more of 6 attention check items distributed throughout the study (e.g., “Please leave this question blank;” “Enter the value equal to 6 minus 1”). Of the remaining 470, cases were further excluded for any one of the following reasons: taking less than half the median completion time of 34.1 min (i.e., less than 17.05 min; n = 14); invalid response style on more than 1 questionnaire (e.g., choosing the same response for all items; n = 11); invalid response to an open-ended text item about personal experiences, not part of the present report (i.e., using no personal pronouns, or nonsensical text; n = 10).
2.3.2. March 2020 sample
These criteria yielded a final sample of 435 participants residing in 46 states (all except Alaska, Montana, North Dakota, and Vermont) and the District of Columbia. The most frequent states were California (11.3%), Florida (10.4%), New York (7.1%), Pennsylvania (7.1%), and Texas (6.5%), also the five most populous states in the U.S. The sample consisted of 230 men (52.9%), 202 women (46.4%), and 3 another gender (0.7%), aged 39.2 years on average ( SD = 11.5; range 20–73). Racial/ethnic self-identification was 75.9% white, 9.4% Black/African-American, 8.0% Asian/Asian-American, 3.0% Hispanic/Latino, 0.2% Native American, and 3.4% multiracial. Median annual household income was $40,000–59,999, distributed as follows: below $20,000 (12.0%), $20,000–39,999 (23.4%), $40,000–59,999 (20.7%), $60,000–79,000 (21.8%), $80,000–99,999 (10.1%), $100,000–119,999 (4.8%) and $120,000 or more (7.1%). Approximately half the sample had less than a bachelor's degree, with education attainment distributed as follows: no diploma (0.7%), high school diploma (26.4%), GED (2.5%), associate's degree (17.0%), bachelor's degree (43.9%), master's degree (8.3%), and doctoral degree (1.1%).
2.3.3. Prospective February 2020 subsample
118 of the individuals in the final March sample had previously participated in an unrelated study in late February and provided valid data, including the same measures of depression and GAD symptoms. Prospective subsample participants did not differ significantly in gender, racial/ethnic identification, income, or education from new participants in March (all p s > .09), but were approximately 3 years older on average ( M = 41.54, SD = 11.19 versus M = 38.34, SD = 11.54), t (433) = 2.60, p = .010.
2.4. Mental health measures
Depressive symptoms (February and March). The Center for Epidemiological Studies Depression Scale (CES-D; Radloff, 1977 ) is a widely-used 20-item general-population measure of depressive symptoms with good psychometric properties. Participants rated how frequently they had experienced symptoms within the previous week (e.g., “I had crying spells,” “I was bothered by things that usually don't bother me”) on a scale from 0 ( rarely or none of the time/less than 1 day ) to 3 ( all of the time/5–7 days) . Reliability was excellent in both February (ɑ = .96) and March (ɑ = .94).
Generalized anxiety disorder symptoms (February and March). The GAD-7 ( Spitzer et al., 2006 ) is a 7-item measure of GAD symptoms over the last 2 weeks. Participants rated how much they had been bothered by, e.g., “Not being able to stop or control worrying,” and “Feeling nervous, anxious, or on edge,” on a scale from 0 ( not at all ) to 3 ( nearly every day ). Validity and reliability were good in past studies (e.g., Spitzer et al., 2006 ), and in this study reliability was excellent in both February (ɑ = .95) and March (ɑ = .93).
Intrusive thoughts (March) . The Experience of Intrusions scale (EIS; Salters-Pedneault et al., 2009 ) is a 5-item measure of the presence of intrusive symptoms, including both frequency and quality (intensity, suddenness, distress, and disruptiveness) of unwanted intrusive thoughts about an index event or topic that can be specified by the researcher. In this study, participants rated intrusive thoughts over the previous 24 h, specifically regarding COVID-19, on scales from 0 to 4. The scale has shown convergent validity with a standard measure of PTSD symptom severity ( r = .63) in an MTurk sample ( Takarangi et al., 2016 ), and reliability in this sample was good (ɑ = .86).
Insomnia (March). The Insomnia Severity Index (ISI; Bastien et al., 2001 ) is a widely-used 7-item measure of sleep difficulties over the previous 2 weeks, including sleep problems (e.g., difficulty falling or staying asleep, or waking up early), dissatisfaction, distress, and interference. Items are scored from 0 to 4 and summed. The ISI has strong psychometric properties ( Bastien et al., 2001 ; Morin et al., 2011 ), and reliability in this sample was excellent (ɑ = .92).
Acute stress (March). The Stress Overload Scale-Short Form (SOS-S; Amirkhan, 2018 ) is a 10-item version of the longer Stress Overload Scale ( Amirkhan, 2012 ), and measures stress within the last week. Total scores are the sum of five items assessing event load (e.g., “felt swamped by your responsibilities”) and five items assessing personal vulnerability (e.g., “felt like nothing was going right”), all scored from 1 ( not at all ) to 5 ( a lot ). The SOS-S has shown good internal reliability and concurrent and predictive validity in diverse community samples ( Amirkhan, 2018 ). Reliability in this sample was excellent (ɑ = .95).
2.5. Social distancing measures
Stay-at-home order status. Participants self-reported whether they had been told to “stay inside your home and avoid social contact by government officials (for example, with a ‘stay at home’ or ‘shelter in place’ order).” Responses were coded 1 for “yes” and 0 for “no.”
Personal distancing behavior. Participants estimated how many times they engaged in each of 12 activities during two time periods: “in the last 3 days,” and “in a typical 3-day period before the coronavirus outbreak.” Items were developed to represent a range of behavioral domains being discussed publicly in late March for limiting virus transmission: leaving one's home; riding public transportation; working from home/staying away from work; shaking hands; sitting/standing within 3 feet of someone not from one's household; hugging/kissing someone not from one's household; using a public restroom; going to a cafe, restaurant, or bar; going to a store; taking a taxi or rideshare service; visiting someone in their home; and having someone visit one's own home. Each item was scored as 1 if the reported last-3-day frequency differed from the pre-virus frequency in the distancing direction (e.g., if the participant reported shaking hands fewer times, or staying away from work more times, in the last 3 days as compared to before). Each behavior was scored as −1 if the reported last-3-day frequency differed in the opposite direction (increased social contact), and it was scored as 0 if the two frequencies were equal. Exploratory factor analyses suggested a single factor solution for all 12 items, and removing any item weakened internal consistency. Thus, all 12 scores were averaged to reflect the extent of each individual's distancing behavior, with possible averages falling between −1 (reduced distancing) and 1 (increased distancing). Reliability was good (ɑ = .80).
2.6. Social resource measures
Social support. Perceived social support was measured with the 24-item Social Provisions Scale (SPS; Cutrona and Russell, 1987 ). On a scale of 1 ( strongly disagree ) to 4 ( strongly agree ), participants rated statements tapping 6 domains of social support in their current relationships (e.g., “There are people I can depend on to help me if I really need it;” “I feel a strong emotional bond with at least one other person”). Responses were summed to provide a global social support score, which had excellent reliability (ɑ = .96).
Social network size. The network size score of the Social Network Index (SNI; Cohen et al., 1997 ) measures the number of all individuals with whom the individual has contact at least once every 2 weeks, within 12 possible social roles (including partners, parents, children, coworkers, neighbors, community group members, and others). The measure is a hybrid of categorical and count-based items, such that the relevance of each social role is established first (e.g., “Do you attend any classes on a regular basis?”), before assessing, if relevant, the degree of social contact within that role over a 2 week time frame (e.g., “How many fellow students or teachers do you talk to at least once every two weeks?”) Given this hybrid structure, internal consistency is not reported for the SNI ( Cohen et al., 1997 ).
2.7. Analytic plan
Preliminary analyses were conducted to describe the sample, including prevalence of clinically significant symptoms, and to examine relevant bivariate relationships (i.e., differences in main study variables based on demographics, bivariate correlations among study variables, and differences in all variables based on stay-at-home status). Main analyses proceeded in three phases. First, to examine cross-sectional hypotheses regarding social distancing correlates of mental health symptoms even in the context of other, more established social factors, both social distancing variables (stay-at-home status and personal distancing behavior) were entered into a series of multiple regression analyses, one for each mental health outcome, together with social resource variables and demographic covariates. Demographic covariates were identified by including all demographics in initial regression models and retaining any demographic variable that was a statistically significant predictor of any outcome variable ( p < .05), and were held constant across models. Second, the hypothesis that depression and GAD symptoms in the population increased from late February to late March was tested with repeated-measures tests of symptoms in the prospective subsample. Third, the hypothesis that social distancing would predict March symptoms, above and beyond social resources and February symptoms, was tested in multiple regression analyses identical to those conducted cross-sectionally in the full sample, but holding constant February symptoms.
3.1. Preliminary analyses
3.1.1. descriptive analyses.
Descriptive statistics for all study variables in the March wave are presented in Table 1 . To assess the prevalence of clinically-relevant symptoms, we examined recommended clinical cutoffs where available. The common cutoff of 16 on the CES-D ( Radloff, 1977 ) indicated that 38.4% of the sample was experiencing at least mild depression; a more stringent cutoff of 20 ( Vilagut et al., 2016 ) identified 27.4% of participants in the clinical range. Recommended cutoffs for the GAD-7 ( Spitzer et al., 2006 ) indicated that 22.8% were experiencing mild symptoms, 15.6% moderate symptoms (suggestive of a potential GAD diagnosis), and 9.0% severe symptoms. The ISI cutoff of 10, for the general population, showed 38.6% were experiencing insomnia symptoms within the clinical range ( Morin et al., 2011 ).
Descriptive statistics and zero-order differences by stay-at-home order status in late March 2020 (N = 435).
| March 2020 Sample Descriptives | Differences by Stay-at-Home Order Status | ||||||
|---|---|---|---|---|---|---|---|
| Mean (SD) | Observed Range | Stay-at-Home Status | (433) | ||||
| Yes | No | ||||||
| (%) | 283 (65.1%) | 152 (34.9%) | |||||
| 0.48 (0.28) | −0.25–1.00 | 0.50 (0.27) | 0.46 (0.29) | 1.45 | .148 | .14 | |
| Social support | 77.81 (14.97) | 30–96 | 78.51 (14.08) | 76.49 (16.48) | 1.34 | .180 | .13 |
| Social network size | 13.67 (8.71) | 0–56 | 13.71 (8.99) | 13.57 (8.18) | 0.17 | .869 | .02 |
| Depression | 14.90 (11.99) | 0–53 | 15.84 (12.43) | 13.13 (10.96) | 2.26 | .025* | .23 |
| GAD | 5.66 (5.50) | 0–21 | 6.18 (5.73) | 4.70 (4.92) | 2.71 | .007** | .28 |
| Intrusive thoughts | 8.26 (4.36) | 0–20 | 8.55 (4.45) | 7.71 (4.14) | 1.92 | .055† | .20 |
| Insomnia | 7.44 (6.11) | 0–27 | 7.77 (6.18) | 6.84 (5.96) | 1.52 | .128 | .15 |
| Acute stress | 22.12 (11.02) | 10–50 | 23.28 (11.77) | 19.97 (9.12) | 3.01 | .003** | .31 |
Note . a Unless otherwise indicated, values are in the format M (SD).
* p < .05, ** p < .01, † p = .055.
3.1.2. Demographic differences in study variables
Older age was associated with lower mental health symptoms of several types (depression, r = −.15; GAD symptoms, r = −.16; acute stress, r = −.16, all p s < .001). Older age was also associated with less personal distancing behavior ( r = −.12, p = .016). Women reported more intrusive thoughts ( M = 9.05, SD = 4.48) than men ( M = 7.50, SD = 4.12), t (430) = 3.73, p < .001, marginally more GAD symptoms ( M = 6.18, SD = 5.66 versus M = 5.16, SD = 5.29), t (430) = 1.94, p = .053, and higher social support ( M = 80.42, SD = 13.76 versus M = 75.62, SD = 15.52), t (430) = 3.38, p = .001. There were no significant racial/ethnic differences in any study variables, whether comparing individual racial/ethnic categories (all p s > .44) or minority status as a binary variable (all p s > .15). Several differences emerged based on income (ANOVA p s ≤ .01). Participants with the lowest annual household income (less than $20,000) were significantly higher in depression than all other income categories (all post-hoc comparison p s < .05), and those with an income of $20,000–39,999 were significantly higher in depression than those in the highest bracket ($120,000 or more), p < .05. Personal distancing behavior, social support, and social network size all increased with income, with differences largest at the extremes. Higher education was associated with a larger social network (ANOVA p < .001), except among doctoral degree holders ( n = 5), whose social networks were significantly smaller than those with master's degrees.
3.1.3. Zero-order associations among study variables
Group comparisons on all study variables by stay-at-home status are presented in Table 1 . More than half of the sample (65.1%; 283 participants) reported being under a stay-at-home order. Participants under a stay-at-home order reported significantly higher depression, GAD symptoms, and acute stress and marginally higher intrusive thoughts, but did not differ in insomnia. Personal distancing behavior, social support, and social network size did not differ based on stay-at-home status. Correlations among all continuous study variables are in Table 2 . Personal distancing behavior was significantly and positively associated with intrusive thoughts, but not with other mental health symptoms in these zero-order analyses. Social support was negatively associated with all symptom types. Social network size was correlated with fewer depressive symptoms but more intrusive thoughts.
Zero-order correlations among study variables in late March 2020 (N = 435).
| Social support | Social network size | Depression | GAD | Intrusive thoughts | Insomnia | Acute stress | |
|---|---|---|---|---|---|---|---|
| Personal distancing behavior | .23** | .38** | .02 | .08 | .23** | −.03 | .06 |
| Social support | – | .40** | −.55** | −.33** | −.10* | −.35** | −.38** |
| Social network size | – | −.17** | −.05 | .12* | −.08 | −.06 | |
| Depression | – | .82** | .53** | .65** | .77** | ||
| GAD | – | .65** | .62** | .71** | |||
| Intrusive thoughts | – | .38** | .49** | ||||
| Insomnia | – | .53** | |||||
| Acute stress | – | ||||||
Note . * p < .05, ** p < .01.
3.2. Main analyses
3.2.1. social distancing and mental health symptoms (march 2020).
We hypothesized that social distancing behavior would be associated with higher symptoms cross-sectionally, above and beyond adaptive effects of social support and social network size. Results of the multiple regression analyses examining this question are depicted in the upper half of Table 3 ; all analyses adjusted for identified demographic effects of age, gender, and income. As expected, social support had relatively strong and independent negative associations with all symptom types. Social network size was independently associated with intrusive thoughts and acute stress; surprisingly, this association was in the positive direction.
Social distancing and social resources as predictors of mental health symptoms in late March 2020 (top) and as predictors of symptom change from February to March 2020 (bottom) .
| Depression | GAD | Intrusive thoughts | Insomnia | Acute stress | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | SE | b | SE | b | SE | b | SE | b | SE | ||||||
| Age | −0.15 | .04 | −.15** | −0.08 | .02 | −.18** | −0.03 | .02 | −.08 | −0.04 | .03 | −.08 | −0.15 | .04 | −.16** |
| Gender | 3.59 | .96 | .15** | 2.14 | .50 | .20** | 2.06 | .41 | .24** | 1.07 | .58 | .09 | 2.32 | .99 | .11* |
| Income | −0.64 | .30 | −.09* | −0.16 | .16 | −.05 | −0.21 | .13 | −.08 | −0.23 | .18 | −.06 | −0.47 | .31 | −.07 |
| Social support | −0.49 | .03 | −.61** | −0.15 | .02 | −.42** | −0.07 | .02 | −.23** | −0.16 | .02 | −.39** | −0.33 | .04 | −.45** |
| Social network size | 0.08 | .06 | .06 | 0.06 | .03 | .09 | 0.07 | .03 | .14** | 0.06 | .04 | .09 | 0.15 | .07 | .12* |
| Stay-at-home status | 3.21 | .97 | .13** | 1.48 | .50 | .13** | 0.66 | .41 | .07 | 1.17 | .58 | .09* | 3.62 | .99 | .16** |
| Distancing behavior | 6.12 | 1.83 | .14** | 2.72 | .95 | .14** | 3.89 | .78 | .25** | 0.73 | 1.09 | .03 | 4.37 | 1.88 | .11* |
| (7, 427) | 37.99** | 16.37** | 10.59** | 10.82** | 17.83** | ||||||||||
| Adjusted R | 0.37 | 0.20 | 0.13 | 0.14 | 0.21 | ||||||||||
| Time 0 Symptoms | 0.69 | .06 | .75** | 0.68 | .06 | .72** | |||||||||
| Age | −0.05 | .06 | −.04 | −0.03 | .03 | −.07 | |||||||||
| Gender | 4.16 | 1.32 | .17** | 1.72 | .65 | .16** | |||||||||
| Income | −0.14 | .41 | −.02 | 0.03 | .20 | .01 | |||||||||
| Social support | −0.13 | .06 | −.15* | −0.06 | .03 | −.16* | |||||||||
| Social network size | −0.02 | .08 | −.01 | 0.01 | .04 | .03 | |||||||||
| Stay-at-home status | 1.10 | 1.25 | .04 | 0.49 | .62 | .04 | |||||||||
| Distancing behavior | 9.91 | 2.50 | .23** | 4.34 | 1.23 | .23** | |||||||||
| (8, 109) | 37.46** | 27.30** | |||||||||||||
| Adjusted R | 0.71 | 0.64 | |||||||||||||
Note . Gender is coded such that 1 = female. Stay-at-home status is coded such that 1 = yes. Time 0 Symptoms refers to the corresponding symptom type at the February 2020 timepoint. * p < .05, ** p < .01.
Stay-at-home status and personal distancing behavior were each significantly and independently associated with mental health symptoms. Being under a stay-at-home order was associated with higher depression, GAD symptoms, insomnia, and acute stress, but not associated with intrusive thoughts. Personal distancing behavior was associated with higher depression, GAD symptoms, intrusive thoughts, and acute stress, but not with insomnia. In sum, both measures of social distancing (stay-at-home status and distancing behavior) were associated independently with concurrent symptoms, and these effects were evident above and beyond the expected, protective effects of social resources. 1
3.2.2. February-to-March mental health symptom change
Our second hypothesis was that mental health symptoms would increase from February to March. Repeated-measures tests using the two prospectively measured symptom types (depression and GAD) in the prospective subsample showed that indeed, depressive symptoms increased between late February and late March, from 12.60 ( SD = 13.14) to 14.78 ( SD = 12.02), t (117) = 3.12, p = .002, d = 0.29. Similarly, GAD symptoms increased during this time period, from M = 4.42 ( SD = 5.55) to M = 5.42 ( SD = 5.28), t (117) = 2.99, p = .003, d = 0.28. Symptom levels in March did not differ between prospective vs. March-only participants [depression M = 14.94, SD = 12.00, t (433) = 0.12, p = .902; GAD M = 5.76, SD = 5.58, t (433) = 0.58, p = .565], suggesting the observed increase was not unique to the prospective sample, but rather might have been detected similarly had the full sample been measured prospectively.
3.2.3. Social distancing and February-to-March symptom change
Our final hypothesis was that magnitudes of prospective symptom increases would be associated with the extent of social distancing, independently of social resources. For both prospectively measured symptom types (depression and GAD), we conducted multiple regression analyses identical to those in the full sample, but adding to each model the corresponding February symptom level as an additional covariate. 2 Results are displayed in the lower half of Table 3 .
Not surprisingly, February symptoms were strong predictors of March symptoms. When accounting for early symptoms, stay-at-home status was no longer significantly associated with March symptoms, and social support was less strongly associated with lower symptoms. However, personal distancing behavior remained significantly positively associated with both depression and GAD symptoms in March. The independent associations between distancing behavior and March depression and GAD symptoms, adjusting for all predictors in the models including respective February symptoms, are depicted in Fig. 1 . Unstandardized coefficients can be consulted to interpret the magnitude of this effect: engaging in all 12 measured distancing behaviors (which would yield a “perfect” distancing score of 1) would account for nearly 10 points in depression severity (on the 60-point CES-D scale), and over 4 points in GAD severity (on the 21-point GAD-7 scale), controlling for all predictors including February symptom levels.

Association between Personal Social Distancing Behaviors and Increases in Depression and Anxiety Symptoms from February to March 2020. Note. March symptom levels are adjusted for all covariates reported in the respective, prospective multiple regression models, including February symptom levels. Distancing behavior: −1 = increased social contact, 0 = no reported change in behaviors from before COVID-19, 1 = distancing behavior reported in all 12 behavioral domains.
4. Discussion
This study examined the mental health effects associated with social distancing, the most broadly visible public health intervention to fight the global spread of COVID-19. In a nationwide sample of U.S. adults at two time points early in the American experience of the pandemic, we found evidence that both governmental stay-at-home orders and individuals’ personal social distancing behavior were associated with symptoms of a range of mental health conditions. In late March 2020, as the pandemic escalated dramatically and states began implementing stay-at-home orders, being subject to those orders was associated with more symptoms of depression, GAD, acute stress, and insomnia. Independently, engaging in personal social distancing behavior was associated with more depression, GAD, acute stress, and intrusive thoughts. These associations with social distancing existed despite individuals’ levels of perceived social support, suggesting that even social resources known to protect mental health do not eliminate the impact of social distancing. Indeed, our approach disentangled the role of social distancing from other important components of the social context of the pandemic, and also identified distinct roles of stay-at-home orders and personal distancing behavior.
These findings replicate early cross-sectional evidence that the COVID-19 pandemic may be impairing mental health in the general population ( Cao et al., 2020 ; Tull et al., 2020 ) and extend them to a broader range of mental health outcomes. Our approach also makes a contribution by examining simultaneous effects of public and private levels of social distancing, showing that both are independently linked with symptom severity. As such, this study extends findings from past, less widespread viral epidemics outside of the U.S. ( Cava et al., 2005 ; Mak et al., 2009 ; Pfefferbaum et al., 2012 ) and from studies of the more severe distancing of quarantine ( Brooks et al., 2020 ; Hawryluck et al., 2004 ).
Importantly, using data available prospectively in mid-to-late February, the present study shows both temporal increases in depression and anxiety symptoms as the presence of COVID-19 grew in the U.S.and a relationship of social distancing to these increases. Cross-sectional approaches (e.g., Cao et al., 2020 ; Tull et al., 2020 ) are agnostic on causal direction: instead of social distancing harming mental health, perhaps people with elevated symptoms are simply more likely to distance. This study does not establish direction of effects or causality, given that distancing behavior was not manipulated or measured in February, but our findings do suggest that distancing was at least associated with worsening mental health course during this period. These models also suggested that perhaps the private, behavioral forms of social distancing may be particularly relevant to worsening mental health, compared to public interventions. A caveat to this possibility, however, is that distancing behaviors may have had more robust effects due to being in place for relatively longer than stay-at-home orders at the time of data collection. Ongoing follow-up studies can help untangle these possibilities. It is also important to note that although prospective analyses showed associations of distancing behavior with symptom change that correspond to clinically-meaningful magnitudes, absolute changes in depression and GAD symptoms, although statistically significant, were relatively modest (2.18 points on the CES-D and 1 point on the GAD-7) and should not be interpreted as evidence of marked clinically-relevant increases across the sample or the general population.
Although this study provides consistent evidence of social distancing associations with five major mental health outcomes, its limitations can guide future research as the pandemic unfolds. Most importantly, even with its longitudinal elements, our design remains correlational, which raises several issues. First is causal direction: the present findings do not rule out the possibility that symptoms (including change in symptoms) affect personal distancing behavior, although this is less likely for stay-at-home order effects, which are externally determined. Second is a number of plausible confounding variables. Stay-at-home orders and personal distancing behaviors have proven to be meaningful, highly salient, and uniquely impactful aspects of the pandemic experience, but they may correlate with other constructs not measured here, such as prevalence of cases in one's geographical area, social norms around distancing, and non-governmental actions (e.g., employer work-from-home policies). A range of pandemic-related experiences that were not measured here are likely implicated in mental health, including personal, family, and community exposure to COVID-19; impact on daily life stressors, including child care and elder care responsibilities; and economic and employment impact, including job loss or working from home. Many of these coincided with social distancing interventions (e.g., stay-at-home orders were enacted earlier in states with more COVID-19 risk, and both forms of distancing involved changes in daily routines, demands, and resources). Thus, social distancing and social resource effects may also reflect associated effects of pandemic-related stressors. 3 Research currently underway, including ongoing longitudinal follow-up in the present study, can determine whether links between mental health and social distancing are better explained by other contemporaneous factors.
As the dynamics of COVID-19 unfold, longitudinal studies will be needed to determine the mechanistic psychological processes that social distancing may either introduce (e.g., isolation), exacerbate (e.g., emotion dysregulation), or disrupt (e.g., relationship quality), as well as specificity to particular symptom outcomes (e.g., depression versus insomnia). This research should also examine moderators of distancing effects, including pre-existing mental health conditions, physical vulnerability to COVID-19, the degree to which distancing impacts ability to work or care for family, and whether distancing essentially means true isolation for some (e.g., those who live alone). Longitudinal work can also address another important question: Do symptoms early in the pandemic represent true phenomena of clinical concern, or normative, non-pathological responses to the initial emergence of a unique and overwhelming event? Of course, experienced symptoms are meaningful regardless of whether they reflect psychiatric abnormality, but for this reason we have emphasized “mental health” as opposed to clinical psychopathology.
The COVID-19 threat increases reliance on online research methods ( Gruber et al., 2020 ). Mechanical Turk, while more demographically diverse than many online and traditional samples ( Buhrmester et al., 2011 ), can have limitations related to participant inattentiveness and lack of researcher control over the study session ( Paolacci and Chandler, 2014 ). We preempted these data quality concerns by following rigorous recruitment and data quality practices ( Buhrmester et al., 2011 ; Paolacci and Chandler, 2014 ; Peer et al., 2014 ). Despite the relative representativeness of our sample on most demographic indicators, the sample should not be considered nationally representative; other characteristics of MTurk participants may limit generalizability (e.g., they may be more liberal, more introverted, and more frequent Internet users than the general population; Paolacci and Chandler, 2014 ; Chandler and Shapiro, 2016 ). Although the sample was relatively demographically diverse overall, it was less so in terms of race/ethnicity. There were no racial/ethnic differences in study variables, which may be a function of statistical power in the present, majority-white sample. However, evidence is building that individuals of marginalized racial and ethnic backgrounds are disproportionately impacted by COVID-19 in terms of contracting the virus, facing severe health outcomes, and death ( Webb Hooper et al., 2020 ), and this may extend to psychological processes. Future research could examine how stressors specific to marginalized groups, including chronic risk factors (e.g., experiences of racism) and acute risk factors (e.g., disproportionate COVID-19 risk and impact to daily life), may impact the relationship between social distancing and mental health symptoms.
Finally, constructs were measured by self-report. While well-suited to measurement of mental health symptoms and perceived social resources, self-report may not correspond with objective governmental distancing initiatives or personal distancing, a construct perhaps especially subject to reporting biases (e.g., social desirability). Moreover, symptom measures vary somewhat in their time frame, e.g., depression within the last week and GAD symptoms within the last 2 weeks. Retaining standard time frames is essential for maintaining psychometric properties and allowing comparison with other studies, but aspects of the pandemic change quickly, and measures with shorter time frames may naturally be more temporally precise with respect to external events.
The present study has several strengths. First, it used a national sample of adults that was fairly representative of the U.S. in terms of age, gender, education, and income. Second, we examined 2 time points that captured the extraordinary period of initial adjustment to COVID-19, beginning well before the pandemic was prominent in awareness and disrupting life in the U.S. on a widespread scale. Third, our inclusion of social support and social network size addressed social distancing in the context of other social factors implicated in mental health. Fourth, we used well-validated measures of specific mental health outcomes, and our sample represented a wide range of most symptom types. Lastly, our novel approach to assessing the extent of social distancing behavior dimensionally appears psychometrically sound based on this initial research, and could be promising for future COVID-19 studies.
The COVID-19 pandemic is expected to have profound mental health effects, which research, policy, and clinical science have been called on to address ( Gruber et al., 2020 ; Pfefferbaum and North, 2020 ). The present findings provide empirical evidence of negative mental health impact to underscore these calls. In the absence of a vaccine, the upcoming year(s) are expected to bring periodic outbreaks and cyclical reinstatements of social distancing recommendations. Social distancing interventions should not be avoided, as they appear critical to controlling the virus; it is for biomedical sciences, public health, and related fields to determine interventions at the public level (e.g., phased state “re-opening” standards) and private level (e.g., encouraging individuals to wear masks) that promise to protect lives. Rather, the present study highlights the possible mental health correlates of virus-containment initiatives, and the need for simultaneous investment into mental health interventions to mitigate these effects. Already-effective interventions for mental health and psychological distress may benefit from more explicit targeting of the role of social disruption in psychological responses during the pandemic, and from increased access to telehealth modalities that allow clinicians to reach those most vulnerable to the mental health impact of the pandemic.
Author statement
Study conceptualization: B. Marroquín and V. Vine. Study design and data collection: B. Marroquín, V. Vine, and R. Morgan. Data analysis and interpretation: B. Marroquín and V. Vine. Drafting and revision of manuscript: B. Marroquín and V. Vine. All authors approved the final manuscript.
This work was supported in part by the Monica Lester Endowment for Psychology at Loyola Marymount University.
Declaration of Competing Interest
The authors have no interests to declare.
1 Results of stepwise versions of these regression models are presented in Supplementary Tables 1 and 2. Social distancing variables explained statistically significant additional variance, compared to models including only demographic covariates and social resources, in March depression, GAD, intrusive thoughts, and acute stress, and in February-to-March changes in depression and GAD.
2 All zero-order correlations in the prospective subsample among social distancing, social resources, depressive symptoms, and GAD symptoms in late March showed the same patterns as in the main sample, including statistical significance. Mirroring findings with March depressive symptoms, February depressive symptoms were correlated with March social support (r = −.66, p < .001) and social network size (r = −.27, p = .003), and not personal distancing behavior (r = −.12, p = .192). February GAD symptoms were correlated with March social support (r = −.49, p < .001) and not personal distancing behavior (r = −.07, p = .425), but unlike March GAD symptoms, February GAD symptoms were significantly correlated with social network size (r = −.19, p = .036).
3 We conducted a series of exploratory analyses to examine potential external factors that might have been associated with stay-at-home orders and personal distancing behavior and might provide alternative explanations for our findings, including personal exposure to COVID-19 and geographical proximity to cases. At the beginning of data collection on March 26, the 86,379 COVID-19 cases in the country represented approximately 0.026% of the U.S. population. Accordingly, when asked, all participants in our sample denied being positive for COVID-19. 395 individuals (90.8%) in our sample reported not knowing any other person who was ill or diagnosed with COVID-19, and 40 (9.2%) reported knowing between 1 and 9 such people. T-tests comparing these groups showed that the latter group experienced higher depressive symptoms and acute stress in March, but including this term in all original regression models resulted in no change to the pattern or significance of findings. To examine geographical proximity, we used cumulative COVID-19 case data for each state on March 26, assigning each participant the number of cases in their state, from 46 (South Dakota) to 6,876 (New Jersey), with an extreme outlier of 39,058 (New York). Correlational analyses (excluding New York participants, whose extreme case values rendered their inclusion statistically inappropriate) indicated that the number of cases in one's state was not significantly associated with any of the study variables, and adding participants' state case count to our original regression analyses did not affect the patterns or statistical significance. Although replicating our regression analyses was impossible among New Yorkers only (n = 31), correlational analyses showed that among New Yorkers more personal distancing behavior was significantly associated with higher depression, GAD symptoms, intrusive thoughts, and acute stress, and was not correlated with social resource variables. Although these analyses represent rough tests of potential alternative explanations related to personal and geographical COVID-19 exposure, together they suggest that neither personal COVID-19 status, the awareness of social contacts with COVID-19, nor the levels of COVID-19 cases in one's state account for our primary findings.
Supplementary material associated with this article can be found, in the online version, at doi: 10.1016/j.psychres.2020.113419 .
Appendix. Supplementary materials
- Amirkhan J.H. Stress overload: a new approach to the assessment of stress. Am. J. Community Psychol. 2012; 49 :55–71. doi: 10.1007/s10464-011-9438-x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Amirkhan J.H. A brief stress diagnostic tool: the Short Stress Overload Scale. Assessment. 2018; 25 :1001–1013. doi: 10.1177/1073191116673173. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bastien C.H., Vallières A., Morin C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001; 2 :297–307. doi: 10.1016/S1389-9457(00)00065-4. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020; 395 :912–920. doi: 10.1016/S0140-6736(20)30460-8. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Buhrmester M., Kwang T., Gosling S.D. Amazon’s Mechanical Turk: a new source of inexpensive, yet high-quality, data? Perspect. Psychol. Sci. 2011; 6 :3–5. doi: 10.1177/1745691610393980. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020; 287 doi: 10.1016/j.psychres.2020.112934. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cava M.A., Fay K.E., Beanlands H.J., McCay E.A., Wignall R. The experience of quarantine for individuals affected by SARS in Toronto. Public Health Nurs. 2005; 22 :398–406. doi: 10.1111/j.0737-1209.2005.220504.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Centers for Disease Control and Prevention, 2020. Coronavirus (COVID-19). https://www.cdc.gov/coronavirus/2019-ncov/ (accessed 21 August 2020).
- Chandler J., Shapiro D. Conducting clinical research using crowdsourced convenience samples. Ann. Rev. Clin. Psych. 2016; 12 :53–81. [ PubMed ] [ Google Scholar ]
- Cohen S. Social relationships and health. Am. Psychol. 2004; 59 :676–684. doi: 10.1037/0003-066X.59.8.676. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cohen S., Doyle W.J., Skoner D.P., Rabin B.S., Gwaltney J.S., Jr. Social ties and susceptibility to the common cold. JAMA. 1997; 277 :1940–1944. doi: 10.1001/jama.1997.03540480040036. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cohen S., Wills T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985; 98 :310–357. doi: 10.1037/0033-2909.98.2.310. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cutrona C.E., Russell D.W. In: Jones W.H., Perlman D., editors. Vol. 1. JAI Press; Greenwich, CT: 1987. The provisions of social relationships and adaptation to stress; pp. 37–67. (Advances in Personal Relationships). [ Google Scholar ]
- Falsetti S.A., Monnier J., Davis J.L., Resnick H.S. Intrusive thoughts in posttraumatic stress disorder. J. Cogn. Psychother. 2002; 16 :127–143. doi: 10.1891/jcop.16.2.127.63993. [ CrossRef ] [ Google Scholar ]
- Gruber, J., Prinstein, M.J., Clark, L.A., Rottenberg, J., Abramowitz, J.S., Albano, A.M., Aldao, A., Borelli, J.L., Davila, J., Forbes, E.E., Gee, D.G., Hall, G.C.N., Hallion, L.S., Hinshaw, S.P., Hofmann, S.G., Hollon, S.D., Joormann, J., Kazdin, A.E., Klein, D.N., Levenson, R.W., MacDonald A.W., III, McKay, D., McLaughlin, K.A., Mendle, J., Miller, A.B., Neblett, E., Nock, M., Olatunji, B.O., Persons, J.B., Rozek, D.C., Schleider, J.L., Slavich, G.M., Teachman, B.A., Vine, V.J., Weinstock, L., 2020. Mental health and clinical psychological science in the time of COVID-19: challenges, opportunities, and a call to action. American Psychologist. Advance online publication. 10.1037/amp0000707. [ PMC free article ] [ PubMed ] [ CrossRef ]
- Harkness, K.L., Hayden, E.P., 2020. The Oxford handbook of stress and mental health. Oxford University Press. 10.1093/oxfordhb/9780190681777.001.0001.
- Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004; 10 :1206–1212. doi: 10.3201/eid1007.030703. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Webb Hooper M., Nápoles A.M., Pérez-Stable E.J. COVID-19 and racial/ethnic disparities. JAMA. 2020; 323 :2466–2467. doi: 10.1001/jama.2020.8598. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kendler K.S., Gardner C.O. Depressive vulnerability, stressful life events and episode onset of major depression: a longitudinal model. Psychol. Med. 2016; 46 :1865–1874. doi: 10.1017/S0033291716000349. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kendler K.S., Hettema J.M., Butera F., Gardner C.O., Prescott C.A. Life event dimensions of loss, humiliation, entrapment, and danger in the prediction of onsets of major depression and generalized anxiety. Arch. Gen. Psychiatry. 2003; 60 :789–796. doi: 10.1001/archpsyc.60.8.789. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mak I.W.C., Chu C.M., Pan P.C., Yiu M.G.C., Chan V.L. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry. 2009; 31 :318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Marroquín, B., Tennen, H., Stanton, A., 2017. Coping, emotion regulation, and well-being: intrapersonal and interpersonal processes, in: The Happy Mind: Cognitive Contributions to Well-Being. pp. 253–274. 10.1007/978-3-319-58763-9_14.
- Morin C.M., Belleville G., Bélanger L., Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011; 34 :601–608. doi: 10.1093/sleep/34.5.601. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Paolacci G., Chandler J. Inside the Turk. Curr. Dir. Psychol. Sci. 2014; 23 :184–188. doi: 10.1177/0963721414531598. [ CrossRef ] [ Google Scholar ]
- Pascual-Vera B., Akin B., Belloch A., Bottesi G., Clark D.A., Doron G., Fernández-Alvarez H., Ghisi M., Gómez B., Inozu M., Jiménez-Ros A., Moulding R., Ruiz M.A., Shams G., Sica C. The cross-cultural and transdiagnostic nature of unwanted mental intrusions. Int. J. Clin. Heal. Psychol. 2019; 19 :85–96. doi: 10.1016/j.ijchp.2019.02.005. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Peer E., Vosgerau J., Acquisti A. Reputation as a sufficient condition for data quality on Amazon Mechanical Turk. Behav. Res. Methods. 2014; 46 :1023–1031. doi: 10.3758/s13428-013-0434-y. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pfefferbaum, B., North, C.S., 2020. Mental health and the Covid-19 pandemic. N. Engl. J. Med.10.1056/NEJMp2008017. [ PubMed ]
- Pfefferbaum B., Schonfeld D., Flynn B.W., Norwood A.E., Dodgen D., Kaul R.E., Donato D., Stone B., Brown L.M., Reissman D.B., Jacobs G.A., Hobfoll S.E., Jones R.T., Herrmann J., Ursano R.J., Ruzek J.I. The H1N1 crisis: a case study of the integration of mental and behavioral health in public health crises. Disaster Med. Public Health Prep. 2012; 6 :67–71. doi: 10.1001/dmp.2012.2. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Radloff L.S. The CES-D scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977; 1 :385–401. doi: 10.1177/014662167700100306. [ CrossRef ] [ Google Scholar ]
- Salters-Pedneault K., Vine V., Mills M.A., Park C., Litz B.T. The Experience of Intrusions scale: a preliminary examination. Anxiety Stress Coping. 2009; 22 :27–37. doi: 10.1080/10615800802403823. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sinha S.S. Trauma-induced insomnia: a novel model for trauma and sleep research. Sleep Med. Rev. 2016; 25 :74–83. doi: 10.1016/j.smrv.2015.01.008. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006; 166 :1092–1097. doi: 10.1001/archinte.166.10.1092. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Takarangi M.K.T., Oulton J.M., Green D.M., Strange D. Boundary restriction for negative emotional images is an example of memory amplification. Clin. Psychol. Sci. 2016; 4 :82–95. doi: 10.1177/2167702615569912. [ CrossRef ] [ Google Scholar ]
- Thoits P.A. Mechanisms linking social ties and support to physical and mental health. J. Health Soc. Behav. 2011; 52 :145–161. doi: 10.1177/0022146510395592. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tull M.T., Edmonds K.A., Scamaldo K.M., Richmond J.R., Rose J.P., Gratz K.L. Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res. 2020; 289 doi: 10.1016/j.psychres.2020.113098. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Uchino B.N. Understanding the links between social support and physical health: a life-span perspective with emphasis on the separability of perceived and received support. Perspect. Psychol. Sci. 2009; 4 :236–255. doi: 10.1111/j.1745-6924.2009.01122.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Van Bavel J.J., Baicker K., Boggio P.S., Capraro V., Cichocka A., Cikara M., Crockett M.J., Crum A.J., Douglas K.M., Druckman J.N., Drury J., Dube O., Ellemers N., Finkel E.J., Fowler J.H., Gelfand M., Han S., Haslam S.A., Jetten J., Kitayama S., Mobbs D., Napper L.E., Packer D.J., Pennycook G., Peters E., Petty R.E., Rand D.G., Reicher S.D., Schnall S., Shariff A., Skitka L.J., Smith S.S., Sunstein C.R., Tabri N., Tucker J.A., van der Linden S., van Lange P., Weeden K.A., Wohl M.J.A., Zaki J., Zion S.R., Willer R. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020; 4 :460–471. doi: 10.1038/s41562-020-0884-z. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vilagut G., Forero C.G., Barbaglia G., Alonso J. Screening for depression in the general population with the Center for Epidemiologic Studies Depression (CES-D): a systematic review with meta-analysis. PLoS ONE. 2016; 11 doi: 10.1371/journal.pone.0155431. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- World Health Organization, 2020. Coronavirus disease (COVID-19) pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed 21 August 2020).
- Worldometer, 2020. COVID-19 coronavirus pandemic. https://www.worldometers.info/coronavirus (accessed 18 May 2020).
- Zhang S.X., Wang Y., Rauch A., Wei F. Unprecedented disruption of lives and work: health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatry Res. 2020; 288 doi: 10.1016/j.psychres.2020.112958. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Exploring COVID-19’s Impact On Undergraduate Nursing Students
- Susan Isherwood University of Calgary
The researchers aimed to assess the effects of the COVID-19 pandemic on nursing education through semi-structured interviews with undergraduate nursing students. The researchers explored themes related to online education, clinical placements, and mental health. Findings revealed that the sudden shift to online learning caused increased stress, and decreased confidence. Clinical placements were affected, leading to missed time and altered learning experiences. Mental health suffered as students faced stressors and challenges brought on by the pandemic. These interviews elucidate the challenges faced by nursing students during the COVID-19 pandemic and provide valuable information for future planning in nursing education during crises.
Copyright (c) 2024 Riley Martens, Mary Hou, Susan Isherwood, Colleen Cuthber

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License .
Authors who publish with this journal agree to the following:
Authors retain copyright and, from 2021 onwards, grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License (CC-BY-NC) that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
Before 2021, a CC BY-NC-ND license applied to all articles.
Developed By
- Français (Canada)
Information
- For Readers
- For Authors
- For Librarians
Papers on Postsecondary Learning and Teaching
ISSN 2560-6050

Uneven geographies of COVID‑19: Reviewing geographical research agendas and concepts from a syndemics perspective
- Butsch, Carsten
- Everts, Jonathan
- Bork-Hüffer, Tabea
Building upon a review of geographic research agendas and concepts related to the uneven geographies of COVID‑19, this first of three articles debates the benefits of geographic analyses to the syndemic approach and, vice versa, of a syndemics perspective to geographic analyses. The syndemics perspective was proposed by critical medical anthropologists. It seeks to deepen the understanding of the structural dimensions and processes that lead to the convergence and cascading of multiple epidemics in specific population groups. Geographers have also highlighted the intersections of multiple health or other crises during COVID‑19, when the pandemic and global health emergency coincided with and escalated existing structural inequalities produced by the climate crisis, environmental degradation, political conflicts and war, socio‑economic disparities and poverty, social divisions, racism, hatred and violence, mental health problems and stress. Geographers have mobilized concepts such as scale, territory, borders and intersectionality to unravel the uneven unfolding and consequences of the global health emergency for diverse population groups. We therefore argue that geography has a lot to contribute to the understanding of the spatial and contextual dimensions of COVID‑19 as a pandemic as well as a syndemic – but it has so far not actively employed the latter concept's analytical lens. Mobilizing the syndemics approach can contribute to more comprehensive accounts of the structural dimensions and processes that continue and cascade in pandemics.

IMAGES
COMMENTS
On a global scale and based on imputations and modeling from survey data of self-reported mental health problems, the Global Burden of Disease (GBD) study 29 estimated that the COVID-19 pandemic has led to a 28% (95% uncertainty interval (UI): 25-30) increase in major depressive disorders and a 26% (95% UI: 23-28) increase in anxiety disorders.
COVID-19 has justifiably raised widespread public concern about mental health worldwide. In the U.S., the pandemic was an unprecedented shock to society at a time when the nation was already ...
The elderly and disabled people living in nursing homes can face extreme mental health issues. However, something as simple as a phone call during the pandemic outbreak can help to console elderly people. COVID‐19 can also result in increased stress, anxiety, and depression among elderly people already dealing with mental health issues.
Mental health professionals can help craft messages to be delivered by trusted leaders. 4. The Covid-19 pandemic has alarming implications for individual and collective health and emotional and ...
On a global scale and based on imputations and modeling from survey data of self-reported mental health problems, the Global Burden of Disease (GBD) study 29 estimated that the COVID-19 pandemic ...
Español. In the first year of the COVID-19 pandemic, global prevalence of anxiety and depression increased by a massive 25%, according to a scientific brief released by the World Health Organization (WHO) today. The brief also highlights who has been most affected and summarizes the effect of the pandemic on the availability of mental health ...
By Mayo Clinic Staff. At the start of the COVID-19 pandemic, life for many people changed very quickly. Worry and concern were natural partners of all that change — getting used to new routines, loneliness and financial pressure, among other issues. Information overload, rumor and misinformation didn't help.
The COVID-19 pandemic affected everyone around the globe. Depending on the country, there have been different restrictive epidemiologic measures and also different long-term repercussions. Morbidity and mortality of COVID-19 affected the mental state of every human being. However, social separation and isolation due to the restrictive measures considerably increased this impact.
The COVID-19 pandemic has had a severe impact on the mental health and wellbeing of people around the world while also raising concerns of increased suicidal behaviour. In addition access to mental health services has been severely impeded. However, no comprehensive summary of the current data on these impacts has until now been made widely ...
The COVID-19 pandemic has profoundly influenced the world. In wave after wave, many countries suffered from the pandemic, which caused social instability, hindered global growth, and harmed mental health. Although research has been published on various mental health issues during the pandemic, some profound effects on mental health are ...
Mental Health During the COVID-19 Pandemic An Urgent Issue. Both SARS-CoV-2 and the COVID-19 pandemic have significantly affected the mental health of adults and children. In a 2021 study, nearly half of Americans surveyed reported recent symptoms of an anxiety or depressive disorder, and 10% of respondents felt their mental health needs were ...
In summary, the COVID-19 pandemic and its countermeasures exuded a complex pattern of effects on physical and mental health, and factors shaping human stress resilience during the pandemic in the ...
COVID-19 pandemic on mental health in the general population, 32 in healthcare workers and 26 in other specific populations. Only three meta-analyses gave pooled effect estimates comparing prevalence of mental health problems before to during the pandemic or during implementation of public health and social measures (PHSMs) (15-17)
Mental health effects of COVID-19. A number of commentators in the popular media have noted that one potential silver-lining of this pandemic has been a mainstreaming of mental health within the broader considerations of the health impact of the pandemic. It is has been noted that mental health needs have never been as central to public discourse as during recent media discussions about the ...
The coronavirus disease 2019 (COVID-19) pandemic has exposed humans to the highest physical and mental risks. Thus, it is becoming a priority to probe the mental health problems experienced during ...
In studies across the world, researchers investigated what else might make people vulnerable to mental health problems during the pandemic. They found a few key factors that put people at risk. For one, people with poor health or chronic diseases tend to have higher symptoms of stress, anxiety, depression, and PTSD, several studies found. Of ...
To minimize the mental health consequences of the COVID-19 pandemic, WHO also recommends that countries: Apply a whole of society approach to promote, protect and care for mental health, including through social and financial protection to safeguard people from domestic violence or impoverishment, and by communicating widely about COVID-19 to ...
Around a third of adults and young people said their mental health has got much worse since March 2020. 58% of people receiving benefits said their mental health was poor. 88% of young people said loneliness made their mental health worse during the pandemic. 1 in 5 adults did not seek support during the pandemic because they didn't think ...
In a survey conducted by the Centers for Disease Control and Prevention from January to June 2021, 37% of students at public and private high schools said their mental health was not good most or all of the time during the pandemic. That included roughly half of girls (49%) and about a quarter of boys (24%). In the same survey, an even larger ...
Most general public surveys link COVID-19 to increased symptoms of depression, anxiety, and stress. Panic buying, binge-watching TV, and other unhealthy behaviors have been reported. Increased ...
Interestingly, similar mental health effects were seen in past containment efforts during infectious disease outbreaks, such as the severe acute respiratory syndrome (SARS) in 2003 [2, 3], the 2009 swine flu pandemic [4, 5], and the 2014-2016 Ebola epidemic . Various studies showed that these outbreaks led to a substantial rise in depression ...
Abstract. Some research has shown how mental health was affected during the COVID-19 pandemic in hospital staff worldwide. However, there is little evidence of the physiological status of healthcare and administrative workers at the first level of medical care.
The pandemic disrupted connections to family, school, and community, which are essential supports for youth mental health. Lessons learned from the pandemic suggest the role of stress and windows of opportunity to build resiliency. Drawing from a policy dialog on the youth mental health crisis conducted by 4 American Academy of Nursing Expert ...
Examination of the experiences of mong mental health clinicians in Canada and the United States during the second phase of the COVID-19 pandemic suggested that although these mental health clinicians certainly reported experiencing psychosocial impacts of the pandemic themselves, these shared experiences with client and general populations did not greatly impact how they understood the SCs.
The loneliness epidemic profoundly affects Gen Z. Despite being hyperconnected through social media, they experience high levels of isolation, worsened by the pandemic.
Social distancing is the most visible public health response to the COVID-19 pandemic, but its implications for mental health are unknown. In a nationwide online sample of 435 U.S. adults, conducted in March 2020 as the pandemic accelerated and states implemented stay-at-home orders, we examined whether stay-at-home orders and individuals' personal distancing behavior were associated with ...
The researchers aimed to assess the effects of the COVID-19 pandemic on nursing education through semi-structured interviews with undergraduate nursing students. The researchers explored themes related to online education, clinical placements, and mental health. Findings revealed that the sudden shift to online learning caused increased stress, and decreased confidence.
Geographers have also highlighted the intersections of multiple health or other crises during COVID‑19, when the pandemic and global health emergency coincided with and escalated existing structural inequalities produced by the climate crisis, environmental degradation, political conflicts and war, socio‑economic disparities and poverty ...