Advertisement

Advancements in Human Embryonic Stem Cell Research: Clinical Applications and Ethical Issues
- Review Article
- Open access
- Published: 19 March 2024
- Volume 21 , pages 379–394, ( 2024 )
Cite this article
You have full access to this open access article

- Soo Jin Park ORCID: orcid.org/0000-0002-7382-230X 1 ,
- Yoon Young Kim ORCID: orcid.org/0000-0003-0671-519X 1 , 3 ,
- Ji Yeon Han ORCID: orcid.org/0000-0002-1007-3188 1 ,
- Sung Woo Kim ORCID: orcid.org/0000-0003-4689-1323 1 ,
- Hoon Kim ORCID: orcid.org/0000-0002-5623-6368 1 , 2 , 3 &
- Seung-Yup Ku ORCID: orcid.org/0000-0002-6423-854X 1 , 2 , 3
2993 Accesses
1 Altmetric
Explore all metrics
Background:
The development and use of human embryonic stem cells (hESCs) in regenerative medicine have been revolutionary, offering significant advancements in treating various diseases. These pluripotent cells, derived from early human embryos, are central to modern biomedical research. However, their application is mired in ethical and regulatory complexities related to the use of human embryos.
This review utilized key databases such as ClinicalTrials.gov, EU Clinical Trials Register, PubMed, and Google Scholar to gather recent clinical trials and studies involving hESCs. The focus was on their clinical application in regenerative medicine, emphasizing clinical trials and research directly involving hESCs.
Preclinical studies and clinical trials in various areas like ophthalmology, neurology, endocrinology, and reproductive medicine have demonstrated the versatility of hESCs in regenerative medicine. These studies underscore the potential of hESCs in treating a wide array of conditions. However, the field faces ethical and regulatory challenges, with significant variations in policies and perspectives across different countries.
Conclusion:
The potential of hESCs in regenerative medicine is immense, offering new avenues for treating previously incurable diseases. However, navigating the ethical, legal, and regulatory landscapes is crucial for the continued advancement and responsible application of hESC research in the medical field. Considering both scientific potential and ethical implications, a balanced approach is essential for successfully integrating hESCs into clinical practice.
Similar content being viewed by others

Is Human Embryonic Stem Cell (HESC) Research Still Necessary Today?

Stem Cells: Embryonic

Avoid common mistakes on your manuscript.
1 Introduction
The field of stem cell research has undergone a significant transformation with the advent of human embryonic stem cells (hESCs). Since their pioneering isolation in 1998, hESCs have been at the forefront of scientific inquiry due to their unique ability for self-renewal and pluripotency [ 1 , 2 ]. This comprehensive review article delves into the advancements, challenges, and ethical considerations surrounding hESCs and their implications for regenerative medicine.
Over the past two decades, the potential of hESCs to revolutionize the treatment of various diseases has been increasingly recognized [ 3 , 4 ]. Their capacity to differentiate into diverse cell types offers promising prospects for repairing or replacing damaged tissues, especially in conditions where current treatments are limited [ 5 , 6 , 7 , 8 ]. However, the journey of hESC research is not without its complexities. Ethical considerations regarding the use of human embryos have sparked intense debates and have had a profound impact on public perception and the regulatory framework governing hESC research [ 9 , 10 ].
The therapeutic applications of hESCs encompass both systemic and localized approaches, including intravenous or intramuscular injections and surgical implantation, sometimes combined with bioscaffolds [ 11 ]. These strategies are broadly classified into transient dosing for temporary therapeutic effects and permanent implantation for long-term tissue repair and regeneration [ 12 , 13 ]. Despite these advancements, challenges in ensuring consistency in hESC properties across different experimental settings continue to pose hurdles in translating laboratory findings into clinical therapies [ 14 , 15 ].
While induced pluripotent stem cells (iPSCs) have emerged as an alternative, hESCs still hold distinct advantages, particularly in the understanding of genetic diseases and human development [ 16 , 17 ]. Despite the ethical complexities and slower pace of clinical research compared to iPSCs, hESCs remain a crucial tool in biomedical research [ 18 , 19 ]. Their unique position in providing insights into early human development and genetic disorders underscores their invaluable role in medical science [ 17 ].
This review aims to provide an in-depth analysis of the current state of clinical trials involving hESCs, emphasizing their role in regenerative medicine. We explore the evolving landscape of hESC research, highlighting the need for ongoing scientific exploration, ethical deliberation, and regulatory guidance to fully realize the therapeutic potential of hESCs in improving patient care and advancing medical science.
2 Methodology
This narrative review was conducted to assess the clinical applications of hESCs. The primary aim was to gather and analyze data from various sources to understand the current state and advancements in hESC research.
For database search, we utilized ClinicalTrials.gov ( https://clinicaltrials.gov/ ) and EU Clinical Trials Register ( https://www.clinicaltrialsregister.eu/ ) for identifying ongoing and completed clinical trials involving hESCs. Also, we used PubMed and Google Scholar to retrieve published clinical trial reports and peer-reviewed articles on hESCs. Studies and trials were included based on their focus on the clinical application of hESCs. Those not directly involving hESCs or outside the scope of clinical application were excluded. The review primarily targeted articles and trials published or conducted in the last five years to maintain contemporary relevance.
For data extraction and analysis, key information extracted included the study title, indication, participant number, study site, study period, study design, and NCT number. This data was organized systematically to provide a clear overview of the current trends and progress in the field of hESC research in clinical applications.
2.1 Overview of clinical trials in hESC research
Figure 1 displays key aspects of hESC clinical trials included in this review. The first clinical trial registration was in 2002, and the largest number of registered trials were in the United States (19, 40.4%), followed by China (8, 17.0%; Fig. 1 A). By disease category, the largest number of trials were related to ophthalmologic conditions (20, 42.6%), followed by neurologic conditions (10, 21.3%), and clinical studies were mainly conducted on diabetes mellitus (7, 14.9%; Fig. 1 B). Figure 1 C shows the number of trial registrations and the cumulative number of clinical studies by year. There has been a sharp increase since 2012. (Fig. 1 C), and by study design, phase 1 or phase 1/2 designs predominate, accounting for 88% (Fig. 1 D). When looking at studies by a specific disease, dry age-related macular degeneration (AMD) is the most common with 8 (18.2%), followed by type 1 diabetes mellitus (T1DM, 7, 15.9%) and Stargardt Macular Dystrophy (SMD, 5, 11.4%).
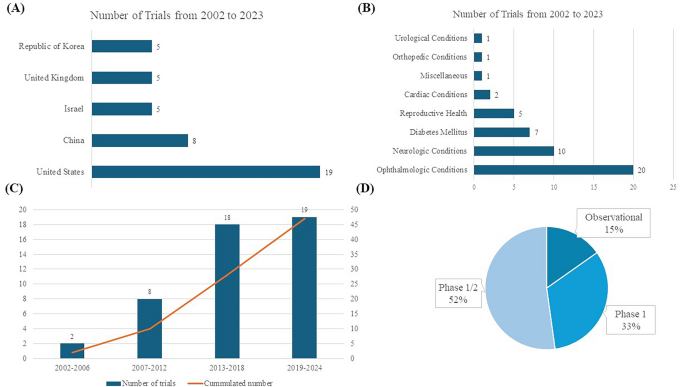
Numbers of trials on human embryonic stem cells ( A ) Global Geographical Distribution of Human Embryonic Stem Cell Clinical Trials ( B ) Distribution of Trials by Disease Category ( C ) Frequency of Trials Across Specific Diseases ( D ) Distribution of Clinical Trials Across Different Phases
2.2 Disease-specific analysis
2.2.1 ophthalmologic diseases.
Retinal degeneration is a significant ophthalmologic disease that affects the eye and vision, including dry AMD, SMD, wet AMD, retinitis pigmentosa (RP), diabetic retinopathy, and myopic macular degeneration, among others [ 20 , 21 , 22 ]. These conditions often lead to severe vision impairment or blindness. Traditional treatments primarily focus on slowing the progression of these diseases but generally fall short of providing substantial visual improvement. For instance, while laser therapy is beneficial in the early stages, there is no established treatment for late-stage dry AMD [ 23 ]. In cases of wet AMD, therapies such as anti-VEGF can be administered through intravitreal infusion (e.g., ranibizumab, bevacizumab, aflibercept, and brolucizumab), yet this disease requires continuous treatment and monitoring due to its chronic nature [ 24 , 25 , 26 , 27 ]. Stem cell therapy, particularly involving retinal pigment epithelium (RPE) degeneration, has emerged as a promising approach in eye diseases [ 28 ]. The RPE is vital for maintaining photoreceptor health and is tasked with recycling photopigments and clearing shed photoreceptor segments [ 29 ]. hESCs have shown significant potential in rescuing photoreceptors and enhancing vision in preclinical macular degeneration models [ 30 ]. One of the initial forays into stem cell therapy using hESCs was directed at treating dry AMD using hESC-derived RPE. Several key factors contributed to this early focus on retinal conditions. Primarily, the unique immune privilege of the eye, reinforced by the blood-ocular barrier, significantly lowers the risk of rejection of transplanted cells—a crucial aspect in the success of any stem cell-based therapy [ 31 , 32 ]. Moreover, the eye's transparency permits the non-invasive tracking of the introduced cells through methods like optical coherence tomography or microperimetry, enabling continuous monitoring and evaluation of the therapy's effectiveness [ 33 ]. The eye's distinct and isolated structure also minimizes the spread of these cells to other body parts, thereby reducing the likelihood of unintended systemic effects [ 34 ]. Furthermore, the absence of synaptic layers in retinal cells aids in their smoother integration [ 29 ]. Lastly, the irreversible progression of many retinal disorders and the absence of adequate existing treatments have necessitated the development of innovative therapeutic strategies, thereby placing retinal ailments at the forefront of hESC research and application.
Dry AMD, a prevalent and progressive ophthalmologic disease affecting elderly patients, is characterized by the degeneration of the RPE layer and impairment of central vision [ 21 ]. The pivotal role of RPE in the pathophysiology of dry AMD makes it a prime target for therapeutic interventions. The potential of stem cells, especially hESCs, in this context, lies in their ability to differentiate into RPE cells, thereby offering the possibility of replacing damaged or degenerated RPE with healthy, functional cells. Preclinical studies in animal models and in vitro experiments have provided substantial evidence supporting the role of stem cells, including hESCs, in treating dry AMD [ 35 , 36 , 37 ].
For example, in Yucatan minipigs, a preclinical study assessed CPCB-RPE1, a hESC-derived retinal pigment epithelium monolayer [ 35 ]. The study successfully placed CPCB-RPE1 implants in the subretinal space without breakage, and histological analysis confirmed the survival of hESC-RPE cells as an intact monolayer for one month [ 35 ]. Another study used differentiated hESC-RPE replacement therapy on albino rabbit eyes induced with NaIO3, employing a 25-gauge transvitreal pars plana vitrectomy (PPV) technique [ 36 ]. Xeno-free hESC-RPE monolayer on a polyester substrate survived and retained functionality for up to four weeks with short-term immunosuppression in a rabbit dry AMD model [ 37 ]. These studies demonstrate the feasibility of generating RPE cells from stem cells and their potential to integrate into the retina, potentially restoring RPE function and rescuing photoreceptors. Also, the critical advantage of hESC-RPE is their reduced risk of uncontrolled proliferation, as they are fully differentiated.
Clinical trials have been conducted to test the safety and feasibility of hESC-derived RPE for dry AMD, as outlined in Table 1 . Dry AMD has been the subject of the most significant number of clinical trials, with studies dating back to 2011 (Table 1 ). The first study involved MA09-hRPE (NCT01344993; NCT01674829; NCT02122159), derived from the MA09 hESC line, a xenograft product with ex vivo exposure to mouse embryonic cells [ 38 ]. Produced by isolating RPE patches when embryoid body formation was confirmed, this treatment was tested in three different dose cohorts (50,000, 100,000, and 150,000 cells) for patients with dry AMD and SMD [ 39 ]. Encouragingly, the study revealed no signs of adverse events like cell proliferation or immune rejection. In addition, the best-corrected visual acuity improved in 10 eyes, and measures related to vision-related quality of life showed enhancements [ 39 ]. In a clinical trial of MA09-hESC-derived RPE cells conducted with an Asian population, which included four participants, there was no evidence of adverse proliferation or tumorigenesis [ 40 ]. Furthermore, one patient experienced improved visual acuity, while the remaining three maintained stable visual acuity throughout the trial [ 40 ]. In the USA, a phase 1/2 clinical study was conducted using CPCB-RPE1, a composite implant consisting of a synthetic parylene substrate and a polarized monolayer of adherent hESC-RPE cells (NCT02590692). This study demonstrated safety and tolerability in legally blind patients with dry AMD [ 41 , 42 ]. However, graft survival remains a significant challenge, influenced by factors like aging of Bruch's membrane, subretinal scarring, para-inflammation, and choroid ischemia [ 33 ].
SMD, a prevalent retinal dystrophy affecting young individuals, is characterized by progressive vision loss, primarily caused by mutations in the ABCA4 gene, which leads to dysfunction of the ABCR protein expressed in retinal photoreceptors [ 43 ]. Currently, there are no established treatments to effectively improve vision in SMD, similar to the situation in dry AMD. Promising outcomes have been observed in preclinical models, including the safe subretinal injection of retinal pigment epithelium (RPE) derived from hESC. This approach was tested in a phase 1 clinical trial in the USA (NCT02941991). The WA-099 hESC line demonstrated the ability to spontaneously differentiate into RPE cells, with subsequent isolation of pigmentation cells. A suspension of these hESC-derived RPE cells, containing 1.0 × 10^6 cells in 0.1 mL, was surgically implanted subretinally in all eyes using a pars plana vitrectomy (PPV) approach [ 44 ]. The study's findings indicated no adverse events during the one-year postoperative follow-up period. Additionally, the treated eyes had no significant improvement in visual acuity [ 44 ]. In China, researchers Li et al. evaluated the Q-CTS-hESC-2 cell line-derived RPE in a 5-year follow-up study on seven patients and reported no significant adverse reactions and some temporary improvements in visual function, though two patients showed a long-term decrease in vision (NCT02749734) [ 45 ]. Sung et al., from the Republic of Korea, reported a 3-year study on Asian patients, also finding no serious adverse events and reporting stable or improved BCVA in some patients (NCT01625559) [ 46 ].
RP is a group of inherited retinal disorders characterized by the progression of vision loss due to photoreceptor degeneration, affecting approximately 1 in 4,000 individuals worldwide [ 47 , 48 ]. A Phase 1/2 clinical trial of RP with monogenic mutations is ongoing (NCT03963154), with interim analysis showing no adverse events in seven patients [ 49 ]. While these studies confirm the long-term safety and tolerability of hESC-RPE cell transplantation, they also highlight the need for further research to improve efficacy, including better patient selection and treatment methodologies, as significant and consistent improvements in visual function are yet to be established.
2.2.2 Neurologic diseases
The utilization of stem cell therapy derived from hESCs in treating neurological disorders is an emerging and promising area of research. As illustrated in Fig. 1 B, neurologic diseases are among the most researched applications in this field. This branch of medical science addresses a diverse spectrum of neurological conditions, including Parkinson's disease (PD), amyotrophic lateral sclerosis (ALS), spinal cord injuries (SCI), and multiple sclerosis. These disorders present considerable treatment challenges, largely due to the complexity of the nervous system and the typically permanent nature of neuronal damage involved. Ongoing studies are displayed in Table 2 .
The first-in-patient clinical trial on neurologic disease was conducted on SCI patients [ 50 ]. Oligodendrocyte progenitor cells (LCTOPC1), which are also nomenclature as AST-OPC1 or GRNOPC1, is the world's first hESC-derived therapy, and the phase 1 trial was approved by US-FDA in 2009, and the first patient was enrolled in 2011 (NCT01217008) [ 50 , 51 ]. Recent 10-year follow-up study results on five participants who received intraparenchymal injections of LCTOPC1 showed no serious adverse effects during follow-up, with 80% of patients showing MRI evidence of tissue matrix formation at the injury site [ 51 ]. This pivotal study, leading to a subsequent cervical dose escalation trial (NCT02302157), demonstrated the safety of hESC-derived therapies using LCTOPC1. In the trial, 25 participants with C4-7 spinal injuries received a single dose of 2, 10, or 20 million LCTOPC1 cells and low-dose tacrolimus for 60 days [ 52 ]. Despite some adverse events, including 29 serious ones, the treatment was well tolerated, with MRI scans showing no significant complications, and at a 1-year follow-up, 96% of participants improved by at least one level of neurological function, and 32% improved by two or more levels [ 52 ].
Additionally, research has shown that neural precursor cells marked by polysialic acid-neural cell adhesion molecule (PSA-NCAM), derived from hESC, can enhance neural tissue integrity in a rat stroke model [ 53 ]. Building on these findings, a phase 1/2a clinical trial (NCT04812431) is currently underway to assess the safety and efficacy of PSA-NCAM( +)-NPC for patients with sub-acute C4-C7 level spinal cord injuries. In this trial, the cells will be delivered intrathecally across five sites, and participants will be monitored for one year and five months as part of a follow-up study.
PD is a neurodegenerative disease characterized primarily by the loss of dopaminergic neurons in the substantia nigra, a region of the brain integral to controlling body movement. This loss leads to the classic symptoms of PD, including tremors, rigidity, bradykinesia, and postural instability [ 54 ]. The potential of hESC-based therapies in PD lies in their ability to differentiate into dopaminergic neurons, the type of cell lost in the disease [ 55 ]. The goal of transplanting hESC-derived cells in PD treatment is to replace the depleted neurons and normalize dopamine levels in the brain, which could help alleviate PD symptoms. MSK-DA01, a midbrain dopamine neuron cell derived from hESCs, is currently undergoing a Phase 1 trial in the United States (NCT04802733). A preclinical study on MSK-DA01 demonstrated successful graft survival and improved behavior in rats with 6-hydroxydopamine-induced lesions, a model for PD. Importantly, these studies revealed no adverse effects related to the graft cells and no unexpected cell proliferation outside the brain, indicating a promising safety profile for this innovative therapy [ 56 ].
STEM-PD, another product consisting of dopaminergic neuronal progenitor cells derived from hESCs, has also been evaluated in a preclinical study [ 57 ]. This study showed the precise stereotactic injection of STEM-PD into a pig model and demonstrated effective innervation of the targeted brain regions. Additionally, this intervention led to a reversal of motor deficits in the pig model of Parkinson's disease, demonstrating the potential efficacy of STEM-PD in addressing the symptoms associated with this neurodegenerative disorder [ 57 ]. Presently, STEM-PD is the subject of a phase 1 clinical trial in the United Kingdom, which is in the process of recruiting eight patients, and this trial marks a significant step in evaluating the safety and potential efficacy of STEM-PD in human subjects, specifically targeting the treatment of PD (NCT05635409).
A research team in China successfully derived dopaminergic neurons from hESCs and demonstrated sustained behavioral improvements over two years in a monkey model of PD [ 58 ]. This significant advancement in stem cell research has led to the registration of a Phase 1 clinical trial (NCT03119636). However, the current status of this trial remains unknown.
ALS, a severe neurodegenerative condition, is characterized by the deterioration of both upper and lower motor neurons (MNs), resulting in the progressive paralysis of muscles controlled by these neurons [ 59 ]. While FDA-approved treatments like riluzole have demonstrated some efficacy in prolonging survival, there remains a significant unmet need for more effective ALS therapies [ 60 ]. Recent evidence points to the involvement of astrocytes in the pathogenesis of ALS [ 61 ]. AstroRx®, a novel cell therapy derived from hESCs, has shown promise in addressing this gap, as evidenced by the outcomes of its recent Phase 1/2a clinical trial [ 62 ]. AstroRx®, administered as a single intrathecal injection, was tested in two cohorts of ALS patients—a low-dose and a high-dose group, each consisting of five patients (NCT03482050). The administration of AstroRx® showed a clinically significant impact lasting for three months post-treatment, with particularly notable effects observed in a group of rapid progressors [ 62 ].
NR1, an hESC-derived neural stem cell, is under investigation for chronic ischemic stroke patients who are 6–60 months post-ischemic subcortical mid-cerebral artery stroke (NCT04631406). Six patients underwent transplantation with NR1, and there was a notable improvement in the Mugl-Meyer motor score. Additionally, all six patients exhibited a transient flair signal that resolved within two months, which correlated with neurological recovery [ 63 ].
2.2.3 Diabetes mellitus
Type 1 Diabetes Mellitus (T1DM) commonly manifests in childhood and adolescence and is marked by a chronic autoimmune condition leading to the loss of insulin-producing beta cells in the pancreas [ 64 ]. Unlike Type 2 DM, which often relates to lifestyle and insulin resistance, T1DM is primarily driven by an autoimmune response [ 64 ]. In stem cell therapy for T1DM, two main strategies have emerged: one involves replacing the missing insulin-producing beta cells, while the other focuses on immunomodulation to safeguard existing beta cells from further autoimmune destruction [ 65 ]. Seven registered clinical trials for stem cell-based treatment of T1DM using hESC are summarized in Table 3 .
Schulz and colleagues described the creation of the VC-01 composite product utilizing pancreatic endoderm cells (PEC-01) obtained from CyT49 hESCs with a retrievable semi-permeable encapsulating device drug delivery system [ 66 ]. VC-02, developed in 2017, is an advanced model featuring multiple large pores across the membrane to facilitate vascularization while maintaining immune isolation [ 67 ]. VC-01 was investigated in phase 1/2 trial (NCT02239354; NCT04678557; NCT02939118) and VC-02 was investigated in phase 1/2 trial (NCT03163511). In the phase 1/2 study of the VC-01 product, immunosuppressants were not administered, leading to a host reaction against the implant, ultimately resulting in its destruction, and the study was terminated [ 68 ]. A Phase 1/2 study involving 17 patients with T1DM was carried out following a modification in the VC-02 device. This study demonstrated successful engraftment and insulin release in 63% of the cases, and as early as six months post-implantation, 35.3% of the participants showed positive C-peptide levels. These results indicate the potential of VC-02 as a viable alternative for T1DM treatment. However, it's important to note that some reported adverse events were primarily related to the surgical procedures of implanting or explanting the device and the side effects of immunosuppression therapy [ 69 ]. VCTX210A represents an innovative approach that uses pancreatic endodermal cells (PEC210A) derived from hESC. These cells have been genetically modified using the CRISPR/Cas9 (Clustered Regularly Interspaced Short Palindromic Repeats/CRISPR-associated protein 9) technology. This modification enhances the cells' survival against the patient's immune system, thereby addressing the challenge of graft versus host disease [ 70 ]. Additionally, VX880, a fully differentiated pancreatic islet cell product derived from hESC designed to treat T1DM, is undergoing clinical investigation (NCT04786262). Interim data analysis from this study has yielded positive results, indicating that the treatment successfully restored insulin production in the first two patients enrolled in the trial [ 71 ].
2.2.4 Female reproductive organ and genitourinary disease
The field of female reproductive organ disorders is increasingly looking towards stem cell therapy and cutting-edge biomedical technologies for potential treatments, as shown in Table 4 . Intravenous injection of hESC-derived mesenchymal cells (hESC-MCs) showed restoration of ovarian function induced by the chemotherapeutic agent in a murine model [ 72 , 73 ]. A product, hESC-MC, has been explored by a Chinese research group for treating moderate to severe intrauterine adhesion (NCT04232592). Additionally, a therapy involving hESC-MC product is currently being investigated as a potential treatment for primary ovarian insufficiency (NCT03877471). Additionally, Table 5 showcases the application of hESC-derived mesenchymal stem cell therapy, specifically MR-MVC-01, which is currently under investigation for treating interstitial cystitis, as per the clinical trial registered under NCT04610359.
2.2.5 Cardiovascular disease
In the field of heart failure treatment, the innovative application of human embryonic stem cells (hESCs) offers a promising alternative to conventional therapies. Table 5 also highlights hESC-derived cardiac progenitor cell-based products in treating heart failure and ischemic heart disease, as illustrated in the clinical trials registered under NCT02057900 and NCT05068674. The ESCORT trial (NCT02057900), conducted in France, marked a pioneering venture in employing hESC-derived cardiomyocytes for heart failure treatment, setting a precedent that has been followed by the HECTOR trial (NCT05068674) in the United States, initiated in 2022. The ESCORT trial, focusing on patients with severe ischemic left ventricular dysfunction, demonstrated the feasibility and safety of using hESC-derived cardiovascular progenitor cells, embedded in a fibrin patch, applied to the damaged heart areas during coronary artery bypass surgery [ 74 ]. The results, including the production of a highly purified batch of progenitor cells and significant symptomatic improvements in patients, though with instances of silent alloimmunization, have laid the groundwork for future explorations in this domain. The HECTOR trial in the U.S. is building upon this foundation with a novel approach, utilizing hESC-derived cardiomyocytes (hESC-CMs) to enhance survival and cardiac function in patients with chronic left ventricular dysfunction secondary to myocardial infarction. This phase I dose-escalation pilot study is designed as an initial safety assessment to determine the maximum tolerated dose (MTD) before proceeding to a phase II randomized, double-blinded, placebo-controlled study. Approximately eighteen patients who are scheduled for cardiac catheterization and meet all inclusion/exclusion criteria will participate in this initial phase. The HECTOR trial represents a significant step forward in the application of hESC-CMs in cardiac therapy, with great anticipation for its potential to revolutionize the treatment of heart failure and related conditions.
2.3 Challenges and ethical considerations
As we explore the burgeoning field of hESC research and its clinical applications, it becomes crucial to examine the accompanying ethical and practical challenges thoroughly. While this area of research offers groundbreaking possibilities in treating various diseases, it is intertwined with complex ethical, legal, and social issues, particularly due to the involvement of human embryos.
2.3.1 Derivation of hESC
In the field of hESC research, the ethical implications surrounding the derivation of these cells from embryos are paramount. hESCs are typically harvested from embryos at the blastocyst stage approximately 5–6 days post-fertilization. This stage of development is critical because it leads to the inevitable destruction of the embryo, a primary ethical concern in this field of research [ 19 , 75 , 76 , 77 ].
Due to their pluripotency, the significant potential of hESCs makes them a valuable asset in understanding disease mechanisms, drug testing, and potential regenerative therapies [ 78 ]. Moreover, hESCs are obtained early in induced pluripotent development, making them crucial for studying human developmental processes and various diseases [ 17 ]. They play a vital role, especially when embryos are discarded after positive preimplantation genetic testing (PGT) results, contributing to our understanding of genetic abnormalities and disease ecology [ 17 ].
Regarding the moral status of the embryo, there are varying views. The Catholic perspective often sees life beginning at fertilization, while Judaism and Islam view the blastocyst as having the potential for life but not as fully alive [ 79 , 80 ]. Hinduism and Buddhism do not provide a clear doctrinal definition of life's beginning, adopting a more philosophical and spiritual perspective [ 81 ].
The use of surplus IVF embryos in hESC research is often defended under the principle of proportionality. This approach favors using them for stem cell research due to the broader potential benefits compared to enhancing IVF techniques [ 17 ]. The utilization of embryos with monogenic defects (PGT-M) or aneuploidies (PGT-A) for deriving disease-specific stem cells is seen as a promising avenue for advancing the understanding of specific diseases and developing targeted treatments [ 9 , 17 ].
In summary, hESC research presents a complex ethical landscape. The scientific and medical benefits of hESCs must be balanced against the moral considerations surrounding the use of human embryos, necessitating a nuanced approach to this rapidly evolving field.
2.3.2 Regulatory issues
In the realm of research involving hESCs, regulatory issues play a crucial role, varying significantly across different countries. Obtaining approval from institutional review boards (IRBs) and adhering to regulations set by authoritative bodies are pivotal steps in developing and progressing hESC-related research and development.
Procedures involving the transfer of stem cells are subject to specific regulations. This encompasses the process of transferring stem cell materials, which requires careful adherence to legal and ethical guidelines [ 15 , 82 ]. It's essential to ensure that the transfer agreements are comprehensive, detailing any restrictions and obligations related to using the materials and associated data [ 83 , 84 ]. Such transfers must respect donor rights and comply with the regulatory frameworks of both the donating and receiving entities.
The process of creating stem cell products that are safe for clinical use involves several critical steps. This includes extensive testing for genetic stability and absence of contaminants, ensuring the cells' identity and functionality, and verifying that they meet the stringent safety standards required for clinical application [ 82 ]. These procedures are designed to safeguard patient safety and ensure the efficacy of the stem cell products.
Overall, the development and research involving hESCs must navigate a complex landscape of regulatory requirements. These regulations are in place to ensure the ethical use of human stem cells, the protection of donor rights, and the safety and efficacy of stem cell-based therapies. Compliance with these regulations is not only a legal requirement but also a cornerstone in maintaining the integrity and credibility of stem cell research.
3 Conclusion
The exploration of hESCs over the past two decades has opened new frontiers in medical science, particularly in the fields of regenerative medicine and cell-based therapies. The landmark discovery and subsequent developments have brought immense potential for understanding and treating a wide range of diseases, from genetic disorders to degenerative conditions.
However, the journey of hESC research is intertwined with a plethora of ethical, legal, and regulatory challenges. The ethical considerations, primarily regarding the use of human embryos, highlight the delicate balance between scientific advancement and moral imperatives. Different religious and cultural perspectives on embryo status underline this debate's complexity. As we have seen, approaches to this issue vary significantly worldwide, influencing the regulatory landscape and research in different countries.
The advancements in hESC research also underscore the importance of robust regulatory frameworks and adherence to ethical standards. From acquiring embryonic materials to developing stem cell-based products for clinical use, each step requires careful consideration of ethical guidelines, safety standards, and regulatory compliance. The involvement of IRBs and adherence to international standards and guidelines are critical in ensuring that the research is conducted responsibly and with the utmost respect for human life and dignity.
Looking ahead, the field of hESC research holds immense promise. With continued technological advancements and a deeper understanding of stem cells' capabilities, we stand on the brink of revolutionary medical breakthroughs. However, the path forward must be navigated with a commitment to ethical principles, regulatory compliance, and public engagement. By upholding these standards, the scientific community can ensure that the benefits of hESC research are realized in a manner that respects human values and contributes positively to human health and well-being.
In conclusion, hESC research represents scientific innovation, ethical reflection, and regulatory prudence. As we continue to advance in this field, it is imperative to maintain a balanced approach that fosters scientific discovery while honoring ethical obligations and regulatory requirements. The future of hESC research, promising as it is, depends on our collective ability to navigate these complex and multifaceted challenges.
Data availability statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Thomson JA, Itskovitz-Eldor J, Shapiro SS, Waknitz MA, Swiergiel JJ, Marshall VS, et al. Embryonic stem cell lines derived from human blastocysts. Science. 1998;282:1145–7.
Article CAS PubMed Google Scholar
Oh SK, Kim HS, Ahn HJ, Seol HW, Kim YY, Park YB, et al. Derivation and characterization of new human embryonic stem cell lines: SNUhES1, SNUhES2, and SNUhES3. Stem Cells. 2005;23:211–9.
Article PubMed Google Scholar
Doğan A. Embryonic stem cells in development and regenerative medicine. Adv Exp Med Biol. 2018;1079:1–15.
Kolios G, Moodley Y. Introduction to stem cells and regenerative medicine. Respiration. 2013;85:3–10.
Jarrige M, Frank E, Herardot E, Martineau S, Darle A, Benabides M, et al. The future of regenerative medicine: cell therapy using pluripotent stem cells and acellular therapies based on extracellular vesicles. Cells. 2021;10:240.
Article CAS PubMed PubMed Central Google Scholar
Kidha DK. Human embryonic stem cell research in transplantation and regenerative medicine: a principlist assessment; 2020.
Kim YY, Ku SY, Liu HC, Cho HJ, Oh SK, Moon SY, et al. Cryopreservation of human embryonic stem cells derived-cardiomyocytes induced by BMP2 in serum-free condition. Rep Sci. 2011;18:252–60.
Kim YY, Min H, Kim H, Choi YM, Liu HC, Ku SY. Differential MicroRNA expression profile of human embryonic stem cell-derived cardiac lineage cells. Tissue Eng Regen Med. 2017;14:163–9.
Douglas T, Savulescu J. Destroying unwanted embryos in research. Talking Point on morality and human embryo research. EMBO Rep. 2009;10:307–12.
Fan R. The ethics of human embryonic stem cell research and the of the family. In: Lee SC, editor. The family, medical decision-making, and biotechnology: Critical reflections on Asian moral perspectives. The MIT Press: Springer; 2007. p. 127–48.
Turksen K. Cell biology and translational medicine. vol. 11. Berlin: Springer; 2021.
Book Google Scholar
Singh MS, Park SS, Albini TA, Canto-Soler MV, Klassen H, MacLaren RE, et al. Retinal stem cell transplantation: balancing safety and potential. Prog Retin Eye Res. 2020;75:100779.
Song MJ, Bharti K. Looking into the future: using induced pluripotent stem cells to build two and three dimensional ocular tissue for cell therapy and disease modeling. Brain Res. 2016;1638:2–14.
Lefkopoulos S. Enhancing reproducibility in human stem cell research. Nat Cell Biol. 2023;25:1237–9.
Ludwig TE, Andrews PW, Barbaric I, Benvenisty N, Bhattacharyya A, Crook JM, et al. ISSCR standards for the use of human stem cells in basic research. Stem Cell Rep. 2023;18:1744–52.
Article CAS Google Scholar
Takahashi K, Tanabe K, Ohnuki M, Narita M, Ichisaka T, Tomoda K, et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 2007;131:861–72.
Salari S, Adashi EY, Keller L, Johnson TRB, Smith GD. Human embryos donated for human embryonic stem cell derivation. Fertil Steril. 2023;119:3–10.
King NM, Perrin J. Ethical issues in stem cell research and therapy. Stem Cell Res Ther. 2014;5:85.
Article PubMed PubMed Central Google Scholar
Banja JD. Ethical considerations in stem cell research on neurologic and orthopedic conditions. PM R. 2015;7:S66-75.
Fleckenstein M, Mitchell P, Freund KB, Sadda S, Holz FG, Brittain C, et al. The progression of geographic atrophy secondary to age-related macular degeneration. Ophthalmology. 2018;125:369–90.
Chakravarthy U, Bailey CC, Johnston RL, McKibbin M, Khan RS, Mahmood S, et al. Characterizing disease burden and progression of geographic atrophy secondary to age-related macular degeneration. Ophthalmology. 2018;125:842–9.
GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;9:e144–60.
Guymer RH, Wu Z, Hodgson LAB, Caruso E, Brassington KH, Tindill N, et al. Subthreshold nanosecond laser intervention in age-related macular degeneration: the LEAD randomized controlled clinical trial. Ophthalmology. 2019;126:829–38.
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355:1419–31.
Rosenfeld PJ, Moshfeghi AA, Puliafito CA. Optical coherence tomography findings after an intravitreal injection of bevacizumab (avastin) for neovascular age-related macular degeneration. Ophthalmic Surg Lasers Imaging. 2005;36:331–5.
Heier JS, Brown DM, Chong V, Korobelnik JF, Kaiser PK, Nguyen QD, et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology. 2012;119:2537–48.
Pearce I, Amoaku W, Bailey C, Downey L, Gale R, Ghanchi F, et al. The changing landscape for the management of patients with neovascular AMD: brolucizumab in clinical practice. Eye (Lond). 2022;36:1725–34.
George SM, Lu F, Rao M, Leach LL, Gross JM. The retinal pigment epithelium: development, injury responses, and regenerative potential in mammalian and non-mammalian systems. Prog Retin Eye Res. 2021;85:100969.
Strauss O. The retinal pigment epithelium in visual function. Physiol Rev. 2005;85:845–81.
Sharma A, Jaganathan BG. Stem cell therapy for retinal degeneration: the evidence to date. Biologics. 2021;15:299–306.
PubMed PubMed Central Google Scholar
Idelson M, Alper R, Obolensky A, Yachimovich-Cohen N, Rachmilewitz J, Ejzenberg A, et al. Immunological properties of human embryonic stem cell-derived retinal pigment epithelial cells. Stem Cell Rep. 2018;11:681–95.
Yamasaki S, Sugita S, Horiuchi M, Masuda T, Fujii S, Makabe K, et al. Low immunogenicity and immunosuppressive properties of human ESC- and iPSC-derived retinas. Stem Cell Rep. 2021;16:851–67.
Qiu TG. Transplantation of human embryonic stem cell-derived retinal pigment epithelial cells (MA09-hRPE) in macular degeneration. NPJ Regen Med. 2019;4:19.
Tomita M, Lavik E, Klassen H, Zahir T, Langer R, Young MJ. Biodegradable polymer composite grafts promote the survival and differentiation of retinal progenitor cells. Stem Cells. 2005;23:1579–88.
Koss MJ, Falabella P, Stefanini FR, Pfister M, Thomas BB, Kashani AH, et al. Subretinal implantation of a monolayer of human embryonic stem cell-derived retinal pigment epithelium: a feasibility and safety study in Yucatán minipigs. Graefes Arch Clin Exp Ophthalmol. 2016;254:1553–65.
Petrus-Reurer S, Bartuma H, Aronsson M, Westman S, Lanner F, Kvanta A. Subretinal transplantation of human embryonic stem cell derived-retinal pigment epithelial cells into a large-eyed model of geographic atrophy. J Vis Exp. 2018.
Ilmarinen T, Thieltges F, Hongisto H, Juuti-Uusitalo K, Koistinen A, Kaarniranta K, et al. Survival and functionality of xeno-free human embryonic stem cell-derived retinal pigment epithelial cells on polyester substrate after transplantation in rabbits. Acta Ophthalmol. 2019;97:e688–99.
Schwartz SD, Hubschman J-P, Heilwell G, Franco-Cardenas V, Pan CK, Ostrick RM, et al. Embryonic stem cell trials for macular degeneration: a preliminary report. Lancet. 2012;379:713–20.
Schwartz SD, Regillo CD, Lam BL, Eliott D, Rosenfeld PJ, Gregori NZ, et al. Human embryonic stem cell-derived retinal pigment epithelium in patients with age-related macular degeneration and Stargardt’s macular dystrophy: follow-up of two open-label phase 1/2 studies. Lancet. 2015;385:509–16.
Song WK, Park KM, Kim HJ, Lee JH, Choi J, Chong SY, et al. Treatment of macular degeneration using embryonic stem cell-derived retinal pigment epithelium: preliminary results in Asian patients. Stem Cell Rep. 2015;4:860–72.
Kashani AH, Lebkowski JS, Rahhal FM, Avery RL, Salehi-Had H, Chen S, et al. One-year follow-up in a phase 1/2a clinical trial of an allogeneic RPE cell bioengineered implant for advanced dry age-related macular degeneration. Transl Vis Sci Technol. 2021;10:13.
Kashani AH, Uang J, Mert M, Rahhal F, Chan C, Avery RL, et al. Surgical method for implantation of a biosynthetic retinal pigment epithelium monolayer for geographic atrophy: experience from a phase 1/2a Study. Ophthalmol Retina. 2020;4:264–73.
Hussain RM, Ciulla TA, Berrocal AM, Gregori NZ, Flynn HW Jr, Lam BL. Stargardt macular dystrophy and evolving therapies. Expert Opin Biol Ther. 2018;18:1049–59.
Brant Fernandes RA, Lojudice FH, Zago Ribeiro L, Santos da Cruz NF, Polizelli MU, Cristovam PC, et al. Transplantation of subretinal stem cell-derived retinal pigment epithelium for Stargardt disease: a phase I clinical trial. Retina. 2023;43:263–74.
Li SY, Liu Y, Wang L, Wang F, Zhao TT, Li QY, et al. A phase I clinical trial of human embryonic stem cell-derived retinal pigment epithelial cells for early-stage Stargardt macular degeneration: 5-years’ follow-up. Cell Prolif. 2021;54:e13100.
Sung Y, Lee MJ, Choi J, Jung SY, Chong SY, Sung JH, et al. Long-term safety and tolerability of subretinal transplantation of embryonic stem cell-derived retinal pigment epithelium in Asian Stargardt disease patients. Br J Ophthalmol. 2021;105:829–37.
Becherucci V, Bacci GM, Marziali E, Sodi A, Bambi F, Caputo R. The new era of therapeutic strategies for the treatment of retinitis pigmentosa: a narrative review of pathomolecular mechanisms for the development of cell-based therapies. Biomedicines. 2023;11:2656.
Lozano B LL, Cervantes A LA. Development of experimental treatments for patients with retinitis pigmentosa. Arch Soc Esp Oftalmol (Engl Ed). 2023;98:646–55.
Monville C, Bertin S, Devisme C, Brazhnikova E, Jaillard C, Walter H, et al. Phase I/II open-label study of implantation into one eye of hESC-derived RPE in patients with retinitis pigmentosa due to monogenic mutation: first safety results. Invest Ophthalmol Vis Sci. 2023;64:3829–929.
Google Scholar
Lebkowski J. GRNOPC1: the world’s first embryonic stem cell-derived therapy. Interview with Jane Lebkowski. Regen Med. 2011;6:11–3.
McKenna SL, Ehsanian R, Liu CY, Steinberg GK, Jones L, Lebkowski JS, et al. Ten-year safety of pluripotent stem cell transplantation in acute thoracic spinal cord injury. J Neurosurg Spine. 2022. https://doi.org/10.3171/2021.12.Spine21622
Fessler RG, Ehsanian R, Liu CY, Steinberg GK, Jones L, Lebkowski JS, et al. A phase 1/2a dose-escalation study of oligodendrocyte progenitor cells in individuals with subacute cervical spinal cord injury. J Neurosurg Spine. 2022;37:812–20.
Kim HS, Choi SM, Yang W, Kim DS, Lee DR, Cho SR, et al. PSA-NCAM(+) neural precursor cells from human embryonic stem cells promote neural tissue integrity and behavioral performance in a rat stroke model. Stem Cell Rev Rep. 2014;10:761–71.
Hayes MT. Parkinson’s Disease and Parkinsonism. Am J Med. 2019;132:802–7.
Sonntag KC, Song B, Lee N, Jung JH, Cha Y, Leblanc P, et al. Pluripotent stem cell-based therapy for Parkinson’s disease: current status and future prospects. Prog Neurobiol. 2018;168:1–20.
Piao J, Zabierowski S, Dubose BN, Hill EJ, Navare M, Claros N, et al. Preclinical efficacy and safety of a human embryonic stem cell-derived midbrain dopamine progenitor product, MSK-DA01. Cell Stem Cell. 2021;28:217-29.e7.
Kirkeby A, Nelander J, Hoban DB, Rogelius N, Bjartmarz H, Storm P, et al. Preclinical quality, safety, and efficacy of a human embryonic stem cell-derived product for the treatment of Parkinson’s disease. STEM-PD Cell Stem Cell. 2023;30:1299-314.e9.
Wang YK, Zhu WW, Wu MH, Wu YH, Liu ZX, Liang LM, et al. Human clinical-grade parthenogenetic ESC-derived dopaminergic neurons recover locomotive defects of nonhuman primate models of Parkinson’s disease. Stem Cell Reports. 2018;11:171–82.
Feldman EL, Goutman SA, Petri S, Mazzini L, Savelieff MG, Shaw PJ, et al. Amyotrophic lateral sclerosis. Lancet. 2022;400:1363–80.
Jaiswal MK. Riluzole and edaravone: a tale of two amyotrophic lateral sclerosis drugs. Med Res Rev. 2019;39:733–48.
Brandebura AN, Paumier A, Onur TS, Allen NJ. Astrocyte contribution to dysfunction, risk and progression in neurodegenerative disorders. Nat Rev Neurosci. 2023;24:23–39.
Gotkine M, Caraco Y, Lerner Y, Blotnick S, Wanounou M, Slutsky SG, et al. Safety and efficacy of first-in-man intrathecal injection of human astrocytes (AstroRx®) in ALS patients: phase I/IIa clinical trial results. J Transl Med. 2023;21:122.
Steinberg GK, Bet A, Williams J, McDonald K, Diaz R, Samos C, et al. First-in-human phase 1/2a study of intracerebral transplantation using embryonic-derived neural stem cells (NR1) for chronic ischemic stroke. Stroke. 2023;54:A147–247.
Article Google Scholar
Acharjee S, Ghosh B, Al-Dhubiab BE, Nair AB. Understanding type 1 diabetes: etiology and models. Can J Diabetes. 2013;37:269–76.
Chen S, Du K, Zou C. Current progress in stem cell therapy for type 1 diabetes mellitus. Stem Cell Res Ther. 2020;11:1–13.
Schulz TC. Concise review: manufacturing of pancreatic endoderm cells for clinical trials in type 1 diabetes. Stem Cells Transl Med. 2015;4:927–31.
Dang HP, Chen H, Dargaville TR, Tuch BE. Cell delivery systems: toward the next generation of cell therapies for type 1 diabetes. J Cell Mol Med. 2022;26:4756–67.
Pullen LC. Stem cell-derived pancreatic progenitor cells have now been transplanted into patients: report from IPITA 2018. Am J Transplant. 2018;18:1581–2.
Shapiro AMJ, Thompson D, Donner TW, Bellin MD, Hsueh W, Pettus J, et al. Insulin expression and C-peptide in type 1 diabetes subjects implanted with stem cell-derived pancreatic endoderm cells in an encapsulation device. Cell Rep Med. 2021;2: 100466.
Ellis CE, Mojibian M, Ida S, Fung VCW, Skovsø S, McIver E, et al. Human A2-CAR T cells reject HLA-A2 + human islets transplanted into mice without inducing graft-versus-host disease. Transplantation. 2023;107:e222–33.
Reichiman TW, Ricordi C, Naji A, Markmann JF, Perkins BA, Wijkstrom M, et al. 836-P: Glucose-dependent insulin production and insulin-independence in type 1 diabetes from stem cell–derived, fully differentiated islet cells—updated data from the VX-880 cinical trial. Diabetes. 2023. https://doi.org/10.2337/db23-836-P
Yoon SY, Yoon JA, Park M, Shin EY, Jung S, Lee JE, et al. Recovery of ovarian function by human embryonic stem cell-derived mesenchymal stem cells in cisplatin-induced premature ovarian failure in mice. Stem Cell Res Ther. 2020;11:255.
Bahrehbar K, Rezazadeh Valojerdi M, Esfandiari F, Fathi R, Hassani SN, Baharvand H. Human embryonic stem cell-derived mesenchymal stem cells improved premature ovarian failure. World J Stem Cells. 2020;12:857–78.
Menasché P, Vanneaux V, Hagège A, Bel A, Cholley B, Parouchev A, et al. Transplantation of human embryonic stem cell-derived cardiovascular progenitors for severe ischemic left ventricular dysfunction. J Am Coll Cardiol. 2018;71:429–38.
de Wert G, Mummery C. Human embryonic stem cells: research, ethics and policy. Hum Reprod. 2003;18:672–82.
Volarevic V, Markovic BS, Gazdic M, Volarevic A, Jovicic N, Arsenijevic N, et al. Ethical and safety issues of stem cell-based therapy. Int J Med Sci. 2018;15:36–45.
Lo B, Parham L. Ethical issues in stem cell research. Endocr Rev. 2009;30:204–13.
Liu G, David BT, Trawczynski M, Fessler RG. Advances in pluripotent stem cells: history, mechanisms, technologies, and applications. Stem Cell Rev Rep. 2020;16:3–32.
Walters L. Human embryonic stem cell research: an intercultural perspective. Kennedy Inst Ethics J. 2004;14:3–38.
Neaves W. The status of the human embryo in various religions. Development. 2017;144:2541–3.
Sivaraman MAF, Noor SNM. Human embryonic stem cell research: ethical views of Buddhist, Hindu and Catholic Leaders in Malaysia. Sci Eng Ethics. 2016;22:467–85.
International Society for Stem Cell Research. Standards for human stem Cell use in research. https://www.isscr.org/s/ISSCR_Standards_09_FINAL.pdf.
Bubela T, Guebert J, Mishra A. Use and misuse of material transfer agreements: lessons in proportionality from research, repositories, and litigation. PLoS Biol. 2015;13:e1002060.
Lovell-Badge R, Anthony E, Barker RA, Bubela T, Brivanlou AH, Carpenter M, et al. ISSCR guidelines for stem cell research and clinical translation: the 2021 update. Stem Cell Rep. 2021;16:1398–408.
Download references
Acknowledgements
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (Grant Number: HI22C1424) and the Grants of the Ministry of ICT Grants and the Ministry of Education, Republic of Korea (2020R1A2C1010293).
Open Access funding enabled and organized by Seoul National University.
Author information
Authors and affiliations.
Department of Obstetrics and Gynecology, Seoul National University Hospital, Seoul, Republic of Korea
Soo Jin Park, Yoon Young Kim, Ji Yeon Han, Sung Woo Kim, Hoon Kim & Seung-Yup Ku
Department of Obstetrics and Gynecology, Seoul National University College of Medicine, 101 Daehak-Ro Jongno-Gu, Seoul, 03080, Republic of Korea
Hoon Kim & Seung-Yup Ku
Institute of Reproductive Medicine and Population, Medical Research Center, Seoul National University, Seoul, Republic of Korea
Yoon Young Kim, Hoon Kim & Seung-Yup Ku
You can also search for this author in PubMed Google Scholar
Contributions
SJP: conceptualization, methodology, formal analysis, resources, data curation, investigations, visualization, Writing—Original Draft, Visualization, project administration, funding acquisition. YYK: methodology, validation, Writing—Review & Editing, Supervision. JYH: methodology, investigation, validation, supervision. SWK: methodology, investigation, validation, supervision. HK: methodology, investigation, validation, supervision. S-YK: conceptualization, methodology, project administration, funding acquisition.
Corresponding author
Correspondence to Seung-Yup Ku .
Ethics declarations
Conflict of interest.
The authors declare nothing to disclose.
Ethical statement
There are no animal experiments carried out for this article.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Park, S.J., Kim, Y.Y., Han, J.Y. et al. Advancements in Human Embryonic Stem Cell Research: Clinical Applications and Ethical Issues. Tissue Eng Regen Med 21 , 379–394 (2024). https://doi.org/10.1007/s13770-024-00627-3
Download citation
Received : 12 December 2023
Revised : 05 January 2024
Accepted : 08 January 2024
Published : 19 March 2024
Issue Date : April 2024
DOI : https://doi.org/10.1007/s13770-024-00627-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Human embryonic stem cells
- Regenerative medicine
- Clinical trials
- Stem cell research
- Find a journal
- Publish with us
- Track your research

Cultural Relativity and Acceptance of Embryonic Stem Cell Research
Article sidebar.
Main Article Content
There is a debate about the ethical implications of using human embryos in stem cell research, which can be influenced by cultural, moral, and social values. This paper argues for an adaptable framework to accommodate diverse cultural and religious perspectives. By using an adaptive ethics model, research protections can reflect various populations and foster growth in stem cell research possibilities.
INTRODUCTION
Stem cell research combines biology, medicine, and technology, promising to alter health care and the understanding of human development. Yet, ethical contention exists because of individuals’ perceptions of using human embryos based on their various cultural, moral, and social values. While these disagreements concerning policy, use, and general acceptance have prompted the development of an international ethics policy, such a uniform approach can overlook the nuanced ethical landscapes between cultures. With diverse viewpoints in public health, a single global policy, especially one reflecting Western ethics or the ethics prevalent in high-income countries, is impractical. This paper argues for a culturally sensitive, adaptable framework for the use of embryonic stem cells. Stem cell policy should accommodate varying ethical viewpoints and promote an effective global dialogue. With an extension of an ethics model that can adapt to various cultures, we recommend localized guidelines that reflect the moral views of the people those guidelines serve.
Stem cells, characterized by their unique ability to differentiate into various cell types, enable the repair or replacement of damaged tissues. Two primary types of stem cells are somatic stem cells (adult stem cells) and embryonic stem cells. Adult stem cells exist in developed tissues and maintain the body’s repair processes. [1] Embryonic stem cells (ESC) are remarkably pluripotent or versatile, making them valuable in research. [2] However, the use of ESCs has sparked ethics debates. Considering the potential of embryonic stem cells, research guidelines are essential. The International Society for Stem Cell Research (ISSCR) provides international stem cell research guidelines. They call for “public conversations touching on the scientific significance as well as the societal and ethical issues raised by ESC research.” [3] The ISSCR also publishes updates about culturing human embryos 14 days post fertilization, suggesting local policies and regulations should continue to evolve as ESC research develops. [4] Like the ISSCR, which calls for local law and policy to adapt to developing stem cell research given cultural acceptance, this paper highlights the importance of local social factors such as religion and culture.
I. Global Cultural Perspective of Embryonic Stem Cells
Views on ESCs vary throughout the world. Some countries readily embrace stem cell research and therapies, while others have stricter regulations due to ethical concerns surrounding embryonic stem cells and when an embryo becomes entitled to moral consideration. The philosophical issue of when the “someone” begins to be a human after fertilization, in the morally relevant sense, [5] impacts when an embryo becomes not just worthy of protection but morally entitled to it. The process of creating embryonic stem cell lines involves the destruction of the embryos for research. [6] Consequently, global engagement in ESC research depends on social-cultural acceptability.
a. US and Rights-Based Cultures
In the United States, attitudes toward stem cell therapies are diverse. The ethics and social approaches, which value individualism, [7] trigger debates regarding the destruction of human embryos, creating a complex regulatory environment. For example, the 1996 Dickey-Wicker Amendment prohibited federal funding for the creation of embryos for research and the destruction of embryos for “more than allowed for research on fetuses in utero.” [8] Following suit, in 2001, the Bush Administration heavily restricted stem cell lines for research. However, the Stem Cell Research Enhancement Act of 2005 was proposed to help develop ESC research but was ultimately vetoed. [9] Under the Obama administration, in 2009, an executive order lifted restrictions allowing for more development in this field. [10] The flux of research capacity and funding parallels the different cultural perceptions of human dignity of the embryo and how it is socially presented within the country’s research culture. [11]
b. Ubuntu and Collective Cultures
African bioethics differs from Western individualism because of the different traditions and values. African traditions, as described by individuals from South Africa and supported by some studies in other African countries, including Ghana and Kenya, follow the African moral philosophies of Ubuntu or Botho and Ukama , which “advocates for a form of wholeness that comes through one’s relationship and connectedness with other people in the society,” [12] making autonomy a socially collective concept. In this context, for the community to act autonomously, individuals would come together to decide what is best for the collective. Thus, stem cell research would require examining the value of the research to society as a whole and the use of the embryos as a collective societal resource. If society views the source as part of the collective whole, and opposes using stem cells, compromising the cultural values to pursue research may cause social detachment and stunt research growth. [13] Based on local culture and moral philosophy, the permissibility of stem cell research depends on how embryo, stem cell, and cell line therapies relate to the community as a whole . Ubuntu is the expression of humanness, with the person’s identity drawn from the “’I am because we are’” value. [14] The decision in a collectivistic culture becomes one born of cultural context, and individual decisions give deference to others in the society.
Consent differs in cultures where thought and moral philosophy are based on a collective paradigm. So, applying Western bioethical concepts is unrealistic. For one, Africa is a diverse continent with many countries with different belief systems, access to health care, and reliance on traditional or Western medicines. Where traditional medicine is the primary treatment, the “’restrictive focus on biomedically-related bioethics’” [is] problematic in African contexts because it neglects bioethical issues raised by traditional systems.” [15] No single approach applies in all areas or contexts. Rather than evaluating the permissibility of ESC research according to Western concepts such as the four principles approach, different ethics approaches should prevail.
Another consideration is the socio-economic standing of countries. In parts of South Africa, researchers have not focused heavily on contributing to the stem cell discourse, either because it is not considered health care or a health science priority or because resources are unavailable. [16] Each country’s priorities differ given different social, political, and economic factors. In South Africa, for instance, areas such as maternal mortality, non-communicable diseases, telemedicine, and the strength of health systems need improvement and require more focus. [17] Stem cell research could benefit the population, but it also could divert resources from basic medical care. Researchers in South Africa adhere to the National Health Act and Medicines Control Act in South Africa and international guidelines; however, the Act is not strictly enforced, and there is no clear legislation for research conduct or ethical guidelines. [18]
Some parts of Africa condemn stem cell research. For example, 98.2 percent of the Tunisian population is Muslim. [19] Tunisia does not permit stem cell research because of moral conflict with a Fatwa. Religion heavily saturates the regulation and direction of research. [20] Stem cell use became permissible for reproductive purposes only recently, with tight restrictions preventing cells from being used in any research other than procedures concerning ART/IVF. Their use is conditioned on consent, and available only to married couples. [21] The community's receptiveness to stem cell research depends on including communitarian African ethics.
c. Asia
Some Asian countries also have a collective model of ethics and decision making. [22] In China, the ethics model promotes a sincere respect for life or human dignity, [23] based on protective medicine. This model, influenced by Traditional Chinese Medicine (TCM), [24] recognizes Qi as the vital energy delivered via the meridians of the body; it connects illness to body systems, the body’s entire constitution, and the universe for a holistic bond of nature, health, and quality of life. [25] Following a protective ethics model, and traditional customs of wholeness, investment in stem cell research is heavily desired for its applications in regenerative therapies, disease modeling, and protective medicines. In a survey of medical students and healthcare practitioners, 30.8 percent considered stem cell research morally unacceptable while 63.5 percent accepted medical research using human embryonic stem cells. Of these individuals, 89.9 percent supported increased funding for stem cell research. [26] The scientific community might not reflect the overall population. From 1997 to 2019, China spent a total of $576 million (USD) on stem cell research at 8,050 stem cell programs, increased published presence from 0.6 percent to 14.01 percent of total global stem cell publications as of 2014, and made significant strides in cell-based therapies for various medical conditions. [27] However, while China has made substantial investments in stem cell research and achieved notable progress in clinical applications, concerns linger regarding ethical oversight and transparency. [28] For example, the China Biosecurity Law, promoted by the National Health Commission and China Hospital Association, attempted to mitigate risks by introducing an institutional review board (IRB) in the regulatory bodies. 5800 IRBs registered with the Chinese Clinical Trial Registry since 2021. [29] However, issues still need to be addressed in implementing effective IRB review and approval procedures.
The substantial government funding and focus on scientific advancement have sometimes overshadowed considerations of regional cultures, ethnic minorities, and individual perspectives, particularly evident during the one-child policy era. As government policy adapts to promote public stability, such as the change from the one-child to the two-child policy, [30] research ethics should also adapt to ensure respect for the values of its represented peoples.
Japan is also relatively supportive of stem cell research and therapies. Japan has a more transparent regulatory framework, allowing for faster approval of regenerative medicine products, which has led to several advanced clinical trials and therapies. [31] South Korea is also actively engaged in stem cell research and has a history of breakthroughs in cloning and embryonic stem cells. [32] However, the field is controversial, and there are issues of scientific integrity. For example, the Korean FDA fast-tracked products for approval, [33] and in another instance, the oocyte source was unclear and possibly violated ethical standards. [34] Trust is important in research, as it builds collaborative foundations between colleagues, trial participant comfort, open-mindedness for complicated and sensitive discussions, and supports regulatory procedures for stakeholders. There is a need to respect the culture’s interest, engagement, and for research and clinical trials to be transparent and have ethical oversight to promote global research discourse and trust.
d. Middle East
Countries in the Middle East have varying degrees of acceptance of or restrictions to policies related to using embryonic stem cells due to cultural and religious influences. Saudi Arabia has made significant contributions to stem cell research, and conducts research based on international guidelines for ethical conduct and under strict adherence to guidelines in accordance with Islamic principles. Specifically, the Saudi government and people require ESC research to adhere to Sharia law. In addition to umbilical and placental stem cells, [35] Saudi Arabia permits the use of embryonic stem cells as long as they come from miscarriages, therapeutic abortions permissible by Sharia law, or are left over from in vitro fertilization and donated to research. [36] Laws and ethical guidelines for stem cell research allow the development of research institutions such as the King Abdullah International Medical Research Center, which has a cord blood bank and a stem cell registry with nearly 10,000 donors. [37] Such volume and acceptance are due to the ethical ‘permissibility’ of the donor sources, which do not conflict with religious pillars. However, some researchers err on the side of caution, choosing not to use embryos or fetal tissue as they feel it is unethical to do so. [38]
Jordan has a positive research ethics culture. [39] However, there is a significant issue of lack of trust in researchers, with 45.23 percent (38.66 percent agreeing and 6.57 percent strongly agreeing) of Jordanians holding a low level of trust in researchers, compared to 81.34 percent of Jordanians agreeing that they feel safe to participate in a research trial. [40] Safety testifies to the feeling of confidence that adequate measures are in place to protect participants from harm, whereas trust in researchers could represent the confidence in researchers to act in the participants’ best interests, adhere to ethical guidelines, provide accurate information, and respect participants’ rights and dignity. One method to improve trust would be to address communication issues relevant to ESC. Legislation surrounding stem cell research has adopted specific language, especially concerning clarification “between ‘stem cells’ and ‘embryonic stem cells’” in translation. [41] Furthermore, legislation “mandates the creation of a national committee… laying out specific regulations for stem-cell banking in accordance with international standards.” [42] This broad regulation opens the door for future global engagement and maintains transparency. However, these regulations may also constrain the influence of research direction, pace, and accessibility of research outcomes.
e. Europe
In the European Union (EU), ethics is also principle-based, but the principles of autonomy, dignity, integrity, and vulnerability are interconnected. [43] As such, the opportunity for cohesion and concessions between individuals’ thoughts and ideals allows for a more adaptable ethics model due to the flexible principles that relate to the human experience The EU has put forth a framework in its Convention for the Protection of Human Rights and Dignity of the Human Being allowing member states to take different approaches. Each European state applies these principles to its specific conventions, leading to or reflecting different acceptance levels of stem cell research. [44]
For example, in Germany, Lebenzusammenhang , or the coherence of life, references integrity in the unity of human culture. Namely, the personal sphere “should not be subject to external intervention.” [45] Stem cell interventions could affect this concept of bodily completeness, leading to heavy restrictions. Under the Grundgesetz, human dignity and the right to life with physical integrity are paramount. [46] The Embryo Protection Act of 1991 made producing cell lines illegal. Cell lines can be imported if approved by the Central Ethics Commission for Stem Cell Research only if they were derived before May 2007. [47] Stem cell research respects the integrity of life for the embryo with heavy specifications and intense oversight. This is vastly different in Finland, where the regulatory bodies find research more permissible in IVF excess, but only up to 14 days after fertilization. [48] Spain’s approach differs still, with a comprehensive regulatory framework. [49] Thus, research regulation can be culture-specific due to variations in applied principles. Diverse cultures call for various approaches to ethical permissibility. [50] Only an adaptive-deliberative model can address the cultural constructions of self and achieve positive, culturally sensitive stem cell research practices. [51]
II. Religious Perspectives on ESC
Embryonic stem cell sources are the main consideration within religious contexts. While individuals may not regard their own religious texts as authoritative or factual, religion can shape their foundations or perspectives.
The Qur'an states:
“And indeed We created man from a quintessence of clay. Then We placed within him a small quantity of nutfa (sperm to fertilize) in a safe place. Then We have fashioned the nutfa into an ‘alaqa (clinging clot or cell cluster), then We developed the ‘alaqa into mudgha (a lump of flesh), and We made mudgha into bones, and clothed the bones with flesh, then We brought it into being as a new creation. So Blessed is Allah, the Best of Creators.” [52]
Many scholars of Islam estimate the time of soul installment, marked by the angel breathing in the soul to bring the individual into creation, as 120 days from conception. [53] Personhood begins at this point, and the value of life would prohibit research or experimentation that could harm the individual. If the fetus is more than 120 days old, the time ensoulment is interpreted to occur according to Islamic law, abortion is no longer permissible. [54] There are a few opposing opinions about early embryos in Islamic traditions. According to some Islamic theologians, there is no ensoulment of the early embryo, which is the source of stem cells for ESC research. [55]
In Buddhism, the stance on stem cell research is not settled. The main tenets, the prohibition against harming or destroying others (ahimsa) and the pursuit of knowledge (prajña) and compassion (karuna), leave Buddhist scholars and communities divided. [56] Some scholars argue stem cell research is in accordance with the Buddhist tenet of seeking knowledge and ending human suffering. Others feel it violates the principle of not harming others. Finding the balance between these two points relies on the karmic burden of Buddhist morality. In trying to prevent ahimsa towards the embryo, Buddhist scholars suggest that to comply with Buddhist tenets, research cannot be done as the embryo has personhood at the moment of conception and would reincarnate immediately, harming the individual's ability to build their karmic burden. [57] On the other hand, the Bodhisattvas, those considered to be on the path to enlightenment or Nirvana, have given organs and flesh to others to help alleviate grieving and to benefit all. [58] Acceptance varies on applied beliefs and interpretations.
Catholicism does not support embryonic stem cell research, as it entails creation or destruction of human embryos. This destruction conflicts with the belief in the sanctity of life. For example, in the Old Testament, Genesis describes humanity as being created in God’s image and multiplying on the Earth, referencing the sacred rights to human conception and the purpose of development and life. In the Ten Commandments, the tenet that one should not kill has numerous interpretations where killing could mean murder or shedding of the sanctity of life, demonstrating the high value of human personhood. In other books, the theological conception of when life begins is interpreted as in utero, [59] highlighting the inviolability of life and its formation in vivo to make a religious point for accepting such research as relatively limited, if at all. [60] The Vatican has released ethical directives to help apply a theological basis to modern-day conflicts. The Magisterium of the Church states that “unless there is a moral certainty of not causing harm,” experimentation on fetuses, fertilized cells, stem cells, or embryos constitutes a crime. [61] Such procedures would not respect the human person who exists at these stages, according to Catholicism. Damages to the embryo are considered gravely immoral and illicit. [62] Although the Catholic Church officially opposes abortion, surveys demonstrate that many Catholic people hold pro-choice views, whether due to the context of conception, stage of pregnancy, threat to the mother’s life, or for other reasons, demonstrating that practicing members can also accept some but not all tenets. [63]
Some major Jewish denominations, such as the Reform, Conservative, and Reconstructionist movements, are open to supporting ESC use or research as long as it is for saving a life. [64] Within Judaism, the Talmud, or study, gives personhood to the child at birth and emphasizes that life does not begin at conception: [65]
“If she is found pregnant, until the fortieth day it is mere fluid,” [66]
Whereas most religions prioritize the status of human embryos, the Halakah (Jewish religious law) states that to save one life, most other religious laws can be ignored because it is in pursuit of preservation. [67] Stem cell research is accepted due to application of these religious laws.
We recognize that all religions contain subsets and sects. The variety of environmental and cultural differences within religious groups requires further analysis to respect the flexibility of religious thoughts and practices. We make no presumptions that all cultures require notions of autonomy or morality as under the common morality theory , which asserts a set of universal moral norms that all individuals share provides moral reasoning and guides ethical decisions. [68] We only wish to show that the interaction with morality varies between cultures and countries.
III. A Flexible Ethical Approach
The plurality of different moral approaches described above demonstrates that there can be no universally acceptable uniform law for ESC on a global scale. Instead of developing one standard, flexible ethical applications must be continued. We recommend local guidelines that incorporate important cultural and ethical priorities.
While the Declaration of Helsinki is more relevant to people in clinical trials receiving ESC products, in keeping with the tradition of protections for research subjects, consent of the donor is an ethical requirement for ESC donation in many jurisdictions including the US, Canada, and Europe. [69] The Declaration of Helsinki provides a reference point for regulatory standards and could potentially be used as a universal baseline for obtaining consent prior to gamete or embryo donation.
For instance, in Columbia University’s egg donor program for stem cell research, donors followed standard screening protocols and “underwent counseling sessions that included information as to the purpose of oocyte donation for research, what the oocytes would be used for, the risks and benefits of donation, and process of oocyte stimulation” to ensure transparency for consent. [70] The program helped advance stem cell research and provided clear and safe research methods with paid participants. Though paid participation or covering costs of incidental expenses may not be socially acceptable in every culture or context, [71] and creating embryos for ESC research is illegal in many jurisdictions, Columbia’s program was effective because of the clear and honest communications with donors, IRBs, and related stakeholders. This example demonstrates that cultural acceptance of scientific research and of the idea that an egg or embryo does not have personhood is likely behind societal acceptance of donating eggs for ESC research. As noted, many countries do not permit the creation of embryos for research.
Proper communication and education regarding the process and purpose of stem cell research may bolster comprehension and garner more acceptance. “Given the sensitive subject material, a complete consent process can support voluntary participation through trust, understanding, and ethical norms from the cultures and morals participants value. This can be hard for researchers entering countries of different socioeconomic stability, with different languages and different societal values. [72]
An adequate moral foundation in medical ethics is derived from the cultural and religious basis that informs knowledge and actions. [73] Understanding local cultural and religious values and their impact on research could help researchers develop humility and promote inclusion.
IV. Concerns
Some may argue that if researchers all adhere to one ethics standard, protection will be satisfied across all borders, and the global public will trust researchers. However, defining what needs to be protected and how to define such research standards is very specific to the people to which standards are applied. We suggest that applying one uniform guide cannot accurately protect each individual because we all possess our own perceptions and interpretations of social values. [74] Therefore, the issue of not adjusting to the moral pluralism between peoples in applying one standard of ethics can be resolved by building out ethics models that can be adapted to different cultures and religions.
Other concerns include medical tourism, which may promote health inequities. [75] Some countries may develop and approve products derived from ESC research before others, compromising research ethics or drug approval processes. There are also concerns about the sale of unauthorized stem cell treatments, for example, those without FDA approval in the United States. Countries with robust research infrastructures may be tempted to attract medical tourists, and some customers will have false hopes based on aggressive publicity of unproven treatments. [76]
For example, in China, stem cell clinics can market to foreign clients who are not protected under the regulatory regimes. Companies employ a marketing strategy of “ethically friendly” therapies. Specifically, in the case of Beike, China’s leading stem cell tourism company and sprouting network, ethical oversight of administrators or health bureaus at one site has “the unintended consequence of shifting questionable activities to another node in Beike's diffuse network.” [77] In contrast, Jordan is aware of stem cell research’s potential abuse and its own status as a “health-care hub.” Jordan’s expanded regulations include preserving the interests of individuals in clinical trials and banning private companies from ESC research to preserve transparency and the integrity of research practices. [78]
The social priorities of the community are also a concern. The ISSCR explicitly states that guidelines “should be periodically revised to accommodate scientific advances, new challenges, and evolving social priorities.” [79] The adaptable ethics model extends this consideration further by addressing whether research is warranted given the varying degrees of socioeconomic conditions, political stability, and healthcare accessibilities and limitations. An ethical approach would require discussion about resource allocation and appropriate distribution of funds. [80]
While some religions emphasize the sanctity of life from conception, which may lead to public opposition to ESC research, others encourage ESC research due to its potential for healing and alleviating human pain. Many countries have special regulations that balance local views on embryonic personhood, the benefits of research as individual or societal goods, and the protection of human research subjects. To foster understanding and constructive dialogue, global policy frameworks should prioritize the protection of universal human rights, transparency, and informed consent. In addition to these foundational global policies, we recommend tailoring local guidelines to reflect the diverse cultural and religious perspectives of the populations they govern. Ethics models should be adapted to local populations to effectively establish research protections, growth, and possibilities of stem cell research.
For example, in countries with strong beliefs in the moral sanctity of embryos or heavy religious restrictions, an adaptive model can allow for discussion instead of immediate rejection. In countries with limited individual rights and voice in science policy, an adaptive model ensures cultural, moral, and religious views are taken into consideration, thereby building social inclusion. While this ethical consideration by the government may not give a complete voice to every individual, it will help balance policies and maintain the diverse perspectives of those it affects. Embracing an adaptive ethics model of ESC research promotes open-minded dialogue and respect for the importance of human belief and tradition. By actively engaging with cultural and religious values, researchers can better handle disagreements and promote ethical research practices that benefit each society.
This brief exploration of the religious and cultural differences that impact ESC research reveals the nuances of relative ethics and highlights a need for local policymakers to apply a more intense adaptive model.
[1] Poliwoda, S., Noor, N., Downs, E., Schaaf, A., Cantwell, A., Ganti, L., Kaye, A. D., Mosel, L. I., Carroll, C. B., Viswanath, O., & Urits, I. (2022). Stem cells: a comprehensive review of origins and emerging clinical roles in medical practice. Orthopedic reviews , 14 (3), 37498. https://doi.org/10.52965/001c.37498
[2] Poliwoda, S., Noor, N., Downs, E., Schaaf, A., Cantwell, A., Ganti, L., Kaye, A. D., Mosel, L. I., Carroll, C. B., Viswanath, O., & Urits, I. (2022). Stem cells: a comprehensive review of origins and emerging clinical roles in medical practice. Orthopedic reviews , 14 (3), 37498. https://doi.org/10.52965/001c.37498
[3] International Society for Stem Cell Research. (2023). Laboratory-based human embryonic stem cell research, embryo research, and related research activities . International Society for Stem Cell Research. https://www.isscr.org/guidelines/blog-post-title-one-ed2td-6fcdk ; Kimmelman, J., Hyun, I., Benvenisty, N. et al. Policy: Global standards for stem-cell research. Nature 533 , 311–313 (2016). https://doi.org/10.1038/533311a
[4] International Society for Stem Cell Research. (2023). Laboratory-based human embryonic stem cell research, embryo research, and related research activities . International Society for Stem Cell Research. https://www.isscr.org/guidelines/blog-post-title-one-ed2td-6fcdk
[5] Concerning the moral philosophies of stem cell research, our paper does not posit a personal moral stance nor delve into the “when” of human life begins. To read further about the philosophical debate, consider the following sources:
Sandel M. J. (2004). Embryo ethics--the moral logic of stem-cell research. The New England journal of medicine , 351 (3), 207–209. https://doi.org/10.1056/NEJMp048145 ; George, R. P., & Lee, P. (2020, September 26). Acorns and Embryos . The New Atlantis. https://www.thenewatlantis.com/publications/acorns-and-embryos ; Sagan, A., & Singer, P. (2007). The moral status of stem cells. Metaphilosophy , 38 (2/3), 264–284. http://www.jstor.org/stable/24439776 ; McHugh P. R. (2004). Zygote and "clonote"--the ethical use of embryonic stem cells. The New England journal of medicine , 351 (3), 209–211. https://doi.org/10.1056/NEJMp048147 ; Kurjak, A., & Tripalo, A. (2004). The facts and doubts about beginning of the human life and personality. Bosnian journal of basic medical sciences , 4 (1), 5–14. https://doi.org/10.17305/bjbms.2004.3453
[6] Vazin, T., & Freed, W. J. (2010). Human embryonic stem cells: derivation, culture, and differentiation: a review. Restorative neurology and neuroscience , 28 (4), 589–603. https://doi.org/10.3233/RNN-2010-0543
[7] Socially, at its core, the Western approach to ethics is widely principle-based, autonomy being one of the key factors to ensure a fundamental respect for persons within research. For information regarding autonomy in research, see: Department of Health, Education, and Welfare, & National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research (1978). The Belmont Report. Ethical principles and guidelines for the protection of human subjects of research.; For a more in-depth review of autonomy within the US, see: Beauchamp, T. L., & Childress, J. F. (1994). Principles of Biomedical Ethics . Oxford University Press.
[8] Sherley v. Sebelius , 644 F.3d 388 (D.C. Cir. 2011), citing 45 C.F.R. 46.204(b) and [42 U.S.C. § 289g(b)]. https://www.cadc.uscourts.gov/internet/opinions.nsf/6c690438a9b43dd685257a64004ebf99/$file/11-5241-1391178.pdf
[9] Stem Cell Research Enhancement Act of 2005, H. R. 810, 109 th Cong. (2001). https://www.govtrack.us/congress/bills/109/hr810/text ; Bush, G. W. (2006, July 19). Message to the House of Representatives . National Archives and Records Administration. https://georgewbush-whitehouse.archives.gov/news/releases/2006/07/20060719-5.html
[10] National Archives and Records Administration. (2009, March 9). Executive order 13505 -- removing barriers to responsible scientific research involving human stem cells . National Archives and Records Administration. https://obamawhitehouse.archives.gov/the-press-office/removing-barriers-responsible-scientific-research-involving-human-stem-cells
[11] Hurlbut, W. B. (2006). Science, Religion, and the Politics of Stem Cells. Social Research , 73 (3), 819–834. http://www.jstor.org/stable/40971854
[12] Akpa-Inyang, Francis & Chima, Sylvester. (2021). South African traditional values and beliefs regarding informed consent and limitations of the principle of respect for autonomy in African communities: a cross-cultural qualitative study. BMC Medical Ethics . 22. 10.1186/s12910-021-00678-4.
[13] Source for further reading: Tangwa G. B. (2007). Moral status of embryonic stem cells: perspective of an African villager. Bioethics , 21(8), 449–457. https://doi.org/10.1111/j.1467-8519.2007.00582.x , see also Mnisi, F. M. (2020). An African analysis based on ethics of Ubuntu - are human embryonic stem cell patents morally justifiable? African Insight , 49 (4).
[14] Jecker, N. S., & Atuire, C. (2021). Bioethics in Africa: A contextually enlightened analysis of three cases. Developing World Bioethics , 22 (2), 112–122. https://doi.org/10.1111/dewb.12324
[15] Jecker, N. S., & Atuire, C. (2021). Bioethics in Africa: A contextually enlightened analysis of three cases. Developing World Bioethics, 22(2), 112–122. https://doi.org/10.1111/dewb.12324
[16] Jackson, C.S., Pepper, M.S. Opportunities and barriers to establishing a cell therapy programme in South Africa. Stem Cell Res Ther 4 , 54 (2013). https://doi.org/10.1186/scrt204 ; Pew Research Center. (2014, May 1). Public health a major priority in African nations . Pew Research Center’s Global Attitudes Project. https://www.pewresearch.org/global/2014/05/01/public-health-a-major-priority-in-african-nations/
[17] Department of Health Republic of South Africa. (2021). Health Research Priorities (revised) for South Africa 2021-2024 . National Health Research Strategy. https://www.health.gov.za/wp-content/uploads/2022/05/National-Health-Research-Priorities-2021-2024.pdf
[18] Oosthuizen, H. (2013). Legal and Ethical Issues in Stem Cell Research in South Africa. In: Beran, R. (eds) Legal and Forensic Medicine. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-32338-6_80 , see also: Gaobotse G (2018) Stem Cell Research in Africa: Legislation and Challenges. J Regen Med 7:1. doi: 10.4172/2325-9620.1000142
[19] United States Bureau of Citizenship and Immigration Services. (1998). Tunisia: Information on the status of Christian conversions in Tunisia . UNHCR Web Archive. https://webarchive.archive.unhcr.org/20230522142618/https://www.refworld.org/docid/3df0be9a2.html
[20] Gaobotse, G. (2018) Stem Cell Research in Africa: Legislation and Challenges. J Regen Med 7:1. doi: 10.4172/2325-9620.1000142
[21] Kooli, C. Review of assisted reproduction techniques, laws, and regulations in Muslim countries. Middle East Fertil Soc J 24 , 8 (2020). https://doi.org/10.1186/s43043-019-0011-0 ; Gaobotse, G. (2018) Stem Cell Research in Africa: Legislation and Challenges. J Regen Med 7:1. doi: 10.4172/2325-9620.1000142
[22] Pang M. C. (1999). Protective truthfulness: the Chinese way of safeguarding patients in informed treatment decisions. Journal of medical ethics , 25(3), 247–253. https://doi.org/10.1136/jme.25.3.247
[23] Wang, L., Wang, F., & Zhang, W. (2021). Bioethics in China’s biosecurity law: Forms, effects, and unsettled issues. Journal of law and the biosciences , 8(1). https://doi.org/10.1093/jlb/lsab019 https://academic.oup.com/jlb/article/8/1/lsab019/6299199
[24] Wang, Y., Xue, Y., & Guo, H. D. (2022). Intervention effects of traditional Chinese medicine on stem cell therapy of myocardial infarction. Frontiers in pharmacology , 13 , 1013740. https://doi.org/10.3389/fphar.2022.1013740
[25] Li, X.-T., & Zhao, J. (2012). Chapter 4: An Approach to the Nature of Qi in TCM- Qi and Bioenergy. In Recent Advances in Theories and Practice of Chinese Medicine (p. 79). InTech.
[26] Luo, D., Xu, Z., Wang, Z., & Ran, W. (2021). China's Stem Cell Research and Knowledge Levels of Medical Practitioners and Students. Stem cells international , 2021 , 6667743. https://doi.org/10.1155/2021/6667743
[27] Luo, D., Xu, Z., Wang, Z., & Ran, W. (2021). China's Stem Cell Research and Knowledge Levels of Medical Practitioners and Students. Stem cells international , 2021 , 6667743. https://doi.org/10.1155/2021/6667743
[28] Zhang, J. Y. (2017). Lost in translation? accountability and governance of Clinical Stem Cell Research in China. Regenerative Medicine , 12 (6), 647–656. https://doi.org/10.2217/rme-2017-0035
[29] Wang, L., Wang, F., & Zhang, W. (2021). Bioethics in China’s biosecurity law: Forms, effects, and unsettled issues. Journal of law and the biosciences , 8(1). https://doi.org/10.1093/jlb/lsab019 https://academic.oup.com/jlb/article/8/1/lsab019/6299199
[30] Chen, H., Wei, T., Wang, H. et al. Association of China’s two-child policy with changes in number of births and birth defects rate, 2008–2017. BMC Public Health 22 , 434 (2022). https://doi.org/10.1186/s12889-022-12839-0
[31] Azuma, K. Regulatory Landscape of Regenerative Medicine in Japan. Curr Stem Cell Rep 1 , 118–128 (2015). https://doi.org/10.1007/s40778-015-0012-6
[32] Harris, R. (2005, May 19). Researchers Report Advance in Stem Cell Production . NPR. https://www.npr.org/2005/05/19/4658967/researchers-report-advance-in-stem-cell-production
[33] Park, S. (2012). South Korea steps up stem-cell work. Nature . https://doi.org/10.1038/nature.2012.10565
[34] Resnik, D. B., Shamoo, A. E., & Krimsky, S. (2006). Fraudulent human embryonic stem cell research in South Korea: lessons learned. Accountability in research , 13 (1), 101–109. https://doi.org/10.1080/08989620600634193 .
[35] Alahmad, G., Aljohani, S., & Najjar, M. F. (2020). Ethical challenges regarding the use of stem cells: interviews with researchers from Saudi Arabia. BMC medical ethics, 21(1), 35. https://doi.org/10.1186/s12910-020-00482-6
[36] Association for the Advancement of Blood and Biotherapies. https://www.aabb.org/regulatory-and-advocacy/regulatory-affairs/regulatory-for-cellular-therapies/international-competent-authorities/saudi-arabia
[37] Alahmad, G., Aljohani, S., & Najjar, M. F. (2020). Ethical challenges regarding the use of stem cells: Interviews with researchers from Saudi Arabia. BMC medical ethics , 21 (1), 35. https://doi.org/10.1186/s12910-020-00482-6
[38] Alahmad, G., Aljohani, S., & Najjar, M. F. (2020). Ethical challenges regarding the use of stem cells: Interviews with researchers from Saudi Arabia. BMC medical ethics , 21(1), 35. https://doi.org/10.1186/s12910-020-00482-6
Culturally, autonomy practices follow a relational autonomy approach based on a paternalistic deontological health care model. The adherence to strict international research policies and religious pillars within the regulatory environment is a great foundation for research ethics. However, there is a need to develop locally targeted ethics approaches for research (as called for in Alahmad, G., Aljohani, S., & Najjar, M. F. (2020). Ethical challenges regarding the use of stem cells: interviews with researchers from Saudi Arabia. BMC medical ethics, 21(1), 35. https://doi.org/10.1186/s12910-020-00482-6), this decision-making approach may help advise a research decision model. For more on the clinical cultural autonomy approaches, see: Alabdullah, Y. Y., Alzaid, E., Alsaad, S., Alamri, T., Alolayan, S. W., Bah, S., & Aljoudi, A. S. (2022). Autonomy and paternalism in Shared decision‐making in a Saudi Arabian tertiary hospital: A cross‐sectional study. Developing World Bioethics , 23 (3), 260–268. https://doi.org/10.1111/dewb.12355 ; Bukhari, A. A. (2017). Universal Principles of Bioethics and Patient Rights in Saudi Arabia (Doctoral dissertation, Duquesne University). https://dsc.duq.edu/etd/124; Ladha, S., Nakshawani, S. A., Alzaidy, A., & Tarab, B. (2023, October 26). Islam and Bioethics: What We All Need to Know . Columbia University School of Professional Studies. https://sps.columbia.edu/events/islam-and-bioethics-what-we-all-need-know
[39] Ababneh, M. A., Al-Azzam, S. I., Alzoubi, K., Rababa’h, A., & Al Demour, S. (2021). Understanding and attitudes of the Jordanian public about clinical research ethics. Research Ethics , 17 (2), 228-241. https://doi.org/10.1177/1747016120966779
[40] Ababneh, M. A., Al-Azzam, S. I., Alzoubi, K., Rababa’h, A., & Al Demour, S. (2021). Understanding and attitudes of the Jordanian public about clinical research ethics. Research Ethics , 17 (2), 228-241. https://doi.org/10.1177/1747016120966779
[41] Dajani, R. (2014). Jordan’s stem-cell law can guide the Middle East. Nature 510, 189. https://doi.org/10.1038/510189a
[42] Dajani, R. (2014). Jordan’s stem-cell law can guide the Middle East. Nature 510, 189. https://doi.org/10.1038/510189a
[43] The EU’s definition of autonomy relates to the capacity for creating ideas, moral insight, decisions, and actions without constraint, personal responsibility, and informed consent. However, the EU views autonomy as not completely able to protect individuals and depends on other principles, such as dignity, which “expresses the intrinsic worth and fundamental equality of all human beings.” Rendtorff, J.D., Kemp, P. (2019). Four Ethical Principles in European Bioethics and Biolaw: Autonomy, Dignity, Integrity and Vulnerability. In: Valdés, E., Lecaros, J. (eds) Biolaw and Policy in the Twenty-First Century. International Library of Ethics, Law, and the New Medicine, vol 78. Springer, Cham. https://doi.org/10.1007/978-3-030-05903-3_3
[44] Council of Europe. Convention for the protection of Human Rights and Dignity of the Human Being with regard to the Application of Biology and Medicine: Convention on Human Rights and Biomedicine (ETS No. 164) https://www.coe.int/en/web/conventions/full-list?module=treaty-detail&treatynum=164 (forbidding the creation of embryos for research purposes only, and suggests embryos in vitro have protections.); Also see Drabiak-Syed B. K. (2013). New President, New Human Embryonic Stem Cell Research Policy: Comparative International Perspectives and Embryonic Stem Cell Research Laws in France. Biotechnology Law Report , 32 (6), 349–356. https://doi.org/10.1089/blr.2013.9865
[45] Rendtorff, J.D., Kemp, P. (2019). Four Ethical Principles in European Bioethics and Biolaw: Autonomy, Dignity, Integrity and Vulnerability. In: Valdés, E., Lecaros, J. (eds) Biolaw and Policy in the Twenty-First Century. International Library of Ethics, Law, and the New Medicine, vol 78. Springer, Cham. https://doi.org/10.1007/978-3-030-05903-3_3
[46] Tomuschat, C., Currie, D. P., Kommers, D. P., & Kerr, R. (Trans.). (1949, May 23). Basic law for the Federal Republic of Germany. https://www.btg-bestellservice.de/pdf/80201000.pdf
[47] Regulation of Stem Cell Research in Germany . Eurostemcell. (2017, April 26). https://www.eurostemcell.org/regulation-stem-cell-research-germany
[48] Regulation of Stem Cell Research in Finland . Eurostemcell. (2017, April 26). https://www.eurostemcell.org/regulation-stem-cell-research-finland
[49] Regulation of Stem Cell Research in Spain . Eurostemcell. (2017, April 26). https://www.eurostemcell.org/regulation-stem-cell-research-spain
[50] Some sources to consider regarding ethics models or regulatory oversights of other cultures not covered:
Kara MA. Applicability of the principle of respect for autonomy: the perspective of Turkey. J Med Ethics. 2007 Nov;33(11):627-30. doi: 10.1136/jme.2006.017400. PMID: 17971462; PMCID: PMC2598110.
Ugarte, O. N., & Acioly, M. A. (2014). The principle of autonomy in Brazil: one needs to discuss it ... Revista do Colegio Brasileiro de Cirurgioes , 41 (5), 374–377. https://doi.org/10.1590/0100-69912014005013
Bharadwaj, A., & Glasner, P. E. (2012). Local cells, global science: The rise of embryonic stem cell research in India . Routledge.
For further research on specific European countries regarding ethical and regulatory framework, we recommend this database: Regulation of Stem Cell Research in Europe . Eurostemcell. (2017, April 26). https://www.eurostemcell.org/regulation-stem-cell-research-europe
[51] Klitzman, R. (2006). Complications of culture in obtaining informed consent. The American Journal of Bioethics, 6(1), 20–21. https://doi.org/10.1080/15265160500394671 see also: Ekmekci, P. E., & Arda, B. (2017). Interculturalism and Informed Consent: Respecting Cultural Differences without Breaching Human Rights. Cultura (Iasi, Romania) , 14 (2), 159–172.; For why trust is important in research, see also: Gray, B., Hilder, J., Macdonald, L., Tester, R., Dowell, A., & Stubbe, M. (2017). Are research ethics guidelines culturally competent? Research Ethics , 13 (1), 23-41. https://doi.org/10.1177/1747016116650235
[52] The Qur'an (M. Khattab, Trans.). (1965). Al-Mu’minun, 23: 12-14. https://quran.com/23
[53] Lenfest, Y. (2017, December 8). Islam and the beginning of human life . Bill of Health. https://blog.petrieflom.law.harvard.edu/2017/12/08/islam-and-the-beginning-of-human-life/
[54] Aksoy, S. (2005). Making regulations and drawing up legislation in Islamic countries under conditions of uncertainty, with special reference to embryonic stem cell research. Journal of Medical Ethics , 31: 399-403.; see also: Mahmoud, Azza. "Islamic Bioethics: National Regulations and Guidelines of Human Stem Cell Research in the Muslim World." Master's thesis, Chapman University, 2022. https://doi.org/10.36837/ chapman.000386
[55] Rashid, R. (2022). When does Ensoulment occur in the Human Foetus. Journal of the British Islamic Medical Association , 12 (4). ISSN 2634 8071. https://www.jbima.com/wp-content/uploads/2023/01/2-Ethics-3_-Ensoulment_Rafaqat.pdf.
[56] Sivaraman, M. & Noor, S. (2017). Ethics of embryonic stem cell research according to Buddhist, Hindu, Catholic, and Islamic religions: perspective from Malaysia. Asian Biomedicine,8(1) 43-52. https://doi.org/10.5372/1905-7415.0801.260
[57] Jafari, M., Elahi, F., Ozyurt, S. & Wrigley, T. (2007). 4. Religious Perspectives on Embryonic Stem Cell Research. In K. Monroe, R. Miller & J. Tobis (Ed.), Fundamentals of the Stem Cell Debate: The Scientific, Religious, Ethical, and Political Issues (pp. 79-94). Berkeley: University of California Press. https://escholarship.org/content/qt9rj0k7s3/qt9rj0k7s3_noSplash_f9aca2e02c3777c7fb76ea768ba458f0.pdf https://doi.org/10.1525/9780520940994-005
[58] Lecso, P. A. (1991). The Bodhisattva Ideal and Organ Transplantation. Journal of Religion and Health , 30 (1), 35–41. http://www.jstor.org/stable/27510629 ; Bodhisattva, S. (n.d.). The Key of Becoming a Bodhisattva . A Guide to the Bodhisattva Way of Life. http://www.buddhism.org/Sutras/2/BodhisattvaWay.htm
[59] There is no explicit religious reference to when life begins or how to conduct research that interacts with the concept of life. However, these are relevant verses pertaining to how the fetus is viewed. (( King James Bible . (1999). Oxford University Press. (original work published 1769))
Jerimiah 1: 5 “Before I formed thee in the belly I knew thee; and before thou camest forth out of the womb I sanctified thee…”
In prophet Jerimiah’s insight, God set him apart as a person known before childbirth, a theme carried within the Psalm of David.
Psalm 139: 13-14 “…Thou hast covered me in my mother's womb. I will praise thee; for I am fearfully and wonderfully made…”
These verses demonstrate David’s respect for God as an entity that would know of all man’s thoughts and doings even before birth.
[60] It should be noted that abortion is not supported as well.
[61] The Vatican. (1987, February 22). Instruction on Respect for Human Life in Its Origin and on the Dignity of Procreation Replies to Certain Questions of the Day . Congregation For the Doctrine of the Faith. https://www.vatican.va/roman_curia/congregations/cfaith/documents/rc_con_cfaith_doc_19870222_respect-for-human-life_en.html
[62] The Vatican. (2000, August 25). Declaration On the Production and the Scientific and Therapeutic Use of Human Embryonic Stem Cells . Pontifical Academy for Life. https://www.vatican.va/roman_curia/pontifical_academies/acdlife/documents/rc_pa_acdlife_doc_20000824_cellule-staminali_en.html ; Ohara, N. (2003). Ethical Consideration of Experimentation Using Living Human Embryos: The Catholic Church’s Position on Human Embryonic Stem Cell Research and Human Cloning. Department of Obstetrics and Gynecology . Retrieved from https://article.imrpress.com/journal/CEOG/30/2-3/pii/2003018/77-81.pdf.
[63] Smith, G. A. (2022, May 23). Like Americans overall, Catholics vary in their abortion views, with regular mass attenders most opposed . Pew Research Center. https://www.pewresearch.org/short-reads/2022/05/23/like-americans-overall-catholics-vary-in-their-abortion-views-with-regular-mass-attenders-most-opposed/
[64] Rosner, F., & Reichman, E. (2002). Embryonic stem cell research in Jewish law. Journal of halacha and contemporary society , (43), 49–68.; Jafari, M., Elahi, F., Ozyurt, S. & Wrigley, T. (2007). 4. Religious Perspectives on Embryonic Stem Cell Research. In K. Monroe, R. Miller & J. Tobis (Ed.), Fundamentals of the Stem Cell Debate: The Scientific, Religious, Ethical, and Political Issues (pp. 79-94). Berkeley: University of California Press. https://escholarship.org/content/qt9rj0k7s3/qt9rj0k7s3_noSplash_f9aca2e02c3777c7fb76ea768ba458f0.pdf https://doi.org/10.1525/9780520940994-005
[65] Schenker J. G. (2008). The beginning of human life: status of embryo. Perspectives in Halakha (Jewish Religious Law). Journal of assisted reproduction and genetics , 25 (6), 271–276. https://doi.org/10.1007/s10815-008-9221-6
[66] Ruttenberg, D. (2020, May 5). The Torah of Abortion Justice (annotated source sheet) . Sefaria. https://www.sefaria.org/sheets/234926.7?lang=bi&with=all&lang2=en
[67] Jafari, M., Elahi, F., Ozyurt, S. & Wrigley, T. (2007). 4. Religious Perspectives on Embryonic Stem Cell Research. In K. Monroe, R. Miller & J. Tobis (Ed.), Fundamentals of the Stem Cell Debate: The Scientific, Religious, Ethical, and Political Issues (pp. 79-94). Berkeley: University of California Press. https://escholarship.org/content/qt9rj0k7s3/qt9rj0k7s3_noSplash_f9aca2e02c3777c7fb76ea768ba458f0.pdf https://doi.org/10.1525/9780520940994-005
[68] Gert, B. (2007). Common morality: Deciding what to do . Oxford Univ. Press.
[69] World Medical Association (2013). World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA , 310(20), 2191–2194. https://doi.org/10.1001/jama.2013.281053 Declaration of Helsinki – WMA – The World Medical Association .; see also: National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. (1979). The Belmont report: Ethical principles and guidelines for the protection of human subjects of research . U.S. Department of Health and Human Services. https://www.hhs.gov/ohrp/regulations-and-policy/belmont-report/read-the-belmont-report/index.html
[70] Zakarin Safier, L., Gumer, A., Kline, M., Egli, D., & Sauer, M. V. (2018). Compensating human subjects providing oocytes for stem cell research: 9-year experience and outcomes. Journal of assisted reproduction and genetics , 35 (7), 1219–1225. https://doi.org/10.1007/s10815-018-1171-z https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6063839/ see also: Riordan, N. H., & Paz Rodríguez, J. (2021). Addressing concerns regarding associated costs, transparency, and integrity of research in recent stem cell trial. Stem Cells Translational Medicine , 10 (12), 1715–1716. https://doi.org/10.1002/sctm.21-0234
[71] Klitzman, R., & Sauer, M. V. (2009). Payment of egg donors in stem cell research in the USA. Reproductive biomedicine online , 18 (5), 603–608. https://doi.org/10.1016/s1472-6483(10)60002-8
[72] Krosin, M. T., Klitzman, R., Levin, B., Cheng, J., & Ranney, M. L. (2006). Problems in comprehension of informed consent in rural and peri-urban Mali, West Africa. Clinical trials (London, England) , 3 (3), 306–313. https://doi.org/10.1191/1740774506cn150oa
[73] Veatch, Robert M. Hippocratic, Religious, and Secular Medical Ethics: The Points of Conflict . Georgetown University Press, 2012.
[74] Msoroka, M. S., & Amundsen, D. (2018). One size fits not quite all: Universal research ethics with diversity. Research Ethics , 14 (3), 1-17. https://doi.org/10.1177/1747016117739939
[75] Pirzada, N. (2022). The Expansion of Turkey’s Medical Tourism Industry. Voices in Bioethics , 8 . https://doi.org/10.52214/vib.v8i.9894
[76] Stem Cell Tourism: False Hope for Real Money . Harvard Stem Cell Institute (HSCI). (2023). https://hsci.harvard.edu/stem-cell-tourism , See also: Bissassar, M. (2017). Transnational Stem Cell Tourism: An ethical analysis. Voices in Bioethics , 3 . https://doi.org/10.7916/vib.v3i.6027
[77] Song, P. (2011) The proliferation of stem cell therapies in post-Mao China: problematizing ethical regulation, New Genetics and Society , 30:2, 141-153, DOI: 10.1080/14636778.2011.574375
[78] Dajani, R. (2014). Jordan’s stem-cell law can guide the Middle East. Nature 510, 189. https://doi.org/10.1038/510189a
[79] International Society for Stem Cell Research. (2024). Standards in stem cell research . International Society for Stem Cell Research. https://www.isscr.org/guidelines/5-standards-in-stem-cell-research
[80] Benjamin, R. (2013). People’s science bodies and rights on the Stem Cell Frontier . Stanford University Press.
Mifrah Hayath
SM Candidate Harvard Medical School, MS Biotechnology Johns Hopkins University
Olivia Bowers
MS Bioethics Columbia University (Disclosure: affiliated with Voices in Bioethics)
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License .
- Search Menu
- Sign in through your institution
- Advance Articles
- Author Guidelines
- Submission Site
- Open Access Options
- Self-Archiving Policy
- Call for Papers
- Why Publish with Us?
- Advertising & Corporate Services
- Reprints, ePrints, Supplements
- About STEM CELLS
- Editorial Board
- Reviewer Guidelines
- Journals on Oxford Academic
- Books on Oxford Academic
Browse issues

Cover image

Volume 42, Issue 7, July 2024
Embryonic stem cells/induced pluripotent stem cells, acquisition of 2c-like totipotency through defined maternal-effect factors.

- View article
- Supplementary data
Re-analysis of single-cell RNA-seq data reveals the origin and roles of cycling myeloid cells

Arp2/3 mediated dynamic lamellipodia of the hPSC colony edges promote liposome-based DNA delivery

Regenerative Medicine
Empagliflozin ameliorates the impaired osteogenic differentiation ability of adipose-derived stem cells in diabetic osteoporosis by activating autophagy.

Modulating the mesenchymal stromal cell microenvironment alters exosome RNA content and ligament healing capacity

Stem Cell Technology: Epigenetics, Genomics, Proteomics, and Metabonomics
Protein crotonylation promotes osteogenic differentiation of periodontal ligament stem cells via the pi3k-akt pathway.

Tissue-Specific Stem Cells
Cortactin controls bone homeostasis through regulating the differentiation of osteoblasts and osteoclasts.

Expression of Concerns
Expression of concern: therapeutic efficacy and fate of bimodal engineered stem cells in malignant brain tumors, expression of concern: stem cells engineered during different stages of reprogramming reveal varying therapeutic efficacies, email alerts.
- Recommend to Your Librarian
- Advertising and Corporate Services
Affiliations
- Online ISSN 1549-4918
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Pioneering Code of Practice released for use of stem cell-based embryo models in research
Media contact: Jacqueline Garget
Published 4 July, 2024

The University of Cambridge, in partnership with the Progress Educational Trust, has led work to create the first ever UK guidelines for the generation and use of stem cell-based embryo models in research.
The guidelines were developed by a Working Group of experts from a range of institutions across the UK, representing world-leading expertise in sciences, law, ethics and regulation.
Stem cell-based embryo models (SCBEMs) are three-dimensional biological structures that mimic aspects of early human embryo development. They can be created in the lab from stem cells, and can provide new insights into critical stages of early human development that are normally inaccessible to researchers.
Embryo model work is expected to lead to new interventions for a range of conditions, including revolutionising treatments for recurrent miscarriage, understanding developmental disorders and improving the success rate of IVF.
Although embryo models are not the same as human embryos, they mimic aspects of early human development - and this has raised ethical concerns.
The previous lack of a regulatory framework for the use of SCBEMs in research has left scientists and research organisations uncertain about the acceptable boundaries of their work, both legally and ethically, and unsupported in their decision-making. Signing up to the SCBEM Code of Practice will remove these obstacles.
The guidelines , released today, provide the first code of practice for the use of stem cell-based embryo models in the UK.
“The new Code of Practice provides processes for decision-making in research using stem cell-based embryo models so that scientists can proceed confidently, while maintaining public trust in this vital area of research.”
Kathy Niakan, Chair of Cambridge Reproduction and Professor of Reproductive Physiology at the University of Cambridge, and member of the SCBEM Code of Practice Working Group.
“We are confident that the Code will enable the UK to continue to lead the world in research into early human development, while ensuring that this research is ethically robust.”
Professor roger sturmey, professor of reproductive medicine at hull york medical school and chair of the scbem code of practice working group., key points of the code.
The new SCBEM Code of Practice sets out standards to make sure that research using SCBEMs is rigorous, upholds ethical principles and maximises the potential benefits. Key to this will be a dedicated Oversight Committee that will review each proposed research project.
The Code recognises that there must be a limit to how long embryo models can be grown in the lab. However, many different types of embryo model are being developed, representing distinct developmental stages and developing at different rates, making it impossible to impose a single fixed limit. Instead, researchers will be required to provide clear justification of the length of their experiments on a case-by-case basis.
The Code prohibits any human SCBEM from being transferred into the womb of a human or animal , or being allowed to develop into a viable organism in the lab.
“Embryo models have huge potential and we want to realise this, while also limiting the risks. The new Code of Practice will allow stem cell-based embryo models to be grown in the lab long enough to gain meaningful biological understanding, but researchers will have to fully justify what they’re doing in scientific and ethical terms,” said Niakan.
How are embryo models useful to research?
Research using embryo models can improve knowledge of human development, including early pregnancy loss and pregnancy disorders, congenital defects and the precursor events that affect adult human health and disease..
The models could also be used for some investigations that are not permitted using human embryos. For example, there are currently significant limitations to clinical trials and the use of many medicines during pregnancy. Models of early development could be helpful to improve options for drug treatments during pregnancy in the future.
Stem cell-based embryo models open new research avenues that can complement, but not replace, the limited studies possible with actual human embryos. The SCBEM Code of Practice states that neither of these areas of research can or should replace the other for the foreseeable future.
How was the Code produced?
The SCBEM Code of Practice Working Group was made up of researchers and practitioners at institutions across the UK, including experts in science, law, ethics and regulation. In drawing up the Code , the team consulted widely with researchers, practitioners, and major funders and regulators of embryo model research, both within the UK and internationally.
The Working Group included researchers and practitioners from the Babraham Institute, Biolawgy, Brighton and Sussex Medical School, the Centre of Medical Law and Ethics at King's College London, the Francis Crick Institute, Hull York Medical School, the Medical Research Council, Newcastle University, University College London, the University of Cambridge, the University of Edinburgh, the University of Exeter and the University of Manchester.
The work was also informed by a public dialogue , held earlier this year, to explore public attitudes towards research involving embryo models.
“Throughout the process of developing the Code of Practice we’ve been keen to engage with as wide a range of stakeholders as possible, including researchers, experts in law and bioethics, regulators and funders.”
Christina Rozeik, Programme Manager of Cambridge Reproduction and member of the SCBEM Code of Practice Project Team.
Rozeik added: “A public dialogue enabled us to include public voices during the development of the Code, taking account of their hopes, concerns and sensitivities around research involving stem cell-based embryo models . Participants were excited by the potential of embryo model research, but also strongly supportive of oversight .”
“Research involving stem cell-based embryo models has enormous potential to improve human knowledge and health, but clearer governance is needed to help researchers work responsibly and maintain public trust. Our Code of Practice addresses this need.”
Sandy Starr, Deputy Director of the Progress Educational Trust (PET) and member of the SCBEM Code of Practice Project Team.
How will the Code be enforced?
The Code is not legislative, but the team proposes that it should be adopted by UK researchers, funders, research organisations, professional societies and publishers.
Widespread use is expected to deter the funding and publication of research that fails to meet the standards set out in the Code . As a result, adherence to the Code will become an essential part of credible science, providing increased transparency and accountability for embryo model research.
Given the rapid pace of research using embryo models, the Code will be reviewed regularly.
“Research using stem cell-based embryo models is very new, and our understanding of the science is rapidly evolving. We’ve taken the opportunity to respond to the current situation, and we’ll continue to update the Code of Practice as the science continues to develop,” said Niakan.
“This guidance takes stem cell-based embryo models out of the grey zone and onto more stable footing so we can fully explore their usefulness, while providing the essential reassurance that this research is being conducted carefully and with appropriate scrutiny.”
Dr Peter Rugg-Gunn, Group Leader and Head of Public Engagement at the Babraham Institute, and member of the SCBEM Code of Practice Working Group.
Creation of the SCBEM Code of Practice (fully titled: Code of Practice for the Generation and Use of Human Stem Cell-Based Embryo Models) was led by Cambridge Reproduction - an interdisciplinary research centre at the University of Cambridge - in partnership with the Progress Educational Trust (PET) - a charity that improves choices for people affected by infertility and genetic conditions.
The work was funded by the BBSRC, the University of Cambridge Impact and Knowledge Exchange fund, and UKRI Sciencewise.
The guidelines can be viewed and downloaded from: www.repro.cam.ac.uk/scbemcode
Images: Top: A growing human embryo model. Credit Naomi Moris/ University of Cambridge. Bottom: Human stem cell-based embryo model. Credit Irene Zorzan and Teresa Rayon, Babraham Institute.
The text in this work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License
Image captions

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Embryonic stem cell research: the relevance of ethics in the progress of science
Affiliation.
- 1 Department of Biomedical Humanities, University of Navarra, Spain. [email protected]
- PMID: 12011787
Experimentation with embryonic stem (ES) cells has become an important breakthrough in medical research. However, it is also a source of controversy, because it requires the destruction of the human embryos used to derive ES cells. This paper deals with some of the ethical issues concerning ES cell research. To begin with, the terms used in the debate on the ethical status of the human embryo need to be defined. Apart from the presumed benefits of ES cell research, we should also consider such issues as the strong opposition to this research by a large part of society, who argue in favour of protecting and respecting human embryos; the fragility and defenseless of human embryos; and the contradiction in terms inherent in the statement that human embryos must be treated with respect. Secondly, we should focus on possible conflicts between the financial, scientific, and ethical aspects of this debate. Thirdly, the significance of social and political debate requires clear and complete information that takes all consequences into account. Finally, the paper suggests how multipotent adult stem cell research may be an optimal and realistic alternative to ES cell research.
PubMed Disclaimer
- Embryonic stem cell research: the relevance of ethics in the progress of science and the moral and ethical quandry of embryonic stem cell research. Fernandez Lamelas MA, Garcia-Mayor R. Fernandez Lamelas MA, et al. Med Sci Monit. 2002 Jun;8(6):LE20. Med Sci Monit. 2002. PMID: 12134780 No abstract available.
- Is the instrumentalization of humans acceptable in contemporary science? Liubarskiene ZV, Darulis Z, Jacobsen R. Liubarskiene ZV, et al. Med Sci Monit. 2006 Dec;12(12):LE23-24. Epub 2006 Nov 23. Med Sci Monit. 2006. PMID: 17136014 No abstract available.
Similar articles
- Ethical (and political) issues in research with human stem cells. Murray TH. Murray TH. Novartis Found Symp. 2005;265:188-96; discussion 196-211. Novartis Found Symp. 2005. PMID: 16050258 Review.
- Stem cells: public policy and ethics. Towns CR, Jones DG. Towns CR, et al. N Z Bioeth J. 2004 Feb;5(1):22-8. N Z Bioeth J. 2004. PMID: 15597489
- Cloning for therapeutic purposes: ethical and policy considerations. Hanson MJ. Hanson MJ. Univ Toledo Law Rev. 2001 Spring;32(3):355-65-. Univ Toledo Law Rev. 2001. PMID: 12627582
- The moral and ethical quandry of embryonic stem cell research. MacQueen BD. MacQueen BD. Med Sci Monit. 2002 May;8(5):ED1-4. Med Sci Monit. 2002. PMID: 12071180 No abstract available.
- Ethical and social considerations of stem cell research. McLaren A. McLaren A. Nature. 2001 Nov 1;414(6859):129-31. doi: 10.1038/35102194. Nature. 2001. PMID: 11689959 Review.
- Stem cells: implications for urology. Lo KC, Whirledge S, Lamb DJ. Lo KC, et al. Curr Urol Rep. 2005 Feb;6(1):49-54. doi: 10.1007/s11934-005-0067-5. Curr Urol Rep. 2005. PMID: 15610697 Review.
- Search in MeSH
LinkOut - more resources
Full text sources.
- International Scientific Literature, Ltd.
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Open access
- Published: 09 July 2024
Applications of extraembryonic tissue-derived cells in vascular tissue regeneration
- Mehdi Amiri Goushki 1 na1 ,
- Zahra Kharat 1 na1 ,
- Mousa Kehtari 3 ,
- Alireza Naderi Sohi 4 ,
- Hana Hanaee Ahvaz 5 ,
- Iman Rad 5 ,
- Simzar HosseinZadeh 6 ,
- Fatemeh Kouhkan 5 &
- Mahboubeh Kabiri ORCID: orcid.org/0000-0003-3123-1365 2
Stem Cell Research & Therapy volume 15 , Article number: 205 ( 2024 ) Cite this article
142 Accesses
Metrics details
Vascular tissue engineering is a promising approach for regenerating damaged blood vessels and developing new therapeutic approaches for heart disease treatment. To date, different sources of cells have been recognized that offer assistance within the recovery of heart supply routes and veins with distinctive capacities and are compelling for heart regeneration. However, some challenges still remain that need to be overcome to establish the full potential application of these cells. In this paper, we review the different cell sources used for vascular tissue engineering, focusing on extraembryonic tissue-derived cells (ESCs), and elucidate their roles in cardiovascular disease. In addition, we highlight the intricate interplay between mechanical and biochemical factors in regulating mesenchymal stem cell (MSC) differentiation, offering insights into optimizing their application in vascular tissues.
Introduction
Despite progressive advances in pharmacological and surgical therapy, cardiovascular diseases remain the leading cause of mortality worldwide [ 1 ]. These diseases typically involve the buildup of fatty deposits within arteries and an increased risk of blood clot formation. The increasing demand for organ transplants and the limited supply of donor organs have resulted in organ shortage crises. Conventional synthetic vascular grafts are incompetent at remodeling and have limited patency, particularly at smaller diameters. This is where tissue engineering has emerged as a promising solution. By combining bioactive cells with biodegradable scaffolds, tissue-engineered vascular grafts can be developed, offering the advantages of growth and self-healing capacity. These features have the potential to overcome the limitations of conventional treatment approaches [ 2 ].
Presently, the treatment of cardiovascular diseases primarily involves a combination of dietary and lifestyle modifications, medical intervention, and surgical procedures, with surgery typically reserved for advanced cases. Surgical interventions include endovascular techniques such as angioplasty and stent placement to widen or clear narrowed blood vessels. Vascular bypass grafting is another surgical method that is employed to circumvent damaged or blocked vessels. This procedure commonly utilizes autologous arteries or veins. However, due to the limited availability of arteries and severe complications associated with their removal, the saphenous vein is more frequently used as an autograft vessel than the arteries [ 3 ]. Nevertheless, the use of autologous vessels also presents certain drawbacks, such as low quality and site morbidity stemming from the extraction process [ 4 ].
Tissue engineering represents a rapidly evolving field with the ambitious goal of creating functional tissues and organs through the integration of cells, biomaterials, and biochemical factors. One of the most promising avenues in tissue engineering is stem cell-based therapy. Stem cells possess the remarkable capacity to differentiate into diverse cell types, making them ideal candidates for regenerating damaged or diseased tissues. The use of stem cells in tissue engineering offers several advantages over traditional therapies. First, stem cells can be obtained from various sources, including bone marrow, adipose tissue, or embryonic tissue. This versatility allows for personalized treatment strategies and reduces the risk of immune rejection. Second, stem cells can be cultivated in vitro, enabling the generation of substantial quantities of cells needed for transplantation. This scalability makes it possible to treat a wide range of patients with different tissue defects [ 5 ].
Stem cell-based therapy has shown promising results in the treatment of a diverse range of conditions, including heart disease, spinal cord injury, and liver failure. For example, in the realm of cardiac tissue engineering, stem cells can differentiate into cardiomyocytes, specialized heart muscle cells, and subsequently be seeded onto a scaffold to create functional heart muscle patches. These engineered patches have the potential to be transplanted into patients with damaged cardiac tissues, offering a promising avenue for enhancing overall cardiac function and potentially restoring heart health [ 6 ].
Among the different sources of stem cells, perinatal stem cells have emerged as a promising source for vascular regeneration due to their unique characteristics and potential applications, including lack of need for invasive procedures to obtain them, high degree of plasticity, immunomodulatory properties, low risk of tumorigenesis, younger and healthier cells compared to other adult stem cells, and angiogenic potential [ 7 ]. These valuable features make perinatal stem cells ideal candidates for regenerating damaged blood vessels and developing new therapeutic approaches for cardiovascular diseases. One of the key advantages of perinatal stem cells is their easy accessibility. Unlike other sources, such as bone marrow or adipose tissue, perinatal stem cells can be obtained noninvasively and do not pose any risk to the mother or baby during childbirth. Such readiness for availability and ethical advantages have contributed to their increasing popularity in research and clinical settings. Furthermore, perinatal stem cells exhibit high proliferative capacity and immunomodulatory properties [ 8 ]. They can be expanded in culture while maintaining their differentiation potential, making them an abundant source for large-scale production of vascular tissues [ 9 ]. Perinatal stem cells exhibit a high degree of plasticity, meaning that they can differentiate into various cardiovascular cell types, including endothelial cells, smooth muscle cells, and fibroblasts, which are crucial for vascular tissue engineering. This versatility allows them to contribute to the formation of functional blood vessels and vascular networks. Additionally, these cells possess immunosuppressive capabilities that allow them to evade immune rejection when transplanted into a recipient [ 7 ]. However, further research is needed to understand their long-term effects, optimize their differentiation protocols, and enhance their therapeutic efficacy. This paper reviews the different cell sources for vascular tissue engineering, focusing on extraembryonic tissue-derived cells.
Functional requirements for vascular grafts
Blood vessel walls typically consist of three main layers. The innermost layer adjacent to the lumen, known as the “tunica intima”, is composed of endothelial cells (ECs) and intimal smooth muscle cells (SMCs). The middle layer, called the “tunica media”, is composed of medial smooth muscle cells. Eventually, the outermost layer, called the “tunica adventitia”, comprises fibroblasts and extracellular matrix (ECM) components as well as microvessels (vasa vasorum), particularly in large blood vessels [ 10 , 11 ] (Fig. 1 ). Although autologous vascular transplantation minimizes immune responses, the high occurrence of occlusion and the need for multiple surgical procedures have restricted the effectiveness of autologous replacement approaches [ 12 ].

Basic structural characteristic of a blood vessel
Vascular graft tissue engineering constitutes a crucial aspect of tissue engineering with the objective of regenerating or generating new blood vessels with the help of bioactive and biocompatible materials [ 13 ].
Synthetic vascular grafts serve as substitutes for autologous vessels under certain conditions. In the long term, these grafts have shown satisfactory outcomes when used in large-diameter arteries (> 8 mm); however, their applicability in small-diameter vessels (< 6 mm) is limited due to unfavorable patency rates [ 14 ]. To address this limitation, attempts have been made to enhance the performance of synthetic grafts. One such approach involves the seeding of autologous endothelial cells onto the luminal surface of synthetic graft vessels, which has been shown to improve patency rates. Nevertheless, even with these improvements, the performance of synthetic grafts has not surpassed that of autologous vessels [ 15 ].
The first engineered blood vessel structures were produced in the mid-1980s by Weinberg and Bell [ 16 ]. Since then, various methods have been adopted to produce similar structures. In general, scaffold-based production methods can be classified into three categories: synthetic polymers, biopolymers, and biodegradable polymers [ 17 ].
Vascular tissue engineering typically entails meeting four fundamental requirements: suitable mechanical properties, blood compatibility, endothelial support, and biodegradability.
Mechanical properties
Tissue-engineered vascular grafts must have specific mechanical characteristics. These include compliance, which allows seamless integration with adjacent vessels, and the appropriate mechanical strength and elasticity to withstand blood pressure without deformation [ 18 ].
Blood compatibility
Blood compatibility refers to the ability of a material or device to interact with blood without causing adverse reactions [ 19 ]. Like other blood-related devices, tissue engineering vascular grafts (TEVGs) share similar mechanisms related to thrombosis; however, there are various antithrombotic strategies for the modification of TEVGs, including the use of antithrombotic agents, platelet inhibitors, or fibrinolysis agents. One effective approach involves surface endothelialization because the vascular endothelium on the inner surface of blood vessels is inherently compatible with blood. Another method is surface passivation, which prevents external surfaces from coming into contact with blood and can be achieved through the use of zwitterionic or hydrophilic polymers [ 18 ].
Endothelial friendliness
The primary goal of vascular graft tissue engineering is to promote neovascularization and the formation of new blood vessels, which mainly depend on the secretion of ECM by adherent endothelial cells. Therefore, an ideally compatible TEVG should guarantee the adhesion of endothelial cells and provide a conducive microenvironment for cell proliferation supported by the presence of growth factors and bioactive molecules [ 18 ].
Several strategies can enhance endothelium friendliness in TEVGs. Some growth factors can be directly incorporated into the polymer solution before electrospinning [ 20 ] or attached to heparin through covalent bonding [ 21 ]. Polydopamine, known for its anchoring properties, can also be utilized to coat the graft surface with growth factors [ 22 ].
However, it is essential to consider the relatively short half-life of growth factors, which can lead to their inactivity. To address this limitation, sustainable release methods have been developed to ensure prolonged release. Another alternative method involves modifying endothelial cells to secrete growth factors. By introducing pDNA to produce growth factors in transfected endothelial cells, both cell viability and ECM production can be significantly increased [ 23 ].
Biodegradability
In vascular graft tissue engineering, the choice of polymer is crucial, and it should ideally be biodegradable to reduce concerns related to immunogenicity and thrombus formation. The biodegradation of the polymer should align with the pace of new blood vessel formation. Premature or delayed degradation may hinder blood vessel formation and exacerbate immunogenicity concerns, respectively. Polycaprolactone (PCL), poly glycolic acid (PGA), and Polylactic acid (PLA) are among the common biodegradable polyesters used in this context. These polymers offer controlled degradation properties, allowing for synchronized tissue regeneration and polymer breakdown [ 24 ].
Since any deficiency in these aspects causes a disturbance in the neovascularization process, all four requirements must be coordinated and work in harmony [ 18 ].
Cell sourcing in vascular tissue engineering
Selecting the right cell source is a crucial step in achieving success in tissue engineering. Considerations should encompass vital characteristics such as the rate of cell survival, proliferation potential, differentiation capabilities, ability to integrate into the host tissue, and ease of accessing these cells (Table 1 ).
Autologous vascular cells
The term “autologous vascular cells” typically refers to endothelial cells and vascular smooth muscle cells sourced directly from the patient’s own body, making them very compatible in terms of immunity. However, the practical application of primary autologous cells presents certain challenges, prompting researchers to explore alternative approaches, such as deriving ECs and vascular smooth muscle cells (VSMCs) from stem cells. These challenges include limitations in cell quantity due to donor age, as well as issues related to poor proliferation and regeneration capacity [ 25 ].
Mesenchymal stem cells (MSCs)
MSCs, also referred to as mesenchymal stromal cells, are the most promising candidates for vascular tissue engineering. These cells are particularly appealing because of their ease of isolation, rapid expansion rate, immune evasion [ 26 ] and potential for differentiation into mesodermal lineages, including osteocytes, chondrocytes, adipocytes, and even nonmesodermal lineages, such as neural cells [ 27 ], hepatocytes [ 28 ] and pneumocytes [ 29 ]. The ability of MSCs to differentiate toward vascular lineages, including ECs and SMCs, coupled with their secretion of paracrine factors, position them as valuable contributors to vascular regeneration [ 30 ]. This versatility and regenerative potential make MSCs a promising avenue for advancing vascular tissue engineering efforts. In the following section, we will highlight three key attributes of MSCs that make them an appealing cell source for VTE treatment.
Progenitor cells
Progenitor cells are descendants of stem cells and require further differentiation to achieve specialization in specific cell types. These cells exhibit a distinct propensity to mature into their intended cell lineage. Progenitor cells are found throughout the body, obviating the necessity of isolating them from vessels. According to previous studies, progenitor cells such as endothelial progenitor cells (EPCs), smooth muscle progenitor cells (SMPCs), and pericytes are effective in vascular repair. During inflammation and shear stress, these cells are activated and begin to differentiate into different types of vascular cells. They also improve vascularization and angiogenesis [ 31 , 32 , 33 ]. However, an inherent challenge arises in their application, particularly in the elderly population, as the quantity of these cells and their differentiation potential diminish with age [ 33 ].
Emergence of Induced Pluripotent Stem cells (iPSCs)
iPSCs, a breakthrough in stem cell biology pioneered by Yamanaka et al., who earned a Nobel Prize in 2012, can differentiate into any cell type, offering vast potential for personalized medicine. Derived from accessible tissues such as skin or blood, iPSCs circumvent ethical issues and reduce immunogenic risks, representing promising advancements in tissue engineering, such as the production of vascular grafts. However, their use is limited by their potential for tumorigenicity, the presence of mitochondrial DNA mutations, and the complex, costly process of cell reprogramming and standardization [ 25 , 34 ].
Extraembryonic perinatal tissues: new putative sources of stem cells
Perinatal stem cells (PSCs) are a remarkable category of stem cells derived from tissues that develop from the 20th week of pregnancy through the 4th week after birth [ 35 ]. While adult stem cells from various tissues hold promise as potential sources for cell therapy applications, certain challenges, including ease of isolation, pluripotency, self-renewal, and ethical considerations, narrow the range of viable tissue sources for cell isolation. Among the commonly sought-after tissues for stem cell extraction, such as adipose tissue and bone marrow, perinatal tissues such as the placenta, amnion, and chorion have proven to be rich sources of stem cells. The stem cells obtained from these perinatal tissues possess highly desirable characteristics, such as ease of access, abundance, noninvasive extraction methods, minimal ethical problems, and reduced immunologic compatibility problems [ 36 ]. Stem cells isolated from perinatal tissue can be broadly categorized into two main groups: hematopoietic stem cells (HSCs) and fetal MSCs. These cells are placed between embryonic and adult cells in terms of their stemness abilities [ 37 ].
Hematopoietic stem cells (HSCs)
HSCs, characterized by their multipotent nature, serve as precursors for various types of blood cells. HSCs isolated from bone marrow have a long history of use in the treatment of hematologic malignancies. However, a significant milestone in the field of stem cell therapy occurred in 1988 when umbilical cord blood cells were first successfully transplanted to treat genetic blood disorders. The patient was a young boy with Fanconi anemia who received cord blood cells, marking a pivotal moment in the therapeutic potential of cord blood stem cells. After this success, subsequent research revealed that cord blood cells exhibit remarkable differentiation capabilities, giving rise to erythroid, myeloid, and lymphoid cell lineages [ 37 ].
Fetal mesenchymal stem cells
In the past, the prevailing belief was that the main source of MSCs was the bone marrow. However, it has become evident that the number of MSCs in the bone marrow is relatively low, and their regenerative capacity diminishes after passage 10–12 [ 38 ]. Therefore, bone marrow-derived MSCs present limitations that restrict their suitability for cell therapy purposes. In contrast, fetal MSCs isolated from perinatal tissue, including the umbilical cord, umbilical cord blood, placental blood, and placenta, do not have these limitations and can be regarded as a valuable alternative for cell therapy purposes [ 39 ]. Fetal MSCs can differentiate into three cardiac lineages: cardiomyocytes, endothelial cells, and smooth muscle cells. Additionally, these cells are able to form capillary structures on Matrigel, while mesenchymal cells isolated from adult sources (bone marrow and adipose tissue) cannot. Therefore, the selection of MSCs from fetal sources, such as the umbilical cord or amniotic membrane/fluid, can be an attractive source of young cells for autologous cell transplantation [ 40 ]. In the following sections, the use of MSCs from perinatal tissues is discussed in more detail.

Stem cells in perinatal tissues
The use of umbilical cord blood in transplantation has a history spanning over 30 years. In addition to cord blood, the placenta and fetal annexes, including the amniotic membrane, chorionic villi, chorionic plate, Wharton jelly of the umbilical cord, decidua, and amniotic fluid, are rich repositories of diverse stem cell types. Among these, one can find trophoblast epithelial stem cells and mesenchymal stromal cells, further underscoring the abundant and varied stem cell resources within perinatal tissues [ 7 ]. The exploration of perinatal stem cell sources offers substantial promise for a broad spectrum of therapeutic applications, notably in the field of cardiovascular diseases. In the subsequent sections, we will delve into the specific applications of these cell sources and elucidate their roles in vascular tissue engineering. (Fig. 2 ).

Various sources of extraembryonic tissue-derived stem cells used in vascular tissue engineering
Amniotic membrane
The amniotic membrane (AM) is the innermost membrane lining the fetal placenta and consists of five distinct layers, including the epithelial layer, which directly interfaces with amniotic fluid and is composed of amniotic epithelium cells (AECs). Beneath the epithelial layer lies the basement membrane, followed by the compact layer. The fibroblast layer is situated beneath the compact layer, and the spongy layer completes the structure. The basic function of the amniotic membrane is to provide a protective and supportive environment, shielding the developing embryo from external threats, potential infections, and harmful toxins [ 41 ]. The membrane has emerged as a suitable candidate for clinical applications, serving as a scaffold for tissue engineering or a carrier for the delivery of various cell types. AM possesses unique biological features, including low immunogenicity, antibacterial capacity, immunomodulation, antiscaring, anti-inflammatory properties, and hemocompatibility, as well as antiangiogenic and proapoptotic qualities, all without presenting ethical challenges [ 42 , 43 , 44 ]. Amniotic epithelial and mesenchymal cells isolated from AMs exhibit stem cell properties and express stemness markers such as Oct3/4, Sox2, Klf4, Nanog, TRA1-60, TA1-81, and SSEA4. Notably, these cells do not display tumorigenic characteristics after transplantation, largely due to the loss of their telomerase activity. Both AECs and amniotic mesenchymal stem cells (AMSCs) possess unique properties, including low immunogenicity, anti-proliferative effects on immune cells, anti-inflammatory properties, proliferation capability, and multipotent differentiation potential into cells with mesodermal, ectodermal, and endodermal lineages, and there is no need for invasive techniques to harvest them because they are discarded after birth [ 42 , 43 ].
Amnion-derived epithelial and mesenchymal cells inhibit tumor growth and invasion through three pathways: the induction of B and T lymphocyte apoptosis through the secretion of soluble factors, including TNF-α, FasL, TRAIL, TGF-β, and macrophage migration-inhibitory factors; the stimulation of cell cycle arrest; and the inhibition of angiogenesis. Therefore, a new line of research has been initiated with a focus on the antiproliferative effects of amniotic epithelial and mesenchymal cells on tumor growth in the last decade [ 42 ].
AECs can integrate into the tumor vascular lumen, differentiate into ECs or smooth muscle cells, reduce dysregulated tumor angiogenesis, enhance vascular perfusion, and subsequently, induce the cytotoxic effects of cisplatin. Since the vascular structure is not repaired because of the interconnected and unstable molecular pathways of the tumor, the vasculature can only be rebuilt within a limited time. Evaluation of the multipotential stem cell features of AECs to monitor the vascular formation abilities of AECs in vitro and in vivo under different conditions confirmed that AECs differentiated into tumor vascular endotheliocytes or pericytes and enhanced tumor vascular integrity to more efficiently kill the tumor during treatment, providing a new approach for rebuilding tumor vascularity [ 45 ].
Amniotic fluid
Amniotic fluid (AF), found within the amnion cavity surrounding the developing fetus, plays a vital role in fetal protection and nourishment during embryogenesis. This fluid consists of water, various chemical substances, and an abundant supply of stem cells (especially amniotic fluid stem cells (AFSCs) and amniotic fluid mesenchymal stem cells (AF-MSCs)). These stem cells exhibit essential stem cell markers, including Oct-4, c-Myc, Sox2, Nanog, and SSEA3, as well as high levels of several MSC markers, including CD29, CD44, CD73, CD90, CD105, CXCR4, stromal cell-derived factor 1 receptor (SDF-1), CD146, CD166, and CD184. Importantly, AFSCs can be safely collected without ethical concerns, either during the second or third trimester of pregnancy or even at later stages. Their unique characteristics combined with their stem cell properties and low immunogenicity make AFSCs highly suitable for various applications in the field of tissue engineering [ 46 ].
The pluripotency of AFSCs falls between that of ASCs and ESCs. Amniotic fluid stem cells exhibit remarkable proliferation capacity, with significant growth observed within just 36 h. Importantly, AFSCs maintain stable telomerase activity and a normal karyotype even after undergoing 250 in vitro amplification cycles [ 47 ].
Human AFSCs can promote vascular development and increase vessel length, area, and thickness in cocultures. These cells can differentiate into ECs, known as AFSC-derived ECs (AFSC-ECs), which have endothelial-like cell functions and can form cohesive vascular networks. A study conducted in 2015 showed that coculturing AFSCs with AFSCs and ECs within a fibrin/PEG matrix had a synergistic effect on various network parameters. The results revealed that the development of robust vessels relied on the presence of both AFSCs-ECs and AFSCs, each contributing to their vasculogenic and perivascular potential, respectively. In addition, fibrin/PEG hydrogels not only promoted capillary-like network formation but also offered advantages in terms of biocompatibility, mechanical stability, and vasculogenesis [ 48 ].
In 2016, Zhang et al. investigated the impact of glial cell line-derived neurotrophic factor (GDNF) on the differentiation of AFSCs into vascular endothelial-like cells. GDNF, known for its role as a neurotrophic factor of dopaminergic neurons, also acts as a tissue morphogen that enhances the differentiation of stem cells. The results indicated that AFSCs express EC markers such as vWF and CD31 after one week of differentiation and can be applied at vascular injury sites to promote angiogenesis. While GDNF improved the capacity of AFSCs to differentiate, these cells did not display the complete vascular morphology of mature ECs [ 47 ].
Human AFSCs can be induced to differentiate into vascular ECs by overexpressing the Ets transcription factors (TFs) Etv2, Fli1, and Erg. These converted amniotic cells successfully acquired an EC-like immunophenotype; however, their functional performance in EC assays was inferior to that of fully mature ECs. Sox17 expression is crucial for the proper functioning of ECs in vascular engraftment. Whereas Ets transcription factors help distinguish EC-like cells from nonvascular amniotic cells, Sox17 increases morphogenesis gene expression and facilitates the integration of transplanted converted cells into injured blood vessels. Therefore, the regulation of the Sox17 gene is essential for the generation of long-lasting, engraftable, and stable ECs following initial EC gene induction by Ets [ 49 ].
In addition, AF-MSCs have shown superior potential compared to BM-MSCs because they can differentiate into multiple cell lineages representing all three embryonic germ layers, such as chondrocytes, ECs, hepatocytes, and neurons, highlighting their remarkable versatility [ 50 ]. The characteristics of amniotic fluid stem cells (AFSCs), amniotic ECs (AECs), and AMSCs are compared in Table 2 , and an overview of research in the field of vascular tissue engineering involving these cells is shown in Table 3 .
The chorion, which lines the inner surface of the trophoblast, is formed from the embryonic mesoderm on the 14th day of human pregnancy, and at this stage, the extracellular space separates it from the amniotic membrane [ 53 ].
Chorionic membrane
The chorionic membrane serves as the connection between the fetus and maternal tissue and is separated from the amniotic membrane by a layer of collagen fibers. Comprising two layers, the mesenchymal layer and the trophoblastic layer, the chorionic membrane contains MSCs. These cells can differentiate into all three germ layers: mesodermal, endodermal, and ectodermal [ 54 ]. Due to its exceptional biomechanical properties and low immunogenicity, the chorionic membrane can be used as a scaffold either independently or in conjunction with an AM for vascular tissue engineering. In the amniochorionic membrane, the epithelial cells of the amniotic membrane and the trophoblast layer of the chorion can be separated and removed through enzymatic solutions and mechanical scraping, resulting in a membrane that supports the growth of ECs and promotes angiogenesis. This unique structure holds significant promise for applications in vascular tissue engineering [ 55 ].
Chorionic villi
Chorionic villi are finger-like projections on the chorion that harbor cells with a multipotent mesenchymal stromal phenotype. Under suitable induction conditions, these cells can differentiate into various cell types, including neurons, cartilage, osteocytes, and adipocytes [ 56 , 57 ]. Elevated levels of hydrogen peroxide in cardiovascular diseases and diabetes can lead to endothelial dysfunction, resulting in increased side effects and immune responses and ultimately the onset of thrombosis and atherosclerosis. Mesenchymal stem/stromal cells derived from the chorionic villi of human term placentae (v-MSCs) are able to protect human ECs against hydrogen peroxide-induced damage. v-MSCs reduce the detrimental effects of hydrogen peroxide on the proliferation, migration, angiogenesis, and permeability of ECs. Additionally, they modulate the expression of genes associated with EC cell function, including those related to survival and apoptosis. These cells hold promise for cell therapy aimed at repairing vascular damage caused by glucose and hydroxide peroxide, thereby reducing the adverse effects of cardiovascular diseases and diabetes [ 58 ].
Using the principle of tissue engineering techniques in conjunction with autologous cells and biodegradable scaffolds opens up possibilities for the fabrication of heart valves, blood vessels, and myocardial structures. Currently, cardiovascular tissue engineering can be a breakthrough for revolutionizing the treatment of congenital heart diseases, particularly among young patients. A significant challenge in treating these individuals is the absence of a suitable replacement structure similar to a cardiovascular valve. The development of a living and growing autologous structure could eliminate a major obstacle in their treatment journey. Advances in high-resolution imaging technologies now enable the early detection of most defects before birth, typically around the 20th week of gestation. To facilitate treatment, it becomes crucial to isolate cells during pregnancy for the subsequent production of tissue engineering implants either at birth or prenatally.
vMSCs hold promise as a suitable cell source for pediatric tissue engineering applications. Schmidt et al. were the first to suggest the possibility of using these cells for in vitro production of living heart valves [ 59 ]. In line with this, a study conducted by Weber et al. involved the extraction of MSCs from chorionic villi that are normally sampled from the applicant and cultivated in vitro. The cells were seeded onto a synthetic biodegradable scaffold to produce heart valve leaflets. The surface of this engineered structure was endothelialized with autologous endothelial progenitor cells derived from amniotic fluid or umbilical cord blood during pregnancy. The resulting tissue exhibited cellular phenotypes, an extracellular matrix composition, and a DNA content comparable to that of its native counterpart. vMSCs are significant for advancing congenital tissue engineering approaches [ 60 ].
vMSCs have also shown promise in the treatment of acute myocardial infarction, one of the most critical heart diseases. It has been proven that first-trimester placental chorion mesenchymal stem cells (fCMSCs) are better at reducing the symptoms of this disease in vivo than third-trimester placental chorion mesenchymal stem cells (tCMSCs) and BM-MSCs. Compared with tCMSCs, fCMSCs express higher levels of proangiogenic genes (PDGFD, VEGFA, and TNC), leading to significantly enhanced tube formation. Moreover, fCMSCs exhibit significantly lower expression of antiangiogenic genes (SPRY1 and ANGPTL1) than tCMSCs. Additionally, the improvement in cardiac function achieved by fCMSCs is significantly greater than that achieved by treatment with both tCMSCs and BM-MSCs [ 61 ].
Chorionic plate
The chorionic plate is composed of the amniochorionic membrane and fetal vessels. As the amniotic membrane is removed, the stem cells of the chorionic plate can be isolated from the area nearest to the umbilical cord. These cells have a mesenchymal phenotype and are able to differentiate into various lineages, including liver, cartilage, adipose, and bone lineages [ 62 ]. The decellularized human chorionic plate holds promise for use as a grafting material and in experimental vascularization studies. Cryopreserved human chorionic plate tissue can be decellularized using a perfusion method involving freeze‒thaw steps and chemical treatments. This approach minimizes the use of chemicals and exposure time. In terms of biocompatibility, when primary human umbilical vein endothelial cells (HUVECs) are cultured on this graft, they demonstrate endothelialization. Furthermore, the structure maintains cell-specific phenotypic and expression patterns [ 63 ].
The route of cell transplantation to damaged tissue is another critical factor in stem cell therapy. Various methods are available for delivering cells to the heart, including intravenous, intracoronary, coronary sinus, and direct epicardial injection. Among these methods, the direct intramuscular injection method is the most effective in terms of the quantity of delivered cells, with approximately 11% of the transferred cells engrafting into the desired area [ 64 ]. Inflammatory cytokines also play a role in the homing and engraftment of stem cells to damaged tissues and organs [ 65 ]. Once they reach the target area and are successfully transplanted, these cells can carry out their biological activities, such as proliferation, differentiation, and apoptosis, to facilitate the regeneration of damaged tissue [ 66 ].
Jung et al. conducted an in vivo study in rats using labeled chorionic plate-derived MSCs (CP-MSCs) to investigate the optimal transplantation route for treating injured livers. They compared direct transplantation, intrasplenic transplantation, and intravenous transplantation via the tail vein (TTP) with a nontransplanted treatment group and concluded that the therapeutic efficacy of the first two methods was superior to that of the TTP group. This outcome underscores the therapeutic ability of CP-MSCs to promote functional recovery of injured tissues and highlights the importance of selecting the appropriate transplantation routes for achieving the best outcome [ 67 ].
Identifying the optimal transplantation route for effective homing of CP-MSCs in cardiovascular diseases remains a significant challenge. Additionally, there is a need to optimize the delivery method to enhance cell engraftment and the survival rate.
Recent studies have shown the advantages of cells derived from the chorionic plate over those derived from the chorionic villi, including greater clonogenic potential and greater expression of cell cycle-related genes, ultimately leading to improved heart function in MI mouse models. Additionally, the exosomes obtained from the culture of these cells show potent angiogenic properties, suggesting that they have valuable potential in vascular tissue engineering [ 68 , 69 ].
In another study, a comparative analysis involving CP-MSCs, ChorionicVilli-MSCs, decidua-derived MSCs, and umbilical cord blood (UCB) MSCs was conducted, focusing on cell proliferation and migration abilities. The findings showed that CP-MSCs had superior performance in these criteria compared to the other cell types. Additionally, CP-MSCs outperformed other groups in regulating macrophage polarization, specifically shifting macrophages from the M1 phenotype to the M2 phenotype [ 62 ]. Notably, compared with CD106-MSCs, CP-MSCs express CD106 markers, which are associated with heightened proliferative capacity and immune regulation potential [ 70 ].
Umbilical cord
The umbilical cord (UC), once considered a biological waste at the time of birth, is now recognized as a perinatal organ that plays a crucial role in facilitating the exchange of nutrients and gases (oxygen and carbon dioxide) between the placenta and the fetus. This remarkable organ, with an average length of 50–60 cm and more than 40 L of blood flow, has emerged as a valuable source of HSCs and MSCs. Importantly, it offers the advantage of being noninvasive and without any ethical concerns. An anatomical cross-section of the umbilical cord revealed that the UC is composed of two arteries and a vein without any branches [ 71 ], which are surrounded by Wharton’s jelly, a gelatinous substance rich in ECM proteins, including collagens, glycosaminoglycans such as hyaluronic acid and chondroitin sulfate, as well as growth factors such as IGF-1 and PDGF [ 72 ]. Wharton’s jelly serves the vital function of preventing blood vessels from clumping and provides flexibility to the cord. The umbilical cord is further enveloped by a membrane consisting of two layers: mesenchymal and epithelial layers.
Umbilical cord stem cells are a rich source of various stem cell types, including endothelial progenitors, epithelial stem cells, MSCs, and HSCs. These stem cells can be isolated from both cord blood and cord tissue and have shown promise in tissue repair through two primary mechanisms: the release of related cytokines and differentiation into specific cell types needed for tissue regeneration [ 71 ].
MSCs derived from Wharton’s jelly (WJ-MSCs) offer several advantages over other sources of MSCs, such as those from the BM. These advantages include a high proliferation rate, a significant capacity for differentiation into various cell types, low immunogenicity, ease of harvesting, and the potential to obtain large quantities of cells during the harvest process [ 71 ].
WJ-MSCs secrete various growth factors and cytokines, including G-CSF, HGF, PDGFAA, TGF-β, IL-6, and IL-8. These secreted factors play crucial roles in immunomodulation, cell proliferation, differentiation, growth, and tissue repair, making WJ-MSCs valuable for clinical applications [ 71 , 73 ].
One notable characteristic of WJ-MSCs is their expression of self-renewal and pluripotency markers, including Oct-4, Sox-2, Nanog, SSEA-4, Tra-1-60, and Tra-1-81. These markers indicate the ability of these cells to maintain their undifferentiated state and their potential to differentiate into various cell lineages [ 74 ]. Although MSCs can be successfully isolated from Wharton’s jelly (WJ), the perivascular space (PRV) and the umbilical membrane (UCM) in UC differ, and they may exhibit variations depending on the specific region of isolation [ 73 ].
The feasibility of using WJ-MSCs as a suitable cell source for cardiovascular tissue engineering was first demonstrated in 2002. Hoerstrup et al. seeded WJ-MSCs onto a bioabsorbable scaffold in a biomimetic flow culture system and demonstrated the feasibility of generating pulmonary artery conduits using WJ-MSCs. Morphological and mechanical analysis revealed that tissue-engineered pulmonary conduits closely resembled native human pulmonary arteries. This research highlighted the potential of human WJ-MSCs as a readily available cell source for tissue engineering applications, eliminating the need to sacrifice intact vascular donor structures [ 75 ].
A more recent study conducted in 2020 investigated the ability of WJ-MSCs seeded on chitosan/hyaluronic acid multilayered films to differentiate into endothelial-like cells. The results were promising, indicating that WJ-MSCs could yield endothelial-like cells in a relatively short time (15 days) in a nontraumatic manner. Such polyelectrolyte films containing an endothelium resulting from the differentiation of MSCs can be used to reduce the risk of graft rejection [ 76 ].
Investigating the synergistic effects of gene and stem cell-based therapy on preventing neointimal formation, a common issue associated with vein graft failure, was first performed by Qingxi Qu et al. In this study, the miRNA-126-3p gene, an EC-specific angiogenic miRNA, was transfected into human UC-MSCs using a lentiviral vector. Therapeutic upregulation of miRNA-126-3p had several positive effects, including preventing restenosis in vein grafts, improving EC function through paracrine mechanisms, repairing dysfunctional endothelium, and reducing neointimal hyperplasia in vein grafts in rats. This improvement was attributed to the synthesis and secretion of various bioactive molecules, such as angiogenic factors, growth factors, and cytokines, by MSCs [ 77 ].
Severe human disorders, such as cardiovascular and peripheral vascular disease, often require the use of vascular grafts. However, the use of autologous vessels such as the saphenous vein of glutaraldehyde-fixed bovine and porcine xenografts is associated with issues such as a limited number of suitable patient vessels and susceptibility to calcification and chronic immune rejection. One suggested approach is the decellularization of human umbilical arteries with inner diameters ranging from 1 to 4 mm. While decellularization removes cellular components and donor antigens, potentially reducing the risk of immune responses, it leaves behind acellular vascular grafts that need to be repopulated with vascular cell populations to become fully functional. In 2018, an efficient method was developed to repopulate decellularized human umbilical arteries (hUAs) with WJ-MSCs. This approach aimed to produce HLA-matched vascular grafts, addressing some of the limitations associated with conventional graft sources [ 78 ]. Vessel bioreactors are commonly used for repopulating vascular grafts under specific conditions, but they often face challenges related to low repopulation efficacy. In an investigation, researchers sought to enhance the repopulation process by culturing human umbilical cord mesenchymal stem cells (hUCMSCs) on decellularized human umbilical arteries in media supplemented with cord blood platelet lysate (CBPL). Mallis et al. reported that CBPL significantly improved cell adhesion, proliferation, and differentiation through the presence of various growth factors, including TGF-β1, FGF, TNF-α, IL-1, IL-3, IL-6, PDGF, and matrix metalloproteases. Moreover, the use of CBPL enabled the differentiation of VSMCs from WJ-MSCs [ 79 ]. In another study by Mallis and colleagues, this approach successfully repopulated decellularized hUAs, leading to an increase in total hydroxyproline and sGAG contents. These results suggest that in vitro production of VSMCs, which involves collagen and sGAG synthesis, may be facilitated by factors such as SOX9, RUNX2, and MSX2 [ 80 ].
The angiogenic effect of MSCs such as WJ-MSCs on HUVECs has been demonstrated in numerous studies. These effects involve stabilizing the EC network and secreting vasculogenic growth factors, including hepatocyte growth factor. In both autogenic and allogenic cell sources, WJ-MSCs have been shown to promote angiogenesis and enhance vascular tube formation when cocultured with ECs for three days [ 81 ].
To ensure the success of endothelialization, it is essential to address challenges such as cell coverage loss due to exposure to physiological levels of shear stress in an active environment. Research has shown that shear stress preconditioning can improve cell retention and enhance the performance of ECs. In one study, HUVECs were preconditioned with shear stress on silk fibroin nanofibrous scaffolds at various time intervals and amplitudes. The results of this research suggest that ECs require sufficient time to acclimate to changing shear stress levels to withstand physiological levels. A gradual increase in shear stress over time can improve EC tolerance to shear stress and enhance the antithrombogenic function of engineered vascular grafts. This process involves an extracellular matrix (ECM)-specific mechanosensitive signaling pathway in which integrin β1, focal adhesion kinase (FAK), and fibronectin (FN) play significant roles [ 82 ].
ECs were used to form a monolayer of cells in the lumen of a vascular graft made of polycaprolactone/gelatin/fibrinogen, which was modified by a thermoforming process and coated with fibronectin and collagen IV. The results of this study showed that human cord blood-derived endothelial cells (hCB-ECs) can proliferate, produce endothelial nitric oxide synthase (eNOS), respond to interleukin 1β through the upregulation of VCAM-1 and ICAM-1, and reduce platelet deposition [ 83 ].
Expanding available resources for autologous to allogeneic (analog) applications in vascular tissue engineering faces a significant challenge due to the expression of human leukocyte antigen class I (HLA I) on the cell surface of ECs, which can lead to antibody-mediated immune responses and graft rejection. Recent advances in the field have used RNA interference (RNAi) to stably silence the expression of HLA I proteins in ECs via lentiviral vectors without affecting the morphological and functional properties of ECs. The silenced ECs were able to maintain the expression of key endothelial markers, including endothelial nitric oxide synthase, von Willebrand factor, CD31, and vascular endothelial cadherin. These markers are essential for maintaining a functional endothelial barrier, regulating blood coagulation, and controlling vessel tone.
Furthermore, HLA I-silenced ECs retained their ability to perform crucial endothelial functions. They are capable of absorbing acetylated low-density lipoprotein (acLDL) and forming capillary-like tube structures when embedded in 3D fibrin gels and exposed to unidirectional flow, similar to nontransduced cells [ 84 ]. The proliferation of ECs is aided by sphingosine-1-phosphate (S1P), an effective additive that also protects Syndecan-1 (SDC1) from shedding, which is important for preventing platelet adhesion. Compared to the controls, their results demonstrated that S1P reduced thrombus formation and enhanced HUVEC proliferation [ 85 ].
From another point of view, the physiological characteristics of conduit endothelialization strategies are inferior to those of native vessels due to the absence of VSMCs, which play a crucial role in vessel structure and function [ 86 ]. As an example of the utilization of smooth muscle cells in vessel engineering, human umbilical artery-derived smooth muscle cells (hUASMCs) were cultured on an electrospun scaffold containing fibrinogen extracted from human umbilical cord blood samples. To enhance the poor elastogenesis property of the scaffold, PCL was incorporated as a reinforcing material [ 87 ].
In 2018, Gökçinar-Yagci and her colleagues attempted to create a fully natural triple-layered vascular construct that mimics all the layers of a blood vessel using natural scaffolds and differentiated vascular cells. In this study, a triple-layered vascular construct was created by combining SMCs and fibroblasts, which were differentiated from perivascular cells (PCs) extracted from the human umbilical cord vein. Collagen type I/elastin/dermatan sulfate was used to form the tunica media, and collagen type I/fibrin was used for the tunica adventitia. Subsequently, HUVECs were seeded onto the construct using the cell sheet engineering method [ 88 ].
While this vascular graft closely resembled native blood vessels with a diameter of less than 5 millimeters, its weak mechanical properties made it unable to withstand the pressure within a blood vessel. To address this limitation, another study introduced a biocompatible electrospun polyurethane (PU) scaffold between the tunica intima and media layers of the construct to provide mechanical reinforcement. Polyurethane nanofibers create a suitable environment for HUVECs, enhancing their tensile strength and elastic modulus. As a result, layers of HUVECs, SMCs, and fibroblasts align with each other, strengthening the graft [ 89 ]. An overview of research in the field of vascular tissue engineering involving cells isolated from the umbilical cord is shown in Table 4 .
The decidua, a tissue in the uterus, is divided into three regions: the basalis, capsularis, and parietalis. The decidua basalis and parietalis are abundant sources of mesenchymal stem cells. These versatile cells can differentiate into various cell types from different germ layers, including lung cells, liver cells, cartilage, adipocytes, neurons, osteoblasts, and skeletal and cardiac myocytes, under laboratory conditions. They have demonstrated effectiveness in the treatment of several diseases, such as breast cancer, multiple sclerosis, and diabetes, and in reducing inflammation in the central nervous system [ 96 , 97 , 98 , 99 ]. Research has indicated that decidual mesenchymal stem cells (DMSCs) are more readily isolated from tissue and more accessible than bone marrow mesenchymal stem cells (BMSCs). Additionally, metabolomics analysis revealed a significant increase in ornithine metabolism, which is related to angiogenesis, in DMSCs.
In vivo studies have shown that the transplantation of DMSCs into murine models of acute myocardial infarction (MI) leads to a significant increase in neovascularization and cardiac remodeling compared to the transplantation of BMSCs. Consequently, compared with BMSCs, DMSCs exhibit superior efficacy in terms of revascularization and cardiac regeneration following MI [ 100 ].
Furthermore, the ability of human decidua basalis mesenchymal stem cells (DBMSCs) to survive and function in an inflammatory environment characterized by a high concentration of lipopolysaccharide has been explored. Inflammatory conditions are known triggers for certain diseases, such as arteriosclerosis. The results of this study indicated that there were no significant differences between the DBMSC-treated group and the control group. This finding suggested that DBMSCs can maintain their activities, including adhesion, proliferation, and migration, even under inflammatory conditions. Therefore, DBMSCs have the potential to be promising candidates for the treatment of inflammatory diseases, including arteriosclerosis [ 101 ].
In a comparative study, the biological characteristics of UCMSCs and MSCs derived from decidua parietalis (DP-MSCs) were investigated. Various features, including cell doubling times, colony formation rates, immune phenotypes, differentiation capacity, and the levels of secreted factors, were assessed for both cell types. Despite DP-MSCs exhibiting increased levels of keratinocyte growth factor, vascular endothelial growth factor, and stem cell factor, UCMSCs exhibited increased proliferation and colony formation rates. Moreover, UC-MSCs exhibited a shorter doubling time than DP-MSCs. Additionally, the concentration of basic fibroblast growth factor in the supernatant of UC-MSCs was notably greater than that in the supernatant of DP-MSCs. Based on these findings, researchers have concluded that UC-MSCs have great potential for effective applications in vascular tissue engineering and regenerative medicine [ 102 ].
Potential clinical application
When exploring cell therapy in clinical trials, it’s crucial to choose diseases for treatment that not only match the cell product’s action mechanism and show promise in preclinical studies but also address severe illnesses lacking effective treatments. This approach is primarily aimed at conditions that are both severely debilitating and critically lacking in medical solutions, underlining the importance of targeting diseases with no current therapy standards [ 103 ].
In cardiovascular treatments, for instance, non-autologous valve or conduit implants often face issues like obstructive tissue growth and calcification. This has led to a shift towards developing autologous, living tissues engineered in vitro, which can regenerate damaged cardiovascular tissue. Among the promising candidates for vascular diseases, placenta-derived cell therapies such as placenta derived adherent stromal cells (PLX-PAD) and Human Placenta-derived Cells (PDA-002) have shown potential, particularly for treating peripheral arterial disease (PAD). Within this area, patient groups are identified based on several factors, including those impacting enrolment and regulatory considerations. PLX-PAD, for example, is seen as particularly suited for critical limb ischemia patients, who face a dire prognosis including high rates of amputation and mortality, and significantly reduced quality of life. These patients, especially that ineligible for revascularization, have no existing treatment options, marking a significant unmet medical need that PLX-PAD aims to address. Early-phase trials in this patient group have shown promising signs of safety and effectiveness, including pain reduction and improved tissue perfusion, providing insights into potentially effective dosages [ 103 , 104 ].
Furthermore, WJ-MSCs have been recognized for their clinical potential in vascular tissue engineering, with successful applications in animal models and human trials. For instance, autologous heart valves derived from human WJ-MSCs have been effectively used in sheep, demonstrating comparable functional and structural qualities to native valves. In a study involving patients with acute myocardial infarction, WJ-MSCs were safely administered and showed significant improvements in heart tissue viability and perfusion, positioning them as a viable alternative to traditional stem cell therapies for heart repair [ 105 , 106 ].
The first human trial to assess the safety of administering UCMSCs through both intra-arterial and intravenous routes in patients with acute ischemic stroke is recruiting. This Phase 1 study has enrolled 14 participants to test the innovative UCMSCs treatment. The trial includes a follow-up period of 12 months and explores a method of administration never before attempted in humans, presenting potential new risks and benefits [ 107 ]. In another study, researchers are investigating the effectiveness of a novel combination therapy using intranasal conditioned medium and intraparenchymal transplantation of UCMSCs to stimulate neurogenesis in patients with acute strokes. This trial features three groups: one receiving the combination therapy, a second receiving only UCMSCs, and a third serving as a control group with standard neurological and neurotrophic drugs. The hypothesis is that the combination therapy will most effectively promote neurogenesis in these patients [ 108 ]. Additionally, a study is set to explore the safety and feasibility of UCMSC catheter transplantation for treating left ventricular dysfunction post-acute myocardial infarction. Slated to start in December 2023 and projected to end in December 2025, this Phase 1 trial will involve 40 patients split into two groups: one receiving the UC-MSC transplantation and the other receiving standard care. The primary focus will be monitoring Major Adverse Cardiac Events (MACE) to evaluate safety during the 12 months following treatment [ 109 ].The advancements in using extra-embryonic Stem Cells in regenerative medicine highlight the diverse therapeutic possibilities these cells might offer. Despite the promise, the outcomes from both pre-clinical and clinical studies are still in early stages and require further clarification. The characteristics and therapeutic potential of extra-embryonic MSCs are not fully understood, necessitating additional research into their role in cell therapy and tissue engineering. Additionally, developing biomaterials compatible with these stem cells, without compromising their regenerative and immune-modulating capabilities, remains a critical area for future research [ 110 ]. Table 5 shows the clinical approaches using extra-embryonic stem cells.
Vascular tissue engineering is a promising approach for regenerating damaged blood vessels and developing new therapeutic strategies for heart diseases. Perinatal stem cells, derived from extraembryonic tissues, have immense potential in addressing the symptoms of cardiovascular diseases due to their angiogenic, immunomodulatory, and endothelialization-promoting properties. Recent studies suggest that not only the perinatal stem cells themselves but also the soluble and insoluble factors they release could play a pivotal role in tissue regeneration. Soluble factors like growth factors (e.g., VEGF, FGF), cytokines (e.g., IL-6, TNF-alpha), and hormones (human Chorionic Gonadotropin, human Placental Lactogen) alongside insoluble factors such as, collagen and fibronectin, may offer a cell-free therapeutic approach. This innovative strategy provides a novel direction for future research that could potentially simplify therapeutic strategies, reduce risks associated with cell-based therapies, and enhance the scalability of treatments. However, more research is required to overcome the existing challenges and to translate these promising findings into effective clinical therapies, which can offer new hope for patients with cardiovascular diseases. In conclusion, the field of vascular tissue engineering, particularly through the innovative use of extraembryonic tissue-derived bioactive factors, is rapidly evolving and holds great promise for the future of cardiovascular disease treatment.
Data availability
Not applicable.
Abbreviations
Acetylated low-density lipoprotein
Amniotic epithelium cells
Amniotic fluid mesenchymal stem cells
Amniotic fluid stem cells
Amniotic fluid stem cell-derived endothelial cells
Amniotic mesenchymal stem cells
Adipose-derived stem cells
Bone marrow mesenchymal stem cells
Ca2+/calmodulin-dependent protein kinase II
Cord blood platelet lysate
Clotting time
Decidual mesenchymal stem/stromal cells
Human Decidual Basalis Mesenchymal Stem Cells
Endothelial cells
Extracellular matrix
Endothelial progenitor cells
- Extraembryonic tissue-derived cells
Expanded polytetrafluoroethylene
Endothelial nitric oxide synthase
Focal adhesion kinase
First-trimester placental chorion mesenchymal stem cells
Glial cell line-derived neurotrophic factor
Mesenchymal stem cell
Myocardial infarction
Induced pluripotent stem cells
Hematopoietic stem cells
Human umbilical vein endothelial cells
Human leukocyte antigen class I
Human umbilical arteries
Human cord blood-derived endothelial cells
Smooth muscle cells
Smooth muscle progenitor cells
Stromal cell-derived factor 1 receptor
Sphingosine-1-phosphate
Vascular Endothelial Growth Factor
Vascular Endothelial Growth Factor receptor-1
Mesenchymal stem/stromal cells derived from chorionic villi
von Willebrand factor
Polycaprolactone
Perivascular cells
Perinatal stem cells
Platelet-Derived Growth Factor
Platelet-derived growth factor receptor
Poly glycolic acid
Polylactic acid
Placenta derived adherent stromal cells
Human Placenta-derived Cells
Prothrombin time
Polyurethane
Activated partial thromboplastin time
RNA interference
Tissue engineering vascular grafts
Transforming growth factorβ
Transcription factors
Third-trimester placental chorion mesenchymal stem cells
Sphingosylphosphorylcholine
Smooth muscle actin
Human umbilical cord
Umbilical cord blood
Umbilical cord pericytes
Umbilical cord mesenchymal stem cells
Vascular smooth muscle cells
Wharton’s jelly mesenchymal stem cells
Zoghbi WA, Duncan T, Antman E, Barbosa M, Champagne B, Chen D et al. Sustainable development goals and the future of Cardiovascular Health: a Statement from the Global Cardiovascular Disease Taskforce. J Am Heart Assoc. 2014;3(5).
Ong CS, Zhou X, Huang CY, Fukunishi T, Zhang H, Hibino N. Tissue engineered vascular grafts: current state of the field. Expert Rev Med Devices. 2017;14(5):383–92.
Article CAS PubMed Google Scholar
Antoniou GA, Chalmers N, Georgiadis GS, Lazarides MK, Antoniou SA, Serracino-Inglott F, et al. A meta-analysis of endovascular versus surgical reconstruction of femoropopliteal arterial disease. J Vasc Surg. 2013;57(1):242–53.
Article PubMed Google Scholar
Weintraub WS, Grau-Sepulveda MV, Weiss JM, O’Brien SM, Peterson ED, Kolm P, et al. Comparative effectiveness of revascularization strategies. N Engl J Med. 2012;366(16):1467–76.
Article CAS PubMed PubMed Central Google Scholar
Kwon SG, Kwon YW, Lee TW, Park GT, Kim JH. Recent advances in stem cell therapeutics and tissue engineering strategies. Biomater Res. 2018;22(1).
Su T, Huang K, Daniele MA, Hensley MT, Young AT, Tang J, et al. Cardiac stem cell Patch Integrated with Microengineered Blood vessels promotes Cardiomyocyte Proliferation and Neovascularization after Acute myocardial infarction. ACS Appl Mater Interfaces. 2018;10(39):33088–96.
de la Torre P, Flores AI. Current status and future prospects of perinatal stem cells. Genes (Basel). 2020;12(1):6.
Silini AR, Masserdotti A, Papait A, Parolini O. Shaping the future of Perinatal cells: lessons from the past and interpretations of the Present. Front Bioeng Biotechnol. 2019;7.
Balbi C, Bollini S. Fetal and perinatal stem cells in cardiac regeneration: moving forward to the paracrine era. Placenta. 2017;59:96–106.
Dan P, Velot É, Decot V, Menu P. The role of mechanical stimuli in the vascular differentiation of mesenchymal stem cells. J Cell Sci. 2015.
Junqueira LCCJ. Basic histology: text & atlas. New York: McGraw-Hill; 2005.
Book Google Scholar
Schmidt CE, Baier JM. Acellular vascular tissues: natural biomaterials for tissue repair and tissue engineering. Biomaterials. 2000;21(22):2215–31.
Benrashid E, McCoy CC, Youngwirth LM, Kim J, Manson RJ, Otto JC, et al. Tissue engineered vascular grafts: origins, development, and current strategies for clinical application. Methods. 2016;99:13–9.
Chlupáč J, Filová E, Bačáková L. Blood vessel replacement: 50 years of development and tissue engineering paradigms in vascular surgery. Physiol Res. 2009;S119–40.
Deutsch M, Meinhart J, Zilla P, Howanietz N, Gorlitzer M, Froeschl A, et al. Long-term experience in autologous in vitro endothelialization of infrainguinal ePTFE grafts. J Vasc Surg. 2009;49(2):352–62.
Weinberg CB, Bell E. A Blood Vessel Model Constructed from Collagen and Cultured Vascular Cells. Science (1979). 1986;231(4736):397–400.
Devillard CD, Marquette CA. Vascular tissue Engineering: challenges and requirements for an Ideal large scale blood vessel. Front Bioeng Biotechnol. 2021;9.
Wu J, Hu C, Tang Z, Yu Q, Liu X, Chen H. Tissue-engineered vascular grafts: balance of the Four Major requirements. Colloid Interface Sci Commun. 2018;23:34–44.
Article CAS Google Scholar
Ratner BD, Horbett TA, Wagner WR. Evaluation of Blood–Materials Interactions. In: Biomaterials Science. Elsevier; 2020. pp. 879–98.
Asiri A, Saidin S, Sani MH, Al-Ashwal RH. Epidermal and fibroblast growth factors incorporated polyvinyl alcohol electrospun nanofibers as biological dressing scaffold. Sci Rep. 2021;11(1):5634.
Henry JJD, Yu J, Wang A, Lee R, Fang J, Li S. Engineering the mechanical and biological properties of nanofibrous vascular grafts for in situ vascular tissue engineering. Biofabrication. 2017;9(3):035007.
Article PubMed PubMed Central Google Scholar
Lee Y, Bin, Shin YM, Lee Jhye, Jun I, Kang JK, Park JC, et al. Polydopamine-mediated immobilization of multiple bioactive molecules for the development of functional vascular graft materials. Biomaterials. 2012;33(33):8343–52.
Liu Y, Lu J, Li H, Wei J, Li X. Engineering blood vessels through micropatterned co-culture of vascular endothelial and smooth muscle cells on bilayered electrospun fibrous mats with pDNA inoculation. Acta Biomater. 2015;11:114–25.
Patel HN, Thai KN, Chowdhury S, Singh R, Vohra YK, Thomas V. In vitro degradation and cell attachment studies of a new electrospun polymeric tubular graft. Prog Biomater. 2015;4(2–4):67–76.
Jouda H, Larrea Murillo L, Wang T. Current progress in Vascular Engineering and its clinical applications. Cells. 2022;11(3):493.
Ankrum JA, Ong JF, Karp JM. Mesenchymal stem cells: immune evasive, not immune privileged. Nat Biotechnol. 2014;32(3):252–60.
Scuteri A, Miloso M, Foudah D, Orciani M, Cavaletti G, Tredici G. Mesenchymal stem cells neuronal differentiation ability: a real perspective for nervous system repair? Curr Stem Cell Res Ther. 2011;6(2):82–92.
Wu XB, Tao R. Hepatocyte differentiation of mesenchymal stem cells. Hepatobiliary Pancreat Dis Int. 2012;11(4):360–71.
HUANG K, KANG X, WANG X, WU S, XIAO J, LI Z, et al. Conversion of bone marrow mesenchymal stem cells into type II alveolar epithelial cells reduces pulmonary fibrosis by decreasing oxidative stress in rats. Mol Med Rep. 2015;11(3):1685–92.
Gu W, Hong X, Potter C, Qu A, Xu Q. Mesenchymal stem cells and vascular regeneration. Microcirculation. 2017;24(1).
Tao J, Cao X, Yu B, Qu A. Vascular Stem/Progenitor cells in Vessel Injury and Repair. Front Cardiovasc Med. 2022;9.
Deng J, Ni Z, Gu W, Chen Q, Nowak WN, Chen T, et al. Single-cell gene profiling and lineage tracing analyses revealed novel mechanisms of endothelial repair by progenitors. Cell Mol Life Sci. 2020;77(24):5299–320.
Gago N, Pérez-López V, Sanz-Jaka JP, Cormenzana P, Eizaguirre I, Bernad A, et al. Age-dependent depletion of human skin-derived progenitor cells. Stem Cells. 2009;27(5):1164–72.
Generali M, Casanova EA, Kehl D, Wanner D, Hoerstrup SP, Cinelli P, et al. Autologous endothelialized small-caliber vascular grafts engineered from blood-derived induced pluripotent stem cells. Acta Biomater. 2019;97:333–43.
Jia H, Caputo M, Ghorbel MT. Stem cells in vascular graft tissue engineering for congenital heart surgery. Interv Cardiol (Lond). 2013;5(6):647–62.
Article Google Scholar
Nur Fariha MMCKTGTAHA. Human chorion-derived stem cells: changes in stem cell properties during serial passage. Cytotherapy. 2011;13(5):582–93.
Zhang Y, Li Z, Liu N. The Stemness of Perinatal stem cells. Perinatal stem cells. Singapore: Springer Singapore; 2019. pp. 27–37.
Chapter Google Scholar
Karahuseyinoglu S, Cinar O, Kilic E, Kara F, Akay GG, Demiralp DÖ, et al. Biology of Stem cells in human umbilical cord stroma: in situ and in Vitro surveys. Stem Cells. 2007;25(2):319–31.
Parolini O, Alviano F, Bagnara GP, Bilic G, Bühring HJ, Evangelista M et al. Concise Review: Isolation and Characterization of Cells from Human Term Placenta: Outcome of the First International Workshop on Placenta Derived Stem Cells. Stem Cells. 2008;26(2):300–11.
Ramkisoensing AA, Pijnappels DA, Askar SFA, Passier R, Swildens J, Goumans MJ, et al. Human embryonic and fetal mesenchymal stem cells differentiate toward three different cardiac lineages in contrast to their adult counterparts. PLoS ONE. 2011;6(9):e24164.
Dadkhah Tehrani F, Firouzeh A, Shabani I, Shabani A. A review on modifications of amniotic membrane for Biomedical Applications. Front Bioeng Biotechnol. 2021;8.
Niknejad H, Yazdanpanah G, Ahmadiani A. Induction of apoptosis, stimulation of cell-cycle arrest and inhibition of angiogenesis make human amnion-derived cells promising sources for cell therapy of cancer. Cell Tissue Res. 2016;363(3):599–608.
Schwab RHM, Goonetilleke M, Zhu D, Kusuma GD, Wallace EM, Sievert W, et al. Amnion epithelial cells — a therapeutic source. Curr Stem Cell Rep. 2021;7(1):13–29.
McDonald C, Siatskas C, Bernard CA. The emergence of amnion epithelial stem cells for the treatment of multiple sclerosis. Inflamm Regen. 2011;31(3):256–71.
Guan L, Zhang A. Amniotic epithelial cells reverse abnormal vascular structure and function in endometrial carcinoma. Int J Clin Exp Pathol. 2019;12(7):2405–24.
CAS PubMed PubMed Central Google Scholar
Jafari A, Rezaei-Tavirani M, Farhadihosseinabadi B, Zali H, Niknejad H. Human amniotic mesenchymal stem cells to promote/suppress cancer: two sides of the same coin. Stem Cell Res Ther. 2021;12(1):126.
Zhang R, Lu Y, Li J, Wang J, Liu C, Gao F, et al. Glial cell line-derived neurotrophic factor induced the differentiation of amniotic fluid-derived stem cells into vascular endothelial-like cells in vitro. J Mol Histol. 2016;47(1):9–19.
Benavides OM, Quinn JP, Pok S, Petsche Connell J, Ruano R, Jacot JG. Capillary-Like Network formation by human amniotic fluid-derived stem cells within Fibrin/Poly(Ethylene Glycol) Hydrogels. Tissue Eng Part A. 2015;21(7–8):1185–94.
Schachterle W, Badwe CR, Palikuqi B, Kunar B, Ginsberg M, Lis R, et al. Sox17 drives functional engraftment of endothelium converted from non-vascular cells. Nat Commun. 2017;8(1):13963.
Tancharoen W, Aungsuchawan S, Pothacharoen P, Markmee R, Narakornsak S, Kieodee J, et al. Differentiation of mesenchymal stem cells from human amniotic fluid to vascular endothelial cells. Acta Histochem. 2017;119(2):113–21.
Kakavand M, Yazdanpanah G, Ahmadiani A, Niknejad H. Blood compatibility of human amniotic membrane compared with heparin-coated ePTFE for vascular tissue engineering. J Tissue Eng Regen Med. 2017;11(6):1701–9.
Weber B, Kehl D, Bleul U, Behr L, Sammut S, Frese L, et al. In vitro fabrication of autologous living tissue-engineered vascular grafts based on prenatally harvested ovine amniotic fluid-derived stem cells. J Tissue Eng Regen Med. 2016;10(1):52–70.
Muench MO, Kapidzic M, Gormley M, Gutierrez AG, Ponder KL, Fomin ME et al. The human chorion contains definitive hematopoietic stem cells from the 15th week of gestation. Development. 2017.
Battula VL, Bareiss PM, Treml S, Conrad S, Albert I, Hojak S, et al. Human placenta and bone marrow derived MSC cultured in serum-free, b-FGF-containing medium express cell surface frizzled-9 and SSEA-4 and give rise to multilineage differentiation. Differentiation. 2007;75(4):279–91.
Shariatzadeh S, Shafiee S, Zafari A, Tayebi T, Yazdanpanah G, Majd A, et al. Developing a pro-angiogenic placenta derived amniochorionic scaffold with two exposed basement membranes as substrates for cultivating endothelial cells. Sci Rep. 2021;11(1):22508.
Ventura Ferreira MS, Bienert M, Müller K, Rath B, Goecke T, Opländer C, et al. Comprehensive characterization of chorionic villi-derived mesenchymal stromal cells from human placenta. Stem Cell Res Ther. 2018;9(1):28.
Chien C, Yen BL, Lee F, Lai T, Chen Y, Chan S, et al. In Vitro differentiation of human placenta-derived multipotent cells into hepatocyte‐like cells. Stem Cells. 2006;24(7):1759–68.
Basmaeil YS, Al Subayyil AM, Khatlani T, Bahattab E, Al-Alwan M, Abomaray FM, et al. Human chorionic villous mesenchymal stem/stromal cells protect endothelial cells from injury induced by high level of glucose. Stem Cell Res Ther. 2018;9(1):238.
Schmidt D, Mol A, Breymann C, Achermann J, Odermatt B, Gössi M et al. Living Autologous Heart valves Engineered from Human prenatally harvested progenitors. Circulation. 2006;114(1_supplement).
Weber B, Zeisberger SM, Hoerstrup SP. Prenatally harvested cells for cardiovascular tissue engineering: fabrication of autologous implants prior to birth. Placenta. 2011;32:S316–9.
Yu S, You X, Liang H, Li Y, Fu Y, Zhang X, et al. First trimester placental mesenchymal stem cells improve cardiac function of rat after myocardial infarction via enhanced neovascularization. Heliyon. 2021;7(1):e06120.
Huang Q, Yang Y, Luo C, Wen Y, Liu R, Li S, et al. An efficient protocol to generate placental chorionic plate-derived mesenchymal stem cells with superior proliferative and immunomodulatory properties. Stem Cell Res Ther. 2019;10(1):301.
Schneider KH, Aigner P, Holnthoner W, Monforte X, Nürnberger S, Rünzler D, et al. Decellularized human placenta chorion matrix as a favorable source of small-diameter vascular grafts. Acta Biomater. 2016;29:125–34.
Hashemzadeh MR, Taghavizadeh Yazdi ME, Amiri MS, Mousavi SH. Stem cell therapy in the heart: Biomaterials as a key route. Tissue Cell. 2021;71:101504.
Penn MS, Mangi AA. Genetic enhancement of Stem Cell Engraftment, Survival, and Efficacy. Circ Res. 2008;102(12):1471–82.
Bai X, Yan Y, Coleman M, Wu G, Rabinovich B, Seidensticker M, et al. Tracking long-term survival of Intramyocardially Delivered Human adipose tissue-derived stem cells using Bioluminescence Imaging. Mol Imaging Biol. 2011;13(4):633–45.
Jung J, Na KH, Lee MJ, Moon J, Kim G, Il, Jang JJ, et al. Efficacy of chorionic plate-derived mesenchymal stem cells isolated from placenta in CCl4-injured rat liver depends on transplantation routes. Tissue Eng Regen Med. 2013;10(1):10–7.
Brown C, McKee C, Bakshi S, Walker K, Hakman E, Halassy S, et al. Mesenchymal stem cells: cell therapy and regeneration potential. J Tissue Eng Regen Med. 2019;13(9):1738–55.
Komaki M, Numata Y, Morioka C, Honda I, Tooi M, Yokoyama N, et al. Exosomes of human placenta-derived mesenchymal stem cells stimulate angiogenesis. Stem Cell Res Ther. 2017;8(1):219.
Yang ZX, Han ZB, Ji YR, Wang YW, Liang L, Chi Y, et al. CD106 identifies a subpopulation of mesenchymal stem cells with Unique Immunomodulatory Properties. PLoS ONE. 2013;8(3):e59354.
Alatyyat SM, Alasmari HM, Aleid OA, Abdel-maksoud MS, Elsherbiny N. Umbilical cord stem cells: background, processing and applications. Tissue Cell. 2020;65:101351.
Beiki B, Zeynali B, Seyedjafari E. Fabrication of a three dimensional spongy scaffold using human Wharton’s jelly derived extra cellular matrix for wound healing. Mater Sci Engineering: C. 2017;78:627–38.
Semenova E, Grudniak MP, Machaj EK, Bocian K, Chroscinska-Krawczyk M, Trochonowicz M, et al. Mesenchymal stromal cells from different parts of umbilical cord: Approach to Comparison & characteristics. Stem Cell Rev Rep. 2021;17(5):1780–95.
Semenov V. Mesenchymal stem cells derived from Wharton’s Jelly and their potential for Cardio-Vascular tissue Engineering. Open Tissue Eng Regen Med J. 2011;4(1):64–71.
Hoerstrup SP, Kadner A, Breymann C, Maurus CF, Guenter CI, Sodian R, et al. Living, autologous pulmonary artery conduits tissue engineered from human umbilical cord cells. Ann Thorac Surg. 2002;74(1):46–52.
Dennaoui H, Chouery E, Harmoush C. Endothelial differentiation of Wharton’s Jelly-derived mesenchymal stem cells seeded on chitosan/hyaluronan multilayer films. Cell Ther Transpl. 2020;9(4):59–67.
Qu Q, Wang L, Bing W, Bi Y, Zhang C, Jing X, et al. miRNA-126-3p carried by human umbilical cord mesenchymal stem cell enhances endothelial function through exosome-mediated mechanisms in vitro and attenuates vein graft neointimal formation in vivo. Stem Cell Res Ther. 2020;11(1):464.
Mallis P, Michalopoulos E, Dinou A, Vlachou MS, Panagouli E, Papapanagiotou A, et al. Development of HLA-matched vascular grafts utilizing decellularized human umbilical artery. Hum Immunol. 2018;79(12):855–60.
Mallis P, Sokolis DP, Katsimpoulas M, Kostakis A, Stavropoulos-Giokas C, Michalopoulos E. Improved Repopulation Efficacy of Decellularized Small Diameter Vascular grafts utilizing the cord blood platelet lysate. Bioengineering. 2021;8(9):118.
Mallis P, Papapanagiotou A, Katsimpoulas M, Kostakis A, Siasos G, Kassi E, et al. Efficient differentiation of vascular smooth muscle cells from Wharton’s jelly mesenchymal stromal cells using human platelet lysate: a potential cell source for small blood vessel engineering. World J Stem Cells. 2020;12(3):203–21.
Kunkanjanawan H, Kunkanjanawan T, Khemarangsan V, Yodsheewan R, Theerakittayakorn K, Parnpai R. A Xeno-Free Strategy for Derivation of Human umbilical vein endothelial cells and Wharton’s Jelly Derived Mesenchymal stromal cells: a feasibility study toward personal cell and vascular based therapy. Stem Cells Int. 2020;2020:1–8.
Liu H, Gong X, Jing X, Ding X, Yao Y, Huang Y, et al. Shear stress with appropriate time-step and amplification enhances endothelial cell retention on vascular grafts. J Tissue Eng Regen Med. 2017;11(11):2965–78.
Ardila D, Liou JJ, Maestas D, Slepian M, Badowski M, Wagner W, et al. Surface Modification of Electrospun Scaffolds for endothelialization of tissue-Engineered vascular grafts using human cord blood-derived endothelial cells. J Clin Med. 2019;8(2):185.
Lau SEDCOMWBSCHABRWMFCBU. Low immunogenic endothelial cells maintain morphological and functional properties required for vascular tissue Engineering. Tissue Eng Part A. 2018;24(5–6):432–47.
Hsia K, Yang MJ, Chen WM, Yao CL, Lin CH, Loong CC, et al. Sphingosine-1-phosphate improves endothelialization with reduction of thrombosis in recellularized human umbilical vein graft by inhibiting syndecan-1 shedding in vitro. Acta Biomater. 2017;51:341–50.
Ghorbel MT, Jia H, Swim MM, Iacobazzi D, Albertario A, Zebele C, et al. Reconstruction of the pulmonary artery by a novel biodegradable conduit engineered with perinatal stem cell-derived vascular smooth muscle cells enables physiological vascular growth in a large animal model of congenital heart disease. Biomaterials. 2019;217:119284.
Woods I, Black A, Molloy EJ, Jockenhoevel S, Flanagan TC. Fabrication of blood-derived elastogenic vascular grafts using electrospun fibrinogen and polycaprolactone composite scaffolds for paediatric applications. J Tissue Eng Regen Med. 2020;term.3100.
Gökçinar-Yagci B, Yersal N, Korkusuz P, Çelebi-Saltik B. Generation of human umbilical cord vein CD146 + perivascular cell origined three-dimensional vascular construct. Microvasc Res. 2018;118:101–12.
Çelebi-Saltik B, Öteyaka MÖ, Gökçinar-Yagci B. Stem cell-based small-diameter vascular grafts in dynamic culture. Connect Tissue Res. 2021;62(2):151–63.
Gu WHXLBANWBSDJXYHYRXXQ. Smooth muscle cells differentiated from human mesenchymal stem cells regulated by microRNA (miR)-503 and mir-222-5p are suitable for vascular tissue engineering. J Biol Chem. 2018;293(21):8089–102.
Sasagawa T, Shimizu T, Yamato M, Okano T. Endothelial colony-forming cells for preparing prevascular three-dimensional cell-dense tissues using cell-sheet engineering. J Tissue Eng Regen Med. 2016;10(9):739–47.
Cathery W, Faulkner A, Jover E, Rodriguez-Arabaolaza I, Thomas AC, Avolio E et al. Umbilical cord pericytes provide a viable alternative to mesenchymal stem cells for neonatal Vascular Engineering. Front Cardiovasc Med. 2021;7.
Muniswami DM, Reddy LVK, Amirtham SM, Babu S, Raj AN, Sen D, et al. Endothelial progenitor/stem cells in engineered vessels for vascular transplantation. J Mater Sci Mater Med. 2020;31(12):119.
Chlupac J, Matejka R, Konarik M, Novotny R, Simunkova Z, Mrazova I, et al. Vascular remodeling of clinically used patches and decellularized pericardial matrices recellularized with autologous or allogeneic cells in a porcine carotid artery model. Int J Mol Sci. 2022;23(6):3310.
Keshi E, Tang P, Weinhart M, Everwien H, Moosburner S, Seiffert N, et al. Surface modification of decellularized bovine carotid arteries with human vascular cells significantly reduces their thrombogenicity. J Biol Eng. 2021;15(1):26.
Macias MI, Grande J, Moreno A, Domínguez I, Bornstein R, Flores AI. Isolation and characterization of true mesenchymal stem cells derived from human term decidua capable of multilineage differentiation into all 3 embryonic layers. Am J Obstet Gynecol. 2010;203(5):495.e9-495.e23.
Abomaray FM, Al Jumah MA, Alsaad KO, Jawdat D, Al Khaldi A, AlAskar AS, et al. Phenotypic and functional characterization of mesenchymal Stem/Multipotent stromal cells from Decidua Basalis of Human Term Placenta. Stem Cells Int. 2016;2016:1–18.
Cerrada A, de la Torre P, Grande J, Haller T, Flores AI, Pérez-Gil J. Human decidua-derived mesenchymal stem cells differentiate into functional alveolar type II-Like cells that synthesize and secrete pulmonary surfactant complexes. PLoS ONE. 2014;9(10):e110195.
Bravo B, Gallego MI, Flores AI, Bornstein R, Puente-Bedia A, Hernández J, et al. Restrained Th17 response and myeloid cell infiltration into the central nervous system by human decidua-derived mesenchymal stem cells during experimental autoimmune encephalomyelitis. Stem Cell Res Ther. 2016;7(1):43.
Chen K, Bai L, Lu J, Chen W, Liu C, Guo E et al. Human decidual mesenchymal stem cells obtained from early pregnancy improve Cardiac Revascularization Postinfarction by activating Ornithine Metabolism. Front Cardiovasc Med. 2022;9.
Alshareef GHMAAMBY. Phenotypic and functional responses of human decidua basalis mesenchymal stem/stromal cells to lipopolysaccharide of gram-negative bacteria. Stem Cells Cloning. 2021;51–69.
Guan Y, Xie Y, Li D, Zhu Y, Zhang X, Feng Y et al. Comparison of biological characteristics of mesenchymal stem cells derived from the human umbilical cord and decidua parietalis. Mol Med Rep. 2019.
Sher N, Ofir R. Clinical Development and commercialization of placenta-derived cell therapy. Perinatal stem cells. Elsevier; 2018. pp. 357–75.
Norgren L, Weiss N, Nikol S, Hinchliffe RJ, Lantis JC, Patel MR, et al. PLX-PAD cell treatment of critical limb ischaemia: rationale and design of the PACE trial. Eur J Vasc Endovasc Surg. 2019;57(4):538–45.
Gao LR, Chen Y, Zhang NK, Yang XL, Liu HL, Wang ZG, et al. Intracoronary infusion of Wharton’s jelly-derived mesenchymal stem cells in acute myocardial infarction: double-blind, randomized controlled trial. BMC Med. 2015;13:1–15.
Kim DW, Staples M, Shinozuka K, Pantcheva P, Kang SD, Borlongan CV. Wharton’s jelly-derived mesenchymal stem cells: phenotypic characterization and optimizing their therapeutic potential for clinical applications. Int J Mol Sci. 2013;14(6):11692–712.
’Hsu S, Shyu WC. Clinical trial.gov NCT04434768. 2020 [cited 2024 Apr 22]. Evaluate the Safety and Explore Efficacy of Umbilical Cord Mesenchymal Stem Cells in Acute Ischemic Stroke. https://clinicaltrials.gov/study/NCT04434768 .
’Agus Aulia M. Clinical trial.gov. 2022 [cited 2024 Apr 22]. Combination of Conditioned Medium and Umbilical Cord-Mesenchymal Stem Cells Therapy for Acute Stroke Infarct. https://clinicaltrials.gov/study/NCT05008588 .
’Shen C. ’LU G. Clinical trials.gov. 2023 [cited 2024 Apr 22]. UC-MSC Transplantation for Left Ventricular Dysfunction After AMI. https://clinicaltrials.gov/study/NCT03902067 .
Malek A, Bersinger NA. Human placental stem cells: biomedical potential and clinical relevance. J Stem Cells. 2011;6(2):75.
PubMed Google Scholar
Download references
Acknowledgements
No funding was received for conducting this study.
Author information
Mehdi Amiri Goushki and Zahra kharat contributed equally to this work as co-first authors.
Authors and Affiliations
Department of Life Science Engineering, Faculty of New Sciences & Technologies, University of Tehran, Tehran, 14395-1561, Iran
Mehdi Amiri Goushki & Zahra Kharat
Department of Biotechnology, College of Science, University of Tehran, Tehran, 14155-6455, Iran
Mahboubeh Kabiri
School of Biology, College of Sciences, University of Tehran, Tehran, 1417614411, Iran
Mousa Kehtari
National Institute of Genetic Engineering and Biotechnology, Tehran, 1497716316, Iran
Alireza Naderi Sohi
Stem Cell Technology Research Center, Tehran, 15856-36473, Iran
Hana Hanaee Ahvaz, Iman Rad & Fatemeh Kouhkan
Department of Tissue Engineering and Regenerative Medicine, School of Advanced Technologies in Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Simzar HosseinZadeh
You can also search for this author in PubMed Google Scholar
Contributions
MK designed the study, supervised the work, and provided comments. MAG and ZK were responsible for creating the tables and figures. ANS, HHA, MKe, IR, SH, MAG, ZK, and FK contributed to drafting the initial manuscript sections and subsequently revised them. MAG and ZK also participated in modifying and proofreading the initial draft. All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Mahboubeh Kabiri .
Ethics declarations
Ethics approval and consent to participate, consent for publication, ai disclosure.
The authors declare that artificial intelligence is not used in this study.
Competing interests
There are no known competing financial interests or personal relationships that influence this paper.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Goushki, M.A., Kharat, Z., Kehtari, M. et al. Applications of extraembryonic tissue-derived cells in vascular tissue regeneration. Stem Cell Res Ther 15 , 205 (2024). https://doi.org/10.1186/s13287-024-03784-3
Download citation
Received : 29 February 2024
Accepted : 06 June 2024
Published : 09 July 2024
DOI : https://doi.org/10.1186/s13287-024-03784-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Vascular tissue regeneration
- perinatal tissues
Stem Cell Research & Therapy
ISSN: 1757-6512
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 06 August 2022
Stem cell-based therapy for human diseases
- Duc M. Hoang ORCID: orcid.org/0000-0001-5444-561X 1 ,
- Phuong T. Pham 2 ,
- Trung Q. Bach 1 ,
- Anh T. L. Ngo 2 ,
- Quyen T. Nguyen 1 ,
- Trang T. K. Phan 1 ,
- Giang H. Nguyen 1 ,
- Phuong T. T. Le 1 ,
- Van T. Hoang 1 ,
- Nicholas R. Forsyth 3 ,
- Michael Heke 4 &
- Liem Thanh Nguyen 1
Signal Transduction and Targeted Therapy volume 7 , Article number: 272 ( 2022 ) Cite this article
76k Accesses
288 Citations
66 Altmetric
Metrics details
- Mesenchymal stem cells
- Stem-cell research
Recent advancements in stem cell technology open a new door for patients suffering from diseases and disorders that have yet to be treated. Stem cell-based therapy, including human pluripotent stem cells (hPSCs) and multipotent mesenchymal stem cells (MSCs), has recently emerged as a key player in regenerative medicine. hPSCs are defined as self-renewable cell types conferring the ability to differentiate into various cellular phenotypes of the human body, including three germ layers. MSCs are multipotent progenitor cells possessing self-renewal ability (limited in vitro) and differentiation potential into mesenchymal lineages, according to the International Society for Cell and Gene Therapy (ISCT). This review provides an update on recent clinical applications using either hPSCs or MSCs derived from bone marrow (BM), adipose tissue (AT), or the umbilical cord (UC) for the treatment of human diseases, including neurological disorders, pulmonary dysfunctions, metabolic/endocrine-related diseases, reproductive disorders, skin burns, and cardiovascular conditions. Moreover, we discuss our own clinical trial experiences on targeted therapies using MSCs in a clinical setting, and we propose and discuss the MSC tissue origin concept and how MSC origin may contribute to the role of MSCs in downstream applications, with the ultimate objective of facilitating translational research in regenerative medicine into clinical applications. The mechanisms discussed here support the proposed hypothesis that BM-MSCs are potentially good candidates for brain and spinal cord injury treatment, AT-MSCs are potentially good candidates for reproductive disorder treatment and skin regeneration, and UC-MSCs are potentially good candidates for pulmonary disease and acute respiratory distress syndrome treatment.
Similar content being viewed by others

Mesenchymal stem cell perspective: cell biology to clinical progress

Mesenchymal stem cell-derived extracellular vesicles for immunomodulation and regeneration: a next generation therapeutic tool?

Next-generation stem cells — ushering in a new era of cell-based therapies
Introduction.
The successful approval of cancer immunotherapies in the US and mesenchymal stem cell (MSC)-based therapies in Europe have turned the wheel of regenerative medicine to become prominent treatment modalities. 1 , 2 , 3 Cell-based therapy, especially stem cells, provides new hope for patients suffering from incurable diseases where treatment approaches focus on management of the disease not treat it. Stem cell-based therapy is an important branch of regenerative medicine with the ultimate goal of enhancing the body repair machinery via stimulation, modulation, and regulation of the endogenous stem cell population and/or replenishing the cell pool toward tissue homeostasis and regeneration. 4 Since the stem cell definition was introduced with their unique properties of self-renewal and differentiation, they have been subjected to numerous basic research and clinical studies and are defined as potential therapeutic agents. As the main agenda of regenerative medicine is related to tissue regeneration and cellular replacement and to achieve these targets, different types of stem cells have been used, including human pluripotent stem cells (hPSCs), multipotent stem cells and progenitor cells. 5 However, the emergence of private and unproven clinics that claim the effectiveness of stem cell therapy as “magic cells” has raised highly publicized concerns about the safety of stem cell therapy. The most notable case involved the injection of a cell population derived from fractionated lipoaspirate into the eyes of three patients diagnosed with macular degeneration, resulting in the loss of vision for these patients. 6 Thus, as regenerative medicine continues to progress and evolve and to clear the myth of the “magic” cells, this review provides a brief overview of stem cell-based therapy for the treatment of human diseases.
Stem cell therapy is a novel therapeutic approach that utilizes the unique properties of stem cells, including self-renewal and differentiation, to regenerate damaged cells and tissues in the human body or replace these cells with new, healthy and fully functional cells by delivering exogenous cells into a patient. 7 Stem cells for cell-based therapy can be of (1) autologous, also known as self-to-self therapy, an approach using the patient’s own cells, and (2) allogeneic sources, which use cells from a healthy donor for the treatment. 8 The term “stem cell” were first used by the eminent German biologist Ernst Haeckel to describe the properties of fertilized egg to give rise to all cells of the organism in 1868. 9 The history of stem cell therapy started in 1888, when the definition of stem cell was first coined by two German zoologists Theodor Heinrich Boveri and Valentin Haecker, 9 who set out to identify the distinct cell population in the embryo capable of differentiating to more specialized cells (Fig. 1a ). In 1902, studies carried out by the histologist Franz Ernst Christian Neumann, who was working on bone marrow research, and Alexander Alexandrowitsch Maximov demonstrated the presence of common progenitor cells that give rise to mature blood cells, a process also known as haematopoiesis. 10 From this study, Maximov proposed the concept of polyblasts, which later were named stem cells based on their proliferation and differentiation by Ernst Haeckel. 11 Maximov described a hematopoietic population presented in the bone marrow. In 1939, the first case report described the transplantation of human bone marrow for a patient diagnosed with aplastic anemia. Twenty years later, in 1958, the first stem cell transplantation was performed by the French oncologist George Mathe to treat six nuclear researchers who were accidentally exposed to radioactive substances using bone marrow transplantation. 12 Another study by George Mathe in 1963 shed light on the scientific community, as he successfully conducted bone marrow transplantation in a patient with leukemia. The first allogeneic hematopoietic stem cell transplantation (HSCT) was pioneered by Dr. E. Donnall Thomas in 1957. 13 In this initial study, all six patients died, and only two patients showed evidence of transient engraftment due to the unknown quantities and potential hazards of bone marrow transplantation at that time. In 1969, Dr. E. Donnall Thomas conducted the first bone marrow transplantation in the US, although the success of the allogeneic treatment remained exclusive. In 1972, the year marked the discovery of cyclosporine (the immune suppressive drug), 14 the first successes of allogeneic transplantation for aplastic anemia and acute myeloid leukemia were reported in a 16-year-old girl. 15 From the 1960s to the 1970s, series of works conducted by Friendenstein and coworkers on bone marrow aspirates demonstrated the relationship between osteogenic differentiation and a minor subpopulation of cells derived from bone marrow. 16 These cells were later proven to be distinguishable from the hematopoietic population and to be able to proliferate rapidly as adherent cells in tissue culture vessels. Another important breakthrough from Friendenstein’s team was the discovery that these cells could form the colony-forming unit when bone marrow was seeded as suspension culture following by differentiation into osteoblasts, adipocytes, and chondrocytes, suggesting that these cells confer the ability to proliferate and differentiate into different cell types. 17 In 1991, combined with the discovery of human embryonic stem cells (hESCs), which will be discussed in the next section, the term “mesenchymal stem cells”, previously known as stromal stem cells or “osteogenic” stem cells, was first coined in Caplan and widely used to date. 18 Starting with bone marrow transplantation 60 years ago, the journey of stem cell therapy has developed throughout the years to become a novel therapeutic agent of regenerative medicine to treat numerous incurable diseases, which will be reviewed and discussed in this review, including neurological disorders, pulmonary dysfunctions, metabolic/endocrine-related diseases, reproductive disorders, skin burns, and cardiovascular conditions).
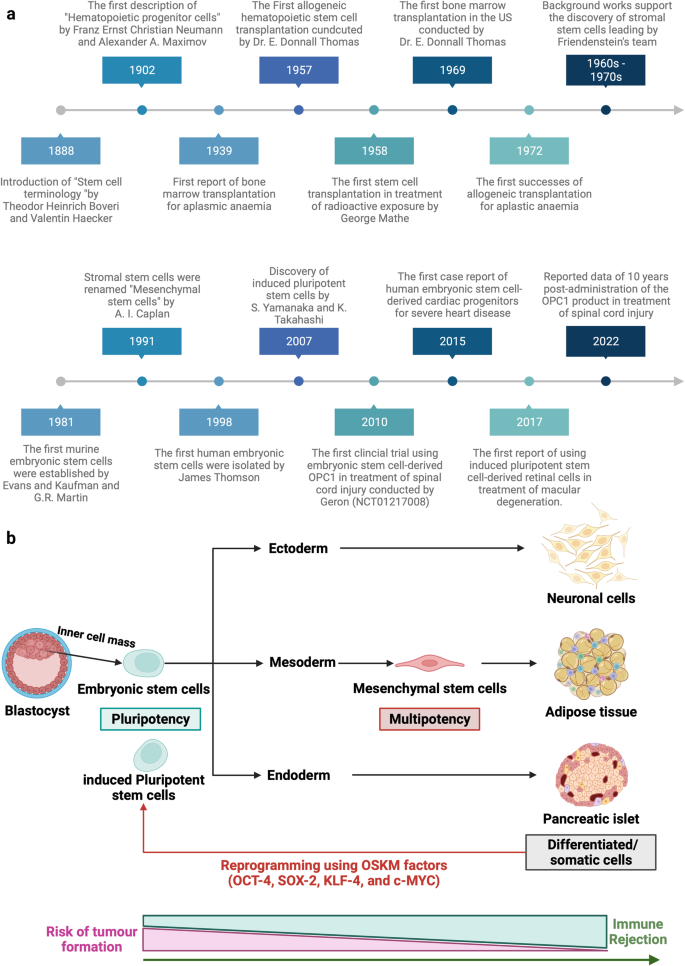
Stem cell-based therapy: the history and cell source. a The timeline of major discoveries and advances in basic research and clinical applications of stem cell-based therapy. The term “stem cells” was first described in 1888, setting the first milestone in regenerative medicine. The hematopoietic progenitor cells were first discovered in 1902. In 1939, the first bone marrow transplantation was conducted in the treatment of aplasmic anemia. Since then, the translation of basic research to preclinical studies to clinical trials has driven the development of stem cell-based therapy by many discoveries and milestones. The isolations of “mesenchymal stem cells” in 1991 following by the discovery of human pluripotent stem cells have recently contributed to the progress of stem cell-based therapy in the treatment of human diseases. b Schematic of the different cell sources that can be used in stem cell-based therapy. (1) Human pluripotent stem cells, including embryonic stem cells (derived from inner cell mass of blastocyst) and induced pluripotent stem cells confer the ability to proliferate indefinitely in vitro and differentiate into numerous cell types of the human body, including three germ layers. (2) Mesenchymal stem cells are multipotent stem cells derived from mesoderm possessing self-renewal ability (limited in vitro) and differentiation potential into mesenchymal lineages. The differentiated/somatic cells can be reprogrammed back to the pluripotent stage using OSKM factors to generate induced pluripotent stem cells. It is important to note that stem cells show a relatively higher risk of tumor formation and lower risk of immune rejection (in the case of mesenchymal stem cells) when compared to that of somatic cells. The figure was created with BioRender.com
In this review, we described the different types of stem cell-based therapies (Fig. 1b ), including hPSCs and MSCs, and provided an overview of their definition, history, and outstanding clinical applications. In addition, we further created the first literature portfolio for the “targeted therapy” of MSCs based on their origin, delineating their different tissue origins and downstream applications with an in-depth discussion of their mechanism of action. Finally, we provide our perspective on why the tissue origin of MSCs could contribute greatly to their downstream applications as a proposed hypothesis that needs to be proven or disproven in the future to further enhance the safety and effectiveness of stem cell-based therapy.
Stem cell-based therapy: an overview of current clinical applications
Cardiovascular diseases.
The clinical applications of stem cell-based therapies for heart diseases have been recently discussed comprehensively in the reviews 19 , 20 and therefore will be elaborated in this study as the focus discussions related to hPSCs and MSCs in the following sections. In general, the safety profiles of stem cell-based therapies are supported by a large body of preclinical and clinical studies, especially adult stem cell therapy (such as MSC-based products). However, clinical trials have not yet yielded data supporting the efficacy of the treatment, as numerous studies have shown paradoxical results and no statistically significant differences in infarct size, cardiac function, or clinical outcomes, even in phase III trials. 21 The results of a meta-analysis showed that stem cells derived from different sources did not exhibit any therapeutic effects on the improvement of myocardial contractility, cardiovascular remodeling, or clinical outcomes. 22 The disappointing results obtained from the clinical trials thus far could be explained by the fact that the administered cells may exert their therapeutic effects via an immune modulation rather than regenerative function. Thus, well-designed, randomized and placebo-controlled phase III trials with appropriate cell-preparation methods, patient selection, follow-up schedules and suitable clinical measurements need to be conducted to determine the efficacy of the treatments. In addition, concerns related to optimum cell source and dose, delivery route and timing of administration, cell distribution post administration and the mechanism of action also need to be addressed. In the following section of this review, we present clinical trials related to MSC-based therapy in cardiovascular disease with the aim of discussing the contradictory results of these trials and analyzing the potential challenges underlying the current approaches.
Digestive system diseases
Gastrointestinal diseases are among the most diagnosed conditions in the developed world, altering the life of one-third of individuals in Western countries. The gastrointestinal tract is protected from adverse substances in the gut environment by a single layer of epithelial cells that are known to have great regenerative ability in response to injuries and normal cell turnover. 23 These epithelial cells have a rapid turnover rate of every 2–7 days under normal conditions and even more rapidly following tissue damage and inflammation. This rapid proliferation ability is possible owing to the presence of a specific stem cell population that is strictly compartmentalized in the intestinal crypts. 24 The gastrointestinal tract is highly vulnerable to damage, tissue inflammation and diseases once the degradation of the mucosal lining layer occurs. The exposure of intestinal stem cells to the surrounding environment of the gut might result in the direct destruction of the stem cell layer or disruption of intestinal functions and lead to overt clinical symptoms. 25 In addition, the accumulation of stem cell defects as well as the presence of chronic inflammation and stress also contributes to the reduction of intestinal stem cell quality.
In terms of digestive disorders, Crohn’s disease (CD) and ulcerative colitis are the two major forms of inflammatory bowel disease (IBD) and represent a significant burden on the healthcare system. The former is a chronic, uncontrolled inflammatory condition of the intestinal mucosa characterized by segmental transmural mucosal inflammation and granulomatous changes. 26 The latter is a chronic inflammatory bowel disease affecting the colon and rectum, characterized by mucosal inflammation initiating in the rectum and extending proximal to the colon in a continuous fashion. 27 Cellular therapy in the treatment of CD can be divided into haematopoietic stem cell-based therapy and MSC-based therapy. The indication and recommendation of using HSCs for the treatment of IBD were proposed in 1995 by an international committee with four important criteria: (1) refractory to immunosuppressive treatment; (2) persistence of the disease conditions indicated via endoscopy, colonoscopy or magnetic resonance enterography; (3) patients who underwent an imminent surgical procedure with a high risk of short bowel syndromes or refractory colonic disease; and (4) patients who refused to treat persistent perianal lesions using coloproctectomy with a definitive stroma implant. 28 In the standard operation procedure, patents’ HSCs were recruited using cyclophosphamide, which is associated with granulocyte colony-stimulating factor (G-CSF), at two different administered concentrations (4 g/m 2 and 2 g/m 2 ). Recently, it was reported that high doses of cyclophosphamide do not improve the number of recruited HSCs but increase the risk of cardiac and bladder toxicity. An interest in using HSCTs in CD originated from case reports that autologous HSCTs can induce sustained disease remission in some 29 , 30 but not all patients 31 , 32 , 33 with CD. The first phase I trial was conducted in Chicago and recruited 12 patients with active moderate to severe CD refractory to conventional therapies. Eleven of 12 patients demonstrated sustained remission after a median follow-up of 18.5 months, and one patient developed recurrence of active CD. 31 The ASTIC trial (the Autologous Stem Cell Transplantation International Crohn Disease) was the first randomized clinical trial with the largest cohort of patients undergoing HSCT for refractory CD in 2015. 34 The early report of the trial showed no statistically significant improvement in clinical outcomes of mobilization and autologous HSCT compared with mobilization followed by conventional therapy. In addition, the procedure was associated with significant toxicity, leading to the suggestion that HSCT for patients with refractory CD should not be widespread. Interestingly, by using conventional assessments for clinical trials for CD, a group reassessed the outcomes of patients enrolled in the ASTIC trial showing clinical and endoscopic benefits, although a high number of adverse events were also detected. 35 A recent systematic review evaluated 18 human studies including 360 patients diagnosed with CD and showed that eleven studies confirmed the improvement of Crohn’s disease activity index between HSCT groups compared to the control group. 36 Towards the cell sources, HSCs are the better sources as they afforded more stable outcomes when compared to that of MSC-based therapy. 37 Moreover, autologous stem cells were better than their allogeneic counterparts. 36 The safety of stem cell-based therapy in the treatment of CD has attracted our attention, as the risk of infection in patients with CD was relatively higher than that in those undergoing administration to treat cancer or other diseases. During the stem cell mobilization process, patient immunity is significantly compromised, leading to a high risk of infection, and requires carefully nursed and suitable antibiotic treatment to reduce the development of adverse events. Taken together, stem cell-based therapy for digestive disease reduced inflammation and improved the patient’s quality of life as well as bowel functions, although the high risk of adverse events needs to be carefully monitored to further improve patient safety and treatment outcomes.
Liver diseases
The liver is the largest vital organ in the human body and performs essential biological functions, including detoxification of the organism, metabolism, supporting digestion, vitamin storage, and other functions. 38 The disruption of liver homeostasis and function might lead to the development of pathological conditions such as liver failure, cirrhosis, cancer, alcoholic liver disease, nonalcoholic fatty liver disease (NAFLD), and autoimmune liver disease (ALD). Orthotropic liver transplantation is the only effective treatment for severe liver diseases, but the number of available and suitable donor organs is very limited. Currently, stem cell-based therapies in the treatment of liver disease are associated with HSCs, MSCs, hPSCs, and liver progenitor cells.
Liver failure is a critical condition characterized by severe liver dysfunctions or decompensation caused by numerous factors with a relatively high mortality rate. Stem cell-based therapy is a novel alternative approach in the treatment of liver failure, as it is believed to participate in the enhancement of liver regeneration and recovery. The results of a meta-analysis including four randomized controlled trials and six nonrandomized controlled trials in the treatment of acute-on-chronic liver failure (ACLF) demonstrated that clinical outcomes of stem cell therapy were achieved in the short term, requiring multiple doses of stem cells to prolong the therapeutic effects. 39 , 40 Interestingly, although MSC-based therapies improved liver functions, including the model of end-stage liver disease score, albumin level, total bilirubin, and coagulation, beneficial effects on survival rate and aminotransferase level were not observed. 41 A randomized controlled trial illustrated the improvement of liver functions and reduction of severe infections in patients with hepatitis B virus-related ACLF receiving allogeneic bone marrow-derived MSCs (BM-MSCs) via peripheral infusion. 42 HSCs from peripheral blood after the G-CSF mobilization process were used in a phase I clinical trial and exhibited an improvement in serum bilirubin and albumin in patients with chronic liver failure without any specific adverse events related to the administration. 43 Taken together, an overview of stem cell-based therapy in the treatment of liver failure indicates the potential therapeutic effects on liver functions with a strong safety profile, although larger randomized controlled trials are still needed to assure the conclusions.
Liver cirrhosis is one of the major causes of morbidity and mortality worldwide and is characterized by diffuse nodular regeneration with dense fibrotic septa and subsequent parenchymal extinction leading to the collapse of liver vascular structure. 44 In fact, liver cirrhosis is considered the end-stage of liver disease that eventually leads to death unless liver transplantation is performed. Stem cell-based therapy, especially MSCs, currently emerges as a potential treatment with encouraging results for treating liver cirrhosis. In a clinical trial using umbilical cord-derived MSCs (UC-MSCs), 45 chronic hepatitis B patients with decompensated liver cirrhosis were divided into two groups: the MSC group ( n = 30) and the control group ( n = 15). 45 The results showed a significant reduction in ascites volume in the MSC group compared with the control. Liver function was also significantly improved in the MSC groups, as indicated by the increase in serum albumin concentration, reduction in total serum bilirubin levels, and decrease in the sodium model for end-stage liver disease score. 45 Similar results were also reported from a phase II trial using BM-MSCs in 25 patients with HCV-induced liver cirrhosis. 46 Consistent with these studies, three other clinical trials targeting liver cirrhosis caused by hepatitis B and alcoholic cirrhosis were conducted and confirmed that MSC administration enhanced and recovered liver functions. 47 , 48 , 49 With the large cohort study as the clinical trial conducted by Fang, the safety and potential therapeutic effects of MSC-based therapies could be further strengthened and confirmed the feasibility of the treatment in virus-related liver cirrhosis. 49 In terms of delivery route, a randomized controlled phase 2 trial suggested that systemic delivery of BM-MSCs does not show therapeutic effects on patients with liver cirrhosis. 50 MSCs are not the only cell source for liver cirrhosis. Recently, an open-label clinical trial conducted in 19 children with liver cirrhosis due to biliary atresia after the Kasai operation illustrated the safety and feasibility of the approach by showing the improvement of liver function after bone marrow mononuclear cell (BMNC) administration assessed by biochemical tests and pediatric end-stage liver disease (PELD) scores. 51 Another study using BMNCs in 32 decompensated liver cirrhosis patients illustrated the safety and effectiveness of BMNC administration in comparison with the control group. 52 Recently, a long-term analysis of patients receiving peripheral blood-derived stem cells indicated a significant improvement in the long-term survival rate when compared to the control group, and the risk of hepatocellular carcinoma formation did not increase. 53 CD133 + HSC infusion was performed in a multicentre, open, randomized controlled phase 2 trial in patients with liver cirrhosis; the results did not support the improvement of liver conditions, and cirrhosis persisted. 54 Notably, these results are in line with a previous randomized controlled study, which also reported that G-CSF and bone marrow-derived stem cells delivered via the hepatic artery did not introduce therapeutic potential as expected. 55 Thus, stem cell-based therapy for liver cirrhosis is still in its immature stage and requires larger trials with well-designed experiments to confirm the efficacy of the treatment.
Nonalcoholic fatty liver disease (NAFLD) is the most common medical condition caused by genetic and lifestyle factors and results in a severe liver condition and increased cardiovascular risk. 56 NAFLD is the hidden enemy, as most patients are asymptomatic for a long time, and their routine life is unaffected. Thus, the detection, identification, and management of NAFLD conditions are challenging tasks, as patients diagnosed with NAFLD often develop nonalcoholic steatohepatitis, cirrhosis, and hepatocellular carcinoma. 57 Although preclinical studies have shown that stem cell administration could enhance liver function in NAFLD models, a limited number of clinical trials were performed in human subjects. Recently, a multi-institutional clinical trial using freshly isolated autologous adipose tissue-derived regenerative cells was performed in Japan to treat seven NAFLD patients. 58 The results illustrated the improvement in the serum albumin level of six patients and prothrombin activity of five patients, and no treatment-related adverse events or severe adverse events were observed. This study illustrates the therapeutic potential of stem cell-based therapy in the treatment of NAFLD.
Autoimmune liver disease (ALD) is a severe liver condition affecting children and adults worldwide, with a female predominance. 59 The condition occurs in genetically predisposed patients when a stimulator, such as virus infection, leads to a T-cell-mediated autoimmune response directed against liver autoantigens. As a result, patients with ALD might develop liver cirrhosis, hepatocellular carcinoma, and, in severe cases, death. To date, HSCT and bone marrow transplantation are the two common stem cell-based therapies exhibiting therapeutic potential for ALD in clinical trials. An interesting report illustrated that haploidentical HSCTs could cure ALD in patients with sickle cells. 60 This report is particularly important, as it illustrates the potential therapeutic approach of using haploidentical HSCTs to treat patients with both sickle cells and ALD. Another case report described a 19-year-old man with a 4-year history of ALD who developed acute lymphoblastic leukemia and required allogeneic bone marrow transplantation from this wholesome brother. 61 The clinical data showed that immunosuppressive therapy for transplantation generated ALD remission in the patient. 62 However, the data also provided valid information related to the sustained remission and the normalization of ASGPR-specific suppressor-inducer T-cell activity following bone marrow transplantation, suggesting that these suppressor functions originated from donor T cells. 61 Thus, it was suggested that if standard immunosuppressive treatment fails, alternative cellular immunotherapy would be a viable option for patients with ALD. Primary biliary cholangitis (PBC), usually known as primary biliary cirrhosis, is a type of ALD characterized by a slow, progressive destruction of small bile ducts of the liver leading to the formation of cirrhosis and accumulation of bile and other toxins in the liver. A pilot, single-arm trial from China recruited seven patents with PBC who had a suboptimal response to ursodeoxycholic acid (UDCA) treatment. 63 These patients received UDCA treatment in combination with three rounds of allogeneic UC-MSCs at 4-week intervals with a dose of 0.5 × 10 6 cells/kg of patient body weight via the peripheral vein. No treatment-related adverse events or severe adverse events were observed throughout the course of the study. The clinical data indicated significant improvement in liver function, including reduction of serum ALP and gamma-glutamyltransferase (GGT) at 48 weeks post administration. The common symptoms of PBC, including fatigue, pruritus, and hypogastric ascites volume, were also reduced, supporting the feasibility of MSC-based therapy in the treatment of PBC, although major limitations of the study were nonrandomized, no control group and small sample size. Another study was conducted in China with ten PBC patients who underwent incompetent UDCA treatment for more than 1 year. These patients received a range of 3–5 allogeneic BM-MSCs/kg body weight by intravenous infusion. 64 Although these early studies have several limitations, such as small sample size, nonrandomization, and no control group, their preliminary data related to safety and efficacy herald the prospects and support the feasibility of stem cell-based therapy in the treatment of ALD.
In summary, the current number of trials for liver disease using stem cell-based therapy has provided fundamental data supporting the safety and potential therapeutic effects in various liver diseases. Unfortunately, due to the small number of trials, several obstacles need to be overcome to prove the effectiveness of the treatments, including (1) stem cell source and dose, (2) administration route, (3) time of intervention, and (4) clinical assessments during the follow-up period. Only by addressing these challenges we will be able to prove, facilitate and promote stem cell-based therapy as a mainstream treatment for liver diseases.
Arthritis is a general term describing cartilage conditions that cause pain and inflammation of the joints. Osteoarthritis (OA) is the most common form of arthritis caused by persistent degeneration and poor recovery of articular cartilage. 65 OA affects one or several diarthrodial joints, such as small joints at the hand and large joints at the knee and hips, leading to severe pain and subsequent reduction in the mobility of patients. There are two types of OA: (1) primary OA or idiopathic OA and secondary OA caused by causative factors such as trauma, surgery, and abnormal joint development at birth. 66 As conventional treatments for OA are not consistent in their effectiveness and might cause unbearable pain as well as long-term rehabilitation (in the case of joint replacement), there is a need for a more reliable, less painful, and curative therapy targeting the root of OA. 67 Thus, stem cell therapy has recently emerged as an alternative approach for OA and has drawn great attention in the regenerative field.
The administration of HSCs has been proven to reduce bone lesions, enhance bone regeneration and stimulate the vascularization process in degenerative cartilage. Attempts were made to evaluate the efficacy of peripheral blood stem cells in ten OA patients by three intraarticular injections. Post-administration analysis indicated a reduction in the WOMAC index with a significant reduction in all parameters. All patients completed 6-min walk tests with an increase of more than 54 meters. MRI analysis indicated an improvement in cartilage thickness, suggesting that cartilage degeneration was reduced post administration. To further enhance the therapeutic potential of HSCT, CD34 + stem cells were proposed to be used in combination with the rehabilitation algorithm, which included three stages: preoperative, hospitalization and outpatient periods. 68 Currently, a large wave of studies has been directed to MSC-based therapy for the treatment of OA due to their immunoregulatory functions and anti-inflammatory characteristics. MSCs have been used as the main cell source in several multiple and small-scale trials, proving their safety profile and potential effectiveness in alleviating pain, reducing cartilage degeneration, and enhancing the regeneration of cartilage structure and morphology in some cases. However, the best source of MSCs, whether from bone marrow, adipose tissue, or umbilical cord, for the management of OA is still a great question to be answered. A systematic review investigating over sixty-one of 3172 articles with approximately 2390 OA patients supported the positive effects of MSC-based therapy on OA patients, although the study also pointed out the fact that these therapeutic potentials were based on limited high-quality evidence and long-term follow-up. 69 Moreover, the study found no obvious evidence supporting the most effective source of MSCs for treating OA. Another systematic review covering 36 clinical trials, of which 14 studies were randomized trials, provides an interesting view in terms of the efficacy of autologous MSC-based therapy in the treatment of OA. 70 In terms of BM-MSCs, 14 clinical trials reported the clinical outcomes at the 1-year follow-up, in which 57% of trials reported clinical outcomes that were significantly better in comparison with the control group. However, strength analysis of the data set showed that outcomes from six trials were low, whereas the outcomes of the remaining eight trials were extremely low. Moreover, the positive evidence obtained from MRI analysis was low to very low strength of evidence after 1-year post administration. 70 Similar results were also found in the outcome analysis of autologous adipose tissue-derived MSCs (AT-MSCs). Thus, the review indicated low quality of evidence for the therapeutic potential of MSC therapy on clinical outcomes and MRI analysis. The low quality of clinical outcomes could be explained by the differences in interventions (including cell sources, cell doses, and administration routes), combination treatments (with hyaluronic acid, 71 peripheral blood plasma, 72 etc.), control treatments and clinical outcome measurements between randomized clinical trials. 73 In addition, the data of the systematic analysis could not prove the better source of MSCs for OA treatment. Taken together, although stem cell-based therapy has been shown to be safe and feasible in the management of OA, the authors support the notion that stem cell-based therapy could be considered an alternative treatment for OA when first-line treatments, such as education, exercise, and body weight management, have failed.
Cancer treatment
Stem cell therapy in the treatment of cancer is a sensitive term and needs to be used and discussed with caution. Clinicians and researchers should protect patients with cancer from expensive and potentially dangerous or ineffective stem cell-based therapy and patients without a cancer diagnosis from the risk of malignancy development. In general, unproven stem cell clinics employed three cell-based therapies for cancer management, including autologous HSCTs, stromal vascular fraction (SVF), and multipotent stem cells, such as MSCs. Allogeneic HSCTs confer the ability to generate donor lymphocytes that contribute to the suppression and regression of hematological malignancies and select solid tumors, a specific condition known as “graft-versus-tumor effects”. 74 However, stem cell clinics provide allogeneic cell-based therapy for the treatment of solid malignancies despite limited scientific evidence supporting the safety and efficacy of the treatment. High-quality evidence from the Cochrane library shows that marrow transplantation via autologous HSCTs in combination with high-dose chemotherapy does not improve the overall survival of women with metastatic breast cancer. In addition, a study including more than 41,000 breast cancer patients demonstrated no significant difference in survival benefits between patients who received HSCTs following high-dose chemotherapy and patients who underwent conventional treatment. 75 Thus, the use of autologous T-cell transplants as monotherapy and advertising stem cell-based therapies as if they are medically approved or preferred treatment of solid tumors is considered untrue statements and needs to be alerted to cancer patients. 76
Over the past decades, many preclinical studies have demonstrated the potential of MSC-based therapy in cancer treatment due to their unique properties. They confer the ability to migrate toward damaged sites via inherent tropism controlled by growth factors, chemokines, and cytokines. MSCs express specific C–X–C chemokine receptor type 4 (CXCR4) and other chemokine receptors (including CCR1, CCR2, CCR4, CCR7, etc.) that are essential to respond to the surrounding signals. 77 In addition, specific adherent proteins, including CD49d, CD44, CD54, CD102, and CD106, are also expressed on the MSC surface, allowing them to attach, rotate, migrate, and penetrate the blood vessel lumen to infiltrate the damaged tissue. 78 Similar to damaged tissues, tumors secrete a wide range of chemoattractant that also attract MSC migration via the CXCL12/CXCR4 axis. Previous studies also found that MSC migration toward the cancer site is tightly controlled by diffusible cytokines such as interleukin 8 (IL-8) and growth factors including transforming growth factor-beta 1 (TGF-β1), 79 platelet-derived growth factor (PDGF), 80 fibroblast growth factor 2 (FGF-2), 81 vascular endothelial growth factor (VEGF), 81 and extracellular matrix molecules such as matrix metalloproteinase-2 (MMP-2). 82 Once MSCs migrate successfully to cancerous tissue, accumulating evidence demonstrates the interaction between MSCs and cancer cells to exhibit their protumour and antitumour effects, which are the major concerns of MSC-based therapy. MSCs are well-known for their regenerative effects that regulate tissue repair and recovery. This unique ability is also attributed to the protumour functions of these cells. A previous study reported that breast cancer cells induce MSC secretion of chemokine (C–C motif) ligand 5 (CCL-5), which regulates the tumor invasion process. 83 , 84 Other studies also found that MSCs secrete a wide range of growth factors (VEGF, basic FGF, HGF, PDGF, etc.) that inhibits apoptosis of cancer cells. 85 Moreover, MSCs also respond to signals released from cancer cells, such as TGF-β, 86 to transform into cancer-associated fibroblasts, a specific cell type residing within the tumor microenvironment capable of promoting tumorigenesis. 87 Although MSCs have been proven to be involved in protumour activities, they also have potent tumor suppression abilities that have been used to develop cancer treatments. It has been suggested that MSCs exhibit their tumor inhibitory effects by inhibiting the Wnt and AKT signaling pathways, 88 reducing the angiogenesis process, 89 stimulating inflammatory cell infiltration, 90 and inducing tumor cell cycle arrest and apoptosis. 91 To date, the exact functions of MSCs in both protumour and antitumor activities are still a controversial issue across the stem cell field. Other approaches exploit gene editing and tissue engineering to convert MSCs into “a Trojan horse” that could exhibit antitumor functions. In addition, MSCs can also be modified to express specific anticancer miRNAs exhibiting tumor-suppressive behaviors. 92 However, genetically modified MSCs are still underdeveloped and require intensive investigation in the clinical setting.
To date, ~25 clinical trials have been registered on ClinicalTrials.gov aimed at using MSCs as a therapeutic treatment for cancer. 93 These trials are mostly phase 1 and 2 studies focusing on evaluating the safety and efficacy of the treatment. Studies exploiting MSC-based therapy have combined MSCs with an oncolytic virus approach. Oncolytic viruses are specific types of viruses that can be genetically engineered or naturally present, conferring the ability to selectively infect cancer cells and kill them without damaging the surrounding healthy cells. 94 A completed phase I/II study using BM-MSCs infected with the oncolytic adenovirus ICOVIR5 in the treatment of metastatic and refractory solid tumors in children and adult patients demonstrated the safety of the treatment and provided preliminary data supporting their therapeutic potential. 95 The same group also reported a complete disappearance of all signs of cancer in response to MSC-based therapy in one pediatric case three years post administration. 96 A reported study in 2019 claimed that adipose-derived MSCs infected with vaccinia virus have the potential to eradicate resistant tumor cells via the combination of potent virus amplification and senitization of the tumor cells to virus infection. 97 However, in a recently published review, a valid question was posed regarding the 2019 study that “do these reported data merit inclusion in the publication record when they were collected by such groups using a dubious therapeutic that was eventually confiscated by US Marshals?” 76
Taken together, cancer research and therapy have entered an innovative and fascinating era with advancements in traditional therapies such as chemotherapy, radiotherapy, and surgery on one hand and stem cell-based therapy on the other hand. Although stem cell-based therapy has been considered a novel and attractive therapeutic approach for cancer treatment, it has been hampered by contradictory results describing the protumour and antitumour effects in preclinical studies. Despite this contradictory reality, the use of stem cell-based therapy, especially MSCs, offers new hope to cancer patients by providing a new and more effective tool in personalized medicine. The authors support the use of MSC-based therapy as a Trojan horse to deliver specific anticancer functions toward cancer cells to suppress their proliferation, eradicate cancer cells, or limit the vascularization process of cancerous tissue to improve the clinical safety and efficacy of the treatment.
Human pluripotent stem cell-based therapy: a growing giant
The discovery of hPSCs, including human embryonic stem cells (hESCs) and human induced pluripotent stem cells (hiPSCs), has revolutionized stem cell research and cell-based therapy. 98 hESCs were first isolated from blastocyst-stage embryos in 1998, 99 followed by breakthrough reprogramming research that converted somatic cells into hiPSCs using just four genetic factors. 100 , 101 Methods have been developed to maintain these cells long-term in vitro and initiate their differentiation into a wide variety of cell types, opening a new era in regenerative medicine, particularly cell therapy to replace lost or damaged tissues.
History of hPSCs
hPSCs are defined as self-renewable cell types that confer the ability to differentiate into various cellular phenotypes of the human body, including three germ layers. 102 Historically, the first pluripotent cell lines to be generated were embryonic carcinoma (EC) cell lines established from human germ cell tumors 103 and murine undifferentiated compartments. 104 Although EC cells are a powerful tool in vitro, these cells are not suitable for clinical applications due to their cancer-derived origin and aneuploidy genotype. 105 The first murine ESCs were established in 1981 based on the culture techniques obtained from EC research. 106 Murine ESCs are derived from the inner cell mass (ICM) of the pre-implantation blastocyst, a unique biological structure that contains outer trophoblast layers that give rise to the placenta and ICM. 107 In vivo ESCs only exist for a short period during the embryo’s development, and they can be isolated and maintained indefinitely in vitro in an undifferentiated state. The discovery of murine ESCs has dramatically changed the field of biomedical research and regenerative medicine over the last 40 years. Since then, enormous investigations have been made to isolate and culture ESCs from other species, including hESCs, in 1998. 99 The success of Thomson et al. in 1998 triggered the great controversy in media and ethical research boards across the globe, with particularly strong objections being raised to the use of human embryos for research purposes. 108 Several studies using hESCs have been conducted demonstrating their therapeutic potential in the clinical setting. However, the use of hESCs is limited due to (1) the ethical barrier related to the destruction of human embryos and (2) the potential risk of immunological rejection, as hESCs are isolated from pre-implantation blastocysts, which are not autologous in origin. To overcome these two great obstacles, several research groups have been trying to develop technology to generate hESCs, including nuclear transfer technology, the well-known strategy that creates Dolly sheep, although the generation of human nuclear transfer ESCs remains technically challenging. 109 Taking a different approach, in 2006, Yamanaka and Takahashi generated artificial PSCs from adult and embryonic mouse somatic cells using four transcription factors ( Oct-3/4 , Sox2 , Klf4 , and c-Myc , called OSKM) reduced from 24 factors. 100 Thereafter, in 2007, Takahashi and colleagues successfully generated the first hiPSCs exhibiting molecular and biological features similar to those of hESCs using the same OSKM factors. 101 Since then, hiPSCs have been widely studied to expand our knowledge of the pathogenesis of numerous diseases and aid in developing new cell-based therapies as well as personalized medicine.
Clinical applications of hPSCs
Since its beginning 24 years ago, hPSC research has evolved momentously toward applications in regenerative medicine, disease modeling, drug screening and discovery, and stem cell-based therapy. In clinical trial settings, the uses of hESCs are restricted by ethical concerns and tight regulation, and the limited preclinical data support their therapeutic potential. However, it is important to acknowledge several successful outcomes of hESC-based therapies in treating human diseases. In 2012, Steven Schwartz and his team reported the first clinical evidence of using hESC-derived retinal pigment epithelium (RPE) in the treatment of Stargardt’s macular dystrophy, the most common pediatric macular degeneration, and an individual with dry age-related macular degeneration. 110 , 111 With a differentiation efficiency of RPE greater than 99%, 5 × 10 4 RPEs were injected into the subretinal space of one eye in each patient. As the hESC source of RPE differentiation was exposed to mouse embryonic stem cells, it was considered a xenotransplantation product and required a lower dose of immunosuppression treatment. This study showed that hESCs improved the vision of patients by differentiating into functional RPE without any severe adverse events. The trial was then expanded into two open-label, phase I/II studies with the published results in 2015 supporting the primary findings. 112 In these trials, patients were divided into three groups receiving three different doses of hESC-derived RPE, including 10 × 10 4 , 15 × 10 4 and 50 × 10 4 RPE cells per eye. After 22 months of follow-up, 19 patients showed improvement in eyesight, seven patients exhibited no improvement, and one patient experienced a further loss of eyesight. The technical challenge of hESC-derived RPE engraftment was an unbalanced proliferation of RPE post administration, which was observed in 72% of treated patients. A similar approach was also conducted in two South Korean patients diagnosed with age-induced macular degeneration and two patients with Stargardt macular dystrophy. 113 The results supported the safety of hESC-derived RPE cells and illustrated an improvement in visual acuity in three patients. Recently, clinical-graded hESC-derived RPE cells were also developed by Chinese researchers under xeno-free culture conditions to treat patients with wet age-related degeneration. 114 As hESC development is still associated with ethical concerns and immunological complications related to allogeneic administration, hiPSC-derived RPE cells have emerged as a potential cell source for macular degeneration. Although RPE differentiation protocols have been developed and optimized to improve the efficacy of hiPSC-derived RPE cells, they are still insufficient, time-consuming and labor intensive. 115 , 116 For clinical application, an efficient differentiation of “primed” to “naïve” state hiPSCs toward the RPE was developed using feeder-free culture conditions utilizing the transient inhibition of the FGF/MAPK signaling pathway. 117 Overexpression of specific transcription factors in hiPSCs throughout the differentiation process is also an interesting approach to generate a large number of RPE cells for clinical use. In a recent study, overexpression of three eye-field transcription factors, including OTX2, PAX6, and MITF , stimulated RPE differentiation in hiPSCs and generated functional RPE cells suitable for transplantation. 118 To date, although reported data from phase I/II clinical trials have been produced enough to support the safety of hESC-derived RPE cells, the treatment is still in its immature stage. Thus, future studies should focus on the development of the cellular manufacturing process of RPE and the subretinal administration route to further improve the outcomes of RPE fabrication and engraftment into the patient’s retina (recommended review 119 ).
Numerous studies have demonstrated that hESC-derived cardiomyocytes exhibit cardiac transcription factors and display a cardiomyocyte phenotype and immature electrical phenotype. In addition, using hPSC-derived cardiomyocytes could provide a large number of cells required for true remuscularization and transplantation. Thus, these cells can be a promising novel therapeutic approach for the treatment of human cardiovascular diseases. In a case report, hESC-derived cardiomyocytes showed potential therapeutic effects in patients with severe heart failure without any subsequent complications. 120 This study was a phase I trial (ESCORT [Transplantation of Human Embryonic Stem Cell-derived Progenitors in Severe Heart Failure] trial) to evaluate the safety of cardiomyocyte progenitor cells derived from hESCs seeded in fibrin gel scaffolds for 10 patients with severe heart failure (NCT02057900). The encouraging results from this study demonstrated the feasibility of producing hESC-derived cardiomyocyte progenitor cells toward clinical-grade standards and combining them with a tissue-engineered scaffold to treat severe heart disease (the first patient of this trial has already reached the 7-year follow-up in October 2021). 121 Currently, the two ongoing clinical trials using hPSC-derived cardiomyocytes have drawn great attention, as their results would pave the way to lift the bar for approving therapies for commercial use. The first trial was conducted by a team led by cardiac surgeon Yoshiki Sawa at Osaka University using hiPSC-derived cardiomyocytes embedded in a cell sheet for engraftment (jRCT2052190081). The trials started first with three patients followed by ten patients to assess the safety of the approach. Once safety is met, the treatment can be sold commercially under Japan’s fast-track system for regenerative medicine. 122 Another trial used a collagen-based construct called BioVAT-HF to contain hiPSC-derived cardiomyocytes. The trial was divided into two parts to evaluate the cell dose: (Part A) recruiting 18 patients and (Part B) recruiting 35 patients to test a broad range of engineered human myocardium (EHM) doses. The expected results from this study will provide the “proof-of-concept” for the use of EHM in the stimulation of heart remuscularization in humans. To date, no adverse events or severe adverse events have been reported from these trials, supporting the safety of the procedure. However, as the number of treated patients was relatively small, limitations in drawing conclusions regarding efficacy are not yet possible. 21 , 123
One of the first clinical trials using hPSC-based therapy was conducted by Geron Corporation in 2010 using hESC-derived oligodendrocyte progenitor cells (OPC1) to treat spinal cord injury (SCI). The results confirmed the safety one year post administration in five participants, and magnetic resonance imaging demonstrated improvement of spinal cord deterioration in four participants. 124 Asterias Biotherapeutic (AST) continued the Geron study by conducting the SCiStar Phase I/IIa study to evaluate the therapeutic effects of AST-OPC1 (NCT02302157). The trial’s results published in clinicaltrials.gov demonstrated significant improvement in running speed, forelimb stride length, forelimb longitudinal deviations, and rear stride frequency. Interestingly, the recently published data of a phase 1, multicentre, nonrandomized, single-group assignment, interventional trial illustrated no evidence of neurological decline, enlarging masses, further spinal cord damage, or syrinx formation in patients 10 years post administration of the OPC1 product. 125 This data set provides solid evidence supporting the safety of OPC1 with an event-free period of up to 10 years, which strengthens the safety profile of the SCiStar trial.
Analysis of the global trends in clinical trials using hPSC-based therapy showed that 77.1% of studies were observational (no cells were administered into patient), and only 22.9% of studies used hPSC-derived cells as interventional treatment. 126 The number of studies using hiPSCs was relatively higher than that using hESCs, which was 74.8% compared to 25.2%, respectively. The majority of observational studies were performed in developed countries, including the USA (41.6%) and France (16.8%), whereas interventional studies were conducted in Asian countries, including China (36.7%), Japan (13.3%), and South Korea (10%). The trends in therapeutic studies were also clear in terms of targeted diseases. The three most studied diseases were ophthalmological conditions, circulatory disorders, and nervous systems. 127 However, it is surprising that the clinical applications of hPSCs have achieved little progress since the first hESCs were discovered worldwide. The relatively low number of clinical trials focusing on using iPSCs as therapeutic agents to administer into patients could be ascribed to the unstable genome of hiPSCs, 128 immunological rejection, 129 and the potential for tumor formation. 130
Mesenchymal stem/stromal cell-based therapy: is it time to consider their origin toward targeted therapy?
Approximately 55 years ago, fibroblast-like, plastic-adherent cells, later named mesenchymal stem cells (MSCs) by Arnold L. Caplan, 18 were discovered for the first time in mouse bone marrow (BM) and were later demonstrated to be able to form colony-like structures, proliferate, and differentiate into bone/reticular tissue, cartilage, and fat. 131 Protocols were subsequently established to directly culture this subpopulation of stromal cells from BM in vitro and to stimulate their differentiation into adipocytes, chondroblasts, and osteoblasts. 132 Since then, MSCs have been found in and derived from different human tissue sources, including adipose tissue (AT), the umbilical cord (UC), UC blood, the placenta, dental pulp, amniotic fluid, etc. 133 To standardize and define MSCs, the International Society for Cell and Gene Therapy (ISCT) set minimal identification criteria for MSCs derived from multiple tissue sources. 134 Among them, MSCs derived from AT, BM, and UC are the most commonly studied MSCs in human clinical trials, 135 and they constitute the three major tissue sources of MSCs that will be discussed in this review.
The discovery of MSCs opened an era during which preclinical studies and clinical trials have been performed to assess the safety and efficacy of MSCs in the treatment of various diseases. The major conclusion of these studies and trials is that MSC-based therapy is safe, although the outcomes have usually been either neutral or at best marginally positive in terms of the clinically relevant endpoints regardless of MSC tissue origin, route of infusion, dose, administration duration, and preconditioning. 136 It is important to note that a solid background of knowledge has been generated from all these studies that has fueled the recent translational research in MSC-based therapy. As MSCs have been intensively studied over the last 55 years and have become the subject of multiple reviews, systematic reviews, and meta-analyses, the objective of this paper is not to duplicate these publications. Rather, we will discuss the questions that both clinicians and researchers are currently exploring with regard to MSC-based therapy, diligently seeking answers to the following:
“With a solid body of data supporting their safety profiles derived from both preclinical and clinical studies, does the tissue origin of MSCs also play a role in their downstream clinical applications in the treatment of different human diseases?”
“Do MSCs derived from AT, BM, and UC exhibit similar efficacy in the treatment of neurological diseases, metabolic/endocrine-related disorders, reproductive dysfunction, skin burns, lung fibrosis, pulmonary disease, and cardiovascular conditions?”
To answer these questions, we will first focus on the most recently published clinical data regarding these targeted conditions, including neurological disorders, pulmonary dysfunctions, metabolic/endocrine-related diseases, reproductive disorders, skin burns, and heart-related diseases, to analyze the potential efficacy of MSCs derived from AT, BM, and UC. Based on the level of clinical improvement observed in each trial, we analyzed the potential efficacy of MSCs derived from each source to visualize the correlation between patient improvement and MSC sources. We will then address recent trends in the exclusive use of MSC-based products, focusing on the efficacy of treatment with MSCs from each of the abovementioned sources, and we will analyze the relationship between the respective efficacies of MSCs from these sources in relation to the targeted disease conditions. Finally, we propose a hypothesis and mechanism to achieve the currently still unmet objective of evaluating the use of MSCs from AT, BM, and UC in regenerative medicine.
An overview of MSC tissue origins and therapeutic potential
In general, MSCs are reported to be isolated from numerous tissue types, but all of these types can be organized into two major sources: adult 137 and perinatal sources 138 (Fig. 2 ). Adult sources of MSCs are defined as tissues that can be harvested or obtained from an individual, such as dental pulp, 139 BM, peripheral blood, 140 AT, 141 lungs, 142 hair, 143 or the heart. 144 Adult MSCs usually reside in specialized structures called stem cell niches, which provide the microenvironment, growth factors, cell-to-cell contacts and external signals necessary for maintaining stemness and differentiation ability. 145 BM was the first adult source of MSCs discovered by Friedenstein 131 and has become one of the most documented and largely used MSC sources to date, followed by AT. BM-MSCs are isolated and cultured in vitro from BM aspirates using a Ficoll gradient-centrifugation method 146 or a red blood cell lysate buffer to collect BM mononuclear cell populations, whereas AT-MSCs are obtained from stromal vascular fractions of enzymatically digested AT obtained through liposuction, 141 lipoplasty, or lipectomy procedures. 147 These tissue collection procedures are invasive and painful for the patient and are accompanied by a risk of infection, although BM aspiration and adipose liposuction are considered safe procedures for BM and AT biopsies. The number of MSCs that can be isolated from these adult tissues varies significantly in a tissue-dependent manner. The percentage of MSCs in BM mononuclear cells ranges from 0.001 to 0.01% following gradient centrifugation. 132 The number of MSCs in AT is at least 500 times higher than that in BM, with approximately 5,000 MSCs per 1 g of AT. Perinatal sources of MSCs consist of UC-derived components, such as UC, Wharton’s jelly, and UC blood, and placental structures, such as the placental membrane, amnion, chorion membrane, and amniotic fluid. 138 The collection of perinatal MSCs, such as UC-MSCs, is noninvasive, as the placenta, UC, UC blood, and amnion are considered waste products that are usually discarded after birth (with no ethical barriers). 148 Although MSCs represent only 10 −7 % the cells found in UC, their higher proliferation rate and rapid population doubling time allow these cells to rapidly replicate and increase in number during in vitro culture. 149 Under standardized xeno-free and serum-free culture platforms, AT-MSCs show a faster proliferation rate and a higher number of colony-forming units than BM-MSCs. 149 UC-MSCs have the fastest population doubling time compared to AT-MSCs and BM-MSCs in both conventional culture conditions and xeno- and serum-free environments. 149 MSCs extracted from AT, BM and UC exhibit all minimal criteria listed by the ISCT, including morphology (plastic adherence and spindle shape), MSC surface markers (95% positive for CD73, CD90 and CD105; less than 2% negative for CD11, CD13, CD19, CD34, CD45, and HLR-DR) and differentiation ability into chondrocytes, osteocytes, and adipocytes. 150
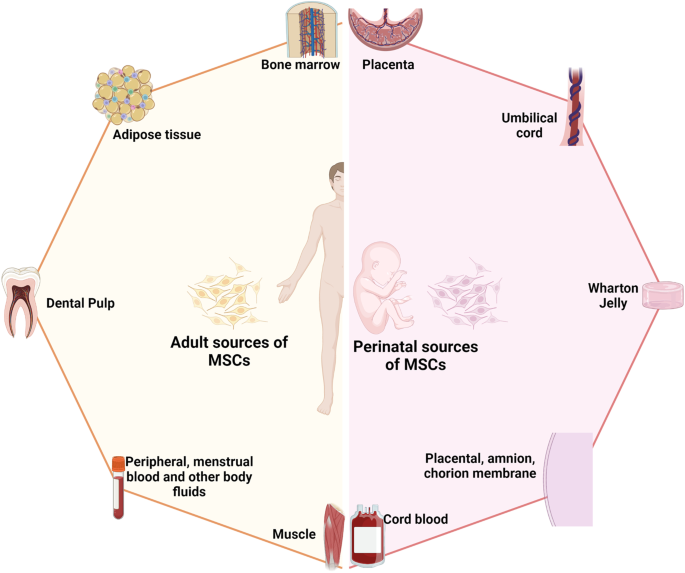
The two major sources of MSCs: adult and perinatal sources. The adult sources of MSCs are specific tissue in human body where MSCs could be isolated, including bone marrow, adipose tissue, dental pulp, peripheral blood, menstrual blood, muscle, etc. The perinatal sources of MSCs consist of umbilical cord-derived components, such as umbilical cord, Wharton’s jelly, umbilical cord blood, and placental structures, such as placental membrane, amnion, chorion membrane, amniotic fluid, etc. The figure was created with BioRender.com
In fact, although MSCs derived from either adult or perinatal sources exhibit similar morphology and the basic characteristics of MSCs, studies have demonstrated that these cells also differ from each other. Regarding immunophenotyping, AT-MSCs express high levels of CD49d and low levels of Stro-1. An analysis of the expression of CD49d and CD106 showed that the former is strongly expressed in AT-MSCs, in contrast to BM-MSCs, whereas CD106 is expressed in BM-MSCs but not in AT-MSCs. 151 Increased expression of CD133, which is associated with stem cell regeneration, differentiation, and metabolic functions, 152 was observed in BM-MSCs compared to MSCs from other sources. 153 A recent study showed that CD146 expression in UC-MSCs was higher than that in AT- and BM-MSCs, 153 supporting the observation that UC-MSCs have a stronger attachment and a higher proliferation rate than MSCs from other sources, as CD146 is a key cell adhesion protein in vascular and endothelial cell types. 154 In terms of differentiation ability, donor-matched BM-MSCs exhibit a higher ability to differentiate into chondrogenic and osteogenic cell types than AT-MSCs, whereas AT-MSCs show a stronger capacity toward the adipogenic lineage. 150 The findings from an in vitro differentiation study indicated that BM-MSCs are prone to osteogenic differentiation, whereas AT-MSCs possess stronger adipogenic differentiation ability, which can be explained by the fact that the epigenetic memory obtained from either BM or AT drives the favored MSC differentiation along an osteoblastic or adipocytic lineage. 155 Interestingly, although UC-MSCs have the ability to differentiate into adipocytes, osteocytes, or chondrocytes, their osteogenic differentiation ability has been proven to be stronger than that of BM-MSCs. 156 The most interesting characteristic of MSCs is their immunoregulatory functions, which are speculated to be related to either cell-to-cell contact or growth factor and cytokine secretion in response to environmental/microenvironmental stimuli. MSCs from different sources almost completely inhibit the proliferation of peripheral blood mononuclear cells (PBMCs) at PBMC:MSC ratios of 1:1 and 10:1. 149 At a higher ratio, BM-MSCs showed a significantly higher inhibitory effect than AT- or UC-MSCs. 153 Direct analysis of the immunosuppressive effects of BM- and UC-MSCs has revealed that these cells exert similar inhibitory effects in vitro with different mechanisms involved. 157 With these conflicting data, the mechanism of action related to the immune response of MSCs from different sources is still poorly understood, and long-term investigations both in preclinical studies and in clinical trial settings are needed to shed light on this complex immunomodulation function.
The great concern in MSC-based therapy is the fate of these cells post administration, especially through different delivery routes, including systemic administration via an intravenous (IV) route or tissue-specific administration, such as dorsal pancreatic administration. It is important to understand the distribution of these cells after injection to expand our understanding of the underlying mechanisms of action of treatments; in addition, this knowledge is required by authorized bodies (the Food and Drug Administration (FDA) in the United States or the regulation of advanced-therapy medicinal products in Europe, No. 1394/2007) prior to using these cells in clinical trials. The preclinical data using various labeling techniques provide important information demonstrating that MSCs do not have unwanted homing that could lead to the incorrect differentiation of the cells or inappropriate tumor formation. In a mouse model, human BM-MSCs and AT-MSCs delivered via an IV route are rapidly trapped in the lungs and then recirculate through the body after the first embolization process, with a small number of infused cells found mainly in the liver after the second embolization. 158 Using the technetium-99 m labeling method, intravenously infused human cells showed long-term persistence up to 13 months in the bone, BM compartment, spleen, muscle, and cartilage. 159 A similar result was reported in baboons, confirming the long-term homing of human MSCs in various tissues post administration. 160 Although the retainment of MSCs in the lungs might potentially reduce their systemic therapeutic effects, 161 it provides a strong advantage when these cells are used in the treatment of respiratory diseases. Local injection of MSCs also revealed their tissue-specific homing, as an injection of MSCs via the renal artery route resulted in the majority of the injected cells being found in the renal cortex. 162 Numerous studies have been conducted to track the migration of administered MSCs in human subjects. Henriksson and his team used MSCs labeled with iron sucrose in the treatment of intervertebral disc degeneration. 163 Their study showed that chondrocytes differentiated from infused MSCs could be detected at the injured intervertebral discs at 8 months but not at 28 months. A study conducted in a patient with hemophilia A using In-oxine-labeled MSCs showed that the majority of the cells were trapped in the lungs and liver 1 h post administration, followed by a reduction in the lungs and an increase in the number of cells in the liver after 6 days. 164 Interestingly, a small proportion of infused MSCs were found in the hemarthrosis site at the right ankle after 24 h, suggesting that MSCs are attracted and migrate to the injured site. The distribution of MSCs was also reported in the treatment of 21 patients diagnosed with type 2 diabetes using 18-FDG-tagged MSCs and visualized using positron emission tomography (PET). 165 The results illustrated that local delivery of MSCs via an intraarterial route is more effective than delivery via an IV route, as MSCs home to the pancreatic head (pancreaticoduodenal artery) or body (splenic artery). Therefore, although the available data related to the biodistribution of infused MSCs are still limited, the results obtained from both preclinical and clinical studies illustrate a comparable set of data supporting results on homing, migration to the injured site, and the major organs where infused MSCs are located. The following comprehensive and interesting reviews are highly recommended. 166 , 167 , 168
To date, 1426 registered clinical trials spanning different trial phases have used MSCs for therapeutic purposes, which is four times the number reported in 2013. 169 , 170 As supported by a large body of preclinical studies and advancements in conducting clinical trials, MSCs have been proven to be effective in the treatment of numerous diseases, including nervous system and brain disorders, pulmonary diseases, 171 cardiovascular conditions, 172 wound healing, etc. The outcomes of MSC-based therapy have been the subject of many intensive reviews and systematic analyses with the solid conclusion that these cells exhibit strong safety profiles and positive outcomes in most tested conditions. 173 , 174 , 175 In addition, the available data have revealed several potential mechanisms that could explain the beneficial effects of MSCs, including their homing efficiency, differentiation potential, production of trophic factors (including cytokines, chemokines, and growth factors), and immunomodulatory abilities. However, it is still not known which MSC types should be used for which diseases, as it seems to be that MSCs exhibit beneficial effects regardless of their sources. 169
Acquired brain and spinal cord injury treatment: BM-MSCs have emerged as key players
The theory that brain cells can never regenerate has been challenged by the discovery of newly formed neurons in the human adult hippocampus or the migration of stem cells in the brain in animal models. 176 These observations have triggered hope for regeneration in the context of neuronal diseases by using exogenous stem cell sources to replenish or boost the stem cell population in the brain. Moreover, the limited regenerative capacity of the brain and spinal cord is an obstacle for traditional treatments of neurodegenerative diseases, such as autism, cerebral palsy, stroke, and spinal cord injury (SCI). As current treatments cannot halt the progression of these diseases, studies throughout the world have sought to exploit cell-based therapies to treat neurodegenerative diseases on the basis of advances in the understanding and development of stem cell technology, including the use of MSCs. Successful stem cell therapy for treating brain disease requires therapeutic cells to reach the injured sites, where they can repair, replace, or at least prevent the deteriorative effects of neuronal damage. 177 Hence, the gold standard of cell-based therapy is to deliver the cells to the target site, stimulate the tissue repair machinery, and regulate immunological responses via either cell-to-cell contact or paracrine effects. 178 Among 315 registered clinical trials using stem cells for the treatment of brain diseases, MSCs and hematopoietic stem cells (HSCs; CD34+ cells isolated from either BM aspirate or UC blood) are the two main cell types investigated, whereas approximately 102 clinical trials used MSCs and 62 trials used HSCs for the treatment of brain disease (main search data from clinicaltrial.gov). MSCs are widely used in almost all clinical trials targeting different neuronal diseases, including multiple sclerosis, 179 stroke, 180 SCI, 181 cerebral palsy, 182 hypoxic-ischemic encephalopathy, 183 autism, 184 Parkinson’s disease, 185 Alzheimer’s disease 185 and ataxia. Among these trials in which MSCs were the major cells used, nearly two-thirds were for stroke, SCI, or multiple sclerosis. MSCs have been widely used in 29 registered clinical trials for stroke, with BM-MSCs being used in 16 of these trials. With 26 registered clinical trials, SCI is the second most common indication for using MSCs, with 16 of these trials using mainly expanded BM-MSCs. For multiple sclerosis, 15 trials employed BM-MSCs among a total of 23 trials conducted for the treatment of this disease. Hence, it is important to note that in neuronal diseases and disorders, BM-MSCs have emerged as the most commonly used therapeutic cells among other MSCs, such as AT-MSCs and UC-MSCs.
The outcomes of the use of BM-MSCs in the treatment of neuronal diseases have been widely reported in various clinical trial types. A review by Zheng et al. indicated that although the treatments appeared to be safe in patients diagnosed with stroke, there is a need for well-designed phase II multicentre studies to confirm the outcomes. 173 One of the earliest trials using autologous BM-MSCs was conducted by Bang et al. in five patients diagnosed with stroke in 2005. The results supported the safety and showed an improved Barthel index (BI) in MSC-treated patients. 186 In a 2-year follow-up clinical trial, 16 patients with stroke received BM-MSC infusions, and the results showed that the treatment was safe and improved clinical outcomes, such as motor impairment scale scores. 187 A study conducted in 12 patients with ischemic stroke showed that autologous BM-MSCs expanded in vitro using autologous serum improved the patient’s modified Rankin Scale (mRS), with a mean lesion volume reduced by 20% at 1 week post cell infusion. 188 In 2011, a modest increase in the Fugl Meyer and modified BI scores was observed after autologous administration of BM-MSCs in patients with chronic stroke. 189 More recently, a prospective, open-label, randomized controlled trial with blinded outcome evaluation was conducted, with 39 patients and 15 patients in the BM-MSC administration and control groups, respectively. The results of this study indicated that autologous BM-MSCs with autologous serum administration were safe, but the treatment led to no improvements at 3 months in modified Rankin Scale (mRS) scores, although leg motor improvement was observed. 180 Researchers explored whether the efficacy of BM-MSC administration was maintained over time in a 5-year follow-up clinical trial. Patients (85) were randomly assigned to either the MSC group or the control group, and follow-ups on safety and efficacy were performed for 5 years, with 52 patients being examined at the end of the study. The MSC group exhibited a significant improvement in terms of decreased mRS scores, whereas the number of patients with an mRS score increase of 0–3 was statistically significant. 187 Although autologous BM-MSCs did not improve the Basel index, mRS, or National Institutes of Health Stroke Scale (NIHSS) score 2 years post infusion, patients who received BM-MSC therapy showed improvement in their motor function score. 190 In addition, a prospective, open-label, randomized controlled trial by Lee et al. showed that autologous BM-MSCs primed with autologous “ischemic” serum significantly improved motor functions in the MSC-treated group. Neuroimaging analysis also illustrated a significant increase in interhemispheric connectivity and ipsilesional connectivity in the MSC group. 191 Recently, a single intravenous infection of allogeneic BM-MSCs has been proven to be safe and feasible in patients with chronic stroke with a significant improvement in BI score and NIHSS score. 192
In two systematic reviews using MSCs for the treatment of SCI, BM-MSCs ( n = 16) and UC-MSCs ( n = 5) were reported to be safe and well-tolerated. 193 , 194 The results indicated significant improvements in the stem cell administration groups compared with the control groups in terms of a composite of the American Spinal Injury Association (ASIA) impairment scale (AIS) grade, AIS grade A, and ASIA sensory scores and bladder function (Table 1 ). However, larger experimental groups with a randomized and multicentre design are needed for further confirmation of these findings. For multiple sclerosis, several early-phase (phase I/II) registered clinical studies have used BM-MSCs. A study compared the potential efficacy of BM-MSC and BM mononuclear cell (BMMNC) transplantation in 105 patients with spastic cerebral palsy. 195 The results showed that the GMFM (gross motor function measure) and the FMFM (fine motor function measure) scores of the BM-MSC transplant group were higher than those of the BMNNC transplant group at 3, 6, and 12 months of assessment. In terms of autism spectrum disorder, a review of 254 children after BMMNC transplantation found that over 90% of patients’ ISAA (Indian Scale for Assessment of Autism) and CARS (Childhood Autism Rating Scale) scores improved. Young patients and those in whom autism spectrum disorder was detected early generally showed better improvement. 196
One of the biggest limitations when using BM-MSCs is the bone marrow aspiration process, as it is an invasive procedure that can introduce a risk of complications, especially in pediatric and elderly patients. 197 Therefore, UC-MSCs have been suggested as an alternative to BM-MSCs and are being studied in clinical trials for the treatment of neurological diseases in approximately 1550 patients throughout the world; however, only three studies have been completed, with data published recently. 198 A recent study showed that UC-MSC administration improved both gross motor function and cognitive skills, assessed using the Activities of Daily Living (ADL), Comprehensive Function Assessment (CFA), and GMFM, in patients diagnosed with cerebral palsy. The improvements peaked 6 months post administration and lasted for 12 months after the first transplantation. 199 In a single-targeted phase I/II clinical trial using UC-MSCs for the treatment of autism, Riordan et al. reported decreases in Autism Treatment Evaluation Checklist (ATEC) and CARS scores for eight patients, but the paper has been retracted due to a violation of the journal’s guidelines. 200 In an open-label, phase I study, UC-MSCs were used as the main cells to treat 12 patients with autism spectrum disorder via IV infusions. It is important to note that five participants developed new class I anti-human leukocyte antigen in response to the specific lot of manufactured UC-MSCs, although these responses did not exhibit any immunological response or clinical manifestations. Only 50% of participants showed improvements in at least two autism-specific measurements. 201 Although not as widely used as BM-MSCs, these trials have demonstrated the efficacy of using UC-MSCs in the treatment of SCIs. In a pilot clinical study, Yang et al. showed that the use of UC-MSCs has the potential to improve disease status through an increase in total ASIA and SCI Functional Rating Scale of the International Association of Neurorestoratology (IANR-SCIFRS) scores, as well as an improvement in pinprick, light touch, motor and sphincter scores. 202 A study of 22 patients with SCIs showed a potential therapeutic effect in 13 patients post UC-MSC infusion. 203 AT-MSCs were also used to treat SCI, with a single case report indicating an improvement in neurological and motor functions in a domestic ferret patient. 204 However, a result obtained from another phase I trial using AT-MSCs showed mild improvements in neurological function in a small number of patients. 205 A phase II, randomized, double-blind, placebo-controlled, single-center, pilot clinical trial using AT-MSCs in the treatment of acute ischemic stroke published a data set that supports the safety of the therapy, although patients who received AT-MSCs showed a nonsignificant improvement after 24 months of follow-up. 206 In all of the above studies, the safety of using either AT-MSCs or UC-MSCs was evaluated, and no significant reactions were reported after infusion.
Therefore, based on the number of recovered patients post-transplantation and the number of recruited patients in large-scale trials using BM-MSCs, it seems that BM-MSCs are the prominent cells in regard to treating neurodegenerative disease with potentially good outcomes (Table 1 ). It is important to note that we do not negate the fact that AT- and UC-MSCs also show positive outcomes in the treatment of neuronal diseases, with numerous ongoing large-scale, multicentre, randomized, and placebo-control trials, 207 , 208 but we suggest alternative and thoughtful decisions regarding which sources of MSCs are best for the treatment of neuronal diseases and degenerative disorders.
Respiratory disease and lung fibrosis: clinical data support UC as a good source of MSCs
In the last decade, significant increases in respiratory disease incidence due to air pollution, smoking behavior, population aging, and recently, respiratory virus infections such as coronavirus disease 2019 (COVID-19) 209 have been observed, leading to substantial burdens on public health and healthcare systems worldwide. Respiratory inflammatory diseases, including bronchopulmonary dysplasia (BPD), chronic obstructive pulmonary disease (COPD), and acute respiratory distress syndrome (ARDS), have recently emerged as three prevalent pulmonary diseases in children and adults. These conditions are usually associated with inflammatory cell infiltration, a disruption of alveolar structural integrity, a reduction in alveolar fluid clearance ability, cytokine release and associated cytokine storms, airway remodeling, and the development of pulmonary fibrosis. Traditional treatments are focused on relieving symptoms and preventing disease progression using surfactants, artificial respiratory support, mechanical ventilation, and antibiotic/anti-inflammatory drugs, with limited effects on the damaged airway, alveolar fluid clearance, and other detrimental effects caused by the inflammatory response. MSCs are known for their immunomodulatory abilities, showing potential in injury reduction and aiding lung recovery after injury. According to ClinicalTrials.gov, from 2017 to date, there have been 159 studies testing the application of MSCs in the treatment of pulmonary diseases, including but not limited to BPD, COPD, and ARDS, suggesting a trend in the use of MSCs as an alternative approach for the treatment of respiratory diseases, especially MSCs from UC as an “off-the-shelf” and allogeneic source.
Extremely premature infants are born with arrested lung development at the canalicular-saccular phases prior to alveolarization and before pulmonary maturation occurs, which results in the development of BPD. 210 These infants require intensive care during the first three months of life using postnatal interventions, including positive pressure mechanical ventilation, external oxygen support, and surfactant infusions, and the newborns have recurrent infections that further compromise normal lung development. 211 To date, 13 clinical trials have been proposed to use UC-MSCs in the treatment of BPD, recruiting ~566 premature infants throughout the world, including Vietnam, Korea, the United States, Spain, Australia, and China. The majority of these trials use UC-derived stem cells for phases I and II, focusing on evaluating the safety and efficacy of stem cell-based therapy. 212 Human UC tissue and its derivative components are considered the most attractive cell sources for MSCs in the treatment of BPD due to the ease of obtaining them, being readily available, with no ethical concerns, low antigenicity, a high cell proliferation rate, and superior regenerative potential. Chang et al. used MSCs derived from UC blood in a phase I dose-escalation clinical trial to treat 9 preterm infants via intratracheal administration to prevent the development of BPD. 213 All 9 preterm infants survived, and only three developed BPD; these infants had significantly decreased BPD severity compared with the historically matched control group. A follow-up study of the same patients after 24 months indicated that only one infant had an E. cloacae infection after discharge at 4 months, with subsequent disseminated intravascular coagulation, which was later proven to be unrelated to the intervention. The remaining eight patients survived with normal pulmonary development and function, suggesting that the therapy was safe. MSCs from UC blood were also used for the treatment of 12 extremely low birthweight preterm patients using the same administration route, which further confirmed the safety of the therapy in the treatment of BPD, although ten of 12 infants still developed severe BPD at 36 weeks. 214 Our group also reported the safety and potential efficacy of using UC-MSCs in the treatment of four preterm infants, and the results supported the safety of UC-MSCs and demonstrated that patients could be weaned from oxygen supply and develop normal lung structure and function. 215 A phase II clinical trial of 66 infants born at 23–28 weeks with a birthweight of 500–1250 g who were recruited and randomized into an MSC-administration group and a control group was conducted. Although the results supported the safety of MSC administration in preterm infants, the efficacy of the treatment was not supported by statistical analysis, potentially due to the small sample size. Subgroup analysis showed that patients with severe BPD born at 23–24 weeks showed a significant improvement in BPD severity, but those born at 25–28 weeks did not. 216 Hence, it is important to conduct controlled phase II clinical trials with larger cohort sizes to further substantiate the efficacy of UC blood-derived MSCs in the treatment of infants with BPD.
With more than 65 million patients worldwide, COPD was the third-leading cause of death in 2020, according to World Health Organization records. COPD is classified as a chronic inflammatory and destructive pulmonary disease characterized by a progressive reduction in lung function. Averyanov et al. performed a randomized, placebo-controlled phase I/IIa study in 20 patients with mild to moderate idiopathic pulmonary fibrosis (IPF). Treatment group patients received two IV doses of allogeneic MSCs (2 × 10 8 cells) every 3 months, and the second group received a placebo. 217 Evaluation tests were performed at weeks 13, 26, 39, and 52. The 6-min walking test distance (6MWTD) results showed that patient fitness improved from week 13 onwards and was maintained until up to the 52nd week. Pulmonary function indicators improved markedly before and after treatment in the treated group but did not change significantly in the placebo group. The goal of MSC therapy in the treatment of COPD is to promote the regeneration of parenchymal cells and alveolar structure and the restoration of lung function. Based on the results of a phase I trial of a commercial BM-MSC product, Prochymal TM , which led to improvements in pulmonary function in treated patients, a multicentre, double-blind, placebo-controlled phase II trial was conducted in 62 patients diagnosed with COPD to determine the safety and potential efficacy of the product. Although the results supported the safety of BM-MSCs, their effectiveness in the treatment of COPD was not assured. No statistically significant differences in FEV 1 or FEV 1% , total lung capacity, or carbon monoxide diffusing capacity were detected after 2 years of follow-up between the two treatment groups. To date, there have been five clinical trials using BM-MSCs as the main stem cells for the treatment of COPD, but the overall clinical outcomes did not demonstrate the potential therapeutic effects of the treatment. 218 , 219 , 220 , 221 , 222 In clinical trial NCT001110252, the results showed that there was an overall reduction in the process of COPD pathological development 3 years after the administration of BM-MSCs, although the trial had a phase I design, with no control group, and evaluated only a small cohort (four patients). 219 To alleviate local inflammatory progression in COPD, Oliveira et al. studied the combination treatment of one-way endobronchial valve (EBV) and BM-MSC intubation. 223 Ten GOLD (Global Initiative for Obstructive Lung Disease) stage C or D patients were equally divided into 2 groups: one group received a dose of 10 8 cells before valve insertion, and the other group received a normal saline infusion. The follow-up time was 90 days. Inflammation was significantly improved as assessed by the CRP (C-reactive protein) index at 30 and 90 days after infusion. In addition, improvements in St. George’s Respiratory Questionnaire (SGRQ) scores indicated improved patient quality of life. Furthermore, an investigation into the homing ability of MSCs in vivo was performed on 9 GOLD patients, from stage A to stage D. Each patient received two 2 × 10 6 BM-MSC/kg IV infusions 1-week apart. 224 The marking of MSCs with indium-111 showed that MSCs were retained in the pulmonary vasculature longer in patients with mild COPD and that the levels of inflammatory mediators improved after 7 days of treatment. The results of the evaluation survey conducted after 1 year showed that the number of COPD exacerbations decreased to six times/year compared to 11 times/year before treatment. In addition, AT-MSCs present in the stromal vascular fraction were used to treat patients with COPD, and no adverse events were observed after 12 months of follow-up, but the clinical improvements post administration were not clear. 225 The results from a phase I clinical trial using AT-MSCs in eight patients with COPD also reported no significant change in pulmonary function test parameters. 226 A study evaluating the use of AT-MSCs as adjunctive therapy for COPD in 12 patients was performed. 227 AT was obtained using standard liposuction, MSCs were isolated, and 150–300 million cells were intravenously infused. The patients showed improvements in quality of life, with improved SGRQ scores after 3 and 6 months of treatment. Recently, UC-MSCs have emerged as potential allogeneic stem cell candidates for the treatment of COPD. 228 In a pilot clinical study, it was demonstrated that allogeneic administration of UC-MSCs in the treatment of COPD was safe and potentially effective. 229 In one study, 20 patients, including 9 at stage C and 11 at stage D per the GOLD classification, with histories of smoking were recruited and received cell-based therapy. The patients who received UC-MSC treatment showed significant reductions in Modified Medical Research Council scores, COPD assessment test scores, and the number of pulmonary exacerbations 6 months post administration. The results of the second trial using UC-MSCs showed that the mean FEV 1 /FVC ratios were increased along with improvements in SGRQ scores and 6MWTDs at three months post administration. 230 Although thorough assessments of the effectiveness of UC-MSCs are still in the early stages, the number of trials using UC-MSCs for the treatment of COPD is increasing steadily, with larger sample sizes and stronger designs (randomized or matched case–control studies), providing a data set strongly supporting the future applications of UC-MSCs. 231
The ongoing pandemic of the 21st century, the COVID-19 pandemic, emerged as a major pulmonary health problem worldwide, with a relatively high mortality rate. Numerous studies, reviews, and systematic analyses have been conducted to discuss and expand our knowledge of the virus and propose different mechanisms by which the virus could alter the immune system. 232 One of the most critical mechanisms is the generation of cytokine storms, which result from the initiation of hyperreactions of the adaptive immune response to viral infection. 233 These cytokine storms are formed by the establishment of waves of hypercytokinaemia generated from overreactive immune cells, which enhance their expression of TNF-α, IL-6, and IL-10, preventing T-lymphocyte recruitment and proliferation and culminating in T-lymphocyte apoptosis and T-cell exhaustion. In COVID-19, once a cytokine storm is formed, it spreads from an initial focal area through the body via circulation, which has been discussed in a comprehensive review by Jamilloux et al. 234 At the time of writing this review, there were 74 clinical trials using MSCs from UC (29 trials; including WJ-derived MSCs (WJ-MSCs) and placenta-derived MSCs (PL-MSCs)), AT (15 trials), and BM (11 trials) (comprehensive review 171 , 235 ). Hence, UC-MSCs have emerged as the most common MSCs for the treatment of COVID-19, with a total of 1047 patients participating in these trials. Among these trials, 15 completed trials using UC-MSCs (including WJ- and PL-MSCs) have been reported, with clinical data from approximately 600 recruited patients. 232 Eight of these 15 studies used allogenic UC-MSC transplantation to treat critically ill patients. 236 A list of case reports using UC-MSCs showed that the treatments were safe and well-tolerated in 14 patients with COVID-19, with the primary outcomes including increased percentages and numbers of T cells, 237 , 238 improved respiratory and renal functions, 239 reductions in inflammatory biomarker levels, 240 and positive outcomes in the PaO 2 /FiO 2 ratio. 240 In a pilot study conducted in ten patients with severe COVID-19, a single dose of UC-MSCs was safe and improved clinical outcomes, although the study did not investigate whether multiple doses of UC-MSCs could further improve the outcomes. 241 Two trials without a control group were conducted in 47 patients, and the results indicated that UC-MSCs were safe and feasible for the treatment of patients with COVID-19. 235 , 242 A single-center, open-label, individually randomized, standard treatment-controlled trial was performed in 41 patients (12 patients assigned to the UC-MSC group), and the results showed that significant improvements in C-reactive protein levels, IL-6 levels, oxygen indices, and lymphocyte numbers were found in the MSC groups. Chest computed tomography (CT) illustrated significant reductions in lung inflammatory responses as reflected by CT findings, the number of lobes involved, and pulmonary consolidation. 238 In a phase I trial conducted in 18 hospitalized patients with COVID-19, UC-MSCs were administered via an IV route in nine patients (five patients with moderate COVID-19 and 4 patients with severe COVID-19) at days 0, 3, and 6, with no treatment-related adverse events or severe adverse events. 243 Only one patient in the UC-MSC group required mechanical ventilation, compared to four patients in the control group. However, the clinical outcomes, such as COVID-19 symptoms, laboratory test results, CT findings of lung damage, and pulmonary function test parameters, were improved in both groups. Interestingly, a 1-year follow-up of the same sample revealed that the patients who received UC-MSC administration improved in terms of whole-lung lesion volume compared to the control group. 244 Moreover, chest CT at 12 months showed significant regeneration of lung tissue in the MSC-administered groups, whereas lung fibrosis was found in all patients in the control group. This finding is of interest because it indicates that a long time is needed to detect the regenerative functions of MSC-based therapy, as the biological process to enhance lung tissue regeneration occurs relatively slowly and requires multiple steps. The effects of UC-MSCs in the attenuation and prevention of the development of cytokine storms were illustrated in an interventional, prospective, three-parallel arm study with two control arms conducted in 30 patients in moderate and critical clinical conditions. 245 The results indicated a significant decrease in proinflammatory cytokines (IFNγ, IL-6, IL-17A, IL-2, and IL-12) and an increase in anti-inflammatory cytokines (IL-10, IL-13, and IL-1ra), suggesting that UC-MSCs might participate in the prevention of cytokine storm development. Lanzoni et al. performed a double-blind, randomized, controlled trial and found that UC-MSC infusions significantly decreased cytokine levels at day 6 and improved survival in patients with COVID-19 with ARDS. In this trial, 24 patients were randomized and assigned 1:1 to receive either MSCs or placebo. 246 MSC treatment was associated with a significant improvement in the survival rate without serious adverse events. To date, other trials conducted using UC-MSCs as the main MSCs provide a solid data set on their safety and efficacy in preventing the development of cytokine storms, reducing the inflammatory response, improving pulmonary function, reducing intensive care unit (ICU) stay duration, enhancing lung tissue regeneration, and reducing lung fibrosis progression. 240 , 247 , 248 , 249 In two large cohort studies (phase I with 210 patients and phase II with 100 patients), the volume of lung lesions and solid component injuries of patients’ lungs were reduced significantly after the administration of UC-MSCs, 250 and clinical symptoms and inflammatory levels were improved. 251 Of the 26 reported clinical trials for the treatment of COVID-19 with MSCs, 1 study used AT-MSCs as the main MSCs. 236 Thirteen COVID-19 adult patients under invasive mechanical ventilation who had received previous antiviral and/or anti-inflammatory treatments (including steroids, lopinavir/ritonavir, hydroxychloroquine, and/or tocilizumab, among others) were treated with allogeneic AT-MSCs. With a mean follow-up time of 16 days after infusion, 9/13 patients’ clinical symptoms improved, and 7/13 patients were intubated. A decrease in inflammatory cytokines and an increase in immunoregulatory cells were also observed in patients, especially in the group of patients with overall clinical improvement. Although there is a lack of clinical efficacy data supporting the use of AT-MSCs in the treatment of patients with COVID-19, AT-MSCs are still potential candidates for inhibiting COVID-19 due to their high secretory activity, strong immune-modulatory effects, and homing ability. 252 , 253 , 254
For ARDS, in a phase IIa trial, 60 patients with moderate to severe disease were randomized into 2 groups. A group of 40 patients received a single infusion of BM-MSCs at a dose of 1 × 10 6 cells/kg body weight, and another 20 patients received a placebo. 255 After 6 and 24 h of infusion, the decrease in plasma inflammatory cytokine levels in the MSC group was significantly greater than that in the placebo group. For severe pulmonary hypertension (PH) associated with BPD (BPD-PH), in a small trial, two preterm infants born at 26–27 weeks of age were intravenously administered heterologous BM-MSCs at a dose of 5 × 10 6 cells per kg of body weight; the treatment reduced oxygen requirements and supported respiration in the infants. 256 The administration of allogeneic AT-MSCs in the treatment of ARDS appeared to be safe and well-tolerated in 12 adult patients, but clinical outcomes were not observed. 257 The results of two patients who received BM-MSCs showed that both patients had improved respiratory function and hemodynamic function and a reduction in multiorgan failure. 258 Although the safety of BM-MSCs was confirmed in a multicentre, open-label, dose-escalation, phase I clinical trial (The Stem cells for ARDS treatment—START trial), 259 no significant improvements were found in a phase II trial, including in respiratory function and ARDS conditions. 260 The safety profile of UC-MSCs is also supported by the findings of a previous phase I clinical trial conducted in 9 patients, which showed that a single IV administration of UC-MSCs was safe and led to positive outcomes in terms of respiratory function and a reduction in the inflammatory response. 261 The findings of this study were also supported by those of the REALIST (Repair of Acute Respiratory Distress with Stromal Cell Administration) trial, which further confirmed the maximum tolerated dose of allogeneic UC-MSCs in patients with moderate to severe ARDS. 262
Although AT- and BM-MSCs have demonstrated therapeutic potential with similar mechanisms of action, UC-MSCs have emerged as potential candidates in the treatment of pulmonary diseases due to their ease of production as “off-the-shelf” products, rapid proliferation, noninvasive isolation methods, and supreme immunological regulation as well as anti-inflammatory effects. 263 However, it is important to note that there is a need to conduct phase III clinical trials with larger cohorts and trials with at least two sources of MSCs in the treatment of pulmonary conditions to further confirm this speculation. 264 Table 2 summarizes several clinical trials with published results discussed in this review.
Endocrine disorders, infertility/reproductive function recovery, and skin burns: should we consider AT-MSCs as the main MSCs based on their origin?
Endocrine disorders.
The human body maintains function and homeostatic regulation via a complex network of endocrine glands that synthesize and release a wide range of hormones. The endocrine system regulates body functions, including heartbeat, bone regeneration, sexual function, and metabolic activity. Endocrine system dysregulation plays a vital role in the development of diabetes, thyroid disease, growth disorder, sexual dysfunction, reproductive malfunction, and other metabolic disorders. The central dogma of regenerative medicine is the use of adult stem cells as a footprint for tissue regeneration and organ renewal. The functions of these stem cells are tightly regulated by microenvironmental stimuli from the nervous system (rapid response) and endocrine signals via hormones, growth factors, and cytokines. This harmonized and orchestrated system creates a symphony of signals that directly regulate tissue homeostasis and repair after injury. The disruption of these complex networks results in an imbalance of tissue homeostasis and regeneration that can lead to the development of endocrine disorders in humans, such as diabetes, sexual hormone deficiency, premature ovarian failure (POF), and Asherman syndrome.
In recent years, obesity and diabetes (type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM)) have been the two biggest challenges in endocrinology research, and the application of MSCs has emerged as a novel approach for therapeutic consideration. T1DM is characterized by the autoimmune destruction of pancreatic β-cells, whereas T2DM is defined as a combination of insulin resistance and pancreatic insulin-producing cell dysfunction. Regenerative medicine seeks to provide an exogenous cell source for replacing damaged or lost β-cells to achieve the goal of stabilizing patients’ blood glucose levels. To date, there are 28 clinical trials using MSCs in the treatment of T1DM ( http://www.clinicaltrials.gov , searched in October 2021), among which three trials were completed using autologous BM-MSCs (NCT01068951), allogeneic BM-MSCs (NCT00690066), and allogeneic AT-MSCs (NCT03920397). Interestingly, UC-MSCs were the most favored MSCs for the remaining trials. All published studies confirmed the safety of MSC therapy in the treatment of T1DM with no adverse events. The first study using autologous BM-MSCs showed that patients who were randomized into the MSC-administration group showed an increase in C-peptide levels in response to a mixed-meal tolerance test (MMTT) in comparison to the control group. 265 Unfortunately, there was no significant improvement in C-peptide levels, HbA1 C or insulin requirements. The use of autologous AT-MSCs in combination with vitamin D was safe and improved HbA1 C levels 6 months post administration. 266 WJ-MSCs were used as the main MSCs for the treatment of new-onset T1DM, which showed a significant improvement in both HbA1 C and C-peptide levels when compared to those of the control group at three and six months post administration. 267 , 268 The combination of allogeneic WJ-MSCs with autologous BM-derived mononuclear cells improved insulin secretion and reduced insulin requirements in patients with T1DM. 269 In terms of T2DM, 23 studies were registered on clinicaltrials.gov (searched in October 2021), with six completed studies (three studies used BM-MSCs and three studies used allogeneic UC-MSCs). Although the number of studies using MSCs for the treatment of T2DM is small, their findings support the safety of MSCs, with no severe adverse events observed during the course of these studies. 270 It was confirmed that MSC therapy potentially reduced fasting blood glucose and HbA1 C levels and increased C-peptide levels. However, these effects were short-term, and multiple doses were required to maintain the MSC effects. Interestingly, the autologous MSC approach in the treatment of patients with diabetes in general is hampered, as both BM-MSCs and AT-MSCs isolated from patients with diabetes showed reduced stemness and functional characteristics. 271 , 272 In addition, the durations of diabetes and obesity are strongly associated with autologous BM-MSC metabolic function, especially mitochondrial respiration, and the accumulation of mitochondrial DNA, which directly interfere with the functions of BM-MSCs and reduce the effectiveness of the therapy. 271 Therefore, the allogeneic approach using MSCs from healthy donors provides an alternative approach for stem cell therapy in the treatment of patients with diabetes.
Infertility and reproductive function recovery
Modern society is increasingly facing the problem of infertility, which is defined as the inability to become pregnant after more than 1 year of unprotected intercourse. 273 This problem has emerged as an important worldwide health issue and social burden. Assisted reproductive techniques and in vitro fertilization technology have recently become the most effective methods for the treatment of infertility in humans, but the use of these approaches is limited, as they cannot be applied in patients with no sperm or those who are unable to support implantation during pregnancy, they are associated with complications, they are time-consuming and expensive, and they are associated with ethical issues in certain territories. 274 Numerous conditions are related to infertility, including POF, nonobstructive azoospermia, endometrial dysfunction, and Asherman syndrome. Recent progress has been illustrated in preclinical studies for the potential applications of stem cell-based therapy for reproductive function recovery, especially recent studies in the field of MSCs, which provide new hope for patients with infertility and reproductive disorders. 275
POF is characterized by a loss of ovarian activity during middle age (before 40 years old) and affects 1–2% of women of reproductive age. 276 Patients diagnosed with POF exhibit oligo-/amenorrhea for at least 4 months, with increased levels of follicle-stimulating hormone (FSH) (>25 IU/L) on two occasions more than 1 month apart. 277 Diverse factors, such as genetic backgrounds, autoimmune disorders, environmental conditions, and iatrogenic and idiopathic situations, have been reported to be the cause of POF. 278 POF can be treated with limited effectiveness via psychosocial support, hormone replacement intervention, and fertility management. 279 MSCs from AT, BM, and UC have been used in the treatment of POF, with improvements in ovarian function in preclinical studies using chemotherapy-induced POF animal models. The early published POF study using BM-MSCs as the main cell source is a single case report in which a perimenopausal woman showed an improvement in follicular regeneration, and increased AMH levels resulted in a successful pregnancy followed by delivery of a healthy infant. 280 A report using autologous BM-MSCs in two women with POF illustrated an increase in baseline estrogen levels and the volume of the treated ovaries along with amelioration of menopausal symptoms. 281 The clinical procedures used in this early trial were invasive, as patients underwent two operations: (1) BM aspiration and (2) laparoscopy. A similar approach was used in two trials conducted in 10 women with POF (age range from 26–33 years old) and 30 patients (age from 18 to 40 years old). 282 A later study investigated two different routes of cell delivery, including laparoscopy and the ovarian artery, but the results have not been reported at this time. 282 Based on the positive outcomes of the mouse model, an autologous stem cell ovarian transplantation (ASCOT) trial was deployed using BM-derived stem cells with encouraging observations of improved ovarian function, as determined by elevated levels of AMH and AFC in 81.3% of participants, six pregnancies, and the successful delivery of three healthy babies. 283 A randomized trial (NCT03535480) was conducted in 20 patients with POF aged less than 39 years to further elaborate on the results of the ASCOT trial. 284 To date, there are no completed trials using AT-MSCs or UC-MSCs in the treatment of patients with POF, limiting the evaluation of these MSCs in the treatment of POF. The speculated reason is that POF is a rare disease, affecting 1% of women younger than 40 years, and with improvements in assisted productive technology, patients have several alternative options to enhance the recovery of reproductive function. 285
Wound healing and skin burns
Burns are the fourth most common injury worldwide, affecting ~11 million people, and are a major cause of death (180,000 patients annually). The severity of burns is defined based on the percentage of surface area burned, burn depth, burn location and patient age, and burns are usually classified into first-, second-, third-, and fourth-degree burns on the basis of their severity. 286 Postburn recovery depends on the severity of the burn and the effectiveness of treatment. Rapid healing may occur over weeks, while alternatively, healing can take months, with the ultimate result being scar formation and disability in patients with severe burns. Different from mechanical injury, burn injury is an invasive progression of damage to tissue at the burn site, including both mechanical damage to the skin surface and biological damage caused by natural apoptosis that prolongs excessive inflammation, oxidative stress, and impaired tissue perfusion. 287 To date, completely reversing the devastating damage of severe burns remains unachievable in medicine, and stem cell therapy provides an alternative option for patients with burn injury. The first case report of the use of BM-MSCs to treat a 45-year-old patient with burns on 40% of their body demonstrated the safety of the therapy and showed partial improvements in vascularization at the wound site and reduced coarse cicatrices. 288 , 289 Later, patients with second- and third-degree burns as well as deep burns were treated using either autologous BM-MSCs or allogeneic BM-MSCs by spraying the MSCs onto the burn sites or adding MSCs over a dermal matrix sheet to cover the wound. The results in these case reports revealed the potential efficacy of MSC-based therapy, which not only enhanced the speed of wound recovery but also reduced pain and improved blood supply without introducing infection. 288 , 290 , 291 In 2017, a study conducted in 60 patients with 10–25% of their total body surface areas burned treated with either autologous BM-MSCs or UC-MSCs showed that both MSC types improved the rate of healing and reduced the hospitalization period. 292 The drawback of BM-MSCs in the treatment of burns is the invasive harvesting method, which causes pain and possible complications in patients. Hence, treatment with allogeneic MSCs obtained from healthy donors is the method of choice, and AT- and UC-MSCs are two suitable candidates for this option. To date, a limited number of clinical trials have been conducted using MSC therapy. These trials have several limitations in trial design, such as a lack of a negative control group and blinding, small sample sizes, and the use of standardized measurement tools for burn injury and wound healing. Currently, AT-MSCs are being used in seven ongoing phase I and II trials in the treatment of burns. Hence, it is important to note that among the most widely studied MSCs, AT-MSCs have advantages over BM-MSCs when obtained from an allogeneic source, while their abilities in burn treatment remain to be determined. The main MSCs that should be used in the regeneration of burn tissue remain undefined (Table 3 ), and we observed the trend that AT-MSCs are more suitable candidates due to their biological nature, which contributes to the generation of keratinocytes and secretion profiles that strongly enhance the skin regeneration process. 293 , 294 , 295 , 296
MSC applications in cardiovascular disease: a promising but still controversial field
In the last two decades, great advancements have been achieved in the development of novel regenerative medicine and cardiovascular research, especially stem cell technology. 297 The discovery of human embryonic stem cells and human induced pluripotent stem cells (hiPSCs) opened a new door for basic research and therapeutic investigation of the use of these cells to treat different diseases. 298 However, the clinical path of hiPSCs and hiPSC-derived cardiomyocytes in the treatment of cardiovascular diseases is limited due to the potential for teratoma formation with hiPSCs and the immaturity of hiPSC-derived cardiomyocytes, which might pose a risk of cancer formation, 299 arrhythmia, and cardiac arrest to patients. 300 A recently emerged stem cell type is adult stem cells/progenitor cells, including MSCs, which can stimulate myocardial repair post administration due to their paracrine effects. Promising results of MSC-based therapy obtained from preclinical studies of cardiac diseases enhance the knowledge and strengthen the clinical research to investigate the safety and efficacy in a clinical trial setting. There are papers that discuss the importance of MSC therapy in the treatment of cardiovascular diseases, with the following references being highly recommended. 301 , 302 , 303 , 304 , 305 , 306 To date, 36 trials have evaluated the therapeutic potential of MSCs in different pathological conditions, with the most prevalent types being BM-MSCs (25 trials), followed by UC-MSCs (7 trials) and AT-MSCs (4 trials). 303 However, the reported results are contradictory and create controversy about the efficacy of the treatments.
One of the first trials using MSCs in the treatment of chronic heart failure was the Cardiopoietic Stem Cell Therapy in Heart Failure (C-CURE) trial, a multicentre, randomized clinical trial that recruited 47 patients. The trial findings supported the safety of BM-MSC therapy and provided a data set that demonstrated improvements in cardiovascular scores along with New York Heart Association functional class, quality of life, and general physical health. 307 Despite these encouraging results in the phase I trial, the treatment failed to achieve the primary outcomes in the phase II/III trial (CHART-1 trial), including no significant improvements in cardiac structure or function or patient quality of life. 308 A positive outcome was also found in a phase I/II, randomized pilot study called the POSEIDON trial, which was the first trial to demonstrate the superior effectiveness of the administration of allogeneic BM-MSCs compared to allogeneic MSCs from other sources. 309 , 310 Published results from the MSC-HF study, with 4 years of follow-up results, 311 , 312 and the TRIDENT study 313 illustrated the positive outcomes of BM-MSCs in the treatment of heart failure. However, a contradictory result from the recently published CONCERT-HF trial demonstrated that the administration of autologous BM-MSCs to patients diagnosed with chronic ischemic heart failure did not improve left ventricular function or reduce scar size at 12 months post administration, but the patient’s quality of life was improved. 314 This observation is similar to that of the TAC-HFT trial 315 but completely different from the reported results of the MSC-HF trial. A comprehensive investigation is still needed to determine the reasons behind these contradictory results. The largest clinical trial to date using BM-MSCs is the DREAM-HF study, which was a randomized, double-blind, placebo-controlled, phase III trial that was conducted at 55 sites across North America and recruited a total of 565 patients with ischemic and nonischaemic heart failure. 172 Although recent reports from the sponsor confirmed that the trial missed its primary endpoint (a reduction in recurrent heart failure-related hospitalization), other prespecified endpoints were met, such as a reduction in overall major adverse cardiac events (including death, myocardial infarction, and stroke). 306 Thus, a complete report from the DREAM-HF trial will provide pivotal data supporting the therapeutic potential of BM-MSCs in the treatment of heart failure and open a new path for the FDA to approve cell-based therapy for cardiovascular diseases.
The early trial using AT-derived cells was the PRECISE trial, which was a phase I, randomized, placebo-controlled, double-blind study that examined the safety and efficacy of adipose-derived regenerative cells (ADRCs) in the treatment of chronic ischemic cardiomyopathy. 316 ADRCs are a homogenous population of cells obtained from the vascular stromal fraction of AT, which contains a small proportion of AT-MSCs. 317 Although the study supported the safety of ADRC administration and illustrated a preserved functional capacity (peak VO 2 ) in the treated group and improvements in heart wall motion, neither poor left ventricle (LV) volume nor poor left ventricular ejection fraction (LVEF) was ameliorated. The follow-up trial of the PRECISE trial, called the ATHENA trial, was conducted in 31 patients, although the study was terminated prematurely because two cerebrovascular events occurred, which were not related to the cell product itself. 318 The results of the study illustrated increases in functional capacity, hospitalization rate, and MLHFQ scores, but the LV volume and LVEF were not significantly different between the two groups. Kastrup and colleagues conducted the first in vitro expanded AT-MSC trial in ten patients with ischemic heart disease and ischemic heart failure in 2017. The results confirmed that ready-to-use AT-MSCs were well-tolerated and potentially effective in the treatment of ischemic heart disease and heart failure. 319 Comparable results of AT-MSCs were also reported from the MyStromalCell Trial, which was a randomized placebo-controlled study. In this trial, 61 patients were randomized at a 2:1 ratio into two groups, with the results showing no significant difference in the primary endpoint, which was a change in the maximal bicycle exercise tolerance test (ETT) score from baseline to 6 months post administration. 320 A 3-year follow-up report from the MyStromalCell Trial confirmed that patients who received AT-MSC administration maintained their preserved exercise capacity and their cardiac symptoms improved, whereas the control group experienced a significant reduction in exercise performance and a worsened cardiovascular condition. 321
UC-MSCs are potential allogeneic cells for the treatment of cardiovascular disease, as they are “ready to use” and easy to isolate, they rapidly proliferate, and they secrete hepatocyte growth factors, 322 which are involved in cardioprotection and cardiovascular regeneration. 323 The pilot study using UC-MSCs in 30 patients with heart failure, called the RIMECARD trial, was the first reported trial for which the results supported the effectiveness of UC-MSCs, as seen in the improved ejection fraction, left ventricular function, functional status, and quality of life in patients administered UC-MSCs. 324 Encouraging results reported from a phase I/II HUC-HEART trial 325 showed improvements in LVEF and reductions in the size of the injured area of the myocardium. However, the opposite observations were also reported from a recently published phase I randomized trial using a combination of UC-MSCs and a collagen scaffold in patients with ischemic heart conditions, in which the size of fibrotic scar tissue was not significantly reduced. 326
Although MSCs from AT, BM, and UC have proven to be safe and feasible in the treatment of cardiovascular diseases, the correlation between the MSC types and their therapeutic potentials is still uncertain because different results have been reported from different clinical trials (Table 4 ). The mechanisms by which MSCs participate in recovery and enhance myocardial regeneration have been discussed comprehensively in a recently published review; 305 , 327 therefore, they will not be discussed in this review. In fact, the challenges of MSC-based therapy in cardiovascular diseases have been clearly described previously, 328 including (1) the lack of an in vitro evaluation of the transdifferentiation potential of MSCs to functional cardiac and endothelial cells, 329 (2) the uncontrollable differentiation of MSCs to undesirable cell types post administration, 330 and (3) the undistinguishable nature of MSCs derived from different sources with various levels of differentiation potential. 331 Therefore, the applications of MSC-based therapy in cardiovascular disease are still in their immature stage, with potential benefits to patients. Thus, there is a need to conduct large-scale, well-designed randomized clinical trials not only to confirm the therapeutic potential of MSCs from various sources but also to enhance our knowledge of cardiovascular regeneration post administration.
Proposed mechanism of BM-MSCs in the treatment of acquired brain and spinal injury
Bones are complex structures constituting a part of the vertebrate skeleton, and they play a vital role in the production of blood cells from HSCs. Similar to the functions of most vertebrate organs, bone function is tightly regulated by its constituents and by long-range signaling from AT and the adrenal glands, parathyroid glands, and nervous system. 332 The central nervous system (CNS) orchestrates the voluntary and involuntary input transmitted by a network of peripheral nerves, which act as the bridge between the nervous system and target organs. The CNS controls involuntary responses via the autonomic nervous system (ANS), consisting of the sympathetic nervous system and the parasympathetic nervous system, and voluntary responses via the somatic nervous system. The ANS penetrates deep into the BM cavity, reaching the regions of hematopoietic activity to deliver neurotransmitters that tightly regulate BM stem cell niches. 333 The BM microenvironment consists of various cell types that participate in the maintenance of HSC niches, which are composed of specialized cells, including BM-MSCs (Fig. 3a ). The release of a specific neurotransmitter, circadian norepinephrine, from the sympathetic nervous system at nerve terminals leads to a reduction in the circadian expression of C–X-C chemokine ligand 12 (CXCL12, which is also known as stromal cell-derived factor-1 (SDF-1)) by Nestin + /NG2 2+ BM-MSCs, resulting in the secretion of HSCs into the peripheral bloodstream. 334 , 335 In fact, BM-MSCs play a significant role in the regulation of HSC quiescence and are closely associated with arterioles and sympathetic nervous system nerve fibers. Nestin-expressing BM-MSCs have been shown to express high levels of SDF-1, stem cell factor (SCF), angiopoietin-1 (Ang-1), interleukin-7, vascular cell adhesion molecule 1 (VCAM-1), and osteopontin (OPN), which are directly involved in the regulation and maintenance of HSC quiescence. 336 The depletion of BM-MSCs in BM leads to the mobilization of HSCs into the peripheral bloodstream and spleen. The findings from a previous study demonstrated that reduced SDF-1 expression in norepinephrine-treated BM-MSCs resulted in the mobilization of CXCR4 + HSCs into circulation. 337 The ability of BM-MSCs to produce SDF-1 is tightly related to their neuronal protective functions. 338 SDF-1 is a member of a chemokine subfamily that orchestrates an enormous diversity of pathways and functions in the CNS, such as neuronal survival and proliferation. The chemokine has two receptors, CXCR4 and CXCR7, that are involved in the pathogenic development of neurodegenerative and neuroinflammatory diseases. 339 In the damaged brain, SDF-1 functions as a stem cell homing signal, and in acquired immune deficiency syndrome (AIDS), SDF-1 has been reported to be involved in the protection of damaged neurons by preventing apoptosis. In a traumatic brain injury model, SDF-1 was found to function as an inhibitor of the caspase-3 pathway by upregulating the Bcl-2/Bax ratio, which in turn protects neurons from apoptosis. 340 Moreover, the release of SDF-1 also facilitates cell recruitment, cell migration, and the homing of neuronal precursor cells in the adult CNS by activating the CXCR4 receptor. 341 , 342 Existing data support that SDF-1 acts as the guiding signal for the regeneration of axon growth in damaged neurons and enhances spinal nerve regeneration. 343 , 344 Hence, the ability of BM-MSCs to express SDF-1 in response to the neuronal environment provides a unique neuronal protective effect that could explain the potential therapeutic efficacy of BM-MSCs in the treatment of neurodegenerative diseases (Fig. 3b ).
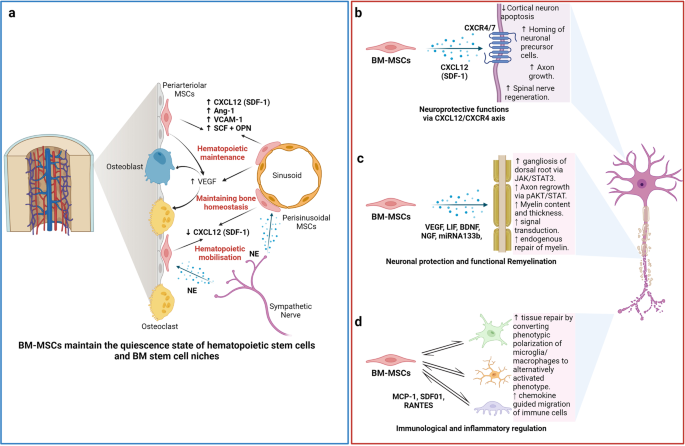
The nature of the “stem niche” of bone marrow-derived mesenchymal stem cells (BM-MSCs) supports their therapeutic potential in neuron-related diseases. a Bone marrow is a complex stem cell niche regulated directly by the central nervous system to maintain bone marrow homeostasis and haematopoietic stem cell (HSC) functions. MSCs in bone marrow respond to the environmental changes through the release of norepinephrine (NE) from the sympathetic nerves that regulate the synthesis of SDF-1 and the migration of HSCs through the sinusoids. The secretion of stem cell factors (SCFs), VCAM-1 and angiotensin-1 from MSCs also plays a significant role in the maintenance of HSCs. b BM-MSCs have the ability to produce and release SDF-1, which directly contributes to neuroprotective functions at the damaged site through interaction with its receptors CXCR4/7, located on the neuronal membrane. c Neuronal protection and the functional remyelination induced by BM-MSCs are also modulated by the release of a wide range of growth factors, including VEGF, BDNF, and NGF, by the BM-MSCs. d BM-MSCs also have the ability to regulate neuronal immune responses by direct interaction or paracrine communication with microglia. Figure was created with BioRender.com
The migration of exogenous MSCs after systemic administration to the brain is limited by the physical blood–brain barrier (BBB), which is a selective barrier formed by CNS endothelial cells to restrict the passage of molecules and cells. The mechanism of molecular movement across the BBB is well established, but how stem cells can bypass the BBB and home to the brain remains unclear. Recent studies have reported that MSCs are able to migrate through endothelial cell sheets by paracellular or transcellular transport followed by migration to the injured or inflammatory site of the brain. 345 , 346 During certain injuries or ischemic events, such as brain injury, stroke, or cerebral palsy, the integrity and efficiency of BBB protection is compromised, which allows MSC migration across the BBB via paracellular transport through the transient formation of interendothelial gaps. 347 CD24 expression has been detected in human BM-MSCs, which are regulated by TGF-β3, 348 allowing them to interact with activated endothelial cells via P-selectin and initiate the tethering and rolling steps of MSCs. 349 Additionally, BM-MSCs express high levels of CXCR4 or CXCR7, 350 , 351 which bind to integrin receptors, such as VLA-4, to activate the integrin-binding process and allow the cells to anchor to endothelial cells, followed by the migration of MSCs through the endothelial cell layer and basement membrane in a process called transmigration. 352 This process is facilitated by the secretion of matrix metalloproteinases (MMPs), which degrade the endothelial basement membrane, allowing BM-MSCs to enter the brain environment. 353 , 354 BM-MSCs can also regulate the integrity of the BBB via the secretion of tissue inhibitor of matrix metalloproteinase-3 (TIMP3), which has been shown to ameliorate the effects of a compromised BBB in traumatic brain injury. 355 The secretion of TIMP3 from MSCs directly blocked vascular endothelial growth factor a (VEGF-a)-induced breakdown of endothelial cell adherent junctions, demonstrating the potential mechanism of BM-MSCs in the regulation of BBB integrity.
The therapeutic applications of BM-MSCs in neurodegenerative conditions have been significantly increased by the demonstration of BM-MSC involvement in axonal and functional remyelination processes. Remyelination is a spontaneous regenerative process occurring in the human CNS to protect oligodendrocytes, neurons, and myelin sheaths from neuronal degenerative diseases. 356 Remyelination is considered a neuroprotective process that limits axonal degeneration by demyelination and neuronal damage. The first mechanism of action of BM-MSCs related to remyelination is the activation of the JAK/STAT3 pathway to regulate dorsal root ganglia development. 357 It was reported that BM-MSCs secrete vascular endothelial growth factor-A (VEGF-A), 358 brain-derived neurotrophic factor (BDNF), interleukin-6, and leukemia inhibitor factor (LIF), which directly function in neurogenesis and neurite growth. 357 VEGF-A is a key regulator of hemangiogenesis during development and bone homeostasis. Postnatally, osteoblast- and MSC-derived VEGF plays a critical role in maintaining and regulating bone homeostasis by stimulating MSC differentiation into osteoblasts and suppressing their adipogenic differentiation. 359 , 360 , 361 To balance osteoblast and adipogenic differentiation, VEGF forms a functional link with the nuclear envelope protein laminin A, which in turn directly regulates the osteoblast and adipocyte transcription factors Runx2 and PPARγ, respectively. 361 , 362 In the brain, VEGF is a potent growth factor mediating angiogenesis, neural migration, and neuroprotection. VEGF-A, secreted from BM-MSCs under in vitro xeno- and serum-free culture conditions, is the most studied member of the VEGF family and is suggested to play a protective role against cognitive impairment, such as in the context of Alzheimer’s disease pathology or stroke. 363 , 364 , 365 Recently, it was reported that the neurotrophic and neuroprotective function of VEGF is mediated through VEGFR2/Flk-1 receptors, which are expressed in the neuroproliferative zones and extend to astroglia and endothelial cells. 366 In animal models of intracerebral hemorrhage and cerebral ischemia, the transfusion of Flk-1-positive BM-MSCs promotes behavioral recovery and anti-inflammatory and angiogenic effects. 367 , 368 Moreover, supplementation with VEGF-A in neuronal disorders enhances intraneural angiogenesis, improves nerve regeneration, and promotes neurotrophic capacities, which in turn increase myelin thickness via the activation of the prosurvival transcription factor nuclear factor-kappa B (NF-kB). This activation, together with the downregulation of Mdm2 and increased expression of the pro-apoptotic transcription factor p53, is considered to be the neuroprotective process associated with an increased VEGF-A level. 369 , 370 , 371 An analysis of microRNA (miRNA) in extracellular vesicles (EVs) secreted from BM-MSCs revealed that BM-MSCs release substantial amounts of miRNA133b, which suppresses the expression of connective tissue growth factor (CTGF) and protects hippocampal neurons from apoptosis and inflammatory injury 372 , 373 , 374 (Fig. 3c ).
In terms of immunoregulatory functions, the administration of human BM-MSCs into immunocompetent mice subjected to SCI or brain ischemia showed that BM-MSCs exhibited a short-term neuronal protective function against neurological damage (Fig. 3d ). Further investigation demonstrated the ability of BM-MSCs to directly communicate with host microglia/macrophages and convert them from phenotypic polarization into alternative activated microglia/macrophages (AAMs), which are key players in axonal extension and the reconstruction of neuronal networks. 375 Other studies have also illustrated that the administration of AAMs directly to the injured spinal cord induced axonal regrowth and functional improvement. 376 The mechanism by which BM-MSCs activate the conversion of microglia/macrophages occurs through two representative macrophage-related chemokine axes, CCL2/CCR2 and CCL-5/CCR5, both of which exhibit acute or chronic elevation following brain injury or SCI. 377 The CCL2/CCR2 axis contributed to the enhancement of inflammatory function, and BM-MSC-mediated induction of CCL2 did not alter the total granulocyte number (Fig. 3d ). Although the chemokine-mediated mechanism of BM-MSCs in the activation of AAMs and enhanced axonal regeneration at the damage sites is evident, the direct mechanism by which the communication between BM-MSCs and the target cells results in these phenomena remains unclear, and further investigation is needed.
BM-MSCs also confer the ability to regulate the inflammatory regulation of the immune cells present in the brain by (1) promoting the polarization of macrophages toward the M2 type, (2) suppressing T-lymphocyte activities, (3) stimulating the proliferation and differentiation of regulatory T cells (Tregs), and (4) inhibiting the activation of natural killer (NK) cells. BM-MSCs secrete glial cell line-derived neurotrophic factor (GDNF), a specific growth factor that contributes directly to the transition of the microglial destructive M1 phenotype into the regenerative M2 phenotype during the neuroinflammatory process. 378 A similar result was also found in AT- 379 and UC-MSCs 380 under neuroinflammation-associated conditions, suggesting that AT-, BM-, and UC-MSCs share the same mechanism in promoting macrophage polarization. In terms of T-lymphocyte suppression, compared to MSCs from AT and BM, UC-MSCs show the strongest potential to inhibit the proliferation of T-lymphocytes by promoting cell cycle arrest (G0/G1 phase) and apoptosis. 381 In addition, UC-MSCs have been proven to be more effective in promoting the proliferation of Tregs 382 and inhibiting NK activation. 383 Although MSCs are well-known for their inflammatory regulatory ability, the mechanism is not exclusive to BM-MSCs, especially in neurological disorders. 384
Proposed mechanism of UC-MSCs in the treatment of pulmonary diseases and lung fibrosis
In contrast to AT-MSCs and BM-MSCs, UC-MSCs have lower expression of major histocompatibility complex I (MHC I) and no expression of MHC II, which prevents the complications of immune rejection. 385 Moreover, as UC is considered a waste product after birth, with the option of noninvasive collection, UC-MSCs are easier to obtain and culture than AD- and BM-MSCs. 386 These advantages of UC-MSCs have contributed to their use in the treatment of pulmonary diseases, especially during the rampant COVID-19 pandemic, as “off-the-shelf” products. Numerous pulmonary diseases have been the subject of applications of UC-MSCs, including BPD, COPD, ARDS, and COVID-19-induced ARDS. In BPD, premature infants are born before the alveolarization process, resulting in arrested lung development and alveolar maturation. Upon administration via an IV route, the majority of exogenous UC-MSCs reach the immature lung and directly interact with immune cells to exert their immunomodulatory properties via cell-to-cell interaction mechanisms (Fig. 4a ). UC-MSCs interact with T cells via the PD-L1 ligand, which binds to the PD-1 inhibitory molecule on T cells, resulting in the suppression of CD3+ T-cell proliferation and effector T-cell responses. 387 In addition, UC-MSCs also express CD54 (ICAM-1), which plays a crucial role in the immunomodulatory functions of T cells. 388 Direct contact between UC-MSCs and macrophages via CD54 expression on UC-MSCs promotes the immune regulation of UC-MSCs via the regulation of phagocytosis by monocytes. 389 Moreover, the contact of UC-MSCs with macrophages during proinflammatory responses increases the secretion of TSG-6 by UC-MSCs, which in turn promotes the inhibitory regulation of CD3+ T cells, macrophages, and monocytes by MSCs. 390 Recently, upregulation of SDF-1 was described in neonatal lung injury, especially in layers of the respiratory epithelium. 391 SDF-1 has been shown to participate in the migration and initiation of the homing process of MSCs via the CXCR4 receptors on their surface. 392 It was reported that UC-MSCs express low levels of CXCR4, allowing them to induce SDF-1-associated migration processes via the Akt, ERK, and p38 signal transduction pathways. 393 Hence, in BPD, the upregulation of SDF-1 together with the homing ability of UC-MSCs strongly supports the therapeutic effects of UC-MSCs in the treatment of BPD. Furthermore, UC-MSCs have the ability to communicate with immune cells via cell-to-cell contact to reduce proinflammatory responses and the production of proinflammatory cytokines (such as TGF-β, INF-γ, macrophage MIF, and TNF-α). The modulation of the human innate immune system by UC-MSCs is mediated by cell–cell interactions via CD54-LFA-1 that switch macrophage polarization processes, promoting the proliferation of M2 macrophages, which in turn reduce inflammatory responses in the immature lung. 394 Moreover, UC-MSCs also have the ability to produce VEGF and hepatocyte growth factors (HGFs), promoting angiogenesis and enhancing lung maturation. 395
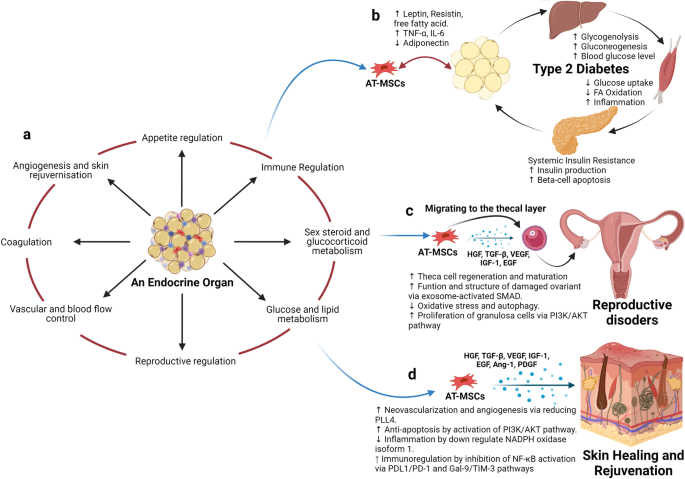
Adipose tissue-derived mesenchymal stem cells (AT-MSCs) and the nature of their tissue of origin support their use in therapeutic applications. a Adipose tissue is considered an endocrine organ, supporting and regulating various functions, including appetite regulation, immune regulation, sex hormone and glucocorticoid metabolism, energy production, the orchestration of reproduction, the control of vascularization, and blood flow, the regulation of coagulation, and angiogenesis and skin regeneration. b In terms of metabolic disorders, such as type 2 diabetes mellitus (T2DM), as adipose tissue is directly involved in the metabolism of glucose and lipids and the regulation of appetite, the detrimental effects of T2DM also alter the functions of AT-MSCs, which in turn, hampers their therapeutic effects. Hence, the use of autologous AT-MSCs is not recommended for the treatment of metabolic disorders, including T2DM, suggesting that allogeneic AT-MSCs from healthy donors could be a better alternative approach. c AT-MSCs are suitable for the treatment of reproductive disorders due to their unique ability to mobilize and home to the thecal layer of the injured ovary, enhance the regeneration and maturation of thecal cells, increase the structure and function of damaged ovaries via exosome-activated SMAD, decrease oxidative stress and autophagy, and increase the proliferation of granulosa cells via PI3K/AKT pathways. These functions are regulated specifically by growth hormones produced by AT-MSCs in response to the surrounding environment, including HGF, TGF-β, IGF-1, and EGF. d AT-MSCs are also good candidates for skin healing and regeneration as their growth factors strongly support neovascularization and angiogenesis by reducing PLL4, increase anti-apoptosis via the activation of PI3K/AKT pathways, regulate inflammation by downregulating NADPH oxidase isoform 1, and increase immunoregulation through the inhibition of NF-κB activation. The figure was created with BioRender.com
COPD is characterized by an increase in hyperinflammatory reactions in the lung, compromising lung function and increasing the development of lung fibrosis. The mechanism by which UC-MSCs contribute to the response to COPD is inflammatory regulation (Fig. 4b ). The administration of UC-MSCs prevented the infiltration of inflammatory cells in peribronchiolar, perivascular, and alveolar septa and switched macrophage polarization to M2. 396 A significant reduction in proinflammatory cytokines, including IL-1β, TNF-α, and IL-8, was also observed following UC-MSC administration. 224 MSCs, including UC-MSCs, have been reported to trigger the production of secretory leukocyte protease inhibitors in epithelial cells through the secretion of HGF and epidermal growth factor (EGF), which is believed to have beneficial effects on COPD. 397 , 398 In addition to their inflammatory regulation ability, UC-MSCs exhibit antimicrobial effects through the inhibition of bacterial growth and the alleviation of antibiotic resistance during Pseudomonas aeruginosa infection. 399 The combination of the regulation of the host immune response and the antimicrobial effects of UC-MSCs may be relevant for the prevention and treatment of COPD exacerbations, as inflammation and bacterial infections are important risk factors that significantly contribute to the morbidity and mortality of patients with COPD. In terms of regenerative functions, UC-MSCs were reported to be able to differentiate into type 2 alveolar epithelial cells in vitro and alleviate the development of pulmonary fibrosis via β-catenin-regulated cell apoptosis. 400 Furthermore, UC-MSCs enhanced alveolar epithelial cell migration and proliferation by increasing matrix metalloproteinase-2 levels and reduced their endogenous inhibitors, tissue inhibitors of matrix metalloproteinases, providing a potential mechanism underlying their anti-pulmonary-fibrosis effects. 401 , 402
In ARDS, especially that associated with COVID-19, the proinflammatory state is initiated by increases in plasma concentrations of proinflammatory cytokines, such as IL-1 beta, IL-7, IL-8, IL-9, IL-10, bFGF, granulocyte colony-stimulating factor (G-CSF), GM-CSF, IFN-γ, and TNF-α. The significant increases in the concentrations of these cytokines in patient plasma suggest the development of a cytokine storm, which is a leading cause of COVID-induced mortality. In addition to the immunomodulatory functions regulated via cell-to-cell interactions between UC-MSCs and immune cells, such as macrophages, monocytes, and T cells, UC-MSCs exert their functions via paracrine effects through the secretion of growth factors, cytokines, and exosomes (Fig. 4c ). The most relevant immunomodulatory function of UC-MSCs is considered to be their inhibition of effector T cells via the induction of T-cell apoptosis and cell cycle arrest by the production of indoleamine 2,3- dioxygenase (IDO), prostaglandin E2 (PGE-2), and TGF-β. Elevated levels of PGE-2 in patients with COVID-19 are reported to be a crucial factor in the initiation of inflammatory regulation by UC-MSCs post administration and prevent the development of cytokine storms by direct inhibition of T- and B lymphocytes. 403 UC-MSCs exert these inhibitory activities through a PGE-2-dependent mechanism. 404 It was reported that UC-MSCs confer the ability to secrete tolerogenic mediators, including TGF-β1, PGE-2, nitric oxide (NO), and TNF-α, which are directly involved in their immunoregulatory mechanism. The secretion of NO from UC-MSCs is reported to be associated with the desensitization of T cells via the IFN-inducible nitric oxide synthase (iNOS) pathways and to stimulate the migration of T cells in close proximity to MSCs that subsequently suppress T-cell sensitivities via NO. 405 Lung infection with viruses usually leads to impairments in alveolar fluid clearance and protein permeability. The administration of UC-MSCs enhances alveolar protection and restores fluid clearance in patients with COVID-19. UC-MSCs secrete growth factors associated with angiogenesis and the regeneration of pulmonary blood vessels and micronetworks, including angiotensin-1, VEGF, and HGF, which also reduce oxidative stress and prevent fibrosis formation in the lungs. These trophic factors have been identified as key players in the modulation of the microenvironment and promote pulmonary repair. Additionally, UC-MSCs are more effective than BM-MSCs in the restoration of impaired alveolar fluid clearance and the permeability of airways in vitro, supporting the use of UC-MSCs in the treatment of patients with pulmonary pneumonia. 406 In the context of pulmonary regeneration, UC-MSCs were shown to inhibit apoptosis and fibrosis in pulmonary tissue by activating the PI3K/AKT/mTOR pathways via the secretion of HGF, which also acts as an inhibitory stimulus that blocks alveolar epithelial-to-mesenchymal transition. 407 , 408 Moreover, UC-MSCs can reverse the process of fibrosis via enhanced expression of macrophage matrix-metallopeptidase-9 for collagen degradation and facilitate alveolar regeneration via Toll-like receptor-4 signaling pathways. 409 UC-MSCs were shown to communicate with CD4+ T cells through HGF induction not only to inhibit their differentiation into Th17 cells, reducing the secretion of IL-17 and IL-22 but also to switch their differentiation into regulatory T cells. 410 , 411 In addition, UC-MSCs conferred the ability to facilitate the number of M2 macrophages and reduce M1 cells via the control of the macrophage polarization process. 412
There are several potential mechanisms of UC-MSCs in the treatment of patients with pulmonary diseases and pneumonia, including the regulation of immune cell function, immunomodulation, the enhancement of alveolar fluid clearance and protein permeability, the modulation of endoplasmic reticulum stress, and the attenuation of pulmonary fibrosis. Hence, based on these discussions, UC-MSCs are recommended as suitable candidates for the treatment of pulmonary disease both in pediatric and adult patients.
Proposed mechanism of AT-MSCs in the treatment of endocrinological diseases, reproductive disorders, and skin burns
Human AT was first viewed as a passive reservoir for energy storage and later as a major site for sex hormone metabolism, the production of endocrine factors (such as adipsin and leptin), and a secretion source of bioactive peptides known as adipokines. 413 It is now clear that AT functions as a complex and highly active metabolic and endocrine organ, orchestrating numerous different biological features 414 (Fig. 5a ). In addition to adipocytes, AT contains hematopoietic-derived progenitor cells, connective tissue, nerve tissue, stromal cells, endothelial cells, MSCs, and pericytes. AT-MSCs and pericytes mobilize from their perivascular locations to aid in healing and tissue regeneration throughout the body. As AT is involved directly in energy storage and metabolism, AT-MSCs are also mediated and regulated by growth factors related to these pathways. In particular, interleukin-6 (IL-6), IL-33, and leptin regulate the maintenance of metabolic activities by increasing insulin sensitivity and preserving homeostasis related to AT. Nevertheless, in the development of obesity and diabetes, omental and subcutaneous AT maintains a low-grade state of inflammation, resulting in the impairment of glucose metabolism and potentially contributing to the development of insulin resistance. 415 In normal AT, direct regulation of Pre-B-cell leukemia homeobox (Pbx)-regulating protein-1 (PREP1) by leptin and thyroid growth factor-beta 1 (TGF-β1) in AT-MSCs and mature adipocytes is involved in the protective function and maintenance of AT homeostasis. However, under diabetic conditions, the balance between the expression of leptin and the secretion of TGF-β1 is compromised, resulting in the malfunction of AT-MSC metabolic activity and the proliferation, differentiation, and maturation of adipocytes. Therefore, the use of autologous AT-MSCs in the treatment of diabetic conditions is not a suitable option, as the functions of AT-MSCs are directly altered by diabetic conditions, which reduces their effectiveness in cell-based therapy (Fig. 5b ).
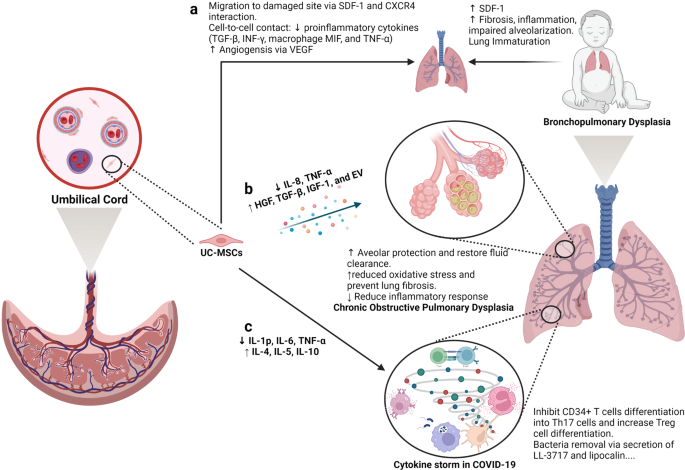
Umbilical cord-derived mesenchymal stem cells (UC-MSCs) are good candidates for the treatment of pulmonary diseases. a Lung immaturity and fibrosis are the major problems of patients with bronchopulmonary dysplasia and lead to increased levels of SDF-1, the development of fibrosis, the induction of the inflammatory response, and the impairment of alveolarization. UC-MSCs are attracted to the damaged lung via the chemoattractant SDF-1, which is constantly released from the immature lung via SDF-1 and CXCR4 communication. Moreover, UC-MSCs reduce the level of proinflammatory cytokines (TGF-β, INF-γ, macrophage MIF, and TNF-α) via a cell-to-cell contact mechanism. The ability of UC-MSCs to produce and secrete VEGF also involves in the regeneration of the immature lung through enhanced angiogenesis. b Upon an exacerbation of chronic obstructive pulmonary disease (COPD), UC-MSCs respond to the surrounding stimuli by reducing IL-8 and TNF-α levels, resulting in the inhibition of the inflammatory response but an increase in the secretion of growth factors participating in the protection of alveoli, fluid clearance and reduced oxidative stress and lung fibrosis, including HGF, TGF-β, IGF-1, and exosomes. c In a similar manner, UC-MSCs prevent the formation of cytokine storms in coronavirus disease 2019 (COVID-19) by inhibiting CD34+ T-cell differentiation into Th17 cells and enhancing the number of regulatory T cells. Moreover, UC-MSCs also have antibacterial activity by secreting LL-3717 and lipocalin. Figure was created with BioRender.com
Preclinical studies and clinical trials have revealed the therapeutic effects of MSCs, in general, and AT-MSCs, in particular, in the management of POF, with relatively high efficacy and enhanced regeneration of the ovaries. Understanding the molecular and cellular mechanisms underlying these effects is the first step in the development of suitable MSC-based therapies for POF. One of the mechanisms by which MSCs exert their therapeutic effects is their ability to migrate to sites of injury, a process known as “homing”. Studies have shown that MSCs from different sources have the ability to migrate to different compartments of the injured ovary. For example, BM-MSCs administered through IV routes migrated mostly to the ovarian hilum and medulla, 416 whereas a significant number of UC-MSCs were found in the medulla. 417 Interestingly, AT-MSCs were found to be engrafted in the theca layers of the ovary but not in the follicles, where they acted as supportive cells to promote follicular growth and the regeneration of thecal layers. 418 The structure and function of the thecal layer have a great impact on fertility, which has been reviewed elsewhere. 419 In brief, the thecal layer consists of two distinct parts, the theca interna, which contains endocrine cells, and the theca externa, which is an outer fibrous layer. The thecal layer contains not only endocrine-derived cells but also vascular- and immune-derived cells, whose functions are to maintain the structural integrity of the follicles, transport nutrients to the inner compartment of the ovary and produce key reproductive hormones such as androgens (testosterone and dihydrotestosterone) and growth factors (morphogenic proteins, e.g., BMPs and TGF-β). 420 As AT-MSCs originate from an endocrine organ, their ability to sense signals and migrate to the thecal layer is anticipated. Additionally, secretome analysis of AT-MSCs showed a wide range of growth factors, including HGF, TBG-β, VEGF, insulin-like growth factor-1 (IGF-1), and EGF, 421 that are directly involved in the restoration of the structure and function of damaged ovaries by stimulating cell proliferation and reducing the aging process of oocytes via the activation of the SIRT1/FOXO1 pathway, a key regulator of vascular endothelial homeostasis. 422 , 423 In POF pathology, autophagy and its correlated oxidative stress contribute to the development of POF throughout a patient’s life. Recently, AT-MSCs were shown to be able to improve the structure and function of mouse ovaries by reducing oxidative stress and inflammation, providing essential data supporting the mechanism of AT-MSCs in the treatment of POF. 424 Several studies have illustrated that AT-MSCs secrete biologically active EVs that regulate the proliferation of ovarian granulosa cells via the PI3K/AKT pathway, resulting in the enhancement of ovarian function. 425 Direct regulation of ovarian cell proliferation modulates the state of these cells, which in turn restores the ovarian reserve. 426 Other mechanisms supporting the effectiveness of MSCs have been carefully reviewed, confirming the therapeutic potential of MSCs derived from different sources 426 (Fig. 5c ).
In the last decade, the number of clinical trials using AT-MSCs in the treatment of chronic skin wounds and skin regeneration has exponentially increased, with data supporting the enhancement of the skin healing processes, the reduction of scar formation, and improvements in skin structure and quality. Several mechanisms are directly linked to the origin of AT-MSCs, including differentiation ability, neovascularization, anti-apoptosis, and immunological regulation. AT is a connective and supportive tissue positioned just beneath the skin layers. AT-MSCs have a strong ability to differentiate into adipocytes, endothelial cells, 427 epithelial cells 428 and muscle cells. 429 The adipogenic differentiation of AT-MSCs is one of the three mesoderm lineages that defines MSC features, and AT-MSCs are likely to be the best MSC type harboring this ability compared to BM- and UC-MSCs. Recent reports detailed that AT-MSCs accelerated diabetic wound tissue closure through the recruitment and differentiation of endothelial cell progenitor cells into endothelial cells mediated by the VEGF-PLCγ-ERK1/ERK2 pathway. 430 Upon injury, the skin must be healed as quickly as possible to prevent inflammation and excessive blood loss. The reparation process occurs through distinct overlapping phases and involves various cell types and processes, including endothelial cells, keratinocyte proliferation, stem cell differentiation, and the restoration of skin homeostasis. 431 Hence, the differentiation ability of AT-MSCs plays a critical role in their therapeutic effect on skin wound regeneration and healing processes. AT-MSCs accelerate wound healing via the production of exosomes that serve as paracrine factors. It was reported that AT-MSCs responded to skin wound injury stimuli by increasing their expression of the lncRNA H19 exosome, which upregulated SOX9 expression via miR-19b, resulting in the acceleration of human skin fibroblast proliferation, migration, and invasion. 432 In addition, the engraftment of AT-MSCs supported wound bed blood flow and epithelialization processes. 433 Anti-apoptosis plays a critical role in AT-MSC-based therapy, as without a microvascular supply network established within 4 days post injury, adipocytes undergo apoptosis and degenerate. Exogenous sources of AT-MSCs mediate anti-apoptosis via IGF-1 and exosome secretion by triggering the activation of PI3K signaling pathways. 434 Another mechanism supporting the therapeutic potential of AT-MSCs is their anti-inflammatory function, which results in the reduction of proinflammatory factors, such as tumor necrosis factor (TNF) and interferon-γ (IFN-γ), and increases the production of the anti-inflammatory factors IL-10 and IL-4. Exosomes from AT-MSCs in response to a wound environment were found to contain high levels of Nrf2, which downregulated wound NADPH oxidase isoform 1 (NOX1), NADPH oxidase isoform 4 (NOX4), IL-1β, IL-6, and TNF-α expression. The anti-inflammatory functions of AT-MSCs are also regulated by their immunomodulatory ability, partially through the inhibition of NF-κB activation in T cells via the PD-L1/PD-1 and Gal-9/TIM-3 pathways, providing a novel target for the acceleration of wound healing 435 (Fig. 5d ).
Therefore, as an endocrine organ in the human body, AT and its derivative stem cells, including AT-MSCs, have shown great potential in the treatment of reproductive disorders and skin diseases. Their potential is supported by mechanisms that are directly related to the nature of AT-MSCs in the maintenance of tissue homeostasis, angiogenesis, anti-apoptosis, and the regulation of inflammatory responses.
The current challenges for MSC-based therapies
Over the past decades, MSC-based research and therapy have made tremendous advancements due to their advantages, including immune evasion, diverse tissue sources for harvesting, ease of isolation, rapid expansion, and cryopreservation as “off-the-shelf” products. However, several important challenges have to be addressed to further enhance the safety profile and efficacy of MSC-based therapy. In our opinion, the most important challenge of MSC-based therapy is the fate of these cells post administration, especially the long-term survival of allogeneic cells in the treatment of certain diseases. Although reported data confirm that the majority of MSCs are trapped in the lung and rapidly removed from the circulation, caution has been raised related to the occurrence of embolism events post infusion, which was proven to be related to MSC-induced innate immune attack (called instant blood-mediated inflammatory reaction). 436 Another related challenge is the homing ability of infused cells, as successful homing at targeted tissue might result in long-term benefits to patients. Other concerns related to MSC-based therapy are the number of dead cells infused into the patients. An interesting study reported that dead MSCs alone still exerted the same immunomodulatory property as live MSCs by releasing phosphatidylserine. 437 This is an interesting observation, as there is always a certain number of dead cells present in the cell-based product, and concerns are always raised related to their effects on the patient’s health. Finally, the hypothesis presented in this review is also a great challenge of the field, which has been proposed for future studies to answer the question: “What is the impact of MSC sources on their downstream application?”. Tables 5 and 6 illustrate the comparative studies that were conducted in preclinical and clinical settings to address the MSC source challenge. Other challenges of MSC-based therapies have been discussed in several reviews and systematic studies, 135 , 185 , 438 , 439 which are highly recommended.
Limitations of the current hypothesis
The proposed hypothesis presented in this review was made based on (1) the calculated number of recovered patients from published clinical trials; (2) the empirical experience of the authors in the treatment of brain-related diseases, 440 pulmonary disorders, 215 and endocrinological conditions; 271 , 441 and (3) the proposed mechanisms by which each type of MSC exhibits its best potential for downstream applications. The authors understand that the approach that we used has a certain level of research bias, as a comprehensive meta-analysis is needed to first confirm the correlation between the origins of MSCs and their downstream clinical outcomes before a complete hypothesis can be made. However, to date, a limited number of clinical trials have been conducted to directly compare the efficacy of MSCs from different sources in treating the same disease, which in turn dampened our analysis to prove this hypothesis. In addition, MSC-based therapy is still in its early stages, as controversy and arguments are still present in the field, including (1) the name of MSCs (medicinal signaling cells vs. MSCs or mesenchymal stromal cells), 442 , 443 (2) the existence of “magic cells” (one cell type for the treatment of all diseases), 444 , 445 (3) the conflicting results from large-scale clinical trials, 135 and (4) the dangerous issues of unauthorized, unproven stem cell therapies and clinics. 446 , 447 Therefore, our hypothesis is proposed at this time to encourage active researchers and clinicians to either prove or disprove it so that future research can strengthen the uses of MSC-based therapies with solid mechanistic study results and clarify results for “one cell type for the treatment of all diseases”.
Another limitation is the knowledge coverage in the field of MSC-based regenerative medicine, as discussed in this study. First, the abovementioned diseases were narrowed to four major disease categories for which MSC-based therapy is widely applied, including neuronal, pulmonary, cardiovascular, and endocrinological conditions. In fact, other diseases also receive great benefits from MSC therapy, including liver cirrhosis, 448 bone regeneration, 360 plastic surgery, 449 autoimmune disease, 450 etc., which are not fully discussed in this review and included in our hypothesis. Recently, the secretome profile of MSCs and its potential application in clinical settings have emerged as a new player in the field, with a recently published comprehensive review including MSC-derived exosomes. 451 , 452 To date, the therapeutic potential of MSCs is believed to be strongly influenced by their secretomes, including growth factors, cytokines, chemokines, and exosomes. 453 However, this body of knowledge is also not fully included in our discussion, as this review focuses on the function and potency of MSCs as a whole with considerations derived from published clinical data. Therefore, the authors believe in and support the future applications of the secreted components derived from MSCs, including exosomes, in the treatment of human diseases. In fact, this potential approach could elevate the uses of MSCs to the next level, where the sources of MSCs could be neglected with advancements in the development of protocols that allow strict control of the secretome profiles of MSCs under specific conditions. 454 , 455 , 456 Finally, strategies that could potentially enhance the therapeutic outcomes of MSC-based therapy, such as the “priming” process, are not discussed in this review. The idea of “priming” MSCs is based on the nature of MSCs, which is similar to the immune cells, 457 that MSCs have proven to be able to “remember” the stimulus from the surrounding environment. 458 , 459 Thus, activating or priming MSCs using certain conditions, such as hypoxia, matrix mechanics, 3D environment, hormones, or inflammatory cytokines, could trigger the memory mechanism of the MSCs in vitro so that these cells are ready to function towards specific therapeutic activities without the need for in vivo activation. 3 , 460
From a cellular and molecular perspective and from our own experience in a clinical trial setting, AD-, BM- and UC-MSCs exhibit different functional activities and treatment effectiveness across a wide range of human diseases. In this paper, we have provided up-to-date data from the most recently published clinical trials conducted in neuronal diseases, endocrine and reproductive disorders, skin regeneration, pulmonary dysplasia, and cardiovascular diseases. The implications of the results and discussions presented in this review and in a very large body of comprehensive and excellent reviews as well as systematic analyses in the literature provide a different aspect and perspective on the use of MSCs from different sources in the treatment of human diseases. We strongly believe that the field of regenerative medicine and MSC-based therapy will benefit from active discussion, which in turn will significantly advance our knowledge of MSCs. Based on the proposed mechanisms presented in this review, we suggest several key mechanistic issues and questions that need to be addressed in the future:
The confirmation and demonstration of the mechanism of action prove that tissue origin plays a significant role in the downstream applications of the originated MSCs.
Is it required that MSCs derived from particular cell sources need to have certain functionalities that are unique to or superior in the original tissue sources?
As mechanisms may rely on the secretion of factors from MSCs, it is important to identify the specific stimuli from the wound environments to understand how MSCs from different sources can exhibit similar functions in the same disease and whether or not MSCs derived from a particular source have stronger effects than their counterparts derived from other tissue sources.
Should we create “universal” MSCs that could be functionally equal in the treatment of all diseases regardless of their origin by modeling their genetic materials?
Can new sources of MSCs from either perinatal or adult tissues better stimulate the innate mechanisms of specific cell types in our body, providing a better tool for MSC-based treatment?
A potential ‘priming’ protocol that allows priming, activating, and switching the potency of MSCs from one source to another with a more appropriate clinical phenotype to treat certain diseases. This idea is potentially relevant to our suggestion that each MSC type could be more beneficial in downstream applications, and the development of such a “priming” protocol would allow us to expand the bioavailability of specific MSC types.
From our clinical perspective, the underlying proposal in our review is to no longer use MSCs for applications while disregarding their sources but rather to match the MSC tissue source to the application, shifting from one cell type for the treatment of all diseases to cell source-specific disease treatments. Whether the application of MSCs from different sources still shows their effectiveness to a certain extent in the treatment of diseases or not, the transplantation of MSCs derived from different sources for each particular disease needs to be further investigated, and protocols need to be established via multicentre, randomized, placebo-controlled phase II and III clinical trials (Fig. 6 ).
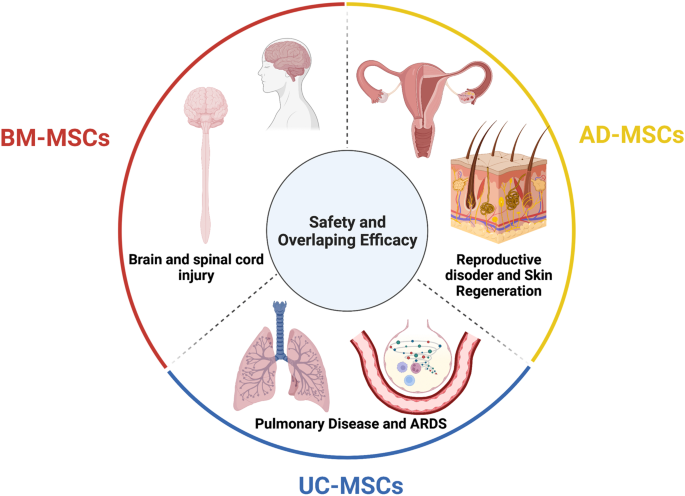
The tissue sources of mesenchymal stem cells (MSCs) contribute greatly to their therapeutic potential, as all MSC types share safety profiles and overlapping efficacy. Although a large body of data and their review and systematic analysis indicated the shared safety and potential efficacy of MSCs derived from different tissue sources, targeted therapies considering MSC origin as an important factor are imperative to enhance the downstream therapeutic effects of MSCs. We suggest that bone marrow-derived MSCs (BM-MSCs) are good candidates for the treatment of brain and spinal cord injury, adipose tissue-derived MSCs (AT-MSCs) are suitable for the treatment of reproductive disorders and skin regeneration, and umbilical cord-derived MSCs (UC-MSCs) could be alternatives for the treatment of pulmonary diseases and acute respiratory distress syndrome (ARDS). Figure was created with BioRender.com
Data availability
All data generated or analyzed in this study are included in this published article.
Mellman, I., Coukos, G. & Dranoff, G. Cancer immunotherapy comes of age. Nature 480 , 480–489 (2011).
Article PubMed PubMed Central CAS Google Scholar
Ancans, J. Cell therapy medicinal product regulatory framework in Europe and its application for MSC-based therapy development. Front. Immunol. 3 , 253 (2012).
Article PubMed PubMed Central Google Scholar
Yin, J. Q., Zhu, J. & Ankrum, J. A. Manufacturing of primed mesenchymal stromal cells for therapy. Nat. Biomed. Eng. 3 , 90–104 (2019).
Article PubMed CAS Google Scholar
O’Brien, T. & Barry, F. P. Stem cell therapy and regenerative medicine. Mayo Clin. Proc. 84 , 859–861 (2009).
Mousaei Ghasroldasht, M., Seok, J., Park, H. S., Liakath Ali, F. B. & Al-Hendy, A. Stem cell therapy: from idea to clinical practice. Int. J. Mol. Sci . 23 , 2850 (2022).
Kuriyan, A. E. et al. Vision loss after intravitreal injection of autologous “stem cells” for AMD. N. Engl. J. Med. 376 , 1047–1053 (2017).
Biehl, J. K. & Russell, B. Introduction to stem cell therapy. J. Cardiovasc. Nurs. 24 , 98–103 (2009). quiz 104-105.
Srijaya, T. C., Ramasamy, T. S. & Kasim, N. H. Advancing stem cell therapy from bench to bedside: lessons from drug therapies. J. Transl. Med. 12 , 243 (2014).
Ramalho-Santos, M. & Willenbring, H. On the origin of the term “stem cell”. Cell Stem Cell 1 , 35–38 (2007).
Konstantinov, I. E. In search of Alexander A. Maximow: the man behind the unitarian theory of hematopoiesis. Perspect. Biol. Med. 43 , 269–276 (2000).
Droscher, A. Images of cell trees, cell lines, and cell fates: the legacy of Ernst Haeckel and August Weismann in stem cell research. Hist. Philos. Life Sci. 36 , 157–186 (2014).
Article PubMed Google Scholar
Jansen, J. The first successful allogeneic bone-marrow transplant: Georges Mathe. Transfus. Med. Rev. 19 , 246–248 (2005).
Blume, K. G. & Weissman, I. L. E. Donnall Thomas (1920-2012). Proc. Natl Acad. Sci. USA 109 , 20777–20778 (2012).
Cheng, M. Hartmann Stahelin (1925-2011) and the contested history of cyclosporin A. Clin. Transpl. 27 , 326–329 (2013).
Article CAS Google Scholar
Thomas, E. D. et al. Aplastic anaemia treated by marrow transplantation. Lancet 1 , 284–289 (1972).
Friedenstein, A. J., Chailakhyan, R. K. & Gerasimov, U. V. Bone marrow osteogenic stem cells: in vitro cultivation and transplantation in diffusion chambers. Cell Tissue Kinet. 20 , 263–272 (1987).
PubMed CAS Google Scholar
Friedenstein, A. J., Chailakhjan, R. K. & Lalykina, K. S. The development of fibroblast colonies in monolayer cultures of guinea-pig bone marrow and spleen cells. Cell Tissue Kinet. 3 , 393–403 (1970).
Caplan, A. I. Mesenchymal stem cells. J. Orthop. Res. 9 , 641–650 (1991).
Bolli, R., Tang, X. L., Guo, Y. & Li, Q. After the storm: an objective appraisal of the efficacy of c-kit+ cardiac progenitor cells in preclinical models of heart disease. Can. J. Physiol. Pharm. 99 , 129–139 (2021).
Liu, C., Han, D., Liang, P., Li, Y. & Cao, F. The current dilemma and breakthrough of stem cell therapy in ischemic heart disease. Front. Cell Dev. Biol. 9 , 636136 (2021).
Zhang, J. et al. Basic and translational research in cardiac repair and regeneration: JACC state-of-the-art review. J. Am. Coll. Cardiol. 78 , 2092–2105 (2021).
Gyongyosi, M., Wojakowski, W., Navarese, E. P., Moye, L. A. & Investigators, A. Meta-analyses of human cell-based cardiac regeneration therapies: controversies in meta-analyses results on cardiac cell-based regenerative studies. Circ. Res. 118 , 1254–1263 (2016).
Okamoto, R., Matsumoto, T. & Watanabe, M. Regeneration of the intestinal epithelia: regulation of bone marrow-derived epithelial cell differentiation towards secretory lineage cells. Hum. Cell 19 , 71–75 (2006).
Gehart, H. & Clevers, H. Tales from the crypt: new insights into intestinal stem cells. Nat. Rev. Gastroenterol. Hepatol. 16 , 19–34 (2019).
Santos, A. J. M., Lo, Y. H., Mah, A. T. & Kuo, C. J. The intestinal stem cell niche: homeostasis and adaptations. Trends Cell Biol. 28 , 1062–1078 (2018).
Roda, G. et al. Crohn’s disease. Nat. Rev. Dis. Prim. 6 , 22 (2020).
Kobayashi, T. et al. Ulcerative colitis. Nat. Rev. Dis. Prim. 6 , 74 (2020).
Gratwohl, A. et al. Autologous hematopoietic stem cell transplantation for autoimmune diseases. Bone Marrow Transpl. 35 , 869–879 (2005).
Kashyap, A. & Forman, S. J. Autologous bone marrow transplantation for non-Hodgkin’s lymphoma resulting in long-term remission of coincidental Crohn’s disease. Br. J. Haematol. 103 , 651–652 (1998).
Hurley, J. M., Lee, S. G., Andrews, R. E. Jr., Klowden, M. J. & Bulla, L. A. Jr. Separation of the cytolytic and mosquitocidal proteins of Bacillus thuringiensis subsp. israelensis. Biochem Biophys. Res. Commun. 126 , 961–965 (1985).
Oyama, Y. et al. Autologous hematopoietic stem cell transplantation in patients with refractory Crohn’s disease. Gastroenterology 128 , 552–563 (2005).
Burt, R. K. et al. Autologous nonmyeloablative hematopoietic stem cell transplantation in patients with severe anti-TNF refractory Crohn disease: long-term follow-up. Blood 116 , 6123–6132 (2010).
Hasselblatt, P. et al. Remission of refractory Crohn’s disease by high-dose cyclophosphamide and autologous peripheral blood stem cell transplantation. Aliment Pharm. Ther. 36 , 725–735 (2012).
Hawkey, C. J. et al. Autologous hematopoetic stem cell transplantation for refractory Crohn disease: a randomized clinical trial. J. Am. Med. Assoc. 314 , 2524–2534 (2015).
Lindsay, J. O. et al. Autologous stem-cell transplantation in treatment-refractory Crohn’s disease: an analysis of pooled data from the ASTIC trial. Lancet Gastroenterol. Hepatol. 2 , 399–406 (2017).
Wang, R. et al. Stem cell therapy for Crohn’s disease: systematic review and meta-analysis of preclinical and clinical studies. Stem Cell Res Ther. 12 , 463 (2021).
Hawkey, C. J. Hematopoietic stem cell transplantation in Crohn’s disease: state-of-the-art treatment. Dig. Dis. 35 , 107–114 (2017).
Si-Tayeb, K., Lemaigre, F. P. & Duncan, S. A. Organogenesis and development of the liver. Dev. Cell 18 , 175–189 (2010).
Xue, R. et al. Clinical performance of stem cell therapy in patients with acute-on-chronic liver failure: a systematic review and meta-analysis. J. Transl. Med. 16 , 126 (2018).
Shi, M. et al. Human mesenchymal stem cell transfusion is safe and improves liver function in acute-on-chronic liver failure patients. Stem Cells Transl. Med. 1 , 725–731 (2012).
Liu, Y., Dong, Y., Wu, X., Xu, X. & Niu, J. The assessment of mesenchymal stem cells therapy in acute on chronic liver failure and chronic liver disease: a systematic review and meta-analysis of randomized controlled clinical trials. Stem Cell Res. Ther. 13 , 204 (2022).
Lin, B. L. et al. Allogeneic bone marrow-derived mesenchymal stromal cells for hepatitis B virus-related acute-on-chronic liver failure: a randomized controlled trial. Hepatology 66 , 209–219 (2017).
Gordon, M. Y. et al. Characterization and clinical application of human CD34+ stem/progenitor cell populations mobilized into the blood by granulocyte colony-stimulating factor. Stem Cells 24 , 1822–1830 (2006).
Arroyo, V. et al. Acute-on-chronic liver failure in cirrhosis. Nat. Rev. Dis. Prim. 2 , 16041 (2016).
Zhang, Z. et al. Human umbilical cord mesenchymal stem cells improve liver function and ascites in decompensated liver cirrhosis patients. J. Gastroenterol. Hepatol. 27 (Suppl 2), 112–120 (2012).
El-Ansary, M. et al. Phase II trial: undifferentiated versus differentiated autologous mesenchymal stem cells transplantation in Egyptian patients with HCV induced liver cirrhosis. Stem Cell Rev. Rep. 8 , 972–981 (2012).
Xu, L. et al. Randomized trial of autologous bone marrow mesenchymal stem cells transplantation for hepatitis B virus cirrhosis: regulation of Treg/Th17 cells. J. Gastroenterol. Hepatol. 29 , 1620–1628 (2014).
Suk, K. T. et al. Transplantation with autologous bone marrow-derived mesenchymal stem cells for alcoholic cirrhosis: Phase 2 trial. Hepatology 64 , 2185–2197 (2016).
Fang, X. et al. A study about immunomodulatory effect and efficacy and prognosis of human umbilical cord mesenchymal stem cells in patients with chronic hepatitis B-induced decompensated liver cirrhosis. J. Gastroenterol. Hepatol. 33 , 774–780 (2018).
Mohamadnejad, M. et al. Randomized placebo-controlled trial of mesenchymal stem cell transplantation in decompensated cirrhosis. Liver Int. 33 , 1490–1496 (2013).
Nguyen, T. L. et al. Autologous bone marrow mononuclear cell infusion for liver cirrhosis after the Kasai operation in children with biliary atresia. Stem Cell Res. Ther. 13 , 108 (2022).
Bai, Y. Q. et al. Outcomes of autologous bone marrow mononuclear cell transplantation in decompensated liver cirrhosis. World J. Gastroenterol. 20 , 8660–8666 (2014).
Guo, C. et al. Long-term outcomes of autologous peripheral blood stem cell transplantation in patients with cirrhosis. Clin. Gastroenterol. Hepatol. 17 , 1175–1182 e1172 (2019).
Newsome, P. N. et al. Granulocyte colony-stimulating factor and autologous CD133-positive stem-cell therapy in liver cirrhosis (REALISTIC): an open-label, randomised, controlled phase 2 trial. Lancet Gastroenterol. Hepatol. 3 , 25–36 (2018).
Spahr, L. et al. Autologous bone marrow mononuclear cell transplantation in patients with decompensated alcoholic liver disease: a randomized controlled trial. PLoS ONE 8 , e53719 (2013).
Maurice, J. & Manousou, P. Non-alcoholic fatty liver disease. Clin. Med. 18 , 245–250 (2018).
Article Google Scholar
Huang, T. D., Behary, J. & Zekry, A. Non-alcoholic fatty liver disease: a review of epidemiology, risk factors, diagnosis and management. Intern. Med. J. 50 , 1038–1047 (2020).
Sakai, Y. et al. Clinical trial of autologous adipose tissue-derived regenerative (stem) cells therapy for exploration of its safety and efficacy. Regen. Ther. 18 , 97–101 (2021).
Mieli-Vergani, G. et al. Autoimmune hepatitis. Nat. Rev. Dis. Primers 4 , 18018 (2018).
Calore, E. et al. Haploidentical stem cell transplantation cures autoimmune hepatitis and cerebrovascular disease in a patient with sickle cell disease. Bone Marrow Transpl. 53 , 644–646 (2018).
Vento, S., Cainelli, F., Renzini, C., Ghironzi, G. & Concia, E. Resolution of autoimmune hepatitis after bone-marrow transplantation. Lancet 348 , 544–545 (1996).
Terziroli Beretta-Piccoli, B., Mieli-Vergani, G. & Vergani, D. Autoimmmune hepatitis. Cell Mol. Immunol. 19 , 158–176 (2022).
Wang, L. et al. Pilot study of umbilical cord-derived mesenchymal stem cell transfusion in patients with primary biliary cirrhosis. J. Gastroenterol. Hepatol. 28 (Suppl 1), 85–92 (2013).
Wang, L. et al. Allogeneic bone marrow mesenchymal stem cell transplantation in patients with UDCA-resistant primary biliary cirrhosis. Stem Cells Dev. 23 , 2482–2489 (2014).
Martel-Pelletier, J. et al. Osteoarthritis. Nat. Rev. Dis. Prim. 2 , 16072 (2016).
Olsson, S., Akbarian, E., Lind, A., Razavian, A. S. & Gordon, M. Automating classification of osteoarthritis according to Kellgren-Lawrence in the knee using deep learning in an unfiltered adult population. BMC Musculoskelet. Disord. 22 , 844 (2021).
Mahmoudian, A., Lohmander, L. S., Mobasheri, A., Englund, M. & Luyten, F. P. Early-stage symptomatic osteoarthritis of the knee—time for action. Nat. Rev. Rheumatol. 17 , 621–632 (2021).
Kubsik-Gidlewska, A. et al. CD34+ stem cell treatment for knee osteoarthritis: a treatment and rehabilitation algorithm. J. Rehabil. Med Clin. Commun. 3 , 1000012 (2018).
Jevotovsky, D. S., Alfonso, A. R., Einhorn, T. A. & Chiu, E. S. Osteoarthritis and stem cell therapy in humans: a systematic review. Osteoarthr. Cartil. 26 , 711–729 (2018).
Wiggers, T. G., Winters, M., Van den Boom, N. A., Haisma, H. J. & Moen, M. H. Autologous stem cell therapy in knee osteoarthritis: a systematic review of randomised controlled trials. Br. J. Sports Med 55 , 1161–1169 (2021).
Han, S. B., Seo, I. W. & Shin, Y. S. Intra-articular injections of hyaluronic acid or steroids associated with better outcomes than platelet-rich plasma, adipose mesenchymal stromal cells, or placebo in knee osteoarthritis: a network meta-analysis. Arthroscopy 37 , 292–306 (2021).
Bastos, R. et al. Intra-articular injections of expanded mesenchymal stem cells with and without addition of platelet-rich plasma are safe and effective for knee osteoarthritis. Knee Surg. Sports Traumatol. Arthrosc. 26 , 3342–3350 (2018).
Molnar, V. et al. Mesenchymal stem cell mechanisms of action and clinical effects in osteoarthritis: a narrative review. Genes 13 , 949 (2022).
Barisic, S. & Childs, R. W. Graft-versus-solid-tumor effect: from hematopoietic stem cell transplantation to adoptive cell therapies. Stem Cells 40 , 556–563 (2022).
Mello, M. M. & Brennan, T. A. The controversy over high-dose chemotherapy with autologous bone marrow transplant for breast cancer. Health Aff. (Millwood) 20 , 101–117 (2001).
Sissung, T. M. & Figg, W. D. Stem cell clinics: risk of proliferation. Lancet Oncol. 21 , 205–206 (2020).
Fu, X. et al. Mesenchymal stem cell migration and tissue repair. Cells 8 , 784 (2019).
Zachar, L., Bacenkova, D. & Rosocha, J. Activation, homing, and role of the mesenchymal stem cells in the inflammatory environment. J. Inflamm. Res. 9 , 231–240 (2016).
de Araujo Farias, V., Carrillo-Galvez, A. B., Martin, F. & Anderson, P. TGF-beta and mesenchymal stromal cells in regenerative medicine, autoimmunity and cancer. Cytokine Growth Factor Rev. 43 , 25–37 (2018).
Ding, W. et al. Platelet-derived growth factor (PDGF)-PDGF receptor interaction activates bone marrow-derived mesenchymal stromal cells derived from chronic lymphocytic leukemia: implications for an angiogenic switch. Blood 116 , 2984–2993 (2010).
Ritter, E. et al. Breast cancer cell-derived fibroblast growth factor 2 and vascular endothelial growth factor are chemoattractants for bone marrow stromal stem cells. Ann. Surg. 247 , 310–314 (2008).
Cronwright, G. et al. Cancer/testis antigen expression in human mesenchymal stem cells: down-regulation of SSX impairs cell migration and matrix metalloproteinase 2 expression. Cancer Res. 65 , 2207–2215 (2005).
Aldinucci, D., Borghese, C. & Casagrande, N. The CCL5/CCR5 axis in cancer progression. Cancers 12 , 1765 (2020).
Karnoub, A. E. et al. Mesenchymal stem cells within tumour stroma promote breast cancer metastasis. Nature 449 , 557–563 (2007).
Kucerova, L., Matuskova, M., Hlubinova, K., Altanerova, V. & Altaner, C. Tumor cell behaviour modulation by mesenchymal stromal cells. Mol. Cancer 9 , 129 (2010).
Schmohl, K. A., Muller, A. M., Nelson, P. J. & Spitzweg, C. Thyroid hormone effects on mesenchymal stem cell biology in the tumour microenvironment. Exp. Clin. Endocrinol. Diabetes 128 , 462–468 (2020).
Mishra, P. J. et al. Carcinoma-associated fibroblast-like differentiation of human mesenchymal stem cells. Cancer Res. 68 , 4331–4339 (2008).
Liu, J., Han, G., Liu, H. & Qin, C. Suppression of cholangiocarcinoma cell growth by human umbilical cord mesenchymal stem cells: a possible role of Wnt and Akt signaling. PLoS ONE 8 , e62844 (2013).
Ho, I. A. et al. Human bone marrow-derived mesenchymal stem cells suppress human glioma growth through inhibition of angiogenesis. Stem Cells 31 , 146–155 (2013).
Sun, Z., Wang, S. & Zhao, R. C. The roles of mesenchymal stem cells in tumor inflammatory microenvironment. J. Hematol. Oncol. 7 , 14 (2014).
Rhee, K. J., Lee, J. I. & Eom, Y. W. Mesenchymal stem cell-mediated effects of tumor support or suppression. Int. J. Mol. Sci. 16 , 30015–30033 (2015).
Liang, W. et al. Mesenchymal stem cells as a double-edged sword in tumor growth: focusing on MSC-derived cytokines. Cell Mol. Biol. Lett. 26 , 3 (2021).
Hmadcha, A., Martin-Montalvo, A., Gauthier, B. R., Soria, B. & Capilla-Gonzalez, V. Therapeutic potential of mesenchymal stem cells for cancer therapy. Front. Bioeng. Biotechnol. 8 , 43 (2020).
Cao, G. D. et al. The oncolytic virus in cancer diagnosis and treatment. Front. Oncol. 10 , 1786 (2020).
Melen, G. J. et al. Influence of carrier cells on the clinical outcome of children with neuroblastoma treated with high dose of oncolytic adenovirus delivered in mesenchymal stem cells. Cancer Lett. 371 , 161–170 (2016).
Garcia-Castro, J. et al. Treatment of metastatic neuroblastoma with systemic oncolytic virotherapy delivered by autologous mesenchymal stem cells: an exploratory study. Cancer Gene Ther. 17 , 476–483 (2010).
Draganov, D. D. et al. Delivery of oncolytic vaccinia virus by matched allogeneic stem cells overcomes critical innate and adaptive immune barriers. J. Transl. Med. 17 , 100 (2019).
Cyranoski, D. How human embryonic stem cells sparked a revolution. Nature 555 , 428–430 (2018).
Thomson, J. A. et al. Embryonic stem cell lines derived from human blastocysts. Science 282 , 1145–1147 (1998).
Takahashi, K. & Yamanaka, S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126 , 663–676 (2006).
Takahashi, K. et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell 131 , 861–872 (2007).
Gepstein, L. Derivation and potential applications of human embryonic stem cells. Circ. Res. 91 , 866–876 (2002).
Andrews, P. W. From teratocarcinomas to embryonic stem cells. Philos. Trans. R. Soc. Lond. B Biol. Sci. 357 , 405–417 (2002).
Finch, B. W. & Ephrussi, B. Retention of multiple developmental potentialities by cells of a mouse testicular teratocarcinoma during prolonged culture in vitro and their extinction upon hybridization with cells of permanent lines. Proc. Natl Acad. Sci. USA 57 , 615–621 (1967).
Ried, T. et al. The consequences of chromosomal aneuploidy on the transcriptome of cancer cells. Biochim Biophys. Acta 1819 , 784–793 (2012).
Evans, M. J. & Kaufman, M. H. Establishment in culture of pluripotential cells from mouse embryos. Nature 292 , 154–156 (1981).
Martin, G. R. Isolation of a pluripotent cell line from early mouse embryos cultured in medium conditioned by teratocarcinoma stem cells. Proc. Natl Acad. Sci. USA 78 , 7634–7638 (1981).
Lo, B. & Parham, L. Ethical issues in stem cell research. Endocr. Rev. 30 , 204–213 (2009).
Wilmut, I., Schnieke, A. E., McWhir, J., Kind, A. J. & Campbell, K. H. Viable offspring derived from fetal and adult mammalian cells. Nature 385 , 810–813 (1997).
Schwartz, S. D. et al. Embryonic stem cell trials for macular degeneration: a preliminary report. Lancet 379 , 713–720 (2012).
Atala, A. Human embryonic stem cells: early hints on safety and efficacy. Lancet 379 , 689–690 (2012).
Schwartz, S. D. et al. Human embryonic stem cell-derived retinal pigment epithelium in patients with age-related macular degeneration and Stargardt’s macular dystrophy: follow-up of two open-label phase 1/2 studies. Lancet 385 , 509–516 (2015).
Song, W. K. et al. Treatment of macular degeneration using embryonic stem cell-derived retinal pigment epithelium: preliminary results in Asian patients. Stem Cell Rep. 4 , 860–872 (2015).
Liu, Y. et al. Human embryonic stem cell-derived retinal pigment epithelium transplants as a potential treatment for wet age-related macular degeneration. Cell Discov. 4 , 50 (2018).
Limnios, I. J., Chau, Y. Q., Skabo, S. J., Surrao, D. C. & O’Neill, H. C. Efficient differentiation of human embryonic stem cells to retinal pigment epithelium under defined conditions. Stem Cell Res. Ther. 12 , 248 (2021).
Foltz, L. P. & Clegg, D. O. Rapid, directed differentiation of retinal pigment epithelial cells from human embryonic or induced pluripotent stem cells. J. Vis. Exp. 128 , e56274 (2017).
Kuroda, T., Ando, S., Takeno, Y., Kishino, A. & Kimura, T. Robust induction of retinal pigment epithelium cells from human induced pluripotent stem cells by inhibiting FGF/MAPK signaling. Stem Cell Res 39 , 101514 (2019).
Dewell, T. E. et al. Transcription factor overexpression drives reliable differentiation of retinal pigment epithelium from human induced pluripotent stem cells. Stem Cell Res. 53 , 102368 (2021).
Dehghan, S., Mirshahi, R., Shoae-Hassani, A. & Naseripour, M. Human-induced pluripotent stem cells-derived retinal pigmented epithelium, a new horizon for cells-based therapies for age-related macular degeneration. Stem Cell Res. Ther. 13 , 217 (2022).
Menasche, P. et al. Human embryonic stem cell-derived cardiac progenitors for severe heart failure treatment: first clinical case report. Eur. Heart J. 36 , 2011–2017 (2015).
Menasche, P. et al. Transplantation of human embryonic stem cell-derived cardiovascular progenitors for severe ischemic left ventricular dysfunction. J. Am. Coll. Cardiol. 71 , 429–438 (2018).
Cyranoski, D. ‘Reprogrammed’ stem cells approved to mend human hearts for the first time. Nature 557 , 619–620 (2018).
Povsic, T. J. & Gersh, B. J. Stem cells in cardiovascular diseases: 30,000-foot view. Cells 10 , 600 (2021).
Romito, A. & Cobellis, G. Pluripotent stem cells: current understanding and future directions. Stem Cells Int. 2016 , 9451492 (2016).
McKenna, S. L. et al. Ten-year safety of pluripotent stem cell transplantation in acute thoracic spinal cord injury. J. Neurosurg. Spine 1 , 1–10 (2022).
Deinsberger, J., Reisinger, D. & Weber, B. Global trends in clinical trials involving pluripotent stem cells: a systematic multi-database analysis. NPJ Regen. Med. 5 , 15 (2020).
Kim, J. Y., Nam, Y., Rim, Y. A. & Ju, J. H. Review of the current trends in clinical trials involving induced pluripotent stem cells. Stem Cell Rev. Rep. 18 , 142–154 (2022).
Ji, P., Manupipatpong, S., Xie, N. & Li, Y. Induced pluripotent stem cells: generation strategy and epigenetic mystery behind reprogramming. Stem Cells Int. 2016 , 8415010 (2016).
Fu, X. The immunogenicity of cells derived from induced pluripotent stem cells. Cell Mol. Immunol. 11 , 14–16 (2014).
Lee, A. S., Tang, C., Rao, M. S., Weissman, I. L. & Wu, J. C. Tumorigenicity as a clinical hurdle for pluripotent stem cell therapies. Nat. Med. 19 , 998–1004 (2013).
Friedenstein, A. J., Piatetzky, S. II & Petrakova, K. V. Osteogenesis in transplants of bone marrow cells. J. Embryol. Exp. Morphol. 16 , 381–390 (1966).
Pittenger, M. F. et al. Multilineage potential of adult human mesenchymal stem cells. Science 284 , 143–147 (1999).
Nombela-Arrieta, C., Ritz, J. & Silberstein, L. E. The elusive nature and function of mesenchymal stem cells. Nat. Rev. Mol. Cell Biol. 12 , 126–131 (2011).
Dominici, M. et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 8 , 315–317 (2006).
Zhou, T. et al. Challenges and advances in clinical applications of mesenchymal stromal cells. J. Hematol. Oncol. 14 , 24 (2021).
Ankrum, J. & Karp, J. M. Mesenchymal stem cell therapy: two steps forward, one step back. Trends Mol. Med. 16 , 203–209 (2010).
Tuan, R. S., Boland, G. & Tuli, R. Adult mesenchymal stem cells and cell-based tissue engineering. Arthritis Res. Ther. 5 , 32–45 (2003).
Witkowska-Zimny, M. & Wrobel, E. Perinatal sources of mesenchymal stem cells: Wharton’s jelly, amnion and chorion. Cell Mol. Biol. Lett. 16 , 493–514 (2011).
Alkhalil, M., Smajilagic, A. & Redzic, A. Human dental pulp mesenchymal stem cells isolation and osteoblast differentiation. Med. Glas. (Zenica) 12 , 27–32 (2015).
Google Scholar
Ouryazdanpanah, N., Dabiri, S., Derakhshani, A., Vahidi, R. & Farsinejad, A. Peripheral blood-derived mesenchymal stem cells: growth factor-free isolation, molecular characterization and differentiation. Iran. J. Pathol. 13 , 461–466 (2018).
PubMed PubMed Central Google Scholar
Francis, M. P., Sachs, P. C., Elmore, L. W. & Holt, S. E. Isolating adipose-derived mesenchymal stem cells from lipoaspirate blood and saline fraction. Organogenesis 6 , 11–14 (2010).
Gong, X. et al. Isolation and characterization of lung resident mesenchymal stem cells capable of differentiating into alveolar epithelial type II cells. Cell Biol. Int. 38 , 405–411 (2014).
Wang, B. et al. Human hair follicle-derived mesenchymal stem cells: Isolation, expansion, and differentiation. World J. Stem Cells 12 , 462–470 (2020).
Pilato, C. A. et al. Isolation and characterization of cardiac mesenchymal stromal cells from endomyocardial bioptic samples of arrhythmogenic cardiomyopathy patients. J. Vis. Exp . 132 , e57263 (2018).
Mannino, G. et al. Adult stem cell niches for tissue homeostasis. J. Cell Physiol. 237 , 239–257 (2022).
Pavlushina, S. V., Orlova, T. G. & Tabagari, D. Z. [Isolation of mononuclear cells from the bone marrow of patients with hemoblastoses using one-step ficoll-verographin density gradient separation]. Eksp. Onkol. 6 , 68–70 (1984).
Schneider, S., Unger, M., van Griensven, M. & Balmayor, E. R. Adipose-derived mesenchymal stem cells from liposuction and resected fat are feasible sources for regenerative medicine. Eur. J. Med Res. 22 , 17 (2017).
Torre, P. & Flores, A. I. Current status and future prospects of perinatal stem cells. Genes 12 , 6 (2020).
Hoang, V. T. et al. Standardized xeno- and serum-free culture platform enables large-scale expansion of high-quality mesenchymal stem/stromal cells from perinatal and adult tissue sources. Cytotherapy 23 , 88–99 (2020).
Mohamed-Ahmed, S. et al. Adipose-derived and bone marrow mesenchymal stem cells: a donor-matched comparison. Stem Cell Res. Ther. 9 , 168 (2018).
Zuk, P. A. et al. Human adipose tissue is a source of multipotent stem cells. Mol. Biol. Cell 13 , 4279–4295 (2002).
Li, Z. CD133: a stem cell biomarker and beyond. Exp. Hematol. Oncol. 2 , 17 (2013).
Petrenko, Y. et al. A comparative analysis of multipotent mesenchymal stromal cells derived from different sources, with a focus on neuroregenerative potential. Sci. Rep. 10 , 4290 (2020).
Wang, Z. & Yan, X. CD146, a multi-functional molecule beyond adhesion. Cancer Lett. 330 , 150–162 (2013).
Xu, L. et al. Tissue source determines the differentiation potentials of mesenchymal stem cells: a comparative study of human mesenchymal stem cells from bone marrow and adipose tissue. Stem Cell Res Ther. 8 , 275 (2017).
Han, I., Kwon, B. S., Park, H. K. & Kim, K. S. Differentiation potential of mesenchymal stem cells is related to their intrinsic mechanical properties. Int. Neurourol. J. 21 , S24–S31 (2017).
Song, Y. et al. Human mesenchymal stem cells derived from umbilical cord and bone marrow exert immunomodulatory effects in different mechanisms. World J. Stem Cells 12 , 1032–1049 (2020).
Lee, R. H. et al. Intravenous hMSCs improve myocardial infarction in mice because cells embolized in lung are activated to secrete the anti-inflammatory protein TSG-6. Cell Stem Cell 5 , 54–63 (2009).
Allers, C. et al. Dynamic of distribution of human bone marrow-derived mesenchymal stem cells after transplantation into adult unconditioned mice. Transplantation 78 , 503–508 (2004).
Devine, S. M., Cobbs, C., Jennings, M., Bartholomew, A. & Hoffman, R. Mesenchymal stem cells distribute to a wide range of tissues following systemic infusion into nonhuman primates. Blood 101 , 2999–3001 (2003).
Fischer, U. M. et al. Pulmonary passage is a major obstacle for intravenous stem cell delivery: the pulmonary first-pass effect. Stem Cells Dev. 18 , 683–692 (2009).
Sierra-Parraga, J. M. et al. Mesenchymal stromal cells are retained in the porcine renal cortex independently of their metabolic state after renal intra-arterial infusion. Stem Cells Dev. 28 , 1224–1235 (2019).
Henriksson, H. B. et al. The traceability of mesenchymal stromal cells after injection into degenerated discs in patients with low back pain. Stem Cells Dev. 28 , 1203–1211 (2019).
Sokal, E. M. et al. Biodistribution of liver-derived mesenchymal stem cells after peripheral injection in a hemophilia A patient. Transplantation 101 , 1845–1851 (2017).
Sood, V. et al. Biodistribution of 18F-FDG-labeled autologous bone marrow-derived stem cells in patients with type 2 diabetes mellitus: exploring targeted and intravenous routes of delivery. Clin. Nucl. Med. 40 , 697–700 (2015).
Sanchez-Diaz, M. et al. Biodistribution of mesenchymal stromal cells after administration in animal models and humans: a systematic review. J. Clin. Med. 10 , 2925 (2021).
Sensebe, L. & Fleury-Cappellesso, S. Biodistribution of mesenchymal stem/stromal cells in a preclinical setting. Stem Cells Int. 2013 , 678063 (2013).
Zhuang, W. Z. et al. Mesenchymal stem/stromal cell-based therapy: mechanism, systemic safety and biodistribution for precision clinical applications. J. Biomed. Sci. 28 , 28 (2021).
Wei, X. et al. Mesenchymal stem cells: a new trend for cell therapy. Acta Pharm. Sin. 34 , 747–754 (2013).
Kouchakian, M. R. et al. The clinical trials of mesenchymal stromal cells therapy. Stem Cells Int. 2021 , 1634782 (2021).
Chen, L. et al. Mesenchymal stem cell-based treatments for COVID-19: status and future perspectives for clinical applications. Cell Mol. Life Sci. 79 , 142 (2022).
Borow, K. M., Yaroshinsky, A., Greenberg, B. & Perin, E. C. Phase 3 DREAM-HF trial of mesenchymal precursor cells in chronic heart failure. Circ. Res. 125 , 265–281 (2019).
Zheng, H. et al. Mesenchymal stem cell therapy in stroke: a systematic review of literature in pre-clinical and clinical research. Cell Transpl. 27 , 1723–1730 (2018).
Rodriguez-Fuentes, D. E. et al. Mesenchymal stem cells current clinical applications: a systematic review. Arch. Med. Res. 52 , 93–101 (2021).
Shi, L. et al. Mesenchymal stem cell therapy for severe COVID-19. Signal Transduct. Target Ther. 6 , 339 (2021).
Carney, B. J. & Shah, K. Migration and fate of therapeutic stem cells in different brain disease models. Neuroscience 197 , 37–47 (2011).
Yao, P., Zhou, L., Zhu, L., Zhou, B. & Yu, Q. Mesenchymal stem cells: a potential therapeutic strategy for neurodegenerative diseases. Eur. Neurol. 83 , 235–241 (2020).
Bonaventura, G. et al. Stem cells: innovative therapeutic options for neurodegenerative diseases? Cells 10 , 1992 (2021).
Mansoor, S. R., Zabihi, E. & Ghasemi-Kasman, M. The potential use of mesenchymal stem cells for the treatment of multiple sclerosis. Life Sci. 235 , 116830 (2019).
Chung, J. W. et al. Efficacy and safety of intravenous mesenchymal stem cells for ischemic stroke. Neurology 96 , e1012–e1023 (2021).
Yamazaki, K., Kawabori, M., Seki, T. & Houkin, K. Clinical trials of stem cell treatment for spinal cord injury. Int. J. Mol. Sci . 21 , 3994 (2020).
Xie, B., Chen, M., Hu, R., Han, W. & Ding, S. Therapeutic evidence of human mesenchymal stem cell transplantation for cerebral palsy: a meta-analysis of randomized controlled trials. Stem Cells Int. 2020 , 5701920 (2020).
McDonald, C. A. et al. Intranasal delivery of mesenchymal stromal cells protects against neonatal hypoxic(-)ischemic brain injury. Int. J. Mol. Sci . 20 , 2449 (2019).
Liu, Q. et al. Rational use of mesenchymal stem cells in the treatment of autism spectrum disorders. World J. Stem Cells 11 , 55–72 (2019).
Fricova, D., Korchak, J. A. & Zubair, A. C. Challenges and translational considerations of mesenchymal stem/stromal cell therapy for Parkinson’s disease. npj Regen. Med. 5 , 20 (2020).
Bang, O. Y., Lee, J. S., Lee, P. H. & Lee, G. Autologous mesenchymal stem cell transplantation in stroke patients. Ann. Neurol. 57 , 874–882 (2005).
Lee, J. S. et al. A long-term follow-up study of intravenous autologous mesenchymal stem cell transplantation in patients with ischemic stroke. Stem Cells 28 , 1099–1106 (2010).
Honmou, O. et al. Intravenous administration of auto serum-expanded autologous mesenchymal stem cells in stroke. Brain 134 , 1790–1807 (2011).
Bhasin, A. et al. Autologous mesenchymal stem cells in chronic stroke. Cerebrovasc. Dis. Extra 1 , 93–104 (2011).
Jaillard, A. et al. Autologous mesenchymal stem cells improve motor recovery in subacute ischemic stroke: a randomized clinical trial. Transl. Stroke Res. 11 , 910–923 (2020).
Lee, J. et al. Efficacy of intravenous mesenchymal stem cells for motor recovery after ischemic stroke: a neuroimaging study. Stroke 53 , 20–28 (2022).
Levy, M. L. et al. Phase I/II study of safety and preliminary efficacy of intravenous allogeneic mesenchymal stem cells in chronic stroke. Stroke 50 , 2835–2841 (2019).
Xu, P. & Yang, X. The efficacy and safety of mesenchymal stem cell transplantation for spinal cord injury patients: a meta-analysis and systematic review. Cell Transpl. 28 , 36–46 (2019).
Liau, L. L. et al. Treatment of spinal cord injury with mesenchymal stem cells. Cell Biosci. 10 , 112 (2020).
Liu, X. et al. Comparative analysis of curative effect of bone marrow mesenchymal stem cell and bone marrow mononuclear cell transplantation for spastic cerebral palsy. J. Transl. Med. 15 , 1–9 (2017).
Sharma, A. K. et al. Cell transplantation as a novel therapeutic strategy for autism spectrum disorders: a clinical study. Am J. Stem Cells 9 , 89 (2020).
Ballen, K. & Kurtzberg, J. Exploring new therapies for children with autism: “Do no harm” does not mean do not try. Stem Cells Transl. Med. 10 , 823–825 (2021).
Reyhani, S., Abbaspanah, B. & Mousavi, S. H. Umbilical cord-derived mesenchymal stem cells in neurodegenerative disorders: from literature to clinical practice. Regen. Med. 15 , 1561–1578 (2020).
Gu, J. et al. Therapeutic evidence of umbilical cord-derived mesenchymal stem cell transplantation for cerebral palsy: a randomized, controlled trial. Stem Cell Res Ther. 11 , 43 (2020).
Retraction. Stem Cells Transl. Med. 10 , 1717 (2021).
Sun, J. M. et al. Infusion of human umbilical cord tissue mesenchymal stromal cells in children with autism spectrum disorder. Stem Cells Transl. Med. 9 , 1137–1146 (2020).
Yang, Y. et al. Repeated subarachnoid administrations of allogeneic human umbilical cord mesenchymal stem cells for spinal cord injury: a phase 1/2 pilot study. Cytotherapy 23 , 57–64 (2021).
Liu, J. et al. Clinical analysis of the treatment of spinal cord injury with umbilical cord mesenchymal stem cells. Cytotherapy 15 , 185–191 (2013).
Przekora, A. & Juszkiewicz, L. The effect of autologous adipose tissue-derived mesenchymal stem cells’ therapy in the treatment of chronic posttraumatic spinal cord injury in a domestic ferret patient. Cell Transpl. 29 , 963689720928982 (2020).
Hur, J. W. et al. Intrathecal transplantation of autologous adipose-derived mesenchymal stem cells for treating spinal cord injury: a human trial. J. Spinal Cord. Med. 39 , 655–664 (2016).
de Celis-Ruiz, E. et al. Final results of allogeneic adipose tissue-derived mesenchymal stem cells in acute ischemic stroke (AMASCIS): a phase II, randomized, double-blind, placebo-controlled, single-center, pilot clinical trial. Cell Transpl. 31 , 9636897221083863 (2022).
Yang, Y. et al. Human umbilical cord mesenchymal stem cells to treat spinal cord injury in the early chronic phase: study protocol for a prospective, multicenter, randomized, placebo-controlled, single-blinded clinical trial. Neural Regen. Res. 15 , 1532–1538 (2020).
de Celis-Ruiz, E. et al. Allogeneic adipose tissue-derived mesenchymal stem cells in ischaemic stroke (AMASCIS-02): a phase IIb, multicentre, double-blind, placebo-controlled clinical trial protocol. BMJ Open 11 , e051790 (2021).
Murray, C. J. L. COVID-19 will continue but the end of the pandemic is near. Lancet 399 , 417–419 (2022).
Thebaud, B. et al. Bronchopulmonary dysplasia. Nat. Rev. Dis. Prim. 5 , 78 (2019).
Mohamed, T., Abdul-Hafez, A., Gewolb, I. H. & Uhal, B. D. Oxygen injury in neonates: which is worse? hyperoxia, hypoxia, or alternating hyperoxia/hypoxia. J. Lung Pulm. Respir. Res. 7 , 4–13 (2020).
Omar, S. A. et al. Stem-cell therapy for bronchopulmonary dysplasia (BPD) in newborns. Cells 11 , 1275 (2022).
Chang, Y. S. et al. Mesenchymal stem cells for bronchopulmonary dysplasia: phase 1 dose-escalation clinical trial. J. Pediatr. 164 , 966–972 e966 (2014).
Powell, S. B. & Silvestri, J. M. Safety of intratracheal administration of human umbilical cord blood derived mesenchymal stromal cells in extremely low birth weight preterm infants. J. Pediatr. 210 , 209–213 e202 (2019).
Nguyen, L. T. et al. Allogeneic administration of human umbilical cord-derived mesenchymal stem/stromal cells for bronchopulmonary dysplasia: preliminary outcomes in four Vietnamese infants. J. Transl. Med. 18 , 398 (2020).
Ahn, S. Y. et al. Stem cells for bronchopulmonary dysplasia in preterm infants: a randomized controlled phase II trial. Stem Cells Transl. Med. 10 , 1129–1137 (2021).
Averyanov, A. et al. First-in-human high-cumulative-dose stem cell therapy in idiopathic pulmonary fibrosis with rapid lung function decline. Stem Cells Transl. Med. 9 , 6–16 (2020).
Ribeiro-Paes, J. T. et al. Unicentric study of cell therapy in chronic obstructive pulmonary disease/pulmonary emphysema. Int. J. Chron. Obstruct Pulmon Dis. 6 , 63–71 (2011).
Stessuk, T. et al. Phase I clinical trial of cell therapy in patients with advanced chronic obstructive pulmonary disease: follow-up of up to 3 years. Rev. Bras. Hematol. Hemoter. 35 , 352–357 (2013).
Weiss, D. J., Casaburi, R., Flannery, R., LeRoux-Williams, M. & Tashkin, D. P. A placebo-controlled, randomized trial of mesenchymal stem cells in COPD. Chest 143 , 1590–1598 (2013).
de Oliveira, H. G. et al. Combined bone marrow-derived mesenchymal stromal cell therapy and one-way endobronchial valve placement in patients with pulmonary emphysema: a phase I clinical trial. Stem Cells Transl. Med. 6 , 962–969 (2017).
Stolk, J. et al. A phase I study for intravenous autologous mesenchymal stromal cell administration to patients with severe emphysema. QJM 109 , 331–336 (2016).
Armitage, J. et al. Mesenchymal stromal cell infusion modulates systemic immunological responses in stable COPD patients: a phase I pilot study. Eur. Respir. J. 51 , 1702369 (2018).
Comella, K. et al. Autologous stromal vascular fraction in the intravenous treatment of end-stage chronic obstructive pulmonary disease: a phase I trial of safety and tolerability. J. Clin. Med. Res. 9 , 701–708 (2017).
Tzilas, V. et al . Prospective phase 1 open clinical trial to study the safety of adipose derived mesenchymal stem cells (ADMSCs) in COPD and combined pulmonary fibrosis and emphysema (CPFE). Eur. Respir. J. 46 , (2015).
Glassberg, M. K., Csete, I., Simonet, E. & Elliot, S. J. Stem cell therapy for COPD: hope and exploitation. Chest 160 , 1271–1281 (2021).
Le Thi Bich, P. et al. Allogeneic umbilical cord-derived mesenchymal stem cell transplantation for treating chronic obstructive pulmonary disease: a pilot clinical study. Stem Cell Res. Ther. 60 , 11 (2020).
Karaoz, E., Kalemci, S. & Ece, F. Improving effects of mesenchymal stem cells on symptoms of chronic obstructive pulmonary disease. Bratisl. Lek. Listy. 121 , 188–191 (2020).
Hoang, D. M., Nguyen, K. T., Nguyen, A. H., Nguyen, B. N. & Nguyen, L. T. Allogeneic human umbilical cord-derived mesenchymal stem/stromal cells for chronic obstructive pulmonary disease (COPD): study protocol for a matched case-control, phase I/II trial. BMJ Open 11 , e045788 (2021).
Xu, R., Feng, Z. & Wang, F. S. Mesenchymal stem cell treatment for COVID-19. EBioMedicine 77 , 103920 (2022).
Khoury, M. et al. Current status of cell-based therapies for respiratory virus infections: applicability to COVID-19. Eur. Respir. J. 55 , 2000858 (2020).
Jamilloux, Y. et al. Should we stimulate or suppress immune responses in COVID-19? Cytokine and anti-cytokine interventions. Autoimmun. Rev. 19 , 102567 (2020).
Feng, Y. et al. Safety and feasibility of umbilical cord mesenchymal stem cells in patients with COVID-19 pneumonia: a pilot study. Cell Prolif. 53 , e12947 (2020).
Primorac, D. et al. Mesenchymal stromal cells: potential option for COVID-19 treatment. Pharmaceutic 13 , 1481 (2021).
Zhang, Y. et al. Intravenous infusion of human umbilical cord Wharton’s jelly-derived mesenchymal stem cells as a potential treatment for patients with COVID-19 pneumonia. Stem Cell Res. Ther. 11 , 207 (2020).
Shu, L. et al. Treatment of severe COVID-19 with human umbilical cord mesenchymal stem cells. Stem Cell Res. Ther. 11 , 361 (2020).
Tao, J. et al. Umbilical cord blood-derived mesenchymal stem cells in treating a critically ill COVID-19 patient. J. Infect. Dev. Ctries 14 , 1138–1145 (2020).
Saleh, M. et al. Cell therapy in patients with COVID-19 using Wharton’s jelly mesenchymal stem cells: a phase 1 clinical trial. Stem Cell Res. Ther. 12 , 410 (2021).
Leng, Z. et al. Transplantation of ACE2(-) mesenchymal stem cells improves the outcome of patients with COVID-19 pneumonia. Aging Dis. 11 , 216–228 (2020).
Guo, Z. et al. Administration of umbilical cord mesenchymal stem cells in patients with severe COVID-19 pneumonia. Crit. Care 24 , 420 (2020).
Meng, F. et al. Human umbilical cord-derived mesenchymal stem cell therapy in patients with COVID-19: a phase 1 clinical trial. Signal Transduct. Target Ther. 5 , 172 (2020).
Shi, L. et al. Human mesenchymal stem cells treatment for severe COVID-19: 1-year follow-up results of a randomized, double-blind, placebo-controlled trial. EBioMedicine 75 , 103789 (2021).
Adas, G. et al. The systematic effect of mesenchymal stem cell therapy in critical COVID-19 patients: a prospective double controlled trial. Cell Transpl. 30 , 9636897211024942 (2021).
Shi, L. et al. Effect of human umbilical cord-derived mesenchymal stem cells on lung damage in severe COVID-19 patients: a randomized, double-blind, placebo-controlled phase 2 trial. Signal Transduct. Targeted Ther. 6 , 58 (2021).
Lanzoni, G. et al. Umbilical cord mesenchymal stem cells for COVID-19 acute respiratory distress syndrome: a double-blind, phase 1/2a, randomized controlled trial. Stem Cells Transl. Med. 10 , 660–673 (2021).
Hashemian, S. R. et al. Mesenchymal stem cells derived from perinatal tissues for treatment of critically ill COVID-19-induced ARDS patients: a case series. Stem Cell Res Ther. 12 , 91 (2021).
Zhu, R. et al. Mesenchymal stem cell treatment improves outcome of COVID-19 patients via multiple immunomodulatory mechanisms. Cell Res. 31 , 1244–1262 (2021).
Shi, L. et al. Effect of human umbilical cord-derived mesenchymal stem cells on lung damage in severe COVID-19 patients: a randomized, double-blind, placebo-controlled phase 2 trial. Signal Transduct. Target Ther. 6 , 58 (2021).
N, O. E., Pekkoc-Uyanik, K. C., Alpaydin, N., Gulay, G. R. & Simsek, M. Clinical experience on umbilical cord mesenchymal stem cell treatment in 210 severe and critical COVID-19 cases in Turkey. Stem Cell Rev. Rep. 17 , 1917–1925 (2021).
Gentile, P., Sterodimas, A., Pizzicannella, J., Calabrese, C. & Garcovich, S. Research progress on mesenchymal stem cells (MSCs), adipose-derived mesenchymal stem cells (AD-MSCs), drugs, and vaccines in inhibiting COVID-19 disease. Aging Dis. 11 , 1191–1201 (2020).
Copcu, H. E. Potential using of fat-derived stromal cells in the treatment of active disease, and also, in both pre- and post-periods in COVID-19. Aging Dis. 11 , 730–736 (2020).
Gentile, P. & Sterodimas, A. Adipose-derived stromal stem cells (ASCs) as a new regenerative immediate therapy combating coronavirus (COVID-19)-induced pneumonia. Expert Opin. Biol. Ther. 20 , 711–716 (2020).
Matthay, M. A. et al. Treatment with allogeneic mesenchymal stromal cells for moderate to severe acute respiratory distress syndrome (START study): a randomised phase 2a safety trial. Lancet Respir. Med. 7 , 154–162 (2019).
Álvarez-Fuente, M. et al. Off-label mesenchymal stromal cell treatment in two infants with severe bronchopulmonary dysplasia: clinical course and biomarkers profile. Cytotherapy 20 , 1337–1344 (2018).
Zheng, G. et al. Treatment of acute respiratory distress syndrome with allogeneic adipose-derived mesenchymal stem cells: a randomized, placebo-controlled pilot study. Respir. Res. 15 , 39 (2014).
Simonson, O. E. et al. In vivo effects of mesenchymal stromal cells in two patients with severe acute respiratory distress syndrome. Stem Cells Transl. Med. 4 , 1199–1213 (2015).
Wilson, J. G. et al. Mesenchymal stem (stromal) cells for treatment of ARDS: a phase 1 clinical trial. Lancet Respir. Med. 3 , 24–32 (2015).
Yip, H. K. et al. Human umbilical cord-derived mesenchymal stem cells for acute respiratory distress syndrome. Crit. Care Med 48 , e391–e399 (2020).
Gorman, E. et al. Repair of acute respiratory distress syndrome by stromal cell administration (REALIST) trial: a phase 1 trial. EClinicalMedicine 41 , 101167 (2021).
Le Thi Bich, P. et al. Allogeneic umbilical cord-derived mesenchymal stem cell transplantation for treating chronic obstructive pulmonary disease: a pilot clinical study. Stem Cell Res. Ther. 11 , 60 (2020).
Wang, M. Y. et al. Current therapeutic strategies for respiratory diseases using mesenchymal stem cells. MedComm 2 , 351–380 (2021).
Carlsson, P. O., Schwarcz, E., Korsgren, O. & Le Blanc, K. Preserved beta-cell function in type 1 diabetes by mesenchymal stromal cells. Diabetes 64 , 587–592 (2015).
Dantas, J. R. et al. Adipose tissue-derived stromal/stem cells + cholecalciferol: a pilot study in recent-onset type 1 diabetes patients. Arch. Endocrinol. Metab. 65 , 342–351 (2021).
PubMed Google Scholar
Joseph, U. A. & Jhingran, S. G. Technetium-99m labeled RBC imaging in gastrointestinal bleeding from gastric leiomyoma. Clin. Nucl. Med. 13 , 23–25 (1988).
Hu, J. et al. Long term effects of the implantation of Wharton’s jelly-derived mesenchymal stem cells from the umbilical cord for newly-onset type 1 diabetes mellitus. Endocr. J. 60 , 347–357 (2013).
Cai, J. et al. Umbilical cord mesenchymal stromal cell with autologous bone marrow cell transplantation in established type 1 diabetes: a pilot randomized controlled open-label clinical study to assess safety and impact on insulin secretion. Diabetes Care 39 , 149–157 (2016).
Huang, Q., Huang, Y. & Liu, J. Mesenchymal stem cells: an excellent candidate for the treatment of diabetes mellitus. Int. J. Endocrinol. 2021 , 9938658 (2021).
Nguyen, L. T. et al. Type 2 diabetes mellitus duration and obesity alter the efficacy of autologously transplanted bone marrow-derived mesenchymal stem/stromal cells. Stem Cells Transl. Med. 10 , 1266–1278 (2021).
Alicka, M., Major, P., Wysocki, M. & Marycz, K. Adipose-derived mesenchymal stem cells isolated from patients with type 2 diabetes show reduced “stemness” through an altered secretome profile, impaired anti-oxidative protection, and mitochondrial dynamics deterioration. J. Clin. Med. 8 , 765 (2019).
Agarwal, A. et al. Male infertility. Lancet 397 , 319–333 (2021).
Farquhar, C. & Marjoribanks, J. Assisted reproductive technology: an overview of Cochrane reviews. Cochrane Database Syst. Rev. 8 , CD010537 (2018).
Chang, Z. et al. Mesenchymal stem cells in preclinical infertility cytotherapy: a retrospective review. Stem Cells Int. 2021 , 8882368 (2021).
Fenton, A. J. Premature ovarian insufficiency: pathogenesis and management. J. Midlife Health 6 , 147–153 (2015).
Coulam, C. B. Premature gonadal failure. Fertil. Steril. 38 , 645–655 (1982).
Huhtaniemi, I. et al. Advances in the molecular pathophysiology, genetics, and treatment of primary ovarian insufficiency. Trends Endocrinol. Metab. 29 , 400–419 (2018).
Torrealday, S., Kodaman, P. & Pal, L. Premature ovarian Insufficiency—an update on recent advances in understanding and management. F1000Res 6 , 2069 (2017).
Gupta, S., Lodha, P., Karthick, M. S. & Tandulwadkar, S. R. Role of autologous bone marrow-derived stem cell therapy for follicular recruitment in premature ovarian insufficiency: review of literature and a case report of world’s first baby with ovarian autologous stem cell therapy in a perimenopausal woman of age 45 year. J. Hum. Reprod. Sci. 11 , 125–130 (2018).
Igboeli, P. et al. Intraovarian injection of autologous human mesenchymal stem cells increases estrogen production and reduces menopausal symptoms in women with premature ovarian failure: two case reports and a review of the literature. J. Med. Case Rep. 14 , 108 (2020).
Ulin, M. et al. Human mesenchymal stem cell therapy and other novel treatment approaches for premature ovarian insufficiency. Reprod. Sci. 28 , 1688–1696 (2021).
Herraiz, S. et al. Autologous stem cell ovarian transplantation to increase reproductive potential in patients who are poor responders. Fertil. Steril. 110 , 496–505 e491 (2018).
Ding, L. et al. Transplantation of UC-MSCs on collagen scaffold activates follicles in dormant ovaries of POF patients with long history of infertility. Sci. China Life Sci. 61 , 1554–1565 (2018).
Wang, M. Y., Wang, Y. X., Li-Ling, J. & Xie, H. Q. Adult stem cell therapy for premature ovarian failure: from bench to bedside. Tissue Eng. Part B Rev. 28 , 63–78 (2022).
Kaddoura, I., Abu-Sittah, G., Ibrahim, A., Karamanoukian, R. & Papazian, N. Burn injury: review of pathophysiology and therapeutic modalities in major burns. Ann. Burns Fire Disasters 30 , 95–102 (2017).
PubMed PubMed Central CAS Google Scholar
Jeschke, M. G. et al. Burn injury. Nat. Rev. Dis. Prim. 6 , 11 (2020).
Rasulov, M. F. et al. First experience of the use bone marrow mesenchymal stem cells for the treatment of a patient with deep skin burns. Bull. Exp. Biol. Med. 139 , 141–144 (2005).
Mansilla, E. et al. Cadaveric bone marrow mesenchymal stem cells: first experience treating a patient with large severe burns. Burns Trauma 3 , 17 (2015).
Xu, Y., Huang, S. & Fu, X. Autologous transplantation of bone marrow-derived mesenchymal stem cells: a promising therapeutic strategy for prevention of skin-graft contraction. Clin. Exp. Dermatol. 37 , 497–500 (2012).
Yoshikawa, T. et al. Wound therapy by marrow mesenchymal cell transplantation. Plast. Reconstr. Surg. 121 , 860–877 (2008).
Abo-Elkheir, W. et al. Role of cord blood and bone marrow mesenchymal stem cells in recent deep burn: a case-control prospective study. Am. J. Stem Cells 6 , 23–35 (2017).
Li, L. et al. Conditioned medium from human adipose-derived mesenchymal stem cell culture prevents UVB-induced skin aging in human keratinocytes and dermal fibroblasts. Int. J. Mol. Sci. 21 , 49 (2019).
Lotfi, M. et al. Adipose tissue-derived mesenchymal stem cells and keratinocytes co-culture on gelatin/chitosan/beta-glycerol phosphate nanoscaffold in skin regeneration. Cell Biol. Int. 43 , 1365–1378 (2019).
Yang, J. A., Chung, H. M., Won, C. H. & Sung, J. H. Potential application of adipose-derived stem cells and their secretory factors to skin: discussion from both clinical and industrial viewpoints. Expert Opin. Biol. Ther. 10 , 495–503 (2010).
Zhou, Y. et al. Combined topical and systemic administration with human adipose-derived mesenchymal stem cells (hADSC) and hADSC-derived exosomes markedly promoted cutaneous wound healing and regeneration. Stem Cell Res. Ther. 12 , 257 (2021).
Arjmand, B. et al. Regenerative medicine for the treatment of ischemic heart disease; status and future perspectives. Front. Cell Dev. Biol. 9 , 704903 (2021).
Denning, C. et al. Cardiomyocytes from human pluripotent stem cells: from laboratory curiosity to industrial biomedical platform. Biochim Biophys. Acta 1863 , 1728–1748 (2016).
Wu, R., Hu, X. & Wang, J. Concise review: optimized strategies for stem cell-based therapy in myocardial repair: clinical translatability and potential limitation. Stem Cells 36 , 482–500 (2018).
Chong, J. J. et al. Human embryonic-stem-cell-derived cardiomyocytes regenerate non-human primate hearts. Nature 510 , 273–277 (2014).
Bagno, L., Hatzistergos, K. E., Balkan, W. & Hare, J. M. Mesenchymal stem cell-based therapy for cardiovascular disease: progress and challenges. Mol. Ther. 26 , 1610–1623 (2018).
Demurtas, J. et al. Stem cells for treatment of cardiovascular diseases: an umbrella review of randomized controlled trials. Ageing Res. Rev. 67 , 101257 (2021).
Gubert, F. et al. Mesenchymal stem cells therapies on fibrotic heart diseases. Int. J. Mol. Sci. 22 , 7447 (2021).
da Silva, J. S. et al. Mesenchymal stem cell therapy in diabetic cardiomyopathy. Cells 11 , 240 (2022).
He, X. et al. Signaling cascades in the failing heart and emerging therapeutic strategies. Signal Transduct. Target Ther. 7 , 134 (2022).
Bolli, R., Solankhi, M., Tang, X. L. & Kahlon, A. Cell therapy in patients with heart failure: a comprehensive review and emerging concepts. Cardiovasc Res. 118 , 951–976 (2022).
Bartunek, J. et al. Cardiopoietic stem cell therapy in heart failure: the C-CURE (cardiopoietic stem Cell therapy in heart failURE) multicenter randomized trial with lineage-specified biologics. J. Am. Coll. Cardiol. 61 , 2329–2338 (2013).
Bartunek, J. et al. Cardiopoietic cell therapy for advanced ischaemic heart failure: results at 39 weeks of the prospective, randomized, double blind, sham-controlled CHART-1 clinical trial. Eur. Heart J. 38 , 648–660 (2017).
Hare, J. M. et al. Comparison of allogeneic vs autologous bone marrow-derived mesenchymal stem cells delivered by transendocardial injection in patients with ischemic cardiomyopathy: the POSEIDON randomized trial. J. Am. Med. Assoc. 308 , 2369–2379 (2012).
Hare, J. M. et al. Randomized comparison of allogeneic versus autologous mesenchymal stem cells for nonischemic dilated cardiomyopathy: POSEIDON-DCM trial. J. Am. Coll. Cardiol. 69 , 526–537 (2017).
Mathiasen, A. B. et al. Bone marrow-derived mesenchymal stromal cell treatment in patients with severe ischaemic heart failure: a randomized placebo-controlled trial (MSC-HF trial). Eur. Heart J. 36 , 1744–1753 (2015).
Mathiasen, A. B. et al. Bone marrow-derived mesenchymal stromal cell treatment in patients with ischaemic heart failure: final 4-year follow-up of the MSC-HF trial. Eur. J. Heart Fail 22 , 884–892 (2020).
Florea, V. et al. Dose comparison study of allogeneic mesenchymal stem cells in patients with ischemic cardiomyopathy (The TRIDENT Study). Circ. Res. 121 , 1279–1290 (2017).
Bolli, R. et al. A Phase II study of autologous mesenchymal stromal cells and c-kit positive cardiac cells, alone or in combination, in patients with ischaemic heart failure: the CCTRN CONCERT-HF trial. Eur. J. Heart Fail 23 , 661–674 (2021).
Heldman, A. W. et al. Transendocardial mesenchymal stem cells and mononuclear bone marrow cells for ischemic cardiomyopathy: the TAC-HFT randomized trial. J. Am. Med. Assoc. 311 , 62–73 (2014).
Perin, E. C. et al. Adipose-derived regenerative cells in patients with ischemic cardiomyopathy: the PRECISE trial. Am. Heart J. 168 , 88–95 e82 (2014).
Han, S., Sun, H. M., Hwang, K. C. & Kim, S. W. Adipose-derived stromal vascular fraction cells: update on clinical utility and efficacy. Crit. Rev. Eukaryot. Gene Expr. 25 , 145–152 (2015).
Henry, T. D. et al. The Athena trials: autologous adipose-derived regenerative cells for refractory chronic myocardial ischemia with left ventricular dysfunction. Catheter Cardiovasc Inter. 89 , 169–177 (2017).
Kastrup, J. et al. Cryopreserved off-the-shelf allogeneic adipose-derived stromal cells for therapy in patients with ischemic heart disease and heart failure—a safety study. Stem Cells Transl. Med. 6 , 1963–1971 (2017).
Qayyum, A. A. et al. Adipose-derived stromal cells for treatment of patients with chronic ischemic heart disease (MyStromalCell Trial): a randomized placebo-controlled study. Stem Cells Int. 2017 , 5237063 (2017).
Qayyum, A. A. et al. Autologous adipose-derived stromal cell treatment for patients with refractory angina (MyStromalCell Trial): 3-years follow-up results. J. Transl. Med. 17 , 360 (2019).
Ngo, A. T. L. et al. Clinically relevant preservation conditions for mesenchymal stem/stromal cells derived from perinatal and adult tissue sources. J. Cell Mol. Med. 25 , 10747–10760 (2021).
Madonna, R., Cevik, C., Nasser, M. & De Caterina, R. Hepatocyte growth factor: molecular biomarker and player in cardioprotection and cardiovascular regeneration. Thromb. Haemost. 107 , 656–661 (2012).
Bartolucci, J. et al. Safety and efficacy of the intravenous infusion of umbilical cord mesenchymal stem cells in patients with heart failure: a phase 1/2 randomized controlled trial (RIMECARD Trial [randomized clinical trial of intravenous infusion umbilical cord mesenchymal stem cells on cardiopathy]). Circ. Res. 121 , 1192–1204 (2017).
Ulus, A. T. et al. Intramyocardial transplantation of umbilical cord mesenchymal stromal cells in chronic ischemic cardiomyopathy: a controlled, randomized clinical trial (HUC-HEART trial). Int. J. Stem Cells 13 , 364–376 (2020).
He, X. et al. Effect of intramyocardial grafting collagen scaffold with mesenchymal stromal cells in patients with chronic ischemic heart disease: a randomized clinical trial. JAMA Netw. Open 3 , e2016236 (2020).
Zhang, Q. et al. Signaling pathways and targeted therapy for myocardial infarction. Signal Transduct. Target Ther. 7 , 78 (2022).
Poomani, M. S. et al. Mesenchymal stem cell (MSCs) therapy for ischemic heart disease: a promising frontier. Glob. Heart 17 , 19 (2022).
Xu, W. et al. Mesenchymal stem cells from adult human bone marrow differentiate into a cardiomyocyte phenotype in vitro. Exp. Biol. Med. 229 , 623–631 (2004).
Jeong, J. O. et al. Malignant tumor formation after transplantation of short-term cultured bone marrow mesenchymal stem cells in experimental myocardial infarction and diabetic neuropathy. Circ. Res. 108 , 1340–1347 (2011).
Denu, R. A. et al. Fibroblasts and mesenchymal stromal/stem cells are phenotypically indistinguishable. Acta Haematol. 136 , 85–97 (2016).
Birbrair, A. & Frenette, P. S. Niche heterogeneity in the bone marrow. Ann. N. Y Acad. Sci. 1370 , 82–96 (2016).
Pinho, S. & Frenette, P. S. Haematopoietic stem cell activity and interactions with the niche. Nat. Rev. Mol. Cell Biol. 20 , 303–320 (2019).
Ono, N. et al. Vasculature-associated cells expressing nestin in developing bones encompass early cells in the osteoblast and endothelial lineage. Dev. Cell 29 , 330–339 (2014).
Sugiyama, T., Kohara, H., Noda, M. & Nagasawa, T. Maintenance of the hematopoietic stem cell pool by CXCL12-CXCR4 chemokine signaling in bone marrow stromal cell niches. Immunity 25 , 977–988 (2006).
Ehninger, A. & Trumpp, A. The bone marrow stem cell niche grows up: mesenchymal stem cells and macrophages move in. J. Exp. Med. 208 , 421–428 (2011).
Golan, K., Kollet, O., Markus, R. P. & Lapidot, T. Daily light and darkness onset and circadian rhythms metabolically synchronize hematopoietic stem cell differentiation and maintenance: the role of bone marrow norepinephrine, tumor necrosis factor, and melatonin cycles. Exp. Hematol. 78 , 1–10 (2019).
Cheng, X. et al. The role of SDF-1/CXCR4/CXCR7 in neuronal regeneration after cerebral ischemia. Front. Neurosci. 11 , 590 (2017).
Zou, Y. R., Kottmann, A. H., Kuroda, M., Taniuchi, I. & Littman, D. R. Function of the chemokine receptor CXCR4 in haematopoiesis and in cerebellar development. Nature 393 , 595–599 (1998).
Mao, W., Yi, X., Qin, J., Tian, M. & Jin, G. CXCL12 inhibits cortical neuron apoptosis by increasing the ratio of Bcl-2/Bax after traumatic brain injury. Int. J. Neurosci. 124 , 281–290 (2014).
Wang, Q. et al. Stromal cell-derived factor 1alpha decreases beta-amyloid deposition in Alzheimer’s disease mouse model. Brain Res. 1459 , 15–26 (2012).
Yellowley, C. CXCL12/CXCR4 signaling and other recruitment and homing pathways in fracture repair. Bonekey Rep. 2 , 300 (2013).
Li, J. et al. CXCL12 promotes spinal nerve regeneration and functional recovery after spinal cord injury. Neuroreport 32 , 450–457 (2021).
Gensel, J. C., Kigerl, K. A., Mandrekar-Colucci, S. S., Gaudet, A. D. & Popovich, P. G. Achieving CNS axon regeneration by manipulating convergent neuro-immune signaling. Cell Tissue Res. 349 , 201–213 (2012).
Matsushita, T. et al. Mesenchymal stem cells transmigrate across brain microvascular endothelial cell monolayers through transiently formed inter-endothelial gaps. Neurosci. Lett. 502 , 41–45 (2011).
Schmidt, A. et al. Mesenchymal stem cells transmigrate over the endothelial barrier. Eur. J. Cell Biol. 85 , 1179–1188 (2006).
Yarygin, K. N. et al. Cell therapy of stroke: do the intra-arterially transplanted mesenchymal stem cells cross the blood-brain barrier? Cells 10 , 2997 (2021).
Schack, L. M. et al. Expression of CD24 in human bone marrow-derived mesenchymal stromal cells is regulated by TGFbeta3 and induces a myofibroblast-like genotype. Stem Cells Int. 2016 , 1319578 (2016).
Ruster, B. et al. Mesenchymal stem cells display coordinated rolling and adhesion behavior on endothelial cells. Blood 108 , 3938–3944 (2006).
Pluchino, N. et al. CXCR4 or CXCR7 antagonists treat endometriosis by reducing bone marrow cell trafficking. J. Cell Mol. Med. 24 , 2464–2474 (2020).
Kowalski, K. et al. Stem cells migration during skeletal muscle regeneration—the role of Sdf-1/Cxcr4 and Sdf-1/Cxcr7 axis. Cell Adh. Migr. 11 , 384–398 (2017).
Liu, L. et al. From blood to the brain: can systemically transplanted mesenchymal stem cells cross the blood-brain barrier? Stem Cells Int. 2013 , 435093 (2013).
Lozito, T. P. & Tuan, R. S. Mesenchymal stem cells inhibit both endogenous and exogenous MMPs via secreted TIMPs. J. Cell Physiol. 226 , 385–396 (2011).
Lozito, T. P., Jackson, W. M., Nesti, L. J. & Tuan, R. S. Human mesenchymal stem cells generate a distinct pericellular zone of MMP activities via binding of MMPs and secretion of high levels of TIMPs. Matrix Biol. 34 , 132–143 (2014).
Menge, T. et al. Mesenchymal stem cells regulate blood-brain barrier integrity through TIMP3 release after traumatic brain injury. Sci. Transl. Med. 4 , 161ra150 (2012).
Franklin, R. J. M. & Ffrench-Constant, C. Regenerating CNS myelin—from mechanisms to experimental medicines. Nat. Rev. Neurosci. 18 , 753–769 (2017).
Brick, R. M., Sun, A. X. & Tuan, R. S. Neurotrophically induced mesenchymal progenitor cells derived from induced pluripotent stem cells enhance neuritogenesis via neurotrophin and cytokine production. Stem Cells Transl. Med. 7 , 45–58 (2018).
Zupanc, H. R. H., Alexander, P. G. & Tuan, R. S. Neurotrophic support by traumatized muscle-derived multipotent progenitor cells: role of endothelial cells and vascular endothelial growth factor-A. Stem Cell Res. Ther. 8 , 226 (2017).
Liu, Y. & Olsen, B. R. Distinct VEGF functions during bone development and homeostasis. Arch. Immunol. Ther. Exp. 62 , 363–368 (2014).
Kangari, P., Talaei-Khozani, T., Razeghian-Jahromi, I. & Razmkhah, M. Mesenchymal stem cells: amazing remedies for bone and cartilage defects. Stem Cell Res. Ther. 11 , 492 (2020).
Liu, Y. et al. Intracellular VEGF regulates the balance between osteoblast and adipocyte differentiation. J. Clin. Investig. 122 , 3101–3113 (2012).
Berendsen, A. D. & Olsen, B. R. How vascular endothelial growth factor-A (VEGF) regulates differentiation of mesenchymal stem cells. J. Histochem Cytochem. 62 , 103–108 (2014).
Garcia, K. O. et al. Therapeutic effects of the transplantation of VEGF overexpressing bone marrow mesenchymal stem cells in the hippocampus of murine model of Alzheimer’s disease. Front. Aging Neurosci. 6 , 30 (2014).
Hohman, T. J., Bell, S. P. & Jefferson, A. L., Alzheimer’s Disease Neuroimaging, I. The role of vascular endothelial growth factor in neurodegeneration and cognitive decline: exploring interactions with biomarkers of Alzheimer disease. JAMA Neurol. 72 , 520–529 (2015).
Zhang, W. et al. Neuroprotective effects of SOX5 against ischemic stroke by regulating VEGF/PI3K/AKT pathway. Gene 767 , 145148 (2021).
Jin, K. et al. Vascular endothelial growth factor (VEGF) stimulates neurogenesis in vitro and in vivo. Proc. Natl Acad. Sci. USA 99 , 11946–11950 (2002).
Bao, X. J. et al. Transplantation of Flk-1+ human bone marrow-derived mesenchymal stem cells promotes behavioral recovery and anti-inflammatory and angiogenesis effects in an intracerebral hemorrhage rat model. Int. J. Mol. Med. 31 , 1087–1096 (2013).
Bao, X. et al. Transplantation of Flk-1+ human bone marrow-derived mesenchymal stem cells promotes angiogenesis and neurogenesis after cerebral ischemia in rats. Eur. J. Neurosci. 34 , 87–98 (2011).
Pelletier, J. et al. VEGF-A promotes both pro-angiogenic and neurotrophic capacities for nerve recovery after compressive neuropathy in rats. Mol. Neurobiol. 51 , 240–251 (2015).
Hobson, M. I., Green, C. J. & Terenghi, G. VEGF enhances intraneural angiogenesis and improves nerve regeneration after axotomy. J. Anat. 197 (Pt 4), 591–605 (2000).
Hayakawa, K. et al. Vascular endothelial growth factor regulates the migration of oligodendrocyte precursor cells. J. Neurosci. 31 , 10666–10670 (2011).
Pei, G., Xu, L., Huang, W. & Yin, J. The protective role of microRNA-133b in restricting hippocampal neurons apoptosis and inflammatory injury in rats with depression by suppressing CTGF. Int. Immunopharmacol. 78 , 106076 (2020).
Xu, H. et al. Mesenchymal stem cell-derived exosomal microRNA-133b suppresses glioma progression via Wnt/beta-catenin signaling pathway by targeting EZH2. Stem Cell Res. Ther. 10 , 381 (2019).
Xin, H. et al. MiR-133b promotes neural plasticity and functional recovery after treatment of stroke with multipotent mesenchymal stromal cells in rats via transfer of exosome-enriched extracellular particles. Stem Cells 31 , 2737–2746 (2013).
Kigerl, K. A. et al. Identification of two distinct macrophage subsets with divergent effects causing either neurotoxicity or regeneration in the injured mouse spinal cord. J. Neurosci. 29 , 13435–13444 (2009).
Knoller, N. et al. Clinical experience using incubated autologous macrophages as a treatment for complete spinal cord injury: phase I study results. J. Neurosurg. Spine 3 , 173–181 (2005).
Yagura, K. et al. The enhancement of CCL2 and CCL5 by human bone marrow-derived mesenchymal stem/stromal cells might contribute to inflammatory suppression and axonal extension after spinal cord injury. PLoS ONE 15 , e0230080 (2020).
Zhong, Z. et al. Bone marrow mesenchymal stem cells upregulate PI3K/AKT pathway and down-regulate NF-kappaB pathway by secreting glial cell-derived neurotrophic factors to regulate microglial polarization and alleviate deafferentation pain in rats. Neurobiol. Dis. 143 , 104945 (2020).
Zhong, Z. et al. Adipose-derived stem cells modulate BV2 microglial M1/M2 polarization by producing GDNF. Stem Cells Dev. 29 , 714–727 (2020).
Dong, B. et al. Exosomes from human umbilical cord mesenchymal stem cells attenuate the inflammation of severe steroid-resistant asthma by reshaping macrophage polarization. Stem Cell Res. Ther. 12 , 204 (2021).
Li, X. et al. Umbilical cord tissue-derived mesenchymal stem cells induce T lymphocyte apoptosis and cell cycle arrest by expression of indoleamine 2, 3-dioxygenase. Stem Cells Int. 2016 , 7495135 (2016).
Wang, A. Y. L. et al. Human Wharton’s jelly mesenchymal stem cell-mediated sciatic nerve recovery is associated with the upregulation of regulatory T cells. Int. J. Mol. Sci. 21 , 6310 (2020).
Noone, C., Kihm, A., English, K., O’Dea, S. & Mahon, B. P. IFN-gamma stimulated human umbilical-tissue-derived cells potently suppress NK activation and resist NK-mediated cytotoxicity in vitro. Stem Cells Dev. 22 , 3003–3014 (2013).
Li, X. et al. Immunomodulatory effects of mesenchymal stem cells in peripheral nerve injury. Stem Cell Res. Ther. 13 , 18 (2022).
Shang, Y., Guan, H. & Zhou, F. Biological characteristics of umbilical cord mesenchymal stem cells and its therapeutic potential for hematological disorders. Front. Cell Dev. Biol. 9 , 570179 (2021).
Mennan, C. et al. Isolation and characterisation of mesenchymal stem cells from different regions of the human umbilical cord. Biomed. Res. Int. 2013 , 916136 (2013).
D’Addio, F. et al. The link between the PDL1 costimulatory pathway and Th17 in fetomaternal tolerance. J. Immunol. 187 , 4530–4541 (2011).
Amable, P. R., Teixeira, M. V., Carias, R. B., Granjeiro, J. M. & Borojevic, R. Protein synthesis and secretion in human mesenchymal cells derived from bone marrow, adipose tissue and Wharton’s jelly. Stem Cell Res. Ther. 5 , 53 (2014).
de Witte, S. F. H. et al. Immunomodulation by therapeutic mesenchymal stromal cells (MSC) is triggered through phagocytosis of MSC by monocytic cells. Stem Cells 36 , 602–615 (2018).
Li, Y. et al. Cell-cell contact with proinflammatory macrophages enhances the immunotherapeutic effect of mesenchymal stem cells in two abortion models. Cell Mol. Immunol. 16 , 908–920 (2019).
De Paepe, M. E., Wong, T., Chu, S. & Mao, Q. Stromal cell-derived factor-1 (SDF-1) expression in very preterm human lungs: potential relevance for stem cell therapy for bronchopulmonary dysplasia. Exp. Lung Res. 46 , 146–156 (2020).
Wynn, R. F. et al. A small proportion of mesenchymal stem cells strongly expresses functionally active CXCR4 receptor capable of promoting migration to bone marrow. Blood 104 , 2643–2645 (2004).
Ryu, C. H. et al. Migration of human umbilical cord blood mesenchymal stem cells mediated by stromal cell-derived factor-1/CXCR4 axis via Akt, ERK, and p38 signal transduction pathways. Biochem Biophys. Res. Commun. 398 , 105–110 (2010).
Yang, C. et al. The biological changes of umbilical cord mesenchymal stem cells in inflammatory environment induced by different cytokines. Mol. Cell Biochem. 446 , 171–184 (2018).
Seedorf, G. et al. Hepatocyte growth factor as a downstream mediator of vascular endothelial growth factor-dependent preservation of growth in the developing lung. Am. J. Physiol. Lung Cell Mol. Physiol. 310 , L1098–L1110 (2016).
Chen, X. Y. et al. Therapeutic potential of human umbilical cord-derived mesenchymal stem cells in recovering from murine pulmonary emphysema under cigarette smoke exposure. Front. Med. 8 , 713824 (2021).
Katsha, A. M. et al. Paracrine factors of multipotent stromal cells ameliorate lung injury in an elastase-induced emphysema model. Mol. Ther. 19 , 196–203 (2011).
Kyurkchiev, D. et al. Secretion of immunoregulatory cytokines by mesenchymal stem cells. World J. Stem Cells 6 , 552–570 (2014).
Ren, Z. et al. Human umbilical-cord mesenchymal stem cells inhibit bacterial growth and alleviate antibiotic resistance in neonatal imipenem-resistant Pseudomonas aeruginosa infection. Innate Immun. 26 , 215–221 (2020).
Liu, J. et al. Type 2 alveolar epithelial cells differentiated from human umbilical cord mesenchymal stem cells alleviate mouse pulmonary fibrosis through beta-catenin-regulated cell apoptosis. Stem Cells Dev. 30 , 660–670 (2021).
Moodley, Y. et al. Human umbilical cord mesenchymal stem cells reduce fibrosis of bleomycin-induced lung injury. Am. J. Pathol. 175 , 303–313 (2009).
Li, D. Y., Li, R. F., Sun, D. X., Pu, D. D. & Zhang, Y. H. Mesenchymal stem cell therapy in pulmonary fibrosis: a meta-analysis of preclinical studies. Stem Cell Res. Ther. 12 , 461 (2021).
Lam, G., Zhou, Y., Wang, J. X. & Tsui, Y. P. Targeting mesenchymal stem cell therapy for severe pneumonia patients. World J. Stem Cells 13 , 139–154 (2021).
Chen, K. et al. Human umbilical cord mesenchymal stem cells hUC-MSCs exert immunosuppressive activities through a PGE2-dependent mechanism. Clin. Immunol. 135 , 448–458 (2010).
Ren, G. et al. Mesenchymal stem cell-mediated immunosuppression occurs via concerted action of chemokines and nitric oxide. Cell Stem Cell 2 , 141–150 (2008).
Loy, H. et al. Therapeutic implications of human umbilical cord mesenchymal stromal cells in attenuating influenza A(H5N1) virus-associated acute lung injury. J. Infect. Dis. 219 , 186–196 (2019).
Gazdhar, A. et al. Targeted gene transfer of hepatocyte growth factor to alveolar type II epithelial cells reduces lung fibrosis in rats. Hum. Gene Ther. 24 , 105–116 (2013).
Wang, W. et al. Therapeutic mechanisms of mesenchymal stem cells in acute respiratory distress syndrome reveal potentials for Covid-19 treatment. J. Transl. Med. 19 , 198 (2021).
Chu, K. A. et al. Reversal of bleomycin-induced rat pulmonary fibrosis by a xenograft of human umbilical mesenchymal stem cells from Wharton’s jelly. Theranostics 9 , 6646–6664 (2019).
Chen, Q. H. et al. Mesenchymal stem cells regulate the Th17/Treg cell balance partly through hepatocyte growth factor in vitro. Stem Cell Res. Ther. 11 , 91 (2020).
Li, L. et al. Human umbilical cord-derived mesenchymal stem cells downregulate inflammatory responses by shifting the Treg/Th17 profile in experimental colitis. Pharmacology 92 , 257–264 (2013).
Zheng, L., Wang, S., Yang, H. & Lyu, X. [Research progress of mesenchymal stem cells attenuating acute respiratory distress syndrome by regulating the balance of M1/M2 macrophage polarization]. Zhonghua Wei Zhong Bing. Ji Jiu Yi Xue 33 , 509–512 (2021).
Fasshauer, M. & Bluher, M. Adipokines in health and disease. Trends Pharm. Sci. 36 , 461–470 (2015).
Kershaw, E. E. & Flier, J. S. Adipose tissue as an endocrine organ. J. Clin. Endocrinol. Metab. 89 , 2548–2556 (2004).
Kurylowicz, A. & Kozniewski, K. Anti-inflammatory strategies targeting metaflammation in type 2 diabetes. Molecules 25 , 2224 (2020).
Liu, J. et al. Homing and restorative effects of bone marrow-derived mesenchymal stem cells on cisplatin injured ovaries in rats. Mol. Cells 37 , 865–872 (2014).
Jalalie, L. et al. Distribution of the CM-Dil-labeled human umbilical cord vein mesenchymal stem cells migrated to the cyclophosphamide-injured ovaries in C57BL/6 mice. Iran. Biomed. J. 23 , 200–208 (2019).
Takehara, Y. et al. The restorative effects of adipose-derived mesenchymal stem cells on damaged ovarian function. Lab. Investig. 93 , 181–193 (2013).
Richards, J. S., Ren, Y. A., Candelaria, N., Adams, J. E. & Rajkovic, A. Ovarian Follicular Theca Cell Recruitment, Differentiation, and Impact on Fertility: 2017 Update. Endocr. Rev. 39 , 1–20 (2018).
Young, J. M. & McNeilly, A. S. Theca: the forgotten cell of the ovarian follicle. Reproduction 140 , 489–504 (2010).
Trzyna, A. & Banas-Zabczyk, A. Adipose-derived stem cells secretome and its potential application in “stem cell-free therapy”. Biomolecules 11 , 878 (2021).
Ding, C. et al. Human amniotic mesenchymal stem cells improve ovarian function in natural aging through secreting hepatocyte growth factor and epidermal growth factor. Stem Cell Res. Ther. 9 , 55 (2018).
Kedenko, L. et al. Genetic polymorphisms at SIRT1 and FOXO1 are associated with carotid atherosclerosis in the SAPHIR cohort. BMC Med. Genet. 15 , 112 (2014).
Shojafar, E., Soleimani Mehranjani, M. & Shariatzadeh, S. M. A. Adipose derived mesenchymal stem cells improve the structure and function of autografted mice ovaries through reducing oxidative stress and inflammation: a stereological and biochemical analysis. Tissue Cell 56 , 23–30 (2019).
Liu, M. et al. Small extracellular vesicles derived from embryonic stem cells restore ovarian function of premature ovarian failure through PI3K/AKT signaling pathway. Stem Cell Res. Ther. 11 , 3 (2020).
Li, Z., Zhang, M., Tian, Y., Li, Q. & Huang, X. Mesenchymal stem cells in premature ovarian insufficiency: mechanisms and prospects. Front. Cell Dev. Biol. 9 , 718192 (2021).
Forghani, A. et al. Differentiation of adipose tissue-derived CD34+/CD31- cells into endothelial cells in vitro. Regen. Eng. Transl. Med 6 , 101–110 (2020).
Baer, P. C. Adipose-derived stem cells and their potential to differentiate into the epithelial lineage. Stem Cells Dev. 20 , 1805–1816 (2011).
Wang, C. et al. Differentiation of adipose-derived stem cells into contractile smooth muscle cells induced by transforming growth factor-beta1 and bone morphogenetic protein-4. Tissue Eng. Part A 16 , 1201–1213 (2010).
Chen, L. et al. Adipose-derived stem cells promote diabetic wound healing via the recruitment and differentiation of endothelial progenitor cells into endothelial cells mediated by the VEGF-PLCgamma-ERK pathway. Arch. Biochem Biophys. 692 , 108531 (2020).
Dekoninck, S. & Blanpain, C. Stem cell dynamics, migration and plasticity during wound healing. Nat. Cell Biol. 21 , 18–24 (2019).
Qian, L., Pi, L., Fang, B. R. & Meng, X. X. Adipose mesenchymal stem cell-derived exosomes accelerate skin wound healing via the lncRNA H19/miR-19b/SOX9 axis. Lab. Investig. 101 , 1254–1266 (2021).
Fujiwara, O. et al. Adipose-derived stem cells improve grafted burn wound healing by promoting wound bed blood flow. Burns Trauma 8 , tkaa009 (2020).
Chen, T. et al. Efficient and sustained IGF-1 expression in the adipose tissue-derived stem cells mediated via a lentiviral vector. J. Mol. Histol. 46 , 1–11 (2015).
Zhou, K. et al. Immunosuppression of human adipose-derived stem cells on T cell subsets via the reduction of NF-kappaB activation mediated by PD-L1/PD-1 and Gal-9/TIM-3 pathways. Stem Cells Dev. 27 , 1191–1202 (2018).
Moll, G. et al. Intravascular mesenchymal stromal/stem cell therapy product diversification: time for new clinical guidelines. Trends Mol. Med. 25 , 149–163 (2019).
He, X. et al. Spontaneous apoptosis of cells in therapeutic stem cell preparation exert immunomodulatory effects through release of phosphatidylserine. Signal Transduct. Target Ther. 6 , 270 (2021).
Lukomska, B. et al. Challenges and controversies in human mesenchymal stem cell therapy. Stem Cells Int. 2019 , 9628536 (2019).
Li, C., Zhao, H. & Wang, B. Challenges for mesenchymal stem cell-based therapy for COVID-19. Drug Des. Devel Ther. 14 , 3995–4001 (2020).
Nguyen Thanh, L. et al. Outcomes of bone marrow mononuclear cell transplantation combined with interventional education for autism spectrum disorder. Stem Cells Transl. Med. 10 , 14–26 (2020).
Nguyen Thanh, L. et al. Can autologous adipose-derived mesenchymal stem cell transplantation improve sexual function in people with sexual functional deficiency? Stem Cell Rev. Rep. 17 , 2153–2163 (2021).
Caplan, A. I. Mesenchymal stem cells: time to change the name! Stem Cells Transl. Med. 6 , 1445–1451 (2017).
de Windt, T. S., Vonk, L. A. & Saris, D. B. F. Response to: Mesenchymal stem cells: time to change the name! Stem Cells Transl. Med. 6 , 1747–1748 (2017).
Boregowda, S. V., Booker, C. N. & Phinney, D. G. Mesenchymal stem cells: the moniker fits the science. Stem Cells 36 , 7–10 (2018).
Masterson, C. & O’Toole, D. The mesenchymal stromal cell magic bullet finds yet another target. Stem Cell Res. Ther. 5 , 82 (2014).
Murray, I. R. et al. Rogue stem cell clinics. Bone Jt. J. 102-B , 148–154 (2020).
Lyons, S., Salgaonkar, S. & Flaherty, G. T. International stem cell tourism: a critical literature review and evidence-based recommendations. Int. Health 14 , 132–141 (2022).
He, C. et al. Mesenchymal stem cell-based treatment in autoimmune liver diseases: underlying roles, advantages and challenges. Ther. Adv. Chronic Dis. 12 , 2040622321993442 (2021).
Bertheuil, N. et al. Adipose mesenchymal stromal cells: definition, immunomodulatory properties, mechanical isolation and interest for plastic surgery. Ann. Chir. Plast. Esthet. 64 , 1–10 (2019).
Chen, Y., Yu, Q., Hu, Y. & Shi, Y. Current research and use of mesenchymal stem cells in the therapy of autoimmune diseases. Curr. Stem Cell Res. Ther. 14 , 579–582 (2019).
Han, Y. et al. The secretion profile of mesenchymal stem cells and potential applications in treating human diseases. Signal Transduct. Target Ther. 7 , 92 (2022).
Rahmani, A. et al. Mesenchymal stem cell-derived extracellular vesicle-based therapies protect against coupled degeneration of the central nervous and vascular systems in stroke. Ageing Res. Rev. 62 , 101106 (2020).
Zhou, W. et al. Single-cell profiles and clinically useful properties of human mesenchymal stem cells of adipose and bone marrow origin. Am. J. Sports Med. 47 , 1722–1733 (2019).
Pachler, K. et al. A good manufacturing practice-grade standard protocol for exclusively human mesenchymal stromal cell-derived extracellular vesicles. Cytotherapy 19 , 458–472 (2017).
Borger, V., Staubach, S., Dittrich, R., Stambouli, O. & Giebel, B. Scaled isolation of mesenchymal stem/stromal cell-derived extracellular vesicles. Curr. Protoc. Stem Cell Biol. 55 , e128 (2020).
Nikfarjam, S., Rezaie, J., Zolbanin, N. M. & Jafari, R. Mesenchymal stem cell derived-exosomes: a modern approach in translational medicine. J. Transl. Med. 18 , 449 (2020).
Monticelli, S. & Natoli, G. Short-term memory of danger signals and environmental stimuli in immune cells. Nat. Immunol. 14 , 777–784 (2013).
Venkatesha, S. et al. Soluble endoglin contributes to the pathogenesis of preeclampsia. Nat. Med. 12 , 642–649 (2006).
Bernardo, M. E. & Fibbe, W. E. Mesenchymal stromal cells: sensors and switchers of inflammation. Cell Stem Cell 13 , 392–402 (2013).
Liu, G. Y. et al. Short-term memory of danger signals or environmental stimuli in mesenchymal stem cells: implications for therapeutic potential. Cell Mol. Immunol. 13 , 369–378 (2016).
Diez-Tejedor, E. et al. Reparative therapy for acute ischemic stroke with allogeneic mesenchymal stem cells from adipose tissue: a safety assessment: a phase II randomized, double-blind, placebo-controlled, single-center, pilot clinical trial. J. Stroke Cerebrovasc. Dis. 23 , 2694–2700 (2014).
Laskowitz, D. T. et al. Allogeneic umbilical cord blood infusion for adults with ischemic stroke: clinical outcomes from a phase I safety study. Stem Cells Transl. Med. 7 , 521–529 (2018).
Jeon, S. R. et al. Treatment of spinal cord injury with bone marrow-derived, cultured autologous mesenchymal stem cells. Tissue Eng. Regenerative Med. 7 , 316–322 (2010).
Park, J. H. et al. Long-term results of spinal cord injury therapy using mesenchymal stem cells derived from bone marrow in humans. Neurosurgery 70 , 1238–1247 (2012).
Saito, F. et al. Administration of cultured autologous bone marrow stromal cells into cerebrospinal fluid in spinal injury patients: a pilot study. Restor. Neurol. Neurosci. 30 , 127–136 (2012).
El-Kheir, W. A. et al. Autologous bone marrow-derived cell therapy combined with physical therapy induces functional improvement in chronic spinal cord injury patients. Cell Transpl. 23 , 729–745 (2014).
Karamouzian, S., Nematollahi-Mahani, S. N., Nakhaee, N. & Eskandary, H. Clinical safety and primary efficacy of bone marrow mesenchymal cell transplantation in subacute spinal cord injured patients. Clin. Neurol. Neurosurg. 114 , 935–939 (2012).
Pal, R. et al. Ex vivo-expanded autologous bone marrow-derived mesenchymal stromal cells in human spinal cord injury/paraplegia: a pilot clinical study. Cytotherapy 11 , 897–911 (2009).
Mendonca, M. V. et al. Safety and neurological assessments after autologous transplantation of bone marrow mesenchymal stem cells in subjects with chronic spinal cord injury. Stem Cell Res. Ther. 5 , 126 (2014).
Vaquero, J. et al. Intrathecal administration of autologous mesenchymal stromal cells for spinal cord injury: safety and efficacy of the 100/3 guideline. Cytotherapy 20 , 806–819 (2018).
Dai, G. et al. Transplantation of autologous bone marrow mesenchymal stem cells in the treatment of complete and chronic cervical spinal cord injury. Brain Res. 1533 , 73–79 (2013).
Jiang, P. C. et al. A clinical trial report of autologous bone marrow-derived mesenchymal stem cell transplantation in patients with spinal cord injury. Exp. Ther. Med. 6 , 140–146 (2013).
Jarocha, D., Milczarek, O., Wedrychowicz, A., Kwiatkowski, S. & Majka, M. Continuous improvement after multiple mesenchymal stem cell transplantations in a patient with complete spinal cord injury. Cell Transpl. 24 , 661–672 (2015).
Huang, L. et al. A randomized, placebo-controlled trial of human umbilical cord blood mesenchymal stem cell infusion for children with cerebral palsy. Cell Transpl. 27 , 325–334 (2018).
Karussis, D. et al. Safety and immunological effects of mesenchymal stem cell transplantation in patients with multiple sclerosis and amyotrophic lateral sclerosis. Arch. Neurol. 67 , 1187–1194 (2010).
Yamout, B. et al. Bone marrow mesenchymal stem cell transplantation in patients with multiple sclerosis: a pilot study. J. Neuroimmunol. 227 , 185–189 (2010).
Mohajeri, M., Farazmand, A., Mohyeddin Bonab, M., Nikbin, B. & Minagar, A. FOXP3 gene expression in multiple sclerosis patients pre- and post mesenchymal stem cell therapy. Iran. J. Allergy Asthma Immunol. 10 , 155–161 (2011).
Odinak, M. M. et al. [Transplantation of mesenchymal stem cells in multiple sclerosis]. Zh . Nevrol. Psikhiatr Im. S S Korsakova 111 , 72–76 (2011).
Bonab, M. M. et al. Autologous mesenchymal stem cell therapy in progressive multiple sclerosis: an open label study. Curr. Stem Cell Res Ther. 7 , 407–414 (2012).
Mohyeddin Bonab, M. et al. Evaluation of cytokines in multiple sclerosis patients treated with mesenchymal stem cells. Arch. Med Res. 44 , 266–272 (2013).
Llufriu, S. et al. Randomized placebo-controlled phase II trial of autologous mesenchymal stem cells in multiple sclerosis. PLoS ONE 9 , e113936 (2014).
Harris, V. K., Vyshkina, T. & Sadiq, S. A. Clinical safety of intrathecal administration of mesenchymal stromal cell-derived neural progenitors in multiple sclerosis. Cytotherapy 18 , 1476–1482 (2016).
Dahbour, S. et al. Mesenchymal stem cells and conditioned media in the treatment of multiple sclerosis patients: clinical, ophthalmological and radiological assessments of safety and efficacy. CNS Neurosci. Ther. 23 , 866–874 (2017).
Meng, M. et al. Umbilical cord mesenchymal stem cell transplantation in the treatment of multiple sclerosis. Am. J. Transl. Res. 10 , 212–223 (2018).
Fernandez, O. et al. Adipose-derived mesenchymal stem cells (AdMSC) for the treatment of secondary-progressive multiple sclerosis: a triple blinded, placebo controlled, randomized phase I/II safety and feasibility study. PLoS ONE 13 , e0195891 (2018).
Alvarez-Fuente, M. et al. Off-label mesenchymal stromal cell treatment in two infants with severe bronchopulmonary dysplasia: clinical course and biomarkers profile. Cytotherapy 20 , 1337–1344 (2018).
Edessy, M. et al. Autologous stem cells therapy, The first baby of idiopathic premature ovarian failure. Acta Med. Int. 3 , 19–23 (2016).
Gabr, H., Elkheir, W. & El-Gazzar, A. Autologous stem cell transplantation in patients with idiopathic premature ovarian failure. J. Tissue Sci. Eng. 7 , 27 (2016).
Bakhtiary, M. et al. Comparison of transplantation of bone marrow stromal cells (BMSC) and stem cell mobilization by granulocyte colony stimulating factor after traumatic brain injury in rat. Iran. Biomed. J. 14 , 142–149 (2010).
Zhou, Z. et al. Comparison of mesenchymal stromal cells from human bone marrow and adipose tissue for the treatment of spinal cord injury. Cytotherapy 15 , 434–448 (2013).
Yousefifard, M. et al. Human bone marrow-derived and umbilical cord-derived mesenchymal stem cells for alleviating neuropathic pain in a spinal cord injury model. Stem Cell Res. Ther. 7 , 36 (2016).
Takahashi, A. et al. Comparison of mesenchymal stromal cells isolated from murine adipose tissue and bone marrow in the treatment of spinal cord injury. Cell Transpl. 27 , 1126–1139 (2018).
Hao, T. et al. Comparison of bone marrow-vs. adipose tissue-derived mesenchymal stem cells for attenuating liver fibrosis. Exp. Ther. Med. 14 , 5956–5964 (2017).
Zare, H., Jamshidi, S., Dehghan, M. M., Saheli, M. & Piryaei, A. Bone marrow or adipose tissue mesenchymal stem cells: Comparison of the therapeutic potentials in mice model of acute liver failure. J. Cell Biochem 119 , 5834–5842 (2018).
Arminan, A. et al. Mesenchymal stem cells provide better results than hematopoietic precursors for the treatment of myocardial infarction. J. Am. Coll. Cardiol. 55 , 2244–2253 (2010).
Gaebel, R. et al. Cell origin of human mesenchymal stem cells determines a different healing performance in cardiac regeneration. PLoS ONE 6 , e15652 (2011).
Dayan, V. et al. Mesenchymal stromal cells mediate a switch to alternatively activated monocytes/macrophages after acute myocardial infarction. Basic Res. Cardiol. 106 , 1299–1310 (2011).
Lopez, Y. et al. Wharton’s jelly or bone marrow mesenchymal stromal cells improve cardiac function following myocardial infarction for more than 32 weeks in a rat model: a preliminary report. Curr. Stem Cell Res. Ther. 8 , 46–59 (2013).
Rasmussen, J. G. et al. Comparison of human adipose-derived stem cells and bone marrow-derived stem cells in a myocardial infarction model. Cell Transpl. 23 , 195–206 (2014).
Abd Emami, B. et al. Mechanical and chemical predifferentiation of mesenchymal stem cells into cardiomyocytes and their effectiveness on acute myocardial infarction. Artif. Organs 42 , E114–E126 (2018).
Omar, A. M., Meleis, A. E., Arfa, S. A., Zahran, N. M. & Mehanna, R. A. Comparative study of the therapeutic potential of mesenchymal stem cells derived from adipose tissue and bone marrow on acute myocardial infarction model. Oman Med. J. 34 , 534–543 (2019).
Download references
Acknowledgements
The authors would like to thank the Vingroup Scientific Research and Clinical Application Fund (grant number: PRO. 19.47) for supporting this work. All figures were created with Biorender.com. This work is supported by the Vingroup Scientific Research and Clinical Application Fund (Grant number: PRO.19.47).
Author information
Authors and affiliations.
Department of Research and Development, Vinmec Research Institute of Stem Cell and Gene Technology, Vinmec Healthcare System, Hanoi, Vietnam
Duc M. Hoang, Trung Q. Bach, Quyen T. Nguyen, Trang T. K. Phan, Giang H. Nguyen, Phuong T. T. Le, Van T. Hoang & Liem Thanh Nguyen
Department of Cellular Therapy, Vinmec High-Tech Center, Vinmec Healthcare System, Hanoi, Vietnam
Phuong T. Pham & Anh T. L. Ngo
Institute for Science & Technology in Medicine, Keele University, Keele, UK
Nicholas R. Forsyth
Department of Biology, Stanford University, Stanford, CA, USA
Michael Heke
You can also search for this author in PubMed Google Scholar
Contributions
D.M.H.: conception and design, manuscript writing, administrative support, data analysis and interpretation, and final approval of the manuscript. P.T.P.: manuscript writing (BM- and UC-MSC sections) and data analysis and interpretation. T.Q.B.: manuscript writing (BM- and UC-MSC sections) and data analysis and interpretation. A.T.L.N.: manuscript writing (UC-MSC section), figure presentation, and data analysis and interpretation. Q.T.N., T.T.K.P., G.H.N., P.T.T.L., and V.T.H.: manuscript writing and data analysis and interpretation. N.R.F. and M.H.: manuscript writing and editing and data analysis and interpretation. L.T.N.: manuscript writing, administrative support, and final approval of the manuscript. All authors have read and approved the article.
Corresponding author
Correspondence to Duc M. Hoang .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Hoang, D.M., Pham, P.T., Bach, T.Q. et al. Stem cell-based therapy for human diseases. Sig Transduct Target Ther 7 , 272 (2022). https://doi.org/10.1038/s41392-022-01134-4
Download citation
Received : 15 March 2022
Revised : 19 July 2022
Accepted : 21 July 2022
Published : 06 August 2022
DOI : https://doi.org/10.1038/s41392-022-01134-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Endothelial progenitor cell-derived extracellular vesicles: the world of potential prospects for the treatment of cardiovascular diseases.
- De-Xin Chen
- Chuang-Hong Lu
Cell & Bioscience (2024)
Adipose-derived stem cell-based optimization strategies for musculoskeletal regeneration: recent advances and perspectives
- Chenrui Yuan
Stem Cell Research & Therapy (2024)
Safety and efficacy of autologous adipose tissue-derived stem cell transplantation in aging-related low-grade inflammation patients: a single-group, open-label, phase I clinical trial
- Ngoc-Huynh Ton Nguyen
- Hao Thanh Phan
- Nhung Hai Truong
Trials (2024)
Unveiling heterogeneity in MSCs: exploring marker-based strategies for defining MSC subpopulations
- Bowei Liang
- Jianyong Xu
Journal of Translational Medicine (2024)
CD317+ MSCs expanded with chemically defined media have enhanced immunological anti-inflammatory activities
Quick links.
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Stem Cell Research and Health Education
Stem cells are being touted as the greatest discovery for the potential treatment of a myriad of diseases in the new millennium, but there is still much research to be done before it will be known whether they can live up to this description. There is also an ethical debate over the production of one of the most valuable types of stem cell: the embryonic form. Consequently, there is public confusion over the benefits currently being derived from the use of stem cells and what can potentially be expected from their use in the future. The health educator’s role is to give an unbiased account of the current state of stem cell research. This paper provides the groundwork by discussing the types of cells currently identified, their potential use, and some of the political and ethical pitfalls resulting from such use.
INTRODUCTION
Stem cells are believed to be one of the greatest untapped resources currently available for the prevention and treatment of many diseases. Inasmuch as current knowledge of stem cells is a combination of scientific reality and cautious speculation, considerable research is required to identify the true, long-term potential for medical advances from these cells. As health resources professionals, communicators, and advocates, 1 health educators are in a position to advance the public dialogue about this promising technology. This article offers a general overview of stem cells, their potential for extending life and improving its overall quality, and some thoughts on the role of health educators with regard to professional and lay audiences.
WHAT ARE STEM CELLS?
Stem cells are template cells found throughout the body that can grow to become cells with specialized functions. 2 – 6 These cells replicate to generate “offspring” cells that can be either stem cells (and hence, self-renewing) or specialized cells (i.e., differentiated cells) that play a specific role—becoming blood, bone, brain, or skin cells, among others. 7 Stem cells, therefore, have the potential to act as repair systems for replacement of damaged cells. 2 – 6 The field in which a great deal of research is currently underway to determine the use of stems cells in the treatment of diseases and injuries is called “regenerative medicine.” Under “normal” conditions stem cells continue to replicate until they receive a signal to differentiate into a specific cell type. 8 When stem cells receive such a signal they first become progenitor cells, and later, the final mature cell type. Determination of the different signals that cause the stem cell to become a specific type rather than just continue to replicate is important (and, in some cases, it is the absence rather than the presence of a signal that is the important factor). 8 The ability of stem cells from one area to differentiate into another completely different type is known as plasticity, and embryonic stem cells appear to be the “most plastic” of the four types discussed below. 2 – 6
Stem cells are described as being of a specific cell line, dependent on the characteristics and location of the original template cells from which all future offspring cells have grown (reflecting the self-renewing capability of the cells). Assuming that no contamination of the cell line occurs as a result of mutations or infections, and no differentiating triggers occur, the cell lines could potentially grow ad infinitum. 2
DIFFERENT TYPES OF STEM CELLS
There are several types of stem cells: embryonic stem cells, fetal stem cells, adult stem cells, embryonic germ cells, and amniotic and umbilical cord stem cells. These stem cell varieties and their distinct properties are discussed below.
Embryonic and Fetal Stem Cells
The development of an organism can be compartmentalized into several stages. 9 Following the union of the egg and sperm, the initial four to five days from conception are characterized by a period of rapid cell division. A “ball” of 50 to 150 cells known as a blastocyst is created, so named because it is a hollow sphere. The blastocyst is composed of three parts: the trophoblast or outer surface, the blastocoel or inner cavity, and the inner cell mass found inside the blastocoel which is composed of stem cells. 9 These inner-lying cells are said to be “embryonic” even though the term embryo does not technically apply until after this initial two-week stage.
The next eight-week stage is characterized by cell growth and multiplication. Following this eight-week stage, the organism has recognizable structures and is classified as a fetus. At this time, embryonic stem cells continue to proliferate and are said to be pluripotent or plastic, meaning that they can differentiate into almost any type of cell that makes up the body. 10 The embryonic stem cell is believed by many scientists to be the most useful for potential medical treatments, but its use is restricted by federal legislation (described later in this article). Existing stem cells for medical research can come from four primary sources: existing stem cell lines, aborted or miscarried fetuses, discarded embryos from fertilization treatments, or cloned embryos. Only the first source can be used in federally funded research programs, however. 11 , 12
The cloning of embryos is another controversial area of research. The cloning of humans to full term is banned almost worldwide. 13 , 14 In some cases, short-term cloning has been performed to allow for the generation and extraction of stem cells, followed by the termination of the cloned embryo by the sixth day after fertilization. Cloning of some animals has been allowed to proceed to full term; the first and most famous example was the work of Scottish scientists resulting in the creation of a sheep known as “Dolly.” 15 That achievement became the driving force for new regulations to prevent a similar event occurring with human cells. The latest evidence suggests that cloned cells do not “reset their longevity clocks,” thus resulting in reduced lifespan. Furthermore, not only is the success rate of cloning low, but the cloned organism is beset with problems, some of which may not become apparent until adulthood, assuming life extends to that age. 16 , 17
For research to occur with embryonic stem cells, the inner cell mass of the blastocyst is extracted (thus destroying the embryo) and grown in cell culture. 18 , 19 This process enables cells to grow on plates coated with a feeder layer that provides anchorage and nutrients. The stem cells become attached to the plate and grow in the nutrient broth (i.e., cell culture media tailored to the specific needs of the cell line being grown). 18 , 19 As the cells proliferate they fill the plate until a point is reached where they would be forced to compete for space and nutrients. Shortly before such competition breaks out, the cultures are replated at the original cell density (meaning that one starting plate could be divided across two or more plates) and the process is repeated. This procedure is known as “passaging.” 20 After several months, the cells will number in the billions without differentiating or changing in any detectable way. They can either be frozen for storage or continue replicating. However, there is some evidence that with continued passaging, a point may be reached in which the cells become less stable with respect to their ability to replicate, differentiate, or avoid mutations. 21 This instability seems to be particularly true when adult and embryonic stem cells are compared (see below).
Fetal stem cells, typically obtained following abortion or miscarriage, are believed to be as pluripotent as their embryonic counterparts, though they occur at a later stage than the true embryonic stem cell. 22 Several biotechnological companies are experimenting with these cells as treatments for a myriad of diseases. For instance, ReNeuron, Inc. (UK) has several cell lines derived from the fetal brain that they are testing for the treatment of neurodegenerative disorders, including stroke, Parkinson’s disease, and Alzheimer’s disease. 23 , 24
Adult Stem Cells
A small number of stem cells can be found in adult humans at specific locations, such as in the bone marrow or the subventricular zone of the brain. 25 , 26 Until the discovery of these and other cells in the central nervous system, it was believed that the brain was the only organ that could not replicate. However, it is now clear that certain regions of the brain may have some limited capability to replace damaged or dead cells as a consequence of endogenous stem cells. 27 , 28
Whereas embryonic stem cells are derived from the inner cell mass of the blastocyst, knowledge of the origin of the adult stem cell is less certain. Its source could potentially be the same, with the adult stem cell being many generations removed from the original source. If this speculation is true, then one would expect the body to have large numbers of these cells, which it does not. It has therefore been suggested that halting of replication is the means by which the number of stem cells found in the organs of the body is limited. 29 The stem cells are said to have entered a state of quiescence, until they receive an activation signal due to cell damage. Determination of the signal that triggers adult stem cells to “wake up” is critical to maximizing their benefit. In addition, identification of what makes the cells quiescent is of considerable merit. One study revealed the presence of a “master switch” that can trigger the change from embryonic to adult stem cell characteristics, suggesting that this signal may originate from the same source. 30
There is considerable debate as to how pluripotent adult stem cells are. The original belief was that they were not as versatile, healthy, or durable as embryonic stem cells because they appeared to be limited to forming only cells of a similar origin (e.g., bone marrow stem cells could only produce blood cells). Consequently, these cells became known as multipotent cells. These characteristics meant that adult stem cells would be harder to manipulate or control compared with embryonic cells. Also, due to their presence in adults, it is likely that the cells could have accumulated abnormalities through continuous exposure of the organism to environmental hazards (such as viruses) or to replication errors. 31 , 32 The latter problems are normally corrected, but with the aging organism, the ability to correct replication errors is believed to diminish. 32 , 33 In the majority of cases, the ability of adult stem cells to replicate also appears to be limited compared with embryonic stem cells, thus reducing their usefulness. 34 However, these cells do have an advantage over embryonic stem cells: theoretically, they can be removed from a patient, grown in culture, and then returned to the patient. 35 Therefore, they would not induce an immunological rejection response that may be seen with embryonic stem cells. 35 , 36 In addition, there is more flexibility in using these cells than human embryonic stem cells, especially with regard to federal funding.
Some research shows that certain adult stem cells can differentiate into a number of varied cell types, including neurons 37 – 39 of the peripheral and central nervous system. However, this observation may not be true of all adult stem cells, and more research is required to determine how useful these cells might be for use in treating human disease and injury.
Most research on adult stem cells is based on mesenchymal cells, i.e., cells from regions originally derived from the mesodermal layer of the embryo. These cells include connective tissue and, in particular, bone marrow and muscles. They are multipotent cells and are a relatively homogeneous population of mononuclear progenitor cells that can be made to differentiate into specific cell lines following environmental cues. Additionally, there are stromal stem cells found in the bone marrow, which are a more heterogeneous population of different cell types with varying degrees of proliferation and differentiation potential. 40 Adult stem cells also can be found in children, in the placenta, and in blood from the umbilical cord. These specialized cells are discussed below.
Embryonic Germ Cells
Germ cells are the precursors to the gametes (egg and sperm) and are therefore found in adult testes and ovaries, and in the areas of the embryo that ultimately differentiate into testes or ovaries. 41 These cells appear to be as pluripotent as other embryonic stem cells. However, they have been found to differentiate spontaneously, which would suggest that there is less control over their development than with other stem cells. 42
Two studies 43 , 44 suggest that adult stem cells can be easily derived from germ cells of both sexes. Further research is needed to explore the validity of this hypothesis, though the findings are certainly intriguing and potentially useful.
Amniotic Fluid (or Placental) and Umbilical Cord Blood Stem Cells
The amniotic fluid that surrounds and protects a developing fetus in its mother’s uterus, as well as the placenta, have also been shown to contain stem cells. 45 An amniocentesis procedure—where amniotic fluid is collected through the insertion of a long, thin needle into a pregnant woman’s abdomen to check for abnormalities, including Down syndrome—is generally considered safe for both the mother and embryo. 46 The collected amniotic fluid is normally discarded once testing is complete, but now that it has been found to contain stem cells, there is potential for further research and storage of such fluid. The current belief is that amniotic fluid contains a mixture of embryonic and adult stem cells. 47 , 48 Testing of these cells has been limited to date. It is believed that they are able to differentiate into a variety of cell types, but it is not known whether they are as pluripotent as other types of stem cells. Some authorities have suggested they could be used as a potential treatment for diabetes. 49
Umbilical cord blood contains low levels of stem cells as well as a number of hematopoietic (blood forming) cells, including lymphocytes and monocytes. There is a considerable amount of research focusing on umbilical cord blood for the treatment of stroke, myocardial infarction, and a variety of blood-related disorders, with some degree of success. 50 – 53 The benefits of such blood have already been demonstrated in the treatment of hematopoietic disorders, with over 6,000 transplants being performed worldwide since it was first used to treat a five-year-old child afflicted with Fanconi anemia in 1988. 50 And there is good experimental evidence that it can help with other disorders as well. 53 , 54 However, it is unclear precisely how these benefits are obtained. Current evidence suggests that in many cases it is not the stem cells per se that provide the benefit, but rather the growth factors these cells release. Some research shows that umbilical cord blood cells do seem to have the ability to become neuronal-like cells in vitro, but do not appear to produce neurons of any significant number in animal models of stroke. 53 , 54
The current research interest in umbilical cord blood cells 53 , 54 has resulted in the formation of many companies worldwide that allow public and private storage of these cells. As a result, at least 18 states have proposed legislation to encourage and inform the public about this potential resource, and in several cases to provide funding for the setting up and/or running of umbilical cord cell banks (see http://www.ncsl.org/programs/health/genetics/geneticsDB.cfm for a searchable database of such legislation). Additionally, official Japanese, European, and Australian banks exist, as well as the many private companies that are currently “getting in on the act.” 55 – 57 This resource could prove to be valuable. Although the potential benefit of these cells still remains relatively unexplored, the practice of banking them already has at least one undeniable benefit: providing donors with a source of their own cells, which considerably reduces the chance of rejection if they ever do need them for medical reasons.
Two other recent papers have demonstrated an additional potential source of adult multipotent stem cells: menstrual blood. 58 , 59
POTENTIAL USES OF STEM CELLS
Adult stem cells derived from bone marrow (i.e., the hematopoietic system) have been used frequently over the past 30 years for successful treatment of numerous blood-based disorders. Current treatments include nuclear radiation exposure and transplantation for the treatment of genetic diseases or cell cancers of the blood and the blood-forming system. 40 , 60 – 63
According to a White House report, there are currently more than 1,200 non-embryonic stem cell clinical trials under way, while none are being performed using embryonic cells. 64 The freeze on federal funding to support embryonic studies, rather than a lack of efficacy, is most likely a major factor behind this statistic. It is important to remember, however, that embryonic stem cell research has never been illegal in the United States; it just cannot be funded from federal sources other than those lines that were approved in August 2001. It is also noteworthy that adult stem cells have been researched for three decades, whereas embryonic stem cell research is considerably more recent, with the first human embryonic stem cell being isolated in 1998 at the University of Wisconsin–Madison by James Thomson. 18 That discovery led to several patents/licenses by the Wisconsin Alumni Research Foundation (WARF), further restricting the use and research of such cells, given the expense of purchasing them. These patents were revoked in April 2007 by the U.S. Patent and Trademark Office, 65 but WARF appealed the decision. In March 2008, WARF’s appeal was upheld. 66 To provide cells to researchers, the National Institutes of Health has established a subsidy that allows the purchase of cell lines approved in August 2001, at much reduced rates, thus resolving some of the previous issues related to their use.
Many of the adult stem cell trials are also oncology studies rather than regenerative medicine studies. 67 , 68 Ongoing clinical studies include phase II trials in which patients suffering from myocardial ischemia have their own adult bone marrow stem cells transplanted into their heart, theoretically increasing revascularization of the affected areas. 69 , 70 Additional cardiac therapies are summarized in a review by Ramos and Hare. 71
A myriad of basic research is underway worldwide on both embryonic and non-embryonic stem cells derived from a number of sources. This research encompasses treatment of various disorders including organ regeneration, cardiovascular improvements, diabetes, and neurodegenerative conditions. They comprise the complete continuum of research from preliminary explorative studies through preclinical and clinical trails. Promising results include the promotion of liver regeneration by bone marrow stem cells in patients with hepatic malignancies, 72 the formation of blood vessels in mice from human embryonic stem cells that have been made to differentiate into endothelial precursor cells, 73 the treatment of stroke and heart ischemia animal models by human umbilical cord blood transplants in rats, 51 , 53 , 54 and the ability of embryonic stem cells to differentiate into functioning heart tissue (myocytes). 74 Adult stem cells also have been used for the latter purpose, but the differentiated cells appear to impair heart function. However, preliminary data from a clinical phase I trial of an intravenous formulation (Provacel) of adult bone marrow–derived mesenchymal stem cells appears to demonstrate some benefit in decreasing subsequent problems among heart attack patients (Schaer, American College of Cardiology’s Innovation in Intervention, March 25, 2007). Also, Yacoub 75 announced that his team has been able to grow a heart valve from bone marrow stem cells using a collagen scaffold. This procedure has yet to be tested to determine if the valve is functional in vivo , but it clearly represents a promising discovery. Similarly, preliminary testing of the recently discovered stem cells in amniotic fluid for treating heart disease has demonstrated some encouraging results that require further study and verification. 76 Unfortunately, transplantation of these cells has been accompanied by a strong immunological response.
Elsewhere, a study using embryonic stem cells has shown considerable improvement in mice specially bred to exhibit symptoms of Sandhoff disease, a childhood disorder. 77 The implanted cells appear to function by replacing the neurons killed by the disease, as well as restoring normal levels of the enzyme hexosaminidase (low levels cause the disease). The disease was found to eventually return, but Lee et al. 78 believe that additional treatments could inhibit recurrence and are conducting further research in this area.
Preliminary findings from other studies involving fetal neural stem cells in culture and in animals have shown rescue of retinal cells after injury or disease. 79 This observation appears to demonstrate a restorative rather than a replacement action by these cells.
In general, considerable research is underway to ensure that the development of treatments involves only those cell types being sought, and that it includes ways of ensuring desired outcomes—i.e., controlling the stem cells so that they form the desired cells and do not proliferate indefinitely, which could lead to malignancy once transplanted. Achieving such outcomes may constitute one of the biggest stumbling blocks to stem cell research. One possible method would be to differentiate the cells before transplantation; Keller 79 has summarized various attempts at this method. Yet, a study involving transplantation of stem cells obtained from the human central nervous system into a primate Parkinsonian model resulted in behavioral improvements and integration of cells without tumor formation. 80 Therefore, predifferentiation of cells before transplant may not be necessary, though further research is required to be sure that this is the case. This avenue of research is likely to see many initiatives, given the anticipated dividends.
Additionally, study of the body’s ability to reject “foreign” tissue is also important because certain embryonic tissue is likely to have the ability to induce a significant immunologic response. Some studies are now suggesting that immature embryonic stem cells and umbilical cord blood cells are not as likely to cause an immunological reaction as differentiated adult stem cells. 81 – 83 With adult stem cells, harvesting from the same patient undergoing the transplant generally eliminates this problem.
A few studies have found that co-transplantation of two or more different types of cells has resulted in a synergistic effect that maintained their survival and execution of beneficial effects. For instance, the co-culture of amniotic epithelial and neural stem cells promoted neuronal differentiation of the latter. 84 Both trophic support and direct contact between the two cell types appeared to have important but independent effects on the neuronal survival and differentiation.
One caveat to consider in stem cell treatment of disease is that the replacement of dying cells by new ones is only a temporary solution because whatever resulted in the death of the cells initially—unless purely intrinsic to the dying cells themselves or only a onetime event—will eventually prove lethal to the new cells, too. This phenomenon has been demonstrated in a paper on fetal tissue grafts for the treatment of Parkinson’s disease. 85 Consequently, calling stem cells a “cure” for diseases is really a misnomer; instead, calling them the “best available treatment” may be more accurate at present. This caveat makes the assumption that stem cell transplants are replacing the dying cells. Studies on stroke models using umbilical cord blood–derived stem cells do not support the idea of replacement, but do show an improvement in the size of the stroke lesion and behavioral markers. 53 , 54 Some of their benefit may be more related to controlling the inflammatory response that causes cell death or to promoting more rapid healing. A study by Capone et al. 86 demonstrated that stem cells do act in this fashion, modifying the microenvironment following stroke to afford neuroprotection, rather than replacing “sick” cells. Similar findings have been observed in other studies, including the eye experiments mentioned previously. Thus, stem cells may help to support the cells that are already present and protect them from further injury or death due to the factors that cause or perpetuate the initial disease or injury. This support in turn leads to another consideration: are pluripotent cells necessarily better than multipotent ones? Assuming that adult stem cells from a specific source (e.g., adult stem cells from the brain) can differentiate into the required replacement cell (e.g., neural cells) or provide the required supporting factors, they do not need to be pluripotent. Therefore, pluripotent (embryonic stem) cells would only be required when adult stem cells are not present or cannot differentiate into the cell of interest or produce the necessary factors to give the desired result. Consequently, research on both pluripotent and multipotent cells would seem to still be necessary. 87
Not only does stem cell research provide direct cell replacement benefits or improve the survivability of “sick” or “injured” cells, it also offers considerable insight on what causes cells to proliferate and differentiate—an important phenomenon to understand in the fight against cancers and in general research dedicated to the development and normal life cycle of cells. 88 – 92 Studies of stem cells could, therefore, have far-reaching implications that are not limited to just disease treatment. 88 – 94 Finally, stem cells could also be used to model organs for the testing of drugs or new surgical techniques—another potentially powerful benefit of stem cell research. 95 , 96
PREDOMINANT CONTROVERSIES ABOUT STEM CELL RESEARCH
There are four main controversies currently surrounding stem cells. Perhaps the most significant involves moral arguments regarding the use of embryonic material to harvest stem cells. The focus of this controversy is on when life begins—which some consider to be at conception—and whether any individual has the right to terminate a life. Strong spiritual and religious beliefs are frequently central to this controversy, and the practice is considered unacceptable by many. One study 97 suggested the possibility of removing one or a few stem cells without harming an in vitro–fertilized embryo prior to implantation, thus maintaining its viability. As of yet, however, it is unclear exactly what impact this action has on the growing organism and whether such studies can be confirmed. Consequently, because of the controversy over when life begins, many countries either ban embryonic stem cell research or severely restrict it. As indicated previously, only those embryonic stem cell lines approved for study in August 2001 can receive federal funding and support in the United States.
Three connected groups of scientists reported success in transforming normal mouse skin cells into embryonic stem cell–like cells via genetic manipulation. 98 – 100 Further research is required to confirm these findings and those of other studies 101 , 102 have translated this technique to human cells. Additionally, the transformed cells are prone to tumorigenesis, and therefore, would not be useful for transplantation in humans in their current form. This technique would not necessarily replace the use of embryo-derived stem cells, as further characterization is necessary to confirm that the cells do possess all of the same characteristics—including the same receptors and response to treatments. Nevertheless, it is a small step in the right direction for those opposed to embryonic sources.
A second controversy surrounding stem cell research is the apparent groundbreaking outcome of studies performed by a research team in South Korea. In 2004, this team reported in Science that they had obtained human embryonic stem cells from the nuclear transfer of oocytes (i.e., the replacement of the nucleus of an egg with that of an already differentiated cell). The following year, this team again reported in Science that they were able to generate patient-specific immune-matched embryonic stem cells for the treatment of diseases. In the end, the data were found to be fraudulent, and some of the female researchers had apparently been coerced to donate their own eggs for the process of obtaining stem cells, a significant ethical breach in the field. 103 As a result of these findings, both papers were retracted in 2005, and significant penalties were imposed on the researchers. This scandal cast a large shadow over the competitiveness in the field and the possible unethical means of obtaining stem cells for research purposes.
A third controversy has to do with stem cells’ alleged potential to produce malignancies once implanted due to their theoretically immortal nature (viewed as such because stem cells can reproduce ad infinitum ). Some research suggests that certain kinds of stem cells could cause cancer because a small number of defective stem cells have been found in tumors, where they may have acted as a seed. 104 Given their ability to proliferate continuously, these cells carry an increased likelihood of mutations, which in turn increases the probability that they will grow out of control and become cancerous. Therefore, their use in treatments could be fraught with problems, at least until a clearer understanding emerges regarding the signals that turn them on and off in their growth cycles. Adult stem cells are normally quiescent, meaning that identification of the process by which mutations occur could prove to be vitally important in preventing transplant tumorigenicity or in preventing cancers altogether.
Interestingly, studies using embryonic carcinoma cells—which are malignant, similar to stem cells, and generally derived from germinal cells—have provided some neurodegenerative improvement in animal models. 105 These cells can be made to differentiate into human neurons under retinoic acid treatment. When this conversion occurs, the cells appear to lose their malignant properties. 105 Once the mechanism for this process has been determined, it could be tested in stem cells, perhaps creating the ability to turn off the malignant characteristics of these cells.
At the same time, another recent study suggested that although stem cells—specifically, those obtained from bone marrow—may look like malignant cells, they do not necessarily function like them. In other words, stem cells may not be cancerous and may not be able to seed tumors. 106 Further research is required to determine whether this is true for all stem cells found in tumors, and whether they are acting as “developmental mimics” or seed tumors.
The fourth main controversy concerns whether adult stem cells are as beneficial as embryonic stem cells. A seminal paper from a group led by Catherine Verfaillie (see Jiang et al. 107 ) reported that adult stem cells from the bone marrow of rats, which they called “multipotent adult progenitor cells” (MAPCs), had the potential to differentiate into almost every type of cell in the body, a claim that previously applied only to embryonic stem cells. Unfortunately, little success has been made in replicating these results. More recent evidence suggests that the paper was flawed, adding further consternation to this area of investigation. 108 , 109 Subsequent research from a number of teams reported that when MAPCs could be successfully isolated from bone marrow using a different technique than that originally proposed, they did have the ability to become any type of blood cell but not other cells. But overall, it is still unclear whether this and other types of adult stem cells are as efficacious as originally proposed. 110 – 112 Criteria that stem cells have to meet to be classified as pluripotent have been proposed, 113 , 114 and few studies have actually met these criteria, with the majority being explained by cell fusion 115 and incorrect interpretation. 111 , 116 Thus, many researchers still believe that embryonic stem cells may provide more benefit due to their hypothetical ability to differentiate into all cell types, though most would prefer both avenues to be explored, acknowledging that adult stem cells could be useful in some circumstances.
Two independent studies by the groups of Yamanaka 101 and Thomson 102 may make this controversy a moot point. Expanding on the mouse studies 98 – 100 mentioned in an earlier section, they reported two similar methods of converting adult human skin cells into embryonic-like stem cells. This was achieved by the insertion of 4 genes that led to the reprogramming of the cells (interestingly, two of the genes differed between the research groups but had similar functions). This research has great potential but requires considerable additional testing to ensure that the embryonic-like stem cells behave in a similar fashion to embryonic stem cells obtained in the “normal” fashion. Additionally, there is the concern that one of the genes the researchers inserted was a cancer gene, which could increase the likelihood for tumorigen-esis using this approach. There is also concern over the retroviruses used to insert the genes, which can have potentially carcinogenic and other detrimental effects due to their ability to randomly insert the gene of interest into the genome. A major bonus of this approach is the ability to take the cells from the patients themselves and therefore reduce the likelihood of transplant rejection. There is also the potential to model a disease more directly by removing the affected cells from a patient and growing them in culture so that they can be characterized and compared with healthy cells. Research by Jaenisch’s group 117 has demonstrated that reprogrammed skin cells can treat the sickle cell anemia mouse model, thus confirming the potentially beneficial effects of such cells.
STATUS OF LEGISLATION ON STEM CELL USE
In the United States, federal funding for embryonic stem cell research from sources such as the National Institutes of Health is restricted by congressional legislation, which mandates that only cell lines approved in August 2001 be used in funded research. At that time, there were more than 60 lines, but only 20 have proven to be viable and available for general use. All of these cell lines have been grown on a mouse fibroblast feeder layer to restrict differentiation and only allow replication. Unfortunately, it has been found that these stem cells are likely contaminated with mouse proteins and sugars that could generate severe immunological responses following transplantation into humans to treat diseases. 118 However, some studies suggest that the proteins and sugars can be removed or cultured out to make the cells safer for human transplantation. 119 Newer procedures that use completely human components have been developed, so any future cell lines are unlikely to have this problem. Research involving adult stem cells is not limited under the current federal restrictions.
The 20 embryonic cell lines that are federally permissible represent only a small fraction of the genetically and immunologically heterogenous population of the world. 120 , 121 This limitation casts doubt over whether any treatments derived from these cell lines will be suitable for treating all of the ethnically diverse populations that exist in the United States and abroad. This limitation is both an incentive for developing additional cell lines and an important factor that should be considered with respect to all types of stem cells. The genetic diversity inherent in the world’s different ethnic groups implies that different ethnicities may respond in different ways to these cell lines. Therefore, any success found with these cells would need to be replicated using cell lines derived from other ethnic groups to determine their general use among the world’s population. 122
In 2006, a congressional bill was proposed to allow research on stem cells derived from embryos discarded after in vitro fertilization treatments. This bill was vetoed by the president based on ethical, moral, and religious concerns. The bill resurfaced following the 2006 midterm elections in which Democrats regained control of the House and Senate, but no change to the veto is likely under the current administration. 123
The restriction on federal funding for embryonic stem cell research led New Jersey to appropriate state funding for research on both embryonic and adult stem cells in early 2004. Ohio had previously proposed funding dedicated to adult stem cell research. The most well known example of funding at the state level is California, which proposed its own legislation in 2004 (Proposition 71) involving the sale of $3 billion in bonds to provide $295 million annually for 10 years to the funding of stem cell research. 124
Since then, several other states have sought endorsement of similar propositions ( Table 1 and Table 2 ). Currently, at least 33 states have specific guidelines with respect to the use of embryos in research, which in several cases (e.g., Arizona, South Dakota, Texas) conform to federal legislation. However, there is considerable variation among these states regarding their support of separate initiatives for stem cell research.
States That Are Encouraging Stem Cell Research
| State | Year | Legislation | Status | Funding |
|---|---|---|---|---|
| California | 2004 | Issuance of bonds to raise money for funding stem cell research | Passed | $3 billion+ over 10 years |
| Connecticut | 2005 | Fund for stem cell research | Passed | $ 100 million over 10 years |
| Florida | 2007 | Recommendation of state money for non-embryonic stem cell research (another bill proposed to provide for embryonic) | Pending | $20 million |
| Hawaii | 2006 | Study and recommendation commissioned by state for the University of Hawaii to investigate “the feasibility of encour aging stem cell research” | Pending | N/A |
| Illinois | 2006 | Illinois Regenerative Medicine Institute | Passed | $ 15 million |
| Indiana | 2005 | Research on fetal stem cells derived from placentas, cord blood, amniotic fluid, or fetal tissue allowed; adult stem cell research center at Indiana University | Passed | $50,000 |
| Iowa | 2007 | Plan to establish Center for Regenerative Medicine; allows embryonic stem cell research | Pending | N/A |
| Maryland | 2006 | Maryland Stem Cell Research Fund (not oocytes) | Passed | $15 million (2007) |
| Massachusetts | 2005 | □ Institute for Stem Cell Research and Regenerative Medicine at University of Massachusetts □ Life Sciences Investment Fund (including stem cell research) | Passed Passed | $1 million $ 10 million |
| Minnesota | 2007 | Currently bans embryo and fetal research; several propos als to support stem cell research using other types (and also embryo) | Pending | N/A |
| New Jersey | 2004 2006 | □ New Jersey Stem Cell Institute □ Issuance of bonds for funding several stem cell–related research facilities in state (ballot-rejected proposal in 2007) | Passed | $23 million $270 million |
| New Mexico | 2007 | Proposal to fund the building of a stem cell research facility, including embryonic research; current legislation prohibits research on live fetus/embryo, but use of fertility treatment excess permitted | Pending | $ 10 million over three years |
| New York | 2006 2007 | □ New York State Institute for Stem Cell Research and Regen erative Medicine □ The Empire State Stem Cell Trust” created for all stem cells | Passed | $300 million over two years $ 100 million in 2007–2008 plus $500 million in 2008–2017 |
| Ohio | 2003 | Adult stem cell research only; Center for Stem Cell and Re generative Medicine | Passed | $ 19.4 million plus $8 million in 2006 |
| South Carolina | 2007 | Bill to allow stem cell research under institutional research board approval | Pending | N/A |
| Virginia | 2006 | Fund to support adult stem cell research | Passed | N/A |
| Washington | 2006 | Life Sciences Discovery Fund; may include funding for stem cell research | Pending | N/A |
| Wisconsin | 2006 | Funding for Stem Cell Products Inc. | Passed | $ 1 million |
Sources: Compiled from various online reports, including www.ncsl.org/programs/health/genetics/embfet.htm , http://isscr.org/public/regions , and “Yahoo! Alerts Health News: Stem Cells” (all last accessed December 7, 2007).
States with Legislation Relating to Embryonic Stem Cell Use
| State | Legislation |
|---|---|
| Arkansas | Research prohibited except on stillborn fetuses |
| Louisiana | Prohibits research on embryos |
| Maine | Research prohibited on in vitro-fertilized embryos; a bill has been proposed for stem cell research this year |
| Michigan | Dead embryos and fetuses available for experimentation by consent |
| Missouri | Prohibits research on live fetus |
| Montana | Prohibits live fetal research |
| Nebraska | Restricted use of money for embryonic stem cell research; a ban on cloning proposed |
| New Hampshire | Prohibits maintenance of unfrozen fertilized embryo beyond 14 days |
| North Dakota | Research (after consent) on embryos from sources other than abortion |
| Oklahoma | Prohibits research on fetus and embryos |
| Pennsylvania | Prohibits research on live fetus and embryos |
| Rhode Island | Prohibits research on in vitro–fertilized embryos post implantation, but pending legislation for embry onic stem cell research with the consent of both parties involved in the creation of the embryo |
| South Dakota | Prohibits destruction of embryos |
| Tennessee | Allows research on aborted fetuses, but requires consent |
| Utah | Prohibits research on aborted fetus or post-implanted embryo |
The International Society for Stem Cell Research recently proposed international guidelines for the use of embryonic tissue to ensure uniform research and experimental practice worldwide. 125 At the core of these guidelines is that embryonic research should be rigorously overseen by sponsoring organizations or regulatory bodies with specific policies and procedures that conform to the recommendations of the scientific community. In all policies, no cloning is to be undertaken to create humans. The society’s policies also recommend the establishment of an institutional oversight committee to review and determine approval of all stem cell research. The use of “chimeras” (i.e., animals created with human cells) is allowed with approval from this committee. Further, the use of any cells donated for research purposes should require consent from those donating them. Regulations pertaining to stem cell use by state and country are kept reasonably up to date at the following websites:
- http://www.ncsl.org/programs/health/genetics/embfet.htm
- http://isscr.org/public/regions
Initially, the federal funding restriction was seen as detrimental to stem cell research. However, some scientists are now suggesting that the restriction has actually opened other funding opportunities that may be more helpful to the research community. As Table 1 shows, federal restrictions have created unprecedented state funding far exceeding any that the National Institutes of Health would likely provide. This alternative funding source has also piqued the interest of pharmaceutical companies. Such companies may be able to position themselves for a larger share of patents and licenses from state-funded research—they already have a near monopoly on drug therapies derived from this research. This apparent paradox was discussed in an opinion piece in The Scientist by Dr. Paul Sanberg. 126
STEM CELL RESEARCH AND HEALTH EDUCATION PRACTICE
Health educators are charged with numerous roles and responsibilities in the public sector. 1 These essential tasks intersect with current and anticipated research involving stem cells. What follows is an iteration of ways in which health educators might be expected to address relevant stem cell knowledge and research issues. Although not exhaustive, the points below highlight the importance of keeping public dialogue about this topic both vibrant and accurate.
Assessing Individual and Community Needs
Health education competencies and subcompetencies in this area include, but are not limited to, selecting valid sources of information about health needs and interests. The debate over stem cell research inevitably becomes enmeshed in moral arguments and political posturing, so it is important that scientifically accurate information and data be made prominent in the public eye. Health educators are positioned to translate technical information and make it accessible to the lay public and other interested consumers. Presently, although there are many avenues of availability for this information in the scientific and medical communities, it is far less available to the general public. What is needed are accurate sources of relevant stem cell data and other information that neither refute scientific discovery nor escalate optimism inappropriately or prematurely.
Planning, Implementing, and Administering Strategies and Programs
The highly diverse nature of the health information consumer includes different levels of health literacy, disparate ethical and moral belief systems, and widely varying learning styles. Health educators are professionally prepared as a group to respond to the needs of these different audiences by identifying individuals and groups who can best benefit from knowledge about stem cell research, incorporating appropriate organizational frameworks, establishing specific learning objectives based on assessment of baseline knowledge, assigning audience-specific modes of education delivery, and developing a program delivery method that includes optimal use of learning technologies.
Health educators are able to assess both knowledge and attitude shifts through the use of well chosen surveys and other assessment instruments. Moreover, health educators can infer needed future activities and programs that build either in a linear or a spiraling fashion on past activities. Stem cell research is a pioneering endeavor, and the knowledge shifts can, therefore, be rapid; the need for recurring data and information sources suitable for general and specific audience consumption is as dynamic as the shifting sands. Health educators are prime candidates for interpreting these changes, putting them in context, and making the necessary and relevant adjustments to the public’s informational needs.
Serving as an Education Resource Person
Health educators should be masters at retrieval of information that can be translated from technical to more audience-friendly language. As with their other resource functions, health educators should be able to match information needs with the appropriate retrieval systems; to select data and data systems commensurate with program needs; and to determine the relevance of various computerized health information resources, access those resources, and employ electronic technology for retrieving references. To enhance the match between information and audience, health educators should be positioned to perform readability assessments using such tools as the SMOG Test, 127 the Flesch Reading Ease Formula, 128 and other indices, 129 thereby increasing the likelihood that relevant information about stem cells will be understood.
Advocating for Education about Stem Cell Research
Health educators are expected to analyze and respond to current and future needs in health education. Particularly pertinent to stem cell research is the analysis of factors (e.g., social, demographic, political) that influence individuals who make decisions about the direction of, and restrictions on, stem cell research. Currently, the wise course may be for health educators to be as politically neutral as possible in organizing and communicating information about stem cell research—standing neither for nor against liberalization of current research postures by the federal government and other entities. Health educators, like any other professional group, are subject to their own biases, including those emanating from personal moral philosophy, ethical principles, or other convictions. Nevertheless, they are obligated to report on stem cell matters factually. They can also serve as advocates for promoting discussions in the public sector, at professional conferences, and in their own scientific literature. Finally, practice standards support health educators’ participation in continuing education on stem cell issues and their development of plans for ongoing professional development.
Stem cell research is a major area in biomedical research, one that could have a far-reaching impact on the overall health of the human race. Many people, professional and lay alike, obtain their knowledge from sources that present personal agendas or dubious interpretations of facts. In this article, we have endeavored to give a fair, balanced, and unbiased view—as much as our personal limits as scientists and individuals permit—of the potential of stem cells. We have also argued that health educators can position themselves to bring some orderliness to the debate about the merits of stem cell research and support a healthy dialogue among lay audiences as well as their own professional peers.

IMAGES
VIDEO
COMMENTS
The multi-disciplinary nature and tremendous potential of the stem cell field has important implications for basic as well as translational research. Recounting these activities will serve to provide an in-depth overview of the field, fostering a further understanding of human stem cell and developmental biology.
Embryonic stem cells are pluripotent cells isolated from the inner cell mass of a blastocyst, the early mammalian embryo that implants into the uterus. Embryonic stem cells self-renew by dividing ...
In addition to organoids, recent advances in stem cell research have even facilitated the development of early embryonic models that mimic human embryos.
Embryonic stem cells (ESCs) are found in the inner cell mass of the human blastocyst, an early stage of the developing embryo lasting from the 4th to 7th day after fertilization. In normal embryonic development, they disappear after the 7th day, and begin to form the three embryonic tissue layers. ESCs extracted from the inner cell mass during the blastocyst stage, however, can be cultured in ...
The greatest therapeutic promise of human embryonic stem cells (hESC) is to generate specialized cells to replace damaged tissue in patients suffering from various degenerative diseases. However, the signaling mechanisms involved in lineage restriction ...
Two papers in Nature now make key advances in this field, showing that human embryonic stem cells 2 or cells reprogrammed from adult tissues 2, 3 can be induced to self-organize in a dish, forming ...
How human embryonic stem cells sparked a revolution. How human embryonic stem cells sparked a revolution. Nature. 2018 Mar 22;555 (7697):428-430. doi: 10.1038/d41586-018-03268-4.
The first isolation of human embryonic stem cells (hESC) reported in the late 90s opened a new window to promising possibilities in the fields of human developmental biology and regenerative medicine. Subsequently, the differentiation of hESC lines into different precursor cells showed their potenti …
Research in human embryonic stem cells (hESCs) is a rapidly developing scientific field. In this study we collect and evaluate a thorough body of data on the current number of publicly disclosed hESC lines and the extent and impact of scientific work involving the use of these cells. These data contribute to the substantiation of the discussion on the current status of hESC research, provide a ...
The use of human embryos for research on embryonic stem (ES) cells is currently high on the ethical and political agenda in many countries. Despite the potential benefit of using human ES cells in the treatment of disease, their use remains controversial because of their derivation from early embryos. Here, we address some of the ethical issues ...
Human embryonic cells possess the ability to become stem cells, which are used in medical research due to two significant features. First, they are unspecialized cells, meaning they can undergo cell division and renew themselves even with long periods of inactivity. Secondly, stem cells are pluripotent, with the propensity to be induced to ...
The development and use of human embryonic stem cells (hESCs) in regenerative medicine have been revolutionary, offering significant advancements in treating various diseases. These pluripotent cells, derived from early human embryos, are central to modern biomedical research. However, their application is mired in ethical and regulatory complexities related to the use of human embryos.
The new guidelines propose three categories of oversight for stem-cell and embryo research (Supplementary Table 1 ): (1) exempt from review by a specialized oversight process, (2) review by a ...
The development and use of human embryonic stem cells (hESCs) in regenerative medicine have been revolutionary, offering significant advancements in treating various diseases. These pluripotent cells, derived from early human embryos, are central to modern biomedical research. However, their application is mired in ethical and regulatory complexities related to the use of human embryos.
The interactions between extra-embryonic tissues and embryonic tissues are crucial to ensure proper early embryo development. However, the understanding of the crosstalk between the embryonic tissues and extra-embryonic tissues is lacking, mainly due to ethical restrictions, difficulties in obtaining natural human embryos, and lack of appropriate in vitro models.
Cultural Relativity and Acceptance of Embryonic Stem Cell Research. ABSTRACT. There is a debate about the ethical implications of using human embryos in stem cell research, which can be influenced by cultural, moral, and social values. This paper argues for an adaptable framework to accommodate diverse cultural and religious perspectives.
A human embryo's legal definition and its entitlement to protection vary greatly worldwide. Recently, human pluripotent stem cells have been used to form in vitro models of early embryos that have challenged legal definitions and raised questions regarding their usage. In this light, we propose a refined legal definition of an embryo, suggest "tipping points" for when human embryo models ...
Human pluripotent stem cells can be used to derive in vitro models recapitulating post-implantation human embryos. While useful for research purposes, such integrated embryo models raise ethical issues that need to be addressed to facilitate ethically appropriate regulations that permit scientific ingenuity and medical progress.
In this collection, we highlight papers published in 2023-2024 across Nature Portfolio and EMBO Press journals on topics including stem cell-based embryo models and organoids, embryonic ...
STEM CELLS focuses on the functional and mechanistic aspects of stem cell biology and the potential of stem cells for therapeutic applications. It publishes key advances in clinical trials and mechanism-based manuscripts with definitive conclusions.
Current state of stem cell-based therapies: an overview. Recent research reporting successful translation of stem cell therapies to patients have enriched the hope that such regenerative strategies may one day become a treatment for a wide range of vexing diseases. In fact, the past few years witnessed, a rather exponential advancement in ...
Participants were excited by the potential of embryo model research, but also strongly supportive of oversight." "Research involving stem cell-based embryo models has enormous potential to improve human knowledge and health, but clearer governance is needed to help researchers work responsibly and maintain public trust.
Experimentation with embryonic stem (ES) cells has become an important breakthrough in medical research. However, it is also a source of controversy, because it requires the destruction of the human embryos used to derive ES cells. This paper deals with some of the ethical issues concerning ES cell …
Part of Nature Outlook: Stem cells. But ethical guidelines on human embryo use have halted most research into these phases of development — until now. This May, the International Society for ...
The ethical implications of stem cell research are often described in terms of risks, side effects, safety, and therapeutic value, which are examples of so-called hard impacts. Hard impacts are typically measurable and quantifiable. To understand the broader spectrum of ethical implications of stem cell research on science and society, it is ...
However, some challenges still remain that need to be overcome to establish the full potential application of these cells. In this paper, we review the different cell sources used for vascular tissue engineering, focusing on extraembryonic tissue-derived cells (ESCs), and elucidate their roles in cardiovascular disease.
Discover how stem cell-based therapy can treat various human diseases, from neurological disorders to skin burns, with the latest clinical trials and research.
Stem cells are believed to be one of the greatest untapped resources currently available for the prevention and treatment of many diseases. Inasmuch as current knowledge of stem cells is a combination of scientific reality and cautious speculation, considerable research is required to identify the true, long-term potential for medical advances from these cells. As health resources ...