Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 09 August 2021

Anti-Black racism in academia and what you can do about it
- Audrey K. Bowden ORCID: orcid.org/0000-0002-5412-3976 1 &
- Cullen R. Buie 2
Nature Reviews Materials volume 6 , pages 760–761 ( 2021 ) Cite this article
16k Accesses
8 Citations
283 Altmetric
Metrics details
The experiences of Black scientists and engineers reveal that science is not a meritocracy. Here is a list of recommendations to combat anti-Black racism in academic institutions.
Racism is an insidious, multifarious social disease. Like cancer, most people do not perceive any issues until there is a catastrophic eruption, such as protesting in the streets over the murder of a Black person by the police. Increasingly, many people claim to be ‘woke’ to the idea of anti-racism; however, combatting anti-Black racism requires more than broad-sweeping ‘diversity, equity and inclusion’ rhetoric — a profound change in the mindset, attitudes and actions of every individual in society is needed, including you.
The experience of Black scholars
The academic community is not immune to society’s racial challenges. Our experiences as scholars cannot be decoupled from our Black identities 1 . Thoughts about how to stay safe, in a society in which violence against our bodies and our minds is a real threat, give rise to fears ( The Fear Black Employees Carry ) that affect our interactions at conferences and on campuses. We personally recall with disgust being racially profiled by hotel security at a scientific conference; being stopped, detailed and questioned for an hour by the police after a long evening of studying at the campus library; and being questioned about the legitimacy of our presence in faculty clubs and on-campus residences. Unfortunately, our experiences are neither unique nor uncommon ( Santa Clara University launches investigation after a Black professor was asked by campus security to prove she lived in her own house ). We have had to learn the hard way how to navigate the unspoken rules of academia, finding our own way into study groups as graduate students or academic collaborations as principal investigators. Some Black peers struggle to master these informal systems, ultimately not completing their PhDs or getting tenure, reinforcing the stereotype that Black scientists are less qualified and making it more difficult for Black scholars to climb through the ranks and thus perpetuating the cycle. Some Black colleagues worry that stereotypes and biased practices keep them from getting published, winning grants, or advancing in their careers despite equal qualifications 2 , 3 . Truth be told, having to work harder to obtain similar opportunities to our colleagues takes an emotional toll 4 , 5 . We are tired.
The racialization of academia
Practices such as creating homework assignments that require students to self-organize into groups, making admissions or hiring decisions based on academic pedigree, or judging articles and proposals on the perceived ‘merit’ of the investigator rather than on the scientific idea are not overtly racist, but their outcomes perpetuate the racialization of academia. That is, one does not need explicitly racist policies to yield racial disparities; it is perhaps more accurate to describe our academic and scientific organizations as racialized rather than racist 6 . If the working definition of racism only considers activities or policies that explicitly discriminate on the basis of race, it is easy to believe that racism does not exist. Yet, like many diseases that quietly invade the body, anti-Black racism has metastasized beneath the surface in the form of goods, benefits and services that are disproportionately allocated along the lines of race, invading the culture of how society operates. For example, providing grant supplements only to those with active awards is not openly racist; however, when you consider that Black principal investigators are funded at a much lower rate than their white colleagues 7 , 8 , the result is less access for Black researchers to these funding opportunities. Similarly, while most hiring policies prevent discrimination on the basis of race, employment is often linked to social networks within an institution. When you consider that fewer Black people have historically been in positions of power at scientific institutions, the result is an inequity of opportunity.
Call to action
Society likes to tout that science is a meritocracy, but science is not a meritocracy because the world is not a meritocracy. Resources, services and benefits allocated within the academic and scientific communities are strongly influenced by race, whether you see it or not. If you are serious about combatting anti-Black racism within your institution, we refer you to the list of recommendations outlined in the Call to action proposed by the organization Black in Engineering , a group of faculty comprising all ranks and types of institution within the USA. Of supreme importance is to approach the document and the task of transformation with an intention — dare we suggest a formal commitment — to act. The Call to action offers several principles to invoke this commitment; here we cite a few of its salient points.
Assume you and your institution have a problem. The Black people around you have been saying it for decades; it is time to listen. If you do not think you have a problem, you are more likely to dismiss suggestions as being irrelevant. Instead, identify aspects of your institution’s policies and structures that are routinely overlooked as being racialized or contributing to racism. How many of your institution’s hires tried to leverage their network to get a job? How diverse was the line-up of your last speaker series, and how were invitees selected (that is, are your people only inviting speakers in their current networks)? If your answers suggest an inequity of opportunity in the way you do things, do something about it.
Accountability
You must hold yourself and your institution accountable. There is little hope for change if there are no consequences for maintaining the status quo or blaming external circumstances, such as a small candidate pool. Do not blame the leaky pipeline — do your part to plug the leaks and prime the pump. We have all seen our institutions enact monumental changes when threatened with the existential crisis of COVID-19. Put that same intensity into adopting new strategies to improve the climate for Black scholars at your institution. Make a bold, public statement that puts your reputation on the line. Tie the need for change to the job description of someone whose compensation depends on enacting change, then set them up to succeed with substantial support from the highest leaders in the organization. Do not overlook that institutional change must include a change in you. Embrace new opportunities to reveal and unlearn your personal biases.
Committed leadership
If the most senior administrators are not committed to fundamental change, it is unlikely that progress made by concerned individuals will ever get institutionalized. Have the most senior person at your institution issue a statement that communicates commitment to change at every level. When necessary, rethink who your leaders are and how they are selected. Make sure that senior leaders are aware that change is coming and that they are on board. Communicate this message not just in value statements but in evaluation processes that reflect the degree to which actions match words. Celebrate success in ways that incentivize others to follow. Most importantly, do not make the few Black people already in your institution do all the work.
Moving the needle on anti-Black racism will be costly, and that should be expected. The toll that anti-Black racism takes on Black people is tremendous, and real justice demands a comparable investment. Do not implement changes that do not cost you anything — an unwillingness to spend money communicates that you do not value the work. Do not wait until you can raise money for new initiatives. Instead, rebalance your current budget to carve out funding. Make the resources available to existing committees that you have under-resourced to take immediate action, or hold contests to crowdsource the best ideas of how to make impactful change. Once you have the ball rolling, it will be easier to raise new funding.
Resilience and creativity
Let’s be honest: when you encounter a research setback, you do not simply throw up your hands in defeat. You redouble your efforts and employ all of your mental faculties to find a solution. The same level of commitment and ingenuity is required to battle anti-Black racism. If you are not in it for the long haul, you should seriously consider not getting involved at all. The more intellectual merit you think you have, the better you should be at coming up with good ideas or recognizing that it may be wise to hire guides who can shepherd your institution in this process.
The time to act is now, and we are waiting. Here is an easy first step: identify what Black staff, faculty or student can you acknowledge, applaud or reward this week for their contributions in building and improving the cultural climate at your institution, then do it.
If you are not part of the solution…
You are the problem. Society likes to believe that the problem of racism will go away with time. History tells a different story; racial progress typically follows on the heels of intense struggle. There is no progress without struggle. Justice takes work — so get to it. Black lives won’t matter in science until they matter to you.
Platt, M. O. We exist. We are your peers. Nat. Rev. Mater. 5 , 783–784 (2020).
Article Google Scholar
Bertrand, M. & Mullainathan, S. Are Emily and Greg more employable than Lakisha and Jamal? A field experiment on labor market discrimination. Am. Econ. Rev. 94 , 991–1013 (2004).
Desai, T. A., Eniola-Adefeso, O., Stevens, K. R., Vazquez, M. & Imoukhuede, P. Perspectives on disparities in scientific visibility. Nat. Rev. Mater. 6 , 556–559 (2021).
Clark, R., Anderson, N. B., Clark, V. R. & Williams, D. R. Racism as a stressor for African Americans: a biopsychosocial model. Am. Psychol. 54 , 805–816 (1999).
Article CAS Google Scholar
Lee, D. B. et al. Psychological pathways from racial discrimination to cortisol in African American males and females. J. Behav. Med. 41 , 208–220 (2018).
Bonilla-Silva, E. Rethinking racism: toward a structural interpretation. Am. Sociol. Rev. 62 , 465–480 (1997).
Hoppe, T. A. et al. Topic choice contributes to the lower rate of NIH awards to African-American/black scientists. Sci. Adv. 5 , eaaw7238 (2019).
Stevens, K. R. et al. Fund Black scientists. Cell 184 , 561–565 (2021).
Download references
Author information
Authors and affiliations.
Department of Biomedical Engineering, Vanderbilt University, Nashville, TN, US
Audrey K. Bowden
Department of Mechanical Engineering, Massachusetts Institute of Technology, Cambridge, MA, US
Cullen R. Buie
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Audrey K. Bowden .
Ethics declarations
Competing interests.
The authors have no competing interests.
Additional information
Related links.
Black in Engineering: https://blackinengineering.org/
Call to action: https://blackinengineering.org/action-item-list/
Santa Clara University launches investigation after a Black professor was asked by campus security to prove she lived in her own house: https://edition.cnn.com/2020/08/24/us/santa-clara-university-black-professor-campus-security-trnd/index.html
The Fear Black Employees Carry: https://hbr.org/2021/04/the-fear-black-employees-carry
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Bowden, A.K., Buie, C.R. Anti-Black racism in academia and what you can do about it. Nat Rev Mater 6 , 760–761 (2021). https://doi.org/10.1038/s41578-021-00361-5
Download citation
Published : 09 August 2021
Issue Date : September 2021
DOI : https://doi.org/10.1038/s41578-021-00361-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Addressing anti-black racism in an academic preterm birth initiative: perspectives from a mixed methods case study.
- Shira P. Rutman
- Natasha Borgen
- Claire D. Brindis
BMC Public Health (2023)
Same storm, different boats: the impact of COVID-19 on Black students and academic staff in UK and US higher education
- Jason Arday
- Christopher Jones
Higher Education (2022)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Research article
- Open access
- Published: 18 November 2020
Racial discrimination and health: a prospective study of ethnic minorities in the United Kingdom
- Ruth A. Hackett ORCID: orcid.org/0000-0002-5428-2950 1 , 2 ,
- Amy Ronaldson 3 ,
- Kamaldeep Bhui 4 ,
- Andrew Steptoe 2 &
- Sarah E. Jackson 2
BMC Public Health volume 20 , Article number: 1652 ( 2020 ) Cite this article
44k Accesses
44 Citations
63 Altmetric
Metrics details
Racism has been linked with poor health in studies in the United States. Little is known about prospective associations between racial discrimination and health outcomes in the United Kingdom (UK).
Data were from 4883 ethnic minority (i.e. non-white) participants in the UK Household Longitudinal Study. Perceived discrimination in the last 12 months on the basis of ethnicity or nationality was reported in 2009/10. Psychological distress, mental functioning, life satisfaction, self-rated health, physical functioning and reports of limiting longstanding illness were assessed in 2009/10 and 2011/12. Linear and logistic regression analyses adjusted for age, sex, income, education and ethnicity. Prospective analyses also adjusted for baseline status on the outcome being evaluated.
Racial discrimination was reported by 998 (20.4%) of the sample. Cross-sectionally, those who reported racial discrimination had a greater likelihood on average of limiting longstanding illness (odds ratio (OR) = 1.78, 95% confidence interval (CI) 1.49; 2.13) and fair/poor self-rated health (OR = 1.50; 95% CI 1.24; 1.82) than those who did not report racial discrimination. Racial discrimination was associated with greater psychological distress ( B = 1.11, 95% CI 0.88; 1.34), poorer mental functioning ( B = − 3.61; 95% CI -4.29; − 2.93), poorer physical functioning ( B = − 0.86; 95% CI -1.50; − 0.27), and lower life satisfaction ( B = − 0.40, 95% CI -0.52; − 0.27). Prospectively, those who reported racial discrimination had a greater likelihood on average of limiting longstanding illness (OR = 1.31, 95% CI 1.01; 1.69) and fair/poor self-rated health (OR = 1.30; 95% CI 1.00; 1.69), than those who did not report racial discrimination. Racial discrimination was associated increased psychological distress ( B = 0.52, 95% CI 0.20; 0.85) and poorer mental functioning ( B = − 1.77; 95% CI -2.70; − 0.83) over two-year follow-up, adjusting for baseline scores.
Conclusions
UK adults belonging to ethnic minority groups who perceive racial discrimination experience poorer mental and physical health than those who do not. These results highlight the need for effective interventions to combat racial discrimination in order to reduce inequalities in health.
Peer Review reports
Discrimination is defined as the differential treatment of an individual based on a socially ascribed characteristic [ 1 ]. In the United Kingdom (UK), the 1965 Race Relations Act [ 2 ] outlawed discrimination on the grounds of colour, nationality and ethnic or national origins. Race remains a protected characteristic under contemporary equality law [ 3 ]. Despite this legislative effort, ethnic inequalities in education, work, health and criminal justice remain [ 4 ].
Discrimination on the basis of ethnic origin is regarded as the most common type of prejudice in Europe, with 64% of adults perceiving racial discrimination to be widespread in a survey of 27,718 people [ 5 ]. In Britain in 2017, 26% of a representative sample described themselves as racially prejudiced [ 6 ], and race continues to be the most common motivator for hate crime incidents [ 7 , 8 ]. Against the backdrop of the vote to leave the European Union (Brexit), hostility towards migrants and the growth in right-wing nationalist movements [ 9 ], these figures reflect a rise in reported racial discrimination in both the UK and Europe [ 5 , 6 ].
A growing body of research has investigated discrimination as a determinant of mental health [ 10 , 11 , 12 ] and to a lesser extent physical health [ 11 ]. In an early meta-analysis of 110 studies, discrimination was linked with poor mental health, including psychological distress and decreased life satisfaction [ 11 ]. A sub-set of 36 studies in the review investigated associations with physical health. Significant associations were detected in a pooled analysis with various outcomes including hypertension and acute cardiovascular responses to laboratory discrimination protocols. A more recent meta-analysis of 328 studies focusing on discrimination and mental health outcomes alone, again observed that those who perceived discrimination had poorer mental health [ 12 ]. This finding was also detected in an independent analysis of 211 cross-sectional studies linking racial discrimination with poor mental health [ 12 ].
Racism is a recognised social determinant of health and a driver of ethnic inequities in health [ 13 ]. It can be understood as a complex, organised system embedded in socio-political and historical contexts, that involves classifying ethnic groups into social hierarchies. These groups are ideologically assigned differential value, which drives disparities in access to power, resources and opportunities [ 14 , 15 ]. It occurs at both structural and individual levels (self-reported experiences of racial discrimination) [ 14 , 15 ].
Several reviews and meta-analyses have focused solely on perceived racial discrimination and health outcomes [ 13 , 16 , 17 , 18 ]. The largest study to date meta-analysed the results from 293 studies and assessed both mental and physical health outcomes [ 16 ]. In this analysis, racial discrimination was associated with poorer overall mental health including greater psychological distress, poorer life satisfaction and poorer general mental functioning in independent analyses. Racism was also linked with poorer general health and poorer physical health overall, though few effects remained significant when looking at specific physical health outcomes in separate analyses.
Racial discrimination at the structural and individual level is theorised to impact health through several mechanisms [ 15 ]. At the structural level racial discrimination may operate through the unfair allocation of societal resources that are determinants of health (e.g. education, employment, housing) [ 14 , 15 ] and through differential access to healthcare, as well as perceived poorer quality of care [ 19 ]. Another mechanism linking racial discrimination and health could be through the dysregulation of stress-related biological processes [ 20 ]. Frequent exposure to racial discrimination is a chronic stressor and has been linked with dysregulated cardiovascular, neuroendocrine and inflammatory processes [ 21 , 22 ] which in turn impact both physical and mental health. Individual health risk (e.g. smoking, alcohol consumption) could link perceived racial discrimination and health, as means of coping with or avoiding discrimination [ 23 , 24 ].
Although a growing number of studies have investigated the link between racial discrimination and health, there are still areas where more research is required. In the 2015 racism meta-analysis of almost 300 studies, only 9% of the data included were prospective [ 16 ]. The authors aimed to compare the effect sizes of the cross-sectional and prospective studies included in their review but were unable to conduct this analysis for the physical outcomes data, emphasising the need for more prospective studies on physical health outcomes in particular.
Further, the literature is dominated by United States (US)-based studies drawn from convenience samples [ 12 , 16 ]. In the latest racism and health meta-analysis, over one third of the articles included were drawn from student samples and only nine (2.7%) of the included studies were UK-based [ 16 ]. This is important as the makeup of ethnic minority groups in the UK differs from that of the US, with those of South Asian backgrounds forming the largest minority group [ 25 ]. In addition, all of the UK studies were cross-sectional in nature and focused on mental health, with physical outcomes such as the number of physical illnesses [ 26 ] and self-rated health [ 27 ] included in only two of the studies.
To date, one UK study has assessed the relationship between racial discrimination and health prospectively. In an analysis of the UK Household Longitudinal Study (UKHLS), the authors found that those who reported racial discrimination had poorer mental functioning scores 4 years later [ 28 ]. They also reported a dose-response relationship between the experience of racial discrimination and mental health, with those who reported racial discrimination at more than one timepoint over a 3-year period experiencing a greater deterioration in mental functioning.
Overall, there is a dearth of prospective evidence on the link between racial discrimination and health in UK samples, particularly in relation to physical health outcomes.
To address these gaps in the literature, the present study set out to assess cross-sectional and prospective associations between racial discrimination and health in a large community-dwelling UK population cohort. Specifically, we were interested in psychological distress, mental functioning and life satisfaction, as indicators of mental health, as well as self-rated health and physical functioning as markers of physical health, along with limiting longstanding illness as an indicator of impairment. We hypothesised that those who perceived racial discrimination would have poorer health across all measures both cross-sectionally and prospectively.
Study population
The current study uses data from UKHLS [ 29 ]. The study began in 2009/10 (wave 1) with follow-ups yearly. This study uses data from waves 1 (2009/10) and 3 (2011/12) of the data collection. The UKHLS consists of a representative sample of the UK population, as well as an ethnic minority boost sample [ 25 , 30 ]. In this study we use data from ‘extra 5 minutes sample’ of over 8000 individuals who had an additional 5 min of questions on issues of importance to ethnicity research including discrimination. The majority of this sample are drawn from ethnic minority groups ( n = 6722), in addition to a smaller comparison group of white participants ( n = 1428) [ 25 ]. We restricted our analyses to those who provided information on racial discrimination at wave 1 ( n = 5707) and self-reported being of non-white ethnicity ( n = 4883). The participants included in our study were significantly older ( p = 0.002) and were less likely to have an educational qualification ( p < 0.001) than those who did not provide data for the study. They were also more likely to be male ( p < 0.001) and of South Asian ethnicity ( p < 0.001) The groups did not differ on income ( p = 0.136). All participants provided fully informed written consent and the University of Essex Ethics Committee granted ethical approval for UKHLS.
Racial discrimination
To measure perceived discrimination, participants were asked whether in the past 12 months, they had (a) felt unsafe, (b) avoided going to or being in, (c) been insulted, called names, threatened or shouted at, or (d) been physically attacked in 7 different settings 1) At school/college/work, 2) On public transport, 3) At or around bus or train stations, 4) In a taxi, 5) Public buildings such as shopping centres or pubs, 6) Outside on the street, in parks or other public places, or 7) At home. If they answered yes to any one of these questions, a follow-up question asked them to choose an attribution for the discrimination from a list of categories including ethnicity, nationality, age, and sex among others. Participants could choose multiple settings and attributions for the perceived discrimination. Those who attributed any experience of discrimination to their ethnicity or nationality are treated as cases of perceived racial discrimination in our analyses. Those who did not perceive any form of discrimination serve as the comparison group in our analyses. Those who reported other (non-racial) forms of discrimination were not included in the analysis. This measure has been used in previous investigations to look at the link between perceived discrimination and health outcomes [ 28 , 31 , 32 ].
Mental health outcomes
We included 3 mental health measures at waves 1 (2009/10) and 3 (2011/12). Psychological distress was assessed using the General Health Questionnaire (GHQ)-12 [ 33 ], in line with previous studies [ 31 , 32 ]. This tool has been validated as a screening tool to detect psychological distress in community samples [ 34 ]. This measure involved ratings of 12 statements including whether the participant had “ Been able to enjoy your normal day to day activities ” or whether they “ Felt constantly under strain ” with binary response options (yes/no). After totalling, the overall score ranged from 0 (least distressed) to 12 (most distressed). The Cronbach’s alpha for the scale was 0.99.
The 12-item short-form health survey (SF-12) mental component summary score was used to measure limitations caused by emotional, mental health and social functioning issues [ 35 ], in keeping with previous studies [ 31 , 32 ]. This tool has been validated for use as a measure of mental functioning in community samples [ 35 , 36 ]. Items included ratings of feelings experienced over the past 4 weeks such as “ Have you felt downhearted or blue ?” or “Accomplished less than you would like” . A total score ranging from 0 (low functioning) to 100 (high functioning) was derived using standard methods [ 37 ]. The Cronbach’s alpha for this scale was 0.98.
One item was used to assess participants’ life satisfaction by asking them how satisfied they were with their “life overall”, on a scale from 1 (completely dissatisfied) to 7 (completely satisfied) [ 38 ]. Single item measures of life satisfaction are widely used in survey studies [ 39 ] This measure has been used in previous investigations to assess the link between discrimination and life satisfaction [ 31 , 32 ].
Impairment outcome
Self-reported limiting longstanding illness at waves 1 (2009/10) and 3 (2011/12) was used as measure of impairment. It was measured using one item “Do you have any long-standing physical or mental impairment, illness or disability?...mean [ing] anything that has … or is likely to trouble you over a period of at least 12 months” with response options of yes or no. Self-reported limiting longstanding illness has been investigated in relation to perceived discrimination in other studies [ 40 , 41 ].
Physical health outcomes
We included 2 measures of physical health that were assessed at waves 1 (2009/10) and 3 (2011/12). The SF-12 physical component summary score was used to measure limitations caused by deficits in physical functioning [ 35 ]. Participants were ask ed “Does your health now limit you a lot, limit you a little or not limit you at all?” in activities such “climbing stairs” or “moving a table, pushing a vacuum cleaner, bowling or playing golf”. Overall scores were derived using standard methods ranging from 0 (low functioning) to 100 (high functioning) [ 37 ]. The Cronbach’s alpha for the scale was 0.98. This tool has been validated for use as a measure of physical functioning in community samples [ 35 , 36 ].
A single item was used to assess self-rated health: “ Would you say your health is … poor/fair/good/very good/excellent?” In keeping with earlier work [ 31 , 32 , 42 ] self-rated health was dichotomised with 0 being “good/very good/excellent” and 1 being “poor/fair”. This single item measure has been shown to have good predictive validity for health outcomes [ 42 ].
Our analyses included covariates that are likely relevant to racial discrimination and physical and mental health. All covariates were assessed at wave 1. Age in years was included as a continuous variable. Self-reported sex was included and coded as male/female. Socioeconomic status is an important contributor to racial disparities in health [ 43 ]. Racial discrimination can compound these inequalities. Therefore, we included education as a 3-level variable, coded as 1 “university degree”, 2 “high school qualification” and 3 “no qualification”. Equivalised monthly household income was computed by dividing total household net income by the modified Organization for Economic Cooperation and Development (OECD) equivalence scale to account for the effects of household size and composition [ 44 ]. The UKHLS samples the 5 main ethnic minority groups in the UK [ 25 , 30 ]: Indian, Pakistani, Bangladeshi, Black African and Black Caribbean. Participants were asked “What is your ethnic group?” with response options standardised in line with the England and Wales 2011 Census [ 25 ]. Response options also accounted for those of “mixed backgrounds”. We included ethnicity as a 6-level variable with these 5 main UK minority groups and 1 additional category of non-white individuals from a range of other minority backgrounds including Chinese, Arab and mixed ethnic backgrounds among others. For our sensitivity analysis, we collapsed ethnicity into a 3-level variable with Indian, Pakistani and Bangladeshi participants coded as “South Asian” Black African and Black Caribbean participants coded as “Black” and other non-white participants coded as “Other”.
Statistical analyses
The characteristics of those who did and those who did not report racial discrimination at wave 1 were compared using Chi-squared tests for categorical variables and independent samples t-tests for continuous variables. Associations between racial discrimination and the mental and physical health measures were assessed using linear regression for continuous outcomes and binary logistic regression for categorical outcomes. For the mental health analyses, psychological distress, mental functioning and life satisfaction were the outcome variables. For the impairment analysis limiting longstanding illness was the outcome variable. For the physical health analyses, physical functioning and self-rated health were the outcome variables. Age, sex, household income, education and ethnicity at wave 1 were adjusted for in all analyses. Baseline (wave 1) score/status on the relevant outcome variable was included as an additional covariate in prospective analyses. Only those with complete case information at wave 1 ( n = 4883) and wave 3 ( n = 2833) were included in the analyses. We tested for interactions between racial discrimination and age, sex, income, education or ethnicity on the mental and physical health outcomes at both waves 1 and 3. No significant effects were detected. Thus, interaction terms were not included in our final reported models.
Results from linear regression analyses are presented as unstandardized B and 95% confidence intervals (95% CI). Results from binary logistic regression analyses are presented as odds ratios (ORs) and 95% CI. The level of significance was set at p < 0.05. Unstandardized Bs and ORs rather than p values should be used to determine the strength of associations. All analyses were conducted using SPSS v.24.
Sensitivity analyses
To test the robustness of our findings, we conducted three sets of sensitivity analyses. In our first, we investigated whether a certain type of discriminatory experience (i.e. feeling unsafe, avoiding somewhere, being insulted or attacked) contributing to the measure of racial discrimination was driving the results. We tested this by removing each type of discriminatory experience from the exposure variable in turn, as has been done in previous investigations [ 31 , 32 , 40 ]. In the second sensitivity analysis, we assessed whether participants who were lost to follow-up differed from those who provided data at both waves, and tested whether this influenced the findings by conducting the cross-sectional analyses (wave 1) including only those who provided follow-up data at wave 3. In our final sensitivity analysis, we assessed whether the associations between racial discrimination and our health outcomes varied depending on ethnic group (South Asian, Black or Other), as there is currently limited evidence in this area outside of the US context [ 16 ].
A total of 4883 participants were included in our analysis and of these 998 (20.4%) reported ethnicity ( n = 854) or nationality ( n = 144) discrimination. The characteristics of the sample at wave 1 in relation to racial discrimination are displayed in Table 1 . Those who perceived racial discrimination were younger on average and were more likely to hold a university degree than those who did not perceive racial discrimination. There were no differences in sex or income, but reports of racial discrimination did vary by ethnic group. Those in the Indian (23.3%) and in the Other ethnic group (24%) were most likely to report experiences of racial discrimination. Further detail on the types of racial discrimination and the settings in which the racial discrimination occurred for the different ethnic groups can be found in Supplementary Table 1 .
Racial discrimination and mental health
The descriptive characteristics of the sample in relation to health outcomes are displayed in Table 2 . The mental health findings from the regression analyses are displayed in the upper panel of Table 3 . Cross-sectionally, those who reported racial discrimination had greater psychological distress ( B = 1.11, 95% CI 0.88; 1.34, p < 0.001), poorer mental functioning ( B = − 3.61; 95% CI -4.29; − 2.93, p < 0.001) and lower life satisfaction ( B = − 0.40, 95% CI -0.52; − 0.27, p < 0.001), than those who did not report racial discrimination, independent of covariates.
In prospective analyses, those who perceived racial discrimination had greater psychological distress 2 years later than those who did not perceive racial discrimination, independent of covariates and baseline psychological distress ( B = 0.52, 95% CI 0.20; 0.85, p = 0.002). We detected an association between racial discrimination and poorer mental functioning ( B = − 1.77; 95% CI -2.70; − 0.83, p < 0.001), independent of covariates and mental functioning at wave 1. In adjusted analyses, those who reported racial discrimination had slightly lower life satisfaction than those who did not report racial discrimination at follow-up (means = 4.77 vs 4.91), but this difference did not reach statistical significance ( p = 0.102).
Racial discrimination, impairment and physical health
The impairment and physical health results are displayed in the lower panel of Table 3 . The cross-sectional findings suggest that independent of covariates, participants who perceived racial discrimination were significantly more likely on average to report having a limiting longstanding illness (OR = 1.78; 95% CI 1.49; 2.13, p < 0.001), and were more likely on average to rate their health as fair/poor (OR = 1.50; 95% CI 1.24; 1.82, p < 0.001) than those who did not perceive racial discrimination. Those who reported racial discrimination also had significantly poorer physical functioning ( B = − 0.86; 95% CI -1.50; − 0.27, p = 0.008) than those who did not report racial discrimination in adjusted analyses.
In prospective analyses, those who reported racial discrimination were significantly more likely on average to have a limiting longstanding illness 2 years later than those who did not report racial discrimination, independent of covariates and limiting longstanding illness at baseline (OR = 1.31; 95% CI 1.01; 1.69, p = 0.039). A greater proportion of those who reported racial discrimination rated their health as fair/poor on average at follow-up than those who did not report racial discrimination (OR = 1.30; 95% CI 1.00; 1.69, p = 0.048) in adjusted analyses. However, we failed to detect a prospective adjusted association between racial discrimination and physical functioning ( p = 0.290).
In the first sensitivity analysis, removing each of the discriminatory experiences from the measure of racial discrimination in turn did not alter any of the cross-sectional results (Table 4 , upper panel). Prospectively, the association between racial discrimination and all the mental health measures and limiting longstanding illness remained the same regardless of the type of discriminatory experience removed from the measure (Table 4 , lower panel). For self-rated health, the association was fairly robust to the type of discriminatory experience, but was slightly attenuated when “feeling unsafe” was removed from the racial discrimination variable ( p = 0.133). Again, for the most part, no significant prospective associations were detected for physical functioning except when “feeling unsafe” was removed from the racial discrimination variable ( p = 0.027).
In the second sensitivity analysis (Supplementary Table 2 ), cross-sectional physical and impairment (lower panel) and mental health (upper panel) findings for those who provided complete data at wave 3 were similar to the full-sample at wave 1.
In our final sensitivity analysis (Supplementary Table 3 ), we assessed whether the associations between racial discrimination and our health outcomes varied depending on ethnic group (South Asian, Black, Other). For the cross-sectional analyses, the findings for psychological distress and mental functioning did not vary by ethnic group. However, for life satisfaction ( B = − 0.23; 95% CI -0.47; 0.02, p = 0.069), limiting longstanding illness (OR = 1.34; 95% CI 0.93; 1.92, p = 0.113), physical functioning ( B = 0.42; 95% CI -0.84; 1.68, p = 0.511), and self-rated health (OR = 1.01; 95% CI 0.67; 1.53, p = 0.955) the findings for the Black group were non-significant, with lower point estimates than when the ethnic groups were combined in the main analysis. For the prospective analyses, there was no group difference for the impairment and physical health outcomes. However, the findings for psychological distress ( B = 0.32; 95% CI -0.18; 0.82, p = 0.207), and mental functioning ( B = − 1.37; 95% CI -2.83; 0.09, p = 0.065), were not significant for the South Asian group, with lower point estimates than in the combined model. Interestingly, for life satisfaction, those in the Other ethnic group had significantly lower life satisfaction at wave 3 ( B = − 0.39; 95% CI -0.69;-0.08, p = 0.013), with greater point estimates than in the combined model. This finding remained non-significant for the South Asian and Black groups.
In this large UK-based prospective sample of ethnic minority participants, we detected associations between racial discrimination and poorer health. Cross-sectionally, those who reported racial discrimination had a greater likelihood on average of limiting longstanding illness and poor self-rated health, than those who did not report racial discrimination. Racial discrimination was associated greater psychological distress, lower life satisfaction, and poorer physical and mental functioning. In prospective analyses, those who reported racial discrimination had a greater likelihood on average of limiting longstanding illness and poor self-rated health than those who did not report racial discrimination. Racial discrimination was associated with greater psychological distress and poorer mental functioning over a two-year follow-up period, regardless of baseline health. No significant prospective associations with physical functioning or life satisfaction were detected.
To our knowledge, this is the first prospective UK-based study to investigate both mental and physical health outcomes in relation to racial discrimination. One earlier analysis of the UKHLS found that those who reported racial discrimination had poorer mental functioning over a 1–4 year follow-up period [ 28 ]. The current study also found a prospective association between racial discrimination and poor mental functioning. Our study builds upon previous findings by additionally showing that this association is independent of baseline mental functioning. We also observed a prospective association with psychological distress, another marker of mental health, with those reporting racial discrimination experiencing an increase in psychological distress over time. We did not detect a prospective association between racial discrimination and poorer life satisfaction. Mean scores trended in this direction but the association did not reach statistical significance. A 2015 longitudinal analysis of the US-based Health and Retirement Study with over 6000 participants also failed to detect a prospective association between racial discrimination and decreases in life satisfaction [ 45 ], and pooled analyses have been unable to investigate prospective associations with life satisfaction due lack of sufficient evidence [ 12 , 16 ]. A possible explanation for this null finding, consistent with earlier work, is that racial discrimination is more strongly associated with negative mental health outcomes such as psychological distress than with positive outcomes such as life satisfaction [ 12 , 16 ]. Another potential reason for these findings relates to duration of follow-up, as review evidence suggests that a recent experience of racial discrimination may be more strongly associated with poor mental health and more weakly related to life satisfaction measures [ 16 ]. Our follow-up period of 2 years was relatively short which may have contributed to these results.
Reviews in the field [ 16 , 17 ] have highlighted the need for more prospective evidence, particularly for physical health outcomes [ 16 ]. We found that participants who reported racial discrimination were more likely to report having a limiting longstanding illness and poorer self-rated health, independent of baseline status. Meta-analytic evidence has demonstrated an association between racism and poor general health and worse physical health outcomes [ 16 ]. We built upon this predominately US-based data (a considerable portion of which used convenience sampling) to demonstrate prospective associations between racial discrimination and physical health outcomes in a representative sample of UK adults from ethnic minority groups. We failed to observe a prospective association between perceived racial discrimination and physical functioning, although participants who reported racial discrimination had slightly lower physical functioning scores prospectively than those who did not report racial discrimination. This lack of association may indicate that ongoing experiences of racial discrimination had already made an impact on physical functioning at the time of wave 1 survey, limiting the scope for further significant decreases in this measure over time, particularly as we took baseline physical functioning into account in our analyses. Another possibility, is that the etiological period involved for a decline in physical functioning may differ from that of mental functioning [ 14 ]. These outcomes were measured using the same tool (SF-12) but only mental functioning was significantly associated with racial discrimination over the follow-up period.
Review evidence based on US data suggests that associations between racial discrimination and health may vary depending on ethnic group [ 16 ]. In our sensitivity analysis, the cross-sectional results for life satisfaction and impairment and physical health outcomes were non-significant for the Black group. Prospectively the findings for psychological distress and mental functioning were non-significant for the South Asian group. Whereas, life satisfaction was found to significantly decline for the Other group over the follow-up period. Taken together these results suggest associations with health outcomes are strongest for South Asian and Other groups cross-sectionally, while prospectively racial discrimination appears to most consistently impact mental health outcomes in Black and Other ethnic groups. These findings should be interpreted with caution due to the likelihood that some of our analyses were underpowered.
In our cross-sectional analyses, we found that those who perceived racial discrimination had poorer mental health, with greater psychological distress, poorer mental functioning and lower life satisfaction. Previous work in UKHLS has demonstrated a cross-sectional association with psychological distress using pooled data across three waves of data collection [ 46 ]. To our knowledge no prior UK-based work has reported on cross-sectional associations with poor mental functioning and low life satisfaction. These findings are consistent with earlier work in other countries [ 12 , 16 , 45 ].
We detected links between racial discrimination and poor physical health and impairment. Specifically, we found that those who reported racial discrimination had poorer self-rated health, poorer physical functioning scores and a greater likelihood of having a limiting longstanding illness than those who did not report racial discrimination. Earlier work using the 1993/1994 UK-based Fourth National Survey of Ethnic Minorities survey reported associations between perceived racial discrimination and poor self-rated health [ 27 , 47 ] and limiting longstanding illness [ 47 ]. Our more recent findings from 2009/2010 suggest that these deleterious associations remain an issue for minorities in the UK.
We detected stronger associations between racial discrimination and health for cross-sectional than for prospective comparisons, in keeping with earlier evidence [ 16 ]. However, cross-sectional work cannot determine whether reports of racial discrimination stimulate poor mental and physical health or whether perceptions of racial discrimination are a manifestation of feeling suboptimal mentally or physically. Our prospective findings therefore add to the field in establishing that racial discrimination predicts poor mental and physical outcomes prospectively, net of baseline associations, supporting the hypothesis that racial discrimination has adverse consequences for future health.
With regard to the pathways through which racial discrimination negatively impacts health, there are several possibilities that could help explain our results. One mechanism linking racial discrimination and health may be through the dysregulation of stress-related biological processes. In response to perceived chronic discrimination, stress processes may be frequently activated, which over time may result in disturbances across multiple biological systems, in line with the theory of allostatic load [ 20 ]. Review evidence indicates discrimination is associated with heightened cardiovascular responses to stress [ 11 , 21 ], though it is unclear whether this translates into an increased risk for clinical hypertension [ 48 ]. Another biological mechanism that may link discrimination and health is through activation of the hypothalamic-pituitary-adrenal (HPA) axis. Several reviews have linked racial discrimination [ 21 , 49 , 50 ] with changes in various cortisol parameters, which in turn have been linked with poorer mental and physical health [ 51 , 52 ]. Deleterious changes in other biological processes such as heightened inflammation [ 22 ] and alterations in DNA methylation of stress-related genes [ 53 ] have been linked with discrimination in recent studies. Alterations in these stress-related biological processes offer a plausible link to negative changes in physical [ 54 , 55 ] and, mental health outcomes [ 51 , 56 ]. Racial discrimination has also been associated with disturbances in neurobiological processes, with alterations observed in brain areas such as the anterior cingulate cortex, prefrontal cortex and amygdala which overlap with pathways associated with poor mental health [ 57 ].
Individual health risk (e.g. smoking, alcohol consumption etc.) could link perceived racial discrimination and poor mental and physical health, either as a method of coping with the negative psychological effect of perceiving racial discrimination (e.g. excessive alcohol consumption as a coping mechanism) or as a barrier to engaging in healthy behaviours (e.g. avoiding a health service perceived to be discriminatory). Racial discrimination has been associated with smoking [ 23 , 58 , 59 ], excessive alcohol consumption [ 23 , 60 ], as well as substance abuse [ 61 , 62 ]. Review evidence has linked discrimination with poor sleep [ 63 ] as well as weight gain in prospective studies [ 24 ]. This individual health risk offers a plausible indirect pathway linking racial discrimination with both poor mental [ 64 , 65 ], as well as physical health outcomes [ 66 ].
Another possibility at the broader structural level is that racial discrimination may impact health through differential access to societal resources such as education, employment, welfare and criminal justice [ 14 , 15 ]. In the UK, a 2016 report documented persistent ethnic disparities in educational attainment, employment, access to fair pay and adequate housing, as well the over-representation of ethnic minorities in the criminal justice system [ 4 ]. Further, data from this report highlight inequalities in access to healthcare among ethnic minority groups [ 4 ]. While meta-analytic evidence indicates that racial discrimination is associated with more negative patient experiences of health services, as well as delaying/not getting healthcare and lack of treatment uptake [ 19 ]. As these factors are social determinants of health in of themselves [ 13 , 14 , 15 ], they may act as a pathway through which perceptions of racial discrimination can act to negatively influence health.
The results of the current study need to be assessed in terms of strengths and limitations. There is a dearth of prospective evidence on the link between racial discrimination and health in UK samples, particularly in relation to physical health. Our large sample of ethnic minority participants allowed us to examine changes in mental and physical health over 2 years, and demonstrated both cross-sectional and prospective associations. We also adjusted statistically for factors that potentially confound associations, including age, sex, socioeconomic status and ethnicity. Although controlling for covariates does not tease out the complexity of the relationships between perceived racial discrimination and these sociodemographic characteristics [ 43 ]. For example, socioeconomic status contributes to racial inequalities in health [ 43 ], while racial discrimination can compound these disparities and can be conceptualised as an indicator of structural racism [ 13 ]; statistical adjusting for socioeconomic status does not capture these relationships.
The study of racism is a complex and contested area of research [ 67 , 68 ] and our study was not without limitations. Our measure of perceived discrimination was not specifically tailored for racial discrimination, as participants in the could attribute their experience to other forms of discrimination as well (e.g. sexism, ageism). There is evidence that the exposure instrument can influence associations between racism and physical and mental health outcomes [ 16 ] . Participants were able to attribute multiple reasons for their report of discrimination, which could have helped to avoid priming and this measure has been used to assess racial discrimination in previous work [ 28 ]. However, it is possible that measures such as the Schedule of Racist Events scale [ 69 ] and the Perceived Racism Scale [ 70 ] with more specific items on racist degradation and experiences of racism in personal and professional contexts could have garnered different results. Further, the self-report individual measure of racial discrimination employed in our study does not capture the structural conditions that shape the varied ways in which racial discrimination operates [ 14 ]. We only assessed perceived racial discrimination at baseline in this study and did not investigate whether racial discrimination experiences were persistent or changed over time.
Racial discrimination was assessed by self-reports of experiences in the past year and was therefore subject to recall bias. Our findings reflect the perception of racial discrimination rather than objective encounters with racial discrimination. It is possible that objective encounters with racism and perceiving one’s self as the target of racial discrimination might have different consequences for health. Experimental studies involving exposure to discriminatory scenarios have been used to investigate the health impact of objective exposures to racial discrimination. However, these studies may not represent a gold standard for the study of the relationship between discrimination and health, as meta-analytic evidence indicates that exposure to a single negative event in a laboratory setting does not negatively influence health [ 12 ].
In conclusion, this study adds to the field by demonstrating cross-sectional and prospective relationships between racial discrimination and both mental and physical health outcomes. With the rise in racial discrimination in the UK [ 6 ] in the aftermath of the Brexit vote [ 9 ] our findings highlight the need to reduce racial discrimination, not only to promote equity, but also to potentially benefit mental and physical health and reduce health inequalities.
Racial discrimination is a complex system that involves assigning ethnic groups differential value, which drives disparities in access to power, resources and opportunities [ 14 , 15 ]. Due to its multi-faceted nature, occurring at both the structural and individual level multiple interventions will be required to tackle this pervasive determinant of health. Historically, raising awareness of racial discrimination has been necessary to promote activism to bring about legislative and social change to improve the position of ethnic minority groups. In terms of public health, there are calls to integrate research about racial discrimination and health into medical teaching in an attempt to tackle structural racism and to highlight the impact racial discrimination has on health [ 71 , 72 ]. As well as strategies to reduce the pervasiveness of racial discrimination in institutional contexts, action through social media may have benefits for individual health too. The Black Lives Matter campaign is an example of a recent social media movement which has drawn attention to the issue of racial discrimination. There is some evidence that campaigns may provide a source of empowerment, particularly in a time where ethnic minority youth participation in traditional civic engagement activities are in decline [ 73 ]. Evidence suggests the Twitter conversation remained Black-led [ 73 ] and that the majority of the 40 million plus tweets were supportive of the movement [ 73 , 74 ]. However, whether social media campaigns positively [ 73 ] or negatively impact minority health [ 75 ] remains the subject of debate. Further, it should be acknowledged that interventions to educate and raise awareness do not tackle the structural macro-level forces that shape the position of ethnic minorities in society. Although, more challenging to address, work is required to identify socio-political processes that generate racial discrimination so attempts can be made to mitigate its effects. Research into the pathways underlying the link between racial discrimination and health are required to develop policy and to target interventions in this field.
Availability of data and materials
The UKHLS datasets analysed during the current study are freely available in the UK Data Service repository https://ukdataservice.ac.uk/
Abbreviations
Confidence Interval
General Health Questionnaire-12
Hypothalamic-pituitary-adrenal
Organization for Economic Cooperation and Development
Short-form Health Survey-12
United Kingdom
The United Kingdom Household Longitudinal Study
United States
Alvarez-Galvez J, Salvador-Carulla L. Perceived discrimination and self-rated health in Europe: evidence from the European social survey (2010). PLoS One. 2013;8:e74252.
Article CAS Google Scholar
The Race Relations Act. 1965. https://www.legislation.gov.uk/ukpga/1965/73/enacted .
The Equality Act. 2010. https://www.legislation.gov.uk/ukpga/2010/15/contents .
Equality and Human Rights Commission. Healing a Divided Britain: the need for a comprehensive race equality strategy. 2016.
Google Scholar
European Union. Discrimination in the EU in 2015. 2015.
Kelley N, Khan O, Sharrock S. Racial prejudice in Britain today. London: NatCen Social Research and Runnymede Trust; 2017.
Home Office. Hate Crime, England and Wales, 2017/18. Statistical Bulletin 20/18. 2018.
Crown Office and Procurator Fiscal Service. Hate Crime in Scotland 2017–18. 2019. https://www.copfs.gov.uk/images/Documents/Statistics/Hate%20Crime%202017-18/Hate%20Crime%20in%20Scotland%202017-18.pdf .
Bhui K, Halvorsrud K, Nazroo J. Making a difference: ethnic inequality and severe mental illness. Br J Psychiatry. 2018;213:574–8.
Article Google Scholar
Goto JB, Couto PFM, Bastos JL. Systematic review of epidemiological studies on interpersonal discrimination and mental health. Cad Saude Publica. 2013;29:445–59.
Pascoe EA, Smart RL. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135:531–54.
Schmitt MT, Branscombe NR, Postmes T, Garcia A. The consequences of perceived discrimination for psychological well-being: a meta-analytic review. Psychol Bull. 2014;140:921–48.
Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32:20–47.
Krieger N. Measures of racism, sexism, heterosexism, and gender Binarism for health equity research: from structural injustice to embodied harm—an Ecosocial analysis. Annu Rev Public Health. 2020;41:37–62.
Williams DR, Mohammed SA. Racism and health I: pathways and scientific evidence. Am Behav Sci. 2013;57. https://doi.org/10.1177/0002764213487340 .
Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, et al. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One. 2015;10:e0138511.
Priest N, Paradies Y, Trenerry B, Truong M, Karlsen S, Kelly Y. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Soc Sci Med 1982. 2013;95:115–27.
Lee DL, Ahn S. The relation of racial identity, ethnic identity, and racial socialization to discrimination-distress: a meta-analysis of black Americans. J Couns Psychol. 2013;60:1–14.
Ben J, Cormack D, Harris R, Paradies Y. Racism and health service utilisation: a systematic review and meta-analysis. PLoS One. 2017;12:e0189900.
McEwen BS. Stress, adaptation, and disease. Allostasis and allostatic load. Ann N Y Acad Sci. 1998;840:33–44.
Lockwood KG, Marsland AL, Matthews KA, Gianaros PJ. Perceived discrimination and cardiovascular health disparities: a multisystem review and health neuroscience perspective. Ann N Y Acad Sci. 2018;1428:170–207.
Kershaw KN, Lewis TT, Diez Roux AV, Jenny NS, Liu K, Penedo FJ, et al. Self-reported experiences of discrimination and inflammation among men and women: the multi-ethnic study of atherosclerosis. Health Psychol Off J Div Health Psychol Am Psychol Assoc. 2016;35:343–50.
Borrell LN, Kiefe CI, Diez-Roux AV, Williams DR, Gordon-Larsen P. Racial discrimination, racial/ethnic segregation, and health behaviors in the CARDIA study. Ethn Health. 2013;18:227–43.
de CO B, Bastos JL, González-Chica DA, Peres MA, Paradies YC. Interpersonal discrimination and markers of adiposity in longitudinal studies: a systematic review. Obes Rev Off J Int Assoc Study Obes. 2017;18:1040–9.
McFall S, Nandi A, Platt L. Understanding society: UK household longitudinal study: user guide to ethnicity and immigration research. 4th ed. Colchester: University of Essex; 2017.
Heim D, Hunter SC, Jones R. Perceived discrimination, identification, social capital, and well-being: relationships with physical health and psychological distress in a U.K. minority ethnic community sample. J Cross-Cult Psychol. 2011;42:1145–64.
Bécares L, Nazroo J, Stafford M. The buffering effects of ethnic density on experienced racism and health. Health Place. 2009;15:700–8.
Wallace S, Nazroo J, Bécares L. Cumulative effect of racial discrimination on the mental health of ethnic minorities in the United Kingdom. Am J Public Health. 2016;106:1294–300.
University of Essex. Institute for Social and Economic Research, NatCen Social Research, Kantar Public. Understanding Society: Waves 1–7, 2009–2016 and Harmonised BHPS: Waves 1–18, 1991–2009. 9th Edition. UK data service; 2017.
Knies G. Understanding society: The UK household longitudinal study, Waves 1–7 (User Guide). University of Essex. Colchester: Institute for Social and Economic Research; 2017.
Hackett RA, Steptoe A, Jackson SE. Sex discrimination and mental health in women: a prospective analysis. Health Psychol Off J Div Health Psychol Am Psychol Assoc. 2019;38:1014–24.
Hackett RA, Steptoe A, Lang RP, Jackson SE. Disability discrimination and well-being in the United Kingdom: a prospective cohort study. BMJ Open. 2020;10:e035714.
Goldberg D, Williams P. A user’s guide to the general health questionnaire. Basingstoke: NFER-Nelson; 1988.
Romppel M, Braehler E, Roth M, Glaesmer H. What is the general health Questionnaire-12 assessing?: dimensionality and psychometric properties of the general health Questionnaire-12 in a large scale German population sample. Compr Psychiatry. 2013;54:406–13.
Ware J, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33.
Cheak-Zamora NC, Wyrwich KW, McBride TD. Reliability and validity of the SF-12v2 in the medical expenditure panel survey. Qual Life Res. 2009;18:727–35.
Ware JE. How to score version 2 of the SF-12 health survey (with a supplement documenting version 1) edition: first. Lincoln, RI: Health Assessment Lab; 2002.
Lucas RE, Donnellan MB. Estimating the reliability of single-item life satisfaction measures: results from four National Panel Studies. Soc Indic Res. 2012;105:323–31.
Dolan P, Peasgood T, White M. Do we really know what makes us happy? A review of the economic literature on the factors associated with subjective well-being. J Econ Psychiatry. 2008;29:94–122.
Jackson SE, Hackett RA, Steptoe A. Associations between age discrimination and health and wellbeing: cross-sectional and prospective analysis of the English longitudinal study of ageing. Lancet Public Health. 2019;4:e200–8.
Jackson SE, Hackett RA, Grabovac I, Smith L, Steptoe A. Perceived discrimination, health and wellbeing among middle-aged and older lesbian, gay and bisexual people: a prospective study. PLoS One. 2019;14:e0216497.
DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. A meta-analysis. J Gen Intern Med. 2006;21:267–75.
Williams DR, Priest N, Anderson N. Understanding associations between race, socioeconomic status and health: patterns and prospects. Health Psychol Off J Div Health Psychol Am Psychol Assoc. 2016;35:407–11.
OECD. What are equivalence scales? 2005.
Sutin AR, Stephan Y, Carretta H, Terracciano A. Perceived discrimination and physical, cognitive, and emotional health in older adulthood. Am J Geriatr Psychiatry Off J Am Assoc Geriatr Psychiatry. 2015;23:171–9.
Nandi A, Luthra R, Benzeval M. Ethnic and racial harassment and mental health: Identifying sources of resilience (No. 2016–14). 2016. https://www.iser.essex.ac.uk/research/publications/working-papers/iser/2016-14 .
Karlsen S, Nazroo JY. Agency and structure: the impact of ethnic identity and racism on the health of ethnic minority people. Sociol Health Illn. 2002;24:1–20.
Dolezsar CM, McGrath JJ, Herzig AJM, Miller SB. Perceived racial discrimination and hypertension: a comprehensive systematic review. Health Psychol Off J Div Health Psychol Am Psychol Assoc. 2014;33:20–34.
Busse D, Yim IS, Campos B, Marshburn CK. Discrimination and the HPA axis: current evidence and future directions. J Behav Med. 2017;40:539–52.
Korous KM, Causadias JM, Casper DM. Racial discrimination and cortisol output: A meta-analysis. Soc Sci Med 1982. 2017;193:90–100.
Adam EK, Quinn ME, Tavernier R, McQuillan MT, Dahlke KA, Gilbert KE. Diurnal cortisol slopes and mental and physical health outcomes: a systematic review and meta-analysis. Psychoneuroendocrinology. 2017;83:25–41.
Hackett RA, Kivimäki M, Kumari M, Steptoe A. Diurnal cortisol patterns, future diabetes, and impaired glucose metabolism in the Whitehall II cohort study. J Clin Endocrinol Metab. 2016;101:619–25.
Santos HP, Nephew BC, Bhattacharya A, Tan X, Smith L, Alyamani RAS, et al. Discrimination exposure and DNA methylation of stress-related genes in Latina mothers. Psychoneuroendocrinology. 2018;98:131–8.
Wang X, Bao W, Liu J, OuYang Y-Y, Wang D, Rong S, et al. Inflammatory markers and risk of type 2 diabetes. Diabetes Care. 2013;36:166–75.
Chida Y, Steptoe A. Greater cardiovascular responses to laboratory mental stress are associated with poor subsequent cardiovascular risk status a meta-analysis of prospective evidence. Hypertension. 2010;55:1026–32.
Slavich GM, Irwin MR. From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychol Bull. 2014;140:774–815.
Berger M, Sarnyai Z. “More than skin deep”: stress neurobiology and mental health consequences of racial discrimination. Stress Amst Neth. 2015;18:1–10.
Bennett GG, Wolin KY, Robinson EL, Fowler S, Edwards CL. Perceived racial/ethnic harassment and tobacco use among African American young adults. Am J Public Health. 2005;95:238–40.
Sims M, Diez-Roux AV, Gebreab SY, Brenner A, Dubbert P, Wyatt S, et al. Perceived discrimination is associated with health behaviours among African-Americans in the Jackson heart study. J Epidemiol Community Health. 2016;70:187–94.
Gilbert PA, Zemore SE. Discrimination and drinking: A systematic review of the evidence. Soc Sci Med 1982. 2016;161:178–94.
Gibbons FX, Gerrard M, Cleveland MJ, Wills TA, Brody G. Perceived discrimination and substance use in African American parents and their children: a panel study. J Pers Soc Psychol. 2004;86:517–29.
Gibbons FX, Etcheverry PE, Stock ML, Gerrard M, Weng C-Y, Kiviniemi M, et al. Exploring the link between racial discrimination and substance use: what mediates? What buffers? J Pers Soc Psychol. 2010;99:785–801.
Slopen N, Lewis TT, Williams DR. Discrimination and sleep: a systematic review. Sleep Med. 2016;18:88–95.
Brennan PL, SooHoo S, Lemke S, Schutte KK. Alcohol use predicts 10-year depressive symptom trajectories in the health and retirement study. J Aging Health. 2016;28:911–32.
Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135:10–9.
Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–52.
Boyd R, Lindo E, Weeks L, McLemore M. On Racism: A New Standard For Publishing On Racial Health Inequities. Health Affairs Blog. 2020. https://www.healthaffairs.org/do/10.1377/hblog20200630.939347/full/ . Accessed 18 Aug 2020.
Kaplan JB, Bennett T. Use of race and ethnicity in biomedical publication. JAMA. 2003;289:2709–16.
Landrine H, Klonoff EA. The schedule of racist events: a measure of racial discrimination and a study of its negative physical and mental health consequences. J Black Psychol. 1996;22:144–68.
McNeilly MD, Anderson NB, Armstead CA, Clark R, Corbett M, Robinson EL, et al. The perceived racism scale: a multidimensional assessment of the experience of White racism among African Americans. Ethn Dis. 1996;6:154–66.
CAS PubMed Google Scholar
Jee-Lyn García J, Sharif MZ. Black lives matter: a commentary on racism and public health. Am J Public Health. 2015;105:e27–30.
Williams DR, Cooper LA. Reducing racial inequities in health: using what we already know to take action. Int J Environ Res Public Health. 2019;16. https://doi.org/10.3390/ijerph16040606 .
Freelon D, McIlwain CD, Clark M. Beyond the Hashtags: #Ferguson, #Blacklivesmatter, and the online struggle for offline justice. SSRN scholarly paper. Rochester, NY: Social Science Research Network; 2016. https://papers.ssrn.com/abstract=2747066 . Accessed 8 Aug 2019.
Ince J, Rojas F, Davis CA. The social media response to black lives matter: how twitter users interact with black lives matter through hashtag use. Ethn Racial Stud. 2017;40:1814–30.
Umaña-Taylor AJ, Tynes BM, Toomey RB, Williams DR, Mitchell KJ. Latino adolescents’ perceived discrimination in online and offline settings: an examination of cultural risk and protective factors. Dev Psychol. 2015;51:87–100.
Download references
Acknowledgements
Not applicable.
This research was funded by the Economic and Social Research Council ( https://esrc.ukri.org/ ), grant number ES/R005990/1. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and affiliations.
Health Psychology Section, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, UK
Ruth A. Hackett
Department of Behavioural Science and Health, University College London, London, UK
Ruth A. Hackett, Andrew Steptoe & Sarah E. Jackson
Department of Psychological Medicine, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, UK
Amy Ronaldson
Centre for Department of Psychiatry & Nuffield Department of Primary Care Health Sciences, University of Oxford, Oxford, UK
Kamaldeep Bhui
You can also search for this author in PubMed Google Scholar
Contributions
RAH conducted the statistical analysis and wrote the manuscript. AR, KB and AS edited and reviewed the manuscript. SJ provided scientific overview, edited and reviewed the manuscript. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Ruth A. Hackett .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval for UKHLS was obtained from the University of Essex Ethics Committee. All participants provided fully informed written consent.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
Supplementary Table 1. Racial discrimination types and settings by ethnic group. Supplementary Table 2. Associations between racial discrimination and health outcomes (complete cases at wave 3). Supplementary Table 3. Cross-sectional and prospective associations between racial discrimination and health outcomes stratified by ethnic group
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hackett, R.A., Ronaldson, A., Bhui, K. et al. Racial discrimination and health: a prospective study of ethnic minorities in the United Kingdom. BMC Public Health 20 , 1652 (2020). https://doi.org/10.1186/s12889-020-09792-1
Download citation
Received : 18 May 2020
Accepted : 29 October 2020
Published : 18 November 2020
DOI : https://doi.org/10.1186/s12889-020-09792-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Discrimination
- Mental health
- Physical health
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Disclaimer » Advertising
- HealthyChildren.org

- Previous Article
- Next Article
Statement of the Problem
Racism as a core determinant of child health, the development of race as a construct, childhood experiences of racism, racism at the intersection of education and child and adolescent health, how pediatricians can address and ameliorate the effects of racism on children and adolescents, optimizing clinical practice, optimizing workforce development and professional education, optimizing systems through community engagement, advocacy, and public policy, optimizing research, conclusions, acknowledgments, section on adolescent health executive committee, 2018–2019, council on community pediatrics executive committee, 2018–2019, committee on adolescence, 2018–2019, the impact of racism on child and adolescent health.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Maria Trent , Danielle G. Dooley , Jacqueline Dougé , SECTION ON ADOLESCENT HEALTH , COUNCIL ON COMMUNITY PEDIATRICS , COMMITTEE ON ADOLESCENCE , Robert M. Cavanaugh , Amy E. Lacroix , Jonathon Fanburg , Maria H. Rahmandar , Laurie L. Hornberger , Marcie B. Schneider , Sophia Yen , Lance Alix Chilton , Andrea E. Green , Kimberley Jo Dilley , Juan Raul Gutierrez , James H. Duffee , Virginia A. Keane , Scott Daniel Krugman , Carla Dawn McKelvey , Julie Michelle Linton , Jacqueline Lee Nelson , Gerri Mattson , Cora C. Breuner , Elizabeth M. Alderman , Laura K. Grubb , Janet Lee , Makia E. Powers , Maria H. Rahmandar , Krishna K. Upadhya , Stephenie B. Wallace; The Impact of Racism on Child and Adolescent Health. Pediatrics August 2019; 144 (2): e20191765. 10.1542/peds.2019-1765
Download citation file:
- Ris (Zotero)
- Reference Manager
The American Academy of Pediatrics is committed to addressing the factors that affect child and adolescent health with a focus on issues that may leave some children more vulnerable than others. Racism is a social determinant of health that has a profound impact on the health status of children, adolescents, emerging adults, and their families. Although progress has been made toward racial equality and equity, the evidence to support the continued negative impact of racism on health and well-being through implicit and explicit biases, institutional structures, and interpersonal relationships is clear. The objective of this policy statement is to provide an evidence-based document focused on the role of racism in child and adolescent development and health outcomes. By acknowledging the role of racism in child and adolescent health, pediatricians and other pediatric health professionals will be able to proactively engage in strategies to optimize clinical care, workforce development, professional education, systems engagement, and research in a manner designed to reduce the health effects of structural, personally mediated, and internalized racism and improve the health and well-being of all children, adolescents, emerging adults, and their families.
Racism is a “system of structuring opportunity and assigning value based on the social interpretation of how one looks (which is what we call ‘race’) that unfairly disadvantages some individuals and communities, unfairly advantages other individuals and communities, and saps the strength of the whole society through the waste of human resources.” 1 Racism is a social determinant of health 2 that has a profound impact on the health status of children, adolescents, emerging adults, and their families. 3 , – 8 Although progress has been made toward racial equality and equity, 9 the evidence to support the continued negative impact of racism on health and well-being through implicit and explicit biases, institutional structures, and interpersonal relationships is clear. 10 Failure to address racism will continue to undermine health equity for all children, adolescents, emerging adults, and their families.
The social environment in which children are raised shapes child and adolescent development, and pediatricians are poised to prevent and respond to environmental circumstances that undermine child health. Pediatrics as a field has yet to systematically address the influence of racism on child health outcomes and to prepare pediatricians to identify, manage, mitigate, or prevent risks and harms. Recognizing that racism has significant adverse effects on the individual who receives, commits, and observes racism, 11 , 12 substantial investments in dismantling structural racism are required to facilitate the societal shifts necessary for optimal development of children in the United States. The American Academy of Pediatrics (AAP) is committed to reducing the ongoing costs and burden of racism to children, the health care system, and society. 13 , 14
Today’s children, adolescents, and emerging adults are increasingly diverse. Strategies to address health and developmental issues across the pediatric life span that incorporate ethnicity, culture, and circumstance are critical to achieving a reduction in health disparities. Accordingly, pediatrics should be at the forefront of addressing racism as a core social determinant. The inclusion of racism is in alignment with the health equity pillar of the AAP strategic plan. 15 In a series of workshops in 2016 during national meetings of pediatricians, 3 strategic actions were identified: (1) development of a task force within the AAP to address racism and other forms of discrimination that impact the health status and outcomes of minority youth, (2) development of a policy statement on racism, and (3) integration of evidence-based anticipatory guidance about racism into Bright Futures . 16
The objective of this policy statement is to provide an evidence-based document focused on the role of racism in child and adolescent development and health outcomes. This policy statement will allow pediatricians to implement recommendations in practice that will better address the factors that make some children more vulnerable than others. 13 The statement also builds on existing AAP policy recommendations associated with other social determinants of health, such as poverty, housing insecurity, child health equity, immigration status, and early childhood adversity. 9 , 17 , – 19
Racism is a core social determinant of health that is a driver of health inequities. 20 , – 22 The World Health Organization defines social determinants of health as “the conditions in which people are born, grow, live, work, and age.” These determinants are influenced by economic, political, and social factors linked to health inequities (avoidable inequalities in health between groups of people within populations and between countries). These health inequities are not the result of individual behavior choices or genetic predisposition but are caused by economic, political, and social conditions, including racism. 23
The impact of racism has been linked to birth disparities and mental health problems in children and adolescents. 6 , 24 , – 30 The biological mechanism that emerges from chronic stress leads to increased and prolonged levels of exposure to stress hormones and oxidative stress at the cellular level. Prolonged exposure to stress hormones, such as cortisol, leads to inflammatory reactions that predispose individuals to chronic disease. 31 As an example, racial disparities in the infant mortality rate remain, 32 and the complications of low birth weight have been associated with perceived racial discrimination and maternal stress. 25 , 33 , 34
Investments in policies to address social determinants of health, such as poverty, have yielded improvements in the health of children. The Food Stamp Program, a War on Poverty initiative first developed in the 1930s during the Great Depression and later revived in the 1960s, is linked to improvements in birth outcomes. 35 Efforts in education, housing, and child health insurance have also led to improved health outcomes for issues such as lead poisoning, injuries, asthma, cancer, neurotoxicity, cardiovascular disease, and mental health problems. 20 , 36 , 37 Expansion of child health insurance has improved health care access for children, with significant gains for African American and Hispanic children in terms of access to well-child, doctor, and dental visits. 38 Despite these improvements, it is important to recognize that children raised in African American, Hispanic, and American Indian populations continue to face higher risks of parental unemployment and to reside in families with significantly lower household net wealth relative to white children in the United States, posing barriers to equal opportunities and services that optimize health and vocational outcomes. 39 , – 45
Juvenile justice involvement is also a critical social determinant of health. Because racial inequity continues to shape the juvenile justice system, this area is a modern example of race being an important determinant of short- and long-term outcomes. The AAP published a statement in 2011 46 focusing on key health issues of justice-involved youth, which was recently revised to include an in-depth discussion on racial and ethnic inequalities for this population. 47 Although the overall rates of youth incarceration have decreased, African American, Hispanic, and American Indian youth continue to be disproportionately represented. 48 While incarcerated, youth experience additional adverse experiences, such as solitary confinement and abuse, that have the potential to undermine socioemotional development and general developmental outcomes. 49 , – 51 Differential treatment of youth offenders on the basis of race shapes an individual’s participation and ultimate function in society. This type of modern racism must be recognized and addressed if the United States seeks to attain health equity. 52
Race as a social construct is rooted in history and remains a mechanism through which social class has been controlled over time. Flawed science was used to solidify the permanence of race, reinforce the notions of racial superiority, and justify differential treatment on the basis of phenotypic differences as people from different parts of the world came in contact with each other. 53 Race emerged as a social classification used to assign dominance of some social classes over others. 53 Scientific, anthropologic, and historical inquiry further solidified race as a social construct. 54 Modern science, however, has demonstrated that there is only 1 biological race and that the clines (phenotypic differences in skin and eye color, hair texture, and bone structure) at the core of early anthropologic research were insufficient to establish different races among human beings. Dr Francis Collins, former director of the National Human Genome Project and presently the director of the National Institutes of Health, has affirmed that humans are 99.9% the same at the level of their genome. 55 Despite this, efforts to collect, organize, and categorize individuals on the basis of the plausibility of the 0.01% human variation remain a force of scientific discovery, innovation, and medical-pharmaceutical collaborations. 56 Rather than focusing on preventing the social conditions that have led to racial disparities, science and society continue to focus on the disparate outcomes that have resulted from them, often reinforcing the posited biological underpinnings of flawed racial categories. 57 Although race used in these ways has been institutionalized, linked to health status, and impeded our ability to improve health and eliminate health disparities, 58 , 59 it remains a powerful measure that must be better measured, carefully used, and potentially replaced to mark progress in pediatric health disparities research. 60 , 61
As such, it is important to examine the historical underpinnings of race used as a tool for subjugation. American racism was transported through European colonization. It began with the subjugation, displacement, and genocide of American Indian populations and was subsequently bolstered by the importation of African slaves to frame the economy of the United States. Although institutions such as slavery were abolished more than a century ago, discriminatory policies, such as Jim Crow laws, were developed to legalize subjugation. As the United States expanded west in North America and into Alaska and the Pacific Islands, the diversity of populations encompassing the United States also expanded. Native Hawaiian and Pacific Islander, Alaskan native, Asian American, and Latino American populations have experienced oppression and similar exclusions from society. 62 , – 65 Although some racial and/or ethnic groups have received reparations 66 and fared better than others over time, remnants of these policies remain in place today and continue to oppress the advancement of people from historically aggrieved groups. 67 , – 72
Through these underpinnings, racism became a socially transmitted disease passed down through generations, leading to the inequities observed in our population today. Although the endemic nature of racism has powerful impacts on perceived and actual health outcomes, it is also important to note that other forms of discrimination (eg, sex, religion, sexual orientation, immigrant status, and disability status) are actively at play and have created a syndemic with the potential to undermine child and family health further. It is important to address racism’s impact on the health and well-being of children, adolescents, and emerging adults to avoid perpetuating a health system that does not meet the needs of all patients. 52 Pediatricians are uniquely positioned to both prevent and mitigate the consequences of racism as a key and trusted source of support for pediatric patients and their families.
Children can distinguish the phenotypic differences associated with race during infancy 73 , – 75 ; therefore, effective management of difference as normative is important in a diverse society. To identify, address, and manage the impacts of racism on child health, it is critical that pediatricians understand 3 key levels through which racism operates: (1) institutional, (2) personally mediated, and (3) internalized. The experience of race is also impacted by other identities that people have related to ethnicity, sex, religious affiliation, immigrant status, family composition, sexuality, disability, and others that must be navigated alongside race. Much of the discussion to date related to the historical underpinnings of race deals with institutionalized (or structural) racism, expressed through patterns of social institutions (eg, governmental organizations, schools, banks, and courts of law) that implicitly or explicitly discriminate against individuals from historically marginalized groups. 22 , 52 , 76 , 77 Children experience the outputs of structural racism through place (where they live), education (where they learn), economic means (what they have), and legal means (how their rights are executed). Research has identified the role of implicit and explicit personally mediated racism (racism characterized by assumptions about the abilities, motives, or intents of others on the basis of race) 78 as a factor affecting health care delivery and general health outcomes. 79 , – 86 The impacts of structural and personally mediated racism may result in internalized racism (internalizing racial stereotypes about one’s racial group). A positive racial identity mediates experiences of discrimination and generates optimal youth development outcomes. 12 , 87 , 88 The importance of a prosocial identity is critical during adolescence, when young people must navigate the impacts of social status and awareness of personally mediated discrimination based on race. 89 , – 91
Although children and adolescents who are the targets of racism experience the most significant impact, bystanders are also adversely affected by racism. As an example, young adults who were bystanders to racism and other forms of victimization as youth experience profound physiologic and psychological effects when asked to recall the memory of a past anchoring event as a victim or bystander that are comparable to those experienced by first responders after a major disaster. Three core features that characterized the abusive event(s) were as follows: (1) an individual gets hurt psychologically or physically, (2) a power differential exists (eg, age, size and/or stature, or status) versus the target individual resulting in domination and erosion of the target’s self-esteem, and (3) the abuse is repetitive, causing stress levels to increase because of anticipation of future events. 11 Internalized negative stereotypes related to race can unconsciously erode self-perception and capacity and may later play out in the form of stereotype threat or the fear of confirming a negative stereotype of one’s race. 91 Stereotype threats can undermine academic and vocational attainment, key developmental milestones for the victim. Underachievement then reinforces the stereotype held by both the perpetrator and victim, further enhancing the vulnerability of the victim and the bystander to repeated acts of overt or covert victimization. These observations suggest that universal interventions to eliminate racism (experienced as a victim or bystander) from the lives of children and to engage in active societal antiracism bystander behavioral intervention may optimize well-being for all children and the adults who care for them. For individual intervention to occur, however, bystanders must identify critical situations, view them as an emergency, develop a sense of personal responsibility, have self-efficacy to succeed with the intervention, perceive the costs of nonintervention as high, and consciously decide to help. 11 , 92 Research has demonstrated that racism has an effect on health across racial groups in communities reporting high levels of racism 93 but that racially diverse environments, such as schools, can benefit all youth by improving cognitive skills such as critical thinking and problem-solving. 94
Educational and vocational attainment are key developmental outcomes that pediatricians monitor to assess for successful growth and development. After accounting for sleep and time spent at home, children spend a significant portion of their time in educational settings. 95 , – 97 Educational achievement is an important predictor of long-term health and economic outcomes for children. Adults with a college degree live longer and have lower rates of chronic disease than those who did not graduate from college. 98 It is critical for pediatricians to recognize the institutional, personally mediated, and internalized levels of racism that occur in the educational setting because education is a critical social determinant of health for children. 99
Disparities in educational access and attainment, along with racism experienced in the educational setting, affect the trajectory of academic achievement for children and adolescents and ultimately impact health. Chronic absenteeism, defined as missing ≥10% of school days in an academic year, is a strong predictor of educational achievement. Chronic absenteeism disproportionately affects children of color, children living in poverty, children with disabilities, and children with chronic diseases. 100 In high school, 21.2% of Hispanic, 23.4% of African American, and 27.5% of American Indian children were chronically absent in 2013–2014 compared with 17.3% of white children. 101 Immigration enforcement and the fear of apprehension by authorities can negatively affect school attendance for Hispanic and black immigrants, thereby perpetuating inequalities in attendance. 102 According to the National Center for Education Statistics, the graduation rate for white students nationally in 2015–2016 was 88% compared with 76% for African American students, 72% for American Indian students, and 79% for Hispanic students. 103 Disparities in chronic absenteeism and high school graduation rates prevent children from realizing the full benefits of educational attainment and can increase the development of chronic disease and reduce overall life expectancy. 104
Although the landmark US Supreme Court case Brown v Board of Education banned government-sponsored segregation and laid a foundation for equal access to a quality public education, the US Department of Education continues to report institutional or structural inequality in educational access and outcomes, 105 even in the most diverse and well-resourced communities in the United States. Students from historically aggrieved groups have less access to experienced teachers, advanced coursework, and resources and are also more harshly punished for minor behavioral infractions occurring in the school setting. 105 They are less likely to be identified for and receive special education services, 106 and in some states, school districts with more nonwhite children receive lower funding at any given poverty level than districts with more white children. 107
Children may also experience personally mediated racism early in their schooling, which may be internalized and ultimately affect their interactions with others. 108 Early teacher-child interactions are important for long-term academic outcomes. The relationship of teacher to student across ages and grade levels influences school adjustment, literacy, math skills, grade point average, and scholastic aptitude test scores. 109 , – 111 Given the critical nature of the student-teacher relationship, it is important to explore how racism and implicit bias affect this dynamic. Student-teacher racial mismatch can impact academic performance, with studies showing that African American children are more likely to receive a worse assessment of their behavior when they have a non-Hispanic white teacher than when they have an African American teacher. 112 This finding may result from racial bias in teachers’ expectations of their students, with data demonstrating that white and other non–African American teachers are more likely than African American teachers to predict that African American students would not finish high school. 113 Similarly, data indicate that teachers may underestimate the ability of African American and Latino students, which can lead to lower grade point averages and fewer years of schooling. 114 African American students who have 1 African American teacher in elementary school are more likely to graduate from high school and enroll in college than their peers who do not have an African American teacher; the proposed mechanism for this improved long-term educational outcome is the exposure to a role model early in the educational experience. 115 These findings indicate the importance of ensuring a diverse teacher workforce, particularly as the population of students in US schools continues to diversify. 116 School racial climate, which refers to norms, curricula, and interactions around race and diversity within the school setting, also impacts educational outcomes for students. 117 Students who had a positive perception of school racial climate had higher academic achievement and fewer disciplinary issues. 118 Racial inequities in school discipline begin early, and school discipline has long-term consequences for children. Although federal civil rights laws prohibit discrimination in the administration of discipline in public schools, the US Government Accountability Office found that African American and American Indian students are overrepresented among students experiencing suspension. 119 Data from the US Department of Education confirm that a disproportionate number of African American children receive more than 1 out-of-school suspension in preschool and overall in kindergarten through grade 12 are suspended 3 times more and expelled 1.9 times more than white students. 120 To mediate the effects of institutional and personally mediated racism in the educational setting and prevent internalized racism, studies show that a positive, strong racial or ethnic identity and parental engagement in families is protective against the negative effects of racial discrimination on academic outcomes. 121 , – 123
Pediatricians and other child health professionals must be prepared to discuss and counsel families of all races on the effects of exposure to racism as victims, bystanders, and perpetrators. 124 , – 126 Pediatricians can implement systems in their practices that ensure that all patients and families know that they are welcome, that they will be treated with mutual respect, and that high-quality care will be delivered regardless of background using the tenets of family- and patient-centered care. 127 To do this, it is critical for pediatricians to examine their own biases. 128 Pediatricians can advocate for community initiatives and collaborate with government and community-based organizations to help redress biases and inequities in the health, justice, and educational systems. These strategies may optimize developmental outcomes and reduce exposure to adverse events that dramatically alter the lived experiences, health, and perceived self-value of youth. 48 , 129 , 130
In practice, pediatricians and other child health care providers encounter children every day who have experienced racism. There are interventions available for use in the medical home that can identify and potentially ameliorate inequities.
Create a culturally safe medical home 131 where the providers acknowledge and are sensitive to the racism that children and families experience by integrating patient- and family-centered communication strategies and evidence-based screening tools that incorporate valid measures of perceived and experienced racism into clinical practice. 132 , – 136
Use strategies such as the Raising Resisters approach during anticipatory guidance to provide support for youth and families to (1) recognize racism in all forms, from subversive to blatant displays of racism; (2) differentiate racism from other forms of unfair treatment and/or routine developmental stressors; (3) safely oppose the negative messages and/or behaviors of others; and (4) counter or replace those messages and experiences with something positive. 137 , 138
Train clinical and office staff in culturally competent care according to national standards for culturally and linguistically appropriate services. 139 , 140
Assess patients for stressors (eg, bullying and/or cyberbullying on the basis of race) 141 and social determinants of health often associated with racism (eg, neighborhood safety, poverty, housing inequity, and academic access) to connect families to resources. 9 , 142 , 143
Assess patients who report experiencing racism for mental health conditions, including signs of posttraumatic stress, anxiety, grief, and depressive symptoms, using validated screening tools and a trauma-informed approach to make referrals to mental health services as needed. 144
Integrate positive youth development approaches, 145 including racial socialization, 123 , 146 to identify strengths and assess youth and families for protective factors, 9 such as a supportive extended family network, that can help mitigate exposure to racist behaviors. 138
Infuse cultural diversity into AAP-recommended early literacy–promotion programs 147 to ensure that there is a representation of authors, images, and stories that reflect the cultural diversity of children served in pediatric practice.
Encourage pediatric practices and local chapters to embrace the challenge of testing best practices using Community Access to Child Health grants and participation in national quality-improvement projects to examine the effectiveness of office-based interventions designed to address the impact of racism on patient outcomes.
Encourage practices and chapters to develop resources for families with civil rights concerns, including medicolegal partnerships and referrals to agencies responsible for enforcing civil rights laws.
Encourage pediatric-serving organizations within local communities, including pediatric practices, hospitals, and health maintenance organizations, to conduct internal quality-assurance assessments that include analyses of quality of care and patient satisfaction by race and to initiate improvement protocols as needed to improve health outcomes and community trust.
Advocate for pediatric training programs that are girded by competencies and subcompetencies related to effective patient and family communication across differences in pediatric populations. 148 , 149
Encourage policies to foster interactive learning communities that promote cultural humility (eg, self-awareness, lifelong commitment to self-evaluation, and commitment to managing power imbalances) 150 , 151 and provide simulation opportunities to ensure new pediatricians are competent to deliver culturally appropriate and patient- and family-centered care. 152 , – 155
Integrate active learning strategies, such as simulation 156 and language immersion, 157 to adequately prepare pediatric residents to serve the most diverse pediatric population to date to exist in the United States 158 and lead diverse and interdisciplinary pediatric care teams. 159
Advocate for policies and programs that diversify the pediatric workforce and provide ongoing professional education for pediatricians in practice as a strategy to reduce implicit biases and improve safety and quality in the health care delivery system. 160 , – 162
Acknowledge that health equity is unachievable unless racism is addressed through interdisciplinary partnerships with other organizations that have developed campaigns against racism. 163 , 164
Engage community leaders to create safe playgrounds and healthy food markets to reduce disparities in obesity and undernutrition in neighborhoods affected by poverty.
Advocate for improvements in the quality of education in segregated urban, suburban, and rural communities designed to better optimize vocational attainment and educational milestones for all students.
Support local educational systems by connecting with and supporting school staff. The AAP Council on School Health provides resources to help physicians engage and interact with their school system and provides guidelines around the role of school physicians and school health personnel. 165 , 166
Advocate for federal and local policies that support implicit-bias training in schools and robust training of educators in culturally competent classroom management to improve disparities in academic outcomes and disproportionate rates of suspension and expulsion among students of color, reflecting a systemic bias in the educational system. 167
Advocate for increased access to support for mental health services in schools designed to help teachers better manage students with disruptive classroom behaviors and to reduce racial disparities in school expulsion. 144 , 168 , 169
Advocate for curricula that are multicultural, multilingual, and reflective of the communities in which children in their practices attend school. 170
Advocate for policies and programs that diversify the teacher workforce to mitigate the effects of the current demographic mismatch of teachers and students that affects academic attitudes and attainment for all students. 115 , 171
Advocate for evidence-based programs that combat racism in the education setting at a population level. 172 , – 174
Encourage community-level advocacy with members of those communities disproportionately affected by racism to develop policies that advance social justice. 19 , 175
Advocate for alternative strategies to incarceration for management of nonviolent youth behavior. 50 , 176 , 177
Collaborate with first responders and community police to enhance positive youth engagement by sharing expertise on child and adolescent development and mental health, considering potential differences in culture, sex, and background. 178
Advocate for fair housing practices, including access to housing loans and rentals that prohibit the persistence of historic “redlining.” 179
Advocate for funding and dissemination of rigorous research that examine the following:
the impact of perceived and observed experiences of discrimination on child and family health outcomes 180 ;
the role of self-identification versus perceived race on child health access, status, and outcomes 52 ;
the impact of workforce development activities on patient satisfaction, trust, care use, and pediatric health outcomes 161 ;
the impact of policy changes and community-level interventions on reducing the health effects of racism and other forms of discrimination on youth development; and
integration of the human genome as a way to identify critical biomarkers that can be used to improve human health rather than continue to classify people on the basis of their minor genetic differences and countries of origin. 55
Achieving decisive public policies, optimized clinical service delivery, and community change with an activated, engaged, and diverse pediatric workforce is critically important to begin untangling the thread of racism sewn through the fabric of society and affecting the health of pediatric populations. Pediatricians must examine and acknowledge their own biases and embrace and advocate for innovative policies and cross-sector partnerships designed to improve medical, economic, environmental, housing, judicial, and educational equity for optimal child, adolescent, and emerging adult developmental outcomes.
Drs Trent, Dooley, and Dougé worked together as a writing team to develop the manuscript outline, conduct the literature search, develop the stated policies, incorporate perspectives and feedback from American Academy of Pediatrics leadership, and draft the final version of the manuscript; and all authors approved the final manuscript as submitted.
This document is copyrighted and is property of the American Academy of Pediatrics and its Board of Directors. All authors have filed conflict of interest statements with the American Academy of Pediatrics. Any conflicts have been resolved through a process approved by the Board of Directors. The American Academy of Pediatrics has neither solicited nor accepted any commercial involvement in the development of the content of this publication.
Policy statements from the American Academy of Pediatrics benefit from expertise and resources of liaisons and internal (AAP) and external reviewers. However, policy statements from the American Academy of Pediatrics may not reflect the views of the liaisons or the organizations or government agencies that they represent.
The guidance in this statement does not indicate an exclusive course of treatment or serve as a standard of medical care. Variations, taking into account individual circumstances, may be appropriate.
All policy statements from the American Academy of Pediatrics automatically expire 5 years after publication unless reaffirmed, revised, or retired at or before that time.
FUNDING: No external funding.
We are grateful for internal review and critical feedback by Drs Benard Dreyer, Olanrewaju Falusi, Renee Jenkins, Judith Palfrey, Krishna Upadhya, Joseph Wright, Jonathan Klein, Janie Ward, Michael Lindsey, Lance Chilton, James Duffee, Andrea Green, Julie Linton, Virginia Keane, Jackie Nelson, Raul Gutierrez, Lase Ajayi, Lee Beers, Nathaniel Beers, Heidi Schumacher, and Tonya Vidal Kinlow.
American Academy of Pediatrics
Maria E. Trent, MD, MPH, FAAP, Chairperson
Robert M. Cavanaugh Jr, MD, FAAP
Amy E. Lacroix, MD, FAAP
Jonathon Fanburg, MD, MPH, FAAP
Maria H. Rahmandar, MD, FAAP
Laurie L. Hornberger, MD, MPH, FAAP
Marcie B. Schneider, MD, FAAP
Sophia Yen, MD, MPH, FAAP
Karen S. Smith
Lance Alix Chilton, MD, FAAP, Chairperson
Andrea E. Green, MD, FAAP
Kimberley Jo Dilley, MD, MPH, FAAP
Juan Raul Gutierrez, MD, FAAP
James H. Duffee, MD, MPH, FAAP
Virginia A. Keane, MD, FAAP
Scott Daniel Krugman, MD, MS, FAAP
Carla Dawn McKelvey, MD, MPH, FAAP
Julie Michelle Linton, MD, FAAP
Jacqueline Lee Nelson, MD, FAAP
Gerri Mattson, MD, FAAP
Donene Feist
Dana Bennett-Tejes, MA, MNM
Cora C. Breuner, MD, MPH, FAAP, Chairperson
Elizabeth M. Alderman, MD, FSAHM, FAAP
Laura K. Grubb, MD, MPH, FAAP
Janet Lee, MD, FAAP
Makia E. Powers, MD, MPH, FAAP
Krishna K. Upadhya, MD, FAAP
Stephenie B. Wallace, MD, FAAP
Liwei L. Hua, MD, PhD – American Academy of Child and Adolescent Psychiatry
Geri D. Hewitt, MD – American College of Obstetricians and Gynecologists
Seema Menon, MD – North American Society of Pediatric and Adolescent Gynecology
Ellie E. Vyver, MD, FRCPC, FAAP – Canadian Pediatric Society
Lauren B. Zapata, PhD, MSPH – Centers for Disease Control and Prevention
Competing Interests
Advertising Disclaimer »
Citing articles via
Email alerts.

Affiliations
- Editorial Board
- Editorial Policies
- Journal Blogs
- Pediatrics On Call
- Online ISSN 1098-4275
- Print ISSN 0031-4005
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Coping With Racism: A Selective Review of the Literature and a Theoretical and Methodological Critique
Elizabeth brondolo.
St. John’s University
Nisha Brady
Melissa pencille, danielle beatty.
University of Pittsburgh Medical Center

Richard J. Contrada
Rutgers, The State University of New Jersey
Racism is a stressor that contributes to racial/ethnic disparities in mental and physical health and to variations in these outcomes within racial and ethnic minority groups. The aim of this paper is to identify and discuss key issues in the study of individual-level strategies for coping with interpersonal racism. We begin with a discussion of the ways in which racism acts as a stressor and requires the mobilization of coping resources. Next, we examine available models for describing and conceptualizing strategies for coping with racism. Third, we discuss three major forms of coping: racial identity development, social support seeking and anger suppression and expression. We examine empirical support for the role of these coping strategies in buffering the impact of racism on specific health-related outcomes, including mental health (i.e., specifically, self-reported psychological distress and depressive symptoms), self-reported physical health, resting blood pressure levels, and cardiovascular reactivity to stressors. Careful examination of the effectiveness of individual-level coping strategies can guide future interventions on both the individual and community levels.
Racism is a stressor that contributes to racial/ethnic disparities in mental and physical health and to variations in health outcomes within racial and ethnic minority groups ( Anderson 1989 ; Clark et al. 1999 ; Mays et al. 2007 ; Paradies 2006 ; Williams and Williams-Morris 2000 ). Racism, in particular, self-reported ethnic or racial discrimination is a highly prevalent phenomenon. Members of most ethnic or racial minority groups report exposure over the course of their lifetime, and recent research indicates that episodes of ethnicity-related maltreatment occur on a weekly basis for some groups (Brondolo et al. 2009). The evidence points consistently to a relationship between self-reported racism and mental health impairments, specifically negative mood and depressive symptoms ( Brondolo et al. 2008 ; Kessler Mickelson and Williams 1999 ; Paradies 2006 ). Some evidence has linked self-reported racism to hypertension and a more consistent body of evidence has linked racism to risk factors for hypertension and/or coronary heart disease ( Brondolo et al. 2003 , 2008 ; Harrell et al. 2003 ; Lewis et al. 2006 ; Peters 2004 ; Steffen and Bowden 2006 ). Racism has also been linked to several other health conditions ( Paradies 2006 ), and to perceived health, which is itself a predictor of all-cause mortality ( Borrell et al. 2007 ; Jackson et al. 1996 ; Schulz et al. 2006 ).
Since racism persists within the US, it is critical to identify the strategies individuals use to cope with this stressor and to evaluate the effectiveness of these strategies. As noted by Fischer & Shaw (1999) , in 1996 the National Advisory Mental Health Council highlighted the importance of investigating individual-level factors that buffer the health effects of discrimination ( Fischer and Shaw 1999 ). Although the knowledge base has grown since 1996, there is an ongoing need for greater understanding of the ways in which individuals can mitigate the health risks associated with racial/ethnic discrimination.
The aim of this paper is to identify and discuss key issues in the study of individual-level strategies for coping with interpersonal racism. It is important to note that we do not intend this review to communicate the idea that the burden of coping with racism should be placed on the shoulders of targeted individuals alone. Eliminating racism and the effects of racism on health will require interventions at all levels: from the individual to the family, community, and nation. Nonetheless, careful examination of the effectiveness of individual-level coping strategies is needed to guide future interventions at both the individual and other levels.
We begin with a discussion of the ways in which racism acts as a stressor and requires the mobilization of coping resources. Next, we examine available models for describing and conceptualizing strategies for coping with racism. Third, we discuss three major approaches to coping: racial identity development, social support seeking, and anger suppression and expression. These coping approaches have received sufficient research attention to permit a systematic review of evidence regarding their effectiveness for both mental and physical health outcomes. In addition, these coping approaches are intuitively plausible as potential buffers of the effects of racism on health, and if shown to be effective, would lend themselves to skills and information-based intervention approaches. We examine empirical support for the role of these coping approaches in buffering the impact of racism on mental health-related outcomes (i.e., specifically, self-reported psychological distress and depressive symptoms), self-reported physical health, resting blood pressure levels, and cardiovascular reactivity to stressors. These outcomes were chosen because they have been among those most consistently identified as correlates of racism ( Paradies 2006 ). Finally, we discuss theoretical and methodological issues that are important to consider when conducting and evaluating research on strategies for coping with racism. Although much of the research on coping with racism has focused on African American samples, we have included the available data on other groups, including individuals of Asian and Latino(a) descent as well.
Definitions
Clark et al. (1999 , p. 805) define racism as “the beliefs, attitudes, institutional arrangements, and acts that tend to denigrate individuals or groups because of phenotypic characteristics or ethnic group affiliation”. Contrada and others (2000, 2001) use the more general term ethnic discrimination to refer to unfair treatment received because of one’s ethnicity, where “ethnicity” refers to various grouping of individuals based on race or culture of origin. We consider racism a special form of social ostracism in which phenotypic or cultural characteristics are used to assign individuals to an outcast status, rendering them targets of social exclusion, harassment, and unfair treatment.
Racism exists at multiple levels, including interpersonal, environmental, institutional, and cultural ( Harrell 2000 ; Jones 1997 , 2000 ; Krieger 1999 ). However, the bulk of empirical research on coping with racism focuses on strategies for coping with interpersonal racism. Interpersonal racism has been defined by Krieger as “directly perceived discriminatory interactions between individuals whether in their institutional roles or as public and private individuals” ( Krieger 1999 , p. 301). Racism may have deleterious effects even when the target does not consciously perceive the maltreatment or attribute it to racism. However, this review considers the effectiveness of individual-level coping strategies employed to address episodes of racism that are both directly experienced and perceived. This focus on an interpersonal approach to examining racism is consistent with much recent work by Smith and colleagues examining the health effects of other psychosocial stressors (e.g., poverty) within an interpersonal context (see, for example, Gallo et al. 2006 ; Ruiz et al. 2006 ; Smith et al. 2003 ).
Types of ethnicity-related maltreatment
Racism/ethnic discrimination can encompass a wide range of acts including social exclusion, workplace discrimination, stigmatization, and physical threat and harassment ( Brondolo et al. 2005a ; Contrada et al. 2001 ). Social exclusion includes a variety of different interactions in which individuals are excluded from social interactions, rejected, or ignored because of their ethnicity or race. Stigmatization can include both verbal and non-verbal behavior directed at the targeted individual that communicates a message that demeans the targeted person (e.g., communicates the idea that the targeted individual must be lazy or stupid because he or she belongs to a particular racial or ethnic group). Workplace discrimination includes acts directed at individuals of a particular race or ethnicity that range from the expression of lowered expectations to a refusal to promote or hire. Threat and harassment can include potential or actual damage to an individual or his or her family or property because of ethnicity or race. Any of these discriminatory acts can be overt, such that the racial bias is made explicit (e.g., when accompanied by racial slurs), or the acts can be covert such that racial bias may not be directly stated but is implicit in the communication ( Taylor and Grundy 1996 ).
Racism as a stressor
A number of conceptual models, including those which consider racism within stress and coping frameworks, have described the ways that racism may confer risk for health impairment ( Anderson et al. 1989 ; Clark et al. 1999 ; Harrell et al. 1998 ; Krieger 1999 ; Mays et al. 2007 ; Outlaw 1993 ; Williams et al. 2003 ). In general, each model emphasizes the need to consider the acute effects of individual incidents of ethnicity-related maltreatment, as well as factors that sustain the damaging effects of these events. They highlight the importance of considering racism as a unique stressor, and as a factor that may interact with other potential race and non-race-related stressors, including low socioeconomic status and neighborhood crime. Racism itself and the environmental conditions associated with racism (e.g., neighborhood segregation) limit access to coping resources. The cumulative effects of acute and sustained stress exposure, combined with limited coping resources are likely to cause perturbations in neuroendocrine and autonomic systems that respond to acute stressors and that maintain or re-establish physiological homeostasis ( Gallo and Matthews 2003 ; McEwen and Lasley 2003 , 2007 ).
From the perspective of the targeted individual, racism is a complex stressor, requiring a range of different coping resources to manage both practical and emotional aspect of the stressor. Features of the racist incident, as well as the corresponding coping demands, may vary depending upon the physical, social, and temporal context of exposure. Targets must cope with the substance of racism, such as interpersonal conflict, blocked opportunities, and social exclusion. They must also manage the emotional consequences, including painful feelings of anger, nervousness, sadness, and hopelessness, and their physiological correlates. Targets may also need to manage their concerns about short and long term effects of racism on other members of their group, including their friends and family members. Indirect effects of racism (e.g., poverty, environmental toxin exposure, changes in family structure) may require additional coping efforts ( Mays et al. 1996 ). A theme that may cut across and link many or even most of the coping tasks posed by racism is the management of damage to self-concept and social identity ( Mellor 2004 ).
Episodes of ethnicity or race-based maltreatment can occur in a number of different venues. The effectiveness of the coping response may vary depending on the context in which the maltreatment occurs. Factors that may influence the choice and effectiveness of a coping strategy include variations in the intensity and nature of the threat, the perceived degree of intentionality of the perpetrator, the potential consequences of the act and of the coping response, the availability of resources to assist the target, and perceptions of the need to repeatedly muster different coping resources and the appraisal of one’s ability to do so ( Richeson and Shelton 2007 ; Scott 2004 ; Scott and House 2005 ; Swim et al. 2003 ).
Different types of coping may be needed at different points in time: in anticipation of potential exposure to ethnicity-related maltreatment, at the time of exposure, following the episode, and when considering longer term implications of persistent or recurring exposure. The strategies that are effective for quickly terminating a specific episode of maltreatment are not necessarily the same as those needed to manage the possibility of longer term exposure. A variety of coping strategies may be needed at each point.
Consequently, one of the most serious challenges facing minority group members is the need to develop a broad range of racism-related coping responses to permit them to respond to different types of situations and to adjust the response depending on factors that might influence the effectiveness of any particular coping strategy. Targets must also develop the cognitive flexibility to implement an appropriate and effective strategy in each of the wide range of situations in which they may be exposed to discrimination, judge the relative costs and benefits of these strategies, and deploy them as needed over prolonged periods of time. This level of coping flexibility is beneficial, but difficult to achieve ( Cheng 2003 ). The perception that one’s coping capacity is not adequate to meet the demands increases the likelihood that ethnicity-related maltreatment will be experienced as a chronic stressor.
Coping with racism: models and measures
There are a number of early models ( Allport 1954 ; Harrell 1979 ) of the different strategies individuals used to respond to racism that have been reviewed in Mellor (2004) . Some of the difficulties with these models are a function of more general problems with models of coping that have been well reviewed elsewhere ( Skinner et al. 2003 ). Other concerns are more specific to the difficulties of developing models for coping with racism.
Most models fail to explicitly incorporate strategies designed to manage the interpersonal conflict associated with ethnicity-related maltreatment as well as with its emotional sequelae. They do not always include strategies both for coping with an acute event (i.e., responding to the perpetrator during episodes of ethnicity-related maltreatment) and for coping with the awareness that race-related maltreatment is likely to be an ongoing stressor. Additionally, it can also be difficult to determine if the coping strategies included in the models are intended to address racism specifically or the various consequences of discrimination, such as unemployment, denial of a job promotion, or poverty.
More recent work has utilized dimensions of coping that are more explicitly tied to theories of stress and coping, including problem-focused coping, emotion-focused coping, approach versus avoidance coping, and social support ( Danoff-Burg et al. 2004 ; Scott 2004 ; Scott and House 2005 ; Thompson Sanders 2006 ). However, as Mellor (2004) points out, many of the strategies included in models of coping responses can only be loosely organized according to available rubrics for categorizing coping strategies. For example, it is unclear how to classify spirituality and Africultural coping, which appear to represent multifaceted strategies with some aspects involving problem-focused coping and others involving emotion-focused coping ( Constantine et al. 2002 ; Lewis-Coles and Constantine 2006 ; Utsey et al. 2000a ). There have been inconsistencies even within specific coping domains. For example, seeking social support when confronted by racism has been considered an approach coping strategy ( Scott 2004 ; Scott and House 2005 ; Thompson Sanders 2006 ), a problem-focused coping strategy ( Noh and Kaspar 2003 ; Plummer and Slane 1996 ), an emotion-focused strategy (such as when seeking emotional social support) ( Tull et al. 2005 ), an avoidance strategy (if it involves venting, but no direct confrontation), and a strategy in an entirely separate category ( Danoff-Burg et al. 2004 ; Swim et al. 2003 ; Utsey et al. 2000b ).
Mellor (2004) suggests an alternate framework for organizing racism-related coping that focuses on the function of the coping strategies versus the content of their focus. His model highlights the importance of distinguishing between tasks that serve to prevent personal injury (e.g., denial, acceptance) from those that are intended to remediate, prevent, or punish racism (e.g., assertiveness, aggressive retaliation). This functional approach may be an important step toward developing more effective models of coping with racism, particularly if the purpose is closely linked to the various specific challenges that face targets of discrimination.
Measurement issues
The development of more comprehensive models is further limited by the small number of instruments available to assess racism-related coping. The Perceived Racism Scale ( McNeilly et al. 1996 ) is one of the only instruments available to assess strategies for coping with racism. It is intended for use with African Americans and measures both exposure to experiences of ethnicity-related maltreatment and coping responses to the exposure. For each venue or domain in which racist events might occur (i.e., job-seeking, educational settings, the health-care system), participants are asked to indicate the cognitive, affective, and behavioral responses used to cope with each experience. Other researchers have used generic coping scales (e.g., the Ways of Coping or the Spielberger Anger Expression Inventory) and modified the presentation to inquire about coping in response to race-related maltreatment (e.g., Brondolo et al. 2005b ).
Each of these measures is subject to the limitations of traditional self-reported trait coping indices ( Lazarus 2000 ). It is difficult to evaluate the timing or circumstances in which the coping response is used. For example, when the Self-Report Coping Scale ( Causey and Dubow 1992 ) is applied to the study of racism-coping (e.g., Scott and House 2005 ), participants indicate the degree to which they use strategies such as externalizing (i.e., getting mad or throwing things) as a response to race-related stress. It is unclear if the item refers to expressing anger at the perpetrator of the racist acts (possibly a problem-focused or approach coping strategy) or discharging anger later when thinking about specific incidents (possibly an emotion-focused coping strategy).
Careful delineation of the timing and function of the coping strategy is valuable, because there may be some strategies that are effective in the short run, but counterproductive if used persistently over time. For example, “keeping it to myself” may be a safe strategy to use as an immediate course of action in a situation in which the target may face immediate retaliation, but may be deleterious once the acute maltreatment has ended. Similarly, there may be strategies that are effective and acceptable in some settings, but not others. Measures which include items assessing both immediate and longer term responses and inquire about the circumstances of exposure to maltreatment are needed.
How do people cope with racism?
There are no population-based epidemiological data on the strategies most commonly used to cope with episodes of ethnicity-related maltreatment at the time of the event. There are very limited population-based data on the strategies used to manage discrimination in general. In a population-based sample of over 4,000 Black and White men and women, participants were asked about the ways they handled episodes of racial discrimination ( Krieger and Sidney 1996 ). Most (69–78% depending on race and gender group) indicated they would “try to do something and talk to others.” Only 17–19% indicated that they would “accept it as a fact of life and talk to others.” Most individuals (86–97%) indicated that they would talk to others whether they took action in response to racism or accepted the racist behavior ( Krieger and Sidney 1996 ). In contrast to the tendency of Black and White Americans to indicate that they would try to do something about racism, other research suggests that Asian immigrants in Canada would prefer to “regard it as a fact of life, avoid it or ignore it” ( Noh et al. 1999 ). The ethnic and national differences in response suggest that the moderating effects of culture and immigration status on racism and coping must be further evaluated in larger ethnically diverse population-based studies.
Evaluating different coping approaches
In the next three sections, we review in detail the data on the effectiveness of three coping approaches that have been considered as responses to racism: racial identity development, social support seeking, and confrontation/anger coping. We restrict the reviews to published, peer-reviewed papers. For each topic area, studies for consideration were identified by accessing all major databases including PsychInfo, ERIC, MEDLINE, and Sociology Abstracts, using both ProQuest and EBSCO search engines. We included thesaurus terms racism, ethnic discrimination, racial discrimination, race discrimination, race-related stress . For a general review, we included the terms: coping, active coping, approach coping, stress-management . For the specific review on racial and ethnic identity, we included the terms: racial identity, ethnic identity, and racial socialization. For the section on social support, we included terms: support, social support, support coping, active coping, approach coping . For the section on anger, we included the terms: confrontation, anger, anger expression, anger suppression, anger management, anger-in, anger-out . We further searched the reference sections of each paper to identify additional studies. We also examined all published work of each author of each paper to determine if additional studies could be identified. Examining the empirical data on these three coping approaches highlights in specific detail some of the methodological issues involved in research investigating effective strategies for coping with racism.
Our evaluation of coping effectiveness focuses on stress-buffering effects. A coping response may be said to buffer stress when, among individuals exposed to the stressor, those who engage in that response (or who engage in it to a greater degree) are less likely to experience a negative outcome than those who do not (or who engage in it to a lesser degree). The relative benefit associated with performing the coping response should be smaller or not at all in evidence among those who are not exposed to the stressor. It should be noted that stress-buffering is not the only manner in which a coping response might confer an advantage. Other models are plausible, including mediational models that describe a causal chain in which exposure to stress promotes performance of the coping response which, in turn, promotes more positive outcomes. However, a focus on stress-buffering is warranted since the aim of the paper is to identify those strategies which might be effective in ameliorating the health effects of exposure to racism, and could form the basis of coping-based interventions. Figure 1 provides a graphical illustration of these different possible pathways.

Different pathways through which coping approaches may offset the effects of racism on mental and physical health.
Racial/ethnic identity as a buffer of the effects of racism on distress
Based on Phinney (1990 , 1996) , Cokley (2007 , p. 225) defines ethnic identity as “the subjective sense of ethnic group membership that involves self-labeling, sense of belonging, preference for the group, positive evaluation of the ethnic group, ethnic knowledge, and involvement in ethnic group activities.” Similarly, racial identity has been defined as “a sense of group or collective identity based on one’s perception that he or she shares a common racial heritage with a particular racial group” ( Helms 1990 , p. 3). There are differences of opinion about the degree to which ethnic and racial identity represent distinct constructs ( Cross and Strauss 1998 ; Helms 1990 ; Phinney and Ong 2007 ). Definitions of both constructs include a focus on shared history, values, and a common heritage. However, those who advocate the study of racial identity as a separate construct suggest that it entails a complex developmental process, reflecting the individual’s attempts to resolve the problems associated with racism directed both at the individual and at the group as a whole.
How could racial or ethnic identity serve as a coping strategy?
Racial and ethnic identity are generally considered individual difference variables, (i.e., an underlying set of schemas that help individuals make sense of and respond to their experiences as a member of their ethnic or racial group) ( Cross and Strauss 1998 ; Helms 1990 ; Phinney and Ong 2007 ). However, researchers explicitly link the process of developing an ethnic identity to other acts that can have stress-buffering effects ( Phinney et al. 2001 ). Some research explicitly frames ethnic identity as a variable possessing characteristics similar to other potential coping responses, capable of buffering the effects of stress exposure (see for example, Lee 2003 ). Despite the ambiguity about the degree to which racial identity can be considered within the domain of coping resources, research on racial identity has a potential impact on public health. If racial identity is mutable, and aspects of racial identity are effective in modifying psychological or psychophysiological responses to racism, those aspects of identity could be incorporated into health communications and could guide racial socialization practices.
Racial/ethnic identity may serve as a coping mechanism in several different ways. Specifically, some aspects of racism may influence the salience of race-related maltreatment and affect the subsequent appraisals of and coping responses to these events ( Oyserman et al. 2003 , Quintana 2007 ). A well-developed racial identity may be associated with historical and experiential knowledge about one’s own group and its social position. In turn this knowledge may help a targeted individual distinguish between actions directed at the person as an individual versus those directed at the person as a member of a particular group ( Cross 2005 ). This can protect targeted individuals from injuries to self-esteem or distress when they are exposed to negative events that may be a function of ethnic discrimination rather than individual characteristics of behavior ( Branscombe et al. 1999 ; Mossakowski 2003 ; Sellers and Shelton 2003 ). Racial socialization could provide an individual with an opportunity to consider possible approaches to this maltreatment and could serve to expedite the implementation of coping responses ( Hughes et al. 2006 ). Ethnic connection and belonging could ameliorate some of the pain of ostracism from other groups.
Appreciating the potential benefits of a well-developed sense of ethnic or racial identity, investigators have generated a large body of research that has examined the nature of racial and ethnic identity, and a smaller body of research that has tested the hypothesis that a strong positive racial or ethnic identity might buffer the effects of racism on mental health/psychological distress. However, the findings to date have been conflicted and present a number of methodological problems that need resolution.
Our review identified 12 published peer-reviewed papers that explicitly tested the hypothesis that ethnic or racial identity buffers the effects of exposure to racism on psychological distress or depression ( Banks and KohnWood 2007 ; Bynum et al. 2007 ; Fischer and Shaw 1999 ; Greene et al. 2006 ; Lee 2003 , 2005 ; Mossakowski 2003 ; Noh et al. 1999 ; Sellers et al. 2003 , 2006 ; Sellers and Shelton 2003 ; Wong et al. 2003 ). Details of the studies, including the samples, measures, and results, are presented in Table 1 . The effects of ethnic identity as a buffer of the relationship of racism to depressive symptoms or psychological distress were tested in samples of African Americans, Filipinos, Koreans, South Asian Indians, and Latino(a)s, with most, but not all, studies employing samples of convenience.
Studies of the buffering effects of racial identity on the relationship of racism to mental physical health indices
Note. AA = African American; MH = mental health; sx = symptoms; discrim. = discrimination; EI = ethnic identity. MIBI = Multidimensional Inventory of Black Identity ( Sellers, Smith, Shelton, Rowley, & Chavous, 1998 ). RaLES Daily Exper. = Daily Life Experiences subscale from the Racism and Life Experience Scales ( Harrell, 1997 ). CES-D = Center for Epidemiological Studies Depression Scale ( Radloff, 1977 ). TERS = Teenager Experience with Racial Socialization Scale ( Stevenson et al., 2002 ). BSI = Brief Symptom Inventory ( Deragotis & Melisarotis, 1983 ). PSS = Perceived Stress Scale ( Cohen & Williamson, 1988 ). RaLES-R - Brief Racism Scale = Brief Racism Scale from the Racism and Life Experiences Scales-Revised ( Harrell, 1997a , 1997b ). SORS-A = Scale of Racial Socialization for Adolescents ( Stevenson, 1994 ). SRE = Schedule of Racist Events ( Landrine & Klonoff, 1996 ). MHI = Mental Health Inventory ( Veit & Ware, 1983 ). MEIM = Multigroup Ethnic Identity Measure ( Phinney, 1992 ); EI = ethnic identity. PDS = Perceived Personal Ethnic Discrimination ( Finch et al., 2000 ). SCL-90 = Symptom Checklist – 90 – Revised ( Deragotis, 1994 ). DLE = Daily Life Experience subscale of the Racism and Life Experience scales ( Harrell, 1994 ). STAI = State–Trait Anxiety Inventory ( Spielberger, 1983 ).
These studies assessed different aspects of ethnic or racial identity and used several different strategies for measuring these dimensions. Some investigators used measures of pride or belonging, including the Multi-Ethnic Identity Measure (MEIM; Phinney 1992 ) or the private regard subscale of the Multidimensional Inventory of Black Identity (MIBI; Sellers et al. 1997 ). Other investigations included measures of racial centrality, a construct involving the degree to which one’s race or ethnicity forms an important part of self-concept ( Sellers et al. 1997 ). Still other studies included aspects of racial identity that refer to the development of preparation for discrimination, including measures of racial socialization. Three studies ( Greene et al. 2006 ; Sellers et al. 2003 ; Wong et al. 2003 ) used longitudinal designs to examine the degree to which racial identity buffers racism-related changes in depression. The remainder used cross sectional, correlational designs. In all the studies, participants completed measures of racial identity, perceived racism and a measure of depression or psychological distress. To test the buffering effects of racial identity, all researchers directly examined the statistical interactions of racial identity and racism on measures of distress, with the exception of those who used path analytic models ( Sellers et al. 2003 ).
These studies provide only very limited evidence for the hypothesis that racial or ethnic identity buffers the effects of racism on psychological distress. Of the 12 studies specifically examining effects of racism on distress or depression, only two found evidence of a buffering effect of racial identity on at least one measure of distress ( Fischer and Shaw 1999 ; Mossakowski 2003 ). One study was a population-based study investigating these issues in Filipino-American adults ( Mossakowski 2003 ). In this study, ethnic identity acted as a buffer only for the predictive effects of a single item measure of discrimination on depressive symptoms. Ethnic identity did not appear to buffer the effects of everyday maltreatment on depressive symptoms. The other study reporting buffering effects on depressive symptoms was a study of African American young adults ( Fischer and Shaw 1999 ). Six studies ( Bynum et al. 2007 ; Fischer and Shaw 1999 ; Lee 2003 , 2005 ; Sellers et al. 2003 ; Wong et al. 2003 ) reported no buffering effects for either distress or depression. Four studies found some evidence that an aspect of ethnic identity (i.e., pride; Lee 2005 ); public regard ( Sellers et al. 2006 ); commitment/centrality ( Noh et al. 1999 ) or positive attitudes towards other cultures ( Banks and Kohn-Wood 2007 ) may intensify the relationship of racism to distress. 1
In contrast, positive main effects of racial identity on distress were obtained in several studies examining dimensions related to ethnic pride or attachment (e.g., positive attachment to one’s ethnic group (i.e., including the MEIM; Phinney 1992 ), the private regard component of the MIBI or the cultural pride dimension of racial socialization or connection to ethnic group) ( Bynum et al. 2007 ; Lee 2005 ; Mossakowski 2003 ; Sellers et al. 2006 ; Wong et al. 2003 ). However, some studies obtained null ( Fischer and Shaw 1999 ; Lee 2003 ; Noh et al. 1999 ; Wong et al. 2003 ) or reverse effects ( Bynum et al. 2007 ). The effects for dimensions such as centrality were more mixed, with some studies reporting that greater racial centrality was associated with less negative mood ( Sellers et al. 2003 ), whereas another study failed to find the same connection ( Sellers et al. 2006 ). In one study a measure that more explicitly assess those aspects of identity that address preparedness for discrimination was associated with increased distress ( Bynum et al. 2007 ).
These main effects analyses suggest that the pride and belonging dimensions of racial identity may produce a more general feeling of well-being. Aspects of racial identity may buffer the effects of other stressors common to the research participants that were not assessed in the study. However, the effects of these positive racial identity dimensions were not sufficient to offset the impact of perceived racism, and in particular everyday maltreatment, on distress and depressive symptoms.
Findings from Lee (2005) suggest a complex relationship of centrality and pride to depression. In this study of Asian young adults, there was a significant main effect of Ethnic Identity (EI)-Pride, such that those with relatively high scores on the ethnic pride dimension of the MEIM (derived from a factor analysis conducted in the same sample) had fewer depressive symptoms than those with low scores. However, among those with high EI-Pride scores, the effects of racism on depressive symptoms were stronger than for those who did not feel a great deal of pride in their ethnic group. This suggests that enhancing pride may reduce depression overall, but may be related to greater symptom reports when individuals are exposed to racism. Racial identity as a buffer of cardiovascular reactivity to race-related stress
There are also two studies that examined racial identity as a moderator or buffer of the relationship of race-related stress to an index of cardiovascular response. These measures of cardiovascular reactivity (CVR) appear to be markers for processes involved in the development of hypertension and coronary heart disease. However, it is difficult to evaluate the meaning of reactivity data in some of these studies, since there are some limitations to the presentations of the existing studies. Clark and Gochett (2006) reported finding an inverse relationship between private regard and cardiac output and stroke volume (measures of sympathetic nervous system influences on the heart) before, during, and after racial and non-racial stressors. The authors interpreted the inverse relationship to suggest higher levels of arousal for those high in private regard; however, analyses directly examining the relationship of identity to the change from baseline are not reported. Similarly, Torres and Bowens (2000) reported positive correlations of the Black Racial Identity Attitude Scale (RIAS-B) internalization attitudes (indicating more acceptance of both Black and Caucasian groups) with systolic blood pressure (SBP) reactivity to both race and non-race related stressors. These findings may indicate that individuals with Black oriented identities (i.e., those who are low on internalization) are better prepared to confront episodes of racism as they expect this maltreatment. However, the data are difficult to interpret, as greater increases in SBP may also indicate greater task engagement and no measures were made of level of effort or involvement. Without data on subjective response to the task, it is difficult to interpret these findings.
In contrast, in a study of the main effect of racial identity on both resting and ambulatory blood pressure (BP), Thompson et al. (2002) found that a transitional racial identity, marked by an intense involvement in in-group activities and an “idealization of African American and African American culture and a devaluation of White culture,” was associated with higher levels of resting and ambulatory BP. The authors suggest that a transitional identity may intensify the perception of racial bias and make race-related conflict more salient, increasing the frequency with which individuals experience interpersonal stress. However, no data were available on the race-related social interactions experienced by the participants.
What accounts for the mixed findings on the effects of racial identity?
The effects of racial identity on mental and physical health are complex, and the data do not support a uniformly positive effect of each aspect of racial or ethnic identity on mental health. The bulk of the evidence suggests that ethnic pride may be associated with fewer depressive symptoms overall, but the results indicate that pride and other aspects of ethnic/racial identity are not sufficient to buffer the effects of racism on depressive symptoms for most (but not all) samples. It is important to note that some aspects of racial identity appear to intensify the relationship of racism to depression.
Ethnic pride may not buffer the pain of race-based ostracism, since social rejection is painful, even when other sources of social connection are available ( Baumeister et al. 2005 ; MacDonald and Leary 2005 ). Further, race-based social rejection or exclusion may heighten the awareness of race-related stereotypes and elicit concerns about stereotype threat. In turn these concerns may evoke feelings of anxiety and shame ( Cohen and Garcia 2005 ; Steele 1997 ). Messages of cultural pride may not be adequate to counteract the emotional consequences of demeaning treatment.
There is also some evidence that ostracism is associated with a decrease in self-awareness and self-regulation ( Baumeister et al. 2005 ; MacDonald and Leary 2005 ). This blunting of self-awareness may help the individual block some of the injury to self-esteem associated with social rejection. However, reductions in self-awareness in response to personal threat may also limit the individual’s ability to access self-related schemas (e.g., racial identity or ethnic pride) that might facilitate coping. Laboratory studies are needed to assess the effects of priming racial salience on responses to acute race-related stressors and to evaluate the effects of increasing versus decreasing self-awareness during these manipulations ( Baumeister et al. 2005 ).
The effects of racial centrality appear to be more variable than the effects of racial/ethnic pride and belonging. There may be circumstances in which drawing attention to race and heightening awareness of potential exposure to racism protect individuals from its harmful effects ( Fischer and Shaw 1999 ), but there is also evidence that racial centrality can intensify distress ( Sellers et al. 2006 ). The awareness that one may be targeted for racism may help individuals gather the strength they need to avoid being denied rights or misjudging their own competence, but this awareness can also be exhausting, elicit distress and anger, and erode some relationships. This is consistent with data on the use of avoidance coping in African Americans reported by Thompson Sanders (2006) . Further work is needed to identify the types and timing of the complex of racial socialization messages that increase awareness without destroying hope or inflicting a costly emotional burden. The nature of these messages may vary by socioeconomic status and parental involvement, and some personality dimensions ( Scott 2003 , 2004 ), and the role of these potential moderators has also not been adequately explored.
There is some evidence that racial identity buffers the effects of racism on self-esteem and some measures of academic performance (e.g., Oyserman et al. 2001 ; Wong et al. 2003 ). Failure to find substantial buffering effects for depression and distress may be a function of the need to match the type of coping strategy with the expected outcome. Racial identity is related to self-concept and pride, and as a consequence may have effects primarily on aspects of functioning that are tied to self-concept versus more global affective states.
The data on the effectiveness of racial identity as a buffer of the relationship of racism to BP or BP reactivity is too limited to support firm conclusions. The findings suggest, however, that measures of racial identity may tap psychological dimensions that influence coping with stressors on a day-to-day basis. These schemas may influence the degree to which individuals are able to engage in challenge or feel they must defend themselves from threat. Both engagement and defensiveness influence cardiovascular dynamics. Continued research on the ways in which racial identity affects appraisals of laboratory tasks and everyday events, and in turn influence cardiovascular and neuroendocrine responses, would be very useful.
Social support as a buffer of the effects of racism on mental and physical health
Social support has been defined as the presence or availability of network members who express concern, love, and care for an individual and provide coping assistance ( Sarason et al. 1983 ). Seeking social support involves communication with others (e.g., family, friends, and community members) about events or experiences. Within the Black community, seeking social support has sometimes been more specifically labeled as “leaning on shoulders” ( Shorter-Gooden 2004 ). This term refers to seeking out and talking to others as a means of coping with racial discrimination.
How might social support buffer the effects of racism on distress?
It is widely accepted that social support is beneficial for physical and psychological health ( Allgower et al. 2001 ; Barnett and Gotlib 1988 ; Symister and Friend 2003 ). A supportive social network promotes a sense of security and connectedness, helping the individual to understand that discrimination is a shared experience. Group members can serve as models, guiding the individual in effective methods for responding to and coping with discrimination. Placing the event in a collective context can also help the individual to feel more connected to his or her ethnic/racial group and can activate racial identity ( Harrell 2000 ; Mellor 2004 ). Greater participation in social activities may help to distract individuals and provide them with positive experiences that may buffer the negative impact of a range of stressors including racism ( Finch and Vega 2003 ).
Seeking social support is commonly used as a coping strategy following a racist incident ( Krieger 1990 ; Krieger and Sidney 1996 ; Lalonde et al. 1995 ; Mellor 2004 ; Shorter-Gooden 2004 ; Swim et al. 2003 ; Thompson Sanders 2006 ; Utsey et al. 2000b ). In Black college students, Swim et al. (2003) found that 68% of the sample discussed a racist incident with their family, friends, or others. In two separate studies, Krieger found that the vast majority of Black individuals sampled reported “talking to others” in response to racial discrimination ( Krieger 1990 ; Krieger and Sidney 1996 ). Furthermore, a majority of Black Canadians reported “seeking advice” and “telling others about the discrimination” in response to a hypothetical situation involving housing rejection based on ethnic discrimination ( Lalonde et al. 1995 ). Although social support is hypothesized to serve as an effective strategy for coping with racism, there has been surprisingly limited empirical research testing this hypothesis.
We are aware of only three empirical tests of the hypothesis that social support buffers the effects of racism on distress ( Fischer and Shaw 1999 ; Noh and Kaspar 2003 ; Thompson Sanders 2006 ), and four studies examining the hypothesis that social support buffers the effects of racism on physical health-related measures (i.e., self-reported health or cardiovascular reactivity to stress) ( Clark 2003 ; Clark and Gochett 2006 ; Finch and Vega 2003 ; McNeilly et al. 1995 ). Diverse ethnic groups were included in the studies. Some studies assessed the tendency to seek social support or guidance in response to racist events ( Noh and Kaspar 2003 ; Thompson Sanders 2006 ), whereas others examined the availability of support (i.e., size of network) or quality of general social support ( Clark 2003 ; Finch and Vega 2003 ; Fischer and Shaw 1999 ; McNeilly et al. 1995 ). Further details of the studies are presented in Table 2 .
Studies of the buffering effects of social support on the relationship of racism to mental or physical health indices
Note. sx = symptoms; discrim. = discrimination. SBP = systolic blood pressure; DBP = diastolic blood pressure. BP = blood pressure. SRE = Schedule of Racist Events ( Landrine & Klonoff, 1996 ). MHI = Mental Health Inventory ( Veit & Ware, 1983 ). CES-D-K = Korean version of the Center for Epidemiologic Studies Depression Scale ( Noh et al., 1998 ; Radloff, 1977 ). CRI = Coping Responses Inventory–Adult Form ( Moos, 1993 ).
The three studies examining the buffering effects of seeking social support on the relationship of racism to distress failed to find positive effects ( Fischer and Shaw 1999 ; Noh and Kaspar 2003 ; Thompson Sanders 2006 ). However, two of these three studies found main effects of social support on depressive symptoms.
The effects are more mixed among the four studies examining the buffering effects of support on a health-related outcome. Finch and Vega (2003) found robust effects of instrumental support on perceived health in a population-based sample of Mexican Americans. Discrimination was not related to health among those with high levels of support, but was associated with poorer health for those with low levels of support. Two studies found buffering effects of support seeking, but only for those who were exposed to low levels of racism ( Clark 2003 ; Clark and Gochett 2006 ). Specifically, Clark (2003) reported that self-reported quantity and quality of social support were associated with reduced DBP reactivity to a non-racial stressor (i.e., mental arithmetic), but only for those who had experienced relatively low levels of racism over the course of their lives. Similarly, in a school-based study, Clark and Gochett (2006) found that youth who indicated that they would “talk to others” had a lower incidence of elevated BP (above 90th percentile) than those who did not endorse this item, but these effects were seen only among those who experienced low levels of racism. In contrast, among those exposed to high levels of racism, “talking to others” was associated with a higher prevalence of elevated BP. Finally, in a laboratory study, McNeilly et al. (1995) reported that providing support (in the form of a supportive confederate) did not reduce cardiovascular reactivity in response to racist provocation (i.e., debating about race-related topics), but did reduce self-reported anger. There are two additional studies that examined the relationship of support to race-related stress in African Americans, but they did not directly test the hypothesis that social support buffers the effects of racism on psychological distress ( Scott and House 2005 ; Utsey et al. 2000a, b ).
Despite the generally null findings of the quantitative studies, two qualitative reports about seeking social support in response to ethnic or racial discrimination suggest beneficial effects. In a diary study of perceived discrimination, participants reported that it was helpful to discuss racist incidents with another person ( Swim et al. 2003 ). Similarly, African American men participating in an African-centered support group for confronting racism reported decreases in levels of anger and frustration. They also reported engaging in fewer interpersonal conflicts with significant others after attending the support group ( Elligan and Utsey 1999 ).
What accounts for the mixed findings on social support?
Overall, the quantitative literature provides minimal support for the hypothesis that social support (either seeking social support or having a supportive network) buffers the impact of racism on psychological health. It also provides very mixed support for the notion that social support buffers racism effects on indices of physical health. There is some suggestion that social support may be helpful at low levels of stress exposure, but exacerbates difficulties at high levels of exposure. Yet, these results are contrary to anecdotal reports or findings from qualitative studies, and largely contrast with the findings from other literatures on the buffering effects of support in the face of other stressors (mostly medical illnesses). What accounts for these variations?
Measures and research design
General difficulties with the social support research have been outlined by Uchino (2006) . Variations in the conceptualization and measurement of social support make the results of studies examining the effects of support as a buffer of the effects of racism on distress or health difficult to interpret. In the studies reviewed, four separate support-related constructs have been studied: seeking support to obtain guidance for ways to manage racism; general support network size, general support network quality, and the proportion of relationships with people of the same ethnicity. The quality of the measurement instruments also varies, with some studies assessing social support seeking using two questions in a self-report survey or diary ( Noh and Kaspar 2003 ; Swim et al. 2003 ).
The research designs of some studies also have some limitations, as cross sectional correlational designs fail to reveal the direction of the effects. In the Clark and Gochett (2006) study, there are some correlations between exposure to higher levels of racism and seeking support, suggesting that the level of support seeking is in fact a function of the degree of stress exposure. Prospective cohort and laboratory studies may be necessary to more clearly distinguish the direction of the relationship between support and distress. Different types of support may be necessary at different points in time, and no studies have examined perceived needs for support at different stages in the experience of ethnicity-related maltreatment. For example, concrete advice and emotional support may be needed at the time of the incident, whereas support focused on meaning and hope may be needed as individuals confront the possibility of more sustained exposure.
Social constraint and facilitation
Some of the failure to find positive effects associated with social support may be a function of issues related to both social constraint and social facilitation. Lepore and Revenson (2007) propose that social constraints limit the effectiveness of certain social support interventions. Seeking support for race-related maltreatment may entail discussions that are anxiety provoking for both the seekers and givers of support. For members of stigmatized groups, discussions of racism may evoke recollections that feel uncontrollable and are stressful. For members of a majority out-group, stereotype threat may be evoked if individuals become concerned about appearing cruel, uncaring, or insensitive when discussing race-related conflict ( Richeson and Shelton 2007 ). Anxiety on the part of both the in-group and out-group members may inhibit effective communication about race-related incidents. When individuals receive messages that tend to minimize or deny aspects of their experience, support seeking may be ineffective and associated with increased versus decreased distress ( Badr and Taylor 2006 ). Research on the dynamics of interracial communication may provide guidance for further research on the types of communication that can minimize social constraints and facilitate inter-racial communication ( Czopp et al. 2006 ; Richeson and Shelton 2005 ).
As Utsey et al. (2002) points out, social facilitation may increase distress when individuals discuss discrimination with other members of their group. The experience of sharing episodes of ethnicity-related maltreatment may arouse greater anger as individuals exchange accounts of their experiences. If the situations appear hopeless or if individuals in the discussion have had negative experiences managing race-related interactions themselves, other negative emotions, including fear, frustration, grief, shame and loss, may also be evoked. Further research is needed to determine how variations in the circumstances in which support is sought and in the content of support message confer different costs and benefits to the target of discrimination. It will be important to understand how best to acknowledge the difficulties and pain associated with exposure to discrimination without eliminating hope or generating additional stress.
Confrontation and anger expression
Race-related maltreatment evokes anger ( Brondolo et al. 2008 ; Broudy et al. 2007 ; Landrine and Klonoff 1996 ). Consequently, many models of coping with racism recognize the need to address the anger evoked by ethnicity-related maltreatment ( Mellor 2004 ), and some of the seminal studies of the effects of racial stress examined anger coping ( Harburg et al. 1979 , 1991 ). Anger coping strategies used in response to ethnicity-related maltreatment may address two goals. The first involves using anger coping strategies, including confrontation, to influence the outcome of the race-related conflict. For example, the expression of anger can be used to motivate the perpetrator to change his or her behavior or to motivate others to take action ( Swim et al. 2003 ). The second goal of anger coping strategies is to manage the emotional burden created by the anger.
Researchers have used several different approaches to assess constructs related to anger expression and confrontation. In some cases, anger coping that involves directly protesting maltreatment has been subsumed under the term confrontation coping ( Noh et al. 1999 ). In other cases, researchers have directly examined the effects of different strategies for anger expression, including outward anger expression (Anger-Out) or anger suppression (Anger-In) (e.g., Dorr et al. 2007 ).
Despite the obvious importance of studying the effects of anger coping, there have been relatively few studies directly addressing these issues. Specifically, there have been two survey studies that examine the effects of confrontation coping as a buffer of the relationship of racism to distress ( Noh et al. 1999 ; Noh and Kaspar 2003 ). There have been five studies examining the effects of anger coping or confrontation as a means of managing racist interactions on BP ( Armstead and Clark 2002 ; Dorr et al. 2007 ; Krieger 1990 ; Krieger and Sidney 1996 ; Steffen et al. 2003 ). Details of these studies are presented in Table 3 .
Studies of the buffering effects of anger expression on the relationship of racism to mental and physical health indices
Note. HTN = Hypertension. ABP = ambulatory blood pressure. BP = blood pressure. SBP = systolic blood pressure. DBP = diastolic blood pressure. MAS = Multidimensional Anger Scale ( Siegel, 1986 ). PRS = Perceived Racism Scale ( McNeilly et al., 1996 ).
In two population-based samples of Asian immigrants, Noh and colleagues examined confrontation coping using measures which include an item assessing direct protests to the perpetrator. In the South Asian sample (i.e., composed largely of Chinese and Vietnamese), Noh and Kaspar (2003) reported no effects of confrontation on the relationship of perceived discrimination to depression. In contrast, in a study of Korean immigrants, the authors reported that personal confrontation coping (i.e., directly protesting or talking to the perpetrator) moderated the effects of discrimination on depression, such that those who were more likely to confront reported less depression in the face of discrimination than those who indicate they are less likely to confront ( Noh et al. 1999 ).
A recent diary study by Hyers (2007) examined costs and benefits associated with confrontation coping, although no measure was made of depression or health. She considered outcomes including rumination-related behaviors (i.e., feelings of emotional upset, regret, wishing to respond differently in the future) and experiences of self-efficacy (i.e., “the perpetrator was educated”) as well as interpersonal conflict. These intermediate outcomes may be predictors of depression over the long run, and potentially serve to maintain the stress associated with the episodes of racism. Hyers reported that when women responded to incidents of racism or sexism with confrontation coping, they were less likely to ruminate and more likely to feel they had been efficacious. Those who did not confront were more likely to report a benefit of avoiding interpersonal conflict; however, it is not clear if the women who did confront actually experienced more conflict.
In five studies using different methodologies, the effects of anger coping on BP levels or reactivity and recovery were examined ( Armstead et al. 1989 ; Dorr et al. 2007 ; Krieger 1990 ; Krieger and Sidney 1996 ; Steffen et al. 2003 ). The results were fairly consistent and are detailed in Table 3 . The main effects analyses indicate that suppressing anger in the face of discrimination is associated with higher levels of BP or poorer cardiovascular recovery from race-related stress exposure. However, there is also some evidence that, for African Americans, expressing anger may be associated with poorer cardiovascular recovery as well.
In two population-based samples, Krieger and colleagues examined the effects of exposure to discrimination and responses to discrimination, contrasting the effects of “doing something about it” with “accepting it as a fact of life”. Among a small sample of Black women, those who reported “doing something about it (discrimination)” were less likely to have a hypertension diagnosis than those who “accepted and kept quiet about it” ( Krieger 1990 ). In Krieger and Sidney (1996) , a large scale population-based study of Black and White individuals, the blood pressure levels of those who reported “doing something about it” were lower than those of individuals who reported “accepting it.” Statistical tests of moderation were not performed, making it difficult to determine if buffering effects were present.
Steffen et al. (2003) reported that trait anger suppression was independently associated with ambulatory DBP in a convenience sample of African Americans. However, neither anger suppression nor expression moderated the effects of racism on ambulatory BP. Armstead et al. (1989) and Dorr et al. (2007) conducted laboratory studies examining the relationship of anger coping to BP response to a racist stressor. Armstead et al. (1989) reported that for Blacks anger suppression was marginally associated with greater SBP at baseline. A style of anger coping in which anger is outwardly expressed was marginally associated with baseline levels of mean arterial pressure and reduced SBP and DBP reactivity to the racist stressor.
In the Dorr et al. study (2007) , African American and European American participants engaged in race and nonrace-related debates facing a European American confederate. Following the tasks participants were given opportunities to express versus inhibit anger. The authors reported that for both African Americans and European Americans, anger inhibition was associated with slower recovery of indices of total peripheral resistance, a measure of vascular response. For African Americans, BP and HR recovery was slower when they were allowed to express their anger than when they were asked to inhibit it, and recovery was also slower than the recovery of EA who were able to express their anger. These effects suggest that anger suppression exacerbates vascular recovery to stress for both groups; whereas outward anger expression exacerbates cardiac and other CV indices of recovery to stress for Blacks.
The authors suggest that one possible explanation for these findings is that anger suppression can lead to rumination if issues are not resolved satisfactorily. However, anger expression may lead to anxiety about retaliation or abandonment if social relations are threatened by direct expression of anger. Both rumination and persistent anxiety may be associated with sustained physiological activation following stress exposure ( Brosschot et al. 2006 ).
What accounts for the variations in the effects of confrontation as a buffer of the effects of racism on depression?
The specific effects of confrontation coping are difficult to interpret, since confrontation coping is subsumed under the general heading of approach coping or problem solving coping and includes items measuring social support seeking as well as “going to the authorities”. Second, the type of confrontation (i.e., hot and angry versus cold and unemotional) is generally not specifically examined, yet laboratory research suggests that the effects of the confrontation depend in part on the emotional quality of the confrontation ( Czopp et al. 2006 ).
Although the limited literature suggests that most Black and White individuals report trying to “do something” about racism ( Krieger and Sidney 1996 ; Plummer and Slane 1996 ; Thompson Sanders 2006 ), diary studies suggest that individuals report thinking about confrontation or indirectly or non-verbally expressing their anger more often than they actually engage in direct anger expression ( Hyers 2007 ). Measures are needed that separate intent from action or more explicitly identify the specific actions taken.
It is also necessary to consider the context in which the conflict occurs when evaluating the effects of anger coping or confrontation. Individuals will hesitate to express anger directly if they believe there will be retaliatory consequences for this anger expression. In any given interaction, individuals with relatively lower levels of power or status are more likely to suppress anger than high power individuals ( Gentry et al. 1973 ). The location of the conflict (i.e., work or social arena) may also influence the choice of coping strategies ( Brondolo et al. 2005b ). Cultural variations in the importance of maintaining relationships may also affect the outcomes associated with confrontation ( Noh et al. 1999 ; Suchday and Larkin 2004 ). Research is needed to clearly differentiate among different types of confrontation strategies and to identify situational and cultural variations in the types of strategies used and their effectiveness.
Some of the health effects of different individual-level coping strategies are likely to be a function of the efficacy of the coping strategies themselves. If the strategies for confrontation and anger coping are effective on some dimensions (e.g., reducing overt expressions of prejudice), but costly on others (e.g., social relations), individuals may not perceive themselves as having appropriate coping resources, making it more likely that they will perceive interracial or race-based maltreatment as stressful. Evaluating a broad range of outcome measures from the target’s perspective (e.g., mental and physical health, rumination, satisfaction with outcome, perceived benefits) is critical. Investigating the perceptions of these different coping strategies from the perspective of others is also important. The growing literature on other’s perceptions of confrontation and other coping strategies ( Czopp et al. 2006 ; Kawakami et al. 2007 ) can provide guidance for future studies on anger coping. More knowledge regarding the perceptions of different coping strategies by individuals of other ethnicities/races can help guide individuals as they weigh the costs and benefits of various responses.
Summary and future directions
The strongest and clearest conclusion that can be drawn from this review is that there is a significant need for further research on strategies for coping with racism. No coping strategy has emerged as a clearly successful strategy for offsetting the mental or physical health impacts of racism. Instead, each approach has some demonstrated strengths, but also considerable side effects or limitations.
Ethnic and racial identity develop to meet multiple needs, including enhancing one’s pride and commitment to one’s cultural group as well as helping individuals develop meaningful strategies for managing discrimination based on racial or ethnic bias. Studies suggest that racial identity, particularly racial or ethnic pride and belonging may have beneficial effects in some circumstances. But these components of identity are not sufficient to ameliorate the effects of racism on the development of depressive symptoms and may increase the detection of threat and the perception of harm.
Involvement with only one type of identity may restrict the individuals’ ability to consider multiple perspectives and learn a range of coping options. Instead, in an increasingly multicultural society, it will be important to understand the best ways to help individuals master the complex psychological tasks involved in maintaining individual, group and national identities, particularly when the values at one level contrast with the values at another. Oyserman has specifically suggested that a “possible selves” approach, encouraging individuals to incorporate aspects of different types of group identities, may be of benefit ( Oyserman et al. 2007 ).
It may be that the strength of this approach is not only in gaining the benefits of having multiple roles, but in the process of mastering the underlying cognitive-affective processes that subserve these identities. Learning to think about oneself as a member of many different groups requires considering multiple perspectives and developing the ability to shift the focus of one’s attention even when experiencing strong emotion. Additionally, individuals must learn to integrate specific individualized information (e.g., about stressors and resources specific to the individual) with larger category-based information (e.g., about stressors and resources conferred because of group membership). In the process of developing an awareness of many possible identities, individuals may also strengthen their own capacity for effective coping in a range of circumstances and increase their ability to draw support from a number of different groups. Similarly, social support appears to be beneficial in a variety of circumstances, but the available data do not support a direct role for non-specific social support as a buffer of the effects of racism on distress. A greater understanding of the types of support beneficial for different phases and dimensions of the experience of racism will be needed to facilitate the development of support-based interventions including, for example, group based stress-management programs.
The clinical literature ( Elligan and Utsey 1999 ; Utsey et al. 2002 ) may provide some guidance for the specific types of support that may be valuable at different points in time. It may be necessary to include communication that is aimed at validating the individual’s experience (i.e., the perception that race-based maltreatment may have occurred), while also offering opportunities to review the circumstances and identify factors that elicited perceptions of threat. This type of support is needed to decrease defensiveness and increase the capacity to clearly articulate specific concerns and develop appropriate strategies to manage the specific threat. But acute problem-focused support may not be sufficient. Support may also be needed to address and ameliorate the painful nature of racism, providing an opportunity to address not only the feelings of anger, but of shame and anxiety as well. Finally, still other forms of support may be needed to provide hope and the motivation and direction to reduce racism and its effects over the long term.
The psychobiological effects of anger suppression among African Americans are among the most consistent findings in the literature on coping with racism. These data suggest that suppressing anger in the face of discrimination is associated with elevated BP or greater BP responses, but the studies have included only African Americans or European Americans. Other data suggest that there may be cultural moderators of these effects, since the association between anger suppression and distress varies depending on the individual’s ethnicity or race.
Yet, it is unclear what the effective alternatives to anger suppression and aggressive confrontation might be. We need better and more detailed answers to the questions: What is the most effective method to protest ethnicity-related maltreatment? How can anger be used to effectively communicate the seriousness of injustice without exhausting the targets of injustice? If individuals suppress anger at the time of the maltreatment, how can they reintroduce the discussion and communicate their concerns and remedy the injustice later? Understanding the predictors of anger suppression and confrontation both at the time of the incident and over the long run is likely to yield insight into the costs and benefits of these different approaches and to suggest more effective strategies.
Since racism and strategies for coping with racism occur within an interpersonal context, it is important to understand how different behaviors are perceived by others. Czopp et al. (2006) indicates that confrontation coping can be very effective in changing a perpetrator’s beliefs and behavior. The different features of the confrontation (e.g., the ethnicity of the confronter, the emotional tone of the message) are associated with variations in the effectiveness of the confrontation in changing behavior and eliciting negative reactions. The literature on coping with racism must be closely integrated with the empirical literature on the perceptions of targeted individuals by members of other racial or ethnic groups ( Kawakami et al. 2007 ). With this knowledge, individuals can make better predictions about the likely outcomes of their efforts to combat racism and to become increasingly effective in their communication.
Cultural norms have changed regarding the acceptability of overtly discriminatory behavior. Social modeling via the media and other methods has been used to communicate more egalitarian values and to deride racist behavior. It may be useful to use similar methods to generate and model strategies for communicating concern and anger about more subtle discriminatory or stigmatizing actions.
There are conceptual and methodological problems with the existing literature that are common to a new research area confronting a complex and disturbing problem. Some difficulties are related to problems in conceptualizing racism-related coping, and developing models that incorporate the different types of strategies needed to accommodate variations in demand across time and across contexts. To date, very few studies have examined the degree to which the effects of racism-related coping strategies vary by context or timing, and very few have examined the degree to which individual difference variables, including the presence of other background stressors or personality dimensions, shape the type of coping choice ( Brondolo et al. 2008 ; Scott 2004 ) or moderate its effectiveness ( Danoff-Burg et al. 2004 ; Scott 2004 ).
Surprisingly, almost no studies have examined variations in the effectiveness of the strategies by the stage of the incident (i.e., in preparation for future difficulties, at the time of the incident or following the termination of the conflict). Additionally, investigations have not adequately separated out the types of strategies most effective for managing the practical consequences of exposure versus the emotional consequences of confronting unjust social exclusion. The development of new measures of racism-related coping that incorporate issues of timing, context, and intent are needed.
Research is also needed to investigate the differential effects of any particular strategy on functioning, affect and health. Some coping strategies, for example, may be effective in limiting exposure to racism, but may have detrimental effects on mental and physical health. Outcomes must also include assessments of the target’s perceptions of effectiveness as well.
Because coping strategies may have side effects, there is a need for more research involving multiple outcome measures. Confrontational coping may have the side effect of creating or exacerbating interpersonal conflict. Anger suppression may have the side effect of increasing rumination. Social support seeking can be distracting or confusing. The results of studies reporting effects that are limited to one or two outcome domains may be misleading regarding the overall effectiveness of the coping responses examined.
In this review, we have chosen to consider a coping strategy as effective if it ameliorates some of the deleterious health effects of racism, specifically effects on depression symptoms or risk factors for hypertension. However, there may be other dimensions of effectiveness worth considering: Does the strategy for coping with racism reduce the incidence of racism over the long run? Does it achieve the personal goals of the target (i.e., to get a job, to avoid exclusion) even it if incurs some consequences as well? Does it decrease fear?
A fuller understanding of the potential benefits of strategies for coping with racism will be facilitated by intervention research. Ultimately, these will have the broadest impact if delivered and evaluated on a community, institutional, or national scale. Public education messages and school-based health promotion activities have the potential of reaching a large and diverse audience. But they will only be as effective as the coping responses that they attempt to promote.
We focused on stress-buffering, which is only one model of the manner in which coping responses may ameliorate the effects of exposure to racism. As shown in Fig. 1 , other plausible models include mediational models that posit simultaneous causal effects of stress on coping and of coping on outcomes. Some of the strategies that we have examined, such as anger expression or racial identity development, may be better considered as responses that emerge as a function of discrimination rather than as coping responses that develop independently of exposure. Developing different strategies may require a substantial effort on the part of the target. Both buffering and mediational models are best examined in large-scale, longitudinal studies, which are in short supply in the published literature.
Early models of coping may have reflected the more general societal view that racial and ethnic discrimination were an immutable feature of life. As legal, economic, and social conditions change, the possibilities for coping with ethnic and racial discrimination will change as well. As new solutions and opportunities develop, the models of these coping strategies will also evolve.
Research on strategies for coping with racism is necessary to empower targeted individuals to develop and choose methods that are effective at reducing discrimination, increasing hope, and buffering the impact of racism on health. As we come to understand a fuller range of consequences of each strategy, we can provide better guidance to help individuals make more informed choices about the ways they wish to cope with racism and protect their health. We hope that this knowledge and the detailed description of the ways in which racism is experienced by the targets will contribute to the elimination of discriminatory behavior.
1 Two additional studies report buffering effects on perceived stress, but not depressive symptoms ( Sellers et al., 2003 ; Sellers et al., 2006 ). Four studies reported buffering effects of racial/ethnicity identity on self-esteem or academic orientation, achievement or efficacy, even when the authors reported that they did not find buffering effects on measures of distress or depression ( Sellers et al., 2003 ; Wong et al., 2003 ) or did not examine effects on depression ( Oyserman & Fryberg, 2006 ; Romero & Roberts, 2003 ). There are also laboratory studies examining the effects of identity on emotional responses to racism-type manipulations ( Ellemers, 1997 ). These provide important insights into the nature of group and individual processes on identity development, but it is not clear that the measures used in these studies are of relevance to the hypothesis that racial/ethnic identity buffers the effects of exposure to racism on clinically significant distress.
Contributor Information
Elizabeth Brondolo, St. John’s University.
Nisha Brady, St. John’s University.
Melissa Pencille, St. John’s University.
Danielle Beatty, University of Pittsburgh Medical Center.
Richard J. Contrada, Rutgers, The State University of New Jersey.
- Allgower A, Wardle J, Steptoe A. Depressive symptoms, social support, and personal health behaviors in young men and women. Health Psychology. 2001; 20 (3):223–227. [ PubMed ] [ Google Scholar ]
- Allport GW. The nature of prejudice. Oxford, England: Addison-Wesley; 1954. [ Google Scholar ]
- Anderson NB. Racial Differences in Stress-Induced Cardiovascular Reactivity and Hypertension: Current Status and Substantive Issues. American Psychological Association. 1989; 105 (1):89–105. [ PubMed ] [ Google Scholar ]
- Anderson NB, Myers HF, Pickering T, Jackson JS. Hypertension in blacks: Psychosocial and Biological perspectives. Journal of Hypertension. 1989; 7 :161–172. [ PubMed ] [ Google Scholar ]
- Armstead CA, Clark R. Assessment of self-reported anger expression in pre- and early-adolescent African Americans: Psychometric considerations. Journal of Adolescence. 2002; 25 (4):365–371. [ PubMed ] [ Google Scholar ]
- Armstead CA, Lawler KA, Gorden G, Cross J, Gibbons J. Relationship of racial stressors to blood pressure responses and anger expression in Black college students. Health Psychology. 1989; 8 (5):541–556. [ PubMed ] [ Google Scholar ]
- Badr H, Taylor CLC. Social constraints and spousal communication in lung cancer. Psycho-Oncology. 2006; 15 (8):673–683. [ PubMed ] [ Google Scholar ]
- Banks KH, Kohn-Wood L. The influence of racial identity profiles on the relationship between racial discrimination and depressive symptoms. Journal of Black Psychology 2007 [ Google Scholar ]
- Barnett PA, Gotlib IH. Psychosocial functioning and depression: Distinguishing among antecedents, concomitants, and consequences. American Psychological Association. 1988; 104 (1):97–126. [ PubMed ] [ Google Scholar ]
- Baumeister RF, DeWall CN, Ciarocco NJ, Twenge JM. Social exclusion impairs self-regulation. Journal of Personality & Social Psychology. 2005; 88 (4):589–604. [ PubMed ] [ Google Scholar ]
- Borrell LN, Jacobs DR, Jr, Williams DR, Pletcher MJ, Houston TK, Kiefe CI. Self-reported racial discrimination and substance use in the coronary artery risk development in adults study. American Journal of Epidemiology. 2007; 20 :1–12. [ PubMed ] [ Google Scholar ]
- Branscombe NR, Schmitt MT, Harvey RD. Perceiving pervasive discrimination among African-Americans: Implications for group identification and well-being. Journal of Personality and Social Psychology. 1999; 77 (1):135–149. [ Google Scholar ]
- Brondolo E, Beatty D, Cubbin C, Weinstein M, Saegert S, Wellington RL, et al. Sociodemographic variations in self-reported racism in a community sample of blacks and latino(a)s. Journal of Applied Social Psychology (in press) [ Google Scholar ]
- Brondolo E, Brady N, Thompson S, Tobin JN, Cassells A, Sweeney M, et al. Perceived racism and negative affect: Analyses of trait and state measures of affect in a community sample. Journal of Social and Clinical Psychology. 2008; 27 (2):150–173. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brondolo E, Kelly KP, Coakley V, Gordon T, Thompson S, Levy E, et al. The Perceived Ethnic Discrimination Questionnaire: development and preliminary validation of a community version. Journal of Applied Social Psychology. 2005; 35 (2):335–365. [ Google Scholar ]
- Brondolo E, Rieppi R, Erickson SA, Bagiella E, Shapiro PA, McKinley P, et al. Hostility, interpersonal interactions, and ambulatory blood pressure. Psychosomatic Medicine. 2003; 65 :1003–1011. [ PubMed ] [ Google Scholar ]
- Brondolo E, Thompson S, Brady N, Appel R, Cassells A, Tobin JN, et al. The relationship of racism to appraisals and coping in a community sample. Ethnicity and Disease. 2005; 15 (4 Suppl 5):S5-14–19. [ PubMed ] [ Google Scholar ]
- Brondolo E, Thompson S, Brady N, Appel R, Cassells A, Tobin JN, et al. The relationship of racism to appraisals and coping in a community sample. Ethnicity and Disease. 2006; 15 (S5):14–19. [ PubMed ] [ Google Scholar ]
- Brosschot JF, Gerin W, Thayer JF. The perseverative cognition hypothesis: A review of worry, prolonged stress-related physiological activation, and health. Journal of Psychosomatic Research. 2006; 60 (2):113–124. [ PubMed ] [ Google Scholar ]
- Broudy R, Brondolo E, Coakley V, Brady N, Cassells A, Tobin J, et al. Perceived ethnic discrimination in relation to daily moods and negative social interactions. Journal of Behavioral Medicine. 2007; 30 (1):31–43. [ PubMed ] [ Google Scholar ]
- Bynum MS, Burton ET, Best C. Racism experiences and psychological functioning in African American college freshmen: Is racial socialization a buffer? Cultural Diversity and Ethnic Minority Psychology. 2007; 13 (1):64–71. [ PubMed ] [ Google Scholar ]
- Causey DL, Dubow EF. Development of a self-report coping measure for elementary school children. Journal of Clinical Child Psychology. 1992; 21 (1):47–59. [ Google Scholar ]
- Cheng C. Cognitive and motivational processes underlying coping flexibility: A dual-process model. Journal of Personality and Social Psychology. 2003; 84 (2):425–438. [ PubMed ] [ Google Scholar ]
- Clark R. Self-reported racism and social support predict blood pressure reactivity in Blacks. Annals of Behavioral Medicine. 2003; 25 (2):127–136. [ PubMed ] [ Google Scholar ]
- Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans. American Psychologist. 1999; 54 (10):805–816. [ PubMed ] [ Google Scholar ]
- Clark R, Gochett P. Interactive effects of perceived racism and coping responses predict a school-based assessment of blood pressure in Black youth. Annals of Behavioral Medicine. 2006; 32 (1):1–9. [ PubMed ] [ Google Scholar ]
- Cohen GL, Garcia J. “I am us”: Negative stereotypes as collective threats. Journal of Personality & Social Psychology. 2005; 89 (4):566–582. [ PubMed ] [ Google Scholar ]
- Cohen S, Williamson GM. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The social psychology of health. Newbury Park, CA: Sage; 1988. [ Google Scholar ]
- Cokley K. Critical issues in the measurement of ethnic and racial identity: A referendum on the state of the field. Journal of Counseling Psychology. 2007; 54 (3):224–234. [ Google Scholar ]
- Constantine MG, Donnelly PC, Myers LJ. Collective self-esteem and africultural coping styles in African American adolescents. Journal of Black Studies. 2002; 32 (6):698–710. [ Google Scholar ]
- Contrada RJ, Ashmore RD, Gary ML, Coups E, Egeth JD, Sewell A, et al. Measures of ethnicity-related stress: Psychometric properties, ethnic group differences, and associations with well-being. Journal of Applied Social Psychology. 2001; 31 :1775–1820. [ Google Scholar ]
- Cross WE., Jr . Ethnicity, race, and identity. Chicago, IL: University of Chicago Press; 2005. [ Google Scholar ]
- Cross WE, Jr, Strauss L. The everyday functions of African American identity. In: Swim JK, Stangor C, editors. Prejudice: The target’s perspective. San Diego, CA: Academic Press; 1998. pp. 267–279. [ Google Scholar ]
- Czopp AM, Monteith MJ, Mark AY. Standing up for a change: reducing bias through interpersonal confrontation. Journal of Personality and Social Psychology. 2006; 90 (5):784–803. [ PubMed ] [ Google Scholar ]
- Danoff-Burg S, Prelow HM, Swenson RR. Hope and life satisfaction in Black college students coping with race-related stress. Journal of Black Psychology. 2004; 30 (2):208–228. [ Google Scholar ]
- Deragotis LR. Symptom Checklist-90-R: Administration, scoring and procedures manual. 3. Minneapolis, MN: National Computer Systems, Inc; 1994. [ Google Scholar ]
- Deragotis LR, Meisarotis N. The Brief Symptom Inventory: An introductory report. Psychological Medicine. 1983; 13 :595–605. [ PubMed ] [ Google Scholar ]
- Dorr N, Brosschot JF, Sollers JJ, III, Thayer JF. Damned if you do, damned if you don’t: The differential effect of expression and inhibition of anger on cardiovascular recovery in Black and White males. International Journal of Psychophysiology. 2007; 66 (2):125–134. [ PubMed ] [ Google Scholar ]
- Ellemers N, Spears R, Doosje B. Sticking together of falling apart: In-group identification as a psychological determinant of group commitment versus individual mobility. Journal of Personality and Social Psychology. 1997; 72 (3):617–626. [ Google Scholar ]
- Elligan D, Utsey SO. Utility of an African-centered support group for African American men confronting societal racism and oppression. Cultural Diversity and Ethnic Minority Psychology. 1999; 41 (3):295–313. [ PubMed ] [ Google Scholar ]
- Finch BK, Kolody B, Vega WA. Perceived discrimination and depression among Mexican-origin adults in California. Journal of Health and Social Behavior. 2000; 41 (3):295–313. [ PubMed ] [ Google Scholar ]
- Finch BK, Vega WA. Acculturation stress, social support, and self-rated health among Latinos in California. Journal of Immigrant Health. 2003; 5 (3):109–117. [ PubMed ] [ Google Scholar ]
- Fischer AR, Shaw CM. African Americans’ mental health and perceptions of racist discrimination: The moderating effects of racial socialization experiences and self-esteem. The Journal of Counseling Psychology. 1999; 46 (3):395–407. [ Google Scholar ]
- Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychological Bulletin. 2003; 129 (1):10–51. [ PubMed ] [ Google Scholar ]
- Gallo LC, Smith TW, Cox C. Socioeconomic status, psychosocial processes, and perceived health: An interpersonal perspective. Annals of Behavioral Medicine. 2006; 31 :109–119. [ PubMed ] [ Google Scholar ]
- Gentry WD, Harburg E, Hauenstein L. Effects of anger expression/inhibition/and guilt on elevated diastolic blood pressure in high/low stress and Black/White females. 1973. pp. 115–116. [ Google Scholar ]
- Greene ML, Way N, Pahl K. Trajectories of perceived adult and peer discrimination among Black, Latino, and Asian American adolescents: Patterns and psychological correlates. Developmental Psychology. 2006; 42 (2):218–238. [ PubMed ] [ Google Scholar ]
- Harburg E, Blakelock EH, Roeper P. Resentful and reflective coping with arbitrary authority and blood pressure: Detroit. Psychosomatic Medicine. 1979; 41 (3):189–202. [ PubMed ] [ Google Scholar ]
- Harburg E, Gleiberman L, Russell M, Cooper ML. Anger-coping styles and blood pressure in Black and White males: Buffalo, New York. Psychosomatic Medicine. 1991; 53 (2):153–164. [ PubMed ] [ Google Scholar ]
- Harrell JP. Analyzing Black coping styles: A supplemental diagnostic system. Journal of Black Psychology. 1979; 5 (2):99–108. [ Google Scholar ]
- Harrell JP, Hall S, Taliaferro J. Physiological responses to racism and discrimination: An assessment of the evidence. American Journal of Public Health. 2003; 93 (2):243–248. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Harrell JP, Merritt MN, Kalu J. Racism, stress and disease. In: Jones RL, editor. African American mental health: Theory, research, and intervention. Hampton, VA: Cobb & Henry Publishers; 1998. pp. 247–280. [ Google Scholar ]
- Harrell SP. A multidimensional conceptualization of racism-related stress: Implications for the well-being of people of color. American Journal of Orthopsychiatry. 2000; 70 (1):42–57. [ PubMed ] [ Google Scholar ]
- Harrell SP. Unpublished manuscript. 1994. The Racism and Life Experience Scale. [ Google Scholar ]
- Harrell SP. Unpublished manuscript. 1997a. The Racism and Life Experiences Scales. [ Google Scholar ]
- Harrell SP. Unpublished manuscript. 1997b. Development and initial validation of scales to measure racism-related stress. [ Google Scholar ]
- Helms JE. An overview of Black racial identity theory. In: Helms JE, editor. Black and White racial identity: Theory, research, and practice. Westport, Conn: Praeger; 1990. pp. 9–32. [ Google Scholar ]
- Horowitz M, Wilner H, Alvarez W. Impact of Events Scale: A measure of subjective stress. Psychosomatic Medicine. 1979; 41 (3):209–218. [ PubMed ] [ Google Scholar ]
- Hughes D, Rodriguez J, Smith EP, Johnson DJ, Stevenson HC, Spicer P. Parents’ ethnic-racial socialization practices: A review of research and directions for future study. Developmental Psychology. 2006; 42 (5):747–770. [ PubMed ] [ Google Scholar ]
- Hyers LL. Resisting prejudice every day: Exploring women’s assertive responses to anti-Black racism, anti-semitism, heterosexism, and sexism. Sex Roles. 2007; 56 (1–2):1–12. [ Google Scholar ]
- Jackson JS, Brown TN, Williams DR, Torres M, Sellers SS, Brown K. Racism and the physical and mental health status of African Americans: A thirteen year national panel study. Ethnicity and Disease. 1996; 6 :132–147. [ PubMed ] [ Google Scholar ]
- Jones CP. Levels of racism: A theoretic framework and a gardener’s tale. American Journal of Public Health. 2000; 90 (8):1212–1215. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jones JM. Prejudice and racism. 2. New York: McGraw Hill; 1997. [ Google Scholar ]
- Kawakami K, Phills CE, Steele JR, Dovidio JF. (Close) distance makes the heart grow fonder: Improving implicit racial attitudes and interracial interactions Through approach behaviors. Journal of Personality & Social Psychology. 2007; 92 (6):957–971. [ PubMed ] [ Google Scholar ]
- Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of Health and Social Behavior. 1999; 40 (3):208–230. [ PubMed ] [ Google Scholar ]
- Krieger N. Racial and gender discrimination: Risk factors for high blood pressure? Social Science and Medicine. 1990; 30 (12):1273–1281. [ PubMed ] [ Google Scholar ]
- Krieger N. Embodying inequality: A review of concepts, measures, and methods for studying health consequences of discrimination. International Journal of Health Services. 1999; 29 :295–352. [ PubMed ] [ Google Scholar ]
- Krieger N, Sidney S. Racial discrimination and blood pressure: The CARDIA study of young Black and White adults. American Journal of Public Health. 1996; 86 (10):1370–1378. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lalonde RN, Majumder S, Parris RD. Preferred responses to situations of housing and employment discrimination. Journal of Applied Social Psychology. 1995; 25 (12):1105–1119. [ Google Scholar ]
- Landrine H, Klonoff EA. The Schedule of Racist Events: A measure of racial discrimination and a study of its negative physical and mental health consequences. Journal of Black Psychology. 1996; 22 :144–168. [ Google Scholar ]
- Lazarus RS. Toward better research on stress and coping. American Psychologist. 2000; 55 :665–673. [ PubMed ] [ Google Scholar ]
- Lee RM. Do ethnic identity and other-group orientation protect against discrimination for Asian Americans? Journal of Counseling Psychology. 2003; 50 (2):133–141. [ Google Scholar ]
- Lee RM. Resilience against discrimination: Ethnic identity and other-group orientation as protective factors for Korean Americans. Journal of Counseling Psychology. 2005; 52 (1):36–44. [ Google Scholar ]
- Lepore S, Revenson TA. Social constraints on disclosure and adjustment to cancer. Social and Personality Psychology Compass. 2007; 1 (1):313–333. [ Google Scholar ]
- Lewis-Coles MaEL, Constantine MG. Racism-related stress, Africultural coping, and religious problem-solving among African Americans. Cultural Diversity and Ethnic Minority Psychology. 2006; 12 (3):433–443. [ PubMed ] [ Google Scholar ]
- Lewis TT, Everson-Rose SA, Powell LH, Matthews KA, Brown C, Karavolos K, et al. Chronic exposure to everyday discrimination and coronary artery calcification in African-American women: the SWAN Heart Study. Psychosomatic Medicine. 2006; 68 (3):362–368. [ PubMed ] [ Google Scholar ]
- MacDonald G, Leary MR. Why does social exclusion hurt? The relationship between social and physical pain. Psychological Bulletin. 2005; 131 (2):202–223. [ PubMed ] [ Google Scholar ]
- Mays VM, Cochran SD, Barnes NW. Race, race-based discrimination and health outcomes among African Americans. Annual Review of Psychology. 2007; 58 :201–225. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mays VM, Coleman LM, Jackson JS. Perceived race-based discrimination, employment status, and job stress in a national sample of Black women: Implications for health outcomes. Journal of Occupational Health Psychology. 1996; 1 :319–329. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- McEwen B, Lasley EN. Allostatic load: When protection gives way to damage. Advances in Mind-Body Medicine. 2003; 19 (1):28–33. [ PubMed ] [ Google Scholar ]
- McEwen B, Lasley EN. Allostatic load: When protection gives way to damage. In: Monat A, Lazarus RS, Reevy G, editors. The Praeger handbook on stress and coping. Vol. 1. Westport, CT: Praeger Publishers/Greenwood Publishing Group; 2007. pp. 99–109. [ Google Scholar ]
- McNeilly MD, Anderson NB, Armstead CA, Clark R, Corbett M, Robinson EL, et al. The Perceived Racism Scale: A multidimensional assessment of the experience of White racism among African Americans. Ethnicity and Disease. 1996; 6 :154–166. [ PubMed ] [ Google Scholar ]
- McNeilly MD, Robinson EL, Anderson NB, Pieper C, Shah A, Toth PS, et al. Effects of racist provocation and social support on cardiovascular reactivity in African American women. International Journal of Behavioral Medicine. 1995; 2 (4):321–338. [ PubMed ] [ Google Scholar ]
- Mellor D. Responses to racism: A taxonomy of coping styles used by aboriginal Australians. American Journal of Orthopsychiatry. 2004; 74 (1):56–71. [ PubMed ] [ Google Scholar ]
- Moos RH. Coping Responses Inventory Adult Form: Professional manual. Odessa, FL: Psychological Assessment Resources; 1993. [ Google Scholar ]
- Mossakowski KN. Coping with perceived discrimination: Does ethnic identity protect mental health? Journal of Health and Social Behavior. 2003; 44 (3):318–331. [ PubMed ] [ Google Scholar ]
- Noh S, Beiser M, Kaspar V, Hou F, Rummens J. Perceived racial discrimination, depression, and coping: A study of Southeast Asian refugees in Canada. Journal of Health and Social Behavior. 1999; 40 :193–207. [ PubMed ] [ Google Scholar ]
- Noh S, Kasper V, Chen X. Measuring depression in Korean Immigrants: Assessing validity of the translated Korean version of the CES-D scale. Cross-Cultural Research: The Journal of Comparative Social Science. 1998; 32 (4):358–377. [ Google Scholar ]
- Noh S, Kaspar V. Perceived discrimination and depression: Moderating effects of coping, acculturation and ethnic support. American Journal of Public Health. 2003; 93 (2):232–238. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Outlaw FH. Stress and coping: The influence of racism on the cognitive appraisal processing of African-Americans. Issues in Mental Health Nursing. 1993; 14 :399–409. [ PubMed ] [ Google Scholar ]
- Oyserman D, Brickman D, Rhodes M. School success, possible selves, and parent school involvement. Family Relations: Interdisciplinary Journal of Applied Family Studies. 2007; 56 (5):479–489. [ Google Scholar ]
- Oyserman D, Fryberg S. The Possible Selves of Diverse Adolescents: Content and Function Across Gender, Race and National Origin. In: Dunkel C, Kerpelman J, editors. Possible selves: Theory, research and applications. Hauppauge, NY: Nova Science Publishers; 2006. pp. 17–39. [ Google Scholar ]
- Oyserman D, Harrison K, Bybee D. Can racial identity be promotive of academic efficacy? International Journal of Behavioral Development. 2001; 25 (4):379–385. [ Google Scholar ]
- Oyserman D, Kemmelmeier M, Fryberg S, Brosh H, Hart-Johnson T. Racial-ethnic self-schemas. Social Psychology Quarterly. 2003; 66 (4):333–347. [ Google Scholar ]
- Quintana SM. Racial and ethnic identity: Developmental perspectives and research. Journal of Counseling Psychology. 2007; 54 (3):259–270. [ Google Scholar ]
- Paradies Y. A systematic review of empirical research on self-reported racism and health. International Journal of Epidemiology. 2006; 35 :888–901. [ PubMed ] [ Google Scholar ]
- Peters RM. Racism and Hypertension Among African Americans. Western Journal of Nursing Research. 2004; 26 (6):612–631. [ PubMed ] [ Google Scholar ]
- Phinney JS. Ethnic identity in adolescents and adults: Review of research. Psychological Bulletin. 1990; 108 (3):499–514. [ PubMed ] [ Google Scholar ]
- Phinney JS. The Multigroup Ethnic Identity Measure: A new scale for use with diverse groups. Journal of Adolescent Research. 1992; 7 :156–176. [ Google Scholar ]
- Phinney JS. When we talk about American ethnic groups, what do we mean? American Psychologist. 1996; 51 :918–927. [ Google Scholar ]
- Phinney JS, Horenczyk G, Liebkind K, Vedder P. Ethnic identity, immigration and well-being: An interactional perspective. Journal of Social Issues. 2001; 57 (3):493–510. [ Google Scholar ]
- Phinney JS, Ong AD. Conceptualization and measurement of ethnic identity: Current status and future directions. Journal of Counseling Psychology. 2007; 54 (3):271–281. [ Google Scholar ]
- Plummer DL, Slane S. Patterns of coping in racially stressful situations. Journal of Black Psychology. 1996; 22 (3):302–315. [ Google Scholar ]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977; 1 (3):385–401. [ Google Scholar ]
- Richeson JA, Shelton NJ. Brief Report: Thin slices of racial bias. Journal of Nonverbal Behavior. 2005; 29 (1):75–86. [ Google Scholar ]
- Richeson JA, Shelton NJ. Negotiating interracial interactions: Costs, consequences and possibilities. 2007; 16 :316–320. [ Google Scholar ]
- Romero AJ, Roberts RE. The impact of multiple dimensions of ethnic identity on discrimination and adolescents’ self-esteem. Journal of Applied Social Psychology. 2003; 33 (11):2288–2305. [ Google Scholar ]
- Ruiz JM, Hamann HA, Coyne J, Compare A. In sickness and in health: Interpersonal risk and resilience in cardiovascular disease. In: Molinari E, Compare A, Parati G, editors. Clinical psychology and heart disease. New York: Springer; 2006. pp. 233–272. [ Google Scholar ]
- Sarason IG, Levine HM, Basham RB, Sarason BR. Assessing social support: The Social Support Questionnaire. Journal of Personality and Social Psychology. 1983; 44 (1):127–139. [ Google Scholar ]
- Sarason IG, Sarason BR, Shearin EN, Pierce GR. A brief measure of social support: Practical and theoretical implications. Journal of Social and Personal Relationships. 1987; 4 (4):497–510. [ Google Scholar ]
- Schulz AJ, Gravlee CC, Williams DR, Israel BA, Mentz G, Rowe Z. Discrimination, Symptoms of Depression, and Self-Rated Health Among African American Women in Detroit: Results from a Longitudinal Analysis. American Journal of Public Health. 2006; 96 (7):1265–1270. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Scott LD., Jr The relation of racial identity and racial socialization to coping with discrimination among African American adolescents. Journal of Black Studies. 2003; 33 (4):520–538. [ Google Scholar ]
- Scott LD., Jr Correlates of coping with perceived discriminatory experiences among African American adolescents. Journal of Adolescence. 2004; 27 (2):123–137. [ PubMed ] [ Google Scholar ]
- Scott LD, Jr, House LE. Relationship of distress and perceived control to coping with perceived racial discrimination among Black youth. Journal of Black Psychology. 2005; 31 (3):254–272. [ Google Scholar ]
- Sellers RM, Caldwell CH, Schmeelk-Cone KH, Zimmerman MA. Racial identity racial discrimination, perceived stress, and psychological distress among African American young adults. Journal of Health and Social Behavior. 2003; 44 (3):302–317. [ PubMed ] [ Google Scholar ]
- Sellers RM, Copeland-Linder N, Martin PP, Lewis RL. Racial identity matters: The relationship between racial discrimination and psychological functioning in African American adolescents. Journal of Research on Adolescence. 2006; 16 (2):187–216. [ Google Scholar ]
- Sellers RM, Rowley SAJ, Chavous TM, Shelton NJ, Smith MA. Multidimensional inventory of Black identity: A preliminary investigation of reliability and constuct validity. Journal of Personality and Social Psychology. 1997; 73 (4):805–815. [ Google Scholar ]
- Sellers RM, Shelton NJ. The role of racial identity in perceived racial discrimination. Journal of Personality and Social Psychology. 2003; 84 (5):1079–1092. [ PubMed ] [ Google Scholar ]
- Sellers RM, Smith MA, Shelton NJ, Rowley SAJ, Chavous TM. Multidimensional model of racial identity: A reconceptualization of African American racial identity. Personality and Social Psychology Review. 1998; 2 (1):18–39. [ PubMed ] [ Google Scholar ]
- Shorter-Gooden K. Multiple resistance strategies: How African American women cope with racism and sexism. Journal of Black Psychology. 2004; 30 (3):406–425. [ Google Scholar ]
- Siegel JM. The Multidimensional Anger Inventory. Journal of Personality and Social Psychology. 1986; 51 (1):191–200. [ PubMed ] [ Google Scholar ]
- Skinner EA, Edge K, Altman J, Sherwood H. Searching for the Structure of Coping: A Review and Critique of Category Systems for Classifying Ways of Coping. Psychological Bulletin. 2003; 129 (2):216. [ PubMed ] [ Google Scholar ]
- Smith TW, Gallo LC, Ruiz JM. Toward a social psychophysiology of cardiovascular reactivity: Interpersonal concepts and methods in the study of stress and coronary disease. In: Suls J, Wallston K, editors. Social psychological foundations of health and illness. Malden, MA: Blackwell; 2003. pp. 335–366. [ Google Scholar ]
- Spielberger CD. Manual for the State–Trait Anxiety Inventory (Form Y) Palo Alto, CA: Consulting Psychologists Press; 1983. [ Google Scholar ]
- Steele CM. A threat in the air: How stereotypes shape intellectual identity and performance. American Psychologist. 1997; 52 (6):613–629. [ PubMed ] [ Google Scholar ]
- Steffen PR, Bowden M. Sleep disturbance mediates the relationship between perceived racism and depressive symptoms. Ethnicity & Disease. 2006; 16 (1):16–21. [ PubMed ] [ Google Scholar ]
- Steffen PR, McNeilly MD, Anderson N, Sherwood A. Effects of perceived racism and anger inhibition on ambulatory blood pressure in African Americans. Psychosomatic Medicine. 2003; 65 (5):746–750. [ PubMed ] [ Google Scholar ]
- Stevenson HC. Validation of the Scale of Racial Socialization for African American adolescents: Steps toward multidimensionality. Journal of Black Psychology. 1994; 20 (4):445–468. [ Google Scholar ]
- Stevenson HC, Jr, Cameron R, Herrero-Taylor T, Davis GY. Development of the Teenager Experience of Racial Socialization scale: Correlates of race-related socialization frequency from the perspective of Black youth. Journal of Black Psychology. 2002; 28 (2):84–106. [ Google Scholar ]
- Suchday S, Larkin KT. Psychophysiological responses to anger provocation among Asian Indian and White men. International Journal of Behavioral Medicine. 2004; 11 (2):71–80. [ PubMed ] [ Google Scholar ]
- Swim JK, Hyers LL, Cohen LL, Fitzgerald DC, Bylsma WH. African American college students’ experiences with everyday racism: Characteristics of and responses to these incidents. Journal of Black Psychology. 2003; 29 (1):38–67. [ Google Scholar ]
- Symister P, Friend R. The influence of social support and problematic support on optimism and depression in chronic illness: A prospective study evaluating self-esteem as a mediator. Health Psychology. 2003; 22 (2):123–129. [ PubMed ] [ Google Scholar ]
- Taylor J, Grundy C. Measuring Black Internalization of White Stereotypes About African Americans: The Nadanolitization Scale. In: Jones RL, editor. The Handbook of Tests and Measurements for Black Populations. Hampton, VA: Cobb & Henry; 1996. pp. 217–226. [ Google Scholar ]
- Thompson HS, Kamarck TW, Manuck SB. The association between racial identity and hypertension in African-American adults: elevated resting and ambulatory blood pressure as outcomes. Ethnicity and Disease. 2002; 12 :20–28. [ PubMed ] [ Google Scholar ]
- Thompson Sanders VL. Coping responses and the experience of discrimination. Journal of Applied Social Psychology. 2006; 36 (5):1198–1214. [ Google Scholar ]
- Thompson Sanders VL. The empirical characteristics of the Multidimensional Racial Identification Scale. Revised. Journal of Research in Personality. 1995; 29 :208–222. [ Google Scholar ]
- Tull ES, Sheu YT, Butler C, Cornelious K. Relationships between Perceived Stress, Coping Behavior and Cortisol Secretion in Women with High and Low Levels of Internalized Racism. Journal of the National Medical Association. 2005; 97 (2):206–212. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Uchino BN. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine. 2006; 29 (4):377–387. [ PubMed ] [ Google Scholar ]
- Utsey SO, Adams EP, Bolden M. Development and initial validation of the Africultural coping systems inventory. Journal of Black Psychology. 2000; 26 (2):194–215. [ Google Scholar ]
- Utsey SO, Chae MH, Brown CF, Kelly D. Effect of ethnic group membership on ethnic identity, race-related stress and quality of life. Cultural Diversity and Ethnic Minority Psychology. 2002; 8 (4):366–377. [ PubMed ] [ Google Scholar ]
- Utsey SO, Ponterotto JG, Reynolds AL, Cancelli AA. Racial discrimination, coping, life satisfaction, and self-esteem among African Americans. Journal of Counseling & Development. 2000; 78 (1):72–80. [ Google Scholar ]
- Veit CT, Ware JE. The structure of psychological distress and well-being in general populations. Journal of Consulting and Clinical Psychology. 1983; 51 (5):730–742. [ PubMed ] [ Google Scholar ]
- Way N. Unpublished Document. 1997. Adult and Peer Discrimination Measure. [ Google Scholar ]
- Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: Findings from community studies. American Journal of Public Health. 2003; 93 (2):200–208. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Williams DR, Williams-Morris R. Racism and mental health: the African American experience. Ethnicity and Health. 2000; 5 :243–268. [ PubMed ] [ Google Scholar ]
- Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology. 1997; 2 (3):335–351. [ PubMed ] [ Google Scholar ]
- Wong CA, Eccles JS, Sameroff A. The influence of ethnic discrimination and ethnic identification on African American adolescents’ school and socioemotional adjustment. Journal of Personality. 2003; 71 (6):1197–1232. [ PubMed ] [ Google Scholar ]
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
April 24, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Exploring how the effects of racism impact sleep in adolescents
by Society for Research in Child Development

Sleep and sleep disturbances have consequences for the development of adolescents and young adults. In a new article, researchers examine sleep during these periods, focusing on the effects of ethnic and racial discrimination. They conclude that improving sleep may boost health for all youth, but especially for those affected by racism.
The article, by researchers at Fordham University and the University of Illinois at Urbana-Champaign, appears in Child Development Perspectives .
"Discrimination based on ethnicity or race is a form of stress, and stress has been implicated in sleep disturbances ," explains Tiffany Yip, professor of psychology at Fordham University and the article's lead author. "Rather than asking young people to 'sleep off' racism, we advocate for creating sleep-promoting programs that have direct benefits for developmental outcomes as well as indirect benefits by disrupting the negative effects of racism."
Parents, teachers, scholars, and educational institutions agree nearly universally that sleep and sleep behaviors are important for the healthy development of young people. Sufficient and good-quality sleep is critical for overall adjustment, developmental milestones, and daily functioning for humans throughout life. Adolescence (ages 12-17) and young adulthood (ages 18-25), which feature significant physical and social changes, are critical periods for sleep health. These are also periods when discrimination is more pronounced.
Although discrimination can be based on many individual and intersecting biases (e.g., gender, sexuality, socioeconomic status , education), the authors chose to focus on discrimination rooted in ethnicity and race because of the well-founded documentation of disparities in sleep by race. In their article, they integrate research linking ethnic and racial discrimination to sleep across a variety of methods and developmental time spans.
Characterizing the ways in which discrimination stress is associated with sleep through direct effects, explanatory pathways, or stress amplification matters because identifying the exact nature of these associations can inform policies and practices related to sleep-focused interventions, the authors say. In addition to being a biological need, science suggests that sleep is also a promotive developmental resource.
For example, sufficient sleep duration and good quality sleep is associated with emotion regulation, learning, and memory consolidation, all important aspects of child adjustment. Moreover, sleep is also a modifiable health behavior with documented health benefits , so improving sleep can disrupt temporal associations between racism and negative effects on development.
The authors highlight various interventions to improve sleep, including school-based sleep hygiene programs, smartphone applications, and cognitive behavioral therapy. Studies show that sleep interventions can improve important components of sleep, such as total sleep duration, sleep quality, and sleep efficiency. Many of these approaches are low in cost.
"Investigations of racism and youth development must consider sleep health," says Jinjin Yan, a postdoctoral research fellow in psychology at Fordham University, who co-authored the article. "A focus on sleep health also holds promise for mitigating the negative developmental effects of ethnic and racial discrimination on mental health, physical health , and academic outcomes."
Explore further
Feedback to editors

Gene linked to epilepsy and autism decoded in new study
11 hours ago

Blood test finds knee osteoarthritis up to eight years before it appears on X-rays

Researchers find pregnancy cytokine levels impact fetal brain development and offspring behavior

Study finds biomarkers for psychiatric symptoms in patients with rare genetic condition 22q
12 hours ago

Clinical trial evaluates azithromycin for preventing chronic lung disease in premature babies
13 hours ago

Scientists report that new gene therapy slows down amyotrophic lateral sclerosis disease progression

Using stem cell-derived heart muscle cells to advance heart regenerative therapy

Analysis identifies 50 new genomic regions associated with kidney cancer risk
14 hours ago

Illusion demystifies the way vision works: Experiments imply brightness perception occurs deeper in brain than thought

How buildings influence the microbiome and human health
Related stories.

Study finds discrimination over time leads to poor sleep
Jul 24, 2023

Study shows a drink before bed can cause reductions in REM sleep
Jan 26, 2024

Study identifies two aspects of sleep related to depression in college student athletes
Jun 5, 2023

U.S. children aged 9 to 13 sleep average of 7.45 hours/Night
Jul 19, 2022

Sleep disorders in parents and children associated with more parental stress, study finds
Jan 25, 2023

Sleep disorders common in chronic migraine
Oct 20, 2022
Recommended for you

Experimental malaria monoclonal antibody protective in Malian children

What happens in the brain when we make decisions about money or food
15 hours ago

International study fills data gap on adolescent mental health

Researchers identify targets in the brain to modulate heart rate and treat depressive disorders
20 hours ago
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
Americans are divided on whether society overlooks racial discrimination or sees it where it doesn’t exist
Ahead of the 60th anniversary of the March on Washington for Black Americans’ civil rights, we asked U.S. adults what they think is the bigger problem when it comes to racial discrimination in the country today.
Pew Research Center conducted this analysis to explore how Americans view racial discrimination in the United States today compared with previous years. This question is a part of a broader study that asked Americans about their views on the Black Lives Matter movement and Martin Luther King Jr.’s legacy .
This analysis is based on a survey of 5,073 U.S. adults conducted April 10-16, 2023. Everyone who took part is a member of the Center’s American Trends Panel (ATP), an online survey panel that is recruited through national, random sampling of residential addresses. Address-based sampling ensures that nearly all U.S. adults have a chance of selection. The survey is weighted to be representative of the U.S. adult population by gender, race, ethnicity, partisan affiliation, education and other categories. Read more about the ATP’s methodology .
Here are the questions used for this analysis , along with responses, and the survey methodology .
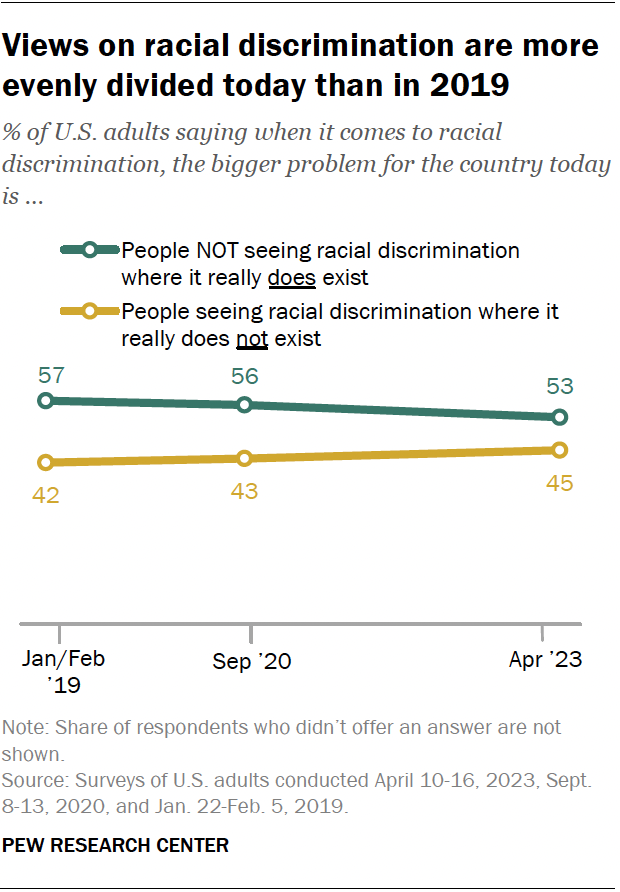
- 53% say people not seeing racial discrimination where it really does exist is the bigger problem.
- 45% point to people seeing racial discrimination where it really doesn’t exist as the larger issue.
Views on this have changed in recent years, according to Pew Research Center surveys. In 2019, 57% said people overlooking racial discrimination was the bigger problem, while 42% pointed to people seeing it where it really didn’t exist. That gap has narrowed from 15 to 8 percentage points.
Americans’ current views on this question differ greatly by:
- Race and ethnicity: 88% of Black adults say people overlooking discrimination is the bigger problem. Smaller majorities of Asian (66%) and Hispanic (58%) adults say the same, as do 45% of White adults.
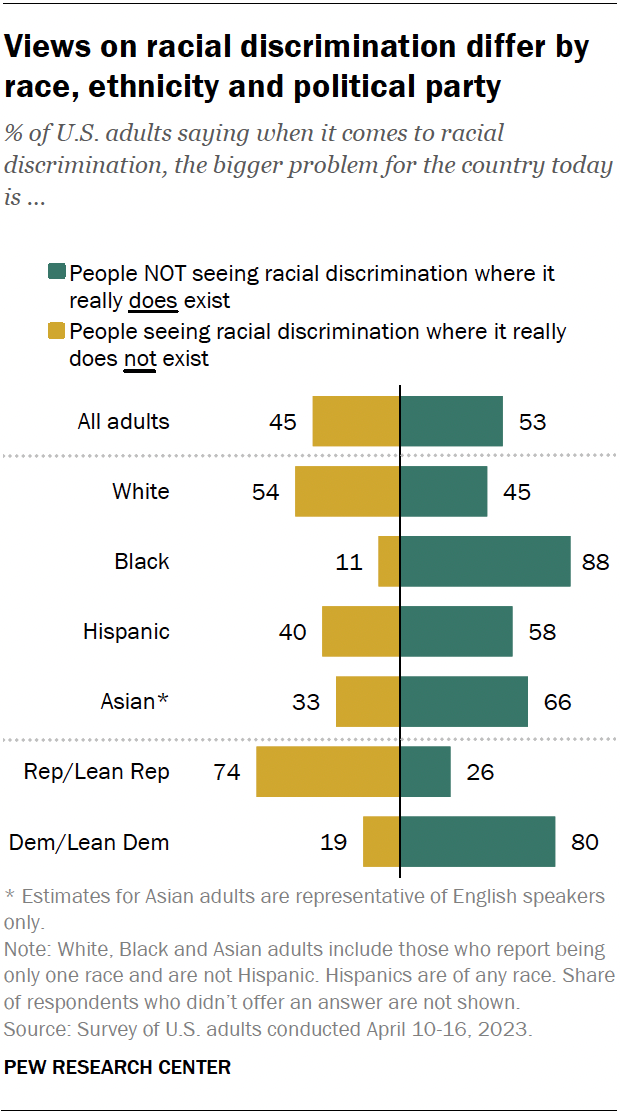
- Partisanship: 80% of Democrats and Democratic-leaning independents say people not seeing racial discrimination where it does exist is the larger issue. About three-quarters (74%) of Republicans and Republican leaners give the opposite answer.
How views on racial discrimination differ within political parties
Majorities of Republicans across age groups say people seeing racial discrimination where it doesn’t exist is the larger issue. But Republicans ages 50 and older are more likely than those under 50 to say this (78% vs. 68%).
Among Democrats, age differences aren’t as large, but there are differences by race and ethnicity. Hispanic Democrats are the most likely to say people seeing discrimination where it doesn’t exist is the bigger problem. Some 29% say this, compared with 20% of Asian Democrats, 19% of White Democrats and 8% of Black Democrats.
Note: Here are the questions used for this analysis , along with responses, and the survey methodology .
- Black Americans
- Discrimination & Prejudice
- Partisanship & Issues
- Racial Bias & Discrimination

Kiley Hurst is a research analyst focusing on social and demographic research at Pew Research Center
A look at Black-owned businesses in the U.S.
8 facts about black americans and the news, black americans’ views on success in the u.s., among black adults, those with higher incomes are most likely to say they are happy, fewer than half of black americans say the news often covers the issues that are important to them, most popular.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Coronavirus (COVID-19)
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy

IMAGES
COMMENTS
Theory and research in cultural psychology highlight the need to examine racism not only "in the head" but also "in the world." Racism is often defined as individual prejudice, but racism is also systemic, existing in the advantages and disadvantages imprinted in cultural artifacts, ideological discourse, and institutional realities that work together with individual biases.
Abstract. This article explores the meanings of racism in the sociology of race/ethnicity and provides a descriptive framework for comparing theories of racism. The authors argue that sociologists use racism to refer to four constructs: (1) individual attitudes, (2) cultural schema, and two constructs associated with structural racism: (3 ...
Racial discrimination is recognised as a key social determinant of health and driver of racial/ethnic health inequities. Studies have shown that people exposed to racism have poorer health outcomes (particularly for mental health), alongside both reduced access to health care and poorer patient experiences. Most of these studies have used cross-sectional designs: this prospective cohort study ...
Residential racial segregation remains a powerful predictor of Black disadvantage. 3,5,9 There is a direct legacy of redlining in health and well-being — preterm birth, cancer, tuberculosis ...
Race plays an important role in how people think, develop, and behave. In the current article, we queried more than 26,000 empirical articles published between 1974 and 2018 in top-tier cognitive, developmental, and social psychology journals to document how often psychological research acknowledges this reality and to examine whether people who edit, write, and participate in the research are ...
Systemic racism is said to occur when racially unequal opportunities and outcomes are inbuilt or intrinsic to the operation of a society's structures. Simply put, systemic racism refers to the processes and outcomes of racial inequality and inequity in life opportunities and treatment. Systemic racism permeates a society's (a) institutional ...
Racism and Health. Racism is an organized social system, in which the dominant racial group, based on an ideology of inferiority, categorizes and ranks people into social groups called "races", and uses its power to devalue, disempower, and differentially allocate valued societal resources and opportunities to groups defined as inferior (13, 140).
Abstract. Since the 1980s, everyday racism has gained ground within the social sciences. However, the. theory of everyday racism has not been properly adopted and, consequently, varies across ...
Some Black colleagues worry that stereotypes and biased practices keep them from getting published, winning grants, or advancing in their careers despite equal qualifications 2, 3. Truth be told ...
Yet, until racism is eliminated, it is important to. Racism, Sociology of 861. investigate how the targets interpret and respond to it in order to understand how racism affects them, ensure their voices are heard, and develop more effective strategies to combat racism itself. Challenges and Future Directions.
Background Racism has been linked with poor health in studies in the United States. Little is known about prospective associations between racial discrimination and health outcomes in the United Kingdom (UK). Methods Data were from 4883 ethnic minority (i.e. non-white) participants in the UK Household Longitudinal Study. Perceived discrimination in the last 12 months on the basis of ethnicity ...
Research papers in languages other than English were excluded. Only peer reviewed articles with empirical data were included. ... Research on racism in healthcare could benefit from sociological research on racism and racialization to explain how overt racism is produced and how racism is normalized and hidden behind supposedly non-racial ...
Objective: The aim of this paper is to provide a systematic review of studies that examine relationships between racial discrimination and trauma in order to further understand the relationship ...
SECTION III: NEW DIRECTIONS IN RACIAL IDENTITY RESEARCH. no. Psychophysiological Stress Responses to Bicultural and Biracial Identity Denial. Analia F. Albuja, ... SECTION IV: IMPLICATIONS OF RESEARCH ON RACE AND RACISM FOR DIVERSITY SCIENCE. no. Diversity (Psychological) Science Training: Challenges, Tensions, and a Call to Action.
In a review and critique of research on race and racism in the digital realm, Jessie Daniels (2013) identified social media platforms—specifically social network sites (SNSs)—as spaces "where race and racism play out in interesting, sometimes disturbing, ways" (Daniels 2013, 702).Since then, social media research has become a salient academic (sub-)field with its own journal (Social ...
Racism is a "system of structuring opportunity and assigning value based on the social interpretation of how one looks (which is what we call 'race') that unfairly disadvantages some individuals and communities, unfairly advantages other individuals and communities, and saps the strength of the whole society through the waste of human resources." 1 Racism is a social determinant of ...
research on racism, discrimination, and prejudice can be thought of in terms of different level of ... This paper reports some of the main findings from a large international study of the ...
Abstract. The study of racism in sociology entails an examination of the social construction of "racial" groups and racial inequalities. Defined as an ideology of racial group superiority that ...
Find relevant calls for papers, read free research summaries, and discover APA journals, scholarly books, and books for kids on race, trauma, and social justice. ... Psychological research has shown that racism and racial discrimination—at both the interpersonal and systemic levels—are barriers to human development and psychological wellbeing.
In this paper, we address the pressing but not sufficiently explored question of how to study racism empirically. Researching racism is a complex and sensitive task (Maiter et al., 2013).Despite, or maybe because of, its tremendous societal significance, researchers studying racism face a multitude of theoretical, empirical, and methodological challenges (Back and Sinha, 2018; Kimmel and ...
Racism, in particular, self-reported ethnic or racial discrimination is a highly prevalent phenomenon. Members of most ethnic or racial minority groups report exposure over the course of their lifetime, and recent research indicates that episodes of ethnicity-related maltreatment occur on a weekly basis for some groups (Brondolo et al. 2009).
"An honest approach to anti-racism involves embracing the limits of our objectivity—in our science, practice, and pedagogy." Increasing diversity in research. Racial disparities in psychological research, including who receives funding from the National Institutes of Health and others, are starting to make headlines. But those findings ...
The main topic of this paper is the racism action towards the main character. The research problems of this paper are the levels of racism that experienced the Black American child and what is the ...
"Investigations of racism and youth development must consider sleep health," says Jinjin Yan, a postdoctoral research fellow in psychology at Fordham University, who co-authored the article.
Pew Research Center conducted this analysis to explore how Americans view racial discrimination in the United States today compared with previous years. This question is a part of a broader study that asked Americans about their views on the Black Lives Matter movement and Martin Luther King Jr.'s legacy.
As we categorized the literature, we built on a theory of the "new racism"—a more covert and hidden racism than that of the past (Bonilla-Silva, 2006; Cross, 2005; Fiske, 1993)—and grouped the articles into two main sections: (1) research that brings to light racism's permanence and significance in the lives of students of Color through manifestations of what we conceptualize as (a ...