Generate accurate APA citations for free
- Knowledge Base
- APA Style 7th edition
- How to write an APA methods section

How to Write an APA Methods Section | With Examples
Published on February 5, 2021 by Pritha Bhandari . Revised on June 22, 2023.
The methods section of an APA style paper is where you report in detail how you performed your study. Research papers in the social and natural sciences often follow APA style. This article focuses on reporting quantitative research methods .
In your APA methods section, you should report enough information to understand and replicate your study, including detailed information on the sample , measures, and procedures used.
Instantly correct all language mistakes in your text
Upload your document to correct all your mistakes in minutes

Table of contents
Structuring an apa methods section.
Participants
Example of an APA methods section
Other interesting articles, frequently asked questions about writing an apa methods section.
The main heading of “Methods” should be centered, boldfaced, and capitalized. Subheadings within this section are left-aligned, boldfaced, and in title case. You can also add lower level headings within these subsections, as long as they follow APA heading styles .
To structure your methods section, you can use the subheadings of “Participants,” “Materials,” and “Procedures.” These headings are not mandatory—aim to organize your methods section using subheadings that make sense for your specific study.
Note that not all of these topics will necessarily be relevant for your study. For example, if you didn’t need to consider outlier removal or ways of assigning participants to different conditions, you don’t have to report these steps.
The APA also provides specific reporting guidelines for different types of research design. These tell you exactly what you need to report for longitudinal designs , replication studies, experimental designs , and so on. If your study uses a combination design, consult APA guidelines for mixed methods studies.
Detailed descriptions of procedures that don’t fit into your main text can be placed in supplemental materials (for example, the exact instructions and tasks given to participants, the full analytical strategy including software code, or additional figures and tables).
Scribbr Citation Checker New
The AI-powered Citation Checker helps you avoid common mistakes such as:
- Missing commas and periods
- Incorrect usage of “et al.”
- Ampersands (&) in narrative citations
- Missing reference entries
Begin the methods section by reporting sample characteristics, sampling procedures, and the sample size.
Participant or subject characteristics
When discussing people who participate in research, descriptive terms like “participants,” “subjects” and “respondents” can be used. For non-human animal research, “subjects” is more appropriate.
Specify all relevant demographic characteristics of your participants. This may include their age, sex, ethnic or racial group, gender identity, education level, and socioeconomic status. Depending on your study topic, other characteristics like educational or immigration status or language preference may also be relevant.
Be sure to report these characteristics as precisely as possible. This helps the reader understand how far your results may be generalized to other people.
The APA guidelines emphasize writing about participants using bias-free language , so it’s necessary to use inclusive and appropriate terms.
Sampling procedures
Outline how the participants were selected and all inclusion and exclusion criteria applied. Appropriately identify the sampling procedure used. For example, you should only label a sample as random if you had access to every member of the relevant population.
Of all the people invited to participate in your study, note the percentage that actually did (if you have this data). Additionally, report whether participants were self-selected, either by themselves or by their institutions (e.g., schools may submit student data for research purposes).
Identify any compensation (e.g., course credits or money) that was provided to participants, and mention any institutional review board approvals and ethical standards followed.
Sample size and power
Detail the sample size (per condition) and statistical power that you hoped to achieve, as well as any analyses you performed to determine these numbers.
It’s important to show that your study had enough statistical power to find effects if there were any to be found.
Additionally, state whether your final sample differed from the intended sample. Your interpretations of the study outcomes should be based only on your final sample rather than your intended sample.
Write up the tools and techniques that you used to measure relevant variables. Be as thorough as possible for a complete picture of your techniques.
Primary and secondary measures
Define the primary and secondary outcome measures that will help you answer your primary and secondary research questions.
Specify all instruments used in gathering these measurements and the construct that they measure. These instruments may include hardware, software, or tests, scales, and inventories.
- To cite hardware, indicate the model number and manufacturer.
- To cite common software (e.g., Qualtrics), state the full name along with the version number or the website URL .
- To cite tests, scales or inventories, reference its manual or the article it was published in. It’s also helpful to state the number of items and provide one or two example items.
Make sure to report the settings of (e.g., screen resolution) any specialized apparatus used.
For each instrument used, report measures of the following:
- Reliability : how consistently the method measures something, in terms of internal consistency or test-retest reliability.
- Validity : how precisely the method measures something, in terms of construct validity or criterion validity .
Giving an example item or two for tests, questionnaires , and interviews is also helpful.
Describe any covariates—these are any additional variables that may explain or predict the outcomes.
Quality of measurements
Review all methods you used to assure the quality of your measurements.
These may include:
- training researchers to collect data reliably,
- using multiple people to assess (e.g., observe or code) the data,
- translation and back-translation of research materials,
- using pilot studies to test your materials on unrelated samples.
For data that’s subjectively coded (for example, classifying open-ended responses), report interrater reliability scores. This tells the reader how similarly each response was rated by multiple raters.
Report all of the procedures applied for administering the study, processing the data, and for planned data analyses.
Data collection methods and research design
Data collection methods refers to the general mode of the instruments: surveys, interviews, observations, focus groups, neuroimaging, cognitive tests, and so on. Summarize exactly how you collected the necessary data.
Describe all procedures you applied in administering surveys, tests, physical recordings, or imaging devices, with enough detail so that someone else can replicate your techniques. If your procedures are very complicated and require long descriptions (e.g., in neuroimaging studies), place these details in supplementary materials.
To report research design, note your overall framework for data collection and analysis. State whether you used an experimental, quasi-experimental, descriptive (observational), correlational, and/or longitudinal design. Also note whether a between-subjects or a within-subjects design was used.
For multi-group studies, report the following design and procedural details as well:
- how participants were assigned to different conditions (e.g., randomization),
- instructions given to the participants in each group,
- interventions for each group,
- the setting and length of each session(s).
Describe whether any masking was used to hide the condition assignment (e.g., placebo or medication condition) from participants or research administrators. Using masking in a multi-group study ensures internal validity by reducing research bias . Explain how this masking was applied and whether its effectiveness was assessed.
Participants were randomly assigned to a control or experimental condition. The survey was administered using Qualtrics (https://www.qualtrics.com). To begin, all participants were given the AAI and a demographics questionnaire to complete, followed by an unrelated filler task. In the control condition , participants completed a short general knowledge test immediately after the filler task. In the experimental condition, participants were asked to visualize themselves taking the test for 3 minutes before they actually did. For more details on the exact instructions and tasks given, see supplementary materials.
Data diagnostics
Outline all steps taken to scrutinize or process the data after collection.
This includes the following:
- Procedures for identifying and removing outliers
- Data transformations to normalize distributions
- Compensation strategies for overcoming missing values
To ensure high validity, you should provide enough detail for your reader to understand how and why you processed or transformed your raw data in these specific ways.
Analytic strategies
The methods section is also where you describe your statistical analysis procedures, but not their outcomes. Their outcomes are reported in the results section.
These procedures should be stated for all primary, secondary, and exploratory hypotheses. While primary and secondary hypotheses are based on a theoretical framework or past studies, exploratory hypotheses are guided by the data you’ve just collected.
Prevent plagiarism. Run a free check.
This annotated example reports methods for a descriptive correlational survey on the relationship between religiosity and trust in science in the US. Hover over each part for explanation of what is included.
The sample included 879 adults aged between 18 and 28. More than half of the participants were women (56%), and all participants had completed at least 12 years of education. Ethics approval was obtained from the university board before recruitment began. Participants were recruited online through Amazon Mechanical Turk (MTurk; www.mturk.com). We selected for a geographically diverse sample within the Midwest of the US through an initial screening survey. Participants were paid USD $5 upon completion of the study.
A sample size of at least 783 was deemed necessary for detecting a correlation coefficient of ±.1, with a power level of 80% and a significance level of .05, using a sample size calculator (www.sample-size.net/correlation-sample-size/).
The primary outcome measures were the levels of religiosity and trust in science. Religiosity refers to involvement and belief in religious traditions, while trust in science represents confidence in scientists and scientific research outcomes. The secondary outcome measures were gender and parental education levels of participants and whether these characteristics predicted religiosity levels.
Religiosity
Religiosity was measured using the Centrality of Religiosity scale (Huber, 2003). The Likert scale is made up of 15 questions with five subscales of ideology, experience, intellect, public practice, and private practice. An example item is “How often do you experience situations in which you have the feeling that God or something divine intervenes in your life?” Participants were asked to indicate frequency of occurrence by selecting a response ranging from 1 (very often) to 5 (never). The internal consistency of the instrument is .83 (Huber & Huber, 2012).
Trust in Science
Trust in science was assessed using the General Trust in Science index (McCright, Dentzman, Charters & Dietz, 2013). Four Likert scale items were assessed on a scale from 1 (completely distrust) to 5 (completely trust). An example question asks “How much do you distrust or trust scientists to create knowledge that is unbiased and accurate?” Internal consistency was .8.
Potential participants were invited to participate in the survey online using Qualtrics (www.qualtrics.com). The survey consisted of multiple choice questions regarding demographic characteristics, the Centrality of Religiosity scale, an unrelated filler anagram task, and finally the General Trust in Science index. The filler task was included to avoid priming or demand characteristics, and an attention check was embedded within the religiosity scale. For full instructions and details of tasks, see supplementary materials.
For this correlational study , we assessed our primary hypothesis of a relationship between religiosity and trust in science using Pearson moment correlation coefficient. The statistical significance of the correlation coefficient was assessed using a t test. To test our secondary hypothesis of parental education levels and gender as predictors of religiosity, multiple linear regression analysis was used.
If you want to know more about statistics , methodology , or research bias , make sure to check out some of our other articles with explanations and examples.
- Normal distribution
- Measures of central tendency
- Chi square tests
- Confidence interval
- Quartiles & Quantiles
Methodology
- Cluster sampling
- Stratified sampling
- Thematic analysis
- Cohort study
- Peer review
- Ethnography
Research bias
- Implicit bias
- Cognitive bias
- Conformity bias
- Hawthorne effect
- Availability heuristic
- Attrition bias
- Social desirability bias
In your APA methods section , you should report detailed information on the participants, materials, and procedures used.
- Describe all relevant participant or subject characteristics, the sampling procedures used and the sample size and power .
- Define all primary and secondary measures and discuss the quality of measurements.
- Specify the data collection methods, the research design and data analysis strategy, including any steps taken to transform the data and statistical analyses.
You should report methods using the past tense , even if you haven’t completed your study at the time of writing. That’s because the methods section is intended to describe completed actions or research.
In a scientific paper, the methodology always comes after the introduction and before the results , discussion and conclusion . The same basic structure also applies to a thesis, dissertation , or research proposal .
Depending on the length and type of document, you might also include a literature review or theoretical framework before the methodology.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
Bhandari, P. (2023, June 22). How to Write an APA Methods Section | With Examples. Scribbr. Retrieved April 9, 2024, from https://www.scribbr.com/apa-style/methods-section/
Is this article helpful?

Pritha Bhandari
Other students also liked, how to write an apa results section, apa format for academic papers and essays, apa headings and subheadings, unlimited academic ai-proofreading.
✔ Document error-free in 5minutes ✔ Unlimited document corrections ✔ Specialized in correcting academic texts
- USC Libraries
- Research Guides
Organizing Your Social Sciences Research Paper
- 6. The Methodology
- Purpose of Guide
- Design Flaws to Avoid
- Independent and Dependent Variables
- Glossary of Research Terms
- Reading Research Effectively
- Narrowing a Topic Idea
- Broadening a Topic Idea
- Extending the Timeliness of a Topic Idea
- Academic Writing Style
- Applying Critical Thinking
- Choosing a Title
- Making an Outline
- Paragraph Development
- Research Process Video Series
- Executive Summary
- The C.A.R.S. Model
- Background Information
- The Research Problem/Question
- Theoretical Framework
- Citation Tracking
- Content Alert Services
- Evaluating Sources
- Primary Sources
- Secondary Sources
- Tiertiary Sources
- Scholarly vs. Popular Publications
- Qualitative Methods
- Quantitative Methods
- Insiderness
- Using Non-Textual Elements
- Limitations of the Study
- Common Grammar Mistakes
- Writing Concisely
- Avoiding Plagiarism
- Footnotes or Endnotes?
- Further Readings
- Generative AI and Writing
- USC Libraries Tutorials and Other Guides
- Bibliography
The methods section describes actions taken to investigate a research problem and the rationale for the application of specific procedures or techniques used to identify, select, process, and analyze information applied to understanding the problem, thereby, allowing the reader to critically evaluate a study’s overall validity and reliability. The methodology section of a research paper answers two main questions: How was the data collected or generated? And, how was it analyzed? The writing should be direct and precise and always written in the past tense.
Kallet, Richard H. "How to Write the Methods Section of a Research Paper." Respiratory Care 49 (October 2004): 1229-1232.
Importance of a Good Methodology Section
You must explain how you obtained and analyzed your results for the following reasons:
- Readers need to know how the data was obtained because the method you chose affects the results and, by extension, how you interpreted their significance in the discussion section of your paper.
- Methodology is crucial for any branch of scholarship because an unreliable method produces unreliable results and, as a consequence, undermines the value of your analysis of the findings.
- In most cases, there are a variety of different methods you can choose to investigate a research problem. The methodology section of your paper should clearly articulate the reasons why you have chosen a particular procedure or technique.
- The reader wants to know that the data was collected or generated in a way that is consistent with accepted practice in the field of study. For example, if you are using a multiple choice questionnaire, readers need to know that it offered your respondents a reasonable range of answers to choose from.
- The method must be appropriate to fulfilling the overall aims of the study. For example, you need to ensure that you have a large enough sample size to be able to generalize and make recommendations based upon the findings.
- The methodology should discuss the problems that were anticipated and the steps you took to prevent them from occurring. For any problems that do arise, you must describe the ways in which they were minimized or why these problems do not impact in any meaningful way your interpretation of the findings.
- In the social and behavioral sciences, it is important to always provide sufficient information to allow other researchers to adopt or replicate your methodology. This information is particularly important when a new method has been developed or an innovative use of an existing method is utilized.
Bem, Daryl J. Writing the Empirical Journal Article. Psychology Writing Center. University of Washington; Denscombe, Martyn. The Good Research Guide: For Small-Scale Social Research Projects . 5th edition. Buckingham, UK: Open University Press, 2014; Lunenburg, Frederick C. Writing a Successful Thesis or Dissertation: Tips and Strategies for Students in the Social and Behavioral Sciences . Thousand Oaks, CA: Corwin Press, 2008.
Structure and Writing Style
I. Groups of Research Methods
There are two main groups of research methods in the social sciences:
- The e mpirical-analytical group approaches the study of social sciences in a similar manner that researchers study the natural sciences . This type of research focuses on objective knowledge, research questions that can be answered yes or no, and operational definitions of variables to be measured. The empirical-analytical group employs deductive reasoning that uses existing theory as a foundation for formulating hypotheses that need to be tested. This approach is focused on explanation.
- The i nterpretative group of methods is focused on understanding phenomenon in a comprehensive, holistic way . Interpretive methods focus on analytically disclosing the meaning-making practices of human subjects [the why, how, or by what means people do what they do], while showing how those practices arrange so that it can be used to generate observable outcomes. Interpretive methods allow you to recognize your connection to the phenomena under investigation. However, the interpretative group requires careful examination of variables because it focuses more on subjective knowledge.
II. Content
The introduction to your methodology section should begin by restating the research problem and underlying assumptions underpinning your study. This is followed by situating the methods you used to gather, analyze, and process information within the overall “tradition” of your field of study and within the particular research design you have chosen to study the problem. If the method you choose lies outside of the tradition of your field [i.e., your review of the literature demonstrates that the method is not commonly used], provide a justification for how your choice of methods specifically addresses the research problem in ways that have not been utilized in prior studies.
The remainder of your methodology section should describe the following:
- Decisions made in selecting the data you have analyzed or, in the case of qualitative research, the subjects and research setting you have examined,
- Tools and methods used to identify and collect information, and how you identified relevant variables,
- The ways in which you processed the data and the procedures you used to analyze that data, and
- The specific research tools or strategies that you utilized to study the underlying hypothesis and research questions.
In addition, an effectively written methodology section should:
- Introduce the overall methodological approach for investigating your research problem . Is your study qualitative or quantitative or a combination of both (mixed method)? Are you going to take a special approach, such as action research, or a more neutral stance?
- Indicate how the approach fits the overall research design . Your methods for gathering data should have a clear connection to your research problem. In other words, make sure that your methods will actually address the problem. One of the most common deficiencies found in research papers is that the proposed methodology is not suitable to achieving the stated objective of your paper.
- Describe the specific methods of data collection you are going to use , such as, surveys, interviews, questionnaires, observation, archival research. If you are analyzing existing data, such as a data set or archival documents, describe how it was originally created or gathered and by whom. Also be sure to explain how older data is still relevant to investigating the current research problem.
- Explain how you intend to analyze your results . Will you use statistical analysis? Will you use specific theoretical perspectives to help you analyze a text or explain observed behaviors? Describe how you plan to obtain an accurate assessment of relationships, patterns, trends, distributions, and possible contradictions found in the data.
- Provide background and a rationale for methodologies that are unfamiliar for your readers . Very often in the social sciences, research problems and the methods for investigating them require more explanation/rationale than widely accepted rules governing the natural and physical sciences. Be clear and concise in your explanation.
- Provide a justification for subject selection and sampling procedure . For instance, if you propose to conduct interviews, how do you intend to select the sample population? If you are analyzing texts, which texts have you chosen, and why? If you are using statistics, why is this set of data being used? If other data sources exist, explain why the data you chose is most appropriate to addressing the research problem.
- Provide a justification for case study selection . A common method of analyzing research problems in the social sciences is to analyze specific cases. These can be a person, place, event, phenomenon, or other type of subject of analysis that are either examined as a singular topic of in-depth investigation or multiple topics of investigation studied for the purpose of comparing or contrasting findings. In either method, you should explain why a case or cases were chosen and how they specifically relate to the research problem.
- Describe potential limitations . Are there any practical limitations that could affect your data collection? How will you attempt to control for potential confounding variables and errors? If your methodology may lead to problems you can anticipate, state this openly and show why pursuing this methodology outweighs the risk of these problems cropping up.
NOTE : Once you have written all of the elements of the methods section, subsequent revisions should focus on how to present those elements as clearly and as logically as possibly. The description of how you prepared to study the research problem, how you gathered the data, and the protocol for analyzing the data should be organized chronologically. For clarity, when a large amount of detail must be presented, information should be presented in sub-sections according to topic. If necessary, consider using appendices for raw data.
ANOTHER NOTE : If you are conducting a qualitative analysis of a research problem , the methodology section generally requires a more elaborate description of the methods used as well as an explanation of the processes applied to gathering and analyzing of data than is generally required for studies using quantitative methods. Because you are the primary instrument for generating the data [e.g., through interviews or observations], the process for collecting that data has a significantly greater impact on producing the findings. Therefore, qualitative research requires a more detailed description of the methods used.
YET ANOTHER NOTE : If your study involves interviews, observations, or other qualitative techniques involving human subjects , you may be required to obtain approval from the university's Office for the Protection of Research Subjects before beginning your research. This is not a common procedure for most undergraduate level student research assignments. However, i f your professor states you need approval, you must include a statement in your methods section that you received official endorsement and adequate informed consent from the office and that there was a clear assessment and minimization of risks to participants and to the university. This statement informs the reader that your study was conducted in an ethical and responsible manner. In some cases, the approval notice is included as an appendix to your paper.
III. Problems to Avoid
Irrelevant Detail The methodology section of your paper should be thorough but concise. Do not provide any background information that does not directly help the reader understand why a particular method was chosen, how the data was gathered or obtained, and how the data was analyzed in relation to the research problem [note: analyzed, not interpreted! Save how you interpreted the findings for the discussion section]. With this in mind, the page length of your methods section will generally be less than any other section of your paper except the conclusion.
Unnecessary Explanation of Basic Procedures Remember that you are not writing a how-to guide about a particular method. You should make the assumption that readers possess a basic understanding of how to investigate the research problem on their own and, therefore, you do not have to go into great detail about specific methodological procedures. The focus should be on how you applied a method , not on the mechanics of doing a method. An exception to this rule is if you select an unconventional methodological approach; if this is the case, be sure to explain why this approach was chosen and how it enhances the overall process of discovery.
Problem Blindness It is almost a given that you will encounter problems when collecting or generating your data, or, gaps will exist in existing data or archival materials. Do not ignore these problems or pretend they did not occur. Often, documenting how you overcame obstacles can form an interesting part of the methodology. It demonstrates to the reader that you can provide a cogent rationale for the decisions you made to minimize the impact of any problems that arose.
Literature Review Just as the literature review section of your paper provides an overview of sources you have examined while researching a particular topic, the methodology section should cite any sources that informed your choice and application of a particular method [i.e., the choice of a survey should include any citations to the works you used to help construct the survey].
It’s More than Sources of Information! A description of a research study's method should not be confused with a description of the sources of information. Such a list of sources is useful in and of itself, especially if it is accompanied by an explanation about the selection and use of the sources. The description of the project's methodology complements a list of sources in that it sets forth the organization and interpretation of information emanating from those sources.
Azevedo, L.F. et al. "How to Write a Scientific Paper: Writing the Methods Section." Revista Portuguesa de Pneumologia 17 (2011): 232-238; Blair Lorrie. “Choosing a Methodology.” In Writing a Graduate Thesis or Dissertation , Teaching Writing Series. (Rotterdam: Sense Publishers 2016), pp. 49-72; Butin, Dan W. The Education Dissertation A Guide for Practitioner Scholars . Thousand Oaks, CA: Corwin, 2010; Carter, Susan. Structuring Your Research Thesis . New York: Palgrave Macmillan, 2012; Kallet, Richard H. “How to Write the Methods Section of a Research Paper.” Respiratory Care 49 (October 2004):1229-1232; Lunenburg, Frederick C. Writing a Successful Thesis or Dissertation: Tips and Strategies for Students in the Social and Behavioral Sciences . Thousand Oaks, CA: Corwin Press, 2008. Methods Section. The Writer’s Handbook. Writing Center. University of Wisconsin, Madison; Rudestam, Kjell Erik and Rae R. Newton. “The Method Chapter: Describing Your Research Plan.” In Surviving Your Dissertation: A Comprehensive Guide to Content and Process . (Thousand Oaks, Sage Publications, 2015), pp. 87-115; What is Interpretive Research. Institute of Public and International Affairs, University of Utah; Writing the Experimental Report: Methods, Results, and Discussion. The Writing Lab and The OWL. Purdue University; Methods and Materials. The Structure, Format, Content, and Style of a Journal-Style Scientific Paper. Department of Biology. Bates College.
Writing Tip
Statistical Designs and Tests? Do Not Fear Them!
Don't avoid using a quantitative approach to analyzing your research problem just because you fear the idea of applying statistical designs and tests. A qualitative approach, such as conducting interviews or content analysis of archival texts, can yield exciting new insights about a research problem, but it should not be undertaken simply because you have a disdain for running a simple regression. A well designed quantitative research study can often be accomplished in very clear and direct ways, whereas, a similar study of a qualitative nature usually requires considerable time to analyze large volumes of data and a tremendous burden to create new paths for analysis where previously no path associated with your research problem had existed.
To locate data and statistics, GO HERE .
Another Writing Tip
Knowing the Relationship Between Theories and Methods
There can be multiple meaning associated with the term "theories" and the term "methods" in social sciences research. A helpful way to delineate between them is to understand "theories" as representing different ways of characterizing the social world when you research it and "methods" as representing different ways of generating and analyzing data about that social world. Framed in this way, all empirical social sciences research involves theories and methods, whether they are stated explicitly or not. However, while theories and methods are often related, it is important that, as a researcher, you deliberately separate them in order to avoid your theories playing a disproportionate role in shaping what outcomes your chosen methods produce.
Introspectively engage in an ongoing dialectic between the application of theories and methods to help enable you to use the outcomes from your methods to interrogate and develop new theories, or ways of framing conceptually the research problem. This is how scholarship grows and branches out into new intellectual territory.
Reynolds, R. Larry. Ways of Knowing. Alternative Microeconomics . Part 1, Chapter 3. Boise State University; The Theory-Method Relationship. S-Cool Revision. United Kingdom.
Yet Another Writing Tip
Methods and the Methodology
Do not confuse the terms "methods" and "methodology." As Schneider notes, a method refers to the technical steps taken to do research . Descriptions of methods usually include defining and stating why you have chosen specific techniques to investigate a research problem, followed by an outline of the procedures you used to systematically select, gather, and process the data [remember to always save the interpretation of data for the discussion section of your paper].
The methodology refers to a discussion of the underlying reasoning why particular methods were used . This discussion includes describing the theoretical concepts that inform the choice of methods to be applied, placing the choice of methods within the more general nature of academic work, and reviewing its relevance to examining the research problem. The methodology section also includes a thorough review of the methods other scholars have used to study the topic.
Bryman, Alan. "Of Methods and Methodology." Qualitative Research in Organizations and Management: An International Journal 3 (2008): 159-168; Schneider, Florian. “What's in a Methodology: The Difference between Method, Methodology, and Theory…and How to Get the Balance Right?” PoliticsEastAsia.com. Chinese Department, University of Leiden, Netherlands.
- << Previous: Scholarly vs. Popular Publications
- Next: Qualitative Methods >>
- Last Updated: Apr 11, 2024 1:27 PM
- URL: https://libguides.usc.edu/writingguide
- Interlibrary Loan and Scan & Deliver
- Course Reserves
- Purchase Request
- Collection Development & Maintenance
- Current Negotiations
- Ask a Librarian
- Instructor Support
- Library How-To
- Research Guides
- Research Support
- Study Rooms
- Research Rooms
- Partner Spaces
- Loanable Equipment
- Print, Scan, Copy
- 3D Printers
- Poster Printing
- OSULP Leadership
- Strategic Plan
Scholarly Articles: How can I tell?
- Journal Information
- Literature Review
- Author and affiliation
- Introduction
- Specialized Vocabulary
Methodology
- Research sponsors
- Peer-review
The methodology section or methods section tells you how the author(s) went about doing their research. It should let you know a) what method they used to gather data (survey, interviews, experiments, etc.), why they chose this method, and what the limitations are to this method.
The methodology section should be detailed enough that another researcher could replicate the study described. When you read the methodology or methods section:
- What kind of research method did the authors use? Is it an appropriate method for the type of study they are conducting?
- How did the authors get their tests subjects? What criteria did they use?
- What are the contexts of the study that may have affected the results (e.g. environmental conditions, lab conditions, timing questions, etc.)
- Is the sample size representative of the larger population (i.e., was it big enough?)
- Are the data collection instruments and procedures likely to have measured all the important characteristics with reasonable accuracy?
- Does the data analysis appear to have been done with care, and were appropriate analytical techniques used?
A good researcher will always let you know about the limitations of his or her research.
- << Previous: Specialized Vocabulary
- Next: Results >>
- Last Updated: Sep 20, 2023 4:01 PM
- URL: https://guides.library.oregonstate.edu/ScholarlyArticle

Contact Info
121 The Valley Library Corvallis OR 97331–4501
Phone: 541-737-3331
Services for Persons with Disabilities
In the Valley Library
- Oregon State University Press
- Special Collections and Archives Research Center
- Undergrad Research & Writing Studio
- Graduate Student Commons
- Tutoring Services
- Northwest Art Collection
Digital Projects
- Oregon Explorer
- Oregon Digital
- ScholarsArchive@OSU
- Digital Publishing Initiatives
- Atlas of the Pacific Northwest
- Marilyn Potts Guin Library
- Cascades Campus Library
- McDowell Library of Vet Medicine

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
11.2 Writing a Research Report in American Psychological Association (APA) Style
Learning objectives.
- Identify the major sections of an APA-style research report and the basic contents of each section.
- Plan and write an effective APA-style research report.
In this section, we look at how to write an APA-style empirical research report , an article that presents the results of one or more new studies. Recall that the standard sections of an empirical research report provide a kind of outline. Here we consider each of these sections in detail, including what information it contains, how that information is formatted and organized, and tips for writing each section. At the end of this section is a sample APA-style research report that illustrates many of these principles.
Sections of a Research Report
Title page and abstract.
An APA-style research report begins with a title page . The title is centered in the upper half of the page, with each important word capitalized. The title should clearly and concisely (in about 12 words or fewer) communicate the primary variables and research questions. This sometimes requires a main title followed by a subtitle that elaborates on the main title, in which case the main title and subtitle are separated by a colon. Here are some titles from recent issues of professional journals published by the American Psychological Association.
- Sex Differences in Coping Styles and Implications for Depressed Mood
- Effects of Aging and Divided Attention on Memory for Items and Their Contexts
- Computer-Assisted Cognitive Behavioral Therapy for Child Anxiety: Results of a Randomized Clinical Trial
- Virtual Driving and Risk Taking: Do Racing Games Increase Risk-Taking Cognitions, Affect, and Behavior?
Below the title are the authors’ names and, on the next line, their institutional affiliation—the university or other institution where the authors worked when they conducted the research. As we have already seen, the authors are listed in an order that reflects their contribution to the research. When multiple authors have made equal contributions to the research, they often list their names alphabetically or in a randomly determined order.
It’s Soooo Cute!
How Informal Should an Article Title Be?
In some areas of psychology, the titles of many empirical research reports are informal in a way that is perhaps best described as “cute.” They usually take the form of a play on words or a well-known expression that relates to the topic under study. Here are some examples from recent issues of the Journal of Personality and Social Psychology .
- “Let’s Get Serious: Communicating Commitment in Romantic Relationships”
- “Through the Looking Glass Clearly: Accuracy and Assumed Similarity in Well-Adjusted Individuals’ First Impressions”
- “Don’t Hide Your Happiness! Positive Emotion Dissociation, Social Connectedness, and Psychological Functioning”
- “Forbidden Fruit: Inattention to Attractive Alternatives Provokes Implicit Relationship Reactance”
Individual researchers differ quite a bit in their preference for such titles. Some use them regularly, while others never use them. What might be some of the pros and cons of using cute article titles?
For articles that are being submitted for publication, the title page also includes an author note that lists the authors’ full institutional affiliations, any acknowledgments the authors wish to make to agencies that funded the research or to colleagues who commented on it, and contact information for the authors. For student papers that are not being submitted for publication—including theses—author notes are generally not necessary.
The abstract is a summary of the study. It is the second page of the manuscript and is headed with the word Abstract . The first line is not indented. The abstract presents the research question, a summary of the method, the basic results, and the most important conclusions. Because the abstract is usually limited to about 200 words, it can be a challenge to write a good one.
Introduction
The introduction begins on the third page of the manuscript. The heading at the top of this page is the full title of the manuscript, with each important word capitalized as on the title page. The introduction includes three distinct subsections, although these are typically not identified by separate headings. The opening introduces the research question and explains why it is interesting, the literature review discusses relevant previous research, and the closing restates the research question and comments on the method used to answer it.
The Opening
The opening , which is usually a paragraph or two in length, introduces the research question and explains why it is interesting. To capture the reader’s attention, researcher Daryl Bem recommends starting with general observations about the topic under study, expressed in ordinary language (not technical jargon)—observations that are about people and their behavior (not about researchers or their research; Bem, 2003). Concrete examples are often very useful here. According to Bem, this would be a poor way to begin a research report:
Festinger’s theory of cognitive dissonance received a great deal of attention during the latter part of the 20th century (p. 191)
The following would be much better:
The individual who holds two beliefs that are inconsistent with one another may feel uncomfortable. For example, the person who knows that he or she enjoys smoking but believes it to be unhealthy may experience discomfort arising from the inconsistency or disharmony between these two thoughts or cognitions. This feeling of discomfort was called cognitive dissonance by social psychologist Leon Festinger (1957), who suggested that individuals will be motivated to remove this dissonance in whatever way they can (p. 191).
After capturing the reader’s attention, the opening should go on to introduce the research question and explain why it is interesting. Will the answer fill a gap in the literature? Will it provide a test of an important theory? Does it have practical implications? Giving readers a clear sense of what the research is about and why they should care about it will motivate them to continue reading the literature review—and will help them make sense of it.
Breaking the Rules
Researcher Larry Jacoby reported several studies showing that a word that people see or hear repeatedly can seem more familiar even when they do not recall the repetitions—and that this tendency is especially pronounced among older adults. He opened his article with the following humorous anecdote (Jacoby, 1999).
A friend whose mother is suffering symptoms of Alzheimer’s disease (AD) tells the story of taking her mother to visit a nursing home, preliminary to her mother’s moving there. During an orientation meeting at the nursing home, the rules and regulations were explained, one of which regarded the dining room. The dining room was described as similar to a fine restaurant except that tipping was not required. The absence of tipping was a central theme in the orientation lecture, mentioned frequently to emphasize the quality of care along with the advantages of having paid in advance. At the end of the meeting, the friend’s mother was asked whether she had any questions. She replied that she only had one question: “Should I tip?” (p. 3).
Although both humor and personal anecdotes are generally discouraged in APA-style writing, this example is a highly effective way to start because it both engages the reader and provides an excellent real-world example of the topic under study.
The Literature Review
Immediately after the opening comes the literature review , which describes relevant previous research on the topic and can be anywhere from several paragraphs to several pages in length. However, the literature review is not simply a list of past studies. Instead, it constitutes a kind of argument for why the research question is worth addressing. By the end of the literature review, readers should be convinced that the research question makes sense and that the present study is a logical next step in the ongoing research process.
Like any effective argument, the literature review must have some kind of structure. For example, it might begin by describing a phenomenon in a general way along with several studies that demonstrate it, then describing two or more competing theories of the phenomenon, and finally presenting a hypothesis to test one or more of the theories. Or it might describe one phenomenon, then describe another phenomenon that seems inconsistent with the first one, then propose a theory that resolves the inconsistency, and finally present a hypothesis to test that theory. In applied research, it might describe a phenomenon or theory, then describe how that phenomenon or theory applies to some important real-world situation, and finally suggest a way to test whether it does, in fact, apply to that situation.
Looking at the literature review in this way emphasizes a few things. First, it is extremely important to start with an outline of the main points that you want to make, organized in the order that you want to make them. The basic structure of your argument, then, should be apparent from the outline itself. Second, it is important to emphasize the structure of your argument in your writing. One way to do this is to begin the literature review by summarizing your argument even before you begin to make it. “In this article, I will describe two apparently contradictory phenomena, present a new theory that has the potential to resolve the apparent contradiction, and finally present a novel hypothesis to test the theory.” Another way is to open each paragraph with a sentence that summarizes the main point of the paragraph and links it to the preceding points. These opening sentences provide the “transitions” that many beginning researchers have difficulty with. Instead of beginning a paragraph by launching into a description of a previous study, such as “Williams (2004) found that…,” it is better to start by indicating something about why you are describing this particular study. Here are some simple examples:
Another example of this phenomenon comes from the work of Williams (2004).
Williams (2004) offers one explanation of this phenomenon.
An alternative perspective has been provided by Williams (2004).
We used a method based on the one used by Williams (2004).
Finally, remember that your goal is to construct an argument for why your research question is interesting and worth addressing—not necessarily why your favorite answer to it is correct. In other words, your literature review must be balanced. If you want to emphasize the generality of a phenomenon, then of course you should discuss various studies that have demonstrated it. However, if there are other studies that have failed to demonstrate it, you should discuss them too. Or if you are proposing a new theory, then of course you should discuss findings that are consistent with that theory. However, if there are other findings that are inconsistent with it, again, you should discuss them too. It is acceptable to argue that the balance of the research supports the existence of a phenomenon or is consistent with a theory (and that is usually the best that researchers in psychology can hope for), but it is not acceptable to ignore contradictory evidence. Besides, a large part of what makes a research question interesting is uncertainty about its answer.
The Closing
The closing of the introduction—typically the final paragraph or two—usually includes two important elements. The first is a clear statement of the main research question or hypothesis. This statement tends to be more formal and precise than in the opening and is often expressed in terms of operational definitions of the key variables. The second is a brief overview of the method and some comment on its appropriateness. Here, for example, is how Darley and Latané (1968) concluded the introduction to their classic article on the bystander effect:
These considerations lead to the hypothesis that the more bystanders to an emergency, the less likely, or the more slowly, any one bystander will intervene to provide aid. To test this proposition it would be necessary to create a situation in which a realistic “emergency” could plausibly occur. Each subject should also be blocked from communicating with others to prevent his getting information about their behavior during the emergency. Finally, the experimental situation should allow for the assessment of the speed and frequency of the subjects’ reaction to the emergency. The experiment reported below attempted to fulfill these conditions (p. 378).
Thus the introduction leads smoothly into the next major section of the article—the method section.
The method section is where you describe how you conducted your study. An important principle for writing a method section is that it should be clear and detailed enough that other researchers could replicate the study by following your “recipe.” This means that it must describe all the important elements of the study—basic demographic characteristics of the participants, how they were recruited, whether they were randomly assigned, how the variables were manipulated or measured, how counterbalancing was accomplished, and so on. At the same time, it should avoid irrelevant details such as the fact that the study was conducted in Classroom 37B of the Industrial Technology Building or that the questionnaire was double-sided and completed using pencils.
The method section begins immediately after the introduction ends with the heading “Method” (not “Methods”) centered on the page. Immediately after this is the subheading “Participants,” left justified and in italics. The participants subsection indicates how many participants there were, the number of women and men, some indication of their age, other demographics that may be relevant to the study, and how they were recruited, including any incentives given for participation.
Figure 11.1 Three Ways of Organizing an APA-Style Method
After the participants section, the structure can vary a bit. Figure 11.1 “Three Ways of Organizing an APA-Style Method” shows three common approaches. In the first, the participants section is followed by a design and procedure subsection, which describes the rest of the method. This works well for methods that are relatively simple and can be described adequately in a few paragraphs. In the second approach, the participants section is followed by separate design and procedure subsections. This works well when both the design and the procedure are relatively complicated and each requires multiple paragraphs.
What is the difference between design and procedure? The design of a study is its overall structure. What were the independent and dependent variables? Was the independent variable manipulated, and if so, was it manipulated between or within subjects? How were the variables operationally defined? The procedure is how the study was carried out. It often works well to describe the procedure in terms of what the participants did rather than what the researchers did. For example, the participants gave their informed consent, read a set of instructions, completed a block of four practice trials, completed a block of 20 test trials, completed two questionnaires, and were debriefed and excused.
In the third basic way to organize a method section, the participants subsection is followed by a materials subsection before the design and procedure subsections. This works well when there are complicated materials to describe. This might mean multiple questionnaires, written vignettes that participants read and respond to, perceptual stimuli, and so on. The heading of this subsection can be modified to reflect its content. Instead of “Materials,” it can be “Questionnaires,” “Stimuli,” and so on.
The results section is where you present the main results of the study, including the results of the statistical analyses. Although it does not include the raw data—individual participants’ responses or scores—researchers should save their raw data and make them available to other researchers who request them. Some journals now make the raw data available online.
Although there are no standard subsections, it is still important for the results section to be logically organized. Typically it begins with certain preliminary issues. One is whether any participants or responses were excluded from the analyses and why. The rationale for excluding data should be described clearly so that other researchers can decide whether it is appropriate. A second preliminary issue is how multiple responses were combined to produce the primary variables in the analyses. For example, if participants rated the attractiveness of 20 stimulus people, you might have to explain that you began by computing the mean attractiveness rating for each participant. Or if they recalled as many items as they could from study list of 20 words, did you count the number correctly recalled, compute the percentage correctly recalled, or perhaps compute the number correct minus the number incorrect? A third preliminary issue is the reliability of the measures. This is where you would present test-retest correlations, Cronbach’s α, or other statistics to show that the measures are consistent across time and across items. A final preliminary issue is whether the manipulation was successful. This is where you would report the results of any manipulation checks.
The results section should then tackle the primary research questions, one at a time. Again, there should be a clear organization. One approach would be to answer the most general questions and then proceed to answer more specific ones. Another would be to answer the main question first and then to answer secondary ones. Regardless, Bem (2003) suggests the following basic structure for discussing each new result:
- Remind the reader of the research question.
- Give the answer to the research question in words.
- Present the relevant statistics.
- Qualify the answer if necessary.
- Summarize the result.
Notice that only Step 3 necessarily involves numbers. The rest of the steps involve presenting the research question and the answer to it in words. In fact, the basic results should be clear even to a reader who skips over the numbers.
The discussion is the last major section of the research report. Discussions usually consist of some combination of the following elements:
- Summary of the research
- Theoretical implications
- Practical implications
- Limitations
- Suggestions for future research
The discussion typically begins with a summary of the study that provides a clear answer to the research question. In a short report with a single study, this might require no more than a sentence. In a longer report with multiple studies, it might require a paragraph or even two. The summary is often followed by a discussion of the theoretical implications of the research. Do the results provide support for any existing theories? If not, how can they be explained? Although you do not have to provide a definitive explanation or detailed theory for your results, you at least need to outline one or more possible explanations. In applied research—and often in basic research—there is also some discussion of the practical implications of the research. How can the results be used, and by whom, to accomplish some real-world goal?
The theoretical and practical implications are often followed by a discussion of the study’s limitations. Perhaps there are problems with its internal or external validity. Perhaps the manipulation was not very effective or the measures not very reliable. Perhaps there is some evidence that participants did not fully understand their task or that they were suspicious of the intent of the researchers. Now is the time to discuss these issues and how they might have affected the results. But do not overdo it. All studies have limitations, and most readers will understand that a different sample or different measures might have produced different results. Unless there is good reason to think they would have, however, there is no reason to mention these routine issues. Instead, pick two or three limitations that seem like they could have influenced the results, explain how they could have influenced the results, and suggest ways to deal with them.
Most discussions end with some suggestions for future research. If the study did not satisfactorily answer the original research question, what will it take to do so? What new research questions has the study raised? This part of the discussion, however, is not just a list of new questions. It is a discussion of two or three of the most important unresolved issues. This means identifying and clarifying each question, suggesting some alternative answers, and even suggesting ways they could be studied.
Finally, some researchers are quite good at ending their articles with a sweeping or thought-provoking conclusion. Darley and Latané (1968), for example, ended their article on the bystander effect by discussing the idea that whether people help others may depend more on the situation than on their personalities. Their final sentence is, “If people understand the situational forces that can make them hesitate to intervene, they may better overcome them” (p. 383). However, this kind of ending can be difficult to pull off. It can sound overreaching or just banal and end up detracting from the overall impact of the article. It is often better simply to end when you have made your final point (although you should avoid ending on a limitation).
The references section begins on a new page with the heading “References” centered at the top of the page. All references cited in the text are then listed in the format presented earlier. They are listed alphabetically by the last name of the first author. If two sources have the same first author, they are listed alphabetically by the last name of the second author. If all the authors are the same, then they are listed chronologically by the year of publication. Everything in the reference list is double-spaced both within and between references.
Appendixes, Tables, and Figures
Appendixes, tables, and figures come after the references. An appendix is appropriate for supplemental material that would interrupt the flow of the research report if it were presented within any of the major sections. An appendix could be used to present lists of stimulus words, questionnaire items, detailed descriptions of special equipment or unusual statistical analyses, or references to the studies that are included in a meta-analysis. Each appendix begins on a new page. If there is only one, the heading is “Appendix,” centered at the top of the page. If there is more than one, the headings are “Appendix A,” “Appendix B,” and so on, and they appear in the order they were first mentioned in the text of the report.
After any appendixes come tables and then figures. Tables and figures are both used to present results. Figures can also be used to illustrate theories (e.g., in the form of a flowchart), display stimuli, outline procedures, and present many other kinds of information. Each table and figure appears on its own page. Tables are numbered in the order that they are first mentioned in the text (“Table 1,” “Table 2,” and so on). Figures are numbered the same way (“Figure 1,” “Figure 2,” and so on). A brief explanatory title, with the important words capitalized, appears above each table. Each figure is given a brief explanatory caption, where (aside from proper nouns or names) only the first word of each sentence is capitalized. More details on preparing APA-style tables and figures are presented later in the book.
Sample APA-Style Research Report
Figure 11.2 “Title Page and Abstract” , Figure 11.3 “Introduction and Method” , Figure 11.4 “Results and Discussion” , and Figure 11.5 “References and Figure” show some sample pages from an APA-style empirical research report originally written by undergraduate student Tomoe Suyama at California State University, Fresno. The main purpose of these figures is to illustrate the basic organization and formatting of an APA-style empirical research report, although many high-level and low-level style conventions can be seen here too.
Figure 11.2 Title Page and Abstract
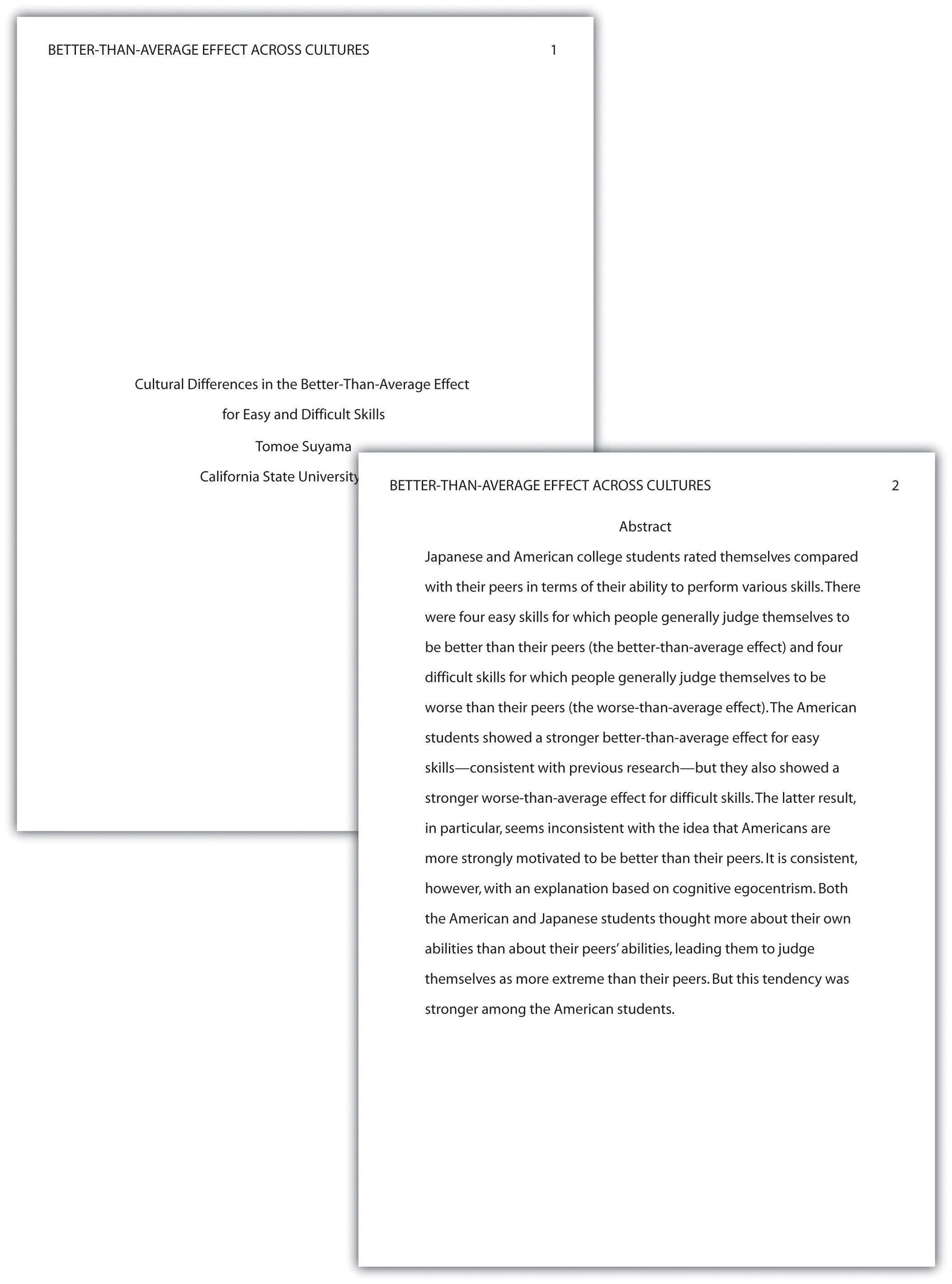
This student paper does not include the author note on the title page. The abstract appears on its own page.
Figure 11.3 Introduction and Method
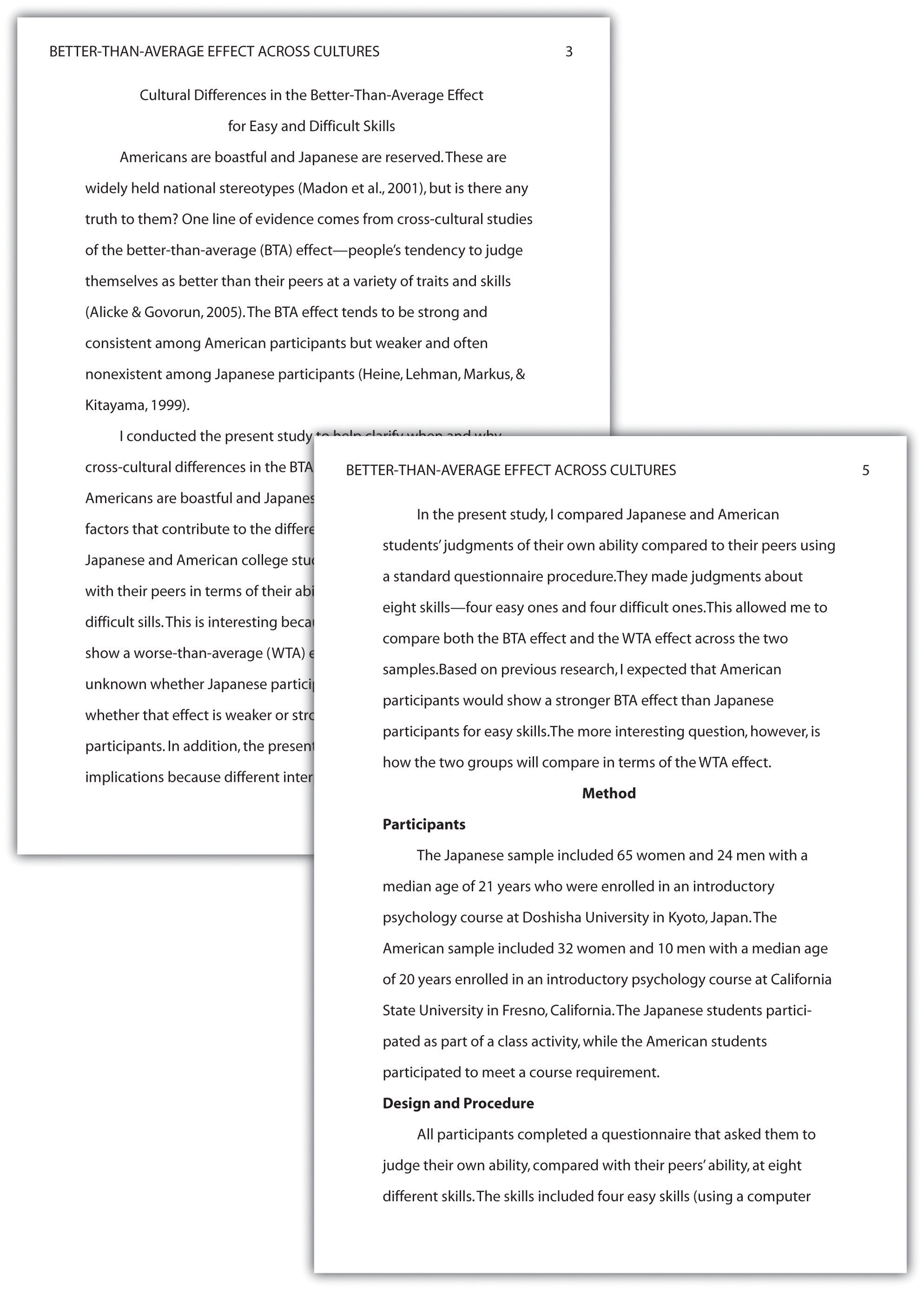
Note that the introduction is headed with the full title, and the method section begins immediately after the introduction ends.
Figure 11.4 Results and Discussion
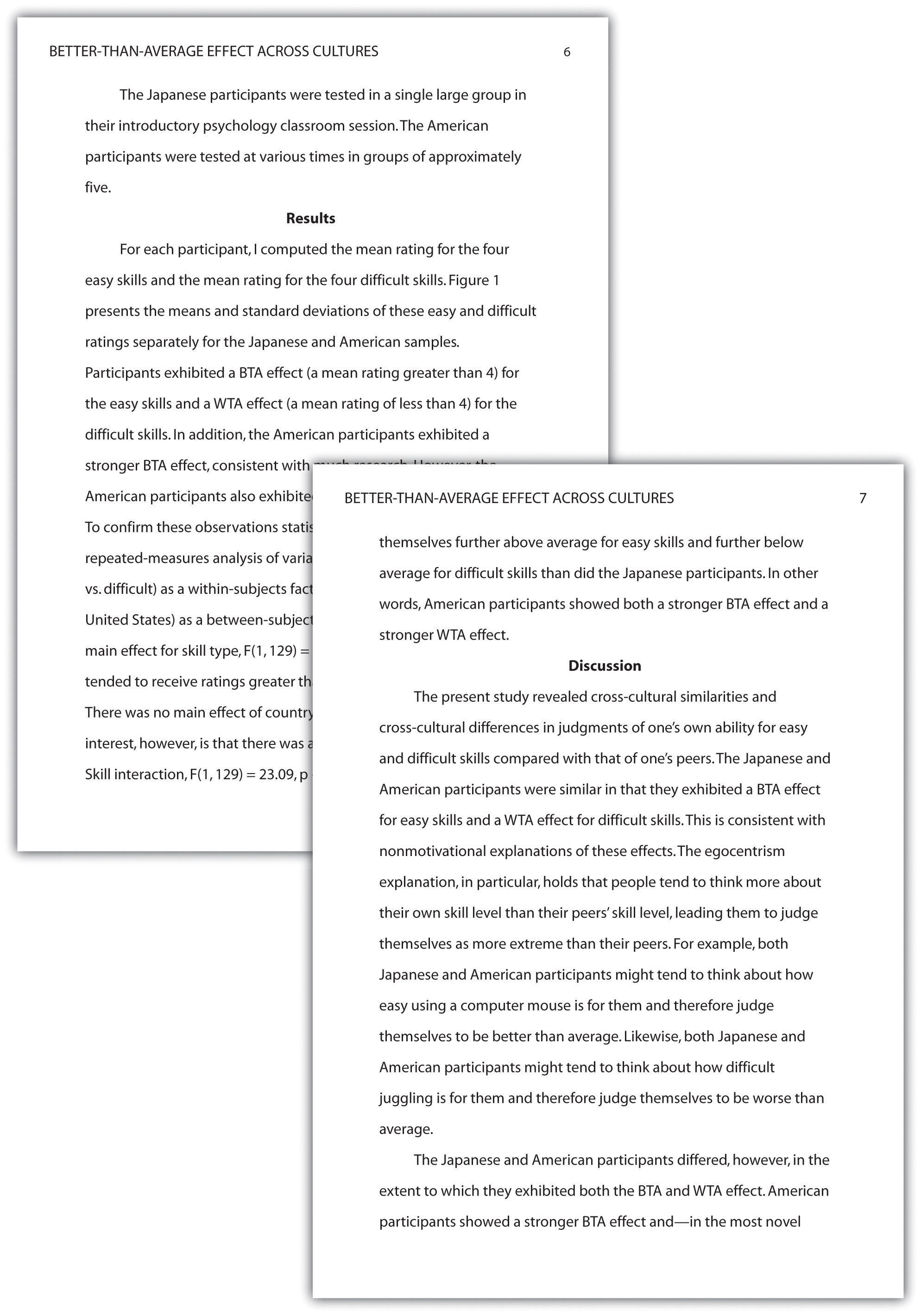
The discussion begins immediately after the results section ends.
Figure 11.5 References and Figure
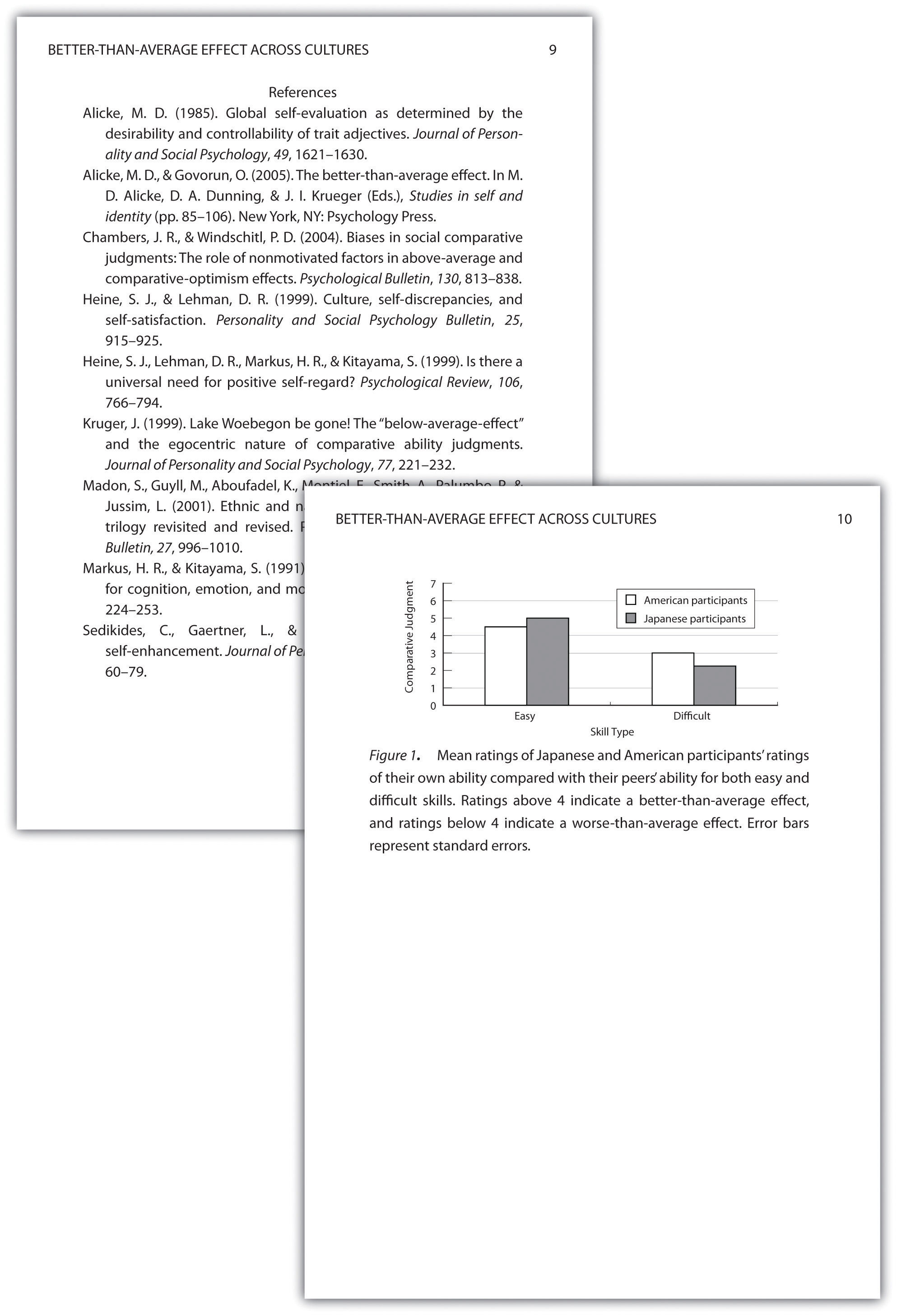
If there were appendixes or tables, they would come before the figure.
Key Takeaways
- An APA-style empirical research report consists of several standard sections. The main ones are the abstract, introduction, method, results, discussion, and references.
- The introduction consists of an opening that presents the research question, a literature review that describes previous research on the topic, and a closing that restates the research question and comments on the method. The literature review constitutes an argument for why the current study is worth doing.
- The method section describes the method in enough detail that another researcher could replicate the study. At a minimum, it consists of a participants subsection and a design and procedure subsection.
- The results section describes the results in an organized fashion. Each primary result is presented in terms of statistical results but also explained in words.
- The discussion typically summarizes the study, discusses theoretical and practical implications and limitations of the study, and offers suggestions for further research.
- Practice: Look through an issue of a general interest professional journal (e.g., Psychological Science ). Read the opening of the first five articles and rate the effectiveness of each one from 1 ( very ineffective ) to 5 ( very effective ). Write a sentence or two explaining each rating.
- Practice: Find a recent article in a professional journal and identify where the opening, literature review, and closing of the introduction begin and end.
- Practice: Find a recent article in a professional journal and highlight in a different color each of the following elements in the discussion: summary, theoretical implications, practical implications, limitations, and suggestions for future research.
Bem, D. J. (2003). Writing the empirical journal article. In J. M. Darley, M. P. Zanna, & H. R. Roediger III (Eds.), The compleat academic: A practical guide for the beginning social scientist (2nd ed.). Washington, DC: American Psychological Association.
Darley, J. M., & Latané, B. (1968). Bystander intervention in emergencies: Diffusion of responsibility. Journal of Personality and Social Psychology, 4 , 377–383.
Research Methods in Psychology Copyright © 2016 by University of Minnesota is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License , except where otherwise noted.
How to Present Results in a Research Paper
- First Online: 01 October 2023
Cite this chapter

- Aparna Mukherjee 4 ,
- Gunjan Kumar 4 &
- Rakesh Lodha 5
616 Accesses
The results section is the core of a research manuscript where the study data and analyses are presented in an organized, uncluttered manner such that the reader can easily understand and interpret the findings. This section is completely factual; there is no place for opinions or explanations from the authors. The results should correspond to the objectives of the study in an orderly manner. Self-explanatory tables and figures add value to this section and make data presentation more convenient and appealing. The results presented in this section should have a link with both the preceding methods section and the following discussion section. A well-written, articulate results section lends clarity and credibility to the research paper and the study as a whole. This chapter provides an overview and important pointers to effective drafting of the results section in a research manuscript and also in theses.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Kallestinova ED (2011) How to write your first research paper. Yale J Biol Med 84(3):181–190
PubMed PubMed Central Google Scholar
STROBE. STROBE. [cited 2022 Nov 10]. https://www.strobe-statement.org/
Consort—Welcome to the CONSORT Website. http://www.consort-statement.org/ . Accessed 10 Nov 2022
Korevaar DA, Cohen JF, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP et al (2016) Updating standards for reporting diagnostic accuracy: the development of STARD 2015. Res Integr Peer Rev 1(1):7
Article PubMed PubMed Central Google Scholar
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 372:n160
Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups | EQUATOR Network. https://www.equator-network.org/reporting-guidelines/coreq/ . Accessed 10 Nov 2022
Aggarwal R, Sahni P (2015) The results section. In: Aggarwal R, Sahni P (eds) Reporting and publishing research in the biomedical sciences, 1st edn. National Medical Journal of India, Delhi, pp 24–44
Google Scholar
Mukherjee A, Lodha R (2016) Writing the results. Indian Pediatr 53(5):409–415
Article PubMed Google Scholar
Lodha R, Randev S, Kabra SK (2016) Oral antibiotics for community acquired pneumonia with chest indrawing in children aged below five years: a systematic review. Indian Pediatr 53(6):489–495
Anderson C (2010) Presenting and evaluating qualitative research. Am J Pharm Educ 74(8):141
Roberts C, Kumar K, Finn G (2020) Navigating the qualitative manuscript writing process: some tips for authors and reviewers. BMC Med Educ 20:439
Bigby C (2015) Preparing manuscripts that report qualitative research: avoiding common pitfalls and illegitimate questions. Aust Soc Work 68(3):384–391
Article Google Scholar
Vincent BP, Kumar G, Parameswaran S, Kar SS (2019) Barriers and suggestions towards deceased organ donation in a government tertiary care teaching hospital: qualitative study using socio-ecological model framework. Indian J Transplant 13(3):194
McCormick JB, Hopkins MA (2021) Exploring public concerns for sharing and governance of personal health information: a focus group study. JAMIA Open 4(4):ooab098
Groenland -emeritus professor E. Employing the matrix method as a tool for the analysis of qualitative research data in the business domain. Rochester, NY; 2014. https://papers.ssrn.com/abstract=2495330 . Accessed 10 Nov 2022
Download references
Acknowledgments
The book chapter is derived in part from our article “Mukherjee A, Lodha R. Writing the Results. Indian Pediatr. 2016 May 8;53(5):409-15.” We thank the Editor-in-Chief of the journal “Indian Pediatrics” for the permission for the same.
Author information
Authors and affiliations.
Clinical Studies, Trials and Projection Unit, Indian Council of Medical Research, New Delhi, India
Aparna Mukherjee & Gunjan Kumar
Department of Pediatrics, All India Institute of Medical Sciences, New Delhi, India
Rakesh Lodha
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Rakesh Lodha .
Editor information
Editors and affiliations.
Retired Senior Expert Pharmacologist at the Office of Cardiology, Hematology, Endocrinology, and Nephrology, Center for Drug Evaluation and Research, US Food and Drug Administration, Silver Spring, MD, USA
Gowraganahalli Jagadeesh
Professor & Director, Research Training and Publications, The Office of Research and Development, Periyar Maniammai Institute of Science & Technology (Deemed to be University), Vallam, Tamil Nadu, India
Pitchai Balakumar
Division Cardiology & Nephrology, Office of Cardiology, Hematology, Endocrinology and Nephrology, Center for Drug Evaluation and Research, US Food and Drug Administration, Silver Spring, MD, USA
Fortunato Senatore
Ethics declarations
Rights and permissions.
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Mukherjee, A., Kumar, G., Lodha, R. (2023). How to Present Results in a Research Paper. In: Jagadeesh, G., Balakumar, P., Senatore, F. (eds) The Quintessence of Basic and Clinical Research and Scientific Publishing. Springer, Singapore. https://doi.org/10.1007/978-981-99-1284-1_44
Download citation
DOI : https://doi.org/10.1007/978-981-99-1284-1_44
Published : 01 October 2023
Publisher Name : Springer, Singapore
Print ISBN : 978-981-99-1283-4
Online ISBN : 978-981-99-1284-1
eBook Packages : Biomedical and Life Sciences Biomedical and Life Sciences (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Turk J Urol
- v.39(Suppl 1); 2013 Sep
How to clearly articulate results and construct tables and figures in a scientific paper?
The writing of the results section of a scientific paper is very important for the readers for clearly understanding of the study. This review summarizes the rules for writing the results section of a scientific paper and describes the use of tables and figures.
Introduction
Medical articles consist of review articles, case reports, and letters to the editor which are prepared with the intention of publishing in journals related to the medical discipline of the author. For an academician to be able to progress in carreer, and make his/her activities known in the academic environment, require preparation of the protocol of his/her academic research article, and acquiring sufficient information, and experience related to the composition of this article. In this review article, the information related to the writing of the ‘Results’ section, and use of tables, and figures will be presented to the attention of the readers.
Writing the ‘Results’ section
The ‘Results’ section is perhaps the most important part of a research article. In fact the authors will share the results of their research/study with their readers. Renown British biologist Thomas Henry Huxley (1825–1895) indicated his feelings as “The great tragedy of science: the slaying of a beautiful hypothesis by an ugly fact.” which emphasizes the importance of accurately, and impressively written results.
In essence results provide a response for the question” What is found in the research performed?”. Therefore, it is the most vital part of the article. As a priority, while drafting the ‘Results’ section of a manuscript one should not firstly write down methods in the ‘Material and Method’ section. The first sentence should give information about the number of patients who met the inclusion criteria, and thus enrolled in the study. [ 1 ] Besides information about the number of patients excluded from the study, and the reasons for exclusion is very important in that they will enlighten the readers, and reviewers who critically evaluate the manuscript, and also reflect the seriousness of the study. On the other hand, the results obtained should be recorded in chronological order, and without any comments. [ 2 ] In this section use of simple present tense is more appropriate. The findings should be expressed in brief, lucid, and explicable words. The writing style should not be boring for the reader. During writing process of a research article, a generally ill-conceived point is that positive, and significant findings are more important, attractive, and valuable, while negative, and insignificant findings are worthless, and less attractive. A scientific research is not performed to confirm a hypothesis, rather to test it. Not only positive, and significant results are worth writing, on the other hand negative or statistically insignificant result which support fallacy of a widely accepted opinion might be valuable. Therefore, all findings obtained during research should be inclıuded in the ‘Results’ section. [ 1 ]
While writing the ‘Results’ section, the sequence of results, tabulated data, and information which will be illustrated as figures should be definitively indicated. In indicating insignificant changes, do not use expressions as “decreased” or “increased”, these words should be reserved for significant changes. If results related to more than one parameter would be reported, it is appropriate to write the results under the subheading of its related parameter so as to facilitate reading, and comprehension of information. [ 2 ] Only data, and information concerning the study in question should be included in the ‘Results’ section. Results not mentioned in this section should not be included in the ‘Discussion’ and ‘Summary’ sections. Since the results obtained by the authors are cited in the ‘Results’ section, any reference should not be indicated in this section. [ 3 ]
In the ‘Results’ section, numerical expressions should be written in technically appropriate terms. The number of digits (1, 2 or 3 digits) to be written after a comma (in Turkish) or a point (in especially American English) should be determined The number of digits written after the punctuation marks should not be changed all throughout the text. Data should be expressed as mean/median ± standard deviation. Data as age, and scale scores should be indicated together with ranges of values. Absolute numerical value corresponding to a percentage must be also indicated. P values calculated in statistical analysis should be expressed in their absolute values. While writing p values of statistically significant data, instead of p<0.05 the actual level of significance should be recorded. If p value is smaller than 0.001, then it can be written as p <0.01. [ 2 ] While writing the ‘Results’ section, significant data which should be recalled by the readers must be indicated in the main text. It will be appropriate to indicate other demographic numerical details in tables or figures.
As an example elucidating the abovementioned topics a research paper written by the authors of this review article, and published in the Turkish Journal of Urology in the year 2007 (Türk Üroloji Dergisi 2007;33:18–23) is presented below:
“A total of 9 (56.2%) female, and 7 (43.8%) male patients with were included in this study. Mean age of all the patients was 44.3±13.8 (17–65) years, and mean dimensions of the adrenal mass was 4.5±3.4 (1–14) cm. Mean ages of the male, and female patients were 44.1 (30–65), and 42.4 (17–64) years, while mean diameters of adrenal masses were 3.2 (1–5), and 4.5 (1–14) cm (p age =0.963, p mass size =0.206). Surgical procedures were realized using transperitoneal approach through Chevron incision in 1 (6.2%), and retroperitoneal approach using flank incision with removal of the 11. rib in 15 (93.7%) patients. Right (n=6; 37.5%), and left (n=2; 12.5%) adrenalectomies were performed. Two (12.5%) patients underwent bilateral adrenalectomy in the same session because of clinical Cushing’s syndrome persisted despite transsphenoidal hipophysectomy. Mean operative time, and length of the hospital stay were 135 (65–190) min, and 3 (2–6) days, respectively. While resecting 11. rib during retroperitoneal adrenalectomy performed in 1 patient, pleura was perforated for nearly 1.5 cm. The perforated region was drained, and closed intraoperatively with 4/0 polyglyctan sutures. The patient did not develop postoperative pneumothorax. In none of the patients postoperative complications as pneumothorax, bleeding, prolonged drainage were seen. Results of histopathological analysis of the specimens retrieved at the end of the operation were summarized in Table 1 .” Table 1. Histopathological examination results of the patients Histopathological diagnosis Men n (%) Women n (%) Total n (%) Adrenal cortical adenoma 5 (31.3) 6 (37.6) 11 (68.8) Pheochromocytoma 1 (6.2) 1 (6.2) 2 (12.6) Ganglioneuroma 1 (6.2) - 1 (6.2) Myelolipoma - 1 (6.2) 1 (6.2) Adrenal carcinoma - 1 (6.2) 1 (6.2) Total 7 (43.7) 9 (56.2) 16 (100) Open in a separate window
Use of tables, and figures
To prevent the audience from getting bored while reading a scientific article, some of the data should be expressed in a visual format in graphics, and figures rather than crowded numerical values in the text. Peer-reviewers frequently look at tables, and figures. High quality tables, and figures increase the chance of acceptance of the manuscript for publication.
Number of tables in the manuscript should not exceed the number recommended by the editorial board of the journal. Data in the main text, and tables should not be repeated many times. Tables should be comprehensible, and a reader should be able to express an opinion about the results just at looking at the tables without reading the main text. Data included in tables should comply with those mentioned in the main text, and percentages in rows, and columns should be summed up accurately. Unit of each variable should be absolutely defined. Sampling size of each group should be absolutely indicated. Values should be expressed as values±standard error, range or 95% confidence interval. Tables should include precise p values, and level of significance as assessed with statistical analysis should be indicated in footnotes. [ 2 ] Use of abbreviations in tables should be avoided, if abbreviations are required they should be defined explicitly in the footnotes or legends of the tables. As a general rule, rows should be arranged as double-spaced Besides do not use pattern coloring for cells of rows, and columns. Values included in tables should be correctly approximated. [ 1 , 2 ]
As an example elucidating the abovementioned topics a research paper written by the authors of this review article, and published in the Turkish Journal of Urology in the year 2007 (Türk Üroloji Dergisi 2007;33:18–23).is shown in Table 1 .
Most of the readers priorly prefer to look at figures, and graphs rather than reading lots of pages. Selection of appropriate types of graphs for demonstration of data is a critical decision which requires artist’s meticulousness. As is the case with tables, graphs, and figures should also disploay information not provided in the text. Bar, line, and pie graphs, scatter plots, and histograms are some examples of graphs. In graphs, independent variables should be represented on the horizontal, and dependent variables on the vertical axis. Number of subjects in every subgroup should be indicated The labels on each axis should be easily understandable. [ 2 ] The label of the Y axis should be written vertically from bottom to top. The fundamental point in writing explanatory notes for graphs, and figures is to help the readers understand the contents of them without referring to the main text. Meanings of abbreviations, and acronyms used in the graphs, and figures should be provided in explanatory notes. In the explanatory notes striking data should be emphasized. Statistical tests used, levels of significance, sampling size, stains used for analyses, and magnification rate should be written in order to facilitate comprehension of the study procedures. [ 1 , 2 ]
Flow diagram can be utilized in the ‘Results’ section. This diagram facilitates comprehension of the results obtained at certain steps of monitorization during the research process. Flow diagram can be used either in the ‘Results’ or ‘Material and Method’ section. [ 2 , 3 ]
Histopathological analyses, surgical technique or radiological images which are considered to be more useful for the comprehension of the text by the readers can be visually displayed. Important findings should be marked on photos, and their definitions should be provided clearly in the explanatory legends. [ 1 ]
As an example elucidating the abovementioned issues, graphics, and flow diagram in the ‘Results’ section of a research paper written by the authors of this review article, and published in the World Journal of Urology in the year 2010 (World J Urol 2010;28:17–22.) are shown in Figures 1 , and and2 2 .

a The mean SHIM scores of the groups before and after treatment. SHIM sexual health inventory for male. b The mean IPSS scores of the groups before and after treatment. IPSS international prostate symptom score

Flowchart showing patients’ progress during the study. SHIM sexual health inventory for male, IIEF international index of erectile function, IPSS international prostate symptom score, QoL quality of life, Q max maximum urinary flow rate. PRV post voiding residual urine volume
In conclusion, in line with the motto of the famous German physicist Albert Einstein (1879–1955). ‘If you are out to describe the truth, leave elegance to the tailor .’ results obtained in a scientific research article should be expressed accurately, and with a masterstroke of a tailor in compliance with certain rules which will ensure acceptability of the scientific manuscript by the editorial board of the journal, and also facilitate its intelligibility by the readers.
How to Write the Methods Section of a Research Manuscript
Affiliation.
- 1 Respiratory Care Services, Arkansas Children's Hospital, Little Rock, Arkansas. [email protected].
- PMID: 37643870
- PMCID: PMC10676260 (available on 2024-12-01 )
- DOI: 10.4187/respcare.11437
The methods section of a manuscript is one of the most important parts of a research paper because it provides information on the validity of the study and credibility of the results. Inadequate description of the methods has been reported as one of the main reasons for manuscript rejection. The methods section must include sufficient detail so that others could repeat the study and reproduce the results. The structure of the methods section should flow logically and chronologically. There are multiple components of methods sections, including study design, materials used, study procedures, and data analysis. Each element must be adequately described and thoroughly detailed to provide an understanding of how the results were obtained and how to interpret the findings. Studies that involved humans or animals must include an ethics statement of approval from the appropriate governing body. The methods section should explain how subjects were identified and should state inclusion and exclusion criteria. All materials used to complete the study should be described in detail, including equipment, drugs, gases, chemicals, treatments, interventions, or other items. Study procedures should outline all steps taken to obtain the results and clearly state the outcome measures. Subheadings might be helpful for organizing the methods section into subsections when there is a considerable amount of information to report. A well-written methods section will guide the reader through the research process and provide adequate information to evaluate study validity and reproduce the work. The purpose of this paper is to provide guidance for writing the methods section of a manuscript.
Keywords: manuscript; methods; publication; research; research paper; science writing; study protocol.
Copyright © 2023 by Daedalus Enterprises.
- Research Design*

Holman Library

Research Guide: Scholarly Journals
Methodology.
- Why Use Scholarly Journals?
- What does "Peer-Reviewed" mean?
- What is *NOT* a Scholarly Journal Article?
- Interlibrary Loan for Journal Articles
- Introduction: Hypothesis/Thesis
- Reading the Citation
- Authors' Credentials
- Literature Review
- Results/Data
- Discussion/Conclusions
- APA Citations for Scholarly Journal Articles
- MLA Citations for Scholarly Journal Articles
Reviewing the methodology section
The image below show the Methods section of the article, where the authors are outlining how they carried out their study.
(click on image to enlarge)

- The Methodology section of the article describes the procedures, or methods, that were used to carry out the research study.
- The methodology the authors follow will vary according to the discipline, or field of study, the research relates to.
- Types of methodology include case studies, scientific experiments, field studies, focus groups, and surveys.
- You may not need to spend much time focusing on the details of this section unless you want to replicate the experiment yourself.
- << Previous: Literature Review
- Next: Results/Data >>
- Last Updated: Mar 15, 2024 1:18 PM
- URL: https://libguides.greenriver.edu/scholarlyjournals
- Privacy Policy
Buy Me a Coffee

Home » Research Methodology – Types, Examples and writing Guide
Research Methodology – Types, Examples and writing Guide
Table of Contents

Research Methodology
Definition:
Research Methodology refers to the systematic and scientific approach used to conduct research, investigate problems, and gather data and information for a specific purpose. It involves the techniques and procedures used to identify, collect , analyze , and interpret data to answer research questions or solve research problems . Moreover, They are philosophical and theoretical frameworks that guide the research process.
Structure of Research Methodology
Research methodology formats can vary depending on the specific requirements of the research project, but the following is a basic example of a structure for a research methodology section:
I. Introduction
- Provide an overview of the research problem and the need for a research methodology section
- Outline the main research questions and objectives
II. Research Design
- Explain the research design chosen and why it is appropriate for the research question(s) and objectives
- Discuss any alternative research designs considered and why they were not chosen
- Describe the research setting and participants (if applicable)
III. Data Collection Methods
- Describe the methods used to collect data (e.g., surveys, interviews, observations)
- Explain how the data collection methods were chosen and why they are appropriate for the research question(s) and objectives
- Detail any procedures or instruments used for data collection
IV. Data Analysis Methods
- Describe the methods used to analyze the data (e.g., statistical analysis, content analysis )
- Explain how the data analysis methods were chosen and why they are appropriate for the research question(s) and objectives
- Detail any procedures or software used for data analysis
V. Ethical Considerations
- Discuss any ethical issues that may arise from the research and how they were addressed
- Explain how informed consent was obtained (if applicable)
- Detail any measures taken to ensure confidentiality and anonymity
VI. Limitations
- Identify any potential limitations of the research methodology and how they may impact the results and conclusions
VII. Conclusion
- Summarize the key aspects of the research methodology section
- Explain how the research methodology addresses the research question(s) and objectives
Research Methodology Types
Types of Research Methodology are as follows:
Quantitative Research Methodology
This is a research methodology that involves the collection and analysis of numerical data using statistical methods. This type of research is often used to study cause-and-effect relationships and to make predictions.
Qualitative Research Methodology
This is a research methodology that involves the collection and analysis of non-numerical data such as words, images, and observations. This type of research is often used to explore complex phenomena, to gain an in-depth understanding of a particular topic, and to generate hypotheses.
Mixed-Methods Research Methodology
This is a research methodology that combines elements of both quantitative and qualitative research. This approach can be particularly useful for studies that aim to explore complex phenomena and to provide a more comprehensive understanding of a particular topic.
Case Study Research Methodology
This is a research methodology that involves in-depth examination of a single case or a small number of cases. Case studies are often used in psychology, sociology, and anthropology to gain a detailed understanding of a particular individual or group.
Action Research Methodology
This is a research methodology that involves a collaborative process between researchers and practitioners to identify and solve real-world problems. Action research is often used in education, healthcare, and social work.
Experimental Research Methodology
This is a research methodology that involves the manipulation of one or more independent variables to observe their effects on a dependent variable. Experimental research is often used to study cause-and-effect relationships and to make predictions.
Survey Research Methodology
This is a research methodology that involves the collection of data from a sample of individuals using questionnaires or interviews. Survey research is often used to study attitudes, opinions, and behaviors.
Grounded Theory Research Methodology
This is a research methodology that involves the development of theories based on the data collected during the research process. Grounded theory is often used in sociology and anthropology to generate theories about social phenomena.
Research Methodology Example
An Example of Research Methodology could be the following:
Research Methodology for Investigating the Effectiveness of Cognitive Behavioral Therapy in Reducing Symptoms of Depression in Adults
Introduction:
The aim of this research is to investigate the effectiveness of cognitive-behavioral therapy (CBT) in reducing symptoms of depression in adults. To achieve this objective, a randomized controlled trial (RCT) will be conducted using a mixed-methods approach.
Research Design:
The study will follow a pre-test and post-test design with two groups: an experimental group receiving CBT and a control group receiving no intervention. The study will also include a qualitative component, in which semi-structured interviews will be conducted with a subset of participants to explore their experiences of receiving CBT.
Participants:
Participants will be recruited from community mental health clinics in the local area. The sample will consist of 100 adults aged 18-65 years old who meet the diagnostic criteria for major depressive disorder. Participants will be randomly assigned to either the experimental group or the control group.
Intervention :
The experimental group will receive 12 weekly sessions of CBT, each lasting 60 minutes. The intervention will be delivered by licensed mental health professionals who have been trained in CBT. The control group will receive no intervention during the study period.
Data Collection:
Quantitative data will be collected through the use of standardized measures such as the Beck Depression Inventory-II (BDI-II) and the Generalized Anxiety Disorder-7 (GAD-7). Data will be collected at baseline, immediately after the intervention, and at a 3-month follow-up. Qualitative data will be collected through semi-structured interviews with a subset of participants from the experimental group. The interviews will be conducted at the end of the intervention period, and will explore participants’ experiences of receiving CBT.
Data Analysis:
Quantitative data will be analyzed using descriptive statistics, t-tests, and mixed-model analyses of variance (ANOVA) to assess the effectiveness of the intervention. Qualitative data will be analyzed using thematic analysis to identify common themes and patterns in participants’ experiences of receiving CBT.
Ethical Considerations:
This study will comply with ethical guidelines for research involving human subjects. Participants will provide informed consent before participating in the study, and their privacy and confidentiality will be protected throughout the study. Any adverse events or reactions will be reported and managed appropriately.
Data Management:
All data collected will be kept confidential and stored securely using password-protected databases. Identifying information will be removed from qualitative data transcripts to ensure participants’ anonymity.
Limitations:
One potential limitation of this study is that it only focuses on one type of psychotherapy, CBT, and may not generalize to other types of therapy or interventions. Another limitation is that the study will only include participants from community mental health clinics, which may not be representative of the general population.
Conclusion:
This research aims to investigate the effectiveness of CBT in reducing symptoms of depression in adults. By using a randomized controlled trial and a mixed-methods approach, the study will provide valuable insights into the mechanisms underlying the relationship between CBT and depression. The results of this study will have important implications for the development of effective treatments for depression in clinical settings.
How to Write Research Methodology
Writing a research methodology involves explaining the methods and techniques you used to conduct research, collect data, and analyze results. It’s an essential section of any research paper or thesis, as it helps readers understand the validity and reliability of your findings. Here are the steps to write a research methodology:
- Start by explaining your research question: Begin the methodology section by restating your research question and explaining why it’s important. This helps readers understand the purpose of your research and the rationale behind your methods.
- Describe your research design: Explain the overall approach you used to conduct research. This could be a qualitative or quantitative research design, experimental or non-experimental, case study or survey, etc. Discuss the advantages and limitations of the chosen design.
- Discuss your sample: Describe the participants or subjects you included in your study. Include details such as their demographics, sampling method, sample size, and any exclusion criteria used.
- Describe your data collection methods : Explain how you collected data from your participants. This could include surveys, interviews, observations, questionnaires, or experiments. Include details on how you obtained informed consent, how you administered the tools, and how you minimized the risk of bias.
- Explain your data analysis techniques: Describe the methods you used to analyze the data you collected. This could include statistical analysis, content analysis, thematic analysis, or discourse analysis. Explain how you dealt with missing data, outliers, and any other issues that arose during the analysis.
- Discuss the validity and reliability of your research : Explain how you ensured the validity and reliability of your study. This could include measures such as triangulation, member checking, peer review, or inter-coder reliability.
- Acknowledge any limitations of your research: Discuss any limitations of your study, including any potential threats to validity or generalizability. This helps readers understand the scope of your findings and how they might apply to other contexts.
- Provide a summary: End the methodology section by summarizing the methods and techniques you used to conduct your research. This provides a clear overview of your research methodology and helps readers understand the process you followed to arrive at your findings.
When to Write Research Methodology
Research methodology is typically written after the research proposal has been approved and before the actual research is conducted. It should be written prior to data collection and analysis, as it provides a clear roadmap for the research project.
The research methodology is an important section of any research paper or thesis, as it describes the methods and procedures that will be used to conduct the research. It should include details about the research design, data collection methods, data analysis techniques, and any ethical considerations.
The methodology should be written in a clear and concise manner, and it should be based on established research practices and standards. It is important to provide enough detail so that the reader can understand how the research was conducted and evaluate the validity of the results.
Applications of Research Methodology
Here are some of the applications of research methodology:
- To identify the research problem: Research methodology is used to identify the research problem, which is the first step in conducting any research.
- To design the research: Research methodology helps in designing the research by selecting the appropriate research method, research design, and sampling technique.
- To collect data: Research methodology provides a systematic approach to collect data from primary and secondary sources.
- To analyze data: Research methodology helps in analyzing the collected data using various statistical and non-statistical techniques.
- To test hypotheses: Research methodology provides a framework for testing hypotheses and drawing conclusions based on the analysis of data.
- To generalize findings: Research methodology helps in generalizing the findings of the research to the target population.
- To develop theories : Research methodology is used to develop new theories and modify existing theories based on the findings of the research.
- To evaluate programs and policies : Research methodology is used to evaluate the effectiveness of programs and policies by collecting data and analyzing it.
- To improve decision-making: Research methodology helps in making informed decisions by providing reliable and valid data.
Purpose of Research Methodology
Research methodology serves several important purposes, including:
- To guide the research process: Research methodology provides a systematic framework for conducting research. It helps researchers to plan their research, define their research questions, and select appropriate methods and techniques for collecting and analyzing data.
- To ensure research quality: Research methodology helps researchers to ensure that their research is rigorous, reliable, and valid. It provides guidelines for minimizing bias and error in data collection and analysis, and for ensuring that research findings are accurate and trustworthy.
- To replicate research: Research methodology provides a clear and detailed account of the research process, making it possible for other researchers to replicate the study and verify its findings.
- To advance knowledge: Research methodology enables researchers to generate new knowledge and to contribute to the body of knowledge in their field. It provides a means for testing hypotheses, exploring new ideas, and discovering new insights.
- To inform decision-making: Research methodology provides evidence-based information that can inform policy and decision-making in a variety of fields, including medicine, public health, education, and business.
Advantages of Research Methodology
Research methodology has several advantages that make it a valuable tool for conducting research in various fields. Here are some of the key advantages of research methodology:
- Systematic and structured approach : Research methodology provides a systematic and structured approach to conducting research, which ensures that the research is conducted in a rigorous and comprehensive manner.
- Objectivity : Research methodology aims to ensure objectivity in the research process, which means that the research findings are based on evidence and not influenced by personal bias or subjective opinions.
- Replicability : Research methodology ensures that research can be replicated by other researchers, which is essential for validating research findings and ensuring their accuracy.
- Reliability : Research methodology aims to ensure that the research findings are reliable, which means that they are consistent and can be depended upon.
- Validity : Research methodology ensures that the research findings are valid, which means that they accurately reflect the research question or hypothesis being tested.
- Efficiency : Research methodology provides a structured and efficient way of conducting research, which helps to save time and resources.
- Flexibility : Research methodology allows researchers to choose the most appropriate research methods and techniques based on the research question, data availability, and other relevant factors.
- Scope for innovation: Research methodology provides scope for innovation and creativity in designing research studies and developing new research techniques.
Research Methodology Vs Research Methods
About the author.
Muhammad Hassan
Researcher, Academic Writer, Web developer
You may also like

How to Cite Research Paper – All Formats and...

Data Collection – Methods Types and Examples

Delimitations in Research – Types, Examples and...


Research Paper Format – Types, Examples and...

Research Process – Steps, Examples and Tips

Research Design – Types, Methods and Examples

How to Write the Methods Section of a Scientific Article
What Is the Methods Section of a Research Paper?
The Methods section of a research article includes an explanation of the procedures used to conduct the experiment. For authors of scientific research papers, the objective is to present their findings clearly and concisely and to provide enough information so that the experiment can be duplicated.
Research articles contain very specific sections, usually dictated by either the target journal or specific style guides. For example, in the social and behavioral sciences, the American Psychological Association (APA) style guide is used to gather information on how the manuscript should be arranged . As with most styles, APA’s objectives are to ensure that manuscripts are written with minimum distractions to the reader. Every research article should include a detailed Methods section after the Introduction.
Why is the Methods Section Important?
The Methods section (also referred to as “Materials and Methods”) is important because it provides the reader enough information to judge whether the study is valid and reproducible.
Structure of the Methods Section in a Research Paper
While designing a research study, authors typically decide on the key points that they’re trying to prove or the “ cause-and-effect relationship ” between objects of the study. Very simply, the study is designed to meet the objective. According to APA, a Methods section comprises of the following three subsections: participants, apparatus, and procedure.
How do You Write a Method Section in Biology?
In biological sciences, the Methods section might be more detailed, but the objectives are the same—to present the study clearly and concisely so that it is understandable and can be duplicated.
If animals (including human subjects) were used in the study, authors should ensure to include statements that they were treated according to the protocols outlined to ensure that treatment is as humane as possible.
- The Declaration of Helsinki is a set of ethical principles developed by The World Medical Association to provide guidance to scientists and physicians in medical research involving human subjects.
Research conducted at an institution using human participants is overseen by the Institutional Review Board (IRB) with which it is affiliated. IRB is an administrative body whose purpose is to protect the rights and welfare of human subjects during their participation in the study.
Literature Search
Literature searches are performed to gather as much information as relevant from previous studies. They are important for providing evidence on the topic and help validate the research. Most are accomplished using keywords or phrases to search relevant databases. For example, both MEDLINE and PubMed provide information on biomedical literature. Google Scholar, according to APA, is “one of the best sources available to an individual beginning a literature search.” APA also suggests using PsycINFO and refers to it as “the premier database for locating articles in psychological science and related literature.”
Authors must make sure to have a set of keywords (usually taken from the objective statement) to stay focused and to avoid having the search move far from the original objective. Authors will benefit by setting limiting parameters, such as date ranges, and avoiding getting pulled into the trap of using non-valid resources, such as social media, conversations with people in the same discipline, or similar non-valid sources, as references.
Related: Ready with your methods section and looking forward to manuscript submission ? Check these journal selection guidelines now!
What Should be Included in the Methods Section of a Research Paper?
One commonly misused term in research papers is “methodology.” Methodology refers to a branch of the Philosophy of Science which deals with scientific methods, not to the methods themselves, so authors should avoid using it. Here is the list of main subsections that should be included in the Methods section of a research paper ; authors might use subheadings more clearly to describe their research.
- Literature search : Authors should cite any sources that helped with their choice of methods. Authors should indicate timeframes of past studies and their particular parameters.
- Study participants : Authors should cite the source from where they received any non-human subjects. The number of animals used, the ages, sex, their initial conditions, and how they were housed and cared for, should be listed. In case of human subjects, authors should provide the characteristics, such as geographical location; their age ranges, sex, and medical history (if relevant); and the number of subjects. In case hospital records were used, authors should include the subjects’ basic health information and vital statistics at the beginning of the study. Authors should also state that written informed consent was provided by each subject.
- Inclusion/exclusion criteria : Authors should describe their inclusion and exclusion criteria, how they were determined, and how many subjects were eliminated.
- Group characteristics (could be combined with “Study participants”) : Authors should describe how the chosen group was divided into subgroups and their characteristics, including the control. Authors should also describe any specific equipment used, such as housing needs and feed (usually for animal studies). If patient records are reviewed and assessed, authors should mention whether the reviewers were blinded to them.
- Procedures : Authors should describe their study design. Any necessary preparations (e.g., tissue samples, drugs) and instruments must be explained. Authors should describe how the subjects were “ manipulated to answer the experimental question .” Timeframes should be included to ensure that the procedures are clear (e.g., “Rats were given XX drug for 14 d”). For animals sacrificed, the methods used and the protocols followed should be outlined.
- Statistical analyses: The type of data, how they were measured, and which statistical tests were performed, should be described. (Note: This is not the “results” section; any relevant tables and figures should be referenced later.) Specific software used must be cited.
What Should not be Included in Your Methods Section?
Common pitfalls can make the manuscript cumbersome to read or might make the readers question the validity of the research. The University of Southern California provides some guidelines .
- Background information that is not helpful must be avoided.
- Authors must avoid providing a lot of detail.
- Authors should focus more on how their method was used to meet their objective and less on mechanics .
- Any obstacles faced and how they were overcome should be described (often in your “Study Limitations”). This will help validate the results.
According to the University of Richmond , authors must avoid including extensive details or an exhaustive list of equipment that have been used as readers could quickly lose attention. These unnecessary details add nothing to validate the research and do not help the reader understand how the objective was satisfied. A well-thought-out Methods section is one of the most important parts of the manuscript. Authors must make a note to always prepare a draft that lists all parts, allow others to review it, and revise it to remove any superfluous information.
m so confused about ma research but now m okay so thank uh so mxh
Mil gracias por su ayuda.
Rate this article Cancel Reply
Your email address will not be published.

Enago Academy's Most Popular Articles

- AI in Academia
- Infographic
- Manuscripts & Grants
- Reporting Research
- Trending Now
Can AI Tools Prepare a Research Manuscript From Scratch? — A comprehensive guide
As technology continues to advance, the question of whether artificial intelligence (AI) tools can prepare…
Abstract Vs. Introduction — Do you know the difference?
Ross wants to publish his research. Feeling positive about his research outcomes, he begins to…

- Old Webinars
- Webinar Mobile App
Demystifying Research Methodology With Field Experts
Choosing research methodology Research design and methodology Evidence-based research approach How RAxter can assist researchers

- Manuscript Preparation
- Publishing Research
How to Choose Best Research Methodology for Your Study
Successful research conduction requires proper planning and execution. While there are multiple reasons and aspects…

Top 5 Key Differences Between Methods and Methodology
While burning the midnight oil during literature review, most researchers do not realize that the…
How to Draft the Acknowledgment Section of a Manuscript
Discussion Vs. Conclusion: Know the Difference Before Drafting Manuscripts

Sign-up to read more
Subscribe for free to get unrestricted access to all our resources on research writing and academic publishing including:
- 2000+ blog articles
- 50+ Webinars
- 10+ Expert podcasts
- 50+ Infographics
- 10+ Checklists
- Research Guides
We hate spam too. We promise to protect your privacy and never spam you.
I am looking for Editing/ Proofreading services for my manuscript Tentative date of next journal submission:

What should universities' stance be on AI tools in research and academic writing?
- Open access
- Published: 12 April 2024
Healthcare team resilience during COVID-19: a qualitative study
- John W. Ambrose 1 ,
- Ken Catchpole 2 ,
- Heather L. Evans 3 ,
- Lynne S. Nemeth 1 ,
- Diana M. Layne 1 &
- Michelle Nichols 1
BMC Health Services Research volume 24 , Article number: 459 ( 2024 ) Cite this article
Metrics details
Resilience, in the field of Resilience Engineering, has been identified as the ability to maintain the safety and the performance of healthcare systems and is aligned with the resilience potentials of anticipation, monitoring, adaptation, and learning. In early 2020, the COVID-19 pandemic challenged the resilience of US healthcare systems due to the lack of equipment, supply interruptions, and a shortage of personnel. The purpose of this qualitative research was to describe resilience in the healthcare team during the COVID-19 pandemic with the healthcare team situated as a cognizant, singular source of knowledge and defined by its collective identity, purpose, competence, and actions, versus the resilience of an individual or an organization.
We developed a descriptive model which considered the healthcare team as a unified cognizant entity within a system designed for safe patient care. This model combined elements from the Patient Systems Engineering Initiative for Patient Safety (SEIPS) and the Advanced Team Decision Making (ADTM) models. Using a qualitative descriptive design and guided by our adapted model, we conducted individual interviews with healthcare team members across the United States. Data were analyzed using thematic analysis and extracted codes were organized within the adapted model framework.
Five themes were identified from the interviews with acute care professionals across the US ( N = 22): teamwork in a pressure cooker , consistent with working in a high stress environment; healthcare team cohesion , applying past lessons to present challenges , congruent with transferring past skills to current situations; knowledge gaps , and altruistic behaviors , aligned with sense of duty and personal responsibility to the team. Participants’ described how their ability to adapt to their environment was negatively impacted by uncertainty, inconsistent communication of information, and emotions of anxiety, fear, frustration, and stress. Cohesion with co-workers, transferability of skills, and altruistic behavior enhanced healthcare team performance.
Working within the extreme unprecedented circumstances of COVID-19 affected the ability of the healthcare team to anticipate and adapt to the rapidly changing environment. Both team cohesion and altruistic behavior promoted resilience. Our research contributes to a growing understanding of the importance of resilience in the healthcare team. And provides a bridge between individual and organizational resilience.
Peer Review reports
Introduction
The COVID-19 pandemic highlighted the complexity and dynamic nature of healthcare systems. It also created a unique opportunity to look at the concept of resilience through the lens of the healthcare team versus the more common approach of situating the concept within the individual or the organization. The early phase of the pandemic was marked by challenges, such as limited access to personal protective equipment, personnel shortages, drug shortages, and increased risks of infection [ 1 , 2 ]. Ensuring patient safety and proper functioning requires coordination and adaptation of the healthcare team and various processes across the health system infrastructure [ 3 , 4 ]. Resilience results from adaptive coordination which enables healthcare systems to maintain routine function in the face of all conditions [ 5 , 6 ].
Resilience in healthcare has been operationalized through resilience engineering, an interdisciplinary aspect of systems engineering focused on promotingpatient safety through the design, implementation, and management of healthcare systems [ 7 , 8 , 9 ] (e.g., how healthcare systems adapt and adjust to maneuver through the daily complexities and challenges to identify effective practices, prevent errors and maintain resilient performance) [ 6 , 8 , 9 , 10 , 11 ]. Resilient performance in healthcare is proposed to be the net result of reaching the threshold of four resilience capabilities within the system: anticipation, the ability to expect and prepare for the unexpected; monitoring, the ability to observe threats to daily system performance; responding, the ability to adapt how the performance is enacted; and learning, the ability to learn from present and past accomplishments within the system [ 12 ]. At present, there is a paucity of research on the resilience of the healthcare team as a cohesive, singular conscious source of knowledge in a highly complex healthcare system. While the resilience of both healthcare systems [ 11 , 13 ] and healthcare workers [ 14 ] has been investigated, there is a gap in knowledge specific to the resilience of the healthcare team as a unified singular consciousness. The circumstances surrounding the COVID-19 pandemic presented a unique opportunity to understand the resilience of the healthcare team in a highly complex system as a singular aware entity within the system; how it acknowledges itself, defines its purpose, and performs under extenuating circumstances. This shifts the emphasis of individual and organization resilience to the resilience in the interconnected healthcare team that extends beyond the boundary of any single person.
The adapted model situates the healthcare team as a cohesive singlular conscious source of knowledge within an intricate and highly complex system [ 15 ]. This model was designed as a bridge between resilience found in individuals within the healthcare system and the organization to emphasize the healthcare team as an aware, unified whole. Our model [ 15 ] combines the existing Systems Engineering Initiative for Patient Safety (SEIPS) model [ 16 ] (version 1), which is based on five domains (organization, person, tasks, technologies, and tools), and environment and the Advanced Team Decision Making Model [ 17 ], which includes components for team performance [ 17 , 18 , 19 ]. Team performance is comprised of team identity, team cognition, team competency, and team metacognition [ 17 , 18 , 19 ]. Team identity describes how the team identifies their purpose to help one another [ 17 ]. Team cognition describes the state of mind of the team, their focus, and common goals [ 17 ]. Team competency describes how well the team accomplishes tasks, and team metacognition describes problem solving and responsibility [ 17 , 19 ], Fig. 1 .
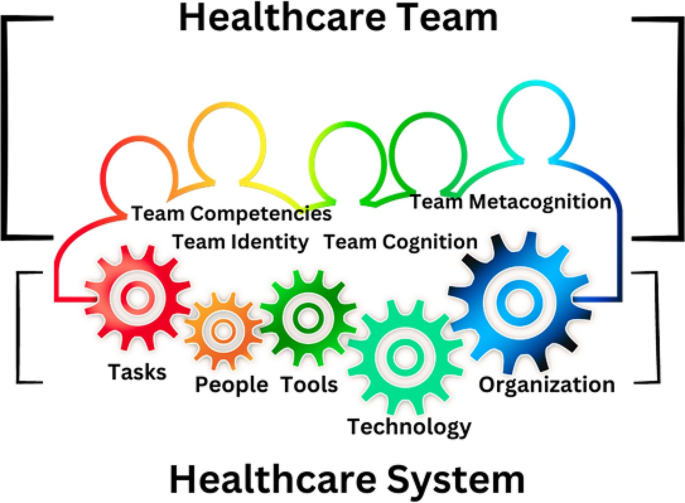
Healthcare Team as a cohesive, singular conscious source of knowledge in a highly complex system. The continuous variegated border represents the singularity and connectedness of the healthcare team within the system. The gears represent the processes, people, technology, and tasks within this highly dynamic healthcare system
The purpose of this qualitative research was to describe resilience in the healthcare team during the COVID-19 pandemic with the healthcare team situated as a singular conscious source of knowledge defined by its collective identity, purpose, competence, and actions. Additionally, we sought to identify factors that may facilitate or hinder the healthcare team from achieving the necessary capabilities to monitor, anticipate, adapt, and learn to meet the standard for resilient performance.
Methodology
A qualitative descriptive design [ 20 , 21 ] was employed. The interview guide was framed using the adapted model to explore various aspects of healthcare team performance (identity, purpose, competence, and cognition). These questions were pilot tested on the first 3 participants and no further changes were needed. Specifically, we aimed to investigate resilience capabilities, decision-making processes, and overall healthcare team performance.
Sampling strategy
A purposive snowball sample was used to identify healthcare team members who worked in U.S. acute care settings between January 2020–December 2020. This sampling method was used to ensure recruitment of participants most likely to have insight into the phenomenon of resilience in the acute care setting.
Inclusion criteria
To explore a wide range of interprofessional experience, participants were recruited across geographic regions and professional roles through personal contacts and social media [ 22 , 23 , 24 , 25 ]. Eligible participants included English-speaking individuals ages 20 and older with a valid personal email address, internet access, and the ability to participate in an online video interview. Potential participants had to be employed full or part-time for any period from January 2020–December 2020 in any of the following acute healthcare environments: emergency room (ER), intensive care unit (ICU), COVID- 19 ICU, COVID-19 floor, gastroenterology inpatient unit, endoscopy suite, operating room (OR), post anesthesia recovery room (PACU), pre-operative holding area, hospital administration, or inpatient medical and/or surgical patient care unit.
Exclusion criteria
Healthcare team members who did not complete the pre-screening survey or failed to schedule an interview were not enrolled.
National recruitment in the U.S
Upon approval by MUSC Institutional Review Board (IRB), registered under Pro00100917, fliers, social media posts on Twitter TM (version 9.34 IOS, San Francisco, California) and Facebook TM (version 390.1 IOS, Menlo Park, CA), and word of mouth were used to initiate recruitment efforts. Interested participants were sent a link to an electronic screening survey explaining the purpose of the study and verifying the respondents’ eligibility to participate. Informed consent was obtained from all subjects.
Data collection
Data were collected via an initial screening questionnaire to determine eligibility. Data were managed using REDCap™ (version 11.2.2) electronic data capture tools hosted at MUSC. Demographic data included age, sex, race, professional role, years of experience, geographic region, patient population served, practice specialty area, and deployment status during the pandemic. Deployment refers to the reassignment of personnel from their primary clinical area to another area to meet the demands of another clinical area without regard for the participant’s clinical expertise. Qualitative data were collected through semi-structured audio video recorded interviews to understand the healthcare team in their natural environment. Recorded interviews were conducted via Microsoft® Teams (version 1.5.00.17261, Microsoft Corporation) from the PIs private office to mitigate the risk of COVID-19 transmission and promote participation across the U.S.
Data monitoring and safety
The quality of the demographic data was monitored to ensure completeness. Potential participants who submitted incomplete responses on the questionnaire were excluded. Interviews were transcribed using software, transcriptions were reviewed and verified for accuracy, and then uploaded to MAXQDA Analytics Pro, Version 2022 (VERBI software) to facilitate data analysis. Transcripts were not returned to the participants. Qualitative codebooks, institutional review board (IRB) logs, and other study records were stored on a secure university server, with access limited to authorized study personnel. Adherence to Consolidated Criteria for Reporting Qualitative Research (COREQ) standards were maintained throughout the study and analysis [ 26 ].
Data analysis
Quantitative analysis.
Demographic data were analyzed using SPSS Statistics for MAC, version 28 (IBM). Both descriptive statistics for the continuous variables of age and years of experience (mean, standard deviation) and frequency tables (age, sex, race, role, geographic region, population served, deployment status) were analyzed.
Qualitative analysis
The Principal Investigator (PI) (JA) and senior mentor (MN) independently coded the interview transcripts. Open coding method was used to identify the categories of data [ 22 , 27 ]. Both a reflexive journal and audit trail were maintained. Codes were identified through induction from participant experiences and verified through weekly consensus meetings, while theoretical deductive analysis was guided by the adapted model and the four resilience capabilities (anticipation, monitoring, responding, learning [ 12 ]. Reflexive thematic analysis (TA) [ 28 , 29 , 30 , 31 ] was used to analyze the coded data and generate themes. Data were collected and categorized into the codebook until no further codes were identified by the PI and research mentor [ 22 , 27 ]. Participant checking was not employed.
Demographics
The eligibility pool was established based on survey completion. Eighty-nine healthcare team members opened the online screening survey; 21 were incomplete and eliminated from the dataset, which left a pool of 68 potential eligible participants. Eligible participants (100%) were contacted by email and phone to determine their interest in completing the study interview. Twenty-two participants completed screening surveys and study interviews between May–September 2021, equating to a 32.5% enrollment rate. Participant interviews lasted between 21 and 91 min with an average of 43 min. None of the interviews were repeated. Participant demographics, including descriptive statistic and role key, are noted in Tables 1 and 2 , respectively.
Five themes were identified: team work in a pressure cooker , healthcare team cohesion , applying past lessons to present challenges , knowledge gaps , and altruistic behaviors .
Teamwork in a pressure cooker
The theme teamwork in a pressure cooker describes the relentless pressures and emotional stressors (e.g., fear, anxiety, frustration, and stress) experienced by the healthcare team from the risks and potential threats associated with COVID-19 contamination and infection. Factors associated with these pressures included risk of COVID-19 exposure, lack of COVID-19 testing, rapid changes to policies and procedures from the standard, personnel shortages, limited physical space, and limited supplies. Exemplary quotes highlighting participant descriptions of these pressures or subthemes are noted in Table 3 .
The healthcare team described an unprecedented level of stress in the workplace as the healthcare team had to adjust to rapidly changing protocols. The lack of protective equipment, shortage of providers to perform patient care and a lack of a familiar clinical routine saturated them in overwhelming pressure and emotions that stuck to them as they navigated uncharted territory. Exemplary quotes highlighting the healthcare team’s descriptions of these emotions are noted in Table 4 .
“It was…uncharted territory for me.” (P1, DIR) “You were stuck in a situation you never— you didn’t know when it was going to end.” (P4, RN PACU) “They have not enough staff—they can’t do it—they—I don’t know what we’re going to do.” (P6, DIR). “When we deployed—trying to get re-accustomed to the changes—with the needs that had to be met was very difficult.” (P10, RN ENDO) “I wasn’t about to sign up for extra time working in under those stressful conditions.” (P17, RN PACU)
The fear of the unknown, combined with the constant need to adapt to rapidly changing circumstances, led to widespread stress, frustration, anxiety, and exhaustion within the healthcare team. This theme was characterized by the constant pressure both inside and outside of work experienced by the healthcare team.
“Driving to the hospital, crying, driving back from the hospital, crying, still doesn’t sum it up— surrounded by people who were just dying. And what could you do?” (P6, DIR) “It was constant. It was terrible. I couldn’t sleep at night. I’d wake up worried.” (P8, ER MD) “It was kind of like just keep sending the Calvary forward—and when one drops, you just walk over them.” (P17, RN PACU) “It was always there—COVID here, COVID there—you never could just completely get away from it. It was basically the center of everybody’s conversation everywhere you went or if you were on the phone with somebody.” (P18, RN COVID ICU) “I was having to call my parents before I’d leave my apartment to go into work— to vent to them and cry— to let out my frustration and my anxiety—and have them essentially convince me to go into work.” (P19, RN ICU). “Working so much— COVID was all that was on my brain—and it was a lot of pressure.” (P22, MGR)
Working during COVID-19 challenged the resilience of the healthcare team in the face of constant fear and uncertainty. The pressure to maintain team performance, while dealing with constant fear associated with the pandemic effected the healthcare team’s resilience.
“I have to tell you that after being in hospital—I don’t feel resilient right now— doing all the things I’ve done—I just want to be out of the hospital— [crying] I can tell you that it will stay with me the rest of my life— It will always stay with me.” (P6, DIR) “I feel like my team has used up all of their resilience. I don’t think there’s much left.” (P8, ER MD)
However, one team member stood out as an exception. They reported the pressures from the environment helped them to make decisions. This demonstrates that environmental pressures affect members of the healthcare team differently. They reported that the pressure and intensity of the situation sharpened their focus and allowed them to make choices more quickly and effectively.
“I make better decisions when I’m under pressure.” (P22, MGR)
Healthcare team cohesion
The theme healthcare team cohesion describes the unique experience of working together during the pandemic that created a means among the healthcare team to form close relationships and unite. This bond was characterized by the emergence of strong interpersonal connections among healthcare professionals during the COVID-19 pandemic. These connections shaped healthcare team relationships and were a factor in the collaborative decision-making processes within healthcare team for their day-to day functions. This cohesive bonding was fueled by the stress and uncertainty of the situation, which brought the healthcare team together illustrated by their solidarity, camaraderie, trust, and empowerment.
“All those decisions, important decisions were made together.” (P7, CRNA) “Everyone felt like they were they were, you know, in a in a battle zone and on the same side—and so that kind of brought people together.” (P8, ER MD) “I think our team worked as one.” (P11, CEO)
Solidarity described the sense of unity evident among the members of the healthcare team. This was characterized by connectedness and a sense of reliance on one another that promoted teamwork and resilience within the team from support both given and received. The sub-theme camaraderie described the close personal connection and support between the healthcare team that went beyond normal social interactions prior to the pandemic. These connections were filled with trust and respect for other healthcare team members.
“I think we were all trying to do the best we could do and help each other do the best they could do—I think early on just camaraderie helped a lot within the department and, you know, just relying on each other for support.” (P8, ER MD) “We knew that we can depend on each other and we all had different skill sets— I think that that was very important—that made us feel secure— rather than going alone.” (P10, RN ENDO) “We [The ICU Nurses] developed a sense of camaraderie that I mean, it’s nothing I’ve ever felt before, like we had to trust each other with our licenses, with our own health—my resiliency came from my coworkers.” (P14, CHG RN) “One of the things that I think the pandemic did in a positive—was—I believe that the teams that I worked for really started to solidify. We leaned on each other. I felt more of a team environment than I had had pre-pandemic—I felt that people were a bit better together. We all needed each other, and we all leaned on each other, and we gave each other support—more so than before COVID- 19.” (P15, CRNA) ”The nurses on the unit were always there for me—they became my friends— my family.” (P19, RN ICU)
The sub theme of empowerment referred to the ability of the healthcare team to confidently make decisions and assume responsibility for their actions within the healthcare setting. This process involved a sense of authority and the ability to exercise agency in decision-making together to respond and adapt to the demands the healthcare team experienced. The combination of solidarity, camaraderie, trust, and empowerment resulted in a strong sense of cohesion within the healthcare team which led to improved relationships and enhanced resilience in their performance.
“I felt that I felt that the team—we all needed each other and we all leaned on each other and we gave each other support—more so than before COVID.” (P15, CRNA) “How do you want to handle this? What’s the plan?—and we collaborated in the true sense of collaboration.” (P15, CRNA) “We just knew that we could count on each other—we knew that we could count on each other at any time if we had questions, because we all worked so closely together during this. We really became a really tight knit group, and it was great.” (P22, MGR)
The benefits of the cohesion found in the healthcare team were significant and apparent during the COVID-19 pandemic. The strengthened relationships and increased resilience allowed for improved communication and collaboration, leading to better patient care and outcomes. Despite these advantages, it was noted by one participant that the relationships developed were not sustained beyond the peak of the pandemic.
“Now that COVID is kind of at bay in our area, it’s kind of gone back to the same way it was— it has not stuck.” (P15, CRNA)
Applying past lessons to present challenges
The theme applying past lessons to present challenges describes how the knowledge and understanding gained from prior participant experiences was used to adapt to the novel clinical and infrastructural challenges faced during the pandemic. Past experiences facilitated the healthcare team to strategize ways to meet the demands of the healthcare system during this time.
Participants described two strategies the healthcare team used to improve the system’s ability to adapt and function effectively: changing roles and deploying personnel. The process of changing roles involved assigning new responsibilities to individuals based on priority-based initiatives, while deployment involved transferring clinical staff from areas with lower patient care needs to those with higher needs to optimize their utilization. Eleven participants (50%) were affected by these strategies. Of these, 73% were assigned to clinical areas for direct patient care, while the remaining 27% underwent a role change to support the operational needs of the system. The participants’ preexisting work relationships, specialized clinical expertise, and leadership abilities helped them adapt to their new clinical and non-clinical roles, which in turn enhanced the resilience of the healthcare team.
“We wanted to make sure that we were putting people into the right area where their skill set could be used the best.” (P1, DIR) “I’m known for moving people forward—I’m also well known for speaking up when I don’t think it is right and there was a lot of stuff that I didn’t think was right— and not only speaking up, I’m also going to come with the solution.” (P6, DIR)
Participants indicated the lessons learned from prior experience positively impacted team performance and improved patient care outcomes. There were two significant examples in the data: the perspective of a nurse who was redeployed to work in an obstetrics unit (P5, ENDO RN) and the perspective of a nursing director (P6, DIR) whose role was changed to develop a program to ensure adequate staffing.
“Because we [the team of interprofessionals] were all very familiar with what we had to do at the task, at handit [the experience of the provision of care] was very fluid—I think it’s because of our years of experience and working with each other for so long that it just worked out very well ”. (P5, ENDO RN) “Staff believed in me when I said I would do something— I could galvanize people because of my reputation of caring for staff, so I was chosen specifically because of my ability to move people forward in spite of things.” (P6, DIR)
Participants identified being assigned to unfamiliar clinical areas or working with unfamiliar patient populations as a barrier that hindered their ability to adapt to clinical situations. The lack of clinical competence among some personnel led to an increase in workload for other healthcare team members, who had to provide additional instruction and guidance on how to complete the task. Decision-makers who deployed nursing staff to a clinical area with higher staffing needs may have believed that the individual nurse had specific clinical skills that would be helpful in that area, and this was not the case.
“She [the patient] felt like it was that he [the new nurse]—really didn’t know what he was doing—not only were we kind of reintroduced to that role of caring for patients where we haven’t been recently, but we’re also in a teaching mode, too, for the new nurses—we had to prioritize how sick the patients were, from basic vital signs to wound dressings to respiratory, and help those new nurses know which to attend to first.” (P10, RN ENDO) “Nurses weren’t really put in a place with enough support and enough resources to be able to do a job, and to do a job that maybe they haven’t done for a few years.” (P10, RN ENDO)
The participants indicated that clinical competencies of a healthcare provider in one patient population may not necessarily be applicable to another patient group. For instance, a neonatal intensive care unit (NICU) nurse who has experience in managing Extra Corporeal Membranous Oxygen (ECMO) in newborns may not have the necessary skills to care for adult ECMO patients in an adult COVID-19 intensive care unit.
“The ECMO nurse was a NICU nurse, so she really could not help me.” (P14, CHG RN)
Knowledge gaps
The theme knowledge gaps refers to the disparity between the existing knowledge of the healthcare team and the knowledge required for the team to effectively respond and adapt to the needs of the healthcare system. The lack of COVID-19 specific knowledge led to gaps in the healthcare team’s understanding, while the lack of communication made it difficult for necessary information to be effectively conveyed and received (e.g., medical logistics, human resources, and other operational policies and procedures). This knowledge gap created a barrier to healthcare team resilience as their capacities to surveil, anticipate, and respond were diminished from the lack of knowledge.
“That [information] is pretty fundamental to how you [the healthcare team] function.” (P17, RN PACU) “I don’t think any amount of preparation could have actually prepared us for how bad COVID was—but we were very, very, very unprepared.” (P18, RN COVID ICU) “It was confusing, it was disruptive to the patients that we had there. They sensed that. And that’s— OK—screw with me, screw with my colleagues, but don’t screw with the patient.” (P21, RN ENDO)
All the participants in leadership roles during the COVID-19 pandemic emphasized the importance of having a thorough understanding of the information and effectively communicating it to the frontline healthcare team members most involved in providing patient care.
“There’s nothing worse than having to learn something in the moment and not being prepared for it.” (P1, DIR) “That made us communicate in multiple ways throughout a day because we all know people learn and adapt it could be in print. It could be in person; it could be a video. We tried to have multiple ways of getting messages out and knowing we needed to repeat messages because this was so unknown, and people were so stressed.” (P11, CEO)
One team member (P13, CRNA), highlighted areas where there were gaps in knowledge in greater detail.
“It was as if the unit was being run by all these sort of substitute teachers that were called in at the last minute. Nobody knew where stuff was—nobody knew what the protocol was—the communication was terrible.” (P13, CRNA)
The cumulative effect from the knowledge gaps contributed to the lack of a practical working knowledge for the healthcare team and affected the healthcare team’s ability to anticipate what needed to be done and adapt their performance to accomplish it. Despite knowledge gaps, healthcare team members reported their capability to learn was facilitated by incremental gains in practical knowledge through their experience over time.
“—people got to be experts at protecting patients and keeping themselves safe.” (P8, ER MD) “I think it kind of was like on the job training at that point, I felt like we were all just trying to survive—learning was like—you went out —then you came back, and you would share how things went.” (P15, CRNA) “You tried to educate yourself so you could be safe.” (P17, RN PACU)
The participant responses received from the leadership (CNO, Directors, and Manager) and front-line personnel (administrative staff, nurses, and physicians) regarding the importance of communication highlighted a difference in perspective. Leadership exhibited a strong commitment toward effective communication and made efforts to ensure all healthcare team members were well informed. On the other hand, the frontline participants indicated instances where communication strategies were not perceived as effective.
“I wasn’t contacted by a manager from the unit or anything to be able to reassure, reassure me that things were being followed through and it should be okay, so that was tough.” (P10, RN ENDO) “It really seemed like there was no communication between—like staffing and the floor—we would get up to the floor and they would say, who are you? What are you doing here? What are we supposed to do with you?” (P20, RN OR)
Altruistic behaviors
The theme altruistic behaviors , encompasses the participants’ perception of their obligation and accountability to their patients and healthcare team, and their steadfastness in supporting the healthcare team even if it meant facing personal or professional repercussions. This readiness to aid the healthcare team and accept consequences showcased their altruism and commitment to the healthcare team. The team’s dedication to both their patients and each other was a primary focus driven by a strong sense of responsibility and obligation.
“I want to be able to look myself in the mirror and feel like I did the right thing—.” (P6, DIR) “My resiliency came from my coworkers. I wanted to come back to work to help them.” (P14, RN COVID ICU) “People really looked out for each other—and people were really kind and compassionate to each other—we all were in this together.” (P15, CRNA) “I’m grateful for the experience that I had and all of the different patients that I was able to help in my time there definitely solidified that being a nurse is what I needed to do—and why I chose the profession is exactly what I should have been doing.” (P19, RN ICU) “You just have to go with what seems right—.” (P22, MGR)
A defining characteristic of this theme was a willingness to endure consequences for the benefit of the healthcare team. These consequences varied from contracting the virus, facing criticism from the healthcare team, to foregoing financial incentives, and even job loss.
“I felt like I was punished for speaking up and I was punished for doing the right thing for patients.” (P6, DIR) “I mean, I literally broke the law so many times. Do you know how many times I started pressors [vasoactive drugs to increase blood pressure] on patients that I had no orders for [because a physician would not enter the ICU]?” (P14, CHG RN)
We identified five key themes based on the coded data; namely teamwork in a pressure cooker , healthcare team cohesion , applying past lessons to present challenges , knowledge gaps , and altruistic behaviors . The researchers propose that stressors arising from the COVID-19 pandemic had an impact on the healthcare team’s resilience. In addition, strong healthcare team cohesion, selfless behaviors among the healthcare team, shared knowledge, and job competence within the healthcare team, enhanced resilient performance.
The healthcare team experienced significant stress and uncertainty, due to the COVID-19 pandemic. This is consistent with previous research that has shown that the unprecedented nature of the pandemic led to challenging working conditions, limited resources, lack of information, and concerns about infecting loved ones [ 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 ]. The collective global impact of COVID-19 on healthcare systems is likely a contributing factor to these stressors [ 45 , 46 , 47 , 48 ].
Our study, along with those conducted by Anjara et al. (2021)[ 49 ] and Kaye-Kauderer et al. (2022) [ 50 ], found that solidarity and camaraderie among healthcare professionals improve resilience. Specifically, Anjara et al. observed increased collaboration among the healthcare professionals they studied in Ireland during the COVID-19 pandemic, while Kaye-Kauderer et al. identified team camaraderie among their sample of front-line healthcare workers from New York. Kinsella et al. (2023) [ 51 ] reported that COVID − 19 offered frontline workers in the UK the opportunity to work together toward a common goal. Potential explanations for these findings align with the concepts of social capital proposed by Coleman [ 52 ] and social identification with other as proposed by Drury [ 54 ]. Coleman suggests an individual’s skills and capabilities are enhanced through their interdependent relationships with others [ 52 ]. Drury found in communities affected by disasters, mutual aid and support emerged from a shared social identity, which serves to strengthen the community [ 53 ]. Brooks et al. (2021) [ 54 ] conducted a study with healthcare, police, and commercial sectors in England. They found it was important for these individuals to receive support from and provide support to their colleagues to mitigate the psychological impact of disaster exposure [ 54 ]. In addition, like our findings, Aufegger and colleague’s 2019 systematic review [ 55 ] found that social support in acute care healthcare teams creates a supportive atmosphere where team members help each other communicate problems, fulfill needs, and deal with stress.
Our results are consistent with those of Liu et al. (2020) [ 32 ] and Banerjee et al. (2021) [ 44 ] who each found that healthcare professionals frequently feel a sense of personal responsibility to overcome challenges. One potential explanation for this may be the influence of collectivism in their cultures. Similarly, our study suggests the sense of camaraderie among healthcare professionals may also contribute to a sense of responsibility and increased altruistic behavior. However, other studies have highlighted different perspectives on healthcare professionals’ sense of responsibility and duty. Godkin and Markwell’s (2003) [ 56 ] revealed that healthcare professionals’ sense of responsibility during the Severe Acute Respiratory Syndrome (SARS) outbreak was dependent on the protective measures and support offered by the healthcare system where most SARS infected patients were hospitalized. More recently, Gray et al. (2021) reported that nurses’ sense of responsibility stems from their ethical obligations, regardless of potential personal or familial risks [ 57 ].
The altruistic behaviors described by our participants helped maintain the performance of the healthcare team. It is too soon to see the long-term impact from working in this high-pressure environment; however, past research by Liu et al. (2012) [ 58 ] and Wu (2009) [ 59 ] demonstrated that “altruistic-risk acceptance” during the SARS outbreak was shown to decrease depressive symptoms among hospital employees in China.
Our research on resilience has important implications for healthcare organizations and professionals. In order to ready themselves for forthcoming events, healthcare systems must emphasize the significance of shared knowledge and its influence on the healthcare team’s ability to foresee and monitor effectively. This knowledge can help the healthcare organization function as a unified entity, rather than as individuals in separate roles or clusters within the organization to improve healthcare team preparedness. Establishing a cohesive, clinically competent healthcare team benefits the organization and the patients served. Measures to enhance social support, improve communication and ensure clinical competence maintain healthcare team resilience.
There are several limitations to consider when interpreting the results of this study. First, the sample was obtained using purposive snowball sampling, which may have introduced sampling bias and may not accurately represent the larger population of healthcare team members who worked during the COVID-19, as 95% of the sample were white. Second, our study did not have equal representation of all interprofessional team members. It is possible that a more heterogenous sample regarding role, race and gender may have introduced additional codes. Additionally, the PI (JA) worked as a Certified Registered Nurse Anesthesiologist (CRNA) in acute care during the pandemic and personal experience may have introduced confirmation bias. Also, the focus of our research was to fill a gap in the existing knowledge of what is known about healthcare team resilience in pandemic disasters, and help to answer if and how it intersects with individual and organizational resilience. It is possible this novel conceptualization of healthcare team as a cohesive singular conscious source of knowledge did not adequately address this.
Steps to ensure rigor and mitigate any potential shortcomings of qualitative data analysis were the maintenance of a reflexive journal, a willingness of the PI to let go of unsupported ideas and constant verification of codes and themes with the research mentor (MN) for coherence and consistency within the coded data, selected methodology and research questions.
Overall, the extracted themes of teamwork in a pressure cooker; healthcare team cohesion; applying past lessons to present challenges; knowledge gaps; and altruistic behaviors illustrate comparable experiences within the healthcare team. As healthcare professionals and organizations continue to navigate the challenges of the COVID-19 pandemic and other crises, our findings provide valuable insights into how team cohesion, along with altruistic behaviors, may enhance resilience capabilities to create and maintain a unified resilient healthcare team.
Data availability
The data for this study are confidential as required by the IRB approval. To protect the anonymity of the participants, the data are not publicly available. Additional information about the research method, Interview questions, informant data, and the study in general can be requested from the corresponding author, J.A.
Berlin G, Singhal S, Lapointe M, Schulz J. Challenges emerge for the US healthcare system as COVID-19 cases rise. 2020;9.
Stevens JP, O’Donoghue A, Horng S, Tabb K. Healthcare’s earthquake: Lessons from complex adaptive systems to develop Covid-19-responsive measures and models. 2020.
Kopach-Konrad R, Lawley M, Criswell M, Hasan I, Chakraborty S, Pekny J, et al. Applying systems Engineering principles in improving Health Care Delivery. J Gen Intern Med. 2007;22(S3):431–7.
Article PubMed PubMed Central Google Scholar
Compton WD, Fanjiang G, Grossman JH, Reid PP. Institute of Medicine (U.S.), National Academy of Engineering. Building a better delivery system: a new engineering/health care partnership [Internet]. Washington, D.C.: National Academies Press; 2005 [cited 2021 Feb 12]. http://public.ebookcentral.proquest.com/choice/publicfullrecord.aspx?p=3378176 .
Hollnagel E, Woods DD. Resilience Engineering concepts and precepts. 1st ed. Boca Raton, FL: CRC Press/Routledge/Taylor & Francis Group; 2006. p. 416.
Google Scholar
Wiig S, O’Hara JK. Resilient and responsive healthcare services and systems: challenges and opportunities in a changing world. BMC Health Serv Res. 2021;21(1):1037.
Nemeth C, Wears RL, Patel S, Rosen G, Cook R. Resilience is not control: healthcare, crisis management, and ICT. Cogn Tech Work. 2011;13(3):189–202.
Article Google Scholar
Hollnagel E. Safety-II in Practice: Developing the Resilience Potentials [Internet]. 1st ed. Routledge; 2017 [cited 2022 May 7]. https://www.taylorfrancis.com/books/9781351780766 .
Braithwaite J, Wears RL, Hollnagel E. Resilient health care: turning patient safety on its head. Int J Qual Health Care. 2015;27(5):418–20.
Article PubMed Google Scholar
Madni AM, Jackson S. Towards a conceptual Framework for Resilience Engineering. IEEE Syst J. 2009;3(2):181–91.
Carthey J. Institutional resilience in healthcare systems. Qual Health Care. 2001;10(1):29–32.
Article CAS PubMed PubMed Central Google Scholar
Hollnagel E. The Four cornerstones of Resilience Engineering. In: Dekker, editor. Resilience engineering perspcetives. E. Hollnagel&S. Ashgate: Farnham, UK; 2009. pp. 117–33.
Fridell M, Edwin S, von Schreeb J, Saulnier DD. Health System Resilience: what are we talking about? A scoping review mapping characteristics and keywords. Int J Health Policy Manag. 2019;9(1):6–16.
Article PubMed Central Google Scholar
Curtin M, Richards HL, Fortune DG. Resilience among health care workers while working during a pandemic: a systematic review and meta synthesis of qualitative studies. Clin Psychol Rev. 2022;95:102173.
Ambrose JW, Layne DM, Catchpole K, Evans H, Nemeth LS. A qualitative protocol to examine Resilience Culture in Healthcare teams during COVID-19. Healthcare. 2021;9(9):1168.
Carayon P, Hundt AS, Karsh B, Gurses AP, Alvarado CJ, Smith M, et al. Work system design for patient safety: the SEIPS model. Qual Saf Health Care. 2006;15(Suppl 1):i50–8.
Thordsen ML, Kyne MM, Klein G, A Model of Advanced Team Decision Making and Performance.: Summary Report: [Internet]. Fort Belvoir, VA: Defense Technical Information Center; 1994 Sep [cited 2021 Feb 13]. http://www.dtic.mil/docs/citations/ADA400497 .
Zsambok CE. Advanced Team Decision Making: A Model and Training Implications.
Klein GA. Sources of power: how people make decisions. MIT Press; 1988.
Doyle L, McCabe C, Keogh B, Brady A, McCann M. An overview of the qualitative descriptive design within nursing research. J Res Nurs. 2020;25(5):443–55.
Siedlecki SL. Understanding descriptive research designs and methods. Clin Nurse Spec. 2020;34(1):8–12.
Crabtree BF, Miller WL. Doing qualitative research. Second. Thousand Oaks, CA: Sage; 1999. p. 406.
Bradley EH, Curry LA, Devers KJ. Qualitative Data Analysis for Health Services Research: developing taxonomy, themes, and theory. Health Serv Res. 2007;42(4):1758–72.
Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13(1):117.
Lincoln Y, Guba E. Naturalistic Inquiry. California: Sage; 1985.
Book Google Scholar
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Saldaña J. The coding manual for qualitative rearchers. Los Angeles, USA: Sage; 2021.
Boyatzis RE. Transforming qualitative information: thematic analysis and code development. Thousand Oaks, CA: SAGE Publications Ltd; 1998.
Braun V, Clarke V. What can thematic analysis offer health and wellbeing researchers? Int J Qualitative Stud Health Well-being. 2014;9(1):26152.
Braun V, Clarke V. Thematic analysis. In: Cooper H, Camic PM, Long DL, Panter AT, Rindskopf D, Sher KJ, editors. APA handbook of research methods in psychology, Vol 2: Research designs: Quantitative, qualitative, neuropsychological, and biological [Internet]. Washington: American Psychological Association; 2012 [cited 2022 May 15]. pp. 57–71. http://content.apa.org/books/13620-004 .
Braun V, Clarke V. Conceptual and design thinking for thematic analysis. Qualitative Psychol. 2022;9(1):3–26.
Liu Y, Zhai Z, Han Y, Liu Y, Liu F, Hu D. Experiences of front-line nurses combating coronavirus disease‐2019 in China: a qualitative analysis. Public Health Nurs. 2020;37(5):757–63.
Catania G, Zanini M, Hayter M, Timmins F, Dasso N, Ottonello G, et al. Lessons from Italian front-line nurses’ experiences during the COVID‐19 pandemic: a qualitative descriptive study. J Nurs Manag. 2021;29(3):404–11.
Croghan IT, Chesak SS, Adusumalli J, Fischer KM, Beck EW, Patel SR et al. Stress, Resilience, and Coping of Healthcare Workers during the COVID-19 Pandemic. Journal of Primary Care and Community Health [Internet]. 2021;12. https://www.scopus.com/inward/record.uri?eid=2-s2.0-85104122303&doi=10.1177%2f21501327211008448&partnerID=40&md5=96ad0164880c9725ce14d534e3c3117
Arnetz JE, Goetz CM, Arnetz BB, Arble E. Nurse reports of stressful situations during the COVID-19 pandemic: qualitative analysis of survey responses. IJERPH. 2020;17(21):8126.
Dagyaran I, Risom SS, Berg SK, Højskov IE, Heiden M, Bernild C, et al. Like soldiers on the front– a qualitative study understanding the frontline healthcare professionals’ experience of treating and caring for patients with COVID-19. BMC Health Serv Res. 2021;21(1):666.
Goh Y, Ow Yong QYJ, Chen TH, Ho SHC, Chee YIC, Chee TT. The impact of COVID-19 on nurses working in a University Health System in Singapore: a qualitative descriptive study. Int J Mental Health Nurs. 2021;30(3):643–52.
LoGiudice JA, Bartos S. Experiences of nurses during the COVID-19 pandemic: a mixed-methods study. AACN Adv Crit Care. 2021;32(1):14–26.
O’Brien JM, Bae FA, Kawchuk J, Reimche E, Abramyk CA, Kitts C et al. We were treading water. Experiences of healthcare providers in Canadian ICUs during COVID-19 visitor restrictions: a qualitative descriptive study.
Perraud F, Ecarnot F, Loiseau M, Laurent A, Fournier A, Lheureux F, et al. A qualitative study of reinforcement workers’ perceptions and experiences of working in intensive care during the COVID-19 pandemic: a PsyCOVID-ICU substudy. Sharma GA, editor. PLoS ONE. 2022;17(3):e0264287.
Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among Health Care professionals during the COVID-19 pandemic. JAMA. 2020;323(21):2133.
Article CAS PubMed Google Scholar
Speroni KG, Seibert DJ, Mallinson RK. Nurses’ perceptions on Ebola Care in the United States, Part 2: a qualitative analysis. JONA: J Nurs Adm. 2015;45(11):544–50.
Sonis J, Pathman DE, Read S, Gaynes BN, Canter C, Curran P, et al. Effects of Healthcare Organization Actions and policies related to COVID-19 on Perceived Organizational Support among U.S. internists: a National Study. J Healthc Manag. 2022;67(3):192–205.
PubMed Google Scholar
Banerjee D, Sathyanarayana Rao TS, Kallivayalil RA, Javed A. Psychosocial Framework of Resilience: navigating needs and adversities during the pandemic, a qualitative exploration in the Indian Frontline Physicians. Front Psychol. 2021;12:622132.
Freudenberg LS, Paez D, Giammarile F, Cerci J, Modiselle M, Pascual TNB, et al. Global impact of COVID-19 on Nuclear Medicine departments: an International Survey in April 2020. J Nucl Med. 2020;61(9):1278–83.
Haldane V, Morgan GT. From resilient to transilient health systems: the deep transformation of health systems in response to the COVID-19 pandemic. Health Policy Plann. 2021;36(1):134–5.
Shrestha N, Shad MY, Ulvi O, Khan MH, Karamehic-Muratovic A, Nguyen USDT, et al. The impact of COVID-19 on globalization. One Health. 2020;11:100180.
Jean WC, Ironside NT, Sack KD, Felbaum DR, Syed HR. The impact of COVID-19 on neurosurgeons and the strategy for triaging non-emergent operations: a global neurosurgery study. Acta Neurochir. 2020;162(6):1229–40.
Anjara S, Fox R, Rogers L, De Brún A, McAuliffe E. Teamworking in Healthcare during the COVID-19 pandemic: a mixed-method study. IJERPH. 2021;18(19):10371.
Kaye-Kauderer H, Loo G, Murrough JW, Feingold JH, Feder A, Peccoralo L, et al. Effects of Sleep, Exercise, and Leadership Support on Resilience in Frontline Healthcare workers during the COVID-19 pandemic. J Occup Environ Med. 2022;64(5):416–20.
Kinsella EL, Muldoon OT, Lemon S, Stonebridge N, Hughes S, Sumner RC. In it together? Exploring solidarity with frontline workers in the United Kingdom and Ireland during COVID-19. Br J Social Psychol. 2023;62(1):241–63.
Coleman JS. Social Capital in the creation of Human Capital. Am J Sociol. 1988;94:S95–120.
Drury J, Carter H, Cocking C, Ntontis E, Tekin Guven S, Amlôt R. Facilitating collective psychosocial resilience in the Public in emergencies: twelve recommendations based on the Social Identity Approach. Front Public Health. 2019;7:141.
Brooks SK, Dunn R, Amlôt R, Rubin GJ, Greenberg N. Protecting the psychological wellbeing of staff exposed to disaster or emergency at work: a qualitative study. BMC Psychol. 2019;7(1):78.
Aufegger L, Shariq O, Bicknell C, Ashrafian H, Darzi A. Can shared leadership enhance clinical team management? A systematic review. LHS. 2019;32(2):309–35.
Godkin D, Markwell H. The Duty to Care of Healthcare Professionals: Ethical Issues and Guidelines for Policy Development. Submitted to SARS Expert Panel Secretariat.:23.
Gray K, Dorney P, Hoffman L, Crawford A. Nurses’ pandemic lives: a mixed-methods study of experiences during COVID-19. Appl Nurs Res. 2021;60:151437.
Liu X, Kakade M, Fuller CJ, Fan B, Fang Y, Kong J, et al. Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Compr Psychiatr. 2012;53(1):15–23.
Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, et al. The psychological impact of the SARS Epidemic on Hospital employees in China: exposure, risk perception, and Altruistic Acceptance of Risk. Can J Psychiatry. 2009;54(5):302–11.
Download references
Acknowledgements
The authors want to thank all the interviewed healthcare team participants for their time and sharing their personal stories and for their continued service during the COVID-19 pandemic. We would also like to acknowledge Ayaba Logan, the Research and Education Informationist, Mohan Madisetti, the MUSC College of Nursing Director of Research, the staff of the MUSC Center for Academic Excellence and the reviewers of this journal for their constructive criticism.
This research (software, transcription services, etc.) was solely funded by the Principal Investigator, J.A.
Author information
Authors and affiliations.
College of Nursing, Medical University of South Carolina, Charleston, SC, USA
John W. Ambrose, Lynne S. Nemeth, Diana M. Layne & Michelle Nichols
Department of Anesthesia and Perioperative Medicine, College of Medicine, Medical University of South Carolina, Charleston, SC, USA
Ken Catchpole
Department of Surgery, College of Medicine, Medical University of South Carolina, Charleston, SC, USA
Heather L. Evans
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization J.A., K.C., L.N., D.L., H.E., and M.N.; methodology J.A. and M.N.; J.A. led the study, recruited the interviewees, conducted interviews, led the data analysis, and drafted the manuscript. J.A., and M.N. conducted the data analyses; review and editing K.C., H.E., D.L., and M.N.; supervision M.N.; research project administration J.A. and M.N.; funding acquisition J.A. All authors reviewed the manuscript.
Corresponding author
Correspondence to John W. Ambrose .
Ethics declarations
Ethics approval and consent to participate.
This study presented no greater than minimal risk to participants and met exempt status per regulatory criteria established by 45 CFR 46.104 and 21 CFR 56.104. The study protocol and all materials were approved by the MUSC Institutional Review Board (IRB), [Pro00100917 ]. All study procedures were followed in accordance with these standards.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ambrose, J.W., Catchpole, K., Evans, H.L. et al. Healthcare team resilience during COVID-19: a qualitative study. BMC Health Serv Res 24 , 459 (2024). https://doi.org/10.1186/s12913-024-10895-3
Download citation
Received : 25 February 2023
Accepted : 25 March 2024
Published : 12 April 2024
DOI : https://doi.org/10.1186/s12913-024-10895-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Resilience Engineering
- Healthcare System
- Healthcare Administration
- Healthcare Team
- Thematic Analysis
- Qualitative Research
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
This paper is in the following e-collection/theme issue:
Published on 11.4.2024 in Vol 26 (2024)
Evaluating the Digital Health Experience for Patients in Primary Care: Mixed Methods Study
Authors of this article:

Original Paper
- Melinda Ada Choy 1, 2 , BMed, MMed, DCH, MD ;
- Kathleen O'Brien 1 , BSc, GDipStats, MBBS, DCH ;
- Katelyn Barnes 1, 2 , BAPSC, MND, PhD ;
- Elizabeth Ann Sturgiss 3 , BMed, MPH, MForensMed, PhD ;
- Elizabeth Rieger 1 , BA, MClinPsych, PhD ;
- Kirsty Douglas 1, 2 , MBBS, DipRACOG, Grad Cert HE, MD
1 School of Medicine and Psychology, College of Health and Medicine, The Australian National University, Canberra, Australia
2 Academic Unit of General Practice, Office of Professional Leadership and Education, ACT Health Directorate, Canberra, Australia
3 School of Primary and Allied Health Care, Monash University, Melbourne, Australia
Corresponding Author:
Melinda Ada Choy, BMed, MMed, DCH, MD
School of Medicine and Psychology
College of Health and Medicine
The Australian National University
Phone: 61 51244947
Email: [email protected]
Background: The digital health divide for socioeconomic disadvantage describes a pattern in which patients considered socioeconomically disadvantaged, who are already marginalized through reduced access to face-to-face health care, are additionally hindered through less access to patient-initiated digital health. A comprehensive understanding of how patients with socioeconomic disadvantage access and experience digital health is essential for improving the digital health divide. Primary care patients, especially those with chronic disease, have experience of the stages of initial help seeking and self-management of their health, which renders them a key demographic for research on patient-initiated digital health access.
Objective: This study aims to provide comprehensive primary mixed methods data on the patient experience of barriers to digital health access, with a focus on the digital health divide.
Methods: We applied an exploratory mixed methods design to ensure that our survey was primarily shaped by the experiences of our interviewees. First, we qualitatively explored the experience of digital health for 19 patients with socioeconomic disadvantage and chronic disease and second, we quantitatively measured some of these findings by designing and administering a survey to 487 Australian general practice patients from 24 general practices.
Results: In our qualitative first phase, the key barriers found to accessing digital health included (1) strong patient preference for human-based health services; (2) low trust in digital health services; (3) high financial costs of necessary tools, maintenance, and repairs; (4) poor publicly available internet access options; (5) reduced capacity to engage due to increased life pressures; and (6) low self-efficacy and confidence in using digital health. In our quantitative second phase, 31% (151/487) of the survey participants were found to have never used a form of digital health, while 10.7% (52/487) were low- to medium-frequency users and 48.5% (236/487) were high-frequency users. High-frequency users were more likely to be interested in digital health and had higher self-efficacy. Low-frequency users were more likely to report difficulty affording the financial costs needed for digital access.
Conclusions: While general digital interest, financial cost, and digital health literacy and empowerment are clear factors in digital health access in a broad primary care population, the digital health divide is also facilitated in part by a stepped series of complex and cumulative barriers. Genuinely improving digital health access for 1 cohort or even 1 person requires a series of multiple different interventions tailored to specific sequential barriers. Within primary care, patient-centered care that continues to recognize the complex individual needs of, and barriers facing, each patient should be part of addressing the digital health divide.
Introduction
The promise of ehealth.
The rapid growth of digital health, sped up by the COVID-19 pandemic and associated lockdowns, brings the promise of improved health care efficiency, empowerment of consumers, and health care equity [ 1 ]. Digital health is the use of information and communication technology to improve health [ 2 ]. eHealth, which is a type of digital health, refers to the use of internet-based technology for health care and can be used by systems, providers, and patients [ 2 ]. At the time of this study (before COVID-19), examples of eHealth used by patients in Australia included searching for web-based health information, booking appointments on the web, participating in online peer-support health forums, using mobile phone health apps (mobile health), emailing health care providers, and patient portals for electronic health records.
Digital health is expected to improve chronic disease management and has already shown great potential in improving chronic disease health outcomes [ 3 , 4 ]. Just under half of the Australian population (47.3%) has at least 1 chronic disease [ 5 ]. Rates of chronic disease and complications from chronic disease are overrepresented among those with socioeconomic disadvantage [ 6 ]. Therefore, patients with chronic disease and socioeconomic disadvantage have a greater need for the potential benefits of digital health, such as an improvement in their health outcomes. However, there is a risk that those who could benefit most from digital health services are the least likely to receive them, exemplifying the inverse care law in the digital age by Hart [ 7 ].
Our Current Understanding of the Digital Health Divide
While the rapid growth of digital health brings the promise of health care equity, it may also intensify existing inequities [ 8 ]. The digital health divide for socioeconomic disadvantage describes a pattern in which patients considered socioeconomically disadvantaged who are already marginalized through poor access to traditional health care are additionally hindered through poor access to digital health [ 9 ]. In Australia, only 67.4% of households in the lowest household income quintile have home internet access, compared to 86% of the general population and 96.9% of households in the highest household income quintile [ 10 ]. Survey-based studies have also shown that even with internet access, effective eHealth use is lower in populations considered disadvantaged, which speaks to broader barriers to digital health access [ 11 ].
The ongoing COVID-19 global pandemic has sped up digital health transitions with the rapid uptake of telephone and video consultations, e-prescription, and the ongoing rollout of e-mental health in Australia. These have supported the continuation of health care delivery while limiting physical contact and the pandemic spread; however, the early evidence shows that the digital health divide remains problematic. A rapid review identified challenges with reduced digital access and digital literacy among the older adults and racial and ethnic minority groups, which are both groups at greater health risk from COVID-19 infections [ 12 ]. An Australian population study showed that the rapid uptake of telehealth during peak pandemic was not uniform, with the older adults, very young, and those with limited English language proficiency having a lower uptake of general practitioner (GP) telehealth services [ 13 ].
To ensure that digital health improves health care outcome gaps, it is essential to better understand the nature and nuance of the digital health divide for socioeconomic disadvantage. The nature of the digital health divide for socioeconomic disadvantage has been explored primarily through quantitative survey data, some qualitative papers, a few mixed methods papers, and systematic reviews [ 11 , 14 - 16 ]. Identified barriers include a lack of physical hardware and adequate internet bandwidth, a reduced inclination to seek out digital health, and a low ability and confidence to use digital health effectively [ 16 ]. The few mixed methods studies that exist on the digital health divide generally triangulate quantitative and qualitative data on a specific disease type or population subgroup to draw a combined conclusion [ 17 , 18 ]. These studies have found digital health access to be associated with education, ethnicity, and gender as well as trust, complementary face-to-face services, and the desire for alternative sources of information [ 17 , 19 ].
What This Work Adds
This project sought to extend previous research by using an exploratory mixed methods design to ensure that the first step and driver of our survey of a larger population was primarily shaped by the experiences of our interviewees within primary care. This differs from the triangulation method, which places the qualitative and quantitative data as equal first contributors to the findings and does not allow one type of data to determine the direction of the other [ 18 ]. We qualitatively explored the experience of digital health for patients with socioeconomic disadvantage and chronic disease and then quantitatively measured some of the qualitative findings via a survey of the Australian general practice patient population. Our key objective was to provide comprehensive primary mixed methods data, describing the experience and extent of barriers to accessing digital health and its benefits, with a focus on the digital health divide. We completed this research in a primary care context to investigate a diverse community-based population with conceivable reasons to seek digital help in managing their health. Findings from this mixed methods study were intended to provide health care providers and policy makers with a more detailed understanding of how specific barriers affect different aspects or steps of accessing digital health. Ultimately, understanding digital health access can influence the future design and implementation of digital health services by more effectively avoiding certain barriers or building in enablers to achieve improved digital health access not only for everyone but also especially for those in need.
Study Design
We conducted a sequential exploratory mixed methods study to explore a complex phenomenon in depth and then measure its prevalence. We qualitatively explored the experience of digital health for patients with chronic disease and socioeconomic disadvantage in the first phase. Data from the first phase informed a quantitative survey of the phenomenon across a wider population in the second phase [ 18 ]. Both stages of research were conducted before the COVID-19 pandemic in Australia.
Recruitment
Qualitative phase participants.
The eligibility criteria for the qualitative phase were as follows: English-speaking adults aged ≥18 years with at least 1 self-reported chronic disease and 1 marker of socioeconomic disadvantage (indicated by ownership of a Health Care Card or receiving a disability pension, unemployment, or a user of public housing). A chronic disease was defined to potential participants as a diagnosed long-term health condition that had lasted at least 6 months (or is expected to last for at least 6 months; examples are listed in Multimedia Appendix 1 ). The markers of socioeconomic disadvantage we used to identify potential participants were based on criteria typically used by local general practices to determine which patients can have lower or no out-of-pocket expenses. Apart from unemployment, the 3 other criteria to identify socioeconomic disadvantage are means-tested government-allocated public social services [ 20 ]. Qualitative phase participants were recruited from May to July 2019 through 3 general practices and 1 service organization that serve populations considered socioeconomically disadvantaged across urban, regional, and rural regions in the Australian Capital Territory and South Eastern New South Wales. A total of 2 recruitment methods were used in consultation with and as per the choice of the participating organizations. Potential participants were either provided with an opportunity to engage with researchers (KB and MAC) in the general practice waiting room or identified by the practice or organization as suitable for an interview. Interested participants were given a detailed verbal and written description of the project in a private space before providing written consent to be interviewed. All interview participants received an Aus $50 (US $32.68) grocery shopping voucher in acknowledgment of their time.
Quantitative Phase Participants
Eligibility for the quantitative phase was English-speaking adults aged ≥18 years. The eligibility criteria for the quantitative phase were deliberately broader than those for the qualitative phase to achieve a larger sample size within the limitations of recruitment and with the intention that the factors of socioeconomic disadvantage and having a chronic disease could be compared to the digital health access of a more general population. The quantitative phase participants were recruited from November 2019 to February 2020. Study information and paper-based surveys were distributed and collected through 24 general practices across the Australian Capital Territory and South Eastern New South Wales regions, with an option for web-based completion.
Ethical Considerations
Qualitative and quantitative phase research protocols, including the participant information sheet, were approved by the Australian Capital Territory Health Human Research Ethics Committee (2019/ETH/00013) and the Australian National University Human Research Ethics Committee (2019/ETH00003). Qualitative phase participants were given a verbal and written explanation of the study, including how and when they could opt out, before they provided written consent. All interview participants received an Aus $50 (US $32.68) grocery shopping voucher in acknowledgment of their time. Quantitative participants were given a written explanation and their informed consent was implied by return of a completed survey. Participants in both phases of the study were told that all their data was deidentified. Consent was implied through the return of a completed survey.
Qualitative Data Collection and Analysis
Participants were purposively sampled to represent a range in age, gender, degree of socioeconomic disadvantage, and experience of digital health. The sampling and sample size were reviewed regularly by the research team as the interviews were being completed to identify potential thematic saturation.
The interview guide was developed by the research team based on a review of the literature and the patient dimensions of the framework of access by Levesque et al [ 21 ]. The framework by Levesque et al [ 21 ] is a conceptualization of health care access comprising 5 service and patient dimensions of accessibility and ability. The patient dimensions are as follows: (1) ability to perceive, (2) ability to seek, (3) ability to reach, (4) ability to pay, and (5) ability to engage [ 21 ]. The key interview topics included (1) digital health use and access, including facilitators and barriers; (2) attitudes toward digital health; and (3) self-perception of digital health skills and potential training. The interview guide was reviewed for face and content validity by the whole research team, a patient advocate, a digital inclusion charity representative, and the general practices where recruitment occurred. The questions and guide were iteratively refined by the research team to ensure relevance and support reaching data saturation. The interview guide has been provided as Multimedia Appendix 1 . The interviews, which took 45 minutes on average, were taped and transcribed. An interview summary sheet and reflective journal were completed by the interviewer after each interview to also capture nonverbal cues and tone.
Interview transcriptions were coded and processed by inductive thematic analysis. Data collection and analysis were completed in parallel to support the identification of data saturation. Data saturation was defined as no significant new information arising from new interviews and was identified by discussion with the research team [ 22 ]. The 2 interviewers (MAC and KB) independently coded the first 5 transcripts and reflected on them with another researcher (EAS) to ensure intercoder validity and reliability. The rest of the interviews were coded independently by the 2 interviewers, who regularly met to reflect on emerging themes and thematic saturation. Data saturation was initially indicated after 15 interviews and subsequently confirmed with a total of 19 interviews. Coding disagreements and theme development were discussed with at least 1 other researcher (EAS, ER, and KD). Thematic saturation and the final themes were agreed upon by the entire research team.
Quantitative Survey Development
The final themes derived in the qualitative phase of the project guided the specific quantitative phase research questions. The final themes were a list of ordered cumulative barriers experienced by participants in accessing digital health and its benefits ( Figure 1 ). The quantitative survey was designed to test the association between barriers to access and the frequency of use of digital health as a proxy measure for digital health access.

In the survey, the participants were asked about their demographic details, health and chronic diseases, knowledge, use and experience of digital health tools, internet access, perception of digital resource affordability, trust in digital health and traditional health services, perceived capability, health care empowerment, eHealth literacy, and relationship with their GP.
Existing scales and questions from the literature and standardized Australian-based surveys were used whenever possible. We used selected questions and scales from the Australian Bureau of Statistics standards, the eHealth Literacy Scale (eHEALS), the eHealth Literacy Questionnaire, and the Southgate Institute for Health Society and Equity [ 17 , 23 - 26 ]. We adapted other scales from the ICEpop Capability Measure for Adults, the Health Care Empowerment Inventory (HCEI), the Patient-Doctor Relationship Questionnaire, and the Chao continuity questionnaire [ 23 , 27 - 29 ]. Where an existing scale to measure a barrier or theme did not exist, the research team designed the questions based on the literature. Our questions around the frequency of digital health use were informed by multiple existing Australian-based surveys on general technology use [ 30 , 31 ]. Most of the questions used a Likert scale. Every choice regarding the design, adaptation, or copy of questions for the survey was influenced by the qualitative findings and decided on by full agreement among the 2 researchers who completed and coded the interviews. A complete copy of the survey is provided in Multimedia Appendix 2 .
Pilot-testing of the survey was completed with 5 patients, 2 experts on digital inclusion, and 3 local GPs for both the paper surveys and web-based surveys via Qualtrics Core XM (Qualtrics LLC). The resulting feedback on face and content validity, functionality of the survey logic, and feasibility of questionnaire completion was incorporated into the final version of the survey.
The survey was offered on paper with a participant information sheet, which gave the patients the option to complete the web-based survey. The survey was handed out to every patient on paper to avoid sampling bias through the exclusion of participants who could not complete the web-based survey [ 32 ].
Quantitative Data Treatment and Analysis
Data were exported from Qualtrics Core XM to an SPSS (version 26; IBM Corp) data set. Data cleaning and screening were undertaken (KB and KO).
Descriptive statistics (number and percentage) were used to summarize participant characteristics, preference measures, and frequency of eHealth use. Significance testing was conducted using chi-square tests, with a threshold of P <.05; effect sizes were measured by the φ coefficient for 2×2 comparisons and Cramer V statistic for all others. Where the cells sizes were too small, the categories were collapsed for the purposes of significance testing. The interpretation of effect sizes was as per the study by Cohen [ 33 ]. The analysis was conducted in SPSS and SAS (version 9.4; SAS Institute).
Participant Characteristics
Participants’ self-reported characteristics included gender, indigenous status, income category, highest level of education, marital status, and language spoken at home.
Age was derived from participant-reported year of birth and year of survey completion as of 2019 and stratified into age groups. The state or territory of residence was derived from the participant-reported postcode. The remoteness area was derived using the postcode reported by the participants and mapped to a modified concordance from the Australian Bureau of Statistics. Occupation-free text responses were coded using the Australian Bureau of Statistics Census statistics level 1 and 2 descriptors. The country of birth was mapped to Australia, other Organisation for Economic Cooperation and Development countries, and non–Organisation for Economic Cooperation and Development countries.
Frequency of eHealth Use
A summary measure of the frequency of eHealth use was derived from the questions on the use of different types of eHealth.
Specifically, respondents were asked if they had ever used any form of web-based health (“eHealth“) and, if so, to rate how often (never, at least once, every now and then, and most days) against 6 types of “eHealth” (searching for health information online, booking appointments online, emailing health care providers, using health-related mobile phone apps, accessing My Health Record, and accessing online health forums). The frequency of eHealth use was then classified as follows:
- High user: answered “most days” to at least 1 question on eHealth use OR answered “every now and then” to at least 2 questions on eHealth use
- Never user: answered “no” to having ever used any form of eHealth OR “never” to all 6 questions on eHealth use
- Low or medium user: all other respondents.
The frequency of eHealth use was reported as unweighted descriptive statistics (counts and percentages) against demographic characteristics and for the elements of each of the themes identified in phase 1.
Overview of Key Themes
Data were reported against the 6 themes from the phase 1 results of preference, trust, cost, structural access, capacity to engage, and self-efficacy. Where the components of trust, cost, capacity to engage, and self-efficacy had missing data (for less than half of the components only), mean imputation was used to minimize data loss. For each theme, the analysis excluded those for whom the frequency of eHealth use was unknown.
Preference measures (survey section D1 parts 1 to 3) asked participants to report against measures with a 4-point Likert scale (strongly disagree, disagree, agree, and strongly agree). Chi-square tests were conducted after the categories were condensed into 2 by combining strongly disagree and as well as combining strongly agree and agree.
Summary measures for trust were created in 4 domains: trust from the eHealth Literacy Questionnaire (survey section D1 parts 4 to 8), trust from Southgate—GPs, specialists, or allied health (survey section D2 parts 1 to 5), trust from Southgate—digital health (survey section D2 parts 6, 7, 9, and 10), and trust from Southgate—books or pamphlets (survey section D2 part 8). The data were grouped as low, moderate, and high trust based on the assigned scores from the component data. Chi-square tests were conducted comparing low-to-moderate trust against high trust for GP, specialists, or allied health and comparing low trust against moderate-to-high trust for book or pamphlet.
Summary measures for cost were created from survey item C10. To measure cost, participants were asked about whether they considered certain items or services to be affordable. These included cost items mentioned in the qualitative phase interviews relating to mobile phones (1 that connects to the internet, 1 with enough memory space to download apps, downloads or apps requiring payment, repairs, and maintenance costs), having an iPad or tablet with internet connectivity, a home computer or laptop (owning, repairs, and maintenance), home fixed internet access, and an adequate monthly data allowance. These 9 items were scored as “yes definitely”=1 or 0 otherwise. Chi-square tests were conducted with never and low or medium eHealth users combined.
Structural Access
Structural access included asking where the internet is used by participants (survey section C8) and factors relating to internet access (survey section C8 parts 1-3) reporting against a 4-point Likert scale (strongly disagree, disagree, agree, and strongly agree). Chi-square tests were conducted with strongly disagree, disagree, agree, or strongly agree, and never, low, or medium eHealth use combined.
Capacity to Engage
Summary measures for capacity to engage were created from survey section E1. To measure the capacity to engage, participants were asked about feeling “settled and secure,” “being independent,” and “achievement and progress” as an adaptation of the ICEpop Capability Measure for Adults [ 27 ], reporting against a 4-point Likert-like scale. Responses were scored from 1 (“I am unable to feel settled and secure in any areas of my life”) to 4 (“I am able to feel settled and secure in all areas of my life”).
The summary capacity measure was derived by the summation of responses across the 3 questions, which were classified into 4 groups, A to D, based on these scores. Where fewer than half of the responses were missing, mean imputation was used; otherwise, the record was excluded. Groups A and B were combined for significance testing.
Self-Efficacy
Summary measures for self-efficacy were adapted from the eHEALS (E3) and the HCEI (E2) [ 23 , 24 ].
Survey section E3—eHEALS—comprised 8 questions, with participants reporting against a 5-point Likert scale for each (strongly disagree, disagree, neither, agree, and strongly agree). These responses were assigned 1 to 5 points, respectively. The summary eHEALS measure was derived by the summation of responses across the 8 questions, which were classified into 5 groups, A to E, based on these scores. Where fewer than half of the responses were missing, mean imputation was used; otherwise, the record was excluded. Groups A to C and D to E were combined for significance testing.
Survey section E2—HCEI—comprised 5 questions, with participants reporting against a 5-point Likert scale for each (strongly disagree, disagree, neither, agree, and strongly agree). Strongly disagree and disagree and neither were combined, and similarly agree and strongly agree were combined for significance testing.
Qualitative Results
The demographic characteristics of the patients that we interviewed are presented in Table 1 .
The key barriers found to accessing digital health included (1) strong patient preference for human-based health services; (2) low trust in digital health services; (3) high financial costs of necessary tools, maintenance, and repairs; (4) poor publicly available internet access options; (5) reduced capacity to engage due to increased life pressures; and (6) low self-efficacy and confidence in using digital health.
Rather than being an equal list of factors, our interviewees described these barriers as a stepped series of cumulative hurdles, which is illustrated in Figure 1 . Initial issues of preference and trust were foundational to a person even when considering the option of digital health, while digital health confidence and literacy were barriers to full engagement with and optimal use of digital health. Alternatively, interviewees who did use digital health had been enabled by the same factors that were barriers to others.
a GP: general practitioner.
b Multiple answers per respondent.
Strong Patient Preference for Human-Based Health Services
Some patients expressed a strong preference for human-based health services rather than digital health services. In answer to a question about how digital health services could be improved, a patient said the following:
Well, having an option where you can actually bypass actually having to go through the app and actually talk directly to someone. [Participant #10]
For some patients, this preference for human-based health services appeared to be related to a lack of exposure to eHealth. These patients were not at all interested in or had never thought about digital health options. A participant responded the following to the interviewer’s questions:
Interviewer: So when...something feels not right, how do you find out what’s going on?
Respondent: I talk to Doctor XX.
Interviewer: Do you ever Google your symptoms or look online for information?
Respondent: No, I have never even thought of doing that actually. [Participant #11]
For other patients, their preference for human-based health care stemmed from negative experiences with technology. These patients reported actively disliking computers and technology in general and were generally frustrated with what they saw as the pitfalls of technology. A patient stated the following:
If computers and internet weren’t so frigging slow because everything is on like the slowest speed network ever and there’s ads blocking everything. Ads, (expletive) ads. [Participant #9]
A patient felt that he was pushed out of the workforce due his inability to keep up with technology-based changes and thus made a decision to never own a computer:
But, you know, in those days when I was a lot younger those sorts of things weren’t about and they’re just going ahead in leaps and bounds and that’s one of the reasons why I retired early. I retired at 63 because it was just moving too fast and it’s all computers and all those sorts of things and I just couldn’t keep up. [Participant #17]
Low Trust in Digital Health Services
Several patients described low trust levels for digital and internet-based technology in general. Their low trust was generally based on stories they had heard of other people’s negative experiences. A patient said the following:
I don’t trust the internet to be quite honest. You hear all these stories about people getting ripped off and I’ve worked too hard to get what I’ve got rather than let some clown get it on the internet for me. [Participant #11]
Some of this distrust was specific to eHealth. For example, some patients were highly suspicious of the government’s motives with regard to digital health and were concerned about the privacy of their health information, which made them hesitant about the concept of a universal electronic health record. In response to the interviewer’s question, a participant said the following:
Interviewer: Are there any other ways you think that eHealth might help you?
Respondent: I’m sorry but it just keeps coming back to me, Big Brother. [Participant #7]
Another participant said the following:
I just would run a mile from it because I just wouldn’t trust it. It wouldn’t be used to, as I said, for insurance or job information. [Participant #16]
High Financial Costs of the Necessary Tools, Maintenance, and Repairs
A wide variety of patients described affordability issues across several different aspects of the costs involved in digital health. They expressed difficulty in paying for the following items: a mobile phone that could connect to the internet, a mobile phone with enough memory space to download apps, mobile phone apps requiring extra payment without advertisements, mobile phone repair costs such as a broken screen, a computer or laptop, home internet access, and adequate monthly data allowance and speeds to functionally use the internet. Current popular payment systems, such as plans, were not feasible for some patients. A participant stated the following:
I don’t have a computer...I’m not in the income bracket to own a computer really. Like I could, if I got one on a plan kind of thing or if I saved up for x-amount of time. But then like if I was going on the plan I’d be paying interest for having it on like lay-buy kind of thing, paying it off, and if it ever got lost or stolen I would still have to repay that off, which is always a hassle. And yeah. Yeah, I’m like financially not in the state where I’m able to...own a computer right now as I’m kind of paying off a number of debts. [Participant #9]
Poor Publicly Available Internet Access Options
Some patients described struggling without home internet access. While they noted some cost-free public internet access points, such as libraries, hotel bars, and restaurants, they often found these to be inconvenient, lacking in privacy, and constituting low-quality options for digital health. A patient stated the following:
...it’s incredibly slow at the library. And I know why...a friend I went to school with used to belong to the council and the way they set it up, they just got the raw end of the stick and it is really, really slow. It’s bizarre but you can go to the X Hotel and it’s heaps quicker. [Participant #15]
In response to the interviewer's question, a participant said the following:
Interviewer: And do you feel comfortable doing private stuff on computers at the library...?
Respondent: Not really, no, but I don’t have any other choice, so, yeah. [Participant #9]
Reduced Capacity to Engage Due to Increased Life Pressures
When discussing why they were not using digital health or why they had stopped using digital health, patients often described significant competing priorities and life pressures that affected their capacity to engage. An unemployed patient mentioned that his time and energy on the internet were focused primarily on finding work and that he barely had time to focus on his health in general, let alone engage in digital health.
Other patients reported that they often felt that their ability to learn about and spend time on digital health was taken up by caring for sick family members, paying basic bills, or learning English. Some patients said that the time they would have spent learning digital skills when they were growing up had been lost to adverse life circumstances such as being in jail:
So we didn’t have computers in the house when I was growing up. And I didn’t know I’ve never...I’ve been in and out of jail for 28 odd years so it sort of takes away from learning from this cause it’s a whole different… it’s a whole different way of using a telephone from a prison. [Participant #11]
Low Self-Efficacy and Confidence in Starting the Digital Health Process
Some patients had a pervasive self-perception of being slow learners and being unable to use technology. Their stories of being unconfident learners seemed to stem from the fact that they had been told throughout their lives that they were intellectually behind. A patient said the following:
The computer people...wouldn’t take my calls because I’ve always been dumb with that sort of stuff. Like I only found out this later on in life, but I’m actually severely numerically dyslexic. Like I have to triple-check everything with numbers. [Participant #7]
Another patient stated the following:
I like went to two English classes like a normal English class with all the kids and then another English class with about seven kids in there because I just couldn’t I don’t know maybe because I spoke another language at home and they sort of like know I was a bit backward. [Participant #6]
These patients and others had multiple missing pieces of information that they felt made it harder to engage in digital health compared to “easier” human-based services. A patient said the following:
Yeah I’ve heard of booking online but I just I don’t know I find it easier just to ring up. And I’ll answer an email from a health care provider but I wouldn’t know where to start to look for their email address. [Participant #11]
In contrast, the patients who did connect with digital health described themselves as independent question askers and proactive people. Even when they did not know how to use a specific digital health tool, they were confident in attempting to and asking for help when they needed it. A patient said the following:
I’m a “I will find my way through this, no matter how long it takes me” kind of person. So maybe it’s more my personality...If I have to ask for help from somewhere, wherever it is, I will definitely do that. [Participant #3]
Quantitative Results
A total of 487 valid survey responses were received from participants across 24 general practices. The participant characteristics are presented in detail in Table S1 in Multimedia Appendix 3 .
The mean age of the participants was approximately 50 years (females 48.9, SD 19.4 years; males 52.8, SD 20.0 years), and 68.2% (332/487) of the participants identified as female. Overall, 34.3% (151/439) of respondents reported never using eHealth, and 53.8% (236/439) reported high eHealth use.
There were statistically significant ( P <.05) differences in the frequency of eHealth use in terms of age group, gender, state, remoteness, highest level of education, employment status, occupation group, marital status, and language spoken at home, with effect sizes being small to medium. Specifically, high eHealth characteristics were associated with younger age, being female, living in an urban area, and being employed.
Table 2 presents the frequency of eHealth use against 3 internet preference questions.
Preference for using the internet and technology in general and for health needs in particular were significantly related to the frequency of eHealth use ( P <.05 for each), with the effect sizes being small to medium.
a Excludes those for whom frequency of eHealth use is unknown.
b Chi-square tests conducted with strongly disagree and disagree combined, and agree and strongly agree combined.
Table 3 presents the frequency of eHealth use against 4 measures of trust.
The degree of trust was not statistically significantly different for the frequency of eHealth use for any of the domains.
b eHLQ: eHealth Literacy Questionnaire.
c Derived from survey question D1, parts 4 to 8. Mean imputation used where ≤2 responses were missing. If >2 responses were missing, the records were excluded.
d Derived from survey question D2, parts 1 to 5. Mean imputation used where ≤2 responses were missing. If >2 responses were missing, the records were excluded.
e Chi-square test conducted comparing low-to-moderate trust against high trust.
f Derived from survey question D2, parts 6, 7, 9, and 10. Mean imputation used where ≤2 responses were missing. If >2 responses were missing, the records were excluded.
g Derived from survey question D2 part 8.
h Chi-square test conducted comparing low trust against moderate-to-high trust.
Affordability of items and services was reported as No cost difficulty or Cost difficulty. eHealth frequency of use responses were available for 273 participants; among those with no cost difficulty , 1% (2/204) were never users, 14.2% (29/204) were low or medium users, and 84.8% (173/204) were high users of eHealth; among those with cost difficulty , 1% (1/69) were never users, 26% (18/69) were low or medium users, and 73% (50/69) were high users. There was a statistically significant difference in the presence of cost as a barrier between never and low or medium eHealth users compared to high users ( χ 2 1 =5.25; P =.02), although the effect size was small.
Table 4 presents the frequency of eHealth use for elements of structural access.
Quality of internet access and feeling limited in access to the internet were significantly associated with frequency of eHealth use ( P <.05), although the effect sizes were small.
b N/A: not applicable (cell sizes insufficient for chi-square test).
c Chi-square tests conducted with strongly disagree and disagree combined, agree and strongly agree combined, and never and low or medium categories combined.
Table 5 presents the frequency of eHealth use against respondents’ capacity to engage.
Capacity to engage was not significantly different for the frequency of eHealth use ( P =.54).
b Derived from survey item E1. Where 1 response was missing, the mean imputation was used. If >1 response was missing, the record was excluded.
c Chi-square tests conducted with groups A and B combined.
Table 6 presents the frequency of eHealth use for elements of self-efficacy.
Statistically significant results were observed for the relationship between self-efficacy by eHEALS (moderate effect size) and frequency of eHealth use as well as for some of the questions from the HCEI (reliance on health professionals or others to access and explain information; small effect size; P <.05).
b eHEALS: eHealth Literacy Scale.
c eHEALS derived from item E3 (8 parts). Where ≤ 4 responses were missing, mean imputation was used. If >4 responses were missing, the records were excluded. Groups A to C as well as groups D to E were combined for the chi-square test.
d Strongly disagree, disagree, neither, and agree or strongly agree combined for significance testing.
Principal Findings
This paper reports on the findings of a sequential exploratory mixed methods study on the barriers to digital health access for a group of patients in Australian family medicine, with a particular focus on chronic disease and socioeconomic disadvantage.
In the qualitative first phase, the patients with socioeconomic disadvantage and chronic disease described 6 cumulative barriers, as demonstrated in Figure 1 . Many nonusers of digital health preferred human-based services and were not interested in technology, while others were highly suspicious of the technology in general. Some digitally interested patients could not afford quality hardware and internet connectivity, a barrier that was doubled by low quality and privacy when accessing publicly available internet connections. Furthermore, although some digitally interested patients had internet access, their urgent life circumstances left scarce opportunity to access digital health and develop digital health skills and confidence.
In our quantitative second phase, 31% (151/487) of the survey participants from Australian general practices were found to have never used a form of digital health. Survey participants were more likely to use digital health tools frequently when they also had a general digital interest and a digital health interest. Those who did not frequently access digital health were more likely to report difficulty affording the financial costs needed for digital access. The survey participants who frequently accessed digital health were more likely to have high eHealth literacy and high levels of patient empowerment.
Comparison With Prior Work
In terms of general digital health access, the finding that 31% (151/487) of the survey participants had never used one of the described forms of eHealth is in keeping with an Australian-based general digital participation study that found that approximately 9% of the participants were nonusers and 17% rarely engaged with the internet at all [ 34 ]. With regard to the digital health divide, another Australian-based digital health divide study found that increased age, living in a lower socioeconomic area, being Aboriginal or Torres Strait Islander, being male, and having no tertiary education were factors negatively associated with access to digital health services [ 17 ]. Their findings correspond to our findings that higher-frequency users of eHealth were associated with younger age, being female, living in an urban area, and being employed. Both studies reinforce the evidence of the digital health divide based on gender, age, and socioeconomic disadvantage in Australia.
With regard to digital health barriers, our findings provide expanded details on the range of digital health items and services that present a cost barrier to consumers. Affordability is a known factor in digital access and digital health access, and it is measured often by general self-report or relative expenditure on internet access to income [ 30 ]. Our study revealed the comprehensive list of relevant costs for patients. Our study also demonstrated factors of cost affordability beyond the dollar value of an item, as interviewees described the struggle of using slow public internet access without privacy features and the risks involved in buying a computer in installments. When we reflected on the complexity and detail of the cost barrier in our survey, participants demonstrated a clear association between cost and the frequency of digital health use. This suggests that a way to improve digital health access for some people is to improve the quality, security, and accessibility of public internet access options as well as to provide free or subsidized hardware, internet connection, and maintenance options for those in need, work that is being done by at least 1 digital inclusion charity in the United Kingdom [ 35 ].
Many studies recognize the factors of eHealth literacy and digital confidence for beneficial digital health access [ 36 ]. Our interviews demonstrated that some patients with socioeconomic disadvantage have low digital confidence, but that this is often underlined by a socially reinforced lifelong low self-confidence in their intellectual ability. In contrast, active users, regardless of other demographic factors, described themselves as innately proactive question askers. This was reinforced by our finding of a relationship between health care empowerment and the frequency of eHealth use. This suggests that while digital health education and eHealth literacy programs can improve access for some patients, broader and deeper long-term solutions addressing socioeconomic drivers of digital exclusion are needed to improve digital health access for some patients with socioeconomic disadvantage [ 8 ]. The deep permeation of socially enforced low self-confidence and lifelong poverty experienced by some interviewees demonstrate that the provision of free hardware and a class on digital health skills can be, for some, a superficial offering when the key underlying factor is persistent general socioeconomic inequality.
The digital health divide literature tends to identify the digital health divide, the factors and barriers that contribute to it, and the potential for it to widen if not specifically addressed [ 16 ]. Our findings have also identified the divide and the barriers, but what this study adds through our qualitative phase in particular is a description of the complex interaction of those barriers and the stepped nature of some of those barriers as part of the individual’s experience in trying to access digital health.
Strengths and Limitations
A key strength of this study is the use of a sequential exploratory mixed methods design. The initial qualitative phase guided a phenomenological exploration of digital health access experiences for patients with chronic disease and socioeconomic disadvantage. Our results in both study phases stem from the patients’ real-life experiences of digital health access. While some of our results echo the findings of other survey-based studies on general digital and digital health participation, our method revealed a greater depth and detail of some of these barriers, as demonstrated in how our findings compare to prior work.
As mentioned previously, the emphasis of this study on the qualitative first phase is a strength that helped describe the interactions between different barriers. The interviewees described their experiences as cumulative unequal stepped barriers rather than as producing a nonordered list of equal barriers. These findings expand on the known complexity of the issue of digital exclusion and add weight to the understanding that improving digital health access needs diverse, complex solutions [ 17 ]. There is no panacea for every individual’s digital health access, and thus, patient-centered digital health services, often guided by health professionals within the continuity of primary care, are also required to address the digital health divide [ 37 ].
While the sequential exploratory design is a strength of the study, it also created some limitations for the second quantitative phase. Our commitment to using the qualitative interview findings to inform the survey questions meant that we were unable to use previously validated scales for every question and that our results were less likely to lead to a normal distribution. This likely affected our ability to demonstrate significant associations for some barriers. We expect that further modeling is required to control for baseline characteristics and determine barrier patterns for different types of users.
One strength of this study is that the survey was administered to a broad population of Australian family medicine patients with diverse patterns of health via both paper-based and digital options. Many other digital health studies use solely digital surveys, which can affect the sample. However, we cannot draw conclusions from our survey about patients with chronic disease due to the limitations of the sample size for these subgroups.
Another sample-based limitation of this study was that our qualitative population did not include anyone aged from 18 to 24 years, despite multiple efforts to recruit. Future research will hopefully address this demographic more specifically.
While not strictly a limitation, we recognize that because this research was before COVID-19, it did not include questions about telehealth, which has become much more mainstream in recent years. The patients may also have changed their frequency of eHealth use because of COVID-19 and an increased reliance on digital services in general. Future work in this area or future versions of this survey should include telehealth and acknowledge the impact of COVID-19. However, the larger concept of the digital health divide exists before and after COVID-19, and in fact, our widespread increased reliance on digital services makes the digital divide an even more pressing issue [ 12 ].
Conclusions
The experience of digital health access across Australian primary care is highly variable and more difficult to access for those with socioeconomic disadvantage. While general digital interest, financial cost, and digital health literacy and empowerment are clear factors in digital health access in a broad primary care population, the digital health divide is also facilitated in part by a stepped series of complex and cumulative barriers.
Genuinely improving digital health access for 1 cohort or even 1 person requires a series of multiple different interventions tailored to specific sequential barriers. Given the rapid expansion of digital health during the global COVID-19 pandemic, attention to these issues is necessary if we are to avoid entrenching inequities in access to health care. Within primary care, patient-centered care that continues to recognize the complex individual needs of, and barriers facing, each patient should be a part of addressing the digital health divide.
Acknowledgments
The authors are thankful to the patients who shared their experiences with them via interview and survey completion. The authors are also very grateful to the general practices in the Australian Capital Territory and New South Wales who kindly gave their time and effort to help organize interviews, administer, and post surveys in the midst of the stress of day-to-day practice life and the bushfires of 2018-2019. The authors thank and acknowledge the creators of the eHealth Literacy Scale, the eHealth Literacy Questionnaire, the ICEpop Capability Measure for Adults, the Health Care Empowerment Inventory, the Patient-Doctor Relationship Questionnaire, the Chao continuity questionnaire, and the Southgate Institute for Health Society and Equity for their generosity in sharing their work with the authors [ 17 , 19 - 25 ]. This study would not have been possible without the support of the administrative team of the Academic Unit of General Practice. This project was funded by the Royal Australian College of General Practitioners (RACGP) through the RACGP Foundation IPN Medical Centres Grant, and the authors gratefully acknowledge their support.
Data Availability
The data sets generated during this study are not publicly available due to the nature of our original ethics approval but are available from the corresponding author on reasonable request.
Authors' Contributions
MAC acquired the funding, conceptualized the project, and organized interview recruitment. MAC and KB conducted interviews and analyzed the qualitative data. EAS, ER, and KD contributed to project planning, supervision and qualitative data analysis. MAC, KB and KO wrote the survey and planned quantitative data analysis. MAC and KB recruited practices for survey administration. KO and KB conducted the quantitative data analysis. MAC and KO, with KB drafted the paper. EAS, ER, and KD helped with reviewing and editing the paper.
Conflicts of Interest
None declared.
Phase 1 interview guide.
Phase 2 survey: eHealth and digital divide.
Phase 2 participant characteristics by frequency of eHealth use.
- Eysenbach G. What is e-health? J Med Internet Res. 2001;3(2):E20. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Iyawa GE, Herselman M, Botha A. Digital health innovation ecosystems: from systematic literature review to conceptual framework. Procedia Comput Sci. 2016;100:244-252. [ FREE Full text ] [ CrossRef ]
- Berrouiguet S, Baca-García E, Brandt S, Walter M, Courtet P. Fundamentals for future mobile-health (mHealth): a systematic review of mobile phone and web-based text messaging in mental health. J Med Internet Res. Jun 10, 2016;18(6):e135. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Shen H, van der Kleij RM, van der Boog PJ, Chang X, Chavannes NH. Electronic health self-management interventions for patients with chronic kidney disease: systematic review of quantitative and qualitative evidence. J Med Internet Res. Nov 05, 2019;21(11):e12384. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Australia's health 2018. Australian Institute of Health and Welfare. 2018. URL: https://www.aihw.gov.au/reports/australias-health/australias-health-2018/contents/table-of-contents [accessed 2024-04-04]
- Australian Institute of Health and Welfare. Chronic Diseases and Associated Risk Factors in Australia, 2006. Canberra, Australia. Australian Institute of Health and Welfare; 2006.
- Hart JT. The inverse care law. The Lancet. Feb 27, 1971;297(7696):405-412. [ CrossRef ]
- Davies AR, Honeyman M, Gann B. Addressing the digital inverse care law in the time of COVID-19: potential for digital technology to exacerbate or mitigate health inequalities. J Med Internet Res. Apr 07, 2021;23(4):e21726. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Choi NG, Dinitto DM. The digital divide among low-income homebound older adults: internet use patterns, eHealth literacy, and attitudes toward computer/internet use. J Med Internet Res. May 02, 2013;15(5):e93. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Household use of information technology. Australian Bureau of Statistics. 2018. URL: https://tinyurl.com/4efm6u92 [accessed 2024-03-24]
- Kontos E, Blake KD, Chou WY, Prestin A. Predictors of eHealth usage: insights on the digital divide from the health information national trends survey 2012. J Med Internet Res. Jul 16, 2014;16(7):e172. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Litchfield I, Shukla D, Greenfield S. Impact of COVID-19 on the digital divide: a rapid review. BMJ Open. Oct 12, 2021;11(10):e053440. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Butler DC, Joshy G, Douglas KA, Sayeed MS, Welsh J, Douglas A, et al. Changes in general practice use and costs with COVID-19 and telehealth initiatives: analysis of Australian whole-population linked data. Br J Gen Pract. Apr 27, 2023;73(730):e364-e373. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Arsenijevic J, Tummers L, Bosma N. Adherence to electronic health tools among vulnerable groups: systematic literature review and meta-analysis. J Med Internet Res. Feb 06, 2020;22(2):e11613. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kontos EZ, Bennett GG, Viswanath K. Barriers and facilitators to home computer and internet use among urban novice computer users of low socioeconomic position. J Med Internet Res. Oct 22, 2007;9(4):e31. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Latulippe K, Hamel C, Giroux D. Social health inequalities and eHealth: a literature review with qualitative synthesis of theoretical and empirical studies. J Med Internet Res. Apr 27, 2017;19(4):e136. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Foley K, Freeman T, Ward P, Lawler A, Osborne R, Fisher M. Exploring access to, use of and benefits from population-oriented digital health services in Australia. Health Promot Int. Aug 30, 2021;36(4):1105-1115. [ CrossRef ] [ Medline ]
- Cresswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA. SAGE Publications; 2007.
- Tappen RM, Cooley ME, Luckmann R, Panday S. Digital health information disparities in older adults: a mixed methods study. J Racial Ethn Health Disparities. Feb 2022;9(1):82-92. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Who can get a card. Services Australia. URL: https://www.servicesaustralia.gov.au/who-can-get-health-care-card?context=21981 [accessed 2023-11-03]
- Levesque JF, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. Mar 11, 2013;12:18. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bryant A, Charmaz K. The SAGE Handbook of Grounded Theory, Paperback Edition. Thousand Oaks, CA. SAGE Publications; 2010.
- Johnson MO, Rose CD, Dilworth SE, Neilands TB. Advances in the conceptualization and measurement of health care empowerment: development and validation of the health care empowerment inventory. PLoS One. 2012;7(9):e45692. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Norman CD, Skinner HA. eHEALS: the eHealth literacy scale. J Med Internet Res. Nov 14, 2006;8(4):e27. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kayser L, Karnoe A, Furstrand D, Batterham R, Christensen KB, Elsworth G, et al. A multidimensional tool based on the eHealth literacy framework: development and initial validity testing of the eHealth Literacy Questionnaire (eHLQ). J Med Internet Res. Feb 12, 2018;20(2):e36. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Standards. Australian Bureau of Statistics. URL: https://www.abs.gov.au/statistics/standards [accessed 2024-04-04]
- Al-Janabi H, Flynn TN, Coast J. Development of a self-report measure of capability wellbeing for adults: the ICECAP-A. Qual Life Res. Feb 2012;21(1):167-176. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Van der Feltz-Cornelis CM, Van Oppen P, Van Marwijk HW, De Beurs E, Van Dyck R. A patient-doctor relationship questionnaire (PDRQ-9) in primary care: development and psychometric evaluation. Gen Hosp Psychiatry. 2004;26(2):115-120. [ CrossRef ] [ Medline ]
- Chao J. Continuity of care: incorporating patient perceptions. Fam Med. 1988;20(5):333-337. [ Medline ]
- Wilson CK, Thomas J, Barraket J. Measuring digital inequality in Australia: the Australian digital inclusion index. JTDE. Jun 30, 2019;7(2):102-120. [ CrossRef ]
- Digital participation: a view of Australia's online behaviours. Australia Post. Jul 2017. URL: https://auspost.com.au/content/dam/auspost_corp/media/documents/white-paper-digital-inclusion.pdf [accessed 2024-04-04]
- Poli A, Kelfve S, Motel-Klingebiel A. A research tool for measuring non-participation of older people in research on digital health. BMC Public Health. Nov 08, 2019;19(1):1487. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences Second Edition. London, UK. Routledge; 1988.
- Borg K, Smith L. Digital inclusion and online behaviour: five typologies of Australian internet users. Behav Inf Technol. Feb 15, 2018;37(4):367-380. [ CrossRef ]
- Mathers A, Richardson J, Vincent S, Joseph C, Stone E. Good Things Foundation COVID-19 response report. Good Things Foundation. 2020. URL: https://tinyurl.com/2peu3kak [accessed 2024-04-04]
- Norman CD, Skinner HA. eHealth literacy: essential skills for consumer health in a networked world. J Med Internet Res. Jun 16, 2006;8(2):e9. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Neves AL, Burgers J. Digital technologies in primary care: implications for patient care and future research. Eur J Gen Pract. Dec 11, 2022;28(1):203-208. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
Edited by T Leung; submitted 03.07.23; peer-reviewed by T Freeman, H Shen; comments to author 16.08.23; revised version received 30.11.23; accepted 31.01.24; published 11.04.24.
©Melinda Ada Choy, Kathleen O'Brien, Katelyn Barnes, Elizabeth Ann Sturgiss, Elizabeth Rieger, Kirsty Douglas. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 11.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.

IMAGES
VIDEO
COMMENTS
To structure your methods section, you can use the subheadings of "Participants," "Materials," and "Procedures.". These headings are not mandatory—aim to organize your methods section using subheadings that make sense for your specific study. Note that not all of these topics will necessarily be relevant for your study.
The methods section should describe what was done to answer the research question, describe how it was done, justify the experimental design, and explain how the results were analyzed. Scientific writing is direct and orderly. Therefore, the methods section structure should: describe the materials used in the study, explain how the materials ...
The results section is where you report the findings of your study based upon the methodology [or methodologies] you applied to gather information. ... In deciding what data to describe in your results section, you must clearly distinguish information that would normally be included in a research paper from any raw data or other content that ...
The methods section describes actions taken to investigate a research problem and the rationale for the application of specific procedures or techniques used to identify, select, process, and analyze information applied to understanding the problem, thereby, allowing the reader to critically evaluate a study's overall validity and reliability.
In this tutorial paper, we will use the term methodological study to refer to any study that reports on the design, conduct, analysis or reporting of primary or secondary research-related reports (such as trial registry entries and conference abstracts). In the past 10 years, there has been an increase in the use of terms related to ...
The methodology section or methods section tells you how the author (s) went about doing their research. It should let you know a) what method they used to gather data (survey, interviews, experiments, etc.), why they chose this method, and what the limitations are to this method. The methodology section should be detailed enough that another ...
One way to write the Methods section of a retrospective clinical study is to address each topic below that applies to your study. The following order works well in many articles. Subjects: Source of the study subjects (for example, chart review, database, patients in a previously reported prospective clinical study).
The results section describes the results in an organized fashion. Each primary result is presented in terms of statistical results but also explained in words. The discussion typically summarizes the study, discusses theoretical and practical implications and limitations of the study, and offers suggestions for further research.
The "Results" section is arguably the most important section in a research manuscript as the findings of a study, obtained diligently and painstakingly, are presented in this section. A well-written results section reflects a well-conducted study. This chapter provides helpful pointers for writing an effective, organized results section.
The results section of the research paper presents the findings of the study. It is the part of the paper where the researcher reports the data collected during the study and analyzes it to draw conclusions. In the results section, the researcher should describe the data that was collected, the statistical analysis performed, and the findings ...
The "Results section" is the third most important anatomical structure of IMRAD (Introduction, Method and Material, Result, And Discussion) frameworks, the almost universally accepted framework in many journals in the late nineteenth century. 3 Before using a structured IMRAD format, research findings in scientific papers were presented in chronological order "First, I saw this, and then ...
The purpose of the methodology section is to accurately and clearly describe the research. design and the procedures undertaken to collect and analyze data, and to present the rationale for ...
The Methods section of a research article is like a roadmap leading to the core of the research, guiding the readers through the actual journey the authors took to reach their destination. In the manuscript, this section contains the essential details for other scientists to replicate the experiments of the study and help the common readers to understand the study better.
The methodology section aims to describe the exact procedures, and rationale for them, when developing a dataset, results, and conclusions in an empirical research study. Therefore,
It describes exactly how data relevant to the study purpose were collected, organized, and analyzed. The methods section describes the process of conducting the study — from how the sample was selected to which statistical methods were used to analyze the data. Authors should clearly name, define, and describe each study variable.
As an example elucidating the abovementioned issues, graphics, and flow diagram in the 'Results' section of a research paper written by the authors of this review article, and published in the World Journal of Urology in the year 2010 (World J Urol 2010;28:17-22.) are shown in Figures 1, and and2 2.
The methods section should explain how subjects were identified and should state inclusion and exclusion criteria. All materials used to complete the study should be described in detail, including equipment, drugs, gases, chemicals, treatments, interventions, or other items. Study procedures should outline all steps taken to obtain the results ...
The Methodology section of the article describes the procedures, or methods, that were used to carry out the research study. The methodology the authors follow will vary according to the discipline, or field of study, the research relates to. Types of methodology include case studies, scientific experiments, field studies, focus groups, and ...
The research methodology is an important section of any research paper or thesis, as it describes the methods and procedures that will be used to conduct the research. It should include details about the research design, data collection methods, data analysis techniques, and any ethical considerations.
What is an introduction? The introduction is a review of the relevant research literature plus identification of a gap in knowledge. It usually has topics similar to these: O Overview of the research topic. O Why the research topic matters. O Previous research specific to this topic. O Where the gap in knowledge is.
The Methods section of a research article includes an explanation of the procedures used to conduct the experiment. For authors of scientific research papers, the objective is to present their findings clearly and concisely and to provide enough information so that the experiment can be duplicated. Research articles contain very specific ...
The purpose of this qualitative research was to describe resilience in the healthcare team during the COVID-19 pandemic with the healthcare team situated as a cognizant, singular source of knowledge and defined by its collective identity, purpose, competence, and actions, versus the resilience of an individual or an organization. Methods
Objective: This study aims to provide comprehensive primary mixed methods data on the patient experience of barriers to digital health access, with a focus on the digital health divide. Methods: We applied an exploratory mixed methods design to ensure that our survey was primarily shaped by the experiences of our interviewees.