Breakthrough Study on Post-Traumatic Stress Disorder
A collaboration of researchers, institutions and databases makes advances on the understanding of the genetic component of ptsd.
- Joseph McClain - [email protected]

Media contact:
- Miles Martin - [email protected]
Published Date
Share this:, article content.
The Psychiatric Genetics Consortium (PGC), a consortium of researchers led by scientists at University of California San Diego School of Medicine has made significant advancements in the understanding of the neurobiology of post-traumatic stress disorder (PTSD), a condition the World Health Organization says affects some 250 million people around the world.
The group recently announced their findings from a genome-wide association study of 1,222,822 people in a paper recently published in the journal Nature Genetics .
Caroline M. Nievergelt, Ph.D., professor of psychiatry at UC San Diego School of Medicine, is the co-first author on the paper, together with Adam X. Maihofer, PhD., an assistant project scientist in Nievergelt’s lab. PGC-PTSD co-chair Murray B. Stein M.D., M.P.H., professor of psychiatry and public health at UC San Diego is also a co-author of the study.
Nievergelt explained that the work confirmed previous neurobiological studies of PTSD and built upon them, identifying 95 loci — positions of genes on a chromosome — significant to PTSD, including 80 new loci.
“As the number of samples has increased, we have gained a better understanding of the genetic factors that contribute to PTSD risk,” Stein said.
The paper underscores the importance of heritability in PTSD risk and notes that the identified genes influence processes related to PTSD symptoms such as stress, fear and threat responses. She said their findings also point to possible associations among PTSD and other mental and physical disorders.
The PGC was formed in 2007, dedicated to finding genes that predispose an individual to psychiatric disorders, such as bipolar disorder or schizophrenia, Nievergelt said. She added that each disorder is addressed by one of 11 working groups, one of which is the PGC for PTSD, which she chairs.
Nievergelt explained that the benefits of research by a consortium extend beyond the hive-mind input of numerous collaborators working toward a common goal. A genome-wide association study (GWAS) examines and compares genomes of a large number of people in a search for genetic markers associated with a specific condition. A GWAS for polygenic disorders such as PTSD necessarily requires an enormous sample size, she noted.
“And no one PI (principal investigator) is able to get nearly enough subjects for a genome-wide association study, so through the consortium we have a large number of collaborators combining data from all over the world,” Nievergelt said.
The PCG for PTSD consortium includes researchers from a wide number of research institutions and universities worldwide. Notable participants include co-chairs Karestan Koenen, Ph.D., from the Harvard Chan School of Public Health and the Broad Institute of MIT, and Kerry Ressler, M.D., Ph.D., of Harvard Medical School and McLean Hospital.
{/exp:typographee}
The brain, DNA, and a fractured glass effect as a PTSD metaphor. Photo by Adobe AI.
The consortium’s database was assembled from various sources, representing a variety of causes and levels of trauma. Nievergelt said the sources included the Marine Resiliency Study, in which U.S. Marine Corps members were assessed before and after going to war, and Army STARRS, a longitudinal study of U.S. Army soldiers. Another is the Grady Trauma Project that includes victims of violent crime, mostly African American individuals from inner cities. Other datasets incorporated into the PGC for PTSD megadata list came from Electronic Health Records (EHRs) and the VA Million Veterans Program. The consortium also incorporated data from Europe and Latin America.
At an appropriate stage, the consortium members agree on a data freeze and begin their examination, seeking to identify specific genes likely to be associated with PTSD. The paper represents “a milestone” in the understanding of the genetic component of PTSD, Nievergelt said.
“It’s the first time that we actually have a very strong genetic signal,” said Maihofer, who analyzed the data. The genetic signal — essentially a mapping of RNA or DNA activity relevant to PTSD — allowed the consortium to pinpoint specific genes and analyze pathways of gene expression for future research or even for eventual treatment strategies, Maihofer explained.
Nievergelt says there are several directions the consortium wants to take in terms of next steps. One is to increase and diversify the sample size. She said the group has received funding from the National Institute of Mental Health to go to Africa and enroll African people in the genetics study, an effort lead by co-chair Koenen. “That will help us improve risk prediction for other people of African ancestry, a group that has been relatively neglected in earlier studies,” Nievergelt noted.
UC San Diego co-authors
Authors affiliated with the University of California San Diego School of Medicine Department of Psychiatry, in addition to first authors Caroline M. Nievergelt and Adam X. Maihofer, are: Dewleen G. Baker, Carol E. Franz, William S. Kremen, Elizabeth A. Mikita, Sonya B. Norman, Matthew S. Panizzon and Murray B. Stein, also affiliated with the UCSD Herbert Wertheim School of Public Health and Human Longevity Science. Other UC San Diego authors are Anders M. Dale, of the Department of Radiology, Department of Neurosciences, and Wesley K. Thompson, of the Herbert Wertheim School of Public Health and Human Longevity Science.
Other noteworthy participants in the study
PGC-PTSD co-chairs:
Kerry J. Ressler, of the Department of Psychiatry at Harvard Medical School; McLean Hospital, and Department of Medicine (Biomedical Genetics), Boston University Chobanian & Avedisian School of Medicine; as well as Karestan C. Koenen, of the Department of Epidemiology at the Harvard T.H. Chan School of Public Health, the Broad Institute of MIT and Harvard, the Stanley Center for Psychiatric Research; and McLean Hospital Developmental Biopsychiatry Research Program.
Writing group members are:
Elizabeth G. Atkinson, Department of Molecular and Human Genetics, Baylor College of Medicine; Chia-Yen Chen, Biogen Inc.,Translational Sciences; Karmel W. Choi, Department of Epidemiology, Harvard T.H. Chan School of Public Health, and the Department of Psychiatry at Massachusetts General Hospital; Jonathan R. I. Coleman, King’s College London, National Institute for Health and Care Research Maudsley Biomedical Research Centre, and King’s College London, Social, Genetic and Developmental Psychiatry Centre, Institute of Psychiatry, Psychology and Neuroscience; Nikolaos P. Daskalakis, Broad Institute of MIT and Harvard, and the Stanley Center for Psychiatric Research in the Department of Psychiatry of Harvard Medical School, and the McLean Hospital, Center of Excellence in Depression and Anxiety Disorders; Laramie E. Duncan, Department of Psychiatry and Behavioral Sciences, Stanford University; Renato Polimanti, VA Connecticut Healthcare Center, and the Department of Psychiatry of Yale University School of Medicine.
Competing interest
Murray B. Stein has in the past three years received consulting income from Aptinyx, atai Life Sciences, BigHealth, Biogen, Bionomics, Boehringer Ingelheim, Delix Therapeutics, EmpowerPharm, Engrail Therapeutics, Janssen, Jazz Pharmaceuticals, Karuna Therapeutics, NeuroTrauma Sciences, Otsuka US, PureTech Health, Sage Therapeutics, and Roche/Genentech. He also has stock options in Oxeia Biopharmaceuticals and EpiVario. Anders M. Dale holds equity in CorTechs Labs and serves on the Scientific Advisory Board of Human Longevity and the Mohn Medical Imaging and Visualization Center, and also receives funding through research grants with General Electric Healthcare. Other authors associated with UCSD declare no competing interests.
Support and funding
Major financial support for the PGC-PTSD was provided by the National Institute of Mental Health (NIMH) grants R01MH106595 and R01MH124847, by the Cohen Veterans Bioscience and by the Stanley Center for Psychiatric Research at the Broad Institute.
Full lists of authors and their affiliations and competing interests, funding/support sources are available on the paper.
"No one PI (principal investigator) is able to get together nearly enough subjects for a genome-wide association study, so through the consortium we have a large number of collaborators combining data from all over the world."
You May Also Like
Creating a “greener,” more connected society, electronic health records unlock genetics of tobacco use disorder, following cellular lineage, stay in the know.
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.
You have been successfully subscribed to the UC San Diego Today Newsletter.
Campus & Community
Arts & culture, visual storytelling.
- Media Resources & Contacts
Signup to get the latest UC San Diego newsletters delivered to your inbox.
Award-winning publication highlighting the distinction, prestige and global impact of UC San Diego.
Popular Searches: Covid-19 Ukraine Campus & Community Arts & Culture Voices
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Expert Review
- Open access
- Published: 17 April 2024
Neuroimaging of posttraumatic stress disorder in adults and youth: progress over the last decade on three leading questions of the field
- Cecilia A. Hinojosa ORCID: orcid.org/0000-0002-2577-6142 1 ,
- Grace C. George 2 &
- Ziv Ben-Zion ORCID: orcid.org/0000-0003-3629-5851 3 , 4 , 5
Molecular Psychiatry ( 2024 ) Cite this article
96 Accesses
20 Altmetric
Metrics details
- Diagnostic markers
- Neuroscience
Almost three decades have passed since the first posttraumatic stress disorder (PTSD) neuroimaging study was published. Since then, the field of clinical neuroscience has made advancements in understanding the neural correlates of PTSD to create more efficacious treatment strategies. While gold-standard psychotherapy options are available, many patients do not respond to them, prematurely drop out, or never initiate treatment. Therefore, elucidating the neurobiological mechanisms that define the disorder can help guide clinician decision-making and develop individualized mechanisms-based treatment options. To this end, this narrative review highlights progress made in the last decade in adult and youth samples on three outstanding questions in PTSD research: (1) Which neural alterations serve as predisposing (pre-exposure) risk factors for PTSD development, and which are acquired (post-exposure) alterations? (2) Which neural alterations can predict treatment outcomes and define clinical improvement? and (3) Can neuroimaging measures be used to define brain-based biotypes of PTSD? While the studies highlighted in this review have made progress in answering the three questions, the field still has much to do before implementing these findings into clinical practice. Overall, to better answer these questions, we suggest that future neuroimaging studies of PTSD should (A) utilize prospective longitudinal designs, collecting brain measures before experiencing trauma and at multiple follow-up time points post-trauma, taking advantage of multi-site collaborations/consortiums; (B) collect two scans to explore changes in brain alterations from pre-to-post treatment and compare changes in neural activation between treatment groups, including longitudinal follow up assessments; and (C) replicate brain-based biotypes of PTSD. By synthesizing recent findings, this narrative review will pave the way for personalized treatment approaches grounded in neurobiological evidence.
Similar content being viewed by others

Distinctively different human neurobiological responses after trauma exposure and implications for posttraumatic stress disorder subtyping
Suji Lee, Sujung Yoon, … In Kyoon Lyoo

Longitudinal volumetric evaluation of hippocampus and amygdala subregions in recent trauma survivors
Ziv Ben-Zion, Nachshon Korem, … Talma Hendler

Neurostructural associations with traumatic experiences during child- and adulthood
Sebastian Siehl, Maurizio Sicorello, … Herta Flor
Introduction
In 2013, the American Psychiatric Association revised the posttraumatic stress disorder (PTSD) criteria in the 5 th edition of its “Diagnostic Statistical Manual of Mental Disorders” (DSM-5). While the DSM-IV classified PTSD under “Anxiety Disorders,” the DSM-5 has repositioned it within a newly established category of “Trauma-and Stressor-Related Disorders.” According to the DSM-5, traumatic events are defined as exposure to actual or threatened death, serious injury, or a threat to the physical integrity of oneself or others, either directly (witnessing trauma) or indirectly (learning that trauma happened to a close relative or friend) [ 1 ]. In addition to trauma exposure (i.e., criterion A), four symptom clusters that characterize the disorder are persistent re-experiencing the trauma (i.e., criterion B), avoiding people, places, or thoughts related to the trauma (i.e., criterion C), negative thoughts and feelings that began or worsened after the trauma (i.e., criterion D); and trauma-related increased in arousal and reactivity (i.e., criterion E). Symptoms must last at least one month, not be caused by drugs or other illnesses, and cause significant functional impairment. The DSM-5 introduced a developmental subtype of PTSD specifically for children aged six years or younger, aligning closely with adult diagnostic criteria. However, it adapts criterion A for this age group, allowing for indirect exposure to trauma, such as through witnessing an event or learning about a traumatic event affecting a parent or caregiver [ 1 ].
Epidemiology and prognosis
Worldwide, up to 70% of the adult population will experience at least one traumatic event (as defined by criterion A) in their lifetime [ 2 ], and the prevalence of PTSD ranges from 2 to 9% [ 3 ]. Indeed, four post-traumatic symptom trajectories have been highlighted in literature: resiliency, recovery, chronic, and delayed onset, the most common being the resiliency trajectory [ 4 , 5 ]. Similarly, childhood trauma exposure is common, with up to two-thirds of youth reported having experienced a traumatic event and almost 5% of trauma-exposed youth meeting the criteria for PTSD [ 6 , 7 , 8 ]. It is important to note that females are more prone to developing PTSD than males [ 9 , 10 ]. This disparity is theorized to be attributed to trauma one is exposed to, with females experiencing more interpersonal violence than males [ 11 ]. However, even when controlling for trauma type, females still exhibit greater PTSD prevalence [ 11 ]. This suggests that biological factors may contribute to this disparity. Given this, more studies are introducing sex as a biological variable to explore this disparity further. For in-depth reviews, see [ 12 , 13 ].
PTSD is a debilitating disorder in many aspects across the lifespan. A PTSD diagnosis contributes to billions in annual productivity loss [ 14 ] and increased medical problems [ 15 ] and is associated with a variety of co-occurring disorders, including substance use disorders [ 16 ], depression, and anxiety [ 17 ]. For individuals diagnosed with PTSD, many treatment options are available. The most empirically supported options are trauma-focused interventions [ 18 ]. Of psychotherapy options available, up to half of the patients who complete treatment will show clinically meaningful improvement [ 19 , 20 , 21 ], and many patients prematurely drop out of treatment before receiving an adequate dose [ 22 ]. Furthermore, many patients fail to seek treatment altogether, especially in marginalized groups [ 23 ]. Given the considerable overlap between PTSD, depression, and anxiety, and because research still has not identified pharmaceutical targets specific for PTSD, sertraline and paroxetine are FDA-approved pharmacological options for PTSD, both with limited efficacy [ 24 ]. Research on using psychedelics to treat PTSD has skyrocketed and looks promising, though more research is needed to determine efficacy and validate safe implementation procedures [ 25 , 26 ]. Psychotherapeutic treatments have shown a greater benefit than pharmacological intervention alone [ 27 ]. Determining the superiority of combining psychotherapy with pharmacological treatment needs further exploration [ 28 ]. To improve the efficacy of current treatment options and to design novel, more efficacious treatment options, we must understand the neural alterations that contribute to the development of PTSD, improve with treatment, and potentially define biotypes of the disorder.
Current narrative review
Given the influx of neuroimaging data published since the first neuroimaging paper using a PTSD sample in 1995 [ 29 ], an extensive library of reviews and meta-analyses has examined this literature [ 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 ]. Our narrative review builds upon this previous literature by exploring progress made in the past decade on three major questions in the field: (1) Which neural alterations serve as predisposing (pre-exposure) risk factors for PTSD development, and which are acquired (post-exposure)? (2) Which neural alterations can predict treatment outcomes and define clinical improvement? and (3) Can neuroimaging measures be used to define brain-based biotypes of PTSD? This review will examine structural and functional magnetic resonance imaging (MRI) literature using univariate, bivariate, and network-based approaches in adult and youth PTSD populations. Following a brief overview of neural alterations in PTSD, we will address each question above by synthesizing current findings, identifying gaps, and discussing limitations. We included articles published in peer-reviewed journals and were found using in-house expertise and searches of databases including PubMed. We will conclude by highlighting the review’s limitations and suggest future directions. Tables 1 – 2 provide an overview of neuroimaging findings for questions 1 and 2 (respectively), and Figs. 1 – 2 illustrate these findings. We will begin by describing different neuroimaging techniques.
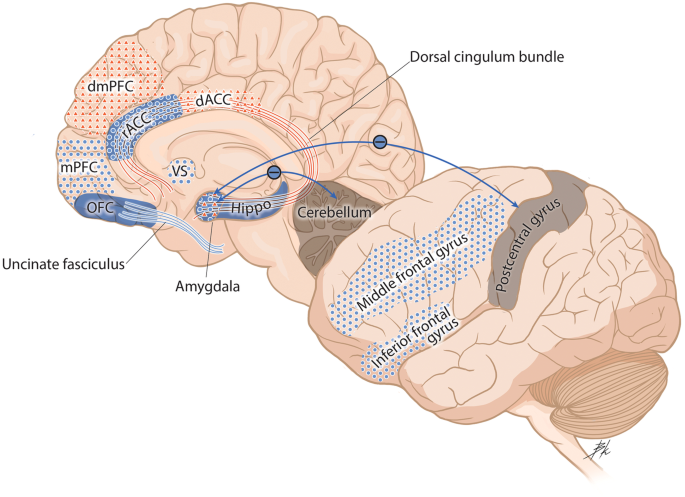
Blue dots represent decreased activation. Red triangles represent increased activation. Solid blue represents decreased volume. Solid blue lines represent decreased structural integrity. Red lines represented increased structural integrity. Functional connectivity findings are depicted with arrows, with blue lines (–) that represent decreased functional connectivity and red lines (+) that represent increased functional connectivity. dACC dorsal anterior cingulate cortex, dmPFC dorsomedial prefrontal cortex, Hippo hippocampus, mPFC medial prefrontal cortex, OFC orbitofrontal cortex, rACC rostral anterior cingulate cortex, VS ventral striatum.
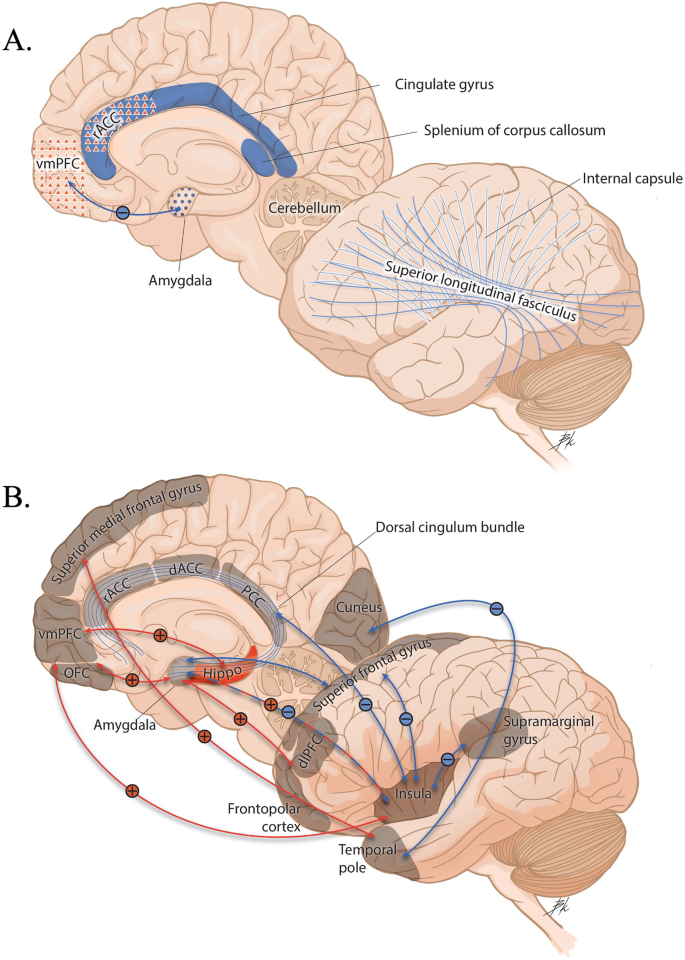
A Brain measures at baseline that predict a positive treatment response. B Brain measures associated with a positive response to treatment. Blue dots represent decreased activation. Red triangles represent increased activation. Solid blue represents decreased volume. Solid red represents greater volume. Solid blue lines represent decreased structural integrity. Functional connectivity findings are depicted with arrows, with blue lines (–) equating to decreased functional connectivity and red lines (+) equating to greater functional connectivity. dACC dorsal anterior cingulate cortex, dlPFC dorsolateral prefrontal cortex, Hippo hippocampus, OFC orbitofrontal cortex, PCC posterior cingulate cortex, rACC rostral anterior cingulate cortex, vmPFC ventromedial prefrontal cortex.
Neuroimaging techniques
Structural techniques.
Structural MRI of PTSD populations typically determines alterations in the morphometry of brain regions in patients versus controls (trauma-exposed non-PTSD [TENC] or healthy controls [HC]). Morphometric measures include subcortical and cortical gray matter volumes, thickness, and white matter microstructure. There are two analysis pipelines one can follow: (1) surface-based, which identifies borders between pial and white matter surfaces, and (2) voxel-based, which labels each voxel in cortical and subcortical tissues and allows for calculating subcortical structures and total intracranial volume [ 41 ]. Thus, structural volume can be measured by contrasting volume inside the pial surface from the white surface and regions, not part of the cortex, or by measuring total cortical labeled voxels. Cortical thickness is measured by contrasting the distance between the pial and the white surface [ 41 ]. Generally, smaller volumes and lower cortical thickness are representative of poorer structural integrity. Diffusion tensor imaging is a structural tool used to measure the structural integrity of white matter tracts via the diffusivity of water molecules along the axial direction of white matter fibers. The pattern of diffusivity can be computed using scalar measures such as fractional anisotropy (FA), whereby lower FA values illustrate a reduced axonal packing density [ 42 ].
Functional techniques
Functional MRI (fMRI) can be used as an indirect proxy to measure brain activation with great spatial and limited temporal resolution. Researchers record activation during the presentation of different tasks designed to induce activation in regions responsible for given functions. There are many different approaches one can take to analyze fMRI data, which can be categorized into three general techniques. The simplest technique is univariate analyses, which examine the activation of single voxels in response to various tasks. As techniques developed with time, more researchers have also included bivariate analyses, which calculate the temporal association of two regions based on activation. This includes task-based and resting-state functional connectivity (FC), which measure spontaneous changes in brain activation during the completion or absence of a task, respectively. Finally, recent years have seen an increase in network-based approaches, which measure activation across many brain regions and networks. Network-based approaches in fMRI studies typically conceptualize the human brain as a network of interconnected functional components that operate in a coordinated dynamic fashion [ 43 ]. By employing such methods, researchers can overcome the limitations of traditional univariate and bivariate approaches by mitigating the bias of preselecting target regions a priori and allowing a more comprehensive investigation of large-scale brain organization (rather than isolated regions or simplistic circuits). In this narrative review, we will focus on the two primary tools for network-based analysis of neuroimaging data in PTSD: (1) independent component analysis (ICA), which isolates individual functional networks within the whole brain, and (2) graph theory methods, which examine properties of networks (e.g., nodes and edges of a graph) and characterize them based on their intercorrelations.
Neural alterations in PTSD
PTSD is the only DSM diagnosis with a known origin (i.e., experiencing trauma). Given the importance of traumatic memory in the development of the disorder, early neuroimaging studies sought to discover alterations in structure and function of brain regions implicated in fear learning and memory (e.g., amygdala and hippocampus) in patients with PTSD compared to controls. These discoveries have created “classical” neurocircuitry models of PTSD that emphasize an inability of cortical regions to successfully regulate subcortical regions important in initiating a fear response [ 33 ]. Research over the last decade has noted diminished structural integrity in areas associated with executive functions, including reduced cortical volumes in the anterior cingulate cortex (ACC) [ 44 , 45 ] and frontal cortical regions [ 44 , 46 ] in PTSD patients and in subcortical structures, including the amygdala and hippocampus (see [ 39 , 47 ] for recent reviews). Furthermore, PTSD patients, compared to controls, have shown reduced white matter integrity in the uncinate fasciculus (UF) [ 48 , 49 , 50 ], corpus callosum, corticospinal tract, and enhanced white matter integrity in the inferior fronto-occipital fasciculus, and inferior temporal gyrus (for review see [ 51 ]), highlighting the structural disconnect between cortical and subcortical regions. Functional studies also support classical neurocircuitry models, with greater amygdala alongside reduced activation in brain regions associated with emotional regulation (e.g., ventromedial prefrontal cortex [vmPFC], inferior, superior, medial frontal gyrus [MFG], ACC, dorsolateral PFC [dlPFC], and dorsomedial PFC [dmPFC]) during emotion-related tasks [ 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 ], extinction recall [ 63 ], and fear generalization [ 64 , 65 ]. Limitations of these classical neurocircuitry models of PTSD include the deficiency of the models to understand the biological bases of PTSD systems holistically rather than focusing on fear processes alone (see [ 35 ] for an in-depth discussion).
Network-level neural alterations in PTSD are present. Specifically, disruptions in connectivity structure or activation profiles within the salience network (SN), default mode network (DMN), and central executive network (CEN) may underlie univariate and bivariate impairments in PTSD patients. For example, hyperarousal and hyperreactivity symptoms were linked to increased activation of the amygdala and dACC, two critical nodes of the SN [ 33 , 66 , 67 ]. Further, intrusive symptoms, impaired fear extinction, and deficits in emotional regulation are associated with decreased activation of the hippocampus and vmPFC, two nodes of the DMN [ 31 , 33 , 68 ]. Decreased activation of nodes within the CEN, such as the IFG and MFG in PTSD, are present [ 32 ].
Numerous neuroimaging studies have employed ICA methodology to test alterations in large-scale networks in adults with PTSD (see reviews [ 69 , 70 , 71 , 72 , 73 , 74 ]). Overall, results are mixed and provide limited support for classical neurocircuitry models of PTSD. Within the DMN, most studies report decreased activation and connectivity at rest in PTSD patients [ 75 , 76 , 77 ], possibly associated with re-experiencing and dissociative symptoms [ 71 , 78 ]. However, one study reported higher integration of the amygdala with the DMN in PTSD patients during a threat-processing task [ 79 ]. Research typically suggests increased activation and connectivity [ 83 , 84 ] within the SN, potentially linked to hyperarousal and hypervigilance symptoms. In contrast, other findings indicate decreased SN connectivity in PTSD [ 48 , 77 ]. The CEN seems to show reduced activation and connectivity among PTSD patients [ 32 , 76 ].
In addition to alterations within each network, some recent evidence points to aberrant connectivity patterns between networks in PTSD. For example, Zhang and colleagues (2015) [ 77 ] reported decreased FC between the SN and DMN, possibly explaining previous contrasting findings regarding the connectivity of the SN in PTSD. As the SN is believed to facilitate the transition between the DMN and CEN in response to external cognitive demands [ 80 ], the reduced connectivity between the SN and DMN might suggest a compromised ability in PTSD to shift between a self-referential state and a cognitive control mode. In another study, PTSD patients showed increased excitatory influence of the executive central network (ECN, like the CEN) on the posterior DMN. Finally, Akiki et al. (2017) [ 71 ] suggested that PTSD is characterized by impaired SN, incapable of DMN-CEN modulation, and weakened top-down regulation of the SN by the CEN.
Several neuroimaging studies of PTSD used graph theory approaches in resting-state data to examine possible alternations in local and global connectivity patterns. One study found that PTSD patients exhibit a transformation from a random or regular network to a “small-world” network, compared to TENC [ 81 ]. The concept of “small-world” networks describes a network topology in which most nodes are not neighbors of one another, but still, nodes can be reached from every other by a small number of steps [ 82 ]. Furthermore, these patients show increased centrality in the DMN and SN [ 81 ] (i.e., amount of nodes with many paths passing through them). Indeed, more severe PTSD symptoms were linked to DMN alteration, including decreased FC strength [ 83 ], decreased functional integration, and increased segregation within the DMN [ 84 ]. Additionally, reduced within-network connectivity and decreased connectional density within a hippocampus-PFC network are associated with more severe re-experiencing symptoms in combat-exposed veterans [ 85 ]. These studies suggest a complex interplay of network alterations in PTSD.
In normative brain development, gray matter volume is shaped like an inverted U, whereby matter increases from birth to childhood, then around early adolescence, starts to decline until adulthood [ 86 ]. This development pattern is due to synaptic proliferation and pruning, which makes the child’s brain more efficient [ 87 ]. White matter generally increases throughout childhood and adolescence and then levels off [ 86 ]. This pattern represents increases in myelination over time to maximize neuronal transmission speed and adjust the timing and synchrony of neural spikes [ 88 ]. In total volume, including gray and white matter, young brains grow in size until late childhood/early adolescence, when they start to asymptote [ 89 ].
In pediatric samples, PTSD and TENC youth typically exhibit overall smaller amygdala [ 90 , 91 , 92 ] and hippocampal volumes [ 91 , 93 ], including smaller CA2/3 hippocampal subfields [ 90 , 94 ]. Studies report that youth with PTSD have smaller vmPFC volumes than TENC or HC youth [ 91 , 95 ]. One study found no differences in the structure of the medial PFC (mPFC) between youth with PTSD and TENC [ 96 ], indicating that more work needs to be done to disentangle how maltreatment and PTSD relate to volume. Heyn and colleagues [ 97 ] (2022) explored sex differences in volume in female and male youth. Female youth with PTSD showed increased volume and surface area in the ventrolateral PFC and frontal pole regions. In contrast, male youth showed smaller volumes of these regions that predicted more severe symptoms one year later [ 97 ]. Additionally, youth with PTSD, compared to controls, had age- and sex-related differences in the UF, inferior longitudinal fasciculus, and cingulum bundle [ 98 ]. Finally, a review found that youth with PTSD had lower FA in the corpus callosum, including the anterior and posterior midbody, the isthmus, and the splenium [ 99 ], and increased PTSD symptoms have been related to lower FA in these regions [ 100 ].
Our comprehension of the typical developmental trajectories of brain function in youth remains limited. Univariate investigations have focused mostly on associations between childhood trauma and brain activation. In the past decade, a movement towards employing consistent brain atlases and pre-processing methods has emerged, particularly for comparing studies with limited sample sizes [ 101 ]. That said, the literature reviewed here will be specific to youth with PTSD and is, therefore, sparse.
In task-based fMRI, greater activation in the amygdala and dACC in response to emotional faces and threatening images have been found in youth with PTSD versus controls [ 102 , 103 ]. Greater activation has been found in the ACC and frontal brain regions in maltreated youth than in HC during the presentation of negative stimuli [ 104 ]. Furthermore, there is an interesting pattern of decreased FC while viewing angry faces and increased FC while viewing happy faces, specifically between the dACC-dmPFC, amygdala-dmPFC, and amygdala-vlPFC [ 102 ]. Youth with PTSD showed increased PCC-vmPFC resting-state FC, which may indicate problems in self-referential tasks or memory consolidation [ 105 ]. In another resting-state study, youth with PTSD showed decreased PCC-hippocampus FC and increased PCC-insula and PCC-cerebellum FC [ 106 ].
Network-based analyses have had limited application in youth PTSD populations. This could be for numerous reasons, including low sample sizes and the novelty of computational imaging methods. The handful of studies that have used ICA and graph theory methods to identify alterations in youth with PTSD have identified a greater anticorrelation between DMN and task-positive network (TPN), indicative of difficulty switching between internal (DMN) and external (TPN) stimuli [ 105 ]. In one study of resting-state whole-brain connectivity in youth exposed to an earthquake, the PTSD group (compared to TENC) showed an increased clustering coefficient and a normalized characteristic path length and local efficiency, suggesting a shift toward regular networks [ 107 ]. Further, the authors found enhanced nodal centralities in the DMN and SN, which may be related to altered processing of negative emotions. They also found reduced centralities in the CEN, which may indicate worse goal-directed behaviors. In contrast, Xu and colleagues (2018) [ 108 ] reported a lower clustering coefficient among youth with PTSD compared to TENC. They further found increases in centralities in the attention and DMN and decreases in the salience and sensorimotor networks [ 109 ].
Question 1: which neural alterations serve as predisposing (pre-exposure) risk factors for PTSD development, and which are acquired (post-exposure)?
An important goal in the PTSD field is to uncover whether the neural alterations in PTSD discussed above are predisposing risk factors that make an individual more susceptible to developing PTSD after experiencing trauma or acquired characteristics of the disorder. Uncovering these distinctions will enable the development of preventative interventions or the creation of more efficacious treatment options that target specific targets affected by the disorder. Many methodological approaches are used to disentangle predisposed from acquired neural alterations in PTSD [ 110 ]. The most methodologically sound techniques include prospective longitudinal studies, which collect neuroimaging data from participants either before trauma exposure or in the early aftermath of trauma and follow these participants at various time points post-trauma. Examples include the Neurobehavioral Moderators of Posttraumatic Disease Trajectories (NMPTDT) [ 111 ] and the Advancing Understanding of Recovery After Trauma (AURORA) studies [ 112 ]. While prospective longitudinal study designs are optimal for answering this question, they are hard to execute as they are often time-consuming, expensive, and have inherently poor participant attrition rates (see [ 111 ]). Further, though it is the goal to recruit participants before or in the early aftermath of trauma, participants may endorse childhood trauma experienced years before study participation, confounding the data collected.
Twin-pair designs have also been used to answer this question. Usually, these studies include monozygotic twin pairs, where one twin has PTSD from combat-related trauma, while their co-twin did not experience combat trauma nor has a PTSD diagnosis. A separate monozygotic twin pair contains a cotwin who experienced combat-related trauma but did not develop PTSD, and their cotwin did not experience combat-related trauma nor develop PTSD [ 113 ]. Again, limitations exist in this design, including an inability to determine whether the findings are attributed to heredity or shared environments.
Lastly, while not optimal, cross-sectional studies that explore brain alterations in three groups, PTSD, TENC, and HC, can provide some insight into whether alterations are PTSD-specific or related to trauma exposure.
Structural neuroimaging
Few structural imaging studies have used prospective longitudinal designs in the past decade. Studies that scanned participants pre-trauma and post-trauma found reduced hippocampal volume [ 68 , 114 ], post-pre-trauma orbitofrontal cortex (OFC) volume, and pre-trauma ventral ACC were related to greater PTSD symptom severity post-trauma [ 115 ]. It is important to highlight that these studies had relatively small sample sizes ( n < 50). One large study ( n = 210) that scanned police recruits found smaller pre-trauma dentate gyrus volume was associated with greater PTSD symptom severity post-trauma and that experiencing more police-related trauma between scan assessments was related to an increase in the volume of the basal nucleus of the amygdala [ 116 ]. It should be noted that the studies reviewed consisted of resilient individuals, with many participants without a PTSD diagnosis.
Numerous recent longitudinal studies have investigated how structural neuroimaging data collected shortly after trauma correlate with or predict PTSD symptoms. Most of these studies supported the hypothesis that decreased hippocampal volume early post-trauma is a risk factor for the development of chronic PTSD [ 117 , 118 , 119 , 120 , 121 ]. However, one study found no associations between hippocampal volume, or any of its subregions, and PTSD symptoms across time [ 122 ]. These differences are likely due to differences in trauma experienced, the timing of neuroimaging measurements, analytic strategy, and other sample characteristics [ 122 ]. Reduced FA of the UF [ 123 , 124 ] and greater FA of the dorsal cingulum [ 125 ] collected early post-trauma predicted greater PTSD symptoms at 3 months, 6 months, and 4 years later (respectively).
Cross-sectional studies comparing three groups - PTSD, TENC, and HC - found reduced hippocampal [ 126 , 127 , 128 ] and right amygdala volume [ 128 ] in the PTSD and TENC groups compared to the HC group. However, one study found that only the PTSD group showed significantly less hippocampal volume compared to the TENC and HC groups [ 129 ]. When examining hippocampal subregions, the CA1 and CA2-3/DG were significantly smaller in PTSD patients than in TENC and HC groups [ 130 ]. Differences in findings may be attributed to different trauma types endured, as has been found previously [ 131 ]. For example, the studies that found differences only in the PTSD group used samples that experienced combat-related trauma [ 129 ] or a terrorist attack [ 130 ] versus the loss of a loved one [ 126 , 127 ] or a natural disaster [ 128 ].
Functional MRI
Using a prospective longitudinal study design, Admon and colleagues (2013) found that service members who exhibited reduced hippocampal volume post-pre-trauma also displayed reduced hippocampus-vmPFC FC, which was related to greater PTSD symptoms post-trauma [ 68 ]. In a separate study from the same research group, the authors found that greater amygdala activation in response to risk anticipation at pre- and post-trauma was related to more PTSD symptoms post-trauma [ 132 ] and reduced nucleus accumbens activation to reward post-trauma was related to greater PTSD symptoms post-trauma [ 132 ]. Zhang and colleagues (2022) [ 133 ] recently used a network-based approach to measure stress-induced connectivity, changing patterns of large-scale brain networks at baseline to the subsequent symptom development post-trauma. In this prospective sample of police trainees, increased coupling between the SN and anterior cerebellum was observed in participants with greater PTSD symptoms (particularly intrusion symptoms) [ 133 ]. Nevertheless, as this work focused on a relatively healthy and resilient sample, future studies in more severe PTSD samples are needed.
Greater hippocampal activation, collected early post-trauma, during fear extinction [ 134 ], but not when looking at fearful versus neutral face stimuli [ 135 ], predicted more severe PTSD symptoms at 3 months post-trauma. In comparison, lesser hippocampal activation during response inhibition predicted greater PTSD symptom severity post-trauma [ 136 ]. Highlighting the unique contribution of the hippocampus in these different constructs. Greater amygdala activation early post-trauma when viewing fearful facial expressions significantly predicted symptoms at 3 [ 137 ] and 12 months post-trauma [ 138 ]. In combat veterans, greater dACC activation to negative images predicted greater PTSD symptom severity four years later [ 125 ]. Similarly, more negative amygdala-cerebellum FC at rest and amygdala-post-central gyrus FC during trauma recall at 2 weeks post-trauma predicted 6-month PTSD symptom severity post-trauma [ 139 ]. In a longitudinal study of n = 171 recent trauma survivors, PTSD severity at 14 months after trauma was associated with decreased neural activity in the ventral striatum (VS) and the amygdala toward rewards versus punishments at 1 month after trauma [ 140 ]. Surprisingly, decreased VS activity and connectivity with the vmPFC were more predictive of PTSD symptoms compared to the amygdala’s activity, highlighting the important role of reward processing in PTSD development or recovery [ 140 ]. Similarly, lesser activation in cortical regions early post-trauma during fear conditioning [ 141 ] and response inhibition [ 142 ] is related to greater PTSD symptoms 3 and 6 month post-trauma, respectively. However, greater dmPFC activation to fearful versus neutral face stimuli early post-trauma was associated with greater PTSD symptoms 3 months later [ 137 ]. Finally, a longitudinal study showed that while FC changes at 3 weeks post-trauma involved the DMN and frontal–limbic–striatal network, only changes in the DMN persisted at the 2 year follow-up [ 143 ].
Using a three-group design, one study examined the neural correlates of memory suppression in PTSD and found that the PTSD and TENC groups exhibited disrupted MFG activation while attempting memory suppression compared to HC, suggesting that disruptions in the MFG are apparent even in those trauma-exposed, regardless of PTSD status [ 144 ]. Regional parameters of the insular lobe, putamen, and precuneus of typhoon-related PTSD patients, TENC, were abnormal compared to HCs [ 145 ].
Recent twin studies have shown that PTSD patients exhibit reduced activation in the rostral ACC and MFG compared to their non-trauma-exposed cotwins and trauma-exposed individuals without PTSD. This diminished response, observed during exposure to trauma-related cues and to surprised faces, indicates that changes in these cortical areas are likely acquired traits of the disorder [ 146 , 147 ].
One study found that increased hippocampal activation to threatening images over one year predicted a non-remitting PTSD trajectory, compared to a remission trajectory and HC groups [ 148 ].
Overall, across longitudinal prospective study designs and studies utilizing three groups, hippocampal alterations (lesser hippocampal volume and function) appear to be a pre-exposure risk factor for the development of PTSD [ 68 , 114 , 116 , 117 , 118 , 119 , 120 , 121 , 126 , 127 , 128 , 129 , 130 , 134 , 135 , 136 ]. Creating interventions that promote hippocampal neurogenesis will be important to use to prevent the development of PTSD early after trauma. Furthermore, alterations in cortical regions such as the vmPFC, ACC, and MFG are apparent early after trauma and predictive of later PTSD symptoms [ 115 , 125 , 137 , 138 , 141 , 142 , 144 , 145 , 146 , 147 ]. As such, interventions introduced early post-trauma that promote greater FC between frontal-limbic networks can potentially strengthen these connections. There are many limitations to the studies reviewed above, including limited sample sizes, many of the longitudinal studies reviewed included participants with sub-threshold PTSD, and there was not much variability concerning trauma type. Thus, the generalizability of the findings across trauma types is questionable. For a pictorial overview of findings, see Fig. 1 .
Question 2: which neural correlates predict treatment outcomes and define treatment improvement?
To date, while trauma-focused cognitive behavioral therapies are gold-standard treatment options for PTSD, many people do not respond well to treatment [ 19 , 20 ]. Uncovering the neural mechanisms that predict symptom improvement and define treatment response will be crucial in helping guide clinician-decision making and provide a more precision-medicine approach to treatment. Given the recent reviews published on this topic [ 40 , 149 , 150 , 151 ], we review studies not included in these reviews, provide an overall summary of findings, and discuss limitations.
Baseline prediction of PTSD symptom improvement
In females who developed PTSD as a result of interpersonal trauma, pre-treatment FA values of the internal capsule, cingulate gyrus, superior longitudinal fasciculus, and splenium of the corpus callosum were positively correlated with changes in PTSD symptoms after cognitive processing therapy [ 152 ]. One study showed that lesser pre-treatment amygdala activation and greater MFG to fearful versus happy facial expressions were associated with a better response to prolonged exposure therapy (PE) [ 153 ]. Furthermore, this study found a greater decrease in the amygdala activation across blocks of fearful facial expression was associated with better symptomatic improvement [ 153 ]. Lower pre-treatment vmPFC-amygdala connectivity during an emotional face-viewing task predicted symptom improvement in individuals with PTSD, an effect that was strongest in individuals who received ketamine (versus midazolam) [ 154 ]. Additionally, this study showed symptom improvement following ketamine was predicted by decreased dACC activity during an emotional conflict regulation task and an increased resting-state FC between the vmPFC and anterior insula [ 154 ]. On the other hand, ketamine did not promote a greater increase in amygdala-mPFC resting-state FC but elicited a stronger transient decrease in vmPFC-amygdala compared to midazolam [ 155 ]. A longitudinal resting-state fMRI study employing support vector machine learning highlighted the precuneus, dmPFC, lingual gyrus, supplementary motor area, and cerebellum showed the highest prognostic remittance value from paroxetine treatment [ 156 ]. Lastly, Korgaonkar and colleagues (2020) found that lower pre-treatment connectivity in the cingulo-opercular, salience, and dorsal attention networks was associated with a better response to trauma-focused cognitive behavioral therapy (TF-CBT) [ 157 ].
Few studies have explored whether neuroimaging measures can predict treatment response in youth diagnosed with PTSD. Decreased pre-treatment activation in the posterior cingulate, mid-cingulate, and hippocampus predicted greater symptom improvement [ 158 ]. Another study trained a support vector machine from brain networks created from an ICA, finding that the bilateral superior temporal gyrus center network distinguished between non-responders and responders to trauma-focused therapies [ 159 ]. This may indicate that auditory processing and social cognition may be important for PTSD remission [ 160 ]. Girls who experienced greater reductions in PTSD symptoms exhibited decreased amygdala-insula connectivity during reappraisal compared to those experiencing milder reductions [ 161 ].
Neuroimaging correlates of PTSD symptom improvement
Increased hippocampal volume appeared in PTSD patients who completed CBT [ 162 ], eye-movement desensitization and realization (EMDR) alone [ 163 ] or paired with a Tetris video game intervention [ 164 ], and in those who remitted following psychotherapy [ 165 ]. Over time, lesser dorsal cingulum FA was found in individuals whose PTSD symptoms decreased after trauma-focused treatment [ 166 ]. Interestingly, recent work reported the normalization of CEN connectivity following cognitive processing therapy for PTSD [ 167 ]. Greater reduction in PTSD symptoms was associated with larger pre- to post-treatment increases in the inferior frontal junction inhibition of the amygdala [ 168 ]. PTSD patients who showed clinical improvement exhibited a reduced relative influence of the anterior insula over motor, affective, and self-other distinction regions [ 169 ]. Upon completion of PE, PTSD patients showed increased pre-post FC in basolateral amygdala-OFC, centromedial amygdala-OFC, and hippocampus-vmPFC. In contrast, TENC saw no significant pre-post changes in connectivity after PE, suggesting that amygdala FC normalized similarly to TENC [ 170 ]. One study showed that a reduction in PTSD symptom severity was associated with decreased connectivity between the visual cortex and temporal lobe regions and increased connectivity between the superior frontal gyrus and temporal pole regions after EMDR and TF-CBT, suggesting minor differences exist in neurophysiological outcome that is therapy-specific, particularly in those who experienced natural-disaster [ 171 ].
Overall, the studies reviewed here and previously published reviews [ 40 , 149 , 150 , 151 ] suggest that treatment non-response in adults was predicted by greater activation in regions responsible for threat detection, lesser activation in emotion regulation, executive function, and contextual processing regions, and altered crosstalk between regions within the DMN and regions important in emotion processing, cognitive function, and salience. In youth, studies are sparse but show a pattern of greater activation in memory-related regions, while lesser connectivity between fear learning-related regions predicted symptom reduction. There are many limitations of the studies reviewed. First, given the stringent inclusion/exclusion criteria many of these intervention studies endorse, their sample sizes are limited. Second, the definition of a responder versus a non-responder to treatment is not objective, and studies define this differently. Third, some variables are not controlled for, making it hard to determine the effect of treatment. For example, no direct comparison exists between groups undergoing different treatment options. Fourth, the analyses are largely ROI-specific. Fifth, no study have examined longitudinal treatment response outcomes. Lastly, many studies did not include a wait-list control group; only one study explored neural differences in treatment response between treatment types. For a pictorial overview of findings, see Fig. 2 .
Question 3: are there neuroimaging-based biotypes that define PTSD?
Psychiatry is moving towards a more precision-medicine approach, aiming to improve objective diagnosis, prediction, and treatment of mental disorders. Currently, to be diagnosed with PTSD, participants need to meet a certain number of symptoms that are largely self-reported and subjective, making the disorder highly heterogeneous [ 172 ]. To overcome the weak link between subjective-based diagnostic methods and objective-based neuroimaging assessments, recent studies have aimed to stratify PTSD to identify consistent subgroups based on objective brain-based markers [ 173 , 174 , 175 ]. Accordingly, Stevens and colleagues (2021) conducted a pioneering study to identify brain-based biotypes of psychiatric vulnerability shortly after trauma [ 176 ]. Using two cohorts from the AURORA longitudinal study of trauma survivors (n = 69 discovery cohort; n = 77 internal replication cohort) [ 112 ], the authors found and replicated three clusters based on early post-trauma brain activity during fMRI tasks assessing threat and reward reactivity, as well as response inhibition. These clusters were associated with distinct clinical trajectories up to 6 months post-trauma, with the group showing increased reactivity to threat and reward experiencing the most severe subsequent PTSD and anxiety symptoms [ 176 ]. In collaboration with Stevens and colleagues, Ben-Zion and colleagues (2023) conducted a conceptual replication of these brain-based biotypes [ 177 ] using a comparable dataset from the NMPTDT longitudinal study of trauma survivors [ 111 ]. While the authors found four clusters based on task-based fMRI data, they were not identical to the previously identified biotypes and were associated with prospective PTSD or anxiety symptoms. While there were many differences between the studies (AURORA and NMPTDT) that could contribute to the non-replication, this study highlights that additional replication studies are needed to identify more stable and generalizable neuroimaging-based biotypes before treatment implications can be fully realized [ 177 , 178 ].
Overall implications, future directions, and limitations
This narrative review aimed at exploring progress made in the past decade on three major questions in the field: (1) Which neural alterations serve as predisposing (pre-exposure) risk factors for PTSD development, and which are acquired (post-exposure)? (2) Which neural alterations can predict treatment outcomes and define clinical improvement? and (3) Can neuroimaging measures be used to define brain-based biotypes of PTSD? We present a synthesis of neuroimaging studies from the past decade in adults and youth with PTSD. Below, we present implications, provide areas of future research to be explored for each question, and highlight the limitations of our narrative review.
In the past decade, neuroimaging research on PTSD has advanced our understanding of the causal pathways of neural alterations within the disorder. However, we still cannot use the current neuroimaging knowledge to predict PTSD symptom trajectories or improve prevention and treatment options. Many of the above findings require replication in larger and more diverse samples with different trauma types across different methodologies. Importantly, future models used to determine the risk of developing trauma-related psychopathology will likely include information regarding demographics, socioeconomic status, and other clinical characteristics; thus, it is important to consider these factors when designing forthcoming studies. In the last ten years, we have seen a surge of longitudinal studies that collect neuroimaging measures early post-trauma and again at subsequent time points. While such studies are resource-intensive, scientists can answer questions not asked before, largely because of the development of large collaborations across multiple sites such as NMPTDT and AURORA research initiatives. The continuation and creation of more collaborations like these, with a focus on the collection of neuroimaging data shortly after trauma (and if possible, even pre-trauma) and at subsequent time points post-trauma, will be crucial in providing evidence to answer the vulnerability versus acquired characteristics of PTSD. To capture the dynamic evolution of the post-traumatic stress response, it is essential to incorporate multiple time points and ensure an adequately long follow-up period post-trauma (e.g., more than a year post-trauma), during which most of the recovery is anticipated.
Much work has been done to determine neural pre-treatment predictors of response and whether treatment normalizes alterations found in the disorder. While we have a relative understanding of potential predictors and changes associated with treatment response, much work still needs to be done to use this information in the clinic. Many of the studies reviewed had small sample sizes, used different treatment options, and samples were not diverse regarding sociodemographic factors and trauma type. Future studies should seek to replicate previous findings with bigger sample sizes, comparisons should be made between treatments, and more community-based samples should be prioritized.
The significant clinical heterogeneity observed in PTSD (and other post-traumatic psychopathologies), coupled with recent advancements in statistical and computational techniques, has spurred the pursuit of identifying homogeneous PTSD subtypes using data-driven methodologies. However, the assumption of distinct and homogeneous subgroups may not be clinically useful or accurately reflect the underlying biology of PTSD. For instance, most clustering methods will invariably produce clusters, even without any inherent data structure, highlighting the importance of differentiating between biologically and clinically relevant subtypes and random data fluctuations or noise [ 179 , 180 ]. Future research aiming to identify brain-based biotypes of PTSD will benefit from global collaborations between research teams, combining unique large-scale datasets and sharing of analytic pipelines (as exemplified recently by Stevens [ 176 ] and Ben-Zion [ 177 ]). Furthermore, subsequent studies will benefit from employing hybrid methodologies that integrate theory- and data-driven approaches Field [195,196] and implementing open science protocols (e.g., preregistration, transparent reporting of all results).
Few investigations explored here explicitly examined sex as a biological variable. As has been recently reviewed [ 13 ], the underlying neurobiological correlates of sex differences in PTSD are unknown. Most of the studies discussed here did not include a direct comparison between males and females. However, a handful of studies did examine female-only or male-only samples, which do not allow for the generalization of findings to the opposite sex. Thus, more studies should examine sex differences in their samples.
We have highlighted findings in youth. Still, much more work is needed to parse better the brain’s natural development versus the impact trauma may have on brain regions. Few studies have explored the questions posed in youth samples. Though resources are a limiting factor, future studies should execute longitudinal study designs that start in youth to determine the role of childhood trauma, potentially before it happens, in the development of trauma-related psychopathology in adulthood. Additionally, genetic and neurobiological studies linking transgenerational PTSD presentation would be beneficial in parsing preventative markers for developing PTSD. Thus, focusing on youth populations would be optimal in answering our first main question.
Limitations
There are notable strengths of this narrative review, including providing a synthesis of neuroimaging studies in both adult and youth samples that explore three leading questions in the PTSD field. Despite these strengths, limitations do exist. First, the authors have tried to include all the pertinent studies to answer the three questions, though a systematic protocol was not used when exploring studies. Second, given the number of studies available to be reviewed, the conclusions drawn from each question are limited. Further, as outlined above, methodological variability exists in the studies reviewed, including differences in scanning parameters and PTSD samples. This variability limits the reliability and validity of the conclusions made. Regardless of these limitations, this review is important as it provides insight into where the field stands on these three questions, highlighting that much research still needs to be conducted to make stronger conclusions.
Despite the limitations of the studies reviewed and of this narrative review, PTSD neuroimagers have made much progress in the last decade and have much more to make, especially in answering questions related to disparities in the development of the disorder and translating the knowledge collected beyond academia, to the communities we serve.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5 TM , 5th ed. Arlington, VA, US: American Psychiatric Publishing, Inc.; 2013. xliv, 947 p. (Diagnostic and statistical manual of mental disorders: DSM-5 TM , 5th ed).
Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, et al. The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychol Med. 2016;46:327–43.
Article CAS PubMed Google Scholar
Paganin W, Signorini S. Biomarkers of post-traumatic stress disorder from emotional trauma: a systematic review. Eur J Trauma Dissociation. 2023;7:100328.
Article Google Scholar
Bonanno GA. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? Psychol Trauma Theory Res Pr Policy. 2008;S:101–13.
Galatzer-Levy IR, Huang SH, Bonanno GA. Trajectories of resilience and dysfunction following potential trauma: a review and statistical evaluation. Clin Psychol Rev. 2018;63:41–55.
Article PubMed Google Scholar
McLaughlin KA, Koenen KC, Hill ED, Petukhova M, Sampson NA, Zaslavsky AM, et al. Trauma exposure and posttraumatic stress disorder in a national sample of adolescents. J Am Acad Child Adolesc Psychiatry. 2013;52:815–830.e14.
Article PubMed PubMed Central Google Scholar
Blom M, Oberink R. The validity of the DSM-IV PTSD criteria in children and adolescents: a review. Clin Child Psychol Psychiatry. 2012;17:571–601.
Ramsdell KD, Smith AJ, Hildenbrand AK, Marsac ML. Posttraumatic stress in school-age children and adolescents: medical providers’ role from diagnosis to optimal management. Pediatr Health Med Ther. 2015;6:167–80.
Google Scholar
Cover KK, Maeng LY, Lebrón-Milad K, Milad MR. Mechanisms of estradiol in fear circuitry: implications for sex differences in psychopathology. Transl Psychiatry. 2014;4:e422–e422.
Article CAS PubMed PubMed Central Google Scholar
Miller-Graff LE, Howell KH. Posttraumatic stress symptom trajectories among children exposed to violence. J Trauma Stress. 2015;28:17–24.
Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol Bull. 2006;132:959–92.
Helpman L, Zhu X, Suarez-Jimenez B, Lazarov A, Monk C, Neria Y. Sex differences in trauma-related psychopathology: a critical review of neuroimaging literature (2014–2017). Curr Psychiatry Rep. 2017;19:104.
Eder-Moreau E, Zhu X, Fisch CT, Bergman M, Neria Y, Helpman L. Neurobiological alterations in females with PTSD: a systematic review. Front Psychiatry. 2022 ;13:862476.
Brunello N, Davidson JR, Deahl M, Kessler RC, Mendlewicz J, Racagni G, et al. Posttraumatic stress disorder: diagnosis and epidemiology, comorbidity and social consequences, biology and treatment. Neuropsychobiology. 2001;43:150–62.
Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Physical Health Conditions Associated with Posttraumatic Stress Disorder in U.S. Older Adults: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Am Geriatr Soc. 2012;60:296–303.
Fani N, Jain J, Hudak LA, Rothbaum BO, Ressler KJ, Michopoulos V. Post-trauma anhedonia is associated with increased substance use in a recently-traumatized population. Psychiatry Res. 2020;285:112777.
Brady KT, Killeen TK, Brewerton T, Lucerini S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J Clin Psychiatry. 2000;61:22–32.
PubMed Google Scholar
Foa EB, Hembree EA, Cahill SP, Rauch SAM, Riggs DS, Feeny NC, et al. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. J Consult Clin Psychol. 2005;73:953–64.
Schottenbauer MA, Glass CR, Arnkoff DB, Tendick V, Gray SH. Nonresponse and dropout rates in outcome studies on PTSD: review and methodological considerations. Psychiatry. 2008;71:134–68.
Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. Am J Psychiatry. 2005 ;162:214–27.
Schnurr PP, Chard KM, Ruzek JI, Chow BK, Resick PA, Foa EB, et al. Comparison of prolonged exposure vs cognitive processing therapy for treatment of posttraumatic stress disorder among US veterans: a randomized clinical trial. JAMA Netw Open. 2022;5:e2136921.
Lewis C, Roberts NP, Gibson S, Bisson JI. Dropout from psychological therapies for post-traumatic stress disorder (PTSD) in adults: systematic review and meta-analysis. Eur J Psychotraumatol. 2020;11:1709709.
Davis RG, Ressler KJ, Schwartz AC, Stephens KJ, Bradley RG. Treatment barriers for low-income, urban african americans with undiagnosed posttraumatic stress disorder. J Trauma Stress. 2008;21:218–22.
Cipriani A, Williams T, Nikolakopoulou A, Salanti G, Chaimani A, Ipser J, et al. Comparative efficacy and acceptability of pharmacological treatments for post-traumatic stress disorder in adults: a network meta-analysis. Psychol Med. 2018;48:1975–84.
Henner RL, Keshavan MS, Hill KP. Review of potential psychedelic treatments for PTSD. J Neurol Sci. 2022;439:120302.
Krediet E, Bostoen T, Breeksema J, van Schagen A, Passie T, Vermetten E. Reviewing the potential of psychedelics for the treatment of PTSD. Int J Neuropsychopharmacol. 2020;23:385–400.
Barawi KS, Lewis C, Simon N, Bisson JI. A systematic review of factors associated with outcome of psychological treatments for post-traumatic stress disorder. Eur J Psychotraumatol. 2020;11:1774240.
Merz J, Schwarzer G, Gerger H. Comparative efficacy and acceptability of pharmacological, psychotherapeutic, and combination treatments in adults with posttraumatic stress disorder: a network meta-analysis. JAMA Psychiatry. 2019;76:904–13.
Bremner JD, Randall P, Scott TM, Bronen RA, Seibyl JP, Southwick SM, et al. MRI-based measurement of hippocampal volume in patients with combat-related posttraumatic stress disorder. Am J Psychiatry. 1995;152:973–81.
Shalev A, Liberzon I, Marmar C. Post-traumatic stress disorder. Longo DL, editor. N Engl J Med. 2017;376:2459–69.
Liberzon I, Abelson JL. Context processing and the neurobiology of post-traumatic stress disorder. Neuron. 2016;92:14–30.
Patel R, Spreng RN, Shin LM, Girard TA. Neurocircuitry models of posttraumatic stress disorder and beyond: a meta-analysis of functional neuroimaging studies. Neurosci Biobehav Rev. 2012;36:2130–42.
Pitman RK, Rasmusson AM, Koenen KC, Shin LM, Orr SP, Gilbertson MW, et al. Biological studies of posttraumatic stress disorder. Nat Rev Neurosci. 2012;13:769–87.
Rauch SL, Shin LM, Phelps EA. Neurocircuitry models of posttraumatic stress disorder and extinction: human neuroimaging research-past, present, and future. Biol Psychiatry. 2006;60:376–82.
Ross MC, Cisler JM. Altered large-scale functional brain organization in posttraumatic stress disorder: A comprehensive review of univariate and network-level neurocircuitry models of PTSD. NeuroImage Clin. 2020;27:102319.
Shin LM, Rauch SL, Pitman RK. Amygdala, medial prefrontal cortex, and hippocampal function in PTSD. Ann N. Y Acad Sci. 2006;1071:67–79.
O’Doherty DCM, Chitty KM, Saddiqui S, Bennett MR, Lagopoulos J. A systematic review and meta-analysis of magnetic resonance imaging measurement of structural volumes in posttraumatic stress disorder. Psychiatry Res Neuroimaging. 2015;232:1–33.
Hinojosa CA. Does hippocampal volume in patients with posttraumatic stress disorder vary by trauma type? Harv Rev Psychiatry. 2022;30:118.
Ben-Zion Z, Korem N, Fine N, Katz S, Siddhanta M, Funaro MC, et al. Structural neuroimaging of hippocampus and amygdala subregions in post-traumatic stress disorder (PTSD): a scoping review. Biol Psychiatry Glob Open Sci [Internet]. 2023 [cited 2023 Aug 29]; Available from: https://www.sciencedirect.com/science/article/pii/S2667174323000812 .
van Rooij SJH, Sippel LM, McDonald WM, Holtzheimer PE. Defining focal brain stimulation targets for PTSD using neuroimaging. Depress Anxiety. 2021. https://doi.org/10.1002/da.23159 .
Backhausen LL, Herting MM, Tamnes CK, Vetter NC. Best practices in structural neuroimaging of neurodevelopmental disorders. Neuropsychol Rev. 2022;32:400–18.
Figley CR, Uddin MN, Wong K, Kornelsen J, Puig J, Figley TD. Potential pitfalls of using fractional anisotropy, axial diffusivity, and radial diffusivity as biomarkers of cerebral white matter microstructure. Front Neurosci [Internet]. 2022 [cited 2023 Sep 14];15. Available from: https://www.frontiersin.org/articles/10.3389/fnins.2021.799576 .
Bassett DS, Sporns O. Network neuroscience. Nat Neurosci. 2017;20:353–64.
Wang X, Xie H, Chen T, Cotton AS, Salminen LE, Logue MW, et al. Cortical volume abnormalities in posttraumatic stress disorder: an ENIGMA-psychiatric genomics consortium PTSD workgroup mega-analysis. Mol Psychiatry. 2021;26:4331–43.
Baldaçara L, Zugman A, Araújo C, Cogo-Moreira H, Lacerda ALT, Schoedl A, et al. Reduction of anterior cingulate in adults with urban violence- related PTSD. J Affect Disord. 2014;168:13–20.
Roy O, Levasseur-Moreau J, Renauld E, Hébert LJ, Leblond J, Bilodeau M, et al. Whole-brain morphometry in Canadian soldiers with posttraumatic stress disorder. Ann NY Acad Sci. 2022;1509:37–49.
Li L, Zhang Y, Zhao Y, Li Z, Kemp GJ, Wu M, et al. Cortical thickness abnormalities in patients with post-traumatic stress disorder: a vertex-based meta-analysis. Neurosci Biobehav Rev. 2022;134:104519.
Koch SBJ, van Zuiden M, Nawijn L, Frijling JL, Veltman DJ, Olff M. Decreased uncinate fasciculus tract integrity in male and female patients with PTSD: a diffusion tensor imaging study. J Psychiatry Neurosci Jpn 2017;42:331–42.
O’Doherty DCM, Ryder W, Paquola C, Tickell A, Chan C, Hermens DF, et al. White matter integrity alterations in post‐traumatic stress disorder. Hum Brain Mapp. 2017;39:1327–38.
Olson EA, Cui J, Fukunaga R, Nickerson LD, Rauch SL, Rosso IM. Disruption of white matter structural integrity and connectivity in posttraumatic stress disorder: A TBSS and tractography study. Depress Anxiety. 2017;34:437–45.
Ju Y, Ou W, Su J, Averill CL, Liu J, Wang M, et al. White matter microstructural alterations in posttraumatic stress disorder: An ROI and whole-brain based meta-analysis. J Affect Disord. 2020;266:655–70.
van Rooij SJH, Rademaker AR, Kennis M, Vink M, Kahn RS, Geuze E. Neural correlates of trauma-unrelated emotional processing in war veterans with PTSD. Psychol Med. 2015;45:575–87.
Mazza M, Tempesta D, Pino MC, Catalucci A, Gallucci M, Ferrara M. Regional cerebral changes and functional connectivity during the observation of negative emotional stimuli in subjects with post-traumatic stress disorder. Eur Arch Psychiatry Clin Neurosci. 2013;263:575–83.
Mazza M, Tempesta D, Pino MC, Nigri A, Catalucci A, Guadagni V, et al. Neural activity related to cognitive and emotional empathy in post-traumatic stress disorder. Behav Brain Res. 2015;282:37–45.
Moser DA, Aue T, Suardi F, Kutlikova H, Cordero MI, Rossignol AS, et al. Violence-related PTSD and neural activation when seeing emotionally charged male–female interactions. Soc Cogn Affect Neurosci. 2015;10:645.
Offringa R, Handwerger Brohawn K, Staples LK, Dubois SJ, Hughes KC, Pfaff DL, et al. Diminished rostral anterior cingulate cortex activation during trauma-unrelated emotional interference in PTSD. Biol Mood Anxiety Disord. 2013;3:1–6.
Stevens JS, Jovanovic T, Fani N, Ely TD, Glover EM, Bradley B, et al. Disrupted amygdala-prefrontal functional connectivity in civilian women with posttraumatic stress disorder. J Psychiatr Res. 2013;47:1469–78.
Killgore WDS, Britton JC, Schwab ZJ, Price LM, Weiner MR, Gold AL, et al. Cortico-limbic responses to masked affective faces across ptsd, panic disorder, and specific phobia. Depress Anxiety. 2014;31:150–9.
Stevens JS, Almli LM, Fani N, Gutman DA, Bradley B, Norrholm SD, et al. PACAP receptor gene polymorphism impacts fear responses in the amygdala and hippocampus. Proc Natl Acad Sci. 2014;111:3158–63.
Neumeister, Feldker P, Heitmann K, Helmich CY, Gathmann R, Becker MPI B, et al. Interpersonal violence in posttraumatic women: brain networks triggered by trauma-related pictures. Soc Cogn Affect Neurosci. 2017;12:555–68.
Xiong K, Zhang Y, Qiu M, Zhang J, Sang L, Wang L, et al. Negative emotion regulation in patients with posttraumatic stress disorder. PLoS ONE. 2013;12:e81957.
Bruce SE, Buchholz KR, Brown WJ, Yan L, Durbin A, Sheline YI. Altered emotional interference processing in the amygdala and insula in women with Post-Traumatic Stress Disorder. NeuroImage Clin 2012;2:43–9.
Garfinkel SN, Abelson JL, King AP, Sripada RK, Wang X, Gaines LM, et al. Impaired contextual modulation of memories in PTSD: an fMRI and psychophysiological study of extinction retention and fear renewal. J Neurosci J Soc Neurosci. 2014;34:13435–43.
Article CAS Google Scholar
Morey RA, Dunsmoor JE, Haswell CC, Brown VM, Vora A, Weiner J, et al. Fear learning circuitry is biased toward generalization of fear associations in posttraumatic stress disorder. Transl Psychiatry. 2015;5:e700.
Diener SJ, Nees F, Wessa M, Wirtz G, Frommberger U, Penga T, et al. Reduced amygdala responsivity during conditioning to trauma-related stimuli in posttraumatic stress disorder. Psychophysiology. 2016;53:1460–71.
Bressler SL, Menon V. Large-scale brain networks in cognition: emerging methods and principles. Trends Cogn Sci. 2010;14:277–90.
Menon V, Uddin LQ. Saliency, switching, attention and control: a network model of insula function. Brain Struct Funct. 2010;214:655–67.
Admon R, Leykin D, Lubin G, Engert V, Andrews J, Pruessner J, et al. Stress-induced reduction in hippocampal volume and connectivity with the ventromedial prefrontal cortex are related to maladaptive responses to stressful military service. Hum Brain Mapp. 2013;34:2808–16.
Bao W, Gao Y, Cao L, Li H, Liu J, Liang K, et al. Alterations in large-scale functional networks in adult posttraumatic stress disorder: A systematic review and meta-analysis of resting-state functional connectivity studies. Neurosci Biobehav Rev. 2021;131:1027–36.
Koch SBJ, van Zuiden M, Nawijn L, Frijling JL, Veltman DJ, Olff M. Aberrant resting-state brain activity in posttraumatic stress disorder: a meta-analysis and systematic review. Depress Anxiety. 2016;33:592–605.
Akiki TJ, Averill CL, Abdallah CG. A network-based neurobiological model of PTSD: evidence from structural and functional neuroimaging studies. Curr Psychiatry Rep. 2017;19:81.
Fenster RJ, Lebois LAM, Ressler KJ, Suh J. Brain circuit dysfunction in post-traumatic stress disorder: from mouse to man. Nat Rev Neurosci. 2018;19:535–51.
Neria Y. Functional neuroimaging in PTSD: from discovery of underlying mechanisms to addressing diagnostic heterogeneity. Am J Psychiatry. 2021;178:128–35.
Norbury A, Seeley SH, Perez-Rodriguez MM, Feder A. Functional neuroimaging of resilience to trauma: convergent evidence and challenges for future research. Psychol Med. 2023;53:3293–305.
Reuveni I, Bonne O, Giesser R, Shragai T, Lazarovits G, Isserles M, et al. Anatomical and functional connectivity in the default mode network of post‐traumatic stress disorder patients after civilian and military‐related trauma. Hum Brain Mapp. 2015;37:589–99.
Shang J, Lui S, Meng Y, Zhu H, Qiu C, Gong Q, et al. Alterations in low-level perceptual networks related to clinical severity in ptsd after an earthquake: a resting-state fMRI study. PLOS ONE. 2014;9:e96834.
Zhang Y, Liu F, Chen H, Li M, Duan X, Xie B, et al. Intranetwork and internetwork functional connectivity alterations in post-traumatic stress disorder. J Affect Disord. 2015 ;187:114–21.
Tursich M, Ros T, Frewen PA, Kluetsch RC, Calhoun VD, Lanius RA. Distinct intrinsic network connectivity patterns of post-traumatic stress disorder symptom clusters. Acta Psychiatr Scand. 2015;132:29–38.
Rabellino D, Tursich M, Frewen PA, Daniels JK, Densmore M, Théberge J, et al. Intrinsic connectivity networks in post-traumatic stress disorder during sub- and supraliminal processing of threat-related stimuli. Acta Psychiatr Scand. 2015;132:365–78.
Menon V. Large-scale brain networks and psychopathology: a unifying triple network model. Trends Cogn Sci. 2011;15:483–506.
Lei D, Li K, Li L, Chen F, Huang X, Lui S, et al. Disrupted functional brain connectome in patients with posttraumatic stress disorder. Radiology. 2015;276:818–27.
Watts DJ, Strogatz SH. Collective dynamics of ‘small-world’ networks. Nature. 1998;393:440–2.
Zhang XD, Yin Y, Hu XL, Duan L, Qi R, Xu Q, et al. Altered default mode network configuration in posttraumatic stress disorder after earthquake: A resting-stage functional magnetic resonance imaging study. Med (Baltim). 2017;96:e7826.
Akiki TJ, Averill CL, Wrocklage KM, Scott JC, Averill LA, Schweinsburg B, et al. Default mode network abnormalities in posttraumatic stress disorder: A novel network-restricted topology approach. NeuroImage. 2018;176:489–98.
Spielberg JM, McGlinchey RE, Milberg WP, Salat DH. Brain network disturbance related to posttraumatic stress and traumatic brain injury in veterans. Biol Psychiatry. 2015;78:210–6.
Giedd JN, Raznahan A, Alexander-Bloch A, Schmitt E, Gogtay N, Rapoport JL. Child psychiatry branch of the national institute of mental health longitudinal structural magnetic resonance imaging study of human brain development. Neuropsychopharmacology. 2015;40:43–9.
Tau GZ, Peterson BS. Normal development of brain circuits. Neuropsychopharmacology. 2010;35:147–68.
Fields RD, Stevens-Graham B. New insights into neuron-glia communication. Science. 2002;298:556–62.
Peterson M, Warf BC, Schiff SJ. Normative human brain volume growth. J Neurosurg Pediatr. 2018;21:478–85.
Jeong HJ, Durham EL, Moore TM, Dupont RM, McDowell M, Cardenas-Iniguez C, et al. The association between latent trauma and brain structure in children. Transl Psychiatry. 2021;11:1–9.
Morey RA, Haswell CC, Hooper SR, De Bellis MD. Amygdala, hippocampus, and ventral medial prefrontal cortex volumes differ in maltreated youth with and without chronic posttraumatic stress disorder. Neuropsychopharmacology. 2016;41:791–801.
Phillips RD, De Bellis MD, Brumback T, Clausen AN, Clarke-Rubright EK, Haswell CC, et al. Volumetric trajectories of hippocampal subfields and amygdala nuclei influenced by adolescent alcohol use and lifetime trauma. Transl Psychiatry. 2021;11:1–13.
Kribakaran S, Danese A, Bromis K, Kempton MJ, Gee DG. Meta-analysis of structural magnetic resonance imaging studies in pediatric posttraumatic stress disorder and comparison with related conditions. Biol Psychiatry Cogn Neurosci Neuroimag. 2020;5:23–34.
Postel C, Viard A, André C, Guénolé F, de Flores R, Baleyte J, et al. Hippocampal subfields alterations in adolescents with post‐traumatic stress disorder. Hum Brain Mapp. 2018;40:1244–52.
Keding TJ, Herringa RJ. Abnormal structure of fear circuitry in pediatric post-traumatic stress disorder. Neuropsychopharmacology. 2015;40:537–45.
Rinne-Albers MA, Boateng CP, van der Werff SJ, Lamers-Winkelman F, Rombouts SA, Vermeiren RR, et al. Preserved cortical thickness, surface area and volume in adolescents with PTSD after childhood sexual abuse. Sci Rep. 2020;10:3266.
Heyn SA, Bailowitz S, Russell JD, Herringa RJ. Sex-based variations of prefrontal structure and longitudinal symptoms in pediatric posttraumatic stress disorder. Depress Anxiety. 2022;39:902–12.
Russell JD, Heyn SA, Dean DC, Herringa RJ. Pediatric PTSD is characterized by age- and sex-related abnormalities in structural connectivity. Neuropsychopharmacol Publ Am Coll Neuropsychopharmacol. 2021;46:2217–23.
Siehl S, Wicking M, Pohlack S, Winkelmann T, Zidda F, Steiger-White F, et al. Structural white and gray matter differences in a large sample of patients with Posttraumatic Stress Disorder and a healthy and trauma-exposed control group: Diffusion tensor imaging and region-based morphometry. NeuroImage Clin. 2020;28:102424.
Rinne-Albers MAW, van der Werff SJA, van Hoof MJ, van Lang ND, Lamers-Winkelman F, Rombouts SA, et al. Abnormalities of white matter integrity in the corpus callosum of adolescents with PTSD after childhood sexual abuse: a DTI study. Eur Child Adolesc Psychiatry. 2016;25:869–78.
Zhang Y, Wei H, Cronin MJ, He N, Yan F, Liu C. Longitudinal atlas for normative human brain development and aging over the lifespan using quantitative susceptibility mapping. NeuroImage. 2018;171:176–89.
Keding TJ, Herringa RJ. Paradoxical prefrontal–amygdala recruitment to angry and happy expressions in pediatric posttraumatic stress disorder. Neuropsychopharmacology. 2016;41:2903–12.
Wolf RC, Herringa RJ. Prefrontal-amygdala dysregulation to threat in pediatric posttraumatic stress disorder. Neuropsychopharmacol Publ Am Coll Neuropsychopharmacol. 2016;41:822–31.
McLaughlin KA, Peverill M, Gold AL, Alves S, Sheridan MA. Child maltreatment and neural systems underlying emotion regulation. J Am Acad Child Adolesc Psychiatry. 2015;54:753–62.
Patriat R, Birn RM, Keding TJ, Herringa RJ. Default-mode network abnormalities in pediatric posttraumatic stress disorder. J Am Acad Child Adolesc Psychiatry. 2016;55:319–27.
Viard A, Mutlu J, Chanraud S, Guenolé F, Egler PJ, Gérardin P, et al. Altered default mode network connectivity in adolescents with post-traumatic stress disorder. NeuroImage Clin. 2019;22:101731.
Suo X, Lei D, Li K, Chen F, Li F, Li L, et al. Disrupted brain network topology in pediatric posttraumatic stress disorder: a resting-state fMRI study. Hum Brain Mapp. 2015;36:3677–86.
Xu J, Chen F, Lei D, Zhan W, Sun X, Suo X, et al. Disrupted functional network topology in children and adolescents with post-traumatic stress disorder. Front Neurosci [Internet]. 2018 [cited 2023 Sep 13];12. Available from: https://www.frontiersin.org/articles/10.3389/fnins.2018.00709 .
Xu J, Chen F, Lei D, Zhan W, Sun X, Suo X, et al. Disrupted functional network topology in children and adolescents with post-traumatic stress disorder. Front Neurosci [Internet]. 2018 [cited 2023 Jul 14];12. Available from: https://www.frontiersin.org/articles/10.3389/fnins.2018.00709 .
Admon R, Milad MR, Hendler T. A causal model of post-traumatic stress disorder: disentangling predisposed from acquired neural abnormalities. Trends Cogn Sci. 2013;17:337–47.
Ben-Zion Z, Fine NB, Keynan NJ, Admon R, Halpern P, Liberzon I, et al. Neurobehavioral moderators of post-traumatic stress disorder (PTSD) trajectories: study protocol of a prospective MRI study of recent trauma survivors. Eur J Psychotraumatology. 2019;10:1683941.
McLean SA, Ressler K, Koenen KC, Neylan T, Germine L, Jovanovic T, et al. The AURORA Study: a longitudinal, multimodal library of brain biology and function after traumatic stress exposure. Mol Psychiatry. 2020;25:283–96.
Pitman RK, Gilbertson MW, Gurvits TV, May FS, Lasko NB, Metzger LJ, et al. Clarifying the origin of biological abnormalities in PTSD through the study of identical twins discordant for combat exposure. Ann NY Acad Sci. 2006;1071:242–54.
Sekiguchi A, Kotozaki Y, Sugiura M, Nouchi R, Takeuchi H, Hanawa S, et al. Resilience after 3/11: structural brain changes 1 year after the Japanese earthquake. Mol Psychiatry. 2015;20:553–4.
Sekiguchi A, Sugiura M, Taki Y, Kotozaki Y, Nouchi R, Takeuchi H, et al. Brain structural changes as vulnerability factors and acquired signs of post-earthquake stress. Mol Psychiatry. 2013;18:618–23.
Koch SBJ, van Ast VA, Kaldewaij R, Hashemi MM, Zhang W, Klumpers F, et al. Larger dentate gyrus volume as predisposing resilience factor for the development of trauma-related symptoms. Neuropsychopharmacol Publ Am Coll Neuropsychopharmacol. 2021;46:1283–92.
Xie H, Erwin MC, Elhai JD, Wall JT, Tamburrino MB, Brickman KR, et al. Relationship of hippocampal volumes and posttraumatic stress disorder symptoms over early post-trauma periods. Biol Psychiatry Cogn Neurosci Neuroimag. 2018;3:968–75.
Quidé Y, Andersson F, Dufour-Rainfray D, Descriaud C, Brizard B, Gissot V, et al. Smaller hippocampal volume following sexual assault in women is associated with post-traumatic stress disorder. Acta Psychiatr Scand. 2018;138:312–24.
Ben-Zion Z, Artzi M, Niry D, Keynan NJ, Zeevi Y, Admon R, et al. Neuroanatomical risk factors for posttraumatic stress disorder in recent trauma survivors. Biol Psychiatry Cogn Neurosci Neuroimag. 2020;5:311–9.
Ben-Zion Z, Korem N, Spiller TR, Duek O, Keynan JN, Admon R, et al. Longitudinal volumetric evaluation of hippocampus and amygdala subregions in recent trauma survivors. Mol Psychiatry. 2023;28:657–67.
Lindgren L, Bergdahl J, Nyberg L. Longitudinal evidence for smaller hippocampus volume as a vulnerability factor for perceived stress. Cereb Cortex. 2016;26:3527–33.
Weis CN, Webb EK, Huggins AA, Kallenbach M, Miskovich TA, Fitzgerald JM, et al. Stability of hippocampal subfield volumes after trauma and relationship to development of PTSD symptoms. NeuroImage. 2021;236:118076.
Harnett NG, Stevens JS, van Rooij SJH, Ely TD, Michopoulos V, Hudak L, et al. Multimodal structural neuroimaging markers of risk and recovery from posttrauma anhedonia: a prospective investigation. Depress Anxiety. 2021;38:79–88.
Fani N, Michopoulos V, van Rooij SJH, Clendinen C, Hardy RA, Jovanovic T, et al. Structural connectivity and risk for anhedonia after trauma: A prospective study and replication. J Psychiatr Res. 2019;116:34–41.
Kennis M, van Rooij SJH, Reijnen A, Geuze E. The predictive value of dorsal cingulate activity and fractional anisotropy on long-term PTSD symptom severity. Depress Anxiety. 2017;34:410–8.
Luo Y, Liu Y, Qin Y, Zhang X, Ma T, Wu W, et al. The atrophy and laterality of the hippocampal subfields in parents with or without posttraumatic stress disorder who lost their only child in China. Neurol Sci J Ital Neurol Soc Ital Soc Clin Neurophysiol. 2017;38:1241–7.
Luo Y, Shan H, Liu Y, Wu L, Zhang X, Ma T, et al. Decreased left hippocampal volumes in parents with or without posttraumatic stress disorder who lost their only child in China. J Affect Disord. 2016;197:223–30.
Zhang L, Lu L, Bu X, Li H, Tang S, Gao Y, et al. Alterations in hippocampal subfield and amygdala subregion volumes in posttraumatic subjects with and without posttraumatic stress disorder. Hum Brain Mapp. 2021;42:2147–58.
van Rooij SJH, Kennis M, Sjouwerman R, van den Heuvel MP, Kahn RS, Geuze E. Smaller hippocampal volume as a vulnerability factor for the persistence of post-traumatic stress disorder. Psychol Med. 2015;45:2737–46.
Postel C, Mary A, Dayan J, Fraisse F, Vallée T, Guillery-Girard B, et al. Variations in response to trauma and hippocampal subfield changes. Neurobiol Stress. 2021;15:100346.
Hinojosa, CA Does Hippocampal Volume in Patients with Posttraumatic Stres…: Harvard Review of Psychiatry. [cited 2023 Aug 2]; Available from: https://journals.lww.com/hrpjournal/Abstract/2022/03000/Does_Hippocampal_Volume_in_Patients_with.3.aspx .
Admon R, Lubin G, Rosenblatt JD, Stern O, Kahn I, Assaf M, et al. Imbalanced Neural Responsivity to Risk and Reward Indicates Stress Vulnerability in Humans. Cereb Cortex. 2013;23:28–35.
Zhang W, Kaldewaij R, Hashemi MM, Koch SBJ, Smit A, van Ast VA, et al. Acute-stress-induced change in salience network coupling prospectively predicts post-trauma symptom development. Transl Psychiatry. 2022;12:1–8.
van Rooij SJH, Ravi M, Ely TD, Michopoulos V, Winters SJ, Shin J, et al. Hippocampal activation during contextual fear inhibition related to resilience in the early aftermath of trauma. Behav Brain Res. 2021;408:113282.
Tanriverdi, Gregory B, Olino DF, Ely TM, Harnett TD, Rooij NG, et al. Hippocampal threat reactivity interacts with physiological arousal to predict PTSD symptoms. J Neurosci. 2022;42:6593–604.
van Rooij SJH, Stevens JS, Ely TD, Hinrichs RC, Michopoulos V, Winters SJ, et al. The role of the hippocampus in predicting future PTSD symptoms in recently traumatized civilians. Biol Psychiatry. 2018;84:106–15.
Wang X, Xie H, Cotton AS, Duval ER, Tamburrino MB, Brickman KR, et al. Preliminary study of acute changes in emotion processing in trauma survivors with PTSD symptoms. PloS One. 2016;11:e0159065.
Stevens JS, Kim YJ, Galatzer-Levy IR, Reddy R, Ely TD, Nemeroff CB, et al. Amygdala reactivity and anterior cingulate habituation predict posttraumatic stress disorder symptom maintenance after acute civilian trauma. Biol Psychiatry. 2017;81:1023–9.
Belleau EL, Ehret LE, Hanson JL, Brasel KJ, Larson CL, deRoon-Cassini TA. Amygdala functional connectivity in the acute aftermath of trauma prospectively predicts severity of posttraumatic stress symptoms. Neurobiol Stress. 2020;12:100217.
Ben-Zion Z, Shany O, Admon R, Keynan NJ, Avisdris N, Balter SR, et al. Neural responsivity to reward versus punishment shortly after trauma predicts long-term development of posttraumatic stress symptoms. Biol Psychiatry Cogn Neurosci Neuroimag. 2022;7:150–61.
Harnett NG, Ference EW, Wood KH, Wheelock MD, Knight AJ, Knight DC. Trauma exposure acutely alters neural function during Pavlovian fear conditioning. Cortex. 2018;109:1–13.
Powers A, Hinojosa CA, Stevens JS, Harvey B, Pas P, Rothbaum BO, et al. Right inferior frontal gyrus and ventromedial prefrontal activation during response inhibition is implicated in the development of PTSD symptoms. Eur J Psychotraumatology. 2022;13:2059993.
Du MY, Liao W, Lui S, Huang XQ, Li F, Kuang WH, et al. Altered functional connectivity in the brain default-mode network of earthquake survivors persists after 2 years despite recovery from anxiety symptoms. Soc Cogn Affect Neurosci. 2015;10:1497–505.
Sullivan DR, Marx B, Chen MS, Depue BE, Hayes SM, Hayes JP. Behavioral and neural correlates of memory suppression in PTSD. J Psychiatr Res. 2019;112:30–7.
Chen HJ, Ke J, Qiu J, Xu Q, Zhong Y, Lu GM, et al. Altered whole-brain resting-state functional connectivity and brain network topology in typhoon-related post-traumatic stress disorder. Ther Adv Psychopharmacol. 2023;13:20451253231175302.
Dahlgren MK, Laifer LM, VanElzakker MB, Offringa R, Hughes KC, Staples-Bradley LK, et al. Diminished medial prefrontal cortex activation during the recollection of stressful events is an acquired characteristic of PTSD. Psychol Med. 2018;48:1128–38.
Hinojosa CA, VanElzakker MB, Hughes KC, Offringa R, Sangermano LM, Spaulding IG, et al. Exaggerated amygdala activation to ambiguous facial expressions is a familial vulnerability factor for posttraumatic stress disorder. J Psychiatr Res. 2022;156:451–9.
George GC, Keding TJ, Heyn SA, Herringa RJ. Longitudinal hippocampal circuit change differentiates persistence and remission of pediatric posttraumatic stress disorder. Depress Anxiety. 2022;39:8–18.
Manthey A, Sierk A, Brakemeier EL, Walter H, Daniels JK Does trauma-focused psychotherapy change the brain? A systematic review of neural correlates of therapeutic gains in PTSD. Eur J Psychotraumatology. 2021;12:1929025.
Malejko K, Abler B, Plener PL, Straub J. Neural correlates of psychotherapeutic treatment of post-traumatic stress disorder: a systematic literature review. Front Psychiatry. 2017;8:85.
Colvonen PJ, Glassman LH, Crocker LD, Buttner MM, Orff H, Schiehser DM, et al. Pretreatment biomarkers predicting PTSD psychotherapy outcomes: A systematic review. Neurosci Biobehav Rev. 2017;75:140–56.
Graziano RC, Vuper TC, Yetter MA, Bruce SE. Treatment outcome of posttraumatic stress disorder: a white matter tract analysis. J Anxiety Disord. 2021;81:102412.
Hinojosa CA, VanElzakker MB, Kaur N, Felicione JM, Charney ME, Bui E, et al. Pre-treatment amygdala activation and habituation predict symptom change in post-traumatic stress disorder. Front Behav Neurosci [Internet]. 2023 [cited 2023 Sep 14];17. Available from: https://www.frontiersin.org/articles/10.3389/fnbeh.2023.1198244 .
Norbury A, Rutter SB, Collins AB, Costi S, Jha MK, Horn SR, et al. Neuroimaging correlates and predictors of response to repeated-dose intravenous ketamine in PTSD: preliminary evidence. Neuropsychopharmacology. 2021;46:2266–77.
Danböck SK, Duek O, Ben-Zion Z, Korem N, Amen SL, Kelmendi B, et al. Effects of a dissociative drug on fronto-limbic resting-state functional connectivity in individuals with posttraumatic stress disorder: a randomized controlled pilot study. Psychopharmacol (Berl). 2024;241:243–52.
Yuan M, Qiu C, Meng Y, Ren Z, Yuan C, Li Y, et al. Pre-treatment resting-state functional MR imaging predicts the long-term clinical outcome after short-term paroxtine treatment in post-traumatic stress disorder. Front Psychiatry [Internet]. 2018 [cited 2024 Feb 11];9. Available from: https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2018.00532 .
Korgaonkar MS, Chakouch C, Breukelaar IA, Erlinger M, Felmingham KL, Forbes D, et al. Intrinsic connectomes underlying response to trauma-focused psychotherapy in post-traumatic stress disorder. Transl Psychiatry. 2020;10:1–11.
Garrett A, Cohen JA, Zack S, Carrion V, Jo B, Blader J, et al. Longitudinal changes in Brain function associated with Symptom Improvement in Youth with PTSD. J Psychiatr Res. 2019;114:161.
Zhutovsky P, Zantvoord JB, Ensink JBM, op den Kelder R, Lindauer RJL, van Wingen GA. Individual prediction of trauma-focused psychotherapy response in youth with posttraumatic stress disorder using resting-state functional connectivity. NeuroImage Clin. 2021;32:102898.
Steuwe C, Daniels JK, Frewen PA, Densmore M, Pannasch S, Beblo T, et al. Effect of direct eye contact in PTSD related to interpersonal trauma: an fMRI study of activation of an innate alarm system. Soc Cogn Affect Neurosci. 2014;9:88–97.
Cisler JM, Sigel BA, Steele JS, Smitherman S, Vanderzee K, Pemberton J, et al. Changes in functional connectivity of the amygdala during cognitive reappraisal predict symptom reduction during trauma-focused cognitive-behavioral therapy among adolescent girls with post-traumatic stress disorder. Psychol Med. 2016;46:1–11.
Levy-Gigi E, Szabó C, Kelemen O, Kéri S. Association among clinical response, hippocampal volume, and FKBP5 gene expression in individuals with posttraumatic stress disorder receiving cognitive behavioral therapy. Biol Psychiatry. 2013;74:793–800.
Bossini L, Santarnecchi E, Casolaro I, Koukouna D, Caterini C, Cecchini F, et al. Morphovolumetric changes after EMDR treatment in drug-naïve PTSD patients. Riv Psichiatr. 2017;52:24–31.
Butler O, Herr K, Willmund G, Gallinat J, Kühn S, Zimmermann P. Trauma, treatment and tetris: video gaming increases hippocampal volume in male patients with combat-related posttraumatic stress disorder. J Psychiatry Neurosci. JPN. 2020;45:279–87.
Butler O, Willmund G, Gleich T, Gallinat J, Kühn S, Zimmermann P. Hippocampal gray matter increases following multimodal psychological treatment for combat‐related post‐traumatic stress disorder. Brain Behav [Internet]. 2018 May [cited 2023 Aug 9];8. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5943737/ .
Kennis M, van Rooij SJH, Tromp DPM, Fox AS, Rademaker AR, Kahn RS, et al. Treatment outcome-related white matter differences in veterans with posttraumatic stress disorder. Neuropsychopharmacol Publ Am Coll Neuropsychopharmacol. 2015;40:2434–42.
Vuper TC, Philippi CL, Bruce SE. Altered resting-state functional connectivity of the default mode and central executive networks following cognitive processing therapy for PTSD. Behav Brain Res. 2021;409:113312.
Fonzo GA, Goodkind MS, Oathes DJ, Zaiko YV, Harvey M, Peng KK, et al. Amygdala and insula connectivity changes following psychotherapy for posttraumatic stress disorder: a randomized clinical trial. Biol Psychiatry. 2021;89:857–67.
Leroy A, Very E, Birmes P, Yger P, Szaffarczyk S, Lopes R, et al. Intrusive experiences in posttraumatic stress disorder: Treatment response induces changes in the directed functional connectivity of the anterior insula. NeuroImage Clin. 2022;34:102964.
Zhu X, Suarez-Jimenez B, Lazarov A, Helpman L, Papini S, Lowell A, et al. Exposure-based therapy changes amygdala and hippocampus resting-state functional connectivity in patients with posttraumatic stress disorder. Depress Anxiety. 2018;35:974–84.
Santarnecchi E, Bossini L, Vatti G, Fagiolini A, La Porta P, Di Lorenzo G, et al. Psychological and brain connectivity changes following trauma-focused CBT and EMDR treatment in single-episode PTSD patients. Front Psychol. 2019;10:129.
Galatzer-Levy IR, Bryant RA. 636,120 ways to have posttraumatic stress disorder. Perspect Psychol Sci J Assoc Psychol Sci. 2013;8:651–62.
Maron-Katz A, Zhang Y, Narayan M, Wu W, Toll RT, Naparstek S, et al. Individual patterns of abnormality in resting-state functional connectivity reveal two data-driven PTSD subgroups. Am J Psychiatry. 2020;177:244–53.
McClellan France J, Jovanovic T. Human fear neurobiology reimagined: can brain-derived biotypes predict fear-based disorders after trauma? Neurosci Biobehav Rev. 2023;144:104988.
Ahrenholtz R, Hiser J, Ross MC, Privratsky A, Sartin-Tarm A, James GA, et al. Unique neurocircuitry activation profiles during fear conditioning and extinction among women with posttraumatic stress disorder. J Psychiatr Res. 2021;141:257–66.
Stevens JS, Harnett NG, Lebois LAM, van Rooij SJH, Ely TD, Roeckner A, et al. Brain-based biotypes of psychiatric vulnerability in the acute aftermath of trauma. Am J Psychiatry. 2021;178:1037–49.
Ben-Zion Z, Spiler TR, Keynan JN, Admon R, Levy I, Liberzon I, et al. Evaluating the evidence for brain-based biotypes of psychiatric vulnerability in the acute aftermath of trauma. Am J Psychiatry. 2023;180:146–154.
Stein MB, Bomyea J. Replicating predictive cluster-based imaging biotypes after trauma: a bridge too far? Am J Psychiatry. 2023;180:114–6.
Liu Y, Hayes DN, Nobel A, Marron JS. Statistical significance of clustering for high-dimension, low-sample size data. J Am Stat Assoc. 2008;103:1281–93.
Dinga R, Schmaal L, Penninx BWJH, van Tol MJ, Veltman DJ, van Velzen L, et al. Evaluating the evidence for biotypes of depression: methodological replication and extension of. NeuroImage Clin. 2019;22:101796.
Download references
Acknowledgements
CAH is supported under an NIAAA Award, K99AA031333. GCG is supported under a NIMH T32 grant, T32MH125786. ZB-Z is supported by Yale University School of Medicine (Dr. Ifat Levy & Dr. Ilan Harpaz-Rotem). We would like to thank Drs. Sanne van Rooij and Jennifer Stevens for providing critical feedback on the manuscript, and Bona Kim, M.A., C.M.I. for creating the figures.
Author information
Authors and affiliations.
Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, Atlanta, GA, USA
Cecilia A. Hinojosa
Department of Psychiatry, McLean Hospital, Belmont, MA, USA
Grace C. George
Department of Comparative Medicine, Yale University School of Medicine, New Haven, CT, USA
Ziv Ben-Zion
Department of Psychiatry, Yale University School of Medicine, New Haven, CT, USA
US Department of Veterans Affairs National Center for PTSD, VA Connecticut Healthcare System, West Haven, CT, USA
You can also search for this author in PubMed Google Scholar
Contributions
CAH was responsible for conceptualization, data curation for all sections, project administration, visualization, validation, writing the original draft, and reviewing and editing the manuscript. GCG helped with data curation for subsections, writing the original draft, and reviewing and editing the manuscript. ZBZ helped with data curation for subsections, writing the original draft, and reviewing and editing the manuscript.
Corresponding author
Correspondence to Cecilia A. Hinojosa .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Hinojosa, C.A., George, G.C. & Ben-Zion, Z. Neuroimaging of posttraumatic stress disorder in adults and youth: progress over the last decade on three leading questions of the field. Mol Psychiatry (2024). https://doi.org/10.1038/s41380-024-02558-w
Download citation
Received : 18 September 2023
Revised : 04 April 2024
Accepted : 08 April 2024
Published : 17 April 2024
DOI : https://doi.org/10.1038/s41380-024-02558-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Article Information
MERS indicates Middle East respiratory syndrome; SARS, severe acute respiratory syndrome.
- Improving the Assessment of COVID-19–Associated Posttraumatic Stress Disorder—Reply JAMA Psychiatry Comment & Response July 1, 2021 Delfina Janiri, MD; Georgios D. Kotzalidis, MD, PhD; Gabriele Sani, MD
- Improving the Assessment of COVID-19–Associated Posttraumatic Stress Disorder JAMA Psychiatry Comment & Response July 1, 2021 Brian P. Marx, PhD; Paula P. Schnurr, PhD; Matthew J. Friedman, MD, PhD
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
- CME & MOC
Janiri D , Carfì A , Kotzalidis GD, et al. Posttraumatic Stress Disorder in Patients After Severe COVID-19 Infection. JAMA Psychiatry. 2021;78(5):567–569. doi:10.1001/jamapsychiatry.2021.0109
Manage citations:
© 2024
- Permissions
Posttraumatic Stress Disorder in Patients After Severe COVID-19 Infection
- 1 Department of Psychiatry, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy
- 2 Department of Geriatrics, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy
- Comment & Response Improving the Assessment of COVID-19–Associated Posttraumatic Stress Disorder—Reply Delfina Janiri, MD; Georgios D. Kotzalidis, MD, PhD; Gabriele Sani, MD JAMA Psychiatry
- Comment & Response Improving the Assessment of COVID-19–Associated Posttraumatic Stress Disorder Brian P. Marx, PhD; Paula P. Schnurr, PhD; Matthew J. Friedman, MD, PhD JAMA Psychiatry
Posttraumatic stress disorder (PTSD) may occur in individuals who have experienced a traumatic event. Previous coronavirus epidemics were associated with PTSD diagnoses in postillness stages, with meta-analytic findings indicating a prevalence of 32.2% (95% CI, 23.7-42.0). 1 However, information after severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is piecemeal. We aimed at filling this gap by studying a group of patients with coronavirus disease 2019 (COVID-19) who sought treatment at the emergency department, most of whom required hospitalization, eventually recovered, and were subsequently referred to a postacute care service for multidisciplinary assessment.
A total of 381 consecutive patients who presented to the emergency department with SARS-CoV-2 and recovered from COVID-19 infection were referred for a postrecovery health check to a postacute care service established April 21, 2020, at the Fondazione Policlinico Universitario Agostino Gemelli IRCCS in Rome, Italy. Patients were offered a comprehensive and interdisciplinary medical and psychiatric assessment, detailed elsewhere, 2 which included data on demographic, clinical, psychopathological, and COVID-19 characteristics. Trained psychiatrists diagnosed PTSD using the criterion-standard Clinician-Administered PTSD Scale for DSM-5 (CAPS-5), reaching a Cohen κ interrater reliability of 0.82. To meet PTSD criteria, in addition to traumatic event exposure (criterion A), patients must have had at least 1 DSM-5 criterion B and C symptom and at least 2 criterion D and E symptoms. Criteria F and G must have been met as well. Additional diagnoses were made through the Structured Clinical Interview for DSM-5 . Participants provided written informed consent, and the study was approved by the Università Cattolica and Fondazione Policlinico Gemelli IRCCS Institutional Ethics Committee.
Data for patients with and without PTSD were compared with the χ 2 test for nominal variables and one-way analysis of variance for continuous variables. Factors significantly associated with PTSD were subjected to a binary logistic regression. P values were 2-tailed, and significance was set at a P value less than .05. Analyses were performed using R version 4 0.0 (The R Foundation).
From April 21 to October 15, 2020, the postacute care service assessed 381 White patients who had recovered from COVID-19 infection within 30 to 120 days, 166 (43.6%) of whom were women. The mean (SD; range) age was 55.26 (14.86; 18-89). During acute COVID-19 illness, most patients were hospitalized (309 of 381 [81.1%]), with a mean (SD) length of hospital stay of 18.41 (17.27) days.
PTSD was found in 115 participants (30.2%). In the total sample, additional diagnoses were depressive episode (66 [17.3%]), hypomanic episode (3 [0.7%]), generalized anxiety disorder (27 [7.0%]), and psychotic disorders (1 [0.2%]). Patients with PTSD were more frequently women (64 [55.7%]), reported higher rates of history of psychiatric disorders (40 [34.8%]) and delirium or agitation during acute illness (19 [16.5%]), and presented with more persistent medical symptoms in the postillness stage (more than 3 symptoms, 72 [62.6%]) ( Table ). Logistic regression specifically identified sex (Wald 1 = 4.79; P = .02), delirium or agitation (Wald 1 = 5.14; P = .02), and persistent medical symptoms (Wald 2 = 12.46; P = .002) as factors associated with PTSD.
This cross-sectional study found a PTSD prevalence of 30.2% after acute COVID-19 infection, which is in line with findings in survivors of previous coronavirus illnesses 1 compared with findings reported after other types of collective traumatic events ( Figure ). 3 - 5 Associated characteristics were female sex, which has been extensively described as a risk factor for PTSD, 1 , 3 , 5 history of psychiatric disorders, and delirium or agitation during acute illness. In the PTSD group, we also found more persistent medical symptoms, often reported by patients after recovery from severe COVID-19. 6
This study had limitations, including the relatively small sample size and cross-sectional design, as PTSD symptom rates may vary over time. Furthermore, this was a single-center study that lacked a control group of patients attending the emergency department for other reasons. Further longitudinal studies are needed to tailor therapeutic interventions and prevention strategies.
Accepted for Publication: January 26, 2021.
Published Online: February 18, 2021. doi:10.1001/jamapsychiatry.2021.0109
Corresponding Author: Delfina Janiri, MD, Department of Psychiatry, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Largo Francesco Vito 1, 00168 Rome, Italy ( [email protected] ).
Author Contributions: Dr Janiri had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design : Janiri, Carfì, Sani.
Acquisition, analysis, or interpretation of data : All authors.
Drafting of the manuscript : Janiri, Kotzalidis, Sani.
Critical revision of the manuscript for important intellectual content : Carfì, Kotzalidis, Bernabei, Landi, Sani.
Statistical analysis : Janiri, Sani.
Administrative, technical, or material support : Carfì.
Supervision : Kotzalidis, Bernabei, Landi, Sani.
Conflict of Interest Disclosures: Dr Sani reports personal fees from Janssen, Angelini Spa, and Lundbeck outside the submitted work. No other disclosures were reported.
Additional Contributions: We thank the Gemelli Against COVID-19 Post-Acute Care Study Group and the patients who contributed their time and effort to participate in this study.
Additional Information: The members of the Gemelli Against COVID-19 Post-Acute Care Study Group are listed in reference 2.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
CASE REPORT article
5-meo-dmt for post-traumatic stress disorder: a real-world longitudinal case study.

- 1 Integrated Research Literacy Group, Draper, UT, United States
- 2 Department of Psychiatry, University of Cambridge, Cambridge, United Kingdom
- 3 Department of Psychology and Neuroscience, Duke University, Durham, NC, United States
- 4 Neuroscience Interdepartmental Program, University of California, Los Angeles, Los Angeles, CA, United States
- 5 Department of Family and Consumer Studies, University of Utah, Salt Lake City, UT, United States
- 6 School of Humanities and Creativity, Sheridan College, Oakville, ON, Canada
- 7 Department of Pediatrics, Division of Pediatric Psychology and Developmental Medicine, Medical College of Wisconsin, Milwaukee, WI, United States
- 8 Children’s Wisconsin, Milwaukee, WI, United States
- 9 The Mission Within, Baja California, Mexico
- 10 Menninger Department of Psychiatry and Behavioral Sciences, Baylor College of Medicine, Houston, TX, United States
- 11 Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX, United States
- 12 Department of Psychiatry, Yale School of Medicine, New Haven, CT, United States
Psychedelic therapy is, arguably, the next frontier in psychiatry. It offers a radical alternative to longstanding, mainstays of treatment, while exciting a paradigm shift in translational science and drug discovery. There is particular interest in 5-methoxy- N,N -dimethyltryptamine (5-MeO-DMT)—a serotonergic psychedelic—as a novel, fast-acting therapeutic. Yet, few studies have directly examined 5-MeO-DMT for trauma- or stress-related psychopathology, including post-traumatic stress disorder (PTSD). Herein, we present the first longitudinal case study on 5-MeO-DMT for chronic refractory PTSD, in a 23-year-old female. A single dose of vaporized bufotoxin of the Sonoran Desert Toad ( Incilius alvarius ), containing an estimated 10−15 mg of 5-MeO-DMT, led to clinically significant improvements in PTSD, with next-day effects. This was accompanied by marked reductions in hopelessness and related suicide risk. Improvements, across all constructs, were sustained at 1-, 3-, 6-, and 12-months follow-up, as monitored by a supporting clinician. The subject further endorsed a complete mystical experience, hypothesized to underly 5-MeO-DMT’s therapeutic activity. No drug-related, serious adverse events occurred. Together, results showed that 5-MeO-DMT was generally tolerable, safe to administer, and effective for PTSD; however, this was not without risk. The subject reported acute nausea, overwhelming subjective effects, and late onset of night terrors. Further research is warranted to replicate and extend these findings, which are inherently limited, non-generalizable, and rely on methods not clinically accepted.
Introduction
5-methoxy- N,N -dimethyltryptamine (5-MeO-DMT) is a natural, short-acting psychoactive indolealkylamine ( 1 ). It was first synthesized in 1936 ( 2 ), later found in several plant (e.g., Dictyoloma incanescens ), fungi (e.g., Amanita citrina ), and animal (e.g., Incilius al var ius ) species ( 2 , 3 ). In humans, 5-MeO-DMT is likely endogenous, with trace amounts detected in urine (2 of 113 people), blood (20 of 39 people), and cerebrospinal fluid (40 of 136 people) ( 2 ). However, various studies contradict this finding ( 2 , 4 ); and its physiological role, if any, remains unclear. Based on ethnographic reports, 5-MeO-DMT may have been used by indigenous cultures, as part of plant extracts and botanical preparations (e.g., yopo or cohoba snuff), specifically for spiritual and ritualistic practices ( 5 , 6 ). These reports date back to ancient People of Mesoamerica ( 5 , 6 ). Yet, there is little evidence to support such claims. Further, contrary to published work, 5-MeO-DMT is not found in traditional or analog ayahuasca ( 7 , 8 ). This points to its use being a more recent phenomenon ( 9 , 10 ).
Regarding its pharmacology, 5-MeO-DMT is a nonselective serotonin (5-HT) receptor agonist ( 11 , 12 ). It also binds to other receptors, including dopamine and serotonin, as well as norepinephrine transporters ( 12 ). The entheogen mildly inhibits 5-HT reuptake, yet exerts no appreciable effects on monoamine release ( 13 ). 5-MeO-DMT has the highest affinity for 5-HT 1A (K i , < 10 nM) over 5-HT 2A (K i , >1,000 nM), with 300–1,000-fold greater selectivity ( 11 , 12 , 14 ). This is notable, given that most serotonergic psychedelics, like LSD and psilocybin, are mediated by 5-HT 2A activation ( 15 ). Other non-5-HT 2A receptors have not been studied as widely ( 16 ). Metabolically, 5-MeO-DMT is processed via oxidative deamination—catalyzed by monoamine oxidase A (MAO A )—into the active metabolite, bufotenine ( 17 ). Use of 5-MeO-DMT with MAO inhibitors (MAOIs), such as antidepressants, can augment and prolong neurochemical and behavioral effects, by blocking biotransformation of 5-MeO-DMT and increasing its exposure ( 18 ). Nonetheless, MAOIs can induce serotonergic toxicity ( 19 ), or ‘serotonin syndrome’, a potentially life-threatening drug reaction caused by excess serotonin in the brain ( 20 ). This can present as shivering or diarrhea, as well as muscle rigidity, high fever, and epileptic seizure. Combining 5-MeO-DMT with harmala alkaloids, short-term MAOIs found in ayahuasca, can also produce toxic interactions, and even death ( 21 ).
There are several routes for administering 5-MeO-DMT. This includes inhalation (~6–20 mg), intranasal (~10 mg), intravenous (~1–3 mg), sublingual (~10 mg), and oral (~30 mg) methods ( 18 , 22 ). Inhalation by vapor is most commonly reported, given its accessibility and relative ease of use, particularly in naturalistic settings ( 6 , 10 ). However, it can lead to intense rapid onset, relative to other dosage forms, like intramuscular injection. The onset, duration, and magnitude of subjective effects, occasioned by 5-MeO-DMT, are both route- and dose-dependent. For example, vaporization induces effects within ~10–15 s and peak experiences within ~2–5 min, resolving within ~25–30 min ( 6 , 22 , 23 ). Conversely, insufflation has a slower onset of action, due to delayed absorption, inducing effects within ~3–4 min and peak experiences within ~35–40 min, resolving within ~60–70 min ( 24 ). Irrespective of route, 5-MeO-DMT produces diverse subjective effects, including visual and auditory hallucinations, distorted time perception, and memory impairment ( 4 ). It also occasions peak mystical experiences comparable to high-dose psilocybin ( 25 ). Ego dissolution, a complete loss of self-identity, is frequently reported, as are profound near-death experiences ( 22 , 25 – 28 ). 5-MeO-DMT can, therefore, be challenging to navigate, with reports of fear, extreme anxiety, and paranoia ( 29 ). Users also describe perceptual isolation, seeing “all white” or “all black” ( 30 ). This contrasts to classic psychedelics, like N,N -DMT and LSD, that produce highly detailed, complex mental imagery. From a clinical standpoint, 5-MeO-DMT shows signals of benefit to mental health and well-being ( 3 , 4 ). However, there is a paucity of evidence in the field, particularly for trauma- and stress-related psychopathology.
Here, in accordance with CARE (CAse REport) guidelines ( 31 ), we present the first real-world, longitudinal case study on 5-MeO-DMT for post-traumatic stress disorder (PTSD). The subject provided written consent for publication and authorized disclosure of private health information. The data presented here were collected by the subject for their own interest and safety, and to monitor their progress over time. We then gained access to and analyzed the data retrospectively. To protect anonymity, the materials are not publicly available. This case study was exempt from ethics review and approval, in line with the Baylor College of Medicine Human Research Protections Manual, including Institutional Review Board procedures.
Subject information
A 23-year-old female presented with chronic refractory PTSD. She reported night terrors, trauma avoidance, negative affect, and hypervigilance. This developed from repeat sexual abuse, spanning six years as an adolescent. There was no relevant family history. Past interventions included variants of cognitive behavioral therapy (CBT), namely prolonged exposure (PE: 10 sessions), cognitive processing therapy (CPT: 12 sessions), and stress inoculation training (SIT: 8 sessions). These techniques targeted feared stimuli, maladaptive beliefs, and stress reactivity, respectively. However, each resulted in marginal improvements. She was then prescribed sertraline (Zoloft: 50 mg daily), a selective serotonin reuptake inhibitor (SSRI), following one week at 25 mg daily. This regimen adhered to pharmacotherapy guidelines for PTSD. Notwithstanding, the subject failed to respond adequately, reporting notable side effects, such as lethargy and disturbed sleep. She was, therefore, tapered off sertraline over the course of four weeks. This led to protracted symptoms and increased night terrors. Eventually, the subject was prescribed trazodone (Desyrel: 75 mg daily), a serotonin antagonist and reuptake inhibitor (SARI), for mixed insomnia. She experienced partial symptom relief and continued taking the medication, accordingly. The subject had no history of psychedelic use; however, she periodically smoked cannabis to manage her anxiety. See Figure 1 for a timeline of events.
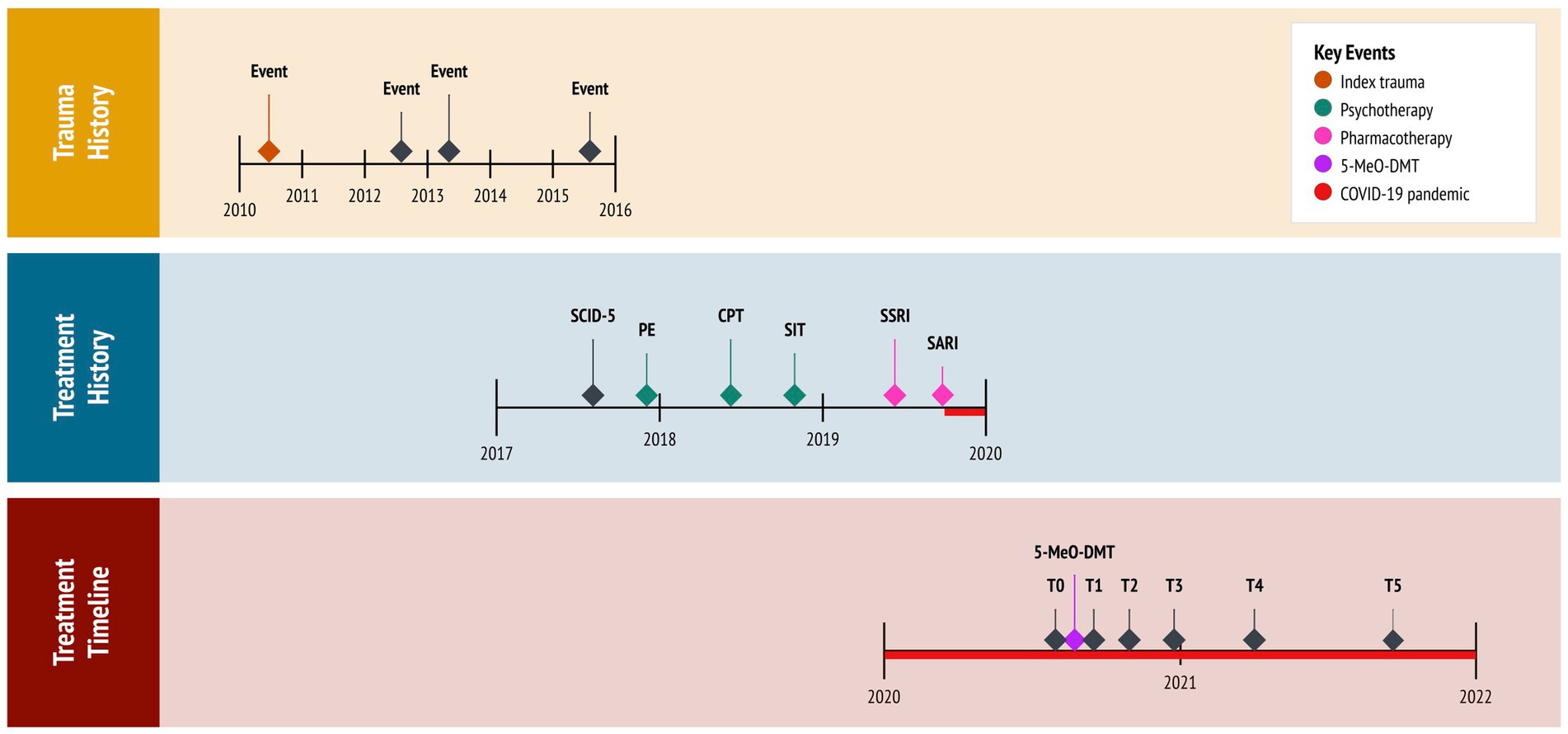
Figure 1 . Timeline of historical and clinical events. 5-MeO-DMT, 5-methoxy- N,N -dimethyltryptamine (experimental treatment); COVID-19, coronavirus disease pandemic; CPT, cognitive processing therapy (cognitive behavioral therapy); PE, prolonged exposure (cognitive behavioral therapy); SARI, serotonin antagonist and reuptake inhibitor (trazadone); SCID-5, Structured Clinical Interview for DSM-5 (diagnostic assessment); SIT, stress inoculation therapy (cognitive behavioral therapy); SSRI, selective serotonin reuptake inhibitor (sertraline); T0, baseline; T1, 24 h follow-up; T2, 1 month follow-up; T3, 3 months follow-up; T4, 6 months follow-up; T5, 12 months follow-up.
The coronavirus (COVID-19) pandemic, restricting social contact with friends and family, further aggravated the subject’s condition. Critically, she desired to end “intense emotional pain” and “chronic sadness.” Isolated in lockdown, desperate for help, and at risk of suicide, the subject pursued self-treatment with 5-MeO-DMT. This was motivated by (1) her resistance to first- and second-line therapies for PTSD, having attempted multiple interventions; (2) evidence on the potential benefits of 5-MeO-DMT for anxiety and trauma, acquired from reading news articles and research studies; (3) new legislation approved in her state (Oregon, Measure 110), which decriminalized the possession of controlled substances, including psychedelics; and (4) access to a trauma-informed 5-MeO-DMT facilitator, to whom a friend referred her to.
Diagnostic assessment
The subject was diagnosed with PTSD at 19 years of age. This was provided by her treating psychiatrist who, at the time, administered the Structured Clinical Interview for DSM-5 (SCID-5) ( 32 ), specifically the PTSD Module. The interview revealed a chronic course with severe PTSD symptoms and comorbid depression. Four years later, the subject pursued 5-MeO-DMT, independent from her psychiatrist, supported by a trauma-informed facilitator. The facilitator had extensive experience with 5-MeO-DMT, who advised on dosing and guided her experience. A licensed clinician, likewise, supported the subject in this pursuit. The clinician administered assessments, monitored her experience, and completed follow-ups. Assessments included the PTSD Checklist for DSM-5 [PCL-5; ( 33 )], the Beck Hopelessness Scale [BHS; ( 34 )] and the Clinical Global Impressions [CGI; ( 35 )] questionnaire. These were used to track the subject’s progress over time, administered prior to 5-MeO-DMT dosing (i.e., at baseline), and again 24 h-, 1 month-, 3 months-, 6 months-, and 12 months later (i.e., at follow-ups). For safety purposes, the clinician took vital signs before, during, and after 5-MeO-DMT dosing. This consisted of blood pressure (mmHg), heart rate (bpm), and peripheral oxygen saturation (SpO 2 ). To assess acute, subjective effects, the Mystical Experiences Questionnaire [MEQ-30; ( 36 )] was administered 3 h post-dosing. The clinician observed the subject for a total of 5 h after her 5-MeO-DMT experience, and conducted follow-ups via phone 24, 36, and 72 h later, before switching to once a month.
PTSD checklist for DSM-5
The PCL-5 is a 20-item measure of PTSD symptoms. It has excellent internal consistency (α = 0.94) ( 33 ), comprising four factors: ‘thought intrusion’, ‘stimuli avoidance’, ‘negative mood and cognitions’, and ‘altered reactivity’. Items are rated on a 5-point scale, with ‘not at all’ (0) and ‘extremely’ (4) as endpoints. The PCL-5 is scored by summing items within a given factor, as well as all items together. Total scores range from 0 to 80. Higher scores reflect greater symptom severity, with 31–33 typically used as the cut-off point for probabilistic PTSD. When monitoring symptoms, a 5–10-point difference indicates reliable change, not due to chance, whereas a 10–20-point difference indicates clinically significant change. The ‘past week’ version of the PCL-5 was utilized in this case study.
Impressions
At baseline, the subject’s total score was 72 of 80 (3.79 ± 0.42), meeting threshold criteria for ‘severe’ PTSD, and a provisional diagnosis. Regarding PCL-5 factors, she scored the highest on ‘altered reactivity’ (4.00 ± 0.00), followed by ‘thought intrusion’ (3.80 ± 0.45), ‘negative mood and cognitions’ (3.71 ± 0.49), and ‘stimuli avoidance’ (3.50 ± 0.71).
Beck hopelessness scale
The BHS is a 20-item measure of hopelessness. It has excellent internal consistency (α = 0.97) ( 37 ), comprising three factors: ‘feelings about the future’, ‘loss of motivation’, and ‘future expectations’. Items are rated on a 2-point scale, using dichotomous ‘true’ (0/1) and ‘false’ (0/1) statements. The BHS is scored by summing items within a given factor, as well as all items together. Total scores range from 0 to 20. Higher scores reflect greater hopelessness, categorized into four levels: ‘normal’ (0–3), ‘mild’ (4–8), ‘moderate’ (9–14), and ‘severe’ (>14). A cut-off score of 9 is frequently used to detect risk of suicidal ideation and behavior.
At baseline, the subject’s total score was 17 of 20 (0.85 ± 0.37), meeting threshold criteria for ‘severe’ hopelessness and suicide risk. Regarding BHS factors, she scored the highest on ‘feelings about the future’, (1.00 ± 0.00) and ‘future expectations’ (1.00 ± 0.00), followed by ‘loss of motivation’ (0.63 ± 0.52).
Clinical global impressions
The CGI is a 3-item measure of global functioning. It was developed for clinical trials, aimed at capturing change after initiating a study drug. The CGI includes three factors. The first factor measures ‘illness severity’, rated on a 7-point scale, anchored by ‘normal and not at all ill’ (1) and ‘among the most extremely ill’ (7). The second factor measures ‘global improvement’, also rated on a 7-point scale, with ‘very much improved’ (1) and ‘very much worse’ (7) as endpoints. Finally, the third factor measures ‘therapeutic response’, rated on a 5-point scale, anchored by ‘marked improvement and no side effects’ (0) and ‘unchanged or worse and side effects outweigh therapeutic effect’ (4). This third factor considers both therapeutic efficacy and drug-related adverse events. A zero is allocated if there is no assessment. Each factor is rated separately, yielding no total scores.
At baseline, the subject’s score for ‘illness severity’, regarding PTSD, was 6 of 7, meeting threshold criteria for ‘severely ill’. In particular, she exhibited disruptive trauma- and stress-related psychopathology, with symptoms considerably impairing her behavior and function. The other two factors, ‘global improvement’ and ‘therapeutic response’, were not assessed at baseline, as they measure changes after treatment.
Therapeutic intervention
5-MeO-DMT was obtained and administered by the subject. The experience occurred in the comfort of her home. Guided by the facilitator, she first set an intention for the experience. “I want to understand and accept the roots of my trauma.” This was designed to help navigate potentially difficult psychedelic states and material, by re-centering the subject’s attention. Next, she engaged in body scan meditation, a specific form of mindfulness practice. This involved deep breathing and mind–body awareness, aimed at relaxation. The subject then inhaled 50 mg of vaporized bufotoxin, derived from the Sonoran Desert Toad ( Incilius alvarius ), slowly and consistently. This was estimated to contain 10–15 mg of 5-MeO-DMT [20–30% of total dried weight ( 38 )]. Using a torch lighter, the bufotoxin was heated in a glass vial until its contents were vaporized. She held the dose for 10 s, exhaled slowly and consistently, and lied down with an eye mask on. Ambient music played in the background. The onset of effects was rapid (15–30 s), with peak effects lasting 10–15 min, resolving within 25–30 min. After the effects had subsided, the subject re-engaged in body scan meditation. She then discussed her experience with the facilitator, integrating newfound insights. Finally, the clinician reviewed the subject’s vital signs and asked about her experience, recording any undesirable reactions. Three hours later, the clinician administered the MEQ-30.
Follow-up and outcomes
5-MeO-DMT was generally tolerated by the subject. Mild nausea was reported, which resolved within 30 min. There were slight increases in systolic blood pressure (126.00 ± 3.54), diastolic blood pressure (89.00 ± 4.24), and heart rate (81.50 ± 4.95), whereas oxygen saturation (97.50 ± 0.71) remained stable. See Table 1 and Figure 2 . Overall, no drug-related, serious adverse events occurred. However, the subject reported “profoundly strong” subjective effects. She described being “instantly blasted” into another dimension. At first, colors were extremely vivid, then morphed into “complete whiteness.” The subject failed to make sense of psychedelic content, stating that visuals were “bright and god-like,” yet vague and fleeting. She also reported increased body temperature and euphoria. “I felt really warm, like my body was melting. It was calm and blissful.” This was accompanied by radical ego dissolution. “I had no identity. I was still alive, but my body was gone. It was quite overwhelming. I just had to surrender.”
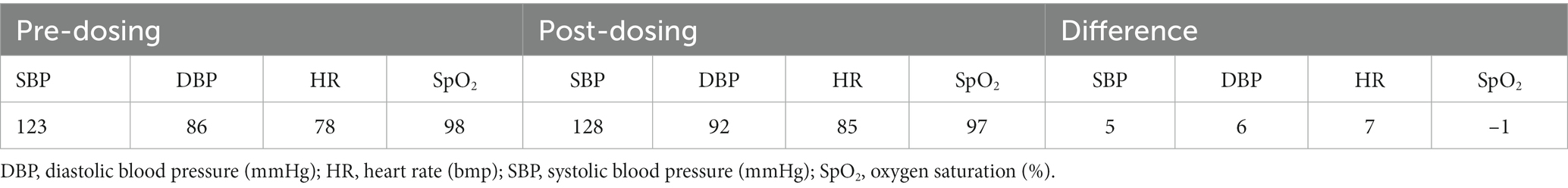
Table 1 . Clinician-reported vital signs.
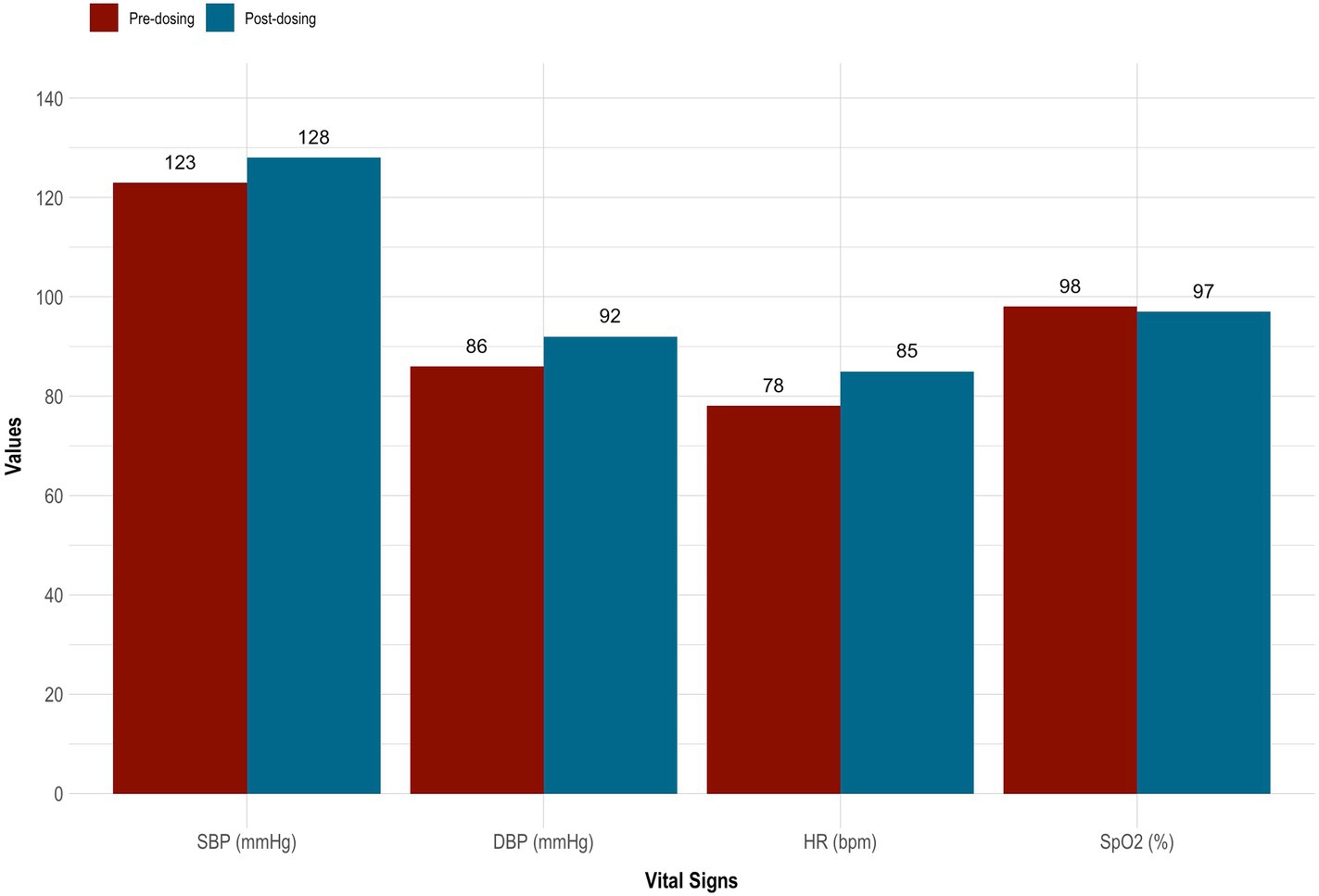
Figure 2 . Vital signs taken before and after 5-MeO-DMT dosing. 5-MeO-DMT, 5-methoxy- N,N -dimethyltryptamine; DBP, diastolic blood pressure (mmHg); HR, heart rate (bmp); SBP, systolic blood pressure (mmHg); SpO 2 , peripheral blood oxygenation (%).
On the MEQ-30, the subject endorsed strong mystical-like effects. Her total score was 135 of 150 (4.47 ± 0.62). She also met criteria for a ‘complete mystical experience’. This was evidenced by scoring ≥60% of the maximum possible scores on all four factors of the MEQ-30: ‘mysticism’ (4.47 ± 0.62 [89.3%]), ‘positive mood’ (4.33 ± 0.75 [86.7%]), ‘transcendence’ (4.67 ± 0.47 [93.3%]), and ‘ineffability; (4.33 ± 0.47 [86.7%]). See Figure 3 for details.
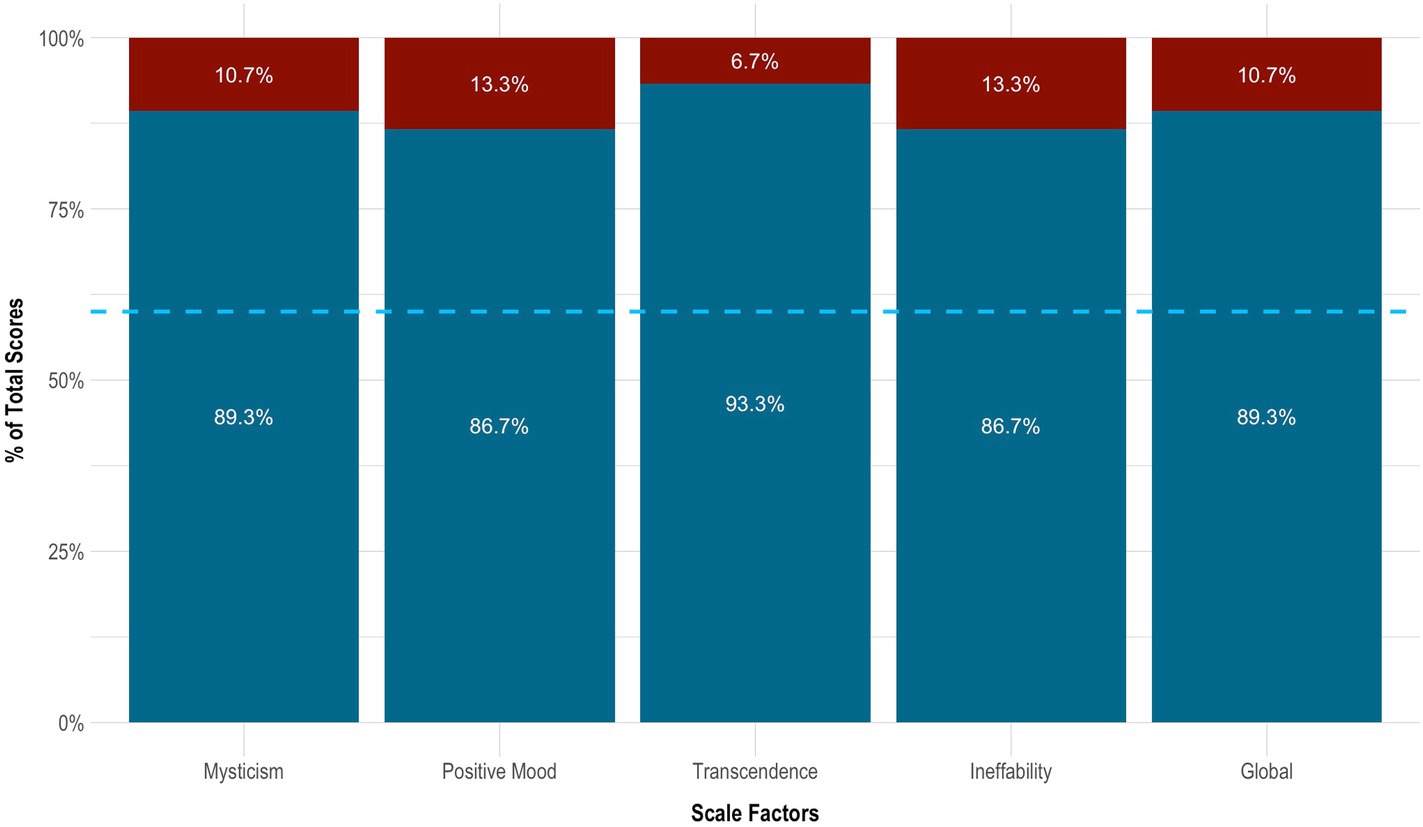
Figure 3 . Mystical effects of 5-MeO-DMT. Blue dotted line indicates the cut-off point for a complete mystical experience (≥60% of total scores across factors). 5-MeO-DMT, 5-methoxy- N,N -dimethyltryptamine; MEQ-30, Mystical Experience Questionnaire.
On the PCL-5, the subject had a clinically significant change in PTSD, which sustained across time. This was evidenced by a ≥ 10-point reduction in total scores from baseline to 24 h (−54 points), 1 month (−49 points), 3 months (−37 points), 6 months (−46 points), and 12 months (−50 points) follow-up. In particular, her symptoms decreased by 75.0% from baseline to 24 h (3.79 ± 0.42 vs. 0.95 ± 0.71), increased by 27.8% from 24 h to 1 month (0.95 ± 0.71 vs. 1.21 ± 0.63), increased by 52.2% from 1 month to 3 months (1.21 ± 0.63 vs. 1.84 ± 0.76), decreased by 25.7% from 3 months to 6 months (1.84 ± 0.76 vs. 1.37 ± 0.68), and finally decreased by 15.4% from 6 months to 12 months (1.37 ± 0.68 vs. 1.16 ± 0.60) follow-up. From baseline to 12 months follow-up, she experienced the greatest improvement in ‘negative mood and cognitions’ (3.71 ± 0.49 vs. 1.10 ± 0.69), followed by ‘thought intrusion’ (3.80 ± 0.45 vs. 1.00 ± 0.71), ‘altered reactivity’ (4.00 ± 0.00 vs. 1.40 ± 0.55), and ‘stimuli avoidance’ (3.50 ± 0.71 vs. 1.00 ± 0.00). See Table 2 and Figures 4A , B .
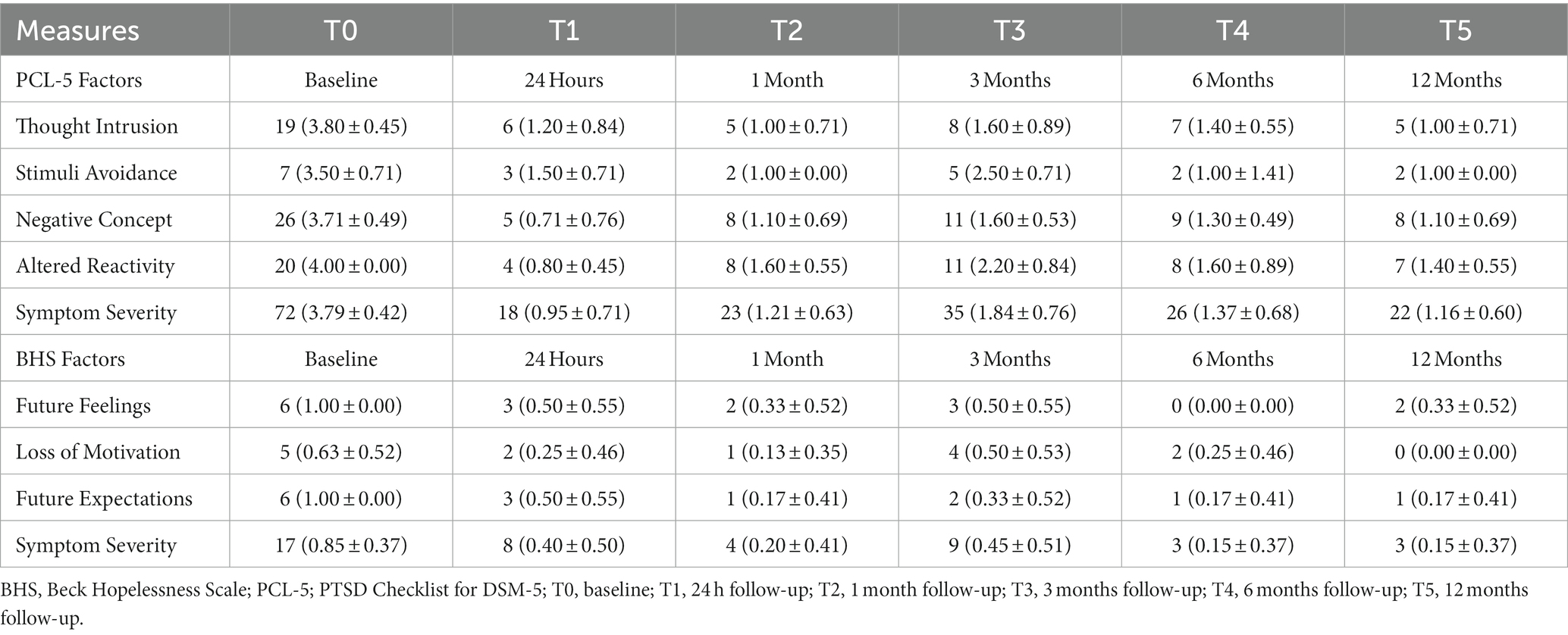
Table 2 . Self-reported outcome measures.
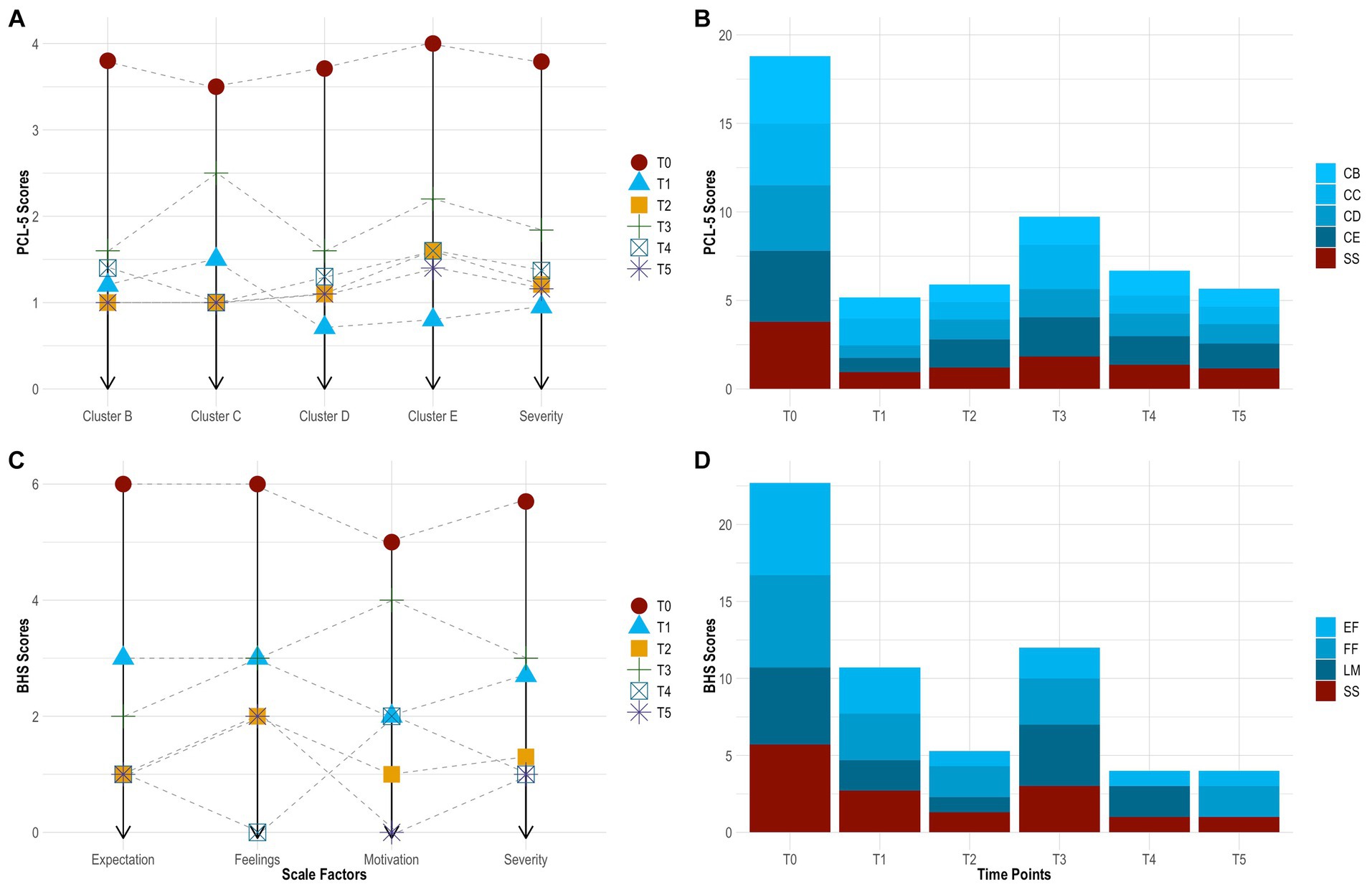
Figure 4 . Change in PTSD symptoms by time point [ (A) , line graph]. Change in PTSD symptoms across time [ (B) , bar chart]. Change in hopelessness symptoms by time point [ (C) line graph]. Change in hopelessness symptoms across time [ (D) , bar chart]. BHS, Beck Hopelessness Scale; CB, cluster B (thought intrusion); CC, cluster C (stimuli avoidance); CD, cluster D (negative mood and cognitions); CE, cluster E (altered reactivity); EF, expectations about the future (hopelessness); FF, feelings about the future (hopelessness); LM, loss of motivation (hopelessness); PCL-5, PTSD Checklist for DSM-5; PTSD, post-traumatic stress disorder; SS, symptom severity; T0, baseline; T1, 24 h follow-up; T2, 1 month follow-up; T3, 3 months follow-up; T4, 6 months follow-up; T5, 12 months follow-up.
On the BHS, the subject showed robust improvement in hopelessness. This also sustained across time. Her symptoms decreased by 52.9% from baseline to 24 h (0.85 ± 0.37 vs. 0.40 ± 0.50), decreased by 50.0% from 24 h to 1 month (0.40 ± 0.50 vs. 0.20 ± 0.41), increased by 125.0% from 1 month to 3 months (0.40 ± 0.50 vs. 0.45 ± 0.51), decreased by 66.7% from 3 months to 6 months (0.45 ± 0.51 vs. 0.15 ± 0.37), and remained stable from 6 months to 12 months (0.15 ± 0.37 vs. 0.15 ± 0.37) follow-up. From baseline to 12 months follow-up, she experienced the greatest improvement in ‘loss of motivation’ (0.63 ± 0.52 vs. 0.00 ± 0.00) and ‘future expectations’ (1.00 ± 0.00 vs. 0.17 ± 0.41), followed by ‘feelings about the future’ (0.63 ± 0.52 vs. 0.33 ± 0.52). Further, the subject had a clinically significant change in suicide risk. This was evidence by scoring ≤9 at 24 h (score = 8), 1 month (score = 4), 3 months (score = 9), 6 months (score = 3), and 12 months (score = 8) follow-up. See Table 2 and Figures 4C , D .
On the CGI, the clinician reported marked reductions in PTSD, which sustained across time. Rated at each time point, she presented as ‘severely ill’ at baseline (score = 6), ‘mildly ill’ at 24 h (score = 3), ‘borderline ill’ at 1 month (score = 2), ‘mildly ill’ at 3 months (score = 3), ‘not at all ill’ at 6 months (score = 1), and ‘not at all ill’ at 12 months (score = 1) follow-up. These ratings considered the clinician’s total experience treating PTSD. Relative to baseline, the subject’s global functioning changed from ‘much improved’ at 24 h post-dosing (score = 2), representing a significant change, with increased functioning and moderate symptoms, to ‘very much improved’ at 12 months follow-up (score = 1), indicating a substantial change, with good functioning and minimal symptoms. This was judged independent from any beliefs about 5-MeO-DMT. Finally, based on drug effect, her therapeutic response was ‘marked’ at 24 h post-dosing (score = 2), with side effects that did not significantly interfere with functioning, and ‘marked’ again at 12 months-follow-up (score = 1), with no side effects. See Table 3 .
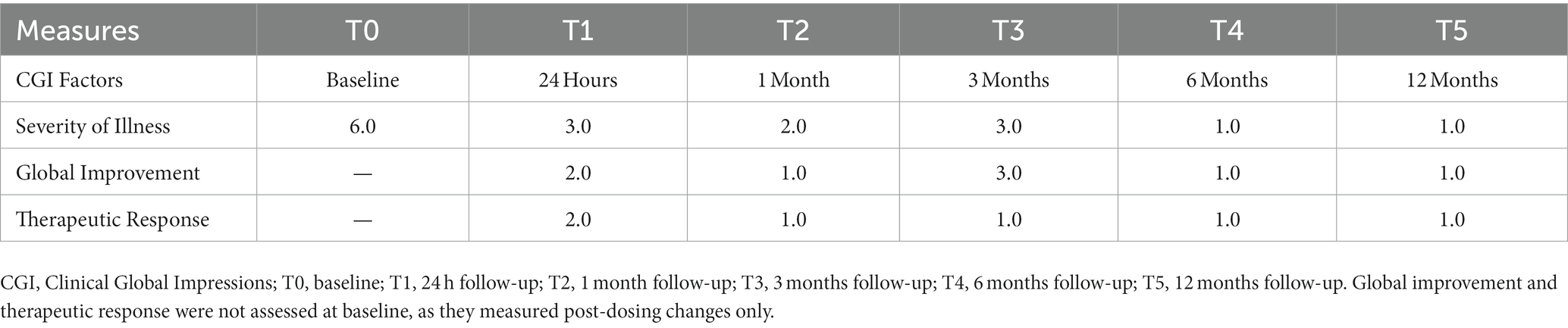
Table 3 . Clinician-reported outcome measures.
In this case study, a single dose of vaporized toad bufotoxin, containing 5-MeO-DMT, led to clinically significant improvements in PTSD, with next-day effects. These gains were sustained at 1-, 3-, 6-, and 12-months follow-up. Moreover, the subject showed striking reductions in hopelessness and related suicide risk. These changes were, likewise, durable across time. Self-reported improvements further reflected clinician-observed changes in global functioning. 5-MeO-DMT was generally tolerated. No drug-related, serious adverse events occurred. However, there were nominal increases in blood pressure and heart rate. This did not extend to oxygen saturation. Subjective effects were also overwhelming. Interestingly, 5-MeO-DMT produced more visual content than previously described ( 30 ). Colors appeared at the beginning of her experience, then faded into transcendent light; the latter being more consistent with literature ( 30 ). The subject’s dose and setting likely impacted her perceptual experience ( 38 ). Regardless, more data is needed to characterize the phenomenology of 5-MeO-DMT, and how this compares to other psychedelics. This is particularly important for optimizing facilitation and harm reduction practices, in helping patients navigate psychedelic states, as well as for targeting PTSD and chronic stress pathology.
Furthermore, the subject endorsed a strong and complete mystical experience. While the mechanism underlying her therapeutic response is unknown, it may be explained, in part, by the epistemological or ‘noetic quality’ of mystical states, occasioned by 5-MeO-DMT ( 39 ). These psychological states are characteristic of psychedelics, namely serotonergic compounds ( 39 ); have been shown to correlate, mediate, and predict therapeutic efficacy ( 40 ); and include feelings of transcendence, ego dissolution, and ineffability as well as unity, love, and peace ( 41 ). Thus, people have rated mystical experiences in their top five most important life events, in terms of personal meaning and spiritual significance, next to giving birth or losing a loved one ( 42 , 43 ). These effects can persist up to 30 years after taking a psychedelic ( 44 ). In the present case study, the subject described the mystical effects of 5-MeO-DMT as both substantial and enduring. “It was the most profound and frightening experience of my life. I saw bright colors. I was connected to all things. I disappeared into space. I smiled for the first time in a long time. I cried and screamed. I forgot about [my] pain and trauma… then relived it. My body had permission to heal. I moved on. It’s hard to put it into words… beautiful and challenging I guess…feeling everything and nothing at once. But it allowed me to view my trauma in a different way. Like a superpower. That insight has stayed with me.” Other possible mechanisms of change, from a psychological standpoint, include re-processing and transforming traumatic material.
This case study aligns with previous findings in the literature. For instance, in a retrospective, epidemiology survey on 5-MeO-DMT ( n = 515; M age = 35.4; male = 79%), 79% of participants with psychiatric disorders reported improved PTSD following 5-MeO-DMT use ( 22 ). Most participants (90%) had moderate-to-strong mystical experiences, while a significant proportion (37%) had challenging ones. In another retrospective, international survey ( n = 99; M age = 37.4; male = 74%), 79% of participants with past or present PTSD, who had used 5-MeO-DMT at least once in their lifetime, reported improved symptomatology ( 45 ). They also endorsed significantly stronger mystical experiences than those who did not experience symptom improvement or regressed. Most recently, Davis et al. ( 46 ) examined ibogaine and 5-MeO-DMT for trauma-related psychological and cognitive impairment, specifically among U.S. Special Operations Forces Veterans ( n = 51; M age = 40.0; male = 96%). They analyzed retrospective data collected 30 days before and 30 days after a clinical psychedelic program in Mexico. The results showed significant and large reductions in depression, suicidal ideation, anxiety, PTSD, and cognitive impairment. Participants additionally reported increased psychological flexibility, which was strongly associated with improvements in all constructs, excluding suicidality.
Other studies have investigated 5-MeO-DMT in naturalistic settings. For example, in an observational group study, using structured dosing protocols, researchers examined clinical correlates of 5-MeO-DMT ( 27 ). Among healthy participants ( n = 362; M age = 47.7; male = 55%), 80% with depression and 79% with anxiety reported spontaneous, unintended reductions in symptoms. This was associated with stronger mystical experiences, as well as higher ratings of spirituality and meaning in life. In another observational study, Uthaug et al. ( 47 ) investigated sub-acute and long-term effects of 5-MeO-DMT on affect and cognition. Among healthy participants ( n = 42; M age = 38.0; male = 60%), ratings of depression, anxiety, and stress decreased 24 h post-intake and reached significance at 4 weeks follow-up. Those who experienced high levels of ego dissolution or oceanic boundlessness, two markers of a mystical experience, displayed lower levels of depression and stress. However, this did not extend to anxiety.
Of note, the subject partially regressed at 3-months follow-up. She reported new onset of night terrors, the nature of which could not be recalled. These night terrors reflect higher scores across all measures at this time point, relative to the others. A phenomenon known as ‘reactivation’, similar to flashbacks, is commonly reported by 5-MeO-DMT users ( 22 , 48 ). This involves re-experiencing parts of a drug-induced state post-administration, which can occur days, weeks, or even months later ( 49 , 50 ). Additionally, the probability of 5-MeO-DMT reactivation increases with being female, dosing in a structured group format, and having a stronger mystical experience ( 48 ). All three of these factors applied to this case study. As such, the subject may have endured a reactivation event following 5-MeO-DMT, presenting as negatively-valenced night terrors. Alternatively, the benefits of 5-MeO-DMT may have only lasted for three months. Despite the partial regression, scores across all measures remained below clinical thresholds, with symptoms naturally remitting overtime. The onset of night terrors was not considered a ‘serious adverse event’, as its association with 5-MeO-DMT could not be definitively concluded. It neither was life-threatening, required intervention or hospitalization, resulted in persistent or significant disability, nor led to the subject’s death.
Strengths and limitations
The longitudinal nature of this case study serves as its primary strength, with repeated observations collected over a 1-year period. Findings are more robust, given the subject’s treatment resistance and disease chronicity, the complexity of this clinical population, and the limitation in available effective, evidence-based interventions. Further, the presence of psychiatric comorbidities, the lack of polypharmacy or medication washout, and the naturalistic setting better reflect patients in the real world. The use of well-validated measures, capturing both subject- and clinician-reported changes, is an additional strength. Notwithstanding, this case study is inherently limited.
First, it describes the presentation, treatment, and follow-up of a single person. Hence, the results cannot be generalized to others with PTSD. Second, the dose of 5-MeO-DMT was estimated by the subject, based on visual inspection. The precise amount cannot be determined, accordingly. Third, the source for obtaining toad bufotoxin, containing the 5-MeO-DMT, is unknown. The compound’s integrity may have been compromised as a result. Fourth, 5-MeO-DMT was self-administered by the subject. This is not considered a suitable clinical or pharmaceutical application, primarily due to safety reasons. Finally, there is no evidence that 5-MeO-DMT, in and of itself, produced therapeutic activity reported in this case study. Facilitation practices, like body scan meditation, for instance, may have confounded the results, magnifying or diminishing therapeutic effects. Findings should, therefore, be interpreted with caution, and only serve to catalyze future research. This is particularly important, as the field is far from establishing clinical efficacy, real-world effectiveness, and standard treatment protocols for 5-MeO-DMT in PTSD and beyond. Additionally, naturalistic psychedelic use has steadily increased over the past decade ( 51 ). This is likely due to media coverage, advances in research, and changes to legislation. It is, thus, critical to balance discussions on 5-MeO-DMT and other psychedelics with clear and careful acknowledgement of safety risks.
Looking ahead, the next logical step is to conduct pilot studies that explore the safety, tolerability, and preliminary efficacy of 5-MeO-DMT for PTSD, in larger and more diverse samples. Including a richer battery of psychometric instruments is highly encouraged. Results could then inform open-label, randomized, and adaptive trials to further characterize 5-MeO-DMT for this patient population; and to explore different therapeutic approaches, including adjunctive psychotherapy, which may augment patient adherence and therapeutic outcomes. Incorporating moderated mediation models, as statistical analyses, is also encouraged in future work. This would allow researchers to control for covariates, like age and gender, while examining potential underlying mechanisms, such as mystical experiences.
This case study is the first to report the longitudinal effects of 5-MeO-DMT for chronic refractory PTSD, complicated by hopelessness and suicidality. The results showed that 5-MeO-DMT offered fast-acting, robust, and sustained improvements in symptomatology, and was generally tolerable and safe to administer. However, this was not without risks, as evidenced by acute nausea, overwhelming subjective effects, and late onset of night terrors. Further research is warranted to replicate and extend these findings, which are inherently limited, non-generalizable, and rely on methods not clinically accepted. This can be achieved through clinical and naturalistic studies, in controlled and uncontrolled environments, to effectively converge on safety, efficacy, effectiveness, and durability of 5-MeO-DMT for PTSD. Evidence can then be leveraged to optimize therapeutic delivery, as well as develop standard clinical practice guidelines.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
AR: Conceptualization, Formal analysis, Project administration, Visualization, Writing – original draft. RK: Investigation, Writing – original draft, Writing – review & editing. PS: Conceptualization, Funding acquisition, Project administration, Supervision, Writing – review & editing. LB: Writing – original draft, Writing – review & editing. RA: Writing – original draft, Writing – review & editing. MK: Writing – original draft, Writing – review & editing. NB: Validation, Writing – review & editing. LJ: Validation, Writing – review & editing. MG: Validation, Writing – review & editing. JB: Supervision, Validation, Writing – review & editing. LA: Conceptualization, Supervision, Validation, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The authors declare that this study received funding from Cubed Biotech. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication. All research in the Department of Psychiatry at the University of Cambridge was supported by the National Institute for Health and Care Research Cambridge Biomedical Research Centre (NIHR203312) and the National Institute for Health and Care Research Applied Research Collaboration East of England. The views expressed are those of the author(s) and not necessarily those of the National Institute for Health and Care Research or the Department of Health and Social Care. LA receives some salary support from the US Department of Veterans Affairs (IK2CX001873) and the American Foundation for Suicide Prevention (YIG-0-004-16).
Acknowledgments
We express our gratitude to the subject, facilitator, and clinician—described in this case study—for collecting and sharing their data; and for their valuable contributions to science, specifically in understanding the potential of 5-MeO-DMT for PTSD and beyond.
Conflict of interest
AR is the Founding Director of the Integrated Research Literacy Group. PS is the Director of Psychological Science at the Integrated Research Literacy Group. He also receives some salary/research support from Cubed Biotech. MK is the Director of Ethnographic Studies at the Integrated Research Literacy Group. JB is the Clinical Advisor to The Mission Within, Journey Colab, Beond, Kaivalya Kollective, Tandava Retreats, Kernel, Woven Science, Brain Health Restoration, and Lionheart Ventures. LA has served as a Consultant, Speaker and/or Advisory Board Member for Guidepoint, Transcend Therapeutics, Beond, Source Research Foundation, Reason for Hope, Beond, The Cohen Foundation, Ampelis, and is owner of NPSYT, PLLC.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer BS declared a shared research group 5 MEO Education with the author JB to the handling editor.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The authors do not condone the illegal use of any psychedelic substance, including 5-MeO-DMT.
1. Pachter, IJ, Zacharias, DE, and Ribeiro, O. Indole alkaloids of Acer saccharinum (the silver maple), Dictyoloma incanescens, Piptadenia colubrina, and Mimosa hostilis. J Org Chem . (1959) 24:1285–7. doi: 10.1021/jo01091a032
CrossRef Full Text | Google Scholar
2. Hoshino, T, and Shimodaira, K. Über die Synthese des Bufotenin-Methly-Äthers (5-Methoxyn-dimethyl-tryptamin) und Bufotenins (Synthesen in Der Indol-Gruppe. XV). Bull Chem Soc Jpn . (1936) 11:221–4. doi: 10.1246/bcsj.11.221
3. Ermakova, AO, Dunbar, F, Rucker, J, and Johnson, MW. A narrative synthesis of research with 5-MeO-DMT. J Psychopharmacol (Oxf) . (2022) 36:273–94. doi: 10.1177/02698811211050543
4. Reckweg, JT, Uthaug, MV, Szabo, A, Davis, AK, Lancelotta, R, Mason, NL, et al. The clinical pharmacology and potential therapeutic applications of 5‐methoxy‐N,N‐dimethyltryptamine (5‐MeO‐DMT). J Neurochem . (2022) 162:128–46. doi: 10.1111/jnc.15587
PubMed Abstract | CrossRef Full Text | Google Scholar
5. Ott, J. Shamanic snuffs or entheogenic errhines . Solothrun, Switzerland: Entheobotanica (2001).
Google Scholar
6. Weil, AT, and Davis, W. Bufo Alvarius : a potent hallucinogen of animal origin. J Ethnopharmacol . (1994) 41:1–8. doi: 10.1016/0378-8741(94)90051-5
7. Lancelotta, R. 5-MeO-DMT has not been found in traditional ayahuasca preparations and the combination of 5-MeO-DMT with MAOIs is dangerous. Hum Psychopharmacol Clin Exp . (2022) 37:e2839. doi: 10.1002/hup.2839
8. Kaasik, H, Souza, RCZ, Zandonadi, FS, Tófoli, LF, and Sussulini, A. Chemical composition of traditional and analog Ayahuasca. J Psychoactive Drugs . (2021) 53:65–75. doi: 10.1080/02791072.2020.1815911
9. VICE TV. (2017). Hamilton Morris learns about the toad ceremonies of the Yaqui tribe. Available at: https://www.youtube.com/watch?v=M5U9D7Y5er4
10. Most, A. Bufo Alvarius : The psychedelic toad of the Sonoran Desert Venom Press (1984).
11. Halberstadt, AL, Nichols, DE, and Geyer, MA. Behavioral effects of α,α,β,β-tetradeutero-5-MeO-DMT in rats: comparison with 5-MeO-DMT administered in combination with a monoamine oxidase inhibitor. Psychopharmacology . (2012) 221:709–18. doi: 10.1007/s00213-011-2616-6
12. Ray, TS. Psychedelics and the human Receptorome. PLoS One . (2010) 5:e9019. doi: 10.1371/journal.pone.0009019
13. Berge, O, Chacho, D, and Hole, K. Inhibitory effect of 5-methoxy- N,N -dimethyltryptamine on the synaptosomal uptake of 5-hydroxytryptamine. Eur J Pharmacol . (1983) 90:293–6. doi: 10.1016/0014-2999(83)90253-4
14. Spencer, DG, Glaser, T, and Traber, J. Serotonin receptor subtype mediation of the interoceptive discriminative stimuli induced by 5-methoxy- N . N -dimethyltryptamine Psychopharmacology (Berl) . (1987) 93:158–66. doi: 10.1007/BF00179927
15. Nutt, D, Spriggs, M, and Erritzoe, D. Psychedelics therapeutics: what we know, what we think, and what we need to research. Neuropharmacology . (2023) 223:109257. doi: 10.1016/j.neuropharm.2022.109257
16. Halberstadt, AL, and Geyer, MA. Multiple receptors contribute to the behavioral effects of Indoleamine hallucinogens. Neuropharmacology . (2011) 61:364–81. doi: 10.1016/j.neuropharm.2011.01.017
17. Vigerelli, H, Sciani, JM, Eula, MAC, Sato, LA, Antoniazzi, MM, Jared, C, et al. Biological effects and biodistribution of Bufotenine on mice. Biomed Res Int . (2018) 2018:1–10. doi: 10.1155/2018/1032638
18. Shen, HW, Jiang, XL, Winter, J, and Yu, AM. Psychedelic 5-Methoxy- N,N -dimethyltryptamine: metabolism, pharmacokinetics, drug interactions, and pharmacological actions. Curr Drug Metab . (2010) 11:659–66. doi: 10.2174/138920010794233495
19. Jiang, XL, Shen, HW, and Yu, AM. Potentiation of 5-methoxy- N,N -dimethyltryptamine-induced hyperthermia by harmaline and the involvement of activation of 5-HT1A and 5-HT2A receptors. Neuropharmacology . (2015) 89:342–51. doi: 10.1016/j.neuropharm.2014.10.013
20. Malcolm, B, and Thomas, K. Serotonin toxicity of serotonergic psychedelics. Psychopharmacology . (2022) 239:1881–91. doi: 10.1007/s00213-021-05876-x
21. Sklerov, J, Levine, B, Moore, KA, King, T, and Fowler, D. A fatal intoxication following the ingestion of 5-Methoxy- N,N -dimethyltryptamine in an Ayahuasca preparation*. J Anal Toxicol . (2005) 29:838–41. doi: 10.1093/jat/29.8.838
22. Davis, AK, Barsuglia, JP, Lancelotta, R, Grant, RM, and Renn, E. The epidemiology of 5-methoxy- N, N -dimethyltryptamine (5-MeO-DMT) use: benefits, consequences, patterns of use, subjective effects, and reasons for consumption. J Psychopharmacol (Oxf) . (2018) 32:779–92. doi: 10.1177/0269881118769063
23. Uthaug, MV, Lancelotta, R, Ortiz Bernal, AM, Davis, AK, and Ramaekers, JG. A comparison of reactivation experiences following vaporization and intramuscular injection (IM) of synthetic 5-methoxy-N,N-dimethyltryptamine (5-MeO-DMT) in a naturalistic setting. J Psychedelic Stud . (2020) 4:104–13. doi: 10.1556/2054.2020.00123
24. Ott, J. Pharmepéna-Psychonautics: human intranasal, sublingual and Oral pharmacology of 5-Methoxy-N, N-Dimethyl-Tryptamine. J Psychoactive Drugs . (2001) 33:403–7. doi: 10.1080/02791072.2001.10399925
25. Barsuglia, JP, Polanco, M, Palmer, R, Malcolm, BJ, Kelmendi, B, and Calvey, T. A case report SPECT study and theoretical rationale for the sequential administration of ibogaine and 5-MeO-DMT in the treatment of alcohol use disorder. Progress Brain Res . (2018):121–58. doi: 10.1016/bs.pbr.2018.08.002
26. Barsuglia, J, Davis, AK, Palmer, R, Lancelotta, R, Windham-Herman, AM, Peterson, K, et al. Intensity of mystical experiences occasioned by 5-MeO-DMT and comparison with a prior psilocybin study. Front Psychol . (2018) 9:2459. doi: 10.3389/fpsyg.2018.02459
27. Davis, AK, So, S, Lancelotta, R, Barsuglia, JP, and Griffiths, RR. 5-methoxy-N,N-dimethyltryptamine (5-MeO-DMT) used in a naturalistic group setting is associated with unintended improvements in depression and anxiety. Am J Drug Alcohol Abuse . (2019) 45:161–9. doi: 10.1080/00952990.2018.1545024
28. Uthaug, MV, Lancelotta, R, Szabo, A, Davis, AK, Riba, J, and Ramaekers, JG. Prospective examination of synthetic 5-methoxy- N,N -dimethyltryptamine inhalation: effects on salivary IL-6, cortisol levels, affect, and non-judgment. Psychopharmacology . (2020) 237:773–85. doi: 10.1007/s00213-019-05414-w
29. Barsuglia, J, Davis, AK, Palmer, R, Lancelotta, R, Windham-Herman, M, Peterson, K, et al. Characterization of mystical experiences occasioned by 5-MeO-DMT- containing toad Bufotoxin and comparison with prior psilocybin studies [internet]. Poster presented at: 3rd International Psychedelic Science Conference. (2017). Oakland, CA.
30. Millière, R, Carhart-Harris, RL, Roseman, L, Trautwein, FM, and Berkovich-Ohana, A. Psychedelics, meditation, and self-consciousness. Front Psychol . (2018) 9:1475. doi: 10.3389/fpsyg.2018.01475
31. Gagnier, JJ, Kienle, G, Altman, DG, Moher, D, Sox, H, Riley, D, et al. The CARE guidelines: consensus-based clinical case reporting guideline development. J Med Case Rep . (2013) 7:223. doi: 10.1186/1752-1947-7-223
32. First, MB, Williams, JBW, Karg, RS, and Spitzer, RL. The structured clinical interview for DSM-5®, clinician version (SCID-5-CV) . Washington DC, United States: The American Psychiatric Association (2016).
33. Blevins, CA, Weathers, FW, Davis, MT, Witte, TK, and Domino, JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress . (2015) 28:489–98. doi: 10.1002/jts.22059
34. Beck, AT, Weissman, A, Lester, D, and Trexler, L. The measurement of pessimism: the hopelessness scale. J Consult Clin Psychol . (1974) 42:861–5. doi: 10.1037/h0037562
35. Guy, W. ECDEU Assessment Manual for Psychopharmacology . Rockville, MD: U.S. Dept. of Health, Education, and Welfare, Public Health Service, Alcohol, Drug abuse, and mental health administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs (1976).
36. MacLean, KA, Leoutsakos, JMS, Johnson, MW, and Griffiths, RR. Factor analysis of the mystical experience questionnaire: a study of experiences occasioned by the hallucinogen psilocybin. J Sci Study Relig . (2012) 51:721–37. doi: 10.1111/j.1468-5906.2012.01685.x
37. Bouvard, M, Charles, S, Guérin, J, Aimard, G, and Cottraux, J. Study of Beck’s hopelessness scale. Valid Factor Anal L’Encephale . (1992) 18:237–40.
PubMed Abstract | Google Scholar
38. Metzner, R. The toad and the jaguar: A field report of underground research on a visionary medicine: Bufo Alvarius and 5-methoxy-dimethyltryptamine . 1st ed. Berkeley, CA: Regent Press (2013).
39. Mosurinjohn, S, Roseman, L, and Girn, M. Psychedelic-induced mystical experiences: an interdisciplinary discussion and critique. Front Psych . (2023) 14:1077311. doi: 10.3389/fpsyt.2023.1077311
40. Ko, K, Knight, G, Rucker, JJ, and Cleare, AJ. Psychedelics, mystical experience, and therapeutic efficacy: a systematic review. Front Psych . (2022) 13:917199. doi: 10.3389/fpsyt.2022.917199
41. Pahnke, WN. The psychedelic mystical experience in the human encounter with death. Harv Theol Rev . (1969) 62:1–21. doi: 10.1017/S0017816000027577
42. Griffiths, RR, Richards, WA, McCann, U, and Jesse, R. Psilocybin can occasion mystical-type experiences having substantial and sustained personal meaning and spiritual significance. Psychopharmacology . (2006) 187:268–83. doi: 10.1007/s00213-006-0457-5
43. Griffiths, RR, Johnson, MW, Carducci, MA, Umbricht, A, Richards, WA, Richards, BD, et al. Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening Cancer: a randomized double-blind trial. J Psychopharmacol (Oxf) . (2016) 30:1181–97. doi: 10.1177/0269881116675513
44. Doblin, R. Pahnke’s “good Friday experiment”: a long-term follow-up and methodological critique. J Transpers Psychol . 23:1–28.
45. Cox, KE, Lancelotta, R, Barsuglia, J, and Davis, AK. 5-MeO-DMT and subjective improvements in post traumatic stress disorder. In: Annual conference of the Maryland Psychological Association . Baltimore, MD: (2018).
46. Davis, AK, Averill, LA, Sepeda, ND, Barsuglia, JP, and Amoroso, T. Psychedelic treatment for trauma-related psychological and cognitive impairment among US special operations forces veterans. Chronic Stress . (2020) 4:247054702093956. doi: 10.1177/2470547020939564
47. Uthaug, MV, Lancelotta, R, van Oorsouw, K, Kuypers, KPC, Mason, N, Rak, J, et al. A single inhalation of vapor from dried toad secretion containing 5-methoxy-N,N-dimethyltryptamine (5-MeO-DMT) in a naturalistic setting is related to sustained enhancement of satisfaction with life, mindfulness-related capacities, and a decrement of psychopathological symptoms. Psychopharmacology . (2019) 236:2653–66. doi: 10.1007/s00213-019-05236-w
48. Ortiz Bernal, AM, Raison, CL, Lancelotta, RL, and Davis, AK. Reactivations after 5-methoxy- N,N -dimethyltryptamine use in naturalistic settings: an initial exploratory analysis of the phenomenon’s predictors and its emotional valence. Front Psych . (2022) 13:1049643. doi: 10.3389/fpsyt.2022.1049643
49. Heaton, RK, and Victor, RG. Personality characteristics associated with psychedelic flashbacks in natural and experimental settings. J Abnorm Psychol . (1976) 85:83–90. doi: 10.1037/0021-843X.85.1.83
50. Matefy, RE, and Krall, RG. An initial investigation of the psychedelic drug flashback phenomena. J Consult Clin Psychol . (1974) 42:854–60. doi: 10.1037/h0037523
51. Glynos, NG, Fields, CW, Barron, J, Herberholz, M, Kruger, DJ, and Boehnke, KF. Naturalistic psychedelic use: a world apart from clinical Care. J Psychoactive Drugs . (2023) 55:379–88. doi: 10.1080/02791072.2022.2108356
Keywords: 5-methoxy- N , N -dimethyltryptamine, 5-MeO-DMT, psychedelic therapy, post-traumatic stress disorder, PTSD, trauma, case report
Citation: Ragnhildstveit A, Khan R, Seli P, Bass LC, August RJ, Kaiyo M, Barr N, Jackson LK, Gaffrey MS, Barsuglia JP and Averill LA (2023) 5-MeO-DMT for post-traumatic stress disorder: a real-world longitudinal case study. Front. Psychiatry . 14:1271152. doi: 10.3389/fpsyt.2023.1271152
Received: 01 August 2023; Accepted: 03 November 2023; Published: 23 November 2023.
Reviewed by:
Copyright © 2023 Ragnhildstveit, Khan, Seli, Bass, August, Kaiyo, Barr, Jackson, Gaffrey, Barsuglia and Averill. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anya Ragnhildstveit, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Case Report
- Open access
- Published: 25 November 2008
A case of PTSD presenting with psychotic symptomatology: a case report
- Georgios D Floros 1 ,
- Ioanna Charatsidou 1 &
- Grigorios Lavrentiadis 1
Cases Journal volume 1 , Article number: 352 ( 2008 ) Cite this article
29k Accesses
4 Citations
1 Altmetric
Metrics details
A male patient aged 43 presented with psychotic symptomatology after a traumatic event involving accidental mutilation of the fingers. Initial presentation was uncommon although the patient responded well to pharmacotherapy. The theoretical framework, management plan and details of the treatment are presented.
Recent studies have shown that psychotic symptoms can be a hallmark of post-traumatic stress disorder [ 1 , 2 ]. The vast majority of the cases reported concerned war veterans although there were sporadic incidents involving non-combat related trauma (somatic or psychic). There is a biological theoretical framework for the disease [ 3 ] as well as several psychological theories attempting to explain cognitive aspects [ 4 ].
Case presentation
A male patient, aged 43, presented for treatment with complaints tracing back a year ago to a traumatic work-related event involving mutilation of the distal phalanges of his right-hand fingers. Main complaints included mixed hallucinations, irritability, inability to perform everyday tasks and depressive mood. No psychic symptomatology was evident before the event to him or his social milieu.
Mental state examination
The patient was a well-groomed male of short stature, sturdy build and average weight. He was restless but not agitated, with a guarded attitude towards the interviewer. His speech pattern was slow and sparse, his voice low. He described his current mood as 'anxious' without being able to provide with a reason. Patient appeared dysphoric and with blunted affect. He was able to maintain a linear train of thought with no apparent disorganization or irrational connections when expressing himself. Thought content centred on his amputated fingers with a semi-compulsive tendency to gaze to his (gloved) hand. The patient was typically lost in ruminations about his accident with a focus on the precise moment which he experienced as intrusive and affectively charged in a negative and painful way. He could remember wishing for his fingers to re-attach to his hand almost as the accident took place. A trigger in his intrusive thoughts was the painful sensation of neuropathic pain from his half-mutilated fingers, an artefact of surgery.
He denied and thoughts of harming himself and demonstrated no signs of aggression towards others. Hallucinations had a predominantly depressive and ego-dystonic character. He denied any perceptual disturbances at the time of the examination. Their appearance was typically during nighttime especially in the twilight. Initially they were visual only, involving shapes and rocks tumbling down towards the patient, gradually becoming more complex and laden with significance. A mixed visual and tactile hallucination of burning rain came afterwards while in the time of examination a tall stranger clad in black and raiding a tall steed would threaten and ridicule the patient. He scored 21 on a MMSE with trouble in the attention, calculation and recall categories. The patient appeared reliable and candid to the extent of his self-disclosure, gradually opening up to the interviewer but displayed a marked difficulty on describing his emotions and memories of the accident, apparently independent of his conscious will. His judgement was adequate and he had some limited Insight into his difficulties, hesitantly attributing them to his accident.
He was married and a father of three (two boys and a girl aged 7–12) He had no prior medical history for mental or somatic problems and received no medication. He admitted to occasional alcohol consumption although his relatives confirmed that he did not present addiction symptoms. He had some trouble making ends meet for the past five years. Due to rampant unemployment in his hometown, he was periodically employed in various jobs, mostly in the construction sector. One of his children has a congenital deformity, underwent several surgical procedures with mixed results and, before the time of the patient's accident, it was likely that more surgery would be forthcoming. The patient's father was a proud man who worked hard but reportedly was victimized by his brothers, they reaping the benefits of his work in the fields by manipulating his own father. He suffered a nervous breakdown attributed to his low economic status after a failed economic endeavour ending in him being robbed of the profits, seven years before the accident. There was no other relevant family history.
Before the accident the patient was a lively man, heavily involved as a participant and organizer in important local social events from a young age. He was respected by his fellow villagers and felt his involvement as a unique source of pride in an otherwise average existence. Prior to his accident, the patient was repeatedly promised a permanent job as a labourer and fate would have it that his appointment was supposedly approved immediately after the accident only to be subsequently revoked. He viewed himself as an exploited man in his previous jobs, much the same way his father was, while he harboured an extreme bitterness over the unavailability of support for his long-standing problems. His financial status was poor, being in sick-leave from his previous job for the last four months following the accident and hoping to receive some compensation. Although his injuries were considered insufficient for disability pension he could not work to his full capacity since the hand affected was his primary one and he was a manual labourer.
Given that the patient clearly suffered a high level of distress as a result of his hallucinatory experiences he was voluntary admitted to the 2nd Psychiatric Department of the Aristotle University of Thessaloniki for further assessment, observation and treatment. A routine blood workup was ordered with no abnormalities. A Rorschach Inkblot Test was administered in order to gain some insight into patient's dynamics, interpersonal relations and underlying personality characteristics while ruling out any malingering or factitious components in the presentation as suggested in Wilson and Keane [ 5 ]. Results pointed to inadequate reality testing with slight disturbances in perception and a difficulty in separating reality from fantasy, leading to mistaken impressions and a tendency to act without forethought in the face of stress. Uncertainty in particular was unbearable and adjustment to a novel environment hard. Cognitive functions (concentration, attention, information processing, executive functions) were impaired possibly due to cognitive inability or neurological disease. Emotion was controlled with a tendency for impulsive behaviour; however there was difficulty in processing and expressing emotions in an adaptive manner. There were distinct patterns of aggression and anger towards others but expressing those patterns was avoided, switching to passivity and denial rather than succumbing to destructive urges or mature competitiveness. Self-esteem was low with feelings of inferiority and inefficiency.
A neurological examination revealed a left VI cranial nerve paresis, reportedly congenital, resulting in diplopia while gazing to the extreme left, which did not significantly affect the patient. The patient had a chronic complaint of occasional vertigo, to which he partly attributed his accident, although the symptoms were not of a persisting nature.
Initial diagnosis at this stage was 'Psychotic disorder NOS' and pharmacological treatment was initiated. An MRI scan of the brain with gadolinium contrast was ordered to rule out any focal neurological lesions. It was performed fifteen days later and revealed no abnormalities.
Patient was placed on ziprasidone 40 mg bid and lorazepam 1 mg bid. He reported an immediate improvement but when the attending physician enquired as to the nature of the improvement the patient replied that in his hallucinations he told the tall raider that he now had a tall doctor who would help him and the raider promptly left (sic). Apparently, the random assignment of a strikingly tall physician had an unexpected positive effect. Ziprasidone gradually increased to 80 mg bid within three days with no notable effect to the perceptual disturbances but with the development of akathisia for which biperiden was added, 1 mg tid. Duloxetine was added, 60 mg once-daily, in a hope that it could have a positive effect to his mood but also to this neuropathic pain which was frequent and demoralising. The patient had a tough time accommodating to the hospital milieu, although the grounds were extended and there was plenty of opportunity for walks and other activities. He preferred to stay in bed sometimes in obvious agony and with marked insomnia. He presented a strong fear for the welfare of his children, which he could not reason for. Due to the apparent inability of ziprasidone to make a dent in the psychotic symptomatology, medication was switched to amisulpride 400 mg bid and the patient was given a leave for the weekend to visit his home. On his return an improvement in his symptoms was reported by him and close relatives, although he still had excessive anxiety in the hospital setting. It was decided that his leave was to be extended and the patient would return for evaluation every third day. After three appointments he had a marked improvement, denied any psychotic symptoms while his sleep pattern improved. A good working relationship was established with his physician and the patient was with a schedule of follow-up appointments initially every fifteen days and following two months, every thirty days. His exit diagnosis was "Psychotic disorder Not Otherwise Specified – PTSD". He remained asymptomatic for five months and started making in-roads in a cognitively-oriented psychotherapeutic approach but unfortunately further trouble befell him, his wife losing a baby and his claim to an injury compensation rejected. He experienced a mood loss and duloxetine was increased to 120 mg per day to some positive effect. His status remains tenuous but he retains a strong will to make his appointments and work with his physician. A case conceptualization following a cognitive framework [ 6 ] is presented in Figure 1 .
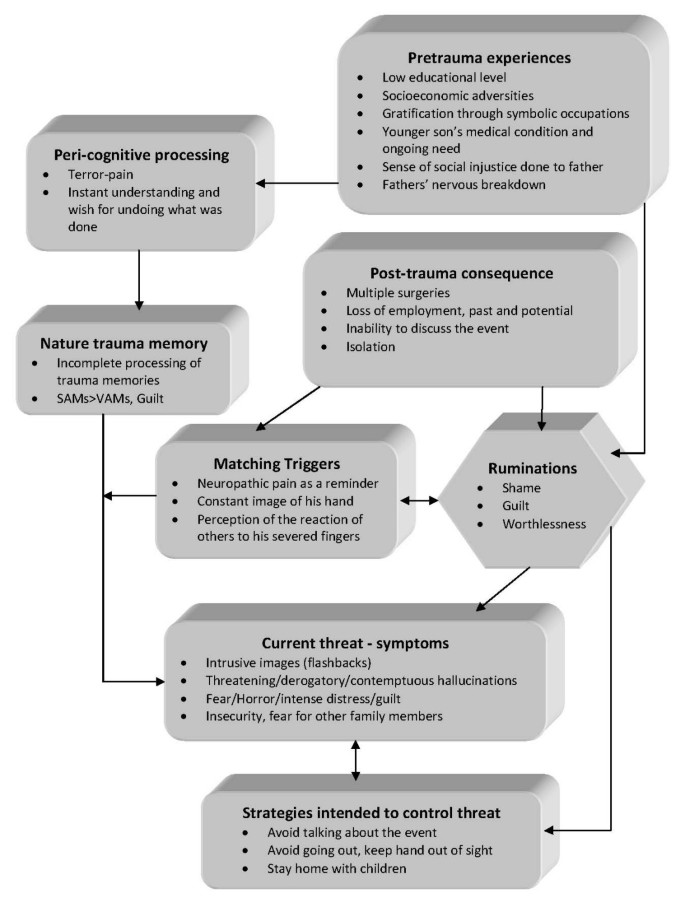
Case formulation – (Persistent PTSD, adapted from Ehlers and Clark [ 6 ] ) . Case formulation following the persistent PTSD model of Ehlers and Clark [ 6 ]. It is suggested that the patient is processing the traumatic information in a way which a sense of immediate threat is perpetuated through negative appraisals of trauma or its consequences and through the nature of the traumatic experience itself. Peri-traumatic influences that operate at encoding, affect the nature of the trauma memory. The memory of the event is poorly elaborated, not given a complete context in time and place, and inadequately integrated into the general database of autobiographical knowledge. Triggers and ruminations serve to re-enact the traumatic information while symptoms and maladaptive coping strategies form a vicious circle. Memories are encoded in the SAM rather than the VAM system, thus preventing cognitive re-appraisal and eventual overcoming of traumatic experience [ 4 ].
The value of a specialized formulation is made clear in complex cases as this one. There is a relationship between the pre-existing cognitive schemas of the individual, thought patterns emerging after the traumatic event and biological triggers. This relationship, best described as a maladaptive cognitive processing style, culminates into feelings of shame, guilt and worthlessness which are unrelated to similar feelings, which emerge during trauma recollection, but nonetheless acts in a positive feedback loop to enhance symptom severity and keep the subject in a constant state of psychotic turmoil. Its central role is addressed in our case formulation under the heading "ruminations" which best describes its ongoing and unrelenting character. The "what if" character of those ruminations may serve as an escape through fantasy from an unbearably stressful cognition. Past experience is relived as current threat and the maladaptive coping strategies serve as negative re-enforcers, perpetuating the emotional suffering.
The psychosocial element in this case report, the patient's involvement with a highly symbolic activity, demonstrates the importance of individualising the case formulation. Apparently the patient had a chronic difficulty in expressing his emotions and integrating into his social surroundings, a difficulty counter-balanced somewhat with his involvement in the local social events which gave him not only a creative way out from any emotional impasse but also status and recognition. His perceived inability to continue with his symbolic activities was not only an indicator of the severity of his troubles but also a stressor in its own right.
Complex cases of PTSD presenting with hallucinatory experiences can be effectively treated with pharmacotherapy and supportive psychotherapy provided a good doctor-patient relationship is established and adverse medication effects rapidly dealt with. A cognitive framework and a Rorschach test can be valuable in deepening the understanding of individuals and obtaining a personalized view of their functioning and character dynamics. A biopsychosocial approach is essential in integrating all aspects of the patients' history in a meaningful way in order to provide adequate help.
Patient's perspective
"My life situation can't seem to get any better. I haven't had any support from anyone in all my life. Leaving home to go anywhere nowadays is hard and I can't seem to be able to stay anyplace else for a long time either. Just getting to the hospital [where the follow-up appointments are held] makes me very nervous, especially the minute I walk in. Can't seem to stay in place at all, just keep pacing while waiting for my appointment. I am only able to open up somewhat to my doctor, whom I thank for his support. Staying in hospital was close to impossible; I was very stressed and particularly concerned for my children, not being able to be close to them. I still need to have them near-by. Getting the MRI scan was also a stressful experience, confined in a small space with all that noise for so long. I succeeded only after getting extra medication.
I hope that things will get better. I don't trust anyone for any help any more; they should have helped me earlier."
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Abbreviations
stands for 'Post Traumatic Stress Disorder'
for 'Verbally Accessible Memory'
for 'Situationally Accessible Memory'
Butler RW, Mueser KT, Sprock J, Braff DL: Positive symptoms of psychosis in posttraumatic stress disorder. Biological Psychiatry. 1996, 39: 839-844. 10.1016/0006-3223(95)00314-2.
Article CAS PubMed Google Scholar
Seedat S, Stein MB, Oosthuizen PP, Emsley RA, Stein DJ: Linking Posttraumatic Stress Disorder and Psychosis: A Look at Epidemiology, Phenomenology, and Treatment. The Journal of Nervous and Mental Disease. 2003, 191: 675-10.1097/01.nmd.0000092177.97317.26.
Article PubMed Google Scholar
Nutt DJ: The psychobiology of posttraumatic stress disorder. J Clin Psychiatry. 2000, 61: 24-29.
CAS PubMed Google Scholar
Brewin CR, Holmes EA: Psychological theories of posttraumatic stress disorder. Clinical Psychology Review. 2003, 23: 339-376. 10.1016/S0272-7358(03)00033-3.
Wilson JP, Keane TM: Assessing Psychological Trauma and PTSD. 2004, The Guilford Press
Google Scholar
Ehlers A, Clark DM: A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 2000, 38: 319-345. 10.1016/S0005-7967(99)00123-0.
Download references
Acknowledgements
The authors wish to acknowledge the valuable support and direction offered by the department's chair, Professor Ioannis Giouzepas who places the utmost importance in creating a suitable therapeutic environment for our patients and a superb learning environment for the SHO's and registrars in his department.
Author information
Authors and affiliations.
2nd Department of Psychiatry, Psychiatric Hospital of Thessaloniki, 196 Langada str., 564 29, Thessaloniki, Greece
Georgios D Floros, Ioanna Charatsidou & Grigorios Lavrentiadis
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Georgios D Floros .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
GF was the attending SHO and the major contributor in writing the manuscript. IC performed the psychological evaluation and Rorschach testing and interpretation. GL provided valuable guidance in diagnosis and handling of the patient. All authors read and approved the final manuscript.

Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Floros, G.D., Charatsidou, I. & Lavrentiadis, G. A case of PTSD presenting with psychotic symptomatology: a case report. Cases Journal 1 , 352 (2008). https://doi.org/10.1186/1757-1626-1-352
Download citation
Received : 12 September 2008
Accepted : 25 November 2008
Published : 25 November 2008
DOI : https://doi.org/10.1186/1757-1626-1-352
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Ziprasidone
- Psychotic Disorder
- Amisulpride
- Hallucinatory Experience
Cases Journal
ISSN: 1757-1626

- Create new account
- Request new password
Search form
Resource center, post traumatic stress disorder case study.

This case study presents information about post traumatic stress disorder in older adults. It is divided into different sections including the history, presentation and examination, diagnosis, case discussion, post traumatic stress disorder explained, take home points, and additional resources.
https://www.hopkinsmedicine.org/gec/studies/ptsd.html#history
- 3,653 Views
- 1 Collections
Related Resources
- Patrick and Gloria Lake- Unfolding Case
- Sherman "Red" Yoder- Unfolding Case
- Henry and Ertha Williams- Unfolding Case
- Judy and Karen Jones- Unfolding Case
- Julia Morales and Lucy Grey- Unfolding Case
User Collections
Related content, start the conversation.
Every registered user can comment on website content.
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Post Traumatic Stress Disorder: PTSD Case Study: One Man's Journey

Abstract This paper is a case study on a client who has been diagnosed with Post Traumatic Stress Disorder (PTSD) from the Vietnam War. A narrative case description is included, which supports the clinical diagnosis and as well as an empirical treatment plan. The treatment plan has included the necessary identifying information with appropriate changes to shield the client’s real identity. The client was referred from the Veteran’s Administrative (VA) hospital in La Jolla, California. As part of the treatment plan the presenting problems will be identified and correlated to the criteria set forth in the Diagnostic and Statistical Manual of Mental Disorders, 4th edition text revision (DSM-IV-TR) multi-axial diagnosis. This case study is based upon a holistic foundation, which includes the inter-connectedness of: the presenting problems, long-term goals, objectives, methods or interventions, treatment length, and measurement of potential outcomes. This paper concludes with a self-critique by the therapist regarding every aspect of the presented case study. Key Words: PTSD, Treatment Plan for Vietnam Vets, Holistic Foundation. Post-Traumatic Stress.
Related Papers
Journal of Traumatic Stress
Steven Silver
Journal of Clinical Psychology
Tracie Shea
Terry Keane
Journal of Consulting and Clinical Psychology
Paul Malloy
Croatian Medical Journal
Goran Arbanas
European Journal of Psychotraumatology
Aleksandra Stevanović
Journal of Aggression, Maltreatment & Trauma
Meredith Landy
Military medicine
Peter Yeomans
While the Veterans Health Administration continues to treat Vietnam War Veterans, approximately two million service men and women have returned from Iraq and Afghanistan. However, our treatments can only be as effective as the quality of our clinical assessment. Disclosure of trauma is facilitated when the type of trauma is present in the sociocultural environment of patient and clinician. Topics that once were deemed too shameful for inquiry, specifically, childhood abuse, domestic violence, sexual abuse, and military sexual trauma are now part of a standard assessment. Similarly, the standard clinical assessment of combat Veterans should include specific queries that address the darkest underside of wartime experiences.
Tracy Simpson
Clinical Psychological Science
Approximately two thirds of veterans with posttraumatic stress disorder (PTSD) remain with the disorder following treatment. Pinpointing the per-symptom effectiveness of treatments in real-world clinical settings can highlight relevant domains for treatment augmentation and development. Baseline and posttreatment assessments of PTSD and depression were performed in 709 veterans with PTSD. PTSD remission was 39.4%. Treatment was least effective for intrusion symptoms and had no effect on flashbacks or on poor recall of traumatic features. Of veterans who remitted, 72.8% still met diagnostic criteria for at least one cluster. Poor clinical effectiveness was noted for depression; only 4.1% of the patients remitted following treatment. Treatments for veterans with PTSD show limited overall effectiveness in real-world settings. Enhancing treatment response may require enhancing provider fidelity and patient compliance with extant treatments or the development of new treatments that speci...
RELATED PAPERS
dhanang soemarmo
Nigerian Journal of International Affairs
Polish Journal of Environmental Studies
Ileana Stoica
Richard RISASI Etutu junior
Emine Bayman
Marina Miraglia
Scholaria: Jurnal Pendidikan dan Kebudayaan
Theodora Sarlotha Nirmala Manu
Darja Rugelj
Marine Drugs
Paz Otero Fuertes
Journal of Clinical Oncology
Dr.Mohammed Baghdadi
Peter J M van Oosterom
Maandblad Voor Accountancy en Bedrijfseconomie
Joost van Buuren
Risto Kuronen
New England Journal of Medicine
Suzanne Oparil
Canadian Journal of Forest Research
Kenneth Anyomi
Oxford University Press
Christopher J Rowe
JIMD reports
Shanti Balasubramaniam
University Museums and Collections Journal
Andrew Simpson
Revista de Lexicografía
Miguel Ángel Puche Lorenzo
Actas Dermo-Sifiliográficas
Dra. Isabel Ogueta
European Journal of Drug Metabolism and Pharmacokinetics
Partner abuse
Sandra Stith
2007 IEEE 19th International Conference on Indium Phosphide & Related Materials
Richard Noetzel
Asian Journal of Chemistry
Nurul Aprilita
Colleen McGahan
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
Post-traumatic stress disorder and GI endoscopy: a case study
- PMID: 8399434
- DOI: 10.1097/00001610-199308000-00005
Post-traumatic stress disorder (PTSD) can be caused by experiencing or witnessing a variety of harsh traumatic events. Rape, burglary, war, torture, violence, and other catastrophic events have been known to precipitate flashbacks, nightmares, and inability to cope with the demands of daily life. The symptoms associated with PTSD can interfere with work, sleep, appetite, relationships, and health. In a Veterans Administration hospital population, PTSD is not an uncommon patient problem: it usually results from witnessing and/or participating in war or military service-related circumstances. This case study describes a 42-year-old man who was a prisoner of war in Vietnam. The form of torture his Vietnamese captors subjected him to presented a challenging situation when he required an endoscopic examination of the upper gastrointestinal tract. The purpose of this case study is to offer suggestions to the GI and endoscopy nursing staff who care for these patients, and to make GI health care providers aware of the special needs of this patient population.
Publication types
- Case Reports
- Duodenogastric Reflux / diagnosis
- Endoscopy, Gastrointestinal / nursing
- Endoscopy, Gastrointestinal / psychology*
- Stress Disorders, Post-Traumatic / psychology*
- Veterans / psychology*
Combat Stress in Pre-modern Europe pp 15–35 Cite as
Post-traumatic Stress Disorder: An Ancient Greek Case Study in Retrospective Diagnosis
- Owen Rees 6
- First Online: 01 November 2022
201 Accesses
2 Altmetric
Part of the book series: Mental Health in Historical Perspective ((MHHP))
Within socio-military history, the diagnosis of post-traumatic stress disorder has aroused a lot of attention, with many scholars claiming its existence in the pre-modern world while sceptics have challenged this claim in no uncertain terms. However, the debates surrounding historic PTSD have been made without due consideration of the wider medical history debates surrounding retrospective diagnosis of biological disease. There is a fundamental methodological challenge in that psychiatric diagnoses frequently emphasise behavioural symptoms, this in turn gives historians a twofold problem: (1) Can we know whether these behavioural symptoms are predominantly characteristic of our own social normality, and thus their observation by clinicians confirms simply antithetical and undesirous behaviours in the modern day? (2) If those same behaviours appeared in another cultural sphere do they still hold the same diagnostic capabilities? This chapter will focus on one such diagnosis, post-traumatic stress disorder, and address some of the pressing methodological issues surrounding such a practice.
This is a preview of subscription content, log in via an institution .
Buying options
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
For discussion on this field of scholarship, and its tradition, see A. Cunningham, ‘Identifying Disease in the Past: Cutting the Gordian Knot’, Asclepio 54, 2002, 13–34; J. Arrizabalaga, ‘Problematizing Retrospective Diagnosis in the History of Disease’, Asclepio 54, 2002, 51–70; K.H. Leven, ‘“At Times These Ancient Facts Seem to Lie Before Me Like a Patient on a Hospital Bed”—Retrospective Diagnosis and Ancient Medical History’, in Manfred Horstmanshoff and Marten Stol (eds), Magic and Rationality in Ancient Near Eastern and Graeco-Roman Medicine (Leiden: Brill, 2004), pp. 369–86; A. Karenberg and F.P. Moog, ‘Next Emperor Please! No End to Retrospective Diagnosis’, Journal of the History of the Neurosciences 13.2, 2004, 143–49.
C. Thumiger, A History of the Mind and Mental Health in Classical Greek Medical Thought (Cambridge: Cambridge University Press, 2017), pp. 2–8.
N.M. Bark, ‘On the History of Schizophrenia: Evidence of Its Existence Before 1800’, New York State Journal of Medicine 88.7, 1988, 374–83; C.V. Haldipur, ‘Madness in Ancient India: Concept of Insanity in Charaka Samhita (first century A.D.)’, Comprehensive Psychiatry 25.3, 1984, 335–44; D.V. Jeste, R. del Carmen, J.B. Lohr, and R.J. Wyatt, ‘Did Schizophrenia Exist Before the Eighteenth Century?’, Comprehensive Psychiatry 26.6, 1985, 493–503; K. Otsuka and A. Sakai, ‘Haizmann’s Madness: The Concept of Bizarreness and the Diagnosis of Schizophrenia’, History of Psychiatry 15.1, 2004, 73–82; M.H. Stone, Healing the Mind: A History of Psychiatry from Antiquity to the Present (New York: W. W. Norton, 1997); H.A. Youssef and F.A. Youssef, ‘Evidence for the Existence of Schizophrenia in Medieval Islamic Society’, History of Psychiatry 7, 1996, 55–62; D. Fraguas, ‘Problems with Retrospective Studies of the Presence of Schizophrenia’, History of Psychiatry 20.1, 2009, 61–71.
Erwin H. Ackerknecht, ‘Psychopathology, Primitive Medicine and Primitive Culture’, Bulletin of the History of Medicine 14.1, 1943, 37.
E. DePoy and S.F. Gilson, Studying Disability: Multiple Theories and Responses (London: Sage, 2011), pp. 9–10, 96–97; Dana Lee Baker, The Politics of Neurodiversity: Why Public Policy Matters (Boulder: Lynne Reiner, 2011), pp. 12–5.
O. Rees, ‘We Need to Talk About Epizelus: PTSD and the Ancient World’, Medical Humanities 46.1, 2020, 46.
Edgar Jones and Simon Wessely, ‘War Syndromes: The Impact of Culture on Medically Unexplained Symptoms’, Medical History 49, 2005, 56.
D. Fraguas, ‘Problems with Retrospective Studies of the Presence of Schizophrenia’, History of Psychiatry 20.1, 2009, 62.
J. Shay, Achilles in Vietnam (New York: Athenaeum, 1994), pp. 166–69; L. Tritle, Melos to My Lai (London: Routledge, 2000), pp. 57–8.
J. Shay, ‘Moral Injury’, Intertexts 16.1, 2012, 57–66.
D. Fraguas, ‘Problems with Retrospective Studies of the Presence of Schizophrenia’, History of Psychiatry 20.1, 2009, 63.
In his follow up book Odysseus in America , 149, he makes the observation that combat adaptations may account of the symptoms of PTSD in the DSM , but equally advised his readers to go and read the list of symptoms themselves.
G.E. Berrios, ‘Classifications in Psychiatry: A Conceptual History’, Australian and New Zealand Journal of Psychiatry 33.2, 1999, 145–60.
C. Thumiger, A History of the Mind and Mental Health in Classical Greek Medical Thought (Cambridge: Cambridge University Press), pp. 72–3.
C. Thumiger, ‘The Early Greek Medical Vocabulary of Insanity’, in William V. Harris (ed), Mental Disorders in the Classical World (Leiden: Brill, 2013), pp. 61–4.
Aretaeus of Cappadocia, On Chronic Diseases , 1.6; Aetius, Iatrika , 6.8; W.V. Harris, ‘Thinking About Mental Disorders in Classical Antiquity’, in William V. Harris (ed), Mental Disorders in the Classical World (Leiden: Brill, 2013), pp. 1–2.
D. Fraguas, ‘Problems with Retrospective Studies of the Presence of Schizophrenia’, History of Psychiatry 20.1, 2009, 64.
J. Shay, Achilles in Vietnam: Trauma and the Undoing of Character (New York: Athenaeum, 1994), xx.
This pan-cultural, universalist model has led at least one team of researchers to use the ancient world to argue that the same is true of treatment: ‘it indicates that modern Western approaches to the psychological treatment of trauma are not entirely culturally dependent and may be applied to the treatment of trauma with patients from different cultural traditions.’—Y. Ustinova and E. Cardeña, ‘Combat Stress Disorders and Their Treatment in Ancient Greece’, Psychological Trauma: Theory, Research, Practice, and Policy 6.6, 2014, 746.
For a historical case study that examines the differing reception of the ‘traumatised’ warrior, see O. Rees, ‘We Need to Talk About Epizelus: PTSD and the Ancient World’, Medical Humanities 46.1, 2020, 46–54.
A. Young, The Harmony of Illusions (Princeton: Princeton University Press, 1995).
L.J. Kirmayer, ‘Confusion of the Senses: Implications of Ethnocultural Variations in Somatoform and Dissociative Disorders for PTSD’, in A.J. Marsella, M.J. Friedman, E.T. Gerrity, and R.M. Scurfield (eds), Ethnocultural Aspects of Posttraumatic Stress Disorder: Issues, Research, and Clinical Applications (Washington, DC: American Psychological Association, 1996), p. 150.
P.J. Bracken, ‘Post-modernity and Post-traumatic Stress Disorder’, Social Science & Medicine 53.6, 2001, 742.
S. O’Brien, Traumatic Events and Mental Health (Cambridge: Cambridge University Press, 1998), p. 5.
N. Metzger, ‘Railway Spine, Shell-shock and Psychological Trauma: The Limits of Retrospective Diagnosis’, in Eve-Marie Becker, Jan Dochhorn, Else Holt (eds), Trauma and Traumatization in Individual and Collective Dimensions: Insights from Biblical Studies and Beyond (Gottingen: Vandenhoek & Ruprecht GmBH, 2014), p. 56.
Jason Crowley, ‘Beyond the Universal Soldier: Combat Trauma in Classical Antiquity’, in P. Meineck and D. Konstan (eds), Combat Trauma and the Ancient Greeks (New York: Palgrave Macmillan, 2014), p. 117.
See for instance Thucydides, History of the Peloponnesian War 2.8, and similar sentiments expressed in the works of poets such as Pindar, fr. 110.
Walid Khalid Abdul-Hamid and Jamie Hacker Hughes, ‘Nothing New under the Sun: Post-traumatic Stress Disorders in the Ancient World’, Early Science and Medicine 19.6, 2014, 549–57.
J. Scurlock and Burton Anderson, Diagnoses in Assyrian and Babylonian Medicine (Chicago: University of Illinois Press, 2005), p. 349.
Ibid., p. 351.
L. Tritle, Melos to My Lai (London: Routledge, 2000), p. 59.
Ibid., p. 56.
Aislinn Melchior, ‘Caesar in Vietnam: Did Roman Soldiers Suffer from Post-traumatic Stress Disorder’, Greece & Rome 58.2, 2011, 216.
Homer, Iliad 16.65; 16.90; 16.836; 17.194; 17.224; 19.269; 20.351; 21.86; 23.5; 23.129.
Diodorus Siculus, Library 15.19.4.
Plutarch, Life of Agesilaus 35.3.
Diodorus Siculus, Library 15.50.5.
J. Roisman, ‘Klearchos in Xenophon’s Anabasis’, Scripta Classica Israelica , 8/9, 1985–1989, 50.
Xenophon, Anabasis 2.6.6.
Xenophon, Anabasis 2.6.7, 10.
Xenophon, Cyropaedia 2.1.22 (Translator Walter Miller, 1914). He repeats this sentiment in his Hellenica , 6.1.6.
Pericles: Plutarch, Life of Pericles 7.1. Alcibiades: Plutarch, Life of Alcibiades 18.1. Heracles: Isocrates, Helen 10.17.
S.S. Monoson, ‘Socrates in Combat: Trauma and Resilience in Plato’s Political Theory’, in P. Meineck and D. Konstan (eds), Combat Trauma and the Ancient Greeks (New York: Palgrave Macmillan, 2014), p. 134; B. Steinbock ‘Sufferings Too Great for Tears: The Destruction of the Athenian Expeditionary Corps in Sicily’, in Melanie Jonasch (ed), The Fight for Greek Sicily Society, Politics, and Landscape (Oxford: Oxbow Books, 2020), pp. 76–8.
Renato D. Alarcón, ‘Culture, Cultural Factors and Psychiatric Diagnosis: Review and Projections’ World Psychiatry 8, 2009, 131–39; Andrew Roderick Gilmoor, Adithy Adithy, and Barbara Regeer, ‘The Cross-Cultural Validity of Post-traumatic Stress Disorder and Post-traumatic Stress Symptoms in the Indian Context: A Systematic Search and Review’ Frontiers in Psychiatry 10.439, 2019; Guerda Nicolas, Anna Wheatley, and Casta Guillaume, ‘Does One Trauma Fit All? Exploring the Relevance of PTSD Across Cultures’, International Journal of Culture and Mental Health 8, 2015, 34–45.
The best discussions of this methodological issue are found in ‘Thinking About Mental Disorders in Classical Antiquity’, in William V. Harris (ed), Mental Disorders in the Classical World (Leiden: Brill, 2013), and C. Thumiger and P.N. Singer, ‘Introduction: Disease Classification and Mental Illness: Ancient and Modern Perspectives’, in C. Thumiger and P.N. Singer (eds), Mental Illness in Ancient Medicine: From Celsus to Paul of Aegina (Leiden: Brill, 2018), 1–32.
Or, as Otto Wahl observed, the common default is to portray a caricatured form of schizophrenia—Otto Wahl, Media Madness: Public Images of Mental Illness (New Brunswick: Rutgers University Press, 1995/2003), pp. 89–90.
C. Thumiger, A History of the Mind and Mental Health in Classical Greek Medical Thought (Cambridge: Cambridge University Press, 2017), p. 48.
B. Simon, ‘“Carving Nature at the Joints”: The Dream of a Perfect Classification of Mental Illness’, in William V. Harris (ed), Mental Disorders in the Classical World (Leiden: Brill, 2013), p. 37.
S. Minsky, W. Vega, T. Miskimen, M. Gara, and J. Escobar, ‘Diagnostic Patterns in Latino, African American, and European American Psychiatric Patients’, Arch Gen Psychiatry 60.6, 2003, 637–44.
Jason Crowley, ‘Beyond the Universal Soldier: Combat Trauma in Classical Antiquity’, in P. Meineck and D. Konstan (eds), Combat Trauma and the Ancient Greeks (New York: Palgrave Macmillan, 2014), pp. 111–12.
B. Liddell and L. Jobson, ‘The Impact of Cultural Differences in Self-representation on the Neural Substrates of Posttraumatic Stress Disorder’, European Journal of Psychotraumatology 7:1, 2016, 1–13, https://doi.org/10.3402/ejpt.v7.30464 , accessed 22 December 21.
Arousal response: K.G. Martinez, J.A. Franco-Chaves, M.R. Milad, and G.J. Quirk, ‘Ethnic Differences in Physiological Responses to Fear Conditioned Stimuli’, PLoS One 9, 12, 2014, e114977, http://dx.doi.org/10.1371/journal.pone.0114977 , accessed 22 December 21.
Amygdala: B. Derntl, U. Habel, S. Robinson, C. Windischberger, I. Kryspin-Exner, R.C. Gur, and E. Moser, ‘Culture But Not Gender Modulates Amygdala Activation During Explicit Emotion Recognition’, BMC Neuroscience 13, 2011, 54; J.Y. Chiao, T. Iidaka, H.L. Gordon, J. Nogawa, M. Bar, E. Aminoff, N. Sadato, and N. Ambady, ‘Cultural Specificity in Amygdala Response to Fear Faces’, Journal of Cognitive Neuroscience 20.12, 2008, 2167–74.
American Psychological Association, Principles of Medical Ethics with Annotations Especially Applicable to Psychiatry (2013 edition), 7.3: ‘it is unethical for a psychiatrist to offer a professional opinion unless he or she has conducted an examination and has been granted proper authorization for such a statement.’
Bibliography
Abdul-Hamid, Walid Khalid, and Jamie Hacker Hughes, ‘Nothing New under the Sun: Post-traumatic Stress Disorders in the Ancient World’, Early Science and Medicine 19.6, 2014, 549–57.
Google Scholar
Ackerknecht, Erwin H., ‘Psychopathology, Primitive Medicine and Primitive Culture’, Bulletin of the History of Medicine 14, 1943, 30–67.
Alarcón, Renato D., ‘Culture, Cultural Factors and Psychiatric Diagnosis: Review and Projections’, World Psychiatry 8, 2009, 131–39.
Article Google Scholar
American Psychological Association, Principles of Medical Ethics with Annotations Especially Applicable to Psychiatry (2013 edition), 7.3.
American Psychiatric Association, Diagnostics and Statistical Manual of Mental Disorders-5 (Washington: American Psychiatric Association, 2019).
Arrizabalaga, J., ‘Problematizing Retrospective Diagnosis in the History of Disease’, Asclepio 54, 2002, 51–70.
Baker, Dana Lee, The Politics of Neurodiversity: Why Public Policy Matters (Boulder: Lynne Reiner, 2011).
Bark, N.M. ‘On the History of Schizophrenia: Evidence of Its Existence Before 1800’, New York State Journal of Medicine 88.7, 1988, 374–83.
Berrios, G.E., ‘Classifications in Psychiatry: A Conceptual History’, Australian and New Zealand Journal of Psychiatry 33.2, 1999, 145–60.
Bracken, P.J., ‘Post-modernity and Post-traumatic Stress Disorder’, Social Science & Medicine 53.6, 2001, 733–43.
Chiao, J.Y., T. Iidaka, H.L. Gordon, J. Nogawa, M. Bar, E. Aminoff, N. Sadato, and N. Ambady, ‘Cultural Specificity in Amygdala Response to Fear Faces’, Journal of Cognitive Neuroscience 20.12, 2008, 2167–74.
Crowley, Jason, ‘Beyond the Universal Soldier: Combat Trauma in Classical Antiquity’, in P. Meineck and D. Konstan (eds), Combat Trauma and the Ancient Greeks (New York: Palgrave Macmillan, 2014), 105–30.
Cunningham, A., ‘Identifying Disease in the Past: Cutting the Gordian Knot’, Asclepio 54, 2002, 13–34.
DePoy, E., and S.F. Gilson, Studying Disability: Multiple Theories and Responses (London: Sage, 2011).
Book Google Scholar
Derntl, B., U. Habel, S. Robinson, C. Windischberger, I. Kryspin-Exner, R.C. Gur, and E. Moser, ‘Culture But Not Gender Modulates Amygdala Activation During Explicit Emotion Recognition’, BMC Neuroscience 13, 2011, 54. https://doi.org/10.1186/1471-2202-13-54
Fraguas, D., ‘Problems with Retrospective Studies of the Presence of Schizophrenia’, History of Psychiatry 20.1, 2009, 61–71.
Gilmoor, Andrew Roderick, Adithy Adithy, and Barbara Regeer, ‘The Cross-Cultural Validity of Post-traumatic Stress Disorder and Post-traumatic Stress Symptoms in the Indian Context: A Systematic Search and Review’, Frontiers in Psychiatry 10.439, 2019, 1–24.
Haldipur, C.V., ‘Madness in Ancient India: Concept of Insanity in Charaka Samhita (1st century A.D.)’, Comprehensive Psychiatry 25.3, 1984, 335–44.
Harris, W.V., ‘Thinking About Mental Disorders in Classical Antiquity’, in William V. Harris (ed), Mental Disorders in the Classical World (Leiden: Brill, 2013), 1–23,
Jeste, D.V., R. del Carmen, J.B. Lohr, and R.J. Wyatt, ‘Did Schizophrenia Exist Before the Eighteenth Century?’ Comprehensive Psychiatry 26.6, 1985, 493–503.
Jones, Edgar, and Simon Wessely, ‘War Syndromes: The Impact of Culture on Medically Unexplained Symptoms’, Medical History 49, 2005, 55–78.
Karenberg, A., and F.P. Moog, ‘Next Emperor Please! No End to Retrospective Diagnosis’, Journal of the History of the Neurosciences 13.2, 2004, 143–49.
Kirmayer, L.J., ‘Confusion of the Senses: Implications of Ethnocultural Variations in Somatoform and Dissociative Disorders for PTSD’, in A.J. Marsella, M.J. Friedman, E.T. Gerrity, and R.M. Scurfield (eds), Ethnocultural Aspects of Posttraumatic Stress Disorder: Issues, Research, and Clinical Applications (Washington, DC: American Psychological Association, 1996), pp. 131–63.
Leven, K.H., ‘“At Times These Ancient Facts Seem to Lie Before Me Like a Patient on a Hospital Bed”—Retrospective Diagnosis and Ancient Medical History,’ in Manfred Horstmanshoff and Marten Stol (eds), Magic and Rationality in Ancient Near Eastern and Graeco-Roman Medicine (Leiden: Brill, 2004), pp. 369–86.
Liddell, B., and L. Jobson, ‘The Impact of Cultural Differences in Self-representation on the Neural Substrates of Posttraumatic Stress Disorder’, European Journal of Psychotraumatology 7.1, 2016, 30464. https://doi.org/10.3402/ejpt.v7.30464 , accessed 22 December 21.
Martinez, K.G., J.A. Franco-Chaves, M.R. Milad, and G.J. Quirk, ‘Ethnic Differences in Physiological Responses to Fear Conditioned Stimuli’, PLoS One 9,12, 2014, e114977. https://doi.org/10.1371/journal.pone.0114977 , accessed 22 December 21.
Metzge, N., ‘Railway Spine, Shell-shock and Psychological Trauma: The Limits of Retrospetcive Diagnosis’, in Eve-Marie Becker, Jan Dochhorn, Else Holt (eds), Trauma and Traumatization in Individual and Collective Dimensions: Insights from Biblical Studies and Beyond (Gottingen: Vandenhoek & Ruprecht GmBH, 2014), pp. 43–61.
Chapter Google Scholar
Minsky, S., W. Vega, T. Miskimen, M. Gara, and J. Escobar, ‘Diagnostic Patterns in Latino, African American, and European American Psychiatric Patients’, Arch Gen Psychiatry 60.6, 2003, 637–44.
Monoson, S.S., ‘Socrates in Combat: Trauma and Resilience in Plato’s Political Theory’, in P. Meineck and D. Konstan (eds), Combat Trauma and the Ancient Greeks (New York: Palgrave Macmillan, 2014), pp. 131–62.
Nicolas, Guerda, Anna Wheatley, and Casta Guillaume, ‘Does One Trauma Fit All? Exploring the Relevance of PTSD Across Cultures’, International Journal of Culture and Mental Health 8, 2015, 34–45.
O’Brien, S., Traumatic Events and Mental Health (Cambridge: Cambridge University Press, 1998).
Otsuka, K., and Sakai, A., ‘Haizmann’s Madness: The Concept of Bizarreness and the Diagnosis of Schizophrenia’, History of Psychiatry 15.1, 2004, 73–82.
Rees, O., ‘We Need to Talk About Epizelus: PTSD and the Ancient World’, Medical Humanities 46.1, 2020, 46–54.
Roisman, J., ‘Klearchos in Xenophon’s Anabasis’, Scripta Classica Israelica , 8–9, 1985–1989, 30–52.
Scurlock, J., and Burton Anderson, Diagnoses in Assyrian and Babylonian Medicine (Chicago: University of Illinois Press, 2005).
Shay, J., Achilles in Vietnam: Trauma and the Undoing of Character (New York: Athenaeum, 1994).
Shay, J., ‘Moral Injury’, Intertexts 16.1, 2012, 57–66.
Simon, B., ‘“Carving Nature at the Joints”: The Dream of a Perfect Classification of Mental Illness’, in William V. Harris (ed), Mental Disorders in the Classical World (Leiden: Brill, 2013), 27–40.
Steinbock, B. ‘Sufferings Too Great for Tears’: The Destruction of the Athenian Expeditionary Corps in Sicily’, in Melanie Jonasch (ed), The Fight for Greek Sicily Society, Politics, and Landscape (Oxford: Oxbow Books, 2020), pp. 73–98.
Stone, M.H. Healing the Mind: A History of Psychiatry from Antiquity to the Present (New York: W. W. Norton, 1997).
Thumiger, C., ‘The Early Greek Medical Vocabulary of Insanity’, in William V. Harris (ed), Mental Disorders in the Classical World (Leiden: Brill, 2013), pp. 61–95.
Thumiger, C., A History of the Mind and Mental Health in Classical Greek Medical Thought (Cambridge: Cambridge University Press, 2017).
Thumiger, C., and P.N. Singer, ‘Introduction. Disease Classification and Mental Illness: Ancient and Modern Perspectives’, in C. Thumiger and P.N. Singer (eds), Mental Illness in Ancient Medicine: From Celsus to Paul of Aegina (Leiden: Brill, 2018), pp. 1–32.
Tritle, L., Melos to My Lai (London: Routledge, 2000).
Wahl, Otto, Media Madness: Public Images of Mental Illness (New Brunswick: Rutgers University Press, 1995/2003).
Young, A., The Harmony of Illusions (Princeton: Princeton University Press, 1995).
Youssef, H.A., and F.A. Youssef, ‘Evidence for the Existence of Schizophrenia in Medieval Islamic Society’, History of Psychiatry 7, 1996, 55–62.
Download references
Acknowledgements
My thanks to my fellow editors for their feedback on this chapter, and also to Dr Jo Edge who read an earlier draft and gave me invaluable comments.
Author information
Authors and affiliations.
Department of History, Politics and Philosophy, Manchester Metropolitan University, Manchester, UK
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Owen Rees .
Editor information
Editors and affiliations.
Kathryn Hurlock
Jason Crowley
Rights and permissions
Reprints and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter.
Rees, O. (2022). Post-traumatic Stress Disorder: An Ancient Greek Case Study in Retrospective Diagnosis. In: Rees, O., Hurlock, K., Crowley, J. (eds) Combat Stress in Pre-modern Europe. Mental Health in Historical Perspective. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-031-09947-2_2
Download citation
DOI : https://doi.org/10.1007/978-3-031-09947-2_2
Published : 01 November 2022
Publisher Name : Palgrave Macmillan, Cham
Print ISBN : 978-3-031-09946-5
Online ISBN : 978-3-031-09947-2
eBook Packages : History History (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Saf Health Work
- v.9(3); 2018 Sep
A Case Study of the Effects of Posttraumatic Stress Disorder on Operational Fire Service Personnel Within the Lancashire Fire and Rescue Service
Associated data.
Lancashire Fire and Rescue Service (LFRS), the subject of this evaluative research document employs 1400 people. 80% of employees are operational firefighters and officers whom operate across a range of duty systems and support functions, providing prevention, protection and emergency response to the communities of Lancashire.
The overarching purpose of this epidemiological study is to assess the prevalence of post-traumatic stress disorder (PTSD) amongst operational LFRS personnel and to analyse the effects upon those who may be suffering from it, whether brought about by a single traumatic event or by repeated exposure to traumatic occurrences over a period of time. A combination of primary and secondary research was carried out. Primary data was collated using two recognised clinical questionnaires and statistical analysis was conducted with the aid of the software package SPSS.
The findings and statistical analysis showed that out of the 100 people surveyed, 30% of respondents had signs of probable distress. Of this quota, 4% showed symptoms of PTSD. The study considers how an organisation can recognise and manage PTSD and provides recommendations to assist in better recognising and managing the associated risks.
Based upon the findings, the authors conclude that the level of PTSD within LFRS is slightly lower than those found in other studies undertaken within the Fire and Rescue Service sector. The paper provides recommendations for future studies and a series of actions for consideration by LFRS senior management to improve PTSD support services for employees.
1. Introduction
1.1. background.
Fire and Rescue Service operational personnel are often exposed to highly pressured, dynamic, and rapidly evolving situations. The work can be extremely demanding, both physically and psychologically [2] . During their careers, most personnel will, at some point, be subjected to particularly traumatic and often tragic events [3] , and evidence suggests that most firefighters' mortality and morbidity are related either directly or indirectly to the stressful nature of their work [4] .
A study undertaken by Dahlan et al [5] reported that past traumatic incidents were the highest ranked source of stress among UK firefighters. For the purpose of this article, the definition of a traumatic event (or incident) is taken to be “an event that involves actual or threatened death or serious injury; a threat to the physical health of self or others in which the person felt frightened, horrified, and helpless” [6] .
Some earlier studies argue that firefighters are at increased risk of developing a variety of psychological, social, and physical reactions [7] , [8] , [9] , [10] , [11] , [12] , one of which is the condition known as post-traumatic stress disorder (PTSD). According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; American Psychiatric Association) [13] , the essential feature of PTSD is the development of characteristic symptoms after exposure to an extremely traumatic event or a stressor, which may manifest in feelings of arousal, intrusion, and avoidance. Linked to this trauma exposure a number of other common health sequelae, such as alcohol and drug abuse, depression, anxiety, and suicide [5] , [14] , are frequently documented
Few empirical studies have systematically examined the cause and effect of work stresses affecting firefighters [5] . However, a number of authors have studied the prevalence rates of PTSD among firefighters and reported wide variances, from 6.5% [15] to 37% [16] , but the sample size, profile, and measures used differed from one report to another [3] .
Baker and Williams [17] also determined that individuals in different ranks reported differing levels of both organizational and operational stress (with those at “Leading Firefighter”, now known as the “Crew Manager” role, reporting the highest levels). Significantly, they also identified that those persons reporting higher levels of psychological distress also reported lower levels of confidence. This then raises the question of a potential link to fireground competency and safety.
Within Lancashire Fire and Rescue Service (LFRS) and neighboring counties, anecdotal evidence suggests that psychological impacts are acknowledged and receive attention through services such as occupational health; however, conditions such as PTSD tend to remain low profile, with minimal visibility and little or no education or awareness being raised among staff. This is a very different situation to the United States where a recent article published in the NFPA Journal [14] , entitled “Trouble in Mind”, highlighted a growing problem of firefighter suicides (c.360 from 2000 to 2013; with a notable increase, more recently, of sixty in both 2012 and 2013). The more worrying aspect, however, is that the information used within the article is based solely on voluntary submissions, and therefore, the actual numbers could be significantly higher. Wilmoth [18] agrees with this standpoint, citing a stigma that makes it difficult for emergency responders to admit to behavioral issues linked to PTSD.
The view that firefighters are “rough and tough and can take on anything that the world can dish out” [19] is a common theme across the evidence base used in the preparation of this article. Haslam and Mallon [15] recognized this situation, explaining that the culture is one of nonadmission, whereas Baker and Williams [17] explain the culture as being one of stoicism and self-discipline, in which the very armor that firefighters use to protect themselves mentally could also be the blocker to maintaining their own mental health. Haslam and Mallon [15] concluded that many respondents felt unable to seek support within the workplace because of the macho image associated with the job; this is a position that is commonly inferred in many case studies [20] , [21] , [22] .
Of equal significance are the organizational impacts that may arise as a result of PTSD cases, such as depression, anxiety, and substance abuse to name a few, going undiagnosed or misdiagnosed [6] . All these can result in extended periods of staff absence, increased health and safety risks, resignations, dismissals, or claims against employers [23] .
This study aims to outline the effects that traumatic events may have on an individual, determine the various factors, which may result in symptoms being exhibited, and specifically consider the prevalence of PTSD within LFRS. It will provide evidence of how the FRS sector locally, nationally, and internationally is prepared to deal with such effects on their staff and assesses the adequacy of the services provided.
To achieve this, the study will focus on the published work on PTSD to provide appropriate definitions and determine signs and symptoms. These may present after traumatic short-term exposure or after repeated exposure to lower level incidents over more prolonged periods [24] . It will consider causal factors and investigate variables, which may or may not result in an individual developing PTSD.
1.2. Study significance
This study investigates the prevalence of PTSD among the operational LFRS personnel. Its significance lies in the insights it offers to the public sector organizations and its management in which their employees deal with traumatic and life-threatening events with the potential health risks of PTSD. The management structure of these organizations need to be aware of the range of the health conditions that might manifest as a result of exposure to these extreme traumatic events and as a result must be able to put into place programs of rehabilitation when necessary.
1.3. The problem
PTSD is defined by the National Institute for Health and Care Excellence [25] as “a disorder that develops in response to a stressful event or situation of exceptionally threatening or catastrophic nature (e.g., assault, road accident, disaster, or rape)”. It is the term used by psychiatrists to describe reactions that clinically cause significant impairment or distress within the functioning of people [6] .
PTSD is clinically diagnosed by meeting the criteria in the DSM-V [26] . According to the DSM-V, the diagnosis of PTSD requires exposure to an event that involved or threatened death, violence, or serious injury. It may be firsthand (primary exposure) but can also result from a third party trauma and the human desire to want to help another, known as secondary stress. Table 1 shows PTSD exposure sources and symptoms.
PTSD exposure sources and symptoms—World Health Organization and DSM-V
DSM-V, Diagnostic and Statistical Manual of Mental Disorders; PTSD, posttraumatic stress disorder.
For a diagnosis to be made, these symptoms need to be impacting significantly on an individual's ability to function with a level of normality [26] for a period longer than 1 month [6] . The characteristics have been recognized in previous studies [28] as frequently manifesting in symptoms of reexperiencing, avoidance, and arousal.
1.4. Study area
Lancashire is a coastal county, bordered to the north by Cumbria, to the south by Merseyside, and to the east by North and West Yorkshire and the metropolitan county of Greater Manchester. It comprises 14 local authority areas, covering 1,189 square miles and has an estimated population of c. 1.5 million people [29] . This study will be conducted with data gathered from a cross section of 1,100 LFRS operational staff who operate countywide from 41 locations on a variety of shift systems see Table 2 :
Table 2
LFRS shift systems
LFRS, Lancashire Fire and Rescue Service.
The shift system worked at each location is depicted within the map shown below in Fig 1 :

LFRS locations and duty systems. LFRS, Lancashire Fire and Rescue Service.
The study compares the prevalence of PTSD levels within the LFRS sample of 150 people against the quoted lifetime prevalence levels of c.10.4% for women and 5% for men [6] (the variance between genders is thought to be due to exposure to different types of events and different ways of coping).
1.5. Study purpose
1.5.1. aims.
- • To determine the extent of the prevalence of PTSD among operational personnel from LFRS.
- • To investigate a range of variables that may affect the development of PTSD.
- • To make recommendations to the LFRS that aims to mitigate threats derived from PTSD among firefighters.
1.5.2. Objectives
- • To gain an understanding of the variations of PTSD among staff from LFRS and the effect of different contributory factors.
- • To use a variety of statistical techniques to present and analyze the variations.
- • To use a range of different modeling techniques to explore the significance of a number of variables.
2. Materials and methods
2.1. literature review.
This literature review explores existing literature on the topic of PTSD and the factors that may lead to its development. The findings of this review shape the remainder of this case study and enable conclusions to be considered alongside the findings of previous studies.
2.1.1. Child involvement
In traumatic events faced by firefighters, a common theme was the involvement of children in incidents. Clohessy and Ehlers [24] identified that such incidents were often perceived as the most stressful and frequently lead to intrusive memories. Boxer and Wild [30] , Baker and Williams [17] , and Haslam and Mallon [15] identified that reports of children being involved/killed were the highest ranked stressors. Haslam and Mallon [15] cited more than 50% of respondents as being emotionally upset when reminded of the incident, with 33% having upsetting thoughts or images and 25% with sleep-related problems. Commonly cited reasons were that “it was a waste of a life” or that “familiarity” was a feature (i.e., the firefighter having children of his/her own). The second most traumatic aspect was purely the witnessing of gore, death, or a human undergoing severe pain and suffering [15] . Frequently respondents in such studies refer to thoughts of “I should have done more” and feelings of guilt and helplessness [28] .
2.1.2. Coping strategies
No one knows in advance how they will react to a particular stressful event, [6] but crisis theory states that when a stressful event takes place, balancing factors can be implemented which can help one regain a sense of equilibrium [31] .
Moran and Colless [32] suggest that coping is the most significant variable in being able to predict an individual's psychological well-being. However, wider factors such as what was happening in a person's life before the event (family difficulties, bereavements etc.) may also play a part in their ability to cope [6] . Equally, it is acknowledged that events which may cause emotional upset to one person may not have the same impact on others and that people will adapt in different ways to their environment [5] .
Moran and Britton [33] found that their sample of emergency workers was in fact “no hardier than most nor did they possess any particular coping styles”. In fact, their research supported the earlier findings of Kessler et al [34] whose study found little evidence to support intervention types that aim to aid coping efforts to master, tolerate, or reduce demands of fire service stress.
Moran [35] surmised that firefighters frequently describe their approach to emergency work as being a case of having a job to do and simply getting on with it. Various writers have referred to this phenomenon as “the employing of a professional armor” [17] or “the trauma membrane” [36] .
Lou [37] suggested that coping behaviors are key factors in the link between managing stress and levels of job satisfaction achieved by individuals. This study provided evidence to support the somewhat logical rationale that a firefighter who can manage his/her stressors is likely to be happier in his work. Dahlan et al [5] drew a similar conclusion that a firefighter's ability to cope is actually more important and relevant to their effectiveness than their levels of personal motivation.
2.1.3. Informal social support
A number of studies have been undertaken to consider the importance of informal social support (i.e., postincident discussions and debriefing) within the FRS context. Fullerton et al [9] suggested that the use of humor can increase social support and relieve stress [38] , [39] . In effect, it acts as a safety valve to release tension. This is a situation that occurs frequently in most fire stations around the country and indeed overseas in developed countries such as Canada [40] .
Interestingly however, while concluding that high levels of social support may ostensibly buffer firefighters from PTSD, Haslam and Mallon [15] identified that in most cases, the respondents relied on their partners to be their listener and relief mechanism. This offers a contrary opinion to the personal view of Meroney [21] who indicated that the stress of the job and associated traumatic effects were somewhat normalized and effects were never discussed at home.
Mitani et al [41] and Prag [42] postulate that social support improves the ability to manage stress and is effective in reducing burnout. It also reduces PTSD symptoms of fire service workers [42] . Boscarino et al [43] and Jonsson and Segesten [44] both support this view.
Conversely, Harris et al [45] consider that seeking treatment for personal mental health issues within the context of coworkers and the workplace, generally, may not be the most conducive way to achieve results, and Dahlan et al [5] found during their study that the fostering of positive attitudes was actually the key contributing factor to their participants' health and well-being. This indicates that there is no firm conclusion as to what is the most useful way to support staff after traumatic incidents happen, and further investigations would be useful.
2.1.4. Common physiological responses
Haslam and Mallon [15] found that PTSD symptoms frequently manifested (33%) in the form of trouble sleeping, bad dreams, and reoccurring nightmares. Interestingly, almost double (65%) shared feelings of rumination, that is, they worried about, or visualized, the same event happening to themselves or members of their family ( [15] ). In the same study, 33% of respondents experienced, or had thoughts of, avoidance (e.g., taking a detour from a particular route to not pass a location or avoid a particular type of activity or smell which may remind them of the event). Such visual stimuli/smells are characteristic of PTSD [15] , [46] .
While Joseph et al [47] and Ingledew and Cooper [48] determined that those exhibiting avoidance behaviors are more likely to be suffering greater psychological distress, Raphael et al [8] explained that avoidance was more likely to be a defense mechanism. Substance abuse and addictive behaviors such as eating, smoking, pornography, extreme exercising, shopping, gambling, and sex/love addiction are other functions commonly cited as being indicative of PTSD [9] , [14] , [19] , [24] .
2.1.5. Age, length of service, and exposure
This factor has two clear viewpoints. The first is that the age and length of service are both protecting mechanisms. Mitani et al [41] reason that fire service workers with a long work history exhibit lower job stressors because they have learned skills that enable them to cope; essentially, they desensitize. They also considered that years of service moderate various job-related stressors which is similar to a view shared by Hytten and Hasle [49] that “seasoned emergency workers possess more effective cognitive and behavioral coping strategies”.
Conversely, there are counter arguments; Corneil [50] reported a positive relationship between years of service and PTSD, while Baker and Williams [17] also found it unsurprising that junior officers (who experienced and responded first to the majority of incidents) reported higher incident-related stress levels.
Moran and Britton [33] found that length of service as a volunteer firefighter was positively associated with both severity and chronicity of psychological reaction, citing possible reasons as less preparatory training or frequency of exposure when compared with the whole-time counterparts.
Contrarily, Beaton et al [12] found no evidence of “seasoning” in their study, nor did they find a correlation between years of service and PTSD.
2.1.6. Selection
Mitchell and Bray [51] posited that selection acts as a factor on PTSD vulnerability, and more attention needs to be paid when selecting new entrants. They shared a view that firefighters are undoubtedly a self-selected occupational group and, therefore, may not be representative of the general population in terms of personalities or coping strategies. Harris and Stacks [52] cite data from the Federal Emergency Management Agency survey that suggests that firefighters are overall a healthy group in terms of predisposition to mental health issues.
2.1.7. Alcohol and substance abuse
The World Health Organization [53] defines substance abuse as the harmful or hazardous use of psychoactive substances including alcohol and illicit drugs. Substance abuse may be regarded as just one of many forms of addiction (highlighted earlier).
Boxer and Wild [30] examined whether a link existed between psychological distress and alcohol use among firefighters. On considering the various stressors used in the self-report instruments, they found that, of the 145 participants, between 33% and 41% showed evidence of significant psychological distress, and of these, 29% had possible or probable problems with alcohol use. This compared to a US adult norm of around 13%. However, when logistic regression analysis was undertaken, no link was established between alcohol use and the 10 most highly ranked work stressors:
- ➢ Hearing that children are in a burning building
- ➢ Being concerned about possible exposure to unknown toxic substances
- ➢ Being concerned about exposure to AIDS, hepatitis, tuberculosis, etc.
- ➢ Believing that reverse prejudice exists toward nonminority groups
- ➢ Being disturbed by tone or intensity of bells
- ➢ Feeling responsible for other peoples' lives
- ➢ Feeling a lack of support from the local government
- ➢ Feeling that the public has the wrong idea of what firefighting work involves
- ➢ Feeling that there is insufficient manpower to deal with the workload
- ➢ Feeling overutilized for emergency medical service runs for nonemergency purposes.
This study failed to examine any further, whether the cumulative effect of repeated exposure could form the underlying reason for the higher levels of alcohol use among firefighters.
By comparison, the National Volunteer Fire Council [19] in the United States undertook a study and, while not directly diagnosing alcoholism among participants, did highlight that 42.5% (male) and 60% (female) respondents had engaged in binge-drinking activities in the previous 30 days. This formed a call for vigilance within the sector.
Boxer and Wild [30] cited a phenomenon known as the “healthy worker effect” that postures that among firefighters, healthier staff enter the workforce and remain employed whereas less healthy personnel may be derepresented either due to sickness or leaving the service, therefore presenting a form of selection bias. In essence, one could then postulate that the real levels of substance abuse may be considerably higher and that the same phenomenon may be applicable to PTSD too.
2.1.8. Formal debriefing/mental health professionals
A “critical incident” can be described as being exposed to personal loss or injury, traumatic stimuli, mission failure, or human error [45] . Such experiences have previously been reported to be capable of overwhelming a firefighter's normal ability to cope [51] , [54] .
Critical incident stress management originated in the United States in the 1980s as a peer support intervention for emergency service workers [6] . One component part of critical incident stress management was Critical Incident Stress Debriefing [54] , also commonly referred to as psychological debriefing [55] or critical incident debriefing (CID) [6] .
CID is a peer counseling group procedure with psychoeducational aspects which aims to deliver information on stress reactions after exposure to critical incident(s) [54] . Ideally, the CID is held between 72 hours and 14 days after incident [6] and aims to prevent psychological damage [56] .
The concept is generally credited to the work of Jeffrey Mitchell [54] and thereafter Mitchell and Everly [57] and is led by one mental health professional, supported by trained sector peers [57] . The seven-step approach [6] , [57] aims to teach the recipients about their stress reaction:
- ➢ Facts
- ➢ Thoughts
- ➢ Reactions
- ➢ Normalization
- ➢ Future planning
- ➢ Coping
- ➢ Disengagement
It also aims to enable individuals and groups to have their needs assessed and receive practical support to reduce psychological distress post exposure [58] . CID aims to promote and facilitate recovery and develop/enhance natural resilience [6] .
Sessions last for 1.5–3 hours and start with materials that the participants are more comfortable discussing before entering into more emotionally intense dialogs. The session is brought to a close with psychoeducational input.
While in widespread use, CID has its critics. Harris et al [45] refer to the rapid increase in the provision of CID services among operational and nonoperational personnel but point out that there is little empirical evidence of the effectiveness of CID, a point also made by Rose et al [58] . Harris et al [45] report a number of studies [59] , [60] , [61] that have made assumptions based on relatively small sample sizes and posture a hypothesis that CID has no effect on PTSD. Similarly, Rose et al [58] cite other such reports [62] , [63] , [64] . These quote variables significantly affect the outcomes, examples being a lack of clarity on which disorders CID is intended to improve; a lack of evidence on the level of disorders which requires large-scale interventions; and a lack of evidence that correlates intervention with outcomes [62] , [63] , [64] .
Rose et al [58] noted that the timing of such a debrief also has relevance because the prevalence of initial distress is much higher than that of PTSD, and therefore, owing to the short timescales involved in delivery, the potential exists that interventions (involving confronting distressing experiences) may be delivered needlessly to participants whose short-term symptoms may otherwise rapidly subside. They expressed a view that the use of single-session debriefing “cannot be recommended in either military or civilian life” and that CID did not prevent the onset of PTSD nor did it reduce any psychological distress, morbidity, depression, or anxiety, instead suggesting that it may increase the risk of PTSD and depression. Their recommendation was an endorsement of the National Institute for Health and Care Excellence (2005) approach of “screen and treat”.
Hytten and Hasle [49] found that there was no difference between those formally debriefed and those who received social support by chatting to colleagues.
Regel and Joseph [6] refute the critics of CID on the basis that only two studies may have had any such relevance, and in both cases, the participants were not of the groups that the interventions were intended for (i.e., one was a fire casualty and one from a road traffic collision). They also refer to flaws in methodologies used for those studies. They instead argue that a number of studies exist which do demonstrate positive outcomes from CID.
2.1.9. Recovery
Regel and Joseph [6] explained a concept of how individuals sometimes deal with their exposure to traumatic events. They likened it to a “hurriedly and poorly packed bag that when banged against something could burst open”, resulting in the psychological effects associated with PTSD. As recognized leading writers in this field, Regel and Joseph [6] explain that persons can “unpack and repack the bag in several ways” to make it better and produce a situation where one can “look into the bag” without any undue distress:
- • Using numbness—a remoteness approach whereby only limited and gradual feelings are encountered;
- • Reconsidering—try to make sense of what happened and rationalize it;
- • Receiving physical and emotional support from others—benefits from informal social support;
- • Monitoring own behavior/avoidance behaviors—confronting a situation but at a scale and speed that are not detrimental;
- • Taking time out to process thoughts fully and avoid “packing the bag too hastily”;
- • Physical exercise—to maintain psychological well-being;
- • Effecting an early return to normal routines and considering new interests—although not so as to distract or prevent healing.
This literature review has examined the concept of PTSD and the various factors that may lead to the condition arising. It has also offered detail on why some people appear to be more at risk of succumbing to PTSD than others and why some are able to cope more effectively in the aftermath of a traumatic event.
Importantly, this review has also provided insight into protective factors, support mechanisms, and the arguments that continue to exist on the benefits and limitations of each.
The areas discussed within this literature review will be considered further in the context of an in-depth analysis into the potential prevalence of PTSD among LFRS staff. It allows for an academic approach to be adopted and enables a comprehensive study into the risk posed to LFRS and the suitability of current arrangements that are in place to manage PTSD risk.
2.2. Methodology
2.2.1. introduction.
The first step was to conduct secondary research on PTSD which was carried out through the university search engine known as Scopus and through various internationally based organizations, such as the World Health Organization, etc. This was to collect various standpoints, opinions, and hypotheses that could be explored.
A level of knowledge and understanding was then reached by the researcher whereby opinions and perspectives could be discussed and either substantiated or rebuffed by virtue of the case studies, reports, and texts that were available. This enabled the researcher to remain objective throughout the study to differentiate fact from supposition or opinion.
The next stage was to conduct quantitative research in the form of questionnaires to establish the prevalence of PTSD within LFRS. Kienzler and Pedersen [65] advise that almost every trauma-related study should include some measures of PTSD symptoms to provide information about how respondents view their symptoms in a context that is not influenced by direct interaction with an interviewer.
It should be noted that although a number of different measures of PTSD exist, no single measure can definitely determine whether or not an individual has PTSD; instead, multiple measures should be administered [66] . Therefore, the adopted methodology was to settle on the use of two recognized clinical questionnaires. Solomon et al [66] stated that with the help of self-report instruments, response accuracy may be increased, especially for those informants who are reluctant to reveal their experiences to another person directly.
While a number of historic USA-derived screening tools were available, the development of culturally sensitive psychological tests and symptom checklists for assessing anxiety and depression is promoted [67] . These include among others the Impact of Event Scale–Revised, the General Health Questionnaire-28 (GHQ-28), the Harvard Trauma Questionnaire, the Hopkins Symptom Checklist-25, and the Posttraumatic Stress Disorder Symptom Scale (PSS). Accordingly, the GHQ-28 and PSS questionnaires were subsequently selected.
2.2.2. General Health Questionnaire
The GHQ-28 [68] is used to indicate psychological well-being and detect possible cases of psychiatric disorders (psychiatric morbidity) [69] . The reason for using this questionnaire was to identify aspects of poor physical health [70] and problems in intimate and family relationships [71] which are frequently associated with PTSD.
The GHQ-28 is commonly used as a community-screening tool and for the detection of nonspecific psychiatric disorders among individuals in primary care settings [65] . It is a self-report instrument comprising four subscales measuring somatic symptoms (physical rather than psychological), anxiety/insomnia, social dysfunction, and severe depression. It has been recommended in previous studies for screening trauma victims [8] , and although developed in the United Kingdom, it has been widely employed in other countries (translated into c.38 languages and >50 validity studies completed) [68] .
A number of different scoring systems can be applied, but for the purposes of this study, the preferred Likert scale was applied (0-1-2-3) [72] to the descriptive answers. This produces a maximum score of 84 across the 28 questions.
2.2.3. Posttraumatic Stress Disorder Symptom Scale
The PSS consists of two pages; the first is essentially a set of “qualifying questions” which lists a set of traumatic events or situations. Page 2 details 17 further questions that diagnose PTSD according to DSM criteria and assess the severity of PTSD symptoms. Questions are grouped around “reexperiencing” (5 questions), “avoidance” (7 questions), and “arousal” (5 questions). Under DSM, PTSD is diagnosed if at least one reexperiencing, three avoidance, and two arousal symptoms are revealed (at a rating of 2 or 3). The exposure had to have taken place more than one month before. As per the GHQ, these questions are answered using the Likert scale with the maximum score across the 17 questions being 51, representing the total severity score [1] . This allows the PSS to be used as either a categorical or dimensional measure. Where this questionnaire differs from the GHQ-28 is in the scoring descriptors of “0 = Not at all”, “1 = Once per week or less/A little bit/Once in a while”, “2 = 2–4 times per week/Somewhat/Half the time”, “3 = 3–5 or more times per week/Very much/Almost Always”; these were altered to reflect the same scoring descriptors used within the GHQ-28. This was to make interpretation and analysis of the results more consistent.
Although the application of the PSS for emergency service workers has been limited in other studies, it is frequently referred to as being used for circumstances such as rape victims; for this reason access to psychometric data for such samples was also very limited; nonetheless, the questionnaire draws some correlations with aspects considered under the GHQ-28. A modified version of this scale exists which includes both frequency and intensity ratings. This allows assessment of symptoms related to multiple traumatic events [66] , and perhaps, this assessment type could also be a useful alternative to the PSS.
2.3. Collection of data
Operational staff were approached during the late 2014 and early 2015 and asked to provide consent to participate. Stations, watches, or groups who offered willingness to participate were then sent copies of the consent form, GHQ-28 and PSS for completion privately and confidentially. To ensure anonymity, completed questionnaires were return mailed in a self-addressed envelope to the authors. From this point, the completed returns were kept securely stored and not shared with third parties.
The aim was to collect 150 responses representing 13.5% of the operational workforce; 100 responses were returned. This number is lower than expected, possibly due to unwillingness to assist in the study because of ongoing industrial action over pension changes within the UK FRS.
Responses came from a cross section of the operational staff; however, it should be noted that LFRS, in common with most other UK FRS, remains a predominantly male environment (c.96%), but no specific reference was made to gender, ethnicity, or age; therefore, these factors will be outside of the scope of this study.
2.4. Analysis of data
Once the data were collated, statistical analysis using a combination of thematic and graphical analysis was then completed. In addition, appropriate for our case study was to use descriptive and summary statistics such as the mean and standard deviation to indicate what the average numbers and variations for different phenomena were, so as to determine if relationships existed.
On completion of the analysis, the findings were then compared with observations from other literature sources to determine how our results fitted with their findings. The outcomes of this analysis are discussed in the remainder of this article along with the conclusions that were drawn.
3. Results and discussion
3.1. general health questionnaire.
Within the range of 0–84, a score of 23 or 24 is deemed to be the threshold for the presence of distress [73] . For this study, a total score of 23 or above has been taken as being the baseline. Of the 100 persons sampled, 30 individuals showed probable signs for the presence of distress (30%). The GHQ results are divided into four sections based on the subject headings within the questionnaire:
- A. Somatic Symptoms
- B. Anxiety/Insomnia
- C. Social Dysfunction
- D. Severe Depression
The results collected have provided ordinal data that produce greater opportunities for analysis because it not only classifies subjects but also ranks them in terms of the degree to which a characteristic is present [74] . Table 3 shows the results of the respective surveys and the analysis following it. Generally, categories 0 and 1 are positive responses i.e., no real change from before, and categories 2 and 3 are negative response i.e., a bigger change than normal.
Table 3
Responses to the General Health Questionnaire (GHQ-28)
Within Section A (Somatic Symptoms), the first four questions tend toward psychological symptoms whereas the other three relate more toward physical symptoms. The questions which provoked the most negative responses were A1, A2, and A3 with question A3 “Feeling run down and out of sorts” and A2 “Been feeling in need of a good tonic” presenting the highest negative responses (26%). Question A5 “Been getting any pains in your head” and A7 “Been having hot or cold spells” received answers of a “0” or “1” (90%) which for the purpose of this survey have been classed as positive responses. In summary, Section A showed that there is a prevalence of more psychological symptoms than physical, and these represent a situation that is worse than the norm.
Within Section B (Anxiety/Insomnia), the first two questions relate to insomnia and the remainder to anxiety. Question B2 “Had difficulty in staying asleep once you are off” had the highest proportion of negative responses (36%) followed by B3 “Felt constantly under strain” and B4 “Been getting edgy and bad-tempered,” both scoring 26%. It is worth noting that B3 scored the highest number of the most negative response “Much more than usual” (10%).
Section C (Social Dysfunction) is a measure of the impact of PTSD on an individual's ability to conduct normal social interactions. For all questions, most responses were positive with respondents either “Better than usual” or “Same as usual” (responses ranging from 82% to 98%). In summary, most responses were of a positive nature when compared with the other sections of the GHQ-28.
Most questions within Section D (Severe Depression) scored a “0” or “1”. Owing to the serious nature of the questions, this is expected. The question with the most notable response was D1, “Been thinking of yourself as a worthless person,” with 30% of respondents scoring a “2” or “3,” which being a significantly higher negative response than normal.
It was also notable that the number of respondents to D6 “Found yourself wishing you were dead and away from it all” had no negative responses, whereas D7 “Found that the idea of taking your own life kept coming into your mind” had two negative responses (termed as “Has crossed my mind”). In summary, the vast majority of responses within this section were of positive nature.
3.2. Posttraumatic Stress Disorder Symptom Scale
Given that the responding group was operational fire service personnel, it was expected that many would answer positively to having experienced or witnessed the “qualifying” situations listed on page 1 of the questionnaire, and indeed, this was so in 100% of occasions.
As previously discussed, the PSS questionnaire's questions can be divided into three sections: reexperiencing, arousal, and avoidance. Table 4 shows the results and analysis of the following categories.
- 0 Not at all
- 1 Once per week or less/a little bit/once in a while
- 2 2–4 times a week/somewhat/half the time
- 3 3–5 or more times a week/very much/almost always
Table 4
Responses to the Posttraumatic Stress Disorder Symptom Scale (PSS) questionnaire
The first five questions summarize the questions relating to reexperiencing from the PSS. Most respondents scored 0, “Not at all” for most questions, with approximately 7% of the sample scoring 2–3 relating to “Rather more than usual” and “Much more than usual”.
For the avoidance questions 6–12, most respondents scored 0, “Not at all”. Approximately 7% of the sample scored 2–3 relating to “Rather more than usual” and “Much more than usual”. This was similar to that seen for the reexperiencing questions.
The arousal questions 13–17 saw the highest number of respondents scoring 2–3 “Rather more than usual” and “Much more than usual” compared with the other sections with approximately 13% of the sample.
For the final part on the questionnaire, the results are given in Table 5 .
Table 5
Positive responses for “Have any of the above problems interfered with the following?”
To summarize, arousal saw the largest variation in responses with more respondents scoring “2” “Rather more than usual” or “3” “Much more than usual” than in the other sections. Reexperiencing saw the least variation with most respondents scoring “0” “Not at all”. These results will be discussed further in the following sections.
The analysis has been divided into two sections, first the GHQ-28 and then the PSS.
3.3. General Health Questionnaire
From looking at the results of the GHQ-28, it was decided to divide the findings into three sections corresponding to physical symptoms, positive emotions, and negative emotions. This was to determine how the most significant symptoms manifest in the most significant emotions. The categories are shown in Table 6 below:
Table 6
Categories applied to GHQ-28 questionnaire results
GHQ, General Health Questionnaire.
To determine the most significant variables, the average number of negative responses from the GHQ-28 has been calculated by adding together those responses that scored ≥2. Standard deviation was then applied to determine which variables were significant. The results are shown in the Table 7 .
Table 7
Application of standard deviation to GHQ-28 results
Any variables that were higher than one standard deviation above the average were considered a warning sign and therefore significant. For sections A and B (symptoms), this affected the following one variable B2, “Had difficulty in staying asleep once you are asleep”, which with a score of 36 was over two standard deviations above the mean. The same methodology was then applied to Section C, Social Dysfunction, and D, Severe Depression (Emotions). For Section C, no variables were found to be significant. In Section D, just one variable was found to be more than one standard deviation above the average. This was (D1), “Been thinking of yourself as a worthless person” with a score of 30. This variable was over two standard deviations above the mean and was, therefore, seen as being very significant.
3.4. Posttraumatic Stress Disorder Symptom Scale
Of the 100 people questioned using the PSS, four people were identified as having symptoms of PTSD. This accounts for 4% of the total sample. All these four people surprisingly did not score significantly in the GHQ-28 as expected (with scores ranging from 9–43). In fact, only two people identified as high risk from the GHQ-28 (scoring 43) went on to show symptoms of PTSD. The other two participants identified in the sample as having PTSD scored GHQ-28 scores of below 10.
The PSS questionnaire is divided into three sections: reexperiencing, avoidance, and arousal. Based on the findings from the literature and results, this analysis aims to see how the different sections of the PSS manifest in people's everyday lives.
Again, to determine the most significant variables, the average number of negative responses from the GHQ-28 has been calculated by adding together those responses that scored ≥2. Standard deviation was then applied to determine which variables were significant. The results are shown in the Table 8 .
Table 8
Application of standard deviation to PSS results
PSS, Posttraumatic Stress Disorder Symptom Scale.
For the reexperiencing section, only one variable question 5 “experiencing physical reactions when reminded of the traumatic event (sweating, increased heart rate)” was significant. For the avoidance section, question 7 “trying to avoid activities or people that remind you of the traumatic event” was significant. For the arousal section, again only one question 14 “feeling irritable or having fits of anger” was significant.
From the results section, counts were also made on each of the variables that were identified as interfering with aspects of everyday life after exposure to a traumatic event. These were “work”, “household duties”, “friendships”, “fun/leisure activities”, “schoolwork”, “family relationships”, “sex life”, “general life satisfaction”, and “overall functioning” as shown in Fig. 2 .

Count of variables interfering with aspects of everyday life.
The variables that showed the highest count and were supported from secondary research were “work”, “family relationships”, and “general life satisfaction”. However, it is seen that sex and education seem to have the lowest count and may suggest that there may be some strategies used to deal with matters of distress.
3.5. Discussion
On completing this research, some interesting observations have been made. The most important being the number of people within LFRS who show signs of distress as highlighted from the GHQ-28 questionnaire and those people who exhibit probable symptoms of PTSD as identified by the PSS questionnaire.
The results from the GHQ-28 highlighted that 30% of the respondents surveyed showed signs of probable distress. If this number was multiplied to represent the number of LFRS employees, approximately 300 operational members of staff could hypothetically be suffering from distress.
Although the research provides evidence that the vulnerability to PTSD does not directly correlate with the GHQ-28 outcomes, it does show that those with poor general health are more susceptible to developing PTSD. This means that potentially 30% of LFRS operational personnel are at risk of developing PTSD.
On analyzing the results of the PSS, four of the 100 people surveyed showed symptoms of PTSD. By scaling these responses up in the same way as for the GHQ-28, LFRS potentially could have approximately 40 cases of PTSD which are presently undiagnosed and untreated, accounting for 4% of the operational workforce. This is lower than what has typically been found in the previously published reports where scores as low as 5% have been obtained [3] .
As the analysis shows, both the GHQ-28 and PSS questionnaires were completed. This was to determine whether general health affected PTSD. The results were inconclusive as of the four people who showed symptoms of PTSD, only two people were identified as high risk from the GHQ-28 (scoring 43). The other two participants identified in the sample as having PTSD scored GHQ-28 scores of below 10. As a result, it was not possible to establish whether general health did influence the development of PTSD symptoms.
The analysis of the results produced some interesting findings. From the GHQ-28, it was determined that emotions affect physical symptoms, supporting the theory that comorbid mental health issues could potentially bring about the development of PTSD.
Interestingly, from a productivity perspective, some of the evidence suggests that the coping strategies used by firefighters are actually more important than their levels of personal motivation, as motivation itself may be directly affected by an individual's ability to cope with the trauma that they witness. Certainly, this survey of LFRS staff highlighted that some will throw themselves into distraction activities (such as sex or education).
LFRS currently adopt an “opt-in” approach to CID; however, this has both advocates and critics. The cultural appetite for engaging in this process is presently limited, and a number of variables exist which may determine the effectiveness of CID such as the timing of the debrief, the duration, or the qualifications, expertise, and training of the facilitator.
The literature review highlighted that CID supporters claim some highly positive outcomes, yet their findings tend not to appear within professional journals. Conversely, several of the less positive studies referred to earlier within this text, which cast doubt over the success of CID, are visible throughout a number of professional medicine and psychology journals. Equally, if no baseline assessment has been undertaken, the outcomes may not be valid, given that the subject may have had existing conditions such as a premorbid personality.
3.6. Recommendations from the study
Current practices within the LFRS are carried out on an optional basis on the part of employees. There is a nonmandatory CID process which employees can take part in if they wish. There is also voluntary counseling service that is available if required and generally, staff is expected to keep an eye on anyone who has recently experienced a traumatic event within the organization.
Based on the findings of both the primary and secondary research completed, this article proposes that LFRS should consider the provision of organizational and leadership practices that aim to mitigate threats derived from PTSD among firefighters; these include the following:
- • Delivery of education packages aimed at increasing awareness of stress and PTSD in order that individuals are able to identify the symptoms in themselves and their colleagues at an early stage.
- • Mental health screening for new entrants to take into account dispositional variables, which may already exist in applicants.
- • Routine screening to facilitate identification and assessment of behavioral issues (such as PTSD) by the means of annual fitness tests and routine medical examinations. This provides a “background reading” for staff in the event of a traumatic event occurring which may require CID or professional health-care involvement.
- • Liaison with the military (using existing associations) to learn from their findings and adapt and introduce training for implementation within LFRS.
- • Revising the workplace significant incident protocol to include automatic directing of affected staff to trained behavioral health experts.
- • An option for immediate access to professional services in the first instance rather than via CID, so as to offer sufferers the earliest and perhaps optimum chance of recovery.
- • Development of a Web/mobile app, similar to Pocket Peer that combines Web training with information on symptom recognition and provides direct links to professional services.
- • As the UK FRS broadens its skill base to adopt new work streams such as Community First Responding, FRSs should recognize that the increased activity levels and exposure to new incident types (many of which may involve children) could have health impacts for staff, both immediate and longer term.
4. Conclusions
The primary research shows that a PTSD problem does exist within LFRS but at a level which is lower than that found in other similar studies and indeed lower than the quoted lifetime prevalence levels of c.10.4% for women and 5% for men. This supports the position of Brown et al [72] that exposure does not automatically mean the development of psychological distress.
From studying the variables that affect PTSD, it can be determined that no conclusive relationship exists between general health and PTSD within LFRS, with the main variables affecting the development of PTSD being emotions which manifest themselves into physical symptoms.
Secondary research has shown that incidents involving children are the most commonly cited factor for the development of PTSD within FRS personnel. Evidence from Haslam and Mallon [15] suggests that this difficulty in dealing with child victims is borne mainly from a sense of identification between the victims and one's own children.
While research suggests that PTSD manifests itself in a person's day-to-day life through reexperiencing, avoidance, and arousal, it was clear from the respondents to this study that arousal was the most significant detriment to a person's everyday life. This was displayed through the existence of anxiety, depression, addictive behaviors, and insomnia.
Conclusions from the secondary research show that although the culture of the UK FRS remains one of required fortitude and endurance, this strength may also present a risk in the form of lower levels of self-reported stress, probably for many years. Based on the primary research undertaken, it is clear that LFRS presently has a number of personnel experiencing adverse psychological and physical reactions, many of which may be going undiagnosed and untreated at the present time.
Where incidents are discussed in the social setting i.e., after incident, they can tend to be done so using humor, so one could argue that the historic culture within the UK FRS actually presents a natural remedy within the workplace. Whereas this may benefit some personnel and help them to contextualize and perhaps “place in a box” that specific occurrence, for others it may place pressure on them to conceal or deny their true feelings again leading to PTSD symptoms going undiagnosed and untreated.
It is clear from the research undertaken that the role of an emergency responder, and specifically a UK firefighter, has the potential for exposure to traumatic sights, smells, and sounds, creating memories which in some cases will last a lifetime. This article supports the continued development of organizational and leadership practices to assist LFRS in planning for, and mitigating against, the inevitable threat that arises from exposure to traumatic incidents.
4.1. Limitations of study and suggestions for future research
One of the limitations of the study was that the intention was to draw findings from a larger sample size than was achieved; national environmental factors (the ongoing industrial dispute) within the sector affected the ability to deliver this. It is therefore a recommendation of this article that a wider study be undertaken, perhaps on a north-west regional footprint to obtain both a wider sample and detect variances between FRS and between firefighters working in urban and rural environments. With the relevant consents, such a study could also consider the implications of gender, age, ethnicity, position within the organizational structure, and whether whole time or retained duty system. This would then allow for the prevalence of PTSD to be compared with sociodemographic factors and any geographical variations.
It should also be noted that the sample used was from within a single county. Lancashire is predominantly rural with several large conurbations. It does not face the same level of challenges and perhaps more serious threats and events as may be seen by some larger metropolitan FRS. As a result, caution should be applied to the current findings when considered in the context of other FRS areas.
To fully appreciate the benefits associated with CID, further research could be undertaken within LFRS (or regionally) to examine more closely the interactions of participants, the outcomes, and the how CID or the involvement of professionals may deliver better outcomes for staff.
Finally, as the nature of a UK firefighter's role continues to evolve with greater exposure via new aspects such as emergency medical response, the exposure to distressing events within our communities also increase. It is recommended that LFRS commission further works to explore the expected implications of such new work streams and the potential impacts to inform the future needs of the service.
Conflicts of interest
All authors have no conflicts of interest to declare.
Acknowledgments
The authors are grateful to the Lancashire Fire and Rescue Service for their kind cooperation that enabled them to pursue this research successfully.
Appendix A Supplementary data related to this article can be found at https://doi.org/10.1016/j.shaw.2017.11.002 .
Appendix A. Supplementary data
The following is the supplementary data related to this article:

IMAGES
VIDEO
COMMENTS
Philip, a 60-year-old who was in a traffic accident (PDF, 294KB) This case example from the European Journal of Psychotraumatology details an assisted self-study application of cognitive therapy for PTSD. Philip developed PTSD and comorbid major depression following a traffic accident. He was treated in six sessions of cognitive therapy with ...
CASE STUDY Victor (post-traumatic stress disorder) Case Study Details. Victor is a 27-year-old man who comes to you for help at the urging of his fiancée. He was an infantryman with a local Marine Reserve unit who was honorably discharged in 2014 after serving two tours of duty in Iraq. His fiancé has told him he has "not been the same ...
Post-traumatic stress disorder (PTSD) is a severe stress reaction that develops in some people after traumatic events, such as accidents, disaster, or physical or sexual violence. ... In conclusion, this case study demonstrates the possibility of using self-study modules in the treatment of PTSD despite the memory and concentration problems ...
Article Content. The Psychiatric Genetics Consortium (PGC), a consortium of researchers led by scientists at University of California San Diego School of Medicine has made significant advancements in the understanding of the neurobiology of post-traumatic stress disorder (PTSD), a condition the World Health Organization says affects some 250 million people around the world.
Post-traumatic stress disorder (PTSD) is a psychiatric condition which may develop after a terrifying event, usually involving a risk to physical integrity or to life, one's own or of other people. ... Our case indicates that peripheral post offices may also be at high risk. The second case is the victim of a terrible accident at work ...
Current treatment strategies for control of trauma-associated symptoms of Post Traumatic Stress Disorder (PTSD) have recently been updated by the Veterans Affairs (VA) and the Department of Defense (DoD, after over a decade of dedicated research. The most recent evidence is compelling that its use of trauma-focused therapies such as Cognitive ...
This case-control study (n = 40) aimed to identify differences in peripheral blood biomarkers, and biomarker combinations, able to distinguish PTSD participants from controls, and examine in a biopsychosocial framework. ... Post-traumatic stress disorder (PTSD) is a debilitating psychiatric condition which may result following exposure to ...
Substance use disorders and post-traumatic stress disorder (PTSD) often co-occur, along with depression and anger. Despite evidence that Prolonged Exposure Therapy is effective for individuals with co-occurring PTSD and SUD when PE is implemented alongside SUD treatment, clinicians have been reluctant to offer PE or other trauma-focused therapies to individuals with co-occurring PTSD and SUD ...
Post-traumatic stress disorder (PTSD) is one of the few neuropsychiatric disorders for which the timing and cause of onset are understood, facilitating research into the underlying mechanisms. In ...
In 2013, the American Psychiatric Association revised the posttraumatic stress disorder (PTSD) criteria in the 5 th edition of its "Diagnostic Statistical Manual of Mental Disorders" (DSM-5 ...
Post-traumatic stress disorder (PTSD) is arguably the most common psychiatric disorder to arise after exposure to a traumatic event. Since its formal introduction in the DSM-III in 1980, knowledge has grown significantly regarding its causes, maintaining mechanisms and treatments. ... Subsequent longitudinal studies indicated that this ...
Posttraumatic stress disorder (PTSD) may occur in individuals who have experienced a traumatic event. Previous coronavirus epidemics were associated with PTSD diagnoses in postillness stages, with meta-analytic findings indicating a prevalence of 32.2% (95% CI, 23.7-42.0). 1 However, information after severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is piecemeal.
Background: Emotional Freedom Techniques (EFT) and Eye Movement Desensitization and Reprocessing (EMDR) have been empirically validated as effective psychotherapeutic interventions for treating Post Traumatic Stress Disorder (PTSD). This single subject design case study is of a survivor of the Twin Towers collapse who was treated for prolonged PTSD complicated by dissociated memories.
Future case studies should consider the use of additional measures, such as the Post Traumatic Cognitions Inventory (PTCI; Foa et al., Reference Foa, Tolin, Ehlers, Clark and Orsillo 1999), and measures for grief response. Measuring grief, low mood and PTSD outcomes in parallel would enable a better understanding of the relationship between ...
Yet, few studies have directly examined 5-MeO-DMT for trauma- or stress-related psychopathology, including post-traumatic stress disorder (PTSD). Herein, we present the first longitudinal case study on 5-MeO-DMT for chronic refractory PTSD, in a 23-year-old female.
Recent studies have shown that psychotic symptoms can be a hallmark of post-traumatic stress disorder [1, 2]. The vast majority of the cases reported concerned war veterans although there were sporadic incidents involving non-combat related trauma (somatic or psychic). ... Case formulation - (Persistent PTSD, adapted from Ehlers and Clark ).
Introduction. Post-traumatic stress disorder (PTSD), also known as the "invisible wound" [] or the "signature illness" [] among Iraq and/or Afghanistan combat veterans, has an estimated prevalence rate of 10%-30% [1-8], with higher rates in those with multiple combat tours [3,7].]. However, most combat veterans do not seek medical care [] often because of stigma [1,2,6,8].
Abstract. Post-traumatic stress disorder (PTSD), previously known as battle fatigue syndrome or shell shock, is a severe mental disturbance condition that is normally triggered by the experience of some frightening/scary events or trauma where a person undergoes some serious physical or mental harm or threatened.
This case study presents information about post traumatic stress disorder in older adults. It is divided into different sections including the history, presentation and examination, diagnosis, case discussion, post traumatic stress disorder explained, take home points, and additional resources.
In Switzerland, since 2014, two psychotherapists obtained 50 licenses on a case-by-case basis and developed a psychedelic-assisted group therapy model utilizing MDMA and LSD for patients suffering from chronic complex post-traumatic stress disorder (C-PTSD), dissociative, and other post-traumatic disorders (Oehen and Gasser, 2022). The authors ...
The case study of Rich (see Case Study 1) demonstrates that the body can be an ally and a catalyst in the process of healing from trauma. Such physical changes often help to resolve the habitual trauma-related responses and provide improved stability to handle future stressors (Ogden et al., 2006).
This paper concludes with a self-critique by the therapist regarding every aspect of the presented case study. Post Traumatic Case Study (PTSD): Case Study; Dick's Journey Descriptive Narrative Dick is a retired military man, in his late fifties, suffering from DSM-IV-TR chronic military-related posttraumatic stress disorder (PTSD).
Post-traumatic stress disorder (PTSD) can be caused by experiencing or witnessing a variety of harsh traumatic events. Rape, burglary, war, torture, violence, and other catastrophic events have been known to precipitate flashbacks, nightmares, and inability to cope with the demands of daily life. ... This case study describes a 42-year-old man ...
Post-traumatic stress disorder, or PTSD, is the psychiatric disorder that can result from the experience or witnessing of traumatic or life-threatening events such as terrorist attack, violent crime and abuse, military combat, natural disasters, serious accidents or violent personal assaults. ... Best case studies in evidence-based research ...
Within socio-military history, the diagnosis of post-traumatic stress disorder has aroused a lot of attention, with many scholars claiming its existence in the pre-modern world while sceptics have challenged this claim in no uncertain terms. ... Rees, O. (2022). Post-traumatic Stress Disorder: An Ancient Greek Case Study in Retrospective ...
Methods. The overarching purpose of this epidemiological study is to assess the prevalence of post-traumatic stress disorder (PTSD) amongst operational LFRS personnel and to analyse the effects upon those who may be suffering from it, whether brought about by a single traumatic event or by repeated exposure to traumatic occurrences over a period of time.
Speaker's Regional Youth Debating Competition 2024 District 11, Round 1 (Match 1)