An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager

Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
A systematic literature review on obesity: Understanding the causes & consequences of obesity and reviewing various machine learning approaches used to predict obesity
Affiliations.
- 1 Centre for Software Technology and Management, Faculty of Information Science and Technology, Universiti Kebangsaan Malaysia (UKM), Bangi, 43600, Selangor, Malaysia.
- 2 Centre for Software Technology and Management, Faculty of Information Science and Technology, Universiti Kebangsaan Malaysia (UKM), Bangi, 43600, Selangor, Malaysia. Electronic address: [email protected].
- 3 RIADI Laboratory, University of Manouba, Manouba, Tunisia; College of Computer Science and Engineering, Taibah University, Medina, Saudi Arabia.
- 4 Center for Artificial Intelligence Technology, Faculty of Information Science and Technology, Universiti Kebangsaan Malaysia (UKM), Bangi, 43600, Selangor, Malaysia.
- PMID: 34426171
- DOI: 10.1016/j.compbiomed.2021.104754
Obesity is considered a principal public health concern and ranked as the fifth foremost reason for death globally. Overweight and obesity are one of the main lifestyle illnesses that leads to further health concerns and contributes to numerous chronic diseases, including cancers, diabetes, metabolic syndrome, and cardiovascular diseases. The World Health Organization also predicted that 30% of death in the world will be initiated with lifestyle diseases in 2030 and can be stopped through the suitable identification and addressing of associated risk factors and behavioral involvement policies. Thus, detecting and diagnosing obesity as early as possible is crucial. Therefore, the machine learning approach is a promising solution to early predictions of obesity and the risk of overweight because it can offer quick, immediate, and accurate identification of risk factors and condition likelihoods. The present study conducted a systematic literature review to examine obesity research and machine learning techniques for the prevention and treatment of obesity from 2010 to 2020. Accordingly, 93 papers are identified from the review articles as primary studies from an initial pool of over 700 papers addressing obesity. Consequently, this study initially recognized the significant potential factors that influence and cause adult obesity. Next, the main diseases and health consequences of obesity and overweight are investigated. Ultimately, this study recognized the machine learning methods that can be used for the prediction of obesity. Finally, this study seeks to support decision-makers looking to understand the impact of obesity on health in the general population and identify outcomes that can be used to guide health authorities and public health to further mitigate threats and effectively guide obese people globally.
Keywords: Diseases; Machine learning; Obesity; Overweight; Risk factors.
Copyright © 2021 The Author(s). Published by Elsevier Ltd.. All rights reserved.
PubMed Disclaimer
Similar articles
- The future of Cochrane Neonatal. Soll RF, Ovelman C, McGuire W. Soll RF, et al. Early Hum Dev. 2020 Nov;150:105191. doi: 10.1016/j.earlhumdev.2020.105191. Epub 2020 Sep 12. Early Hum Dev. 2020. PMID: 33036834
- Identification of Risk Factors Associated with Obesity and Overweight-A Machine Learning Overview. Chatterjee A, Gerdes MW, Martinez SG. Chatterjee A, et al. Sensors (Basel). 2020 May 11;20(9):2734. doi: 10.3390/s20092734. Sensors (Basel). 2020. PMID: 32403349 Free PMC article.
- Data-driven modeling and prediction of blood glucose dynamics: Machine learning applications in type 1 diabetes. Woldaregay AZ, Årsand E, Walderhaug S, Albers D, Mamykina L, Botsis T, Hartvigsen G. Woldaregay AZ, et al. Artif Intell Med. 2019 Jul;98:109-134. doi: 10.1016/j.artmed.2019.07.007. Epub 2019 Jul 26. Artif Intell Med. 2019. PMID: 31383477 Review.
- The effect of weight management interventions that include a diet component on weight-related outcomes in pregnant and postpartum women: a systematic review protocol. Spencer L, Rollo M, Hauck Y, MacDonald-Wicks L, Wood L, Hutchesson M, Giglia R, Smith R, Collins C. Spencer L, et al. JBI Database System Rev Implement Rep. 2015 Jan;13(1):88-98. doi: 10.11124/jbisrir-2015-1812. JBI Database System Rev Implement Rep. 2015. PMID: 26447010
- Screening and Interventions for Childhood Overweight [Internet]. Whitlock EP, Williams SB, Gold R, Smith P, Shipman S. Whitlock EP, et al. Rockville (MD): Agency for Healthcare Research and Quality (US); 2005 Jul. Rockville (MD): Agency for Healthcare Research and Quality (US); 2005 Jul. PMID: 20722132 Free Books & Documents. Review.
- Comparing the Efficacy of Digital and In-Person Weight Loss Interventions for Patients with Obesity and Glycemic Disorders: Evidence from a Randomized Non-Inferiority Trial. Moravcová K, Sovová M, Ožana J, Karbanová M, Klásek J, Kolasińska AB, Sovová E. Moravcová K, et al. Nutrients. 2024 May 16;16(10):1510. doi: 10.3390/nu16101510. Nutrients. 2024. PMID: 38794747 Free PMC article. Clinical Trial.
- Prevalence of Obesity and Dental Caries in High School Adolescents during the First Decade of Saudi Vision 2030: A Cross-Sectional Study. Farsi DJ, Farsi NJ, Elkhodary HM, Alattas LK, Alshaikh AB, Farsi NM. Farsi DJ, et al. Children (Basel). 2024 May 8;11(5):563. doi: 10.3390/children11050563. Children (Basel). 2024. PMID: 38790558 Free PMC article.
- Common mental disorders in Brazilian adolescents: association with school characteristics, consumption of ultra-processed foods and waist-to-height ratio. Gratão LHA, Silva TPRD, Rocha LL, Jardim MZ, Oliveira TRPR, Cunha CF, Mendes LL. Gratão LHA, et al. Cad Saude Publica. 2024 May 17;40(4):e00068423. doi: 10.1590/0102-311XEN068423. eCollection 2024. Cad Saude Publica. 2024. PMID: 38775572 Free PMC article.
- Anemia Status Changes Among Patients With Obesity Following Bariatric Surgery. Soheilipour F, Eskandari D, Abolghasemi J. Soheilipour F, et al. Cureus. 2024 May 17;16(5):e60500. doi: 10.7759/cureus.60500. eCollection 2024 May. Cureus. 2024. PMID: 38764702 Free PMC article.
- Cardiovascular Benefits of GLP-1 Receptor Agonists in Patients Living with Obesity or Overweight: A Meta-analysis of Randomized Controlled Trials. de Oliveira Almeida G, Nienkötter TF, Balieiro CCA, Pasqualotto E, Cintra JB, Carvalho HCP, Silva ALS, Kabariti JC, Minucci BS, Bertoli ED, Guida CM. de Oliveira Almeida G, et al. Am J Cardiovasc Drugs. 2024 Jul;24(4):509-521. doi: 10.1007/s40256-024-00647-3. Epub 2024 May 11. Am J Cardiovasc Drugs. 2024. PMID: 38734847
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Elsevier Science
- Genetic Alliance
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Loading metrics
Open Access
Perspective
The Perspective section provides experts with a forum to comment on topical or controversial issues of broad interest.
See all article types »
Obesity research: Moving from bench to bedside to population
* E-mail: [email protected]
Affiliation Diabetes Research Program, Department of Medicine, New York University Grossman School of Medicine, New York, New York, United States of America
- Ann Marie Schmidt

Published: December 4, 2023
- https://doi.org/10.1371/journal.pbio.3002448
- Reader Comments
Globally, obesity is on the rise. Research over the past 20 years has highlighted the far-reaching multisystem complications of obesity, but a better understanding of its complex pathogenesis is needed to identify safe and lasting solutions.
Citation: Schmidt AM (2023) Obesity research: Moving from bench to bedside to population. PLoS Biol 21(12): e3002448. https://doi.org/10.1371/journal.pbio.3002448
Copyright: © 2023 Ann Marie Schmidt. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: AMS received funding from U.S. Public Health Service (grants 2P01HL131481 and P01HL146367). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The author has declared that no competing interests exist.
Abbreviations: EDC, endocrine disruptor chemical; GIP, gastric inhibitory polypeptide; GLP1, glucagon-like peptide 1; HFCS, high-fructose corn syrup
This article is part of the PLOS Biology 20th anniversary collection.
Obesity is a multifaceted disorder, affecting individuals across their life span, with increased prevalence in persons from underrepresented groups. The complexity of obesity is underscored by the multiple hypotheses proposed to pinpoint its seminal mechanisms, such as the “energy balance” hypothesis and the “carbohydrate–insulin” model. It is generally accepted that host (including genetic factors)–environment interactions have critical roles in this disease. The recently framed “fructose survival hypothesis” proposes that high-fructose corn syrup (HFCS), through reduction in the cellular content of ATP, stimulates glycolysis and reduces mitochondrial oxidative phosphorylation, processes that stimulate hunger, foraging, weight gain, and fat accumulation [ 1 ]. The marked upswing in the use of HFCS in beverages and foods, beginning in the 1980s, has coincided with the rising prevalence of obesity.
The past few decades of scientific progress have dramatically transformed our understanding of pathogenic mechanisms of obesity ( Fig 1 ). Fundamental roles for inflammation were unveiled by the discovery that tumor necrosis factor-α contributed to insulin resistance and the risk for type 2 diabetes in obesity [ 2 ]. Recent work has ascribed contributory roles for multiple immune cell types, such as monocytes/macrophages, neutrophils, T cells, B cells, dendritic cells, and mast cells, in disturbances in glucose and insulin homeostasis in obesity. In the central nervous system, microglia and their interactions with hypothalamic neurons affect food intake, energy expenditure, and insulin sensitivity. In addition to cell-specific contributions of central and peripheral immune cells in obesity, roles for interorgan communication have been described. Extracellular vesicles emitted from immune cells and from adipocytes, as examples, are potent transmitters of obesogenic species that transfer diverse cargo, including microRNAs, proteins, metabolites, lipids, and organelles (such as mitochondria) to distant organs, affecting functions such as insulin sensitivity and, strikingly, cognition, through connections to the brain [ 3 ].
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
Basic, clinical/translational, and epidemiological research has made great strides in the past few decades in uncovering novel components of cell-intrinsic, intercellular, and interorgan communications that contribute to the pathogenesis of obesity. Both endogenous and exogenous (environmental) stressors contribute to the myriad of metabolic perturbations that impact energy intake and expenditure; mediate innate disturbances in the multiple cell types affected in obesity in metabolic organelles and organs, including in immune cells; and impair beneficial interkingdom interactions of the mammalian host with the gut microbiome. The past few decades have also witnessed remarkable efforts to successfully treat obesity, such as the use of the incretin agonists and bariatric surgery. Yet, these and other strategies may be accompanied by resistance to weight loss, weight regain, adverse effects of interventions, and the challenges of lifelong implementation. Hence, through leveraging novel discoveries from the bench to the bedside to the population, additional strategies to prevent obesity and weight regain post-weight loss, such as the use of “wearables,” with potential for implementation of immediate and personalized behavior modifications, may hold great promise as complementary strategies to prevent and identify lasting treatments for obesity. Figure created with BioRender.
https://doi.org/10.1371/journal.pbio.3002448.g001
Beyond intercellular communication mediated by extracellular vesicles, the discovery of interactions between the host and the gut microbiome has suggested important roles for this interkingdom axis in obesity. Although disturbances in commensal gut microbiota species and their causal links to obesity are still debated, transplantation studies have demonstrated relationships between Firmicutes/Bacteroidetes ratios and obesity [ 4 ]. Evidence supports the concept that modulation of gut microbiota phyla modulates fundamental activities, such as thermogenesis and bile acid and lipid metabolism. Furthermore, compelling discoveries during the past few decades have illustrated specific mechanisms within adipocytes that exert profound effects on organismal homeostasis, such as adipose creatine metabolism, transforming growth factor/SMAD signaling, fibrosis [ 5 ], hypoxia and angiogenesis, mitochondrial dysfunction, cellular senescence, impairments in autophagy, and modulation of the circadian rhythm. Collectively, these recent discoveries set the stage for the identification of potential new therapeutic approaches in obesity.
Although the above discoveries focus largely on perturbations in energy metabolism (energy intake and expenditure) as drivers of obesity, a recently published study suggests that revisiting the timeline of obesogenic forces in 20th and 21st century society may be required. The authors tracked 320,962 Danish schoolchildren (born during 1930 to 1976) and 205,153 Danish male military conscripts (born during 1939 to 1959). Although the overall trend of the percentiles of the distributions of body mass index were linear across the years of birth, with percentiles below the 75th being nearly stable, those above the 75th percentile demonstrated a steadily steeper rise the more extreme the percentile; this was noted in the schoolchildren and the military conscripts [ 6 ]. The authors concluded that the emergence of the obesity epidemic might have preceded the appearance of the factors typically ascribed to mediating the obesogenic transformation of society by several decades. What are these underlying factors and their yet-to-be-discovered mechanisms?
First, in terms of endogenous factors relevant to individuals, stressors such as insufficient sleep and psychosocial stress may impact substrate metabolism, circulating appetite hormones, hunger, satiety, and weight gain [ 7 ]. Reduced access to healthy foods rich in vegetables and fruits but easy access to ultraprocessed ingredients in “food deserts” and “food swamps” caused excessive caloric intake and weight gain in clinical studies [ 8 ]. Second, exogenous environmental stresses have been associated with obesity. For example, air pollution has been directly linked to adipose tissue dysfunction [ 9 ], and ubiquitous endocrine disruptor chemicals (EDCs) such as bisphenols and phthalates (found in many items of daily life including plastics, food, clothing, cosmetics, and paper) are linked to metabolic dysfunction and the development of obesity [ 10 ]. Hence, factors specific to individuals and their environment may exacerbate their predisposition to obesity.
In addition to the effects of exposure to endogenous and exogenous stressors on the risk of obesity, transgenerational (passed through generations without direct exposure of stimulant) and intergenerational (direct exposure across generations) transmission of these stressors has also been demonstrated. A leading proposed mechanism is through epigenetic modulation of the genome, which then predisposes affected offspring to exacerbated responses to obesogenic conditions such as diet. A recent study suggested that transmission of disease risk might be mediated through transfer of maternal oocyte-derived dysfunctional mitochondria from mothers with obesity [ 11 ]. Additional mechanisms imparting obesogenic “memory” may be evoked through “trained immunity.”
Strikingly, the work of the past few decades has resulted in profound triumphs in the treatment of obesity. Multiple approved glucagon-like peptide 1 (GLP1) and gastric inhibitory polypeptide (GIP) agonists [ 12 ] (alone or in combinations) induce highly significant weight loss in persons with obesity [ 13 ]. However, adverse effects of these agents, such as pancreatitis and biliary disorders, have been reported [ 14 ]. Therefore, the long-term safety and tolerability of these drugs is yet to be determined. In addition to pharmacological agents, bariatric surgery has led to significant weight loss as well. However, efforts to induce weight loss through reduction in caloric intake and increased physical activity, pharmacological approaches, and bariatric surgery may not mediate long-term cures in obesity on account of resistance to weight loss, weight regain, adverse effects of interventions, and the challenges of lifelong implementation of these measures.
Where might efforts in combating obesity lie in the next decades? At the level of basic and translational science, the heterogeneity of metabolic organs could be uncovered through state-of-the-art spatial “omics” and single-cell RNA sequencing approaches. For example, analogous to the deepening understanding of the great diversity in immune cell subsets in homeostasis and disease, adipocyte heterogeneity has also been suggested, which may reflect nuances in pathogenesis and treatment approaches. Further, approaches to bolster brown fat and thermogenesis may offer promise to combat evolutionary forces to hoard and store fat. A better understanding of which interorgan communications may drive obesity will require intensive profiling of extracellular vesicles shed from multiple metabolic organs to identify their cargo and, critically, their destinations. In the three-dimensional space, the generation of organs-on-a-chip may facilitate the discovery of intermetabolic organ communications and their perturbations in the pathogenesis of obesity and the screening of new therapies.
Looking to prevention, recent epidemiological studies suggest that efforts to tackle obesity require intervention at multiple levels. The institution of public health policies to reduce air pollution and the vast employment of EDCs in common household products could impact the obesity epidemic. Where possible, the availability of fresh, healthy foods in lieu of highly processed foods may be of benefit. At the individual level, focused attention on day-to-day behaviors may yield long-term benefit in stemming the tide of obesity. “Wearable” devices that continuously monitor the quantity, timing, and patterns of food intake, physical activity, sleep duration and quality, and glycemic variability might stimulate on-the-spot and personalized behavior modulation to contribute to the prevention of obesity or of maintenance of the weight-reduced state.
Given the involvement of experts with wide-ranging expertise in the science of obesity, from basic science, through clinical/translational research to epidemiology and public health, it is reasonable to anticipate that the work of the next 2 decades will integrate burgeoning multidisciplinary discoveries to drive improved efforts to treat and prevent obesity.
Acknowledgments
The author is grateful to Ms. Latoya Woods of the Diabetes Research Program for assistance with the preparation of the manuscript and to Ms. Kristen Dancel-Manning for preparation of the Figure accompanying the manuscript.
- View Article
- PubMed/NCBI
- Google Scholar
Introduction to Obesity
Cite this chapter.

- Imran Alam MBBS,BSc,FRCS(Glas),FRCSEd,MD 2 &
- Sanjay Agrawal MS, FRCSEd, FRCSGlasg, FRCS 3 , 4
5051 Accesses
Obesity is defined as an abnormal or excessive accumulation of fat that may impair health. According to World Health Organization (WHO), any individual with a body mass index (BMI) greater than or equal to 30 kg/m 2 is obese and severe or class III obesity is defined as a BMI equal to or greater than 40 kg/m 2 ; this term is also used for individuals with a BMI between 30 and 39.9 kg/m 2 who have significant comorbidities. National Institute of Clinical Excellence (NICE) has recommended bariatric surgery for such individuals. The prevalence of severe obesity has increased significantly in the last two to three decades. Mexico and United States of America have highest prevalence in the world and United Kingdom is leading in Europe. BMI is used as a surrogate for adiposity. There are other methods like bioimpedance analysis, dual-energy x-ray absorptiometry (DEXA), hydrometry, computed tomography (CT), magnetic resonance imaging (MRI) and others but for all clinical and interventional purposes, BMI is used as a measure of obesity.
Fat is the main source of stored energy and it also secretes number of hormones and cytokines. Excess central fat deposition is associated with increased risk of morbidity and mortality. Overweight (BMI of 25 kg/m 2 to 29.9 kg/m 2 ) is associated with increased risk of comorbidities such as type 2 diabetes mellitus, cardiovascular diseases, respiratory disorders, infertility, certain forms of cancers, psychological and social problems; and the risk of these comorbidities increases significantly with further increase in BMI. The cost of treating obesity and associated comorbidity is causing significant burden on the health system. Conservative treatment has a high failure rate. Bariatric surgery performed primarily for weight reduction also causes resolution/remission of associated comorbidities.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or Ebook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others

Strengths and Limitations of BMI in the Diagnosis of Obesity: What is the Path Forward?
Li Z, Bowerman S, Heber D. Health ramifications of the obesity epidemic. Surg Clin North Am. 2005;85(4):681–701. 4.
Article PubMed Google Scholar
Falaschetti E, Malbut K, Primatesta P. Health Survey for England 2000: the general health of older people and their use of health services. London: The Stationery Office; 2002. Available from: http://discover.ukdataservice.ac.uk/Catalogue/?sn=4487&type=Data%20catalogue .
Google Scholar
NICE clinical guidelines Obesity: Guidance on the prevention, identification, assessment and management of overweight and obesity in adults and children. Issued: December 2006 (last modified: January 2010). NICE 2002. http://www.evidence.nhs.uk/search?q=obesity%20surgery%202002%20NICE&ps=30 . Available from: http://www.nice.org.uk/guidance/cg43/resources/guidance-obesity-pdf .
MacLean LD, Rhode BM, Forse RA, et al. Late results of vertical banded gastroplasty for morbid and super obesity. Surgery. 1990;107(1):20–7.
CAS PubMed Google Scholar
Bray GA. Definition, measurement, and classification of the syndromes of obesity. Int J Obes. 1978;2(2):99–112.
Organization for Economic Co-operation and Development. Obesity update. 2014. http://www.oecd.org/health/obesity-update.htm .
Marie N, Fleming T, Robinson M, Thomson B, Graetz N, Margono G, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980—2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–81.
Article Google Scholar
Health Survey England 2012. www.hscic.gov.uk/catalogue/PUB13218 .
Foresight. Tackling obesities: future choices [Internet]. London: Government Office for Science and Department of Health; 2007. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/287937/07–1184x-tackling-obesities-future-choices-report.pdf .
Pischon T, Boeing H, Hoffmann K, Bergmann M, Schulze MB, Overvad K. General and abdominal adiposity and risk of death in Europe. N Engl J Med. 2008;359:2105–20.
Article CAS PubMed Google Scholar
National Audit Office. Tackling obesity in England. Part 2; p. 16. Report by the comptroller and auditor general HC 220 Session 2000–2001: 15 February 2001. Available from: http://www.nao.org.uk/wp-content/uploads/2001/02/0001220.pdf .
Campbell IW, Haslam D. Chapter 1: What is obesity? In: Campbell IW, Haslam D, editors. Your questions answered-obesity. Edinburgh: Churchill Livingstone; 2005. p. 6. ISBN 0433074534.
Nightingale CM, Rudnicka AR, Owen CG, Cook DG, Whincup PH. Patterns of body size and adiposity among UK children of South Asian, black African-Caribbean and white European origin: Child Heart And health Study in England (CHASE Study). Int J Epidemiol. 2011;40(1):33–44.
Article PubMed Central PubMed Google Scholar
Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010;363(23):2211–9.
Botti TJ. Chapter 1: An irreconcilable conflict of interest 1607–1762. In: Botti T, editor. Envy of the world. An irreconcilable conflict of interest. New York: Algora Pub; 2006. p. 1607–762. ISBN 0875864317.
Tulsa World. MetLife expands beyond ‘slow growth’ U.S. market. [Internet]. 2010 [cited 14 March 2011]:1. Available from: http://www.tulsaworld.com/business/metlife-expands-beyond-slow-growth-u-s-market/image_5d394721-ff35–5512–9adf-6cbb55f497bc.html .
MetLife. MetLife and Fidelity introduce new retirement income solution: a variable annuity designed to provide lifetime income for those nearing or in retirement [Internet]. 2009. Available from: http://personal.fidelity.com/myfidelity/InsideFidelity/NewsCenter/mediadocs/metlife_income_solution.pdf .
Harrison GG. Height-weight tables. Ann Intern Med. 1985;103(6 (Pt 2)):989–94.
Metropolitan MLF. 1983 metropolitan height and weight table. Stat Bull Metrop Life Found. 1983;64(1):3–9.
Deitel M, Dixon J. Comorbidities of morbid obesity and determination of optimal weight. In: Deitel M, Dixon J, Gagner M, Madan A, Himpens J, editors. Handbook of obesity surgery. 1st ed. Toronto: FD-Communications; 2010. ISBN 978–0-9684426–5-4.
Hatoum IJ, Kaplan LM. Advantages of percent weight loss as a method of reporting weight loss after Roux-en-Y gastric bypass. Obesity (Silver Spring). 2013;21(8):1519–25.
Deitel M, Greenstein RJ. Recommendations for reporting weight loss. Obes Surg. 2003;13(2):159–60.
Health and social care information center. Statistics on obesity, physical activity and diet—England, 2014 [Internet]. London: Health and social care information center; 2014. Available from: http://www.hscic.gov.uk/catalogue/PUB13648/Obes-phys-acti-diet-eng-2014-rep.pdf .
Ali AT, Crowther NJ. Body fat distribution and insulin resistance. S Afr Med J. 2005;95(11):878–80.
Pouliet MC, Despres JP, Lemieux S, Moorjani S, Bouchard C, Tremblay A, et al. Waist circumference and abdominal sagittal diameter: best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women. Am J Cardiol. 1994;73(7):460–8.
Lean MEJ. Clinical handbook of weight management. London: Martin Dunitz, Ltd.; 1998.
Han TS, van Leer EM, Seidell JC, Lean ME. Waist circumference action levels in the identification of cardiovascular risk factors: prevalence study in a random sample. BMJ. 1995;311(7017):1401–5.
Article PubMed Central CAS PubMed Google Scholar
Marlowe F, Apicella C, Reed D. Men’s preferences for women’s profile waist-to-hip ratio in two societies. Evol Hum Behav. 2005;26:458–68.
Sun G, French CR, Martin GR, Younghusband B, Green RC, Xie YG, et al. Comparison of multifrequency bioelectrical impedance analysis with dual-energy X-ray absorptiometry for assessment of percentage body fat in a large, healthy population. Am J Clin Nutr. 2005;81(1):74–8.
Goodsitt MM. Evaluation of a new set of calibration standards for the measurement of fat content via DPA and DXA. Med Phys. 1992;19:35–44.
Rothney MP, Brychta RJ, Schaefer EV, Chen KY, Skarulis MC. Body composition measured by dual-energy X-ray absorptiometry half-body scans in obese adults. Obesity (Silver Spring). Am J Clin Nutr. 1995;61(2):274–8.
Jensen MD, Sheedy PF. Measurement of abdominal and visceral fat with computed tomography and dual-energy x-ray absorptiometry. Am J Nutr. 1995;61(2):274–8.
CAS Google Scholar
Hu FB. Measurements of adiposity and body composition. In: Hu FB, editor. Obesity epidemiology. New York City: Oxford University Press; 2008. p. 53–83.
Fujioka S, Matsuzawa Y, Tokunaga K, Tarui S. Contribution of intra-abdominal fat accumulation to the impairment of glucose and lipid metabolism in human obesity. Metabolism. 1987;36(1):54–9.
Abate N, Garg A, Peshock RM, Stray Gundersen J, Adams-Huet B, Grundy SM. Relationship of generalized and regional adiposity to insulin sensitivity in men with NIDDM. Diabetes. 1996;45(12):1684–93.
Lemieux S, Prud’homme D, Bouchard C, Tremblay A, Després JP. A single threshold value of waist girth identifies normal-weight and overweight subjects with excess visceral adipose tissue. Am J Clin Nutr. 1996;64(5):685–93.
DHHS. Results of the Healthy Communities Survey. Tasmania, Tasmanian Public and Environment Health Service, Tasmania. Department of Health and Human Services. 1998. Available from: http://www.dhhs.tas.gov.au/__data/assets/pdf_file/0009/81747/Tasmanian_food_and_nutrition_policy_2004.pdf .
Download references
Author information
Authors and affiliations.
Department of Surgery, Royal Albert Edwards Infirmary, WWL NHS Foundation Trust, Wigan, UK
Imran Alam MBBS,BSc,FRCS(Glas),FRCSEd,MD
Bariatric Surgery Unit, Homerton University Hospital, London, UK
Sanjay Agrawal MS, FRCSEd, FRCSGlasg, FRCS ( Consultant Surgeon Honorary Senior Lecturer )
Blizard Institute, Barts and The London School of Medicine and Dentistry, Queen Mary, University of London, London, UK
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Imran Alam MBBS,BSc,FRCS(Glas),FRCSEd,MD .
Editor information
Editors and affiliations.
Homerton University Hospital, London, United Kingdom
Sanjay Agrawal
Rights and permissions
Reprints and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Alam, I., Agrawal, S. (2016). Introduction to Obesity. In: Agrawal, S. (eds) Obesity, Bariatric and Metabolic Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-04343-2_1
Download citation
DOI : https://doi.org/10.1007/978-3-319-04343-2_1
Publisher Name : Springer, Cham
Print ISBN : 978-3-319-04342-5
Online ISBN : 978-3-319-04343-2
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Open access
- Published: 14 April 2004
Obesity: An overview on its current perspectives and treatment options
- Srinivas Nammi 1 , 3 ,
- Saisudha Koka 1 ,
- Krishna M Chinnala 2 &
- Krishna M Boini 1 , 3
Nutrition Journal volume 3 , Article number: 3 ( 2004 ) Cite this article
88k Accesses
4 Altmetric
Metrics details
Obesity is a multi-factorial disorder, which is often associated with many other significant diseases such as diabetes, hypertension and other cardiovascular diseases, osteoarthritis and certain cancers. The management of obesity will therefore require a comprehensive range of strategies focussing on those with existing weight problems and also on those at high risk of developing obesity. Hence, prevention of obesity during childhood should be considered a priority, as there is a risk of persistence to adulthood. This article highlights various preventive aspects and treatment procedures of obesity with special emphasis on the latest research manifolds.
Peer Review reports
Introduction
Obesity can be described as the "New World Syndrome". Its prevalence is on continuous rise in all age groups of many of the developed countries in the world. Statistical data reveals that the problem of obesity has increased from 12–20% in men and from 16–25% in women over the last ten years [ 1 ]. Recent studies suggest that nearly 15–20% of the middle aged European population are obese [ 2 ] and that in USA alone it is responsible for as many as 3,00,000 premature deaths each year [ 3 ]. Obese patients have been associated with increased risk of morbidity and mortality relative to those with ideal body weight [ 4 ]. Even modest weight reduction in the range of 5–10% of the initial body weight is associated with significant improvements in a wide range of co-morbid conditions [ 5 – 9 ]. Obesity, which was once viewed as the result of lack of will power, or a lifestyle "choice" – the choice to overeat and under exercise, is now being considered more appropriately by the modern world as a chronic disease, which requires effective strategies for its management.
Obesity, in simple terms, may be defined as a state of imbalance between calories ingested versus calories expended which would lead to excessive or abnormal fat accumulation. Body Mass Index (BMI) is a measure of weight corrected for height and which reflects the total body fat and has been the most accepted parameter for defining over weight [ 10 ].
Optimal BMI increases with age. WHO also classified over weight according to BMI [ 11 ]. There is a very good correlation between BMI and the percentage of body fat in large populations.
Percent Body fat = 1.2 (BMI) + 0.23 (age) - 10.8 (gender) - 5.4
Where gender = '1' for men and '0' for women.
It follows from this equation that for a given height and weight, the percentage of body fat is about 10% higher in women compared to men. The reason for this could be that in women, the excess body fat is usually distributed as subcutaneous fat and is mainly peripheral (thighs, buttocks, breasts) where as in men there is a relative excess of body fat stored in abdominal cavity as abdominal subcutaneous fat.
New classifications of over weight may be based on cut-off points for simple anthropometric measures such as waist hip ratio, total adiposity and intra-abdominal fatness. There exists a correlation between increased BMI, mortality due to allied risks which is depicted in Fig. 1
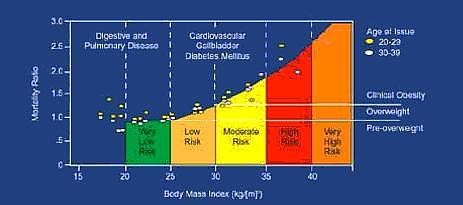
Correlation between increased BMI and risk of mortality
Aetiology of obesity
Obesity is not a single disorder but a heterogeneous group of conditions with multiple causes each of which is ultimately expressed as obese phenotype. Obesity involves complex aetiological links between the genetic, metabolic and neural frameworks on one hand and behavior, food habits, physical activity and socio-cultural factors on the other (Table 1 ).
Genetic considerations
Although obesity had a genetic component, it is not a simple genetic disorder. There is an underlying genetic predisposition to obesity on to which environmental factors are layered. The discovery of 'ob' gene, which was mapped to chromosome 7, has led to a renewed interest in understanding the patho-biological basis of genetic predisposition in obesity. The 'ob' gene codes a hormone called leptin, a 167 amino acid protein and was supposed to be produced in white and brown adipose tissue and placenta [ 12 ]. The leptin receptors are concentrated in hypothalamus and belong to the same class of IL-2 and growth hormone receptors [ 13 ]. Any mutation of 'ob' gene leads to improper coding of leptin, which further results in obesity [ 14 ]. The effects of the 'ob' gene are mediated through effects on both energy intake and energy expenditure. Obesity can also be considered as a "complex trait" as many other genes coding proteins like apolipoprotein B, D, E, β 3 -adrenergic receptor [ 15 ], dopamine D 2 -receptor, tumor necrosis factor (TNF), glucocorticoid receptor etc. are associated with it. So far, 200 genes, gene markers and chromosomal regions have been associated with human obesity [ 16 ].
Neurobiology
Two neurotransmitters neuropeptide Y (NPY) and serotonin (5-HT) are found to play a major role in body weight regulation. NPY is a 36 amino acid peptide, which is concentrated mainly in the hypothalamus; a region crucial to regulation of appetite [ 17 ] has emerged as a possible key neurotransmitter candidate for the regulation of energy homeostasis. Increased NPY activity has been found in the hypothalamus of obese rodents [ 18 ]. NPY increases food in-take through its interaction with a unique Y5 subtype of NPY receptor and hence Y5 receptor antagonists could be effective in the treatment of obesity [ 19 ].
The inhibitory actions of 5-HT on food in-take have been localized to the hypothalamic para ventricular nucleus (PVN), the site at which NPY is most active in inducing feeding behavior [ 20 ]. 5-HT induced reduction in food in-take is mediated by post-synaptic 5-HT IB receptors. The hypophagic actions of 5-HT may be mediated at least partly through the NPY pathway. For example, 5-HT antagonist which stimulates feeding increases NPY concentrations in the arcuate and para ventricular nuclei of the hypothalamus [ 21 ]. Similarly, a 5-HT agonist, which reduces food intake significantly, reduces NPY concentrations in the hypothalamic para ventricular nucleus. Corticotrophin releasing factor (CRF) which also causes weight loss by reducing appetite and act in opposing to NPY on the regulation of energy balances. Cholecystokinin (CCK), a neurotransmitter present in the brain plays a physiological role as a meal termination (satiety) signal between the two receptors such as CCK A and CCK B , CCK acted at CCK A receptors [ 22 ]. Hence, CCK A agonist could also be useful in the treatment of obesity.
Environmental factors
These factors play a critical role in the development of obesity by unmasking genetic or metabolic susceptibilities. Environmental influences act via an increase in energy intake or a decrease in energy expenditure with little physical activity and hence there is increased likelihood of becoming obese. Sedentary behaviors, notably television watching, car ownership also contributes to the risk of obesity. The role of passive over consumption [ 23 ], eating disorders, and preference for high carbohydrate diet also play an important role in increasing the risk of obesity. Other food habits like smoking and alcohol consumption lowers body weight and results in higher BMI respectively.
Psycho-social impact
A number of individual characteristics may place individuals at increased risk of obesity. Restrained eating also plays a role in aetiology of obesity. Restrained eaters report more food carvings and binge eating [ 24 ]. One of the characteristic features of dietary restraints is the tendency towards disinhibited eating in particular circumstances. Restrained eaters may be more susceptible to the availability of highly palatable foods, which act as a stimulus for excess food consumption.
Obesity-associated diseases and risk factors
Cardiovascular diseases (cvd).
Hypertension
Coronary heart disease
Cerebrovascular disease
Varicose veins
Deep venous thrombosis
The increased risk of CVD is 2-fold in women of BMI 25–28.9 kg/m 2 and 3.6 fold for BMI in 29 kg/m 2 or more. In males a 10% increase in body weight increases risk of CVD by 38%, where as 20% weight risk corresponds with 86% increased risk. Blood pressure is increased by 6 mm systole and 4 mm diastole for a 10% gain in body fat. Hyper tension is prevalent in obese adults at a rate of 2.9 fold than non-obese population and weight reduction reduces risk of developing hyper tension [ 25 ].
Respiratory diseases
Sleep apnoea
Hypoventilation syndrome
There are a number of ways in which obesity affects lung function [ 26 ]. An increased amount of fat in the chest wall and abdomen limits respiratory excursion reducing lung volume. As the obesity worsens, so do the apnoeic episodes resulting in frequent awakening and the resultant sleep deprivation produces daytime somnolence.
Metabolic disorders
Hyperlipidemia
Diabetes mellitus
Insulin resistance
Menstrual irregularities
There is a consistent graded relationship between increased BMI and prevalence of NIDDM and insulin resistance [ 27 ]. Over 10 to 15 million Americans with type 2 diabetes are obese [ 28 ]. A mean weight loss of 7% weight reduces risk of developing type 2 diabetes by more than 55% [ 29 ]. BMI above 35 kg/m 2 increases the risk by 93 fold in women and by 42 fold in men. Obesity is associated with lipid disorders in which elevated levels of cholesterol, triglycerides, LDL-cholesterol and low levels of HDL-cholesterol are observed. For every 1 kg of weight loss, there is a corresponding reduction by about 1% in HDL and reduction by 3% of triglycerides. It has been observed that modest weight loss reduces lipid abnormalities [ 30 ] and diabetes mellitus [ 31 ].
Gastrointestinal disorders
Fatty liver and cirrhosis
Haemorrhoids
Colorectal cancer
Gall bladder disease is the most common gastrointestinal disorder in obese individuals. Obese women have a 2.7 fold increase in the prevalence of gall bladder disease. There is an increased risk of gallstones in individuals having BMI of 20 kg/m 2 or more. The mortality rates of cancer of the stomach and pancreas were higher in obese individuals.
Malignancies
Breast cancer
Endometrial Cancer
Prostrate Cancer
Cervical Cancer
Obese women have higher incidence of endometrial, ovarian, cervical and postmenopausal breast cancer, while obese men have incidents of prostrate cancer.
However, it remains to be confirmed whether these malignancies occur as a result of hormonal changes associated with obesity or due to specific dietary pattern.
Miscellaneous
Arthritis and bone mass
Stress is associated with the consumption of high fat foods and leads to weight gain. Obesity is also associated with osteoarthritis of hip and knee although in some cases, mechanical stress associated with obesity leads to osteoarthritis [ 32 ]. Obese women have a higher risk of obstetric complication and have increased risk of caesarean delivery due to variety of foetal size. Recently, an increased risk of neural tube defects especially spinabifida has been reported in women with BMI greater than 29 kg/m 2 .
Prevention of obesity
Obesity is a serious, chronic medical condition, which is associated with a wide range of debilitating and life threatening conditions. The fact that obesity prevalence continues to increase at an alarming rate in almost all regions of the world is of major concern. Hence, an effective control of obesity requires the development of coherent strategies that tackle the main issues related to preventing:
i) The development of over weight in normal weight individuals
ii) The progression of over weight to obesity in those who are already over weight
iii) Weight regain in those who have been over weight or obese in the past but who have since lost weight and
iv) Further worsening of a condition already established.
The prevention of obesity involves action at several levels i) Primary ii) Secondary iii) Tertiary [ 33 ]. Objective of primary prevention is to decrease the number of new cases, secondary prevention is to lower the rate of established cases in the community and tertiary prevention is to stabilize or reduce the amount of disability associated with the disorder. When the attention is focused on the multi-factorial condition such as coronary heart disease (CHD), primary prevention of this involves national programmes to control blood cholesterol levels and secondary prevention deals with reducing CHD risk in those with existing elevated blood cholesterol levels while tertiary action would be associated with preventing re-infarction in those who had a previous heart attack. However, this classification system for prevention of obesity results in a great deal of ambiguity and confusion. To avoid this, the US institute of medicine [ 34 ] has proposed alternative classification of system. The new system separates prevention efforts into 3 levels. Universal (or) public health measures (directed at every one in the population), selective (for a sub-group who may have an above average risk of developing obesity) and indicated (targeted at high risk individuals who may have a detectable amount of excess weight which fore-shadows obesity). However, preventive measures for any disorder may not be helpful in all cases hence, proper management strategies can be integrated along with prevention programmes.
Management of obesity
Management include both weight control or reducing excess body weight and maintaining that weight loss, as well as, initiating other measures to control associated risk factors. Periodic evaluation for obesity should be done by the measurement of BMI, measurement of waist circumference etc., to assess risk factors. Based on the evaluation, appropriate treatment can be suggested. Treatment may consist of modification of diet, increased physical activity, behavioral therapy, and in certain circumstances weight loss medication and surgery.
Dietary therapy
Restrictions of calories represent the first line therapy in all cases except in cases with pregnancy, lactation, terminal illness, anorexia nervosa, cholelithiasis and osteoporosis. Low calorie diets (LCD), which provide 100–1500 kcal/day, resulted in weight loss of 8% of baseline body weight over six months but on long run most of the lost weight is regained [ 35 ].
Very low calories diets (VLCD), which provide 300–800 kcal/day, can be useful in severely obese patients under strict medical supervision. They are found to produce 13% weight loss over six months, i.e. they produce greater initial weight loss than LCDs, however, the long-term (>1 year) weight loss by VLCD's is not found superior to that of the LCDs.
Meal replacement programmes and formula diets can be used as an effective tool in weight management [ 36 ]. Optifast, Medifast are available through physians or hospitals as part of packaged weight-reduction programmes. These products appear to be safe, but maintenance of weight loss over the long term is difficult.
Other over the counter (OTC) variations to formula diets includes Slimfast and Ultra slimfast. The consumer is instructed to drink the formulations and use it to replace one or two meals.
Fat substitutes like Olestra (Olean), which is a non-digestible, non-caloric fat, can be used in food preparations taken by obese patients.
It has been observed that calorie restriction alone has remarkable effects compared to exercise alone [ 37 – 39 ]. A loss of 5% initial weight achieved with diet and exercise is associated with significant improvement in glycylated haemoglobin A IC and that diet control can be useful to treat co morbidities of obesity such as diabetes [ 40 ].
Physical activity
All individuals can benefit from regular exercise [ 41 ]. Physical activity, which increases energy expenditure, has a positive role in reducing fat storage and adjusting energy balance in obese patients. Various exercises preceded and followed by short warm up and cool down sessions help to decrease abdominal fat, prevent loss of muscle mass. Studies revealed that patients who exercise regularly had increased cardio vascular fitness [ 42 , 43 ] along with betterment in their mental and emotional status. Hence a minimum of 30 minutes exercise is recommended for people of all ages [ 44 ] as part of comprehensive weight loss therapy.
Behaviour therapy
Behaviour therapy is a useful adjunct when incorporated into treatment for weight loss and weight maintenance. Patients need to be trained in gaining self-control of their eating habits. Behaviour modification programmes which seek to eliminate improper eating behaviours (eating while watching TV, eating too rapidly, eating when not hungry etc.,) include individual or group counseling of patients.
Self-help groups (weight watchers, Nutri-System) use a program of diet, education and self-monitoring like maintenance of logbook, keeping an account of food intake etc are beneficial.
Pharmacotherapy
Drug treatment is advised only for subjects with BMI > 27 and with associated risk factors or with a BMI > 30 [ 45 ] and thus at medical risk because of their obesity. It should not be used for "cosmetic" weight loss. Weight loss medications should be used only as an adjunct to dietary and exercise regimes coupled with a program of behavioural treatment and nutritional counseling.
Pharmacological approaches in obesity treatment
Most available weight loss medications are "appetite–suppressant" medications. The initial drugs used for appetite suppression were amphetamine [ 46 ], metamphetamine and phenmetrazine (Preludin) and are no longer used in treatment of obesity because of their high potential for abuse.
Inhibitors of 5-hyroxytryptamine (5-HT) reuptake, fenfluramine and dexfenfluramine were licensed for obesity but proved to cause pulmonary hyper tension and increased valvular heart disease [ 47 ] and have been withdrawn from the market. Drugs like phendimetrazine (Plegine), diethylpropion (Tenuate), phentermine (Lonamin) etc., are being marketed but have been classified as controlled substances and are recommended for short-term use only.
The newest agents available for weight loss are sibutramine (Meredia) and orlistat (Xenical). They are the only weight loss medications approved by the US Food and Drug Administration (FDA) for long-term use [ 48 ] in significantly obese patients, although their safety and effectiveness have not been established for use beyond one year.
Sibutramine is the serotonin and norepinephrine re-uptake inhibitor, which induces decreased food intake and increased thermogensis [ 49 – 52 ]. In clinical trials, sibutramine showed a statistical improvement in amount of weight lost versus placebo [ 53 ]. It limits decline of metabolic rate that typically accompanies weight loss [ 54 ]. However, this agent is contraindicated in-patient with known seizure disorders, high blood pressure, congestive heart failure (CHF) a history of myocardial infraction and arrhythmias.
Orlistat is a potent and irreversible inhibitor of gastric, pancreatic lipases. It blocks the digestion of approximately 30% of the ingested dietary triglycerides. Studies proved that it produces 5% more weight loss than in control groups [ 55 ]. It is now available on prescription as Xenical ® (Orlistat-120 mg). The most commonly reported side effects include oily stools, soft stool [ 56 ], and increased defecation and decreased absorption of fat-soluble vitamins (A, D, E and K). Hence, patient may be recommended intake of fat-soluble vitamins [ 57 ] along with it. When used in conjugation with diet it was found to improve glycemic control and cardiovascular disorders [ 58 , 59 ].
In general, monotherapy in obese patients produced sub-optimal weight loss [ 60 ] but the use of more than one weight loss medication at a time (combined drug therapy) is not approved [ 61 ] and hence such an off-label use of combinations of drugs for weight loss is not recommended except as part of a research study.
Drugs under development
There has been a wide search for effective drugs for the treatment of obesity. Some of the promising drug development research areas are mentioned below.
Amylin is a peptide secreted with insulin in response to food intake that shares many other properties with established adiposity signals like insulin and leptin. Its circulating levels can be correlated with body fat. Preclinical studies have shown that amylin complements the effects of insulin in mealtime glucose regulation via several effects, which include a suppression of post meal glucagon secretion, a decrease in gastric emptying, and a decrease in food intake [ 62 ]. The drug pramlintide, a synthetic analogue of amylin is currently in phase III trials.
11β-hydroxysteroid dehydrogenase type-1 (11β-HSD-1) is an enzyme that increases cortisol levels in adipocytes. Studies on mice lacking gene for 11β-HSD-1 suggest that they are resistant to diet induced obesity [ 63 ]. An 11β-HSD-1 inhibitor being developed by Biovitrum is currently in clinical testing.
Stimulation of β 3 adrenoreceptors (β 3 -ARs) by selective agonists improves insulin action and stimulates energy metabolism. In animals, chronic β 3 -AR agonist treatment causes body weight reduction, which is almost entirely due to decrease in body fat [ 64 ]. At least a dozen pharmaceutical companies are in the process of developing β 3 -AR drugs, some of which are already in human testing. AD9677 a β-adrenoceptor agonist is in phase II trails.
The botanical P57 is an extract of steroidal glycosides derived from South African Cactus . The potent appetite suppression may occur via the melanocortin-4 (MCR-4) saponins from the Platycodi radix and Salacia reticulata have been shown to inhibit pancreatic lipase, producing weight loss and reduction of fatty liver in laboratory animals [ 65 ]. Currently, P57 is in Phase II testing and Table 2 summarizes some other important drugs union are under clinical trials for the treatment of obesity.
Apart from drug treatment, surgery is also indicated when BMI is exceedingly high (>40 kg/m 2 or >30 kg/m 2 with obesity-related medical co-morbidities) and when other treatment modalities have failed [ 66 ]. The most popular surgical procedures used for treatment of severe obesities involve gastric portioning or gastroplasty and gastric by-pass. The gastroplasty procedures create a small gastric pouch, which is drained through a narrow calibrated stoma [ 67 , 68 ]. The intake of solids is therefore considerably limited. Gastric by-pass surgery creates a larger pouch emptied by an anastomosis directly into the jejunum, bypassing the duodenum. It is considered now as the most effective and safe surgery for morbid obesity [ 69 , 70 ]. This technique induces weight loss by combining restricted intake and a moderate degree of malabsorbtion [ 71 ]. Initial loss of weight is greater after this procedure than following gastroplasty [ 72 ].
Gastric and nutritional complications [ 73 ] may be serious implications of the surgery. Nutritional deficiencies and intractable vomiting are frequently associated with surgery. Surgical treatments for obesity resolve most co-morbidities of severe obesity such as hypertension [ 74 , 75 ], serum lipid levels [ 76 ] and diabetes mellitus [ 77 , 78 ].
Obesity is not a social condition but is a rampant disease. Obesity cannot be overviewed as just a matter of overeating and lack of will power but must be considered as a major genetic aetiology modified by environment and should be treated vigorously in the same manner that we now apply to other diseases. A better understanding of the aetiological determinants in individual subjects will provide a basis for more rational intervention to prevent this recalcitrant public health problem. With the increasing awareness and ongoing research in this area there is a considerable reason for optimism that the next coming years will bring better treatment for the obese.
Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL: Over weight and obesity in the United States: Prevalence and trends, 1960–1994. Int J Obes Relat Metab Disord. 1998, 22: 39-47. 10.1038/sj.ijo.0800541.
Article CAS PubMed Google Scholar
Bjorntorp P: Obesity. Lancet. 1997, 350: 423-426. 10.1016/S0140-6736(97)04503-0.
US Department of Health and Human Services. Office of the Surgeon General: The surgeon General's call to action to prevent and decrease overweight and obesity. Rockville MD: United States Department of Health and Human Services. 2001
Google Scholar
Manson JE, Willett WC, Stamfer MJ, Colditz GA, Hunter DJ, Hankinson SE, Hennekens CH, Speizer FE: Body weight and mortality among women. N Eng J Med. 1995, 333: 677-685. 10.1056/NEJM199509143331101.
Article CAS Google Scholar
Blackburn GL: Effect of degree of weight loss on health benefits. Obes Res. 1995, 3: 211s-216s.
Article PubMed Google Scholar
World Health Organization: Obesity: Preventing and managing the global epidemic. World Health Organisation Geneva. 2000
Goldstein DJ: Beneficial health effects of a modest weight loss. Int J Obes Relat Metab Disord. 1992, 16: 397-415.
CAS PubMed Google Scholar
Bosello O, Armellini F, Zamboni M, Fitchet M: The benefits of modest weight loss in type-II diabetes. Int J Obes Relat Metab Disord. 1997, 21: S10-S13.
PubMed Google Scholar
Wing RR, Koeske R, Epstein LH, Nowalk MP, Gooding W, Becker D: Long term effects of modest weight loss in type-II diabetic patients. Arch Intern Med. 1987, 147: 1749-1753. 10.1001/archinte.147.10.1749.
Taylor RW, Keil D, Gold EJ, Williams SM, Goulding A: Body mass index, waist girth and waist-to-hip ratio as indexes of total and regional adiposity in women: evaluation using receiver operating characteristic curves. Am J Clin Nutr. 1998, 67: 44-49.
Jacob CS, Katherine MH: Assessing obesity classification and epidemology. Br Med Bull. 1997, 2: 239-
Zhang YY, Proencea R, Maffei M, Barone M, Leopold L, Friedman JM: Positional clone of the mouse obese gene and its human homologue. Nature. 1994, 372: 425-432. 10.1038/372425a0.
Auwerx J, Stales B: Leptin. Lancet. 1998, 351: 732-742. 10.1016/S0140-6736(97)06348-4.
Article Google Scholar
Andersson LB: Genes and obesity. Ann Med. 1996, 28: 5-7.
Arner P: The β 3 -adrenergic receptor – a cause & cure of obesity. N Engl J Med. 1995, 333: 382-383. 10.1056/NEJM199508103330612.
Chagnon YC, Perusse L, Weisnagel SJ, Rankinen T, Bouchard C: The human obesity gene map: the 1999 update. Obes Res. 2000, 8: 89-117.
Dryden S, Frankish H, Wang Q, Williams G: Neuropeptide Y and energy balance, one way ahead for the treatment of obesity?. Eur J Clin Invest. 1994, 24: 293-308.
Flier JS, Flier EM: Obesity and the hypothalamus: Novel peptides for new pathways. Cell. 1998, 92: 437-440. 10.1016/S0092-8674(00)80937-X.
Friedman JM: The alphabet of weight control. Nature. 1997, 385: 119-120. 10.1038/385119a0.
Shor Posnar G, Grinker JA, Marinescu C: Hypothalamic serotonin in the control of meal patterns and macronutrient selection. Brain Res Bull. 1986, 17: 663-671. 10.1016/0361-9230(86)90198-X.
Dryden S, Frankish H, Wang Q, Williams G: The serotonin antagonist methysergide increase NPY synthesis and secretion in the hypothalamus of rat. Brain Res. 1995, 699: 12-18. 10.1016/0006-8993(95)00841-D.
Boosalis MG, Gemayel N, Lee A, Bray GA, Laine L, Cohen H: Cholecystokinin and satiety: effect of hypothalamic obesity and gastric bubble insertion. Am J Physiol. 1992, 262: R241-244.
Spiegelman BM, Flier JS: Adipogenesis and obesity: round in out the big picture. Cell. 1996, 87: 377-389. 10.1016/S0092-8674(00)81359-8.
Wadley J: Dietary restraint and binge eating behaviour. Anal Modif. 1980, 4: 647-660.
Tuck ML, Sowers J, Dornfeld L, Kledzik G, Maxwell M: The effect of weight reduction on blood pressure, plasma rennin activity, and plasma aldosterone levels in obese patients. N Engl J Med. 1981, 304: 930-933.
Kolarzyk E, Kiec E, Wiater M: Effect of obesity on the ventilatory capacity of the respiratory system. I. Relation between basic spirometric indicators: vital capacity (VC) and forced expiratory volume (FEV1) and obesity. Med Pr. 1985, 36: 87-95.
Rahilly OS: Non insulin dependent diabetes mellitus: the gathering storm. Br Med J. 1997, 314: 955-960.
Ford ES, Giles WH, Dietz WH: Prevalence of the metabolic syndrome among US adults: findings from the Third National health and Nutrition Examination survey. J Amer Med Assoc. 2002, 287: 356-359. 10.1001/jama.287.3.356.
Franz MJ, Bantle JP, Beebe CA, Brunzell JD, Chiasson JL, Garg A, Holzmeister LA, Hoogwerf B, Mayer_Davis E, Mooradian AD, Purnell JQ, Wheeler M: Evidence based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes care. 2002, 25: 148-198.
Dattilo AM, Kris-Etherton PM: Effects of weight reduction on blood lipids and lipoproteins: a meta-analysis. Am J Clin Nutr. 1992, 56: 320-328.
Anonymous: UK Prospective study on maturity onset diabetes. I. Effect of diet and sulphonylurea, insulin or biguainide therapy on fasting plasma glucose and body weight over one year. Diabetologia. 1983, 24: 404-411.
Davis MA, Neuhaus JM, Ettinger WH, Mueller WH: Body fat distributions and osteoarthritis. Am J Epidemiol. 1990, 132: 701-707.
Timothy PG: Key issues in the prevention of obesity. Br Med Bull. 1997, 53: 359-388.
US Institute of medicine: Reducing risks of mental disorders. Frontiers for preventive intervention research. 1994, Washington, National Academy Press
Wadden TA: Treatment of obesity by moderate and severe caloric restriction results of clinical research tracts. Ann Intern Med. 1993, 119: 688-693.
Ashley JM, St Jeor ST, Schrage JP, Perumean_Chaney SE, Gilbertson MC, McCall NL, Bovee V: Weight control in the physician's office. Arch Intern Med. 2001, 161: 1599-1604. 10.1001/archinte.161.13.1599.
Anderssen S, Holme I, Urdal P, Hjermann I: Diet and exercise intervention have favourable effects on blood pressure in hypertensives: The Oslo Diet and Exercise Study (ODES). Blood Press. 1995, 4: 343-349.
Bertram SR, Venter I, Stewart RI: Weight loss in obese women – exercise vs dietary education. S Afr Med J. 1990, 78: 15-18.
Wood PD, Stefanick ML, Dreon DM, Frey-Hewitt B, Garay SC, Williams PT, Superko HR, Fortman SP, Albers JJ, Vranizan KM, et al: Changes in plasma lipids and lipoproteins in overweight men during weight loss through dieting as compared with exercise. N Engl J Med. 1988, 319: 1173-1179.
Ditschuneit HH, Flechtner-Mors M, Johnson TD, Adler G: Metabolic and weight loss effects of a long term dietary intervention in obese patients. Am J Clin Nutr. 1999, 69: 198-204.
US Department of Health and Human services: Leading health indicators. Overweight and obesity. Healthy people 2010 (Conference ed. in two volumes). DC. US Department of Health and Human Services, Washington. 2000, 24-45.
Wyatt HR, Wing RR, Hill JO: The National weight control registry. In: Evaluation & Management of obesity. Edited by: Bessesen DH, Kushner RF. 2002, Philadelphia, Hanley & Belfus Inc, 199-224.
Schoeller DA, Shay K, Kushner RF: How much physical activity is needed to minimize weight gain in previously obese women?. Am J Clin Nutr. 1997, 66: 551-556.
Physical Activity and Health: A Report of the surgeon General PA. US Department of Health and Human services. 1996
National Institutes of Health (NHLBI): Clinical guidelines on the identification, evaluation and treatment of overweight and obesity in adults. The evidence report Washington D.C. National Institute of Health, Obese Res. 1998, 6: 51s-201s.
Lessof MH, Myerson A: Benzedrine sulfate as an aid to be the treatment of obesity. N Engl J Med. 1938, 218: 119-205.
Connolly HM, Crary JL, McGoon MD, Hensud DD, Edwards BS, Edwards WD: Valvular heart disease associated with fenfluramine – phentermine. N Engl J Med. 1997, 337: 783-10.1056/NEJM199708283370901.
James WP, Astrup A, Finer N, Hilsted J, Kopelman P, Rossner S, Saris WH, Van Gaal LF: Effect of sibutramine on weight maintenance after weight loss: a randomised trial. STORM Study Group. Sibutramine Trial of Obesity Reduction and Maintenance. Lancet. 2000, 356: 2119-2125. 10.1016/S0140-6736(00)03491-7.
Mun EC, Blackbur GL, Matthews JB: Current status of medical and surgical therapy for obesity. Gastroenterology. 2001, 120: 669-681.
Rolls BJ, Shide DJ, Thorwart ML, Ulbrecht JS: Sibutramine reduces food intake in non-dieting women with obesity. Obes Res. 1998, 6: 1-11.
Hansen DL, Toubro S, Stock MJ, Macdonald IA, Astrup A: Thermogenic effects of sibutramine in humans. Am J Clin Nutr. 1998, 68 : 1180-1186.
Seagle HM, Bessesen DH, Hill JO: Effects of sibutramine on resting metabolic rate and weight loss in over weight women. Obes Res. 1998, 6: 115-121.
Astrup A, Toubro S: When, for whom and how to use sibutramine?. Int J Obes Relat Metab Disord. 2001, 25 (Suppl 4): 52-57. Review
Luque CA: Sibutramine: a serotonin-norepinephrine reuptake inhibitor for the treatment of obesity. Ann Pharmacother. 1999, 33: 968-978. 10.1345/aph.18319.
Sjostrom L, Rissonen A, Andersen T, Boldrin M, Golay A, Koppeschaar HP, Krempf M: Randomised placebo-controlled trial of orlistat for weight loss and prevention of weight in obese patients. European Multicenter Orlistat study group. Lancet. 1998, 352: 167-172. 10.1016/S0140-6736(97)11509-4.
Hill JO, Hauptman J, Anderson JW, Fujioka K, O'Neil PM, Smith DK, Zavoral JH, Aronne LJ: Orlistat, a lipase inhibitor, for weight maintenance after conventional dieting: a 1-year study. Am J Clin Nutr. 1999, 69: 1108-1116.
Mc Duffie JR, Calis KA, Booth SL, Uwaifo GI, Yanovski JA: Effects of orlistat on fat soluble vitamins in obese adolescents. Pharmacotherapy. 2002, 22: 814-822.
Hollander PA, Elbein SC, Hirsch IB, Kelley D, McGill J, Taylor T, Weiss SR, Crockett SE, Kaplan RA, Comstock J, Lucas CP, Lodewick PA, Canovatchel W, Chung J, Hauptman J: Role of orlistat in the treatment of obese patients with type-2 diabetes. A 1-year randomized double blind study. Diabetes care. 1998, 21: 1288-1294.
Davidson MH, Hauptman J, DiGirolamo M, Foreyt JP, Halsted CH, Heber D, Heimburger DC, Lucas CP, Robbins DC, Chung J, Heymsfield SB: Weight control and risk factor reduction in obese subjects treated for 2 years with orlistat: a randomized controlled trial. J Amer Med Assoc. 1999, 281: 235-242. 10.1001/jama.281.3.235.
Wadden TA, Berkowitz RI, Sarwer DB, Prus-Wisniewski R, Steinberg C: Benefits of lifestyle modification in the pharmacologic treatment of obesity: a randomized trial. Arch Intern Med. 2001, 161: 218-227. 10.1001/archinte.161.2.218.
NHLBI: Prescription medication for treatment of obesity. [ http://www.niddk.nih.gov/health/nutrit/nutrit.htm ]
Rushing PA, Hagan MM, Seeley RJ, Lutz TA, Woods SC: Amylin: a novel action in the brain to reduce body weight. Endocrinology. 2000, 141: 850-853. 10.1210/en.141.2.850.
Stewart PM, Tomlinson JW: Cortisol, 11 beta-hydroxysteroid dehydrogenase type 1 and central obesity. Trends Endocrinol Metab. 2002, 13: 94-96. 10.1016/S1043-2760(02)00566-0.
Clapham JC, Arch JRS, Tadayyon M: Anti-obesity drugs: a critical review of current therapies and future opportunities. Pharmacol Ther. 2001, 89: 81-121. 10.1016/S0163-7258(00)00105-4.
Anonymous: P 57 and food intake. obesity Meds and Research News. 2000
Anonymous: NIH Conference. Gastrointestinal surgery for severe obesity. Consensus Development Conference Panel. Ann Intern Med. 1991, 115: 956-961.
Karl JG: Overview of surgical techniques for treating obesity. Am J Clin Nutr. 1992, 55: 552s-555s.
Ashley S, Bird DL, Sugden G, Royston CM: Vertical banded gastroplasty for the treatment of morbid obesity. Br J Surg. 1993, 80: 1421-1423.
Shikora SA, Benotti PN, Forre RA: Surgical Treatment of Obesity. In: Obesity, pathophysiology, psychology and treatment. Edited by: Blackburn GL, Kanders BS. 1994, New York Chapman & Hall, 264-282.
Sagar PM: Surgical treatment of morbid obesity. Br J Surg. 1995, 82: 732-739.
Lonroth H, Dalenback J, Haglind E, Josefsson K, Olbe L, Fagevik Olsen M, Lundell L: Vertical banded gastroplasty by laparoscopic technique in the treatment of morbid obesity. Surg Laparosc Endosc. 1996, 6: 102-107. 10.1097/00019509-199604000-00004.
Salmon PA, McArdle MO: The rationale and results of gastroplasty/gastric by-pass. Obes Surg. 1992, 2: 61-68. 10.1381/096089292765560565.
Seehra H, Macc Dermatt N, Lascelles RG, Taylor TV: Wernicke's encephalapathy after vertical banded gastroplasty for morbid obesity. Br Med J. 1996, 312: 434-
Foley EF, Benotti PN, Borlase BC, Hollingshead J, Blackburn GL: Impact of gastric restrictive surgery on hypertension in the morbidly obese. Am J Surg. 1992, 163: 294-297. 10.1016/0002-9610(92)90005-C.
Carson JL, Ruddy ME, Duff AE, Holmes NJ, Cody RP, Brolin RE: The effect of gastric bypass surgery on hypertension in the morbidity obese patients. Arch Intern Med. 1994, 154: 193-200. 10.1001/archinte.154.2.193.
Olsson SA, Petersson BG, Sorbris R, Nilsson-Ehle P: Effects of weight reduction after gastroplasty on glucose and lipid metabolism. Am J Clin Nutr. 1984, 40: 1273-1280.
Herbst CA, Hughes TA, Gwynne JT, Buckwalter JA: Gastric bariatric operation in insulin treated adults. Surgery. 1984, 95: 209-214.
Pories WJ, Swanson MS, MacDonald KG, Long SB, Morris PG, Brown BM, Barakat HA, deRamon RA, Israel G, Dolezal JM: Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. 1995, 222: 339-350.
Article CAS PubMed PubMed Central Google Scholar
Download references
Author information
Authors and affiliations.
Pharmacology Division, Department of Pharmaceutical Sciences, Andhra University, Visakhapatnam, 530003, Andhra Pradesh, India
Srinivas Nammi, Saisudha Koka & Krishna M Boini
University College of Pharmaceutical Sciences, Kakatiya University, Warangal, 506009, Andhra Pradesh, India
Krishna M Chinnala
Department of Physiology, University of Tuebingen, D 72076, Tuebingen, Germany
Srinivas Nammi & Krishna M Boini
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Srinivas Nammi .
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Rights and permissions.
Reprints and permissions
About this article
Cite this article.
Nammi, S., Koka, S., Chinnala, K.M. et al. Obesity: An overview on its current perspectives and treatment options. Nutr J 3 , 3 (2004). https://doi.org/10.1186/1475-2891-3-3
Download citation
Received : 28 February 2004
Accepted : 14 April 2004
Published : 14 April 2004
DOI : https://doi.org/10.1186/1475-2891-3-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Anorexia Nervosa
- Sibutramine
- Gall Bladder Disease

Nutrition Journal
ISSN: 1475-2891
- General enquiries: [email protected]
- Search Menu
- Sign in through your institution
- Advance Articles
- Editor's Choice
- Author Guidelines
- Submission Site
- Open Access Options
- Self-Archiving Policy
- About Journal of Molecular Cell Biology
- Society affiliations
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Obesity: causes, consequences, treatments, and challenges.
- Article contents
- Figures & tables
- Supplementary Data
Obesity: causes, consequences, treatments, and challenges, Journal of Molecular Cell Biology , Volume 13, Issue 7, July 2021, Pages 463–465, https://doi.org/10.1093/jmcb/mjab056
- Permissions Icon Permissions
Obesity has become a global epidemic and is one of today’s most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer ( Bluher, 2019 ).
Obesity is mainly caused by imbalanced energy intake and expenditure due to a sedentary lifestyle coupled with overnutrition. Excess nutrients are stored in adipose tissue (AT) in the form of triglycerides, which will be utilized as nutrients by other tissues through lipolysis under nutrient deficit conditions. There are two major types of AT, white AT (WAT) and brown AT, the latter is a specialized form of fat depot that participates in non-shivering thermogenesis through lipid oxidation-mediated heat generation. While WAT has been historically considered merely an energy reservoir, this fat depot is now well known to function as an endocrine organ that produces and secretes various hormones, cytokines, and metabolites (termed as adipokines) to control systemic energy balance. Studies over the past decade also show that WAT, especially subcutaneous WAT, could undergo ‘beiging’ remodeling in response to environmental or hormonal perturbation. In the first paper of this special issue, Cheong and Xu (2021) systematically review the recent progress on the factors, pathways, and mechanisms that regulate the intercellular and inter-organ crosstalks in the beiging of WAT. A critical but still not fully addressed issue in the adipose research field is the origin of the beige cells. Although beige adipocytes are known to have distinct cellular origins from brown and while adipocytes, it remains unclear on whether the cells are from pre-existing mature white adipocytes through a transdifferentiation process or from de novo differentiation of precursor cells. AT is a heterogeneous tissue composed of not only adipocytes but also nonadipocyte cell populations, including fibroblasts, as well as endothelial, blood, stromal, and adipocyte precursor cells ( Ruan, 2020 ). The authors examined evidence to show that heterogeneity contributes to different browning capacities among fat depots and even within the same depot. The local microenvironment in WAT, which is dynamically and coordinately controlled by inputs from the heterogeneous cell types, plays a critical role in the beige adipogenesis process. The authors also examined key regulators of the AT microenvironment, including vascularization, the sympathetic nerve system, immune cells, peptide hormones, exosomes, and gut microbiota-derived metabolites. Given that increasing beige fat function enhances energy expenditure and consequently reduces body weight gain, identification and characterization of novel regulators and understanding their mechanisms of action in the beiging process has a therapeutic potential to combat obesity and its associated diseases. However, as noticed by the authors, most of the current pre-clinical research on ‘beiging’ are done in rodent models, which may not represent the exact phenomenon in humans ( Cheong and Xu, 2021 ). Thus, further investigations will be needed to translate the findings from bench to clinic.
While both social–environmental factors and genetic preposition have been recognized to play important roles in obesity epidemic, Gao et al. (2021) present evidence showing that epigenetic changes may be a key factor to explain interindividual differences in obesity. The authors examined data on the function of DNA methylation in regulating the expression of key genes involved in metabolism. They also summarize the roles of histone modifications as well as various RNAs such as microRNAs, long noncoding RNAs, and circular RNAs in regulating metabolic gene expression in metabolic organs in response to environmental cues. Lastly, the authors discuss the effect of lifestyle modification and therapeutic agents on epigenetic regulation of energy homeostasis. Understanding the mechanisms by which lifestyles such as diet and exercise modulate the expression and function of epigenetic factors in metabolism should be essential for developing novel strategies for the prevention and treatment of obesity and its associated metabolic diseases.
A major consequence of obesity is type 2 diabetes, a chronic disease that occurs when body cannot use and produce insulin effectively. Diabetes profoundly and adversely affects the vasculature, leading to various cardiovascular-related diseases such as atherosclerosis, arteriosclerotic, and microvascular diseases, which have been recognized as the most common causes of death in people with diabetes ( Cho et al., 2018 ). Love et al. (2021) systematically review the roles and regulation of endothelial insulin resistance in diabetes complications, focusing mainly on vascular dysfunction. The authors review the vasoprotective functions and the mechanisms of action of endothelial insulin and insulin-like growth factor 1 signaling pathways. They also examined the contribution and impart of endothelial insulin resistance to diabetes complications from both biochemical and physiological perspectives and evaluated the beneficial roles of many of the medications currently used for T2D treatment in vascular management, including metformin, thiazolidinediones, glucagon-like receptor agonists, dipeptidyl peptidase-4 inhibitors, sodium-glucose cotransporter inhibitors, as well as exercise. The authors present evidence to suggest that sex differences and racial/ethnic disparities contribute significantly to vascular dysfunction in the setting of diabetes. Lastly, the authors raise a number of very important questions with regard to the role and connection of endothelial insulin resistance to metabolic dysfunction in other major metabolic organs/tissues and suggest several insightful directions in this area for future investigation.
Following on from the theme of obesity-induced metabolic dysfunction, Xia et al. (2021) review the latest progresses on the role of membrane-type I matrix metalloproteinase (MT1-MMP), a zinc-dependent endopeptidase that proteolytically cleaves extracellular matrix components and non-matrix proteins, in lipid metabolism. The authors examined data on the transcriptional and post-translational modification regulation of MT1-MMP gene expression and function. They also present evidence showing that the functions of MT1-MMP in lipid metabolism are cell specific as it may either promote or suppress inflammation and atherosclerosis depending on its presence in distinct cells. MT1-MMP appears to exert a complex role in obesity for that the molecule delays the progression of early obesity but exacerbates obesity at the advanced stage. Because inhibition of MT1-MMP can potentially lower the circulating low-density lipoprotein cholesterol levels and reduce the risk of cancer metastasis and atherosclerosis, the protein has been viewed as a very promising therapeutic target. However, challenges remain in developing MT1-MMP-based therapies due to the tissue-specific roles of MT1-MMP and the lack of specific inhibitors for this molecule. Further investigations are needed to address these questions and to develop MT1-MMP-based therapeutic interventions.
Lastly, Huang et al. (2021) present new findings on a critical role of puromycin-sensitive aminopeptidase (PSA), an integral non-transmembrane enzyme that catalyzes the cleavage of amino acids near the N-terminus of polypeptides, in NAFLD. NAFLD, ranging from simple nonalcoholic fatty liver to the more aggressive subtype nonalcoholic steatohepatitis, has now become the leading chronic liver disease worldwide ( Loomba et al., 2021 ). At present, no effective drugs are available for NAFLD management in the clinic mainly due to the lack of a complete understanding of the mechanisms underlying the disease progress, reinforcing the urgent need to identify and validate novel targets and to elucidate their mechanisms of action in NAFLD development and pathogenesis. Huang et al. (2021) found that PSA expression levels were greatly reduced in the livers of obese mouse models and that the decreased PSA expression correlated with the progression of NAFLD in humans. They also found that PSA levels were negatively correlated with triglyceride accumulation in cultured hepatocytes and in the liver of ob/ob mice. Moreover, PSA suppresses steatosis by promoting lipogenesis and attenuating fatty acid β-oxidation in hepatocytes and protects oxidative stress and lipid overload in the liver by activating the nuclear factor erythroid 2-related factor 2, the master regulator of antioxidant response. These studies identify PSA as a pivotal regulator of hepatic lipid metabolism and suggest that PSA may be a potential biomarker and therapeutic target for treating NAFLD.
In summary, papers in this issue review our current knowledge on the causes, consequences, and interventions of obesity and its associated diseases such as type 2 diabetes, NAFLD, and cardiovascular disease ( Cheong and Xu, 2021 ; Gao et al., 2021 ; Love et al., 2021 ). Potential targets for the treatment of dyslipidemia and NAFLD are also discussed, as exemplified by MT1-MMP and PSA ( Huang et al., 2021 ; Xia et al., 2021 ). It is noted that despite enormous effect, few pharmacological interventions are currently available in the clinic to effectively treat obesity. In addition, while enhancing energy expenditure by browning/beiging of WAT has been demonstrated as a promising alternative approach to alleviate obesity in rodent models, it remains to be determined on whether such WAT reprogramming is effective in combating obesity in humans ( Cheong and Xu, 2021 ). Better understanding the mechanisms by which obesity induces various medical consequences and identification and characterization of novel anti-obesity secreted factors/soluble molecules would be helpful for developing effective therapeutic treatments for obesity and its associated medical complications.
Bluher M. ( 2019 ). Obesity: global epidemiology and pathogenesis . Nat. Rev. Endocrinol . 15 , 288 – 298 .
Google Scholar
Cheong L.Y. , Xu A. ( 2021 ). Intercellular and inter-organ crosstalk in browning of white adipose tissue: molecular mechanism and therapeutic complications . J. Mol. Cell Biol . 13 , 466 – 479 .
Cho N.H. , Shaw J.E. , Karuranga S. , et al. ( 2018 ). IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045 . Diabetes Res. Clin. Pract . 138 , 271 – 281 .
Gao W. , Liu J.-L. , Lu X. , et al. ( 2021 ). Epigenetic regulation of energy metabolism in obesity . J. Mol. Cell Biol . 13 , 480 – 499 .
Huang B. , Xiong X. , Zhang L. , et al. ( 2021 ). PSA controls hepatic lipid metabolism by regulating the NRF2 signaling pathway . J. Mol. Cell Biol . 13 , 527 – 539 .
Loomba R. , Friedman S.L. , Shulman G.I. ( 2021 ). Mechanisms and disease consequences of nonalcoholic fatty liver disease . Cell 184 , 2537 – 2564 .
Love K.M. , Barrett E.J. , Malin S.K. , et al. ( 2021 ). Diabetes pathogenesis and management: the endothelium comes of age . J. Mol. Cell Biol . 13 , 500 – 512 .
Ruan H.-B. ( 2020 ). Developmental and functional heterogeneity of thermogenic adipose tissue . J. Mol. Cell Biol . 12 , 775 – 784 .
Xia X.-D. , Alabi A. , Wang M. , et al. ( 2021 ). Membrane-type I matrix metalloproteinase (MT1-MMP), lipid metabolism, and therapeutic implications . J. Mol. Cell Biol . 13 , 513 – 526 .
Author notes
Shanghai Diabetes Institute, Shanghai Key Laboratory of Diabetes Mellitus, Shanghai Clinical Center for Diabetes, Shanghai Jiao Tong University Affiliated Sixth People's Hospital, Shanghai 200233, China E-mail: [email protected]
| Month: | Total Views: |
|---|---|
| October 2021 | 130 |
| November 2021 | 124 |
| December 2021 | 74 |
| January 2022 | 81 |
| February 2022 | 149 |
| March 2022 | 125 |
| April 2022 | 146 |
| May 2022 | 128 |
| June 2022 | 123 |
| July 2022 | 115 |
| August 2022 | 101 |
| September 2022 | 123 |
| October 2022 | 183 |
| November 2022 | 199 |
| December 2022 | 151 |
| January 2023 | 191 |
| February 2023 | 298 |
| March 2023 | 466 |
| April 2023 | 545 |
| May 2023 | 632 |
| June 2023 | 831 |
| July 2023 | 388 |
| August 2023 | 559 |
| September 2023 | 495 |
| October 2023 | 515 |
| November 2023 | 477 |
| December 2023 | 394 |
| January 2024 | 444 |
| February 2024 | 504 |
| March 2024 | 525 |
| April 2024 | 661 |
| May 2024 | 664 |
| June 2024 | 464 |
| July 2024 | 100 |
Email alerts
Citing articles via, affiliations.
- Online ISSN 1759-4685
- Copyright © 2024 Chinese Academy of Sciences
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

Introduction
Ebooks + books, suggested websites.
- What is obesity?
Obesity is a chronic condition defined by an excess amount of body fat. It indicates a weight greater than what is considered healthy.
Obesity has been more precisely defined by the National Institutes of Health (the NIH) as a BMI (Body Mass Index) of 30 and above. (A BMI of 30 is about 30 pounds overweight.) The BMI, a key index for relating body weight to height, is a person's weight in kilograms (kg) divided by their height in meters (m) squared.
MedicineNet
Image Credit: picserver.org
- What Causes Obesity?
- Health Risks Linked to Obesity
- Childhood Obesity
- Treatments for Obesity
The balance between calorie intake and energy expenditure determines a person's weight. If a person eats more calories than he or she burns (metabolizes), the person gains weight (the body will store the excess energy as fat). If a person eats fewer calories than he or she metabolizes, he or she will lose weight. Therefore, the most common causes of obesity are overeating and physical inactivity. Ultimately, body weight is the result of genetics, metabolism, environment, behavior, and culture.
- Genetics. A person is more likely to develop obesity if one or both parents are obese. Genetics also affect hormones involved in fat regulation.
- Overeating. Overeating leads to weight gain, especially if the diet is high in fat.
- A diet high in simple carbohydrates. The role of carbohydrates in weight gain is not clear. Carbohydrates increase blood glucose levels, which in turn stimulate insulin release by the pancreas, and insulin promotes the growth of fat tissue and can cause weight gain.
- Frequency of eating. The relationship between frequency of eating (how often you eat) and weight is somewhat controversial. There are many reports of overweight people eating less often than people with normal weight. Scientists have observed that people who eat small meals four or five times daily, have lower cholesterol levels and lower and/or more stable blood sugar levels than people who eat less frequently. One possible explanation is that small frequent meals produce stable insulin levels, whereas large meals cause large spikes of insulin after meals.
- Physical inactivity. Sedentary people burn fewer calories than people who are active. The National Health and Nutrition Examination Survey (NHANES) showed a strong correlations between physical inactivity and weight gain in both sexes.
- Medications. Medications associated with weight gain include certain antidepressants, anticonvulsants, some diabetes medications, certain hormones such as oral contraceptives, and most corticosteroids. Some high blood pressure medications and antihistamines cause weight gain.
- Psychological factors. For some people, emotions influence eating habits. Many people eat excessively in response to emotions such as boredom, sadness, stress, or anger.
- Diseases such as hypothyroidism, insulin resistance, polycystic ovary syndrome, and Cushing's syndrome are also contributors to obesity.
Excess weight may increase the risk for many health problems, including
- type 2 diabetes
- high blood pressure
- heart disease and strokes
- certain types of cancer
- sleep apnea
- osteoarthritis
- fatty liver disease
- kidney disease
- pregnancy problems, such as high blood sugar during pregnancy, high blood pressure, and increased risk for cesarean delivery (C-section)
National Institute of Diabetes ad Digestive Kidney Diseases
In the United States, the percentage of children and adolescents affected by obesity has more than tripled since the 1970s. Data from 2015-2016 show that nearly 1 in 5 school age children and young people (6 to 19 years) in the United States has obesity.
Many factors contribute to childhood obesity, including:
- Metabolism—how your body changes food and oxygen into energy it can use.
- Eating and physical activity behaviors.
- Community and neighborhood design and safety.
- Short sleep duration.
- Negative childhood events
Genetic factors are difficult to change. However, people and places can play a role in helping children achieve and maintain a healthy weight. Changes in the environments where young people spend their time—like homes, schools, and community settings—can make it easier for youth to access nutritious foods and be physically active. Schools can adopt policies and practices that help young people eat more fruits and vegetables, eat fewer foods and beverages that are high in added sugars or solid fats, and increase daily minutes of physical activity. These kinds of school-based and after-school programs and policies can be cost-effective and even cost-saving.
Centers for Disease Control and Prevention
There are countless weight-loss strategies available but many are ineffective and short-term, particularly for those who are morbidly obese. Among the morbidly obese, less than 5 percent succeed in losing a significant amount of weight and maintaining the weight loss with non-surgical programs — usually a combination of dieting, behavior modification therapy and exercise.
People do lose weight without surgery, however, particularly when they work with a certified health care professional to develop an effective and safe weight-loss program. Most health insurance companies don't cover weight-loss surgery unless you first make a serious effort to lose weight using non-surgical approaches.
Many people participate in a combination of the following therapies:
1. Dietary Modification
2. Behavior Modification
3. Exercise
4. Medications
USFC Health
Explore library databases .
Discover eBook collections or find print books/materials through the catalog for each campus:
CDC-Centers for Disease Control and Prevention
Genomics and health.
The Endocrine Society
This site serves as the one-stop clearinghouse for the general public seeking information on the key scientific trends and advancements that may one day lead to a slimmer, fitter America.
Mayo Clinic
Complications of Obesity
Obesity Society
Research. Education. Action.
The State of Obesity
National School Breakfast and Lunch Program: 70th Anniversary
World Health Organization
General information on obesity and childhood obesity, including global strategy on diet, physical activity and health.
Academy of Nutritionist and Dietetics
- Time to Act on Obesity
A visual breakdown of why some individuals are resistant to maintaining weight loss through diet and exercise alone.
- Last Updated: Jun 18, 2024 12:05 PM
- URL: https://libguides.cccneb.edu/obesity
Obesity Research Paper

View sample obesity research paper. Browse research paper examples for more inspiration. If you need a health research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.
Obesity has increasingly been identified as a critical global public health concern. This focus on obesity as a health priority raises complex bioethical issues. These include how obesity is defined and categorized, the implications of the centrality of personal responsibility in medical and public health approaches, how competing ethical frames impact social justice concerns, and the growing “moral panic” concerning obesity. A critical examination of how obesity is defined as a medical problem suggests that ethical approaches could be more productive if obesity were addressed as a social problem with medical consequences, rather than emphasizing it as a medical problem with social consequences.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% off with 24start discount code, introduction.
There has been a dramatic rise in the prevalence of obesity globally in the last three decades, and the World Health Organization (WHO) estimates around 11 % of the world’s total population is obese (WHO 2012). Obesity is seen as a major public health concern because it is widely recognized as a precipitating factor in the parallel emergence of chronic diseases as a primary cause of death in many countries. Obesity is often reported as a major drain on medical systems, and the growing obesity rates in developing countries are often cited as especially worrying in this regard. From a bioethics perspective, the focus on obesity as a health priority raises complex issues. This entry highlights inter-related and key bioethical dimensions of contemporary concerns around and approaches to obesity, including the means by which people are categorized as obese or not, the medicalization of obesity as a disease that needs to be treated, implications of the centrality of individual responsibility in medical and public health approaches, obesity as a social justice issue, and media and growing “moral panic.”
Obesity is most simply defined as an excess of adipose (fat) tissue, usually with negative health effects. However, this definition is problematic. Medically, as discussed below, the science of obesity is increasingly suggesting that many people can be both obese and healthy. However, “obese” and “obesity” are terms that have also entered everyday media and other public discourses in ways that are mostly negative and imply ill-health and disease. The growing assumption that obesity is defined as a negative characteristic is historically and culturally particular, in marked contrast to cross-cultural records that describe plump bodies as powerful, sexy, social, abundant, fertile, and certainly healthy (Brewis 2011a).
Ethical Dimensions
The Categorization of Obesity. A definition of obesity based upon the notion of excess body fat requires measurement against a standard of what constitutes “normal.” Given that human bodies are highly ecologically flexible and vary in averages across populations, the imposition of a single standard for classification as obese raises some complex bioethical issues. The most widely employed means to classify people as obese, and then assess variation in population levels of obesity, is through use of body mass index (BMI).
BMI does not directly measure body fat; rather, it is a proxy measure using the ratio of mass (weight) relative to height. Using statistical methods and prescriptive and risk models, four basic categories of weight (underweight, normal, overweight, obese) have been identified and are now widely applied, from the doctor’s office to large public health interventions. These standard categories are arbitrarily defined through cutoff points related to morbidity and mortality rates found in large-scale epidemiological studies, with obesity normally set at a BMI of 30 or higher.
While BMI as a measure of obesity is sometimes useful, particularly in clinical studies, because of both individual and population variation, this mapping of weight to health risk is not precise or even especially predictive. For example, there is growing evidence that many people clinically defined as obese prove to be metabolically healthy even as they are advised by doctors they need to lose weight, and that the level of obesity at which conditions like diabetes and heart disease become more prevalent differs across populations. Moreover, BMI does not discriminate between muscle mass, bone, connective tissue, and amount types of adipose tissue, obscuring accurate measurement of total body fat. As a result, people with highly-developed musculature are labeled obese by the measure, even when they have low levels of actual body fat. Further, some populations have greater bone density on average or shorter leg bone length resulting in falsely high BMI scores (Hruschka et al. 2013). For example, for decades there has been a public health concern focused on very high obesity risk in Pacific Island populations, but more recent studies have shown that the disease correlates of obesity emerge at higher levels of adiposity in comparison to other groups. Hence, the common standard for categorizing obesity probably misassigns a significant number of people and accordingly implies health risks where none may exist (and vice versa). Additionally, women have a higher percentage of body fat than men, and weight tends to increase in both genders as individuals age. Attempts to address the weaknesses in BMI classifications have resulted in alternative methods that more accurately measure the amount and distribution of body fat, but these use technologies or expertise that are difficult to implement in real-world settings.
Defining Obesity as a Disease. Defining obesity against a set standard of what is a normal or healthy level of body fat leads to an emphasis on prevention and cure, and underscores obesity as (1) a problem, with (2) an identifiable cause (diagnosis), and that (3) requires evaluation, intervention, management, and control. The central bioethical issue is this: regardless of how people are classified into an obese category, once so categorized it is generally assumed that labeling a person as unhealthy is warranted and medical or other intervention is necessary. Certainly, obesity has become increasingly identified as a major factor and index of ill-health over the last two decades. This culminated in the formal recognition of obesity as a disease by the American Medical Association in 2013, even in the absence of other risk factors or clinical symptoms. The growing medicalization of obesity as a condition explains why highly invasive and often risky medical treatments for obesity, such as bariatric surgery, are on the rise. The emphasis on excess weight as a health problem also negatively impacts how people view and relate to their own and others’ bodies and in ways that create emotional and social distress related to failing to meet social prescriptions for an ideal or acceptable body size.
Levels of Analyses and Ultimate Causation. Current scientific evidence on the causes of obesity can be analyzed at different levels, often working iteratively and in feedback with each other. At the genetic level, some individuals have a predisposition toward higher weights, weight gain, and difficulty in weight loss, related to genetic variants in appetite, metabolism, and activity. At the individual level, obesity is the result of excess calorie intake over calories expended through physical activity, but individual-level factors such as income, education level, ethnicity, age, and gender also predict differential risks of being obese, as does use of certain medications or comorbidities such as depression. Institutional factors such as health care access also matter.
At the community, neighborhood, or regional level, obesity risk accrues differently based solely on where people live. One factor in this pattern is the rapid urbanization of the world’s population: urbanization is associated with higher rates of obesity, and an increasing majority of humans live in cities. This correlation is due, in part, to the low cost of high density foods, changes in activity with the move to urban settings and structural and economic barriers to healthier lifestyles (Metzl and Hansen 2014). Further, within those cities, specific locales and their inhabitants’ lifestyles vary based upon social, spatial, and economic factors. The built environment of a particular locale is one example of how the physical expression of social, spatial, and economic factors relates to obesity prevalence: walkability, public transportation, access to fresh foods, safety, parks, light and shade, access to healthcare, and density all help shape obesity risk. For example, barriers in transportation and distance may make it difficult for residents to access healthy foods, while the perception by residents that the place they live in is unsafe or of poor quality may limit opportunities to be physically active. Social and economic factors also influence residential effects, including social exclusion, discrimination, and diminished economic infrastructure. Efforts to address residential effects often evoke stakeholder objections, as these efforts may inhibit personal choice, stigmatize neighborhood residents, or create changes that conflict with personal lifestyles and cultural values (ten Have et al. 2011).
Education and wealth, and most especially poverty, are also implicated in obesity risk. The relationship between income and obesity is complex and varies depending on the economic development of the resident country. Most nations, even the poorest, demonstrate some level of obesity, even in the presence of food shortages and undernutrition. The combination of under and over nutrition increases the likelihood of obesity and has significant implications in terms of health risks and negative health effects. As poorer nations become increasingly urbanized and industrialized, these problems are exacerbated, particularly as low income countries have fewer healthcare resources to meet the challenges posed by chronic conditions associated with obesity. This “dual burden” is also evident in middle-income countries: as economic changes at both the household and national level occur, families with a dual burden of having overweight and underweight individuals become increasingly prevalent.
Evidence suggests that income and obesity also rise together as inexpensive food becomes easily accessible. However, this trend reverses at the point where the apparent social costs of obesity outweigh the advantages. In middle to high-income countries, obesity tends to be inversely correlated with socioeconomic status, meaning that the highest obesity rates are found in those populations with the lowest incomes and with the lowest levels of educational achievement (Brewis 2011a). At a national level, BMI appears to rise in the early and accelerated phases of economic development due to a complex set of factors including urban migration, a shift from traditional occupations, and increased technology. At the individual level, poverty is contextual, demonstrating a complex residential pattern, with both rural and urban poverty linked to lower education and higher obesity.
While there have been some efforts to develop community-level interventions in line with increasing recognition of these upstream causes of obesity risk, medical and public health interventions continue to give the most attention to individual behavior change. The standard treatment model, often shared by clinicians and patients alike, is that the individual must lose excess weight by eating less and/or exercising more. This is despite decades of evidence that most such behavioral change strategies eventually fail to result in weight lost, and often serve to promote weight regain (Brewis 2011a).
Obesity and Social Justice Considerations. The role of proximate and ultimate factors discussed above means that obesity can be framed as a social justice issue, not solely a medical one. This suggests a very different course, emphasis, and pathway for public health interventions. Policies that seek to restrict behavior (passively or actively) can disproportionately affect the poor, the rural, and the malnourished. Of critical importance is who designs, implements, and evaluates these efforts. How do these interventions ethically impact personal physical health while promoting equality and maintaining individual autonomy? If population-level interventions are not necessarily individually beneficial and may in fact have psychosocial and cultural costs with their own negative health consequences, should public health entities intervene at all? These are some of the ethical issues that arise when the focus moves away from considering obesity fundamentally a medical problem to thinking about obesity at the aggregate level.
The challenge is to consider both the ultimate (structural) as well as the proximate factors (nutrition, activity, and medical conditions) that shape obesity risk when developing obesity policy and interventions. Identifying the causes of obesity, when coupled with how it is defined, becomes important in the ethical frame used to intervene. To date, there have been multiple framings in approaches to combat the rise of obesity. These ethical frames are not mutually exclusive and often coexist within a particular approach. Understanding the ethical platform from which programs spring will enable better understanding of the consequences (intentional or unintentional), successes, and failures. Identifying obesity as a health problem is more than defining disease, biomedical risk, and treatment; assigning responsibility – individual or otherwise – becomes part of the equation. The increasing prevalence of obesity on a global scale is accompanied by concerns that society is harmed in some way. This sense of harm in turn is linked to the notion of blame. How responsibility and blame are assigned varies with different ethical frames.
Framing Obesity Solutions
Emphasis on Individual Responsibility. The notion of individual responsibility has dominated the discourse surrounding the obesity crisis and efforts to contain the problem. Individual responsibility is rooted in notions of individual autonomy based within a moralistic theory of personal determination. Morality frames emphasize the threat to social values and economic stability by focusing on personal choice and the impact these choices have on society (Boero 2012). A morality frame advances notions of normal, ideal, virtue, right, and wrong. In this frame, obesity is related to personal failings – a lack of self-discipline, restraint, rationality, and moral failings attributed to poor life choices (gluttony, sloth, and a lack of adherence to personal improvement). Obesity, therefore, is self-induced and harm is self-inflicted. Because the individual is responsible for their health and body, blame is personal and can take the form of value imperatives about who is obese or overweight and who is responsible. Interventions and public health campaigns using this frame focus on problem awareness, promote better individual health behaviors, and encourage personal responsibility. Interventions range from educational efforts to weight loss programs, “fat taxes” (on calorie or fat dense foods), and increased insurance rates for individuals with high BMIs. This type of framing, when used in conjunction with a medical definition of obesity, places the focus of the intervention on achieving a physical ideal body weight and ignores the psychosocial dimensions of health, even as it places responsibility upon the individual (as psychologically weak or morally lax). Stigmatization, discrimination, and negative self-image are the result, which have their own negative health consequences (Sagay 2013; Puhl and Heuer 2010).
Biomedical and Public Health Frames. The biomedical frame uses the language of risk to intervene and regulate the body in order to promote health or, more usually, decrease illness or disease. Obesity in this frame is seen as pathologic – a biological condition to be monitored, treated, and cured. The body is understood to be the recipient of treatment, a somewhat passive vessel that needs management by healthcare professionals (Sagay 2013). De-emphasizing personal responsibility can be helpful in decreasing stigma, but medicalization also promotes stigmatization by labeling obese bodies as sick. Framing obesity in terms of mortality and morbidity imparts urgency and authority to the issue. The locus for intervention is on proximate factors and responsibility remains with the individual-aspatient, though the medical system is a crucial partner in terms of defining the problem and determining and managing treatment. Generally individual and small-scale interventions focused on dietary choice, activity, and medical/surgical interventions are utilized in this context. However, the biomedical frame informs larger policy issues resulting in industry and governmental regulations generally rooted in economic analyses, such as differential insurance rates for individuals based upon weight, corporate programs to incentivize weight reduction or dietary choice, bans or taxes on sugar-sweetened beverages, and regulation of nutritional information on food products.
A public health frame assigns responsibility to the government (local, state, and federal). Public health entities are most often located within governments and are charged with setting standards, regulating and protecting public safety and promoting health, and minimizing or preventing public harm while at the same time ensuring individual liberty, privacy, and public access to needed resources. This equation differs internationally as notions of individual and public health are culturally constituted. In general, obesity is seen as a threat to public health and the approach taken is to reduce the threat, generally combining individual and systemic approaches to address the issue. Ethical approaches in this frame deal with the differential distribution of obesity across groups and subpopulations as prevalence and risk manifest variably within cultural groups, gender, socioeconomic status, etc. Financial triggers (incentives & disincentives), built environment changes that alter lifestyle options (slowing elevators, car-free zoning, food banning), and informational campaigns are often used or suggested within a public health intervention. Issues of justice and fairness can be particularly problematic in this framing as the dual focus of public health creates a tension between liberty and protection. Obesity at the individual level includes social and economic disparities as well as discrimination and psychological stress from weight bias. Addressing these issues within the systemic frames of government, business, and infrastructure (including larger social forces) can contribute to stigmatization, discrimination, and differential opportunities and access.
Thus, in practice, there is a smorgasbord of antiobesity efforts, structured within multiple framings – moralistic, biomedical, and public health – that tend to be disconnected from each other. Even assuming a universal definition of obesity and its determinants exists, the ethics of policy interventions still needs to be addressed. At the heart of the ethics, debate is concerned over individual choice, autonomy, and the exacerbation of stigma and discrimination. Rephrasing the two previous ethical questions might then ask: What are the individual’s essential rights and responsibilities concerning weight? Secondly, what is the responsibility of the government in providing healthy, safe environments for its citizens?
This tension between rights and responsibilities (individual, societal, and governmental) plays out differently globally. The body (and body size) is understood as a “domain of liberty and autonomy” (Tirosh 2014, p. 1801), but the expression of these values is differentially understood across societies. When seen as a lifestyle issue, obesity remains focused at the individual and local levels, to be dealt with through small-scale interventions in select populations to encourage individuals to control their weight and make healthier choices (moralistic frame). These types of interventions tend to ignore the complexity of factors (and responsibilities) underlying obesity and keep responsibility (and blame) with the individual. Growing public discourse has revolved around policy changes to combat the “rising epidemic” of obesity. Public health officials have supported this groundswell of opinion through campaigns to promote the adoption of a healthy lifestyle, emphasizing a diet high in fruits, vegetables, complex carbohydrates, and lean proteins and sufficient exercise – efforts that highlight personal choice and responsibility. Much of the work on prevention and intervention at this level has had mixed results. Even among public health practitioners who seek to address structural components underlying obesity, the political weight of the morality frame leads them to use “code language” such as “make the healthy choice, the easy choice.” Essentially structural changes are presented as changes enabling personal choice.
At a governmental level, rising healthcare costs in conjunction with rising obesity rates globally and concerns over the efficacy of individual-level interventions are frequently cited as an impetus for governmental strategies and policies to guide widespread interventions, primarily through legislation. Governmental interventions are influenced by the culture, political system, economics, and traditions of the nations involved, resulting in a spectrum of policies and programs globally. Efforts range from health education to restrictive taxes on unhealthy foods and beverages, with a goal of shaping behavior by restricting or coercing individual choice. In the European Union (EU), a concerted effort is being made to encourage voluntary action on the part of industry partners to alter nutrition and activity environments. Voluntary efforts to support decision-making through evidence-based information, self-regulation of product claims (labeling, advertisements) through the proposed establishment of an industry code of conduct, food redistribution (surplus fruits/vegetables) focused on children 4–12 years old, reformulation of foods to decrease sugar, fat, and salt, and sustainable urban transportation facilities to promote physical activity/ public infrastructure (Commission of the European Communities 2007) are examples of this type of intervention. In the USA, taxation of SSBs and calorie-dense foods has been implemented (or attempted), most notably in New York City and the Navajo Nation. China, Britain, and Mexico have all passed or attempted to enact legislation that aims to regulate behavior with an eye to reducing the economic burden of healthcare. Often, particular populations are targeted for interventions, as evidence indicates that obesity is more prevalent in these groups. Unfortunately, these efforts can take the form of value imperatives about who is obese or overweight and who is responsible, encouraging the spread of stigmatization and victimization (Puhl and Heuer 2010).
Some initiatives have sought to create structural or environmental changes to address the inequities, disparities, and deficits implicated in obesity (public health framing with social justice focus). Policies attempting to reduce the unequal distribution of resources, barriers to healthy foods and activities, and social and economic inequities can be found in new regulations requiring enhanced visibility and simplified nutritional labeling; limitations on commercial advertising of high density, low-nutrient foods to children; venue-specific banning of “unhealthy items” such as high-fat items in restaurants or SSBs in school vending machines; and limiting the proximity of fast-food restaurants to schools (Kass et al. 2014; ten Have et al. 2011). These types of initiatives still impact personal choice and liberty and have resulted in public debates regarding the role of government in regulating health. Impacting broader economic and social structures is more challenging from the local level, though increasingly tools like health impact assessments and health in all policies are being used to provide more equity in land use decisions, and have even been used to evaluate local minimum wage, affordable housing, and supplemental nutrition policies. Criticisms of obesity policies have ranged from concerns over the inhibition of individual autonomy, the expansion of the paternalistic “nanny” state (and subsequent economic burden), and the inequitable treatment and stigmatization of low-income populations.
Ethical discussions concerning interventions that limit choice or coerce behavior tend to be centered on arguments about legitimacy and utility. Legitimacy focuses on the value to society in instituting a particular policy or practice. Generally, the discussion revolves around the role of paternalism (soft or hard) in promoting the general welfare of the individual. Paternalism is best viewed as a sliding scale that ranges from promoting informed choice (information campaigns) through implementation of incentives (free or reduced costs, tax benefits, etc.) and ultimately various forms of coercion (bans, taxation). Utility looks at the cost-benefit ratio: is a policy or intervention likely to succeed and does it offer enough benefit to offset the reduction in choice, liberty, or privacy. Because there is little cohesion in how data is collected internationally, making evidence based comparisons of the effectiveness of different types of interventions is difficult. In general, arguments made for coercive policies are rooted in the premise that obesity is associated with higher morbidity and attendant higher costs of treatment. As previously noted, this is by no means a validated conclusion and therefore the utility of such efforts is suspect.
An example of this trade-off is the call for school districts to restrict soft drinks on school campuses. This type of intervention may have the unintended consequence of reducing the school’s revenue stream, resulting in less money available for student education or extra-curricular activities. Obesity prevalence is associated with poverty and disadvantage, disproportionately impacting precisely those communities whose schools need funding the most. Reduced funding may lead to a reduction in programming and healthy food options, elimination of physical education or play equipment, poor food quality to reduce costs, increased sedentism, and reduced educational opportunities (Crooks 2003). The result may be an environmental trade-off of biological costs for social benefits – poorer nutritional quality in order to provide education for all students and thus hopefully propel the students out of poverty.
Another example is the call to use social pressure tactics, similar to antismoking campaigns, to leverage public opinion toward acceptance of stringent governmental regulations. The trade-off here is to focus on increased legitimacy at the expense of utility. This type of intervention operates at the individual, acute, and proximate level and does not address any of the underlying structural conditions. Couched as “stigmatization lite” the argument is that overweight and obese individuals do not recognize their “problem” and need to be awakened to reality. Unfortunately increasing stigmatization of the individual has not been demonstrated to positively impact behavior change; rather, it produces the opposite impact. Discrimination is implicated in stress induced physiological responses associated with obesity that not only negatively impact health but also discourage potential participation in health-related activities. Beyond this, how is the level of stigma “titrated?” Increasing antiobesity thinking may contribute to the moral panic over the rise in obesity rates (Campos et al. 2006).
Stigmatization And Moral Panic
Obesity and Weight-related Stigma. Any discussion on bioethics needs to address the issue of stigmatization (and resulting victimization and discrimination) of obese individuals. Placing the responsibility for one’s weight on the individual has led to sanctioned discrimination in the form of diminished access to goods, services, and employment opportunities and higher healthcare costs for obese individuals. Obesity has even been used as evidence in child abuse cases and other legal interventions. Despite multiple framings of obesity as a medical and public health problem, the persistent focus on individual responsibility and autonomy continues to direct the understanding of obesity through the lens of morality – a platform for value imperatives and subsequent stigmatization.
Obesity stigma must be addressed within the social and structural conditions that produce it. That is, there must be recognition that even a focus on ultimate factors (zoning laws, bans, taxation, urban renewal) can have unintended consequences resulting in increased discrimination. In the past, public health concerns were often the result of an external agent (bacterial or viral agent, poor sanitation, cigarettes, etc.), allowing the focus of interventions to remain external to the body/self. However, weight (and excess weight) is rooted in the body itself – it is a domain of the self. Eating and movement are necessary components of life and are seen as highly personal, as one chooses what, when, and how to eat, move, and function bodily within personal environments. Because these activities are necessary (one cannot stop eating, for example), efforts have focused on changing personal decisions related to eating and activity. Attempts to alter these bodily functions with an external agent (medication, surgery) have had mixed results, but as long as eating and activity are categorized as personal choices, stigmatization will remain a factor.
Media and Corporate Roles. The “moral panic” that has resulted from the framing of obesity as an epidemic has produced a media onslaught. This begs the question of whether the media is reflecting this panic or creating it. Popular media promotes a thin ideal body size (particularly for women), while continuing to also promote the sale of obesogenic products. Fast food and junk food advertisements, product placement in movies, casting of thin ideal body types, and disparaging characterizations of obese characters are prevalent throughout multiple media formats. Visual representations of obese bodies that employ “de-evolution tropes” (which portray the human species as degenerating from more fit ancestors) are common. Media use (screen time) is certainly associated with increased snacking and requests for caloriedense foods and decreased activity and altered sleep patterns (American Academy of Pediatrics 2011).
The increasing documentation of these negative social and physical impacts of media treatment of obesity has led to a mishmash of corporate efforts and legislative calls to action. For example, the Disney Corporation has announced that it will no longer advertise “junk foods” on its television channel. However, Disney continues to promote thin body ideals in its movie and cartoon heroines. McDonald’s has been criticized for targeting children with “toy” gifts in their high fat and sugar Happy Meals. Several European Union countries have instituted restrictions on food advertising aimed at very young children. The impacts of the media on obesity risk and stigma bring to the fore the ongoing ethical conundrum concerning the extent to which governments should have control over media that promote unhealthy behaviors or stigmatization. Issues of free speech, government regulation, and equal access to opportunity and goods have all been cited as deterrents to government regulation of advertising and media. Combining this with a moralistic frame that castigates large bodies as personal failures and the bioethical landscape is messy indeed.
Obesity arises through individual behaviors shaped within varied epigenetic, cognitive, sociocultural, physical, material, political, and other institutional structures and environments. Bioethically, based on the discussion above, this entry suggests that obesity is perhaps more productively addressed as a social problem with medical consequences rather than a medical problem with social consequences. Competing frames of obesity, whether medically or otherwise problematized or not (moralistic, medical/ healthcare, public health, governmental), are rooted in concerns about the ethical behavior of members within the group, not about the larger social, economic, and political domains. Social justice models for obesity intervention rightly focus on the role of the built environment, but rarely tackle the ultimate determinants like poverty, education, and discrimination. Many complex bioethical questions remain: Is it possible to account for acute and chronic dimensions as well as proximate and ultimate factors and mitigate some of the unintended, negative consequences of interventions? How can health policies and interventions ethical approaches be constructed to take into account the very real social dimensions of weight and the body? If health is a public good, what are the ethical implications of not intervening?
Ultimately, being obese is both a private and public matter. While an individual’s weight is the result of multiple individual and biosocial components, the individual’s body is subject to public scrutiny and – increasingly – public regulation. The consequences of public efforts, both intended and unintended, need to be critically examined within the context of how obesity is defined as a problem, the frame used to address the problem as defined, and then how, with whom, and at what level various prevention and intervention efforts are implemented.
Bibliography :
- American Academy of Pediatrics. (2011). Policy statement – children, adolescents, obesity, and the media. Pediatrics, 128(1), 201–208.
- Boero, N. (2012). Killer fat: Media, medicine, and morals in the American “Obesity Epidemic.” New Brunswick: Rutgers University Press.
- Brewis, A. (2011a). Obesity: Cultural and biocultural perspectives. New Brunswick: Rutgers University Press.
- Campos, P., Saguy, A., Ernsberger, P., Oliver, E., & Gaesser, G. (2006). The epidemiology of overweight and obesity: Public health crisis or moral panic? International Journal of Epidemiology, 35, 55–60.
- Commission of the European Communities. (2007). A strategy for Europe on nutrition, overweight and obesity related health issues. Brussels, SEC. 706–7.
- Crooks, D. (2003). Nutrition and the sale of snack foods. Medical Anthropology Quarterly, 17(2), 182–199.
- Hruschka, D. J., Rush, E., & Brewis, A. (2013). Population differences in the relationship between height, weight, and adiposity: An application of Burton’s model. American Journal of Physical Anthropology, 151, 68–76.
- Kass, N., Hecht, K., Paul, A., & Birnbach, K. (2014). Ethics and obesity prevention: Ethical considerations in 3 approaches to reducing consumption of sugar-sweetened beverages. Public Health Ethics, 104(5), 787–795.
- Metzl, J., & Hansen, H. (2014). Structural competency: Theorizing a new medical engagement with stigma and inequality. Social Science & Medicine, 103, 126–133.
- Puhl, R., & Heuer, C. (2010). Obesity stigma: Important considerations for public health. Framing Health Matters, 100(6), 1019–1028.
- Sagay, A. (2013). What’s wrong with fat? Oxford: Oxford University Press.
- ten Have, M., de Beaufort, I. D., Teixera, P. J., Mackenbach, J. P., & van der Heide, A. (2011). Ethics and prevention of overweight and obesity: An inventory. Obesity Reviews, 12, 669–679.
- Tirosh, Y. (2014). Three comments on paternalism in public health. Connecticut Law Review, 46(5), 1795–1816.
- World Health Organization. (2012). Obesity and overweight: fact sheets. World Health Organization. Retrieved from https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight
- Brewis, A. (2011b). Obesity: Cultural and biocultural perspectives. New Brunswick: Rutgers University Press.
- Puhl, R. M., & Heuer, C. A. (2009). The stigma of obesity: A review and update. Obesity, 17(5), 941–964.
- Saguy, A. (2012). What’s wrong with fat? Oxford: Oxford University Press.
ORDER HIGH QUALITY CUSTOM PAPER

Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Gender- and obesity-specific association of co-exposure to personal care product and plasticizing chemicals and short sleep duration among adults: evidence from the national health and nutrition examination survey 2011–2016.

1. Introduction
2. materials and methods, 2.1. study population, 2.2. biomeasure of personal care product and plasticizing chemicals (pcppcs), 2.3. sleep duration, 2.4. covariates, 2.5. statistical analysis, 2.5.1. logistic regression, 2.5.2. weighted quantile sum regression, 2.5.3. bayesian kernel machine regression, 2.6. sensitivity analysis, 3.1. baseline characteristics of the study population, 3.2. distributions of urinary pcppcs, 3.3. association between pcppc exposures and short sleep duration by gender and obesity-specific status: logistic regression findings, 3.4. association between pcppc mixture and short sleep duration by gender- and obesity-specific status: wqs regression findings, 3.5. association between pcppc mixture and short sleep duration by gender and obesity: bkmr findings, 3.6. sensitivity analysis findings, 4. discussion, 4.1. principle findings, 4.2. comparison with other studies, 4.2.1. gender-specific differences, 4.2.2. obesity-specific differences, 4.3. research implications, 4.4. strengths and limitations, 5. conclusions, supplementary materials, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- Watson, N.F.; Badr, M.S.; Belenky, G.; Bliwise, D.L.; Buxton, O.M.; Buysse, D.; Dinges, D.F.; Gangwisch, J.; Grandner, M.A.; Kushida, C.; et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep 2015 , 38 , 843–844. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Khubchandani, J.; Price, J.H. Short Sleep Duration in Working American Adults, 2010–2018. J. Community Health 2020 , 45 , 219–227. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Altevogt, B.M.; Colten, H.R. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem ; National Academies Press (US): Washington, DC, USA, 2006. [ Google Scholar ]
- Grandner, M.A.; Chakravorty, S.; Perlis, M.L.; Oliver, L.; Gurubhagavatula, I. Habitual sleep duration associated with self-reported and objectively determined cardiometabolic risk factors. Sleep Med. 2014 , 15 , 42–50. [ Google Scholar ] [ CrossRef ]
- Itani, O.; Jike, M.; Watanabe, N.; Kaneita, Y. Short sleep duration and health outcomes: A systematic review, meta-analysis, and meta-regression. Sleep Med. 2017 , 32 , 246–256. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Beydoun, H.A.; Beydoun, M.A.; Jeng, H.A.; Zonderman, A.B.; Eid, S.M. Bisphenol-A and Sleep Adequacy among Adults in the National Health and Nutrition Examination Surveys. Sleep 2016 , 39 , 467–476. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sears, C.G.; Braun, J.M. Urinary phthalate metabolite concentrations and adolescent sleep duration. Environ. Epidemiol. 2021 , 5 , e134. [ Google Scholar ] [ CrossRef ]
- Shiue, I. Urinary arsenic, pesticides, heavy metals, phthalates, polyaromatic hydrocarbons, and polyfluoroalkyl compounds are associated with sleep troubles in adults: USA NHANES, 2005-2006. Environ. Sci. Pollut. Res. Int. 2017 , 24 , 3108–3116. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zhou, R.; Zhang, L.; Yan, J.; Sun, Y.; Jiang, H. Association of sleep problems with urinary concentrations of personal care and consumer product chemicals: A nationally representative, population-based study. Environ. Sci. Pollut. Res. Int. 2023 , 30 , 14533–14544. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Fatima, Y.; Doi, S.A.; Najman, J.M.; Mamun, A.A. Exploring Gender Difference in Sleep Quality of Young Adults: Findings from a Large Population Study. Clin. Med. Res. 2016 , 14 , 138–144. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Luo, J.; Zhu, G.; Zhao, Q.; Guo, Q.; Meng, H.; Hong, Z.; Ding, D. Prevalence and risk factors of poor sleep quality among Chinese elderly in an urban community: Results from the Shanghai aging study. PLoS ONE 2013 , 8 , e81261. [ Google Scholar ] [ CrossRef ]
- Cho, K.H.; Cho, E.H.; Hur, J.; Shin, D. Association of Sleep Duration and Obesity According to Gender and Age in Korean Adults: Results from the Korea National Health and Nutrition Examination Survey 2007-2015. J. Korean Med. Sci. 2018 , 33 , e345. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Fan, Y.; Zhang, L.; Wang, Y.; Li, C.; Zhang, B.; He, J.; Guo, P.; Qi, X.; Zhang, M.; Guo, C.; et al. Gender differences in the association between sleep duration and body mass index, percentage of body fat and visceral fat area among chinese adults: A cross-sectional study. BMC Endocr. Disord. 2021 , 21 , 247. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ren, L.; Chang, L.; Kang, Y.; Zhao, Y.; Chen, F.; Pei, L. Gender-Specific Association Between Sleep Duration and Body Mass Index in Rural China. Front. Endocrinol. (Lausanne) 2022 , 13 , 877100. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kishman, E.E.; Breneman, C.B.; Sparks, J.R.; Wang, X. Associations between Sleep and Body Composition in Older Women and the Potential Role of Physical Function. Sleep Biol. Rhythms. 2023 , 21 , 175–183. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Do, M.T.; Chang, V.C.; Mendez, M.A.; de Groh, M. Urinary bisphenol A and obesity in adults: Results from the Canadian Health Measures Survey. Health Promot Chronic Dis Prev Can 2017 , 37 , 403–412. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Shankar, A.; Teppala, S.; Sabanayagam, C. Urinary bisphenol a levels and measures of obesity: Results from the national health and nutrition examination survey 2003-2008. Int. Sch. Res. Not. Endocrinol. 2012 , 2012 , 965243. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Fan, J.; Ding, C.; Gong, W.; Yuan, F.; Zhang, Y.; Feng, G.; Song, C.; Liu, A. Association of Sleep Duration and Overweight/Obesity among Children in China. Int. J. Environ. Res. Public Health 2020 , 17 , 1962. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hatcher, K.M.; Smith, R.L.; Chiang, C.; Li, Z.; Flaws, J.A.; Mahoney, M.M. Association of phthalate exposure and endogenous hormones with self-reported sleep disruptions: Results from the Midlife Women’s Health Study. Menopause 2020 , 27 , 1251–1264. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hatcher, K.M.; Smith, R.L.; Li, Z.; Flaws, J.A.; Davies, C.R.; Mahoney, M.M. Preliminary findings reveal that phthalate exposure is associated with both subjective and objective measures of sleep in a small population of midlife women. Maturitas 2022 , 157 , 62–65. [ Google Scholar ] [ PubMed ]
- Wu, X.; Liu, S.; Wen, L.; Tan, Y.; Zeng, H.; Liang, H.; Weng, X.; Wu, Y.; Yao, H.; Fu, Y.; et al. Association between phthalates and sleep problems in the U.S. adult females from NHANES 2011-2014. Int. J. Environ. Health Res. 2023 , 34 , 1961–1976. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zamora, A.N.; Peterson, K.E.; Goodrich, J.M.; Téllez-Rojo, M.M.; Song, P.X.K.; Meeker, J.D.; Dolinoy, D.C.; Torres-Olascoaga, L.A.; Cantoral, A.; Jansen, E.C. Associations between exposure to phthalates, phenols, and parabens with objective and subjective measures of sleep health among Mexican women in midlife: A cross-sectional and retrospective analysis. Environ. Sci. Pollut. Res. Int. 2023 , 30 , 65544–65557. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Spiegel, K.; Leproult, R.; Colecchia, E.F.; L’Hermite-Balériaux, M.; Nie, Z.; Copinschi, G.; Cauter, E.V. Adaptation of the 24-h growth hormone profile to a state of sleep debt. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2000 , 279 , R874–R883. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kim, W.; Lee, J.; Ha, J.; Jo, K.; Lim, D.J.; Lee, J.M.; Chang, S.A.; Kang, M.I.; Kim, M.H. Association between Sleep Duration and Subclinical Thyroid Dysfunction Based on Nationally Representative Data. J. Clin. Med. 2019 , 8 , 2010. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Han, L.; Wang, Q. Association between organophosphorus insecticides exposure and the prevalence of sleep problems in the US adults: An analysis based on the NHANES 2007-2018. Ecotoxicol. Environ. Saf. 2023 , 255 , 114803. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zamora, A.N.; Watkins, D.J.; Peterson, K.E.; Jansen, E.C. Association between pesticide exposure and sleep health among a representative sample of US adults: Evidence from NHANES 2009-2014. BMC Public Health 2021 , 21 , 2199. [ Google Scholar ] [ CrossRef ]
- NCHS. About the National Health and Nutrition Examination Survey. Available online: https://www.cdc.gov/nchs/nhanes/about_nhanes.htm (accessed on 25 May 2023).
- Silva, M.J.; Samandar, E.; Preau, J.L., Jr.; Reidy, J.A.; Needham, L.L.; Calafat, A.M. Quantification of 22 phthalate metabolites in human urine. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2007 , 860 , 106–112. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- NCHS. Lab Methods for 2,4-Dichlorophenol, 2,5-Dichlorophenol. Available online: https://wwwn.cdc.gov/nchs/data/nhanes/2011-2012/labmethods/pp_g_met.pdf (accessed on 25 May 2023).
- NCHS. Lab Methods for Benzophenone-3, Bisphenol A, Methyl-, Ethyl-, Propyl-, and Butyl Parabens, Triclosan. Available online: https://wwwn.cdc.gov/nchs/data/nhanes/2011-2012/labmethods/eph_g_met.pdf (accessed on 25 May 2023).
- NCHS. Lab Methods for Metabolites of Phthalates and Phthalate Alternatives. Available online: https://wwwn.cdc.gov/nchs/data/nhanes/2011-2012/labmethods/phthte_g_met.pdf (accessed on 25 May 2023).
- NCHS. Laboratory Procedure Manual for Personal Care and Consumer Product Chemicals and Metabolites. Available online: https://wwwn.cdc.gov/nchs/data/nhanes/2013-2014/labmethods/EPHPP_H_MET.pdf (accessed on 25 May 2023).
- NCHS. Laboratory Procedure Manual for Phthalates and Plasticizers Metabolites. Available online: https://wwwn.cdc.gov/nchs/data/nhanes/2013-2014/labmethods/PHTHTE_H_MET_Phthalates.pdf (accessed on 25 May 2023).
- NCHS. Laboratory Procedure Manual for Personal Care and Consumer Product Chemicals and Metabolites. Available online: https://wwwn.cdc.gov/nchs/data/nhanes/2015-2016/labmethods/EPHPP_I_MET.pdf (accessed on 25 May 2023).
- NCHS. Laboratory Procedure Manual for Phthalates and Phthalate Alternative Metabolites. Available online: https://wwwn.cdc.gov/nchs/data/nhanes/2015-2016/labmethods/PHTHTE_I_MET.pdf (accessed on 25 May 2023).
- Shih, Y.-H.; Howe, C.G.; Scannell Bryan, M.; Shahriar, M.; Kibriya, M.G.; Jasmine, F.; Sarwar, G.; Graziano, J.H.; Persky, V.W.; Jackson, B.; et al. Exposure to metal mixtures in relation to blood pressure among children 5–7 years old: An observational study in Bangladesh. Environ. Epidemiol. 2021 , 5 , e135. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zhang, Y.; Dong, T.; Hu, W.; Wang, X.; Xu, B.; Lin, Z.; Hofer, T.; Stefanoff, P.; Chen, Y.; Wang, X.; et al. Association between exposure to a mixture of phenols, pesticides, and phthalates and obesity: Comparison of three statistical models. Environ. Int. 2019 , 123 , 325–336. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Carrico, C.; Gennings, C.; Wheeler, D.C.; Factor-Litvak, P. Characterization of weighted quantile sum regression for highly correlated data in a risk analysis setting. J. Agric. Biol. Environ. Stat. 2015 , 20 , 100–120. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Czarnota, J.; Gennings, C.; Colt, J.S.; De Roos, A.J.; Cerhan, J.R.; Severson, R.K.; Hartge, P.; Ward, M.H.; Wheeler, D.C. Analysis of Environmental Chemical Mixtures and Non-Hodgkin Lymphoma Risk in the NCI-SEER NHL Study. Environ. Health Perspect. 2015 , 123 , 965–970. [ Google Scholar ] [ CrossRef ]
- Bobb, J.F.; Valeri, L.; Claus Henn, B.; Christiani, D.C.; Wright, R.O.; Mazumdar, M.; Godleski, J.J.; Coull, B.A. Bayesian kernel machine regression for estimating the health effects of multi-pollutant mixtures. Biostatistics 2015 , 16 , 493–508. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Watanabe, M.; Kikuchi, H.; Tanaka, K.; Takahashi, M. Association of short sleep duration with weight gain and obesity at 1-year follow-up: A large-scale prospective study. Sleep 2010 , 33 , 161–167. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Singh, M.; Drake, C.L.; Roehrs, T.; Hudgel, D.W.; Roth, T. The association between obesity and short sleep duration: A population-based study. J. Clin. Sleep Med. 2005 , 1 , 357–363. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Dong, R.; Zhou, T.; Chen, J.; Zhang, M.; Zhang, H.; Wu, M.; Li, S.; Zhang, L.; Chen, B. Gender- and Age-Specific Relationships Between Phthalate Exposures and Obesity in Shanghai Adults. Arch. Environ. Contam. Toxicol. 2017 , 73 , 431–441. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chailurkit, L.O.; Aekplakorn, W.; Ongphiphadhanakul, B. The Association of Serum Bisphenol A with Thyroid Autoimmunity. Int. J. Environ. Res. Public Health 2016 , 13 , 1153. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Skarha, J.; Mínguez-Alarcón, L.; Williams, P.L.; Korevaar, T.I.M.; de Poortere, R.A.; Broeren, M.A.C.; Ford, J.B.; Eliot, M.; Hauser, R.; Braun, J.M. Cross-sectional associations between urinary triclosan and serum thyroid function biomarker concentrations in women. Environ. Int. 2019 , 122 , 256–262. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mong, J.A.; Cusmano, D.M. Sex differences in sleep: Impact of biological sex and sex steroids. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2016 , 371 , 20150110. [ Google Scholar ] [ CrossRef ]
- Barrett-Connor, E.; Dam, T.T.; Stone, K.; Harrison, S.L.; Redline, S.; Orwoll, E. The association of testosterone levels with overall sleep quality, sleep architecture, and sleep-disordered breathing. J. Clin. Endocrinol. Metab. 2008 , 93 , 2602–2609. [ Google Scholar ] [ CrossRef ]
- Bigambo, F.M.; Zhang, M.; Zhang, J.; Yang, X.; Yu, Q.; Wu, D.; Wang, X.; Xia, Y. Exposure to a mixture of personal care product and plasticizing chemicals in relation to reproductive hormones and menarche timing among 12–19 years old girls in NHANES 2013–2016. Food Chem. Toxicol. 2022 , 170 , 113463. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zimberg, I.Z.; Dâmaso, A.; Del Re, M.; Carneiro, A.M.; de Sá Souza, H.; de Lira, F.S.; Tufik, S.; de Mello, M.T. Short sleep duration and obesity: Mechanisms and future perspectives. Cell Biochem. Funct. 2012 , 30 , 524–529. [ Google Scholar ] [ CrossRef ] [ PubMed ]
Click here to enlarge figure
| Overall (N = 3012) | Short Sleep (N = 1118) | Adequate Sleep (N = 1894) | p-Value | |
|---|---|---|---|---|
| Gender | 0.042 | |||
| Male | 1451 (48.2) | 566 (50.6) | 885 (46.7) | |
| Female | 1561 (51.8) | 552 (49.4) | 1009 (53.3) | |
| Age (Year) (mean (SD)) | 39.70 (11.79) | 40.44 (11.65) | 39.26 (11.85) | 0.008 |
| Race (%) | <0.001 | |||
| Mexican | 413 (13.7) | 137 (12.3) | 276 (14.6) | |
| Hispanic | 329 (10.9) | 126 (11.3) | 203 (10.7) | |
| White | 1068 (35.5) | 355 (31.8) | 713 (37.6) | |
| Black | 690 (22.9) | 330 (29.5) | 360 (19.0) | |
| Asian | 395 (13.1) | 123 (11.0) | 272 (14.4) | |
| Multi-racial | 117 (3.9) | 47 (4.2) | 70 (3.7) | |
| Education (%) | 0.002 | |||
| Less than 9th grade | 180 (6.0) | 58 (5.2) | 122 (6.4) | |
| 9–11th grade | 360 (12.0) | 141 (12.6) | 219 (11.6) | |
| High school | 638 (21.2) | 248 (22.2) | 390 (20.6) | |
| College | 981 (32.6) | 396 (35.4) | 585 (30.9) | |
| Graduate or above | 853 (28.3) | 275 (24.6) | 578 (30.5) | |
| Marital status (%) | <0.001 | |||
| Married | 1837 (61.0) | 646 (57.8) | 1191 (62.9) | |
| Never married | 760 (25.2) | 281 (25.1) | 479 (25.3) | |
| Separated, widowed, divorced | 415 (13.8) | 191 (17.1) | 224 (11.8) | |
| PIR (%) | 0.479 | |||
| No poverty | 2318 (77.0) | 852 (76.2) | 1466 (77.4) | |
| Poverty | 694 (23.0) | 266 (23.8) | 428 (22.6) | |
| Food insecurity (%) | 0.547 | |||
| No | 2034 (67.5) | 747 (66.8) | 1287 (68.0) | |
| Yes | 978 (32.5) | 371 (33.2) | 607 (32.0) | |
| Waist circumference (mean (SD)) | 98.89 (17.08) | 100.64 (17.49) | 97.86 (16.75) | <0.001 |
| Abdominal obesity (%) | 0.06 | |||
| No | 1375 (45.7) | 485 (43.4) | 890 (47.0) | |
| Yes | 1637 (54.3) | 633 (56.6) | 1004 (53.0) | |
| BMI (kg/m ) (mean (SD)) | 29.42 (7.13) | 30.09 (7.41) | 29.03 (6.93) | <0.001 |
| General obesity (%) | 0.001 | |||
| No | 1826 (60.6) | 634 (56.7) | 1192 (62.9) | |
| Yes | 1186 (39.4) | 484 (43.3) | 702 (37.1) | |
| Physical activity (%) | <0.001 | |||
| Yes | 1168 (38.8) | 480 (42.9) | 688 (36.3) | |
| No | 1844 (61.2) | 638 (57.1) | 1206 (63.7) | |
| Cotinine (mean (SD)) | 61.67 (130.71) | 77.38 (148.56) | 52.40 (117.99) | <0.001 |
| Creatinine (mean (SD)) | 131.66 (86.37) | 139.31 (88.89) | 127.14 (84.55) | <0.001 |
| PCPPCs | Female (N = 1561) | Male (N = 1451) | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Phenols | ||||
| BZP | 0.98 (0.87, 1.10) | 0.734 | 1.04 (0.90, 1.20) | 0.631 |
| BPA | 1.39 (1.04, 1.84) | 0.024 | 1.47 (1.11, 1.94) | 0.007 |
| TCS | 1.18 (1.04, 1.35) | 0.012 | 1.02 (0.90, 1.17) | 0.728 |
| 2, 5-DCP | 1.02 (0.90, 1.16) | 0.724 | 1.09 (0.96, 1.25) | 0.185 |
| 2, 4-DCP | 1.12 (0.92, 1.36) | 0.246 | 1.04 (0.85, 1.28) | 0.679 |
| Parabens | ||||
| MeP | 1.17 (0.99, 1.38) | 0.073 | 1.02 (0.87, 1.19) | 0.834 |
| PrP | 1.03 (0.91, 1.17) | 0.650 | 0.98 (0.86, 1.11) | 0.748 |
| Phthalate metabolites | ||||
| MCNP | 1.56 (1.18, 2.06) | 0.002 | 1.40 (1.07, 1.84) | 0.015 |
| MCOP | 1.59 (1.30, 1.94) | <0.001 | 1.37 (1.13, 1.67) | 0.001 |
| MECPP | 1.54 (1.14, 2.08) | 0.005 | 1.38 (1.02, 1.87) | 0.034 |
| MnBP | 1.29 (0.96, 1.73) | 0.087 | 1.16 (0.86, 1.57) | 0.323 |
| MCPP | 1.62 (1.31, 2.01) | <0.001 | 1.44 (1.17, 1.77) | 0.001 |
| MEP | 1.01 (0.84, 1.22) | 0.903 | 1.12 (0.93, 1.35) | 0.218 |
| MEHHP | 1.59 (1.20, 2.13) | 0.002 | 1.34 (1.00, 1.78) | 0.048 |
| MiBP | 1.40 (1.02, 1.94) | 0.039 | 1.07 (0.79, 1.46) | 0.662 |
| MEOHP | 1.57 (1.17, 2.13) | 0.003 | 1.50 (1.11, 2.03) | 0.009 |
| MBzP | 1.56 (1.20, 2.04) | 0.001 | 1.17 (0.91, 1.51) | 0.207 |
| PCPPCs | General Obesity (N = 1186) | No General Obesity (N = 1826) | Abdominal Obesity (N = 1637) | No Abdominal Obesity (N = 1375) | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Phenols | ||||||||
| BZP | 1.00 (0.86, 1.15) | 0.989 | 0.99 (0.88, 1.11) | 0.833 | 0.98 (0.87, 1.10) | 0.722 | 0.99 (0.86, 1.13) | 0.851 |
| BPA | 1.33 (0.97, 1.80) | 0.072 | 1.45 (1.12, 1.89) | 0.005 | 1.44 (1.11, 1.86) | 0.006 | 1.37 (1.00, 1.87) | 0.047 |
| TCS | 1.05 (0.91, 1.22) | 0.493 | 1.15 (1.02, 1.30) | 0.022 | 1.09 (0.96, 1.23) | 0.206 | 1.12 (0.98, 1.29) | 0.090 |
| 2, 5-DCP | 1.08 (0.94, 1.24) | 0.273 | 1.03 (0.91, 1.16) | 0.682 | 1.06 (0.94, 1.19) | 0.341 | 1.04 (0.90, 1.20) | 0.612 |
| 2, 4-DCP | 1.06 (0.86, 1.31) | 0.584 | 1.09 (0.91, 1.32) | 0.353 | 1.08 (0.91, 1.30) | 0.378 | 1.07 (0.85, 1.34) | 0.555 |
| Parabens | ||||||||
| MeP | 1.01 (0.85, 1.20) | 0.883 | 1.06 (0.92, 1.22) | 0.402 | 1.11 (0.95, 1.28) | 0.180 | 0.98 (0.84, 1.14) | 0.751 |
| PrP | 0.92 (0.81, 1.06) | 0.259 | 1.02 (0.92, 1.13) | 0.741 | 1.00 (0.89, 1.12) | 0.993 | 0.96 (0.85, 1.08) | 0.483 |
| Phthalate metabolites | ||||||||
| MCNP | 1.65 (1.20, 2.26) | 0.002 | 1.32 (1.03, 1.69) | 0.027 | 1.56 (1.19, 2.04) | 0.001 | 1.38 (1.05, 1.83) | 0.023 |
| MCOP | 1.59 (1.26, 2.00) | <0.001 | 1.38 (1.16, 1.64) | <0.001 | 1.62 (1.34, 1.97) | <0.001 | 1.31 (1.07, 1.61) | 0.008 |
| MECPP | 1.48 (1.06, 2.08) | 0.020 | 1.38 (1.05, 1.81) | 0.023 | 1.50 (1.12, 2.01) | 0.006 | 1.41 (1.04, 1.93) | 0.029 |
| MnBP | 1.38 (1.00, 1.91) | 0.054 | 1.06 (0.81, 1.37) | 0.677 | 1.29 (0.98, 1.70) | 0.065 | 1.08 (0.80, 1.46) | 0.623 |
| MCPP | 1.76 (1.37, 2.27) | <0.001 | 1.39 (1.15, 1.67) | 0.001 | 1.83 (1.48, 2.27) | <0.001 | 1.26 (1.03, 1.56) | 0.026 |
| MEP | 1.05 (0.86, 1.29) | 0.610 | 1.05 (0.87, 1.24) | 0.670 | 1.07 (0.90, 1.28) | 0.429 | 1.05 (0.86, 1.29) | 0.618 |
| MEHHP | 1.41 (1.02, 1.94) | 0.036 | 1.46 (1.12, 1.89) | 0.005 | 1.46 (1.11, 1.93) | 0.008 | 1.48 (1.10, 1.99) | 0.010 |
| MiBP | 1.32 (0.93, 1.87) | 0.119 | 1.09 (0.83, 1.45) | 0.533 | 1.42 (1.05, 1.93) | 0.022 | 0.98 (0.71, 1.34) | 0.895 |
| MEOHP | 1.48 (1.06, 2.07) | 0.021 | 1.49 (1.13, 1.95) | 0.004 | 1.47 (1.10, 1.96) | 0.009 | 1.60 (1.17, 2.18) | 0.003 |
| MBzP | 1.44 (1.09, 1.92) | 0.011 | 1.22 (0.97, 1.54) | 0.089 | 1.41 (1.11, 1.80) | 0.005 | 1.22 (0.94, 1.60) | 0.137 |
| Variables | Model | OR (95%CI) | p-Value |
|---|---|---|---|
| Female | |||
| Model 1 | 1.44 (1.20, 1.72) | <0.001 | |
| Model 2 | 1.24 (1.02, 1.50) | 0.031 | |
| Model 3 | 1.55 (1.13, 2.11) | 0.006 | |
| Male | |||
| Model 1 | 1.27 (1.06, 1.53) | 0.011 | |
| Model 2 | 1.24 (1.03, 1.50) | 0.026 | |
| Model 3 | 1.38 (1.03, 1.83) | 0.029 | |
| General obesity | |||
| Model 1 | 1.36 (1.10, 1.68) | 0.005 | |
| Model 2 | 1.20 (0.96, 1.52) | 0.111 | |
| Model 3 | 1.40 (1.02, 1.92) | 0.037 | |
| No general obesity | |||
| Model 1 | 1.28 (1.09, 1.52) | 0.003 | |
| Model 2 | 1.18 (1.00, 1.40) | 0.047 | |
| Model 3 | 1.36 (1.06, 1.75) | 0.015 | |
| Abdominal obesity | |||
| Model 1 | 1.53 (1.28, 1.83) | <0.001 | |
| Model 2 | 1.40 (1.17, 1.69) | <0.001 | |
| Model 3 | 1.76 (1.33, 2.34) | <0.001 | |
| No abdominal obesity | |||
| Model 1 | 1.06 (0.88, 1.27) | 0.546 | |
| Model 2 | 1.00 (0.82, 1.22) | 0.983 | |
| Model 3 | 1.30 (0.95, 1.78) | 0.106 |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Bigambo, F.M.; Sun, J.; Zhu, C.; Zheng, S.; Xu, Y.; Wu, D.; Xia, Y.; Wang, X. Gender- and Obesity-Specific Association of Co-Exposure to Personal Care Product and Plasticizing Chemicals and Short Sleep Duration among Adults: Evidence from the National Health and Nutrition Examination Survey 2011–2016. Toxics 2024 , 12 , 503. https://doi.org/10.3390/toxics12070503
Bigambo FM, Sun J, Zhu C, Zheng S, Xu Y, Wu D, Xia Y, Wang X. Gender- and Obesity-Specific Association of Co-Exposure to Personal Care Product and Plasticizing Chemicals and Short Sleep Duration among Adults: Evidence from the National Health and Nutrition Examination Survey 2011–2016. Toxics . 2024; 12(7):503. https://doi.org/10.3390/toxics12070503
Bigambo, Francis Manyori, Jian Sun, Chun Zhu, Songshan Zheng, Yang Xu, Di Wu, Yankai Xia, and Xu Wang. 2024. "Gender- and Obesity-Specific Association of Co-Exposure to Personal Care Product and Plasticizing Chemicals and Short Sleep Duration among Adults: Evidence from the National Health and Nutrition Examination Survey 2011–2016" Toxics 12, no. 7: 503. https://doi.org/10.3390/toxics12070503
Article Metrics
Supplementary material.
ZIP-Document (ZIP, 962 KiB)
Further Information
Mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- Introduction
- Conclusions
- Article Information
T2D indicates type 2 diabetes.
a The combined total of patients is not necessarily a sum of the individuals from each of the groups because individuals could be prescribed both glucagon-like peptide 1 receptor agonists (GLP-1RAs) and insulins or metformin during the study period.
b The combined total of patients is not necessarily a sum of the individuals from each of the groups because individuals could be prescribed both insulins and metformin during the study period.
Patients were followed up for as along as 15 years after the index event for both groups. Hazard ratios (HRs) rates were calculated using a Cox proportional hazards model with censoring applied. Overall risk equals the number of patients with outcomes during the follow-up time window divided by number of patients in the group at the beginning of the time window. For each outcome, the groups were separately propensity-score matched for covariates related to the outcome, and the outcome was compared between the matched groups. Each eligible individual was followed up from the index event until the occurrence of the outcomes, death, loss to follow-up, or 15 years after the index event, whichever occurred first.
Kaplan-Meier survival analysis was used. Each eligible individual was followed up from the index event until the occurrence of the outcomes, death, loss to follow-up, or 15 years after the index event, whichever occurred first.
Patients were followed up for as long as 15 years after the index event for both groups. Hazard ratios (HRs) were calculated using a Cox proportional hazards model with censoring applied. Overall risk equals the number of patients with outcomes during the follow-up time window divided by the number of patients in the group at the beginning of the time window. For each outcome, the groups were separately propensity-score matched for covariates related to the outcome, and the outcome was compared between the matched groups. Each eligible individual was followed up from the index event until the occurrence of the outcomes, death, loss to follow-up, or 15 years after the index event, whichever occurred first.
eAppendix. Database
eTable 1. Clinical diagnosis, and other codes used in the platform that are used to determine the status of variables for study population definitions, exposures, outcomes, and those for propensity-score matching for groups
eTable 2. Characteristics of the GLP-1RA/no insulin group and insulin/no GLP-1RA group before and after matched for baseline covariates related to esophageal cancer for the study populations of patients with T2D and no history of any OAC
eTable 3. Characteristics of the GLP-1RA/no insulin group and insulin/no GLP-1RA group before and after matched for covariates related to breast cancer for the study populations of women (age 55 and older) with T2D and no history of any OAC
eTable 4. Characteristics of the GLP-1RA/no insulin group and insulin/no GLP-1RA group before and after matched for covariates related to endometrial cancer for the study populations of women with T2D and no history of any OAC
eTable 5. Characteristics of the GLP-1RA/no insulin group and insulin/no GLP-1RA group before and after matched for covariates related to gallbladder cancer for the study populations of patients with T2D and no history of any OAC
eTable 6. Characteristics of the GLP-1RA/no insulin group and insulin/no GLP-1RA group before and after matched for covariates related to stomach cancer for the study populations of patients with T2D and no history of any OAC
eTable 7. Characteristics of the GLP-1RA/no insulin group and insulin/no GLP-1RA group before and after matched for covariates related to kidney cancer for the study populations of patients with T2D and no history of any OAC
eTable 8. Characteristics of the GLP-1RA/no insulin group and insulin/no GLP-1RA group before and after matched for covariates related to liver cancer for the study populations of patients with T2D and no history of any OAC
eTable 9. Characteristics of the GLP-1RA/no insulin group and insulin/no GLP-1RA group before and after matched for covariates related to ovarian cancer for the study populations of women with T2D and no history of any OAC
eTable 10. Characteristics of the GLP-1RA/no insulin group and insulin/no GLP-1RA group before and after matched for covariates related to pancreatic cancer for the study populations of patients with T2D and no history of any OAC
eTable 11. Characteristics of the GLP-1RA/no insulin group and insulin/no GLP-1RA group before and after matched for covariates related to thyroid cancer for the study populations of patients with T2D and no history of any OAC
eTable 12. Characteristics of the GLP-1RA/no insulin group and insulin/no GLP-1RA group before and after matched for covariates related to meningioma for the study populations of patients with T2D and no history of any OAC
eTable 13. Characteristics of the GLP-1RA/no insulin group and insulin/no GLP-1RA group before and after matched for covariates related to multiple myeloma for the study populations of patients with T2D and no history of any OAC
eTable 14. Characteristics of the GLP-1RA/no metformin group and metformin/no GLP-1RA group before and after matched for covariates related to esophageal cancer for the study populations of patients with T2D and no history of any OAC
eTable 15. Characteristics of the GLP-1RA/no metformin group and metformin/no GLP-1RA group before and after matched for covariates related to breast cancer for the study populations of women (age 55 and older) with T2D and no history of any OAC
eTable 16. Characteristics of the GLP-1RA/no metformin group and metformin/no GLP-1RA group before and after matched for covariates related to colorectal cancer for the study populations of patients with T2D and no history of any OAC
eTable 17. Characteristics of the GLP-1RA/no metformin group and metformin/no GLP-1RA group before and after matched for covariates related to endometrial cancer for the study populations of women with T2D and no history of any OAC
eTable 18. Characteristics of the GLP-1RA/no metformin group and metformin/no GLP-1RA group before and after matched for covariates related to gallbladder cancer for the study populations of patients with T2D and no history of any OAC
eTable 19. Characteristics of the GLP-1RA/no metformin group and metformin/no GLP-1RA group before and after matched for covariates related to stomach cancer for the study populations of patients with T2D and no history of any OAC
eTable 20. Characteristics of the GLP-1RA/no metformin group and metformin/no GLP-1RA group before and after matched for covariates related to kidney cancer for the study populations of patients with T2D and no history of any OAC
eTable 21. Characteristics of the GLP-1RA/no metformin group and metformin/no GLP-1RA group before and after matched for covariates related to liver cancer for the study populations of patients with T2D and no history of any OAC
eTable 22. Characteristics of the GLP-1RA/no metformin group and metformin/no GLP-1RA group before and after matched for covariates related to ovarian cancer for the study populations of women with T2D and no history of any OAC
eTable 23. Characteristics of the GLP-1RA/no metformin group and metformin/no GLP-1RA group before and after matched for covariates related to pancreatic cancer for the study populations of patients with T2D and no history of any OAC
eTable 24. Characteristics of the GLP-1RA/no metformin group and metformin/no GLP-1RA group before and after matched for covariates related to thyroid cancer for the study populations of patients with T2D and no history of any OAC
eTable 25. Characteristics of the GLP-1RA/no metformin group and metformin/no GLP-1RA group before and after matched for covariates related to meningioma for the study populations of patients with T2D and no history of any OAC
eTable 26. Characteristics of the GLP-1RA/no metformin group and metformin/no GLP-1RA group before and after matched for covariates related to multiple myeloma for the study populations of patients with T2D and no history of any OAC
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Wang L , Xu R , Kaelber DC , Berger NA. Glucagon-Like Peptide 1 Receptor Agonists and 13 Obesity-Associated Cancers in Patients With Type 2 Diabetes. JAMA Netw Open. 2024;7(7):e2421305. doi:10.1001/jamanetworkopen.2024.21305
Manage citations:
© 2024
- Permissions
Glucagon-Like Peptide 1 Receptor Agonists and 13 Obesity-Associated Cancers in Patients With Type 2 Diabetes
- 1 Center for Science, Health, and Society, Case Western Reserve University School of Medicine, Cleveland, Ohio
- 2 Center for Artificial Intelligence in Drug Discovery, Case Western Reserve University School of Medicine, Cleveland, Ohio
- 3 Case Comprehensive Cancer Center, Case Western Reserve University School of Medicine, Cleveland, Ohio
- 4 Departments of Internal Medicine, Pediatrics, and Population and Quantitative Health Sciences and the Center for Clinical Informatics Research and Education, The MetroHealth System, Cleveland, Ohio
Question Is there clinical evidence supporting the potential benefits of glucagon-like peptide receptor agonists (GLP-1RAs) for the prevention of 13 obesity-associated cancers (OACs)?
Findings This cohort study of more than 1.6 million patients with type 2 diabetes (T2D) who had no prior diagnosis of 13 OACs found that patients with T2D treated with GLP-1RAs vs insulin had a significant risk reduction in 10 of 13 OACs, including esophageal, colorectal, endometrial, gallbladder, kidney, liver, ovarian, and pancreatic cancer as well as meningioma and multiple myeloma. No decrease in cancer risk was associated with GLP-1RAs compared with metformin.
Meaning This study provides clinical data suggesting that GLP-1RAs may reduce the risk of specific OACs compared with insulins.
Importance Thirteen human malignant neoplasms have been identified as obesity-associated cancers (OACs), ie, the presence of excess body fat is associated with increased risk of developing cancer and worse prognosis in patients with these specific tumors. The glucagon-like peptide receptor agonist (GLP-1RA) class of pharmaceuticals are effective agents for the treatment of type 2 diabetes (T2D) and for achieving weight loss, but the association of GLP-1RAs with the incident risk of 13 OACs is unclear.
Objective To compare the incident risk of each of the 13 OACs in patients with T2D who were prescribed GLP-1RAs vs insulins or metformin.
Design, Setting, and Participants This retrospective cohort study was based on a nationwide multicenter database of electronic health records (EHRs) of 113 million US patients. The study population included 1 651 452 patients with T2D who had no prior diagnosis of OACs and were prescribed GLP-1RAs, insulins, or metformin during March 2005 to November 2018. Data analysis was conducted on April 26, 2024.
Exposures Prescription of GLP-1RAs, insulins, or metformin.
Main Outcomes and Measures Incident (first-time) diagnosis of each of the 13 OACs occurring during a 15-year follow-up after the exposure was examined using Cox proportional hazard and Kaplan-Meier survival analyses with censoring applied. Hazard ratios (HRs), cumulative incidences, and 95% CIs were calculated. All models were adjusted for confounders at baseline by propensity-score matching baseline covariates.
Results In the study population of 1 651 452 patients with T2D (mean [SD] age, 59.8 [15.1] years; 827 873 [50.1%] male and 775 687 [47.0%] female participants; 5780 [0.4%] American Indian or Alaska Native, 65 893 [4.0%] Asian, 281 242 [17.0%] Black, 13 707 [0.8%] Native Hawaiian or Other Pacific Islander, and 1 000 780 [60.6%] White participants), GLP-1RAs compared with insulin were associated with a significant risk reduction in 10 of 13 OACs, including in gallbladder cancer (HR, 0.35; 95% CI, 0.15-0.83), meningioma (HR, 0.37; 95% CI, 0.18-0.74), pancreatic cancer (HR, 0.41; 95% CI, 0.33-0.50), hepatocellular carcinoma (HR, 0.47; 95% CI, 0.36-0.61), ovarian cancer (HR, 0.52; 95% CI, 0.03-0.74), colorectal cancer (HR, 0.54; 95% CI, 0.46-0.64), multiple myeloma (HR, 0.59; 95% CI, 0.44-0.77), esophageal cancer (HR, 0.60; 95% CI, 0.42-0.86), endometrial cancer (HR, 0.74; 95% CI, 0.60-0.91), and kidney cancer (HR, 0.76; 95% CI, 0.64-0.91). Although not statistically significant, the HR for stomach cancer was less than 1 among patients who took GLP-1RAs compared with those who took insulin (HR, 0.73; 95% CI, 0.51-1.03). GLP-1RAs were not associated with a reduced risk of postmenopausal breast cancer or thyroid cancer. Of those cancers that showed a decreased risk among patients taking GLP-1RAs compared with those taking insulin, HRs for patients taking GLP-1RAs vs those taking metformin for colorectal and gallbladder cancer were less than 1, but the risk reduction was not statistically significant. Compared with metformin, GLP-1RAs were not associated with a decreased risk of any cancers, but were associated with an increased risk of kidney cancer (HR, 1.54; 95% CI, 1.27-1.87).
Conclusions and Relevance In this study, GLP-1RAs were associated with lower risks of specific types of OACs compared with insulins or metformin in patients with T2D. These findings provide preliminary evidence of the potential benefit of GLP-1RAs for cancer prevention in high-risk populations and support further preclinical and clinical studies for the prevention of certain OACs.
Thirteen human malignant neoplasms have been identified as obesity-associated cancers (OAC), ie, the presence of excess body fat is associated with increased risk of developing cancer and worse prognosis in patients with these specific tumors. 1 Obesity also contributes to insulin resistance and type 2 diabetes (T2D), which may further increase the risk and worsen the prognosis of the OACs. 2 , 3
The glucagon-like peptide 1 receptor agonist (GLP-1RA) class of pharmaceuticals are highly effective agents for the treatment of T2D and for achieving weight loss. 4 - 9 GLP-1RAs have further been shown to reduce the risk of adverse cardiovascular outcomes in patients with obesity 10 and to contribute to the resolution of nonalcoholic steatohepatitis. 11 Because of their efficacy in controlling T2D, obesity, and related comorbidities, we hypothesized that these agents might reduce the risk of the OACs. We recently reported that GLP-1RAs were associated with lower risks for colorectal cancer, 12 an OAC. Otherwise, clinical evidence of the potential clinical benefits of GLP-1RA in preventing OAC has not been systematically assessed. Here we conducted a nationwide multicenter retrospective cohort study in patients with T2D who were prescribed GLP-1RAs vs insulins or metformin to determine whether GLP-1RAs were associated with changes in the risk of each of 13 OACs, including esophageal, breast, colorectal, endometrial, gallbladder, stomach, kidney, ovarian, pancreatic, and thyroid cancer as well as hepatocellular carcinoma, meningioma, and multiple myeloma. 1
We used the TriNetX platform to access deidentified electronic health records (EHRs) of 113 million patients from 64 health care organizations across 50 states, covering diverse age, racial and ethnic, income, and insurance groups and clinical settings. 13 , 14 The platform’s built-in analytic functions allow patient-level analyses, while only reporting population-level data. The platform has been used for retrospective cohort studies. 15 - 26 Similar to this study, we have examined the association of GLP-1RAs with colorectal cancer incidence in patients with T2D 12 and the associations of GLP-1RA (semaglutide) with suicidal ideations 27 and with cannabis use in patients with obesity and those with T2D. 28 The MetroHealth System institutional review board determined that the research as described in this study was not human participant research and institutional review board approval and informed consent were not required. This cohort study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
Available data elements of EHRs include extensive information on demographics, diagnoses ( International Statistical Classification of Diseases and Related Health Problems, Tenth Revision ), medications (Anatomical Therapeutic Chemical and medical prescription normalized medical prescription or RxNorm), procedures ( Current Procedural Terminology ), laboratory tests (Logical Observation Identifiers Names and Codes), genomics, visits, and socioeconomic and lifestyle information. The data on the analytic platform have been expanded to include oncology-specific data from cancer registry data from North American Association of Central Cancer Registries (NAACCR) records and other data resources. 14
Self-reported sex, race, and ethnicity data from contributing health care systems are mapped by according to Office of Management and Budget standards into (1) race, American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or Other Pacific Islander, White, and unknown race; and (2) ethnicity, Hispanic or Latinx, not Hispanic or Latinx, or unknown ethnicity. All covariates are either binary, categorical, or continuous but essentially guaranteed to exist. Age is guaranteed to exist. Missing sex values are represented using “unknown sex.” The missing data for race and ethnicity are presented as “unknown race” or “unknown ethnicity.” For other variables, including medical conditions, procedures, laboratory tests, and socioeconomic determinants of health, the value is either present or absent so missing is not pertinent.
The study population comprised 1 651 452 patients with a diagnosis of T2D who had medical encounters with health care organizations and were prescribed GLP-1RAs vs insulin or metformin between March 2005 and November 2018 and had no history of any of the 13 OACs. The study population was divided into exposure and comparison groups. For comparing GLP-1RAs with insulins, the study population was divided into a GLP-1RA/no insulin group (48 983 patients prescribed a GLP-1RA but not insulins) and a insulin/no GLP-1RA group (1 044 745 patients prescribed insulins but not GLP-1RAs). For comparing GLP-1RAs with metformin, the study population was divided into a GLP-1RA/no metformin group (32 365 patients prescribed a GLP-1RA but not metformin) and a metformin/no GLP-1RA group (856 160 patients prescribed metformin but not GLP-1RAs) ( Figure 1 ).
The 13 OACs are esophageal, breast, colorectal, endometrial, gallbladder, stomach, kidney, ovarian, pancreatic, and thyroid cancer as well as hepatocellular carcinoma, meningioma, and multiple myeloma. 1 Each of the 13 OACs was examined as a separate outcome in groups that were propensity-score matched for covariates related to the specific OAC. For each OAC outcome, the exposure and comparison groups (ie, GLP-1RA/no insulin vs insulin/no GLP-1RA groups and GLP-1RA/no metformin vs metformin/no GLP-1RA groups) were propensity-score matched (1:1 using nearest neighbor greedy matching) for baseline covariates related to the specific OAC, including demographic characteristics (age, sex, race, and ethnicity); adverse socioeconomic determinants of health; family and personal history of cancer; genetic susceptibility to cancer; preexisting medical conditions, including obesity and overweight; and medical procedures, including cancer screening, bariatric surgery, and prior prescription of antidiabetes medications. Each eligible individual was followed up from the index event (the first prescription of GLP-1RAs, insulins, or metformin during March 2005 to November 2018) until the occurrence of the outcomes, death, loss to follow-up, or 15 years after the index event, whichever occurred first. Cox proportional hazard analyses were used to compare rates of time to events on a daily basis during the follow-up time after the index event. Hazard ratios (HRs) and 95% CIs were calculated. Cumulative incidences were estimated using the Kaplan-Meier survival analysis. All models are adjusted for confounders at baseline by propensity-score matching baseline covariates.
The data were collected and analyzed on April 26, 2024, within the analytics platform. All statistical analyses in this study, including propensity-score matching, Kaplan-Meier survival analysis, and Cox proportional hazard analysis were done using built-in functions within the platform that are implemented using Survival version 3.2-3 in R version 4.0.2 (R Project for Statistical Computing) and libraries and utilities for data science and statistics in Python version 3.7 (Python Software Foundation) and Java version 11.0.16 (Oracle). Details of clinical codes for eligibility criteria, treatment strategies, outcomes, and baseline covariates are in eTable 1 in Supplement 1 .
The study population included 1 651 452 patients with T2D (mean [SD] age, 59.8 [15.1] years; 827 873 [50.1%] male and 775 687 [47.0%] female participants; 5780 [0.4%] American Indian or Alaska Native, 65 893 [4.0%] Asian, 281 242 [17.0%] Black, 13 707 [0.8%] Native Hawaiian or Other Pacific Islander, and 1 000 780 [60.6%] White participants). For comparing GLP-1RAs with insulins in patients with T2D, the study population included 1 093 728 patients with T2D who had no prior diagnosis of any OAC and were prescribed GLP-1RAs or insulins but not both between March 2005 and November 2018. The GLP-1RA/no insulin group (n = 48 983) compared with the insulin/no GLP-1RA group (n = 1 044 475) was younger; included more women and White participants; had a higher prevalence of family history of cancer, obesity or overweight, medical encounters for cancer screening, and prior prescriptions of other antidiabetic agents, including insulins, metformin, dipeptidyl peptidase 4 (DPP-4) inhibitors, sodium-glucose cotransporter 2 (SGLT2) inhibitors, sulfonylureas, thiazolidinediones, and α-glucosidase inhibitors. For each OAC outcome, the GLP-1RA/no insulin and the insulin/no GLP-1RA groups were separately matched for covariates associated with the OAC. The Table shows the characteristics of the GLP-1RA/no insulin and insulin/no GLP-1RA groups before and after propensity-score matching for covariates related to colorectal cancer. The characteristics of the exposure and comparison groups before and after matching for each of the other 12 OACs are in eTables 2 to 13 in Supplement 1 .
Compared with insulins, GLP-1RAs were associated with a significantly lower risk of 10 of the 13 OACs, including gallbladder cancer (HR, 0.35; 95% CI, 0.15-0.83), meningioma (HR, 0.37; 95% CI, 0.18-0.74), pancreatic cancer (HR, 0.41; 95% CI, 0.33-0.50), hepatocellular carcinoma (HR, 0.47; 95% CI, 0.36-0.61), ovarian cancer (HR, 0.52; 95% CI, 0.03-0.74), colorectal cancer (HR, 0.54; 95% CI, 0.46-0.64), multiple myeloma (HR, 0.59; 95% CI, 0.44-0.77), esophageal cancer (HR, 0.60; 95% CI, 0.42-0.86), endometrial cancer (HR, 0.74; 95% CI, 0.60-0.91), and kidney cancer (HR, 0.76; 95% CI, 0.64-0.91). The HR for stomach cancer among patients taking GLP-1RAs vs those taking insulin was less than 1, but it was not statistically significant (HR, 0.73; 95% CI, 0.51-1.03). GLP-1RAs were not associated with risk of postmenopausal breast cancer or thyroid cancer ( Figure 2 ). Figure 3 shows the cumulative incidences of colorectal cancer and liver cancer comparing GLP-1RAs with insulins. The mean (SD) follow-up time for the outcome of colorectal cancer was 2074.7 (435.3) days for the GLP-1RA/no insulin group and 1981.8 (471.1) days for the insulin/no GLP-1RA group. The mean (SD) follow-up time for the outcome of liver cancer was 2023.1 (1112.6) days for the GLP-1RA/no insulin group and 2037.9 (766.4) days for the insulin/no GLP-1RA group.
For comparing GLP-1RAs with metformin in patients with T2D, the study population included 888 525 patients with T2D who had no prior diagnosis of any OAC and were prescribed GLP-1RAs or metformin but not both between March 2005 and November 2018. For each OAC outcome, the GLP-1RA/no metformin group (n = 32 365) and the metformin/no GLP-1RA group (n = 856 160) were separately matched for covariates related to the OAC (eTables 14-26 in Supplement 1 ). Compared with metformin, GLP-1RAs were not associated with a lower risk of colorectal cancer, gallbladder cancer, and meningioma but were associated with an increased risk of kidney cancer ( Figure 4 ). Figure 3 shows the cumulative incidences of colorectal cancer and liver cancer by comparing GLP-1RAs with metformin. The mean (SD) follow-up time for the outcome of colorectal cancer was 1967.2 (592.2) days for the GLP-1RA/no metformin group and 2101.6 (576.0) days for metformin/no GLP-1RA group. The mean (SD) follow-up time for the outcome of liver cancer was 1970.9 (426.0) days for the GLP-1RA/no metformin group and 2129.8 (514.7) days for metformin/no GLP-1RA group.
Using a data platform 29 to analyze more than 15 years of longitudinal EHRs of a US population-based cohort of more than 100 million individuals, we found that in patients with T2D who had no history of any OAC, GLP-1RAs compared with insulins were associated with a significant risk reduction in 10 of 13 OACs, including esophageal, colorectal, kidney, pancreatic, gallbladder, ovarian, endometrial, and liver cancers as well as meningioma and multiple myeloma. Decreased risk reduction that did not reach statistical significance was also noted for stomach cancer. Of those cancers that showed decreased risk of GLP-1RAs compared with insulin, risk reduction was also noted for GLP-1RAs relative to metformin for colorectal cancer, gallbladder, and meningiomas, although these findings were not statistically significant.
Our observations on the reduction in the incidence of OACs in patients with T2D treated with GLP-1RAs compare favorably with the OAC-reducing effects of intensive lifestyle intervention (ILI) observed in the Look AHEAD trial (Action for Health in Diabetes) 30 and with the results of metabolic-bariatric surgery as recently reported in the SPLENDID (Surgical Procedure and Long-term Effectiveness In Neoplastic Disease Incidence and Death) trial. 31 The Look AHEAD study, a randomized clinical trial in which 4859 patients with T2D and overweight or obesity (age, 45-76 years; median follow-up, 11 years) were randomized to an ILI or diabetes support and education group, found a 16% reduction in risk for OAC (HR, 0.84; 95% CI, 0.68-1.04). 30 The SPLENDID trial, a matched cohort study, compared 5053 patients with obesity with 25 265 nonsurgical matched controls, with a median age of 46 years and median follow-up of 6.1 years, showed an OAC risk reduction of 32%, (HR, 0.68; 95% CI, 0.53-0.87). 31
A recent 9-year follow-up population-based historical cohort study 32 conducted in Israel reported a decrease (although not statistically significant) in incidence of pancreatic cancer (HR, 0.50; 95% CI, 0.15-1.71) in patients with T2D treated with GLP-1RAs compared with insulin. 32 Our US population-based study, with 15 years of follow-up and a larger sample size, now extends these observations, suggesting that treatment of patients with T2D with GLP-1RAs vs insulin is associated with a significantly decreased incidence of pancreatic cancer (HR, 0.41; 95% CI, 0.33-0.50).
In contrast to the risk reduction shown for most of the OACs, thyroid cancer showed no statistically different risk in patients treated with GLP-1RAs compared with insulins. Studies in rodents indicate that GLP-1RAs promote thyroid C-cell hyperplasia and medullary thyroid carcinoma (MTC) by a GLP-1R mediated increase in calcitonin synthesis. 33 High levels of fasting serum insulin and insulin resistance are associated with an increased risk of thyroid cancer. 34 Although clinical evidence for an association of thyroid cancer with the use of GLP-1RAs has been reported as inconclusive, 35 the findings from our study together with previous reports of insulins promoting cancer growth suggest that GLP-1RAs might be associated with increased risk of thyroid cancer. Our results are further supported by a recent report 36 by the French National Health Cancer Data System showing that the use of GLP-1RAs for 1 to 3 years was associated with increased risk of all thyroid cancers (adjusted HR, 1.78; 95% CI 1.04-3.05). 36 These studies support the package warnings included with GLP-1RAs that these agents are contraindicated in patients with multiple endocrine neoplasia syndrome type 2 and that patients should be counseled regarding the potential risk of MTC and symptoms of thyroid tumors.
Kidney cancers showed an increased risk with GLP-1RA treatment relative to that with metformin (HR, 1.54; 95% CI 1.27-1.87) but a decrease relative to insulin (HR, 0.76; 95% CI 0.64-0.91). GLP-1RAs have direct effects on kidney function mediated by GLP-1Rs in renal vasculature; however, these are not associated with increased mitogenesis, 37 and to our knowledge, there have been no previous reports of kidney cancers with the use of GLP1-RAs. These divergent risks require further clinical and mechanistic studies for full evaluation. Nonetheless, they suggest the need for continued monitoring in patients being treated with GLP-1RAs.
Our study, with follow-up over 15 years, found no signs of increase or decrease in risk for breast cancer in postmenopausal women with T2D being treated with GLP-1RAs compared with those being treated with insulin or metformin. GLP-1RAs have been shown to reduce the growth of murine and human breast cancer cell lines in vitro and in vivo murine models. 38 However, a meta-analysis of more than 50 randomized clinical trials, evaluating GLP-1RAs in women aged between 45 to 70 years and followed up from 24 weeks to 7.5 years, showed no differences in benign, premalignant, or malignant breast neoplasms in patients treated with GLP-1RAs compared with other antidiabetic agents or placebos. 39 A more recent population-based cohort study of 44 984 women 40 years and older treated with GLP-1RAs or other antidiabetic agents for a mean of 3.5 years showed no overall significant difference in the risk for breast cancer occurrence. However, an increased risk (HR, 2.66; 95% CI, 1.32-5.38) was noted for those treated between 2 to 3 years with a return to null after more than 3 years’ treatment. 40 Interestingly, the SPLENDID trial of bariatric surgery for weight reduction, which found an overall 32% risk reduction for OACs, showed no significant difference among women for incidence of overall or postmenopausal breast cancer. 31 This lack of effect on breast cancer risk needs to be further investigated to determine the impact of longer duration of therapy as well as to more fully understand the relation between GLP-1RAs and estrogen metabolism. The lack of breast cancer risk reduction by GLP-1RAs and the similar lack of protection by bariatric surgery may also suggest the possibility that factors determining the incidence of breast cancer in patients with overweight or obesity may have been initiated long before intervention with GLP-1RAs and/or bariatric surgery and therefore require earlier intervention to affect risk reduction. The concept that early intervention might reduce breast cancer incidence is supported by the observation that both pregnancy and breastfeeding reduce the incidence of breast cancer. 41 , 42
Our study has several limitations. First, this is a retrospective observational study of patient EHRs, which has inherent limitations including overdiagnosis, underdiagnosis, and misdiagnosis; unmeasured or uncontrolled confounders; and biases. Although we controlled for an extensive list of variables, these limitations and biases could not be fully eliminated; therefore, no causal inferences can be drawn. Second, patients in our study represented those who had medical encounters with health care systems contributing to the data platform. Although both the exposure and comparison groups were drawn from the same EHR database and from the same time period, which should not significantly affect the HR calculations, results from the platform need to be validated in other EHR databases and analytics platforms. Third, the status of incident cancer was based on the presence of first-ever diagnosis codes of OACs documented in patient EHRs, which also included oncology-specific data from cancer registry data, such as NAACCR records. However, it is unknown how well cancer diagnoses are captured in patient EHRs. For this study, the main interest was the relative risk (or HR) of cancer diagnosis. Since all patients in the study population were drawn from the same health care organizations in the data platform, cancer underdiagnosis, misdiagnosis, or overdiagnosis should not have a substantial impact on the relative risk analysis. Fourth, the built-in functions did not allow us to control for variables (eg, weight loss) that occurred after the index event and to identify individual patient data, which precludes our ability to correlate risk reduction with a degree of weight loss, which was demonstrated to be particularly important in the SPLENDID bariatric study. 25 In addition, we could not explicitly control for health care utilization and insurance type although the study population included patients who had medical encounters with health care organizations and were withdrawn from the same 64 health care organizations in the network. Finally, due to the lack of patients’ medication adherence information in EHRs, we used intention-to-treat (medication prescriptions) as a causal contrast of interest regardless of whether the individuals adhered to their medications and the duration of the medication use.
In this study of patients with T2D who were cancer free at baseline, taking GLP-1RAs compared with insulin was associated with a lower risk of 10 of 13 OACs. The potential cancer-preventative effects of OACs by GLP-1RAs warrant further long-term studies as well as studies of individual newer and possibly more effective antidiabetic and weight loss agents as well as those with multihormone agonist activities. Studies are also warranted to evaluate the preventive effects of these agents on non-OACs. In addition, the associations of the GLP-1RA targeted pharmacologic agents with cancer risk should be compared with the use of ILI and metabolic-bariatric surgery for the control of obesity and diabetes. As noted previously, it will be important to correlate these associations with the control of T2D and obesity. Moreover, given that T2D and overweight or obesity have negative impacts on patients during cancer therapy, GLP-1RAs should be evaluated for control of these comorbid conditions during cancer therapy as well as for secondary prevention to delay cancer recurrence.
Accepted for Publication: May 9, 2024.
Published: July 5, 2024. doi:10.1001/jamanetworkopen.2024.21305
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2024 Wang L et al. JAMA Network Open .
Corresponding Authors: Nathan A. Berger, MD, Center for Science, Health, and Society, Case Comprehensive Cancer Center ( [email protected] ), and Rong Xu, PhD, Center for Artificial Intelligence in Drug Discovery, Case Western Reserve University School of Medicine, 10900 Euclid Ave, Cleveland, OH 44106 ( [email protected] ).
Author Contributions: Dr Xu and Ms Wang had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Xu, Berger.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Xu, Berger.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Wang, Xu.
Obtained funding: Xu, Berger.
Administrative, technical, or material support: Xu, Kaelber, Berger.
Supervision: Xu, Kaelber, Berger.
Conflict of Interest Disclosures: Drs Kaelber and Berger reported receiving grants from the National Institutes of Health (NIH) during the conduct of the study. No other disclosures were reported.
Funding/Support: We acknowledge support from National Cancer Institute Case Comprehensive Cancer Center (grant Nos. CA221718 and CA043703), American Cancer Society (grant No. RSG-16-049-01–MPC), The Landon Foundation–American Association for Cancer Research (award No. 15-20-27-XU), NIH Director’s New Innovator Award Program (award No. DP2HD084068), National Institute on Aging (grant Nos. AG057557, AG061388, AG062272, and AG07664), and the National Institute on Alcohol Abuse and Alcoholism (grant No. AA029831).
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Singapore Med J
- v.64(3); 2023 Mar
- PMC10071857

The impact of obesity: a narrative review
Benjamin chih chiang lam.
1 Family and Community Medicine, Khoo Teck Puat Hospital, Singapore
2 Integrated Care for Obesity and Diabetes, Khoo Teck Puat Hospital, Singapore
Amanda Yuan Ling Lim
3 Singapore Association for the Study of Obesity, Singapore
4 Division of Endocrinology, Department of Medicine, National University Hospital, Singapore
Soo Ling Chan
5 Division of Endocrinology, Department of Medicine, Ng Teng Fong General Hospital, Singapore
Mabel Po Shan Yum
6 Psychology Service, Khoo Teck Puat Hospital, Singapore
Natalie Si Ya Koh
7 Department of Cardiology, National Heart Centre, Singapore
Eric Andrew Finkelstein
8 Health Services and Systems Research, Duke-NUS Medical School, Singapore
Obesity is a disease with a major negative impact on human health. However, people with obesity may not perceive their weight to be a significant problem and less than half of patients with obesity are advised by their physicians to lose weight. The purpose of this review is to highlight the importance of managing overweight and obesity by discussing the adverse consequences and impact of obesity. In summary, obesity is strongly related to >50 medical conditions, with many of them having evidence from Mendelian randomisation studies to support causality. The clinical, social and economic burdens of obesity are considerable, with these burdens potentially impacting future generations as well. This review highlights the adverse health and economic consequences of obesity and the importance of an urgent and concerted effort towards the prevention and management of obesity to reduce the burden of obesity.
INTRODUCTION
The prevalence of obesity has increased significantly over the last two decades worldwide, including in Singapore, a multiethnic Southeast Asian country.[ 1 , 2 ] Recent national health surveys of adult Singaporeans suggest a continuation of this rising trend after a brief period of stabilisation.[ 3 ] Obesity, which is characterised by excessive adiposity, is not benign.
Obesity predisposes affected individuals to a large array of diseases that are often interconnected, leading to an increased risk of simple (two comorbid diseases) and complex (four or more comorbid diseases) multimorbidity in these individuals, when compared to people with healthy weight.[ 4 ] For example, in a large Finnish cohort of 114,657 people aged 16–78 years, with a mean follow-up of 12.1 years, people with obesity were five times more likely to develop simple multimorbidity and 12 times more likely to develop complex multimorbidity, with stronger associations found in people with more severe obesity.[ 4 ] This dose–response relationship between obesity and multimorbidity is also observed in other populations, including Asian populations.[ 5 , 6 ] In Singapore, the proportion of disability-adjusted life years, a composite measure of all health loss within a population, contributed by overweight and obesity, increased from 3.9% in 1990 to 6.4% in 2017, making it the fifth leading risk factor affecting health in Singapore.[ 7 ] Hence, obesity is a disease with a major negative impact on human health and has become a major global and regional health problem.
However, according to international surveys and interviews, people with obesity may not perceive their weight to be a significant problem,[ 8 ] with evidence also suggesting that less than half of patients with obesity are advised by their physicians to lose weight.[ 9 , 10 ] Hence, the purpose of this narrative review, as part of a series on obesity, is to highlight the importance of managing overweight and obesity by presenting and summarising the latest evidence on the adverse consequences and impact of obesity [ Figure 1 ]. The causal role of excess adiposity on obesity-related conditions (as established by the many epidemiological evidence already described in literature) will be explored. In addition, data from Singapore, if any, will be included in the review for each section, with the review on the economic burden of overweight and obesity focusing on Singapore.

Diagram shows a summary of the diseases and conditions associated with obesity and the potential impacts. *Supported by mendelian randomisation studies. T1DM: type 1 diabetes mellitus, T2DM: type 2 diabetes mellitus
EVIDENCE FOR CAUSAL ROLE OF EXCESS ADIPOSITY ON OBESITY-RELATED DISEASES
The hypertrophy of adipose tissue is associated with proinflammatory adipokine production and macrophage infiltration. In addition, the failure of adipose tissue to continually expand leads to lipotoxicity and ectopic fat deposition in lean tissues such as the heart, liver, pancreas and kidneys.[ 11 , 12 ] These phenomena contribute to a proinflammatory and insulin-resistant milieu and, together with increased mechanical stress due to increased adipose tissue mass,[ 11 , 13 ] are the main pathophysiological mechanisms responsible for the development of multiple medical conditions. Hence, there are reasonable pathways to link outcome to exposure (i.e. plausibility), one of the principles useful for establishing a causal relationship.[ 14 ]
This causal role of obesity is further supported by evidence from Mendelian randomisation (MR) studies. MR is an analytical technique involving genetic variants that are associated with exposures (risk factors such as obesity) as instrumental variables to investigate the effects of these exposures on an outcome of interest (e.g. a disease).[ 15 ] Since these genetic variants are fixed, randomly allocated at conception and temporally precede the outcome, MR is less likely to be subject to bias, confounding and reverse causation, which are frequent in conventional observational studies.[ 15 ] ’BMI’, ’obesity’, ’Mendelian randomisation’, ’Mendelian randomization’ and the outcome of interest (e.g. ’diabetes’) were used as search terms, and all studies relevant to this review were considered. These obesity-related diseases, with evidence for the causal role of obesity (plausible biological mechanisms and MR studies), and the various impacts of obesity will be discussed next.
Diabetes mellitus, dyslipidaemia and hypertension
As highlighted, obesity leads to insulin resistance. Additionally, elevated free fatty acid from the adipose tissues and ectopic fat deposition cause pancreatic β-cell dysfunction.[ 16 , 17 ] Hence, the various pathological mechanisms synergistically exacerbate the onset of type 2 diabetes mellitus (T2DM). In particular, visceral fat deposition plays an important role in the development of T2DM.[ 18 ] Hepatic fat worsens hepatic insulin resistance, while pancreatic fat affects insulin secretion and glucose tolerance.[ 18 ] In a meta-analysis of MR studies, genetically predicted higher body mass index (BMI) was consistently associated with T2DM, with a combined odds ratio (OR) of 2.03 (95% confidence interval [CI] 1.88–2.19) per 1 standard deviation increase in BMI.[ 19 ] In Singapore, multiple observational studies confirm the increased risk of T2DM with increasing BMI in all major ethnic groups,[ 20 , 21 , 22 ] although there might be ethnic-specific sensitivity to the effects of increasing adiposity.[ 23 ]
There is also increasing evidence for the role of obesity in the increased incidence of type 1 diabetes mellitus (T1DM), with studies from North America and the UK suggesting an increasing prevalence of overweight and obesity in people with T1DM.[ 24 ] It has been hypothesised that obesity-induced insulin resistance may be responsible for the accelerated loss of pancreatic β cells through excessive stimulation[ 25 ] and a chronic proinflammatory state.[ 26 ] This causal role is supported by MR studies, although the evidence is not as consistent (compared to obesity and T2DM), with high heterogeneity between the studies.[ 19 ]
Obesity is associated with dyslipidaemia, which is characterised by increased triglycerides (TGs) and free fatty acids, decreased high-density lipoprotein-cholesterol (HDL-C) with HDL dysfunction and increased low-density lipoprotein cholesterol (LDL-C), in particular, small dense LDL-C, which is particularly atherogenic.[ 27 ] The underlying mechanisms involve hepatic fat accumulation, insulin resistance and chronic inflammation.[ 27 , 28 ] In a recent MR study based on participants from the UK Biobank, genetically predicted higher BMI was significantly associated with dyslipidaemia (low HDL-C levels).[ 29 ] In Singapore, in a multiethnic sample of 4,723 adult participants, elevated TG was more common in people with obesity, with the prevalence of elevated TG increasing with higher BMI and waist-to-hip ratio (WHR),[ 20 ] consistent with the evidence.
Hypertension is more than twice as prevalent in people with obesity compared to people with normal weight.[ 30 ] The mechanisms for obesity-induced hypertension are varied (involving adipokines, cytokines, free fatty acids, insulin, the rennin–angiotensin–aldosterone system) and interconnected, with the final common pathways being endothelial dysfunction, extracellular fluid overload and sympathetic nervous system activation.[ 30 , 31 ] Hence, obesity is an established risk factor for hypertension, and its causal role is supported by MR studies,[ 19 , 32 ] particularly that of higher adiposity with a more unfavourable metabolic profile (higher visceral and ectopic fat).[ 32 ] In Singapore, the increased prevalence of hypertension with higher BMI and WHR is consistent, especially in males.[ 20 ]
Nonalcoholic fatty liver disease
Nonalcoholic fatty liver disease (NAFLD) is a condition in which fat accumulates in the liver in the absence of excessive alcohol consumption. Genetic variants that increase hepatic fat content have been shown to be associated with increased liver enzymes, hepatocellular damage and fibrosis, suggesting that hepatic fat accumulation mediates the development of liver fibrosis, independent of inflammation.[ 33 ] Hence, NAFLD may lead to nonalcoholic steatohepatitis (NASH), and ultimately, cirrhosis or hepatocellular carcinoma.
The prevalence of NAFLD has risen in tandem with the global epidemic of obesity, with NAFLD now being the most common cause of chronic liver disease worldwide.[ 34 ] A meta-analysis of MR studies confirms the causal effect of obesity on NAFLD,[ 19 ] with central adiposity (waist circumference) having the strongest relationship (OR 2.93, 95% CI 1.85–4.63) among the various obesity measures.[ 35 ] In Singapore, studies consistently show that participants with evidence of NAFLD have significantly higher BMI and waist circumference.[ 36 , 37 ]
Cardiovascular diseases
The association between obesity and increased incidence of cardiovascular diseases such as heart failure, coronary heart disease and stroke has long been established.[ 38 ] For example, based on pooled data from 97 prospective cohort studies involving 1.8 million participants, the hazard ratio (HR) for each 5 kg/m 2 higher BMI was 1.27 (95% CI 1.23–1.31) for coronary heart disease and 1.18 (95% CI 1.14–1.22) for stroke after adjustment for potential confounders.[ 39 ] Additional adjustment for diabetes mellitus, hypertension and dyslipidaemia reduced the HRs to 1.15 (95% CI 1.12–1.18) and 1.04 (95% CI 1.01–1.08) for coronary heart disease and stroke, respectively, suggesting that 46% (95% CI 42%–50%) of the excess risk of BMI for coronary heart disease and 76% (95% CI 65%–91%) for stroke were mediated by these conditions,[ 39 ] which are common in people with obesity.[ 4 , 30 ]
Obesity itself leads to an increased risk of these cardiovascular events, likely via mechanisms such as the secretion of adipokines, proinflammatory cytokines and hypofibrinolytic factors, that together could lead to increased oxidative stress and endothelial dysfunction resulting in atherosclerosis.[ 40 ] Additionally, excessive adiposity results in haemodynamic alterations via various neurohormonal and metabolic abnormalities, causing left ventricular (LV) hypertrophy and subsequent dysfunction, leading to LV failure. LV failure, facilitated by pulmonary arterial hypertension from hypoxia due to obstructive sleep apnoea (OSA) and/or obesity hypoventilation syndrome (OHS), may subsequently lead to right ventricular failure.[ 41 ] This causal role of obesity is supported by multiple MR studies,[ 19 , 29 , 32 ] with the strongest association between BMI and heart failure, followed by BMI and coronary artery disease, then BMI and stroke.[ 19 , 32 ]
Another obesity-related cardiovascular disease is atrial fibrillation (AF), with evidence suggesting that obesity is an independent risk factor for AF, even after accounting for OSA.[ 41 ] Also, studies have demonstrated a strong graded association between higher BMI and the risk of persistent AF and higher BMI, with increased risk of postablation AF.[ 41 ] The mechanisms linking obesity and AF are complex and incompletely understood, with increased left atrial and ventricular abnormalities, altered haemodynamics, increased epicardial and pericardial fat, inflammation, and metabolic and neurohormonal abnormalities being the potential causal mechanisms.[ 41 ] This causal relationship is similarly supported by MR studies which consistently show that genetically predicted BMI is associated with AF.[ 19 , 32 , 42 ]
In Singapore, a longitudinal study involving 2,605 Chinese participants found that the adjusted HR for cardiovascular and stroke mortality was highest in the group with obesity (BMI ≥30 kg/m 2 ) among those aged ≥65 years,[ 43 ] which is consistent with the association between obesity and increased incidence of cardiovascular diseases.
Obstructive sleep apnoea and hypoventilation syndrome
The increased intra-abdominal and intrathoracic pressure as a result of excessive adiposity impedes inflation of the lung, which can significantly affect the lung function, thereby leading to hypoventilation and ventilation–perfusion imbalance.[ 44 ] A constellation of obesity, daytime hypoventilation characterised by hypercapnia and hypoxaemia, and sleep-disordered breathing, without an alternative cause for hypoventilation, is known as OHS, with an estimated prevalence of 8%–20% in patients with obesity who were referred to sleep centres for evaluation of sleep-disordered breathing.[ 45 ]
The most common sleep-disordered breathing in such patients and people with obesity is OSA, as fat accumulation around the upper airways predisposes to the collapse of these airways.[ 44 ] About 50% of people with OSA have obesity, and approximately 40%–90% of people who are overweight suffer from OSA.[ 44 , 45 ] Consistent with epidemiological observations and genetic correlation (between OSA and BMI), an MR study shows that genetically predicted BMI is strongly associated with OSA, supporting the causal effect of BMI on OSA.[ 46 ] In Singapore, a study based on 587 Chinese participants reported that people with OSA had significantly higher BMI, and also BMI remained an important predictor of OSA after adjusting for hypertension and smoking,[ 47 ] in line with the overall evidence.
Polycystic ovary syndrome
Obesity is strongly associated with polycystic ovary syndrome (PCOS),[ 48 ] which is characterised by reproductive dysfunction (oligo-amenorrhoea, infertility), hyperandrogenism (hirsutism, acne, androgenic alopecia and biochemical hyperandrogenism) and a polycystic ovarian morphology (high antral follicle counts or increased ovarian volume).[ 49 ] Up to 88% of women with PCOS are overweight or obese,[ 48 ] with a meta-analysis showing that women with obesity had a twofold to threefold higher risk for PCOS when compared to women without obesity.[ 50 ] The pathogenesis of PCOS involves primarily insulin resistance, with the ensuing secondary hyperinsulinaemia resulting in enhanced steroidogenesis in the ovaries, particularly androgen production.[ 48 ] Hence, the insulin-resistant milieu associated with obesity can lead to the development of PCOS. This causal effect of obesity on PCOS is supported by MR studies,[ 32 , 51 ] with one MR study suggesting that this effect is predominantly metabolic in nature.[ 32 ] In Singapore, a study based on a multiethnic population of 389 participants reported that women with PCOS had significantly higher BMI compared to women without PCOS,[ 52 ] consistent with the evidence.
Cognitive impact and dementia
Experimental studies have shown that cellular mechanisms such as oxidative stress and inflammation can affect the brain structure and function.[ 53 ] Obesity is an established risk factor for dementia,[ 54 ] and has been associated with cognitive impairment[ 55 , 56 ] and decreased grey matter volume linked with executive functioning.[ 53 , 57 ] However, while MR studies have found causal relationships between BMI and grey matter volumes,[ 58 ] evidence for BMI and dementia has so far not been significant.[ 32 , 58 , 59 ] In Singapore, a longitudinal analysis of 1,519 cognitively normal older persons (>55 years) of Chinese ethnicity showed that central obesity was associated with a higher risk of developing mild cognitive impairment,[ 60 ] consistent with the overall evidence that higher adiposity has a negative impact on the brain.
Chronic kidney disease
Excess adiposity results in pathological processes such as lipotoxicity, inflammation, oxidative stress and activation of the renin–angiotensin–aldosterone system, leading to glomerular and tubular injuries (obesity-induced nephropathy).[ 61 ] Multiple MR studies have confirmed this causal relationship between obesity and kidney disease,[ 32 , 62 , 63 ] including one study conducted in an East Asian population using BMI-associated variants validated in East Asia.[ 63 ] In Singapore, longitudinal gain in adiposity was associated with progressive renal decline in a prospective multiethnic cohort with T2DM, suggesting that increasing adiposity would lead to adverse renal outcomes over time.[ 64 ]
Obesity is known to be associated with 13 types of cancers: oesophageal adenocarcinoma, renal cell carcinoma, postmenopausal breast cancer, endometrial cancer, colorectal cancer, meningioma, multiple myeloma, and cancer of the gastric cardia, liver, gallbladder, pancreas, ovary and thyroid.[ 65 ] In Singapore, these obesity-associated cancers make up four out of the top five cancers affecting women (breast, colorectal, endometrial and ovarian) and two of the top five cancers affecting men (colorectal and liver).[ 66 ] Potential mechanisms of increased cancer risk in obesity include hyperinsulinaemia, chronic inflammation and oestrogen excess.[ 67 ] This causal role of obesity in cancer is supported by MR studies,[ 19 , 32 ] particularly for cancers of the digestive system, with all of them (oesophageal, colorectal, gastric, liver, gallbladder, pancreas) positively associated with genetically predicted BMI based on a meta-analysis of MR studies.[ 19 ]
Depression and anxiety
The prevalence of depression is much higher among people with obesity than that in the general population.[ 68 , 69 ] Similarly, anxiety occurs more frequently in people who are overweight or obese compared to people with normal weight, and the relationship is stronger among those who are more severely obese.[ 70 , 71 , 72 ] Research findings consistently show that people with obesity frequently suffer from psychological issues ranging from stress associated with weight-related issues, perceived weight discrimination and stigmatisation to body image dissatisfaction.[ 68 , 69 ] Additionally, there is evidence that the dysfunctional adipose tissues present in obesity result in metabolic abnormalities, such as altered glucocorticoid, adipokine, insulin, leptin and inflammatory signalling, which either directly or indirectly impact the control of emotions and mood.[ 73 , 74 ] Hence, the causal relationship between obesity and depression/anxiety is likely to have both psychological and biological components. This is supported by MR studies which demonstrate the relationship between genetically predicted BMI (and fat mass) and depression,[ 75 , 76 , 77 ] even when using a genetic instrument that omits the metabolic consequences of higher BMI.[ 75 ]
In Singapore, a study based on 83 patients with obesity at a weight management clinic reported that the prevalence of anxiety symptoms and depressive symptoms was 28% and 11%, respectively,[ 78 ] suggesting that symptoms of depression and anxiety are highly prevalent in people with obesity in Singapore and are higher than the national prevalence of depression and anxiety,[ 79 ] consistent with international data.
Severe coronavirus disease-19
The dysfunctional physiological milieu of obesity has been associated with altered lymphoid tissue integrity, shifts in leukocyte populations and proinflammatory profiles, such that immune responses and pathogen defence are impaired.[ 80 ] This is demonstrated in previous influenza outbreaks[ 81 ] and the current coronavirus disease 2019 (COVID-19) pandemic, where obesity (high adiposity) is a major risk factor for severe COVID-19 (death and hospitalisation), as supported by multiple epidemiological studies worldwide[ 82 ] and MR studies[ 83 , 84 , 85 , 86 ] using data from the COVID-19 Host Genetics Initiative (an international collaboration that aims to uncover the genetic determinants of outcomes related to COVID-19 susceptibility and severity). In Singapore, where the COVID-19 mortality rate is low (<0.001),[ 87 ] a subgroup analysis of younger (<60 years) COVID-19 patients found that a BMI ≥25 kg/m 2 was significantly associated with the need for low-flow supplemental oxygen and mechanical ventilation,[ 88 ] consistent with observations internationally.
Other diseases
Other diseases with established epidemiological and strong MR evidence include asthma,[ 32 ] gastro-oesophageal reflux disease,[ 19 , 32 ] diverticular disease,[ 19 , 32 ] gallstone disease,[ 19 , 32 ] Crohn's disease,[ 19 , 89 ] osteoarthritis,[ 32 , 90 ] intervertebral degeneration (including back pain and sciatica),[ 91 , 92 ] peripheral arterial disease,[ 19 , 32 ] venous thromboembolism,[ 19 , 32 ] deep vein thrombosis,[ 19 , 32 ] aortic valve stenosis,[ 19 ] atopic dermatitis,[ 93 ] psoriasis,[ 32 ] gout[ 32 ] and rheumatoid arthritis.[ 32 ]
IMPACT ON MOTHER AND CHILD
Maternal obesity has been associated with adverse outcomes, including increased mortality, for both mother and child.[ 94 ] Mothers with obesity are more likely to develop pregnancy complications such as gestational hypertension, preeclampsia, gestational diabetes mellitus and thromboembolic disease, with a higher risk of preterm delivery, caesarian section, stillbirth, intrauterine growth retardation and foetus that is large for gestational age.[ 94 , 95 , 96 ] In an MR study, genetically elevated maternal BMI was associated with higher offspring birthweight, supporting a causal relationship.[ 97 ] These adverse outcomes can lead to complications and disability, with increased birth weight being associated with childhood adiposity and metabolic disorders during life.[ 94 ] Hence, the impact of obesity may extend beyond the current generation (mother) to the next generation (child). In Singapore, findings from the Growing Up in Singapore Towards Healthy Outcomes (GUSTO) study, a prospective mother–offspring birth cohort, showed that pre-pregnancy BMI and maternal obesity were associated with child size and adiposity[ 98 ] and childhood obesity,[ 99 ] respectively, confirming the generational impact of obesity.
PSYCHOSOCIAL IMPACT
Obesity negatively impacts health-related quality of life, with greater degrees of obesity associated with greater impairments.[ 100 , 101 , 102 ] While most individuals often report significant difficulties with physical and occupational functioning, many also experience problems with social functioning, such as social withdrawal[ 103 ] and social isolation.[ 104 ] This could be due to perceived negative attitudes and discrimination towards people with obesity, increased self-consciousness and self-blame for being overweight.[ 69 , 104 ] People with obesity, especially females, are often dissatisfied with their body image, which is exacerbated by society's expectation of thinness, with the degree of dissatisfaction positively correlated with the amount of excess weight.[ 102 , 105 , 106 ] Taken together, obesity can negatively impact an individual's self-esteem,[ 69 ] thereby affecting self-efficacy,[ 107 ] possibly resulting in a vicious circle and downward spiral.
ECONOMIC IMPACT
There are substantially higher healthcare utilisation and medical costs among people who are overweight or obese due to treatment of medical conditions caused by excess adiposity and for direct obesity treatments, which may include weight loss surgeries and medications.[ 108 ] In addition to direct medical costs, there is also an increase in indirect costs as a result of increased absenteeism (workdays missed due to illness or injury) and presenteeism (reduced productivity while working).[ 109 ]
The economic burden of overweight and obesity has been well described and quantified in North America,[ 108 , 110 ] Europe,[ 111 , 112 , 113 , 114 ] Brazil,[ 115 ] Australia,[ 116 , 117 ] China[ 118 ] and Saudi Arabia,[ 119 ] with an estimated cost of 0.8%–2.4% of gross domestic product (GDP) in 2019 based on eight countries.[ 120 ] As for Singapore, a recent study has attempted to quantify the economic burden of overweight and obesity.[ 121 ] Using econometric methods and cross-sectional data from the Singapore Epidemiology of Eye Diseases (SEED) cohort, which includes measured height and weight, self-reported healthcare utilisation and absenteeism/presenteeism (based on a modified version of the Work Productivity Activity Impairment questionnaire), the incremental per capita and aggregate direct and indirect costs of excess weight among a multiethnic population of older adults (aged 40–80) were estimated.
Among Chinese, individuals who were overweight missed one additional workday per year compared to those who were of normal weight. Individuals in the obese category had SGD720 per year greater medical expenditures, but missed workdays were not statistically different from those in the normal weight category. Among Indians, differences were not significant between normal and overweight categories, but Indians in the obese category incurred an additional SGD310 per year in absenteeism costs than those of normal weight. For Malays, no significant differences by BMI category were identified.[ 121 ]
In aggregate, the predicted total medical expenditures attributable to overweight and obesity in Singapore were estimated to be SGD178 million, representing 1.6% of Singapore's total healthcare expenditures (SGD11,300 million in 2019). This figure is on the low end of published estimates, which range between 2.9% and 9.7% of the total healthcare spending.[ 121 ] Including absenteeism increases this estimate to SGD261 million, although this estimate is likely to be conservative because it does not include costs for presenteeism (reduced productivity while working), retraining, injuries or other costs resulting from excess weight in the workplace.[ 121 ] By ethnicity, Malays are responsible for 19% of the total costs of excess weight, even though they make up only 12% of the Singapore population.[ 121 ] This disproportionate burden is consistent with the disproportionately higher rates of overweight and obesity among Malays.[ 3 ]
LIMITATIONS OF REVIEW
First, this review discussed mainly the impact of adult obesity, with a focus on diseases that have shown a strong relationship with obesity, especially those supported by MR studies. Hence, the impact of paediatric obesity is not discussed and not all diseases have been covered. Second, not all the diseases supported by evidence from MR studies were discussed in detail. Nonetheless, they are listed in the section ’Other diseases’ and included in Figure 1 . Third, interventional studies which show significant weight loss-improving health outcomes were not discussed. These studies, by showing the positive impact of weight loss, would have further supported the negative impact of obesity. Lastly, while there are some MR studies based on Asian cohorts, the majority of MR studies were based on genetic data derived from individuals of European ancestry or large cohorts that were predominantly European. Hence, the inference of causality may be limited in non-European populations.
As discussed, obesity is strongly related to more than 50 medical conditions [summarised in Figure 1 ], with evidence from MR studies to support causality for many of these conditions. Based on the 2017 Global Burden of Diseases study, the top four causes (cardiovascular diseases, cancers, musculoskeletal disorders and mental disorders) of disability-adjusted life years in Singapore account for more than 50% of the total burden,[ 7 ] with many of the common conditions in these four causes related to obesity. Hence, the clinical, social and economic burdens of obesity are considerable, potentially impacting future generations as well. This review, therefore, highlights the importance of an urgent and concerted effort towards the prevention and management of obesity to reduce the burden of obesity.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.

IMAGES
VIDEO
COMMENTS
Introduction. Obesity is an increasing, global public health issue. ... The 2013 White Paper from the American Nurse Practitioners Foundation on the Prevention and Treatment of Obesity considers a food diary as an important evidence‐based nutritional intervention in aiding weight loss (ANPF). ... Obesity Research & Clinical Practice, 9 (5 ...
The present study conducted a systematic literature review to examine obesity research and machine learning techniques for the prevention and treatment of obesity from 2010 to 2020. Accordingly, 93 papers are identified from the review articles as primary studies from an initial pool of over 700 papers addressing obesity.
Introduction. Obesity is a medical condition de ned as disproportionate fat . ... In this research, the prevalence rate of obesity and overweight was 30.4%, 7.7% of them were obese, and 22.7% were ...
Recent research has established the physiology of weight regulation, the pathophysiology that leads to unwanted weight gain with establishment of a higher body-weight set point, and the defense of the overweight and obese state even when reasonable attempts in lifestyle improvement are made. This knowledge has informed our approach to obesity as a chronic disease.
In the United States, overweight and obesity are chronic diseases that contribute to excess morbidity and mortality. Despite public health efforts, these disorders are on the rise, and their consequences are burgeoning. 1 The Centers for Disease Control and Prevention report that during 2017 to 2018, the prevalence of obesity in the United States was 42.4%, which was increased from the ...
Obesity has become a global epidemic and is one of today's most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer (Bluher, 2019).Obesity is mainly caused by imbalanced energy intake and expenditure due to a ...
The present study conducted a systematic literature review to examine obesity research and machine learning techniques for the prevention and treatment of obesity from 2010 to 2020. Accordingly, 93 papers are identified from the review articles as primary studies from an initial pool of over 700 papers addressing obesity. Consequently, this ...
Introduction. With the acceleration of industrialization and urbanization worldwide, obesity has become the highest incidence of chronic diseases, affecting approximately 650 million individuals. 1 Obesity and overweight are global health problems and have been associated with a variety of diseases such as diabetes, cardiovascular diseases, tumors, skeletal diseases, and digestive system ...
This article is part of the PLOS Biology 20th anniversary collection. Obesity is a multifaceted disorder, affecting individuals across their life span, with increased prevalence in persons from underrepresented groups. The complexity of obesity is underscored by the multiple hypotheses proposed to pinpoint its seminal mechanisms, such as the ...
1 Definition of Obesity. Obesity is defined as an increase in number and size of fat cells (body fat) compared to lean body mass. In clinical practice, body mass index (BMI) is used to both define and classify obesity. A person with a BMI of 25-29.9 kg/m 2 is said to be overweight and any individual with BMI ≥30 kg/m 2, obese (Table 1 ).
Obesity is defined as an excess of body fat (increased fat cell size and number) relative to lean body mass [ 1 ]. Clinically, obesity is defined on the basis of BMI. Any person with BMI between 25 and 29.9 kg/m 2 is termed overweight and any individual with BMI 30 kg/m 2 or more is classified as obese (see Table 1.1) [ 2 ].
This paper provid es a comprehensive overview of the obesity epidemic, examining its causes, consequences, and potential solutions. It explores the complex interplay of genetic, environmental, and ...
Introduction. Obesity is linked with elevated risk of non-communicable diseases (NCDs) [].An increasing trend in obesity prevalence since the early 1980s has posed a significant population health burden across the globe [] while obesity prevalence varies by region and country [1, 3].Country-specific trends in obesity are generally tracked using longitudinal panel or repeated cross-sectional ...
The Obesity Society (TOS) first published a position statement on obe-sity as a disease in 2008 (1). This statement reflected the thoughtful deliberations and consensus of Society members that was published in the same year (2). In 2016, an updated in-house position paper affirmed the 2008 declaration, stating, "TOS recommits to its position ...
Thus, the management of obesity through exercise, nutrition, supplementation, and medical intervention are at the forefront of research. The purpose of this review is to examine the current literature as it pertains to the prevalence, theories, medical consequences, management, and future research directions in the study of obesity. Further, this
Obesity is a multi-factorial disorder, which is often associated with many other significant diseases such as diabetes, hypertension and other cardiovascular diseases, osteoarthritis and certain cancers. The management of obesity will therefore require a comprehensive range of strategies focussing on those with existing weight problems and also on those at high risk of developing obesity ...
Obesity has become a global epidemic and is one of today's most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer (Bluher, 2019).Obesity is mainly caused by imbalanced energy intake and expenditure due to a ...
States obesity is estimated to cause an excess 111,909 to 365,000 death per year, while 1 million (7.7%) of deaths in the European Union are attributed to excess weight . [9,10] Classification: Obesity is a medical condition in which excess body fat has accumulated to the extent that it may have an adverse effect on health. [11]
Introduction. What is obesity? Obesity is a chronic condition defined by an excess amount of body fat. It indicates a weight greater than what is considered healthy. Obesity has been more precisely defined by the National Institutes of Health (the NIH) as a BMI (Body Mass Index) of 30 and above. (A BMI of 30 is about 30 pounds overweight.)
1. Introduction. Obesity is a complex, multifactorial, and largely preventable disease (), affecting, along with overweight, over a third of the world's population today (2,3).If secular trends continue, by 2030 an estimated 38% of the world's adult population will be overweight and another 20% will be obese ().In the USA, the most dire projections based on earlier secular trends point to ...
View sample obesity research paper. ... Introduction. There has been a dramatic rise in the prevalence of obesity globally in the last three decades, and the World Health Organization (WHO) estimates around 11 % of the world's total population is obese (WHO 2012). Obesity is seen as a major public health concern because it is widely ...
There is limited evidence about the gender- and obesity-specific effects of personal care product and plasticizing chemicals (PCPPCs) on short sleep duration in adults. We evaluated the gender- and obesity-specific association of co-exposure to PCPPCs and short sleep duration among adults aged 20-60 years using the National Health and Nutrition Examination Survey (NHANES) 2011-2016, a ...
Introduction. Obesity in children and adolescents is a global health issue with increasing prevalence in low-income and middle-income countries (LMICs) as well as a high prevalence in many high-income countries. 1 Obesity during childhood is likely to continue into adulthood and is associated with cardiometabolic and psychosocial comorbidity as well as premature mortality.2, 3, 4 The provision ...
T2D indicates type 2 diabetes. a The combined total of patients is not necessarily a sum of the individuals from each of the groups because individuals could be prescribed both glucagon-like peptide 1 receptor agonists (GLP-1RAs) and insulins or metformin during the study period.. b The combined total of patients is not necessarily a sum of the individuals from each of the groups because ...
INTRODUCTION. The prevalence of obesity has increased significantly over the last two decades worldwide, including in Singapore, a multiethnic Southeast Asian country.[1,2] Recent national health surveys of adult Singaporeans suggest a continuation of this rising trend after a brief period of stabilisation.[] Obesity, which is characterised by excessive adiposity, is not benign.