An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager

Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
A case report of complete remission of acute myeloid leukemia combined with DNMT3A, FLT3-TKD , and IDH2 gene mutations and active pulmonary tuberculosis treated with homeharringtonine + venetoclax + azacytidine
Affiliation.
- 1 Department of Oncology and Hematology, Hangzhou Red Cross Hospital, Hangzhou, Zhejiang, China.
- PMID: 37384044
- PMCID: PMC10294669
- DOI: 10.3389/fmed.2023.1180757
In March 2022, a 58-year-old man was admitted to the local hospital for nausea and vomiting. His blood routine indicated that he had leukocytosis and anemia. The patient was diagnosed with acute myeloid leukemia (AML)-M5b accompanied by DNMT3A, FLT3-TKD , and IDH2 mutations, chest CT revealed pulmonary tuberculosis (TB). Acid-fast bacillus (AFB) was detected in sputum. The patient then received anti-TB treatment with isoniazid + rifampicin + pyrazinamide + ethambutol. On April 8, he was transferred to our hospital's Hematology Department after three consecutive negative sputum smears. He was administered the VA (Venetoclax + Azacytidine) regimen of anti-leukemia treatment and also received levofloxacin + isohydrazide + pyrazinamide + ethambutol anti-TB treatment. After one course of VA therapy, there was no remission in the bone marrow. Therefore, the patient received the HVA (Homeharringtonine + Venetoclax + Azacytidine) regimen of anti-leukemia treatment. On May 25, the bone marrow smear revealed that the original mononuclear cells were 1%. Moreover, bone marrow flow cytometry revealed the absence of any abnormal cells. mNGS showed DNMT3A (mutation rate 44.7%), but no mutations were detected in FLT3-TKD and IDH2. The patient then received the HVA regimen three consecutive times, resulting in complete remission. Repeated chest CT examinations revealed progressive regression of pulmonary TB foci, no AFB was detected in the sputum. This AML patient with DNMT3A, FLT3-TKD, and IDH2 mutations and active TB is difficult to treat. It is very necessary for him to administer prompt anti-leukemia treatment under the premise of active anti-TB treatment. The HVA regimen is effective for this patient.
Keywords: DNMT3A mutation; FLT3-TKD mutation; IDH2 mutation; active pulmonary tuberculosis; acute myeloid leukemia; complete remission; homeharringtonine.
Copyright © 2023 Ji, Yang, Xu and Xu.
PubMed Disclaimer
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Similar articles
- Targeting FLT3 Mutation in Acute Myeloid Leukemia: Current Strategies and Future Directions. Fedorov K, Maiti A, Konopleva M. Fedorov K, et al. Cancers (Basel). 2023 Apr 15;15(8):2312. doi: 10.3390/cancers15082312. Cancers (Basel). 2023. PMID: 37190240 Free PMC article. Review.
- [Venetoclax and azacitidine induced cytogenetic response in an elderly patient with IDH2- and DNMT3A-mutated refractory acute myeloid leukemia]. Kunisada K, Matsuoka A, Yoshida S, Taoka T. Kunisada K, et al. Rinsho Ketsueki. 2022;63(12):1621-1625. doi: 10.11406/rinketsu.63.1621. Rinsho Ketsueki. 2022. PMID: 36653133 Japanese.
- Profiling of somatic mutations and fusion genes in acute myeloid leukemia patients with FLT3-ITD or FLT3-TKD mutation at diagnosis reveals distinct evolutionary patterns. Guan W, Zhou L, Li Y, Yang E, Liu Y, Lv N, Fu L, Ding Y, Wang N, Fang N, Liu Q, Wang B, Li F, Zhang J, Wang M, Wang L, Jing Y, Li Y, Yu L. Guan W, et al. Exp Hematol Oncol. 2021 Apr 9;10(1):27. doi: 10.1186/s40164-021-00207-4. Exp Hematol Oncol. 2021. PMID: 33836835 Free PMC article.
- [Detection of point mutation at second tyrosine kinase domain of FLT3 gene in acute myeloid leukemia]. Wang LH, Wang M, Zhou CL, Chen S, Zhang XW, Xing HY, Wang JX. Wang LH, et al. Zhonghua Xue Ye Xue Za Zhi. 2005 Jun;26(6):335-8. Zhonghua Xue Ye Xue Za Zhi. 2005. PMID: 16185475 Chinese.
- [Agranulocytosis due to anti-tuberculosis drugs including isoniazid (INH) and rifampicin (RFP)--a report of four cases and review of the literature]. Shishido Y, Nagayama N, Masuda K, Baba M, Tamura A, Nagai H, Akagawa S, Kawabe Y, Machida K, Kurashima A, Komatsu H, Yotsumoto H. Shishido Y, et al. Kekkaku. 2003 Nov;78(11):683-9. Kekkaku. 2003. PMID: 14672045 Review. Japanese.
- Carrimycin in the treatment of acute promyelocytic leukemia combined with pulmonary tuberculosis: A case report. Yang FY, Shao L, Su J, Zhang ZM. Yang FY, et al. World J Clin Cases. 2024 Jan 26;12(3):623-629. doi: 10.12998/wjcc.v12.i3.623. World J Clin Cases. 2024. PMID: 38322455 Free PMC article.
- Papaemmanuil E, Gerstung M, Bullinger L, Gaidzik VI, Paschka P, Roberts ND, et al. . Genomic classification and prognosis in acute myeloid leukemia. N Engl J Med. (2016) 374:2209–21. 10.1056/NEJMoa1516192 - DOI - PMC - PubMed
- Loghavi S, Zuo Z, Ravandi F, Kantarjian HM, Bueso-Ramos C, Zhang L, et al. . Clinical features of de novo acute myeloid leukemia with concurrent DNMT3A, FLT3 and NPM1 mutations. J Hematol Oncol. (2014) 7:74. 10.1186/s13045-014-0074-4 - DOI - PMC - PubMed
- Bezerra MF, Lima AS, Piqué-Borràs MR, Silveira DR, Coelho-Silva JL, Pereira-Martins DA, et al. . Co-occurrence of DNMT3A, NPM1, FLT3 mutations identifies a subset of acute myeloid leukemia with adverse prognosis. Blood. (2020) 135:870–5. 10.1182/blood.2019003339 - DOI - PubMed
- Jia Z-X, Chao H-Y, Liu J, Cai X-H, Qin W, Wu P, et al. . Coexisting mutations in IDH1/2-mutated acute myeloid leukemia. J Exp Hematol. (2019) 27:1440–8. 10.19746/j.cnki.issn.1009-2137.2019.05.014 - DOI - PubMed
- Xu Q, Li Y, Lv N, Jing Y, Xu Y, Li Y, et al. . Correlation between isocitrate dehydrogenase gene aberrations and prognosis of patients with acute myeloid leukemia: a systematic review and meta-analysis. Clin Cancer Res. (2017) 23:4511–22. 10.1158/1078-0432.CCR-16-2628 - DOI - PubMed
Publication types
- Search in MeSH
Related information
Grants and funding, linkout - more resources, full text sources.
- Europe PubMed Central
- Frontiers Media SA
- PubMed Central
Miscellaneous
- NCI CPTAC Assay Portal

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Leukemia Research Results and Study Updates
See Advances in Leukemia Research for an overview of recent findings and progress, plus ongoing projects supported by NCI.
Treatment options for people with acute myeloid leukemia (AML) have expanded yet again. On July 20, FDA approved quizartinib (Vanflyta) combined with chemotherapy as a first-line treatment for AML with a specific change in the FLT3 gene.
Giving the drug blinatumomab (Blincyto) after standard chemotherapy substantially increased survival for infants with an aggressive form of acute lymphoblastic leukemia (ALL), a recent study showed. If confirmed in larger studies, the treatment may become standard therapy for infants with ALL caused by KMT2A rearrangements.
Treatment with revumenib caused complete remission in about one-third of participants in an early-phase clinical trial involving patients who’d had many prior treatments. Revumenib is part of a new class of targeted drugs known as menin inhibitors.
An NCI-funded clinical trial has shown that treatment-related early deaths in people with a rare leukemia can be dramatically reduced. How did they do it? In part, by establishing a help desk staffed by experts in treating APL.
FDA has approved zanubrutinib (Brukinsa) for chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL) based on results from two clinical trials. In both trials, the drug, which blocks a protein called BTK, was more effective and caused fewer side effects than other treatments.
The immunotherapy drug blinatumomab (Blincyto) extends life for people with acute lymphoblastic leukemia who are in remission, even those with no signs of disease after initial treatment, a trial has found.
For some people with acute myeloid leukemia (AML) that has a mutation in the IDH1 gene, combining ivosidenib (Tibsovo) with the chemotherapy drug azacitidine may be a new treatment option, according to results from a large clinical trial.
Removing immune cells called naive T cells from donated stem cells before they are transplanted may prevent chronic graft-versus-host disease (GVHD) in people with leukemia, a new study reports. The procedure did not appear to increase the likelihood of patients’ cancer returning.
A Children’s Oncology Group trial shows that the combination of all-trans retinoic acid and arsenic trioxide is highly effective in children with acute promyelocytic leukemia. The therapy avoids or minimizes the use of conventional chemotherapy.
The CAR T-cell therapy Tecartus has become the first such treatment approved by FDA to treat adults with acute lymphoblastic leukemia (ALL). The approval is for patients whose cancer has not responded to treatment or returned after treatment.
FDA has approved belumosudil (Rezurock) for the treatment of chronic graft-versus-host disease (GVHD). The approval covers the use of belumosudil for people 12 years and older who have already tried at least two other therapies.
FDA has approved a new form of asparaginase called Rylaze. The drug was developed to help alleviate shortages of Erwinia asparaginase, a key part of treatment for children and adults with acute lymphoblastic leukemia.
In a small study, vemurafenib (Zelboraf) and rituximab (Rituxan) helped 85% of participants stay in remission for nearly 3 years. The study involved 30 people with hairy cell leukemia that had come back after or had not responded to previous treatment.
People with blood cancers seem to be less protected by COVID-19 vaccines than those with other cancers and people without cancer, three new studies suggest. Experts believe this limited effectiveness is likely due to patients’ weakened immune systems.
For people with acute myeloid leukemia and related cancers, a new study shows whole-genome sequencing could replace a series of conventional tests used to help guide decisions about treatment.
The results of two trials establish blinatumomab (Blincyto) as a new standard treatment for children and young adults with high-risk relapsed B-cell acute lymphoblastic leukemia after remission has been achieved and before a stem cell transplant.
For adults with CML who are in a sustained deep molecular remission, stopping treatment with a tyrosine kinase inhibitor is safe and improves their quality of life, a study shows. But researchers cautioned that these patients must be closely monitored.
Two rediscovered drugs, bisantrene and brequinar, slowed the growth of acute myeloid leukemia in studies of mice. The drugs blocked the activity of a protein called FTO, killing cancer stem cells and helping the immune system attack the cancer.
Maintenance therapy with CC-486 extended overall survival of adults with the blood cancer acute myeloid leukemia (AML) in a large clinical trial. CC-486 is a pill form of another cancer therapy called azacitidine (Vidaza).
For children and young adults with certain relapsed B-cell acute lymphoblastic leukemia (B-ALL), the immunotherapy drug blinatumomab is superior to standard chemotherapy, an NCI-sponsored Children’s Oncology Group trial shows.
People with relapsed or refractory acute myeloid leukemia (AML) with FLT3 gene mutations treated with gilteritinib had improved survival, higher rates of remission, and fewer side effects than those treated with chemotherapy, a recent trial found.
Only 1.5% of children with acute lymphoblastic leukemia who skipped radiation had a recurrence in the central nervous system, according to a recent trial. The therapy, which is intended to prevent such a recurrence, can have devastating side effects.
The Food and Drug Administration has approved venetoclax (Venclexta) in combination with obinutuzumab (Gazyva) for the initial treatment of adults with chronic lymphocytic leukemia or small lymphocytic lymphoma.
New findings from a clinical trial of the drug tagraxofusp confirm its efficacy against the rare blood cancer blastic plasmacytoid dendritic cell neoplasm (BPDCN).
In this trial, patients with hairy cell leukemia who have disease-related symptoms that require treatment, and who have not been treated or have had only one prior treatment with cladribine, will be randomly assigned to receive cladribine with either concurrent rituximab or rituximab at least 6 months after completing cladribine therapy.
A clinical trial found that an intensive treatment regimen developed specifically for children with acute lymphoblastic leukemia is also effective for older adolescents and young adults with the disease.
FDA has approved venetoclax (Venclexta) and glasdegib (Daurismo) for use in people with acute myeloid leukemia aged 75 and older and those with health conditions that prevent them from receiving the intensive chemotherapy regimen that is the standard initial treatment.
Two new studies show how the drugs venetoclax (Venclexta) and azacitidine (Vidaza) team up to block the unique metabolism of leukemia stem cells and may explain why the drug combination is effective against acute myeloid leukemia.
A clinical trial showed that ibrutinib plus rituximab is superior to standard treatment for patients age 70 and younger with untreated chronic lymphocytic leukemia (CLL). Findings were announced at the American Society of Hematology annual meeting.
The FDA has approved moxetumomab pasudotox (Lumoxiti), a bacterial toxin–based drug, for the treatment of some patients with hairy cell leukemia (HCL). Moxetumomab is approved to treat patients with HCL who have already undergone at least two lines of standard treatments.
The FDA has approved ivosidenib (Tibsovo) for the treatment of adults with acute myeloid leukemia (AML) that has a specific mutation in a gene called IDH1. Ivosidenib becomes the first FDA-approved IDH1-targeted treatment.
FDA expanded the approval of venetoclax (Venclexta) for people with chronic lymphocytic leukemia (CLL) to include those whose cancer has progressed after previous treatment, regardless of whether their cancer cells have the deletion 17p gene alteration.
This NCI-funded Children’s Oncology Group trial tested the addition of nelarabine (Arranon) to standard treatment for children and young adults with T-cell acute lymphoblastic leukemia (T-ALL).
People diagnosed with hairy cell leukemia (HCL) may have an effective new treatment option, a type of drug called an immunotoxin. Read more about how this treatment, moxetumomab pasudotox, fared in a phase 3 clinical trial in patients with advanced HCL.
A new study has identified a possible strategy for improving the efficacy of a toxin-based cancer treatment, moxetumomab pasudotox, in some patients with acute lymphoblastic leukemia (ALL).
An NCI-funded study has found significant differences in the genetics of acute myeloid leukemia in younger and older patients. The findings could help guide the development of treatments tailored specifically for childhood AML.
On December 22, FDA approved an update to the label of nilotinib (Tasignia) that states that some patients with CML who are taking nilotinib and whose cancer has been in remission for an extended period can safely stop taking it.
Interim results from an ongoing clinical trial show that patients with relapsed or refractory chronic lymphocytic leukemia treated with rituximab plus venetoclax have longer progression-free survival compared with patients treated with chemotherapy.
In a unique clinical trial, a group of oncologists with experience treating acute promyelocytic leukemia are making themselves available around the clock to help clinicians at hospitals across the country treat their APL patients.
On November 9, the FDA approved dasatinib (Sprycel®) for the treatment of children with chronic myelogenous leukemia (CML) whose cancer cells express the Philadelphia chromosome and whose disease is in a relatively early stage, known as the chronic phase.
FDA has approved gemtuzumab ozogamicin (Mylotarg™) for adults with newly diagnosed CD33-positive AML and patients 2 years and older with CD33-positive AML who have experienced a relapse or whose disease has not responded to initial treatment.
FDA has approved inotuzumab (Besponsa®) for some adults with B-cell acute lymphoblastic leukemia (ALL). The approval covers patients with B-cell ALL whose disease has relapsed or is refractory to standard chemotherapy.
FDA has approved tisagenlecleucel (Kymriah™), a type of immunotherapy called CAR T-cell therapy, for some children and young adults with advanced acute lymphoblastic leukemia (ALL).
FDA has approved two new treatments for some adult patients with acute myeloid leukemia (AML): enasidenib (Idhifa®), which targets the IDH2 protein; and liposomal cytarabine-daunorubicin CPX-351 (Vyxeos®), a two-drug chemotherapy combination encapsulated in liposomes.
FDA changed its accelerated approval of blinatumomab (Blincyto) for some patients with acute lymphoblastic leukemia to a full approval and expanded the approved indications for its use.
The FDA has approved a new formulation of rituximab, Rituxan Hycela, that reduces treatment administration time for patients with several types of blood cancer.
The FDA has approved midostaurin for patients with newly diagnosed acute myeloid leukemia (AML) with mutations in the FLT3 gene. The approval also covers several rare conditions.
Results from a large phase III clinical trial suggest that a highly intensive preparatory regimen should be used for younger patients with acute myeloid leukemia or myelodysplastic syndromes preparing to undergo an allogeneic stem cell transplant.
Patients with previously treated acute lymphoblastic leukemia who received blinatumomab, which encourages the immune system to kill cancer cells, lived longer and experienced fewer side effects than patients given standard chemotherapy.
- DOI: 10.1016/j.heliyon.2024.e32450
- Corpus ID: 270568797
Washed Microbiota Transplantation in an Elderly Patient with Lymphocytic Leukemia and Clostridioides difficile Infection: A Case Report Illustrating a Triumph Over Complexity
- Xinyu Zhang , Yuan Li , +3 authors Xia Ding
- Published in Heliyon 1 June 2024
33 References
Concept, breakthrough, and future of colonic transendoscopic enteral tubing, washed microbiota transplantation for clostridioides difficile infection: a national multicenter real‐world study, from microbial technology to microbiota medicine as a clinical discipline: sustainable development goal, gut microbiota changes associated with clostridioides difficile infection and its various treatment strategies, colonic transendoscopic enteral tubing is a new pathway to microbial therapy, colonic drainage, and host–microbiota interaction research, faecal microbiota transplantation for first or second clostridioides difficile infection (earlyfmt): a randomised, double-blind, placebo-controlled trial., systematic review of guidelines for the diagnosis and treatment of clostridioides difficile infection, washed preparation of faecal microbiota changes the transplantation related safety, quantitative method and delivery, clinical practice guidelines for fecal microbiota transplantation in korea, european society of clinical microbiology and infectious diseases: 2021 update on the treatment guidance document for clostridioides difficile infection in adults., related papers.
Showing 1 through 3 of 0 Related Papers
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
A rare onset of t-lymphoid blast crisis in chronic myeloid leukemia with two distinct blast populations, share and cite.
Mongia, A.; Romano, F.; Ciullini Mannurita, S.; Peruzzi, B.; Bencini, S.; Parrini, D.; Fasano, L.; Fanelli, A. A Rare Onset of T-Lymphoid Blast Crisis in Chronic Myeloid Leukemia with Two Distinct Blast Populations. Hematol. Rep. 2024 , 16 , 413-420. https://doi.org/10.3390/hematolrep16030040
Mongia A, Romano F, Ciullini Mannurita S, Peruzzi B, Bencini S, Parrini D, Fasano L, Fanelli A. A Rare Onset of T-Lymphoid Blast Crisis in Chronic Myeloid Leukemia with Two Distinct Blast Populations. Hematology Reports . 2024; 16(3):413-420. https://doi.org/10.3390/hematolrep16030040
Mongia, Alessandra, Francesca Romano, Sara Ciullini Mannurita, Benedetta Peruzzi, Sara Bencini, Daniela Parrini, Laura Fasano, and Alessandra Fanelli. 2024. "A Rare Onset of T-Lymphoid Blast Crisis in Chronic Myeloid Leukemia with Two Distinct Blast Populations" Hematology Reports 16, no. 3: 413-420. https://doi.org/10.3390/hematolrep16030040
Article Metrics
Article access statistics, supplementary material.
ZIP-Document (ZIP, 417 KiB)
Further Information
Mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
CASE REPORT article
Acute pulmonary embolism combined with acute myocardial infarction as the first manifestation of acute leukemia: a case report.

- 1 Department of Cardiology, The Affiliated Hospital of Southwest Medical University, Luzhou, China
- 2 Department of Respiratory and Critical Care Medicine, The Affiliated Hospital of Southwest Medical University, Luzhou, China
- 3 Inflammation & Allergic Diseases Research Unit, The Affiliated Hospital of Southwest Medical University, Luzhou, China
Thrombotic complications in acute myeloid leukemia (AML) are uncommon due to coagulation dysfunction and thrombocytopenia. We report a unique case of AML presenting as concomitant pulmonary embolism and atypical acute myocardial infarction. A 67-year-old male experienced persistent bilateral chest pain. Despite an unremarkable electrocardiogram, elevated D-dimer and mildly increased troponin T levels prompted further investigation, leading to the diagnosis of simultaneous pulmonary embolism and acute myocardial infarction. The patient underwent percutaneous coronary intervention and received triple antithrombotic therapy. However, antithrombotic therapy was discontinued following a sharp decline in hemoglobin and platelet counts, and the patient subsequently developed persistent fever. AML was diagnosed via bone marrow biopsy. Chemotherapy was not initiated due to the patient's deteriorating condition, and he ultimately succumbed to presumed intracranial bleeding.

Introduction
Thrombotic complications in acute myeloid leukemia (AML) are rare due to coagulopathy and thrombocytopenia. Paradoxically, thrombocytopenia and thrombosis can coexist, leading to treatment dilemmas, as thrombosis may be fatal and become the primary cause of death. Additionally, concomitant arterial and venous embolisms are seldom reported in association with AML. This case is notable for the simultaneous occurrence of acute pulmonary embolism (PE) and acute myocardial infarction (AMI) as the initial manifestation of AML, which was treated with antithrombotic therapy until the final diagnosis of acute leukemia. Atypical clinical presentations of acute myocardial infarction may signify early-stage AML.
A 67-year-old male patient was admitted to the hospital with a complaint of bilateral chest pain and weakness lasting for five days. The patient reported that the pain was persistent, albeit tolerable, and not associated with exercise or breath. He denied experiencing symptoms such as cough, dyspnea, diaphoresis, or lower limb edema. His pertinent medical history included a well-controlled hypertension for three years and a recent weight loss of 10 kg over the past year. The patient was a non-smoker and reported infrequent alcohol consumption.
The patient's vital signs upon admission were within normal limits, with a blood pressure of 115/72 mmHg, a heart rate of 80 bpm, a respiratory rate of 18 bpm, and an oxygen saturation (SpO2) of 98% while breathing room air. Physical examination revealed scattered moist rales across the bilateral lower lung fields. Cardiac and abdominal examinations were unremarkable, with no evidence of edema in the lower extremities.
The results of the complete blood count (CBC) revealed a white blood cell count of 8.51 × 10 9 /L, a hemoglobin level of 114 g/L, and a platelet count of 96 × 10 9 /L. The coagulation panel showed a prothrombin time (PT) of 12.6 s, a D-dimer level of 94.83 ug/ml [normal range (NR) 0–0.5], a fibrinogen level of 6.53 mg/dl (NR 1.8–3.5), fibrinogen degradation products (FDP) level of 270.70 ug/ml (NR 0–5), and antithrombin III (ATIII) level of 83% (NR 80–120). The cardiac marker showed a high-sensitive troponin T level of 0.357 μg/l (NR 0–0.014). Liver and renal function tests were unremarkable, while procalcitonin levels were elevated at 0.29 ng/ml (NR 0–0.05).
The electrocardiogram showed no ST segment changes but a Q wave in lead III ( Figure 1 ). The computed tomography (CT) of the chest revealed a 1.0 × 1.1 cm solid nodule in the right upper lobe of the lung, with a shallow lobulated edge, and mild to moderate homogeneous enhancement, and exudation in the lower lobe of the lungs, mild bilateral pleural effusion. CT angiography showed embolization in the left upper branches of the pulmonary arteries and bilateral lower pulmonary arteries ( Figure 2 ). However, no thrombus was found in the lower limb veins. Pulmonary embolism was diagnosed, and the patient was given 0.6 ml enoxaparine subcutaneously every 12 h for anticoagulation.
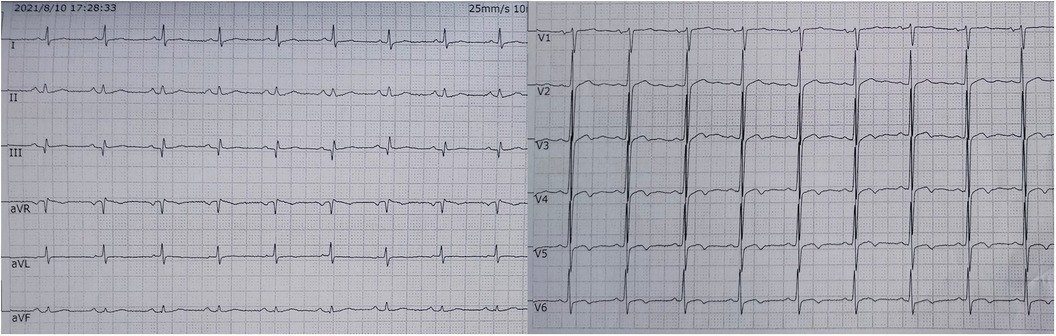
Figure 1 . The electrocardiogram showed no ST segment changes but a Q wave in lead III.
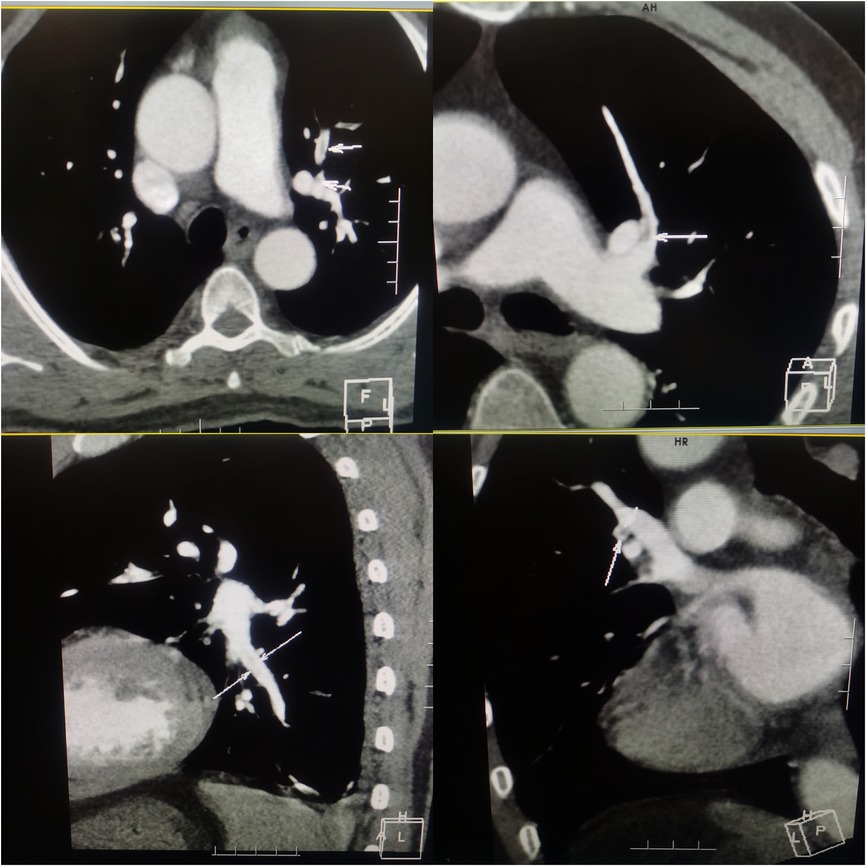
Figure 2 . Computered tomography angiography of chest showing embolization in the left upper branches and bilateral lower pulmonary arteries.
Initially, acute coronary syndrome was not considered due to the absence of angina and no ST segment change in the electrocardiogram. However, moderate stenosis in the left coronary artery was identified by CT angiography. Subsequent coronary angiography revealed occlusion in the middle segments of the left circumflex artery (LCX), 50% stenosis in the middle segment of the left anterior descending artery, and 80% stenosis in the middle segment of the right coronary artery. A drug-eluting stent (DES) was successfully implanted in the middle segment of the LCX, achieving thrombolysis in myocardial infarction (TIMI) grade III flow ( Figure 3 ). The patient was given 100 mg aspirin with 75 mg clopidogrel daily for antiplatelet aggregation and 20 mg atorvastatin to stabilize the plaque after the procedure. To identify the cause of concomitant thrombosis in the pulmonary arteries and coronary artery, autoantibody spectrum, anticardiolipin antibody, tumor markers of the respiratory system, rheumatoid factor, and immunoglobulin levels were tested, but no abnormalities were found.
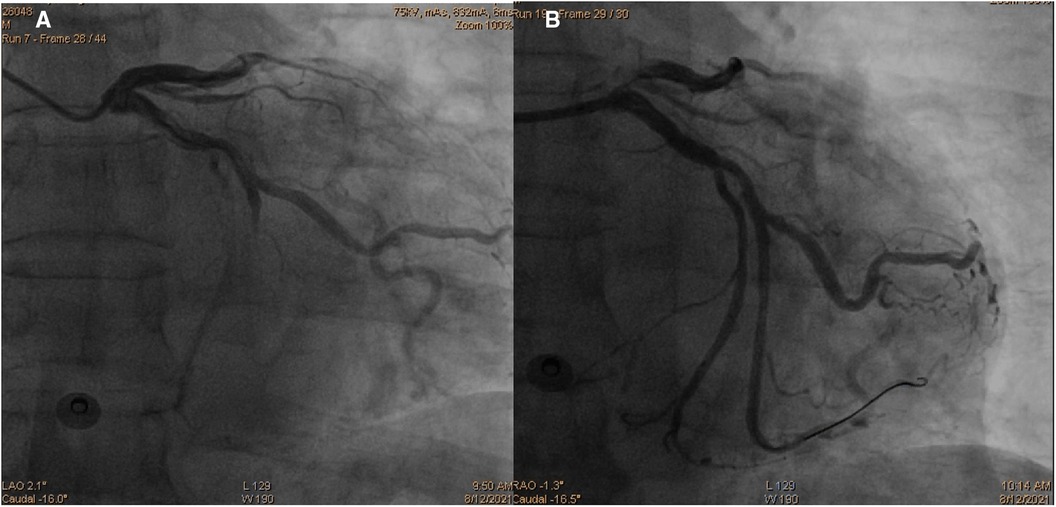
Figure 3 . Coronary angiography images demonstrating occlusion in the middle segments of the left circumflex artery ( A ) and revascularization of the left circumflex artery after percutaneous coronary intervention ( B ).
On the second day of hospitalization, the patient's hemoglobin level decreased to 106 g/L, and platelet counts dropped to 55 × 10 9 /L. Furthermore, the D-dimer levels increased, and urinary occult blood was detected. Suspecting heparin-induced thrombocytopenia, the patient's medication was switched from enoxaparin to rivaroxaban, with a daily dose of 10 mg. Following the switch, the urinary occult blood became negative on two consecutive tests. On the third day, the patient developed a fever, and piperacillin sodium, tazobactam, and cephalotazidine moxifloxacin were administered to treat the infection. Hepatitis virus screening and autoimmune hepatitis tests, along with tests for antibodies to EB virus, cytomegalovirus, rubella virus, and herpes simplex virus, galactomannan tests, and blood bacterial cultures were all negative.
On the sixth day of hospitalization, pancytopenia with 13% blasts was detected in the patient's peripheral blood. The following day, ecchymosis was observed at the vein puncture site on the wrist, and the white blood cell counts dropped to 2.61 × 10 9 /L, with hemoglobin at 61 g/L and platelets at 8 × 10 9 /L, with 17% blasts. The coagulation panel revealed disseminated intravascular coagulation, as evidenced by a prolonged PT (22.8 s), elevated D-dimer levels (>20.00 μg/ml), and decreased fibrinogen levels (5.03 mg/dl), with FDP levels >150.00 μg/Ml and normal ATIII level (88%). The Coombs test was negative. Following consultation with a hematologist, aspirin, clopidogrel, and rivaroxaban were discontinued, and red cell and platelet transfusions were administered, resulting in platelet counts increasing to 37 × 10 9 /L and PT decreasing to 15.2 s. Fortunately, no fresh ecchymosis or massive hemorrhage occurred. A bone marrow smear revealed hyperplasia of nucleated cells with necrotic cell remnants, confirming the diagnosis of acute myeloid leukemia (AML). The bone marrow biopsy showed a large amount of necrosis in the bone marrow tissue, with hyperactive proliferation of blasts in the necrotic part and few megakaryocytes and lymphocytes ( Figure 4 ). Immunophenotyping was not performed due to few nucleated cells. Immunohistochemical examination revealed CD117 (−), CD34 (−), MPO (granulocyte+), CD68/PG-M1 (+), CD71 (nucleated red blood cell+), CD61 (megakaryocyte+), CD3 (−), CD20 (-), CK-L (−), TTF-1 (−), NapsinA (−), CK7 (−), PSA (−), and P504s (−).
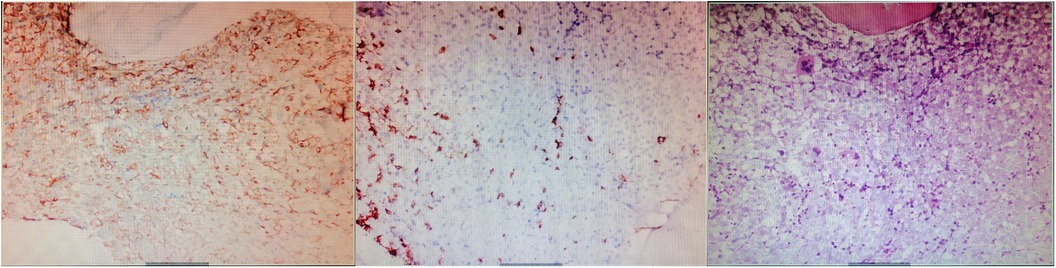
Figure 4 . Immuohistochemical stainin of bone marrow biopsy (×200). The results showed a large amount of necrosis in the bone marrow tissue, with hyperactive proliferation of blasts in the necrotic part and few megakaryocytes and lymphocytes.
Despite the initial improvement, the patient's condition deteriorated in the following days, with persistent fever and unstable hemodynamics. The platelet count fell to 6 × 10 9 /L, and chemotherapy was not initiated due to the worsening condition. On the 16th day of admission, the patient lost consciousness, and his heart rate gradually decreased, with blood pressure eventually collapsing, leading to presumed cerebral bleeding and subsequent death.
Thrombosis is a rare and atypical complication of acute leukemia that may lead to misdiagnosis and improper treatment at the early stages of the disease. In this case, an elderly male patient presented with acute PE combined with AMI, received percutaneous coronary intervention (PCI) and triple antithrombotic therapy. However, the progressive decline in hemoglobin and platelet count suggested hematological disease, and the patient was ultimately diagnosed with AML. This case is relatively rare clinically since anemia and bleeding are common initial presentations, as normal bone marrow hematopoietic function is inhibited by leukemic cell proliferation and thrombocytopenia. In the literature, the association of venous thromboembolic events with hematological malignancies is well documented ( 1 ). However, limited data is available for arterial thromboembolism (ATE), ATE like stroke, acute myocardial infarction, or lower extremity arterial embolism ( 2 , 3 ), and arteriovenous thrombosis ( 3 ) have been sparsely reported in leukemia.
This patient had a rapid onset and short course of chest pain, with no risk factors for PE before. When PE and AMI coexist in the setting of thrombocytopenia, it suggests that the nature of arteriovenous thrombosis is driven by underlying pathology rather than seeming diseases. Althouth the mechanism of thrombosis in acute leukemia is not yet clear, several pathogenic mechanisms have been proposed. Leukemic blasts express procoagulant proteins (such as tissue factor, TF) which can induce activation of the coagulation cascade and platelet aggregation. In addition, inflammatory cytokines (tumor necrosis factor- α and interleukin-1b) and microparticles secreted by leukemic cells stimulate the expression of the prothrombotic phenotype of platelets and leukocytes ( 4 ). Meanwhile, they promote the upregulation of TF and plasminogen activator inhibitor type 1 expression and the downregulation of thrombomodulin in endothelial cells ( 5 ). Besides, leukocytosis and leukostasis resulting from high blast cell count increased blood viscosity which impede blood flow ( 6 ). Moreover, it's worth noting that chemotherapy further promotes thrombus formation which is related to blasts'death and release of procoagulant factors in the circulation ( 7 ). Other reasons related to thrombosis include venous catheter procedures or infections ( 8 ). It has been reported that anticoagulant factor protein C, protein S, and ATIII decreased in varying degrees in leukemia patients ( 9 ). In this patient, the leukocyte count was normal with no blasts in peripheral blood at admission. The patient neither received chemotherapy nor underwent any invasive procedure before. Antiphospholipid antibody syndrome was excluded by negative anticardiolipin antibody test. Hypercoagulable and inflammatory state caused by blasts and pulmonary infection, combined with coexist atherosclerosis lesion might promote the simultaneous PE and AMI. Besides, although no change of ATIII level was observed, it's a limitation that other anticoagulant factors were not detected in this case, it was speculated that some anticoagulation defects might have given rise to thrombosis in leukemia.
Concomitant AMI and PE are rare and often require double antiplatelet (DAPT) and anticoagulant therapy to reduce new thrombotic events. Unfractionated heparin or low molecular weight heparin (LMWH) is recommended in the acute phase to rapidly extinguish thrombin and fibrin clot generation, which further prevents thrombus extension. Direct oral anticoagulants (DOACs) have been shown to be as effective as conventional treatment for venous thromboembolism ( 10 ). However, in the setting of leukemia with thrombocytopenia, triple antithrombotic therapy is worth exploring, as leukemia-related thrombocytopenia, platelet dysfunction, and systemic coagulation abnormalities increase the risk of bleeding. Unfortunately, despite recent guidelines addressing the management of VTE in cancer patients ( 11 ), there are no unambiguous data in dealing with thrombosis in the leukemic population. LMWH is still the standard treatment for VTE in leukemia, while data for DOACs is lacking since AML patients with thrombocytopenia were often excluded in prospective randomized trials ( 12 ). For patients with thrombocytopenia, dosing of anticoagulation should be modulated according to platelet count: Full therapeutic dose with LMWH should be considered in patients with platelet count >50 × 10 9 /L. In patients with persistent, severe thrombocytopaenia (<50 × 10 9 /L), for acute VTE at high risk of recurrence (within 30 days), platelet transfusions should be considered to maintain a count >50 × 10 9 /L and to continue a full dose anticoagulation. Anticoagulation must be withheld with platelets <25 × 10 9 /L ( 13 ).
PCI and following DAPT is the standard therapy for AMI patients. However, managing concomitant bleeding risk caused by antithrombotic drugs and stent thrombosis secondary to drug withdrawal due to bleeding events is challenging for treating patients with thrombocytopenia. Although the incidence of stent thrombosis was not significantly different between the two groups in a meta-analysis of all-cause mortality of PCI patients with or without baseline thrombocytopenia, gastrointestinal bleeding, intracranial hemorrhage, and hemorrhagic stroke after PCI were significantly higher than those of patients with normal platelets ( 14 ). To reduce bleeding risk, some experts suggest using bare metal stents or drug-eluting balloons to shorten the time of DAPT ( 15 ). Besides, the type of antiplatelet drugs and time of DAPT should be adjusted according to the platelet count: If the platelet count exceeds 10,000/ µl, aspirin can be used, while adding clopidogrel when count exceeds 30,000/ µl. If the platelet count is less than 50,000/ µl, the duration of DAPT should be 2 weeks after PTCA, 4 weeks after bare metal stenting, and 6 months after the second and third generation DES implantation. However, Prasugrel, Ticagrelor, and glycoprotein IIb/IIIa antagonists are not recommended ( 16 ). According to EHA guidelines, in secondary prevention of ATE in patients with platelets between 50 and 70 × 10 9 /L, single antiplatelet therapy (SAPT) is recommended, but be withheld if platelets <25 × 10 9 /L ( 13 ). If the platelet count is lower than 20 × 10 9 /L or the patient has fever, leukocytosis, sudden decrease of platelet count or other blood coagulation disorders, prophylactic platelet transfusion is required ( 17 ). In this case, the patient received DES implantation and was treated with a standard dose of enoxaparin and DAPT without knowing the existence of leukemia. However, on the second day after PCI, enoxaparin was replaced by rivaroxaban due to platelet decline. On the fourth day after PCI, antithrombotic drugs were discontinued due to a sharp drop in hemoglobin and platelets. Platelet transfusion was given when the platelet count was 8,000/ μl for bleeding prevention. The patient did not develop massive hemorrhage despite low platelets nor stent thrombosis without antithrombotic therapy until he died of irreversible bone marrow necrosis and possible intracranial bleeding. Thus, closely observing changes in the platelet count and timely adjusting the strategy according to the platelet value is crucial. Moreover, multidisciplinary management is also important in tackling the patient's complex situation.
The initial symptoms of AML may not be typical, and thrombotic complications such as acute pulmonary embolism and acute myocardial infarction are rare but can present and lead to treatment dilemmas, further increasing the mortality of AML. It is essential to further elucidate the specific mechanism of arteriovenous thrombosis in the context of thrombocytopenia. Since there is no standard therapy, the strategy should be carefully evaluated based on individual characteristics and should involve multidisciplinary management.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
ZS: Writing – original draft, Writing – review & editing. LS: Writing – original draft. LY: Writing – original draft. LD: Writing – review & editing. ZW: Writing – review & editing. PQ: Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Rashidi A, Silverberg ML, Conkling PR, Fisher SI. Thrombosis in acute promyelocytic leukemia. Thrombo Res . (2013)131(4):281–9. doi: 10.1016/j.thromres.2012.11.024
CrossRef Full Text | Google Scholar
2. Muñiz AE. Myocardial infarction and stroke as the presenting symptoms of acute myeloid leukemia. J Emerg Med . (2012)42(6):651–4. doi: 10.1016/j.jemermed.2009.04.061
3. Hashemi A, Gerges F, Naqvi HR, Kotlar I, Moscatelli S, Hashemi A, et al. A rare presentation of an elderly patient with acute lymphocytic leukemia and platelet count of zero associated with ST-elevation myocardial infarction, pulmonary thromboembolism in the setting of SARS-CoV 2:a case report. Egypt Heart J . (2021)73(1):39. doi: 10.1186/s43044-021-00162-9
PubMed Abstract | CrossRef Full Text | Google Scholar
4. Horowitz NA, Brenner B. Thrombosis in hematological malignancies: mechanisms and implications. Thromb Res . (2020)191:S58–62. doi: 10.1016/S0049-3848(20)30398-4
5. Rickles FR, Falanga A, Montesinos P, Sanz MA, Brenner B, Barbui T. Bleeding and thrombosis in acute leukemia: what does the future of therapy look like? Thromb Res . (2007)120(SUPPL.2):99–106. doi: 10.1016/S0049-3848(07)70137-8
6. Manogna D, Sham R. Acute myocardial infarction as initial manifestation of acute myeloid leukemia: a rare manifestation of leukostasis. Cureus . (2020)12(8):e9551. doi: 10.7759/cureus.9551
7. Herrmann J, Yang EH, Alliescu CA. Vascular toxicities of cancer therapies: the old and the new-an evolving avenue. Circulation . (2016)133(13):1272–89. doi: 10.1161/CIRCULATIONAHA.115.018347
8. Del Principe MI, Del Principe D, Venditti A. Thrombosis in adult patients with acute leukemia. Curr Opin Oncol . (2017)29(6):448–54. doi: 10.1097/CCO.0000000000000402
9. Dixit A, Kannan M, Mahapatra M, Choudhry VP, Saxena R. Roles of protein C, protein S, and antithrombin III in acute leukemia. Am J Hematol . (2006)81(3):171–4. doi: 10.1002/ajh.20546
10. Streiff MB, Agnelli G, Connors JM, Crowther M, Eichinger S, Lopes R, et al. Guidance for the treatment of deep vein thrombosis and pulmonary embolism. J Thromb and Thrombolys . (2016)41(1):32–67. doi: 10.1007/s11239-015-1317-0
11. Falanga A, Ay C, Di Nisio M, Gerotziafas G, Jara-Palomares L, Langer F, et al. Venous thromboembolism in cancer patients: ESMO clinical practice guideline. Ann Oncol . (2023)34(5): 452–67. doi: 10.1016/j.annonc.2022.12.014
12. Falanga A, Gal GL, Carrier M, Abdel-Razeq H, Ay C, Martin AJM, et al. Management of cancer-associated thrombosis: unmet needs and future perspectives. TH Open . (2021)5(3):e376–86. doi: 10.1055/s-0041-1736037
13. Falanga A, Leader A, Ambaglio C, Bagoly Z, Castaman G, Elalamy I, et al. EHA Guidelines on management of antithrombotic treatments in thrombocytopenic patients with cancer. HemaSphere . (2022)6(8):e750. doi: 10.1097/HS9.0000000000000750
14. Long MY, Ye ZL, Zheng J, Chen WX, Li L. Dual anti-platelet therapy following percutaneous coronary intervention in a population of patients with thrombocytopenia at baseline: a meta-analysis. BMC Pharmacol Toxicol . (2020)21(1):31. doi: 10.1186/s40360-020-00409-2
15. Iliescu CA, Grines CL, Herrmann J, Yang EH, Cilingiroglu M, Charitakis K, et al. SCAI Expert consensus statement: evaluation, management, and special considerations of cardio-oncology patients in the cardiac catheterization laboratory (endorsed by the cardiological society of India, and sociedad latino Americana de cardiologıa intervention). Catheter Cardio Inte . (2016)87(5): E202–23. doi: 10.1002/ccd.26379
16. McCarthy CP, Steg G, Bhatt DL. The management of antiplatelet therapy in acute coronary syndrome patients with thrombocytopenia: a clinical conundrum. Eur Heart J . (2017)38(47):3488–92. doi: 10.1093/eurheartj/ehx531
17. Iliescu C, Durand JB, Kroll M. Cardiovascular interventions in thrombocytopenic cancer patients. Tex Heart Inst J . (2011)38(3):259–60.21720465
PubMed Abstract | Google Scholar
Keywords: acute myocardial infarction, pulmonary embolism, acute myeloid leukemia, thrombocytopenia, percutaneous coronary intervention
Citation: Zheng S, Luo S, Luo Y, Liu D, Zheng W and Peng Q (2023) Acute pulmonary embolism combined with acute myocardial infarction as the first manifestation of acute leukemia: a case report. Front. Cardiovasc. Med. 10:1259548. doi: 10.3389/fcvm.2023.1259548
Received: 17 July 2023; Accepted: 31 August 2023; Published: 13 September 2023.
Reviewed by:
© 2023 Zheng, Luo, Luo, Liu, Zheng and Peng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shuzhan Zheng [email protected] ; [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Acute myeloid leukemia discovery tackles drug-resistant gene mutations
IU School of Medicine Jun 20, 2024

Reuben Kapur, PhD
INDIANAPOLIS — Indiana University School of Medicine researchers and their collaborators have uncovered molecular insights expected to enhance treatment options for acute myeloid leukemia (AML), a rare and severe blood and bone marrow cancer. With a new chemical compound engineered to overcome drug-resistant gene mutations not targeted by current treatments, the researchers aim to provide a new alternative with longer-lasting effects and improve outcomes for future patients battling this aggressive disease.
Although it’s considered a rare cancer, acute myeloid leukemia is one of the most common types of leukemia in adults. Individuals with AML have genetic mutations that cause an excess amount of abnormal blood cells , and their prognosis worsens if left untreated. The five-year survival rate for adults with AML is about 3 0% .
In a recent study published in the Journal of Clinical Investigation (JCI) , researchers identified inhibitors, or blocking agents, that target FLT3 gene mutations, the most common mutation in acute myeloid leukemia .
“Despite the widespread occurrence and clinical importance of FLT3 mutations in causing AML, treatment options tailored to this genetic anomaly are scarce,” said Baskar Ramdas, PhD , assistant research professor of pediatrics at the IU School of Medicine and co-first author of the study. “Our goal was to identify new and powerful inhibitors targeting the mutations, particularly those resistant to currently approved FDA options.”
FDA-approved drugs like q uizartinib and c renolanib are currently used to target FLT3 mutations, but some leukemia patients develop resistance to the se treatments . In their latest study, t he scientists identified two new inhibitors that effectively target FLT3 mutations, including secondary mutations that were previously drug resistant.
“ P inpointing where other treatments were causing resistance or relapse led to the development of a new lead compound that will hopefully be a more effective drug in the long run,” said Reuben Kapur , PhD , director of the IU School of Medicine’s Herman B Wells Center for Pediatric Research , co-leader of Hematopoiesis and Hematologic Malignancies program at the Indiana University Melvin and Bren Simon Comprehensive Cancer Center and co-author of the study. “Our preclinical study results have shown incredible promise, and we’re excited to keep the momentum going so AML patients can have more resilient options .”
T he study’s co-author Herman Sintim , PhD , Richard B. Wetherill Professor of Chemistry and Drug Discovery and Distinguished Professor in Chemistry in the James Tarpo Jr. and Margaret Tarpo Department of Chemistry at Purdue University engineered the patent-pending compound named HSN748 for impending clinical use .
Si n tim said the strong preliminary data made possible by collaboration between Purdue and IU subsequently attracted funding from the National Institutes of Health. This support enables the evaluation of HSN748 across different cancer models and enhanc es its prospects for further development funding . These next steps will be primarily managed by the compound ’s license holder KinaRx , an e arly - stage biotechnology company that aims to develop innovative solutions to cancers that have become resistant to existing drugs and get them into the market. Sintim is also the co-founder of KinaRx , and will continue to work closely with Kapur , a scientific advisory board member at the company .
“This academic-industry collaboration between KinaRx , Purdue and IU will continue as we continue determining the mutational backgrounds that are most sensitive to our lead compound HSN748 ,” Sintim said. “As the drug progresses to the next phase of clinical trials, the company would like to increase the collaboration to clinicians, including leukemia specialists at IU.”
Additional study authors include Ruchi Pandey , Rahul Kanumuri , Santhosh Kumar Pasupuleti , Sheng Liu, Jun Wan and Laura S. Haneline of IU ; Neetu Dayal , Elizabeth Larocque , Elizabeth Ruth Fei Y. Chu , Rodrigo Mohallem , Saniya Virani, Gaurav Chopra and Uma K. Aryal of Purdue ; Rena Lapidus and Ashkan Emadi of the University of Maryland; and Chrysi Kanellopoulou , Frederick W . Holtsberg and M Javad Aman of KinaRx , Inc.
About the IU School of Medicine
The IU School of Medicine is the largest medical school in the U.S. and is annually ranked among the top medical schools in the nation by U.S. News & World Report. The school offers high-quality medical education, access to leading medical research and rich campus life in nine Indiana cities, including rural and urban locations consistently recognized for livability. According to the Blue Ridge Institute for Medical Research, the IU School of Medicine ranks No. 13 in 2023 National Institutes of Health funding among all public medical schools in the country.
Writer: Jackie Maupin, [email protected]
Sources: Baskar Ramdas, [email protected]; Reuben Kapur, [email protected]; Herman Sintim, [email protected]
For more news, visit the IU School of Medicine Newsroom: medicine.iu.edu/news
Follow us on X: @IUMedSchool
SEARCH THE NEWSROOM
Subscribe to the news.
We've added you to our mailing list!
Sorry, there was a problem
Media Contacts
Related news.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Case Reports
An extremely delayed cytogenetic response to interferon-α in a patient with chronic myeloid leukaemia.
- AJ Whiteway
Translocation (2;8)(p12;q24) in blastic transformation of atypical chronic myeloid leukemia
Quick links.
- Explore articles by subject
- Guide to authors
- Editorial policies
- ASH Foundation
- Log in or create an account
- Publications
- Diversity Equity and Inclusion
- Global Initiatives
- Resources for Hematology Fellows
- American Society of Hematology
- Hematopoiesis Case Studies
Case Study: 47-Year-Old Woman With New-Onset AML and Leukostasis
- Agenda for Nematology Research
- Precision Medicine
- Genome Editing and Gene Therapy
- Immunologic Treatment
- Research Support and Funding
A 47-year-old woman presents to the emergency department complaining of fatigue and shortness of breath. She reports a two-week history of worsening exercise tolerance and a rather abrupt onset of shortness of breath over the past several hours. The patient has no major past medical history and works as an architect. Prior to this illness, she exercised three to four times weekly. Her breathing appears somewhat labored. Physical examination is notable for tachycardia, tachypnea, an erythematous rash on her chest and back, and scattered ecchymosis on the extremities. Her laboratory results reveal the following:
| White blood cells | 174.1 × 10 /L | 4 x 10 /L – 10 × 10 /L |
| Hemoglobin | 7.3 g/dL | 14 – 18 g/dL |
| Platelet count | 24 × 10 /L | 150 × 10 /L – 450 × 10 /L |
White blood cell (WBC) differential is notable for 89 percent blasts. Peripheral blood smear shows a vast majority of cells are large blasts with occasional cytoplasmic granules and pseudopodia. Bone marrow aspiration and biopsy is performed, revealing a hypercellular marrow involved with monocytic-appearing blasts comprising 80 percent of bone marrow cellularity. Cytogenetics reveal t(6;11)(q27;q23) present in 19 out of 20 metaphase cells. Molecular studies show wild-type CEPBA and NPM1 genes and a FLT3-ITD mutation (FMS-like tyrosine kinase 3, internal tandem duplication) is present. She is admitted to the hospital to initiate induction chemotherapy for acute myeloid leukemia (AML).
Following acute cytoreductive strategies to treat pulmonary complications of leukostasis, which of the following FDA-approved induction regimens is most likely to result in long-term overall survival?
- 7+3 chemotherapy with infusional cytarabine and an anthracycline (daunorubicin or idarubicin) plus gemtuzumab ozogamicin
- 7+3 chemotherapy with infusional cytarabine and an anthracycline (daunorubicin or idarubicin), plus etoposide
- 7+3 chemotherapy with infusional cytarabine and an anthracycline (daunorubicin or idarubicin), plus midostaurin
- 7+3 chemotherapy with infusional cytarabine and an anthracycline (daunorubicin or idarubicin), plus sorafenib
The correct answer is (C), 7+3 chemotherapy with infusional cytarabine and an anthracycline (daunorubicin or idarubicin), plus midostaurin. The patient is a younger adult woman with no prior medical history who presents with de novo AML with t(6;11) as well as a FLT3 -ITD mutation. Her clinical presentation is explained by her anemia (fatigue), thrombocytopenia (ecchymoses), and extreme leukocytosis (pulmonary leukostasis). Her cytogenetics reveal an 11q23 translocation, associated with therapy-related AML secondary to topoisomerase II inhibitors (such as etoposide and anthracyclines), which she does not have given her lack of prior history of such exposures, and monocytic differentiation of the leukemia, which she does have on the basis of her morphology. Monocytic differentiation may increase the chance of leukemic blasts infiltrating into tissues, which may result in leukemia cutis (likely based on her exam), gingival hyperplasia, and a higher likelihood of central nervous system involvement. Her very high WBC count is likely a result of her FLT3 -ITD mutation, which is associated with extreme elevations in the WBC count at presentation, a shorter WBC doubling time, and an increased likelihood of relapse following consolidation therapy. Midostaurin is a newly developed inhibitor of FLT3 that is FDA-approved, along with standard 7+3 combination chemotherapy, for the induction therapy of FLT3 mutation-positive AML. This is based on a multicenter phase III trial of 717 adult patients with newly-diagnosed FLT3 mutation-positive AML who were randomized to either standard 7+3 induction chemotherapy plus placebo or 7+3 induction chemotherapy plus midostaurin (on days 8 through 21, following chemotherapy). After a median of 59 months of follow-up, median overall survival was superior in the midostaurin group (75 months vs. 26 months), with a hazard ratio for death of 0.78.
While induction therapy with midostaurin has not been directly compared to such therapy with gemtuzumab ozogamicin (answer choice A), etoposide (answer choice B), or sorafenib (answer choice D), studies have examined the impact of adding etoposide to 7+3 and no benefit over 7+3 alone has been found. Sorafenib is a multi-tyrosine kinase inhibitor with activity against FLT3, and small studies have suggested a possible role for this drug in the management of patients with FLT3 mutation-positive AML, but more investigation is necessary, and the agent is not currently FDA-approved for this purpose. Gemtuzumab ozogamicin is a recombinant anti-CD33 monoclonal antibody linked to a cytotoxic agent. It had initially been approved by the FDA for use in older adults (age >60) with AML in first relapse, but it has since been pulled from the U.S. market following a more recent randomized trial showing no benefit from adding gemtuzumab ozogamicin to standard induction in younger adults with newly diagnosed AML. Trials are ongoing investigating other possible uses of this agent.
Case study submitted by Hanny Al-Samkari, MD, of Massachusetts General Hospital, Dana-Farber Cancer Institute, Harvard University, Boston, MA
- Stone RM, Mandrekar SJ, Sanford BL, et al. Midostaurin plus Chemotherapy for Acute Myeloid Leukemia with a FLT3 Mutation . N Engl J Med. 2017; doi:10.1056/NEJMoa1614359. [Epub ahead of print].
- Bishop JF, Lowenthal RM, Joshua D, et al. Etoposide in acute nonlymphocytic leukemia. Australian Leukemia Study Group . Blood. 1990; 75:27-32.
- Röllig C, Serve H, Hüttmann A, et al. Addition of sorafenib versus placebo to standard therapy in patients aged 60 years or younger with newly diagnosed acute myeloid leukaemia (SORAML): a multicentre, phase 2, randomised controlled trial . Lancet Oncol. 2015; 16:1691-1699.
- Petersdorf SH, Kopecky KJ, Slovak M, et al. A phase 3 study of gemtuzumab ozogamicin during induction and postconsolidation therapy in younger patients with acute myeloid leukemia . Blood. 2013; 121:4854-4860.
American Society of Hematology. (1). Case Study: 47-Year-Old Woman With New-Onset AML and Leukostasis. Retrieved from https://www.hematology.org/education/trainees/fellows/case-studies/female-with-new-onset-aml-and-leukostasis .
American Society of Hematology. "Case Study: 47-Year-Old Woman With New-Onset AML and Leukostasis." Hematology.org. https://www.hematology.org/education/trainees/fellows/case-studies/female-with-new-onset-aml-and-leukostasis (label-accessed June 28, 2024).
"American Society of Hematology." Case Study: 47-Year-Old Woman With New-Onset AML and Leukostasis, 28 Jun. 2024 , https://www.hematology.org/education/trainees/fellows/case-studies/female-with-new-onset-aml-and-leukostasis .
Citation Manager Formats
- Share full article

A 2022 Supreme Court opinion.
Supported by
The Gun Lobby’s Hidden Hand in the 2nd Amendment Battle
In the battle to dismantle gun restrictions, raging in America’s courts even as mass shootings become commonplace, one name keeps turning up in the legal briefs and judges’ rulings: William English, Ph.D.
A little-known political economist at Georgetown University, Dr. English conducted a largest-of-its-kind national survey that found gun owners frequently used their weapons for self-defense. That finding has been deployed by gun rights activists to notch legal victories with far-reaching consequences.
He has been cited in a landmark Supreme Court case that invalidated many restrictions on guns, and in scores of lawsuits around the country to overturn limits on assault weapons, high-capacity magazines and the carrying of firearms. His findings were also offered in another Supreme Court case this term, with a decision expected this month.
Dr. English seems at first glance to be an impartial researcher interested in data-driven insights. He has said his “scholarly arc” focuses on good public policy, and his lack of apparent ties to the gun lobby has lent credibility to his work.
But Dr. English’s interest in firearms is more than academic: He has received tens of thousands of dollars as a paid expert for gun rights advocates, and his survey work, which he says was part of a book project, originated as research for a National Rifle Association-backed lawsuit, The New York Times has found.
He has also increasingly drawn scrutiny in some courts over the reliability and integrity of his unpublished survey, which is the core of his research, and his refusal to disclose who paid for it. Other researchers say that the wording of some questions could elicit answers overstating defensive gun use, and that he cherry-picked pro-gun responses.

The Bruen decision in 2022 upended Second Amendment law by sweeping away any modern-day gun restrictions that could not be tied to a historical antecedent. The ruling led to a surge in firearms cases — to an annual average of 680 today compared with 122 in the decade before. Pro-gun rulings have also risen: The 74 issued last year make up a quarter of all such rulings since 2000, according to researchers at the University of Southern California. Courts have struck down restrictions on high-capacity magazines in Oregon, handgun purchases in Maryland and assault weapons in California.

Dr. English’s brief in the Bruen case.
Here’s an example of that missing context.

The paper quotes a survey question, omitting the setup to it, which is highlighted below in blue.
Many policymakers recognize that a large number of people participate in shooting sports but question how often guns are used for self-defense. Have you ever defended yourself or your property with a firearm, even if it was not fired or displayed? Please do not include military service, police work, or work as a security guard.
Other questions followed the same pattern of omission. This one, about AR-15-style rifles, included text before and after the question in the version respondents saw, but not in the paper.
Some have argued that few gun owners actually want or use guns that are commonly classified as ‘assault weapons.’ Have you ever owned an AR-15 or similarly styled rifle? You can include any rifles of this style that have been modified or moved to be compliant with local law. Answering this will help us establish how popular these types of firearms are.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
Advertisement
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Iran J Ped Hematol Oncol
- v.4(4); 2014
A Case Report: Acute Myeloid Leukemia (FAB M7)
R masoumi-dehshiri.
1 Nutrition and Food Security Research Centre, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
2 Hematology and oncology Research Center, Shahid Sadoughi University of Medical Sciences and Health Services, Yazd, Iran.
H Neamatzadeh
H zare-zardeini.
Acute myeloid leukemia (AML-M7) is a type of pediatric AML accounting for 3–10% of primary childhood AML and children may present with a broad variety of symptoms including low-grade fever, diarrhea, easy bruising, failure to gain weight and life-threatening conditions. We report a rare case of AML .A 26-month-old boy who presented with weakness and fatigue. He was diagnosed as a case of AMLM-7 on the basis of peripheral blood finding, bone marrow examination report and immune phenotyping.
Introduction
Acute myeloid leukemia (AML) is the most common acute leukemia in adults [ , ]. In the United States and Europe, the incidence has been stable at 3 to 5 cases per 100,000 populations [ - ]. In contrast, AML accounts for less than 10 percent of acute leukemia's in children less than 10 years of age.AML comprises a type of hematologic malignancies with variable outcomes and characterized by a clonal proliferation of myeloid precursors with a reduced capacity to differentiate into more mature cellular elements. As a result, there is an accumulation of leukemic blasts or immature forms in the bone marrow, peripheral blood, and occasionally in other tissues, with a variable reduction in the production of normal red blood cells, platelets, and mature granulocytes ( 5 )
The un-differentiated myeloid cells show chromosomal abnormalities in about 55% of cases of adult AML [ 6 ]. Translocations are used for disease classification [ 6 , 7 ]. Although a presumptive diagnosis of AML can be made via examination of the peripheral blood smear when there are circulating leukemic blasts, a definitive diagnosis usually requires an adequate bone marrow aspiration. A portion of the biopsy can be submitted in saline or preferably culture medium and crushed in the flow cytometry laboratory to isolate a blast cell suspension for analysis [ 8 ].
The French-American-British classification (FAB) Classification sub-types of AML based on morphology and cytochemical staining with immunophenotypic data in some instances. Types (M0, M1, M2, and M3) are predominantly granulocytic and differ according to the extent of maturation. M4 is both granulocytic and monocytic, with at least 20%monocytic cells, whereas M5 is predominantly monocytic (at least 50% monocytic cells). M6 shows primarily differentiation with dysplastic features including megaloblastic changes, M7 is acute megakaryocytic leukemia (AML-M7) identified by the presence of megakaryocytic antigens demonstrated by flow cytometry or immunohistochemistry or the presence of platelet peroxides [ 9 ].
Case report
A 26-month-old boy patient from Iran who was admitted 9 month ago to the shahid sadoughi hospital that presenting with neutropenia associated with anemia and thrombocytopenia. There was no history of any hematological disorder. On examination; the patient had pallor and splenic enlargement, measuring 23 cm in ultrasonography.
Physical examination was otherwise unremarkable. The patient had been suffering from recurrent febrile episodes and nocturnal sweats with weakness and fatigue. Morphology and Immunophenotyping Peripheral blood cells were examined by an automated hematologic analyzer (Sysmex, XE-5000, Vienna, Austria).
Peripheral blood smear examination showed normocytic normochromic red blood cells including few nucleated red blood cells, white blood cells showed left, shift with significant number ofblast that suggestive of acute leukemia.Many giant platelets and platelet aggregates were seen. The leukocyte differential count was eosinophils5%, lymphocytes 62%, and neutrophils 31%and band forms 1%. Coagulation tests showed a prolonged prothrombin time of 16.3 sec (reference range, 10.2 to 13.8), a normal activated partial thromboplastin time, a normal fibrinogen and an increased D-dimer concentration of 4.96 mg/mL (reference range, 0 to 0.35). Bone marrow smears were stained with Wright-Giemsa and analyzed according to routine clinical laboratory procedures. Bone marrow aspiration and biopsy showed increased abnormal megakaryocytic, Monolobated and multinucleated megakaryocytic with hyper chromatic and pleomorphic nuclei were seen and showed the leukemic cells were positive for CD13 , CD33, CD42 and CD61 and negative for CD3, CD5, CD7, CD20, CD22 and human leukocyte antigen-DR. The biochemical parameters such as uric acid, bilirubin, creatinine, liver enzymes were normal. Serum LDH was slightly raised. The diagnosis was confirmed as AML-M7 as the blasts were positivefor CD42 and CD61 (megakaryocyte specific antigen) along with myeloid markers CD13 and CD33. Based on this diagnosis and with respect to the patient’s severely compromised overall condition, therapy withal-trans retinoic acid (ATRA, 10 mg/kg) was initiated, followed by cytarabine- and anthracycline-based induction polychemotherapy after 5 days and died four months after diagnosis.
The incidence of acute leukemia is approximately 2.3 per 100000 people per year.AML M-7 is a rare subtype of leukemia and represents 1.2% of cases of adult leukemia, compared to 3-10% of childhood leukemia ( 10 ).It is classified under M-7 in the French-American-British classification ( 11 ).
The patient was a 26 month years old male. Clinical features are not different from other type of AML but organomegaly is noted infrequently in adults. In our patient symptoms of anemia that is progressive weakness and diabetic were symptoms. Cytopenias are usually present but 30% of patients have platelet counts >100000/uL but in our case who had low platelet count (40x109/L). Osteosclerotic and osteolytic lesions have been described in few case reports [ 12 , 13 , 14 ].
The diagnosis depends on the expression of at least one platelet antigen (CD41, CD42b, and CD61) on the leukemic cells [ 13 , 14 ].In our patient bone marrow aspiration was done that showed increased abnormal megakaryocytic, Monolobated and multinucleated megakaryocytic with hyper chromatic and pleomorphic nuclei were seen and showed the leukemic cells were positive for CD13, D33,CD42 and CD61 and negative for CD3, CD5, CD7, CD20, CD22, and human leukocyte antigen-DR.Cytogenetic analysis was not carried out in this case. AML M 7 may present as de novo leukemia, secondary leukemia after chemotherapy, or transformed myeloproliferative disorders and myelodysplastic syndromes [ 15 ]. This report describes a presentation of AML M7 with thrombocytopenia. Although, nonspecific, cytogenetic abnormalities are more frequent (>90%) in AMLM-7 than in other subtypes of AML ( 14 ). The prognosis is significantly poor in AML M7 with megakaryocytic blast crisis. AML M7 by itself is an adverse prognostic factor for disease-free survival. However remission and long term survival are common in children with AML M7 specially in children with Down syndrome ( 15 , 16 ). This patient had partial recovery and clinically stable for several days with symptomatic treatment despite poor prognosis of AML-M7 and died four months after diagnosis.
AML M7 is a rare manifestation, patients with acute megakaryoblastic leukemia validated by a review of morphologic and immunophenotyping data is the largest comprehensive series with cytogenetic data to assess their frequencies and to emphasize the differences between M7 developing in infancy and adulthood. We conclude acute megakaryocytic leukemia should be considered in the differential diagnosis of undifferentiated acute leukemia with low platelet count.
Acknowledgements
We thank the participating children and all of the teachers (Shahid Sadoughi University of Medical Sciences and Health Services, Yazd, ran).
Conflict of interest
The authors have no conflict of interest.

COMMENTS
Official journal of the Myelodysplastic Syndromes Foundation. Leukemia Research Reports (LRR), a companion title to Leukemia Research, is a peer-reviewed publication devoted to the rapid publication of short, high-quality papers related to a broad scope of therapeutic areas of hematology, including …. View full aims & scope.
1.7 CiteScore. Official journal of the Myelodysplastic Syndromes Foundation. Leukemia Research Reports (LRR), a companion title to Leukemia Research, is a peer-reviewed publication devoted to the rapid publication of short, high-quality papers related to a broad scope of therapeutic areas of hematology, including …. View full aims & scope.
Relapsed acute myeloid leukemia. Discussion of Management. Dr. Andrew M. Brunner: This 49-year-old man had a subtype of AML that had arisen de novo, with a normal male karyotype and mutations in ...
Chronic lymphocytic leukemia (CLL) is one of the most common types of leukemia among adults in the United States and is still considered incurable. 1,2 It affects B and T lymphocytes as well as natural killer cells, but the majority of CLL cases diagnosed are of the B-cell phenotype. 3 CLL results from the uncontrolled clonal growth of small B lymphocytes in a manner that often leads to the ...
The phase 1-2 HGB-206 study is evaluating the efficacy and safety of LentiGlobin for sickle cell disease, and an unprespecified interim analysis of the results is now reported in the Journal. 8 ...
Read the latest Research articles from Leukemia. ... Case Report (2) Debate Round Table (53) ... (BC), emanating from chronic myeloid leukemia (CML), is a fatal disease with limited treatment ...
BACKGROUND. Acute leukemia in newborns is also known as neonatal or congenital leukemia (CL) and is a rare disease with an incidence rate of 1-5 per 1000000 live births. After birth, infants with CL exhibit infiltrative cutaneous nodules, hepatosplenomegaly, thrombocytopenia, and immature leukocytes in the peripheral blood.
Lenalidomide induced secondary Acute Lymphoblastic Leukemia in a Multiple Myeloma patient: A case-report. Dr. Saqib Raza Khan, Dr. Muhammad Tariq, Dr. Sidra Malik Fayyaz, Salman Muhammad Soomar, Dr. Munira Moosajee. Article 100315. View PDF.
NCI-funded researchers are working to advance our understanding of how to treat leukemia. With progress in both targeted therapies and immunotherapies, leukemia treatment has the potential to become more effective and less toxic. This page highlights some of the latest research in leukemia, including clinical advances that may soon translate ...
Leukemia is one of the leading journals in hematology and oncology. It covers all aspects of the research and treatment of leukemia and allied diseases. Studies of normal hemopoiesis are covered ...
The study is part of a comprehensive CLL characterization approved by the Internal Review Board of the Centro di Riferimento Oncologico di Aviano (Approvals n. IRB-05-2010, n. IRB-05-2015 and n ...
The patient was diagnosed with acute myeloid leukemia (AML)-M5b accompanied by DNMT3A, FLT3-TKD , and IDH2 mutations, chest CT re … A case report of complete remission of acute myeloid leukemia combined with DNMT3A, FLT3-TKD , and IDH2 gene mutations and active pulmonary tuberculosis treated with homeharringtonine + venetoclax + azacytidine
Pure erythroid leukemia (PEL) is an extremely rare type of acute myeloid leukemia (AML), accounting for fewer than 1% of all AML cases. A 72-year-old man presented with severe fatigue. His bone marrow aspiration contained myeloperoxidase negative abnormal cells that were aggregating and depicting epithelial adhesion, suggesting the possibility of solid tumor metastasis. His general condition ...
2. Case presentation. A 58-year-old man was admitted to a local hospital in March 2022 due to nausea and vomiting. His blood test results showed that he had a white blood cell count (WBC) of 25.3 × 10 9 /L, hemoglobin (HB) 65 g/L, and platelet (PLT) 190 × 10 9 /L. At the time, the doctor considered the possibility of acute leukemia.
Posted: December 10, 2019. For children and young adults with certain relapsed B-cell acute lymphoblastic leukemia (B-ALL), the immunotherapy drug blinatumomab is superior to standard chemotherapy, an NCI-sponsored Children's Oncology Group trial shows. Gilteritinib Improves Survival in AML with FLT3 Mutations.
Considering that the present study was a case report without a control group, our conclusions would be more robust if supported in multicenter clinical research. Table 1. Literature review of the treatment regimens for patients with AML complicated with T-LBL ... early T-cell precursor acute lymphoblastic leukemia or mixed phenotype acute ...
In such a consideration, therefore, our new publication, the Leukemia Research Reports is committing to support an open access rapid online publication of case reports, brief communications ...
Objective This study aims to elucidate the clinical features observed in cases of pediatric acute myeloid leukemia (AML) initially presenting with cardiac tamponade and to share treatment experiences.
Leukemia Research Reports. Volume 14, 2020, 100222. A case report and case review: Chronic myeloid leukemia (CML) blast phase with myelomastocytic differentiation ... Myelomastocytic blast cell crisis in resistant tyrosine kinase inhibitor chronic myelogenous leukemia: case report and review of literature. Cureus, 11 (5) (2019), p.
@article{Zhang2024WashedMT, title={Washed Microbiota Transplantation in an Elderly Patient with Lymphocytic Leukemia and Clostridioides difficile Infection: A Case Report Illustrating a Triumph Over Complexity}, author={Xinyu Zhang and Yuan Li and Bo Li and Jing Wu and Junmei Zhang and Xia Ding}, journal={Heliyon}, year={2024}, url={https://api ...
Chronic myeloid leukemia (CML) is a myeloproliferative neoplasm characterized by bone marrow expansion and the proliferation of one or more myeloid cell lineages, predominantly driven by the expression of the constitutively active fusion product tyrosine kinase BCR:ABL1. Rarely, CML patients directly develop a blast crisis (BC), mostly of myeloid origin. CML at blast crisis with a T-cell ...
This article is part of the Research Topic Case Reports in Thrombosis: 2023 View all 9 articles. Acute pulmonary embolism combined with acute myocardial infarction as the first manifestation of acute leukemia: a case report. Shuzhan Zheng 1* Sha Luo 1 Yong Luo 1 Dan Liu 2,3 Wenwu Zheng 1 Qing Peng 1. 1 Department of Cardiology, ...
Abstract. We report two cases of chronic myeloid leukaemia (CML) with extreme thrombocytosis. The first patient was a 65-year-old man who presented with prolonged history of upper abdominal discomfort, anorexia and two episodes of recent gum bleeds without fever or other bleeding manifestations. He was a chronic smoker with no other comorbidities.
INDIANAPOLIS — Indiana University School of Medicine researchers and their collaborators have uncovered molecular insights expected to enhance treatment options for acute myeloid leukemia (AML), a rare and severe blood and bone marrow cancer. With a new chemical compound engineered to overcome drug-resistant gene mutations not targeted by current treatments, the researchers aim to provide a ...
Translocation (2;8) (p12;q24) in blastic transformation of atypical chronic myeloid leukemia. SK Ma. KL Au. LC Chan. Case Report 01 Apr 1997. Leukemia ( Leukemia) ISSN 1476-5551 (online) ISSN 0887 ...
Immunostainings allowed to specify the type of leukemia (71.4%). In one case, diagnosis was made on blood smear and flow cytometry was performed on fresh blood samples. All cases corresponded to acute myeloid leukemia. Karyotype was abnormal in 4 cases (66.7%), including one free trisomy 21, two mosaic trisomy 21 and one chromosome 15 deletion.
Blood. 2013; 121:4854-4860. A 47-year-old woman presents to the emergency department complaining of fatigue and shortness of breath. She reports a two-week history of worsening exercise tolerance and a rather abrupt onset of shortness of breath over the past several hours.
Dr. English's 2021 brief in the Bruen case debuted his "National Firearms Survey," one of two gun studies he had posted just days earlier on the Social Science Research Network site, where ...
All articles published in Leukemia Research Reports are peer-reviewed and indexed in PubMed/PubMed Central and Scopus. They are fully citable through digital object identifiers (DOI) and rapidly available online via ScienceDirect, the world's leading online content platform. ... Case Reports must present an abstract, should not exceed 1,500 ...
Discussion. The incidence of acute leukemia is approximately 2.3 per 100000 people per year.AML M-7 is a rare subtype of leukemia and represents 1.2% of cases of adult leukemia, compared to 3-10% of childhood leukemia ( 10 ).It is classified under M-7 in the French-American-British classification ( 11 ). The patient was a 26 month years old ...