Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character

Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Eating Disorders: Current Knowledge and Treatment Update
- B. Timothy Walsh , M.D.
Search for more papers by this author
Although relatively uncommon, eating disorders remain an important concern for clinicians and researchers as well as the general public, as highlighted by the recent depiction of Princess Diana’s struggles with bulimia in “The Crown.” This brief review will examine recent findings regarding the diagnosis, epidemiology, neurobiology, and treatment of eating disorders.

Eight years ago, DSM-5 made major changes to the diagnostic criteria for eating disorders. A major problem in DSM-IV ’s criteria was that only two eating disorders, anorexia nervosa and bulimia nervosa, were officially recognized. Therefore, many patients presenting for treatment received the nonspecific diagnostic label of eating disorder not otherwise specified (EDNOS), which provided little information about the nature of the patient’s difficulties. This problem was addressed in several ways in DSM-5 (see DSM-5 Feeding and Eating Disorder list). The diagnostic criteria for anorexia nervosa and bulimia nervosa were slightly expanded to capture a few more patients in each category. But two other changes had a greater impact in reducing the use of nonspecific diagnoses.
The first of these was the addition of binge eating disorder (BED), which had previously been described in an appendix of DSM-IV . BED is the most common eating disorder in the United States, so its official recognition in DSM-5 led to a substantial reduction in the need for nonspecific diagnoses.
DSM-5 Feeding and Eating Disorder
Rumination Disorder
Avoidant/restrictive food intake disorder
Anorexia nervosa
Bulimia nervosa
Binge-eating disorder
Other specified feeding or eating disorder
Unspecified feeding or eating disorder
The second important change was the combination of the DSM-IV section titled “Feeding and Eating Disorders of Infancy or Early Childhood” with “Eating Disorders” to form an expanded section, “Feeding and Eating Disorders.” This change thereby included three diagnostic categories: pica, rumination disorder, and feeding disorder of infancy or early childhood. Pica and rumination disorder are infrequently diagnosed.
The other category, feeding disorder of infancy or early childhood, was rarely used and had been the subject of virtually no research since its inclusion in DSM-IV . The Eating Disorders Work Group responsible for reviewing the criteria for eating disorders for DSM-5 realized that there was a substantial number of individuals, many of them children, who severely restricted their food intake but did not have anorexia nervosa. For example, after a severe bout of vomiting after eating, some individuals attempt to prevent a recurrence by no longer eating at all, leading to potentially serious nutritional disturbances. No diagnostic category in DSM-IV existed for such individuals. Therefore, the DSM-IV category, feeding disorder of infancy or early childhood, was expanded and retitled “avoidant/restrictive food intake disorder” (ARFID). Combined, these changes led to a substantial reduction in the need for nonspecific diagnostic categories for eating disorders.
In the course of assessing the impact of the recommended changes in the diagnostic criteria for eating disorders, the Eating Disorders Work Group became aware of another group of individuals presenting for clinical care whose symptoms did not quite fit any of the existing or proposed categories. These were individuals, many of them previously overweight or obese, who had lost a substantial amount of weight and developed many of the signs and symptoms characteristic of anorexia nervosa. However, at the time of presentation, their weights remained within or above the normal range, therefore not satisfying the first diagnostic criterion for anorexia nervosa. The work group recommended that a brief description of such individuals be included in the DSM-5 diagnostic category that replaced DSM-IV ’s EDNOS: “other specified feeding and eating disorders” (OSFED); this description was labeled atypical anorexia nervosa. The degree to which the symptoms, complications, and course of individuals with atypical anorexia nervosa resemble and differ from those of individuals with typical anorexia nervosa remains an important focus of current research.
Epidemiology
Although eating disorders contribute significantly to the global burden of disease, they remain relatively uncommon. A study published in September 2018 by Tomoko Udo, Ph.D., and Carlos M. Grilo, Ph.D., in Biological Psychiatry examined data from a large, nationally representative sample of over 36,000 U.S. adults 18 years of age and older surveyed using a lay-administered diagnostic interview in 2012-2013. The 12-month prevalence estimates for anorexia nervosa, bulimia nervosa, and BED were 0.05%, 0.14%, and 0.44%, respectively. Although the relative frequencies of these disorders were similar to those described in prior studies, the absolute estimates were somewhat lower for unclear reasons. Consistent with clinical experience and prior reports, the eating disorders, especially anorexia nervosa and bulimia nervosa, were more prevalent among women (though men are also affected). Although eating disorders occurred across all ethnic and racial groups, there were fewer cases of anorexia nervosa among non-Hispanic and Hispanic Black respondents than among non-Hispanic White respondents. Consistent with long-standing clinical impression, individuals with lifetime anorexia nervosa reported higher incomes.
Finally, when BED was under consideration for official recognition in DSM-5 , some critics suggested that, since virtually everyone occasionally overeats, BED was an example of the misguided tendency of DSM to pathologize normal behavior. The low prevalence of BED reported in the study by Udo and Grilo documents that, when carefully assessed, BED affects only a minority of individuals and is therefore distinct from normality.
A subject of some debate and substantial uncertainty is whether the incidence of eating disorders (the number of new cases a year) is increasing. Some studies, such as that of Udo and Grilo, have found that the lifetime rates of eating disorders among older individuals are lower than those among younger individuals, suggesting that the frequency of eating disorders may be increasing. However, this might also reflect more recent awareness and knowledge of eating disorders. Other studies that conducted multiple examinations of the frequency of eating disorders in the same settings over time appear to suggest that, in the last several decades, the incidence of anorexia nervosa has remained roughly stable, whereas the incidence of bulimia nervosa has decreased. Presumably, this reflects changes in the sociocultural environment such as an increased acceptance of being overweight and reduced pressure to engage in inappropriate compensatory measures such as self-induced vomiting after binge eating.
The COVID-19 pandemic has impacted virtually every facet of life across the world and has produced severe financial, medical, and psychological stresses. Preliminary research suggests that such stresses have exacerbated the symptoms of individuals with preexisting eating disorders and have led to increased binge eating in the general population. Hopefully, these trends will improve with successful control of the pandemic.
Neurobiology
Much recent research on the mechanisms underlying the development and persistence of eating disorders has focused on the processing of rewarding and nonrewarding/punishing stimuli. Several studies have suggested that individuals with anorexia nervosa are less able to distinguish among stimuli with varying probabilities of obtaining a reward. Other studies suggest that, when viewing images of food during MRI scanning, individuals with anorexia nervosa tend to show less activation of brain reward areas than do controls. Such deficits may be related to disturbances in dopamine function in areas of the brain known to be involved in reward processing. Research based on emerging methods in computational psychiatry suggests that individuals with anorexia nervosa may be particularly sensitive to learning from punishment; for example, they may be very quick to learn what stimuli lead to a decrease in the amount of a reward. Conceivably, they may learn that eating high-fat foods prevents weight loss and produces undesirable weight gain, and they begin to avoid such foods. These studies, and a range of others, focus on probing basic brain mechanisms and how they may be disrupted in anorexia nervosa. A challenge for this “bottom-up” approach is to determine how exactly disturbances in such mechanisms are related to the eating disturbances characteristic of anorexia nervosa.
Other recent studies take a “top-down” approach, focusing on the neural circuitry underlying the persistent maladaptive choices made by individuals with anorexia nervosa when they decide what foods to eat. Such research successfully captures the well-established avoidance of high-fat foods by individuals with anorexia nervosa and has documented that such individuals utilize different neural circuits in making decisions about what to eat than do healthy individuals. These results are consistent with suggestions that the impressive persistence of anorexia nervosa in many individuals may be due to the establishment of automatic, stereotyped, and habitual behavior surrounding food choice. A challenge for such top-down research strategies is to determine how these maladaptive patterns develop so rapidly and become so ingrained.
Research on the neurobiology underlying bulimia nervosa is broadly similar. Although the results are complex, individuals with bulimia nervosa appear to find food stimuli more rewarding, and there are indications of disturbances in reward responsiveness to sweet tastes. Several studies have documented impairments in impulse control assessed using behavioral paradigms such as the Stroop Task. In this task, individuals are presented with a word naming a color (for example, “red”) but asked to name the color of the letters spelling the word (for example, the letters r, e, and d are green). Increased difficulties in performing such tasks have been described in individuals with bulimia nervosa and linked to reduced prefrontal cortical thickness.
It has long been known that eating disorders tend to run in families, and there has been strong evidence that this in part reflects the genes that individuals inherit from their parents. In recent decades, it has become clear that the risk of developing most complex human diseases, including obesity, hypertension, and eating disorders is related to many genes, each one of which contributes a small amount to the risk. Because the contribution of a single gene is so small, the DNA from a very large number of individuals with and without the disorder needs to be examined. For instance, genomewide association studies (GWAS) in schizophrenia have examined tens of thousands of individuals with schizophrenia and over 100,000 controls and identified well over 100 genetic loci that contribute to the risk of developing schizophrenia.
GWAS examining the genetic risk for eating disorders are under way but to date have focused primarily on anorexia nervosa. The Psychiatric Genetics Consortium has collected information from 10,000 to 20,000 individuals with anorexia nervosa and over 50,000 controls and has, so far, identified eight loci that contribute to the genetic risk for this disorder. In addition, this work has identified genetic correlations between anorexia nervosa and a range of other disorders known to be comorbid with anorexia nervosa such as anxiety disorders as well as a negative genetic correlation with obesity. These data suggest that the genetic risk for anorexia nervosa is based on a complex interplay between loci associated with a range of psychological and metabolic/anthropometric traits.
Although there have been no dramatic developments in our knowledge of how best to treat individuals with eating disorders, there have been some significant and useful advances in recent years.
For anorexia nervosa, arguably the most significant advance in treatment in the last quarter century has been family-based treatment for adolescents. In this approach, sometimes referred to as the “Maudsley method,” the family, guided by the therapist, becomes the primary agent of change and responsible for ensuring that eating behavior normalizes and weight increases. This approach differs markedly from prior treatment strategies that assumed parental involvement was not helpful or even detrimental. Family-based treatment is now widely viewed as a treatment of first choice for adolescents with anorexia nervosa and has also been adapted to treat bulimia nervosa.
Family-based treatment can be quite challenging for parents. The entire family is asked to attend treatment sessions, and one session early in treatment includes a family meal during which the parents are charged with the difficult task of persuading the adolescent to consume more food than he/she had intended. An alternative but related model, termed “parent-focused treatment,” has recently been explored in a few studies. In this approach, parents meet with a therapist without the affected adolescent or other members of the family and receive guidance regarding how to help the adolescent to alter his or her behavior following techniques virtually identical to those provided in traditional family-based treatment. Several small studies have examined this approach, and results suggest similar effectiveness. Although more research is needed, these findings suggest that parent-focused treatment may be an attractive alternative to family-based treatment for many parents and practitioners.
The COVID-19 pandemic has led to a dramatic acceleration in the provision of psychiatric care remotely, including family-based treatment. Work on providing family-based treatment via videoconference had begun prior to the arrival of COVID-19, as this specialized form of care is not widely available, and its provision via HIPAA-compliant video links would offer a substantial increase in accessibility. Several small studies suggested that remote provision of family-based treatment is feasible and likely to be efficacious. The restrictions imposed by COVID-19 on face-to-face contact have accelerated the remote delivery of family-based treatment; hopefully, new research will document its effectiveness. It should be noted, however, that, in most cases, local contact with a medical professional who can directly measure weight and oversee the patient’s physical state is required.
The treatment of adults with anorexia nervosa, who typically developed the disorder as teenagers and have been ill for five or more years, remains challenging. Structured behavioral interventions, such as those available in specialized inpatient, day program, or residential centers, typically lead to significant weight restoration and psychological and physiological improvement. However, the rate of relapse following acute care remains substantial. Furthermore, most adult patients with anorexia nervosa are very reluctant to accept treatment in such structured programs. A recent helpful development is evidence that olanzapine, at a dose of 5 mg/day to 10 mg/day, assists modestly with weight gain in adult outpatients with anorexia nervosa and is associated with few significant side effects. Unfortunately, it does not address core psychological symptoms and must be viewed as adjunctive to standard care.
There have been fewer recent developments in the treatment of patients with bulimia nervosa and of BED. For bulimia nervosa, cognitive-behavioral therapy remains the mainstay psychological treatment, and SSRIs continue to be the first-choice class of medication. For BED, multiple forms of psychological treatment are associated with substantial improvement in binge eating, and, in 2015, the FDA approved the use of the stimulant lisdexamfetamine (Vyvanse) for individuals with BED. Unlike most psychological treatments, lisdexamfetamine is associated with modest weight loss but has effects on pulse and blood pressure that may be of concern, especially for older individuals.
Also noteworthy are the development and application of new forms of psychological treatment for individuals with eating disorders. These include dialectical behavior therapy (DBT), acceptance and commitment therapy (ACT), and integrative cognitive-affective therapy (ICAT). Although only a few controlled studies have examined the effectiveness of these treatments, anecdotal information and the results of these studies suggest that such methods may be useful alternatives to more established interventions.
Conclusions
Eating disorders remain uncommon but clinically important problems characterized by persistent disturbances in eating or eating-related behavior. Cutting-edge research focuses on neurobiology and genetics, utilizing novel and rapidly evolving methodology. There have been modest advances in treatment approaches, including the COVID-19 pandemic’s acceleration of treatment delivery via video-link. Future studies will hopefully clarify the nature of ARFID and of atypical anorexia nervosa and lead to the development of more effective interventions, especially for individuals with long-standing eating disorders. ■
Additional Resources
Walsh BT. Diagnostic Categories for Eating Disorders: Current Status and What Lies Ahead. Psychiatr Clin North Am . 2019; 42(1):1-10.
Udo T, Grilo CM. Prevalence and Correlates of DSM-5 -Defined Eating Disorders in a Nationally Representative Sample of U.S. Adults. Biol Psychiatry . 2018; 84(5):345-354.
Van Hoeken D, Hoek HW. Review of the Burden of Eating Disorders: Mortality, Disability, Costs, Quality of Life, and Family Burden. Curr Opin Psychiatry . 2020; 33(6):521-527.
Bernardoni F, Geisler D, King JA, et al. Altered Medial Frontal Feedback Learning Signals in Anorexia Nervosa. Biol Psychiatry . 2018; 83(3):235-243.
Frank GKW, Shott ME, DeGuzman MC. The Neurobiology of Eating Disorders. Child Adolesc Psychiatr Clin N Am . 2019; 28(4):629-640.
Steinglass JE, Berner LA, Attia E. Cognitive Neuroscience of Eating Disorders. Psychiatr Clin North Am . 2019; 42(1):75-91.
Bulik CM, Blake L, Austin J. Genetics of Eating Disorders: What the Clinician Needs to Know. Psychiatr Clin North Am . 2019; 42(1):59-73.
Attia E, Steinglass JE, Walsh BT, et al. Olanzapine Versus Placebo in Adult Outpatients With Anorexia Nervosa: A Randomized Clinical Trial. Am J Psychiatry . 2019; 176(6):449-456.
Le Grange D, Hughes EK, Court A, et al. Randomized Clinical Trial of Parent-Focused Treatment and Family-Based Treatment for Adolescent Anorexia Nervosa. J Am Acad Child Adolesc Psychiatry . 2016; 55(8):683-92.
Pisetsky EM, Schaefer LM, Wonderlich SA, et al. Emerging Psychological Treatments in Eating Disorders. Psychiatr Clin North Am . 2019; 42:219-229.
B. Timothy Walsh, M.D., is a professor of psychiatry at the Columbia University Irving Medical Center and the founding director of the Columbia Center for Eating Disorders at the New York State Psychiatric Institute. He is the co-editor of the Handbook of Assessment and Treatment of Eating Disorders from APA Publishing.
Dr. Walsh reports receiving royalties or honoraria from UpToDate, McGraw-Hill, the Oxford University Press, the British Medical Journal, the Johns Hopkins Press, and Guidepoint Global

BRIEF RESEARCH REPORT article
Mentalizing in psychotherapeutic processes of patients with eating disorders.

- 1 Department of Psychosomatic Medicine und Psychotherapy, Center for Mental Health, Faculty of Medicine, University of Freiburg, Freiburg im Breisgau, Germany
- 2 Department of Consultation Psychiatry and Psychosomatics, University Hospital Zürich, Zürich, Switzerland
Background: Improvement in the capacity to mentalize (i.e., reflective functioning/RF) is considered both, an outcome variable as well as a possible change mechanism in psychotherapy. We explored variables related to (in-session) RF in patients with an eating disorder (ED) treated in a pilot study on a Mentalization-Based Treatment (MBT) - oriented day hospital program. The research questions were secondary and focused on the psychotherapeutic process: What average RF does the group of patients show in sessions and does it change over the course of a single session? Are differences found between sections in which ED symptomatology is discussed and those in which it is not? Does RF increase after MBT-type interventions?
Methods: 1232 interaction segments from 77 therapy sessions of 19 patients with EDs were rated for RF by reliable raters using the In-Session RF Scale. Additionally, content (ED symptomatology yes/no) and certain MBT interventions were coded. Statistical analysis was performed by mixed models.
Results: Patients showed a rather low RF, which increased on average over the course of a session. If ED symptomatology was discussed, this was associated with significantly lower RF, while MBT-type interventions led to a significant increase in RF.
Conclusions: Results suggest that in-session mentalizing can be stimulated by MBT-typical interventions. RF seems to be more impaired when disorder-specific issues are addressed. Further studies have to show if improving a patient´s ability to mentalize their own symptoms is related to better outcomes.
1 Introduction
Mentalizing describes the ability to perceive and understand oneself and others (one’s own behavior/the behavior of others) in relation to inner states, feelings, intentions and desires ( 1 ). The capacity to mentalize is important for self-regulation (including the regulation of impulses and affect), as well as the regulation of relationships ( 1 ). Therefore, improved mentalizing (operationalized as Reflective Functioning/RF) is discussed both as an desirable outcome of psychotherapy as well as a change mechanism in psychotherapeutic processes ( 2 – 4 ). It was also suggested that a better ability to mentalize is associated with better therapeutic alliances and reduces the risk of treatment drop-out ( 5 , 6 ). This is an obvious consideration, as a patient who is able to reflect on the mental state of his/her therapist will find it easier not to experience a behavior or intervention as directed against him/herself. To improve mentalizing is the main focus in Mentalization Based Treatment (MBT), an approach originally developed for the treatment of borderline personality disorder – a disorder in which mentalizing is considerably impaired ( 7 , 8 ). More recently, MBT was adapted for the use in other mental disorders with impairment in mentalizing ( 9 ), including eating disorders ( 10 , 11 ).
RF can be described along different dimensions: It can be related to the self or another person, has a cognitive or affective focus, be implicit or explicit and related to something observable vs. internal mental states ( 4 ). Additionally, RF is not only a skill that people have more or less. Mentalizing in a given situation also depends on the context - for example, on the emotional relevance of a given session or the level of arousal induced in the relationship with another individual, including the therapist ( 7 ). For instance, high emotional arousal will lead to a fight or flight reaction instead of mentalizing. Therefore, the overall capacity to mentalize a person shows (e.g. in a structured interview like the Adult Attachment Interview), might differ from RF in a specific situation. Such a specific situation are psychotherapy sessions, in which RF is expected to be improved by therapeutic interventions. “In-session” RF (which can be measured with the In-Session-RF-Scale, see below) will depend on the relationship between the patient and the therapist, the topics discussed, the interventions of the therapist and several other factors that might influence the situation (e.g. events prior to the session: if a patient had a conflict with her partner) ( 12 ). Furthermore, RF might be impaired concerning the symptoms a patient has. “Symptom specific RF” was defined by Rudden et al. as the ability to reflect on the underlying meaning and affect- or relationship-related function of a symptom ( 13 ).
Overall, RF-related process research is in its infancy, although a better understanding of the factors that stimulate mentalizing in sessions and if and how mentalizing is related to productive psychotherapeutic processes is urgently needed. Previous research was able to find a relationship between interventions that are intended to increase RF and higher RF in the respective session (e.g. 14 – 16 ). Better RF in a session in turn predicted lower emotional arousal in patients with borderline personality disorder ( 14 ). Furthermore, an increase in in-session RF (positive deviation from the individual baseline-level) was shown to be related to less interpersonal problems and a reduction of depressive symptoms in patients with depression and anxiety treated with cognitive-behavior therapy ( 17 ).
Eating disorders (EDs) like anorexia nervosa (AN) and bulimia nervosa (BN) primarily affect girls and women in the first half of their lives. AN and BN can easily become chronic with fluctuating courses, and are associated with serious mental and physical consequences ( 18 ). Treatment outcomes are not satisfactory, with remission rates barely reaching 50% in adults ( 19 ). AN, in particular, carries high mortality rates ( 20 ). At the core of psychopathology are difficulties in regulating negative affect ( 21 ), along with weight and shape concerns ( 22 ). These issues contribute to problematic eating behaviors (restrictive and/or binge eating) and inappropriate compensatory behaviors to prevent weight gain. Maintaining factors include affect intolerance, unfavorable interpersonal interactions, consequences of malnutrition, and habit formation ( 23 ). Psychotherapeutic treatment is challenging because of a high ambivalence regarding change ( 24 ) and a strong wish for autonomy, while feeling needy and dependent on important others ( 25 ). In the majority of studies RF in individuals with ED was found to be impaired, including RF as shown in psychotherapy sessions ( 26 , 27 ). This is consistent with the fact that problems with the regulation of self-esteem, emotions and impulses on one hand and relationships on the other are at the core of ED psychopathology ( 18 ). Therefore, an adapted MBT-approach (MBT-ED) which focuses on an improvement in the capacity to mentalize might be helpful also in the treatment of individuals with an ED. However, there are only few pilot studies evaluating such an approach ( 11 , 28 , 29 ) and one randomized controlled study which included patients with an ED and features of a borderline-personality disorder ( 30 ). All of these studies have methodological limitations (observational studies, high drop-out rates) limiting the conclusions which can be drawn from them.
We developed a MBT manual for the treatment of eating disorders ( 11 , 31 ) and - as a first step - conducted an observational proof-of-concept study in a day hospital setting ( 11 ). Results were promising and showed that the program was well accepted by the patients (drop-out rate: 13.2%) and lead to significant reductions in eating pathology (EDE total score) and difficulties with emotion regulation as well as an improvement in RF ( 11 ), although overall outcome in ED symptomatology did not differ when compared to a historical matched control group.
The goal of this study, which followed an exploratory approach, is to support a better understanding of processes related to RF in psychotherapy sessions. To this end, we propose to answer the following questions that may inform future research: What is the average RF score of patients during individual MBT-ED sessions? Does RF change over the course of a single session? Are there differences in RF between parts of a therapy session in which eating disorder symptoms are discussed and those in which they are not? Are certain MBT-type interventions associated with increases in RF during the same during the same session sequence? Although the study - due to the few process studies in patients with eating disorders on this topic - was primarily exploratory in nature, we had some expectations based on previous findings. We expected a level of RF below the average values for health individuals. We further expected that MBT-type interventions will be associated with an increase in RF and that RF in average will increase over the course of a session (as we analyzed MBT-oriented sessions with corresponding objectives).
2.1 Study design – original study
The original “proof-of-concept”-study was prospective and observational. It was approved by the local ethics committee (No 448/17) and conducted in a day hospital, which provides an MBT-ED program for six patients with an ED at a time. All consecutively admitted patients with an ED over a period of 2 years were asked to take part in the study. In this time period, 38 out of 40 ED-patients admitted could be included. Inclusion criteria were a diagnosis of anorexia nervosa (AN), bulimia nervosa (BN) or other specified feeding and eating disorders (OSFED) according to DSM-5 (mental diagnoses were given after a SCID-5 interview), age ≥ 18, BMI ≥ 14.5 kg/m² and an indication for day hospital treatment ( 11 ). Exclusion criteria were psychoses, substance dependency, bipolar disorder, organic brain disease, dementia, severe somatic illness or acute suicidal ideation. The multimodal treatment program includes two MBT individual sessions per week (50 min, 25 min) and a one-weekly MBT-group therapy session besides further components [e.g. art and body therapy, work with an eating diary; for details see ( 11 )]. Therapists were trained in MBT and supervised by a certified MBT supervisor. Individual sessions were videotyped and assessed for MBT adherence which included feed back to the therapist after every 4th session. Main time points of assessment were admission, discharge and follow up assessments three and twelve months after discharge.
2.2 Process study
Every second patient was asked to take part in a process study (not every patient could be included due to the high effort involved). To study psychotherapeutic processes, we focused on individual treatment sessions. The second session and every forth of following sessions were included and transcribed according to the rules of Mergenthaler ( 32 ). Session transcripts were divided into 3-minute sequences. Thus, a therapy session of about 50 minutes yields 17 coded segments, with a time variable ranging from 3 to 51 by 3. Each sequence of the included sessions was rated for RF using the In-Session-Reflective Functioning-Scale ( 12 ). The scale ranges from -1 (refusing to use RF) and 0 (no RF) to values between 1 and 9 (1-4 low RF, 5 = normal RF, 6-9 high RF). The ratings were conducted by two trained and reliable raters (ICC = .81 ( 27 );). In addition to RF, the content of a sequence was coded. It was coded in terms of a focus on eating symptomatology (1 = yes/defined as sequences with a focus on ED symptoms vs. 0 = no/sequences without this focus) and if two types of MBT- interventions were used in the respective time segment: „demand”-interventions (prompting a patient to reflect on or explore a topic in more detail) and empathic validation (actively validating the emotional experience reported by a patient) (1 = yes/sequences with MBT intervention; 0 = no/sequences without MBT intervention).
We decided to exclude the last six minutes of each session from the analysis, because of typically very low RF (tested with mixed model: -0.64 RF compared to the other time segments; p < 0.0001), potentially changing the trajectory to non-linear. We considered the last minutes (talking out/saying goodbye, appointments, organizational issues) therefore as not representative of the psychotherapy process and the capacity of a patient to mentalize.
2.3 Psychometric measures
Eating psychopathology was measured with the Eating Disorder Examination Interview (EDE) interview ( 33 , 34 ) and the Eating Disorder Inventory self-report questionnaire (EDI-2) ( 35 , 36 ), general psychopathology with the Symptom-Check-List (SCL-90-R) ( 37 ), see also ( 11 ). In the original study, time points of measurement were admission, discharge as well as three and twelve month after discharge.
2.4 Statistical analysis
In order to account for the hierarchical structure of the data, we used mixed models to estimate linear trends of RF within sessions and it’s relations to session process. The analyses were computed with R (V4.2.2) and the package lme4 (V.1.1-32; Syntax see Table 1 ; REML estimation).
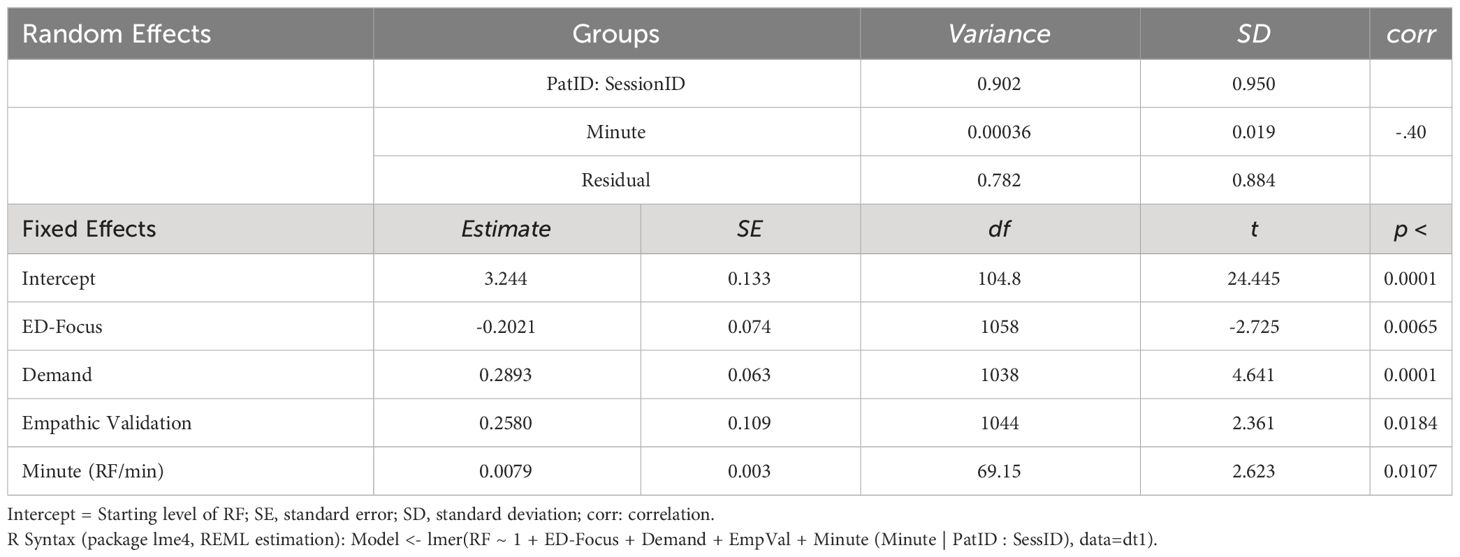
Table 1 Results of mixed model.
19 patients were included in the study. 77 sessions and 1232 session sequences were available for the analysis. For a sample description see Table 2 .
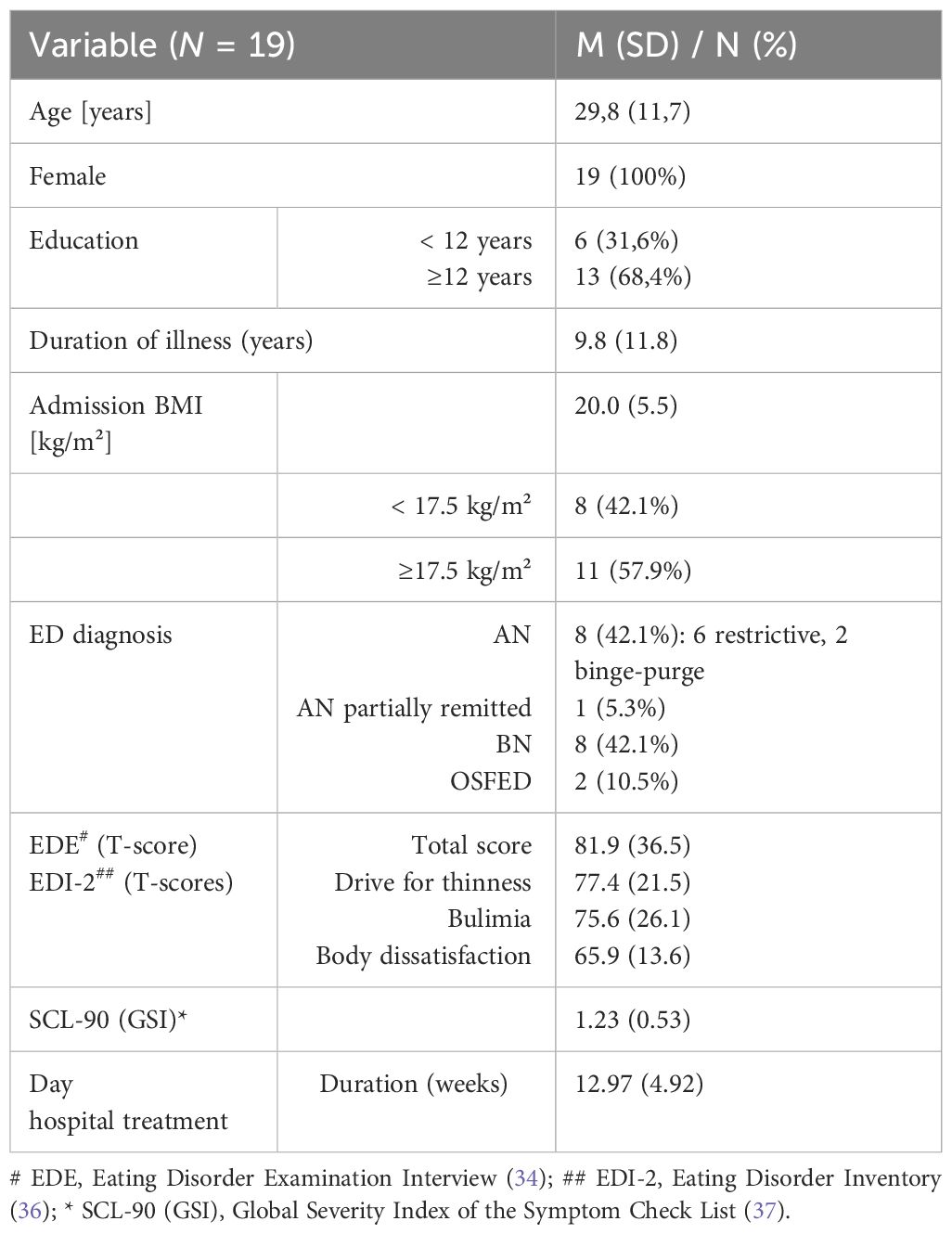
Table 2 Sample description.
Overall, patients showed a low level of RF in sessions (M = 3.48). It did not differ between patients with a BMI below 18.5 kg/m² (M = 3.54; N = 9) and those with a BMI of 18.5-25 kg/m² (M = 3.47; N = 8). Two patients with a BMI > 25 kg/m² had a lower RF (M = 2.50; N = 2). On average, RF increased over the course of a session (Intercept = 3.24, slope = +0.0079/min = +0.48/50min), see Table 1 . Talking about eating-disorder related themes was associated with significantly lower RF (-0.20) within the respective, 3-minute long sequences of the sessions. Demand-interventions were positively associated with higher RF (+ 0.29) within the respective 3-minute sequence, this also applied to empathic validation (+ 0.26). Table 1 shows the formula and the estimates of the mixed model. For an illustration and better understanding, a constructed trajectory of a singe case is visualized in Figure 1 .
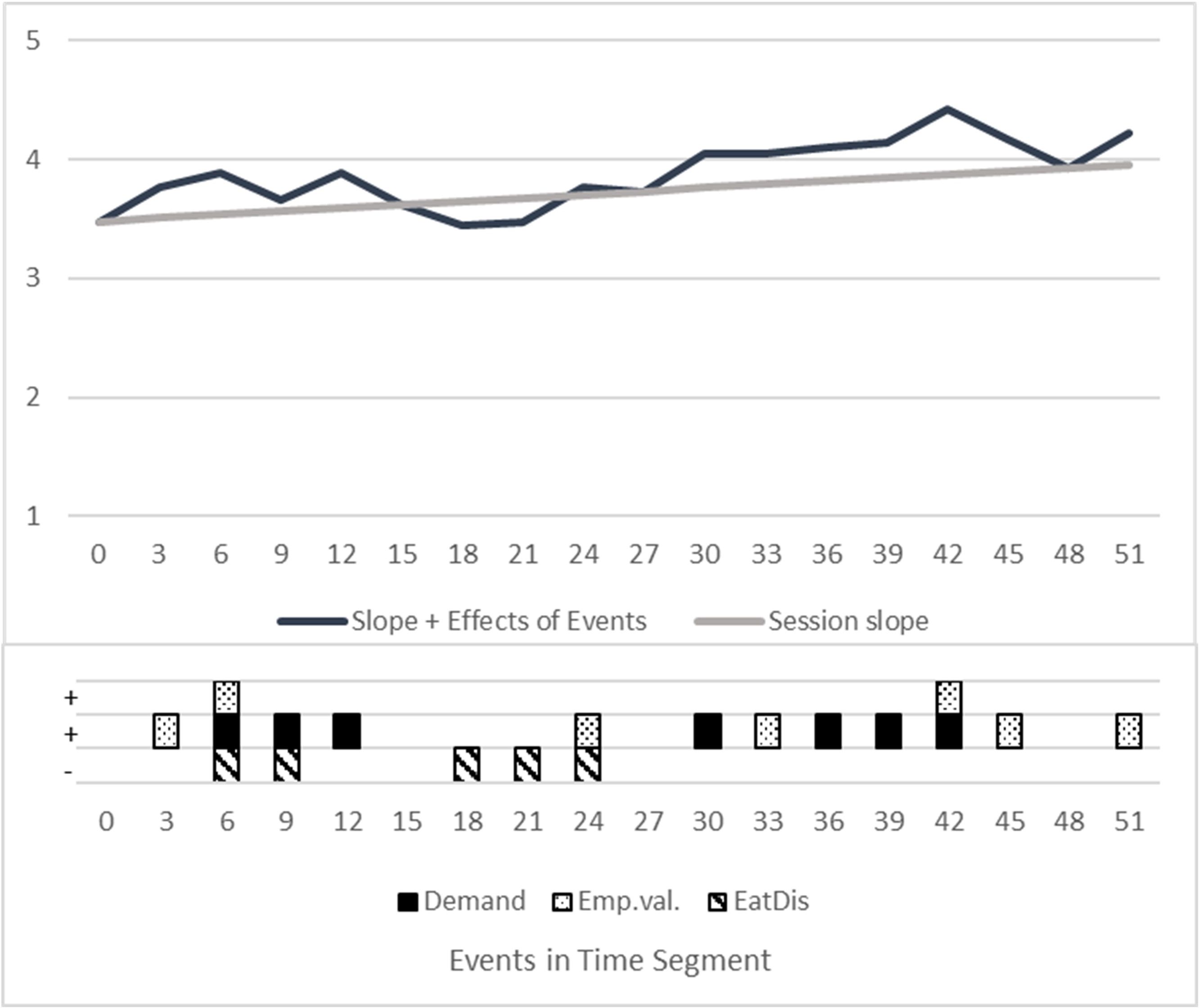
Figure 1 Visualization of a constructed therapy session. Constructed trajectory, showing the estimated impact of interventions on RF with a hypothetical pattern of interventions and ED focus. “Session slope”: RF Mean session trajectory with intercept = 3.48 RF and estimated increase of 0.48 RF (from minute 1 to minute 50). “Events”: Estimation of fixed effects directly in the segment of occurrence. Slope + Effects of Events: Mean course PLUS effects of all events / interventions. X-Axis/Time: Divided into the rated segments of 3 minutes. Squares with patterns: Constructed occurrences of interventions, coded yes=1, no = 0. Random Effects: Not shown, as this is a constructed single case. Random intercepts and slopes differ individually.
4 Discussion
The average RF shown in the sessions was low ( 38 , 39 ). This is consistent with preliminary findings in patients with EDs ( 10 , 26 ). It has to be taken into account that we assessed in-session RF, which depends on the process in each session and interventions used by the therapist. However, if we understand a psychotherapeutic session as a situation in which RF is usually challenged, average in-session RF will be an indicator for the overall capacity to mentalize ( 17 ). Talia et al. ( 12 ) found a moderate correlation between In-Session-RF and RF as assessed with the Adult Attachment Interview (AAI), probably due to the less standardized situation in therapy sessions (the AAI is a structured interview that uses so-called “demand” questions to stimulate RF). Nevertheless, patients with higher RF ratings in the AAI, showed also a better capacity to mentalize in psychotherapy sessions.
We found that RF increased over the course of a session. This might reflect a process of increasing reflection in this session, which would be intended in an MBT-oriented treatment ( 7 , 40 ). However, we cannot rule out that the finding is unspecific and for example due to the typical structure of a psychotherapy session: At the beginning the focus is on getting into contact and establishing a safe atmosphere, before more challenging topics are discussed. However, despite the general increase in RF, there could be fluctuations in RF that depend, for example, on the extent to which a patient feels perceived by their therapist and considers their interventions to be credible and trustworthy ( 41 , 42 ).
In terms of content, RF was lower in transcript sequences in which symptomatology was discussed. This could mean that mentalizing might „break in” when disorder-specific topics are addressed and be interpreted as a reduced capacity to reflect on the function and meaning of symptoms. It is an important question, if this correlation changes over the course of a successful treatment (that psychotherapy leads to an increase in RF in the context of eating-disorder related themes) and if such an improvement in symptom-related RF is finally related to outcome. This would need to be investigated in a larger prospective study in the future. As mentioned in the introduction, symptom-specific RF was previously shown to be relevant for change: A study on patients with panic disorder, the Cornell-Penn-Study, found that an increase in panic-specific RF in cognitive-behavioral as well as psychodynamic psychotherapy mediated a better treatment outcome ( 43 , 44 ).
Finally, we found that sequences with demand interventions or empathic validation showed increased mentalizing in the patient. Although we did not study the time sequence (if patients mentalized directly following these interventions), the finding suggest that both interventions might simulate RF. This would be a replication of previous findings, where could be shown that that MBT-type interventions in cognitive-behavioral and psychodynamic treatments of AN were associated with an increase in in-session RF ( 15 ). Interestingly, both interventions are correlated with a similar increase in RF, although they differ in terms of their aim and might work through different mechanisms: While demand-interventions intend to directly stimulate RF, empathic validation is used to give the patient a feeling of being understood and intends to validate his experience emotionally. This is considered to be a necessary base for mentalizing, especially in situations, in which a patient is emotionally challenged ( 42 ).
The study has several limitations, which include the small sample size (which did not allow to analyze for influences of weight status) and the heterogeneous group of patients with an ED. An a priori power analysis was not conducted, power and sample size depended on the design of the primary study. Exploratory data analyses revealed no consistent pattern of non-linear trajectories. Therefore, we decided to model linear trajectories only. The sample consisted of women only. There is no baseline assessment of RF, e. g. with the Adult Attachment Interview and the RF-Rating-Scale, measuring by overall capacity of the patients to mentalize. Interventions like “demand” and “empathic validation” could be considered rather “unspecific” interventions without the context of the situation in which they are used and we did not assess a lot of other therapeutic interventions that might or might not contribute to RF.
In summary, we were able to show that RF in psychotherapy sessions with patients with an ED is not only context-dependent, but also depends on the content discussed. The ability to mentalize appears to be particularly impaired when disorder-specific topics (relating to food, body and weight) are addressed. Future studies should answer the question of whether a therapeutic focus on mentalizing eating disorder-specific experiences and beliefs during a session and an improvement in symptom-specific RF is a significant mediator of treatment success.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the local ethics committee of the University of Freiburg, No 448/17. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AZ: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing. IL: Data curation, Investigation, Project administration, Writing – review & editing. KE: Data curation, Investigation, Writing – review & editing. LS: Resources, Writing – review & editing. SE: Supervision, Writing – review & editing. CL: Writing – review & editing. AH: Conceptualization, Data curation, Formal Analysis, Methodology, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. We are thankful for receiving research grants to conduct the study: The work was supported by the Heidehofstiftung GmbH Stuttgart (Project No 59055.03.1/2.17; 59055.03.2/4.18; 59055.03.3/4.19). We acknowledge support by the Open Access Publication Fund of the University of Freiburg.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Fonagy P, Gergely G, Jurist E, Target M. Affect regulation, mentalization, and the development of the self . New York: Other Press (2002).
Google Scholar
2. Katznelson H. Reflective functioning: a review. Clin Psychol Rev . (2014) 34:107–17. doi: 10.1016/j.cpr.2013.12.003
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Lüdemann J, Rabung S, Andreas S. Systematic review on mentalization as key factor in psychotherapy. Int J Environ Res Public Health . (2021) 18:9161. doi: 10.3390/ijerph18179161
4. Luyten P, Campbell C, Allison E, Fonagy P. The mentalizing approach to psychopathology: state of the art and future directions. Annu Rev Clin Psychol . (2020) 16:297–325. doi: 10.1146/annurev-clinpsy-071919-015355
5. Ekeblad A, Falkenström F, Holmqvist R. Reflective functioning as predictor of working alliance and outcome in the treatment of depression. J Consult Clin Psychol . (2016) 84:67–78. doi: 10.1037/ccp0000055
6. Katznelson H, Falkenström F, Daniel SIF, Lunn S, Folke S, Pedersen SH, et al. Reflective functioning, psychotherapeutic alliance, and outcome in two psychotherapies for bulimia nervosa. Psychother (Chic) . (2020) 57:129–40. doi: 10.1037/pst0000245
CrossRef Full Text | Google Scholar
7. Bateman A, Fonagy P. Mentalization-based treatment for personality disorders: A practical guide . Oxford: Oxford University Press (2016). doi: 10.1093/med:psych/9780199680375.001.0001
8. Levy KN, Meehan KB, Kelly KM, Reynoso JS, Weber M, Clarkin JF, et al. Change in attachment patterns and reflective function in a randomized control trial of transference-focused psychotherapy for borderline personality disorder. J Consult Clin Psychol . (2006) 74:1027–40. doi: 10.1037/0022-006X.74.6.1027
9. Bateman A, Fonagy P. Handbook of mentalizing in mental health practice . 2nd edition. Washington: American Psychiatric Association Publishing (2019).
10. Robinson P, Skaderud F. “Eating disorders.,”. In: Handbook of mentalizing in mental health practice . American Psychiatric Association Publishing, Washington (2019). p. 369–86.
11. Zeeck A, Endorf K, Euler S, Schaefer L, Lau I, Flösser K, et al. Implementation of mentalization-based treatment in a day hospital program for eating disorders-A pilot study. Eur Eat Disord Rev . (2021) 29:783–801. doi: 10.1002/erv.2853
12. Talia A, Miller-Bottome M, Katznelson H, Pedersen SH, Steele H, Schröder P, et al. Mentalizing in the presence of another: Measuring reflective functioning and attachment in the therapy process. Psychother Res . (2019) 29:652–65. doi: 10.1080/10503307.2017.1417651
13. Rudden M, Milrod B, Target M, Ackerman S, Graf E. Reflective functioning in panic disorder patients: a pilot study. J Am Psychoanal Assoc . (2006) 54:1339–43. doi: 10.1177/00030651060540040109
14. Kivity Y, Levy KN, Kelly KM, Clarkin JF. In-session reflective functioning in psychotherapies for borderline personality disorder: The emotion regulatory role of reflective functioning. J Consult Clin Psychol . (2021) 89:751–61. doi: 10.1037/ccp0000674
15. Meier AF, Zeeck A, Taubner S, Gablonski T, Lau I, Preiter R, et al. Mentalization-enhancing therapeutic interventions in the psychotherapy of anorexia nervosa: An analysis of use and influence on patients’ mentalizing capacity. Psychother Res . (2023) 33:595–607. doi: 10.1080/10503307.2022.2146542
16. Möller C, Karlgren L, Sandell A, Falkenström F, Philips B. Mentalization-based therapy adherence and competence stimulates in-session mentalization in psychotherapy for borderline personality disorder with co-morbid substance dependence. Psychother Res . (2017) 27:749–65. doi: 10.1080/10503307.2016.1158433
17. Babl A, Berger T, Decurtins H, Gross I, Frey T, Caspar F, et al. A longitudinal analysis of reflective functioning and its association with psychotherapy outcome in patients with depressive and anxiety disorders. J Couns Psychol . (2022) 69:337–47. doi: 10.1037/cou0000587
18. Treasure J, Duarte TA, Schmidt U. Eating disorders. Lancet . (2020) 395:899–911. doi: 10.1016/S0140-6736(20)30059-3
19. Herpertz S, Fichter M, Herpertz-Dahlmann B, Hilbert A, Tuschen-Caffier B, Vocks S, et al. S3-Leitinie Diagnostik und Behandlung der Essstörungen . Zweite Auflage. Berlin: Springer Verlag (2019). doi: 10.1007/978-3-662-59606-7
20. Arcelus J. Mortality rates in patients with anorexia nervosa and other eating disorders: A meta-analysis of 36 studies. Arch Gen Psychiatr . (2011) 68:724. doi: 10.1001/archgenpsychiatry.2011.74
21. Lavender JM, Wonderlich SA, Engel SG, Gordon KH, Kaye WH, Mitchell JE. Dimensions of emotion dysregulation in anorexia nervosa and bulimia nervosa: A conceptual review of the empirical literature. Clin Psychol Rev . (2015) 40:111–22. doi: 10.1016/j.cpr.2015.05.010
22. Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behav Res Ther . (2003) 41:509–28. doi: 10.1016/S0005-7967(02)00088-8
23. Treasure J, Willmott D, Ambwani S, Cardi V, Clark Bryan D, Rowlands K, et al. Cognitive interpersonal model for anorexia nervosa revisited: the perpetuating factors that contribute to the development of the severe and enduring illness. J Clin Med . (2020) 9(3):630. doi: 10.3390/jcm9030630
24. Zipfel S, Giel KE, Bulik CM, Hay P, Schmidt U. Anorexia nervosa: aetiology, assessment, and treatment. Lancet Psychiatry . (2015) 2:1099–111. doi: 10.1016/S2215-0366(15)00356-9
25. Jewell T, Collyer H, Gardner T, Tchanturia K, Simic M, Fonagy P, et al. Attachment and mentalization and their association with child and adolescent eating pathology: A systematic review. Int J Eat Disord . (2016) 49:354–73. doi: 10.1002/eat.22473
26. Simonsen CB, Jakobsen AG, Grøntved S, Kjaersdam Telléus G. The mentalization profile in patients with eating disorders: a systematic review and meta-analysis. Nord J Psychiatry . (2020) 74:311–22. doi: 10.1080/08039488.2019.1707869
27. Zeeck A, Taubner S, Gablonski TC, Lau I, Zipfel S, Herzog W, et al. In-session-reflective-functioning in anorexia nervosa: an analysis of psychotherapeutic sessions of the ANTOP study. Front Psychiatry . (2022) 13:814441. doi: 10.3389/fpsyt.2022.814441
28. Sonntag M, Russell J. The mind-in-mind study: A pilot randomised controlled trial that compared modified mentalisation based treatment with supportive clinical management for patients with eating disorders without borderline personality disorder. Eur Eat Disord Rev . (2022) 30:206–20. doi: 10.1002/erv.2888
29. Balestrieri M, Zuanon S, Pellizzari J, Zappoli-Thyrion E, Ciano R. ResT-MBT. Mentalization in eating disorders: a preliminary trial comparing mentalization-based treatment (MBT) with a psychodynamic-oriented treatment. Eat Weight Disord . (2015) 20:525–8. doi: 10.1007/s40519-015-0204-1
30. Robinson P, Hellier J, Barrett B, Barzdaitiene D, Bateman A, Bogaardt A, et al. The NOURISHED randomised controlled trial comparing mentalisation-based treatment for eating disorders (MBT-ED) with specialist supportive clinical management (SSCM-ED) for patients with eating disorders and symptoms of borderline personality disorder. BMCTrials . (2016) 17(1):549. doi: 10.1186/s13063-016-1606-8
31. Zeeck A, Floesser K, Euler S. Mentalisierungsbasierte therapie für essstörungen. Psychotherapeut . (2018) 63:129–34. doi: 10.1007/s00278-018-0273-5
32. Mergenthaler E. Die Transkription von Gespraechen- eine Zusammenstellung von Regeln mit einem Beispieltranskript . 4the edition. Ulm: Ulmer Textbank (2017).
33. Fairburn C, Cooper P. The eating disorder examination. In: Fairburn CG, Wilson GT, editors. Binge eating. Nature, assessment, and treatment , 12th ed. Guilford Press, New York (1993). p. 317–60.
34. Hilbert A, Tuschen-Caffier B, Karwautz A, Niederhofer H, Munsch S. Eating Disorder Examination-Questionnaire: Evaluation der deutschsprachigen Übersetzung. Diagnostica . (2007) 53:144–54. doi: 10.1026/0012-1924.53.3.144
35. Garner D. Eating disorder inventory - 2. Professional manual . Odessa Florida, USA: Psychological Assessment Ressources (1991).
36. Meermann R, Napierski CH, Schulenkorf EM. EDI-muenster - selbstbeurteilungsfragebogen fuer essst”rungen. In: Therapie der Magersucht und Bulimia Nervosa. Ein klinischer Leitfaden fuer den Praktiker . Walter de Gruyter, Berlin, New York (1987). doi: 10.1515/9783110859140
37. Franke G. Die symptom-check-liste von derogatis (SCL-90-R). Deutsche version - manual . Goettingen: Hogrefe (2002).
38. Fonagy P, Target M, Steele H, Steele M. Reflective-functioning manual, version 5.0, for application to adult attachment interviews . London: University College London (1998). doi: 10.1037/t03490-000
39. Karlsson R, Kermott A. Reflective-functioning during the process in brief psychotherapies. Psychother (Chic) . (2006) 43:65–84. doi: 10.1037/0033-3204.43.1.65
40. Zeeck A, Euler S. Mentalisieren bei essstoerungen . Stuttgart: Klett-Cotta (2023).
41. Milesi A, De Carli P, Locati F, Campbell C, Fonagy P, Parolin L. How can I trust you? The role of facial trustworthiness in the development of Epistemic and Interpersonal Trust. Hum Dev . (2023) 67(2):57-68. doi: 10.1159/000530248
42. Fonagy P, Allison E. The role of mentalizing and epistemic trust in the therapeutic relationship. Psychother (Chic) . (2014) 51:372–80. doi: 10.1037/a0036505
43. Keefe JR, Huque ZM, DeRubeis RJ, Barber JP, Milrod BL, Chambless DL. In-session emotional expression predicts symptomatic and panic-specific reflective functioning improvements in panic-focused psychodynamic psychotherapy. Psychother (Chic) . (2019) 56:514–25. doi: 10.1037/pst0000215
44. Barber JP, Milrod B, Gallop R, Solomonov N, Rudden MG, McCarthy KS, et al. Processes of therapeutic change: Results from the Cornell-Penn Study of Psychotherapies for Panic Disorder. J Couns Psychol . (2020) 67:222–31. doi: 10.1037/cou0000417
Keywords: menatlization based treatment, intervention, in-session, eating disorder, psychotherapy
Citation: Zeeck A, Lau I, Endorf K, Schaefer L, Euler S, Lahmann C and Hartmann A (2024) Mentalizing in psychotherapeutic processes of patients with eating disorders. Front. Psychiatry 15:1367863. doi: 10.3389/fpsyt.2024.1367863
Received: 09 January 2024; Accepted: 04 April 2024; Published: 19 April 2024.
Reviewed by:
Copyright © 2024 Zeeck, Lau, Endorf, Schaefer, Euler, Lahmann and Hartmann. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Almut Zeeck, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Eating disorders
Affiliations.
- 1 Institute of Psychiatry, Psychology and Neuroscience, King's College London, London, UK. Electronic address: [email protected].
- 2 Institute of Psychiatry, Psychology and Neuroscience, King's College London, London, UK; Serviço de Psiquiatria e Saúde Mental, Hospital de Santa Maria, Centro Hospitalar Universitário Lisboa Norte, Lisbon, Portugal.
- 3 Institute of Psychiatry, Psychology and Neuroscience, King's College London, London, UK; South London and Maudsley NHS Foundation Trust, London, UK.
- PMID: 32171414
- DOI: 10.1016/S0140-6736(20)30059-3
Eating disorders are disabling, deadly, and costly mental disorders that considerably impair physical health and disrupt psychosocial functioning. Disturbed attitudes towards weight, body shape, and eating play a key role in the origin and maintenance of eating disorders. Eating disorders have been increasing over the past 50 years and changes in the food environment have been implicated. All health-care providers should routinely enquire about eating habits as a component of overall health assessment. Six main feeding and eating disorders are now recognised in diagnostic systems: anorexia nervosa, bulimia nervosa, binge eating disorder, avoidant-restrictive food intake disorder, pica, and rumination disorder. The presentation form of eating disorders might vary for men versus women, for example. As eating disorders are under-researched, there is a great deal of uncertainty as to their pathophysiology, treatment, and management. Future challenges, emerging treatments, and outstanding research questions are addressed.
Copyright © 2020 Elsevier Ltd. All rights reserved.
Publication types
- Research Support, Non-U.S. Gov't
- Diagnosis, Differential
- Feeding and Eating Disorders* / diagnosis
- Feeding and Eating Disorders* / physiopathology
- Feeding and Eating Disorders* / psychology
- Feeding and Eating Disorders* / therapy
- Nutritional Status
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 17 March 2022
Binge eating disorder
- Katrin E. Giel ORCID: orcid.org/0000-0003-0938-4402 1 , 2 ,
- Cynthia M. Bulik ORCID: orcid.org/0000-0001-7772-3264 3 , 4 , 5 ,
- Fernando Fernandez-Aranda ORCID: orcid.org/0000-0002-2968-9898 6 , 7 , 8 ,
- Phillipa Hay 9 , 10 ,
- Anna Keski-Rahkonen 11 ,
- Kathrin Schag 1 , 2 ,
- Ulrike Schmidt 12 , 13 &
- Stephan Zipfel 1 , 2
Nature Reviews Disease Primers volume 8 , Article number: 16 ( 2022 ) Cite this article
7475 Accesses
68 Citations
193 Altmetric
Metrics details
- Feeding behaviour
- Limbic system
- Psychiatric disorders
Binge eating disorder (BED) is characterized by regular binge eating episodes during which individuals ingest comparably large amounts of food and experience loss of control over their eating behaviour. The worldwide prevalence of BED for the years 2018–2020 is estimated to be 0.6–1.8% in adult women and 0.3–0.7% in adult men. BED is commonly associated with obesity and with somatic and mental health comorbidities. People with BED experience considerable burden and impairments in quality of life, and, at the same time, BED often goes undetected and untreated. The aetiology of BED is complex, including genetic and environmental factors as well as neuroendocrinological and neurobiological contributions. Neurobiological findings highlight impairments in reward processing, inhibitory control and emotion regulation in people with BED, and these neurobiological domains are targets for emerging treatment approaches. Psychotherapy is the first-line treatment for BED. Recognition and research on BED has increased since its inclusion into DSM-5; however, continuing efforts are needed to understand underlying mechanisms of BED and to improve prevention and treatment outcomes for this disorder. These efforts should also include screening, identification and implementation of evidence-based interventions in routine clinical practice settings such as primary care and mental health outpatient clinics.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
92,52 € per year
only 92,52 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others

Sleep dysregulation in binge eating disorder and “food addiction”: the orexin (hypocretin) system as a potential neurobiological link

Genetics and neurobiology of eating disorders

What pharmacological interventions are effective in binge-eating disorder? Insights from a critical evaluation of the evidence from clinical trials
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5 350–353 (American Psychiatric Association, 2013).
World Health Organization. ICD-11: International Classification of Diseases 11th Revision. ICD https://icd.who.int/ (2019).
Treasure, J. et al. Anorexia nervosa. Nat. Rev. Dis. Primers 1 , 15074 (2015).
PubMed Google Scholar
Zipfel, S., Giel, K. E., Bulik, C. M., Hay, P. & Schmidt, U. Anorexia nervosa: aetiology, assessment, and treatment. Lancet Psychiatry 2 , 1099–1111 (2015).
Keski-Rahkonen, A. & Mustelin, L. Epidemiology of eating disorders in Europe: prevalence, incidence, comorbidity, course, consequences, and risk factors. Curr. Opin. Psychiatry 29 , 340–345 (2016).
Hoek, H. W. Review of the worldwide epidemiology of eating disorders. Curr. Opin. Psychiatry 29 , 336–339 (2016).
Udo, T. & Grilo, C. M. Prevalence and correlates of DSM-5-defined eating disorders in a nationally representative sample of U.S. adults. Biol. Psychiatry 84 , 345–354 (2018).
PubMed PubMed Central Google Scholar
Agh, T. et al. Epidemiology, health-related quality of life and economic burden of binge eating disorder: a systematic literature review. Eat. Weight. Disord. 20 , 1–12 (2015). This systematic review highlights what is known about quality of life and burden of people affected by BED .
Dawes, A. J. et al. Mental health conditions among patients seeking and undergoing bariatric surgery: a meta-analysis. JAMA 315 , 150–163 (2016).
CAS PubMed Google Scholar
NCD Risk Factor Collaboration. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 387 , 1377–1396 (2016).
Google Scholar
World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 894 (WHO, 2000).
National Institute for Health and Care Excellence. Eating disorders: recognition and treatment (full guideline). NICE https://www.nice.org.uk/guidance/ng69/evidence/full-guideline-pdf-161214767896 (2017).
Herpertz, S. et al. S3-Leitlinie Diagnostik und Behandlung der Essstörungen. AWMF https://www.awmf.org/uploads/tx_szleitlinien/051-026l_S3_Essstoerung-Diagnostik-Therapie_2020-03.pdf (2018).
Gonzalez-Muniesa, P. et al. Obesity. Nat. Rev. Dis. Primers 3 , 17034 (2017).
Santomauro, D. F. et al. The hidden burden of eating disorders: an extension of estimates from the Global Burden of Disease Study 2019. Lancet Psychiatry 8 , 320–328 (2021). This paper, based on studies from the Global Burden of Disease (GBD) dataset provides up-to-date evidence on epidemiology and burden caused by eating disorders including BED, providing so far unrepresented GBD data .
Stice, E., Marti, C. N. & Rohde, P. Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. J. Abnorm. Psychol. 122 , 445–457 (2013).
Kessler, R. C. et al. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol. Psychiatry 73 , 904–914 (2013).
Keski-Rahkonen, A. Epidemiology of binge eating disorder: prevalence, course, comorbidity, and risk factors. Curr. Opin. Psychiatry 34 , 525–531 (2021).
Mitchison, D. et al. DSM-5 full syndrome, other specified, and unspecified eating disorders in Australian adolescents: prevalence and clinical significance. Psychol. Med. 50 , 981–990 (2020).
Olsen, E. M., Koch, S. V., Skovgaard, A. M. & Strandberg-Larsen, K. Self-reported symptoms of binge-eating disorder among adolescents in a community-based Danish cohort–a study of prevalence, correlates, and impact. Int. J. Eat. Disord. 54 , 492–505 (2021).
Glazer, K. B. et al. The course of eating disorders involving bingeing and purging among adolescent girls: prevalence, stability, and transitions. J. Adolesc. Health 64 , 165–171 (2019).
Meule, A. The psychology of overeating: food and the culture of consumerism. Food Cult. Soc. 19 , 735–736 (2016).
Streatfeild, J. et al. Social and economic cost of eating disorders in the United States: evidence to inform policy action. Int. J. Eat. Disord. 54 , 851–868 (2021).
Silén, Y. et al. Detection, treatment, and course of eating disorders in Finland: a population-based study of adolescent and young adult females and males. Eur. Eat. Disord. Rev. 29 , 720–732 (2021).
Coffino, J. A., Udo, T. & Grilo, C. M. Rates of help-seeking in US adults with lifetime DSM-5 eating disorders: prevalence across diagnoses and differences by sex and ethnicity/race. Mayo Clin. Proc. 94 , 1415–1426 (2019).
Abbott, S., Dindol, N., Tahrani, A. A. & Piya, M. K. Binge eating disorder and night eating syndrome in adults with type 2 diabetes: a systematic review. J. Eat. Disord. 6 , 36 (2018).
Brownley, K. A. et al. Binge-eating disorder in adults: a systematic review and meta-analysis. Ann. Intern. Med. 165 , 409–420 (2016).
Wassenaar, E., Friedman, J. & Mehler, P. S. Medical complications of binge eating disorder. Psychiatr. Clin. North. Am. 42 , 275–286 (2019).
Harris, S. R., Carrillo, M. & Fujioka, K. Binge-eating disorder and type 2 diabetes: a review. Endocr. Pract. 27 , 158–164 (2021).
Tate, A. E. et al. Association and familial coaggregation of type 1 diabetes and eating disorders: a register-based cohort study in Denmark and Sweden. Diabetes Care 44 , 1143–1150 (2021).
Zhang, J. et al. Pilot study of the prevalence of binge eating disorder in non-alcoholic fatty liver disease patients. Ann. Gastroenterol. 30 , 664–669 (2017).
CAS PubMed PubMed Central Google Scholar
Forlano, R. et al. Binge-eating disorder is associated with an unfavorable body mass composition in patients with non-alcoholic fatty liver disease. Int. J. Eat. Disord. 54 , 2025–2030 (2021).
Cremonini, F. et al. Associations among binge eating behavior patterns and gastrointestinal symptoms: a population-based study. Int. J. Obes. 33 , 342–353 (2009).
CAS Google Scholar
Thornton, L. M. et al. Binge-eating disorder in the Swedish national registers: somatic comorbidity. Int. J. Eat. Disord. 50 , 58–65 (2017).
Kimmel, M. C., Ferguson, E. H., Zerwas, S., Bulik, C. M. & Meltzer-Brody, S. Obstetric and gynecologic problems associated with eating disorders. Int. J. Eat. Disord. 49 , 260–275 (2016).
Udo, T. & Grilo, C. M. Psychiatric and medical correlates of DSM-5 eating disorders in a nationally representative sample of adults in the United States. Int. J. Eat. Disord. 52 , 42–50 (2019). This paper provides a recent and comprehensive description of common co-occurring conditions with eating disorders based on a representative population sample .
Udo, T., Bitley, S. & Grilo, C. M. Suicide attempts in US adults with lifetime DSM-5 eating disorders. BMC Med. 17 , 120–123 (2019).
Fernandez-Aranda, F. et al. Impulse control disorders in women with eating disorders. Psychiatry Res. 157 , 147–157 (2008).
Jimenez-Murcia, S. et al. Pathological gambling in eating disorders: prevalence and clinical implications. Compr. Psychiatry 54 , 1053–1060 (2013).
Nazar, B. P. et al. The risk of eating disorders comorbid with attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Int. J. Eat. Disord. 49 , 1045–1057 (2016).
Schmidt, F., Körber, S., de Zwaan, M. & Müller, A. Impulse control disorders in obese patients. Eur. Eat. Disord. Rev. 20 , e144–e147 (2012).
Lydecker, J. A. & Grilo, C. M. Psychiatric comorbidity as predictor and moderator of binge-eating disorder treatment outcomes: an analysis of aggregated randomized controlled trials. Psychol. Med. https://doi.org/10.1017/S0033291721001045 (2021).
Article PubMed Google Scholar
West, C. E., Goldschmidt, A. B., Mason, S. M. & Neumark-Sztainer, D. Differences in risk factors for binge eating by socioeconomic status in a community-based sample of adolescents: findings from Project EAT. Int. J. Eat. Disord. 52 , 659–668 (2019).
Braun, J. et al. Trauma exposure, DSM-5 posttraumatic stress, and binge eating symptoms: results from a nationally representative sample. J. Clin. Psychiatry 80 , 19m12813 (2019).
Coffino, J. A., Udo, T. & Grilo, C. M. The significance of overvaluation of shape or weight in binge-eating disorder: results from a national sample of U.S. adults. Obesity 27 , 1367–1371 (2019).
& Borg, S. L. et al. Relationships between childhood abuse and eating pathology among individuals with binge-eating disorder: examining the moderating roles of self-discrepancy and self-directed style. Eat. Disord. https://doi.org/10.1080/10640266.2020.1864588 (2021).
Hazzard, V. M., Bauer, K. W., Mukherjee, B., Miller, A. L. & Sonneville, K. R. Associations between childhood maltreatment latent classes and eating disorder symptoms in a nationally representative sample of young adults in the United States. Child. Abus. Negl. 98 , 104171 (2019).
Hazzard, V. M., Loth, K. A., Hooper, L. & Becker, C. B. Food insecurity and eating disorders: a review of emerging evidence. Curr. Psychiatry Rep. 22 , 74–70 (2020).
& Hazzard, V. M. et al. Past-year abuse and eating disorder symptoms among U.S. college students. J. Interpers. Violence https://doi.org/10.1177/08862605211005156 (2021).
Masheb, R. M. et al. DSM-5 eating disorder prevalence, gender differences, and mental health associations in United States military veterans. Int. J. Eat. Disord. 54 , 1171–1180 (2021).
de Beaurepaire, R. Binge eating disorders in antipsychotic-treated patients with schizophrenia: prevalence, antipsychotic specificities, and changes over time. J. Clin. Psychopharmacol. 41 , 114–120 (2021).
Goode, R. W. et al. Binge eating and binge-eating disorder in Black women: a systematic review. Int. J. Eat. Disord. 53 , 491–507 (2020).
Marques, L. et al. Comparative prevalence, correlates of impairment, and service utilization for eating disorders across US ethnic groups: implications for reducing ethnic disparities in health care access for eating disorders. Int. J. Eat. Disord. 44 , 412–420 (2011).
Perez, M., Ohrt, T. K. & Hoek, H. W. Prevalence and treatment of eating disorders among Hispanics/Latino Americans in the United States. Curr. Opin. Psychiatry 29 , 378–382 (2016).
Kamody, R. C., Grilo, C. M. & Udo, T. Disparities in DSM-5 defined eating disorders by sexual orientation among US adults. Int. J. Eat. Disord. 53 , 278–287 (2020).
Nagata, J. M., Ganson, K. T. & Austin, S. B. Emerging trends in eating disorders among sexual and gender minorities. Curr. Opin. Psychiatry 33 , 562–567 (2020).
Beccia, A. L., Baek, J., Austin, S. B., Jesdale, W. M. & Lapane, K. L. Eating-related pathology at the intersection of gender, gender expression, sexual orientation, and weight status: an intersectional Multilevel Analysis of Individual Heterogeneity and Discriminatory Accuracy (MAIHDA) of the Growing Up Today Study cohorts. Soc. Sci. Med. 281 , 114092 (2021).
Cheah, S. L., Jackson, E., Touyz, S. & Hay, P. Prevalence of eating disorder is lower in migrants than in the Australian-born population. Eat. Behav. 37 , 101370 (2020).
Burt, A., Mitchison, D., Doyle, K. & Hay, P. Eating disorders amongst Aboriginal and Torres Strait Islander Australians: a scoping review. J. Eat. Disord. 8 , 73 (2020).
Puhl, R. & Suh, Y. Health consequences of weight stigma: implications for obesity prevention and treatment. Curr. Obes. Rep. 4 , 182–190 (2015).
Donnelly, B. et al. Neuroimaging in bulimia nervosa and binge eating disorder: a systematic review. J. Eat. Disord. 6 , 3 (2018).
Strubbe, J. H. & Woods, S. C. The timing of meals. Psychol. Rev. 111 , 128–141 (2004).
Berthoud, H. R. & Morrison, C. The brain, appetite, and obesity. Annu. Rev. Psychol. 59 , 55–92 (2008).
Rosenbaum, M. & Leibel, R. L. 20 years of leptin: role of leptin in energy homeostasis in humans. J. Endocrinol. 223 , T83–T96 (2014).
Muller, T. D. et al. Glucagon-like peptide 1 (GLP-1). Mol. Metab. 30 , 72–130 (2019).
Yu, Y., Fernandez, I. D., Meng, Y., Zhao, W. & Groth, S. W. Gut hormones, adipokines, and pro- and anti-inflammatory cytokines/markers in loss of control eating: a scoping review. Appetite 166 , 105442 (2021).
Hernandez, D., Mehta, N. & Geliebter, A. Meal-related acyl and des-acyl ghrelin and other appetite-related hormones in people with obesity and binge eating. Obesity 27 , 629–635 (2019).
Munsch, S., Biedert, E., Meyer, A. H., Herpertz, S. & Beglinger, C. CCK, ghrelin, and PYY responses in individuals with binge eating disorder before and after a cognitive behavioral treatment (CBT). Physiol. Behav. 97 , 14–20 (2009).
Voon, V. Cognitive biases in binge eating disorder: the hijacking of decision making. CNS Spectr. 20 , 566–573 (2015).
Avena, N. M., Bocarsly, M. E., Hoebel, B. G. & Gold, M. S. Overlaps in the nosology of substance abuse and overeating: the translational implications of “food addiction”. Curr. Drug Abus. Rev. 4 , 133–139 (2011).
& Steward, T. et al. What difference does it make? Risk-taking behavior in obesity after a loss is associated with decreased ventromedial prefrontal cortex activity. J. Clin. Med. 8 , 1551 (2019).
PubMed Central Google Scholar
Hege, M. A. et al. Attentional impulsivity in binge eating disorder modulates response inhibition performance and frontal brain networks. Int. J. Obes. 39 , 353–360 (2015).
Wolz, I. et al. Subjective craving and event-related brain response to olfactory and visual chocolate cues in binge-eating and healthy individuals. Sci. Rep. 7 , 41736 (2017).
Balodis, I. M. et al. Divergent neural substrates of inhibitory control in binge eating disorder relative to other manifestations of obesity. Obesity 21 , 367–377 (2013).
Frank, G. K. W., Shott, M. E., Stoddard, J., Swindle, S. & Pryor, T. L. Association of brain reward response with body mass index and ventral striatal-hypothalamic circuitry among young women with eating disorders. JAMA Psychiatry 78 , 1123–1133 (2021).
Leehr, E. J. et al. Emotion regulation model in binge eating disorder and obesity–a systematic review. Neurosci. Biobehav. Rev. 49 , 125–134 (2015).
Ansell, E. B., Grilo, C. M. & White, M. A. Examining the interpersonal model of binge eating and loss of control over eating in women. Int. J. Eat. Disord. 45 , 43–50 (2012).
Iceta, S. et al. Cognitive function in binge eating disorder and food addiction: a systematic review and three-level meta-analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry 111 , 110400 (2021).
Giel, K. E., Teufel, M., Junne, F., Zipfel, S. & Schag, K. Food-related impulsivity in obesity and binge eating disorder–a systematic update of the evidence. Nutrients 9 , 1170 (2017).
Kessler, R. M., Hutson, P. H., Herman, B. K. & Potenza, M. N. The neurobiological basis of binge-eating disorder. Neurosci. Biobehav. Rev. 63 , 223–238 (2016). This review provides a comprehensive synthesis of the neurobiological findings in BED and develops hyopotheses for neurobiological pathomechanisms in the development and maintenance of BED .
Schag, K., Schonleber, J., Teufel, M., Zipfel, S. & Giel, K. E. Food-related impulsivity in obesity and binge eating disorder–a systematic review. Obes. Rev. 14 , 477–495 (2013).
Mallorqui-Bague, N. et al. Impulsivity and cognitive distortions in different clinical phenotypes of gambling disorder: profiles and longitudinal prediction of treatment outcomes. Eur. Psychiatry 61 , 9–16 (2019).
& Lozano-Madrid, et al.Impulsivity, emotional dysregulation and executive function deficits could be associated with alcohol and drug abuse in eating disorders. J. Clin. Med. 9 , 1936 (2020).
CAS PubMed Central Google Scholar
Grant, J. E. & Chamberlain, S. R. Neurocognitive findings in young adults with binge eating disorder. Int. J. Psychiatry Clin. Pract. 24 , 71–76 (2020).
Oliva, R., Morys, F., Horstmann, A., Castiello, U. & Begliomini, C. Characterizing impulsivity and resting-state functional connectivity in normal-weight binge eaters. Int. J. Eat. Disord. 53 , 478–488 (2020).
Lucas, I. et al. Neuropsychological learning deficits as predictors of treatment outcome in patients with eating disorders. Nutrients 13 , 2145 (2021).
Schag, K. et al. Food-related impulsivity assessed by longitudinal laboratory tasks is reduced in patients with binge eating disorder in a randomized controlled trial. Sci. Rep. 11 , 8225 (2021).
Dingemans, A. E., van Son, G. E., Vanhaelen, C. B. & van Furth, E. F. Depressive symptoms rather than executive functioning predict group cognitive behavioural therapy outcome in binge eating disorder. Eur. Eat. Disord. Rev. 28 , 620–632 (2020).
Mestre-Bach, G., Fernandez-Aranda, F., Jimenez-Murcia, S. & Potenza, M. N. Decision-making in gambling disorder, problematic pornography use, and binge-eating disorder: similarities and differences. Curr. Behav. Neurosci. Rep. 7 , 97–108 (2020).
Amlung, M. et al. Delay discounting as a transdiagnostic process in psychiatric disorders: a meta-analysis. JAMA Psychiatry 76 , 1176–1186 (2019).
Appelhans, B. M. et al. Inhibiting food reward: delay discounting, food reward sensitivity, and palatable food intake in overweight and obese women. Obesity 19 , 2175–2182 (2011).
Tang, J., Chrzanowski-Smith, O. J., Hutchinson, G., Kee, F. & Hunter, R. F. Relationship between monetary delay discounting and obesity: a systematic review and meta-regression. Int. J. Obes. 43 , 1135–1146 (2019).
Steward, T. et al. Delay discounting of reward and impulsivity in eating disorders: from anorexia nervosa to binge eating disorder. Eur. Eat. Disord. Rev. 25 , 601–606 (2017).
Steward, T. et al. Delay discounting and impulsivity traits in young and older gambling disorder patients. Addict. Behav. 71 , 96–103 (2017).
Miranda-Olivos, R. et al. The neural correlates of delay discounting in obesity and binge eating disorder. J. Behav. Addict. 10 , 498–507 (2021).
Fowler, S. & Bulik, C. Family environment and psychiatric history in women with binge eating disorder and obese controls. Behav. Change 14 , 106–112 (1997).
Hudson, J. et al. Familial aggregation of binge-eating disorder. Arch. Gen. Psychiatry 63 , 313–319 (2006).
Javaras, K. N. et al. Familiality and heritability of binge eating disorder: results of a case-control family study and a twin study. Int. J. Eat. Disord. 41 , 174–179 (2008).
Mitchell, K. S. et al. Binge eating disorder: a symptom-level investigation of genetic and environmental influences on liability. Psychol. Med. 40 , 1899–1906 (2010).
Reichborn-Kjennerud, T., Bulik, C., Tambs, K. & Harris, J. Genetic and environmental influences on binge eating in the absence of compensatory behaviours: a population-based twin study. Int. J. Eat. Disord. 36 , 307–314 (2004).
Manfredi, L., Accoto, A., Couyoumdjian, A. & Conversi, D. A systematic review of genetic polymorphisms associated with binge eating disorder. Nutrients 13 , 848 (2021).
Micioni Di Bonaventura, E. et al. The melanocortin system behind the dysfunctional eating behaviors. Nutrients 12 , 3502 (2020).
Qasim, A. et al. Gain-of-function variants in the melanocortin 4 receptor gene confer susceptibility to binge eating disorder in subjects with obesity: a systematic review and meta-analysis. Obes. Rev. 20 , 13–21 (2019).
Hübel, C. et al. One size does not fit all. Genomics differentiates among anorexia nervosa, bulimia nervosa, and binge-eating disorder. Int. J. Eat. Disord. 54 , 785–793 (2021). This study uses data from the UK Biobank to present the first molecular genetic evidence that the underlying biology differs between binge-type eating disorders, including bulimia nervosa and binge-eating disorder and anorexia nervosa, and these differences can be captured at the genomic level .
Dinan, T. G. & Cryan, J. F. The impact of gut microbiota on brain and behaviour: implications for psychiatry. Curr. Opin. Clin. Nutr. Metab. Care 18 , 552–558 (2015).
Basolo, A. et al. Effects of underfeeding and oral vancomycin on gut microbiome and nutrient absorption in humans. Nat. Med. 26 , 589–598 (2020).
David, L. A. et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature 505 , 559–563 (2014).
Wu, G. D. et al. Linking long-term dietary patterns with gut microbial enterotypes. Science 334 , 105–108 (2011).
Ridaura, V. K. et al. Gut microbiota from twins discordant for obesity modulate metabolism in mice. Science 341 , 1241214 (2013).
Chen, L. L. et al. Gut microbiota in psychiatric disorders: a systematic review. Psychosom. Med. 83 , 679–692 (2021).
Reed, K. K., Abbaspour, A., Bulik, C. M. & Carroll, I. M. The intestinal microbiota and anorexia nervosa: cause or consequence of nutrient deprivation? Curr. Opin. Endocr. Metab. Res. 19 , 46–51 (2021).
Herman, A. & Bajaka, A. The role of the intestinal microbiota in eating disorders–bulimia nervosa and binge eating disorder. Psychiatry Res. 300 , 113923 (2021).
Alcock, J., Maley, C. C. & Aktipis, C. A. Is eating behavior manipulated by the gastrointestinal microbiota? Evolutionary pressures and potential mechanisms. Bioessays 36 , 940–949 (2014).
van de Wouw, M., Schellekens, H., Dinan, T. G. & Cryan, J. F. Microbiota-gut-brain axis: modulator of host metabolism and appetite. J. Nutr. 147 , 727–745 (2017).
Glenny, E. M., Bulik-Sullivan, E. C., Tang, Q., Bulik, C. M. & Carroll, I. M. Eating disorders and the intestinal microbiota: mechanisms of energy homeostasis and behavioral influence. Curr. Psychiatry Rep. 19 , 51 (2017).
Madison, A. & Kiecolt-Glaser, J. K. Stress, depression, diet, and the gut microbiota: human–bacteria interactions at the core of psychoneuroimmunology and nutrition. Curr. Opin. Behav. Sci. 28 , 105–110 (2019).
Rantala, M. J., Luoto, S., Krama, T. & Krams, I. Eating disorders: an evolutionary psychoneuroimmunological approach. Front. Psychol. 10 , 2200 (2019).
Leyrolle, Q. et al. Specific gut microbial, biological, and psychiatric profiling related to binge eating disorders: a cross-sectional study in obese patients. Clin. Nutr. 40 , 2035–2044 (2021).
Reas, D. L. Public and healthcare professionals’ knowledge and attitudes toward binge eating disorder: a narrative review. Nutrients 9 , 1267 (2017).
Kazdin, A. E., Fitzsimmons-Craft, E. E. & Wilfley, D. E. Addressing critical gaps in the treatment of eating disorders. Int. J. Eat. Disord. 50 , 170–189 (2017).
Kornstein, S. G. Epidemiology and recognition of binge-eating disorder in psychiatry and primary care. J. Clin. Psychiatry 78 (Suppl. 1), 3–8 (2017).
Wolfe, B. E., Baker, C. W., Smith, A. T. & Kelly-Weeder, S. Validity and utility of the current definition of binge eating. Int. J. Eat. Disord. 42 , 674–686 (2009).
Lindvall Dahlgren, C. & Wisting, L. Transitioning from DSM-IV to DSM-5: a systematic review of eating disorder prevalence assessment. Int. J. Eat. Disord. 49 , 975–997 (2016).
Dakanalis, A., Colmegna, F., Riva, G. & Clerici, M. Validity and utility of the DSM-5 severity specifier for binge-eating disorder. Int. J. Eat. Disord. 50 , 917–923 (2017).
Grilo, C. M., Ivezaj, V. & White, M. A. Evaluation of the DSM-5 severity indicator for binge eating disorder in a clinical sample. Behav. Res. Ther. 71 , 110–114 (2015).
Ali, K. et al. Perceived barriers and facilitators towards help-seeking for eating disorders: a systematic review. Int. J. Eat. Disord. 50 , 9–21 (2017).
Bohon, C. Binge eating disorder in children and adolescents. Child. Adolesc. Psychiatr. Clin. N. Am. 28 , 549–555 (2019).
Citrome, L. Binge eating disorder revisited: what’s new, what’s different, what’s next. CNS Spectr. 24 , 4–13 (2019).
Morgan, J. F., Reid, F. & Lacey, J. H. The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ 319 , 1467–1468 (1999).
Parker, K. & Brennan, L. Measurement of disordered eating in bariatric surgery candidates: a systematic review of the literature. Obes. Res. Clin. Pract. 9 , 12–25 (2015).
Klein, D. A., Sylvester, J. E. & Schvey, N. A. Eating disorders in primary care: diagnosis and management. Am. Fam. Physician 103 , 22–32 (2021).
O’Loghlen, E., Grant, S. & Galligan, R. Shame and binge eating pathology: a systematic review. Clin. Psychol. Psychother. https://doi.org/10.1002/cpp.2615 (2021).
Alberti, K. G. et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120 , 1640–1645 (2009).
Heriseanu, A. I., Hay, P., Corbit, L. & Touyz, S. Grazing in adults with obesity and eating disorders: a systematic review of associated clinical features and meta-analysis of prevalence. Clin. Psychol. Rev. 58 , 16–32 (2017).
Pope, H. G. Jr. et al. Binge eating disorder: a stable syndrome. Am. J. Psychiatry 163 , 2181–2183 (2006).
Wadden, T. A., Brownell, K. D. & Foster, G. D. Obesity: responding to the global epidemic. J. Consult. Clin. Psychol. 70 , 510–525 (2002).
Kass, A. E. et al. Universal prevention efforts should address eating disorder pathology across the weight spectrum: implications for screening and intervention on college campuses. Eat. Behav. 25 , 74–80 (2017).
Ewart-Pierce, E., Mejia Ruiz, M. J. & Gittelsohn, J. “Whole-of-community” obesity prevention: a review of challenges and opportunities in multilevel, multicomponent interventions. Curr. Obes. Rep. 5 , 361–374 (2016).
Swinburn, B., Egger, G. & Raza, F. Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prev. Med. 29 , 563–570 (1999).
Booth, S. L. et al. Environmental and societal factors affect food choice and physical activity: rationale, influences, and leverage points. Nutr. Rev. 59 , S21–S39; discussion S57–S65 (2001).
Micha, R. et al. Effectiveness of school food environment policies on children’s dietary behaviors: a systematic review and meta-analysis. PLoS ONE 13 , e0194555 (2018).
Pike, K. M. et al. Antecedent life events of binge-eating disorder. Psychiatry Res. 142 , 19–29 (2006).
Stice, E., Desjardins, C. D., Rohde, P. & Shaw, H. Sequencing of symptom emergence in anorexia nervosa, bulimia nervosa, binge eating disorder, and purging disorder and relations of prodromal symptoms to future onset of these disorders. J. Abnorm. Psychol. 130 , 377–387 (2021).
Harrer, M. et al. Internet interventions for mental health in university students: a systematic review and meta-analysis. Int. J. Methods Psychiatr. Res. 28 , e1759 (2019).
Le, L. K., Barendregt, J. J., Hay, P. & Mihalopoulos, C. Prevention of eating disorders: a systematic review and meta-analysis. Clin. Psychol. Rev. 53 , 46–58 (2017).
Stice, E., Onipede, Z. A. & Marti, C. N. A meta-analytic review of trials that tested whether eating disorder prevention programs prevent eating disorder onset. Clin. Psychol. Rev. 87 , 102046 (2021).
Hay, P. et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of eating disorders. Aust. N. Z. J. Psychiatry 48 , 977–1008 (2014).
Hilbert, A., Hoek, H. W. & Schmidt, R. Evidence-based clinical guidelines for eating disorders: international comparison. Curr. Opin. Psychiatry 30 , 423–437 (2017).
Peat, C. M. et al. Comparative effectiveness of treatments for binge-eating disorder: systematic review and network meta-analysis. Eur. Eat. Disord. Rev. 25 , 317–328 (2017).
Hay, P. J. et al. Inpatient versus outpatient care, partial hospitalisation and waiting list for people with eating disorders. Cochrane Database Syst. Rev. 1 , CD010827 (2019).
Fairburn, C. G. Cognitive Behavior Therapy and Eating Disorders (Guilford Press, 2008).
Wilfley, D. E., Mackenzie, K. R., Welch, R. R., Ayres, V. E. & Weissman, M. M. Interpersonal Psychotherapy for Group (Basic Books, 2008).
Safer, D. L., Telch, C. F. & Chen, E. Y. Dialectical Behavior Therapy for Binge Eating and Bulimia (Guilford Press, 2009).
Wilson, G. T. & Zandberg, L. J. Cognitive-behavioral guided self-help for eating disorders: effectiveness and scalability. Clin. Psychol. Rev. 32 , 343–357 (2012).
Kenny, T. E., Carter, J. C. & Safer, D. L. Dialectical behavior therapy guided self-help for binge-eating disorder. Eat. Disord. 28 , 202–211 (2020).
Hilbert, A. et al. Meta-analysis of the efficacy of psychological and medical treatments for binge-eating disorder. J. Consult. Clin. Psychol. 87 , 91–105 (2019).
Wilson, G. T., Wilfley, D. E., Agras, W. S. & Bryson, S. W. Psychological treatments of binge eating disorder. Arch. Gen. Psychiatry 67 , 94–101 (2010).
Hilbert, A. et al. Long-term efficacy of psychological treatments for binge eating disorder. Br. J. Psychiatry 200 , 232–237 (2012).
Rozakou-Soumalia, N., Darvariu, S. & Sjogren, J. M. Dialectical behaviour therapy improves emotion dysregulation mainly in binge eating disorder and bulimia nervosa: a systematic review and meta-analysis. J. Pers. Med. 11 , 931 (2021).
Lammers, M. W., Vroling, M. S., Crosby, R. D. & van Strien, T. Dialectical behavior therapy adapted for binge eating compared to cognitive behavior therapy in obese adults with binge eating disorder: a controlled study. J. Eat. Disord. 8 , 27 (2020).
Vall, E. & Wade, T. D. Predictors of treatment outcome in individuals with eating disorders: a systematic review and meta-analysis. Int. J. Eat. Disord. 48 , 946–971 (2015). This review and meta-analysis provides comprehensive information on predictors of outcome in the treatment of eating disorders .
Grilo, C. M., Thompson-Brenner, H., Shingleton, R. M., Thompson, D. R. & Franko, D. L. Clinical moderators and predictors of cognitive-behavioral therapy by guided-self-help versus therapist-led for binge-eating disorder: analysis of aggregated clinical trials. Int. J. Eat. Disord. 54 , 1875–1880 (2021).
Hazzard, V. M. et al. Treatment outcomes of psychotherapy for binge-eating disorder in a randomized controlled trial: examining the roles of childhood abuse and post-traumatic stress disorder. Eur. Eat. Disord. Rev. 29 , 611–621 (2021).
Hilbert, A. et al. Meta-analysis on the long-term effectiveness of psychological and medical treatments for binge-eating disorder. Int. J. Eat. Disord. 53 , 1353–1376 (2020). This meta-analysis synthesizes current evidence on the efficacy of psychotherapy and pharmacotherapy for the treatment of BED .
Ghaderi, A. et al. Psychological, pharmacological, and combined treatments for binge eating disorder: a systematic review and meta-analysis. PeerJ 6 , e5113 (2018).
Reas, D. L. & Grilo, C. M. Psychotherapy and medications for eating disorders: better together? Clin. Ther. 43 , 17–39 (2021).
Heo, Y. A. & Duggan, S. T. Lisdexamfetamine: a review in binge eating disorder. CNS Drugs 31 , 1015–1022 (2017).
Gasior, M. et al. A phase 3, multicenter, open-label, 12-month extension safety and tolerability trial of lisdexamfetamine dimesylate in adults with binge eating disorder. J. Clin. Psychopharmacol. 37 , 315–322 (2017).
Hudson, J. I., McElroy, S. L., Ferreira-Cornwell, M. C., Radewonuk, J. & Gasior, M. Efficacy of lisdexamfetamine in adults with moderate to severe binge-eating disorder: a randomized clinical trial. JAMA Psychiatry 74 , 903–910 (2017).
Grilo, C. M. et al. Efficacy and safety of dasotraline in adults with binge-eating disorder: a randomized, placebo-controlled, fixed-dose clinical trial. CNS Spectr. 26 , 481–490 (2021).
McElroy, S. L. et al. Efficacy and safety of dasotraline in adults with binge-eating disorder: a randomized, placebo-controlled, flexible-dose clinical trial. J. Clin. Psychiatry 81 , 19m13068 (2020).
Palavras, M. A., Hay, P., Filho, C. A. & Claudino, A. The efficacy of psychological therapies in reducing weight and binge eating in people with bulimia nervosa and binge eating disorder who are overweight or obese–a critical synthesis and meta-analyses. Nutrients 9 , 299 (2017).
Munsch, S., Meyer, A. H. & Biedert, E. Efficacy and predictors of long-term treatment success for cognitive-behavioral treatment and behavioral weight-loss-treatment in overweight individuals with binge eating disorder. Behav. Res. Ther. 50 , 775–785 (2012).
Ulian, M. D. et al. Effects of health at every size(R) interventions on health-related outcomes of people with overweight and obesity: a systematic review. Obes. Rev. 19 , 1659–1666 (2018).
Grilo, C. M. et al. Randomized controlled trial testing the effectiveness of adaptive “SMART” stepped-care treatment for adults with binge-eating disorder comorbid with obesity. Am. Psychol. 75 , 204–218 (2020).
Palavras, M. A. et al. Integrated weight loss and cognitive behavioural therapy (CBT) for the treatment of recurrent binge eating and high body mass index: a randomized controlled trial. Eat. Weight. Disord. 26 , 249–262 (2021).
David, L. A., Sijercic, I. & Cassin, S. E. Preoperative and post-operative psychosocial interventions for bariatric surgery patients: a systematic review. Obes. Rev. 21 , e12926 (2020).
Kops, N. L. et al. Preoperative binge eating and weight loss after bariatric surgery: a systematic review and meta-analysis. Obes. Surg. 31 , 1239–1248 (2021).
Spirou, D., Raman, J. & Smith, E. Psychological outcomes following surgical and endoscopic bariatric procedures: a systematic review. Obes. Rev. 21 , e12998 (2020).
Taba, J. V. et al. The development of feeding and eating disorders after bariatric surgery: a systematic review and meta-analysis. Nutrients 13 , 2396 (2021).
Masheb, R. M., Dorflinger, L. M., Rolls, B. J., Mitchell, D. C. & Grilo, C. M. Binge abstinence is associated with reduced energy intake after treatment in patients with binge eating disorder and obesity. Obesity 24 , 2491–2496 (2016).
Pacanowski, C. R. et al. Weight change over the course of binge eating disorder treatment: relationship to binge episodes and psychological factors. Obesity 26 , 838–844 (2018).
Preuss, H., Pinnow, M., Schnicker, K. & Legenbauer, T. Improving inhibitory control abilities (ImpulsE)–a promising approach to treat impulsive eating? Eur. Eat. Disord. Rev. 25 , 533–543 (2017).
Schag, K. et al. IMPULS: impulsivity-focused group intervention to reduce binge eating episodes in patients with binge eating disorder–a randomised controlled trial. Psychother. Psychosom. 88 , 141–153 (2019).
Eichen, D. M., Matheson, B. E., Appleton-Knapp, S. L. & Boutelle, K. N. Neurocognitive treatments for eating disorders and obesity. Curr. Psychiatry Rep. 19 , 62 (2017).
Ince, B. et al. Can we change binge eating behaviour by interventions addressing food-related impulsivity? A systematic review. J. Eat. Disord. 9 , 38 (2021).
Raman, J., Hay, P., Tchanturia, K. & Smith, E. A randomised controlled trial of manualized cognitive remediation therapy in adult obesity. Appetite 123 , 269–279 (2018).
Brockmeyer, T. et al. Approach bias modification training in bulimia nervosa and binge-eating disorder: a pilot randomized controlled trial. Int. J. Eat. Disord. 52 , 520–529 (2019).
Chami, R. et al. Targeting binge eating in bulimia nervosa and binge eating disorder using inhibitory control training and implementation intentions: a feasibility trial. Psychol. Med. https://doi.org/10.1017/S0033291720002494 (2020).
Giel, K. E., Speer, E., Schag, K., Leehr, E. J. & Zipfel, S. Effects of a food-specific inhibition training in individuals with binge eating disorder–findings from a randomized controlled proof-of-concept study. Eat. Weight. Disord. 22 , 345–351 (2017).
Lewer, M. et al. Effects of a cognitive-behavioral exposure-based body image therapy for overweight females with binge eating disorder: a pilot study. J. Eat. Disord. 5 , 43 (2017).
Schyns, G., van den Akker, K., Roefs, A., Houben, K. & Jansen, A. Exposure therapy vs lifestyle intervention to reduce food cue reactivity and binge eating in obesity: a pilot study. J. Behav. Ther. Exp. Psychiatry 67 , 101453 (2020).
Low, T. L., Ho, R., Ho, C. & Tam, W. The efficacy of virtual reality in the treatment of binge-purging eating disorders: a meta-analysis. Eur. Eat. Disord. Rev. 29 , 52–59 (2021).
Manzoni, G. M. et al. Virtual reality-enhanced cognitive-behavioral therapy for morbid obesity: a randomized controlled study with 1 year follow-up. Cyberpsychol Behav. Soc. Netw. 19 , 134–140 (2016).
Peterson, C. B. et al. Comparing integrative cognitive-affective therapy and guided self-help cognitive-behavioral therapy to treat binge-eating disorder using standard and naturalistic momentary outcome measures: a randomized controlled trial. Int. J. Eat. Disord. 53 , 1418–1427 (2020).
Runfola, C. D. et al. A pilot open trial of UNITE-BED: a couple-based intervention for binge-eating disorder. Int. J. Eat. Disord. 51 , 1107–1112 (2018).
Chao, A. M. et al. Effects of liraglutide and behavioral weight loss on food cravings, eating behaviors, and eating disorder psychopathology. Obesity 27 , 2005–2010 (2019).
Da Porto, A. et al. Dulaglutide reduces binge episodes in type 2 diabetic patients with binge eating disorder: a pilot study. Diabetes Metab. Syndr. 14 , 289–292 (2020).
Dalton, B., Bartholdy, S., Campbell, I. C. & Schmidt, U. Neurostimulation in clinical and sub-clinical eating disorders: a systematic update of the literature. Curr. Neuropharmacol. 16 , 1174–1192 (2018).
Dalton, B., Campbell, I. C. & Schmidt, U. Neuromodulation and neurofeedback treatments in eating disorders and obesity. Curr. Opin. Psychiatry 30 , 458–473 (2017).
Zeng, B. Y. et al. Efficacy and acceptability of noninvasive brain stimulation interventions for weight reduction in obesity: a pilot network meta-analysis. Int. J. Obes. 45 , 1705–1716 (2021).
Max, S. M., Plewnia, C., Zipfel, S., Giel, K. E. & Schag, K. Combined antisaccade task and transcranial direct current stimulation to increase response inhibition in binge eating disorder. Eur. Arch. Psychiatry Clin. Neurosci. 271 , 17–28 (2021).
Gordon, G., Brockmeyer, T., Schmidt, U. & Campbell, I. C. Combining cognitive bias modification training (CBM) and transcranial direct current stimulation (tDCS) to treat binge eating disorder: study protocol of a randomised controlled feasibility trial. BMJ Open 9 , e030023 (2019).
WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol. Med. 28 , 551–558 (1998).
Topp, C. W., Ostergaard, S. D., Sondergaard, S. & Bech, P. The WHO-5 well-being index: a systematic review of the literature. Psychother. Psychosom. 84 , 167–176 (2015).
Ware, J. Jr, Kosinski, M. & Keller, S. D. A 12-item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med. Care 34 , 220–233 (1996).
Bohn, K. & Fairburn, C. in Cognitive Behavior Therapy and Eating Disorders: The Clinical Impairment Assessment Questionnaire (CIA). Appendix III (ed. Fairburn, C. G.) (Guilford Press, 2008).
Sepulveda, A. R., Whitney, J., Hankins, M. & Treasure, J. Development and validation of an Eating Disorders Symptom Impact Scale (EDSIS) for carers of people with eating disorders. Health Qual. Life Outcomes 6 , 28 (2008).
Li, N., Mitchison, D., Touyz, S. & Hay, P. Cross-sectional comparison of health-related quality of life and other features in people with and without objective and subjective binge eating using a general population sample. BMJ Open 9 , e024227 (2019).
Le, L. K. et al. Burden and health state utility values of eating disorders: results from a population-based survey. Psychol. Med. 51 , 130–137 (2021). This paper provides important data on the burden associated with BED, which is based on a representative population sample .
Tannous, W. K. et al. The economic cost of bulimia nervosa and binge eating disorder: a population-based study. Psychol. Med. https://doi.org/10.1017/S0033291721000775 (2021).
Watson, H. J. et al. A register-based case-control study of health care utilization and costs in binge-eating disorder. J. Psychosom. Res. 108 , 47–53 (2018).
Hart, L. M., Granillo, M. T., Jorm, A. F. & Paxton, S. J. Unmet need for treatment in the eating disorders: a systematic review of eating disorder specific treatment seeking among community cases. Clin. Psychol. Rev. 31 , 727–735 (2011).
Hay, P. et al. General practitioner and mental healthcare use in a community sample of people with diagnostic threshold symptoms of bulimia nervosa, binge-eating disorder, and other eating disorders. Int. J. Eat. Disord. 53 , 61–68 (2020).
Gearhardt, A. N. & Schulte, E. M. Is food addictive? A review of the science. Annu. Rev. Nutr. 41 , 387–410 (2021).
Hebebrand, J. et al. “Eating addiction”, rather than “food addiction”, better captures addictive-like eating behavior. Neurosci. Biobehav. Rev. 47 , 295–306 (2014).
van Hoeken, D. & Hoek, H. W. Review of the burden of eating disorders: mortality, disability, costs, quality of life, and family burden. Curr. Opin. Psychiatry 33 , 521–527 (2020).
Giel, K., Schmidt, U., Fernandez-Aranda, F. & Zipfel, S. The neglect of eating disorders. Lancet 388 , 461–462 (2016).
Schmidt, U. et al. Eating disorders: the big issue. Lancet Psychiatry 3 , 313–315 (2016).
Bulik, C. et al. The Binge Eating Genetics Initiative (BEGIN) study. BMC Psychiatry 20 , 307 (2020).
Bulik, C. M. et al. The Eating Disorders Genetics Initiative (EDGI): study protocol. BMC Psychiatry 21 , 234 (2021).
Krug, I. et al. A proof-of-concept study applying machine learning methods to putative risk factors for eating disorders: results from the multi-centre European project on healthy eating. Psychol. Med. https://doi.org/10.1017/S003329172100489X (2021).
Leme, A. C. B. et al. Impact of strategies for preventing obesity and risk factors for eating disorders among adolescents: a systematic review. Nutrients 12 , 3134 (2020).
Wilfley, D. E. et al. Training models for implementing evidence-based psychological treatment: a cluster-randomized trial in college counseling centers. JAMA Psychiatry 77 , 139–147 (2020).
Taylor, C. B., Fitzsimmons-Craft, E. E. & Graham, A. K. Digital technology can revolutionize mental health services delivery: the COVID-19 crisis as a catalyst for change. Int. J. Eat. Disord. 53 , 1155–1157 (2020).
Herman, B. K. et al. Development of the 7-item binge-eating disorder screener (BEDS-7). Prim. Care Companion CNS Disord. https://doi.org/10.4088/PCC.15m01896 (2016).
Article PubMed PubMed Central Google Scholar
Gormally, J., Black, S., Daston, S. & Rardin, D. The assessment of binge eating severity among obese persons. Addict. Behav. 7 , 47–55 (1982).
van Strien, T., Frijters, J. E. R., Bergers, G. P. A. & Defares, P. B. The Dutch Eating Behaviour Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int. J. Eat. Disord. 5 , 295–315 (1986).
Fairburn, C. G. & Beglin, S. J. Eating Disorder Examination Questionnaire (6.0). in Cognitive Behaviour Therapy and Eating Disorders (ed. Fairburn, C. G.) (Guilford Press, 2008).
Garner, D. Eating Disorder Inventory-3 (EDI-3) Professional Manual (PAR, 2004).
Maguen, S. et al. Screen for disordered eating: improving the accuracy of eating disorder screening in primary care. Gen. Hosp. Psychiatry 50 , 20–25 (2018).
Stunkard, A. J. & Messick, S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J. Psychosom. Res. 29 , 71–83 (1985).
Yanovski, S. Z., Marcus, M. D., Wadden, T. A. & Walsh, B. T. The Questionnaire on Eating and Weight Patterns-5: an updated screening instrument for binge eating disorder. Int. J. Eat. Disord. 48 , 259–261 (2015).
Fairburn, C. G., Cooper, Z., & O’Connor, M. in Cognitive Behaviour Therapy and Eating Disorders (ed. Fairburn, C. G.) (Guilford Press, 2008).
First, M. B., Williams, J. B. W., Karg, R. S. & Spitzer, R. L. Structured Clinical Interview for DSM-5–Research Version (SCID-5 for DSM-5, Research Version; SCID-5-RV) (American Psychiatric Association, 2015).
Stunkard, A. J. Eating patterns and obesity. Psychiatr. Q. 33 , 284–295 (1959).
Hamburger, W. W. Emotional aspects of obesity. Med. Clin. North. Am. 35 , 483–499 (1951).
American Psychiatric Association. Diagnostic and statistical manual of mental disorders 3rd edn (American Psychiatric Association, 1980).
American Psychiatric Association. Diagnostic and statistical manual of mental disorders 4th edn (American Psychiatric Association, 1994).
Kolar, D. R., Rodriguez, D. L., Chams, M. M. & Hoek, H. W. Epidemiology of eating disorders in Latin America: a systematic review and meta-analysis. Curr. Opin. Psychiatry 29 , 363–371 (2016).
Smink, F. R., van Hoeken, D., Oldehinkel, A. J. & Hoek, H. W. Prevalence and severity of DSM-5 eating disorders in a community cohort of adolescents. Int. J. Eat. Disord. 47 , 610–619 (2014).
Faravelli, C. et al. Clinical epidemiology of eating disorders: results from the Sesto Fiorentino study. Psychother. Psychosom. 75 , 376–383 (2006).
Bagaric, M., Touyz, S., Heriseanu, A., Conti, J. & Hay, P. Are bulimia nervosa and binge eating disorder increasing? Results of a population-based study of lifetime prevalence and lifetime prevalence by age in South Australia. Eur. Eat. Disord. Rev. 28 , 260–268 (2020).
De Silva, A., Salem, V., Matthews, P. M. & Dhillo, W. S. The use of functional MRI to study appetite control in the CNS. Exp. Diabetes Res. 2012 , 764017 (2012).
Heal, D. J. & Smith, S. L. Prospects for new drugs to treat binge-eating disorder: insights from psychopathology and neuropharmacology. J. Psychopharmacol. https://doi.org/10.1177/02698811211032475 (2021).
Quilty, L. C., Allen, T. A., Davis, C., Knyahnytska, Y. & Kaplan, A. S. A randomized comparison of long acting methylphenidate and cognitive behavioral therapy in the treatment of binge eating disorder. Psychiatry Res. 273 , 467–474 (2019).
Download references
Acknowledgements
U.S. acknowledges salary support from the National Institute of Health Research (NIHR) Mental Health Biomedical Research Centre (BRC) at the South London and Maudsley NHS Foundation Trust and King’s College London. She is also supported by an NIHR Senior Investigator Award. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. C.M.B. is supported by NIMH (R01MH120170, R01MH124871, R01MH119084, R01MH118278, R01 MH124871); Brain and Behavior Research Foundation Distinguished Investigator Grant; Swedish Research Council (Vetenskapsrådet, award 538-2013-8864); Lundbeck Foundation (grant no. R276-2018-4581). S.Z. was supported by the publicly funded project INTERBED (01GV0601) of the German Federal Ministry of Education and Research (Bundesministerium für Bildung und Forschung (BMBF)). F.F.-A. is supported by CERCA Programme/Generalitat de Catalunya for institutional support, and by research grants from PERIS (SLT006/17/00246), Instituto Salud Carlos III (PI17/01167, PI20/132, CIBERobn) and EU-H2020 grants (Eat2beNICE/H2020-SFS-2016-2, ref. 728018; and PRIME/H2020-SC1-BHC-2018-2020, ref. 847879) and COST Action (CA19115). K.S. is supported by a grant from the Margarete von Wrangell Program by the Federal Ministry of Science and Education Baden-Württemberg. K.E.G. acknowledges grants from the Federal Ministry of Education and Research (BMBF) (01KG2009) and the German Research Foundation (DFG) (GI 878/4-1). The authors thank the patient for anonymously sharing personal experiences of BED.
Author information
Authors and affiliations.
Department of Psychosomatic Medicine and Psychotherapy, Medical University Hospital Tübingen, Tübingen, Germany
Katrin E. Giel, Kathrin Schag & Stephan Zipfel
Center of Excellence for Eating Disorders (KOMET), Tübingen, Germany
Department of Psychiatry, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
Cynthia M. Bulik
Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden
Department of Nutrition, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
Department of Psychiatry, Bellvitge University Hospital-IDIBELL, Barcelona, Spain
Fernando Fernandez-Aranda
Ciber Fisiopatología Obesidad y Nutrición (CIBERObn), Instituto Salud Carlos III, Madrid, Spain
Department of Clinical Sciences, School of Medicine and Health Sciences, University of Barcelona, Barcelona, Spain
Translational Health Research Institute, Western Sydney University, Sydney, NSW, Australia
Phillipa Hay
Camden and Campbelltown Hospitals, SWSLHD, Campbelltown, NSW, Australia
Department of Public Health, University of Helsinki, Helsinki, Finland
Anna Keski-Rahkonen
Section of Eating Disorders, Department of Psychological Medicine, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, London, UK
- Ulrike Schmidt
South London and Maudsley NHS Foundation Trust, London, UK
You can also search for this author in PubMed Google Scholar
Contributions
Introduction (K.E.G.); Epidemiology (A.K.-R.); Mechanisms/pathophysiology (C.M.B. and F.F.-A.); Diagnosis, screening and prevention (K.S., K.E.G. and S.Z.); Management (P.H. and U.S.); Quality of life (P.H.); Outlook (K.E.G.); Overview of Primer (K.E.G.).
Corresponding author
Correspondence to Katrin E. Giel .
Ethics declarations
Competing interests.
C.M.B. received a grant from Shire, was a member of the Shire Scientific Advisory Board, acted as a consultant for Idorsia, received a grant from Lundbeckfonden, acted as an author for and received a grant from Pearson, and was a member of the Equip Health Inc. Clinical Advisory Board. F.F.-A. received consultancy honorarium from Novo Nordisk and an editorial honorarium as editor-in-chief from Wiley. P.H. is a consultant to Takeda Pharmaceuticals, receives or has received sessional fees and lecture fees from the Australian Medical Council, Therapeutic Guidelines publication, and New South Wales Institute of Psychiatry, and royalties/honoraria from Hogrefe and Huber, McGraw Hill Education, Blackwell Scientific Publications, BioMed Central and PLOS Medicine, and has received research grants from the NHMRC and ARC. She is Chair of the National Eating Disorders Collaboration Steering Committee in Australia and was a member of the ICD-11 Working Group for Eating Disorders and was Chair of the Clinical Practice Guidelines Project Working Group (Eating Disorders) of RANZCP. All views expressed in this paper are her own. All other authors declare no competing interests.
Peer review
Peer review information.
Nature Reviews Disease Primers thanks M. Fennig, A. C. Grammer, C. Segura-Garcia, F. Thomas, D. Wilfey and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Giel, K.E., Bulik, C.M., Fernandez-Aranda, F. et al. Binge eating disorder. Nat Rev Dis Primers 8 , 16 (2022). https://doi.org/10.1038/s41572-022-00344-y
Download citation
Accepted : 28 January 2022
Published : 17 March 2022
DOI : https://doi.org/10.1038/s41572-022-00344-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
The cost of the perfect body: influence mechanism of internalization of media appearance ideals on eating disorder tendencies in adolescents.
BMC Psychology (2024)
Experiences of living with binge eating disorder and facilitators of recovery processes: a qualitative study
- Marit Fjerdingren Bremer
- Lisa Garnweidner-Holme
- Marianne Molin
Journal of Eating Disorders (2023)
SipNose-topiramate: a potential novel approach to binge eating management
- Ayala Kobo-Greenhut
- Adit Zohar-Beja
A randomised controlled feasibility study of food-related computerised attention training versus mindfulness training and waiting-list control for adults with overweight or obesity: the FOCUS study
- Daniela Mercado
- Jessica Werthmann
The social epidemiology of binge-eating disorder and behaviors in early adolescents
- Jason M. Nagata
- Zacariah Smith-Russack
- Kyle T. Ganson
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
Eating Disorders
What are eating disorders.
There is a commonly held misconception that eating disorders are a lifestyle choice. Eating disorders are actually serious and often fatal illnesses that are associated with severe disturbances in people’s eating behaviors and related thoughts and emotions. Preoccupation with food, body weight, and shape may also signal an eating disorder. Common eating disorders include anorexia nervosa, bulimia nervosa, and binge-eating disorder.
What are the signs and symptoms of eating disorders?
Anorexia nervosa.
Anorexia nervosa is a condition where people avoid food, severely restrict food, or eat very small quantities of only certain foods. They also may weigh themselves repeatedly. Even when dangerously underweight, they may see themselves as overweight.
There are two subtypes of anorexia nervosa: a "restrictive " subtype and a "binge-purge " subtype.
- In the restrictive subtype of anorexia nervosa, people severely limit the amount and type of food they consume.
- In the binge-purge subtype of anorexia nervosa, people also greatly restrict the amount and type of food they consume. In addition, they may have binge-eating and purging episodes—eating large amounts of food in a short time followed by vomiting or using laxatives or diuretics to get rid of what was consumed.
Anorexia nervosa can be fatal. It has an extremely high death (mortality) rate compared with other mental disorders. People with anorexia are at risk of dying from medical complications associated with starvation. Suicide is the second leading cause of death for people diagnosed with anorexia nervosa.
If you or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide & Crisis Lifeline at 988 or chat at 988lifeline.org . In life-threatening situations, call 911.
Symptoms include:
- Extremely restricted eating
- Extreme thinness (emaciation)
- A relentless pursuit of thinness and unwillingness to maintain a normal or healthy weight
- Intense fear of gaining weight
- Distorted body image, a self-esteem that is heavily influenced by perceptions of body weight and shape, or a denial of the seriousness of low body weight
Other symptoms may develop over time, including:
- Thinning of the bones (osteopenia or osteoporosis)
- Mild anemia and muscle wasting and weakness
- Brittle hair and nails
- Dry and yellowish skin
- Growth of fine hair all over the body (lanugo)
- Severe constipation
- Low blood pressure
- Slowed breathing and pulse
- Damage to the structure and function of the heart
- Brain damage
- Multiorgan failure
- Drop in internal body temperature, causing a person to feel cold all the time
- Lethargy, sluggishness, or feeling tired all the time
- Infertility
Bulimia nervosa
Bulimia nervosa is a condition where people have recurrent and frequent episodes of eating unusually large amounts of food and feeling a lack of control over these episodes. This binge-eating is followed by behavior that compensates for the overeating such as forced vomiting, excessive use of laxatives or diuretics, fasting, excessive exercise, or a combination of these behaviors. People with bulimia nervosa may be slightly underweight, normal weight, or over overweight.
- Chronically inflamed and sore throat
- Swollen salivary glands in the neck and jaw area
- Worn tooth enamel and increasingly sensitive and decaying teeth as a result of exposure to stomach acid
- Acid reflux disorder and other gastrointestinal problems
- Intestinal distress and irritation from laxative abuse
- Severe dehydration from purging of fluids
- Electrolyte imbalance (too low or too high levels of sodium, calcium, potassium, and other minerals) which can lead to stroke or heart attack
Binge-eating disorder
Binge-eating disorder is a condition where people lose control over their eating and have reoccurring episodes of eating unusually large amounts of food. Unlike bulimia nervosa, periods of binge-eating are not followed by purging, excessive exercise, or fasting. As a result, people with binge-eating disorder often are overweight or obese. Binge-eating disorder is the most common eating disorder in the U.S.
- Eating unusually large amounts of food in a specific amount of time, such as a 2-hour period
- Eating even when you're full or not hungry
- Eating fast during binge episodes
- Eating until you're uncomfortably full
- Eating alone or in secret to avoid embarrassment
- Feeling distressed, ashamed, or guilty about your eating
- Frequently dieting, possibly without weight loss
Avoidant restrictive food intake disorder
Avoidant restrictive food intake disorder (ARFID), previously known as selective eating disorder, is a condition where people limit the amount or type of food eaten. Unlike anorexia nervosa, people with ARFID do not have a distorted body image or extreme fear of gaining weight. ARFID is most common in middle childhood and usually has an earlier onset than other eating disorders. Many children go through phases of picky eating, but a child with ARFID does not eat enough calories to grow and develop properly, and an adult with ARFID does not eat enough calories to maintain basic body function.
- Dramatic restriction of types or amount of food eaten
- Lack of appetite or interest in food
- Dramatic weight loss
- Upset stomach, abdominal pain, or other gastrointestinal issues with no other known cause
- Limited range of preferred foods that becomes even more limited (“picky eating” that gets progressively worse)
What are the risk factors for eating disorders?
Eating disorders can affect people of all ages, racial/ethnic backgrounds, body weights, and genders. Eating disorders frequently appear during the teen years or young adulthood but may also develop during childhood or later in life.
Researchers are finding that eating disorders are caused by a complex interaction of genetic, biological, behavioral, psychological, and social factors. Researchers are using the latest technology and science to better understand eating disorders.
One approach involves the study of human genes. Eating disorders run in families. Researchers are working to identify DNA variations that are linked to the increased risk of developing eating disorders.
Brain imaging studies are also providing a better understanding of eating disorders. For example, researchers have found differences in patterns of brain activity in women with eating disorders in comparison with healthy women. This kind of research can help guide the development of new means of diagnosis and treatment of eating disorders.
How are eating disorders treated?
It is important to seek treatment early for eating disorders. People with eating disorders are at higher risk for suicide and medical complications. People with eating disorders can often have other mental disorders (such as depression or anxiety) or problems with substance use. Complete recovery is possible.
Treatment plans are tailored to individual needs and may include one or more of the following:
- Individual, group, and/or family psychotherapy
- Medical care and monitoring
- Nutritional counseling
- Medications
Psychotherapies
Family-based therapy, a type of psychotherapy where parents of adolescents with anorexia nervosa assume responsibility for feeding their child, appears to be very effective in helping people gain weight and improve eating habits and moods.
To reduce or eliminate binge-eating and purging behaviors, people may undergo cognitive behavioral therapy (CBT), which is another type of psychotherapy that helps a person learn how to identify distorted or unhelpful thinking patterns and recognize and change inaccurate beliefs.
Evidence also suggests that medications such as antidepressants, antipsychotics, or mood stabilizers may also be helpful for treating eating disorders and other co-occurring illnesses such as anxiety or depression. The Food and Drug Administration’s (FDA) website has the latest information on medication approvals, warnings, and patient information guides.
How can I find a clinical trial for an eating disorder?
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. The goal of clinical trials is to determine if a new test or treatment works and is safe. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
To learn more or find a study, visit:
- NIMH’s Clinical Trials webpage : Information about participating in clinical trials
- Clinicaltrials.gov: Current Studies on Eating Disorders : List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
Where can I learn more about eating disorders?
Free brochures and shareable resources.
- Eating Disorders: About More Than Food : A brochure about the common eating disorders anorexia nervosa, bulimia nervosa, and binge-eating disorder, and various approaches to treatment. Also available en español .
- Let’s Talk About Eating Disorders : An infographic with facts that can help shape conversations around eating disorders. Also available in en español .
- Shareable Resources on Eating Disorders : Help support eating disorders awareness and education in your community. Use these digital resources, including graphics and messages, to spread the word about eating disorders.
- Mental Health Minute: Eating Disorders : Take a mental health minute to watch this video on eating disorders.
- Let’s Talk About Eating Disorders with NIMH Grantee Dr. Cynthia Bulik : Learn about the signs, symptoms, treatments, and the latest research on eating disorders.
Research and statistics
- NIMH Eating Disorders Research Program : This program supports research on the etiology, core features, longitudinal course, and assessment of eating disorders.
- Journal Articles : References and abstracts from MEDLINE/PubMed (National Library of Medicine).
- Statistics: Eating Disorders
Last Reviewed: January 2024
Unless otherwise specified, the information on our website and in our publications is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.
- Open access
- Published: 26 April 2024
Moderating effect of self-esteem between perfectionism and avoidant restrictive food intake disorder among Lebanese adults
- Roni Chaaya 1 ,
- Rabih Hallit 2 , 3 , 4 ,
- Diana Malaeb 5 ,
- Fouad Sakr 6 ,
- Mariam Dabbous 6 ,
- Sami El Khatib 7 , 8 ,
- Feten Fekih-Romdhane 9 , 10 na1 ,
- Souheil Hallit 2 , 11 na1 &
- Sahar Obeid 1 na1
BMC Psychiatry volume 24 , Article number: 325 ( 2024 ) Cite this article
82 Accesses
Metrics details
Avoidant Restrictive Food Intake Disorder (ARFID) is a new diagnosis added to the DSM-5 characterized by pathological eating habits without body image disturbances. Previous findings demonstrated a general association between high levels of perfectionism and low levels of self-esteem in association with general eating disorders. However, research is scant when it comes to ARFID specifically. Subsequently, although self-esteem is seen to moderate the association between perfectionism and general eating disorders, this research study aims to explore the same moderation but with ARFID specifically.
For this study, 515 Lebanese adults from the general Lebanese population were recruited from all over Lebanon, 60.1% of which were females. The Arabic version of the Big Three Perfectionism Scale– Short Form (BTPS-SF) was used to measure self-critical, rigid and narcissistic perfectionism; the Avoidant/Restrictive Food Intake Disorder screen (NIAS) was used to score the ARFID variable; the Arabic-Single Item Self-Esteem (A-SISE) was the scale used to measure self-esteem.
Across the different perfectionism types, self-esteem was seen to moderate the association between narcissistic perfectionism and ARFID (Beta = − 0.22; p =.006). At low (Beta = 0.77; p <.001), moderate (Beta = 0.56; p <.001) and high (Beta = 0.36; p =.001) levels of self-esteem, higher narcissistic perfectionism was significantly associated with higher ARFID scores.
This study brought to light some crucial clinical implications that highlight the need for interventions that help in the enhancement of self-esteem in patients with high perfectionism and ARFID. This study suggests that clinicians and healthcare professionals should focus more on risk factors influencing the development and maintenance of ARFID-like symptoms.
Peer Review reports
Introduction
Avoidant Restrictive Food Intake Disorder (ARFID), a diagnosis first introduced in the fifth version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), is distinguished by abnormal eating patterns without the body image disturbances characteristic of other eating disorders [ 1 , 2 ]. More specifically, those diagnosed with ARFID fail to fulfill their nutritional requirements due to reasons unrelated to self-image worries, weight gain fears or medical or cultural concerns [ 3 ]. This disordered eating behavior can be associated with (1) being disinterested in food; (2) having a heightened visual, olfactory, or gustatory sensitivity to food; (3) exhibiting avoidance of potential consequences, such as choking that may arise from eating [ 3 ]. Unlike other eating disorders, ARFID is characterized by the absence of any fear related to weight gain [ 4 ]. Patients with ARFID are characterized by their inability to meet their nutritional requirements, with food avoidance being their primary characteristic [ 4 ]. Another distinction to make between ARFID on one hand, and anorexia nervosa and bulimia nervosa on the other hand, is the absence of body image disturbances [ 4 ]. Unlike other eating disorders, ARFID patients seek to improve their food intake habits and to gain weight; however, they find themselves unable to act upon this desire [ 4 ]. In addition, a distinction between ARFID patient and picky eaters should be made, where the former have clinically significant impairments in their eating habits, avoiding food to a degree where their energy is depleted, and their nutritional needs are not met [ 4 ]. Therefore, compared to anorexia and bulimia nervosa, patients with ARFID do not struggle with overevaluation of their weight nor do they have disturbances with their body image [ 2 ]. Individuals with ARFID commonly express apprehension regarding negative consequences of eating, such as the fear of choking or nausea, and being concerned about the immediate adverse effects of eating [ 5 ]. Moreover, while binge eating disorder is identified by frequent occurrences of uncontrollable overeating, on a weekly basis, accompanied with significant distress, ARFID is distinguished by limited food consumption, leading to deficiencies in nutrient-intake [ 2 ].
The diagnosis of ARFID can be established in people across all age groups whose restrictive eating patterns result in an insufficient nutritional intake, weight loss, an increased reliance on nutritional supplements, and an impairment in psychosocial functioning [ 6 ]. Additionally, medical abnormalities can ensue from ARFID such as abdominal pain and amenorrhea in females [ 3 ], as well as malnutrition and bradycardia [ 7 ]. Selective eating behaviors during childhood have been linked to the development of ARFID; however, limited research is available regarding the longitudinal trajectory of ARFID and its ultimate outcome [ 7 ]. Furthermore, anxiety disorders, autism spectrum disorders, and attention deficit and hyperactivity disorders have been shown to be comorbid with ARFID [ 7 ]. Depression, suicidal ideations, self-harm, and weight loss also correlated with symptoms of ARFID [ 8 ].
With ARFID being a disorder that is associated with both physical health complications as well as concurrent psychiatric conditions, recent findings have emerged regarding its treatment [ 9 , 10 ]. Primarily, Cognitive Behavioral Therapeutic approach specialized for the treatment of children, adolescents, and adults with ARFID (CBT-AR) was developed [ 9 , 10 ]. CBT-AR spans 20 to 30 sessions across four stages. The first stage consists of psycho-educating the patient about ARFID and allowing them to self-monitor their eating habits [ 9 , 10 ]. The second stage involves planning the treatment, explaining nutritional deficiencies, identifying new foods that the patient can try to counteract these deficiencies while promoting weight gain and improving overall wellbeing [ 9 , 10 ]. In stage 3, the therapist addresses the patient’s maintaining mechanisms while practicing exposure during and in-between sessions [ 9 , 10 ]. Finally, in stage 4, the patient’s progress is discussed, and a relapse prevention plan is created [ 9 , 10 ]. In this context, in a study conducted on patients aged 10–17, CBT-AR was reported to have notable enhancements in ARFID symptoms, including the introduction of new foods into the patients’ diets and significant weight gain [ 9 ]. While following the same 4-stage approach, another study implemented the CBT-AR among adults aged 18 to 55 years [ 10 ]. Concordant with the outcomes observed in children and adolescents, adults who underwent CBT-AR demonstrated substantial decrease in their ARFID symptoms [ 10 ]. This improvement was accompanied by notable weight gain and the incorporation of new foods into their diets [ 10 ]. Both mentioned studies proved the feasibility, acceptability and proof-of-concept of CBT-AR as being an efficacious treatment for children, adolescents [ 9 ] and adults [ 10 ] with ARFID.
On another hand, in children and adolescents, Family-Based Therapy (FBT) that is specialized to patients with ARFID, has been shown to be efficient through parental empowerment and psychoeducation on eating behaviors and nutrition [ 11 ]. In the latter case, exposure exercises were led by parents at home with the patient, leading to reduced stress [ 11 ]. A different study pointed out that, unlike other eating disorders, the treatment of ARFID should prioritize behavioral and nutritional strategies of treatment [ 4 ]. Additionally, the study also noted variations in treatment between short-term and long-term ARFID patients. Thus, short-term patients, having had healthy eating habits prior to the development of ARFID, can relate to a remembered standard of healthy eating through behavioral experiments and the help of a dietician [ 4 ]. On the contrary, therapy with long-term patients requires the minimization of certain symptoms rather than entirely removing the disorder [ 4 ]. Therefore, gaining more insight into the mechanisms underlying the development of ARFID might help advance knowledge on its prevention and intervention. In this study, we are focusing on the relationship between perfectionism and ARFID.
The development of ARFID symptoms has the most diverse etiology among all eating disorders, with a history of picky eating being one contributing factor [ 12 ]. Typical selective / picky eating is set apart from ARFID through the absence of substantial nutritional or psychosocial consequences [ 13 ], not always impacting weight status [ 6 ]. Yet, in severe cases of picky eating, the development of ARFID symptoms ensues, contributing to malnourishment, weight loss and psychosocial complications [ 6 ], with individuals rigidly rejecting any kind of novel foods, becoming more selective with age [ 12 ]. Individuals exhibiting selective eating behaviors have demonstrated cognitive and behavioral rigidities, including limited interests, perfectionism and challenges dealing with unfamiliar or new situations [ 14 ]. With selective eating behaviors being associated with ARFID and with cognitive and behavioral rigidity, case studies have shown that individuals with ARFID tend to exhibit this form of rigidity as well [ 14 ]. Perfectionism, which is a cognitive or behavioral contributor to the maintenance of psychopathology [ 15 ], has been seen in individuals exhibiting ARFID symptoms in the form of rigidity as to how food is prepared or presented or showing aversive responses to the sensory properties of food [ 14 ]. Concordantly, perfectionism was seen to be associated with both behavioral and cognitive food restraints [ 16 ].
It is important to highlight that perfectionism is a varied construct with different forms, one of which is described by the inclination to project one’s own perfectionistic standards onto others in a manner that is demanding and overly critical [ 17 ]. This other-oriented perfectionism is commonly referred to as ‘narcissistic perfectionism’ [ 17 ]. Researchers aimed to elucidate this phenomenon by developing a model illustrating that narcissistic perfectionism encompasses traits such as grandiosity, entitlement, high expectations from others and perfectionism directed towards others [ 17 ].
Self-esteem as a moderator
As for self-esteem, it is synonymous with one’s personal evaluation of their own self-worth [ 18 ]. Low self-esteem manifests itself in a sense of hopelessness to change, affecting the adherence to therapy of patients with eating disorders. It also comes in the form of determination in achieving success in areas that matter to them, such as weight regulation and body shape; hence, making it more challenging to exhibit change in these specific areas [ 19 ]. In contrast, a study conducted in Saudi Arabia found no significant association between self-esteem and eating disorders [ 20 ]. On another hand, in patients with ARFID specifically, one study found that they tend to have higher self-esteem compared to patients with anorexia nervosa [ 21 ]. This can be attributed to the fact that ARFID patients struggle to find the desire to eat, rather than presenting body dissatisfaction or fear of gaining weight [ 4 ]. However, compared to those who eat freely, avoidant eaters tend to have lower levels of self-esteem [ 22 ]. Another study concluded that psychological distress, such as depressive symptoms and low self-esteem, acts as a risk factor that contributes to restrictive eating behaviors in adolescents, allowing for the maintenance and escalation of symptoms [ 23 ]. Studies have also demonstrated the moderating effect of low self-esteem between the negative affect associated with social rejection and restrictive eating behaviors, while high self-esteem acted as a protective factor moderating the relationship between the affective consequences of social rejection and restrictive eating [ 24 ].
As previously discussed, in patients with ARFID symptoms specifically, picky eating was shown to be associated with perfectionism [ 14 ]. Neophobia, which is defined as avoidance and unwillingness to try or eat new food [ 25 ], is a common characteristic seen in patients displaying symptoms of ARFID [ 13 ]. This neophobic tendency has been associated with lower self-esteem scores [ 26 ]. In elaboration, adult patients diagnosed with ARFID might feel the need to hide their eating patterns out of fear of being perceived as immature [ 27 ]. They may also refrain from eating in social settings to prevent drawing attention to their perfectionistic food preferences [ 27 ]. This avoidance behavior hinders their abilities to form new relationships, leading to social isolation and increased neophobia [ 27 ]. With social isolation being associated with low self-esteem [ 28 ] we can assume that the picky eating and neophobic characteristics of people with ARFID contribute to the low self-esteem in these individuals. It can also be assumed that it is this neophobic tendency, which is hindering these people’s ability to socialize, is reinforcing the perfectionistic selective eating behaviors seen in ARFID patients.
The present study
To our knowledge, due to the scarce literature on ARFID in Lebanon, this would be the first study focusing on ARFID specifically in light of the two other variables among a sample of Lebanese participants. When discussing eating disorders, it is essential to comprehend the cultural factors that contribute towards their etiology [ 20 ], including in Arab countries and cultural background. In Saudi Arabia for instance, an Islamic nation, people adopt the teachings of the Holy Quran that advocates for restrictive eating behaviors [ 20 ]. In addition, food is perceived with high respect among Arab people, carrying a robust social, religious, and cultural significance [ 29 ]. Therefore, in an Arab country, where food is viewed highly, having ARFID can be perceived as impairing and challenging [ 29 ]. In a study conducted on a Saudi sample, the findings demonstrated the absence of a significant distinction in eating habits between Saudis who adopt an Arab-oriented lifestyle compared to those who are more Western-oriented [ 20 ]. Additionally, the study found no significant associations between eating disorders on one hand, and self-esteem and the use of social media on the other hand [ 20 ]. A different study showed a significant association between eating disturbances and increased exposure to Western media [ 30 ]. Therefore, the exploration of ARFID along with its associated characteristics and tendencies would aid in filling up the gaps in the literature, specifically within the Arab context.
More specifically, within the Lebanese context, a better understanding is needed regarding how perfectionism and self-esteem correlate with increased levels of avoidant and restrictive eating behaviors, and how self-esteem can moderate this relationship as well. In this study, our objective was to assess the moderating effect of self-esteem between perfectionism and ARFID symptoms [ 18 ]. Therefore, it is expected that self-esteem will moderate this association.
Study design
Using Google Forms, a questionnaire was developed and disseminated thought a variety of messaging platforms, such as WhatsApp, Instagram, and Facebook Messenger. Through a snowball sampling, 515 participants were recruited in this cross-sectional between February and March of 2023. To be eligible for participation, individuals needed to be Lebanese citizens residing in Lebanon and be 18 years old or older. Considering that an online survey was created for this study, internet access was a necessity, alongside a willingness to partake in the research study. Participants who declined to complete the questionnaire were excluded from the study. The assessment tools provided in the questionnaire were presented in a randomized order to mitigate any potential order-related biases. Participants were assured confidentiality and anonymity, while agreeing to complete the questionnaire voluntarily without any form of compensation. The average time required to fill out the questionnaire was around 20 min.
Minimal sample size calculation
We used G*Power software to determine the sample size. The minimum required sample size was 457 participants, considering an alpha error of 5%, a power of 95%, a minimal model R-square of 5% (effect size of 5%) and allowing 9 predictors to be included in the model.
Instruments
The questionnaire consisted of self-report scales. It also comprised of questions about sociodemographic details such as age, sex, education level, living area, marital status and Household Crowding Index (HCI), which is calculated by dividing the total count of people living in a household, excluding a newborn child, by the total number of rooms in that household, excluding the kitchen and bathrooms [ 31 ]. Participants self-reported their height and weight to compute their Body Mass Index (BMI) [ 32 ]. Three questions about physical activity intensity (1 = light activity to 5 = Heavy breathing and constant sweating), duration (1 = < 10 min to 4 = 30 or more minutes), and frequency (1 = less than once a month to 5 = daily or almost daily) were used to calculate a physical activity index by multiplying the three values (yielding a maximum score of 100). Higher scores reflect greater physical activity [ 33 ]. Regarding their perceived financial burden, respondents were asked to answer one question “How much pressure do you feel with regard to your personal financial situation in general?” on a scale from 1 to 10, with 10 referring to overwhelming pressure. The following measures have been used:
The big three perfectionism scale– short form (BTPS-SF)
The BTPS-SF, validated in Lebanon [ 34 ], is an abridged, 16-item scale of the 45-item BTPS, scored on a 7-point Likert scale from 1 (disagree strongly) to 7 (agree strongly) [ 35 ]. It includes three primary factors of perfectionism that tend to be overarching, namely rigid, self-critical, and narcissistic perfectionism [ 35 ]. Rigid perfectionism, characterized by the expectation of flawless performance from oneself [ 36 ], includes 4 items such as “I have a strong need to be perfect” [ 35 ]. The second factor, self-critical perfectionism, which is defined as having negative reactions to performance that is flawed and that others expect perfection from oneself [ 37 ], consists of 6 items such as “The idea of making a mistake frightens me” [ 35 ]. Narcissistic perfectionism, on the other hand, refers to the expectation of perfection from others in an overly critical and entitled manner [ 36 ], and consists of 6 items such as “I expect those close to me to be perfect” [ 35 ]. In this study, the internal reliability values were as follows: rigid perfectionism ( ω = 0.85 / α = 0.85), self-critical perfectionism ( ω = 0.86 / α = 0.86) and narcissistic perfectionism ( ω = 0.83 / α = 0.83).
Avoidant/restrictive food intake disorder screen (NIAS)
Validated in Lebanon [ 29 ], the Arabic version of the NIAS was used to screen for ARFID symptoms [ 29 ]. This 9-item scale is scored on a 6-point Likert scale labeled from “strongly disagree” to “strongly agree”, with a total score ranging from 0 to 45, calculated by summing all 9 items [ 38 ]. It is composed of three factors– Picky eating, Appetite and Fear– each consisting of three items [ 29 ]. Subscale scores range from 0 to 15 and are calculated by summing their respective 3 items [ 38 ]. The higher the score on the NIAS, the more avoidant/restrictive the eating behavior is [ 39 ]. Cutoff values of ≥ 10, ≥ 9, and/or ≥ 10 have been proposed for capturing individuals who fit the NIAS dimensions: Picky eating, Appetite, and Fear respectively [ 39 ] ( ω = 0.88 and α = 0.88 in this study).
The arabic-single item self-esteem (A-SISE)
The Arabic version of the Single Item Self-Esteem scale was used for this study, which consists of a 5-point Likert scale ranging from 1 ( not at all true to me ) to 5 ( very true of me ). The only item in this scale is “I have high self-esteem” [ 40 ]. The scale is validated in the Lebanese population and has been proven to be a valid and reliable instrument for the measurement of self-esteem [ 40 ].
Statistical analysis
Data analysis was performed using SPSS software. The database contained no missing data. Reliability analysis of all scales and subscales was conducted by recording McDonald’s omega and Cronbach’s alpha values. The ARFID score was normally distributed (skewness and kurtosis values between ± 1) [ 41 ]. The Student t test was used to compare two means. Pearson’s correlation test was used to correlate two scores. The PROCESS Macro v3.4 model 1 (add-on for SPSS) [ 42 ] was used to conduct moderation models to examine the potential moderating effect of self-esteem (moderator) on the relationship between perfectionism (independent variable) and avoidant restrictive eating (dependent variable). Variables that demonstrated a p <.25 in the bivariate analysis were subsequently selected for inclusion in the moderation analysis as confounding factors. P <.05 denoted a statistically significant relationship.
Sociodemographic and other characteristics of the sample
Five hundred fifteen adults participated in this study, with a mean age of 27.55 ± 10.92 years and 60.1% females. Other descriptive statistics of the sample can be found in Table 1 . Furthermore, 17 (3.3%) had positive screen on any NIAS subscale (≥ 10 NIAS-picky eating, ≥ 9 NIAS-appetite, and ≥ 10 NIAS-fear).
Bivariate analysis of factors associated with avoidant restrictive eating
The results of the bivariate analysis of factors associated with avoidant restrictive eating are summarized in Tables 2 and 3 . The results showed that higher BMI ( r = −.12) was significantly associated with lower avoidant restrictive eating, whereas higher rigid ( r =.18), self-critical ( r =.24) and narcissistic ( r =.29) perfectionism were significantly associated with higher avoidant restrictive eating.
Moderation analysis
The results of the moderation analysis are summarized in Table 4 . Results were adjusted over body mass index. Higher perfectionism was significantly associated with higher avoidant restrictive eating in all three models. The interaction narcissistic perfectionism by self-esteem was significantly associated with ARFID scores (Beta = − 0.22; p =.006). At low (Beta = 0.77; p <.001), moderate (Beta = 0.56; p <.001) and high (Beta = 0.36; p =.001) levels of self-esteem, higher narcissistic perfectionism was significantly associated with higher ARFID scores (Table 5 ). The same results were found in the total sample, males and females separately.
The aim of this study was primarily to explore the moderating role of self-esteem in the association between perfectionism and ARFID symptoms. It was seen that high perfectionism scores were associated with more avoidant restrictive eating, consistent with the findings of other studies [ 16 , 43 ]. Through a moderation analysis of three different models, self-esteem was shown to moderate the effect of narcissistic perfectionism, but not self-critical and rigid perfectionism, on ARFID symptoms. In other words, higher levels of narcissistic perfectionism were significantly associated with higher levels of ARFID at low, moderate, and high self-esteem levels. With perfectionism often observed in individuals with ARFID symptoms manifesting as rigidity in food presentation [ 14 ], and considering narcissistic perfectionism as perfectionism directed towards others [ 17 ], we can explore the association between elevated levels of narcissistic perfectionism and ARFID. This association may stem from the notion that individuals with ARFID could demonstrate perfectionistic tendencies in how food is presented or prepared, alongside exhibiting aversive responses to the sensory attributes of food. Thus, based on the results of this study, it can be concluded that both self-esteem and perfectionism are related to ARFID, in agreement with the findings of other studies that showed a positive association between self-esteem and restrained eating [ 44 ] and between perfectionism and restrictive eating patterns [ 43 , 45 ].
Previous findings illustrated that low self-esteem [ 21 , 46 ] and high perfectionism [ 21 ] were characteristic of Anorexia Nervosa rather than ARFID in children and adolescents. This can be highlighted by the fact that people with ARFID have more long-term symptoms compared to those with Anorexia, leading the former to habituate to their symptoms over time [ 46 ]. The current study, however, demonstrated that these two variables, low self-esteem, and high perfectionism, are factors contributing to high ARFID scores in adults. The high levels of perfectionism seen in this study in individuals with ARFID can be explained by the rigidity exhibited by those who display selective eating behaviors, considering that perfectionism acts as a cognitive and behavioral risk factor contributing to the maintenance of ARFID symptoms [ 14 , 15 ]. On another hand, the low self-esteem seen in individuals displaying ARFID symptoms in this study can be attributed to the association that exists between neophobia, a common tendency seen in ARFID patients [ 13 ], and low self-esteem [ 25 ].
In this study, higher levels of rigid, self-critical, and narcissistic perfectionism were seen to be associated with higher avoidant restrictive eating. Even in the presence of high levels of self-esteem, perfectionism still correlated with high NIAS scores. However, lower perfectionism scores are commonly witnessed in ARFID patients compared to those with anorexia or bulimia nervosa [ 47 ]. Thus, it is important to imply that perfectionism differs based on the profile of the eating disorder being studied and context-dependent on the eating disorder [ 47 ]. Behavioral restrictions in eating have been related to greater levels of self-critical perfectionism. This is seen as problematic considering the physical consequences of these behavioral restrictions [ 16 ]. Additionally, self-critical perfectionism was seen to negatively relate to improvements in therapy [ 48 ]. Self-critical perfectionism has also been negatively correlated with mindfulness eating, adding proof to why someone with high self-critical perfectionism might engage in restrictive eating behaviors [ 49 ]. Both self-critical and rigid perfectionism have been associated with a greater likelihood of developing eating disorders, and a rise in mental illnesses [ 50 ]. In a different study, rigid perfectionism was found to be a risk factor for the development of eating disorders in general [ 51 ]. On another hand, narcissistic perfectionism has not been seen to be associated with eating attitudes in a different study [ 50 ]. Despite that research about the association between perfectionism and ARFID is scant, it can be deduced that the former is related to higher disordered eating generally, and restrictive eating behaviors specifically [ 16 ]. Therefore, future research should focus on mitigating the symptoms of ARFID through interventions that target both perfectionism and self-esteem, as well as studying the role of body dissatisfaction in the triadic model explored in this study between the three variables.
Furthermore, in the present study, self-esteem was found to be a moderator between perfectionism and restrictive eating behaviors. Previous studies have shown that self-esteem plays a moderating role in the relationship between body dissatisfaction (which is linked to perfectionism) and restrained eating [ 44 ]. Although body dissatisfaction is not a characteristic of ARFID [ 4 ], the moderating effect of self-esteem was witnessed between perfectionism and restrained eating in this study. Higher levels of self-esteem [ 21 , 46 ] and lower levels of perfectionism [ 21 ] were seen in patients with ARFID compared to those with Anorexia Nervosa, which can suggest that high levels of self-esteem contributes to minimizing the impact of perfectionism on the development of ARFID symptoms compared to low levels.
Limitations
The male-to-female ratio in this study was disproportionate, which might have given rise to biases in the results of the study. Another limitation is the derivation of the results from self-report scales, giving rise to the possibility of social desirability affecting the scores and influencing the outcome of the study [ 18 ]. This study consisted of a non-clinical sample of participants [ 16 ]. The snowball technique method used to recruit participants predisposes us to a selection bias; therefore, our sample does not represent the general Lebanese population. Finally, this study used the perfectionism scale that is limited to three subscales; other perfectionism dimensions also exist, such as personal standards, concern over mistakes, parental expectations, doubting of actions, and organization [ 52 ]. Future research can also explore different perfectionism dimensions other than the three used in this study which can also provide a more detailed, comprehensive understanding of their relationship with ARFID.
This study adds to the missing literature on the triadic model delineating the moderating role of self-esteem between perfectionism and ARFID. Additionally, this study brought to light some crucial clinical implications that highlight the need for interventions, which would help enhance self-esteem in patients with high perfectionism and ARFID. This study suggests that clinicians and healthcare professionals should focus more on risk factors influencing the development and maintenance of ARFID-like symptoms. Based on the results of this study, by implementing interventions that work on improving people’s self-esteem or the management of perfectionistic tendencies, symptoms of ARFID are likely to be reduced. Additionally, awareness sessions should be implemented within the Lebanese context to highlight the risk factors that contribute to ARFID and provide tips on how to manage these symptoms to enhance one’s eating habits. Therefore, it is crucial to improve the self-esteem of people exhibiting ARFID symptoms and those reporting high levels of perfectionism. An experimental approach to this study would also be beneficial by integrating a clinical ARFID sample alongside a healthy control group which can provide a deeper comprehension of the studied associations; thus, enhancing the validity of the findings in clinical settings.
Data availability
All data generated or analyzed during this study are not publicly available due the restrictions from the ethics committee, but are available upon a reasonable request from the corresponding author.
Barney A, Bruett LD, Forsberg S, Nagata JM. Avoidant Restrictive Food Intake Disorder (ARFID) and body image: a case report. J Eat Disorders. 2022;10(1):61.
Article Google Scholar
Hay P, Mitchison D, Collado AEL, González-Chica DA, Stocks N, Touyz S. Burden and health-related quality of life of eating disorders, including Avoidant/Restrictive Food Intake Disorder (ARFID), in the Australian population. J Eat Disorders. 2017;5(1):21.
Van Buuren L, Fleming CAK, Hay P, Bussey K, Trompeter N, Lonergan A, et al. The prevalence and burden of avoidant/restrictive food intake disorder (ARFID) in a general adolescent population. J Eat Disorders. 2023;11(1):104.
Zimmerman J, Fisher M. Avoidant/Restrictive food intake disorder (ARFID). Curr Probl Pediatr Adolesc Health Care. 2017;47(4):95–103.
Article PubMed Google Scholar
Zohar AH, Zamir M, Lev-Ari L, Bachner-Melman R. Too healthy for their own good: orthorexia nervosa and compulsive exercise in the community. Eat Weight Disorders. 2023;28(1):55.
Zickgraf HF, Franklin ME, Rozin P. Adult picky eaters with symptoms of avoidant/restrictive food intake disorder: comparable distress and comorbidity but different eating behaviors compared to those with disordered eating symptoms. J Eat Disorders. 2016;4(1):26.
Thomas JJ, Lawson EA, Micali N, Misra M, Deckersbach T, Eddy KT. Avoidant/Restrictive food intake disorder: a three-Dimensional Model of Neurobiology with implications for etiology and treatment. Curr Psychiatry Rep. 2017;19(8):54.
Article PubMed PubMed Central Google Scholar
Duncombe Lowe K, Barnes TL, Martell C, Keery H, Eckhardt S, Peterson CB, et al. Youth with Avoidant/Restrictive food intake disorder: examining differences by Age, Weight Status, and Symptom Duration. Nutrients. 2019;11(8):1955.
Thomas JJ, Becker KR, Kuhnle MC, Jo JH, Harshman SG, Wons OB, et al. Cognitive-behavioral therapy for avoidant/restrictive food intake disorder: feasibility, acceptability, and proof‐of‐concept for children and adolescents. Int J Eat Disord. 2020;53(10):1636–46.
Thomas JJ, Becker KR, Breithaupt L, Murray HB, Jo JH, Kuhnle MC, et al. Cognitive-behavioral therapy for adults with avoidant/restrictive food intake disorder. J Behav Cogn Therapy. 2021;31(1):47.
Family-Based Therapy for Avoidant Restrictive Food Intake Disorder. Families facing Food Neophobias. In: Loeb KL, Le Grange D, Lock J, editors. Family Therapy for Adolescent Eating and Weight disorders. Routledge; 2015, 276–96.
Nitsch A, Knopf E, Manwaring J, Mehler PS. Avoidant/Restrictive Food Intake Disorder (ARFID): its medical complications and their treatment—an emerging area. Current pediatrics reports. (Philadelphia PA). 2021;9(2):21–9.
Google Scholar
Zickgraf HF, Murray HB, Kratz HE, Franklin ME. Characteristics of outpatients diagnosed with the selective/neophobic presentation of avoidant/restrictive food intake disorder. Int J Eat Disord. 2019;52(4):367–77.
Zickgraf HF, Richard E, Zucker NL, Wallace GL. Rigidity and sensory sensitivity: independent contributions to selective eating in children, adolescents, and young adults. J Clin Child Adolesc Psychol. 2022;51(5):675–87.
Morris L, Mansell W. A systematic review of the relationship between rigidity/flexibility and transdiagnostic cognitive and behavioral processes that maintain psychopathology. J Experimental Psychopathol. 2018;9(3):204380871877943.
Solomon-Krakus S, Uliaszek AA, Sabiston CM. The differential associations between self-critical perfectionism, personal standards perfectionism, and facets of restrictive eating. Pers Indiv Differ. 2022;184:111178.
Nealis LJ, Sherry SB, Lee-Baggley DL, Stewart SH, Macneil MA. Revitalizing narcissistic perfectionism: evidence of the reliability and the validity of an emerging construct. J Psychopathol Behav Assess. 2016;38(3):493–504.
Puttevils L, Vanderhasselt M, Vervaet M. Investigating transdiagnostic factors in eating disorders: does self-esteem moderate the relationship between perfectionism and eating disorder symptoms? Eur Eat Disorders Rev. 2019;27(4):381–90.
Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: a transdiagnostic theory and treatment. Behav Res Ther. 2003;41(5):509–28.
Melisse B, Blankers M, de Beurs E, van Furth EF. Correlates of eating disorder pathology in Saudi Arabia: BMI and body dissatisfaction. J Eat Disorders. 2022;10(1):1–126.
Keery H, LeMay-Russell S, Barnes TL, Eckhardt S, Peterson CB, Lesser J, et al. Attributes of children and adolescents with avoidant/restrictive food intake disorder. J Eat Disorders. 2019;7(1):31.
Sfeir E, Haddad C, Salameh P, Sacre H, Hallit R, Akel M, et al. Binge eating, orthorexia nervosa, restrained eating, and quality of life: a population study in Lebanon. Eat Weight Disorders. 2021;26(1):145–58.
Haynos AF, Watts PD, Loth AWPD, Pearson KAPD, Neumark-Stzainer CMPD. Ph.D. Factors Predicting an escalation of restrictive eating during adolescence. J Adolesc Health. 2016;59(4):391–6.
Beekman JB, Stock ML, Howe GW. Stomaching rejection: self-compassion and self-esteem moderate the impact of daily social rejection on restrictive eating behaviours among college women. Psychol Health. 2017;32(11):1348–70.
Maiz E, Balluerka N. Trait anxiety and self-concept among children and adolescents with food neophobia. Food Res Int. 2018;105:1054–9.
Shariff ZM, Yasin ZM. Correlates of children’s eating attitude test scores among primary School Children. Percept Mot Skills. 2005;100(2):463–72.
Nicholas JK, Tilburg MAL, Pilato I, Erwin S, Rivera-Cancel AM, Ives L, et al. The diagnosis of avoidant restrictive food intake disorder in the presence of gastrointestinal disorders: opportunities to define shared mechanisms of symptom expression. Int J Eat Disord. 2021;54(6):995–1008.
Teneva N, Lemay EP. Projecting loneliness into the past and future: implications for self-esteem and affect. Motiv Emot. 2020;44(5):772–84.
Fekih-Romdhane F, Hallit R, Malaeb D, Sakr F, Dabbous M, Sawma T, et al. Psychometric properties of an arabic translation of the Nine Item Avoidant/Restrictive Food Intake Disorder Screen (NIAS) in a community sample of adults. J Eat Disorders. 2023;11(1):1–10.
Melisse B, de Beurs E, van Furth EF. Eating disorders in the arab world: a literature review. J Eat Disorders. 2020;8(1):1–59.
Melki IS, Beydoun HA, Khogali M, Tamim H, Yunis KA, National Collaborative Perinatal Neonatal Network. Household crowding index: a correlate of socioeconomic status and inter-pregnancy spacing in an urban setting. J Epidemiol Community Health (1979). 2004;58(6):476–80.
A healthy lifestyle - WHO recommendations. 2010; https://www.who.int/europe/news-room/fact-sheets/item/a-healthy-lifestyle---who-recommendations .
Kimberly Anne Weary-Smith. Validation of the Physical Activity Index (PAI) as a measure of total activity load and total kilocalorie expenditure during submaximal treadmill walkingProQuest Dissertations Publishing; 2007.
Fekih-Romdhane F, Rogoza R, Hallit R, Malaeb D, Sakr F, Dabbous M, et al. Psychometric properties of an arabic translation of the Big Three Perfectionism Scale–Short Form (BTPS-SF) in a community sample of adults. BMC Psychiatry. 2023;23(1):932.
Feher A, Smith MM, Saklofske DH, Plouffe RA, Wilson CA, Sherry SB. The Big Three Perfectionism Scale–Short Form (BTPS-SF): development of a brief self-report measure of Multidimensional Perfectionism. J Psychoeducational Assess. 2020;38(1):37–52.
Smith MM, Saklofske DH, Stoeber J, Sherry SB. The Big Three Perfectionism Scale: a New measure of perfectionism. J Psychoeducational Assess. 2016;34(7):670–87.
Dunkley DM, Zuroff DC, Blankstein KR. Self-critical perfectionism and daily affect: dispositional and situational influences on stress and coping. J Pers Soc Psychol. 2003;84(1):234–52.
Zickgraf HF, Ellis JM. Initial validation of the Nine Item Avoidant/Restrictive Food Intake disorder screen (NIAS): a measure of three restrictive eating patterns. Appetite. 2018;123:32–42.
Burton Murray H, Dreier MJ, Zickgraf HF, Becker KR, Breithaupt L, Eddy KT, et al. Validation of the nine item ARFID screen (NIAS) subscales for distinguishing ARFID presentations and screening for ARFID. Int J Eat Disord. 2021;54(10):1782–92.
Fekih-Romdhane F, Bitar Z, Rogoza R, Sarray El Dine A, Malaeb D, Rashid T, et al. Validity and reliability of the arabic version of the self-report single-item self-esteem scale (A-SISE). BMC Psychiatry. 2023;23(1):351.
Hair J Jr, Hair JF Jr, Hult GTM, Ringle CM, Sarstedt M. A primer on partial least squares structural equation modeling (PLS-SEM). Sage; 2021.
Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. Guilford; 2017.
Sanchez-Ruiz MJ, El-Jor C, Abi Kharma J, Bassil M, Zeeni N. Personality, emotion-related variables, and media pressure predict eating disorders via disordered eating in Lebanese university students. Eat Weight Disorders. 2019;24(2):313–22.
Kong F, Zhang Y, You Z, Fan C, Tian Y, Zhou Z. Body dissatisfaction and restrained eating: Mediating effects of Self-Esteem. Social Behav Personality. 2013;41(7):1165–70.
Schwarz HC, Gairrett RL, Aruguete MS, Gold ES. Eating attitudes, body dissatisfaction, and perfectionism in female college athletes. North Am J Psychol. 2005;7(3):345.
Lieberman M, Houser ME, Voyer A, Grady S, Katzman DK. Children with avoidant/restrictive food intake disorder and anorexia nervosa in a tertiary care pediatric eating disorder program: a comparative study. Int J Eat Disord. 2019;52(3):239–45.
Vacca M, Ballesio A, Lombardo C. The relationship between perfectionism and eating-related symptoms in adolescents: a systematic review. Eur Eat Disorders Rev. 2021;29(1):32–51.
van der Kaap-Deeder J, Smets J, Boone L. The impeding role of self-critical perfectionism on Therapeutic Alliance during Treatment and eating disorder symptoms at Follow-up in patients with an eating disorder. Psychol Belg. 2016;56(2):101–10.
Miley M, Egan H, Wallis D, Mantzios M. Orthorexia nervosa, mindful eating, and perfectionism: an exploratory investigation. Eat Weight Disorders. 2022;27(7):2869–78.
Merhy G, Moubarak V, Hallit R, Obeid S, Hallit S. The indirect role of orthorexia nervosa and eating attitudes in the association between perfectionism and muscle dysmorphic disorder in Lebanese male University students - results of a pilot study. BMC Psychiatry. 2023;23(1):55.
Woropay-Hordziejewicz NA, Buźniak A, Lawendowski R, Atroszko PA. Compulsive study behaviors are Associated with Eating disorders and have independent negative effects on Well-Being: a structural equation Model Study among young musicians. Sustain (Basel Switzerland). 2022;14(14):8617.
Frost RO, Marten P, Lahart C, Rosenblate R. The dimensions of perfectionism. Cogn Therapy Res. 1990;14:449–68.
Download references
Acknowledgements
The authors would like to thank all participants.
Author information
Feten Fekih-Romdhane, Souheil Hallit and Sahar Obeid are last coauthors.
Authors and Affiliations
School of Arts and Sciences, Social and Education Sciences Department, Lebanese American University, Jbeil, Lebanon
Roni Chaaya & Sahar Obeid
School of Medicine and Medical Sciences, Holy Spirit University of Kaslik, Jounieh, P.O. Box 446, Lebanon
Rabih Hallit & Souheil Hallit
Department of Infectious Disease, Bellevue Medical Center, Mansourieh, Lebanon
Rabih Hallit
Department of Infectious Disease, Notre Dame des Secours University Hospital, Postal code 3, Byblos, Lebanon
College of Pharmacy, Gulf Medical University, Ajman, United Arab Emirates
Diana Malaeb
School of Pharmacy, Lebanese International University, Beirut, Lebanon
Fouad Sakr & Mariam Dabbous
Department of Biomedical Sciences, School of Arts and Sciences, Lebanese International University, Bekaa, Lebanon
Sami El Khatib
Center for Applied Mathematics and Bioinformatics (CAMB), Gulf University for Science and Technology (GUST), Hawally, Kuwait
The Tunisian Center of Early Intervention in Psychosis, Department of Psychiatry “Ibn Omrane”, Razi hospital, 2010, Manouba, Tunisia
Feten Fekih-Romdhane
Faculty of Medicine of Tunis, Tunis El Manar University, Tunis, Tunisia
Applied Science Research Center, Applied Science Private University, Amman, Jordan
Souheil Hallit
You can also search for this author in PubMed Google Scholar
Contributions
FFR, SO and SH designed the study; RC drafted the manuscript; SH carried out the analysis and interpreted the results; FS, MD and DM collected the data. RH reviewed the paper for intellectual content; all authors reviewed the final manuscript and gave their consent.
Corresponding authors
Correspondence to Souheil Hallit or Sahar Obeid .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval for this study was obtained from the ethics committee of the School of Pharmacy at the Lebanese International University (2023RC-014-LIUSOP). Written informed consent was obtained from all subjects; the online submission of the soft copy was considered equivalent to receiving a written informed consent. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Chaaya, R., Hallit, R., Malaeb, D. et al. Moderating effect of self-esteem between perfectionism and avoidant restrictive food intake disorder among Lebanese adults. BMC Psychiatry 24 , 325 (2024). https://doi.org/10.1186/s12888-024-05762-8
Download citation
Received : 18 September 2023
Accepted : 12 April 2024
Published : 26 April 2024
DOI : https://doi.org/10.1186/s12888-024-05762-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Restrictive eating
- Restrained eating
- Self-esteem
- Perfectionism
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Research Note
- Open access
- Published: 25 April 2024
Evaluating Night-Eating Syndrome in bariatric surgery patients: A cross-sectional study
- Sarah Almuammar 1 ,
- Elham Aljaaly 2 ,
- Lama Alqarni 3 ,
- Hadeel Alazwari 3 ,
- Ruba Alsubhi 3 &
- Nouf Alatawi 3
BMC Research Notes volume 17 , Article number: 118 ( 2024 ) Cite this article
99 Accesses
Metrics details
Night-Eating Syndrome (NES) is a complex eating disorder that has gained recognition in the context of bariatric surgery. However, its prevalence and associated factors in this specific patient population remain understudied, particularly in the Saudi Arabian context.
This cross-sectional study was conducted at King Abdulaziz University Hospital in Jeddah, Saudi Arabia, from June to November 2022. Adult patients who had undergone bariatric surgery with a postoperative follow-up of 6 months were included. NES was assessed using the Night Eating Questionnaire (NEQ).
A total of 154 patients were enrolled in the study, with a mean age of 38.8 ± 11.4 years. The mean BMI before surgery was 44.8 ± 8.2 kg/m 2 , which reduced to 28.9 ± 5.8 kg/m 2 post-surgery. Of these, 52 patients (33.8%) met the criteria for NES based on NEQ scores. The prevalence of NES was significantly higher among female patients, with 35 out of 83 females (42.2%) compared to 17 out of 71 males (23.9%) experiencing NES. While NES was not significantly associated with age, nationality, diet adherence, BMI, or surgery type, chronic diseases—particularly diabetes—emerged as significant risk factors for NES in post-bariatric surgery patients.
NES is a prevalent concern among post-bariatric surgery patients, with distinct associations with gender and chronic diseases, particularly diabetes. This study provides valuable insights into NES prevalence and its risk factors in the Saudi Arabian context, highlighting the importance of addressing eating disorders within the framework of bariatric surgery care.
Peer Review reports
The prevalence of bariatric surgery has seen a steady increase impacting the lives of over 14.6 million individuals [ 1 ]. For patients with class II and III obesity, bariatric surgery represents a transformative journey, leading to significant weight loss and substantial improvements in physical health [ 2 ]. Notable one-year post-surgery outcomes include reduced waist circumference, lower glucose and insulin levels, decreased free fatty acids and triglycerides, and a modest increase in high-density lipoprotein levels [ 3 ]. However, this path to weight reduction often intersects with the challenges posed by eating disorders.
A formal diagnosis of eating disorders has been linked to post-bariatric surgery patients, some resorting to spontaneous or forced vomiting as a means of weight control [ 4 ]. Cravings, more prevalent in this group than in healthy-weight controls, add another layer of complexity [ 5 ]. Furthermore, night-eating disorders have surfaced as a noteworthy concern post-surgery, with patients describing symptoms persisting for up to eight years following the procedure [ 6 ]. The foundational work of Stunkard et al. [ 7 ] introduced the concept of Night-Eating Syndrome (NES), characterized by minimal breakfast intake, consumption of over 25% of daily calories after dinner, and disrupted sleep patterns. Mood disorders, poor sleep quality, metabolic syndromes, obesity, and eating disorders are among the factors associated with NES [ 8 ]. To diagnose NES, specific criteria must be met, including the consumption of at least 25% of daily intake after dinner and nighttime awakenings occurring at least twice a week for a minimum of three months [ 9 ]. NES has been found to affect 1.5% of the general population in the United States and 1.5% of adult Omani residents [ 10 , 11 ].
Recent studies highlight the challenge of NES in post-bariatric patients, with an observed increase in NES behaviors two to three years post-surgery [ 12 , 13 , 14 , 15 ]. A retrospective analysis in Bahrain linked eating disorder behaviors with diminished postoperative weight outcomes, emphasizing the importance of addressing these behaviors [ 16 ]. Variability in NES prevalence has been documented, ranging from 1.9 to 8.9% depending on the diagnostic criteria, which underscores the complexity of diagnosing and managing NES [ 17 ]. While these studies underscore the importance of understanding nighttime eating habits and their impact on the outcomes of weight-loss therapy, only a limited number of investigations have been conducted in Saudi Arabia, examining the relationship between NES and postoperative prognosis.
The present study aims to bridge this knowledge gap by investigating the prevalence and risk factors associated with NES in patients who underwent bariatric surgery at King Abdulaziz University Hospital in Saudi Arabia.
Study design
This cross-sectional study employed a self-administered, web-based survey through Google Forms. The study was conducted in collaboration with the Family Medicine Department and the Obesity Clinic at the Medical Nutrition Unit of King Abdulaziz University Hospital in Jeddah, Saudi Arabia, from June to November 2022.
Study participants
The study included adult men and women who had undergone bariatric surgery, were 18 years of age or older, and had a postoperative follow-up period of 1 year. Pregnant women in the postoperative phase were excluded from the study.
Study instrument
The survey encompassed thorough inquiries into the following areas:
Demographics and clinical history : Participants were requested to provide details regarding their age, gender, and nationality. Furthermore, they were asked about any chronic medical conditions, including hypertension, dyslipidemia, and diabetes mellitus type 2.
Anthropometric measurements : Respondents were required to report their height in centimeters (cm) and their weight in kilograms (kg), both before the bariatric procedure and one-year post-procedure.
Type of bariatric procedure : Information was collected on the specific bariatric surgery procedure undergone by the participants.
Night Eating Questionnaire (NEQ) : The NEQ was employed as a primary diagnostic tool to identify the presence and severity of Night Eating Syndrome (NES) among participants. This questionnaire is a validated self-report instrument designed to capture the distinctive behaviors and patterns associated with NES. It comprises multiple items that ask respondents about their eating habits, specifically focusing on the timing and quantity of food consumption. Key aspects evaluated by the NEQ include the proportion of daily caloric intake consumed after the evening meal, incidents of nocturnal eating (defined as waking during the night to eat), mood fluctuations related to eating times, and sleep disturbances influenced by eating patterns. A critical threshold, a global NEQ score of 25 or higher, was adopted based on established diagnostic criteria to identify individuals likely to have NES.
Statistical analyses
Data analysis was performed using SPSS software, version 20 (IBM, Armonk, New York, USA). Descriptive statistics were applied to summarize mean, standard deviation, and to provide frequency counts and percentages for categorical variables. The chi-squared test was utilized for examining associations among categorical variables, and the Mann–Whitney U test for analyzing continuous data. Spearman’s test was used for correlation analysis. Multivariate logistic regression analysis was carried out to identify factors independently associated with NES among participants. This analysis incorporated variables selected for their potential relevance to NES, with odds ratios calculated at a 95% confidence interval. A P value of less than 0.05 was considered statistically significant for all tests.
Ethical considerations
This study received approval from the Research Ethics Committee of the Unit of Biomedical Ethics at the Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia (Approval Number: 322 − 22). Prior to participation, all individuals gave their written informed consent, adhering to the ethical guidelines and ensuring the confidentiality and anonymity of their responses.
Participant characteristics
In our assessment of 371 individuals, 154 patients were identified as meeting the study’s inclusion criteria. The demographic breakdown revealed 83 patients (53.9%) were female, and 130 patients (84.4%) were of Saudi nationality. The mean age of participants was 38.8 ± 11.4 years. Prior to undergoing bariatric procedures, the average weight of these individuals was 125.1 ± 29.0 kg, which significantly decreased to 80.5 ± 18.1 kg following the procedures. Correspondingly, the mean Body Mass Index (BMI) was reduced from 44.8 ± 8.2 kg/m² to 28.9 ± 5.8 kg/m². Sleeve gastrectomy was the predominant bariatric procedure, conducted on 131 patients (85.1%). Chronic diseases were reported by 109 patients (70.8%), with hypertension being the most commonly reported condition by 44 patients (28.8%). Furthermore, 41 patients (26.6%) reported adherence to a post-procedure diet (Table 1 ).
Factors associated with night-eating syndrome
Of the participants, 52 (33.8%) scored 25 or higher on the NEQ, indicating the presence of NES. Analysis showed non-significant negative correlations between NEQ scores and age, sex, as well as pre- and post-procedure weights and BMIs (Table 2 ). Notably, the prevalence of NES was significantly higher among female patients, with 35 females (42.2%) affected, compared to males, where 41 (57.8%) were found to have NES ( P = 0.017). Among chronic conditions, diabetes was significantly associated with NES ( P = 0.025), unlike other conditions examined in this study (Table 3 ).
Multivariable regression analysis model
The logistic regression analysis identified significant determinants of NES (Table 4 ). Being female was associated with an elevated risk of NES (OR: 2.33; 95% CI: 1.05–5.19; P = 0.030), and the presence of chronic diseases significantly increased the risk of NES (OR: 32.95; 95% CI: 2.33–464.44; P = 0.010). Specifically, diabetes mellitus was associated with a higher prevalence of NES (OR: 2.63; 95% CI: 1.23–5.88; P = 0.013).
This study aimed to evaluate the prevalence of NES in patients who had undergone bariatric surgery at King Abdulaziz University Hospital. Our findings shed light on the prevalence rates and associated factors of NES in this specific patient population and contribute to the growing body of knowledge on eating disorders post-bariatric surgery.
According to the NEQ, our study identified that 33.8% of patients in our sample met the criteria for NES. This prevalence rate aligns with previous research findings in the field. For instance, a study conducted in the United States found that 25% of overweight and obese patients exhibited NES symptoms after bariatric surgery [ 15 ]. However, variations in NES prevalence across studies may be attributed to differences in sample sizes and diagnostic criteria used for NES assessment.
Our study further delved into the demographic characteristics of patients with NES. The mean age of patients with NES in our study was 38.8 years, which is in line with similar studies that have reported relatively young ages among NES-affected individuals [ 18 , 19 ]. This finding aligns with epidemiologic data indicating that NES tends to be less frequent among individuals over 65 years of age [ 11 ].
An intriguing finding in our study was the significantly higher prevalence of NES among female patients compared to male patients. This observation echoes the outcomes of previous investigations [ 15 , 20 ] and reflects the well-established fact that women are more prone to developing eating disorders [ 21 ].
A notable finding in our study was the association between NES and chronic illnesses, particularly diabetes. A previous study conducted in the United States on patients with obesity and type 2 diabetes also identified NES as the most prevalent eating disorder in this population [ 22 ]. This reinforces the relationship between NES and metabolic conditions, as well as the impact of NES on dietary adherence and mood [ 23 ]. Furthermore, our study revealed that the majority of patients with NES underwent sleeve gastrectomy (90.3%). However, we found no significant relationship between NES prevalence and the type of bariatric procedure.
While our study explored various factors, including age, nationality, diet adherence, BMI, and type of bariatric procedure, we did not find any significant associations between these factors and the presence of NES. These results corroborate the findings of previous studies [ 24 , 25 ]. Our study suggests that NES prevalence among post-bariatric surgery patients may not be strongly influenced by these demographic or clinical factors.
While our study offers valuable insights, it is essential to acknowledge its limitations. As a cross-sectional study, it is susceptible to recall bias. Moreover, the reliance on self-reported data through a questionnaire may introduce inaccuracies. To address these limitations, future research in this area should consider longitudinal designs and incorporate clinical assessments to provide a more comprehensive understanding of NES in post-bariatric surgery patients.
In conclusion, our study contributes to the understanding of NES prevalence and risk factors among patients who have undergone bariatric surgery. The complex relationship between NES, demographic factors, and clinical variables necessitates further research to elucidate its underlying mechanisms and develop targeted interventions. Recognizing NES as part of postoperative care is essential for optimizing long-term outcomes and quality of life for this patient population. Moreover, our findings underscore the importance of continued research in the evolving field of bariatric surgery outcomes and eating disorders.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Welbourn R, Hollyman M, Kinsman R, et al. Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the fourth ifso global registry report 2018. Obes Surg. 2019;29:782–95. https://doi.org/10.1007/s11695-018-3593-1 .
Article PubMed Google Scholar
Cohn I, Raman J, Sui Z. Patient motivations and expectations prior to bariatric surgery: a qualitative systematic review. Obes Rev. 2019;20:1608–18. https://doi.org/10.1111/obr.12919 .
Fraszczyk E, Luijten M, Spijkerman AMW, et al. The effects of bariatric surgery on clinical profile, DNA methylation, and ageing in severely obese patients. Clin Epigenetics. 2020;12:14. https://doi.org/10.1186/s13148-019-0790-2 .
Article CAS PubMed PubMed Central Google Scholar
Conceicao EM, Utzinger LM, Pisetsky EM. Eating disorders and problematic eating behaviours before and after bariatric surgery: characterization, assessment and association with treatment outcomes. Eur Eat Disord Rev. 2015;23:417–25. https://doi.org/10.1002/erv.2397 .
Article PubMed PubMed Central Google Scholar
Crowley NM, LePage ML, Goldman RL, O’Neil PM, Borckardt JJ, Byrne TK. The food craving questionnaire-trait in a bariatric surgery seeking population and ability to predict post-surgery weight loss at six months. Eat Behav. 2012;13:366–70. https://doi.org/10.1016/j.eatbeh.2012.07.003 .
Taba JV, Suzuki MO, Nascimento FSD, et al. The development of feeding and eating disorders after bariatric surgery: a systematic review and meta-analysis. Nutrients. 2021;13. https://doi.org/10.3390/nu13072396 .
Stunkard AJ, Grace WJ, Wolff HG. The night-eating syndrome; a pattern of food intake among certain obese patients. Am J Med. 1955;19:78–86. https://doi.org/10.1016/0002-9343(55)90276-x .
Article CAS PubMed Google Scholar
Shoar S, Naderan M, Mahmoodzadeh H, Shoar N, Lotfi D. Night eating syndrome: a psychiatric disease, a sleep disorder, a delayed circadian eating rhythm, and/or a metabolic condition? Expert Rev Endocrinol Metab. 2019;14:351–58. https://doi.org/10.1080/17446651.2019.1657006 .
Allison KC, Lundgren JD, O’Reardon JP, et al. Proposed diagnostic criteria for night eating syndrome. Int J Eat Disord. 2010;43:241–7. https://doi.org/10.1002/eat.20693 .
Tozzi F, Thornton LM, Klump KL, et al. Symptom fluctuation in eating disorders: correlates of diagnostic crossover. Am J Psychiatry. 2005;162:732–40. https://doi.org/10.1176/appi.ajp.162.4.732 .
Rand CS, Macgregor AM, Stunkard AJ. The night eating syndrome in the general population and among postoperative obesity surgery patients. Int J Eat Disord. 1997;22:65–9.
Nasirzadeh Y, Kantarovich K, Wnuk S, et al. Binge eating, loss of control over eating, emotional eating, and night eating after bariatric surgery: results from the toronto bari-psych cohort study. Obes Surg. 2018;28:2032–39. https://doi.org/10.1007/s11695-018-3137-8 .
Unal S, Sevincer GM, Maner AF. [prediction of weight regain after bariatric surgery by night eating, emotional eating, eating concerns, depression and demographic characteristics]. Turk Psikiyatri Derg. 2019;30:31–41.
PubMed Google Scholar
Ivezaj V, Lawson JL, Lydecker JA, Duffy AJ, Grilo CM. Examination of night eating and loss-of-control eating following bariatric surgery. Eat Weight Disord. 2022;27:207–13. https://doi.org/10.1007/s40519-021-01156-x .
Brancati GE, Barbuti M, Calderone A, et al. Prevalence and psychiatric comorbidities of night-eating behavior in obese bariatric patients: preliminary evidence for a connection between night-eating and bipolar spectrum disorders. Eat Weight Disord. 2022;27:1695–704. https://doi.org/10.1007/s40519-021-01306-1 .
Al Khalifa K, Al Ansari A. Quality of life, food tolerance, and eating disorder behavior after laparoscopic gastric banding and sleeve gastrectomy - results from a middle eastern center of excellence. BMC Obes. 2018;5:44. https://doi.org/10.1186/s40608-018-0220-6 .
Allison KC, Wadden TA, Sarwer DB, et al. Night eating syndrome and binge eating disorder among persons seeking bariatric surgery: prevalence and related features. Obes (Silver Spring). 2006;14(Suppl 2):S77–82. https://doi.org/10.1038/oby.2006.286 .
Article Google Scholar
Nolan LJ, Geliebter A. Food addiction is associated with night eating severity. Appetite. 2016;98:89–94. https://doi.org/10.1016/j.appet.2015.12.025 .
Vinai P, Ferri R, Anelli M, et al. New data on psychological traits and sleep profiles of patients affected by nocturnal eating. Sleep Med. 2015;16:746–53. https://doi.org/10.1016/j.sleep.2014.12.020 .
Petroni ML, Barbanti FA, Bonadonna R, et al. Dysfunctional eating in type 2 diabetes mellitus: a multicenter Italian study of socio-demographic and clinical associations. Nutr Metab Cardiovasc Dis. 2019;29:983–90. https://doi.org/10.1016/j.numecd.2019.06.006 .
Qian J, Wu Y, Liu F, et al. An update on the prevalence of eating disorders in the general population: a systematic review and meta-analysis. Eat Weight Disord. 2022;27:415–28. https://doi.org/10.1007/s40519-021-01162-z .
Gonzalez JS, Hood KK, Esbitt SA, Mukherji S, Kane NS, Jacobson A. Psychiatric and psychosocial issues among individuals living with diabetes. Diabetes in America 3rd edition. 2018.
Allison KC, Crow SJ, Reeves RR, et al. Binge eating disorder and night eating syndrome in adults with type 2 diabetes. Obes (Silver Spring). 2007;15:1287–93. https://doi.org/10.1038/oby.2007.150 .
Silen Y, Keski-Rahkonen A. Worldwide prevalence of dsm-5 eating disorders among young people. Curr Opin Psychiatry. 2022;35:362–71. https://doi.org/10.1097/YCO.0000000000000818 .
Ozsoy Z, Demir E. Which bariatric procedure is the most popular in the world? A bibliometric comparison. Obes Surg. 2018;28:2339–52. https://doi.org/10.1007/s11695-018-3163-6 .
Download references
Acknowledgements
Not applicable.
This research received no specific funding from any external source. All authors contributed their time and resources voluntarily.
Author information
Authors and affiliations.
Family Medicine Department, Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia
Sarah Almuammar
Clinical Nutrition Department, Faculty of Applied Medical Sciences, King Abdulaziz University, Jeddah, Saudi Arabia
Elham Aljaaly
Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia
Lama Alqarni, Hadeel Alazwari, Ruba Alsubhi & Nouf Alatawi
You can also search for this author in PubMed Google Scholar
Contributions
Sarah AlMuammar provided overall supervision and guidance. Elham Aljaaly conducted data analysis and contributed to the study design. Lama Alqarniwrote the manuscript and conducted data collection. Hadeel Alazwari contributed to manuscript writing and data analysis. Ruba Alsubhi conducted the literature review. Nouf Alatawi assisted with the literature review and data validation. All authors reviewed and approved the final manuscript.
Corresponding author
Correspondence to Sarah Almuammar .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Institutional Review Board of King Abdulaziz University. The participants provided electronic informed consent prior to participating in the study. Participants were informed that their participation in the study was voluntary and that they could withdraw at any time. Confidentiality and anonymity of the participants were ensured throughout the study.
Consent for publication
Competing interests.
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Almuammar, S., Aljaaly, E., Alqarni, L. et al. Evaluating Night-Eating Syndrome in bariatric surgery patients: A cross-sectional study. BMC Res Notes 17 , 118 (2024). https://doi.org/10.1186/s13104-024-06774-z
Download citation
Received : 07 November 2023
Accepted : 15 April 2024
Published : 25 April 2024
DOI : https://doi.org/10.1186/s13104-024-06774-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Night-eating syndrome
- Bariatric surgery
- Eating disorders
- Public health
BMC Research Notes
ISSN: 1756-0500
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Why Aren't Our Girls and Women Eating?
There are some unique reasons why females diet..
Posted April 27, 2024 | Reviewed by Pam Dailey
- Anorexic women often experience shame and seek to numb this feeling.
- They attempt to numb the shame with perfectionism.
- The vicious cycle of shame and perfectionism should be addressed in therapy.
What is going on with our girls, teens, and women? Why are eating and weight such hot topics? Why do so many females feel that dieting and losing weight are such major accomplishments? I am referring to females of all ages who engage in the relentless pursuit of thinness and take pride in dietary restraint. Being a healthy weight is certainly important, but focusing on dieting and restraining food intake does in many cases lead to eating disorders like anorexia nervosa which are extremely resistant to treatment. In addition, they are associated with depression , isolation, and health problems.
The thinking among professionals who are treating females with eating disorders seems to be concentrated on the treatment of depression and anxiety while also working on cognitive restructuring, particularly around such negative thoughts as, "I will be seen as a glutton if I gain a pound." Therapists also tend to work in conjunction with nutritionists who aim to normalize healthy eating habits to restore body weight. Additionally, the therapy often includes a physician who monitors physical health.
More recent research particularly that of Howard et al. (2023) has had a very interesting and unique focus. I found this research particularly refreshing because it adds an additional lens from which to view anorexia nervosa and dietary restraint in general. I think this perspective has been largely overlooked in the treatment of females with eating and body image issues. Howard et al. (2023) interviewed 11 females over the age of 18 who were receiving outpatient treatment for anorexia nervosa in a community eating-disorders service. They were assessed with the Eating Disorder Examination Questionnaire, a demographics questionnaire, and a face-to-face interview.
The focus of the study was on the relationship between anorexia and the self-conscious emotions of shame and perfectionism . The findings indicated that anorexia was clearly driven in part by the vicious cycle of shame and perfectionism. The relationship was as follows: Anorexics tend to deal with their feelings of shame by striving for perfectionism. It is not entirely clear why these women were so full of shame, although those who had a history of trauma reported experiencing shame prior to perfectionism. The women who did not report a history of trauma were either unsure of which feeling came first or sometimes reported that perfectionism preceded shame. Regardless of the directionality of these two self-conscious emotions, they coexisted to form a vicious cycle for these women. Many reported trying to minimize feelings of shame by setting high standards for themselves. In this group, perfectionism was centered around the body and dietary restraint. They were striving for the perfect body by controlling their eating. And recovery was particularly difficult for several reasons, including the need to be perfect at recovery.
While the findings may have implications for the successful treatment of anorexics, there are several limitations of this study. The sample size was small. We also do not know if the same degree of shame and perfectionism would be found in younger and older females who are not in treatment or who are at different stages of their eating disorder. The most important question is whether or not the shame-perfectionism cycle precedes the development of body image and eating issues or if this cycle is preceded by the development of full-blown anorexia nervosa. We could learn the answers to these questions by replicating this study with both a large control group and a large number of females of all ages pretreatment, during treatment, and during recovery. In the meantime, issues of shame and perfectionism should be addressed with females who present with body image issues and eating/dieting issues.
Howard,T.L.M.,Williams.M.O.Woodward.,D.&Fox, J.R.E. (2023)The relationship between shame, perfectionism, and Anorexia Nervosa:A grounded theory study. Psychology and Psychotherapy:Theory, Research, and Practice, 96,40-55.

Barbara Greenberg, Ph.D., is a clinical psychologist who specializes in the treatment of adolescents and their well-intentioned but exhausted parents.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Eat Disord

Risk factors for eating disorders: findings from a rapid review
Sarah barakat.
1 InsideOut Institute for Eating Disorders, University of Sydney, Sydney Local Health District, Sydney, Australia
4 Faculty of Medicine and Health, Charles Perkins Centre (D17), InsideOut Institute, University of Sydney, Level 2, Sydney, NSW 2006 Australia
Siân A. McLean
2 School of Psychology and Public Health, La Trobe University, Melbourne, Australia
Emma Bryant
3 Healthcare Management Advisors, Melbourne, Australia
Stephen Touyz
Sarah maguire, associated data.
Not applicable—all citations provided.
Risk factors represent a range of complex variables associated with the onset, development, and course of eating disorders. Understanding these risk factors is vital for the refinement of aetiological models, which may inform the development of targeted, evidence-based prevention, early intervention, and treatment programs. This Rapid Review aimed to identify and summarise research studies conducted within the last 12 years, focusing on risk factors associated with eating disorders.
The current review forms part of a series of Rapid Reviews to be published in a special issue in the Journal of Eating Disorders, funded by the Australian Government to inform the development of the National Eating Disorder Research and Translation Strategy 2021–2031. Three databases were searched for studies published between 2009 and 2021, published in English, and comprising high-level evidence studies (meta-analyses, systematic reviews, moderately sized randomised controlled studies, moderately sized controlled-cohort studies, or population studies). Data pertaining to risk factors for eating disorders were synthesised and outlined in the current paper.
A total of 284 studies were included. The findings were divided into nine main categories: (1) genetics, (2) gastrointestinal microbiota and autoimmune reactions, (3) childhood and early adolescent exposures, (4) personality traits and comorbid mental health conditions, (5) gender, (6) socio-economic status, (7) ethnic minority, (8) body image and social influence, and (9) elite sports. A substantial amount of research exists supporting the role of inherited genetic risk in the development of eating disorders, with biological risk factors, such as the role of gut microbiota in dysregulation of appetite, an area of emerging evidence. Abuse, trauma and childhood obesity are strongly linked to eating disorders, however less conclusive evidence exists regarding developmental factors such as role of in-utero exposure to hormones. Comorbidities between eating disorders and mental health disorders, including personality and mood disorders, have been found to increase the severity of eating disorder symptomatology. Higher education attainment, body image-related factors, and use of appearance-focused social media are also associated with increased risk of eating disorder symptoms.
Eating disorders are associated with multiple risk factors. An extensive amount of research has been conducted in the field; however, further studies are required to assess the causal nature of the risk factors identified in the current review. This will assist in understanding the sequelae of eating disorder development and in turn allow for enhancement of existing interventions and ultimately improved outcomes for individuals.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40337-022-00717-4.
Plain English summary
Research into the risk factors associated with eating disorders (EDs) is necessary in order to better understand the reasons why people develop EDs and to inform programs which aim to reduce these risk factors. In the current study we reviewed studies published between 2009 and 2021 which had researched risk factors associated with EDs. This study is one review of a wider Rapid Review series conducted as part the development of Australia’s National Eating Disorders Research and Translation Strategy 2021–2031. The findings from this review are grouped into nine main risk factor categories. These include (1) genetics, (2) gastrointestinal microbiota and autoimmune reactions, (3) childhood and early adolescent exposures, (4) personality traits and comorbid mental health conditions, (5) gender, (6) socio-economic status, (7) ethnic minority, (8) body image and social influence, and (9) elite sports. Further research is needed to better understand the relationship between the risk factors, in particular the ways in which they may interact with each other and whether they cause the ED or are just associated with the ED.
Introduction
Eating disorders (ED) are complex psychiatric conditions associated with significant psychological and physical impairment. Individuals with EDs are at greater risk of suicide attempts, mortality, and poorer quality of life relative to both the general population and individuals with other psychiatric conditions [ 1 – 3 ]. Central to addressing the pervasive nature of EDs is understanding the circumstances which make individuals more vulnerable to developing these psychiatric conditions. The development of an ED is dependent on a myriad of variables ranging from sociocultural, to biological and genetic, and psychological factors. Despite the variation and complexity present in the aetiology of EDs, efforts have been made by researchers to identify risk factors which commonly predict onset [ 4 – 6 ]. Understanding the range of risk factors and their potential contribution to onset of an ED is crucial to identifying at risk groups and providing effective screening and prevention programs, as well as targeted interventions [ 7 , 8 ].
EDs can be severe and are often chronic in nature, particularly if not addressed in a timely manner. A recent study of ED patients identified an average delay of 5.28 years between ED symptom onset and treatment-seeking [ 9 ]. A factor considered to contribute to this delay is health professionals’ lack of awareness of indicators of disordered eating behaviours, meaning EDs often go unrecognised by treating clinicians [ 10 ]. Identification of risk factors for EDs offers an opportunity for targeted education of health professionals to assist in distinguishing patterns of psychosocial, biological, and genetic vulnerabilities for disordered eating even in the absence of any overt weight or dietary concerns [ 11 ].
Knowledge of the risk factors for EDs offers the opportunity for early identification of high-risk groups and in turn a timely and tailored response via avenues such as public policy development or initiation of targeted prevention programs [ 12 ]. Prevention and early intervention programs based upon aetiological models may help to prevent movement along the spectrum from at-risk to full threshold disorder [ 13 ]. Additionally, EDs are complex psychiatric conditions with a somewhat limited range of efficacious evidence-based interventions [ 14 , 15 ]. In addition, a significant number of patients with EDs do not respond to current evidence-based treatments [ 16 – 20 ]. As such, attempts to better understand the role of risk factors in aetiological and causal pathways of EDs are necessary in order to form more nuanced conceptualisations of these illnesses. This may inform the development of more effective treatments, especially for those with persistent and chronic course [ 21 ].
The current Rapid Review paper forms part of a series of reviews commissioned by the Australian Federal Government to inform the Australian National Eating Disorders Research and Translation Strategy 2021–2031[ 22 ]. This paper aims to identify and explore the risk factors associated with EDs by summarising the existing evidence related to aetiological underpinnings. Importantly, the review is inclusive of research which considers risk factors to be either causal in nature or associated with the onset of ED.
The Australian Government Commonwealth Department of Health funded the InsideOut Institute for Eating Disorders (IOI) to develop the Australian Eating Disorders Research and Translation Strategy 2021–2031 [ 1 ] under the Psych Services for Hard to Reach Groups initiative (ID 4-8MSSLE). The strategy was developed in partnership with state and national stakeholders including clinicians, service providers, researchers, and experts by lived experience (including consumers and families/carers). Developed through a two-year national consultation and collaboration process, the strategy provides the roadmap to establishing EDs as a national research priority and is the first disorder-specific strategy to be developed in consultation with the National Mental Health Commission. To inform the strategy, IOI commissioned Healthcare Management Advisors (HMA) to conduct a series of RRs to broadly assess all available peer-reviewed literature on the six DSM-5 listed EDs.
A RR Protocol [ 23 ] was utilised to swiftly synthesise evidence in order to guide public policy and decision-making [ 24 ]. This approach has been adopted by several leading health organisations including the World Health Organisation [ 25 ] and the Canadian Agency for Drugs and Technologies in Health Rapid Response Service [ 26 ], to build a strong evidence base in a timely and accelerated manner, without compromising quality. A RR is not designed to be as comprehensive as a systematic review – it is purposive rather than exhaustive and provides actionable evidence to guide health policy [ 27 ].
The RR is a narrative synthesis and sought to adhere to the PRISMA guidelines [ 28 ]. It is divided by topic area and presented as a series of papers. Three research databases were searched: ScienceDirect, PubMed and Ovid/Medline. To establish a broad understanding of the progress made in the field of EDs, and to capture the largest evidence base from the past 12 years (originally 2009–2019, but expanded to include the preceding two years), the eligibility criteria for included studies into the rapid review were kept broad. Therefore, included studies were published between 2009 and 2021, in English, and conducted within Western healthcare systems or health systems comparable to Australia in terms of structure and resourcing. The initial search and review process was conducted by three reviewers between 5 December 2019 and 16 January 2020. The re-run for the years 2020–2021 was conducted by two reviewers at the end of May 2021.
The RR had a translational research focus with the objective of identifying evidence relevant to developing optimal care pathways. Searches therefore used a Population, Exposure, Outcome (PEO) approach [ 29 ] whereby search terms are specified to identify literature relating to the population or group of interest (i.e., individuals of any age or background with the propensity to develop and eating disorder), exposure to the risk factors that are associated with the development of an eating disorder, and the outcome of interest (i.e., the development of an eating disorder). By using the three PEO components to guide the search strategy, the PEO approach aims to facilitate a thorough and systematic examination of existing literature. Purposive sampling focused on high-level evidence studies such as: meta-analyses; systematic reviews; moderately sized randomised controlled studies (RCTs) ( n > 50); moderately sized controlled-cohort studies ( n > 50), or population studies ( n > 500). However, the diagnoses ARFID and UFED necessitated a less stringent eligibility criterion due to a paucity of published articles. As these diagnoses are newly captured in the DSM-5 (released in 2013, within the allocated search timeframe), the evidence base is emerging and fewer studies have been conducted. Thus, smaller studies (n = < 20) and narrative reviews were also considered and included. Grey literature, such as clinical or practice guidelines, protocol papers (without results) and Masters’ theses or dissertations, was excluded. Other sources (which may not be replicable when applying the current methodology) included the personal libraries of authors, yielding four additional studies (see Additional File 1 ). This extra step was conducted in line with the PRISMA-S: an extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews [ 30 ].
Full methodological details including eligibility criteria, search strategy and terms and data analysis are published in a separate protocol paper [ 31 ]. The full RR included a total of 1320 studies (see Additional File 1 for PRISMA flow diagram). Data from included studies relating to risk factors for EDs were synthesised and are presented in the current review.
The Rapid Review identified 284 studies for inclusion in the ‘Risk Factors’ category. When referring to ‘risk factors’ in this review, we are not always referring to causal risk factors. Accordingly, some of the risk factors included in this review are correlated or associated with increased risk of an ED, without evidence of causation. As the aim of a Rapid Review is to broadly synthesise findings, we did not narrow to studies only providing evidence regarding the causal relationship of risk factors. Rather, the current review focused on a range of research including prospective, experimental and correlational studies to identify a large number of potential correlates which have risk capacity for EDs. According to the Kraemer et al. (2001) criteria, this review covers research related to the following technical terms: “correlate” (a measure associated with the outcome), “risk factor” (a measure which precedes the outcome), and “causal risk factor” (a risk factor, which when manipulated, causes a change in the outcome) [ 32 ]. Therefore, the factors identified in this review are associated or predictive factors, unless in cases where a causative link has been demonstrated. A summary of the key risk factors associated with EDs is provided in Table Table1 1 and are discussed in this section. Results are subdivided into nine categories: (1) genetics, (2) gastrointestinal microbiota and autoimmune reactions, (3) childhood and early adolescent exposures, (4) personality traits and comorbid mental health conditions, (5) gender, (6) socio-economic status, (7) ethnic minority, (8) body image and social influence, and (9) elite sports. A full list of included studies for this topic, including population, aims, design, and outcome measures is available in Additional File 1 .
Risk factors associated with EDs
ED eating disorder; AN anorexia nervosa; BN bulimia nervosa; BED binge eating disorder; EDNOS eating disorder not otherwise specified; BMI body mass index; AN-BP anorexia nervosa (binge-purge subtype); PD personality disorder; ARFID avoidant restrictive food intake disorder; AN-R anorexia nervosa (restrictive subtype); A-AN atypical AN
1. Genetics: endocrines and neurotransmitters
Genetic risk factors and polymorphisms (variations in gene expression), relating to core EDs have been widely studied. Research conducted within twins and family groups as well as large-scale genomic studies have indicated a genetic component to risk of Anorexia Nervosa (AN), Bulimia Nervosa (BN) and Binge Eating Disorder (BED) [ 33 ]. Incidence rates in individuals with a parent with a history of ED have been found to be over twice as high compared to individuals with parents with no history of an ED [ 34 ]. Familial studies have demonstrated a strong genetic association for AN in particular. An individual is 11 times more likely to develop AN if they have a relative with the disorder as compared to someone with no family history. Similarly, an individual is 9.6 times more likely to develop BN, and 2.2 times more likely to develop BED if they have a relative with the disorder [ 33 ]. Evidence of genetic risk factors for other EDs is growing [ 33 ], although there have been no genetic studies to date conducted with Avoidant Restrictive Food Intake Disorder (ARFID) [ 35 ].
Anorexia nervosa and bulimia nervosa
Genetic factors have been shown to strongly contribute to both AN and BN [ 36 ]. There is evidence to suggest approximately half of the genetic factors implicated in AN and BN are shared between the disorders, with the remaining 50% being unique to one or the other [ 36 ]. An older study of Norwegian twins found some support for different features of AN being more heritable than others; having found weight/shape concern to have greater genetic association than low BMI and amenorrhea [ 37 ]. In contrast the landmark 2019 study by two international genome-wide association consortiums found that both metabolic and anthropometric related genetic loci associated with BMI lowering alleles have strong correlations with AN [ 38 ].
Hereditary patterns of EDs have been shown to disproportionately affect females [ 34 ]. In a sample of adolescent twins aged 15 to 17, Baker et al. (2009) found females were at greater genetic risk for disordered eating than males [ 39 ]. This is consistent with earlier evidence suggesting drive for thinness and body dissatisfaction showed lower heritability in males [ 40 ]. Baker et al. [ 39 ] found that only half of the genetic risk factors predicting drive for thinness and body dissatisfaction in females predicted the same traits in males. A possible explanation for this difference was offered in a study of French and German cohorts whereby inherited variations in an estrogen receptor gene (ESR1) significantly increased risk of restrictive eating and subsequently development of AN restrictive subtype (AN-R) [ 41 ].

Comorbidities
Genetic risk has been implicated in co-occurrence of EDs and other psychiatric diagnoses. Genetic associations have been found between Attention-Deficit/Hyperactivity Disorder (ADHD) and all EDs, with the strongest correlation to binge/purge-type ED behaviours [ 42 , 43 ]. Strong positive genetic associations have also been identified between AN and other psychiatric comorbidities, including Obsessive Compulsive Disorder (OCD), major depressive disorder, suicidality, schizophrenia, neuroticism, autism, and neurodevelopmental delay [ 44 – 48 ]. Genetic risk for comorbid AN and Generalised Anxiety Disorder (GAD) has also been identified [ 46 , 47 ].
The contribution of comorbid mental health disorders to ED risk and outcomes are further discussed in Sect. Results and in another topic paper of the Rapid Review, ‘Psychiatric Comorbidities and Medical Complications.’
Genes and polymorphisms
Several genomic studies have attempted to locate specific gene loci implicated in the development of EDs. See Table Table2 2 for a summary of genes and polymorphisms identified in ED genomic studies. A recent genome-wide association study published in 2021 has suggested that there is a distinct difference in the underlying biology between binge-type EDs (BN and BED) and AN. The study reported that both BN and BED shared genomic variant with overweight and obesity, whereas the directions of these associations were reversed for AN [ 49 ].
Genes and polymorphisms identified in the development of EDs
ED eating disorder; AN anorexia nervosa; BN bulimia nervosa, BED binge eating disorder
Genetic susceptibility to AN was explored in a landmark meta-analysis of 33 datasets from international genome-wide association studies. Watson et al. [ 38 ] compared the DNA of almost 17,000 individuals with AN to the DNA of 55,000 people without AN around the world. Eight loci associated with significant risk of developing AN were identified [ 38 , 50 ], including genetic correlations with certain psychiatric, anthropometric, and metabolic traits, as well as physical activity. Positive associations were found for physical activity, anxiety and schizophrenia disorders, and HDL cholesterol. Negative associations were found for metabolic (including glycemic), lipid, and anthropometric traits including fat mass, fat-free mass, BMI, obesity, type 2 diabetes, fasting insulin, insulin resistance, and leptin [ 48 ]. Analysis of causality revealed a bi-directional relationship between potential AN genes and risk for low body mass index (BMI). However, there is stronger evidence that low-BMI-causing alleles increase risk of AN than there is for AN-risk genes leading to low BMI [ 38 ].
A study of Norwegian adolescents found an association between poor appetite and undereating, and the COMT gene, which is responsible for regulating dopamine levels through the production of the COMT enzyme [ 51 ]. Brain studies of patients with AN have indicated that, due to disturbances in regular serotonin and dopamine reward pathways, individuals with AN may use restricted eating as a mechanism to reduce anxiety [ 52 ]. In one study of patients with AN and BN, mutations in genes with heightened expression in brain tissue (CNTF, NTRK) were associated with a higher minimum lifetime BMI and earlier ED onset [ 53 ].
Six genetic polymorphisms have been associated with the development of BN in people with obesity [ 54 ]. Of the six genetic polymorphisms, three are thought to be related to the neuroendocrine receptors of dopamine, serotonin, and cannabinoid. This association is supported by evidence that genetic variations which lead to low dopamine production and neurotransmission are associated with an increased risk of binge/purge type EDs [ 55 ]. The remaining three polymorphisms identified in BN aetiology were associated with an estrogen receptor, the production of an enzyme expressed in brain tissue, and the FTO gene (which has a role in BMI regulation) [ 54 ]. While dopamine and serotonin receptor genes (DRD2 and SLC6A4, respectively) are implicated in the development of both BN and BED, differing polymorphisms in these genes appear to be associated with increased risk of developing one disorder over the other [ 54 ]. Further, triallelic 1 variations in a serotonin receptor allele (5-HTTLPR) have also been observed to contribute to compulsive personality traits and the development of AN, BN, and eating disorder not otherwise specified (EDNOS) [ 56 , 57 ]. A polymorphism of the oxytocin receptor gene (OXT-R) was also found to distinguish between risk of onset for restricting type EDs or binge/purge type EDs, indicating the potential role of oxytocin in the development and maintenance of EDs [ 58 ]. Additional research has identified an association between a polymorphism in a neurotransmitter inhibition gene (HTR1B) and an increased risk of developing BN as well as greater severity of AN symptoms, including low BMI [ 59 ].
Expression of genes associated with the production of appetite and weight control endocrines (leptin, melanocortin, and neurotrophin) are thought to have a role in ED development and severity [ 45 ]. A case–control study by Zeeland et al. [ 60 ] found a significant number of AN participants with a polymorphism in a cholesterol metabolism gene (EPHX2), which was also associated with lower BMI (see Table Table2). 2 ). Yilmaz et al. (2014) examined 20 single-nucleotide polymorphisms 2 (SNPs) in the endocrine system genes in a sample of individuals with BN (n = 745) and AN (n = 245). Although no significant differences were observed between either ED diagnosis or control participants, two SNPs associated with regulation of BMI were found to have an impact on disease severity (See Table Table2) 2 ) [ 61 ].
Consequences of variations in endocrine signalling in individuals with ED also include reduced capacity for interoception 3 particularly relating to gastric interoception. A systematic review of interoception in individuals with ED found the strongest correlations were observed in individuals with AN who consistently had lower gastric interoception relating to satiety and self-reported fullness, while individuals with BN were found to have lower pain interoception resulting in higher pain thresholds. However, researchers were unable to ascertain whether lack of gastric interoception in individuals with AN was a result of conscious processing of satiety cues or disruptions in endocrine signalling [ 62 ].
Non-shared vs. shared environments
A Swedish study of female monozygotic (identical) and dizygotic (fraternal) twins aged between 20 and 47 found that nonshared environmental factors between twins had a greater impact on ED risk than shared environmental factors [ 36 ]. This finding was further supported by a study of an Australian twin sample, which concluded that nonshared environmental factors contributed to the genetic factors associated with weight loss behaviours and overeating behaviours in AN and BN, respectively [ 63 ]. Shared environmental factors were not observed to have an impact on disordered eating behaviours [ 63 ].
Exposure to childhood trauma has been linked to polymorphisms in genes expressed in the glucocorticoid receptor pathway which are associated with increased risk of developing BN, binge eating, and loss of control over eating [ 51 , 64 – 66 ]. This finding is supported by research conducted by Monteleone et al. [ 67 ], who found significantly lower levels of cortisol in individuals with AN and BN with a history of childhood maltreatment than healthy controls and those ED patients with no history of childhood trauma. Exposure to childhood trauma was also found to interact with gene expression through creating higher levels of DNA methylation 4 in women with BN [ 68 ]. Analysis of evidence from seven studies found a strong additive effect for serotonin transporter 5-HTTLPR polymorphism combined with childhood experiences of physical and sexual abuse in the development of BN [ 69 ]. Childhood trauma and abuse as a risk factor for EDs, particularly related to environmental influence, will be further discussed in Sect. Results .
Binge eating disorder
Variation in genes linked to appetite and satiety modulating hormones such as ghrelin are often implicated in the development of BED, as well as several genes related to regulation of BMI and fat storage. A study of 4,360 adolescents aged 14 or 16 found that frequency of binge eating was associated with expression of a polymorphism in the FTO gene, thought to play a role in BMI and obesity [ 70 ]. Further, mutations of the MC4R gene, involved in metabolism and feeding, is also associated with BED and obesity [ 71 , 72 ].
As previously discussed, polymorphisms in genes responsible for the production of neuroendocrine receptors such as dopamine and serotonin are also commonly associated with BN and BED [ 54 ]. Reward responses to food have long been implicated in the development and perpetuation of BED. The expression of two alleles in the dopamine D2 receptor has been found to be positively associated with BED in a sample of 230 individuals with obesity [ 73 ]. The authors concluded that expressions of these alleles was associated with hypersensitivity to reward, likely having a causal relationship with BED [ 73 ]. In a study of female twins in the US, increased binge eating frequency was also found to be associated with genetic factors related to the personality traits neuroticism and conscientiousness [ 74 ].
Night eating syndrome
Genetic research relating to Night Eating Syndrome (NES) is less developed than the primary EDs. Work in animal models has implicated variants of the VGF, a gene responsible for production of a neuropeptide precursor in NES aetiology [ 75 , 76 ]. One familial study was identified assessing the heritability of NES involving families where at least one parent had obesity. Night eating symptoms in mothers were strongly associated with similar behaviours in their sons and daughters, while no such correlation was observed for fathers [ 77 ]. Interestingly, the association was slightly stronger in sons (r = 0.19) than in daughters (r = 0.15), whereas heritability relationships are typically stronger in female offspring in other ED diagnoses [ 34 , 77 ]. This finding was further supported by evidence from a Swedish twin registry study where males were more likely to endorse night eating traits associated with genetic factors, while females were more likely to endorse binge eating [ 76 ]. Further research is required to understand any potential genetic risk factors associated with NES.
There is considerable evidence pointing to genetic risk in the development of EDs, with the highest heritability conferred for AN [ 33 , 34 ]. Females are also at greater genetic risk for disordered eating in comparison to males [ 39 ]. When considering the specific genetic variations thought to contribute to increased ED risk, genetic associations have been found between EDs and other psychiatric comorbidities, however the type of comorbidity differs according to the ED diagnosis. For binge-type EDs (BN and BED) strongest genetic correlations are observed with ADHD [ 42 , 43 ] whilst AN has strong correlations with OCD, MDD, suicidality, schizophrenia, neuroticism, autism, and neurodevelopmental delay [ 44 – 48 ]. In a similar manner, genetic correlations with metabolic traits appear to differ between ED diagnoses, such that BN and BED have been found to share genomic variants with overweight and obesity [ 49 ] whereas potential AN genes uphold a bi-directional relationship with low BMI [ 38 ]. Genes associated with other metabolic functions, including appetite and weight control endocrines (leptin, melanocortin, neurotrophin) have also been implicated in ED development and severity, however fewer differences between ED diagnoses are apparent. Polymorphisms in the genetic loci responsible for neurotransmitters associated with reward processing and appetite regulation hormones, including dopamine, serotonin, and cannabinoid have been identified as a risk factor across several ED diagnoses including AN, BN, and EDNOS [ 45 , 50 – 62 ]. Additionally, genetic polymorphisms in the glucocorticoid receptor pathway responsible for the stress response have been linked to individuals who have experienced trauma and are associated with increased risk for BN [ 51 , 65 , 66 ].
2. Gastrointestinal microbiota and autoimmune reactions
Gastrointestinal microbiota.
The role of gut microbiota and immune system reactions in the development and perpetuation of EDs is an emerging field, however is receiving growing attention. Endocrines produced in the gastrointestinal (GI) tract communicate with the brain to regulate functions of appetite and satiety. Given the role of these functions in EDs, it is thought that dysregulation of the gut microbiome may be partially responsible for ED psychopathology [ 78 – 80 ]. A review of evidence on the gut microbiome suggests that the growth cycle of gut bacteria and their metabolites 5 may contribute to patterns of accelerated and/or prolonged satiety in AN and periodic lack of satiation in BN [ 78 ]. In a study of 33 AN patients undergoing refeeding, Hanachi et al. [ 81 ] found the AN patients to have significant gut microbial dysbiosis compared with 22 healthy controls.
Several studies of AN have investigated the role of a protein (CIpB) produced by the Escherichia Coli ( E. Coli ) bacteria. The CIpB protein has a similar structure to the human hormone responsible for simulating secretion of satiation peptide YY. The peptide YY has been detected in high levels in the blood plasma of individuals with AN compared to healthy controls [ 78 , 82 , 83 ]. Peptide YY levels have also been found to be elevated among individuals with AN-R as compared to those with AN-BP and healthy controls [ 84 ]. Intestinal infections and chronic inflammation can lead to large increases in the number of E. coli bacteria in the GI tract, therefore increasing the levels of peptide YY and potentially increasing risk of ED [ 83 ]. The CIpB protein produced by E. Coli also prompts an immune reaction whereby autoantibodies are created. The position on the receptor for this autoantibody has been shown to differentiate between risk for BN and BED or AN [ 78 ]. Despite such emerging evidence indicating a role for gut microbiome dysregulation in EDs, researchers consider much of the evidence to be in an observational phase or using murine models 6 and lacking the capacity to explain aspects of ED pathology [ 79 , 85 ].
Autoimmune and autoinflammatory diseases
Gut microbiota are also known to interact with autoimmune responses, which have been investigated as a potential risk factor for EDs. In a large population-based cohort study, autoimmune and autoinflammatory diseases were identified as a significant predictor in the development of EDs and were associated with a 36% increased chance of developing AN. Interestingly, risk of BN and EDNOS was much higher at 73% and 72%, respectively [ 86 ]. Among a sample of patients hospitalised for EDs in Finland, higher prevalence of type 1 diabetes and Crohn’s disease was observed compared with healthy controls [ 87 ]. A recent meta-analysis has also identified a bidirectional association between coeliac disease and EDs. In particular, patients with AN are at a significantly greater risk of coeliac disease than healthy adults without AN [ 88 ]. Further, researchers argue that symptoms of ED commonly mimic those of chronic inflammatory GI and endocrine disease, including inflammatory bowel disease and diabetes type 1 and 2, emphasising the importance of screening for possible co-occurrence [ 89 ]. Unlike the vast majority of other risk factors associated with EDs, autoimmune and autoinflammatory diseases represented a greater risk for male participants as compared to females [ 86 ].
As a type of autoimmune disease, diabetes is commonly associated with EDs. There is a substantial evidence base indicating an increased prevalence of disordered eating behaviours among individuals with both type 1 and type 2 diabetes [ 90 , 91 ]. However, much of the evidence is observational and there are limitations in distinguishing between avoidance of certain food groups due to presence of an ED versus a feature of diabetes management [ 92 , 93 ]. Nevertheless, high rates of ED behaviours not related to food restriction (e.g., excessive exercise, vomiting, and laxative abuse) have been observed in adolescents and adults with diabetes [ 94 , 95 ]. Insulin manipulation or restriction has also been observed in adolescents with diabetes resulting in poor glycaemic control and poorer outcomes [ 89 , 90 , 94 – 96 ]. Interestingly, a study of adults has revealed that weight/shape overvaluation was lower in participants with diabetes (31.5%) compared to those who did not have diabetes (41.2%). The authors suggest that this may indicate that BED, as an ED for which weight/shape overvaluation is not a diagnostic criteria, may be of particular concern among adults with diabetes [ 97 ].
In terms of biological risk factors, evidence has largely focused upon proteins produced by gut bacteria, which have been implicated in dysregulation of appetite and satiety in individuals with EDs. The metabolites of gut bacteria are thought to play a role in disordered eating patterns, including prolonged satiety in AN and periodic absence of satiety in BN [ 78 – 80 ]. For example, a protein produced by E. Coli bacteria has been found to mimic the structure of the satiation peptide YY, a protein that is higher in individuals with AN as compared to healthy controls [ 83 , 84 ]. Findings such as these have led researchers to consider intestinal infections and chronic inflammation as a potential risk factor for EDs. However, research in this field is emerging, with further studies needed to better understand the association between gut microbiome dysregulation and EDs. Large studies have indicated that having an autoimmune or autoinflammatory disease, such as Crohn’s disease, inflammatory bowel disease, diabetes type 1 and 2, and coeliac disease, is also significantly associated with increased risk of BN and EDNOS, and to a lesser extent, AN [ 90 – 95 ].
3. Childhood and early adolescent experiences
A range of childhood experiences have been linked to the development of EDs later in life, including in-utero exposures, family dynamics and parental characteristics, childhood weight, and experiences of abuse and trauma.
In utero exposures
There is evidence to suggest that exposure to certain levels of hormones during foetal development could increase risk of ED development later in life. In a large cohort study of women in the UK, daughters whose mothers had a lifetime diagnosis of BN were found to have been exposed to high levels of prenatal testosterone in the womb, which was implicated in an increased risk of BN and binge eating [ 98 ]. However, a large multinational twin study was unable to find any link to in utero exposure to sex hormones and ED onset later in life [ 99 ].
Research has indicated that in-utero exposure to high levels of cortisol through maternal stress is associated with later development of ED [ 100 , 101 ]. A further study in the UK found that individuals who were born preterm had an increased risk of ED associated with structural brain alterations linked to underdevelopment [ 102 ]. Additional risk factors include the use of substances during pregnancy (e.g., nicotine) and maternal illness leading to malnutrition (e.g., anaemia), which have also been linked to an increased risk of AN and BN in the child later in life [ 103 ].
Risk factors conferred during foetal development are further supported by findings that risk of BED is associated with high weight at birth or being large for gestational age, while AN was associated with low weight at birth. No significant foetal developmental risk factors have been identified for BN [ 104 ]. Moreover, stressful events experienced by mothers in the year prior or during pregnancy, in particular the death of a close relative in the six months preceding pregnancy, have been shown to have an impact on the development of feeding or EDs in infants and toddlers [ 105 ]. Feeding issues in babies of mothers who had an ED diagnosis during pregnancy were also noted in this cohort [ 106 ].
A recent systematic review identified an association between AN and older maternal age, preterm birth (< 32 weeks), lower birth size, and maternal health complications (e.g., preeclampsia, eclampsia). The review also reported an association between BN and maternal stress during pregnancy [ 107 ].
There appears to be an impact of pregnancy upon the eating behaviours of women with an ED diagnosis. One study has found that ED behaviours across diagnoses tended to improve significantly during the pregnancy period, although this may not be maintained after [ 108 ]. It has also been reported that pregnancy is associated with remission of BN but an increased risk of BED onset [ 109 , 110 ]. Women with a history of psychosocial adversities have been found to possess a significantly greater risk for BN during pregnancy [ 111 ].
Family dynamics and parental characteristics
Research has shown that children are more likely to develop an ED if their parents display characteristics commonly associated with ED psychopathology, such as drive for thinness and perfectionism [ 112 ]. Specifically, maternal history of an ED has been shown to be associated with higher rates of emotional eating in children as young as four years old [ 113 ]. The children of women with lifetime AN have also been found to exhibit deficits in cognitive functioning, including social understanding, visual-motor function, planning, and abstract reasoning [ 114 ].
Additionally, Larsen et al. [ 115 ] reported that general parental psychiatric illness is associated with increased risk of BN and EDNOS. The authors also identified the experience of childhood adversity and significant family disruption as significant risk factors for development of BN and EDNOS. Interestingly, no associations between childhood adversities and risk of AN could be identified by authors, although a separate study identified maternal depressive symptoms as a predictor of AN [ 116 ].
Adopted individuals have also been identified as having a greater risk of binge eating and extreme weight loss behaviours, as well as increased risk of a lifetime diagnosis of an ED [ 117 ]. Other parental characteristics which have been associated with ED behaviours include high maternal BMI at 16 weeks’ gestation and when their child is eight years old, high maternal education attainment, and low parental self-esteem [ 118 – 120 ].
Individuals’ perceptions of the quality and nature of their parental relationship has been investigated as a potential risk factor for development of an ED. Research has found that female individuals diagnosed with AN or BN report significantly lower perceived emotional connectedness prior to disorder onset than their healthy sisters. In a family-based study of 332 female individuals, low emotional connectedness conferred a greater risk of developing BN over AN-R [ 121 ]. Further, females who report low maternal warmth have a higher risk of developing binge/purge type EDs [ 122 ]. Low parental warmth appears to be a risk factor for ED development in females but not males [ 123 ]. A study of AN patients and their healthy siblings found that both siblings in these families perceived low maternal care and high maternal overprotection. Siblings affected by AN developed insecure attachment compared with their siblings and had higher preoccupation with relationships, while healthy siblings were able to develop secure attachment and low need for approval and high self-transcendence [ 124 ]. Other risk factors include an oppressive parental relationship and childhood unhappiness [ 122 ].
Parents’ communication about food, as well as parental eating behaviours, have been shown to be a significant risk factor for EDs in their children. Several studies have found that exposure to disordered eating behaviours such as dietary restriction in parents is likely to have an impact on the early development on EDs in children, beyond the influence of genetics [ 125 , 126 ]. One study identified maternal distress as a mediating factor in the relationship between maternal ED and infant feeding difficulties [ 127 ]. Maternal dieting and poor communication among family members have also been associated with long-term risk for restrictive disordered eating [ 128 ]. Conversely, parental conversations regarding healthy eating, rather than dieting or weight, and regular family meals were found to be protective against development of EDs among child and adolescent samples in Europe and the US [ 129 , 130 ]. Parental pressure to eat, early negative experiences with food, and high disgust sensitivity were found to predict picky eating behaviours associated with ARFID. Parental encouragement around food in childhood was observed as a protective factor. Being male was also found to be a significant risk factor for adult picky eating behaviour and potential ARFID [ 131 ].
The experience of stressful life events, including bereavement, separation from family members, or involvement in an accident have been found to have an impact on ED development, in particular BN and BED. The occurrence of three or more events in combination with external criticism of weight or shape has been shown to be significant predictors in the year prior to BN onset [ 132 ]. No significant differences were observed between BN and BED in terms of the number or types of events experienced prior to onset [ 133 ].
Childhood weight
Research on the association between childhood weight and risk of eating pathology in later years is ambiguous. Several studies have reported that higher weight during childhood poses an increased risk of developing an ED in later years, including among culturally and linguistically diverse (CALD) individuals, as well as males [ 134 – 138 ]. Analysis of specific ED behaviours among adolescents in the US between 1999 and 2010 found that ED symptomatology and weight/shape concern persisted beyond adolescence for individuals who were overweight. Contrastingly, for non-overweight individuals, unhealthy weight control behaviours and body dissatisfaction decreased over time [ 139 ]. Other studies have found that adolescents with a weight history in the overweight range experience a significantly greater drop in BMI, higher levels of ED psychopathology and comorbid mental health difficulties, and take much longer to be identified than adolescents without a history of overweight [ 140 ], 141 .
Contrastingly, explorations of the association between weight history and AN specifically have found that low baseline BMI is a significant risk factor for development of both atypical AN and AN [ 38 , 142 , 143 ].
It has been suggested that parental perception of their child as being overweight may be a more powerful predictor of ED development than the child’s weight itself [ 118 , 144 , 145 ]. The significant impact of parental behaviours on ED risk has been supported by a study comparing individuals with BN to healthy controls and individuals with other psychiatric conditions. While being overweight or obese in childhood was identified as a risk factor, high maternal expectations and negative parental attitudes about weight and obesity in childhood were more strongly associated with the onset of BN among participants [ 146 , 147 ]. These risk factors are also associated with onset of BED [ 148 ]. Negative parental attitude towards childhood weight, including parental teasing about weight, has been shown to have a strong positive association with ED behaviours in both males and females, in particular binge eating behaviours [ 146 , 149 , 150 ]. Parental comments about their child’s weight and eating behaviours are also significantly associated with increased drive for thinness and body dissatisfaction [ 151 , 152 ].
Abuse and trauma
Experience of childhood trauma and abuse has been consistently identified as a non-specific risk factor for the development of EDs, although these experiences are more strongly associated with binge-purge type disorders such as BN, BED, and AN-BP [ 153 – 157 ]. Evidence from several studies suggests that emotional abuse is a significant predictor of binge/purge symptomology in women, while sexual abuse and physical neglect were associated with symptoms in men [ 158 – 160 ]. Sexual harassment has also been identified as a risk factor for EDs however little is known about the causal relationship or the role of mediating factors [ 161 ]. Attempts to investigate the association between types of childhood trauma and specific ED diagnoses have found that emotional abuse is a risk factor for all core ED symptoms [ 162 ]. A large-scale study of young adults in the US found that participants who reported multiple types of maltreatment in childhood were almost twice as likely to report binge eating and skipping meals as compared to those who reported no or low maltreatment [ 163 ]. Verbally abusive fathers have been shown to be strongly associated with AN-BP and BN, and verbally abusive mothers influence the development of BN [ 164 ].
Studies conducted in groups of women with obesity have found relationships between binge eating and childhood abuse and neglect. The severity of the abuse, rather than the type of abuse, appears to have a role in the development of BED and severity of food addiction [ 165 , 166 ]. A recent study has found that childhood food neglect is associated with increased risk for BN and BED even after adjusting for other adverse experiences and financial difficulties experienced during childhood [ 167 ]. A study on the impact of childhood emotional abuse and ED risk found that low self-perception and self-esteem caused by the abuse contributed to an increased risk of BED and NES [ 168 ]. Further, individuals with both an ED diagnosis and a history of childhood trauma and abuse have been found to have increased risk of lifetime suicide attempts [ 169 , 170 ].
The experience of childhood bullying has been found to increase risk of AN, and to a lesser extent BN, in children and adolescents [ 171 – 173 ]. However, increased risk of EDs was not found to carry on into early adulthood [ 171 ]. Weight-based teasing has also been associated with emotional eating, eating in the absence of hunger, and disordered eating attitudes and behaviours [ 174 ]. Consistent with existing evidence, an observational study of 182 adolescents receiving treatment for EDs found bullying was the most common form of trauma experienced by patients [ 175 ]. Assessment of the impact of cyberbullying also found the experience predicted onset of AN, BN, and EDNOS in a group of individuals with an ED diagnosis and increased ED symptomology and depression among a group of high-risk individuals [ 176 ]. Exposure to online content and risk of ED development is discussed further in Sect. Gender .
An overview of the evidence regarding the impact of early experiences in terms of ED risk has identified a range of factors starting from the in-utero environment through to adolescence. In-utero exposure to high levels of testosterone, cortisol, or substances have been associated with increased risk of EDs [ 98 – 100 , 102 , 103 ]. There is also evidence to linking high birth weight to BED and low birth weight to AN [ 104 ]. Weight persists as a risk factor throughout childhood and adolescence, with research findings that high maternal expectations and negative parental attitudes about weight are also associated with ED risk. The quality and nature of one’s parental relationship is considered another risk factor for EDs, such that lower ratings of parental warmth or emotional connectedness have been reported by individuals with AN and BN as compared to their healthy siblings [ 121 – 124 ]. Experiences of childhood adversity, significant family disruption, childhood trauma (including neglect and emotional or sexual abuse) are well-documented risk factors, with evidence suggesting that they are most likely to contribute to the development of binge/purge type disorders (AN-BP, BN, BED, PD) [ 115 , 153 – 156 ]. Researchers have also suggested that the link between EDs and trauma is likely to be underestimated due to non-disclosure [ 207 ].
4. Personality traits and comorbid mental health conditions
Traits such as anxiety, perfectionism and obsessive-compulsivity are frequently associated with increased risk of EDs and may play a substantial role in the severity of symptoms, response to treatment, and risk of relapse [ 178 ].
Perfectionism, impulsivity, compulsiveness, and avoidance motivation
Rather than being linked to diagnostic type, a meta-analysis of personality traits (Farstad et al., 2016) found a more robust association with specific behaviours and symptomatology. Studies have shown that relative to controls, individuals with ED have elevated levels of perfectionism (setting of excessively high standards for performance, accompanied by overly critical self-evaluation); neuroticism (tendency to experience negative effects such as anger, anxiety, self-consciousness, irritability, emotional instability, and depression); impulsivity, particularly negative urgency (tendency to engage in impulsive behaviour when experiencing strong negative emotion); compulsivity (tendency toward overcontrolled behaviour); avoidance motivation (tendency to move away from or avoid situations associated with punishment); sensitivity to social rewards; introversion; and self-directedness (goal-oriented behaviour) [ 178 – 186 ].
Perfectionistic traits are common in both AN and BN. A systematic review and meta-analysis concluded that individuals with AN tended to place greater emphasis on high personal standards, while individuals with BN were more likely to perceive high levels of parental criticism [ 178 ]. The contribution of perfectionism to ED symptomatology (including dietary restriction and shape and weight overvaluation) was further supported by Joyce et al. [ 180 ] in a community-based sample of women. The study was inconclusive as to whether perfectionism was the cause of the ED symptoms. However, a significant positive association between perfectionism and weight and shape overvaluation was observed [ 180 ].
Among a sample of adolescent females recruited from an ED service in Australia, researchers found both a direct relationship between perfectionism and AN symptoms as well as an indirect relationship when mediated by depression [ 187 ]. The two different relationships were found to be equally viable, further supporting the notion of a reciprocity of symptoms between anxiety, depression, and AN, which are preceded by perfectionism.
In a 10-year follow-up study of university-aged adults in the US perfectionism was associated with the onset of AN, BN, and EDNOS and found to contribute significantly to disorder maintenance [ 188 ]. The tendency toward perfectionism in AN has been linked to a trait of vulnerable narcissism, ‘hiding the self,’ described as an unwillingness to show one’s faults or needs to others. The ability to exhibit control over emotional needs and relationships was correlated with AN-R in a comparison study involving individuals with AN and BN. However, the cross-sectional design was unable to determine whether this trait preceded AN-R and the sample size was relatively small [ 189 ].
Obsessiveness has also been found to be strongly associated with AN. Among a clinical sample of patients with AN and atypical AN, obsessiveness was positively correlated with a drive for thinness, a key aspect of AN symptomatology. The study did not find any significant differences between AN and atypical AN in terms of obsessive behaviours [ 190 ].
Studies seeking to assess personality traits contributing to differences in clinical presentation between restricting and binge/purge ED subtypes conclude that alexithymia – the inability to identify or verbally describe feelings or emotions – plays a role in the emotional dysregulation displayed by both AN-R and BN patients [ 191 , 192 ]. Higher levels of alexithymia have been associated with greater risk of re-hospitalisation in a three-year follow-up study of women with both AN and BN [ 193 ]. Prefit et al.’s [ 194 ] meta-analysis of studies into EDs and associated personality traits found lack of emotional awareness and inability to regulate emotions leading to maladaptive ED symptomology was not diagnosis specific [ 194 ]. Findings from the meta-analysis support Brown et al. (2018), suggesting a need for emotion-focused treatment approaches such as dialectical behaviour therapy (DBT) [ 192 , 195 ].
While binge/purge presentations are consistently associated with impulsivity and greater emotional dysregulation [ 196 , 197 ], one study demonstrated no significant differences in ability to regulate emotions between AN-R and BN patients with high levels of alexithymia [ 192 ]. However, in another study involving clinical samples of AN-R, AN-BP and BN patients, individuals with AN-R were found to have fewer fluctuations in mood than individuals with AN-BP and BN. Only in groups exhibiting binge/purge symptomology were these behaviours observed as a method for alleviating negative affect [ 198 ]. Similarly, among a group of 139 female college students, lower impulsivity in addition to lower self-esteem was found to be associated with AN risk [ 199 ]. A recent systemic review has warned that due to methodological limitations in the studies conducted to date, there is insufficient evidence to support the characterisation of AN and BN as being low and high in impulsivity, respectively [ 200 ].
Individuals with binge/purge subtypes EDs, including AN-BP, BN, BED and various OSFEDs, have been found to have higher levels of avoidance motivation, impulsivity, emotional dysregulation, anxiety, depression, and paranoia than healthy controls [ 178 ]. Within a clinical sample of AN patients, individuals displaying binge/purge symptoms were more likely to engage in non-suicidal self-injurious behaviour and have lower self-directedness and co-operation than individuals with AN only [ 201 ]. However, the literature is inconclusive as to whether these traits contribute to ED onset or are symptoms of it.
Several studies have observed high levels of impulsivity in individuals with BN, with these individuals commonly displaying negative urgency, lack of planning and sensation seeking. Farstadt et al. (2016) in their meta-analysis also argue a role for compulsiveness (i.e., the tendency towards overcontrolled behaviour), suggesting that the interaction of personality traits such as impulsiveness and compulsiveness can have implications for ED symptomology and disorder severity [ 161 , 180 , 183 , 184 ]. In this manner, impulsivity was found to have a significant impact on the types of ED symptomatology displayed by the individual and clinical presentation [ 178 , 195 ]. In contrast, Waxman [ 195 ] found no significant differences in impulsivity between ED diagnoses. Waxman [ 195 ] suggested that while there is a lack of evidence from longitudinal studies to determine conclusively that impulsivity is a risk factor in the development of ED, evidence from studies using proxy measures such as delinquency found these behaviours preceded BN onset. One further study has reported an association between NES and impulse control disorder [ 202 ]. It has also been suggested that impulsivity and addiction-like mechanisms may explain the association between ED psychopathology and both high-risk sexual behaviours and substance misuse [ 203 , 204 ].
A study of 83 sister pairs found participants with a lifetime ED diagnosis displayed higher levels of internalising behavioural issues (social withdrawal, anxiety, depression) and/or externalising behavioural problems (aggression and delinquency) than their healthy sisters [ 205 ]. Internalising behaviours were found to be a strong predictor for AN-R, while externalising behaviours were strongly associated with later onset of bulimic symptoms and BN [ 205 ].
Two models illustrating risk of bulimic behaviours among young females have attempted to account for both the role of personality traits and traditional ED concepts of the ‘thin ideal’ [ 206 ]. Pearson’s integrated model of risk combines the ‘state-based’ pathway, which shows binge eating as an impulsive lack of control behaviour and purging as a compulsive correction, and the ‘trait-based’ pathway, which emphasises negative urgency as a consistent tendency toward impulsivity and stress alleviation through binge eating. The ‘trait-based’ pathway also considers the role of inherited ED risk and predisposing childhood exposures [ 206 ]. Pearson et al. argue that integration of the ‘trait-based’ model considers the important role of heritability and negative urgency that is absent from the Stice model [ 207 ]. Further investigation of disease models of bulimic behaviour by Dakanalis et al. [ 208 ] indicate that risk factors are more complex than can be mapped by the dual pathway model, citing bi-directional relationship between dietary restriction and negative affect.
Negative urgency has also been found to be an independent predictor of food addiction among individuals displaying binge-eating symptomology [ 209 ]. A further study by Utschig et al. [ 210 ] indicated that fear of negative evaluation from others is a predictor for body dissatisfaction and pressure to be thin, contributing to an internalised ‘thin ideal’ in individuals with BN and feeding into the state-based model. Fear of negative evaluation is considered an aspect of social anxiety and relates to heightened sensitivity to social rewards, a trait found to be elevated across ED diagnoses [ 178 , 210 ].
Personality disorders
The central role of certain personality traits in the perpetuation and potential development of ED symptomology reflects established relationships between some personality disorders and EDs [ 211 – 213 ]. Comorbidity studies have found borderline personality disorder (BPD) to most commonly occur with BN and other binge/purge ED subtypes [ 212 ]. This finding is supported by research on personality traits in EDs where avoidant behaviours and low emotion regulation flexibility are elevated in bulimic-type disorders and also a core feature of BPD [ 178 , 212 , 214 ]. However, some researchers argue that the co-occurrence of EDs and personality disorders may have been inflated in previous studies [ 215 ]. In a sample of 132 females with ED, prevalence of any personality disorder was 21%, lower than in other studies where reported figures were between 27 and 95% [ 215 ]. However, findings from von Lojewski et al. [ 215 ] were consistent with existing evidence that BPD traits were significantly associated with binge/purge EDs compared with AN-R. Individuals with comorbid BPD and ED were also more likely to report self-induced vomiting as compared to any other personality disorder. Co-occurrence of EDs and BPD has also been associated with increased risk of engaging in non-suicidal, self-injurious behaviours within a clinical sample [ 212 ]. Meta-analysis of 20 studies published between 1987 and 2010 found comorbidity of BPD with EDNOS (now OSFED) to be 38%, and 29% with BED. Researchers indicated that ED and personality disorder comorbidity are more common among individuals with AN and BN than BED and EDNOS [ 216 ]. However, among patients with BED or EDNOS, avoidant personality disorders were found to be the most common, followed by BPD [ 216 ]. It should however be noted that two of three studies identified by the Rapid Review concerning ED and personality disorders were restricted to relatively small clinical samples without control groups. They were also limited by their cross-sectional design in their capacity to investigate the temporal relationships between disorders.
Anxiety, mood disorders and psychiatric comorbidities
Co-occurring and preceding mental health conditions, particularly those with shared genetic and experiential influences such as anxiety and mood disorders, are also risk factors for EDs. While it is difficult to assess which condition precedes the other without use of prospective study designs [ 217 ] these relationships have been widely studied in AN and BN, and there is some evidence for anxiety and mood disorders including depression and bipolar disorder preceding ED symptomatology. Evidence from a three-year prospective study of 615 pairs of twins in the US suggests elevated risk for AN is associated with higher levels of depression and anxiety in combination with a high drive for thinness, rather than either risk factor alone [ 218 ]. There is less conclusive evidence on the relationship between BN, anxiety, and depression although some preliminary research was identified indicating several key symptoms were shared between the three disorders [ 219 ].
Mood disorders
In clinical ED populations, prevalence of mood disorders is frequently high [ 220 ]. In one study, major depressive disorder (MDD) was found to affect 64% of individuals with AN-R and over 75% of binge/purge ED subtypes (AN-BP, BN). Sequencing of disorder onset found that mood disorders preceded ED onset in a third of the AN-R cases and 40% of the AN-BP/BN cases. The remaining comorbid cases were either co-occurring or onset following ED diagnosis. These findings from Godart et al. [ 220 ] indicate that depressive disorders can be both a predictor and consequence of ED, as well as a comorbidity caused by malnutrition further complicating management and treatment of EDs.
Assessment of the temporal relationship between depression and disordered eating in an eight-year longitudinal study found depressive symptoms predicted increases in BN behaviours, which in turn predicted increases in depressive symptoms [ 221 ]. These findings indicate there may be a reciprocal relationship between the two conditions. A reciprocal relationship was also identified in a larger cohort of adolescent females where individuals who reported depressive symptoms were twice as likely to engage in overeating and binge eating at four-year follow-up, and individuals reporting overeating and binge eating were also more likely to report depressive symptoms at follow-up [ 222 ].
Anxiety disorders
There is evidence to suggest that anxiety is the most commonly occurring comorbidity with ED [ 223 ]. Childhood anxiety disorders have repeatedly been found to precede the onset of an ED, particularly AN [ 224 – 228 ]. Studies have identified a greater incidence of childhood obsessive–compulsive traits in individuals diagnosed with AN in comparison to control groups without an ED [ 177 ]. Micali et al. [ 211 ] conducted a longitudinal study of 231 young people diagnosed with OCD over a nine year period. Of the 126 participants who completed the follow up assessment, 12.7% had a diagnosis of an ED. Such findings highlight predictive value of childhood anxiety disorders in the later development of EDs, especially AN.
A reciprocal relationship between GAD and AN was indicated in a large twin study by Thornton et al. [ 229 ] whereby having GAD significantly increased likelihood of AN and having AN significantly increased likelihood of GAD. The group with AN and GAD had the lower mean adult BMI than both AN only and GAD only groups and healthy controls. These findings indicate the presence of comorbid mental health conditions may exacrerbate EDs and increases severity of symptoms. Sihvola et al. (2009) found co-occurrence of MDD and GAD at age 14 was strongly associated with onset of ED at follow-up (age 17). Weaker associations were observed for both MDD and GAD alone [ 230 ].
Ciarma and Mathew [ 231 ] investigated the relationship between social anxiety disorder (SAD) and disordered eating among adults aged between 18 and 35 living in the community. This study found self-esteem and stress reactivity resulting from interpersonal conflict to be partial mediators, indicating that ED symptoms can be elicited by heightened responses to stress from social conflict and negative self-view. However, the partial mediation effect observed indicated that other unidentified factors may also have a role in the relationship. A further study of adolescents found evidence of a bidirectional relationship whereby depression and anxiety were risk factors for disordered eating behaviours, which in turn led to increased depression and anxiety [ 232 ].
Prevalence of social anxiety was also found to be high among a separate clinical sample of Australian adults with an ED, where 42% were found to have social phobia. It was also the most commonly diagnosed anxiety disorder within each of the ED subtypes, including 33% of those diagnosed with BN, 26% for AN and 25% for EDNOS. Investigations into the temporal relationship between ED diagnosis and anxiety disorder have found many individuals have anxiety prior to their ED diagnosis [ 225 – 227 ]. However, in one systematic review, this was supported only by the included retrospective case–control and cohort studies, and was not supported by evidence from prospective studies included in the review [ 227 ]. This discrepancy highlights the potential role of recall bias that may be present across studies relating to anxiety and EDs [ 227 ]. OCD and SAD also tend to precede onset of ED, and BN in adolescence may increase risk of SAD and panic disorders in adulthood [ 233 ].
In some individuals, shame has been found to predict later onset of BN and social anxiety, indicating a shared risk factor for both conditions [ 234 ]. Impaired psychosocial functioning and capacity to maintain interpersonal relationships associated with shame or shyness was also found to predict ED onset among adolescents in the US [ 235 ].
Psychiatric comorbidities of ED diagnoses other than AN/BN
Evidence relating to mental health comorbidities for EDs other than AN and BN is less developed. Studies conducted investigating BED and NES are confined to clinical samples with cross-sectional designs, highlighting a need for further work in this area, especially considering the high prevalence of psychiatric comorbidities detected in individuals with these diagnoses. Among patients receiving treatment for BED, 74% had a lifetime psychiatric disorder diagnosis, and 43% had a current diagnosis [ 236 ]. In a population of overweight and obese patients with severe mental illness, 25% were diagnosed with NES and 6% with BED [ 237 ]. Other studies measuring NES in patient samples with depression and bipolar disorder (BD) found the prevalence to be 32.5% and 8.8% respectively [ 238 , 239 ]. Higher prevalence of NES was detected in both depression and BD groups compared with healthy controls, indicating increased risk among these individuals.
ED and BD comorbidities are also commonly reported in research, with association between BD and BN/BED considered particularly significant, although the casual and temporal relationships between the disorders are not well understood [ 240 – 242 ]. While it is likely that some risk factors are shared, lack of data regarding disorder onset limits commentary on the relative risk BD confers to the development of ED [ 241 ]. One review found incidence of BD to be 4.7 times higher in individuals with BN, 3.6 times higher in individuals with BED and 3.5 times higher for binge/purge ED subtypes overall. Due to the low prevalence of AN and BD in the general population, an accurate estimation of this comorbidity is difficult to obtain [ 241 , 243 ]. BD in individuals with ED is associated with increased severity of core symptoms including body dissatisfaction, weight/shape concern, eating concern, impulse regulation, interoceptive awareness and perfectionism [ 244 ]. Mood instability is also significantly higher in individuals with a BD/ED comorbidity compared to those with BD alone. Systematic review of BD and its clinical correlates by McDonald et al. [ 245 ] suggests this finding indicates shared aetiology between ED and BD through emotional dysregulation.
ADHD and autism spectrum disorders
There is an emerging body of literature exploring associations between EDs and attention-deficit hyperactivity disorder (ADHD) and autism spectrum disorders (ASDs), however few have examined the conditions as risk factors in the development of ED. A 2016 meta-analysis of twelve studies found a three-fold increased risk of ED among individuals with ADHD [ 246 ]. Similarly, a 2020 matched cohort screening study found the same three-fold increase—almost one third of children and adolescents with ADHD were at risk of ED, compared to 12% of healthy controls. Here, BMI was a statistically significant predictor of risk [ 247 ]. Impulsivity and inattention symptoms of childhood ADHD have been positively associated with the development of overeating and bulimic-type behaviours in adolescence [ 248 ]. A longitudinal study of a large sample of adolescents reported that the onset of emotional and behavioural issues, including those associated with ADHD and conduct disorder, was observed to occur prior to the onset of disordered eating behaviours [ 249 ].
A 2013 systematic review found elevated rates of ASDs in ED populations compared with healthy controls, however, six of the eight studies in this review were based on longitudinal research using the same community sample [ 250 ]. The authors suggested a need to integrate appropriate, well-structured ASD assessment tools into routine care of ED service users, with the prevalence of ASD traits potentially contributing to ‘high treatment resistance to conventional therapies’ [ 250 ]. Dell’ Osso et al. [ 251 ] tested such an instrument in a sample of 138 individuals meeting DSM-5 criteria for an ED and 160 controls. They found significantly higher autism spectrum traits in participants with EDs, particularly verbal and non-verbal communication, inflexibility and adherence to routine, and restricted interest and rumination. Individuals with restrictive EDs were more likely to display ASD traits. Similarly, as part of a large, population-based prospective study of women and their children, Schaumberg et al. (2021) found autistic-like social communication difficulties during middle childhood were associated with BN symptoms during adolescence in both males and females [ 252 ]. They also discovered that misattribution of faces as sad or angry at 8.5 years of age was associated with a diagnosis of AN and purging behaviours at age 14. Contrarily, Dinkler et al. [ 253 ] in their prospective twin cohort study found no association between traits of autism in nine-year-old children and a later AN diagnosis, as well as noting a marked elevation in restricted/repetitive behaviour and interests only in the subgroup of individuals with acute AN. They questioned previous reports of elevated prevalence of ASD in AN and instead wondered if autistic traits may be best conceptualised as an epiphenomenon of the acute phase of AN.
Post-traumatic stress disorder
Although there is a large body of evidence relating to childhood trauma and abuse as a risk factor for the development of ED, few studies were identified investigating the role of post-traumatic stress disorder (PTSD) specifically as a risk factor. No distinction was made in the search methodology for this review between complex trauma and early childhood adverse events, with all studies captured under the search term ‘risk factors.’ Studies presented in this section, focused on the link between diagnosed PTSD and development of ED.
Results from two cohort studies observed an association between PTSD and severity of ED symptoms as well as relatively high prevalence rates within sample populations [ 254 , 255 ]. Among a patient sample in Sweden who had experienced trauma either prior to ED onset, after onset or within a year of onset, lifetime prevalence of PTSD was observed to be 24.1% [ 255 ]. An almost identical PTSD prevalence was found within a smaller ethnically diverse sample of obese women with BED in the US, at 24% [ 254 ]. Analysis of the impact of timing of trauma exposure on ED symptom severity in the Swedish sample found the association was only significant in the group who had experienced trauma in the same year of their ED diagnosis [ 255 ]. This analysis was not undertaken in the US study. Brewerton et al. [ 256 ] assessed adults entering ED treatment at seven US sites and found 49.3% had PTSD. It was found that individuals who were significantly more symptomatic had a higher propensity towards binge-type disorders and reported worse quality of life than those without PTSD. Co-occurrence of PTSD and AN was reported by Reyes-Rodriguez et al. (2011) as part of their cross-sectional study of 753 women with AN. They found 13.7% of the sample of AN patients also met criteria for PTSD with childhood sexual traumas being the most common traumatic event associated with the diagnosis [ 257 ].
Evidence from three studies relating to EDs in veteran populations—a meta-analysis (Barlett and Mitchell [ 259 ]); a retrospective chart review (Forman-Hoffman et al. [ 258 ]); and a retrospective cohort study of female veterans (Mitchell et al. [ 260 ])—found an association between increased ED prevalence and PTSD and trauma. Through a telephone interview with 1004 veterans, Formann-Hoffman et al. [ 258 ] determined that 16% of their sample had a lifetime ED with many of the cases also experiencing comorbid PTSD or lifetime sexual trauma. However, increased risk for ED among the veteran population could not be solely attributed to trauma, as unhealthy weight control behaviours are also common in this population due to strict weight and fitness requirements within the military [ 259 – 261 ].
The prevalence of personality traits appear to differ according to the ED diagnostic category. Elevated levels of perfectionism are common amongst AN and BN, obsessiveness strongly associated with AN, and binge/purge presentations consistently associated with impulsivity and greater emotional dysregulation, whereas lack of emotional awareness is not ED specific and common amongst most ED diagnoses [ 178 – 183 , 196 ]. Although co-occurrence of ED and personality disorders has been consistently identified in studies of comorbidity (e.g., BPD and binge/purge EDs), mood and anxiety disorders represent the most common psychiatric comorbidities in individuals with EDs (e.g., MDD affects over 75% of binge/purge EDs, SAD affects 42% of adults with an ED) [ 212 , 220 , 223 , 225 – 227 ]. There is also good evidence to suggest that the presence of a diagnosable childhood anxiety disorder (e.g., OCD) precedes the onset of an ED later in life [ 177 , 211 ]. Other psychological factors which appear to contribute to the risk of EDs include diagnoses of PTSD, ADHD, or ASD [ 246 , 250 , 254 ].
5. Gender differences
EDs impact a higher number of females with greater symptom severity. While common risk factors are shared across genders, such as low self-esteem and high shape/weight concern, males have been identified as less likely to engage in severe dieting behaviours compared with their female counterparts [ 262 , 263 ].
Puberty is a period of significant risk for ED development in both males and females. Research has implicated increased production of sex hormones during puberty, in particular estrogen, in the onset of EDs [ 264 ]. Evidence has consistently demonstrated that early onset of puberty is strongly associated with increased risk for ED development in both young males and females. Favaro et al. [ 265 ] linked earlier age of menarche with a younger mean age of onset of AN and BN. It has been suggested that if an individual experiences changes to their body shape, associated with menarche, at an earlier time than their peers, this may lead to heightened body dissatisfaction and which in turn may contribute to early the onset of EDs.
Despite the commonality between males and females in terms of the risk of ED development posed by puberty, it had been suggested that bodily changes experienced during this time possess a stronger impact for females as compared to males. It is thought that changes to one’s body shape move females further away from the thin ideal, whereas the changes for males move them closer to ideals around muscularity [ 266 ]. These findings have been supported by a cohort study, which found that bulimic symptoms and body dissatisfaction were associated with early puberty in females and late puberty in males [ 267 ]. Similarly, having a higher BMI comparative to peers has been associated with ED risk among teenage girls but not boys in a US school cohort [ 265 ].
Comorbidity
Research into gender differences has found that an equal proportion of male and female adolescents with an ED experience comorbid anxiety or depression [ 268 ]. A further four-year retrospective study in male adolescents with a diagnosed ED supported the assertion that comorbid anxiety and depression posed considerable ED risk to males [ 269 ]. Research has also identified increased prevalence of compulsive disorders, including gambling and substance use, among males as compared to females in a cohort of individuals at risk of ED [ 270 ]. While male ED risk has been associated with compulsive and depressive symptoms in these studies, evidence presented in a longitudinal study of adolescents found depression to be associated with higher ED symptomology in 12-year-old girls but not in boys [ 271 ]. Further research into EDs and depression in males is required to clarify the impact of this association.
Gender roles
Gender roles have been investigated as a potential contributor to ED risk. Exposure to media ideals has been found to be associated with increased body dissatisfaction and ED symptomology in university-aged males [ 272 ]. Research has also indicated that increased femininity in heterosexual males is negatively associated with muscle dissatisfaction [ 273 ]. Weak associations have also been found between femininity in women and eating pathology and body satisfaction. Among both sexes, masculinity was found to have a significant negative relationship with eating pathology, also conferring modest protection to body dissatisfaction [ 273 ].
Interactions between societal gender roles and sexual orientation is also known to play a role in ED risk with researchers suggesting that greater social body image pressures are present among gay males. A systematic review of disordered eating among sexual minority individuals has reported that elevated ED symptomology exists across all LGBTQI + groups as compared to heterosexual males and females [ 274 ]. A further study of men aged 18 to 35 found that disordered eating and body dissatisfaction was higher in gay and bisexual men compared to heterosexual men, as was susceptibility to social messaging around body image [ 275 ]. The occurrence of body image disorders has also been found to be higher among sexual minorities as compared to heterosexual samples [ 276 ]. A recent study involving a sample of transgender and gender non-binary individuals reported that increased internalised transphobia was associated with increased likelihood of disordered eating symptoms [ 277 ]. There is insufficient evidence currently available to separate risk of engagement in specific types of ED behaviours according on sexual identity [ 274 ].
The literature indicates that whilst both males and females are susceptible to risk factors for EDs such as early puberty onset and elevated weight/shape concerns, it appears that these factors have a stronger impact upon females as compared to males in terms of risk of developing disordered eating behaviours and psychopathology (e.g., severe dieting, bulimic symptoms and body dissatisfaction) [ 292 , 294 , 297 – 300 ]. Recent findings also indicate that LGBTQI + groups are at a higher risk of ED symptomology and body image disorders as compared to heterosexual individuals [ 305 – 307 ].
6. Socio-economic status
Despite the pervasive view that EDs disproportionately affect more affluent groups, evidence suggests that disordered eating behaviours occur at similar rates across all income levels and regardless of employment status [ 278 ]. Differences between socio-economic status (SES) seem to emerge in the types of disordered eating. Specifically, a positive correlation has been reported between non-fulltime workers and binge eating and purging behaviours. Also, a trade or certificate qualification has been shown to be positively associated with strict dieting as compared to groups with no higher education [ 278 ]. In contrast, a large study conducted in Sweden failed to find a relationship between social class and household income and incidence of EDs in females. However, in males, lower household income was associated with increased risk of BN and EDNOS, although the study observed a very low rate of BN in males [ 279 ].
Recent studies in the US have found low food security to be a predictor for disordered eating behaviours [ 280 ]. Among higher SES adolescents, binge eating behaviours were associated with weight-related teasing by family members [ 281 ]. In an adult sample, experience of low food security was more common among individuals with BN and BED as compared to healthy weight controls [ 282 ]. Lower food security in these individuals was associated with more frequent binge eating episodes and, in individuals with BN, unhealthy compensatory behaviours [ 282 ].
High levels of parental education have also been identified as a predictor of EDs [ 119 , 283 ]. Higher educational attainment by both parents as well as maternal grandparents has been associated with higher incidence of AN, BN, and EDNOS equally across diagnoses in females [ 279 , 284 ]. In males a positive association was found between parental education and AN, but not for BN or EDNOS [ 279 ].
Research into sociocultural risk factors for EDs suggests that income has little impact on overall ED risk although available evidence points to specific indicators that have an influence [ 278 ]. Higher education attainment is associated with restrictive ED behaviours, while experience of food insecurity is associated with binge-type behaviours and EDs [ 279 , 282 , 284 ].
7. Ethnic minority
Although there is no evidenced association between ethnic background and the risk of ED onset, specific aspects of ED psychopathology do appear to differ between ethnic groups [ 285 , 286 ]. A cohort study of females aged between nine and 22 years old found those with an ED were more likely to be non-Hispanic White, come from well-educated households, and be well-educated themselves [ 287 ]. A recent study of a treatment-seeking community sample in US found that Black individuals displayed higher rates of BED as compared to other ethnic groups, however overall Asian and Black individuals were less likely to report ED symptoms than White individuals [ 288 ]. Significantly higher thin ideal internalisation has been observed among Asian-American participants as compared with other groups [ 285 ]. Additionally, the association between fear of losing control of eating and depressive symptoms has been found to be stronger in Asian and Pacific Islander minorities than other ethnic groups [ 289 ]. In a study comparing thin-ideal internalisation among young Australian and Malaysian women, a stronger association between body dissatisfaction and restrained eating practices was observed in the Australian sample [ 286 ].
Further investigation of ethnic minority status has implicated perceived ethnic discrimination as a risk factor in ED development. In a cohort of college students, perceived discrimination based upon one’s ethnicity was associated with increased prevalence of key ED symptoms including restraint, weight/shape concern, body dissatisfaction and bulimia [ 290 ]. Perceived discrimination was also found to increase drive for muscularity among males in the sample but not drive for thinness among females. These findings indicate a potentially growing risk for ED in CALD individuals [ 290 ].
A small body of evidence was identified in the current RR regarding the association between ethnic minority status and ED risk. Of the studies reviewed, unique associations have been found between particular ethnic groups and specific aspects of ED psychopathology. For example, in comparison to other ethnic groups, higher rates of BED have been observed in Black-Americans and greater thin ideal internalisation in Asian-Americans [ 286 , 289 ]. Given that a significant proportion of ED research has been conducted using White/Caucasian participants, greater research efforts are needed to better understand the features of EDs in ethnically diverse groups.
8. Body image and social influence
Weight/shape concern, overvaluation of weight/shape and drive for thinness, referred to here using the term body image concerns, are key concepts in ED [ 291 , 292 ]. Along with the social and cultural factors that contribute to body image concerns, these concerns have been extensively investigated as risk factors for the development of EDs. Research in this area has been concentrated among women and girls whose body image concerns are characterised by a focus on low body weight and the thin-ideal [ 293 ], but greater recent focus on men and boys with regard to the muscular/lean ideal has been seen due to increasing recognition of muscle orientated EDs in males. Engagement with particular environments that shape social norms for appearance and promote pursuit of the ideal body shape or weight, or involvement in certain activities with a culture of strict dieting and excessive exercise is encouraged, such as college level or professional sports, are also well studied risk factors in ED literature.
Body image and appearance ideals
Studies using prospective designs have found evidence for body image concerns predicting development of EDs and ED behaviours. In an eight-year longitudinal study of adolescent girls, higher levels of perceived pressure to be thin, thin-ideal internalisation, and body dissatisfaction were significant predictors of later onset ED (BN, BED, and purging disorder) [ 294 ]. Among an adolescent sample, dissatisfaction with weight and shape, but not overvaluation or preoccupation, was a predictor of onset of an ED after 12 months [ 295 ]. The authors suggest that while body dissatisfaction may impart risk for ED development, the other body image-related constructs of overvaluation and preoccupation, may indicate presence of ED psychopathology. A systematic review of the impact of anti-obesity public health messages has found that endorsement of thin ideals and drive for thinness are exacerbated in response to exposure to messages which are stigmatising towards individuals who are overweight or obese [ 296 ]. In a large longitudinal sample of adolescent boys and girls, body image concerns predicted binge eating over 5 years to young adulthood [ 297 ] and persistent disordered eating 10 years later among both males and females [ 298 ], and body dissatisfaction, preoccupation with body weight and shape, and overvaluation predicted increases in disordered eating 15 years later, particularly in females [ 299 ]. Similarly, in a cohort of this sample characterised as having BMI in the overweight category, higher body image concerns predicted prevalence and onset of disordered eating (binge eating and extreme weight control behaviours) over five years [ 300 ]. Findings for body image concern as a risk factor for development of AN are mixed. In this regard, a systematic review of 46 longitudinal studies by Glashouwer et al. [ 301 ] with a pooled sample of 4,928 patients with AN was unable to definitively determine whether body dissatisfaction was a causal factor in disorder onset.
Media, social media, and the internet
The impact of media depictions of appearance ideals on ED symptoms have been examined with studies of varying methodologies. A meta-analysis of laboratory-based experimental studies found that viewing idealised images resulted in a small but non-significant increase in body dissatisfaction. However, exposure to these images was found to have a greater impact on groups considered at high-risk for developing EDs [ 302 ]. Of note, there were no differences observed in the impact of these images based on gender, indicating that men and women are equally affected by media portrayals of idealised bodies [ 302 ].
Among 574 women aged between 14 and 36, social expectations to be thin were found to mediate the relationship between protective self-presentation and disordered eating [ 303 ]. This finding aligns with research on exposure to negative parental attitudes regarding weight to be a risk factor in the later development of ED, discussed previously [ 118 , 303 ].
As with traditional media, the effects of portrayal of idealised bodies on the internet and on social media has been explored. Among young women, use of social media was found to impact weight and shape concerns [ 304 ] and among a predominantly female sample of participants with AN, use of appearance-focused social media was found to be associated with higher levels of ED symptoms [ 305 ]. A systematic review found that general internet use was associated with body image and eating concerns [ 306 ]. Further exploration of problematic internet use suggested excessive use of social media was associated with increased risk of AN and BN, while video gaming was associated with risk of BED [ 307 ]. However, recent proliferation of pro-AN or pro-ED websites and social media networks may create online environments that are more detrimental to the health of individuals at risk of ED than other forms of media. Even among females with normal BMI and no history of ED, one week of exposure to pro-ED website content resulted in a significant reduction (20%) in calorie intake among participants compared to groups who were exposed to other website content including health and fitness websites [ 308 ]. Dangers associated with pro-ED websites is not restricted to females, with a content analysis study finding that up to 25% of participants on pro-AN forums are male, suggesting that these sites may have a substantive negative impact with males engaged with these sites expressing negative experiences including body dissatisfaction [ 309 ].
Body image concerns are a well-known risk factor for EDs. High levels of body dissatisfaction and internalisation of the thin ideal have been found to be predictors of ED onset, whereas related constructs of overvaluation and preoccupation with weight and shape are considered to reflect current ED psychopathology [ 270 – 277 ]. Exposure to the thin ideal via either traditional media or social media is associated with greater risk of an ED, with evidence suggesting that both males and females are equally impacted by this content [ 278 – 283 ].
9. Elite sports, female athlete triad, and excessive exercise
Engagement in activities that accept or promote strict dieting practices and endorsement of low body fat has the potential to contribute to development and maintenance of ED symptoms [ 310 ]. Consistent with this, EDs among elite and college/university level athletes were observed at higher rates than in non-athlete comparison groups [ 311 ], although no difference in prevalence of EDs was found between athletes engaged in sports with an emphasis on aesthetics and/or weight and athletes engaged in sports without this focus. The female athlete triad (FAT), characterised by low energy availability (through increased physical activity or dietary restriction), amenorrhea and low mineral bone density, is considered a consequence of training for elite level sports and pursuit of lean physiques [ 312 ]. Features of FAT have also been observed in elite para-athletes (n = 260) with no difference in risk between genders or sport type [ 313 ].
In relation to ED behaviours, among elite athletes (n = 224), high prevalence of clinically significant ED symptomology (22.8%) has also been found [ 314 ].Similarly, in a sample of college level female gymnasts and swimmers (n = 325), 4.6% (n = 15) engaged in intentional vomiting, 1.5% (n = 5) used laxatives and 2.5% (n = 8) used diuretics for weight control. Additionally, 10.5% (n = 3.4) engaged in binge eating two or more times a week, while almost all participants engaged in binge eating once a week, 96.6% (n = 314) [ 315 ]. However, in a smaller UK sample of male and female gymnasts (n = 51) no purging behaviours were observed, although 31% of male gymnasts in this group scored highly on ED self-report questionnaires [ 316 ].
However, other studies have not found these differences between athlete and non-athlete groups. For example, a cohort study comparing elite and non-elite athletes to controls (n = 725) was also unable to find any differences between the three groups in terms of ED behaviours. However, it did highlight distinct differences associated with social pressures and influences on body image and weight in athletes versus non-athletes. There is some evidence to suggest that unlike female athletes, male athletes are not at greater risk of developing EDs than non-athletes [ 317 ]. Evidence from a meta-analysis of 31 studies of ED athletes indicated that, with the exception of wrestling, male athletes were not at greater risk of disordered eating than non-athletes. Although, researchers noted that studies were heterogenous and measurements were impacted by the potential inappropriateness of ED assessment tools for male populations [ 318 ].
Among non-elite populations, recognising excessive physical activity or exercise levels among women in the community is particularly important in risk assessment of ED, as these individuals were found to be 2.5 times as likely to have an ED diagnosis than non-excessively exercising individuals [ 319 ]. Furthermore, participation in activities promoting lean body types such as yoga and pilates has also been highlighted as a potential risk factor for ED development. However, in a large cohort study (n = 2,287) of young adults no association was found between participating in yoga and pilates and ED symptomology among female subjects but increased risk of unhealthy and extreme weight control behaviours as well as binge eating was observed in males [ 320 ]. Further research is required to understand the unique associations identified in this study.
Similar to athletic settings, other physical activity pursuits take place in environments that may promote ED symptoms. A systematic review and meta-analysis observed higher rates of ED among dancers, where dancers were found to have three times greater risk of having AN or EDNOS but not BN, than the general population and risk was particularly heightened among ballet dancers [ 321 ].
Involvement in elite sports is a potential risk factor for disordered eating behaviours among both male and female athletes [ 311 – 317 ]. Increased attention should be paid towards excessive exercise by non-elite populations in the community as risk factor for EDs and to support screening and early intervention activities [ 318 – 320 ].
This review to aimed to summarise recent peer-reviewed evidence relating to risk factors associated with EDs. An extensive number of research studies were identified, exploring a multitude of risk factors. For the purposes of this review, the research findings were broadly characterised into nine primary categories: (1) genetics, (2) gastrointestinal microbiota and autoimmune reactions, (3) childhood and early adolescent experiences, (4) personality traits and comorbid mental health conditions, (5) gender, (6) socio-economic status, (7) ethnic minority, (8) body image and social influence, (9) and elite sports.
Identification of the recent evidence relating to key risk factors offers valuable knowledge to researchers, clinicians, and policy makers, such that it may inform the development of evidence-based approaches for the care and treatment of individuals with EDs. An understanding of risk factors is essential for the development and refinement of aetiological models [ 8 ]. In a recent review of existing models of disordered eating, Pennesi and Wade [ 21 ] reported that very few of the existing theoretical models (18.5%) have informed the development of effective interventions. The authors call upon researchers to use empirically supported risk-factors to modify existing theories, which then can inform prevention and treatment interventions [ 21 ].
The findings of the current review can be used to determine which risk factors are differentially appropriate targets for prevention, early intervention, and/or treatment efforts [ 322 ]. For example, modifiable risk factors such as negative parental comments towards weight and eating behaviours may be best approached using targeted prevention parenting programs to assist with modelling of healthy eating patterns and family dialogue. There is evidence to suggest targeted prevention programs addressing early signs of disordered eating in adolescents (e.g., the Body Project, StudentBodies2-BED ) are effective in significantly reducing future onset of EDs [ 323 , 324 ]. They represent a targeted, efficient way of addressing modifiable risk factors rather than approaching the population as a whole in a largely non-specific manner.
Identifying risk factors which are less amenable to modification, such as genetic risk factors and autoimmune conditions, may represent an opportunity for enhanced screening measures to recognise early signs of disordered eating prior to onset of full ED diagnosis. Research has identified low levels of screening and poor detection rates of EDs by health practitioners, in particular non-stereotypical presentations of EDs in primary care settings [ 325 – 327 ]. A noteworthy outcome of the current review pertains to the growing field of evidence supporting increased risk of EDs within the sexual minority groups as compared to heterosexual samples. Given the high levels stigma surrounding both LGBTQI and EDs, particularly for young males, it is of particular importance that clinicians thoroughly assess for disordered eating behaviours within sexual minority groups [ 328 , 329 ]. Accordingly, the findings of this review may offer an opportunity for advances in the development of resources (e.g., screening instruments) to assist practitioners in recognising evidenced risk factors for EDs.
Finally, awareness of comorbid psychiatric illnesses or personality traits may inform targets for treatment interventions, including as specific programs for individuals with comorbid personality disorders and ED. Enhanced Cognitive Behaviour Therapy (CBT-e) offers an example of the way in which comorbid psychological traits, considered to be “external” to the ED itself, can be addressed to create a more efficacious, tailored treatment for patients [ 330 ]. The inclusion of additional treatment targets to address comorbid psychological mechanisms (clinical perfectionism, core low self-esteem, and interpersonal problems) allows for cognitive behaviour therapy treatment to meet the needs of non-responders for whom comorbid psychopathology may have interfered with their treatment response [ 331 ].
Additionally, given the search strategy of the review adopted a timeline which overlaps between two versions of the Diagnostic and Statistical Manual of Mental Disorders [ 332 ], namely Version 4 and 5 (i.e., DSM-IV and DSM-5), our findings were able to highlight inconsistences in the degree of research conducted across various ED diagnoses. In particular, the findings demonstrate that considerably less is known about the risk factors associated with EDs which were recently included as formal diagnoses in the DSM-5, including ARFID, BED, rumination disorder, and pica, highlighting the need for more focused research efforts to be put towards these diagnoses.
In this review, gaps in the existing literature were identified. Many of the research studies included in the review adopted a cross-sectional study design and therefore focused upon associations and correlations between EDs and potential risk factors. Consequently, some studies were limited in their capacity to delineate temporal or causal relationships, or how in fact the associations connect the factor with the illnesses. For example, although an understanding of psychiatric comorbidities of EDs (e.g., perfectionism, impulsivity etc.) provides value, without longitudinal research it is difficult to disentangle whether these traits contribute to ED onset or are symptoms of it. Similarly, identification of trauma and abuse as a risk factor for eating disorders needs further clarification as this association has been described for many other mental health conditions such as anxiety and depression [ 333 ], and is not likely a specific association to eating disorders. Additionally, several of the studies included in the current review were not able to distinguish between factors related to onset and factors related to maintenance in EDs, which represents an important differentiation of different classes of risk factors and their influence [ 207 ]. It is possible that some of the constructs reviewed in the present paper have a role as maintenance factors, even if they may not have a role as a causal risk factor. An understanding of whether one psychiatric condition precedes another can assist clinicians in treatment planning and inform sequencing of treatment targets. Taken together, these considerations represent a limitation in our ability to understand the implications of these identified risk factors. For risk factors which have relied heavily upon cross-sectional studies, future research is encouraged to adopt experimental or prospective study designs to better capture the nature of the variable being examined.
Several of the studies included in the review examined risk factors in isolation from one another and thus assessment of their association with EDs occurred as though they were independent contributors of risk. This is markedly distinct from real world environments in which EDs develop in response to a multitude of risk factors and consequently, weakens the ecological validity of the reported findings. An understanding of the ways in which various risk factors interact with each other (e.g., whether they are cumulative in nature), is necessary to form a detailed conceptualisation of illness profiles for both clinicians and researchers, which can in turn inform the development of targeted interventions. Conversely, in the absence of this information, the mechanisms of change are less clear. Future research would benefit from adopting an approach towards risk factors as co-occurring, interactional variables as opposed to a siloed view.
Given the attempt to summarise peer-reviewed ED literature in a broad-reaching and prompt manner, there are some limitations of the review. First broad search terms, required to fulfil the purpose of the large series of rapid reviews, of which this paper forms part, were used to collate evidence, which may have compromised the specificity of the included studies for individual ED diagnoses and/or phenotypes and individual risk factors. Additionally, research studies were excluded if they reported on unpublished data, implementation research, or if they were observational studies; and included studies were mostly limited to those conducted in Western cultures with high-resource health systems. Finally, having a specified time period for the review meant that seminal studies conducted prior to the start date were not included.
Conclusions
This review has identified risk factors for which a substantial evidence-base exists as well as emerging areas requiring further investigation (e.g., ADHD) and ED diagnoses where there is less available evidence (e.g., BED, ARFID). A broad review of the literature has been provided, however future studies are required which critique the strength of evidence of the causal nature of these risk factors.
Acknowledgements
The authors would like to thank and acknowledge the hard work of Healthcare Management Advisors (HMA) who were commissioned to undertake the Rapid Review. Additionally, the authors would like to thank all members of the consortium and consultation committees for their advice, input, and considerations during the development process. Further, a special thank you to the carers, consumers and lived experience consultants that provided input to the development of the Rapid Review and wider national Eating Disorders Research & Translation Strategy. Finally, thank you to the Australian Government—Department of Health for their support of the current project.
Abbreviations
Author contributions.
PM, ST and SM oversaw the Rapid Review process; AL carried out and wrote the initial review; SB, SMC and EB wrote the first manuscript; all authors edited and approved the final manuscript.
The RAPID REVIEW was in-part funded by the Australian Government Department of Health in partnership with other national and jurisdictional stakeholders. As the organisation responsible for overseeing the National Eating Disorder Research & Translation Strategy, InsideOut Institute commissioned Healthcare Management Advisors to undertake the RAPID REVIEW as part of a larger, ongoing, project. Role of Funder: The funder was not directly involved in informing the development of the current review.
Availability of data and materials
Declarations.
Not applicable.
ST receives royalties from Hogrefe and Huber, McGraw Hill and Taylor and Francis for published books/book chapters. He has received honoraria from the Takeda Group of Companies for consultative work, public speaking engagements and commissioned reports. He has chaired their Clinical Advisory Committee for Binge Eating Disorder. He is the Editor in Chief of the Journal of Eating Disorders. ST is a committee member of the National Eating Disorders Collaboration as well as the Technical Advisory Group for Eating Disorders. AL undertook work on this RAPID REVIEW while employed by HMA. A/Prof Sarah Maguire is a guest editor of the special issue “Improving the future by understanding the present: evidence reviews for the field of eating disorders.”
1 having three different alleles at the same locus.
2 Polymorphism is a DNA sequence variation.
3 perception or awareness of sensations inside the body.
4 DNA methylation is a process that controls the expression/suppression of a gene without changing the genetic sequence.
5 Small molecules formed in or necessary for metabolism.
6 Models using rates and mice.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Phillip aouad, robert boakes.
5 School of Psychology, Faculty of Science, University of Sydney, Sydney, NSW Australia
Leah Brennan
6 School of Psychology and Public Health, La Trobe University, Melbourne, VIC Australia
Susan Byrne
7 School of Psychology, Western Australia, Perth, Australia
Belinda Caldwell
8 Eating Disorders Victoria, Melbourne, VIC Australia
Shannon Calvert
9 Perth, WA Australia
Bronny Carroll
David castle.
10 Medicine, Dentistry and Health Sciences, University of Melbourne, Melbourne, VIC Australia
Ian Caterson
11 School of Life and Environmental Sciences, University of Sydney, Sydney, NSW Australia
Belinda Chelius
12 Eating Disorders Queensland, Brisbane, QLD Australia
13 Sydney Local Health District, New South Wales Health, Sydney, Australia
Simon Clarke
14 Westmead Hospital, Sydney, NSW Australia
Janet Conti
15 Translational Health Research Institute, Western Sydney University, Sydney, NSW Australia
Lexi Crouch
16 Brisbane, QLD Australia
Genevieve Dammery
Natasha dzajkovski, jasmine fardouly.
17 School of Psychology, University of New South Wales, Sydney, NSW Australia
Carmen Felicia
18 University of Sydney, Sydney, NSW Australia
John Feneley
19 New South Wales Health, Sydney, NSW Australia
Amber-Marie Firriolo
Nasim foroughi, mathew fuller-tyszkiewicz.
20 School of Psychology, Faculty of Health, Deakin University, Geelong, VIC Australia
Anthea Fursland
21 School of Population Health, Faculty of Health Sciences, Curtain University, Perth, Australia
Veronica Gonzalez-Arce
Bethanie gouldthorp.
22 Hollywood Clinic, Ramsay Health Care, Perth, Australia
Kelly Griffin
Scott griffiths.
23 Melbourne School of Psychological Sciences, University of Melbourne, Victoria, Australia
Ashlea Hambleton
Amy hannigan.
24 Queensland Eating Disorder Service, Brisbane, QLD Australia
25 Hunter New England Local Health District, Sydney, NSW Australia
26 St Vincent’s Hospital Network Local Health District, Sydney, NSW Australia
Phillipa Hay
27 Brain and Mind Centre, University of Sydney, Sydney, Australia
Francis Kay-Lambkin
28 School of Medicine and Public Health, University of Newcastle, Sydney, NSW Australia
Michael Kohn
29 Westmead Hospital, Sydney, Australia
Eyza Koreshe
Isabel krug.
30 Healthcare Management Advisors, Victoria, Australia
Jake Linardon
Randall long.
31 College of Medicine and Public Health, Flinders University, Adelaide, SA Australia
Amanda Long
32 Exchange Consultancy, Redlynch, NSW Australia
Sloane Madden
33 Eating Disorders Service, Children’s Hospital at Westmead, Sydney, NSW Australia
Danielle Maloney
Sian mclean.
34 The Bouverie Centre, School of Psychology and Public Health, La Trobe University, Victoria, Australia
Thy Meddick
35 Clinical Excellence Queensland, Mental Health Alcohol and Other Drugs Branch, Brisbane, QLD Australia
Jane Miskovic-Wheatley
Deborah mitchison, richard o’kearney.
36 College of Health and Medicine, Australian National University, Canberra, ACT Australia
Shu Hwa Ong
Roger paterson.
37 ADHD and BED Integrated Clinic, Melbourne, VIC Australia
Susan Paxton
38 Department of Psychology and Counselling, La Trobe University, Melbourne, VIC Australia
Melissa Pehlivan
Genevieve pepin.
39 School of Health and Social Development, Faculty of Health, Deakin University, Geelong, VIC Australia
Andrea Phillipou
40 Swinburne Anorexia Nervosa (SWAN) Research Group, Centre for Mental Health, School of Health Sciences, Swinburne University, Melbourne, VIC Australia
Judith Piccone
41 Children’s Health Queensland Hospital and Health Service, Brisbane, QLD Australia
Rebecca Pinkus
Bronwyn raykos.
42 Centre for Clinical Interventions, Western Australia Health, Perth, WA Australia
Paul Rhodes
Elizabeth rieger, sarah rodan, karen rockett, janice russell.
43 Central Clinical School Brain and Mind Research Institute, University of Sydney, Sydney, NSW Australia
Haley Russell
Fiona salter.
44 Ramsay Health Care, Perth, Australia
Susan Sawyer
45 Department of Paediatrics, The University of Melbourne, Melbourne, Australia
Beth Shelton
46 National Eating Disorders Collaboration, Melbourne, VIC Australia
Urvashnee Singh
47 The Hollywood Clinic Hollywood Private Hospital, Ramsey Health, Perth, Australia
Sophie Smith
48 Sydney, NSW Australia
Evelyn Smith
Karen spielman, sarah squire.
49 The Butterfly Foundation, Sydney, Australia
Juliette Thomson
Marika tiggemann.
50 College of Education, Psychology and Social Work, Flinders University, Adelaide, SA Australia
Ranjani Utpala
Lenny vartanian, andrew wallis.
51 Eating Disorder Service, The Sydney Children’s Hospital Network, Westmead Campus, Sydney, Australia
Warren Ward
52 Department of Psychiatry, University of Queensland, Brisbane, Australia
Sarah Wells
53 University of Tasmania, Hobart, TAS Australia
Eleanor Wertheim
Simon wilksch, michelle williams.
54 Royal Hobart, Tasmanian Health Service, Hobart, TAS Australia
- Open access
- Published: 15 November 2022
Conceptualizing eating disorder recovery research: Current perspectives and future research directions
- Heather Hower 1 , 2 ,
- Andrea LaMarre 3 ,
- Rachel Bachner-Melman 4 , 5 ,
- Erin N. Harrop 6 ,
- Beth McGilley 7 &
- Therese E. Kenny 8
Journal of Eating Disorders volume 10 , Article number: 165 ( 2022 ) Cite this article
4466 Accesses
3 Citations
6 Altmetric
Metrics details
How we research eating disorder (ED) recovery impacts what we know (perceive as fact) about it. Traditionally, research has focused more on the “what” of recovery (e.g., establishing criteria for recovery, reaching consensus definitions) than the “how” of recovery research (e.g., type of methodologies, triangulation of perspectives). In this paper we aim to provide an overview of the ED field’s current perspectives on recovery, discuss how our methodologies shape what is known about recovery, and suggest a broadening of our methodological “toolkits” in order to form a more complete picture of recovery.
This paper examines commonly used methodologies in research, and explores how incorporating different perspectives can add to our understanding of the recovery process. To do this, we (1) provide an overview of commonly used methodologies (quantitative, qualitative), (2) consider their benefits and limitations, (3) explore newer approaches, including mixed-methods, creative methods (e.g., Photovoice, digital storytelling), and multi-methods (e.g., quantitative, qualitative, creative methods, psycho/physiological, behavioral, laboratory, online observations), and (4) suggest that broadening our methodological “toolkits” could spur more nuanced and specific insights about ED recoveries. We propose a potential future research model that would ideally have a multi-methods design, incorporate different perspectives (e.g., expanding recruitment of diverse participants, including supportive others, in study co-creation), and a longitudinal course (e.g., capturing cognitive and emotional recovery, which often comes after physical). In this way, we hope to move the field towards different, more comprehensive, perspectives on ED recovery.
Our current perspectives on studying ED recovery leave critical gaps in our knowledge about the process. The traditional research methodologies impact our conceptualization of recovery definitions, and in turn limit our understanding of the phenomenon. We suggest that we expand our range of methodologies, perspectives, and timeframes in research, in order to form a more complete picture of what is possible in recovery; the multiple aspects of an individual’s life that can improve, the greater number of people who can recover than previously believed, and the reaffirmation of hope that, even after decades, individuals can begin, and successfully continue, their ED recovery process.
Plain English summary
How we research eating disorder (ED) recovery impacts what we know (perceive as fact) about it. In this paper we aim to provide an overview of the ED field’s current perspectives on recovery, discuss how our methodologies shape what is known about recovery, and suggest a broadening of our methodological “toolkits” in order to form a more complete picture of recovery. To do this, we (1) provide an overview of commonly used methodologies (quantitative, qualitative), (2) consider their benefits and limitations, (3) explore newer approaches, including mixed-methods, creative methods (e.g., Photovoice, digital storytelling), and multi-methods (e.g., quantitative, qualitative, creative methods, psycho/physiological, behavioral, laboratory, online observations), and (4) propose a potential future research model with a multi-methods design, incorporating different perspectives (e.g., increasing recruitment of diverse participants, including supportive others in study co-creation), and a longitudinal course (e.g., capturing cognitive recovery, which often comes after physical). In this way, we seek to expand our picture of what is possible in recovery; the multiple aspects of an individual’s life that can improve, the greater number of people who can recover than previously believed, and the reaffirmation of hope that, even after decades, individuals can begin and continue their ED recovery process.
How we research the process of eating disorder (ED) recovery impacts what we know (perceive as fact) about this process. Traditionally, research has focused more on the “what” of recovery (e.g., establishing criteria for recovery, connecting research and clinical experiences, reaching consensus definitions) than the “how” of recovery research (e.g., timing and framing of ED recovery items and measures, type of methodologies, triangulation of perspectives). Given that our “ways of looking” are inextricably tied to what we are looking at [ 1 ] it is important to step back and investigate how research methods shape what we can know about a phenomenon of interest. This exploration can offer insight into missing pieces of the analytic puzzle (e.g., the current gaps in our knowledge), and invite novel ways of researching ED recovery (e.g., incorporating different perspectives).
ED recovery research that is published in peer-reviewed journals most frequently uses quantitative (numerical, “objective”) Footnote 1 statistical methods, or qualitative (descriptive, “subjective”) interview methods, in order to convey their findings. In this paper, we provide an overview of commonly used methods and outline key analytic features of various types of analyses that fit within these broader method categories. We also present an examination of these commonly used methods, reflecting on the benefits and limitations of each, and what each allows us to know, or not know, about ED recovery. Following this overview, we explore mixed-methods (quantitative and qualitative), creative methods (e.g., Photovoice, digital storytelling), and multi-methods (e.g., quantitative, qualitative, creative methods, psycho/physiological, behavioral, laboratory, online observations), which may provide directions for future research, and enable new understandings of ED recovery.
Importantly, we are not suggesting that researchers abandon these commonly used quantitative or qualitative methods or that one approach is inherently better than others. Rather, we are recommending a broadening of our methodological “toolkits,” to increase the clarity of purpose of our studies, along with an alignment of the methods used. This may enable the development of more nuanced and specific insights about ED recoveries that take into account context, varied perspectives, and different positionalities. In this paper we thus aim to provide an overview of the ED field’s current perspectives on recovery, illuminate how those perspectives are necessarily informed by our methodological choices, and recommend broadening our methodological “toolkits” in order to form a more complete picture about what can be known as possible in recovery.
Ontological and epistemological stances in ED recovery research
The goal or purpose of ED recovery research depends largely on the ontological (the “what” of research) and the epistemological (the “how” of research) stances endorsed by the researcher [ 2 , 3 ]. This is often considered to be foundational in qualitative research, but is less frequently named in quantitative approaches. We give a brief overview of these stances here, because how a researcher views the world will inevitably impact the goal of the research and the methodological approaches used. In this way, we cannot present a discussion of recovery methodologies without also considering ontology and epistemology.
Ontological stance refers to what we believe can be known [ 4 , 5 ]. From a realist perspective, there is a single objective truth which exists [ 6 ]. On the other side, a relativist perspective suggests that there is no singular reality outside of human practices [ 7 ]. Researchers can therefore vary along this spectrum in terms of their assumptions about what knowledge exists.
Epistemology refers to how we can come to know this information [ 8 ]. For example, positivism argues that we can come to understand or know an objective reality through rigorous scientific practices [ 9 , 10 ]. This is the foundation of the scientific approach and what has often been referred to as the “hard sciences.” Recently, there has been a shift in which individuals from this perspective acknowledge that data collection and interpretation may be imperfect and influenced by researcher characteristics; what is now known as post-positivism [ 11 ].
Many of the quantitative approaches that will be discussed in this paper come from a post-positivist framework in that they assume there is an objective recovery “truth” that can be uncovered if we are rigorous in our approach and seek to minimize bias. On the other side, there are contextualist [ 12 ] and constructionist [ 13 ] epistemologies. Contextualism situates knowledge and the people who create it (e.g., participants, researchers) in a broader context, acknowledging that no one person can know everything. Constructionism argues that meaning is multiple, socially-constructed, and connected to wider systems of power. In this way, there is no one definition or understanding of a phenomenon.
The ontological/epistemological stance and research assumptions that dictate the approaches we take in turn inform debates on recovery. Those coming from different traditions will thus have different views of what can be known about the phenomenon. For example, the frames of (post)positivism typically underlie quantitative research, and researchers coming from this perspective have long been calling for a clear, consistent, and applicable definition of recovery (e.g., [ 14 , 15 , 16 , 17 ]). However, no overall consensus definition has been reached to date, which has several implications from a (post)positivist perspective. This lack of conceptual clarity, and between-study differences in measurement approaches, impact our ability to compare the findings between studies, including reported recovery rates, which can vary dramatically, depending upon the definitions and clinical groups used (e.g., [ 14 , 15 , 18 , 19 ]).
The belief that there is a need for a singular definition is one way of understanding the utility of recovery and may be useful for some groups. The intent of our paper, though, is not to provide a statement about what a consensus definition might be. Rather, we are offering a more diverse view of methodological perspectives (which stem from various ontological and epistemological stances) and ideas that might allow for forward movement in the field. In a dialectal format, this can involve both movement toward and away from consensus, including perspectives which do not seek to identify a single recovery definition. These paths are sometimes polarized, indicating that research aiming for (provisional) consensus is incompatible with research pushing into new areas. We suggest that both can be simultaneously pursued, acknowledging that one does not discount the other.
ED recovery research approaches: A brief overview
Quantitative research stemming from (post)positivist perspectives has tended to emphasize “objective” illness and recovery criteria that can be measured and compared in the lab/treatment, such as body mass index (BMI) (e.g., [ 20 ]), and behavioral/cognitive symptoms (e.g., [ 21 , 22 ]). For example, scores of validated ED measures such as the Eating Attitudes Test (EAT) [ 23 ] are frequently subdivided into “threshold” (criteria met for a probable clinical diagnosis) or “subthreshold” (diagnostic criteria unlikely to be met). Changes in measurable physical, behavioral, and symptomatic criteria are characteristic of the medical model of recovery, with a growing body of research suggesting that such approaches may not fit as well with lived experience perspectives [ 24 , 25 ].
In a systematic review of 126 studies looking at predictors of ED outcomes [ 26 ], symptom remission was used as a key outcome in over 80% of studies. This may differ from the “process” recovery criteria typically used in clinical settings, where the individual’s progress in therapy (e.g., how they navigate their recovery, showing improvements in not only symptoms, but also psychosocial functioning) may affect the extent to which they are deemed “recovered.”
A key element of these different definitions hinges on the extent to which symptom remission is considered an important first step in recovery. This point has often been promoted as self-evident, but is inconsistent with some orientations to recovery. For instance, a recovery model orientation, which has been noted to be potentially resonant with EDs (e.g., [ 27 ]) starts with an emphasis on a person’s goals and contexts, rather than assuming that symptom remission is a first step. This does not mean that “anything goes"; a recovery model promotes collaboration and discussion in exploring what recovery means and does for the person seeking it [ 28 , 29 ].
More recently, researchers have suggested that in alignment with this recovery model, it may be possible to continue to exhibit some symptoms (e.g., behaviors), but have improvement in other areas (e.g., improved psychosocial functioning, QOL), and still feel that one is in ED recovery (e.g., [ 27 , 29 , 30 , 31 , 32 , 33 , 34 , 35 ]). ED advocacy groups led by people with lived experience are also beginning to support approaches to harm reduction within ED recovery circles, such as those promoted by Nalgona Positivity Pride. Indeed, there are now several ED-specific, standardized measures of functioning and QOL that can provide more insight in this area, including the Eating Disorders Quality of Life (EDQOL) [ 36 ], Quality of Life for Eating Disorders (QOL ED) [ 37 ], Health-Related Quality of Life in Eating Disorders Questionnaire (HeRQoLED) [ 38 ], Eating Disorders Quality of Life Scale (EDQLS) [ 39 ], and, more recently, the Eating Disorders Recovery Questionnaire (EDRQ) [ 40 ]. In addition to assessing QOL from a quantitative perspective, QOL can also be explored qualitatively, allowing it to be contextualized against the landscape of participants’ lives.
What is considered to “matter” in ED recovery definitions thus far also differs to some extent according to who is asked. Researchers, clinicians, and people with lived experience (individuals and supportive others such as parents, family, partners, friends, mentors) may emphasize different criteria for ED recovery [ 41 ]. Further, these categories are not distinct; people may simultaneously occupy multiple positionalities at once, such as researchers and/or clinicians who also have lived experience of ED. While a consensus definition among clinicians is arguably becoming a more plausible goal [ 16 ], there may still be significant divergence of opinion between the larger clinical, research, and lived experience spaces [ 18 ]. Nevertheless, Bachner-Melman et al. [ 42 ] also found a broad area of overlap in the perspectives of people with lived experience of an ED, family members, and ED therapists, on what recovery encompasses. They proposed a questionnaire to measure four aspects of ED recovery that were agreed on by these overlapping perspectives: lack of symptoms, acceptance of self and body, social and emotional connection, and physical health [ 20 ].
Lived experience, including personally having lived with an ED, as well as being a “support” for someone with an ED (e.g., parents, family, partners, friends, mentors), necessarily informs a particular person’s ED recovery definition and provides an additional lens on the same construct. Thus, individuals who have lived through an ED may have a different view of recovery to that of their “supports” (e.g., improved psychosocial functioning, QOL, vs. medical stability, decreases in behaviors, and vice versa). However, the recovery priorities of individuals and “supports” may also align. For example, recent studies have indicated that both individuals and parents/families place high value on increased body acceptance and independence in the individual’s recovery process [ 43 , 44 ]. In addition, there is a relatively new resource for partners of those with ED, which focuses on understanding, supporting, and connecting with the partner on shared recovery goals [ 45 ]. In the book “Loving Someone with an Eating Disorder,” Dana Harron includes perspective-taking exercises to help the person understand their partner’s struggle, strategies for dealing with mealtime challenges, up-to-date facts about EDs, and self-care tips to help the person maintain healthy boundaries [ 45 ].
Conceptual and methodological challenges in ED recovery research
Related to the above, researchers face a number of conceptual and methodological questions when exploring ED recovery. For example, whether or not recovery should be considered per individual ED, or trans-diagnostically, is an important question in the recovery definition literature. Bardone-Cone et al. [ 15 ] suggest that a transdiagnostic approach is most appropriate, given that diagnoses can shift, and symptoms can fluctuate over time. Indeed, longitudinal studies have indicated that participants report receiving a single ED diagnosis at one point in time, however, over their lifetime, they would have met criteria for two, three, or four “different” ED diagnoses at different times (e.g., [ 46 ]). Anecdotally, our co-authors have also noted this when recruiting participants for research. Instead of necessitating an overall cessation of ED symptoms within one diagnostic category in the traditional categorical approach, a transdiagnostic approach could rather focus on improving the status of individual symptoms (e.g., frequency of restricting, binging) as a marker of individual “recovery.”
Beyond differences in being able to compare clinical groups across research findings, we might also consider who is most commonly included in these recovery studies (and who is not). There are many significant logistical barriers to receiving an ED diagnosis and related treatment worldwide. Indeed, practical barriers include: cost, insurance coverage, rurality, transportation, work or education schedules, and lack of available childcare, which disproportionately affects people from potentially disadvantaged groups (e.g., [ 47 , 48 , 49 , 50 ]). The process of recovery itself invokes privilege (e.g., who is able to be diagnosed, who has access to formal treatment, and who is recovering in the “right way”). For example, EDs may be missed, or diagnoses delayed, in those who do not fit the stereotypical picture of a person with an ED, including those in larger, or non-emaciated, bodies [ 51 , 52 ].
The majority of the studies thus far on ED recovery definitions are therefore composed predominantly of non-diverse participant samples who have the means to overcome the barriers to treatment access (i.e., predominantly White, thin, socioeconomically privileged, cisgender women, drawn primarily from clinical settings). Indeed, there has been comparatively little research on other populations with EDs (e.g., cis men, trans and nonbinary people, children, elders, higher weight individuals, individuals with binge eating disorder [BED], comorbidities, or late onset), as these groups often do not have access to the diagnoses and treatments that are the gateway to research study participation. These limitations determine whose recoveries we can learn about, and excludes other experiences [ 18 , 53 , 54 ].
Traditionally, those with lived experience have not been invited to co-design recovery research, limiting study participation and the diversity of representation. Even when recovery research includes non-clinical samples, methodology choices impact who is selected for participation. For example, studies that exclude potential participants with BMIs above certain levels (e.g., BMIs that are considered “overweight” or “obese”) exclude many ED recovery experiences automatically, limiting the view of what “recovery” looks like.
Additionally, the specific terminology of “recovery” may not resonate with all people experiencing life beyond an ED [ 55 ], causing some potential participants to self-select out of such studies. Some people with lived experience note that the term “recovery” is prescribed and carries preconceptions [ 56 , 57 ]. Indeed, there are nuances and connotations involved with the use of the word “recovery.” Some individuals may consider themselves “in recovery” (on a continuous journey), while others may consider themselves “recovered” (having moved past the ED completely). In this way, the meaning of “recovery” can indicate both a process and a state [ 58 ]. Stringent criteria for including people in studies as “recovered” may pre-define the group with whom recovery is being explored. Other terminology, such as severe and enduring anorexia nervosa (SEAN), and severe and enduring eating disorders (SEED), emphasize more chronic conditions. However, these terms are not always helpful for people experiencing longer-lasting ED, as they may insinuate that healthcare providers (or the patient) have given up hope for recovery [ 59 , 60 , 61 , 62 ].
Given that “recovery” as a term does not resonate with all [ 55 , 63 , 64 , 65 ], using other terms, including non-clinical ones (e.g., “getting better”, “healing”) to refer to these experiences may increase the diversity of experiences in the literature. As we will explain, these methodological features matter in recovery research because they significantly impact what we can know about ED recovery, and for whom.
Positioning ourselves
We come into this work from various vantage points; we name our positionalities here, since researchers’ subjectivity inevitably shapes their research and interpretations [ 66 ]. Engaging with the subjective, rather than presuming objectivity is the most ethical and effective stance in research, and can invite opportunities to uncover new and different knowledge [ 67 ]. The authors bring research and clinical lenses to bear on this work; some of us are primarily or exclusively researchers in the ED field, whereas others also practice clinically. We come from Global North countries, and all of us are White. We were thus trained in scientific traditions that privilege certain ways of knowing and doing that reflect the English and White dominant landscape of academia. While most of us benefit from thin privilege, able-bodied privilege, and cis-hetero privilege, our authorship team also includes those with non-binary, queer, fat, and chronically ill identities. Some of us have lived experience with ED, and have used this to inform our research and clinical practice. Some of us are newer to the ED field, whereas others have been working in the field for over 30 years. While we are different in some ways, our sameness centers around the academic privilege we have to access, interpret and navigate these literatures and their methodologies.
Overview and analysis of ED research methods
Below we provide an overview of the commonly used quantitative and qualitative research methods, along with tables that illustrate examples of the different types of analyses that fit within these broader methodological categories. We also analyze the benefits and limitations of each method, focusing on what we can learn from them and identifying relevant gaps in the literature.
Quantitative methods
As noted above, quantitative methods typically stem from a (post)positivist ontological/epistemological stance, which inherently affects how data are interpreted and understood. This is a core consideration of how we in turn can view the findings. This approach aims to provide “objective” results [ 68 ]; in this case, it is “recovery by the numbers.” It allows for the measurement of results through data, relying on a systematic approach of empirical investigation, and based on the assumption that there is a singular recovery definition which can be known. Researchers use statistical models, computational techniques, and mathematics to develop and test specific hypotheses. The types of quantitative analyses range from relatively simple descriptive/comparative measures to more complex multivariate measures and multi-level designs (which are all influenced by their study samples, assessments, and testable hypotheses). Data can be collected from the traditional in-person research study (or through video conferencing), or alternatively, from participant surveys (e.g., online, phone, mail, text).
Different types of quantitative methods have been employed in ED recovery research (see Table 1 ). Descriptive studies focus on the “how/what/when/where,” rather than the “why” (e.g., examining aspects of recovery definitions [ 69 ]), and comparative studies have a procedure to conclude that one variable is better than another (e.g., comparing different recovery definitions for agreement [ 70 ]). Univariate analyses examine the statistical characteristics of a single variable (e.g., dichotomous yes/no variable differences between recovery groups on a single measure [ 33 ], continuous range variable differences between recovery groups on multiple measures [ 71 ]), while bivariate analyses determine the empirical relationship between two variables (X and Y) (e.g., relationships between recovery attitudes and related variables [ 72 ]). Multivariate analyses aim to determine the best combination of all possible variables to test the study hypothesis (e.g., comparing recovery and healthy control groups across different recovery scores [ 73 ]).
According to (post)positivist stances, these quantitative methods have the anticipated or theoretical benefits of enabling researchers to reach higher sample sizes (increases generalizability), randomize participants (reduces bias), and replicate results (validates data). In practice, though, generalizability extends only to the sample that is recruited (as noted above, in most cases, thin, White women), and randomization within that sample thus does not increase the diversity of results. The relative focus on “novel” research means that replication studies are not conducted to the degree we would hope or expect.
In addition, quantitative methods limit what can be known about any particular individual. For example, numbers can tell us a person’s standardized assessment scores, but they do not include the detailed descriptions of the individual’s experiences. They also reduce recovery to a single experience which may overlook the tremendous diversity in lived experiences. Similarly, while statistical analyses can account for contextual confounding variables, they cannot tell us the broader factors which influence the delivery and the function of interventions.
Qualitative methods
Overall, qualitative methods offer the potential to engage deeply with phenomenon of interest, often stemming from non-positivist epistemological stances (e.g., constructionist, feminist). While qualitative methods are commonly critiqued for small sample sizes, in a qualitative paradigm, small samples allow researchers to dig into the nuances illustrated in participants’ stories, strengthening study findings. The aim of qualitative research is in-depth, contextualized analysis, rather than generalizations. Qualitative methods often, but not always, involve interacting directly with participants in the form of interviews or focus groups. However, qualitative research can also involve analyses of existing textual or image data, such as blog or social media posts, or news articles. A core feature of qualitative research is the researchers’ focus on exploring meaning in voiced or textual data, vs. using only quantitative measures.
Despite shared features, qualitative methods vary enormously in terms of data collection and analysis types. This is due in part to the differences in theoretical basis, epistemologies, ontologies, and paradigms that inform what meaning researchers perceive as possible to achieve. Some (e.g., [ 74 ]) draw on the concepts of “big Q” and “small q” to differentiate in broad terms between the qualitative methods [ 75 ]. Briefly, “big Q” methods invite and acknowledge researcher subjectivity, whereas “small q” approaches attempt to aim at more “objective interpretation,” [ 76 ], which is more similar to (post)positivist approaches. Further, “big Q” approaches tend to delve into the connections between knowledge production, analysis, and sociocultural contexts in which research takes place, whereas “small q” approaches tend to focus more on descriptive, groundwork-laying analysis for quantitative methods to provide generalizability [ 76 ]. Neither approach is inherently “better;” they are designed to achieve distinct findings.
Some of the qualitative methods that have been commonly used to explore ED recovery experiences are summarized in Table 2 . Note that these are not the only methods used. Some (particularly earlier) studies, describe their methods as “qualitative,” without specifying the exact type(s) of analysis. The differences between these various types of methods are at times subtle.
Discourse Analysis (DA) focuses on language not as just a route to content, but as powerful in and of itself (e.g., analysis of talk about recovery) [ 77 , 78 ]. Within DA, Linguistic Analysis adds a focus on language present in the text, with more of an emphasis on terms used, and their connotations (e.g., explorations of Internet message board communications about recovery) [ 79 ]. Also within DA, Narrative-Discursive Analysis adds a focus on social power (e.g., analysis of recovery interviews with a gender lens [ 80 ]), alongside an emphasis on stories (individual and broader, social stories). Narrative Approaches emphasize the story (e.g., analyses of participant writing, life-history), and situates recovery within the broader culture [ 31 , 81 , 82 , 83 , 84 ]). Phenomenological and Phenomenographic Approaches, including Interpretive Phenomenological Analysis (IPA) aim to get in “close” to participant embodied experiences (e.g., focus on recovery self-process in specific groups such as men, former patients, people in recovery from AN specifically [ 85 , 86 , 87 ]). Grounded Theory emphasizes context-specific “ground-up” theory developed from participant responses (e.g., development of cyclical, phase, and process models of recovery in/outside of treatment contexts [ 65 , 88 , 89 , 90 , 91 ]). Thematic Analysis (TA) is aimed at developing patterns/themes based on data (e.g., exploring patterns in experiences of recovery [ 92 , 93 , 94 ]) and can look quite different depending on the type of thematic analysis employed, ranging from more descriptive to more analytical. Content Analysis summarizes and organizes experiences amongst a particular group in a particular context (e.g., describing the content of interviews with specific groups, for example, athletes, or exploring the content of a particular stage of recovery, such as late-stage recovery [ 95 , 96 , 97 , 98 , 99 ]).
It is also possible to use different qualitative methods to explore similar phenomenon. For example, a constructivist grounded theory exploration of people who have received treatment for AN may focus on theorizing what ED recovery processes are occurring for this particular group [ 99 , 100 ]. An IPA of this same group, meanwhile, may emphasize the development of a set of themes relating to shared perspectives on what the experience felt like [ 101 , 102 ].
Qualitative methods can thus provide detailed descriptions of a wide diversity of lived experiences. This enables us to have a broader perspective of what is possible in recovery. Additionally, these methods allow us to consider the contextual factors which influence the delivery and the function of interventions. A potential further benefit is the individual’s own process of reflecting on their changes in recovery (via study participation), which may provide insight and encouragement for continuing on their path.
Critiques of qualitative methods tend to center around the concept of generalizability, though as noted this is not typically the goal of qualitative approaches. As noted above, quantitative studies, which typically focus on a person’s ED standardized assessment scores, and account for contextual confounding variables through statistical analyses, theoretically generate findings which can be applied to other populations from the study sample. However, as we have indicated, extrapolation of the results of mostly homogenous groups (e.g., predominantly White, thin, socioeconomically privileged, cisgender women, drawn primarily from clinical settings) falsely assumes that the course and outcomes will be the same for all.
Exploration of mixed-methods, creative methods, and multi-methods research
While ED recovery researchers have primarily conducted either quantitative or qualitative studies, some have integrated alternative or multiple methods in their designs. Below we explore some of these methods, which may enable new understandings of ED recovery. These include mixed-methods (usually a weaving of quantitative and qualitative), creative methods (e.g., Photovoice, digital storytelling), and multi-methods (e.g., complementary combinations of quantitative, qualitative, creative methods, psycho/physiological, behavioral, laboratory, online observations).
Mixed-methods (weaving of quantitative and qualitative)
It has been argued that mixed-methods allow us to weave together our quantitative and qualitative insights by acknowledging the benefits and limits of both designs. Cluster analysis intends to combine these methods with the goal of maximizing benefits [ 103 ]. For the qualitative aspects of the analysis, data is coded to themes using one of the qualitative methods, and each individual unit of data (e.g., person) is coded for the presence or absence of each theme. For the quantitative aspects of the analysis, data is plotted to identify different clusters of individuals, and then these clusters are interpreted via statistical methods. Cluster analysis aims to provide greater insight into groups of individuals, and potentially elucidate different clusters of “recovery definitions.” However, the qualitative analysis in this approach is inherently reductionistic (e.g., people are coded to create a quantitative measure), which aligns with the post-positivist stance associated with quantitative analyses. From this view, the approaches are not actually integrated; rather they are complimentary. Indeed, it may not be possible to truly integrate them when they emerge from different epistemological stances. We suggest, however, that integration is not needed.
Bachner-Melman et al. [ 42 ] used exploratory factor analysis to identify four factors that mapped onto ED recovery which had general agreement between participants with a lifetime ED diagnosis, healthy family members, and ED clinicians; (1) lack of symptomatic behavior, (2) acceptance of self and body, (3) social and emotional connection, and (4) physical health. These factors were then confirmed using confirmatory factor analysis. Utilizing more than one method thus expands our perspectives of ED recovery, allowing us to broaden our understanding of what can be known about recovery. Yet as noted above, we caution readers in viewing mixed-method approaches as an overall panacea; the approach tends to be more (post)positivist, and aims to quantify experiences, which may not be the goal for researchers from other stances. Again, this is not to say that the approach is without merit, but that it is important to acknowledge what it aims to do (or know).
Creative methods (photovoice, digital/verbal storytelling, collages, drawings)
Quantitative and qualitative methods are, of course, not the only options at the disposal of researchers interested in exploring ED recovery. Some researchers have elected to take creative approaches to research, seeking to explore recovery in different ways. Potentially, such methods enable researchers to “see” facets of recovery phenomenon that are less evident in methods that primarily hinge on either words or numbers [ 57 ]. To date, ED recovery researchers have used creative methods such as Photovoice [ 104 , 105 ], which aims to involve participants in the process of generating and analyzing research data [ 106 ]. This method may be particularly useful for generating disseminable results, with a view towards change in policy settings for the benefit of people in recovery [ 104 ].
Another creative method, digital storytelling [ 57 , 107 ], encourages participants to “story themselves” at a particular moment in time. This may enable the creation of more nuanced, rich, and person-centered depictions of recovery; the participant’s voice is centered in a way that may be less feasible in research that seeks to generate patterns across several participants’ accounts [ 107 ]. Like Photovoice, digital stories can also be used to work toward enhancing understandings of recovery amongst people who do not have lived experience (e.g., healthcare providers) [ 57 ].
Other creative methods include the use of collages, verbal storytelling, drawing,and more [ 108 , 109 , 110 ]. Placing the decision about which creative method to use in the hands of research participants may also enable a redressing of traditional power dynamics in research that position the researcher as the ultimate decision-maker [ 57 ].
Multi-methods (complimentary use of multiple methods)
Given that ED recovery is a complex phenomenon, one approach to exploring it is the use of a multi-method research design, including different complimentary types of analyses (e.g., quantitative, qualitative, creative methods, psycho/physiological, behavioral, laboratory, online observations), and ideally from different perspectives (e.g., individuals, “supports,” clinicians, researchers, policy makers, and other stakeholders). Broadening our methodological “toolkits” may allow for more nuanced and specific insights about ED recoveries, taking into account context, varied perspectives, and positionalities.
Several studies of ED symptom assessment have employed multi-method designs thus far, and each of these has the potential to contribute a piece of the “ED recovery puzzle.” For example, Stewart et al. [ 111 ] conducted a mixed method investigation of the experiences young people, parents, and clinicians had of online ED treatment during COVID-19. They used a mixed quantitative (Likert scale rating questions) and qualitative (free text entry questions) survey which they analyzed using a summary approach (quantitative) and reflexive thematic analysis (qualitative). Leehr and colleagues [ 112 ] analyzed binge eating episodes under negative mood conditions via electroencephalography (EEG) and eye tracking (ET) in a laboratory.
Bartholome et al. [ 113 ] combined standardized instrument interviews, laboratory investigations, and ecological momentary assessment (EMA) to collect data on binge eating episodes in participants with BED. In order to examine underlying mechanisms of the somatic sensation of “feeling fat,” Mehak and Racine [ 114 ] used multiple methods of self-reports, EMA, heart rate variability, laboratory measurements of BMI, dual energy X-ray absorptiometry (DEXA) scans, and clothing sizes.
Technological advances can offer more in-depth information about the recovery process, and could be utilized further in research studies. For example, EMA allows for moment by moment collection of data on phenomenon of interest. This can include biological functions (e.g., heart rate), as well as feelings and behaviors in an individual’s daily life. This approach provides a more “real time” look into experiences (versus having to recall such experiences later on in a survey, or in an interview). In the case of ED recovery, future research can explore the answer to the question of what “active” recovery looks like on a daily basis for individuals via EMA (e.g., what challenges do individuals encounter; how does it impact their behavior/feelings?).
Other technological laboratory tools, such as fMRI, DEXA, and other scanning techniques, can add visual information about the current physical state of recovery (and any related functional “scars” from the ED). It may be helpful in future studies to provide this feedback so individuals can have an accurate picture of the medical status of their body, and make adjustments (e.g., take Vitamin D to increase bone density).
Additional methodological approaches/considerations
Co-design with different perspectives in ed recovery research.
We believe it will be helpful to incorporate different perspectives in ED recovery research for many reasons. For example, expanding who is included in our studies, what identities are represented, and those with both formal and informal treatment, will increase the participant representation, relevance, and generalizability of the findings [ 53 ]. This in turn will allow us to know more about the process of recovery for different individuals and groups, and will broaden our conceptualization of the phenomenon. Ideally, future research will include individuals with lived experiences and their “supports” (e.g., parents, families, partners, friends, mentors), as well as clinicians and researchers, in co-designing studies that could identify and assess aspects of ED recovery that are important to all of the constituents.
Longitudinal research design
We also underscore the need for an extended duration of studies in order to better understand the longitudinal course and outcome of individuals in ED recovery. This design will allow us to compare recovery operalizations vs. subsequent relapse rates, to track how perspectives of recovery develop and change over time (via quantitative, qualitative and mixed-method measures), and how these in turn affect an individual’s identity (e.g., [ 15 ]).
There are several areas of potential future longitudinal research. For example, follow-up on cognitive recovery (which we know tends to occur later (e.g., [ 43 ]), and how related timelines for this may impact subsequent relapse rates, tracking recovery changes over time with mixed or multi-methods designs in underrepresented populations (e.g., Atypical Anorexia (AAN) [ 115 ]), and holding on to hope, with more longitudinal data indicating that recovery is possible, even after decades (e.g., [ 59 ]).
Future research directions
Based on the above studies, we suggest some potential areas for future research, ideally incorporating multi-method designs to provide different perspectives on ED recovery. Recently, several themes have been identified in the literature as promising lines of research that may improve our understanding of ED, and increase the clinical application of findings.
Predictors of outcomes
Within quantitative research, Bardone-Cone et al. [ 15 ] note that predictors of outcomes, biological/neuropsychological techniques, and a focus on the SEAN population are newer, more nuanced, areas of investigation. In their systematic review and meta-analysis of predictors of ED treatment outcomes (at end of treatment [EoT], and follow-up), Vall and Wade [ 26 ] reported that the most robust predictor at both time frames was greater symptom change earlier in treatment. Other baseline predictors of better outcomes included: higher BMI, fewer binge/purge behaviors, more functional relationships (e.g., with family, friends), and greater motivation to recover. Of note, it is important to understand that higher BMI is in the context of a “higher” thin BMI, as most people with BMI > 25 are not included in studies of recovery. This is another example of how our methods and design choices impact what we can know.
Relatedly, one potential area for future ED quantitative predictor research is to build a Risk Calculator (RC), which is a statistical tool that identifies risk factors, and determines how likely an event is to happen for a particular person [ 116 ]. Physicians have used RCs clinically across an array of medical conditions, including stroke [ 117 ] and cancer [ 118 ]. There has been a recent turn toward integrating RCs into charting psychiatric disorder outcomes and treatment approaches; they have been used for psychosis [ 116 ], depression [ 119 ], and bipolar disorder [ 120 , 121 , 122 , 123 ]. This same technique could be applied to build a RC for personalized risk of ED onset/relapse, utilizing variables collected in research/treatment. A statistical combination of factors that reliably predict the non-occurrence of ED relapse could be a valuable addition to, predictor of, or even criterion, for full recovery. As part of these research initiatives, it will be important for researchers to employ diverse and longitudinal methods in order to obtain long-term, dynamic data.
In line with this, narrative qualitative analysis may be useful in elucidating predictors/risk factors for individuals. In this way, the (narrative) story that the person tells themselves about their recovery, and what was helpful to them, also has importance alongside any quantitative measures. Indeed, this perspective perhaps has more personal meaning, especially in contexts where minute changes identifiable through quantitative studies may be less relevant in the daily lives of their ED recovery.
Biological and neurological markers
Recent developments in the understanding of biological and neurological markers have enabled us to parse out what features may be involved with the ED “state” (which resolves with recovery), what features may onset premorbid to the ED (and will potentially continue after recovery), and what features may be “scars” (consequences of the ED). In their functional Magnetic Resonance Imaging (fMRI) study on participants who had recovered from AN, Fuglset et al. [ 124 ] reported increased activation in visual processing regions in anticipation of seeing images of food, with corresponding reduced activation in decision-making regions. While they found some normalization of the brain regions during recovery, other differences related to longer periods of starvation that appear later in life remained (residual “scars”).
Future quantitative research which incorporates longitudinal designs following the same participant cohort may elucidate more closely the timepoints during which the “state” and “scar” markers begin to emerge, in order to provide earlier interventions. In this instance, qualitative longitudinal studies could be beneficial here too. For example, participant narrative descriptions of ongoing biological changes in their recovery (e.g., feeling hungrier, not being able to tolerate hunger as well) not only reaffirm that people are noticing these internal bio markers, but provide the opportunity for them to discuss their day to day experiences of these lasting changes.
Recovery criteria
From a post-positivist perspective, there has been a longstanding call for standardized ED recovery criteria, typically involving weight, behavioral, and cognitive criteria (e.g., [ 14 , 15 , 16 , 17 ]). Drawing from the above, we suggest that research looking into recovery criteria may benefit from more diverse methodological approaches which pull from a variety of sources (e.g., clinicians, researchers, individuals with lived experience). For example, BMI has historically been used as an indicator of recovery status because it is readily obtained by ED researchers (and clinicians). While weight monitoring can be helpful in specific cases (e.g., those who are severely underweight or have lost a lot of weight in a short period of time), it is limited in use. Namely, BMI is insufficient to determine medical stabilization, it fails to take into account individual differences, and it can have negative impacts on treatment when individuals are discharged on the basis of weight alone [ 125 ]. Given these concerns, future research could discontinue the use of BMI as the “core” recovery criterion, as suggested by Kenny and Lewis [ 126 ], and instead focus on other variables that are more indicative of recovery over follow-up (e.g., Vall and Wade’s systematic review and meta-analysis findings of early symptom change during treatment as the most robust predictor of outcomes) [ 26 ].
Similarly, standardized assessments (e.g., EDE-Q, EDE, ED-LIFE) have been the “go-to” for assessing recovery outcomes in comparison to statistical norms. However, these measures are often developed by clinicians/researchers (thus reflecting what they feel is important in recovery) and in line with particular therapeutic modalities (e.g., the EDE-Q has a cognitive orientation). Thus, scores on these measures may not always match the person’s particular recovery aims and goals, nor the relative importance of particular behaviors in their lives. Employing these measures as a part of multi-methods designs with other types of assessments for comparison may offer the potential to think differently about these measures, and their role in assessing outcomes. We also suggest the need for measures co-designed with folks with lived experience and which reflect the diverse recovery elements described in qualitative studies (e.g., [ 33 ]).
The recovery process
Future research could compile more comprehensive lived experience narratives of changes in thought patterns through the recovery journeys (e.g., descriptions of how the “ED” voice began to leave, if ED voice is a relevant construct for the person), which could provide a more realistic timeline of this portion of the process for individuals and their “supports.” To begin to employ these kinds of measures in a way that opens up new possibilities, it would also be important to explore whether the ED-related ideas being measured resonate with the person whose recovery is being explored. Co-design processes may also be particularly relevant here, inviting people in recovery to be a part of research teams and take a role in determining the kinds of measures that could be used to assess recovery.
As years of ED behaviors and thoughts tend to impair different areas of psychosocial functioning (e.g., relationships, school/work, recreation, household duties), improvement in these areas, along with related QOL, tends to also lag behind physical recovery (e.g., [ 43 ]). Future research could further elaborate the timelines for which recovery in the different areas occurs, both from a group (e.g., through life story, narrative, or thematic analysis), and an individual (e.g., personal recording of recovery progress, case study approach) level. This approach offers a shift in methodological perspective, providing opportunity to conceptualize recovery differently.
Other areas for future consideration
Several studies (and informal support groups) have successfully employed recovered mentors, providing hope in recovery (e.g., [ 127 ]). Future research could examine more of the nuances of the mentorship role, including the characteristics of the mentor, the stage of recovery that the individual is in, and the dynamics of the mentor relationship. Further, taking a truly co-designed approach and, in particular, working with those who have not been included and heard in either treatment or research (not only more diverse participants, but their “supports,” including mentors), could offer new insight into recovery processes. Indeed, going forwards, we need to conduct our research differently if we want to incorporate the perspectives of those that we do not usually hear from.
Another area of study has developed around online (e.g., social media) use among those who are at risk for developing an ED, struggling with an ED, and those who are on the path to ED recovery. Analyses of online websites, blogs, and social media posts, along with their related potentially triggering content, have been conducted (e.g., [ 128 ]). However, on a positive note, this medium allows us to explore other methodological possibilities, including potentially focusing on reducing participant burden, and engaging with content from spaces where people are more “organically” describing these experiences, to get a sense of recovery outside of a clinical perspective. One possibility for future research is to combine the use of EMA with exposure to a range of different ED blog content (e.g., from triggering to supportive posts), in order to provide more proximal individual reaction information (e.g., EMA before exposure, EMA at exposure time, EMA after exposure time).
Proposed future research model: Dialectical movement towards and away from a consensus
The aim of this paper is to offer a more diverse view of methodological perspectives (which stem from various ontological and epistemological stances) and ideas that might allow for forward movement in the field. As noted above, in a dialectal format, this can involve both movement toward and away from a consensus, including perspectives which do not seek to identify a single recovery definition. We believe that both can be simultaneously pursued, acknowledging that one does not discount the other. We have outlined several potential areas to explore which do not necessarily depend upon a consensus definition. Here, for balance, we would like to propose a future research model that could guide us in a direction that may eventually lead to a consensus definition–or definition s . In effect, we are advocating for: (1) transparency in researchers’ epistemological stances; (2) more varied approaches to research in order to “see” different aspects of recovery experiences; and (3) collaboration between researchers and other stakeholders to generate new methodological approaches and insights about recovery.
Our proposed future research model is detailed in Table 3 . Based upon the studies we cited above, we suggest a multi-methods design (e.g., quantitative, qualitative, creative methods, psycho/physiological, behavioral, laboratory, online observations), which incorporates different perspectives (e.g., expanding recruitment of participants that have been less represented in the literature, including “supportive” others), and extends the duration of studies to provide a more longitudinal outlook (e.g., capturing cognitive recovery, and improvement in psychosocial functioning/QOL, which often comes later, and noting how definitions of recovery may change over time for people). In this way, we hope to move the field towards different, more nuanced, and comprehensive perspectives on ED recovery.
In conclusion, we would like to encourage a creative, transparent, and thoughtful approach to ED recovery methodology, that considers what each of the methods allows us to engage with, or not, as the case may be. What we can (and do) know about recovery is intricately tied to our methodological and study design choices, which all have limits. Within this context, while there is a benefit to current pushes in the field to “come to consensus,“ these consensus definitions will necessarily leave out some people and experiences. This is especially the case for those who have not been meaningfully included in the research we have conducted to reach this consensus (e.g., people with lived experience, “non-traditional” patients, patients without access to treatment). Since there are so many different facets of recovery experiences, using different methodologies is imperative to develop a more complete understanding.
Indeed, it is important to acknowledge how the centrality of the method that is chosen to define ED recovery in turn influences how researchers and clinicians understand recovery, and how one moves towards it. New insights into recovery processes may depend on new methods of investigation. Thus, we suggest that some potential areas for future research ideally employ multi-method designs (e.g., quantitative, qualitative, creative methods, psycho/physiological, behavioral, laboratory, online observations), incorporate different perspectives (e.g., expanding recruitment of participants that have been less represented in the literature, including supportive others) and extend the duration of studies to provide a more longitudinal outlook (e.g., capturing cognitive recovery, which often comes later, and noting how definitions of recovery may change over time for people). In this way, we hope to move the field towards different, more nuanced, and comprehensive perspectives on ED recovery.
Availability of data and materials
Not applicable.
There are debates about the degree to which research can ever be truly objective or whether this is desirable. Here, we use objective and subjective in quotation marks to signal broader perceptions about these processes.
Abbreviations
Anorexia nervosa
Binge eating disorder
Body mass index
Bulimia Nervosa
Connectedness, hope and optimism, identity, meaning in life, empowerment
Dual energy X-ray absorptiometry
Eating attitudes test
- Eating disorders
Eating Disorders Recovery Endorsement Questionnaire
Eating Disorders Recovery Questionnaire
Eating Disorders Quality of Life Scale
Eating Disorders Quality of Life
Electroencephalography
Ecological momentary assessment
Eye tracking
Functional magnetic resonance imaging
Generalized estimating equations
Health-Related Quality of Life in Eating Disorders Questionnaire
Hierarchical linear models
Interpretive phenomenological analysis
Multivariate analysis of variance
National Institutes of Health
Risk calculator
Substance Abuse and Mental Health Services Administration
Severe and enduring anorexia nervosa
Severe and enduring eating disorder
Quality of life for eating disorders
Barad K. Meeting the Universe Halfway. Durham: Duke University Press; 2007.
Book Google Scholar
Slevitch L. Qualitative and quantitative methodologies compared: ontological and epistemological perspective. J Qual Assur Hosp Tour. 2011;12(1):73–81.
Article Google Scholar
Tuli F. The basis of distinction between qualitative and quantitative research in social science: reflection on ontological, epistemological and methodological perspectives. Ethiop J Educ Sci. 2010;6(1).
Duncan C, Cloutier JD, Bailey PH. Concept analysis: the importance of differentiating the ontological focus. J Adv Nurs. 2007;58(3):293–300.
Article PubMed Google Scholar
Hofweber T. Logic and ontology. In: Zalta EN, editor. The Stanford encyclopedia of philosophy. Stanford: The Metaphysics Research Lab, Center for the Study of Language and Information; 2021.
Google Scholar
Hupcey JE, Penrod J. Concept analysis: examining the state of the science. Res Theory Nurs Pract. 2005;19(2):197–208.
Wilson J. Thinking with concepts. Cambridge: Cambridge University Press; 1963.
Setup M, Ram N. Epistemology. In: Zalta EN, editor. The Stanford encyclopedia of philosophy. Stanford: The Metaphysics Research Lab, Center for the Study of Language and Information; 2020.
Macionis JJ, Gerber LM, Sociology (7th Canadian). Pearson, Canada: Pearson Canada; 2011.
Larrain J. The concept of ideology. London: Hutchison; 1979.
Phillips DC, Burbules NC. Postpositivism and educational research. Lanham & Boulder: Rowman & LIttlefield Publishers; 2000.
Stanley J. Knowledge and practical interests. New York: Oxford University Press; 2005.
Cakir M. Constructivist approaches to learning in science and their implications for science pedagogy: a literature review. Int J Environ Sci Educ. 2008;3(4):193–206.
Bardone-Cone AM, Harney MB, Maldonado CR, Lawson MA, Robinson DP, Smith R, et al. Defining recovery from an eating disorder: conceptualization, validation, and examination of psychosocial functioning and psychiatric comorbidity. Behav Res Ther. 2010;48(3):194–202.
Bardone-Cone AM, Hunt RA, Watson HJ. An overview of conceptualizations of eating disorder recovery, recent findings, and future directions. Curr Psychiatry Rep. 2018;20(9):79.
Wade TD, Lock J. Developing consensus on the definition of remission and recovery for research. Int J Eat Disord. 2020;53(8):1204–8.
Attia E, Blackwood KL, Guarda AS, Marcus MD, Rothman DJ. Marketing residential treatment programs for eating disorders: a call for transparency. Psychiatr serv. 2016;67(6):664–6.
McGilley BS. J. Recipe for recovery: necessary ingredients for the client’s and clinician’s Success. In: Maine M, Bunnell, editors. New York: Elsevier; 2010.
Noordenbos G. Which criteria for recovery are relevant according to eating disorder patients and therapists? Eat Disord. 2011;19(5):441–51.
Solmi M, Wade TD, Byrne S, Del Giovane C, Fairburn CG, Ostinelli EG, et al. Comparative efficacy and acceptability of psychological interventions for the treatment of adult outpatients with anorexia nervosa: a systematic review and network meta-analysis. Lancet Psychiatry. 2021;8(3):215–24.
Treasure J, Duarte TA, Schmidt U. Eating disorders. Lancet. 2020;395(10227):899–911.
Waller G, Raykos B. Behavioral interventions in the treatment of eating disorders. Psychiatr Clin North Am. 2019;42(2):181–91.
Garner DM, Garfinkel PE. The eating attitudes test: an index of the symptoms of anorexia nervosa. Psychol Med. 1979;9(2):273–9.
Kenny TE, Trottier K, Lewis S. Lived experience perspectives on a model of eating disorder recovery in a sample of predominantly white women: a mixed method study. J Eat Disord. 2022;10(1):1–19.
McDonald S, Williams AJ, Barr P, McNamara N, Marriott M. Service user and eating disorder therapist views on anorexia nervosa recovery criteria. Psychol Psychother. 2021;94(3):721–36.
Article PubMed PubMed Central Google Scholar
Vall E, Wade TD. Predictors of treatment outcome in individuals with eating disorders: a systematic review and meta-analysis. Int J Eat Disord. 2015;48(7):946–71.
Dawson L, Rhodes P, Touyz S. “Doing the impossible”: the process of recovery from chronic anorexia nervosa. Qual Health Res. 2014;24(4):494–505.
Anthony WA. Recovery from mental illness: the guiding vision of the mental health service system in the 1990s. Psychosoc Rehabilit J. 1993;24(9):159–68.
Wetzler S, Hackmann C, Peryer G, Clayman K, Friedman D, Saffran K, et al. A framework to conceptualize personal recovery from eating disorders: a systematic review and qualitative meta-synthesis of perspectives from individuals with lived experience. Int J Eat Disord. 2020;53(8):1188–203.
Jarman M, Walsh S. Evaluating recovery from anorexia nervosa and bulimia nervosa: integrating lessons learned from research and clinical practice. Clin Psychol Rev. 1999;19(7):773–88.
Dawson L, Rhodes P, Touyz S. Defining recovery from anorexia nervosa: a Delphi study to determine expert practitioners’ views. Adv Eat Disord: Theory Res Pract. 2015;3:165–76.
’t Slof-OpLandt MCT, Dingemans AE, de la Torre YRJ, van Furth EF. Self-assessment of eating disorder recovery: absence of eating disorder psychopathology is not essential. Int J Eat Disord. 2019;52(8):956–61.
de Vos JA, Radstaak M, Bohlmeijer ET, Westerhof GJ. Having an eating disorder and still being able to flourish? Examination of pathological symptoms and well-being as two continua of mental health in a clinical sample. Front Psychol. 2018;9:2145.
Emanuelli F, Waller G, Jones-Chester M, Ostuzzi R. Recovery from disordered eating: sufferers’ and clinicians’ perspectives. Eur Eat Disord Rev. 2012;20(5):363–72.
Noordenbos G, Seubring A. Criteria for recovery from eating disorders according to patients and therapists. Eat Disord. 2006;14(1):41–54.
Engel SG, Wittrock DA, Crosby RD, Wonderlich SA, Mitchell JE, Kolotkin RL. Development and psychometric validation of an eating disorder-specific health-related quality of life instrument. Int J Eat Disord. 2006;39(1):62–71.
Abraham SF, Brown T, Boyd C, Luscombe G, Russell J. Quality of life: eating disorders. Aust N Z J Psychiatry. 2006;40(2):150–5.
Las Hayas C, Quintana JM, Padierna A, Bilbao A, Munoz P, Madrazo A, et al. The new questionnaire health-related quality of life for eating disorders showed good validity and reliability. J Clin Epidemiol. 2006;59(2):192–200.
Adair CE, Marcoux GC, Cram BS, Ewashen CJ, Chafe J, Cassin SE, et al. Development and multi-site validation of a new condition-specific quality of life measure for eating disorders. Health Qual Life Outcomes. 2007;5:23.
Bachner-Melman R, Lev-Ari L, Zohar AH, Linketsky M. The Eating Disorders Recovery Questionnaire: psychometric properties and validity. Eat Weight Disord. 2021;26(8):2633–43.
Noordenbos G. When have eating disordered patients recovered and what do the DSM-IV criteria tell about recovery? Eat Disord. 2011;19(3):234–45.
Bachner-Melman R, Lev-Ari L, Zohar AH, Lev SL. Can recovery from an eating disorder be measured? Toward a standardized questionnaire. Front Psychol. 2018;9:2456.
Accurso EC, Sim L, Muhlheim L, Lebow J. Parents know best: caregiver perspectives on eating disorder recovery. Int J Eat Disord. 2020;53(8):1252–60.
Richmond TK, Woolverton GA, Mammel K, Ornstein RM, Spalding A, Woods ER, et al. How do you define recovery? A qualitative study of patients with eating disorders, their parents, and clinicians. Int J Eat Disord. 2020;53(8):1209–18.
Harron D. Loving Someone with an Eating Disorder. Oakland: New Harbinger Publications, Inc.; 2019.
Milos G, Spindler A, Schnyder U, Fairburn CG. Instability of eating disorder diagnoses: prospective study. Br J Psychiatry. 2005;187:573–8.
Becker AE, Franko DL, Speck A, Herzog DB. Ethnicity and differential access to care for eating disorder symptoms. Int J Eat Disord. 2003;33(2):205–12.
Cachelin FM, Rebeck R, Veisel C, Striegel-Moore RH. Barriers to treatment for eating disorders among ethnically diverse women. Int J Eat Disord. 2001;30(3):269–78.
Cachelin FM, Striegel-Moore RH. Help seeking and barriers to treatment in a community sample of Mexican American and European American women with eating disorders. Int J Eat Disord. 2006;39(2):154–61.
Ali K, Farrer L, Fassnacht DB, Gulliver A, Bauer S, Griffiths KM. Perceived barriers and facilitators towards help-seeking for eating disorders: a systematic review. Int J Eat Disord. 2017;50(1):9–21.
Lebow J, Sim LA, Kransdorf LN. Prevalence of a history of overweight and obesity in adolescents with restrictive eating disorders. J Adolesc Health. 2015;56(1):19–24.
Harrop EN, Mensinger JL, Moore M, Lindhorst T. Restrictive eating disorders in higher weight persons: a systematic review of atypical anorexia nervosa prevalence and consecutive admission literature. Int J Eat Disord. 2021;54(8):1328–57.
Egbert AH, Hunt RA, Williams KL, Burke NL, Mathis KJ. Reporting racial and ethnic diversity in eating disorder research over the past 20 years. Int J Eat Disord. 2022;55(4):455–62.
Mikhail ME, Klump KL. A virtual issue highlighting eating disorders in people of black/African and indigenous heritage. Int J Eat Disord. 2021;54(3):459–67.
Conti JE. Recovering identity from anorexia nervosa: women’s constructions of their experiences of recovery from anorexia nervosa over 10 years. J Constructivist Psychol. 2018;31(1):72–94.
Kenny TE, Thomassin K, Trottier K, Lewis SP. Views on the term ‘recovery’ in a sample of primarily white treatment-experienced women with lived eating disorder experience. Int J Eat Disord. Under Review.
LaMarre A, Rice C. Healthcare providers’ engagement with eating disorder recovery narratives: opening to complexity and diversity. Med Humanit. 2020;47:78–86.
Fava GA. The concept of recovery in affective disorders. Psychother Psychosom. 1996;65(1):2–13.
Eddy KT, Tabri N, Thomas JJ, Murray HB, Keshaviah A, Hastings E, et al. Recovery from anorexia nervosa and bulimia nervosa at 22-year follow-up. J Clin Psychiatry. 2017;78(2):184–9.
Dawson L, Rhodes P, Touyz S. The recovery model and anorexia nervosa. Aust N Z J Psychiatry. 2014;48(11):1009–16.
Touyz S, Hay P. Severe and enduring anorexia nervosa (SE-AN): in search of a new paradigm. J Eat Disord. 2015;3:26.
Calugi S, Milanese C, Sartirana M, El Ghoch M, Sartori F, Geccherle E, et al. The eating disorder examination questionnaire: reliability and validity of the Italian version. Eat Weight Disord. 2017;22(3):509–14.
LaMarre A, Rice C, Rinaldi J tracing fatness through the eating disorder assemblage. Thickening fat, 1st Edition: Routledge; 2019. pp. 64–76.
Shohet MN, Anorexia. “Full” and “struggling.” Genres Recover Ethos. 2008;35(3):344–82.
Musolino C, Warin M, Wade T, Gilchrist P. Developing shared understandings of recovery and care: a qualitative study of women with eating disorders who resist therapeutic care. J Eat Disord. 2016;4:36.
Malterud K. Qualitative research: standards, challenges, and guidelines. Lancet. 2001;358(9280):483–8.
Gough B, Madill A. Subjectivity in psychological science: from problem to prospect. Psychol Methods. 2012;17(3):374–84.
Matthews B, Ross L. Research methods. a practical guide for the social sciences. Harlow: Pearson Education; 2010.
Couturier J, Lock J. What is recovery in adolescent anorexia nervosa? Int J Eat Disord. 2006;39(7):550–5.
Ackard DM, Richter SA, Egan AM, Cronemeyer CL. What does remission tell us about women with eating disorders? Investigating applications of various remission definitions and their associations with quality of life. J Psychosom Res. 2014;76(1):12–8.
Cogley CB, Keel PK. Requiring remission of undue influence of weight and shape on self-evaluation in the definition of recovery for bulimia nervosa. Int J Eat Disord. 2003;34(2):200–10.
Dimitropoulos G, McCallum L, Colasanto M, Freeman VE, Gadalla T. The effects of stigma on recovery attitudes in people with anorexia nervosa in intensive treatment. J Nerv Ment Dis. 2016;204(5):370–80.
Bachner-Melman R, Zohar AH, Ebstein RP. An examination of cognitive versus behavioral components of recovery from anorexia nervosa. J Nerv Ment Dis. 2006;194(9):697–703.
Braun VC, Can V. I use TA? Should I use TA? Should I not use TA? Comparing reflexive thematic analysis and other pattern-based qualitative analytic approaches. Couns Psychother Res. 2021;21(1):37–47.
Kidder LH, Fine M. Qualitative and quantitative methods: when stories converge. Eval Policy. 1987;1987(35):57–75.
Clarke V. Navigating the messy swamp of qualitative research: are generic reporting standards the answer? In: Levitt HM, editor. Reporting qualitative research in psychology: how to meet APA Style journal article reporting standards, revised edition. Washington: American Psychological Association; 2020.
Hardin PK. Social and cultural considerations in recovery from anorexia nervosa: a critical poststructuralist analysis. ANS Adv Nurs Sci. 2003;26(1):5–16.
Keski-Rahkonen A, Tozzi F. The process of recovery in eating disorder sufferers’ own words: an Internet-based study. Int J Eat Disord. 2005;37(Suppl):S80-6 discussion S7-9.
Maison H, Bailey L, Clarke S, Treasure J, Anderson G, Kohn M. Un/imaginable future selves: a discourse analysis of in-patients’ talk about recovery from an eating disorder. Eur Eat Disord Rev. 2011;19(a):25–36.
Moulding N. Gendered intersubjectivities in narratives of recovery from an eating disorder. J Women Soc Work. 2016;31(1):70–83.
LaMarre A, Rice C. Normal eating is counter-cultural: embodied experiences of eating disorder recovery. J Commun Appl Soc Psychol. 2016;26:136–49.
Matusek JA, Knudson RM. Rethinking recovery from eating disorders: spiritual and political dimensions. Qual Health Res. 2009;19(5):697–707.
Patching J, Lawler J. Understanding women’s experiences of developing an ED and recovery: a life-history approach. Nurs Inq. 2009;12(1):10–21.
Redenbach J, Lawler J. Recovery from disordered eating: what life histories reveal. Contemp Nurse. 2003;15(1–2):148–56.
Bjork T, Wallin K, Pettersen G. Male experiences of life after recovery from an eating disorder. Eat Disord. 2012;20(5):460–8.
Bjork T, Ahlstrom G. The patient’s perception of having recovered from an eating disorder. Health Care Women Int. 2008;29(8):926–44.
Jenkins J, Ogden J. Becoming ‘whole’ again: a qualitative study of women’s views of recovering from anorexia nervosa. Eur Eat Disord Rev. 2012;20(1):e23–31.
D’Abundo M, Chally P. Struggling with recovery: participant perspectives on battling an eating disorder. Qual Health Res. 2004;14(8):1094–106.
Krentz A, Chew J, Arthur N. Can J Couns. 2005;39(2):118–35.
Lamoureux MMH, Bottorff JL. “Becoming the real me”: Recovering from anorexia nervosa. Heatlh Care for Women International. 2005;26:170–88.
Woods S. Untreated recovery from eating disorders. Adolescence. 2004;39(154):361–71.
PubMed Google Scholar
Hay PJ, Cho K. A qualitative exploration of influences on the process of recovery from personal written accounts of people with anorexia nervosa. Women Health. 2013;53(7):730–40.
LaMarre A, Rice C. Hashtag recovery: #eating disorder recovery on instagram. Soc Sci. 2017;6(3):68.
Lord VM, Reiboldt W, Gonitzke D, Parker E, Peterson C. Experiences of recovery in binge-eating disorder: a qualitative approach using online message boards. Eat Weight Disord. 2018;23(1):95–105.
Arthur-Cameselle JN, Quatromoni PA. A qualitative analysis of female college athletes’ eating disorder recovery experiences. Sport Psychol. 2014;28:334–46.
Lindgren BM, Enmark A, Bohman A, Lundstrom M. A qualitative study of young women’s experiences of recovery from bulimia nervosa. J Adv Nurs. 2015;71(4):860–9.
Nilsson K, Hagglof B. Patient perspectives of recovery in adolescent onset anorexia nervosa. Eat Disord. 2006;14(4):305–11.
Pettersen G, Thune-Larsen KB, Wynn R, Rosenvinge JH. Eating disorders: challenges in the later phases of the recovery process: a qualitative study of patients’ experiences. Scand J Caring Sci. 2013;27(1):92–8.
Charmaz K. The power of constructivist grounded theory for critical inquiry. Res Methods Eval. 2016;23(1):34–45.
Williams K, King J, Fox JR. Sense of self and anorexia nervosa: a grounded theory. Psychol Psychother. 2016;89(2):211–28.
Smith JA. Reflecting on the development of interpretive phenomenological analysis and its contribution to qualitative research in psychology. Qual Res Psychol. 2008;1(1):39–54.
Fox AP, Larkin M, Leung N. The personal meaning of eating disorder symptoms: an interpretative phenomenological analysis. J Health Psychol. 2011;16(1):116–25.
Henry D, Dymnicki AB, Mohatt N, Allen J, Kelly JG. Clustering methods with qualitative data: a mixed-methods approach for prevention research with small samples. Prev Sci. 2015;16(7):1007–16.
Saunders JF, Eaton AA. Social comparisons in eating disorder recovery: using photovoice to capture the sociocultural influences on women’s recovery. Int J Eat Disord. 2018;51(12):1361–6.
Saunders JF, Eaton AA, Aguilar S. From self(ie)-objectification to self-empowerment: the meaning of selfies on social media in eating disorder recovery. Comput Human Beh. 2020;111:106420.
Wang C, Burris MA. Photovoice: concept, methodology, and use for participatory needs assessment. Health Educ Behav. 1997;24(3):369–87.
LaMarre A, Rice C. Embodying critical and corporeal methodology: digital storytelling With young women in eating disorder recovery. Forum Qual Soc Res. 2016;17:2.
Bartel H. A ‘Girls’ Illness?’ Using narratives of eating disorders in men and boys in healthcare education and research. In: Arts based health care research: a multidisciplinary perspective. Cham: Springer; 2022. p. 69-84.
Proszynski J. Interior designs: demolition and reconstruction of the self in eating disorder recovery through transformable collage book making (Doctoral dissertation, Pratt Institute). 2022.
Marzola E, Abbate-Daga G, Gramaglia C, Amianto F, Fassino S, Mobini S (ReviewingEditor). A qualitative investigation into anorexia nervosa: The inner perspective. Cogent Psychol 2015;2:1. https://doi.org/10.1080/23311908.2015.1032493 .
Stewart C, Konstantellou A, Kassamali F, McLaughlin N, Cutinha D, Bryant-Waugh R, et al. Is this the ‘new normal’? A mixed method investigation of young person, parent and clinician experience of online eating disorder treatment during the COVID-19 pandemic. J Eat Disord. 2021;9(1):78.
Leehr EJ, Schag K, Dresler T, Grosse-Wentrup M, Hautzinger M, Fallgatter AJ, et al. Food specific inhibitory control under negative mood in binge-eating disorder: Evidence from a multimethod approach. Int J Eat Disord. 2018;51(2):112–23.
Bartholome LT, Raymond NC, Lee SS, Peterson CB, Warren CS. Detailed analysis of binges in obese women with binge eating disorder: Comparisons using multiple methods of data collection. Int J Eat Disord. 2006;39(8):685–93.
Mehak A, Racine SE. Understanding “feeling fat” and its underlying mechanisms: the importance of multimethod measurement. Int J Eat Disord. 2020;53(9):1400–4.
Harrop E. “Maybe i really am too fat to have an eating disorder”: A mixed methods study of weight stigma and healthcare experiences in a diverse sample of patients with atypical anorexia (Doctoral dissertation). Seattle: University of Washington; 2020.
Fusar-Poli P, Rutigliano G, Stahl D, Davies C, Bonoldi I, Reilly T, et al. Development and validation of a clinically based risk calculator for the transdiagnostic prediction of psychosis. JAMA Psychiatry. 2017;74(5):493–500.
Nobel L, Mayo NE, Hanley J, Nadeau L, Daskalopoulou SS. MyRisk_stroke calculator: a personalized stroke risk assessment tool for the general population. J Clin Neurol. 2014;10(1):1–9.
Gail MH, Brinton LA, Byar DP, Corle DK, Green SB, Schairer C, et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst. 1989;81(24):1879–86.
Perlis RH. Pharmacogenomic testing and personalized treatment of depression. Clin Chem. 2014;60(1):53–9.
Hafeman DM, Merranko J, Goldstein TR, Axelson D, Goldstein BI, Monk K, et al. Assessment of a person-level risk calculator to predict new-onset bipolar spectrum disorder in youth at familial risk. JAMA Psychiatry. 2017;74(8):841–7.
Birmaher B, Merranko JA, Goldstein TR, Gill MK, Goldstein BI, Hower H, et al. A risk calculator to predict the individual risk of conversion from subthreshold bipolar symptoms to bipolar disorder I or II in youth. J Am Acad Child Adolesc Psychiatry. 2018;57(10):755–63 e4.
Birmaher B, Merranko JA, Gill MK, Hafeman D, Goldstein T, Goldstein B, et al. Predicting personalized risk of mood recurrences in youths and young adults with bipolar spectrum disorder. J Am Acad Child Adolesc Psychiatry. 2020;59(10):1156–64.
Goldstein TR, Merranko J, Hafeman D, Gill MK, Liao F, Sewall C, et al. A risk calculator to predict suicide attempts among individuals with early-onset bipolar disorder. Bipolar Disord. 2022.
Fuglset TS, Landro NI, Reas DL, Ro O. Functional brain alterations in anorexia nervosa: a scoping review. J Eat Disord. 2016;4:32.
Phillipou A, Beilharz F. Should we shed the weight criterion for anorexia nervosa? Aust N Z J Psychiatry. 2019;53(6):501–2.
Kenny TE, Lewis SP. Reconceptualizing recovery: integrating lived experience perspectives into traditional eating disorder recovery frameworks. Psychiatr Serv. 2021;72(8):966–8.
Ramjan LM, Hay P, Fogarty S. Benefits of a mentoring support program for individuals with an eating disorder: a proof of concept pilot program. BMC Res Notes. 2017;10(1):709.
Wolf M, Thies F, Kordy H. Language use in eating disorder blogs: psychological implications of social online activity. J Lang Soc Psychol. 2013;32(2):212–26.
Download references
Acknowledgements
The authors wish to thank our colleagues in ED recovery.
None received.
Author information
Authors and affiliations.
Department of Psychiatry, Eating Disorders Center for Treatment and Research, University of California at San Diego School of Medicine, 4510 Executive Drive, San Diego, CA, 92121, USA
Heather Hower
Department of Health Services, Policy, and Practice, Hassenfeld Child Innovation Institute, Brown University School of Public Health, 121 South Main Street, Providence, RI, 02903, USA
School of Psychology, Massey University, North Shore, Private Bag 102-904, Auckland, 0632, New Zealand
Andrea LaMarre
Clinical Psychology Graduate Program, Ruppin Academic Center, 4025000, Emek-Hefer, Israel
Rachel Bachner-Melman
School of Social Work, Hebrew University of Jerusalem, Mt. Scopus, 9190501, Jerusalem, Israel
Graduate School of Social Work, University of Denver, 2148 S High Street, Denver, CO, 80208, USA
Erin N. Harrop
University of Kansas School of Medicine, 1010 N Kansas St, Wichita, KS, 67214, USA
Beth McGilley
Department of Psychology, Clinical Child and Adolescent Psychology, University of Guelph, 50 Stone Road East, Guelph, ON, N1G 2W1, Canada
Therese E. Kenny
You can also search for this author in PubMed Google Scholar
Contributions
HH contributed to the conceptualization of the manuscript, the writing and editing of the abstract, introduction, quantitative text and table, mixed-methods, creative methods, multi-methods, future research, and conclusions sections, EndNote reference library/citations, formatting of the manuscript, and overall final revisions. AL contributed to the conceptualization of the manuscript, the writing and editing of the abstract, introduction, qualitative text and table, mixed-methods, creative methods, and conclusion sections, and overall final revisions. RBM contributed to the conceptualization of the manuscript, the writing and editing of the abstract, introduction, quantitative, and qualitative sections, and overall final revisions. EH contributed to the conceptualization of the manuscript, the writing and editing of the abstract, introduction, qualitative text and table sections, and overall final revisions. BM contributed to the conceptualization of the manuscript, the writing and editing of the abstract, introduction, qualitative, and mixed-methods sections, and overall final revisions. TK contributed to the conceptualization of the manuscript, the writing and editing of the epistemology and ontology sections, and discussion of these concepts through other sections, as well as overall final revisions. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Heather Hower .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
RBM is a Senior Editor of this Journal. All other authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hower, H., LaMarre, A., Bachner-Melman, R. et al. Conceptualizing eating disorder recovery research: Current perspectives and future research directions. J Eat Disord 10 , 165 (2022). https://doi.org/10.1186/s40337-022-00678-8
Download citation
Received : 05 September 2022
Accepted : 25 October 2022
Published : 15 November 2022
DOI : https://doi.org/10.1186/s40337-022-00678-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Quantitative research
- Qualitative research
- Multi-methods research
Journal of Eating Disorders
ISSN: 2050-2974
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
DSM-5 Feeding and Eating Disorder. The second important change was the combination of the DSM-IV section titled "Feeding and Eating Disorders of Infancy or Early Childhood" with "Eating Disorders" to form an expanded section, "Feeding and Eating Disorders.". This change thereby included three diagnostic categories: pica, rumination ...
The nine item avoidant/restrictive food intake disorder screen (NIAS) is a short and practical assessment tool specific to ARFID with three ARFID phenotypes such as "Picky eating," "Fear," and "Appetite". This... Hakan Öğütlü, Meryem Kaşak, Uğur Doğan, Hana F. Zickgraf and Mehmet Hakan Türkçapar. Journal of Eating Disorders ...
Eating disorders (ED) such as anorexia nervosa, bulimia nervosa and binge eating disorders lead to higher physical and psychological morbidity, disabilities, and mortality rates . The prevalence of eating disorder is increasing, with the lifetime prevalence between 3.3 and 18.6% among women and between 0.8 and 6.5% among men [ 2 ].
Advances and the current status of evidence‐based treatment and outcomes for the main eating disorders, anorexia nervosa, bulimia nervosa and BED are discussed with focus on first‐line psychological therapies. Deficits in knowledge and directions for further research are highlighted, particularly with regard to treatments for BED and ARFID ...
Eating disorders (ED), especially Anorexia Nervosa (AN), are internationally reported to have amongst the highest mortality and suicide rates in mental health. With limited evidence for current pharmacological and/or psychological treatments, there is a grave responsibility within health research to better understand outcomes for people with a lived experience of ED, factors and interventions ...
Methods. This article provides a state-of-the-art review of current neurobiological research in eating disorders in children, adolescents and young adults up to 25 years of age when brain structure has generally matured to adult levels while avoiding effects from aging or illness chronicity. 5 The US National Library of Medicine database PubMed was searched for brain research studies done in ...
Aims and scope. Journal of Eating Disorders is the first open access, peer-reviewed journal publishing leading research in the science and clinical practice of eating disorders. It disseminates research that provides answers to the important issues and key challenges in the field of eating disorders and to facilitate translation of evidence ...
Eating disorders are disabling, deadly, and costly mental disorders that considerably impair physical health and disrupt psychosocial functioning. Disturbed attitudes towards weight, body shape, and eating play a key role in the origin and maintenance of eating disorders. Eating disorders have been increasing over the past 50 years and changes in the food environment have been implicated.
Introduction. Eating disorders have their peak onset in adolescence and a severe impact on physical and mental health (Qian et al., Citation 2022).At the core of eating disorders is concern over eating, shape, weight and their control (Fairburn et al., Citation 2003b).Disordered eating behaviours may consist of overeating or insufficient food intake and be associated with compensatory ...
Meet the Editor. Ruth Weissman is a Walter Crowell University Professor of Social Sciences, Emerita, at Wesleyan University, USA. She is a clinical psychologist with research expertise in eating and weight disorders. Her scholarship focuses on reducing the burden of suffering associated with eating and weight problems, and past projects have included work on defining and classifying eating ...
Eating psychopathology was measured with the Eating Disorder Examination Interview (EDE) interview (33, 34) and the Eating Disorder Inventory self-report questionnaire (EDI-2) (35, 36), general psychopathology with the Symptom-Check-List (SCL-90-R) , see also . In the original study, time points of measurement were admission, discharge as well ...
Recent research on eating disorders has highlighted the complexity of these conditions including the significance of early period intervention measures in treatment, the role of genetics and social factors, and the impact of the COVID-19 pandemic. Eating disorders are associated with a range of negative health outcomes, including malnutrition ...
A comprehensive review of eating disorders in children and adolescents, covering the causes, diagnosis, treatment, and prevention of these complex conditions. Published by Sage, a leading publisher of social science research.
Eating disorders are disabling, deadly, and costly mental disorders that considerably impair physical health and disrupt psychosocial functioning. Disturbed attitudes towards weight, body shape, and eating play a key role in the origin and maintenance of eating disorders. Eating disorders have been increasing over the past 50 years and changes ...
Furthermore, our study might provide an impetus for research into binge-eating disorder and OSFED, which have received less attention than other eating disorders. The current study drew on the GBD epidemiological dataset and modelled prevalence and burden for eating disorders. Although GBD is the most comprehensive epidemiological study ...
Objective Mealtimes are a period of heightened distress for individuals with eating disorders. Patients frequently display maladaptive coping strategies, such as hiding food and using distraction techniques to avoid eating. The aim of this systematic review is to evaluate the evidence for meal support interventions as a first-line intervention for eating disorders. Method Six databases were ...
Abstract. Binge eating disorder (BED) is characterized by regular binge eating episodes during which individuals ingest comparably large amounts of food and experience loss of control over their ...
There are many forms of EDs, which are described in the Diagnostic and Statistical Manual of Mental Disorders (DSM) and International Classification of Diseases and Related Health Problems (ICD) classifications. The most widely used classification is the DSM classification. EDs appeared in 1980 within the DSM-III, their criteria were revised in 1987, and evolved over time with DSM-IV in 1994 ...
A Singapore-based study by Ho et al ( 3) found that 7.4% of females (aged 12-26 years) are at risk of developing an eating disorder. Eating disorders are serious illnesses and have the highest mortality rate among all psychiatric disorders, with mortality stemming from both the physical and psychiatric complications.
Eating disorders are serious mental illnesses that can lead to severe complications, including death. Common eating disorders include anorexia nervosa, bulimia nervosa, and binge-eating disorder. Behaviors associated with eating disorders can vary in type and severity and include actions such as binge-eating, purging, and restricting food intake.
In recent years there has been an increase in qualitative eating disorder research [] which explores the experiences of persons living with eating disorders.However, a number of these studies struggle to grasp the importance of conducting qualitative research in natural settings [2, 3].Much of this qualitative research has also been grounded in traditional research paradigms, and therefore ...
In life-threatening situations, call 911. Symptoms include: Extremely restricted eating. Extreme thinness (emaciation) A relentless pursuit of thinness and unwillingness to maintain a normal or healthy weight. Intense fear of gaining weight. Distorted body image, a self-esteem that is heavily influenced by perceptions of body weight and shape ...
Avoidant Restrictive Food Intake Disorder (ARFID) is a new diagnosis added to the DSM-5 characterized by pathological eating habits without body image disturbances. Previous findings demonstrated a general association between high levels of perfectionism and low levels of self-esteem in association with general eating disorders. However, research is scant when it comes to ARFID specifically.
Night-Eating Syndrome (NES) is a complex eating disorder that has gained recognition in the context of bariatric surgery. However, its prevalence and associated factors in this specific patient population remain understudied, particularly in the Saudi Arabian context. This cross-sectional study was conducted at King Abdulaziz University Hospital in Jeddah, Saudi Arabia, from June to November 2022.
In the present review, the results show that the main factors associated with eating disorders were psychological-type with a prevalence of the factor inherent the dissatisfaction with body image ( 16 ─ 18, 21, 25, 27, 29, 31, 32, 35 ). Literature refers that dissatisfaction with body image increases significantly in adolescence due to ...
Eating disorders (ED) such as anorexia nervosa, bulimia nervosa and binge eating disorders lead to higher physical and psychological morbidity, disabilities, and mortality rates [].The prevalence of eating disorder is increasing, with the lifetime prevalence between 3.3 and 18.6% among women and between 0.8 and 6.5% among men [].Risk factors such as dieting and body dissatisfaction have been ...
Howard et al. (2023) interviewed 11 females over the age of 18 who were receiving outpatient treatment for anorexia nervosa in a community eating-disorders service.
This study is one review of a wider Rapid Review series conducted as part the development of Australia's National Eating Disorders Research and Translation Strategy 2021-2031. The findings from this review are grouped into nine main risk factor categories. These include (1) genetics, (2) gastrointestinal microbiota and autoimmune reactions ...
Background How we research eating disorder (ED) recovery impacts what we know (perceive as fact) about it. Traditionally, research has focused more on the "what" of recovery (e.g., establishing criteria for recovery, reaching consensus definitions) than the "how" of recovery research (e.g., type of methodologies, triangulation of perspectives). In this paper we aim to provide an ...