- Share full article
Advertisement
Supported by
student opinion

How Is the Coronavirus Outbreak Affecting Your Life?
How are you staying connected and sane in a time of social distancing?

By Jeremy Engle
Find all our Student Opinion questions here.
Note: The Times Opinion section is working on an article about how the coronavirus outbreak has disrupted the lives of high school students. To share your story, fill out this form .
The coronavirus has changed how we work , play and learn : Schools are closing, sports leagues have been canceled, and many people have been asked to work from home.
On March 16, the Trump administration released new guidelines to slow the spread of the coronavirus, including closing schools and avoiding groups of more than 10 people, discretionary travel, bars, restaurants and food courts.
How are you dealing with these sudden and dramatic changes to how we live? Are you practicing social distancing — and are you even sure what that really means?
In “ Wondering About Social Distancing? ” Apoorva Mandavilli explains the term and offers practical guidance from experts:
What is social distancing? Put simply, the idea is to maintain a distance between you and other people — in this case, at least six feet. That also means minimizing contact with people. Avoid public transportation whenever possible, limit nonessential travel, work from home and skip social gatherings — and definitely do not go to crowded bars and sporting arenas. “Every single reduction in the number of contacts you have per day with relatives, with friends, co-workers, in school will have a significant impact on the ability of the virus to spread in the population,” said Dr. Gerardo Chowell, chair of population health sciences at Georgia State University. This strategy saved thousands of lives both during the Spanish flu pandemic of 1918 and, more recently, in Mexico City during the 2009 flu pandemic.
The article continues with expert responses to some common questions about social distancing. Here are excerpts from three:
I’m young and don’t have any risk factors. Can I continue to socialize? Please don’t. There is no question that older people and those with underlying health conditions are most vulnerable to the virus, but young people are by no means immune. And there is a greater public health imperative. Even people who show only mild symptoms may pass the virus to many, many others — particularly in the early course of the infection, before they even realize they are sick. So you might keep the chain of infection going right to your own older or high-risk relatives. You may also contribute to the number of people infected, causing the pandemic to grow rapidly and overwhelm the health care system. If you ignore the guidance on social distancing, you will essentially put yourself and everyone else at much higher risk. Experts acknowledged that social distancing is tough, especially for young people who are used to gathering in groups. But even cutting down the number of gatherings, and the number of people in any group, will help. Can I leave my house? Absolutely. The experts were unanimous in their answer to this question. It’s O.K. to go outdoors for fresh air and exercise — to walk your dog, go for a hike or ride your bicycle, for example. The point is not to remain indoors, but to avoid being in close contact with people. You may also need to leave the house for medicines or other essential resources. But there are things you can do to keep yourself and others safe during and after these excursions. When you do leave your home, wipe down any surfaces you come into contact with, disinfect your hands with an alcohol-based sanitizer and avoid touching your face. Above all, frequently wash your hands — especially whenever you come in from outside, before you eat or before you’re in contact with the very old or very young. How long will we need to practice social distancing? That is a big unknown, experts said. A lot will depend on how well the social distancing measures in place work and how much we can slow the pandemic down. But prepare to hunker down for at least a month, and possibly much longer. In Seattle, the recommendations on social distancing have continued to escalate with the number of infections and deaths, and as the health system has become increasingly strained. “For now, it’s probably indefinite,” Dr. Marrazzo said. “We’re in uncharted territory.”
Abdullah Shihipar writes in an Opinion essay, “ Coronavirus and the Isolation Paradox ,” that while social distancing is required to prevent infection, loneliness can make us sick:
A paradox of this moment is that while social distancing is required to contain the spread of the coronavirus, it may also contribute to poor health in the long run. So while physical isolation will be required for many Americans who have Covid-19 or have been exposed to it, it’s important that we don’t let such measures cause social and emotional isolation, too. The Health Resources and Services Administration cautions that loneliness can be as damaging to health as smoking 15 cigarettes a day. Feelings of isolation and loneliness can increase the likelihood of depression, high blood pressure, and death from heart disease. They can also affect the immune system’s ability to fight infection — a fact that’s especially relevant during a pandemic. Studies have shown that loneliness can activate our fight-or-flight function, causing chronic inflammation and reducing the body’s ability to defend itself from viruses.
The essay continues:
For solutions, we can look to countries where people have been dealing with coronavirus for some time. As the BBC reported, people in China are turning to creative means to stay connected. Some are streaming concerts and gym classes. Others are organizing virtual book-club meetings. In Wuhan, people gathered at their windows to shout “Wuhan, jiayou!” which translates to “Keep fighting, Wuhan!” A business owner packed 200 meals for medical workers, while a villager in a neighboring province donated 15,000 masks to those in need. For those of us who know people, especially elderly people, who may be isolated, get connected. Check in daily and look for ways to spend time together, either through a FaceTime or WhatsApp call, through collaborative gaming or just by using the telephone.
It concludes:
It may provide some comfort to know that thousands of other people are going through the same thing, and as in China, collective coping strategies will emerge. TikTok videos, memes, stories, essays and poems about living in isolation will all become part of the culture. We could come out of this feeling more connected to each other than before.
Students, read ONE of the articles in its entirety, then tell us:
How is the coronavirus affecting your life — physically, socially and emotionally? What changes have you, your friends, family and community experienced? What has been the most difficult aspect for you?
How is the coronavirus outbreak disrupting your middle or high school experience? Has your school been closed? If so, what does your education look and feel like now? If not, are you worried about your school closing? Does your school have a plan in place if it does?
Are you and your family practicing any forms of social distancing? If yes, which ones and why? Will you practice more social distancing now that you have read this article?
How are you staying connected and sane in a time of social distancing? How have you been staying in touch with your social groups? What new routines have you developed?
What helps you deal with all the changes brought about by the coronavirus outbreak? How do you cope with feelings of isolation and loneliness? Do any of the coping strategies suggested by Mr. Shihipar resonate with you? What strategies would you recommend to others?
Students 13 and older are invited to comment. All comments are moderated by the Learning Network staff, but please keep in mind that once your comment is accepted, it will be made public.
Jeremy Engle joined The Learning Network as a staff editor in 2018 after spending more than 20 years as a classroom humanities and documentary-making teacher, professional developer and curriculum designer working with students and teachers across the country. More about Jeremy Engle
- Newsletters
Site search
- Israel-Hamas war
- 2024 election
- Kate Middleton
- TikTok’s fate
- Supreme Court
- All explainers
- Future Perfect
Filed under:
Read these 12 moving essays about life during coronavirus
Artists, novelists, critics, and essayists are writing the first draft of history.
Share this story
- Share this on Facebook
- Share this on Twitter
- Share this on Reddit
- Share All sharing options
Share All sharing options for: Read these 12 moving essays about life during coronavirus
/cdn.vox-cdn.com/uploads/chorus_image/image/66606035/1207638131.jpg.0.jpg)
The world is grappling with an invisible, deadly enemy, trying to understand how to live with the threat posed by a virus . For some writers, the only way forward is to put pen to paper, trying to conceptualize and document what it feels like to continue living as countries are under lockdown and regular life seems to have ground to a halt.
So as the coronavirus pandemic has stretched around the world, it’s sparked a crop of diary entries and essays that describe how life has changed. Novelists, critics, artists, and journalists have put words to the feelings many are experiencing. The result is a first draft of how we’ll someday remember this time, filled with uncertainty and pain and fear as well as small moments of hope and humanity.
At the New York Review of Books, Ali Bhutto writes that in Karachi, Pakistan, the government-imposed curfew due to the virus is “eerily reminiscent of past military clampdowns”:
Beneath the quiet calm lies a sense that society has been unhinged and that the usual rules no longer apply. Small groups of pedestrians look on from the shadows, like an audience watching a spectacle slowly unfolding. People pause on street corners and in the shade of trees, under the watchful gaze of the paramilitary forces and the police.
His essay concludes with the sobering note that “in the minds of many, Covid-19 is just another life-threatening hazard in a city that stumbles from one crisis to another.”
Writing from Chattanooga, novelist Jamie Quatro documents the mixed ways her neighbors have been responding to the threat, and the frustration of conflicting direction, or no direction at all, from local, state, and federal leaders:
Whiplash, trying to keep up with who’s ordering what. We’re already experiencing enough chaos without this back-and-forth. Why didn’t the federal government issue a nationwide shelter-in-place at the get-go, the way other countries did? What happens when one state’s shelter-in-place ends, while others continue? Do states still under quarantine close their borders? We are still one nation, not fifty individual countries. Right?
Award-winning photojournalist Alessio Mamo, quarantined with his partner Marta in Sicily after she tested positive for the virus, accompanies his photographs in the Guardian of their confinement with a reflection on being confined :
The doctors asked me to take a second test, but again I tested negative. Perhaps I’m immune? The days dragged on in my apartment, in black and white, like my photos. Sometimes we tried to smile, imagining that I was asymptomatic, because I was the virus. Our smiles seemed to bring good news. My mother left hospital, but I won’t be able to see her for weeks. Marta started breathing well again, and so did I. I would have liked to photograph my country in the midst of this emergency, the battles that the doctors wage on the frontline, the hospitals pushed to their limits, Italy on its knees fighting an invisible enemy. That enemy, a day in March, knocked on my door instead.
In the New York Times Magazine, deputy editor Jessica Lustig writes with devastating clarity about her family’s life in Brooklyn while her husband battled the virus, weeks before most people began taking the threat seriously:
At the door of the clinic, we stand looking out at two older women chatting outside the doorway, oblivious. Do I wave them away? Call out that they should get far away, go home, wash their hands, stay inside? Instead we just stand there, awkwardly, until they move on. Only then do we step outside to begin the long three-block walk home. I point out the early magnolia, the forsythia. T says he is cold. The untrimmed hairs on his neck, under his beard, are white. The few people walking past us on the sidewalk don’t know that we are visitors from the future. A vision, a premonition, a walking visitation. This will be them: Either T, in the mask, or — if they’re lucky — me, tending to him.
Essayist Leslie Jamison writes in the New York Review of Books about being shut away alone in her New York City apartment with her 2-year-old daughter since she became sick:
The virus. Its sinewy, intimate name. What does it feel like in my body today? Shivering under blankets. A hot itch behind the eyes. Three sweatshirts in the middle of the day. My daughter trying to pull another blanket over my body with her tiny arms. An ache in the muscles that somehow makes it hard to lie still. This loss of taste has become a kind of sensory quarantine. It’s as if the quarantine keeps inching closer and closer to my insides. First I lost the touch of other bodies; then I lost the air; now I’ve lost the taste of bananas. Nothing about any of these losses is particularly unique. I’ve made a schedule so I won’t go insane with the toddler. Five days ago, I wrote Walk/Adventure! on it, next to a cut-out illustration of a tiger—as if we’d see tigers on our walks. It was good to keep possibility alive.
At Literary Hub, novelist Heidi Pitlor writes about the elastic nature of time during her family’s quarantine in Massachusetts:
During a shutdown, the things that mark our days—commuting to work, sending our kids to school, having a drink with friends—vanish and time takes on a flat, seamless quality. Without some self-imposed structure, it’s easy to feel a little untethered. A friend recently posted on Facebook: “For those who have lost track, today is Blursday the fortyteenth of Maprilay.” ... Giving shape to time is especially important now, when the future is so shapeless. We do not know whether the virus will continue to rage for weeks or months or, lord help us, on and off for years. We do not know when we will feel safe again. And so many of us, minus those who are gifted at compartmentalization or denial, remain largely captive to fear. We may stay this way if we do not create at least the illusion of movement in our lives, our long days spent with ourselves or partners or families.
Novelist Lauren Groff writes at the New York Review of Books about trying to escape the prison of her fears while sequestered at home in Gainesville, Florida:
Some people have imaginations sparked only by what they can see; I blame this blinkered empiricism for the parks overwhelmed with people, the bars, until a few nights ago, thickly thronged. My imagination is the opposite. I fear everything invisible to me. From the enclosure of my house, I am afraid of the suffering that isn’t present before me, the people running out of money and food or drowning in the fluid in their lungs, the deaths of health-care workers now growing ill while performing their duties. I fear the federal government, which the right wing has so—intentionally—weakened that not only is it insufficient to help its people, it is actively standing in help’s way. I fear we won’t sufficiently punish the right. I fear leaving the house and spreading the disease. I fear what this time of fear is doing to my children, their imaginations, and their souls.
At ArtForum , Berlin-based critic and writer Kristian Vistrup Madsen reflects on martinis, melancholia, and Finnish artist Jaakko Pallasvuo’s 2018 graphic novel Retreat , in which three young people exile themselves in the woods:
In melancholia, the shape of what is ending, and its temporality, is sprawling and incomprehensible. The ambivalence makes it hard to bear. The world of Retreat is rendered in lush pink and purple watercolors, which dissolve into wild and messy abstractions. In apocalypse, the divisions established in genesis bleed back out. My own Corona-retreat is similarly soft, color-field like, each day a blurred succession of quarantinis, YouTube–yoga, and televized press conferences. As restrictions mount, so does abstraction. For now, I’m still rooting for love to save the world.
At the Paris Review , Matt Levin writes about reading Virginia Woolf’s novel The Waves during quarantine:
A retreat, a quarantine, a sickness—they simultaneously distort and clarify, curtail and expand. It is an ideal state in which to read literature with a reputation for difficulty and inaccessibility, those hermetic books shorn of the handholds of conventional plot or characterization or description. A novel like Virginia Woolf’s The Waves is perfect for the state of interiority induced by quarantine—a story of three men and three women, meeting after the death of a mutual friend, told entirely in the overlapping internal monologues of the six, interspersed only with sections of pure, achingly beautiful descriptions of the natural world, a day’s procession and recession of light and waves. The novel is, in my mind’s eye, a perfectly spherical object. It is translucent and shimmering and infinitely fragile, prone to shatter at the slightest disturbance. It is not a book that can be read in snatches on the subway—it demands total absorption. Though it revels in a stark emotional nakedness, the book remains aloof, remote in its own deep self-absorption.
In an essay for the Financial Times, novelist Arundhati Roy writes with anger about Indian Prime Minister Narendra Modi’s anemic response to the threat, but also offers a glimmer of hope for the future:
Historically, pandemics have forced humans to break with the past and imagine their world anew. This one is no different. It is a portal, a gateway between one world and the next. We can choose to walk through it, dragging the carcasses of our prejudice and hatred, our avarice, our data banks and dead ideas, our dead rivers and smoky skies behind us. Or we can walk through lightly, with little luggage, ready to imagine another world. And ready to fight for it.
From Boston, Nora Caplan-Bricker writes in The Point about the strange contraction of space under quarantine, in which a friend in Beirut is as close as the one around the corner in the same city:
It’s a nice illusion—nice to feel like we’re in it together, even if my real world has shrunk to one person, my husband, who sits with his laptop in the other room. It’s nice in the same way as reading those essays that reframe social distancing as solidarity. “We must begin to see the negative space as clearly as the positive, to know what we don’t do is also brilliant and full of love,” the poet Anne Boyer wrote on March 10th, the day that Massachusetts declared a state of emergency. If you squint, you could almost make sense of this quarantine as an effort to flatten, along with the curve, the distinctions we make between our bonds with others. Right now, I care for my neighbor in the same way I demonstrate love for my mother: in all instances, I stay away. And in moments this month, I have loved strangers with an intensity that is new to me. On March 14th, the Saturday night after the end of life as we knew it, I went out with my dog and found the street silent: no lines for restaurants, no children on bicycles, no couples strolling with little cups of ice cream. It had taken the combined will of thousands of people to deliver such a sudden and complete emptiness. I felt so grateful, and so bereft.
And on his own website, musician and artist David Byrne writes about rediscovering the value of working for collective good , saying that “what is happening now is an opportunity to learn how to change our behavior”:
In emergencies, citizens can suddenly cooperate and collaborate. Change can happen. We’re going to need to work together as the effects of climate change ramp up. In order for capitalism to survive in any form, we will have to be a little more socialist. Here is an opportunity for us to see things differently — to see that we really are all connected — and adjust our behavior accordingly. Are we willing to do this? Is this moment an opportunity to see how truly interdependent we all are? To live in a world that is different and better than the one we live in now? We might be too far down the road to test every asymptomatic person, but a change in our mindsets, in how we view our neighbors, could lay the groundwork for the collective action we’ll need to deal with other global crises. The time to see how connected we all are is now.
The portrait these writers paint of a world under quarantine is multifaceted. Our worlds have contracted to the confines of our homes, and yet in some ways we’re more connected than ever to one another. We feel fear and boredom, anger and gratitude, frustration and strange peace. Uncertainty drives us to find metaphors and images that will let us wrap our minds around what is happening.
Yet there’s no single “what” that is happening. Everyone is contending with the pandemic and its effects from different places and in different ways. Reading others’ experiences — even the most frightening ones — can help alleviate the loneliness and dread, a little, and remind us that what we’re going through is both unique and shared by all.
Will you help keep Vox free for all?
At Vox, we believe that clarity is power, and that power shouldn’t only be available to those who can afford to pay. That’s why we keep our work free. Millions rely on Vox’s clear, high-quality journalism to understand the forces shaping today’s world. Support our mission and help keep Vox free for all by making a financial contribution to Vox today.
We accept credit card, Apple Pay, and Google Pay. You can also contribute via
Next Up In Culture
Sign up for the newsletter today, explained.
Understand the world with a daily explainer plus the most compelling stories of the day.
Thanks for signing up!
Check your inbox for a welcome email.
Oops. Something went wrong. Please enter a valid email and try again.
Lead pollution anywhere is a public health threat everywhere

Multigenerational housing is coming back in a big way
Biden wants to campaign on housing. He also sort of has to.
Want a 32-hour workweek? Give workers more power.

The harrowing “Quiet on Set” allegations, explained

The chaplain who doesn’t believe in God
4 Ways That the Pandemic Changed How We See Ourselves

A fter more than two years of pandemic life , it seems like we’ve changed as people. But how? In the beginning, many wished for a return to normal, only to realize that this might never be possible—and that could be a good thing. Although we experienced the same global crisis, it has impacted people in extremely different ways and encouraged us to think more deeply about who we are and what we’re looking for.
Isolation tested our sense of identity because it limited our access to in-person social feedback. For decades, scientists have explored how “the self is a social product.” We interpret the world through social observation. In 1902, Charles Cooley invented the concept “the looking glass self.” It explains how we develop our identity based on how we believe other people see us, but also try to influence their perceptions , so they see us in the way we’d like to be seen. If we understand who we are based on social feedback, what happened to our sense of self under isolation?
Here are four ways that the pandemic changed how we see ourselves.
When lockdown started, our identities felt less stable, but we adjusted back over time
In crisis, our self-concept was challenged. A December 2020 study by Guido Alessandri and colleagues, which was published in Identity: An International Journal of Theory and Research , measured how Italians reacted to the first week of the COVID-19 lockdown in March 2020 by evaluating how their self-concept clarity—the extent to which they have a consistent sense of self—affected their negative emotional response to the sudden lockdown.
Self-concept clarity represents “how much you have [clearly defined who you are] in your mind … not in this moment but in general,” explains Alessandri, a psychology professor at the Sapienza University of Rome. While generally people have high self-concept clarity, those with depression or personality disorders usually experience lower levels. “The lockdown threatened people’s self-concept. The very surprising result was that people with higher self-concept clarity [were] more reactive” and experienced a greater increase in negative affect than those with lower self-concept clarity.
In Alessandri’s study, people eventually returned to their initial stages of self-concept clarity, but it took longer than expected due to the shock and distress of the pandemic. This reflects a concept called emotional inertia , where emotional states are “resistant to change” and take some time to return to a baseline level. At the beginning of the pandemic, we questioned what we believed to be true about ourselves, but since then, we’ve adjusted to this new world.
Many people were forced to adopt new social roles, but the discomfort they felt depends on how important that role is to them
Our identities are not fixed; we hold several different social roles within our family, workplace, and friend groups, which naturally change over time. But in isolation, many of our social roles had to involuntarily change , from “parents homeschooling children [to] friends socializing online and employees working from home.”
As we adapted to a new way of life, a study published in September 2021 in PLOS One found that people who experienced involuntary social role disruptions because of COVID-19 reported increased feelings of inauthenticity—which could mean feeling disconnected from their true self because of their current situation. It was challenging for people to suddenly change their routines and feel like themselves in the midst of a crisis.
But the study also uncovered that “this social role interruption affects people’s sense of authenticity only to the extent that the role is important to you,” says co-author Jingshi (Joyce) Liu, a lecturer in marketing at the City campus of the University of London. If being a musician is central to your identity, for example, it’s more likely that you would feel inauthentic playing virtual shows on Zoom, but if your job isn’t a big part of who you are, you may not be as affected.
To feel more comfortable in their new identity, people can start accepting their new sense of self without trying to go back to who they once were
Over the last two years, our mindset and control over the roles we occupy in many facets of life helped determine how virtual learning and remote work affected us. “We are very sensitive to our environment,” Liu says. “[The] disruption of who we are will nonetheless feed into how we feel about our own authenticity.” But we can do our best to accept these changes and even form a new sense of self. “[If] I incorporated virtual teaching as a part of my self-identity, I [may not] need to change my behavior to go back to classroom teaching for me to feel authentic. I simply just adapt or expand the definition of what it means to be a teacher,” she adds. Similarly, if you’re a therapist, you can expand your understanding of what consulting with patients looks like to include video and phone calls.
During the pandemic, many people have made voluntary role changes, like choosing to become parents, move to a new city or country, or accept a new job. Previous research by Ibarra and Barbulescu (2010) shows that although these voluntary role changes may temporarily cause a sense of inauthenticity, they eventually tend to result in a feeling of authenticity because people are taking steps to be true to themselves or start a new chapter. “The authenticity will be restored as people adapt to their new identity,” Liu says.
Our identities have changed, so it’s important to be authentic with how we present ourselves online and offline
We have more power than we may realize to navigate a crisis by accepting that it’s OK to change. But it’s important to act in a way that’s true to ourselves. “People have a perception of the true self … They have some idea of who they truly are,” Liu says. “When you lend that to the [looking glass self], I think people would feel most inauthentic when they are performing to others in a way that is inconsistent with how they are [thinking and feeling internally],” which can happen on social media.
In isolation , when we didn’t have access to the same level of social feedback as normal, social media in some cases became a lifeline and a substitute for our self-presentation. The pandemic inspired people to take space away from the Internet and others to become increasingly dependent on it for their social wellbeing. “[Our unpublished data shows] that time spent on social media increased people’s sense of inauthenticity, perhaps because social media entails a lot of impression management [and] people are heavily editing themselves on these platforms,” Liu says.
With all that we’ve experienced, many of us have fundamentally changed as people. “In the same way which the first lockdown required us to [self-regulate] and adhere to new social norms, these changes that we’re experiencing now require another self-regulation effort to understand what is happening,” Alessandri says. “We don’t expect that people will simply get back to their previous [lives]—I don’t think this is possible. I think we have to negotiate a new kind of reality.”
The more we accept that we are no longer the same people after this crisis, the easier it will be for us to reconcile who we are now and who we want to become.
More Must-Reads From TIME
- Jane Fonda Champions Climate Action for Every Generation
- Biden’s Campaign Is In Trouble. Will the Turnaround Plan Work?
- Why We're Spending So Much Money Now
- The Financial Influencers Women Actually Want to Listen To
- Breaker Sunny Choi Is Heading to Paris
- Why TV Can’t Stop Making Silly Shows About Lady Journalists
- The Case for Wearing Shoes in the House
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]
You May Also Like
- COVID-19 and your mental health
Worries and anxiety about COVID-19 and its impact can be overwhelming. Learn ways to cope during this pandemic.
The COVID-19 pandemic may have brought many changes to how you live your life, and with it, at times, uncertainty, altered daily routines, financial pressures and social isolation. You may worry about getting sick, how long the pandemic will last, whether your job will be affected and what the future will bring. Information overload, rumors and misinformation can make your life feel out of control and make it unclear what to do.
During the COVID-19 pandemic, you may experience stress, anxiety, fear, sadness and loneliness. And mental health disorders, including anxiety and depression, can worsen.
Surveys show a major increase in the number of U.S. adults who report symptoms of stress, anxiety, depression and insomnia during the pandemic, compared with surveys before the pandemic. Some people have increased their use of alcohol or drugs, thinking that can help them cope with their fears about the pandemic. In reality, using these substances can worsen anxiety and depression.
People with substance use disorders, notably those addicted to tobacco or opioids, are likely to have worse outcomes if they get COVID-19 . That's because these addictions can harm lung function and weaken the immune system, causing chronic conditions such as heart disease and lung disease, which increase the risk of serious complications from COVID-19 .
For all of these reasons, it's important to learn self-care strategies and get the care you need to help you cope.
Self-care strategies
Self-care strategies are good for your mental and physical health and can help you take charge of your life. Take care of your body and your mind and connect with others to benefit your mental health.
Take care of your body
Be mindful about your physical health:
- Get enough sleep. Go to bed and get up at the same times each day. Stick close to your typical sleep-wake schedule, even if you're staying at home.
- Participate in regular physical activity. Regular physical activity and exercise can help reduce anxiety and improve mood. Find an activity that includes movement, such as dance or exercise apps. Get outside, such as a nature trail or your own backyard.
- Eat healthy. Choose a well-balanced diet. Avoid loading up on junk food and refined sugar. Limit caffeine as it can aggravate stress, anxiety and sleep problems.
- Avoid tobacco, alcohol and drugs. If you smoke tobacco or if you vape, you're already at higher risk of lung disease. Because COVID-19 affects the lungs, your risk increases even more. Using alcohol to try to cope can make matters worse and reduce your coping skills. Avoid taking drugs to cope, unless your doctor prescribed medications for you.
- Limit screen time. Turn off electronic devices for some time each day, including 30 to 60 minutes before bedtime. Make a conscious effort to spend less time in front of a screen — television, tablet, computer and phone.
- Relax and recharge. Set aside time for yourself. Even a few minutes of quiet time can be refreshing and help to settle your mind and reduce anxiety. Many people benefit from practices such as deep breathing, tai chi, yoga, mindfulness or meditation. Soak in a bubble bath, listen to music, or read or listen to a book — whatever helps you relax. Select a technique that works for you and practice it regularly.
Take care of your mind
Reduce stress triggers:
- Keep your regular routine. Maintaining a regular daily schedule is important to your mental health. In addition to sticking to a regular bedtime routine, keep consistent times for meals, bathing and getting dressed, work or study schedules, and exercise. Also set aside time for activities you enjoy. This predictability can make you feel more in control.
- Limit exposure to news media. Constant news about COVID-19 from all types of media can heighten fears about the disease. Limit social media that may expose you to rumors and false information. Also limit reading, hearing or watching other news, but keep up to date on national and local recommendations. Look for reliable sources, such as the U.S. Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
- Stay busy. Healthy distractions can get you away from the cycle of negative thoughts that feed anxiety and depression. Enjoy hobbies that you can do at home, such as reading a book, writing in a journal, making a craft, playing games or cooking a new meal. Or identify a new project or clean out that closet you promised you'd get to. Doing something positive to manage anxiety is a healthy coping strategy.
- Focus on positive thoughts. Choose to focus on the positive things in your life, instead of dwelling on how bad you feel. Consider starting each day by listing things you are thankful for. Maintain a sense of hope, work to accept changes as they occur and try to keep problems in perspective.
- Use your moral compass or spiritual life for support. If you draw strength from a belief system, it can bring you comfort during difficult and uncertain times.
- Set priorities. Don't become overwhelmed by creating a life-changing list of things to achieve while you're home. Set reasonable goals each day and outline steps you can take to reach those goals. Give yourself credit for every step in the right direction, no matter how small. And recognize that some days will be better than others.
Connect with others
Build support and strengthen relationships:
Make connections. If you work remotely from home or you need to isolate yourself from others for a period of time due to COVID-19 , avoid social isolation. Find time each day to make virtual connections by email, texts, phone or video chat. If you're working remotely from home, ask your co-workers how they're doing and share coping tips. Enjoy virtual socializing and talking to those in your home.
If you're not fully vaccinated, be creative and safe when connecting with others in person, such as going for walks, chatting in the driveway and other outdoor activities, or wearing a mask for indoor activities.
If you are fully vaccinated, you can more safely return to many indoor and outdoor activities you may not have been able to do because of the pandemic, such as gathering with friends and family. If you are in an area with a high number of people with COVID-19 in the hospital, the CDC recommends wearing a mask indoors in public or outdoors in crowded areas or in close contact with unvaccinated people. For unvaccinated people, outdoor activities that allow plenty of space between you and others pose a lower risk of spread of the COVID-19 virus than indoor activities do.
- Do something for others. Find purpose in helping the people around you. Helping others is an excellent way to help ourselves. For example, email, text or call to check on your friends, family members and neighbors — especially those who are older. If you know someone who can't get out, ask if there's something needed, such as groceries or a prescription picked up.
- Support a family member or friend. If a family member or friend needs to be quarantined at home or in the hospital due to COVID-19 , come up with ways to stay in contact. This could be through electronic devices or the telephone or by sending a note to brighten the day, for example.
Avoid stigma and discrimination
Stigma can make people feel isolated and even abandoned. They may feel depressed, hurt and angry when friends and others in their community avoid them for fear of getting COVID-19 .
Stigma harms people's health and well-being in many ways. Stigmatized groups may often be deprived of the resources they need to care for themselves and their families during a pandemic. And people who are worried about being stigmatized may be less likely to get medical care.
People who have experienced stigma related to COVID-19 include people of Asian descent, health care workers, people with COVID-19 and those released from quarantine. People who are stigmatized may be excluded or shunned, treated differently, denied job and educational opportunities, and be targets of verbal, emotional and physical abuse.
You can reduce stigma by:
- Getting the facts about COVID-19 from reputable sources such as the CDC and WHO
- Speaking up if you hear or see inaccurate statements about COVID-19 and certain people or groups
- Reaching out to people who feel stigmatized
- Showing support for health care workers
Recognize what's typical and what's not
Stress is a normal psychological and physical reaction to the demands of life. Everyone reacts differently to difficult situations, and it's normal to feel stress and worry during a crisis. But multiple challenges, such as the effects of the COVID-19 pandemic, can push you beyond your ability to cope.
Many people may have mental health concerns, such as symptoms of anxiety and depression during this time. And feelings may change over time.
Despite your best efforts, you may find yourself feeling helpless, sad, angry, irritable, hopeless, anxious or afraid. You may have trouble concentrating on typical tasks, changes in appetite, body aches and pains, or difficulty sleeping or you may struggle to face routine chores.
When these signs and symptoms last for several days in a row, make you miserable and cause problems in your daily life so that you find it hard to carry out normal responsibilities, it's time to ask for help.
Get help when you need it
Hoping mental health problems such as anxiety or depression will go away on their own can lead to worsening symptoms. If you have concerns or if you experience worsening of mental health symptoms, ask for help when you need it, and be upfront about how you're doing. To get help you may want to:
- Call or use social media to contact a close friend or loved one — even though it may be hard to talk about your feelings.
- Contact a minister, spiritual leader or someone in your faith community.
- Contact your employee assistance program, if your employer has one, and ask for counseling or a referral to a mental health professional.
- Call your primary care professional or mental health professional to ask about appointment options to talk about your anxiety or depression and get advice and guidance. Some may provide the option of phone, video or online appointments.
- Contact organizations such as the National Alliance on Mental Illness (NAMI), the Substance Abuse and Mental Health Services Administration (SAMHSA), or the Anxiety and Depression Association of America for help and guidance on information and treatment options.
If you're feeling suicidal or thinking of hurting yourself, seek help. Contact your primary care professional or a mental health professional. Or contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline , available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential.
Continue your self-care strategies
You can expect your current strong feelings to fade when the pandemic is over, but stress won't disappear from your life when the health crisis of COVID-19 ends. Continue these self-care practices to take care of your mental health and increase your ability to cope with life's ongoing challenges.
- How stress affects your health. American Psychological Association. https://www.apa.org/helpcenter/stress-facts. Accessed Oct. 19, 2021.
- Taking care of your emotional health. Centers for Disease Control and Prevention. https://emergency.cdc.gov/coping/selfcare.asp. Accessed Oct. 19, 2021.
- COVID-19 resource and information guide. National Alliance on Mental Illness. https://www.nami.org/Support-Education/NAMI-HelpLine/COVID-19-Information-and-Resources/COVID-19-Resource-and-Information-Guide. Accessed Oct. 19, 2021.
- Combating bias and stigma related to COVID-19. American Psychological Association. https://www.apa.org/topics/covid-19-bias. Accessed Oct. 19, 2021.
- #HealthyAtHome—Mental health. World Health Organization. www.who.int/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome---mental-health. Accessed Oct. 19, 2021.
- Your healthiest self: Emotional wellness toolkit. National Institutes of Health. https://www.nih.gov/health-information/emotional-wellness-toolkit. Accessed Oct. 19, 2021.
- Coping with stress. Centers for Disease Control and Prevention. www.cdc.gov/mentalhealth/stress-coping/cope-with-stress/. Accessed Oct. 19, 2021.
- Manage stress. U.S. Department of Health and Human Services. https://health.gov/myhealthfinder/topics/health-conditions/heart-health/manage-stress. Accessed March 20, 2020.
- Health effects of cigarette smoking. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/index.htm#respiratory. Accessed March 25, 2020.
- Sawchuk CN (expert opinion). Mayo Clinic. March 27, 2020.
- Holman EA, et al. The unfolding COVID-19 pandemic: A probability-based, nationally representative study of mental health in the U.S. Science Advances. 2020; doi:10.1126/sciadv.abd5390.
- Wang QQ, et al. COVID-19 risk and outcomes in patients with substance use disorders: Analyses from electronic health records in the United States. Molecular Psychiatry. 2020; doi:10.1038/s41380-020-00880-7.
- Ettman CK, et al. Prevalence of depression symptoms in U.S. adults before and during the COVID-19 pandemic. JAMA Network Open. 2020; doi:10.1001/jamanetworkopen.2020.19686.
- Czeisler ME, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24-30, 2020. Centers for Disease Control and Prevention. Morbidity and Mortality Weekly Report. https://www.cdc.gov/mmwr/volumes/69/wr/mm6932a1.htm. Accessed Oct. 12, 2020.
- Social stigma associated with COVID-19. World Health Organization. https://www.who.int/docs/default-source/coronaviruse/covid19-stigma-guide.pdf. Accessed Oct. 20, 2021.
- Yashadhana A, et al. Pandemic-related racial discrimination and its health impact among non-Indigenous racially minoritized peoples in high-income contexts: A systematic review. Health Promotion International. 2021; doi:10.1093/heapro/daab144.
- Participate in outdoor and indoor activities. Centers for Disease Control and Prevention. www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/outdoor-activities.html. Accessed Nov. 16, 2021.
- When you've been fully vaccinated. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/fully-vaccinated.html. Accessed Nov. 16, 2021.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and coronavirus
- COVID-19 and pets
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- COVID-19 drugs: Are there any that work?
- Long-term effects of COVID-19
- COVID-19 tests
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 travel advice
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to take your pulse
- How to measure your respiratory rate
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
Related information
- The new work-life balancing act (podcast) - Related information The new work-life balancing act (podcast)
- COVID-19 pandemic's mental health toll (podcast) - Related information COVID-19 pandemic's mental health toll (podcast)
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.
Read our research on: Abortion | Podcasts | Election 2024
Regions & Countries

In Their Own Words, Americans Describe the Struggles and Silver Linings of the COVID-19 Pandemic
The outbreak has dramatically changed americans’ lives and relationships over the past year. we asked people to tell us about their experiences – good and bad – in living through this moment in history..
Pew Research Center has been asking survey questions over the past year about Americans’ views and reactions to the COVID-19 pandemic. In August, we gave the public a chance to tell us in their own words how the pandemic has affected them in their personal lives. We wanted to let them tell us how their lives have become more difficult or challenging, and we also asked about any unexpectedly positive events that might have happened during that time.
The vast majority of Americans (89%) mentioned at least one negative change in their own lives, while a smaller share (though still a 73% majority) mentioned at least one unexpected upside. Most have experienced these negative impacts and silver linings simultaneously: Two-thirds (67%) of Americans mentioned at least one negative and at least one positive change since the pandemic began.
For this analysis, we surveyed 9,220 U.S. adults between Aug. 31-Sept. 7, 2020. Everyone who completed the survey is a member of Pew Research Center’s American Trends Panel (ATP), an online survey panel that is recruited through national, random sampling of residential addresses. This way nearly all U.S. adults have a chance of selection. The survey is weighted to be representative of the U.S. adult population by gender, race, ethnicity, partisan affiliation, education and other categories. Read more about the ATP’s methodology .
Respondents to the survey were asked to describe in their own words how their lives have been difficult or challenging since the beginning of the coronavirus outbreak, and to describe any positive aspects of the situation they have personally experienced as well. Overall, 84% of respondents provided an answer to one or both of the questions. The Center then categorized a random sample of 4,071 of their answers using a combination of in-house human coders, Amazon’s Mechanical Turk service and keyword-based pattern matching. The full methodology and questions used in this analysis can be found here.
In many ways, the negatives clearly outweigh the positives – an unsurprising reaction to a pandemic that had killed more than 180,000 Americans at the time the survey was conducted. Across every major aspect of life mentioned in these responses, a larger share mentioned a negative impact than mentioned an unexpected upside. Americans also described the negative aspects of the pandemic in greater detail: On average, negative responses were longer than positive ones (27 vs. 19 words). But for all the difficulties and challenges of the pandemic, a majority of Americans were able to think of at least one silver lining.
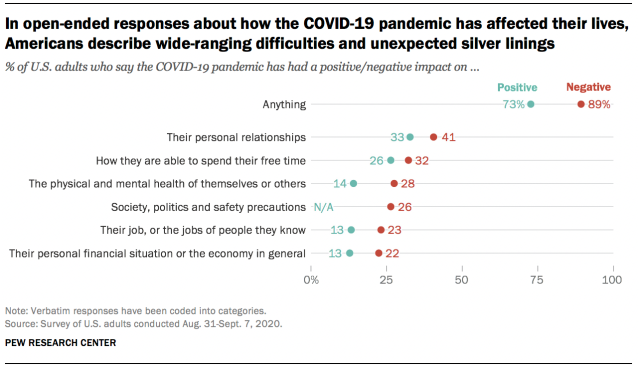
Both the negative and positive impacts described in these responses cover many aspects of life, none of which were mentioned by a majority of Americans. Instead, the responses reveal a pandemic that has affected Americans’ lives in a variety of ways, of which there is no “typical” experience. Indeed, not all groups seem to have experienced the pandemic equally. For instance, younger and more educated Americans were more likely to mention silver linings, while women were more likely than men to mention challenges or difficulties.
Here are some direct quotes that reveal how Americans are processing the new reality that has upended life across the country.
Sign up for our weekly newsletter
Fresh data delivered Saturday mornings
About Pew Research Center Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .

Illustration by Tomi Um
The Pandemic's Effects on Everyday Life
Boston College researchers are exploring COVID-19's impact on life as we know it. Here’s a look at just some of the important questions they’re asking—and answering.

Is remote work here to stay?
As many as 60 percent of U.S. employees are estimated to have worked remotely at some point during the pandemic, a shift that could lead to “profound transformations in mindsets around work and life as we know it,” said Assistant Professor of Sociology Wen Fan. In a project funded by the National Science Foundation, Fan is exploring the changing nature of work and remote workers’ experiences and preferences, as well as disparities in remote-working conditions and work-family balance by gender, socioeconomic status, and race/ethnicity, which could inform social policies moving forward. Though the team has just begun analyzing the data, Fan says one respondent’s thoughts—“It’s a fickle thing, sometimes you love it, sometimes you hate it”— captures the overall sentiment so far.

Are kids now spending too much time with screens?
When schools and daycares closed abruptly, kids began spending much more time engaged with cell phones and computers.“Screens are the babysitter of last resort,” said BC psychologist Joshua Hartshorne, coauthor of the study “Screen Time as an Index of Family Distress.” Whereas lower screen-time rates before the pandemic were thought to be a function of well- informed parenting, it’s now clear that they were also due to well-resourced parenting, he said. The next phase of the project, funded by the National Science Foundation, will examine whether screen time is actually problematic for child development.

Can we safely reuse PPE?
The pandemic revealed a severe national shortage of personal protective equipment (PPE). So when the CDC made the unprecedented recommendation to reuse N95 respirators, a team from the Connell School’s new Doctor of Nursing Practice program— Jacqueline Sly, Beth McNutt-Clarke, Nanci Haze, and Allan Thomas—created a three-minute YouTube video and guide illustrating how to don, doff, store, and then redon the masks. Their materials are now part of clinical orientation for nursing students, and the team also shared their guidelines and experiences training their colleagues in them in American Nurse and Nursing Management .

What does science say about masks?
Masks are the most important public-health tool for containing the pandemic, according to BC Law School Associate Professor Dean Hashimoto. His new book, The Case for Masks , presents situations in which wearing (or not wearing) face coverings directly affected how many people got sick. One case study focuses on the Mass General Brigham healthcare network, where Hashimoto is the chief medical officer for occupational health services. When the network required patients and 78,000 employees at its hospitals to mask up last March, there was a linear decline in COVID-19 cases among healthcare workers.

Has language development been affected?
For kids, the pandemic has meant time away from school and friends. To find out if this would affect language development, BC psychologist Joshua Hartshorne and a University of Maryland colleague created the KidTalk app ( kidtalkscrapbook.org ), a tool that allows parents to record conversations and track their children’s speech development. The data could be used by policymakers to support families after the pandemic. “The more we understand how this affects children,” Hartshorne said, “the better we can plan.”

What happens when the earth goes quiet?
There’s been much less human activity during the pandemic lockdowns—so much so that scientists recorded a drop of up to 50 percent in human-induced seismic vibrations of the earth beneath us in early 2020. Associate Professor of Earth and Environmental Sciences Alan Kafka was one of seventy-six scientists from two dozen countries who reported these results in Science . “It is culturally quieter, so we can explore the finer details of natural seismic phenomena that might otherwise be hidden,” said Kafka, who shared data from BC’s Weston Observatory, as well as from two seismometers on campus.
For more pandemic-related research from across Boston College, see sites.bc.edu/responding-to-covid-19 .
More Stories

Menstrual Care with a Conscience
Katie Diasti ’19 is creating earth-friendly and toxin-free pads and tampons.

Breaking the Cycle
Professor Catherine Taylor is testing strategies to prevent spanking and its negative outcomes.

A Billion to None
Reeves Wiedeman ’08 traces the rise and fall of the new-economy darling WeWork.

Hockey for All
Former NWHL player Blake Bolden ’13 is determined to diversify the sport she loves.
How to Write About Coronavirus in a College Essay
Students can share how they navigated life during the coronavirus pandemic in a full-length essay or an optional supplement.
Writing About COVID-19 in College Essays

Getty Images
Experts say students should be honest and not limit themselves to merely their experiences with the pandemic.
The global impact of COVID-19, the disease caused by the novel coronavirus, means colleges and prospective students alike are in for an admissions cycle like no other. Both face unprecedented challenges and questions as they grapple with their respective futures amid the ongoing fallout of the pandemic.
Colleges must examine applicants without the aid of standardized test scores for many – a factor that prompted many schools to go test-optional for now . Even grades, a significant component of a college application, may be hard to interpret with some high schools adopting pass-fail classes last spring due to the pandemic. Major college admissions factors are suddenly skewed.
"I can't help but think other (admissions) factors are going to matter more," says Ethan Sawyer, founder of the College Essay Guy, a website that offers free and paid essay-writing resources.
College essays and letters of recommendation , Sawyer says, are likely to carry more weight than ever in this admissions cycle. And many essays will likely focus on how the pandemic shaped students' lives throughout an often tumultuous 2020.
But before writing a college essay focused on the coronavirus, students should explore whether it's the best topic for them.
Writing About COVID-19 for a College Application
Much of daily life has been colored by the coronavirus. Virtual learning is the norm at many colleges and high schools, many extracurriculars have vanished and social lives have stalled for students complying with measures to stop the spread of COVID-19.
"For some young people, the pandemic took away what they envisioned as their senior year," says Robert Alexander, dean of admissions, financial aid and enrollment management at the University of Rochester in New York. "Maybe that's a spot on a varsity athletic team or the lead role in the fall play. And it's OK for them to mourn what should have been and what they feel like they lost, but more important is how are they making the most of the opportunities they do have?"
That question, Alexander says, is what colleges want answered if students choose to address COVID-19 in their college essay.
But the question of whether a student should write about the coronavirus is tricky. The answer depends largely on the student.
"In general, I don't think students should write about COVID-19 in their main personal statement for their application," Robin Miller, master college admissions counselor at IvyWise, a college counseling company, wrote in an email.
"Certainly, there may be exceptions to this based on a student's individual experience, but since the personal essay is the main place in the application where the student can really allow their voice to be heard and share insight into who they are as an individual, there are likely many other topics they can choose to write about that are more distinctive and unique than COVID-19," Miller says.
Opinions among admissions experts vary on whether to write about the likely popular topic of the pandemic.
"If your essay communicates something positive, unique, and compelling about you in an interesting and eloquent way, go for it," Carolyn Pippen, principal college admissions counselor at IvyWise, wrote in an email. She adds that students shouldn't be dissuaded from writing about a topic merely because it's common, noting that "topics are bound to repeat, no matter how hard we try to avoid it."
Above all, she urges honesty.
"If your experience within the context of the pandemic has been truly unique, then write about that experience, and the standing out will take care of itself," Pippen says. "If your experience has been generally the same as most other students in your context, then trying to find a unique angle can easily cross the line into exploiting a tragedy, or at least appearing as though you have."
But focusing entirely on the pandemic can limit a student to a single story and narrow who they are in an application, Sawyer says. "There are so many wonderful possibilities for what you can say about yourself outside of your experience within the pandemic."
He notes that passions, strengths, career interests and personal identity are among the multitude of essay topic options available to applicants and encourages them to probe their values to help determine the topic that matters most to them – and write about it.
That doesn't mean the pandemic experience has to be ignored if applicants feel the need to write about it.
Writing About Coronavirus in Main and Supplemental Essays
Students can choose to write a full-length college essay on the coronavirus or summarize their experience in a shorter form.
To help students explain how the pandemic affected them, The Common App has added an optional section to address this topic. Applicants have 250 words to describe their pandemic experience and the personal and academic impact of COVID-19.
"That's not a trick question, and there's no right or wrong answer," Alexander says. Colleges want to know, he adds, how students navigated the pandemic, how they prioritized their time, what responsibilities they took on and what they learned along the way.
If students can distill all of the above information into 250 words, there's likely no need to write about it in a full-length college essay, experts say. And applicants whose lives were not heavily altered by the pandemic may even choose to skip the optional COVID-19 question.
"This space is best used to discuss hardship and/or significant challenges that the student and/or the student's family experienced as a result of COVID-19 and how they have responded to those difficulties," Miller notes. Using the section to acknowledge a lack of impact, she adds, "could be perceived as trite and lacking insight, despite the good intentions of the applicant."
To guard against this lack of awareness, Sawyer encourages students to tap someone they trust to review their writing , whether it's the 250-word Common App response or the full-length essay.
Experts tend to agree that the short-form approach to this as an essay topic works better, but there are exceptions. And if a student does have a coronavirus story that he or she feels must be told, Alexander encourages the writer to be authentic in the essay.
"My advice for an essay about COVID-19 is the same as my advice about an essay for any topic – and that is, don't write what you think we want to read or hear," Alexander says. "Write what really changed you and that story that now is yours and yours alone to tell."
Sawyer urges students to ask themselves, "What's the sentence that only I can write?" He also encourages students to remember that the pandemic is only a chapter of their lives and not the whole book.
Miller, who cautions against writing a full-length essay on the coronavirus, says that if students choose to do so they should have a conversation with their high school counselor about whether that's the right move. And if students choose to proceed with COVID-19 as a topic, she says they need to be clear, detailed and insightful about what they learned and how they adapted along the way.
"Approaching the essay in this manner will provide important balance while demonstrating personal growth and vulnerability," Miller says.
Pippen encourages students to remember that they are in an unprecedented time for college admissions.
"It is important to keep in mind with all of these (admission) factors that no colleges have ever had to consider them this way in the selection process, if at all," Pippen says. "They have had very little time to calibrate their evaluations of different application components within their offices, let alone across institutions. This means that colleges will all be handling the admissions process a little bit differently, and their approaches may even evolve over the course of the admissions cycle."
Searching for a college? Get our complete rankings of Best Colleges.
10 Ways to Discover College Essay Ideas

Tags: students , colleges , college admissions , college applications , college search , Coronavirus
2024 Best Colleges

Search for your perfect fit with the U.S. News rankings of colleges and universities.
College Admissions: Get a Step Ahead!
Sign up to receive the latest updates from U.S. News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
Ask an Alum: Making the Most Out of College

You May Also Like
How to decide if an mba is worth it.
Sarah Wood March 27, 2024

What to Wear to a Graduation
LaMont Jones, Jr. March 27, 2024

FAFSA Delays Alarm Families, Colleges
Sarah Wood March 25, 2024

Help Your Teen With the College Decision
Anayat Durrani March 25, 2024

Toward Semiconductor Gender Equity
Alexis McKittrick March 22, 2024

March Madness in the Classroom
Cole Claybourn March 21, 2024

20 Lower-Cost Online Private Colleges
Sarah Wood March 21, 2024

How to Choose a Microcredential
Sarah Wood March 20, 2024

Basic Components of an Online Course
Cole Claybourn March 19, 2024

Can You Double Minor in College?
Sarah Wood March 15, 2024


- < Previous
Home > History Community Special Collections > Remembering COVID-19 Community Archive > Community Reflections > 21

Community Reflections
My life experience during the covid-19 pandemic.
Melissa Blanco Follow
Document Type
Class Assignment
Publication Date
Affiliation with sacred heart university.
Undergraduate, Class of 2024
My content explains what my life was like during the last seven months of the Covid-19 pandemic and how it affected my life both positively and negatively. It also explains what it was like when I graduated from High School and how I want the future generations to remember the Class of 2020.
Class assignment, Western Civilization (Dr. Marino).
Recommended Citation
Blanco, Melissa, "My Life Experience During the Covid-19 Pandemic" (2020). Community Reflections . 21. https://digitalcommons.sacredheart.edu/covid19-reflections/21
Creative Commons License

Since September 23, 2020
Included in
Higher Education Commons , Virus Diseases Commons
To view the content in your browser, please download Adobe Reader or, alternately, you may Download the file to your hard drive.
NOTE: The latest versions of Adobe Reader do not support viewing PDF files within Firefox on Mac OS and if you are using a modern (Intel) Mac, there is no official plugin for viewing PDF files within the browser window.
Advanced Search
- Notify me via email or RSS
- Expert Gallery
- Collections
- Disciplines
Author Corner
- SelectedWorks Faculty Guidelines
- DigitalCommons@SHU: Nuts & Bolts, Policies & Procedures
- Sacred Heart University Library
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley - PMC COVID-19 Collection

Family in the Age of COVID‐19
Jay l. lebow.
1 Editor, Family Process, Family Institute at Northwestern, Evanston IL
The coronavirus has had a profound effect on the world in a multitude of ways. By the time this appears (written in mid‐April 2020), we probably will have some better sense of its ultimate impact. This essay centers on only one meaning of its effects: How it has impacted family life.
First and foremost, the COVID‐19 outbreak is a great human tragedy. In the long progression of human suffering, there have been other momentous times of loss, ranging from wars to genocides to massive oppression to other pandemics, but never one so widespread across such an interconnected world. Many people have died; still, more are critically ill. World economies and social structures suffer, and with this comes vulnerabilities to totalitarian and authoritarian politics in many countries.
Having said that, reactions to COVID‐19 also present a once in a lifetime international social experiment about family life, perhaps the most widespread social experiment of all time. Not only have individuals and families been dealing with threats to their health from COVID‐19 itself by trying to avoid and survive infection, but there have also been so many special meanings for families. For many, there, very directly, is the loss of family members (with those losses often occurring in ways removed from family contact that are in this era unusual). For almost everyone, there are anxieties and other feelings related to such potential losses (Weingarten & Worthen, 2018 ). Combine this with the other problems (e.g., increased unemployment and financial vulnerability) that accompany the pandemic, dealing with loss and possible loss are ubiquitous (Walsh, 2019 ).
Beyond such direct impacts of the virus, there are indirect effects. We are living through an intense period for family life, governed by a unique set of very strong external boundaries. Physical contact and close emotional contact have been mandated in many places by orders to remain within living units. This makes for powerful shared processes. It also makes for sometimes painful, intentional choices about who is in close contact with whom, that is, who is included within the boundary of close contact and who is excluded. To quote Dickens, “It was the best of times; It was the worst of times” (Dickens, 2014 ), a moment in which stories of heroic family closeness and resilience (Walsh, 2016 ) and unmitigated family stress and conflict both are prevalent. Enactments having to do with key processes within families can be expected to frequently emerge, moments that have long been described by structural family therapists as filled with possibilities for both gains and deterioration (Minuchin, 1974 ).
COVID‐19 also has plunged most of us full tilt into the already emerging world of virtual connection. Contacts beyond the nuclear family unit are almost exclusively by videoconferencing, phone, or app. With this change, it does seem that geography is now becoming far less a factor in our interconnected world. Zoom across an ocean or to next door does not differ much from each other. Yet, there is a difference between virtual and in‐person contact. Again, there are both the yin and yang of this, both the challenge of loss of connection and new possibilities for connection (Fishbane, 2019 ). Future social science will sure tell us how this has been experienced and its impact.
There have also been additional tests for those families that already face special challenges. What is the impact on families that already have members or subsystems in which there are individual or relational difficulties that are now cutoff from much of the outside world? Clearly, additional risks are evident in couples and families already at risk of violence, conflict, or other forms of relational difficulty. Not surprisingly, early data from China point to an increase in divorce rates during their period of lockdown (Prasso, 2019 ). Additional difficulties also likely emerge for families who have been dealing with troubled family members with the help of others that is now absent (McFarlane, 2016 ). Similarly, there are new and different opportunities for conflict in divorced and remarried families, where the frequency of contact between parents and children often already is at issue (Ganong & Coleman, 2018 ; Lebow, 2019a , 2019b ; Papernow, 2018 ). In other families, what looked to be successful processes of family transition, such as young adults leaving home to establish their own identities, have been suddenly radically reversed, engendering a myriad of problematic possibilities. And as virtual communication becomes the norm, what do families do about connecting with those who lack the necessary technology or technological skill to do so? There also is a challenge for those who depend on rituals for connection, be it church or Alcoholics Anonymous meetings or family dinners, that are now disrupted. Research shows that the maintenance of such regular and dependable rituals can be central in distinguishing those who become casualties from those who remain resilient through difficult times (Bennett, Wolin, Reiss, & Teitelbaum, 1987 ; Imber‐Black, Roberts, & Whiting, 1988 ). It also has already emerged that this virus is fatal far more often in some groups, such as African Americans, than in others. As is frequently the case in terrible events, effects are more pronounced for those who have the least financial resources. Crises like this one call further attention to profound underlying issues surrounding the impact of income inequality and racism in society (Anderson, McKenny, & Stevenson, 2019 ; Watson, 2019 ).
On the clinical front, COVID‐19 has prompted a vast expansion in telehealth practices and a considerable evolution in the methods and ethics for practice delivered through technology. For those who do couple and family therapy, the issues raised are complex and there has been limited guidance from earlier writing and presentations about these methods (Caldwell et al., 2017 ; Hertlein, Blumer, & Mihaloliakos, 2015 ; Hertlein & Piercy, 2012 ; Pickens et al., 2020 ). How to establish appointments with some members of a family at a distance? How to guarantee the privacy of the members of a family who are in treatment from those who are not? How to adapt therapies that involve young children? 1 What have been the initial offerings of a few about telehealth and online intervention in relational therapies (Connolly, Miller, Lindsay, & Bauer, 2020 ; Forgatch & Kjøbli, 2016 ; Georgia Salivar, Rothman, Roddy, & Doss, 2018 ; Owen, 2019 ; Roddy, Nowlan, & Doss, 2017 ; Traube et al., 2019 ; Tsami, Lerman, & Toper‐Korkmaz, 2019 ) have suddenly become the predominant methods of practice.
All these specific questions about the clinical practice of couple and family therapy also lead to larger empirical questions. Are relational therapies delivered at a distance as effective as in‐person therapy? What impact do teletherapy treatments or computer and app‐mediated prevention programs have on relational life and individual well‐being in this time? How are therapy processes, such as alliance formation, impacted (Davis & Hsieh, 2019 )? Do some forms of couple and family therapy or therapist methods of practice export to telehealth better than others (Russell & Breunlin, 2019 )? Are there alterations in practice that are needed for the most effective telehealth practice? Several studies already point to the benefits of online methods (Connolly et al., 2020 ; Owen, 2019 ; Traube et al., 2019 ; Tsami et al., 2019 ), but what can we learn from this vastly expanded context?
All told, these are highly stressful and most interesting times. Clinical experience already points to emerging trends. It will be fascinating to see what family science finds to be the short‐ and long‐term effects of these times and the impact of our methods of intervention during it.
1 The good news for those with a systemic focus is that this question about therapy with children can only be answered by including parents in therapy; thus, a systemic goal of parent involvement in all cases may be furthered by the evolution of this medium.
- Anderson, R. E. , McKenny, M. C. , & Stevenson, H. C. (2019). EMBRace: Developing a racial socialization intervention to reduce racial stress and enhance racial coping among black parents and adolescents . Family Process , 58 ( 1 ), 53–67. 10.1111/famp.12412. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bennett, L. A. , Wolin, S. J. , Reiss, D. , & Teitelbaum, M. A. (1987). Couples at risk for transmission of alcoholism: Protective influences . Family Process , 26 ( 1 ), 111–129. [ PubMed ] [ Google Scholar ]
- Caldwell, B. E. , Bischoff, R. J. , Derrig‐Palumbo, K. A. , & Liebert, J. D. (2017). Best practices in the online practice of couple and family therapy [PDF file]. Retrieved April 10, 2020 from https://www.aamft.org/Documents/Products/AAMFT_Best_Practices_for_Online_MFT.pdf . [ Google Scholar ]
- Connolly, S. L. , Miller, C. J. , Lindsay, J. A. , & Bauer, M. S. (2020). A systematic review of providers’ attitudes toward telemental health via videoconferencing . Clinical Psychology: Science and Practice . 10.1111/cpsp.12311. [ CrossRef ] [ Google Scholar ]
- Davis, S. D. , & Hsieh, A. L. (2019). What does it mean to be a common factors informed family therapist? Family Process , 58 ( 3 ), 629–640. 10.1111/famp.12477. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dickens, C. (2014). A tale of two cities . Minneapolis, MN: First Avenue Editions. [ Google Scholar ]
- Fishbane, M. D. (2019). Healing intergenerational wounds: An integrative relational‐neurobiological approach . Family Process , 58 ( 4 ), 796–818. 10.1111/famp.12488. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Forgatch, M. S. , & Kjøbli, J. (2016). Parent management training—oregon model: Adapting intervention with rigorous research . Family Process , 55 ( 3 ), 500–513. 10.1111/famp.12224. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ganong, L. , & Coleman, M. (2018). Studying stepfamilies: Four eras of family scholarship . Family Process , 57 ( 1 ), 7–24. 10.1111/famp.12307. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Georgia Salivar, E. J. , Rothman, K. , Roddy, M. K. , & Doss, B. D. (2018). Relative cost effectiveness of in‐person and internet interventions for relationship distress . Family Process , 59 ( 1 ), 66–80. 10.1111/famp.12414. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hertlein, K. M. , Blumer, M. L. C. , & Mihaloliakos, J. H. (2015). Marriage and family counselors’ perceived ethical issues related to online therapy . The Family Journal , 23 ( 1 ), 5–12. 10.1177/1066480714547184. [ CrossRef ] [ Google Scholar ]
- Hertlein, K. M. , & Piercy, F. P. (2012). Essential elements of internet infidelity treatment . Journal of Marital and Family Therapy , 38 , 257–270. 10.1111/j.1752-0606.2011.00275.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Imber‐Black, E. , Roberts, J. , & Whiting, R. A. (Eds.) (1988). Rituals in families and family therapy . New York: W. W. Norton & Co Inc. [ Google Scholar ]
- Lebow, J. L. (2019a). Current issues in the practice of integrative couple and family therapy . Family Process , 58 ( 3 ), 610–628. 10.1111/famp.12473. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lebow, J. L. (2019b). Treating the difficult divorce: A practical guide for psychotherapists . Washington, DC: American Psychological Association. [ Google Scholar ]
- McFarlane, W. R. (2016). Family Interventions for Schizophrenia and the Psychoses: A Review . Family Process , 55 ( 3 ), 460–482. 10.1111/famp.12235. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Minuchin, S. (1974). Families & family therapy . Oxford, UK: Harvard U. Press. [ Google Scholar ]
- Owen, N. (2019). Feasibility and acceptability of using telehealth for early intervention parent counselling . Advances in Mental Health , 18 ( 1 ), 39–49. 10.1080/18387357.2019.1679026. [ CrossRef ] [ Google Scholar ]
- Papernow, P. L. (2018). Clinical guidelines for working with stepfamilies: What family, couple, individual, and child therapists need to know . Family Process , 57 ( 1 ), 25–51. 10.1111/famp.12321. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pickens, J. C. , Morris, N. , & Johnson, D. J. (2020). The digital divide: Couple and family therapy programs’ integration of teletherapy training and education . Journal of Marital and Family Therapy , 46 ( 2 ), 186–200. 10.1111/jmft.12417. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Prasso, S . (2019) China’s divorce spike is a warning to rest of locked‐down world . Bloomberg Businessweek. March 31, 2020. [ Google Scholar ]
- Roddy, M. K. , Nowlan, K. M. , & Doss, B. D. (2017). A randomized controlled trial of coach contact during a brief online intervention for distressed couples . Family Process , 56 ( 4 ), 835–851. 10.1111/famp.12262. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Russell, W. P. , & Breunlin, D. C. (2019). Transcending therapy models and managing complexity: Suggestions from integrative systemic therapy . Family Process , 58 ( 3 ), 641–655. 10.1111/famp.12482. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Traube, D. E. , Hsiao, H.‐Y. , Rau, A. , Hunt‐O'Brien, D. , Lu, L. , & Islam, N. (2019). Advancing home based parenting programs through the use of telehealth technology . Journal of Child and Family Studies , 29 ( 1 ), 44–53. 10.1007/s10826-019-01458-w. [ CrossRef ] [ Google Scholar ]
- Tsami, L. , Lerman, D. , & Toper‐Korkmaz, O. (2019). Effectiveness and acceptability of parent training via telehealth among families around the world . Journal of Applied Behavior Analysis , 52 ( 4 ), 1113–1129. 10.1002/jaba.645. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Walsh, F. (2016). Applying a family resilience framework in training, practice, and research: Mastering the art of the possible . Family Process , 55 ( 4 ), 616–632. 10.1111/famp.12260. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Walsh, F. (2019). Loss and bereavement in families: A systemic framework for recovery and resilience. In Fiese B. H., Celano M., Deater‐Deckard K., Jouriles E. N. & Whisman M. A. (Eds.), APA handbook of contemporary family psychology: Foundations, methods, and contemporary issues across the lifespan (Vol. 1 , pp. 649–663). Washington, DC: American Psychological Association. [ Google Scholar ]
- Watson, M. F. (2019). Social justice and race in the united states: Key issues and challenges for couple and family therapy . Family Process , 58 ( 1 ):23–33. 10.1111/famp.12427. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Weingarten, K. , & Worthen, M. (2018). The solace of an uncertain future: Acute illness, the self, and self‐care . Family Process , 57 ( 2 ), 572–586. 10.1111/famp.12347. [ PubMed ] [ CrossRef ] [ Google Scholar ]
How COVID-19 pandemic changed my life

Table of Contents
Introduction
The COVID-19 pandemic is one of the biggest challenges that our world has ever faced. People around the globe were affected in some way by this terrible disease, whether personally or not. Amid the COVID-19 pandemic, many people felt isolated and in a state of panic. They often found themselves lacking a sense of community, confidence, and trust. The health systems in many countries were able to successfully prevent and treat people with COVID-19-related diseases while providing early intervention services to those who may not be fully aware that they are infected (Rume & Islam, 2020). Personally, this pandemic has brought numerous changes and challenges to my life. The COVID-19 pandemic affected my social, academic, and economic lifestyle positively and negatively.

Social and Academic Changes
One of the changes brought by the pandemic was economic changes that occurred very drastically (Haleem, Javaid, & Vaishya, 2020). During the pandemic, food prices started to rise, affecting the amount of money my parents could spend on goods and services. We had to reduce the food we bought as our budgets were stretched. My family also had to eliminate unhealthy food bought in bulk, such as crisps and chocolate bars. Furthermore, the pandemic made us more aware of the importance of keeping our homes clean, especially regarding cooking food. Lastly, it also made us more aware of how we talked to other people when they were ill and stayed home with them rather than being out and getting on with other things.
Furthermore, COVID-19 had a significant effect on my academic life. Immediately, measures to curb the pandemic were announced, such as closing all learning institutions in the country; my school life changed. The change began when our school implemented the online education system to ensure that we continued with our education during the lockdown period. At first, this affected me negatively because when learning was not happening in a formal environment, I struggled academically since I was not getting the face-to-face interaction with the teachers I needed. Furthermore, forcing us to attend online caused my classmates and me to feel disconnected from the knowledge being taught because we were unable to have peer participation in class. However, as the pandemic subsided, we grew accustomed to this learning mode. We realized the effects on our performance and learning satisfaction were positive, as it seemed to promote emotional and behavioral changes necessary to function in a virtual world. Students who participated in e-learning during the pandemic developed more ownership of the course requirement, increased their emotional intelligence and self-awareness, improved their communication skills, and learned to work together as a community.
If there is an area that the pandemic affected was the mental health of my family and myself. The COVID-19 pandemic caused increased anxiety, depression, and other mental health concerns that were difficult for my family and me to manage alone. Our ability to learn social resilience skills, such as self-management, was tested numerous times. One of the most visible challenges we faced was social isolation and loneliness. The multiple lockdowns made it difficult to interact with my friends and family, leading to loneliness. The changes in communication exacerbated the problem as interactions moved from face-to-face to online communication using social media and text messages. Furthermore, having family members and loved ones separated from us due to distance, unavailability of phones, and the internet created a situation of fear among us, as we did not know whether they were all right. Moreover, some people within my circle found it more challenging to communicate with friends, family, and co-workers due to poor communication skills. This was mainly attributed to anxiety or a higher risk of spreading the disease. It was also related to a poor understanding of creating and maintaining relationships during this period.
Positive Changes
In addition, this pandemic has brought some positive changes with it. First, it had been a significant catalyst for strengthening relationships and neighborhood ties. It has encouraged a sense of community because family members, neighbors, friends, and community members within my area were all working together to help each other out. Before the pandemic, everybody focused on their business, the children going to school while the older people went to work. There was not enough time to bond with each other. Well, the pandemic changed that, something that has continued until now that everything is returning to normal. In our home, it strengthened the relationship between myself and my siblings and parents. This is because we started spending more time together as a family, which enhanced our sense of understanding of ourselves.

The pandemic has been a challenging time for many people. I can confidently state that it was a significant and potentially unprecedented change in our daily life. By changing how we do things and relate with our family and friends, the pandemic has shaped our future life experiences and shown that during crises, we can come together and make a difference in each other’s lives. Therefore, I embrace wholesomely the changes brought by the COVID-19 pandemic in my life.
- Haleem, A., Javaid, M., & Vaishya, R. (2020). Effects of COVID-19 pandemic in daily life. Current medicine research and practice , 10 (2), 78.
- Rume, T., & Islam, S. D. U. (2020). Environmental effects of COVID-19 pandemic and potential strategies of sustainability. Heliyon , 6 (9), e04965.
- ☠️ Assisted Suicide
- Affordable Care Act
- Breast Cancer
- Genetic Engineering

Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.

Asking the internet about birth control

‘Harvard Thinking’: Facing death with dignity

Novel teamwork, promising results for glioblastoma treatment
When even grief is taken away.
COVID-19 isolation has undercut the human need for collective mourning, expert says
Alvin Powell
Harvard Staff Writer
Illustration by Eddie Edwards
With more than 500,000 dead, the COVID-19 pandemic has created a nation touched by grief, compounded by the trauma of job loss, financial trouble, and everyday confusion, a mix that a Harvard psychologist said creates a complex and troubling picture of the country’s emotional landscape.
Christy Denckla, a research fellow at the Stanley Center for Psychiatric Research at the Broad Institute of MIT and Harvard and a postdoctoral fellow in the Harvard T.H. Chan School of Public Health’s Department of Epidemiology, said that with so many having died from the pandemic, few Americans at this point haven’t either lost a loved one to COVID-19 or at least know someone who has. Those losses amid an infectious disease mean the practices that society has developed over centuries — vigils for the dying, wakes, funerals, and other end-of-life rituals — that bring people together to mourn and support those closest to the deceased, are disrupted or suspended entirely.
Such rituals, she said, were created to help those involved acknowledge and process their loss, while giving and gaining support from loved ones. The rituals provide a language through which to talk about pain and sadness and provide strength and hope when needed most. Those facing pandemic-enforced isolation instead may have trouble processing what has happened, particularly if it occurs together with job loss or other displacements.
“We’re sort of in a perfect storm, we worry, for long-term, clinically impairing conditions.” Christy Denckla
“In the mental health community, there is concern — there is a lot of concern — about the impact this is having,” Denckla said. “We are forced now to grieve alone and oftentimes in isolation. Parts of grieving happen alone, but parts of grieving happen in community, and, in the absence of that community, I am concerned with how people are coping with this loss right now.”
Denckla, whose work focuses on resilience following exposure to trauma, spoke Tuesday at a Facebook Live event, “The Coronavirus Pandemic: Grieving and Mental Health,” sponsored by The Forum at Harvard T.H. Chan School of Public Health and PRX’s The World.
More like this

We may duck a surge from variant that sent Britain reeling
Feeling more anxious and stressed? You’re not alone

Marking the passing of a grim pandemic milestone for the nation

Seeded amid the many surprises of COVID times, some unexpected positives

Newest vaccine emerges amid a ‘more complicated pandemic’
Denckla said the long-term impact of the current situation may be something called prolonged grief disorder, in which people who are isolated and cut off from the normal grieving process find their lives impaired over time by unresolved grief.
“We’re sort of in a perfect storm, we worry, for long-term, clinically impairing conditions,” Denckla said.
The situation may be exacerbated in communities of color which have suffered even more from the pandemic. Denckla said she’s particularly concerned about the long-term impact on children who’ve lost parents, and those who are vulnerable who lost providers who supported them.
Denckla pointed out that the COVID-19 deaths have occurred on top of those that would normally occur, yet mourning has become complicated for everyone. This is also happening at a time when the U.S. mental health system is operating at capacity, Denckla said. Though the pandemic era’s rise of telehealth is seen as improving access to mental health services, Denckla said that her colleagues report being inundated by the demand for services.
“There has been so much loss during this time. People have lost jobs, lost livelihoods, lost celebrations — I’ve been to a few Zoom weddings — birthdays, holidays,” Denckla said.
Denckla said that compounded stressors increase risk for an array of mental health conditions, such as anxiety, depression, suicidal thoughts, hopelessness, loss of interest in pleasurable activities, and interpersonal conflict.
“The [increased] burden on couples, on parents, on children and families has been quite remarkable; relationships are stressed,” Denckla said. “These compounded stressors are troubling.”
On the plus side, Denckla acknowledged that technology combined with creativity has provided an alternate outlet for many. Facebook posts about lost loved ones give friends and relatives a chance to express grief and support, while Zoom gatherings provide a way to be with each other, even if not in the same room.
Denckla said hospital clergy in some cases have donned protective gear and allowed loved ones to connect via video with dying loved ones when pandemic rules prohibit in-person visits. What is unknown, Denckla said, is how effective a substitute these digital practices are and whether they can help mitigate potential problems in the future.
Another hopeful development, she said, is the attention the pandemic has brought to the issue of mourning. With loss on such a scale, an issue that is often skirted in public discourse has been brought more centrally into the spotlight, with one organization proposing a White House office on bereavement care, another a bereavement bill of rights that allows relatives to see a body and details that the body be treated with respect. And yet all is not dour.
“What we’ve learned is that we are surprisingly resilient,” Denckla. “What I’m inspired by now is the collective conversation about the importance of grief, about the rights of the bereaved, about transforming social policy around loss and support, which can go a long way to reducing inequity.”
Share this article
You might like.
Only a fraction of it will come from an expert, researchers say

In podcast episode, a chaplain, a bioethicist, and a doctor talk about end-of-life care

Researchers cite ‘academic medicine’ as key factor in success
College accepts 1,937 to Class of 2028
Students represent 94 countries, all 50 states
Pushing back on DEI ‘orthodoxy’
Panelists support diversity efforts but worry that current model is too narrow, denying institutions the benefit of other voices, ideas
So what exactly makes Taylor Swift so great?
Experts weigh in on pop superstar's cultural and financial impact as her tours and albums continue to break records.
MINI REVIEW article
Covid-19: emergence, spread, possible treatments, and global burden.

- 1 Department of Pharmacology, Manipal College of Pharmaceutical Sciences, Manipal Academy of Higher Education, Manipal, India
- 2 Department of Health Sciences, School of Education and Health, Cape Breton University, Sydney, NS, Canada
The Coronavirus (CoV) is a large family of viruses known to cause illnesses ranging from the common cold to acute respiratory tract infection. The severity of the infection may be visible as pneumonia, acute respiratory syndrome, and even death. Until the outbreak of SARS, this group of viruses was greatly overlooked. However, since the SARS and MERS outbreaks, these viruses have been studied in greater detail, propelling the vaccine research. On December 31, 2019, mysterious cases of pneumonia were detected in the city of Wuhan in China's Hubei Province. On January 7, 2020, the causative agent was identified as a new coronavirus (2019-nCoV), and the disease was later named as COVID-19 by the WHO. The virus spread extensively in the Wuhan region of China and has gained entry to over 210 countries and territories. Though experts suspected that the virus is transmitted from animals to humans, there are mixed reports on the origin of the virus. There are no treatment options available for the virus as such, limited to the use of anti-HIV drugs and/or other antivirals such as Remdesivir and Galidesivir. For the containment of the virus, it is recommended to quarantine the infected and to follow good hygiene practices. The virus has had a significant socio-economic impact globally. Economically, China is likely to experience a greater setback than other countries from the pandemic due to added trade war pressure, which have been discussed in this paper.
Introduction
Coronaviridae is a family of viruses with a positive-sense RNA that possess an outer viral coat. When looked at with the help of an electron microscope, there appears to be a unique corona around it. This family of viruses mainly cause respiratory diseases in humans, in the forms of common cold or pneumonia as well as respiratory infections. These viruses can infect animals as well ( 1 , 2 ). Up until the year 2003, coronavirus (CoV) had attracted limited interest from researchers. However, after the SARS (severe acute respiratory syndrome) outbreak caused by the SARS-CoV, the coronavirus was looked at with renewed interest ( 3 , 4 ). This also happened to be the first epidemic of the 21st century originating in the Guangdong province of China. Almost 10 years later, there was a MERS (Middle East respiratory syndrome) outbreak in 2012, which was caused by the MERS-CoV ( 5 , 6 ). Both SARS and MERS have a zoonotic origin and originated from bats. A unique feature of these viruses is the ability to mutate rapidly and adapt to a new host. The zoonotic origin of these viruses allows them to jump from host to host. Coronaviruses are known to use the angiotensin-converting enzyme-2 (ACE-2) receptor or the dipeptidyl peptidase IV (DPP-4) protein to gain entry into cells for replication ( 7 – 10 ).
In December 2019, almost seven years after the MERS 2012 outbreak, a novel Coronavirus (2019-nCoV) surfaced in Wuhan in the Hubei region of China. The outbreak rapidly grew and spread to neighboring countries. However, rapid communication of information and the increasing scale of events led to quick quarantine and screening of travelers, thus containing the spread of the infection. The major part of the infection was restricted to China, and a second cluster was found on a cruise ship called the Diamond Princess docked in Japan ( 11 , 12 ).
The new virus was identified to be a novel Coronavirus and was thus initially named 2019-nCoV; later, it was renamed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) ( 13 ), and the disease it causes is now referred to as Coronavirus Disease-2019 (COVID-19) by the WHO. The virus was suspected to have begun its spread in the Huanan seafood wholesale market in the Wuhan region. It is possible that an animal that was carrying the virus was brought into or sold in the market, causing the spread of the virus in the crowded marketplace. One of the first claims made was in an article published in the Journal of Medical Virology ( 14 ), which identified snakes as the possible host. A second possibility was that pangolins could be the wild host of SARS-CoV-2 ( 15 ), though the most likely possibility is that the virus originated from bats ( 13 , 16 – 19 ). Increasing evidence and experts are now collectively concluding the virus had a natural origin in bats, as with previous such respiratory viruses ( 2 , 20 – 24 ).
Similarly, SARS and MERS were also suspected to originate from bats. In the case of MERS, the dromedary camel is an intermediate host ( 5 , 10 ). Bats have been known to harbor coronaviruses for quite some time now. Just as in the case of avian flu, SARS, MERS, and possibly even HIV, with increasing selection and ecological pressure due to human activities, the virus made the jump from animal to man. Humans have been encroaching increasingly into forests, and this is true over much of China, as in Africa. Combined with additional ecological pressure due to climate change, such zoonotic spillovers are now more common than ever. It is likely that the next disease X will also have such an origin ( 25 ). We have learned the importance of identification of the source organism due to the Ebola virus pandemic. Viruses are unstable organisms genetically, constantly mutating by genetic shift or drift. It is not possible to predict when a cross-species jump may occur and when a seemingly harmless variant form of the virus may turn into a deadly strain. Such an incident occurred in Reston, USA, with the Reston virus ( 26 ), an alarming reminder of this possibility. The identification of the original host helps us to contain future spreads as well as to learn about the mechanism of transmission of viruses. Until the virus is isolated from a wild animal host, in this case, mostly bats, the zoonotic origin will remain hypothetical, though likely. It should further be noted that the virus has acquired several mutations, as noted by a group in China, indicating that there are more than two strains of the virus, which may have had an impact on its pathogenicity. However, this claim remains unproven, and many experts have argued otherwise; data proving this are not yet available ( 27 ). A similar finding was reported from Italy and India independently, where they found two strains ( 28 , 29 ). These findings need to be further cross-verified by similar analyses globally. If true, this finding could effectively explain why some nations are more affected than others.
Transmission
When the spread of COVID-19 began ( Figure 1 ), the virus appeared to be contained within China and the cruise ship “Diamond Princess,” which formed the major clusters of the virus. However, as of April 2020, over 210 countries and territories are affected by the virus, with Europe, the USA, and Iran forming the new cluster of the virus. The USA ( Figure 2 ) has the highest number of confirmed COVID-19 cases, whereas India and China, despite being among the most population-dense countries in the world, have managed to constrain the infection rate by the implementation of a complete lockdown with arrangements in place to manage the confirmed cases. Similarly, the UK has also managed to maintain a low curve of the graph by implementing similar measures, though it was not strictly enforced. Reports have indicated that the presence of different strains or strands of the virus may have had an effect on the management of the infection rate of the virus ( 27 – 29 ). The disease is spread by droplet transmission. As of April 2020, the total number of infected individuals stands at around 3 million, with ~200,000 deaths and more than 1 million recoveries globally ( 30 , 34 ). The virus thus has a fatality rate of around 2% and an R 0 of 3 based on current data. However, a more recent report from the CDC, Atlanta, USA, claims that the R 0 could be as high as 5.7 ( 35 ). It has also been observed from data available from China and India that individuals likely to be infected by the virus from both these countries belong to the age groups of 20–50 years ( 36 , 37 ). In both of these countries, the working class mostly belongs to this age group, making exposure more likely. Germany and Singapore are great examples of countries with a high number of cases but low fatalities as compared to their immediate neighbors. Singapore is one of the few countries that had developed a detailed plan of action after the previous SARS outbreak to deal with a similar situation in the future, and this worked in their favor during this outbreak. Both countries took swift action after the outbreak began, with Singapore banning Chinese travelers and implementing screening and quarantine measures at a time when the WHO recommended none. They ordered the elderly and the vulnerable to strictly stay at home, and they ensured that lifesaving equipment and large-scale testing facilities were available immediately ( 38 , 39 ). Germany took similar measures by ramping up testing capacity quite early and by ensuring that all individuals had equal opportunity to get tested. This meant that young, old, and at-risk people all got tested, thus ensuring positive results early during disease progression and that most cases were mild like in Singapore, thus maintaining a lower death percentage ( 40 ). It allowed infected individuals to be identified and quarantined before they even had symptoms. Testing was carried out at multiple labs, reducing the load and providing massive scale, something which countries such as the USA did quite late and India restricted to select government and private labs. The German government also banned large gatherings and advocated social distancing to further reduce the spread, though unlike India and the USA, this was done quite late. South Korea is another example of how a nation has managed to contain the spread and transmission of the infection. South Korea and the USA both reported their first COVID-19 cases on the same day; however, the US administration downplayed the risks of the disease, unlike South Korean officials, who constantly informed their citizens about the developments of the disease using the media and a centralized messaging system. They also employed the Trace, Test, and Treat protocol to identify and isolate patients fast, whereas the USA restricted this to patients with severe infection and only later broadened this criterion, like many European countries as well as India. Unlike the USA, South Korea also has universal healthcare, ensuring free diagnostic testing.
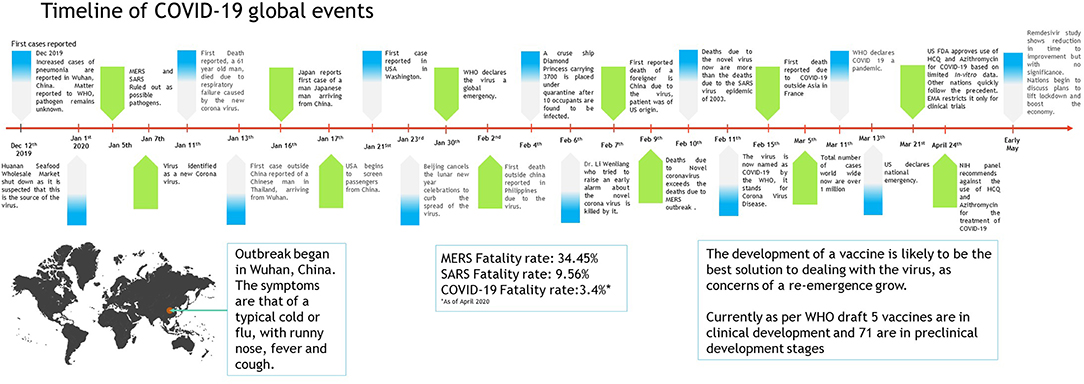
Figure 1 . Timeline of COVID-19 progression ( 30 – 32 ).
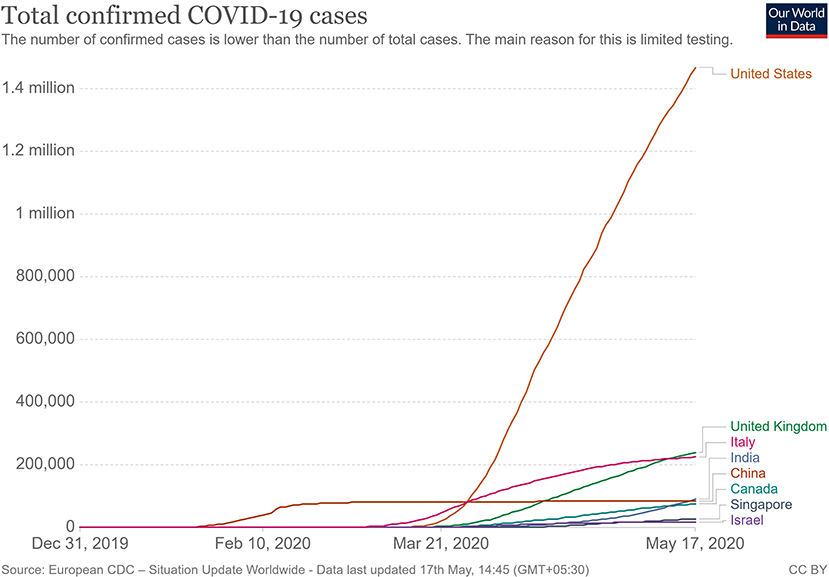
Figure 2 . Total confirmed COVID 19 cases as of May 2020 ( 33 ).
The main mode of transmission of 2019-nCoV is human to human. As of now, animal-to-human transfer has not yet been confirmed. Asymptomatic carriers of the virus are at major risk of being superinfectors with this disease, as all those infected may not develop the disease ( 41 ). This is a concern that has been raised by nations globally, with the Indian government raising concerns on how to identify and contain asymptomatic carriers, who could account for 80% of those infected ( 42 ). Since current resources are directed towards understanding the hospitalized individuals showing symptoms, there is still a vast amount of information about asymptomatic individuals that has yet to be studied. For example, some questions that need to be answered include: Do asymptomatic individuals develop the disease at any point in time at all? Do they eventually develop antibodies? How long do they shed the virus for? Can any tissue of these individuals store the virus in a dormant state? Asymptomatic transmission is a gray area that encompasses major unknowns in COVID-19.
The main route of human-to-human transmission is by droplets, which are generated during coughing, talking, or sneezing and are then inhaled by a healthy individual. They can also be indirectly transmitted to a person when they land on surfaces that are touched by a healthy individual who may then touch their nose, mouth, or eyes, allowing the virus entry into the body. Fomites are also a common issue in such diseases ( 43 ).
Aerosol-based transmission of the virus has not yet been confirmed ( 43 ). Stool-based transmission via the fecal-oral route may also be possible since the SARS-CoV-2 has been found in patient feces ( 44 , 45 ). Some patients with COVID-19 tend to develop diarrhea, which can become a major route of transmission if proper sanitation and personal hygiene needs are not met. There is no evidence currently available to suggest intrauterine vertical transmission of the disease in pregnant women ( 46 ).
More investigation is necessary of whether climate has played any role in the containment of the infection in countries such as India, Singapore, China, and Israel, as these are significantly warmer countries as compared with the UK, the USA, and Canada ( Figure 2 ). Ideally, a warm climate should prevent the virus from surviving for longer periods of time on surfaces, reducing transmissibility.
Pathophysiology
On gaining entry via any of the mucus membranes, the single-stranded RNA-based virus enters the host cell using type 2 transmembrane serine protease (TMPRSS2) and ACE2 receptor protein, leading to fusion and endocytosis with the host cell ( 47 – 49 ). The uncoated RNA is then translated, and viral proteins are synthesized. With the help of RNA-dependant RNA polymerase, new RNA is produced for the new virions. The cell then undergoes lysis, releasing a load of new virions into the patients' body. The resultant infection causes a massive release of pro-inflammatory cytokines that causes a cytokine storm.
Clinical Presentation
The clinical presentation of the disease resembles beta coronavirus infections. The virus has an incubation time of 2–14 days, which is the reason why most patients suspected to have the illness or contact with an individual having the illness remain in quarantine for the said amount of time. Infection with SARS-CoV-2 causes severe pneumonia, intermittent fever, and cough ( 50 , 51 ). Symptoms of rhinorrhoea, pharyngitis, and sneezing have been less commonly seen. Patients often develop acute respiratory distress syndrome within 2 days of hospital admission, requiring ventilatory support. It has been observed that during this phase, the mortality tends to be high. Chest CT will show indicators of pneumonia and ground-glass opacity, a feature that has helped to improve the preliminary diagnosis ( 51 ). The primary method of diagnosis for SARS-CoV-2 is with the help of PCR. For the PCR testing, the US CDC recommends testing for the N gene, whereas the Chinese CDC recommends the use of ORF lab and N gene of the viral genome for testing. Some also rely on the radiological findings for preliminary screening ( 52 ). Additionally, immunodiagnostic tests based on the presence of antibodies can also play a role in testing. While the WHO recommends the use of these tests for research use, many countries have pre-emptively deployed the use of these tests in the hope of ramping up the rate and speed of testing ( 52 – 54 ). Later, they noticed variations among the results, causing them to stop the use of such kits; there was also debate among the experts about the sensitivity and specificity of the tests. For immunological tests, it is beneficial to test for antibodies against the virus produced by the body rather than to test for the presence of the viral proteins, since the antibodies can be present in larger titers for a longer span of time. However, the cross-reactivity of these tests with other coronavirus antibodies is something that needs verification. Biochemical parameters such as D-dimer, C-reactive protein, and variations in neutrophil and lymphocyte counts are some other parameters that can be used to make a preliminary diagnosis; however, these parameters vary in a number of diseases and thus cannot be relied upon conclusively ( 51 ). Patients with pre-existing diseases such as asthma or similar lung disorder are at higher risk, requiring life support, as are those with other diseases such as diabetes, hypertension, or obesity. Those above the age of 60 have displayed the highest mortality rate in China, a finding that is mirrored in other nations as well ( Figure 3 ) ( 55 ). If we cross-verify these findings with the population share that is above the age of 70, we find that Italy, the United Kingdom, Canada, and the USA have one of the highest elderly populations as compared to countries such as India and China ( Figure 4 ), and this also reflects the case fatality rates accordingly ( Figure 5 ) ( 33 ). This is a clear indicator that aside from comorbidities, age is also an independent risk factor for death in those infected by COVID-19. Also, in the US, it was seen that the rates of African American deaths were higher. This is probably due to the fact that the prevalence of hypertension and obesity in this community is higher than in Caucasians ( 56 , 57 ). In late April 2020, there are also claims in the US media that young patients in the US with COVID-19 may be at increased risk of stroke; however, this is yet to be proven. We know that coagulopathy is a feature of COVID-19, and thus stroke is likely in this condition ( 58 , 59 ). The main cause of death in COVID-19 patients was acute respiratory distress due to the inflammation in the linings of the lungs caused by the cytokine storm, which is seen in all non-survival cases and in respiratory failure. The resultant inflammation in the lungs, served as an entry point of further infection, associated with coagulopathy end-organ failure, septic shock, and secondary infections leading to death ( 60 – 63 ).
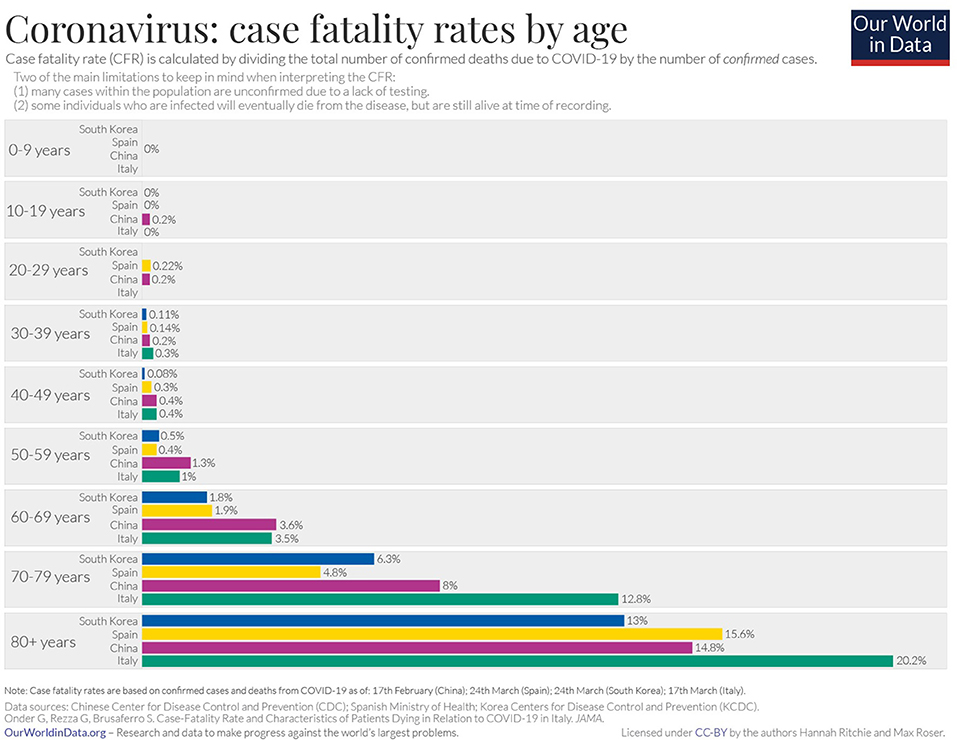
Figure 3 . Case fatality rate by age in selected countries as of April 2020 ( 33 ).
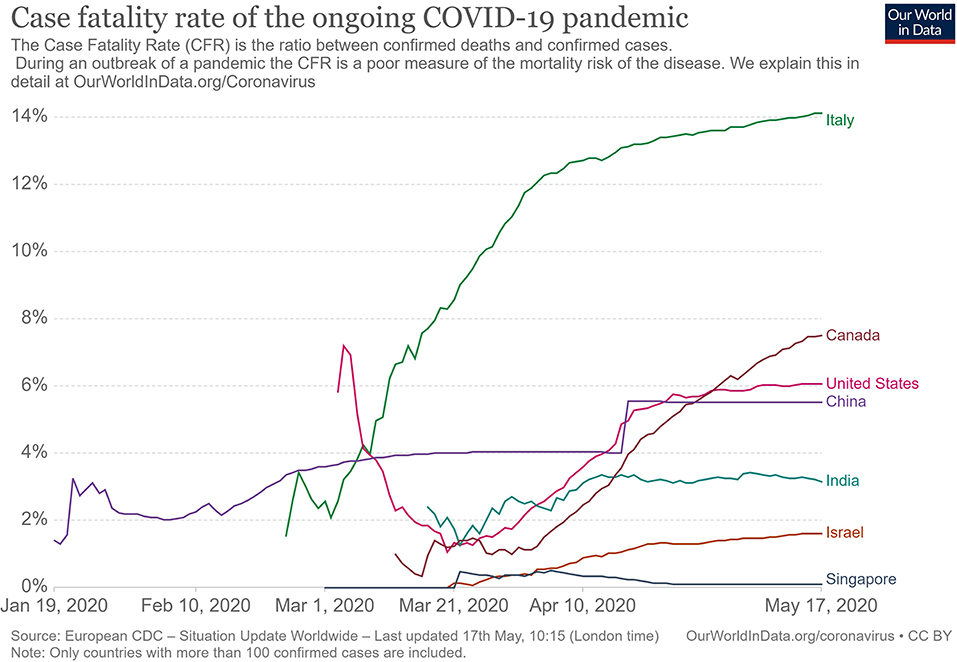
Figure 4 . Case fatality rate in selected countries ( 33 ).
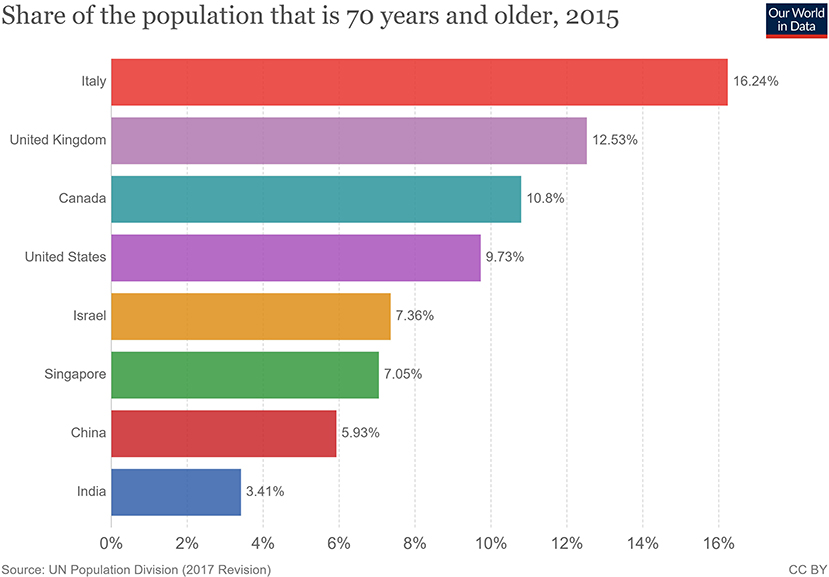
Figure 5 . Population share above 70 years of age ( 33 ).
For COVID-19, there is no specific treatment available. The WHO announced the organization of a trial dubbed the “Solidarity” clinical trial for COVID-19 treatments ( 64 ). This is an international collaborative study that investigates the use of a few prime candidate drugs for use against COVID-19, which are discussed below. The study is designed to reduce the time taken for an RCT by over 80%. There are over 1087 studies ( Supplementary Data 1 ) for COVID-19 registered at clinicaltrials.gov , of which 657 are interventional studies ( Supplementary Data 2 ) ( 65 ). The primary focus of the interventional studies for COVID-19 has been on antimalarial drugs and antiviral agents ( Table 1 ), while over 200 studies deal with the use of different forms of oxygen therapy. Most trials focus on improvement of clinical status, reduction of viral load, time to improvement, and reduction of mortality rates. These studies cover both severe and mild cases.
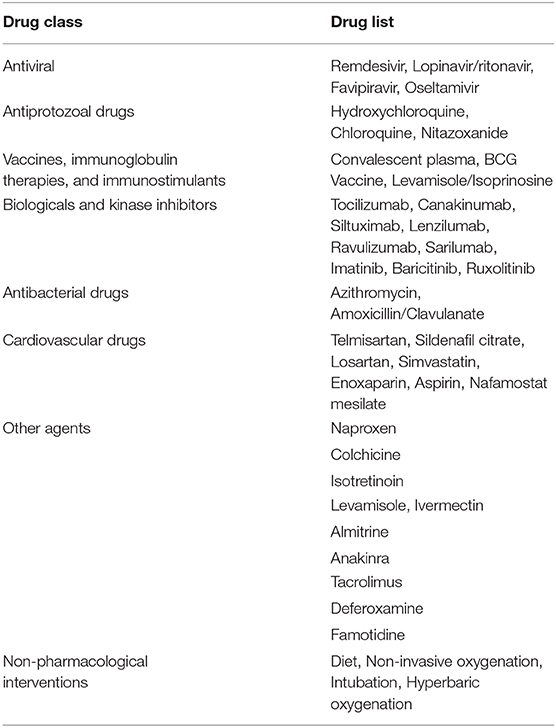
Table 1 . List of therapeutic drugs under study for COVID-19 as per clinical trials registered under clinicaltrials.gov .
Use of Antimalarial Drugs Against SARS-CoV-2
The use of chloroquine for the treatment of corona virus-based infection has shown some benefit in the prevention of viral replication in the cases of SARS and MERS. However, it was not validated on a large scale in the form of a randomized control trial ( 50 , 66 – 68 ). The drugs of choice among antimalarials are Chloroquine (CQ) and Hydroxychloroquine (HCQ). The use of CQ for COVID-19 was brought to light by the Chinese, especially by the publication of a letter to the editor of Bioscience Trends by Gao et al. ( 69 ). The letter claimed that several studies found CQ to be effective against COVID-19; however, the letter did not provide many details. Immediately, over a short span of time, interest in these two agents grew globally. Early in vitro data have revealed that chloroquine can inhibit the viral replication ( 70 , 71 ).
HCQ and CQ work by raising the pH of the lysosome, the cellular organelle that is responsible for phagocytic degradation. Its function is to combine with cell contents that have been phagocytosed and break them down eventually, in some immune cells, as a downstream process to display some of the broken proteins as antigens, thus further enhancing the immune recruitment against an antigen/pathogen. The drug was to be administered alone or with azithromycin. The use of azithromycin may be advocated by the fact that it has been seen previously to have some immunomodulatory role in airway-related disease. It appears to reduce the release of pro-inflammatory cytokines in respiratory illnesses ( 72 ). However, HCQ and azithromycin are known to have a major drug interaction when co-administered, which increases the risk of QT interval prolongation ( 73 ). Quinine-based drugs are known to have adverse effects such as QT prolongation, retinal damage, hypoglycemia, and hemolysis of blood in patients with G-6-PD deficiency ( 66 ). Several preprints, including, a metanalysis now indicate that HCQ may have no benefit for severe or critically ill patients who have COVID-19 where the outcome is need for ventilation or death ( 74 , 75 ). As of April 21, 2020, after having pre-emptively recommended their use for SARS-CoV-2 infection, the US now advocates against the use of these two drugs based on the new data that has become available.
Use of Antiviral Drugs Against SARS-CoV-2
The antiviral agents are mainly those used in the case of HIV/AIDS, these being Lopinavir and Ritonavir. Other agents such as nucleoside analogs like Favipiravir, Ribavirin, Remdesivir, and Galidesivir have been tested for possible activity in the prevention of viral RNA synthesis ( 76 ). Among these drugs, Lopinavir, Ritonavir, and Remdesivir are listed in the Solidarity trial by the WHO.
Remdesivir is a nucleotide analog for adenosine that gets incorporated into the viral RNA, hindering its replication and causing chain termination. This agent was originally developed for Ebola Virus Disease ( 77 ). A study was conducted with rhesus macaques infected with SARS-CoV-2 ( 78 ). In that study, after 12 h of infection, the monkeys were treated with either Remdesivir or vehicle. The drug showed good distribution in the lungs, and the animals treated with the drug showed a better clinical score than the vehicle group. The radiological findings of the study also indicated that the animals treated with Remdesivir have less lung damage. There was a reduction in viral replication but not in virus shedding. Furthermore, there were no mutations found in the RNA polymerase sequences. A randomized clinical control study that became available in late April 2020 ( 79 ), having 158 on the Remdesivir arm and 79 on the placebo arm, found that Remdesivir reduced the time to recovery in the Remdesivir-treated arm to 11 days, while the placebo-arm recovery time was 15 days. Though this was not found to be statistically significant, the agent provided a basis for further studies. The 28-days mortality was found to be similar for both groups. This has now provided us with a basis on which to develop future molecules. The study has been supported by the National Institute of Health, USA. The authors of the study advocated for more clinical trials with Remdesivir with a larger population. Such larger studies are already in progress, and their results are awaited. Remdesivir is currently one of the drugs that hold most promise against COVID-19.
An early trial in China with Lopinavir and Ritonavir showed no benefit compared with standard clinical care ( 80 ). More studies with this drug are currently underway, including one in India ( 81 , 82 ).
Use of Convalescent Patient Plasma
Another possible option would be the use of serum from convalescent individuals, as this is known to contain antibodies that can neutralize the virus and aid in its elimination. This has been tried previously for other coronavirus infections ( 83 ). Early emerging case reports in this aspect look promising compared to other therapies that have been tried ( 84 – 87 ). A report from China indicates that five patients treated with plasma recovered and were eventually weaned off ventilators ( 84 ). They exhibited reductions in fever and viral load and improved oxygenation. The virus was not detected in the patients after 12 days of plasma transfusion. The US FDA has provided detailed recommendations for investigational COVID-19 Convalescent Plasma use ( 88 ). One of the benefits of this approach is that it can also be used for post-exposure prophylaxis. This approach is now beginning to be increasingly adopted in other countries, with over 95 trials registered on clinicaltrials.gov alone, of which at least 75 are interventional ( 89 ). The use of convalescent patient plasma, though mostly for research purposes, appears to be the best and, so far, the only successful option for treatment available.
From a future perspective, the use of monoclonal antibodies for the inhibition of the attachment of the virus to the ACE-2 receptor may be the best bet. Aside from this, ACE-2-like molecules could also be utilized to attach and inactivate the viral proteins, since inhibition of the ACE-2 receptor would not be advisable due to its negative repercussions physiologically. In the absence of drug regimens and a vaccine, the treatment is symptomatic and involves the use of non-invasive ventilation or intubation where necessary for respiratory failure patients. Patients that may go into septic shock should be managed as per existing guidelines with hemodynamic support as well as antibiotics where necessary.
The WHO has recommended that simple personal hygiene practices can be sufficient for the prevention of spread and containment of the disease ( 90 ). Practices such as frequent washing of soiled hands or the use of sanitizer for unsoiled hands help reduce transmission. Covering of mouth while sneezing and coughing, and disinfection of surfaces that are frequently touched, such as tabletops, doorknobs, and switches with 70% isopropyl alcohol or other disinfectants are broadly recommended. It is recommended that all individuals afflicted by the disease, as well as those caring for the infected, wear a mask to avoid transmission. Healthcare works are advised to wear a complete set of personal protective equipment as per WHO-provided guidelines. Fumigation of dormitories, quarantine rooms, and washing of clothes and other fomites with detergent and warm water can help get rid of the virus. Parcels and goods are not known to transmit the virus, as per information provided by the WHO, since the virus is not able to survive sufficiently in an open, exposed environment. Quarantine of infected individuals and those who have come into contact with an infected individual is necessary to further prevent transmission of the virus ( 91 ). Quarantine is an age-old archaic practice that continues to hold relevance even today for disease containment. With the quarantine being implemented on such a large scale in some countries, taking the form of a national lockdown, the question arises of its impact on the mental health of all individuals. This topic needs to be addressed, especially in countries such as India and China, where it is still a matter of partial taboo to talk about it openly within the society.
In India, the Ministry of Ayurveda, Yoga, and Naturopathy, Unani, Siddha and Homeopathy (AYUSH), which deals with the alternative forms of medicine, issued a press release that the homeopathic, drug Arsenicum album 30, can be taken on an empty stomach for 3 days to provide protection against the infection ( 92 ). It also provided a list of herbal drugs in the same press release as per Ayurvedic and Unani systems of medicine that can boost the immune system to deal with the virus. However, there is currently no evidence to support the use of these systems of medicine against COVID-19, and they need to be tested.
The prevention of the disease with the use of a vaccine would provide a more viable solution. There are no vaccines available for any of the coronaviruses, which includes SARS and MERS. The development of a vaccine, however, is in progress at a rapid pace, though it could take about a year or two. As of April 2020, no vaccine has completed the development and testing process. A popular approach has been with the use of mRNA-based vaccine ( 93 – 96 ). mRNA vaccines have the advantage over conventional vaccines in terms of production, since they can be manufactured easily and do not have to be cultured, as a virus would need to be. Alternative conventional approaches to making a vaccine against SARS-CoV-2 would include the use of live attenuated virus as well as using the isolated spike proteins of the virus. Both of these approaches are in progress for vaccine development ( 97 ). Governments across the world have poured in resources and made changes in their legislation to ensure rapid development, testing, and deployment of a vaccine.
Barriers to Treatment
Lack of transparency and poor media relations.
The lack of government transparency and poor reporting by the media have hampered the measures that could have been taken by healthcare systems globally to deal with the COVID-19 threat. The CDC, as well as the US administration, downplayed the threat and thus failed to stock up on essential supplies, ventilators, and test kits. An early warning system, if implemented, would have caused borders to be shut and early lockdowns. The WHO also delayed its response in sounding the alarm regarding the severity of the outbreak to allow nations globally to prepare for a pandemic. Singapore is a prime example where, despite the WHO not raising concerns and banning travel to and from China, a country banned travelers and took early measures, thus managing the outbreak quite well. South Korea is another example of how things may have played out had those measures by agencies been taken with transparency. Increased transparency would have allowed the healthcare sector to better prepare and reduced the load of patients they had to deal with, helping flatten the curve. The increased patient load and confusion among citizens arising from not following these practices has proved to be a barrier to providing effective treatments to patients with the disease elsewhere in the world.
Lack of Preparedness and Protocols
Despite the previous SARS outbreak teaching us important lessons and providing us with data on a potential outbreak, many nations did not take the important measures needed for a future outbreak. There was no allocation of sufficient funds for such an event. Many countries experienced severe lack of PPE, and the lockdown precautions hampered the logistics of supply and manufacturing of such essential equipment. Singapore and South Korea had protocols in place and were able to implement them at a moment's notice. The spurt of cases that Korea experienced was managed well, providing evidence to this effect. The lack of preparedness and lack of protocol in other nations has resulted in confusion as to how the treatment may be administered safely to the large volume of patients while dealing with diagnostics. Both of these factors have limited the accessibility to healthcare services due to sheer volume.
Socio-Economic Impact
During the SARS epidemic, China faced an economic setback, and experts were unsure if any recovery would be made. However, the global and domestic situation was then in China's favor, as it had a lower debt, allowing it to make a speedy recovery. This is not the case now. Global experts have a pessimistic outlook on the outcome of this outbreak ( 98 ). The fear of COVID-19 disease, lack of proper understanding of the dangers of the virus, and the misinformation spread on the social media ( 99 ) have caused a breakdown of the economic flow globally ( 100 ). An example of this is Indonesia, where a great amount of fear was expressed in responses to a survey when the nation was still free of COVID-19 ( 101 ). The pandemic has resulted in over 2.6 billion people being put under lockdown. This lockdown and the cancellation of the lunar year celebration has affected business at the local level. Hundreds of flights have been canceled, and tourism globally has been affected. Japan and Indonesia are estimated to lose over 2.44 billion dollars due to this ( 102 , 103 ). Workers are not able to work in factories, transportation in all forms is restricted, and goods are not produced or moved. The transport of finished products and raw materials out of China is low. The Economist has published US stock market details indicating that companies in the US that have Chinese roots fell, on average, 5 points on the stock market as compared to the S&P 500 index ( 104 ). Companies such as Starbucks have had to close over 4,000 outlets due to the outbreak as a precaution. Tech and pharma companies are at higher risk since they rely on China for the supply of raw materials and active pharmaceutical ingredients. Paracetamol, for one, has reported a price increase of over 40% in India ( 104 – 106 ). Mass hysteria in the market has caused selling of shares of these companies, causing a tumble in the Indian stock market. Though long-term investors will not be significantly affected, short-term traders will find themselves in soup. Politically, however, this has further bolstered support for world leaders in countries such as India, Germany, and the UK, who are achieving good approval ratings, with citizens being satisfied with the government's approach. In contrast, the ratings of US President Donald Trump have dropped due to the manner in which the COVID-19 pandemic was handled. These minor impacts may be of temporary significance, and the worst and direct impact will be on China itself ( 107 – 109 ), as the looming trade war with the USA had a negative impact on the Chinese and Asian markets. The longer production of goods continues to remain suspended, the more adversely it will affect the Chinese economy and the global markets dependent on it ( 110 ). If this disease is not contained, more and more lockdowns by multiple nations will severely affect the economy and lead to many social complications.
The appearance of the 2019 Novel Coronavirus has added and will continue to add to our understanding of viruses. The pandemic has once again tested the world's preparedness for dealing with such outbreaks. It has provided an outlook on how a massive-scale biological event can cause a socio-economic disturbance through misinformation and social media. In the coming months and years, we can expect to gain further insights into SARS-CoV-2 and COVID-19.
Author Contributions
KN: conceptualization. RK, AA, JM, and KN: investigation. RK and AA: writing—original draft preparation. KN, PN, and JM: writing—review and editing. KN: supervision.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to acknowledge the contributions made by Dr. Piya Paul Mudgal, Assistant Professor, Manipal Institute of Virology, Manipal Academy of Higher Education towards inputs provided by her during the drafting of the manuscript.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2020.00216/full#supplementary-material
Supplementary Data 1, 2. List of all studies registered for COVID-19 on clinicaltrials.gov .
1. McIntosh K, Dees JH, Becker WB, Kapikian AZ, Chanock RM. Recovery in tracheal organ cultures of novel viruses from patients with respiratory disease. Proc Natl Acad Sci USA. (1967) 57:933–40. doi: 10.1073/pnas.57.4.933
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Esper F, Weibel C, Ferguson D, Landry ML, Kahn JS. Evidence of a novel human coronavirus that is associated with respiratory tract disease in infants and young children. J Infect Dis. (2005) 191:492–8. doi: 10.1086/428138
3. Stöhr K. A multicentre collaboration to investigate the cause of severe acute respiratory syndrome. Lancet. (2003) 361:1730–3. doi: 10.1016/S0140-6736(03)13376-4
4. Peiris JSM, Lai ST, Poon LLM, Guan Y, Yam LYC, Lim W, et al. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet. (2003) 361:1319–25. doi: 10.1016/S0140-6736(03)13077-2
5. Zumla A, Hui DS, Perlman S. Middle East respiratory syndrome. Lancet. (2015) 386:995–1007. doi: 10.1016/S0140-6736(15)60454-8
6. Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus ADME, Fouchier RAM. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. (2012) 367:1814–20. doi: 10.1056/NEJMoa1211721
7. Perlman S, Netland J. Coronaviruses post-SARS: update on replication and pathogenesis. Nat Rev Microbiol. (2009) 7:439–50. doi: 10.1038/nrmicro2147
8. Li W, Moore MJ, Vasllieva N, Sui J, Wong SK, Berne MA, et al. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. (2003) 426:450–4. doi: 10.1038/nature02145
9. Ge X-Y, Li J-L, Yang X-L, Chmura AA, Zhu G, Epstein JH, et al. Isolation and characterization of a bat SARS-like coronavirus that uses the ACE2 receptor. Nature. (2013) 503:535–8. doi: 10.1038/nature12711
10. Wang M, Hu Z. Bats as animal reservoirs for the SARS coronavirus: Hypothesis proved after 10 years of virus hunting. Virol Sin. (2013) 28:315–7. doi: 10.1007/s12250-013-3402-x
11. Diamond Princess Cruise Ship in Japan Confirms 99 New Coronavirus Cases | World news | The Guardian. Available online at: https://www.theguardian.com/world/2020/feb/17/coronavirus-japan-braces-for-hundreds-more-cases-as-another-china-city-locked-down (accessed February 17, 2020).
Google Scholar
12. Diamond Princess Coronavirus & Quarantine Updates - Notices & Advisories - Princess Cruises. Available online at: https://www.princess.com/news/notices_and_advisories/notices/diamond-princess-update.html (accessed February 17, 2020).
13. Gorbalenya AE, Baker SC, Baric RS, Groot RJ, de Drosten C, Gulyaeva AA, et al. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. (2020) 5:536–44. doi: 10.1038/s41564-020-0695-z
14. Ji W, Wang W, Zhao X, Zai J, Li X. Homologous recombination within the spike glycoprotein of the newly identified coronavirus may boost cross-species transmission from snake to human. J Med Virol . (2020) 7:jmv.25682. doi: 10.1002/jmv.25682
15. Cyranoski D. Did pangolins spread the China coronavirus to people? Nature . (2020) doi: 10.1038/d41586-020-00364-2
CrossRef Full Text | Google Scholar
16. Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. (2020) 395:565–74. doi: 10.1016/S0140-6736(20)30251-8
17. Wassenaar TM, Zou Y. 2019_nCoV: Rapid classification of betacoronaviruses and identification of traditional Chinese medicine as potential origin of zoonotic coronaviruses. Lett Appl Microbiol. (2020) 70:324–48. doi: 10.1111/lam.13285
18. Velavan TP, Meyer CG. The Covid-19 epidemic. Trop Med Int Heal . (2020) 25:278–80. doi: 10.1111/tmi.13383
19. Guarner J. Three Emerging Coronaviruses in Two Decades. Am J Clin Pathol . (2020) 153:420–21. doi: 10.1093/ajcp/aqaa029
20. Li W, Shi Z, Yu M, Ren W, Smith C, Epstein JH, et al. Bats are natural reservoirs of SARS-like coronaviruses. Science. (2005) 310:676–9. doi: 10.1126/science.1118391
21. Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. (2020) 579:270–3. doi: 10.1038/s41586-020-2012-7
22. Menachery VD, Yount BL, Debbink K, Agnihothram S, Gralinski LE, Plante JA, et al. A SARS-like cluster of circulating bat coronaviruses shows potential for human emergence. Nat Med. (2015) 21:1508–13. doi: 10.1038/nm.3985
23. COVID-19 Coronavirus Epidemic has a Natural Origin—ScienceDaily. Available online at: https://www.sciencedaily.com/releases/2020/03/200317175442.htm (accessed April 22, 2020).
24. Andersen KG, Rambaut A, Lipkin WI, Holmes EC, Garry RF. The proximal origin of SARS-CoV-2. Nat Med . (2020) 26:450–2. doi: 10.1038/s41591-020-0820-9
25. Prioritizing Diseases for Research and Development in Emergency Contexts. Available online at: https://www.who.int/activities/prioritizing-diseases-for-research-and-development-in-emergency-contexts (accessed April 22, 2020).
26. Albariño CG, Guerrero LW, Jenks HM, Chakrabarti AK, Ksiazek TG, Rollin PE, et al. Insights into Reston virus spillovers and adaption from virus whole genome sequences. PLoS ONE. (2017) 12:e0178224. doi: 10.1371/journal.pone.0178224
27. Yao H, Lu X, Chen Q, Xu K, Chen Y, Cheng L, et al. Patient-derived mutations impact pathogenicity of SARS-CoV-2. medRxiv. (2020). doi: 10.2139/ssrn.3578153
28. Stefanelli P, Faggioni G, Lo Presti A, Fiore S, Marchi A, Benedetti E, et al. Whole genome and phylogenetic analysis of two SARS-CoV-2 strains isolated in Italy in January and February 2020: additional clues on multiple introductions and further circulation in Europe. Eurosurveillance. (2020) 25:2000305. doi: 10.2807/1560-7917.ES.2020.25.13.2000305
29. Yadav P, Potdar V, Choudhary M, Nyayanit D, Agrawal M, Jadhav S, et al. Full-genome sequences of the first two SARS-CoV-2 viruses from India. Indian J Med Res. (2020) 151:200–9. doi: 10.4103/ijmr.IJMR_663_20
30. WHO | Coronavirus disease 2019 (COVID-19) Situation Report – 26. Beijing (2020). Available online at: http://www.nhc.gov.cn/xcs/yqtb/list_gzbd.shtml (accessed February 16, 2020).
31. WHO | Middle East Respiratory Syndrome Coronavirus (MERS-CoV). World Health Organization (2020).
32. WHO | Summary of Probable SARS Cases With Onset of Illness From 1 November 2002 to 31 July 2003. World Health Organization (2015).
33. Worldometer. Coronavirus cases. Worldometer. (2020) 1−22.
34. Update on the Outbreak of New Coronavirus Pneumonia as of 24 hours on 15 February. Beijing (2020). Available online at: http://www.nhc.gov.cn/xcs/yqtb/list_gzbd.shtml (accessed February 16, 2020).
35. Sanche S, Lin YT, Xu C, Romero-Severson E, Hengartner N, Ke R. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. (2020) 26. doi: 10.3201/eid2607.200282
36. 83% of India's Coronavirus Patients Are Below the Age of 50: Health ministry data - India News. Available online at: https://www.indiatoday.in/india/story/83-of-india-s-coronavirus-patients-are-below-the-age-of-50-health-ministry-data-1663314-2020-04-04 (accessed April 23, 2020).
37. 42% of Coronavirus Patients in 21-40 age bracket: Govt. Available online at: https://economictimes.indiatimes.com/news/politics-and-nation/42-of-coronavirus-patients-in-21-40-age-bracket-govt/articleshow/74987254.cms (accessed April 23, 2020).
38. Why COVID-19 Case Counts Are so Low in Singapore Hong Kong and Taiwan | Advisory Board Daily Briefing. Available online at: https://www.advisory.com/daily-briefing/2020/03/19/asian-countries (accessed April 29, 2020).
39. Coronavirus: Why so Few Deaths Among Singapore's 14000 Covid-19 Infections? | South China Morning Post. Available online at: https://www.scmp.com/weekasia/health-environment/article/3081772/coronavirus-why-so-few-deaths-among-singapores-14000 (accessed April 29, 2020).
40. Stafford N. Covid-19: Why Germany's case fatality rate seems so low. BMJ. (2020) 7:369. doi: 10.1136/bmj.m1395
41. Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, et al. Transmission of 2019-NCOV infection from an asymptomatic contact in Germany. N Engl J Med . (2020) 382:970–1. doi: 10.1056/NEJMc2001468
42. Coronavirus pandemic | 80% of COVID-19 Cases Either Asymptomatic or Show Mild Symptoms. Health ministry - Moneycontrol.com. Available online at: https://www.moneycontrol.com/news/india/coronavirus-pandemic-80-of-covid-19-cases-either-asymptomatic-or-show-mild-symptoms-health-ministry-5170631.html (accessed April 24, 2020).
43. WHO | Q&A on Coronaviruses. Available online at: https://www.who.int/news-room/q-a-detail/q-a-coronaviruses (accessed February 16, 2020).
44. Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med . (2020) 382:929–36. doi: 10.1056/NEJMoa2001191
45. Yeo C, Kaushal S, Yeo D. Enteric involvement of coronaviruses: is faecal–oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol Hepatol. (2020) 5:335–37. doi: 10.1016/S2468-1253(20)30048-0
46. Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. (2020) 395:809–15. doi: 10.1016/S0140-6736(20)30360-3
47. Fehr AR, Perlman S. Coronaviruses: An overview of their replication and pathogenesis. In: Coronaviruses: Methods and Protocols (New York: Springer), 1–23. doi: 10.1007/978-1-4939-2438-7_1
48. Chen Y, Liu Q, Guo D. Emerging coronaviruses: Genome structure, replication, and pathogenesis. J Med Virol. (2020) 92:418–23. doi: 10.1002/jmv.25681
49. Hoffmann M, Kleine-Weber H, Schroeder S, Mü MA, Drosten C, Pö S. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. (2020) 181:271–80. doi: 10.1016/j.cell.2020.02.052
50. Cheng VCC, Chan JFW, To KKW, Yuen KY. Clinical management and infection control of SARS: Lessons learned. Antiviral Res. (2013) 100:407–19. doi: 10.1016/j.antiviral.2013.08.016
51. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
52. Udugama B, Kadhiresan P, Kozlowski HN, Malekjahani A, Osborne M, Li VYC, et al. Diagnosing COVID-19: the disease and tools for detection. ACS Nano . (2020) 14:3822–35. doi: 10.1021/acsnano.0c02624
53. Testing, | CDC,. Available online at: https://www.cdc.gov/coronavirus/2019-ncov/testing/index.html (accessed April 29, 2020).
54. Advice on the Use of Point-of-Care Immunodiagnostic Tests for COVID-19. Available online at: https://www.who.int/news-room/commentaries/detail/advice-on-the-use-of-point-of-care-immunodiagnostic-tests-for-covid-19 (accessed April 29, 2020).
55. Zhang Yanping. The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) — China, 2020. (2020) Available online at: http://weekly.chinacdc.cn/en/article/id/e53946e2-c6c4-41e9-9a9bfea8db1a8f51 (accessed February 18, 2020).
56. Petersen R, Pan L, Blanck HM. Racial and ethnic disparities in adult obesity in the United States: CDC's tracking to inform state and local action. Prev Chronic Dis. (2019) 16:180579. doi: 10.5888/pcd16.180579
57. Wang L, Southerland J, Wang K, Bailey BA, Alamian A, Stevens MA, et al. Ethnic differences in risk factors for obesity among adults in California, the United States. (2017) 2017:2427483. doi: 10.1155/2017/2427483
58. Covid-19 Causes Sudden Strokes in Young Adults Doctors Say - CNN. Available online at: https://edition.cnn.com/2020/04/22/health/strokes-coronavirus-young-adults/index.html (accessed April 24, 2020).
59. Wang J, Hajizadeh N, Moore EE, McIntyre RC, Moore PK, Veress LA, et al. Tissue plasminogen activator (tPA) treatment for COVID-19 associated acute respiratory distress syndrome (ARDS): a case series. J Thromb Haemost . (2020) 1–4. doi: 10.1111/jth.14828
60. Lancet T, Medicine R. Comment Understanding pathways to death in patients with. Lancet Respir Med. (2020) 2019:2019–21. doi: 10.1016/S2213-2600(20)30165-X
61. Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA . (2020) 323:1775–6. doi: 10.1001/jama.2020.4683
62. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. (2020) 395:1054–62. doi: 10.1016/S0140-6736(20)30566-3
63. Doctors Warn COVID-19 Might Cause Strokes in Young Adults. Available online at: https://nypost.com/2020/04/23/doctors-warn-covid-19-might-cause-strokes-in-young-adults/ (accessed April 24, 2020).
64. “Solidarity” Clinical Trial for COVID-19 Treatments. Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov/solidarity-clinical-trial-for-covid-19-treatments (accessed April 23, 2020).
65. Search, of: COVID-19 - List Results - ClinicalTrials.gov . Available online at: https://www.clinicaltrials.gov/ct2/results?cond=COVID-19&term=&cntry=&state=&city=&dist= (accessed May 1, 2020).
66. De Wilde AH, Jochmans D, Posthuma CC, Zevenhoven-Dobbe JC, Van Nieuwkoop S, Bestebroer TM, et al. Screening of an FDA-approved compound library identifies four small-molecule inhibitors of Middle East respiratory syndrome coronavirus replication in cell culture. Antimicrob Agents Chemother. (2014) 58:4875–84. doi: 10.1128/AAC.03011-14
67. Tai DYH. Pharmacologic treatment of SARS: current knowledge and recommendations. Ann Acad Med Singapore. (2007) 36:438–43.
PubMed Abstract | Google Scholar
68. Sheahan TP, Sims AC, Leist SR, Schäfer A, Won J, Brown AJ, et al. Comparative therapeutic efficacy of remdesivir and combination lopinavir, ritonavir, and interferon beta against MERS-CoV. Nat Commun. (2020) 11:222. doi: 10.1038/s41467-019-13940-6
69. Gao J, Tian Z, Yang X. Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Biosci Trends. (2020) 14:72–73. doi: 10.5582/bst.2020.01047
70. Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M, et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. (2020) 30:269–71. doi: 10.1038/s41422-020-0282-0
71. Vincent MJ, Bergeron E, Benjannet S, Erickson BR, Rollin PE, Ksiazek TG, et al. Chloroquine is a potent inhibitor of SARS coronavirus infection and spread. Virol J. (2005) 2:1–0. doi: 10.1186/1743-422X-2-69
72. Cramer CL, Patterson A, Alchakaki A, Soubani AO. Immunomodulatory indications of azithromycin in respiratory disease: a concise review for the clinician. Postgrad Med. (2017) 129:493–9. doi: 10.1080/00325481.2017.1285677
73. Plaquenil™ Hydroxychloroquine Sulfate Tablets USP Description. Available online at: http://www.cdc.gov/malaria (accessed April 21, 2020).
74. Magagnoli J, Narendran S, Pereira F, Cummings T, Hardin JW, Sutton SS, et al. Outcomes of hydroxychloroquine usage in United States veterans hospitalized with Covid-19. medRxiv. (2020) doi: 10.1101/2020.04.16.20065920
75. Shamshirian A, Hessami A, Heydari K, Alizadeh-Navaei R, Ebrahimzadeh MA, Ghasemian R, et al. Hydroxychloroquine Versus COVID-19: A Rapid Systematic Review and Meta-Analysis. medRxiv. (2020) doi: 10.1101/2020.04.14.20065276
76. Li G, De Clercq E. Therapeutic options for the 2019 novel coronavirus (2019-nCoV). Nat Rev Drug Discov . (2020) 19:149–50. doi: 10.1038/d41573-020-00016-0
77. Warren TK, Jordan R, Lo MK, Ray AS, Mackman RL, Soloveva V, et al. Therapeutic efficacy of the small molecule GS-5734 against Ebola virus in rhesus monkeys. Nature. (2016) 531:381–5. doi: 10.1038/nature17180
78. Williamson BN, Feldmann F, Schwarz B, Meade-White K, Porter DP, Schulz J, et al. Clinical benefit of remdesivir in rhesus macaques infected with SARS-CoV-2. bioRxiv. (2020) doi: 10.1101/2020.04.15.043166
79. Wang Y, Zhang D, Du G, Du R, Zhao J, Jin Y, et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. (2020) 395:1569–78. doi: 10.1016/S0140-6736(20)31022-9
80. Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, et al. A trial of lopinavir–ritonavir in adults hospitalized with severe covid-19. N Engl J Med . (2020) 382:1787–99. doi: 10.1056/NEJMoa2001282
81. Search, of: Lopinavir, Ritonavir, | COVID - List Results - ClinicalTrials.gov . Available online at: https://clinicaltrials.gov/ct2/results?term=Lopinavir%2CRitonavir&cond=COVID&draw=4&rank=22#rowId21 (accessed April 23, 2020).
82. Bhatnagar T, Murhekar M, Soneja M, Gupta N, Giri S, Wig N, et al. Lopinavir/ritonavir combination therapy amongst symptomatic coronavirus disease 2019 patients in India: protocol for restricted public health emergency use. Indian J Med Res. (2020) 151:184–9. doi: 10.4103/ijmr.IJMR_502_20
83. Yeh K-M, Chiueh T-S, Siu LK, Lin J-C, Chan PKS, Peng M-Y, et al. Experience of using convalescent plasma for severe acute respiratory syndrome among healthcare workers in a Taiwan hospital. J Antimicrob Chemother. (2005) 56:919–22. doi: 10.1093/jac/dki346
84. Shen C, Wang Z, Zhao F, Yang Y, Li J, Yuan J, et al. Treatment of 5 critically Ill patients with COVID-19 with convalescent plasma. JAMA . (2020) 323:1582–9. doi: 10.1001/jama.2020.4783
85. Cao W, Liu X, Bai T, Fan H, Hong K, Song H, et al. High-dose intravenous immunoglobulin as a therapeutic option for deteriorating patients with coronavirus disease 2019. Open Forum Infect Dis . (2020) 7:1–6. doi: 10.1093/ofid/ofaa102
86. Bloch EM, Shoham S, Casadevall A, Sachais BS, Shaz B, Winters JL, et al. Deployment of convalescent plasma for the prevention and treatment of COVID-19. J Clin Invest . (2020) 138745:1–22. doi: 10.1172/JCI138745
87. Ye M, Fu D, Ren Y, Wang F, Wang D, Zhang F, et al. Treatment with convalescent plasma for COVID-19 patients in Wuhan, China. J Med Virol. (2 020) doi: 10.1002/jmv.25882
88. Recommendations for Investigational COVID-19 Convalescent Plasma | FDA. Available online at: https://www.fda.gov/vaccines-blood-biologics/investigational-new-drug-ind-or-device-exemption-ide-process-cber/recommendations-investigational-covid-19-convalescent-plasma (accessed April 23, 2020).
89. Search, of: plasma | Interventional Studies | COVID - List Results - ClinicalTrials.gov . Available online at: https://clinicaltrials.gov/ct2/results?term=plasma&cond=COVID&Search=Apply&age_v=&gndr=&type=Intr&rslt= (accessed April 23, 2020).
90. Infection Prevention and Control. Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/infection-prevention-and-control (accessed February 17, 2020).
91. Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med . (2020) 27:taaa020. doi: 10.1093/jtm/taaa020
92. Press Information Bureau AYUSH Advisory for Corona virus. Press Inf Bereau. Available online at: https://pib.gov.in/PressReleasePage.aspx?PRID=1600895 (accessed February 17, 2020).
93. CanSino, Biologics : China Announces First Human Trials of Covid-19 Vaccine | MarketScreener,. Available online at: https://www.marketscreener.com/CANSINO-BIOLOGICS-INC-59318312/news/CanSino-Biologics-China-announces-first-human-trials-of-Covid-19-vaccine-30183232/ (accessed April 7, 2020).
94. Safety, and Immunogenicity Study of 2019-nCoV Vaccine (mRNA-1273) for Prophylaxis SARS CoV-2 Infection - Full Text View - ClinicalTrials.gov . Available online at: https://clinicaltrials.gov/ct2/show/NCT04283461 (accessed April 7, 2020).
95. NIH, Clinical Trial of Investigational Vaccine for COVID-19 Begins | National Institutes of Health (NIH),. Available at: https://www.nih.gov/news-events/news-releases/nih-clinical-trial-investigational-vaccine-covid-19-begins (accessed April 7, 2020).
96. Novel, Coronavirus vaccine manufacturing contract signed — The Jenner Institute,. Available online at: https://www.jenner.ac.uk/about/news/novel-coronavirus-vaccine-manufacturing-contract-signed (accessed April 7, 2020).
97. Xie L, Sun C, Luo C, Zhang Y, Zhang J, Yang J, et al. SARS-CoV-2 and SARS-CoV Spike-RBD structure and receptor binding comparison and potential implications on neutralizing antibody and vaccine development. bioRxiv [Preprint]. (2020). doi: 10.1101/2020.02.16.951723
98. The Global Economic Impact of the Coronavirus Outbreak – Harvard Gazette. Available online at: https://news.harvard.edu/gazette/story/2020/02/the-global-economic-impact-of-the-coronavirus-outbreak/ (accessed February 17, 2020).
99. Shimizu K. 2019-nCoV, fake news, and racism. Lancet . (2020) 395:685–6. doi: 10.1016/S0140-6736(20)30357-3
100. ROHDE RODNEY. 2019 Novel Coronavirus (2019-nCoV) Update: Uncoating the Virus. Am Soc Microbiol. (2020). Available online at: https://asm.org/Articles/2020/January/2019-Novel-Coronavirus-2019-nCoV-Update-Uncoating
101. Virus-free Indonesia more threatened by COVID-19 than Singapore Malaysia: Survey - World - The Jakarta Post. Available online at: https://www.thejakartapost.com/news/2020/02/18/virus-free-indonesia-more-threatened-by-covid-19-than-singapore-malaysia-survey.html (accessed February 18, 2020).
102. Japan, May Lose $1,.29 Billion in Tourism Revenue Due to COVID-19 Outbreak | The Japan Times. Available online at: https://www.japantimes.co.jp/news/2020/02/16/business/economy-business/japan-lose-billion-tourism-revenue-covid19-outbreak/#.XkvxX0fitPY (accessed February 18, 2020).
103. Coronavirus's Effect on Tourism Will Carry Into 2021 Experts Say - Bloomberg. Available online at: https://www.bloomberg.com/news/articles/2020-02-13/coronavirus-s-effect-on-tourism-will-carry-into-2021-experts-say (accessed February 18, 2020).
104. The, week in charts - The cost of covid-19 | Graphic detail | The Economist,. Available online at: https://www.economist.com/graphic-detail/2020/02/14/the-cost-of-covid-19 (accessed February 17, 2020).
105. coronavirus: Covid-19 Impact: Pharma Companies Feel the Pain as Prices of Key Inputs Shoot Up - The Economic Times. Available online at: https://economictimes.indiatimes.com/industry/healthcare/biotech/pharmaceuticals/covid-19-impact-pharma-companies-feel-the-pain-as-prices-of-key-inputs-shoot-up/articleshow/74144044.cms?from=mdr (accessed February 17, 2020).
106. Coronavirus Outbreak: Paracetamol Prices Jump 40% In India As Coronavirus Shuts Down China. Available online at: https://www.ndtv.com/india-news/coronavirus-outbreak-paracetamol-prices-jump-40-in-india-as-coronavirus-shuts-down-china-2181480 (accessed February 18, 2020).
107. The coronavirus could cripple China's economy for longer than Wall Street wants to believe | Business Insider India. Available online at: https://www.businessinsider.in/international/news/the-coronavirus-could-cripple-chinas-economy-for-longer-than-wall-street-wants-to-believe/articleshow/74162183.cms (accessed February 17, 2020).
108. Viral Slowdown - How China's Coronavirus Epidemic Could Hurt the World Economy | Leaders | The Economist. Available online at: https://www.economist.com/leaders/2020/02/13/how-chinas-coronavirus-epidemic-could-hurt-the-world-economy (accessed February 17, 2020).
109. China's Economic Battle With COVID-19 | The ASEAN Post. Available online at: https://theaseanpost.com/article/chinas-economic-battle-covid-19 (accessed February 17, 2020).
110. The Coronavirus Could Cost China's Economy $60 Billion this Quarter. - CNN. Available online at: https://edition.cnn.com/2020/01/31/economy/china-economy-coronavirus/index.html (accessed February 18, 2020).
Keywords: 2019-nCoV, COVID-19, SARS-CoV-2, coronavirus, pandemic, SARS
Citation: Keni R, Alexander A, Nayak PG, Mudgal J and Nandakumar K (2020) COVID-19: Emergence, Spread, Possible Treatments, and Global Burden. Front. Public Health 8:216. doi: 10.3389/fpubh.2020.00216
Received: 21 February 2020; Accepted: 11 May 2020; Published: 28 May 2020.
Reviewed by:
Copyright © 2020 Keni, Alexander, Nayak, Mudgal and Nandakumar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Krishnadas Nandakumar, mailnandakumar77@gmail.com
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

IMAGES
COMMENTS
Reading time: 3 min (864 words) The COVID-19 pandemic has led to a dramatic loss of human life worldwide and presents an unprecedented challenge to public health, food systems and the world of work. The economic and social disruption caused by the pandemic is devastating: tens of millions of people are at risk of falling into extreme poverty ...
From lifestyle changes to better eating habits, people are using this time to get healthier in many areas. Since the pandemic started, nearly two-thirds of the survey's participants (62%) say ...
Feelings of isolation and loneliness can increase the likelihood of depression, high blood pressure, and death from heart disease. They can also affect the immune system's ability to fight ...
The World Health Organisation (WHO) has declared the coronavirus disease 2019 (COVID-19) a pandemic. Covid-19 has affected and still affecting our life in many ways. Covid-19 has rapidly affected our day to day life, businesses, disrupted the world trade and movements. Identification of the disease at an early stage is vital to control the ...
'COVID-19 has shown that people do value local food networks. You saw informal markets, and adaptable businesses springing up and driving things ahead,' Benton says. However it remains to be seen how permanent or widespread any move towards more seasonal, localized produce supply chains will be, without any dedicated support or state ...
The days dragged on in my apartment, in black and white, like my photos. Sometimes we tried to smile, imagining that I was asymptomatic, because I was the virus. Our smiles seemed to bring good ...
The United States' unemployment rate rose from 3.5 percent in February 2020 to a record high of 14.7 percent in April 2020, but as of November 2020 it was back down to 6.7 percent. In November 2020, 21.8 percent of U.S. people with jobs teleworked due to the pandemic. The majority of school-age children in the United States have attended ...
As we adapted to a new way of life, a study published in September 2021 in PLOS One found that people who experienced involuntary social role disruptions because of COVID-19 reported increased ...
During the COVID-19 pandemic, you may experience stress, anxiety, fear, sadness and loneliness. And mental health disorders, including anxiety and depression, can worsen. Surveys show a major increase in the number of U.S. adults who report symptoms of stress, anxiety, depression and insomnia during the pandemic, compared with surveys before ...
1. Introduction. The coronavirus disease 2019 (COVID-19) pandemic has led to unprecedented changes in people's daily lives, with implications for mental health and well-being [1-4], both at the level of a given country's population, and when considering specific vulnerable groups [5-7].In order to mitigate the untoward impact of the pandemic (including lockdown) and support mental health ...
The outbreak has dramatically changed Americans' lives and relationships over the past year. We asked people to tell us about their experiences - good and bad - in living through this moment in history. Pew Research Center has been asking survey questions over the past year about Americans' views and reactions to the COVID-19 pandemic.
Presently the impacts of COVID-19 in daily life are extensive and have far reaching consequences. These can be divided into various categories: Closure of places for entertainment such as movie and play theatres, sports clubs, gymnasiums, swimming pools, and so on. This COVID-19 has affected the sources of supply and effects the global economy.
The Pandemic's Effects on Everyday Life. Boston College researchers are exploring COVID-19's impact on life as we know it. Here's a look at just some of the important questions they're asking—and answering. Is remote work here to stay? As many as 60 percent of U.S. employees are estimated to have worked remotely at some point during the ...
Students can choose to write a full-length college essay on the coronavirus or summarize their experience in a shorter form. To help students explain how the pandemic affected them, The Common App ...
My content explains what my life was like during the last seven months of the Covid-19 pandemic and how it affected my life both positively and negatively. It also explains what it was like when I graduated from High School and how I want the future generations to remember the Class of 2020. Class assignment, Western Civilization (Dr. Marino).
Click here 👆 to get an answer to your question ️ How COVID 19 affect in our life? Essay. nimmaladinesh9327 nimmaladinesh9327 17.09.2020 English Secondary School answered How COVID 19 affect in our life? Essay See answer Advertisement
Family in the Age of COVID‐19. The coronavirus has had a profound effect on the world in a multitude of ways. By the time this appears (written in mid‐April 2020), we probably will have some better sense of its ultimate impact. This essay centers on only one meaning of its effects: How it has impacted family life.
The COVID-19 pandemic caused increased anxiety, depression, and other mental health concerns that were difficult for my family and me to manage alone. Our ability to learn social resilience skills, such as self-management, was tested numerous times. One of the most visible challenges we faced was social isolation and loneliness.
March 2, 2021 5 min read. Illustration by Eddie Edwards. With more than 500,000 dead, the COVID-19 pandemic has created a nation touched by grief, compounded by the trauma of job loss, financial trouble, and everyday confusion, a mix that a Harvard psychologist said creates a complex and troubling picture of the country's emotional landscape.
The outbreak of the coronavirus disease 2019 (COVID-19) has created a global health crisis that had a deep impact on the way we perceive our world and our everyday lives. Not only has the rate of contagion and patterns of transmission threatened our sense of agency, but the safety measures to contain the spread of the virus also required social ...
In this new study, researchers from the Cleveland Clinic will use tools that they developed from earlier NIH-supported projects to study how COVID-19 affects the brain. They will focus on fatigue, headaches, loss of smell or taste, and memory loss, or "brain fog.". They will also look at more serious but less common complications, such as ...
COVID-19: Emergence, Spread, Possible Treatments, and Global Burden. The Coronavirus (CoV) is a large family of viruses known to cause illnesses ranging from the common cold to acute respiratory tract infection. The severity of the infection may be visible as pneumonia, acute respiratory syndrome, and even death.