A systematic literature review to clarify the concept of vaccine hesitancy
Affiliations.
- 1 Radboud University Medical Center, Radboud Institute for Health Sciences, Primary and Community Care, Nijmegen, the Netherlands. [email protected].
- 2 Radboud University Medical Center, Radboud Institute for Health Sciences, Primary and Community Care, Nijmegen, the Netherlands.
- 3 Behavioural Science Institute, Radboud University, Nijmegen, the Netherlands.
- 4 Radboud University Medical Center, Radboud Institute for Health Sciences, IQ Healthcare, Nijmegen, the Netherlands.
- PMID: 35995837
- DOI: 10.1038/s41562-022-01431-6
Vaccine hesitancy (VH) is considered a top-10 global health threat. The concept of VH has been described and applied inconsistently. This systematic review aims to clarify VH by analysing how it is operationalized. We searched PubMed, Embase and PsycINFO databases on 14 January 2022. We selected 422 studies containing operationalizations of VH for inclusion. One limitation is that studies of lower quality were not excluded. Our qualitative analysis reveals that VH is conceptualized as involving (1) cognitions or affect, (2) behaviour and (3) decision making. A wide variety of methods have been used to measure VH. Our findings indicate the varied and confusing use of the term VH, leading to an impracticable concept. We propose that VH should be defined as a state of indecisiveness regarding a vaccination decision.
© 2022. The Author(s), under exclusive licence to Springer Nature Limited.

Publication types
- Systematic Review
- Research Support, Non-U.S. Gov't
- Patient Acceptance of Health Care*
- Research Design
- Vaccination
- Vaccination Hesitancy*
- Vaccination Refusal
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- News & Views
- Published: 23 November 2022
Defining and measuring vaccine hesitancy
- Heidi J. Larson ORCID: orcid.org/0000-0002-8477-7583 1 , 2
Nature Human Behaviour volume 6 , pages 1609–1610 ( 2022 ) Cite this article
5563 Accesses
34 Citations
4 Altmetric
Metrics details
- Health policy
- Science, technology and society
When the term ‘vaccine hesitancy’ first appeared, it was deemed ambiguous and difficult to measure. A systematic review of published articles on vaccine hesitancy suggests it should be defined as a state of indecisiveness regarding a vaccination decision, independently of behaviour, and that it needs new modes of analysis and measurement.
Vaccine hesitancy has become a household term in the wake of the COVID-19 pandemic, with more people in the world thinking about vaccines than perhaps at any time in our history. The term ‘hesitancy’ was already gaining traction in vaccine discussions in the decade before COVID-19 erupted, and had become a growing topic of research and public health concern: the World Health Organization (WHO) had already named vaccine hesitancy as one of the top ten global health threats in 2019.

But what does vaccine hesitancy really mean? And how useful is it in terms of actionable measures to address it? In a recent article in Nature Human Behaviour — an extensive review of over 400 articles — Bussink-Voorend and colleagues 1 investigate how the concept of vaccine hesitancy is characterized and measured. They find that vaccine hesitancy is operationalized in a number of ways, and conclude that it is therefore not a practicable concept.
This comprehensive review and analysis updates the field beyond a previous 2014 systematic review 2 , and is not the first to question the usefulness and specificity of the term vaccine hesitancy — a liminal state of uncertainty in making a vaccination decision. Early references cited in the paper challenged various characterizations of vaccine hesitancy as being an unspecific and ambiguous notion 3 in need of a clear definition 4 . Bussink-Voorend et al. make a strong case for distinguishing between hesitancy and behaviour, and argue that including behaviour within a definition of vaccine hesitancy is not tenable. This disputes the 2014 WHO Sage Working group definition of vaccine hesitancy as a behavioural phenomenon; however, it is also a point made in Maya Goldenberg’s recent book Vaccine Hesitancy 5 , which similarly rejects the definition of vaccine hesitancy as a behaviour. In their conclusion, Bussink-Voorend et al. propose that vaccine hesitancy should be defined as “a state of indecisiveness regarding a vaccination decision.”
For a concrete example of the distinction between vaccine hesitancy as a psychological state and a behaviour, we can look to the recent example of the French health pass 6 . A survey of a representative sample of French adults asked respondents how they felt after getting a COVID-19 vaccine: “Were you relieved? Did you feel regret? Or were you angry?” Between March and September 2021, they discovered a striking increase in the proportion of people feeling regret or anger after COVID-19 vaccination. Even more telling was the finding that the number of people who had doubts about the vaccine — despite being vaccinated — increased from 44% to 61% after the government introduced the health pass. This suggests that many vaccinated people remained in a psychological state of indecisiveness. Thus, the health pass encouraged vaccination but did not reduce hesitancy, confirming the importance of distinguishing between vaccine hesitancy and behaviour.
This is also in agreement with a recent narrative review of vaccine hesitancy, which discusses the many different influencing factors along the path of decision-making towards accepting, delaying or refusing a vaccine 7 . Vaccine hesitancy is not a static state; instead, vaccine decision-making is a journey with ups and downs, and changes over time with different influences and nudges along the path that sometimes prompt hesitancy and sometimes nudge a positive intention to vaccinate. In the case of COVID-19 vaccines, the constantly evolving information environment — including new information (and misinformation), changing guidance and requirements, and a volatile and changing epidemic context that affected risk perceptions and the felt need (or not) for vaccination — were all factors that have prompted changing sentiments around the vaccines, sometimes prompting eagerness and at other times hesitancy, delays or outright refusal of vaccination.
The dynamic nature of vaccine hesitancy is not discussed in Bussink-Voorend et al.’s review. Nonetheless, in their conclusions the authors argue that vaccine hesitancy is “a psychological state of being undecided,” and psychological states are dynamic by nature. This changing, even volatile, and emotive nature of vaccine hesitancy also requires new disciplines of analysis beyond the public health, social science and biomedical studies reviewed in the paper. ‘Big data’ analyses, such as those from computer science and engineering, are crucial when it comes to analysing and measuring the dynamic and viral nature of hesitancy 8 .
Overall, as discussed in Bussink-Voorend’s review and in related literature, the distinction between the affective nature of vaccine hesitancy in the context of decision-making, and it being a behaviour, is crucial. Vaccine hesitancy is not a behaviour.
Where does this leave us in terms of research and measurement of vaccine hesitancy? Maybe we are asking the wrong questions and need to look at the new realities of contested science, challenged governments and publics armed with their own notions of evidence.
Bussink-Voorend, D., Hautvast, J. L. A., Vandeberg, L., Visser, O. & Hulscher, M. E. J. L. Nat. Hum. Behav . https://doi.org/10.1038/s41562-022-01431-6 (2022).
Larson, H. J., Jarrett, C., Eckersberger, E., Smith, D. M. D. & Paterson, P. Vaccine 32 , 2150–2159 (2014).
Article Google Scholar
Peretti-Watel P., Larson H. J., Ward J. K., Schulz W. S. & Verger P. PLoS Curr . 7 , ecurrents.outbreaks.6844c80ff9f5b273f34c91f71b7fc289 (2015).
Bedford, H. et al. Vaccine 36 , 6556–6558 (2018).
Goldenberg, M. Vaccine Hesitancy: Public Trust, Expertise, and the War on Science (Univ. Pittsburgh Press, 2021).
Ward, J. K. et al. Nat. Med. 28 , 232–235 (2022).
Article CAS Google Scholar
Larson, H. J., Gakidou, E. & Murray, C. J. L. N. Engl. J. Med. 387 , 58–65 (2022).
Sear, R., Leahy, R., Restrepo, N. J., Lupu, Y. & Johnson, N. (2022) Machine learning reveals adaptive COVID-19 narratives in online anti-vaccination network. In Proc. 2021 Conf. of the Computational Social Science Society of the Americas (eds Yang, Z. & von Briesen, E.) 164–175 (Springer, 2022).
Download references
Author information
Authors and affiliations.
Infectious Disease Epidemiology, London School of Hygiene & Tropical Medicine, London, UK
Heidi J. Larson
Institute for Health Metrics and Evaluation, University of Washington, Seattle, WA, USA
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Heidi J. Larson .
Ethics declarations
Competing interests.
H.J.L.’s research group has received grants from the Bill & Melinda Gates Foundation, GSK, Hong Kong Government, Johnson & Johnson, MacArthur Foundation, Merck, NIHR (UK) and UNICEF.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Larson, H.J. Defining and measuring vaccine hesitancy. Nat Hum Behav 6 , 1609–1610 (2022). https://doi.org/10.1038/s41562-022-01484-7
Download citation
Published : 23 November 2022
Issue Date : December 2022
DOI : https://doi.org/10.1038/s41562-022-01484-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Between now and later: a mixed methods study of hpv vaccination delay among chinese caregivers in urban chengdu, china.
- Vivian Wan-Cheong Yim
- Qianyun Wang
BMC Public Health (2024)
Understanding the role of risk preferences and perceptions in vaccination decisions and post-vaccination behaviors among U.S. households
- Jianhui Liu
- Bachir Kassas
- Zhifeng Gao
Scientific Reports (2024)
Social Processes and COVID-19 Vaccination of Children of Hesitant Mothers
- Don E. Willis
- Rachel S. Purvis
- Pearl A. McElfish
Journal of Community Health (2024)
Institutional trust is a distinct construct related to vaccine hesitancy and refusal
- Sekoul Krastev
- Oren Krajden
BMC Public Health (2023)
COVID-19 vaccine refusal associated with health literacy: findings from a population-based survey in Korea
- Inmyung Song
- Soo Hyun Lee
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Europe PMC requires Javascript to function effectively.
Either your web browser doesn't support Javascript or it is currently turned off. In the latter case, please turn on Javascript support in your web browser and reload this page.
Search life-sciences literature (43,904,411 articles, preprints and more)
- Full text links
- Citations & impact
- Similar Articles
A systematic literature review to clarify the concept of vaccine hesitancy.
Author information, affiliations.
- Bussink-Voorend D 1
- Hautvast JLA 1
- Vandeberg L 2
- Hulscher MEJL 3
ORCIDs linked to this article
- Hulscher MEJL | 0000-0002-2160-4810
- Vandeberg L | 0000-0002-7229-2378
- Bussink-Voorend D | 0000-0002-9873-1404
Nature Human Behaviour , 22 Aug 2022 , 6(12): 1634-1648 https://doi.org/10.1038/s41562-022-01431-6 PMID: 35995837
Abstract
Full text links .
Read article at publisher's site: https://doi.org/10.1038/s41562-022-01431-6
References
Articles referenced by this article (385)
Progress Toward Regional Measles Elimination - Worldwide, 2000-2019.
Patel MK , Goodson JL , Alexander JP Jr , Kretsinger K , Sodha SV , Steulet C , Gacic-Dobo M , Rota PA , McFarland J , Menning L , Mulders MN , Crowcroft NS
MMWR Morb Mortal Wkly Rep, (45):1700-1705 2020
MED: 33180759
Economic Costs of Measles Outbreak in the Netherlands, 2013-2014.
Suijkerbuijk AW , Woudenberg T , Hahne SJ , Nic Lochlainn L , de Melker HE , Ruijs WL , Lugner AK
Emerg Infect Dis, (11):2067-2069 2015
MED: 26488199
The economic cost of measles: Healthcare, public health and societal costs of the 2012-13 outbreak in Merseyside, UK.
Ghebrehewet S , Thorrington D , Farmer S , Kearney J , Blissett D , McLeod H , Keenan A
Vaccine, (15):1823-1831 2016
MED: 26944712
Inpatient morbidity and mortality of measles in the United States.
Chovatiya R , Silverberg JI
PLoS One, (4):e0231329 2020
MED: 32343688
Resurgence of measles in the United States: how did we get here?
Feemster KA , Szipszky C
Curr Opin Pediatr, (1):139-144 2020
MED: 31790030
Resurgence of Measles in Europe: A Systematic Review on Parental Attitudes and Beliefs of Measles Vaccine.
Wilder-Smith AB , Qureshi K
J Epidemiol Glob Health, (1):46-58 2020
MED: 32175710
Barriers to childhood immunization in sub-Saharan Africa: A systematic review.
Bangura JB , Xiao S , Qiu D , Ouyang F , Chen L
BMC Public Health, (1):1108 2020
MED: 32664849
Bibliometric analysis of global scientific literature on vaccine hesitancy in peer-reviewed journals (1990-2019).
BMC Public Health, (1):1252 2020
MED: 32807154
The Long Road Toward COVID-19 Herd Immunity: Vaccine Platform Technologies and Mass Immunization Strategies.
Frederiksen LSF , Zhang Y , Foged C , Thakur A
Front Immunol, 1817 2020
MED: 32793245
Herd Immunity: Understanding COVID-19.
Randolph HE , Barreiro LB
Immunity, (5):737-741 2020
MED: 32433946
Citations & impact
Impact metrics, citations of article over time, alternative metrics.

Smart citations by scite.ai Smart citations by scite.ai include citation statements extracted from the full text of the citing article. The number of the statements may be higher than the number of citations provided by EuropePMC if one paper cites another multiple times or lower if scite has not yet processed some of the citing articles. Explore citation contexts and check if this article has been supported or disputed. https://scite.ai/reports/10.1038/s41562-022-01431-6
Article citations, exploring human papillomavirus vaccine hesitancy among college students and the potential of virtual reality technology to increase vaccine acceptance: a mixed-methods study..
Yoon S , Kim H , An J , Jin SW
Front Public Health , 12:1331379, 13 Feb 2024
Cited by: 0 articles | PMID: 38414894 | PMCID: PMC10896851
"Every Time It Comes Time for Another Shot, It's a Re-Evaluation": A Qualitative Study of Intent to Receive COVID-19 Boosters among Parents Who Were Hesitant Adopters of the COVID-19 Vaccine.
Moore R , Purvis RS , Willis DE , Li J , Langner J , Gurel-Headley M , Kraleti S , Curran GM , Macechko MD , McElfish PA
Vaccines (Basel) , 12(2):171, 07 Feb 2024
Cited by: 0 articles | PMID: 38400154 | PMCID: PMC10892107
Perceived impact of discussions with a healthcare professional on patients' decision regarding COVID-19 vaccine.
Charmasson A , Ecollan M , Jaury P , Partouche H , Frachon A , Pinot J
Hum Vaccin Immunother , 20(1):2307735, 12 Feb 2024
Cited by: 0 articles | PMID: 38346925 | PMCID: PMC10863372
COVID-19 Vaccine Acceptance and Hesitancy among Nurses in Thailand: Implications, Challenges, and Future Prospects for Attitudes and Vaccine Literacy.
Butsing N , Maneesriwongul W , Visudtibhan PJ , Leelacharas S , Kittipimpanon K
Vaccines (Basel) , 12(2):142, 29 Jan 2024
Cited by: 0 articles | PMID: 38400126 | PMCID: PMC10892553
The impact of risk perception and institutional trust on COVID-19 vaccine hesitancy in China.
Chen G , Yao Y , Zhang Y , Zhao F
Hum Vaccin Immunother , 20(1):2301793, 28 Jan 2024
Cited by: 0 articles | PMID: 38282324 | PMCID: PMC10826627
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Understanding the determinants of vaccine hesitancy and vaccine confidence among adolescents: a systematic review.
Cadeddu C , Castagna C , Sapienza M , Lanza TE , Messina R , Chiavarini M , Ricciardi W , de Waure C
Hum Vaccin Immunother , 17(11):4470-4486, 02 Sep 2021
Cited by: 21 articles | PMID: 34473589 | PMCID: PMC8828162
Review Free full text in Europe PMC
Qualitative Assessment of Vaccine Hesitancy in Romania.
Miko D , Costache C , Colosi HA , Neculicioiu V , Colosi IA
Medicina (Kaunas) , 55(6):E282, 17 Jun 2019
Cited by: 17 articles | PMID: 31213037 | PMCID: PMC6631779
Vaccine Hesitancy in Rural Pediatric Primary Care.
Mical R , Martin-Velez J , Blackstone T , Derouin A
J Pediatr Health Care , 35(1):16-22, 01 Oct 2020
Cited by: 5 articles | PMID: 33010996 | PMCID: PMC7527836
Determinants of COVID-19 vaccine hesitancy and uptake in sub-Saharan Africa: a scoping review.
Deml MJ , Githaiga JN
BMJ Open , 12(11):e066615, 18 Nov 2022
Cited by: 6 articles | PMID: 36400736 | PMCID: PMC9676416
COVID-19 Vaccine Hesitancy in Pakistan: A Mini Review of the Published Discourse.
Khalid S , Usmani BA , Siddiqi S
Front Public Health , 10:841842, 31 May 2022
Cited by: 6 articles | PMID: 35712302 | PMCID: PMC9194092
Funding
Funders who supported this work.
ZonMw (1)
Evaluating interventions to stimulate acceptance of nip vaccinations: the role of deliberation on experiences and values..
DR Hautvast, Radboudumc
Grant ID: 839190002
1 publication
Europe PMC is part of the ELIXIR infrastructure
Peer Reviewed
Vaccine hesitancy in online spaces: A scoping review of the research literature, 2000-2020
Article metrics.
CrossRef Citations
Altmetric Score
PDF Downloads
We review 100 articles published from 2000 to early 2020 that research aspects of vaccine hesitancy in online communication spaces and identify several gaps in the literature prior to the COVID-19 pandemic. These gaps relate to five areas: disciplinary focus; specific vaccine, condition, or disease focus; stakeholders and implications; research methodology; and geographical coverage. Our findings show that we entered the global pandemic vaccination effort without a thorough understanding of how levels of confidence and hesitancy might differ across conditions and vaccines, geographical areas, and platforms, or how they might change over time. In addition, little was known about the role of platforms, platforms’ politics, and specific sociotechnical affordances in the spread of vaccine hesitancy and the associated issue of misinformation online.
Media, Inequality and Change Center, Annenberg School for Communication, University of Pennsylvania, USA
Communication, Journalism, & Media, Suffolk University, USA
MINDS (Management in Networked and Digital Societies), Kozminski University, Poland
Center for Constructive Communication, Massachusetts Institute of Technology, USA
School of Computer Science, University College Dublin, Ireland
Digital Health Lab, Meedan, USA
Tecnologico de Monterrey, Mexico
Digital Democracies Institute, Simon Fraser University, Canada
Paul G. Allen School of Computer Science & Engineering, University of Washington, USA


Research Questions
- RQ1: How was vaccine hesitancy—defined as “delay in acceptance or refusal of vaccination despite availability of vaccination services” (MacDonald & the SAGE Working Group on Vaccine Hesitancy, 2015, p. 4161)—in online spaces studied in the academic literature from 2000 to 2020?
- RQ2: What were the research gaps in the academic literature in relation to this area of investigation as of early 2020?
Essay Summary
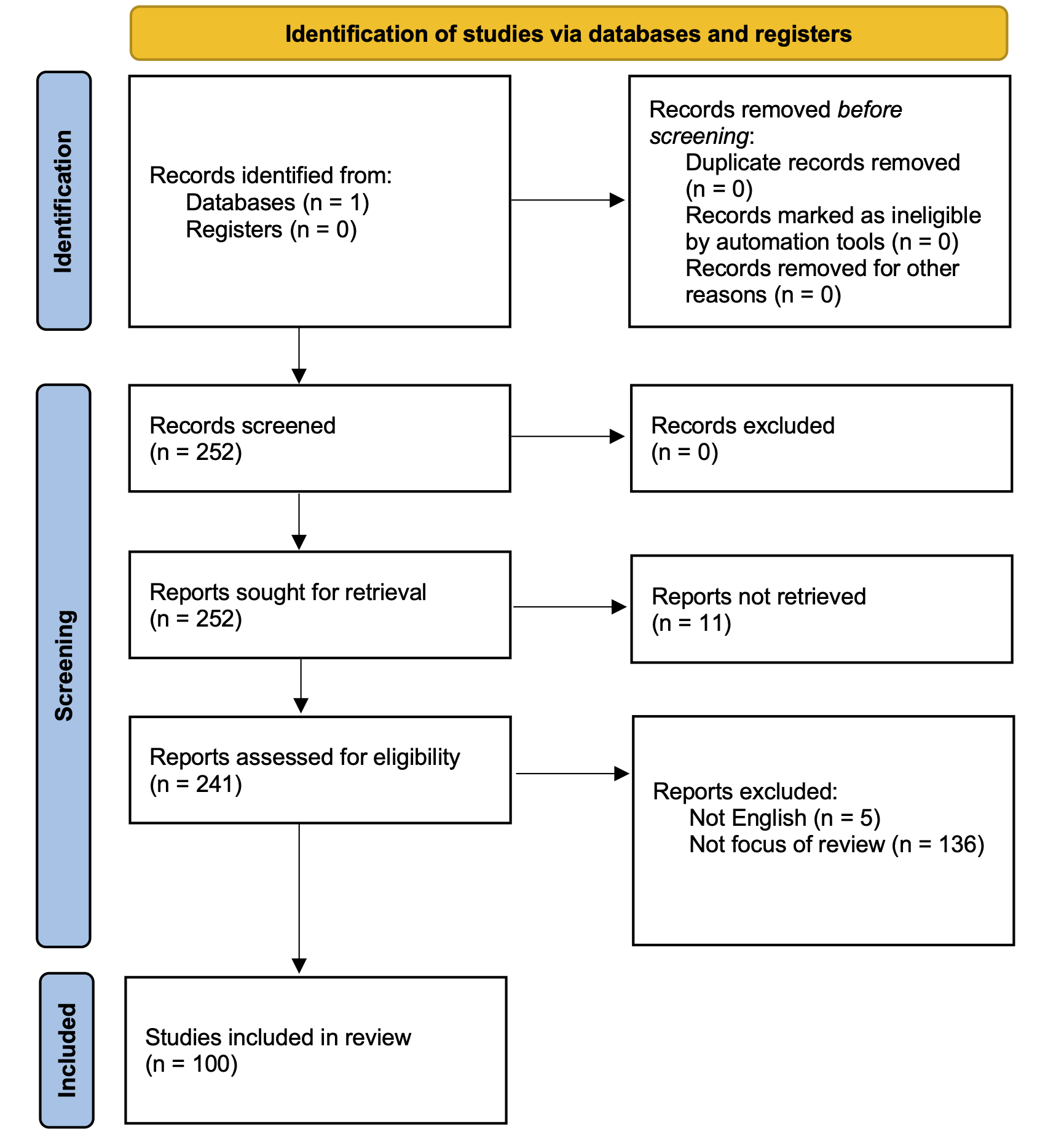
- We searched the Web of Science database for articles researching aspects of vaccine hesitancy in online spaces. Of 236 articles selected for analysis, 100 were determined relevant to our research interest and content analyzed by human coders.
- We identified gaps in the academic literature pertaining to vaccine hesitancy and the associated issue of online misinformation prior to the pandemic in five areas: disciplinary focus; specific vaccine, condition, or disease focus; geographical focus; stakeholders and implications; research methodology.
- Although this literature has greatly expanded, as of early 2020 it had yet to fully grapple with key dimensions of how vaccine hesitancy may be expressed in online discourse, specifically how online vaccine hesitancy differs across diseases, digital spaces, and local contexts, and how it might change over time. In addition, as of early 2020 very little appeared in the literature about the role of social media platforms in preventing and addressing the spread of vaccine hesitancy and online misinformation.
- Most of the articles we analyzed were produced within the field of public health research. In general, more interdisciplinary research is needed.
Implications
Globally and with increasing intensity during the present COVID-19 pandemic, efforts have been taken to address adherence to vaccine implementation across a spectrum of vaccine confidence levels, where low levels can contribute to hesitancy to vaccinate, and, potentially, the spread of related misinformation. Our research examines the lower end of the vaccine confidence spectrum, focusing on vaccine hesitancy and related challenges. 1 Researchers have used both the term “vaccine hesitancy” and the term “vaccine confidence” to refer to sentiments about vaccines, “hesitancy” drawing attention to negative sentiments and “confidence” inclusive of positive sentiments. We use the term “vaccine hesitancy,” which we operationalize as search terms used in our scoping review, such as “refusal,” “skepticism,” and “critical” (see Methods), referring to sentiments expressing the lower end of what has been studied as a spectrum of confidence levels (de Figueiredo et al., 2020; Larson, 2020; Orenstein et al., 2015).
Though vaccine hesitancy, misinformation, and online environments offer different sets of issues, health officials and researchers acknowledge important overlaps, as achieving broad acceptance of vaccines requires understanding information ecosystems (Berman, 2020; Larson, 2020). Vaccine hesitancy also has associated challenges that are specific to different vaccines, including COVID-19 vaccines, yet the persistence of varying degrees of confidence in vaccines more broadly is an ongoing challenge, and online environments have long been gathering points where vaccine rumors and myths are shared (Burki, 2020).
In this article, we conduct a scoping review 2 Unlike systematic reviews, scoping reviews seek to identify concepts and characteristics across extant literature rather than seeking to answer a specific question about a topic related to that literature (Munn et al., 2018). of the existing academic research on online vaccine hesitancy and suggest directions for future research. Though we acknowledge that vaccine hesitancy and the related issue of vaccine misinformation are not exclusively or most importantly online problems, our review provides a valuable snapshot of the state of research on this growing area of concern (RQ1), including potential research gaps (RQ2), prior to the COVID-19 pandemic. Given the impact of the pandemic on global dialogues about vaccination adherence, including effective communication to promote vaccination among diverse communities, it is useful to create a baseline for future research that can address challenges to vaccine uptake related to the present pandemic and future diseases. Our review also can serve as a point of comparison for understanding how the present pandemic tests prior research findings and influences future research.
Our review covers two decades in which research focusing on vaccine hesitancy online emerged and steadily evolved. In the early 2000s, researchers studied vaccine information on websites and even at this earliest stage of online research noted the prevalence of “misleading or inaccurate information” (article ID 19), the spread of anecdotal accounts of vaccine dangers, and the misrepresentation of the science behind vaccines (ID 6). Though we did not use the term “misinformation” in our database search string (see Methods), search results show that the relationship between online vaccine hesitancy and the quality of online information is a persistent concern in the research literature, and our review frequently encountered articles referencing “misinformation” (e.g., IDs 21, 60, 98, 104, 106, 138, 195) or expressing concerns for the accuracy of information (IDs 15, 23, 157).
With the emergence of participatory “Web 2.0” websites and technologies enabling Internet users to generate content and interact with each other via social media, researchers recognized the potential for the public spread of private concerns about vaccines (ID 10), which challenges the information-gatekeeping power of health professionals (ID 3). Research in the 2010s increasingly examined the sources of information about vaccines and network dynamics that help these sources spread information, finding that vaccine hesitancy is prevalent online (IDs 21, 73, 131) but often circulates in small but active and cohesive subgroups of Internet users (IDs 60, 92, 109, 244, 225). Researchers also have increasingly recognized nuances among different forms of vaccine hesitancy (IDs 34, 98) and have explored the power of storytelling vs. the power of facts and statistics prevalent on official health sites (IDs 23, 45, 138, 165, 187). Conclusions increasingly have urged monitoring and moderating social media platforms to stop the spread of misinformation (IDs 178, 243).
Our review identifies gaps in this literature in five areas:
- Disciplinary focus
- Disease and vaccine focus
- Geographical focus
- Stakeholders and implications
- Research methodology
In terms of disciplinary focus, a majority of the articles we analyzed were published in journals in the field of public health and medicine and focus on understanding how people share information about vaccines online. Articles identified online discourse that may contribute to vaccine hesitancy (ID 127); analyzed which subpopulations of users are likely to amplify vaccine misinformation (ID 15); investigated whether search engines return quality information sources (ID 83). These analyses aim to develop tactics and tools to help public health officials surveil in real-time public opinions and attitudes toward immunization and leverage online media to better communicate their messages.
Only 35 of the 100 articles we looked at examined vaccine hesitancy in relation to a specific disease and vaccine, most prominently measles, mumps, rubella (MMR), and the human papillomavirus (HPV), while 65 analyzed generic vaccine hesitancy or hesitancy across multiple diseases. The predominance of general studies is concerning because interventions should take account of the unique characteristics of specific vaccines and diseases.
Most articles we reviewed were conducted by Western research institutions and focused on vaccine hesitancy within Western contexts. We removed non-English articles prior to content analysis, but even considering this limitation of our review, the predominately Western focus in the extant research is clear. One consequence of this Western focus in the available research may be that the field becomes primarily aimed at developing vaccine-related digital communication strategies while overlooking issues of access to vaccines. Also, such strategies may be inappropriate in regions grappling with diseases not prominent in the West, such as polio.
In part due to the prominence of the field of public health in the extant research, health authorities and professionals are most often identified as top stakeholders in addressing vaccine hesitancy and online misinformation. Proposed actions for this category of stakeholders include getting involved in online groups that spread misinformation (ID 60); including stories alongside scientific facts in communication efforts (ID 209); and adopting “vaccine ambassador” programs, in which community members or health professionals share reliable information with select audiences to promote vaccine confidence and adherence (ID 23).
Though health professionals intervene at the nexus of vaccines, information, and patients, the dynamics of how information spreads involve a broader set of issues, such as online platforms’ politics and sociotechnical affordances and coordinated efforts by actors external to the doctor-patient relationship. These dynamics also involve a broader set of stakeholders, such as platforms, news media organizations, and policymakers who can intervene at a structural level. These stakeholders are prominent in media studies, sociology, human-computer interaction, political science, and other fields positioned to make valuable contributions to research on vaccine hesitancy and misinformation online.
In terms of research methodology, few of the articles we reviewed made causal inferences. It is therefore difficult to confirm underlying factors in the online spread of vaccine hesitancy and related misinformation, or to recommend concrete strategies. We also found few studies focused on changes in expressions of vaccine hesitancy over time, beyond the ebb and flow (volume) of online activity, a finding that is likely connected to platform restrictions on access to data. Yet, in order to identify effective interventions, it is imperative to understand the long-term growth of online communities, how they connect to other communities, and how issue framings evolve.
Finally, as of early 2020, little attention had been paid to social media platforms beyond Facebook and Twitter that are well-known for playing major roles in the distribution and amplification of online misinformation, such as YouTube and Reddit (Cinelli et al., 2020; Kaiser et al., 2021; Li et al., 2020). Research has begun to fill this gap, but more work needs to be done to understand persistent, platform-specific challenges, though recommendations for action abound: enhancing surveillance of misinformation; removing sources, as well as information; stepping up platform self-regulation; and engaging lawmakers, activists, and others in policy interventions (see, for example, Chou et al., 2020; Rutschman, 2020).
The core takeaway of this review is that research on vaccine hesitancy in online spaces would benefit from the continued and strengthened participation of disciplines that can offer a range of research approaches to online communication dynamics, including but not limited to anthropology, media and communications, human-computer interaction, information science, sociology, STS, and political science. Such participation would harness the strengths of these disciplines in research on specific practices, sociotechnical affordances, and structural factors—such as media policymaking, platform and media economics, and socioeconomic variables—that play roles in addressing and adequately responding to vaccine hesitancy and related misinformation in online and offline spaces during the present pandemic and future health crises. After presenting our findings, we suggest and elaborate five directions for future research.
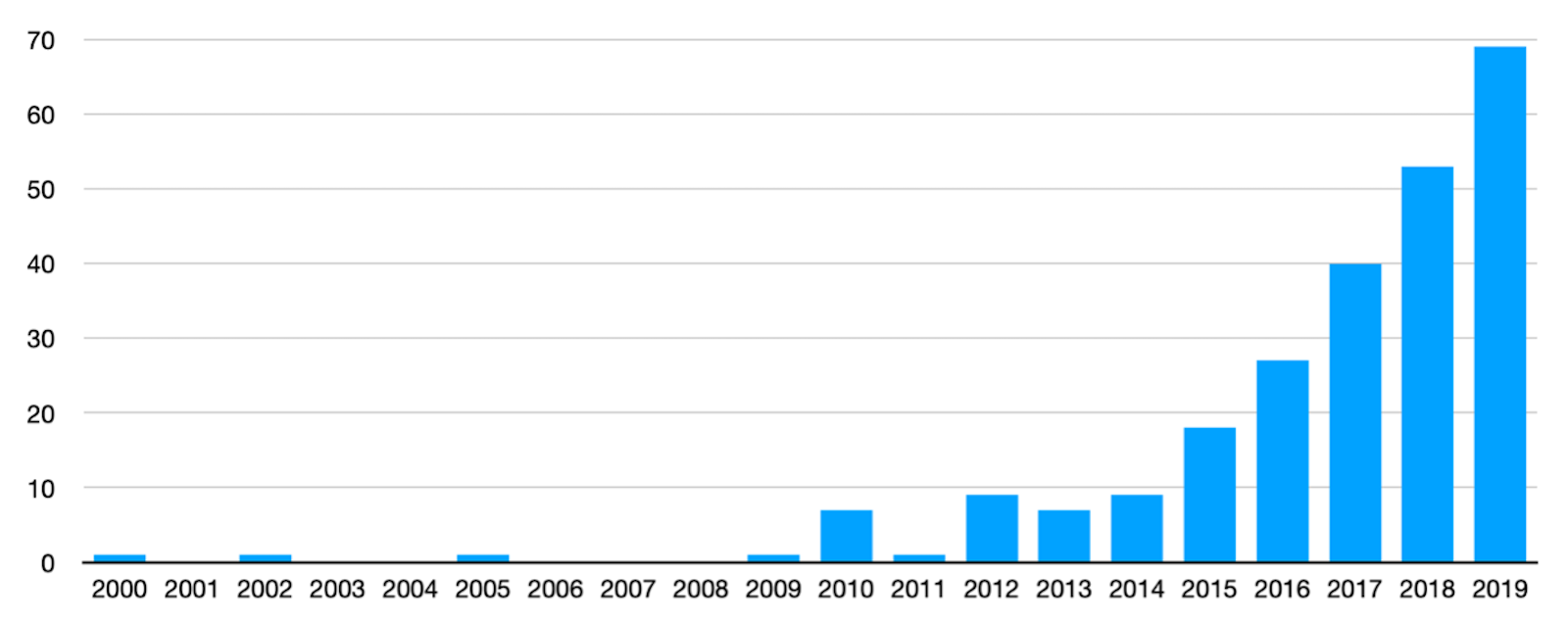
Finding 1: Research on vaccine hesitancy is a rapidly growing field.
Our search of the Web of Science database surfaced 252 articles researching aspects of vaccine hesitancy that referenced online spaces, the earliest of which was published in 2000. We note that the publication rate begins to climb in 2010, rising to 69 articles in 2019. 3 A search using the same terms on April 17, 2021, showed that 182 articles were published between 2020 and early 2021, more than double the pace of publications in 2019. The rise to prominence of social media platforms Facebook and Twitter (both launched to the general public in 2006) coincides with this increased research interest in online spaces.
Of 236 articles selected for analysis (see Methods), 100 were determined relevant to our research interest as primarily focused on vaccine hesitancy in online spaces. Table 1 breaks down these 100 articles by digital platform analyzed.
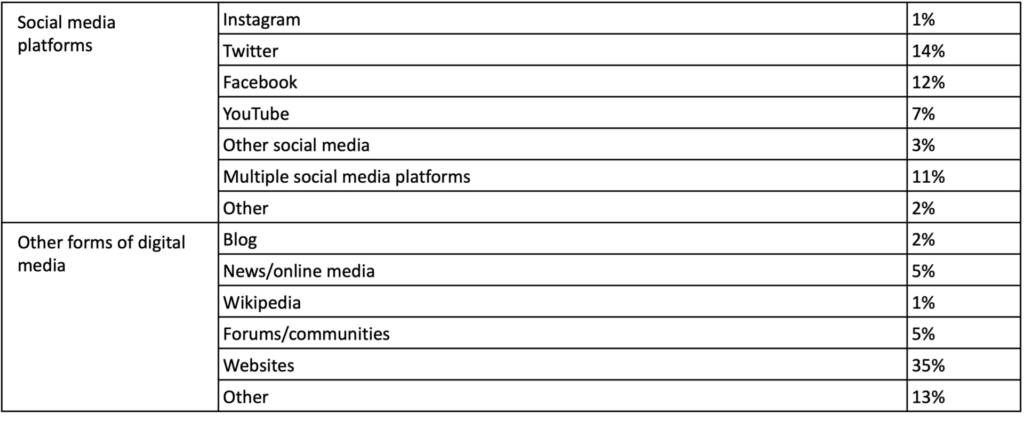
Finding 2: Research is dominated by public health field, with a focus on how people talk about vaccines.
The majority of these articles appear in academic journals focusing on public health and medicine (76 percent). Few articles make causal inferences (9 percent). Table 2 shows the research focus 5 Intercoder reliability testing resulted in low coder agreement for “research focus” and “stakeholders” variables; see Methods. of the articles, which most often demonstrates interest in how people in online spaces talk about vaccines and vaccinations.
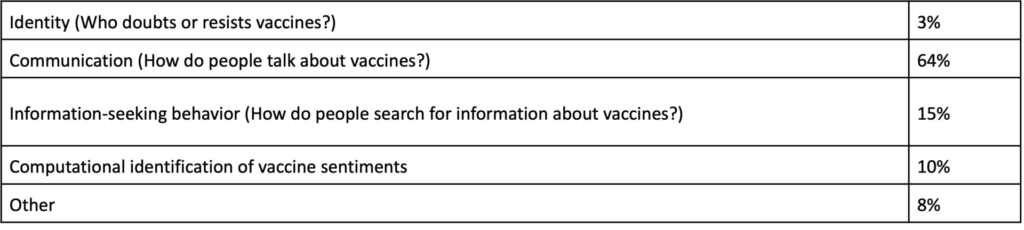
Table 3 shows the main stakeholders (n = 139) in the articles. Researchers most often indicate that their studies have conclusions relevant to medical professionals and the public health sector. These conclusions often focus on steps medical practitioners should take to counter misinformation about vaccines.
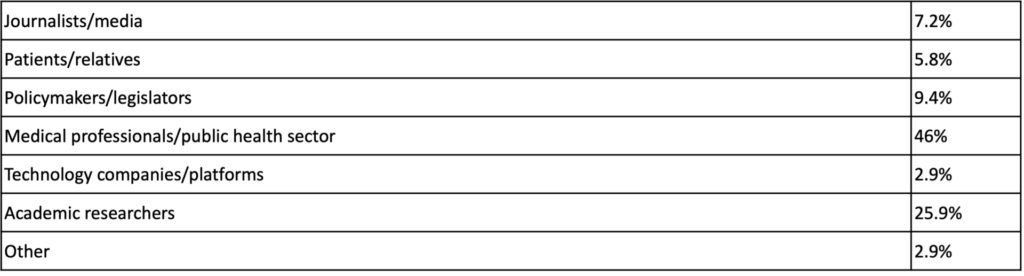
The majority of stakeholders identified in articles published by public health journals are medical professionals (51 percent; n = 110), with academic researchers comprising 22 percent of stakeholders in these articles. In journals from other fields, academic researchers are identified as stakeholders 41 percent of the time, while medical professionals are identified as stakeholders only 28 percent of the time (n = 29).
Finding 3: Additional gaps include demographic groups, terminology, geography, and disease- or vaccine-specific research.
Very few articles include a focus on gender (11 percent), ethnicity (4 percent), or age (7 percent). When authors focus on gender, they usually study women’s communication around vaccinations (e.g., in the context of Facebook groups). More research focused on these demographics and others would aid efforts to develop more relevant response approaches tailored to different social contexts.
We also note a wide variance in the terminology used for people who are doubtful of or otherwise resistant to vaccines. “Anti-vaccine” or “anti-vaccination” is the most common term found in these articles (55 percent), followed by “vaccine hesitancy” (25 percent) and “vaccine critical” (7 percent). Authors occasionally use the terms interchangeably although they represent different concepts: “Vaccine hesitancy” reflects individuals or communities who may experience challenges related to confidence, complacency, or knowledge and awareness, while “anti-vaccination” reflects active opposition to vaccines. A preferable framework involves terminology broader than these categorizations but not often used in social media contexts: the spectrum of “vaccine confidence” (Larson, 2020).
Seventy-eight percent of the time, countries listed by Web of Science as the origin for the 252 articles originally returned by our search are located in North America or Western Europe (254 out of 325 instances). 6 Web of Science uses addresses of author institutions to populate a “countries/regions” field used in our assessment.
Finally, 35 percent of the articles relevant for our review (n = 100) focus on a specific vaccine or disease, with the most prominent diseases being the human papillomavirus (HPV) and the vaccine for mumps, measles, and rubella (MMR).
Directions for research
This scoping review suggests multiple directions for research to address online vaccine hesitancy and related vaccine misinformation. At a minimum, future reviews should examine how the present pandemic has changed the state of this research. In addition, we suggest the following directions for research.
- Broadening the scope . One direction of research that would address multiple gaps in the present literature is interdisciplinary comparative research on online vaccine hesitancy across national, regional, local, and cultural contexts. Not only would such research help close gaps in our understanding of how vaccine hesitancy in online spaces differs from one vaccine and disease to another, but it also would provide opportunities for new research beyond Western contexts. Such research, well established in political science and media and cultural studies, also is capable of denaturalizing structural influences, such as economic, political, and media system dynamics, that encourage and amplify the online sharing of misinformation. Our review has noted that the extant research has over the years begun to engage more with the online sources of information rather than the quality of the information itself; interdisciplinary, comparative research is capable of bringing into view an additional set of structural sources or influences that can be addressed through policy interventions.
- Methods . The existing research would be enhanced by qualitative, ethnographic fieldwork. Our review shows that information sharing behaviors rather than the identities of those who share information, including social milieus important to those identities, have been the most prominent focus of research. Researchers have used surveys to gather views on vaccines, but ethnographic fieldwork is capable of enhancing our understanding of how vaccine hesitancy relates, on a day-to-day basis, to a variety of social factors and how these factors relate to the online sharing of vaccine information. This fine-grained, nuanced fieldwork could inform intervention strategies that complement or even move beyond the prominent debate in the extant research over the effectiveness of facts vs. stories in encouraging vaccine uptake.
- Different communities . More research is needed on the different communities that exist within every society and that differ with regard to their vulnerability to vaccine misinformation, as well as where and how they encounter it. Investigations into the role of gender, race, religious/spiritual beliefs and political ideology could highlight different online information pathways. These communities are not necessarily clearly delineated from one another but overlap; understanding these intersections is important when it comes to effective communication and outreach.
- Longitudinal research . Most studies in our review that analyzed social media focused on a certain point in time or excluded time from their analyses. Longitudinal research is needed in order to highlight changes over time, identify patterns and discursive moments, and assess the impact of platform actions such as de-platforming bad actors.
- Access and data. The gaps that our review finds in research on certain types of social media, research over time, and research on platform specific-interventions point to the broader, persistent issue of constraints on researcher access to online spaces and the challenges posed by frequently changing data formats and algorithms. These issues – so ubiquitous that they risk becoming invisible and uncritically accepted – often are left unsaid in research; by cataloging how researchers have encountered and addressed them, future literature reviews could contribute to the development of better research strategies and methods.
For our scoping review of the academic literature, we follow procedures outlined by Moher et al. (2009): identify relevant articles in a database; check these articles against other sources; screen out duplicates; assess articles for eligibility; and include the final list in the meta-assessment. Figure 2 shows our process as a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart (Page et al., 2021).
Through discussion, experimentation, and comparison with different libraries of articles, we developed a string of search terms that surfaced a list of articles roughly commensurate with articles found in other databases. This search string operationalizes the concept of vaccine hesitancy by including terms related to research on the lower end of the spectrum of vaccine confidence, such as “refusal,” “denial,” and “skepticism:”
((“anti-vaccination” OR “anti-vaccine” OR “anti-vax” OR “vaccine hesitancy” OR “vaccine reluctance” OR “vaccine refusal” OR “anti-vaxxer” OR “anti-vaxx” OR “vaccine denial” OR “vaccine skepticism” OR “vaccine critical”) AND (“internet” OR “online” OR “social network analysis” OR “social network sites” OR “social media” OR “social networking” OR “Web 2.0” OR “websites”))
We chose the Web of Science Core Collection database for our scoping review due to its widely recognized quality, providing some assurance that the articles included in our review are well-researched and impactful. 7 Web of Science developed the “impact factor” commonly used to assess the academic influence of journals (Garfield, 1994). However, the Scopus database also is prominent in literature reviews. As there are differences in coverage (Martín-Martín et al., 2021; Visser et al., 2021), we compared search results between the two databases and found 20 additional items indexed by Scopus from 2000 to the end of 2019 (roughly corresponding to our Web of Science search’s time period) relevant to our study, three of which could not be accessed. A content analysis of these items found nothing that would significantly alter our findings, though we note a higher prevalence of articles from the field of computer science – most published in conference and workshop proceedings – among the additional Scopus articles (7 of 17 items) than among our relevant Web of Science articles (5 of 100 items).
Using our search string in Web of Science’s title, abstract, and keywords field surfaced 252 articles on Feb. 12, 2020, approximately one month prior to the beginning of widespread COVID-19 precautions in the United States. After removing from this list inaccessible articles and articles not written in English, our final list for analysis included 236 articles. The full text of each of these articles was screened for inclusion in our findings.
Our codebook includes 24 variables, 11 of which require manual coding. Intercoder reliability testing involved 10 coders. Due to the difficulty of achieving high levels of agreement with such a large number of coders, a subset of three coders developed a shared codesheet for a 10 percent subsample of the articles. The other seven coders coded each of these articles separately, without access to the shared codesheet, and checked their coding against it, making changes when they agreed with the shared codesheet.
Final intercoder agreement (Holsti’s) exceeded 0.75 for most variables, except for “stakeholders” (0.51 and 0.64 for two categorical variables sharing the same set of categories, as multiple stakeholders were allowed, coded in order of appearance in each article); and “research focus” (0.6). Coding for multiple stakeholders was complicated by requiring coders to enter codes in the order in which stakeholders appeared in each article; this complication does not affect the coders’ ability to categorize stakeholders, and so we believe reliability for the stakeholders variable is higher than indicated. With regard to research focus, although articles focusing on how people talk about vaccines (communication) clearly dominated our corpus of research articles, at times coders found that some of these articles aimed to shed light on who these people are (identity) or primarily were about computational methods used to study them. We include findings for these two variables in our article, with the caution that intercoder reliability fell short of high confidence for them.
After intercoder reliability testing concluded, we randomly distributed the remaining 90 percent of the articles to our coders for final coding. We used SPSS software to generate descriptive statistics from the results of this coding.
- / Public Health
Cite this Essay
Neff, T., Kaiser, J., Pasquetto, I., Jemielniak, D., Dimitrakopoulou, D., Grayson, S., Gyenes, N., Ricaurte, P., Ruiz-Soler, J., & Zhang, A. (2021). Vaccine hesitancy in online spaces: A scoping review of the research literature, 2000-2020. Harvard Kennedy School (HKS) Misinformation Review . https://doi.org/10.37016/mr-2020-82
Bibliography
Berman, J. M. (2020). Anti-vaxxers: How to challenge a misinformed movement . MIT Press.
Burki, T. (2020). The online anti-vaccine movement in the age of COVID-19. The Lancet Digital Health, 2 (10), e504-e505. https://doi.org/10.1016/S2589-7500(20)30227-2
Chou, W. S., & Gaysynsky, A., & Cappella, J. N. (2020). Where we go from here: Health misinformation on social media. American Journal of Public Health, 110 (S3), S273–S275. https://doi.org/10.2105/AJPH.2020.305905
Cinelli, M., Quattrociocchi, W., Galeazzi, A., Valensise, C. M., Brugnoli, E., Schmidt, A. L., Zola, P., Zollo, F., & Scala, A. (2020). The COVID-19 social media infodemic. Nature Scientific Reports , 10 , 1–10. https://doi.org/10.1038/s41598-020-73510-5
de Figueiredo, A., Simas, C., Karafillakis, E., Paterson, P., & Larson, H. J. (2020). Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: A large-scale retrospective temporal modelling study. Lancet, 396 (10255), 898–908. https://doi.org/10.1016/S0140-6736(20)31558-0
Garfield, E. (1994). The Clarivate Analytics impact factor. Clarivate. https://clarivate.com/webofsciencegroup/essays/impact-factor/
Kaiser, J., Rauchfleisch, A., & Córdova, Y. (2021). Fighting Zika with honey: An analysis of YouTube’s video recommendations on Brazilian YouTube. International Journal of Communication, 15 , 1244–1262. https://ijoc.org/index.php/ijoc/article/view/14802
Larson, H. J. (2020). Stuck: How vaccine rumours start – and why they don’t go away. Oxford University Press.
Li, H. O., Bailey, A., Huynh, D., & Chan, J. (2020). YouTube as a source of information on COVID-19: A pandemic of misinformation? BMJ Global Health , 5 (5), 1–6. https://doi.org/10.1136/bmjgh-2020-002604
MacDonald, N. E., & the SAGE Working Group on Vaccine Hesitancy. (2015). Vaccine hesitancy: Definition, scope and determinants. Vaccine, 33 (34), 4161–4164. https://doi.org/10.1016/j.vaccine.2015.04.036
Martín-Martín, A., Thelwall, M., Orduna-Malea, E., & López-Cózar, E. D. (2021). Google Scholar, Microsoft Academic, Scopus, Dimensions, Web of Science, and OpenCitations’ COCI: A multidisciplinary comparison of coverage via citations. Scientometrics , 126 , 871–906. https://doi.org/10.1007/s11192-020-03690-4
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLOS Medicine, 6 (7), 1–6. https://doi.org/10.1371/journal.pmed.1000097
Munn, Z., Peters, M. D. J., Stern, C., Tufanaru, C., McArthur, A., & Aromataris, E. (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology, 18 (143), 1–7. https://doi.org/10.1186/s12874-018-0611-x
Orenstein, W. A., Gellin, B. G., Beigi, R. H., Despres, S., Lynfield, R., Maldonado, Y., Mouton, C., Rawlins, W., Rothholz, M. C., Smith, N., Thompson, K., Torres, C., Kasisomayajula, V., & Hosbach, P. (2015). Assessing the state of vaccine confidence in the United States: Recommendations from the National Vaccine Advisory Committee. Public Health Reports, 150 (6), 573–595. https://doi.org/10.1177/003335491513000606
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffman, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., McGuinness, L. A., Stewart, L. A., Thomas, J., Tricco, A. C., Welch, V. A., Whiting, P., & Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372 (71), 1–9. http://dx.doi.org/10.1136/bmj.n71
Rutschman, A. S. (2020). Facebook’s latest attempt to address vaccine misinformation – and why it’s not enough (Legal Studies Research Paper No. 2020-35). Health Affairs Blog, Saint Louis University. https://scholarship.law.slu.edu/faculty/544/
Visser, M., van Eck, N. J., & Waltman, L. (2021). Large-scale comparison of bibliographic data sources: Scopus, Web of Science, Dimensions, Crossref, and Microsoft Academic. Quantitative Science Studies, 2 (1), 20–41. https://doi.org/10.1162/qss_a_00112
Dariusz Jemielniak’s work on this project was possible thanks to a grant No. OSPOSTRATEG-II/0007/2020-00 from Polish National Center for Research and Development.
Javier Ruiz-Soler’s work was supported by funding from the Canada 150 Research Chairs Program and the Social Science and Humanities Research Council of Canada.
Dimitra Dimitrakopoulou received funding from the European Union’s Horizon 2020 research and innovation program under the Marie Skłodowska-Curie grant agreement No. 844167.
Siobhan Grayson’s contributions were made possible thanks to an Irish-U.S. Fulbright scholarship awarded by the Fulbright Commission.
Competing Interests
The authors report no conflicts of interest.
The authors have no ethics approvals to declare that are relevant to the content of this article.
This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided that the original author and source are properly credited.
Data Availability
All materials needed to replicate this study are available via the Harvard Dataverse: https://doi.org/10.7910/DVN/MACUIS
Acknowledgements
This project emerged from the Misinformation Working Group at the Berkman Klein Center for Internet & Society, Harvard University. This article also greatly benefited from our reviewers’ insightful comments and suggestions.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Public Health
COVID-19 Vaccine Hesitancy in the United States: A Systematic Review
Farah yasmin.
1 Department of Internal Medicine, Dow University of Health Sciences, Karachi, Pakistan
Hala Najeeb
Abdul moeed, unaiza naeem, muhammad sohaib asghar.
2 Department of Internal Medicine, Dow University Ojha Hospital, Karachi, Pakistan
Najeeb Ullah Chughtai
3 Department of General Surgery, Liaquat National Hospital and Medical College, Karachi, Pakistan
Zohaib Yousaf
4 Department of Internal Medicine, Hamad Medical Corporation, Doha, Qatar
Binyam Tariku Seboka
5 Department of Public Health, Dilla University, Dilla, Ethiopia
Irfan Ullah
6 Department of Community Medicine, Kabir Medical College, Peshawar, Pakistan
Chung-Ying Lin
7 Institute of Allied Health Sciences, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan, Taiwan
Amir H. Pakpour
8 Department of Nursing, School of Health and Welfare, Jönköping University, Jönköping, Sweden
Associated Data
The original contributions presented in the study are included in the article/ Supplementary Material , further inquiries can be directed to the corresponding author/s.
Vaccine hesitancy in the US throughout the pandemic has revealed inconsistent results. This systematic review has compared COVID-19 vaccine uptake across US and investigated predictors of vaccine hesitancy and acceptance across different groups. A search of PUBMED database was conducted till 17th July, 2021. Articles that met the inclusion criteria were screened and 65 studies were selected for a quantitative analysis. The overall vaccine acceptance rate ranged from 12 to 91.4%, the willingness of studies using the 10-point scale ranged from 3.58 to 5.12. Increased unwillingness toward COVID-19 vaccine and Black/African Americans were found to be correlated. Sex, race, age, education level, and income status were identified as determining factors of having a low or high COVID-19 vaccine uptake. A change in vaccine acceptance in the US population was observed in two studies, an increase of 10.8 and 7.4%, respectively, between 2020 and 2021. Our results confirm that hesitancy exists in the US population, highest in Black/African Americans, pregnant or breastfeeding women, and low in the male sex. It is imperative for regulatory bodies to acknowledge these statistics and consequently, exert efforts to mitigate the burden of unvaccinated individuals and revise vaccine delivery plans, according to different vulnerable subgroups, across the country.
Introduction
Vaccines are critical in lowering disease-specific mortality rates ( 1 ) and the long-standing control of the COVID-19 pandemic is pivoted upon the development and uptake of the vaccine ( 2 ). Vaccines currently recommended and authorized in the US are BNT162b2 (Pfizer-BioNTech), mRNA-1273 (Moderna), Johnson & Johnson/Janssen ( 3 ) with the challenge now shifting from finding an effective cure to ensuring its implementation ( 4 ).
The US Centers for Disease Control and Prevention acclaims vaccination as one of the leading success stories of public health in the twentieth century ( 1 ) and a similar feat is now being aimed for the novel coronavirus. As part of Operation Warp Speed, the US administration alongside manufacturers and developers exerted efforts and by January 2021, hoped to deliver 300 million doses of a safe and effective vaccine for COVID-19 ( 5 ). By mid-January 2021, there were around 13 million persons who had COVID-19 vaccine initiated in the US ( 6 ) and while these numbers were promising, the vaccination process has been met with an undesirable, although not unusual, phenomenon well-known as “vaccine hesitancy.” Defined by the World Health Organization as “the delay in the acceptance or refusal to vaccinate despite the availability of vaccine services” ( 7 ), the term vaccine “hesitant” is preferred over “pro” and “anti” vaccination to avoid polarization and, as it insinuates that the minds can be persuaded toward acceptance ( 8 ).
Since the inception of vaccines in medical practice in the 1800s ( 9 ), the public has not always concurred to getting vaccinated albeit many people have complied in face of apparent death and indisposition ( 1 ). Frequent outbreak of vaccine-preventable diseases in the US, such as 1,282 confirmed cases of measles in the United States in 2019 ( 8 ), can be ascribed to reduced vaccination and hence vaccine hesitancy, the latter ranked by the WHO as the top threat to global health in 2019 ( 1 ).
According to a global study, 72% of people would take the COVID-19 vaccine if deemed safe and effective, but willingness varies between countries ( 10 ). When studied under the framework of the 5C model of psychological antecedents that drive vaccine acceptance: confidence, constraints, complacency, calculation, and collective responsibility, the US population indicated 54% vaccine acceptance, a value that divulges vaccine skepticism ( 11 ). The US population has demonstrated inconsistent results over the period as between April 1–14 and November 25–December 8, 2020, the percentage who stated they were somewhat or very likely to get vaccinated declined from 74 to 56% ( 12 ). The percentage of US adults intending to get vaccinated has seen a u-shaped pattern with results showing changes between September and December 2020, which correspond to pre-authorization and post-authorization dates in the US, respectively ( 7 ). Conversely, another national representative survey revealed the vaccine hesitancy to have a longitudinal decline of 10.8% points between October 2020 and March 2021 ( 13 ).
COVID-19 vaccine receptivity in the US has varied between states and subgroups. In mid-October 2020, acceptance rates ranged from 38% in the Northeast to 49% in the West ( 14 ). Vaccine hesitancy in the general population has been correlated with certain factors including gender, age, race, socioeconomic status, education level, and US-based surveys disclose important findings. Women have lower intentions than men to be vaccinated ( 14 ) and as of a study from April to December 2020, the self-reported likelihood of getting COVID-19 vaccination was lower among females than males (51 vs. 62%) ( 12 ).
The cohort comprising of vaccine-hesitant individuals can be large enough to diminish the COVID-19 vaccine's potential to provide population immunity ( 15 ). Impediments to vaccination involve concerns including fear of side effects, inadequate information, short duration of immunity ( 14 ) forgoing vaccination due to lack of insurance or financial resources ( 16 ). Safety and effectiveness of the vaccine are the most pivotal detriments of hesitancy ( 4 ) while for some, especially marginalized factions, dissatisfaction with the health system owing to past experiences of discrimination, systematic racism deters them from vaccination ( 17 ).
Vaccine hesitancy is not a singular problem but attributed to various underlying causes that differ across time and communities ( 1 ). Recent results have shown somewhat reduced hesitancy, corresponding to the dates of vaccine approval and mass roll-out ( 13 ) and it is speculated that as the pandemic becomes more “real” to the Americans, vaccine acceptance can improve. Being one of the representative countries hardest hit by COVID-19, estimating vaccine hesitancy in the U.S could be important for future vaccine promotion and herd immunity ( 18 ). This systematic review aims to broaden the scope of discussion by studying factors coupled with vaccine hesitancy in the US population and the study's findings will be beneficial not only for COVID-19 vaccination coverage but also improving the existing healthcare system's preparedness for routine and emergency vaccination. Furthermore, our results will be imperative in helping strategize policies for tackling antagonism and for developing a thorough vaccine delivery plan.
The review was performed following PRISMA guidelines. Papers published in MEDLINE (PubMed), Cochrane library, and Google Scholar assessing COVID-19 vaccine hesitancy/vaccine uptake/ vaccine acceptance in the English language were eligible for inclusion in the review. The inclusion criteria were: (1) peer-reviewed published articles indexed in PubMed; (2) survey studies among the general population, healthcare workers, minority and religious communities, students, or patients (3) the major aim of the study was to evaluate COVID-19 vaccine acceptance/uptake/hesitancy in the US population only and (4) publication language was English. The exclusion criteria were: (1) the article did not aim to evaluate COVID-19 vaccine acceptance/hesitancy/uptake in the US population; (2) publication language was not English.
A search was carried out till 17th July 2021 using the following search strategy: (COVID * vaccine * hesitancy [Title/Abstract]) OR (COVID * vaccine acceptance [Title/Abstract])) OR (COVID * vaccine * hesitancy [Title/Abstract])) OR (COVID * intention to vaccinate * [Title/Abstract]) OR (COVID vaccine * accept * [Title/Abstract]).
Articles were screened by abstracts and titles. Studies shortlisted were cohort studies and cross-sectional studies that assessed COVID-19 vaccine acceptance over a certain time period, specific for each study, respectively. Studies drew comparison between vaccine acceptance and vaccine hesitance in the population surveyed. After selection, data extraction for the following items was conducted: title and date of the study, study period/duration, the target population of the study (e.g., general public, students, healthcare workers, patients, religious groups, and minority groups), region of US where the study took place, population characteristics i.e., sample size, % female, mean age, % Whites, the definition of vaccine acceptance in the study, overall acceptance rate, acceptance rate by education level, factors relating to vaccine acceptance, and factors relating to vaccine hesitancy. Overall vaccine acceptance (%) was taken from each study as deduced, corresponding to the definition of vaccine acceptance presented in the study. A forest plot was also constructed using Microsoft Excel version 2018 to demonstrate the overall prevalence of COVID-19 vaccine acceptance in the United States.
The search string provided in the Supplementary Material retrieved 784 records, of which 65 were included in the quantitative synthesis of observational studies on vaccine acceptance in the United States (US). Figure 1 illustrates the four-step selection process as per the PRISMA guidelines ( 19 ).

PRISMA guidelines flow chart.
Characteristics of the Literature
The sample size of the selected studies ranged from 25 to 73,650, with a total of 3,13,998 individuals. Out of the 65 studies (67 surveys), 31 of them reported the study region, of which nine were conducted in New York City (NYC). Of the 50 studies reporting female sex %, 38 of them had a percentage >50. Acceptance was measured as somewhat likely, extremely likely, and willingness to take the vaccine. The majority of the surveys that reported race and ethnicity, had a predominant non-Hispanic white population. Vaccine acceptance was presented as percentages in 61 studies, whereas the remaining four studies reported means. Four of the studies used a point scale system to measure the likelihood of receiving the COVID-19 vaccine. Silva et al. ( 20 ) made use of a 10-point scale ranging from 1- extremely unlikely and 10- extremely likely, whereas Meier et al. ( 21 ), Rhodes et al. ( 22 ), and Dorman et al. ( 7 ) used a 7-point scale. Detailed studies characteristics are present in Table 1 .
Characteristics of the literature.
COVID-19 Vaccine Acceptance Rates
Vaccine acceptance rates varied from a low of 12% to a high of 91.4%. In 48 from 63 surveys, readiness to get vaccinated was ≥50%. The mean and standard deviation of acceptance rate by Silva et al. was 7 (3.12); meanwhile, the willingness of studies using the 10-point scale ranged from 3.58 to 5.12.
COVID-19 Vaccine Acceptance Stratified per Region
A total of 32 studies included the geographical location of the survey, comprising data of 20 states out of a possible 50. Overall, a low of 12% was observed in New York City in the Orthodox Jewish community, whereas a high of 90.1% was reported in Kansas among employees and students at the University of Kansas Medical Centre. Figure 2 illustrates the geographical average COVID-19 vaccine acceptance percentage reported in each state. Classifying vaccine acceptance per the four regions in the United States shows New England division of Northeast, West North Central of Midwest, Mountain division of West, and the whole of the South, except West South Central, had a low percentage of states with vaccine acceptance figures, however, in the Mid Atlantic division of Northeast, all three states had surveys conducted, making it the only division with 100 percent data availability. Supplementary Table 1 states the percentage acceptance by each state, with Kansas reporting a high of 89.6%.

COVID-19 vaccine acceptance rates of United States.
COVID-19 Vaccine Acceptance Stratified per Respondents' Population
Apart from the studies with the general population, 18 surveys took place in a healthcare setting, including patients, workers and, students. From these 18, eight highlighted patients' attitudes toward the COVID-19 vaccine. Amongst patients, two surveys on solid organ transplant (SOT) recipients showed their hesitance toward the vaccine owing to lack of data and concerns of its safety in transplant recipients (56.10 and 31.63% acceptance). Other than SOT recipients, studies report willingness in patients with chronic disease, multiple sclerosis, dialysis, and cancer which showed a positive response toward the COVID-19 vaccine. Of these, patients suffering from chronic disease reported the highest acceptance rate of 85%. Healthcare workers and students (dental and medical) showed a varying attitude toward the vaccine as acceptance ranged from a low of 45% in nursing home staff to a high of 90.10% in staff and students at the University of Kansas Medical Centre.
Three surveys were carried out in religious communities, two in Jewish and one in the Amish community. The Amish community had an alarmingly low acceptance rate of 25%, whereas the Jewish people had 12 and 65.3%, with the latter being of greater significance due to the large sample size. Two surveys carried out in New York highlighted the increased hesitance toward the vaccine by pregnant women. Amongst pregnant women, an acceptance rate of 44.3 and 58.35% was reported, whereas 76.2% of non-pregnant women were inclined to take up the COVID-19 vaccine. Studies on vaccine acceptance in inmates and those discharged from prison found a 20, 44.9, and, 66.5% acceptance rate in women recently released from prison, inmates from four states, and a California state prison, respectively, with the latter being significant with a sample size of 97,779. Furthermore, a survey on tobacco and marijuana users showed a low vaccine uptake rate of 49.1%. In all four of these studies, Blacks/African Americans were correlated with increased unwillingness toward the COVID-19 vaccine. Figure 3 summarizes the percentage of vaccine acceptance in different population groups. Figure 4 demonstrates the pooled prevalence of COVID-19 vaccine acceptance in the United States with the pooled prevalence being 71.42%.

COVID-19 vaccine acceptance stratified per-respondents' population.

Pooled prevalence of COVID-19 vaccine acceptance in the United States.
Factors Associated With Vaccine Acceptance and Hesitance
Several factors were identified as leading to low or high vaccine acceptance. From the 65 studies, sex was mentioned in 22 surveys, race in 31, age in 16, education level in 19, and income status in 4. The male sex and individuals with a college degree or higher education were significantly associated with higher vaccine acceptance rates in all surveys reporting these variables. Furthermore, non-Hispanic Blacks were correlated with having the lowest vaccine acceptance in all 31 surveys whereas Whites and Asians showed a positive attitude toward uptake of the COVID-19 vaccination. People aged >45 years were linked with an increased approval of the vaccine compared to the younger population in 15 out of the 16 surveys. Respondents from lower-income backgrounds were less inclined to get vaccinated in all four studies. Apart from these significant predictors of behavior toward a vaccine, other factors that contributed to vaccine hesitancy included uncertainty about the vaccine safety and side effects entailing after its administration, religious reasons, and a lack of trust in the healthcare system. A comprehensive data evaluation of the studies is included in Table 1 .
Changes in COVID-19 Vaccine Acceptance Over Time
Two studies investigated the change in acceptance of the COVID-19 vaccine by surveying the population twice. Daly et al. conducted the first round of the survey in October 2020, followed by the second one in March 2021. Percentage acceptance rose by 10.8% from 54 to 64.8%. Furthermore, Szilagyi et al. carried out their surveys in November-December 2020 and April 2021 with 56.2 and 74.1% accepting the vaccine, respectively, marking a rise of 7.9%. However, an overall change in readiness for uptake of the vaccine was notable; the predictors of hesitance remained the same throughout time. African/American Blacks and females were the leading predictors of low acceptance in both studies. Daly et al. also correlated younger age and lower-income with the increased unwillingness of the COVID-19 vaccine.
The emergence of the B.1.617.2 (Delta) variant has put the United States on the forefront in the total number of COVID-19 cases countrywide ( 76 ). Studies have shown that a two-dose regime of any available vaccine significantly reduces a poor prognosis of COVID-19 ( 77 ). The rapid advent of efficacious vaccines for coronavirus is a projection of leaps in the field of medicine toward the goal of herd immunity. This, however, is threatened by the globally persistent but a re-emerging phenomenon of vaccine hesitancy and anti-vaccination, as experienced for vaccine-preventable diseases such as poliovirus and rubella. Despite a population of 59.9% receiving at least one dose of the COVID-19 vaccine ( 78 ), analyzing vaccine hesitancy is imperative to strategize vaccine delivery plans to procure maximum vaccine coverage and limit the spread of pathogens to the immunocompromised individuals and children who cannot be vaccinated.
In this systematic review, predictors of vaccine hesitancy and acceptance are studied across the U.S in the general population, pregnant women, immunocompromised individuals, students, healthcare workers, racial groups, and demographic characteristics. Factors associated with vaccine hesitancy are vastly different before and after the availability of vaccines. Before the roll-out of COVID-19 vaccines in mid-December 2020, major concerns across all the population groups were focused on the safety, effectiveness, and cost of the vaccine ( 38 , 63 ). As the death toll peaked in the US, and with more publicly available data of vaccine trials, there was a considerable trend shift in the attitudes toward receiving a vaccination ( 33 ).
Thirty-three studies from a pool of 62 gathered vaccine acceptance rates from the general population, ranging from 91.4% ( 52 ) to a surprising low of 4.6% ( 7 ). Besides the difference in the timeline of each study, hesitancy was mainly driven by the lack of education and understanding of the process of vaccine development. As pharmaceutical companies develop multiple vaccines for the emerging strains, the expedited process of approval has raised concerns about its effectiveness ( 52 ), explaining their preferred choice of mRNA vaccines as opposed to any available vaccines ( 18 ).
Eleven studies report ethical and racial groups' unwillingness which stems from the deep-seated mistrust in the healthcare system. A study by Willis et al. conducted between July and August 2020 showed that one in every four Blacks/African Americans and Hispanics were hesitant to receive the COVID-19 vaccine, while COVID-19 vaccine hesitancy was highest among Black/African American respondents (50.00%), followed by Hispanic/Latinx respondents (19.18%), and White respondents (18.37%) ( 15 ). An online survey from March 2021 revealed a significant decline in vaccine hesitancy amongst the Black race ( 14 ). Black/African Americans have been reported to consistently depict suspicion toward the vaccine, with similar patterns observed previously with the influenza vaccines. These can be traced back to the Tuskegee Syphilis study which mishandled hundreds of Black individuals and has institutionalized racial discrimination since then ( 34 , 79 ). Consistent with the findings of observational studies, Blacks/African American race were more susceptible to SARS-CoV-2 than White Americans race; if contracted, the percentage of hospitalization and mortality was significantly higher ( 80 ). A survey that studied COVID-19 vaccine acceptance in sexual and gender minority (SGM) group reported the least willingness in individuals who identified as Black; insensitivity from government representatives toward movements such as Black Lives Matter has deepened racial and economic disparity ( 20 ). Vaccine hesitancy in this minority group can be further explained by the pre-existing disparities with healthcare professionals, unavailability of healthcare services, and underrepresentation in clinical trials ( 7 , 38 , 64 ). Maximum vaccine coverage can be achieved by building trust in the government and medical services; Black/African Americans and Hispanic healthcare workers can contribute to foster trust in the system. As many belong to the low-income strata, health insurance can help recover the losses. Providing maximum transparency in COVID-19 trials through informed consent, ensuring maximum representation, and consistent access to healthcare during and after the pandemic is likely to improve turnout at vaccination centers. Entrusting distribution and vaccine manufacturing to businesses owned by Blacks will be a step toward positive vaccine trends. However, Blacks and Hispanics can only be freed from centuries of structural racism and classism in fields outside of medicine through consistent cultural policies across the US ( 34 , 64 , 79 ).
Two studies report COVID-19 vaccine acceptance percentages in religious minorities in the US; an average willingness of 25% in Amish families of the Holmes County in Ohio ( 56 ) and 12% in Jewish Orthodox individuals in NY ( 30 ). Previous studies have shown that outbreaks of measles, rubella, and poliovirus have significantly affected the Amish community in Ohio, reflecting their lack of concern regarding the severity of the disease ( 81 ). Similar to findings of previous surveys conducted for Amish families, concerns about the adverse effects of COVID-19 vaccines were recognized as a major factor for vaccine hesitancy. Other predictors of unwillingness included avoiding dependence on the government, while some conservative families were not convinced as the bishop did not levy importance to it ( 56 , 82 ). Local governments in Pennsylvania, Ohio, and Indiana have set up vaccination facilities at health departments to increase turnout ( 30 ). However, an effective approach to spreading COVID-19 vaccine awareness and destigmatizing it in the Amish community will have to be in conjunction with the church leadership, and the Old Order Amish families which were unaffected by the religious doctrine ( 82 ). On the contrary, shared accommodation amongst the Jewish community in NY has increased the incidence of COVID-19, especially in the Chasidish sect. Regardless of the likelihood of contracting coronavirus, negative vaccine trends in Chasidish respondents in Brooklyn were observed ( 83 ). However, factors affecting their vaccination status; the belief that natural immunity was more beneficial, and the mistrust in physicians in the US, among other reasons put them on the priority list of strategizing distribution plans and approaches ( 30 ).
Individuals from ethnic minority groups or persons suffering from substance use disorders or mental illnesses are frequently incarcerated. The lack of stable housing, food supplies, and subpar treatment facilities delay diagnosis, which increases the risk of diseases like COVID-19 ( 68 ). Vaccine acceptance rates were relatively moderately high, ranging from 44 to 66% ( 45 , 68 ) in prisons while 49% in smokers ( 29 ). Consistent with previous surveys, hesitancy in prisoners originated from health illiteracy and the perception that a COVID-19 vaccine was unnecessary ( 68 ). In individuals who have been exposed to marijuana and/or tobacco, low acceptance was governed by demographic characteristics and if they lived alone or with a family of more than 5 people. This could be explained by the notion that living alone meant no exposure to SARS-CoV-2 while living with a larger family meant greater coronavirus exposure, and hence natural immunity ( 29 ). Although California, Washington, and Texas have recognized the importance of vaccinating detained residents and have put them on the priority list, distrust in government facilities revokes any efforts made.
As experienced in the 2009 H1N1 influenza pandemic, a survey administered among reproductive-aged women from January 7, 2021, to January 29, 2021, established non-pregnant respondents to be most likely to accept vaccination, followed by breastfeeding responders with pregnant responders had the lowest vaccine acceptance ( 43 ). The lack of research of COVID-19 vaccines in pregnant women and females has raised major concerns related to its safety to the fetus, with many non-pregnant women considering disruption to the menstrual cycle and infertility a side effect ( 43 ). Future research should be geared toward pregnant and breastfeeding women who make up a large proportion of the population of the US.
Frontline healthcare workers and paramedics across the globe were the first to receive the COVID vaccine. Of the 9 studies reported in this systematic review, vaccine acceptance is one of the highest (60–90%) in most studies. Nursing staff showed the least willingness to vaccination (<50%) in multiple surveys which were conducted as vaccines were rolled out ( 30 , 71 ). This results from the level of medical education in each group, and prospects about its long-term safety. The ethical duty of healthcare workers to not harm their patients makes relying on personal protective equipment insufficient and obligates them to urge staff and patients to receive the vaccine. COVID-19 poses a serious threat to immunocompromised patients, and upon hospitalization, such patients have an early mortality rate of 25% ( 26 ). In a population suffering from chronic illnesses, patients with multiple sclerosis have been included in trials, and thus show an acceptance rate between 60 and 70% ( 24 , 74 ). However, skepticism regarding vaccines was greatly observed in solid organ transplant (SOT) patients (31% acceptance) ( 39 ) compared to hemodialysis patients (49% acceptance) ( 65 ). SOT patients suffer from comorbidities such as chronic kidney disease and diabetes. Immunosuppressive drugs reduce hyper inflammation in SOT patients, but if infected with SARS-COV-2, risk bacterial and fungal co-infection as innate and adaptive immunity is compromised ( 84 ). Of the fundamental 5Cs that determine vaccine coverage, decreased confidence and medical mistrust correlated with the lack of research in SOT respondents ( 39 ). Suboptimal humoral responses were recorded with two-dose regimes of COVID-19 vaccines in organ transplant recipients. Therefore, three doses of COVID-19 vaccines are being recommended to obtain recommended antibody titers ( 85 ).
The vaccine acceptance rates in the US vary by demographic characteristics, including age, geographical location, sex, and household income. While the country of origin of the vaccine has minimal contribution in encouraging or dissuading people from vaccination ( 23 ), statistics from March 2021 relay that vaccine hesitancy in the US was highest in low socioeconomic respondents belonging to households earning $50,000 or less, among those without a degree adults, or those aged 18–39 years ( 13 ). Significant generational difference in vaccine hesitancy is shown as Baby Boomers and Gen X have lower odds of vaccine hesitancy compared to Millennials ( 86 ). In a study from 18 to 64-year-old Tennessee adults, a positive response was received regarding vaccine safety, efficacy, importance, and benefit ( 38 ). In a different clinical study comprising U.S. adults aged 65 and older, 63.6% of participants reported they were very willing to receive a COVID-19 vaccine ( 33 ). This is possibly governed by the social media exposure to each generation; Gen Z and Millennials are more likely to be technologically advanced as compared to Baby Boomer and Gen X. Therefore, health information could be easily obtained from social media platforms such as Facebook and Twitter. A skewed display of factually incorrect information on social media and an individual's tendency to be vulnerable to social media's emotional appeal often becomes the gist of the decision made by a lot of individuals ( 87 ). Furthermore, a positive trend in vaccine acceptance among males vs. females ( 71 ), could be a result of a sampling bias thereof.
Medical mistrust is likely to improve if public health campaigns are run by health experts, CDC, or the WHO. Endorsements of COVID-19 vaccines by political figures is seen as politicizing a requirement of today, such as promotion of unapproved hydroxychloroquine by the US president wreaked havoc amongst the healthcare workers ( 88 ). Mandating vaccination in workplaces but also banning entry of unvaccinated individuals to public spaces may contribute as a factor of vaccine acceptance ( 89 ). Given the disproportionate willingness in the low-economic strata, efforts should be made to make the vaccine more accessible to them, by promoting health insurance. A study revealed only 35% of individuals were willing to pay $50 or more for the coronavirus vaccine. Therefore, adopting a unified policy of a no-cost follow-up after vaccination as introduced by a few states can remove financial barriers ( 73 ). The expedited process of COVID-19 vaccine testing and the cases of adverse events of a vaccine contributed significantly to vaccine hesitance. This mandates the role of media and pharmaceutical companies to deliver information that can be easily interpreted by the general population ( 88 ).
This systematic review reports a multitude of populations, and analyses percentages by regions in the US. However, the pooled percentages are subjected to spectrum bias since percentages for general population are pooled with terminally ill or marginalized groups. Percentage of COVID-19 vaccine acceptance is liable to random error as published studies were carried out at different phases of the coronavirus peak. Another limitation worth noting is that it does not provide a timeline change in the vaccine hesitancy across all groups, and thus does not record the change in vaccine enthusiasm. Lastly, vaccine acceptance percentages by states should be interpreted logically as demographic characteristics differ across the region.
This study confirms that demographic characteristics played an important role in positive trends in vaccine acceptance, with the male sex showing higher acceptance of the COVID-19 vaccine. Least willingness was identified in the Black/African American population, and pregnant or breastfeeding women. Therefore, pharmaceutical companies and the US government must acknowledge the COVID-19 vaccine hesitancy that exists across the country. Increased hospitalization and adverse effects of COVID-19 in non-vaccinated individuals identify as potential threats to the economic and social stability of the country and aim to increase the divide. The willingness rates of vaccination are alarming in ethnic and sexual and gender minority groups, urging the need for outreach campaigns to prevent a COVID-19 outbreak in a susceptible population. Restoring trust in medical professionals and vaccines requires a strategical approach to overcome the racial injustice in the system, while timely implementation of vaccine delivery plans remains a challenge as new strains of coronavirus emerge as potential threats to the healthcare system.
Data Availability Statement
Author contributions.
FY: conception of the study, primary drafting of the work, final approval, and agreeing to the accuracy of the work. HN: conception of the study, major drafting of the work, final approval, and agreeing to the accuracy of the work. AM: conception of the study, drafting of the work, final approval, and agreeing to the accuracy of the work. UN: drafting of the work, final approval, and agreeing to the accuracy of the work. MA: conception of the study, critical revision of the work, final approval, and agreeing to the accuracy of the work. NC, ZY, BS, IU, C-YL, and AP: critical revision of the work, final approval, and agreeing to the accuracy of the work. All authors have read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.770985/full#supplementary-material
April 10, 2024
Spring quarter 2022 Tier 1 pilot grant awardees report final impact of funded projects

The purpose of the Tier 1 pilot grant program is to support researchers in laying an interdisciplinary foundation for a future project to generate proof-of-concept. Reported project outcomes and findings for each of the awards are detailed in the following tabs.
Patient acceptability of clinical suggestion of social needs automatically identified from clinical notes in the electronic health record
Investigators Andrea Hartzler, Department of Biomedical Informatics & Medical Education Angad Singh, Department of Family Medicine Patrick Wedgeworth, Department of Biomedical Informatics & Medical Education Kevin Lybarger, Department of Biomedical Informatics & Medical Education Serena Xie, Department of Biomedical Informatics & Medical Education Herbie Duber, Department of Emergency Medicine Brian Wood, Department of Medicine
Project summary Identifying patients’ social needs is a first critical step for health systems to address social determinants of health (SDoH). Yet, SDoH screening is underused since it relies on arduous clinician entry and patient-entered questionnaires in the electronic health record (EHR). While these methods identify a subset of patients with social needs, they primarily capture patients who are already engaged in healthcare and don’t scale for enterprise-wide population health management, especially when considering patient populations who may need the greatest level of outreach. Emerging CMS mandates for health systems to report SDoH data as a quality metric for federal level tracking will only amplify the need to address barriers to screening. Innovative strategies could bolster screening efforts by filling data gaps for a fuller picture of upstream social factors impacting the health of the population.
We investigated autosuggestion as a novel strategy that surfaces social needs information previously documented in clinical notes in the EHR. The free text of clinical notes contains rich detail about patients’ social needs, but this SDoH data is scattered across patient encounters, difficult to find, and thus remains underutilized. Natural language processing (NLP) makes it technically feasible to automatically extract SDoH from clinical notes with high accuracy. With this automated approach “SDoH autosuggestion” in mind, our team envisions a future in which the EHR surfaces SDoH automatically extracted from clinical notes, and pre-fills those social needs as auto-suggestions for users to accept/reject in clinical tools, such as Epic flowsheets, MyChart, health equity dashboards. Although SDoH autosuggestion could help facilitate and scale up social needs screening, SDoH data is sensitive. This study addresses how patients would feel about having their EHR mined for data to identify social needs.
The purpose of this project was to illuminate the voice of patients regarding potential use of SDoH auto-suggestion in health care. Below we describe key findings and achievements for the two aims that address this objective. This project enabled multidisciplinary collaboration among domain experts, community advisers with lived experience, two PhD students, and a clinical informatics fellow.
Aim 1. Co–produce inclusive study materials with clinical and community champions
- Convened a five-member board of community advisors with professional and lived experience for 3 workshops to: 1) produce recruitment materials and storyboards that explain SDoH auto suggest to patients with varied digital literacy, 2) analyze data together, and 3) create dissemination plans.
- Conducted key informant interviews with 8 interdisciplinary domain experts to vet and refine the interview study design and recruitment plan – the expertise of these “clinical champions” spans primary care, emergency medicine, health equity, NLP, and human-computer interaction.
- Convened meetings with subgroup of five clinical champions for data analysis and manuscripts.
- Collaborated with clinical and community champions on a publication in the Journal of the American Medical Informatics Association published in the special issue on NLP and SDoH.
- Demonstrated an effective model of “multi stakeholder co-production” for future research.
Aim 2. Interview patients about their acceptability of SDoH auto-suggestion
- Partnered with four clinics serving underrepresented and hard-to-reach patient populations.
- Interviewed 16 patients who experience social needs about their acceptability, concerns and recommendations for future implementation of SDoH auto suggestion.
- We used storyboard scenarios to explain how SDoH autosuggestion could work in future care in which NLP-extracted SDoH data extracted from a patient’s clinical notes could be presented in the EHR to healthcare providers for employment, housing stability, food insecurity and substance use domains.
- Most participants found SDoH autosuggestion acceptable, with greater acceptability of SDoH domains perceived as more health-related (i.e., substance use) compared to others (i.e., employment).
- Concerns that participants raised focused on tradeoffs between potential risks of data inaccuracies, privacy/security threats, promotion of stigma and bias and impaired patient-provider relationships.
- Participants recommended that future implementation of automated SDoH systems foster transparency, patient autonomy and empathetic clinical communication about social needs.
- These findings add critical perspective of patients on careful consideration of how automated SDoH systems are implemented and used in clinical care and strategies to safeguard risks.
- Dissemination for Aim 2 to date has included an oral presentation and submission of a manuscript to the American Medical Informatics Association, which is under review.
Understanding the Impacts of Washington Paid Family Leave Policy on American Indian and Alaska Native Birthing Parents and Newborns
Investigators Teresa Abrahamson-Richards, School of Social Work Jennifer Romich, School of Social Work Rose James, Urban Indian Health Institute
Project summary This project intended to lay the foundation for future research into Paid Family and Medical Leave (PFML) access among American Indian and Alaska Native (AIAN) Washingtonians. Both paid and unpaid parental leave have been consistently associated with positive perinatal outcomes in a variety of studies. However, little is known about access, uptake, and outcomes among AIAN people. Furthermore, intersections between state level policy-making and Tribal sovereignty are also unexplored in this area. As stated in our original project abstract: “Washington’s PFML went into effect on January 1, 2020 and is available to eligible workers in the state who have a qualifying family or medical event such as welcoming a new child. This project will undertake a community-engaged study design process, conduct preliminary analyses, and enable the researchers to acquire the necessary quantitative data to conduct a future study examining birth outcomes among first time AIAN birthing parents.”
We began meeting with community partners at the beginning of the grant period. The partners in these groups included nurses, home visitors, representatives from community social services organizations/nonprofits, public health professionals, and others who work directly with AIAN families during the perinatal period. These partners expressed enthusiasm for the potential to learn about PFML, and overall parental leave access, among AIAN families. However, they also talked about a broader framing to contextualize this work. In addition to these meetings, we also met with researchers to gain insights into appropriate study designs and with state partners to learn more about PFML policy development vis a vis Tribes and AIAN populations.
The initial analysis on pre-PFML employment trends and likely PFML eligibility was completed. The analysis focuses on the proportion of AIAN birthing parents in 2013- 2016 whose work hours would have made them eligible for PFML under the future policy’s rules as well as the employment and earnings of these families pre- and post-birth. The analysis also examines how these trends differ by urban versus rural locality and education status. Preliminary results were presented at one conference in April 2023 and to community partners, as approved by the state of Washington.
Another goal of this work was to design a follow-on quantitative study of PFML access and birth outcomes among AIAN Washingtonians using merged Employment Security Department PFML data and Department of Health birth record data. Based on community partner feedback, we determined that more initial research was needed into the holistic perinatal experiences and needs of working AIAN parents in the state welcoming a new child. In line with this, and with community partner involvement, we designed a qualitative study with the aim to learn about (1) individuals’ in-depth experiences of parental leave type and duration, (2) positive aspects and challenges related to parental leave access, (3) AIAN mothers’ situated perspectives on parental leave design and adequacy, and (4) visions and recommendations for future parental leave policymaking. Preliminary results from these interviews have been presented to community partners, and will be included alongside our initial quantitative findings funded through this Tier 1 population health grant in the manuscript that is under development.
This pilot grant ultimately enabled us to do deep work with our community for the benefit of family health and well-being into the future. By far the most exciting outcome is the community partner enthusiasm for the work, the generation of preliminary results and policy context to share with them and the interest in continued partnership moving forward.
Examining share pantry/refrigerator safety and potential as a hyper-local alternate means of food assistance in the Puget Sound
Investigators Emily Hovis, Department of Environmental & Occupational Health Sciences Joe Graham, Washington State Department of Health Tania Busch Isaksen, Department of Environmental & Occupational Health Sciences
Project summary As a result of the COVID-19 pandemic, many communities and individuals began providing food in neighborhood pantries/refrigerators to help feed their neighbors. These “share pantries” are generally small, unattended, open‐access food pantries that may or may not include refrigerated foods. Donations are provided by members of a community and generally use a “take what you need, leave what you can” model. Anecdotal evidence suggests that some shared pantries and community refrigerators may provide unsafe food (such as home-prepared foods, unpackaged foods, and food held at improper temperatures). Access to safe and wholesome food, regardless of whether donated or purchased, is an expectation for all Washingtonians. For this reason, our primary project focus was to evaluate the safety of shared pantries/refrigerators within the context of existing food rules. Our secondary focus was to analyze existing locations and gather user data to better understand where they are, who is using them, and why.
We mapped 286 pantries and 12 community refrigerators within the project area of Puget Sound using publicly available information from websites such as littefreepantry.com and freedge.com. A random subset of these sites was visited for in-person safety assessments, including 118 pantries and 12 community refrigerators. The majority of sites were located at private residences in King County, with non-profit organizations being the second most common site. Also, with few exceptions, the sites are located within 1 mile of public transportation.
Interestingly, we identified that a large proportion of sites (33% of fridges and 18% of pantries) were no longer operating at the time of the field visit. The characteristics that contribute to the long-term viability of shared pantries as a community resource is something that we are interested in exploring in the future. In particular, if certain operational models (private residence vs. community organization) are more successful for long-term success.
We conducted safety assessments during the hottest period of the year, from August – October 2022. Inadequate temperature control was identified as the most significant food safety risk at community refrigerator sites, with 75% of refrigerator ambient temperatures greater than 41°F (excluding data from one unplugged refrigerator). Other food safety risks included moldy/decaying food present (55%), food in torn/open containers (40%), presence of leftovers/partially eaten food (25%), potential cross-contamination due to improper animal protein storage (15%), and the presence of home prepared food (10%). Dented/rusty cans (33%) and non-commercially packaged/unlabeled foods (32%) were identified as the most common food safety risks observed at pantry sites. Insects and rodents were identified to be another common risk observed in 29% of pantries. Improper door construction seems to be a common contributing factor, which may lead to pest entry. Our findings suggest there are safety concerns associated with this type of food sharing, but opportunities exist for community education to help improve safety at these sites.
Development and Evaluation of a Culturally-informed Food Insecurity Screening Protocol with American Indian Adults: Evidence from Northern Navajo Medical Center
Investigators Amanda M. Fretts, Department of Epidemiology Terra Yabeny, Navajo Department of Health Preyanka Makadia, Northern Navajo Medical Center Cassandra Nguyen, Washington State University Partnerships for Native Health
Project summary Food insecurity (i.e., insufficient access to nutritious food) is a pressing public health concern among American Indian people. Recent reports indicate that more than 46% of American Indian households have experienced food insecurity during the past year. To address this, Indian Health Services (IHS) encourages providers to screen patients for food insecurity to identify households that can be referred to federal or Tribal food assistance programs. The IHS currently utilizes a 2-question food insecurity screener that asks if the food patients buy does not last, or if they worry about food running out before they have money to buy more. Though these questions are approved and recommended for use in healthcare settings in the USA, providers at the IHS Northern Navajo Medical Center found that the 2-question screener is stigmatizing for many patients given the deficit-oriented wording of the questions; the questions make some patients feel uncomfortable and they refuse to complete the screener. Providers at the IHS Northern Navajo Medical Center are interested in identifying an alternate set of strengths-based screener questions that focus on patients’ capacity to maintain food security, while opening a dialogue about opportunities to access food through non-market activities (e.g., farming, foraging, hunting), community resources, and/or food assistance programs.
This pilot project comprised two phases. The first phase was a qualitative phase that included brief 20-minute interviews with patients at the IHS Northern Navajo Medical Center. Patients who enrolled in the study provided feedback on the existing two question food insecurity screener currently being used at IHS, as well as an alternate set of (strengths-based) food security screening questions. In total, we enrolled 25 participants in Phase 1. Interviews were recorded. An external service was used to transcribe all interviews. We analyzed the transcripts using a basic content analysis approach to gather insights and common sentiments about the existing and alternate food insecurity screening questions. Findings from the interviews informed the second phase of the study.
During Phase 2, 97 participants completed both food insecurity questions (i.e., the two question food insecurity screener currently being used at IHS and alternate set of food insecurity questions developed/refined during Phase 1). Agreement between responses on the screeners were compared to assess whether the new screener could validly replace the existing screener.
Most participants in the study (both Phase 1 and Phase 2) were less than 65 years old, identified as female, had no or some college experience, and lived in households with children and incomes below $50,000 per year. Over 60% of participants were classified as food insecure based on responses to the 2 question food insecurity screener currently being used at IHS. During the interviews, many respondents reported a high prevalence of food insecurity in the community and felt that discussing food access with providers at the IHS Northern Navajo Medical Center was valuable. However, interviewees felt the questions on the IHS-approved Food Insecurity Screener are confusing and may produce shame or embarrassment for some respondents. Most respondents felt that screening would be best if providers took the time to discuss food security with sensitivity and with the support of visual aids. Participants felt that discussing food choices with a focus on composition and portions was more comfortable than the format of the current IHS screener.
The alternate screener that we developed included three questions with visual aids. High risk of food insecurity was classified affirmatively if participants indicated that the amount of food usually available was either “Always not enough” or “sometimes not enough” or if they indicated they did not eat “Almost only healthy and traditional Southwest foods” and felt average or unhappy about the kinds of foods they ate. When this classification criteria were used, the Pearson correlation coefficient between the two screeners (i.e., the 2 question food insecurity screener currently being used at IHS and the alternate set of questions developed during Phase 1) was only moderate. More work is needed to better understand the discordant findings.
We are currently focusing on dissemination activities. In September 2023, we gave a one hour learning session (for CME credit) to providers and staff at the Northern Navajo Medical Center. We have additional presentations scheduled in November 2023 for Navajo Department of Health and Navajo Nation Human Research Review Board. We are also in the process of scheduling a data work session with relevant Tribal programs.
A Framework for Prioritizing Urban Green Space Protection and Restoration to Improve Health
Investigators Kristin Hayman, School of Marine & Environmental Affairs Jeremy Hess, Department of Environmental & Occupational Health Sciences Phillip Levin, School of Marine & Environmental Affairs Josh Lawler, School of Environmental & Forest Sciences Jamie Robertson, The Nature Conservancy, Washington Julie Fox, Washington State Department of Health Buffi LaDue, Washington State Department of Health Allison Ertl, Washington State Department of Health Christopher Ahmed, Washington State Department of Health Marnie Boardman, Washington State Department of Health
Project summary The purpose of our project is to work with public health and conservation practitioners to develop and implement a framework for identifying locations across the Puget Sound region where protection and restoration of urban green space have the greatest potential to promote health and wellbeing, abate environmental health disparities, and further environmental resilience.
The team conducted an extensive literature review of over 100 peer-reviewed journal articles. Via this literature review, they investigated the dose-responses of a suite of health outcomes to green space, with a major take-away that very few dose-responses between green space and health outcomes have been identified by the literature to date.
Via the literature review, the team also selected three focal health metrics that are affected by green space and conveyed via direct contact with green space: all-cause mortality, depression and self-reported health status. They pulled data from the Environmental Health Disparities Index and the Center for Disease Control and Prevention (CDC) as proxies for the sensitivity of populations in each census tract to the focal health metrics.
The team also pulled data from the Stormwater Heat Map to estimate green space density in each census tract. Further, they used green space density per census tract as a proxy for the average exposure of populations in each census tract to green space. They pulled data from the US Census Bureau to estimate population in each census tract, and then prioritized census tracts and created heat maps of the Puget Sound region that depict the relative priority of each census tract.
Establishing a rural Food Equity Collaborative to increase healthy food retail options for Latinos in WA
Investigators Barbara Baquero, Department of Health Systems and Population Health Elizabeth Torres, Northwest Communities Education Center/Radio KDNA Ria Francisco, Department of Health Systems and Population Health
Project summary Through this community-based participatory research project, the University of Washington Health Promotion Research Center and Northwest Communities Education Center (NCEC)/ Radio KDNA, conducted formative research to: 1) establish an academic-community Collaborative to advance Latino food equity in rural WA; and 2) examine the contextual factors (geographical, epidemiological, socio-cultural, socio-economic, ethical, legal, political) that would influence healthy food retail promotions for Latinos in rural WA.
Both objectives were accomplished through the following tasks:
- Completed a literature review on academic and gray literature and publicly available sources to draft a summary report on contextual factors (geographical, epidemiological, cultural, economic, legal, ethical, political) that would influence healthy food retail promotions for Latinos in Yakima, Benton and Franklin counties.
- Completed 14 informational interviews with 18 individuals and utilized a combination of inductive and deductive methods to conduct thematic analysis.
- Established a Food Research and Equity Collaborative (FrEsCo) of nine community leaders from Yakima Health District, Yakima Valley Partners in Education (Heritage University), 211, People for People, Yakima School District Fresh Fruit and Vegetable Program, Yakima Valley Farmworkers Clinic Snap Ed, Toppenish Community Chest, and Benton-Franklin Health District representing a multi-sectoral team addressing intersecting community priorities with thoughtful, inclusive solutions.
- Completed training with health educators at Radio KDNA who conducted food retail audits at a sample of 10% of all tiendas across Yakima, Benton, and Franklin (n=9)
Eighteen interviews were completed across 14 organizations. The themes that emerged:
- Transportation is a barrier to accessing services.
- Food is not affordable with current living wages.
- Tiendas (Latino small retail stores) are a comfortable way to purchase culturally relevant foods.
- Communities share wealth of knowledge and resources through informal networks.
- Intersecting structural and social factors emerged as the most important, persistent and complex to address. For example, limited transportation services in these areas affect access to foods, combined with lower wages in rural areas, limit the ability to afford healthier foods.
- Immigration status prevents undocumented residents from accessing government services such as SNAP, despite the fact they participate in the agricultural workforce of the region.
- The strong community ties within the Latino community and access to tiendas, where culturally relevant foods were available for purchase, were leveraging resources to support Latinos.
- Tiendas served as a safe, familiar, affordable setting where Latinos buy healthier food while feeling connected socially and culturally and could be an effective setting for a nutrition intervention.
Understanding mechanisms of social determinants of health and symptoms in adults with subarachnoid hemorrhage
Investigators Eeeseung Byun, Department of Biobehavioral Nursing and Health Informatics Michael Levitt, Department of Neurological Surgery Maria Bleil, Department of Child, Family & Population Health Nursing
Project summary The goals of our study were 1) Aim 1: to explore the relationship between individual-level social determinants of health (e.g., demographics and socio-economic status) and symptoms (sleep disturbance, fatigue, and impaired cognition) in subarachnoid hemorrhage (SAH) survivors as well as the potential mechanistic role of inflammation in explaining any observed associations and 2) Aim 2: to examine demographics and socio-economic status in SAH patients admitted to Harborview Medical Center in 2021, a potential site for a large grant application, as well as to develop relationships with other potential recruitment sites.
For Aim 1, we conducted a secondary data analysis based on a previous study that examined symptoms (sleep disturbance, fatigue, and impaired cognition) and inflammation (Toll-Like Receptor 4 [TLR4] messenger RNA [mRNA] expression and plasma concentrations of Tumor Necrosis Factor-alpha [TNFα] and Interleukins [IL1β and IL6]) in the first 6 months after SAH in 43 SAH survivors. The findings indicate that demographics and socio-economic status (e.g., age, gender, race/ethnicity, education, employment, and income) were associated with symptoms (e.g., sleep disturbance, fatigue, and impaired cognition) in SAH survivors over 6 months post-SAH. In addition, inflammatory biomarkers (e.g., TLR4 mRNA, TNFα, IL1β, and IL6) were associated with symptoms (e.g., sleep disturbance, fatigue, and impaired cognition). Inflammatory biomarkers also moderated the relationship between social determinants of health (e.g., age, gender, race/ethnicity, education, employment, and income) and symptoms, which indicates that the effect of social determinants of health on symptoms may differ based on the degree of inflammation after SAH. Further studies, with a large sample size, an extended follow- up period, and rigorous measures of social determinants of health are warranted to confirm the associations of social determinants of health, symptoms, and inflammation in people with SAH.
For Aim 2, we reviewed 80 medical charts of aneurysmal SAH patients admitted to Harborview Medical Center in 2021 and examined their demographics and socio-economic status (e.g., race/ethnicity, gender, marital status, education, employment, insurance, areas of living, and social support) and clinical characteristics (e.g., severity of SAH and comorbidity). Our findings indicate that SAH patients at Harborview had diverse demographics and socio-economic status, indicating that Harborview is an excellent recruitment site for a future large grant application. In addition, we have been disseminating research findings related to social determinants of health in SAH at international and national scientific meetings and initiated a network of potential collaborators. We will further foster interdisciplinary research collaboration and initiatives with a high potential for further research related to social determinants of health in people with SAH.
PrEParing for the future: preferences for HIV pre-exposure prophylaxis products and delivery models among cisgender men, transgender, and non-binary persons in Seattle, Washington
Investigators David Katz, Department of Global Health Lauren Violette, Department of Epidemiology Jodi Greathouse, Department of Global Health
Project summary he primary aims of this project were to 1) design and pilot a discrete choice experiment (DCE) to identify HIV pre-exposure prophylaxis (PrEP) product and delivery preferences of cisgender men who have sex with men, transgender persons, and non-binary people, and 2) describe and identify characteristics associated with preferences for PrEP product attributes and delivery models.
The DCE design process spanned from April to August 2022. We used a combination of current literature, expert opinion, and previously conducted qualitative research to guide attribute and level development. Ngene and SAS were used to program the experiment. The final DCE was piloted by the study team, translated, and programmed into REDCap in both English and Spanish. We enrolled 325 participants from the Public Health – Seattle & King County (PHSKC) Sexual Health Clinic between August 2022 and December 2023. The majority (87%) of participants identified as cisgender men, while 10% identified as non-binary or genderqueer, and 2% were transgender women. Over half (67%) had previously used (20%) or were currently using (47%) PrEP, while 30% were PrEP-naive.
Final analyses for the primary outcomes of this project will be completed and summarized in a manuscript by Summer 2024. Depending on availability, we may also present these data at a “Work in Progress” meeting with a UW Center for AIDS Research (CFAR) working group or core. These data will be disseminated to our project collaborators at the PHSKC Sexual Health Clinic to enhance their existing PrEP services and plan for implementation of new PrEP products. Our DCE can also serve as a tool for local community organizations and partners to tailor PrEP delivery to their clients. As such, we plan to create a one-page summary with key takeaways of our study to disseminate to other local stakeholders including, but not limited to, the UW CFAR, community-based organizations in King County, and the Washington State Department of Health. Finally, Lauren Violette, the project co-investigator, will use this DCE design to explore PrEP delivery preferences among similar populations in Boston during a post-doctoral fellowship within the Department of Population Medicine at Harvard Medical School.
Residential Segregation and Pediatric Injury and Violence in Seattle, Spokane, and Tacoma
Investigators Chelsea Hicks, Department of Pediatrics Frederick Rivara, Department of Pediatrics Abril Harris, School of Social Work Rebecca Walter, Department of Real Estate Monica Vavilala, Department of Anesthesiology & Pain Medicine Qian Qiu, Department of Pediatrics Tony Escobar, Mary Bridge Children’s Hospital Timothy Bax, Sacred Heart Medical Center
Project summary The original project proposal defined three aims: (1) Create a model of the relationship between residential segregation, the built environment and pediatric injury exposure through a scoping review. (2) Quantify present day association between residential segregation and pediatric injury and violence outcomes in three Washington state cities (Seattle, Tacoma, Spokane). (3) Identify potential interventions through moderating and mediating mechanisms in the relationship between residential segregation and pediatric injury and violence.
Progress toward each aim is as follows:
- The research team conducted a systematic literature review that included approximately 25 journals and databases. Over the course of several months over 3,000 articles were screened for inclusion. We dual abstracted data from 34 eligible studies and conducted quality assessments of the studies. Our team is currently in the process of finishing a manuscript to be submitted to a peer reviewed journal on the associations other studies have found between geographic location, built environment and pediatric injury or violence outcomes.
- In partnership with Harborview Medical Center, Sacred Heart Medical Center (Spokane) and Mary Bridge Children’s Hospital (Tacoma), we received pediatric injury data from their trauma registries for patients from years 2012-202l (Seattle) and 2015-2021 (Spokane and Tacoma). The team used trauma registry data from Harborview Medical Center, Mary Bridge Children’s Hospital, and Sacred Heart Medical Center to identify residential zip codes in these cities of youth treated at these hospitals for injuries and violence. While it was initially believed we could acquire access to the residential addresses to geocode into census tracts, there were difficulties in receiving this data due to personal health information concerns. We thus were forced to rely on zip code data. Using the available hospital data and the American Community Survey (ACS) data, we did not find any association of sociodemographic characteristics of the zip code and the injury rates. This was due to the fact that injury rates were relatively low per zip code and there was a lack of variation in injury rates at the zip code level. However, this research project and analysis did lend to methodological insights to improve measuring injury and violence outcomes at the environment level while noting limitations in existing data formats.
- Based on the null findings at the zip code level, we identified that the methods that are typically used to measure mediating and moderating mechanisms were unfeasible for our variables of residential segregation and pediatric injury and violence at the zip code level and a more granular unit of analysis is required for future research.
Piloting a Strategy to Improve Pediatric Inpatient Guideline Adherence in Migori, Kenya
Investigators Megan Coe, Department of Child, Family, and Population Health Nursing Sarah Gimbel, Departments of Global Health and Child, Family, and Population Health Nursing Arianna Rubin Means, Department of Global Health Beth Kolko, Department of Human Centered Design & Engineering Benson Singa, Kenya Medical Research Institute Ann Van Haney, Department of Global Health
Project summary This pilot study used participatory approaches to identify and tailor an implementation strategy aimed at improving pediatric hospital care in Migori, Kenya. In Aim 1, a nominal group technique approach was used to match potential interventions to identified barriers and select a strategy to pilot. This strategy was then tailored to the needs of the health care workers using an iterative design process (Aim 2). After piloting, we evaluated the usability and feasibility of the piloted strategy for ongoing use through mixed methods data collection and analysis (Aim 3).
Aim 1 of the project was completed in August 2022. A targeted implementation strategy was selected using participatory techniques with seven staff members from Migori County Referral Hospital. First, preliminary results of an earlier qualitative study conducted at the site were presented to the participants. This study had identified barriers and facilitators of use of pediatric treatment guidelines. Four challenges that came out strongly in the qualitative results and were modifiable at the facility-level were identified and participants ranked them on their likelihood of change and potential for impact. There was consensus among participant that the focus of this pilot should be the challenge: Health care workers rely on nutritionists to handle many tasks related to nutrition. If the nutritionist is not available this can delay guideline adherent care (especially at night/weekends).
The group was then presented with examples of strategies that were mapped to the specific barriers that had been identified in the qualitative study. They brainstormed to identify specific strategies that would be relevant to their setting. Six ideas were generated by the group. Participants ranked these options on three criteria (acceptability, feasibility, and impact), had a discussion about these options, and then reached consensus on an idea to pilot: Develop a summary of key information from the Integrated Management of Acute Malnutrition and other guidelines, merge them, and agree how they will be delivered by staff. Our team decided to call this idea the Team Approach to Malnutrition Services (TeAMS) Toolkit.
Based on the outcome of Aim 1, the study team refined plans for the pilot study and ethics approval for the remainder of the study was granted in February 2023. In Aim 2, an iterative design process was used to identify the content and features that health care workers at the facility preferred in the TeAMS Toolkit. Twenty participants completed pre-pilot surveys describing their experience and competence in caring for children with malnutrition. Between April and July 20203, 18 one-on-one design sessions were held with participants, consisting of interactive activities to guide refinement of the TeAMS Toolkit. The toolkit was designed to support staff by: (1) offering guidance on teamwork and clarifying team member roles and (2) consolidating recommendations from national guidelines so that health workers have easier access to the information they need to fulfil their roles. This is accomplished in four sections: Teamwork Skills, Team Member Roles and Responsibilities, Key Information from IMAM, Monitoring and Documentation. The TeAMS Toolkit was launched at the facility in September 2023 and a 10-week pilot period commenced.
At the conclusion of the TeAMS Toolkit pilot in November 2023, 29 participants completed a post-pilot survey. In addition, one focus group discussion and six in-depth interviews were conducted with participants. Among 19 participants with both pre- and post- data, mean scores for frequency of completing seven of eight tasks related to malnutrition increased, however changes in perceived competence scores on these tasks were variable (some increasing and some decreasing). While the survey data did not show increases in competence, during qualitative interviews several participants described additional staff being able to initiate feedings for children with malnutrition by utilizing the information on Toolkit posters. Responses to five out of six items assessing teamwork perceptions increased between the pre- to post-pilot surveys. This aligned with sentiments shared in the interviews describing improved teamwork and information sharing among staff. One participant stated: “I used to think it is a nutritionist duty, but currently I can also initiate [feeding]. …I have learnt that for success then, it has to be teamwork.”
Among all participants who completed the post-pilot survey, the mean System Usability Score for the TeAMS Toolkit was 77.4 on a 100-point scale, which can be interpreted as good system usability. The SUS score has two dimensions – usability and learnability. The mean score on the 8 usability questions was 3.3 out of 4, while the mean score on the two learnability questions was 2.3 out of 4. In interviews, participants noted the ease of use of most of the content in the TeAMS Toolkit, but often requested additional training opportunities to support development of knowledge and skills related to the TeAMS Toolkit. On three questions related to the feasibility of continuing implementation of the TeAMS Toolkit within the facility, mean scores among staff within the Paediatric Ward ranged from 4.29 to 4.71; where 4 indicates agreement and 5 indicates strong agreement that it would be possible to continue implementation of the Toolkit.
Exploring Multicultural and Multilingual Methods in Developing Dialog-Based Health Technologies
Investigators Weichao Yuwen, School of Nursing & Healthcare Leadership, UW Tacoma Trevor Cohen, Department of Biomedical Informatics and Medical Education Magaly Ramirez, Department of Health Systems and Population Health Serena Jinchen Xie, Department of Biomedical Informatics and Medical Education
Project summary In the United States, over 20 million family caregivers self-identified as having a racial or ethnic minority background spend on average more than 20 hours per week providing unpaid care to a care receiver. In addition, at least one-third of caregivers speak a language other than English at home. Existing barriers that prevent these marginalized caregivers from accessing services include a lack of culturally sensitive and linguistically appropriate programs of care. On-demand digital health technologies delivering interventions through text-based dialogs could be cost-effective solutions to support family caregivers. Recent innovations in machine learning and artificial intelligence (AI) have the potential to automate labor-intensive work such as language translation. However, these technologies, if used without careful intention, can increase biases and existing imbalances for marginalized groups. To our knowledge, there has not been the development of efficient multilingual AI language models in the health domain. We proposed to conduct a literature review of multicultural and multilingual model development methods in developing health dialogs (aim 1) and perform pilot training using an existing caregiver-domain-specific dataset in English to translate to and train in Spanish (aim 2).
We established an interdisciplinary research team consisting of faculty members, undergraduate students, pre-doctoral and post-doctoral trainees from nursing, biomedical informatics, and public health. The team conducted a narrative review on the topic of multilingual model for health dialog development and exploring the capabilities and limitations of large multilingual language models like mBERT and XLM-R. We submitted an abstract of the preliminary results to the American Medical Informatics Association Annual Symposium (AMIA 2023), and plan to submit the review for publication this summer. In addition, we conducted preliminary exploration of our existing dataset for machine translation and training, and used the results in a grant application to the National Institute of Health (NIH), which is currently under review. The team was recently awarded an Emergent Innovation Grant from the Rita & Alex Hillman Foundation for a pilot project building on this project.
More information about the Population Health Initiative pilot grant program, tiering and upcoming deadlines can be found by visiting our funding page .
What is population health?
Population health is a broad concept encompassing not only the elimination of diseases and injuries, but also the intersecting and overlapping factors that influence health.
Population Health Twitter
Events calendar, be boundless, connect with us:.
© 2024 University of Washington | Seattle, WA

IMAGES
COMMENTS
Vaccine hesitancy (VH) is considered a top-10 global health threat. The concept of VH has been described and applied inconsistently. This systematic review aims to clarify VH by analysing how it is operationalized. We searched PubMed, Embase and PsycINFO databases on 14 January 2022. We selected 422 studies containing operationalizations of VH ...
Vaccine hesitancy (VH) is considered a top-10 global health threat. The concept of VH has been described and applied inconsistently. This systematic review aims to clarify VH by analysing how it ...
This systematic review aims to clarify VH by analysing how it is operationalized and proposes that VH should be defined as a state of indecisiveness regarding a vaccination decision. Vaccine hesitancy (VH) is considered a top-10 global health threat. The concept of VH has been described and applied inconsistently. This systematic review aims to clarify VH by analysing how it is operationalized.
When the term 'vaccine hesitancy' first appeared, it was deemed ambiguous and difficult to measure. A systematic review of published articles on vaccine hesitancy suggests it should be defined ...
Vaccine hesitancy (VH) is considered a top-10 global health threat. The concept of VH has been described and applied inconsistently. This systematic review... Toggle navigation. Rankings; Articles . Article search; Cited-by search; Sections . ... A systematic literature review to clarify the concept of vaccine hesitancy.
Introduction. The World Health Organization designated vaccine hesitancy and vaccine confidence as among the most pressing issues in global health (World Health Organization, 2019).Although some have defined vaccine hesitancy as delay in acceptance or refusal of vaccines despite availability of vaccine services (MacDonald, 2015), it may be more helpful to characterize hesitancy as a set of ...
This website requires cookies, and the limited processing of your personal data in order to function. By using the site you are agreeing to this as outlined in our privacy notice and cookie policy.privacy notice and cookie policy.
A literature review on vaccine hesitancy showed that the number of articles on adolescent and adult vaccines increased from 2007 to 2012, with publications on the HPV vaccine (approved in 2006 ...
Methods. A systematic review of descriptive and analytic studies was conducted using specific key word searches to identify literature containing information about interventions directed at vaccine hesitancy. The search was done using PubMed, Global Health, and Science Direct databases.
Background Vaccination, albeit a necessity in the prevention of infectious diseases, requires appropriate strategies for addressing vaccine hesitancy at an individual and community level. However, there remains a glaring scarcity of available literature in that regard. Therefore, this review aims to scrutinize globally tested interventions to increase the vaccination uptake by addressing ...
2 Figure 25: Effect of dialogue based, incentive based, multi-component, reminder / recall and other interventions on uptake of combined childhood vaccinations; Evidence from the peer reviewed literature
A systematic literature review to clarify the concept of vaccine hesitancy ... W. M. Bibliometric analysis of global scientific literature on vaccine hesitancy in peer-reviewed journals (1990-2019). BMC Public Health 20, 1252 (2020). ... S. B. & Podsakoff, N. P. Recommendations for creating better concept definitions in the organizational ...
ing the vaccine hesitancy. However, there is a paucity of critical synthesis of all these interventions across the globe and contextual summarization to guide program managers and policy makers in implementing appropri-ate strategies to address vaccine hesitancy. erefore, this review aims to analyze globally tested interventions
In this article, we conduct a scoping review 2 Unlike systematic reviews, scoping reviews seek to identify concepts and characteristics across extant literature rather than seeking to answer a specific question about a topic related to that literature (Munn et al., 2018). of the existing academic research on online vaccine hesitancy and suggest ...
Abstract. Vaccine hesitancy in the US throughout the pandemic has revealed inconsistent results. This systematic review has compared COVID-19 vaccine uptake across US and investigated predictors of vaccine hesitancy and acceptance across different groups. A search of PUBMED database was conducted till 17th July, 2021.
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Understanding vaccine hesitancy of nurses; Assessing drivers of HPV vaccine hesitancy; ... The team conducted an extensive literature review of over 100 peer-reviewed journal articles. Via this literature review, they investigated the dose-responses of a suite of health outcomes to green space, with a major take-away that very few dose ...