Clinical Presentation: Case History # 1 Ms. C is a 35 year old white female. She came to Neurology Clinic for evaluation of her long-term neurologic complaints. The patient relates that for many years she had noticed some significant changes in neurologic functions, particularly heat intolerance precipitating a stumbling gait and a tendency to fall. Her visual acuity also seemed to change periodically during several years. Two months ago the patient was working very hard and was under a lot of stress. She got sick with a flu and her neurologic condition worsened. At that time, she could not hold objects in her hands, had significant tremors and severe exhaustion. She also had several bad falls. Since that time she had noticed arthralgia on the right and subsequently on the left side of her body. Then, the patient abruptly developed a right hemisensory deficit after several days of work. The MRI scan was performed at that time and revealed a multifocal white matter disease - areas of increased T2 signal in both cerebral hemispheres. Spinal tap was also done which revealed the presence of oligoclonal bands in CSF. Visual evoked response testing was abnormal with slowed conduction in optic nerves. (Q.1) (Q. 2) (Q.3) Today, the patient has multiple problems related to her disease: she remains weak and numb on the right side; she has impaired urinary bladder function which requires multiple voids in the mornings, and nocturia times 3. She became incontinent and now has to wear a pad during the day. (Q.4) She also has persistent balance problems with some sensation of spinning, and she is extremely fatigued. REVIEW OF SYSTEMS is also significant for a number of problems related to her suspected MS. The patient has a tendency to aspirate liquids and also solids. (Q.5) (Q.6) She complains of tinnitus which is continuous and associated with hearing loss, more prominent on the left. She has decreased finger dexterity and weakness of the hands bilaterally. She also complains of impaired short-term memory and irritability. FAMILY HISTORY is significant for high blood pressure, cancer and heart disease in the immediate family. PERSONAL HISTORY is significant for mumps and chicken pox as a child, and anemia and allergies with hives later in life. She also had a tubal ligation. NEUROLOGIC EXAMINATION: Cranial Nerve II - disks are sharp and of normal color. Funduscopic examination is normal. Cranial Nerves III, IV, VI - no extraocular motor palsy or difficulties with smooth pursuit or saccades are seen. Remainder of the cranial nerve exam is normal except for decreased hearing on the left, and numbness in the right face, which extends down into the entire right side. The Weber test reveals greater conductance to the right. Rinne's test reveals air greater than bone bilaterally. (Q.7) The palate elevates well. Swallow appears to be intact. Tongue movements are slowed, but tongue power appears to be intact. Motor examination reveals relatively normal strength in the upper extremities throughout. However, rapid alternating movements are decreased in both upper extremities and the patient has dysdiadochokinesia in the left hand. (Q.8) Mild paraparesis is noted in both legs without severe spasticity. Deep tendon reflexes are +2 and symmetrical in the arms, +3 at the ankles and at the knees. Bilateral extensor toe sign are present. Sensory exam reveals paresthesia on the right to touch and decreased pin sensation on the right diffusely. The patient has mild vibratory sense loss in the distal lower extremities. Romberg's is negative. (Q.9) Tandem gait is mildly unstable. Ambulation index is 7.0 seconds for 25 feet. (The patient takes 7.0 seconds to walk 25 feet.) Diagnosis: Multiple Sclerosis with laboratory support. © John W.Rose, M.D., Maria Houtchens, MSIII, Sharon G. Lynch, M.D.

Diagnosis and management of multiple sclerosis: case studies
Affiliation.
- 1 Multiple Sclerosis Program, Department of Neurology, University of Texas Southwestern Medical Center, 5323 Harry Hines Boulevard, Dallas, TX 75390-9036, USA.
- PMID: 16684629
- DOI: 10.1016/j.ncl.2006.01.002
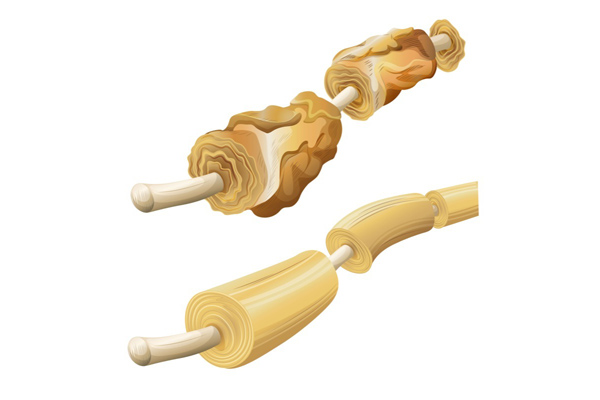
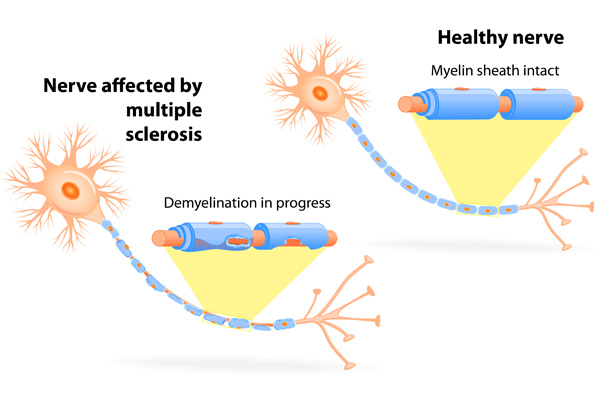
Although substantial capabilities have emerged in the ability to globally manage patients who have MS, clinicians continue to be confronted with formidable challenges. Reduction in disease activity and its impact on dis-ability progression remains the central objective of disease-modifying therapy and most current MS research initiatives. Nevertheless, the principal factors that determine the day-to-day limitations on functional capabilities(activities of daily living, work performance, quality of life, and so forth)are a derivative of the pathophysiology of the disease process itself. The substrate for these limitations is inherent in the pathology of demyelination and axonal dysfunction. Identifying measures that can optimize the performance and fidelity of axonal conduction mechanisms may translate into a reduction in MS-related symptoms. Chronic neurologic disease management (with MS representing a signature example) can be optimized when all members of the care team (including patients and their families) collaborate in the co-ordination of interdisciplinary care models that address all aspects of suffering.
Publication types
- Case Reports
- Adjuvants, Immunologic / therapeutic use*
- Anti-Inflammatory Agents / therapeutic use*
- Brain / pathology
- Diagnosis, Differential
- Disease Progression
- Interferon beta-1b
- Interferon-beta / therapeutic use*
- Magnetic Resonance Imaging
- Middle Aged
- Multiple Sclerosis / drug therapy*
- Multiple Sclerosis / pathology*
- Multiple Sclerosis, Relapsing-Remitting / pathology
- Multiple Sclerosis, Relapsing-Remitting / therapy
- Optic Neuritis / pathology
- Adjuvants, Immunologic
- Anti-Inflammatory Agents
- Interferon-beta

- © 2017
Case Studies in Multiple Sclerosis
- Paul S. Giacomini 0
McGill University , MONTREAL, Canada
You can also search for this editor in PubMed Google Scholar
- A collection of case studies illustrating the complex, unpredictable nature of multiple sclerosis and its many presentations and disease courses
- Case studies submitted from clinicians from some of the world's leading neurology departments
- Edited by Dr Paul Giacomini of McGill University, a leading expert in the field of multiple sclerosis
- Includes supplementary material: sn.pub/extras
19k Accesses
2 Citations
1 Altmetric
- Table of contents
About this book
Editors and affiliations, about the editor, bibliographic information.
- Publish with us
Buying options
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Other ways to access
This is a preview of subscription content, log in via an institution to check for access.
Table of contents (19 chapters)
Front matter, clinically isolated syndrome, optic neuritis.
- Mahtab Ghadiri
Early Multiple Sclerosis
Disease-modifying therapies.
- Anne-Marie Trudelle
Management of relapses with corticosteroids
Established relapsing-remitting multiple sclerosis, breakthrough disease.
- Chris Eckstein
Progressive multifocal leukoencephalopathy
Induction therapy, primary progressive multiple sclerosis, diagnosing primary progressive multiple sclerosis.
- Scott D. Newsome
Symptomatic care in primary progressive multiple sclerosis
Secondary progressive multiple sclerosis, diagnosing secondary progressive multiple sclerosis.
- Sarah Morrow
Walking disability in multiple sclerosis
Cognitive impairment, pediatric multiple sclerosis and related disorders, acute disseminated encephalomyelitis.
- Sunita Venkateswaran
- Case studies
- Clinically isolated syndrome
- Multiple sclerosis
- Primary progressive multiple sclerosis
- Relapse remitting multiple sclerosis
Paul S. Giacomini
Book Title : Case Studies in Multiple Sclerosis
Editors : Paul S. Giacomini
DOI : https://doi.org/10.1007/978-3-319-31190-6
Publisher : Adis Cham
eBook Packages : Medicine , Medicine (R0)
Copyright Information : Springer International Publishing Switzerland 2017
Softcover ISBN : 978-3-319-31188-3 Published: 21 October 2016
eBook ISBN : 978-3-319-31190-6 Published: 06 October 2016
Edition Number : 1
Number of Pages : XVII, 149
Number of Illustrations : 14 b/w illustrations
Topics : Neurology , Neuroradiology , Primary Care Medicine
Policies and ethics
- Find a journal
- Track your research
- Campus Directory
- Current Students
- Faculty & Staff

Multiple Sclerosis Case Study
Janet has experienced periodic episodes of tingling in her extremities, dizziness, and even episodes of blindness. After 12 years, doctors have finally given her a diagnosis. Follow Janet through her journey and find out why her disease is so difficult to diagnose.
Module 3: Multiple Sclerosis

Janet, age 22, was preparing for her 6-week postpartum checkup...
MS - Page 1
Three years later, at 34, Janet awoke to a prickly tingling feeling...
MS - Page 2
The neurologist made a diagnosis of multiple sclerosis based on the MRI...
MS - Page 3
Case Summary
Summary of the Case
MS - Summary

Answers to Case Questions
MS - Answers

Professionals
Health Professionals Introduced in Case
MS - Professionals
Additional Links
Optional Links to Explore Further
- Future Leaders in Neurology
- ACTRIMS 2024
- Treating NMOSD: What's Next?

- Conferences
- Publications
Patient Case #1: 37-Year-Old Female With RRMS
- Gabriel Pardo, MD, FAAN
Expert neurologists review treatment options for a young female with relapsing remitting multiple sclerosis (RRMS).

EP: 1 . Advances in the Management of Relapsing-Remitting Multiple Sclerosis (RRMS)

EP: 2 . Unmet Needs in the RRMS Treatment Landscape

EP: 3 . Generic Disease-Modifying Therapies (DMTs) in RRMS
Ep: 4 . fda approval process for rrms therapies, ep: 5 . treatment selection in rrms.

EP: 6 . Generic DMTs as First-Line Treatment in RRMS
Ep: 7 . patient case #1: 37-year-old female with rrms, ep: 8 . switching dmts in patients with rrms, ep: 9 . patient case #2: 36-year-old female with rrms with lesions in the spine and brain, ep: 10 . treatment options for a patient with rrms and psoriasis, ep: 11 . use of generic dmts in clinical practice in rrms, ep: 12 . challenges in use of generic dmts for treatment of ms, ep: 13 . the future of rrms treatment, ep: 14 . recommendations for rrms management.
Ahmed Zayed Obeidat MD, PhD: The first case we’re going to talk about is a 37-year-old female with 2 young children. We’re going to talk about some factors about what you would select as a treatment. The patient presented to the neurology clinic for first time with fatigue, weakness, tremors in the right hand, so that’s 1 side. And then medical history was significant for previous numbness and tingling in the lower extremity which was both and the result spontaneously about 2 years ago—not an uncommon scenario where people had maybe a pinched disc or something and they didn’t get medical attention because it went away on a physical exam. She had mild right upper extremity weakness and then increased tone in her right hand, already with increased tone, and some mild intention tremor. That’s important to keep in mind. And then gait was stable but had some hyperreflexia on examination. So those are some of the symptoms she presented with.
You did an MRI, and there were some lesions consistent with demyelination, and then spinal fluid showed unique oligoclonal bands. So, the diagnosis was consistent with what appears to be a relapsing remitting MS [multiple sclerosis].I’ll start with you, Dr Dukkipati. What’s your impression of this case and the initial treatment recommendation? How would you treat this patient?
Ravi Dukkipati, MD: Based on the vignette given, this is a relatively young woman, still of childbearing age with 2 young children, who I’m presuming is fairly active, and by all means has relapsing remitting multiple sclerosis based on the clinical presentation. And the brain MRI demonstrates multiple areas of demyelination, which is concerning, and I would characterize this woman as having a moderate disease burden both clinically and radiographically.
This is the type of patient whom I would not hesitate in terms of being aggressive from the beginning because the concern is that time is brain matter. And so, I generally don’t start new patients on platform therapies any longer, so the real decision-making in my mind would be between one of the oral therapies vs monoclonal antibodies with a patient like this or natalizumab.
Ahmed Zayed Obeidat MD, PhD: Dr Pardo?
Gabriel Pardo, MD, FAAN: Yes, I completely agree. I think there are some concerning signs already in this patient. I assume she’s right-hand dominant just by statistics and that’s where she has most of her symptoms. She already has dexterity problems spasticity problems weakness problems, and it’s not harboring good things for the future. The burden of disease seems to be high, and the diagnosis is straightforward. So, I am concerned about this patient. I think that there is no time to waste with platform therapies; there is no doubt about that.
Other elements we were discussing to individualize the decision-making along with the patient will be, as Dr Dukkipati mentioned, as she is still of childbearing age, is she planning on having more children? That will be a very important aspect in the counseling of this patient regarding the selection of the different agents that we have. And each one of them will have different characteristics in that regard. Some of them will allow her to be treated with 4 courses and then be free of treatment if she is able to delay pregnancy for 2 years, for example, maybe 2½ years 1½ years, or 18 months. Or she might imply the decision of having to stop treatment to pursue pregnancy with the risk of a potential rebound if she does not become pregnant promptly. So, a lot of elements again become important in individual patients, and for this patient, we’ll have to get that in the conversation to be able to counsel her in addition. But from the get-go, I am concerned about the patient, and she should definitely be on high-efficacy therapies. There’s no time to beat around the bush.
Ahmed Zayed Obeidat MD, PhD: Yes, and I agree because as you mentioned, there are already signs of incomplete recovery. There are signs of maybe brain stem involvement here, right? There’s a tremor, there is maybe cerebellar involvement. And that’s concerning when we think about her young age and that it was previously untreated for probably over 2 years because the first episode was over 2 years ago with what appears to be transgressed myelitis, which is again another spinal cord involvement which carries a poor prognosis sometimes. So I would do the same. I would start with a highly effective therapy for her. And then maybe, again, considering other factors; when she wants, if she wants more children, when the plan is. And we’ll work around many of these factors.
So I’m going to tell you a little bit of what happened. Maybe she was not started on highly effective therapy. So despite receiving disease-modifying therapy [DMT], she had 2 more relapses in the past year. She reported increased fatigue, difficulty with memory and concentration. And her exam showed right-sided weakness and wrist reflexes are still there, but more weakness. Another MRI of the brain shows multiple new and enhancing lesions while on a disease-modifying therapy, suggestive of ongoing disease activity. Her fatigue and memory issues are interfering with job performance. Now her symptoms are starting to affect her day-to-day and then maybe threatening her job or maybe could result in her losing her job. So this is now even more concerning. So now the patient comes back to you and asks, “How would you monitor? How would you treat me? What else can I do?" Dr Dukkipati, I’ll start with you for this one now, and then we’ll see what Dr Pardo has to say.
Ravi Dukkipati, MD: Well, this is clearly the worst-case scenario, what we had talked about earlier. This woman unfortunately is progressing. Clinically she’s had several relapses. She’s exhibiting signs of progression and her MRI studies clearly demonstrate a very active disease, involving both the brain and the spinal cord. Now, we don’t necessarily know what her initial disease-modifying therapy was, but clearly, she’s failing with that initial therapy. And this patient would need close monitoring both clinically and radiographically and imminent or immediate change or escalation of therapy to a different class.
Ahmed Zayed Obeidat MD, PhD: Dr Pardo, do you agree, and do you have any other additional thoughts?
Gabriel Pardo, MD, FAAN: Absolutely. I agree completely. And just this case highlights the fact that in addition to our selection of the disease-modifying therapy, we need to be always in tune with the patient’s needs and the fact that MS is multifaceted, it has a lot of manifestations, and that it does require comprehensive management of the disease. We need to go beyond the selection of the DMT. We need to explore all these other possibilities.
The threat of potentially losing her job has tremendous social, familial, and personal implications. And it brings then the conversation of the complementary things that we do to the DMTs, which are symptom management and trying to improve function, something that we also need to monitor closely. It is not just the markers that we use for failing a treatment as clearly evident in this case with relapses, and new MRI additions, but all these other ancillary ways of assessing how the patient is functioning and what else should we do, and can we do to improve that function, and to improve the ability of the patient to continue to live their life the best they can?
Ahmed Zayed Obeidat MD, PhD: Yes, and what strikes me in this case is also that she had 2 relapses in the past year, so she was left to relapse again after 1 relapse. So we didn’t have to even wait for that, right? You see 1 relapse, and for me, it’s sufficient to just switch to a different mechanism of action, and in this case, perhaps going higher; something with known higher efficacy.
Transcript edited for clarity
Episode 112: Exploring Dimethyl Fumarate to Treat Friedreich Ataxia
NeurologyLive® Friday 5 — April 5, 2024
Episode 111: Reviewing ACTRIMS 2024
NeuroVoices: Francesco Saccà, MD, PhD, on Crossing Over Dimethyl Fumarate in Friedriech Ataxia

Kyverna Publishes Promising First Case Reports of CAR-T Cell Therapy in Progressive Multiple Sclerosis
2 Commerce Drive Cranbury, NJ 08512
609-716-7777
- Open access
- Published: 10 April 2024
“So at least now I know how to deal with things myself, what I can do if it gets really bad again”—experiences with a long-term cross-sectoral advocacy care and case management for severe multiple sclerosis: a qualitative study
- Anne Müller ORCID: orcid.org/0000-0002-2456-2492 1 ,
- Fabian Hebben ORCID: orcid.org/0009-0003-6401-3433 1 ,
- Kim Dillen 1 ,
- Veronika Dunkl 1 ,
- Yasemin Goereci 2 ,
- Raymond Voltz 1 , 3 , 4 ,
- Peter Löcherbach 5 ,
- Clemens Warnke ORCID: orcid.org/0000-0002-3510-9255 2 &
- Heidrun Golla ORCID: orcid.org/0000-0002-4403-630X 1
on behalf of the COCOS-MS trial group represented by Martin Hellmich
BMC Health Services Research volume 24 , Article number: 453 ( 2024 ) Cite this article
Metrics details
Persons with severe Multiple Sclerosis (PwsMS) face complex needs and daily limitations that make it challenging to receive optimal care. The implementation and coordination of health care, social services, and support in financial affairs can be particularly time consuming and burdensome for both PwsMS and caregivers. Care and case management (CCM) helps ensure optimal individual care as well as care at a higher-level. The goal of the current qualitative study was to determine the experiences of PwsMS, caregivers and health care specialists (HCSs) with the CCM.
In the current qualitative sub study, as part of a larger trial, in-depth semi-structured interviews with PwsMS, caregivers and HCSs who had been in contact with the CCM were conducted between 02/2022 and 01/2023. Data was transcribed, pseudonymized, tested for saturation and analyzed using structuring content analysis according to Kuckartz. Sociodemographic and interview characteristics were analyzed descriptively.
Thirteen PwsMS, 12 caregivers and 10 HCSs completed interviews. Main categories of CCM functions were derived deductively: (1) gatekeeper function, (2) broker function, (3) advocacy function, (4) outlook on CCM in standard care. Subcategories were then derived inductively from the interview material. 852 segments were coded. Participants appreciated the CCM as a continuous and objective contact person, a person of trust (92 codes), a competent source of information and advice (on MS) (68 codes) and comprehensive cross-insurance support (128 codes), relieving and supporting PwsMS, their caregivers and HCSs (67 codes).
Conclusions
Through the cross-sectoral continuous support in health-related, social, financial and everyday bureaucratic matters, the CCM provides comprehensive and overriding support and relief for PwsMS, caregivers and HCSs. This intervention bears the potential to be fine-tuned and applied to similar complex patient groups.
Trial registration
The study was approved by the Ethics Committee of the University of Cologne (#20–1436), registered at the German Register for Clinical Studies (DRKS00022771) and in accordance with the Declaration of Helsinki.
Peer Review reports
Introduction
Multiple sclerosis (MS) is the most frequent and incurable chronic inflammatory and degenerative disease of the central nervous system (CNS). Illness awareness and the number of specialized MS clinics have increased since the 1990s, paralleled by the increased availability of disease-modifying therapies [ 1 ]. There are attempts in the literature for the definition of severe MS [ 2 , 3 ]. These include a high EDSS (Expanded disability Status Scale [ 4 ]) of ≥ 6, which we took into account in our study. There are also other factors to consider, such as a highly active disease course with complex therapies that are associated with side effects. These persons are (still) less disabled, but may feel overwhelmed with regard to therapy, side effects and risk monitoring of therapies [ 5 , 6 ].
Persons with severe MS (PwsMS) develop individual disease trajectories marked by a spectrum of heterogeneous symptoms, functional limitations, and uncertainties [ 7 , 8 ] manifesting individually and unpredictably [ 9 ]. This variability can lead to irreversible physical and mental impairment culminating in complex needs and daily challenges, particularly for those with progressive and severe MS [ 5 , 10 , 11 ]. Such challenges span the spectrum from reorganizing biographical continuity and organizing care and everyday live, to monitoring disease-specific therapies and integrating palliative and hospice care [ 5 , 10 ]. Moreover, severe MS exerts a profound of social and economic impact [ 9 , 12 , 13 , 14 ]. PwsMS and their caregivers (defined in this manuscript as relatives or closely related individuals directly involved in patients’ care) often find themselves grappling with overwhelming challenges. The process of organizing and coordinating optimal care becomes demanding, as they contend with the perceived unmanageability of searching for, implementing and coordinating health care and social services [ 5 , 15 , 16 , 17 ].
Case management (CM) proved to have a positive effect on patients with neurological disorders and/or patients with palliative care needs [ 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 ]. However, a focus on severe MS has been missed so far Case managers primarily function as: (1) gatekeeper involving the allocation of necessary and available resources to a case, ensuring the equitable distribution of resources; as (2) broker assisting clients in pursuing their interests, requiring negotiation to provide individualized assistance that aligns as closely as possible with individual needs and (3) advocate working to enhance clients’ individual autonomy, to advocate for essential care offers, and to identify gaps in care [ 25 , 26 , 27 , 28 , 29 ].
Difficulties in understanding, acting, and making decisions regarding health care-related aspects (health literacy) poses a significant challenge for 54% of the German population [ 30 ]. Additionally acting on a superordinate level as an overarching link, a care and case management (CCM) tries to reduce disintegration in the social and health care system [ 31 , 32 ]. Our hypothesis is that a CCM allows PwsMS and their caregivers to regain time and resources outside of disease management and to facilitate the recovery and establishment of biographical continuity that might be disrupted due to severe MS [ 33 , 34 ].
Health care specialists (HCSs) often perceive their work with numerous time and economic constraints, especially when treating complex and severely ill individuals like PwsMS and often have concerns about being blamed by patients when expectations could not be met [ 35 , 36 ]. Our hypothesis is that the CCM will help to reduce time constraints and free up resources for specialized tasks.
To the best of our knowledge there is no long-term cross-sectoral and outreaching authority or service dedicated to assisting in the organization and coordination of the complex care concerns of PwsMS within the framework of standard care addressing needs in health, social, financial, every day and bureaucratic aspects. While some studies have attempted to design and test care programs for persons with MS (PwMS), severely affected individuals were often not included [ 37 , 38 , 39 ]. They often remain overlooked by existing health and social care structures [ 5 , 9 , 15 ].
The COCOS-MS trial developed and applied a long-term cross-sectoral CCM intervention consisting of weekly telephone contacts and monthly re-assessments with PwsMS and caregivers, aiming to provide optimal care. Their problems, resources and (unmet) needs were assessed holistically including physical health, mental health, self-sufficiency and social situation and participation. Based on assessed (unmet) needs, individual care plans with individual actions and goals were developed and constantly adapted during the CCM intervention. Contacts with HCSs were established to ensure optimal care. The CCM intervention was structured through and documented in a CCM manual designed for the trial [ 40 , 41 ].
Our aim was to find out how PwsMS, caregivers and HCSs experienced the cross-sectoral long-term, outreaching patient advocacy CCM.
This study is part of a larger phase II, randomized, controlled clinical trial “Communication, Coordination and Security for people with severe Multiple Sclerosis (COCOS-MS)” [ 41 ]. This explorative clinical trial, employing a mixed-method design, incorporates a qualitative study component with PwsMS, caregivers and HCSs to enrich the findings of the quantitative data. This manuscript focuses on the qualitative data collected between February 2022 and January 2023, following the Consolidated Criteria for Reporting Qualitative Research (COREQ) guidelines [ 42 ].
Research team
Three trained authors AM, KD and FH (AM, female, research associate, M.A. degree in Rehabilitation Sciences; KD, female, researcher, Dr. rer. medic.; FH, male, research assistant, B.Sc. degree in Health Care Management), who had no prior relationship with patients, caregivers or HCSs conducted qualitative interviews. A research team, consisting of clinical experts and health services researchers, discussed the development of the interview guides and the finalized category system.
Theoretical framework
Interview data was analyzed with the structuring content analysis according to Kuckartz. This method enables a deductive structuring of interview material, as well as the integration of new aspects found in the interview material through the inductive addition of categories in an iterative analysis process [ 43 ].
Sociodemographic and interview characteristics were analyzed descriptively (mean, median, range, SD). PwsMS, caregivers and HCSs were contacted by the authors AM, KD or FH via telephone or e-mail after providing full written informed consent. Participants had the option to choose between online interviews conducted via the GoToMeeting 10.19.0® Software or face-to-face. Peasgood et al. (2023) found no significant differences in understanding questions, engagement or concentration between face-to-face and online interviews [ 44 , 45 ]. Digital assessments were familiar to participants due to pandemic-related adjustments within the trial.
Out of 14 PwsMS and 14 caregivers who were approached to participate in interviews, three declined to complete interviews, resulting in 13 PwsMS (5 male, 8 female) and 12 caregiver (7 male, 5 female) interviews, respectively (see Fig. 1 ). Thirty-one HCSs were contacted of whom ten (2 male, 8 female) agreed to be interviewed (see Fig. 2 ).
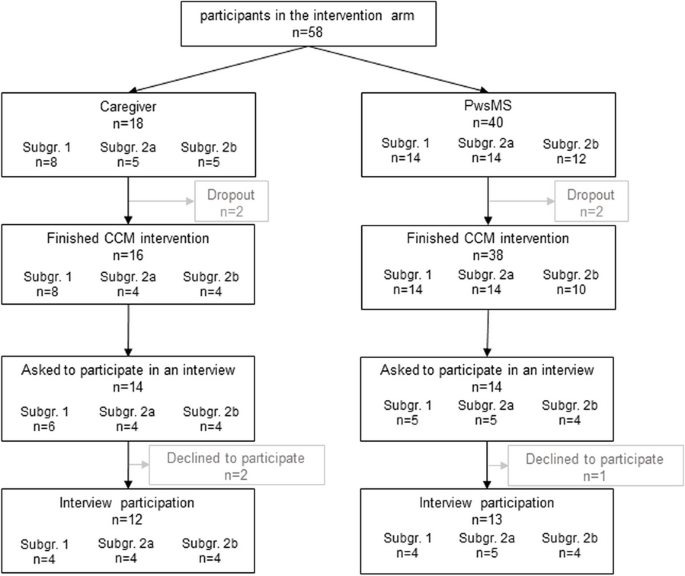
Flowchart of PwsMS and caregiver participation in the intervention group of the COCOS-MS trial. Patients could participate with and without a respective caregiver taking part in the trial. Therefore, number of caregivers does not correspond to patients. For detailed inclusion criteria see also Table 1 in Golla et al. [ 41 ]
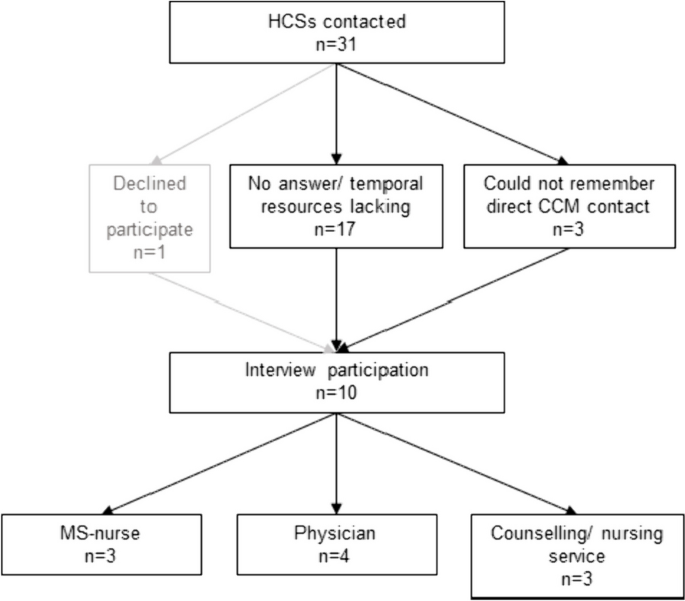
Flowchart of HCSs interview participation
Setting and data collection
Interviews were carried out where participants preferred, e.g. at home, workplace, online, and no third person being present. In total, we conducted 35 interviews whereof 7 interviews face-to-face (3 PwsMS, 3 caregivers, 1 HCS).
The research team developed a topic guide which was meticulously discussed with research and clinical staff to enhance credibility. It included relevant aspects for the evaluation of the CCM (see Tables 1 and 2 , for detailed topic guides see Supplementary Material ). Patient and caregiver characteristics (covering age, sex, marital status, living situation, EDSS (patients only), subgroup) were collected during the first assessment of the COCOS-MS trial and HCSs characteristics (age, sex, profession) as well as interview information (length and setting) were collected during the interviews. The interview guides developed for this study addressed consistent aspects both for PwsMS and caregivers (see Supplementary Material ):
For HCSs it contained the following guides:
Probing questions were asked to get more specific and in-depth information. Interviews were carried out once and recorded using a recording device or the recording function of the GoToMeeting 10.19.0® Software. Data were pseudonymized (including sensitive information, such as personal names, dates of birth, or addresses), audio files were safely stored in a data protection folder. The interview duration ranged from 11 to 56 min (mean: 23.9 min, SD: 11.1 min). Interviews were continued until we found that data saturation was reached. Audio recordings were transcribed verbatim by an external source and not returned to participants.
Data analysis
Two coders (AM, FH) coded the interviews. Initially, the first author (AM) thoroughly reviewed the transcripts to gain a sense of the interview material. Using the topic guide and literature, she deductively developed a category system based on the primary functions of CM [ 25 , 26 , 27 , 28 , 29 ]. Three interviews were coded repeatedly for piloting, and inductive subcategories were added when new themes emerged in the interview material. This category system proved suitable for the interview material. The second coder (FH) familiarized himself with the interview material and category system. Both coders (AM, FH) independently coded all interviews, engaging in discussions and adjusting codes iteratively. The finalized category system was discussed and consolidated in a research workshop and within the COCOS-MS trial group and finally we reached an intercoder agreement of 90% between the two coders AM and FH, computed by the MAXQDA Standard 2022® software.
We analyzed sociodemographic and interview characteristics using IBM SPSS Statistics 27® and Excel 2016®. Transcripts were managed and analyzed using MAXQDA Standard 2022®.
Participants were provided with oral and written information about the trial and gave written informed consent. Ethical approvals were obtained from the Ethics Committee of the University of Cologne (#20–1436). The trial is registered in the German Register for Clinical Studies (DRKS) (DRKS00022771) and is conducted under the Declaration of Helsinki.
Characteristics of participants and interviews
PwsMS participating in an interview were mainly German (84.6%), had a mean EDSS of 6.8 (range: 6–8) and MS for 13.5 years (median: 14; SD: 8.1). For detailed characteristics see Table 3 .
Most of the interviewed caregivers (9 caregivers) were the partners of the PwsMS with whom they lived in the same household. For further details see Table 3 .
HCSs involved in the study comprised various professions, including MS-nurse (3), neurologist (2), general physician with further training in palliative care (1), physician with further training in palliative care and pain therapist (1), housing counselling service (1), outpatient nursing service manager (1), participation counselling service (1).
Structuring qualitative content analysis
The experiences of PwsMS, caregivers and HCSs were a priori deductively assigned to four main categories: (1) gatekeeper function, (2) broker function, (3) advocacy function [ 25 , 26 , 27 , 28 , 29 ] and (4) Outlook on CCM in standard care, whereas the subcategories were developed inductively (see Fig. 3 ).
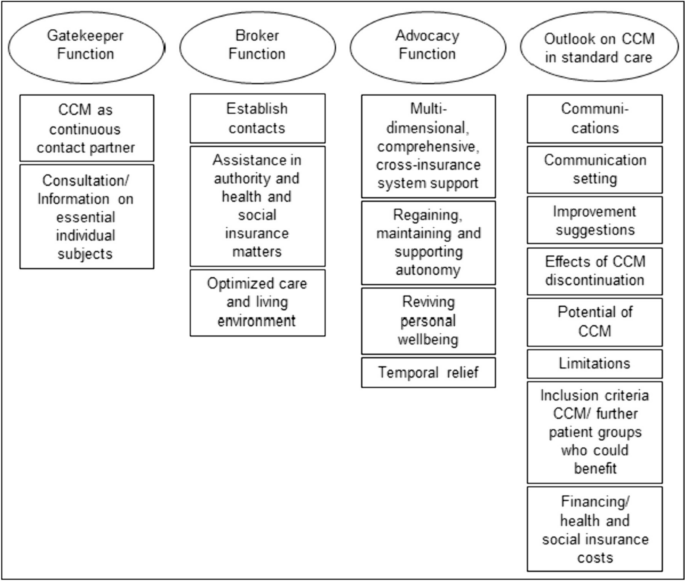
Category system including main and subcategories of the qualitative thematic content analysis
The most extensive category, housing the highest number of codes and subcodes, was the “ Outlook on CCM in standard care ” (281 codes). Following this, the category “ Advocacy Function ” contained 261 codes. The “ Broker Function ” (150 codes) and the “ Gatekeeper Function ” (160 codes) constituted two smaller categories. The majority of codes was identified in the caregivers’ interviews, followed by those of PwsMS (see Table 4 ). Illustrative quotes for each category and subcategory can be found in Table 5 .
Persons with severe multiple sclerosis
In the gatekeeper function (59 codes), PwsMS particularly valued the CCM as a continuous contact person . They appreciated the CCM as a person of trust who was reliably accessible throughout the intervention period. This aspect, with 41 codes, held significant importance for PwsMS.
Within the broker function (44 codes), establishing contact was most important for PwsMS (22 codes). This involved the CCM as successfully connecting PwsMS and caregivers with physicians and therapists, as well as coordinating and arranging medical appointments, which were highly valued. Assistance in authority and health and social insurance matters (10 codes) was another subcategory, where the CCM encompassed support in communication with health insurance companies, such as improving the level of care, assisting with retirement pension applications, and facilitating rehabilitation program applications. Optimized care (12 codes) resulted in improved living conditions and the provision of assistive devices through the CCM intervention.
The advocacy function (103 codes) emerged as the most critical aspect for PwsMS, representing the core of the category system. PwsMS experienced multidimensional, comprehensive, cross-insurance system support from the CCM. This category, with 43 statements, was the largest within all subcategories. PwsMS described the CCM as addressing their concerns, providing help, and assisting with the challenges posed by the illness in everyday life. The second-largest subcategory, regaining, maintaining and supporting autonomy (25 codes), highlighted the CCM’s role in supporting self-sufficiency and independence. Reviving personal wellbeing (17 codes) involved PwsMSs’ needs of regaining positive feelings, improved quality of life, and a sense of support and acceptance, which could be improved by the CCM. Temporal relief (18 codes) was reported, with the CCM intervention taking over or reducing tasks.
Within the outlook on CCM in standard care (84 codes), eight subcategories were identified. Communications was described as friendly and open (9 codes), with the setting of communication (29 codes) including the frequency of contacts deemed appropriate by the interviewed PwsMS, who preferred face-to-face contact over virtual or telephone interactions. Improvement suggestions for CCM (10 codes) predominantly revolved around the desire for the continuation of the CCM beyond the trial, expressing intense satisfaction with the CCM contact person and program. PwsMS rarely wished for better cooperation with the CCM. With respect to limitations (7 codes), PwsMS distinguished between individual limitations (e.g. when not feeling ready for using a wheelchair) and overriding structural limitations (e.g. unsuccessful search for an accessible apartment despite CCM support). Some PwsMS mentioned needing the CCM earlier in the course of the disease and believed it would beneficial for anyone with a chronic illness (6 codes).
In the gatekeeper function (75 codes), caregivers highly valued the CCM as a continuous contact partner (33 codes). More frequently than among the PwsMS interviewed, caregivers valued the CCM as a source of consultation/ information on essential individual subjects (42 codes). The need for basic information about the illness, its potential course, treatment and therapy options, possible supportive equipment, and basic medical advice/ information could be met by the CCM.
Within the broker function (63 codes), caregivers primarily experienced the subcategory establish contacts (24 codes). They found the CCM as helpful in establishing and managing contact with physicians, therapists and especially with health insurance companies. In the subcategory assistance in authority and health and social insurance matters (22 codes), caregivers highlighted similar aspects as the PwsMS interviewed. However, there was a particular emphasis on assistance with patients' retirement matters. Caregivers also valued the optimization of patients’ care and living environment (17 codes) in various life areas during the CCM intervention, including improved access to assistive devices, home modification, and involvement of a household support and/ or nursing services.
The advocacy function, with 115 codes, was by far the broadest category . The subcategory multidimensional, comprehensive, cross-insurance system support represented the largest subcategory of caregivers, with 70 statements. In summary, caregivers felt supported by the CCM in all domains of life. Regaining, maintaining and supporting autonomy (11 codes) and reviving personal wellbeing (8 codes) in the form of an improved quality of life played a role not only for patients but also for caregivers, albeit to a lower extend. Caregivers experienced temporal relief (26 codes) as the CCM undertook a wide range of organizational tasks, freeing up more needed resources for their own interests.
For the Outlook on CCM in standard care , caregivers provided various suggestions (81 codes). Similar to PwsMS, caregivers felt that setting (home based face-to-face, telephone, virtual) and frequency of contact were appropriate (10 codes, communication setting ) and communications (7 codes) were recognized as open and friendly. However, to avoid conflicts between caregiver and PwsMS, caregivers preferred meeting the CCM separately from the PwsMS in the future. Some caregivers wished the CCM to specify all services it might offer at the beginning, while others emphasized not wanting this. Like PwsMS, caregivers criticized the CCM intervention being (trial-related) limited to one year, regardless of whether further support was needed or processes being incomplete (13 codes, improvement suggestions ). After the CCM intervention time had expired, the continuous contact person and assistance were missed and new problems had arisen and had to be managed with their own resources again (9 codes, effects of CCM discontinuation ), which was perceived as an exhausting or unsolvable endeavor. Caregivers identified analogous limitations (8 codes), both individual and structural. However, the largest subcategory, was the experienced potential of CCM (27 codes), reflected in extremely high satisfaction with the CCM intervention. Like PwsMS, caregivers regarded severe chronically ill persons in general as target groups for a CCM (7 codes) and would implement it even earlier, starting from the time of diagnosis. They considered a CCM to be particularly helpful for patients without caregivers or for caregivers with limited (time) resources, as it was true for most caregivers.
Health care specialists
In the gatekeeper function (26 codes) HCSs particularly valued the CCM as a continuous contact partner (18 codes). They primarily described their valuable collaboration with the CCM, emphasizing professional exchange between the CCM and HCSs.
Within the broker function (43 codes), the CCM was seen as a connecting link between patients and HCSs, frequently establishing contacts (18 codes). This not only improved optimal care on an individual patient level (case management) but also at a higher, superordinate care level (care management). HCSs appreciated the optimized care and living environment (18 codes) for PwsMS, including improved medical and therapeutic access and the introduction of new assistive devices. The CCM was also recognized as providing assistance in authority and health and social matters (7 codes) for PwsMS and their caregivers.
In the advocacy function (43 codes), HCSs primarily reported temporal relief through CCM intervention (23 codes). They experienced this relief, especially as the CCM provided multidimensional, comprehensive, and cross-insurance system support (15 codes) for PwsMS and their caregivers. Through this support, HCSs felt relieved from time intensive responsibilities that may not fall within their area of expertise, freeing up more time resources for their actual professional tasks.
The largest category within the HCSs interviews was the outlook on CCM in standard care (116 codes). In the largest subcategory, HCSs made suggestions for further patient groups who could benefit (38 codes) from a CCM. Chronic neurological diseases like neurodegenerative diseases (e.g. amyotrophic lateral sclerosis), typical and atypical Parkinson syndromes were mentioned. HCSs considered the enrollment of the CCM directly after the diagnosis of these complex chronic diseases. Additionally, chronic progressive diseases in general or oncological diseases, which may also run chronically, were regarded worthwhile for this approach. HCSs also provided suggestions regarding improvement (21 codes). They wished e.g. for information or contact when patients were enrolled to the CCM, regular updates, exchange and collaborative effort. On the other hand, HCSs reported, that their suggestions for improvement would hardly be feasible due to their limited time resources. Similar to patients and caregivers, HCSs experienced structural limits (13 codes), which a CCM could not exceed due to overriding structural limitations (e.g. insufficient supply of (household) aids, lack of outreach services like psychotherapists, and long processing times on health and pension insurers' side). HCSs were also asked about their opinions on financial resources (14 codes) of a CCM in standard care. All interviewed HCSs agreed that CCM would initially cause more costs for health and social insurers, but they were convinced of cost savings in the long run. HCSs particularly perceived the potential of the CCM (20 codes) through the feedback of PwsMS, highlighting the trustful relationship enabling individualized help for PwsMS and their caregivers.
Persons with severe multiple sclerosis and their caregivers
The long-term cross-sectoral CCM intervention implemented in the COCOS-MS trial addressed significant unmet needs of PwsMS and their caregivers which previous research revealed as burdensome and hardly or even not possible to improve without assistance [ 5 , 6 , 9 , 10 , 33 , 35 , 46 ]. Notably, the CCM service met the need for a reliable, continuous contact partner, guiding patients through the complexities of regulations, authorities and the insurance system. Both, PwsMS and their caregivers highly valued the professional, objective perspective provided by the CCM, recognizing it as a source of relief, support and improved care in line with previous studies [ 37 , 47 ]. Caregivers emphasized the CCM’s competence in offering concrete assistance and information on caregiving and the fundamentals of MS, including bureaucratic, authority and insurances matters. On the other hand, PwsMS particularly appreciated the CCMs external reflective and advisory function, along with empathic social support tailored to their individual concerns. Above all, the continuous partnership of trust, available irrespective of the care sector, was a key aspect that both PwsMS and their caregivers highlighted. This consistent support was identified as one of the main components in the care of PwsMS in previous studies [ 5 , 33 , 35 ].
As the health literacy is inadequate or problematic for 54% of the German population and disintegration in the health and social care system is high [ 30 , 31 , 32 ], the CCM approach serves to enhance health literacy and reduce disintegration of PwsMS and their caregivers by providing cross-insurance navigational guidance in the German health and social insurance sector on a superordinate level. Simultaneously PwsMS and caregivers experienced relief and gained more (time) resources for all areas of life outside of the disease and its management, including own interests and establishing biographical continuity. This empowerment enables patients to find a sense of purpose beyond their illness, regain autonomy, and enhance social participation, reducing the feeling of being a burden to those closest to them. Such feelings are often experienced as burdensome and shameful by PwsMS [ 6 , 48 , 49 , 50 ]. Finding a sense of purpose beyond the illness also contributes to caregivers perceiving their loved ones not primarily as patient but as individuals outside of the disease, reinforcing valuable relationships such as partners, siblings, or children, strengthening emotional bonds. These factors are also highly relevant and well-documented in a suicide-preventive context, as the suicide rate is higher in persons diagnosed with neurological disorders [ 19 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 ] and the feeling of being a burden to others, loss of autonomy, and perceived loss of dignity are significant factors in patients with severe chronic neurological diseases for suicide [ 50 , 57 ].
The temporal relief experienced by the CCM was particularly significant for HCSs and did not only improve the satisfaction of HCSs but also removed unfulfilled expectations and concerns about being blamed by patients when expectations could not be met, which previous studied elaborated [ 35 , 36 ]. Moreover, the CCM alleviated the burden on HCSs by addressing patients’ concerns, allowing them to focus on their own medical responsibilities. This aspect probably reduced the dissatisfaction that arises when HCSs are expected to address issues beyond their medical expertise, such as assistive devices, health and social insurance, and the organization and coordination of supplementary therapies, appointments, and contacts [ 35 , 36 , 61 ]. Consequently, the CCM reduced difficulties of HCSs treating persons with neurological or chronical illnesses, which previous research identified as problematic.
HCSs perceive their work as increasingly condensed with numerous time and economic constraints, especially when treating complex and severely ill individuals like PwsMS [ 36 ]. This constraint was mentioned by HCSs in the interviews and was one of the main reasons why they were hesitant to participate in interviews and may also be an explanation for a shorter interview duration than initially planned in the interview guides. The CCM’s overarching navigational competence in the health and social insurance system was particularly valued by HCSs. The complex and often small-scale specialties in the health and social care system are not easily manageable or well-known even for HCSs, and dealing with them can exceed their skills and time capacities [ 61 ]. The CCM played a crucial role in keeping (temporal) resources available for what HCSs are professionally trained and qualified to work on. However, there remains a challenge in finding solutions to the dilemma faced by HCSs regarding their wish to be informed about CCM procedures and linked with each other, while also managing the strain of additional requests and contact with the CCM due to limited (time) resources [ 62 ]. Hudon et al. (2023) suggest that optimizing time resources and improving exchange could involve meetings, information sharing via fax, e-mail, secure online platforms, or, prospectively, within the electronic patient record (EPR). The implementation of an EPR has shown promise in improving the quality of health care and time resources, when properly implemented [ 63 , 64 ]. The challenge lies ineffective information exchange between HCSs and CCM for optimal patient care. The prospect of time saving in the long run and at best for a financial incentive, e.g., when anchoring in the Social Security Code, will help best to win over the HCSs.If this crucial factor can be resolved, there is a chance that HCSs will thoroughly accept the CCM as an important pillar, benefiting not only PwsMS but also other complex patient groups, especially those with long-term neurological or complex oncological conditions that might run chronically.
Care and case management and implications for the health care system
The results of our study suggest that the cross-sectoral long-term advocacy CCM in the COCOS-MS trial, with continuous personal contacts at short intervals and constant reevaluation of needs, problems, resources and goals, is highly valued by PwsMS, caregivers, and HCSs. The trial addresses several key aspects that may have been overlooked in previous studies which have shown great potential for the integration of case management [ 17 , 47 , 62 , 65 , 66 ]. However, they often excluded the overriding care management, missed those patient groups with special severity and complexity who might struggle to reach social and health care structures independently or the interventions were not intended for long-term [ 22 , 37 ]. Our results indicate that the CCM intervention had a positive impact on PwsMS and caregivers as HCSs experienced them with benefits such as increased invigoration, reduced demands, and enhanced self-confidence. However, there was a notable loss experienced by PwsMS and caregivers after the completion of the CCM intervention, even if they had stabilized during the intervention period. The experiences of optimized social and health care for the addressed population, both at an individual and superordinate care level, support the integration of this service into standard care. Beyond the quantitatively measurable outcomes and economic considerations reported elsewhere [ 16 , 20 , 21 ], our results emphasize the importance of regaining control, self-efficacy, self-worth, dignity, autonomy, and social participation. These aspects are highlighted as preventive measures in suicidal contexts, which is particularly relevant for individuals with severe and complex illnesses [ 19 , 50 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 ]. Our findings further emphasize the societal responsibilities to offer individuals with severe and complex illnesses the opportunity to regain control and meaningful aspects of life, irrespective of purely economic considerations. This underscores the need for a comprehensive evaluation that not only takes into account quantitative measures but also the qualitative aspects of well-being and quality of life when making recommendations of a CCM in standard care.
The study by J. Y. Joo and Huber (2019) highlighted that CM interventions aligned with the standards of the Case Management Society of America varied in duration, ranging from 1 month to 15.9 years, and implemented in community- or hospital-based settings. However, they noted a limitation in understanding how CM processes unfold [ 67 ]. In contrast, our trial addressed this criticism by providing transparent explanations of the CCM process, which also extends to a superordinate care management [ 40 , 41 ]. Our CCM manual [ 40 ] outlines a standardized and structured procedure for measuring and reevaluating individual resources, problems, and unmet needs on predefined dimensions. It also identifies goals and actions at reducing unmet needs and improving the individual resources of PwsMS and caregivers. Importantly, the CCM manual demonstrates that the CCM process can be structured and standardized, while accounting for the unique aspects of each individual’s serious illness, disease courses, complex needs, available resources, and environmental conditions. Furthermore, the adaptability of the CCM manual to other complex chronically ill patient groups suggests the potential for a standardized approach in various health care settings. This standardized procedure allows for consistency in assessing and addressing the individual needs of patients, ensuring that the CCM process remains flexible while maintaining a structured and goal-oriented framework.
The discussion about the disintegration in the social and health care system and the increasing specialization dates back to 2009 [ 31 , 32 ]. Three strategies were identified to address this issue: (a) “driver-minimizing” [Treiberminimierende], (b) “effect-modifying” [Effektmodifizierende] and (c) “disintegration-impact-minimizing” [Desintegrationsfolgenminimierende] strategies. “Driver-minimizing strategies” involve comprehensive and radical changes within the existing health and social care system, requiring political and social pursuit. “Disintegration-impact-minimizing strategies” are strategies like quality management or tele-monitoring, which are limited in scope and effectiveness. “Effect-modifying strategies”, to which CCM belongs, acknowledges the segmentation within the system but aims to overcome it through cooperative, communicative, and integrative measures. CCM, being an “effect-modifying strategy”, operates the “integrated segmentation model” [Integrierte Segmentierung] rather than the “general contractor model” [Generalunternehmer-Modell] or “total service provider model” [Gesamtdienstleister-Modell] [ 31 , 32 ]. In this model, the advantage lies in providing an overarching and coordinating service to link different HCSs and services cross-sectorally. The superordinate care management aspect of the CCM plays a crucial role in identifying gaps in care, which is essential for future development strategies within the health and social care system. It aims to find or develop (regional) alternatives to ensure optimal care [ 17 , 23 , 24 , 68 , 69 ], using regional services of existing health and social care structures. Therefore, superordinate care management within the CCM process is decisive for reducing disintegration in the system.
Strengths and limitations
The qualitative study results of the explorative COCOS-MS clinical trial, which employed an integrated mixed-method design, provide valuable insights into the individual experiences of three leading stakeholders: PwsMS, caregivers and HCSs with a long-term cross-sectoral CCM. In addition to in-depth interviews, patient and caregiver reported outcome measurements were utilized and will be reported elsewhere. The qualitative study’s strengths include the inclusion of patients who, due to the severity of their condition (e.g. EDSS mean: 6.8, range: 6–8, highly active MS), age (mean: 53.9 years, range: 36–73 years) family constellations, are often underrepresented in research studies and often get lost in existing social and health care structures. The study population is specific to the wider district region of Cologne, but the broad inclusion criteria make it representative of severe MS in Germany. The methodological approach of a deductive and inductive structuring content analysis made it possible to include new findings into an existing theoretical framework.
However, the study acknowledges some limitations. While efforts were made to include more HCSs, time constraints on their side limited the number of interviews conducted and might have biased the results. Some professions are underrepresented in the interviews. Complex symptoms (e.g. fatigue, ability to concentrate), medical or therapeutic appointments and organization of the everyday live may have been reasons for the patients’ and caregivers’ interviews lasting shorter than initially planned.
The provision of functions of a CCM, might have pre-structured the answers of the participants.
At current, there is no support system for PwsMS, their caregivers and HCSs that addresses their complex and unmet needs comprehensively and continuously. There are rare qualitative insights of the three important stakeholders: PwsMS, caregivers and HCSs in one analysis about a supporting service like a CCM. In response to this gap, we developed and implemented a long-term cross-sectoral advocacy CCM and analyzed it qualitatively. PwsMS, their caregivers and HCSs expressed positive experiences, perceiving the CCM as a source of relief and support that improved care across various aspects of life. For patients, the CCM intervention resulted in enhanced autonomy, reviving of personal wellbeing and new established contacts with HCSs. Caregivers reported a reduced organizational burden and felt better informed, and HCSs experienced primarily temporal relief, allowing them to concentrate on their core professional responsibilities. At a higher level of care, the study suggests that the CCM contributed to a reduction in disintegration within the social and health care system.
The feedback from participants is seen as valuable for adapting the CCM intervention and the CCM manual for follow-up studies, involving further complex patient groups such as neurological long-term diseases apart from MS and tailoring the duration of the intervention depending on the complexity of evolving demands.
Availability of data and materials
Generated and/or analyzed datasets of participants are available from the corresponding author on reasonable request to protect participants. Preliminary partial results have been presented as a poster during the EAPC World Congress in June 2023 and the abstract has been published in the corresponding abstract booklet [ 70 ].
Abbreviations
Amyotrophic lateral sclerosis
- Care and case management
Case management
Central nervous system
Communication, Coordination and security for people with multiple sclerosis
Consolidated criteria for reporting qualitative research
German register for clinical studies
Extended disability status scale
Electronic patient record
Quality of life
Multiple sclerosis
Koch-Henriksen N, Magyari M. Apparent changes in the epidemiology and severity of multiple sclerosis. Nat Rev Neurol. 2021;17:676–88. https://doi.org/10.1038/s41582-021-00556-y .
Article PubMed Google Scholar
Ellenberger D, Flachenecker P, Fneish F, Frahm N, Hellwig K, Paul F, et al. Aggressive multiple sclerosis: a matter of measurement and timing. Brain. 2020;143:e97. https://doi.org/10.1093/brain/awaa306 .
Article PubMed PubMed Central Google Scholar
Edmonds P, Vivat B, Burman R, Silber E, Higginson IJ. Loss and change: experiences of people severely affected by multiple sclerosis. Palliat Med. 2007;21:101–7. https://doi.org/10.1177/0269216307076333 .
Kurtzke JF. Rating neurologic impairment in multiple rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology. 1983;33(11):1444–52.
Article CAS PubMed Google Scholar
Galushko M, Golla H, Strupp J, Karbach U, Kaiser C, Ernstmann N, et al. Unmet needs of patients feeling severely affected by multiple sclerosis in Germany: a qualitative study. J Palliat Med. 2014;17:274–81. https://doi.org/10.1089/jpm.2013.0497 .
Borreani C, Bianchi E, Pietrolongo E, Rossi I, Cilia S, Giuntoli M, et al. Unmet needs of people with severe multiple sclerosis and their carers: qualitative findings for a home-based intervention. PLoS One. 2014:e109679. https://doi.org/10.1371/journal.pone.0109679 .
Yamout BI, Alroughani R. Multiple Sclerosis. Semin Neurol. 2018;38:212–25. https://doi.org/10.1055/s-0038-1649502 .
Nissen N, Lemche J, Reestorff CM, Schmidt M, Skjerbæk AG, Skovgaard L, et al. The lived experience of uncertainty in everyday life with MS. Disabil Rehabil. 2022;44:5957–63. https://doi.org/10.1080/09638288.2021.1955302 .
Strupp J, Hartwig A, Golla H, Galushko M, Pfaff H, Voltz R. Feeling severely affected by multiple sclerosis: what does this mean? Palliat Med. 2012;26:1001–10. https://doi.org/10.1177/0269216311425420 .
Strupp J, Voltz R, Golla H. Opening locked doors: Integrating a palliative care approach into the management of patients with severe multiple sclerosis. Mult Scler J. 2016;22:13–8.
Article CAS Google Scholar
Kraft AK, Berger K. Kernaspekte einer bedarfsgerechten Versorgung von Patienten mit Multipler Sklerose : Inanspruchnahme ambulanter Leistungen und „shared decision making“ [Core aspects of a needs-conform care of patients with multiple sclerosis : Utilization of outpatient services and shared decision making]. Nervenarzt. 2020;91:503–10. https://doi.org/10.1007/s00115-020-00906-z .
Doshi A, Chataway J. Multiple sclerosis, a treatable disease. Clin Med (Lond). 2017;17:530–6. https://doi.org/10.7861/clinmedicine.17-6-530 .
Kobelt G, Thompson A, Berg J, Gannedahl M, Eriksson J. New insights into the burden and costs of multiple sclerosis in Europe. Mult Scler. 2017;23:1123–36. https://doi.org/10.1177/1352458517694432 .
Conradsson D, Ytterberg C, Engelkes C, Johansson S, Gottberg K. Activity limitations and participation restrictions in people with multiple sclerosis: a detailed 10-year perspective. Disabil Rehabil. 2021;43:406–13. https://doi.org/10.1080/09638288.2019.1626919 .
Sorensen PS, Giovannoni G, Montalban X, Thalheim C, Zaratin P, Comi G. The Multiple Sclerosis Care Unit. Mult Scler J. 2019;5:627–36.
Article Google Scholar
Tan H, Yu J, Tabby D, Devries A, Singer J. Clinical and economic impact of a specialty care management program among patients with multiple sclerosis: a cohort study. Mult Scler. 2010;16:956–63. https://doi.org/10.1177/1352458510373487 .
Article CAS PubMed PubMed Central Google Scholar
Oeseburg B, Wynia K, Middel B, Reijneveld SA. Effects of case management for frail older people or those with chronic illness: a systematic review. Nurs Res. 2009;58:201–10.
Aiken LS, Butner J, Lockhart CA, Volk-Craft BE, Hamilton G, Williams FG. Outcome evaluation of a randomized trial of the PhoenixCare intervention: program of case management and coordinated care for the seriously chronically ill. J Palliat Med. 2006;9:111–26. https://doi.org/10.1089/jpm.2006.9.111 .
Kuhn U, Düsterdiek A, Galushko M, Dose C, Montag T, Ostgathe C, Voltz R. Identifying patients suitable for palliative care—a descriptive analysis of enquiries using a Case Management Process Model approach. BMC Res Notes. 2012;5:611. https://doi.org/10.1186/1756-0500-5-611 .
Leary A, Quinn D, Bowen A. Impact of proactive case management by multiple sclerosis specialist nurses on use of unscheduled care and emergency presentation in multiple sclerosis: a case study. Int J MS Care. 2015;17:159–63. https://doi.org/10.7224/1537-2073.2014-011 .
Strupp J, Dose C, Kuhn U, Galushko M, Duesterdiek A, Ernstmann N, et al. Analysing the impact of a case management model on the specialised palliative care multi-professional team. Support Care Cancer. 2018;26:673–9. https://doi.org/10.1007/s00520-017-3893-3 .
Wynia K, Annema C, Nissen H, de Keyser J, Middel B. Design of a Randomised Controlled Trial (RCT) on the effectiveness of a Dutch patient advocacy case management intervention among severely disabled Multiple Sclerosis patients. BMC Health Serv Res. 2010;10:142. https://doi.org/10.1186/1472-6963-10-142 .
Ewers M, Schaeffer D, editors. Case Management in Theorie und Praxis. Bern: Huber; 2005.
Google Scholar
Neuffer M. Case Management: Soziale Arbeit mit Einzelnen und Familien. 5th ed. Weinheim, Basel: Beltz Juventa; 2013.
Case Management Society of America. The standards of practice for case management. 2022.
Deutsche Gesellschaft für Care und Case Management e.V., editor. Case Management Leitlinien: Rahmenempfehlung, Standards und ethische Grundlagen. 2nd ed. Heidelberg: Medhochzwei; 2020.
Monzer M. Case Management Grundlagen. 2nd ed. Heidelberg: Medhochzwei; 2018.
Wissert M. Grundfunktionen und fachliche Standards des Unterstützungsmanagements. Z Gerontol Geriat. 1998;31(5):331–7.
Wissert M. Tools und Werkzeuge beim Case Management: Die Hilfeplanung. Case Manag. 2007;1:35–7.
Schaeffer D, Berens E-M, Vogt D. Health literacy in the German population. Dtsch Arztebl Int. 2017;114:53–60. https://doi.org/10.3238/arztebl.2017.0053 .
Pfaff H, Schulte H. Der onkologische Patient der Zukunft. Onkologe. 2012;18:127–33. https://doi.org/10.1007/s00761-011-2201-y .
Pfaff H, Kowalski C, Ommen O. Modelle zur Analyse von Integration und Koordination im Versorgungssystem. In: Ameldung, Sydow, Windeler, editor. Vernetzung im Gesundheitswesen: Wettbewerb und Kooperation. Stuttgart: Kohlhammer Verlag; 2009. p. 75–90.
Golla H, Mammeas S, Galushko M, Pfaff H, Voltz R. Unmet needs of caregivers of severely affected multiple sclerosis patients: A qualitative study. Palliat Support Care. 2015;13(6):1685–93.
Golla H, Galushko M, Pfaff H, Voltz R. Multiple sclerosis and palliative care - perceptions of severely affected multiple sclerosis patients and their health professionals: a qualitative study. BMC Palliat Care. 2014;13:11. https://doi.org/10.1186/1472-684x-13-11 .
Golla H, Galushko M, Pfaff H, Voltz R. Unmet needs of severely affected multiple sclerosis patients: the health professionals’ view. Palliat Med. 2012;26:139–51. https://doi.org/10.1177/0269216311401465 .
Methley AM, Chew-Graham CA, Cheraghi-Sohi S, Campbell SM. A qualitative study of patient and professional perspectives of healthcare services for multiple sclerosis: implications for service development and policy. Health Soc Care Community. 2017;25:848–57. https://doi.org/10.1111/hsc.12369 .
Kalb R, Costello K, Guiod L. Case management services to meet the complex needs of patients with multiple sclerosis in the community—the successes and challenges of a unique program from the national multiple sclerosis society. US Neurology. 2019;15:27–31.
Krüger K, Fricke LM, Dilger E-M, Thiele A, Schaubert K, Hoekstra D, et al. How is and how should healthcare for people with multiple sclerosis in Germany be designed?-The rationale and protocol for the mixed-methods study Multiple Sclerosis-Patient-Oriented Care in Lower Saxony (MS-PoV). PLoS One. 2021;16:e0259855. https://doi.org/10.1371/journal.pone.0259855 .
Ivancevic S, Weegen L, Korff L, Jahn R, Walendzik A, Mostardt S, et al. Effektivität und Kosteneffektivät von Versorgungsmanagement-Programmen bei Multipler Sklerose in Deutschland – Eine Übersichtsarbeit. Akt Neurol. 2015;42:503–8. https://doi.org/10.1055/s-0035-1564111 .
Müller A, Dillen K, Dojan T, Ungeheuer S, Goereci Y, Dunkl V, et al. Development of a long-term cross-sectoral case and care management manual for patients with severe multiple sclerosis and their caregivers. Prof Case Manag. 2023;28:183–93. https://doi.org/10.1097/NCM.0000000000000608 .
Golla H, Dillen K, Hellmich M, Dojan T, Ungeheuer S, Schmalz P, et al. Communication, Coordination, and Security for People with Multiple Sclerosis (COCOS-MS): a randomised phase II clinical trial protocol. BMJ Open. 2022;12:e049300. https://doi.org/10.1136/bmjopen-2021-049300 .
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–57. https://doi.org/10.1093/intqhc/mzm042 .
Kuckartz U. Qualitative Inhaltsanalyse: Methoden, Praxis, Computerunterstützung. 4th ed. Weinheim: Beltz Juventa; 2018.
Akyirem S, Ekpor E, Aidoo-Frimpong GA, Salifu Y, Nelson LE. Online interviews for qualitative health research in Africa: a scoping review. Int Health. 2023. https://doi.org/10.1093/inthealth/ihad010 .
Peasgood T, Bourke M, Devlin N, Rowen D, Yang Y, Dalziel K. Randomised comparison of online interviews versus face-to-face interviews to value health states. Soc Sci Med. 2023;323:115818. https://doi.org/10.1016/j.socscimed.2023.115818 .
Giordano A, Cimino V, Campanella A, Morone G, Fusco A, Farinotti M, et al. Low quality of life and psychological wellbeing contrast with moderate perceived burden in carers of people with severe multiple sclerosis. J Neurol Sci. 2016;366:139–45. https://doi.org/10.1016/j.jns.2016.05.016 .
Joo JY, Liu MF. Experiences of case management with chronic illnesses: a qualitative systematic review. Int Nurs Rev. 2018;65(1):102–1113.
Freeman J, Gorst T, Gunn H, Robens S. “A non-person to the rest of the world”: experiences of social isolation amongst severely impaired people with multiple sclerosis. Disabil Rehabil. 2020;42:2295–303. https://doi.org/10.1080/09638288.2018.1557267 .
National Institute for Health and Care Excellence. Multiple sclerosis: Management of multiple sclerosis in primary and secondary care. 2014.
Erdmann A, Spoden C, Hirschberg I, Neitzke G. The wish to die and hastening death in amyotrophic lateral sclerosis: A scoping review. BMJ Support Palliat Care. 2021;11:271–87. https://doi.org/10.1136/bmjspcare-2020-002640 .
Erlangsen A, Stenager E, Conwell Y, Andersen PK, Hawton K, Benros ME, et al. Association between neurological disorders and death by suicide in Denmark. JAMA. 2020;323:444–54. https://doi.org/10.1001/jama.2019.21834 .
Kalb R, Feinstein A, Rohrig A, Sankary L, Willis A. Depression and suicidality in multiple sclerosis: red flags, management strategies, and ethical considerations. Curr Neurol Neurosci Rep. 2019;19:77. https://doi.org/10.1007/s11910-019-0992-1 .
Feinstein A, Pavisian B. Multiple sclerosis and suicide. Mult Scler. 2017;23:923–7. https://doi.org/10.1177/1352458517702553 .
Marrie RA, Salter A, Tyry T, Cutter GR, Cofield S, Fox RJ. High hypothetical interest in physician-assisted death in multiple sclerosis. Neurology. 2017;88:1528–34. https://doi.org/10.1212/WNL.0000000000003831 .
Gauthier S, Mausbach J, Reisch T, Bartsch C. Suicide tourism: a pilot study on the Swiss phenomenon. J Med Ethics. 2015;41:611–7. https://doi.org/10.1136/medethics-2014-102091 .
Fischer S, Huber CA, Imhof L, MahrerImhof R, Furter M, Ziegler SJ, Bosshard G. Suicide assisted by two Swiss right-to-die organisations. J Med Ethics. 2008;34:810–4. https://doi.org/10.1136/jme.2007.023887 .
Strupp J, Ehmann C, Galushko M, Bücken R, Perrar KM, Hamacher S, et al. Risk factors for suicidal ideation in patients feeling severely affected by multiple sclerosis. J Palliat Med. 2016;19:523–8. https://doi.org/10.1089/jpm.2015.0418 .
Spence RA, Blanke CD, Keating TJ, Taylor LP. Responding to patient requests for hastened death: physician aid in dying and the clinical oncologist. J Oncol Pract. 2017;13:693–9. https://doi.org/10.1200/JOP.2016.019299 .
Monforte-Royo C, Villavicencio-Chávez C, Tomás-Sábado J, Balaguer A. The wish to hasten death: a review of clinical studies. Psychooncology. 2011;20:795–804. https://doi.org/10.1002/pon.1839 .
Blanke C, LeBlanc M, Hershman D, Ellis L, Meyskens F. Characterizing 18 years of the death with dignity act in Oregon. JAMA Oncol. 2017;3:1403–6. https://doi.org/10.1001/jamaoncol.2017.0243 .
Methley A, Campbell S, Cheraghi-Sohi S, Chew-Graham C. Meeting the mental health needs of people with multiple sclerosis: a qualitative study of patients and professionals. Disabil Rehab. 2017;39(11):1097-105. https://doi.org/10.1080/09638288.2016.1180547 .
Hudon C, Bisson M, Chouinard M-C, Delahunty-Pike A, Lambert M, Howse D, et al. Implementation analysis of a case management intervention for people with complex care needs in primary care: a multiple case study across Canada. BMC Health Serv Res. 2023;23:377. https://doi.org/10.1186/s12913-023-09379-7 .
Beckmann M, Dittmer K, Jaschke J, Karbach U, Köberlein-Neu J, Nocon M, et al. Electronic patient record and its effects on social aspects of interprofessional collaboration and clinical workflows in hospitals (eCoCo): a mixed methods study protocol. BMC Health Serv Res. 2021;21:377. https://doi.org/10.1186/s12913-021-06377-5 .
Campanella P, Lovato E, Marone C, Fallacara L, Mancuso A, Ricciardi W, Specchia ML. The impact of electronic health records on healthcare quality: a systematic review and meta-analysis. Eur J Public Health. 2016;26:60–4. https://doi.org/10.1093/eurpub/ckv122 .
García-Hernández M, González de León B, Barreto-Cruz S, Vázquez-Díaz JR. Multicomponent, high-intensity, and patient-centered care intervention for complex patients in transitional care: SPICA program. Front Med (Lausanne). 2022;9:1033689. https://doi.org/10.3389/fmed.2022.1033689 .
Meisinger C, Stollenwerk B, Kirchberger I, Seidl H, Wende R, Kuch B, Holle R. Effects of a nurse-based case management compared to usual care among aged patients with myocardial infarction: results from the randomized controlled KORINNA study. BMC Geriatr. 2013. https://doi.org/10.1186/1471-2318-13-115 .
Joo JY, Huber DL. Case management effectiveness on health care utilization outcomes: a systematic review of reviews. West J Nurs Res. 2019;41:111–33. https://doi.org/10.1177/0193945918762135 .
Stergiopoulos V, Gozdzik A, Misir V, Skosireva A, Connelly J, Sarang A, et al. Effectiveness of housing first with intensive case management in an ethnically diverse sample of homeless adults with mental illness: a randomized controlled trial. PLoS One. 2015;10:e0130281. https://doi.org/10.1371/journal.pone.0130281 .
Löcherbach P, Wendt R, editors. Care und Case Management: Transprofessionelle Versorgungsstrukturen und Netzwerke. 1st ed. Stuttgart: Kohlhammer; 2020.
EAPC2023 Abstract Book. Palliat Med. 2023;37:1–302. https://doi.org/10.1177/02692163231172891 .
Download references
Acknowledgements
We would like to thank all the patients, caregivers and health care specialists who volunteered their time to participate in an interview and the trial, Carola Janßen for transcribing the interviews, Fiona Brown for translating the illustrative quotes and Beatrix Münzberg, Kerstin Weiß and Monika Höveler for data collection in the quantitative study part.
COCOS-MS Trial Group
Anne Müller 1 , Fabian Hebben 1 , Kim Dillen 1 , Veronika Dunkl 1 , Yasemin Goereci 2 , Raymond Voltz 1,3,4 , Peter Löcherbach 5 , Clemens Warnke 2 , Heidrun Golla 1 , Dirk Müller 6 , Dorthe Hobus 1 , Eckhard Bonmann 7 , Franziska Schwartzkopff 8 , Gereon Nelles 9 , Gundula Palmbach 8 , Herbert Temmes 10 , Isabel Franke 1 , Judith Haas 10 , Julia Strupp 1 , Kathrin Gerbershagen 7 , Laura Becker-Peters 8 , Lothar Burghaus 11 , Martin Hellmich 12 , Martin Paus 8 , Solveig Ungeheuer 1 , Sophia Kochs 1 , Stephanie Stock 6 , Thomas Joist 13 , Volker Limmroth 14
1 Department of Palliative Medicine, Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
2 Department of Neurology, Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
3 Center for Integrated Oncology Aachen Bonn Cologne Düsseldorf (CIO ABCD), University of Cologne, Cologne, Germany
4 Center for Health Services Research (ZVFK), University of Cologne, Cologne, Germany
5 German Society of Care and Case Management e.V. (DGCC), Münster, Germany
6 Institute for Health Economics and Clinical Epidemiology (IGKE), Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
7 Department of Neurology, Klinikum Köln, Cologne, Germany
8 Clinical Trials Centre Cologne (CTCC), Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
9 NeuroMed Campus, MedCampus Hohenlind, Cologne, Germany
10 German Multiple Sclerosis Society Federal Association (DMSG), Hannover, Germany
11 Department of Neurology, Heilig Geist-Krankenhaus Köln, Cologne, Germany
12 Institute of Medical Statistics and Computational Biology (IMSB), Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
13 Academic Teaching Practice, University of Cologne, Cologne, Germany
14 Department of Neurology, Klinikum Köln-Merheim, Cologne, Germany
Open Access funding enabled and organized by Projekt DEAL. This work was supported by the Innovation Funds of the Federal Joint Committee (G-BA), grant number: 01VSF19029.
Author information
Authors and affiliations.
Department of Palliative Medicine, Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
Anne Müller, Fabian Hebben, Kim Dillen, Veronika Dunkl, Raymond Voltz & Heidrun Golla
Department of Neurology, Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
Yasemin Goereci & Clemens Warnke
Center for Integrated Oncology Aachen Bonn Cologne Düsseldorf (CIO ABCD), University of Cologne, Cologne, Germany
Raymond Voltz
Center for Health Services Research, University of Cologne, Cologne, Germany
German Society of Care and Case Management E.V. (DGCC), Münster, Germany
Peter Löcherbach
You can also search for this author in PubMed Google Scholar
- Anne Müller
- , Fabian Hebben
- , Kim Dillen
- , Veronika Dunkl
- , Yasemin Goereci
- , Raymond Voltz
- , Peter Löcherbach
- , Clemens Warnke
- , Heidrun Golla
- , Dirk Müller
- , Dorthe Hobus
- , Eckhard Bonmann
- , Franziska Schwartzkopff
- , Gereon Nelles
- , Gundula Palmbach
- , Herbert Temmes
- , Isabel Franke
- , Judith Haas
- , Julia Strupp
- , Kathrin Gerbershagen
- , Laura Becker-Peters
- , Lothar Burghaus
- , Martin Hellmich
- , Martin Paus
- , Solveig Ungeheuer
- , Sophia Kochs
- , Stephanie Stock
- , Thomas Joist
- & Volker Limmroth
Contributions
HG, KD, CW designed the trial. HG, KD obtained ethical approvals. HG, KD developed the interview guidelines with help of the CCM (SU). AM was responsible for collecting qualitative data, developing the code system, coding, analysis of the data and writing the first draft of the manuscript, thoroughly revised and partly rewritten by HG. FH supported in collecting qualitative data, coding and analysis of the interviews. KD supported in collecting qualitative data. AM, FH, KD, VD, YG, RV, PL, CW, HG discussed and con-solidated the finalized category system. AM, FH, KD, VD, YG, RV, PL, CW, HG read and commented on the manuscript and agreed to the final version.
Authors’ information
Not applicable.
Corresponding author
Correspondence to Anne Müller .
Ethics declarations
Ethics approval and consent to participate.
Participants were provided with oral and written information about the trial and provided written informed consent. Ethical approval was obtained from the Ethics Committee of the University of Cologne (#20–1436). The trial is registered in the German Register for Clinical Studies (DRKS) (DRKS00022771) and is conducted under the Declaration of Helsinki.
Consent for publication
Competing interests.
Clemens Warnke has received institutional support from Novartis, Alexion, Sanofi Genzyme, Janssen, Biogen, Merck and Roche. The other authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Müller, A., Hebben, F., Dillen, K. et al. “So at least now I know how to deal with things myself, what I can do if it gets really bad again”—experiences with a long-term cross-sectoral advocacy care and case management for severe multiple sclerosis: a qualitative study. BMC Health Serv Res 24 , 453 (2024). https://doi.org/10.1186/s12913-024-10851-1
Download citation
Received : 23 November 2023
Accepted : 11 March 2024
Published : 10 April 2024
DOI : https://doi.org/10.1186/s12913-024-10851-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cross-sectoral
- Qualitative research
- Health care specialist
- Severe multiple sclerosis
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]

Case Study: Use of Disease-Modifying Therapy in Elderly Patients With Multiple Sclerosis
With the advent of disease-modifying therapies, the life span of patients with multiple sclerosis has increased dramatically.
CM is a 65-year-old female presenting to the neurology clinic with a past medical history of relapsing/remitting multiple sclerosis (MS). Her initial symptoms at diagnosis were sensory loss in her left leg and optic neuritis.
After diagnosis, it was decided to start disease-modifying therapy (DMT) on interferon beta-1a. CM remained on this therapy for 13 years. She suffered from multiple relapses, including a relapse that resulted in hospitalization and steroid treatments.
The MRI results showed multiple enhancing lesions. The provider switched therapy to fingolimod. After 7 years of fingolimod therapy, CM suffered another severe relapse, resulting in hospitalization requiring treatment with SoluMedrol.
After multiple severe relapses and complications surrounding a car accident, CM is no longer ambulatory. She is in an assisted living facility, has an indwelling catheter, and has multiple reoccurring infections. Her EDSS score is 8.
In 2021, the provider discontinued all DMTs due to the risk of infection outweighing the benefits of prevention of relapses and disease progression due to the high EDSS score.
Today, a year later, she is presenting to the neurology clinic with the question of whether to restart a DMT to prevent relapses.What is your recommendation to the provider?
Mental Status
- Oriented to person, place, and time.
- Follows 3 step commands.
- Attention: normal.
- Concentration: normal.
- Speech: normal
- Level of consciousness: alert
- Knowledge: good.
- Able to name object. Able to read. Normal comprehension.
- Nurse advocate: She has good cognitive function and can feed herself if her meal is set up for her, uses her arms for daily tasks that are important for her quality of life.
- Gait: wheelchair bound
Coordination
Finger to nose coordination: normal
- Left deltoid: 4/5
- Right wrist flexion: 4/5
- Right wrist extension: 4/5
- Right interossei: 4/5
- Right abdominals: 1/5
- Left abdominals: 0/5
- AST, ALT, WBC – Within normal limits
- CrCl – 94 mL/min
- JCVaB – Negative
Medications
- Baclofen 10 mg oral BID
- Bupropion XL 300 mg QD
- Eliquis 5 mg QD
- Sulfamethoxazole-trimethoprim 400/80 mg as needed
Immunizations
Up to date on all vaccines.
MS is an autoimmune disease characterized by inflammation, demyelination, and axonal degeneration. MS primarily affects women with a ratio of 3:1 compared to men with an initial diagnosis age ranging from 20 to 40 years. 1
According to the International Advisory Committee on Clinical Trials of MS, there are 4 main disease courses—clinically isolated syndrome (CIS), relapsing/remitting MS (RRMS), secondary progressive MS (SPMS), and primary progressive MS (PPMS). RRMS is the most common disease course, with approximately 85% of patients initially diagnosed in this stage. Patients with RRMS form cycles between relapses followed by periods of complete or partial recovery. 1
With the advent of DMTs, the life span of patients with MS has increased dramatically. Approximately 25% of patients with MS are adults over 65 years of age. 2
Health care providers face unique challenges in treating an elderly patient with MS. Elderly patients suffer from age-related and MS-related comorbidities with the disease course shifting from an inflammatory to a neurodegenerative phenotype. Among older adults, limited data exist for prescribing patterns of DMTs.
A retrospective longitudinal cohort study examined the prescribing patterns of DMTs in older adults with MS. 3 The study cohort consisted of 12,922 patients with MS aged 60 years and older, with 2455 patients receiving DMT therapy.
The most commonly prescribed DMTs were injectables (10.46%), orals (6.06%), and infusions (2.40%). The authors concluded nearly 1 in 5 older adults with MS were prescribed DMTs, with injectables being the most common form.
CMs condition has deteriorated over time and her EDSS score is currently 8. Clinical trials routinely exclude patients of CM’s age and with her degree of disability.
Hence, health care providers face a lack of knowledge of the safety and efficacy of DMTs in the elderly population. Often, providers will discontinue treatment because of increased risk and decreased benefit to the patient.
CM and her nurse advocate favor preserving and maintaining her quality of life. CM is still very functional cognitively and has fine upper extremity mobility.
Because future relapses could affect CM’s quality of life—after discussions with the patient, and the patient advocate—the provider decided to initiate CM on diroximel fumarate. Although the platform therapies of glatiramer acetate and interferon-beta1a are safest in the elderly population, CM was not interested in any injectable forms.
DMTs can cause varying degrees of lymphopenia, which is classified as grade 1 (mild lymphopenia) ALC < lower limit of normal to 800/mm 3 , grade 2 (moderate lymphopenia) ALC < 800–500/mm 3 , grade 3 (severe lymphopenia) ALC < 500–200/mm 3 and grade 4 < 200/mm 3 .
In the general population, lymphopenia is associated with increased risk of hospitalization and increased risk of infection-related death. 4 In patients with MS, this increased risk of infection is likely to be elevated due to comorbidities and the immunocompromised state.
Diroximel fumarate is used to treat both RRMS and active SPMS. 5 It has an unknown mechanism of action but does activate the nuclear factor (erythroid-derived 2)-like 2 (Nrf2) pathway reducing cellular oxidative stress.
CM is at a high risk of infection due to her baseline wheelchair status, prior infections, and indwelling catheter. In clinical trials with dimethyl fumarate (has the same active metabolite as diroximel fumarate), mean lymphocyte counts decreased by 30% during the first year of treatment, and then remained stable thereafter. 5
CM requires close monitoring—she will need CBC including lymphocyte count at baseline, and every 6 months thereafter, and MRI at baseline and then for routine monitoring. 5 If CM exhibits any disease activity (either clinical or on radiograph) after initiating diroximel fumarate, the provider should stop the medication due to the altered risk versus benefit scenario. Diroximel fumarate can cause liver toxicity—serum aminotransferase, alkaline phosphates, and total bilirubin levels must be checked before initiation and during treatment as clinically indicated.
The starting dose of diroximel fumarate is 231 mg twice a day orally. 5 The dose is increased to 462 mg twice a day after 7 days.
The pharmacist should counsel CM to take the medication with a meal or snack containing no more than 700 calories and 30 grams of fat to reduce flushing. Although diroximel fumarate causes less GI distress compared to dimethyl fumarate, CM should be counseled on abdominal pain, diarrhea, and nausea.5
PML is an opportunistic infection caused by the JC virus in immunocompromised patients. CM has tested negative for the JCV virus, but she should be counseled on the signs and symptoms of PML which include progressive weakness on one side of the body or clumsiness of limbs, visual changes, changes in memory, and orientation leading to confusion and personality changes. Patients may also develop herpes zoster or other opportunistic infections while on therapy.
The safety and efficacy of live or live-attenuated vaccines with diroximel fumarate has not been assessed. 5 According to the National MS Society guidelines, no adjustments are required with diroximel fumarate and COVID-19 vaccine administration. 6
About the Authors
Justin Bivona is a specialty clinical pharmacist working in multiple sclerosis and rare diseases at the Outpatient Pharmacy Services (OPS).
Bisni Narayanan, PharmD, MS is the supervisor for operations at OPS. OPS is a specialty pharmacy integrated within the Yale New Health System.
- What is MS? National Multiple Sclerosis Society 2022. Accessed on Nov 17, 2022. What is MS? | National Multiple Sclerosis Society (nationalmssociety.org)
- Vaughn CB, Jakimovski D, Kavak KS, et al. Epidemiology and treatment of multiple sclerosis in elderly populations. Nat Rev Neurol. 2019;15(6):329-342
- Talwar A, Earla JR, Hutton GJ, et al. Prescribing of disease modifying agents in older adults with multiple sclerosis. Mult Scler Relat Disord. 2022;57:103308
- Warny M, Helby J, Nordestgaard BG, et al. Lymphopenia and risk of infection and infection-related death in 98,344 individuals from a prospective Danish population-based study. PLoS Med. 2018;15(11):e1002685.
- Vumerity [package insert] Biogen; 2019
- COVID-19 VACCINE GUIDANCE FOR PEOPLE LIVING WITH MS. National Multiple Sclerosis Society. 2022. Accessed on Nov 17, 2022. COVID-19 Vaccine Guidance for People Living with MS | National MS Society | National Multiple Sclerosis Society .

Public Health Matters: Seacrest Studios’ Impact on Children’s Hospitals and Healing Through Broadcasting
Study: Inappropriate Diagnosis of Community-Acquired Pneumonia is Common

Pharmacy Focus: Limited Series - Celebrity Endorsements in Public Health

Anticholinergic Medications in Older Adults and Strategies for Safe Deprescribing

More Research Needed for Treatment of Clozapine-Resistant Schizophrenia
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

To Measure MS Progression, Monitor the Cervical Lymph Nodes
—researchers in finland concluded that deep cervical lymph node diameter is feasible as a biomarker for multiple sclerosis disease course..
Erin Kello, PhD
An accessible biomarker that tracks disease activity and progression in multiple sclerosis (MS) could lead to more-informed treatment decisions, which would help to put patients on a path to better outcomes.
Previous research, in both humans and mice, has hinted that deep cervical lymph nodes (CLNs) are the locus of the autoimmune response in individuals with MS. Building on this information, the authors of a new study, published online ahead of print in Multiple Sclerosis and Related Disorders, evaluated whether CLN diameter could serve as a biomarker for monitoring MS progression and activity. 1

Characteristics of the study population This retrospective cohort study identified patients from the Finnish MS register who had received a follow-up evaluation at the Helsinki University Hospital outpatient neurology clinic. 1 Patients between 17 and 45 years of age with relapsing-remitting MS (RRMS) who received magnetic resonance imaging (MRI) of the head between January 2017 and December 2020 were eligible for the study.
In terms of treatment, the highly active RRMS cohort (ha-RRMS-stable, n=26) used highly effective disease-modifying treatments (DMTs). In this cohort, MRIs were taken before patients started DMTs. Patients using glatiramer acetate or beta-interferon were classified as having active RRMS (a-RRMS-stable, n=23); some MRIs in this group were taken during active treatment.
The RRMS relapse cohort included 64 patients with a head MRI taken within 1 month of a clinical relapse. Of the relapse patients, 26 had follow-up MRIs (r-RRMS-follow-up cohort). A fourth cohort, RRMS-stable, included the 72 patients in the a-RRMS-stable, ha-RRMS-stable, and r-RRMS-follow-up cohorts (3 patients who appeared in 2 groups were excluded). Age and sex-matched controls (n=52) were selected from patients who underwent an MRI for primary headache syndrome at the Helsinki University Hospital outpatient neurology clinic within the same time frame as MS patients.
All cohorts were filtered for the following exclusionary criteria: “cancer, neuroimmunological or neuroinflammatory diseases, previous history of notable infectious diseases, sinusitis in the head MRI analyzed, previous history of neck or head pathology, or use of per oral corticosteroids.” 1 Clinical and demographic characteristics were collected from hospital medical records. The primary outcome measure was to determine the feasibility of using deep CLN diameter as a biomarker for the MS disease course, by evaluating the relationship between CLN diameter and disease activity.
Evidence backs up the authors’ hypothesis Several correlations between CLN diameter and clinical features of MS were identified. For one, a significant inverse correlation was found between the Expanded Disability Status Scale (EDSS) score recorded during the initial MRI and right-sided CLN diameter after roughly 2 years of follow-up in the stable RRMS versus control cohorts (correlation coefficient -0.305; P =.009). A significant inverse correlation was also found between patient age and the diameter of the largest CLN in the stable RRMS cohort (correlation coefficient -0.206; P =.031). In the same cohort, disease duration (decrease of 0.011 mm every month) and change in EDSS (decrease of 0.518 mm for every unit) at follow-up significantly predicted the diameter of the largest CLN.
The median diameter of the right-sided ( P =.012), left-sided ( P =.017), and largest CLN ( P =.003) were reduced in the RRMS-relapse group compared to controls. CLN diameter was also reduced in patients further along in the disease course. Among the 22 participants with stable RRMS who were more than 5 years from their diagnosis, 9% had abnormally large (over 10 mm) CLN diameters, compared to 26% (n=50) of patients who were less than 5 years from diagnosis and 50% of controls. In the stable RRMS cohort, EDSS ( P =.003) and diameter of the largest CLN ( P =.033) at the time of the initial MRI significantly predicted change in EDSS at follow-up.
What are the main take-aways? The study wasn’t without its limitations, of course, the main one being the retrospective nature of the analysis, which didn’t allow for patients with undisclosed infections—including the common cold—to be excluded at the time of the MRI. The authors were also mindful of raising the following possibilities: “Comparing lymph node diameter in deep cervical versus other lymph node compartments in MS patients is a relevant topic for future studies,” they wrote. “Interestingly, CD20 monoclonal antibodies deplete cervical intranodal memory B cells as shown for neuromyelitis optica spectrum disorder patients, and the possible effect of B cell depletion on CLN size in MS is also to be further addressed.” 1
Sini Laakso, MD, PhD, of the Department of Neurology, Helsinki University Hospital, and the study’s corresponding author, told MedPage Today: “Deep cervical lymph nodes are the site of antigen drainage from the central nervous system, and suspected to thus be the main site where autoimmune reactions are programmed in relapsing-remitting MS. Our study explored, to our understanding for the first time, whether the diameter of these lymph nodes correlates to disease states in MS. We found that, indeed, deep cervical lymph node diameter is altered both during an acute relapse and when the patient has entered a secondarily progressive disease state.”
Clinically, Dr. Laakso says, these results suggest that a measure of CLN diameter could be included in MS care. “In the future,” she notes, “by including a simple measure of cervical lymph node diameter to the analysis of the routine follow-up head MRIs that are performed usually every year to patients with MS, neurologists could have an additional tool to predict disease states without any extra costs."
Published: April 05, 2024
- 1. Tuulasvaara A, Kurdo G, Martola J, Laakso SM. Cervical lymph node diameter reflects disease progression in multiple sclerosis. Mult Scler Relat Disord . 2024 Feb 11. doi:10.1016/j.msard.2024.105496. [Epub ahead of print]
Multiple sclerosis: familial risk and heritability, ms progression independent of relapse activity: new insights, progressive multiple sclerosis: the search for new strategies to improve cognition, in patients with ms, can pain phenotype predict physical activity levels, cognitive decline in ms linked to multiple cortical regions, multiple sclerosis: the role of genetic variation in progression, ms disease-modifying therapies: how prescribing patterns have changed.
.jpg)

- Immune signatures may predict MS course, treatment response
Findings may offer insights toward options for personalized care

by Margarida Maia, PhD | April 10, 2024
Share this article:
Researchers have identified three distinct immune signatures in the blood of people with early multiple sclerosis (MS) that seem to be linked to specific disease trajectories and response to treatment, potentially offering a path to personalized care.
“These findings represent a pivotal shift towards precision medicine in MS,” Heinz Wiendl, MD said in a press release . “By understanding the individual immune system variations among patients, we can move closer to personalized treatment plans that are more effective and have fewer side effects.” Wiendl, who heads the Department of Neurology with Institute of Translational Neurology at the University of Münster in Germany, co-led the study, “ Multiple sclerosis endophenotypes identified by high-dimensional blood signatures are associated with distinct disease trajectories ,” which was published in Science Translational Medicine.
MS is an autoimmune disease where the immune system attacks the protective covering of nerve fibers in the brain and spinal cord, causing a range of symptoms . Which ones manifest and how they change as the disease progresses varies widely from patient to patient.
While many treatment options are available, the selection of one is made based on certain parameters of disease activity and severity, and ignores variations in the underlying immune responses that drive the condition. This is mostly because there’s still a gap in understanding how specific immune signatures may predict the course of disease or which patients are most likely to respond to specific medications.
Receptor may link gut microbiome to immune system in MS: Study
Assessing ms immune signatures.
“Ascertaining a patient’s blood immune signature before immunomodulatory treatment initiation may facilitate prediction of clinical disease trajectories and enable personalized treatment decisions,” wrote researchers at the University of Münster, who collaborated with the German Competence Network Multiple Sclerosis to analyze data from 309 patients with early MS whose symptoms started less than two years before and who hadn’t received any previous treatment.
The researchers assessed each participant’s immune signatures in detail by counting the number of multiple types of circulating immune cells. Then, using machine learning and algorithms to cluster data sets and discover hidden patterns, they identified three different endophenotypes, that is, MS subgroups, defined by distinct immune signatures.
These signatures remained stable in individual patients for up to nine years, indicating they are intrinsic to each person’s disease. They were also confirmed in an independent group of 232 patients with early MS.
“Our data demonstrate that early MS consists of different immunological endophenotypes characterized by distinct cellular signatures, potentially reflecting differential immunological pathways involved in disease pathogenesis,” wrote the researchers, who then looked at whether the three immune signatures were associated with distinct disease trajectories.
Patients with one signature had higher inflammatory disease activity with multiple relapses in the first year, more frequent use of high-efficacy medications, higher number of inflammatory brain lesions, and a rapid accumulation of disability. Another group had markers that indicated greater structural damage in the brain and disease severity, with increased disability at the start of the study, impaired cognition, and higher levels of nerve damage biomarkers.
This led the researchers to name the groups “inflammatory” and “degenerative.” The third needs more details to be fully characterized.
Along with distinct disease courses, patients in each group differed in how they responded to certain MS treatments. For example, interferon-based medications didn’t work well for those in the inflammatory endophenotype, who progressed more rapidly and showed greater MRI activity over up to four years of follow-up than patients with the same signature treated with glatiramer acetate, which is sold as Copaxone , among others, and Tecfidera (dimethyl fumarate).
“Our study not only challenges the current treatment paradigm, but also helps to provide a practical tool for clinicians to predict disease progression and treatment response,” said Luisa Klotz, MD, who co-led the study from the University of Münster.
Checking a patient’s blood for a specific immune signature before starting treatment could help personalize care and improve clinical outcomes. “This could significantly improve the quality of life for individuals living with MS,” Klotz said.
About the Author


Recent Posts
- Enrollment full in trial of Scone device for overactive bladder
- New assay measures molecular immune response to EBV
Recommended reading
Astrocytes, much like immune cells, can drive inflammation in MS

Crocin supplement seen to reduce signs of inflammation in MS
In pilot trial, Ocrevus failed to reduce MS inflammation in meninges
Subscribe to our newsletter.
Get regular updates to your inbox.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
April 2, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Early cortical remyelination has a neuroprotective effect in multiple sclerosis, study shows
by Marie Simon, Paris Brain Institute
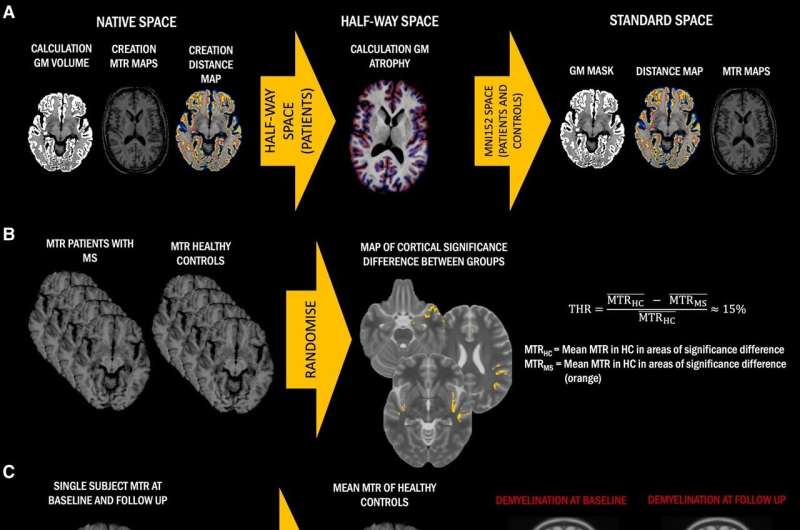
Multiple sclerosis is a heterogeneous disease whose manifestations vary considerably from patient to patient and whose course appears, on the surface, unpredictable. Hence, it is crucial to identify the factors that drive disability progression.
In a new study published in Brain , researchers at Paris Brain Institute show that spontaneous remyelination of nerve fibers in the cortex has a neuroprotective effect in patients with shorter disease duration and minor lesions: it halves the risk of worsening symptoms five years later. These results will be crucial for targeted patient recruitment in future clinical trials—in which researchers will test drugs that promote myelin repair.
Multiple sclerosis (MS) is an inflammatory disease in which the immune system attacks myelin, the protective sheath of nerve fibers. This abnormality causes brain and spinal cord lesions, which are associated with motor, sensory, or cognitive disorders.
In the absence of treatments capable of targeting the causes of MS, researchers at Paris Brain Institute are looking at remyelination—the body's ability to spontaneously regenerate the myelin sheath —and its effects on the course of the disease.
"We are studying remyelination in the cerebral cortex—also known as gray matter—which includes the cell bodies of neurons. Indeed, several studies indicate that remyelination is more extensive and complete in the cortex than in the white matter, made up of axons," Prof. Benedetta Bodini (AP-HP), neurologist and co-author of the study, explains.
"We place high hopes in the study of this biological process. But when we compare the level of cortical remyelination in different patients or evaluate the efficacy of molecules likely to promote myelin repair, we run into a major problem: it's very difficult to see myelin with conventional MRI."
Innovative use of imaging
To overcome this problem, the team uses magnetization transfer imaging (MTI). "This technique is not new, but until today, it was mainly used to observe white matter —a brain region where the signal is blurred by other processes, such as inflammation. We are the first to use MTI to study cortical remyelination! In this context, the technique makes it possible to quantify myelin very precisely and to monitor the evolution of lesions in each patient," the clinician adds.
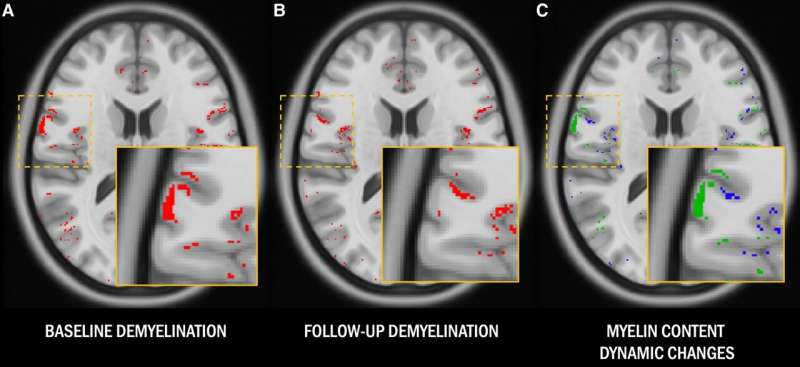
Armed with this new tool, Prof. Bodini and her colleague Andrea Lazzaratto (AP-HP, Sorbonne University), the study's first author, set an ambitious goal: to identify the conditions under which myelin was likely to degenerate or rebuild.
"One of the major challenges of this research is that patients are very different. Even when they have the same form of MS and the same number of lesions, one will have a moderate disability. In contrast, the other will experience very severe symptoms that progress rapidly.
"In short, the number and size of lesions cannot be used to deduce a patient's disability, and vice versa. To try and better explain these differences, we examined their remyelination dynamics over the long term," Lazzarotto says.
The effects of remyelination in question
The team, in collaboration with the European MAGNIMS network, recruited 140 patients with multiple sclerosis (37 with a clinically isolated syndrome, 71 with a relapsing-remitting form, 32 with a progressive form) and 84 healthy people in four European neurological centers—Graz, Milan, Paris and Siena. Each participant received a clinical assessment at the start of the study and after five years. An imaging examination was also performed at baseline and after one year.
The researchers' results show that cortical remyelination occurred spontaneously in half the patients, regardless of age, duration of disease or form of MS they had. Most importantly, in patients with short disease duration and limited cortical lesions, significant remyelination was associated with low neurodegeneration after one year and half the risk of disability worsening after five years. Conversely, patients who did not remyelinate much were less well after five years, even without having experienced an inflammatory relapse characteristic of the disease.
"These new data indicate that cortical remyelination has a neuroprotective effect and is a key mechanism in contributing to clinical disability," Lazzarotto says. "Even if it is not an optimal biological process—new myelin is not always as tough as the original one—it is likely sufficient to protect axons, to the point of delaying the progression of the disease."
According to the researchers, magnetization transfer imaging could be used in future clinical trials to select patients who could best benefit from remyelinating drugs. In addition, MTI is easier to use and less expensive than positron emission tomography (PET) for quantifying myelin.
"The day we have an effective and safe remyelinating treatment, we will know that it is necessary to use it from the very first symptoms, at the same time as immunomodulating or immunosuppressive drugs," Prof. Bodini concludes. "Time is myelin! In eligible patients, the benefits might be very significant."
Explore further
Feedback to editors

Artificial intelligence can help people feel heard, study finds
29 minutes ago

A new diagnostic model offers hope for Alzheimer's
56 minutes ago

New study validates prediction rules for pediatric intra-abdominal and traumatic brain injuries

Chemicals stored in home garages linked to amyotrophic lateral sclerosis risk

In the drive to deprescribe, heartburn drug study teaches key lessons

Researchers identify new genetic risk factors for persistent HPV infections

New AI method captures uncertainty in medical images

Survey of mental health and exposure to blasts reveals differences among displaced people who remained in Ukraine

Scientists use wearable technology to detect stress levels during sleep

Scientists discover groups of spinal cord neurons that allow for brain-independent motor learning
Related stories.

New model of multiple sclerosis correlates demyelination with evolution of cognitive and motor abilities
May 3, 2023

Pregnancy hormone repairs myelin damage in MS mouse model
Jun 15, 2023

Can this medication reverse multiple sclerosis? Brain biomarker shows it can
Jun 12, 2023

Flashing lights may provide vital first test of multiple sclerosis drug success
Dec 16, 2019

β-NMN delays myelin aging and enhances myelin repair in the aged mouse brain by targeting SIRT2
Apr 29, 2022

Mechanisms identified to restore myelin sheaths after injury or in multiple sclerosis
Aug 24, 2020
Recommended for you

Researchers identify safety of a potential new treatment to manage complications from sickle cell disease
2 hours ago

Decoding spontaneous thoughts from the brain via machine learning
3 hours ago

Study lays the basis for new perspectives on gastrointestinal diseases
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
- Reference Manager
- Simple TEXT file
People also looked at
Opinion article, emotional dyscontrol in multiple sclerosis: an opinion article.

- Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy
Highlights:
• Emotional dyscontrol is often underdiagnosed in patients with MS. The lack of consensus regarding classification and diagnostic criteria necessitates a more detailed definition of emotional dyscontrol and standardized diagnostic questionnaires.
• Emotional dyscontrol is frequently underreported. The presence of stigma surrounding emotional dyscontrol often results in individuals refraining from reporting it to parents and clinicians. Increasing awareness in clinical settings by incorporating the assessment of emotional dyscontrol within the clinical evaluation of this condition is necessary.
• Knowledge about the specific domains of social cognition affected in MS is still limited. Personalized assessment for specific social cognitive deficits using standardized tasks for evaluating different domains of theory of mind or emotion recognition is recommended.
• Knowledge about the links between deficits in different domains of social cognition, specific neurological damage, neurochemical changes, and emotional dysregulation is limited. A personalized characterization of these aspects in relation to each other is suggested at the patient level.
• Deficits in specific social cognitive domains, including emotion recognition and theory of mind, are thought to underscore limited social interactions and emotional dyscontrol, which impact social and psychological quality of life of individuals with multiple sclerosis. Recognizing and addressing these issues may enhance the general well-being of individuals with MS.
Introduction
The overall quality of life and wellbeing of individuals with multiple sclerosis (MS) are dramatically affected by cognitive deficits (present in 40%−70% of patients), and impairments in the domains of social cognition further contribute to affecting their lives (see Cotter et al., 2016 for a systematic review and meta-analysis). Social cognition deficits encompass challenges in emotion recognition and theory of mind, which, in turn, are also directly linked to the emotional dyscontrol observed in certain MS patients ( Cotter et al., 2016 ).
Emotional dyscontrol refers to difficulties in regulating emotions underlying episodes of inappropriate or exaggerated emotional responses, including uncontrollable laughing, crying, or anger that appear to be disproportionate to the context ( Arciniegas and Wortzel, 2018 ).
Emotional dyscontrol is common in mental disorders, including schizophrenia, bipolar disorder, borderline personality disorder ( Sharma and McClellan, 2021 ), as well as in traumatic and non-traumatic brain injuries ( Annoni et al., 2006 ; Bryant et al., 2022 ), and neurological disorders, including MS ( Wortzel et al., 2008 ; Finegan et al., 2019 ). For example, a study observed that 73% of the participants with MS reported symptoms of emotional dyscontrol in the month preceding enrollment ( Feinstein and Feinstein, 2001 ). Moreover, 8%−46% of patients with MS also receive a diagnosis of pathological laughter and crying-a disorder of affect characterizing several neurological disorders, characterized by difficulty controlling emotional expressions of laugher and crying, exaggerated in response to the actual emotional valence of contextual information- usually in later stages of the disease ( Feinstein et al., 1997 ; Parvizi et al., 2006 ; Hanna et al., 2016 ; Luhoway et al., 2019 ). Importantly, it has been pointed out that even though they clearly have a profound negative impact on the patient's wellbeing, emotional dysfunctions are somehow still underreported to clinicians, underdiagnosed, and undertreated ( Luhoway et al., 2019 ). Among the possible reasons of these problems, stigma surrounding these conditions, inconsistency among definitions, and a lack of standardized assessment tools have been suggested ( Luhoway et al., 2019 ).
In individuals with MS, emotional dyscontrol often manifests as a profound and foolish apathy (called “emotional blunting”) both toward others and various aspects of everyday life, boosts of laughter that appear senseless and lack any apparent cause, and episodes of irritability, sadness, and tearfulness without apparent reasons ( Feinstein and Feinstein, 2001 ).
In MS, emotional dyscontrol is believed to act as a mediator for the effects of the disease on neuropsychiatric disturbances ( Prakash et al., 2019 ), thereby indicating it as a potential intermediate phenotype. Indeed, MS patients have an increased lifetime risk for neuropsychiatric disturbances, including major depression, and symptoms of depression and anxiety, which often manifest in comorbidity with emotional dyscontrol ( Prakash et al., 2019 ; Schirda et al., 2020 ). Even though some patients with MS do not fully meet the criteria for the diagnosis of a mental disorder, the coexistence of emotional dyscontrol with depressive and/or anxiety symptoms has been shown to significantly affect the degree of psychological stress and the quality of life of MS patients ( Feinstein and Feinstein, 2001 ).
This evidence highlights the importance of deepening scientific knowledge about emotional dyscontrol in patients with MS, emphasizing the need to further research in this area with the aim of developing targeted interventions to address these problems and improve the quality of life for patients with MS.
Exploring the relationship between multiple sclerosis and emotional dyscontrol
MS is a chronic inflammatory, demyelinating, and neurodegenerative disease that affects the central nervous system of young adults ( Filippi et al., 2018 ). It is characterized by damage to nerve fibers and axonal pathology, as well as microstructural changes and brain atrophy, resulting in a diverse range of symptoms ( Feinstein et al., 1997 ; Hanna et al., 2016 ). These symptoms can affect various parts of the body and cause both physical and cognitive impairments of varying severity, depending on the brain region involved and the degree of demyelination ( Zagon and McLaughlin, 2017 ; Filippi et al., 2018 ).
The exact etiological mechanisms underlying emotional dyscontrol in MS ere not fully understood because, to date, this aspect has been poorly explored. One of the main obstacles to research in this area is that, in addition to the psychiatric manifestations of MS, many patients develop psychological problems in reaction to the disease ( Haussleiter et al., 2009 ). Reactive psychological problems have been challenging to distinguish and separate from the psychopathology directly related to the morphological changes that occur in the brains of MS patients ( Haussleiter et al., 2009 ).
Nevertheless, because brain demyelination and inflammation processes typical of MS can affect neural pathways involved in emotional regulation, they might also underlie the emotional dyscontrol observed in patients ( Krause et al., 2009 ). The structural and functional integrity within the ventral paralimbic network, responsible for emotion regulation, the dorsal paralimbic network, facilitating conscious perception and intentional emotional control, and the cerebellum, which is interconnected with and regulates both networks, may be compromised in neurological disorders, including MS; these mechanisms have been hypothesized to underlie emotional dyscontrol ( Wortzel et al., 2008 ).
Furthermore, in MS patients, emotional dyscontrol has been shown to significantly correlate with specific cognitive indices of executive functions, such as, for example, Stroop test, divided attention, and verbal fluency ( Feinstein et al., 1999 ; Berneiser et al., 2014 ; Pfaff et al., 2021 ). As these indices rely on frontal lobe functioning, this evidence linking executive dysfunctions with emotional dyscontrol is in line with the hypothesis of a prefrontal involvement in the mechanisms underlying emotional dyscontrol in MS patients ( Feinstein et al., 1999 ).
Theory of mind and facial emotion recognition in MS patients
A recent meta-analysis has revealed significant impairments in overall theory of mind abilities, and its cognitive and affective components in all subtypes of MS, including primary-progressive, secondary-progressive, and relapsing-remitting MS ( Lin et al., 2021 ). The same meta-analysis also revealed impairments in emotion recognition, which were not exhibited homogeneously across patients with different subtypes of MS ( Lin et al., 2021 ).
Indeed, in MS, emotional dyscontrol has been shown to be associated with difficulties in recognizing facial expressions, linked to the use of inappropriate eye-gaze strategies to decode facial emotions ( Henry et al., 2009 , 2011 ; Krause et al., 2009 ; Banati et al., 2010 ; Berneiser et al., 2014 ). One study, investigating a cohort of 52 patients with different types of MS, found that 21% of them had developed significant facial emotion recognition impairments ( Polet et al., 2023 ). These deficits appeared to be particularly pronounced for negative emotions, mainly fear and anger ( Henry et al., 2009 , 2011 ; Berneiser et al., 2014 ; Pfaff et al., 2021 ), but also sadness ( Krause et al., 2009 ; Berneiser et al., 2014 ; Pfaff et al., 2021 ) and disgust ( Lin et al., 2021 ). Deficits in recognition of surprise and neutral faces were also reported ( Lin et al., 2021 ; Pfaff et al., 2021 ).
The heightened impairment of patients with MS in experiencing fear and anger has been hypothesized to be related with abnormalities in the structure and function of bilateral and right amygdala ( Green et al., 2018 ; Pitteri et al., 2019 ).
Moreover, it has been hypothesized that emotion recognition deficits in MS patients might result also from temporal white matter lesions, which could impair the transmission of information from temporal visual processing areas, important for facial processing, to frontal regulation areas, such as the ventro-lateral prefrontal cortex that selectively activates when observing the eye region and controls facial emotion recognition ( Krause et al., 2009 ).
The difficulties in emotional dimensions do not appear to be influenced by the severity of physical disability or the duration of the disease ( Pfaff et al., 2021 ). However, facial emotion recognition deficits have been shown to be more frequent and severe in progressive forms ( Polet et al., 2023 ). In line with this evidence, a recent study has compared emotion recognition performance of patients with relapsing-remitting MS with that of individuals affected by secondary-progressive MS, suggesting that emotion recognition dysfunctions might be a sign of MS progression ( Argento et al., 2022 ). Additionally, the authors observed that emotion recognition deficits were linked to poorer cognitive performance (i.e., verbal learning and memory, abstract reasoning, executive function efficiency, and overall cognitive impairment) only in relapsing-remitting MS patients ( Argento et al., 2022 ). On the opposite, in the secondary-progressive MS patients, emotion recognition deficits strongly correlated with psychological aspects, such as perceived fatigue, anxiety, depression, and anger but not with cognitive performance ( Argento et al., 2022 ). In particular, only in these subgroup of MS patients, high levels of anger (trait, state, and expression), lowered the ability to decode other's emotion during the Reading the Mind in the Eyes test.
Overall, it has been hypothesized that patients with the secondary-progressive form might experience more emotional dysregulations than those with relapsing-remitting MS, as they develop difficulties both in managing their own emotions and in recognizing the emotions of others ( Argento et al., 2022 ). Interestingly, fatigue and impairment in social cognition have been linked to reduced function in the right prefrontal and anterior cingulate cortex, as well as damage to frontal white matter fibers ( Neuhaus et al., 2018 ). Similar neurological alterations might characterize patients with secondary-progressive MS experiencing emotional dyscontrol.
The most severe emotional dysregulations appear to affect severely physically disabled patients, probably due to more extensive brain damage, coupled with more severe cognitive impairments, particularly in verbal fluency, verbal learning, and auditory recall ( Feinstein et al., 1997 ; Hanna et al., 2016 ). These severely ill patients are more prone to exhibiting pathological laughter and crying.
The brain lesions causing the latter condition are very heterogenous; dysfunctions in a cortico-limbic-subcortico-thalamo-ponto-cerebellar network have been hypothesized, where symptoms mirror both direct effects of lesions occurring in crucial brain arears and indirect effects where these areas are not lesioned but are influenced by functionally connected lesioned areas (a mechanisms termed diaschisis) ( Klingbeil et al., 2021 ). A bilateral network has been proposed, where a loss of control by cortical areas on two affected neural systems, one involved in emotional regulation and the other involved in volitional control, takes place ( Klingbeil et al., 2021 ).
The above scientific data suggest that emotional dyscontrol in MS patients follows different paths in the context of psychological and/or neurological conditions and is influenced by the type and anatomical localization of brain lesions.
Emotional dyscontrol significantly affects the overall quality of life of patients affected by MS ( Phillips et al., 2014 ). It has been proposed that emotional control abilities should be investigated in MS to consider potential targeted interventions for correcting emotional dyscontrol, if present, with the ultimate goal of enhancing the patient's quality of life ( Phillips et al., 2014 ). Other authors have highlighted that interventions should be considered also when such disabilities do not reach the severity necessary to be considered pathological, that is, fulfilling a psychiatric diagnosis ( Feinstein and Feinstein, 2001 ).
Indeed, emotional dysfunctions might be linked to social functioning impairments negatively effecting overall wellbeing. The diminished ability of MS patients with emotional dysfunctions to interpret facial expressions could, in part, underlie alterations of their social interaction abilities. In fact, the ability to identify emotional expressions allows exhibiting appropriate behavioral responses and is pivotal for proper social interaction ( Muratori et al., 2024 ). However, knowledge about the specific domains of social cognition affected in MS is still limited ( Neuhaus et al., 2018 ). A better characterization of the social cognition deficits underpinning emotional dyscontrol and their neural correlates is necessary to understand whether different paths of dyscontrol stem from deficits in different domains of social cognition associated with different neurological deficits and/or patterns of brain lesion. This understanding is crucial not only for distinguishing emotional dyscontrol between different subtypes of MS, but also between patients form the same subgroup with diverse clinical symptoms.
Overall, the scientific literature concerning the relation between MS, emotional dyscontrol, and quality of life of patients suggests that emotion recognition should receive more attentions in clinical setting, be incorporated within the clinical evaluation of this disease, and treated.
Tailored interventions aimed at improving deficits in social cognition skills, such as, for example, emotion recognition training or mindfulness meditation, might be considered as potential treatments for reducing emotion dysregulation and improve social functioning and quality of life for patients affected by MS ( Schirda et al., 2020 ). For example, a computerized social cognition training has been shown effective in improving recognition of facial emotions ( Schoeneman Patel et al., 2022 ). At last, pharmacological treatments have been shown to be effective for treating pathological laughing and crying ( Wortzel et al., 2008 ; Husbands and Talbot, 2022 ) and might be beneficial also for treating emotional dyscontrol in MS.
Author contributions
MP: Writing – original draft. SP: Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Annoni, J. M., Staub, F., Bruggimann, L., Gramigna, S., and Bogousslavsky, J. (2006). Emotional disturbances after stroke. Clin. Exp. Hypertens . 28, 243–249. doi: 10.1080/10641960600549173
Crossref Full Text | Google Scholar
Arciniegas, D. B., and Wortzel, H. S. (2018). “Emotional dyscontrol,” in Textbook of Traumatic Brain Injury , eds. J. M. M., Silver, D.B. Arciniegas (Washington, DC: American Psychiatric Pub. Inc.). doi: 10.1176/appi.books.9781615372645.js18
Argento, O., Piacentini, C., Bossa, M., and Nocentini, U. (2022). Emotional recognition and its relation to cognition, mood and fatigue in relapsing-remitting and secondary progressive multiple sclerosis. Int. J. Environ. Res. Public Health 19:16408. doi: 10.3390/ijerph192416408
PubMed Abstract | Crossref Full Text | Google Scholar
Banati, M., Sandor, J., Mike, A., Illes, E., Bors, L., Feldmann, A., et al. (2010). Social cognition and Theory of Mind in patients with relapsing-remitting multiple sclerosis. Eur. J. Neurol . 17, 426–433. doi: 10.1111/j.1468-1331.2009.02836.x
Berneiser, J., Wendt, J., Grothe, M., Kessler, C., Hamm, A. O., Dressel, A., et al. (2014). Impaired recognition of emotional facial expressions in patients with multiple sclerosis. Mult. Scler. Relat. Disord . 3, 482–488. doi: 10.1016/j.msard.2014.02.001
Bryant, B. R., Richey, L. N., Jahed, S., Heinzerling, A., Stevens, D. A., Pace, B. D., et al. (2022). Behavioral and emotional dyscontrol following traumatic brain injury: a systematic review of neuroimaging and electrophysiological correlates. J. Acad. Consult. Liaison Psychiatry . 63, 579–598. doi: 10.1016/j.jaclp.2022.05.004
Cotter, J., Firth, J., Enzinger, C., Kontopantelis, E., Yung, A. R., Elliott, R., et al. (2016). Social cognition in multiple sclerosis: a systematic review and meta-analysis. Neurology 87, 1727–1736. doi: 10.1212/WNL.0000000000003236
Feinstein, A., and Feinstein, K. (2001). Depression associated with multiple sclerosis. Looking beyond diagnosis to symptom expression. J. Affect Disord . 66, 193–198. doi: 10.1016/S0165-0327(00)00298-6
Feinstein, A., Feinstein, K., Gray, T., and O'Connor, P. (1997). Prevalence and neurobehavioral correlates of pathological laughing and crying in multiple sclerosis. Arch. Neurol . 54, 1116–1121. doi: 10.1001/archneur.1997.00550210050012
Feinstein, A., O'Connor, P., Gray, T., and Feinstein, K. (1999). Pathological laughing and crying in multiple sclerosis: a preliminary report suggesting a role for the prefrontal cortex. Mult. Scler . 5, 69–73. doi: 10.1177/135245859900500201
Filippi, M., Bar-Or, A., Piehl, F., Preziosa, P., Solari, A., Vukusic, S., et al. (2018). Multiple sclerosis. Nat. Rev. Dis. Primers 4:43. doi: 10.1038/s41572-018-0041-4
Finegan, E., Chipika, R. H., Li Hi Shing, S., Hardiman, O., and Bede, P. (2019). Pathological crying and laughing in motor neuron disease: pathobiology, screening, intervention. Front. Neurol . 10:260. doi: 10.3389/fneur.2019.00260
Green, R., Adler, A., Banwell, B. L., Fabri, T. L., Yeh, E. A., Collins, D. L., et al. (2018). Involvement of the amygdala in memory and psychosocial functioning in pediatric-onset multiple sclerosis. Dev. Neuropsychol . 43, 524–534. doi: 10.1080/87565641.2018.1485679
Hanna, J., Feinstein, A., and Morrow, S. A. (2016). The association of pathological laughing and crying and cognitive impairment in multiple sclerosis. J. Neurol. Sci . 361, 200–203. doi: 10.1016/j.jns.2016.01.002
Haussleiter, I. S., Brüne, M., and Juckel, G. (2009). Psychopathology in multiple sclerosis: diagnosis, prevalence and treatment. Ther. Adv. Neurol. Disord . 2, 13–29. doi: 10.1177/1756285608100325
Henry, A., Tourbah, A., Chaunu, M. P., Rumbach, L., Montreuil, M., Bakchine, S., et al. (2011). Social cognition impairments in relapsing-remitting multiple sclerosis. J. Int. Neuropsychol. Soc . 17, 1122–1131. doi: 10.1017/S1355617711001147
Henry, J. D., Phillips, L. H., Beatty, W. W., McDonald, S., Longley, W. A., Joscelyne, A., et al. (2009). Evidence for deficits in facial affect recognition and theory of mind in multiple sclerosis. J. Int. Neuropsychol. Soc . 15, 277–285. doi: 10.1017/S1355617709090195
Husbands, E., and Talbot, K. (2022). Pathological laughter and crying in neurological disorders: recognition and treatment. Pract. Neurol . 22, 486–490. doi: 10.1136/pn-2021-003301
Klingbeil, J., Wawrzyniak, M., Stockert, A., Brandt, M. L., Schneider, H. R., Metelmann, M., et al. (2021). Pathological laughter and crying: insights from lesion network-symptom-mapping. Brain 144, 3264–3276. doi: 10.1093/brain/awab224
Krause, M., Wendt, J., Dressel, A., Berneiser, J., Kessler, C., Hamm, A. O., et al. (2009). Prefrontal function associated with impaired emotion recognition in patients with multiple sclerosis. Behav. Brain Res . 205, 280–285. doi: 10.1016/j.bbr.2009.08.009
Lin, X., Zhang, X., Liu, Q., Zhao, P., Zhong, J., Pan, P., et al. (2021). Social cognition in multiple sclerosis and its subtypes: a meta-analysis. Mult. Scler. Relat. Disord . 52:102973. doi: 10.1016/j.msard.2021.102973
Luhoway, J. A., Sharma, M., Menon, S., Rosehart, H., and Morrow, S. A. (2019). Posterior fossa lesion load and pathological laughing and crying in multiple sclerosis. Int. J. MS Care . 21, 135–142. doi: 10.7224/1537-2073.2018-016
Muratori, P., Palumbo, S., Vellucci, S., Mariotti, V., Billeci, L., Levantini, V., et al. (2024). Deficits in emotion recognition and processing in children with high callous-unemotional traits: the role of the MAOA gene. Eur. Child Adolesc. Psychiatry. Ahead of print. doi: 10.1007/s00787-024-02397-8
Neuhaus, M., Bagutti, S., Yaldizli, Ö., Zwahlen, D., Schaub, S., Frey, B., et al. (2018). Characterization of social cognition impairment in multiple sclerosis. Eur. J. Neurol . 25, 90–96. doi: 10.1111/ene.13457
Parvizi, J., Arciniegas, D. B., Bernardini, G. L., Hoffmann, M. W., Mohr, J. P., Rapoport, M. J., et al. (2006). Diagnosis and management of pathological laughter and crying. Mayo. Clin. Proc . 81, 1482–1486. doi: 10.4065/81.11.1482
Pfaff, L., Gounot, D., Chanson, J. B., de Seze, J., and Blanc, F. (2021). Emotional experience is increased and emotion recognition decreased in multiple sclerosis. Sci. Rep . 11:21885. doi: 10.1038/s41598-021-01139-z
Phillips, L. H., Henry, J. D., Nouzova, E., Cooper, C., Radlak, B., Summers, F., et al. (2014). Difficulties with emotion regulation in multiple sclerosis: Links to executive function, mood, and quality of life. J. Clin. Exp. Neuropsychol . 36, 831–842. doi: 10.1080/13803395.2014.946891
Pitteri, M., Genova, H., Lengenfelder, J., DeLuca, J., Ziccardi, S., Rossi, V., et al. (2019). Social cognition deficits and the role of amygdala in relapsing remitting multiple sclerosis patients without cognitive impairment. Mult. Scler. Relat. Disord . 29, 118–123. doi: 10.1016/j.msard.2019.01.030
Polet, K., Hesse, S., Joly, H., Cohen, M., Morisot, A., Kullmann, B., et al. (2023). Facial emotion impairment in multiple sclerosis is linked to modifying observation strategies of emotional faces. Mult. Scler. Relat. Disord . 69:104439. doi: 10.1016/j.msard.2022.104439
Prakash, R. S., Schirda, B., Valentine, T. R., Crotty, M., and Nicholas, J. A. (2019). Emotion dysregulation in multiple sclerosis: impact on symptoms of depression and anxiety. Mult. Scler. Relat. Disord . 36:101399. doi: 10.1016/j.msard.2019.101399
Schirda, B., Duraney, E., Lee, H. K., Manglani, H. R., Andridge, R. R., Plate, A., et al. (2020). Mindfulness training for emotion dysregulation in multiple sclerosis: a pilot randomized controlled trial. Rehabil. Psychol . 65, 206–218. doi: 10.1037/rep0000324
Schoeneman Patel, S. E., Haut, K. M., Guty, E., Dodell-Feder, D., Saxena, A., Nahum, M., et al. (2022). Social cognition training improves recognition of distinct facial emotions and decreases misattribution errors in healthy individuals. Front. Psychiat . 13:1026418. doi: 10.3389/fpsyt.2022.1026418
Sharma, A., and McClellan, J. (2021). Emotional and behavioral dysregulation in severe mental illness. Child Adolesc. Psychiatr. Clin. N. Am . 30, 415–429. doi: 10.1016/j.chc.2020.10.010
Wortzel, H. S., Oster, T. J., Anderson, C. A., and Arciniegas, D. B. (2008). Pathological laughing and crying: epidemiology, pathophysiology and treatment. CNS Drugs . 22, 531–545. doi: 10.2165/00023210-200822070-00001
Zagon, I. S., and McLaughlin, P. J. (2017). Multiple Sclerosis: Perspectives in Treatment and Pathogenesis . Brisbane (AU): Codon Publications. doi: 10.15586/codon.multiplesclerosis.2017
Keywords: emotional dyscontrol, social cognition, emotion recognition, multiple sclerosis, theory of mind
Citation: Palumbo M and Palumbo S (2024) Emotional dyscontrol in multiple sclerosis: an opinion article. Front. Behav. Neurosci. 18:1376021. doi: 10.3389/fnbeh.2024.1376021
Received: 24 January 2024; Accepted: 01 April 2024; Published: 10 April 2024.
Reviewed by:
Copyright © 2024 Palumbo and Palumbo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sara Palumbo, sara.palumbo@unipi.it
This article is part of the Research Topic
Reviews in Emotional and Behavioral Dyscontrol in Neurological Disorders

Egyptian Journal of Hospital Medicine Journal / Egyptian Journal of Hospital Medicine / Vol. 94 No. 1 (2024) / Articles (function() { function async_load(){ var s = document.createElement('script'); s.type = 'text/javascript'; s.async = true; var theUrl = 'https://www.journalquality.info/journalquality/ratings/2404-www-ajol-info-ejhm'; s.src = theUrl + ( theUrl.indexOf("?") >= 0 ? "&" : "?") + 'ref=' + encodeURIComponent(window.location.href); var embedder = document.getElementById('jpps-embedder-ajol-ejhm'); embedder.parentNode.insertBefore(s, embedder); } if (window.attachEvent) window.attachEvent('onload', async_load); else window.addEventListener('load', async_load, false); })();
Article sidebar.

Article Details
The journal owns copyright.
Main Article Content
Executive functions impairment in patients with multiple sclerosis in relation to lesion burden in mri: a case-control study, asmaa said mohamed said, hussein al oleimy rezk al sheikh, abozaid abdullah abd elaal khodir, raghdaa abdelkhalek abdelhalem, aya shaaban mohammed gadallah, amina mohammed nagah mohammed.
Background : Multiple Sclerosis (MS) is a chronic demyelinating autoimmune disease impacting the central nervous system. It manifests through various neurological dysfunctions, including cognitive impairments, especially in executive functions.
Objective : This study aimed to explore the relationship between executive function impairment and lesion burden in MS as evidenced by MRI.
Results : The MS patients demonstrated lower scores in the five words test (learning median score 4 vs. 5, p<0.001; recall median score 4.5 vs. 5, p<0.001) and Stroop Color-Word Test (SCWT) (median score in color naming 73.5 vs. 82.5, p=0.001). MRI assessments revealed a median of 6 lesions, predominantly in the parietal (84.8%) and frontal (78.3%) lobes. A significant positive correlation was found between the number of lesions and color test score (r=0.493, p=0.001) and a negative correlation with recall score (r=-0.334, p=0.023).
Conclusions: The study demonstrated that there was a relationship between executive functions impairment in MS and lesion burden in MRI. This can be observed through significant difference between MS patients and healthy control group in tests of working memory and inhibition. Also, our findings suggest that site, number of lesions and brain atrophy in MRI correlated significantly with tests of working memory and inhibition.
AJOL is a Non Profit Organisation that cannot function without donations. AJOL and the millions of African and international researchers who rely on our free services are deeply grateful for your contribution. AJOL is annually audited and was also independently assessed in 2019 by E&Y.
Your donation is guaranteed to directly contribute to Africans sharing their research output with a global readership.
- For annual AJOL Supporter contributions, please view our Supporters page.
Journal Identifiers

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Clin Med (Lond)
- v.20(4); 2020 Jul
Clinical presentation and diagnosis of multiple sclerosis
Leeds Centre for Neurosciences, Leeds, UK
The diagnosis of multiple sclerosis (MS) is through clinical assessment and supported by investigations. There is no single accurate and reliable diagnostic test. MS is a disease of young adults with a female predominance. There are characteristic clinical presentations based on the areas of the central nervous system involved, for example optic nerve, brainstem and spinal cord. The main pattern of MS at onset is relapsing–remitting with clinical attacks of neurological dysfunction lasting at least 24 hours. The differential diagnosis includes other inflammatory central nervous system disorders. Magnetic resonance imaging of the brain and lumbar puncture are the key investigations. New diagnostic criteria have been developed to allow an earlier diagnosis and thus access to effective disease modifying treatments.
- The diagnosis of multiple sclerosis is a clinical diagnosis supported by investigation findings.
- There is no single sensitive and specific diagnostic test for multiple sclerosis.
- The principle of dissemination of lesions in time and space underpins the diagnosis.
- Eighty-five per cent of people with multiple sclerosis have a relapsing-remitting course at onset.
- New diagnostic criteria aim to allow an earlier, accurate diagnosis.
Introduction
Multiple sclerosis (MS) is an inflammatory demyelinating central nervous system (CNS) disease. Its onset is typically in adults with peak age at onset between 20–40 years. There is a female predominance of up to 3:1. The course of MS is relapsing–remitting (RRMS) at onset in 85% with episodes of neurological dysfunction followed by complete or incomplete recovery. Fifteen per cent of people present with a gradually progressive disease course from onset known as primary progressive MS (PPMS). A single episode in isolation with no previous clinical attacks in someone who does not fulfil the diagnostic criteria for MS is known as clinically isolated syndrome (CIS). Over time, people with RRMS can develop gradually progressive disability called secondary progressive MS (SPMS). This usually occurs at least 10–15 years after disease onset. These descriptions of clinical disease course are still used in practice (Fig (Fig1). 1 ). However, increased understanding of MS and its pathology has led to new definitions focused on disease activity (based on clinical or magnetic resonance imaging (MRI) findings) and disease progression. 1

Multiple sclerosis disease course.
Clinical presentation
MS is a CNS disease characterised by demyelinating lesions in regions including the optic nerves, brainstem, cerebellum, periventricular and spinal cord. Histopathology also shows widespread involvement of the cerebral grey matter, although this is not well appreciated on conventional MRI. The clinical features of an MS attack depend on the areas of the brain or spinal cord involved. As this is an inflammatory condition, the onset of symptoms of an attack in RRMS is usually gradual and can evolve over days. Sudden onset with symptoms maximal at onset would be much more suggestive of a vascular event. A clinical attack must last at least 24 hours in the absence of fever or infection. In primary progressive MS, symptoms would be expected to have a gradual and insidious onset over at least 12 months by the time of diagnosis.
A common first presentation of RRMS is with unilateral optic neuritis characterised by gradual onset monocular visual loss, pain on moving the eye and altered colour vision. Visual loss rarely progresses beyond 2 weeks from the onset. Visual recovery usually takes longer than 2 weeks and may not recover to baseline. On examination, visual acuity is typically reduced, there may be a relative afferent pupillary defect, a central scotoma or impaired colour vision. On funduscopy, the optic disc may appear normal (retrobulbar neuritis) or swollen acutely, and may become pale and atrophic over time following the attack.
An inflammatory lesion in the spinal cord causes a myelitis that is usually partial and presents with gradual onset sensory and motor symptoms of the limbs. Evolution is over hours to days. The severity of myelitis can vary from a mild sensory syndrome to a severe disabling attack causing tetraparesis. A lesion in the cervical cord can cause Lhermitte's phenomenon with an electric shock-like sensation down the neck and back on flexing the neck. This can be a useful clue to the diagnosis. Thoracic cord lesions can cause a tight band-like sensation around the trunk or abdomen often described as the ‘MS hug’. In severe cases this has been misinterpreted as being due to a cardiac event. On examination, signs can include sensory signs of reduced fine touch, vibration sense and joint position sense. There may be a sensory level. Motor signs are typical of an upper motor neuron lesion with increased tone or spasticity, pyramidal weakness and hyperreflexia with extensor plantar responses. Myelitis may be partial causing a hemi-cord syndrome or partial Brown-Séquard.
Brainstem syndromes can present with diplopia, oscillopsia, facial sensory loss, vertigo and dysarthria. Typical findings include an isolated sixth nerve palsy, gaze evoked nystagmus or an internuclear ophthalmoplegia. Bilateral internuclear ophthalmoplegia is pathognomonic of MS.
The diagnosis of MS is based on the clinical features of the attacks including the history and examination findings. The guiding principle of the diagnosis is that of dissemination in time (DIT) and dissemination in space (DIS). There is no single diagnostic laboratory test for MS. The diagnosis is based on the clinical findings supported by investigations.
Investigations
Magnetic resonance imaging.
MRI has been increasingly used to support the diagnosis of MS and to look for any atypical features suggesting an alternative diagnosis. Brain and spinal cord MRI are used to determine dissemination in space (DIS) and for evidence of dissemination in time (DIT) in patients with a typical CIS. DIS can be demonstrated by one or more MRI T2-hyperintense lesions that are characteristic of MS in two or more of four areas of the CNS: periventricular; cortical or juxtacortical; infratentorial; and the spinal cord. DIT can be demonstrated by the simultaneous presence of gadolinium-enhancing and non-enhancing lesions at any time or a new T2 lesion or gadolinium-enhancing lesion on follow-up MRI. 2
Cerebrospinal fluid
Cerebrospinal fluid (CSF) examination remains a valuable diagnostic test, particularly when clinical and MRI evidence is insufficient to confirm the diagnosis of MS. There has been a major change in the most recent MS diagnostic criteria in that oligoclonal bands in the CSF can be used as a surrogate marker of DIT to confirm the diagnosis of RRMS in people with CIS and MRI evidence of DIS. 3 CSF findings are also important when there is a progressive course from onset (PPMS) and when there are any atypical clinical or imaging findings. Evidence of intrathecal antibody synthesis (ie oligoclonal bands in the CSF but not in a paired serum sample) supports the diagnosis of MS. An elevated CSF protein >1.0 g/L or significant pleocytosis >50 cells/mm³ or the presence of neutrophils would suggest an alternative diagnosis.
Visually evoked potentials and optical coherence tomography
Visually evoked potentials (VEPs) were historically included in MS diagnostic criteria with an abnormal VEP (delayed but with a well preserved waveform) being used as objective evidence of a second lesion if the clinical presentation did not include the visual pathway. 4,5 In the 2017 criteria, it was recommended that further studies are needed to determine the role of VEPs and optical coherence tomography (OCT) in supporting the diagnosis of MS and VEPs are not included in the criteria. 3 In clinical practice VEPs can be useful, for example in a patient with a progressive spinal cord syndrome and normal brain MRI.
Differential diagnosis
The differential diagnosis of MS is wide and varies depending on the site of presentation eg optic nerve or spinal cord. It is important for the clinician to be vigilant for atypical clinical findings or investigation results. 6,7 Non-specific symptoms with white matter lesions on the MRI can be a common cause of misdiagnosis of common disorders, such as migraine or small vessel vascular disease in the elderly.
Other CNS inflammatory diseases including neuromyelitis optica spectrum disorder (NMOSD), myelin oligodendrocyte glycoprotein (MOG) antibody-associated disease and acute disseminated encephalomyelitis (ADEM) are important differential diagnoses as the treatment approaches are different. Several other rarer inflammatory, infective and metabolic conditions should also be considered (Table (Table1 1 ).
Differential diagnosis of multiple sclerosis
CADASIL = cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy; CNS = central nervous system.
NMOSD is an inflammatory CNS syndrome distinct from MS that can be associated with serum aquaporin-4 immunoglobulin G antibodies (AQP4-IgG). 8 NMOSD is stratified by serologic testing into NMOSD with or without AQP4-IgG. NMOSD presents with severe episodes of complete transverse myelitis and/or severe episodes of optic neuritis with incomplete recovery or a brainstem syndrome of the area postrema causing nausea and vomiting or hiccups. More stringent clinical criteria with additional neuroimaging findings, are required for diagnosis of NMOSD without AQP4-IgG or when serologic testing is unavailable. The myelitis is usually extensive on MRI with a T2 spinal cord lesion extending over three or more spinal segments (longitudinally extensive transverse myelitis (LETM)). Brain lesions in NMO are located in areas of high expression of aquaporin 4, including the hypothalamus, medulla, and other brainstem areas. Oligoclonal bands in the CSF are detected in 10–20% of patients with NMO.
MOG antibody disease is associated with pathogenic serum antibodies against myelin oligodendrocyte glycoprotein. 9 Most are AQP4-IgG-seronegative. The presentation is varied ranging from isolated optic neuritis to classic NMO to ADEM. It affects both children and adults and there is no sex predominance. The disease can relapse, but medium-term immunosuppression is usually effective. Permanent disability is less frequent than in NMOSD associated with positive AQP4 antibodies. Sphincter and sexual dysfunction are common as the transverse myelitis involves the conus.
ADEM tends to present with a subacute encephalopathy with altered level of consciousness, behaviour or cognitive function. It often follows an infectious illness and is most common in children. It was initially thought to be a monophasic condition, but some patients experience recurrence of their initial ADEM symptoms. Around 60% of children with ADEM have MOG antibodies. MRI typically shows symmetrical multifocal or diffuse brain lesions (Table (Table1 1 ).
Diagnostic criteria
Diagnostic criteria for MS have been developed since the first description of MS as ‘La sclérose en plaques disséminées’ by Charcot in 1868. He described a triad of nystagmus, intention tremor and scanning speech. Clinical criteria were supplemented by CSF, MRI and evoked potentials in the Poser criteria in 1983. 4 With the more widespread availability of MRI, the McDonald criteria were developed by the International Panel on Diagnosis of Multiple Sclerosis in 2001 giving increasing weight to MRI in the diagnosis of MS. 5 There have been subsequent revisions of these criteria in 2005 and 2010 with the most recent revision in 2017 (Table (Table2 2 ). 3 The new criteria allow for an earlier diagnosis of MS in patients experiencing a typical clinically isolated syndrome. Earlier diagnosis of MS has become much more important with the availability of highly effective disease modifying treatments (DMTs) for MS. However, the benefits of earlier diagnosis have to be balanced with the risks of misdiagnosis. 10 The 2017 position paper addresses concerns about the potential for misdiagnosis, particularly with misinterpretation of non-specific symptoms and non-specific MRI findings. The development of the 2017 McDonald criteria was informed by the new MRI criteria for diagnosing MS proposed by the European Magnetic Resonance Imaging in Multiple Sclerosis (MAGNIMS) network. 1,2
2017 McDonald criteria for the diagnosis of multiple sclerosis in patients with an attack at onset 3
a = no additional tests are required to demonstrate dissemination in space and time. However, unless MRI is not possible, brain MRI should be obtained in all patients in whom the diagnosis of multiple sclerosis is being considered. In addition, spinal cord MRI or CSF examination should be considered in patients with insufficient clinical and MRI evidence supporting multiple sclerosis, with a presentation other than a typical clinically isolated syndrome, or with atypical features. If imaging or other tests (eg CSF) are undertaken and are negative, caution needs to be taken before making a diagnosis of multiple sclerosis, and alternative diagnoses should be considered. CNS = central nervous system; CSF = cerebrospinal fluid; MRI = magnetic resonance imaging.
The diagnosis of MS is still based on a combination of clinical, MRI and laboratory (eg CSF) findings. The diagnostic criteria are designed to be used for patients with typical clinical presentations and should not be applied in cases where MRI changes are incidentally identified in asymptomatic individuals. In that situation, cases are referred to as radiologically isolated syndrome (RIS). The risk of misdiagnosis may have harmful consequences if patients are started on DMTs inappropriately, for example, some MS DMTs can worsen outcomes for patients with NMO spectrum disorders.
The aim of the criteria is to make an earlier and accurate diagnosis of MS and lessen the period of uncertainty for the patient and clinician. This enables appropriate management including confirmation of the diagnosis for the patient and access to effective disease modifying treatments.
The clinical diagnosis of MS is based on history and examination providing evidence of typical neurological dysfunction. Dissemination in time and space can be demonstrated clinically but MRI is now routinely used to confirm the diagnosis. With a single episode, or clinically isolated syndrome, MRI evidence can allow an earlier diagnosis using new diagnostic criteria. Over-interpretation of non-specific symptoms and non-specific white matter lesions on MRI can lead to misdiagnosis. The differential diagnosis of MS includes other CNS inflammatory conditions such as NMOSD, ADEM and MOG antibody-related disease. It is important to differentiate these conditions as the treatment approach is different. CNS infections, metabolic conditions and vascular disease also need to be considered. There are now highly effective DMTs for MS and an accurate, timely diagnosis is crucial to ensure appropriate access to treatment.
News Center
Uncovering the culprits of neurodegenerative disorders .

This story w as published in the April 2024 issue of the Breakthroughs newsletter.
The World Health Organization estimates that 50 million people worldwide are affected by neurodegenerative disorders – primarily characterized by motor neuron dysfunction and loss – and that number is expected to rise as our population ages.
Recent studies from Feinberg scientists have uncovered new insights into these disorders, elucidating the mechanisms behind Alzheimer’s disease, Parkinson’s disease and amyotrophic lateral sclerosis, or ALS.
RNA’s role in brain cell death
A study published in Nature Communications showed that RNA interference may play a key role in Alzheimer’s disease. For the first time, scientists identified short strands of toxic RNAs that contribute to brain cell death and DNA damage in Alzheimer’s and aged brains. Short strands of protective RNAs are decreased during aging, the scientists reported, which may allow Alzheimer’s to develop.
Alzheimer’s disease, which is expected to affect about 6.7 million patients in the U.S. in 2023, results in a substantial loss of brain cells. But the events that cause neuron death remain poorly understood.
“Nobody has ever connected the activities of RNAs to Alzheimer’s,” said corresponding study author Marcus Peter, PhD , the Tom D. Spies Professor of Cancer Metabolism and a professor of Medicine in the Division of Hematology and Oncology . “We found that in aging brain cells, the balance between toxic and protective sRNAs shifts toward toxic ones.”

In the study, scientists analyzed mouse models of Alzheimer’s disease , the brains of young and old mice, induced pluripotent stem cell-derived neurons from normal individuals (both young and aged) and from patients living with Alzheimer’s disease, as well as the brains of a group of older individuals over 80 with memory capacity similar to individuals 50 to 60 years old, and multiple human brain-derived neuron-like cell lines treated with amyloid beta fragments, a possible trigger of Alzheimer’s.
The findings may lay the foundation for a new avenue of treating Alzheimer’s and potentially other neurodegenerative diseases.
“Our data support the idea that stabilizing or increasing the amount of protective short RNAs in the brain could be an entirely new approach to halt or delay Alzheimer’s or neurodegeneration in general,” Peter said.
Mutated protein linked to aggressive Parkinson’s
Parkinson’s disease is the second-most common neurodegenerative disorder in the U.S., after Alzheimer’s disease. The National Institutes of Neurological Disorders and Stroke estimates that as many as one million Americans are living with Parkinson’s. Motor dysfunction, a hallmark of Parkinson’s, is caused by the progressive loss of dopaminergic neurons in the midbrain.
Feinberg investigators led by Dimitri Krainc, MD, PhD, found that a mutated protein expressed in lysosomes may contribute to Parkinson’s disease, according to a study published in the Journal of Cell Biology.

Lysosomes, organelles that function as recycling plants inside cells, have previously been associated with several neurodegenerative diseases, including Parkinson’s disease, according to Krainc, the Aaron Montgomery Ward Professor and chair of the Davee Department of Neurology and senior author of the study.
Krainc and his collaborators used live-cell microscopy to investigate the role of VPS13C, a gene linked to a rare and aggressive form of early-onset Parkinson’s disease, in regulating lysosomal function in dopaminergic neurons derived from human-induced pluripotent stem cells.
“We found that VPS13C regulates lysosomal health in dopaminergic neurons, the primary cell type that is affected in Parkinson’s disease,” said Krainc, who also directs the Simpson Querrey Center for Neurogenetics . “We further discovered that VPS13C regulates lysosomal maintenance through the interaction with a ‘helper protein’ called Rab10. When this protein is present on the lysosomal membrane together with VPS13C, it keeps lysosomes functional and healthy.”
Mutations in VPS13C lead to its loss of function in patient-derived dopaminergic neurons, according to the study.
“The loss of VPS13C function that is seen in Parkinson’s neurons causes lysosomes to become larger and form more contacts with each other. This disrupts the ability of lysosomes to move throughout neurons and respond to cellular stress,” Krainc said. “Furthermore, lysosomes become less efficient in breaking down unwanted debris and other cellular components that need to be recycled which in turn leads to dysfunction and degeneration of dopaminergic neurons.”
Now, Krainc and his colleagues hope to target VPS13C to restore lysosome dysfunction in Parkinson’s disease, representing a potential new avenue toward treatment for the condition.
Understanding mechanisms behind ALS
Recent studies from the laboratory of Evangelos Kiskinis, PhD , associate professor in the Ken and Ruth Davee Department of Neurology’s Division of Neuromuscular Disease and of Neuroscience, have uncovered novel cellular mechanisms that are involved in two types of genetic amyotrophic lateral sclerosis, or ALS.
The findings, published in Science Advances, improve the understanding of ALS, a progressive neurodegenerative disease that attacks motor neurons in the brain and spinal cord, and provides support for the future development of targeted therapies.

An estimated 32,000 individuals are currently living with ALS in the U.S., according to the Les Turner ALS Foundation . There are two types of ALS: sporadic (non-genetic), which makes up more than 90 percent of all ALS cases, and familial (genetic).
In the Science Advances study, the Kiskinis team studied a type of familial ALS caused by a repeat genetic sequence of the C9ORF72 gene, which is the most common genetic cause of ALS.
According to Kiskinis, healthy individuals may have 20 repeats of C9ORF72 in their genome, while patients with ALS can have thousands. These repeats are transcribed and translated through non-canonical pathways which produce irregular RNAs and dipeptides (molecules with two amino acids bonded by a peptide) in neurons.
Kiskinis’ team hypothesized that this cascading effect is what leads to gain-of-function toxicity in motor neurons in this type of ALS. This prompted them to investigate the mechanisms that make these repeated dipeptides (R-DPRs) increasingly toxic.
Using computational and experimental techniques, the investigators found that R-DPRs have a strong binding affinity for RNA molecules. Then, they used a technique called crosslinking immunoprecipitation, or CLIP-seq, to isolate specific RNA fragments and found that R-DPRs bind exclusively to ribosomal RNAs. Specifically, the poly-GR dipeptide binds to ribosomal RNA, which impairs ribosomal homeostasis, a process essential for cell differentiation and the overall makeup of a cell.
Using these findings, the investigators then designed an RNA “bait,” which tricks poly-GR into binding with something that appears to be ribosomal RNA —or in this case, the bait. In both in vivo models and in induced pluripotent stem cell neurons derived from patients with C9ORF72 mutations, the bait molecule inhibited toxicity.
“We showed using multiple different approaches that the molecule we designed — the ‘bait’ —binds very highly and specifically to this poly-GR protein, and in binding to it prevents it from binding to ribosomal RNA and prevents it from going into the nucleus, which is where it becomes most toxic,” Kiskinis said. “It serves as a proof of principle to the idea that an RNA molecule that has these ‘bait’ capacities can be therapeutic and it also strengthens the hypothesis that a lot of the toxicity from the C9ORF72 mutation is associated with impairing ribosomal biology.”
The investigators are now optimizing the chemistry of the bait molecule and aim to test it in other models of ALS, according to Kiskinis.
These studies demonstrate the breadth of research happening at Feinberg across neurodegenerative diseases. Continued research will inform breakthroughs in the field and improve the understanding of and future treatment for these complex diseases.
Read more April Breakthroughs content.
Related Posts
Developing tools to explore dna methylation, potential therapeutic target for small cell lung cancer discovered, novel mechanism supports antitumor response and t-cell survival.
Comments are closed.
Type above and press Enter to search. Press Esc to cancel.

IMAGES
VIDEO
COMMENTS
Clinical Presentation: Case History # 1. Ms. C is a 35 year old white female. She came to Neurology Clinic for evaluation of her long-term neurologic complaints. The patient relates that for many years she had noticed some significant changes in neurologic functions, particularly heat intolerance precipitating a stumbling gait and a tendency to ...
The mean age of onset is from 28 to 31 years. The age of onset varies among the clinical subtypes (phenotypes). RRMS has an earlier onset, averaging between 25 and 29 years, with SPMS presenting at a mean age between 40 and 49 years of age. The estimated male to female ratio is 1.4-2.3 to 1.
This case report involved one patient; having more participants in this case study would have produced more information for analysis. Longer treatment durations are shown to be more effective in chronic conditions. ... Doig J, Premkumar K. The effects of massage therapy on multiple sclerosis patients' quality of life and leg function. Evid ...
Oct 2017. Case Studies in Multiple Sclerosis. pp.27-32. A 28-year-old woman with known relapsing-remitting multiple sclerosis (RRMS) for 2 years was seen in the emergency room for a subacute onset ...
The PROs, related to domains that most care to multiple sclerosis patients (case study) defined by the PROMOPROMS initiative (manual ability, bladder functions, motor, cognitive, psychosocial fatigue, anxiety, and depression, quality of life), are currently used to measure disease progression and the efficacy of treatments (drugs and/or ...
Stanford Center for Continuing Medical Education, Multiple Sclerosis: Case Studies on the Importance of Early Diagnosis and Optimal Treatment, 12/20/2022 12:00:00 AM - 12/19/2025 11:59:00 PM, Internet Enduring Material sponsored by Stanford University School of Medicine. Presented by the Stanford University School of Medicine Department of Neurology and Center for Continuing Medical Education ...
Abstract. Although substantial capabilities have emerged in the ability to globally manage patients who have MS, clinicians continue to be confronted with formidable challenges. Reduction in disease activity and its impact on dis-ability progression remains the central objective of disease-modifying therapy and most current MS research initiatives.
Multiple sclerosis (MS) is the most common disabling neurologic disease in people ages 18 to 60, second overall only to trauma. This prevalence is more than matched by the complexity of the disease, which is compounded by the dearth of definitive evidence to guide clinical decision making and leaves physicians to rely on their judgment and anecdotal experience.
A collection of case studies illustrating the complex, unpredictable nature of multiple sclerosis and its many presentations and disease courses. Case studies submitted from clinicians from some of the world's leading neurology departments. Edited by Dr Paul Giacomini of McGill University, a leading expert in the field of multiple sclerosis.
Patient 2drelapsing remitting multiple sclerosis on disease-modifying therapy with breakthrough relapses A 39-year-old woman suffers an episode of optic neuritis and is found to have multiple white matter lesions consistent with MS on MRI. A course of intravenous (IV) steroids is given with subsequent recovery of vision after 2 weeks.
Figure 2.Histology showed an active demyelinating multiple sclerosis (MS) lesion corresponding to immunopathological pattern II. Arrows indicate the sharply demarcated inflammatory subcortical plaque on the left; the cerebral cortex is present on the right [H&E stain, ×10 (A)].Axons were preserved within the lesion [Bielschowsky silver stain, ×10 (B)], whereas myelin was lost [proteolipid ...
Multiple Sclerosis (MS) is a chronic, inflammatory, demyelinating disease of CNS that afects cerebral cortex and grey matter including basal ganglia and Cerebellar cortex [1]. MS prevails in a total of 2.8 million people worldwide according to a study conducted in 2020 with an estimation of one person being diagnosed with MS every five minutes [2].
Multiple Sclerosis Case Study. Janet has experienced periodic episodes of tingling in her extremities, dizziness, and even episodes of blindness. After 12 years, doctors have finally given her a diagnosis. Follow Janet through her journey and find out why her disease is so difficult to diagnose.
Lunde HMB, Assmus J, Myhr K-M, Bø L, Grytten N. Survival and cause of death in multiple sclerosis: a 60-year longitudinal population study. J Neurol Neurosurg Psychiatry . 2017;88(8):621-625. doi ...
Ahmed Zayed Obeidat MD, PhD: The first case we're going to talk about is a 37-year-old female with 2 young children. We're going to talk about some factors about what you would select as a treatment. The patient presented to the neurology clinic for first time with fatigue, weakness, tremors in the right hand, so that's 1 side.
Multiple sclerosis (MS) is an incurable, heterogeneous, chronic, degenerative, demyelinating, immune-mediated neurological disease of the central nervous system. 1,2 Indeed, the disease burden of MS affects the physical, mental, emotional, psychosocial, and spiritual dimensions of the patient and their family. A plethora of studies highlight the symptoms, stressors, financial demands, and ...
This study is part of a larger phase II, randomized, controlled clinical trial "Communication, Coordination and Security for people with severe Multiple Sclerosis (COCOS-MS)" [].This explorative clinical trial, employing a mixed-method design, incorporates a qualitative study component with PwsMS, caregivers and HCSs to enrich the findings of the quantitative data.
A CASE STUDY OF MULTIPLE SCLEROSIS (MS) YEAR/BLOCK . YEAR 1 BLOCK 3 2017/2018 . ... patients are more likely than controls to have EBV-specific cytotoxic T cells. MS patients are .
With the advent of disease-modifying therapies, the life span of patients with multiple sclerosis has increased dramatically. CM is a 65-year-old female presenting to the neurology clinic with a past medical history of relapsing/remitting multiple sclerosis (MS).
A case-control study from Sweden examined familial risk and heritability of MS through 2 major phenotypes: relapsing onset and primary progressive. ... In older patients with multiple sclerosis ...
1 Introduction. Pain, fatigue, depression and anxiety are common symptoms in people newly diagnosed with multiple sclerosis (pwMS) (1-5).This can limit family, social, recreational and work-related activities and negatively influence quality of life (6, 7).Preventative programmes for newly diagnosed pwMS are frequently recommended (4, 8, 9) and their effectiveness have been documented by ...
I NTRODUCTION. Multiple sclerosis (MS) is a chronic progressive disease that destroys the central nervous system myelin, thereby affecting the sensory and motor function. 1 This disease is determined with periods of worsening and recovery. 2 It is one of the most common neurological disorder and cause disability in young people. 3 It is also one of the most important life-changing diseases ...
A clinical trial testing SpineX's Scone neuromodulation device for treating a neurogenic, or overactive, bladder, a common symptom of multiple sclerosis (MS), has finished enrolling patients ...
by Margarida Maia, PhD April 10, 2024. Researchers have identified three distinct immune signatures in the blood of people with early multiple sclerosis (MS) that seem to be linked to specific ...
The team, in collaboration with the European MAGNIMS network, recruited 140 patients with multiple sclerosis (37 with a clinically isolated syndrome, 71 with a relapsing-remitting form, 32 with a ...
INTRODUCTIONThe overall quality of life and well-being of individuals with multiple sclerosis (MS) are dramatically affected by cognitive deficits (present in 40-70% of patients), and impairments in the domains of social cognition further contribute to affecting their lives (see Cotter et al., 2016, for a systematic review and meta-analysis) (1). Social cognition deficits encompass challenges ...
Background: Long-term neurological conditions include multiple sclerosis, Parkinson's-related diseases, and motor neurone disease. National and international guidelines recommend a palliative approach for advancing neurological disease, but there is little research describing and comparing the palliative care needs of these patients side by side. Objective: The aim of this study was to ...
Background: Multiple Sclerosis (MS) is a chronic demyelinating autoimmune disease impacting the central nervous system.It manifests through various neurological dysfunctions, including cognitive impairments, especially in executive functions. Objective: This study aimed to explore the relationship between executive function impairment and lesion burden in MS as evidenced by MRI.
Bilateral internuclear ophthalmoplegia is pathognomonic of MS. The diagnosis of MS is based on the clinical features of the attacks including the history and examination findings. The guiding principle of the diagnosis is that of dissemination in time (DIT) and dissemination in space (DIS). There is no single diagnostic laboratory test for MS.
In the study, scientists analyzed mouse models of Alzheimer's disease , the brains of young and old mice, induced pluripotent stem cell-derived neurons from normal individuals (both young and aged) and from patients living with Alzheimer's disease, as well as the brains of a group of older individuals over 80 with memory capacity similar to individuals 50 to 60 years old, and multiple ...