Advertisement

Empirical studies of factors associated with child malnutrition: highlighting the evidence about climate and conflict shocks
- Original Paper
- Open access
- Published: 21 May 2020
- Volume 12 , pages 1241–1252, ( 2020 )
Cite this article
You have full access to this open access article

- Molly E. Brown ORCID: orcid.org/0000-0001-7384-3314 1 ,
- David Backer 2 ,
- Trey Billing 2 ,
- Peter White 3 ,
- Kathryn Grace 4 ,
- Shannon Doocy 5 &
- Paul Huth 2
15k Accesses
27 Citations
37 Altmetric
Explore all metrics
Children who experience poor nutrition during the first 1000 days of life are more vulnerable to illness and death in the near term, as well as to lower work capacity and productivity as adults. These problems motivate research to identify basic and underlying factors that influence risks of child malnutrition. Based on a structured search of existing literature, we identified 90 studies that used statistical analyses to assess relationships between potential factors and major indicators of child malnutrition: stunting, wasting, and underweight. Our review determined that wasting, a measure of acute malnutrition, is substantially understudied compared to the other indicators. We summarize the evidence about relationships between child malnutrition and numerous factors at the individual, household, region/community, and country levels. Our results identify only select relationships that are statistically significant, with consistent signs, across multiple studies. Among the consistent predictors of child malnutrition are shocks due to variations in climate conditions (as measured with indicators of temperature, rainfall, and vegetation) and violent conflict. Limited research has been conducted on the relationship between violent conflict and wasting. Improved understanding of the variables associated with child malnutrition will aid advances in predictive modeling of the risks and severity of malnutrition crises and enhance the effectiveness of responses by the development and humanitarian communities.
Similar content being viewed by others
Conflict and Climate Factors and the Risk of Child Acute Malnutrition Among Children Aged 24–59 Months: A Comparative Analysis of Kenya, Nigeria, and Uganda
Conflict and Child Malnutrition: a Systematic Review of the Emerging Quantitative Literature
Exposure to conflict and child health outcomes: evidence from a large multi-country study
Avoid common mistakes on your manuscript.
1 Introduction
Malnutrition is preventable, yet remains a major public health challenge. This condition affects one in five children and contributes to nearly half of all deaths during childhood globally (Black et al. 2013 ). Children who have poor nutrition during their first 1000 days of life attain lower levels of education and have lower work capacity and productivity as adults. Malnourished children also face increased likelihoods of being overweight, of developing chronic illnesses such as cardiovascular disease, diabetes and cancer, and of suffering from mental health issues later in life (Haddad et al. 1994 ; Hoddinott et al. 2013 ). After having suffered of malnutrition during early childhood, girls face increased likelihoods of having children that are born too early or underweight (UNSCN 2010 ).
Given the serious repercussions for survival, health, and well-being, anticipating and addressing the circumstances under which children become malnourished is vital. Various development and humanitarian interventions focus on fostering healthy communities where children are better protected and able to recover from nutrient deficits (Collins et al. 2006 ). To facilitate those interventions, assessments of food security conducted by organizations such as the Famine Early Warning Systems Network (FEWS NET) and the Integrated Food Security Phase Classification (IPC) initiative have sought to project the future status of at-risk countries and issue alerts about impending and ongoing crises months in advance, aiming to ensure enough lead time for the coordination and implementation of appropriate responses (Brown et al. 2007 ; Funk et al. 2019 ; IPC 2012 ). Assessments that focus on early warning have advantages relative to relying on measuring the prevalence of malnutrition in a community, which can detect a crisis only after it emerges (Maxwell et al. 2020 ). Assessments such as FEWS NET and IPC, however, do not gauge, much less substantiate, associations between malnutrition at an individual level and relevant factors. Statistically modelling these empirical relationships is integral to detecting vulnerabilities, diagnosing their sources, and directing assistance.
In this article, we consolidate what has been learned from published studies that used statistical analysis of empirical data to examine relationships between malnutrition among children and a large array of individual-, household-, community-, regional- and national-level variables. Our literature review is guided by two main questions: (1) Which variables were consistently associated with child malnutrition? (2) What types of quantitative empirical data and statistical methods have been used to analyse the nature of the relationship between these variables and child malnutrition? Answering these questions results in a summary of drivers of malnutrition, clarifies the strengths and limitations of existing studies, and suggests potential directions for further research, which may include a formal meta-analysis.
Our review considers studies in which the outcomes of interest included at least one of three major indicators of malnutrition, formalized in international standards (WHO 2020 ). Wasting (low weight for height) indicates an acute decline in nutritional status experienced by a normally well-nourished child. This decline usually involves rapid and substantial weight loss. Stunting (low height for age), by contrast, indicates a chronic, long-term nutritional deficit, the effects of which are potentially irreversible (Kennedy et al. 2015 ). Children who suffer wasting regularly over time may also develop stunting (Hoddinott et al. 2008 ). Underweight (low weight for age), on the other hand, can reflect wasting, stunting, or both (WHO 2010 ).
The breadth of our review provides a more expansive picture of the findings from the empirical research about malnutrition, according to statistical modelling of quantitative data. In the process, we can compare the state of knowledge about factors associated with the different indicators of malnutrition. Our expectation is that the findings of the review will improve awareness of which factors yield consistent findings and emphasize how particular relationships can vary across different measures of malnutrition.
At the same time, we have a specific interest in the variables associated with wasting. The acute nature of this condition presents a distinct challenge in practice. Prompt, effective interventions, with the potential to mitigate the risk of wasting, depend on the existence of reliable guidance about factors that tend to be associated with changes in individuals’ nutritional status in the short term. Insights from such a review may help inform interventions that are focused on reversing weight loss trajectories in children before malnutrition becomes a persistent condition.
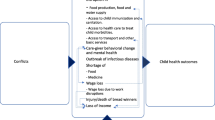
Finally, we spotlight the role of external shocks experienced by individuals, households and communities, especially those caused by exposures to environmental and societal forces. Disasters due to climate extremes (e.g., drought) and violent conflict (e.g., civil war) are regularly attributed as the primary causes – acting independently and in interaction – of crises such as famines resulting in prevalence spikes in the rate of acute malnutrition. The urgency of understanding the role of these shocks has been magnified as complex emergencies are becoming more common and lasting longer (Lautze and Raven-Roberts 2006 ; Young et al. 2004 ). Policies resulting in timely action are needed to reduce the impact of these crises on children, families, and the communities in which they live (Ghobarah et al. 2003 ; Hillbruner and Moloney 2012 ).
We start by presenting the methods we used to isolate and code relevant studies that were included in our review. Next, we summarize the results of our review. In the concluding section, we discuss the results in the context of the broader literature, with particular attention to studies about the relationship between malnutrition and climate extremes, conflict events, and their interactions.
We conducted a search of the American Economic Association’s EconLit database in January 2019. EconLit indexes six types of materials: journal articles, books, book chapters, dissertations, working papers, and book reviews. The coverage features nearly 1 million articles from over 1000 journals published in 74 countries, dating from 1969 to the present ( https://www.aeaweb.org/econlit/content ). Many of the topics covered by the material indexed in EconLit relate to child malnutrition, including Health and Economic Development (JEL code I15), Health and Inequality (JEL code I14), Health, Government Policy, and Regulation (JEL code I16), Welfare, Wellbeing and Poverty (JEL code I3), Fertility, Family Planning, Child Care, Children, and Youth (JEL code J13), Agricultural Economics (JEL code Q1), and Renewable Resources and Conservation (JEL code Q2) (see http://www.aeaweb.org/econlit/jelCodes.php for a complete list of topics covered by EconLit). We sought to identify articles indexed by EconLit that quantitatively assess potential factors, with explicit statistical tests, in relation to child malnutrition. We therefore conducted separate searches using “malnutrition,” “wasting,” “wasted,” “stunting,” “stunted,” “underweight,” and “undernourishment” as key words. In addition, we paired each of these key words with “child” when conducting searches. In total, the searches yielded a set of 688 articles.
Within this set, we then selected articles relevant to our review. We therefore searched for any mentions of “child wast*” (166 articles), “child stunt*” (104 articles), and “child under*” (39 articles) in the article titles and abstracts. Certain articles referenced multiple search terms. We thus selected 209 potentially relevant articles. Finally, we scanned the titles and abstracts of these remaining articles with the following criteria:
use of quantitative and/or numerically coded qualitative data within a statistical analysis.
dependent variable(s) in the analysis must be some variant(s) of child malnutrition.
testing of statistical relationship between child malnutrition and one or more independent variables.
Some of the reasons for excluding articles include:
article not published in an English-language academic journal (for reasons of feasibility in conducting the review).
title and/or abstract indicating that the study is unrelated to our review (e.g., food waste).
title and/or abstract indicating that the study is peripheral to our objective (e.g., global narratives regarding child health).
title and/or abstract not mentioning quantitative data analysis.
quantitative analysis referred to in abstract concerning adult malnutrition Articles evaluating adult nutrition (e.g., of the mother during pregnancy) as a factor for child malnutrition were retained.
quantitative analysis referred to in title and/or abstract concerning not concerning relationships between child nutrition prevalence and any of its factors.
quantitative analysis referred to in the title and/or abstract considering child malnutrition as an independent, and not a dependent variable.
Our approach using the inclusion and exclusion criteria yielded a sample of 61 articles from EconLit.
We further augmented the sample with 29 articles from beyond the EconLit database. These additional articles: (1) cited articles from the EconLit sample, (2) were cited by those articles, and/or (3) involved authors of those articles. All the additional articles satisfied the inclusion and exclusion criteria stated above. The final sample therefore consists of a total of 90 articles (see supplementary Table S 1 for details).
2.1 Coding of article variables
Information pertaining to each article was coded according to the following: the data used (location, timing, panel vs. cross-section, sample size); statistical methods of analysis; and the dependent and independent variables considered. Only the main statistical results in a given article were coded; other results (e.g., exploratory subgroup tests, robustness checks, and sensitivity analyses) were not included. Dependent variables were grouped into three categories: wasting (W, continuous weight-for-height z-score and/or binary indicator for wasted), stunting (S, continuous height-for-age z-score and/or binary indicator for stunted), and underweight (U, continuous weight-for-age z-score and/or binary indicator for underweight) (de Onis and Blössner 2003 ). Each combination of a dependent variable and an independent variable in a given article was coded with both the sign and the level of reported statistical significance of the relationship as evaluated in the analysis. Most of the reviewed studies focus on the sign of relationships; few studies pay close attention to the magnitude of effect sizes. P -values were not always reported in all articles, reflecting differences in standards across journals and fields. The coding categorized each relationship as significant if the p value was smaller than or equal to 0.05. These instances were marked as 1. All other instances were marked as 0. The coding also noted instances of p -values less than (or equal to) 0.01 and 0.001 (supplementary materials; (Finlay and Agresti 1986 )). Supplementary Table S 2 provides a list of all variables reported in all 90 reviewed articles, along with their reported statistical significance.
Across the sample of reviewed studies, more than 300 independent variables were found. Independent variables about the same factor, even if operationalized differently, were consolidated into a factor category to facilitate comparison across studies (Phalkey et al. 2015 ). Supplementary Table S 3 lists all variables analysed in the reviewed studies that comprise our factor categories, and which papers they came from.
The findings of the studies included in our review enabled each factor to be characterized as follows:
Risk factor – a majority of reviewed studies examining a given type of malnutrition report a significant ( p ≤ 0.05) positive relationship with the independent variables (i.e., a greater extent or probability of malnutrition as a function of increasing values of the independent variable).
Mitigating factor – a majority of reviewed studies examining a given type of malnutrition report a significant (p ≤ 0.05) negative relationship with the independent variables (i.e., a lower extent or probability of malnutrition as a function of increasing values of the independent variable).
Inconclusive factor – a majority of studies examining a given type of malnutrition report either an inconsistent sign of the relationship with the independent factor, or a relationship that is not statistically significant ( p > 0.05).
In order to facilitate comparison and the policy and other practical applications of the analysis, factors were grouped according to the scale they concern: child, household, region/community, or country (Smith et al. 2005 ).
Relationships between a given type of malnutrition and a given factor may have been evaluated in only one study. While all relationships appearing in the main statistical analysis of each study were coded and documented (Table S2 ), only factors evaluated in multiple studies were reported in the results. All studies were treated equally, regardless of scope, scale of the analysis, magnitude of effect sizes, and level of significance reported. The results of the analysis offer a general summary and mapping of results to capture patterns in the existing research. No statistical assessment of the importance of factors across publications (“effect size” in the meta-analysis literature) is provided in the interest of reflecting the broadest possible sample of studies.
Wasting and underweight have been studied less often than stunting (Table 1 ). Just over 34% of the reviewed studies modelled wasting. Slightly more studies operationalized this outcome with a binary variable (whether or not children were wasted, as a status based on exceeding a given threshold) than with a z-score (extent of deviation from international standards, along a continuous scale that captures a spectrum of outcomes in a process of becoming undernourished). Under 5% of the reviewed articles used both operationalizations of wasting in their analysis. Similarly, underweight appeared in 34% of the reviewed studies. In these studies, the operationalization was most often a z-score, rather than a binary variable. Meanwhile, 81% of the articles used stunting as a dependent variable; a z-score was most common for stunting as well.
3.1 Factors evaluated as affecting child nutrition
A total of 49 factors were evaluated in relation to wasting, stunting, and/or underweight by multiple studies (Fig. 1 ). This list includes 12 factors measured at the individual level; 25 factors measured at the household level (including five factors pertaining to mothers); eight factors measured at the region/community level; and four factors measured at the country level (Table S3 ). Analysis of disaggregated data at the individual and/or household level featured in 89% of the reviewed articles. Most analyses did not include any covariates measured at the regional/community or country levels (e.g., (Ekbrand and Halleröd 2018 )). Thus, fewer articles are available with which to evaluate the consistency of relationships of factors at the regional/community and country levels than at the individual and household levels. Of the 49 factors, 18 have been evaluated by multiple studies in relation to each of the three standard measures of child malnutrition (Fig. 1 ). The subsequent presentation of results is restricted to instances of prevailing evidence of statistically significant relationships indicating risk factors or mitigating factors, according to a majority of relevant reviewed studies.
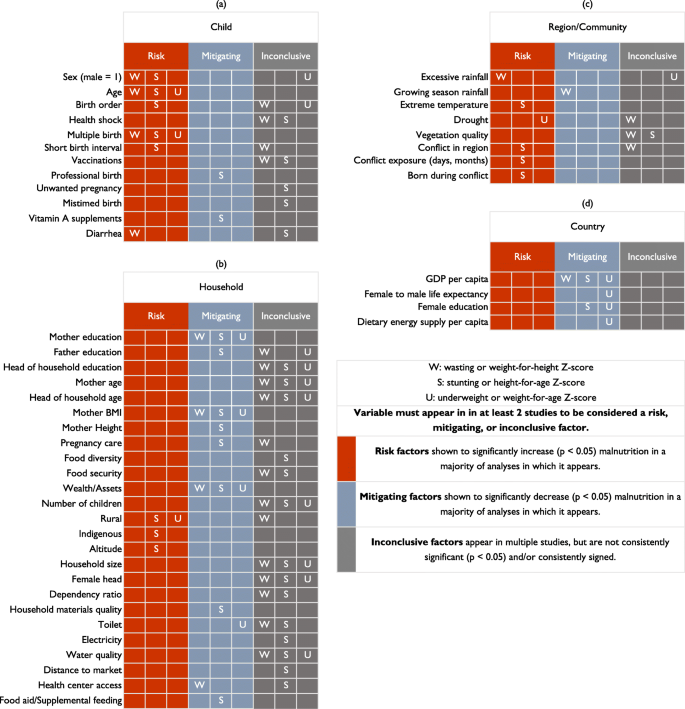
Summary of results from statistical analyses of relationships between indicators of child malnutrition and: a child-specific factors, b household-level factors, c region/community-level factors, and d country-level factors. Note: We limit the results reflected in this figure to factors that are evaluated in the main statistical analyses reported in at least two of the 90 reviewed articles. Details of which study was included in each factor can be found in Supplementary Table S 3
Eight of the 12 factors measured at the level of individual children exhibited statistically significant relationships for the following factors: child’s sex and age, if they were a multiple at birth (twin, triplet, etc.), and diarrhea status (Fig. 1a ). Seven of the 10 factors evaluated in relation to stunting exhibited statistically significant associations. These associations identified five risk factors: child’s sex and age, their birth order, if they were a multiple at birth, and short birth interval. Two mitigating factors were also identified: if a professionally trained assistant was present at the birth and if Vitamin A supplements had been used. The results indicated that two of the four factors evaluated in relation to underweight were statistically significant risk factors: child’s age and if they were a multiple at birth. According to our review, therefore, all three anthropometric measures of malnutrition were associated with two individual-level risk factors: age and multiple at birth.
Of the 25 household-level factors, just four of the 17 factors exhibited statistically significant associations: mother’s education, mother’s BMI, wealth/assets, and access to a health care center (Fig. 1b ). All were evaluated as being mitigating factors. Eleven of the 25 factors evaluated in relation to stunting yielded statistically significant associations. The relationships identified three risk factors: rural, indigenous, and altitude. In addition, eight mitigating factors were identified: mother’s education, father’s education, mother’s BMI, mother’s height, pregnancy care, wealth/assets, quality of household materials, and food aid or supplemental feeding. Five of the 13 factors evaluated in relation to underweight yielded statistically significant associations. Only one relationship identified a risk factor: rural residence. Four mitigating factors were also identified: mother’s education, mother’s BMI, wealth/assets, and quality of toilet. According to our review, therefore, all three anthropometric measures were associated with three household-level risk factors: mother’s education (either years of education or specific levels relative to no education), mother’s BMI, and wealth/assets (encompassing different indices).
The eight factors measured at the region/community level is split between measuring features of the environment, including climate conditions, and features related to conflict (Fig. 1c ). Wasting had a statistically significant association with excessive rainfall as a risk factor and growing season rainfall as a mitigating factor. Stunting had a statistically significant association with extreme temperatures as a risk factor. Underweight only exhibited a statistically significant association with drought as a risk factor. Several of the reviewed studies analysed vegetation quality, employing either the normalized difference vegetation index (NDVI) or the enhanced vegetation index (EVI), with varying operationalizations. In particular, vegetation quality during the previous growing season has been evaluated in multiple studies of both wasting and stunting, yielding findings that vary by context. Statistically significant associations were observed between stunting and three factors that reflect distinctive operationalizations of the role of conflict. Conflict in the surrounding region, conflict exposure (days or months), and whether a child was born during a conflict were all identified as risk factors for stunting.
At the country level, national per capita GDP was identified as a mitigating factor for wasting, stunting, and underweight (Fig. 1d ). Female education (encompassing national rates of female literacy and female secondary enrolment) was identified as a mitigating factor for stunting and underweight. Both the national average female-to-male life expectancy ratio and the dietary energy supply per capita were identified as mitigating factors for underweight.
3.2 Statistical methods
About 60% of the reviewed studies employed standard variations of multivariate regression techniques, such as linear, generalized linear (e.g., logit), or multilevel models. Only 5% of studies used explicit multilevel statistical techniques, modelling simultaneously the relationships between malnutrition and covariates at the individual, household, and regional/community levels (e.g., (Ekbrand and Halleröd 2018 )). Other studies that did not estimate multilevel models instead included covariates aggregated to higher levels, introduced dummy variables for geographic regions, or adjusted for within-spatial-unit correlation via clustered standard errors (e.g., (Rashad and Sharaf 2018 )). Five articles used quantile regression, which fits a model through quantiles of the dependent variable, rather than the mean (e.g., (Asfaw 2018 )). This approach has the advantage of allowing for heterogeneous treatment effects for different segments of the distribution of child malnutrition. For example, a given factor may exhibit a stronger association with weight-for-height z-scores for children who are undernourished (i.e., the left tail of the distribution), relative the association observed for children whose nutrition status is near the center of the distribution.
A majority of reviewed studies relied on cross-sectional analysis of either data from single surveys or a pooled dataset comprising multiple cross-sectional surveys. Just five of the studies capitalized on panel data involving repeated waves of data collection for the same children or households over time. The remaining studies employed a diversity of approaches, including time-series analysis of repeated cross-sections of countries or subnational regions. Among the reviewed studies, the most common source of malnutrition measures was Demographic and Health Survey (DHS) data (27 studies). Five of the reviewed studies used Living Standards and Measurements Survey (LSMS) data. The remaining studies employed other country-specific surveys, with India’s National Family Health Survey (4 studies) and Ethiopia’s Rural Household Survey (2 studies) featuring in multiple cases.
In terms of causal identification strategies, 17% of the reviewed studies directly leveraged the availability of data collected from repeated measurement over time, estimating either unit-level fixed effects or difference-in-differences models (e.g., (Lucas and Wilson 2013 )). A further 9% of articles featured an instrumental variables strategy (e.g., (Yamano et al. 2005 )) and another 6% of articles resorted to matching techniques (e.g., propensity score) to control for selection bias and minimize problems of sample imbalance. The remaining studies exhibited a variety of other approaches, including decomposition analysis (Block et al. 2004 ; Rodriguez 2016 ) and a regression discontinuity design (Ali and Elsayed 2018 ).
Among the reviewed studies, attention to the temporal relationship between malnutrition and potential factors was limited and uneven, constraining the ability to ascertain any general patterns. The lack of such examination of the impact of climate and conflict shocks is especially conspicuous. A common approach has been to measure deviations in conditions during the survey period relative to long-run average conditions, within a suitable sub-national geographic area surrounding the survey cluster. The implicit assumption is that the deviations in conditions exert a contemporaneous impact on malnutrition. Select studies used models specifying factors with time lags. For example, Johnson and Brown (Johnson and Brown 2014 ) tested one- and two-year lagged measures of shocks in vegetation, but the results of these estimations were not presented because the observed effects were not statistically significant. Kinyoki et al. ( 2016 ) tested lags measures of conflict during the three months prior to survey and the period from 3 to 12 months prior to the survey, finding that both variables have statistically significant associations with wasting and stunting. Howell et al. (Howell et al. 2018 ) tested yearly lagged values of conflict days and deaths in an analyses of stunting and wasting. Another approach in studies that have modelled the effects of conflict shocks on child malnutrition is cohort analysis. The effect of the shock is gauged based on birth timing relative to the shock, evaluating how the “during” shock cohort differs from the “before” shock and “after” shock cohorts (Grace et al. 2015 ).
3.3 Geographical coverage
Nearly 80% of the reviewed studies focused on a single country or even just one sub-national geographic area within a country. The country that features the most often was India, in 13% of the studies. Ethiopia was second (10%), followed by Guatemala and Kenya (6% each). Nineteen of the reviewed studies (21%) analysed data from multiple countries. The studies with the most extensive geographic scope covered 166 countries (Smith and Haddad 2015 ), 63 countries (Smith and Haddad 2001 ), and 41 countries (Kimenju and Qaim 2016 ). The analysis in each of these studies was conducted at the country level.
The shortage of comparative analysis within individual studies, the limited scope of geographic coverage among multiple studies that examined the same factors, and the lack of comparability of the studies that did examine the same factors in different country settings restricts understanding of the generalizability of observed relationships. Of interest, no comparative studies have been conducted to analyse the consistency of the relationship between child malnutrition and conflict across multiple country settings.
4 Discussion and conclusions
We conducted a review of 90 studies involving statistical analyses of empirical data to examine relationships of child malnutrition to factors measured at the individual, household, regional/community and national levels. Our main purpose was to consolidate understanding about the tendencies of findings to date and the design and extent of existing research. A main strength of our review was the wide scope, with respect to the number of studies included, the multiple measures of malnutrition reflected in the analyses reported in these studies, and the volume of factors evaluated in those analyses. The review by Phalkey et al. (Phalkey et al. 2015 ) takes a similar approach on fewer (15) studies and considered seven categories (agriculture, crops, weather, livelihood, demographics, morbidity, and diet). These categories were simply reported statistically significant, or not (Phalkey et al. 2015 ). The present review achieves a broader coverage of the literature, includes description of risk and mitigating factors, and highlights possible differences in relationships across the types of malnutrition. The approach used in the present review departs from a formal meta-analytical approach (Borenstein et al. 2011 ). Our approach allowed us to include a large number of studies, irrespective of statistical designs, choice of variables, and modelling approaches. Meta-analysis published elsewhere will be useful in confirming trends reported here.
Specifically, our review reveals that wasting is understudied as a measure of child malnutrition. Instead, far more attention has been paid to stunting. Another main observation is that many of the factors evaluated in relation to the different types of child malnutrition yielded inconclusive results or were not analysed in multiple studies. According to the prevailing evidence, select factors were associated with all three types of child malnutrition: age of child and multiple births are risk factors, while mother’s education, mother’s BMI, household wealth/assets, and national GDP per capita are mitigating factors. A single factor is associated with both wasting and stunting (child’s sex as a categorical variable) and two factors with both stunting and underweight (rural household, national female education level), while 23 factors are associated with only one of the types of malnutrition.
Previous research summarising determinants of child nutritional status identified factors similar to those in our review. For example, Smith et al. (Smith et al. 2005 ) list a number of individual- and household-level factors that seem important to nutritional status, including whether the child has had diarrhoea, mother’s education, mother’s nutritional status, feeding practices, sanitary conditions, wealth, and medical care. Many of these factors exhibit significant associations in the studies included in our review, which identifies other risk and mitigating factors as well.
The present review explicitly captures findings about the role of climate and conflict conditions, while other recent reviews about child malnutrition overlook these conditions (Jones et al. 2013 ; Leroy et al. 2015 ; (Wrottesley et al. 2015 )). Among the studies we reviewed, climate conditions are widely included in analyses, most often measured with indicators of precipitation, temperature, and vegetation. Measures of conflict conditions – activity in the surrounding region, extent of exposure, and birth during an affected period – are also included more selectively in analyses (Akresh et al. 2012 ; Delbiso et al. 2017 ). The prevailing evidence indicates that climate shocks involving excessive rainfall, extreme temperatures, and drought are among the risk factors for wasting, stunting, and underweight, respectively, while conflict emerged as a risk factor for stunting. Additional relationships between certain types of malnutrition and certain forms of external shocks may exist, but the evidence from our review is either inconclusive or only reflects single studies (Table S2 ).
Our results are consistent with existing research showing that climate-related shocks, such as droughts or floods, are detrimental to food security, especially of rural populations (Table S3 ) (Cooper et al. 2019 ; Douxchamps et al. 2016 ; Grace et al. 2014 ; Murali and Afifi 2014 ). Our review reveals that excessive rainfall is a risk factor and growing season rainfall is a mitigating factor. Excessive rainfall represents an extreme event, with the potential for natural disasters (e.g., floods) that can be damaging to health, well-being, and economic production. By comparison, growing season rainfall captures conditions during critical periods of agricultural productivity, when above-average precipitation logically tends to be beneficial to food security (Cooper et al. 2019 ; Funk et al. 2008 ). Another study found that households located in regions that experienced a drier-than-average year reported one more month of food insecurity than households experiencing wetter-than-average years (Niles and Brown 2017 ). Our review also found that stunting was associated with both extremely cold temperatures (Skoufias and Vinha 2012 ) and extremely hot temperatures (Jacoby et al. 2014 ) as risk factors. Other existing studies suggest that high temperatures and heat waves tend to be important for understanding food security (Phalkey et al. 2015 ; Bain et al. 2013 ; Grace et al. 2012 ). In addition, we found that the results for vegetation quality differ across countries. For example, Johnson and Brown (Johnson and Brown 2014 ) find vegetation quality during the previous growing season to be a statistically significant mitigating factor for wasting in Mali, but not Benin, Burkina Faso, or Guinea, while Shively et al. (Shively et al. 2015 ) did not find a statistically significant relationship between wasting and this factor in Nepal.
In comparison to the literature using climate variables, analyses of relationships between child malnutrition and conflict shocks are limited in number. Foundations for such studies exist in the literature about the effect of conflict on food security and public health. For example, Akresh et al. ( 2011 , (Akresh et al. 2012 )) and Bundervoet et al. ( 2009 ) showed that children in conflict-affected settings exhibit signs of stunting, with similar effects for children born before or during wartime. These results, however, have not translated into interventions that take advantage of data on climate and conflict, despite the increasing availability of sources with granular detail (Dunn 2018 ; Jones et al. 2010 ; Raleigh et al. 2010 ). Our review also highlights the lack of attention in existing research to the relationship between conflict and wasting. We view this gap as warranting attention given the acute nature of this type of malnutrition, which could plausibly be influenced by the sort of shock that conflict represents.
Another important consideration is that climate and conflict shocks can coincide – and influence one another. These potential intersections and interactions suggest possible causal pathways of child malnutrition. Multiple theories address the impact of climate shocks on the emergence of armed conflict, which cannot be decisively established (Hsiang and Burke 2014 ). Food security and nutrition may also be a key mediating factors in the nexus between climate and conflict. For example, Buhaug et al. (Buhaug et al. 2015 ) model a process in which climate shocks cause in a first stage to an increase of local food prices, which then lead to conflict during a second stage. They find evidence of a strong climate impact at the first stage, but a weak and inconsistent one at the second stage. Their argument is that the effect of food prices on conflict is likely conditional on local “socioeconomic and political contexts.” This explanation is consistent with findings of studies on the relationship between food prices and urban unrest (Berazneva and Lee 2013 ; Hendrix and Haggard 2015 ).
Our review indicates that empirical research evaluating the joint effects of environmental and political conditions on risks of malnutrition unfortunately remains the exception (Fig. 1 and Tables S 2 and S 3 ). Few studies on malnutrition have considered both climate and conflict simultaneously. A meta-analysis of nutrition surveys in Ethiopia from 2000 to 2017 concluded that droughts increase the prevalence of wasting, but the impact of conflict is less certain (Delbiso et al. 2017 ). Other research suggests that the effects of climate extremes and conflict should exacerbate one another, pushing conditions beyond a tipping point and contributing to complex emergencies. In the famines of the twentieth Century caused primarily by drought or flood, concurrent conflict often served to escalate the environmental crisis and exacerbate mortality (Devereux 2000 ). This finding is consistent with Sen’s (Sen 1981 ) seminal argument that no famines with exclusively natural causes have been observed in the modern era. Sen (Sen 1981 ) argues that contemporary societies should be able to respond more effectively to potential famines caused by droughts or other natural events, except when hampered by failures in social, economic, and political institutions. Crises arising with one type of shock may be eased by stored food or relief supplies, whereas the coincidence of both types of shocks undermines those responses. For example, conflict blocked aid from reaching populations at risk of malnutrition amid droughts in Ethiopia during the 1980s and in Somalia in 2011 (Hillbruner and Moloney 2012 ; Maxwell and Fitzpatrick 2012 ). More generally, conflict diminishes the capacity of households and communities to cope with other stresses and shocks (Raleigh et al. 2015 ).
Among the main challenges to achieving improvements in the detailed, rigorous analysis of relationships between child malnutrition and conflict is the availability of data. Surveys that serve as the source of data on nutrition are conducted in conflict-affected areas. The insecure nature of these conditions, however, can make data collection less frequent, extensive, and reliable, reducing their scope, scale, and quality. Also, the relevant surveys rarely collect information about direct conflict exposure at the individual or household level. Instead, studies that evaluate conflict as a factor usually resort to making inferences from analysis using event data. These data offer consistent precision of georeferencing of events only to the level of first- or at best second-order administrative divisions (Raleigh et al. 2010 ), rather than specific point locations or even small areas. Appropriately integrating these data on conflict into analysis requires a multilevel modelling approach (Gelman and Hill 2006 ), which can account for potential influences at the regional level, as well as other levels (individual, household, community). Such an approach can be complemented by reasonable theoretical arguments that children residing within regions experiencing conflict (and possibly affected neighbouring regions) are more vulnerable to suffering effects on malnutrition, through various causal pathways. Given that the direct exposure to conflict events is not measured, compounded by events being infrequent in most settings, the evaluated relationships are likely to be difficult to detect. Encountering such difficulties in the analysis of climate factors is less likely because of the greater geographic granularity of the available data, a more balanced distribution of conditions, and clearer, more direct pathways of influence of local conditions on individuals and households.
Ultimately, examining the state of knowledge about factors associated with acute and chronic child malnutrition holds the potential to help advance an ongoing agenda of scientific inquiry with practical applications that have important real-world consequences. Recent technological developments in mobile devices and remote sensing, communications coverage (including cell phone and Internet networks), and the ability to transmit large amounts of information rapidly improve the potential of designing and implementing more timely protective interventions (GSMA 2015 ). Considerable opportunities exist for identifying where, when, how, and why proven policy and public health interventions should be implemented (Collins et al. 2006 ), especially to gauge the local impact of climate and conflict shocks. Our review contributes to capabilities of isolating intervention points in ways that can improve strategies (Wrottesley et al. 2015 ; Walker et al. 2015 ). Further evidence from studies spanning multiple countries and time periods is needed to bolster the foundations for designing interventions (Dilley 2000 ). Pertinent data are increasingly available, including from sources (e.g., the World Food Program’s Food Aid Information System) that can be used to study the effectiveness of international aid and humanitarian assistance in relation to vulnerabilities to malnutrition.
Akresh, R., Lucchetti, L., & Thirumurthy, H. (2012). Wars and child health: Evidence from the Eritrean--Ethiopian conflict. Journal of Development Economics, 99 , 330–340.
Article Google Scholar
Akresh, R., Verwimp, P., & Bundervoet, T. (2011). Civil war, crop failure, and child stunting in Rwanda. Economic Development and Cultural Change, 59 , 777–810.
Ali, F. R. M., & Elsayed, M. A. A. (2018). The effect of parental education on child health: Quasi-experimental evidence from a reduction in the length of primary schooling in Egypt. Health Economics, 27 , 649–662.
Asfaw, A. A. (2018). The distributional effect of investment in early childhood nutrition: A panel quantile approach. World Development, 110 , 63–74.
Bain, L.E., Awah, P.K., Geraldine, N., Kindong, N.P., Siga, Y., Bernard, N., Tanjeko, A.T., 2013. Malnutrition in sub--Saharan Africa: Burden, causes and prospects. Pan Afr. Med. J. 15.
Berazneva, J., & Lee, D. R. (2013). Explaining the African food riots of 2007--2008: An empirical analysis. Food Policy, 39 , 28–39.
Black, R.E., Victora, C.G., Walker, S.P., Bhutta, Z.A., Christian, P., De Onis, M., Ezzati, M., Grantham-McGregor, S., Katz, J., Martorell, R., others, 2013. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet, 382 : 427–451.
Block, S. A., Kiess, L., Webb, P., Kosen, S., Moench-Pfanner, R., Bloem, M. W., & Timmer, C. P. (2004). Macro shocks and micro outcomes: Child nutrition during Indonesia’s crisis. Economics and Human Biology, 2 , 21–44.
Borenstein, M., Hedges, L. V., Higgins, J. P., & Rothstein, H. R. (2011). Introduction to meta-analysis . Chichester: John Wiley & Sons.
Google Scholar
Brown, M. E., Funk, C., Galu, G., & Choularton, R. (2007). Earlier famine warning possible using remote sensing and models. EOS. Transactions of the American Geophysical Union, 88 , 381–382.
Buhaug, H., Benjaminsen, T. A., Sjaastad, E., & Theisen, O. M. (2015). Climate variability, food production shocks, and violent conflict in sub-Saharan Africa. Environmental Research Letters, 10 , 125015.
Bundervoet, T., Verwimp, P., & Akresh, R. (2009). Health and civil war in rural Burundi. Journal of Human Resources, 44 , 536–563.
Collins, S., Dent, N., Binns, P., Bahwere, P., Sadler, K., & Hallam, A. (2006). Management of severe acute malnutrition in children. Lancet, 368 , 1992–2000.
Cooper, M., Brown, M. E., Azzarri, C., & Meinzen-Dick, R. (2019). Hunger, nutrition, and precipitation: Evidence from Ghana and Bangladesh. Population and Environment, 41 , 151–208. https://doi.org/10.1007/s11111-019-00323-8 .
de Onis, M., & Blössner, M. (2003). The World Health Organization global database on child growth and malnutrition: Methodology and applications. International Journal of Epidemiology, 32 , 518–526.
Delbiso, T. D., Rodriguez-Llanes, J. M., Donneau, A.-F., Speybroeck, N., & Guha-Sapir, D. (2017). Drought, conflict and children’s undernutrition in Ethiopia 2000--2013: a meta-analysis. Bulletin of the World Health Organization, 95 , 94–102.
Devereux, S., 2000. Famine in the twentieth century. Institute of Development Studies.
Dilley, M. (2000). Warning and intervention: What kind of information does the response community need from the early warning community . Office of US Foreign Disaster Assistance, Washington DC: USAID.
Douxchamps, S., Van Wijk, M. T., Silvestri, S., Moussa, A. S., Quiros, C., Ndour, N. Y. B., Buah, S., Somé, L., Herrero, M., Kristjanson, P., Ouedraogo, M., Thornton, P. K., Van Asten, P., Zougmoré, R., & Rufino, M. C. (2016). Linking agricultural adaptation strategies, food security and vulnerability: Evidence from West Africa. Regional Environmental Change, 16 , 1305–1317. https://doi.org/10.1007/s10113-015-0838-6 .
Dunn, G. (2018). The impact of the Boko haram insurgency in Northeast Nigeria on childhood wasting: A double-difference study. Conflict and Health, 12 , 6.
Ekbrand, H., & Halleröd, B. (2018). The more gender equity, the less child poverty? A multilevel analysis of malnutrition and health deprivation in 49 low-and middle-income countries. World Development, 108 , 221–230.
Finlay, B., Agresti, A., 1986. Statistical methods for the social sciences. Dellen.
Funk, C. C., Dettinger, M. D., Michaelsen, J. C., Verdin, J. P., Brown, M. E., Barlow, M., & Hoell, A. (2008). The warm ocean dry Africa dipole threatens food insecure Africa, but could be mitigated by agricultural development. Proceedings of the National Academy of Sciences, 105 , 11081–11086. https://doi.org/10.1073/pnas.0708196105 .
Funk, C., Shukla, S., Thiaw, W.M., Rowland, J., Hoell, A., McNally, A., Husak, G., Novella, N., Budde, M., Peters-Lidard, C., others, 2019. Recognizing the famine early warning systems network: Over 30 years of drought early warning science advances and partnerships promoting global food security. Bulletin of the American Meteorological Society 100 : 1011–1027.
Gelman, A., & Hill, J. (2006). Data analysis using regression and multilevel/ hierarchical models . London: Cambridge University Press.
Book Google Scholar
Ghobarah, H. A., Huth, P., & Russett, B. (2003). Civil wars kill and maim people-long after the shooting stops. The American Political Science Review, 97 , 189–202. https://doi.org/10.1017/S0003055403000613 .
Grace, K., Davenport, F., Funk, C., & Lerner, A. M. (2012). Child malnutrition and climate in sub-Saharan Africa: An analysis of recent trends in Kenya. Applied Geography, 35 , 405–413.
Grace, K., Brown, M., & McNally, A. (2014). Examining the link between food prices and food insecurity: A multi-level analysis of maize price and birthweight in Kenya. Food Policy, 46 , 56–65. https://doi.org/10.1016/j.foodpol.2014.01.010 .
Grace, K., Davenport, F., Hanson, H., Funk, C., & Shukla, S. (2015). Linking climate change and health outcomes: Examining the relationship between temperature, precipitation and birth weight in Africa. Global Environmental Change, 35 , 125–137.
GSMA, 2015. The Mobile economy 2014, URL: http://www. gsmamobileeconomylatinamerica. com/GSMA_Mobile_Economy_ LatinAmerica_2014. pdf. London, UK.
Haddad, L., Kennedy, E., & Sullivan, J. (1994). Choice of indicators for food security and nutrition monitoring. Food Policy, 19 , 329–343.
Hendrix, C. S., & Haggard, S. (2015). Global food prices, regime type, and urban unrest in the developing world. Journal of Peace Research, 52 , 143–157.
Hillbruner, C., Moloney, G., 2012. When early warning is not enough - lessons learned from the 2011 Somalia famine. Glob. Food Sec. https://doi.org/10.1016/j.gfs.2012.08.001
Hoddinott, J., Maluccio, J. A., Behrman, J. R., Flores, R., & Martorell, R. (2008). Effect of a nutrition intervention during early childhood on economic productivity in Guatemalan adults. Lancet, 371 , 411–416.
Hoddinott, J., Alderman, H., Behrman, J. R., Haddad, L., & Horton, S. (2013). The economic rationale for investing in stunting reduction. Maternal & Child Nutrition, 9 , 69–82.
Howell, E., Waidmann, T., Holla, N., Birdsall, N., Jiang, K., 2018. The impact of civil conflict on child malnutrition and mortality, Nigeria, 2002–2013. Cent. Glob. Dev. Work. Pap.
Hsiang, S. M., & Burke, M. (2014). Climate, conflict, and social stability: What does the evidence say? Clim. Change, 123 , 39–55.
IPC (2012). Integrated food security phase classification technical manual version 2.0: evidence and standards for better food security decisions. . Food and Agriculture Organization (FAO), Rome.
Jacoby, H.G., Rabassa, M.J., Skoufias, E., 2014. Weather and child health in rural Nigeria.
Johnson, K. B., & Brown, M. E. (2014). Environmental risk factors and child nutritional status and survival in a context of climate variability and change. Applied Geography, 54 , 209–221. https://doi.org/10.1016/j.apgeog.2014.08.007 .
Jones, A. D., Ngure, F. M., Pelto, G., & Young,. S. L. (2013). What are we assessing when we measure food security? A compendium and review of current metrics. Advances in Nutrition, 4 , 481–505.
Jones, L., Jaspars, S., Pavanello, S., Ludi, E., Slater, R., Grist, N., Mtisi, S. (2010). Responding to a changing climate: Exploring how disaster risk reduction, social protection and livelihoods approaches promote features of adaptive capacity.
Kennedy, E., Branca, F., Webb, P., Bhutta, Z., & Brown, R. (2015). Setting the scene: An overview of issues related to policies and programs for moderate and severe acute malnutrition. Food and Nutrition Bulletin, 36 , S9–S14.
Kimenju, S. C., & Qaim, M. (2016). The nutrition transition and indicators of child malnutrition. Food Secur., 8 , 571–583.
Kinyoki, D. K., Berkley, J. A., Moloney, G. M., Odundo, E. O., Kandala, N,. & Noor, A. M. (2016). Space--time mapping of wasting among children under the age of five years in Somalia from 2007 to 2010. Spatial and Spatio-temporal Epidemiology, 16 , 77–87.
Lautze, S., & Raven-Roberts, A. (2006). Violence and complex humanitarian emergencies: Implications for livelihoods models. Disasters, 30 , 383–401.
Leroy, J. L., Ruel, M., Frongillo, E. A., Harris, J., & Ballard, T. J. (2015). Measuring the food access dimension of food security: a critical review and mapping of indicators. Food and Nutrition Bulletin, 36 , 167–195.
Lucas, A. M., & Wilson, N. L. (2013). Adult antiretroviral therapy and child health: Evidence from scale-up in Zambia. The American Economic Review, 103 , 456–461.
Maxwell, D., & Fitzpatrick, M. (2012). The 2011 Somalia famine: Context, causes, and complications. Global Food Security, 1 , 5–12.
Maxwell, D., Khalif, A., Hailey, P., Checchi, F., 2020. Determining famine: Multi-dimensional analysis for the twenty-first century. Food Policy in press.
Murali, J., & Afifi, T. (2014). Rainfall variability, food security and human mobility in the Janjgir-Champa district of Chhattisgarh state. India. Clim. Dev., 6 , 28–37. https://doi.org/10.1080/17565529.2013.867248 .
Niles, M., Brown, M.E., 2017. A multi-country assessment of factors related to smallholder food security in varying rainfall conditions. Sci. Rep.
Phalkey, R. K., Aranda-Jan, C., Marx, S., Höfle, B., & Sauerborn, R. (2015). Systematic review of current efforts to quantify the impacts of climate change on undernutrition. Proceedings of the National Academy of Sciences, 112 , E4522–E4529.
Article CAS Google Scholar
Raleigh, C., Linke, A., Hegre, H., & Karlsen, J. (2010). Introducing ACLED – Armed conflict location and event data. Journal of Peace Research, 47 , 651–660.
Raleigh, C., Choi, H. J., & Kniveton, D. (2015). The devil is in the details: An investigation of the relationships between conflict, food price and climate across Africa. Global Environmental Change, 32 , 187–199.
Rashad, A. S., & Sharaf, M. F. (2018). Economic growth and child malnutrition in Egypt: New evidence from national demographic and health survey. Social Indicators Research, 135 , 769–795.
Rodriguez, L. (2016). Intrahousehold inequalities in child rights and well-being. A barrier to progress? World Development, 83 , 111–134.
Sen, A. K. (1981). Poverty and famines: An essay on entitlements and deprivation . Oxford: Clarendon Press.
Shively, G., Sununtnasuk, C., & Brown, M. E. (2015). Environmental variability and child growth in Nepal. Health Place in press, 35 , 37–51. https://doi.org/10.1016/j.healthplace.2015.06.008 .
Skoufias, E., & Vinha, K. (2012). Climate variability and child height in rural Mexico. Economics and Human Biology, 10 , 54–73.
Smith, L. C., & Haddad, L. (2001). How important is improving food availability for reducing child malnutrition in developing countries? Agricultural Economics, 26 , 191–204.
Smith, L. C., & Haddad, L. (2015). Reducing child undernutrition: Past drivers and priorities for the post-MDG era. World Development, 68 , 180–204.
Smith, L. C., Ruel, M. T., & Ndiaye, A. (2005). Why is child malnutrition lower in urban than in rural areas? Evidence from 36 developing countries. World Development, 33 , 1285–1305.
UNSCN. (2010). Sixth report on the world nutrition situation . Italy: Rome.
Walker, S. P., Chang, S. M., Wright, A., Osmond, C., & Grantham-McGregor, S. M. (2015). Early childhood stunting is associated with lower developmental levels in the subsequent generation of children. The Journal of Nutrition, 145 , 823–828. https://doi.org/10.3945/jn.114.200261 .
Article CAS PubMed Google Scholar
WHO (2010). Nutrition Landscape Information System (NLIS) country profile indicators: interpretation guide.
WHO (2020) Severe acute malnutrition. Nutrition topics. United Nations World Health Organization.
Wrottesley, S. V., Lamper, C., & Pisa, P. T. (2015). Review of the importance of nutrition during the first 1000 days: Maternal nutritional status and its associations with fetal growth and birth, neonatal and infant outcomes among African women. Journal of Developmental Origins of Health and Disease, 7 , 144–162. https://doi.org/10.1017/S2040174415001439 .
Article PubMed Google Scholar
Yamano, T., Alderman, H., & Christiaensen, L. (2005). Child growth, shocks, and food aid in rural Ethiopia. American Journal of Agricultural Economics, 87 , 273–288.
Young, H., Borrel, A., Holland, D., & Salama, P. (2004). Public nutrition in complex emergencies. Lancet, 364 , 1899–1909.
Download references
Author information
Authors and affiliations.
Department of Geographical Sciences, University of Maryland, 7251 Preinkert Drive, 2181 LeFrak Hall, College Park, MD, 20742, USA
Molly E. Brown
Department of Government & Politics and Center for International Development and Conflict Management, University of Maryland, 2117 Chincoteague Hall, 7401 Preinkert Drive, College Park, MD, 20142, USA
David Backer, Trey Billing & Paul Huth
Department of Political Science, Auburn University, 7080 Haley Center, Auburn, AL, 36849, USA
Peter White
Department of Geography, Environment, and Society, Minnesota Population Center, University of Minnesota, Minneapolis, MN, 55455, USA
Kathryn Grace
International Health, Johns Hopkins University, 615 N. Wolfe Street, Room E8132, Baltimore, MD, 21205, USA
Shannon Doocy
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Molly E. Brown .
Ethics declarations
Conflict of interest.
The authors declared that they have no conflict of interest.
Electronic supplementary material
(PDF 128 kb)
(PDF 69 kb)
(DOCX 16 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Brown, M.E., Backer, D., Billing, T. et al. Empirical studies of factors associated with child malnutrition: highlighting the evidence about climate and conflict shocks. Food Sec. 12 , 1241–1252 (2020). https://doi.org/10.1007/s12571-020-01041-y
Download citation
Received : 07 July 2019
Accepted : 30 April 2020
Published : 21 May 2020
Issue Date : December 2020
DOI : https://doi.org/10.1007/s12571-020-01041-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Food security
- Undernutrition
- Literature review
- Find a journal
- Publish with us
- Track your research
- Research article
- Open access
- Published: 13 November 2020
Ending malnutrition in all its forms requires scaling up proven nutrition interventions and much more: a 129-country analysis
- Nick Scott 1 , 2 ,
- Dominic Delport 1 ,
- Samuel Hainsworth 1 ,
- Ruth Pearson 1 ,
- Christopher Morgan 1 , 3 , 4 ,
- Shan Huang 1 ,
- Jonathan K. Akuoku 5 ,
- Ellen Piwoz 6 ,
- Meera Shekar 5 ,
- Carol Levin 7 ,
- Mike Toole 1 &
- Caroline SE Homer 1
BMC Medicine volume 18 , Article number: 356 ( 2020 ) Cite this article
11k Accesses
28 Citations
37 Altmetric
Metrics details
Sustainable Development Goal (SDG) 2.2 calls for an end to all forms of malnutrition, with 2025 targets of a 40% reduction in stunting (relative to 2012), for wasting to occur in less than 5% of children, and for a 50% reduction in anaemia in women (15–49 years). We assessed the likelihood of countries reaching these targets by scaling up proven interventions and identified priority interventions, based on cost-effectiveness.
For 129 countries, the Optima Nutrition model was used to compare 2019–2030 nutrition outcomes between a status quo (maintained intervention coverage) scenario and a scenario where outcome-specific interventions were scaled up to 95% coverage over 5 years. The average cost-effectiveness of each intervention was calculated as it was added to an expanding package of interventions.
Of the 129 countries modelled, 46 (36%), 66 (51%) and 0 (0%) were on track to achieve the stunting, wasting and anaemia targets respectively. Scaling up 18 nutrition interventions increased the number of countries reaching the SDG 2.2 targets to 50 (39%), 83 (64%) and 7 (5%) respectively. Intermittent preventative treatment of malaria during pregnancy (IPTp), infant and young child feeding education, vitamin A supplementation and lipid-based nutrition supplements for children produced 88% of the total impact on stunting, with average costs per case averted of US$103, US$267, US$556 and US$1795 when interventions were consecutively scaled up, respectively. Vitamin A supplementation and cash transfers produced 100% of the total global impact on prevention of wasting, with average costs per case averted of US$1989 and US$19,427, respectively. IPTp, iron and folic acid supplementation for non-pregnant women, and multiple micronutrient supplementation for pregnant women produced 85% of the total impact on anaemia prevalence, with average costs per case averted of US$9, US$35 and US$47, respectively.
Conclusions
Prioritising nutrition investment to the most cost-effective interventions within the country context can maximise the impact of funding. A greater focus on complementing nutrition-specific interventions with nutrition-sensitive ones that address the social determinants of health is critical to reach the SDG targets.
Peer Review reports
Undernutrition contributes to an estimated 45% of child deaths globally [ 1 ]. Stunting (height-for-age more than two standard deviations below the World Health Organization (WHO) Child Growth Reference Standards median) and wasting (weight-for-height more than two standard deviations below the WHO Child Growth Standards median) are associated with higher risk of severe illness and death. Other forms of undernutrition affect child brain development, impairing learning and future earning capacity [ 2 ]. Together, these conditions increase child mortality, exacerbate poverty, create entrenched intergenerational disadvantage and hinder the economic future of a country. The Sustainable Development Goals (SDGs) target 2.2 calls for ending malnutrition in all its forms [ 3 ]. Progress is tracked by four nutritional indicators; stunting and wasting levels in children under 5 years of age, anaemia in women of reproductive age (15–49 years) and overweight among children under five. There is an aspiration to achieve, by 2025, a 40% relative reduction in stunting (to a global prevalence of approximately 15%), a reduction in child wasting to < 5% prevalence, and a 50% relative reduction in anaemia in women (to a global prevalence of approximately 15%), with 2012 as the baseline year. [ 3 ]. Several analyses have shown that despite improvements in child stunting and wasting over the last two decades [ 4 ], most countries are not on track to reach the SDG 2.2 undernutrition targets [ 5 ].
Today there exists a suite of proven nutrition interventions that address the immediate causes of undernutrition, widely referred to as “nutrition-specific interventions”. It is well-established that non-nutritional factors affect nutritional status, including subclinical inflammation and untreated infections, environmental pathogen exposure, gender inequality and women’s lack of agency and empowerment. Policies and interventions to address these underlying factors, such as health systems strengthening, improved water, sanitation and hygiene (WASH) and women’s empowerment, are called “nutrition-sensitive” because they address underlying social, environmental and health-related nutrition determinants, and improvements in nutritional status may result when these interventions are implemented at scale (as illustrated in UNICEF’s conceptual framework [ 6 ]).
Evidence for the impact of nutrition-specific interventions comes from systematic reviews and meta-analyses of findings from randomised controlled efficacy and effectiveness studies that are summarised in the WHO guidelines [ 7 , 8 ] and multiple Lancet nutrition series (2008 [ 9 ], 2013 [ 10 ], 2019 [ 11 ]). The cost and marginal impact of policies and interventions to address underlying determinants is less amenable to controlled study, and information about their role is primarily based on quantitative decomposition analyses of cross-sectional data collected over time [ 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 ]. This asymmetry in the evidence base makes it difficult to model and compare the cost-effectiveness of these different types of interventions or to measure their complementary impacts; however, in recent years, the number of studies to address this evidence gap is increasing. An additional challenge is that data on coverage of most proven nutrition interventions is lacking, making it difficult to assess baselines and progress towards implementing interventions [ 22 ].
Previous work has estimated the cost and impact of scaling up evidence-based nutrition interventions. In 2010, Horton and colleagues [ 23 ] estimated that it would cost US$10.3 billion per annum globally to scale up the 13 nutrition interventions from the 2008 Lancet series [ 9 ], and that doing so could reduce stunting by 20% and the prevalence of severe acute malnutrition by 50%. In 2013, Bhutta and colleagues [ 10 ] estimated that it would cost US$9.6 billion per annum to scale up 10 nutrition-specific interventions in 34 countries (90% of the world’s stunting burden), and that this could reduce stunting by 20% and the prevalence of severe wasting by 61%. In 2017, Shekar and colleagues [ 24 ] provided an investment framework for reaching the SDG 2.2 undernutrition targets (and the global nutrition target of 50% of infants < 6 months exclusively breastfed by 2025 [ 25 ]). They estimated that the world needs US$70 billion over 10 years to invest in high-impact nutrition-specific interventions in order to reach these targets, combined with continued improvements in WASH and other underlying determinants [ 26 ].
Investment cases and costing estimates for nutrition interventions are vital for their adoption; however, budget constraints mean that countries will not be able to scale up all available nutrition interventions. Decisions must be made about how to prioritise interventions, and countries will benefit from knowing what the most cost-effective strategies are to maximise the impact of limited funds. Optima Nutrition [ 27 ] is a mathematical model that estimates the impact of scaling up combinations of 18 different nutrition interventions on stunting, wasting and mortality in children under five and anaemia in women of reproductive age. These interventions are included in the model based on systematic reviews, meta-analyses and the findings of multiple Lancet series; each intervention has been shown in isolation to lead to improved nutrition outcomes. The model also includes an economic component and can generate average cost-effectiveness estimates for interventions.
This first aim of this study was to expand the scope of previous analyses by estimating the progress that could be made towards the SDG 2.2 undernutrition targets by scaling up 18 nutrition interventions (for which there is currently evidence of effectiveness) within 129 individual low- and middle-income countries (LMICs). The second aim was to estimate which interventions countries should prioritise, to provide countries guidance on how to maximise impact when investment is limited.
The Optima Nutrition model
The Optima Nutrition model tracks the number of women of reproductive age (15–49 years) in a population, who can become pregnant and give birth. After birth, children are tracked until 5 years of age across five age bands and are categorised according to their mother’s breastfeeding practices, family economic status, height-for-age (stunting) status, weight-for-height (wasting) status and anaemia status (Additional file 1 : Fig. A1) [ 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 ]. Children in the model can die from a range of specific causes, with the relative risks of dying from each cause related to the child’s breastfeeding, stunting, wasting and anaemia status according to global published estimates.
Several risk factors for stunting in children are modelled: birth outcomes (preterm birth and/or a child being born small for gestational age [SGA]), stunting at a younger age band, sub-optimal feeding practices (age-appropriate breastfeeding and complementary foods) and incidence of diarrhoea (Additional file 1 : Fig. A2). In addition, anaemia in women of reproductive age is modelled to be a risk factor for sub-optimal birth outcomes, birth outcomes and diarrhoea incidence are modelled to be risk factors for wasting and sub-optimal breastfeeding is modelled to be a risk factor for diarrhoea incidence.
In the model, interventions can improve nutritional outcomes directly or indirectly by reducing risk factors. For example, changes to breastfeeding practices can reduce diarrhoea incidence which indirectly reduces stunting. Changing the coverage of an intervention among its target population leads to changes in projected nutrition outcomes based global estimates of intervention effectiveness (Additional file 1 : Fig. A2). The cost of achieving a given intervention coverage is calculated by multiplying the number of beneficiaries by the intervention’s estimated unit cost per beneficiary (see below).
Eighteen nutrition interventions were considered in this study based on the available literature and global recommendations (Tables 1 , 2 , and 3 ). These include various nutrition supplements for pregnant women, micronutrient supplements for children under five, treatment of severe acute malnutrition for children, lipid-based nutrition supplements for children 6–23 months at risk of food insecurity and/or poor growth, treatment of diarrhoea for children, nutrition education and interventions for reducing malaria.
A detailed model description is available in Additional file 1 , as well as the Optima Nutrition user guide [ 80 ].
Population and epidemiological data
For 129 countries (selected based on data availability), population and epidemiological data inputs, including baseline data on stunting, wasting and anaemia, were sourced from global datasets and are summarised in Additional file 1 , Table B1. The main sources were Demographic and Health Survey (DHS) data [ 37 ], Multiple Indicator Cluster Survey (MICS) reports [ 81 ], the World Bank Group [ 32 , 33 ], WHO [ 82 ], United Nations Joint Child Malnutrition Estimates (UN-JME) [ 38 ], the Global Burden of Disease study [ 39 ] and the academic literature [ 41 , 83 ]. Where country-specific estimates of epidemiological data were not available, estimates (based on regional averages) were taken from the Lives Saved Tool (LiST) [ 28 , 29 , 34 ]
The SDG baseline year (2012) prevalence of stunting and wasting in children were taken from the UN-JME [ 38 ] and baseline prevalence of anaemia in women was taken from the Global Burden of Disease study [ 39 ]. Annual rates of reduction in undernutrition for each country were obtained from the 2017 Global Burden of Disease SDG indicator projections [ 39 ] and applied to baseline (2012) estimates. The Global Burden of Disease study uses statistical methods to project each indicator based on past trends (1990–2017), correlates of these trends with socioeconomic development factors, and expected trends in these socioeconomic development factors [ 84 ].
Country-specific inputs are provided in Additional file 2 .
Intervention coverage data
The coverage of interventions (Table 2 ) was estimated for 2018 for each country from DHS [ 37 ] and MICS [ 81 ] data. For interventions not directly contained in these surveys, estimates were taken from the LiST [ 34 ] model, which creates coverage estimates based on other nationally representative household surveys. For interventions not in DHS, MICS or LiST, baseline coverage was modelled to be zero.
Intervention cost data
The unit costs of interventions are difficult to estimate because many interventions are integrated within health systems and delivered simultaneously with other health services. Therefore, for this study, we made simple estimates of the country-specific unit costs of each intervention (i.e., the cost per beneficiary) that included costs associated with eight different domains. These were the costs associated with commodities, supply chain and health provider time, as well as fractional costs associated with the additional infrastructure/equipment, health information systems, health financing policy, governance and additional health programme costs that would be required for their expansion.
An ingredient-based approach was used to estimate global commodity costs (estimated from either the WHO International Drug Price Indicator Guide [ 68 ] or UNICEF supply cost estimates [ 71 ]) and country-specific health provider time requirements (taken from the OneHealth tool [ 66 ] and Bhutta et al. (2013) supplement [ 10 ], with per capita gross domestic product (GDP) for each country used as a country-specific proxy for salary).
Country-specific supply chain costs were estimated similarly to Stenberg and colleagues’ [ 70 ], who grouped 73 countries into five categories based on “Logistics System Condition”, and estimated a mark-up percentage to apply to commodities for countries in each group (ranging from 8 to 50% for drugs and other commodities and 14–63% specifically for insecticide-treated bednets). The additional countries in this study were allocated into the five groups by determining an approximate range of GDP per capita for each group (higher GDP per capita is assumed to be associated with better logistics system conditions).
The fractional costs associated with the remaining five domains were estimated based on Stenberg and colleagues’ [ 85 ] work estimating the financing needs of health system expansion to achieve universal health care. They estimated that costs associated with infrastructure and equipment, health information systems, health financing policy, governance and additional health programme costs would comprise 51% of the total costs (i.e. commodities, health provider time and supply chain costs only account for 49% of all costs). Therefore, the overall (country-specific) unit cost for each intervention was calculated by inflating the commodity, health provider time and supply chain costs by ~ 100%.
Costs are presented in 2017 US$ with details for each intervention in Table 3 . Discounting is not included.
Status quo scenario: maintained existing investment
The model was run without changes to intervention coverage, thus including only continued current trends in stunting and wasting in children and anaemia in women (based on annual rates of reduction for each country, obtained from the 2017 Global Burden of Disease SDG indicator projections [ 78 ] and applied to baseline (2012) estimates). The models were projected from 2019 to 2030, and progress was measured against the SDG targets.
Maximum impact scenario
For each country, a projection was run where a 5-year period was used to linearly scale up all interventions from their baseline estimated coverage in 2019 to 95% coverage of their target population in 2024, which was maintained in the model until 2030. The effect sizes of interventions were assumed to be the same across countries as insufficient evidence is available on how they vary by setting.
Intervention expansion pathways
For each country, scenarios were run with each of the 18 interventions scaled up one at a time to 95% coverage over a 5-year period (2019–2024) and maintained until 2030. In each scenario, the total additional cost and impact on each indicator (stunting, wasting, anaemia) was recorded and compared to the status quo, with the average cost-effectiveness of each intervention calculated as the additional cost divided by the number of cases averted over the period 2019–2030 (e.g. average cost per stunting case averted). For each country and indicator, the single most cost-effective intervention was identified.
To identify the second most cost-effective intervention, the results above are inadequate as the effects of scaling interventions together will not be additive. This is because intervention effectiveness measures are based on relative reductions in nutritional outcomes, and so to avoid overestimating combined impact, the second intervention is modelled against a new baseline where the first intervention has already reduced a risk factor or outcome. This is consistent with other nutrition models [ 29 , 86 ]. Therefore, to identify the next most cost-effective intervention for each indicator, the process above was repeated but with each of the remaining 17 interventions scaled up one at a time to 95% coverage, alongside the most cost-effective intervention, with outcomes compared to the scenario of only the most cost-effective intervention being scaled up.
This methodology was repeated to identify a sequence of interventions for each indicator that represent a prioritisation for inclusion in an overall package of interventions.
Uncertainty bounds
Univariate uncertainty analyses were conducted to generate uncertainty intervals for the estimated impact (obtained by running projections using the lower and upper bounds of their effect size estimates) and costs (lower bounds based on commodity costs of interventions only, and upper bounds assuming double the non-commodity costs) of all interventions and countries.
Sensitivity analyses
Univariate sensitivity analyses were used to explore a variety of alternate analyses including the following: the possible impact if only nutrition-sensitive interventions were considered (i.e. excluding cash transfers, intermittent preventative treatment of malaria during pregnancy (IPTp), long-lasting insecticide-treated bed nets (LLINs)), comparison against the extended 2030 global targets [ 87 ] (50% reduction in the number of stunted children, wasting in children < 3%, 50% reduction on anaemia in women); and sub-analyses for low-income, lower-middle-income and upper-middle-income countries.
The estimated 2018 prevalence of undernutrition derived for the 129 countries varied significantly by country and indicator, but was generally highest in south and central Africa (Fig. 1 ). Under-five stunting prevalence was highest in Burundi at 57% (global average 25%), under-five wasting prevalence was highest in South Sudan at 24% (global average 6%) and anaemia prevalence among women was highest in Yemen at 71% (global average 29%).

Estimated 2018 prevalence of stunting in children under 5 (top left), wasting in children under 5 (top right) and anaemia in women of reproductive age (bottom left)
Under the status quo (i.e. no change to current trends), 46 (34%) of the 129 countries were on track to achieve a 40% in reduction in stunting by 2025, 66 (51%) were on track to reduce wasting to below 5% by 2025 and 0 (0%) were on track to reduce anaemia by 50% by 2025.
Scaling up all 18 nutrition interventions to 95% coverage reduced the cumulative number of children reaching age five stunted or wasted between 2019 and 2030 by 42.1 million and 13.8 million respectively, and averted 476 million cases of anaemia. With all interventions scaled up, the global number of children under five who were stunted in 2030 was 20% lower than the status quo scenario in 2030, and the prevalence of wasting in children and anaemia in women in 2030 were reduced by an average of 14% and 22%, respectively, compared to 2030 prevalence in the status quo scenario. With all interventions scaled up, an additional 4, 17 and 7 countries were projected to reach the stunting, wasting and anaemia targets respectively (Fig. 2 , with projected stunting prevalence in Fig. 3 ).

Countries that are projected to reach targets under that status quo (green), in the maximum impact scenario (orange) or not at all (red). Panels show targets for stunting in children under five (top left), wasting in children under five (to-right) and anaemia in women of reproductive age (bottom left)
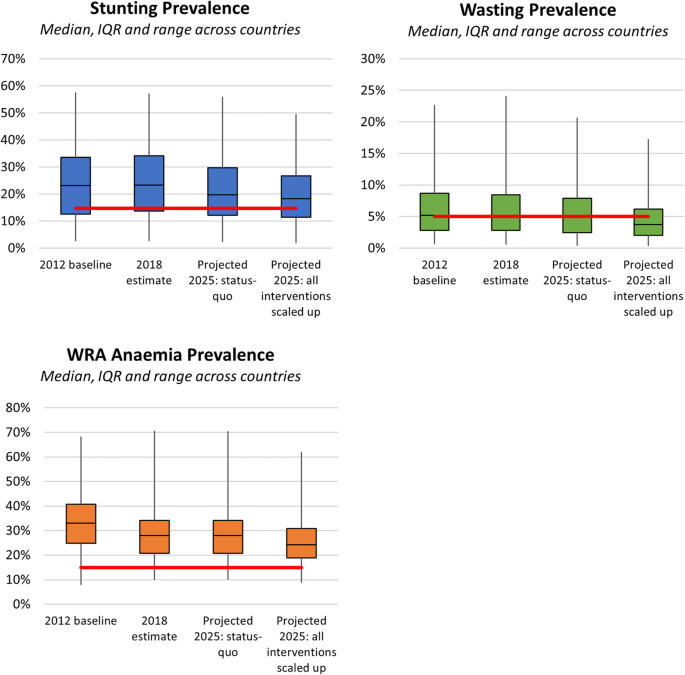
Projected changes to nutrition indicators under the status quo and maximal impact scenarios for individual countries. Boxplots show the median and inter-quartile range of indicators across countries, with tails representing the maximum and minimum values. The red line represents the relevant 2025 target at a global level. a Stunting prevalence among children under five. b Wasting prevalence among children under five. c Anaemia prevalence among women of reproductive age. Abbreviations: IQR, inter-quartile range; WRA, women of reproductive age
Scaling up all interventions was estimated to cost an additional $458 billion between 2019 and 2030; however, the majority of the total possible impact came from only a few interventions (Fig. 4 ). At an aggregate global level, the model estimated that scaling up IPTp (in regions with malaria), infant and young child feeding (IYCF) education, vitamin A supplementation and lipid-based nutrition supplements produced 88% of the total global impact on stunting and cost US$19.75 billion between 2019 and 2030, with average costs per case averted of US$103, US$267, US$556 and US$1795 when interventions were consecutively added, respectively (Table 4 ). In a sensitivity analysis, we estimate that if IYCF were more than 2.1 times our unit cost estimate, then the order of IYCF and vitamin A supplementation would be reversed. Country-specific estimates are provided in Additional file 2 .
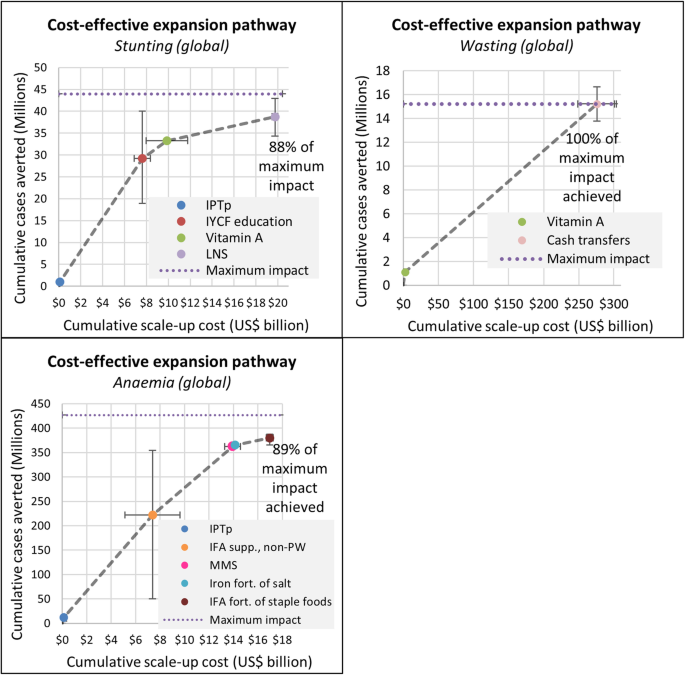
Cost-effective expansion pathway for reducing the prevalence of stunting in children under five (top left), wasting in children under five (top right) and anaemia in women of reproductive age (bottom left). The additional cost and impact at sequential steps are calculated by taking continued status quo outcomes 2019–2030 aggregated over all countries, and sequentially increasing intervention coverage in all countries from baseline to 95% over a 5-year period (2019–2024). Variations in prioritisation exist for individual countries (Additional file 2 ). Maximum impact is the total cases averted across all countries when all 18 interventions were scaled up simultaneously. Abbreviations: IFA, iron and folic acid; IFA supp., iron and folic acid supplementation; IPTp, intermittent preventative treatment of malaria during pregnancy; IYCF, infant and young child feeding; LNS, lipid-based nutrition supplements; MMS, multiple micronutrient supplementation; PW, pregnant women
At an aggregate global level, scaling up vitamin A supplementation and cash transfers produced 100% of the total impact on wasting and cost US$275.97 billion between 2019 and 2030 (predominantly for cash transfers), with average costs per case averted of US$1989 and US$19,427 when interventions were consecutively added, respectively (Table 4 ). Note that while the treatment of severe acute malnutrition (SAM) intervention is effective at preventing mortality from wasting, in the model it had no impact on wasting prevalence (Table 1 and “ Discussion ”).
At an aggregate global level, scaling up IPTp, iron and folic acid (IFA) supplementation for non-pregnant women, multiple micronutrient supplementation for pregnant women produced 89% of the total impact on anaemia and cost US$16.98 billion between 2019 and 2030, with average costs per case averted of US$9, US$35, US$47, US$71 and US$194 when interventions were consecutively added, respectively (Table 3 ). Iron fortification of salt and iron and folic acid fortification of staple foods were the next most cost-effective for reducing anaemia.
There were important differences between countries as to which interventions were the most cost-effective, which were driven largely by differences in the data inputs such as risk of malaria (countries without malaria receive no benefit from IPTp or LLINs), prevalence of breastfeeding (higher breastfeeding prevalence reducing the impact of IYCF education), incidence of diarrhoea (less diarrhoea meaning reduced impact of vitamin A supplementation), the proportion of small and preterm births (smaller impact of supplements for pregnant women) and unit cost assumptions. However, despite differences in the prioritisation of interventions between settings, the finding that the majority of the total impact came from a select few interventions remained true.
Sub-analyses indicate that the majority of the cost and impact is in low-income countries, rather than lower-middle- or upper-middle-income countries (Table 5 , based on World Bank classifications). Similar results were found when progress was assessed against the 2030 targets. If only nutrition-specific interventions were included in the analysis (i.e. excluding cash transfers, IPTp, LLINs), then a smaller impact was achieved, particularly for wasting and anaemia, highlighting the benefits of these interventions.
Using the Optima Nutrition model, scaling up 18 evidence-based nutrition interventions to 95% coverage across 129 countries could lead to 42 million fewer stunted children between 2019 and 2030 and a 20% reduction in the number of children stunted in 2030, and reduce the 2030 prevalence of wasting in children and anaemia in women by an average of 14% and 22% respectively. This work expands previous analyses by identifying a subset of interventions that are the most cost-effective and contribute the greatest impact towards the SDG undernutrition indicators; these interventions should be prioritised in the context of limited financial resources. These models also highlight the need to consider a broader set of interventions to address food systems and social determinants of health in order to reach the SDG targets, for example agriculture interventions and interventions for poverty alleviation, food security, WASH and women’s empowerment. This is consistent with previous studies that have recognised the that nutrition-specific interventions alone will not help countries reach SDG targets, highlighting the need for investments in evidence-based nutrition-sensitive interventions [ 5 , 10 , 18 , 23 , 24 , 88 ].
For reducing stunting, IPTp, IYCF education and vitamin A supplementation were the most cost-effective interventions globally. IPTp can lead to improved birth outcomes in areas with malaria risk [ 66 ], therefore reducing stunting risk, but it was its low cost rather than high impact that made it the most cost-effective intervention—even at high coverage it produced limited total gains. IYCF education can improve breastfeeding and complementary feeding behaviours [ 45 ], which can reduce diarrhoea [ 45 ] and stunting [ 89 ]. Importantly, relevant and high-quality education must be delivered that includes support for breastfeeding at a local and national level, combined with enabling activities such as countries implementing WHO codes for breast-milk substitutes [ 90 ]. The next most cost-effective intervention for stunting was vitamin A supplementation [ 91 ]. Vitamin A supplementation has been implemented at scale in many countries already to both reduce mortality and prophylactically reduce diarrhoea incidence, and this study provides evidence to continue expansion of this intervention to countries where this is not already the case.
For reducing wasting, vitamin A supplementation was identified as the most cost-effective intervention. Vitamin A supplementation can reduce diarrhoea incidence, a risk factor for wasting, and is therefore preventative. While the treatment of SAM intervention is effective at preventing mortality from wasting [ 10 , 59 ], in the model it had no impact on wasting prevalence. This is because the intervention is defined as treating children until they reach a weight-for-height of three standard deviations below the WHO Child Growth Standards median, at which point their mortality risks are significantly reduced but they are still defined as being wasted for purposes of the SDG target (i.e. children who are severely wasted are treated to become only moderately wasted, but wasted nonetheless). Cash transfers were identified as the next most cost-effective intervention, but with a cost per case averted six times higher than vitamin A supplementation. Cash transfers is an example of a social protection intervention primarily intended to help households meet basic needs; however, this study provides evidence of its potential benefit for nutrition. For anaemia, it is not surprising that IPTp, IFAS for non-pregnant women and multiple micronutrient supplements for pregnant women were the most cost-effective given their low unit costs and high impacts (Table 1 ).
The results of this study are consistent with previous work, but expand the intervention and country sets, and also consider intervention prioritisation. Other studies have estimated that scaling up subsets of these 18 nutrition interventions could lead to approximately a 20% reduction in stunting in children [ 23 , 24 ] (~ 65 million cases averted globally [ 24 ]). The consistency of impact projections is not surprising because the effect estimates for interventions (Table 1 ), as well as the causal pathways and risk factors used in the Optima Nutrition model (Figure A2), are based on the same evidence base as other models used for these analyses (e.g. LiST [ 92 , 93 ]). A recent study also estimated that 45% and 35% of 105 LMICs analysed were likely to reach the stunting and wasting targets respectively [ 94 ], which is consistent with our analysis if we constrain to the same set of countries. Our cost estimate of approximately $42 billion per annum to scale up all 18 interventions was more than previous estimates ($10.3 billion [ 23 ] and $9.6 billion [ 10 ] per annum, and $70 billion over 10 years [ 24 ]), because, as well as including additional high-cost interventions (e.g. cash transfers), our unit costs are up to twice as high due to the fractional costs associated with infrastructure and health system strengthening. Where comparisons are available, the cost-effectiveness estimates for individual interventions are approximately in line with World Bank estimates (e.g. $266 and $467 per stunting case averted for vitamin A and IYCF education respectively [ 24 ], and $10–62 per anaemia case averted with IPTp and micronutrient supplements for women [ 24 ]).
Between countries, different intervention priorities may be needed based on differences in baseline nutrition indicators, baseline intervention coverages, intervention effect sizes and intervention costs. In this analysis, effect estimates for interventions and baseline intervention coverage did not have an impact on between-country variation in cost-effectiveness. This is because intervention effect sizes were assumed to apply across all settings, a limitation of this study due to lack of evidence indicating otherwise, and because a linear cost-coverage relationship was used, meaning that baseline intervention coverage affected the impact that could be achieved with further scale-up but not cost-effectiveness. In this analysis, country-specific unit costs were calculated for interventions; however, between countries the intervention costs were largely scaled in proportion to one another (e.g. the human resource component costs were scaled according to the GDP) meaning that the relative costs were generally unchanged. Therefore, the greatest driver of between-country differences was baseline nutrition indicators, highlighting the importance of tailoring interventions to target areas or risk factors that drive the greatest burden (e.g. IYCF education was a higher priority in settings with lower baseline breastfeeding prevalence).
Major areas of current and future research are to define a broader set of interventions that can indirectly improve nutrition indicators, and to quantify their costs and benefits. For example, there is evidence that animal-sourced foods may reduce stunting [ 95 , 96 ], but there are limited studies linking agriculture and food system interventions to changes in nutritional indicators. Addressing the known underlying determinants of undernutrition is also critical. For example, improving gender equity and ensuring women can choose when and how many children they have can improve financial security and reduce poverty [ 97 , 98 ], both of which are correlated with poor nutritional outcomes. However, defining interventions to empower women and quantifying their effect sizes, which will be highly context specific, remains a challenge.
Implications of the COVID-19 pandemic
The COVID-19 pandemic is expected to have profound impacts on countries’ ability to achieve the SDG targets [ 99 ]. Recent estimates suggest that globally there could be a 14.3% increase in the prevalence of moderate or severe wasting among children under five in 2020, or 6.7 million additional children with wasting, compared with projections for 2020 without COVID-19 [ 100 ]. The implications for stunting are less clear, as it is a chronic condition and would therefore depend on the duration of the pandemic and associated disruptions.
In this study, the subset of interventions identified as the most cost-effective is based on pre-COVID-19 estimates of nutrition indicator trends, baseline intervention coverages and intervention unit costs. In particular, short-term changes to the unit costs (e.g. if commodities are more difficult to procure, if there are additional personal protective equipment costs or if services are delivered differently), if large enough and disproportionate across interventions, may lead to changes in the prioritisation of interventions. Further work is required to identify how to prioritise interventions to address the acute impacts of COVID-19, and this is currently being undertaken by the Standing Together for Nutrition consortium [ 101 ]. Once the immediate impacts of COVID-19 are managed, costs may revert to pre-pandemic levels, but at this point, we cannot predict when this will occur.
Limitations
This study has a number of limitations. The effect sizes of interventions may be overestimated as they were taken from meta-analyses that included an overrepresentation of randomised controlled trials. The modelled impact is therefore based on the assumption that interventions could be implemented as effectively observed in controlled conditions, and delivered precisely to their target populations, which is not likely to be the case. Therefore, our lower-bound estimates, which were derived from the lower-bound impact estimates, may be closer to the actual achievable impact when accounting for loss of effectiveness when moving from trials to scaled up programmes. Effect estimates were assumed to apply across all settings, due to lack of evidence indicating otherwise, but in reality, some populations will respond to them differently. We did not assume any complementary effects of interventions when implemented together, and applied consecutive independent relative reductions, but it is unclear whether there are cumulative benefits (or diminishing returns) to layering interventions.
It is unclear how feasible it would be to scale some of these interventions to high coverage, particularly within 5 years. The coverage of interventions was assumed to be constant in the status quo, but may naturally increase as health systems are strengthened, which would mean we have overestimated the impact of scaling up these interventions (but the cost-effectiveness would remain as estimated). Similarly, changes in projected populations sizes, GDP growth, poverty and other indicators may influence the baseline (status quo) projection, and hence the results. Where no intervention coverage data was available, we assumed a baseline zero coverage, which would also mean we have overestimated the impact of scale-up if some coverage already existed.
There are limitations to the model structure. For example, the model is based on the risk factor structure / causal pathway outlined in Figure A2 based on evidence available to support and quantify each relationship. Optima Nutrition is a global model and as such relies on a high threshold of evidence for interventions and/or risk factors to be included (i.e. typically meta-analyses of randomised controlled trials). This means that some interventions, particularly those that impact risk areas not in Figure A2, may be being overlooked where trial data are unpublished or no meta-analysis exists because few published trials are available.
While costing studies exist for selected interventions in selected countries, nothing is currently available at a global level that could be adapted across the 129 settings that were modelled. Therefore, we generated simple unit cost estimates that attempted to include the different costing domains, but individual country-specific costing studies could more precisely account for staffing, infrastructure, logistic and other overhead costs and improve the accuracy of cost and cost-effectiveness estimates. We also assumed that the unit costs of interventions would remain constant with scale, which may not be the case as economies of scale may reduce marginal costs as coverage increases and saturation effects may decrease marginal costs as coverage becomes high.
Population and epidemiological data inputs came largely from global data sets, and for some countries, this required imputing regional values or using modelled data where estimates were missing. This also does not account for differences within each country by geographic location or wealth quintile, or temporal differences such as seasonality that may be associated with wasting but not captured in DHS or MICS surveys as a result of survey timing. In the main results, we have rolled-up country estimates to derive global progress; however, there is a great deal of subnational variation in progress and our supplementary results may be more useful for individual countries than whether or not global targets are reached.
Of the 129 countries modelled, 46 (34%) were on track to achieve a 40% in reduction in stunting by 2025, 66 (51%) were on track to reduce wasting to below 5% by 2025, and 0 (0%) were on track to reduce anaemia by 50% by 2025. Scaling up 18 nutrition interventions globally could reduce stunting, wasting and anaemia by 20%, 14% and 22% respectively, and increase the number of countries on track to achieve the SDG 2.2 targets to 50 (39%), 83 (64%) and 7 (5%) respectively. The majority of the total impact was the result of only nine interventions, which suggests that they should be prioritised in the context of limited budgets.
Availability of data and materials
Model inputs and parameters are available in the supplementary material.
Abbreviations
Demographic and Health Survey
Gross domestic product
Iron and folic acid
Infant and young child feeding
Inter-quartile range
Intermittent preventative treatment of malaria during pregnancy
Lives Saved Tool
Long-lasting insecticide-treated bed nets
Moderate acute malnutrition
Multiple Indicator Cluster Survey
Sustainable Development Goal
Small for gestational age
Severe acute malnutrition
United Nations Joint Child Malnutrition Estimates
water, sanitation and hygiene
World Health Organization
Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, De Onis M, Ezzati M, Grantham-McGregor S, Katz J, Martorell R, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427–51.
Article PubMed Google Scholar
Daelmans B, Darmstadt GL, Lombardi J, Black MM, Britto PR, Lye S, Dua T, Bhutta ZA, Richter LM. Early childhood development: the foundation of sustainable development. Lancet. 2017;389(10064):9–11.
United Nations: Transforming our world: the 2030 Agenda for Sustainable Development. Accessed 1 February 2020 from: http://www.un.org/ga/search/view_doc.asp?symbol=A/RES/70/1&Lang=E .
Stevens GA, Finucane MM, Paciorek CJ, Flaxman SR, White RA, Donner AJ, Ezzati M. Nutrition Impact Model Study Group: Trends in mild, moderate, and severe stunting and underweight, and progress towards MDG 1 in 141 developing countries: a systematic analysis of population representative data. Lancet. 2012;380(9844):824–34.
Article PubMed PubMed Central Google Scholar
UNICEF. The State of the World’s Children 2019. In: Children, Food and Nutrition: Growing well in a changing world. New York: UNICEF; 2019. Accessed 1 February 2020 from: https://www.unicef.org/reports/state-of-worlds-children-2019 .
Google Scholar
United Nations Children’s Fund. UNICEF’s approach to scaling up nutrition for mothers and their children. In: Discussion paper. New York: Programme Division, UNICEF; 2015. Accessed 16 March 2020 from: https://www.unicef.org/nutrition/files/Unicef_Nutrition_Strategy.pdf .
World Health Organization: WHO recommendations on maternal health: guidelines approved by the WHO Guidelines Review Committee. Geneva. Accessed 1 February 2020 from: https://www.who.int/maternal_child_adolescent/documents/maternal-health-recommendations/en/ .
World Health Organization: WHO recommendations on child health: guidelines approved by the WHO Guidelines Review Committee. Geneva. Accessed 1 February 2020 from: https://www.who.int/maternal_child_adolescent/documents/child-health-recommendations/en/ .
Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K, Giugliani E, Haider BA, Kirkwood B, Morris SS, Sachdev H. What works? Interventions for maternal and child undernutrition and survival. Lancet. 2008;371(9610):417–40.
Bhutta ZA, Das JK, Rizvi A, Gaffey MF, Walker N, Horton S, Webb P, Lartey A, Black RE, Group TLNIR. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet. 2013;382(9890):452–77.
Popkin BM, Corvalan C, Grummer-Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet. 2019;395(10217):65–74.
Ganpule-Rao AV, Roy D, Karandikar BA, Yajnik CS, Rush EC. Food Access and Nutritional Status of Rural Adolescents in India: Pune Maternal Nutrition Study. Am J Prev Med. 2020;58(5):728–35.
Ogunniyi AI, Mavrotas G, Olagunju KO, Fadare O, Adedoyin R. Governance quality, remittances and their implications for food and nutrition security in Sub-Saharan Africa. World Dev. 2020;127:104752.
Article Google Scholar
Young MF, Nguyen P, Tran LM, Avula R, Menon P. A Double Edged Sword? Improvements in Economic Conditions over a Decade in India Led to Declines in Undernutrition as Well as Increases in Overweight among Adolescents and Women. J Nutr. 2020;150(2):364–72.
PubMed Google Scholar
Argaw A, Hanley-Cook G, De Cock N, Kolsteren P, Huybregts L, Lachat C. Drivers of Under-Five Stunting Trend in 14 Low-and Middle-Income Countries since the Turn of the Millennium: A Multilevel Pooled Analysis of 50 Demographic and Health Surveys. Nutrients. 2019;11(10):2485.
Article PubMed Central Google Scholar
Hirvonen K, Hoddinott J. Agricultural production and children's diets: Evidence from rural Ethiopia. Agric Econ. 2017;48(4):469–80.
Rosenberg AM, Maluccio JA, Harris J, Mwanamwenge M, Nguyen PH, Tembo G, Rawat R. Nutrition-sensitive agricultural interventions, agricultural diversity, food access and child dietary diversity: Evidence from rural Zambia. Food Policy. 2018;80:10–23.
Ruel MT, Alderman H. Maternal, Group CNS: Nutrition-sensitive interventions and programmes: how can they help to accelerate progress in improving maternal and child nutrition? Lancet. 2013;382(9891):536–51.
Alderman H, Headey DD. How important is parental education for child nutrition? World Dev. 2017;94:448–64.
Headey D, Hoddinott J, Park S. Drivers of nutritional change in four South Asian countries: a dynamic observational analysis. Matern Child Nutr. 2016;12:210–8.
Bill and Melinda Gates Foundation: The Goalkeepers Report 2019. Accessed 13 Mar 2020 from: https://www.gatesfoundation.org/goalkeepers/ .
Gillespie S, Haddad L, Mannar V, Menon P, Nisbett N. Maternal, Group CNS: The politics of reducing malnutrition: building commitment and accelerating progress. Lancet. 2013;382(9891):552–69.
Horton S, Shekar M, McDonald C, Mahal A, Brooks J. Scaling Up Nutrition: What Will it Cost? Directions in Development Series. Washington, DC: World Bank; 2010.
Shekar M, Kakietek J, Dayton Eberwein J, Walters D. An investment framework for nutrition: reaching the global targets for stunting, anemia, breastfeeding, and wasting. Washington DC: The World Bank; 2017.
Book Google Scholar
World Health Organization: Comprehensive Implementation Plan on Maternal, Infant and Young Child Nutrition. Geneva: WHO. Accessed 16 March 2020 from: http://apps.who.int/iris/bitstream/10665/113048/1/WHO_NMH_NHD_14.1_eng.pdf?ua=1 .
Smith LC, Haddad L. Reducing child undernutrition: past drivers and priorities for the post-MDG era. World Dev. 2015;68:180–204.
Pearson R, Killedar M, Petravic J, Kakietek JJ, Scott N, Grantham KL, Stuart RM, Kedziora DJ, Kerr CC, Skordis-Worrall J. Optima Nutrition: an allocative efficiency tool to reduce childhood stunting by better targeting of nutrition-related interventions. BMC Public Health. 2018;18(1):384.
Walker N, Tam Y, Friberg IK. Overview of the lives saved tool (LiST). BMC Public Health. 2013;13(Suppl 3):S1.
Winfrey W, McKinnon R, Stover J. Methods used in the lives saved tool (LiST). BMC Public Health. 2011;11(3):S32.
Hazel E, Gilroy K, Friberg I, Black RE, Bryce J, Jones G. Comparing modelled to measured mortality reductions: applying the Lives Saved Tool to evaluation data from the Accelerated Child Survival Programme in West Africa. Int J Epidemiol. 2010;39(Suppl 1):i32–9.
Larsen DA, Friberg IK, Eisele TP. Comparison of Lives Saved Tool model child mortality estimates against measured data from vector control studies in sub-Saharan Africa. BMC Public Health. 2011;11(S3):S34.
World Bank Group: Population Estimates and Projections. Accessed 11 Sep 2019 from: https://datacatalog.worldbank.org/dataset/population-estimates-and-projections . 2019.
World Bank Group: Development Indicators. Accessed 11 Sep 2019 from: https://databank.worldbank.org/source/world-development-indicators . 2019.
LiST: Lives Saved Tool (LiST). Accessed 16 March 2020: https://www.livessavedtool.org/ .
Guerra CA, Gikandi PW, Tatem AJ, Noor AM, Smith DL, Hay SI, Snow RW. The limits and intensity of Plasmodium falciparum transmission: implications for malaria control and elimination worldwide. PLoS Med. 2008;5(2):e38.
Lee AC, Katz J, Blencowe H, Cousens S, Kozuki N, Vogel JP, Adair L, Baqui AH, Bhutta ZA, Caulfield LE. National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle-income countries in 2010. Lancet Glob Health. 2013;1(1):e26–36.
USAID: Demographic and Health Surveys (DHS). Accessed 11 Sep 2019 from: https://dhsprogram.com/data/ .
UNICEF, WHO, The World Bank: Joint Child Malnutrition Estimates. Accessed 16 March 2020 from: https://data.unicef.org/resources/dataset/malnutrition-data/ .
Institute for Health Metrics and Evaluation (IHME): Globa Burden of Disease Study. Accessed 11 Sep 2019 from: http://ghdx.healthdata.org/gbd-results-tool .
Stevens GA, Finucane MM, De-Regil LM, Paciorek CJ, Flaxman SR, Branca F, Pena-Rosas JP, Bhutta ZA, Ezzati M. Nutrition Impact Model Study Group (Anemia): Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for1995–2011: a systematic analysis of population-representative data. Lancet Glob Health. 2017;1(1):e16–25.
Walker CLF, Rudan I, Liu L, Nair H, Theodoratou E, Bhutta ZA, O'Brien KL, Campbell H, Black RE. Global burden of childhood pneumonia and diarrhoea. Lancet. 2013;381(9875):1405–16.
Katz J, Lee AC, Kozuki N, Lawn JE, Cousens S, Blencowe H, Ezzati M, Bhutta ZA, Marchant T, Willey BA. Mortality risk in preterm and small-for-gestational-age infants in low-income and middle-income countries: a pooled country analysis. Lancet. 2013;382(9890):417–25.
Olofin I, McDonald CM, Ezzati M, Flaxman S, Black RE, Fawzi WW, Caulfield LE, Danaei G, Study NIM. Associations of suboptimal growth with all-cause and cause-specific mortality in children under five years: a pooled analysis of ten prospective studies. PLoS One. 2013;8(5):e64636.
Article CAS PubMed PubMed Central Google Scholar
NEOVITA Study Group. Timing of initiation, patterns of breastfeeding, and infant survival: prospective analysis of pooled data from three randomised trials. Lancet Glob Health. 2016;4(4):e266–75.
Lamberti LM, Walker CLF, Noiman A, Victora C, Black RE. Breastfeeding and the risk for diarrhea morbidity and mortality. BMC Public Health. 2011;11(3):1.
Lamberti LM, Zakarija-Grković I, Walker CLF, Theodoratou E, Nair H, Campbell H, Black RE. Breastfeeding for reducing the risk of pneumonia morbidity and mortality in children under two: a systematic literature review and meta-analysis. BMC Public Health. 2013;13(3):S18.
Christian P, Lee SE, Donahue Angel M, Adair LS, Arifeen SE, Ashorn P, Barros FC, Fall CH, Fawzi WW, Hao W. Risk of childhood undernutrition related to small-for-gestational age and preterm birth in low-and middle-income countries. Int J Epidemiol. 2013;42(5):1340–55.
Child Health Epidemiology Reference Group. Moderate to Severe, but Not Mild, Maternal Anemia Is Associated with Increased Risk of Small-for-Gestational-Age Outcomes. J Nutr. 2011;142(2):358–62.
Article CAS Google Scholar
Xiong X, Buekens P, Alexander S, Demianczuk N, Wollast E. Anemia during pregnancy and birth outcome: a meta-analysis. Am J Perinatol. 2000;17(03):137–46.
Article CAS PubMed Google Scholar
Langendorf C, Roederer T, de Pee S, Brown D, Doyon S, Mamaty A-A, Touré LW-M, Manzo ML, Grais RF. Preventing acute malnutrition among young children in crises: a prospective intervention study in Niger. PLoS Med. 2014;11(9):e1001714.
Hutton EK, Hassan ES. Late vs early clamping of the umbilical cord in full-term neonates: systematic review and meta-analysis of controlled trials. JAMA. 2007;297(11):1241–52.
Sinha B, Chowdhury R, Upadhyay RP, Taneja S, Martines J, Bahl R, Sankar MJ. Integrated interventions delivered in health systems, home, and community have the highest impact on breastfeeding outcomes in low-and middle-income countries. J Nutr. 2017;147(11):2179S–87S.
CAS PubMed Google Scholar
Panjwani A, Heidkamp R. Complementary feeding interventions have a small but significant impact on linear and ponderal growth of children in low-and middle-income countries: a systematic review and meta-analysis. J Nutr. 2017;147(11):2169S–78S.
Boundy EO, Dastjerdi R, Spiegelman D, Fawzi WW, Missmer SA, Lieberman E, Kajeepeta S, Wall S, Chan GJ. Kangaroo mother care and neonatal outcomes: a meta-analysis. Pediatrics. 2016;137(1):e20152238.
Lawn JE, Mwansa-Kambafwile J, Horta BL, Barros FC. Cousens S: ‘Kangaroo mother care’to prevent neonatal deaths due to preterm birth complications. Int J Epidemiol. 2010;39(Suppl 1):i144–54.
De-Regil LM, Suchdev PS, Vist GE, Walleser S, Peña-Rosas JP. Home fortification of foods with multiple micronutrient powders for health and nutrition in children under two years of age. Evid Based Child Health Cochrane Rev J. 2013;8(1):112–201.
Munos MK, Walker CLF, Black RE. The effect of oral rehydration solution and recommended home fluids on diarrhoea mortality. Int J Epidemiol. 2010;39(Suppl 1):i75–87.
Walker CLF, Black RE. Zinc for the treatment of diarrhoea: effect on diarrhoea morbidity, mortality and incidence of future episodes. Int J Epidemiol. 2010;39(Suppl 1):i63–9.
Lenters LM, Wazny K, Webb P, Ahmed T, Bhutta ZA. Treatment of severe and moderate acute malnutrition in low- and middle-income settings: a systematic review, meta-analysis and Delphi process. BMC Public Health. 2013;13(Suppl 3):S23.
Imdad A, Mayo-Wilson E, Herzer K, Bhutta ZA. Vitamin A supplementation for preventing morbidity and mortality in children from six months to five years of age. Cochrane Database Syst Rev. 2017;3:CD008524.
Ota E, Hori H, Mori R, Tobe-Gai R, Farrar D. Antenatal dietary education and supplementation to increase energy and protein intake. Cochrane Database Syst Rev. 2015;6:CD000032.
Hofmeyr GJ, Lawrie TA, Atallah ÁN, Torloni MR. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst Rev. 2018;10:CD001059.
Peña-Rosas JP, De-Regil LM, Garcia-Casal MN, Dowswell T. Daily oral iron supplementation during pregnancy. Cochrane Database Syst Rev. 2015;7:CD004736.
Fernández-Gaxiola AC, De-Regil LM. Intermittent iron supplementation for reducing anaemia and its associated impairments in menstruating women. Cochrane Database Syst Rev. 2011;12:CD009218.
Radeva-Petrova D, Kayentao K, ter Kuile FO, Sinclair D, Garner P. Drugs for preventing malaria in pregnant women in endemic areas: any drug regimen versus placebo or no treatment. Cochrane Database Syst Rev. 2014;10:CD000169.
Eisele TP, Larsen D, Steketee RW. Protective efficacy of interventions for preventing malaria mortality in children in Plasmodium falciparum endemic areas. Int J Epidemiol. 2010;39(Suppl 1):i88–i101.
Keats EC, Haider BA, Tam E, Bhutta ZA. Multiple-micronutrient supplementation for women during pregnancy. Cochrane Database Syst Rev. 2019;3:CD004905.
Barkley JS, Wheeler KS, Pachón H. Anaemia prevalence may be reduced among countries that fortify flour. Br J Nutr. 2015;114(2):265–73.
Blencowe H, Cousens S, Modell B, Lawn J. Folic acid to reduce neonatal mortality from neural tube disorders. Int J Epidemiol. 2010;39(Suppl 1):i110–21.
UNICEF: UNICEF global nutrition database. Accessed 16 March 2020 from: https://data.unicef.org/topic/nutrition/vitamin-a-deficiency/ .
Ghauri K, Horton S, Spohrer R, Garrett G. Food Fortification Cost Model. Unpublished manuscript. Washington, DC: Global Alliance for Improved Nutrition; 2016.
Food Fortification Initiative. Accessed 16 March 2020 from: http://www.ffinetwork.org/ .
UNICEF: State of the World's Children 2017 Statistical Tables. Accessed 11 Sep 2019 from: https://data.unicef.org/resources/state-worlds-children-2017-statistical-tables/ .
Avenir Health: OneHealth Tool. Available from: https://www.avenirhealth.org/software-onehealth.php .
World Health Organization: WHO-CHOICE Results of Unit Costs for patient services for the 14 GBD Regions. Accessed 11 Sep 2019 from: https://www.who.int/choice/costs/unit_regions/en/ .
World Health Organization: International Drug Price Indicator Guide. Accessed 11 Sep 2019 from: http://apps.who.int/medicinedocs/documents/s21982en/s21982en.pdf .
Horton S. The economics of food fortification. J Nutr. 2006;136(4):1068–71.
Stenberg K, Axelson H, Sheehan P, Anderson I, Gülmezoglu AM, Temmerman M, Mason E, Friedman HS, Bhutta ZA, Lawn JE. Advancing social and economic development by investing in women's and children's health: a new Global Investment Framework. Lancet. 2014;383(9925):1333–54.
UNICEF Supply Division: Supply costs for nutrition. Accessed 11 Sep 2019 from: https://www.unicef.org/supply/index_59714.html .
Optima Consortium for Decisions Science: Optima Nutrition User Guide. Accessed 1 February 2020 from: http://optimamodel.com/nutrition/documents.html .
UNICEF: Multiple Indicator Cluster Surveys (MICS). Accessed 11 Sep 2019 from: https://mics.unicef.org/surveys .
World Health Organization: WHO Global Health Observatory. Accessed 11 Sep 2019 from: http://apps.who.int/gho/data/node.main .
Say L, Chou D, Gemmill A, Tunçalp Ö, Moller A-B, Daniels J, Gülmezoglu AM, Temmerman M, Alkema L. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2(6):e323–33.
Lozano R, Fullman N, Abate D, Abay SM, Abbafati C, Abbasi N, Abbastabar H, Abd-Allah F, Abdela J, Abdelalim A. Measuring progress from 1990 to 2017 and projecting attainment to 2030 of the health-related Sustainable Development Goals for 195 countries and territories: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):2091–138.
Stenberg K, Hanssen O, Edejer TT-T, Bertram M, Brindley C, Meshreky A, Rosen JE, Stover J, Verboom P, Sanders R. Financing transformative health systems towards achievement of the health Sustainable Development Goals: a model for projected resource needs in 67 low-income and middle-income countries. Lancet Glob Health. 2017;5(9):e875–87.
Engle-Stone R, Perkins A, Clermont A, Walker N, Haskell MJ, Vosti SA, Brown KH. Estimating lives saved by achieving dietary micronutrient adequacy, with a focus on vitamin a intervention programs in Cameroon. J Nutr. 2017;147(11):2194S–203S.
World Health Organization and UNICEF: The extension of the 2025 maternal, infant and young child nutrition targets to 2030. Discussion paper. Geneva: World Health Organization 2018. Accessed 1 February 2020 from: https://www.who.int/nutrition/global-target-2025/discussion-paper-extension-targets-2030.pdf .
Heidkamp RA, Clermont A, Walker N. How Can We Reach World Health Assembly 2025 Nutrition Targets? Using the Lives Saved Tool to Support Strategic Planning by the Nutrition Sector in Low-and Middle-Income Countries. FASEB J. 2017;31(Suppl 1):312.314.
Imdad A, Yakoob MY, Bhutta ZA. Impact of maternal education about complementary feeding and provision of complementary foods on child growth in developing countries. BMC Public Health. 2011;11(3):1.
World Health Organization: International Code of Marketing of Breast-milk Substitutes. Geneva 1981, ISBN 92 4 154160 1. Accessed 24 September 2020 from: https://www.who.int/nutrition/publications/code_english.pdf .
Imdad A, Yakoob MY, Sudfeld C, Haider BA, Black RE, Bhutta ZA. Impact of vitamin A supplementation on infant and childhood mortality. BMC Public Health. 2011;11(Suppl 3):S20.
Chola L, Pillay Y, Barron P, Tugendhaft A, Kerber K, Hofman K. Cost and impact of scaling up interventions to save lives of mothers and children: taking South Africa closer to MDGs 4 and 5. Glob Health Action. 2015;8(1):27265.
Alderman H, Nguyen PH, Menon P. Progress in reducing child mortality and stunting in India: an application of the Lives Saved Tool. Health Policy Plan. 2019;34(9):667–75.
Local Burden of Disease Child Growth Failure Collaborators. Mapping child growth failure across low-and middle-income countries. Nature. 2020;577(7789):231.
Headey D, Hirvonen K, Hoddinott J. Animal sourced foods and child stunting. Am J Agric Econ. 2018;100(5):1302–19.
Choudhury S, Headey DD. Household dairy production and child growth: Evidence from Bangladesh. Econ Hum Biol. 2018;30:150–61.
Canning D, Schultz TP. The economic consequences of reproductive health and family planning. Lancet. 2012;380(9837):165–71.
Carr B, Gates MF, Mitchell A, Shah R. Giving women the power to plan their families. Lancet. 2012;380(9837):80–2.
Akseer N, Kandru G, Keats EC, Bhutta ZA. COVID-19 pandemic and mitigation strategies: implications for maternal and child health and nutrition. Am J Clin Nutr. 2020;112(2):251–6.
Headey D, Heidkamp R, Osendarp S, Ruel M, Scott N, Black R, Shekar M, Bouis H, Flory A, Haddad L. Impacts of COVID-19 on childhood malnutrition and nutrition-related mortality. Lancet. 2020;396(10250):519–21.
Standing Together for Nutrition consortium: Accessed 10 August 2020 from: https://micronutrientforum.org/standing-together-for-nutrition/ .
Download references
Acknowledgements
We are grateful to David P Wilson and Jolene Skordis for useful discussions. The authors acknowledge the support provided to the Burnet Institute by the Victorian Government Operational Infrastructure Support Program.
National Health and Medical Research Council of Australia. The funders had no role in study design, data collection and analysis, or decision to publish.
Author information
Authors and affiliations.
Maternal, Child and Adolescent Health Program, Burnet Institute, Melbourne, Australia
Nick Scott, Dominic Delport, Samuel Hainsworth, Ruth Pearson, Christopher Morgan, Shan Huang, Mike Toole & Caroline SE Homer
School of Public Health and Preventative Medicine, Monash University, Melbourne, Australia
School of Population and Global Health, University of Melbourne, Melbourne, Australia
Christopher Morgan
Jhpiego, Baltimore, MD, USA
World Bank Group, Washington DC, USA
Jonathan K. Akuoku & Meera Shekar
Nutrition Global Development Program, Bill and Melinda Gates Foundation, Seattle, USA
Ellen Piwoz
Department of Global Health, University of Washington, Seattle, USA
Carol Levin
You can also search for this author in PubMed Google Scholar
Contributions
NS conceived the study, designed the methods, performed the literature review and drafted the manuscript. DD collated the data and ran the analyses. NS, SHa, RP, MS and JKA designed the model. NS, DD, SHa and RP built the model. NS, DD, SHu, CM, MT and CH interpreted the results and revised the methods. EP and MS provided critical review of results and interpretation. CL provided critical review of costings. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Nick Scott .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
Detailed model description and additional model parameters.
Additional file 2.
Country-specific model inputs and country-specific model results.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Scott, N., Delport, D., Hainsworth, S. et al. Ending malnutrition in all its forms requires scaling up proven nutrition interventions and much more: a 129-country analysis. BMC Med 18 , 356 (2020). https://doi.org/10.1186/s12916-020-01786-5
Download citation
Received : 15 July 2020
Accepted : 16 September 2020
Published : 13 November 2020
DOI : https://doi.org/10.1186/s12916-020-01786-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Economic analysis
- Mathematical model
- Optima Nutrition
- Sustainable Development Goals
BMC Medicine
ISSN: 1741-7015
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Hunger and...
Hunger and malnutrition in the 21st century
Food for thought, click here to read other articles in this collection.
- Related content
- Peer review
- Patrick Webb , professor 1 ,
- Gunhild Anker Stordalen , policy advocate 2 ,
- Sudhvir Singh , policy researcher 2 ,
- Ramani Wijesinha-Bettoni , United Nations 3 ,
- Prakash Shetty , professor 4 ,
- Anna Lartey , director of nutrition 3
- 1 Friedman School of Nutrition Science and Policy, Tufts University, Boston, Massachusetts, USA
- 2 EAT Forum, Oslo, Norway
- 3 Food and Agriculture Organization of the United Nations, Ringgold Standard Institution, Rome, Italy
- 4 MS Swaminathan Research Foundation, Ringgold Standard Institution, Chennai, India
- Correspondence to: P Webb patrick.webb{at}tufts.edu
Despite record food output globally, hunger is still with us. Patrick Webb and colleagues argue that key policy actions are urgently needed to tackle this scourge and must focus on improving diet quality for all
Today’s world is characterised by the coexistence of agricultural bounty and widespread hunger and malnutrition. 1 Recent years have seen a reversal of a decades old trend of falling hunger, alongside the re-emergence of famine. 1 National and global evidence shows that ensuring an adequate food supply is still an important contribution to eradicating hunger. However, generating more food in the form of staple grains or tubers is not enough. Good nutrition and an end to hunger both require everyone to have an appropriate diet. How can that be achieved?
Characterising the problem
A recent report for the World Committee on Food Security argued that “malnutrition in all its forms—not only hunger, but also micronutrient deficiencies, as well as overweight and obesity—is … a critical challenge not only in the developing but also in the developed countries. Resolving malnutrition requires a better understanding of the determinants and processes that influence diets.” 1 Malnutrition ranges from extreme hunger and undernutrition to obesity ( box 1 ). 2 3 Furthermore, malnutrition is found in all countries, irrespective of their economic development, where people lack high quality diets. 4 5 6 Thus, solutions to hunger and to all forms of malnutrition need to focus on ensuring an adequate supply of food, but equally, on the quality of diets.
Terms and definitions 1 2 3
Hunger is characterised in many ways. It encompasses individual sensations and household behavioural responses, food scarcity (actual or feared) and national food balance sheets that focus on supply of energy (kilocalories) in any country in relation to a minimum threshold of need. The food balance sheet approach is the only standard of measurement used globally. It is based on data collated by the Food and Agriculture Organization of the United Nations. This organisation has replaced its previous use of the word “hunger” in describing this metric with the phrase “chronic undernourishment”. This today is defined as “a person’s inability to acquire enough food to meet daily minimum dietary energy requirements during 1 year” 1
Malnutrition— An all inclusive term that represents all manifestations of poor nutrition. It can mean any or all forms of undernutrition, overweight, and obesity
Undernutrition —Refers to any form of nutritional deficiency, particularly those manifest in maternal underweight, child stunting, child wasting, or micronutrient deficiencies. It does not include reference to overweight and obesity
Maternal underweight— A body mass index (BMI) of <18.5 among women of reproductive age. This typically reflects chronic energy deficiency coupled with a lack of other key macronutrients or micronutrients, ill health, or energy expenditure higher than consumption. A prevalence >20% indicates a serious public health problem
Child stunting —Height for age ≤ −2 standard deviations of the median for children aged 6-59 months, according to World Health Organization child growth standards
Child wasting— Weight for height ≤ −2 standard deviations of the median for children aged 6-59 months, according to WHO child growth standards
Micronutrient deficiencies— A lack of various key vitamins and minerals leads to a range of symptoms that are of global concern. These include anaemia due to iron deficiency and risk of child mortality associated with clinical vitamin A deficiency. Such deficiencies are measured in several ways, including biomarkers (assessed using blood, serum, urine, etc), clinical manifestations, or proxy measures of diet quality
Overweight and obesity —For non-pregnant adults, a BMI ≥25 represents being overweight. The threshold for obesity is a BMI ≥30. Child obesity is of increasing concern and was included in the latest global nutrition goals for 2030 (“no increase in childhood obesity”) 4
Today, risk factors for ill health associated with poor quality diets are the main causes of the global burden of disease. 5 6 Low quality diets lack key vitamins, minerals (micronutrients), and fibre or contain too many calories, saturated fats, salt, and sugar. 7 In 2010, dietary risk factors combined with physical inactivity accounted for 10% of the global burden of disease (measured as disability adjusted life years, which reflect the number of years lost due to ill health, disability, or early death). 8 By 2015, six of the top 11 global risk factors were related to diet, including undernutrition, high body mass index (BMI), and high cholesterol. 9 10 Where governments have invested the economic gains derived from rising productivity in safety nets and services accessible to the poor, this has resulted in national growth. 11 12 13 However, where poverty persists, including in rich nations, hunger also persists.
Several faces of hunger
Hunger is a broad unscientific term that relates to nutrition and health outcomes in various ways. The proportion of people defined as hungry over the long term (usually termed “chronically undernourished”) fell from 18.6% globally in 1990-2002 to under 11% in 2014-16 ( table 1 ). That was a decline of 211 million people while the world’s population increased by 2 billion. 2 Big gains were made in large countries like China and in Brazil, Ethiopia, and Bangladesh ( box 2 ). South America was particularly successful, reducing undernourishment by over 50% in 25 years. 1 Such gains were made possible largely by rapid reduction of poverty, rising levels of literacy, and health improvements that reduced preventable child mortality. 17
Numbers (millions) and prevalence (%) of people with chronic undernourishment, stunting, and wasting* by year and geographical region 2 14
- View inline
Successful resolution of undernutrition: Brazil, Ethiopia, and Bangladesh
Hunger (chronic undernourishment) has remained static at around 800 million people for several decades. This is largely because of rising populations in fragile states and the escalation of armed conflict in numerous parts of the world. 1 2 Nevertheless, child undernutrition has been falling. In 2000, roughly 200 million children under 5 years of age were stunted, but this has fallen to less than 151 million today. Rapid improvements in nutrition have been concentrated in several large nations, which have shown the way with policy success stories
• Brazil saw its prevalence of child stunting decline from 37% in 1974–1975 to 7% in 2006-7. 17 It achieved these gains through a sustained commitment to expand access to maternal and child health services (reaching into previously underserved geographical regions). This was coupled with large scale investment in social reform and safety net programmes that supported a narrowing of the income gap (through equitable poverty reduction), rising numbers of girls in school, declining fertility, and greater stability in income flows and food consumption among the poor. Stable food consumption was achieved through food supplementation targeted at mothers and children, and with cash transfers targeted at the poorest groups. All of this was helped by improved stability of governance. Few of these actions focused explicitly on nutrition, but many were driven by a policy agenda called “zero hunger.” Even with recent economic challenges and changes of government, the gains made over past decades persist
• Ethiopia has faced famines many times between the 1980s and the early 2000s. It has also reduced child stunting from 58% in 2000 to <40% by 2014. 18 Although this figure is still unacceptably high, it represents a fall of about 1.2% a year. 19 Ethiopia also increased enrolment and retention of girls in schools during this period, increased agricultural productivity, and implemented a huge employment based safety net (one of the largest social protection programmes in Africa). However, two other important drivers improved nutrition in this period. Firstly, a move by government to treat nutrition as a multisector challenge (met by numerous line ministry responsibilities) and, secondly, improved sanitation, focused on eradicating open defecation, which was a major impediment to health and the retention of nutrients in the diet 18 19
• Bangladesh is a modern nutrition superstar. It emerged from famine in the 1970s. Successive governments have worked alongside an unusually vibrant non-governmental sector to deal with underlying problems and visible symptoms of malnutrition. While service delivery remains generally weak, widespread targeted interventions were combined with a variety of nutritional measures that deal with underlying problems. 20 Such actions included economic growth policies aimed at the poor, girls’ education, improved sanitation, and a significant turnaround in the agricultural sector, which moved Bangladesh from being a net importer of food to a significant exporter. 18 21 As a result, child stunting fell from almost 57% in 1997 to around 36% in 2014 18 19
However, despite such progress the world still has unacceptably high numbers of undernourished people. Of the roughly 800 million undernourished, 780 million are in low income countries, especially in sub-Saharan Africa and South Asia. 1 The continents of Africa and Asia have the greatest number of people living in extreme poverty, and it is here that extreme hunger and poverty together present the greatest risk of famine.
Famine is the most acute face of hunger. Over 70 million people died in famines during the 20th century. 22 23 24 Most deaths occurred in human induced crises, in which political mismanagement, armed conflict, and discrimination of marginalised political or ethnic groups compounded the effects of environmental shocks, such as droughts or locust invasions. 25 Deaths from famine fell from the mid-1980s onwards. However, as of 2017 four countries were again struggling to cope: Somalia, Yemen, South Sudan, and Nigeria. 26 In each case, instability induced by conflict, terrorism, drought and decades of failed governance have left over 20 million people facing famine, including 1.4 million children “at imminent risk of death.” 27
A major cause of mortality in famines is children becoming severely wasted. Around 52 million children were wasted in 2016, of whom around 70% (36 million) resided in Asia ( table 1 ). 14 Roughly 12.6% of deaths among children under 5 are attributed to wasting worldwide. 28 Although wasting has declined, progress has been slow and some countries have seen a rise, including Pakistan and India. 29 Many of the drivers of wasting are often the same as for stunting—namely, low birth weight, lack of exclusive breast feeding, poor hygiene and sanitation, and infectious disease. 30 While wasting is one sign of acute hunger, stunting (being too short for one’s age) represents chronic distress. Around 151 million preschool children were stunted in 2017, down from 200 million at the turn of the 20th century. 14 Improvements were made in east Asia, including China (today reporting a prevalence of only 6% compared with the global mean of 23%) and Bangladesh as well as in Latin America ( table 1 ). 31 Nevertheless, South Asia and East and Central Africa all still had rates over 32% in 2017.
Coexisting forms of malnutrition related to diet
The coexistence of multiple forms of malnutrition is a global phenomenon. That is, wasting often coexists with stunting in the same geographical areas, and can be found simultaneously in children. 32 For example, around 9% of children in India exhibit both conditions, while the rate in parts of Ghana is reported to be >3%. 32 33 Many countries with a high prevalence of stunting have made limited progress in achieving annual average rates of reduction required to meet global targets. For example, Timor Leste needs an annual reduction of around 5% to reduce stunting by 40% by 2030, but its current reduction rate is barely above zero. 9 Ethiopia also needs an annual average rate of reduction of 5%, but continues to remain at 3%.
Part of the reason for slow progress lies in overlapping micronutrient deficiencies. Inadequate supply of energy and protein both impair a child’s growth, but micronutrient deficiencies also have a role. It has been estimated that roughly 2 billion people, or about 29% of the world’s population, faced micronutrient deficiencies in 2010. 34 35 36 37 Micronutrient deficiencies are also widely present in high income countries. For example, childhood anaemia in 2010 was 26% in the Russian Federation and in Georgia, and 16%, on average, across the European Union. 38
Obesity is conventionally associated with food excess, but it is also associated with micronutrient deficiencies and even with daily hunger, as shown for Malaysia, 39 Canada, 40 and Iran. 41 Indeed, people with obesity can be prone to deficiencies of micronutrients, such as zinc, iron, and vitamins A, C, D, and E. 42 43 44 45 46 Between 1990 and 2010, the prevalence of adults with a high BMI in sub-Saharan Africa tripled. At the same time, hypertension increased by 60%, and the prevalence of high blood glucose rose nearly 30%. 47 The prevalence of overweight and obesity among South Asian women is almost the same today as the prevalence of underweight. 6 Pacific and Caribbean islands and countries in the Middle East and Central America have reached extremely high rates of adult overweight and obesity. Some have a prevalence as high as 80% (eg, Tonga, 84% for men, 88% for women). 48
Many countries today face the dual burden of rising rates of female obesity with continuing high rates of maternal underweight. The latter matters because of ill effects on the mother and on the unborn child. Roughly 30% of stunting by a child’s 3rd birthday can be attributed to being born small for gestational age, which is linked to nutrition before birth and health problems of the mother. 28 Not only is maternal underweight still more prevalent than overweight in rural parts of South Asia and sub-Saharan Africa but adult female underweight rose recently in Senegal, Madagascar, and Mali, mainly in urban settings. 49
Thus, actions are needed in all countries around the world to deal with undernutrition, micronutrient deficiencies, and overweight and obesity simultaneously. No country is exempt. “Triple duty” investments are needed everywhere because wealth and food sufficiency will not in themselves resolve the problems of low quality of diets.
Effective actions to tackle hunger and malnutrition
In 2016, the world hit a new record by producing over 2.5 billion metric tons of cereal grains—up from 1.8 billion tons 20 years earlier. 50 But hunger persists because an increased supply of food alone is neither the solution to hunger nor an answer to malnutrition. Countries that have made recent progress in reducing hunger and improving nutrition have a core set of common characteristics. Firstly, they tend to be politically stable countries that have pursued relatively equitable growth policies (not only increasing wealth for some but reducing poverty overall). Secondly, they employ targeted safety nets for the poor and invest in accessible services (education, clean water, healthcare). Thirdly, they assume responsibility for responding to shocks (economic, environmental, or due to conflict) in timely ways that mitigate human suffering.
Successful actions typically include a mix of targeted so called nutrition specific programming (aimed at preventing or resolving defined nutrition and health problems in individuals) and nutrition sensitive interventions for the whole population that deal with the underlying causes. 9 32 35 Table 2 provides details of evidence based policies and programmes in a variety of sectors, which are known to reduce hunger and deal with malnutrition. 32 In food and agriculture, these may include national price support interventions that increase the supply and accessibility of nutrient rich foods (often perishables, like dairy, fruits and fresh meats), coupled with technical and financial support for women farmers to produce nutrient rich vegetables in their gardens. In health, national policies to support accessible high quality services are critical to ensuring antenatal and postnatal care, particularly combined with targeted nutrition, exclusive breast feeding, and infant feeding messaging. Measures directed at underweight mothers are important for good birth outcomes, as well as varied forms of micronutrient supplementation. 1 In other words, the quality of services, scale of coverage, and the singling out of nutritionally vulnerable demographic groups are all keys to success. 20 47
Examples of actions to tackle hunger and malnutrition across sectors 3 20 47 51
Good nutrition and eradication of hunger comes at a price, but pays for itself in the longer term. Donor funding for nutrition sensitive programmes rose between 2003 and 2015, from 11.8% to 19.4%, reaching around $19bn (£14bn, €16bn) in 2015. 48 Such assistance is deemed to be effective, in that a 10% increase in overall nutrition sensitive aid delivers an estimated 1.1% “decrease in hunger” (measured as chronic undernourishment). 48 The World Bank has argued that a “priority package” of evidence based nutritional interventions that could be readily scaled up would require roughly $23bn over a decade, or $5 per child. 51 52 The World Bank emphasises that while international donor agencies should increase spending to achieve global nutrition goals, national governments and citizens themselves need to increase spending and act appropriately. The role of individuals and families comes largely in the form of preferences and constraints. 52 People make choices that shape dietary patterns and physical activity but also the uptake of healthcare services, spending on smoking and hygiene, as well as investments in schooling for their children and agricultural productivity (if farmers).
The value of such large investments to future human and economic development has long been understood in high income countries, such as Europe and the United States. European countries deploy a wide range of policies to combat residual hunger. These include promoting more diverse local food production and diversified diets, the latter “encouraged through nutrition education targeting school children and mothers of young children.” 38 The United States also supports large state food provisioning through nutrition programmes aimed at women and children. For example, spending on the federal food stamp programme in 2017 reached $68bn ($126 per person). 53 Similarly, spending on the Women Infants and Children programme, which targets low income families nutritionally at risk with food supplements, nutrition education, and health system referrals, reached $6.5bn in 2017. 54
Conclusions
The sustainable development goals require all countries and their citizens to act together to end hunger and all forms of malnutrition by 2030. 13 Setting targets is a good first step, but actions need to follow quickly. Urgent attention to achieve such goals is seriously overdue. Policy action must be designed to reduce malnutrition in all its forms, and be adequately funded. Measures must be evidence based, implemented at scale, and include both broad based and targeted actions aimed at the most nutritionally vulnerable people. The evidence to support such actions is growing, but it is already plentiful and compelling; there is no need for delay. The rapidly escalating threats posed by malnutrition represent a planetary challenge on a par with poverty and climate change. An appropriate response at the required scale is top priority for decision makers globally. It cannot wait.
Key messages
Despite record levels of food production globally, hunger and many forms of malnutrition still affect billions of people
While traditionally associated with a lack of food, hunger, and malnutrition (which includes overweight and obesity as well as undernutrition) are associated with low quality diets
Poor diet quality is a problem in every country—high and low income alike. A high quality diet meets most key nutrient needs, mainly through nutrient rich foods
Securing high quality diets for all, comprising sufficiency, diversity, balance, and safety, is necessary to resolve hunger and malnutrition in all its forms
Policy makers must urgently implement evidence based, cost effective actions that have a triple purpose: eradicate hunger, resolve all forms of undernutrition, and tackle obesity
Governments must consider how policies across multiple sectors influence the functioning of food systems from farm to fork. They must identify changes that will help all consumers to have healthy diets
The challenge is huge, but the urgency has never been so great
Contributors and sources: The authors have diverse subject expertise and policy experience relating to hunger, food insecurity, diets and nutrition. Some authors have a medical or agriculture background, while others have training and experience in policy analysis, nutrition and humanitarian action. PW and GAS were both members of the Global Futures Council on Food Security and Agriculture of the World Economic Forum. PW and AL advise the Global Panel on Agriculture and Food Systems for Nutrition. SS is a contributing author to the upcoming EAT Lancet Commission on Healthy Diets from Sustainable Food Systems. Data used are all in the public domain, and are derived from nationally representative surveys, United Nations agency analyses, or peer reviewed publications. PW, GAS and AL were involved in manuscript concept and design. All authors were involved in drafting and editing the manuscript; critically revised the manuscript for important intellectual content and approved the final manuscript and the authorship list. PW is the guarantor.
Competing interests: We have read and understood BMJ policy on declaration of interests and have no relevant interests to declare.
Provenance and peer review: Commissioned; externally peer reviewed.
This article is one of a series commissioned by The BMJ . Open access fees for the series were funded by Swiss Re, which had no input into the commissioning or peer review of the articles. The BMJ thanks the series advisers, Nita Forouhi and Dariush Mozaffarian, for valuable advice and guiding selection of topics in the series.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- ↵ High Level Panel of Experts. Second note on critical and emerging issues for food security and nutrition. High level panel of experts on food security and nutrition of the Committee on World Food Security. Rome, Italy. 2017. http://www.fao.org/fileadmin/user_upload/hlpe/hlpe_documents/Critical-Emerging-Issues-2016/HLPE_Note-to-CFS_Critical-and-Emerging-Issues-2nd-Edition__27-April-2017_.pdf
- ↵ Food and Agriculture Organization of the United Nations/International Fund for Agricultural Development/World Food Programme. State of food insecurity in the world 2017. Rome, Italy, 2017. https://www.wfp.org/content/2017-state-food-security-and-nutrition-world-sofi-report
- ↵ Pangaribowo EM, Gerber N, Torero M. 2013. Food and nutrition security indicators: a review. FOODSECURE working paper 04. Report for the European Union's Seventh Framework Programme FP7/2007-2011 under grant agreement n° 290693. http://www3.lei.wur.nl/WECRGeneral/FoodSecurePublications/05_Pangaribowo%20Gerber%20Torero_FNS%20Indicators.pdf
- ↵ International Food Policy Research Institute. Global nutrition report 2016: from promise to impact: ending malnutrition by 2030. Washington, DC, USA; 2016. http://www.ifpri.org/publication/global-nutrition-report-2016-promise-impact-ending-malnutrition-2030
- Sutherland J ,
- Dangour AD ,
- Shankar B ,
- Global panel
- ↵ World Health Organization. Healthy diet. WHO Fact Sheet N°394. Geneva, Switzerland; 2015. http://www.who.int/en/news-room/fact-sheets/detail/healthy-diet
- Flaxman AD ,
- GBD 2015 Risk Factors Collaborators.
- WHO Multicentre Growth Reference Study Group
- ↵ Roser M, Ortiz-Ospina E. Global extreme poverty. 2017. http://ourworldindata.org/extreme-poverty
- ↵ World Bank. Understanding poverty; 2016. http://www.worldbank.org/en/understanding-poverty
- ↵ International Food Policy Research Institute. Global Nutrition Report 2017: Nourishing the SDGs . Washington, DC, USA, 2017. http://165.227.233.32/wp-content/uploads/2017/11/Report_2017-2.pdf
- ↵ UNICEF, World Health Organization and World Bank. Joint child malnutrition estimates: levels and trends (2018 edition). New York, NY, 2018. http://www.who.int/nutgrowthdb/estimates/en/
- de Onís M ,
- Monteiro C ,
- de Onis M ,
- ↵ International Food Policy Research Institute. Global nutrition report 2014: Actions and accountability to advance nutrition and sustainable development . 2017. http://globalnutritionreport.org/the-report/
- Gillespie S ,
- van den Bold M ,
- Stories of Change Study Team
- ↵ Headey D. Nutrition in Ethiopia: an emerging success story? Ethiopia strategic support program. Research Note 40. Ethiopian Development Research Institute, International Food Policy Research Institute, 2015. http://ebrary.ifpri.org/utils/getfile/collection/p15738coll2/id/129266/filename/129477.pdf
- Alderman H ,
- Maternal and Child Nutrition Study Group
- ↵ Nisbett N, Davis P, Yosef S, Akhtar N. Bangladesh’s story of change in nutrition: strong improvements in basic and underlying determinants with an unfinished agenda for direct community level support. Glob Food Secur 2017;13:21-9. doi: 10.1016/j.gfs.2017.01.005 .
- Griffiths M
- ↵ Famine Early Warning Systems Network. Acute food insecurity: near term (February-May 2017). Washington, DC, USA, 2017. http://fews.net/east-africa/somalia/alert/may-9-2017
- von Braun J ,
- ↵ Hasell J, Roser M. Our world in data. Famines, 2015. https://ourworldindata.org/famines
- ↵ United Nations Office for the Coordination of Humanitarian Affairs. Famine response and prevention North-East Nigeria, South Sudan, Somalia and Yemen. New York, NY, 2017. https://docs.unocha.org/sites/dms/Documents/FAMINE_press_handout_Final.pdf
- Victora CG ,
- Walker SP ,
- Dasgupta R ,
- Prendergast AJ ,
- Humphrey JH
- Hoddinott J ,
- Tesfaye R ,
- McDonald CM ,
- Flaxman S ,
- Nutrition Impact Model Study
- Massiot E ,
- Arsenault JE ,
- Stevens GA ,
- Finucane MM ,
- De-Regil LM ,
- Nutrition Impact Model Study Group (Anaemia)
- Andersson M ,
- Karumbunathan V ,
- Zimmermann MB
- Wessells KR ,
- ↵ Food and Agriculture Organization of the United Nations. Europe and Central Asia regional overview of food insecurity: the food insecurity transition. Budapest, Hungary, 2017. http://www.fao.org/3/a-i6877e.pdf
- Shariff ZM ,
- Francis D ,
- Burnier D ,
- Dorosty AR ,
- Eshraghian M
- ↵ Greenberg H, Deckelbaum RJ. Diet and non-communicable diseases: an urgent need for new paradigms. In: Eggersdorfer M, Kraemer K, Cordaro JB, et al, eds. Good nutrition: perspectives for the 21st century . Karger, 2016. https://www.karger.com/Article/Pdf/452379
- Fleming T ,
- Robinson M ,
- Franklin B ,
- Puckett S ,
- Macklin J ,
- White-Means S
- Vedovato GM ,
- Surkan PJ ,
- Jones-Smith J ,
- García OP ,
- Ronquillo D ,
- del Carmen Caamaño M ,
- Bhutta ZA ,
- Lancet Nutrition Interventions Review Group, the Maternal and Child Nutrition Study Group
- Saravia-Matus S ,
- Gomez y Paloma S
- Jaacks LM ,
- Slining MM ,
- ↵ Food and Agriculture Organization of the United Nations. Food outlook: biannual report on global food markets. Rome, Italy, 2016. http://www.fao.org/3/a-I5703E.pdf
- Kakietek J ,
- Eberwein JD ,
- ↵ Hoddinot J, Rosegrant M, Torero M. 2012. Investments to reduce hunger and undernutrition. Copenhagen Consensus 2012 challenge paper: hunger and malnutrition. http://www.copenhagenconsensus.com/sites/default/files/hungerandmalnutrition.pdf
- ↵ United States Department of Agriculture. Supplemental nutrition assistance program participation and costs (as of 4 May 2018). https://fns-prod.azureedge.net/sites/default/files/pd/SNAPsummary.pdf
- ↵ United States Department of Agriculture. Women, infants and children (WIC): WIC funding and program data. https://www.fns.usda.gov/wic/wic-funding-and-program-data
- Research article
- Open access
- Published: 29 July 2020
Factors associated with malnutrition in children < 5 years in western Kenya: a hospital-based unmatched case control study
- Edwin Gudu 1 , 2 ,
- Mark Obonyo 2 ,
- Victor Omballa 3 ,
- Elvis Oyugi 2 ,
- Cecilia Kiilu 4 ,
- Jane Githuku 2 ,
- Zeinab Gura 5 &
- James Ransom ORCID: orcid.org/0000-0001-6528-3994 6
BMC Nutrition volume 6 , Article number: 33 ( 2020 ) Cite this article
35k Accesses
3 Citations
Metrics details
Globally, under-nutrition accounts for > 3 million deaths annually among children < 5 years, with Kenya having ~ 35,000 deaths. This study aimed to identify factors associated with malnutrition in children aged < 5 years in western Kenya.
We conducted a hospital-based unmatched case-control study between May and June 2017. Cases were defined as children aged 6–59 months with either z-score for weight-for-height ≤ −2SD or ≥ +2SD; weight-for-age ≤ −2SD or ≥ +2SD; or height-for-age ≤ −2SD. Controls were children aged 6–59 months with age-appropriate anthropometric measurements. Cases were consecutively recruited while systematic random sampling was used to select controls. Data from interviews and clinical records were collected and entered into Epi-Info, which was used to run unconditional logistic regression analyses.
A total of 94 cases and 281 controls were recruited. Of the cases, 84% (79/94) were under-nourished. Mother not having attended ante-natal clinic (OR = 7.9; 95% CI: 1.5–41.2), deworming (OR = 0.8; 95% CI: 0.4–1.2), and pre-lacteal feeding (OR = 1.8; 95% CI: 1.1–3.0) were associated with under-nutrition. Delayed developmental milestones (AOR = 13.9; 95% CI: 2.8–68.6); low birth weight (AOR = 3.3; 95% CI: 1.4–7.6), and paternal lack of formal education (AOR = 4.9; 95% CI: 1.3–18.9) were independently associated with under-nutrition.
Proper pre-natal care, child feeding practices and deworming programs should be enhanced to reduce pediatric malnutrition.
Peer Review reports
Malnutrition refers to a state of either under-nutrition or over-nutrition. Under-nutrition occurs when the diet a person consumes does not meet their body’s requirement for growth and development whereas over-nutrition occurs when a person consumes too many calories [ 1 ]. Good nutrition and feeding practices are critical to a child’s growth and development especially during the first two years of life [ 2 ]. Under-nutrition impairs a child’s immunity, which can lead to recurrent infections, and impaired physical and cognitive development [ 3 ].
Under-nutrition is a major cause of morbidity and mortality especially, in low-to-middle-income (LMIC) countries. Globally, malnutrition contributes to more than 3 million deaths among children < 5 years annually [ 4 ]. UNICEF estimates that in Kenya, 239,446 children suffer from moderate acute malnutrition (MAM) and 2600 children suffer from severe acute malnutrition (SAM). Under-nutrition also contributes to about 35,000 deaths among children < 5 years each year in Kenya [ 4 ]. Stunting has also been linked to development of non-communicable diseases and lower adult productivity later in life. Children < 5 years who are prone to recurrent infectious diseases such as diarrheal illnesses, respiratory tract infections, tuberculosis and malaria often have under-nutrition as a co-morbidity [ 5 ].
The Kenya Demographic Health Survey 2014 reports that 26% of children < 5 years are stunted, 4% are wasted, and 11% are underweight. Malnutrition remains a public health concern in western Kenya. According to the survey 25.2% of children < 5 years are stunted while 8.2% are severely stunted [ 6 ]. This means that 1 in 4 children suffer from chronic under-nutrition. Therefore, identifying factors associated with malnutrition (especially under-nutrition) is vital in preventing the development of long-term deleterious effects.
This study aimed to identify clinical, demographic, and socio-economic factors associated with malnutrition in children < 5 years for public health action.
The study was carried out at Alupe Sub-County Hospital. The hospital is a level 4 hospital located in Angorom ward, Teso South Sub-County in Busia County serving a catchment population of 34,321 persons (Fig. 1 ) [ 7 ].
Map of Busia County, Western Kenya showing the constituent sub-counties including Teso South sub-county. Map source: Commission on Revenue Allocation-Kenya
Study design
We conducted a facility-based unmatched case control study carried out between May 2017 and June 2017. We chose an unmatched design due to the more limited number of cases and the inconsistency and lack of some documentation of the data available in the records at the hospital. The study population consisted of all children < 5 years attending the child welfare clinic and the outpatient clinic within the hospital during the study period.
Case definitions
Under-nourished child was defined as a child aged 6–59 months attending the hospital as an inpatient or outpatient whose anthropometric measurements were not appropriate for their age with z-scores (weight-for-height [WHZ], weight-for-age [WAZ], height-for-age [HAZ]) of <= − 2 SD. WAZ score from the WHO charts were used to define presence of under-nutrition [ 8 ].
A participant was classified as stunted if HAZ score was <−2SD and severely stunted if HAZ score was <−3SD. Wasting was defined as WHZ score < −2SD while severe wasting was WHZ score < −3SD. Any participant with WAZ score < −2SD was classified underweight.
Mid upper arm circumference (MUAC) calculations
For the MUAC cut-points to determine whether a child was under- or over-nourished, we used the cut-points of any child with MUAC < 126 mm was classified under-nourished [ 8 ].
Definition of controls
Any child aged 6–59 months attending the hospital as an inpatient or outpatient whose anthropometric measurements are appropriate for their age with z-scores between -2SD and + 2SD [ 9 ].
Sample size determination
The sample size was calculated using statistical software Epi Info® version 7.2.0. The study assumed a 95% confidence interval, 80% power, 10% wasting among controls [ 10 ], and the ratio of cases to controls of 1:3. Using these assumptions, the minimum sample size was 375 (94 cases and 282 controls).
Selection of cases and controls
The cases were sampled consecutively due to the low number seen each day for eligible children enrolled for nutritional support in welfare clinic. The sampling occurred via the data entered into the MoH Child Health Logbook, which would have each presenting child’s age, MUAC, and other information indicative of over-, under-, or at-level nutrition. The controls were selected through systematic random sampling from the data in the logbook. The average number of children < 5 years visiting the outpatient section of the child welfare clinic daily was used as a sampling frame. This was determined by obtaining the number of children visiting the out-patient clinic between April and June of three preceding years before the study. The study was conducted during weekdays within the duration of the study period hence the number of controls to be enrolled in the study on any single day was pre-determined. Using the average number of patients seen each day at the clinic and number of controls to be enrolled in the study each day, a sampling interval was determined, and the first control was picked randomly between one and the sampling interval. The sampling interval was then added to enroll the remaining controls. Any eligible participant whose legal parent/guardian did not give oral consent was replaced by the next available participant whose legal parent/guardian consented to the study.
Data collection
Triage was carried out by the hospital staffs as is the norm and all critically and severely ill patients were urgently attended to by the hospital clinicians as per procedures and guidelines of the hospital. The weight was measured using electronic digital weighing scale (Seca®). For height/length, children < 2 years were measured lying down (recumbent length) while those who were > =2 years were measured standing up. For MUAC and head circumference, a non-stretch tape was used.
A pre-tested trans-adapted interviewer-administered questionnaire was used for each study participant to obtain demographic, clinical, nutritional, social and economic information. This questionnaire was adapted from a survey sheet used in Guinea [ 11 ]. (Each patient was de-identified by a unique code to ensure their privacy and maintenance of confidentiality.)
Data management
Data entry, cleaning, validation and analysis was done using Microsoft Excel (Microsoft, Seattle, WA, USA), and Epi info version 7 (CDC, Atlanta, GA, USA). Anthropometric data was analyzed using WHO Anthro® software version 3.2.2 (WHO Anthro®) to assess nutritional indicators like weight-for-length/weight-for-height (wasting), weight-for-age (underweight or overweight), length-for-age/height-for-age (stunting), MUAC-for-age, and HC-for-age. The software then provided the z-scores based on gender, age and the anthropometric measurements. We calculated measures of central tendency and dispersion for the continuous variables and proportions for categorical variables. For univariable analysis, we calculated odds ratios (OR), 95% confidence intervals (CI), chi-square statistics and p -values. Variables with p-value ≤0.05 were statistically significant. We carried out unconditional logistic regression with variables that had p-values of < 0.2 at univariable analysis. A backward elimination stepwise method was used to identify independent factors associated with malnutrition. During model building, any variable that caused an insignificant increase in deviance on removal from the model were left out of the model while the variable that caused a significant increase in deviance on removal were retained in the model. All variables removed from the model when a backward stepwise method was performed and those known to be potential cofounders or factors associated with malnutrition from previous studies were tested for confounding, any of the mentioned variables that had a more than ten percentage change (> 10%) between the crude and adjusted odds ratio was considered as a confounder. The final model after testing for all biologically and statistically plausible interactions had only variables with p -value ≤0.05.

Description of the study participants
There were 375 participants (94 cases and 281 controls), with median age of 16 months (IQR 10, 22), and 51% (191/375) male. Males were 57% (54/94) of cases and 49% (137/281) of controls.
Nutritional status of cases
Of the cases, 84% (79/94) were under-nourished and 16% (15/94) over-nourished. Among those that were under-nourished, by assessing the WHZ score, 20% (16/79) were wasted while 9% (7/79) were severely wasted. Among the same group, using WAZ score, 39% (31/79) were underweight while 29% (23/79) were severely underweight. Using the HAZ score among the under-nourished, 46% (36/79) were stunted while 38% (30/79) were severely stunted.
Univariable and multivariable analysis of factors associated with under-nutrition
On univariable analysis, socio-demographic factors like high birth order of five or more (OR = 2.3; 95% CI: 0.9–6.0), living in urban areas (OR = 1.9; 95% CI: 0.8–4.3), children whose mothers had no formal education (OR = 2.0; 95% CI 0.9–4.4), those whose fathers had no formal education (OR = 4.6; 95% CI: 1.4–15.0) and those who came from large family sizes of more than 6 occupants (OR = 1.8; 95% CI: 1.1–3.0) had higher odds of developing under-nutrition.
Pre-natal maternal factors were also shown to increase odds of developing under-nutrition. These included: participants whose mothers’ did not attend antenatal clinic (ANC) at least once (OR = 7.9; 95% CI: 1.5–41.6), participants whose mothers who did not attend 4 ANC visits as recommended by WHO (OR = 1.6; 95% CI: 0.9–2.7) and those whose mothers had illness during pregnancy (OR = 1.7; 95% CI: 1.0–2.8). The participants who were born preterm (OR = 2.0; 95% CI: 0.6–7.4) and those with low birth weight (OR = 2.8; 95% CI: 1.2–6.2) had higher odds of under-nutrition compared to term babies and those with normal birth weights.
Post-natal factors such as failure to complete or not being up-to-date on immunizations as per the national immunization schedule (OR = 2.2; 95% CI: 0.7–7.2) and human immunodeficiency virus (HIV) sero-exposure (OR = 1.4; 95% CI: 0.6–3.5) and delayed developmental milestones (OR = 18.9; 95% CI: 4.1–87.5) also increased the odds of developing under-nutrition. The participants who were eligible for deworming and had been dewormed at least once were protected from under-nutrition (OR = 0.8; 95% CI: 0.4–1.2). Infant and young child feeding practices also affected nutritional status of the participants. During the study period, 24% (89/375) of the participants were receiving pre-lacteal feeds increased their odds of under-nutrition (OR 1.8; 95% CI: 1.0–3.1). Exclusive breastfeeding for 6 months as recommended by the WHO was also widely practiced with 72% (271/375) of the participant’s parents adhering to this guideline. Forty percent (149/375) of the participant’s parents still used bottle with nipple for feeding, while 31% (116/375) ceased breastfeeding before the recommended 2 years of age. However, during the study period, there was no statistically significant association between duration of exclusive breastfeeding for the first six months of life (OR = 1.1; 95% CI 0.6–2.0), cessation of breastfeeding at less than 2 years (OR = 0.6; 95% CI 0.2–1.7) or bottle with nipple feeding (OR = 0.9; 95% CI 0.5–1.5) and developing under-nutrition.
Economic factors of the families also affected the nutritional status of the participants. Those whose mothers were unemployed had higher chances of under-nutrition (OR = 1.8; 95% CI 1.0–3.1) whereas those families with an average monthly income of above 5000 Kenya shillings (KES) were protective of under-nutrition (OR 0.7; 95% CI 0.4–1.2) (Table 1 ).
On multivariable analysis, delayed developmental milestones (AOR = 13.9; 95% CI: 2.8–68.6); low birth weight (AOR = 3.3; 95% CI: 1.4–7.6) and paternal lack of formal education (AOR = 4.9; 95% CI: 1.3–18.9) were found to be independently associated with under-nutrition.
The study identified various factors affecting nutritional status among children < 5 years which need to be adequately addressed. This included both pre-natal and post-natal factors as well as infant and young child feeding practices. Therefore, consistent follow-up of pregnant mothers from the antenatal period and post-natal care of the children < 5 years needs to be enhanced.
Among the undernourished, we found that stunting was the most common form of malnutrition, followed by children who were underweight and wasting being the least common among the study population. Stunting was common among cases of under-nutrition and over-nutrition alike. Stunting is a chronic form of malnutrition that results from prolonged non-adherence to proper dietary requirements to meet the body’s physiological needs. These findings were similar to those of a demographic and health survey carried out in the Western Kenya in 2014 [ 6 ]. Other studies carried out in Burundi and Uganda also had similar findings [ 12 , 13 ].
Deworming of children > 1 year of age was also found to be protective of under-nutrition. This finding was in line with another study done in India among pre-school children which showed substantial weight gain among children who were dewormed [ 14 ]. This is because intestinal nematodes affect absorption of both micro and macronutrients which are vital for a child’s growth. However, current systematic reviews show little benefit is derived from mass deworming. They show that children found to be worm infested are the ones that gain weight more significantly compared to non-worm infested children [ 15 , 16 ].
Proper breastfeeding practices for children are advocated for by WHO [ 17 ]. Children that are breastfed up to 2 years of age show quicker linear growth than those breastfed for shorter durations [ 2 ]. Feeding practices such as bottle with nipple feeding, breastfeeding within thirty minutes of delivery, exclusive breast feeding for 6 months and cessation of breastfeeding at 2 years were also assessed during the study. However, they were not statistically significantly associated with under-nutrition. In contrast, the giving of pre-lacteal feeds adversely affected nutritional status and predisposed the children to under-nutrition. This has also been shown by other studies [ 18 , 19 , 20 ]. This could be because pre-lacteal feeding affects the quality and quantity of breastfeeding which in turn affects the nutritional intake by the child. As such, proper education on feeding practices during post-natal period should be enhanced.
Children with under-nutrition were also shown to be more likely to have delayed developmental milestones. This finding was consistent with other studies [ 21 , 22 , 23 ]. This could be because they lack the macro and micronutrients necessary for normal growth and development. Children with prematurity and low birth weight also had higher odds of under-nutrition. These findings were similar from a review done in several countries [ 24 ]. This could be because they require more nutrients for catch-up growth which if not provided in adequate quantities leave them vulnerable to develop under-nutrition. These children should therefore be followed up more closely.
We also found that lack of parental formal education was linked to development of under-nutrition with paternal illiteracy being shown to have a greater influence. This finding concurred with other studies [ 20 , 25 ]. This could be because the community being a patriarchal society, the fathers control the family’s resources. As such, lack of formal education could mean no formal employment and by extension no regular source of income to provide for their families.
Our study also showed that the cases of over-nutrition were also high, compared to findings of other studies in Kenya, despite the hospital serving a population of predominantly low socio-economic status [ 26 ]. This clearly points to the double burden of malnutrition that is supported by other literature based on a critical review done in other lower middle income countries [ 27 ]. This is a new development over the last couple of decades that needs to be further explored to halt and decrease the burden of cases of over-nutrition.
During the study period, children aged less than 12 months were more likely to be over-nourished. This finding was similar to another study carried out in Kenya in 2009 [ 28 ]. This could be because younger children are more likely to receive more attention and feeding effort from their parents as compared to older children. Male gender was also positively associated with over-nutrition. A study carried out in Kenya in 2016 had similar findings [ 29 ]. This could probably be due to the value and cultural preferences placed on the male child. As such, they are likely to be better fed as compared to the girl child. This has also been shown in other Sub-Saharan African countries [ 30 ].
Children who came from households in urban areas and those who came from families with higher average monthly income had higher odds of over-nutrition. This finding was similar to other studies [ 28 ]. This could be due to the higher levels of income which increase their ability to provide more than enough nutrition for their growing children.
Maternal lack of formal education also increased the chances of developing over-nutrition. This finding was contrary with other studies carried out in Sub-Saharan Africa [ 30 ]. High birth weight was also linked to increased chances of over-nutrition. This has also been shown by other studies [ 30 , 31 ]. However, the exact mechanism of this link has not yet been clearly described.
We conducted a hospital-based case-control study and as such, its findings cannot be generalized to the entire population of under-five children in Western Kenya. The data collected on some of the variables could be susceptible to recall bias more so if the child was brought in by a guardian. Another limitation of the study was that the study relied on participants’ self-reported data, which was prone to recall bias and social desirability bias and interviewer bias due to the retrospective tracking of information beyond the advantages of case control study. The other limitation was that since it was a case–control study, which means it cannot establish the relationship between exposure and disease. Anthropometric measures and their technical errors are another limitation because it can result in misclassification of children’s nutritional status. However, we gave strict attention to the study procedures, including the process of training the research team and workers at the hospital, standardization of anthropometric measurements, and close and supportive supervision throughout the field activities to minimize biases.
Proper pre-natal care, child feeding practices and deworming programs should be enhanced. As such, we recommend that close monitoring especially of children more likely to be malnourished should be enhanced. This can be done by providing job aids to providers to help them talk to parents about adherence to key recommended practices such as appropriate feeding, continuous auditing of patient outcomes, and better use of data for improved decision-making should be implemented at these facilities.
Proper infant and young child feeding practices and deworming should be emphasized. Provider advocacy and better health education to parents should be intensified in the region for better outcomes. The hospital in conjunction with Busia County Government should organize for regular outreach to the community targeting pregnant and lactating mothers, strengthen deworming programs for children > 1 year and all children with delayed developmental milestones. It should also organize for health advocacy camps targeting the parents with children < 5 years to educate them on the proper infant and young child feeding practices.
Availability of data and materials
All data generated or analyzed during this study are available upon request to the corresponding author.
Abbreviations
Moderate Acute Malnutrition
Mid Upper Arm Circumference
Weight for Height Z-score
Weight for Age Z-score
Height for Age Z-score
Standard Deviation
Adjusted Odds Ratio
Confidence Interval
UNICEF, Progress for children, in UNICEF. 2016.
Google Scholar
Onyango AW, Esrey SA, Krammer MS. Continued breastfeeding and child growth in the second year of life: a prospective cohort study in western Kenya. Lancet. 1999;354(9195):2041–5.
Article CAS Google Scholar
Services, J.C.o.I.C.s, Orphan Nutrition. 2017.
Fanzo J, Hawkes C, Udomkesmalee E, Afshin A, Allemandi L, Assery O, Baker P, Battersby J, Bhutta Z, Chen K, Corvalan C. Global Nutrition Report. 2019.
Intitute, I.F.P.R. Global nutrition report. Washington DC: International Food Policy Research Intitute; 2015.
Statistics, K.N.B.o. 2014 Kenya Demographic and Health Survey. Nairobi: Kenya National Beaureau of statistics; 2015.
System KHI. DHIS2, in DHIS2; 2016.
Van den Broeck J, Willie D, Younger N. The World Health Organization child growth standards: expected implications for clinical andepidemiological research. 2009;247–51.
Organization, W.H. World Health Organization (WHO) - global database on child growth and malnutrition. 2017.
Shikur B. The relationship between malaria and malnutrition among under five children in Adami Tulu District, south-Central Ethiopia: a case-control study. Addis Ababa: Addis Ababa University College of health sciences; 2014.
Sory DI, Sory D, N’fanly C, Ibrahima D, Mamoudou BE, Moussa C, et al. Neonatal mortality associated with the referral of low birth weight newborns to the Institute of Child Nutrition and Health (INSE). Open J Pediatrics. 2019;9(4):287–95.
Article Google Scholar
Yiga, P. E. T. E. R. (2016). Child Growth and Determinant Factors: A Case Study of Burundi. Unpublished dissertation. Universiteit Gent.
Gilbert H. An investigation on factors associated with malnutrition among underfive children in Nakaseke and Nakasongola districts, Uganda. BMC Pediatr. 2015;15:(134):134.
Shally A, Peto R, Pande V. Effects of deworming on malnourished preschool children in India. PLoS Negl Trop Dis. 2008;2(4):223.
Taylor R. Deworming school children in developing countries. Cochrane: Cochrane Library; 2015.
Tim A. Deworming delusions? Mass drug administration in east African schools. J Biosoc Sci. 2016;48:116–47.
Organization, W.H. Indicators for assessing breastfeeding practices. Geneva: World Health Organization; 1991.
Nayak R, Mallapur D. Determinants of nutritional status in under five children- a cross sectional study. Ann Commun Health. 2014;2(2):26–9.
Wagaye F, Tariku A. Undernutrition and associated factors among children aged 6-59 months in east Belesa District, Northwest Ethiopia: a community based cross-sectional study. BMC Public Health. 2016;16(506):1–10.
Asfaw M, Lamessa D. Prevalence of undernutrition and associated factors among children aged between six to fifty nine months in Bule Hora district, South Ethiopia. BMC Public Health. 2015;15(41):41.
AA. Children at risk for developmental delay can be recognized by stunting, being underweight, ill health, little maternal schooling or high gravidity. NIH Public Access. 2010;51(6):652–9.
Hyun P. The impact of nutritional status and longitudinal recovery of motor and cognitive milestones in internationally adopted children. Int J Environ Res Public Health. 2010;8:105–16.
Deepti D. A community-based study on growth and development of under-five children in an Urbanized Village of South Delhi. J Trop Pediatr. 2016;62:446–56.
Christian P, Lee S. Risk of childhood undernutrition related to small-for-gestational age and preterm birth in low- and middle-income countries. Int J Epidemiol. 2013;42:1340–55.
Zaida H, Luis S. Cross-Sectional Study of Malnutrition and Associated Factors among School Aged Children in Rural and Urban Settings of Fogera and Libo Kemkem Districts, Ethiopia; 2014.
Hoffman D, Cacciola T, Barrios P, Simon J. Temporal changes and determinants of childhood nutritional status in Kenya and Zambia. J Health Popul Nutr. 2017;36(1):27.
Tzioumis E, Adair LS. Childhood dual burden of under- and overnutrition in low- and middle-income countries: A critical review. Food Nutr Bull. 2014;35(2):230–43.
Constance G. Childhood overweight and obesity among Kenyan pre-school children: association with maternal and early child nutritional factors. Public Health Nutr. 2009;13(4):496–503.
Ole Tankoi EO, Asito SA, Adoka S. Determinants of Malnutrition among Children Aged 6–59 Months in Trans-Mara East Sub-County, Narok County, Kenya. Int J Public Health Saf. 2016;1(116):2.
Keino S. Determinants of stunting and overweight among young children and adolescents in sub-Saharan Africa. Food Nutr Bull. 2014;35(2):167–78.
Qiao Y. Birth weight and childhood obesity: a 12-country study. Int J Obes Suppl. 2015;5:74–9.
Download references
Acknowledgements
We would like to appreciate the participants whose data were used in this study. We also acknowledge Alupe Sub-County Hospital and Busia County Government.
This study was fully funded by Kenya Field Epidemiology and Laboratory Training Program. The funding body of this study did not participate in the design or conclusion of the study.
Author information
Authors and affiliations.
Ministry of Health, Moi Teaching and Referral Hospital, Eldoret, Kenya
Ministry of Health, Field Epidemiology & Laboratory Training Program, Nairobi, Kenya
Edwin Gudu, Mark Obonyo, Elvis Oyugi & Jane Githuku
Center for Global Health Research, Kenya Medical Research Institute, Nairobi, Kenya
Victor Omballa
West Pokot County Health Department, Kapenguria, West Pokot, Kenya
Cecilia Kiilu
Ministry of Health, Division for Human Resource for Health Development, Nairobi, Kenya
Zeinab Gura
Piret Partners Consulting, 611 Pennsylvania Avenue SE, Unit 358, Washington, DC, 20003, USA
James Ransom
You can also search for this author in PubMed Google Scholar
Contributions
EG, MO, JG, EO, and JR conceived the study, EG collected data, EG, VO, EO, CK, JG, ZG, and MO analyzed the data and drafted the manuscript. All authors helped with the interpretation of the results, read, critically reviewed and approved the final manuscript.
Corresponding author
Correspondence to James Ransom .
Ethics declarations
Ethics approval and consent to participate.
Ethical clearance was sought from Institutional Review Ethics Committee Moi University/Moi teaching and Referral Hospital under reference FAN: IREC 1870. Permission for the study was also sought from the County health department and the hospital administration. During the interviews informed oral consent was obtained from parents/legal guardians of all study participants after explaining the objectives of the study. The authors used oral consent to accommodate the low literacy rates in the populations served by this hospital in Alupe. Measures were taken to assure confidentiality of the information provided during these interviews and codes were used to de-classify personal identifying information of study participants. Measures were taken to assure collected data were properly stored and secured and only accessible to the investigators.
Consent for publication
This study was based on patient records, thus consent for publication was not applicable.
Competing interests
The authors declare that they have no personal or financial competing interests that may bias publication of this manuscript.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Gudu, E., Obonyo, M., Omballa, V. et al. Factors associated with malnutrition in children < 5 years in western Kenya: a hospital-based unmatched case control study. BMC Nutr 6 , 33 (2020). https://doi.org/10.1186/s40795-020-00357-4
Download citation
Received : 09 July 2019
Accepted : 18 June 2020
Published : 29 July 2020
DOI : https://doi.org/10.1186/s40795-020-00357-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Nutrition
ISSN: 2055-0928
- General enquiries: [email protected]
- Research article
- Open access
- Published: 21 February 2019
Malnutrition and its associated factors: a cross-sectional study with children under 2 years in a suburban area in Angola
- João B. Humbwavali ORCID: orcid.org/0000-0002-0422-1084 1 , 2 ,
- Camila Giugliani 2 ,
- Luciana N. Nunes 2 ,
- Susana V. Dalcastagnê 2 &
- Bruce B. Duncan 2
BMC Public Health volume 19 , Article number: 220 ( 2019 ) Cite this article
28k Accesses
11 Citations
4 Altmetric
Metrics details
The prevalence of child malnutrition in Angola is still very high, and little is known about its associated factors. The aim of this study was to identify these factors in children under 2 years in a suburban area of the country’s capital city.
We used data from a cross-sectional population-based study conducted in 2010. The outcomes studied were stunting and underweight. Multivariable analysis was conducted; prevalence ratios were estimated by Poisson regression with robust variance using a hierarchical model.
Of the children studied ( N = 749), 232 [32.0% (95% CI: 28.7–35.5%)] were stunted and 109 [15.1% (95% CI: 12.6–17.9%)] were underweight. In multivariable analysis, occurrence of diarrhea (PR 1.39 [95% CI: 1.07–1.87]) and the death of other children in the household (PR 1.52 [95% CI: 1.01–2,29]) were associated with stunting and underweight, respectively. In the model composed only of distal and intermediate factors, the primary caregiver not being the mother increased the prevalence of stunting by 42% (PR 1.42 [95% CI: 1.10–1.84], and a mother’s working outside the house while not being self-employed was associated with its reduced prevalence (PR 0.55 [95% CI: 0.34–0.89]). In the intermediate model, each additional month of delay in the onset of prenatal care increased the relative prevalence of underweight by 20% (PR 1.20 [95% CI: 1.03–1.40]).
Conclusions
Despite the high prevalence rates of stunting and underweight, relatively few risk factors were identified for these conditions, suggesting that collective exposures are likely to play a major role in causing malnutrition in Angola. The individual factors identified can be useful for the development of strategies to deal with this public health problem.
Peer Review reports
It is known that good nutrition is a key driver in achieving a satisfactory level of human development. The World Health Organization (WHO) estimated in a recent report that there are 178 million undernourished children in the world, 20 million of whom suffer from severe malnutrition; undernutrition contributing to 3.5 to 5 million annual deaths among children under 5 years [ 1 ].
The monitoring of the goals against hunger set by the Millennium Development Goals ended in 2015 with the goals not having been met [ 2 ]. In Sub-Saharan Africa, the slow pace of progress in fighting hunger over the years is particularly worrisome [ 3 ]. This region still holds the highest prevalence of undernourishment for any region, having the number of undernourished people even increased by 44 million between 1990 and 92 and 2014–16 [ 2 ].
Some factors associated with malnutrition have been identified in the literature. In the global context, food security, mother and child care (fertility rate and maternal literacy), characteristics of the health services and environment, and potential resources (national and domestic income) were factors explaining the variability in the prevalence of malnutrition among children under 5 years of age in developing countries [ 4 ].
Angola, located on the south Atlantic coast of West Africa, is one of the largest and richest countries in the sub Saharan Africa. Its total population, in the census carried out in 2014, was around 25 million inhabitants [ 5 ]. After a long civil war, which ended in 2002, the country’s health system is still being rebuilt. In this context, health data of the Angolan population, often obtained through estimates made by nongovernmental organizations operating with the government and health services, are scarce, and scant primary data exist in terms of the determinants of malnutrition. Knowledge of this information is important for proper policy planning to address this problem in a context-specific manner. Thus, the present study aims to describe the nutritional status of children under 2 years of age in a suburban area of Angola, and to identify the factors associated with the occurrence of malnutrition in this population.
We carried out a cross-sectional population-based study, linked to a larger project entitled “Developing primary health care services in Angola: a proposal for evaluation of the Community Health Workers Program”, whose data were collected from August 1 to September 26 of 2010 [ 6 ]. The study site, Cacuaco, located in the suburban region of Luanda, was chosen because it was the first municipality to implement the Angolan Community Health Workers Program. The estimated population in Cacuaco is 700,000 inhabitants, distributed over an area of 572 km 2 (population density of 1.2 inhabitants per km 2 ).
Participants were recruited in four neighborhoods, which were selected based on the criteria: neighborhood map availability, authorization by resident committees and researchers’ security. The neighborhoods were divided into micro areas, each with 100 households. One house in each micro area was randomly selected as the starting point, and every third house to the right of the index house was visited by the interviewers.
Children under 2 years of age and their mothers were eligible. The exclusion criteria were: mothers who lived for less than 1 year at the study site or who did not live with the child. In the case of more than one child under 2 years of age in the same household, only the oldest was included, since in the original study there was an intention to take advantage of the children’s exposure time to the public health interventions that were being implemented in the area. In case of twins, the child selected was the one born first. In the original study, a sample of 700 children was calculated as necessary, considering the prevalence estimation of main endpoints studied (e.g. children’s low body mass index-for-age and low height-for-age). With this sample size and considering point estimators varying from 10 to 40 percentage points, 95% confidence intervals of < 2.5 percentage points on either side would be attained, considering a conglomerate effect of 1.5. To attain relative risks of the size seen in previous investigations of determinants in other African countries and in Bangladesh [ 7 , 8 ] for the outcome “malnutrition”, assuming a 5% α-error, power of 80% and the same conglomerate effect, a sample size ranging from 348 to 574 would be necessary.
The Angolan interviewers underwent 5 days of intensive training, after which four teams were assembled, each consisting of a field coordinator, four interviewers, and an area supervisor. A structured questionnaire was applied to the mother and additional data were obtained from pregnancy and child health cards (an English version of the questionnaire is provided in Additional file 1 ). Standardized anthropometric measurements were obtained by properly trained field coordinators with Tanita® digital scales and custom-made wooden stadiometers.
The outcomes investigated were stunting (low stature for age) and underweight (low weight for age), using the WHO definition of two or more Z scores below the median [ 9 ]. Exposure variables surveyed through the questionnaires included: sociodemographic characteristics, economic conditions, living conditions, health situation of the mother, the child and other children in the household, and the use of health services by the mother and the child.
The economic condition was assessed indirectly by means of a score, based on a previous study conducted in Ghana [ 10 ], to stratify the participating families into categories of a more or less favored economic situation. Scores were given for certain household characteristics (house building material, piped water, electric light, presence of a refrigerator and of a toilet inside the house) totaling values from 0 to 10.
The questionnaires were coded, scanned and entered into the database using the Teleform® software. In the data analysis, descriptive statistics were initially performed, followed by multivariable analyses using a hierarchical model based on the existing literature [ 11 ]. In this model, the exposure variables were classified into levels (distal, intermediate and proximal) considering their proximity to the dependent variable, according to the conceptual basis for possible interrelationships involving the factors under study [ 12 ]. As outcomes had high prevalence (greater than 10%), Poisson regression was employed [ 13 ] in order to have a better estimate of prevalence ratios and their respective confidence intervals. Moreover, we chose the robust variance model, also known as modified Poisson regression, because it can give a better estimate of the variability of the coefficient estimator when applied to binary outcome variables [ 14 ]. At each level of the hierarchical model, the variables were adjusted in relation to the others at the same level. Those with a p -value < 0.20 were carried forward to adjust the analyses in the next level. The p-value for statistical significance was 0.05. Statistical analyses were performed with the Statistical Package for the Social Sciences (SPSS) software version 18.0. Missing data were not considered in the analyses, resulting in successive losses in the sample across the levels of the multivariable model.
The study was approved by the Ethics Committee of the Federal University of Rio Grande do Sul (register number 2008045) and by the Provincial Health Department of Luanda, Angola. The interviews were preceded by the signing of an informed consent form by the mother.
We visited 1360 houses in 49 micro areas of the four selected neighborhoods. Forty-two (5.7%) children whose mothers had lived for less than 1 year at the study site or who did not live with the child were excluded, 111 (15.0%) were lost after three consecutive visits at different days and times, and 10 (1.4%) mothers refused to participate. The final sample included 749 children and their mothers. Table 1 shows the sociodemographic characteristics, as well as the housing conditions and some health features of the study population, together with their crude association with the studied outcomes.
Table 2 shows the nutritional status of children, according to anthropometric data measured on the day of the visit, indicating the Z scores for length-for-age and weight-for-age. Considering a Z score below − 2, 232 (32%; 95% CI: 28.7–35.5%) were stunted and 109 (15.1%; 95% CI: 12.6–17.9) were underweight. In Table 2 , it is also possible to observe the proportions of severely malnourished children, considering a Z score below − 3.
Tables 3 and 4 show the prevalence ratios (PR) for the studied outcomes, adjusted for the predictors, according to the hierarchical model. For underweight (Table 3 ), greater gestational age at the onset of prenatal care was the only factor in distal or intermediate models presenting an association. At the proximal level, only the occurrence of death of other children in the household was associated with the outcome. A non-maternal primary caregiver, female sex of the child, and diarrhea during the last 15 days all presented non-statistically significant PRs greater than 1.3. For stunting (Table 4 ), in distal and intermediate models, mother’s current occupation, with a global p -value of 0.109, followed to the next level. In the intermediate model, a mother’s working but not being self-employed was associated with a prevalence 45% lower while the primary caregiver not being the mother was associated with a prevalence 42% higher. In the proximal model, only the occurrence of diarrhea in the last 15 days was associated with the outcome.
In our study, the prevalence rates of stunting and underweight in children under 2 years of age was 32 and 15.1%, respectively. Regarding malnutrition’s associated factors, we found, after adjustment for predictors, the occurrence of death of other children and greater gestational age at the onset of prenatal care as risk factors for underweight, and the presence of diarrhea in the last two weeks, as well as mother’s working but not being self-employed and primary caregiver not being the mother, as predictors in the case of stunting.
The prevalence of stunting found in this study, considered high according to WHO standards [ 15 ], was slightly higher than that found in the United Nations Children’s Fund (UNICEF) survey conducted in Angola in 2009 (29%), whereas the one found for underweight, considered medium by WHO, was slightly lower (16%) [ 16 ]. More recent data released by the Joint Malnutrition Estimates in 2016 show estimates of 4.9% (4.6% in urban area) and 37.6% (31.8% in urban area) of underweight and stunting in Angola, respectively [ 17 ].
In the African region, existing data show that the continent has been making slow progress in reducing stunting over time. From 2000 to 2015, although stunting prevalence among children under 5 decreased from 38 to 32%, the number of stunted children increased from 50.4 million to 58.5 million [ 17 ]. Considering that the first of six global targets set by Member States in the 65th World Health Assembly, to be achieved by 2025, is to reduce by 40% the number of stunted children, then the region is not making a good response [ 17 ].
Our findings showed that children of mothers with a history of at least one death among the previous children had a higher prevalence of underweight. This variable seems to reflect the number of people living in the house, since mothers with deceased children had a higher average number of people living in the household (6.99 vs. 6.22, p < 0.001; univariate analysis, data not shown). In this case, our finding is in line with other studies in different countries that found that children of mothers with more children (indirectly reflecting more people living in the household) have more malnutrition [ 7 , 18 , 19 , 20 ]. We found that early onset of prenatal care protected children from being underweight, like other studies, in Ghana and in Brazil, that showed that improved access to prenatal care was associated with a lower prevalence of malnutrition [ 21 , 22 ].
We also observed the association of diarrhea in the last two weeks with stunting, but not with underweight, partially corroborating with studies in Ethiopia [ 7 ] and Bangladesh [ 8 ]. The mother’s occupation (another in relation to self-employed) obtained statistical significance in the intermediate model. In any case, mothers with other occupations (with formal employment or students), who are not self-employed nor housewives, usually have more resources, both financial and related to organization of daily life, which could influence the nutritional status of their children. Hien and Hoa found an independent association of maternal occupation (peasant mothers) with a higher risk of malnutrition [ 18 ]. In our analysis, the main caregiver (the mother compared to another) presented statistical significance in the intermediate model ( p = 0.007), suggesting that the presence of the mother taking care of the child has a protective role in relation to malnutrition.
We identified two risk factors not mentioned in other studies – mother working in a non self-employed position and non maternal caretaker. This is an original contribution of our study, which probably makes more sense in the modern life style and in the urban setting, and it highlights the need to discuss about the best strategies to help mothers to better structure and organize their lives in the postpartum period, such as having a protected maternal leave followed by formal job opportunities.
Unlike other studies [ 18 , 20 , 22 , 23 ] we have not identified low birth weight as a determinant of malnutrition, possibly because the data collected was self-reported, therefore with reduced reliability. We also did not find an association of maternal schooling nor of economic situation with the evaluated outcomes, like other authors did [ 7 , 11 , 19 , 20 , 21 , 22 ]. It is likely that our population is very homogeneous in economic terms, and that the difference in years of school, in the context studied, does not represent a real difference in the life of families, given the low quality of education in general. We did not find any association with the child’s sex, contrasting with two studies that have identified the male sex as a risk factor for malnutrition [ 7 , 8 , 24 ].
Our study has some limitations. It is important to note that, although the study had a sample of 749 mothers and children, in many of the variables, the N was much smaller, and this would impair the multivariable model. Thus, a few variables, such as exclusive breastfeeding below 6 months ( N = 269), were not included in the model due to the small number of observations. In addition, the occurrence of successive losses in the sample can be observed in the multivariable analysis, due to missing values in one or another variable.
Despite these limitations, this is an unprecedented work whose findings bring relevant contributions to the health policies focused on improving the nutritional status of children in Angola and in other countries with similar contexts. Our results point to the importance of strengthening family planning policies and to the need for improvement in primary health care and sanitation, because of the high prevalence of malnutrition found, especially stunting, which has been associated with the occurrence of diarrhea in the last two weeks. Due to the study’s cross-sectional design, we cannot affirm causality, so it is possible that children with recent diarrhea have had repeated episodes previously, leading to chronic malnutrition and stunting. Or that due to pre-existing nutritional deficits, these children are more vulnerable to infections that lead to diarrhea. According to Rissin et al. (2006), malnutrition can be considered a timely disease of recurrent infectious diseases, and in this view, recurrent diarrhea has been shown to be a potential determinant of malnutrition, due to the decreased nutrient absorption imposed on the organism [ 25 ].
It is also worth mentioning that the studied population was collectively exposed to several factors that may influence their nutritional status. Aside from lack of access to quality primary care and education, as mentioned previously, these include endemic malaria, precarious sanitation and lack of food. These exposures, because of their almost universal character in the context of our study, were not measured. Therefore, we do not know how much they are involved with the high prevalence of malnutrition at the study site, but the fact that we identified relatively few individual risk factors speaks in favor of the importance of collective exposures. Nevertheless, it is important to highlight the effort of revitalization of the Municipal Health System in Cacuaco [ 26 ], whose deployment began in 2007, including the Community Health Workers Program [ 6 , 27 ]. The findings concerning this suburban area in Luanda cannot be generalized to the whole country, but they provide a scenario that is probably similar to other suburban areas in Angola, especially those surrounding the capital city. Additionally, these results shall be insightful for other countries as well, especially in Sub-Saharan Africa, where resembling contexts are likely to be found.
We are currently living the post 2015 development era, and estimates of child malnutrition are useful for monitoring progress towards the Sustainable Development Goals, in particular “ending hunger, achieving food security, and improving nutrition and promoting sustainable agriculture” [ 2 ]. In Africa, the variation in stunting prevalence was 40.5% (1980) [ 26 ] to 32% (2015) [ 17 ]. According to prominent researchers, investing in interventions aimed at improving physical growth and mental health of children is important not only to reduce the prevalence of malnutrition but also to avoid its negative functional consequences throughout the life cycle [ 28 ] and to be able to build a favorable human capital [ 29 ].
Our findings also cause reflection on the nutritional transition, a worldwide trend. It is important to note that food insecurity is complex, leading to recurrent malnutrition and hunger crises, but also to overeating and eating errors, which can lead to overweight and obesity. Therefore, it is necessary to be alert to the double burden of malnutrition caused by the vicious circle of poverty, hunger and food insecurity, facing its determinants and prioritizing the implementation of public policies that can prevent such illnesses, as is being pointed out in this study.
The high prevalence of stunting and underweight found in this study enable us to conclude that malnutrition is still an important problem among children under 2 years in Angola. The absence of strong individual risk factors in our study suggests that a combination of life course factors, particularly those associated with pregnancy and birth, which we could not accurately measure, and collective exposures, over which individuals have little control, likely play a predominant role. Thus, a joint and coordinated effort between government, community, and nongovernmental organizations operating in the country is necessary to improve the nutritional status of children, focusing on effective programs and policies that reinforce the removal of collective risk factors such as lack of safe water and basic sanitation, and the provision of adequate and accessible education and health services to the population to enable effective health education actions as well as prevention and treatment of child malnutrition at the individual level.
Abbreviations
Body mass index
Prevalence ratio
Statistical package for the social sciences
United nations children’s fund
World health organization
World Health Organization. Essential nutrition actions: improving maternal, newborn, infant and young child health and nutrition. Geneva: WHO; 2013 [accessed in 2019 11 Jan]. Available from: http://apps.who.int/iris/bitstream/10665/84409/1/9789241505550_eng.pdf .
United Nations. Food and Agriculture Organization, International Fund for Agricultural Development, World Food Programme. The state of food insecurity in the world: meeting the 2015 international hunger targets: taking stock of uneven progress. Rome: FAO; 2015 [accessed in 2019 14 Jan]. Available from: http://www.fao.org/3/a-i4646e.pdf .
Requejo JH, Bryce J, Barros AJD, Berman P, Bhutta Z, Chopra M, et al. Countdown to 2015 and beyond: fulfilling the health agenda for women and children. Lancet. 2015;385:466–76.
Article Google Scholar
Frongillo EA, de Onis M. Hanson KM (1997) socioeconomic and demographic factors are associated with worldwide patterns of stunting and wasting of children. J Nutr. 1997;127:2302–9.
Article CAS Google Scholar
ANGOP Angolan Press Agency [Angola: Angolan population reaches 25 million inhabitants, according to definitive census data] News from 2016, 23 Mar [accessed in 2019 18 Jan]. Available from: http://www.angop.ao/angola/pt_pt/noticias/sociedade/2016/2/12/Angola-Populacao-angolana-atinge-milhoes-habitantes-segundo-dados-definitivos-censo,790199af-5cb1-43e2-8583-def58f1873c2.html .
Humbwavali JB, Giugliani C, Duncan BB, Harzheim E, Lavor ACH, Lavor MC, et al. Health and health Care of Mothers and Children in a suburban area of Luanda, Angola. J Community Health. 2014;39:617–26.
Asfaw M, Wondaferash M, Taha M, Dube L. Prevalence of undernutrition and associated factors among children aged between six to fifty nine months in Bule Hora district, South Ethiopia. BMC Public Health. 2015;15:–41.
Ahmed AMS, Ahmed T, Roy SK, Alam N, Hossain MI. Determinants of undernutrition in children under 2 years of age from rural Bangladesh. Indian Pediatr. 2012;49:821–4.
World Health Organization. WHO Child Growth Standards: Length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: Methods and development. Geneva: WHO; 2006 [accessed in 2019 14 Jan]. Available from: https://www.who.int/childgrowth/standards/Technical_report.pdf
Krefis AC, Schwarz NG, Nkrumah B, Acquah S, Loag W, Sarpong N, et al. Principal component analysis of socioeconomic factors and their association with malaria in children from the Ashanti region, Ghana. Malar J. 2010;9:201.
Aerts D, Drachler ML, Giugliani ERJ. Determinants of growth retardation in southern Brazil. Cad Saúde Pública. 2004;20:1182–90.
Victora CCG, Huttly SRS, Fuchs SCS, Olinto MMTA. The role of conceptual frameworks in epidemiological analysis: a hierarchical approach. Int J Epidemiol. 1997;26(1):224–7.
Coutinho LMS, Scazufca M, Menezes PR. Métodos para estimar razão de prevalência em estudos de corte transversal. Rev Saúde Pública. 2008;42:992–8.
Barros AJD, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3:21.
World Health Organization [internet]. Nutrition Landscape Information System (NLiS). Geneva: Nutrition; 2016 [accessed in 2019 14 Jan]. Available from: http://www.who.int/nutrition/nlis/en/ .
United Nations Children’s Fund. The state of the world’s children 2016: a fair chance for every child. New York: UNICEF; 2016 [accessed in 2019 14 Jan]. Available from: https://www.unicef.org/publications/files/UNICEF_SOWC_2016.pdf
United Nations Children’s Fund, World Health Organization, World Bank Joint Child Malnutrition Estimates (JME). [accessed in 2019 11 Jan]. Available from: https://data.worldbank.org/indicator/SH.STA.MALN.ZS?locations=AO
Hien N, Hoa N. Nutritional status and determinants of malnutrition in children under three years of age in Nghean, Vietnam. Pak J Nutr. 2009;8:958–64.
Drachler ML, Andersson MCS, Leite JCC, Marshall T, Aerts DRGC, Freitas PF, et al. Social inequality and other determinants of height in children: a multilevel analysis. Cad Saúde Pública. 2003;19:1815–25.
Vitolo MR, Gama CM, Bortolini GA, Campagnolo PDB, Drachler ML. Some risk factors associated with overweight, stunting and wasting among children under 5 years old. J Pediatr. 2008;84:251–7.
Van de Poel E, Hosseinpoor AR, Jehu-Appiah C, Vega J, Speybroeck N. Malnutrition and the disproportional burden on the poor: the case of Ghana. Int J Equity Health. 2007;6:21.
Oliveira VA, Assis AMO, Pinheiro SMC, Barreto ML. Determinants of weight and linear growth deficits in children under two years of age. Rev Saúde Pública. 2006;40:874–82.
Mamiro PS, Kolsteren P, Roberfroid D, Tatala S, Opsomer AS, Van Camp JH. Feeding practices and factors contributing to wasting, stunting, and iron-deficiency anaemia among 3-23-month old children in Kilosa district, rural Tanzania. J Health Popul Nutr. 2005;23:222–30.
PubMed Google Scholar
Rakotomanana H, Gates GE, Hildebrand D, Stoecker BJ. Determinants of stunting in children under 5 years in Madagascar. Matern Child Nutr. 2017;13:e12409.
Rissin A. [Malnutrition in children under five in the state of Pernambuco: an analysis of hierarchized causal relations] [dissertation]. Recife, PE: Universidade Federal de Pernambuco; 2003.
Angola (2008). Ministry of Health. [National Direction of Public Health. Revitalization of Municipal Health Services to Accelerate the Reduction of Maternal and Child Mortality]. Luanda: Ministry of Health; 2008.
Giugliani C, Duncan BB, Harzheim E, Lavor ACH, Lavor MC, Machado MMT, et al. Community health workers programme in Luanda, Angola: an evaluation of the implementation process. Hum Resour Health. 2014;12:68.
Onis M, Frongillo EA. Blössner M. Is malnutrition declining? An analysis of changes in levels of child malnutrition since 1980. Bull World Health Organ. 2000;78:1222–33.
PubMed PubMed Central Google Scholar
Victora CG, Adair L, Fall C, Hallal PC, Martorell R, Richter L, et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet. 2008;371:340–57.
Download references
Acknowledgements
We thank the Provincial Health Department of Luanda for the collaboration in data collection, and all the women and children whose participation has enabled this study.
This study has been financed by the Brazilian Commission for the Improvement of Higher Education Personnel (CAPES), through a scholarship to the PhD student JBH. The original broader study has been financed by the Brazilian National Council of Scientific and Technological Development (CNPq PROAFRICA) and the Brazilian Institute for Health Technology Assessment (IATS). These funding bodies had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
Data and material availability declaration: the database and study materials are available under request directly to the authors.
Author information
Authors and affiliations.
Superior Institute of Health Sciences (ISCISA), Agostinho Neto University, Avenida 4 de Fevereiro, 77, Luanda, Angola
João B. Humbwavali
Post-Graduation Program in Epidemiology, Federal University of Rio Grande do Sul (UFRGS), Rua Ramiro Barcellos, 2400/2° andar, CEP, Porto Alegre, RS, 90035-003, Brazil
João B. Humbwavali, Camila Giugliani, Luciana N. Nunes, Susana V. Dalcastagnê & Bruce B. Duncan
You can also search for this author in PubMed Google Scholar
Contributions
JBH and CG have participated in study conception, data collection, data analysis and manuscript preparation. LNN has participated in data analysis and manuscript preparation. SVD has collaborated with data bases organization, data analysis and manuscript preparation. BBD has supervised the whole study, since its conception, and has participated in manuscript preparation. All authors have read and approved the manuscript.
Corresponding author
Correspondence to João B. Humbwavali .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Ethics Committee of the Federal University of Rio Grande do Sul (register number 2008045) and by the Provincial Health Department of Luanda, Angola. The interviews were preceded by the signing of an informed consent form by the mother.
Consent for publication
Included in the informed consent form signed by participants.
Competing interests
None to declare.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
Study Questionnaire. Structured questionnaire applied to participant mothers in data collection. The questionnaire was applied by trained interviewers. Anthropometric information was collected by field coordinators, who also revised the whole content of the interview and finalized the questionnaires. (PDF 576 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Humbwavali, J.B., Giugliani, C., Nunes, L.N. et al. Malnutrition and its associated factors: a cross-sectional study with children under 2 years in a suburban area in Angola. BMC Public Health 19 , 220 (2019). https://doi.org/10.1186/s12889-019-6543-5
Download citation
Received : 09 July 2018
Accepted : 14 February 2019
Published : 21 February 2019
DOI : https://doi.org/10.1186/s12889-019-6543-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Malnutrition
- Infant nutrition disorders
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
REVIEW article
The intertwined relationship between malnutrition and poverty.

- 1 Division of Women and Child Health, Aga Khan University, Karachi, Pakistan
- 2 Robinson Research Institute, Adelaide Medical School, University of Adelaide, Adelaide, SA, Australia
Despite social and economic development, the burden of malnutrition across the globe remains unacceptably high. A vital relationship exists between nutritional status, human capital, and economic standing. Malnutrition adversely affects the physiological and mental capacity of individuals; which in turn hampers productivity levels, making them and their respective countries more susceptible to poverty. A two-way link exists between malnutrition and poverty, creating a vicious cycle with each fueling the other. Malnutrition produces conditions of poverty by reducing the economic potential of the population and likewise, poverty reinforces malnutrition by increasing the risk of food insecurity. The aim of the paper is to describe the interconnection between malnutrition and poverty, and to highlight how both serve as the cause and consequence of each other. The paper also discusses ways to move ahead to tackle these issues in a parallel manner rather than in separate silos.
Introduction
Malnutrition relates to a deficiency, excess, or imbalance of energy and other macro and micro-nutrients. It comprises of varying degrees of under- or over- nutrition, which leads to changes in body composition, body function, and clinical outcomes. In other words, malnutrition is an all-inclusive term that represents all manifestations of poor nutrition and ranges from extreme hunger and undernutrition to obesity ( 1 , 2 ). Despite social and economic development, the burden of malnutrition across the globe remains unacceptably high ( 2 ), recent data suggests that ~800 million people are undernourished, out of which 780 million reside in low-to-middle income countries, especially in Sub-Saharan Africa and South Asia ( 2 ). In 2015, inadequate food intake and poor dietary quality were responsible directly or indirectly for causing ill-health with six of the top 11 global risk factors being associated with dietary imbalances ( 2 ) and in 2017, 11 million deaths and 255 million disability-adjusted life years (DALYs) were attributable to dietary risk factors ( 3 ). Children under the age of 5 years are highly vulnerable to malnutrition with estimates suggesting that in 2019, globally 144 million children under the age of five were stunted (short for his/her age), 47 million wasted (thin for his/her height) and 38 million overweight (abnormal or excess bodyweight) ( 4 ). In adults, obesity is becoming more prevalent worldwide with ~38.9% of the adult population being either overweight or obese ( 5 ). Paradoxically, even though women have a higher prevalence (15.1%) of obesity than men (11%) ( 5 ); millions of women around the world are still underweight and one-third of women of reproductive age are estimated to have anemia ( 5 ).
Malnutrition has long been linked to poverty as higher rates of malnutrition are found in areas with chronic poverty ( 6 ). The impact of poverty on individuals can be seen through multiple manifestations and includes poor nutritional status, food insecurity, vulnerability to disease, reduced productivity levels, and compromised physical and intellectual development. Additionally, people living in poverty are unable to access necessities including nutritious food, hygienic environment, appropriate shelter, and adequate health care ( 7 ). Therefore, it would not be incorrect to suggest that even though malnutrition is a global phenomenon, those living in poverty face a higher burden. The question that now arises is whether malnutrition is a cause or consequence of poverty. The relationship between the nutritional status and economic standing has been further explored through the course of this paper.
The World Bank has set the International Poverty Line at $1.90 per person per day using 2011 Purchasing Power Parity (PPP) conversion factors ( 8 ). Therefore, households with a per capita income or expenditure less than the standard poverty line are defined as being poor ( 9 ). This makes income level the prime indicator for poverty, however with the passage of time, the need for re-conceptualizing poverty is becoming more evident as poverty is complex and multifaceted. Therefore, the conceptualization of poverty should not be limited to average income and wealth only but should encompass various other deprivations that are often experienced by people living in poverty. The global Multidimensional Poverty Index (MPI) is an international measure of acute poverty covering over 100 developing countries; created by the Oxford Poverty and Human Development Initiative (OPHI) and the United Nations Development Programme (UNDP) in 2010 ( 10 ). The global MPI steps away from the traditional view of poverty being solely limited to average income and wealth; to a more holistic view that highlights the need for using multiple indicators to account for various issues faced by people as a consequence of poverty ( 10 ). Through this index, poverty is portrayed to be a deprivation of basic amenities that restricts individuals from leading a good and healthy life ( 11 ) and takes into account the systemic disparities within a country and stretches the boundaries of poverty beyond the shortage of material assets to a concept that encompasses multiple deprivations, including but not limited to: assets, living standards, education, sanitation and hygiene, health and nutrition ( 10 ).
Since the 1990s, it is estimated that the proportion of the world's population living in extreme poverty has declined by more than a half ( 8 ). In 2015, 10% of the world's population lived under the poverty line; compared to nearly 36% in 1990 ( 8 ). Unfortunately, despite the overall decline in global poverty, progress has been uneven and disproportionate with the majority of the world's poor residing predominantly in Sub-Saharan Africa and South Asia ( 8 ). In 2015, 736 million people lived in extreme conditions of poverty with half of them i.e., 368 million residing only in five countries of India, Nigeria, Democratic Republic of Congo, Ethiopia, and Bangladesh ( 8 ). This illustrates that certain countries especially those afflicted by conflict, poor governance, and natural disasters continue to experience a skewed burden of poverty.
To analyze the vital linkages between poverty and malnutrition; it is important to highlight the growing evidence that health outcomes including malnutrition are driven by social determinants of health i.e., the conditions and circumstances in which people live, learn, work, and even play have a significant impact on their health ( 12 ). This interconnection between people's conditions and circumstances and their health can be displayed using the concept of poverty and food insecurity. The term “food insecurity” refers to a situation in which people do not have adequate physical, social or economic access to sufficient and nutritious food ( 13 ). Broadly, food insecurity is assessed using four dimensions i.e., food availability, access to food, stability of supply and safe, and healthy food utilization ( 14 ). Food insecurity may occur at various levels including regional, national, household, or individual. Poverty and food insecurity are deeply related, as poverty may adversely affect the social determinants of health and may create unfavorable conditions in which people might experience unreliable food supply ( 13 ). Food is a major household expenditure for the poor households ( 15 ). Data from African countries indicate that close to half of household income is spent on food: Nigeria (56.4%) ( 16 ); Kenya (46.7%), Cameroon (45.6%), Algeria (42.5%) ( 17 ). Similarly, within high-income countries, low-income households spend a significant proportion of their income on food: Ireland (14–33%), USA (28.8–42.6%) ( 17 , 18 ). In comparison, the wealthiest households in the USA spend a much lower 6.5–9.2% of household income on food ( 17 ). Despite spending a large proportion of their household income on food, many poor households continue to remain food insecure because of their insufficient, irregular, and fluctuating incomes ( 2 , 13 ).
Poverty, Food Insecurity and Double Burden of Malnutrition
A vital relationship exists between malnutrition and poverty. Poverty creates unstable and unfavorable conditions that may contribute to fueling the problem of malnutrition ( 7 ). People living in poverty often face financial limitations, which hinders their ability to access safe, sufficient, and nutritious food ( 7 ). Food insecurity compromises people's ability to acquire the amount of food needed to fulfill the bodily requirement of calories and without sufficient calorie intake, an individual may not be able to build up energy or strength to carry out everyday life activities and this also hampers the capacity and productivity to earn ( 19 ). While people living in poverty may require a greater quantity of food than they cursrently have, it is important to take into consideration that appropriate intake of nutrients and quality of food is equally important ( 19 ). Poverty can contribute to worsening malnutrition by compromising the quality of food intake and bolstering hidden hunger which is the deficiency of essential vitamins and minerals. The burden of obesity has extended beyond wealthier, developed nations and has now also become a feature of the developing world ( 16 ). Poverty leads to financial constraints that in turn lead to the consumption of cheap, high-energy staple foods, primarily carbohydrates, and fats rather than nutritionally dense food. Through the consumption of carbohydrates and fats, energy levels spike; but nutritional quality becomes compromised. The consequence of this is reduced nutritional quality and nutrient deficiencies. Poverty plays a significant role in regulating access and preference of foods ( 13 , 16 ), and this is evident in studies that showcase that when people living in poverty get a chance to spend relatively more on food; they often prefer to buy better tasting food, rather than good quality food ( 19 ).
The deficiency of micronutrients or “hidden hunger” is an important component of malnutrition ( 13 ). Micronutrient deficiencies can exists in all age groups and in any socioeconomic bracket. Iron, folate, vitamin A, iodine, and zinc deficiencies are among the most common and widespread micronutrient deficiencies among women and children in low- and middle- income countries and many of these micronutrient deficiencies co-exist. Assessing the relationship between malnutrition and poverty, requires consideration of micronutrient deficiencies. While macro- and micro- nutrient deficiencies may cause suboptimal mental and physical development, recurrent infections and growth retardation ( 20 , 21 ); micro-nutrient deficiencies may also result in adverse birth outcomes including low birth weight babies ( 22 , 23 ). To date, ~20 million babies are born with low birth weight each year and there is growing evidence of the connections between slow growth in height early in life and impaired health and educational and economic performance later in life ( 5 , 24 ). Low birth weight in babies can contribute to the vicious cycle of malnutrition since maternal nutrition status especially maternal stature has been reported to be inversely associated with offspring mortality, underweight, and stunting in infancy and childhood ( 22 , 23 ). Moreover, the importance of adequate intake of micronutrients can be noted in children born to mothers with sufficient amounts of iodine during pregnancy ( 19 ), as these children tend to complete one-third or one-half a year more schooling than children born to mothers with inadequate amount of iodine during pregnancy ( 19 ). It has been suggested that if every mother took iodine capsules during pregnancy then this could improve educational attainment among children in Central and Southern Africa ( 19 ).
Briefly put, the double burden of malnutrition and the importance of micro-nutrients should be recognized when analyzing the malnutrition-poverty cycle. There is a growing need to reimagine the concept of malnutrition and development experts and policy makers should make strides to account for the inherent complexities of both concepts in order to develop successful and sustainable nutritional strategies ( 19 ).
Malnutrition: Cause or Consequence of Poverty?
The question that now arises is whether malnutrition is a cause or consequence of poverty and vice versa? To elaborate upon this, it is important to highlight the relationship of human capital with nutrition and poverty.
Human capital is an integral asset of any country and the process of developing human capital begins from infancy and continues throughout the course of an individual's life ( 25 ). Nutritional status has a profound impact on human capital. The reasoning is simple, improved nutritional status is vital for escaping poverty, as good health is needed to increase productivity levels, contribute to economic growth, and improve a country's overall welfare ( 6 ). Without adequate nutrition, human capital starts to decline. This is because malnutrition negatively impacts physical and mental development, intellectual capacity, productivity, and the economic potential of an individual ( 25 ). As a consequence, economic stability is threatened, making a country more vulnerable to poverty. Poverty contributes to the problem of food insecurity which is referred to as a “resourced-constrained” or “poverty related” condition. Although the populations affected by poverty and food insecurity overlap; it is important to note that not all people living in poverty are food insecure and that this problem also exists in people living above the poverty line. Moreover, poverty also contributes in creating conditions of micro-nutrient deficiencies and hidden hunger. These factors exacerbate the issue of malnutrition and makes individuals more vulnerable to other health concerns. Irregular and unstable food supply along with low quality of food due to insufficient or inadequate nutrient intake can compromise immunity and make individuals more susceptible to infections. Additionally, if infected, matters tend to become worse because infections may further reduce nutritional and health status, thereby aggravating malnutrition and reinforcing its cycle with poverty ( 25 , 26 ).
A vicious cycle exists through which both poverty and malnutrition fuel and reinforce each other ( 25 ). Globally, the poorest countries are the countries bearing the highest burden of malnutrition. Nutritional imbalances reduce work capacity and human capital; and this makes countries more susceptible to poverty. Furthermore, malnutrition is also a consequence of poverty, as poverty increases food insecurity and hidden hunger; which contributes to the problem of malnutrition. This makes both these elements a cause and a consequence of each other. Establishing a linear relationship between the two would overlook the complexities and nuances that exist within the framework of this topic.
What Will be the Next Steps?
In order to progress socially and economically, there is an urgent need to recognize the burden of poverty and malnutrition and to take immediate steps to break the ongoing cycle. To achieve this target, it is important to understand what factors feed and reinforce it.
The cycle of poverty and malnutrition appears to be intergenerational. Evidence suggests that malnourished women are at a higher risk of having malnourished children and this creates an intergenerational effect ( 6 ). It is imperative to intervene early in life in order to maximize the effectiveness of interventions and break the cycle. The Lancet Nutrition Series ( 27 ) modeled the effect of 10 evidence based nutrition specific interventions on lives saved in the 34 countries that have 90% of the world's children with stunted growth. The series also examined the effect of various delivery platforms and delivery options using community health workers to engage poor populations and promote behavior change, access to and uptake of these interventions. Findings suggest that the current total of deaths in children younger than 5 years can be reduced by 15% if populations can access these 10 evidence-based nutrition interventions at 90% coverage. These nutrition specific interventions included salt iodization, multiple micronutrient supplementation in pregnancy (includes iron-folate), calcium supplementation in pregnancy, energy-protein supplementation in pregnancy, vitamin A supplementation in childhood, zinc supplementation in childhood, breastfeeding promotion, complementary feeding education, complementary food supplementation, and management of severe acute malnutrition in children. The findings also support the use of various community engagement and delivery strategies that can help reach poor segments of the population at greatest risk in order to make a difference ( 27 ). In other words, the interventions need to reach the poorest of the poor to break the cycle of malnutrition and poverty and should also incorporate disease and infection prevention as a part of their strategy ( 25 ).
Considering the inter-linkages described above between malnutrition and poverty, nutrition specific interventions need to be augmented with nutrition sensitive interventions in order to accelerate the progress of reducing malnutrition. Nutrition sensitive interventions are those that address intermediate and underlying causes of malnutrition and help to improve access to nutritious food, clean water and sanitation, education and employment, and health care etc. Large scale nutrition programs focusing on evidence based nutrition interventions should also target key underlying determinants of nutrition including poverty in order to enhance the coverage and effectiveness of nutrition-specific interventions. These include interventions in the sectors of agriculture, social safety nets, early child development, education, and women's empowerment. Women's empowerment is instrumental in not only improving malnutrition but general well-being ( 28 ). Hence, a parallel focus on nutrition sensitive and nutrition specific interventions has the potential to greatly accelerate progress in not only the areas of nutrition but also break the intergenerational cycle of malnutrition and poverty ( 29 ). More recently, bio-fortification and agricultural biodiversity are also considered to have the potential to cater to the issues of poverty and malnutrition in a parallel manner ( 30 ). In developing countries, bio-fortification could focus on improving quality of coarse cereals, as well as fodders along with community participatory approaches to enhance agricultural biodiversity. This approach not only could contribute to a reduction in malnutrition and poverty, but reduce food insecurity and improve sustainability ( 31 , 32 ), though further research is needed in the domain ( 30 , 31 ). Income disparity is also a factor that allows the malnutrition-poverty cycle to persist. In fact, a country may experience economic growth, but still have widespread poverty and high levels of malnutrition. This is because income inequality translates as health inequality; as the income gap grows, so does health disparity ( 7 , 13 , 25 ). Furthermore, gender inequities have also been associated with both poverty and malnutrition as a result of lower opportunities for women in the fields of education and employment. A recent analysis based on data from 49 low- and middle-income countries assessing the relationship between gender equity and malnutrition and health suggests that gender equity in education and employment decreases child malnutrition and is an important determinant in nutrition and access to health care ( 33 ). Therefore, any attempt to improve global nutritional status and to achieve the targets set by the “2030 Agenda for Sustainable Development” requires a focus on alleviating poverty and simultaneously focusing on agriculture, social safety nets, early child development, education, and strengthening women's position in society ( 34 – 37 ).
Nutritional interventions should be designed in an all-rounded, holistic manner. It would be fruitful to involve multiple stakeholders including health, education, agriculture, water, sanitation and hygiene, gender and economics. To ensure sustainability, nutritional interventions should be context-specific and should also be cost-effective since these issues concern low and middle income countries.
Ending poverty in all its forms is the first of the 17 Sustainable Development Goals and ending hunger, reducing food insecurity and improved nutrition and agriculture is the second goal. Furthermore, at least 12 of the 17 goals contain indicators that are highly relevant to nutrition. Poverty and malnutrition are deeply interrelated, with each fuelling the other and hence it is imperative to tackle both issues simultaneously rather than in parallel silos. A two-way link exists, with both elements being the cause and consequence of each other. This vicious cycle remains a prime public health concern and immediate strides need to be made against it. For a sustainable improvement in nutritional outcomes, the battle against poverty and malnutrition has to be fought on all fronts, to achieve a healthier and more equitable society.
Author Contributions
All authors contributed to the study and the write-up.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Soeters P, Bozzetti F, Cynober L, Forbes A, Shenkin A, Sobotka L. Defining malnutrition: a plea to rethink. Clin Nutr. (2017) 36:896–901. doi: 10.1016/j.clnu.2016.09.032
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Webb P, Stordalen GA, Singh S, Wijesinha-Bettoni R, Shetty P, Lartey A. Hunger and malnutrition in the 21st century. BMJ . (2018) 361:k2238. doi: 10.1136/bmj.k2238
3. Afshin A, Sur PJ, Fay KA, Cornaby L, Ferrara G, Salama JS, et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet . (2019) 393:1958–72. doi: 10.1016/S0140-6736(19)30041-8
4. UNICEF WHO WBG. Levels and Trends in Child Malnutrition UNICEF-WHO-World Bank Group Joint Child Malnutrition Estimates: Key Findings of the 2020 Edition . Geneva (2020).
Google Scholar
5. Development Initiatives. Global Nutrition Report: Shining a Light to Spur Action on Nutrition . Bristol: Development Initiatives (2018).
6. Setboonsarng S. Child Malnutrition as a Poverty Indicator: An Evaluation in the Context of Different Development Interventions in Indonesia . Tokyo: ADB Institute Discussion Papers (2005).
7. Peña M, Bacallao J. Malnutrition and poverty. Annu Rev Nutr. (2002) 22:241–53. doi: 10.1146/annurev.nutr.22.120701.141104
8. The World Bank. Poverty . (2019). Available online at: https://www.worldbank.org/en/topic/poverty/overview (accessed January 3, 2019).
9. Heltberg R. Malnutrition, poverty, and economic growth. Health Econ. (2009) 18(S1):S77–88. doi: 10.1002/hec.1462
CrossRef Full Text | Google Scholar
10. Oxford Poverty and Human Development Initiative and UNDP. Global Multidimensional Poverty Index 2019: Illuminating Inequalities . Oxford (2019).
11. Knech A. Understanding and fighting poverty–Amartya Sen's capability approach and related theories. Soc Change Rev. (2012) 10:153–76. doi: 10.2478/scr-2013-0016
12. WHO. Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health: Commission on Social Determinants of Health final report . Geneva: World Health Organization (2008).
13. Tanumihardjo SA, Anderson C, Kaufer-Horwitz M, Bode L, Emenaker NJ, Haqq AM, et al. Poverty, obesity, and malnutrition: an international perspective recognizing the paradox. J Am Diet Assoc. (2007) 107:1966–72. doi: 10.1016/j.jada.2007.08.007
14. Mundial B. Biofuels: Prospects, Risks and Opportunities . Washington, DC: The State of Food and Agriculture (2008).
15. Schanzenback D, Nunn R, Bauer L, Mumford M. Where Does All the Money Go: Shifts in Household Spending Over the Past 30 Years . Washington, DC: The Brookings Institute (2016).
16. Delisle H, Batal M. The double burden of malnutrition associated with poverty. Lancet. (2016) 387:2504–5. doi: 10.1016/S0140-6736(16)30795-4
17. World Economic Forum. Which Countries Spend the Most on Food? This Map Will Show You . Dublin (2016). Available online at: https://www.weforum.org/agenda/2016/12/this-map-shows-how-much-each-country-spends-on-food/ (accessed April 24, 2020).
18. Safefood. What Is the Cost of a Healthy Food Basket in the Republic of Ireland in 2018? Dublin (2019).
19. Banerjee A, Duflo E. More than 1 billion people are hungry in the world. Foreign Policy . (2011). p. 66–72.
20. WHO. Nutritional Landscape Information System: Country Profile Indicators - Interpretation Guide . Geneva: World Health Organization (2010).
21. World Health Organization. UNICEF-WHO-The World Bank: Joint Child Malnutrition Estimates: Levels and Trends . Geneva (2019).
PubMed Abstract | Google Scholar
22. Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, De Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. (2013) 382:427–51. doi: 10.1016/S0140-6736(13)60937-X
23. Özaltin E, Hill K, Subramanian S. Association of maternal stature with offspring mortality, underweight, and stunting in low-to middle-income countries. JAMA . (2010) 303:1507–16. doi: 10.1001/jama.2010.450
24. Dewey KG, Begum K. Long-term consequences of stunting in early life. Maternal Child Nutr . (2011) 7:5–18. doi: 10.1111/j.1740-8709.2011.00349.x
25. Vorster HH. The link between poverty and malnutrition: a South African perspective. Health SA Gesondheid. (2010) 15:1–6. doi: 10.4102/hsag.v15i1.435
26. Thompson B, Cohen MJ, Meerman J. World food insecurity and malnutrition: scope, trends, causes and consequences. In: Thompson B, Cohen MJ, editors. The Impact of Climate Change and Bioenergy on Nutrition . Springer (2012). p. 21–41.
27. Bhutta ZA, Das JK, Rizvi A, Gaffey MF, Walker N, Horton S, et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet . (2013) 382:452–77. doi: 10.1016/S0140-6736(13)60996-4
28. Van den Bold M, Quisumbing AR, Gillespie S. Women's Empowerment and Nutrition: An Evidence Review . Washington, DC: International Food Policy Research Institute (2013).
29. Ruel MT, Alderman H, Maternal Group CNS. Nutrition-sensitive interventions and programmes: how can they help to accelerate progress in improving maternal and child nutrition? Lancet . (2013) 382:536–51. doi: 10.1016/S0140-6736(13)60843-0
30. Johns T, Eyzaguirre PB. Biofortification, biodiversity and diet: a search for complementary applications against poverty and malnutrition. Food Policy. (2007) 32:1–24. doi: 10.1016/j.foodpol.2006.03.014
31. Hunter D, Özkan I, Moura de Oliveira Beltrame D, Samarasinghe WLG, Wasike VW, Charrondière UR, et al. Enabled or disabled: is the environment right for using biodiversity to improve nutrition? Front Nutr. (2016) 3:14. doi: 10.3389/fnut.2016.00014
32. Kennedy G, Stoian D, Hunter D, Kikulwe E. Agricultural Biodiversity for Healthy, Diverse Diets . Rome: Bioversity International (2016).
33. Ekbrand H, Halleröd B. The more gender equity, the less child poverty? A multilevel analysis of malnutrition and health deprivation in 49 low-and middle-income countries. World Dev. (2018) 108:221–30. doi: 10.1016/j.worlddev.2018.01.028
34. Doss CR. Women and agricultural productivity: reframing the issues. Dev Policy Rev. (2018) 36:35–50. doi: 10.1111/dpr.12243
35. Fernandez RM. SDG3 good health and well-being: integration and connection with other SDGs. In: Leal Filho W, Wall T, Azul AM, Brandli L, Özuyar PG, editors. Good Health and Well-Being . Springer Nature (2020). p. 629–36.
36. Ishikawa M, Yokoyama T, Sagehashi M, Kunugita N, Miura H. Diagnosing the double burden of malnutrition using estimated deviation values in low-and lower-middle-income countries. PLoS ONE. (2018) 13:e0208525. doi: 10.1371/journal.pone.0208525
37. Leal Filho W, Tripathi SK, Andrade Guerra J, Giné-Garriga R, Orlovic Lovren V, Willats J. Using the sustainable development goals towards a better understanding of sustainability challenges. Int J Sustain Dev World Ecol. (2019) 26:179–90. doi: 10.1080/13504509.2018.1505674
Keywords: malnutrition, poverty, undernutrition, obesity, food insecurity
Citation: Siddiqui F, Salam RA, Lassi ZS and Das JK (2020) The Intertwined Relationship Between Malnutrition and Poverty. Front. Public Health 8:453. doi: 10.3389/fpubh.2020.00453
Received: 07 January 2020; Accepted: 21 July 2020; Published: 28 August 2020.
Reviewed by:
Copyright © 2020 Siddiqui, Salam, Lassi and Das. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jai K. Das, jai.das@aku.edu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

Ibom Medical Journal Journal / Ibom Medical Journal / Vol. 17 No. 1 (2024) / Articles (function() { function async_load(){ var s = document.createElement('script'); s.type = 'text/javascript'; s.async = true; var theUrl = 'https://www.journalquality.info/journalquality/ratings/2405-www-ajol-info-ibom'; s.src = theUrl + ( theUrl.indexOf("?") >= 0 ? "&" : "?") + 'ref=' + encodeURIComponent(window.location.href); var embedder = document.getElementById('jpps-embedder-ajol-ibom'); embedder.parentNode.insertBefore(s, embedder); } if (window.attachEvent) window.attachEvent('onload', async_load); else window.addEventListener('load', async_load, false); })();
Article sidebar.

Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License .
Ibom Medical Journal retains copyright.
Main Article Content
Morbidity pattern of underfives with moderate acute malnutrition in southern nigeria, f okpokowuruk, b nwazuluoke.
Background: Moderate acute malnutrition (MAM) is a leading cause of childhood morbidity and mortality globally. The morbidity pattern of underfives with this condition is yet to be described.
Objective: To describe the morbidity pattern of underfives with MAM.
Method: A cross sectional study was conducted in two Primary Health Centres in Uruan Local Government Area of Akwa Ibom State. Caregivers’ brought children aged 6- 59 months to the health facilities following community mobilization. Eligible children were recruited into the study after obtaining parental consent. A validated proforma was used to obtain the biodata and symptoms of common illnesses in the children. A general physical examination, anthropometric measurements and systemic examination were performed.
Results: A total of 162 children were recruited into the study. Their mean (±SD) age was 20.4 ± 13.0 months. Over 70% of them were 6 - 23 months of age. Their mean (±SD) length/height was 77.3 ± 29.6 cm, mean (±SD) weight was 8.3 ± 3.4 kg and mean (±SD) mid upper arm circumference was 12.4 ± 4.5 cm. The main symptoms noted in the children were; fever 99 (61.1%), cough 84 (51.9%), weight loss 81 (50.0%), diarrhoea 40 (24.7%) and vomiting 40 (24.7%) while pallor 77 (47.5%), lymphadenopathy 56 (34.6%), hair changes 49 (30.2%), skin changes 27 (16.6%) were the main signs in them.
Conclusion: The main symptomatology of underfives with MAM were fever, cough and weight loss while pallor, lymphadenopathy and hair changes were the topmost signs. This morbidity pattern is related to interactions between malnutrition and infection in childhood.
AJOL is a Non Profit Organisation that cannot function without donations. AJOL and the millions of African and international researchers who rely on our free services are deeply grateful for your contribution. AJOL is annually audited and was also independently assessed in 2019 by E&Y.
Your donation is guaranteed to directly contribute to Africans sharing their research output with a global readership.
- For annual AJOL Supporter contributions, please view our Supporters page.
Journal Identifiers

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 15 October 2018
Protein, malnutrition and wasting disorders
The impact of using a malnutrition screening tool in a hospital setting: a mixed methods study
- Doris Eglseer 1 ,
- Daniela Schoberer 1 ,
- Ruud Halfens 2 &
- Christa Lohrmann 1
European Journal of Clinical Nutrition volume 73 , pages 284–292 ( 2019 ) Cite this article
809 Accesses
7 Citations
Metrics details
Background/Objectives
Malnutrition risk screening represents a crucial starting point for the successful management of malnourished patients. This study was conducted to (1) examine the effect of the use of a malnutrition screening tool on process indicators of nutritional care and (2) explore healthcare professionals’ perceptions and opinions regarding this tool.
A mixed methods design was used. A controlled pretest–posttest study was conducted to carry out quantitative analyses, and semi-structured, qualitative interviews were held. Quantitative data were analysed with descriptive statistics, Chi-squared tests, Student’s t -tests and Kruskal–Wallis H tests, using SPSS 23. Qualitative data were analysed by performing a qualitative content analysis using MAXQDA 12. Two comparable hospitals participated in the study, representing one intervention group (IG) and one control group (CG). The Graz Malnutrition Screening Tool (GMS) was implemented and used in the IG for at least 1 month, while the CG received no intervention.
The use of the screening tool positively correlated with significant improvements in the process indicators of nutritional care after 1 month, in terms of the number of nutritional interventions and the frequency of documentation of the diagnosis and the patient’s weight and height. The content of the interviews revealed that nearly all professionals involved perceived the overall screening process positively. Few barriers were identified.
Conclusions
The results of this study show that the use of a screening tool has a positive, short-term impact on the hospital’s process quality of nutritional care. Ongoing efforts are required to sustainably maintain these positive changes. During this process, positive attitudes, nomination of motivated ‘opinion-leaders’ and concerted management support are helpful facilitators.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
251,40 € per year
only 20,95 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Interrater reliability of routine screening for risk of malnutrition with the Mini Nutritional Assessment Short-Form in hospital

Incidence and criteria used in the diagnosis of hospital-acquired malnutrition in adults: a systematic review and pooled incidence analysis
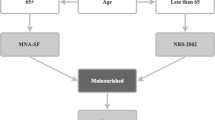
A multi-center survey on hospital malnutrition and cachexia in Slovenia
Thomas MN, Kufeldt J, Kisser U, Hornung HM, Hoffmann J, Andraschko M, et al. Effects of malnutrition on complication rates, length of hospital stay, and revenue in elective surgical patients in the G-DRG-system. Nutrition. 2016;32:249–54. https://doi.org/10.1016/j.nut.2015.08.021 .
Article PubMed Google Scholar
Felder S, Lechtenboehmer C, Bally M, Fehr R, Deiss M, Faessler L, et al. Association of nutritional risk and adverse medical outcomes across different medical inpatient populations. Nutrition. 2015;31:1385–93. https://doi.org/10.1016/j.nut.2015.06.007 .
Lew CC, Yandell R, Fraser RJ, Chua AP, Chong MF, Miller M. Association between malnutrition and clinical outcomes in the intensive care unit: a systematic review. J Parenter Enteral Nutr. 2016. https://doi.org/10.1177/0148607115625638 .
Article Google Scholar
Khalatban-Soltani S, Marques-Vidal P. The economic cost of hospital malnutrition in Europe; a narrative review. Clin Nutr ESPEN. 2015;10:e89–94.
Guerra RS, Sousa AS, Fonseca I, Pichel F, Restivo MT, Ferreira S, et al. Comparative analysis of undernutrition screening and diagnostic tools as predictors of hospitalisation costs. J Hum Nutr Diet. 2016;29:165–73. https://doi.org/10.1111/jhn.12288 .
Article CAS PubMed Google Scholar
Raynaud-Simon A, Revel-Delhom C, Hebuterne X. Clinical practice guidelines from the French Health High Authority: nutritional support strategy in protein-energy malnutrition in the elderly. Clin Nutr. 2011;30:312–9. https://doi.org/10.1016/j.clnu.2010.12.003 .
Group DMS. Guideline on malnutrition. In: Kruizenga H, Beijer S, Hulsman-de Waal G, Jonkers-Schultema C, Klos M, Remijnse-Meester W, et al., editors. Recognising, diagnosing and treating malnutrition in adults. Dutch Malnutrition Steering Group. Guidline on malnutrition. 2017. p. 36.
NICE. Nutrition support for adults: oral nutrition support, enteral tube feeding and parenteral nutrition. https://www.nice.org.uk/guidance/cg32/chapter/About-this-guideline . 2013.
Mueller C, Compher C, Ellen DM. A.S.P.E.N. clinical guidelines: nutrition screening, assessment, and intervention in adults. J Parenter Enter Nutr. 2011;35:16–24. https://doi.org/10.1177/0148607110389335 .
Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, Bischoff SC, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr. 2017;36:49–64. https://doi.org/10.1016/j.clnu.2016.09.004 .
Bueche J, Charney P, Pavlinac J, Skipper A, Thompson E, Myers E, et al. Nutrition care process and model part I: the 2008 update. J Am Diet Assoc. 2008;108:1113–7. https://doi.org/10.1016/j.jada.2008.04.027 .
Kondrup J, Allison SP, Elia M, Vellas B, Plauth M. ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003;22:415–21.
Article CAS Google Scholar
Cederholm T, Bosaeus I, Barazzoni R, Bauer J, Van Gossum A, Klek S, et al. Diagnostic criteria for malnutrition—an ESPEN Consensus Statement. Clin Nutr. 2015;34:335–40. https://doi.org/10.1016/j.clnu.2015.03.001 .
Eglseer D, Halfens RJ, Lohrmann C. Is the presence of a validated malnutrition screening tool associated with better nutritional care in hospitalized patients? Nutrition. 2017;37:104–11. https://doi.org/10.1016/j.nut.2016.12.016 .
White JV, Guenter P, Jensen G, Malone A, Schofield M. Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Parenter Enter Nutr. 2012;36:275–83. https://doi.org/10.1177/0148607112440285 .
Pirkle CM, Dumont A, Zunzunegui MV. Medical recordkeeping, essential but overlooked aspect of quality of care in resource-limited settings. Int J Qual Health Care. 2012;24:564–7. https://doi.org/10.1093/intqhc/mzs034 .
Tappenden KA, Quatrara B, Parkhurst ML, Malone AM, Fanjiang G, Ziegler TR. Critical role of nutrition in improving quality of care: an interdisciplinary call to action to address adult hospital malnutrition. J Acad Nutr Diet. 2013;113:1219–37. https://doi.org/10.1016/j.jand.2013.05.015 .
Smith PC. Performance measurement for health system improvement: experiences, challenges and prospects. Cambridge University Press; New York. 2009.
Donabedian A. The quality of care. How can it be assessed? JAMA. 1988;260:1743–8.
Mainz J. Defining and classifying clinical indicators for quality improvement. Int J Qual Health Care. 2003;15:523–30. https://doi.org/10.1093/intqhc/mzg081
Omidvari AH, Vali Y, Murray SM, Wonderling D, Rashidian A. Nutritional screening for improving professional practice for patient outcomes in hospital and primary care settings. Cochrane Database Syst Rev. 2013;CD005539. https://doi.org/10.1002/14651858.CD005539.pub2 .
Green SM, James EP. Barriers and facilitators to undertaking nutritional screening of patients: a systematic review. J Hum Nutr Diet. 2013;26:211–21. https://doi.org/10.1111/jhn.12011 .
Borglin G. The value of mixed methods for researching complex interventions. Oxon: Routledge; 2015.
Google Scholar
Creswell JW. A concise introduction to mixed methods research. Sage Publications; Los Angeles. 2014.
Polit DF, Beck CT. Nursing research: generating and assessing evidence for nursing practice. 10th ed. Philadelphia: Lippincott Williams & Wilkins; 2015.
Roller RE, Eglseer D, Eisenberger A, Wirnsberger GH. The Graz Malnutrition Screening (GMS): a new hospital screening tool for malnutrition. Br J Nutr. 2016;115:650–7. https://doi.org/10.1017/s0007114515004924 .
Released IC. IBM SPSS statistics for Windows. Version 23.0. Armonk, NY: IBM Corp.; 2015.
Neuendorf K. The content analysis guidebook. 2nd ed. California: SAGE Publications, Inc.; 2017.
Schreier M. Qualitative content analysis in practice. 1st ed. London: SAGE Publications Ltd.; 2012.
GmbH VS-C-S MAXQDA, software for qualitative data analysis. 1989–2018.
Leistra E, van Bokhorst-de van der Schueren MA, Visser M, van der Hout A, Langius JA, Kruizenga HM. Systematic screening for undernutrition in hospitals: predictive factors for success. Clin Nutr. 2014;33:495–501. https://doi.org/10.1016/j.clnu.2013.07.005 .
Keller HH, Vesnaver E, Davidson B, Allard J, Laporte M, Bernier P, et al. Providing quality nutrition care in acute care hospitals: perspectives of nutrition care personnel. J Hum Nutr Diet. 2014;27:192–202. https://doi.org/10.1111/jhn.12170 .
Green SM, James EP, Latter S, Sutcliffe M, Fader MJ. Barriers and facilitators to screening for malnutrition by community nurses: a qualitative study. J Hum Nutr Diet. 2014;27:88–95. https://doi.org/10.1111/jhn.12104 .
Rasmussen HH, Kondrup J, Staun M, Ladefoged K, Lindorff K, Jorgensen LM, et al. A method for implementation of nutritional therapy in hospitals. Clin Nutr. 2006;25:515–23. https://doi.org/10.1016/j.clnu.2006.01.003 .
Eide HD, Halvorsen K, Almendingen K. Barriers to nutritional care for the undernourished hospitalised elderly: perspectives of nurses. J Clin Nurs. 2015;24:696–706. https://doi.org/10.1111/jocn.12562 .
Boaz A, Baeza J, Fraser A. Effective implementation of research into practice: an overview of systematic reviews of the health literature. BMC Res Notes. 2011;4:212 https://doi.org/10.1186/1756-0500-4-212 .
Article PubMed PubMed Central Google Scholar
Flodgren G, Parmelli E, Doumit G, Gattellari M, O’Brien MA, Grimshaw J, et al. Local opinion leaders: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2011;CD000125. https://doi.org/10.1002/14651858.CD000125.pub4 .
DeLegge MH, Kelly AT. State of nutrition support teams. Nutr Clin Pract. 2013;28:691–7. https://doi.org/10.1177/0884533613507455 .
Hvas CL, Farrer K, Donaldson E, Blackett B, Lloyd H, Forde C, et al. Quality and safety impact on the provision of parenteral nutrition through introduction of a nutrition support team. Eur J Clin Nutr. 2014;68:1294–9. https://doi.org/10.1038/ejcn.2014.186 .
Cong MH, Li SL, Cheng GW, Liu JY, Song CX, Deng YB, et al. An interdisciplinary nutrition support team improves clinical and hospitalized outcomes of esophageal cancer patients with concurrent chemoradiotherapy. Chin Med J. 2015;128:3003–7. https://doi.org/10.4103/0366-6999.168963 .
Tappenden KA, Quatrara B, Parkhurst ML, Malone AM, Fanjiang G, Ziegler TR. Critical role of nutrition in improving quality of care: an interdisciplinary call to action to address adult hospital malnutrition. J Parenter Enter Nutr. 2013;37:482–97. https://doi.org/10.1177/0148607113484066 .
Download references
Author information
Authors and affiliations.
Institute of Nursing Science, Medical University of Graz, Graz, Austria
Doris Eglseer, Daniela Schoberer & Christa Lohrmann
Department of Health Services Research, CAPHRI, Maastricht University, Maastricht, The Netherlands
Ruud Halfens
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Doris Eglseer .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Ethics approval
Ethical approval was obtained from the responsible ethics committee (29-270 ex 16/17). The hospitals participated on a voluntary basis, and all responsible persons (medical and nursing hospital directors) gave their written informed consent. The persons interviewed agreed orally to participate in the interviews. Following the recommendations of the ethics committee, it was not necessary to obtain the informed consent from the patients because we only collected routine data.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Eglseer, D., Schoberer, D., Halfens, R. et al. The impact of using a malnutrition screening tool in a hospital setting: a mixed methods study. Eur J Clin Nutr 73 , 284–292 (2019). https://doi.org/10.1038/s41430-018-0339-z
Download citation
Received : 17 May 2018
Revised : 29 August 2018
Accepted : 26 September 2018
Published : 15 October 2018
Issue Date : February 2019
DOI : https://doi.org/10.1038/s41430-018-0339-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Mapping evidence on malnutrition screening tools for children under 5 years in sub-saharan africa: a scoping review protocol.
- Tlharihani Phisac Maphosa
- Delarise Maud Mulqueeny
- Tivani P. Mashamba-Thompson
Systematic Reviews (2020)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Latest information

- High contrast
- About UNICEF
- Our Chad team
- Partnerships
- Convention of the Rights of the Child
- Press center

Search UNICEF
In liwa, lac province, mariam has overcome malnutrition., "my child suffered a lot from malnutrition. now i'm relieved to see her smile, eat and play again" alimé, a mother of three..

One-year-old Mariam sits with her mother on a hospital bed at the UNICEF-supported clinic in Liwa, Lac province. Her face exudes vitality, and her mother, Alimé Saleh, also looks happy. Alimé and her daughter live in Kandom, a village about twenty kilometers from Liwa.
Mariam was admitted in the therapeutic nutrition unit of the Liwa health center a week earlier. Alimé explains that she first spent eight days at the Kandom health center with her baby, before being transferred to Liwa in a vehicle.
"My daughter was vomiting and had fever and diarrhea. She was also crying all day long and I didn't know what to do," says Alimé. "We spent eight days at the Kandom health center, but my daughter's health was still not improving," she adds.
At the Liwa clinic, the nurses diagnosed severe acute malnutrition, indicating that Mariam's life was in danger. They immediately administered her a drip to replace the fluids she had lost due to repeated diarrhea, and her condition was regularly monitored.

My child has suffered a lot from malnutrition. Now I'm relieved to see her smile, eat and play again. Alimé Saleh
Mariam has received milk, medicines and therapeutic foods that helped her recover. In addition to the children being treated, the center supports mothers with soap, bed sheets and three meals a day.
As baby Mariam gradually recovers, more and more women arrive every day, carrying sick babies in their arms. Most of them come to the clinic as a last resort, after unsuccessfully trying local remedies and traditional healing methods.

The majority of the cases we receive arrive with many complications. Mothers keep their children at home for a long time, and only come to us when they are already in a critical condition. Gilbert Sylnone, a pediatrician at ALIMA, a UNICEF NGO partner.
UNICEF supports malnutrition prevention and treatment in Liwa by providing care, medicines and therapeutic food, thanks to funding from the Central Emergency Response Fund (CERF), European Civil Protection and Humanitarian Aid Operations (ECHO) and the World Bank.
Related topics
More to explore, lac, a province plagued by child malnutrition in chad.
Alima, a 7-month-old orphan, is fighting for her survival.
When conflict drives children into malnutrition.
'' The nurses take good care of us, and my child's health has improved." Raoda, a Sudanese refugee in Adre, Eastern Chad
How preconceived ideas about breastfeeding put Hassan's life
"A healthy child is a blessing for his family and community," says Sadia, a 35-year-old mother.
The path to healing: Issaka’s story
"I was convinced that the disease would take my son away," Arafa, a mother of seven.

IMAGES
VIDEO
COMMENTS
Background. Malnutrition is a health condition resulting from eating food that contains either insufficient or too many calories, carbohydrates, vitamins, proteins or minerals. 1,2 It is a state of under- or overnutrition, evidenced by a deficiency or an excess of essential nutrients. 3 Good nutrition is the basic need for children to thrive, grow, learn, play and participate.
Moreover, although recent research on determinants of malnutrition has added considerable new evidence, the impact of ageing-related changes on the long-term development of malnutrition, still needs further elucidation. One example is the ageing gut and its altered microbiome, which have gained attention in the last years.
The number of people affected by malnutrition is startling. Globally, an estimated 149 million children are stunted (chronically undernourished) and 50 million are acutely undernourished (wasted), 1 with undernutrition a direct or underlying cause in 45% of all child deaths. 2 In addition, 40 million children under 5 years are overweight and ...
Malnutrition articles from across Nature Portfolio. ... Research Highlights 18 May 2023 Journal of Perinatology. Volume: 43, P: 823-826. Kidney disease as a medical complication of eating disorders.
Key Points. Malnutrition is a common, under-recognised and undertreated condition in hospital patients. Disease-related malnutrition arises due to reduced dietary intake, malabsorption, increased nutrient losses or altered metabolic demands. Wide-ranging changes in physiological function occur in malnourished patients leading to increased rates ...
Malnutrition is a serious problem with a negative impact on the quality of life and the evolution of patients, contributing to an increase in morbidity, length of hospital stay, mortality, and health spending. ... Over time, different nutritional assessment methods have been used, some complicated and expensive, used mainly in research, and ...
Malnutrition remains prevalent and existing health problem globally 1,2,3.Particularly Undernutrition is a major public health issue in low and middle income countries 2,4,5,6.Across regions there ...
This triple burden of malnutrition is a major public health challenge. The numbers speak for themselves: 51% of the world's population over five years of age is predicted to be obese or ...
Children who experience poor nutrition during the first 1000 days of life are more vulnerable to illness and death in the near term, as well as to lower work capacity and productivity as adults. These problems motivate research to identify basic and underlying factors that influence risks of child malnutrition. Based on a structured search of existing literature, we identified 90 studies that ...
Background Sustainable Development Goal (SDG) 2.2 calls for an end to all forms of malnutrition, with 2025 targets of a 40% reduction in stunting (relative to 2012), for wasting to occur in less than 5% of children, and for a 50% reduction in anaemia in women (15-49 years). We assessed the likelihood of countries reaching these targets by scaling up proven interventions and identified ...
However, it is very challenging to determine if malnutrition can be considered a cause or consequence of poverty ( Siddiqui et al. ). Individuals living in poverty have limited access to necessities such as clean water, hygiene, and healthy food products. The consequences of poverty on individuals include food insecurity, poor health, and ...
Malnutrition Increase Risk of Infection. A vicious relationship between malnutrition and infectious diseases has been long established. Malnutrition causes an exponential decrease in the chances of survival per exposure to any fatal infectious disease while non-fatal and subclinical infections may impair the process of growth ().Published research revealed that malnourished children have a ...
All titles and abstracts were screened to determine inclusion eligibility and full articles were independently assessed according to inclusion/exclusion criteria. For inclusion, papers had to cover research on at least one of the following topics: the problem of malnutrition, its determinants, its effects, and intervention research on malnutrition.
Despite record food output globally, hunger is still with us. Patrick Webb and colleagues argue that key policy actions are urgently needed to tackle this scourge and must focus on improving diet quality for all Today's world is characterised by the coexistence of agricultural bounty and widespread hunger and malnutrition.1 Recent years have seen a reversal of a decades old trend of falling ...
Background Globally, under-nutrition accounts for > 3 million deaths annually among children < 5 years, with Kenya having ~ 35,000 deaths. This study aimed to identify factors associated with malnutrition in children aged < 5 years in western Kenya. Methods We conducted a hospital-based unmatched case-control study between May and June 2017. Cases were defined as children aged 6-59 months ...
Four malnutrition diagnostic tools are currently in use today in adults: Subjective Global Assess-ment, the Mini Nutritional Assessment, the Academy of Nutrition and Dietet-ics/American Society for Parenteral and Enteral Nutrition malnutrition consen-sus characteristics, and the Global Leadership Initiative on Malnutrition criteria.
The prevalence of child malnutrition in Angola is still very high, and little is known about its associated factors. The aim of this study was to identify these factors in children under 2 years in a suburban area of the country's capital city. We used data from a cross-sectional population-based study conducted in 2010. The outcomes studied were stunting and underweight.
Introduction. As studies show, malnutrition is one of the risk factors responsible for non-communicable diseases (NCDs) globally. 1 2 About one-third of people in any community have at least one form of malnutrition, which includes disorders caused by excessive and/or imbalanced intake, leading to obesity and overweight, and disorders caused by deficient intake of energy or nutrients, leading ...
1 Division of Women and Child Health, Aga Khan University, Karachi, Pakistan; 2 Robinson Research Institute, Adelaide Medical School, University of Adelaide, Adelaide, SA, Australia; Despite social and economic development, the burden of malnutrition across the globe remains unacceptably high. A vital relationship exists between nutritional status, human capital, and economic standing.
1) Malnutrition: In this study it refers to the lesser intake. of food for children in terms of quality and quantity to. maintain optimum health. 2) Mother of Under Five Children: In this study it ...
Malnutrition is a global problem. Millions of people are suffering from different forms of malnutrition. In fact, 1.9 billion adults are overweight or obese while 462 million are underweight. Among children, 52 million under-fives are suffering from wasting, where they have a low weight for height. Around one in ten children are born with low ...
Malnutrition refers to deficiencies or excesses in nutrient intake, imbalance of essential nutrients or impaired nutrient utilization. The double burden of malnutrition consists of both undernutrition and overweight and obesity, as well as diet-related noncommunicable diseases. Undernutrition manifests in four broad forms: wasting, stunting ...
Nutritional therapy (NT) based on a controlled protein intake represents a cornerstone in managing chronic kidney disease (CKD). However, if a CKD patient is at the same time affected by cancer, oncologists and nutritionists tend to suggest a dietary regimen based on high protein intake to avoid catabolism and malnutrition. International guidelines are not clear when we consider onco ...
There is increasing evidence in children suffering from Severe Acute Malnutrition (SAM) that there is disruption of the gut microbiome and low gut microbiota diversity, which may be contributing factors to poor outcomes during nutritional treatment and recovery. The gut microbiome of children with SAM has been demonstrated to have a lower production of beneficial short chain fatty acids, which ...
All titles and abstracts were screened to determine inclusion eligibility and full articles were independently assessed according to inclusion/exclusion criteria. For inclusion, papers had to cover research on at least one of the following topics: the problem of malnutrition, its determinants, its effects, and intervention research on malnutrition.
Background: Moderate acute malnutrition (MAM) is a leading cause of childhood morbidity and mortality globally.The morbidity pattern of underfives with this condition is yet to be described. Objective: To describe the morbidity pattern of underfives with MAM. Method: A cross sectional study was conducted in two Primary Health Centres in Uruan Local Government Area of Akwa Ibom State.
In this issue of Pediatric Research Holgerson et al. report measurements of plasma glucose-regulatory hormones in 225 very preterm infants (VPIs) showing that these hormone levels were minimally ...
Malnutrition risk screening represents a crucial starting point for the successful management of malnourished patients. This study was conducted to (1) examine the effect of the use of a ...
At the Liwa clinic, the nurses diagnosed severe acute malnutrition, indicating that Mariam's life was in danger. They immediately administered her a drip to replace the fluids she had lost due to repeated diarrhea, and her condition was regularly monitored.
Today's world is characterised by the coexistence of agricultural bounty and widespread hunger and malnutrition. 1 Recent years have seen a reversal of a decades old trend of falling hunger, alongside the re-emergence of famine. 1 National and global evidence shows that ensuring an adequate food supply is still an important contribution to ...