Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.

Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: Third trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
5X Challenge
Thanks to generous benefactors, your gift today can have 5X the impact to advance AI innovation at Mayo Clinic.

Obstetric and Newborn Care I
10.02 key terms related to fetal positions.
a. “Lie” of an Infant.
Lie refers to the position of the spinal column of the fetus in relation to the spinal column of the mother. There are two types of lie, longitudinal and transverse. Longitudinal indicates that the baby is lying lengthwise in the uterus, with its head or buttocks down. Transverse indicates that the baby is lying crosswise in the uterus.
b. Presentation/Presenting Part.
Presentation refers to that part of the fetus that is coming through (or attempting to come through) the pelvis first.
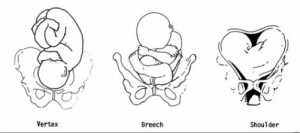
(1) Types of presentations (see figure 10-1). The vertex or cephalic (head), breech, and shoulder are the three types of presentations. In vertex or cephalic, the head comes down first. In breech, the feet or buttocks comes down first, and last–in shoulder, the arm or shoulder comes down first. This is usually referred to as a transverse lie.
(2) Percentages of presentations.
(a) Head first is the most common-96 percent.
(b) Breech is the next most common-3.5 percent.
(c) Shoulder or arm is the least common-5 percent.
(3) Specific presentation may be evaluated by several ways.
(a) Abdominal palpation-this is not always accurate.
(b) Vaginal exam–this may give a good indication but not infallible.
(c) Ultrasound–this confirms assumptions made by previous methods.
(d) X-ray–this confirms the presentation, but is used only as a last resort due to possible harm to the fetus as a result of exposure to radiation.
c. Attitude.
This is the degree of flexion of the fetus body parts (body, head, and extremities) to each other. Flexion is resistance to the descent of the fetus down the birth canal, which causes the head to flex or bend so that the chin approaches the chest.
(1) Types of attitude (see figure 10-2).
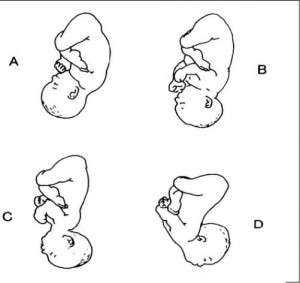
(a) Complete flexion. This is normal attitude in cephalic presentation. With cephalic, there is complete flexion at the head when the fetus “chin is on his chest.” This allows the smallest cephalic diameter to enter the pelvis, which gives the fewest mechanical problems with descent and delivery.
(b) Moderate flexion or military attitude. In cephalic presentation, the fetus head is only partially flexed or not flexed. It gives the appearance of a military person at attention. A larger diameter of the head would be coming through the passageway.
(c) Poor flexion or marked extension. In reference to the fetus head, it is extended or bent backwards. This would be called a brow presentation. It is difficult to deliver because the widest diameter of the head enters the pelvis first. This type of cephalic presentation may require a C/Section if the attitude cannot be changed.
(d) Hyperextended. In reference to the cephalic position, the fetus head is extended all the way back. This allows a face or chin to present first in the pelvis. If there is adequate room in the pelvis, the fetus may be delivered vaginally.
(2) Areas to look at for flexion.
(a) Head-discussed in previous paragraph, 10-2c(1).
(b) Thighs-flexed on the abdomen.
(c) Knees-flexed at the knee joints.
(d) Arches of the feet-rested on the anterior surface of the legs.
(e) Arms-crossed over the thorax.
(3) Attitude of general flexion. This is when all of the above areas are flexed appropriately as described.
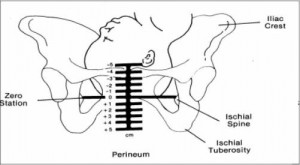
d. Station.
This refers to the depth that the presenting part has descended into the pelvis in relation to the ischial spines of the mother’s pelvis. Measurement of the station is as follows:
(1) The degree of advancement of the presenting part through the pelvis is measured in centimeters.
(2) The ischial spines is the dividing line between plus and minus stations.
(3) Above the ischial spines is referred to as -1 to -5, the numbers going higher as the presenting part gets higher in the pelvis (see figure10-3).
(4) The ischial spines is zero (0) station.
(5) Below the ischial spines is referred to +1 to +5, indicating the lower the presenting part advances.
e. Engagement.
This refers to the entrance of the presenting part of the fetus into the true pelvis or the largest diameter of the presenting part into the true pelvis. In relation to the head, the fetus is said to be engaged when it reaches the midpelvis or at a zero (0) station. Once the fetus is engaged, it (fetus) does not go back up. Prior to engagement occurring, the fetus is said to be “floating” or ballottable.
f. Position.
This is the relationship between a predetermined point of reference or direction on the presenting part of the fetus to the pelvis of the mother.
(1) The maternal pelvis is divided into quadrants.
(a) Right and left side, viewed as the mother would.
(b) Anterior and posterior. This is a line cutting the pelvis in the middle from side to side. The top half is anterior and the bottom half is posterior.
(c) The quadrants never change, but sometimes it is confusing because the student or physician’s viewpoint changes.
NOTE: Remember that when you are describing the quadrants, view them as the mother would.
(2) Specific points on the fetus.
(a) Cephalic or head presentation.
1 Occiput (O). This refers to the Y sutures on the top of the head.
2 Brow or fronto (F). This refers to the diamond sutures or anterior fontanel on the head.
3 Face or chin presentation (M). This refers to the mentum or chin.
(b) Breech or butt presentation.
1 Sacrum or coccyx (S). This is the point of reference.
2 Breech birth is associated with a higher perinatal mortality.
(c) Shoulder presentation.
1 This would be seen with a transverse lie.
2. Scapula (Sc) or its upper tip, the acromion (A) would be used for the point of reference.
(3) Coding of positions.
(a) Coding simplifies explaining the various positions.
1 The first letter of the code tells which side of the pelvis the fetus reference point is on (R for right, L for left).
2 The second letter tells what reference point on the fetus is being used (Occiput-O, Fronto-F, Mentum-M, Breech-S, Shoulder-Sc or A).
3 The last letter tells which half of the pelvis the reference point is in (anterior-A, posterior-P, transverse or in the middle-T).

(b) Each presenting part has the possibility of six positions. They are normally recognized for each position–using “occiput” as the reference point.
1 Left occiput anterior (LOA).
2 Left occiput posterior (LOP).
3 Left occiput transverse (LOT).
4 Right occiput anterior (ROA).
5. Right occiput posterior (ROP).
6 Right occiput transverse (ROT).
(c) A transverse position does not use a first letter and is not the same as a transverse lie or presentation.
1 Occiput at sacrum (O.S.) or occiput at posterior (O.P.).
2 Occiput at pubis (O.P.) or occiput at anterior (O.A.).
(4) Types of breech presentations (see figure10-4).
(a) Complete or full breech. This involves flexion of the fetus legs. It looks like the fetus is sitting in a tailor fashion. The buttocks and feet appear at the vaginal opening almost simultaneously.
A–Complete. B–Frank. C–Incomplete.
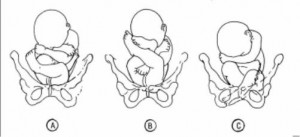
(b) Frank and single breech. The fetus thighs are flexed on his abdomen. His legs are against his trunk and feet are in his face (foot-in-mouth posture). This is the most common and easiest breech presentation to deliver.
(c) Incomplete breech. The fetus feet or knees will appear first. His feet are labeled single or double footing, depending on whether 1 or 2 feet appear first.
(5) Observations about positions (see figure 10-5).
(a) LOA and ROA positions are the most common and permit relatively easy delivery.
(b) LOP and ROP positions usually indicate labor may be longer and harder, and the mother will experience severe backache.
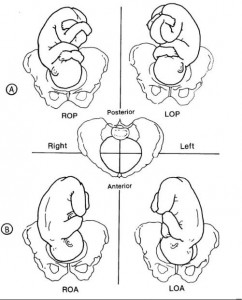
(c) Knowing positions will help you to identify where to look for FHT’s.
1 Breech. This will be upper R or L quad, above the umbilicus.
2 Vertex. This will be lower R or L quad, below the umbilicus.
(d) An occiput in the posterior quadrant means that you will feel lumpy fetal parts, arms and legs (see figure 10-5 A). If delivered in that position, the infant will come out looking up.
(e) An occiput in the anterior quadrant means that you will feel a more smooth back (see figure 10-5 B). If delivered in that position, the infant will come out looking down at the floor.
Distance Learning for Medical and Nursing Professionals
Need to talk? Call 1800 882 436. It's a free call with a maternal child health nurse. *call charges may apply from your mobile
Is it an emergency? Dial 000 If you need urgent medical help, call triple zero immediately.
Share via email
There is a total of 5 error s on this form, details are below.
- Please enter your name
- Please enter your email
- Your email is invalid. Please check and try again
- Please enter recipient's email
- Recipient's email is invalid. Please check and try again
- Agree to Terms required
Error: This is required
Error: Not a valid value
Presentation and position of baby through pregnancy and at birth
9-minute read
If you are concerned about your baby’s movements, contact your doctor or midwife for advice immediately.
- If you baby is in a breech presentation, your doctor may recommend trying a technique called an external cephalic version to try and move your baby while they are still in the uterus for an easier birth.
What does presentation and position mean?
Presentation refers to the part of your baby’s body that is facing downwards in the direction of the birth canal.
Position refers to where your baby’s occiput (the bottom part of the back of their head) is in relation to your body.
If your baby is in a breech presentation , then position refers to where your baby’s sacrum (lower back) is in relation to your body.
People — including medical professionals — sometimes use these terms incorrectly. Sometimes when speaking about babies in breech presentation, the word ‘position’ will be used to refer to their presentation. For example, you may read information or hear people say ‘breech position’ instead of ‘breech presentation’.
What are the different types of presentation my baby could be in during pregnancy and birth?
Most babies present headfirst, also known as cephalic presentation. Most babies that are headfirst will be vertex presentation. This means that the crown of their head sits at the opening of your birth canal.
In rare cases, your baby can be headfirst but in face or brow presentation, which may not be suitable for vaginal birth.

If your baby is in a breech presentation, their feet or bottom will be closest to your birth canal. The 3 most common types of breech presentation are:
- frank or extended breech — where your baby’s legs are straight up in front of their body, with their feet up near their face
- complete or flexed breech — where your baby is in a sitting position with their legs crossed in front of their body and their feet near their bottom
- footling breech — where one or both of your baby’s feet are hanging below their bottom, so the foot or feet are coming first
Read more on breech presentation .
What are the different positions my baby could be in during pregnancy and birth?
If your baby is headfirst, the 3 main types of presentation are:
- anterior – when the back of your baby’s head is at the front of your belly
- lateral – when the back of your baby’s head is facing your side
- posterior – when the back of your baby’s head is towards your back

How will I know what presentation and position my baby is in?
Your doctor or midwife can usually work out your baby’s presentation by feeling your abdomen. They may also double check it with a portable ultrasound. Your baby’s presentation is usually checked around 36 weeks .
Your doctor or midwife will also confirm your baby’s head position in labour by examining your belly and using an ultrasound , and they may also do a vaginal examination . During the vaginal examination they are feeling for certain ridges on your baby’s head called sutures and fontanelles that help them work out which way your baby is positioned.
What is the ideal presentation and position for baby to be in for a vaginal birth?
For a vaginal birth, your baby will ideally be headfirst with the back of their head at the front of your belly, also known as being in the anterior position. This position is best for labour and birth since it means that the smallest part of your baby’s head goes down the birth canal first.

When does a baby usually get in the ideal presentation and position for birth?
Your baby will usually be in a headfirst position by 37 weeks of pregnancy. Around 3 in every 100 babies will be in breech presentation after 37 weeks.
Your baby’s position can change with your contractions during labour as they move down the birth canal, so their exact position can change during labour.
What are my options if baby isn't in the ideal presentation or position for a vaginal birth?
If your baby is in a breech presentation, your doctor may recommend a technique called an external cephalic version (ECV) to try and move your baby while they are still in the uterus . An ECV involves your doctor using their hands to apply pressure on your belly and help turn your baby to a headfirst position. It has a 1 in 2 chance of success and is a safe option in most pregnancies.
There is no evidence to show that alternative therapies, such as exercises, acupuncture or chiropractic treatments, help your baby change from a breech presentation to headfirst.
If your baby remains breech, your doctor may discuss having a breech vaginal birth. Not all doctors and hospitals offer this option. They may also suggest you birth your baby with a planned caesarean section .
If your baby’s presentation is headfirst but the position of your baby’s head is not ideal for labour, it can lead to a longer labour, and potential complications . The position of your baby’s head will often change as your labour progresses. If it doesn’t, sometimes you can still give birth without assistance, or you may need your doctor to help turn your baby’s head or help your birth with a vacuum or forceps .
Any procedure or decision for a type of birth will only go ahead with your consent . You will be able to discuss all the options with your doctor, and based on your preferences for yourself and your baby’s safety, make a decision together .
Resources and support
The Royal Australian and New Zealand College of Obstetrics and Gynaecology has a factsheet about the options available to you if your baby is in a breech presentation at the end of your pregnancy .
Mercy Perinatal has information on external cephalic version (ECV) safety and benefits if your baby is in a breech presentation at the end of your pregnancy.
The Women’s Hospital has information about the different presentations and positions your baby could be in, and how it can affect your birthing experience.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call . Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content .
Last reviewed: October 2023
Related pages
External cephalic version (ecv), malpresentation, breech pregnancy, search our site for.
- Foetal Version
- Breech Presentation
Need more information?
Top results
Breech presentation and turning the baby
In preparation for a safe birth, your health team will need to turn your baby if it is in a bottom first ‘breech’ position.
Read more on WA Health website

Breech Presentation at the End of your Pregnancy
Breech presentation occurs when your baby is lying bottom first or feet first in the uterus (womb) rather than the usual head first position. In early pregnancy, a breech position is very common.
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website

External Cephalic Version for Breech Presentation - Pregnancy and the first five years
This information brochure provides information about an External Cephalic Version (ECV) for breech presentation
Read more on NSW Health website

When a baby is positioned bottom-down late in pregnancy, this is called the breech position. Find out about 3 main types and safe birthing options.
Read more on Pregnancy, Birth & Baby website

Malpresentation is when your baby is in an unusual position as the birth approaches. Sometimes it’s possible to move the baby, but a caesarean maybe safer.
Labour complications
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
ECV is a procedure to try to move your baby from a breech position to a head-down position. This is performed by a trained doctor.
Having a baby
The articles in this section relate to having a baby – what to consider before becoming pregnant, pregnancy and birth, and after your baby is born.
Anatomy of pregnancy and birth - pelvis
Your pelvis helps to carry your growing baby and is tailored for vaginal births. Learn more about the structure and function of the female pelvis.
Planned or elective caesarean
There are important things to consider if you are having a planned or elective caesarean such as what happens during and after the procedure.
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Call us and speak to a Maternal Child Health Nurse for personal advice and guidance.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Government Accredited with over 140 information partners
We are a government-funded service, providing quality, approved health information and advice
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
© 2024 Healthdirect Australia Limited
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.

- Mammary Glands
- Fallopian Tubes
- Supporting Ligaments
- Reproductive System
- Gametogenesis
- Placental Development
- Maternal Adaptations
- Menstrual Cycle
- Antenatal Care
- Small for Gestational Age
- Large for Gestational Age
- RBC Isoimmunisation
- Prematurity
- Prolonged Pregnancy
- Multiple Pregnancy
- Miscarriage
- Recurrent Miscarriage
- Ectopic Pregnancy
- Hyperemesis Gravidarum
- Gestational Trophoblastic Disease
- Breech Presentation
- Abnormal lie, Malpresentation and Malposition
- Oligohydramnios
- Polyhydramnios
- Placenta Praevia
- Placental Abruption
- Pre-Eclampsia
- Gestational Diabetes
- Headaches in Pregnancy
- Haematological
- Obstetric Cholestasis
- Thyroid Disease in Pregnancy
- Epilepsy in Pregnancy
- Induction of Labour
- Operative Vaginal Delivery
- Prelabour Rupture of Membranes
- Caesarean Section
- Shoulder Dystocia
- Cord Prolapse
- Uterine Rupture
- Amniotic Fluid Embolism
- Primary PPH
- Secondary PPH
- Psychiatric Disease
- Postpartum Contraception
- Breastfeeding Problems
- Primary Dysmenorrhoea
- Amenorrhoea and Oligomenorrhoea
- Heavy Menstrual Bleeding
- Endometriosis
- Endometrial Cancer
- Adenomyosis
- Cervical Polyps
- Cervical Ectropion
- Cervical Intraepithelial Neoplasia + Cervical Screening
- Cervical Cancer
- Polycystic Ovary Syndrome (PCOS)
- Ovarian Cysts & Tumours
- Urinary Incontinence
- Genitourinary Prolapses
- Bartholin's Cyst
- Lichen Sclerosus
- Vulval Carcinoma
- Introduction to Infertility
- Female Factor Infertility
- Male Factor Infertility
- Female Genital Mutilation
- Barrier Contraception
- Combined Hormonal
- Progesterone Only Hormonal
- Intrauterine System & Device
- Emergency Contraception
- Pelvic Inflammatory Disease
- Genital Warts
- Genital Herpes
- Trichomonas Vaginalis
- Bacterial Vaginosis
- Vulvovaginal Candidiasis
- Obstetric History
- Gynaecological History
- Sexual History

Obstetric Examination
- Speculum Examination
- Bimanual Examination
- Amniocentesis
- Chorionic Villus Sampling
- Hysterectomy
- Endometrial Ablation
- Tension-Free Vaginal Tape
- Contraceptive Implant
- Fitting an IUS or IUD
Original Author(s): Minesh Mistry Last updated: 12th November 2018 Revisions: 7
- 1 Introduction
- 2 Preparation
- 3 General Inspection
- 4 Abdominal Inspection
- 5.1 Fundal Height
- 5.3 Presentation
- 5.4 Liquor Volume
- 5.5 Engagement
- 6 Fetal Auscultation
- 7 Completing the Examination
The obstetric examination is a type of abdominal examination performed in pregnancy.
It is unique in the fact that the clinician is simultaneously trying to assess the health of two individuals – the mother and the fetus.
In this article, we shall look at how to perform an obstetric examination in an OSCE-style setting.
Introduction
- Introduce yourself to the patient
- Wash your hands
- Explain to the patient what the examination involves and why it is necessary
- Obtain verbal consent
Preparation
- In the UK, this is performed at the booking appointment, and is not routinely recommended at subsequent visits
- Patient should have an empty bladder
- Cover above and below where appropriate
- Ask the patient to lie in the supine position with the head of the bed raised to 15 degrees
- Prepare your equipment: measuring tape, pinnard stethoscope or doppler transducer, ultrasound gel
General Inspection
- General wellbeing – at ease or distressed by physical pain.
- Hands – palpate the radial pulse.
- Head and neck – melasma, conjunctival pallor, jaundice, oedema.
- Legs and feet – calf swelling, oedema and varicose veins.
Abdominal Inspection
In the obstetric examination, inspect the abdomen for:
- Distension compatible with pregnancy
- Fetal movement (>24 weeks)
- Surgical scars – previous Caesarean section, laproscopic port scars
- Skin changes indicative of pregnancy – linea nigra (dark vertical line from umbilicus to the pubis), striae gravidarum (‘stretch marks’), striae albicans (old, silvery-white striae)
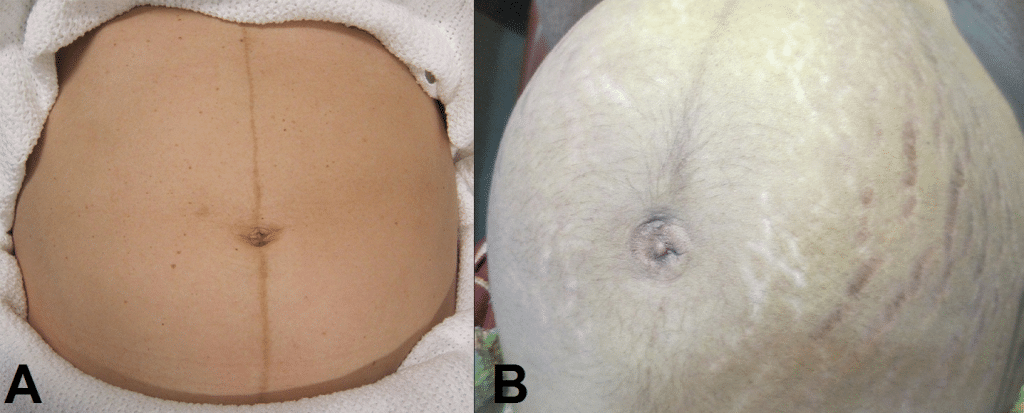
Fig 1 – Skin changes in pregnancy. A) Linea nigra. B) Striae gravidarum and albicans.
Ask the patient to comment on any tenderness and observe her facial and verbal responses throughout. Note any guarding.
Fundal Height
- Use the medial edge of the left hand to press down at the xiphisternum, working downwards to locate the fundus.
- Measure from here to the pubic symphysis in both cm and inches. Turn the measuring tape so that the numbers face the abdomen (to avoid bias in your measurements).
- Uterus should be palpable after 12 weeks, near the umbilicus at 20 weeks and near the xiphisternum at 36 weeks (these measurements are often slightly different if the woman is tall or short).
- The distance should be similar to gestational age in weeks (+/- 2 cm).
- Facing the patient’s head, place hands on either side of the top of the uterus and gently apply pressure
- Move the hands and palpate down the abdomen
- One side will feel fuller and firmer – this is the back. Fetal limbs may be palpable on the opposing side
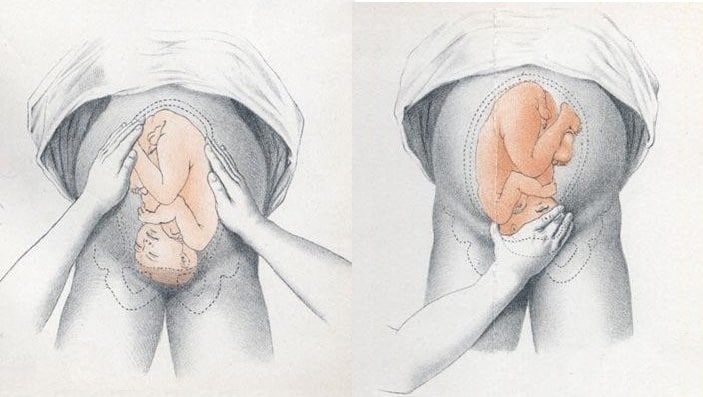
Fig 2 – Assessing fetal lie and presentation.
Presentation
- Palpate the lower uterus (below the umbilicus) to find the presenting part.
- Firm and round signifies cephalic, soft and/or non-round suggests breech. If breech presentation is suspected, the fetal head can be often be palpated in the upper uterus.
- Ballot head by pushing it gently from one side to the other.
Liquor Volume
- Palpate and ballot fluid to approximate volume to determine if there is oligohydraminos/polyhydramnios
- When assessing the lie, only feeling fetal parts on deep palpation suggests large amounts of fluid
- Fetal engagement refers to whether the presenting part has entered the bony pelvis
- Note how much of the head is palpable – if the entire head is palpable, the fetus is unengaged.
- Engagement is measured in 1/5s
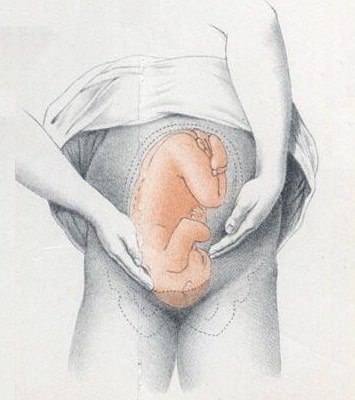
Fig 3 – Assessing fetal engagement.
Fetal Auscultation
- Hand-held Doppler machine >16 weeks (trying before this gestation often leads to anxiety if the heart cannot be auscultated).
- Pinard stethoscope over the anterior shoulder >28 weeks
- Feel the mother’s pulse at the same time
- Should be 110-160bpm (>24 weeks)
Completing the Examination
- Palpate the ankles for oedema and test for hyperreflexia (pre-eclampsia)
- Thank the patient and allow them to dress in private
- Summarise findings
- Blood pressure
- Urine dipstick
- Hands - palpate the radial pulse.
- Skin changes indicative of pregnancy - linea nigra (dark vertical line from umbilicus to the pubis), striae gravidarum ('stretch marks'), striae albicans (old, silvery-white striae)
- One side will feel fuller and firmer - this is the back. Fetal limbs may be palpable on the opposing side
Found an error? Is our article missing some key information? Make the changes yourself here!
Once you've finished editing, click 'Submit for Review', and your changes will be reviewed by our team before publishing on the site.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.15(1); 2023 Jan

Fetus-in-Fetu: A Differential Diagnosis of Neonatal Fetiform Encysted Abdominal Mass
Muhammad c jihwaprani.
1 Medicine and Surgery, Sulaiman Al Rajhi University, Al Bukayriyah, SAU
Ahmed A Mousa
Ali a mohamed.
2 Pediatrics, Maternity and Children Hospital, Buraydah, SAU
Yousef Alkouz
3 Obstetrics and Gynecology, Maternity and Children Hospital, Buraydah, SAU
Inas H Bahlawan
4 Medicine and Surgery, International University of Africa, Khartoum, SDN
Fetus-in-fetu (FIF) is a rare embryological anomaly in which an encysted fetiform mass develops within the infant or adult host body. It mainly occurs intraabdominal. There are embryo-pathogenetic debates over whether it belongs to the spectrum of highly differentiated teratomas or is a parasitic twinning from a monozygotic monochorionic diamniotic pregnancy. The presence of vertebral segments and an encapsulating cyst can reliably distinguish FIF from teratoma. The diagnosis may be initially made by imaging modalities such as computed tomography (CT) and magnetic resonance imaging (MRI), and a confirmatory diagnosis made by histopathology of the excised mass. Our center experienced a case of a male neonate presented after emergency cesarean delivery at 40-week gestation with the suspicion of an intraabdominal mass identified antenatally. Antenatal ultrasonography at 34 weeks gestation suggested the presence of an intraabdominal cystic mass measuring 6.5 cm with a hyperechoic focus. A follow-up MRI performed after the delivery showed a well-defined mass with the cystic formation in the left abdominal region with a centrally located fetiform structure. Vertebral bodies and long limb bones were visualized. The diagnosis of FIF was initially made preoperatively by the characteristic findings of imaging studies. Laparotomy was scheduled on day 6, revealing a large encysted mass with fetiform content. FIF should be considered a possible differential diagnosis of neonatal encysted fetiform mass. Routine antenatal imaging permits more frequent antenatal detection with earlier workup and management.
Introduction
Fetus-in-fetu (FIF) is an extremely rare congenital anomaly in which a vertebrate fetus-like mass is situated within the body of its fully developed host. Two main hypotheses on the pathogenesis of FIF have been described. The "included-twin" or "parasitic-twin" theory suggests that FIF arises from an anomalous monozygotic monochorionic diamniotic twin pregnancy. The malformed fetus becomes entrapped within its twin while dependent on its blood supply via persistent anastomosis of vitelline circulation [ 1 , 2 ]. Alternative theory, the "teratoma-spectrum" theory, suggests that FIF arises as a highly differentiated mature fetiform teratoma. Teratoma is a type of germ cell neoplasm consisting of at least two of three germ layers, i.e. endoderm, mesoderm, and ectoderm. FIF usually presents as a localized swelling that may compress adjacent structures due to the growing mass effect. Diagnosis can be provisionally made by imaging studies such as plain radiography, ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI), which are confirmed by exploratory laparotomy and complete surgical excision of the mass.
Case presentation
A full-term male neonate born to a 21-year-old primigravida presented with a swelling in the left abdomen. The baby was previously delivered via emergency cesarean section due to prolonged labor at 40 weeks gestation. Apgar's score was 9 both at 1 and 5 minutes. His birth weight was 3500 grams. The mother did not have any significant previous history of medical illness before and during pregnancy. There was no history of radiation exposure. She was not a smoker. There was no medication history apart from the prescribed antenatal supplements.
During the antenatal period, the mother underwent antenatal ultrasonography (USG) at 29+3-week gestation, which suggested the presence of a congenital anomaly. The USG showed an intraabdominal mass in a single viable developing fetus with a cephalic presentation. The estimated weight of the fetus was 1413 grams and the amniotic fluid level (AFL) was 4.3 centimeters at the largest sack. A follow-up USG was scheduled at 34 weeks of gestation, demonstrating an intra-abdominal cystic mass of unknown origin measuring 6.5 centimeters and a hyperechoic focus measuring 4.5 centimeters. The mass pushed the left kidney anteriorly and medially, resulting in left renal pelvic dilatation. The estimated fetal weight was 2745 grams in cephalic presentation with an AFL of 6.3 centimeters.
The complete neonatal examination was remarkable for a distended abdomen with a palpable midline abdominal mass. Laboratory investigation revealed serum α-fetoprotein (AFP) of 3000 nanograms/milliliter (normal: 0-5.8 nanogram/milliliter) and β-human chorionic gonadotropin of 3.16 mIU/liter (normal: 0-5.3 mIU/liter). All other values including complete blood count, urea, electrolytes, and liver function tests were within normal ranges. A plain baby-gram X-Ray (Figure 1 ) demonstrated a midline abdominal mass with multiple ectopic calcified structures indicating bones. Abdominal USG (Figure 2 ) revealed a well-defined cystic structure in the center of the abdomen to the left side measuring around 80 x 50 millimeters with heterogenous soft tissue content, which is highly suggestive of a non-viable fetus inside a cyst, with an empty skull, vertebrae, and limbs. Correspondingly, the MRI showed a well-defined cystic mass in the left abdomen anterior to the left kidney with a centrally located fetus (Figure (Figure3 3 A and B). Multiple long-shaped hyperintensities that correspond to fetal limbs were also observed. Vertebral bodies were visualized on axial T1-weighted MRI which indicates spina bifida. The mass compresses and displaces the bowel loop anteriorly and to the right side (Figure (Figure3 3 B). The head was not visualized well with a well-defined cystic structure abutting the cervical spine may be due to hydrocephaly or myelomeningocele. Those findings were consistent with a malformed fetus located in the body of its twin, suggesting the diagnosis of FIF.

USG: ultrasonography

MRI: magnetic resonance imaging
Exploratory laparotomy was scheduled at the age of six days with a left upper abdominal incision, revealing a large encysted mass (Figure 4 A). The cyst was mobilized from the left colon, left renal vein, and left ureter, and is excised completely. Dissection of the cyst revealed fetus-like structures (Figure 4 B and C) with limb buds visible and anencephalic features. The postoperative period at the neonatal intensive care unit was uneventful, and the baby was discharged at the age of nine days old. A subsequent follow-up visit at six months showed a normally developing infant with no recurrence of the soft tissue mass at the site of surgery. Measurement of serum AFP also demonstrated a regression compared to the preoperative level, measuring around 39 nanograms/milliliter.

FIF is a rare developmental anomaly with a prevalence of less than one in 500,000 births. It has a slight male preponderance (2 male: 1 female) [ 3 ]. Despite the two pathogenetic controversies on whether FIF represents a distinct pathogenetic entity (the parasitic-twin theory) or is a part of the fetiform teratoma spectrum (the teratoma-spectrum theory), distinguishing FIF from teratoma is extremely important. That is because even mature cystic teratoma carries a risk of malignancy from 3.5% to as high as 6.67%, while immature teratoma should be regarded as malignant [ 4 , 5 ]. In contrast, there were only two known cases of malignant recurrences in the case of FIF [ 6 , 7 ]. The fetiform mass in FIF is genetically identical to its host body and is usually single, although the case of multiple FIF masses in a single host has also been reported [ 8 ]. The differences between FIF and teratoma are summarized in (Table (Table1 1 ).
FIF: fetus-in-fetu
| Fetus-in-fetu | Teratoma | |
| Definition | Congenital anomaly in which a vertebrate fetus-like mass is entrapped within the body of its fully developed host | Germ cell neoplasm due to disorganized pluripotent cell proliferation, contents are derived off of >2/3 germ layers |
| Common sites | Abdominal, retroperitoneal | Ovaries, testes |
| Size | Variable, usually 5-8 centimeters | Usually large (>6 centimeters ) |
| Cyst surrounding the fetiform mass | Yes | No |
| Vascular pedicle | Connected to the host by a small number of relatively large vascular pedicles | No vascular pedicle. Usually has a wider attachment site with multiple small blood vessels. |
| Anatomical structures | Grossly recognizable, well-formed. Mostly acardiac and anencephalic | Occasional, disorganized. E.g. cartilage, hair, respiratory mucosa, teeth, and intestinal mucosa. |
| Axial skeletal segments | Its presence is pathognomonic | Not present |
| Risk of malignant change/recurrence | Extremely low | Immature: High if left untreated Mature: 3.5-6.67% |
| Staging of the tumor | Not required | Required |
| α-fetoprotein level | Elevated (typically >3000 nanogram/milliliter) | Not elevated |
| Management | Surgical excision is curative. An early operation is needed if the mass effect compromises organ functions. | Early surgical excision (risk of malignant transformation if delayed) |
Most cases of FIF occur retroperitoneally in the abdominal region (80%). This may be explained by the fact that vitelline circulation embryologically develops into the superior mesenteric artery that is located retroperitoneally. However, its occurrence in other areas has also been reported, including intracranial [ 9 ], intrahepatic [ 10 ], intrathoracic [ 11 ], oral cavity [ 12 ], sacrococcygeal [ 13 ], and undescended testis [ 14 ].
The diagnostic findings favoring FIF over teratoma include the presence of axial skeleton and limb buds on imaging modalities. Willis et al. regarded the presence of a vertebral column as one of the important diagnostic criteria of FIF [ 15 ]. The presence of vertebrae indicates an organized embryological development that has developed notochord, the precursor of vertebral bones, during the primitive streak stage. In contrast, teratomata develop as a result of disorganized and uncontrolled pluripotent cell replication, thus vertebral segmentation and organogenesis are not usually found [ 1 , 16 ]. In the neonate, other differential diagnoses should include meconium pseudocyst, which is the result of meconium peritonitis caused by prenatal bowel perforation. In females of reproductive age, ectopic pregnancy should also be considered as a potential differential diagnosis of the fetiform mass [ 17 ].
Spencer et al. have proposed that the diagnosis of FIF requires at least one of the following conditions met [ 2 ]: (1) it is enclosed within a distinct cyst; (2) it is partially or entirely covered in normal skin; (3) it has anatomical structures that are grossly recognizable; (4) it is connected to the host by a small number of relatively large blood vessels; and (5) it is either positioned immediately next to one of the sites where conjoined twins attached, or be connected to the neural tube or the gastrointestinal system.
Antenatal diagnosis of FIF is made possible by the advancement in imaging modalities. A plain radiograph can sufficiently secure the tentative diagnosis of FIF when the vertebral column and long limb bones are visualized. USG may visualize the fetiform mass and delineate the presence of a cyst enclosing it. More advanced imaging modalities such as CT and MRI can further aid in the diagnosis. In addition to the identification of long bones and vertebral segments, they can establish the exact relationship with the surrounding structures and the mass effect it has caused, e.g. compression and displacement. Laboratory investigations typically reveal an elevated AFP, typically ≥3000 nanograms/milliliter, further supporting the diagnosis of FIF [ 18 ]. Consequently, postoperative follow-up for FIF should include the serial measurement of AFP, showing a significant decrease after complete excision of the fetiform mass [ 19 ].
Conclusions
In conclusion, FIF should be considered as a differential diagnosis in a neonate presenting with an encysted fetiform mass. Early diagnosis is made more frequently nowadays due to antenatal routine imaging such as USG. Further imaging modalities such as CT or MRI can reliably differentiate FIF from teratoma by the presence of the encapsulating cyst, vertebral organization, and limb bones in the fetiform mass. The condition should also be differentiated from ectopic pregnancy in adult females and meconium pseudocyst in neonates. Despite its benign nature, post-operative follow-up with serum AFP and imaging modalities may be necessary.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is a Transverse Baby Position?
Why It Happens, How to Turn Your Baby, and Tips for a Safe Delivery
Causes and Risk Factors
Turning the fetus, complications, frequently asked questions.
A transverse baby position, also called transverse fetal lie, is when the fetus is sideways—at a 90-degree angle to your spine—instead of head up or head down. This development means that a vaginal delivery poses major risks to both you and the fetus.
Sometimes, a transverse fetus will turn itself into the head-down position before you go into labor. Other times, a healthcare provider may be able to turn the position.
If a transverse fetus can't be turned to the right position before birth, you're likely to have a cesarean section (C-section).
This article looks at causes and risk factors for a transverse baby position. It also covers how it's diagnosed and treated, the possible complications, and how you can plan ahead for delivery.
Marko Geber / Getty Images
How Common Is Transverse Baby Position?
An estimated 2% to 13% of babies are in an unfavorable position at delivery —meaning they're not in the head-down position .
Certain physiological issues can lead to a transverse fetal lie. These include:
- A bicornuate uterus : The uterus has a deep V in the top that separates the uterus into two sides; it may only be able to hold a near-term fetus sideways.
- Oligohydramnios or polyhydramnios : Abnormally low or high amniotic fluid volume (respectively).
Several risk factors can make it more likely for the fetus to be in a transverse lie, such as:
- The placenta being in an unusual position, such as blocking the opening to the cervix ( placenta previa ), which doesn't allow the fetus to reach the head-down position
- Going into labor early, before the fetus has had a chance to get into the right position
- Being pregnant with twins or other multiples, as the uterus is crowded and may not allow for much movement
- An abnormal pelvic structure that limits fetal movement
- Having a cyst or fibroid tumor blocking the cervix
Transverse fetal positioning is also more common after your first pregnancy.
It’s not uncommon for a fetus to be in a transverse position during the earlier stages of pregnancy. In most cases, though, they shift on their own well before labor begins. The transverse fetal position doesn't cause any signs or symptoms.
Healthcare professionals diagnose a transverse lie through an examination called Leopold’s Maneuvers. That involves feeling your abdomen to determine the fetal position. It's usually confirmed by an ultrasound.
You may also discover a transverse fetal lie during a routine ultrasound.
Timing of Transverse Position Diagnosis
The ultrasound done at your 36-week checkup lets your healthcare provider see the fetal position as you get closer to labor and delivery. If it's still a transverse lie at that time, your medical team will look at options for the safest labor and delivery.
Approximately 97% of deliveries involve a fetus positioned with the head down, in the best position to slide out. That makes a vaginal delivery easier and safer.
A transverse position only happens in about 1% of deliveries. In that position, the shoulder, arm, or trunk of the fetus may present first. This isn't a good scenario for either of you because a vaginal delivery is nearly impossible.
In these cases, you have two options:
- Turning the fetal position
- Having a C-section
If the fetus is in a transverse lie late in pregnancy, you or your healthcare provider may be able to change the position. Turning into the proper head-down position may help you avoid a C-section.
Medical Options
A healthcare provider can use one of the following techniques to attempt re-positioning a fetus:
- External cephalic version (ECV) : This procedure typically is performed at or after 36 weeks of pregnancy; involves using pressure on your abdomen where the fetal head and buttocks are.
- Webster technique : This is a chiropractic method in which a healthcare professional moves your hips to allow your uterus to relax and make more room for the fetus to move itself. (Note: No evidence supports this method.)
A 2020 study reported a 100% success rate for trained practitioners who used turning to change a transverse fetal lie. Real-world success rates are closer to 60%.
At-Home Options
You may be able to encourage a move out of the transverse position at home. You can try:
- Getting on your hands and knees and gently rocking back and forth
- Lying on your back with your knees bent and feet flat on the floor, then pushing your hips up in the air (bridge pose)
- Talking or playing music to stimulate the fetus to become more active
- Applying some cold to your abdomen where the fetal head is, which may make them want to move away from it
These methods may or may not work for you. While there's anecdotal evidence that they sometimes work, they haven't been researched.
Talk to your healthcare provider before attempting any of these techniques to ensure you're not doing anything unsafe.
Can Babies Go Back to Transverse After Being Turned?
Even if the fetus does change position or is successfully moved, it is possible that it could return to a transverse position prior to delivery.
Whether your child is born via C-section or is successfully moved so you can have a vaginal delivery, potential complications remain.
Cesarean Sections
C-sections are extremely common and are generally safe for both you and the fetus. Still, some inherent risks are associated with the procedure, as there are with any surgery.
The transverse position can force the surgeon to make a different type of incision, as the fetal lie may be right where they'd usually cut. Possible C-section complications for you can include:
- Increased bleeding
- Bladder or bowel injury
- Reactions to medicines
- Blood clots
- Death (very rare)
In rare cases, a C-section can result in potential complications for the baby , including:
- Breathing problems, if fluid needs to be cleared from their lungs
Most C-sections are safe and result in a healthy baby and parent. In some situations, a surgical delivery is the safest option available.
Vaginal Delivery
If the fetus is successfully moved out of the transverse lie position, you'll likely be able to deliver it vaginally. However, a few complications are possible even after the fetus has been moved:
- Labor typically takes longer.
- Your baby’s face may be swollen and appear bruised for a few days.
- The umbilical cord may be compressed, potentially causing distress and leading to a C-section.
Studies suggest that ECV is safe, effective, and may help lower the C-section rate.
Planning Ahead
As with any birth, if you experience a transverse fetal position, you should work with your healthcare provider to develop a delivery plan. If the transverse position has been maintained throughout the pregnancy, the medical team will evaluate the position at about 36 weeks and make plans accordingly.
Remember that even if the fetal head is down late in pregnancy, things can change quickly during labor and delivery. That means it's worthwhile to discuss options for different types of delivery in case they become necessary.
A transverse baby position, or transverse fetal lie, is the term for a fetus that's lying sideways in the uterus. Vaginal delivery usually isn't possible in these cases.
If the fetus is in this position near the time of delivery, the options are to turn it to make vaginal delivery possible or to have a C-section. A trained healthcare provider can use turning techniques. You may also be able to get the fetus to turn at home with some simple techniques.
Both C-section and vaginal delivery pose a risk of certain complications. However, these problems are rare and the vast majority of deliveries end with a healthy baby and parent.
A Word From Verywell
Pregnancy comes with many unknowns, and the surprises can continue up through labor and delivery.
Talking to your healthcare provider early on about possible scenarios can give you time to think about possible outcomes. This helps to avoid a situation where you’re considering risks and benefits during labor when quick decisions need to be made.
Ideally, a baby should be in the cephalic position (head down) at 32 weeks. If not, a doctor will examine the fetal position at around the 36-week mark and determine what should happen next to ensure a smooth delivery. Whether this involves a cesarian section will depend on the specific case.
Less than 1% of babies are born in the transverse position. In many cases, a doctor might recommend a cesarian delivery to ensure a more safe delivery. The risk of giving birth in the transverse lie position is greater before a due date or if twins or triplets are also born.
A planned cesarian section, or C-section, is typically performed in the 39th week of gestation. This is done so the fetus is given enough time to grow and develop so that it is healthy.
In some cases, a doctor may perform an external cephalic version (ECV) to change a transverse fetal lie. This involves the doctor using their hands to apply firm pressure to the abdomen so the fetus is moved into the cephalic (head-down) position.
Most attempts of ECV are successful, but there is a chance the fetus can move back to its previous position; in these cases, a doctor can attempt ECV again.
The American College of Obstetricians and Gynecologists. If your baby is breech .
Tempest N, Lane S, Hapangama D. Babies in occiput posterior position are significantly more likely to require an emergency cesarean birth compared with babies in occiput transverse position in the second stage of labor: a prospective observational study . Acta Obstet Gynecol Scand . 2020;99(4):537-545. doi:10.1111/aogs.13765
National Institutes of Health, U.S. National Library of Medicine: MedlinePlus. Congenital uterine anomalies .
Figueroa L, McClure EM, Swanson J, et al. Oligohydramnios: a prospective study of fetal, neonatal and maternal outcomes in low-middle income countries . Reprod Health. 2020;17 (article 19). doi:10.1186/s12978-020-0854-y
National Institutes of Health, U.S. National Library of Medicine: MedlinePlus. Placenta previa .
National Institutes of Health, U.S. National Library of Medicine: MedlinePlus. Your baby in the birth canal .
Van der Kaay DC, Horsch S, Duvekot JJ. Severe neonatal complication of transverse lie after preterm premature rupture of membranes . BMJ Case Rep . 2013;bcr2012008399. doi:10.1136/bcr-2012-008399
Oyinloye OI, Okoyomo AA. Longitudinal evaluation of foetal transverse lie using ultrasonography . Afr J Reprod Health ; 14(1):129-133.
Nishikawa M, Sakakibara H. Effect of nursing intervention program using abdominal palpation of Leopold’s maneuvers on maternal-fetal attachment . Reprod Health 2013;10 (article 12). doi.org/10.1186/1742-4755-10-12
National Institutes of Health, U.S. National Library of Medicine: MedlinePlus. Delivery presentations .
Dalvi SA. Difficult deliveries in Cesarean section . J Obstet Gynaecol India . 2018;68(5):344-348. doi:10.1007/s13224-017-1052-x
Zhi Z, Xi L. Clinical analysis of 40 cases of external cephalic version without anesthesia . J Int Med Res . 2021;49(1):300060520986699. doi:10.1177/0300060520986699
National Institutes of Health, U.S. National Library of Medicine: MedlinePlus. Questions to ask your doctor about labor and delivery .
Nemours KidsHealth. Cesarean sections .
By Elizabeth Yuko, PhD Yuko has a doctorate in bioethics and medical ethics and is a freelance journalist based in New York.

What you need to know about fetal abdominal masses
With routine antenatal ultrasound and advances in ultrasound technology, fetal intra-abdominal cystic masses are recognized more often and are better characterized than in the past.
How Individually Identifying More HPV Types Enables Better Patient Management and More Precise Care

HIV Roundtable: Adolescents and issues around care, adherence, and privacy
In this last episode, our panel discusses this patient population and the challenges around keeping them in the continuum of care.
The Importance of Including Hemoglobinopathies as a Part of Carrier Screening Panels

Policies implementation linked to increased 12-month contraception coverage
In a recent study, rates of 12-month or longer contraceptive supply were increased by the implementation of a 12-month contraceptive supply policy.

Study links solid organ transplant to adverse pregnancy outcomes
In a recent study, the odds of adverse pregnancy outcomes were significantly increased in pregnancies of women with solid organ transplants.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

Malpresentation and Malposition of the Fetus
Obie Editorial Team
A malpresentation or malposition of the fetus is when the fetus is in any abnormal position, other than vertex (head down) with the occiput anterior or posterior.
The following are considered malpresentations or malpositions:
Unstable lie
- Transverse presentation
- Oblique presentation
Face presentation
Brow presentation
Shoulder presentation
High head at term
- Prolapsed arm
The cause of a malpresentation can often not be clearly identified but it can be associated with the following:
- Preterm pregnancy
- Uterine anomalies
- Pelvic tumors eg f ibroids
- Placenta previa
- Grandmultiparty
- Contracted maternal pelvis
- Multiple gestation
- Too much amniotic fluyid (polyhydramnios)
- Short umbilical cord
- Fetal anomalies (e.g. anencephaly, hydro-cephalus)
- Abnormal fetal motor ability
There is an increased risk of neonatal and maternal complications associated with a malpresentation including neonatal and maternal trauma. If delivery is indicated, doing a cesarean delivery can significantly decrease the risk of complications.
Transverse lie
Oblique lie
In most cases of a normal vertex (head down) presentation, the baby's head is flexed with the chin close to the baby's chest. In these cases, the presenting part is the occiput, the posterior part of the baby's head. If the baby's head is more but not completekly extended then the baby's brow presents towards the vagina. A brow presentation is rare, maybe happening in about 1 in 2,000 births, more likely in pwomen with their second or subsequent births. A baby with a brow presentation can only deliver vaginally if the head flexes or extends.
Prolapsed arm
Popular Pregnancy Resources

New! Get Our Childbirth Course

Due Date Calculator

Boy or Girl? Find Out!

Early Pregnancy Symptoms

Brown, Green or Blue Eyes? Predict!

Ultrasound Measurements Explained
Pregnancy Week by Week

- About Merck
- Merck Careers
Toward the end of pregnancy, the fetus moves into position for birth. Normally, the position of a fetus is facing rearward (toward the woman’s back) with the face and body angled to one side and the neck flexed, and presentation is head first.

COMMENTS
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
Cephalic occiput posterior. Your baby is head down with their face turned toward your belly. This can make delivery a bit harder because the head is wider this way and more likely to get stuck ...
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one ...
Once the fetus is engaged, it (fetus) does not go back up. Prior to engagement occurring, the fetus is said to be "floating" or ballottable. f. Position. This is the relationship between a predetermined point of reference or direction on the presenting part of the fetus to the pelvis of the mother. (1) The maternal pelvis is divided into ...
Posterior position is formally known as "occiput posterior" because the back of your baby's skull (occipital bone) is in the back (posterior) of your pelvis. In the frank breech presentation, both the baby's legs are extended so that the feet are up near the face. This is the most common type of breech presentation.
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse. Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position. Abnormal fetal lie, presentation, or position may occur with. Fetopelvic disproportion (fetus too large for the pelvic inlet)
If your baby is headfirst, the 3 main types of presentation are: anterior - when the back of your baby's head is at the front of your belly. lateral - when the back of your baby's head is facing your side. posterior - when the back of your baby's head is towards your back. Top row: 'right anterior — left anterior'.
Presentation of twins in Der Rosengarten ("The Rose Garden"), a German standard medical text for midwives published in 1513. In obstetrics, the presentation of a fetus about to be born specifies which anatomical part of the fetus is leading, that is, is closest to the pelvic inlet of the birth canal.According to the leading part, this is identified as a cephalic, breech, or shoulder presentation.
Normally, the presentation is vertex (head first), and the position is occiput anterior (facing toward the pregnant person's spine) and with the face and body angled to one side and the neck flexed. Variations in fetal presentations include face, brow, breech, and shoulder. Occiput posterior position (facing forward, toward the mother's pubic ...
Lie. Facing the patient's head, place hands on either side of the top of the uterus and gently apply pressure. Move the hands and palpate down the abdomen. One side will feel fuller and firmer - this is the back. Fetal limbs may be palpable on the opposing side. Fig 2 - Assessing fetal lie and presentation.
Fetal lie refers to the relationship between the long axis of the fetus with respect to the long axis of the mother. The possibilities include a longitudinal lie, a transverse lie, and, on occasion, an oblique lie. Fetal presentation is a reference to the part of the fetus that is overlying the maternal pelvic inlet.
Head Down, Facing Up (Cephalic, Occiput Posterior Presentation) In this position, baby is still head down towards the cervix, but is facing its mama's front side. This position is also known as "sunny side up," and is associated with uncomfortable back labor and a longer delivery. While not as ideal as a cephalic presentation, it's very ...
Follow Step 5 - a complementary diagnostic procedure after performing the Leopold Maneuver. e, position, presentation and attitudeStep 1First maneuverFundal gripUsing both hands and facing the pregnant woman, palpate the upper a. domen by putting both hands on the top of the uterus, called the fundus.Use this maneuver to.
Fetal position reflects the orientation of the fetal head or butt within the birth canal. The bones of the fetal scalp are soft and meet at "suture lines." Over the forehead, where the bones meet, is a gap, called the "anterior fontanel," or "soft spot." This will close as the baby grows during the 1st year of life, but at birth, it is open.
Toward the end of pregnancy, the fetus moves into position for delivery. Normally, the presentation is vertex (head first), and the position is occiput anterior (facing toward the pregnant patient's spine) with the face and body angled to one side and the neck flexed. Abnormal presentations include face, brow, breech, and shoulder. Occiput ...
Fetus-in-fetu (FIF) is an extremely rare congenital anomaly in which a vertebrate fetus-like mass is situated within the body of its fully developed host. Two main hypotheses on the pathogenesis of FIF have been described. The "included-twin" or "parasitic-twin" theory suggests that FIF arises from an anomalous monozygotic monochorionic ...
Approximately 97% of deliveries involve a fetus positioned with the head down, in the best position to slide out. That makes a vaginal delivery easier and safer. A transverse position only happens in about 1% of deliveries. In that position, the shoulder, arm, or trunk of the fetus may present first. This isn't a good scenario for either of you ...
The urinary system is the most common site of abdominal masses; however, we will not consider the kidneys, ureter, and bladder in this review. Management is conservative and depends on mass size, symptoms, and presence of complications. Masses greater than 4 cm to 5 cm are associated with a risk of torsion approaching 50% to 78% and typically ...
A malpresentation or malposition of the fetus is when the fetus is in any abnormal position, other than vertex (head down) with the occiput anterior or posterior. ... If the baby's head is more but not completekly extended then the baby's brow presents towards the vagina. A brow presentation is rare, maybe happening in about 1 in 2,000 births ...
Toward the end of pregnancy, the fetus moves into position for delivery. Normally, the presentation is vertex (head first), and the position is occiput anterior (the fetus faces toward the pregnant person's spine) with the face and body angled to one side and the neck flexed. Abnormal presentations include face, brow, breech, and shoulder.
Normal Position and Presentation of the Fetus. Toward the end of pregnancy, the fetus moves into position for birth. Normally, the position of a fetus is facing rearward (toward the woman's back) with the face and body angled to one side and the neck flexed, and presentation is head first. In these topics. Labor.