A Letter To My Pregnant Self

TLDR: In this personal essay, a mother reflects on her journey by writing a letter to her past pregnant self to assure her—and other mothers-to-be—about the wonder of motherhood.
Dear Pregnant Self,
You know I am not one for the cheesy stuff—I’m not a very romantic person. I don’t like Hallmark cards. I don’t even like Valentine’s Day.
So you know that I’m not prone to overstatement when I say this:
You are about to meet the love of your life.
That growing bump that you’ve been patting for the past few months, looking at in the mirror, wondering about? That’s the love of your life in there. I know it sounds cheesy, and if I knew any other way to describe it, I would. But sometimes, it turns out, the cheesiest things in the world are also the truest. I know you’ve had other loves in your life, but not like this one. There is nothing more pure and strong than this, there just isn’t. Agape love, the Ancient Greeks called it—a universal, unconditional love that transcends, no matter the circumstances.
I look at my birth photos now and it seems amazing to me that there was ever a time I didn’t know him. Before he was born, I didn’t have any sense of who I thought he might be or my hopes for him, other than that he would be happy. When he was born, I remember looking at him in total amazement, just thinking, “Who are you?”
The not knowing? That’s one of the sweetest parts.
So I’m not going to give you any of this "sleep when the baby sleeps" business. (Although seriously, sleep when the baby sleeps . People aren’t just making this advice up.)
I’m not going to tell you to enjoy every minute, because I know there will be days where you just feel raw and hormonal and weepy and not yourself and neither triumphant nor very joyful.
And I won’t tell you not to worry , either, because that’s simply not possible.
“When will I stop being afraid?” I tearfully asked my mom weeks after his birth, knocked over by this newfound combination of love and terror. “Oh honey,” she said. “You never will.”
Once, several years before I got pregnant or was even thinking about it, I asked a male coworker what it was like to have kids. “It’s like having your heart outside your body, running around in the world,” he said cheerfully. “That sounds so scary,” I said. “Oh, it is,” he said, still smiling. “And absolutely worth it.”
What I will tell you is to have long dinners with your closest friends—friends that have kids, friends that don’t. Friends that are married, friends that aren’t. They’re all going to be so important in this next stage of your life, even though it might take a bit more planning to see them after the baby is born.
If you’re a traveling sort, definitely take a trip. It doesn’t have to be a huge, over-the-top journey, just something fun to tide you over. (Although you can absolutely travel with babies. It just isn’t as convenient.)
But of all the things that keep you up at night as you wonder about this new world of motherhood , don’t worry about not loving him enough. That part will be easier than anything you’ve ever done before. Because like I said, you’re about to meet the love of your life.

Want evidence-based health & wellness advice for fertility, pregnancy, and postpartum delivered to your inbox?
Your privacy is important to us. By subscribing you agree to our Privacy Policy and Terms & Conditions . This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Anna Gannon
Meditation Guide
Anna Gannon is an intuitive meditation and yoga teacher.
Related Articles

Can You Go Down a Waterslide While Pregnant?

Can You Donate Plasma During Pregnancy?

Everything To Know About Prenatal Yoga

8 People You Need in Your Pregnancy Support Crew - article body template
Everything to Know About Prenatal Yoga

These Are the 8 People You Need in Your Pregnancy Support Crew

Is Papaya Safe During Pregnancy? Yes, If You Follow a Few Guidelines

Can You Use a Massage Chair During Pregnancy?

6 Pregnancy Self-Care Tips for Expectant Moms
Get the newsletter.
Evidence-based health and wellness resources for fertility, pregnancy and postpartum.
CONFIDENCE, COMMUNITY, AND JOY
- Skincare Ingredients A-Z
- Skin Concerns
- Hair Removal
- Moisturizers
- Tools and Techniques
- Hair Concerns
- Hair Styling
- Fashion Trends
- What to Wear
- Accessories
- Clothing and Apparel
- Celebrities
- Product and Brand News
- Trends and Innovation
- Amazon Picks
- Gift Guides
- Product Reviews
- Mental Health and Mood
- The Byrdie Team
- Editorial Guidelines
- Editorial Policy
- Terms of Use and Policies
- Privacy Policy
- The Self-Expression Issue Overview Cover Story Arden Cho Has Found Her Light The B Side Get to Know Arden's Glam Team: Hairstylist TerraRose Puncerelli and MUA Sang Jeon
- 25 Products We're Using to Bring Our Favorite Summer Trends to Life
- Is This the End of Hotness as We Know it?
- *If You're Looking for the Next Big Jeans Trend, You Won't Find It
- 15 Matching Sets That'll Carry You Through the Summer Months
- Elevate Your Spring/Summer Look With These Not-So-Basic Denim Skirts
- These Trending Luxury Pieces for Summer Are Actually Worth the Buy
- Praise for the Silly Little Tattoo
- We’re In Our Brow Decorating Era
- The Watercolor Manicure Trend Will Transform Your Nails into a Monet
- The Varsity Trend Is the Retro-Sporty Alternative to Athleisure This Summer
- We're Wearing Highlighter Everywhere But Our Cheeks
- Powder Puffs Are Trending—Here's How to Use Them For Flawless Makeup
- 3 Important Life Lessons My Unexpected Pregnancy Taught Me About Self-Love
- Is This the End of the "Cool Girl" Beauty Brand?
Three Important Life Lessons My Unexpected Pregnancy Taught Me About Self-Love
:max_bytes(150000):strip_icc():format(webp)/aimee-3-c5d7984be2de4300a8e02aaac71a3cc3.jpg)
I've never trusted myself in life until now. Let me explain.
I'm 28 years old, the oldest child to immigrant parents, and I have had an awesome career thus far. I'm in a loving, long-term relationship with my best friend in the universe. I've traveled, moved, and taken care of myself and others. Still, up until now, I've never fully trusted myself with my decisions or happiness. It took a lot for me to admit that—especially in writing—but it's a realization that has made me proud of myself in my newest life phase as a soon-to-be mom.
I found out I was pregnant in late 2022, which, at the time, hit me like a ton of bricks. The holiday season; end-of-year commitments; and the shocking, life-altering view of a positive pregnancy test staring me in the eyes hit me hard. Morning sickness, fatigue, and loss of appetite also came down on me like an avalanche.
I've always dreamed of a family, and my partner and I would fantasize about what that day would look like when it came. We've had our baby names picked out for years and always joked about which of us would be the buttoned-up parent versus the jokester. Still, nothing could prepare us for the day that the thought we'd stored away in our memory boxes was becoming a reality. I always thought the day I learned I was pregnant would open a dumpster fire of second-guessing and self-doubt. Yes, I've experienced those questionable thoughts since finding out, but they haven't plagued me and consumed my life and brain as anticipated.
As a natural overthinker and people pleaser, I thought I'd be in for a mentally miserable, guilt-ridden pregnancy, fearful of all the possibilities and opinions. Instead, I’ve experienced an extreme sense of calm, and having honest conversations with myself has put me in the best mental state I've been in for a long time. I've looked in the mirror a few times and thought: What is wrong with me? As though this new chapter wouldn't be valid unless it was met with extreme angst.
"A woman may feel calm or nervous during pregnancy for several psychological reasons, including hormonal and circumstantial factors," says licensed psychologist Carolyn Rubenstein, PhD. "Aside from hormones, factors such as a woman's support system, financial situation, and overall health can also affect how a woman feels during pregnancy."
Pregnancy is challenging and looks different for everyone. Still, honoring a few truths of my own have helped me process this significant life change in a valuable way, making the good days great and the bad days feel more manageable. It's shown me the true meaning of giving myself grace and practicing gratitude, and I'm a better person because of it.
Ahead, find the three life-changing lessons I've learned so far that have gotten me the closest to feeling real self-love for the first time in—dare I say—ever?
Meet the Expert
- Carolyn Rubenstein , Ph.D., is a licensed psychologist and wellness consultant based in Boca Raton, Florida.
Transition Is Consistent, and Change Is Temporary
One of the first things I felt when finding out I was pregnant was the incoming of a huge life transition. Everyone tells you how much your life will change, but few people talk about these changes positively and optimistically. I was initially scared, but that changed when a close friend reminded me that most things in life—pregnancy included—are temporary. Bringing a life into the world is a huge deal, met with many emotions, but it isn't the only life transition you'll experience.
I had fears of my body changing, fears of my home being different, and fears of learning new things. Reminding myself that these phases will evolve has helped me work through them. "When faced with major life changes like pregnancy, it's common to feel overwhelmed and anxious about unknowns," Rubenstein says. "However, there are ways to shift your mindset and approach these changes with a more positive outlook." Rubenstein says reframing your thinking to focus on opportunities and growth is a great way to cope with change, which I've found valuable at the most uncertain times thus far.
The positive outweighs my fears when I think of how I've grown as a person in the past few months. I've used moments of uncertainty to better inform and educate my decisions. I've found a voice to advocate for myself in situations where I'd usually retreat, one of the significant self-improvement indicators in my book. This has taught me that I am a work in progress and will continue to be beyond pregnancy and motherhood.
Self-Care Is Critical
Aimee Simeon
In addition to reframing your thoughts, Rubenstein says practicing mindfulness and self-care—whatever that means to you—can help you better navigate significant life transitions. "Prioritizing self-care, such as rest, mindful eating, fitness, and participating in activities that bring you joy, can help you stay grounded and centered during this time," she says.
I've found this step critical in evolving during these past months. One year before getting pregnant, I was diagnosed with PCOS. I was physically and mentally burned out, and my self-esteem and comfort in my body were at an all-time low. Desperate to feel at home in my skin and manage my symptoms, I embarked on a journey to find my "thing" in the wellness world.
I discovered the healing powers of therapy, acupuncture, and movement tapping as a release. What started as a mission to balance my hormones turned into finding a source of joy where I could be with myself and feel happier for it.
Waking up in the morning and dedicating time to my body taught me the power of movement and the value of carving out time to be alone each day to feel more centered. Taking time each day for myself helped me feel less stressed and more connected and attuned to my mental health.
Having a new family member in our household will mean less solo time for the foreseeable future. Still, acknowledging the impact intentional solo time had on me motivates me to make it a nonnegotiable part of my routine instead of one that feels jeopardized when our baby is earthside. I want to show my daughter that her mom knows the importance of resetting and caring for herself so that she can show up for others.
Rubenstein says movement is beneficial, but you aren't limited to just working out. "Take time for yourself and do things you enjoy. This could be reading a book, taking a relaxing bath, or getting a prenatal massage," she says. Pregnancy has reminded me to relish in the moments of "nothing", including a midday nap, my favorite snack, or a weekend spent repotting plants—all things I may have deprived myself of before.
Connecting with myself in these moments that may otherwise feel mundane has increased my feelings of peace and happiness, showing me that comfort lies within when you allow yourself to feel it. Plus, there's nothing like extreme fatigue and nausea to remind you to slow the f down and smell the roses.
Embrace the Positive
I've often wondered if my positivity could be considered toxic or naive, but it's neither. "During pregnancy, the body undergoes significant hormonal changes, including increased levels of estrogen and progesterone, which can impact brain function and emotional regulation," Rubenstein says. "Hormonal changes during pregnancy can cause alterations in brain regions involved in emotional processing, social cognition, and memory. For example, some pregnant women have increased activity in the amygdala, a brain region associated with emotional processing and stress response."
I, by no means, have a perfect life, but practicing gratitude has helped me feel fortunate during this time. I'm grateful to my body for allowing me to be healthy enough to have made it this far. I'm also thankful for my small but mighty support system of friends and family, who are always around to talk or listen as I navigate this new chapter. I realize this is a huge privilege I do not take for granted.
Society has conditioned many of us, especially Black women, to embrace struggle and hustle, but doing so has only made me regularly feel stressed out, unhappy, and physically unwell. Talking myself out of this negative rut has been the ultimate radical act of self-love and one I fully intend to teach my daughter.
Creating life has taught me that, ultimately, life will throw you challenges, but it's genuinely up to us not to let them define who we are. This is a huge realization for me, since I'm someone who would typically let even the slightest mistake send me into a spiral of self-loathing and doubt. Instead, my priorities have shifted to making sure that I am mentally well before anything else, which has improved my life in all areas. Call me crazy or toxically optimistic, but basking in moments of gratitude and appreciating everything going well has put a lot into perspective.
Relinquish Self-Doubt
Before this current chapter in my life, self-reassurance was something I lacked. I questioned my outfit choices, looked to others to validate career moves, and didn't think to make a significant (or minor) life choice without fearing the opinions of my peers and family.
Pregnancy has taught me the most beautiful lesson that I am in control of nothing but myself. I can't control the outcomes of every transition in life, but I can control how I work through them and what I take from each process. I've learned to trust my instincts, listen to my body, and prioritize my mental health in a way that doesn't feel forced because it's the "cool" thing to do.
Instead, it's taught me to relinquish doubt and embrace control by loving myself. It's unlocked a new sense of optimism that will allow me to show up as my best for myself and my family; I'm forever grateful for that transition.
Related Stories
4 Black Women on Moving Cross-Country and Starting New Lives During the Pandemic
"Be the Storm": A Look at What Power Means at Every Age
8 Women Share the Ups and Downs of Living Alone During a Pandemic
I Lived It: Ending My Longterm Relationship During a Global Pandemic
Why Can’t "Smart Girl" and "Beauty Girl" Go Hand in Hand?
Exclusive: Meena Harris Is Changing the World, One T-Shirt at a Time
"I Finally Feel Relief": 11 Healthcare Workers on the Emotional Journey to Vaccination
From ER Nurses to Small Business Owners: 7 Real Stories of Pandemic Trauma
Shay Mitchell Is Pursuing Happiness on Her Terms
Get to Know Shay's BTS Team: Hairstylist Dimitris Giannetos and Stylist Shalev Lavàn
Editors’ Picks: The Best New Beauty Products We Discovered At Home
I Got a Haircut During My Wedding to Connect with My Higher-Self
How I Quit Drinking and Started Listening to My Body
9 Women Open Up About What It's Really Like to Have Anxiety
Why I Let Go of My Perfect Relationship
What People Don't Know About Love After a Toxic Relationship
Understanding what pregnancy feels like if you’ve never had this experience can be difficult. Here, we’ve answered some of your burning questions on this topic, including “What does being pregnant feel like?” and “How does being pregnant make you feel?”
- When to Start
- Due Date Calculator
- Prenatal Care Costs
What Does It Feel Like To Be Pregnant?
Being pregnant is a life-changing experience for many women — but it’s one that’s hard to comprehend if you have never been pregnant before. The idea of growing another human inside of you for nine months is a feeling only certain women can experience and, as much as they try, it’s hard to explain in words exactly what pregnancy is like.
Still, people often ask: What does it feel like to be pregnant? How does it feel to be pregnant, and what can you expect from a pregnancy experience?
These questions tend to come from women who are interested in becoming pregnant or are thinking they might be pregnant, but they can also come from men who are curious about what their wives, spouses, friends and other loved ones go through during this process. While every pregnancy is different, we’ve tried to describe in general terms what it is like to be pregnant below — to help all those who are curious understand this beautiful process in more detail.
Remember, it’s always best to speak with your doctor if you are curious about pregnancy or think you might be pregnant. They can offer the best medical advice for your situation.
What Does It Feel Like to Be Pregnant?
While some of the questions about what pregnancy feels like come from curious outsiders, others ask “What does being pregnant feel like?” for a more serious reason — they think they might be pregnant.
The first symptoms of pregnancy are different for everyone, and so is what being pregnant feels like for each individual. Perhaps you feel nauseous, tired and cranky, or maybe you think your breasts are tenderer than they usually are. Maybe you’ve missed your period this month.
Panic alarms may be going off inside your head, prompting you to ask, “What does it feel like when you get pregnant?”
It’s common to hope you can determine whether you are pregnant simply from side effects , but the most effective way to find out you are pregnant will always be through a pregnancy test. You can pick one up from your local drugstore or go to your doctor to receive a professional blood or urine test.
In the meantime, you may want to identify some of these side effects — how you will feel when you are pregnant. Here are a few early pregnancy symptoms that you may want to look out for during this time:
- Morning sickness, or nausea at any time of the day
- Cramps or headache
- Slight bleeding
- Food aversions or cravings
- Breast tenderness
- Mood swings
- Faintness or dizziness
- Missed period
Sometimes, women wonder what being pregnant feels like because they simply “feel different” and have a hunch they are pregnant. The abovementioned side effects can be due to many things other than pregnancy but, if you are not feeling like yourself or feel like something is “off,” you may be finding out for yourself what pregnancy “feels” like.
If you are experiencing any of these signs and wondering “How do you feel when you’re pregnant?” remember that a pregnancy test is the best way to confirm any possible pregnancy.
What Being Pregnant Feels Like as Your Baby Grows
Once you have your answer to the question, “How do you feel in early pregnancy?” you are probably just as curious to know the answer to this question: “What does it feel like being pregnant as your baby continues to grow?” After all, this is the one of the biggest questions from people curious about the pregnancy process; carrying a living human being inside of you is such a foreign idea to those who haven’t experienced it themselves.
Again, every woman’s pregnancy is unique, and only you will be able to know what it is like to be pregnant in your later trimesters. For many women, the earlier side effects of pregnancy lessen as they enter their second and third trimesters , but that’s not the case for everyone. Sometimes, the side effects of early pregnancy are replaced with more constant side effects that a woman can’t alleviate until her baby is born.
When you carry a child inside of you, your body reacts in certain ways. A lot of your energy is going toward creating this child, and you can’t expect your body to feel the same as it did when you were not pregnant. In addition to the symptoms listed above, you may also feel:
- The constant urge to urinate, a lot
- Fatigue and muscle soreness from carrying an ever-growing child inside of you
- Irritability due to difficulty sleeping and getting comfortable with an expanding stomach
- Mood swings due to changing hormones
- Constipation and other upset stomach
- Heartburn and backache
Don’t forget: All of what you feel during your pregnancy will likely seem trivial compared to the experience of labor and delivery .
Of course, what pregnancy feels like for some women will be easier than for others — but it’s important to be aware of these potential side effects if you are considering becoming pregnant in the near future. Having all the information before you get started will help you have the appropriate expectations for your pregnancy journey and understand that everything you are feeling during this time is normal.
What is it Like to Be Pregnant?
Typically, when you ask women, “What does being pregnant feel like?” they’ll say it is the most beautiful thing they have ever experienced. It’s a powerful feeling, to grow a child from nothing to a tiny human, and many are so happy with the end result that they may gloss over some of the harder parts of pregnancy.
But, before you become pregnant yourself, you need to understand: While many say it’s worth it in the end, pregnancy is very hard , comes with certain risks and possible complications, and should not be seen as anything less than a great commitment of your mind and body.
In addition to the physical challenges of pregnancy, there are a few mental and emotional challenges that many women have to cope with. The hormones of pregnancy can cause extreme mood swings that are often not helped by the stress of pregnancy and preparing to bring a little one into your family. While these mood swings are normal, they can be overwhelming for someone who doesn’t know how it feels to be pregnant.
If you are pregnant, you may feel:
- Stressed at the all the preparations needed for a baby
- Tired from the physical challenges of pregnancy
- Worried about your baby’s future, especially if you did not plan to become pregnant at this time in your life
- Misunderstood by unsupportive partners
- Panicked about how your life is going to change
- Depressed about your situation, whether due to personal circumstances or antenatal depression
While every woman’s experience is different, and it’s difficult to predict exactly what it will be, knowing the answer to the question “How do you feel when you are pregnant?” beforehand can help you better prepare yourself for the challenges and experience awaiting you. Remember, if you find yourself overwhelmed during your pregnancy or worried that you’re not feeling the way you “should,” this is completely normal — and you do have options.
If being pregnant feels like an unexpected, unwanted but unavoidable thing in your life, you always have unplanned pregnancy options such as abortion and adoption. Don’t ever let anyone tell you what you should feel during pregnancy; focus on yourself and your emotions, and don’t be afraid to reach out for support from loved ones and counselors, should you need it.
My Birth Story: Moms Share Their Birth Experiences
What to expect birth stories, jump to your week of pregnancy.

Essay on Pregnancy
Students are often asked to write an essay on Pregnancy in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Pregnancy
What is pregnancy.
Pregnancy is when a baby grows inside a woman’s womb or uterus. It starts when a sperm from a man joins with a woman’s egg. This tiny new life is called an embryo at first, and then a fetus as it gets bigger. A full pregnancy usually lasts about nine months.
Stages of Pregnancy
Pregnancy has three parts called trimesters. Each trimester is about three months long. In the first, the baby’s body is forming. During the second, the baby grows bigger and stronger. In the last trimester, the baby gets ready to be born.
Changes in the Mother
A pregnant woman’s body changes a lot. She may feel tired, have morning sickness, and her belly will grow as the baby does. She needs to eat healthy foods, get checkups, and take care of herself to help her baby grow strong.
The Birth of the Baby
When the baby is ready to be born, the mother will feel labor pains. This is when her body tells her it’s time for the baby to come out. The baby will come out through the birth canal, and the family will welcome a new member.
250 Words Essay on Pregnancy
Pregnancy is the time when a baby grows inside a mother’s womb. It starts when a sperm from the father joins with an egg from the mother. This can happen through a natural process when parents are trying to have a baby, or through medical help if they are having trouble.
Pregnancy lasts about nine months and is divided into three parts, called trimesters. In the first trimester, the baby is just starting to form. The mother might feel tired and sick. The second trimester is often easier. The baby grows bigger, and the mother can feel it move. In the last part, the third trimester, the baby gets ready to be born. The mother’s belly is very big, and she might feel uncomfortable and excited to meet her baby.
Health During Pregnancy
It’s important for the mother to take care of herself and the baby. Eating healthy food, going to the doctor for check-ups, and staying away from bad habits like smoking or drinking alcohol are all very important. These things help the baby grow strong and healthy.
Having the Baby
When the baby is ready to come out, the mother will feel pains called contractions. This is when the baby is pushing to get out of the womb. The mother will go to a hospital or a birthing center where doctors or nurses will help her give birth. After the baby is born, it’s a happy time for the family as they welcome the new member.
Pregnancy is a special time when a new life is being made. It’s full of changes, care, and excitement as families prepare for a new baby.
500 Words Essay on Pregnancy
Pregnancy is the time when a baby grows inside a woman’s womb or uterus. It starts when a sperm from a man joins with an egg from a woman. This is called fertilization. The fertilized egg then attaches to the wall of the uterus. This is the beginning of a nine-month journey, which we divide into three parts called trimesters.
The Three Trimesters
The first trimester is from week one to the end of week 12. During this time, the baby is called an embryo. It’s a critical time because all the baby’s organs start to form. The mother might feel very tired and sick as her body changes.
The second trimester is from week 13 to the end of week 26. The baby is now called a fetus. This is when the mother can feel the baby moving. The baby’s skin is thin and red, and its bones start to harden.
The third trimester is from week 27 until the birth. The baby grows bigger and stronger. It can now blink, dream, and even listen to sounds. The mother’s belly is very big, and she might feel uncomfortable and excited to meet her baby.
Changes in the Mother’s Body
A woman’s body goes through many changes during pregnancy. She might gain weight and feel different emotions. Her belly will grow as the baby grows. She will also visit the doctor often to make sure she and the baby are healthy. These visits are called prenatal care.
Healthy Habits for Pregnancy
It’s important for a mother to take care of herself during pregnancy. Eating healthy foods and staying away from harmful substances like cigarettes and alcohol are very important. Taking vitamins, getting rest, and doing gentle exercises can help keep the mother and baby healthy.
When the baby is ready to be born, the mother will feel contractions. These are like very strong belly aches that come and go. They mean the baby is pushing its way out. Birth usually happens in a hospital, but some choose to have their babies at home. Doctors, nurses, or midwives help the mother during birth.
After the Baby is Born
After the baby is born, it’s a time for joy and celebration. The mother will keep taking care of herself and the baby. The baby will need to eat often and sleep a lot. The mother might feel many emotions and get tired, but it’s important to ask for help if she needs it.
Pregnancy is a special time when a new life is growing. It brings changes and new responsibilities. It’s important for the mother to take good care of herself and get ready for the arrival of her baby. With support from family, friends, and doctors, she can look forward to the birth of her child. When the baby finally arrives, it’s the start of a new adventure for the whole family.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on My Own Philosophy Of Education
- Essay on My Parents My Hero
- Essay on My Parents Sacrifice For Me
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.


Experiences of pregnancy
When talking about their experiences of pregnancy, most people described it as life-changing, and discussed both its physical and emotional aspects. Some women enjoyed being pregnant and said they ‘didn’t have any problems’. Others found the experience of pregnancy more challenging, whether for physical or emotional reasons or a combination of both. Some men also talked about their emotional experiences during their partner’s pregnancy.
Common changes women talked about were altering their diets, looking and feeling different, craving certain foods, and experiencing fatigue and nausea. Some were surprised about how exhausted they felt. Many women experienced physical pain or discomfort during pregnancy, including sciatica, restless legs syndrome, deep vein thrombosis, headaches, fluid retention, heightened sensitivity to smell and heat, and tender larger breasts. When pregnant with twins, women felt that their changes and discomforts doubled. A few women loved the physical experience of being pregnant and embraced their new shape. Others felt ‘uncomfortable’ and described being unprepared for the physical dimensions of pregnancy.
> Click here to view the transcript
I went to the physio but they couldn’t push it in, they just said, “It’s the position that the baby’s in, there’s nothing you can do about it and try not to move,” [laughs].
Often women struggled to accept they were experiencing a ‘normal’ pregnancy because they felt so bad physically. Several women with more than one child said their second or later pregnancies were harder, particularly due to having to care for other children. Coping with nausea was more difficult when women had older children, experienced a lack of support, or when they had demanding or inflexible jobs. Some partners helped by providing practical support, including Ajay, a migrant father of one, who learned to cook when his wife was unwell during early pregnancy.
I found it immensely difficult on the train of a morning going into town. My GP gave me this recommendation to carry a plastic bag in my handbag so I that I always had something to throw up into if I needed to. It just places this pressure on you that I had never felt before, and I remember feeling like I didn’t want to be pregnant anymore. If this is what being pregnant is like I don’t want it, you can have it back. And my mum said to me, “You know, it’s only six more weeks and then you should feel better”, and the thought of six more weeks felt like a lifetime. The thought of just getting through the day felt like a lifetime.
So it was very draining, just very difficult – and again it placed a strain on the relationship with my husband because on the weekends he’d say, “Do you want to go out, do you want to go to a café, would you like to do this, would you like to do that?” and I said, “I don’t want to do anything, I just want to be at home with a bucket in my tracksuit pants [laughs] doing nothing”, because I just felt rotten. And you inevitably compare yourself to other people and the very early pre-birthing classes that I went to, they were talking about the importance of healthy eating and exercise and other pregnant ladies would say, “I go swimming four times a week”, and “I’m walking and I’m doing this”, and I thought, ‘I’m lucky if I can make to the letterbox and back’.
The physical and emotional aspects of pregnancy were intertwined for many women. Chelsea, a mother of one, described wondering if her nausea was caused by her anxiety or if it was the other way around. Others experienced a sense of disconnection between being pregnant and their day-to-day lives. Loretta described having difficulty focusing in formal work meetings while feeling her baby’s hiccoughs inside her: ‘That’s something I will never forget, just thinking – these two worlds are not matching in any way and I don’t know how they’re ever going to’. A few women mentioned social expectations to be happy, positive and ‘glowing’ during pregnancy.
And I can see that it’s a sacrifice. I’ve got a newfound respect for pregnant women and I will from now on question when they tell you how happy they are whether that is true because that’s the perception I gained before falling pregnant that pregnancy is lovely and exciting and sure, on many levels it is but the physical changes that happen to you and the daily aches you have.
And how sleep gets disturbed to the point that for me going to bed is actually the least pleasant part of the day because I feel breathless and I feel dizzy and I don’t feel comfortable and I can’t sleep.
I feel like nobody told me that, as if they either kept it to themselves, surely I’m not the only one going through these symptoms.
And I feel like the pregnancy affects my productivity. I’m always very goal-oriented person so to come home and not having energy to do what I would have normally done. Or not being able to walk somewhere as fast as I would have liked or as far.
Women talked about how the novelty of the experience of a first pregnancy distracted them from thinking about parenthood. Zara explained how she felt during her first pregnancy: ‘I think the whole time the focus was on the practical matters and I didn’t really give a lot of thought at all to the emotional consequences or realities of what it would mean to become a mother’. As a result, many women described being unprepared for life with a new baby – yet said they were not sure anyone could have prepared them.
A sense of vulnerability and responsibility for their unborn child was described by some women, while others remembered marvelling at having a baby growing inside them. Pregnancy brought emotional ambivalence for women such as Susanne who had always wanted to become a mother, but found pregnancy challenging and felt ‘miserable’.
I felt good for like a week. I’m like, ‘I can totally do this pregnant thing,’ and I just had this feeling, I just had this ridiculous idea that I’d be a bump and I’d be rosy and glowing and I could still walk and I could wear those tops to show off the belly.
I put on 10 kilos within about 30 seconds of being pregnant. I now know that it’s because I developed a form of arthritis which messes with your metabolism, whatever. So I had ongoing health issues throughout the whole thing, but I had no idea. So I couldn’t do any exercise, I could hardly walk, I could definitely not run, and I was emotionally… I’ve really bad psoriasis and the type of arthritis that I get is psoriatic arthritis. So it’s connected to psoriasis. I’d never had it before, never been diagnosed before, but looking back I’ve had it since I was a kid, it just wasn’t that serious. So the flare-ups went sort of undetected in an arthritis context.
The type of psoriasis and arthritis that I get is triggered by an immune system overloaded stress on your body which is exactly what pregnancy is [laughs]. So looking back that started pretty much straightaway, that achiness and, yeah, that beached whale thing.
So it was a really awful pregnancy and I felt really conflicted through the whole thing because this is all I wanted my whole life, and not only is this what I wanted my whole life but I left a heterosexual relationship and a heterosexual identity to be true to myself and I still am managing to have this amazing gift and living my dream and I am hating every single second of it.
A number of people related emotional distress during pregnancy to past experiences of depression and anxiety, or childhood experiences. When pregnant with her second child, Maree was worried about unconsciously repeating the favouritism she thought her parents had shown towards her younger sibling. Others experienced anxiety, stress, or antenatal depression related to the pregnancy itself (see talking points under the theme ‘Perinatal depression and anxiety’).

From my previous experience as a mental health worker, I started to spot warning signs that I needed to have some kind of communication. Because I think that the first step in anything, when you think that there’s something going wrong with your head, because that’s the first thing people spot, the first thing to do is to actually talk to people about it. So we’ve had a very open communication with my partner, and we’ve been able to talk a lot about the way that I’ve been feeling. And I’ve also been quite lucky, that I have quite a tight-knit group of male friends who are actually the partners of – my partner has a mum’s group, so there’s probably six mums who hang out every week with the kids, and they’ve all grown up together.
And the dads have actually got a tight bond now. And without trying to scare the males into having sort of bonding and talking sessions, that’s what we’ve been doing, and it’s been really useful. Because it’s not just me who’s been going through this, there’s been a couple of other guys who are in a similar situation of just stress, panic, fear, all of those sorts of things, coming out into the open. I think it’s the fear of the unknown, and wondering whether you can actually cope with having another child. There’s always an assumption that a guy can cope with everything that’s thrown at him and there’s not so much availability for support networks.
And there’s an assumption that a guy can get through this without any help. And yeah, I don’t feel strong enough to be able to do that. I’ve broken down a number of times. And by that I mean lots of crying and thinking that I can’t do it and I don’t have enough mental strength to get through the situation. But being able to express that has been very, very useful. As I got closer to the time of the birth I was much more excited about the birth.
A number of people experienced significant life events, including losing jobs, relationship breakdowns, family violence, or moving interstate or overseas, including to escape war. These experiences significantly contributed to emotional distress in pregnancy. Melanie described how a difficult relationship with her mother became more complicated after finding out that her mother had lung cancer. Tolai migrated from Afghanistan to Australia during very late pregnancy.

Parents described a range of complications during pregnancy involving the mother’s health, the baby’s health, or both. These included ectopic pregnancy, bleeding, placental problems, ‘incompetent cervix’, gestational diabetes, severe nausea (hyperemesis gravidum), ovarian cysts, high blood pressure and pre-eclampsia. Two people experienced problems with their babies, including supraventricular tachycardia (SVT) and gastroschisis.
The emotional impact of these experiences ranged from a sense of inconvenience through to significant distress. Erin described a range of complications including gestational diabetes in her fourth pregnancy and bleeding for over half of her sixth pregnancy due to a hematoma within her uterus.
So they could see that I had a sub-chorionic haematoma, which is like a blood sac next to the gestational sac. That was – it was bigger than the baby at that stage. And they said, “Prepare yourself for the worst, because the bleed could push the foetus out”. And there was nothing they could do really. It is what it is. So I was going on and I was just bleeding all the time and, you know, being pregnant and bleeding does your head. I know what it was like when I was bleeding when I had my fourth child. It was horrendous, you know. You just can’t relax. But, I mean, there was a break there. It wasn’t happening all the time, whereas this was constant bleeding and it was awful.
I couldn’t function. I just felt like I was walking on eggshells all the time. It was like, ‘Can you either just make up your mind, are you going to stay or are you going to go, but don’t have this constant’. Because going to the toilet was doing my head. It was a constant reminder that things were not normal. And there’d be days where all of a sudden it would just be a huge bleed, and I’d think, ‘Oh God, is this it’? You know, it was awful. So I could never relax. I was always just really tense, which is not a good thing to be when you’ve got five other kids to look after as well and life to continue.
Prenatal testing results that fostered fears about a baby’s health were stressful for people. Despite Chorionic Villus Sampling (CVS) revealing that Sarah M’s baby did not have Down Syndrome, she continued to have ‘morbid thoughts’ about her pregnancy. Loretta’s first child was diagnosed with a genetic condition while she was pregnant with her second, making her anxious about her unborn daughter. Rarer or more serious complications were experienced by some women, sometimes with a risk of stillbirth or a threat to their own health or fertility. These included extremely rare conditions such as placenta percreta. A few women were hospitalised for part of their pregnancies. Surgery for an ectopic pregnancy left Jane, who is now a mother of twins, unable to conceive, leading her and her partner to undergo IVF (which was successful).
So after that I had to heal and it was emotionally difficult, but it was just one more thing. We just kind of kept it aside – so that was pretty horrible. So we kept trying, once I’d recovered. It took a few months, because I was just so lacking in iron, and we started trying again and then just couldn’t, because I’d lost one fallopian tube. So, I really felt violated and brutalised and it was hard. But, you know, we really wanted to have children.
So my mother had said she would help us and she gave us some money so we would be able to afford to do IVF and we did three IUIs, which weren’t successful and even though my husband has this amazingly high, fantastic sperm count, it just didn’t work. So we had to try IVF and we only did two cycles and the first time we had two implanted and it didn’t work and at that point I thought we’ve got to give this all we could do. I’m always on the internet, so I’d known the statistics on how hard it was going to be at my age, because by then I was 41, 42, while we were doing this and anything over 35 can be very difficult. Over 40 you are incredibly lucky.
So I thought we’ve just got to go all out. We can’t keep affording to do this forever. So we found a woman, through a friend of mine, through word of mouth. Found this woman who was a Chinese herbalist and naturopath and I’d read that acupuncture is really good for IVF. So she had me on all these potions and things I had to drink, herbal remedies and, acupuncture quite a lot and – that cost us thousands too. But I think it really made the difference. So three months later, from the first IVF we went again.
Further Information:
Talking Points Experiences of pre-term birth, special care, stillbirth and death of a baby Experiences of conceiving, IVF, surrogacy and adoption Talking Points under the theme ‘Perinatal depression and anxiety’
Other resources
COPE: Expecting a baby

Personal Narrative: My First Experience When I Was Pregnant
How did I find out I was pregnant? The beginning of 2016 I had been talking to this boy named Rodney and we had been getting really serious with other about being in a relationship. April came and my mother did like the fact that I was staying with him; she wanted me to get on birth control because she didn’t want me to have any babies yet. I agreed to the birth control there were many to choose from I was scared of needle so I didn’t do it that way , I took the easy way and got the patch. With the patch you wear it for three weeks and the fourth week you have your period. Later that month Rodney took me to prom and we had so much fun with each other. We were really in a relationship by then, May is here now and I have just turned the Big 18. That means I …show more content…
I felt really bad because we were arguing the night before. After his surgery I had finally made it down there, the doctors told him that he need to walk so as me and him was walking I had told him I thought I was pregnant. He looked at me and said I had a feeling you was pregnant because of the pain you had been feeling and you not having your period. I didn’t think he was gone be happy about it but he was. I still kind of doubted it because of the birth control. We decide that I need to take a pregnancy test so we went to my house and got me sister and her friend and told them. My sister’s friend was a little older than me so I got her to get the test for me. Rodney and I went back to his house and I took the test and waited for the results. It was Positive; I never felt so many emotions at one time before. All I could think was what my mother was going to say, how I was going to tell her. I showed Rodney and he was happy but because I didn’t know what to do all I did was cried. I called and told my sister and they came right over and she was happy but I just
Personal Narrative: My First OB Clinical
This past Thursday was the first OB clinical day and I was assigned the post partum unit. I was paired with Nurse Donna, who was full of information. Originally we had three couplets, with one baby in the nursrey. As the day went on and families were discharged, all our patients had gone home so we gained three other patients from two other nurses so they could go home for the day. I was able to give two moms their TDAP (tetanus, diptheria, and pertusis) vaccines and learned a new trick when it comes to giving intramuscular shots. Donna told me to have the patient hang her arm down by her side and wiggle her fingers. This not only had the patient concentrating on something other than the shot they were about to get, but it helped activate the
Personal Narrative: My Clinical Experience
I had such a great day at clinical yesterday. I was finally able to see a vaginal delivery and that entire process. When I arrived in the morning, the mom had just received Cytotec, to help induce labor and ripen her cervix. She was forty-one weeks and zero. Around ten thirty in the morning, she asked for her epidural to manage her pain. We bolused her with fifteen hundred milliliters of lactated ringers to prevent hypotension. Shane was the certified registered nurse anesthesiologist (CRNA) who administered the epidural. It was very cool watching him administer all the needed pain relief medication before he administered the epidural to make sure that it would be placed in the epidural space in the spine. Then administered a small test dose, waited till a few blood pressures were taken, then administered the remaining about through an epidural pump. After the epidural was administered, I was able to administer her foley catheter. I was so happy that I was finally able to place one. I learned a few tricks from Maura (my nurse) as well. She taught me that it was easier to take the top off of the lubricant syringe and to place the tip of the foley inside of the syringe, that way it will not wiggle around and become unsterile. She also taught me to grab from the bottom of the labia and pull up, that way it ensures that I will have a clear entrance to
Why Adoption Is Wrong?
It was late February in 1998 when I found out I was expecting another child. I was 16 years old. It should have been a happy day it was my daughter’s 1st birthday party and everyone was there. The house was full of family and friends and smelled of chill and cake. Please don’t get me wrong, it was a happy day for the most part until I found out I was pregnant. Scared and not knowing what to do, I kept this what most would call exciting news to myself. You see I was dating a man and he was not a very nice person he was mentally and physically abusive to me most of our relationship and he was the soon to be father. A month or so went by after I told him and we were both somewhat excited him more than I. I was more scared then anything. He managed to get himself into some legal trouble and was sent away for a long time. Where did that leave me? I was scared to death
Personal Narrative: My Experience With My Female Birth
My one true goal in life was always to be a mother. I was thirty years old and had underwent over four surgeries on my female organs. I had finally given up hope that I may ever get pregnant and it not ultimately end in a miscarriage.
Personal Narrative: To The Woman Who Birthed Me
Hey Nandi, just letting you know that you're a really amazing person. Honestly you're a unique person there is no other person I could meet on the planet that could out weight your personality. I've decided that since the day I was born, BAM, mother-child bond. You've always been a strong woman you've done everything from working two jobs, to go our every school events, and handling our family problems. You're extremely happy even in bad situations and your not afraid to show us discipline that has an impact. You're a woman of few words but when you do open your mouth something extraordinary comes out. You fight for us, love us, your kind to all people, help raise strong people by putting reality in front of us since we were little. The most valuable lesson you've taught me so far is, life's going to be extremely difficult at times but you have to be strong, because you are strong, you can fight, and if you go down swinging better make worth your while. Couldn't ask for a better woman in my life.
Personal Narrative: My Prenatal Development
My prenatal development was normal. There were not any concerns or worries about my development. My mom had a fairly normal pregnancy other than preeclampsia. Preeclampsia is a medical condition in women who have not experienced high blood pressure, and developed in during a pregnancy (Preeclampsia and Eclampsia, 2016). High protein levels in urine and swelling of the hands, legs and feet are other symptoms of preeclampsia. My mom had an ultrasound at fourteen weeks. She did not have any other testing like an amniocentesis or chorionic villus sampling. It was unnecessary.
Personal Narrative: The 2nd Trimester Stage Of Development
I decided to discuss the second trimester stage of development because for me, with both of my pregnancies, that is when I started to get really excited about having a baby. There is the whole scare of losing the baby in the first trimester but also that’s when I started to feel the baby move, both times in the 16th week, when the baby, and myself, grew the most (I gained 8 pounds in the 5th month with both pregnancies), and when I got so heavy I had to walk instead of run, it was actually faster from about 18 weeks on. Babycenter.com says that the fetus of 14 weeks of age is the size of a lemon, 3 ½ inches long and weighing 1 ½ ounces, while parents.com says it’s the same weight and length but the size of a peach. At 27 weeks both sites said the babies are at 2+ pounds, 9.25-14 inches long and either the size of a head of cauliflower or a sock monkey (which wasn’t fun to look at when your trying to picture a cute little baby). On page 96 of the textbook in Figure 5.8 it is confirmed that after the 16th week the mother may start to feel the baby move. The fetus is also forming small hairs all over the body, including the scalp, and the lungs are beginning to
Personal Narrative: The Mother Of One
Alexus Casidy is out of her teenage years and now twenty, with a whole life ahead. The name Alexus may be a common but, the story of how it was picked, was not. Her father named her after a nurse at a Psychiatric Hospital, that he said was pretty. Not only did he name her after a nurse but, he chose the spelling of the car, Alexus. She grew up with her two younger siblings in Beloit WI, and I am yet to wonder if her sibling’s names have a comical story behind theirs as well. My peer went to high school at Beloit Memorial, graduating in 2015. Where she was an active cheerleading and softball player, also where she met her boyfriend, of three years, Ryan. Most don’t see that she is a mother, student, girlfriend, and employee; holding many different roles in all statuses. Alexus studies at UW Rock County and is undecided with fulfilling her dreams for becoming a children’s nurse or a teacher. Also, is hard-working employee at the factory Prent Corporation in Janesville, WI as an Inspector Packer. Where the money pays for the house her and her boyfriend own, with their one year old, Brooks.
Personal Narrative: My First Clinical
My first clinical I felt my greatest accomplishment was not being shy and hesitant. The first day we had clinical was the first day that I got the opportunity to float to another floor, I was very nervous at first. Going into a new place for anyone is different at first because you don’t know what to expect. I think what made my experience so great was the endoscopy nurses and doctors, they were some of the nicest and helpful people I’ve met so far. I got a wonderful opportunity to learn next to the doctors doing the procedures and also see other roles of the healthcare team like the nurse anesthesiologist.
Today was the second day of my 6-week placement at Ward 3A-Logan Hospital, I have originally been paired with a demand casual pool RN, however, the said RN is not confident enough to handle me as her student nurse at the time. After the scrum at 7am, and the handover on the 4-bed bay + sides, I politely ask her if I could take one patient as it was one of the instructions of my CF during the orientation on day 1, but I was answered with “I’m not really familiar with the area and I’m from the demand casual pool...” Having sighted my CF at the corridors, I excused myself from the RN and discussed the matter to my CF, and she allowed me to be buddied with a very good EN, informing me that “she is an EN” before letting me to the bay and introducing me to my new buddy EN.
Personal Narrative: My Postpartum Trauma
It was 3 years ago when I was diagnosed with Pectus Excavatum, a condition in which the breastbone sinks into the chest. 1 in every 400 births have it. My condition over the years began to get worse, reducing my ability to participate in sports. The feeling of being exhausted everyday started to hit me as time passed. After finally being diagnosed, my mom took the initiative to schedule my surgery date on June 8,2015. I had asked myself “What if something goes wrong?”, over and over creating this emotion of vulnerability inside me. This feeling that I had never fallen victim to, brought me to a time of reflection. Reflection on the life that I had lived up to that point. The question "What if I don't make it out of this? Is not a common question for someone my age, at least I don't know anyone who has had to ask this of themselves.
Personal Narrative: My Clinical Experiences
This week I had rotation at Genesis and also Cumberland Hall. Genesis was very different that what I expected. When I think of a “rehab” I think of people all sitting around with major withdrawal symptoms, a very strict schedule, multiple one-on-one session, and with no smoke breaks. At Genesis, throughout the day the client was able to do their own thing until the scheduled group session and smoke breaks. I was placed on the male unit and I was very surprise of the self-awareness that I experienced. Just listening men talk and tell their stories brought on a whole new prospective and quickly changed the image of the addict stereotype. While I was there we also established that all the clients was first timers and all fathers, and afterwards I was able to sit and think about how grateful I am to have my father who’s not an addict. I have had the luxury of always having a clean and sober father; which I had taking for granted.
My first clinical was a good experience because I learned a lot. I would say my first day involved experiences that I was expected to learn but also ones I didn’t. I learned that getting up at 5am in the morning really isn’t as bad as you think, once you get your coffee paid of course. As well as the drive from Valpo to St. Mary only talks about 20 mins. As soon as I arrived at the hospital, I expected to learn about what we as student nurse would be doing, as well as that since it was the first day, learn are way around the hospital. I wasn’t to nervous about going to a hospital for clinical, but as Soon as I stepped on the oncology unit I got a little nervous. It hit me that I was no longer just practicing vital and providing base care to
Personal Narrative: Growing Up With A New Baby
It’s August 13, 1975. Mom left the house 2 days ago, and she came back today with a new baby. He doesn’t look like a newborn, he has none of my parents features, and well he looks kind of weird. But, I guess I have really never seen a newborn and I mean the kids at school call me weird so maybe we are exactly the same. I can tell from the start that we are going to be great friends, but I just can’t help it when he cries I get so annoyed. It’s like he is doing it on purpose. Mom and Dad left the house a few minutes after they got home and I didn’t see them for another 5 days. All I heard from them was, “ There is food in the fridge. Should be enough to last you a few days. Take care of this one. Lord knows we don’t need any more trouble than we are already in.” How could they just leave me here with this annoying little brat? lts evident that Mom and Dad don’t care about me or my little brother.
Personal Narrative: My Goal For Clinical Experiences
My goal for clinical experiences is to apply what I have learned throughout my semesters to a clinical setting. I want to become more competent in my skills. I want to be able to look at a patient and identify clues that help me create a focus assessment. I also want to be able to use the patient medication to identify some adverse effects to create a preventative plan of care. My goals are to become more structured with my care plans. I want to make them more patient centered and more focused on initial issues that the patient might have then move it towards preventive methods instead of having my preventative methods first . I also want to become more confident in preparing and starting IV. I know that perfecting starting an IV will come
Related Topics
- Menstrual cycle
Personal Narrative Essay: The Story Of My Pregnancy
This is the story of my pregnancy. The night I found out I was pregnant I got a funny feeling in my stomach, and I wasn’t sure what was going on. I told my mom what was going on, but she was already suspecting I was pregnant and already had a test ready for me to take. I took the test and the results was positive. I cried because I was scared and in shock. I showed my mom and I called my boyfriend Damonte to tell him the news. He was in shock and scared of how his mom was going to react. My mom already agreed to tell his mom. The next day I went to the doctor and she confirmed the test was right. I was indeed pregnant, she said I needed an emergency ultrasound. So, she set that appointment up for the next morning. After my appointment my mom called my boyfriend’s mother to tell her the news because I was scared. I didn’t know how she was going to react. We found out that she already suspected as well and wanted to see me after we got back. So, when we got home my boyfriend’s mother Jendie came and got me from my house. I had previously texted my boyfriend when our moms were on the phone to let him know she wasn’t mad at all and he could relax a little bit. Everyone got their shock of the news and seemed happy that …show more content…
I have a high pain tolerance, so it took all day for me to start feeling my contractions and I eventually needed an epidural. Thirty-six hours later I was fully dilated, and it was time to start pushing. The doctors gave me the option to watch myself give birth and I did so with my mom, my boyfriend, and his mom by my side at 3:35 PM my son was born and fully healthy thank god. My son is five and a half months old now. He is my motivation, a big reason why I’m getting my diploma. I am so happy to be a mom and Damonte is so happy about being a dad. We have fallen more in love with each other
Summary Of The Glass Castle By Jeannette Walls
The next day came and my mom said that he had made it through the night, so I was really happy so I could go see him again! I had a basketball scrimmage that morning in Van Wert though, so I thought that I would be able to go and see him after that. But when I got out of the scrimmage I looked at my phone and my mom had texted me that he had passed. It was one of the toughest days ever. That was really hard for me to get through my head that he wouldn’t be with us anymore.
Book Report On The Glass Castle By Jeannette Walls
She was freaking out, of course, but my dad stayed calm. They talked for awhile and when he got off the phone, he said, “Your mother said I can either bring you home right now or I’m calling the cops!” I told my dad to let her call the cops. He called her back, told her what I said, and they hung up. About ten minutes later, the cops were calling my dad.
Personal Narrative: R Bend's Shoes
Even though I knew that my mom understood that I was in pain, that didn’t stop me from complaining. Once my mom pulled into the parking lot of the emergency room, she faced the next challenge. Getting me out of the booster seat. I know that my mom loves me and was not trying to put me in pain, but boy did that hurt! I cried and cried as she took me into the emergency room.
9/11: A Short Story
We went to the attendance office to pull him out of class and they said they couldn’t because they were outside and my Dad was starting to get mad because my Mom was about to give birth to my little brother any minute and my Dad could not miss it. We finally got him out of class and we flew to the hospital. When we got there we went straight to a room because my dad had to go to my mom because she was having a baby. While we were in the waiting room we watched T.V on a big flat screen T.V. We sat in there for about four hours waiting, it was like watching paint dry it was the longest time of my life. Justin and I were watching some Zeke and Luther and the doctor comes in and says “Do you want to see your baby brother”.
Personal Narrative: My Trip To Six Flags
New Plans One Saturday morning, I woke up at seven in the morning to go to an amusement park called Six Flags. The plans had been made days ago, my two older sisters, my brother, a friend of ours and I would be going to Six Flags and spend the entire day there. As I got up after finally getting my alarm to finally shut up I walked over to the bathroom to take a shower when I realized that the ground was spinning, in my eyes at least, I had a vile taste in the back of my throat. I quickly fell back onto my bed feeling like if I hadn’t
Personal Narrative: Celiac Disease
It was the middle of summer when it happened. I was about 9 years old and my mom and dad had just called me into my mom’s room. I had had a medical procedure about a couple of weeks before hand so I wasn’t surprised when they said it was about the results. They started talking to me about the results when they finally told me the main thing that had showed up.
Monologue The Crucible
I got away with it for awhile but the guilt overran me and I told my mom a day later. She wasn’t mad or disappointed but glad I finally told the truth and sometimes it’s better to tell the truth.
Personal Narrative: Misdiagnose
So, like any other teenage girl, I told my mom. She was worried, so the next day she took me to the doctor. I sat there
Foster Care Narrative
We found out that it, is a boy and he would be born in the fall. Each day got better since we heard the news, but I still couldn’t be with my mom. I was never close to her, I’ve always been a daddy's girl, but going to foster care changed that. I have gotten closer to my mom and now my dad and I can’t talk about what we used to
Summary Of The Pregnancy Project By Gaby Rodriguez
Gaby Rodriguez spent her senior year with a fake pregnant belly on her body. She was told her entire life that she was going to end up just like the rest of her family: pregnant as a teen in high school. Defying all stereotypes, and working hard to disprove them, she used her year-long senior project to change everyone’s minds. The Pregnancy Project by Gaby Rodriguez is a realistic, eye-opening story that all teenagers should read. One of the things that makes it such a good book is the rawness you feel the whole time.
The Pregnancy Project By Gaby Rodriguez
The two novels, “The Pregnancy Project” written by Gaby Rodriguez and the novel “Turning 15 and On The Road to Freedom” both share the same meaning. Both authors of the novels write about taking action. In the short novel, “Turning 15 and On The Road to Freedom”, Lynda Blackmon Lowery helps to the march for the right to vote. Many people took action and sacrificed a lot to help others approve Selma’s voting rights. In the novel of “The Pregnancy Project” Gaby Rodriguez illustrates her Senior Year Project which showed how stereotypical people can be.
Personal Narrative Essay: Becoming A Single Mother
I waited a few weeks the flu like symptoms, sick stomach, sensitive skin, random headaches; finally giving in and went and bought a test. When it came back positive I was in disbelief. I made my appointment at our local pregnancy center to get my confirmation letter. The confirmation letter is required to go visit an actual OBGYN. The appointment was two days before my twentieth birthday, I also had to inform the father of the child I was carrying.
Personal Narrative: The Day I Gave Birth To My Daugther
My mom and sister started running around getting things ready because it was time to head out to the hospital it was bbay time. My contractions werent that bad till i got in thecar ride it was horrible i remeber i almost started crying from the excrutiating pain i was in. I remember getting to the hospital and 2 hours later doctors and nurses where rushing and it was because
Personal Narrative Essay: Becoming A Father In My Life
Becoming a father in my life was the best thing that has ever happened to me. Living for someone else and not just yourself is a special feeling. Knowing that it is your sole duties in life are now to love, provide, teach, mentor, discipline and love some more. I always hear people say “ Im don 't think I 'm ready to be a parent.” and to be honest I do not think anyone is ready to be a parent.
Personal Narrative Essay: Growing Up In My Life
Then 9 months later on February 16, 1999, at 3:10 am my precious son came out of my womb and placed on my chest. It was the most amazing experience ever, but also extremely exhausting thing ever! I was in the hospital for about another week till the doctor told me to go home, funny thing is that I got discharged on my birthday February 21, 1999, which I turned 16. At first, it felt like being a mother was easy, but in reality, it wasn 't because I also had to go to school plus he would always wake me up in the middle of the night, and be in an extreme of exhaustion. I started missing school more and more till I finally dropped out.
More about Personal Narrative Essay: The Story Of My Pregnancy
Related topics.
- English-language films
- Open access
- Published: 10 November 2023
Women’s experiences of social support during pregnancy: a qualitative systematic review
- Mona Al-Mutawtah 1 , 2 ,
- Emma Campbell 1 ,
- Hans-Peter Kubis 1 &
- Mihela Erjavec 1
BMC Pregnancy and Childbirth volume 23 , Article number: 782 ( 2023 ) Cite this article
5305 Accesses
4 Citations
15 Altmetric
Metrics details
Social support during pregnancy can alleviate emotional and physical pressures, improving the well-being of mother and child. Understanding women's lived experiences and perceptions of social support during pregnancy is imperative to better support women. This systematic review explores and synthesises the qualitative research on women's experiences of social support during pregnancy.
Databases PubMed, CINAHL, MEDLINE, APA PsycInfo and Scopus were searched with no year limit. Eligible studies included pregnant women or women who were up to one year postpartum and were assessed on their experiences of social support during pregnancy. The data were synthesised using the thematic synthesis approach.
Fourteen studies were included with data from 571 participating women across ten countries; two studies used focus groups, and 12 used interviews to collect their data. Four main themes were developed ('a variety of emotional support', 'tangible and intangible instrumental support', 'traditional rituals and spiritual support', and 'the all-encompassing natal home'), and six sub-themes ('female network connections', 'care and affection from the husband', 'dissatisfaction with relationships', 'financial support from the husband and family', 'practical support from family and friends', 'health information support').
Conclusions
This systematic review sheds light on women’s experiences of social support during pregnancy. The results indicate a broad variety of emotional support experienced and valued by pregnant women from different sources. Additionally, women expressed satisfaction and dissatisfaction with tangible and intangible support forms. It was also highlighted that spirituality played an essential role in reducing stress and offering coping mechanisms for some, whereas spirituality increased stress levels for others.
Peer Review reports
For some women, pregnancy is considered a time of joy, but it also involves many well-being, social, and physical changes (e.g., emotional, physiological, and relational changes). These changes during pregnancy can present many challenges [ 1 , 2 , 3 ]. For example, Yin et al. [ 4 ] conducted a systematic review to investigate the prevalence of antenatal depression during pregnancy across several continents. The results showed that the prevalence rates of any antenatal depression were 20.7%, and 15% of pregnant women experienced major antenatal depression, which is higher than general population 14.5% [ 5 ]. Other challenges reported in the existing literature are related to unplanned pregnancy, mood instability, physical health problems, financial problems, and a lack of social support during pregnancy [ 6 , 7 , 8 , 9 ]. For example, social support during pregnancy reportedly helps to alleviate the pressures of the pregnant women’s emotional and physical changes, and suggests to improve the mother and child’s well-being [ 10 , 11 , 12 ].
The conceptualisation of social support
There is a wide range of literature connected to social support from many perspectives and disciplines over many decades of research [ 13 , 14 , 15 , 16 ]. Social support has broadly been outlined as a complex, multi-dimensional concept that can be defined as assistance provided by a person’s social network and involves the provision of emotional and physical support [ 16 , 17 ]. However, from a traditional psychological perspective, Cohen and Wills [ 13 ] describe social support as support from social networks that can influence health through two pathways (direct effects and stress buffering). The direct-effect hypothesis suggests that social support can improve health regardless of whether the environment is stressful or not [ 18 ]. Further, it contributes to a sense of belonging and stability, resulting in improved self-esteem and reduced stress and mental health disorders [ 19 ]. Alternatively, the stress-buffering hypothesis posits that support may buffer against unhealthy reactions and provide the individual with access to additional resources that will enhance their capacity to cope with stressful events in two ways:
Perceived support can prevent a psychological or physiological stress reaction from arising when a potentially stressful event occurs. Consequently, perceived support may increase the perception that individuals can cope with negative events.
Perceived social support can intervene between the event of a stress reaction and the onset of a pathological process by reducing the stress reaction [ 19 , 20 ].
Social support during pregnancy
Kroelinger and Oths [ 21 ] explored the role of social support in wanted and unwanted pregnancies. The results indicated that unwanted pregnancies are strongly influenced by factors such as support from partners, the partner’s stability and status, and their feelings towards pregnancy. Therefore, Kroelinger and Oths highlights the potential role of a partner’s social support during pregnancy and shows how the lack of a partner’s support, particularly their emotional and practical support, can negatively affect women’s experiences by leading them to experience the pregnancy as unwanted. However, although, the relationship between a partner’s social support and whether a pregnancy is desirable seems simple, a person may decide that they want the pregnancy while it progresses based on certain discoveries, experiences, or events that are unrelated to the social support they receive from their partner. For example, parental social support can buffer the negative impacts of an unsupportive partner [ 22 ].
Likewise, Rini et al. [ 23 ] aimed to assess their experiences of the quality and quantity of social support they received from their partners, referred to as social support effectiveness (SSE). It focused on three functional types of social support: practical, emotional, and informational support. Greater SSE from partners predicted less anxiety during the second to third trimesters [ 23 ]. In addition, a recent systematic review of social support during pregnancy sought to investigate the relationship between social support and mental illness during pregnancy. A significant positive correlation between low social support and antenatal depression (14/15 papers), antenatal anxiety (6/8 papers), and self-harm (3/4 papers) was found [ 6 ]. Although these studies stressed that social support directly affects mental health, the pregnant women’s feelings, attitudes, perspectives, and past pregnancy experiences may mediate the relationship between a partner’s social support and the pregnant person’s anxiety [ 24 ]. This aligns with several studies that showed that those who perceive adequate social support during pregnancy are less likely to report stress, distress, or symptoms associated with anxiety and depression [ 25 , 26 , 27 ].
The above evidence demonstrates that social support may influence women’s experiences during pregnancy. However, more recent research has also incorporated contextual and situational factors associated with the COVID-19 pandemic. Since December 2019, the COVID-19 pandemic has affected almost all countries and territories and cases of COVID-19 increased exponentially worldwide [ 28 ]. Recent research by Meaney et al. [ 29 ] aimed to assess pregnant women’s perceptions and satisfaction with social support from an online survey conducted with 573 pregnant women during the pandemic from the US, Ireland, and the UK. The authors illustrated that a reduction in perceived social support that resulted from the lack of access to antenatal care during the COVID-19 pandemic increased negative feelings such as sadness, anxiety, and loneliness during pregnancy for these women. Although this kind of research can help healthcare providers determine strategies to help women during stressful times, further research is required to identify the types of social support (e.g., emotional, instrumental, etc.) that were most affected by the pandemic.
In conclusion, the existing literature affirms that social support during pregnancy plays a role in women’s well-being and physical health (amongst other areas). However, most of these studies primarily employed quantitative approaches [ 21 , 23 , 30 , 31 , 32 ]. This indicates that the existing studies would have been unable to capture any wider contextual factors which may also shape women’s experiences, the emotional aspects of social support, or experiential aspects of the topic [ 33 ]. Therefore, qualitative synthesis can provide an in-depth understanding of precious women’s experiences and perceptions of social support during pregnancy.
Overall aim
This systematic review sought to analyse and synthesise all available qualitative evidence about women’s experiences of social support during pregnancy.
Research question
According to Stern et al. [ 34 ] and Butler et al. [ 35 ], to formulate a good question, the four elements of the PICo (with a lowercase o) (as P referred to participants; I referred to phenomenon of interest; Co referred to context) mnemonic framework must be incorporated to identify the keywords to use in the review question. Table 1 outlines how the review research question was formulated using this framework.
Therefore, the research question developed via the PICo framework [ 35 ] was: How do women experience the social support provided to them during pregnancy?
Search strategy
An extensive literature search was conducted using five electronic databases: PubMed, CINAHL Plus with full text, MEDLINE, APA PsycInfo, and Scopus between May 2022- February 2023. Shea et al. [ 49 ] notes that at least two databases should be searched for systematic reviews and meta-analyses; however, utilising more databases can yield more comprehensive and accurate results.
In addition, the Boolean connectors AND and OR were utilised to combine the following MeSH and search terms: “qualitative research”, “qualitative”, “qualitative method”, “interview”, “focus group”, “social support”, “psychosocial support systems”, “emotional support”, “family support”, “practical support”, “information support”, “pregnancy”, “pregnant”. Furthermore, following Butler et al. [ 35 ], a manual screening of the reference lists of all included studies was performed to identify additional potential studies.
In addition, the Enhancing the Transparency of the Reported Comprehensive Qualitative Research Statement (ENTREQ), was used to increase transparency (see Additional file 1 ) [ 50 ].
Inclusion and exclusion criteria
The included studies met the following criteria:
Original qualitative studies published in English-language peer-reviewed journals with no year limit.
The participants were mainly adult women over 18, although two papers included two pregnant women aged 17 in their samples.
The participants were pregnant women or women who had given birth and were assessed on their experience of social support during pregnancy.
The participants were pregnant women that were not specifically recruited because of pre-existing health issues or mental illness, as these conditions may affect their social support experiences.
The exclusion criteria:
Pregnant under age 17.
Specific sub-groups of pregnant women (e.g., pregnant with HIV, diabetes, intellectual disabilities and visually impaired).
Social support in breastfeeding.
Unpublished and grey studies.
Theses and secondary research sources (e.g., reviews).
Data extraction
As part of the review process, researchers can extract descriptive data (e.g., details of setting or context) and outcome data (e.g., results or conclusions) from the selected studies [ 51 ]. The critical information needed to extract the context and participants are the study setting, country, population, and participant characteristics. The information needed to describe the research design and methods is the methods for data collection, analysis, and findings [ 50 , 51 ]. The information we included in Table 2 offers an overview of this data about the studies included in this review. A total of 14 international studies spanning 1990 to 2022 have been selected, from the United States ( n = 5), Canada ( n = 1), Bangladesh ( n = 1), Indonesia ( n = 1), Iran ( n = 1), Pakistan ( n = 1), India ( n = 1), Zambia ( n = 1), Nigeria ( n = 1) and the UK ( n = 1). In total, 571 adult women participated; two studies used focus groups and 12 used interviews to collect their data.
Quality appraisal
A quality assessment of the studies included was conducted using the Critical Appraisal Skills Programme for Qualitative Studies Checklist (CASP). The CASP tool is endorsed by both Cochrane and the World Health Organization for the qualitative synthesis of evidence [ 61 ]. According to Butler et al. [ 35 ], the scoring system for the answers to each question was Yes = 1, Can’t tell = 0.5, and No = 0 points; high-quality papers earned 9–10 points, moderate-quality papers, 7.5–9, and low-quality papers, less than 7.5. The first author (MA) was the first appraiser and a second independent reviewer (MP) evaluated five randomised studies to verify the robustness of the process [ 62 ]. Next, the results were compared, and the reviewers’ assessments were found to be similar across the sample studies. Table 2 summarises the results of the critical appraisal.
Data and thematic synthesis
Thematic synthesis, developed by Thomas and Harden [ 63 ], was used to generate new insights from the primary studies. This approach consists of three stages: coding the text, developing descriptive themes, and generating analytical themes. This method provides an explicit process for reducing qualitative data by utilising different reporting styles, such as thin descriptions and multiple quotations [ 62 , 64 ]. Each article’s results section was stored on a Word file and manually analysed using free line-by-line analysis. Then, these free codes were organised into related areas to construct descriptive themes, and, ultimately, these were developed into analytical themes [ 65 ]. The coding process was conducted inductively, and all of the preliminary codes and the descriptive and analytical themes were discussed and refined by the independent reviewer (EC), between July and September 2022. The themes were also further discussed under supervision for expert supervisory input, review, and iterative development (ME, PH, & EC). This process supported the quality of the theme generation. After this iterative process, four main themes and six sub-themes were developed from 126 codes.
Search outcome
A total of 1,597 articles were identified by the initial search. After 107 duplicates and 148 unsuitable studies were removed, 762 titles and abstracts were screened and a further 652 were excluded. The full text of 110 articles was retrieved and screened by the first author for eligibility and 99 articles did not meet the inclusion criteria. After reviewing the reference lists of the remaining studies, two additional studies that met the inclusion criteria were identified. One final study was found while writing the first draft that met the inclusion criteria. Thus, a total of 14 qualitative studies were reviewed with the research teams, who decided to include all 14 in this systematic review. The PRISMA Flow Diagram shows a detailed description of the study selection process (Fig. 1 ).
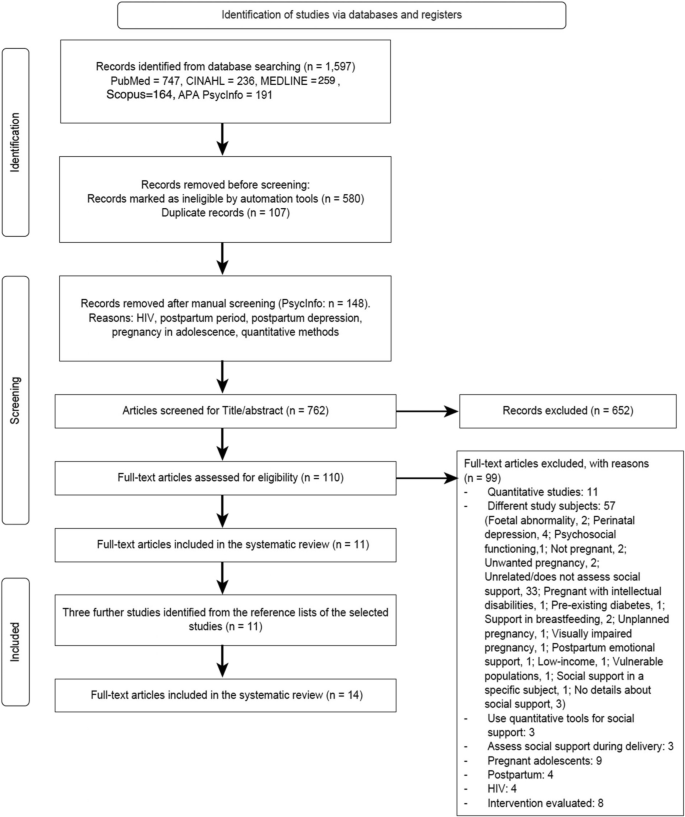
PRISMA diagram outlining the search process
Results of the thematic synthesis
The four main themes (see Fig. 2 ) generated through the thematic synthesis are “a variety of emotional support”, “tangible and intangible instrumental support”, “traditional rituals and spiritual support”, and “the all-encompassing natal home”. Each of the main themes and sub-themes is discussed below in more detail.
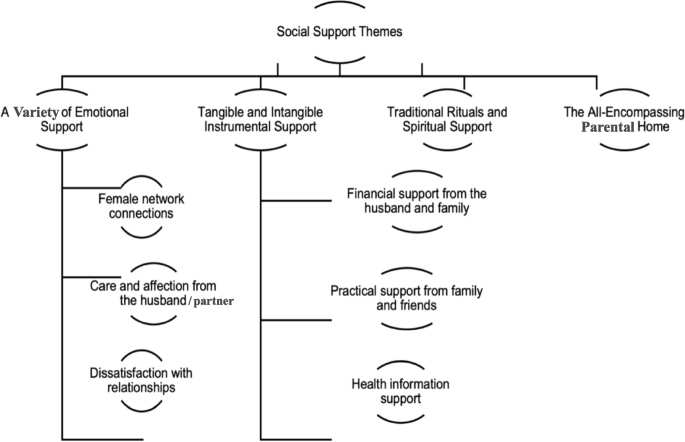
Analytical themes
A variety of emotional support
This main theme describes women’s experiences of emotional support during pregnancy. The data from the included papers illustrated that the participants experienced increased emotional support during pregnancy from their female networks and marital relationships [ 10 , 36 , 38 , 40 , 42 , 43 , 44 , 45 , 46 , 47 , 48 ]. For some, the experience of emotional support existed across a variety, including some women who reported dissatisfaction.
Female network connections
This sub-theme offers insight into a range of sources from which the women had previously gained emotional support during pregnancy. The participants highlighted that they gained emotional support through their connections with other females within their social networks [ 10 , 36 , 38 , 39 , 40 , 46 ]. Female emotional support could be afforded by family members (e.g., mothers, grandmothers, sisters, or sisters-in-law) or other female friends and neighbours. Pregnant women described emotional support as the act of women expressing care, sharing, and expressing feelings and supportive words, and listening to them. Some women also referenced how their mothers offered emotional support during the perinatal period and how they perceived this support as essential throughout their pregnancy.
“There are enough people around me to talk to and support, (but) mainly I would tell my mother about everything. She has been very supportive throughout” [ 46 ] .
“Sister-in-law told me: ‘Do not get afraid, nothing will happen,’ when I felt the pain, she told me, ‘Do not worry, nothing will happen’” [ 10 ] .
Moreover, some women mentioned that during the COVID-19 pandemic, when social restrictions were in place, receiving gifts from loved ones expressed love and care between the female relatives and friends and the pregnant women.
“Due to social restrictions, Kelly’s mother and sisters sent a stroller and a car seat to celebrate her pregnancy” [ 36 ] .
In addition to receiving gifts during Covid-19, some women revealed that connecting via social media with both pregnant and non-pregnant friends helped them to alleviate their stress and ensured that they were not alone during this challenging time.
“Cause like my husband was great support too, but to communicate with someone who is more in your shoes is helpful” [ 36 ] .
The above shows how the women’s connections with others offered a variety of emotional support both before and during the Covid-19 pandemic.
Care and affection from the husband/ partner
This sub-theme outlines a range of emotional support that the women experienced from their husband or partner during pregnancy. This was sometimes described as how their husband’s paid attention to them, encouraged them with supportive words, and allowed them space to discuss their concerns of the pregnancy [ 36 , 37 , 40 , 41 , 42 , 44 , 45 , 47 ].
“I feel lucky that I have somebody that’s willing to let me go take a bath and not be consumed in playing a video game or something. He was always listening to what I needed” [ 41 ] .
In addition, this shows that some husbands met women’s needs when they were patient during pregnancy, avoiding any conflict or arguments [ 43 ]. Meanwhile, husbands prevented their pregnant wives from having to do hard manual labour, such as working in a factory, as an expression of affection and care [ 45 ]. Care can also be exemplified through the husband taking care of their wives’ diets.
“My husband is so loving and caring; he takes care for my diet, he brings me ½ kg milk and fruits on daily basis” [ 44 ] .
Dissatisfaction with relationships
This sub-theme gives insights into the other end of the spectrum, showing how some women experienced a lack of emotional support during pregnancy (highlighted in 6 of the 14 studies included) [ 38 , 39 , 40 , 44 , 47 , 48 ]. For example, some women discussed how their husbands or partners were less caring and did not focus on their health or the health of their babies. There was also dissatisfaction when their husbands did not understand any emotional changes that they may have experienced.
“My husband does not ask me what the doctor said about me and baby’s condition; when I come back from the doctor’s clinic, he is careless” [ 44 ] .
Furthermore, women without close family and friends or who live far from them described themselves as lonely or helpless [ 38 , 39 , 44 , 47 ].
“I know almost no one here. I met a woman, but she moved, and now there’s no one” [ 38 ] .
Tangible and intangible instrumental support
This main theme illustrates a range of instrumental social support that the women experienced during pregnancy. As part of this theme, tangible support refers to material aids, e.g., the provision of money or goods and behavioural acts, such as helping with household chores [ 18 , 66 ]. Alternatively, intangible support describes directive guidance, such as information, advice, constructive feedback, and affirmation about the women’s health during pregnancy [ 67 ]. The first and second subthemes, “financial support from the husband and family” and “practical support from family and friends” relate to tangible support, and the third, “health information support”, to intangible support.
Financial support from the husband and family
This sub-theme describes how some of the participants appeared to be satisfied with their financial situation and the financial support they received from their husbands or families. However, this was not true of all women; some were dissatisfied with the financial support available to them. The source of financial support varied but included the participants’ husbands and parents and grandparents [ 10 , 37 , 40 , 42 , 44 , 48 ]. One of the participants expressed how her husband’s financial support uplifts her mood.
“I want him to buy baby items for the baby or he gives me money to buy. This makes me feel good because it shows that he is concerned about my situation” [ 37 ] .
Practical support from family and friends
For this sub-theme, the women’s husbands and in-laws were referred to as sources of practical help. Some women also mentioned their mothers and friends, although the participants rarely asked them for practical support [ 10 , 36 , 37 , 38 , 39 , 43 , 44 , 45 , 46 ]. Forms of practical support included helping with household chores, cooking, childcare, shopping, and taking the pregnant person to their antenatal appointments. Women perceived their husbands as providers of many aspects of practical support during pregnancy, particularly assisting with daily housework, taking them to natal clinics, and providing childcare for their children [ 10 , 37 , 45 , 46 ]. These tasks were also mentioned in connection to other family members, such as the women’s mothers, and friends.
“My husband used to help me with things I could not do. For example, carrying water for cows” [ 10 ] .
“When I was vomiting for the first few months, three different friends used to cook different dishes for me every day; they looked after me so well” [ 46 ].
Furthermore, some participants highlighted how their family and friends provided practical support during the COVID-19 pandemic. They talked about how their loved ones helped them with grocery shop and run errands.
“They’ll call and be like, ‘Do you need me to get you anything? I’m at the store, that way you don’t have to go out” [ 36 ].
Health information support
This sub-theme provides insight into how healthcare professionals were considered sources of information and advice, in addition to people such as mothers, friends, and pregnancy group members. This included positive feedback to normalise the pregnant person’s experience, information about the foetus’s health condition, nutrition advice and information about delivery [ 10 , 36 , 38 , 39 , 40 , 45 , 46 , 48 ].
Some participants never mentioned healthcare providers as routine sources of information support but occasionally referred to them when describing acute problems related to pregnancy, the health of the foetus, or delivery information [ 40 , 45 , 46 ]. Other women, especially mothers, were routine sources of information and advice.
“My mother had 11 children, out of which seven survive… therefore she gave all advice (during pregnancy). And I followed her advice” [ 46 ] .
During the Covid-19 pandemic, some pregnant women faced a lack of informational support from healthcare providers about the Covid-19 virus and lockdown regulations. This led them to rely upon their pregnancy group peers to discuss concerns online through social media. For example, Charvat et al. [ 36 ] referred to the following quotes by two participants:
“They don’t really tell me [anything]. And [my obstetrician] makes me feel comfortable as he tells me not to worry. He says I’m not high-risk, etc. But no, my OB doesn’t talk much about the actual virus.”
These examples give an overview of the different forms and sources of health information support in the context of the Covid-19 pandemic and beyond.
Traditional rituals and spiritual support
This main theme refers to any culturally specific support (i.e., to avoid certain types of foods or exercises and to go out at noon) or any cultural or traditional practices during pregnancy that centre the well-being of the mother and child [ 10 , 36 , 38 , 40 , 45 , 48 ]. The examples presented below will demonstrate how the women reported various forms of such support, including advice on movement and exercise, traditional foods, and avoiding evil spirits [ 10 , 38 ]. These forms of support usually came from grandmothers, mothers, sisters-in-law, and aunts, as some participants mentioned in Edmonds’s et al. [ 10 ] study:
“You cannot go out at noon, evening, dawn, and night. Evil spirits will catch you.” “She (sister-in-law) forbade me to move in a clumsy way. She told me to be careful about movement and timing of movement.”
Spiritual support, in the context of this review, refers to relying on the ‘higher spiritual being’ (as some participants called it God and others called it Allah) to protect and reduce stress and pain during pregnancy via prayers from the pregnant women and their husbands, mothers, and grandmothers. The concept of spiritual support signifies the religious dimension of a relationship with a preferred power (e.g., God, Allah, or Brahman) [ 48 ]. All pregnant women in the selected studies highlighted God as a form of spiritual support, mentioning trusting God, praying to God to reduce stress, and faith in God’s protection [ 10 , 36 , 38 , 40 , 45 , 48 ].
“Prayer and supplication to God help me calm down and reduce my stress” [ 48 ] .
Spiritual support was not only experienced by the pregnant women but was a shared relational experience among them, their husbands, and other close family members. During the Covid-19 pandemic, faith in God was a type of support that one participant mentioned.
“When asked how she feels about the information she has received from her doctors, Becka said, ‘Confused. Nothing set in stone… Yeah, the information I get is all over the place. And so, I mean, the best I can do is keep myself protected and hope to God that it keeps me protected’” [ 36 ] .
Moreover, some participants reported religious group support during their pregnancy, mainly through counselling and financial support. The religious group support gave these women a sense of security and gave them the strength to persevere through this difficult time. It also gave them a sense of purpose, knowing that they had a support system, and that God was in control.
The all-encompassing parental home
The final main theme refers to how the participants expressed their experiences of social support within their family homes. For example, the parental home is the home of the pregnant woman’s parents, which usually, as the participants revealed, was the setting in which all their needs were met during pregnancy. This theme was developed from three studies assessing social support in Pakistan, India, and Bangladesh [ 10 , 44 , 46 ]. Most of the women from these countries mentioned their parental home as an integral part of their lives and described their parental home as a place where they feel happy and relaxed and receive more care.
“My parents thought if I will be there [in-laws’ house], I will have to work, so I won’t be able to take rest also, that is why they [my parents] brought me here” [ 46 ] .
The review affirmed that during pregnancy, women tend to spend more time in their parental homes, as their families often look after them in terms of chores, cooking, and cleaning [ 10 ].
This review sought to analyse and synthesise all available qualitative evidence about women’s experiences of social support during pregnancy. The participants in the included studies described a broad variety of social support experiences, including emotional, instrumental, and informational support. Four main themes were generated: “a variety of emotional support”, “tangible and intangible instrumental support”, “traditional rituals and spiritual support”, and “the all-encompassing parental home”.
This review found that pregnant people received emotional support from a diverse range of people within their social networks, gaining helpful support in terms of coping mechanisms and the regulation of stress during pregnancy and the COVID pandemic [ 10 , 36 , 42 , 43 , 45 , 46 ]. These findings align with Rini et al. [ 23 ], who found that emotional and intimate support from the marital relationship and the husband supports adjustment during pregnancy and increases well-being. Kolker et al. [ 68 ] also found that emotional support was particularly critical during the pandemic, as many women experienced isolation and loneliness. The lack of physical connection with family and friends due to the pandemic caused many women to experience higher levels of stress, anxiety, and feelings of loneliness. Women’s emotions are regulated through social support and their relationships, which, in turn, may reduce emotional exhaustion during pregnancy due to the fear of childbirth or fears of having a child born with illness [ 69 , 70 ]. The importance of emotional support (e.g., listening and affectionate interactions) is evident and consistent with the findings of this review [ 10 , 36 , 41 ].
Conversely, this review also highlighted a lack of or dissatisfaction with the emotional support that some of the participants experienced [ 38 , 39 , 40 , 44 , 47 , 48 ]. Insufficient family support harmed pregnant women’s maternal behaviour and health. For example, Fernandez and Newby [ 71 ] used interviews to explore the extent to which pregnant women of Mexican descent in the United States were supported by their families and partners. Their results indicated an association between family support and the circumstances of the pregnancy. Women without cohabiting relationships with the baby’s father before becoming pregnant received less emotional support from their families, particularly their mothers. These women were, therefore, less likely to look forward to prenatal care, adopt a healthy behaviour (e.g., smoking), or be excited about giving birth to their babies.
This finding also highlights the importance of instrumental support, such as financial, informational, and practical support during pregnancy. As it revealed that a lack of financial support increased stress and dissatisfaction, while the provision of this support increased feelings of safety, emotional support, and being cared for and not alone [ 10 , 40 , 42 , 44 , 48 ]. Therefore, although instrumental (e.g., financial, or informational) support may be seen as merely practical support, these types of behaviours may make the woman feel that she is loved, cared for, and supported: that she matters [ 37 ]. Thus, the practical aspects of social support may not be considered separate categories of support but occasionally interacting forms of social support.
Dissatisfaction with the husband’s or partner’s practical support also was found as part of the thematic synthesis [ 43 , 44 ]. However, when considering the role of practical support, a gap in the literature appears regarding many cultural factors. For instance, many studies argue that culture should be considered when trying to understand perceived satisfaction or dissatisfaction with the support given [ 72 , 73 , 74 ]. For example, in Western cultures, fathers’ roles have evolved from being only breadwinners to partners who play an active role in all aspects of their children’s lives [ 41 ]. However, women in Middle Eastern cultures (Saudi Arabia and Iran) are assumed to be primarily responsible for traditionally feminine tasks and homemaking, including attending to children’s needs, cleaning, and cooking, whereas men are the key breadwinners and are responsible for traditionally masculine tasks, such as making money, and home repairs [ 75 , 76 ]. This is an important argument as cross-cultural differences or the impact of culture on pregnant women’s perceptions were not considered in most of the studies included in this review, which might be one of its critical limitations.
The included studies highlighted how important informational support was for women to understand or make sense of their health-related experiences and gather information during pregnancy. This included positive feedback to normalise their experience, information about the foetus’s health condition and nutrition advice. Gist-Mackey et al. [ 77 ] suggested that informational support has previously been determined vital during times of uncertainty and stress (such as pregnancy and COVID-19 pandemic), supporting other literature affirming that informational support can decrease stress, anxiety, and ambiguity among pregnant women [ 78 , 79 ].
The theme of traditional rituals and spiritual support was also generated as part of the thematic synthesis. This was considered to take several different forms, such as prayers and advice on traditional food and avoiding evil spirits [ 10 , 36 , 38 , 40 , 45 , 48 ]. The role of traditional cultural customs, values, and beliefs has been explored in the existing literature. For instance, Ayaz and Efe [ 80 ] described how some people in Turkey believe that, if the pregnant woman eats quince during pregnancy, the baby will be born with dimples. However, the overall results of this review indicated that some pregnant women perceived traditional rituals as a way to show concern and care [ 10 , 36 , 38 ]. Prayer was a form of spiritual support that the participants in the included studies relied on during pregnancy to reduce stress and seek protection [ 10 , 36 , 38 , 45 ]. However, the role of spirituality and varying spiritual beliefs regarding the experience of stress may also be culturally influenced and shaped. In the current literature, the stress-buffering impact of spirituality may be higher among people from more conservative, religious cultures (e.g., Iranians), compared with those who are less religious, less conservative cultures. For example, a study conducted in Iran found that spirituality can reduce stress, particularly stress related to pregnancy [ 81 ]. It is also important to acknowledge that the role of spiritual support may have not only positive effects; as Mann et al. [ 82 ] emphasise, spirituality was associated with increased perceived stress among pregnant Hispanic people living in the US. The most likely explanation lies in the phenomenon of reverse causation (women with higher levels of stress seek comfort in religion). Therefore, the impact of spirituality on perceived stress may also be affected by the culture, among other broad factors (i.e., social, cognitive, personal, emotional, situational, or demographic factors).
During pregnancy, the parental home appeared important, with visits to this home described as motivated by the desire to reduce the pregnant person’s workload [ 10 , 44 , 46 ]. The benefits of visiting the parental home were often related to the women being surrounded by their families, who offered social and practical support. The finding that pregnant women experienced yearning for their parental homes can be explained by the theory of the collectivism/ individualism dichotomy as this theme arose from three studies performed in collectivist cultures (India, Bangladesh, and Pakistan). The theory of the collectivism/individualism dichotomy argues that individualistic cultures prioritise the needs of individuals over the needs of the group as a whole. Collectivist cultures are characterised by strong emotional bonds and social relationships between society members, especially mothers, whereas individualistic cultures have weaker emotional bonds [ 76 , 83 ]. Individuals from more collectivistic backgrounds reported feeling less alone and experiencing more social support from their families than those from individualistic backgrounds [ 84 , 85 ]. Therefore, further studies on individualistic cultures are needed to confirm these findings. However, they are consistent, from a broad psychological perspective, with the stress-buffering model, which emphasises that social support may buffer stress and contribute to a sense of belonging and stability, resulting in improved self-esteem and reduced stress [ 28 , 86 , 87 , 88 ].

Strengths and limitations
This review is the first one to consider qualitative research on women’s experiences of social support during pregnancy, which may inform future research designs. Additionally, it examines women's experiences of social support from all over the world and takes a rigorous and systematic approach. It reveals how social support and other factors impact women's well-being during pregnancy and what types of support they value. This review also provides insight into pregnant experiences during COVID-19 and provides some preliminary findings derived from recent research. However, the failure to conduct a sufficiently exhaustive search for studies is a potential limitation of any review, including this one [ 89 ]. Also, the small number of studies in this review curtail the richness and depth of the analysis of individual subjective meanings, making the findings difficult to generalise. Although the generalisation of qualitative findings is not typically the aim of qualitative research, generalisation does allow the analysis to be transferred to other contexts and settings [ 33 ]. Moreover, most of the included papers were from low-income countries; thus, future studies are needed to examine women’s experiences in wealthy countries.
Implications
Healthcare providers (e.g., nurses, psychologists, or social workers) should raise awareness about the importance of providing pregnant women with the required social support (e.g., emotional, instrumental, and informational) through their social circles, including the husband, mother, father, and female networks. Healthcare providers should tailor social support interventions to meet individualised needs as women’s needs may differ. For example, Dennis et al. [ 90 ] found that women who participated in breastfeeding peer support interventions valued emotional support most and were less focused on education and informational support, although many social support interventions focus on informational and educational aspects [ 91 ]. Interventions are most effective when they are developed based on the needs of the target population [ 92 ]. It is therefore important for healthcare providers to not adopt a one-size-fits-all approach, but rather tailor their services and interventions in order to meet the specific and diverse needs of women within their communities, based on research and data analysis results. Moreover, healthcare providers need to screen pregnant women to know what they value in receiving support and assess their level of emotional and practical support during pregnancy. This screening should be followed by encouraging the inclusion of the key support people (friends, family members, and partners) throughout pregnancy [ 43 , 47 ]. Yawn et al. [ 93 ] concluded that 654 of 1,897 women had elevated screening scores indicative of depression. This is significant as it shows that many women needed additional help and resources for mental health issues. Mental health screenings can provide valuable information to help identify those needing extra support. Thus, by integrating formal mental health screening into a wider assessment and taking into account the factors highlighted in this study, health professionals could achieve a more person-centred, holistic, and effective provision.
Additionally, policymakers and other relevant stakeholders should consider a community-based social support program for pregnant women as a means of helping them cope with the challenges of pregnancy. By providing such programs, we can facilitate a more comprehensive approach to maternal care, acknowledging that emotional and social support is an essential component of the well-being of a pregnant woman.
This systematic review provides insight into women’s experiences of social support during pregnancy. The results indicate that pregnant women experienced and valued a wide variety of emotional support from different sources, including their female networks, husbands, families, and parents. Furthermore, women experienced a mixture of tangible and intangible support and reported satisfaction and dissatisfaction with these kinds of support. In addition, the review highlighted the role of spirituality and how this was sometimes perceived as reducing stress and offering a coping mechanism, whilst for others, spirituality increased the stress experience. Overall, the results of this review provide insight into a range of experiences associated with social support in pregnancy.
Availability of data and materials
The datasets used and/or analysed during the current study are available.
from the corresponding author on reasonable request.
Abbreviations
Social support effectiveness
Coronavirus disease 2019
United Kingdom
United States of America
Enhancing the Transparency of the Reported Comprehensive Qualitative Research Statement
Medical Subject Headings
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Critical Analysis Skills Programme
Ayano G, Tesfaw G, Shumet S. Prevalence and determinants of antenatal depression in Ethiopia: a systematic review and meta-analysis. PLoS ONE. 2019;14:e0211764.
Article CAS PubMed PubMed Central Google Scholar
Marca-Ghaemmaghami PL, Ehlert U. Stress during pregnancy: experienced stress, stress hormones, and protective factors. Eur Psychol. 2015;20:102–19.
Article Google Scholar
Ross LE, Sellers EM, Gilbert Evans SE, Romach MK. Mood changes during pregnancy and the postpartum period: development of a biopsychosocial model. Acta Psychiatr Scand. 2004;109:457–66.
Article CAS PubMed Google Scholar
Yin X, Sun N, Jiang N, Xu X, Gan Y, Zhang J, et al. Prevalence and associated factors of antenatal depression: systematic reviews and meta-analyses. Clin Psychol Rev. 2021;83:101932.
Article PubMed Google Scholar
World Health Organization. Depression. Geneva, Switzerland: WHO; 2021.
Google Scholar
Bedaso A, Adams J, Peng W, Sibbritt D. Prevalence and determinants of low social support during pregnancy among Australian women: a community-based cross-sectional study. Reprod Health. 2021;18:158.
Article PubMed PubMed Central Google Scholar
Li H, Bowen A, Bowen R, Balbuena L, Feng C, Bally J, et al. Mood instability during pregnancy and postpartum: a systematic review. Arch Women’s Ment Health. 2020;23:29–41.
Carvalho MECC, Lima LC, Terceiro CAdL, Pinto DRL, Silva MN, Cozer GA, et al. Low back pain during pregnancy. Braz J Anesthesiol. 2017;67:266–70.
Geller PA. Pregnancy as a stressful life event. CNS Spectr. 2004;9:188–97.
Edmonds JK, Paul M, Sibley LM. Type, content, and source of social support perceived by women during pregnancy: evidence from Matlab. Bangladesh J Health Popul Nutr. 2011;29:163–73.
PubMed Google Scholar
Faramarzi M, Pasha H. The role of social support in prediction of stress during pregnancy. J Babol Univ Med Sci. 2015;17:52–60.
Maharlouei N. The importance of social support during pregnancy. Women’s Health Bull. 2016;3:1.
Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98:310–57.
Hutchison C. Social support: factors to consider when designing studies that measure social support. J Adv Nurs. 1999;29:1520–6.
Langford CPH, Bowsher J, Maloney JP, Lillis PP. Social support: a conceptual analysis. J Adv Nurs. 1997;25:95–100.
Taylor SE, Sherman DK, Kim HS, Jarcho J, Takagi K, Dunagan MS. Culture and social support: who seeks it and why? J Pers Soc Psychol. 2004;87:354–62.
Sofaer S. Qualitative methods: what are they and why use them? Health Serv Res. 1999;34:1101.
CAS PubMed PubMed Central Google Scholar
Friedman HS. The Oxford handbook of health psychology. Oxford: Oxford University Press; 2011.
Book Google Scholar
Rodriguez MS, Cohen S. Social support. In: Friedman H, editor. Encyclopedia of mental health. San Diego: Academic Press; 1998. p. 535–44.
Cohen S, Underwood S, Gottlieb B. Social support measures and interventionb. New York: Oxford University Press; 2000.
Kroelinger CD, Oths KS. Partner support and pregnancy wantedness. Birth. 2000;27:112–9.
Phillips CR. Family-centered maternity care. Sudbury, MA: Jones & Bartlett Learning; 2003.
Rini C, Schetter CD, Hobel CJ, Glynn LM, Sandman CA. Effective social support: antecedents and consequences of partner support during pregnancy. Pers Relatsh. 2006;13:207–29.
Albarracín D, Johnson BT, Zanna MP. The handbook of attitudes. New York, NY: Psychology Press; 2014.
Asselmann E, Kunas SL, Wittchen H-U, Martini J. Maternal personality, social support, and changes in depressive, anxiety, and stress symptoms during pregnancy and after delivery: a prospective-longitudinal study. PLoS ONE. 2020;15:e0237609.
Friedman LE, Gelaye B, Sanchez SE, Williams MA. Association of social support and antepartum depression among pregnant women. J Affect Disord. 2020;264:201–5.
Moshki M, Cheravi K. Relationships among depression during pregnancy, social support and health locus of control among Iranian pregnant women. Int J Soc Psychiatry. 2016;62:148–55.
Pokhrel S, Chhetri R. A literature review on impact of COVID-19 pandemic on teaching and learning. Higher Education for the Future. 2021;8:133–41.
Meaney S, Leitao S, Olander EK, Pope J, Matvienko-Sikar K. The impact of COVID-19 on pregnant womens’ expereiences and perceptions of antenatal maternity care, social support, and stress-resuction strategies. Women and Birth. 2022;35:307–16.
Reid KM, Taylor MG. Social support, stress, and maternal postpartum depression: a comparison of supportive relationships. Soc Sci Res. 2015;54:246–62.
Khoury JE, Atkinson L, Bennett T, Jack SM, Gonzalez A. COVID-19 and mental health during pregnancy: the importance of cognitive appraisal and social support. J Affect Disord. 2021;282:1161–9.
Al-Amer RM, Malak MZ, Darwish MM. Self-esteem, stress, and depressive symptoms among Jordanian pregnant women: social support as a mediating factor. Women Health. 2022;62:412–20.
Braun V, Clarke V. Thematic analysis: a practical guide. London: Sage; 2021.
Stern C, Jordan Z, McArthur A. Developing the review question and inclusion criteria. AJN Am J Nurs. 2014;114:53–6.
Butler A, Hall H, Copnell B. A guide to writing a qualitative systematic review protocol to enhance evidence-based practice in nursing and health care. Worldviews Evid Based Nurs. 2016;13:241–9.
Charvat E, Horstman HK, Jordan E, Leverenz A, Okafor B. Navigating pregnancy during the COVID-19 pandemic: the role of social support in communicated narrative sense-making. J Fam Commun. 2021;21:167–85.
Chongo C, Ngoma CM. Pregnant women’s perception on provision of support during pregnancy and childbirth. Standard Res J Nurs Midwifery. 2014;1(1):1–5.
La CL. Familia: methodological issues in the assessment of perinatal social support for Mexicanas living in the United States. Soc Sci Med. 2001;53:1303–20.
Darvill R, Skirton H, Farrand P. Psychological factors that impact on women’s experiences of first-time motherhood: a qualitative study of the transition. Midwifery. 2010;26:357–66.
Eapen DJ, Wambach K, Domian EW. A qualitative description of pregnancy-related social support experiences of low-income women with low birth weight infants in the midwestern United States. Matern Child Health J. 2019;23:1473–81.
Eddy BP, Fife ST. Active husband involvement during pregnancy: a grounded theory. Fam Relat. 2021;70:1222–37.
Giblin PT, Poland ML, Ager JW. Effects of social supports on attitudes, health behaviors and obtaining prenatal care. J Community Health. 1990;15:357–68.
John-Akinola YO, Babatunde OO, Desmennu AT. Perspectives of women about social support provided by men during pregnancy: a qualitative study. Matern Child Health J. 2022;26:1255–60.
Naz S, Muhammad D, Ahmad A, Ali P. Pregnant women perceptions regarding their husbands and in-laws’ support during pregnancy: a qualitative study. Pan Afr Med J. 2021;39:229.
Puspitasari N, Sulistyorini Y. Exploring factors on quality of life of pregnant women: a qualitative study. Int J Nurs Educ. 2021;13:101–6.
Raman S, Srinivasan K, Kurpad A, Dwarkanath P, Ritchie J, Worth H. ‘My mother…my sisters… and my friends’: sources of maternal support in the perinatal period in urban India. Midwifery. 2014;30:130–7.
Reszel J, Peterson WE, Moreau D. Young women’s experiences of expected health behaviors during pregnancy: the importance of emotional support. J Community Health Nurs. 2014;31:198–211.
Shakeri M, Mahfoozpour S, Alimohamadzadeh K, Molaei B, Zanjani NC. The concept of social support from the perspective of pregnant mothers: a phenomenological study. J Qual Res Health Sci. 2021;10:204–12.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ (Clinical research ed). 2017;358:j4008.
Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12:181.
Munn Z, Tufanaru C, Aromataris E. JBI’s systematic reviews: data extraction and synthesis. AJN Am J Nurs. 2014;114:49–54.
Schaefer C, Coyne JC, Lazarus RS. The health-related functions of social support. J Behav Med. 1981;4:381–406.
Tilden VP. The relation of life stress and social support to emotional disequilibrium during pregnancy. Res Nurs Health. 1983;6:167–74.
Norbeck JS, Tilden VP. Life stress, social support and emotional disequilibrium in complications of pregnancy: a prospective, multivariate study. J health Soc Behav. 1983;1:30–47.
McDowell I. Measuring health: a guide to raing scales and questionnaires. USA: Oxford University Press; 2006.
Pescosolido BA. Illness careers and network ties: a conceptual model of utilization and compliance. Adv Med Soc. 1991;2:164–81.
Cutrona CE, Suhr JA. Social support communication in the context of marriage: An analysis of couples’ supportive interactions. 1994: 113–35.
House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241:540–5.
Weber K, Johnson A, Corrigan M. Communicating emotional support and its relationship to feelings of being understood, trust, and self-disclosure. Commun Res Rep. 2004;21:316–23.
Cwikel J, Segal-Engelchin D, Niego L. Addressing the needs of new mothers in a multi-cultural setting: an evaluation of home visiting support for new mothers-Mom to Mom (Negev). Psychology Health edicine. 2018;23:517–24.
Long HA, French DP, Brooks JM. Optimising the value of the critical appraisal skills programme (CASP) tool for quality appraisal in qualitative evidence synthesis. Res Methods Med Health Sci. 2020;1:31–42.
McHale S, Astin F, Neubeck L, Dawkes S, Hanson CL. A systematic review and thematic synthesis exploring how a previous experience of physical activity influences engagement with cardiac rehabilitation. Eur J Cardiovasc Nurs. 2020;19:31–43.
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8:45.
Noyes J, Booth A, Flemming K, Garside R, Harden A, Lewin S, Pantoja T, Hannes K, Cargo M, Thomas J. Cochrane Qualitative and Implementation methods group guidance series—paper 3: methods for assessing methodological limitations, data extraction and synthesis, and confidence in synthesized qualitative findings. J Clin Epidemiol. 2018;97:49–58.
Booth A, Noyes J, Flemming K, Gerhaudus A, Wahlster P, Van der Wilt GJ, Mozygemba K, Refolo P, Sacchini D, Tummers M, Rehfuess E. Duidance on choosing qualitative evidence synthesis methods for use in health technology assessments of complex interventions. Bremen (DE): Integrate-HTA. 2016: 1–38.
Feld H, Barnhart S, Wiggins AT, Ashford K. Social support reduces the risk of unintended pregnancy in low-income population. Public Health Nurs. 2021;38:801–9.
Qutteina Y, Nasrallah C, James-Hawkins K, Nur AA, Yount KM, Hennink M, Rahim HF. Social resources and Arab women’s perinatal mental health: a systematic review. Women Birth. 2018;31(5):386–97.
Kolker S, Biringer A, Bytautas J, Blumenfeld H, Kukan S, Carroll JC. Pregnant during the COVID-19 pandemic: an exploration of patients’ lived experiences. BMC Pregnancy Childbirth. 2021;21(1):1–13.
Magee S, Nakisbendi K. The pregnancy countdown book: nine months of practical tips, useful advice, and uncensored truths. Philadelphia: Quirk Books; 2006.
Pluut H, Ilies R, Curşeu PL, Liu Y. Social support at work and at home: dual-buffering effects in the work-family conflict process. Organ Behav Hum Decis Process. 2018;146:1–13.
Fernández LE, Newby A. Family support and pregnancy behavior among women in two border Mexican cities. Front Norte. 2010;22:7–34.
Lee YT, McCauley CR, Draguns JG. Personality and person perception across cultures. London, England: Psychology Press; 2013.
Saleh IM, Khine MS. Attitude research in science education: classic and contemporary measurements. Charlotte, NC: IAP; 2011.
Maio G, Verplanken B, Haddock G. The psychology of attitudes and attitude change. London: Sage; 2018.
Habib RR, Nuwayhid IA, Yeretzian JS. Paid work and domestic labor in disadvantaged communities on the outskirts of beirut, lebanon. Sex Roles. 2006;55:321–9.
Georgas J, Berry JW, van de Vijver FJR, Kağitçibaşi Ç, Poortinga Y. Families across cultures: a 30-nation psychological study. Cambridge: Cambridge University Press; 2006.
Gist-Mackey AN, Wiley ML, Erba J. You’re doing great. Keep doing what you’re doing”: socially supportive communication during first-generation college students’ socialization. Commun Educ. 2018;67:52–72.
Fitzpatrick JJ, Wallace M. Encyclopedia of nursing research. New York, NY: Springer; 2006.
Mangaleshwari MN. Personality style, anxiety sensitivity and perceived social support among the pregnant women. M.Phil in Clinical Psychology, Osmania University, 2013.
Ayaz S, Efe SY. Potentially harmful traditional practices during pregnancy and postpartum. Eur J Contracept Reprod Health Care. 2008;13:282–8.
Dolatian M, Mahmoodi Z, Dilgony T, Shams J, Zaeri F. The structural model of spirituality and psychological well-being for pregnancy-specific stress. J Relig Health. 2017;56:2267–75.
Mann JR, Mannan J, Quiñones LA, Palmer AA, Torres M. Religion, spirituality, social support, and perceived stress in pregnant and postpartum hispanic women. J Obstet Gynecol Neonatal Nurs. 2010;39:645–57.
Sharifian F. The Routledge handbook of language and culture. London: Routledge; 2015.
Goodwin R, Hernandez PS. Perceived and received social support in two cultures: collectivism and support among british and Spanish students. J Soc Pers Relatsh. 2000;17:282–91.
Sagrestano LM, Feldman P, Rini CK, Woo G, Dunkel-Schetter C. Ethnicity and social support during pregnancy. Am J Community Psychol. 1999;27:869–98.
Jiang QJ. Medical psychology. Beijing: People’s Health Press; 2005.
Kawachi I, Berkman LF. Social ties and mental health. J Urban Health. 2001;78:458–67.
Lakey B, Cohen S. Social support theory and measurement. In: Cohen S, Underwood LG, Gottlieb BH, editors. Social support measurement and intervention: a guide for health and social scientists. New York: Oxford University Press; 2000. p. 29–52.
Chapter Google Scholar
Cooper H, Hedges LV, Valentine JC. The handbook of research synthesis and meta-analysis. New York: Russell Sage Foundation; 2019.
Dennis CL, Hodnett E, Gallop R, Chalmers B. The effect of peer support on breast-feeding duration among primiparous women: a randomized controlled trial. CMAJ. 2002;166:21–8.
PubMed PubMed Central Google Scholar
Small R, Taft AJ, Brown SJ. The power of social connection and support in improving health: lessons from social support interventions with childbearing women. BMC Public Health. 2011;11(Suppl 5):S4.
Renfrew MJ, Pokhrel S, Quigley M, McCormick F, Fox-Rushby J, Dodds R, et al. Preventing disease and saving resources: the potential contribution of increasing breastfeeding rates in the UK. United Kingdom: UNICEF; 2012.
Yawn BP, Dietrich AJ, Wollan P, Bertram S, Graham D, Huff J, Kurland M, Madison S, Pace WD, Practices T. TRIPPD: a practice-based network effectiveness study of postpartum depression screening and management. Ann Family Med. 2012;10(4):320–9.
Download references
Acknowledgements
Thank you to Matthew for helping with quality appraisal of five studies.
This study was supported by PhD funding to the first author awarded by Kuwait University.
Author information
Authors and affiliations.
School of Human and Behavioural Sciences, Bangor University, Bangor, UK
Mona Al-Mutawtah, Emma Campbell, Hans-Peter Kubis & Mihela Erjavec
Community Medicine- Clinical Psychology, Kuwait University, Kuwait City, Kuwait
Mona Al-Mutawtah
You can also search for this author in PubMed Google Scholar
Contributions
MA was responsible for the study inception and design, data interpretation, conducted the searches, screening, quality appraisal, data extraction, analysis and synthesis, and wrote the final manuscript. EC provided guidance on methodology and study design, reviewed and revised the initial coding and analytical themes, and edited the manuscript. HK and ME contributed to the study design, advised on methodology and study inclusion, reviewed analytical themes, and edited the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Mona Al-Mutawtah .
Ethics declarations
Ethics approval and consent to participate.
There was no contact with human participants in this systematic review, and therefore no ethical approval was required.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. .
Enhancing the transparency in reporting the synthesis of qualitative research: the ENTREQ statement.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Al-Mutawtah, M., Campbell, E., Kubis, HP. et al. Women’s experiences of social support during pregnancy: a qualitative systematic review. BMC Pregnancy Childbirth 23 , 782 (2023). https://doi.org/10.1186/s12884-023-06089-0
Download citation
Received : 27 March 2023
Accepted : 27 October 2023
Published : 10 November 2023
DOI : https://doi.org/10.1186/s12884-023-06089-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Social support
- Systematic review
- Qualitative research
- Thematic synthesis
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
We use cookies to enhance our website for you. Proceed if you agree to this policy or learn more about it.
- Essay Database >
- Essay Examples >
- Essays Topics >
- Essay on Children
Essay On Pregnant Womens Health
Type of paper: Essay
Topic: Children , Family , Pregnancy , Parents , Women , Health , Education , Food
Words: 1700
Published: 02/22/2020
ORDER PAPER LIKE THIS
This paper will talk about pregnancy. It will give the physical and the psychological changes that the pregnant mother will experience throughout the period of pregnancy. Pregnancy is a journey will ensure the safe delivery of the baby while maintaining the mother in a healthy condition. The paper will also talk about the tests that the pregnant mother will undergo during the period of pregnancy because in this period the mother faces many risks of getting a disease basing on the previous pregnancies or developing conditions. The diet that the pregnant mother uses in the period is also of vital importance and the paper will give what the mother will eat during and after pregnancy to ensure the health of the baby is good. It will also give what the mother should not eat that may pose a risk to the mother and the baby. A special connection exists between the mother and the unborn baby and the paper will give how they connect. Finally, the paper will give the summary of the changes that the mother will go through in the three trimesters.
Introduction
Becoming a mother is the most exciting time in a woman’s life. Pregnancy is an amazing journey and a pregnant woman experiences many changes both physical and emotional changes. The changes will totally have an impact on the woman’s life from relationships to the way she eats and the choices she makes at home and work. All the changes and the choices are to ensure the mother and the baby are safe. Pregnancy involves many sacrifices because the mother must put the needs of someone else above her own. The woman must have emotional readiness to receive the baby and be ready to become a mother. She also has day-to-day needs of the house even though the husband may help. The woman must change her lifestyle to accommodate the child. Every pregnancy has some risks of problems. The causes of the problems may be because of the conditions the mother has or conditions developed during the pregnancy. The problems also include being pregnant with more than one baby. They affect the health of the other and the baby.
There are prenatal tests that the pregnant woman undergoes before delivery. The first test is first to determine if the pregnancy is there. Screening tests are necessary because it helps in detecting the disease or a condition in the early stages before it develops into a bigger problem. Early detection of a disease is easy to treat. During the early stages of pregnancy, the doctor will to the pregnant woman and asks her general questions about her family history, social history, general health and previous pregnancies. For example, if the pregnant woman had diabetes in the previous pregnancy, she will require close monitoring to ensure safe delivery. If also, the woman has a social problem like domestic violence, a special help to her is important. The weight and height checks occur during the early stages of pregnancy. This is to see if the mother is underweight or overweight which increases the potential of developing problems during pregnancy. The assessment of the growth of the baby occurs during the antenatal checks. This happens by use of a tape measure from the top of the womb to the pubic bone. The blood pressure of the mother is also an important aspect of the health of the mother during pregnancy. Blood pressure of pregnant mothers tends to increase during pregnancy. This affects the unborn baby and may even lead to death of the fetus. Examination of the baby`s position must also happen. This occurs at about week 36 of pregnancy. This is to ensure that the baby is lying in the breech position. Urine tests include the tests on protein, glucose and bacteria. Test on protein in the urine indicates the existence of pre-eclampsia. Glucose testing is a test for sugars and it is an initial check for diabetes. Blood tests check for anemia, Rhesus factor, infections and hemoglobin disorders. The infections checked for include HIV status, syphilis and hepatitis B (Mattison, 2013). The checks on hemoglobin disorders will detect the presence of any disorder like anemia. Ultra sound scan happens to give the images of the unborn baby. Two scans normally happen: during the early pregnancy to work out on the due date of the baby delivery and later in the pregnancy to show if there are any developing problems with the baby.Screening for downs syndrome must also happen during the pregnancy period. Down`s syndrome is a genetic chromosome disorder that babies are born with.
Eating well during pregnancy is important because it ensures the health of the mother and the development of the unborn baby occurs. A pregnant mother should consume 300 calories a day than she did before becoming pregnant (Lammi-keefe, 2008). Nausea and vomiting may make eating difficult during the first months of pregnancy but the mother should try eating a well balance diet. The mother needs to eat variety of foods to get the nutrients for the nourishment of the baby. A healthy diet for the mother includes carbohydrates, proteins, vitamins, fats, plenty of water and minerals. The proteins ensure the blood production and cell growth. The best sources for proteins include eggs, fish, peanut butter and lean meat. The carbohydrates provide daily energy for the mother. The sources include bread, potatoes, fruits, vegetables, rice and cereals. Vitamins promote the formation of red blood cells, healthy skin, assistance in iron formation and growth of bones. The minerals important for the pregnant mother include iron, which is important in the production of red blood cells to prevent anemia. The foods rich in iron include spinach and lean red meat. The fats act as store for energies and the foods rich in fats include dairy products, meat, margarine and peanut butter. There are foods and drinks that the mother must avoid during pregnancy.The mother should take no amount of alcohol consumption. The alcohol is not good for the development of the baby. Seafood is a great source of omega 3 fatty acids and proteins necessary for the brain development. However, there are fish that contain high levels of mercury that leads to the damage of the baby`s developing nervous system. The mother should avoid this. Undercooked meat is not also good for the mother and the developing baby. Unpasteurized food products are posing as risk to the health of the mothers. The pregnant mothers should avoid eating the unpasteurized foods because they lead to foodborne illness.
Mother and fetus connection
The baby becomes a living being from conception time and reacts to the changes to the changes in the environment of the mother`s womb. The physical, emotion, food intake and psychological condition of the mother are factors that affect the baby.What the mother takes as food influences the development of the baby. A pregnant woman shares physical effects with the baby by the hormones and chemicals in her bloodstream. If the mother is stressed the baby reacts to the emotions the mother experiences by being restless. The babies in the womb communicate, perceive and learn at multiple levels. They are very aware and sensitive of their mothers experience and the environment. For example, playing loud music affects the baby in the womb and they respond by kicking. The baby seeks tenders, happiness, delight and laughter. Each pregnant mother develops way to bond with the baby in the stomach
Summary of the changes during pregnancy
Pregnancy lasts for about forty weeks if you count from the first day of the last normal period. The summary are in weeks trimesters and the mother has the following changes:
First trimester (week 1- week 12)
During this period, the body of the mother undergoes many changes. The hormonal changes affect almost every organ of the mother. The changes include extreme tiredness, tender swollen breasts, morning sickness, mood swings, constipation, weight loss/gain, heartburn and vomiting.
Second trimester (Weeks 13- week 28)
This trimester is not difficult like the first trimester. The abdomen is expanding during this trimester and the mother begins to feel the baby move. The mother experiences aches on thigh, groin and back pains. The stretch marks begin to appear on the breasts, buttocks and thighs. The skin around the nipples begins to dampen and become dark. The mother feels itchy on the abdomen, soles of feet and palms (Tulman &Fawcett, 2003). There is loss of appetite and likelihood of vomiting. The ankles face and the ankles become swollen. This is leads to an increase in weight.
Third trimester (Week 29- week 40)
This is the homestretch. The discomforts in the second trimester may continue in this trimester. In this trimester, breathing becomes difficult and the mother has to go to the bathroom many times. This is because the baby is growing bigger and it puts pressure on the organs. The tender breasts sometimes start leaking pre-milk called colostrum. The belly button sticks out and the woman experiences sleepless nights. Heartburns are also a characteristic in this trimester. There are contractions, which are signs of false or real labor. Hemorrhoids may also occur in this trimester. When the due date approaches, the cervix becomes thinner and softer through a process called effacing. This process helps the birth canal to open.
Lammi-Keefe, C. J., Couch, S. C., & Philipson, E. H. (2008). Handbook of nutrition and pregnancy. Totowa, N.J: Humana Press. Mattison, D. R. (2013). Clinical pharmacology during pregnancy. Amsterdam: Academic Press. Tulman, L., & Fawcett, J. (2003). Women's health during and after pregnancy: A theory- based study of adaptation to change. New York: Springer Pub. Co.

Cite this page
Share with friends using:
Removal Request

Finished papers: 1038
This paper is created by writer with
ID 266842643
If you want your paper to be:
Well-researched, fact-checked, and accurate
Original, fresh, based on current data
Eloquently written and immaculately formatted
275 words = 1 page double-spaced

Get your papers done by pros!
Other Pages
Suppression reports, complaint reports, grill reports, vicinity reports, cone reports, coil reports, funeral reports, cockpit reports, birthday college essays, truancy essays, vladimir putin essays, dunning essays, switcher essays, dropping out of high school essays, save our planet essays, desalination of water essays, jerry falwell essays, trainspotting essays, holy basil essays, xanthan essays, throne of blood essays, essay on qualitative data, essay on utilization management, course work on accounting, free essay on circle of courage, sermon on the mount research papers example, where is the corpse essay samples, u s political parties and the electoral process research paper, sample creative writing on american history, sample essay on comparison between the butter battle and gullivers travels, free violence against women creative writing sample, free essay about raving fans, good example of leadership at general electric corporation term paper, good the challenge research paper example, sample essay on global warming and its causes, myrtle beach essay, sample essay on senate bill 492 licensure for optometrist practice, free essay about levinasian ethics and social theory, free american patriotic music term paper example, sample essay on group development, good example of essay on law of contracts, youth in conflict with law essays example, conflict management styles quiz essays example.
Password recovery email has been sent to [email protected]
Use your new password to log in
You are not register!
By clicking Register, you agree to our Terms of Service and that you have read our Privacy Policy .
Now you can download documents directly to your device!
Check your email! An email with your password has already been sent to you! Now you can download documents directly to your device.
or Use the QR code to Save this Paper to Your Phone
The sample is NOT original!
Short on a deadline?
Don't waste time. Get help with 11% off using code - GETWOWED
No, thanks! I'm fine with missing my deadline

Improving writing skills since 2002
(855) 4-ESSAYS
Type a new keyword(s) and press Enter to search
My pregnancy experience.
- Word Count: 933
- Approx Pages: 4
- View my Saved Essays
- Downloads: 27
- Grade level: High School
- Problems? Flag this paper!
Before my pregnancy I had heard different types of stories about pregnancy, labor, and delivery. Some of the stories were good and some of the stories were bad. Therefore, in my mind I expected to feel a certain way when I found out I was going to be a mother. All sorts of questions were running through my head. "Are the stories true about pregnancy?", "Will I feel like that?", "Will the labor hurt that bad?", and most of all "Am I ready to be a mother?" Well, I guess all I could do was wait and find out for myself. Instead my pregnancy, labor, and delivery were an experience that I never anticipated and will never forget. When I found out I was two months pregnant, I had all sorts of emotions run through my body. I thought about the consequences I was going to have to face such as what my mother would say or think when she found out I was pregnant, especially at the age of 18. I also thought about what my family would say and how they might disapprove of the situation. I also knew that the activities I enjoyed doing with my friends and family would have to stop. Five months later, I finally had the courage to tell my mother that I was pregnant. I knew my mother would be disappointed and upset at the news. But to my surprise she became very happy and supportive of throughout my pregnancy so was my family. I also stopped engaging in some of my old activities such as going to ceremonies, hanging out with friends late at night, and family occasions, but continued to make myself do other things such as go to school, work, and start a closer relationship with my mother. . During my pregnancy, I thought I would be very miserable. Sometimes I read articles on pregnancy through the Internet and magazines. I read that pregnant women can do unhealthy things to themselves such as weight gain before birth and after birth or high blood pressure and thought all these actions would be terrible.
- Page 1 of 3
Essays Related to My Pregnancy Experience
1. life or liberty.

These groups generally only believe in ending the pregnancy early in case such as certain death caused by pregnancy, such as ectopic pregnancy. ... This is a belief that I have always had and that ultimately was cemented by my own experience. I found myself unprepared for a pregnancy shortly after high school in my late teens. ... Luckily I had the freedom to choose to end my pregnancy. ... Sharing my experience with friends over the years always opens up lines of communication with many of them that have gone through the same experience, or have known someone who has. ...
- Word Count: 1267
- Approx Pages: 5
- Grade Level: High School
2. Teenage Pregnancy

Teenage Pregnancy The subject of teenage pregnancy is a very personal subject for me because one of my best friends is currently pregnant. ... So the topic of teenage pregnancy is very relevant in my life right now and something that I would like to research to help out my friend, and friends in the future. ... And looking into the experiences that I am having right now with my friend I am actually noticing how much a child actually costs. ... In my opinion I believe that if everybody is more educated everywhere, just not in inner cities then maybe the teenage pregnancy rate would g...
- Word Count: 930
3. Difficult Pregnancy

Difficult pregnancy, stronger faith, trust in God my experience brought all of these things together. ... My pregnancy was very stressful and the stress lasted throughout the next five month's. ... My sister became pepper in her early months of pregnancy and she appeared to have a glow around her. ... Many women have babies and never experience this kind of problem. ... Can a difficult pregnancy develop a stronger faith? ...
- Word Count: 1578
- Approx Pages: 6
4. right to choose

Based upon my personal experience and ability to refute opposing views, I believe every woman, no matter what race, marital status, or age, has the right to her own reproductive self-determination and privacy of the decisions she makes. ... If not for freedom of choice my friend Jamie would not be where she is today. ... She is also thankful that the option of terminating the pregnancy was available to her. ... These are done by inducing pregnancy and then severing the fetus' cerebrum when delivered. ... In an ectopic pregnancy, the egg becomes implanted in one of the woman's fal...
- Word Count: 963
5. Teenage Pregnancy

Teen Pregnancy Everyday more than 3,000 girls find out they"re pregnant. ... Most teen mothers are less likely to graduate from high school and their kids are often born at low birth weight or experience health and development problems. ... "The media also plays a big role in the teenage sex and pregnancy. ... Easy access to contraception's help reduce the cost of teen pregnancy. ... I know how much it cost because I get the shot and for now my insurance plan covers it until I am 18 then I"m going to have to play for it which gets expensive. ...
- Word Count: 1001
6. Pregnancy - A Letter to My Son

The purpose of this letter is to provide you with all the information about my pregnancy, the process of giving birth to you, and include all the factors that I believe affected your overall development. ... That feeling of confusion and depression I was experiencing, I now know were influenced by different domains; social-emotional and social-cultural factors, and perhaps some biological factors, too. ... I have to admit my temper got worse the first few months of pregnancy; I felt like I hated your father, everything seemed to irritate me. ... I can tell you, that after the third month afte...
- Word Count: 1627
- Approx Pages: 7
7. Birth Control and Teen Pregnancy

The young couple would lose precious years of experiencing successes, failures, and teenage life in itself. ... My story is first-hand proof to how the typical parent acts when going through "the talk." My parents sat me down in my high school years, to tell me to "save myself for the married years.... As much as my heart was pounding along with the alarming thoughts in my head as to what they were going to say, I finally caught enough breath and nerve to release my secretive information. ... Teen pregnancy rates have dropped in recent years. ...
- Word Count: 1691
8. Teen Pregnancy

She took a pregnancy test and when the pregnancy test came out positive, she kept it a secret and explored her possible options. ... Her pregnancy not only affected her, but her family as well. The social problem focused on in the film is, teenage pregnancy. ... There are just so many people and things affected by teen pregnancies. ... Like, "what if my parents find out or my partner's parents, we could get in trouble with the law." ...
- Word Count: 1829
9. Teen Pregnancies

Statistics about teen pregnancies are indicators of a societal problem. ... A fair number of pregnancies result from such foolishness. ... Initial sex experiences outside of marriage are often disciplinary because of high anxiety and guilt levels. ... What are my true feelings about this person? Are my partner and I able to communicate? ...
- Word Count: 1385
- Has Bibliography
- Open access
- Published: 03 August 2023
Lived experiences of pregnant and parenting adolescents in Africa: A scoping review
- Anthony Idowu Ajayi 1 ,
- Sherine Athero 1 ,
- Winstoun Muga 1 &
- Caroline W. Kabiru 1
Reproductive Health volume 20 , Article number: 113 ( 2023 ) Cite this article
3398 Accesses
1 Citations
11 Altmetric
Metrics details
Previous studies have not synthesized existing literature on the lived experiences of pregnant and parenting adolescents (aged 10–19) in Africa. Such evidence synthesis is needed to inform policies, programs, and future research to improve the well-being of the millions of pregnant or parenting adolescents in the region. Our study fills this gap by reviewing the literature on pregnant and parenting adolescents in Africa. We mapped existing research in terms of their substantive focus, and geographical distribution. We synthesized these studies based on thematic focus and identified gaps for future research.
We used a three-step search strategy to find articles, theses, and technical reports reporting primary research published in English between January 2000 and June 2021 in PubMed, Jstor, AJOL, EBSCO Host, and Google Scholar. Three researchers screened all articles, including titles, abstracts, and full text, for eligibility. Relevant data were extracted using a template designed for the study. Overall, 116 studies met the inclusion criteria and were included in the study. Data were analyzed using descriptive and thematic analyses.
Research on pregnant and parenting adolescents is limited in volume and skewed to a few countries, with two-fifths of papers focusing on South Africa (41.4%). Most of the studies were African-led (81.9%), received no funding (60.3%), adopted qualitative designs (58.6%), and were published between 2016 and 2021 (48.3%). The studies highlighted how pregnancy initiates a cycle of social exclusion of girls with grave implications for their physical and mental health and social and economic well-being. Only 4.3% of the studies described an intervention. None of these studies employed a robust research design (e.g., randomized controlled trial) to assess the intervention’s effectiveness. Adolescent mothers' experiences (26.7%) and their education (36.2%) were the most studied topics, while repeat pregnancy received the least research attention.
Research on issues affecting pregnant and parenting adolescents is still limited in scope and skewed geographically despite the large burden of adolescent childbearing in many African countries. While studies have documented how early pregnancy could result in girls' social and educational exclusion, few interventions to support pregnant and parenting adolescents exist. Further research to address these gaps is warranted.
Peer Review reports
Introduction
One group of young people that has received limited attention in sexual and reproductive health and rights research is pregnant and parenting adolescents (aged 10–19). This group of adolescents faces daunting challenges as they navigate parenthood, care for their babies, and improve their lives [ 1 , 2 , 3 ]. Many forfeit their future aspirations, including their educational goals and skills acquisition, with significant implications for their health and well-being, as well as that of their offspring [ 4 , 5 , 6 ].
Girls who become pregnant outside marriage often face stigma because of widespread socio-cultural and religious beliefs that sex should only occur in marriage [ 7 ]. As a result, some face an an hostile home environment or move away from home to reside with their partners [ 8 ]. Further, girls who become pregnant while in school are often forced to drop out of school [ 9 ]. This situation initiates a cycle of events culminating in their social exclusion. Social exclusion of pregnant and parenting adolescents can jeopardize the immediate and future health and well-being of young mothers. Patton et.al. argues that adolescence offers huge opportunities to alter negative and harmful trajectories that can jeopardize their future health. In their Lancet Commission, they demonstrate that investing in adolescent health, education and family would yield a triple dividend of benefits in the development of capabilities during adolescence, future adult-health trajectories, and secure welfare of the next generation [ 10 ].
Despite the existence of school reentry policies in most African countries that should facilitate reentry, available estimates show that a vast majority of pregnant and parenting adolescents are out of school even though they would like to return to school [ 11 ]. The few that manage to return to school describe the school environment as hostile, discriminatory, and inflexible [ 12 ]. Teachers unfairly target them, resulting in them dropping out or infrequently attending school [ 13 ].
Adolescent pregnancy and parenthood are also associated with child marriage, as these adolescents may be forced to move in with or get married to their partners [ 14 , 15 ]. For some adolescent girls who become pregnant outside of wedlock, marriage serves as the only option to escape the associated stigma and social exclusion, enhance their status in the community or get financial support to care for their children [ 16 ]. However, child marriage can expose adolescent mothers to mental problems [ 17 ], school dropout [ 18 ], and intimate partner violence [ 19 ].
The social exclusion of pregnant and parenting adolescents has grave implications for gender equality. Because they rarely return to school [ 11 ], pregnant and parenting adolescents are unable to achieve their educational goals, which has consequences for their participation in the labor force [ 4 ]. Ultimately, this disenfranchises them and their children. Even though there are review studies on adolescent sexual and reproductive health, experience of adolescent mothers affected by HIV, and adolescent mental health in Africa [ 20 , 21 ], there is limited attention to the lived experiences of pregnant and parenting adolescents. Given the unique challenges facing this cohort of adolescents, it is pertinent to review the literature to identify gaps in research on this population. Also, noting that a quarter of adolescent girls are either pregnant or parenting in the region, there is a need to target this population for interventions [ 22 ].
A review of existing studies will inform our knowledge of what interventions exist to improve their health and well-being as well as their socioeconomic and education empowerment and identify areas to prioritize for interventions. Our scoping review addresses this gap, drawing on the social exclusion framework [ 23 ], and aims to answer three questions: (1) What is the profile of research on the lived experiences of pregnant and parenting adolescents in terms of research designs, geographical distribution and substantive focus, including motherhood, and experiences in the community and schools? (2) How does early childbearing impact pregnant and parenting adolescents’ mental health? (3) What interventions are reaching adolescent mothers to improve their health and socioeconomic wellbeing?
A scoping review is the appropriate design for the study given we aim to explore the breadth and extent of the literature, map and summarize the evidence, and inform future research, of the broader objective of this review.
Search strategy
Guided by the Joanna Briggs Institute (JBI) methodological approach, we searched for peer-reviewed papers and grey literature published between January 2000 and June 2021 on pregnant and parenting adolescents. Grey literature was limited to theses. The search was limited to documents published in the English language and focusing on African countries. A three-step search strategy was used to ensure our search was comprehensive. First, we conducted a limited PubMed search to identify medical subject heading (MesH) terms for pregnant adolescents, adolescent mothers, and adolescent fathers. We analyzed the text words in the title, abstracts, and index terms in the articles from the initial search. We then created search terms for the study using the results of our analysis. In the second step, we searched PubMed, Jstor, AJOL, EBSCO Host, and Google scholar. After removing duplicates from the initial articles, we identified review studies found during our search. We reviewed the reference lists of these review articles and identified articles from the list that met our inclusion criteria. A detailed sample of PubMed search is provided in Additional file 1 .
Eligibility criteria
We included articles focusing on pregnant and parenting adolescents (married and unmarried) published in English between January 2000 and June 2021. As we aimed to identify gaps in research on pregnant and parenting adolescents with a specific focus on the challenges they face and interventions to address them, we only included articles that focused on parenting adolescents' well-being, including school reentry, livelihood, and repeat pregnancy, contraceptive use, mental health, motherhood challenges and care-seeking practices, and programs reaching pregnant and parenting adolescents. We excluded studies focusing on maternal health care services utilization, obstetric outcomes and adolescent pregnancy rate and risk factors to have a manageable number of articles and because previous systematic review studies have explored these topics [ 24 , 25 , 26 ] (Table 1 ).
Study selection
Two reviewers independently screened the articles' titles and abstracts to assess their eligibility. Articles were included if they met the pre-specified inclusion criteria and if both reviewers agreed. When there was disagreement, a discussion was held with a third reviewer to resolve it. Figure 1 presents the PRISMA flow diagram demonstrating the process of article screening, inclusion, and exclusion. The initial search yielded a total of 427 articles, from which we removed 188 duplicates. After screening abstracts and titles, we excluded 112 articles that did not meet the eligibility criteria. We assessed the full text of a total of 127 articles and further removed 11 articles that did not meet the eligibility criteria, leaving 116 articles in our analysis.
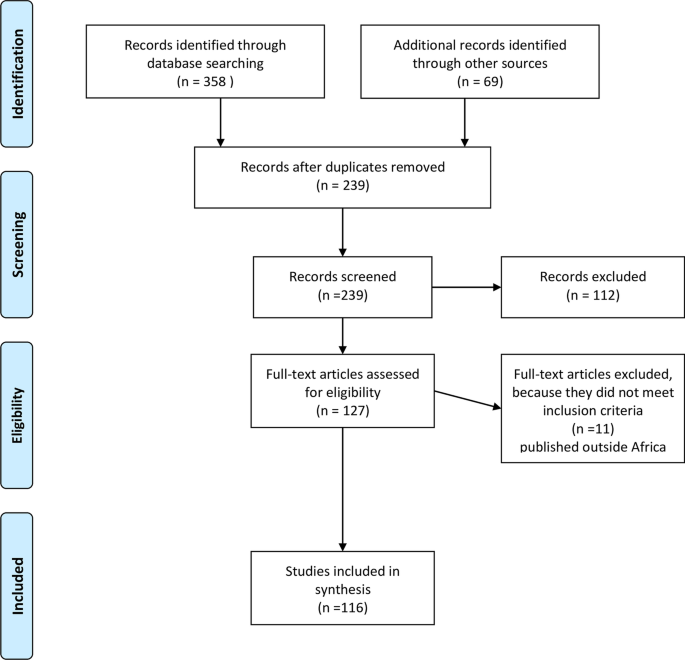
Overview of the articles selection process
Data extraction and charting
We developed a data extraction template using Microsoft Excel. Three members of the research team completed the data extraction. Specifically, we extracted the country of affiliation of the first and last authors, country of study and sub-region, year of publication, journal of publication, study design, study objectives, key findings, and funder. We also classified the articles into common themes, including contraceptive use, mental health, lived experiences, education, social support, motherhood, care-seeking practices, and repeat pregnancy and HIV. One member of the research team reviewed samples of the extracted data for quality assurance.
Evidence synthesis
We synthesized the data using descriptive statistics and content analysis. Descriptive analysis was used to describe the studies in terms of geographic distribution, year of publication, thematic focus, and research design. We summarized the key findings under the themes generated.
Overall, 116 studies met the inclusion criteria and were included in the study. About half of the studies were published between 2016 and 2021 (48.3%). The studies were conducted in 17 African countries, and two-fifth of them focused on South Africa (41.4%) (Fig. 2 ). As shown in Table 2 , most of the studies were African-led (81.9%). Only a few of the studies (4.3%) described an intervention, and none of these intervention studies employed a robust research design (e.g., randomized controlled trial design) to assess its effectiveness and impact. Qualitative methodology was the most commonly used study design (58.6%), enabling a deeper understanding of adolescent mothers' challenges. Adolescent mothers' experiences (26.7%) and their education (36.2%) were the most studied topics, while repeat pregnancy received the least research attention. Close to two in three studies did not receive any funding; 30.2% received external funding, while 9.5% had local funding. Organizations and agencies in the United States funded 37.1% of studies (n = 35) that received external funding. The United Kingdom (14.3%), Netherlands (14.3), Sweden (11.4%), and Canada (8.6%) governments were also prominent funders of research on pregnant and parenting adolescents in Africa.
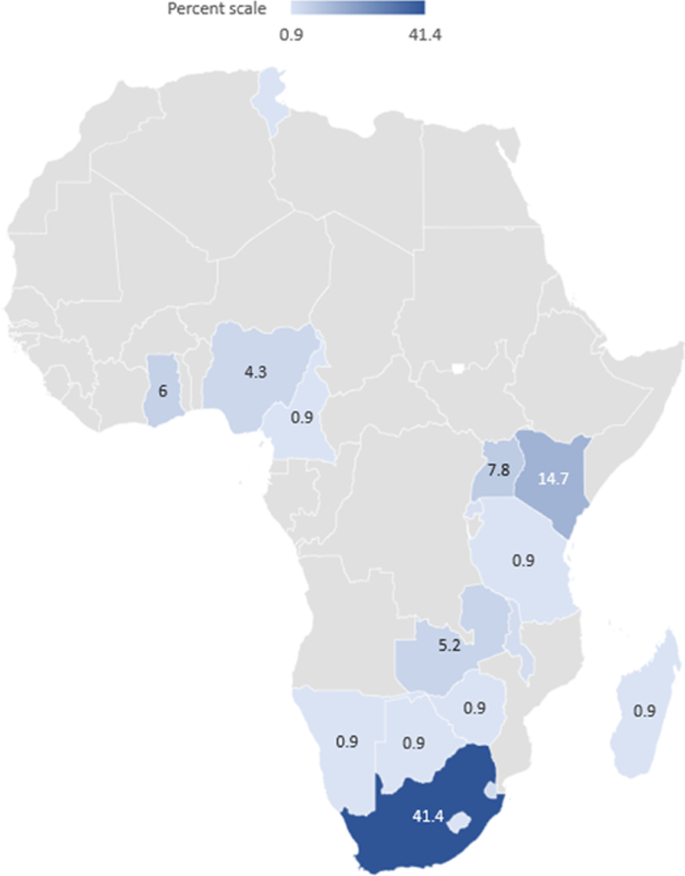
Geographical distribution of studies of adolescent mothers
Partners, parents and community reactions to and support for pregnant and parenting adolescents
Partners, parents and community reactions to and support for pregnant and parenting adolescents were the areas that have received the most research attention [ 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 ]. However, eighteen of the 30 studies were conducted in South Africa. Most adolescent girls described their pregnancy as unintended [ 28 , 29 ] and owing to transactional sex to meet their basic needs, sexual violence and exploitation, and lack of accurate information on methods of preventing pregnancy. A few adolescents wanted to become pregnant to command respect from people. Most were still in school when they became pregnant—many experienced denials of paternity [ 30 , 31 ]. Boys were reported to deny paternity because they thought admitting it would jeopardize their educational and employment opportunities. As a result, adolescent mothers had limited support from the boys or their parents. Adolescent girls’ reactions to their pregnancy ranged from disappointment, anger, regret, and anxiety, for many, to a personal sense of satisfaction, happiness, and accomplishment, for a few [ 32 ].
Family reactions to adolescent pregnancy and motherhood were largely negative [ 30 , 31 , 33 ] and ranged from anger, disappointment, abandonment, rejection, and physical and emotional violence. In studies in Ghana and South Africa, parents and guardians of adolescent mothers were upset in the initial stages when they heard the news of the pregnancy, but they subsequently turned the initial emotion into forgiveness and acceptance. Lack of support from families, friends, and society was reported in Nigeria [ 33 ]. In Swaziland [ 32 ] and South Africa [ 34 ], adolescent pregnancy strained relationships with fathers, but mothers provided emotional and material support [ 32 ].
Adolescent mothers were noted to experience extreme hardship, educational disruption, stigma, stress, loneliness, guilt, and harsh treatment from family, schools, hospitals, and community members [ 35 , 36 ]. They also faced financial constraints and food insecurity, prompting some to take up menial jobs. They faced unfavorable health [ 37 ] and school systems [ 38 ] emanating from discrimination by health workers, abuse and mockery from teachers, and stigma from peers [ 35 ]. This, in return, restricted them from effectively managing their schoolwork and parenting roles and resulted in delays in healthcare seeking and poor performance in school. Their pregnancy was seen as a major impediment to their education and career aspirations. Others were forced into early marriages and left feeling rejected. The negative treatment of pregnant and parenting adolescents was associated with skill gaps in handling parenting adolescent needs among key stakeholders, including parents, teachers, and service providers. Positive experiences included parenting adolescents’ views of their children as a source of meaning and the aspirations they had for their children [ 39 ]. Also, despite these challenges, adolescent mothers in South Africa were more likely to report parental support [ 28 ].
Only four studies focused on the experiences of adolescent fathers [ 40 , 41 , 42 , 43 ] and were conducted in South Africa. Peer influence, misconceptions about contraceptives, multiple partners, and low education attainment were associated with adolescent fatherhood. The studies found that adolescent fathers' own experience of absent fathers gave them a strong sense of responsibility towards their children and partners, but they faced financial constraints and were emotionally, psychologically, and socioeconomically overwhelmed by parental responsibilities. Adolescent fatherhood was related to stress and feelings of low confidence due to stigma related to becoming a father too early. Some had to work to support their children.
School reentry policies and experiences of adolescent mothers in school
Forty-two studies focused on school reentry policies and adolescent mothers' experiences in school [ 5 , 7 , 11 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 ]. These studies are mainly from South Africa (19 publications), Kenya (11 publications), Zambia (six publications), Ghana (two publications), Eswatini (one publication), Tanzania (one publication), Namibia (one publication), and Ghana (one publication). The review shows that most countries studied have school reentry policies in place while others are in the process of drafting or finalizing a policy [ 60 ]. In Kenya, there is a school reentry policy, but key stakeholders are unfamiliar with the provisions within the policy and are unable to fully implement policy [ 49 ]. Thus, 98% of adolescent mothers were reported to be out of school [ 56 ]. A lack of proper monitoring systems to ascertain conformity with the guidelines and limited circulation to headteachers and principals were noted [ 60 ]. In Zambia, pregnant girls were reported to drop out of school voluntarily or involuntarily as soon as the pregnancy is visible. On return to school, they experienced discrimination, mockery, abuse, humiliation, labeling, and isolation from teachers, peers, friends, classmates, and community members [ 7 ]. Their social exclusion resulted in low self-esteem, identity crises, poor academic performance, alcohol use, truancy, and running away from home [ 7 ]. Parents and adolescent mothers lacked information about the school reentry policy and guidelines resulting in the limited implementation of the policy [ 80 ]. Also, preference for boys’ education and poverty affected adolescent mothers' education with parents not willing or lacking resources to fund their education [ 57 , 80 ].
While most adolescent mothers wanted to reenter school, they were constrained with child care responsibilities coupled with various contextual barriers, including financial burden, lack of emotional and social support, culture, lack of policy guidelines, fear of the school being ostracized by the community, fear of having mothers at school, and political factors, which impeded their full reintegration in school and impacted negatively on their school performance [ 11 , 56 , 60 ]. These contextual barriers suppressed the implementation of school reentry policies, especially in very conservative communities. Prevailing negative factors such as childcare responsibilities, poor economic background, and unsympathetic teachers and schoolmates made it difficult for adolescent mothers to reintegrate back into school [ 60 ]. Almost all adolescent mothers indicated that financial support for school fees and other expenses is critical for their reentry back to school. Only a few mentioned the need for childcare support. A study in Kenya found that school environment, teacher encouragement, school clubs, school sponsors, attitudes of other learners, the attitude of the school principal, teacher parenting program, curriculum, guidance and counseling services, opportunities to take part in activities and perform duties, motivational talks by resource persons, time for arrival and departure from school are factors facilitating the education of adolescent mothers [ 79 ].
In South Africa, however, many adolescent mothers returned to school. But, there were concerns that they return too early, as early as the first two months of postpartum [ 63 ]. Their return to school was fraught with challenges like limited support, social stigma, verbal abuse, and discrimination, resulting in many quitting schools or not succeeding with schooling [ 46 , 48 ]. Adolescent mothers also struggled with balancing childcare with school demands [ 45 ]. But teachers were aware of their constitutional right to education and painstakingly protected this right [ 47 ].
Mental health
Few studies have focused on the mental health of pregnant and parenting adolescents. Except for two studies, the rest were published between 2015 and 2021 [ 20 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 ]. They concentrated on Zimbabwe [ 87 ], Nigeria [ 81 , 85 ], South Africa [ 86 , 92 , 95 ], Kenya [ 83 , 91 , 93 ], Uganda [ 82 , 88 ], Rwanda [ 94 ], and Lesotho [ 90 ]. One study looked at data from across sub-Saharan Africa [ 16 ], while one focused on global data[ 84 ]. Except for one intervention study, all these studies described the mental health challenges faced by pregnant, and parenting adolescents (including suicidal ideation, stress, anxiety, hearing voices, depression), the key stressors increasing their risk to mental distress, and challenges they experienced in accessing care.
These studies demonstrate that pregnant and parenting adolescents face high levels of depression, stress, and anxiety, heightened by their social exclusion, poverty, intimate partner violence, rejection by partners and parents after becoming pregnant, stigma from the community, chronic illnesses like HIV, and childhood vulnerabilities. The prevalence of depression ranged from 13% in Zimbabwe [ 87 ], 16% in South Africa [ 92 ], 48% in Rwanda [ 94 ], and 33% [ 93 ], and 53% [ 91 ] in Kenya. Common risk factors for depression included physical violence, verbal abuse, intimate partner violence [ 92 ], low family income, psychoactive substances [ 91 ], having experienced stressful life events, being diagnosed with HIV/AIDS, absence of social support, abandonment by a partner, absence of both parents during childhood [ 93 ], social insecurity, negative perception of teenage pregnancy, and bad relationships within families [ 87 ]. Protective factors included partner support [ 92 ]. Postpartum depression among adolescent mothers was associated with parental distress, weight/body shape disturbances, economic income, and parental-child dysfunctional interaction [ 94 ].
Negative service providers’ attitudes and stigma towards mental illness [ 85 ] and adolescent pregnancy, lack of confidentiality, and logistic and environmental challenges prevented the use of mental health services [ 86 ]. The lack of an all-inclusive approach to address adolescent parents’ multiple needs, including inadequate capacity and training for healthcare providers on handling their needs, was another challenge. Limited evidence exists on the effectiveness of psychosocial interventions on mental health disorders, prevention or treatment of common mental illnesses for adolescent mothers, particularly from low- or middle-income countries to inform effective intervention strategies for mental health illnesses.
Motherhood challenges and care-seeking practices
A few studies focused on the challenges faced by adolescent mothers and care-seeking behaviors [ 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 ]. These studies were conducted in Uganda, South Africa, Swaziland, and Ghana with one study focusing on sub-Saharan Africa. The findings highlighted adolescent mothers' limited knowledge and skills about newborn/childcare practices. They often resorted to practices deemed harmful to their children [ 102 ], such as applying hot towels heated with hot stones to children's umbilical stump [ 102 , 104 ]. Further, early motherhood was noted to strip adolescent girls of their agency and expose them to the stigma that compounds their barriers to accessing care during and after pregnancy. As a result, adolescent mothers may face more challenges during pregnancy and early motherhood than adult mothers.
Contraception
Only seven studies focused on contraception among parenting adolescents [ 82 , 108 , 109 , 110 , 111 , 112 , 113 ], four were published between 2001 and 2004, and two were published in 2020. These studies focused on contraceptive knowledge, attitude, perceptions, and use and were conducted in Cameroon, Nigeria, South Africa, Malawi, and Uganda. The studies highlighted low contraceptive uptake or the use of less effective methods like periodic abstinence, herbal concoctions, and vaginal douching [ 108 ]. However, in Uganda, Muyama et al. [ 82 ] reported a relatively high uptake of contraceptives among adolescent mothers, influenced by the desire to return to school [ 82 ]. The findings in terms of contraceptive knowledge were mixed with the study conducted in Nigeria, showing that contraceptive knowledge is poor. In contrast, the study in Cameroon found that most adolescent mothers had heard about contraceptives [ 111 ]. A study in South Africa reported several barriers to contraceptive use among parenting adolescents, including fear of side effects, partner rejection, providers' attitudes, and shortage of contraceptive supplies [ 112 ].
Repeat pregnancy
Just three studies focused on repeat pregnancy among adolescent mothers, and all were conducted in South Africa [ 114 , 115 , 116 ]. The prevalence of repeat pregnancy in South Africa ranged from 17.6% to 19.9%. A history of spontaneous abortion, contraceptive use, a higher level of education, and emotional support were protective against repeat pregnancy. However, HIV-positive status, having more than one sexual partner and having a partner that is at least five years older were risk factors for repeat pregnancy. Adolescent mothers who received medical, psychosocial, educational, and family planning support experienced lower repeat pregnancy rates.
Programs reaching pregnant and parenting adolescents
Five studies described programs targeting adolescent mothers [ 117 , 118 , 119 , 120 , 121 ]. Two of these five papers reported on one program—the Teenage Mothers project—implemented in Uganda [ 120 , 121 ]. The program used an iterative, bottom-up, participatory approach to co-design an intervention to improve the psychological and social well-being of unmarried adolescent mothers. The program encompassed five intervention components: community awareness-raising, teenage mother support groups, formal education and income generation, counseling, and advocacy. The program was evaluated using qualitative research, and the findings suggest that it contributed to the teenage mothers' well-being and supportive social environment and community norms towards their future opportunities. Results also suggested that the program increased agency, improved coping with early motherhood and related stigma, continued education, and increased income generation. However, the program was not effective in changing community norms regarding out-of-wedlock sex and pregnancy [ 120 ].
Another study in Kenya used young mothers' clubs to increase adolescent mothers' knowledge of family planning and postpartum hemorrhage [ 118 ]. Young mothers participating in the program met weekly to share experiences and solutions to their challenges while receiving health education from health facility staff and community health workers.
Another intervention was implemented in Malawi to improve adolescent mothers' well-being and promote the healthy upbringing of their children. The program was informed by a literature review and consultation with key stakeholders. A safe space was created to share the daily challenges faced by adolescent mothers. Key stakeholders were brought to teach mothers about various topics like brain development, hygiene, and nutrition. Their children were provided with early childhood education and stimulation activities for up to two and a half years. Lastly, there was a community advocacy component to ensure the continued support of adolescent mothers.
As part of the fourth intervention, adolescent mothers in South Africa were introduced to kangaroo mother care to improve their childcare practices [ 119 ]. Kangaroo mother care is the practice of skin-to-skin contact between an infant and parent and has been found to improve growth and decrease the morbidity and mortality of low-birth-weight and premature infants [ 119 ]. Adolescent mothers in this intervention reported positive feelings about the kangaroo mother care. They also reported positive interactions with nurses, doctors, and other mothers and were pleased with the physical, emotional, social, and discharge support they received. However, they considered kangaroo mother care boring because they would just sit with their babies and do nothing.
Ours is the first study to our knowledge to synthesize existing literature on the experiences of pregnant and parenting adolescents in Africa. Research on pregnant and parenting adolescents is generally limited in volume and skewed to a few countries despite most countries recording a high prevalence of adolescent childbearing. The bulk of research on these adolescents is from two countries (South Africa and Kenya), underscoring the gaps in the geographical distribution of research on the issue in the region. These two countries are by far not the ones with the highest prevalence of adolescent childbearing in Africa. The significant research attention on the issues in these countries could make the issues facing pregnant and parenting adolescents more prominent to policymakers. Kenya, for example, formulated and released National Guidelines for School Reentry in Early Learning and Basic Education in 2020 [ 122 ]. Without the significant research attention on the issue in Kenya, this may have been impossible.
Despite the limited research attention on the experiences of pregnant and parenting adolescents, more recently, there appears to be increasing research attention given that about half of the studies were conducted between 2016 and 2021. Researchers' apparent growing interest in this population of adolescents bodes well for future research and investments in programs to improve their well-being. If the current interest in pregnant and parenting adolescents continues, there is a possibility for filling research gaps and addressing the wide geographical gaps in its distribution.
Unlike research on adolescent sexual and reproductive health in general [ 123 ], affiliated African authors led a vast majority of research on pregnant and parenting adolescents’ experiences and challenges. Adolescent sexual and reproductive has received significant research attention given it is one of the global development priority topics. Ending HIV, child marriage, female genital mutilation, early and unintended pregnancy, and increasing contraceptive uptake among adolescents are important global health priorities that have received significant research and program investments. However, issues affecting adolescent mothers have received limited focus, including funding and program investments. It is not surprising that most studies on pregnant and parenting adolescents did not receive any funding. The low representation of global north researchers in publications on these adolescents’ experiences and challenges may reflect the limited research funds available on these issues. Given that millions of girls in the region become pregnant every year, it is important that issues affecting them, particularly their education and skill empowerment, prevention of repeat pregnancy, mental health, and prevention of partner and non-partner violence, gain global attention. Empowering pregnant and parenting adolescents is key to realizing Sustainable Development Goal 5—Achieve gender equality and empower all women and girls. It is, therefore, imperative that global development partners and governments invest in research and programs to improve their health and well-being.
Our review demonstrates that pregnant and parenting adolescents, particularly girls, face several social, education, health, and motherhood challenges, including stigma, poor mental health, low contraceptive uptake, repeat pregnancy, lack of support, hostile school environment. Yet limited studies report on interventions to address these challenges. Such overwhelming neglect suggests that the suffering and social exclusion of this population of adolescents will continue, resulting in their disempowerment, poverty, and exacerbation of gender inequality. However, it is important to note that there is a range of experiences across the continent and challenges faced by adolescent parents varies hugely depending on the context [ 63 ]. For example, adolescent mothers are more likely to return to school in South Africa compared to Kenya, suggesting differential experiences of adolescent mothers in both settings [ 11 , 63 ]. Also, some countries have formulated school reentry policies to address hostile school environments and facilitate adolescent mothers’ return to school.
While most studies focus on pregnant and parenting adolescents’ lived experiences and education, topics like contraceptive uptake, repeat pregnancy, intimate partner violence, mental health, and interventions to demonstrate what works in improving overall well-being and empowerment have received limited attention. Even though a few studies described an intervention, none used robust research designs to assess their effectiveness. Gaps exist in terms of understanding what works to empower adolescent mothers educationally and economically. Overall, evidence on scalable and cost-effective programmatic responses for adolescent mothers' education and economic empowerment is lacking in sub-Saharan Africa. Also lacking are studies documenting the complex nature of adolescent fatherhood and its impacts on their health and socioeconomic well-being. Overall, the studies were limited in scope and geographical distribution. There is a need for studies on lived experiences of pregnant and parenting adolescents in many African countries where no such studies exist. Future studies should document the positive experiences of pregnant and parenting adolescents and especially young fathers.
Limitations
Our study is not without limitations. The articles reviewed are limited to those published in English. Excluding publications written in other languages may have potentially limited the number of studies reviewed. Our search was also limited to online sources and might have missed out on manuscripts not published online. We also did not assess the quality of the studies included. Lastly, since our search was completed in 2021, there is a need for future studies to update this review to keep pace with the evolving research on the topic.
Our review shows that research on lived experiences of pregnant and parenting adolescents is limited in scope and geographical coverage. While studies have documented how early pregnancy could result in girls' social and educational exclusion, few interventions to support and empower pregnant and parentings adolescents exist. Further research is warranted on repeat pregnancy, contraceptive uptake, and exposure to violence among pregnant and parenting adolescents. Further, research on what works to empower these adolescents is needed.
Data availability
All data analysed are in the article.
The United Nations Population Fund. Motherhood in childhood: facing the challenge of adolescent pregnancy. New York: UNFPA; 2014.
Google Scholar
Gomez AM, Arteaga S, Ingraham N, Arcara J, Villaseñor E. It’s not planned, but is it okay? The acceptability of unplanned pregnancy among young people. Womens Health Issues. 2018;28(5):408–14.
Article PubMed PubMed Central Google Scholar
Hanna B. Negotiating motherhood: the struggles of teenage mothers. J Adv Nurs. 2001;34(4):456–64.
Article PubMed CAS Google Scholar
Yazdkhasti M, Pourreza A, Pirak A, Abdi F. Unintended pregnancy and its adverse social and economic consequences on health system: a narrative review article. Iran J Public Health. 2015;44(1):12.
PubMed PubMed Central Google Scholar
Gyan C. The effects of teenage pregnancy on the educational attainment of girls at Chorkor, a suburb of Accra. J Educ Soc Res. 2013;3(3):53.
Rosenberg M, Pettifor A, Miller WC, Thirumurthy H, Emch M, Afolabi SA, et al. Relationship between school dropout and teen pregnancy among rural South African young women. Int J Epidemiol. 2015;44(3):928–36.
Nkwemu S, Jacobs CN, Mweemba O, Sharma A, Zulu JM. “They say that I have lost my integrity by breaking my virginity”: experiences of teen school going mothers in two schools in Lusaka Zambia. BMC Public Health. 2019;19(1):62.
Ajayi AI, Akpan W, Goon DT, Nwokocha EE, Adeniyi OV. Tough love: socio-cultural explanations for deadly abortion choices among Nigerian undergraduate students: health. Afr J Phys Activity Health Sci. 2016;22(31):711–24.
Human Rights Watch. Leave No Girl Behind in Africa: Discrimination in Education against Pregnant Girls and Adolescent Mothers. 2018. https://www.hrw.org/report/2018/06/14/leave-no-girl-behind-africa/discrimination-education-against-pregnant-girls-and . Accessed 17 July 2021.
Patton GC, Sawyer SM, Santelli JS, Ross DA, Afifi R, Allen NB, et al. Our future: a Lancet commission on adolescent health and wellbeing. Lancet. 2016;387(10036):2423–78.
Undie C-C, Birungi H, Odwe G, Obare F. Expanding access to secondary school education for teenage mothers in Kenya: A baseline study report. 2015.
Karimi E. Challenges experienced by young mother learners upon reentry to formal primary school. Oslo: Faculty of Educational Sciences, University of Oslo; 2015.
Undie C, Birungi H. Are School Principals ‘the Bad Guys’? Nuancing the narrative of school re‐entry policy implementation in Kenya. In: Okwany A, Wazir R, editors. Changing Social Norms to Universalize Girls' Education in East Africa: Lessons from a Pilot Project. 2016. p. 166.
Menon J, Kusanthan T, Mwaba S, Juanola L, Kok M. ‘Ring’your future, without changing diaper–Can preventing teenage pregnancy address child marriage in Zambia? PLoS ONE. 2018;13(10): e0205523.
Article PubMed PubMed Central CAS Google Scholar
Steinhaus M, Hinson L, Rizzo AT, Gregowski A. Measuring social norms related to child marriage among adult decision-makers of young girls in Phalombe and Thyolo, Malawi. J Adolesc Health. 2019;64(4):S37–44.
Schaffnit SB, Wamoyi J, Urassa M, Dardoumpa M, Lawson DW. When marriage is the best available option: perceptions of opportunity and risk in female adolescence in Tanzania. Glob Public Health. 2020;16:1–14.
Gage AJ. Association of child marriage with suicidal thoughts and attempts among adolescent girls in Ethiopia. J Adolesc Health. 2013;52(5):654–6.
Article PubMed Google Scholar
Sekine K, Hodgkin ME. Effect of child marriage on girls’ school dropout in Nepal: Analysis of data from the Multiple Indicator Cluster Survey 2014. PLoS ONE. 2017;12(7): e0180176. https://doi.org/10.1371/journal.pone.0180176 .
Ahinkorah BO, Onayemi OM, Seidu A-A, Awopegba OE, Ajayi AI. Association between girl-child marriage and intimate partner violence in Sub-Saharan Africa: insights from a multicountry analysis of demographic and health surveys. J Interpers Violence. 2021. https://doi.org/10.1177/08862605211005139 .
Roberts KJ, Smith C, Cluver L, Toska E, Sherr L. Understanding mental health in the context of adolescent pregnancy and HIV in sub-Saharan Africa: a systematic review identifying a critical evidence gap. AIDS Behav. 2021;25:2094–107.
Toska E, Laurenzi CA, Roberts KJ, Cluver L, Sherr L. Adolescent mothers affected by HIV and their children: a scoping review of evidence and experiences from sub-Saharan Africa. Glob Public Health. 2020;15(11):1655–73.
UNICEF. Early childbearing and teenage pregnancy rates by country New York, United States: UNICEF; 2021. https://data.unicef.org/topic/child-health/adolescent-health/ . Accessed 16 July 2021.
Sen A. Social exclusion: concept, application, and scrutiny. Manila: Asian Development Bank; 2000.
Fasula AM, Chia V, Murray CC, Brittain A, Tevendale H, Koumans EH. Socioecological risk factors associated with teen pregnancy or birth for young men: a scoping review. J Adolesc. 2019;74:130–45.
Yakubu I, Salisu WJ. Determinants of adolescent pregnancy in sub-Saharan Africa: a systematic review. Reprod Health. 2018;15(1):15. https://doi.org/10.1186/s12978-018-0460-4 .
Amjad S, MacDonald I, Chambers T, Osornio-Vargas A, Chandra S, Voaklander D, et al. Social determinants of health and adverse maternal and birth outcomes in adolescent pregnancies: a systematic review and meta-analysis. Paediatr Perinat Epidemiol. 2019;33(1):88–99.
Mngadi PT, Zwane IT, Ahlberg BM, Ransjö-Arvidson AB. Family and community support to adolescent mothers in Swaziland. J Adv Nurs. 2003;43(2):137–44.
Mjwara N, Maharaj P. Becoming a mother: perspectives and experiences of young women in a South African Township. Cult Health Sex. 2018;20(2):129–40. https://doi.org/10.1080/13691058.2017.1334963 .
Gyesaw NYK, Ankomah A. Experiences of pregnancy and motherhood among teenage mothers in a suburb of Accra, Ghana: a qualitative study. Int J Women’s Health. 2013;5:773–80. https://doi.org/10.2147/IJWH.S51528 .
Article Google Scholar
Kaufman CE, De Wet T, Stadler J. Adolescent pregnancy and parenthood in South Africa. Stud Fam Plann. 2001;32(2):147–60.
Govender D, Naidoo S, Taylor M. “I have to provide for another life emotionally, physically and financially”: understanding pregnancy, motherhood and the future aspirations of adolescent mothers in KwaZulu-Natal South, Africa. BMC Pregnancy Childbirth. 2020;20(1):620. https://doi.org/10.1186/s12884-020-03319-7 .
Ntinda K, Thwala SLK, Dlamini TP. Lived experiences of school-going early mothers in Swaziland. J Psychol Afr. 2016;26(6):546–50.
Melvin AO, Uzoma UV. Adolescent mothers’ subjective well-being and mothering challenges in a Yoruba community, southwest Nigeria. Soc Work Health Care. 2012;51(6):552–67.
Mashala P, Esterhuizen R, Basson W, Nel K. Qualitative exploration of the experiences and challenges of adolescents during pregnancy. J Psychol Afr. 2012;22(1):49–55.
Naidoo J, Muthukrishna N, Nkabinde R. The journey into motherhood and schooling: narratives of teenage mothers in the South African context. Int J Incl Educ. 2021;25(10):1125–39.
Dzotsi HT, Oppong Asante K, Osafo J. Challenges associated with teenage motherhood in Ghana: a qualitative study. Vulnerable Child Youth Stud. 2020;15(1):85–96.
Amod Z, Halana V, Smith N. School-going teenage mothers in an under-resourced community: lived experiences and perceptions of support. J Youth Stud. 2019;22(9):1255–71.
Taffa N, Matthews Z. Teenage pregnancy experiences in rural Kenya. Int J Adolesc Med Health. 2003;15(4):331–40.
Van Zyl L, van Der Merwe M, Chigeza S. Adolescents’ lived experiences of their pregnancy and parenting in a semi-rural community in the Western Cape. Soc Work. 2015;51(2):151–73.
Swartz S, Bhana A. Teenage tata: Voices of young fathers in South Africa. 2009.
Chideya Y, Williams F. Adolescent fathers: exploring their perceptions of their role as parent. Social Work/Maatskaplike Werk. 2013;49(2).
Matlakala F, Makhubele J, Mashilo M. Challenges of teenage fathers towards fatherhood in Vaalbank, Mpumalanga province. Gender Behav. 2018;16(3):12013–20.
De Wet N, Amoo EO, Odimegwu C. Teenage pregnancy in South Africa: where are the young men involved? S Afr J Child Health. 2018;2018(1):s44–50.
Shefer T, Bhana D, Morrell R. Teenage pregnancy and parenting at school in contemporary South African contexts: deconstructing school narratives and understanding policy implementation. Perspect Educ. 2013;31(1):1–10.
Ngabaza S, Shefer T. Policy commitments vs. lived realities of young pregnant women and mothers in school, Western Cape, South Africa. Reprod Health Matt. 2013;21(41):106–13.
Matlala SF, Nolte A, Temane M. Secondary school teachers’ experiences of teaching pregnant learners in Limpopo province, South Africa. S Afr J Educ. 2014;34(4):1.
Theron L, Dunn N. Coping strategies for adolescent birth-mothers who return to school following adoption. S Afr J Educ. 2006;26(4):491–9.
Chigona A, Chetty R. Girls’ education in South Africa: Special consideration to teen mothers as learners. Journal of education for international development. 2007.
Omwancha KM. The implementation of an educational re-entry policy for girls after teenage pregnancy: a case study of public secondary schools in the Kuria District, Kenya. 2012.
Ngabaza S. An exploratory study of experiences of parenting among a group of school-going adolescent mothers in a South African township. Cape Town: University of the Western Cape; 2010.
Simelane Q, Thwala S, Mamba T. An assessment of the implementation of the re-entry policy for girls in Swaziland: school practices and implications for policy development. Probl Educ 21st Century. 2013;56:115.
Runhare T, Mulaudzi O, Dzimiri P, Vandeyar S. Democratisation of formal schooling for pregnant teenagers in South Africa and Zimbabwe: smoke and mirrors in policy. Gender Behav. 2014;12(2):6382–95.
Nyariro MP. Re-conceptualizing school continuation & re-entry policy for young mothers living in an urban slum context in Nairobi, Kenya: a participatory approach. Stud Soc Justice. 2018;12(2):310–28.
Mwanza MN. Factors that influence the use of the education re-entry policy for adolescent mothers in Monze, Zambia. 2018.
Maluli 1 F, Bali T. Exploring experiences of pregnant and mothering secondary school students in Tanzania. 2014.
Walgwe EL, LaChance NT, Birungi H, Undie C-C. Kenya: Helping adolescent mothers remain in school through strengthened implementation of school re-entry policies. 2016.
Zuilkowski SS, Henning M, Zulu J, Matafwali B. Zambia’s school re-entry policy for adolescent mothers: examining impacts beyond re-enrollment. Int J Educ Dev. 2019;64:1–7.
Tarus CBK. The level of awareness of re–entry policy of teenage mothers in public secondary schools in Kenya. Am J Humanit Soc Sci Res. 2020;4(2):249–63.
Mbugua NW. Stakeholders’roles in implementing the readmission policy on adolescent mothers in public secondary schools in Kikuyu District, Kiambu County, Kenya. Kenya: The Catholic University of Eastern Africa; 2015.
Birungi H, Undie C-C, MacKenzie I, Katahoire A, Obare F, Machawira P. Education sector response to early and unintended pregnancy: A review of country experiences in Sub-Saharan Africa. 2015.
Shaningwa LM. The educationally-related challenges faced by teenage mothers on returning to school: a Namibian case study. Grahamstown: Rhodes University; 2007.
McCadden DT. An Assessment of the Impact of Zambia’s School Re-Entry Policy on Female Educational Attainment and Adolescent Fertility. Washington: Georgetown University; 2015.
Jochim J, Groves A, Cluver L. When do adolescent mothers return to school? Timing across rural and urban South Africa. S Afr Med J. 2020;110(9):850–4.
Bhana D, Morrell R, Shefer T, Ngabaza S. South African teachers’ responses to teenage pregnancy and teenage mothers in schools. Cult Health Sex. 2010;12(8):871–83.
Nelima WA. Bending the private-public gender norms: negotiating schooling for young mothers from low-income households in Kenya. Hague: International Institute of Social Studies; 2011.
Madhavan S, Thomas KJ. Childbearing and schooling: New evidence from South Africa. Comp Educ Rev. 2005;49(4):452–67.
Achoka JS, Njeru FM. De-stigmatizing teenage motherhood: towards achievement of universal basic education in Kenya. J Emerg Trends Educ Res Policy Stud. 2012;3(6):887–92.
Bhana D, Clowes L, Morrell R, Shefer T. Pregnant girls and young parents in South African schools. Agenda. 2008;22(76):78–90.
Chilisa B. National policies on pregnancy in education systems in Sub-Saharan Africa: the case of Botswana. Gend Educ. 2002;14(1):21–35. https://doi.org/10.1080/09540250120098852 .
Grant MJ, Hallman KK. Pregnancy-related school dropout and prior school performance in KwaZulu-Natal, South Africa. Stud Fam Plan. 2008;39(4):369–82.
Malahlela MK, Chireshe R. Educators’ perceptions of the effects of teenage pregnancy on the behaviour of the learners in South African secondary schools: implications for teacher training. J Soc Sci. 2013;37(2):137–48.
Maputle M, Lebese R, Khoza L. Perceived challenges faced by mothers of pregnant teenagers who are attending a particular school in Mopani District, Limpopo Province, South Africa. Int J Educ Sci. 2015;10(1):142–8.
Mashishi N, Makoelle T. Inclusion or exclusion ramifications of teenage pregnancy: a comparative analysis of Namibia and South African Schools Pregnancy Policies. Mediterr J Soc Sci. 2014;5(14):374.
Matshotyana Z. Experiences of parenting learners with regards to learner pregnancy policy. Cape Town: University of the Western Cape; 2010.
Mcambi SJ. Exploring young women's experiences of teenage motherhood in schools: a gendered perspective 2010.
Nkabinde RN. The geographies of schooling and motherhood: narratives of teen mothers in KwaZulu-Natal 2014.
Nkani FN, Bhana D. No to bulging stomachs: male principals talk about teenage pregnancy at schools in Inanda. Durban Agenda. 2010;24(83):107–13.
Pillay N. Pathways to school completion for young mothers: are we winning the fight? South Afr J Child Health. 2018;2018(1):s15–8.
Jumba LK, Githinji F. School factors which enhance the schooling of teen mothers in secondary school in Kenya: a Case of Trans-Nzoia West Sub-County. J Art Soc Sci. 2018;2(1).
Mwanza MN. Factors that influence the use of the education re-entry policy for adolescent mothers in Monze, Zambia. The Hague: International Institute of Social Studies; 2018.
Kola L, Abiona D, Adefolarin AO, Ben-Zeev D. Mobile phone use and acceptability for the delivery of mental health information among perinatal adolescents in nigeria: survey study. JMIR Mental Health. 2021;8(1): e20314.
Muyama DL, Musaba MW, Opito R, Soita DJ, Wandabwa JN, Amongin D. Determinants of postpartum contraception use among teenage mothers in Eastern Uganda: a cross-sectional study. Open Access J Contracept. 2020;11:187.
Musyimi CW, Mutiso VN, Nyamai DN, Ebuenyi I, Ndetei DM. Suicidal behavior risks during adolescent pregnancy in a low-resource setting: a qualitative study. PLoS ONE. 2020;15(7): e0236269.
Laurenzi CA, Gordon S, Abrahams N, du Toit S, Bradshaw M, Brand A, et al. Psychosocial interventions targeting mental health in pregnant adolescents and adolescent parents: a systematic review. Reprod Health. 2020;17:1–15.
Kola L, Bennett IM, Bhat A, Ayinde OO, Oladeji BD, Abiona D, et al. Stigma and utilization of treatment for adolescent perinatal depression in Ibadan Nigeria. BMC Pregnancy Childbirth. 2020;20:1–8.
Field S, Honikman S, Abrahams Z. Adolescent mothers: a qualitative study on barriers and facilitators to mental health in a low-resource setting in Cape Town, South Africa. Afr J Primary Health Care Fam Med. 2020;12(1):1–9.
Mbawa M, Vidmar J, Chingwaru C, Chingwaru W. Understanding postpartum depression in adolescent mothers in Mashonaland Central and Bulawayo Provinces of Zimbabwe. Asian J Psychiatr. 2018;32:147–50.
Kaye DK. Negotiating the transition from adolescence to motherhood: coping with prenatal and parenting stress in teenage mothers in Mulago hospital, Uganda. BMC Public Health. 2008;8(1):1–6.
BeLue R, Schreiner AS, Taylor-Richardson K, Murray-Kolb LE, Beard JL. What matters most: an investigation of predictors of perceived stress among young mothers in Khayelitsha. Health Care Women Int. 2008;29(6):638–48.
Yako E. A comparative study of adoloscents’ perceived stress and health outcomes among adolescent mothers and their infants in Lesotho. Curationis. 2007;30(1):15–25.
Kimbui E, Kuria M, Yator O, Kumar M. A cross-sectional study of depression with comorbid substance use dependency in pregnant adolescents from an informal settlement of Nairobi: drawing implications for treatment and prevention work. Ann Gen Psychiatry. 2018;17(1):1–15.
Govender D, Naidoo S, Taylor M. Antenatal and postpartum depression: prevalence and associated risk factors among adolescents’ in KwaZulu-Natal, South Africa. Depression Res Treat. 2020. https://doi.org/10.1155/2020/5364521 .
Osok J, Kigamwa P, Vander Stoep A, Huang K-Y, Kumar M. Depression and its psychosocial risk factors in pregnant Kenyan adolescents: a cross-sectional study in a community health Centre of Nairobi. BMC Psychiatry. 2018;18(1):1–10.
Niyonsenga J, Mutabaruka J. Factors of postpartum depression among teen mothers in Rwanda: a cross-sectional study. J Psychosomatic Obstet Gynecol. 2020;42:356.
Mokwena JP, Govender S, Setwaba MB. Health and well-being among teenage mothers in a rural South African community. J Psychol Afr. 2016;26(5):428–31.
Sodi EE. Psychological impact of teenage pregnancy on pregnant teenagers 2010.
Govender D, Taylor M, Naidoo S. Adolescent pregnancy and parenting: perceptions of healthcare providers. J Multidiscip Healthc. 2020;13:1607.
Ruzibiza Y. ‘They are a shame to the community…’stigma, school attendance, solitude and resilience among pregnant teenagers and teenage mothers in Mahama refugee camp, Rwanda. Glob Public Health. 2020;16:763.
Kululanga LI, Kadango A, Lungu G, Jere D, Ngwale M, Kumbani LC. Knowledge deficit on health promotion activities during pregnancy: the case for adolescent pregnant women at Chiladzulu District, Malawi. BMC Pregnancy Childbirth. 2020;20(1):1–9.
Atuyambe L, Mirembe F, Annika J, Kirumira EK, Faxelid E. Seeking safety and empathy: adolescent health seeking behavior during pregnancy and early motherhood in central Uganda. J Adolesc. 2009;32(4):781–96.
Atuyambe L, Mirembe F, Tumwesigye NM, Annika J, Kirumira EK, Faxelid E. Adolescent and adult first time mothers’ health seeking practices during pregnancy and early motherhood in Wakiso district, central Uganda. Reprod Health. 2008;5(1):1–11.
Twintoh RF, Anku PJ, Amu H, Darteh EKM, Korsah KK. Childcare practices among teenage mothers in Ghana: a qualitative study using the ecological systems theory. BMC Public Health. 2021;21(1):1–12.
Pillay N. ‘There is no more future for me? Like really, are you kidding?’: agency and decision-making in early motherhood in an urban area in Johannesburg, South Africa. Glob Health Action. 2021;14(1):1886456.
Kabwijamu L, Waiswa P, Kawooya V, Nalwadda CK, Okuga M, Nabiwemba EL. Newborn care practices among adolescent mothers in Hoima District, Western Uganda. PLoS ONE. 2016;11(11): e0166405.
Naidoo S, Taylor M, Govender D. Nurses’ perception of the multidisciplinary team approach of care for adolescent mothers and their children in Ugu, KwaZulu-Natal. Afr J Primary Health Care Fam Med. 2019;11(1):1–11.
Mngadi PT. Adolescent pregnancy and parenthood in Swaziland: quality of care, community support and health care service needs: Institutionen för folkhälsovetenskap/Department of Public Health Sciences; 2006.
Yeboah M. Social support and access to prenatal health services: a study of pregnant teenagers in Cape Coast, Ghana. J Sci Technol. 2012;32(1):68–78.
Adonis T. Family planning among teenage mother in a cameroonian centre. Afr J Reprod Health. 2001;5(2):105.
Ehlers V. Adolescent mothers’ knowledge and perceptions of contraceptives in Tshwane, South Africa. Health SA Gesondheid. 2003;8(1):13–25.
Ehlers VJ. Adolescent mothers’ utilization of contraceptive services in South Africa. Int Nurs Rev. 2003;50(4):229–41.
Olaseha I, Ajuwon A, Onyejekwe O. Reproductive health knowledge and use of contraceptives among adolescent mothers in a sub-urban community in Oyo State, Nigeria. Afr J Med Med Sci. 2004;33(2):139–43.
PubMed CAS Google Scholar
Govender D, Naidoo S, Taylor M. “My partner was not fond of using condoms and I was not on contraception”: understanding adolescent mothers’ perspectives of sexual risk behaviour in KwaZulu-Natal, South Africa. BMC Public Health. 2020;20(1):1–17.
Machira K, Palamuleni ME. Health care factors influencing teen mothers’ use of contraceptives in Malawi, Ghana. Med J. 2017;51(2):88–93.
Mphatswe W, Maise H, Sebitloane M. Prevalence of repeat pregnancies and associated factors among teenagers in KwaZulu-Natal, South Africa. Int J Gynaecol Obstet. 2016;133(2):152–5. https://doi.org/10.1016/j.ijgo.2015.09.028 . ( Epub 2016/03/08 ).
Govender D, Naidoo S, Taylor M. Scoping review of risk factors of and interventions for adolescent repeat pregnancies: a public health perspective. Afr J Prim Health Care Fam Med. 2018;10(1):e1–10. https://doi.org/10.4102/phcfm.v10i1.1685 . ( Epub 2018/06/27 ).
Govender D, Naidoo S, Taylor M. Prevalence and risk factors of repeat pregnancy among South African adolescent females. Afr J Reprod Health. 2019;23(1):73–87.
PubMed Google Scholar
Dzabala N, Kachingwe M, Chikowe I, Chidandale C, van der Haar L. Using evidence and data to design an intervention in the Project Community Model for fostering health and wellbeing among adolescent mothers and their children. Front Public Health. 2021. https://doi.org/10.3389/fpubh.2021.584575 .
Ndirangu G, Gichangi A, Kanyuuru L, Otai J, Mulindi R, Lynam P, et al. Using young mothers’ clubs to improve knowledge of postpartum hemorrhage and family planning in informal settlements in Nairobi, Kenya. J Commun Health. 2015;40(4):692–8.
Robertson AE, Crowley T. Adolescent mothers’ lived experiences whilst providing continuous kangaroo mother care: a qualitative study. Health SA Gesondheid. 2020. https://doi.org/10.4102/hsag.v25i0.1450 . ( Epub 2020-01-20 ).
Leerlooijer JN, Bos AER, Ruiter RAC, van Reeuwijk MAJ, Rijsdijk LE, Nshakira N, et al. Qualitative evaluation of the Teenage Mothers Project in Uganda: a community-based empowerment intervention for unmarried teenage mothers. BMC Public Health. 2013;13(1):816. https://doi.org/10.1186/1471-2458-13-816 .
Leerlooijer JN, Kok G, Weyusya J, Bos AER, Ruiter RAC, Rijsdijk LE, et al. Applying Intervention Mapping to develop a community-based intervention aimed at improved psychological and social well-being of unmarried teenage mothers in Uganda. Health Educ Res. 2014;29(4):598–610. https://doi.org/10.1093/her/cyu020 .
Ministry of Education Republic of Kenya. National Guidelines for school re-entry in Early Learning and Basic Education, 220. Nairobi: Ministry of Education; 2021.
Ajayi AI, Otukpa EO, Mwoka M, Kabiru CW, Ushie BA. Adolescent sexual and reproductive health research in sub-Saharan Africa: a scoping review of substantive focus, research volume, geographic distribution and Africa-led inquiry. BMJ Glob Health. 2021;6(2): e004129. https://doi.org/10.1136/bmjgh-2020-004129 .
Download references
This research was made possible through funding to the African Population and Health Research Center from the Swedish International Development Cooperation Agency for the Challenging the Politics of Social Exclusion project (Sida Contribution No. 12103). CK’s writing time was partially covered by a grant from the International Development Research Centre (IDRC) for the Action to empower adolescent mothers in Burkina Faso and Malawi to improve their sexual and reproductive health project (Grant No. 109813 – 001). The views expressed herein do not necessarily represent those of IDRC or its Board of Governors or Sida.
Author information
Authors and affiliations.
Sexual, Reproductive, Maternal, New-Born, Child, and Adolescent Health (SRMNCAH) Unit, African Population and Health Research Center, Nairobi, Kenya
Anthony Idowu Ajayi, Sherine Athero, Winstoun Muga & Caroline W. Kabiru
You can also search for this author in PubMed Google Scholar
Contributions
AIA and CWK conceptualized the study. AIA, SA, and WM conducted the search and data extraction. All authors contributed to drafting and reviewing the paper.
Corresponding author
Correspondence to Anthony Idowu Ajayi .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was not obtained for this study because it is based on a review of publicly available articles and does not involve human subjects.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Sample search terms.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ajayi, A.I., Athero, S., Muga, W. et al. Lived experiences of pregnant and parenting adolescents in Africa: A scoping review. Reprod Health 20 , 113 (2023). https://doi.org/10.1186/s12978-023-01654-4
Download citation
Received : 25 May 2022
Accepted : 26 July 2023
Published : 03 August 2023
DOI : https://doi.org/10.1186/s12978-023-01654-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Social exclusion
- Lived experiences
- Pregnant and parenting adolescents
- Adolescent mothers
- Girls empowerment
Reproductive Health
ISSN: 1742-4755
- General enquiries: [email protected]
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
Reproductive rights in America
What abortion politics has to do with new rights for pregnant workers.

Selena Simmons-Duffin

Employers are required to make accommodations for pregnant women and new moms like time off for doctor's appointments. Thomas Trutschel/Photothek via Getty Images hide caption
Employers are required to make accommodations for pregnant women and new moms like time off for doctor's appointments.
This week, attorneys general from 17 Republican-led states sued the Equal Employment Opportunity Commission over something they say is an "abortion accommodation mandate."
Here are four things to know about the latest battle in the war over abortion between Republican-led states and the Biden administration.
1. The law in question is about protections for pregnant workers.
First, a little background: In 2015, a survey found that nearly 1 in 4 women went back to work just two weeks after giving birth.
It took about ten years for a bill protecting pregnant workers to get through Congress, and in 2022, not long after Roe v. Wade was overturned, the Pregnant Workers Fairness Act passed with bipartisan support. The law requires employers with at least 15 employees to accommodate workers who are pregnant with things like extra bathroom breaks, time off for prenatal appointments, a chair for sitting during a shift. It also says employers have to accommodate workers after they give birth.
Even though lawmakers from both parties think pregnancy protections are a good thing, abortion politics have overshadowed the news of those new rights. It all comes down to one line in the law and the word "abortion" in the regulation.
The law says employers should make "reasonable accommodations" for pregnant workers during and after "pregnancy, childbirth and related medical conditions." The new rule EEOC put out to implement the law includes abortion in a lengthy list of "related medical conditions," along with everything from ectopic pregnancy to anxiety to varicose veins.
2. Abortion entered the chat and about 100,000 people chimed in on the regulations.
Political and religious groups that oppose abortion rights took notice of the inclusion of "abortion" in the list of related medical conditions, as did the lead Republican co-sponsor of the law , Sen. Bill Cassidy of Louisiana. Some 54,000 people commented on the proposed rule objecting to the inclusion of abortion, according to the EEOC's analysis in the final rule, while 40,000 people commented in support of abortion's inclusion. (The agency noted that most of these were nearly identical "form comments" driven by advocacy groups).
In the end, "abortion" remained on the list. In its analysis, the agency explained that abortion's inclusion is consistent with longstanding interpretation of civil rights laws and courts' rulings. In the final rule, the EEOC says the law "does not require any employee to have – or not to have – an abortion, does not require taxpayers to pay for any abortions, and does not compel health care providers to provide any abortions." The rule also notes that unpaid time off for appointments is the most likely accommodation that would be sought by workers having abortions.
3. The lawsuit + the politics of the lawsuit
Within days of the rule being published in the Federal Register , a coalition of 17 Republican-led states filed suit. "The implications of mandating abortion accommodations are immense: covered employers would be required to support and devote resources, including by providing extra leave time, to assist employees' decision to terminate fetal life," the lawsuit reads .
The lawsuit was filed on Thursday in federal court in Eastern Arkansas. The plaintiffs ask the court to put a hold on the effective date of the final rule pending judicial review, and to temporarily block the enforcement of – and ultimately vacate – the rule's "abortion-accommodation mandate."
Arkansas and Tennessee are the two states leading the lawsuit. In a statement , Arkansas Attorney General Tim Griffin said: "This is yet another attempt by the Biden administration to force through administrative fiat what it cannot get passed through Congress."
Griffin said the rule is a "radical interpretation" of the new pregnancy protection law that would leave employers subject to federal lawsuits if they don't give employees time off for abortions, even if abortions are illegal in those states. "The PWFA was meant to protect pregnancies, not end them," he said.
Women's advocates see the politics of the lawsuit as well. "It's no coincidence that this organized, partisan effort is occurring in states that have some of the highest maternal mortality rates in the country," Jocelyn Frye of the National Partnership for Women & Families wrote in a statement . "Any attempt to dismantle these protections will have serious consequences for women's health, working families, and the ability for women to thrive in the workplace."
Greer Donley is a law professor at the University of Pittsburgh who submitted a comment on the proposed regulation defending the inclusion of abortion. She points out that this is the latest in a string of legal challenges from anti-abortion groups fighting the Biden administration's efforts to protect abortion using federal agencies.
"You can really see this in a suite of [abortion] lawsuits – including the two that were heard in the Supreme Court this term, one involving the FDA's regulation of mifepristone and one involving the Biden administration's interpretation of EMTALA ," she observes, and guesses a legal challenge will also come in response to the newly announced privacy protections for patients who've had abortions. "You have a Supreme Court that is overwhelmingly anti-abortion and overwhelmingly anti-administrative state – those two things in tandem are not a good thing for the Biden administration."
4. In the meantime, pregnant workers have new rights.
At the moment, until a judge says otherwise, the new protections for pregnant workers are already in effect. The EEOC has a guide for pregnant workers about their new rights under the law and how to file charges against their employers. It's also holding trainings for human resource professionals on how to comply with the law.
Complaints have already started to roll in. In a statement to NPR, EEOC spokesperson Victor Chen wrote that in the first three months that the law was in effect, the agency received nearly 200 charges alleging a violation of the Pregnant Workers Fairness Act, which works out to nearly two a day.
- pregnancy discrimination
- Abortion rights
Essay About Being Pregnant

Show More My experience of being pregnant was mostly eventful. There were a lot of things people told me that they shouldn’t have. For instance, having constipation while being pregnant and getting hemorrhoids, that never occurred in my nine months. It was a waste of being fearful for nine months. There were also things that mothers should have told me. For instance, how it actually feels when your baby is moving or kicking. When my baby moved or kicked it was the weirdest feeling ever; it was not pleasant. Most Mothers call it a beautiful thing but don’t necessary describe how an active baby feels inside your belly. While being pregnant you get a lot of different experiences. No pregnancy is the same, I must say. Even though pregnancy can be very rewarding, the Nine Months of Pregnancy can be eventful and emotional. It can be a long dreadful experience, a wonderful experience, or it can be both dreadful and wonderful. First off, pregnancy can be a long dreadful experience. For instance, nine months of pregnancy is a long time to carry a baby. It felt like it took forever for my son to come out. I was so impatient to see him; I was ready to see what and who he was going to look like. In another instance, I had morning sickness in the beginning of my pregnancy, for the first two months. Unlike most mothers, I didn’t do a lot of throwing up. I constantly felt bad. I had to switch between …show more content… I tried my best to enjoy every moment and do as much as I can to make it the best experience it can be. I took plenty advice into consideration and I nod my head yes to not so helpful advice out of respect. Nine Months of Pregnancy can be a long, dreadful experience, a wonderful experience, or it can be both dreadful and wonderful at the same time. I would advise documenting every moment. It’s always good to go back and remember some of the things you have experienced rather good or
Related Documents
Essay on transitioning to parenthood.
There are an equal amount of difficulties as well as enjoyment in being a new parent. Adamsons states that parenthood is the most common experience experienced by individual in the US (Adamsons 160). Parents should anticipate new challenges and lifestyles after the arrival of the baby. Arrival of the baby also puts a marital strain on the relationship between the spouse/partner. Family system is also influence by the addition of another baby.…
Analysis Of 'Maternity Rolls' By Heather Kuttai
The readings for today’s lesson were chapters 3 and 4 from the book “Maternity Rolls” by Heather Kuttai. The chapters tell Kuttai’s journey through pregnancy and childbirth. From what Kuttai states, it seems as if pregnancy was a very difficult time for her, emotionally and physically. It was difficult emotionally because although Kuttai and her spouse were very excited to be pregnant, not everyone was equally excited for or supportive of them. Kuttai states “I saw the man ultrasounds as many opportunities to see the sex, but I was terribly disappointed when my ultrasound technician refused to pass this knowledge on to our doctor, and therefore on to us.…
Pregnancy After Age 35 Summary
The reading, Pregnancy after Age 35 by Dominique Roe-Sepowitz, details the personal accounts of a happily married couple and their struggles with pregnancy. The wife and her husband had everything in place and followed all recommendations and advice for how to get pregnant efficiently and effectively. They did not rush their decision to get pregnant and decided to pursue their careers and accomplish personal goals in their professions prior to having a child. They both had secure, well-paying jobs, and were finally in a position where they felt confident they could provide emotionally and financially for a newborn. However, they now dealt with the issue of pregnancy after the age of thirty-five.…
Pro Life Research Paper
Yes, pregnancy is going to be hard at times, but life is hard. However, pregnancy is not a disease, so why do people treat it like one? A medical condition is often defined as an injury, disease, or disorder. Pregnancy is not…
Iman Carraway Research Paper
Imani Crawford The Unexpected I would like to tell you about my pregnancy. I am 19 years old and my pregnancy was unexpected. I have been confronted with not only finding out about the pregnancy , but what it is doing to my body and the consequences of being a teen parent. I am having to struggle with choosing to complete my high school diploma or working to save for my baby’s future.…
Neonatal Abstinence Syndrome Essay
Help for the hopeless Pain can be very intense it may seem perfectly reasonable to want something that would make it stop and find some relief. It is a complicated issue, but there has to be some balance and responsibility when consuming painkillers. According to the centers for Disease control and prevention, nearly 2 million Americans abused prescription painkillers in 2013, with 44 people dying from an overdose each day (D’ Amora). Although, these are devastating news; this is not the worse part. An unborn child has to suffer the sad consequence of a pregnant woman who is addicted to these types of pills.…
How Do Myths Affect A Baby?
Myths have been around for centuries and as decades go by more of them are being created. Many choose to believe that myths are true and will incorporate them into their daily lives. A very common group of people who tend to listen to myths are pregnant women. People have different myths and beliefs on how you should act when you are pregnant, but how do these choices effect a baby? Pregnant women want what is best for their child so they follow every rule in the book to make sure that their baby is born healthy.…
Robotic Baby Experience Essay
The baby didn’t affect much of anything because, at the time my sleep schedule was already atrocious, I wasn’t in school because it was the weekend, I only get to spend time with my friends while at school, and I don’t do sports. I gave up nothing while doing this assignment because my life is nonexistent while out of school. I was emotionally not phased, although there were times when I couldn’t figure out what the baby needed so I got frustrated. While I had the baby I had some people laugh at me, (mainly friends) while others gave me a look of pity.…
Patient Interview Research Paper
I asked her how she thought her last pregnancy went overall and how it went compared to her previous pregnancies. She responded with she thought it went well overall, but there were a couple problems that occurred. She said about 7 weeks before I was born she was having really bad false labor contractions, so her doctors had her come in so they could run tests to make sure it was real labor. They were concerned because nothing would help the contractions and they were not disappearing. They sent her home telling her to just go for a really long walk and it should just go away.…
Personal Narrative: My Birth Story
My Birth Story Birth stories have a lasting impact on expectant mothers. Recognizing the influence of birth stories is a key component of informal communication of knowledge about childbirth for expectant mothers. The goals of the birth story interview and discussion are to provide an opportunity to explore the sharing of a birth story as a critical way of knowing within the family and community, and also to promote understanding of the prenatal period and taking-on of the parental role. The topic of storytelling is important to nurses and families, as it allows the integration of the nurses’ experiences into their future nursing practice, which may be invaluable in facilitating authentic and meaningful connections with their patients.…
Personal Narrative: My Life As A Teen Mom
It was the end of my junior year rolling into my final year of high school. It was absolutely devastating. I thought my life was over until I saw her for the first time. Pregnancy is so beautiful and such a special aspect of life. “God’s purpose will always prevail”, this is a quote I always look up to, because I believe all things happen for a reason.…
Postpartum Depression Informative Speech
The joys of a new baby are numerous for couples, it’s an addition to your family, a new person to love; but a new child also means new responsibilities, a new found source of stress and in some cases depression for the new moms. The particular type of depression I’m referring to is known as postpartum depression. When moms give birth to their babies, their body limits the release of certain hormones, and can cause the new moms to feel sluggish, tired and even depressed. The depression is common for most women, and last for around two weeks, typically starting around the second, or third day after the birth of their baby. This is whats known as the “postpartum baby blues” but those that last longer and are more severe are what 's referred…
Personal Narrative Essay: Giving Birth to my First Child
I used to think that giving birth was overrated and believed that the emotional rollercoaster leading up the birth was insincere. In my opinion, giving birth had always seemed frightening, long and most of all painful. Surprisingly, my whole outlook on giving birth and its emotional impact changed when I gave birth to my first child, Joy. I remember the day as if it was yesterday, despite the fact that it took place almost nine years ago.…
Narrative Essay On Becoming A Mother
As I got further into my pregnancy I grew in such a cute way because I only gained belly weight. I looked as if I had a basketball in my tummy. I was so big, I was unable to stand without stumbling and I was unable to see my feet. My babies were growing healthy and my doctor had my preterm labor under control. My…
Having A New Born Baby Essay
When the new born body has come home the parents will get a lack of sleep and the baby will be unsettled. Due to lack of sleep the parents will be on ledge and be stressed out. Because the mother has been pregnancy for 9 months her hormones will be all over the place and due to the new born born baby in the house it…
Related Topics
Ready to get started.
- Create Flashcards
- Mobile apps
- Cookie Settings
Trump says it’s up to states whether to punish, monitor women for abortions
Former president Donald Trump said in an interview published Tuesday that he would not intervene in state decisions on abortion policy, including in situations where states seek to monitor women’s pregnancies and prosecute those who violate abortion bans.
Trump also declined during the interview with Time magazine to commit to veto any additional federal restrictions if they were to come to his desk upon a possible return to the White House.
Asked by Time if he would be comfortable with states prosecuting women for having abortions outside limited periods permitted by state laws, Trump suggested the federal government should have no role.
“It’s irrelevant whether I’m comfortable or not,” Trump said. “It’s totally irrelevant, because the states are going to make those decisions.”
Trump’s comments highlight the fraught politics of the stance on abortion that he outlined earlier this month.
Trump announced on social media that policy should be left to the states, after months of mixed signals about his position. Trump has consistently taken credit for overturning Roe v. Wade — three of the justices who ruled on the case were appointed by him — yet has distanced himself from the political repercussions of the decision.
Shortly after Trump articulated his states-rights stance this month, Arizona’s Supreme Court revived an 1864 law passed before it was granted statehood that forbids abortions except to save a mother’s life and punishes providers with prison time. In that case, Trump said the state had gone too far.
During the Time interview, however, Trump repeatedly emphasized his support for state autonomy, at least in concept.
When asked, for instance, about the federal Republican-sponsored Life at Conception Act, which would grant “full legal rights to embryos,” Trump said: “I’m leaving everything up to the states.”
He declined to say whether he would veto such a bill, suggesting he wouldn’t be presented with that decision.
“I don’t have to do anything about vetoes,” Trump said, “because we now have it back in the states.”
Asked by Time if states should monitor women’s pregnancies to detect whether they get abortions after a ban takes effect, Trump said: “I think they might do that.”
“Again, you’ll have to speak to the individual states,” he said. “Look, Roe v. Wade was all about bringing it back to the states.”
Democrats have sought to make abortion the dominant issue in the 2024 elections, highlighting Trump’s role in appointing the three conservative Supreme Court justices who helped overturn a constitutional right to abortion in 2022, and legislation pushed by Republican lawmakers to ban or severely restrict access to the procedure.
President Biden’s campaign seized on the Time interview after it was published Tuesday.
Biden campaign manager Julie Chavez Rodriguez said Trump’s latest remarks are proof that reproductive health care is at stake in the election.
“Donald Trump’s latest comments leave little doubt: if elected he’ll sign a national abortion ban, allow women who have an abortion to be prosecuted and punished, allow the government to invade women’s privacy to monitor their pregnancies, and put IVF and contraception in jeopardy nationwide,” Rodriguez said in a statement. “Simply put: November’s election will determine whether women in the United States have reproductive freedom, or whether Trump’s new government will continue its assault to control women’s health care decisions.”
Trump declined to answer directly when asked by Time if he thinks women should be able to obtain the abortion pill mifepristone .
“Well, I have an opinion on that, but I’m not going to explain. I’m not gonna say it yet.” He said he would announce his position “probably over the next week.” When pressed for an answer, Trump sought more time. “I will be making a statement on that over the next 14 days.”
Trump spoke with writer Eric Cortellessa at his home in Florida on April 12 and had a follow-up phone interview April 27, the magazine reported. On Tuesday it published a story about the interview along with a transcript .
The interview comes as Republicans brace for fallout from their newly pushed restrictions.
Florida’s ban on abortion after six weeks of pregnancy takes effect this week, one of the strictest in the nation.
The Republican-led Arizona Senate is expected to vote on a repeal of the state’s near total abortion ban after the state Supreme Court ruled a Civil War-era bill can take effect following the overturning of Roe v. Wade . Arizona’s House last week voted to repeal the law, after prominent antiabortion Republicans such as Senate candidate Kari Lake reversed course on the issue .
Trump, who once described himself as “very pro-choice,” said in 2000 that he would “indeed support a ban.” As a candidate, Trump struggled to adopt a position to fully satisfy leading members of the antiabortion movement while shielding himself and Republicans from blowback at the ballot box.
During the GOP nominating contests, Trump declined to take a firm stance on federal legislation and criticized Florida’s six-week abortion ban as a “terrible mistake.” In a CNN town hall last year, Trump would not say whether he would sign a federal abortion ban. Instead he said the antiabortion movement was in a “very good negotiating position” after the Supreme Court overturned Roe.
As president, Trump backed a 20-week abortion ban that did not have the votes to pass Congress and at the time conflicted with Roe, which gave Americans nationwide a right to abortion until a fetus was viable outside the womb, often pegged at roughly 24 weeks of pregnancy.
After publication of the Time interview Tuesday, Trump celebrated the piece while speaking to reporters outside the courtroom in New York, where he is on trial.
“I want to thank the Time magazine,” he said. “They did a cover story, which is very nice.”
“It’s at least 60 percent correct, which is all I could ask for,” Trump said, without identifying anything that he might say were inaccuracies. Trump walked away and ignored questions shouted by reporters.
Isaac Arnsdorf contributed to this report.
U.S. abortion access, reproductive rights
Tracking abortion access in the United States: Since the Supreme Court struck down Roe v. Wade , the legality of abortion has been left to individual states. The Washington Post is tracking states where abortion is legal, banned or under threat.
Abortion and the election: Voters in about a dozen states could decide the fate of abortion rights with constitutional amendments on the ballot in a pivotal election year. Biden supports legal access to abortion , and he has encouraged Congress to pass a law that would codify abortion rights nationwide. After months of mixed signals about his position, Trump said the issue should be left to states . Here’s how Biden and Trump’s abortion stances have shifted over the years.
New study: The number of women using abortion pills to end their pregnancies on their own without the direct involvement of a U.S.-based medical provider rose sharply in the months after the Supreme Court eliminated a constitutional right to abortion , according to new research.
Abortion pills: The Supreme Court seemed unlikely to limit access to the abortion pill mifepristone . Here’s what’s at stake in the case and some key moments from oral arguments . For now, full access to mifepristone will remain in place . Here’s how mifepristone is used and where you can legally access the abortion pill .
- States where abortion is on the ballot in the 2024 election April 15, 2024 States where abortion is on the ballot in the 2024 election April 15, 2024
- States where abortion is legal, banned or under threat April 9, 2024 States where abortion is legal, banned or under threat April 9, 2024
- Trump says it’s up to states whether to punish, monitor women for abortions April 30, 2024 Trump says it’s up to states whether to punish, monitor women for abortions April 30, 2024

Florida abortion clinics squeeze in as many patients as possible ahead of 6-week ban
JACKSONVILLE, Fla. — Abortion clinics in Florida say they have been trying to see as many patients as possible before the state's ban on abortions after six weeks takes effect Wednesday.
In Jacksonville, a clinic called A Woman’s Choice provided around double its usual volume of abortions Monday, according to Amber Gavin, its vice president of advocacy and operations.
The waiting room has been so crowded that patients' companions were asked to stay in their cars or drop people off to free up space, Gavin said. Parking spaces were also scarce, prompting some patients to park off-site and walk to the clinic.
“Tomorrow is going to look very different,” Kelly Flynn, CEO of A Woman’s Choice, said Tuesday. “A lot of patients will come in for the consult and be told that we can’t see them.”
Florida's new restriction, which takes effect just after midnight on Wednesday, makes it a felony to perform or actively participate in an abortion after six weeks of pregnancy. Because gestation is counted from a woman's last period, that leaves her around two weeks after a missed period to realize she is pregnant and complete the process to terminate the pregnancy, which in Florida requires two in-person visits to a clinic, 24 hours apart.
The ban has exceptions for rape, incest and human trafficking up to 15 weeks of pregnancy. Abortions can also be provided after six weeks if there's a fatal fetal abnormality, a woman's life is at stake or she faces “substantial and irreversible” physical impairment.
Candace Dye, the owner of A Woman’s World Medical Center in Fort Pierce, Florida, said phones were ringing off the hook last week as patients tried to book appointments.
“We usually only do like 50, 60 patients in one month,” Dye said. “This month is going to be over 100.”
The waiting room at A Hialeah Woman’s Care Center in Miami-Dade County was also full Tuesday. The abortion clinic, which serves a working-class community with a sizable immigrant population, had to turn away some patients Monday.
Abortion providers said many patients are confused about the state's restrictions and timelines.
Dr. Marian Sampson, a provider at Planned Parenthood of Southwest and Central Florida, said some patients were shocked that Monday was the last day to initiate the abortion process for those who are more than six weeks pregnant, given Florida's two-appointment requirement. (Come Wednesday, patients will need to show up to clinics a few days before the six-week mark to be eligible.)
Other patients, she said, were not aware that Florida had banned abortion after 15 weeks of pregnancy in 2022, or thought that the new law would outlaw abortion entirely and that "traveling out of state will lead to possible criminal repercussions."
That is not the case. Given that some abortions will still be permissible in Florida, clinics said they plan to keep operating for now.
“It’s just going to be a day-by-day learning process in how we can reframe how we’re doing the work,” Flynn said. “We are not going to close. We’re going to stay open and we’re going to fight our way through this.”
Patients who are more than six weeks pregnant will be given information about how to obtain abortions in a different state, said Dr. Daniel Sacks, a provider at Presidential Women’s Center in West Palm Beach.
Sacks said his approach has been to make patients aware of the deadline without rushing them.
“We don’t want to push anybody to make a decision that they’re not ready to make,” he said. “It’s presented as, ‘You’re X number of weeks. Should you decide you want to terminate, you would have to do so by the 30th of this month or go out of state.’”
Gov. Ron DeSantis signed Florida’s six-week ban a year ago, in April 2023, but legal challenges held it up until the state Supreme Court issued a ruling earlier this month.
Anti-abortion groups have been eagerly awaiting the ban.
“This is a historic moment. On May 1, Florida becomes a sanctuary for life,” said Mat Staver, founder and chairman of the Florida-based Liberty Counsel, a legal organization that opposes abortion rights.
Staver noted that Florida’s ban sets aside $25 million to expand the Florida Pregnancy Care Network, a group of so-called crisis pregnancy centers. These types of centers aim to convince pregnant women not to have abortions, and offer them counseling and supplies like car seats and diapers. Some have been known to provide inaccurate or misleading information .
Florida's abortion policies could change once more after November, when residents will vote on a proposed amendment to the state's constitution that would enshrine abortion access.
"I am optimistic that we will have the votes," Flynn said. "In the meantime, we are really talking to patients and explaining to them how important this is to get out and vote."
Marissa Parra and Juliette Arcodia reported from Jacksonville, Florida; Bracey Harris from Jackson, Mississippi; and Aria Bendix from New York City. Carmen Sesin contributed reporting from Miami.
Marissa Parra is a national correspondent for NBC News based in Miami, Florida.
Bracey Harris is a national reporter for NBC News, based in Jackson, Mississippi.
Aria Bendix is the breaking health reporter for NBC News Digital.
- Live In The D
- Newsletters
Maternal deaths are 3 times higher in Black women, doctors say
There are several ways women can reduce their risk of pregnancy-related complications.
The advertiser paid a fee to promote this sponsored article and may have influenced or authored the content. The views expressed in this article are those of the advertiser and do not necessarily reflect those of this site or affiliated companies.
Pregnancy and childbirth can be an incredibly joyful experience, but for some women, it can cause fear about possible complications.
Doctors say maternal deaths are three times higher for Black women and more than half of these deaths are preventable. Detroit Medical Center obstetrics specialists recognize the disparity in pregnancy-related complications in Black versus white women and have made complex pregnancies a high priority every day.
Dr. Rebecca Jameson, an obstetrician gynecologist with the DMC, said there are many factors that come into play when we talk about the disparity in pregnancy-related complications in Black women.
“There can be huge differences in access to quality care and higher likelihood of chronic diseases due to family history and genetics,” she said. “(There are) other social factors like lack of insurance and health care, lack of transportation, housing, and lack of quality food in some neighborhoods.”
Some of the chronic diseases that can increase the risk of pregnancy-related complications are hypertension, cardiovascular disease, obesity and diabetes, all of which are seen more commonly in Black women.
Reducing the risk
While many social factors beg for structural and societal change, there are ways women can reduce their individual risks right now, according to Jameson.
“These are getting regular preventive visits -- prior to pregnancy -- with a gynecologist or a primary care provider and managing any chronic diseases with lifestyle changes or medication prescribed by a physician,” she said.
Jameson said one unique thing obstetricians need to do more of is have a patient schedule an appointment for preconception counseling.
“We can talk about their individual risks, how that would impact their pregnancy and help create goals to improve their health prior to pregnancy,” she said.
During pregnancy, women should have regular prenatal visits with a nurse midwife, an obstetrician or a maternal-fetal medicine (high-risk OB) doctor. They should make sure before they deliver that they choose a facility that will meet their needs.
“For some women, the hospitals closest to their homes may not have the resources to manage some of these high-risk conditions, so they will want to make sure with their doctor or midwife that the facility will be able to manage their obstetrical care,” Jameson said.
Deciding on a doula
Doulas are non-clinical professional caregivers that provide emotional and physical support before, during and after delivery.
Jameson said while doulas do not provide medical advice, they can be crucial advocates during pregnancy and postpartum care. They can provide many benefits to patients to make it safer for moms and babies.
“Some of the benefits we see are fewer C-sections, less anxiety and depression, better pain relief during labor, and better communication between the pregnant patient and their providers,” Jameson said. “Having a doula means women are two times less likely to have a birth complication, four times less likely to have a low birthweight baby, more likely to breastfeed, and more likely to be satisfied with the care they received.”
Most insurance plans, including Medicaid, cover doula services. Women should call their insurance provider to find out which groups are covered.
Making a birth plan
Jameson said making a birth plan can be a great jumping off point for women.
“We use them a lot,” she said. “Ask your provider if they have a birth plan form that outlines what is offered at their facility. Go over this plan in the office so that you can talk about which things are safe. This helps us to know what the environment should be in the labor room, identify any support persons you would like present, pain control options, monitoring options, and physical movement during labor.”
The most important thing, Jameson said, is to be flexible with the plan, because things can change very quickly in the delivery room. She said the goal, above all, is to have a healthy mom and baby.
“Make sure you have a provider you can trust so they can discuss how things are changing and what that means for your baby and your care,” Jameson said.
To learn more about the DMC birthing centers or to find an OB-GYN that will meet your needs, click or tap here .
RELATED STORIES
Would you know symptoms of a heart issue what about your personal risks, chest pain can be scary. here are some signs it could warrant a visit with a cardiologist..
Click here to take a moment and familiarize yourself with our Community Guidelines.
Recommended Videos

COMMENTS
Relationships. Image courtesy of @msvaniarios. TLDR: In this personal essay, a mother reflects on her journey by writing a letter to her past pregnant self to assure her—and other mothers-to-be—about the wonder of motherhood. Dear Pregnant Self, You know I am not one for the cheesy stuff—I'm not a very romantic person. I don't like ...
In the essay "What Pregnant Women Won't Tell You - Ever", Elyse Anders talks about the downsides of pregnancy. ... During the first trimester of pregnancy plenty of pregnant women experience bleeding, it's normal, it's just from the fertilized egg implanting itself into the uterus, or other reasons, such as sex, hormone changes, or an ...
The physical and emotional changes of pregnancy and, then, labor, birth, and breastfeeding play vital roles in guiding women on the journey of becoming a mother. Standard prenatal care and medicalized labor and birth interfere in powerful ways with nature's plan and, consequently, women's ability to negotiate this journey.
Voices. Three Important Life Lessons My Unexpected Pregnancy Taught Me About Self-Love. By. Aimee Simeon. Published on 05/16/23 08:00AM. I've never trusted myself in life until now. Let me explain. I'm 28 years old, the oldest child to immigrant parents, and I have had an awesome career thus far. I'm in a loving, long-term relationship with my ...
Cramps or headache. Slight bleeding. Food aversions or cravings. Breast tenderness. Mood swings. Faintness or dizziness. Missed period. Sometimes, women wonder what being pregnant feels like because they simply "feel different" and have a hunch they are pregnant. The abovementioned side effects can be due to many things other than pregnancy ...
My Birth Story: Moms Share Their Birth Experiences. Every birth story is unique — that's why we asked moms from all over the world to share their experiences of how they welcomed their little ones into the world. No two stories in this series are the same, but each one powerfully illustrates the beauty of birth.
Women with diabetes experience a sense of objectification during pregnancy; combined with a lack of control; and the awareness of having an unwell, high-risk body. They also refer to an exaggerated sense of responsibility, constant worry, pressure, and feelings of self-reproach (Berg, 2005; Berg & Honkasalo, 2000 ).
Pregnancy and Motherhood While on the Tenure Track. Lucia Taylor discusses the realities of life in academe. I am Spanish citizen who came to the United States six years ago with a scholarship to enroll in a Master of Language Pedagogy and teach at the University of Utah. My plan was to stay for a year and then move back to Spain where I could ...
Maternity and pregnancy involve significant biopsychosocial changes in the lives of women. Pregnant women undergo hormonal changes, such as increased cortisol, the effects of which include fatigue, disruptive sleep, anxiety, and poor memory (Ziomkiewicz et al., 2019).In addition, their self-perception and self-efficacy are influenced by their emotional state, expectations, and idealization of ...
Pregnancy is when a baby grows inside a woman's womb or uterus. It starts when a sperm from a man joins with a woman's egg. This tiny new life is called an embryo at first, and then a fetus as it gets bigger. A full pregnancy usually lasts about nine months.
As a pregnancy trainer who prepares pregnant women for childbirth, the author wrote her personal childbirth story with an autoethnographic narrative method. Her aim is to help motivate pregnant women preparing for childbirth, health-care professionals preparing those pregnant women, and birthing staff. Keywords: autoethnography, childbirth ...
Parents described a range of complications during pregnancy involving the mother's health, the baby's health, or both. These included ectopic pregnancy, bleeding, placental problems, 'incompetent cervix', gestational diabetes, severe nausea (hyperemesis gravidum), ovarian cysts, high blood pressure and pre-eclampsia.
My prenatal development was normal. There were not any concerns or worries about my development. My mom had a fairly normal pregnancy other than preeclampsia. Preeclampsia is a medical condition in women who have not experienced high blood pressure, and developed in during a pregnancy (Preeclampsia and Eclampsia, 2016).
Being pregnant was one of the most joyous moments of my life. I was able to bring a human being into this world, and to be able to wake up next to her everyday automatically puts a smile on my face and makes me a happier person. I am very grateful to call her mines. The pregnancy experience for me was a little hectic and also self-learning ...
Pregnancy, an experience that is very hard and painful, but leads to the most amazing thing any person can have, a child. Knowing you have a life growing inside is an amazing, life changing experience for pregnant woman, even for the men, and although the woman may not always feel their best along the journey they'll know it was all worth it in the end.
It's been a crazy emotional roller coaster for me, especially being young and still living at home. When I found out I was pregnant, I didn't know what to do. I was scared to tell the father of my baby, but more terrified to tell my parents. I had plans for my future that did not involve having a baby. This is my experience of being in ...
Personal Narrative Essay: The Story Of My Pregnancy. 829 Words4 Pages. This is the story of my pregnancy. The night I found out I was pregnant I got a funny feeling in my stomach, and I wasn't sure what was going on. I told my mom what was going on, but she was already suspecting I was pregnant and already had a test ready for me to take.
The participants were mainly adult women over 18, although two papers included two pregnant women aged 17 in their samples. ... This included positive feedback to normalise the pregnant person's experience, information about the foetus's health condition, nutrition advice and information about delivery [10, 36, 38,39,40, 45, 46, 48].
Essay On Pregnant Womens Health. Type of paper: Essay. Topic: Children, Family, Pregnancy, Parents, Women, Health, Education, Food. Pages: 6. Words: 1700. Published: 02/22/2020. ORDER PAPER LIKE THIS. This paper will talk about pregnancy. It will give the physical and the psychological changes that the pregnant mother will experience throughout ...
The example essays in Kibin's library were written by real students for real classes. To protect the anonymity of contributors, we've removed their names and personal information from the essays. When citing an essay from our library, you can use "Kibin" as the author.
Essays Related to My Pregnancy Experience. 1. Life or Liberty. These groups generally only believe in ending the pregnancy early in case such as certain death caused by pregnancy, such as ectopic pregnancy. ... This is a belief that I have always had and that ultimately was cemented by my own experience.
Background Previous studies have not synthesized existing literature on the lived experiences of pregnant and parenting adolescents (aged 10-19) in Africa. Such evidence synthesis is needed to inform policies, programs, and future research to improve the well-being of the millions of pregnant or parenting adolescents in the region. Our study fills this gap by reviewing the literature on ...
4 things to know about the latest abortion lawsuit from Republican states : Shots - Health News A new regulation to protect the rights of pregnant workers is the subject of an anti-abortion ...
All week, TODAY will be sharing stories to raise awareness of what it is like to experience infertility. In the last 13 years, 37-year-old Emily Westerfield has delivered 10 healthy babies ...
A ban on abortions after six weeks of pregnancy took effect in Florida on Wednesday. Before that, the state had been a refuge for abortion access in the South. More than 9,000 people traveled to ...
Essay About Being Pregnant. My experience of being pregnant was mostly eventful. There were a lot of things people told me that they shouldn't have. For instance, having constipation while being pregnant and getting hemorrhoids, that never occurred in my nine months. It was a waste of being fearful for nine months.
Trump's comments to Time magazine highlight the fraught politics of the stance on abortion that he outlined earlier this month.
Staver noted that Florida's ban sets aside $25 million to expand the Florida Pregnancy Care Network, a group of so-called crisis pregnancy centers. These types of centers aim to convince ...
Pregnancy and childbirth can be an incredibly joyful experience, but for some women, it can cause fear about possible complications. Doctors say maternal deaths are three times higher for Black ...
Three officers were killed in a shooting while attempting to serve a warrant at a home in Charlotte, North Carolina, including one deputy US Marshal and two local task force officers, authorities say.