
- Majors & Careers
- Online Grad School
- Preparing For Grad School
- Student Life

Top 10 Best PhD in Medicine Programs

Dreaming of making the latest breakthrough medical discoveries? Whether you’re interested in neuroscience , psychology, or microbiology, a PhD in medicine will give you advanced skills and in-depth medical science knowledge to propel the medical field forward. You’ll feel equipped to conduct innovative research and perhaps even make important discoveries!
Out of all PhD programs, a PhD in medical science will prepare you for some of the world’s highest-paid roles. After all, the average yearly salary of a doctorate-holder in medicine is $153,000 . The best part? You’ll graduate and embark on a career that will make a difference.
Doctorates in medicine are in high demand, and you might even find — we’ll cover all the highlights in our list of doctorate degrees in medicine.
Table of Contents
Best PhD in Medicine Programs and Schools
Harvard university.
Ph.D. Program in Virology

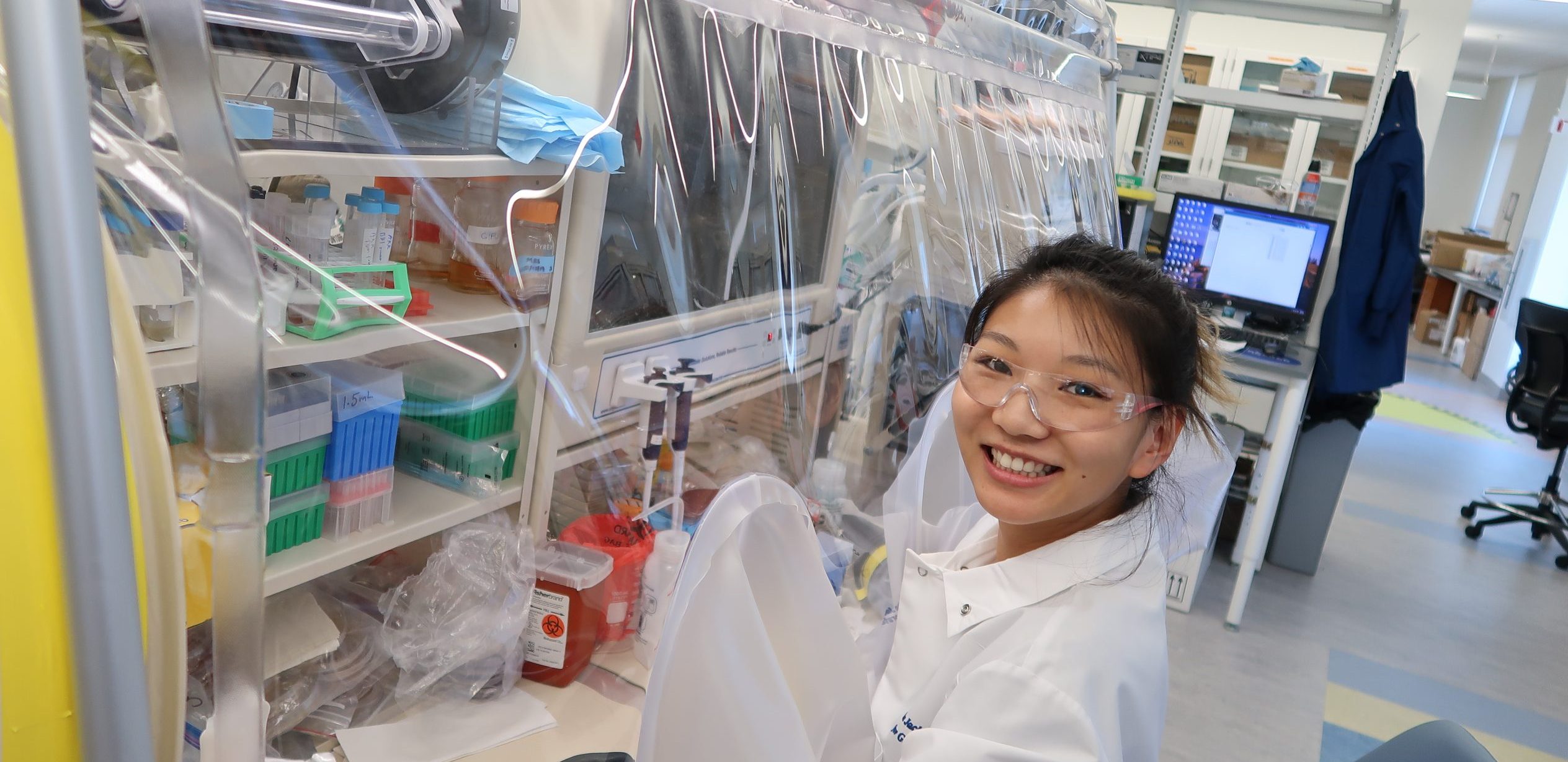
Harvard University offers one of the most dynamic types of doctorate degrees in medicine — the virology PhD. The Ivy League school has produced countless world-renowned virology researchers who have invented valuable vaccines and treatments. This virology PhD program involves small student groups for stronger faculty and student relationships.
- Courses/research areas : Molecular genetics, viruses and immunity interaction, and rational antiviral drug design
- Duration : 5 years
- Tuition : Full funding
- Financial aid: Full tuition & stipend support, health insurance, child support, parent support, and emergency fund
- Acceptance rate: 5%
- Location: Cambridge, Massachusetts
Stanford University, Institute of Stem Cell Biology and Regenerative Medicine
Graduate Program in Stem Cell Biology & Regenerative Medicine

Stanford is one of the world’s leading research centers in stem cell biology and regenerative medicine. In this program, you’ll have multiple options to meet the course requirements by passing substitute courses or through oral or written exams.
- Courses : Stem cells & human development, chemistry of biological processes, and advanced cell biology
- Tuition : Full tuition funding and stipend
- Financial aid : Grants, fellowships, stipend and tuition support, travel allowance, insurance
- Location : Stanford, California
Johns Hopkins University, School of Medicine
Cellular and Molecular Medicine Program

Johns Hopkins is one of the biggest names in medicine globally and the only institution with a surviving CMM program (Cellular & Molecular Medicine) funded by the Lucille Markey Foundation. In this doctorate program, you’ll research cellular and molecular biology with a focus on the practical diagnosis and treatment of diseases instead of a pure scientific emphasis.
- Courses : Molecular biology & genomics, cellular/molecular basis of disease, and immunology principles
- Duration : 3 years+
- Financial aid: Full funding, health insurance, fellowships, teaching assistantships, research assistantships, and grants
- Acceptance rate : 11.1%
- Location : Baltimore, Maryland
Harvard-MIT, Harvard Medical School
MEMP Ph.D. Program

Massachusetts Institute of Technology (MIT) and Harvard University are two of the world’s most acclaimed research universities. They’ve collaborated to offer this unique combined PhD program in MEMP (Medical Engineering and Medical Physics) to advance research and innovation in medical diagnosis, treatment, and patient care. Students can choose one of the program’s 11 concentrations to create a personalized curriculum.
- Courses : Molecular diagnostics & bioinformatics, cellular & molecular immunology, and genetics in modern medicine
- Duration : 5.7 years average
- Financial aid : Full funding for tuition, stipend & health insurance, research assistantships, teaching assistantships, and fellowships
- Acceptance rate: 5-7%
- Location : Cambridge/Boston, Massachusetts
The University of California Berkeley, School of Public Health
Ph.D. Infectious Diseases & Immunity

The University of California Berkeley is ranked #2 among top public schools and is committed to student diversity, demonstrated by its dedicated Office for Graduate Diversity. This PhD is a unique program with its multidisciplinary and integrated focus on host-pathogen environmental interactions.
- Courses : Molecular basis of bacterial pathogenesis, epidemiology & control of infectious diseases, and advanced cell biology
- Duration : 5.5 years average
- Tuition : $14,442 per academic year
- Financial aid : Fellowships, scholarships, grants, work-study, and loans
- Acceptance rate : 17.5%
- Location : Berkeley, California
The University of Pennsylvania, Biomedical Graduate Studies Division
Cellular & Molecular Biology (CAMB) Graduate Group

The University of Pennsylvania’s BGS (Biomedical Graduate Studies) division has around 900 PhD students — 25% belong to underrepresented minorities, and 58% are female. The CAMB Graduate Group is a unique interdisciplinary research program offering six specialized medical discipline areas and world-class facilities.
- Courses : Regulation of the genome, cell & molecular biology, and data analysis for life sciences
- Financial aid: Full funding, including tuition, fees, and stipend, as well as fellowships and grants
- Acceptance rate: 9%
- Location : Philadelphia, Pennsylvania
Yale University, School of Medicine
Investigative Medicine Program

Yale School of Medicine is well-known for its eminent faculty and one of the world’s largest medical libraries. This PhD program specializes in investigative medicine, allowing you to develop high-level creative and analytical skills. It also prepares you with the knowledge to conduct both laboratory-based and clinically based patient-oriented medical research.
- Courses : Topics in human investigation, ethics issues in biomedical research, and methods in clinical research.
- Duration : 3-4 years
- Financial aid : Grants, loans, and fellowships.
- Acceptance rate : 7%
- Location : New Haven, Connecticut
The University of California San Francisco, Department of Epidemiology & Biostatistics
Doctoral Program in Epidemiology & Translational Science

The University of California San Francisco is an innovative research institution focusing exclusively on medicine across education, research, and patient care. As a result, it has some of the highest rankings by the US & News Report in various medical disciplines. The program allows you to choose between 17 concentration areas, including cancer epidemiology, global health, and bioinformatics.
- Courses : Biostatistics, epidemiological methods, and clinical epidemiology.
- Tuition : $11,442 per academic year
- Financial aid : Fellowships, student employment, grants, teaching assistantships, and research assistantships.
- Acceptance rate : 4%
- Location : San Francisco, California
Columbia University, Irving Medical Center
Ph.D. Pathobiology and Mechanisms of Disease Program

Columbia University is home to several well-known medical research schools. It’s also located close to many scientific institutions, providing valuable collaboration opportunities. This program allows students to pursue in-depth research in basic sciences while focusing on knowledge application at the clinical and patient care levels.
- Courses : Biochemistry, cell & molecular biology, molecular genetics, and mechanisms of human disease.
- Duration : 3 years
- Tuition : $25,248 per semester
- Financial aid: Training grants, loans, student employment, and awards.
- Location : New York City, New York
Cornell University, Weill Cornell Medicine Graduate School of Medical Sciences
Ph.D. Cell and Development Biology

Cornell University’s Weill Cornell Medicine Graduate School has over 330 capable faculty members and $275 million in research funds. A reputable program, it involves a lab rotation, allowing each student to pass through three different laboratories before deciding on a research focus area.
- Courses : Molecular genetics, biochemistry & structural biology, and quantitative understanding in biology.
- Tuition : Refer tuition page
- Financial aid : Scholarships, health insurance, and travel support.
- Acceptance rate: 11%
- Location : New York, New York
What Do You Need to Get a PhD in Medicine?
You’ll typically need a master’s degree to be eligible to apply for a PhD in medicine. Some universities also require your master’s to include certain subjects.
As part of your application, the selection committee will generally ask to see:
- Official transcripts from your undergraduate and master’s degrees
- Practical experience
- Resume or CV
- Personal statement
- Letters of reference
Preparing for a Medicine Doctorate Program
Research programs early to determine the specializations you’re interested in. Then, read up on each subject as much as possible and keep up with developments in the field. It’s also a good idea to research your potential mentors. You can also build your network by joining aspirant and professional groups with similar interests.
You’ll find different types of medical doctor degrees online based on the core area of study, such as:
- Ph.D. Healthcare Administration
- Ph.D. Epidemiology
- Ph.D. Public Health
- Ph.D. Health Informatics
- Ph.D. Health Research & Policy
In addition to your preferred specialization, assess programs based on funding options, faculty, accreditation, proximity, and cost of living.
Why Get a Doctorate Degree in Medicine
A doctorate of medicine helps you work in high-level scientific, academic, and research positions within the medical field. On average, professionals with a doctorate in medicine have a salary of $153,000 a year.
You’ll also learn several important skills through a PhD in medicine, including:
- Research, analysis, and problem-solving skills for the medical discipline
- Critical and innovative thinking
- Oral and written communication skills
- Information management skills
- Leadership skills
Some of the most common roles and average salaries for PhD-holders in medicine are:
- Clinical Research Manager ( $78,566 )
- Chief Executive Officer ( $156,335 )
- Postdoctoral Research Associate ( $52,270 )
- Technical Director ( $124,783 )
- Physician/Doctor for Emergency Room ( $249,174 )
What is the Average Cost & Duration of a PhD in Medicine?
The total cost for a PhD in medicine varies between $60,000 and $200,000, based on various factors. The program usually takes 3-6 years to complete.
The Difference Between an MD and a PhD for Medical Doctors
An MD is a practicing degree that equips doctors with high-level knowledge and skills to treat patients. A PhD is a research degree that helps you discover new medical knowledge or prepare for academic and management roles.
Key Takeaways
A PhD in medicine can take your career to the highest level and allow you to earn a lucrative salary. Not only is medicine a prestigious field, but it also fosters your ability to make valuable contributions to society. Check out each program on our list and think about which speaks out to your career goals and values. Then, put together a winning application !
Still not sure which program is right for you? Take a look at other options with our guides to the highest paying PhDs and the best 1-year PhD online programs .
Frequently Asked Questions
How many years is a phd in medicine.
A PhD in Medicine can take between three and six years to complete.
Is a PhD the Same as a Medical Doctor?
A medical doctor does not necessarily need a PhD, as they can qualify with a medical degree. Additionally, a PhD is usually a research degree, not as focused on patient care.
Is a PhD Higher than an MD?
No. Both PhD and MD degrees are doctorate qualifications, but usually with different applications.
Can a PhD be a Medical Doctor?
You can be qualified as a medical doctor without a PhD in medicine, though a doctor can pursue a PhD if they wish. However, an MD degree, which is also a doctoral degree in medicine, is generally more useful for medical practitioners.
Who Makes More Money, a PhD or MD?
There’s not much difference between an MD and PhD regarding benefits and earning potential. However, an MD may attract a slightly higher salary as practitioners are popular and in high demand. While a PhD salary can be comparable, there may not be as many academic and research positions available.
What Can You Do with a PhD in Medicine?
A PhD in medicine qualifies you to hold well-respected positions in academic research centers or teaching hospitals. Additionally, you can continue as a medical practitioner at a higher level.
What is a Doctorate in Medicine (MD) program?
An MD is a graduate program designed for already-qualified surgeons and physicians. It involves rigorous clinical training and coursework to prepare medical professionals for a more advanced level of specialization.

Lisa Marlin
Lisa is a full-time writer specializing in career advice, further education, and personal development. She works from all over the world, and when not writing you'll find her hiking, practicing yoga, or enjoying a glass of Malbec.
- Lisa Marlin https://blog.thegradcafe.com/author/lisa-marlin/ 30+ Best Dorm Room Essentials for Guys in 2024
- Lisa Marlin https://blog.thegradcafe.com/author/lisa-marlin/ 12 Best Laptops for Computer Science Students
- Lisa Marlin https://blog.thegradcafe.com/author/lisa-marlin/ ACBSP Vs AACSB: Which Business Program Accreditations is Better?
- Lisa Marlin https://blog.thegradcafe.com/author/lisa-marlin/ BA vs BS: What You Need to Know [2024 Guide]
Top 10 Best Master’s in Astrophysics Programs
Top 10 best phd in immunology programs, related posts.

How New Grads Research Companies to Find Jobs

Experience Paradox: Entry-Level Jobs Demand Years in Field

Grad Trends: Interest in Artificial Intelligence Surges

Applying to Big Tech This Year? Here’s How to Ace It.

73% of job seekers believe a degree is needed for a well-paying role–but is it?

Tech Talent Crunch: Cities with More Jobs Than Workers

Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Recent Posts
- How Many Grad Schools Should I Apply To?
- Last Mile Education Fund Paves the Way for Tech Students, Offers Lifeline Grants
- When to Apply for Grad School: Easy Monthly Timeline [2025-2026]
- 30+ Best Dorm Room Essentials for Guys in 2024
- Best Laptop for Programming Students in 2024

© 2024 TheGradCafe.com All rights reserved
- Partner With Us
- Results Search
- Submit Your Results
- Write For Us
- Administrators
- MD-PhD Program Interview Committee
- MSTP Faculty
- MSTP Faculty by Discipline
- Current Students
- MD-PhD Advisory Committee
- Student Council
- Students Perspectives on, Inclusion, Diversity and Equity at Yale (SPIDEY)
- Peer Advising by Senior Students (PASS)
- Mentoring and Peer Advice from Recent Trainees (MPART)
- Faculty Mentoring
- Career Development
- Useful Links
- Parental Support and Relief
- MD-PhD House System
- Important Dates & Deadlines
- Application Process
- Financial Support
- Life at Yale
- Frequently Asked Questions
- Who we are: Goals & Committees
- What We Do: Current D&I Initiatives
- Resources for Support
- Resources for Self-Education
- Yale BioMed Amgen Scholars Program
- MD-PhD Timeline
- Responsible Conduct of Research (RCR)
- Clinical Activities
- Research Activities
- Leadership & Research Management Certificate
- Annual Program Retreat
- Perspectives of Women in Science Lectures
- Grant-writing workshops
- Teaching Requirements & Opportunities
- Thriving in the Training Environment
- Where To Go For Help
- Physician-Scientist Specialty Shadowing Opportunities
- 2019 Newsletters
- 2020 Newsletters
- 2021 Newsletters
- 2022 Newsletters
- Residency Matches
- Student Publications
- PhDs Conferred
- Fellowships Awarded
INFORMATION FOR
- Residents & Fellows
- Researchers
MD-PhD Program
Our mission.
Our mission is to provide students with integrated training in clinical medicine and research that qualifies them to perform at the highest standards as rigorous clinicians and scientists; to create a diverse and inclusive physician-scientist community to support and mentor trainees along axes of personal identity, clinical discipline and research domain; to cultivate the characteristics of curiosity, creativity, compassion and service in our trainees; and to develop skills associated with success in a broad range of physician-scientist research careers through experiential learning.
Our commitment to diversity & inclusion
Director's welcome: yale md-phd program, message from the director.
Whether you are a prospective or current student, alumnus, faculty or staff member, you are here because of a shared interest in how physician-scientists can advance patient care through their unique and rigorous training in both clinical medicine and research.
Here at Yale, we have world-class scientists and clinicians engaged in basic, translational and clinical research that runs from sub-atomic bonds to the bonds that hold society together, and everything in between. Our students come from diverse backgrounds, with different scientific and clinical interests, but share the desire to make an impact through their work and practice. Our program has didactic, clinical and research opportunities within divisions, departments and schools that span the entire University. I am glad to report that the Yale System still lives and continues to promote a culture of independence of thought, creativity, mission and service among our collaborative students and faculty. I am very proud of our past and current students who do groundbreaking research that leads to advances in medicine.
I hope you take a moment to learn more about our program from these web pages, or by contacting any of our students, faculty or staff. If you are a student who is ready to accept the challenges, responsibilities and rewards of preparing for a career that makes a positive impact on human health and well-being, I invite you to apply to our MD-PhD program. We hope that you will become part of the Yale MD-PhD family, and join us in celebrating our 50th anniversary in 2020!
With warm regards,
Barbara Kazmierczak, MD PhD Professor of Medicine & Microbial Pathogenesis Gustavus and Louise Pfeiffer Research Foundation MD-PhD Program Director
Our websites may use cookies to personalize and enhance your experience. By continuing without changing your cookie settings, you agree to this collection. For more information, please see our University Websites Privacy Notice .
School of Medicine
Medical Education
M.d./ph.d. program.
- Applying to the M.D./Ph.D. Program
- M.D./Ph.D. Program Blog
- M.D./Ph.D. Student Profiles
- M Delta Curriculum for M.D./Ph.D. Students
- M.D./Ph.D. Student Publications
- M.D./Ph.D. Student Government
UConn’s M.D./Ph.D. program provides students with an intellectually stimulating and highly integrated educational experience leading to completion of both the M.D. and Ph.D. degrees. With many alumni matched to highly competitive residencies, the UConn M.D./Ph.D. program prepares its graduates for successful careers in both medicine and science.
The mission of our M.D./Ph.D. program is to prepare individuals of outstanding potential for productive careers as physician-scientists. The program emphasizes the development of skills necessary to become a highly competent and caring physician and to perform, evaluate, and communicate the results of independent research in the biomedical sciences.
Furthermore, we strongly believe in the importance of diversity, equity, and inclusion in science and medicine. Essential to this is our giving opportunities for students of all backgrounds including underrepresented minority groups, disadvantaged backgrounds, and those with disabilities. We are committed to provide individualized support for students from underrepresented or underprivileged backgrounds.
Our program is dedicated to high quality medical and graduate education tailored to the needs of the individual student. We are a close-knit community of students, faculty, and staff. Collegiality and mentorship are key aspects of the program.
Dedication to Diversity
The M.D./Ph.D. program at UConn Health is fully dedicated to making an environment that is inclusive and accepting of all of our students. To this end, we value diversity in all its forms, and encourage people of all backgrounds to apply to join our community of learning.
We believe that having a wide range of lived experiences adds value to the discussions we have with one another. As future healthcare providers and researchers, understanding differences in lifestyles and cultures help us provide the best care for our patients. The program works towards having a diverse environment to encourage dialogue and strengthen our understanding. Through this, we aim to add diverse and culturally competent physician-scientists to the work force.
We also emphasize outreach to underrepresented communities in our surrounding area through a variety of programs. These programs provide mentorship and education about the career paths in science and medicine, including physician-scientists. Through these, we aim to spread awareness and encourage diversity in the science and medical field in the future.
We welcome you to explore the many ways in which the UConn M.D./Ph.D. program, the School of Medicine, and the Graduate School work to ensure that UConn is a safe and welcoming environment for all. We also ask you to reach out to us with any questions about the M.D./Ph.D. program’s commitment to diversity, equity, and inclusion.
Program Structure
M.D./Ph.D. students matriculate for the first 18 months with the regular M.D. students before they pursue their graduate studies, taking four years to complete their Ph.D., and then return for clinical clerkships. During the first two years, in addition to completing the preclinical requirements of the medical school curriculum, students pursue select graduate school coursework and two to three laboratory rotations. Incoming M.D./Ph.D. students have the option to complete their first laboratory rotation the summer before matriculation.

There is an emphasis in continuity of clinical education, providing opportunity to practice clinical skills on patients from the start of medical school and throughout the graduate phase, better preparing students to excel in clinical rotations. Students remain actively involved in the program during all phases of their training via weekly research club, symposiums, leadership opportunities, and other events.
As part of the longitudinal clinical experience, students are required to continue clinical activities in community service clinics or in specialty clinics for a half day per month during the graduate phase in order to maintain their clinical skills. Following successful completion of requirements for the Ph.D. degree, students return to medical school to complete two years of clinical training.
For a full breakdown of program structure, see our page on the M Delta Curriculum for M.D./Ph.D. Students.
UConn School of Medicine is one of the nation's leading public medical schools, featuring a modern, case-based learning curriculum, early clinical experience, and state-of-the-art facilities for clinical simulation, virtual and cadaverial anatomy education
M.D./Ph.D. students engage in UConn School of Medicine’s industry-leading M Delta curriculum.
Learn more about UConn School of Medicine’s curriculum.
Graduate Education
During the graduate phase, students pursue intensive thesis research in one of seven areas of concentration (AOC) in biomedical science and complete additional coursework required by their AOC. The Biomedical Science AOCs are:
- Cell Biology
- Genetics & Developmental Biology
- Molecular Biology and Biochemistry
- Neuroscience
- Skeletal Biology and Regeneration
- Systems Biology
The Jackson Laboratory for Genomic Medicine
The Jackson Laboratory (JAX) offers collaborative research training opportunities for our students in mammalian genetics and genomic medicine on our UConn Health campus. Our students have the option to complete lab rotations and perform their Ph.D. thesis research with a JAX faculty member at the Jackson Laboratory on our Farmington, CT campus at UConn Health, if the JAX faculty member has an appointment as a faculty member of the UConn Graduate School. Learn more about the cooperative Ph.D. program and JAX-GM.

External Fellowship Awards
Tuition waivers and full stipend funding are guaranteed throughout the entire length of our program. For the 2024-2025 academic year the stipend is $39,100. Many of our students succeed in obtaining fellowship grants, such as several of UConn and/or Jackson's Labs T32/T90 Training Programs, NIH F30 Fellowships, and American Heart Association awards. We provide extensive support for trainee grant applications including a mock study section with senior faculty members to prepare our students for success. To read about some of our current student fellowships success stories, read our M.D./Ph.D. student blog.
Residency Placement
Our students routinely match to physician-scientist training programs (PSTPs) and other competitive residencies in a broad range of specialties all over the country. For more details, check out our M.D./Ph.D. Program fact sheet and M.D./Ph.D. student blog .
To learn more about the success of our our past and current students, see our M.D./Ph.D. student blog , Student Profile page, and M.D./Ph.D. Program fact sheet.
Applications
Applicants should have substantive research experience, a strong academic record, and prior clinical exposures. Applicants must complete the online AMCAS application, indicate on their application that they are applying to the UConn M.D./Ph.D. program, and complete the M.D./Ph.D. essay. Learn more about applying to the UConn PhD Program.
Contact Information
| Kim Dodge-Kafka, Ph.D. Email: | Ms. Tracy Dieli Email: Ms. Diane Starosciak |
M.D./Ph.D. Program News & Blog
- Congratulations Keaven Caro on F30 Award
- Congratulations to MD-PhD M4 students on their Match!
- Congratulations to Justin and Cullen on T90/T32 appointments!
- MD/PhD Program Director’s Innovative Approach to Heart Disease
- MD/PhD Candidate Rachel Cohn Awarded F30 Fellowship from NIA
- Congratulations to our new MD-PhD Graduates!
What It's Like to Do an MD-PhD Program
New section.
Two medical students answer questions about what it's like to do an MD-PhD program.

Elias (Eli) Wisdom
Undergraduate: Pacific University, Oregon Major: BS, Biology Medical school: Oregon Health & Science University (OHSU) Anticipated Graduation Year: 2028 Bio: Eli Wisdom is an MD-PhD student at Oregon Health & Science University (OHSU) studying the molecular mechanisms of Parkinson’s Disease. He grew up in the small rural town of La Grande, Oregon, where he gained a deep appreciation for community and service and a fascination with the natural world. At Pacific University, he completed his degree in Biology while also playing varsity baseball. After graduating, he was as an Associate in Neuroscience at Yale School of Medicine for two years before starting an MD-PhD program. Outside of school, he enjoys competing in triathlons, camping, and spending time with family.

Sreya Sanyal
Undergraduate: New Jersey Institute of Technology Major: Biology & History Double Major Medical school: Rutgers Robert Wood Johnson Medical School Anticipated Graduation Year: 2031 Bio: Sreya Sanyal is a MD-PhD student at Robert Wood Johnson Medical School and Princeton University. She is Bengali, and she aspires to become a laboratory principal investigator in the field of oncology. Outside of academia, she enjoys singing, cooking, going to museums, and lifting at the gym.
Why did you decide to pursue an MD-PhD program?
Eli: As an undergraduate student, I found my first biomedical research experience to be quite thrilling, and seriously considered pursuing a career in research. Medical school had surfaced as an opportunity, too, as I was deeply passionate about serving others and caring for the sick, but I felt that basic science research was the backbone of advancing clinical care. I first learned about combined MD-PhD programs during my senior year when I was taking part in a summer research program at another academic institute. I learned that in a dual-degree program, I could become rigorously trained as a research scientist and as a physician — and could do both in my future career. To learn more, I reached out to a few physician-scientists who shared how much they loved their careers. In the clinic, their patients and associated medical problems provided new ideas for exploration in the laboratory. And in the laboratory, the insights they gained could inform the way they treated their patients. Sreya: I’ve wanted to become an oncologist ever since I was 11 and my mother died from gastric cancer. When I shadowed hematologist oncologists in academic settings, I became more interested in their work in clinical trials and research. Entering college, I explored translational research through my undergraduate biomedical engineering lab experiences. As I met more people in the field of drug development and oncology, I realized that I wanted to be at the cutting edge of this work, but I still had the desire to see patients. Through a lot of soul searching and luck, I was able to embark on a career in medical research by pursuing an MD-PhD. Using my training as a physician-scientist, I plan to establish my own lab or work in other ways to improve translational research in the oncological space.
What kinds of career options does the MD-PhD program give you?
Eli: From my experience, rigorous training in medicine and scientific research prepares you best for a career in academic medicine. This often means working at a large teaching hospital, where you have an opportunity to conduct independent scientific research, care for patients, and teach students. While it can differ depending on the medical specialty or the individual, a typical physician-scientist may spend 80% of their time conducting research and 20% caring for patients. However, there are many other career paths available to MD-PhD graduates. Students may also pursue careers working for private research organizations, pharmaceutical and biotechnology companies, or government agencies. Sreya: In my experience as an MD-PhD student interested in oncology, I have a wide array of career options to explore. As a clinician-scientist, I can lead research teams and conduct studies in cancer biology, treatment approaches, and translational medicine. In these roles, I can also mentor students interested in my field, allowing me to advance scientific knowledge while shaping the next generation of researchers. Alternatively, I could directly impact patients' lives by increasing my clinical time spent as an oncologist, developing personalized treatment plans, and contributing to clinical trials. The pharmaceutical and biotechnology industries also present exciting opportunities for me where I would be able to work on drug development, clinical research, or medical affairs, playing an essential role in bringing innovative therapies to market. With my combined medical and research expertise, I am well-equipped to make a meaningful difference in oncology through various rewarding career paths.
What type of research experience did you have before entering the program?
Eli: I attended a liberal arts college where students engaged in scientific research through 2- to 4-month long classes, which were combined lecture and laboratory experiences. Building on excitement from these courses, I pursued a summer research internship at a large biomedical research institute the summer prior to my senior year. I loved this initial exposure to working in a high-powered scientific research center. From working in state-of-the-art reach laboratories, to solving scientific problems in creative ways, and watching physicians bounce between research and patient care — I was hooked. Sreya: Before starting my current program, I had two significant research experiences. First, I worked in a lab that focused on creating materials for drug delivery in the field of biomedical engineering. We used special gels to deliver important substances to specific parts of the body, which had significant effects on the surrounding tissues, such as promoting blood vessel growth and blocking certain enzymes. I spent about ten hours a week for three years in this lab and contributed to three published papers.
Secondly, I worked at a research institute where I studied mice that were genetically modified to show signs of anthrax toxin exposure. These modified toxins could be controlled to specifically target tumor cells in the body. I dedicated forty hours a week to this research, and as a result, we have two research papers in progress for publication
How did you prepare to apply to MD-PhD programs?
Eli: Since I had played varsity baseball throughout college (which was impactful training in its own right), I had limited time for research as an undergraduate. So, I decided to pursue an extended research position before applying to MD-PhD programs. After sending several emails to laboratories across the U.S. and applying to many formal postbacc research programs, I took a two-year job as a postgraduate researcher at an academic research institute. During my time working on a project in a laboratory, I also volunteered at the connected hospital. This allowed me to experience what it was like to conduct independent research during the first part of my day, then care for patients in the afternoon. This experience only confirmed my deeply held passions for both medicine and science, but also exposed me to the challenges that both careers entailed. I felt much more confident in my decision to pursue a dual-degree knowing these insights.
What is your favorite part about being an MD-PhD student?
Eli: Thus far, my favorite part of my training has been directly experiencing the intersection of clinical care and research. During the first two years of the MD-PhD, I was mainly focused on medical school courses and preparing for the first board exam. But now, as I am beginning my PhD, I am realizing how medical school has broadened my perspective. When I read research papers or craft a plan to tackle a hypothesis, I feel empowered with the knowledge I learned in my didactic medical school courses. For example, during one of my PhD research rotations, a scientist was having difficulty delivering a therapeutic to the brains of the mice they were studying. Immediately I recalled from my medical school courses how mannitol could be co-infused to transiently open the blood-brain barrier for drug delivery. It could easily be translated to this scenario. Similarly, my experiences with clinic patients have benefited from my MD-PhD training. Often, it can be as simple as the ability to explain to a patient or their family, the exact mechanism of a drug and the reason it could be effective for their ailment. Or, informing them about current basic science efforts in the field or current clinical trials they might be eligible for. As I advance further into my training, I am eager to see how clinical care and laboratory research can become even more intertwined. Sreya: I am very excited to learn new techniques and approaches to my field of interest. I am also glad that for MD-PhD students in my program, there is a huge emphasis on lifestyle and work/life balance. Many students in my program have become engaged, or married, and are starting families, while many medical students may feel pressure to push these milestones off. Being an MD-PhD student is a huge commitment, so I am especially grateful for all of the personal and professional support my program has to offer.
What do you wish you’d known before you started the program?
Eli: I wish I had known how important it would be to keep an open mind about the research topics that interested me most. I began the MD-PhD program with a rigid focus on a certain topic, thinking that it was the only topic that gave me real excitement. It was also the topic I was most versed in and comfortable in. But during my medical school courses, I was suddenly overwhelmed with several fascinating questions and problems that all seemed equally thrilling. It took a fair bit of mental wrestling with myself to broaden my own research interests and muster up the courage to explore a field I was fascinated with even if I didn’t have the most experience in it quite yet. Luckily, MD-PhD programs are usually quite supportive of students exploring new topics of interest and are eager to see you follow your motivations.
Sreya: One of the most important aspects to consider for MD-PhD students is the idea that this path is a marathon, not a sprint. There is a lot of temptation to overload on clubs, leadership, research, etc., to keep pace with MD colleagues, but in the long run, an MD-PhD is about the quality and depth of training. It’s important to build healthy habits, strong social relationships, and enjoy activities in a sustainable manner, since MD-PhD students have to do another graduate degree on top of medical training.
What advice would you give a student considering an MD-PhD program?
Eli: My advice is to accrue as many experiences as you can in medicine and research before applying. Through these, you can understand if pursuing both an MD and a PhD is the best fit for you, or, if you’d be completely satisfied pursuing a career with only training in one discipline. If you can, shadow physicians at both large academic hospitals and private practices. This can teach you if you’d enjoy treating patients daily and give you insight into how your experience will vary based on the setting. Seek out research experiences as early as possible. This may be difficult to procure, but having a longitudinal research experience that encompasses the successes and failures of science will inform you if this should be your future career. If you can, ask for opportunities to experience what it’s like to write a grant or an academic research article. These are not easy to write, yet they encompass a significant amount of time for professional physician-scientists, so, it is important to learn if you’d enjoy (or at least tolerate) the academic writing load. Lastly, don’t be intimidated by the amount time it takes to complete an MD-PhD. Yes, it is longer than most post-graduate training and takes up a significant portion of your early life. But it is a unique and worthy career path that is much needed in service to society. Sreya: My advice to anyone considering an MD-PhD would be to get both a variety and depth of research experiences. As a student, it’s very easy to continue down a path you already started, but you must try to explore before you commit to any one approach. MD-PhD programs appreciate students who know what they would like to research and the only way to discover this is to pursue broad research experiences. That said, once you find what drives and excites you, it’s important to stick with it and maintain good relationships with your PIs and mentors. It’s a small world among physician-scientists, so depth of work and networking will help you achieve and further your goals. Above all, remember that an MD-PhD is not necessary to do research as a physician. The goal of an MD-PhD is to provide the specific training needed to conduct research above and beyond what a physician alone can do. In this case, you must really be sure that research is fulfilling and allows you to achieve your career goals when applying to programs, as they will ask you about your aspirations.
- @AAMCpremed
Translating Pre-Medical Experiences into Clinical Skills
Michael Foster | May 3, 2023
Your time before medical school is golden. It is a unique time to explore where your passions lie (both within and beyond medicine) and lay a strong foundation of the inter- and intrapersonal skills needed for you to be the best physician you can be. The best advice is simple: challenge yourself, be honest, and have fun! […]
The AAMC offers trusted resources and services to help you navigate the journey from premed to residency and beyond.
Our PhD and Doctoral Programs
- Studies & Further Education
- PhD & Doctoral Programs
Are you looking for a Ph.D. position? Our next Ph.D. Call starts on 15.10.2024

Training the next generation of young scientists is a long tradition of ours!
MedUni Vienna has been training doctors and young researchers since 1365 and can therefore look back on a long tradition in research and education. Here you can work closely with respected academics and researchers while taking your first independent steps as a scientist. As a young researcher, you’ll be part of a research team from the very beginning and develop your first original project with guidance from a supervisor. Your work will shape the knowledge base of tomorrow’s doctors and have a positive influence on the lives of many people. Medical research is meaningful and rewarding work for anyone who is enthusiastic about science and research. You’ll acquire a deep understanding of your field and its methods and develop important transferable skills you’ll need to succeed in the future. The university and the Alumni club offer excellent networking and training opportunities. At the end of your studies, you’ll write your dissertation, and after a successful defense, you’ll be rewarded with your Ph.D. and be recognized as a fully trained scientist (R2-R3 researcher profile EU level). The doctoral program is full-time and linked to employment at MedUni Vienna.
A Ph.D. is the basis of a successful career in research, education, medicine, or any research-orientated position in the public or private sector.
Depending on your educational background, you can focus your studies on basic or clinical research. For more detail on our interdisciplinary Ph.D. and doctoral programs, please click on the links to respective postgraduate training programs. Become a part of our constant endeavour to keep humanity vital and healthy!
Click here for general information on doctoral studies at the Medical University of Vienna.
UN 094 PhD – Doctor of Philosophy (UN094)
Joint phd studies, the doctoral programme of applied medical science (un790), contact us.
We have collected all information about our PhD studies for you in our FAQ section . Please contact us directly by Email for any questions left unanswered and make an appointment with us. We will be pleased to provide you with information on any arising questions from recruiting to details about the complete academic calendar.
Our office is located in the Study Departement Building of the Medical University Vienna at the following address :
Währinger Straße 25a A-1090 Vienna, Austria
Contact for general inquiries
Dieter Breitenbaum Vesna Dominkovic
P: +43 (0)1 40160-21029 P: +43 (0)1 40160-21030
Contact for PhD Call recruiting
Stephanie Danzinger P: +43 (0)1 40160-21033
We use cookies
We use cookies that are technically necessary for the functionality of our website, but also cookies for functional, marketing and analysis purposes to optimise the user experience on our site. With your consent to the cookies, data is processed both by us and by third-party providers, some of which are based in third countries (e.g. the USA). You can find more information about the tools and the partners in our data protection declaration, in which we also explain exactly what data transfer to the USA can mean. You can individually adjust or revoke your cookie settings at any time if you wish.
These cookies are necessary for the basic functions of the website. You can block or delete them in your browser settings, but you then run the risk that some parts of the website will not function properly.
- PHPSESSID Technically necessary cookie from the web server. storage duration: session
- fe_typo_user_live Used by TYPO3 as function for user administration. storage duration: session
Necessary to obtain consent for certain cookies and thus for the use of certain tools.
- cookieUser Used to recognise the browser and its cookie history (consent or rejection of particular cookies with date und time) by an anonymised identification number. storage duration: 1 years
- fcc_cookie_consent Cookie Consent storage duration: 1 years
- fcc_cookie_consent_minified Cookie Consent storage duration: 1 years
- cookie_matomo Cookie Consent storage duration: 1 years
To track users on your website(s) or app(s), the default Matomo Tracking code in JavaScript uses 1st party cookies, which are set on the domain of your website.
- pk_ses short lived cookies used to temporarily store data for the visit storage duration: 30 minutes
- pk_id used to store a few details about the user such as the unique visitor ID storage duration: 13 months
MEMP PhD Program
Hst’s memp phd program, is this program a good fit for me.
HST’s Medical Engineering and Medical Physics (MEMP) PhD program offers a unique curriculum for engineers and scientists who want to impact patient care by developing innovations to prevent, diagnose, and treat disease. We're committed to welcoming applicants from a wide range of communities, backgrounds, and experiences.
How is HST’s MEMP PhD program different from other PhD programs?
As a MEMP student, you’ll choose one of 11 technical concentrations and design an individualized curriculum to ground yourself in the foundations of that discipline. You’ll study medical sciences alongside MD students and become fluent in the language and culture of medicine through structured clinical experiences. You’ll select a research project from among laboratories at MIT, Harvard, affiliated hospitals and research institutes , then tackle important questions through the multiple lenses of your technical discipline and your medical training. As a result, you will learn how to ask better questions, identify promising research areas, and translate research findings into real-world medical practice.
What degree will I earn?
You’ll earn a PhD awarded by MIT or by the Harvard Faculty of Arts and Sciences.
What can I do with this degree?
Lead pioneering efforts that translate technical work into innovations that improve human health and shape the future of medicine.
How long will it take me to earn a PhD in HST’s MEMP program?
Similar to other PhD programs in MIT's School of Engineering, the average time-to-degree for MEMP PhD students is less than six years.

What are the degree requirements?
Science / engineering.
Choose one of the established concentration areas and select four courses from the approved list for the chosen area. Current MEMP concentration areas are:
- Aeronautics & Astronautics
- Biological Engineering
- Brain & Cognitive Sciences
- Chemical Engineering
- Computer Science
- Electrical Engineering
- Materials Science & Engineering
- Mechanical Engineering
- Nuclear Engineering
Harvard MEMPs fulfill Basic Science/Engineering Concentration and Qualifying Exam through their collaborating department (SEAS or Biophysics).
Biomedical Sciences and Clinical Requirements
Biomedical sciences core.
- HST030 or HST034: Human Pathology
- HST160: Genetics in Modern Medicine
- HST090: Cardiovascular Pathophysiology
Restricted Electives - two full courses required*
- HST010: Human Anatomy
- HST020: Musculoskeletal Pathophysiology*
- HST100: Respiratory Pathophysiology**
- HST110: Renal Pathophysiology**
- HST130: Introduction to Neuroscience
- HST162: Molecular Diagnostics and Bioinformatics*
- HST164: Principles of Biomedical Imaging*
- HST175: Cellular & Molecular Immunology
* May combine two half-courses to count as one full course **Must choose at least one of HST100, HST110
Clinical Core
- HST201: Intro. to Clinical Medicine I and HST202: Intro. to Clinical Medicine II
- HST207: Intro. to Clinical Medicine
PhD Thesis Guide
Letter of intent #1:.
Research advisor and topic. Due by April 30 of 2nd year.
Letter of Intent #2:
Tentative thesis committee. Due by April 30 of 3rd year.
Thesis proposal:
Defended before thesis committee. Due by April 30 of 4th year.
Final Thesis:
Public defense and submission of final thesis document.
Harvard MEMPs must an electronic copy of the final thesis including the signed cover sheet. Harvard MEMPs should not register for HST.ThG.
Qualifying Exam
TQE: Technical qualification based on performance in four concentration area courses and Pathology
OQE: Oral examination to evaluate ability to integrate information from diverse sources into a coherent research proposal and to defend that proposal
Professional Skills
Hst500: frontiers in (bio)medical engineering and physics.
Required spring of first year
HST590: Biomedical Engineering Seminar
Required fall semester of first year. Minimum of four semesters required; one on responsible conduct of research and three electives. Topics rotate.
Required for all MEMP students. (Biophysics students may substitute MedSci 300 for HST590 term on responsible conduct of research.)
Professional Perspectives
Required once during PhD enrollment
What can I expect?
You’ll begin by choosing a concentration in a classical discipline of engineering or physical science. During your first two years in HST, you’ll complete a series of courses to learn the fundamentals of your chosen area.
In parallel, you’ll become conversant in the biomedical sciences through preclinical coursework in pathology and pathophysiology, learning side-by-side with HST MD students.
With that foundation, you’ll engage in truly immersive clinical experiences, gaining a hands-on understanding of clinical care, medical decision-making, and the role of technology in medical practice. These experiences will help you become fluent in the language and culture of medicine and gain a first-hand understanding of the opportunities for — and constraints on — applying scientific and technological innovations in health care.
You’ll also take part in two seminar classes that help you to integrate science and engineering with medicine, while developing your professional skills. Then you’ll design an individualized professional perspectives experience that allows you to explore career paths in an area of your choice: academia, medicine, industry, entrepreneurship, or the public sector.
A two-stage qualifying examination tests your proficiency in your concentration area, your skill at integrating information from diverse sources into a coherent research proposal, and your ability to defend that research proposal in an oral presentation.
Finally, as the culmination of your training, you’ll investigate an important problem at the intersection of science, technology, and medicine through an individualized thesis research project, with opportunities to be mentored by faculty in laboratories at MIT, Harvard, and affiliated teaching hospitals.
Interested in applying? Learn about the application process here.
HST MEMP grad Carmen Martin Alonso looks ahead to a bright future as a medical researcher

Study at Cambridge
About the university, research at cambridge.
- Undergraduate courses
- Events and open days
- Fees and finance
- Postgraduate courses
- How to apply
- Postgraduate events
- Fees and funding
- International students
- Continuing education
- Executive and professional education
- Courses in education
- How the University and Colleges work
- Term dates and calendars
- Visiting the University
- Annual reports
- Equality and diversity
- A global university
- Public engagement
- Give to Cambridge
- For Cambridge students
- For our researchers
- Business and enterprise
- Colleges & departments
- Email & phone search
- Museums & collections
- Course Directory
PhD in Medicine
Postgraduate Study
- Why Cambridge overview
- Chat with our students
- Cambridge explained overview
- The supervision system
- Student life overview
- In and around Cambridge
- Leisure activities
- Student union
- Music awards
- Student support overview
- Mental health and wellbeing
- Disabled students
- Language tuition
- Skills training
- Support for refugees
- Courses overview
- Department directory
- Qualification types
- Funded studentships
- Part-time study
- Research degrees
- Visiting students
- Finance overview
- Fees overview
- What is my fee status?
- Part-time fees
- Application fee
- Living costs
- Funding overview
- Applying for University funding
- Doctoral training programmes
- External funding and loans
- Colleges overview
- College listing overview
- Accommodation
- Applying overview
- Before you apply
- Entry requirements
- Application deadlines
- How do I apply? overview
- Application fee overview
- Application fee waiver
- Life Science courses
- Terms and conditions
- Continuing students
- Disabled applicants
- Supporting documents overview
- Academic documents
- Finance documents
- Evidence of competence in English
- AI and postgraduate applications
- Terms and Conditions
- Applicant portal and self-service
- After you apply overview
- Confirmation of admission
- Student registry
- Previous criminal convictions
- Deferring an application
- Updating your personal details
- Appeals and Complaints
- Widening participation
- Postgraduate admissions fraud
- International overview
- Immigration overview
- ATAS overview
- Applying for an ATAS certificate
- Current Cambridge students
- International qualifications
- Competence in English overview
- What tests are accepted?
- International events
- International student views overview
- Akhila’s story
- Alex’s story
- Huijie’s story
- Kelsey’s story
- Nilesh’s story
- Get in touch!
- Events overview
- Upcoming events
- Postgraduate Open Days overview
- Discover Cambridge webinars
- Virtual tour
- Research Internships
- How we use participant data
- Postgraduate Newsletter
Primary tabs
- Overview (active tab)
- Requirements
- How To Apply
Doctoral studies are carried out by science postgraduates, medical students combining clinical training with the PhD, and clinically qualified doctors undertaking scientific training. The research covers the whole spectrum of medical science from basic biology to clinical therapies.
Along with the specific research training provided in the laboratory in which they work, students receive further training within the department in the form of postgraduate workshops concentrating on research techniques, research seminars both on the Addenbrooke's site and elsewhere in the University, and postgraduate student seminars dealing with generic skills such as intellectual property rights, writing a thesis or paper, and entrepreneurship.
Candidates wishing to take a shorter course of research and write a thesis for the master's after one year may apply for the MPhil in Medical Sciences.
Learning Outcomes
Those who wish to progress to a PhD after completing an MPhil will be required to satisfy their potential supervisor, Head of Department and the Faculty Degree Committee that they have the skills and ability to achieve the higher degree.
The Postgraduate Virtual Open Day usually takes place at the end of October. It’s a great opportunity to ask questions to admissions staff and academics, explore the Colleges virtually, and to find out more about courses, the application process and funding opportunities. Visit the Postgraduate Open Day page for more details.
See further the Postgraduate Admissions Events pages for other events relating to Postgraduate study, including study fairs, visits and international events.
Key Information
3-4 years full-time, 4-7 years part-time, study mode : research, doctor of philosophy, department of medicine, course - related enquiries, application - related enquiries, course on department website, dates and deadlines:.
Some courses can close early. See the Deadlines page for guidance on when to apply.
Easter 2025
Michaelmas 2025, easter 2026, funding deadlines.
These deadlines apply to applications for courses starting in Michaelmas 2025, Lent 2026 and Easter 2026.
Similar Courses
- MD (Doctor of Medicine) MD
- Medical Science (Medicine) MPhil
- Clinical Medicine Wellcome Trust PhD
- Infection and Immunity PhD
- Medical Science (Medical Genetics) MPhil
Postgraduate Admissions Office
- Admissions statistics
- Start an application
- Applicant Self-Service
At a glance
- Bringing a family
- Current Postgraduates
- Cambridge Students' Union (SU)
University Policy and Guidelines
Privacy Policy
Information compliance
Equality and Diversity
Terms of Study
About this site
About our website
Privacy policy
© 2024 University of Cambridge
- Contact the University
- Accessibility
- Freedom of information
- Privacy policy and cookies
- Statement on Modern Slavery
- University A-Z
- Undergraduate
- Postgraduate
- Research news
- About research at Cambridge
- Spotlight on...
Navigation auf uzh.ch
Faculty of Medicine
Quicklinks und sprachwechsel, main navigation, md-phd-programm, table of contents, general information, admission requirements, program structure, study guide and curriculum, interfaculty md-phd committee impk.
The MD-PhD Program enables medical students and graduates (in addition to their regular degree in medicine, dentistry, or veterinary medicine) to gain a basic natural science education which allows them to conduct regular doctoral studies at the Science Faculty of UZH, without previously attaining an MSc degree in natural science. The program serves as an entry point for medical students and graduates into the Life Science Zurich Graduate School. The role of the MD-PhD program is to select eligible candidates and to coordinate their integrated science education. The program consists of original research (doctoral thesis) as well as of curricular content (propaedeutic studies).
The MD-PhD is oriented exclusively toward Master students and graduates of degree courses in human medicine, veterinary medicine or dentistry. The MD-PhD program can be entered as MD-PhD Track I in parallel to the medical Master studies at UZH. Applicants to the Track II program must hold a Master's degree from a university in human medicine, veterinary medicine or dentistry.
The MD-PhD program is supervised by an Interfaculty steering committee (IMPK), which consists of representatives of the Faculty of Science, the Faculty of Medicine, and the Vetsuisse Faculty.
Track I: The Track I MD-PhD program is open to students who are enrolled in a medical Master program at UZH, with at least good grades during their Bachelor studies.
Track II: Students who have earned at least a Master’s degree in human medicine, veterinary medicine or dentistry. We recommend that candidates enter the program no later than five years after completing their medical degree. Admission of applicants from outside Europe is subject to the recognition of their degree by the Admission Office of UZH.
Graduates of other fields such as biology, pharmacy, or biochemistry are not admitted.
In addition to fulfilling the requirements of the regular doctoral studies at the Science Faculty, MD-PhD students are required to earn additional ECTS credit points in the framework of the MD-PhD propaedeutic studies.
Track I: The propaedeutic studies are entered in parallel to the medical Master studies at UZH. The doctoral dissertation is conducted after earning the medical Master degree.
Track II: Both propaedeutic studies and doctoral dissertation are conducted after attaining a medical Master degree (human medicine, veterinary medicine, dentistry).
The doctoral dissertation must be carried out in one of the research groups of UZH affiliated to the Life Science Zurich Graduate School. Students must endeavor independently to secure a position in a host laboratory.
The study guides for students and supervisors as well as the curriculum of the propaedeutic studies can be downloaded on the right.
3 years minimum
Dr. sc. nat.
The doctorate is conducted in the frame of one of the PhD programs of the Life Science Graduate School (MNF).
Regulations: https://www.mnf.uzh.ch/de/studium/reglemente/phd.html (in German)
Medical doctorate degrees (Dr. med., Dr. med. dent., Dr. med. vet.) are not awarded in the framework of the MD-PhD program. They have to be obtained separately from the respective faculties.
The MD-PhD program is supervised by an Interfaculty steering committee (IMPK), which consist of representatives of the Faculty of Science, the Faculty of Medicine, and the Vetsuisse Faculty.
The responsibilities of the IMPK include:
- Supervision and coordination of the MD-PhD program
- Supervision and coordination of the MSc Medical Biology program
- MD-PhD program
- Clinical Science
- Biomedical Ethics & Law
- Epidemiology and Biostatistics
Current members:
- Prof. Dr. Adriano Aguzzi (President, supervision MD-PhD)
- Prof. Dr. Nicole Joller (Vice President, supervision MSc Medical Biology)
- Prof. Dr. Felix Beuschlein
- Prof. Dr. Urs Greber
- Prof. Dr. Johannes Loffing
- Prof. Dr. Bjoern Menze
- Prof. Dr. Anne Müller
- Prof. Dr. Christian Münz
- Prof. Dr. Chantal Pauli
- Prof. Dr. Hanspeter Nägeli (Vetsuisse representative)
- Prof. Dr. Nikola Biller-Andorno (representative for Biomedical Ethics & Law)
- Prof. Dr. Milo Puhan (representative for Epidemiologie und Biostatistik)
- Prof. Dr. Beatrix Latal (representative for Clinical Science)
Artemi Bendandi, Coordinator E-mail: [email protected]
Weiterführende Informationen

Study guides
Study guide MD-PhD until 2021
Study guide MD-PhD from 2022
Information for Supervisors
Propaedeutic Studies
Application deadlines
• 15. Juni
• 15. Dezember
Confirmation of Host Laboratory
National MD-PhD Scholarship
https://www.samw.ch/en/Funding/MD-PhD-Program.html
Open MD-PhD position
PhD position at University Heart Center

Medicine MPhil/PhD
London, Bloomsbury and London, Hampstead (Royal Free Hospital)
A full or part-time research degree at the UCL Division of Medicine offers broad research training opportunities under the supervision of academics who are world experts in their fields. Collaborative interactions between scientists, clinicians and healthcare industries at national and international levels provide our students with excellent networking opportunities and career prospects.
UK tuition fees (2024/25)
Overseas tuition fees (2024/25), programme starts, applications accepted.
- Entry requirements
A first or an upper second-class UK Bachelor’s degree in an appropriate subject, or an overseas qualification of an equivalent standard or a recognised taught Master’s degree.
The English language level for this programme is: Level 3
UCL Pre-Master's and Pre-sessional English courses are for international students who are aiming to study for a postgraduate degree at UCL. The courses will develop your academic English and academic skills required to succeed at postgraduate level.
Further information can be found on our English language requirements page.
Equivalent qualifications
Country-specific information, including details of when UCL representatives are visiting your part of the world, can be obtained from the International Students website .
International applicants can find out the equivalent qualification for their country by selecting from the list below. Please note that the equivalency will correspond to the broad UK degree classification stated on this page (e.g. upper second-class). Where a specific overall percentage is required in the UK qualification, the international equivalency will be higher than that stated below. Please contact Graduate Admissions should you require further advice.
About this degree
The multidisciplinary Division of Medicine combines excellent facilities with world-leading scientific and clinical expertise directed towards better understanding and treatment of human disease.
Research students benefit from a training environment that fosters collaboration across the interface between basic science, clinical practice within our associated hospitals, and the pharmaceutical and healthcare industries.
During your research degree, you will be able to select training courses to develop a wide variety of transferable research, teaching, and leadership skills. There will also be opportunities to put these skills into practice in laboratory and teaching environments. We aim to enhance not only your research project, but also your communication skills and career prospects.
You will receive regular guidance and support from your project supervisors and from an independent thesis committee across your full registration period.
Who this course is for
We aim to recruit the best graduates in science and medicine from across the world with a genuine passion and talent for biomedical research.
What this course will give you
This programme offers you the following benefits and opportunities.
- You join the multidisciplinary Division of Medicine, which trains and inspires the next generation of leading biomedical scientists and clinicians.
- An excellent educational experience and unrivalled opportunities for interdisciplinary research, networking, career development and employment across the biomedical and healthcare sectors.
- Networking and career opportunities from our academics' international collaborative links with academic and commercial organisations.
- A unique springboard for ambitious clinicians and scientists.
The foundation of your career
Through close collaborations between scientists and clinicians in a wide range of clinical disciplines, a research degree in the Division of Medicine provides a unique springboard for ambitious clinicians and scientists. Our alumni have progressed to senior leadership positions in many areas of academia, the health services and industry.
Employability
A PhD from the UCL Division of Medicine is internationally recognised as a high achievement. Our graduates are expected to be independent thinkers that bring rigorous expertise to solving complex problems.
Recent graduates have taken up clinical, academic, postdoctoral, and scientific advisory positions in the public and private sectors, nationally and internationally.
The Division runs several seminar programmes that attract high-profile national and international external speakers, as well as a student-led 'Presenting Outstanding Papers' group/seminar series.
There is also an annual day retreat away from the university, where we discuss ideas and hear presentations from staff and students across the entire Division.
Students are encouraged to present their results at a major national or international conference at least once during their project period.
Our academics have numerous national and international collaborative links with academic and commercial organisations. These provide students with broad opportunities for networking and career development.
Teaching and learning
Most of your research will be carried out independently with guidance provided by your supervisory team and Thesis Committee. There will also be a series of training requirements that you will need to complete in the early stages of the programme. Your supervisory team will provide guidance on appropriate training requirements relevant to your proposed area of research.
Your first milestone will be to upgrade from MPhil to the PhD degree. For this, you will submit and present a report (upgrade viva). You will also need to give an oral presentation for which all members of the Division will be invited to attend. In your final year, you submit a thesis covering your research and discuss this at a formal interview known as a viva examination.
Most of your time will be spent conducting independent research, alongside regular meetings with your supervisory team and Thesis Committee, and completing your training requirements. We also encourage you to attend relevant research events at UCL and elsewhere.
Research areas and structure
The biomedical disciplines represented within the research departments and institutes of the UCL Division of Medicine include:
- Advanced Biomedical Imaging
- Amyloidosis
- Clinical Kidney Disease
- Computational Medicine
- Dialysis and Physiology
- Drug Design
- Experimental Inflammation
- Experimental Nephrology
- Fibrosis and Tissue Repair
- Genetics and Genomics
- Human Health and Performance
- Immunosenescense and Ageing
- Intensive Care Medicine
- Liver and Pancreaticobiliary Cancer
- Liver tissue engineering
- Medical Imaging
- Metabolism and Inflammation
- Nuclear Medicine
- Obesity and Metabolism
- Radiochemistry
- Regenerative Medicine
- Respiratory Medicine
- Rheumatology
- Transplantation
- Urological Biology
Research environment
Our world-class undergraduate and postgraduate courses attract the best students from all over the world and train the next generation of basic and clinical scientists and practitioners. Over 200 postgraduate students are enrolled on our PhD programme at any given time.
The UCL Division of Medicine forms one of the most sizeable concentrations of biomedical scientists in Europe in one of the world's leading universities. Our aims are:
- To educate, train, and inspire the next generation of scientists and clinicians.
- To be at the international forefront of biomedical research from lab bench to bedside.
- To attract, retain and develop the most gifted biomedical researchers and teachers at all levels.
- To develop and deliver outstanding patient care together with UCL’s partner hospitals.
Our research aims to understand the basis of disease, and to develop better diagnostics and treatments for diseases with an emphasis on experimental medicine. In the REF 2021 Clinical Medicine unit of assessment, we are ranked first in the UK for our impact and research environment.
Our clinical mission is to provide the highest quality medical care, as practitioners of medicine and leaders of the NHS, and to work in partnership with patients to fulfil our research and teaching missions. The Division’s clinical academics are active as physicians in partner hospitals, with programmes of national and international standing in major medical specialities.
The full-time registration period for a PhD is three years.
You initially register for an MPhil. In your first few months, you discuss and agree a deliverable plan and timeline for your research project with your supervisors. This plan can be revised as new results are obtained.
You will be eligible to upgrade to PhD registration in year two (at around 12-18 months). The assessment is a written report and oral exam following an upgrade presentation. You will also present your work to your group and to the Division when you upgrade from MPhil to PhD registration in year two.
After three years, you can apply for 'completing research status' if you have completed your research and you are focused on writing your thesis.
The part-time registration period for a PhD is five years.
You are initially registered for an MPhil. In your first few months, you discuss and agree a deliverable plan and timeline for your research project with your supervisors. This plan can be revised as new results are obtained.
You are eligible to upgrade to PhD registration in years two to three (at around 15-30 months). The assessment is a written report and oral exam following an upgrade presentation. You also present your work to your group and to the Division during the upgrade process.
After five years, you can apply for 'completing research status' if you have completed your research and you are focused on writing your thesis.
Accessibility
Details of the accessibility of UCL buildings can be obtained from AccessAble accessable.co.uk . Further information can also be obtained from the UCL Student Support and Wellbeing Services team .
Fees and funding
Fees for this course.
| Fee description | Full-time | Part-time |
|---|---|---|
| Tuition fees (2024/25) | £6,035 | £3,015 |
| Tuition fees (2024/25) | £34,400 | £17,200 |
The tuition fees shown are for the year indicated above. Fees for subsequent years may increase or otherwise vary. Where the programme is offered on a flexible/modular basis, fees are charged pro-rata to the appropriate full-time Master's fee taken in an academic session. Further information on fee status, fee increases and the fee schedule can be viewed on the UCL Students website: ucl.ac.uk/students/fees .
Additional costs
Your research degree may be subject to an Additional Fee Element (AFE). The AFE (also known as bench fees) is an additional cost, incurred by yourself or your sponsor. It is levied to cover the costs related to consumables, equipment and materials etc. which are not included in the tuition fee. As each research project is unique, the AFE is calculated on an individual basis and is determined by your academic supervisor.
You should discuss finding support for these costs with your proposed primary supervisor.
For more information on additional costs for prospective students please go to our estimated cost of essential expenditure at Accommodation and living costs .
Funding your studies
Research council and charity studentships and fellowships are occasionally available for MPhil/PhD students. Opportunities may also exist for studentships funded via the UCL Division of Medicine, the Faculty of Medical Sciences, and UCL doctoral training programmes. These are usually advertised on major medical research funding sites and findaphd.com when they become available.
For a comprehensive list of the funding opportunities available at UCL, including funding relevant to your nationality, please visit the Scholarships and Funding website .
Students are advised to apply at least 2 months before their proposed start date. Those applying for scholarship funding (particularly overseas applicants) should take note of application deadlines.
You should identify and contact potential supervisors and agree on a project before making your application. While there is often some flexibility, deadlines and start dates may be dictated by funding arrangements, so check with the department, academic unit or funder to see if you need to consider these when preparing your application. Applicants who are not restricted by external funding terms and conditions (e.g. self-funding) may start on any of the designated start dates available during the academic year.
Your references must be from individuals unconnected to your proposed supervisory team.
Please note that you may submit applications for a maximum of two graduate programmes (or one application for the Law LLM) in any application cycle.
Choose your programme
Please read the Application Guidance before proceeding with your application.
Year of entry: 2024-2025
Got questions get in touch.

Division of Medicine
UCL is regulated by the Office for Students .
Prospective Students Graduate
- Graduate degrees
- Taught degrees
- Taught Degrees
- Applying for Graduate Taught Study at UCL
- Research degrees
- Research Degrees
- Funded Research Opportunities
- Doctoral School
- Funded Doctoral Training Programmes
- Applying for Graduate Research Study at UCL
- Teacher training
- Teacher Training
- Early Years PGCE courses
- Primary PGCE courses
- Secondary PGCE courses
- Further Education PGCE programme
- How to apply
- The IOE approach
- Teacher training in the heart of London
- Why choose UCL?
- Entrepreneurship
- Inspiring facilities and resources
- Careers and employability
- Your global alumni community
- Your wellbeing
- Postgraduate Students' Association
- Your life in London
- Accommodation
- Funding your Master's

PhD Programs
You are creative, curious and passionate about basic research? You would like to live in the oldest university town in Germany and work at one of the famous Max Planck Institutes? You would enjoy doing research in a supportive, stimulating and diverse environment?
We welcome graduate students from all over the world and a wide range of disciplines. Because Max Planck Institutes cannot confer PhD degrees, our students are simultaneously enrolled at Heidelberg University and receive their doctorate from one of the university’s faculties ( Biosciences Faculty , Chemistry Faculty , Physics Faculty ). These faculties have their own specific requirements, which students must fulfill.
PhD students at the institute perform research work and write a thesis under the supervision of a scientist who leads a research group in one of the institute’s departments. Students are usually enrolled in a graduate program. We offer access to a number of graduate schools, such as the Max Planck School Matter to Life , the IMRPS-QD or other graduate schools of Heidelberg University. Most group leaders are associated with one or more of these graduate schools. Joining a graduate school makes you part of the Heidelberg life science community and gives you opportunities for scientific and social exchange outside of the institute.
For students who are not enrolled in a structured PhD program we offer support and guidance through individual Thesis Advisory Committees (TAC). The TAC monitors the progress and development of the PhD student and provides advice to both the student and his/her supervisor. The TAC members are also available for one-to-one consultations with the student and can become an important networking partner. Our PhD students can contact their committee members for personal discussions at any time.
For more information about the different PhD programs and the application procedure, please follow the links provided below. Alternatively, you may also directly contact the head of the department or group leader of the program you’re interested in. Just send an e-mail including your CV and a short description of your interests and expertise to establish first contact. Feel free to contact the PhD representatives or scientific coordinator with any general questions about working at our institute.

PhD Life at the Institute
Graduate Schools in Heidelberg
IMPRS Quantum Dynamics in Physics, Chemistry and Biology

Max Planck School Matter to Life
- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram
Stanford Medicine welcomes a new cohort of PhD students
More than 130 new graduate students in 16 specialties received a warm welcome — and lab coats — as they began their doctoral studies at Stanford Medicine.
September 27, 2024 - By Hanae Armitage

Lloyd Minor addresses the new cohort of PhD students. Steve Fisch
One hundred and thirty-six students — in 16 specialties, from health policy and structural biology to epidemiology and genetics — eagerly pushed their arms through the sleeves of crisp white lab coats embroidered with their name and their field of study. Then they stepped, one by one, onto a stage; paused for a photo; and stepped off as newly minted, lab-coat-wearing doctoral students.
The ceremony, held Sept. 25 at the at the Li Ka Shing Center for Learning and Knowledge on the Stanford Medicine campus, commemorated the beginning of the students’ journeys toward PhDs in biomedical sciences.
Speakers throughout the event, including Lloyd Minor , MD, dean of the School of Medicine and vice president for medical affairs at Stanford University, emphasized the advantage of conducting research within an environment designed to support and encourage collaboration among departments and schools.
“One of the things that brought me to Stanford Medicine12 years ago was the fact that we are an academic medical center that is so well integrated with the rest of Stanford University,” Minor said. “Just across the street is the engineering school, and on the other side is the biology department. We have about 1,100 hospital beds and tertiary care facilities offering premier care to the sickest of sick patients.”
“The opportunity to pursue scientific inquiry from the very, very fundamental level all the way up through translation into clinical trials and patient care — those opportunities exist right here on our campus,” he added. “And you’re going to be a part of making sure those opportunities become the realities of the future.”

Incoming PhD students don their lab coats for the first time. Steve Fisch
Graduate advice
A panel of students and faculty members welcomed the fledgling researchers and discussed the ins and outs of how to succeed as new graduate students.
Their advice: Stop comparing yourself to others; don’t be afraid to talk to faculty members outside of your lab; seek help, whether personal or professional, when you need it; and enjoy the perks of campus, among other practical pearls of wisdom.
New graduate students rotate through labs, eventually choosing one in which they’ll pursue their PhD. Ellen Yeh , PhD, associate professor of pathology and of microbiology and immunology, emphasized the importance of finding the right “fit” during that process.
“Do people say hi to each other in the morning? Do they talk science? Do they know not just about their own projects, but about other projects in the lab? That can give you a sense of how collegial and unified the community is,” Yeh said.
“The one that’s hard to assess, but really important…is conflict. Do people challenge each other? And when they challenge each other, where is it on the spectrum of too-nice or a-little-too-spicy?” she added. “That often is a little harder to get at, but that’s the type of thing that can make or break a PhD once you’re past the honeymoon phase.”
Ted Graves , PhD, associate professor of radiation oncology, agreed: “You want to know that you can coexist with [the principal investigator], that you feel supported by them, that you have a good relationship with them and that there’s an element of trust there,” he said. “It’s getting to know the science, as well as getting to know the people in the lab and seeing if it would be a comforting home for you.”

Sheri Krams, senior associate dean of graduate education and postdoctoral affairs, celebrates with entering PhD students. Steve Fisch
Taking initiative — and chances
Graduate students often bring an ingenuity and refreshing take that invigorates a lab, Graves said. “They’re the ones coming to us with these great ideas that we haven’t thought about, and potentially forging new collaborations and new directions.”
Even if the ideas don’t work, that’s OK, Yeh said. She’s looking for “active learners” or students who are curious and want to improve on projects and learn in real time. Did you get a wonky result? Don’t just bring it to the principal investigator and ask what to do. Come up with a few hypotheses yourself.
“Even if none of those hypotheses turn out to be the [right] one, at least you tried … and that practice of iterating and trying to be active in your learning will eventually get you to the answer or to the right next step,” she said.
As the ceremony came to a conclusion, Minor led the new researchers in a pledge that affirmed their commitment to truth through science; rigorous research; and an inclusive, supportive lab environment.
What’s the key to success? Graduate student Claire Chiang summed it up succinctly: “Work hard, do your best…and ask questions.”

About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
The majestic cell
How the smallest units of life determine our health

- Education Home
- Medical Education Technology Support
- Graduate Medical Education
- Medical Scientist Training Program
- Public Health Sciences Program
- Continuing Medical Education
- Clinical Performance Education Center
- Center for Excellence in Education
- Research Home
- Office for Research
- Services for Researchers
- Research Departments
- Research Centers
- Research Core Facilities
- Research News
- Research Faculty Directory
- Clinical Home
- Anesthesiology
- Dermatology
- Emergency Medicine
- Family Medicine
- Neurosurgery
- Obstetrics & Gynecology
- Ophthalmology
- Orthopaedic Surgery
- Otolaryngology
- Physical Medicine & Rehabilitation
- Plastic Surgery, Maxillofacial, & Oral Health
- Psychiatry & Neurobehavioral Sciences
- Radiation Oncology
- Radiology & Medical Imaging
- UVA Health: Patient Care
- Diversity Home
- Diversity Overview
- Student Resources
- GME Trainee Resources
- Faculty Resources
- Community Resources
Tajie Harris, PhD, Awarded $2.6 Million to Study How the Immune System Benefits the Brain
September 5, 2024 by [email protected] | Leave a Comment
Congrats to Tajie Harris, who was awarded a five-year $2.6 million grant from the National Institute of Neurological Disorders and Stroke, titled “Caspase-8 mediated control of CNS infection.” Visit this link to learn more about her lab’s work!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
- BIG Seminars
- Neurodegenerative Disease Research Coalition
- News and Events
- Uncategorized
Outstanding Fully Funded 40+ PhD Opportunities at Top European Universities in Natural Sciences and Engineering Disciplines

🌟 Exciting PhD Opportunities Available!
🎓Outstanding Fully Funded 40+ PhD Opportunities at Top European Universities in Natural Sciences and Engineering Disciplines
🌟 Are you looking to elevate your PhD studies in a vibrant environment?
🌟We invite applications for PhD positions across a diverse range of fields, including Mathematics, Programming & AI, Computational Biology, User Design, Structural Engineering, Physics, Machine Learning, Battery Technology, Chemistry, Immunology, Electrolysis, and many more, empowering candidates from around the world to engage in groundbreaking research.
🌟We are excited to announce a fully funded 40+ scholarship programmes at some of Europe’s prestigious universities!
🇩🇪 Berlin Mathematical School 🇩🇪 Technical University of Munich 🇩🇪 University Hospital Tübingen 🇩🇪 Karlsruhe Institute of Technology 🇩🇪 Heidelberg University (HBIGS) 🇩🇪 Charles University 🇫🇷 Aix-Marseille Université 🇪🇸 Barcelona Supercomputing Center 🇪🇸 Universitat Politècnica de Catalunya (UPC) - Barcelona Tech 🇪🇸 Universitat de Barcelona 🇪🇸 CIC energiGUNE 🇵🇹 Ventient Portugal 🇳🇴 NTNU - Norwegian University of Science and Technology 🇳🇴 University of Bergen 🇳🇴 UiT - The Arctic University of Norway 🇦🇹 Medical University of Vienna 🇮🇸 University of Iceland 🇧🇭 Swansea University 🇫🇮 Fundació Hospital Universitari Vall d'Hebron - Institut de recerca 🇨🇭 Paul Scherrer Institut Villigen 🇳🇱 Wetsus - European Centre of Excellence for Sustainable Water Technology 🇪🇸 AMADE Research Group 🇫🇷 Université Paris Cité 🇮🇹 Eco Recycling Societa A Responsabilita Limitata
Apply now for the following doctoral (PhD) studies in diverse fields at esteemed European universities:-
PhD Student in Mathematics, Berlin Mathematical School (Germany)
PhD Student in Acoustic and mechanical metamaterials for biomedical and energy harvesting applications – ‘MetacMed’, University of Leeds (United Kingdom)
PhD Student in Programming model for edge to cloud through swarm methodologies, Barcelona Supercomputing Center (Spain)
PhD Student in IntelliWind project on AI-based maintenance planning for wind farms,
Technical University of Munich (Germany)
PhD Student in Computational Biology of Nucleic Acid Modifications, International PhD Programme (IPP) Mainz (Germany)
PhD Student in user centered design of new digital navigational tools, NTNU_Norwegian University of Science and Technology (Norway)
PhD Student in the field of Immunoimaging, University Hospital Tübingen (Germany)
PhD Student in Synthesis of enzyme-mimicking hybrid nanomaterials, Karlsruhe Institute of Technology (Germany)
PhD Student in “An in-vitro human model to study MOGAD physiopathology”, Fundació Hospital Universitari Vall d'Hebron- Institut de recerca (Spain)
PhD Student in Secretory proteins in genome stability, International PhD Programme (IPP) Mainz (Germany)
PhD Student in “Towards more sustainable FRP strengthened concrete structures through novel strategies preventing flexural debonding. Effect of temperature & load distribution conditions”, AMADE research group (Spain)
PhD Student in Design, manufacturing and testing of “living” cellular microfluidic sensors, Swansea University (United Kingdom)
PhD Research Fellow in Reservoir Physics, University of Bergen (Norway)
PhD Fellow in Satellite Altimetry to Characterize Sea Ice Ridges, UiT The Arctic University of Norway (Norway)
PhD Student in "in vivo characterization of highly specialized RNAs - bacterial riboswitches", Heidelberg University_HBIGS Heidelberg Biosciences International Graduate School (Germany)
PhD Student in Machine Learning for Medical Image Analysis, Medical University of Vienna (Austria)
PhD Student in observational cosmology, University of Iceland (Iceland)
PhD Student in developing battery digitalisation methods for parameter identification, NTNU_Norwegian University of Science and Technology (Norway)
PhD Student in control and machine learning for sustainable battery recycling, Chalmers University of Technology (Sweden)
PhD Student in Physics-Informed Machine Learning for Quantum Chemistry, Aix-Marseille Université (France)
PhD Student in designing and developing novel stimuli-responsive metallic and hydrogel materials, embedded with antibacterial peptides, Universitat Politècnica de Catalunya (UPC)- BarcelonaTECH (Spain)
PhD Research Fellow in Data Analytics in Maritime Logistics, University of South-Eastern Norway (Norway)
PhD Student in Correlative Atom Probe Tomography and Electron Tomography for 3D Sub-Nanometer Analysis of InGaN-based Nano-Emitters, CEA (France)
PhD Student in structural and surface modification of biodegradable zinc alloys for biomedical applications, Universitat Politècnica de Catalunya (UPC)- BarcelonaTECH (Spain)
PhD Student in Enhanced wind turbine lifetime management through automated data processing and bespoke sensing, Ventient Portugal (Portugal)
PhD Student in Substance Flow Analysis (SFA) for regional nutrient management, NTNU Norwegian University of Science and Technology (Norway)
PhD Student in Computational and Theoretical Chemistry, Universitat de Barcelona (Spain)
PhD Research Fellow in Fish Immunology, University of Bergen (Norway)
PhD Student in Development of Sustainable Decoupled Electrolysers of Redox Mediators, CIC energiGUNE (Spain)
PhD Student in transient operando spectroscopy of supported metal catalysts, Paul Scherrer Institut Villigen (Switzerland)
PhD Student in Numerical Linear Algebra and High Performance Computing, Charles University in Prague (Czech Republic)
PhD Student in Geodynamics, Université Paris Cité (France)
PhD Student in neurobiology and electrophysiology, Institute of Neurosciences (Spain)
PhD Research Fellow in Deep Sea Biology, University of Bergen (Norway)
PhD Student in X-ray imaging - Multiscale characterization of mineralized biological tissue, Paul Scherrer Institut Villigen (Switzerland)
PhD Student in Recycling process for inorganic and PSK-based IPVs, Eco Recycling Societa A Responsabilita Limitata (Italy)
PhD Student in Creation and application of charged nano bubbles, Wetsus - European centre of excellence for sustainable water technology (Netherlands)
PhD Student in Nuclear pore complex biogenesis, Heidelberg Biosciences International Graduate School_ Heidelberg University (Germany)
Don't miss the opportunity to engage in cutting-edge research and advance your academic journey in Europe.
#EURAXESSAfrica #PhD #DoctoralStudy #PhDPositions #Europe #StudyInEurope #HigherEducation #ResearchOpportunities #BerlinMathematicalSchool #UniversityofLeeds #BarcelonaSupercomputingCenter #TechnicalUniversityofMunich #NTNU #KarlsruheInstituteofTechnology #SwanseaUniversity #UniversityofBergen #CEA #PaulScherrerInstitut #Wetsus
- Introduction
- Conclusions
- Article Information
eTable 1. SARS-CoV-2 RT-PCR testing practices for weekly and symptomatic respiratory swabs, whole genome sequencing methods, and SARS-CoV-2 serologic testing assays by study site
eTable 2. COVID-19 symptoms included in the weekly survey by study site
eTable 3. Characteristics of participants aged 5-17 years by laboratory-confirmed SARS-CoV-2 infection, Sept 4, 2022 – January 31, 2023
eTable 4. Bivalent COVID-19 vaccine effectiveness against laboratory-confirmed SARS-CoV-2 infection among children and adolescents aged 5-17 years, sensitivity analysis restricted to Arizona study sites only
eFigure. Whole genome sequencing results for a subset of laboratory-confirmed SARS-CoV-2 respiratory specimens, September 4, 2022 – January 31, 2023eTables
eContributions
eReferences
Data sharing statement
- Neonatal Outcomes After COVID-19 Vaccination in Pregnancy JAMA Original Investigation February 6, 2024 This cohort study evaluates the risks of neonatal adverse events after exposure to COVID-19 vaccination during pregnancy. Mikael Norman, MD, PhD; Maria C. Magnus, PhD; Jonas Söderling, PhD; Petur B. Juliusson, MD, PhD; Lars Navér, MD, PhD; Anne K. Örtqvist, MD, PhD; Siri Håberg, MD, PhD; Olof Stephansson, MD, PhD
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Feldstein LR , Britton A , Grant L, et al. Effectiveness of Bivalent mRNA COVID-19 Vaccines in Preventing SARS-CoV-2 Infection in Children and Adolescents Aged 5 to 17 Years. JAMA. 2024;331(5):408–416. doi:10.1001/jama.2023.27022
Manage citations:
© 2024
- Permissions
Effectiveness of Bivalent mRNA COVID-19 Vaccines in Preventing SARS-CoV-2 Infection in Children and Adolescents Aged 5 to 17 Years
- 1 Coronavirus and Other Respiratory Viruses Division, National Center for Immunization and Respiratory Diseases, US Centers for Disease Control and Prevention, Atlanta, Georgia
- 2 Division of Allergy and Infectious Diseases, Department of Medicine, University of Washington, Seattle
- 3 University of Arizona, Tucson
- 4 Department of Public Health Science, University of Miami, Miami, Florida
- 5 Children’s Research Institute, Seattle, Washington
- 6 University of Utah Health, Salt Lake City
- 7 Abt Associates Inc, Rockville, Maryland
- 8 Division of Infectious Diseases, Department of Internal Medicine, University of Michigan, Ann Arbor
- 9 Department of Epidemiology, School of Public Health, University of Michigan, Ann Arbor
- 10 Baylor Scott and White Health, Temple, Texas
- 11 Marshfield Clinic Research Institute, Marshfield, Wisconsin
- 12 Kaiser Permanente Center for Health Research, Portland, Oregon
- 13 St Luke’s Regional Health Care System, Duluth, Minnesota
- Original Investigation Neonatal Outcomes After COVID-19 Vaccination in Pregnancy Mikael Norman, MD, PhD; Maria C. Magnus, PhD; Jonas Söderling, PhD; Petur B. Juliusson, MD, PhD; Lars Navér, MD, PhD; Anne K. Örtqvist, MD, PhD; Siri Håberg, MD, PhD; Olof Stephansson, MD, PhD JAMA
Question What is the effectiveness of the bivalent COVID-19 vaccines among children and adolescents aged 5 to 17 years?
Findings In this prospective cohort study including 2959 participants aged 5 to 17 years, vaccine effectiveness against laboratory-confirmed SARS-CoV-2 infection was 54.0% and vaccine effectiveness against symptomatic COVID-19 was 49.4%.
Meaning During a period when the Omicron BA.4/5 sublineages were the predominant circulating variants, children and adolescents received protection against SARS-CoV-2 infection and symptomatic COVID-19 from the bivalent COVID-19 vaccines compared with those who were unvaccinated or received only the monovalent COVID-19 vaccine.
Importance Bivalent mRNA COVID-19 vaccines were recommended in the US for children and adolescents aged 12 years or older on September 1, 2022, and for children aged 5 to 11 years on October 12, 2022; however, data demonstrating the effectiveness of bivalent COVID-19 vaccines are limited.
Objective To assess the effectiveness of bivalent COVID-19 vaccines against SARS-CoV-2 infection and symptomatic COVID-19 among children and adolescents.
Design, Setting, and Participants Data for the period September 4, 2022, to January 31, 2023, were combined from 3 prospective US cohort studies (6 sites total) and used to estimate COVID-19 vaccine effectiveness among children and adolescents aged 5 to 17 years. A total of 2959 participants completed periodic surveys (demographics, household characteristics, chronic medical conditions, and COVID-19 symptoms) and submitted weekly self-collected nasal swabs (irrespective of symptoms); participants submitted additional nasal swabs at the onset of any symptoms.
Exposure Vaccination status was captured from the periodic surveys and supplemented with data from state immunization information systems and electronic medical records.
Main Outcome and Measures Respiratory swabs were tested for the presence of the SARS-CoV-2 virus using reverse transcriptase–polymerase chain reaction . SARS-CoV-2 infection was defined as a positive test regardless of symptoms. Symptomatic COVID-19 was defined as a positive test and 2 or more COVID-19 symptoms within 7 days of specimen collection. Cox proportional hazards models were used to estimate hazard ratios for SARS-CoV-2 infection and symptomatic COVID-19 among participants who received a bivalent COVID-19 vaccine dose vs participants who received no vaccine or monovalent vaccine doses only. Models were adjusted for age, sex, race, ethnicity, underlying health conditions, prior SARS-CoV-2 infection status, geographic site, proportion of circulating variants by site, and local virus prevalence.
Results Of the 2959 participants (47.8% were female; median age, 10.6 years [IQR, 8.0-13.2 years]; 64.6% were non-Hispanic White) included in this analysis, 25.4% received a bivalent COVID-19 vaccine dose. During the study period, 426 participants (14.4%) had laboratory-confirmed SARS-CoV-2 infection. Among these 426 participants, 184 (43.2%) had symptomatic COVID-19, 383 (89.9%) were not vaccinated or had received only monovalent COVID-19 vaccine doses (1.38 SARS-CoV-2 infections per 1000 person-days), and 43 (10.1%) had received a bivalent COVID-19 vaccine dose (0.84 SARS-CoV-2 infections per 1000 person-days). Bivalent vaccine effectiveness against SARS-CoV-2 infection was 54.0% (95% CI, 36.6%-69.1%) and vaccine effectiveness against symptomatic COVID-19 was 49.4% (95% CI, 22.2%-70.7%). The median observation time after vaccination was 276 days (IQR, 142-350 days) for participants who received only monovalent COVID-19 vaccine doses vs 50 days (IQR, 27-74 days) for those who received a bivalent COVID-19 vaccine dose.
Conclusion and Relevance The bivalent COVID-19 vaccines protected children and adolescents against SARS-CoV-2 infection and symptomatic COVID-19. These data demonstrate the benefit of COVID-19 vaccine in children and adolescents. All eligible children and adolescents should remain up to date with recommended COVID-19 vaccinations.
Although rates of SARS-CoV-2–related hospitalizations and death among children and adolescents are lower than rates in adults, 1 severe disease can still occur and lead to hospitalization, life-threatening complications (such as multisystem inflammatory syndrome in children), 2 - 5 and postinfection sequelae. 6 - 8 As of December 31, 2023, there have been at least 911 COVID-19–associated deaths among individuals aged 5 to 17 years in the US. 9
The Omicron variant was more transmissible and included lineages with greater potential to evade vaccine-induced immunity than previous variants. 10 - 12 To provide protection against the Omicron variant, the US Food and Drug Administration authorized use of the bivalent mRNA COVID-19 vaccine, which was composed of ancestral and Omicron BA.4/5 strains. 13 On September 1, 2022, the bivalent mRNA COVID-19 vaccine was recommended for persons aged 12 years or older (to be administered ≥2 months after completion of any monovalent primary series or monovalent booster dose authorized by the Food and Drug Administration), and on October 12, 2022, the bivalent COVID-19 vaccine was recommended for children aged 5 to 11 years. 14 , 15
Although data have shown that bivalent mRNA COVID-19 vaccination among adults is effective at reducing the risk of COVID-19, 16 - 20 including severe outcomes, limited data exist on the effectiveness of bivalent COVID-19 vaccine doses among children and adolescents. Available studies are limited by small sample size and a short duration of follow-up and reliance on voluntary testing. 21 , 22 Understanding how well children and adolescents are protected by a bivalent COVID-19 vaccine dose is important for informing public health strategies, especially in the context of updated vaccine formulations and emergence of new variants.
During a period in which the Omicron BA.4/5 sublineages and subsequent Omicron lineages were predominant, this analysis used merged data from 3 prospective cohort studies to estimate vaccine effectiveness of authorized COVID-19 bivalent vaccines against laboratory-confirmed SARS-CoV-2 infection and symptomatic COVID-19 among children and adolescents aged 5 to 17 years.
From September 4, 2022, to January 31, 2023, we conducted an analysis across 6 sites in the US to estimate COVID-19 vaccine effectiveness among children and adolescents aged 5 to 17 years by combining data from 3 prospective cohort studies (Pediatric Research Observing Trends and Exposures in COVID-19 Timelines [PROTECT], CASCADIA, and Community Vaccine Effectiveness [CoVE], which is an expansion of the Household Influenza Vaccine Evaluation [HIVE] cohort). 23 - 25 Children and adolescents living in Arizona, Michigan, Oregon, Texas, Utah, and Washington, including individuals from the same household, were eligible for inclusion.
Written informed consent was obtained from the parents or guardians of the enrolled children and assent was obtained from children and adolescents aged 7 to 17 years. This study was reviewed by the US Centers for Disease Control and Prevention and approved by the institutional review boards at participating sites, or under a reliance agreement with the Abt Associates institutional review board, and was conducted in a manner consistent with applicable federal law and policy of the Centers for Disease Control and Prevention. 26 - 30
Each participant or a parent or legal guardian (on behalf of the participant) completed an enrollment survey regarding demographics, household characteristics, chronic medical conditions, COVID-19 vaccination history, and prior SARS-CoV-2 infection. Participants were resurveyed at regular intervals to capture up-to-date demographic information.
As part of the demographic information, race and ethnicity were collected because vaccine uptake and risk of SARS-CoV-2 infection may vary by race and ethnicity. This information was reported by each participant or a parent or legal guardian using predefined race and ethnicity categories.
Blood specimens were collected from participants who consented to phlebotomy. Weekly surveillance was conducted for COVID-19 symptoms. Participants were asked to self-collect (performed by the parent, legal guardian, child, or adolescent) upper respiratory specimens weekly, irrespective of symptoms. To optimally capture all infections, participants were instructed to collect an additional respiratory specimen upon onset of symptoms if outside the timing of their regular weekly specimen collection (swab).
All respiratory specimens were tested for the presence of the SARS-CoV-2 virus using multiplex reverse transcriptase–polymerase chain reaction (RT-PCR) (eTable 1 in Supplement 1 ). Specimens that failed molecular testing due to contamination or that were misidentified or had a cycle threshold value in the inconclusive range were considered negative. Whole-genome sequencing was attempted on all SARS-CoV-2 infection–positive specimens with an adequate viral quantity in the CASCADIA and CoVE studies and on a representative subset in the PROTECT study. 31 - 34
Available serum specimens were tested for the presence of antinucleocapsid IgG using a qualitative IgG enzyme-linked immunosorbent assay or quantitative Meso Scale Discovery VPLEX assays (eTable 1 in Supplement 1 ). For the Meso Scale Discovery assay, antinucleocapsid IgG titers were compared with a standard curve provided by the manufacturer to determine titer quantity. Specimens below the lower limit of quantitation per assay insert were set to a value of half the lower limit. Per the assay insert, specimens were determined to have detectable antinucleocapsid IgG if they had a titer equal to or greater than 5000 AU/mL.
COVID-19 vaccination status was captured from enrollment, weekly, and monthly surveys (self-report); vaccine cards provided by the participant; and from queries of the state immunization information systems and electronic medical records when available. Vaccination data included vaccination dates, number of doses, and manufacturer. If discrepant information was recorded across multiple data sources, information from the electronic medical record and state immunization information systems was used preferentially over self-reported information.
SARS-CoV-2 infection was defined as a positive RT-PCR test regardless of symptoms. Symptomatic COVID-19 was defined as a positive RT-PCR test and 2 or more COVID-19 symptoms reported within 7 days before or after the specimen collection date. The surveyed list of COVID-19 symptoms varied by study cohort (eTable 2 in Supplement 1 ).
Prior SARS-CoV-2 infection was defined as a positive RT-PCR test from a specimen collected during study enrollment but before the start of the study period, self-report of infection prior to enrollment or start of the study period (whichever occurred later), or a positive antinucleocapsid SARS-CoV-2 antibody. Time since prior SARS-CoV-2 infection was defined as less than 4 months, 4 months to less than 6 months, 6 months to less than 12 months, 12 months or longer, and no prior infection. Dates of prior SARS-CoV-2 infection were imputed for 146 participants (4.9%) who only had serological results and, therefore, did not have dates associated with prior SARS-CoV-2 infection. Imputation was done using results from linear regression models, in which the baseline nucleocapsid blood draw date and the numeric nucleocapsid values served as the predictors for the date of prior infection among study participants with known prior infection dates (eMethods in Supplement 1 ).
Descriptive statistics comparing participants who had SARS-CoV-2 infection during the study period vs participants who remained uninfected included frequency (proportion) for categorical variables and median (IQR) for continuous variables. The P values were calculated using χ 2 tests for categorical variables and Wilcoxon tests for continuous variables at the .01 level. The Andersen-Gill extension of the Cox proportional hazards model with time-varying vaccination status was used to estimate the hazard ratios for first occurrence of SARS-CoV-2 infection in each participant, comparing participants who received a bivalent COVID-19 vaccine dose (>7 days after receipt) vs those who did not receive a bivalent COVID-19 vaccine dose (either unvaccinated or received monovalent COVID-19 vaccine doses only). 35
Multivariable models used L2 regularization to adjust for potential confounders, 36 specifically age, sex, race, ethnicity, underlying health conditions, time since prior SARS-CoV-2 infection, geographic site, 7-day average of COVID-19 cases per 100 000 by site (local incidence was modeled as a continuous linear variable), and proportion of circulating variants by site (categorized by those containing the spike substitution R346T). 37 The L2-regularized models used bootstrap resampling by household to estimate the 95% CIs and account for household clustering because 30.6% of households had 2 or more children and adolescents included in the analysis. 38
Person-time was calculated as the total number of days under surveillance for a given vaccination status during the study period. The study period started on September 4, 2022, for children and adolescents aged 12 to 17 years and on October 16, 2022, for children aged 5 to 11 years. Surveillance ended on the date of a participant’s first positive RT-PCR test result for SARS-CoV-2 infection, the participant’s study withdrawal date, 18th birthday, or at the end of the study period (January 31, 2023). For the participants who enrolled in 1 of the cohorts after the start of the study period, time at risk started at their enrollment or at 6 weeks after SARS-CoV-2 infection if recently infected prior to enrollment.
Surveillance weeks were not censored for missing specimen result (eg, participant skipped a weekly swab) or if there were problems with specimen testing. The 2 weeks after a monovalent COVID-19 primary vaccine dose and the week after bivalent and monovalent COVID-19 booster vaccine doses were excluded from person-time. COVID-19 vaccine effectiveness was calculated as vaccine effectiveness = (1 − hazard ratio) × 100.
In the primary analysis, the effectiveness of a dose of bivalent COVID-19 vaccine compared with no vaccine or monovalent only doses was estimated against laboratory-confirmed SARS-CoV-2 infection (inclusive of asymptomatic and symptomatic infections) and symptomatic COVID-19. For the outcome of laboratory-confirmed SARS-CoV-2 infection, the estimates were also stratified by age group (5-11 years and 12-17 years) and prior SARS-CoV-2 infection status. In a secondary analysis, the effectiveness of bivalent COVID-19 vaccine was estimated stratified by time since bivalent vaccination (7-60 days or 61-150 days) compared with no vaccine or monovalent doses received 180 or more days ago.
Two sensitivity analyses for vaccine effectiveness were conducted. The first analysis restricted the reference category to only participants who received a monovalent COVID-19 vaccine dose. The second analysis restricted to only participants from the Arizona study sites because they constituted 52% of the study population and had low coverage for the bivalent COVID-19 vaccine.
All analyses were conducted using SAS software version 9.4 (SAS Institute Inc) or R software version 4.1.2 (R Foundation for Statistical Computing).
Between September 4, 2022, and January 31, 2023, a total of 2959 participants were included in the analyses ( Table 1 ). The median adherence to weekly upper respiratory specimen collection (swabbing) throughout the study period was 93.8% (IQR, 84%-100%). Overall, 47.8% of the participants were female, the median age was 10.6 years (IQR, 8.0-13.2 years), the majority were non-Hispanic White (64.6%), 25.4% had received a bivalent COVID-19 vaccine dose, and 61.7% had self-reported or confirmed SARS-CoV-2 infection prior to the study period ( Table 1 ).
During the study period, 426 participants (14.4%) had a laboratory-confirmed SARS-CoV-2 infection (eTable 3 in Supplement 1 ); of those with SARS-CoV-2 infection, 184 (43.2%) had symptomatic COVID-19 ( Table 1 ). Participants living in Michigan (20.2%; 24/119) and those without documented prior SARS-CoV-2 infection (22.5%; 255/1134) had the highest proportion of in-study SARS-CoV-2 infection. Of the 426 participants with SARS-CoV-2 infection, 238 (56.0%) had genetic sequencing results. Of the 238 participants with genetic sequencing results, the most prevalent lineages were BA.4 or BA.5 (50.0%), BQ.1.1 (36.5%), XBB (5.9%), and BA.2 (3.8%) (eFigure in Supplement 1 ).
Participants living in Oregon had the highest uptake of bivalent COVID-19 vaccine (56.2%; 246/438), whereas those living in Texas had the lowest (2.4%; 3/124). Participants reporting Hispanic ethnicity had lower bivalent COVID-19 vaccine uptake (17.1%; 87/509) compared with non-Hispanic participants of all races (27.1%; 665/2450). Participants with 1 or more chronic medical conditions had higher uptake of bivalent COVID-19 vaccine (34.5%; 154/447) compared with those without a chronic medical condition (23.8%; 598/2512). Of the 2207 participants who did not receive a bivalent COVID-19 vaccine dose, 535 (24.2%) were unvaccinated and 1672 (75.8%) received at least 1 monovalent COVID-19 vaccine dose.
Of the 426 participants with SARS-CoV-2 infection, 383 (89.9%) were either unvaccinated or received monovalent COVID-19 vaccine doses only (1.38 infections per 1000 person-days) and 43 (10.1%) received a bivalent COVID-19 vaccine dose (0.84 infections per 1000 person-days) ( Table 2 ). Compared with being unvaccinated or receiving only monovalent COVID-19 vaccine doses, the adjusted vaccine effectiveness of a bivalent COVID-19 vaccine dose was 54.0% (95% CI, 36.6%-69.1%) against laboratory-confirmed SARS-CoV-2 infection ( Table 2 ). The median number of observation days after COVID-19 vaccination was 276 (IQR, 142-350 days) for those who received any monovalent COVID-19 vaccine doses and 50 (IQR, 27-74 days) for those who received a bivalent COVID-19 vaccine dose.
When stratified by age, the adjusted bivalent COVID-19 vaccine effectiveness was 58.3% (95% CI, 34.0%-76.5%) for children aged 5 to 11 years and 47.5% (95% CI, 18.2%-71.9%) for children and adolescents aged 12 to 17 years ( Table 3 ). Among children aged 5 to 11 years, the median number of observation days after COVID-19 vaccination was 221 (IQR, 140-349 days) for those who received any monovalent COVID-19 vaccine doses and 44 (IQR, 24-66 days) for those who received a bivalent COVID-19 vaccine dose. Among children and adolescents aged 12 to 17 years, the median number of observation days after COVID-19 vaccination was 313 (IQR, 241-404 days) for those who received any monovalent COVID-19 vaccine doses and 59 (IQR, 32-87 days) for those who received a bivalent COVID-19 vaccine dose.
Of the 184 participants with symptomatic COVID-19, 164 (89.1%) were either unvaccinated or received monovalent COVID-19 vaccine doses only (0.59 infections per 1000 person-days) and 20 (10.9%) received a bivalent COVID-19 vaccine dose (0.39 infections per 1000 person-days) ( Table 2 ). The adjusted vaccine effectiveness of a bivalent COVID-19 vaccine dose against symptomatic COVID-19 was 49.4% (95% CI, 22.2%-70.7%). Among participants with symptomatic COVID-19, the median number of observation days after vaccination was 276 (IQR, 142-350 days) for those who received any monovalent COVID-19 vaccine doses and 50 (IQR, 27-74 days) for those who received a bivalent COVID-19 vaccine dose.
Compared with participants who did not receive the COVID-19 vaccine or received monovalent only doses 180 days or more ago, the adjusted vaccine effectiveness of a bivalent COVID-19 vaccine dose against SARS-CoV-2 infection was 51.3% (95% CI, 23.6%-71.9%) 7 to 60 days after vaccination and was 62.4% (95% CI, 38.5%-81.1%) 61 to 150 days after vaccination. The median number of observation days after vaccination was 350 (IQR, 303-392 days) for monovalent COVID-19 vaccine doses administered 180 days or more ago, 34 (IQR, 20-47 days) for a bivalent COVID-19 vaccine dose administered 7 to 60 days ago, and 81 (IQR, 70-95 days) for a bivalent COVID-19 vaccine dose administered 61 to 150 days ago.
Among participants who had prior SARS-CoV-2 infection before the start of the study, the adjusted effectiveness of bivalent COVID-19 vaccine against SARS-CoV-2 infection was 63.6% (95% CI, 33.0%-84.0%) ( Table 3 ). Among participants with no prior SARS-CoV-2 infection, COVID-19 vaccine effectiveness was 47.2% (95% CI, 26.7%-67.8%) ( Table 3 ). Among participants with prior SARS-CoV-2 infection, the median number of observation days after COVID-19 vaccination was 288 (IQR, 156-357 days) for monovalent doses and 47 (IQR, 25-71 days) for a bivalent dose. Among participants without prior SARS-CoV-2 infection, the median number of observation days after COVID-19 vaccination was 241 (IQR, 127-334 days) for monovalent doses and 54 (IQR, 29-78 days) for a bivalent dose.
In a sensitivity analysis restricting the reference group to persons who had received at least 1 dose of monovalent COVID-19 vaccine (ie, excluding unvaccinated individuals), the adjusted vaccine effectiveness of bivalent COVID-19 vaccine against SARS-CoV-2 infection was 56.3% (95% CI, 40.5%-70.1%) and was 51.1% (95% CI, 26.9%-72.1%) against symptomatic COVID-19 ( Table 2 ). In a subsequent sensitivity analysis restricted to participants from the Arizona study site, the adjusted bivalent COVID-19 vaccine effectiveness was 51.5% (95% CI, 20.3%-77.2%) (eTable 4 in Supplement 1 ).
In this analysis of data from 3 prospective cohort studies in the US, children and adolescents aged 5 to 17 years who received an mRNA bivalent COVID-19 vaccine dose were less likely to be infected with SARS-CoV-2 than those who were unvaccinated or who received only monovalent COVID-19 vaccine doses. The vaccine effectiveness of a bivalent COVID-19 vaccine dose against SARS-CoV-2 infection was not significantly different when stratified by age group (5-11 years vs 12-17 years).
There was no observed waning 61 to 150 days after receipt of a bivalent COVID-19 vaccine dose, although there may not have been sufficient follow-up time to assess waning. Nevertheless, these results suggest that, during a period when the Omicron BA.4/5 sublineages were the predominant circulating variants, bivalent COVID-19 vaccines provided protection against SARS-CoV-2 infection and symptomatic COVID-19 among children and adolescents.
We conducted several sensitivity analyses to address potential confounding, including using an alternative reference category and restricting the analysis only to participants from the Arizona study site because they constituted half of all study participants. We found the bivalent COVID-19 vaccine effectiveness estimates from these analyses to be consistent with the overall estimate. We also examined COVID-19 vaccine effectiveness by prior SARS-CoV-2 infection status to determine whether hybrid immunity from both vaccination and prior infection provided greater protection than COVID-19 vaccination alone. 39 , 40 Even though the bivalent COVID-19 vaccine effectiveness estimate among those with reported SARS-CoV-2 infection or with evidence of prior SARS-CoV-2 infection was higher than among those without prior SARS-CoV-2 infection, the difference was not statistically significant.
These findings are consistent with the limited other data available on protection provided by the bivalent vaccine for children and adolescents. In a study by Lin et al 21 among children aged 5 to 11 years, effectiveness of the bivalent COVID-19 vaccine 2 months after receipt was 47.3% (95% CI, −17.9% to 76.4%). The estimate for vaccine effectiveness 1 month after receipt of a bivalent COVID-19 vaccine dose (76.7% [95% CI, 45.7 to 90.0]) by Lin et al 21 was higher than the estimate (51.3% [95% CI, 23.6% to 71.9%]) in the current study for those who received a bivalent COVID-19 vaccine dose within 7 to 60 days. However, the 95% CIs overlap, and the difference in vaccine effectiveness may be due to different sites and study periods.
In addition, the current multistate study followed up participants through January 31, 2023, whereas Lin et al 21 followed up North Carolina residents until January 6, 2023. National surveillance data 37 show increased circulation of variants other than BA.4/5 during those 4 weeks, and it is possible that the bivalent COVID-19 vaccine may not be as protective against those variants (eg, XBB), thus decreasing the vaccine effectiveness estimate for the entire study period.
This study had many strengths, including almost 3000 participants enrolled from 6 diverse sites across multiple states in the US. Participants collected weekly swabs regardless of symptoms, which greatly reduces the risk of missing an asymptomatic SARS-CoV-2 infection, and adherence to weekly swabbing was high (median, 94%). Weekly and quarterly surveys, as well as data from the state immunization information systems and electronic medical records, ensured detailed and complete information on potential confounding variables and vaccination status. Although there was no observed waning 61 to 150 days after receipt of the bivalent COVID-19 vaccine dose, the 95% CIs were wide because of small sample size and this analysis could not examine vaccine waning beyond 150 days. The continuation of the participant cohorts will present future opportunities for examination of longer-term waning patterns to support future vaccine decision-making.
There are several important limitations of this study. First, RT-PCR testing methods and the list of COVID-19 symptoms surveyed varied by cohort; therefore, some differences in the definition of SARS-CoV-2 infection or symptomatic COVID-19 may be present.
Second, weekly or symptomatic RT-PCR testing prior to the analytic study start date for estimation of prior SARS-CoV-2 infection history was only available among a subset of participants. To address this concern, we incorporated serological data to identify additional prior SARS-CoV-2 infections. The sensitivity and specificity of the serological assays varied by cohort site and, due to antinucleocapsid SARS-CoV-2 antibody waning, the assays may not have detected some prior infections.
Third, social desirability or recall bias may have affected self- or parent-report of prior SARS-CoV-2 infection when RT-PCR and serological test results were unavailable, and self- or parent-reported vaccination status when data were unavailable from the state immunization information systems and electronic medical records.
Fourth, our analysis did not account for the social vulnerability index and immunocompromised status, which may be associated with vaccine uptake and risk of SARS-CoV-2 infection.
Fifth, limited sample sizes resulted in imprecise subgroup estimates and precluded us from examining vaccine effectiveness against symptomatic COVID-19 and vaccine waning by age group.
The bivalent COVID-19 vaccine protected children and adolescents against SARS-CoV-2 infection and symptomatic COVID-19. These data demonstrate the benefit of COVID-19 vaccine in children and adolescents. All eligible children and adolescents should remain up to date with recommended COVID-19 vaccinations.
Accepted for Publication: December 11, 2023.
Corresponding Author: Leora R. Feldstein, PhD, US Centers for Disease Control and Prevention, 1600 Clifton Rd NE, Atlanta, GA 30329 ( [email protected] ).
Author Contributions: Drs Feldstein and Britton had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Feldstein, Britton, Grant, Wiegand, Babu, Briggs Hagen, Burgess, Caban-Martinez, Chu, Englund, Hegmann, Lutrick, Martin, Meece, Midgley, Monto, Phillips, Saydah, Smith, Vandermeer, Yoon, Naleway.
Acquisition, analysis, or interpretation of data: Feldstein, Britton, Grant, Wiegand, Ruffin, Babu, Briggs Hagen, Burgess, Caban-Martinez, Chu, Ellingson, Englund, Hegmann, Jeddy, Lauring, Martin, Mathenge, Meece, Midgley, Monto, Newes-Adeyi, Odame-Bamfo, Olsho, Phillips, Rai, Saydah, Steinhardt, Tyner, Vaughan, Yoon, Gaglani, Naleway.
Drafting of the manuscript: Feldstein, Britton, Wiegand, Babu, Hegmann, Martin, Vandermeer.
Critical review of the manuscript for important intellectual content: Feldstein, Britton, Grant, Wiegand, Ruffin, Babu, Briggs Hagen, Burgess, Caban-Martinez, Chu, Ellingson, Englund, Hegmann, Jeddy, Lauring, Lutrick, Martin, Mathenge, Meece, Midgley, Monto, Newes-Adeyi, Odame-Bamfo, Olsho, Phillips, Rai, Saydah, Smith, Steinhardt, Tyner, Vaughan, Yoon, Gaglani, Naleway.
Statistical analysis: Feldstein, Grant, Wiegand, Odame-Bamfo, Smith.
Obtained funding: Briggs Hagen, Burgess, Chu, Englund, Lutrick, Martin, Midgley, Olsho, Phillips, Yoon.
Administrative, technical, or material support: Feldstein, Britton, Ruffin, Caban-Martinez, Chu, Ellingson, Englund, Hegmann, Jeddy, Lauring, Martin, Meece, Midgley, Monto, Newes-Adeyi, Olsho, Phillips, Rai, Steinhardt, Vandermeer, Vaughan, Yoon.
Supervision: Feldstein, Britton, Briggs Hagen, Burgess, Chu, Englund, Hegmann, Jeddy, Martin, Meece, Olsho, Phillips, Yoon, Gaglani.
Conflict of Interest Disclosures: Dr Caban-Martinez reported receiving grants from the Florida Firefighter Cancer Initiative and the Florida Department of Health. Dr Chu reported receiving personal fees from AbbVie, Vindico, Ellume, Medscape, Merck, Clinical Care Options, Cataylst Medical Education, Vir, Pfizer, and Prime Education. Dr Englund reported receiving personal fees from AbbVie, AstraZeneca, Merck, Meissa Vaccines, Moderna, Sanofi Pasteur, Pfizer, Ark Biopharma, GSK (formerly GlaxoSmithKline), and Shinogi. Dr Hegmann reported being the editor of the American College of Occupational and Environmental Medicine practice guidelines. Ms Jeddy reported being an employee of Abt Associates. Dr Lauring reported receiving personal fees from Roche and Sanofi and receiving grants from the Flu Lab and the Burroughs Wellcome Fund. Dr Martin reported receiving grants from Merck. Dr Monto reported receiving personal fees from Roche. Dr Newes-Adeyi reported being an employee of Abt Associates. Dr Olsho reported being an employee of Abt Associates and a study participant in CASCADIA. Dr Phillips reported receiving personal fees from Novavax. Ms Rai reported being an employee of Abt Associates. Dr Vaughan reported being an employee of Abt Associates. Dr Yoon reported receiving personal fees from Novavax. Dr Gaglani reported serving as co-chair of the infectious diseases and immunization committee and the respiratory syncytial virus taskforce lead for the Texas Pediatric Society and the Texas Chapter of the American Academy of Pediatrics. No other disclosures were reported.
Funding/Support: This study was supported by the National Center for Immunization and Respiratory Diseases, US Centers for Disease Control and Prevention under contracts 75D30121C12297 (Kaiser Foundation Hospitals), 75D30122C13149 (University of Michigan), 75D30120C08150 (Abt Associates Inc), and 75D30122C14188 (University of Arizona) and by the National Institute of Allergy and Infectious Diseases (contract 75N93021C00015).
Role of the Funder/Sponsor: The US Centers for Disease Control and Prevention, but not the National Institute of Allergy and Infectious Diseases, collaborated with partner sites to design and conduct the study; managed, analyzed, and interpreted the data; prepared, reviewed, and approved the manuscript; and had a role in the decision to submit the manuscript for publication.
Disclaimer: The findings and conclusions are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention.
Data Sharing Statement: See Supplement 2 .
Additional Contributions: There is an extensive list of additional contributions listed in the eContributions section in Supplement 1 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

IMAGES
VIDEO
COMMENTS
The PhD program in epidemiology and clinical research will provide methodologic and interdisciplinary training that will equip students to carry out cutting-edge epidemiologic research. The program trains students in the tools of modern epidemiology, with heavy emphases on statistics, computer science, genetics, genomics, and bioinformatics.
The Harvard/MIT MD-PhD Program at Harvard Medical School (HMS) has been sponsored in part by the National Institutes of Health (NIH) through its Medical Scientist Training Program (MSTP) since 1974. All MD-PhD student applicants to our program compete on equal footing for MSTP support, regardless of scientific interest.
There are nine HMS-based PhD programs. Students in these programs are all enrolled in the Graduate School of Arts and Sciences (GSAS): Biomedical Informatics. Biological and Biomedical Sciences ... The Division of Medical Sciences is the administrative centralized home for all Harvard PhD students located at HMS. There are many resources ...
The average MD-PhD program length, according to the AAMC report, is eight years. So, in attending an MD-PhD program, you're doubling your time in medical school. When factoring in residency training and, for those who have aims on fellowship, an MD-PhD student's training can extend well beyond a decade. "The best advice I got was once you ...
Yale University, School of Medicine. Investigative Medicine Program. Yale School of Medicine is well-known for its eminent faculty and one of the world's largest medical libraries. This PhD program specializes in investigative medicine, allowing you to develop high-level creative and analytical skills.
Before You Apply. The MD-PhD Program seeks students with a deep passion and commitment to a dual physician-scientist career. Our admissions process assesses the potential of our applicants to become physician-scientist leaders who are committed to both providing compassionate, cutting-edge patient care and expanding the boundaries of biomedical ...
Diversity and inclusion are central to the mission of the Yale MD-PhD Program. By fostering diversity of persons, groups, views and academic disciplines, we strive to enrich academic discourse and create a welcoming, vibrant community. As students and faculty who value diversity and inclusion, we are committed to enacting these values in our ...
Mailing Address. M.D./Ph.D. Program. UConn Health. 263 Farmington Avenue. Farmington, CT 06030-3906. Email: [email protected]. UConn's combined M.D./Ph.D. program provides students with a highly integrated educational experience leading to completion of both the M.D. and Ph.D. degrees. Students pursue intensive thesis research in one of seven ...
According to a study of MD-PhD program outcomes, nearly 80 percent of graduates are following career paths consistent with the goals of their training, including working as full-time faculty in academic medical centers or for the NIH, research institutes, industry, and federal agencies. Those in academia spend between 50 and 80 percent of their ...
MD-PhD The Harvard/MIT MD-PhD Program at Harvard Medical School (HMS), sponsored primarily by the National Institutes of Health (NIH) through its Medical Scientist Training Program (MSTP) since 1974, provides fellowship support for selected and highly qualified students who have elected to pursue both the MD and PhD degrees. The overall mission is to train the next generation of premier and ...
Icahn Mount Sinai offers three PhD programs to choose from—and endless research opportunities. Explore your next step now. Our PhD in Biomedical Sciences is highly personalized, preparing you to succeed as an independent researcher in your choice of seven multidisciplinary training areas, including artificial intelligence, immunology, cancer ...
The MD-PhD Program at the Icahn School of Medicine at Mount Sinai prepares you for a thriving career as a physician-scientist. In our highly personalized, National Institutes of Health (NIH)-funded Medical Scientist Training Program (MSTP), you select your own multidisciplinary training area in Biomedical Sciences or Neuroscience, corresponding curriculum, and thesis research preceptor.
Elias (Eli) Wisdom. Undergraduate: Pacific University, Oregon Major: BS, Biology Medical school: Oregon Health & Science University (OHSU) Anticipated Graduation Year: 2028 Bio: Eli Wisdom is an MD-PhD student at Oregon Health & Science University (OHSU) studying the molecular mechanisms of Parkinson's Disease. He grew up in the small rural town of La Grande, Oregon, where he gained a deep ...
The objectives of the PhD in Epidemiology program are to train students to master current quantitative methods, obtain broad knowledge of major human disease epidemiology, and become expert in a specific disease or health status topic. The 28-credit (minimum) PhD in Epidemiology program is offered primarily as a full-time degree program, and ...
Our office is located in the Study Departement Building of the Medical University Vienna at the following address: Währinger Straße 25a. A-1090 Vienna, Austria. Contact for general inquiries. Dieter Breitenbaum. Vesna Dominkovic. P: +43 (0)1 40160-21029. P: +43 (0)1 40160-21030. Contact for PhD Call recruiting.
With over 150 universities featured in international rankings, the U.S. has some of the best business schools, medical schools, and engineering schools. Universities and colleges in the U.S. are well known for academic flexibility and ways to customize your study experience with optional studies and extracurricular activities.
How is HST's MEMP PhD program different from other PhD programs? As a MEMP student, you'll choose one of 11 technical concentrations and design an individualized curriculum to ground yourself in the foundations of that discipline. You'll study medical sciences alongside MD students and become fluent in the language and culture of medicine ...
PhD in Medicine. Doctoral studies are carried out by science postgraduates, medical students combining clinical training with the PhD, and clinically qualified doctors undertaking scientific training. The research covers the whole spectrum of medical science from basic biology to clinical therapies.
The MD-PhD is oriented exclusively toward Master students and graduates of degree courses in human medicine, veterinary medicine or dentistry. The MD-PhD program can be entered as MD-PhD Track I in parallel to the medical Master studies at UZH. Applicants to the Track II program must hold a Master's degree from a university in human medicine ...
The Medical Scientist Training Program at Baylor College of Medicine is designed for highly motivated students. The successful applicant should have both an excellent scholastic record and sustained potential in research. Exposure to both laboratory bench work and clinical care in private practice, academic medicine or emergency room experience ...
The Doctor of Medicine-Doctor of Philosophy (MD-PhD) is a dual doctoral program for physician-scientists, combining the professional training of the Doctor of Medicine degree with the research program of the Doctor of Philosophy degree.. In the United States, the National Institutes of Health currently provides 50 medical schools with Medical Scientist Training Program grants that ...
Over 200 postgraduate students are enrolled on our PhD programme at any given time. ... Our clinical mission is to provide the highest quality medical care, as practitioners of medicine and leaders of the NHS, and to work in partnership with patients to fulfil our research and teaching missions. The Division's clinical academics are active as ...
Our institute is a major center for fundamental research at the intersection of chemistry, physics, biology and material sciences. We strive to create knowledge with long-term relevance to basic medical science, focusing on molecular and cellular mechanisms and structures. Our institute enjoys worldwide recognition and is headed by scientists ...
Lloyd Minor addresses the new cohort of PhD students. Steve Fisch One hundred and thirty-six students — in 16 specialties, from health policy and structural biology to epidemiology and genetics — eagerly pushed their arms through the sleeves of crisp white lab coats embroidered with their name and their field of study.
Tajie Harris, PhD, Awarded $2.6 Million to Study How the Immune System Benefits the Brain September 5, 2024 by [email protected] | Leave a Comment Congrats to Tajie Harris, who was awarded a five-year $2.6 million grant from the National Institute of Neurological Disorders and Stroke, titled "Caspase-8 mediated control of CNS infection."
PhD Student in Machine Learning for Medical Image Analysis, Medical University of Vienna (Austria) PhD Student in observational cosmology, University of Iceland (Iceland) PhD Student in developing battery digitalisation methods for parameter identification, NTNU_Norwegian University of Science and Technology (Norway)
Key Points. Question What is the effectiveness of the bivalent COVID-19 vaccines among children and adolescents aged 5 to 17 years?. Findings In this prospective cohort study including 2959 participants aged 5 to 17 years, vaccine effectiveness against laboratory-confirmed SARS-CoV-2 infection was 54.0% and vaccine effectiveness against symptomatic COVID-19 was 49.4%.