- Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- HIV and AIDS
- Hypertension
- Mental disorders
- Top 10 causes of death
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- Data collection tools
- Global Health Observatory
- Insights and visualizations
- COVID excess deaths
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal

Impact of COVID-19 on people's livelihoods, their health and our food systems
Joint statement by ilo, fao, ifad and who.
The COVID-19 pandemic has led to a dramatic loss of human life worldwide and presents an unprecedented challenge to public health, food systems and the world of work. The economic and social disruption caused by the pandemic is devastating: tens of millions of people are at risk of falling into extreme poverty, while the number of undernourished people, currently estimated at nearly 690 million, could increase by up to 132 million by the end of the year.
Millions of enterprises face an existential threat. Nearly half of the world’s 3.3 billion global workforce are at risk of losing their livelihoods. Informal economy workers are particularly vulnerable because the majority lack social protection and access to quality health care and have lost access to productive assets. Without the means to earn an income during lockdowns, many are unable to feed themselves and their families. For most, no income means no food, or, at best, less food and less nutritious food.
The pandemic has been affecting the entire food system and has laid bare its fragility. Border closures, trade restrictions and confinement measures have been preventing farmers from accessing markets, including for buying inputs and selling their produce, and agricultural workers from harvesting crops, thus disrupting domestic and international food supply chains and reducing access to healthy, safe and diverse diets. The pandemic has decimated jobs and placed millions of livelihoods at risk. As breadwinners lose jobs, fall ill and die, the food security and nutrition of millions of women and men are under threat, with those in low-income countries, particularly the most marginalized populations, which include small-scale farmers and indigenous peoples, being hardest hit.
Millions of agricultural workers – waged and self-employed – while feeding the world, regularly face high levels of working poverty, malnutrition and poor health, and suffer from a lack of safety and labour protection as well as other types of abuse. With low and irregular incomes and a lack of social support, many of them are spurred to continue working, often in unsafe conditions, thus exposing themselves and their families to additional risks. Further, when experiencing income losses, they may resort to negative coping strategies, such as distress sale of assets, predatory loans or child labour. Migrant agricultural workers are particularly vulnerable, because they face risks in their transport, working and living conditions and struggle to access support measures put in place by governments. Guaranteeing the safety and health of all agri-food workers – from primary producers to those involved in food processing, transport and retail, including street food vendors – as well as better incomes and protection, will be critical to saving lives and protecting public health, people’s livelihoods and food security.
In the COVID-19 crisis food security, public health, and employment and labour issues, in particular workers’ health and safety, converge. Adhering to workplace safety and health practices and ensuring access to decent work and the protection of labour rights in all industries will be crucial in addressing the human dimension of the crisis. Immediate and purposeful action to save lives and livelihoods should include extending social protection towards universal health coverage and income support for those most affected. These include workers in the informal economy and in poorly protected and low-paid jobs, including youth, older workers, and migrants. Particular attention must be paid to the situation of women, who are over-represented in low-paid jobs and care roles. Different forms of support are key, including cash transfers, child allowances and healthy school meals, shelter and food relief initiatives, support for employment retention and recovery, and financial relief for businesses, including micro, small and medium-sized enterprises. In designing and implementing such measures it is essential that governments work closely with employers and workers.
Countries dealing with existing humanitarian crises or emergencies are particularly exposed to the effects of COVID-19. Responding swiftly to the pandemic, while ensuring that humanitarian and recovery assistance reaches those most in need, is critical.
Now is the time for global solidarity and support, especially with the most vulnerable in our societies, particularly in the emerging and developing world. Only together can we overcome the intertwined health and social and economic impacts of the pandemic and prevent its escalation into a protracted humanitarian and food security catastrophe, with the potential loss of already achieved development gains.
We must recognize this opportunity to build back better, as noted in the Policy Brief issued by the United Nations Secretary-General. We are committed to pooling our expertise and experience to support countries in their crisis response measures and efforts to achieve the Sustainable Development Goals. We need to develop long-term sustainable strategies to address the challenges facing the health and agri-food sectors. Priority should be given to addressing underlying food security and malnutrition challenges, tackling rural poverty, in particular through more and better jobs in the rural economy, extending social protection to all, facilitating safe migration pathways and promoting the formalization of the informal economy.
We must rethink the future of our environment and tackle climate change and environmental degradation with ambition and urgency. Only then can we protect the health, livelihoods, food security and nutrition of all people, and ensure that our ‘new normal’ is a better one.
Media Contacts
Kimberly Chriscaden
Communications Officer World Health Organization
Nutrition and Food Safety (NFS) and COVID-19
- Share full article
Advertisement
Supported by
student opinion
How Is the Coronavirus Outbreak Affecting Your Life?
How are you staying connected and sane in a time of social distancing?

By Jeremy Engle
Find all our Student Opinion questions here.
Note: The Times Opinion section is working on an article about how the coronavirus outbreak has disrupted the lives of high school students. To share your story, fill out this form .
The coronavirus has changed how we work , play and learn : Schools are closing, sports leagues have been canceled, and many people have been asked to work from home.
On March 16, the Trump administration released new guidelines to slow the spread of the coronavirus, including closing schools and avoiding groups of more than 10 people, discretionary travel, bars, restaurants and food courts.
How are you dealing with these sudden and dramatic changes to how we live? Are you practicing social distancing — and are you even sure what that really means?
In “ Wondering About Social Distancing? ” Apoorva Mandavilli explains the term and offers practical guidance from experts:
What is social distancing? Put simply, the idea is to maintain a distance between you and other people — in this case, at least six feet. That also means minimizing contact with people. Avoid public transportation whenever possible, limit nonessential travel, work from home and skip social gatherings — and definitely do not go to crowded bars and sporting arenas. “Every single reduction in the number of contacts you have per day with relatives, with friends, co-workers, in school will have a significant impact on the ability of the virus to spread in the population,” said Dr. Gerardo Chowell, chair of population health sciences at Georgia State University. This strategy saved thousands of lives both during the Spanish flu pandemic of 1918 and, more recently, in Mexico City during the 2009 flu pandemic.
The article continues with expert responses to some common questions about social distancing. Here are excerpts from three:
I’m young and don’t have any risk factors. Can I continue to socialize? Please don’t. There is no question that older people and those with underlying health conditions are most vulnerable to the virus, but young people are by no means immune. And there is a greater public health imperative. Even people who show only mild symptoms may pass the virus to many, many others — particularly in the early course of the infection, before they even realize they are sick. So you might keep the chain of infection going right to your own older or high-risk relatives. You may also contribute to the number of people infected, causing the pandemic to grow rapidly and overwhelm the health care system. If you ignore the guidance on social distancing, you will essentially put yourself and everyone else at much higher risk. Experts acknowledged that social distancing is tough, especially for young people who are used to gathering in groups. But even cutting down the number of gatherings, and the number of people in any group, will help. Can I leave my house? Absolutely. The experts were unanimous in their answer to this question. It’s O.K. to go outdoors for fresh air and exercise — to walk your dog, go for a hike or ride your bicycle, for example. The point is not to remain indoors, but to avoid being in close contact with people. You may also need to leave the house for medicines or other essential resources. But there are things you can do to keep yourself and others safe during and after these excursions. When you do leave your home, wipe down any surfaces you come into contact with, disinfect your hands with an alcohol-based sanitizer and avoid touching your face. Above all, frequently wash your hands — especially whenever you come in from outside, before you eat or before you’re in contact with the very old or very young. How long will we need to practice social distancing? That is a big unknown, experts said. A lot will depend on how well the social distancing measures in place work and how much we can slow the pandemic down. But prepare to hunker down for at least a month, and possibly much longer. In Seattle, the recommendations on social distancing have continued to escalate with the number of infections and deaths, and as the health system has become increasingly strained. “For now, it’s probably indefinite,” Dr. Marrazzo said. “We’re in uncharted territory.”
Abdullah Shihipar writes in an Opinion essay, “ Coronavirus and the Isolation Paradox ,” that while social distancing is required to prevent infection, loneliness can make us sick:
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
8 Lessons We Can Learn From the COVID-19 Pandemic
BY KATHY KATELLA May 14, 2021

Note: Information in this article was accurate at the time of original publication. Because information about COVID-19 changes rapidly, we encourage you to visit the websites of the Centers for Disease Control & Prevention (CDC), World Health Organization (WHO), and your state and local government for the latest information.
The COVID-19 pandemic changed life as we know it—and it may have changed us individually as well, from our morning routines to our life goals and priorities. Many say the world has changed forever. But this coming year, if the vaccines drive down infections and variants are kept at bay, life could return to some form of normal. At that point, what will we glean from the past year? Are there silver linings or lessons learned?
“Humanity's memory is short, and what is not ever-present fades quickly,” says Manisha Juthani, MD , a Yale Medicine infectious diseases specialist. The bubonic plague, for example, ravaged Europe in the Middle Ages—resurfacing again and again—but once it was under control, people started to forget about it, she says. “So, I would say one major lesson from a public health or infectious disease perspective is that it’s important to remember and recognize our history. This is a period we must remember.”
We asked our Yale Medicine experts to weigh in on what they think are lessons worth remembering, including those that might help us survive a future virus or nurture a resilience that could help with life in general.
Lesson 1: Masks are useful tools
What happened: The Centers for Disease Control and Prevention (CDC) relaxed its masking guidance for those who have been fully vaccinated. But when the pandemic began, it necessitated a global effort to ensure that everyone practiced behaviors to keep themselves healthy and safe—and keep others healthy as well. This included the widespread wearing of masks indoors and outside.
What we’ve learned: Not everyone practiced preventive measures such as mask wearing, maintaining a 6-foot distance, and washing hands frequently. But, Dr. Juthani says, “I do think many people have learned a whole lot about respiratory pathogens and viruses, and how they spread from one person to another, and that sort of old-school common sense—you know, if you don’t feel well—whether it’s COVID-19 or not—you don’t go to the party. You stay home.”
Masks are a case in point. They are a key COVID-19 prevention strategy because they provide a barrier that can keep respiratory droplets from spreading. Mask-wearing became more common across East Asia after the 2003 SARS outbreak in that part of the world. “There are many East Asian cultures where the practice is still that if you have a cold or a runny nose, you put on a mask,” Dr. Juthani says.
She hopes attitudes in the U.S. will shift in that direction after COVID-19. “I have heard from a number of people who are amazed that we've had no flu this year—and they know masks are one of the reasons,” she says. “They’ve told me, ‘When the winter comes around, if I'm going out to the grocery store, I may just put on a mask.’”
Lesson 2: Telehealth might become the new normal
What happened: Doctors and patients who have used telehealth (technology that allows them to conduct medical care remotely), found it can work well for certain appointments, ranging from cardiology check-ups to therapy for a mental health condition. Many patients who needed a medical test have also discovered it may be possible to substitute a home version.
What we’ve learned: While there are still problems for which you need to see a doctor in person, the pandemic introduced a new urgency to what had been a gradual switchover to platforms like Zoom for remote patient visits.
More doctors also encouraged patients to track their blood pressure at home , and to use at-home equipment for such purposes as diagnosing sleep apnea and even testing for colon cancer . Doctors also can fine-tune cochlear implants remotely .
“It happened very quickly,” says Sharon Stoll, DO, a neurologist. One group that has benefitted is patients who live far away, sometimes in other parts of the country—or even the world, she says. “I always like to see my patients at least twice a year. Now, we can see each other in person once a year, and if issues come up, we can schedule a telehealth visit in-between,” Dr. Stoll says. “This way I may hear about an issue before it becomes a problem, because my patients have easier access to me, and I have easier access to them.”
Meanwhile, insurers are becoming more likely to cover telehealth, Dr. Stoll adds. “That is a silver lining that will hopefully continue.”
Lesson 3: Vaccines are powerful tools
What happened: Given the recent positive results from vaccine trials, once again vaccines are proving to be powerful for preventing disease.
What we’ve learned: Vaccines really are worth getting, says Dr. Stoll, who had COVID-19 and experienced lingering symptoms, including chronic headaches . “I have lots of conversations—and sometimes arguments—with people about vaccines,” she says. Some don’t like the idea of side effects. “I had vaccine side effects and I’ve had COVID-19 side effects, and I say nothing compares to the actual illness. Unfortunately, I speak from experience.”
Dr. Juthani hopes the COVID-19 vaccine spotlight will motivate people to keep up with all of their vaccines, including childhood and adult vaccines for such diseases as measles , chicken pox, shingles , and other viruses. She says people have told her they got the flu vaccine this year after skipping it in previous years. (The CDC has reported distributing an exceptionally high number of doses this past season.)
But, she cautions that a vaccine is not a magic bullet—and points out that scientists can’t always produce one that works. “As advanced as science is, there have been multiple failed efforts to develop a vaccine against the HIV virus,” she says. “This time, we were lucky that we were able build on the strengths that we've learned from many other vaccine development strategies to develop multiple vaccines for COVID-19 .”
Lesson 4: Everyone is not treated equally, especially in a pandemic
What happened: COVID-19 magnified disparities that have long been an issue for a variety of people.
What we’ve learned: Racial and ethnic minority groups especially have had disproportionately higher rates of hospitalization for COVID-19 than non-Hispanic white people in every age group, and many other groups faced higher levels of risk or stress. These groups ranged from working mothers who also have primary responsibility for children, to people who have essential jobs, to those who live in rural areas where there is less access to health care.
“One thing that has been recognized is that when people were told to work from home, you needed to have a job that you could do in your house on a computer,” says Dr. Juthani. “Many people who were well off were able do that, but they still needed to have food, which requires grocery store workers and truck drivers. Nursing home residents still needed certified nursing assistants coming to work every day to care for them and to bathe them.”
As far as racial inequities, Dr. Juthani cites President Biden’s appointment of Yale Medicine’s Marcella Nunez-Smith, MD, MHS , as inaugural chair of a federal COVID-19 Health Equity Task Force. “Hopefully the new focus is a first step,” Dr. Juthani says.
Lesson 5: We need to take mental health seriously
What happened: There was a rise in reported mental health problems that have been described as “a second pandemic,” highlighting mental health as an issue that needs to be addressed.
What we’ve learned: Arman Fesharaki-Zadeh, MD, PhD , a behavioral neurologist and neuropsychiatrist, believes the number of mental health disorders that were on the rise before the pandemic is surging as people grapple with such matters as juggling work and childcare, job loss, isolation, and losing a loved one to COVID-19.
The CDC reports that the percentage of adults who reported symptoms of anxiety of depression in the past 7 days increased from 36.4 to 41.5 % from August 2020 to February 2021. Other reports show that having COVID-19 may contribute, too, with its lingering or long COVID symptoms, which can include “foggy mind,” anxiety , depression, and post-traumatic stress disorder .
“We’re seeing these problems in our clinical setting very, very often,” Dr. Fesharaki-Zadeh says. “By virtue of necessity, we can no longer ignore this. We're seeing these folks, and we have to take them seriously.”
Lesson 6: We have the capacity for resilience
What happened: While everyone’s situation is different (and some people have experienced tremendous difficulties), many have seen that it’s possible to be resilient in a crisis.
What we’ve learned: People have practiced self-care in a multitude of ways during the pandemic as they were forced to adjust to new work schedules, change their gym routines, and cut back on socializing. Many started seeking out new strategies to counter the stress.
“I absolutely believe in the concept of resilience, because we have this effective reservoir inherent in all of us—be it the product of evolution, or our ancestors going through catastrophes, including wars, famines, and plagues,” Dr. Fesharaki-Zadeh says. “I think inherently, we have the means to deal with crisis. The fact that you and I are speaking right now is the result of our ancestors surviving hardship. I think resilience is part of our psyche. It's part of our DNA, essentially.”
Dr. Fesharaki-Zadeh believes that even small changes are highly effective tools for creating resilience. The changes he suggests may sound like the same old advice: exercise more, eat healthy food, cut back on alcohol, start a meditation practice, keep up with friends and family. “But this is evidence-based advice—there has been research behind every one of these measures,” he says.
But we have to also be practical, he notes. “If you feel overwhelmed by doing too many things, you can set a modest goal with one new habit—it could be getting organized around your sleep. Once you’ve succeeded, move on to another one. Then you’re building momentum.”
Lesson 7: Community is essential—and technology is too
What happened: People who were part of a community during the pandemic realized the importance of human connection, and those who didn’t have that kind of support realized they need it.
What we’ve learned: Many of us have become aware of how much we need other people—many have managed to maintain their social connections, even if they had to use technology to keep in touch, Dr. Juthani says. “There's no doubt that it's not enough, but even that type of community has helped people.”
Even people who aren’t necessarily friends or family are important. Dr. Juthani recalled how she encouraged her mail carrier to sign up for the vaccine, soon learning that the woman’s mother and husband hadn’t gotten it either. “They are all vaccinated now,” Dr. Juthani says. “So, even by word of mouth, community is a way to make things happen.”
It’s important to note that some people are naturally introverted and may have enjoyed having more solitude when they were forced to stay at home—and they should feel comfortable with that, Dr. Fesharaki-Zadeh says. “I think one has to keep temperamental tendencies like this in mind.”
But loneliness has been found to suppress the immune system and be a precursor to some diseases, he adds. “Even for introverted folks, the smallest circle is preferable to no circle at all,” he says.
Lesson 8: Sometimes you need a dose of humility
What happened: Scientists and nonscientists alike learned that a virus can be more powerful than they are. This was evident in the way knowledge about the virus changed over time in the past year as scientific investigation of it evolved.
What we’ve learned: “As infectious disease doctors, we were resident experts at the beginning of the pandemic because we understand pathogens in general, and based on what we’ve seen in the past, we might say there are certain things that are likely to be true,” Dr. Juthani says. “But we’ve seen that we have to take these pathogens seriously. We know that COVID-19 is not the flu. All these strokes and clots, and the loss of smell and taste that have gone on for months are things that we could have never known or predicted. So, you have to have respect for the unknown and respect science, but also try to give scientists the benefit of the doubt,” she says.
“We have been doing the best we can with the knowledge we have, in the time that we have it,” Dr. Juthani says. “I think most of us have had to have the humility to sometimes say, ‘I don't know. We're learning as we go.’"
Information provided in Yale Medicine articles is for general informational purposes only. No content in the articles should ever be used as a substitute for medical advice from your doctor or other qualified clinician. Always seek the individual advice of your health care provider with any questions you have regarding a medical condition.
More news from Yale Medicine

Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:

In Their Own Words, Americans Describe the Struggles and Silver Linings of the COVID-19 Pandemic
The outbreak has dramatically changed americans’ lives and relationships over the past year. we asked people to tell us about their experiences – good and bad – in living through this moment in history..
Pew Research Center has been asking survey questions over the past year about Americans’ views and reactions to the COVID-19 pandemic. In August, we gave the public a chance to tell us in their own words how the pandemic has affected them in their personal lives. We wanted to let them tell us how their lives have become more difficult or challenging, and we also asked about any unexpectedly positive events that might have happened during that time.
The vast majority of Americans (89%) mentioned at least one negative change in their own lives, while a smaller share (though still a 73% majority) mentioned at least one unexpected upside. Most have experienced these negative impacts and silver linings simultaneously: Two-thirds (67%) of Americans mentioned at least one negative and at least one positive change since the pandemic began.
For this analysis, we surveyed 9,220 U.S. adults between Aug. 31-Sept. 7, 2020. Everyone who completed the survey is a member of Pew Research Center’s American Trends Panel (ATP), an online survey panel that is recruited through national, random sampling of residential addresses. This way nearly all U.S. adults have a chance of selection. The survey is weighted to be representative of the U.S. adult population by gender, race, ethnicity, partisan affiliation, education and other categories. Read more about the ATP’s methodology .
Respondents to the survey were asked to describe in their own words how their lives have been difficult or challenging since the beginning of the coronavirus outbreak, and to describe any positive aspects of the situation they have personally experienced as well. Overall, 84% of respondents provided an answer to one or both of the questions. The Center then categorized a random sample of 4,071 of their answers using a combination of in-house human coders, Amazon’s Mechanical Turk service and keyword-based pattern matching. The full methodology and questions used in this analysis can be found here.
In many ways, the negatives clearly outweigh the positives – an unsurprising reaction to a pandemic that had killed more than 180,000 Americans at the time the survey was conducted. Across every major aspect of life mentioned in these responses, a larger share mentioned a negative impact than mentioned an unexpected upside. Americans also described the negative aspects of the pandemic in greater detail: On average, negative responses were longer than positive ones (27 vs. 19 words). But for all the difficulties and challenges of the pandemic, a majority of Americans were able to think of at least one silver lining.
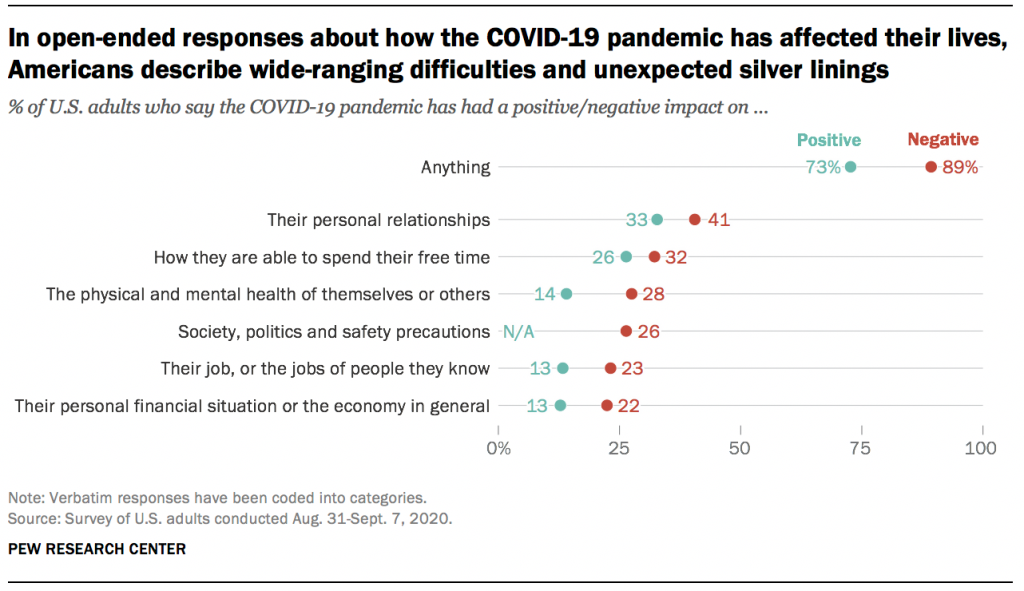
Both the negative and positive impacts described in these responses cover many aspects of life, none of which were mentioned by a majority of Americans. Instead, the responses reveal a pandemic that has affected Americans’ lives in a variety of ways, of which there is no “typical” experience. Indeed, not all groups seem to have experienced the pandemic equally. For instance, younger and more educated Americans were more likely to mention silver linings, while women were more likely than men to mention challenges or difficulties.
Here are some direct quotes that reveal how Americans are processing the new reality that has upended life across the country.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
© 2024 Pew Research Center

Illustration by Tomi Um
The Pandemic's Effects on Everyday Life
Boston College researchers are exploring COVID-19's impact on life as we know it. Here’s a look at just some of the important questions they’re asking—and answering.

Is remote work here to stay?
As many as 60 percent of U.S. employees are estimated to have worked remotely at some point during the pandemic, a shift that could lead to “profound transformations in mindsets around work and life as we know it,” said Assistant Professor of Sociology Wen Fan. In a project funded by the National Science Foundation, Fan is exploring the changing nature of work and remote workers’ experiences and preferences, as well as disparities in remote-working conditions and work-family balance by gender, socioeconomic status, and race/ethnicity, which could inform social policies moving forward. Though the team has just begun analyzing the data, Fan says one respondent’s thoughts—“It’s a fickle thing, sometimes you love it, sometimes you hate it”— captures the overall sentiment so far.

Are kids now spending too much time with screens?
When schools and daycares closed abruptly, kids began spending much more time engaged with cell phones and computers.“Screens are the babysitter of last resort,” said BC psychologist Joshua Hartshorne, coauthor of the study “Screen Time as an Index of Family Distress.” Whereas lower screen-time rates before the pandemic were thought to be a function of well- informed parenting, it’s now clear that they were also due to well-resourced parenting, he said. The next phase of the project, funded by the National Science Foundation, will examine whether screen time is actually problematic for child development.

Can we safely reuse PPE?
The pandemic revealed a severe national shortage of personal protective equipment (PPE). So when the CDC made the unprecedented recommendation to reuse N95 respirators, a team from the Connell School’s new Doctor of Nursing Practice program— Jacqueline Sly, Beth McNutt-Clarke, Nanci Haze, and Allan Thomas—created a three-minute YouTube video and guide illustrating how to don, doff, store, and then redon the masks. Their materials are now part of clinical orientation for nursing students, and the team also shared their guidelines and experiences training their colleagues in them in American Nurse and Nursing Management .

What does science say about masks?
Masks are the most important public-health tool for containing the pandemic, according to BC Law School Associate Professor Dean Hashimoto. His new book, The Case for Masks , presents situations in which wearing (or not wearing) face coverings directly affected how many people got sick. One case study focuses on the Mass General Brigham healthcare network, where Hashimoto is the chief medical officer for occupational health services. When the network required patients and 78,000 employees at its hospitals to mask up last March, there was a linear decline in COVID-19 cases among healthcare workers.

Has language development been affected?
For kids, the pandemic has meant time away from school and friends. To find out if this would affect language development, BC psychologist Joshua Hartshorne and a University of Maryland colleague created the KidTalk app ( kidtalkscrapbook.org ), a tool that allows parents to record conversations and track their children’s speech development. The data could be used by policymakers to support families after the pandemic. “The more we understand how this affects children,” Hartshorne said, “the better we can plan.”

What happens when the earth goes quiet?
There’s been much less human activity during the pandemic lockdowns—so much so that scientists recorded a drop of up to 50 percent in human-induced seismic vibrations of the earth beneath us in early 2020. Associate Professor of Earth and Environmental Sciences Alan Kafka was one of seventy-six scientists from two dozen countries who reported these results in Science . “It is culturally quieter, so we can explore the finer details of natural seismic phenomena that might otherwise be hidden,” said Kafka, who shared data from BC’s Weston Observatory, as well as from two seismometers on campus.
For more pandemic-related research from across Boston College, see sites.bc.edu/responding-to-covid-19 .
More Stories

Menstrual Care with a Conscience
Katie Diasti ’19 is creating earth-friendly and toxin-free pads and tampons.

Breaking the Cycle
Professor Catherine Taylor is testing strategies to prevent spanking and its negative outcomes.

A Billion to None
Reeves Wiedeman ’08 traces the rise and fall of the new-economy darling WeWork.

Hockey for All
Former NWHL player Blake Bolden ’13 is determined to diversify the sport she loves.
- COVID-19 and your mental health
Worries and anxiety about COVID-19 can be overwhelming. Learn ways to cope as COVID-19 spreads.
At the start of the COVID-19 pandemic, life for many people changed very quickly. Worry and concern were natural partners of all that change — getting used to new routines, loneliness and financial pressure, among other issues. Information overload, rumor and misinformation didn't help.
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020.
Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19. And you're not alone if you've coped with the stress in less than healthy ways, such as substance use.
But healthier self-care choices can help you cope with COVID-19 or any other challenge you may face.
And knowing when to get help can be the most essential self-care action of all.
Recognize what's typical and what's not
Stress and worry are common during a crisis. But something like the COVID-19 pandemic can push people beyond their ability to cope.
In surveys, the most common symptoms reported were trouble sleeping and feeling anxiety or nervous. The number of people noting those symptoms went up and down in surveys given over time. Depression and loneliness were less common than nervousness or sleep problems, but more consistent across surveys given over time. Among adults, use of drugs, alcohol and other intoxicating substances has increased over time as well.
The first step is to notice how often you feel helpless, sad, angry, irritable, hopeless, anxious or afraid. Some people may feel numb.
Keep track of how often you have trouble focusing on daily tasks or doing routine chores. Are there things that you used to enjoy doing that you stopped doing because of how you feel? Note any big changes in appetite, any substance use, body aches and pains, and problems with sleep.
These feelings may come and go over time. But if these feelings don't go away or make it hard to do your daily tasks, it's time to ask for help.
Get help when you need it
If you're feeling suicidal or thinking of hurting yourself, seek help.
- Contact your healthcare professional or a mental health professional.
- Contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline , available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential.
If you are worried about yourself or someone else, contact your healthcare professional or mental health professional. Some may be able to see you in person or talk over the phone or online.
You also can reach out to a friend or loved one. Someone in your faith community also could help.
And you may be able to get counseling or a mental health appointment through an employer's employee assistance program.
Another option is information and treatment options from groups such as:
- National Alliance on Mental Illness (NAMI).
- Substance Abuse and Mental Health Services Administration (SAMHSA).
- Anxiety and Depression Association of America.
Self-care tips
Some people may use unhealthy ways to cope with anxiety around COVID-19. These unhealthy choices may include things such as misuse of medicines or legal drugs and use of illegal drugs. Unhealthy coping choices also can be things such as sleeping too much or too little, or overeating. It also can include avoiding other people and focusing on only one soothing thing, such as work, television or gaming.
Unhealthy coping methods can worsen mental and physical health. And that is particularly true if you're trying to manage or recover from COVID-19.
Self-care actions can help you restore a healthy balance in your life. They can lessen everyday stress or significant anxiety linked to events such as the COVID-19 pandemic. Self-care actions give your body and mind a chance to heal from the problems long-term stress can cause.
Take care of your body
Healthy self-care tips start with the basics. Give your body what it needs and avoid what it doesn't need. Some tips are:
- Get the right amount of sleep for you. A regular sleep schedule, when you go to bed and get up at similar times each day, can help avoid sleep problems.
- Move your body. Regular physical activity and exercise can help reduce anxiety and improve mood. Any activity you can do regularly is a good choice. That may be a scheduled workout, a walk or even dancing to your favorite music.
- Choose healthy food and drinks. Foods that are high in nutrients, such as protein, vitamins and minerals are healthy choices. Avoid food or drink with added sugar, fat or salt.
- Avoid tobacco, alcohol and drugs. If you smoke tobacco or if you vape, you're already at higher risk of lung disease. Because COVID-19 affects the lungs, your risk increases even more. Using alcohol to manage how you feel can make matters worse and reduce your coping skills. Avoid taking illegal drugs or misusing prescriptions to manage your feelings.
Take care of your mind
Healthy coping actions for your brain start with deciding how much news and social media is right for you. Staying informed, especially during a pandemic, helps you make the best choices but do it carefully.
Set aside a specific amount of time to find information in the news or on social media, stay limited to that time, and choose reliable sources. For example, give yourself up to 20 or 30 minutes a day of news and social media. That amount keeps people informed but not overwhelmed.
For COVID-19, consider reliable health sources. Examples are the U.S. Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
Other healthy self-care tips are:
- Relax and recharge. Many people benefit from relaxation exercises such as mindfulness, deep breathing, meditation and yoga. Find an activity that helps you relax and try to do it every day at least for a short time. Fitting time in for hobbies or activities you enjoy can help manage feelings of stress too.
- Stick to your health routine. If you see a healthcare professional for mental health services, keep up with your appointments. And stay up to date with all your wellness tests and screenings.
- Stay in touch and connect with others. Family, friends and your community are part of a healthy mental outlook. Together, you form a healthy support network for concerns or challenges. Social interactions, over time, are linked to a healthier and longer life.
Avoid stigma and discrimination
Stigma can make people feel isolated and even abandoned. They may feel sad, hurt and angry when people in their community avoid them for fear of getting COVID-19. People who have experienced stigma related to COVID-19 include people of Asian descent, health care workers and people with COVID-19.
Treating people differently because of their medical condition, called medical discrimination, isn't new to the COVID-19 pandemic. Stigma has long been a problem for people with various conditions such as Hansen's disease (leprosy), HIV, diabetes and many mental illnesses.
People who experience stigma may be left out or shunned, treated differently, or denied job and school options. They also may be targets of verbal, emotional and physical abuse.
Communication can help end stigma or discrimination. You can address stigma when you:
- Get to know people as more than just an illness. Using respectful language can go a long way toward making people comfortable talking about a health issue.
- Get the facts about COVID-19 or other medical issues from reputable sources such as the CDC and WHO.
- Speak up if you hear or see myths about an illness or people with an illness.
COVID-19 and health
The virus that causes COVID-19 is still a concern for many people. By recognizing when to get help and taking time for your health, life challenges such as COVID-19 can be managed.
- Mental health during the COVID-19 pandemic. National Institutes of Health. https://covid19.nih.gov/covid-19-topics/mental-health. Accessed March 12, 2024.
- Mental Health and COVID-19: Early evidence of the pandemic's impact: Scientific brief, 2 March 2022. World Health Organization. https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1. Accessed March 12, 2024.
- Mental health and the pandemic: What U.S. surveys have found. Pew Research Center. https://www.pewresearch.org/short-reads/2023/03/02/mental-health-and-the-pandemic-what-u-s-surveys-have-found/. Accessed March 12, 2024.
- Taking care of your emotional health. Centers for Disease Control and Prevention. https://emergency.cdc.gov/coping/selfcare.asp. Accessed March 12, 2024.
- #HealthyAtHome—Mental health. World Health Organization. www.who.int/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome---mental-health. Accessed March 12, 2024.
- Coping with stress. Centers for Disease Control and Prevention. www.cdc.gov/mentalhealth/stress-coping/cope-with-stress/. Accessed March 12, 2024.
- Manage stress. U.S. Department of Health and Human Services. https://health.gov/myhealthfinder/topics/health-conditions/heart-health/manage-stress. Accessed March 20, 2020.
- COVID-19 and substance abuse. National Institute on Drug Abuse. https://nida.nih.gov/research-topics/covid-19-substance-use#health-outcomes. Accessed March 12, 2024.
- COVID-19 resource and information guide. National Alliance on Mental Illness. https://www.nami.org/Support-Education/NAMI-HelpLine/COVID-19-Information-and-Resources/COVID-19-Resource-and-Information-Guide. Accessed March 15, 2024.
- Negative coping and PTSD. U.S. Department of Veterans Affairs. https://www.ptsd.va.gov/gethelp/negative_coping.asp. Accessed March 15, 2024.
- Health effects of cigarette smoking. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/index.htm#respiratory. Accessed March 15, 2024.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed March 15, 2024.
- Your healthiest self: Emotional wellness toolkit. National Institutes of Health. https://www.nih.gov/health-information/emotional-wellness-toolkit. Accessed March 15, 2024.
- World leprosy day: Bust the myths, learn the facts. Centers for Disease Control and Prevention. https://www.cdc.gov/leprosy/world-leprosy-day/. Accessed March 15, 2024.
- HIV stigma and discrimination. Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/basics/hiv-stigma/. Accessed March 15, 2024.
- Diabetes stigma: Learn about it, recognize it, reduce it. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/features/diabetes_stigma.html. Accessed March 15, 2024.
- Phelan SM, et al. Patient and health care professional perspectives on stigma in integrated behavioral health: Barriers and recommendations. Annals of Family Medicine. 2023; doi:10.1370/afm.2924.
- Stigma reduction. Centers for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/od2a/case-studies/stigma-reduction.html. Accessed March 15, 2024.
- Nyblade L, et al. Stigma in health facilities: Why it matters and how we can change it. BMC Medicine. 2019; doi:10.1186/s12916-019-1256-2.
- Combating bias and stigma related to COVID-19. American Psychological Association. https://www.apa.org/topics/covid-19-bias. Accessed March 15, 2024.
- Yashadhana A, et al. Pandemic-related racial discrimination and its health impact among non-Indigenous racially minoritized peoples in high-income contexts: A systematic review. Health Promotion International. 2021; doi:10.1093/heapro/daab144.
- Sawchuk CN (expert opinion). Mayo Clinic. March 25, 2024.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and respiratory illness
- COVID-19 and pets
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- Long-term effects of COVID-19
- COVID-19 tests
- COVID-19 drugs: Are there any that work?
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 travel advice
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to measure your respiratory rate
- How to take your pulse
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
Related information
- Mental health: What's normal, what's not - Related information Mental health: What's normal, what's not
- Mental illness - Related information Mental illness
Your gift holds great power – donate today!
Make your tax-deductible gift and be part of the cutting-edge research and care that's changing medicine.
Read these 12 moving essays about life during coronavirus
Artists, novelists, critics, and essayists are writing the first draft of history.
by Alissa Wilkinson

The world is grappling with an invisible, deadly enemy, trying to understand how to live with the threat posed by a virus . For some writers, the only way forward is to put pen to paper, trying to conceptualize and document what it feels like to continue living as countries are under lockdown and regular life seems to have ground to a halt.
So as the coronavirus pandemic has stretched around the world, it’s sparked a crop of diary entries and essays that describe how life has changed. Novelists, critics, artists, and journalists have put words to the feelings many are experiencing. The result is a first draft of how we’ll someday remember this time, filled with uncertainty and pain and fear as well as small moments of hope and humanity.
- The Vox guide to navigating the coronavirus crisis
At the New York Review of Books, Ali Bhutto writes that in Karachi, Pakistan, the government-imposed curfew due to the virus is “eerily reminiscent of past military clampdowns”:
Beneath the quiet calm lies a sense that society has been unhinged and that the usual rules no longer apply. Small groups of pedestrians look on from the shadows, like an audience watching a spectacle slowly unfolding. People pause on street corners and in the shade of trees, under the watchful gaze of the paramilitary forces and the police.
His essay concludes with the sobering note that “in the minds of many, Covid-19 is just another life-threatening hazard in a city that stumbles from one crisis to another.”
Writing from Chattanooga, novelist Jamie Quatro documents the mixed ways her neighbors have been responding to the threat, and the frustration of conflicting direction, or no direction at all, from local, state, and federal leaders:
Whiplash, trying to keep up with who’s ordering what. We’re already experiencing enough chaos without this back-and-forth. Why didn’t the federal government issue a nationwide shelter-in-place at the get-go, the way other countries did? What happens when one state’s shelter-in-place ends, while others continue? Do states still under quarantine close their borders? We are still one nation, not fifty individual countries. Right?
- A syllabus for the end of the world
Award-winning photojournalist Alessio Mamo, quarantined with his partner Marta in Sicily after she tested positive for the virus, accompanies his photographs in the Guardian of their confinement with a reflection on being confined :
The doctors asked me to take a second test, but again I tested negative. Perhaps I’m immune? The days dragged on in my apartment, in black and white, like my photos. Sometimes we tried to smile, imagining that I was asymptomatic, because I was the virus. Our smiles seemed to bring good news. My mother left hospital, but I won’t be able to see her for weeks. Marta started breathing well again, and so did I. I would have liked to photograph my country in the midst of this emergency, the battles that the doctors wage on the frontline, the hospitals pushed to their limits, Italy on its knees fighting an invisible enemy. That enemy, a day in March, knocked on my door instead.
In the New York Times Magazine, deputy editor Jessica Lustig writes with devastating clarity about her family’s life in Brooklyn while her husband battled the virus, weeks before most people began taking the threat seriously:
At the door of the clinic, we stand looking out at two older women chatting outside the doorway, oblivious. Do I wave them away? Call out that they should get far away, go home, wash their hands, stay inside? Instead we just stand there, awkwardly, until they move on. Only then do we step outside to begin the long three-block walk home. I point out the early magnolia, the forsythia. T says he is cold. The untrimmed hairs on his neck, under his beard, are white. The few people walking past us on the sidewalk don’t know that we are visitors from the future. A vision, a premonition, a walking visitation. This will be them: Either T, in the mask, or — if they’re lucky — me, tending to him.
Essayist Leslie Jamison writes in the New York Review of Books about being shut away alone in her New York City apartment with her 2-year-old daughter since she became sick:
The virus. Its sinewy, intimate name. What does it feel like in my body today? Shivering under blankets. A hot itch behind the eyes. Three sweatshirts in the middle of the day. My daughter trying to pull another blanket over my body with her tiny arms. An ache in the muscles that somehow makes it hard to lie still. This loss of taste has become a kind of sensory quarantine. It’s as if the quarantine keeps inching closer and closer to my insides. First I lost the touch of other bodies; then I lost the air; now I’ve lost the taste of bananas. Nothing about any of these losses is particularly unique. I’ve made a schedule so I won’t go insane with the toddler. Five days ago, I wrote Walk/Adventure! on it, next to a cut-out illustration of a tiger—as if we’d see tigers on our walks. It was good to keep possibility alive.
At Literary Hub, novelist Heidi Pitlor writes about the elastic nature of time during her family’s quarantine in Massachusetts:
During a shutdown, the things that mark our days—commuting to work, sending our kids to school, having a drink with friends—vanish and time takes on a flat, seamless quality. Without some self-imposed structure, it’s easy to feel a little untethered. A friend recently posted on Facebook: “For those who have lost track, today is Blursday the fortyteenth of Maprilay.” ... Giving shape to time is especially important now, when the future is so shapeless. We do not know whether the virus will continue to rage for weeks or months or, lord help us, on and off for years. We do not know when we will feel safe again. And so many of us, minus those who are gifted at compartmentalization or denial, remain largely captive to fear. We may stay this way if we do not create at least the illusion of movement in our lives, our long days spent with ourselves or partners or families.
- What day is it today?
Novelist Lauren Groff writes at the New York Review of Books about trying to escape the prison of her fears while sequestered at home in Gainesville, Florida:
Some people have imaginations sparked only by what they can see; I blame this blinkered empiricism for the parks overwhelmed with people, the bars, until a few nights ago, thickly thronged. My imagination is the opposite. I fear everything invisible to me. From the enclosure of my house, I am afraid of the suffering that isn’t present before me, the people running out of money and food or drowning in the fluid in their lungs, the deaths of health-care workers now growing ill while performing their duties. I fear the federal government, which the right wing has so—intentionally—weakened that not only is it insufficient to help its people, it is actively standing in help’s way. I fear we won’t sufficiently punish the right. I fear leaving the house and spreading the disease. I fear what this time of fear is doing to my children, their imaginations, and their souls.
At ArtForum , Berlin-based critic and writer Kristian Vistrup Madsen reflects on martinis, melancholia, and Finnish artist Jaakko Pallasvuo’s 2018 graphic novel Retreat , in which three young people exile themselves in the woods:
In melancholia, the shape of what is ending, and its temporality, is sprawling and incomprehensible. The ambivalence makes it hard to bear. The world of Retreat is rendered in lush pink and purple watercolors, which dissolve into wild and messy abstractions. In apocalypse, the divisions established in genesis bleed back out. My own Corona-retreat is similarly soft, color-field like, each day a blurred succession of quarantinis, YouTube–yoga, and televized press conferences. As restrictions mount, so does abstraction. For now, I’m still rooting for love to save the world.
At the Paris Review , Matt Levin writes about reading Virginia Woolf’s novel The Waves during quarantine:
A retreat, a quarantine, a sickness—they simultaneously distort and clarify, curtail and expand. It is an ideal state in which to read literature with a reputation for difficulty and inaccessibility, those hermetic books shorn of the handholds of conventional plot or characterization or description. A novel like Virginia Woolf’s The Waves is perfect for the state of interiority induced by quarantine—a story of three men and three women, meeting after the death of a mutual friend, told entirely in the overlapping internal monologues of the six, interspersed only with sections of pure, achingly beautiful descriptions of the natural world, a day’s procession and recession of light and waves. The novel is, in my mind’s eye, a perfectly spherical object. It is translucent and shimmering and infinitely fragile, prone to shatter at the slightest disturbance. It is not a book that can be read in snatches on the subway—it demands total absorption. Though it revels in a stark emotional nakedness, the book remains aloof, remote in its own deep self-absorption.
- Vox is starting a book club. Come read with us!
In an essay for the Financial Times, novelist Arundhati Roy writes with anger about Indian Prime Minister Narendra Modi’s anemic response to the threat, but also offers a glimmer of hope for the future:
Historically, pandemics have forced humans to break with the past and imagine their world anew. This one is no different. It is a portal, a gateway between one world and the next. We can choose to walk through it, dragging the carcasses of our prejudice and hatred, our avarice, our data banks and dead ideas, our dead rivers and smoky skies behind us. Or we can walk through lightly, with little luggage, ready to imagine another world. And ready to fight for it.
From Boston, Nora Caplan-Bricker writes in The Point about the strange contraction of space under quarantine, in which a friend in Beirut is as close as the one around the corner in the same city:
It’s a nice illusion—nice to feel like we’re in it together, even if my real world has shrunk to one person, my husband, who sits with his laptop in the other room. It’s nice in the same way as reading those essays that reframe social distancing as solidarity. “We must begin to see the negative space as clearly as the positive, to know what we don’t do is also brilliant and full of love,” the poet Anne Boyer wrote on March 10th, the day that Massachusetts declared a state of emergency. If you squint, you could almost make sense of this quarantine as an effort to flatten, along with the curve, the distinctions we make between our bonds with others. Right now, I care for my neighbor in the same way I demonstrate love for my mother: in all instances, I stay away. And in moments this month, I have loved strangers with an intensity that is new to me. On March 14th, the Saturday night after the end of life as we knew it, I went out with my dog and found the street silent: no lines for restaurants, no children on bicycles, no couples strolling with little cups of ice cream. It had taken the combined will of thousands of people to deliver such a sudden and complete emptiness. I felt so grateful, and so bereft.
And on his own website, musician and artist David Byrne writes about rediscovering the value of working for collective good , saying that “what is happening now is an opportunity to learn how to change our behavior”:
In emergencies, citizens can suddenly cooperate and collaborate. Change can happen. We’re going to need to work together as the effects of climate change ramp up. In order for capitalism to survive in any form, we will have to be a little more socialist. Here is an opportunity for us to see things differently — to see that we really are all connected — and adjust our behavior accordingly. Are we willing to do this? Is this moment an opportunity to see how truly interdependent we all are? To live in a world that is different and better than the one we live in now? We might be too far down the road to test every asymptomatic person, but a change in our mindsets, in how we view our neighbors, could lay the groundwork for the collective action we’ll need to deal with other global crises. The time to see how connected we all are is now.
The portrait these writers paint of a world under quarantine is multifaceted. Our worlds have contracted to the confines of our homes, and yet in some ways we’re more connected than ever to one another. We feel fear and boredom, anger and gratitude, frustration and strange peace. Uncertainty drives us to find metaphors and images that will let us wrap our minds around what is happening.
Yet there’s no single “what” that is happening. Everyone is contending with the pandemic and its effects from different places and in different ways. Reading others’ experiences — even the most frightening ones — can help alleviate the loneliness and dread, a little, and remind us that what we’re going through is both unique and shared by all.
Most Popular
The caribbean has a defense system against deadly hurricanes — but it’s vanishing, the supreme court’s disastrous trump immunity decision, explained, the supreme court also handed down a hugely important first amendment case today, do other democrats actually poll better against trump than biden, 5 terrible reasons for biden to stay in the race, today, explained.
Understand the world with a daily explainer plus the most compelling stories of the day.
More in Culture

Chappell Roan spent 7 years becoming an overnight success

The Spotify conspiracy theories about "Espresso," explained

Tiktok is full of bad health “tricks”

How the UFC explains the USA

Kevin Costner’s ego and the strange road to Horizon

Hawk Tuah Girl, explained by straight dudes

What about Kamala?

Food is no longer a main character on The Bear

Should Biden drop out? The debate, explained.

How white victimhood is shaping a second Trump term

If it’s 100 degrees out, does your boss have to give you a break? Probably not.
I Thought We’d Learned Nothing From the Pandemic. I Wasn’t Seeing the Full Picture

M y first home had a back door that opened to a concrete patio with a giant crack down the middle. When my sister and I played, I made sure to stay on the same side of the divide as her, just in case. The 1988 film The Land Before Time was one of the first movies I ever saw, and the image of the earth splintering into pieces planted its roots in my brain. I believed that, even in my own backyard, I could easily become the tiny Triceratops separated from her family, on the other side of the chasm, as everything crumbled into chaos.
Some 30 years later, I marvel at the eerie, unexpected ways that cartoonish nightmare came to life – not just for me and my family, but for all of us. The landscape was already covered in fissures well before COVID-19 made its way across the planet, but the pandemic applied pressure, and the cracks broke wide open, separating us from each other physically and ideologically. Under the weight of the crisis, we scattered and landed on such different patches of earth we could barely see each other’s faces, even when we squinted. We disagreed viciously with each other, about how to respond, but also about what was true.
Recently, someone asked me if we’ve learned anything from the pandemic, and my first thought was a flat no. Nothing. There was a time when I thought it would be the very thing to draw us together and catapult us – as a capital “S” Society – into a kinder future. It’s surreal to remember those early days when people rallied together, sewing masks for health care workers during critical shortages and gathering on balconies in cities from Dallas to New York City to clap and sing songs like “Yellow Submarine.” It felt like a giant lightning bolt shot across the sky, and for one breath, we all saw something that had been hidden in the dark – the inherent vulnerability in being human or maybe our inescapable connectedness .
More from TIME
Read More: The Family Time the Pandemic Stole
But it turns out, it was just a flash. The goodwill vanished as quickly as it appeared. A couple of years later, people feel lied to, abandoned, and all on their own. I’ve felt my own curiosity shrinking, my willingness to reach out waning , my ability to keep my hands open dwindling. I look out across the landscape and see selfishness and rage, burnt earth and so many dead bodies. Game over. We lost. And if we’ve already lost, why try?
Still, the question kept nagging me. I wondered, am I seeing the full picture? What happens when we focus not on the collective society but at one face, one story at a time? I’m not asking for a bow to minimize the suffering – a pretty flourish to put on top and make the whole thing “worth it.” Yuck. That’s not what we need. But I wondered about deep, quiet growth. The kind we feel in our bodies, relationships, homes, places of work, neighborhoods.
Like a walkie-talkie message sent to my allies on the ground, I posted a call on my Instagram. What do you see? What do you hear? What feels possible? Is there life out here? Sprouting up among the rubble? I heard human voices calling back – reports of life, personal and specific. I heard one story at a time – stories of grief and distrust, fury and disappointment. Also gratitude. Discovery. Determination.
Among the most prevalent were the stories of self-revelation. Almost as if machines were given the chance to live as humans, people described blossoming into fuller selves. They listened to their bodies’ cues, recognized their desires and comforts, tuned into their gut instincts, and honored the intuition they hadn’t realized belonged to them. Alex, a writer and fellow disabled parent, found the freedom to explore a fuller version of herself in the privacy the pandemic provided. “The way I dress, the way I love, and the way I carry myself have both shrunk and expanded,” she shared. “I don’t love myself very well with an audience.” Without the daily ritual of trying to pass as “normal” in public, Tamar, a queer mom in the Netherlands, realized she’s autistic. “I think the pandemic helped me to recognize the mask,” she wrote. “Not that unmasking is easy now. But at least I know it’s there.” In a time of widespread suffering that none of us could solve on our own, many tended to our internal wounds and misalignments, large and small, and found clarity.
Read More: A Tool for Staying Grounded in This Era of Constant Uncertainty
I wonder if this flourishing of self-awareness is at least partially responsible for the life alterations people pursued. The pandemic broke open our personal notions of work and pushed us to reevaluate things like time and money. Lucy, a disabled writer in the U.K., made the hard decision to leave her job as a journalist covering Westminster to write freelance about her beloved disability community. “This work feels important in a way nothing else has ever felt,” she wrote. “I don’t think I’d have realized this was what I should be doing without the pandemic.” And she wasn’t alone – many people changed jobs , moved, learned new skills and hobbies, became politically engaged.
Perhaps more than any other shifts, people described a significant reassessment of their relationships. They set boundaries, said no, had challenging conversations. They also reconnected, fell in love, and learned to trust. Jeanne, a quilter in Indiana, got to know relatives she wouldn’t have connected with if lockdowns hadn’t prompted weekly family Zooms. “We are all over the map as regards to our belief systems,” she emphasized, “but it is possible to love people you don’t see eye to eye with on every issue.” Anna, an anti-violence advocate in Maine, learned she could trust her new marriage: “Life was not a honeymoon. But we still chose to turn to each other with kindness and curiosity.” So many bonds forged and broken, strengthened and strained.
Instead of relying on default relationships or institutional structures, widespread recalibrations allowed for going off script and fortifying smaller communities. Mara from Idyllwild, Calif., described the tangible plan for care enacted in her town. “We started a mutual-aid group at the beginning of the pandemic,” she wrote, “and it grew so quickly before we knew it we were feeding 400 of the 4000 residents.” She didn’t pretend the conditions were ideal. In fact, she expressed immense frustration with our collective response to the pandemic. Even so, the local group rallied and continues to offer assistance to their community with help from donations and volunteers (many of whom were originally on the receiving end of support). “I’ve learned that people thrive when they feel their connection to others,” she wrote. Clare, a teacher from the U.K., voiced similar conviction as she described a giant scarf she’s woven out of ribbons, each representing a single person. The scarf is “a collection of stories, moments and wisdom we are sharing with each other,” she wrote. It now stretches well over 1,000 feet.
A few hours into reading the comments, I lay back on my bed, phone held against my chest. The room was quiet, but my internal world was lighting up with firefly flickers. What felt different? Surely part of it was receiving personal accounts of deep-rooted growth. And also, there was something to the mere act of asking and listening. Maybe it connected me to humans before battle cries. Maybe it was the chance to be in conversation with others who were also trying to understand – what is happening to us? Underneath it all, an undeniable thread remained; I saw people peering into the mess and narrating their findings onto the shared frequency. Every comment was like a flare into the sky. I’m here! And if the sky is full of flares, we aren’t alone.
I recognized my own pandemic discoveries – some minor, others massive. Like washing off thick eyeliner and mascara every night is more effort than it’s worth; I can transform the mundane into the magical with a bedsheet, a movie projector, and twinkle lights; my paralyzed body can mother an infant in ways I’d never seen modeled for me. I remembered disappointing, bewildering conversations within my own family of origin and our imperfect attempts to remain close while also seeing things so differently. I realized that every time I get the weekly invite to my virtual “Find the Mumsies” call, with a tiny group of moms living hundreds of miles apart, I’m being welcomed into a pocket of unexpected community. Even though we’ve never been in one room all together, I’ve felt an uncommon kind of solace in their now-familiar faces.
Hope is a slippery thing. I desperately want to hold onto it, but everywhere I look there are real, weighty reasons to despair. The pandemic marks a stretch on the timeline that tangles with a teetering democracy, a deteriorating planet , the loss of human rights that once felt unshakable . When the world is falling apart Land Before Time style, it can feel trite, sniffing out the beauty – useless, firing off flares to anyone looking for signs of life. But, while I’m under no delusions that if we just keep trudging forward we’ll find our own oasis of waterfalls and grassy meadows glistening in the sunshine beneath a heavenly chorus, I wonder if trivializing small acts of beauty, connection, and hope actually cuts us off from resources essential to our survival. The group of abandoned dinosaurs were keeping each other alive and making each other laugh well before they made it to their fantasy ending.
Read More: How Ice Cream Became My Own Personal Act of Resistance
After the monarch butterfly went on the endangered-species list, my friend and fellow writer Hannah Soyer sent me wildflower seeds to plant in my yard. A simple act of big hope – that I will actually plant them, that they will grow, that a monarch butterfly will receive nourishment from whatever blossoms are able to push their way through the dirt. There are so many ways that could fail. But maybe the outcome wasn’t exactly the point. Maybe hope is the dogged insistence – the stubborn defiance – to continue cultivating moments of beauty regardless. There is value in the planting apart from the harvest.
I can’t point out a single collective lesson from the pandemic. It’s hard to see any great “we.” Still, I see the faces in my moms’ group, making pancakes for their kids and popping on between strings of meetings while we try to figure out how to raise these small people in this chaotic world. I think of my friends on Instagram tending to the selves they discovered when no one was watching and the scarf of ribbons stretching the length of more than three football fields. I remember my family of three, holding hands on the way up the ramp to the library. These bits of growth and rings of support might not be loud or right on the surface, but that’s not the same thing as nothing. If we only cared about the bottom-line defeats or sweeping successes of the big picture, we’d never plant flowers at all.
More Must-Reads from TIME
- Welcome to the Noah Lyles Olympics
- Melinda French Gates Is Going It Alone
- What to Do if You Can’t Afford Your Medications
- How to Buy Groceries Without Breaking the Bank
- Sienna Miller Is the Reason to Watch Horizon
- Why So Many Bitcoin Mining Companies Are Pivoting to AI
- The 15 Best Movies to Watch on a Plane
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]
What Life Was Like for Students in the Pandemic Year

- Share article
In this video, Navajo student Miles Johnson shares how he experienced the stress and anxiety of schools shutting down last year. Miles’ teacher shared his experience and those of her other students in a recent piece for Education Week. In these short essays below, teacher Claire Marie Grogan’s 11th grade students at Oceanside High School on Long Island, N.Y., describe their pandemic experiences. Their writings have been slightly edited for clarity. Read Grogan’s essay .
“Hours Staring at Tiny Boxes on the Screen”
By Kimberly Polacco, 16
I stare at my blank computer screen, trying to find the motivation to turn it on, but my finger flinches every time it hovers near the button. I instead open my curtains. It is raining outside, but it does not matter, I will not be going out there for the rest of the day. The sound of pounding raindrops contributes to my headache enough to make me turn on my computer in hopes that it will give me something to drown out the noise. But as soon as I open it up, I feel the weight of the world crash upon my shoulders.
Each 42-minute period drags on by. I spend hours upon hours staring at tiny boxes on a screen, one of which my exhausted face occupies, and attempt to retain concepts that have been presented to me through this device. By the time I have the freedom of pressing the “leave” button on my last Google Meet of the day, my eyes are heavy and my legs feel like mush from having not left my bed since I woke up.
Tomorrow arrives, except this time here I am inside of a school building, interacting with my first period teacher face to face. We talk about our favorite movies and TV shows to stream as other kids pile into the classroom. With each passing period I accumulate more and more of these tiny meaningless conversations everywhere I go with both teachers and students. They may not seem like much, but to me they are everything because I know that the next time I am expected to report to school, I will be trapped in the bubble of my room counting down the hours until I can sit down in my freshly sanitized wooden desk again.
“My Only Parent Essentially on Her Death Bed”
By Nick Ingargiola, 16
My mom had COVID-19 for ten weeks. She got sick during the first month school buildings were shut. The difficulty of navigating an online classroom was already overwhelming, and when mixed with my only parent essentially on her death bed, it made it unbearable. Focusing on schoolwork was impossible, and watching my mother struggle to lift up her arm broke my heart.
My mom has been through her fair share of diseases from pancreatic cancer to seizures and even as far as a stroke that paralyzed her entire left side. It is safe to say she has been through a lot. The craziest part is you would never know it. She is the strongest and most positive person I’ve ever met. COVID hit her hard. Although I have watched her go through life and death multiple times, I have never seen her so physically and mentally drained.
I initially was overjoyed to complete my school year in the comfort of my own home, but once my mom got sick, I couldn’t handle it. No one knows what it’s like to pretend like everything is OK until they are forced to. I would wake up at 8 after staying up until 5 in the morning pondering the possibility of losing my mother. She was all I had. I was forced to turn my camera on and float in the fake reality of being fine although I wasn’t. The teachers tried to keep the class engaged by obligating the students to participate. This was dreadful. I didn’t want to talk. I had to hide the distress in my voice. If only the teachers understood what I was going through. I was hesitant because I didn’t want everyone to know that the virus that was infecting and killing millions was knocking on my front door.
After my online classes, I was required to finish an immense amount of homework while simultaneously hiding my sadness so that my mom wouldn’t worry about me. She was already going through a lot. There was no reason to add me to her list of worries. I wasn’t even able to give her a hug. All I could do was watch.
“The Way of Staying Sane”
By Lynda Feustel, 16
Entering year two of the pandemic is strange. It barely seems a day since last March, but it also seems like a lifetime. As an only child and introvert, shutting down my world was initially simple and relatively easy. My friends and I had been super busy with the school play, and while I was sad about it being canceled, I was struggling a lot during that show and desperately needed some time off.
As March turned to April, virtual school began, and being alone really set in. I missed my friends and us being together. The isolation felt real with just my parents and me, even as we spent time together. My friends and I began meeting on Facetime every night to watch TV and just be together in some way. We laughed at insane jokes we made and had homework and therapy sessions over Facetime and grew closer through digital and literal walls.
The summer passed with in-person events together, and the virus faded into the background for a little while. We went to the track and the beach and hung out in people’s backyards.
Then school came for us in a more nasty way than usual. In hybrid school we were separated. People had jobs, sports, activities, and quarantines. Teachers piled on work, and the virus grew more present again. The group text put out hundreds of messages a day while the Facetimes came to a grinding halt, and meeting in person as a group became more of a rarity. Being together on video and in person was the way of staying sane.
In a way I am in a similar place to last year, working and looking for some change as we enter the second year of this mess.
“In History Class, Reports of Heightening Cases”
By Vivian Rose, 16
I remember the moment my freshman year English teacher told me about the young writers’ conference at Bread Loaf during my sophomore year. At first, I didn’t want to apply, the deadline had passed, but for some strange reason, the directors of the program extended it another week. It felt like it was meant to be. It was in Vermont in the last week of May when the flowers have awakened and the sun is warm.
I submitted my work, and two weeks later I got an email of my acceptance. I screamed at the top of my lungs in the empty house; everyone was out, so I was left alone to celebrate my small victory. It was rare for them to admit sophomores. Usually they accept submissions only from juniors and seniors.
That was the first week of February 2020. All of a sudden, there was some talk about this strange virus coming from China. We thought nothing of it. Every night, I would fall asleep smiling, knowing that I would be able to go to the exact conference that Robert Frost attended for 42 years.
Then, as if overnight, it seemed the virus had swung its hand and had gripped parts of the country. Every newscast was about the disease. Every day in history, we would look at the reports of heightening cases and joke around that this could never become a threat as big as Dr. Fauci was proposing. Then, March 13th came around--it was the last day before the world seemed to shut down. Just like that, Bread Loaf would vanish from my grasp.
“One Day Every Day Won’t Be As Terrible”
By Nick Wollweber, 17
COVID created personal problems for everyone, some more serious than others, but everyone had a struggle.
As the COVID lock-down took hold, the main thing weighing on my mind was my oldest brother, Joe, who passed away in January 2019 unexpectedly in his sleep. Losing my brother was a complete gut punch and reality check for me at 14 and 15 years old. 2019 was a year of struggle, darkness, sadness, frustration. I didn’t want to learn after my brother had passed, but I had to in order to move forward and find my new normal.
Routine and always having things to do and places to go is what let me cope in the year after Joe died. Then COVID came and gave me the option to let up and let down my guard. I struggled with not wanting to take care of personal hygiene. That was the beginning of an underlying mental problem where I wouldn’t do things that were necessary for everyday life.
My “coping routine” that got me through every day and week the year before was gone. COVID wasn’t beneficial to me, but it did bring out the true nature of my mental struggles and put a name to it. Since COVID, I have been diagnosed with severe depression and anxiety. I began taking antidepressants and going to therapy a lot more.
COVID made me realize that I’m not happy with who I am and that I needed to change. I’m still not happy with who I am. I struggle every day, but I am working towards a goal that one day every day won’t be as terrible.
Coverage of social and emotional learning is supported in part by a grant from the NoVo Foundation, at www.novofoundation.org . Education Week retains sole editorial control over the content of this coverage. A version of this article appeared in the March 31, 2021 edition of Education Week as What Life Was Like for Students in the Pandemic Year

Sign Up for The Savvy Principal
Edweek top school jobs.


Sign Up & Sign In

- Research article
- Open access
- Published: 02 June 2021
How do you feel during the COVID-19 pandemic? A survey using psychological and linguistic self-report measures, and machine learning to investigate mental health, subjective experience, personality, and behaviour during the COVID-19 pandemic among university students
- Cornelia Herbert ORCID: orcid.org/0000-0002-9652-5586 1 ,
- Alia El Bolock 1 , 2 &
- Slim Abdennadher 2
BMC Psychology volume 9 , Article number: 90 ( 2021 ) Cite this article
117k Accesses
34 Citations
Metrics details
The WHO has raised concerns about the psychological consequences of the current COVID-19 pandemic, negatively affecting health across societies, cultures and age-groups.
This online survey study investigated mental health, subjective experience, and behaviour (health, learning/teaching) among university students studying in Egypt or Germany shortly after the first pandemic lockdown in May 2020. Psychological assessment included stable personality traits, self-concept and state-like psychological variables related to (a) mental health (depression, anxiety), (b) pandemic threat perception (feelings during the pandemic, perceived difficulties in describing, identifying, expressing emotions), (c) health (e.g., worries about health, bodily symptoms) and behaviour including perceived difficulties in learning. Assessment methods comprised self-report questions, standardized psychological scales, psychological questionnaires, and linguistic self-report measures. Data analysis comprised descriptive analysis of mental health, linguistic analysis of self-concept, personality and feelings, as well as correlational analysis and machine learning. N = 220 (107 women, 112 men, 1 = other) studying in Egypt or Germany provided answers to all psychological questionnaires and survey items.
Mean state and trait anxiety scores were significantly above the cut off scores that distinguish between high versus low anxious subjects. Depressive symptoms were reported by 51.82% of the student sample, the mean score was significantly above the screening cut off score for risk of depression. Worries about health (mental and physical health) and perceived difficulties in identifying feelings, and difficulties in learning behaviour relative to before the pandemic were also significant. No negative self-concept was found in the linguistic descriptions of the participants, whereas linguistic descriptions of feelings during the pandemic revealed a negativity bias in emotion perception. Machine learning (exploratory) predicted personality from the self-report data suggesting relations between personality and subjective experience that were not captured by descriptive or correlative data analytics alone.
Despite small sample sizes, this multimethod survey provides important insight into mental health of university students studying in Egypt or Germany and how they perceived the first COVID-19 pandemic lockdown in May 2020. The results should be continued with larger samples to help develop psychological interventions that support university students across countries and cultures to stay psychologically resilient during the pandemic.
Peer Review reports
Only in a few month, the COVID-19 epidemic developed into a serious pandemic affecting all countries around the globe. Physical and social distancing and global lockdown of public, social, and work life was and still is a necessity in many countries to fight the pandemic without vaccine. Scientific progress in understanding the behaviour of the virus has grown rapidly since the outbreak of the pandemic, while scientific understanding of the psychological consequences of the pandemic is still at a developing stage. Empirical studies investigating mental health, well-being, subjective experience and behaviour during the COVID-19 pandemic are currently underway and several survey studies from several countries have meanwhile been published. First published surveys investigated the mental health of Covid-19 survivors or of health care professionals enrolled in the treatment of COVID-19 patients [ 1 , 2 ]. Moreover, first observations from surveys investigating psychological reactions of the general population in the hot spot countries immediately after the outbreak of the COVID-19 pandemic in 2020 have meanwhile been published e.g., [ 3 , 4 , 5 ]. The results suggest a significant increase in mental ill health among populations during the first few months of the COVID-19 pandemic, supporting earlier observations from previous epi- and pandemics [ 6 ]. The World Health Organization (WHO) expects mental health burdens in the general population to be particularly pronounced in people who have already been at risk of or suffering from affective disorders before the pandemic (see for an overview [ 7 , 8 ]). Similarly, patients in general as well as patients with a chronic mental disorder in particular, are expected to suffer from impairments in mental health and well-being due to their medical and psychotherapeutic treatment being reduced or cancelled as a consequence of the pandemic lockdown [ 8 ]. In addition, health care professionals involved in the treatment of COVID-19 patients as well as workers with system-relevant jobs are supposed to be at special risk of developing stress-related symptoms and diseases such as post-traumatic stress disorder, chronic fatigue, anxiety, and depressive disorder [ 1 , 2 , 8 ].
However, the current COVID-19 pandemic is not just threatening specific parts of the population. On the contrary. The spread of the virus around the world, its exponential increase in infection probability, and its high lethality bear constant threats for whole societies and for each individual as the pandemic is still evident now, one year after the pandemic outbreak.
Therefore, according to the WHO, primary mental health prevention targeting either the general public or specific population groups should be an indispensable goal of crisis management of the current COVID-19 pandemic [ 8 ] comprising all age-groups from youth, adolescence to adulthood.
Notably, fighting the COVID-19 pandemic currently still requires behaviour change in everybody including daily behaviour (work, business, family, and leisure) as well as changes in health behaviour and social behaviour. In each country so far, the COVID-19 pandemic lockdowns affected daily behaviour routines including work, business, family, and leisure time activities. The COVID-19 pandemic lockdowns started in China in January 2020 and only a few months later, lockdowns followed in many countries around the globe including Germany and Egypt in March 2020. Crucially, in all countries, the first lockdowns came by far and large unexpected to the population. The restrictions in daily life and behaviour may therefore not be tolerated equally well by everybody. Accordingly, health care professionals and the WHO have suggested that counseling programs supporting and assisting people in behaviour change need to become part of the COVID-19 pandemic prevention initiatives [ 8 , 9 ] to avoid unnecessary mental health burdens in the general public.
However, in order to successfully support mental health, well-being, and behaviour in those social domains of life most seriously affected by the current COVID-19 pandemic, a better scientific understanding is required of how individual people experience and psychologically react to the current COVID-19 pandemic, how they think, feel, suffer and cope with the situation, and how they are handling threat perception, how they perceive and regulate emotions and behaviour [ 10 ].
Academia and education are two social and public domains that have been seriously affected by the pandemic lockdown in every country. Concerning Germany, in March 2020 the different states of Germany decided to postpone all academic teaching at higher education institutions to an indefinite period. The universities’ infrastructure including libraries were closed and students were not allowed to come to the university. Similarly, concerning Egypt, public and private universities responded in a similar manner as mandated by the government by closing the campus for students and switching all teaching activities to e-learning. Teaching courses including classes, laboratory courses, seminars, preparatory and induction courses were suspended for the summer term 2020. Teaching during the summer term was announced to be offered as online e-learning format. The lockdown situation in the two countries was thus almost identical for university students concerning the aspects of their social and academic life.
Working at home without any possibility of coming to the university campus and not being able of attending to lectures and courses face-to-face together with peers, tutors, and teachers require from students to learn and adapt to new behaviour rules. Psychologically, pandemics increase uncertainty [ 11 ]. Uncertainty causes stress and increases the risk for mental ill health if it conflicts with behaviour routines and habits [ 11 ]. Despite most of the students being digital natives, the abrupt switch from face-to-face communication to digital, computer-assisted forms of teaching and sole reliance on digital interaction as the only means of social interaction might not be tolerated mentally and physically equally well by all students. Whether the current pandemic situation and its consequences are experienced as a threat may depend on the students’ individual character, i.e., the student’s personality and self-concept as well as his/her current cognitive, affective, and motivational state.
Recent observations from published survey studies among Chinese students after the lockdown reported an increase in general anxiety within about 25% of the student participants. Anxiety symptoms ranged from mild to moderate to severe anxiety [ 3 ]. Moreover, pandemic self-isolation was found to be associated with complex patterns of psychopathology amongst students including an increase in symptoms of obsessive–compulsive disorder, hypochondria, depression, and neurasthenia [ 4 ]. Meanwhile published survey studies from several countries in Europe and across the world support negative changes in mental health among university students immediately after the first lockdowns in 2020, specifically in relation with quarantine and self-isolation [ 12 , 13 , 14 , 15 , 16 ].
Nationwide surveys conducted before the COVID-19 pandemic already reported elevated mental health problems and stress-related symptoms including anxiety and depression among university students [ 17 , 18 , 19 , 20 , 21 ], and this, although university students across countries might belong to the young educated low-risk population. In a recent online study including N = 185 university students studying in Germany, 36.6% of the students (women and men) reported to experience depressive symptoms, 41.83% (women and men) reported high levels of state anxiety, and mental stress due to excessive demands and uncertainty in finances, job, or social relationships [ 21 ]. This prevalence of academic stress and mental health burdens have been found among university students all over the globe [ 17 , 18 , 19 , 20 ], including Egypt [ 22 , 23 ].
Thus, as a population group, university students may be particularly vulnerable to stress-related lifestyle changes affecting mental health that are associated with the current COVID-19 pandemic. Individual differences in mental health may also exist and influence how the students perceive and how well they adapt and cope with the current COVID-19 pandemic situation and to what degree they are motivated to change their behaviour in response to the pandemic consequences in social and academic life and teaching. Psychological theories and models of behaviour change, e.g., Health Belief Model, Transtheoretical Model, or Social Cognitive Theory [ 24 , 25 , 26 ], all agree in that individual factors, specifically those related to emotion- and self-regulation can explain how people perceive themselves, whether and why they change their behaviour and why others do not. Threat perception has been suggested to play an outstanding role [ 27 ], because pandemics threaten the whole person, i.e. our self and the self-concept. Personality traits although considered stable may play a critical role in threat perception, in mental health and behaviour because they influence and modulate the person’s feelings, beliefs, and the person’s trust in one’s own self-regulatory abilities required to change one’s own behaviour [ 27 ]. Moreover, stable personality traits and a positive self-concept are considered general important stress buffers and protectors of mental health, whereas neuroticisms, trait anxiety, difficulties in describing and identifying feelings as well as an overall negative self-concept are considered significant risk factors of mental ill-health, specifically of anxiety disorder and depressive disorder [ 28 , 29 , 30 ].
These examples underscore the complexity and dynamics of how individual traits and state-like individual psychological factors as well as characteristics of the situation interact and influence subjective experience and behaviour. Methodologically, this raises questions of how interactions between situation, person and behaviour can best be assessed, investigated, modeled and predicted in relation to the COVID-19 pandemic in which little empirical evidence is available so far and different aggregated data measures of qualitative and quantitative origin might be used to best capture the internal personal variables of interest (e.g., feelings, worries, self-concept, or personality traits) that provide insight into the subjective experience and the perceived changes in health and behaviour of individual persons behaving in the context of the COVID-19 pandemic.
Computational modeling and machine learning have been already successfully applied in the field of pandemic research to predict transmission rates of the virus based on global behavioural changes of the general population [ 31 ]. These approaches require huge data sets (big data). In health behaviour research, first attempts have been made to apply computational models to data sets comprising smaller sample sizes to model behaviour of individuals, for instance, in response to behavioural interventions supporting health prevention [ 32 ]. These computational models build on psychological theories of human behaviour. Character Computing is one of these psychologically-driven approaches, whose computational models include stable character traits (e.g., personality, self-concept) and cognitive, affective, and motivational state variables and behavioural indicators as input to take into consideration the dynamic interactions between situation (S), person (P) and behaviour (B) (for an overview, see [ 33 , 34 , 35 ] and Fig. 1 ). The computational models are not fixed but can be improved and extended, e.g., by ontologies [ 36 ] or automated data processing, the more empirical evidence and data is available [ 32 , 33 , 34 , 35 ].
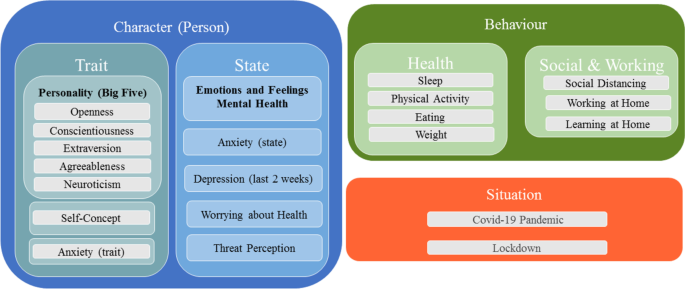
Illustration of the dynamic relationships between situation, a person’s character (traits and states), and behaviour change
Aim of this online survey study
Based on the challenges of the COVID-19 pandemic outlined above, this online survey study is aimed at contributing to the scientific understanding of the psychological consequences of the pandemic by investigating mental health, subjective experience, and behaviour among university students studying in Egypt or Germany after the first pandemic lockdown in May 2020. As outlined above, university students may be particularly sensitive to lifestyle changes related to the COVID-19 pandemic, negatively affecting the students’ mental health, their subjective experience and behaviour. Moreover, as also explained above, the students’ personality traits and self-concept might constitute important stable psychological variables that could influence mental health as well as subjective experience and behaviour related to the COVID-19 pandemic. Therefore, to fully capture these psychological aspects, psychological assessment included a number of psychological variables ranging from stable personality traits and self-concept to state-like psychological variables sensitive to situational change and related to (a) mental health (current depressive symptoms and state anxiety), (b) pandemic threat and emotion perception including current feelings, (c) worries about health including perceived changes in paying attention to bodily symptoms, and (d) self-reported perceived changes in health behaviour (weight, eating, sleeping, physical activity), social and learning behaviour (difficulties in self-regulated learning). To capture all aspects summarized under (a)–(d), the assessment methods comprised a mix of self-report tools (survey items, standardized psychometric scales, psychological questionnaires, and linguistic self-report measures).
Data analysis included (a) descriptive analysis for prevalence estimation of mental health variables, (b) linguistic analysis of self-concept, personality and feelings during the pandemic and (c) correlational analysis and machine learning tools. Machine learning tools were used for exploratory purpose only to further explore the idea of whether machine learning algorithms could despite small sample sizes be trained to predict stable personality traits from the self-report data of the students. Knowing whether stable personality traits (that due to their stability cannot easily be changed by health care interventions) can be predicted from the students’ self-report data could help develop individualized health care interventions that take the students’ personality development into account. The online survey was distributed among university students studying at universities in Egypt and also in Germany. Both countries were equally affected by the lockdowns in May 2020. With respect to the already published survey studies (see above), all attesting an increase in mental ill health among university students during the COVID-19 pandemic the following main research questions were addressed:
RQ1 Mental health: Can the present online survey study confirm high state anxiety and depressive symptoms reported in previous studies in the current sample of university students during the time period of the first COVID-19 pandemic lockdown in May 2020? Crucially, are the self-reported symptoms of anxiety and depression when assessed on standardized psychological screening and assessments tools beyond the cut off scores of clinical samples, and comparable or even higher than the prevalence rates reported in pre-pandemic surveys?
RQ2 Threat perception and worries about health: Do university students report to experience threat, negative feelings and worries about health during the COVID-19 pandemic?
RQ3 Emotion perception: Do university students report to perceive difficulties in emotion perception in the time period of the first pandemic lockdown relative to before the pandemic?
RQ4 Health behaviour, social behaviour and learning: Do university students report to perceive changes in health behaviour (e.g., weight, eating, sleeping, physical activity, paying attention to bodily symptoms), and do they report to experience difficulties in self-regulation during learning (teaching), and in social behaviour in the time period of the first pandemic lockdown?
RQ5 Self-concept and personality: Do university students report a positive or a negative self-concept? Are mental health variables correlated with the students’ personality?
RQ6 Exploratory analysis: Can machine learning despite small data sample sizes predict stable personality traits from the self-report data of the students?
Participants
The survey study was designed and conducted by the Department of Applied Emotion and Motivation Psychology of Ulm University and administered via Ulm University and LimeSurvey software ( https://www.limesurvey.org/de/ ). The survey was advertised among others via the university’s international office to reach specifically students studying in Egypt. The survey was provided in English language (i.e., the academic language), and proficiency in English language was a prerequisite for taking part in the study. Participants were fully debriefed about the purpose of the survey, participation was voluntary and anonymous (see ethics statement). After registration, participants answered questions about their language proficiency, age, gender, their university, study year, and their living situation (alone, with friends or family). Only university students who were aged 18 years and older, and who provided informed consent were able to participate in the study. The survey items were structured in blocks of items and questionnaires: sociodemographic (1), personality (Big-Five) and anxiety (state and trait) (2), survey items about teaching, survey items about health including the linguistic task (self-concept) (3–4), and finally, emotion perception and depression screening (5). The blocking of the serial order of these topics lead to partial drop-outs across the survey, particularly across blocks (see below).
An overview of the complete study-design is provided in the flow-diagram in Fig. 2 . An overview of the online survey items and questionnaires can be found in the Additional file 1 .
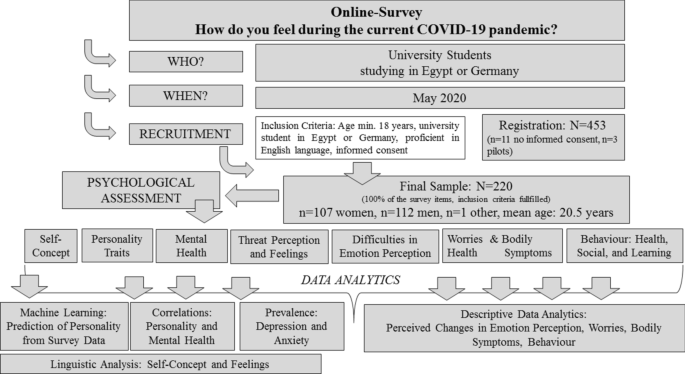
Design of the survey including data collection and recruitment of participants and data analytics. Please see sections ““ Aim of this online survey study ” and “ Methods ” for detailed explanation
Study sample, survey drop-out and missing data
In total, N = 453 university students registered for the study and answered the inclusion and exclusion criteria. Of these, n = 3 were pilots and n = 11 participants did not give informed consent or did not explicitly state that they want to get their data published in scientific research, and were therefore excluded from the study sample. N = 439 volunteers (n = 215 men, n = 219 women, n = 5 did prefer not to name their gender; mean age : 20.69 years, SD = 2.87 years) completed the sociodemographic questions. Of these, n = 19 (4.3%) did not report to study in Germany or Egypt and were excluded. Of the 420 university students who reported to study in Egypt or Germany, n = 325 participants (n = 167 men, n = 156 women, n = 2 did prefer not to name their gender; mean age : 20.38 years, SD = 1.76 years, range: 18–33 years) filled in the personality and anxiety questionnaires only, while n = 220 participants (n = 112 men, n = 107 women, n = 1 did prefer not to name the gender; mean age : 20.45 years, SD = 1.88 years, range: 18–33 years) completed the entire survey. This corresponds to a survey completion rate of 0.49 (division of the number of participants who complete the entire survey (n = 220) by the total number of participants who register for the survey (n = 453)). This rate falls within the rate expected for online surveys (20–50%).
Analysis of the drop-outs (including e.g., univariate measures of variance (ANOVA)), showed no difference in age between the groups (i.e., the sample who filled in the sociodemographic items only (n = 95) versus the sample who filled in the personality and anxiety questionnaires only (n = 105) versus the final sample (n = 220), F (417,2) = 1.72, p = .18. In addition, the student samples did not differ with respect to gender, i.e., the % of the number of women and men. Analysis of anxiety and personality scores likewise suggests that the final sample and the sample who dropped-out after filling in the personality or anxiety questionnaires (n = 220 versus n = 105) did not differ in state anxiety or in the scores on any of the Big-Five personality dimension. (state anxiety: F (323,1) = 1.77, p > .18; Openness: F (323,1) = 0.16, p > .69; Conscientiousness: F (323,1) = 2.82, p > .13; Extraversion: F (332,1) = 0.94, p > .33; Agreeableness: F (323,1) = .062, p > .43; Neuroticism: F (323,1) = 1.22, p > .27). Mean scores of trait anxiety differed between the final sample and the sample who dropped out (n = 220: mean : 46.02, SD = 11.2, range : 26–79 vs. n = 105: mean : 49.02, SD = 10.98, range : 26–77, F (323,1) = 5.78, p = .017). However, using median tests (which are less susceptible to outliers) showed no significant difference in the distribution of trait anxiety scores between the samples (median-test = 1.59, p = .21), see Fig. 3 for an overview.
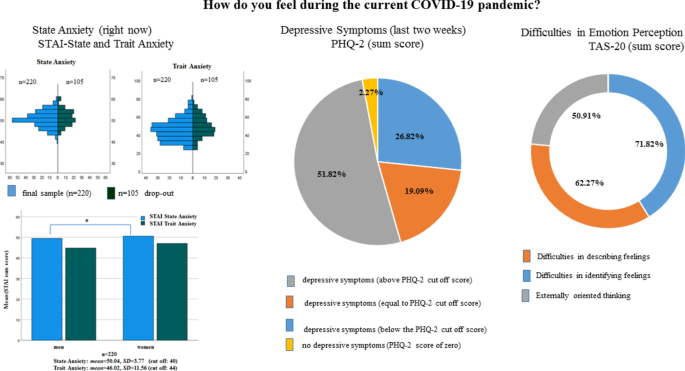
State and Trait Anxiety distributions across the final sample and drop outs (left upper column). Mean state and trait anxiety scores in women and man in the final sample (left lower column), significant results ( p < .05) are illustrated by lines and cross. Percentage of students reporting depressive symptoms (middle column). Right column: Percentage of students reporting changes in emotion perception on the TAS-20 questionnaire and subscales after the COVID-19 pandemic outbreak
The survey was programmed such that it produced as little missing data as possible. Therefore, missing data of single items in a questionnaire or in a block of open items could be excluded and missing scores were therefore not imputed. Regarding the self-generated prompts, participants were free to answer the prompts (self-concept and feeling descriptions). Inspection of the data shows that in the full sample, 5 participants did not fill in all of self-descriptive prompts, leaving open 1, 2 or 3 of the descriptions, respectively.
Measures: survey items and questionnaires
The online survey included several self-report measures comprising a mix of single items with open and closed questions, standardized psychometric scales, and standardized psychological questionnaires. The section below and Table 1 provide an overview of the survey items, questionnaire measures and hypotheses grouped according to the psychological domains and research questions of interest (for an overview, see also RQ1–RQ6 in the section “ Aim of this online survey study ”).
Mental health: anxiety (trait/state), current depressive symptoms (last 2 weeks)
As illustrated in Table 1 , the participants anxiety proneness including trait and state anxiety as well as their current self-reported depressive symptoms (last 2 weeks) were assessed with psychological questionnaires including the Spielberger Trait and State Inventory (STAI, [ 37 ]), and the Patient Health Questionnaire (PHQ-2, [ 38 ]). The STAI is available in many different languages and has shown similar values of internal consistencies among university students from European and Arabic countries [ 39 ]. Whereas the trait scale of the STAI asks for how one generally feels, the instruction of the state scale of the STAI asks for how one feels right now. The PHQ-2 has proven to be a robust screening for depressive symptoms across different cultures including European and Arabic countries [ 40 ]. It asks for the presence of depressive symptoms over a time period of the last two weeks.
Threat perception, feelings, and perceived difficulties in emotion perception during the COVID-19 pandemic
Threat perception as well as discrete emotions and feelings in response to the COVID-19 pandemic situation were assessed by single survey items. Specifically, these items asked the participants about how the current COVID-19 pandemic situation makes them feel in terms of valence (positive/pleasant-negative/unpleasant), arousal (low/calm-high/aroused), and dominance (feeling in or out of control of the situation). The 9-point Self-Assessment Manikin scales (SAM, [ 41 ]) were used for valence, arousal and dominance assessment. The SAM scales are one of the most robust and frequently used scales for the unbiased, non-verbal assessment of emotions and feelings on the three dimensions of emotions including valence, arousal and dominance [ 41 ]. In accordance with the literature [ 41 ], the SAM scales ranged from 1 (negative/unpleasant, low arousal/calm, out of control) to 9 (positive/pleasant, high arousal/aroused, in control). In addition, we asked the participants to indicate which kind of discrete emotions they experienced in response to the COVID-19 pandemic. Participants could choose among six discrete emotions (sad, anxious, angry, disgusted, happy, surprised, or neutral). In addition, participants were given five prompts to describe their current feelings in response to the COVID-19 pandemic situation (“I feel ….”). In order to assess potential difficulties in emotion perception, participants filled in the Toronto Alexithymia Scale (TAS-20; [ 42 ]), which comprises the three subscales “Difficulty Describing Feelings”, “Difficulty Identifying Feelings”, and “Externally-Oriented Thinking”. Since we were interested in perceived changes since the pandemic outbreak, participants were instructed to answer each item of the TAS-20 questionnaire relative to before the pandemic.
Worries about health and perceived changes in behaviour during the COVID-19 pandemic
Worries about health, perceived changes in paying attention to bodily symptoms (e.g., taste, smell, cardiovascular, respiration/breathing, appetite/eating/drinking), as well as perceived changes in health behaviour (weight, eating behaviour, sleep and physical activity behaviour) as well as perceived difficulties in social behaviour (social distancing) and self-regulatory learning (i.e., difficulties in paying attention to the content provided by e-learning, difficulties in studying with the same effort as before the pandemic situation) were assessed via single survey items. The single item questions that asked for worries and perceived changes in behaviour could be answered with “yes” or “no”; “yes” meaning an increase and “no” meaning no change in relation to before the pandemic. The items on health behaviour included items asking in both directions, e.g., whether one eats more or less, sleeps more or less, exercises more or less than before the pandemic. The single item questions of paying attention to bodily symptoms could be answered on 10-point Likert scales such that change scores could be calculated based on the participants’ answers allowing evaluation of the degree of change as increase, decrease or no change during the pandemic situation in relation to before the pandemic (see Table 1 for an overview).
Personality and self-concept
As illustrated in Table 1 , the participants’ personality traits were assessed with the Big Five Personality Inventory (BFI-40, [ 43 ]). The BFI-40 is a standardized self-report measure that has been validated in different cultural populations and age groups [ 44 ]. The self-concept was assessed using a modified short version of the twenty statements tests (TST, [ 45 ]). The TST is a cross-cultural tool for the assessment of different facets of the self-concept including actual, ideal, and ought selves. In the present study, participants had to generate self-descriptions for the actual self only. In line with the instruction of the TST [ 45 ], participants were asked to provide five words to the prompts “I am ….” in order to describe themselves.
Mental health: anxiety (trait and state) and current depressive symptoms
In line with previous pre-pandemic surveys among university students (see Background for an overview), we expected a high prevalence of anxiety and depressive symptoms in the present sample of university students irrespective of their culture or country in which they study. Prevalence rates for self-reported current depressive symptoms assessed with the screening tool of the PHQ-2 asking for depressive symptoms in the last 2 weeks (PHQ-2 items: item1: “little interest or pleasure in doing things”; item 2: “feeling down, depressed or hopeless”) and state anxiety (asking for how one feels right now) might be expected to be even higher than prevalence rates reported in previous surveys before the pandemic situation.
Threat perception, feelings, and difficulties in emotion perception
We expected threat perception to the COVID-19 pandemic to be associated with self-reported unpleasantness, feelings of moderate to high levels of arousal, self-reported perceived lack of dominance (feeling less in control of the situation) on the Self-Assessment Manikin (SAM) scales. In addition, we expected self-reports of feelings of anger, sadness, and anxiety towards the pandemic as assessed by the survey items assessing discrete emotions. We also explored whether students report to perceive changes in emotion perception since the pandemic outbreak relative to before the pandemic outbreak. Specifically, we explored whether participants report difficulties in describing and identifying feelings and report externally oriented thinking on the TAS-20 as potential maladaptive adaptions in coping with the pandemic lockdown. As mentioned above, the instruction of the TAS-20 items asked the participants to answer the items in relation to before the pandemic.
Worries about health, perceived changes in behaviour during the COVID-19 pandemic
We expected that the majority of students will report to be more worried about their mental and physical health than before the pandemic. Moreover, we expected a higher awareness of bodily symptoms (i.e., paying more attention to perceived changes in smell, taste, cardiovascular functions, breathing/respiration, and appetite/eating/drinking) relative to before the pandemic. Given that the lockdown in every country had effects on the students’ work and leisure time activities, we also expected that participants will report changes in health behaviour including a decrease in regular physical activity compared to before the pandemic lockdown including self-reported changes in eating- and sleeping behaviour and weight. We also expected difficulties in learning and social behaviour (see Table 1 ).
Moreover, we examined how university students see themselves (self-concept). In particular, we explored whether the students would report a positive or negative self-concept and compared their linguistic descriptions of the self to their descriptions of their current feelings pandemic-related feelings (“I feel …) and their personality. Regarding personality, we explored whether stable psychological personality traits (Big Five and trait anxiety) would be correlated with state anxiety and depressive symptoms and the students’ perceived changes in emotion perception. Finally, we examined for exploratory purpose, whether machine learning could predict the students’ personality traits from their reports (for details see “Data Analysis” section).
Descriptive analyses and statistics
To answer the hypotheses outlined above, the participants’ answers (questionnaires, single items) were analysed descriptively to provide insight into how many students on average reported anxiety and depressive symptoms as well as how many students reported to perceive changes in subjective experience (threat perception, difficulties in emotion perception, worries about health, bodily symptoms) and behaviour (health, social, learning). Analysis of the questionnaires (PHQ-2, STAI, TAS-20, BFI-40) followed the guidelines and manuals and were calculated as sum scores or mean scores (non-normalized). For the PHQ-2, STAI and TAS-20, cut off scores are available from the literature (see “ Results ” section). These cut off scores were also used in the present study to discriminate between high versus low trait anxiety, high versus low state anxiety, depressive symptoms, and difficulties in emotion perception. Means and standard deviations were calculated for all questionnaire data and for the closed survey items using Likert scales or the SAM scales. The questionnaire data and answers to the survey items were tested statistically for significance by means of non-parametric or parametric statistical tests as appropriate. The respective test statistics are presented in brackets in the “ Results ” sections. Given the drop-out across blocks of the survey (see section about Sample size, survey drop-out and missing data), the results for each scale, item or questionnaire were calculated for the available sample who filled in the questions and the final sample (n = 220) who filled in the complete survey and who reported to study in Egypt or Germany. P values are reported uncorrected and two tailed if not otherwise specified. The SPSS software (IBM SPSS Statistics Software, Version 27) was used for all statistical testing including correlation analysis (see below).
Correlational analysis
Correlation analyses (Pearson) were used to assess the relationships between the Big Five personality traits (BFI-40), mental health variables (STAI: trait and state anxiety, PHQ2: screening for depressive symptoms), and difficulties in emotion perception (TAS-20). P values are reported uncorrected and two tailed if not otherwise specified.
Linguistic analysis of self-concept and feelings
The open-ended linguistic answers assessing the self-concept (“I am …”) and feelings in response to the pandemic (“I feel …”) were analysed with computer-assisted text analysis tools including Linguistic Inquiry of Word Count (LIWC; [ 46 ]). The dictionary of the LIWC software contains words and word stems, grouped into semantic categories related to psychological constructs. The categories provided by the LIWC allow the assessment of the polarity of words (positive or negative). The LIWC analysis produces reliably results with about 500 words and more. Therefore, in the present study, words generated by each participant were accumulated across participants and entered as a whole text corpus for words generated for the prompts “I am …” (self-concept) or for the prompt “I feel …” (feelings in response to the pandemic), respectively. This allows the evaluation of the self-concept and current pandemic feelings of the university sample as a whole. For the linguistic analysis no statistic testing was performed.
Machine learning (exploratory analysis)
Machine learning (ML) was used for exploratory purpose only and the ML algorithms were chosen to combine the different psychological variables that were descriptively analysed in order to explore whether individual personality traits including the Big Five and trait anxiety can be predicted and classified by automated machine learning tools. To this end, the questionnaire scores and answers to the different survey items were preprocessed according to the following procedure: the participants’ Big Five personality traits from the BFI-40, the state and trait anxiety scores (from the STAI including for each individual, a difference score for self-reported trait and state anxiety), depression (PHQ-2), perceived changes regarding difficulties in emotion perception (TAS-20) as well as the participants’ answers on the SAM scales for threat perception (e.g., valence, arousal, dominance) were normalized (z-scores). The participants’ answers to the discrete emotions elicited during the pandemic, difference scores assessing increase in current anxiety (difference score comparing STAI state vs. STAI trait) as well as the participants’ answers to the survey items asking for worries and perceived changes in health and behaviour were labeled as positive or negative or set to zero if the students reported no change. The answers to the survey items asking for perceived changes in paying attention to bodily sensations/symptoms were combined to a total score denoting the total perceived changes in attention towards bodily sensations/symptoms and the total change was labeled as positive or negative depending on whether attention increased or decreased relative to before the pandemic or set to zero if there was no change. Sociodemographic variables such as country or university were no contribution factors in prediction and classification. After data preprocessing and data labeling, the dataset for machine learning comprised continuous features and discrete categorical features. The whole dataset was denoted “X” and the continuous or discrete features were denoted “y” in the feature matrix. The machine learning libraries of the Python software package ( https://www.python.org/ ) were used for automated data analysis. Data analysis was based on regression models. Gradient Boosting Regression (GBR) and Support Vector Regression (SVR) were chosen for the regression models. The principle of Gradient Boosting Regression is to build multiple regression models based on decision trees. Decision tree models are supervised machine learning algorithms that have tree structures that recursively break down the dataset into smaller datasets through branching operations while comparing the final node results with the target values. Decision tree models provide the best fit for small sample sizes to avoid overfitting the data. The same holds true for support vector machine algorithms. Support Vector Regressions (SVR) aim at finding the best fitting line in continuous data within a predefined threshold error. The evaluation of the accuracy of the prediction is evaluated based on the root mean squared error (RMSE). Depending on the type of data to be predicted, RMSE within 10–20% of the range is considered a good result. Especially with human self-report, data accuracies are usually much lower than in other more deterministic domains of machine learning e.g., natural language processing or bioinformatics. One reason for the lower accuracies in human behaviour data is the higher variance in the data itself [ 47 ]. To account for this, we accepted a RMSE of up to 16.6% as sufficient for the decision that the data can be predicted by the model accurately.
We used the classical train/test split approach with a ratio of 8:2. Train/test split is a common validation approach frequently used in ML studies including those with smaller sample sizes [for a critical review see [ 48 ]). No k-fold cross validation (CV) approach was chosen as it has been shown that k-fold CV can lead to overestimation especially with small sample sizes, whereas train/test split and nested CV approaches have been shown to be equally reliable even with small sample sizes [ 48 ]. We also performed hyperparameter tuning, an algorithm frequently used and recommended in machine learning to choose and select during training the best model while avoiding biasing the data, and the number of features and the feature-to-sample ratio) was kept in an optimal range (less features than samples) for avoiding overfitting [ 48 ].
Descriptive data analytics
Mental health: anxiety (trait and state) and depressive symptoms.
The mean state and trait anxiety scores of the university students who completed the entire survey and who studied in Egypt or in Germany (n = 220) were above the cut off scores that according to the literature distinguishes between high versus low anxious subjects [ 49 ]. The mean state anxiety score as measured with the STAI inventory was significantly above the cut of score of 40 (n = 220, mean : 50.04, SD = 3.77; T = 39.47, df = 219, cut off: 40, p < 0.001). A cut off score below or above a score of 44 in the trait STAI scale differentiates between low trait anxious and high anxiety prone individuals [ 49 ]. The mean score for trait anxiety was significantly higher than this cut off score (n = 220, mean: 46.02, SD = 11.56; T = 2.60, df = 219, cut off: 44, p < 0.01). Given the drop-out of n = 105 students, the analysis of the mean state and trait anxiety scores were recalculated for the final sample including those students who dropped out. The analysis showed that also in this larger sample of n = 325 students the cut off scores were significantly above the cut off scores (state anxiety: n = 325; mean : 50.23, SD = 3.75; T = 49.13, df = 324, cut off: 40, p < 0.001; trait anxiety: n = 325; mean : 47.08, SD = 11.52; T = 4.72, df = 324, cut off: 44, p < 0.001) and in addition, trait anxiety scores (trait) did not differ significantly between women and men in this sample (trait anxiety: n = 325; mean-woman : 47.94, SD = 11.82; men: 45.96, SD = 10.91; F (321,1) = 2.45, p > 0.12). However, women reported higher state anxiety scores than men. This difference in state anxiety scores between women and men was significant (state anxiety: n = 325; mean-woman : 50.81, SD = 3.62; men: 49.63, SD = 3.79; F (321,1) = 8.08, p < 0.005) and was also significant in the n = 220 sample. There was no significant difference in state anxiety scores between students studying in Egypt or Germany, neither in the n = 220 sample nor in the sample comprising n = 325 students (n = 220, state anxiety: Egypt- mean : 50.16, SD = 3.75, Germany- mean : 49.08, SD = 3.86, Mann – Whitney-U = -1.39, p = 0.16; n = 325, state anxiety: Egypt- mean = 50.32, SD = 3.70, Germany- mean : 49.45, SD = 4.22, Mann – Whitney-U = -1.24, p = 0.22). However, students studying in Egypt reported higher trait anxiety compared to the students studying in Germany (n = 325, trait anxiety: Egypt- mean : 47.62, SD = 11.60, Germany- mean : 42.24, SD = 9.75, n = 220, trait anxiety: Egypt- mean : 46.49, SD = 11.57, Germany- mean : 42.40, SD = 10.93), but this difference was not significant in the final sample (n = 220, Mann – Whitney-U = − 1.39, p = 0.16). The results are illustrated and summarized in Fig. 3 .
For the PHQ-2 screening for depressive symptoms a sum score greater than 3 on both items is associated with depression proneness [ 38 ]. In the sample of university students who completed the entire survey and therefore had filled in the PHQ-2 depression screening, the mean sum score was mean: 3.48, SD = 1.58, and significantly above the cut off score ( T = 4.51, df = 219, cut off = 3, p < 0.0001). 51.82% (n = 114) of the students had sum scores greater than the cut off (> 3), and 19.09% (n = 42) had a sum score of 3 (cut off). Only 26.82% (n = 59) of the sample scored below the PHQ-2 cut off score (< 3), and only 2.27% (n = 5) did report to not suffer from loss of interest or pleasure in doing things (PHQ-2 item 1) or from feeling down, depressed or hopeless during the last two weeks (PHQ-2 item 1) (see Fig. 3 for an overview on state anxiety and depressive symptoms). The PHQ-2 scores did not differ between students studying in Egypt or Germany (n = 220, Egypt- mean : 3.51, SD = 1.56, Germany- mean : 3.24, SD = 1.79, Mann – Whitney-U = − 0.643, p = 0.52) nor did they differ between women and men (n = 220, woman- mean : 3.48, SD = 1.54, men- mean : 3.47, SD = 1.63, F (217,1) = 0.00, p = 0.98).
Descriptive analysis of the items assessing threat perception (SAM; Self-Assessment Manikin scales ranging from 1 (unpleasant, not aroused, or no control) to 9 (pleasant, very highly aroused, in control)) showed that, the students (n = 220) felt slightly unpleasant ( mean : 4.19, SD = 1.97). In addition, 55% (n = 120) of the final study sample (n = 220) reported a score from 1 to 4, i.e., from high unpleasantness to moderate unpleasantness on the 9-point SAM valence scale. On average, the students did not feel much in or out of control of the situation ( mean : 5.07, SD = 2.41) on the 9-point SAM scale for dominance. Nevertheless, 37.55% of the study sample reported a score from 1 (no control) to 4 (loss of control) on the SAM scale for dominance. Mean physiological arousal was rated as moderate ( mean : 5.40, SD = 2.22). However, 50% of the university students (n = 110) reported an arousal score of 6 (aroused) to 9 (very high arousal) on the SAM arousal scale. Given the drop-out of students, comparisons of the ratings (valence, arousal, or control) were performed between samples (n = 220 and n = 59 who completed the ratings but did not fill in the entire survey). This showed that the ratings did not differ between the samples ( Mann – Whitney-U -tests, all p > 0.70). From the set of discrete emotions (including sadness, anger, fear, disgust, happiness, surprise, or neutral emotions), 66.8% reported to feel not neutral, 93.2% reported to feel not happy, 56.4% reported to feel sad, 75.9% reported to feel angry, 92.3% reported to feel surprised, 87.7% reported to feel disgusted, and 52.7% reported to feel afraid by the current pandemic situation. The distribution of “yes” versus “no” answers differed significantly for the categories feel neutral, happy, surprised, disgusted, or angry, respectively, (non-parametric test for binomial distribution: all p < 0.001). From all students who completed these items (n = 277) the same significant results were obtained for the answers concerning discrete emotions.
16.88% of the students of the final sample (n = 220) had a total TAS-20 score greater than the critical TAS-20 cut off score (TAS-20 cut off > 60, [ 30 ]). From the three subscales of the TAS-20 questionnaire, changes in self-reported difficulties in emotion perception in relation to the pandemic as compared to before the pandemic were reported by 62.27% (n = 137) for items belonging to the subscale “Difficulty describing feelings”, and by 71.82% (n = 158) for the items belonging to the subscale “Difficulty identifying feelings” and by 50.91% (n = 112) for the items belonging to the subscale “Externally Orienting Thinking”. The distributions of the TAS-20 scores of the three subscales did not differ between students studying in Egypt or Germany ( Mann – Whitney-U , all p > 0.50). However, woman (n = 107) reported higher scores on the subscales “Difficulties identifying feeling” compared to men (n = 112), F (217,1) = 217.1, p = 0.035.
Worries about health
In the final sample who completed the survey (n = 220), 65.5% (n = 144 students) of the study sample reported to worry about their mental health more due to the COVID-19 pandemic than before the pandemic, whereas 34.5% (n = 76) answered to worry not more than before the pandemic. 71.4% (n = 157) of the students reported to worry more about their physical health than before the pandemic, whereas 28.6% (n = 63) answered to worry not more about their physical health than before the pandemic. The distributions of “yes” versus “no” differed significantly for both, worries about mental and physical health, respectively (non-parametric test for binomial distribution: all p < 0.001) and this also held true when considering all students who filled in these items (n = 227). Self-reported worries about mental health and physical health were significantly related (χ2 = 100.43, df = 2, p < 0.001). 65% (n = 143 of n = 220) reported to worry in both domains (mental health and physical health) more than before the pandemic and this also held true when considering all students who filled in these items (n = 227), see Fig. 4 a.
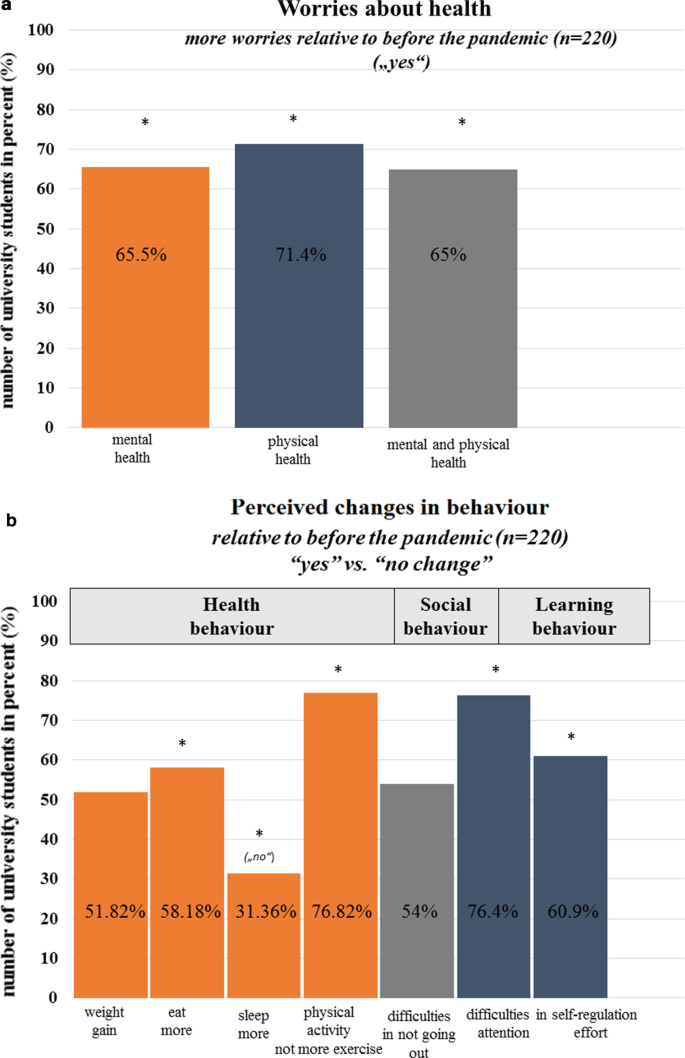
a Worries about mental health or physical health or both (mental and physical health). The cross represents significant results, p < .05. b Perceived changes in health behaviour including weight, eating, sleeping, and physical activity. The cross represents significant results, p < .05
Behaviour: health
Across health behaviour domains (weight, eating, sleep, physical activity), 52.3%, 58.2%, 31.8%, and 76.4% of the study sample (n = 220) reported to have gained weight, to eat more than before the pandemic and to not sleep more or exercise more than before the pandemic situation. The distributions of “yes” versus “no” answers were significantly different for the domains of eating, sleep and exercise/physical activity (non-parametric test for binomial distribution: eat, sleep, exercise/physical activity all p < 0.001) and this again held true when considering all students who filled in the items (n = 227). Paying attention to bodily sensations and symptoms (i.e., changes in taste, smell, appetite/eating/drinking, cardiovascular functions, breathing/respiration) did however not change significantly relative to before the pandemic outbreak. On average, on Likert scales ranging from 1 (“decrease”) to 5 (“no change”) to 10 (“increase”), participants reported not to pay more attention to or to be more aware of bodily sensations and symptoms than before the pandemic (smell: mean : 5.18, SD = 1.21, taste: mean : 5.15, SD = 1.27, bodily symptoms: mean : 5.84, SD = 1.74, cardiac symptoms: mean : 5.78, SD = 1.66, breathing: mean : 5.77, SD = 1.64, eating and drinking/appetite: mean : 5.52, SD = 2.09). The answers on these rating scales did not differ between students studying in Egypt or Germany (all p > 0.16), but comparisons between women and men showed that women scored significantly higher on the scale asking for attention to bodily symptoms than men (woman- mean : 6.18, SD = 1.90, men- mean : 5.50, SD = 1.53, F (217,1) = 8.50, p > 0.002). This again held true when considering all students who filled in the items (n = 227).
Behaviour: social distancing and learning
Being asked about their social situation of self-isolation, teaching and learning behaviour, 54% of the student sample (n = 220) replied to have difficulties in not going out during the pandemic. 76.4% replied to have difficulties in self-regulated learning, being unable of focusing their attention on the teaching content. Of these students, 60.9% replied to have difficulties in studying with the same self-regulatory effort because of being anxiously preoccupied with the current pandemic situation (see Fig. 4 b). The distributions of “yes” versus “no” answers were significantly different for the domains of learning (non-parametric test for binomial distribution: eat, sleep, exercise/physical activity all p < 0.002) and this again held true when considering all students who filled in these items (n = 305, all p < 0.001).
Linguistic self-concept and self-descriptions of current feelings
Linguistic self-descriptions (“I am …”) showed a positivity bias. Overall, more positive words than negative words were used by the students to describe themselves (see Fig. 5 ). As mentioned above, linguistic analysis of the university students’ self-descriptions about how the current COVID-19 pandemic situation makes them feel (“I feel …”) showed the reverse pattern with more negative words than positive words being used by the study sample to complete the prompt “I feel ….” (see Fig. 5 ). In addition, Fig. 6 shows the most prominent examples, i.e., the words most often used by the students to describe their feelings during the pandemic.in the prompt “I feel …”.
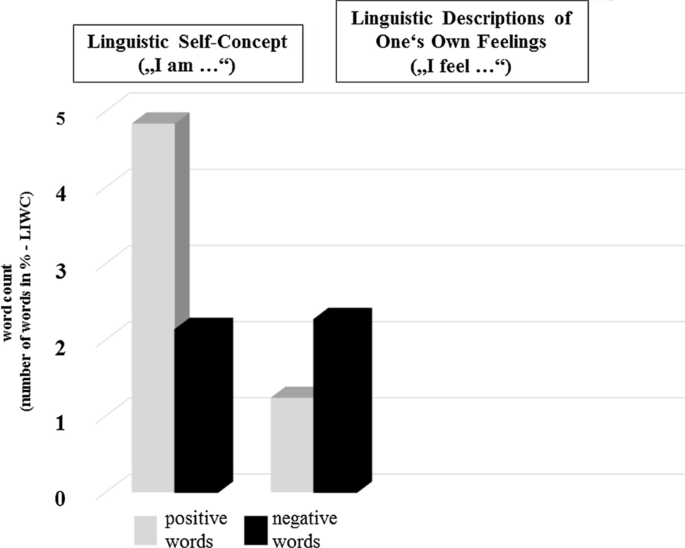
Percentage of negative and positive words. Left column: Self-concept: “I am …”. Right column: Current feelings during the pandemic “I feel …”
Summary of the words most often used by the university students to describe their feelings in response to the pandemic
Personality: Big Five
The final student sample (n = 220) scored low on the BFI-40 subscales for extraversion ( mean : 24.5, SD = 5.65), neuroticism ( mean : 25.37, SD = 6.51), and reported moderate scores on the conscientiousness scale ( mean : 30.69, SD = 6.07), the openness scale ( mean : 36.85, SD = 5.07), and the agreeableness scale ( mean : 33.42, SD = 4.50) and as described earlier (see section “ Study sample, survey drop-out and missing data ”), the BFI-40 scores of the samples (n = 220 vs. n = 105 who dropped-out) did not differ in the five personality dimensions. The Big Five personality traits were significantly correlated with self-reported depressive and anxiety symptoms as well as with the self-reported difficulties in emotion perception. Table 2 shows a summary of the correlations between measures of personality traits (BFI-40), trait anxiety (STAI-trait scale), state anxiety (STAI-state scale), self-reported depressive symptoms (PHQ-2), and perceived difficulties in emotion perception (TAS-20) as obtained from the final sample (n = 220).
Automated data analytics, machine learning (exploratory)
The university students’ personality traits (Big Five) and trait anxiety could be predicted from the psychological variables (trait and state) summarized in Table 3 through feature importance extraction by Support Vector Regression. The table and the numbers in percent show the major contributing factors to the prediction of the respective trait listed in the left column (under “Measure”). Table 4 shows the prediction accuracy suggesting that prediction of all trait attributes have similar error rates.
The COVID-19 pandemic is taking its toll. Concerns have been raised by the WHO (2020) [ 8 ], that the COVID-19 pandemic will cause “a considerable degree of fear, worry and concern in the population” (cited from WHO, 2020 [ 8 ]) and that stress and anxiety as well as depression will increase considerably during the COVID-19 pandemic, rendering affective disorders a public mental health concern of the COVID-19 pandemic [ 8 ]. In the present survey, mental health (depressive symptoms, state and trait anxiety), subjective experience (threat perception, current feelings, perceived difficulties in emotion perception, worries about health during the pandemic) as well as perceived changes in behaviour (related to health, social behaviour and learning/teaching) was assessed among university students studying in Egypt or Germany, respectively. The survey was administered in May 2020, shortly after the lockdown in these countries. Going beyond previous surveys, the students’ self-concept and the Big Five of human personality were additionally assessed to explore psychological patterns between personality traits, mental health, and perceived changes in subjective experience by means of correlation analysis and machine learning.
Mental health among university students
Regarding pandemic risk groups, previous cross-cultural pre-pandemic surveys have shown high prevalence rates of anxiety and depression among university students across countries [ 17 , 18 , 19 , 20 , 21 , 22 , 50 , 51 , 52 , 53 ]. Therefore, the WHO’s concerns about the psychological consequences of the COVID-19 pandemic on mental health and well-being might affect university students as a population group as well. The results obtained from this sample of university students who study in Egypt or Germany during the first lockdown period confirm these concerns. In particular, the results confirm previous pre-pandemic results about mental health of university students and they seem to confirm the concerns of the WHO regarding mental health and threat perception during the current pandemic. The mean state anxiety score (assessed with standardized questionnaires including the Spielberger Trait-State Anxiety Inventory, STAI) was significantly above the cut off score that, according to the literature [ 34 ], discriminate high from low anxious subjects. In addition, state anxiety scores were significantly higher in woman than man. Moreover, 51.82% (n = 114) of the students had sum scores greater than the cut off (> 3), and 19.09% (n = 42) had a sum score of 3 (cut off). Only 26.82% (n = 59) of the sample scored below the PHQ-2 cut off score (< 3), and only 2.27% (n = 5) did report to not suffer from loss of interest or pleasure in doing things (PHQ-2 item 1) or from feeling down, depressed or hopeless during the last two weeks (PHQ-2 item 1), and self-reported depressive symptom did not differ among students studying in Egypt or Germany or in woman or men (see Fig. 3 for an overview on state anxiety and depressive symptoms). Thus, in total, 51.82% and 19.09% of the final student sample (n = 220) reported depressive symptoms at and above the cut off score for depressive symptoms [ 38 ], thus feeling depressed or hopeless and reporting a loss of interest and pleasure in the items of the PHQ-2 questionnaire during most of the days of the last 2 weeks of the COVID-19 pandemic. Prevalence rates from previous surveys among university students reported a prevalence of anxiety symptoms or depressive symptoms above 35% among university students before the pandemic (e.g., for depression or anxiety [ 17 , 18 , 19 , 20 , 21 , 22 , 50 , 51 , 52 , 53 ]). A recent online study [ 21 ], including N = 185 university students studying in Germany found that 36.6% of the university students (women and men) report experiencing depressive symptoms, 41.83% (women and men) reported experiencing high levels of state anxiety, and all students reported experiencing stress due to excessive demands and uncertainty in finances, job, or social relationships. These prevalence rates have actually been found in cohort studies including university students all over the globe, irrespective of culture before the outbreak of the pandemic [ 17 , 18 , 19 , 20 , 21 , 22 , 50 , 51 , 52 , 53 ]. In relation to these pre-pandemic prevalence rates, the prevalence of state anxiety and of depressive symptoms in the current sample seem to have more than doubled during the pandemic time period.
The scores for state anxiety need to be seen in relation to the results obtained for trait anxiety. As mentioned above, trait anxiety scores were even higher in those students who dropped-out, however state anxiety scores did not differ across students who completed the survey and those who did not. Students with high state anxiety during the pandemic may be at special risk of suffering from anxiety proneness in the long run. Therefore, surveys among university students should be continued to further explore the development of anxiety and particularly also of depressive symptoms during the current pandemic as well as the comorbidity of anxiety with depressive symptoms as a consequence of the COVID-19 pandemic. Very recent surveys among university students from Greece (Europe) and the United States conducted in a similar time period (during the first lockdowns in these countries) report similar high percentage numbers of anxiety, depression and mental health burdens [ 12 , 13 ]). Given that the STAI asks for feelings of stress, worry, discomfort, experienced on a day to day basis one could expect changes in other psychological domains as well (see below).
Threat perception and perceived difficulties in emotion perception
Being asked about their feelings during the pandemic, 55% of the students reported unpleasantness and 37.55% of the students rated to be in loss of control of the situation, and about 50% reported moderate to high physiological arousal. Moreover, university students reported a mix of discrete emotions in response to the pandemic. In particular, there was a significant loss of happiness, and a change in feelings of surprise, disgust and anger. In line with this, as illustrated in Fig. 5 , linguistic analysis of the participants’ answers to the questions “I feel …” also suggest a negativity bias in the linguistic descriptions of the students’ feelings: In summary, there was more intense use of negative than positive words to describe one’s feelings in response to the pandemic. Thus, feelings of threat and negative emotions were also reflected in the self-generated linguistic answers of the students, supporting a general increase in anxiety during the first period of the COVID-19 pandemic among university students. Similarly, and in line with the scores obtained from the depression screening instrument (PHQ-2), linguistic analysis of the questions “I feel …” revealed a high percentage of words such as feeling depressed, down or hopeless (see Fig. 6 ). Thus, anxiety and depression related words were amongst the most frequently used words when participants were asked to describe in their own words, how the current COVID-19 pandemic situation makes them feel. The study sample also reported to have perceived difficulties in emotion perception during the pandemic. Using the three subscales of the Toronto Alexithymia Scale (TAS-20), the participants were instructed to rate whether they experience difficulties in emotion perception relative to before the pandemic situation. Especially difficulties in identifying and describing feelings were reported. Moreover, the sum scores of the TAS-20 were significantly correlated with the students’ anxiety scores and the intensity of self-reported depressive symptoms (see Table 2 ). Taken together, these results are of particular interest in light of discussions which mental health interventions might help university students to cope with the threat provoked by the pandemic situation. Given that previous research has shown that high scores on the TAS-20 promote psychopathology [ 28 , 29 ], the reports of the students about them perceiving difficulties in identifying one’s feelings in response to the pandemic situation relative to before the pandemic outbreak should be taken seriously and investigated in further studies in larger student cohorts.
Worries about health and health behaviour during the COVID-19 pandemic
Moreover, the university students’ worries about health should be taken seriously. Chronic worrying is a sign of chronic distress and constitutes a risk factor of later development of general anxiety disorder [ 54 ]. In the current study, 65.5% of the final student sample (n = 220) reported being worried about their mental health and 71.4% reported to worry about their physical health more often than before the pandemic. The majority of the student sample did, however, not report to pay more attention to bodily sensations or symptoms (taste, smell, cardiovascular, respiration/breathing) than before the pandemic. However, worries about mental and physical health were accompanied by perceived changes in health behaviour. The percentage of “yes” and “no”-answers differed significantly for changes in health behaviour related to eating and physical activity behaviour since the outbreak of the pandemic. We did not ask the students for their eating behaviour or their physical activity level before the pandemic. Thus, the questions asking for perceived changes during relative to before the pandemic might have the potential of a memory bias. Nevertheless, pre-pandemic surveys report that up to 30% of university students do not exercise at a regular basis and do not meet the WHO’s weekly or daily physical activity recommendations (for an overview see [ 55 ]). The present results suggest a reduction in physical activity during the pandemic and physical inactivity and sedentarism are among the major risk factors promoting negative lifestyle-related diseases in the long run [ 55 ].
Learning behaviour during the COVID-19 pandemic
The pandemic might have negative effects on student’s teaching and learning behaviour. In the present sample of university students, difficulties in teaching and learning were reported by the majority of students. One interpretation of these results is, that pandemic situations such as the current COVID-19 pandemic are characterized by uncertainty, fear, and threat, i.e., factors that are known to impact self-regulation. Previous research has shown that self-regulation is negatively related with threat perception [ 27 ] because responding to fear, anxiety and to threatening events depletes top-down control and self-regulatory resources [ 56 , 57 ] that are also required for academic performance. In line with this, students reported having difficulties in focusing and concentrating on the teaching content during the current COVID-19 pandemic situation (see Fig. 4 b). Self-learning formats such as e-learning may accentuate these effects.
Self-concept and personality of university students, and machine learning
When asked to describe themselves with a modified version of the TST asking for descriptions of the students’ “actual self”, positive word use outweighed negative word use. When the student sample was considered as a whole, linguistic analysis of word use (see Fig. 5 ) supported a clear bias towards positivity that also accords with previous results that seeing yourself in a positive light correlates with positive self-descriptions and preferential processing of positive words [ 58 , 59 , 60 , 61 ]. Although this result must be seen in relation to a general positivity bias in written and spoken language (most languages having more positive than negative words [ 62 ], the analysis of word use suggests that the pandemic situation at the time of the survey did not provoke a threat to the self-concept of this university student sample and this, although linguistic analysis of the answers to the prompt that asked for feelings during the pandemic (see also Fig. 5 ) revealed a negativity bias as immediate negative responses to the pandemic situation in line with the results observed for the survey items asking for threat perception. Symptoms of state anxiety and current depressive symptoms may therefore reflect temporary changes of the university students to the pandemic situation that however occur immediately in response to the pandemic lockdown.
Psychological theories agree that individual factors such as one’s personality are correlated with subjective experience, well-being, mental health, and behaviour, e.g., [ 63 , 64 ]. In line with this, analyses showed correlations between the Big Five (BFI-40) personality traits and the university students’ self-reported symptoms of anxiety, depression and their perceived difficulties in emotion perception. Statistically, correlation analysis, linear regression analysis, multivariate structural equation models, mediator analysis, or moderator analysis may all be feasible statistical methods to describe the relationship between psychological variables. However, in the present study we attempted to apply supervised machine learning algorithms that are built on regression models to further explore whether personality traits were not only correlated with mental health variables but could be predicted from the self-reported subjective experience of the participants obtained from this survey’s multimethod assessment. The observed results are promising despite the relatively small datasets used for training and prediction. The algorithms provided relatively accurate models for the prediction of personality traits from self-report data. As illustrated in Table 3 , neuroticism as one of the big five personality traits (shown to be related to mental ill health [ 63 , 64 ]) and in the present study sample significantly correlated with both, self-reported anxiety and depressive symptoms (see Table 2 ) could best be predicted by changes in current anxiety (threat perception, difference scores state vs trait anxiety), by the students’ self-reported trait and state anxiety, by their self-reported perceived difficulties in emotion perception (describing one’s feelings reported on the TAS-20), by self-reported changes in physical health behaviour (eating) and by self-reported difficulties in social distancing. Very recent results from surveys investigating the role of personality factors during the current COVID-19 pandemic also found that people’s self-reported psychological perceptions of and reactions towards the pandemic also depend on stable personality traits including the Big Five (for an overview [ 65 ]). Interestingly, there is also evidence that expression on personality traits such as the Big Five can change in conjunction with mental ill health [ 66 ]. Our results and these recent results suggest that future studies exploring the psychological consequences of the COVID-19 pandemic should include the assessment of personality traits in their anamnestic exploration of mental health and self-reported experience.
Limitations
The present study adds to the evidence reported in the literature about the negative consequences of the current COVID-19 pandemic on mental health and well-being of university students. By using a mix of self-report measures it allows detailed insight into the subjective experiences associated with the pandemic in this population group in the psychological domains of mental health, health behaviour change and learning. However, some limitations already discussed in the sections above should be stressed. First, there was a high drop-out whose percentage was within the upper range of the expected drop-out rates for online surveys (20–50%). Although drop-outs were statistically assessed and compared to the final sample as far as appropriate, suggesting no bias by age or gender or the student’s personality, the drop-out reduced the final sample size reducing the power of the study. Thus, further data is required to demonstrate the generalizability of the present observations and to further explore possible cultural differences. In the present study sample, the reported significant differences between gender and students studying in Egypt or Germany might be tentative due to the small study samples. Power calculations suggest an ideal sample size of about N = 271 (90% confidence) or N = 385 (95% confidence) participants (margin of error of 5%). Although this sample size was reached in the beginning, it was reduced by the successive drop-out across the blocks of survey items. Second, statistics revealed significant results for the quantitative measures, however, the results of the linguistic tasks (self-concept and feeling prompts) could be reported only descriptively. The LIWC software was used for linguistic analysis. This allowed word categorization with high accuracy and validity [ 46 ] providing interesting insight that otherwise might have gone unnoticed and confirmed the results obtained from quantitative measures. Third, due to the small sample size the machine learning approach is exploratory and challenged by limitations. While machine learning tools have already been applied in many domains of psychology (e.g., in the domain of Affective Computing and Health Psychology), their use is still relatively under investigated in studies using psychology data obtained from multimethod approaches as the current one [ 67 ]. Existing studies using machine learning for analyzing personality- and behaviour-related data, mainly target personality prediction from larger datasets (e.g., [ 68 ]). In the present study, we followed guidelines and recommendations from existing machine learning studies discussing possible solutions for application of machine learning tools with small sample sizes (see for an overview [ 69 , 70 , 71 ]), using sample size of about 200 and support vector machines (SVM similar to SVR used in our study) for estimation of depressive symptoms, for personality trait and perceived stress prediction based on sample sizes ranging from 150 to 250 participants [ 69 , 70 , 71 ], as in the present study. In line with these previous studies applying machine learning tools to smaller sample sizes, we applied machine learning to a mix of measures that captured subjective experience in relation to the current COVID-19 pandemic situation in line with the recommendations from psychologically-driven computational approaches that suggest to include trait and state measures for prediction [ 25 , 26 ]. Nevertheless, the present approach is exploratory and application of machine learning to small sample sizes need to be critically discussed, e.g., for a detailed discussion see [ 48 ], as it can lead to overfitting or overestimation. One recommendation to avoid such problems with small sample sizes is to use nested cross validation and control feature-to-sample ratio [ 48 ]. It will be interesting to follow-up the present ML results in future COVID-19 survey studies and use additional data collected during the course of the pandemic for validation and training in order to confirm the results from ML in hopefully larger samples, supporting the combination of machine learning and classical data analytics in the domain of psychology.
This survey investigated the subjective experience of university students studying in Egypt or Germany during the COVID-19 pandemic in May 2020, i.e., in the time period after the first pandemic lockdown in the countries. Perceived changes in all psychological domains including state anxiety, depressive symptoms, threat perception, emotion perception, worries about health and behaviour (health, social distancing, and learning) were reported in the majority of students taking part in the survey. Recent COVID-10 surveys report similar high prevalence rates among university students across the globe [ 3 , 4 , 12 , 13 ]. Although the results of this survey are tentative, the multimethod approach of this survey, using multiple scales, descriptive, correlational, and linguistic analysis, provides a valuable contribution to previously published COVID-19 studies. Moreover, the approach of combining descriptive analysis with machine learning should and could be followed-up in larger samples during the second period of the current pandemic. Crucially, despite the small sample size, the present results of self-reported anxiety and depressive symptoms among university students, that also seem to be supported by recent surveys including university students from other countries [ 3 , 4 , 12 , 13 ] should be taken serious as they suggest that there is an urgent need to develop interventions that help prevent mental health among university students in order to avoid negative consequences in health and learning behaviour in response to the pandemic and provide health care to those students who might be at special risk of mental ill health.
Questionnaire/survey
The questionnaires and self-assessment scales used in this study are standardized questionnaires and standardized scales whose references are cited in the manuscript in brackets. The single survey questions e.g., health and teaching have been developed for the purpose of this survey and are summarized in Table 1 in the manuscript. An overview of the online survey can be found in the supplement of this manuscript.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. Due to the informed consent form in which the possibility of raw data being published online was not explicitly stated, the raw data cannot be made accessible in online repositories.
Abbreviations
BFI five inventory [ 43 ]
Decision tree regression
Gradient Boosting Regression
Linguistic inquiry of word count [ 46 ]
Personal Health Questionnaire 2 [ 38 ]
Root mean squared error
Self-Assessment Manikin scales [ 41 ]
Spielberger Trait State Anxiety Inventory [ 37 ]
Support Vector Regression
Toronto Alexithymia Scale [ 42 ]
World Health Organization
Bohlken J, Schömig F, Lemke MR, Pumberger M, Riedel-Heller SG. COVID-19-Pandemie: Belastungen des medizinischen Personals [COVID-19 pandemic: stress experience of healthcare workers—a short current review]. Psychiatr Prax. 2020;47:190–7. https://doi.org/10.1055/a-1159-5551 .
Article PubMed PubMed Central Google Scholar
Petzold MB, Plag J, Ströhle A. Umgang mit psychischer Belastung bei Gesundheitsfachkräften im Rahmen der Covid-19-Pandemie [Dealing with psychological distress by healthcare professionals during the COVID-19 pandemia]. Nervenarzt. 2020;91:417–21. https://doi.org/10.1007/s00115-020-00905-0 .
Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. https://doi.org/10.1016/j.psychres.2020.112934 .
Chen B, Sun J, Feng Y. How have COVID-19 isolation policies affected young people’s mental health? – Evidence from Chinese College Students. Front Psychol. 2020. https://doi.org/10.3389/fpsyg.2020.01529 .
Rodríguez-Rey R, Garrido-Hernansaiz H, Collado S. Psychological impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Front Psychol. 2020. https://doi.org/10.3389/fpsyg.2020.01540 .
Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–20. https://doi.org/10.1016/S0140-6736(20)30460-8 .
Talevi D, Socci V, Carai M, Carnaghi G, Faleri S, Trebbi E, Di Bernardo A, Capelli F, Pacitti F. Mental health outcomes of the CoViD-19 pandemic. Riv Psichiatr. 2020;55:137–44. https://doi.org/10.1708/3382.33569 .
Article PubMed Google Scholar
World Health Organization (2020). Mental health and COVID-19. https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/technical-guidance/mental-health-and-covid-19 . Accessed 29 June 2020.
Betsch C. How behavioural science data helps mitigate the COVID-19 crisis. Nat Hum Behav. 2020. https://doi.org/10.1038/s41562-020-0866-1 .
van Bavel JJ, Baicker K, Boggio PS, Capraro V, Cichocka A, Cikara M, Crockett MJ et al. Using social and behavioural science to support COVID-19 pandemic response; 2020. https://www.nature.com/articles/s41562-020-0884-z . Accessed 28 June 2020.
Greco V, Roger D. Uncertainty, stress, and health. Personal Individ Differ. 2003;34:1057–68. https://doi.org/10.1016/s0191-8869(02)00091-0 .
Article Google Scholar
Patsali ME, Mousa DPV, Papadopoulou EV, Papadopoulou KK, Kaparounaki CK, Diakogiannis I, Fountoulakis KN. University students’ changes in mental health status and determinants of behavior during the COVID-19 lockdown in Greece. Psychiatry Res. 2020;292:113298.
Son C, Hegde S, Smith A, Wang X, Sasangohar F. Effects of COVID-19 on college students’ mental health in the United States: interview survey study. J Med Internet Res. 2020;22(9):e21279.
Wathelet M, Duhem S, Vaiva G, Baubet T, Habran E, Veerapa E, Debien C, Molenda S, Horn M, Grandgenèvre P, Notredame CE. Factors associated with mental health disorders among university students in France confined during the COVID-19 pandemic. JAMA Netw Open. 2020;3(10):e2025591.
Kaparounaki CK, Patsali ME, Mousa DPV, Papadopoulou EV, Papadopoulou KK, Fountoulakis KN. University students’ mental health amidst the COVID-19 quarantine in Greece. Psychiatry Res. 2020;290:113111.
Sahu P. Closure of universities due to coronavirus disease 2019 (COVID-19): impact on education and mental health of students and academic staff. Cureus. 2020;12(4):e7541.
PubMed PubMed Central Google Scholar
Duffy A, Saunders KE, Malhi GS, Patten S, Cipriani A, McNevin SH, MacDonald E, Geddes J. Mental health care for university students: a way forward? Lancet Psychiatry. 2019;6(11):885–7.
Storrie K, Ahern K, Tuckett A. A systematic review: students with mental health problems—a growing problem. Int J Nurs Pract. 2010;16(1):1–6.
Brown JSL. Student mental health: some answers and more questions. J Ment Health. 2018;27:193–6. https://doi.org/10.1080/09638237.2018.1470319 .
Ibrahim AK, Kelly SJ, Adams CE, Glazebrook C. A systematic review of studies of depression prevalence in university students. J Psychiatr Res. 2013;47:391–400. https://doi.org/10.1016/j.jpsychires.2012.11.015 .
Herbert C, Meixner F, Wiebking C, Gilg V. Regular physical activity, short-term exercise, mental health, and well-being among university students: the results of an online and a laboratory study. Front Psychol. 2020;11:509. https://doi.org/10.3389/fpsyg.2020.00509 .
El-Gilany AH, Amro M, Eladawi N, Khalil M. Mental health status of medical students: a single faculty study in Egypt. J Nerv Ment Dis. 2019;207(5):348–54.
Abdallah AR, Gabr HM. Depression, anxiety and stress among first year medical students in an Egyptian public university. Int Res J Med Med Sci. 2014;2(1):11–9.
Google Scholar
Champion VL, Skinner CS. The health belief model. Health Behav Health Educ Theory Res Pract. 2008;4:45–65.
Bandura A. Social cognitive theory of self-regulation. Organ Behav Hum Decis Process. 1991;50(2):248–87.
Prochaska JO, Johnson S, Lee P. The trans theoretical model of behavior change. In: Shumaker SA, Ockene JK, Riekert KA, editors. The handbook of health behavior change. Berlin: Springer; 2009. p. 59–83.
Fernandes O, Portugal LCL, Alves RCS, Campagnoli RR, Mocaiber I, David IPA, Erthal FCS, Volchan E, de Oliveira L, Pereira MG. How you perceive threat determines your behaviour. Front Hum Neurosci. 2013;7:632.
Honkalampi K, Hintikka J, Tanskanen A, Lehtonen J, Viinamäki H. Depression is strongly associated with alexithymia in the general population. J Psychosom Res. 2000;48:99–104. https://doi.org/10.1016/S0022-3999(99)00083-5 .
Marchesi C, Brusamonti E, Maggini C. Are alexithymia, depression, and anxiety distinct constructs in affective disorders? J Psychosom Res. 2000;49:43–9. https://doi.org/10.1016/S0022-3999(00)00084-2 .
Beck AT. Cognitive therapy and the emotional disorders. London: Penguin; 1979.
Verelst F, Willem L, Beutels P. Behavioural change models for infectious disease transmission: a systematic review (2010–2015). J R Soc Interface. 2016. https://doi.org/10.1098/rsif.2016.0820 .
Spruijt-Metz D, Hekler E, Saranummi N, Intille S, Korhonen I, Nilsen W, Rivera DE, et al. Building new computational models to support health behaviour change and maintenance: new opportunities in behavioural research. Transl Behav Med. 2015;5:335–46. https://doi.org/10.1007/s13142-015-0324-1 .
Herbert, C. An experimental-psychological approach for the development of character computing. In: Character computing (pp. 17–38). Springer, Cham; 2020.
El Bolock A, Abdennadher S, Herbert C. Applications of character computing from psychology to computer science. In: Character computing. Springer, Cham; 2020. p. 53–71.
Herbert C, El Bolock A, Abdennadher S. A psychologically driven, user-centered approach to character modeling. In: Character computing. Springer, Cham; 2020. p. 39–51.
El Bolock A, Herbert C, Abdennadher S. CCOnto: towards an ontology-based model for character computing. In: International conference on research challenges in information science. Springer, Cham; 2020. p. 529–535.
Spielberger CD. State-trait anxiety inventory for adults. 1983.
Löwe B, Kroenke K, Gräfe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosom Res. 2005;58(2):163–71.
Bahammam MA. Validity and reliability of an Arabic version of the state-trait anxiety inventory in a Saudi dental setting. Saudi Med J. 2016;37(6):668.
AlHadi AN, AlAteeq DA, Al-Sharif E, Bawazeer HM, Alanazi H, AlShomrani AT, Shuqdar RM, AlOwaybil R. An arabic translation, reliability, and validation of patient health questionnaire in a Saudi sample. Ann Gen Psychiatry. 2017;16(1):32.
Bradley MM, Lang PJ. Measuring emotion: the self-assessment manikin and the semantic differential. J Behav Therapy Exp Psychiatry. 1994;25(1):49–59.
Bagby RM, Ayearst LE, Morariu RA, Watters C, Taylor GJ. The Internet administration version of the 20-item Toronto Alexithymia Scale. Psychol Assess. 2014;26(1):16.
John OP, Donahue EM, Kentle RL. Big five inventory. J Personal Soc Psychol. 1991. https://doi.org/10.1037/t07550-000 .
Schmitt DP, Allik J, McCrae RR, Benet-Martínez V. The geographic distribution of Big Five personality traits: patterns and profiles of human self-description across 56 nations. J Cross Cult Psychol. 2007;38(2):173–212.
Rees A, Nicholson N. The twenty statements test. Essential guide to qualitative methods in organizational research. 2004. p. 86–97.
Pennebaker JW, Francis ME, Booth RJ. Linguistic inquiry and word count: LIWC 2001. Mahway Lawrence Erlbaum Assoc. 2001;71(2001):2001.
Guo Y, Graber A, McBurney RN, Balasubramanian R. Sample size and statistical power considerations in high-dimensionality data settings: a comparative study of classification algorithms. BMC Bioinform. 2010;11(1):447.
Vabalas A, Gowen E, Poliakoff E, Casson AJ. Machine learning algorithm validation with a limited sample size. PLoS ONE. 2019;14(11):e0224365.
Julian LJ. Measures of anxiety: state-trait anxiety inventory (STAI), beck anxiety inventory (BAI), and hospital anxiety and depression scale-anxiety (HADS-A). Arthritis Care Res. 2011;63(Suppl. 11):467–72.
Auerbach RP, Alonso J, Axinn WG, Cuijpers P, Ebert DD, Green JG, et al. Mental disorders among college students in the world health organization world mental health surveys. Psychol Med. 2016;46:2955–70. https://doi.org/10.1017/S0033291716001665 .
Auerbach RP, Mortier P, Bruffaerts R, Alonso J, Benjet C, Cuijpers P, et al. WHO world mental health surveys international college student project: prevalence and distribution of mental disorders. J Abnorm Psychol. 2018;127:623–38. https://doi.org/10.1037/abn0000362 .
January J, Madhombiro M, Chipamaunga S, Ray S, Chingono A, Melanie A. Prevalence of depression and anxiety among undergraduate university students in low- and middle-income countries: a systematic review protocol; 2018. https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-018-0723-8 . Accessed 29 June 2020.
Stock C, Kücük N, Miseviciene I, Guillén-Grima F, Petkeviciene J, Aguinaga-Ontoso I, Krämer A. Differences in health complaints among university students from three European countries. Prev Med. 2003;37:535–43.
Andrews G, Hobbs MJ, Borkovec TD, Beesdo K, Craske MG, Heimberg RG, Rapee RM, Ruscio AM, Stanley MA. Generalized worry disorder: a review of DSM-IV generalized anxiety disorder and options for DSM-V. Depress Anxiety. 2010;27:134–47. https://doi.org/10.1002/da.20658 .
World Health Organization. Physical activity; 2020. https://www.who.int/dietphysicalactivity/pa/en/ . Accessed 29 June 2020.
Wagner DD, Heatherton TF. Self-regulatory depletion increases emotional reactivity in the amygdala. Social Cogn Affect Neurosci. 2013;8:410–7. https://doi.org/10.1093/scan/nss082 .
Hoyle RH. Personality and self-regulation: trait and information-processing perspectives. J Pers. 2006;74(6):1507–26.
Diener E, Diener C. Most people are happy. Psychol Sci. 1996;7(3):181–5.
Herbert C, Junghofer M, Kissler J. Event related potentials to emotional adjectives during reading. Psychophysiology. 2008;45:487–98. https://doi.org/10.1111/j.1469-8986.2007.00638.x .
Herbert C, Kissler J, Junghöfer M, Peyk P, Rockstroh B. Processing of emotional adjectives: evidence from startle EMG and ERPs. Psychophysiology. 2006;43:197–206. https://doi.org/10.1111/j.1469-8986.2006.00385.x .
Watson LA, Dritschel B, Obonsawin MC, Jentzsch I. Seeing yourself in a positive light: brain correlates of the self-positivity bias. Brain Res. 2007;1152:106–10.
Dodds PS, Clark EM, Desu S, Frank MR, Reagan AJ, Williams JR, Mitchell L, et al. Human language reveals a universal positivity bias. Proc Natl Acad Sci USA. 2015;112:2389–94. https://doi.org/10.1073/pnas.1411678112 .
Hayes N, Joseph S. Big 5 correlates of three measures of subjective well-being. Personal Individ Differ. 2003;34(4):723–7.
Jylhä P, Isometsä E. The relationship of neuroticism and extraversion to symptoms of anxiety and depression in the general population. Depress Anxiety. 2006;23(5):281–9.
Jorm AF, Christensen H, Henderson AS, Jacomb PA, Korten AE, Rodgers B. Predicting anxiety and depression from personality: is there a synergistic effect of neuroticism and extraversion? J Abnorm Psychol. 2000;109(1):145.
Karsten J, Penninx BW, Riese H, Ormel J, Nolen WA, Hartman CA. The state effect of depressive and anxiety disorders on big five personality traits. J Psychiatr Res. 2012;46(5):644–50.
Stachl C, Pargent F, Hilbert S, Harari GM, Schoedel R, Vaid S, Bühner M. Personality research and assessment in the era of machine learning. Eur J Personal. 2019;34(5):613–31.
Azucar D, Marengo D, Settanni M. Predicting the Big 5 personality traits from digital footprints on social media: a meta-analysis. Personal Individ Differ. 2018;124:150–9.
Singh C. Using data analysis and machine learning for studying and predicting depression in users on social media. Doctoral dissertation, Carleton University; 2020.
Marouf AA, Ashrafi AF, Ahmed T, Emon T. A machine learning based approach for mapping personality traits and perceived stress scale of undergraduate students. Int J Mod Educ Comput Sci. 2019;11(8):42.
Tandera T, Suhartono D, Wongso R, Prasetio YL. Personality prediction system from facebook users. Procedia Comput Sci. 2017;116:604–11.
Download references
Acknowledgements
Not applicable.
Open Access funding enabled and organized by Projekt DEAL. This study was funded by the DAAD/BMBF (principal investigators: CH, SA) and by the budgetary resources of the Department of Applied Emotion and Motivation Psychology, and the open access publication fund of Ulm University. The funding bodies played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and affiliations.
Applied Emotion and Motivation Psychology, Institute of Psychology and Education, Faculty of Engineering, Computer Science and Psychology, Ulm University, Albert Einstein Allee 47, 89081, Ulm, Germany
Cornelia Herbert & Alia El Bolock
Computer Science Department, Faculty of Media Engineering and Technology, German University in Cairo - GUC, New Cairo City, Egypt
Alia El Bolock & Slim Abdennadher
You can also search for this author in PubMed Google Scholar
Contributions
CH conceptualized and designed the study and the survey. CH was involved in data recruitment, in data preprocessing and CH performed data analytics for descriptive and correlational data and results (descriptive data analytics, statistical analysis), and CH interpreted the result, CH supervised the machine learning part, created figures and tables and drafted and wrote the manuscript and revised it for scientific content. AB helped in the survey, performed the machine learning part, the machine learning part was also supervised by SA. All authors read and approved the manuscript.
Corresponding author
Correspondence to Cornelia Herbert .
Ethics declarations
Ethics approval and consent to participate.
The present survey follows ethical guidelines: all students took part voluntarily in the survey. They gave written informed consent prior to filling out the survey. The participants were fully debriefed about the purpose of the study. They were informed that they will be questioned about their health, teaching and learning behaviour, and their subjective experience with the current COVID-19 pandemic situation. They were informed that they can withdraw from the study at any time during the survey without giving reasons or without negative consequences on confidentiality. They were debriefed in detail about data privacy. No individual ethics approval was submitted before the start of the survey. The survey contains questionnaires that are part of online studies that had received approval in previous studies of the corresponding author by the local ethics committee of Ulm University.
Consent for publication
This manuscript does not contain any individual person’s data.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
. An overview of the online survey items and questionnaires.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Herbert, C., El Bolock, A. & Abdennadher, S. How do you feel during the COVID-19 pandemic? A survey using psychological and linguistic self-report measures, and machine learning to investigate mental health, subjective experience, personality, and behaviour during the COVID-19 pandemic among university students. BMC Psychol 9 , 90 (2021). https://doi.org/10.1186/s40359-021-00574-x
Download citation
Received : 12 August 2020
Accepted : 26 April 2021
Published : 02 June 2021
DOI : https://doi.org/10.1186/s40359-021-00574-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Corona virus
- Personality
- Mental health
- Emotion perception
- Self-concept
- Linguistic analysis
- Machine learning
- Character computing
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]

How COVID-19 Affects the Brain
Share this article
An online risk calculator could help doctors predict, and hopefully prevent, brain-related complications in COVID-19 patients.
What you need to know
An NIH-funded study is developing an online risk calculator to help doctors predict which COVID-19 patients will develop brain-related complications. The study will also look at how COVID-19 causes these complications.
What is this research about?
Scientists and doctors do not fully understand how COVID-19 causes problems with the brain or why these problems occur in some patients and not others. In this new study, researchers from the Cleveland Clinic will use tools that they developed from earlier NIH-supported projects to study how COVID-19 affects the brain. They will focus on fatigue, headaches, loss of smell or taste, and memory loss, or “brain fog.” They will also look at more serious but less common complications, such as epilepsy and stroke.
What are the researchers doing?
The researchers are analyzing data from the hospital records of thousands of patients who tested positive for COVID-19 and were enrolled in the Cleveland Clinic COVID-19 Registry and Biobank. These records have information on a patient’s age, race and ethnicity, and social determinants of health, which are the conditions in a person’s environment that can affect health and wellbeing. The hospital records also include a patient’s COVID-19 symptoms and how seriously ill the patient was, and whether the patient smokes or has serious health conditions such as cancer, diabetes, heart disease, and high blood pressure.
The researchers will first find out how many of these patients developed problems with the brain while they had COVID-19 or after they recovered. They will then use computer programs to compare patient information and find out whether problems with the brain are more common in any specific group of patients . They will also find out whether any combination of factors increased the risk of problems with the brain. The researchers will use this information to develop a new computer program that predicts whether new patients are more likely to have problems with the brain based on their own demographic and health information.
The researchers plan to expand the study to include health information from large datasets at the Mayo Clinic and the University of Campinas in Brazil. This will help ensure that the risk calculator is accurate for diverse groups and can be used globally.
Why is this research important?
An effective online risk calculator and information on how COVID-19 affects the brain could help doctors predict and possibly prevent neurological complications in people who have COVID-19. The researchers plan to develop risk calculators for other short- and long-term complications of COVID-19 to help improve medical care for this disease.
Where can I go to learn more?
Neurological Complications of COVID-19 Are Focus of New NIH Grant Supplement to Cleveland Clinic Researchers .
- Learn more about this project from Cleveland Clinic.
Taking a Closer Look at COVID-19’s Effects on the Brain .
- In this blog post, NIH Director Francis Collins, M.D., Ph.D., discusses research by NIH scientists to better understand how COVID-19 affects brain function.
Neurological Complications of COVID-19 and NINDS Clinical Research .
- In this video, Avindra Nath, M.D., of the National Institute of Neurological Disorders and Stroke (NINDS) discusses how COVID-19 affects the brain.
NIH Launches Database to Track Neurological Symptoms Associated with COVID-19 .
- Read about NIH’s database for tracking how COVID-19 affects the brain, spinal cord, and nerves.
NIH Study Uncovers Blood Vessel Damage and Inflammation in COVID-19 Patients’ Brains but No Infection .
- Read about research by NIH scientists designed to better understand how COVID-19 affects the brain.
CombatCOVID.HHS.Gov .
- Find out more about COVID-19 and opportunities to participate in clinical trials.
Jehi, L. (2020). A nomogram to predict seizure outcomes after resective epilepsy surgery. NIH RePORTER. Retrieved February 8, 2021, from https://reporter.nih.gov/project-details/10181321#description
Cleveland Clinic. (2020). Neurological complications of COVID-19 are focus of new NIH grant supplement to Cleveland Clinic researchers . Retrieved February 8, 2021, from https://consultqd.clevelandclinic.org/neurological-complications-of-covid-19-are-focus-of-new-nih-grant-supplement-to-cleveland-clinic-researchers/

News and Stories
Read stories about the efforts underway to prevent, detect, and treat COVID-19 and its effects on our health.
NIH COVID-19 Resources by Topic
COVID-19 research information and resources by topic from NIH institutes and centers
- High Contrast
- Increase Font
- Decrease Font
- Default Font
- Turn Off Animations
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

The Effect of COVID-19 on Education
Jacob hoofman.
a Wayne State University School of Medicine, 540 East Canfield, Detroit, MI 48201, USA
Elizabeth Secord
b Department of Pediatrics, Wayne Pediatrics, School of Medicine, Pediatrics Wayne State University, 400 Mack Avenue, Detroit, MI 48201, USA
COVID-19 has changed education for learners of all ages. Preliminary data project educational losses at many levels and verify the increased anxiety and depression associated with the changes, but there are not yet data on long-term outcomes. Guidance from oversight organizations regarding the safety and efficacy of new delivery modalities for education have been quickly forged. It is no surprise that the socioeconomic gaps and gaps for special learners have widened. The medical profession and other professions that teach by incrementally graduated internships are also severely affected and have had to make drastic changes.
- • Virtual learning has become a norm during COVID-19.
- • Children requiring special learning services, those living in poverty, and those speaking English as a second language have lost more from the pandemic educational changes.
- • For children with attention deficit disorder and no comorbidities, virtual learning has sometimes been advantageous.
- • Math learning scores are more likely to be affected than language arts scores by pandemic changes.
- • School meals, access to friends, and organized activities have also been lost with the closing of in-person school.
The transition to an online education during the coronavirus disease 2019 (COVID-19) pandemic may bring about adverse educational changes and adverse health consequences for children and young adult learners in grade school, middle school, high school, college, and professional schools. The effects may differ by age, maturity, and socioeconomic class. At this time, we have few data on outcomes, but many oversight organizations have tried to establish guidelines, expressed concerns, and extrapolated from previous experiences.
General educational losses and disparities
Many researchers are examining how the new environment affects learners’ mental, physical, and social health to help compensate for any losses incurred by this pandemic and to better prepare for future pandemics. There is a paucity of data at this juncture, but some investigators have extrapolated from earlier school shutdowns owing to hurricanes and other natural disasters. 1
Inclement weather closures are estimated in some studies to lower middle school math grades by 0.013 to 0.039 standard deviations and natural disaster closures by up to 0.10 standard deviation decreases in overall achievement scores. 2 The data from inclement weather closures did show a more significant decrease for children dependent on school meals, but generally the data were not stratified by socioeconomic differences. 3 , 4 Math scores are impacted overall more negatively by school absences than English language scores for all school closures. 4 , 5
The Northwest Evaluation Association is a global nonprofit organization that provides research-based assessments and professional development for educators. A team of researchers at Stanford University evaluated Northwest Evaluation Association test scores for students in 17 states and the District of Columbia in the Fall of 2020 and estimated that the average student had lost one-third of a year to a full year's worth of learning in reading, and about three-quarters of a year to more than 1 year in math since schools closed in March 2020. 5
With school shifted from traditional attendance at a school building to attendance via the Internet, families have come under new stressors. It is increasingly clear that families depended on schools for much more than math and reading. Shelter, food, health care, and social well-being are all part of what children and adolescents, as well as their parents or guardians, depend on schools to provide. 5 , 6
Many families have been impacted negatively by the loss of wages, leading to food insecurity and housing insecurity; some of loss this is a consequence of the need for parents to be at home with young children who cannot attend in-person school. 6 There is evidence that this economic instability is leading to an increase in depression and anxiety. 7 In 1 survey, 34.71% of parents reported behavioral problems in their children that they attributed to the pandemic and virtual schooling. 8
Children have been infected with and affected by coronavirus. In the United States, 93,605 students tested positive for COVID-19, and it was reported that 42% were Hispanic/Latino, 32% were non-Hispanic White, and 17% were non-Hispanic Black, emphasizing a disproportionate effect for children of color. 9 COVID infection itself is not the only issue that affects children’s health during the pandemic. School-based health care and school-based meals are lost when school goes virtual and children of lower socioeconomic class are more severely affected by these losses. Although some districts were able to deliver school meals, school-based health care is a primary source of health care for many children and has left some chronic conditions unchecked during the pandemic. 10
Many families report that the stress of the pandemic has led to a poorer diet in children with an increase in the consumption of sweet and fried foods. 11 , 12 Shelter at home orders and online education have led to fewer exercise opportunities. Research carried out by Ammar and colleagues 12 found that daily sitting had increased from 5 to 8 hours a day and binge eating, snacking, and the number of meals were all significantly increased owing to lockdown conditions and stay-at-home initiatives. There is growing evidence in both animal and human models that diets high in sugar and fat can play a detrimental role in cognition and should be of increased concern in light of the pandemic. 13
The family stress elicited by the COVID-19 shutdown is a particular concern because of compiled evidence that adverse life experiences at an early age are associated with an increased likelihood of mental health issues as an adult. 14 There is early evidence that children ages 6 to 18 years of age experienced a significant increase in their expression of “clinginess, irritability, and fear” during the early pandemic school shutdowns. 15 These emotions associated with anxiety may have a negative impact on the family unit, which was already stressed owing to the pandemic.
Another major concern is the length of isolation many children have had to endure since the pandemic began and what effects it might have on their ability to socialize. The school, for many children, is the agent for forming their social connections as well as where early social development occurs. 16 Noting that academic performance is also declining the pandemic may be creating a snowball effect, setting back children without access to resources from which they may never recover, even into adulthood.
Predictions from data analysis of school absenteeism, summer breaks, and natural disaster occurrences are imperfect for the current situation, but all indications are that we should not expect all children and adolescents to be affected equally. 4 , 5 Although some children and adolescents will likely suffer no long-term consequences, COVID-19 is expected to widen the already existing educational gap from socioeconomic differences, and children with learning differences are expected to suffer more losses than neurotypical children. 4 , 5
Special education and the COVID-19 pandemic
Although COVID-19 has affected all levels of education reception and delivery, children with special needs have been more profoundly impacted. Children in the United States who have special needs have legal protection for appropriate education by the Individuals with Disabilities Education Act and Section 504 of the Rehabilitation Act of 1973. 17 , 18 Collectively, this legislation is meant to allow for appropriate accommodations, services, modifications, and specialized academic instruction to ensure that “every child receives a free appropriate public education . . . in the least restrictive environment.” 17
Children with autism usually have applied behavioral analysis (ABA) as part of their individualized educational plan. ABA therapists for autism use a technique of discrete trial training that shapes and rewards incremental changes toward new behaviors. 19 Discrete trial training involves breaking behaviors into small steps and repetition of rewards for small advances in the steps toward those behaviors. It is an intensive one-on-one therapy that puts a child and therapist in close contact for many hours at a time, often 20 to 40 hours a week. This therapy works best when initiated at a young age in children with autism and is often initiated in the home. 19
Because ABA workers were considered essential workers from the early days of the pandemic, organizations providing this service had the responsibility and the freedom to develop safety protocols for delivery of this necessary service and did so in conjunction with certifying boards. 20
Early in the pandemic, there were interruptions in ABA followed by virtual visits, and finally by in-home therapy with COVID-19 isolation precautions. 21 Although the efficacy of virtual visits for ABA therapy would empirically seem to be inferior, there are few outcomes data available. The balance of safety versus efficacy quite early turned to in-home services with interruptions owing to illness and decreased therapist availability owing to the pandemic. 21 An overarching concern for children with autism is the possible loss of a window of opportunity to intervene early. Families of children and adolescents with autism spectrum disorder report increased stress compared with families of children with other disabilities before the pandemic, and during the pandemic this burden has increased with the added responsibility of monitoring in-home schooling. 20
Early data on virtual schooling children with attention deficit disorder (ADD) and attention deficit with hyperactivity (ADHD) shows that adolescents with ADD/ADHD found the switch to virtual learning more anxiety producing and more challenging than their peers. 22 However, according to a study in Ireland, younger children with ADD/ADHD and no other neurologic or psychiatric diagnoses who were stable on medication tended to report less anxiety with at-home schooling and their parents and caregivers reported improved behavior during the pandemic. 23 An unexpected benefit of shelter in home versus shelter in place may be to identify these stressors in face-to-face school for children with ADD/ADHD. If children with ADD/ADHD had an additional diagnosis of autism or depression, they reported increased anxiety with the school shutdown. 23 , 24
Much of the available literature is anticipatory guidance for in-home schooling of children with disabilities rather than data about schooling during the pandemic. The American Academy of Pediatrics published guidance advising that, because 70% of students with ADHD have other conditions, such as learning differences, oppositional defiant disorder, or depression, they may have very different responses to in home schooling which are a result of the non-ADHD diagnosis, for example, refusal to attempt work for children with oppositional defiant disorder, severe anxiety for those with depression and or anxiety disorders, and anxiety and perseveration for children with autism. 25 Children and families already stressed with learning differences have had substantial challenges during the COVID-19 school closures.
High school, depression, and COVID-19
High schoolers have lost a great deal during this pandemic. What should have been a time of establishing more independence has been hampered by shelter-in-place recommendations. Graduations, proms, athletic events, college visits, and many other social and educational events have been altered or lost and cannot be recaptured.
Adolescents reported higher rates of depression and anxiety associated with the pandemic, and in 1 study 14.4% of teenagers report post-traumatic stress disorder, whereas 40.4% report having depression and anxiety. 26 In another survey adolescent boys reported a significant decrease in life satisfaction from 92% before COVID to 72% during lockdown conditions. For adolescent girls, the decrease in life satisfaction was from 81% before COVID to 62% during the pandemic, with the oldest teenage girls reporting the lowest life satisfaction values during COVID-19 restrictions. 27 During the school shutdown for COVID-19, 21% of boys and 27% of girls reported an increase in family arguments. 26 Combine all of these reports with decreasing access to mental health services owing to pandemic restrictions and it becomes a complicated matter for parents to address their children's mental health needs as well as their educational needs. 28
A study conducted in Norway measured aspects of socialization and mood changes in adolescents during the pandemic. The opportunity for prosocial action was rated on a scale of 1 (not at all) to 6 (very much) based on how well certain phrases applied to them, for example, “I comforted a friend yesterday,” “Yesterday I did my best to care for a friend,” and “Yesterday I sent a message to a friend.” They also ranked mood by rating items on a scale of 1 (not at all) to 5 (very well) as items reflected their mood. 29 They found that adolescents showed an overall decrease in empathic concern and opportunity for prosocial actions, as well as a decrease in mood ratings during the pandemic. 29
A survey of 24,155 residents of Michigan projected an escalation of suicide risk for lesbian, gay, bisexual, transgender youth as well as those youth questioning their sexual orientation (LGBTQ) associated with increased social isolation. There was also a 66% increase in domestic violence for LGBTQ youth during shelter in place. 30 LGBTQ youth are yet another example of those already at increased risk having disproportionate effects of the pandemic.
Increased social media use during COVID-19, along with traditional forms of education moving to digital platforms, has led to the majority of adolescents spending significantly more time in front of screens. Excessive screen time is well-known to be associated with poor sleep, sedentary habits, mental health problems, and physical health issues. 31 With decreased access to physical activity, especially in crowded inner-city areas, and increased dependence on screen time for schooling, it is more difficult to craft easy solutions to the screen time issue.
During these times, it is more important than ever for pediatricians to check in on the mental health of patients with queries about how school is going, how patients are keeping contact with peers, and how are they processing social issues related to violence. Queries to families about the need for assistance with food insecurity, housing insecurity, and access to mental health services are necessary during this time of public emergency.
Medical school and COVID-19
Although medical school is an adult schooling experience, it affects not only the medical profession and our junior colleagues, but, by extrapolation, all education that requires hands-on experience or interning, and has been included for those reasons.
In the new COVID-19 era, medical schools have been forced to make drastic and quick changes to multiple levels of their curriculum to ensure both student and patient safety during the pandemic. Students entering their clinical rotations have had the most drastic alteration to their experience.
COVID-19 has led to some of the same changes high schools and colleges have adopted, specifically, replacement of large in-person lectures with small group activities small group discussion and virtual lectures. 32 The transition to an online format for medical education has been rapid and impacted both students and faculty. 33 , 34 In a survey by Singh and colleagues, 33 of the 192 students reporting 43.9% found online lectures to be poorer than physical classrooms during the pandemic. In another report by Shahrvini and colleagues, 35 of 104 students surveyed, 74.5% students felt disconnected from their medical school and their peers and 43.3% felt that they were unprepared for their clerkships. Although there are no pre-COVID-19 data for comparison, it is expected that the COVID-19 changes will lead to increased insecurity and feelings of poor preparation for clinical work.
Gross anatomy is a well-established tradition within the medical school curriculum and one that is conducted almost entirely in person and in close quarters around a cadaver. Harmon and colleagues 36 surveyed 67 gross anatomy educators and found that 8% were still holding in-person sessions and 34 ± 43% transitioned to using cadaver images and dissecting videos that could be accessed through the Internet.
Many third- and fourth-year medical students have seen periods of cancellation for clinical rotations and supplementation with online learning, telemedicine, or virtual rounds owing to the COVID-19 pandemic. 37 A study from Shahrvini and colleagues 38 found that an unofficial document from Reddit (a widely used social network platform with a subgroup for medical students and residents) reported that 75% of medical schools had canceled clinical activities for third- and fourth-year students for some part of 2020. In another survey by Harries and colleagues, 39 of the 741 students who responded, 93.7% were not involved in clinical rotations with in-person patient contact. The reactions of students varied, with 75.8% admitting to agreeing with the decision, 34.7% feeling guilty, and 27.0% feeling relieved. 39 In the same survey, 74.7% of students felt that their medical education had been disrupted, 84.1% said they felt increased anxiety, and 83.4% would accept the risk of COVID-19 infection if they were able to return to the clinical setting. 39
Since the start of the pandemic, medical schools have had to find new and innovative ways to continue teaching and exposing students to clinical settings. The use of electronic conferencing services has been critical to continuing education. One approach has been to turn to online applications like Google Hangouts, which come at no cost and offer a wide variety of tools to form an integrative learning environment. 32 , 37 , 40 Schools have also adopted a hybrid model of teaching where lectures can be prerecorded then viewed by the student asynchronously on their own time followed by live virtual lectures where faculty can offer question-and-answer sessions related to the material. By offering this new format, students have been given more flexibility in terms of creating a schedule that suits their needs and may decrease stress. 37
Although these changes can be a hurdle to students and faculty, it might prove to be beneficial for the future of medical training in some ways. Telemedicine is a growing field, and the American Medical Association and other programs have endorsed its value. 41 Telemedicine visits can still be used to take a history, conduct a basic visual physical examination, and build rapport, as well as performing other aspects of the clinical examination during a pandemic, and will continue to be useful for patients unable to attend regular visits at remote locations. Learning effectively now how to communicate professionally and carry out telemedicine visits may better prepare students for a future where telemedicine is an expectation and allow students to learn the limitations as well as the advantages of this modality. 41
Pandemic changes have strongly impacted the process of college applications, medical school applications, and residency applications. 32 For US medical residencies, 72% of applicants will, if the pattern from 2016 to 2019 continues, move between states or countries. 42 This level of movement is increasingly dangerous given the spread of COVID-19 and the lack of currently accepted procedures to carry out such a mass migration safely. The same follows for medical schools and universities.
We need to accept and prepare for the fact that medial students as well as other learners who require in-person training may lack some skills when they enter their profession. These skills will have to be acquired during a later phase of training. We may have less skilled entry-level resident physicians and nurses in our hospitals and in other clinical professions as well.
The COVID-19 pandemic has affected and will continue to affect the delivery of knowledge and skills at all levels of education. Although many children and adult learners will likely compensate for this interruption of traditional educational services and adapt to new modalities, some will struggle. The widening of the gap for those whose families cannot absorb the teaching and supervision of education required for in-home education because they lack the time and skills necessary are not addressed currently. The gap for those already at a disadvantage because of socioeconomic class, language, and special needs are most severely affected by the COVID-19 pandemic school closures and will have the hardest time compensating. As pediatricians, it is critical that we continue to check in with our young patients about how they are coping and what assistance we can guide them toward in our communities.
Clinics care points
- • Learners and educators at all levels of education have been affected by COVID-19 restrictions with rapid adaptations to virtual learning platforms.
- • The impact of COVID-19 on learners is not evenly distributed and children of racial minorities, those who live in poverty, those requiring special education, and children who speak English as a second language are more negatively affected by the need for remote learning.
- • Math scores are more impacted than language arts scores by previous school closures and thus far by these shutdowns for COVID-19.
- • Anxiety and depression have increased in children and particularly in adolescents as a result of COVID-19 itself and as a consequence of school changes.
- • Pediatricians should regularly screen for unmet needs in their patients during the pandemic, such as food insecurity with the loss of school meals, an inability to adapt to remote learning and increased computer time, and heightened anxiety and depression as results of school changes.
The authors have nothing to disclose.

IMAGES
COMMENTS
Presently the impacts of COVID-19 in daily life are extensive and have far reaching consequences. These can be divided into various categories: Closure of places for entertainment such as movie and play theatres, sports clubs, gymnasiums, swimming pools, and so on. This COVID-19 has affected the sources of supply and effects the global economy.
The World Health Organisation (WHO) has declared the coronavirus disease 2019 (COVID-19) a pandemic. Covid-19 has affected and still affecting our life in many ways. Covid-19 has rapidly affected our day to day life, businesses, disrupted the world trade and movements. Identification of the disease at an early stage is vital to control the ...
Reading time: 3 min (864 words) The COVID-19 pandemic has led to a dramatic loss of human life worldwide and presents an unprecedented challenge to public health, food systems and the world of work. The economic and social disruption caused by the pandemic is devastating: tens of millions of people are at risk of falling into extreme poverty ...
From lifestyle changes to better eating habits, people are using this time to get healthier in many areas. Since the pandemic started, nearly two-thirds of the survey's participants (62%) say ...
Feelings of isolation and loneliness can increase the likelihood of depression, high blood pressure, and death from heart disease. They can also affect the immune system's ability to fight ...
'COVID-19 has shown that people do value local food networks. You saw informal markets, and adaptable businesses springing up and driving things ahead,' Benton says. However it remains to be seen how permanent or widespread any move towards more seasonal, localized produce supply chains will be, without any dedicated support or state ...
1. Introduction. The coronavirus disease 2019 (COVID-19) pandemic has led to unprecedented changes in people's daily lives, with implications for mental health and well-being [1-4], both at the level of a given country's population, and when considering specific vulnerable groups [5-7].In order to mitigate the untoward impact of the pandemic (including lockdown) and support mental health ...
The CDC reports that the percentage of adults who reported symptoms of anxiety of depression in the past 7 days increased from 36.4 to 41.5 % from August 2020 to February 2021. Other reports show that having COVID-19 may contribute, too, with its lingering or long COVID symptoms, which can include "foggy mind," anxiety, depression, and post ...
The outbreak has dramatically changed Americans' lives and relationships over the past year. We asked people to tell us about their experiences - good and bad - in living through this moment in history. Pew Research Center has been asking survey questions over the past year about Americans' views and reactions to the COVID-19 pandemic.
The Pandemic's Effects on Everyday Life. Boston College researchers are exploring COVID-19's impact on life as we know it. Here's a look at just some of the important questions they're asking—and answering. Is remote work here to stay? As many as 60 percent of U.S. employees are estimated to have worked remotely at some point during the ...
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020. Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19.
Read these 12 moving essays about life during coronavirus. Artists, novelists, critics, and essayists are writing the first draft of history. A woman wearing a face mask in Miami. Alissa Wilkinson ...
The United States' unemployment rate rose from 3.5 percent in February 2020 to a record high of 14.7 percent in April 2020, but as of November 2020 it was back down to 6.7 percent. In November 2020, 21.8 percent of U.S. people with jobs teleworked due to the pandemic. The majority of school-age children in the United States have attended ...
Students can choose to write a full-length college essay on the coronavirus or summarize their experience in a shorter form. To help students explain how the pandemic affected them, The Common App ...
Alex, a writer and fellow disabled parent, found the freedom to explore a fuller version of herself in the privacy the pandemic provided. "The way I dress, the way I love, and the way I carry ...
She was all I had. I was forced to turn my camera on and float in the fake reality of being fine although I wasn't. The teachers tried to keep the class engaged by obligating the students to ...
Physical distancing due to the COVID‐19 outbreak can have drastic negative effects on the mental health of the elderly and disabled individuals. Physical isolation at home among family members can put the elderly and disabled person at serious mental health risk. It can cause anxiety, distress, and induce a traumatic situation for them.
Family in the Age of COVID‐19. The coronavirus has had a profound effect on the world in a multitude of ways. By the time this appears (written in mid‐April 2020), we probably will have some better sense of its ultimate impact. This essay centers on only one meaning of its effects: How it has impacted family life.
Background The WHO has raised concerns about the psychological consequences of the current COVID-19 pandemic, negatively affecting health across societies, cultures and age-groups. Methods This online survey study investigated mental health, subjective experience, and behaviour (health, learning/teaching) among university students studying in Egypt or Germany shortly after the first pandemic ...
Click here 👆 to get an answer to your question ️ How COVID 19 affect in our life? Essay. nimmaladinesh9327 nimmaladinesh9327 17.09.2020 English Secondary School answered How COVID 19 affect in our life? Essay See answer Advertisement
In this new study, researchers from the Cleveland Clinic will use tools that they developed from earlier NIH-supported projects to study how COVID-19 affects the brain. They will focus on fatigue, headaches, loss of smell or taste, and memory loss, or "brain fog.". They will also look at more serious but less common complications, such as ...
The transition to an online education during the coronavirus disease 2019 (COVID-19) pandemic may bring about adverse educational changes and adverse health consequences for children and young adult learners in grade school, middle school, high school, college, and professional schools. The effects may differ by age, maturity, and socioeconomic ...
How covid 19 affect your life as a student? give me a simple and small essay pa helppppp nonsense the best brainliest See answers Bereavement, isolation, loss of income and fear are triggering mental health conditions or exacerbating existing ones. Many people may be facing increased levels of alcohol and drug use, insomnia, and anxiety ...