Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 13 July 2021

Systematic review and meta-analysis of depression, anxiety, and suicidal ideation among Ph.D. students
- Emily N. Satinsky 1 ,
- Tomoki Kimura 2 ,
- Mathew V. Kiang 3 , 4 ,
- Rediet Abebe 5 , 6 ,
- Scott Cunningham 7 ,
- Hedwig Lee 8 ,
- Xiaofei Lin 9 ,
- Cindy H. Liu 10 , 11 ,
- Igor Rudan 12 ,
- Srijan Sen 13 ,
- Mark Tomlinson 14 , 15 ,
- Miranda Yaver 16 &
- Alexander C. Tsai 1 , 11 , 17
Scientific Reports volume 11 , Article number: 14370 ( 2021 ) Cite this article
89k Accesses
79 Citations
817 Altmetric
Metrics details
- Epidemiology
- Health policy
- Quality of life
University administrators and mental health clinicians have raised concerns about depression and anxiety among Ph.D. students, yet no study has systematically synthesized the available evidence in this area. After searching the literature for studies reporting on depression, anxiety, and/or suicidal ideation among Ph.D. students, we included 32 articles. Among 16 studies reporting the prevalence of clinically significant symptoms of depression across 23,469 Ph.D. students, the pooled estimate of the proportion of students with depression was 0.24 (95% confidence interval [CI], 0.18–0.31; I 2 = 98.75%). In a meta-analysis of the nine studies reporting the prevalence of clinically significant symptoms of anxiety across 15,626 students, the estimated proportion of students with anxiety was 0.17 (95% CI, 0.12–0.23; I 2 = 98.05%). We conclude that depression and anxiety are highly prevalent among Ph.D. students. Data limitations precluded our ability to obtain a pooled estimate of suicidal ideation prevalence. Programs that systematically monitor and promote the mental health of Ph.D. students are urgently needed.
Similar content being viewed by others

Prevalence of depression among Chinese university students: a systematic review and meta-analysis
A repeated cross-sectional analysis assessing mental health conditions of adults as per student status during key periods of the COVID-19 epidemic in France
Relationship between depression and quality of life among students: a systematic review and meta-analysis
Introduction.
Mental health problems among graduate students in doctoral degree programs have received increasing attention 1 , 2 , 3 , 4 . Ph.D. students (and students completing equivalent degrees, such as the Sc.D.) face training periods of unpredictable duration, financial insecurity and food insecurity, competitive markets for tenure-track positions, and unsparing publishing and funding models 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 —all of which may have greater adverse impacts on students from marginalized and underrepresented populations 13 , 14 , 15 . Ph.D. students’ mental health problems may negatively affect their physical health 16 , interpersonal relationships 17 , academic output, and work performance 18 , 19 , and may also contribute to program attrition 20 , 21 , 22 . As many as 30 to 50% of Ph.D. students drop out of their programs, depending on the country and discipline 23 , 24 , 25 , 26 , 27 . Further, while mental health problems among Ph.D. students raise concerns for the wellbeing of the individuals themselves and their personal networks, they also have broader repercussions for their institutions and academia as a whole 22 .
Despite the potential public health significance of this problem, most evidence syntheses on student mental health have focused on undergraduate students 28 , 29 or graduate students in professional degree programs (e.g., medical students) 30 . In non-systematic summaries, estimates of the prevalence of clinically significant depressive symptoms among Ph.D. students vary considerably 31 , 32 , 33 . Reliable estimates of depression and other mental health problems among Ph.D. students are needed to inform preventive, screening, or treatment efforts. To address this gap in the literature, we conducted a systematic review and meta-analysis to explore patterns of depression, anxiety, and suicidal ideation among Ph.D. students.
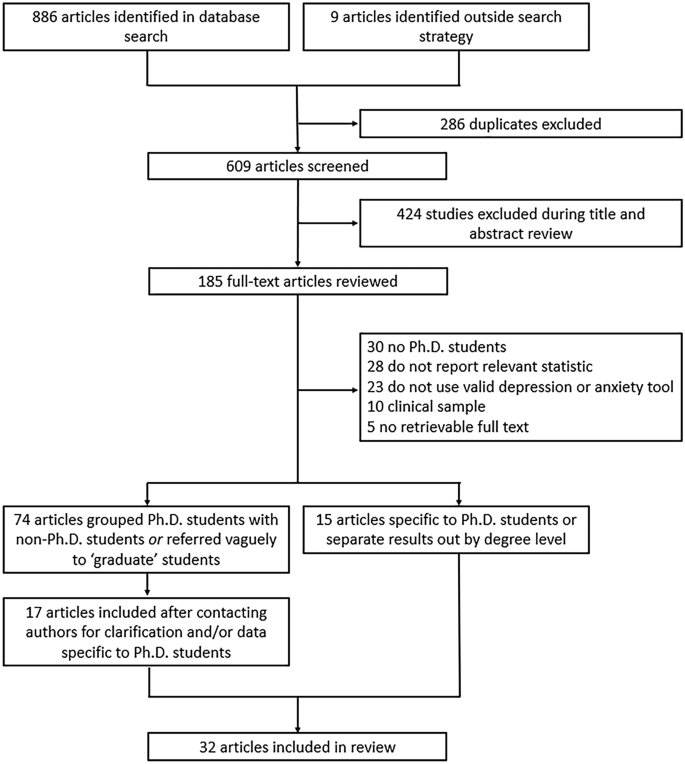
Flowchart of included articles.
The evidence search yielded 886 articles, of which 286 were excluded as duplicates (Fig. 1 ). An additional nine articles were identified through reference lists or grey literature reports published on university websites. Following a title/abstract review and subsequent full-text review, 520 additional articles were excluded.
Of the 89 remaining articles, 74 were unclear about their definition of graduate students or grouped Ph.D. and non-Ph.D. students without disaggregating the estimates by degree level. We obtained contact information for the authors of most of these articles (69 [93%]), requesting additional data. Three authors clarified that their study samples only included Ph.D. students 34 , 35 , 36 . Fourteen authors confirmed that their study samples included both Ph.D. and non-Ph.D. students but provided us with data on the subsample of Ph.D. students 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 . Where authors clarified that the sample was limited to graduate students in non-doctoral degree programs, did not provide additional data on the subsample of Ph.D. students, or did not reply to our information requests, we excluded the studies due to insufficient information (Supplementary Table S1 ).
Ultimately, 32 articles describing the findings of 29 unique studies were identified and included in the review 16 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 (Table 1 ). Overall, 26 studies measured depression, 19 studies measured anxiety, and six studies measured suicidal ideation. Three pairs of articles reported data on the same sample of Ph.D. students 33 , 38 , 45 , 51 , 53 , 56 and were therefore grouped in Table 1 and reported as three studies. Publication dates ranged from 1979 to 2019, but most articles (22/32 [69%]) were published after 2015. Most studies were conducted in the United States (20/29 [69%]), with additional studies conducted in Australia, Belgium, China, Iran, Mexico, and South Korea. Two studies were conducted in cross-national settings representing 48 additional countries. None were conducted in sub-Saharan Africa or South America. Most studies included students completing their degrees in a mix of disciplines (17/29 [59%]), while 12 studies were limited to students in a specific field (e.g., biomedicine, education). The median sample size was 172 students (interquartile range [IQR], 68–654; range, 6–6405). Seven studies focused on mental health outcomes in demographic subgroups, including ethnic or racialized minority students 37 , 41 , 43 , international students 47 , 50 , and sexual and gender minority students 42 , 54 .
In all, 16 studies reported the prevalence of depression among a total of 23,469 Ph.D. students (Fig. 2 ; range, 10–47%). Of these, the most widely used depression scales were the PHQ-9 (9 studies) and variants of the Center for Epidemiologic Studies-Depression scale (CES-D, 4 studies) 63 , and all studies assessed clinically significant symptoms of depression over the past one to two weeks. Three of these studies reported findings based on data from different survey years of the same parent study (the Healthy Minds Study) 40 , 42 , 43 , but due to overlap in the survey years reported across articles, these data were pooled. Most of these studies were based on data collected through online surveys (13/16 [81%]). Ten studies (63%) used random or systematic sampling, four studies (25%) used convenience sampling, and two studies (13%) used multiple sampling techniques.
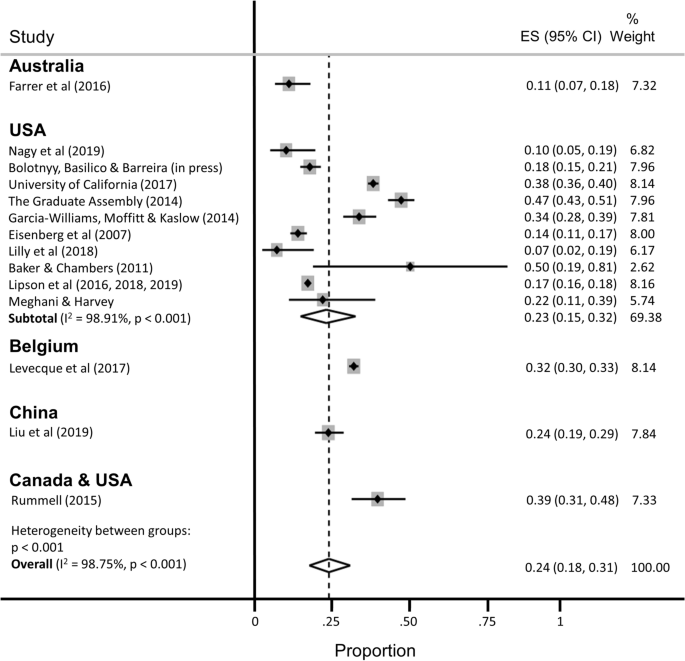
Pooled estimate of the proportion of Ph.D. students with clinically significant symptoms of depression.
The estimated proportion of Ph.D. students assessed as having clinically significant symptoms of depression was 0.24 (95% confidence interval [CI], 0.18–0.31; 95% predictive interval [PI], 0.04–0.54), with significant evidence of between-study heterogeneity (I 2 = 98.75%). A subgroup analysis restricted to the twelve studies conducted in the United States yielded similar findings (pooled estimate [ES] = 0.23; 95% CI, 0.15–0.32; 95% PI, 0.01–0.60), with no appreciable difference in heterogeneity (I 2 = 98.91%). A subgroup analysis restricted to the studies that used the PHQ-9 to assess depression yielded a slightly lower prevalence estimate and a slight reduction in heterogeneity (ES = 0.18; 95% CI, 0.14–0.22; 95% PI, 0.07–0.34; I 2 = 90.59%).
Nine studies reported the prevalence of clinically significant symptoms of anxiety among a total of 15,626 Ph.D. students (Fig. 3 ; range 4–49%). Of these, the most widely used anxiety scale was the 7-item Generalized Anxiety Disorder scale (GAD-7, 5 studies) 64 . Data from three of the Healthy Minds Study articles were pooled into two estimates, because the scale used to measure anxiety changed midway through the parent study (i.e., the Patient Health Questionnaire-Generalized Anxiety Disorder [PHQ-GAD] scale was used from 2007 to 2012 and then switched to the GAD-7 in 2013 40 ). Most studies (8/9 [89%]) assessed clinically significant symptoms of anxiety over the past two to four weeks, with the one remaining study measuring anxiety over the past year. Again, most of these studies were based on data collected through online surveys (7/9 [78%]). Five studies (56%) used random or systematic sampling, two studies (22%) used convenience sampling, and two studies (22%) used multiple sampling techniques.
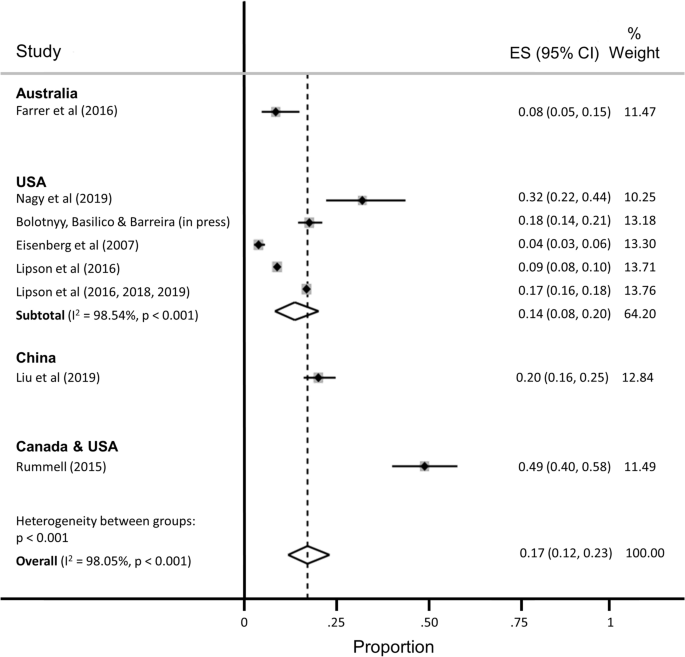
Pooled estimate of the proportion of Ph.D. students with clinically significant symptoms of anxiety.
The estimated proportion of Ph.D. students assessed as having anxiety was 0.17 (95% CI, 0.12–0.23; 95% PI, 0.02–0.41), with significant evidence of between-study heterogeneity (I 2 = 98.05%). The subgroup analysis restricted to the five studies conducted in the United States yielded a slightly lower proportion of students assessed as having anxiety (ES = 0.14; 95% CI, 0.08–0.20; 95% PI, 0.00–0.43), with no appreciable difference in heterogeneity (I 2 = 98.54%).
Six studies reported the prevalence of suicidal ideation (range, 2–12%), but the recall windows varied greatly (e.g., ideation within the past 2 weeks vs. past year), precluding pooled estimation.
Additional stratified pooled estimates could not be obtained. One study of Ph.D. students across 54 countries found that phase of study was a significant moderator of mental health, with students in the comprehensive examination and dissertation phases more likely to experience distress compared with students primarily engaged in coursework 59 . Other studies identified a higher prevalence of mental ill-health among women 54 ; lesbian, gay, bisexual, transgender, and queer (LGBTQ) students 42 , 54 , 60 ; and students with multiple intersecting identities 54 .
Several studies identified correlates of mental health problems including: project- and supervisor-related issues, stress about productivity, and self-doubt 53 , 62 ; uncertain career prospects, poor living conditions, financial stressors, lack of sleep, feeling devalued, social isolation, and advisor relationships 61 ; financial challenges 38 ; difficulties with work-life balance 58 ; and feelings of isolation and loneliness 52 . Despite these challenges, help-seeking appeared to be limited, with only about one-quarter of Ph.D. students reporting mental health problems also reporting that they were receiving treatment 40 , 52 .
Risk of bias
Twenty-one of 32 articles were assessed as having low risk of bias (Supplementary Table S2 ). Five articles received one point for all five categories on the risk of bias assessment (lowest risk of bias), and one article received no points (highest risk). The mean risk of bias score was 3.22 (standard deviation, 1.34; median, 4; IQR, 2–4). Restricting the estimation sample to 12 studies assessed as having low risk of bias, the estimated proportion of Ph.D. students with depression was 0.25 (95% CI, 0.18–0.33; 95% PI, 0.04–0.57; I 2 = 99.11%), nearly identical to the primary estimate, with no reduction in heterogeneity. The estimated proportion of Ph.D. students with anxiety, among the 7 studies assessed as having low risk of bias, was 0.12 (95% CI, 0.07–0.17; 95% PI, 0.01–0.34; I 2 = 98.17%), again with no appreciable reduction in heterogeneity.
In our meta-analysis of 16 studies representing 23,469 Ph.D. students, we estimated that the pooled prevalence of clinically significant symptoms of depression was 24%. This estimate is consistent with estimated prevalence rates in other high-stress biomedical trainee populations, including medical students (27%) 30 , resident physicians (29%) 65 , and postdoctoral research fellows (29%) 66 . In the sample of nine studies representing 15,626 Ph.D. students, we estimated that the pooled prevalence of clinically significant symptoms of anxiety was 17%. While validated screening instruments tend to over-identify cases of depression (relative to structured clinical interviews) by approximately a factor of two 67 , 68 , our findings nonetheless point to a major public health problem among Ph.D. students. Available data suggest that the prevalence of depressive and anxiety disorders in the general population ranges from 5 to 7% worldwide 69 , 70 . In contrast, prevalence estimates of major depressive disorder among young adults have ranged from 13% (for young adults between the ages of 18 and 29 years in the 2012–2013 National Epidemiologic Survey on Alcohol and Related Conditions III 71 ) to 15% (for young adults between the ages of 18 and 25 in the 2019 U.S. National Survey on Drug Use and Health 72 ). Likewise, the prevalence of generalized anxiety disorder was estimated at 4% among young adults between the ages of 18 and 29 in the 2001–03 U.S. National Comorbidity Survey Replication 73 . Thus, even accounting for potential upward bias inherent in these studies’ use of screening instruments, our estimates suggest that the rates of recent clinically significant symptoms of depression and anxiety are greater among Ph.D. students compared with young adults in the general population.
Further underscoring the importance of this public health issue, Ph.D. students face unique stressors and uncertainties that may put them at increased risk for mental health and substance use problems. Students grapple with competing responsibilities, including coursework, teaching, and research, while also managing interpersonal relationships, social isolation, caregiving, and financial insecurity 3 , 10 . Increasing enrollment in doctoral degree programs has not been matched with a commensurate increase in tenure-track academic job opportunities, intensifying competition and pressure to find employment post-graduation 5 . Advisor-student power relations rarely offer options for recourse if and when such relationships become strained, particularly in the setting of sexual harassment, unwanted sexual attention, sexual coercion, and rape 74 , 75 , 76 , 77 , 78 . All of these stressors may be magnified—and compounded by stressors unrelated to graduate school—for subgroups of students who are underrepresented in doctoral degree programs and among whom mental health problems are either more prevalent and/or undertreated compared with the general population, including Black, indigenous, and other people of color 13 , 79 , 80 ; women 81 , 82 ; first-generation students 14 , 15 ; people who identify as LGBTQ 83 , 84 , 85 ; people with disabilities; and people with multiple intersecting identities.
Structural- and individual-level interventions will be needed to reduce the burden of mental ill-health among Ph.D. students worldwide 31 , 86 . Despite the high prevalence of mental health and substance use problems 87 , Ph.D. students demonstrate low rates of help-seeking 40 , 52 , 88 . Common barriers to help-seeking include fears of harming one’s academic career, financial insecurity, lack of time, and lack of awareness 89 , 90 , 91 , as well as health care systems-related barriers, including insufficient numbers of culturally competent counseling staff, limited access to psychological services beyond time-limited psychotherapies, and lack of programs that address the specific needs either of Ph.D. students in general 92 or of Ph.D. students belonging to marginalized groups 93 , 94 . Structural interventions focused solely on enhancing student resilience might include programs aimed at reducing stigma, fostering social cohesion, and reducing social isolation, while changing norms around help-seeking behavior 95 , 96 . However, structural interventions focused on changing stressogenic aspects of the graduate student environment itself are also needed 97 , beyond any enhancements to Ph.D. student resilience, including: undercutting power differentials between graduate students and individual faculty advisors, e.g., by diffusing power among multiple faculty advisors; eliminating racist, sexist, and other discriminatory behaviors by faculty advisors 74 , 75 , 98 ; valuing mentorship and other aspects of “invisible work” that are often disproportionately borne by women faculty and faculty of color 99 , 100 ; and training faculty members to emphasize the dignity of, and adequately prepare Ph.D. students for, non-academic careers 101 , 102 .
Our findings should be interpreted with several limitations in mind. First, the pooled estimates are characterized by a high degree of heterogeneity, similar to meta-analyses of depression prevalence in other populations 30 , 65 , 103 , 104 , 105 . Second, we were only able to aggregate depression prevalence across 16 studies and anxiety prevalence across nine studies (the majority of which were conducted in the U.S.) – far fewer than the 183 studies included in a meta-analysis of depression prevalence among medical students 30 and the 54 studies included in a meta-analysis of resident physicians 65 . These differences underscore the need for more rigorous study in this critical area. Many articles were either excluded from the review or from the meta-analyses for not meeting inclusion criteria or not reporting relevant statistics. Future research in this area should ensure the systematic collection of high-quality, clinically relevant data from a comprehensive set of institutions, across disciplines and countries, and disaggregated by graduate student type. As part of conducting research and addressing student mental health and wellbeing, university deans, provosts, and chancellors should partner with national survey and program institutions (e.g., Graduate Student Experience in the Research University [gradSERU] 106 , the American College Health Association National College Health Assessment [ACHA-NCHA], and HealthyMinds). Furthermore, federal agencies that oversee health and higher education should provide resources for these efforts, and accreditation agencies should require monitoring of mental health and programmatic responses to stressors among Ph.D. students.
Third, heterogeneity in reporting precluded a meta-analysis of the suicidality outcomes among the few studies that reported such data. While reducing the burden of mental health problems among graduate students is an important public health aim in itself, more research into understanding non-suicidal self-injurious behavior, suicide attempts, and completed suicide among Ph.D. students is warranted. Fourth, it is possible that the grey literature reports included in our meta-analysis are more likely to be undertaken at research-intensive institutions 52 , 60 , 61 . However, the direction of bias is unpredictable: mental health problems among Ph.D. students in research-intensive environments may be more prevalent due to detection bias, but such institutions may also have more resources devoted to preventive, screening, or treatment efforts 92 . Fifth, inclusion in this meta-analysis and systematic review was limited to those based on community samples. Inclusion of clinic-based samples, or of studies conducted before or after specific milestones (e.g., the qualifying examination or dissertation prospectus defense), likely would have yielded even higher pooled prevalence estimates of mental health problems. And finally, few studies provided disaggregated data according to sociodemographic factors, stage of training (e.g., first year, pre-prospectus defense, all-but-dissertation), or discipline of study. These factors might be investigated further for differences in mental health outcomes.
Clinically significant symptoms of depression and anxiety are pervasive among graduate students in doctoral degree programs, but these are understudied relative to other trainee populations. Structural and clinical interventions to systematically monitor and promote the mental health and wellbeing of Ph.D. students are urgently needed.
This systematic review and meta-analysis follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) approach (Supplementary Table S3 ) 107 . This study was based on data collected from publicly available bibliometric databases and did not require ethical approval from our institutional review boards.
Eligibility criteria
Studies were included if they provided data on either: (a) the number or proportion of Ph.D. students with clinically significant symptoms of depression or anxiety, ascertained using a validated scale; or (b) the mean depression or anxiety symptom severity score and its standard deviation among Ph.D. students. Suicidal ideation was examined as a secondary outcome.
We excluded studies that focused on graduate students in non-doctoral degree programs (e.g., Master of Public Health) or professional degree programs (e.g., Doctor of Medicine, Juris Doctor) because more is known about mental health problems in these populations 30 , 108 , 109 , 110 and because Ph.D. students face unique uncertainties. To minimize the potential for upward bias in our pooled prevalence estimates, we excluded studies that recruited students from campus counseling centers or other clinic-based settings. Studies that measured affective states, or state anxiety, before or after specific events (e.g., terrorist attacks, qualifying examinations) were also excluded.
If articles described the study sample in general terms (i.e., without clarifying the degree level of the participants), we contacted the authors by email for clarification. Similarly, if articles pooled results across graduate students in doctoral and non-doctoral degree programs (e.g., reporting a single estimate for a mixed sample of graduate students), we contacted the authors by email to request disaggregated data on the subsample of Ph.D. students. If authors did not reply after two contact attempts spaced over 2 months, or were unable to provide these data, we excluded these studies from further consideration.
Search strategy and data extraction
PubMed, Embase, PsycINFO, ERIC, and Business Source Complete were searched from inception of each database to November 5, 2019. The search strategy included terms related to mental health symptoms (e.g., depression, anxiety, suicide), the study population (e.g., graduate, doctoral), and measurement category (e.g., depression, Columbia-Suicide Severity Rating Scale) (Supplementary Table S4 ). In addition, we searched the reference lists and the grey literature.
After duplicates were removed, we screened the remaining titles and abstracts, followed by a full-text review. We excluded articles following the eligibility criteria listed above (i.e., those that were not focused on Ph.D. students; those that did not assess depression and/or anxiety using a validated screening tool; those that did not report relevant statistics of depression and/or anxiety; and those that recruited students from clinic-based settings). Reasons for exclusion were tracked at each stage. Following selection of included articles, two members of the research team extracted data and conducted risk of bias assessments. Discrepancies were discussed with a third member of the research team. Key extraction variables included: study design, geographic region, sample size, response rate, demographic characteristics of the sample, screening instrument(s) used for assessment, mean depression or anxiety symptom severity score (and its standard deviation), and the number (or proportion) of students experiencing clinically significant symptoms of depression or anxiety.
Risk of bias assessment
Following prior work 30 , 65 , the Newcastle–Ottawa Scale 111 was adapted and used to assess risk of bias in the included studies. Each study was assessed across 5 categories: sample representativeness, sample size, non-respondents, ascertainment of outcomes, and quality of descriptive statistics reporting (Supplementary Information S5 ). Studies were judged as having either low risk of bias (≥ 3 points) or high risk of bias (< 3 points).
Analysis and synthesis
Before pooling the estimated prevalence rates across studies, we first transformed the proportions using a variance-stabilizing double arcsine transformation 112 . We then computed pooled estimates of prevalence using a random effects model 113 . Study specific confidence intervals were estimated using the score method 114 , 115 . We estimated between-study heterogeneity using the I 2 statistic 116 . In an attempt to reduce the extent of heterogeneity, we re-estimated pooled prevalence restricting the analysis to studies conducted in the United States and to studies in which depression assessment was based on the 9-item Patient Health Questionnaire (PHQ-9) 117 . All analyses were conducted using Stata (version 16; StataCorp LP, College Station, Tex.). Where heterogeneity limited our ability to summarize the findings using meta-analysis, we synthesized the data using narrative review.
Woolston, C. Why mental health matters. Nature 557 , 129–131 (2018).
Article ADS CAS Google Scholar
Woolston, C. A love-hurt relationship. Nature 550 , 549–552 (2017).
Article Google Scholar
Woolston, C. PhD poll reveals fear and joy, contentment and anguish. Nature 575 , 403–406 (2019).
Article ADS CAS PubMed Google Scholar
Byrom, N. COVID-19 and the research community: The challenges of lockdown for early-career researchers. Elife 9 , e59634 (2020).
Article PubMed PubMed Central Google Scholar
Alberts, B., Kirschner, M. W., Tilghman, S. & Varmus, H. Rescuing US biomedical research from its systemic flaws. Proc. Natl. Acad. Sci. USA 111 , 5773–5777 (2014).
Article ADS CAS PubMed PubMed Central Google Scholar
McDowell, G. S. et al. Shaping the future of research: A perspective from junior scientists. F1000Res 3 , 291 (2014).
Article PubMed Google Scholar
Petersen, A. M., Riccaboni, M., Stanley, H. E. & Pammoli, F. Persistence and uncertainty in the academic career. Proc. Natl. Acad. Sci. USA 109 , 5213–5218 (2012).
Leshner, A. I. Rethinking graduate education. Science 349 , 349 (2015).
National Academies of Sciences Engineering and Medicine. Graduate STEM Education for the 21st Century (National Academies Press, 2018).
Google Scholar
Charles, S. T., Karnaze, M. M. & Leslie, F. M. Positive factors related to graduate student mental health. J. Am. Coll. Health https://doi.org/10.1080/07448481.2020.1841207 (2021).
Riddle, E. S., Niles, M. T. & Nickerson, A. Prevalence and factors associated with food insecurity across an entire campus population. PLoS ONE 15 , e0237637 (2020).
Article CAS PubMed PubMed Central Google Scholar
Soldavini, J., Berner, M. & Da Silva, J. Rates of and characteristics associated with food insecurity differ among undergraduate and graduate students at a large public university in the Southeast United States. Prev. Med. Rep. 14 , 100836 (2019).
Clark, U. S. & Hurd, Y. L. Addressing racism and disparities in the biomedical sciences. Nat. Hum. Behav. 4 , 774–777 (2020).
Gardner, S. K. The challenges of first-generation doctoral students. New Dir. High. Educ. 2013 , 43–54 (2013).
Seay, S. E., Lifton, D. E., Wuensch, K. L., Bradshaw, L. K. & McDowelle, J. O. First-generation graduate students and attrition risks. J. Contin. High. Educ. 56 , 11–25 (2008).
Rummell, C. M. An exploratory study of psychology graduate student workload, health, and program satisfaction. Prof. Psychol. Res. Pract. 46 , 391–399 (2015).
Salzer, M. S. A comparative study of campus experiences of college students with mental illnesses versus a general college sample. J. Am. Coll. Health 60 , 1–7 (2012).
Hysenbegasi, A., Hass, S. & Rowland, C. The impact of depression on the academic productivity of university students. J. Ment. Health Policy Econ. 8 , 145–151 (2005).
PubMed Google Scholar
Harvey, S. et al. Depression and work performance: An ecological study using web-based screening. Occup. Med. (Lond.) 61 , 209–211 (2011).
Article CAS Google Scholar
Eisenberg, D., Golberstein, E. & Hunt, J. B. Mental health and academic success in college. BE J. Econ. Anal. Policy 9 , 40 (2009).
Lovitts, B. E. Who is responsible for graduate student attrition--the individual or the institution? Toward an explanation of the high and persistent rate of attrition. In: Annual Meeting of the American Education Research Association (New York, 1996). Available at: https://eric.ed.gov/?id=ED399878.
Gardner, S. K. Student and faculty attributions of attrition in high and low-completing doctoral programs in the United States. High. Educ. 58 , 97–112 (2009).
Lovitts, B. E. Leaving the Ivory Tower: The Causes and Consequences of Departure from Doctoral Study (Rowman & Littlefield Publishers, 2001).
Rigler Jr, K. L., Bowlin, L. K., Sweat, K., Watts, S. & Throne, R. Agency, socialization, and support: a critical review of doctoral student attrition. In: Proceedings of the Third International Conference on Doctoral Education: Organizational Leadership and Impact , University of Central Florida, Orlando, (2017).
Golde, C. M. The role of the department and discipline in doctoral student attrition: Lessons from four departments. J. High. Educ. 76 , 669–700 (2005).
Council of Graduate Schools. PhD Completion and Attrition: Analysis of Baseline Program Data from the PhD Completion Project (Council of Graduate Schools, 2008).
National Research Council. A Data-Based Assessment of Research-Doctorate Programs in the United States (The National Academies Press, 2011).
Akhtar, P. et al. Prevalence of depression among university students in low and middle income countries (LMICs): A systematic review and meta-analysis. J. Affect. Disord. 274 , 911–919 (2020).
Mortier, P. et al. The prevalence of suicidal thoughts and behaviours among college students: A meta-analysis. Psychol. Med. 48 , 554–565 (2018).
Article CAS PubMed Google Scholar
Rotenstein, L. S. et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: A systematic review and meta-analysis. JAMA 316 , 2214–2236 (2016).
Tsai, J. W. & Muindi, F. Towards sustaining a culture of mental health and wellness for trainees in the biosciences. Nat. Biotechnol. 34 , 353–355 (2016).
Levecque, K., Anseel, F., De Beuckelaer, A., Van der Heyden, J. & Gisle, L. Work organization and mental health problems in PhD students. Res. Policy 46 , 868–879 (2017).
Nagy, G. A. et al. Burnout and mental health problems in biomedical doctoral students. CBE Life Sci. Educ. 18 , 1–14 (2019).
Garcia-Williams, A., Moffitt, L. & Kaslow, N. J. Mental health and suicidal behavior among graduate students. Acad. Psychiatry 28 , 554–560 (2014).
Sheldon, K. M. Emotionality differences between artists and scientists. J. Res. Pers. 28 , 481–491 (1994).
Lightstone, S. N., Swencionis, C. & Cohen, H. W. The effect of bioterrorism messages on anxiety levels. Int. Q. Community Health Educ. 24 , 111–122 (2006).
Clark, C. R., Mercer, S. H., Zeigler-Hill, V. & Dufrene, B. A. Barriers to the success of ethnic minority students in school psychology graduate programs. School Psych. Rev. 41 , 176–192 (2012).
Eisenberg, D., Gollust, S. E., Golberstein, E. & Hefner, J. L. Prevalence and correlates of depression, anxiety, and suicidality among university students. Am. J. Orthopsychiatry 77 , 534–542 (2007).
Farrer, L. M., Gulliver, A., Bennett, K., Fassnacht, D. B. & Griffiths, K. M. Demographic and psychosocial predictors of major depression and generalised anxiety disorder in Australian university students. BMC Psychiatry 16 , 241 (2016).
Lipson, S. K., Zhou, S., Wagner, B. III., Beck, K. & Eisenberg, D. Major differences: Variations in undergraduate and graduate student mental health and treatment utilization across academic disciplines. J. Coll. Stud. Psychother. 30 , 23–41 (2016).
Lilly, F. R. W. et al. The influence of racial microaggressions and social rank on risk for depression among minority graduate and professional students. Coll. Stud. J. 52 , 86–104 (2018).
Lipson, S. K., Raifman, J., Abelson, S. & Reisner, S. L. Gender minority mental health in the U.S.: Results of a national survey on college campuses. Am. J. Prev. Med. 57 , 293–301 (2019).
Lipson, S. K., Kern, A., Eisenberg, D. & Breland-Noble, A. M. Mental health disparities among college students of color. J. Adolesc. Health 63 , 348–356 (2018).
Baker, A. J. L. & Chambers, J. Adult recall of childhood exposure to parental conflict: Unpacking the black box of parental alienation. J. Divorce Remarriage 52 , 55–76 (2011).
Golberstein, E., Eisenberg, D. & Gollust, S. E. Perceived stigma and mental health care seeking. Psychiatr. Serv. 59 , 392–399 (2008).
Hindman, R. K., Glass, C. R., Arnkoff, D. B. & Maron, D. D. A comparison of formal and informal mindfulness programs for stress reduction in university students. Mindfulness 6 , 873–884 (2015).
Hirai, R., Frazier, P. & Syed, M. Psychological and sociocultural adjustment of first-year international students: Trajectories and predictors. J. Couns. Psychol. 62 , 438–452 (2015).
Lee, J. S. & Jeong, B. Having mentors and campus social networks moderates the impact of worries and video gaming on depressive symptoms: A moderated mediation analysis. BMC Public Health 14 , 1–12 (2014).
Corral-Frias, N. S., Velardez Soto, S. N., Frias-Armenta, M., Corona-Espinosa, A. & Watson, D. Concurrent validity and reliability of two short forms of the mood and anxiety symptom questionnaire in a student sample from Northwest Mexico. J. Psychopathol. Behav. Assess. 41 , 304–316 (2019).
Meghani, D. T. & Harvey, E. A. Asian Indian international students’ trajectories of depression, acculturation, and enculturation. Asian Am. J. Psychol. 7 , 1–14 (2016).
Barry, K. M., Woods, M., Martin, A., Stirling, C. & Warnecke, E. A randomized controlled trial of the effects of mindfulness practice on doctoral candidate psychological status. J. Am. Coll. Health 67 , 299–307 (2019).
Bolotnyy, V., Basilico, M. & Barreira, P. Graduate student mental health: lessons from American economics departments. J. Econ. Lit. (in press).
Barry, K. M., Woods, M., Warnecke, E., Stirling, C. & Martin, A. Psychological health of doctoral candidates, study-related challenges and perceived performance. High. Educ. Res. Dev. 37 , 468–483 (2018).
Boyle, K. M. & McKinzie, A. E. The prevalence and psychological cost of interpersonal violence in graduate and law school. J. Interpers. Violence 36 , 6319-6350 (2021).
Heinrich, D. L. The causal influence of anxiety on academic achievement for students of differing intellectual ability. Appl. Psychol. Meas. 3 , 351–359 (1979).
Hish, A. J. et al. Applying the stress process model to stress-burnout and stress-depression relationships in biomedical doctoral students: A cross-sectional pilot study. CBE Life Sci. Educ. 18 , 1–11 (2019).
Jamshidi, F. et al. A cross-sectional study of psychiatric disorders in medical sciences students. Mater. Sociomed. 29 , 188–191 (2017).
Liu, C. et al. Prevalence and associated factors of depression and anxiety among doctoral students: The mediating effect of mentoring relationships on the association between research self-efficacy and depression/anxiety. Psychol. Res. Behav. Manag. 12 , 195–208 (2019).
Sverdlik, A. & Hall, N. C. Not just a phase: Exploring the role of program stage on well-being and motivation in doctoral students. J. Adult Contin. Educ. 26 , 1–28 (2019).
University of California Office of the President. The University of California Graduate student Well-Being Survey Report (University of California, 2017).
The Graduate Assembly. Graduate Student Happiness & Well-Being Report (University of California at Berkeley, 2014).
Richardson, C. M., Trusty, W. T. & George, K. A. Trainee wellness: Self-critical perfectionism, self-compassion, depression, and burnout among doctoral trainees in psychology. Couns. Psychol. Q. 33 , 187-198 (2020).
Radloff, L. S. The CES-D Scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1 , 385–401 (1977).
Spitzer, R. L., Kroenke, K., Williams, J. B. W. & Lowe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 166 , 1092–1097 (2006).
Mata, D. A. et al. Prevalence of depression and depressive symptoms among residents physicians: A systematic review and meta-analysis. JAMA 314 , 2373–2383 (2015).
Gloria, C. T. & Steinhardt, M. A. Flourishing, languishing, and depressed postdoctoral fellows: Differences in stress, anxiety, and depressive symptoms. J. Postdoct. Aff. 3 , 1–9 (2013).
Levis, B. et al. Patient Health Questionnaire-9 scores do not accurately estimate depression prevalence: Individual participant data meta-analysis. J. Clin. Epidemiol. 122 , 115-128.e111 (2020).
Tsai, A. C. Reliability and validity of depression assessment among persons with HIV in sub-Saharan Africa: Systematic review and meta-analysis. J. Acquir. Immune Defic. Syndr. 66 , 503–511 (2014).
Baxter, A. J., Scott, K. M., Vos, T. & Whiteford, H. A. Global prevalence of anxiety disorders: A systematic review and meta-regression. Psychol. Med. 43 , 897–910 (2013).
Ferrari, A. et al. Global variation in the prevalence and incidence of major depressive disorder: A systematic review of the epidemiological literature. Psychol. Med. 43 , 471–481 (2013).
Hasin, D. S. et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry 75 , 336–346 (2018).
US Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health (Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, 2020).
Kessler, R. C. et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 62 , 593–602 (2005).
Working Group report to the Advisory Committee to the NIH Director. Changing the Culture to End Sexual Harassment (U. S. National Institutes of Health, 2019).
National Academies of Sciences Engineering and Medicine. Sexual Harassment of Women: Climate, Culture, and Consequences in Academic Sciences, Engineering, and Medicine (The National Academies Press, 2018).
Wadman, M. A hidden history. Science 360 , 480–485 (2018).
Hockfield, S., Magley, V. & Yoshino, K. Report of the External Review Committee to Review Sexual Harassment at Harvard University (External Review Committee to Review Sexual Harassment at Harvard University, 2021).
Bartlett, T. & Gluckman, N. She left Harvard. He got to stay. Chronicle High. Educ. 64 , A14 (2021). Available at: https://www.chronicle.com/article/she-left-harvard-he-got-to-stay/.
Tseng, M. et al. Strategies and support for Black, Indigenous, and people of colour in ecology and evolutionary biology. Nat. Ecol. Evol. 4 , 1288–1290 (2020).
Williams, D. R. et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: Results from the National Survey of American Life. Arch. Gen. Psychiatry 64 , 305–315 (2007).
Wu, A. H. Gender bias in rumors among professionals: An identity-based interpretation. Rev. Econ. Stat. 102 , 867–880 (2020).
Kessler, R. C. Epidemiology of women and depression. J. Affect. Disord. 74 , 5–13 (2003).
Mattheis, A., Cruz-Ramirez De Arellano, D. & Yoder, J. B. A model of queer STEM identity in the workplace. J. Homosex 67 , 1839–1863 (2020).
Semlyen, J., King, M., Varney, J. & Hagger-Johnson, G. Sexual orientation and symptoms of common mental disorder or low wellbeing: Combined meta-analysis of 12 UK population health surveys. BMC Psychiatry 16 , 1–19 (2016).
Lark, J. S. & Croteau, J. M. Lesbian, gay, and bisexual doctoral students’ mentoring relationships with faculty in counseling psychology: A qualitative study. Couns. Psychol. 26 , 754–776 (1998).
Jaremka, L. M. et al. Common academic experiences no one talks about: Repeated rejection, imposter syndrome, and burnout. Perspect Psychol Sci 15 , 519–543 (2020).
Allen, H. K. et al. Substance use and mental health problems among graduate students: Individual and program-level correlates. J. Am. Coll. Health https://doi.org/10.1080/07448481.2020.1725020 (2020).
Turner, A. & Berry, T. Counseling center contributions to student retention and graduation: A longitudinal assessment. J. Coll. Stud. Dev. 41 , 627–636 (2000).
Dyrbye, L. N., Thomas, M. R. & Shanafelt, T. D. Medical student distress: Causes, consequences, and proposed solutions. Mayo Clin. Proc. 80 , 1613–1622 (2005).
Tija, J., Givens, J. L. & Shea, J. A. Factors associated with undertreatment of medical student depression. J. Am. Coll. Health 53 , 219–224 (2005).
Dearing, R., Maddux, J. & Tangney, J. Predictors of psychological help seeking in clinical and counseling psychology graduate students. Prof. Psychol. Res. Pract. 36 , 323–329 (2005).
Langin, K. Amid concerns about grad student mental health, one university takes a novel approach. Science https://doi.org/10.1126/science.caredit.aay7113 (2019).
Guillory, D. Combating anti-blackness in the AI community. arXiv , arXiv:2006.16879 (2020).
Galán, C. A. et al. A call to action for an antiracist clinical science. J. Clin. Child Adolesc. Psychol 50 , 12-57 (2021).
Wyman, P. A. et al. Effect of the Wingman-Connect upstream suicide prevention program for air force personnel in training: A cluster randomized clinical trial. JAMA Netw Open 3 , e2022532 (2020).
Knox, K. L. et al. The US Air Force Suicide Prevention Program: Implications for public health policy. Am. J. Public Health 100 , 2457–2463 (2010).
Inclusive Climate Subcommittee of the Government Department Climate Change Committee. Government Department Climate Change: Final Report and Recommendations (Government Department, Harvard University, 2019).
Inclusive Climate Subcommittee of the Government Department Climate Change Committee. Government Department Climate Survey Report (Government Department, Harvard University, 2019).
Magoqwana, B., Maqabuka, Q. & Tshoaedi, M. “Forced to care” at the neoliberal university: Invisible labour as academic labour performed by Black women academics in the South African university. S. Afr. Rev. Sociol. 50 , 6–21 (2019).
Jones, H. A., Perrin, P. B., Heller, M. B., Hailu, S. & Barnett, C. Black psychology graduate students’ lives matter: Using informal mentoring to create an inclusive climate amidst national race-related events. Prof. Psychol. Res. Pract. 49 , 75–82 (2018).
Mathur, A., Meyers, F. J., Chalkley, R., O’Brien, T. C. & Fuhrmann, C. N. Transforming training to reflect the workforce. Sci. Transl. Med. 7 , 285 (2015).
Scharff, V. Advice: Prepare your Ph.D.s for diverse career paths. Chronicle High. Educ. 65 , 30 (2018).
Beattie, T. S., Smilenova, B., Krishnaratne, S. & Mazzuca, A. Mental health problems among female sex workers in low- and middle-income countries: A systematic review and meta-analysis. PLoS Med. 17 , e1003297 (2020).
Ismail, Z. et al. Prevalence of depression in patients with mild cognitive impairment: A systematic review and meta-analysis. JAMA Psychiatry 74 , 58–67 (2017).
Lim, G. Y. et al. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci. Rep. 8 , 1–10 (2018).
Article ADS Google Scholar
Jones-White, D. R., Soria, K. M., Tower, E. K. B. & Horner, O. G. Factors associated with anxiety and depression among U.S. doctoral students: Evidence from the gradSERU survey. J. Am. Coll. Health https://doi.org/10.1080/07448481.2020.1865975 (2021).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 151 , 264–269 (2009).
Helmers, K. F., Danoff, D., Steinert, Y., Leyton, M. & Young, S. N. Stress and depressed mood in medical students, law students, and graduate students at McGill University. Acad. Med. 72 , 708–714 (1997).
Rabkow, N. et al. Facing the truth: A report on the mental health situation of German law students. Int. J. Law Psychiatry 71 , 101599 (2020).
Bergin, A. & Pakenham, K. Law student stress: Relationships between academic demands, social isolation, career pressure, study/life imbalance and adjustment outcomes in law students. Psychiatr. Psychol. Law 22 , 388–406 (2015).
Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 25 , 603–605 (2010).
Freeman, M. F. & Tukey, J. W. Transformations related to the angular and the square root. Ann. Math. Stat. 21 , 607–611 (1950).
Article MathSciNet MATH Google Scholar
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Control Clin. Trials 7 , 177–188 (1986).
Wilson, E. B. Probable inference, the law of succession, and statistical inference. J. Am. Stat. Assoc. 22 , 209–212 (1927).
Newcombe, R. G. Two-sided confidence intervals for the single proportion: Comparison of seven methods. Stat. Med. 17 , 857–872 (1998).
Higgins, J. P. T. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21 , 1539–1558 (2002).
Kroenke, K., Spitzer, R. L. & Williams, J. B. W. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 16 , 606–613 (2001).
Download references
Acknowledgements
We thank the following investigators for generously sharing their time and/or data: Gordon J. G. Asmundson, Ph.D., Amy J. L. Baker, Ph.D., Hillel W. Cohen, Dr.P.H., Alcir L. Dafre, Ph.D., Deborah Danoff, M.D., Daniel Eisenberg, Ph.D., Lou Farrer, Ph.D., Christy B. Fraenza, Ph.D., Patricia A. Frazier, Ph.D., Nadia Corral-Frías, Ph.D., Hanga Galfalvy, Ph.D., Edward E. Goldenberg, Ph.D., Robert K. Hindman, Ph.D., Jürgen Hoyer, Ph.D., Ayako Isato, Ph.D., Azharul Islam, Ph.D., Shanna E. Smith Jaggars, Ph.D., Bumseok Jeong, M.D., Ph.D., Ju R. Joeng, Nadine J. Kaslow, Ph.D., Rukhsana Kausar, Ph.D., Flavius R. W. Lilly, Ph.D., Sarah K. Lipson, Ph.D., Frances Meeten, D.Phil., D.Clin.Psy., Dhara T. Meghani, Ph.D., Sterett H. Mercer, Ph.D., Masaki Mori, Ph.D., Arif Musa, M.D., Shizar Nahidi, M.D., Ph.D., Arthur M. Nezu, Ph.D., D.H.L., Angelo Picardi, M.D., Nicole E. Rossi, Ph.D., Denise M. Saint Arnault, Ph.D., Sagar Sharma, Ph.D., Bryony Sheaves, D.Clin.Psy., Kennon M. Sheldon, Ph.D., Daniel Shepherd, Ph.D., Keisuke Takano, Ph.D., Sara Tement, Ph.D., Sherri Turner, Ph.D., Shawn O. Utsey, Ph.D., Ron Valle, Ph.D., Caleb Wang, B.S., Pengju Wang, Katsuyuki Yamasaki, Ph.D.
A.C.T. acknowledges funding from the Sullivan Family Foundation. This paper does not reflect an official statement or opinion from the County of San Mateo.
Author information
Authors and affiliations.
Center for Global Health, Massachusetts General Hospital, Boston, MA, USA
Emily N. Satinsky & Alexander C. Tsai
San Mateo County Behavioral Health and Recovery Services, San Mateo, CA, USA
Tomoki Kimura
Department of Epidemiology and Population Health, Stanford University, Palo Alto, CA, USA
Mathew V. Kiang
Center for Population Health Sciences, Stanford University School of Medicine, Palo Alto, CA, USA
Harvard Society of Fellows, Harvard University, Cambridge, MA, USA
Rediet Abebe
Department of Electrical Engineering and Computer Science, University of California Berkeley, Berkeley, CA, USA
Department of Economics, Hankamer School of Business, Baylor University, Waco, TX, USA
Scott Cunningham
Department of Sociology, Washington University in St. Louis, St. Louis, MO, USA
Department of Microbiology, Immunology, and Molecular Genetics, Institute for Quantitative and Computational Biosciences, University of California Los Angeles, Los Angeles, CA, USA
Xiaofei Lin
Departments of Newborn Medicine and Psychiatry, Brigham and Women’s Hospital, Boston, MA, USA
Cindy H. Liu
Harvard Medical School, Boston, MA, USA
Cindy H. Liu & Alexander C. Tsai
Centre for Global Health, Edinburgh Medical School, Usher Institute, University of Edinburgh, Edinburgh, Scotland, UK
Department of Psychiatry, University of Michigan, Ann Arbor, MI, USA
Department of Global Health, Institute for Life Course Health Research, Stellenbosch University, Cape Town, South Africa
Mark Tomlinson
School of Nursing and Midwifery, Queens University, Belfast, UK
Fielding School of Public Health, Los Angeles Area Health Services Research Training Program, University of California Los Angeles, Los Angeles, CA, USA
Miranda Yaver
Mongan Institute, Massachusetts General Hospital, Boston, MA, USA
Alexander C. Tsai
You can also search for this author in PubMed Google Scholar
Contributions
A.C.T. conceptualized the study and provided supervision. T.K. conducted the search. E.N.S. contacted authors for additional information not reported in published articles. E.N.S. and T.K. extracted data and performed the quality assessment appraisal. E.N.S. and A.C.T. conducted the statistical analysis and drafted the manuscript. T.K., M.V.K., R.A., S.C., H.L., X.L., C.H.L., I.R., S.S., M.T. and M.Y. contributed to the interpretation of the results. All authors provided critical feedback on drafts and approved the final manuscript.
Corresponding authors
Correspondence to Emily N. Satinsky or Alexander C. Tsai .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Satinsky, E.N., Kimura, T., Kiang, M.V. et al. Systematic review and meta-analysis of depression, anxiety, and suicidal ideation among Ph.D. students. Sci Rep 11 , 14370 (2021). https://doi.org/10.1038/s41598-021-93687-7
Download citation
Received : 31 March 2021
Accepted : 24 June 2021
Published : 13 July 2021
DOI : https://doi.org/10.1038/s41598-021-93687-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
How to improve academic well-being: an analysis of the leveraging factors based on the italian case.
- Alice Tontodimamma
- Emiliano del Gobbo
- Antonio Aquino
Quality & Quantity (2024)
Suicidal affective risk among female college students: the impact of life satisfaction
- Dawei Huang
- Xianbin Wang
Current Psychology (2024)
A single-center assessment of mental health and well-being in a biomedical sciences graduate program
- Sarah K. Jachim
- Bradley S. Bowles
- Autumn J. Schulze
Nature Biotechnology (2023)
Mental Health Problems Among Graduate Students in Turkey: a Cross-Sectional Study
- Cafer Kılıç
- Faika Şanal Karahan
International Journal for the Advancement of Counselling (2023)
A study in University of Ruhuna for investigating prevalence, risk factors and remedies for psychiatric illnesses among students
- Patikiri Arachchige Don Shehan Nilm Wijesekara
Scientific Reports (2022)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed, affiliation.
- 1 Thomas Jefferson University Hospital
- PMID: 28613597
- Bookshelf ID: NBK430847
Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest. The American Psychiatric Association’s Diagnostic Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) classifies the depressive disorders into:
Disruptive mood dysregulation disorder
Major depressive disorder
Persistent depressive disorder (dysthymia)
Premenstrual dysphoric disorder
Depressive disorder due to another medical condition
The common features of all the depressive disorders are sadness, emptiness, or irritable mood, accompanied by somatic and cognitive changes that significantly affect the individual’s capacity to function.
Because of false perceptions, nearly 60% of people with depression do not seek medical help. Many feel that the stigma of a mental health disorder is not acceptable in society and may hinder both personal and professional life. There is good evidence indicating that most antidepressants do work but the individual response to treatment may vary.
Copyright © 2024, StatPearls Publishing LLC.
PubMed Disclaimer
Conflict of interest statement
Disclosure: Suma Chand declares no relevant financial relationships with ineligible companies.
Disclosure: Hasan Arif declares no relevant financial relationships with ineligible companies.
- Continuing Education Activity
- Introduction
- Epidemiology
- Pathophysiology
- History and Physical
- Treatment / Management
- Differential Diagnosis
- Enhancing Healthcare Team Outcomes
- Review Questions
Similar articles
- Depression (Nursing). Chand SP, Arif H, Kutlenios RM. Chand SP, et al. 2023 Jul 17. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. 2023 Jul 17. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 33760492 Free Books & Documents.
- Letter to the Editor: CONVERGENCES AND DIVERGENCES IN THE ICD-11 VS. DSM-5 CLASSIFICATION OF MOOD DISORDERS. Cerbo AD. Cerbo AD. Turk Psikiyatri Derg. 2021;32(4):293-295. doi: 10.5080/u26899. Turk Psikiyatri Derg. 2021. PMID: 34964106 English, Turkish.
- Mood Disorder. Sekhon S, Gupta V. Sekhon S, et al. 2023 May 8. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. 2023 May 8. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 32644337 Free Books & Documents.
- [The difference between depression and melancholia: two distinct conditions that were combined into a single category in DSM-III]. Ohmae S. Ohmae S. Seishin Shinkeigaku Zasshi. 2012;114(8):886-905. Seishin Shinkeigaku Zasshi. 2012. PMID: 23012851 Review. Japanese.
- [Psychiatric and psychological aspects of premenstrual syndrome]. Limosin F, Ades J. Limosin F, et al. Encephale. 2001 Nov-Dec;27(6):501-8. Encephale. 2001. PMID: 11865558 Review. French.
- Salik I, Marwaha R. StatPearls [Internet] StatPearls Publishing; Treasure Island (FL): 2022. Sep 19, Electroconvulsive Therapy. - PubMed
- Singh R, Volner K, Marlowe D. StatPearls [Internet] StatPearls Publishing; Treasure Island (FL): 2023. Jun 12, Provider Burnout. - PubMed
- Ormel J, Kessler RC, Schoevers R. Depression: more treatment but no drop in prevalence: how effective is treatment? And can we do better? Curr Opin Psychiatry. 2019 Jul;32(4):348-354. - PubMed
- Pham TH, Gardier AM. Fast-acting antidepressant activity of ketamine: highlights on brain serotonin, glutamate, and GABA neurotransmission in preclinical studies. Pharmacol Ther. 2019 Jul;199:58-90. - PubMed
- Namkung H, Lee BJ, Sawa A. Causal Inference on Pathophysiological Mediators in Psychiatry. Cold Spring Harb Symp Quant Biol. 2018;83:17-23. - PubMed
Publication types
- Search in PubMed
- Search in MeSH
- Add to Search
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- NCBI Bookshelf

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Advertisement
Major Depressive Disorder: Advances in Neuroscience Research and Translational Applications
- Open access
- Published: 13 February 2021
- Volume 37 , pages 863–880, ( 2021 )
Cite this article
You have full access to this open access article

- Zezhi Li 1 , 2 ,
- Meihua Ruan 3 ,
- Jun Chen 1 , 5 &
- Yiru Fang ORCID: orcid.org/0000-0002-8748-9085 1 , 4 , 5
50k Accesses
128 Citations
16 Altmetric
Explore all metrics
A Correction to this article was published on 17 May 2021
This article has been updated
Major depressive disorder (MDD), also referred to as depression, is one of the most common psychiatric disorders with a high economic burden. The etiology of depression is still not clear, but it is generally believed that MDD is a multifactorial disease caused by the interaction of social, psychological, and biological aspects. Therefore, there is no exact pathological theory that can independently explain its pathogenesis, involving genetics, neurobiology, and neuroimaging. At present, there are many treatment measures for patients with depression, including drug therapy, psychotherapy, and neuromodulation technology. In recent years, great progress has been made in the development of new antidepressants, some of which have been applied in the clinic. This article mainly reviews the research progress, pathogenesis, and treatment of MDD.
Similar content being viewed by others

Introduction
Neuroimaging advance in depressive disorder.

The cellular and molecular basis of major depressive disorder: towards a unified model for understanding clinical depression
Avoid common mistakes on your manuscript.
Major depressive disorder (MDD) also referred to as depression, is one of the most severe and common psychiatric disorders across the world. It is characterized by persistent sadness, loss of interest or pleasure, low energy, worse appetite and sleep, and even suicide, disrupting daily activities and psychosocial functions. Depression has an extreme global economic burden and has been listed as the third largest cause of disease burden by the World Health Organization since 2008, and is expected to rank the first by 2030 [ 1 , 2 ]. In 2016, the Global Burden of Diseases, Injuries, and Risk Factors Study demonstrated that depression caused 34.1 million of the total years lived with disability (YLDs), ranking as the fifth largest cause of YLD [ 3 ]. Therefore, the research progress and the clinical application of new discoveries or new technologies are imminent. In this review, we mainly discuss the current situation of research, developments in pathogenesis, and the management of depression.
Current Situation of Research on Depression
Analysis of published papers.
In the past decade, the total number of papers on depression published worldwide has increased year by year as shown in Fig. 1 A. Searching the Web of Science database, we found a total of 43,863 papers published in the field of depression from 2009 to 2019 (search strategy: TI = (depression$) or ts = ("major depressive disorder$")) and py = (2009 – 2019), Articles). The top 10 countries that published papers on the topic of depression are shown in Fig. 1 B. Among them, researchers in the USA published the most papers, followed by China. Compared with the USA, the gap in the total number of papers published in China is gradually narrowing (Fig. 1 C), but the quality gap reflected by the index (the total number of citations and the number of citations per paper) is still large, and is lower than the global average (Fig. 1 D). As shown in Fig. 1 E, the hot research topics in depression are as follows: depression management in primary care, interventions to prevent depression, the pathogenesis of depression, comorbidity of depression and other diseases, the risks of depression, neuroimaging studies of depression, and antidepressant treatment.
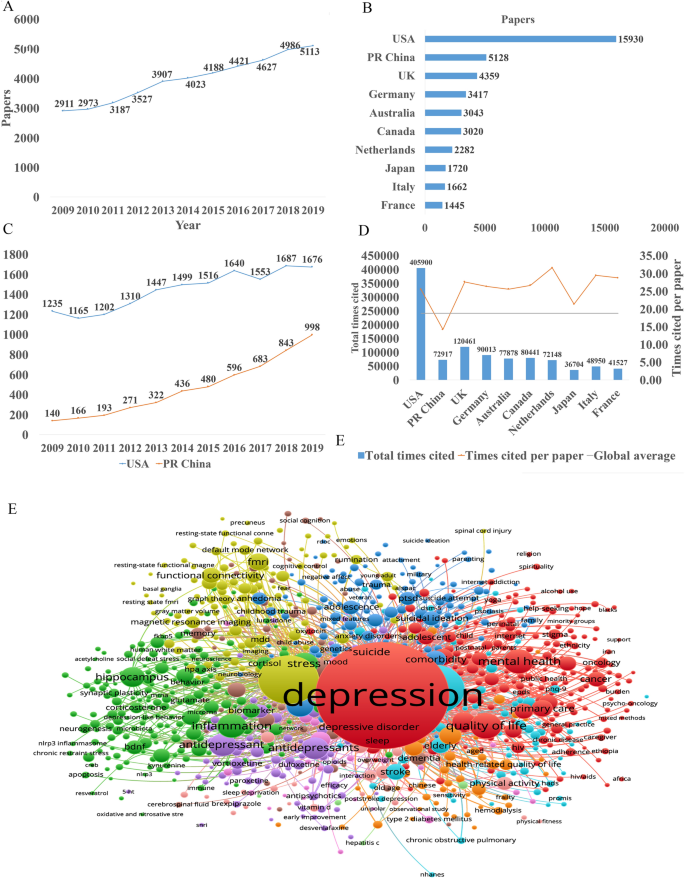
Analysis of published papers around the world from 2009 to 2019 in depressive disorder. A The total number of papers [from a search of the Web of Science database (search strategy: TI = (depression$) or ts = ("major depressive disorder$")) and py = (2009 – 2019), Articles)]. B The top 10 countries publishing on the topic. C Comparison of papers in China and the USA. D Citations for the top 10 countries and comparison with the global average. E Hot topics.
Analysis of Patented Technology Application
There were 16,228 patent applications in the field of depression between 2009 and 2019, according to the Derwent Innovation Patent database. The annual number and trend of these patents are shown in Fig. 2 A. The top 10 countries applying for patents related to depression are shown in Fig. 2 B. The USA ranks first in the number of depression-related patent applications, followed by China. The largest number of patents related to depression is the development of antidepressants, and drugs for neurodegenerative diseases such as dementia comorbid with depression. The top 10 technological areas of patents related to depression are shown in Fig. 2 C, and the trend in these areas have been stable over the past decade (Fig. 2 D).
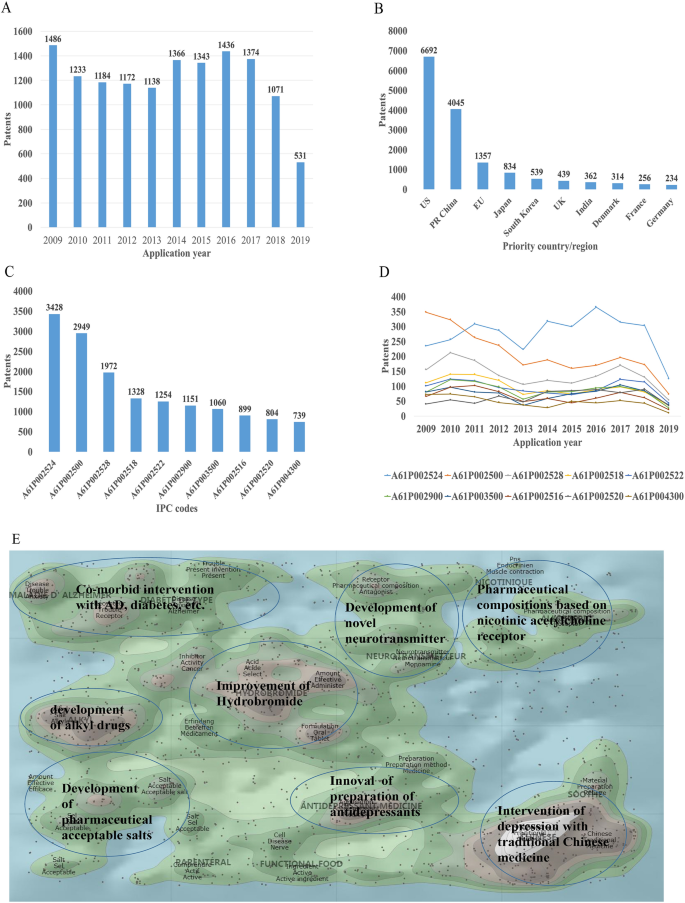
Analysis of patented technology applications from 2009 to 2019 in the field of depressive disorder. A Annual numbers and trends of patents (the Derwent Innovation patent database). B The top 10 countries/regions applying for patents. C The top 10 technological areas of patents. D The trend of patent assignees. E Global hot topic areas of patents.
Analysis of technical hotspots based on keyword clustering was conducted from the Derwent Innovation database using the "ThemeScape" tool. This demonstrated that the hot topic areas are as follows (Fig. 2 E): (1) improvement for formulation and the efficiency of hydrobromide, as well as optimization of the dosage; intervention for depression comorbid with AD, diabetes, and others; (3) development of alkyl drugs; (4) development of pharmaceutical acceptable salts as antidepressants; (5) innovation of the preparation of antidepressants; (6) development of novel antidepressants based on neurotransmitters; (7) development of compositions based on nicotinic acetylcholine receptors; and (8) intervention for depression with traditional Chinese medicine.
Analysis of Clinical Trial
There are 6,516 clinical trials in the field of depression in the ClinicalTrials.gov database, and among them, 1,737 valid trials include the ongoing recruitment of subjects, upcoming recruitment of subjects, and ongoing clinical trials. These clinical trials are mainly distributed in the USA (802 trials), Canada (155), China (114), France (93), Germany (66), UK (62), Spain (58), Denmark (41), Sweden (39), and Switzerland (23). The indications for clinical trials include various types of depression, such as minor depression, depression, severe depression, perinatal depression, postpartum depression, and depression comorbid with other psychiatric disorders or physical diseases, such as schizophrenia, epilepsy, stroke, cancer, diabetes, cardiovascular disease, and Parkinson's disease.
Based on the database of the Chinese Clinical Trial Registry website, a total of 143 clinical trials for depression have been carried out in China. According to the type of research, they are mainly interventional and observational studies, as well as a small number of related factor studies, epidemiological studies, and diagnostic trials. The research content involves postpartum, perinatal, senile, and other age groups with clinical diagnosis (imaging diagnosis) and intervention studies (drugs, acupuncture, electrical stimulation, transcranial magnetic stimulation). It also includes intervention studies on depression comorbid with coronary heart disease, diabetes, and heart failure.
New Medicine Development
According to the Cortellis database, 828 antidepressants were under development by the end of 2019, but only 292 of these are effective and active (Fig. 3 A). Large number of them have been discontinued or made no progress, indicating that the development of new drugs in the field of depression is extremely urgent.
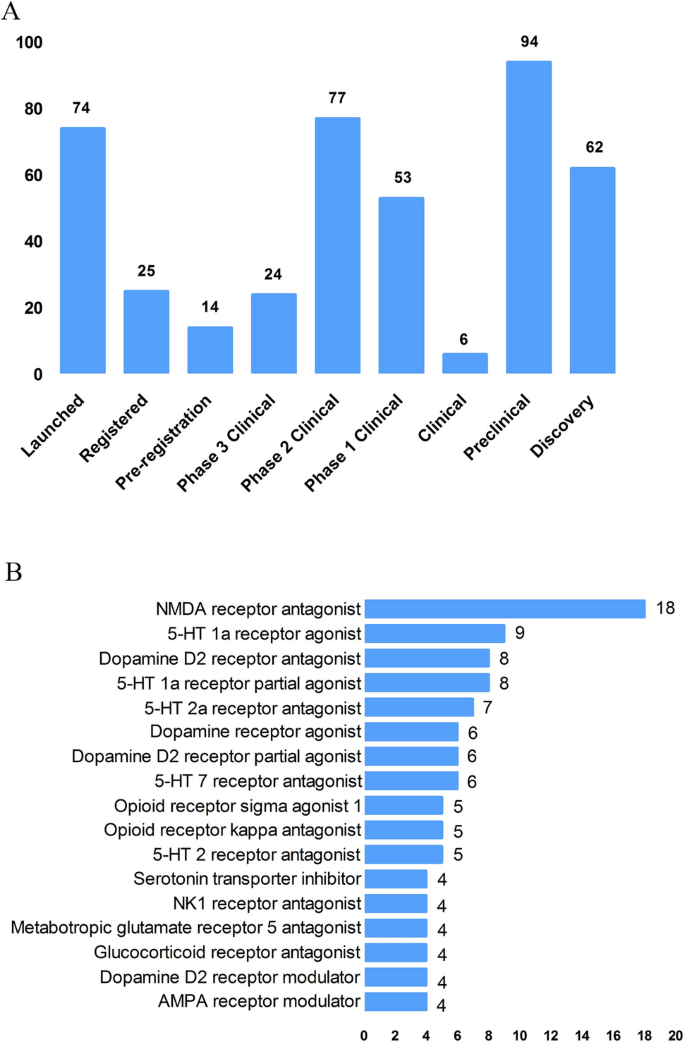
New medicine development from 2009 to 2019 in depressive disorder. A Development status of new candidate drugs. B Top target-based actions.
From the perspective of target-based actions, the most common new drugs are NMDA receptor antagonists, followed by 5-HT targets, as well as dopamine receptor agonists, opioid receptor antagonists and agonists, AMPA receptor modulators, glucocorticoid receptor antagonists, NK1 receptor antagonists, and serotonin transporter inhibitors (Fig. 3 B).
Epidemiology of Depression
The prevalence of depression varies greatly across cultures and countries. Previous surveys have demonstrated that the 12-month prevalence of depression was 0.3% in the Czech Republic, 10% in the USA, 4.5% in Mexico, and 5.2% in West Germany, and the lifetime prevalence of depression was 1.0% in the Czech Republic, 16.9% in the USA, 8.3% in Canada, and 9.0% in Chile [ 4 , 5 ]. A recent meta-analysis including 30 Countries showed that lifetime and 12-month prevalence depression were 10.8% and 7.2%, respectively [ 6 ]. In China, the lifetime prevalence of depression ranged from 1.6% to 5.5% [ 7 , 8 , 9 ]. An epidemiological study demonstrated that depression was the most common mood disorder with a life prevalence of 3.4% and a 12-month prevalence of 2.1% in China [ 10 ].
Some studies have also reported the prevalence in specific populations. The National Comorbidity Survey-Adolescent Supplement (NCS-A) survey in the USA showed that the lifetime and 12-month prevalence of depression in adolescents aged 13 to 18 were 11.0% and 7.5%, respectively [ 11 ]. A recent meta-analysis demonstrated that lifetime prevalence and 12-month prevalence were 2.8% and 2.3%, respectively, among the elderly population in China [ 12 ].
Neurobiological Pathogenesis of Depressive Disorder
The early hypothesis of monoamines in the pathophysiology of depression has been accepted by the scientific community. The evidence that monoamine oxidase inhibitors and tricyclic antidepressants promote monoamine neurotransmission supports this theory of depression [ 13 ]. So far, selective serotonin reuptake inhibitors and norepinephrine reuptake inhibitors are still the first-line antidepressants. However, there remain 1/3 to 2/3 of depressed patients who do not respond satisfactorily to initial antidepressant treatment, and even as many as 15%–40% do not respond to several pharmacological medicines [ 14 , 15 ]. Therefore, the underlying pathogenesis of depression is far beyond the simple monoamine mechanism.
Other hypotheses of depression have gradually received increasing attention because of biomarkers for depression and the effects pharmacological treatments, such as the stress-responsive hypothalamic pituitary adrenal (HPA) axis, neuroendocrine systems, the neurotrophic family of growth factors, and neuroinflammation.
Stress-Responsive HPA Axis
Stress is causative or a contributing factor to depression. Particularly, long-term or chronic stress can lead to dysfunction of the HPA axis and promote the secretion of hormones, including cortisol, adrenocorticotropic hormone, corticotropin-releasing hormone, arginine vasopressin, and vasopressin. About 40%–60% of patients with depression display a disturbed HPA axis, including hypercortisolemia, decreased rhythmicity, and elevated cortisol levels [ 16 , 17 ]. Mounting evidence has shown that stress-induced abnormality of the HPA axis is associated with depression and cognitive impairment, which is due to the increased secretion of cortisol and the insufficient inhibition of glucocorticoid receptor regulatory feedback [ 18 , 19 ]. In addition, it has been reported that the increase in cortisol levels is related to the severity of depression, especially in melancholic depression [ 20 , 21 ]. Further, patients with depression whose HPA axis was not normalized after treatment had a worse clinical response and prognosis [ 22 , 23 ]. Despite the above promising insights, unfortunately previous studies have shown that treatments regulating the HPA axis, such as glucocorticoid receptor antagonists, do not attenuate the symptoms of depressed patients [ 24 , 25 ].
Glutamate Signaling Pathway
Glutamate is the main excitatory neurotransmitter released by synapses in the brain; it is involved in synaptic plasticity, cognitive processes, and reward and emotional processes. Stress can induce presynaptic glutamate secretion by neurons and glutamate strongly binds to ionotropic glutamate receptors (iGluRs) including N-methyl-D-aspartate receptors (NMDARs) and α-amino-3-hydroxy-5-methyl-4-isoxazole-propionic acid receptors (AMPARs) [ 26 ] on the postsynaptic membrane to activate downstream signal pathways [ 27 ]. Accumulating evidence has suggested that the glutamate system is associated with the incidence of depression. Early studies have shown increased levels of glutamate in the peripheral blood, cerebrospinal fluid, and brain of depressed patients [ 28 , 29 ], as well as NMDAR subunit disturbance in the brain [ 30 , 31 ]. Blocking the function of NMDARs has an antidepressant effect and protects hippocampal neurons from morphological abnormalities induced by stress, while antidepressants reduce glutamate secretion and NMDARs [ 32 ]. Most importantly, NMDAR antagonists such as ketamine have been reported to have profound and rapid antidepressant effects on both animal models and the core symptoms of depressive patients [ 33 ]. On the other hand, ketamine can also increase the AMPAR pathway in hippocampal neurons by up-regulating the AMPA glutamate receptor 1 subunit [ 34 ]. Further, the AMPAR pathway may be involved in the mechanism of antidepressant effects. For example, preclinical studies have indicated that AMPAR antagonists might attenuate lithium-induced depressive behavior by increasing the levels of glutamate receptors 1 and 2 in the mouse hippocampus [ 35 ].
Gamma-Aminobutyric Acid (GABA)
Contrary to glutamate, GABA is the main inhibitory neurotransmitter. Although GABA neurons account for only a small proportion compared to glutamate, inhibitory neurotransmission is essential for brain function by balancing excitatory transmission [ 36 ]. Number of studies have shown that patients with depression have neurotransmission or functional defects of GABA [ 37 , 38 ]. Schür et al ., conducted a meta-analysis of magnetic resonance spectroscopy studies, which showed that the brain GABA level in depressive patients was lower than that in healthy controls, but no difference was found in depressive patients in remission [ 39 ]. Several postmortem studies have shown decreased levels of the GABA synthase glutamic acid decarboxylase in the prefrontal cortex of patients with depression [ 40 , 41 ]. It has been suggested that a functional imbalance of the GABA and glutamate systems contributes to the pathophysiology of depression, and activation of the GABA system might induce antidepressant activity, by which GABA A receptor mediators α2/α3 are considered potential antidepressant candidates [ 42 , 43 ]. Genetic mouse models, such as the GABA A receptor mutant mouse and conditional the Gad1-knockout mouse (GABA in hippocampus and cerebral cortex decreased by 50%) and optogenetic methods have verified that depression-like behavior is induced by changing the level of GABA [ 44 , 45 ].
Neurotrophin Family
The neurotrophin family plays a key role in neuroplasticity and neurogenesis. The neurotrophic hypothesis of depression postulates that a deficit of neurotrophic support leads to neuronal atrophy, the reduction of neurogenesis, and the destruction of glia support, while antidepressants attenuate or reverse these pathophysiological processes [ 46 ]. Among them, the most widely accepted hypothesis involves brain-derived neurotrophic factor (BDNF). This was initially triggered by evidence that stress reduces the BDNF levels in the animal brain, while antidepressants rescue or attenuate this reduction [ 47 , 48 ], and agents involved in the BDNF system have been reported to exert antidepressant-like effects [ 49 , 50 ]. In addition, mounting studies have reported that the BDNF level is decreased in the peripheral blood and at post-mortem in depressive patients, and some have reported that antidepressant treatment normalizes it [ 51 , 52 ]. Furthermore, some evidence also showed that the interaction of BDNF and its receptor gene is associated with treatment-resistant depression [ 15 ].
Recent studies reported that depressed patients have a lower level of the pro-domain of BDNF (BDNF pro-peptide) than controls. This is located presynaptically and promotes long-term depression in the hippocampus, suggesting that it is a promising synaptic regulator [ 53 ].
Neuroinflammation
The immune-inflammation hypothesis has attracted much attention, suggesting that the interactions between inflammatory pathways and neural circuits and neurotransmitters are involved in the pathogenesis and pathophysiological processes of depression. Early evidence found that patients with autoimmune or infectious diseases are more likely to develop depression than the general population [ 54 ]. In addition, individuals without depression may display depressive symptoms after treatment with cytokines or cytokine inducers, while antidepressants relieve these symptoms [ 55 , 56 ]. There is a complex interaction between the peripheral and central immune systems. Previous evidence suggested that peripheral inflammation/infection may spread to the central nervous system in some way and cause a neuroimmune response [ 55 , 57 ]: (1) Some cytokines produced in the peripheral immune response, such as IL-6 and IL-1 β, can leak into the brain through the blood-brain barrier (BBB). (2) Cytokines entering the central nervous system act directly on astrocytes, small stromal cells, and neurons. (3) Some peripheral immune cells can cross the BBB through specific transporters, such as monocytes. (4) Cytokines and chemokines in the circulation activate the central nervous system by regulating the surface receptors of astrocytes and endothelial cells at the BBB. (5) As an intermediary pathway, the immune inflammatory response transmits peripheral danger signals to the center, amplifies the signals, and shows the external phenotype of depressive behavior associated with stress/trauma/infection. (6) Cytokines and chemokines may act directly on neurons, change their plasticity and promote depression-like behavior.
Patients with depression show the core feature of the immune-inflammatory response, that is, increased concentrations of pro-inflammatory cytokines and their receptors, chemokines, and soluble adhesion molecules in peripheral blood and cerebrospinal fluid [ 58 , 59 , 60 ]. Peripheral immune-inflammatory response markers not only change the immune activation state in the brain that affects explicit behavior, but also can be used as an evaluation index or biological index of antidepressant therapy [ 61 , 62 ]. Li et al . showed that the level of TNF-α in patients with depression prior to treatment was higher than that in healthy controls. After treatment with venlafaxine, the level of TNF-α in patients with depression decreased significantly, and the level of TNF-α in the effective group decreased more [ 63 ]. A recent meta-analysis of 1,517 patients found that antidepressants significantly reduced peripheral IL-6, TNF-α, IL-10, and CCL-2, suggesting that antidepressants reduce markers of peripheral inflammatory factors [ 64 ]. Recently, Syed et al . also confirmed that untreated patients with depression had higher levels of inflammatory markers and increased levels of anti-inflammatory cytokines after antidepressant treatment, while increased levels of pro-inflammatory cytokines were found in non-responders [ 62 ]. Clinical studies have also found that anti-inflammatory cytokines, such as monoclonal antibodies and other cytokine inhibitors, may play an antidepressant role by blocking cytokines. The imbalance of pro-inflammatory and anti-inflammatory cytokines may be involved in the pathophysiological process of depression.
In addition, a recent study showed that microglia contribute to neuronal plasticity and neuroimmune interaction that are involved in the pathophysiology of depression [ 65 ]. When activated microglia promote inflammation, especially the excessive production of pro-inflammatory factors and cytotoxins in the central nervous system, depression-like behavior can gradually develop [ 65 , 66 ]. However, microglia change polarization as two types under different inflammatory states, regulating the balance of pro- and anti-inflammatory factors. These two types are M1 and M2 microglia; the former produces large number of pro-inflammatory cytokines after activation, and the latter produces anti-inflammatory cytokines. An imbalance of M1/M2 polarization of microglia may contribute to the pathophysiology of depression [ 67 ].
Microbiome-Gut-Brain Axis
The microbiota-gut-brain axis has recently gained more attention because of its ability to regulate brain activity. Many studies have shown that the microbiota-gut-brain axis plays an important role in regulating mood, behavior, and neuronal transmission in the brain [ 68 , 69 ]. It is well established that comorbidity of depression and gastrointestinal diseases is common [ 70 , 71 ]. Some antidepressants can attenuate the symptoms of patients with irritable bowel syndrome and eating disorders [ 72 ]. It has been reported that gut microbiome alterations are associated with depressive-like behaviors [ 73 , 74 ], and brain function [ 75 ]. Early animal studies have shown that stress can lead to long-term changes in the diversity and composition of intestinal microflora, and is accompanied by depressive behavior [ 76 , 77 ]. Interestingly, some evidence indicates that rodents exhibit depressive behavior after fecal transplants from patients with depression [ 74 ]. On the other hand, some probiotics attenuated depressive-like behavior in animal studies, [ 78 ] and had antidepressant effects on patients with depression in several double-blind, placebo-controlled clinical trials [ 79 , 80 ].
The potential mechanism may be that gut microbiota can interact with the brain through a variety of pathways or systems, including the HPA axis, and the neuroendocrine, autonomic, and neuroimmune systems [ 81 ]. For example, recent evidence demonstrated that gut microbiota can affect the levels of neurotransmitters in the gut and brain, including serotonin, dopamine, noradrenalin, glutamate, and GABA [ 82 ]. In addition, recent studies showed that changes in gut microbiota can also impair the gut barrier and promote higher levels of peripheral inflammatory cytokines [ 83 , 84 ]. Although recent research in this area has made significant progress, more clinical trials are needed to determine whether probiotics have any effect on the treatment of depression and what the potential underlying mechanisms are.
Other Systems and Pathways
There is no doubt that several other systems or pathways are also involved in the pathophysiology of depression, such as oxidant-antioxidant imbalance [ 85 ], mitochondrial dysfunction [ 86 , 87 ], and circadian rhythm-related genes [ 88 ], especially their critical interactions ( e.g. interaction between the HPA and mitochondrial metabolism [ 89 , 90 ], and the reciprocal interaction between oxidative stress and inflammation [ 2 , 85 ]). The pathogenesis of depression is complex and all the hypotheses should be integrated to consider the many interactions between various systems and pathways.
Advances in Various Kinds of Research on Depressive Disorder
Genetic, molecular, and neuroimaging studies continue to increase our understanding of the neurobiological basis of depression. However, it is still not clear to what extent the results of neurobiological studies can help improve the clinical and functional prognosis of patients. Therefore, over the past 10 years, the neurobiological study of depression has become an important measure to understand the pathophysiological mechanism and guide the treatment of depression.
Genetic Studies
Previous twin and adoption studies have indicated that depression has relatively low rate of heritability at 37% [ 91 ]. In addition, environmental factors such as stressful events are also involved in the pathogenesis of depression. Furthermore, complex psychiatric disorders, especially depression, are considered to be polygenic effects that interact with environmental factors [ 13 ]. Therefore, reliable identification of single causative genes for depression has proved to be challenging. The first genome-wide association studies (GWAS) for depression was published in 2009, and included 1,738 patients and 1,802 controls [ 92 , 93 ]. Although many subsequent GWASs have determined susceptible genes in the past decade, the impact of individual genes is so small that few results can be replicated [ 94 , 95 ]. So far, it is widely accepted that specific single genetic mutations may play minor and marginal roles in complex polygenic depression. Another major recognition in GWASs over the past decade is that prevalent candidate genes are usually not associated with depression. Further, the inconsistent results may also be due to the heterogeneity and polygenic nature of genetic and non-genetic risk factors for depression as well as the heterogeneity of depression subtypes [ 95 , 96 ]. Therefore, to date, the quality of research has been improved in two aspects: (1) the sample size has been maximized by combining the data of different evaluation models; and (2) more homogenous subtypes of depression have been selected to reduce phenotypic heterogeneity [ 97 ]. Levinson et al . pointed out that more than 75,000 to 100,000 cases should be considered to detect multiple depression associations [ 95 ]. Subsequently, several recent GWASs with larger sample sizes have been conducted. For example, Okbay et al . identified two loci associated with depression and replicated them in separate depression samples [ 98 ]. Wray et al . also found 44 risk loci associated with depression based on 135,458 cases and 344,901 controls [ 99 ]. A recent GWAS of 807,553 individuals with depression reported that 102 independent variants were associated with depression; these were involved in synaptic structure and neural transmission, and were verified in a further 1,507,153 individuals [ 100 ]. However, even with enough samples, GWASs still face severe challenges. A GWAS only marks the region of the genome and is not directly related to the potential biological function. In addition, a genetic association with the indicative phenotype of depression may only be part of many pathogenic pathways, or due to the indirect influence of intermediate traits in the causal pathway on the final result [ 101 ].
Given the diversity of findings, epigenetic factors are now being investigated. Recent studies indicated that epigenetic mechanisms may be the potential causes of "loss of heritability" in GWASs of depression. Over the past decade, a promising discovery has been that the effects of genetic information can be directly influenced by environment factors, and several specific genes are activated by environmental aspects. This process is described as interactions between genes and the environment, which is identified by the epigenetic mechanism. Environmental stressors cause alterations in gene expression in the brain, which may cause abnormal neuronal plasticity in areas related to the pathogenesis of the disease. Epigenetic events alter the structure of chromatin, thereby regulating gene expression involved in neuronal plasticity, stress behavior, depressive behavior, and antidepressant responses, including DNA methylation, histone acetylation, and the role of non-coding RNA. These new mechanisms of trans-generational transmission of epigenetic markers are considered a supplement to orthodox genetic heredity, providing the possibility for the discovery of new treatments for depression [ 102 , 103 ]. Recent studies imply that life experiences, including stress and enrichment, may affect cellular and molecular signaling pathways in sperm and influence the behavioral and physiological phenotypes of offspring in gender-specific patterns, which may also play an important role in the development of depression [ 103 ].
Brain Imaging and Neuroimaging Studies
Neuroimaging, including magnetic resonance imaging (MRI) and molecular imaging, provides a non-invasive technique for determining the underlying etiology and individualized treatment for depression. MRI can provide important data on brain structure, function, networks, and metabolism in patients with depression; it includes structural MRI (sMRI), functional MRI (fMRI), diffusion tensor imaging, and magnetic resonance spectroscopy.
Previous sMRI studies have found damaged gray matter in depression-associated brain areas, including the frontal lobe, anterior cingulate gyrus, hippocampus, putamen, thalamus, and amygdala. sMRI focuses on the thickness of gray matter and brain morphology [ 104 , 105 ]. A recent meta-analysis of 2,702 elderly patients with depression and 11,165 controls demonstrated that the volumes of the whole brain and hippocampus of patients with depression were lower than those of the control group [ 106 ]. Some evidence also showed that the hippocampal volume in depressive patients was lower than that of controls, and increased after treatment with antidepressants [ 107 ] and electroconvulsive therapy (ECT) [ 108 ], suggesting that the hippocampal volume plays a critical role in the development, treatment response, and clinical prognosis of depression. A recent study also reported that ECT increased the volume of the right hippocampus, amygdala, and putamen in patients with treatment-resistant depression [ 109 ]. In addition, postmortem research supported the MRI study showing that dentate gyrus volume was decreased in drug-naive patients with depression compared to healthy controls, and was potentially reversed by treatment with antidepressants [ 110 ].
Diffusion tensor imaging detects the microstructure of the white matter, which has been reported impaired in patients with depression [ 111 ]. A recent meta-analysis that included first-episode and drug-naïve depressive patients showed that the decrease in fractional anisotropy was negatively associated with illness duration and clinical severity [ 112 ].
fMRI, including resting-state and task-based fMRI, can divide the brain into self-related regions, such as the anterior cingulate cortex, posterior cingulate cortex, medial prefrontal cortex, precuneus, and dorsomedial thalamus. Many previous studies have shown the disturbance of several brain areas and intrinsic neural networks in patients with depression which could be rescued by antidepressants [ 113 , 114 , 115 , 116 ]. Further, some evidence also showed an association between brain network dysfunction and the clinical correlates of patients with depression, including clinical symptoms [ 117 ] and the response to antidepressants [ 118 , 119 ], ECT [ 120 , 121 ], and repetitive transcranial magnetic stimulation [ 122 ].
It is worth noting that brain imaging provides new insights into the large-scale brain circuits that underlie the pathophysiology of depressive disorder. In such studies, large-scale circuits are often referred to as “networks”. There is evidence that a variety of circuits are involved in the mechanisms of depressive disorder, including disruption of the default mode, salience, affective, reward, attention, and cognitive control circuits [ 123 ]. Over the past decade, the study of intra-circuit and inter-circuit connectivity dysfunctions in depression has escalated, in part due to advances in precision imaging and analysis techniques [ 124 ]. Circuit dysfunction is a potential biomarker to guide psychopharmacological treatment. For example, Williams et al . found that hyper-activation of the amygdala is associated with a negative phenotype that can predict the response to antidepressants [ 125 ]. Hou et al . showed that the baseline characteristics of the reward circuit predict early antidepressant responses [ 126 ].
Molecular imaging studies, including single photon emission computed tomography and positron emission tomography, focus on metabolic aspects such as amino-acids, neurotransmitters, glucose, and lipids at the cellular level in patients with depression. A recent meta-analysis examined glucose metabolism and found that glucose uptake dysfunction in different brain regions predicts the treatment response [ 127 ].
The most important and promising studies were conducted by the ENIGMA (Enhancing NeuroImaging Genetics through Meta Analysis) Consortium, which investigated the human brain across 43 countries. The ENIGMA-MDD Working Group was launched in 2012 to detect the structural and functional changes associated with MDD reliably and replicate them in various samples around the world [ 128 ]. So far, the ENIGMA-MDD Working Group has collected data from 4,372 MDD patients and 9,788 healthy controls across 14 countries, including 45 cohorts [ 128 ]. Their findings to date are shown in Table 1 [ 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 ].
Objective Index for Diagnosis of MDD
To date, the clinical diagnosis of depression is subjectively based on interviews according to diagnostic criteria ( e.g. International Classification of Diseases and Diagnostic and Statistical Manual diagnostic systems) and the severity of clinical symptoms are assessed by questionnaires, although patients may experience considerable differences in symptoms and subtypes [ 138 ]. Meanwhile, biomarkers including genetics, epigenetics, peripheral gene and protein expression, and neuroimaging markers may provide a promising supplement for the development of the objective diagnosis of MDD, [ 139 , 140 , 141 ]. However, the development of reliable diagnosis for MDD using biomarkers is still difficult and elusive, and all methods based on a single marker are insufficiently specific and sensitive for clinical use [ 142 ]. Papakostas et al . showed that a multi-assay, serum-based test including nine peripheral biomarkers (soluble tumor necrosis factor alpha receptor type II, resistin, prolactin, myeloperoxidase, epidermal growth factor, BDNF, alpha1 antitrypsin, apolipoprotein CIII, brain-derived neurotrophic factor, and cortisol) yielded a specificity of 81.3% and a sensitivity of 91.7% [ 142 ]. However, the sample size was relatively small and no other studies have yet validated their results. Therefore, further studies are needed to identify biomarker models that integrate all biological variables and clinical features to improve the specificity and sensitivity of diagnosis for MDD.
Management of Depression
The treatment strategies for depression consist of pharmacological treatment and non-pharmacological treatments including psychotherapy, ECT [ 98 ], and transcranial magnetic stimulation. As psychotherapy has been shown to have effects on depression including attenuating depressive symptoms and improving the quality of life [ 143 , 144 ]; several practice guidelines are increasingly recommending psychotherapy as a monotherapy or in combination with antidepressants [ 145 , 146 ].
Current Antidepressant Treatment
Antidepressants approved by the US Food and Drug Administration (FDA) are shown in Table 2 . Due to the relatively limited understanding of the etiology and pathophysiology of depression, almost all the previous antidepressants were discovered by accident a few decades ago. Although most antidepressants are usually safe and effective, there are still some limitations, including delayed efficacy (usually 2 weeks) and side-effects that affect the treatment compliance [ 147 ]. In addition, <50% of all patients with depression show complete remission through optimized treatment, including trials of multiple drugs with and without simultaneous psychotherapy. In the past few decades, most antidepressant discoveries focused on finding faster, safer, and more selective serotonin or norepinephrine receptor targets. In addition, there is an urgent need to develop new approaches to obtain more effective, safer, and faster antidepressants. In 2019, the FDA approved two new antidepressants: Esketamine for refractory depression and Bresanolone for postpartum depression. Esmolamine, a derivative of the anesthetic drug ketamine, was approved by the FDA for the treatment of refractory depression, based on a large number of preliminary clinical studies [ 148 ]. For example, several randomized controlled trials and meta-analysis studies showed the efficacy and safety of Esketamine in depression or treatment-resistant depression [ 26 , 149 , 150 ]. Although both are groundbreaking new interventions for these debilitating diseases and both are approved for use only under medical supervision, there are still concerns about potential misuse and problems in the evaluation of mental disorders [ 151 ].
To date, although several potential drugs have not yet been approved by the FDA, they are key milestones in the development of antidepressants that may be modified and used clinically in the future, such as compounds containing dextromethorphan (a non-selective NMDAR antago–nist), sarcosine (N-methylglycine, a glycine reuptake inhibitor), AMPAR modulators, and mGluR modulators [ 152 ].

Neuromodulation Therapy
Neuromodulation therapy acts through magnetic pulse, micro-current, or neural feedback technology within the treatment dose, acting on the central or peripheral nervous system to regulate the excitatory/inhibitory activity to reduce or attenuate the symptoms of the disease.
ECT is one of most effective treatments for depression, with the implementation of safer equipment and advancement of techniques such as modified ECT [ 153 ]. Mounting evidence from randomized controlled trial (RCT) and meta-analysis studies has shown that rTMS can treat depressive patients with safety [ 154 ]. Other promising treatments for depression have emerged, such as transcranial direct current stimulation (tDCS) [ 155 ], transcranial alternating current stimulation (tACS)[ 156 ], vagal nerve stimulation [ 157 ], deep brain stimulation [ 158 ] , and light therapy [ 159 ], but some of them are still experimental to some extent and have not been widely used. For example, compared to tDCS, tACS displays less sensory experience and adverse reactions with weak electrical current in a sine-wave pattern, but the evidence for the efficacy of tACS in the treatment of depression is still limited [ 160 ]. Alexander et al . recently demonstrated that there was no difference in efficacy among different treatments (sham, 10-Hz and 40-Hz tACS). However, only the 10-Hz tACS group had more responders than the sham and 40-Hz tACS groups at week 2 [ 156 ]. Further RCT studies are needed to verify the efficacy of tACS. In addition, the mechanism of the effect of neuromodulation therapy on depression needs to be further investigated.
Precision Medicine for Depression
Optimizing the treatment strategy is an effective way to improve the therapeutic effect on depression. However, each individual with depression may react very differently to different treatments. Therefore, this raises the question of personalized treatment, that is, which patients are suitable for which treatment. Over the past decade, psychiatrists and psychologists have focused on individual biomarkers and clinical characteristics to predict the efficiency of antidepressants and psychotherapies, including genetics, peripheral protein expression, electrophysiology, neuroimaging, neurocognitive performance, developmental trauma, and personality [ 161 ]. For example, Bradley et al . recently conducted a 12-week RCT, which demonstrated that the response rate and remission rates of the pharmacogenetic guidance group were significantly higher than those of the non-pharmacogenetic guidance group [ 162 ].
Subsequently, Greden et al . conducted an 8-week RCT of Genomics Used to Improve Depression Decisions (GUIDED) on 1,167 MDD patients and demonstrated that although there was no difference in symptom improvement between the pharmacogenomics-guided and non- pharmacogenomics-guided groups, the response rate and remission rate of the pharmacogenomics-guided group increased significantly [ 163 ].
A recent meta-analysis has shown that the baseline default mode network connectivity in patients with depression can predict the clinical responses to treatments including cognitive behavioral therapy, pharmacotherapy, ECT, rTMS, and transcutaneous vagus nerve stimulation [ 164 ]. However, so far, the biomarkers that predict treatment response at the individual level have not been well applied in the clinic, and there is still a lot of work to be conducted in the future.
Future Perspectives
Although considerable progress has been made in the study of depression during a past decade, the heterogeneity of the disease, the effectiveness of treatment, and the gap in translational medicine are critical challenges. The main dilemma is that our understanding of the etiology and pathophysiology of depression is inadequate, so our understanding of depression is not deep enough to develop more effective treatment. Animal models still cannot fully simulate this heterogeneous and complex mental disorder. Therefore, how to effectively match the indicators measured in animals with those measured in genetic research or the development of new antidepressants is another important challenge.
Change history
17 may 2021.
A Correction to this paper has been published: https://doi.org/10.1007/s12264-021-00694-9
Dadi AF, Miller ER, Bisetegn TA, Mwanri L. Global burden of antenatal depression and its association with adverse birth outcomes: an umbrella review. BMC Public Health 2020, 20: 173
Article PubMed PubMed Central Google Scholar
Zhu S, Zhao L, Fan Y, Lv Q, Wu K, Lang X. Interaction between TNF-alpha and oxidative stress status in first-episode drug-naive schizophrenia. Psychoneuroendocrinology 2020, 114: 104595
Article CAS PubMed Google Scholar
Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390: 1211–1259
Article Google Scholar
Andrade L, Caraveo-Anduaga JJ, Berglund P, Bijl RV, De Graaf R, Vollebergh W, et al. The epidemiology of major depressive episodes: results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys. Int J Methods Psychiatr Res 2003, 12: 3–21
Article PubMed Google Scholar
Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health 2013, 34: 119–138
Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep 2018, 8: 2861
Liu J, Yan F, Ma X, Guo HL, Tang YL, Rakofsky JJ, et al. Prevalence of major depressive disorder and socio-demographic correlates: Results of a representative household epidemiological survey in Beijing, China. J Affect Disord 2015, 179: 74–81
Zhang YS, Rao WW, Cui LJ, Li JF, Li L, Ng CH, et al. Prevalence of major depressive disorder and its socio-demographic correlates in the general adult population in Hebei province, China. J Affect Disord 2019, 252: 92–98
Ma X, Xiang YT, Cai ZJ, Li SR, Xiang YQ, Guo HL, et al. Prevalence and socio-demographic correlates of major depressive episode in rural and urban areas of Beijing, China. J Affect Disord 2009, 115: 323–330
Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry 2019, 6: 211–224
Avenevoli S, Swendsen J, He JP, Burstein M, Merikangas KR. Major depression in the national comorbidity survey-adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry 2015, 54(37–44): e32
Google Scholar
Wang F, Zhang QE, Zhang L, Ng CH, Ungvari GS, Yuan Z, et al. Prevalence of major depressive disorder in older adults in China: A systematic review and meta-analysis. J Affect Disord 2018, 241: 297–304
Krishnan V, Nestler EJ. The molecular neurobiology of depression. Nature 2008, 455: 894–902
Article CAS PubMed PubMed Central Google Scholar
Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry 2006, 163: 1905–1917
Li Z, Zhang Y, Wang Z, Chen J, Fan J, Guan Y, et al. The role of BDNF, NTRK2 gene and their interaction in development of treatment-resistant depression: data from multicenter, prospective, longitudinal clinic practice. J Psychiatr Res 2013, 47: 8–14
Murphy BE. Steroids and depression. J Steroid Biochem Mol Biol 1991, 38: 537–559
Pariante CM, Lightman SL. The HPA axis in major depression: classical theories and new developments. Trends Neurosci 2008, 31: 464–468
Keller J, Gomez R, Williams G, Lembke A, Lazzeroni L, Murphy GM Jr, et al. HPA axis in major depression: cortisol, clinical symptomatology and genetic variation predict cognition. Mol Psychiatry 2017, 22: 527–536
Gomez RG, Fleming SH, Keller J, Flores B, Kenna H, DeBattista C, et al. The neuropsychological profile of psychotic major depression and its relation to cortisol. Biol Psychiatry 2006, 60: 472–478
Lamers F, Vogelzangs N, Merikangas KR, de Jonge P, Beekman AT, Penninx BW. Evidence for a differential role of HPA-axis function, inflammation and metabolic syndrome in melancholic versus atypical depression. Mol Psychiatry 2013, 18: 692–699
Nandam LS, Brazel M, Zhou M, Jhaveri DJ. Cortisol and major depressive disorder-translating findings from humans to animal models and back. Front Psychiatry 2019, 10: 974
Owashi T, Otsubo T, Oshima A, Nakagome K, Higuchi T, Kamijima K. Longitudinal neuroendocrine changes assessed by dexamethasone/CRH and growth hormone releasing hormone tests in psychotic depression. Psychoneuroendocrinology 2008, 33: 152–161
Mickey BJ, Ginsburg Y, Sitzmann AF, Grayhack C, Sen S, Kirschbaum C, et al. Cortisol trajectory, melancholia, and response to electroconvulsive therapy. J Psychiatr Res 2018, 103: 46–53
Stetler C, Miller GE. Depression and hypothalamic-pituitary-adrenal activation: a quantitative summary of four decades of research. Psychosom Med 2011, 73: 114–126
Aubry JM. CRF system and mood disorders. J Chem Neuroanat 2013, 54: 20–24
Correia-Melo FS, Leal GC, Vieira F, Jesus-Nunes AP, Mello RP, Magnavita G, et al. Efficacy and safety of adjunctive therapy using esketamine or racemic ketamine for adult treatment-resistant depression: A randomized, double-blind, non-inferiority study. J Affect Disord 2020, 264: 527–534
Duman RS, Voleti B. Signaling pathways underlying the pathophysiology and treatment of depression: novel mechanisms for rapid-acting agents. Trends Neurosci 2012, 35: 47–56
Sanacora G, Zarate CA, Krystal JH, Manji HK. Targeting the glutamatergic system to develop novel, improved therapeutics for mood disorders. Nat Rev Drug Discov 2008, 7: 426–437
Hashimoto K. The role of glutamate on the action of antidepressants. Prog Neuropsychopharmacol Biol Psychiatry 2011, 35: 1558–1568
Gray AL, Hyde TM, Deep-Soboslay A, Kleinman JE, Sodhi MS. Sex differences in glutamate receptor gene expression in major depression and suicide. Mol Psychiatry 2015, 20: 1057–1068
Chandley MJ, Szebeni A, Szebeni K, Crawford JD, Stockmeier CA, Turecki G, et al. Elevated gene expression of glutamate receptors in noradrenergic neurons from the locus coeruleus in major depression. Int J Neuropsychopharmacol 2014, 17: 1569–1578
Musazzi L, Treccani G, Mallei A, Popoli M. The action of antidepressants on the glutamate system: regulation of glutamate release and glutamate receptors. Biol Psychiatry 2013, 73: 1180–1188
Kadriu B, Musazzi L, Henter ID, Graves M, Popoli M, Zarate CA Jr. Glutamatergic Neurotransmission: Pathway to Developing Novel Rapid-Acting Antidepressant Treatments. Int J Neuropsychopharmacol 2019, 22: 119–135
Beurel E, Grieco SF, Amadei C, Downey K, Jope RS. Ketamine-induced inhibition of glycogen synthase kinase-3 contributes to the augmentation of alpha-amino-3-hydroxy-5-methylisoxazole-4-propionic acid (AMPA) receptor signaling. Bipolar Disord 2016, 18: 473–480
Gould TD, O’Donnell KC, Dow ER, Du J, Chen G, Manji HK. Involvement of AMPA receptors in the antidepressant-like effects of lithium in the mouse tail suspension test and forced swim test. Neuropharmacology 2008, 54: 577–587
Duman RS, Sanacora G, Krystal JH. Altered Connectivity in Depression: GABA and Glutamate Neurotransmitter Deficits and Reversal by Novel Treatments. Neuron 2019, 102: 75–90
Ghosal S, Hare B, Duman RS. Prefrontal Cortex GABAergic Deficits and Circuit Dysfunction in the Pathophysiology and Treatment of Chronic Stress and Depression. Curr Opin Behav Sci 2017, 14: 1–8
Fee C, Banasr M, Sibille E. Somatostatin-positive gamma-aminobutyric acid interneuron deficits in depression: Cortical microcircuit and therapeutic perspectives. Biol Psychiatry 2017, 82: 549–559
Schur RR, Draisma LW, Wijnen JP, Boks MP, Koevoets MG, Joels M, et al. Brain GABA levels across psychiatric disorders: A systematic literature review and meta-analysis of (1) H-MRS studies. Hum Brain Mapp 2016, 37: 3337–3352
Guilloux JP, Douillard-Guilloux G, Kota R, Wang X, Gardier AM, Martinowich K, et al. Molecular evidence for BDNF- and GABA-related dysfunctions in the amygdala of female subjects with major depression. Mol Psychiatry 2012, 17: 1130–1142
Karolewicz B, Maciag D, O’Dwyer G, Stockmeier CA, Feyissa AM, Rajkowska G. Reduced level of glutamic acid decarboxylase-67 kDa in the prefrontal cortex in major depression. Int J Neuropsychopharmacol 2010, 13: 411–420
Lener MS, Niciu MJ, Ballard ED, Park M, Park LT, Nugent AC, et al. Glutamate and gamma-aminobutyric acid systems in the pathophysiology of major depression and antidepressant response to ketamine. Biol Psychiatry 2017, 81: 886–897
Chen X, van Gerven J, Cohen A, Jacobs G. Human pharmacology of positive GABA-A subtype-selective receptor modulators for the treatment of anxiety. Acta Pharmacol Sin 2019, 40: 571–582
Ren Z, Pribiag H, Jefferson SJ, Shorey M, Fuchs T, Stellwagen D, et al. Bidirectional homeostatic regulation of a depression-related brain state by gamma-aminobutyric acidergic deficits and ketamine treatment. Biol Psychiatry 2016, 80: 457–468
Kolata SM, Nakao K, Jeevakumar V, Farmer-Alroth EL, Fujita Y, Bartley AF, et al. Neuropsychiatric phenotypes produced by GABA reduction in mouse cortex and hippocampus. Neuropsychopharmacology 2018, 43: 1445–1456
Duman RS, Li N. A neurotrophic hypothesis of depression: role of synaptogenesis in the actions of NMDA receptor antagonists. Philos Trans R Soc Lond B Biol Sci 2012, 367: 2475–2484
Albert PR, Benkelfat C, Descarries L. The neurobiology of depression—revisiting the serotonin hypothesis. I. Cellular and molecular mechanisms. Philos Trans R Soc Lond B Biol Sci 2012, 367: 2378–2381
Li K, Shen S, Ji YT, Li XY, Zhang LS, Wang XD. Melatonin augments the effects of fluoxetine on depression-like behavior and hippocampal BDNF-TrkB signaling. Neurosci Bull 2018, 34: 303–311
Zhang JJ, Gao TT, Wang Y, Wang JL, Guan W, Wang YJ, et al. Andrographolide exerts significant antidepressant-like effects involving the hippocampal BDNF system in mice. Int J Neuropsychopharmacol 2019, 22: 585–600
Wang JQ, Mao L. The ERK pathway: Molecular mechanisms and treatment of depression. Mol Neurobiol 2019, 56: 6197–6205
Chiou YJ, Huang TL. Serum brain-derived neurotrophic factors in taiwanese patients with drug-naive first-episode major depressive disorder: Effects of antidepressants. Int J Neuropsychopharmacol 2017, 20: 213–218
CAS PubMed Google Scholar
Youssef MM, Underwood MD, Huang YY, Hsiung SC, Liu Y, Simpson NR, et al. Association of BDNF Val66Met polymorphism and brain BDNF levels with major depression and suicide. Int J Neuropsychopharmacol 2018, 21: 528–538
Kojima M, Matsui K, Mizui T. BDNF pro-peptide: physiological mechanisms and implications for depression. Cell Tissue Res 2019, 377: 73–79
Jeon SW, Kim YK. Inflammation-induced depression: Its pathophysiology and therapeutic implications. J Neuroimmunol 2017, 313: 92–98
Miller AH, Raison CL. The role of inflammation in depression: from evolutionary imperative to modern treatment target. Nat Rev Immunol 2016, 16: 22–34
Zhao G, Liu X. Neuroimmune advance in depressive disorder. Adv Exp Med Biol 2019, 1180: 85–98
Li Z, Wang Z, Zhang C, Chen J, Su Y, Huang J, et al. Reduced ENA78 levels as novel biomarker for major depressive disorder and venlafaxine efficiency: Result from a prospective longitudinal study. Psychoneuroendocrinology 2017, 81: 113–121
Ambrosio G, Kaufmann FN, Manosso L, Platt N, Ghisleni G, Rodrigues ALS, et al. Depression and peripheral inflammatory profile of patients with obesity. Psychoneuroendocrinology 2018, 91: 132–141
Mao R, Zhang C, Chen J, Zhao G, Zhou R, Wang F, et al. Different levels of pro- and anti-inflammatory cytokines in patients with unipolar and bipolar depression. J Affect Disord 2018, 237: 65–72
Enache D, Pariante CM, Mondelli V. Markers of central inflammation in major depressive disorder: A systematic review and meta-analysis of studies examining cerebrospinal fluid, positron emission tomography and post-mortem brain tissue. Brain Behav Immun 2019, 81: 24–40
Haroon E, Daguanno AW, Woolwine BJ, Goldsmith DR, Baer WM, Wommack EC, et al. Antidepressant treatment resistance is associated with increased inflammatory markers in patients with major depressive disorder. Psychoneuroendocrinology 2018, 95: 43–49
Syed SA, Beurel E, Loewenstein DA, Lowell JA, Craighead WE, Dunlop BW, et al. Defective inflammatory pathways in never-treated depressed patients are associated with poor treatment response. Neuron 2018, 99(914–924): e913
Li Z, Qi D, Chen J, Zhang C, Yi Z, Yuan C, et al. Venlafaxine inhibits the upregulation of plasma tumor necrosis factor-alpha (TNF-alpha) in the Chinese patients with major depressive disorder: a prospective longitudinal study. Psychoneuroendocrinology 2013, 38: 107–114
Kohler CA, Freitas TH, Stubbs B, Maes M, Solmi M, Veronese N, et al. Peripheral alterations in cytokine and chemokine levels after antidepressant drug treatment for major depressive disorder: systematic review and meta-analysis. Mol Neurobiol 2018, 55: 4195–4206
Innes S, Pariante CM, Borsini A. Microglial-driven changes in synaptic plasticity: A possible role in major depressive disorder. Psychoneuroendocrinology 2019, 102: 236–247
Sochocka M, Diniz BS, Leszek J. Inflammatory response in the CNS: Friend or foe? Mol Neurobiol 2017, 54: 8071–8089
Zhang L, Zhang J, You Z. Switching of the microglial activation phenotype is a possible treatment for depression disorder. Front Cell Neurosci 2018, 12: 306
Sandhu KV, Sherwin E, Schellekens H, Stanton C, Dinan TG, Cryan JF. Feeding the microbiota-gut-brain axis: diet, microbiome, and neuropsychiatry. Transl Res 2017, 179: 223–244
Gonzalez-Arancibia C, Urrutia-Pinones J, Illanes-Gonzalez J, Martinez-Pinto J, Sotomayor-Zarate R, Julio-Pieper M, et al. Do your gut microbes affect your brain dopamine? Psychopharmacology (Berl) 2019, 236: 1611–1622
Article CAS Google Scholar
Kennedy PJ, Cryan JF, Dinan TG, Clarke G. Irritable bowel syndrome: a microbiome-gut-brain axis disorder? World J Gastroenterol 2014, 20: 14105–14125
Whitehead WE, Palsson O, Jones KR. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: what are the causes and implications? Gastroenterology 2002, 122: 1140–1156
Ruepert L, Quartero AO, de Wit NJ, van der Heijden GJ, Rubin G, Muris JW. Bulking agents, antispasmodics and antidepressants for the treatment of irritable bowel syndrome. Cochrane Database Syst Rev 2011: CD003460.
Marin IA, Goertz JE, Ren T, Rich SS, Onengut-Gumuscu S, Farber E, et al. Microbiota alteration is associated with the development of stress-induced despair behavior. Sci Rep 2017, 7: 43859
Zheng P, Zeng B, Zhou C, Liu M, Fang Z, Xu X, et al. Gut microbiome remodeling induces depressive-like behaviors through a pathway mediated by the host’s metabolism. Mol Psychiatry 2016, 21: 786–796
Curtis K, Stewart CJ, Robinson M, Molfese DL, Gosnell SN, Kosten TR, et al. Insular resting state functional connectivity is associated with gut microbiota diversity. Eur J Neurosci 2019, 50: 2446–2452
O’Mahony SM, Marchesi JR, Scully P, Codling C, Ceolho AM, Quigley EM, et al. Early life stress alters behavior, immunity, and microbiota in rats: implications for irritable bowel syndrome and psychiatric illnesses. Biol Psychiatry 2009, 65: 263–267
Garcia-Rodenas CL, Bergonzelli GE, Nutten S, Schumann A, Cherbut C, Turini M, et al. Nutritional approach to restore impaired intestinal barrier function and growth after neonatal stress in rats. J Pediatr Gastroenterol Nutr 2006, 43: 16–24
Hao Z, Wang W, Guo R, Liu H. Faecalibacterium prausnitzii (ATCC 27766) has preventive and therapeutic effects on chronic unpredictable mild stress-induced depression-like and anxiety-like behavior in rats. Psychoneuroendocrinology 2019, 104: 132–142
Messaoudi M, Violle N, Bisson JF, Desor D, Javelot H, Rougeot C. Beneficial psychological effects of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in healthy human volunteers. Gut Microbes 2011, 2: 256–261
Rudzki L, Ostrowska L, Pawlak D, Malus A, Pawlak K, Waszkiewicz N, et al. Probiotic Lactobacillus Plantarum 299v decreases kynurenine concentration and improves cognitive functions in patients with major depression: A double-blind, randomized, placebo controlled study. Psychoneuroendocrinology 2019, 100: 213–222
Foster JA, McVey Neufeld KA. Gut-brain axis: how the microbiome influences anxiety and depression. Trends Neurosci 2013, 36: 305–312
Mittal R, Debs LH, Patel AP, Nguyen D, Patel K, O’Connor G, et al. Neurotransmitters: The critical modulators regulating gut-brain axis. J Cell Physiol 2017, 232: 2359–2372
Diviccaro S, Giatti S, Borgo F, Barcella M, Borghi E, Trejo JL, et al. Treatment of male rats with finasteride, an inhibitor of 5alpha-reductase enzyme, induces long-lasting effects on depressive-like behavior, hippocampal neurogenesis, neuroinflammation and gut microbiota composition. Psychoneuroendocrinology 2019, 99: 206–215
Kiecolt-Glaser JK, Wilson SJ, Bailey ML, Andridge R, Peng J, Jaremka LM, et al. Marital distress, depression, and a leaky gut: Translocation of bacterial endotoxin as a pathway to inflammation. Psychoneuroendocrinology 2018, 98: 52–60
Lindqvist D, Dhabhar FS, James SJ, Hough CM, Jain FA, Bersani FS, et al. Oxidative stress, inflammation and treatment response in major depression. Psychoneuroendocrinology 2017, 76: 197–205
Czarny P, Wigner P, Galecki P, Sliwinski T. The interplay between inflammation, oxidative stress, DNA damage, DNA repair and mitochondrial dysfunction in depression. Prog Neuropsychopharmacol Biol Psychiatry 2018, 80: 309–321
Xie X, Yu C, Zhou J, Xiao Q, Shen Q, Xiong Z, et al. Nicotinamide mononucleotide ameliorates the depression-like behaviors and is associated with attenuating the disruption of mitochondrial bioenergetics in depressed mice. J Affect Disord 2020, 263: 166–174
Wang XL, Yuan K, Zhang W, Li SX, Gao GF, Lu L. Regulation of circadian genes by the MAPK pathway: Implications for rapid antidepressant action. Neurosci Bull 2020, 36: 66–76
Xie X, Shen Q, Yu C, Xiao Q, Zhou J, Xiong Z, et al. Depression-like behaviors are accompanied by disrupted mitochondrial energy metabolism in chronic corticosterone-induced mice. J Steroid Biochem Mol Biol 2020, 200: 105607
Zhang LF, Shi L, Liu H, Meng FT, Liu YJ, Wu HM, et al. Increased hippocampal tau phosphorylation and axonal mitochondrial transport in a mouse model of chronic stress. Int J Neuropsychopharmacol 2012, 15: 337–348
Flint J, Kendler KS. The genetics of major depression. Neuron 2014, 81: 1214
Sullivan PF, de Geus EJ, Willemsen G, James MR, Smit JH, Zandbelt T, et al. Genome-wide association for major depressive disorder: a possible role for the presynaptic protein piccolo. Mol Psychiatry 2009, 14: 359–375
Dunn EC, Brown RC, Dai Y, Rosand J, Nugent NR, Amstadter AB, et al. Genetic determinants of depression: recent findings and future directions. Harv Rev Psychiatry 2015, 23: 1–18
Major Depressive Disorder Working Group of the Psychiatric GC, Ripke S, Wray NR, Lewis CM, Hamilton SP, Weissman MM, et al. A mega-analysis of genome-wide association studies for major depressive disorder. Mol Psychiatry 2013, 18: 497–511.
Levinson DF, Mostafavi S, Milaneschi Y, Rivera M, Ripke S, Wray NR, et al. Genetic studies of major depressive disorder: why are there no genome-wide association study findings and what can we do about it? Biol Psychiatry 2014, 76: 510–512
Sullivan PF, Agrawal A, Bulik CM, Andreassen OA, Borglum AD, Breen G, et al. Psychiatric genomics: An update and an agenda. Am J Psychiatry 2018, 175: 15–27
Schwabe I, Milaneschi Y, Gerring Z, Sullivan PF, Schulte E, Suppli NP, et al. Unraveling the genetic architecture of major depressive disorder: merits and pitfalls of the approaches used in genome-wide association studies. Psychol Med 2019, 49: 2646–2656
Okbay A, Baselmans BM, De Neve JE, Turley P, Nivard MG, Fontana MA, et al. Genetic variants associated with subjective well-being, depressive symptoms, and neuroticism identified through genome-wide analyses. Nat Genet 2016, 48: 624–633
Wray NR, Ripke S, Mattheisen M, Trzaskowski M, Byrne EM, Abdellaoui A, et al. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nat Genet 2018, 50: 668–681
Howard DM, Adams MJ, Clarke TK, Hafferty JD, Gibson J, Shirali M, et al. Genome-wide meta-analysis of depression identifies 102 independent variants and highlights the importance of the prefrontal brain regions. Nat Neurosci 2019, 22: 343–352
Ormel J, Hartman CA, Snieder H. The genetics of depression: successful genome-wide association studies introduce new challenges. Transl Psychiatry 2019, 9: 114
Uchida S, Yamagata H, Seki T, Watanabe Y. Epigenetic mechanisms of major depression: Targeting neuronal plasticity. Psychiatry Clin Neurosci 2018, 72: 212–227
Yeshurun S, Hannan AJ. Transgenerational epigenetic influences of paternal environmental exposures on brain function and predisposition to psychiatric disorders. Mol Psychiatry 2019, 24: 536–548
van Eijndhoven P, van Wingen G, Katzenbauer M, Groen W, Tepest R, Fernandez G, et al. Paralimbic cortical thickness in first-episode depression: evidence for trait-related differences in mood regulation. Am J Psychiatry 2013, 170: 1477–1486
Peng W, Chen Z, Yin L, Jia Z, Gong Q. Essential brain structural alterations in major depressive disorder: A voxel-wise meta-analysis on first episode, medication-naive patients. J Affect Disord 2016, 199: 114–123
Geerlings MI, Gerritsen L. Late-life depression, hippocampal volumes, and hypothalamic-pituitary-adrenal axis regulation: A systematic review and meta-analysis. Biol Psychiatry 2017, 82: 339–350
Maller JJ, Broadhouse K, Rush AJ, Gordon E, Koslow S, Grieve SM. Increased hippocampal tail volume predicts depression status and remission to anti-depressant medications in major depression. Mol Psychiatry 2018, 23: 1737–1744
Joshi SH, Espinoza RT, Pirnia T, Shi J, Wang Y, Ayers B, et al. Structural plasticity of the hippocampus and amygdala induced by electroconvulsive therapy in major depression. Biol Psychiatry 2016, 79: 282–292
Gryglewski G, Baldinger-Melich P, Seiger R, Godbersen GM, Michenthaler P, Klobl M, et al. Structural changes in amygdala nuclei, hippocampal subfields and cortical thickness following electroconvulsive therapy in treatment-resistant depression: longitudinal analysis. Br J Psychiatry 2019, 214: 159–167
Boldrini M, Santiago AN, Hen R, Dwork AJ, Rosoklija GB, Tamir H, et al. Hippocampal granule neuron number and dentate gyrus volume in antidepressant-treated and untreated major depression. Neuropsychopharmacology 2013, 38: 1068–1077
Liang S, Wang Q, Kong X, Deng W, Yang X, Li X, et al. White matter abnormalities in major depression biotypes identified by diffusion tensor imaging. Neurosci Bull 2019, 35: 867–876
Chen G, Guo Y, Zhu H, Kuang W, Bi F, Ai H, et al. Intrinsic disruption of white matter microarchitecture in first-episode, drug-naive major depressive disorder: A voxel-based meta-analysis of diffusion tensor imaging. Prog Neuropsychopharmacol Biol Psychiatry 2017, 76: 179–187
Brakowski J, Spinelli S, Dorig N, Bosch OG, Manoliu A, Holtforth MG, et al. Resting state brain network function in major depression - Depression symptomatology, antidepressant treatment effects, future research. J Psychiatr Res 2017, 92: 147–159
Dutta A, McKie S, Downey D, Thomas E, Juhasz G, Arnone D, et al. Regional default mode network connectivity in major depressive disorder: modulation by acute intravenous citalopram. Transl Psychiatry 2019, 9: 116
Meyer BM, Rabl U, Huemer J, Bartova L, Kalcher K, Provenzano J, et al. Prefrontal networks dynamically related to recovery from major depressive disorder: a longitudinal pharmacological fMRI study. Transl Psychiatry 2019, 9: 64
Muller VI, Cieslik EC, Serbanescu I, Laird AR, Fox PT, Eickhoff SB. Altered brain activity in unipolar depression revisited: Meta-analyses of neuroimaging studies. JAMA Psychiatry 2017, 74: 47–55
Connolly CG, Ho TC, Blom EH, LeWinn KZ, Sacchet MD, Tymofiyeva O, et al. Resting-state functional connectivity of the amygdala and longitudinal changes in depression severity in adolescent depression. J Affect Disord 2017, 207: 86–94
Godlewska BR, Browning M, Norbury R, Igoumenou A, Cowen PJ, Harmer CJ. Predicting treatment response in depression: The role of anterior cingulate cortex. Int J Neuropsychopharmacol 2018, 21: 988–996
Goldstein-Piekarski AN, Staveland BR, Ball TM, Yesavage J, Korgaonkar MS, Williams LM. Intrinsic functional connectivity predicts remission on antidepressants: a randomized controlled trial to identify clinically applicable imaging biomarkers. Transl Psychiatry 2018, 8: 57
Leaver AM, Vasavada M, Joshi SH, Wade B, Woods RP, Espinoza R, et al. Mechanisms of antidepressant response to electroconvulsive therapy studied with perfusion magnetic resonance imaging. Biol Psychiatry 2019, 85: 466–476
Miskowiak KW, Macoveanu J, Jorgensen MB, Stottrup MM, Ott CV, Jensen HM, et al. Neural response after a single ECT session during retrieval of emotional self-referent words in depression: A randomized, sham-controlled fMRI study. Int J Neuropsychopharmacol 2018, 21: 226–235
Du L, Liu H, Du W, Chao F, Zhang L, Wang K, et al. Stimulated left DLPFC-nucleus accumbens functional connectivity predicts the anti-depression and anti-anxiety effects of rTMS for depression. Transl Psychiatry 2018, 7: 3
Williams LM. Defining biotypes for depression and anxiety based on large-scale circuit dysfunction: a theoretical review of the evidence and future directions for clinical translation. Depress Anxiety 2017, 34: 9–24
Williams LM. Precision psychiatry: a neural circuit taxonomy for depression and anxiety. Lancet Psychiatry 2016, 3: 472–480
Williams LM, Korgaonkar MS, Song YC, Paton R, Eagles S, Goldstein-Piekarski A, et al. Amygdala reactivity to emotional faces in the prediction of general and medication-specific responses to antidepressant treatment in the randomized iSPOT-D trial. Neuropsychopharmacology 2015, 40: 2398–2408
Hou Z, Gong L, Zhi M, Yin Y, Zhang Y, Xie C, et al. Distinctive pretreatment features of bilateral nucleus accumbens networks predict early response to antidepressants in major depressive disorder. Brain Imaging Behav 2018, 12: 1042–1052
De Crescenzo F, Ciliberto M, Menghini D, Treglia G, Ebmeier KP, Janiri L. Is (18)F-FDG-PET suitable to predict clinical response to the treatment of geriatric depression? A systematic review of PET studies. Aging Ment Health 2017, 21: 889–894
Schmaal L, Pozzi E, T CH, van Velzen LS, Veer IM, Opel N, et al. ENIGMA MDD: seven years of global neuroimaging studies of major depression through worldwide data sharing. Transl Psychiatry 2020, 10: 172.
Schmaal L, Veltman DJ, van Erp TG, Samann PG, Frodl T, Jahanshad N, et al. Subcortical brain alterations in major depressive disorder: findings from the ENIGMA Major Depressive Disorder working group. Mol Psychiatry 2016, 21: 806–812
Schmaal L, Hibar DP, Samann PG, Hall GB, Baune BT, Jahanshad N, et al. Cortical abnormalities in adults and adolescents with major depression based on brain scans from 20 cohorts worldwide in the ENIGMA Major Depressive Disorder Working Group. Mol Psychiatry 2017, 22: 900–909
Frodl T, Janowitz D, Schmaal L, Tozzi L, Dobrowolny H, Stein DJ, et al. Childhood adversity impacts on brain subcortical structures relevant to depression. J Psychiatr Res 2017, 86: 58–65
Renteria ME, Schmaal L, Hibar DP, Couvy-Duchesne B, Strike LT, Mills NT, et al. Subcortical brain structure and suicidal behaviour in major depressive disorder: a meta-analysis from the ENIGMA-MDD working group. Transl Psychiatry 2017, 7: e1116
Tozzi L, Garczarek L, Janowitz D, Stein DJ, Wittfeld K, Dobrowolny H, et al. Interactive impact of childhood maltreatment, depression, and age on cortical brain structure: mega-analytic findings from a large multi-site cohort. Psychol Med 2020, 50: 1020–1031
de Kovel CGF, Aftanas L, Aleman A, Alexander-Bloch AF, Baune BT, Brack I, et al. No alterations of brain structural asymmetry in major depressive disorder: An ENIGMA consortium analysis. Am J Psychiatry 2019, 176: 1039–1049
Ho TC, Gutman B, Pozzi E, Grabe HJ, Hosten N, Wittfeld K, et al. Subcortical shape alterations in major depressive disorder: Findings from the ENIGMA major depressive disorder working group. Hum Brain Mapp 2020.
Han LKM, Dinga R, Hahn T, Ching CRK, Eyler LT, Aftanas L, et al. Brain aging in major depressive disorder: results from the ENIGMA major depressive disorder working group. Mol Psychiatry 2020.
van Velzen LS, Kelly S, Isaev D, Aleman A, Aftanas LI, Bauer J, et al. White matter disturbances in major depressive disorder: a coordinated analysis across 20 international cohorts in the ENIGMA MDD working group. Mol Psychiatry 2020, 25: 1511–1525
Lv X, Si T, Wang G, Wang H, Liu Q, Hu C, et al. The establishment of the objective diagnostic markers and personalized medical intervention in patients with major depressive disorder: rationale and protocol. BMC Psychiatry 2016, 16: 240
Fabbri C, Hosak L, Mossner R, Giegling I, Mandelli L, Bellivier F, et al. Consensus paper of the WFSBP Task Force on Genetics: Genetics, epigenetics and gene expression markers of major depressive disorder and antidepressant response. World J Biol Psychiatry 2017, 18: 5–28
Li Z, Zhang C, Fan J, Yuan C, Huang J, Chen J, et al. Brain-derived neurotrophic factor levels and bipolar disorder in patients in their first depressive episode: 3-year prospective longitudinal study. Br J Psychiatry 2014, 205: 29–35
Gong Q, He Y. Depression, neuroimaging and connectomics: a selective overview. Biol Psychiatry 2015, 77: 223–235
Papakostas GI, Shelton RC, Kinrys G, Henry ME, Bakow BR, Lipkin SH, et al. Assessment of a multi-assay, serum-based biological diagnostic test for major depressive disorder: a pilot and replication study. Mol Psychiatry 2013, 18: 332–339
Kolovos S, Kleiboer A, Cuijpers P. Effect of psychotherapy for depression on quality of life: meta-analysis. Br J Psychiatry 2016, 209: 460–468
Park LT, Zarate CA Jr. Depression in the primary care setting. N Engl J Med 2019, 380: 559–568
Health N C C F M . Depression: The treatment and management of depression in adults (updated edition) 2010.
Qaseem A, Barry MJ, Kansagara D. Clinical Guidelines Committee of the American College of P. Nonpharmacologic versus pharmacologic treatment of adult patients with major depressive disorder: A clinical practice guideline from the american college of physicians. Ann Intern Med 2016, 164: 350–359
Dodd S, Mitchell PB, Bauer M, Yatham L, Young AH, Kennedy SH, et al. Monitoring for antidepressant-associated adverse events in the treatment of patients with major depressive disorder: An international consensus statement. World J Biol Psychiatry 2018, 19: 330–348
Cristea IA, Naudet F. US Food and Drug Administration approval of esketamine and brexanolone. Lancet Psychiatry 2019, 6: 975–977
Zheng W, Cai DB, Xiang YQ, Zheng W, Jiang WL, Sim K, et al. Adjunctive intranasal esketamine for major depressive disorder: A systematic review of randomized double-blind controlled-placebo studies. J Affect Disord 2020, 265: 63–70
Popova V, Daly EJ, Trivedi M, Cooper K, Lane R, Lim P, et al. Efficacy and safety of flexibly dosed esketamine nasal spray combined with a newly initiated oral antidepressant in treatment-resistant depression: A Randomized Double-Blind Active-Controlled Study. Am J Psychiatry 2019, 176: 428–438
Turner EH. Esketamine for treatment-resistant depression: seven concerns about efficacy and FDA approval. Lancet Psychiatry 2019, 6: 977–979
Murrough JW, Abdallah CG, Mathew SJ. Targeting glutamate signalling in depression: progress and prospects. Nat Rev Drug Discov 2017, 16: 472–486
Gill SP, Kellner CH. Clinical practice recommendations for continuation and maintenance electroconvulsive therapy for depression: Outcomes from a review of the evidence and a consensus workshop held in Australia in May 2017. J ECT 2019, 35: 14–20
McClintock SM, Reti IM, Carpenter LL, McDonald WM, Dubin M, Taylor SF, et al. Consensus recommendations for the clinical application of repetitive transcranial magnetic stimulation (rTMS) in the treatment of depression. J Clin Psychiatry 2018, 79.
Chase HW, Boudewyn MA, Carter CS, Phillips ML. Transcranial direct current stimulation: a roadmap for research, from mechanism of action to clinical implementation. Mol Psychiatry 2020, 25: 397–407
Alexander ML, Alagapan S, Lugo CE, Mellin JM, Lustenberger C, Rubinow DR, et al. Double-blind, randomized pilot clinical trial targeting alpha oscillations with transcranial alternating current stimulation (tACS) for the treatment of major depressive disorder (MDD). Transl Psychiatry 2019, 9: 106
Akhtar H, Bukhari F, Nazir M, Anwar MN, Shahzad A. Therapeutic efficacy of neurostimulation for depression: Techniques, current modalities, and future challenges. Neurosci Bull 2016, 32: 115–126
Zhou C, Zhang H, Qin Y, Tian T, Xu B, Chen J, et al. A systematic review and meta-analysis of deep brain stimulation in treatment-resistant depression. Prog Neuropsychopharmacol Biol Psychiatry 2018, 82: 224–232
Li X, Li X. The antidepressant effect of light therapy from retinal projections. Neurosci Bull 2018, 34: 359–368
Shekelle PG, Cook IA, Miake-Lye IM, Booth MS, Beroes JM, Mak S. Benefits and harms of cranial electrical stimulation for chronic painful conditions, depression, anxiety, and insomnia: A systematic review. Ann Intern Med 2018, 168: 414–421
Kessler RC. The potential of predictive analytics to provide clinical decision support in depression treatment planning. Curr Opin Psychiatry 2018, 31: 32–39
Bradley P, Shiekh M, Mehra V, Vrbicky K, Layle S, Olson MC, et al. Improved efficacy with targeted pharmacogenetic-guided treatment of patients with depression and anxiety: A randomized clinical trial demonstrating clinical utility. J Psychiatr Res 2018, 96: 100–107
Greden JF, Parikh SV, Rothschild AJ, Thase ME, Dunlop BW, DeBattista C, et al. Impact of pharmacogenomics on clinical outcomes in major depressive disorder in the GUIDED trial: A large, patient- and rater-blinded, randomized, controlled study. J Psychiatr Res 2019, 111: 59–67
Long Z, Du L, Zhao J, Wu S, Zheng Q, Lei X. Prediction on treatment improvement in depression with resting state connectivity: A coordinate-based meta-analysis. J Affect Disord 2020, 276: 62–68
Download references
Acknowledgments
This review was supported by the National Basic Research Development Program of China (2016YFC1307100), the National Natural Science Foundation of China (81930033 and 81771465; 81401127), Shanghai Key Project of Science & Technology (2018SHZDZX05), Shanghai Jiao Tong University Medical Engineering Foundation (YG2016MS48), Shanghai Jiao Tong University School of Medicine (19XJ11006), the Sanming Project of Medicine in Shenzhen Municipality (SZSM201612006), the National Key Technologies R&D Program of China (2012BAI01B04), and the Innovative Research Team of High-level Local Universities in Shanghai.
Author information
Authors and affiliations.
Clinical Research Center and Division of Mood Disorders of Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, 200030, China
Zezhi Li, Jun Chen & Yiru Fang
Department of Neurology, Ren Ji Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, 200127, China
Shanghai Institute of Nutrition and Health, Shanghai Information Center for Life Sciences, Chinese Academy of Science, Shanghai, 200031, China
Meihua Ruan
Center for Excellence in Brain Science and Intelligence Technology, Chinese Academy of Science, Shanghai, 200031, China
Shanghai Key Laboratory of Psychotic Disorders, Shanghai, 201108, China
Jun Chen & Yiru Fang
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Yiru Fang .
Ethics declarations
Conflicts of interest.
The authors declare no conflicts of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Li, Z., Ruan, M., Chen, J. et al. Major Depressive Disorder: Advances in Neuroscience Research and Translational Applications. Neurosci. Bull. 37 , 863–880 (2021). https://doi.org/10.1007/s12264-021-00638-3
Download citation
Received : 30 May 2020
Accepted : 30 September 2020
Published : 13 February 2021
Issue Date : June 2021
DOI : https://doi.org/10.1007/s12264-021-00638-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Major depressive disorder
- Pathogenesis
- Find a journal
- Publish with us
- Track your research
Depression Research Paper

This sample depression research paper features: 5700 words (approx. 19 pages), an outline, and a bibliography with 7 sources. Browse other research paper examples for more inspiration. If you need a thorough research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.

Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% off with 24start discount code.
Even for professionals the use of the term depression can vary. In 1987, Kendall and colleagues noted that “The professional use of the term depression has several levels of reference: symptom, syndrome, nosologic disorder . . . . Depression itself can be a symptom – for example, being sad. As a syndrome, depression is a constellation of signs and symptoms that cluster together . . . . The syndrome of depression is itself a psychological dysfunction but can also be present, in secondary ways, in other diagnosed disorders. Finally, for depression to be a nosologic category careful diagnostic procedures are required during which other potential diagnostic categories are excluded. The presumption, of course, is that a discrete nosologic entity will ultimately prove to be etiologically distinct from other discrete entities, with associated differences likely in course, prognosis, and treatment response.” It is this likely nosologic disorder of depression that we will discuss.
I. Definition of Depression
A. symptoms of depression, b. comorbidity: the relationship between depression and anxiety, ii. diagnostic classification, a. major depressive disorder, b. dysthymic disorder, c. bipolar i disorder, d. bipolar ii disorder, e. cyclothymic disorder, iii. exploratory categories of depressive disorders, a. premenstrual dysphoric disorder, b. minor depressive disorder, c. recurrent brief depressive disorder, d. mixed anxiety-depressive disorder, iv. epidemiology, a. prevalence, 1. national prevalence, 2. international prevalence, b. age differences, c. sex and ethnic differences, d. environmental correlates, v. etiological theories of depression, a. psychological theories, 1. psychoanalytic approaches, 2. interpersonal approaches, 3. cognitive approaches, b. biological theories, 1. genetic approaches, 2. neurotransmitter approaches, vi. protective factors, a. social support, b. coping styles.
Any definition of depression must begin with the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). The DSM-IV represents the official diagnostic classification system of the American Psychiatric Association and provides the criteria that are used to diagnosis depression. These criteria consist of the symptoms of depression. In order to make a diagnosis of depression, at least five out of nine possible symptoms must be present. These include (1) depressed mood; (2) diminished pleasure or interest in activities; (3) significant weight loss or weight gain; (4) insomnia or hypersomnia; (5) agitation; (6) fatigue or loss of energy; (7) thoughts of worthlessness or inappropriate guilt; (8) diminished concentration ability; and (9) thoughts of death or suicide.
Symptoms of depression may vary according to an individual’s age and culture. Children who are depressed, for instance, may express symptoms of irritability rather than sadness. They may also fail to make expected weight gains rather than lose weight. On the other end of the age continuum, older adults are more likely than younger adults to experience symptoms such as loss of appetite, loss of interest, and thoughts of death. Cultural differences also exist in report of depressive symptoms. One study, for example, found that depressed Jewish patients reported more somatic symptoms, and less guilt, than did non-Jewish patients. Another study that examined depressive symptomatology in American, Korean, Philippine, and Taiwanese college students found that Taiwanese students reported the lowest numbers of somatic symptoms and the highest numbers of affective symptoms. The other ethnic groups reporting similar levels of these symptoms. One’s age and culture thus seems to affect how depression is expressed.
Comorbidity refers to the occurrence of more than one disorder at the same time. Although researchers and clinicians generally acknowledge depression as a distinct disorder, it does overlap with a variety of other difficulties. Much current research on this overlap has focused on the relationship between anxiety and depression. This is not surprising, given the high rates of comorbidity found in studies of the two disorder types. For example, one study found that 63% of a group of patients with panic disorder also experienced major depression. One possible explanation provided for such overlap lies in the concept of “negative affectivity.” In 1984, Watson and Clark described individuals with high levels of negative affectivity as having a tendency “to be distressed and upset and have a negative view of self, whereas those low on the dimension are relatively content and secure and satisfied with themselves.” Other characteristics of high negative affectivity include nervousness, tension, worry, anger, scorn, revulsion, guilt, self-dissatisfaction, rejectedness, and sadness.
Both anxiety and depression seem to consist of high negative affectivity. There are however, important differences between depression and anxiety. While both depression and anxiety are characterized by high levels of negative affect, only depression is related to lowered levels of positive affect. Thus, depressed individuals tend to display both high negative affect and low positive affect, whereas anxious individuals display high negative affect and may or may not have lowered positive affect–the level of positive affect is unrelated to one’s anxiety state. Research on negative affect as a link between anxiety and depression is continuing at a rapid pace.
Earlier we noted the DSM-IV. The DSM-IV is the most widely used classification scheme for psychiatric disorders in North America. According to this manual, there are five types of mood disorders that include depression as a significant component. These are (1) Major Depressive Disorder; (2) Dysthymic Disorder; (3) Bipolar I Disorder; (4) Bipolar II Disorder; and (5) Cyclothymic Disorder. Each of these classifications differs in terms of etiology, course, and symptomatology.
For a diagnosis of Major Depressive Disorder (MDD), DSM-IV specifies that at least five symptoms must occur for a period of at least 2 weeks. Chief among these symptoms is depressed mood that occurs most of the day, nearly every day for at least 2 weeks, or significantly diminished interest or pleasure in virtually all activities most of the day, nearly every day for the 2-week period.
MDD can be further classified according to severity (i.e., mild, moderate, severe without psychotic features, severe with psychotic features), course (e.g., single episode versus recurrent episodes), and presentation (e.g., with catatonic features, with melancholic features). Psychotic features of depression include such experiences as delusions (i.e., false beliefs) and hallucinations (i.e., sensory experiences that have no basis in reality). A delusion, for example, would be a person who believes that she is dead. Catatonic features of depression involve psychomotor disturbances such as excessive movement or stupor. Melancholic features include the inability to experience pleasure even when good things happen and a lack of interest in previously pleasurable activities. No matter what the specific characteristics of a given individual’s disturbance, MDD is, by definition, extremely distressing to the sufferer and is associated with significant impairment in important areas of the person’s life (e.g., at work, home or school).
Dysthymic Disorder is characterized by a chronic depressed mood that lasts at least 2 years in adults and at least 1 year in children and adolescents. This depressed mood is accompanied by at least two of the following six depressive symptoms: (1) poor appetite or overeating; (2) insomnia or hypersomnia; (3) low energy or fatigue; (4) low self-esteem; (5) poor concentration or difficulty making decisions; and (6) feelings of hopelessness. As fewer depressive symptoms are required to make a diagnosis, Dysthymic Disorder is often considered a milder form of depression than MDD. However, it can be just as upsetting to the sufferer and can cause just as much impairment. In addition, Dysthymic Disorder may occur in combination with episodes of major depression. When Dysthymic Disorder occurs along with major depression, the individual is considered to be suffering from a “double depression.” The co-occurrence of MDD and dysthymia is not uncommon.
The hallmark characteristic of Bipolar I Disorder is mania. According to DSM-IV, a manic episode is characterized by elevated, expansive, or irritable mood that is persistent and distinctly different from normal elevated or irritable moods. This period is accompanied by at least three of seven possible symptoms. These symptoms include (1) inflated self-esteem; (2) a decreased need for sleep; (3) unusual talkativeness; (4) the feeling that one’s thoughts are racing; (5) increased distractibility; (6) increased activity; (7) involvement in pleasurable but potentially harmful activities (e.g., sexual indiscretions).
Bipolar I Disorder is typically recurrent; according to DSM-IV, additional episodes occur in more than 90% of individuals who have had a single manic episode. The manic episodes of those with Bipolar I Disorder are often intermixed with periods of depression. Like those with MDD, people with Bipolar I Disorder may exhibit psychotic, catatonic, and melancholic features as part of either their mania or their depression.
Bipolar II Disorder is characterized by periods of hypomania intermixed with periods of depression. Hypomanic episodes are characterized by the same symptoms as manic episodes. However, hypomanic episodes are shorter (e.g., 4 days in duration) and are associated with less impairment. While manic episodes may include psychotic features, interrupt daily functioning, and require hospitalization, hypomanic episodes typically do not. The depression experienced as part of Bipolar II Disorder, however, can be just as severe as that experienced in MDD and Bipolar I Disorder.
Cyclothymic disorder is characterized by hypomanic periods intermixed with depressive periods that are not as severe as those experienced in MDD, Bipolar I Disorder, and Bipolar II Disorder. In Cyclothymia, the periods of mood disturbance may alternate rapidly, with little respite from affective difficulties. For a diagnosis of Cyclothymia these periods of shifting moods must be problematic for at least 2 years in adults and at least i year in children and adolescents.
In addition to the five official diagnoses, DSM-IV has denoted four classifications for further study that include depression as a significant component. Such classifications are not yet considered to be disorders and more information is needed on factors such as symptom presentation, etiology, and degree of impairment to sufferers before these might be considered disorders in their own right. Nevertheless, these may represent serious problems and even though they are currently exploratory, we describe them here. They are: (1) Premenstrual Dysphoric Disorder; (2) Minor Depressive Disorder; (3) Recurrent Brief Depressive Disorder; and (4) Mixed Anxiety-Depressive Disorder.
Premenstrual Dysphoric Disorder is characterized by several hallmark symptoms of depression (e.g., decreased interest in usual activities, depressed mood, difficulty sleeping or sleeping too much) in addition to symptoms such as affective lability, feelings of being overwhelmed or out of control, and food cravings. In order to meet the criteria that have been proposed for this diagnosis, such symptoms must have occurred during the late luteal phase of most of a woman’s menstrual cycles in the past year. As a number of authors have pointed out, such a classification has potentially serious social, political, and legal ramifications for women. For example, some have argued that if this classification is adopted as an orificial diagnosis then women might be stigmatized as more unstable than or inferior to men. Arguments such as this keep the classification of Premenstrual Dysphoric Disorder a topic of considerable debate.
Minor Depressive Disorder is characterized by fewer depressive symptoms than are seen in MDD. The level of impairment is also less than that associated with MDD. To meet the proposed criteria for Minor Depressive Disorder, a person must demonstrate either a depressed mood or loss of interest and two additional symptoms of a Major Depressive Episode. If this classification were included in future DSM editions as a disorder, it would constitute a residual category to be used only after the other mood disorders have been ruled out.
The principle difference between Recurrent Brief Depressive Disorder and MDD is one of duration. Recurrent Brief Depressive Disorder is characterized by periods of depression that meet all of the criteria for a Major Depressive Episode except for the duration requirement. While in major depressive episodes, symptoms must last at least 2 weeks, in recurrent brief depressive episodes, symptoms must last at least 2 but less than 14 days. In addition, these brief episodes must occur at least once a month for 12 months to meet criteria for the classification of Recurrent Brief Depressive Disorder. Recurrent Brief Depressive Disorder is quite similar to MDD in its age of onset and family incidence rates, thus raising questions as to whether this should be considered a distinct disorder.
The impetus behind a mixed anxious-depressed category lies in the finding that there are many people suffering from symptoms of anxiety and depression who do not meet criteria for any DSM anxiety or mood disorder, but who are nonetheless significantly impaired by their difficulties. The classification of Mixed Anxiety-Depressive Disorder is characterized by a dysphoric mood for at least 1 month in addition to at least four additional symptoms that primarily reflect anxiety (e.g., mind going blank, worry, hypervigilance). The primary argument in favor of adopting this proposed disorder is that it would cover the large number of people who have significant impairment linked to depression and anxiety but who do not fall into any currently existing diagnostic category. The primary argument against this classification is that people suffering from both depression and anxiety could in fact be categorized into already existing disorders with the use of more precise assessment methods.
Epidemiology refers to information about the incidence and prevalence of disorders in a population. A prevalence rate refers to the number of people who have a given disorder during a particular time period (e.g., the percentage of people in given location diagnosed with MDD within a 1-year period of time). An incidence rate refers to the number of new cases of a disorder which occur during a given time period (e.g., the number of people diagnosed with Dysthymic Disorder during April 1996). Because the distribution of a disorder can be examined to determine whether it correlates with other factors, epidemiological information can be important for understanding some of the possible causes and correlates of depression.
Two recent large-scale surveys of psychopathology in the United States have provided differing prevalence data on depression. Using diagnostic criteria from the revised 3rd Edition of the DSM (DSM-III-R), the Epidemiologic Catchment Area (ECA) study examined the rates of depression in five sites: New Haven, Baltimore, St. Louis, Los Angeles, and Durham. The ECA study found the lifetime prevalence of major depression (i.e., the number of people experiencing major depression during any point in life) to be 4.9% and the lifetime prevalence of dysthymia to be 3.2%. Alternatively, the National Comorbidity Survey (NCS) reported much higher prevalence rates: 14.9% for lifetime major depression and 6.4% for dysthymia. The discrepancies between these two studies may be accounted for by the different assessment instruments used, slightly different diagnostic criteria employed, and different age ranges studied (i.e., the ECA sample was 18 years of age or older, whereas the NCS sample ranged in age from 15 to 54 years). According to the ECA study, prevalence rates for bipolar disorders were much lower; lifetime prevalence of these disorders was .8% for Bipolar I and .5% for Bipolar II. The NCS lifetime prevalence for manic episode was somewhat higher: 1.6 %. Even though these epidemiological studies reported somewhat discrepant rates, they are in agreement that mood disorders are relatively common in the United States.
A number of studies have examined the community prevalence of major depression in countries besides the United States. International lifetime prevalence rates vary widely, from a low of 3.3% in Seoul to a high of 15.1% among New Zealand residents aged 25 to 46. While such differences may indeed reflect true international differences in the occurrence of depression, other factors such as cultural differences in the sensitivity of the instruments used to assess disorder and different sample ages may also account for this range. In prevalence studies focusing on bipolar illness, ranges from .07% in Sweden to 7% in Ireland have been reported. Most studies, however, place prevalence at about 1% for bipolar illnesses, consistent with data from the ECA and NCS studies.
The ECA study also reported incidence rates of depression for various age groups. For men, major depression was highest among those aged 18 to 29. A large decline in incidence was noted for men aged 45 and older. For women, the incidence of major depression was highest in the group aged 30 to 44 and did not decline until age 65.
According to the ECA study, lifetime prevalence rates of major depression, dysthymia, and all mood disorders are approximately twice as high for women as for men. Women’s lifetime rates were 7.0%, 4.1%, and 10.2%, respectively, while rates for men were 2.6%, 2.2 %, and 5.2 %, respectively. These differences occur across a variety of ethnic groups (e.g., African American, Hispanic, Caucasian) even when differences in education, income, and occupations are controlled. Sex differences are also found in countries besides the United States. While sex differences in depression are among the most stable of findings across studies, no sex differences in the rates of bipolar disorder are reliably found.
Although sex difference in the incidence of depression occur across different ethnic groups, there are some differences among these groups overall. For instance, the ECA study found higher rates of Major Depression and Dysthymia among Caucasians and Hispanics than among African Americans. However, few difference in the rates of bipolar disorders among the three groups were found.
The ECA study also examined a number of environmental correlates of depression and bipolar disorders. This study found that people who were separated or divorced had higher 1-year prevalence rates of major depression (6.3%) than those who were never married (2.8%), currently married (2.1%), or widowed (2.1%). This was also true of those with bipolar disorders, although the rates for those separated or divorced versus never married were nearly identical (1.7% versus 1.6%). The 1-year prevalence rate of major depression was also higher among the unemployed than the employed (3.4% versus 2.2%), but the rate was nearly identical for those with bipolar disorders (1.1% versus 1.0%). In addition, the ECA study found higher rates of major depression among white-collar workers and those with at least 12 years of education, but lower rates of depression among those with annual incomes of $15,000 or more. Consistent with the major depression findings, bipolar disorders were also less prevalent among those with annual incomes of $15,000 or more. Bipolar disorders were also found to be the most prevalent among none-white-collar workers with less than 12 years of education. Overall, these socioeconomic status differences were quite small.
A variety of different psychological theories of the causes of depression have been proposed. These can be grouped in psychoanalytic, interpersonal, and cognitive.
The first psychoanalytic writers to theorize about the etiology of depression were Sigmund Freud and his student, Karl Abraham. As would be expected, there are a number of similarities in the theories proposed by Freud and Abraham. First, both Freud and Abraham believed that some people are predisposed to experience depression. For Abraham, this predisposition consisted of anatomical anomalies that allowed a person to experience a great deal of oral eroticism. For Freud, this predisposition consisted of narcissistic object choices (e.g., object choices which are so similar to the self that love of the object is truly love of self). Second, both believed that a predisposition to experience depression was not, in and of itself, enough to cause depression. In order to experience a depression, a predisposed individual must also experience the loss of a loved object (e.g., through death or rejection).
Despite these basic similarities, the two theorists diverge somewhat on how depression occurs once a loss has been experienced. For Abraham, the loss of a loved object in a person predisposed to depression triggers a regression to the oral stage of psychosexual development. Such a regression is meant to achieve three purposes: (1) to increase pleasure; (2) to hold on to the object through oral incorporation; and (3) to discharge one’s aggressive impulses on to the object. Such a regression manifests itself most saliently in the depressive symptoms of eating too much or too little. For Freud, the loss of a loved object possesses different implications. Since the lost object was a narcissistic choice and thus represented the self, loss of the object means loss of the self. This loss of self triggers feelings of anger and depression. The energy associated with these negative feelings is withdrawn from the lost object and brought inward, in a process called introjection. Thus, depression as conceptualized by Freud is often summarized as “anger turned inward.” For Freud, the difference between sadness and “true” depression was the difference between “this is awful” and “I am awful.” Freud further extended his theory to account for the mania characteristic of bipolar depressive disorders. He hypothesized that, once the feelings of anger and depression over loss of the object are resolved, the energy associated with these negative feelings is freed for other purposes. In a person with bipolar disorder, this freed energy is used to zealousy search for new objects, thus accounting for the symptoms of mania.
More recent psychoanalytic theorists have focused on the superego’s role in depression. Some theorists, for example, have suggested that depression is distinguished from other states such as shame, apathy, or resentment by the presence of guilt. As guilt results only from an intrapsychic conflict of the superego, the superego is necessarily implicated in depression. One result of these differences in etiological focus has been the proposition of two forms of depression: anaclitic and introjective. Anaclitic depression is characterized by feelings of helplessness, inferiority, and being unloved. Anaclitic depression is proposed to be associated with the earlier stages of development and is most closely associated with the theorizing of Abraham and Freud. Alternatively, introjective depression focuses on feelings of unworthiness and failure to measure up to expectations and standards. It is associated with later stages of development, and more closely aligned with the works of later psychoanalytic theorists. Although much of psychoanalytic theory has been criticized on grounds that it has not been empirically tested, the distinction between anaclitic and introjectire depressions has been empirically examined and found to be valid. Psychoanalytic theorists have accounted for the development of bipolar disorders as well. Most notable amongst these theorists is Melanie Klein, who expanded upon the work of Freud.
Interpersonal approaches to the etiology and maintenance of depression focus on the interplay between a depressed person and his or her relations with others. Empirical research in this area has taken several directions. For example, some researchers focus on the role of social skills in depression, asking such questions as whether depressed people have poor social skills and whether the lack of such skills results in decreased reinforcement from others and consequent depression. Other research has evaluated the types of communications depressed people emit (e.g., sadness, hopelessness) and the effects these communications have on others. If others find the communications of depressed persons aversive, they will likely avoid such persons, which may then exacerbate depressive symptoms such as isolation and loneliness. Still others address the interplay between stress, social support, and depression. All of these lines of research have found some support; interpersonal research highlights the fact that depression is caused by a multitude of factors in interplay with one another.
Much of the research converges on the theoretical idea that depression is maintained by a vicious cycle that is caused by disruptions in interpersonal interactions. For instance, many depressed individuals quite understandably seek out social support from others. If this support does not alleviate the negative feelings, further support is sought. This intensified support seeking, however, has the paradoxical effect of pushing away those who have been supportive. That is, as individuals begin to feel that their support capacity has been exhausted they pull back from the depressed person, leading to an even further intensification of social support seeking, and the further distancing of potentially supportive people.
Interpersonal factors in the etiology of bipolar depressive disorders have not received as much research attention as such factors in unipolar depressive disorders. Nonetheless, persons with both types of depressive disorders seem to have difficulties in retaining social support. Indeed, in one recent study, people with bipolar disorder perceived their social supports as less available to them and as less adequate in the amount of support received than people in a community sample. Furthermore, perceptions of social support availability seemed to decrease as the duration of illness increased. Thus, it seems likely that social support plays a role in bipolar as well as unipolar depressive disorders.
Currently, cognitive approaches are among the most widely studied theories in the etiology of depression. One of the most influential of these theories was proposed by Aaron Beck in 1967. Beck argued that all individuals possess cognitive structures called schemas that guide the ways information in the environment is attended to and interpreted. Such schemas are determined from childhood by our interactions with the external world. For example, a child who is constantly criticized may begin to believe she is worthless. She might then begin to interpret every failure experience as further evidence of her worthlessness. If this negative processing of information is not changed, it will become an enduring part of her cognitive organization, that is, a schema. When this schema is activated (e.g., by a poor grade on a test or any other failure experience), it will predispose her to depressive feelings (e.g., I’m no good). Beck stated that, as a result of this faulty information processing, depressed persons demonstrate a cognitive triad of negative thoughts about themselves, the world, and the future. He further extended his argument to include the manic phases of bipolar depressive disorders. Beck stated that such phases are characterized by a manic triad of irrationally positive thoughts about oneself, the world, and the future. Like the depressive triad in unipolar depressive disorders, the manic triad in bipolar depressive disorders was hypothesized to lead to the symptoms of mania, such as inflated selfesteem and extremely elevated mood.
There is widespread agreement that depression can be caused by different factors. Some theorists have argued that dysfunctional cognitions cause only a subset of depressions. Termed the “negative cognition” subtype, this type of depression is brought about by either the kinds of schemas discussed by Aaron Beck or by dysfunctional attributional patterns that lead depressed people to take responsibility for the occurrence of negative events, and to avoid taking responsibility for positive events. This dysfunctional attributional pattern can lead to a sense of hopelessness that results in a “hopelessness depression,” a component of negative cognition depression.
Although there are a variety of biologically based theories of depression, they can be broken down into two general approaches: genetic and neurotransmitter.
Genetic approaches suggest that depression is the result of inheriting genes that predispose to occurrence of depression. Three types of studies that are used to investigate genetic inheritance of depression illustrate this approach. These studies consist of family studies, twin studies, and adoption studies. In a typical family study, families with a depressed member are interviewed to determine how many other family members have or had an affective disorder. In twin studies, the concordance rate of affective disorder between monozygotic and dizygotic twin pairs is compared. Because monozygotic twins have identical genes, if genetic theories are correct then concordance rates of depression should be higher than for dizygotic twins (who have similar but not identical genes). In adoption studies, two strategies are most often used. In the first, the rate of depressive disorder in the biological parents of adopted persons with and without affective disorders is compared. In the second, the rate of depressive disorders is compared between adopted children with and without affectively disordered biological parents. Adoption studies have an advantage over family and twin studies, as the effects of environment on affective disorder are reduced in this design. However, adoption studies constitute the least-used approach to investigating genetic factors in depression; the difficulty of obtaining complete records on adoptees and their biological parents makes this design quite prohibitive.
Despite design differences, all three genetic approaches to the etiology of depression have yielded similar results: depression is heritable to at least some degree. A recent review of the research literature, for example, found rates of affective disorders among first-degree relatives of unipolar-disordered individuals ranging from 11.8% to 32.2%. Rates of affective disorders among first-degree relatives of bipolardisordered individuals ranged from 10.6% to 33.1%. Rates of affective disorder among first-degree relatives of normal individuals ranged from 4.8% to 6.3. In twin studies of unipolar and bipolar depression, concordance rates ranged from .04 to 1.0 for monozygotic twins, and from 0.0 to .43 to dizygotic twins, with the majority of studies reviewed reporting no concordance for dizygotic twins. The results of genetic investigations clearly suggest that there is a genetic component to depression, although the exact nature and functioning of this component is thus far still unknown.
Research on brain chemistry as an etiological factor in unipolar depression has focused on two monoamine neurotransmitters: norepinephrine (NE) and serotonin (5-HT). Initially, researchers believed that depression was due to a lack of NE in the brain, and later, to a lack of both NE and 5-HT. However, several difficulties with these hypotheses arose: (1) While the effects of antidepressants on monoamine levels start within hours of taking the medication, decreased depression levels do not become apparent until weeks later. (2) Some drugs that do not affect monoamine levels alleviate depression. (3) Some drugs that increase monoamine levels do not alleviate depression. Thus, researchers have directed their efforts to investigating more complicated relations between these neurotransmitters and depression. Recent efforts have included the study of receptor site hyposensitivity, relationships between NE and 5-HT, and relationships between. 5-HT and the neurotransmitter dopamine (DA).
Research on brain chemistry as in etiological factor in bipolar depression has followed much the same course as such research on unipolar depression. Initially, researchers believed that the mania characteristic of bipolar disorders was due to excesses of the neurotransmitters NE and 5-HT, exactly opposite the belief for depression. However, difficulties arose with this hypothesis, including findings that (1) lithium, the medical treatment of choice for bipolar disorder which seems to affect both NE and 5-HT, was effective at controlling both depression and mania, and (2) both depression and mania may be characterized by lower levels of 5-HT. Thus, as with unipolar depression, researchers of bipolar depression have begun investigating more complicated relationships between bipolar depression and neurotransmitters. Similar to the recent efforts concerning unipolar depression, researchers have investigated interactions between 5-HT and DA, interactions between NE and DA, and receptor site hypersensitivity. These types of investigations represent promising areas of research in elucidating the multifaceted etiology of depression. Certainly, biology and psychology are implicated in the causes of depression, both unipolar and bipolar forms.
Given the potentially devastating effects of depression, many researchers have devoted their efforts to studying factors that decrease the likelihood of becoming depressed or decrease the amount of time spent in depressive episodes. Among the most widely studied of such protective factors are social support and coping styles.
There are numerous facets to the concept of social support. For example, social support can be conceived as the number of persons one can rely on for support. Social support can also be conceived as the amount of support received, regardless of the number of persons one receives support from. In addition, socially supportive relationships can be conceptualized on a continuum of quality from very poor to very good. Examination of all these facets has proven important in understanding relationships between depression and social support.
Overall, people in contact with numerous socially supportive persons are less likely to have mental health difficulties, including depression. In addition, those who perceive a great deal of support from others are less likely to be negatively affected by stressors that might lead to depression. For people who have become depressed, having a confidant such as a spouse or best friend and a supportive family is related to greater success in treatment. The quality of such relationships is also important to treatment. In one study, for example, depressed persons with good-quality confidant relationships needed shorter periods of treatment than those with poor-quality confidant relationships.
The effects of social support for people with bipolar depressive disorders have not been as well studied as the effects for people with unipolar depressive disorders. Nonetheless, research suggests that social support is indeed beneficial for people with bipolar disorders. In one study, for example, a great deal of available social support was related to fewer psychological symptoms, better social adjustment, and better overall functioning.
Ways of coping with stressors can be roughly divided into two categories: approach strategies and avoidance strategies. Approach strategies are characterized by identifying the problematic situation, devising reasonable solutions to it, an implementing those solutions. Avoidance strategies include trying not to think about the problem, wishing the problem did not exist, and fantasizing about life without the problem. Overall, approach strategies seem to help people cope with stressors that might otherwise lead to depression. In addition, use of approach strategies is associated with better treatment outcome for those who become depressed. Conversely, people who use avoidance strategies to cope with stress seem more likely to become depressed and to have poorer treatment outcomes.
As with the effects of social support, research on coping styles among people with bipolar depressive disorders is scarce. Nonetheless, one recent study that examined differences in coping between high- and low-functioning people with bipolar disorders suggested that avoidant coping styles are associated with poorer functioning. Thus, relationships between coping styles and bipolar depressive disorders and coping and unipolar depressive disorders may be similar.
Bibliography:
- Beck, A. T. (1967). Depression: Causes and treatment. Philadelphia: University of Pennsylvania Press.
- Beckham, E. E., & Leber W. R. (1995). (Eds.). Handbook of depression (2nd ed. ). New York: Guilford Press.
- Cicchetti, D., & Toth, S. L. (1992). (Eds.). Developmental perspectives on depression. Rochester, NY: University of Rochester Press.
- Craig, K. D., & Dobson, K. S. (1995). (Eds.). Anxiety and depression in children and adults. Thousand Oaks, CA: Sage.
- Kendall, P. C., Hollon, S. D., Beck, A. T., Hammen, C. L., & Ingram, R. E. (1987). Issues and recommendations regarding use of the Beck Depression Inventory. Cognitive Therapy and Research, 11,289-299.
- Ingrain, R. E., Miranda, J., & Segal, Z. V. (in press). Cognitive vulnerability to depression. New York: Guilford Press.
- Robins, L. N., & Regier, D. A. (1991). (Eds.). Psychiatric disorders in America. New York: The Free Press.
ORDER HIGH QUALITY CUSTOM PAPER

- Introduction
- Conclusions
- Article Information
Outcomes are estimated from bivariate and multivariable generalized estimating equation models. aOR, indicates adjusted odds ratio; GAD-7, Generalized Anxiety Disorder 7-item scale; PHQ-9, Patient Health Questionnaire 9-item scale; whiskers, 95% CIs.
eTable 1. Survey Instruments
eTable 2. Prevalence of Exposure Over Time
eTable 3. Prevalence of Outcomes Over Time by Exposure Group
eTable 4. E-Value Calculation for Association Between Puberty Blockers or Gender-Affirming Hormones and Mental Health Outcomes
eTable 5. Examining Association Between Puberty Blockers or Gender-Affirming Hormones and Mental Health Outcomes Separately
eTable 6. Bivariate Model Restricted to Youths Ages 13 to 17 Years
eTable 7. Multivariable Model Restricted to 90 Youths Ages 13 to 17 Years
eTable 8. Sensitivity Analyses using Patient Health Questionnaire 8-item Scale Score of 10 or Greater for Moderate to Severe Depression
eFigure 1. Schematic of Generalized Estimating Equation Model
eFigure 2. Association Between Receipt of Gender-Affirming Hormones or Puberty Blockers and Mental Health Outcomes
eReferences
- Medical Groups Defend Patient-Physician Relationship and Access to Adolescent Gender-Affirming Care JAMA Medical News & Perspectives April 19, 2022 This Medical News article discusses physicians’ advocacy to protect patients and the patient-physician relationship amid efforts by politicians to limit access or criminalize gender-affirming care. Bridget M. Kuehn, MSJ
- As Laws Restricting Health Care Surge, Some US Physicians Choose Between Fight or Flight JAMA Medical News & Perspectives June 13, 2023 In this Medical News article, 13 physicians and health care experts spoke with JAMA about the increasing efforts to criminalize evidence-based medical care in the US. Melissa Suran, PhD, MSJ
- Data Errors in eTables 2 and 3 JAMA Network Open Correction July 26, 2022
- Improving Mental Health Among Transgender and Gender-Diverse Youth JAMA Network Open Invited Commentary February 25, 2022 Brett Dolotina, BS; Jack L. Turban, MD, MHS
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Tordoff DM , Wanta JW , Collin A , Stepney C , Inwards-Breland DJ , Ahrens K. Mental Health Outcomes in Transgender and Nonbinary Youths Receiving Gender-Affirming Care. JAMA Netw Open. 2022;5(2):e220978. doi:10.1001/jamanetworkopen.2022.0978
Manage citations:
© 2024
- Permissions
Mental Health Outcomes in Transgender and Nonbinary Youths Receiving Gender-Affirming Care
- 1 Department of Epidemiology, University of Washington, Seattle
- 2 Department of Psychiatry and Behavioral Sciences, University of Washington, Seattle
- 3 School of Medicine, University of Washington, Seattle
- 4 Department of Psychiatry and Behavioral Medicine, Department of Adolescent and Young Adult Medicine, Seattle Children’s Hospital, Seattle, Washington
- 5 University of California, San Diego School of Medicine, Rady Children's Hospital
- 6 Division of Adolescent Medicine, Department of Pediatrics, Seattle Children’s Hospital, Seattle, Washington
- Invited Commentary Improving Mental Health Among Transgender and Gender-Diverse Youth Brett Dolotina, BS; Jack L. Turban, MD, MHS JAMA Network Open
- Medical News & Perspectives Medical Groups Defend Patient-Physician Relationship and Access to Adolescent Gender-Affirming Care Bridget M. Kuehn, MSJ JAMA
- Medical News & Perspectives As Laws Restricting Health Care Surge, Some US Physicians Choose Between Fight or Flight Melissa Suran, PhD, MSJ JAMA
- Correction Data Errors in eTables 2 and 3 JAMA Network Open
Question Is gender-affirming care for transgender and nonbinary (TNB) youths associated with changes in depression, anxiety, and suicidality?
Findings In this prospective cohort of 104 TNB youths aged 13 to 20 years, receipt of gender-affirming care, including puberty blockers and gender-affirming hormones, was associated with 60% lower odds of moderate or severe depression and 73% lower odds of suicidality over a 12-month follow-up.
Meaning This study found that access to gender-affirming care was associated with mitigation of mental health disparities among TNB youths over 1 year; given this population's high rates of adverse mental health outcomes, these data suggest that access to pharmacological interventions may be associated with improved mental health among TNB youths over a short period.
Importance Transgender and nonbinary (TNB) youths are disproportionately burdened by poor mental health outcomes owing to decreased social support and increased stigma and discrimination. Although gender-affirming care is associated with decreased long-term adverse mental health outcomes among these youths, less is known about its association with mental health immediately after initiation of care.
Objective To investigate changes in mental health over the first year of receiving gender-affirming care and whether initiation of puberty blockers (PBs) and gender-affirming hormones (GAHs) was associated with changes in depression, anxiety, and suicidality.
Design, Setting, and Participants This prospective observational cohort study was conducted at an urban multidisciplinary gender clinic among TNB adolescents and young adults seeking gender-affirming care from August 2017 to June 2018. Data were analyzed from August 2020 through November 2021.
Exposures Time since enrollment and receipt of PBs or GAHs.
Main Outcomes and Measures Mental health outcomes of interest were assessed via the Patient Health Questionnaire 9-item (PHQ-9) and Generalized Anxiety Disorder 7-item (GAD-7) scales, which were dichotomized into measures of moderate or severe depression and anxiety (ie, scores ≥10), respectively. Any self-report of self-harm or suicidal thoughts over the previous 2 weeks was assessed using PHQ-9 question 9. Generalized estimating equations were used to assess change from baseline in each outcome at 3, 6, and 12 months of follow-up. Bivariate and multivariable logistic models were estimated to examine temporal trends and investigate associations between receipt of PBs or GAHs and each outcome.
Results Among 104 youths aged 13 to 20 years (mean [SD] age, 15.8 [1.6] years) who participated in the study, there were 63 transmasculine individuals (60.6%), 27 transfeminine individuals (26.0%), 10 nonbinary or gender fluid individuals (9.6%), and 4 youths who responded “I don’t know” or did not respond to the gender identity question (3.8%). At baseline, 59 individuals (56.7%) had moderate to severe depression, 52 individuals (50.0%) had moderate to severe anxiety, and 45 individuals (43.3%) reported self-harm or suicidal thoughts. By the end of the study, 69 youths (66.3%) had received PBs, GAHs, or both interventions, while 35 youths had not received either intervention (33.7%). After adjustment for temporal trends and potential confounders, we observed 60% lower odds of depression (adjusted odds ratio [aOR], 0.40; 95% CI, 0.17-0.95) and 73% lower odds of suicidality (aOR, 0.27; 95% CI, 0.11-0.65) among youths who had initiated PBs or GAHs compared with youths who had not. There was no association between PBs or GAHs and anxiety (aOR, 1.01; 95% CI, 0.41, 2.51).
Conclusions and Relevance This study found that gender-affirming medical interventions were associated with lower odds of depression and suicidality over 12 months. These data add to existing evidence suggesting that gender-affirming care may be associated with improved well-being among TNB youths over a short period, which is important given mental health disparities experienced by this population, particularly the high levels of self-harm and suicide.
Transgender and nonbinary (TNB) youths are disproportionately burdened by poor mental health outcomes, including depression, anxiety, and suicidal ideation and attempts. 1 - 5 These disparities are likely owing to high levels of social rejection, such as a lack of support from parents 6 , 7 and bullying, 6 , 8 , 9 and increased stigma and discrimination experienced by TNB youths. Multidisciplinary care centers have emerged across the country to address the health care needs of TNB youths, which include access to medical gender-affirming interventions, such as puberty blockers (PBs) and gender-affirming hormones (GAHs). 10 These centers coordinate care and help youths and their families address barriers to care, such as lack of insurance coverage 11 and travel times. 12 Gender-affirming care is associated with decreased rates of long-term adverse outcomes among TNB youths. Specifically, PBs, GAHs, and gender-affirming surgeries have all been found to be independently associated with decreased rates of depression, anxiety, and other adverse mental health outcomes. 13 - 16 Access to these interventions is also associated with a decreased lifetime incidence of suicidal ideation among adults who had access to PBs during adolescence. 17 Conversely, TNB youths who present to care later in adolescence or young adulthood experience more adverse mental health outcomes. 18 Despite this robust evidence base, legislation criminalizing and thus limiting access to gender-affirming medical care for minors is increasing. 19 , 20
Less is known about the association of gender-affirming care with mental health outcomes immediately after initiation of care. Several studies published from 2015 to 2020 found that receipt of PBs or GAHs was associated with improved psychological functioning 21 and body satisfaction, 22 as well as decreased depression 23 and suicidality 24 within a 1-year period. Initiation of gender-affirming care may be associated with improved short-term mental health owing to validation of gender identity and clinical staff support. Conversely, prerequisite mental health evaluations, often perceived as pathologizing by TNB youths, and initiation of GAHs may present new stressors that may be associated with exacerbation of mental health symptoms early in care, such as experiences of discrimination associated with more frequent points of engagement in a largely cisnormative health care system (eg, interactions with nonaffirming pharmacists to obtain laboratory tests, syringes, and medications). 25 Given the high risk of suicidality among TNB adolescents, there is a pressing need to better characterize mental health trends for TNB youths early in gender-affirming care. This study aimed to investigate changes in mental health among TNB youths enrolled in an urban multidisciplinary gender clinic over the first 12 months of receiving care. We also sought to investigate whether initiation of PBs or GAHs was associated with depression, anxiety, and suicidality.
This cohort study received approval from the Seattle Children’s Hospital Institutional Review Board. For youths younger than age 18 years, caregiver consent and youth assent was obtained. For youths ages 18 years and older, youth consent alone was obtained. The 12-month assessment was funded via a different mechanism than other survey time points; thus, participants were reconsented for the 12-month survey. The study follows the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
We conducted a prospective observational cohort study of TNB youths seeking care at Seattle Children’s Gender Clinic, an urban multidisciplinary gender clinic. After a referral is placed or a patient self-refers, new patients, their caregivers, or patients with their caregivers are scheduled for a 1-hour phone intake with a care navigator who is a licensed clinical social worker. Patients are then scheduled for an appointment at the clinic with a medical provider.
All patients who completed the phone intake and in-person appointment between August 2017 and June 2018 were recruited for this study. Participants completed baseline surveys within 24 hours of their first appointment and were invited to complete follow-up surveys at 3, 6, and 12 months. Youth surveys were used to assess most variables in this study; caregiver surveys were used to assess caregiver income. Participation and completion of study surveys had no bearing on prescribing of PBs or GAHs.
We assessed 3 internalizing mental health outcomes: depression, generalized anxiety, and suicidality. Depression was assessed using the Patient Health Questionnaire 9-item scale (PHQ-9), and anxiety was assessed using the Generalized Anxiety Disorder 7-item scale (GAD-7). We dichotomized PHQ-9 and GAD-7 scores into measures of moderate or severe depression and anxiety (ie, scores ≥10). 26 , 27 Self-harm and suicidal thoughts were assessed using PHQ-9 question 9 (eTable 1 in the Supplement ).
Participants self-reported if they had ever received GAHs, including estrogen or testosterone, or PBs (eg, gonadotropin-releasing hormone analogues) on each survey. We conducted a medical record review to capture prescription of androgen blockers (eg, spironolactone) and medications for menstrual suppression or contraception (ie, medroxyprogesterone acetate or levonorgestrel-releasing intrauterine device) during the study period.
We a priori considered potential confounders hypothesized to be associated with our exposures and outcomes of interest based on theory and prior research. Self-reported gender was ascertained on each survey using a 2-step question that asked participants about their current gender and their sex assigned at birth. If a participant’s self-reported gender changed across surveys, we used the gender reported most frequently by a participant (3 individuals identified as transmasculine at baseline and as nonbinary on all follow-up surveys). We collected data on self-reported race and ethnicity (available response options were Arab or Middle Eastern; Asian; Black or African American; Latinx; Native American, American Indian, or Alaskan Native or Native Hawaiian; Pacific Islander; and White), age, caregiver income, and insurance type. Race and ethnicity were assessed as potential covariates owing to known barriers to accessing gender-affirming care among transgender youth who are members of minority racial and ethnic groups. For descriptive statistics, Asian and Pacific Islander groups were combined owing to small population numbers. We included a baseline variable reflecting receipt of ongoing mental health therapy other than for the purpose of a mental health assessment to receive a gender dysphoria diagnosis. We included a self-report variable reflecting whether youths felt their gender identity or expression was a source of tension with their parents or guardians. Substance use included any alcohol, marijuana, or other drug use in the past year. Resilience was measured by the Connor-Davidson Resilience Scale (CD-RISC) 10-item score developed to measure change in an individual’s state resilience over time. 28 Resilience scores were dichotomized into high (ie, ≥median) and low (ie, <median). Prior studies of young adults in the US reported mean CD-RISC scores ranging from 27.2 to 30.1. 29 , 30
We used generalized estimating equations to assess change in outcomes from baseline at each follow-up point (eFigure 1 in the Supplement ). We used a logit link function to estimate adjusted odds ratio (aOR) for the association between variables and each mental health outcome. We initially estimated bivariate associations between potential confounders and mental health outcomes. Multivariable models included variables that were statistically significant in bivariate models. For all outcomes and models, statistical significance was defined as 95% CIs that did not contain 1.00. Reported P values are based on 2-sided Wald test statistics.
Model 1 examined temporal trends in mental health outcomes, with time (ie, baseline, 3, 6, and 12 months) modeled as a categorical variable. Model 2 estimated the association between receipt of PBs or GAHs and mental health outcomes adjusted for temporal trends and potential confounders. Receipt of PBs or GAHs was modeled as a composite binary time-varying exposure that compared mean outcomes between participants who had initiated PBs or GAHs and those who had not across all time points (eTable 2 in the Supplement ). All models used an independent working correlation structure and robust standard errors to account for the time-varying exposure variable.
We performed several sensitivity analyses. Because our data were from an observational cohort, we first considered the degree to which they were sensitive to unmeasured confounding. To do this, we calculated the E-value for the association between PBs or GAHs and mental health outcomes in model 2. The E-value is defined as the minimum strength of association that a confounder would need to have with both exposure and outcome to completely explain away their association (eTable 4 in the Supplement ). 31 Second, we performed sensitivity analyses on several subsets of youths. We separately examined the association of PBs and GAHs with outcomes of interest, although we a priori did not anticipate being powered to detect statistically significant outcomes owing to our small sample size and the relatively low proportion of youths who accessed PBs. We also conducted sensitivity analyses using the Patient Health Questionnaire 8-item scale (PHQ-8), in which the PHQ-9 question 9 regarding self-harm or suicidal thoughts was removed, given that we analyzed this item as a separate outcome. Lastly, we restricted our analysis to minor youths ages 13 to 17 years because they were subject to different laws and policies related to consent and prerequisite mental health assessments. We used R statistical software version 3.6.2 (R Project for Statistical Computing) to conduct all analyses. Data were analyzed from August 2020 through November 2021.
A total of 169 youths were screened for eligibility during the study period, among whom 161 eligible youths were approached. Nine youths or caregivers declined participation, and 39 youths did not complete consent or assent or did not complete the baseline survey, leaving a sample of 113 youths (70.2% of approached youths). We excluded 9 youths aged younger than 13 years from the analysis because they received different depression and anxiety screeners. Our final sample included 104 youths ages 13 to 20 years (mean [SD] age, 15.8 [1.6] years). Of these individuals, 84 youths (80.8%), 84 youths, and 65 youths (62.5%) completed surveys at 3, 6, and 12 months, respectively.
Our cohort included 63 transmasculine youths (60.6%), 27 transfeminine youths (26.0%), 10 nonbinary or gender fluid youths (9.6%), and 4 youths who responded “I don’t know” or did not respond to the gender identity question on all completed questionnaires (3.8%) ( Table 1 ). There were 4 Asian or Pacific Islander youths (3.8%), 3 Black or African American youths (2.9%); 9 Latinx youths (8.7%); 6 Native American, American Indian, or Alaskan Native or Native Hawaiian youths (5.8%); 67 White youths (64.4%); and 9 youths who reported more than 1 race or ethnicity (8.7%). Race and ethnicity data were missing for 6 youth (5.8%).
At baseline, 7 youths had ever received PBs or GAHs (including 1 youth who received PBs, 4 youths who received GAHs, and 2 youths who received both PBs and GAHs). By the end of the study, 69 youths (66.3%) had received PBs or GAHs (including 50 youths who received GAHs only [48.1%], 5 youths who received PBs only [4.8%], and 14 youths who received PBs and GAHs [13.5%]), while 35 youths had not received either PBs or GAHs (33.7%) (eTable 3 in the Supplement ). Among 33 participants assigned male sex at birth, 17 individuals (51.5%) had received androgen blockers, and among 71 participants assigned female sex at birth, 25 individuals (35.2%) had received menstrual suppression or contraceptives by the end of the study.
A large proportion of youths reported depressive and anxious symptoms at baseline. Specifically, 59 individuals (56.7%) had baseline PHQ-9 scores of 10 or more, suggesting moderate to severe depression; there were 22 participants (21.2%) scoring in the moderate range, 11 participants (10.6%) in the moderately severe range, and 26 participants (25.0%) in the severe range. Similarly, half of participants had a GAD-7 score suggestive of moderate to severe anxiety at baseline (52 individuals [50.0%]), including 20 participants (19.2%) scored in the moderate range, and 32 participants (30.8%) scored in the severe range. There were 45 youths (43.3%) who reported self-harm or suicidal thoughts in the prior 2 weeks. At baseline, 65 youths (62.5%) were receiving ongoing mental health therapy, 36 youths (34.6%) reported tension with their caregivers about their gender identity or expression, and 34 youths (32.7%) reported any substance use in the prior year. Lastly, we observed a wide range of resilience scores (median [range], 22.5 [1-38], with higher scores equaling more resiliency). There were no statistically significant differences in baseline characteristics by gender.
In bivariate models, substance use was associated with all mental health outcomes ( Table 2 ). Youths who reported any substance use were 4-fold as likely to have PHQ-9 scores of moderate to severe depression (aOR, 4.38; 95% CI, 2.10-9.16) and 2-fold as likely to have GAD-7 scores of moderate to severe anxiety (aOR, 2.07; 95% CI, 1.04-4.11) or report thoughts of self-harm or suicide in the prior 2 weeks (aOR, 2.06; 95% CI, 1.08-3.93). High resilience scores (ie, ≥median), compared with low resilience scores (ie, <median), were associated with lower odds of moderate or severe anxiety (aOR, 0.51; 95% CI, 0.26-0.999).
There were no statistically significant temporal trends in the bivariate model or model 1 ( Table 2 and Table 3 ). However, among all participants, odds of moderate to severe depression increased at 3 months of follow-up relative to baseline (aOR, 2.12; 95% CI, 0.98-4.60), which was not a significant increase, and returned to baseline levels at months 6 and 12 ( Figure ) prior to adjusting for receipt of PBs or GAHs.
We also examined the association between receipt of PBs or GAHs and mental health outcomes in bivariate and multivariable models (eFigure 2 in the Supplement ). After adjusting for temporal trends and potential confounders ( Table 4 ), we observed that youths who had initiated PBs or GAHs had 60% lower odds of moderate to severe depression (aOR, 0.40; 95% CI, 0.17-0.95) and 73% lower odds of self-harm or suicidal thoughts (aOR, 0.27; 95% CI, 0.11-0.65) compared with youths who had not yet initiated PBs or GAHs. There was no association between receipt of PBs or GAHs and moderate to severe anxiety (aOR, 1.01; 95% CI, 0.41-2.51). After adjusting for time-varying exposure of PBs or GAHs in model 2 ( Table 4 ), we observed statistically significant increases in moderate to severe depression among youths who had not received PBs or GAHs by 3 months of follow-up (aOR, 3.22; 95% CI, 1.37-7.56). A similar trend was observed for self-harm or suicidal thoughts among youths who had not received PBs or GAHs by 6 months of follow-up (aOR, 2.76; 95% CI, 1.22-6.26). Lastly, we estimated E-values of 2.56 and 3.25 for the association between receiving PGs or GAHs and moderate to severe depression and suicidality, respectively (eTable 4 in the Supplement ). Sensitivity analyses obtained comparable results and are presented in eTables 5 through 8 in the Supplement .
In this prospective clinical cohort study of TNB youths, we observed high rates of moderate to severe depression and anxiety, as well as suicidal thoughts. Receipt of gender-affirming interventions, specifically PBs or GAHs, was associated with 60% lower odds of moderate to severe depressive symptoms and 73% lower odds of self-harm or suicidal thoughts during the first year of multidisciplinary gender care. Among youths who did not initiate PBs or GAHs, we observed that depressive symptoms and suicidality were 2-fold to 3-fold higher than baseline levels at 3 and 6 months of follow-up, respectively. Our study results suggest that risks of depression and suicidality may be mitigated with receipt of gender-affirming medications in the context of a multidisciplinary care clinic over the relatively short time frame of 1 year.
Our findings are consistent with those of prior studies finding that TNB adolescents are at increased risk of depression, anxiety, and suicidality 1 , 11 , 32 and studies finding long-term and short-term improvements in mental health outcomes among TNB individuals who receive gender-affirming medical interventions. 14 , 21 - 24 , 33 , 34 Surprisingly, we observed no association with anxiety scores. A recent cohort study of TNB youths in Dallas, Texas, found that total anxiety symptoms improved over a longer follow-up of 11 to 18 months; however, similar to our study, the authors did not observe statistically significant improvements in generalized anxiety. 22 This suggests that anxiety symptoms may take longer to improve after the initiation of gender-affirming care. In addition, Olson et al 35 found that prepubertal TNB children who socially transitioned did not have increased rates of depression symptoms but did have increased rates of anxiety symptoms compared with children who were cisgender. Although social transition and access to gender-affirming medical care do not always go hand in hand, it is noteworthy that access to gender-affirming medical care and supported social transition appear to be associated with decreased depression and suicidality more than anxiety symptoms.
Time trends were not significant in our study; however, it is important to note that we observed a transient and nonsignificant worsening in mental health outcomes in the first several months of care among all participants and that these outcomes subsequently returned to baseline by 12 months. This is consistent with findings from a 2020 study 36 in an academic medical center in the northwestern US that observed no change in TNB adolescents’ GAD-7 or PHQ-9 scores from intake to first follow-up appointment, which occurred a mean of 4.7 months apart. Given that receipt of PBs or GAHs was associated with protection against depression and suicidality in our study, it could be that delays in receipt of medications is associated with initially exacerbated mental health symptoms that subsequently improve. It is also possible that mental health improvements associated with receiving these interventions may have a delayed onset, given the delay in physical changes after starting GAHs.
Few of our hypothesized confounders were associated with mental health outcomes in this sample, most notably receipt of ongoing mental health therapy and caregiver support; however, this is not surprising given that these variables were colinear with baseline mental health, which we adjusted for in all models. Substance use was the only variable associated with all mental health outcomes. In addition, youths with high baseline resilience scores were half as likely to experience moderate to severe anxiety as those with low scores. This finding suggests that substance use and resilience may be additional modifiable factors that could be addressed through multidisciplinary gender-affirming care. We recommend more granular assessment of substance use and resilience to better understand support needs (for substance use) and effective support strategies (for resilience) for TNB youths in future research.
This study has a number of strengths. This is one of the first studies to quantify a short-term transient increase in depressive symptoms experienced by TNB youths after initiating gender-affirming care, a phenomenon observed clinically by some of the authors and described in qualitative research. 37 Although we are unable to make causal statements owing to the observational design of the study, the strength of associations between gender-affirming medications and depression and suicidality, with large aOR values, and sensitivity analyses that suggest that these findings are robust to moderate levels of unmeasured confounding. Specifically, E-values calculated for this study suggest that the observed associations could be explained away only by an unmeasured confounder that was associated with both PBs and GAHs and the outcomes of interest by a risk ratio of 2-fold to 3-fold each, above and beyond the measured confounders, but that weaker confounding could not do so. 31
Our findings should be interpreted in light of the following limitations. This was a clinical sample of TNB youths, and there was likely selection bias toward youths with supportive caregivers who had resources to access a gender-affirming care clinic. Family support and access to care are associated with protection against poor mental health outcomes, and thus actual rates of depression, anxiety, and suicidality in nonclinical samples of TNB youths may differ. Youths who are unable to access gender-affirming care owing to a lack of family support or resources require particular emphasis in future research and advocacy. Our sample also primarily included White and transmasculine youths, limiting the generalizability of our findings. In addition, the need to reapproach participants for consent and assent for the 12-month survey likely contributed to attrition at this time point. There may also be residual confounding because we were unable to include a variable reflecting receipt of psychotropic medications that could be associated with depression, anxiety, and self-harm and suicidal thought outcomes. Additionally, we used symptom-based measures of depression, anxiety, and suicidality; further studies should include diagnostic evaluations by mental health practitioners to track depression, anxiety, gender dysphoria, suicidal ideation, and suicide attempts during gender care. 2
Our study provides quantitative evidence that access to PBs or GAHs in a multidisciplinary gender-affirming setting was associated with mental health improvements among TNB youths over a relatively short time frame of 1 year. The associations with the highest aORs were with decreased suicidality, which is important given the mental health disparities experienced by this population, particularly the high levels of self-harm and suicide. Our findings have important policy implications, suggesting that the recent wave of legislation restricting access to gender-affirming care 19 may have significant negative outcomes in the well-being of TNB youths. 20 Beyond the need to address antitransgender legislation, there is an additional need for medical systems and insurance providers to decrease barriers and expand access to gender-affirming care.
Accepted for Publication: January 10, 2022.
Published: February 25, 2022. doi:10.1001/jamanetworkopen.2022.0978
Correction: This article was corrected on July 26, 2022, to fix minor errors in the numbers of patients in eTables 2 and 3 in the Supplement.
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2022 Tordoff DM et al. JAMA Network Open .
Corresponding Author: Diana M. Tordoff, MPH, Department of Epidemiology, University of Washington, UW Box 351619, Seattle, WA 98195 ( [email protected] ).
Author Contributions : Diana Tordoff had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Diana Tordoff and Dr Wanta are joint first authors. Drs Inwards-Breland and Ahrens are joint senior authors.
Concept and design: Collin, Stepney, Inwards-Breland, Ahrens.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Tordoff, Wanta, Collin, Stepney, Inwards-Breland.
Critical revision of the manuscript for important intellectual content: Wanta, Collin, Stepney, Inwards-Breland, Ahrens.
Statistical analysis: Tordoff.
Obtained funding: Inwards-Breland, Ahrens.
Administrative, technical, or material support: Ahrens.
Supervision: Wanta, Inwards-Breland, Ahrens.
Conflict of Interest Disclosures: Diana Tordoff reported receiving grants from the National Institutes of Health National Institute of Allergy and Infectious Diseases unrelated to the present work and outside the submitted work. No other disclosures were reported.
Funding/Support: This study was supported Seattle Children’s Center for Diversity and Health Equity and the Pacific Hospital Preservation Development Authority.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Share full article
Advertisement
The Morning
Americans’ struggle with mental health.
We explore why rates of anxiety and depression are higher than they were before the pandemic.

By Ellen Barry
I cover mental health.
It is no mystery why rates of anxiety and depression in the United States climbed in 2020, at the height of the pandemic. But then life began a slow return to normal. Why haven’t rates of distress returned to normal, too?
Self-reported anxiety and depression have declined from the peak they reached in November 2020, when 42.6 percent of adults said they had symptoms, according to the Household Pulse Survey, a Census Bureau tool that measures well-being. Since then, that figure has declined to 20.7 percent. That’s still double the 11 percent of Americans who said the same thing before the pandemic.
In today’s newsletter, I’ll explain why. Researchers say a big reason for this stubbornly elevated distress is young people, whose low mood was not linked to the pandemic.
A youth epidemic
The share of young adults reporting anxiety and depression had been rising for about a decade before Covid struck. That continued throughout the pandemic — and did not ease as quickly when vaccines became available.
This is likely because their symptoms were tied to problems other than the virus, like economic precarity, the housing crisis, social isolation and political turmoil, said Emma Adam, a psychologist at Northwestern. “There’s so many things affecting adolescents and young adults that are about uncertainty with their future,” Adam said. “And that hasn’t changed.”
Age, of course, tracks with income. Adam’s team found that people between the ages of 18 and 39 were half as likely to live in their own home as their counterparts over 40. That means they were especially vulnerable to inflation, rent increases and job loss — just as they faced big decisions like whether to have children or own a home.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
ORIGINAL RESEARCH article
Evolution and emerging trends in depression research from 2004 to 2019: a literature visualization analysis.

- 1 School of Traditional Chinese Medicine, Beijing University of Chinese Medicine, Beijing, China
- 2 School of Life Sciences, Beijing University of Chinese Medicine, Beijing, China
Depression has become a major threat to human health, and researchers around the world are actively engaged in research on depression. In order to promote closer research, the study of the global depression knowledge map is significant. This study aims to map the knowledge map of depression research and show the current research distribution, hotspots, frontiers, and trends in the field of depression research, providing researchers with worthwhile information and ideas. Based on the Web of Science core collection of depression research from 2004 to 2019, this study systematically analyzed the country, journal, category, author, institution, cited article, and keyword aspects using bibliometric and data visualization methods. A relationship network of depression research was established, highlighting the highly influential countries, journals, categories, authors, institutions, cited articles, and keywords in this research field. The study identifies great research potential in the field of depression, provides scientific guidance for researchers to find potential collaborations through collaboration networks and coexistence networks, and systematically and accurately presents the hotspots, frontiers, and shortcomings of depression research through the knowledge map of global research on depression with the help of information analysis and fusion methods, which provides valuable information for researchers and institutions to determine meaningful research directions.
Introduction
Health issues are becoming more and more important to people due to the continuous development of health care. The social pressures on people are becoming more and more pronounced in a social environment that is developing at an increasing rate. Prolonged exposure to stress can have a negative impact on brain development ( 1 ), and depression is one of the more typical disorders that accompany it. Stress will increase the incidence of depression ( 2 ), depression has become a common disease ( 3 ), endangering people's physical health. Depression is a debilitating mental illness with mood disorders, also known as major depression, clinical depression, or melancholia. In human studies of the disease, it has been found that depression accounts for a large proportion of the affected population. According to the latest data from the World Health Organization (WHO) statistics in 2019, there are more than 350 million people with depression worldwide, with an increase of about 18% in the last decade and an estimated lifetime prevalence of 15% ( 4 ), it is a major cause of global disability and disease burden ( 5 ), and depression has quietly become a disease that threatens hundreds of millions of people worldwide.
Along with the rise of science communication research, the quantification of science is also flourishing. As a combination of “data science” and modern science, bibliometrics takes advantage of the explosive growth of research output in the era of big data, and uses topics, authors, publications, keywords, references, citations, etc. as research targets to reveal the current status and impact of the discipline more accurately and scientifically. Whereas, there is not a wealth of bibliometric studies related to depression. Fusar-Poli et al. ( 6 ) used bibliometrics to systematically evaluate cross-diagnostic psychiatry. Hammarström et al. ( 7 ) used bibliometrics to analyze the scientific quality of gender-related explanatory models of depression in the medical database PubMed. Tran et al. ( 8 ) used the bibliometric analysis of research progress and effective interventions for depression in AIDS patients. Wang et al. ( 9 ) used bibliometric methods to analyze scientific studies on the comorbidity of pain and depression. Shi et al. ( 10 ) performed a bibliometric analysis of the top 100 cited articles on biomarkers in the field of depression. Dongping et al. ( 11 ) used bibliometric analysis of studies on the association between depression and gut flora. An Chunping et al. ( 12 ) analyzed the literature on acupuncture for depression included in PubMed based on bibliometrics. Yi and Xiaoli ( 13 ) used a bibliometric method to analyze the characteristics of the literature on the treatment of depression by Chinese medicine in the last 10 years. Zhou and Yan ( 14 ) used bibliometric method to analyze the distribution of scientific and technological achievements on depression in Peoples R China. Guaijuan ( 15 ) performed a bibliometric analysis of the interrelationship between psoriasis and depression. Econometric analysis of the relationship between vitamin D deficiency and depression was performed by Yunzhi et al. ( 16 ) and Shauni et al. ( 17 ) performed a bibliometric analysis of domestic and international research papers on depression-related genes from 2003 to 2007. A previous review of depression-related bibliometric studies revealed that there is no bibliometric analysis of global studies in the field of depression, including country network analysis, journal network analysis, category network analysis, author network analysis, institutional network analysis, literature co-citation analysis, keyword co-presentation analysis, and cluster analysis.
The aim of this study was to conduct a comprehensive and systematic literature-based data mining and metrics analysis of depression-related research. More specifically, this analysis focuses on cooperative network and co-presentation analysis, based on the 36,477 papers included in the Web of Science Core Collection database from 2004 to 2019, and provides an in-depth analysis of cooperative network, co-presentation network, and co-citation through modern metrics and data visualization methods. Through the mining of key data, the data correlation is further explored, and the results obtained can be used to scientifically and reasonably predict the depression-related information. This study aims to show the spatial and temporal distribution of research countries, journals, authors, and institutions in the field of depression in a more concise manner through a relational network. A deeper understanding of the internal structure of the research community will help researchers and institutions to establish more accurate and effective global collaborations, in line with the trend of human destiny and globalization. In addition, the study will allow for the timely identification of gaps in current research. A more targeted research direction will be established, a more complete picture of the new developments in the field of depression today will be obtained, and the research protocol will be informed for further adjustments. The results of these analyses will help researchers understand the evolution of this field of study. Overall, this paper uses literature data analysis to find research hotspots in the field of depression, analyze the knowledge structure within different studies, and provide a basis for predicting research frontiers. This study analyzed the literature in the field of depression using CiteSpace 5.8.R2 (64-bit) to analyze collaborative networks, including country network analysis, journal network analysis, category network analysis, researcher network analysis, and institutional network analysis using CiteSpace 5.8.R2 (64-bit). In addition, literature co-citation, keyword co-presentation, and cluster analysis of depression research hotspots were also performed. Thus, exploring the knowledge dimensions of the field, quantifying the research patterns in the field, and uncovering emerging trends in the field will help to obtain more accurate and complete information. The large amount of current research results related to depression will be presented more intuitively and accurately with the medium of information technology, and the scientific evaluation of research themes and trend prediction will be provided from a new perspective.
Data Sources
The data in this paper comes from the Web of Science (WoS) core collection. The time years were selected as 2004–2019. First, the literature was retrieved after entering “depression” using the title search method. A total of 73,829 articles, excluding “depression” as “suppression,” “decline,” “sunken,” “pothole,” “slump,” “low pressure,” “frustration.” The total number of articles with other meanings such as “depression” was 5,606, and the total number of valid articles related to depression was 68,223. Next, the title search method was used to search for studies related to “major depressive disorder” not “depression,” and a total of 8,070 articles were retrieved. For the two search strategies, a total of 76,293 records were collected. The relevant literature retrieved under the two methods were combined and exported in “plain text” file format. The exported records included: “full records and references cited.” CiteSpace processed the data to obtain 41,408 valid records, covering all depression-related research articles for the period 2004–2019, and used this as the basis for analysis.
Processing Tools
CiteSpace ( 18 ), developed by Chao-Mei Chen, a professor in the School of Information Science and Technology at Drexel University, is a Java-based program with powerful data visualization capabilities and is one of the most widely used knowledge mapping tools. The software version used in this study is CiteSpace 5.8.R2 (64-bit).
Methods of Analysis
This study uses bibliometrics and data visualization as analytical methods. First, the application of bibliometrics to the field of depression helped to identify established and emerging research clusters, demonstrating the value of research in this area. Second, data visualization provides multiple perspectives on the data, presenting correlations in a clearer “knowledge graph” that can reveal underestimated and overlooked trends, patterns, and differences ( 19 ). CiteSpace is mainly based on the “co-occurrence clustering idea,” which extracts the information units (keywords, authors, institutions, countries, journals, etc.) in the data by classification, and then further reconstructs the data in the information units to form networks based on different types and strengths of connections (e.g., keyword co-occurrence, author collaboration, etc.). The resulting networks include nodes and links, where the nodes represent the information units of the literature and the links represent the existence of connections (co-occurrence) between the nodes. Finally, the network is measured, statistically analyzed, and presented in a visual way. The analysis needs to focus on: the overall structure of the network, key nodes and paths. The key evaluation indicators in this study are: betweenness centrality, year, keyword frequency, and burst strength. Betweenness centrality (BC) is the number of times a node acts as the shortest bridge between two other nodes. The higher the number of times a node acts as an “intermediary,” the greater its betweenness centrality. Betweenness centrality is a measure of the importance of articles found and measured by nodes in the network by labeling the category (or authors, journals, institutions, etc.) with purple circles. There may be many shortest paths between two nodes in the network, and by counting all the shortest paths of any two nodes in the network, if many of the shortest paths pass through a node, then the node is considered to have high betweenness centrality. In CiteSpace, nodes with betweenness centrality over 0.1 are called critical nodes. Year, which represents the publication time of the article. Frequency, which represents the number of occurrences. Burst strength, an indicator used to measure articles with sudden rise or sudden decline in citations. Nodes with high burst strength usually represent a shift in a certain research area and need to be focused on, and the burst article points are indicated in red. The nodes and their sizes and colors are first analyzed initially, and further analyzed by betweenness centrality indicators for evaluation. Each node represents an article, and the larger the node, the greater the frequency of the keyword word and the greater the relevance to the topic. Similarly, the color of the node represents time: the warmer the color, the more recent the time; the colder the color, the older the era; the node with a purple outer ring is a node with high betweenness centrality; the color of each annual ring can determine the time distribution: the color of the annual ring represents the corresponding time, and the thickness of one annual ring is proportional to the number of articles within the corresponding time division; the dominant color can reflect the relative concentration of the emergence time; the node The appearance of red annual rings in the annual rings means hot spots, and the frequency of citations has been or is still increasing rapidly.
Large-Scale Assessment
Country analysis.
During the period 2004–2019, a total of 157 countries/territories have conducted research on depression, which is about 67.38% of 233 countries/territories worldwide. This shows that depression is receiving attention from many countries/regions around the world. Figure 1 shows the geographical distribution of published articles for 157 countries. The top 15 countries are ranked according to the number of articles published. Table 1 lists the top 15 countries with the highest number of publications in the field of depression worldwide from 2004 to 2019. These 15 countries include 4 Asian countries (Peoples R China, Japan, South Korea, Turkey), 2 North American countries (USA, Canada), 1 South American country (Brazil), 7 European countries (UK, Germany, Netherlands, Italy, France, Spain, Sweden), and 1 Oceania country (Australia).
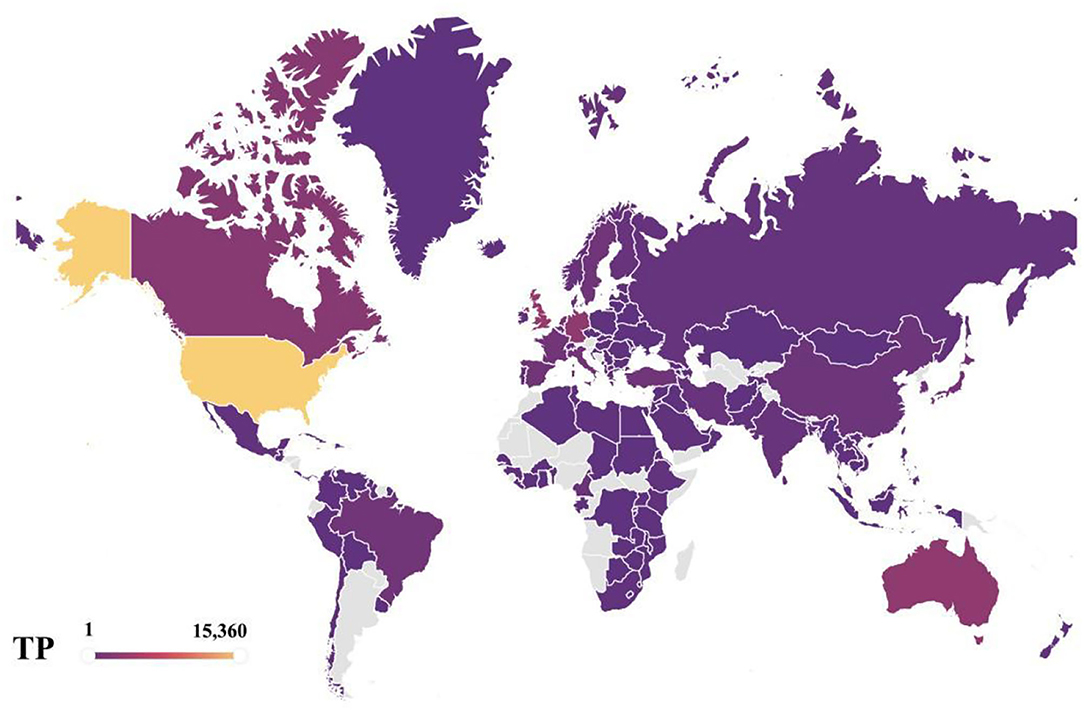
Figure 1 . Geographical distributions of publications, 2004–2019.
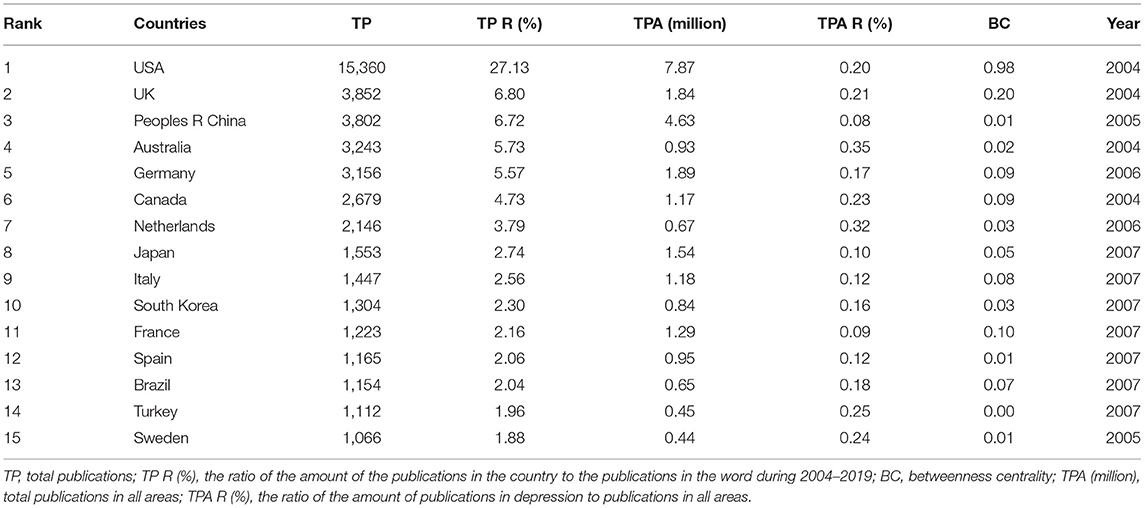
Table 1 . The top 15 productive countries.
Overall, the main distribution of these articles is in USA and some European countries, such as UK, Germany, Netherlands, Italy, France, Spain, and Sweden. This means that these countries are more interested and focused on research on depression compared to others. The total number of publications across all research areas in the Web of Science core collection is similar to the distribution of depression research areas, with the trend toward USA, UK, and Peoples R China as leading countries being unmistakable, and USA has been a leader in the field of depression, with far more articles published than any other country. It can also be seen that USA is the country with the highest betweenness centrality in the network of national collaborations analyzed in this paper. USA research in the field of depression is closely linked to global research, and is an important part of the global collaborative network for depression research. As of 2019, the total number of articles published in depression performance research in USA represents 27.13% of the total number of articles published in depression worldwide, which is ~4 times more than the second-place country, UK, which is far ahead of other countries. Peoples R China, as the third most published country, has a dominant number of articles, but its betweenness centrality is 0.01, reflecting the fact that Peoples R China has less collaborative research with other countries, so Peoples R China should strengthen its foreign collaborative research and actively establish global scientific research partnerships to seek development and generate breakthroughs in cooperation. The average percentage of scientific research on depression in each country is about 0.19%, also highlighting the urgent need to address depression as one of the global human health problems. The four Asian countries included in the top 15 countries are Peoples R China, Japan, South Korea, and Turkey, with Peoples R China ranking third with 6.72% of the total number of all articles counted. The distribution may be explained by the fact that Peoples R China is the largest developing country with a rapid development rate as the largest. Along with the steady rise in the country's economic power, people are creating economic benefits and their health is becoming a consumable commodity. The lifetime prevalence and duration of depression varies by country and region ( 2 ), but the high prevalence and persistence of depression worldwide confirms the increasing severity of the disease worldwide. The WHO estimates that more than 300 million people, or 4.4% of the world's population, suffer from depression ( 20 ), with the number of people suffering from depression increasing at a patient rate of 18.4% between 2005 and 2015. Depression, one of the most prevalent mental illnesses of our time, has caused both physical and psychological harm to many people, and it has become the leading cause of disability worldwide today, and in this context, there is increased interest and focus on research into depression. It is expected that a more comprehensive understanding of depression and finding ways to prevent and cope with the occurrence of this disease can help people get rid of the pain and shadow brought by depression, obtain a healthy and comfortable physical and mental environment and physical health, and make Chinese contributions to the cause of human health. Undoubtedly, the occurrence of depressive illnesses in the context of irreversible human social development has stimulated a vigorous scientific research environment on depression in Peoples R China and other developing countries and contributed to the improvement of research capacity in these countries. Moreover, from a different perspective, the geographical distribution of articles in this field also represents the fundamental position of the country in the overall scientific and academic research field.
Growth Trend Analysis
Figure 2 depicts the distribution of 38,433 articles from the top 10 countries in terms of the number of publications and the trend of growth during 2004–2019.
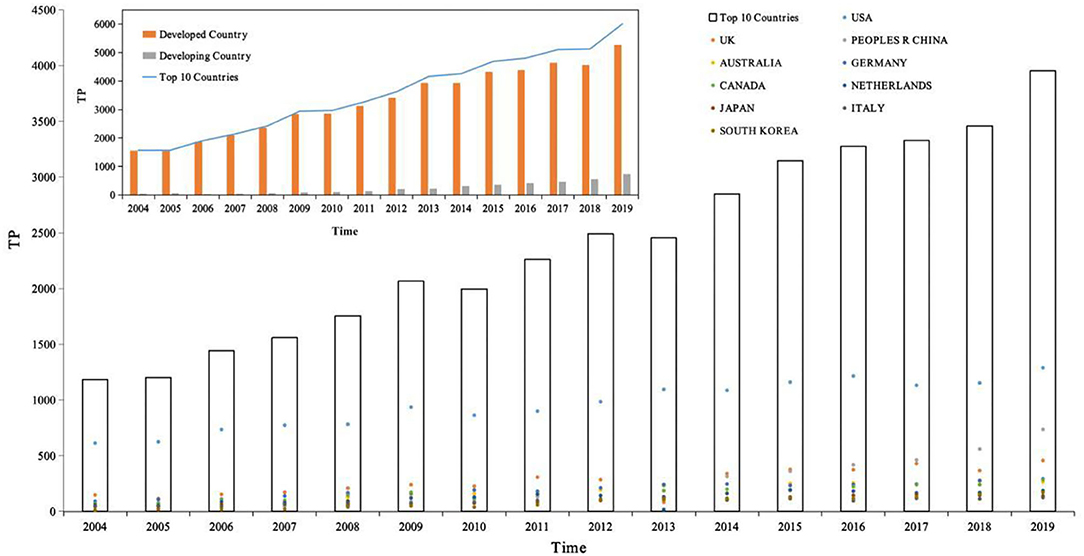
Figure 2 . The distribution of publications in top 10 productive countries, 2004–2019. Source: author's calculation. National development classification criteria refer to “Human Development Report 2020” ( 21 ).
First, the number of articles published per year for the top 10 countries in terms of productivity was counted and then the white bar chart in Figure 2 was plotted, with the year as the horizontal coordinate and total publications as the vertical coordinate, showing the distribution of the productivity of articles in the field of depression per year. The total number of publications for the period 2004–2019 is 38,433. Based on the white bars and line graphs in Figure 2 , we can divide this time period into three growth periods. The number of publications in each growth period is calculated based on the number of publications per year. As can be seen from the figure, the period 2004–2019 can be divided into three main growth periods, namely 2004–2009, 2010–2012, and 2013–2019, the first growth period being from 2004 to 2009, the number of publications totaled 6,749, accounting for 23.97% of all publications; from 2010 to 2012, the number of publications totaled 8,236, accounting for 17.56% of all publications; and from 2013 to 2019, the number of publications totaled 22,473, accounting for 58.47% of all publications. Of these, 2006 was the first year of sharp growth with an annual growth rate of 19.97%, 2009 was the second year of sharp growth with an annual growth rate of 17.64%, and 2008 was the third year of sharp growth with an annual growth rate of 16.09%. In the last 5 years, 2019 has also shown a sharp growth trend with a growth rate of 14.34%. Notably, in 2010 and 2013, there was negative growth with the growth rate of −3.39 and −1.45%. In the last 10 years, depression research has become one of the most valuable areas of human research. It can also be noted that the number of publications in the field of depression in these 10 countries has been increasing year after year.
Second, the analysis is conducted from the perspective of national development, divided into developed and developing countries, as shown in the orange bar chart in Figure 2 , where the horizontal coordinate is year and the vertical coordinate is total publications, comparing the article productivity variability between developed and developing countries. The top 10 most productive countries in the field of depression globally include nine developed countries and one developing country, respectively. During the period 2004–2019, 34,631 papers were published in developed countries and 3,802 papers were published in developing countries, with developed countries accounting for 90.11% of the 38,433 articles and developing countries accounting for 9.89%, and the total number of publications in developed countries was about 9 times higher than that in developing countries. During the period 2004–2019, the number of publications in developed countries showed negative growth in 2 years (2010 and 2013) with growth rates of −3.39 and −1.45%, respectively. The rest of the years showed positive growth with growth rates of 1.52% (2005), 19.97 (2006), 8.11 (2007), 12.70 (2008), 17.64 (2009), 13.22 (2011), 10.17 (2012), 16.09 (2014), 10.46 (2015), 4.10 (2016), 1.59 (2017), 3.91 (2018), and 14.34 (2019), showing three periods of positive growth: 2004–2009, 2011–2012, and 2014–2019, with the highest growth rate of 19.97% in 2006. Recent years have also shown a higher growth trend, with a growth rate of 14.34% in 2019. It is worth noting that developing countries have been showing positive growth in the number of articles in the period 2004–2019, with annual growth rates of 81.25 (2005), 17.24 (2006), 35.29 (2007), 19.57 (2008), 65.45 (2009), 13.19 (2010), 29.13 (2011), 54.89 (2012), 12.14 (2013), 36.36 (2014), 14.92 (2015), 16.02 (2016), 10.24 (2017), 21.17 (2018), and 31.37 (2019), with the highest growth rate of 81.25% in 2005. In the field of depression research, developed countries are still the main force and occupy an important position.
Further, 10 countries with the highest productivity in the field of depression are compared, total publications in the vertical coordinate, and the colored scatter plot contains 10 colored dots, representing 10 different countries. On the one hand, the variability of the contributions of different countries in the same time frame can be compared horizontally. On the other hand, it is possible to compare vertically the variability of the growth of different countries over time. Among them, USA, with about 40.29% of the world's publications in the field of depression, has always been a leader in the field of depression with its rich research results. Peoples R China, as the only developing country, ranks 3rd in the top 10 countries with high production of research papers in the field of depression, and Peoples R China's research in the field of depression has shown a rapid growth trend, and by 2016, it has jumped to become the 2nd largest country in the world, with the number of published papers increasing year by year, which has a broad prospect and great potential for development.
Distribution of Periodicals
Table 2 lists the top 15 journals in order of number of journal co-citations. In the field of depression, the top 15 cited journals accounted for 19.06% of the total number of co-citations, nearly one in five of the total number of journal co-citations. In particular, the top 3 journals were ARCH GEN PSYCHIAT (ARCHIVES OF GENERAL PSYCHIATRY), J AFFECT DISORDERS (JOURNAL OF AFFECTIVE DISORDERS), and AM J PSYCHIAT (AMERICAN JOURNAL OF PSYCHIATRY), with co-citation counts of 20,499, 20,302, and 20,143, with co-citation rates of 2.09, 2.07, and 2.06%, respectively. The main research area of ARCH GEN PSYCHIAT is Psychiatry; the main research area of the journal J AFFECT DISORDERS is Neurosciences and Neurology, Psychiatry; AM J PSYCHIAT is the main research area of Psychiatry, and the three journals have “psychiatry” in common, making them the most frequently co-cited journals in the field of depression.
Table 2 . The top 15 co-cited journals.
Figure 3 shows the network relationship graph of the cited journals from 2004 to 2019. The figure takes g-index as the selection criteria, the scale factor k = 25 to include more nodes. Each node of the graph represents each journal, the node size represents the number of citation frequencies, the label size represents the size of the betweenness centrality of the journal in the network, and the links between journals represent the co-citation relationships. The journal co-citation map reflects the structure of the journals, indicating that there are links between journals and that the journals include similar research topics. These journals included research topics related to neuroscience, psychiatry, neurology, and psychology. The journal with betweenness centrality size in the top 1 was ARCH GEN PSYCHIAT, with betweenness centrality size of 0.07, and impact shadows of 14.48. ARCH GEN PSYCHIAT, has research themes of Psychiatry. In all, these journals in Figure 3 occupy an important position in the journal's co-citation network and have strong links with other journals.
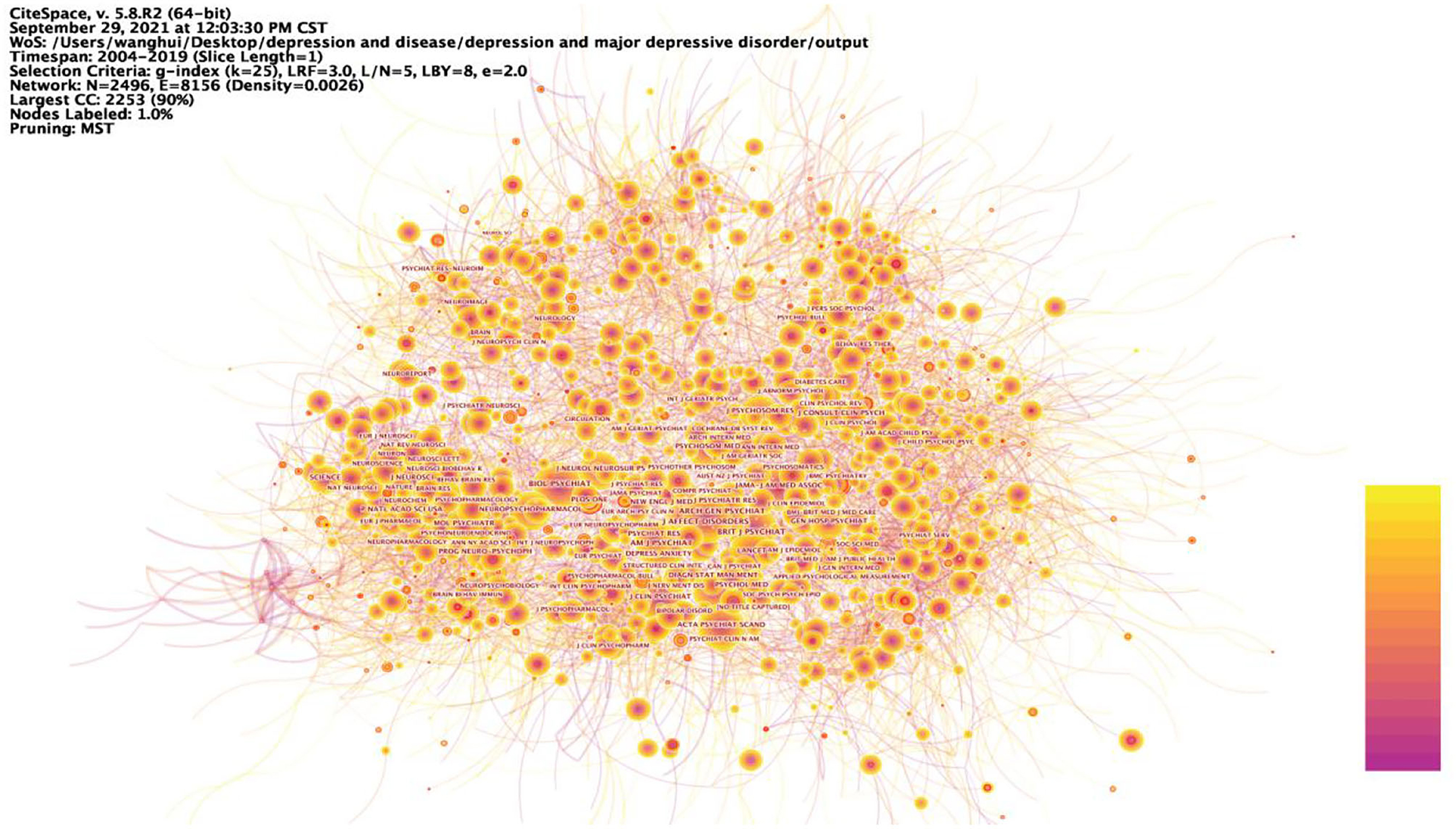
Figure 3 . Prominent journals involved in depression. The betweenness centrality of a node in the network measures the importance of the position of the node in the network. Two types of nodes may have high betweenness centrality scores: (1) Nodes that are highly connected to other nodes, (2) Nodes are positioned between different groups of nodes. The lines represent the link between two different nodes.
Distribution of Categories
Table 3 lists the 15 most popular categories in the field of depression research during the period 2004–2019. In general, the main disciplines involved are neuroscience, psychology, pharmacy, medicine, and health care, which are closely related to human life and health issues. Of these, psychiatry accounted for 20.78%, or about one-five, making it the most researched category. The study of depression focuses on neuroscience, reflecting the essential characteristics of depression as a category of mental illness and better reflecting the fact that depression is an important link in the human public health care. In addition, Table 3 shows that the category with the highest betweenness centrality is Neuroscience, followed by Public, Environment & Occupational Health, and then Pharmacology & Pharmacy, with betweenness centrality of 0.16, 0.13, and 0.11, respectively. It is found that the research categories of depression are also centered on disciplines such as neuroscience, public health and pharmacology, indicating that research on depression requires a high degree of integration of multidisciplinary knowledge and integration of information from various disciplines in order to have a more comprehensive and in-depth understanding of the depression.
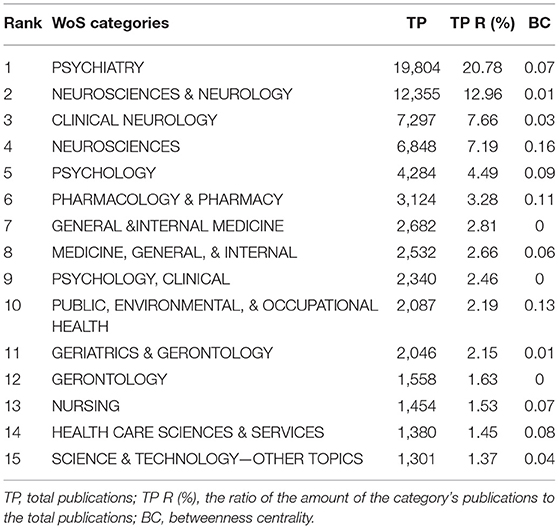
Table 3 . The top 15 productive categories, 2004–2019.
Figure 4 shows the nine categories with the betweenness centrality in the category research network, with Neuroscience being the node with the highest betweenness centrality in this network, meaning that Neuroscience is most strongly linked to all research categories in the field of depression research. Depression is a debilitating psychiatric disorder with mood disorders. It is worth noting that the development of depression not only has psychological effects on humans, but also triggers many somatic symptoms that have a bad impact on their daily work and life, giving rise to the second major mediating central point of research with public health as its theme. The somatization symptoms of depression often manifest as abnormalities in the cardiovascular system, and many studies have looked at the pathology of the cardiovascular system in the hope of finding factors that influence the onset of depression, mechanisms that trigger it or new ways to treat it. Thus, depression involves not only the nervous system, but also interacts with the human cardiovascular system, for example, and the complexity of depression dictates that the study of depression is an in-depth study based on complex systems.
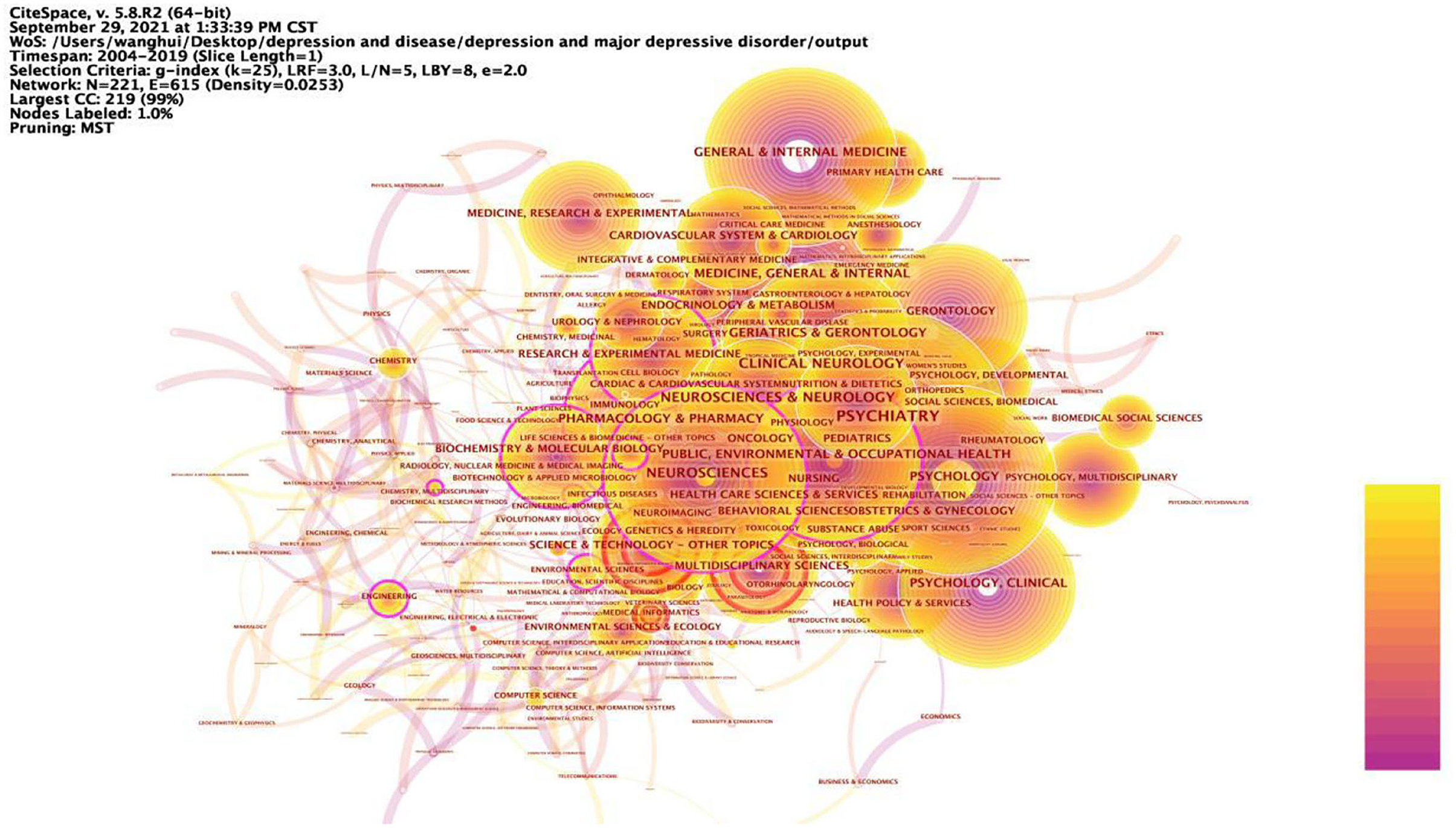
Figure 4 . Prominent categories involved in depression, 2004–2019. The betweenness centrality of a node in the network measures the importance of the position of the node in the network. Two types of nodes may have high betweenness centrality scores: (1) Nodes that are highly connected to other nodes, (2) Nodes are positioned between different groups of nodes. The lines represent the link between two different nodes.
Author Statistics
The results of the analysis showed that there were many researchers working in the field of depression over the past 16 years, and 63 of the authors published at least 30 articles related to depression. Table 4 lists the 15 authors with the highest number of articles published. It includes the rank of the number of articles published, author, country, number of articles published in depression-related studies, total number of articles included in Web of Science, total number of citations, average number of citations, and H-index. According to the statistics, seven of the top 15 authors are from USA, three from the Netherlands, one from Canada, one from Australia, one from New Zealand, one from Italy, and one from Germany. From this, it can be seen that these productive authors are from developed countries, thus it can be inferred that developed countries have a better research environment, more advanced research technology and more abundant research funding. The evaluation indicators in the author co-occurrence network are frequency, betweenness centrality and time of first appearance. The higher the frequency, i.e., the higher the number of collaborative publications, the more collaboration, the higher the information dissemination rate, the three authors with the highest frequency in this author co-occurrence network are MAURIZIO FAVA, BRENDA W. J. H. PENNINX, MADHUKAR H. TRIVEDI; the higher the betweenness centrality, i.e., the closer the relationship with other authors, the more collaboration, the higher the information dissemination rate, the three authors with the highest betweenness centrality are the three authors with the highest betweenness centrality are MICHAEL E. THASE, A. JOHN RUSH; the time of first appearance, i.e., the longer the influence generated by the author's research, the higher the information dissemination rate; in addition, the impact factor and citations can also reflect the information dissemination efficiency of the authors.
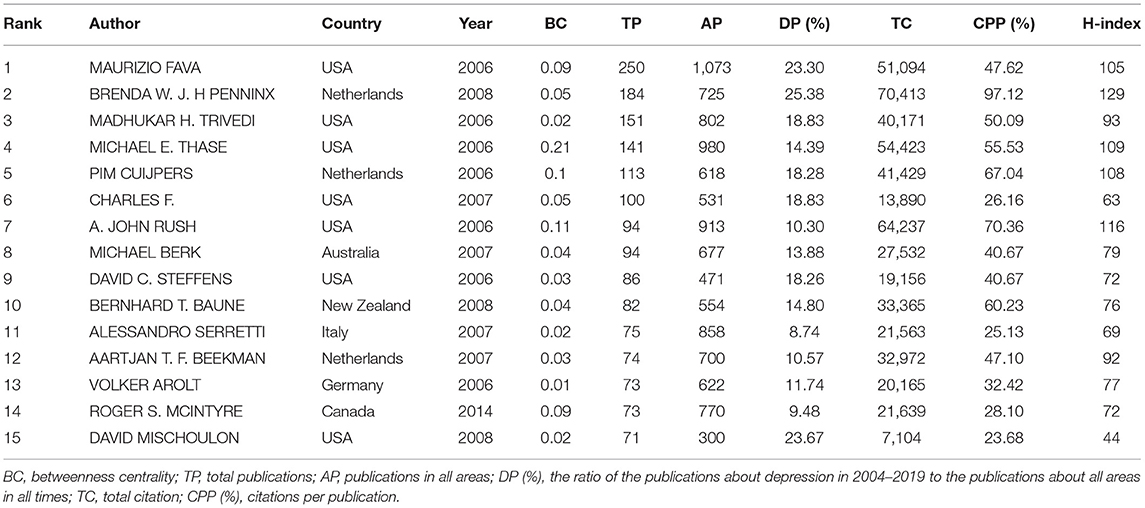
Table 4 . The top 15 authors in network of co-authorship, 2004–2019.
The timezone view ( Figure 5 ) in the author co-occurrence network clearly shows the updates and interactions of author collaborations, for example. All nodes are positioned in a two-dimensional coordinate with the horizontal axis of time, and according to the time of first posting, the nodes are set in different time zones, and their positions are sequentially upward with the time axis, showing a left-to-right, bottom-up knowledge evolution diagram. The time period 2004–2019 is divided into 16 time zones, one for each year, and each circle in the figure represents an author, and the time zone in which the circle appears is the year when the author first published an article in the data set of this study. The closer the color, the warmer the color, the closer the time, the colder the color, the older the era, the thickness of an annual circle, and the number of articles within the corresponding time division is proportional, the dominant color can reflect the relative concentration of the emergence time, the nodes appear in the annual circle of the red annual circle, that is, on behalf of the hot spot, the frequency of being cited was or is still increasing sharply. Nodes with purple outer circles are nodes with high betweenness centrality. The time zone view demonstrates the growth of author collaboration in the field, and it can be found from the graph that the number of author collaborations increases over time, and the frequency of publications in the author collaboration network is high; observe that the thickness of the warm annual rings in the graph is much greater than the thickness of the cold annual rings, which represents the increase of collaboration in time; there are many authors in all time zones, which indicates that there are many research collaborations and achievements in the field, and the field is in a period of collaborative prosperity. The linkage relationship between the sub-time-periods can be seen by the linkage relationship between the time periods, and it can be found from the figure that there are many linkages in the field in all time periods, which indicates that the author collaboration in the field of depression research is strong.
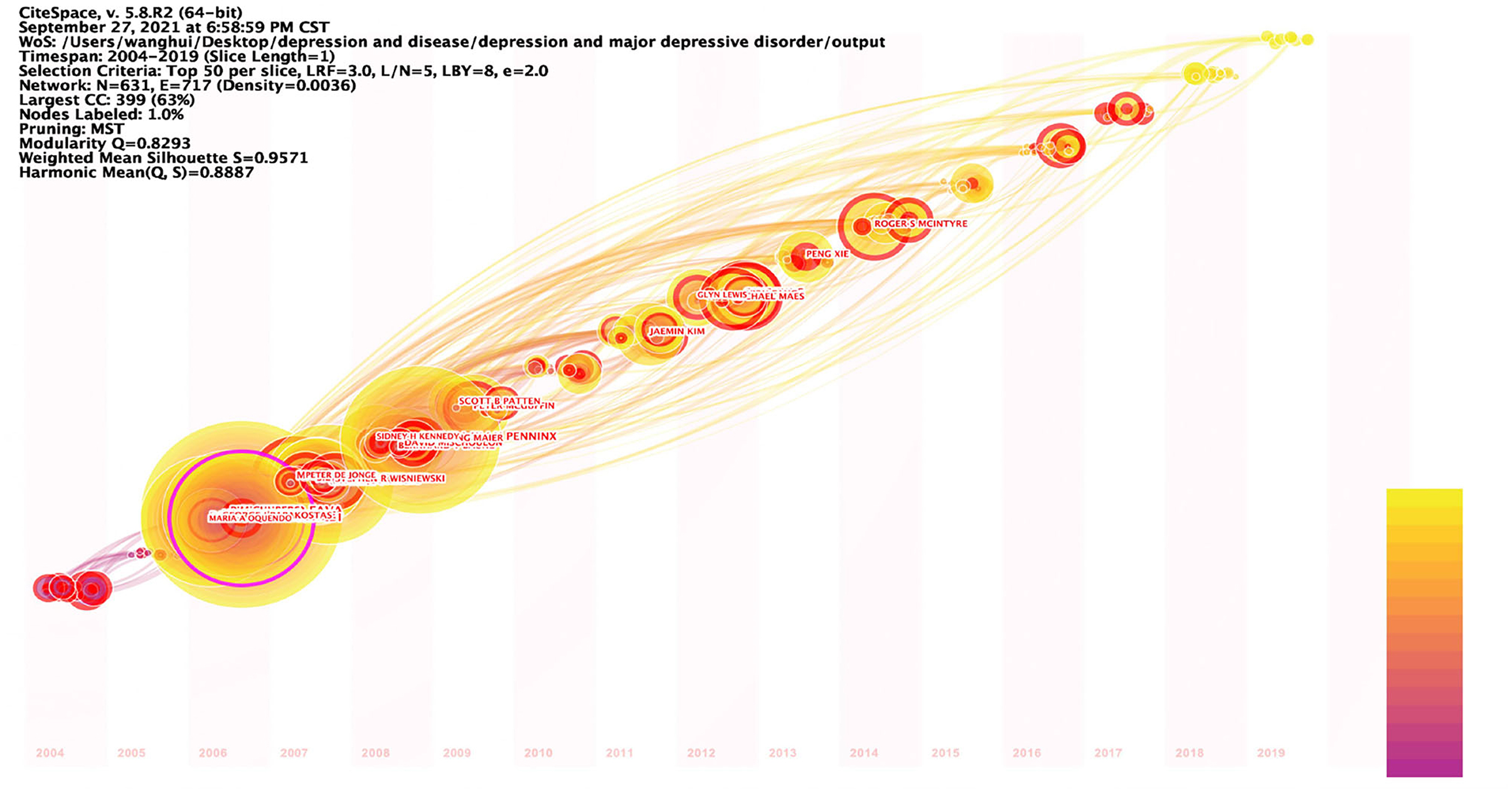
Figure 5 . Timezone view of the author's co-existing network in depression, 2004–2019. The circle represents the author, the time zone in which the circle appears is the year in which the author first published in this study dataset, the radius of the circle represents the frequency of appearance, the color represents the different posting times, the lines represent the connections between authors, and the time zone diagram shows the evolution of author collaboration.
Institutional Statistics
Table 5 lists the top 15 research institutions in network of co-authors' institutions. These include 10 American research institutions, two Netherlands research institutions, one UK research institution, one Canadian research institution and one Australian research institution, all of which, according to the statistics, are from developed countries. Of these influential research institutions, 66.7% are from USA. Figure 6 shows the collaborative network with these influential research institutions as nodes. Kings Coll London (0.2), Univ Michigan (0.17), Univ Toronto (0.15), Stanford Univ (0.14), Univ Penn (0.14), Univ Pittsburgh (0.14), Univ Melbourne (0.12), Virginia Commonwealth Univ (0.12), Columbia Univ (0.1), Duke Univ (0.1), Massachusetts Gen Hosp (0.1), Vrije Univ Amsterdam (0.1), with betweenness centrality >0.1. Kings Coll London has a central place in this collaborative network and is influential in the field of depression research. Table 6 lists the 15 institutions with the strong burst strength. The top 3 institutions are all from USA. Univ Copenhagen, Univ Illinois, Harvard Med Sch, Boston Univ, Univ Adelaide, Heidelberg Univ, Univ New South Wales, and Icahn Sch Med Mt Sinai have had strong burst strength in recent years. It suggests that these institutions may have made a greater contribution to the field of depression over the course of this year and more attention could be paid to their research.
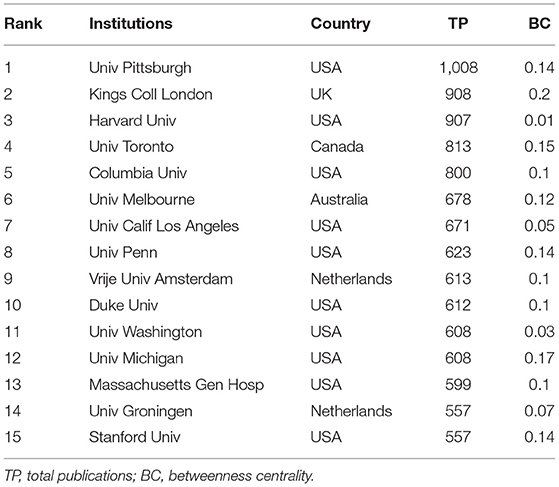
Table 5 . The top 15 institutions in network of co-authors' institutions, 2004–2019.
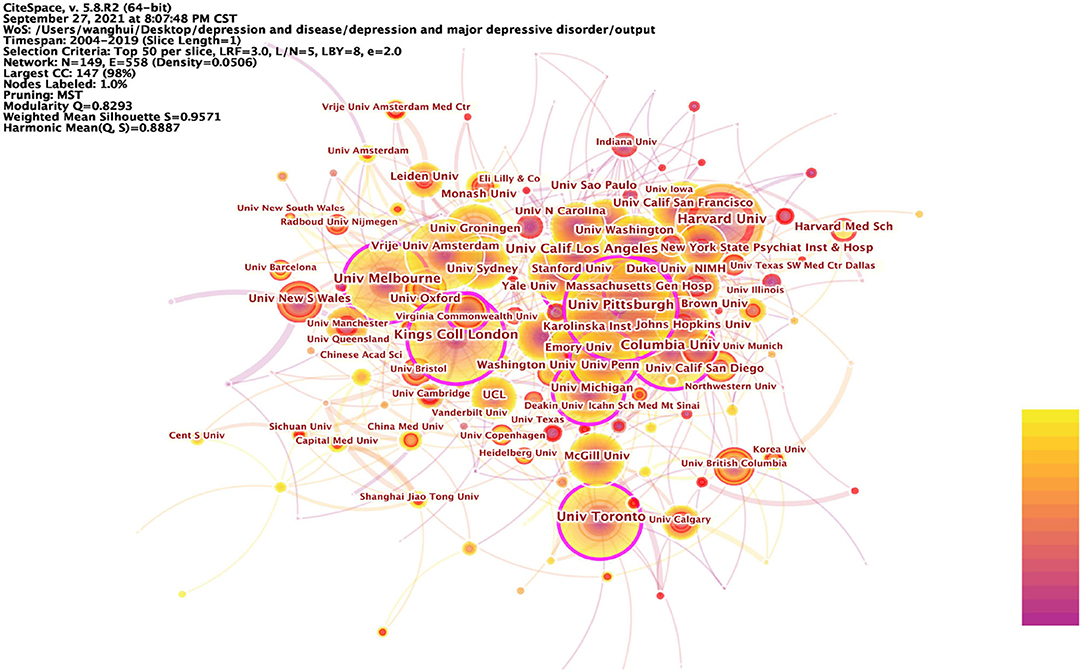
Figure 6 . Prominent institutions involved in depression, 2004–2019. The betweenness centrality of a node in the network measures the importance of the position of the node in the network. Two types of nodes may have high betweenness centrality scores: (1) Nodes that are highly connected to other nodes, (2) Nodes are positioned between different groups of nodes. The lines represent the link between two different nodes.
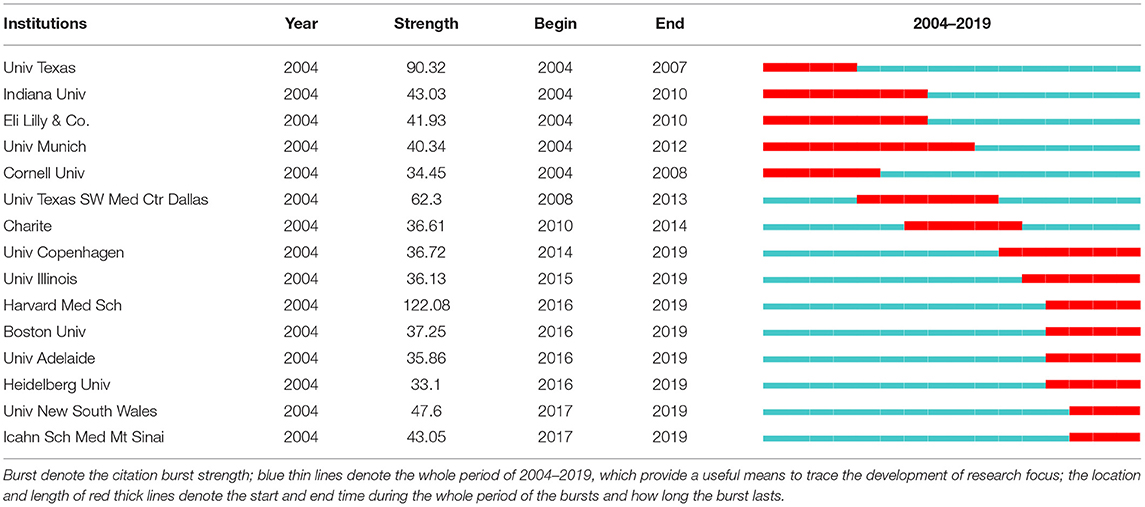
Table 6 . The top 15 institutions with the strongest citation bursts, 2004–2019.
Summing up the above analysis, it can be seen that the research institutions in USA are at the center of the depression research field, are at the top of the world in terms of quantity and quality of research, and are showing continuous growth in vitality. Research institutions in USA, as pioneers among all research institutions, lead and drive the development of depression research and play an important role in cutting-edge research in the field of depression.
Article Citations
Table 7 lists the 16 articles that have been cited more than 1,000 times within the statistical range of this paper from 2004 to 2019. As can be seen from the table, the most cited article was written by Dowlati et al. from Canada and published in BIOLOGICAL PSYCHIATRY 2010, which was cited 2,556 times. In addition, 11 of these 16 highly cited articles were from the USA. Notably, two articles by Kroenke, K as first author appear in this list, ranked 7th and 11th, respectively. In addition, there are three articles from Canada, one article from Switzerland, and one article from the UK. And interestingly, all of these countries are developed countries. It can be reflected that developed countries have ample research experience and high quality of research in the field of depression research. On the other hand, it also reflects that depression is a key concern in developed countries. These highly cited articles provide useful information to many researchers and are of high academic and exploratory value.
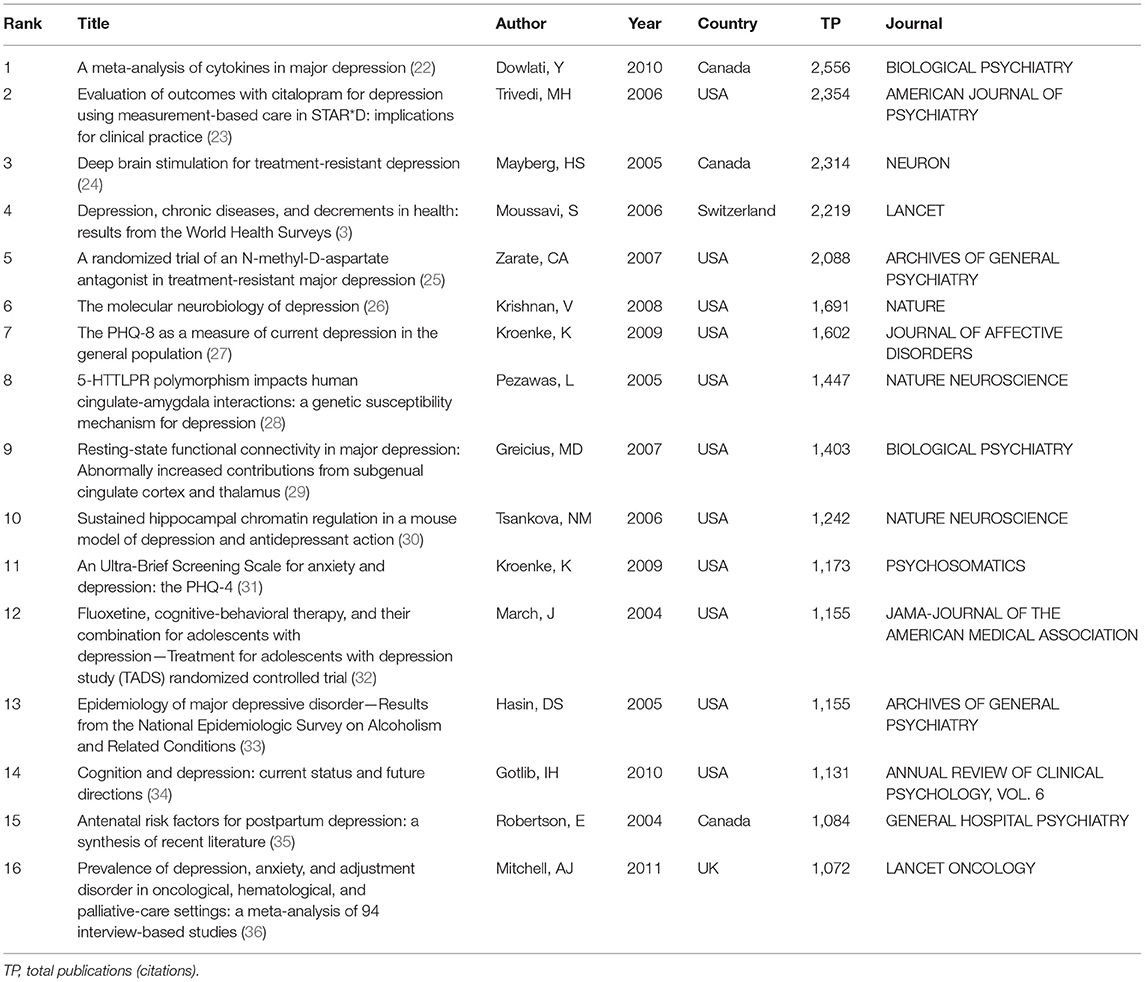
Table 7 . The top 15 frequency cited articles, 2004–2019.
Research Hotspots Ang Frontiers
Keyword analysis.
The keyword analysis of depression yielded the 25 most frequent keywords in Table 8 and the keyword co-occurrence network in Figure 7 . Also, the data from this study were detected by burst, the 25 keywords with the strongest burst strength were obtained in Table 9 . These results bring out the popular and cutting-edge research directions in the field clearly.
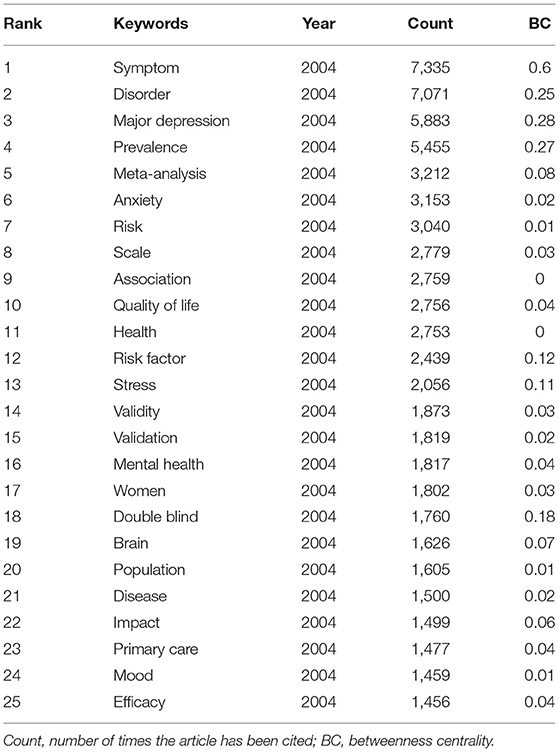
Table 8 . Top 25 frequent keywords in the period of 2004–2019.
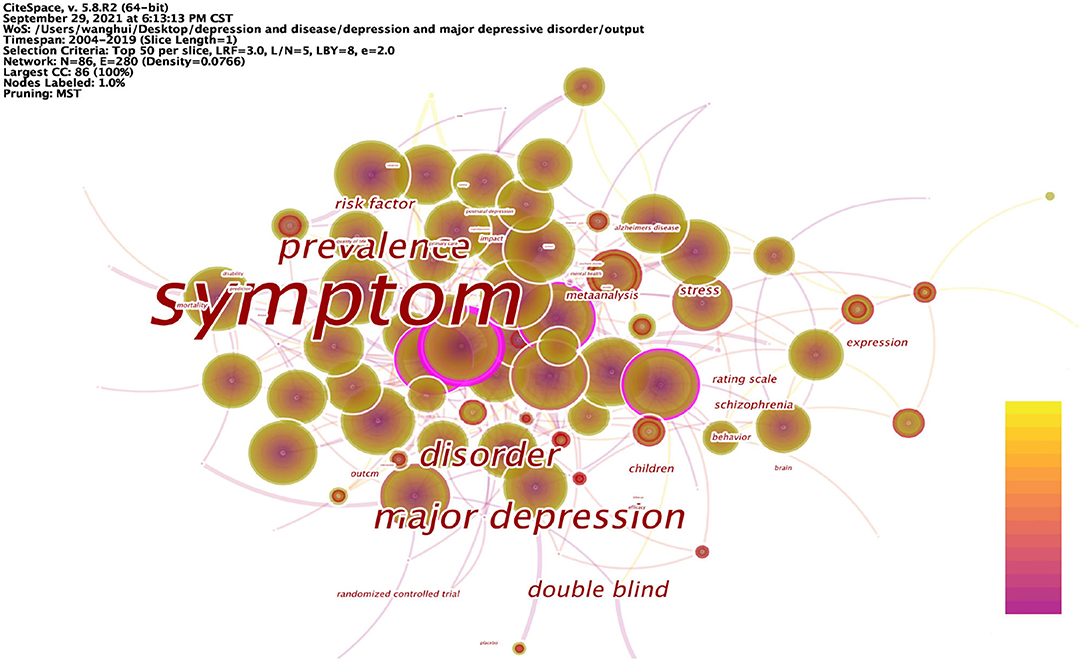
Figure 7 . Keyword co-occurrence network in depression, 2004–2019.

Table 9 . Top 25 keywords with strongest citation bursts in the period of 2004–2019.
The articles on depression during 2004–2019 were analyzed in 1-year time slices, and the top 25 keywords with the highest frequency of occurrence were selected from each slice to obtain the keyword network shown in Table 8 . The top 25 keywords with the highest frequencies were: symptom, disorder, major depression, prevalence, meta-analysis, anxiety, risk, scale, association, quality of life, health, risk factor, stress, validity, validation, mental health, women, double blind, brain, population, disease, impact, primary care, mood, and efficacy. High-frequency nodes respond to popular keywords and are an important basis for the field of depression research.
Figure 7 shows the co-occurrence network mapping of keywords regarding depression research. Each circle in the figure is a node representing a keyword, and the greater the betweenness centrality, the more critical the position of the node in the network. The top 10 keywords in terms of betweenness centrality are: symptom (0.6), major depression (0.28), prevalence (0.27), disorder (0.25), double blind (0.18), risk factor (0.12), stress (0.11), children (0.1), schizophrenia (0.1), and expression (0.1). Nodes with high betweenness centrality reflect that the keyword forms a co-occurrence relationship with multiple other keywords in the domain. A higher betweenness centrality indicates that it is more related to other keywords, and therefore, the node plays an important role in the study. Relatively speaking, these nodes represent the main research directions in the field of depression; they are also the key research directions in this period, and to a certain extent, represent the research hotspots in this period.
Burst detection was performed on the keywords, and the 25 keywords with the strongest strength were extracted, as shown in Table 9 . These keywords contain: fluoxetine, community, follow up, illness, psychiatric disorder, dementia, trial, placebo, disability, serotonin reuptake inhibitor, myocardial infarction, hospital anxiety, antidepressant treatment, late life depression, United States, epidemiology, major depression, model, severity, adolescent, people, prefrontal cortex, management, meta-analysis, and expression. The keywords that burst earlier include fluoxetine (2004), community (2004), follow up (2004), illness (2004), and psychiatric disorder (2004), are keywords that imply that researchers focused on themes early in the field of depression. As researchers continue to explore, the study of depression is changing day by day, and the keywords that have burst in recent years are people (2015), prefrontal cortex (2016), management (2016), meta-analysis (2017), and expression (2017). Reflecting the fact that depression research in recent years has mainly focused on human subjects, the focus has been on the characterization of populations with depression onset. The relationship between depression and the brain has aroused the curiosity of researchers, what exactly are the causes that trigger depression and what are the effects of depression for the manifestation of depression have caused a wide range of discussions in the research community, and the topics related to it have become the most popular studies and have been the focus of research in recent years. All of these research areas showed considerable growth, indicating that research into this area is gaining traction, suggesting that it is becoming a future research priority. The keywords with the strongest burst strength are fluoxetine (111.2), community (110.08), antidepressant treatment (94.28), severity (88.35), meta-analysis (86.42), people (85.33), and follow up (84.46). The rapid growth of research based on these keywords indicates that these topics are the most promising and interesting. The keywords that has been around the longest burst are follow up (2004–2013), model (2013–2019), hospital anxiety (2008–2013), severity (2014–2019), and psychiatric disorder (2004–2008), researchers have invested a lot of research time in these research directions, making many research results, and responding to the exploratory value and significance of research on these topics. At the same time, the longer duration of burst also proves that these research directions have research potential and important value.
Research Hotspots
Hotspots must mainly have the characteristics of high frequency, high betweenness centrality, strong burst, and time of emergence can be used as secondary evaluation indicators. The higher the number of occurrences, the higher the degree of popularity and attention. The higher betweenness centrality means the greater the influence and the higher the importance. Nodes with strong burst usually represent key shift nodes and need to be focused on. The time can be dynamically adjusted according to the target time horizon of the analysis. Thus, based on the results of statistical analysis, it is clear that the research hotspots in the field of depression can be divided into four main areas: etiology (external factors, internal factors), impact (quality of life, disease symptoms, co-morbid symptoms), treatment (interventions, drug development, care modalities), and assessment (population, size, symptoms, duration of disease, morbidity, mortality, effectiveness).
Risk factors for depression include a family history of depression, early life abuse and neglect, and female sexuality and recent life stressors. Physical illnesses also increase the risk of depression, particularly increasing the prevalence associated with metabolic (e.g., cardiovascular disease) and autoimmune disorders.
Research on the etiology of depression can be divided into internal and external factors. In recent years, researchers have increasingly focused on the impact of external factors on depression. Depression is influenced by environmental factors related to social issues, such as childhood experiences, social interactions, and lifestyles. Adverse childhood experiences are risk factors for depression and anxiety in adolescence ( 37 ) and are a common pathway to depression in adults ( 38 ). Poor interpersonal relationships with classmates, family, teachers, and friends increase the prevalence of depression in adolescents ( 39 ). Related studies assessed three important, specific indicators of the self-esteem domain: social confidence, academic ability, and appearance ( 40 ). The results suggest that these three dimensions of self-esteem are key risk factors for increased depressive symptoms in Chinese adolescents. The vulnerability model ( 41 ) suggests that low self-esteem is a causal risk factor for depression, and low self-esteem is thought to be one of the main causes of the onset and progression of depression, with individuals who exhibit low self-esteem being more likely to develop social anxiety and social withdrawal, and thus having a sense of isolation ( 42 ), which in turn leads to subsequent depression. Loneliness predicts depression in adolescents. Individuals with high levels of loneliness experience more stress and tension from psychological and physical sources in their daily lives, which, combined with insufficient care from society, can lead to depression ( 43 ). A mechanism of association exists between life events and mood disorders, with negative life events being directly associated with depressive symptoms ( 44 ). In a cross-sectional study conducted in Shanghai, the prevalence of depression was higher among people who worked longer hours, and daily lifestyle greatly influenced the prevalence of depression ( 45 ). A number of studies in recent years have presented a number of interesting ideas, and they suggest that depression is related to different environmental factors, such as temperature, sunlight hours, and air pollution. Environmental factors have been associated with suicidal behavior. Traffic noise is a variable that triggers depression and is associated with personality disorders such as depression ( 46 ). The harmful effects of air pollution on mental health, inhalation of air pollutants can trigger neuroinflammation and oxidative stress and induce dopaminergic neurotoxicity. A study showed that depression was associated with an increase in ambient fine particulate matter (PM2.5) ( 47 ).
Increased inflammation is a feature of many diseases and even systemic disorders, such as some autoimmune diseases [e.g., type 1 diabetes ( 48 ) or rheumatoid arthritis ( 49 )] and infectious diseases [e.g., hepatitis and sepsis ( 50 )], are associated with an inflammatory response and have been found to increase the risk of depression. A growing body of evidence supports a bidirectional association between depression and inflammatory processes, with stressors and pathogens leading to excessive or prolonged inflammatory responses when combined with predisposing factors (e.g., childhood adversity and modifying factors such as obesity). The resulting illnesses (e.g., pain, sleep disorders), depressive symptoms, and negative health (e.g., poor diet, sedentary lifestyle) may act as mediating pathways leading to inflammation and depression. In terms of mechanistic pathways, cytokines induce depression by affecting different mood-related processes. Elevated inflammatory signals can dysregulate the metabolism of neurotransmitters, damaging neurons, and thus altering neural activity in the brain. In addition cytokines can modulate depression by regulating hormone levels. Inflammation can have different effects on different populations depending on individual physiology, and even lower levels of inflammation may have a depressive effect on vulnerable individuals. This may be due to lower parasympathetic activity, poorer sensitivity to glucocorticoid inhibitory feedback, a greater response to social threat in the anterior oral cortex or amygdala and a smaller hippocampus. Indeed, these are all factors associated with major depression that can affect the sensitivity to the inhibitory consequences of inflammatory stimuli.
Depression triggers many somatization symptoms, which can manifest as insomnia, menopausal syndrome, cardiovascular problems, pain, and other somatic symptoms. There is a link between sleep deprivation and depression, with insomnia being a trigger and maintenance of depression, and more severe insomnia and chronic symptoms predicting more severe depression. Major depression is considered to be an independent risk factor for the development of coronary heart disease and a predictor of cardiovascular events ( 51 ). Patients with depression are extremely sensitive to pain and have increased pain perception ( 52 ) and is associated with an increased risk of suicide ( 53 , 54 ), and generally the symptoms of these pains are not relieved by medication.
Studies have shown that depression triggers an inflammatory response, promoting an increase in cytokines in response to stressors vs. pathogens. For example, mild depressive symptoms have been associated with an amplified and prolonged inflammatory response ( 55 , 56 ) following influenza vaccination in older adults and pregnant women. Among women who have recently given birth, those with a lifetime history of major depression have greater increases in both serum IL-6 and soluble IL-6 receptors after delivery than women without a history of depression ( 57 ). Pro-inflammatory agents, such as interferon-alpha (IFN-alpha), for specific somatization disorders [e.g., hepatitis C or malignant melanoma ( 58 , 59 )], although effective for somatic disorders, pro-inflammatory therapy often leads to psychiatric side effects. Up to 80% of patients treated with IFN-α have been reported to suffer from mild to moderate depressive symptoms.
Clinical trials have shown better antidepressant treatment with anti-inflammatory drugs compared to placebo, either as monotherapy ( 60 , 61 ) or as an add-on treatment ( 62 – 65 ) to antidepressants ( 66 , 67 ). However, findings like whether NSAIDs can be safely used in combination with antidepressants are controversial. Patients with depression often suffer from somatic co-morbidities, which must be included in the benefit/risk assessment. It is important to consider the type of medication, duration of treatment, and dose, and always balance the potential treatment effect with the risk of adverse events in individual patients. Depression, childhood adversity, stressors, and diet all affect the gut microbiota and promote gut permeability, another pathway that enhances the inflammatory response, and effective depression treatment may have profound effects on mood, inflammation, and health. Early in life gut flora colonization is associated with hypothalamic-pituitary-adrenal (HPA) axis activation and affects the enteric nervous system, which is associated with the risk of major depression, gut flora dysbiosis leads to the onset of TLR4-mediated inflammatory responses, and pro-inflammatory factors are closely associated with depression. Clinical studies have shown that in the gut flora of depressed patients, pro-inflammatory bacteria such as Enterobacteriaceae and Desulfovibrio are enriched, while short-chain fatty acid producing bacteria are reduced, and some of these bacterial taxa may transmit peripheral inflammation into the brain via the brain-gut axis ( 68 ). In addition, gut flora can affect the immune system by modulating neurotransmitters (5-hydroxytryptamine, gamma-aminobutyric acid, norepinephrine, etc.), which in turn can influence the development of depression ( 69 ). Therefore, antidepressant drugs targeting gut flora are a future research direction, and diet can have a significant impact on mood by regulating gut flora.
As the molecular basis of clinical depression remains unclear, and treatments and therapeutic effects are limited and associated with side effects, researchers have worked to discover new treatment modalities for depression. High-amplitude low-frequency musical impulse stimulation as an additional treatment modality seems to produce beneficial effects ( 70 ). Studies have found electroconvulsive therapy to be one of the most effective antidepressant treatment therapies ( 71 ). Physical exercise can promote molecular changes that lead to a shift from a chronic pro-inflammatory to an anti-inflammatory state in the peripheral and central nervous system ( 72 ). Aromatherapy is widely used in the treatment of central nervous system disorders ( 73 ). By activating the parasympathetic nervous system, qigong can be effective in reducing depression ( 74 ). The exploration of these new treatment modalities provides more reference options for the treatment of depression.
Large-scale assessments of depression have found that the probability of developing depression varies across populations. Depression affects some specific populations more significantly, for example: adolescents, mothers, and older adults. Depression is one of the disorders that predispose to adolescence, and depression is associated with an increased risk of suicide among college students ( 75 ). Many women develop depression after childbirth. Depression that develops after childbirth is one of the most common complications for women in the postpartum period ( 76 ). The health of children born to mothers who suffer from postpartum depression can also be adversely affected ( 77 ). Depression can cause many symptoms within the central nervous system, especially in the elderly population ( 78 ).
Furthermore, one of the most consistent findings of the association between inflammation and depression is the elevated levels of peripheral pro-inflammatory markers in depressed individuals, and peripheral pro-inflammatory marker levels can also be used as a basis for the assessment of depressed patients. Studies have shown that the following pro-inflammatory markers have been found to be at increased levels in depressed individuals: CRP ( 79 , 80 ), IL-6 ( 22 , 79 , 81 , 82 ), TNF–α, and interleukin-1 receptor antagonist (IL-1ra) ( 79 , 82 ), however, this association is not unidirectional and the subsequent development of depression also increases pro-inflammatory markers ( 82 , 83 ). These biomarkers are of great interest, and depressed patients with increased inflammatory markers may represent a relatively drug-resistant population.
Frontier Analysis
The exploration and analysis of frontier areas of depression were based on the results of the analysis of the previous section on keywords. According to the evaluation index and analysis idea of this study, the frontier research topics need to have the following four characteristics: low to medium frequency, strong burst, high betweenness centrality, and the research direction in recent years. Therefore, combining the results of keyword analysis and these characteristics, it can be found that the frontier research on depression also becomes clear.
Research on Depression Characterized by Psychosexual Disorders
Exploration of biological mechanisms based on depression-associated neurological disorders and analysis of depression from a neurological perspective have always been the focus of research. Activation of neuroinflammatory pathways may contribute to the development of depression ( 84 ). A research model based on the microbial-gut-brain axis facilitates the neurobiology of depression ( 85 ). Some probiotics positively affect the central nervous system due to modulation of neuroinflammation and thus may be able to modulate depression ( 86 ). The combination of environmental issues and the neurobiological study of depression opens new research directions ( 46 ).
Research on Relevant Models of Depression
How to develop a model that meets the purpose of the study determines the outcome of the study and has become the direction that researchers have been exploring in recent years. Martínez et al. ( 87 ) developed a predictive model to assess factors that modify the treatment pathway for postpartum depression. Nie et al. ( 88 ) extended the work on predictive modeling of treatment-resistant depression to establish a predictive model for treatment-resistant depression. Rational modeling methods and behavioral testing facilitate a more comprehensive exploration of depression, with richer studies and more scientifically valid findings.
Research and Characterization of the Depressed Patient Population
Current research on special groups and depression has received much attention. In a study of a group of children, 4% were found to suffer from depression ( 89 ). The diagnosis and treatment of mental health disorders is an important component of pediatric care. Second, some studies of populations with distinct characteristics have been based primarily on female populations. Maternal perinatal depression is also a common mental disorder with a prevalence of over 10% ( 90 ). In addition, geriatric depression is a chronic and specific disorder ( 91 ). Studies based on these populations highlight the characteristics of the disorder more directly than large-scale population explorations and are useful for conducting extended explorations from specific to generalized.
Somatic Comorbidities Associated With Depression
Depression often accompanies the onset and development of many other disorders, making the study of physical comorbidities associated with depression a new landing place for depression research. Depression is a complication of many neurological or psychopathological disorders. Depression is a common co-morbidity of glioblastoma multiforme ( 92 ). Depression is an important disorder associated with stroke ( 93 ). Chronic liver disease is associated with depression ( 94 ). The link between depressive and anxiety states and cancer has been well-documented ( 95 ). In conclusion, depression is associated with an increased risk of lung, oral, prostate, and skin cancers, an increased risk of cancer-specific death from lung, bladder, breast, colorectal, hematopoietic system, kidney, and prostate cancers, and an increased risk of all-cause mortality in lung cancer patients. The early detection and effective intervention of depression and its complications has public health and clinical implications.
Research on Mechanisms of Depression
Research based on the mechanisms of depression includes the study of disease pathogenesis, the study of drug action mechanisms, and the study of disease treatment mechanisms. Research on the pathogenesis of depression has focused more on the study of the hypothalamic-pituitary-adrenal axis. Social pressure can change the hypothalamic-pituitary-adrenal axis ( 96 ). Studies on the mechanism of action of drugs are mostly based on their effects on the central nervous system. The antidepressant effects of Tanshinone IIA are mediated by the ERK-CREB-BDNF pathway in the hippocampus of mice ( 97 ). Research on the mechanisms of depression treatment has also centered on the central nervous system. It has been shown that the vagus nerve can transmit signals to the brain that can lead to a reduction in depressive behavior ( 98 ).
In this study, based on the 2004–2019 time period, this wealth of data is effectively integrated through data analysis and processing to reproduce the research process in a particular field and to co-present global trends in homogenous fields while organizing past research.
Journals that have made outstanding contributions in this field include ARCH GEN PSYCHIAT, J AFFECT DISORDERS and AM J PSYCHIAT. PSYCHIATRY, NEUROSCIENCES & NEUROLOGY and CLINICAL NEUROLOGY are the three most popular categories. The three researchers with the highest number of articles were MAURIZIO FAVA (USA), BRENDA W. J. H. PENNINX (NETHERLANDS) and MADHUKAR H TRIVEDI (USA). Univ Pittsburgh (USA), Kings Coll London (UK) and Harvard Univ (USA) are three of the most productive and influential research institutions. A Meta-Analysis of Cytokines in Major Depression, Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: Implications for clinical practice and Deep brain stimulation for treatment-resistant depression are key articles. Through keyword analysis, a distribution network centered on depression was formed. Although there are good trends in the research on depression, there are still many directions to be explored in depth. Some recommendations regarding depression are as follows.
(1) The prevention of depression can be considered by focusing on treating external factors and guiding the individual.
Faced with the rising incidence of depression worldwide and the difficulty of treating depression, researchers can think more about how to prevent the occurrence of depression. Depressed moods are often the result of stress, not only social pressures on the individual, but also environmental pressures in the developmental process, which in turn have an unhealthy relationship with the body and increase the likelihood of depression. The correlation between external factors and depression is less well-studied, but the control of external factors may be more effective in the short term than in the long term, and may be guided by self-adjustment to avoid major depressive disorder.
(2) The measurement and evaluation of the degree of depression should be developed in the direction of precision.
In the course of research, it has been found that the Depression Rating Scale is mostly used for the detection and evaluation of depression. This kind of assessment is more objective, but it still lacks accuracy, and the research on measurement techniques and methods is less, which is still at a low stage. Patients with depression usually have a variety of causes, conditions, and duration of illness that determine the degree of depression. Therefore, whether these scales can truly accurately measure depression in depressed patients needs further consideration. Accurate measurement is an important basis for evidence-based treatment of depression, and thus how to achieve accurate measurement of depression is a research direction that researchers can move toward.
Therefore, there is an urgent need for further research to address these issues.
A systematic analysis of research in the field of depression in this study concludes that the distribution of countries, journals, categories, authors, institutions, and citations may help researchers and research institutions to establish closer collaboration, develop appropriate publication plans, grasp research hotspots, identify valuable research ideas, understand current emerging research, and determine research directions. In addition, there are still some limitations that can be overcome in future work. First, due to the lack of author and address information in older published articles, it may not be possible to accurately calculate their collaboration; second, although the data scope of this paper is limited to the Web of Science, it can adequately meet our objectives.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
HW conceived and designed the analysis, collected the data, performed the analysis, and wrote the paper. XT, XW, and YW conceived and designed the analysis. All authors contributed to the article and approved the submitted version.
This work was supported by the National Natural Science Foundation of China under Grant No. 81973495.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. (2009) 10:434–45. doi: 10.1038/nrn2639
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health. (2013) 34:119–38. doi: 10.1146/annurev-publhealth-031912-114409
3. Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. (2007) 370:851–8. doi: 10.1016/S0140-6736(07)61415-9
4. Peter Heutink MR. The genetics of MDD – a review of challenges and opportunities. J Depress Anxiety. (2014) 3:150. doi: 10.4172/2167-1044.1000150
CrossRef Full Text | Google Scholar
5. Melchior M, Caspi A, Milne BJ, Danese A, Poulton R, Moffitt TE. Work stress precipitates depression and anxiety in young, working women and men. Psychol Med. (2007) 37:1119–29. doi: 10.1017/S0033291707000414
6. Fusar-Poli P, Solmi M, Brondino N, Davies C, Chae C, Politi P, et al. Transdiagnostic psychiatry: a systematic review. World Psychiatry. (2019) 18:192–207. doi: 10.1002/wps.20631
7. Hammarström A, Lehti A, Danielsson U, Bengs C, Johansson EE. Gender-related explanatory models of depression: a critical evaluation of medical articles. Public Health. (2009) 123:689–93. doi: 10.1016/j.puhe.2009.09.010
8. Tran BX, Ho RCM, Ho CSH, Latkin CA, Phan HT, Ha GH, et al. Depression among patients with HIV/AIDS: research development and effective interventions (gapresearch). Int J Environ Res Public Health. (2019) 16:1772. doi: 10.3390/ijerph16101772
9. Wang XQ, Peng MS, Weng LM, Zheng YL, Zhang ZJ, Chen PJ. Bibliometric study of the comorbidity of pain and depression research. Neural Plast. (2019) 2019:1657498. doi: 10.1155/2019/1657498
10. Shi S, Gao Y, Sun Y, Liu M, Shao L, Zhang J, et al. The top-100 cited articles on biomarkers in the depression field: a bibliometric analysis. Psychol Heal Med. (2020) 26:533–42. doi: 10.1080/13548506.2020.1752924
11. Dongping G, Ami D, Ranran D, Yuan Y, Xiaobei S, Xiaoyao W, et al. A study of the relationship between depression and intestinal flora based on bibliometrics. China Med Her. (2017) 14:173–6.
12. Chunping A, Haiyan W, Nina H, Pinghui H. Bibiometrics analysis of acupuncture for treating depression based on GoPubMed. J Clin Acupunct Moxibustion. (2017) 33:54–7.
13. Yi Y, Xiaoli W. Bibiometrics analysis of acupuncture for treating depression based on GoPubMed. Mod Chinese Med. (2012) 14:35–8. doi: 10.13313/j.issn.1673-4890.2012.09.013
CrossRef Full Text
14. Zhou X, Yan F. Analysis on scientific and technological achievements in the field of depression during 1999-2017. J Prev Med Inf. (2019) 35:777–82.
15. Guaijuan W. Bibliometric analysis of literatures of psoriasis and depression based on GoPubmed. J Dermatol Venereol. (2017) 39:391–4.
16. Yunzhi C, Jie G, Yihui C, Chen G, Chen W, Wang H, et al. A Bibliometric analysis on research of vitamin D deficiency and depression caused. J Guiyang Coll Tradit Chinese Med. (2016) 38:32–5.
17. Shaoni L, Shumin R, Chunhui Z, Yongxiao T, Qizheng Z. Bibliometric analysis of depression-related genes. Chinese J Med Libr Inf Sci. (2009) 18:75–8.
18. Chen C. CiteSpace II: detecting and visualizing emerging trends and transient patterns in scientific literature. J Am Soc Inf Sci Technol. (2014) 57:359–77. doi: 10.1002/asi.20317
19. Elgendi M. Scientists need data visualization training. Nat Biotechnol. (2017) 35:990–1. doi: 10.1038/nbt.3986
20. World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates (2017).
Google Scholar
21. World Health Organization. Human Development Report 2020 (2020).
22. Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, et al. A meta-analysis of cytokines in major depression. Biol Psychiatry. (2010) 67:446–57. doi: 10.1016/j.biopsych.2009.09.033
23. Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR * D: implications for clinical practice. Am J Psychiatry. (2006) 163:28–40. doi: 10.1176/appi.ajp.163.1.28
24. Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C, et al. Deep brain stimulation for treatment-resistant depression. Neuron. (2005) 45:651–60. doi: 10.1016/j.neuron.2005.02.014
25. Zarate CA, Jr., Singh JB, Carlson PJ, Brutsche NE, Ameli R, et al. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry . (2006) 67:793–802. doi: 10.1001/archgenpsychiatry.2010.90
26. Krishnan V, Nestler EJ. The molecular neurobiology of depression. Nature. (2008) 455:894–902. doi: 10.1038/nature07455
27. Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. (2009) 114:163–73. doi: 10.1016/j.jad.2008.06.026
28. Pezawas L, Meyer-Lindenberg A, Drabant EM, Verchinski BA, Munoz KE, Kolachana BS, et al. 5-HTTLPR polymorphism impacts human cingulate-amygdala interactions: a genetic susceptibility mechanism for depression. Nat Neurosci. (2005) 8:828–34. doi: 10.1038/nn1463
29. Greicius MD, Flores BH, Menon V, Glover GH, Solvason HB, Kenna H, et al. Resting-state functional connectivity in major depression: abnormally increased contributions from subgenual cingulate cortex and thalamus. Biol Psychiatry. (2007) 62:429–37. doi: 10.1016/j.biopsych.2006.09.020
30. Tsankova NM, Berton O, Renthal W, Kumar A, Neve RL, Nestler EJ. Sustained hippocampal chromatin regulation in a mouse model of depression and antidepressant action. Nat Neurosci. (2006) 9:519–25. doi: 10.1038/nn1659
31. Kroenke K, Spitzer RL, Williams JBW, Löwe B. An Ultra-Brief Screening Scale for anxiety and depression: the PHQ−4. Psychosomatics. (2009) 50:613–21. doi: 10.1016/s0033-3182(09)70864-3
32. March J, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, et al. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents with Depression Study (TADS) randomized controlled trial. J Pediatr. (2005) 146:145. doi: 10.1016/j.jpeds.2004.10.032
33. Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder. Arch Gen Psychiatry. (2005) 62:1097. doi: 10.1001/archpsyc.62.10.1097
34. Gotlib IH, Joormann J. Cognition and depression: current status and future directions. Annu Rev Clin Psychol. (2010) 6:285–312. doi: 10.1146/annurev.clinpsy.121208.131305
35. Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. (2004) 26:289–95. doi: 10.1016/j.genhosppsych.2004.02.006
36. Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. (2011) 12:160–74. doi: 10.1016/S1470-2045(11)70002-X
37. Wang D, Jiang Q, Yang Z, Choi JK. The longitudinal influences of adverse childhood experiences and positive childhood experiences at family, school, and neighborhood on adolescent depression and anxiety. J Affect Disord. (2021) 292:542–51. doi: 10.1016/j.jad.2021.05.108
38. LeMasters K, Bates LM, Chung EO, Gallis JA, Hagaman A, Scherer E, et al. Adverse childhood experiences and depression among women in rural Pakistan. BMC Public Health. (2021) 21:400. doi: 10.1186/s12889-021-10409-4
39. Zhao Y, Zhao Y, Lee YT, Chen L. Cumulative interpersonal relationship risk and resilience models for bullying victimization and depression in adolescents. Pers Individ Dif. (2020) 155:109706. doi: 10.1016/j.paid.2019.109706
40. Zhou J, Li X, Tian L, Huebner ES. Longitudinal association between low self-esteem and depression in early adolescents: the role of rejection sensitivity and loneliness. Psychol Psychother Theor Res Pract. (2020) 93:54–71. doi: 10.1111/papt.12207
41. Butler AC, Hokanson JE, Flynn HA. A comparison of self-esteem lability and low trait self-esteem as vulnerability factors for depression. J Pers Soc Psychol. (1994) 66:166–77. doi: 10.1037/0022-3514.66.1.166
42. Watson J, Nesdale D. Rejection sensitivity, social withdrawal, and loneliness in young adults. J Appl Soc Psychol. (2012) 42:1984–2005. doi: 10.1111/j.1559-1816.2012.00927.x
43. Teo AR, Marsh HE, Forsberg CW, Nicolaidis C, Chen JI, Newsom J, et al. Loneliness is closely associated with depression outcomes and suicidal ideation among military veterans in primary care. J Affect Disord. (2018) 230:42–9. doi: 10.1016/j.jad.2018.01.003
44. Sarubin N, Goerigk S, Padberg F, Übleis A, Jobst A, Erfurt L, et al. Self-esteem fully mediates positive life events and depressive symptoms in a sample of 173 patients with affective disorders. Psychol Psychother Theor Res Pract. (2020) 93:21–35. doi: 10.1111/papt.12205
45. Li Z, Dai J, Wu N, Jia Y, Gao J, Fu H. Effect of long working hours on depression and mental well-being among employees in Shanghai: the role of having leisure hobbies. Int J Environ Res Public Health. (2019) 16:4980. doi: 10.3390/ijerph16244980
46. Díaz J, López-Bueno JA, López-Ossorio JJ, Gónzález JL, Sánchez F, Linares C. Short-term effects of traffic noise on suicides and emergency hospital admissions due to anxiety and depression in Madrid (Spain). Sci Total Environ. (2020) 710:136315. doi: 10.1016/j.scitotenv.2019.136315
47. Fan SJ, Heinrich J, Bloom MS, Zhao TY, Shi TX, Feng WR, et al. Ambient air pollution and depression: a systematic review with meta-analysis up to 2019. Sci Total Environ . (2020) 701:134721. doi: 10.1016/j.scitotenv.2019.134721
48. Korczak DJ, Pereira S, Koulajian K, Matejcek A, Giacca A. Type 1 diabetes mellitus and major depressive disorder: evidence for a biological link. Diabetologia. (2011) 54:2483–93. doi: 10.1007/s00125-011-2240-3
49. Dickens C, McGowan L, Clark-Carter D, Creed F. Depression in rheumatoid arthritis: a systematic review of the literature with meta-analysis. Psychosom Med. (2002) 64:52–60. doi: 10.1097/00006842-200201000-00008
50. Benros ME, Waltoft BL, Nordentoft M, Ostergaard SD, Eaton WW, Krogh J, et al. Autoimmune diseases and severe infections as risk factors for mood disorders a nationwide study. JAMA Psychiatry. (2013) 70:812–20. doi: 10.1001/jamapsychiatry.2013.1111
51. Charlson FJ, Stapelberg NJC, Baxter AJ, Whiteford HA. Should global burden of disease estimates include depression as a risk factor for coronary heart disease? BMC Med. (2011) 9:47. doi: 10.1186/1741-7015-9-47
52. Velly AM, Mohit S. Epidemiology of pain and relation to psychiatric disorders. Prog Neuro Psychopharmacol Biol Psychiatry. (2018) 87:159–67. doi: 10.1016/j.pnpbp.2017.05.012
53. Razali SM, Khalib AQ. Pain symptoms in Malay patients with major depression. Asian J Psychiatr. (2012) 5:297–302. doi: 10.1016/j.ajp.2012.02.015
54. Bahk WM, Park S, Jon DI, Yoon BH, Min KJ, Hong JP. Relationship between painful physical symptoms and severity of depressive symptomatology and suicidality. Psychiatry Res. (2011) 189:357–61. doi: 10.1016/j.psychres.2011.01.009
55. Glaser R, Robles TF, Sheridan J, Malarkey WB, Kiecolt-Glaser JK. Mild depressive symptoms are associated with amplified and prolonged inflammatory responses after influenza virus vaccination in older adults. Arch Gen Psychiatry. (2003) 60:1009–14. doi: 10.1001/archpsyc.60.10.1009
56. Christian LM, Franco A, Iams JD, Sheridan J, Glaser R. Depressive symptoms predict exaggerated inflammatory responses to an in vivo immune challenge among pregnant women. Brain Behav Immun. (2010) 24:49–53. doi: 10.1016/j.bbi.2009.05.055
57. Maes M, Ombelet W, De Jongh R, Kenis G, Bosmans E. The inflammatory response following delivery is amplified in women who previously suffered from major depression, suggesting that major depression is accompanied by a sensitization of the inflammatory response system. J Affect Disord. (2001) 63:85–92. doi: 10.1016/S0165-0327(00)00156-7
58. Friebe A, Horn M, Schmidt F, Janssen G, Schmid-Wendtner MH, Volkenandt M, et al. Dose-dependent development of depressive symptoms during adjuvant interferon-α treatment of patients with malignant melanoma. Psychosomatics . (2010) 51:466–73. doi: 10.1016/s0033-3182(10)70738-6
59. Eggermont AM, Suciu S, Santinami M, Testori A, Kruit WH, Marsden J, et al. Adjuvant therapy with pegylated interferon alfa-2b versus observation alone in resected stage III melanoma: final results of EORTC 18991, a randomised phase III trial. Lancet. (2008) 372:117–26. doi: 10.1016/S0140-6736(08)61033-8
60. Tyring S, Gottlieb A, Papp K, Gordon K, Leonardi C, Wang A, et al. Etanercept and clinical outcomes, fatigue, and depression in psoriasis: double-blind placebo-controlled randomised phase III trial. Lancet. (2006) 367:29–35. doi: 10.1016/S0140-6736(05)67763-X
61. Iyengar RL, Gandhi S, Aneja A, Thorpe K, Razzouk L, Greenberg J, et al. NSAIDs are associated with lower depression scores in patients with osteoarthritis. Am J Med . (2013) 126:1017.e11–8. doi: 10.1016/j.amjmed.2013.02.037
62. Müller N, Schwarz MJ, Dehning S, Douhe A, Cerovecki A, Goldstein-Müller B, et al. The cyclooxygenase-2 inhibitor celecoxib has therapeutic effects in major depression: results of a double-blind, randomized, placebo controlled, add-on pilot study to reboxetine. Mol Psychiatry. (2006) 11:680–4. doi: 10.1038/sj.mp.4001805
63. Akhondzadeh S, Jafari S, Raisi F, Nasehi AA, Ghoreishi A, Salehi B, et al. Clinical trial of adjunctive celecoxib treatment in patients with major depression: a double blind and placebo controlled trial. Depress Anxiety. (2009) 26:607–11. doi: 10.1002/da.20589
64. Abbasi SH, Hosseini F, Modabbernia A, Ashrafi M, Akhondzadeh S. Effect of celecoxib add-on treatment on symptoms and serum IL-6 concentrations in patients with major depressive disorder: Randomized double-blind placebo-controlled study. J Affect Disord. (2012) 141:308–14. doi: 10.1016/j.jad.2012.03.033
65. Majd M, Hashemian F, Hosseinib SM, Shariatpanahi MV, Sharifid A. A randomized, double-blind, placebo-controlled trial of celecoxib augmentation of sertraline in treatment of drug-naive depressed women: a pilot study. Iran J Pharm Res. (2015) 14:891–9. doi: 10.22037/ijpr.2015.1637
66. Warner-Schmidt JL, Vanover KE, Chen EY, Marshall JJ, Greengard P. Antidepressant effects of selective serotonin reuptake inhibitors (SSRIs) are attenuated by antiinflammatory drugs in mice and humans. Proc Natl Acad Sci USA. (2011) 108:9262–7. doi: 10.1073/pnas.1104836108
67. Uher R, E TK, Tracy D, Wolfgang M, Ole M, Joanna H, et al. An inflammatory biomarker as a differential predictor of outcome of depression treatment with escitalopram and nortriptyline. Am J Psychiatry. (2014) 171:1278–86. doi: 10.1176/appi.ajp.2014.14010094
68. Simpson CA, Diaz-Arteche C, Eliby D, Schwartz OS, Simmons JG, Cowan CSM. The gut microbiota in anxiety and depression – a systematic review. Clin Psychol Rev. (2021) 83:101943. doi: 10.1016/j.cpr.2020.101943
69. Yang Z, Li J, Gui X, Shi X, Bao Z, Han H, et al. Updated review of research on the gut microbiota and their relation to depression in animals and human beings. Mol Psychiatry. (2020) 25:2759–72. doi: 10.1038/s41380-020-0729-1
70. Sigurdardóttir GA, Nielsen PM, Rønager J, Wang AG. A pilot study on high amplitude low frequency–music impulse stimulation as an add-on treatment for depression. Brain Behav. (2019) 9:e01399. doi: 10.1002/brb3.1399
71. Maffioletti E, Gennarelli M, Gainelli G, Bocchio-Chiavetto L, Bortolomasi M, Minelli A. BDNF genotype and baseline serum levels in relation to electroconvulsive therapy effectiveness in treatment-resistant depressed patients. J ECT. (2019) 35:189–94. doi: 10.1097/YCT.0000000000000583
72. Ignácio ZM, da Silva RS, Plissari ME, Quevedo J, Réus GZ. Physical exercise and neuroinflammation in major depressive disorder. Mol Neurobiol. (2019) 56:8323–35. doi: 10.1007/s12035-019-01670-1
73. Lu Z, Zhang T, Wang X, Wang J, Shen J, Xiao Z, et al. Zwitterionic polymer-based nanoparticles encapsulated with linalool for regulating central nervous system. ACS Biomater Sci Eng. (2020) 6:442–9. doi: 10.1021/acsbiomaterials.9b01451
74. Koo JW, Chaudhury D, Han MH, Nestler EJ. Role of mesolimbic brain-derived neurotrophic factor in depression. Biol Psychiatry. (2019) 86:738–48. doi: 10.1016/j.biopsych.2019.05.020
75. Seppälä EM, Bradley C, Moeller J, Harouni L, Nandamudi D, Brackett MA. Promoting mental health and psychological thriving in university students: a randomized controlled trial of three well-being interventions. Front Psychiatry. (2020) 11:590. doi: 10.3389/fpsyt.2020.00590
76. Weissman M, Olfson M. Depression in women: implications for health care research. Science. (1995) 269:799–801. doi: 10.2105/AJPH.2020.305798
77. Savory K, Garay SM, Sumption LA, Kelleher JS, Daughters K, Janssen AB, et al. Prenatal symptoms of anxiety and depression associated with sex differences in both maternal perceptions of one year old infant temperament and researcher observed infant characteristics. J Affect Disord. (2020) 264:383–92. doi: 10.1016/j.jad.2019.11.057
78. Eraydin IE, Mueller C, Corbett A, Ballard C, Brooker H, Wesnes K, et al. Investigating the relationship between age of onset of depressive disorder and cognitive function. Int J Geriatr Psychiatry. (2019) 34:38–46. doi: 10.1002/gps.4979
79. Howren MB, Lamkin DM, Suls J. Associations of depression with c-reactive protein, IL-1, and IL-6: a meta-analysis. Psychosom Med. (2009) 71:171–86. doi: 10.1097/PSY.0b013e3181907c1b
80. Wium-Andersen MK, Ørsted DD, Nielsen SF, Nordestgaard BG. Elevated C-reactive protein levels, psychological distress, and depression in 73131 individuals. JAMA Psychiatry. (2013) 70:176–84. doi: 10.1001/2013.jamapsychiatry.102
81. Liu Y, Ho RCM, Mak A. Interleukin (IL)-6, tumour necrosis factor alpha (TNF-α) and soluble interleukin-2 receptors (sIL-2R) are elevated in patients with major depressive disorder: a meta-analysis and meta-regression. J Affect Disord. (2012) 139:230–9. doi: 10.1016/j.jad.2011.08.003
82. Dahl J, Ormstad H, Aass HCD, Malt UF, Bendz LT, Sandvik L, et al. The plasma levels of various cytokines are increased during ongoing depression and are reduced to normal levels after recovery. Psychoneuroendocrinology. (2014) 45:77–86. doi: 10.1016/j.psyneuen.2014.03.019
83. Khandaker GM, Pearson RM, Zammit S, Lewis G, Jones PB. Association of serum interleukin 6 and C-reactive protein in childhood with depression and psychosis in young adult life a population-based longitudinal study. JAMA Psychiatry. (2014) 71:1121–8. doi: 10.1001/jamapsychiatry.2014.1332
84. Zhang Z, xuan, Li E, Yan J, ping, Fu W, Shen P, Tian SW, et al. Apelin attenuates depressive-like behavior and neuroinflammation in rats co-treated with chronic stress and lipopolysaccharide. Neuropeptides. (2019) 77:101959. doi: 10.1016/j.npep.2019.101959
85. Tian P, O'Riordan KJ, Lee Y, kun, Wang G, Zhao J, Zhang H, et al. Towards a psychobiotic therapy for depression: Bifidobacterium breve CCFM1025 reverses chronic stress-induced depressive symptoms and gut microbial abnormalities in mice. Neurobiol Stress. (2020) 12:100216. doi: 10.1016/j.ynstr.2020.100216
86. Paiva IHR, Duarte-Silva E, Peixoto CA. The role of prebiotics in cognition, anxiety, and depression. Eur Neuropsychopharmacol. (2020) 34:1–18. doi: 10.1016/j.euroneuro.2020.03.006
87. Martínez P, Vöhringer PA, Rojas G. Barreiras de acesso a tratamento para mães com depressão pós-parto em centros de atenção primária: Um modelo preditivo. Rev Lat Am Enfermagem. (2016) 24:e2675. doi: 10.1590/1518-8345.0982.2675
88. Nie Z, Vairavan S, Narayan VA, Ye J, Li QS. Predictive modeling of treatment resistant depression using data from STARD and an independent clinical study. PLoS ONE. (2018) 13:e0197268. doi: 10.1371/journal.pone.0197268
89. Elmore AL, Crouch E. The Association of adverse childhood experiences with anxiety and depression for children and youth, 8 to 17 years of age. Acad Pediatr. (2020) 20:600–8. doi: 10.1016/j.acap.2020.02.012
90. Cheng B, Wang X, Zhou Y, Li J, Zhao Y, Xia S, et al. Regional cerebral activity abnormality in pregnant women with antenatal depression. J Affect Disord. (2020) 274:381–8. doi: 10.1016/j.jad.2020.05.107
91. Senel B, Özel-Kizil ET, Sorgun MH, Tezcan-Aydemir S, Kirici S. Transcranial sonography imaging of brainstem raphe, substantia nigra and cerebral ventricles in patients with geriatric depression. Int J Geriatr Psychiatry. (2020) 35:702–11. doi: 10.1002/gps.5287
PubMed Abstract | CrossRef Full Text
92. Mugge L, Mansour TR, Crippen M, Alam Y, Schroeder J. Depression and glioblastoma, complicated concomitant diseases: a systemic review of published literature. Neurosurg Rev. (2020) 43:497–511. doi: 10.1007/s10143-018-1017-2
93. Allida S, Kl C, Cf H, Lang H, House A, Ml H. Pharmacological, psychological, and non-invasive brain stimulation interventions for treating depression after stroke. Cochrane Database Syst Rev. (2020) 1:CD003437. doi: 10.1002/14651858.CD003437.pub4
94. Lee K, Otgonsuren M, Younoszai Z, Mir HM, Younossi ZM. Association of chronic liver disease with depression: a population-based study. Psychosomatics. (2013) 54:52–9. doi: 10.1016/j.psym.2012.09.005
95. Wang YH, Li JQ, Shi JF, Que JY, Liu JJ, Lappin JM, et al. Depression and anxiety in relation to cancer incidence and mortality: a systematic review and meta-analysis of cohort studies. Mol Psychiatry. (2020) 25:1487–99. doi: 10.1038/s41380-019-0595-x
96. Colaianna M, Schiavone S, Zotti M, Tucci P, Morgese MG, Bäckdahl L, et al. Neuroendocrine profile in a rat model of psychosocial stress: relation to oxidative stress. Antioxida Redox Signal. (2013) 18:1385–99. doi: 10.1089/ars.2012.4569
97. Lu J, Zhou H, Meng D, Zhang J, Pan K, Wan B, et al. Tanshinone IIA Improves depression-like behavior in mice by activating the ERK-CREB-BDNF signaling pathway. Neuroscience. (2020) 430:1–11. doi: 10.1016/j.neuroscience.2020.01.026
98. McVey Neufeld KA, Bienenstock J, Bharwani A, Champagne-Jorgensen K, Mao YK, West C, et al. Oral selective serotonin reuptake inhibitors activate vagus nerve dependent gut-brain signalling. Sci Rep. (2019) 9:14290. doi: 10.1038/s41598-019-50807-8
Keywords: depression, major depressive disorder, bibliometrics, visual analysis, knowledge graphs, CiteSpace
Citation: Wang H, Tian X, Wang X and Wang Y (2021) Evolution and Emerging Trends in Depression Research From 2004 to 2019: A Literature Visualization Analysis. Front. Psychiatry 12:705749. doi: 10.3389/fpsyt.2021.705749
Received: 06 May 2021; Accepted: 05 October 2021; Published: 29 October 2021.
Reviewed by:
Copyright © 2021 Wang, Tian, Wang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yun Wang, wangyun@bucm.edu.cn
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
How to determine the capacity of a person with depression who requests voluntary assisted dying

A new paper by Sam Boyle , written with colleagues Andrew McGee and Felicity Wood, addresses the important question of whether someone who has depression could qualify for voluntary assisted dying (VAD). The authors point out that there is common but mistaken assumption that those who request VAD while they are depressed cannot have capacity to request it. As Boyle and his colleagues argue, this assumption contravenes the law on how capacity assessments should proceed. Firstly, there is always a presumption that a patient making a medical decision has capacity to make that decision. This presumption is retained in VAD legislation. Secondly, the law is clear that capacity can’t be decided by whether someone has a particular illness, nor whether we think the person is making a good decision or not. What the law requires is an assessment of the person’s decision-making ability, that is, whether they are able to understand information about a decision, use and weigh that information to make a decision, and communicate the decision in some way. That is all. Provided a person can do those things, whether they have depression or any other mental condition, the law allows them to decide for themselves. Therefore, provided a person with depression can do those things, under Australian law, they should be found to have capacity to request VAD.
The authors acknowledge that the idea of a person with depression accessing VAD may be concerning to some people. However, they argue that excluding people with a particular illness from making certain decisions is inherently problematic, and something that the law has been at pains to avoid. Importantly, the authors point out that depression is not a single phenomenon. It can have varying cognitive symptoms, and can be anything from very mild to very severe. This variation means that a person with depression may have capacity to request VAD, or they may not. Boyle and colleagues argue that when a person with depression requests VAD, there must be a careful, individual assessment of the person’s decision-making abilities. Anything else risks contravening the law.
How to determine the capacity of a person with depression who requests voluntary assisted dying is available online .
Sakana AI’s ‘AI Scientist’ conducts research autonomously, challenging scientific norms
- Share on Facebook
- Share on LinkedIn
Join our daily and weekly newsletters for the latest updates and exclusive content on industry-leading AI coverage. Learn More
Sakana AI , in collaboration with scientists from the University of Oxford and the University of British Columbia, has developed an artificial intelligence system that can conduct end-to-end scientific research autonomously. This breakthrough, named “ The AI Scientist ,” promises to completely transform the process of scientific discovery.
The AI Scientist automates the entire research lifecycle, from generating novel ideas to writing full scientific manuscripts. “We propose and run a fully AI-driven system for automated scientific discovery, applied to machine learning research,” the team reports in their newly released paper .
Introducing The AI Scientist: The world’s first AI system for automating scientific research and open-ended discovery! https://t.co/8wVqIXVpZJ From ideation, writing code, running experiments and summarizing results, to writing entire papers and conducting peer-review, The AI… pic.twitter.com/SJuat9a2Uw — Sakana AI (@SakanaAILabs) August 13, 2024
This innovative system uses large language models (LLMs) to mimic the scientific process. It can generate research ideas, design and execute experiments, analyze results, and even perform peer review of its own papers. The researchers claim that The AI Scientist can produce a complete research paper for approximately $15 in computing costs.
The dawn of AI-driven discovery: A new era in scientific research
In their study, published on the preprint server arXiv , the researchers detail how The AI Scientist was tested on tasks in machine learning research, including developing new techniques for diffusion models, transformer-based language models, and analyzing learning dynamics. According to the team, the system produced papers that “exceed the acceptance threshold at a top machine learning conference as judged by our automated reviewer.”
This development represents a significant leap in AI capabilities, moving beyond narrow task-specific applications to a more general scientific problem-solving approach. The AI Scientist’s ability to navigate the entire research process autonomously suggests a level of reasoning and creativity previously thought to be the exclusive domain of human researchers.
The implications of such a system are profound and multifaceted. On one hand, it could dramatically accelerate the pace of scientific discovery by allowing continuous, round-the-clock research without human limitations. This could lead to rapid advancements in fields like drug discovery, materials science, and climate change mitigation.
? Stoked to share The AI-Scientist ?? – our end-to-end approach for conducting research with LLMs including ideation, coding, experiment execution, paper write-up & reviewing. Blog ?: https://t.co/kBwAgvXDjZ Paper ?: https://t.co/XvkwWfQhyi Code ?: https://t.co/hXlXjxFAD9 … https://t.co/bPB37b9RUY pic.twitter.com/mHn6ShzaiA — Robert Lange (@RobertTLange) August 13, 2024
Balancing act: Human intuition vs. AI efficiency in the lab
However, the automation of scientific research raises critical questions about the future role of human scientists. While AI may excel at processing vast amounts of data and identifying patterns, human intuition, creativity, and ethical judgment remain crucial in steering scientific inquiry towards meaningful and beneficial outcomes. The challenge will be in finding the right balance between AI-driven efficiency and human-guided purpose in scientific research.
Moreover, the system’s ability to conduct research at such a low cost could have significant economic implications for academic institutions and the broader scientific community. This could potentially lead to a restructuring of how research is funded and conducted, with implications for employment in the scientific sector.
The researchers themselves acknowledge the potential risks associated with such powerful AI systems. They explain in their paper, saying, “The AI Scientist current capabilities, which will only improve, reinforces that the machine learning community needs to immediately prioritize learning how to align such systems to explore in a manner that is safe and consistent with our values.”
Ethical considerations: Navigating the uncharted waters of AI-led science
This admission from the researchers underscores the importance of developing robust ethical frameworks and safeguards alongside technological advancements. As AI systems become more capable of independent scientific inquiry, ensuring they operate in ways that benefit humanity and align with our values becomes increasingly critical.
The open-sourcing of The AI Scientist’s code allows for broader scrutiny and development by the scientific community, which could help address some of these concerns. It also enables researchers to build upon this technology, potentially leading to even more advanced AI-driven scientific discovery systems in the future.
As the scientific community grapples with the implications of this technology, it’s clear that the process of scientific discovery is on the cusp of a profound transformation.
The challenge now lies in harnessing the power of AI-driven research while preserving the irreplaceable elements of human scientific inquiry — creativity, intuition, and ethical consideration — that have driven progress for centuries.
Stay in the know! Get the latest news in your inbox daily
By subscribing, you agree to VentureBeat's Terms of Service.
Thanks for subscribing. Check out more VB newsletters here .
An error occured.
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Suma P. Chand ; Hasan Arif .
Affiliations
Last Update: July 17, 2023 .
- Continuing Education Activity
Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest. The American Psychiatric Association’s Diagnostic Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) classifies the depressive disorders into Disruptive mood dysregulation disorder; Major depressive disorder; Persistent depressive disorder (dysthymia); Premenstrual dysphoric disorder; and Depressive disorder due to another medical condition. The common features of all the depressive disorders are sadness, emptiness, or irritable mood, accompanied by somatic and cognitive changes that significantly affect the individual’s capacity to function. This activity reviews the evaluation and management of depression and the role of interprofessional team members in collaborating to provide well-coordinated care and enhance patient outcomes.
- Review the risk factors for depression.
- Describe DSM V criteria for the diagnosis of depression.
- Summarize the treatment of depression.
- Outline the evaluation and management of depression and the role of interprofessional team members in collaborating to provide well-coordinated care and enhance patient outcomes.
- Introduction
Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest. [1] [2] The American Psychiatric Association’s Diagnostic Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) classifies the depressive disorders into:
- Disruptive mood dysregulation disorder
- Major depressive disorder
- Persistent depressive disorder (dysthymia)
- Premenstrual dysphoric disorder
- Depressive disorder due to another medical condition
The common features of all the depressive disorders are sadness, emptiness, or irritable mood, accompanied by somatic and cognitive changes that significantly affect the individual’s capacity to function. [3]
Because of false perceptions, nearly 60% of people with depression do not seek medical help. Many feel that the stigma of a mental health disorder is not acceptable in society and may hinder both personal and professional life. There is good evidence indicating that most antidepressants do work but the individual response to treatment may vary.
The etiology of major depressive disorder is multifactorial with both genetic and environmental factors playing a role. First-degree relatives of depressed individuals are about 3 times as likely to develop depression as the general population; however, depression can occur in people without family histories of depression. [4] [5]
Some evidence suggests that genetic factors play a lesser role in late-onset depression than in early-onset depression. There are potential biological risk factors that have been identified for depression in the elderly. Neurodegenerative diseases (especially Alzheimer disease and Parkinson disease), stroke, multiple sclerosis, seizure disorders, cancer, macular degeneration, and chronic pain have been associated with higher rates of depression. Life events and hassles operate as triggers for the development of depression. Traumatic events such as the death or loss of a loved one, lack or reduced social support, caregiver burden, financial problems, interpersonal difficulties, and conflicts are examples of stressors that can trigger depression.
- Epidemiology
Twelve-month prevalence of major depressive disorder is approximately 7%, with marked differences by age group. The prevalence in 18- to 29-year-old individuals is threefold higher than the prevalence in individuals aged 60 years or older. Females experience 1.5- to 3-fold higher rates than males beginning in early adolescence. In the US, depression affects nearly 17 million adults but these numbers are gross underestimates as many have not even come to medical attention.
- Pathophysiology
The underlying pathophysiology of major depressive disorder has not been clearly defined. Current evidence points to a complex interaction between neurotransmitter availability and receptor regulation and sensitivity underlying the affective symptoms.
Clinical and preclinical trials suggest a disturbance in central nervous system serotonin (5-HT) activity as an important factor. Other neurotransmitters implicated include norepinephrine (NE), dopamine (DA), glutamate, and brain-derived neurotrophic factor (BDNF).
The role of CNS 5-HT activity in the pathophysiology of major depressive disorder is suggested by the therapeutic efficacy of selective serotonin reuptake inhibitors (SSRIs). Research findings imply a role for neuronal receptor regulation, intracellular signaling, and gene expression over time, in addition to enhanced neurotransmitter availability.
Seasonal affective disorder is a form of major depressive disorder that typically arises during the fall and winter and resolves during the spring and summer. Studies suggest that seasonal affective disorder is also mediated by alterations in CNS levels of 5-HT and appears to be triggered by alterations in circadian rhythm and sunlight exposure.
Vascular lesions may contribute to depression by disrupting the neural networks involved in emotion regulation—in particular, frontostriatal pathways that link the dorsolateral prefrontal cortex, orbitofrontal cortex, anterior cingulate, and dorsal cingulate. Other components of limbic circuitry, in particular, the hippocampus and amygdala, have been implicated in depression.
- History and Physical
The investigation into depressive symptoms begins with inquiries of the neurovegetative symptoms which include changes in sleeping patterns, appetite, and energy levels. Positive responses should elicit further questioning focused on evaluating for the presence of the symptoms which are diagnostic of major depression. These are the 9 symptoms listed in the DSM-5 . Five must be present to make the diagnosis (one of the symptoms should be depressed mood or loss of interest or pleasure):
- Sleep disturbance
- Interest/pleasure reduction
- Guilt feelings or thoughts of worthlessness
- Energy changes/fatigue
- Concentration/attention impairment
- Appetite/weight changes
- Psychomotor disturbances
- Suicidal thoughts
- Depressed mood
All patients with depression should be evaluated for suicidal risk. Any suicide risk must be given prompt attention which could include hospitalization or close and frequent monitoring.
Other areas of investigation include:
- Past medical history and family medical history, and current medications
- Social history with a focus on stressors and the use of drugs and alcohol
- History and physical examination to rule out organic causes of depression. Depressive symptoms and their severity are also evaluated with the help of questionnaires such as the Beck's Depression Inventory (BDI), Hamilton Depression Scale (Ham-D), and Zung Self Rating Depression Scale
The diagnosis of depression is based on history and physical findings. No diagnostic laboratory tests are available to diagnose major depressive disorder. Laboratory studies are, however, useful to exclude medical illnesses that may present as major depressive disorder. [6] [7] [8] These laboratory studies might include the following:
- Complete blood cell (CBC) count
- Thyroid-stimulating hormone (TSH)
- Vitamin B-12
- Rapid plasma reagin (RPR)
- Electrolytes, including calcium, phosphate, and magnesium levels
- Blood urea nitrogen (BUN) and creatinine
- Liver function tests (LFTs)
- Blood alcohol level
- Blood and urine toxicology screen
- Arterial blood gas (ABG)
- Dexamethasone suppression test (Cushing disease, but also positive in depression)
- Cosyntropin (ACTH) stimulation test (Addison disease)
- Computed tomography (CT) scanning or magnetic resonance imaging (MRI) of the brain should be considered if organic brain syndrome or hypopituitarism is included in the differential diagnosis
- Treatment / Management
Medication alone and brief psychotherapy (cognitive-behavioral therapy, interpersonal therapy) alone can relieve depressive symptoms. Combination therapy has also been associated with significantly higher rates of improvement in depressive symptoms; increased quality of life; and better treatment compliance. There is also empirical support for the ability of CBT to prevent relapse. [9] [10]
Electroconvulsive therapy is useful for patients who are not responding well to medications or are suicidal. [11] [1]
Medications
- Selective serotonin reuptake inhibitors (SSRIs)
- Serotonin/norepinephrine reuptake inhibitors (SNRIs)
- Atypical antidepressants
- Serotonin-Dopamine Activity Modulators (SDAMs)
- Tricyclic antidepressants (TCAs)
- Monoamine oxidase inhibitors (MAOIs)
- Selective serotonin reuptake inhibitors (SSRIs): SSRIs have the advantage of ease of dosing and low toxicity in overdose. They are also the first-line medications for late-onset depression.
- SSRIs include: Citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, sertraline, vilazodone, vortioxetine
- Serotonin/norepinephrine reuptake inhibitors (SNRIs): SNRIs, which include venlafaxine, desvenlafaxine, duloxetine, and levomilnacipran can be used as first-line agents, particularly in patients with significant fatigue or pain syndromes associated with the episode of depression. SNRIs also have an important role as second-line agents in patients who have not responded to SSRIs.
- Atypical antidepressants: Atypical antidepressants include bupropion, mirtazapine, nefazodone, and trazodone. They have all been found to be effective in monotherapy in major depressive disorder and may be used in combination therapy for more difficult to treat depression.
- Serotonin-Dopamine Activity Modulators (SDAMs): SDAMs include brexpiprazole and aripiprazole. SDAMs act as a partial agonist at 5-HT1A and dopamine D2 receptors at similar potency, and as an antagonist at 5-HT2A and noradrenaline alp Brexpiprazole is indicated as adjunctive therapy for major depressive disorder (MDD).
- Tricyclic antidepressants (TCAS): TCAs include the following: Amitriptyline, clomipramine, desipramine, doxepin, imipramine, nortriptyline, protriptyline, trimipramine. TCAs have a long record of efficacy in the treatment of depression. They are used less commonly because of their side-effect profile and their considerable toxicity in overdose.
- Monoamine oxidase inhibitors (MAOIs): MAOIs include isocarboxazid, phenelzine, selegiline, and tranylcypromine. These agents are widely effective in a broad range of affective and anxiety disorders. Because of the risk of hypertensive crisis, patients on these medications must follow a low-tyramine diet. Other adverse effects can include insomnia, anxiety, orthostasis, weight gain, and sexual dysfunction.
Electroconvulsive Therapy (ECT)
ECT is a highly effective treatment for depression. Onset of action may be more rapid than that of drug treatments, with benefit often seen within 1 week of commencing treatment. A course of ECT (usually up to 12 sessions) is the treatment of choice for patients who do not respond to drug therapy, are psychotic, or are suicidal or dangerous to themselves. Thus, the indications for the use of ECT include the following:
- Need for a rapid antidepressant response Failure of drug therapies
- History of a good response to ECT
- Patient preference
- High risk of suicide
- High risk of medical morbidity and mortality
Although advances in brief anesthesia and neuromuscular paralysis have improved the safety and tolerability of ECT, this modality poses numerous risks, including those associated with general anesthesia, postictal confusion, and, more rarely, short-term memory difficulties .
Psychotherapy
Cognitive Behavior Therapy and Interpersonal Therapy are evidence-based psychotherapies that have been found to be effective in the treatment of depression.
Cognitive-behavioral therapy (CBT)
CBT is a structured, and didactic form of therapy that focuses on helping individuals identify and modify maladaptive thinking and behavior patterns (16 to 20 sessions). It is based on the premise that patients who are depressed exhibit the “cognitive triad” of depression, which includes a negative view of themselves, the world, and the future. Patients with depression also exhibit cognitive distortions that help to maintain their negative beliefs. CBT for depression typically includes behavioral strategies (i.e., activity scheduling), as well as cognitive restructuring to change negative automatic thoughts and addressing maladaptive schemas.
There is evidence supporting the use of CBT with individuals of all ages. It is also considered being efficacious for the prevention of relapse. It is particularly valuable for elderly patients, who may be more prone to problems or side effects with medications.
Mindfulness-based cognitive therapy (MBCT) was designed to reduce relapse among individuals who have been successfully treated for an episode of recurrent major depressive disorder. The primary treatment component is mindfulness training. MBCT specifically focuses on ruminative thought processes as being a risk factor for relapse. Research indicates that MBCT is effective in reducing the risk of relapse in patients with recurrent depression, especially in those with the most severe residual symptoms. Interpersonal therapy (IPT)
Interpersonal Therapy (IPT)
Interpersonal therapy (IPT) is a time-limited (typically 16 sessions) treatment for major depressive disorder. IPT draws from attachment theory and emphasize the role of interpersonal relationships, focusing on current interpersonal difficulties. Specific areas of emphasis include grief, interpersonal disputes, role transitions, and interpersonal deficits.
- Differential Diagnosis
- Adjustment disorders
- Chronic Fatigue syndrome
- Dissociative disorders
- Illness anxiety disorders
- Hypoglycemia
- Hypopituitarism
- Schizoaffective disorders
- Schizophrenia
- Somatic symptom disorders
Major depression has very high morbidity and mortality contributing to high rates of suicide. Even though effective drug treatment is available, nearly 50% may not initially respond. Complete remission is not common but at least 40% achieve partial remission in 12 months.
However, relapses are common and many patients require a variety of treatments to control the symptoms. The quality of life of most patients with depression is poor.
Depression accounts for nearly 40,000 cases of suicide each year in the US. The highest rate of suicides is in older men.
- Enhancing Healthcare Team Outcomes
Depression is a very common disorder encountered by the nurse practitioner, primary care provider, psychiatrist, and mental health worker, coordinating as an interprofessional healthcare team. The disorder has extremely high morbidity including the risk of suicide. All healthcare workers should be knowledgeable about this disorder and refer the patient to a psychiatrist if there is a risk of self-harm.
Education plays an important role in the successful treatment of major depressive disorder. This would include the education of the family and the patient. Lack of accurate information and misperceptions of the illness as a personal weakness or failings leads to painful stigmatization and avoidance of the diagnosis by many of those affected. Patients should know the rationale behind the choice of treatment, potential adverse effects, and expected results.
The involvement of the pharmacist in the treatment plan can enhance medication compliance and referral for psychotherapy. The pharmacist can also check that dosing is appropriate, that there are no significant interactions, and counsel on adverse effects. Engaging family members can be a critical component of a treatment plan. Family members are helpful informants, can ensure medication compliance, be a big source of social support and can encourage patients to change behaviors that perpetuate depression (e.g., inactivity).
Patients with moderate to severe depression should also be seen by a social worker or case management nurse to ensure that they have a support system and finances for treatment. If there is a concern, the person managing the case should present the issues to the interprofessional team so that a plan can be developed to get the patient the care they need. Overall, depression is managed by an interprofessional team dedicated to the management of mental health disorders. Open communication between all the members of the interprofessional team is the key to lowering the morbidity of the disorder. [Leve 5]
The outcomes for patients with depression are guarded. There is no cure and the condition has frequent relapses and remissions, leading to a poor quality of life. [3] [12] [13]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Suma Chand declares no relevant financial relationships with ineligible companies.
Disclosure: Hasan Arif declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Chand SP, Arif H. Depression. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Depression (Nursing). [StatPearls. 2024] Depression (Nursing). Chand SP, Arif H, Kutlenios RM. StatPearls. 2024 Jan
- Letter to the Editor: CONVERGENCES AND DIVERGENCES IN THE ICD-11 VS. DSM-5 CLASSIFICATION OF MOOD DISORDERS. [Turk Psikiyatri Derg. 2021] Letter to the Editor: CONVERGENCES AND DIVERGENCES IN THE ICD-11 VS. DSM-5 CLASSIFICATION OF MOOD DISORDERS. Cerbo AD. Turk Psikiyatri Derg. 2021; 32(4):293-295.
- Mood Disorder. [StatPearls. 2024] Mood Disorder. Sekhon S, Gupta V. StatPearls. 2024 Jan
- Review [The difference between depression and melancholia: two distinct conditions that were combined into a single category in DSM-III]. [Seishin Shinkeigaku Zasshi. 2012] Review [The difference between depression and melancholia: two distinct conditions that were combined into a single category in DSM-III]. Ohmae S. Seishin Shinkeigaku Zasshi. 2012; 114(8):886-905.
- Review [Psychiatric and psychological aspects of premenstrual syndrome]. [Encephale. 2001] Review [Psychiatric and psychological aspects of premenstrual syndrome]. Limosin F, Ades J. Encephale. 2001 Nov-Dec; 27(6):501-8.
Recent Activity
- Depression - StatPearls Depression - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
COMMENTS
In this paper, we describe and present the vast, fragmented, and complex literature related to this topic. This review may be used to guide practice, public health efforts, policy, and research related to mental health and, specifically, depression. ... This paper discusses key areas in depression research; however, an exhaustive discussion of ...
1. Introduction. The World Health Organization [] estimates that 264 million people worldwide were suffering from an anxiety disorder and 322 million from a depressive disorder in 2015, corresponding to prevalence rates of 3.6% and 4.4%.While their prevalence varies slightly by age and gender [], they are among the most common mental disorders in the general population [2,3,4,5,6].
Econometric analysis of the relationship between vitamin D deficiency and depression was performed by Yunzhi et al. and Shauni et al. performed a bibliometric analysis of domestic and international research papers on depression-related genes from 2003 to 2007. A previous review of depression-related bibliometric studies revealed that there is ...
The paper gives a complete overview of what is known about therapies for depression. ... we have developed a 'Meta-analytic Research Domain' (MARD) of all randomized trials of psychological treatments of depression. ... Depression in most studies was moderate to severe. Response (50 % improvement between baseline and endpoint) was the main ...
Authors of papers were contacted for clarification when data was missing or unclear. ... with most research on depression focusing on the 5-HT 1A receptor [11, 34].
Molecular Psychiatry - Advances in depression research: second special issue, 2020, with highlights on biological mechanisms, clinical features, co-morbidity, genetics, imaging, and treatment
In all, 16 studies reported the prevalence of depression among a total of 23,469 Ph.D. students (Fig. 2; range, 10-47%).Of these, the most widely used depression scales were the PHQ-9 (9 studies ...
In this essay, we have briefly reviewed a selected range of key discoveries that neuroscientific research has made on the topic of depressive disorders in the last decades. We have shown that depression has been linked to a wide range of abnormalities on different levels of neuroscientific description ranging from molecules and cells to brain ...
Our lack of knowledge cannot be put down to a scarcity of research in existing treatments. In the past decades, more than 500 randomised trials have examined the effects of antidepressant medications, and more than 600 trials have examined the effects of psychotherapies for depression (although comparatively few are conducted for early-onset depression).
Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest. The American Psychiatric Association's Diagnostic Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) classifies the depressive disorders into: The common features of all the depressive disorders are sadness, emptiness, or irritable mood ...
Depression is common, costly, debilitating, and associated with increased risk of suicide. It is one of the leading global public health problems. Although existing available pharmacological treatments can be effective, their onset of action can take up to 6 weeks, side-effects are common, and recovery can require treatment with multiple different agents. Although psychosocial interventions ...
Analysis of published papers around the world from 2009 to 2019 in depressive disorder. A The total number of papers [from a search of the Web of Science database (search strategy: TI = (depression$) or ts = ("major depressive disorder$")) and py = (2009-2019), Articles)].B The top 10 countries publishing on the topic.C Comparison of papers in China and the USA.
This article summarizes data on the prevalence and diagnosis of depression as well as findings from research regarding recovery and relapse from depression. It also offers a summary of models of ...
Analysis of published papers around the world from 2009 to 2019 in depressive disorder. A The total number of papers [from a search of the Web of Science database (search strategy: TI = (depression$) or ts = ("major depressive disorder$")) and py = (2009-2019), Articles)].B The top 10 countries publishing on the topic.C Comparison of papers in China and the USA.
Abstract. Major depression is a mood disorder characterized by a sense of inadequacy, despondency, decreased activity, pessimism, anhedonia and sadness where these symptoms severely disrupt and ...
Depression is a leading cause of disability worldwide (World Health Organization [WHO], 2020), with a 12-month prevalence in the United States of approximately 7% and a lifetime prevalence of approximately 16% (Kessler et al., 2003).While 40%-60% of the affected individuals will experience single-episode, non-recurrent depression followed by high-end-state functioning (Eaton et al., 2008 ...
The complete interview took about 1.5 hours and consisted of two parts: first, the Expectations of Therapy Interview, and second, a semi-structured diagnostic interview, the Kiddie-Schedule for Affective Disorders and Schizophrenia (K-SADS; Delmo, Weiffenbach, Gabriel, Stadler, & Poustka, 2001; Kaufman et al., 1997). The purpose of the second ...
The research is done on both gender, male and female. 29 students are female and. male students are 112. This portion of research is to check whether female students can have more chances. of ...
Increasing evidence suggests that diet may influence risk of depression. 1-3 Despite extensive data linking ultraprocessed foods (UPF; ie, energy-dense, palatable, and ready-to-eat items) with human disease, 4 evidence examining the association between UPF consumption and depression is scant. Prior studies have been hampered by short-term dietary data 1,2 and a limited ability to account for ...
These variables were considered clinically relevant to major depression. 61-63 Sensitivity analyses were conducted to examine if potential outliers, research designs and low-quality studies, affected the pooled effect sizes. The minimum number of studies was set at three studies for the main and subgroup analyses, and 10 for meta-regression.
This sample depression research paper features: 5700 words (approx. 19 pages), an outline, and a bibliography with 7 sources. Browse other research paper examples for more inspiration. If you need a thorough research paper written according to all the academic standards, you can always turn to our experienced writers for help.
This is one of the first studies to quantify a short-term transient increase in depressive symptoms experienced by TNB youths after initiating gender-affirming care, a phenomenon observed clinically by some of the authors and described in qualitative research. 37 Although we are unable to make causal statements owing to the observational design ...
Self-reported anxiety and depression have declined from the peak they reached in November 2020, when 42.6 percent of adults said they had symptoms, according to the Household Pulse Survey, a ...
Introduction. Depression affects more than two hundred sixty million people across the world and is a leading cause of disability ().The estimated prevalence of depressive disorders in 2016 was 3,627 per 100,000 and in the last decade the number of all-age years lived with disability (YLDs) increased of 14% (2,3).Resulting from a complex interaction of social, psychological and biological ...
Econometric analysis of the relationship between vitamin D deficiency and depression was performed by Yunzhi et al. and Shauni et al. performed a bibliometric analysis of domestic and international research papers on depression-related genes from 2003 to 2007. A previous review of depression-related bibliometric studies revealed that there is ...
A new paper by Sam Boyle, written with colleagues Andrew McGee and Felicity Wood, addresses the important question of whether someone who has depression could qualify for voluntary assisted dying (VAD). The authors point out that there is common but mistaken assumption that those who request VAD while they are depressed cannot have capacity to request it.
The researchers claim that The AI Scientist can produce a complete research paper for approximately $15 in computing costs. The dawn of AI-driven discovery: A new era in scientific research.
Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest. The American Psychiatric Association's Diagnostic Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) classifies the depressive disorders into Disruptive mood dysregulation disorder; Major depressive disorder; Persistent depressive ...