Your web browser is outdated and may be insecure
The RCN recommends using an updated browser such as Microsoft Edge or Google Chrome

Non-medical prescribers
Types of nurse prescriber.
Nurses, Midwives, Pharmacists and other allied healthcare professionals (AHPs) who have completed an accredited prescribing course and registered their qualification with their regulatory body, are able to prescribe.
The two main types are:
- Community Practitioner Nurse Prescribers (CPNP)
These are nurses who have successfully completed a Nursing and Midwifery Council (NMC) Community Practitioner Nurse Prescribing course (also known as a v100 or v150 course) and are registered as a CPNP with the NMC. The majority of nurses who have done this course are district nurses and public health nurses (previously known as health visitors), community nurses and school nurses. They are qualified to prescribe only from the Nurse Prescribers Formulary (NPF) for Community Practitioners. This formulary contains appliances, dressings, pharmacy (P), general sales list (GSL) and thirteen prescription only medicines (POMs).
- Independent Prescribers (IP)
Independent prescribers are nurses who have successfully completed an NMC Independent Nurse Prescribing Course (also known as a v200 or v300 course) and are registered with the NMC as an IP. They are able to prescribe any medicine provided it is in their competency to do so. This includes medicines and products listed in the BNF, unlicensed medicines and all controlled drugs in schedules two - five.
Those who have successfully completed the supplementary part of the prescribing course are also able to prescribe against a clinical management plan. Supplementary prescribing is described by the Medicines and Healthcare products Regulatory Agency (MHRA) as:
"a voluntary partnership between an Independent Prescriber (IP-er) and a supplementary prescriber (SP-er)," (e.g. nurse, pharmacist) "to implement an agreed patient-specific clinical management plan (CMP) with the patient's agreement."
The RCN acknowledges that some nurse prescribers are registered midwives.
Nurse independent prescribers and controlled drugs: changes to the Misuse of Drugs Regulations
The Misuse of Drugs Regulations covers all of the UK except Northern Ireland. This legislation divides controlled drugs (CDs) into five schedules corresponding to their therapeutic usefulness and misuse potential.
On 23 April 2012 changes to these regulations allowed nurses and midwives who are qualified as nurse independent prescribers to prescribe all controlled drugs listed in schedules two-five where it is clinically appropriate and within their professional competence (except for cocaine, diamorphine and dipipanone for the treatment of addiction). Changes also allowed nurse independent prescribers to mix any controlled drugs listed in schedules two-five prior to administration with another medicine for patients who need drugs intravenously.
Amendments to the Misuse of Drugs Regulations (Northern Ireland) 2002 were introduced on 10 May 2012 to allow a nurse independent prescriber and a pharmacist independent prescriber to prescribe controlled drugs as described.
Pharmacists and Allied Healthcare Professionals
There are two types of prescribers:
- An independent prescriber is a practitioner, who is responsible and accountable for the assessment of patients with undiagnosed or diagnosed conditions and can make prescribing decisions to manage the clinical condition of the patient.
- A supplementary prescriber is a practitioner who prescribes within an agreed patient specific clinical management plan (CMP), agreed in partnership by a supplementary prescriber with a doctor or dentist.
The table below is a brief summary of what IPs and SPs can prescribe (this does not include CPNP).
In general, an IP can prescribe any medicine for any condition within their clinical competence, whilst a SP may prescribe any medicine within their clinical competence that is included in the patient specific CMP.
| Independent Prescriber (IP) | Supplementary Prescriber (SP) (Nurses, Midwives and Pharmacists only | |
| Controlled Drugs (CDs) | Yes - CDs Schedule 2 to 5, except diamorphine, dipipanone | Yes - CDs Schedule 2 to 5, except diamorphine, dipipanone or cocaine for treatment of addiction |
| Unlicensed medicines | Yes -provided they are competent and take responsibility for doing so. May vary for Nurse prescribers in Scotland see the | Yes - covered by the CMP |
| Off label/off-licence prescribing | Yes - should only be prescribed where it is best practice to do so and | Yes - covered by the CMP |
| Private prescribing | Yes - for any medicine within their competence | Yes - for any medicine covered by the CMP |
Nurse prescribers and RCN indemnity
Become a nurse prescriber, further information.
RCN resources
Medicines Management : RCN Library subject guide
From the NMC website:
The NMC Code
Standards of Proficiency for Nurse and Midwife Prescribers (pre-2019). Please note that from November 2021 the NMC accepted the Royal Pharmaceutical Society’s Prescribing Competency Framework as their standards of competency for prescribing practice. All approved prescribing programmes must meet the new standards by 1 September 2022.
Other resources:
Medicines and Healthcare products Regulatory Agency (MHRA ) can provide information on legislation and medicines and medical devices
NICE Medicines and Prescribing Centre provides support for medicines and prescribing.
Country-specific guidance is also available at the following websites by searching for ‘nurse prescribing':
England: Department of Health
Northern Ireland: Department of Health
Scotland: NHS Scotland
Wales: Welsh Government
Read our advice on medicines management, immunisation, revalidation, practice standards and mental health.
See our A-Z of advice. These guides will help you answer many of your questions about work.
Page last updated - 29/12/2023
Your Spaces
- RCNi Profile
- Steward Portal
- RCN Foundation
- RCN Library
- RCN Starting Out
Work & Venue
- RCNi Nursing Jobs
- Work for the RCN
- RCN Working with us
Further Info
- Manage Cookie Preferences
- Modern slavery statement
- Accessibility
- Press office
Connect with us:
© 2024 Royal College of Nursing
Our systems are now restored following recent technical disruption, and we’re working hard to catch up on publishing. We apologise for the inconvenience caused. Find out more: https://www.cambridge.org/universitypress/about-us/news-and-blogs/cambridge-university-press-publishing-update-following-technical-disruption
We use cookies to distinguish you from other users and to provide you with a better experience on our websites. Close this message to accept cookies or find out how to manage your cookie settings .
Login Alert
- > Independent and Supplementary Prescribing
- > Non-medical prescribing: an overview
Book contents
- Frontmatter
- List of contributors
- Foreword to the second edition
- Preface to the second edition
- 1 Non-medical prescribing: an overview
- 2 Non-medical prescribing in a multidisciplinary team context
- 3 Consultation skills and decision making
- 4 Legal aspects of independent and supplementary prescribing
- 5 Ethical issues in independent and supplementary prescribing
- 6 Psychology and sociology of prescribing
- 7 Applied pharmacology
- 8 Monitoring skills
- 9 Promoting concordance in prescribing interactions
- 10 Evidence-based prescribing
- 11 Extended/supplementary prescribing: a public health perspective
- 12 Calculation skills
- 13 Prescribing in practice: how it works
- 14 Minimising the risk of prescribing error
1 - Non-medical prescribing: an overview
Published online by Cambridge University Press: 10 January 2011
In 1986, recommendations were made for nurses to take on the role of prescribing. The Cumberlege report, Neighbourhood nursing: a focus for care (Department of Health and Social Security (DHSS) 1986), examined the care given to clients in their homes by district nurses (DNs) and health visitors (HVs). It was identified that some very complicated procedures had arisen around prescribing in the community and that nurses were wasting their time requesting prescriptions from the general practitioner (GP) for such items as wound dressings and ointments. The report suggested that patient care could be improved and resources used more effectively if community nurses were able to prescribe as part of their everyday nursing practice, from a limited list of items and simple agents agreed by the DHSS.
Following the publication of this report, the recommendations for prescribing and its implications were examined. An advisory group was set up by the Department of Health (DoH) to examine nurse prescribing (DoH 1989). Dr June Crown was the Chair of this group.
The following is taken from the Crown report:
Nurses in the community take a central role in caring for patients in their homes. Nurses are not, however, able to write prescriptions for the products that are needed for patient care, even when the nurse is effectively taking professional responsibility for some aspects of the management of the patient. However experienced or highly skilled in their own areas of practice, nurses must ask a doctor to write a prescription. It is well known that in practice a doctor often rubber stamps a prescribing decision taken by a nurse. […]
Access options
Save book to kindle.
To save this book to your Kindle, first ensure [email protected] is added to your Approved Personal Document E-mail List under your Personal Document Settings on the Manage Your Content and Devices page of your Amazon account. Then enter the ‘name’ part of your Kindle email address below. Find out more about saving to your Kindle .
Note you can select to save to either the @free.kindle.com or @kindle.com variations. ‘@free.kindle.com’ emails are free but can only be saved to your device when it is connected to wi-fi. ‘@kindle.com’ emails can be delivered even when you are not connected to wi-fi, but note that service fees apply.
Find out more about the Kindle Personal Document Service .
- Non-medical prescribing: an overview
- By Molly Courtenay , Matt Griffiths
- Edited by Molly Courtenay , University of Surrey , Matt Griffiths , University of the West of England, Bristol
- Foreword by June Crown
- Book: Independent and Supplementary Prescribing
- Online publication: 10 January 2011
- Chapter DOI: https://doi.org/10.1017/CBO9780511861123.003
Save book to Dropbox
To save content items to your account, please confirm that you agree to abide by our usage policies. If this is the first time you use this feature, you will be asked to authorise Cambridge Core to connect with your account. Find out more about saving content to Dropbox .
Save book to Google Drive
To save content items to your account, please confirm that you agree to abide by our usage policies. If this is the first time you use this feature, you will be asked to authorise Cambridge Core to connect with your account. Find out more about saving content to Google Drive .

- Clinical articles
- CPD articles
- CPD Quizzes
- Expert advice
- Clinical placements
- Study skills
- Clinical skills
- University life
- Person-centred care
- Career advice
- Reflective accounts
- Practice-related feedback
- Patient view
- Revalidation articles
- Cancer Nursing Practice
- Emergency Nurse
- Learning Disability Practice
- Mental Health Practice
- Nurse Researcher
- Nursing Children and Young People
- Nursing Management
- Nursing Older People
- Nursing Standard
- Primary Health Care
- CPD webinars on-demand
- Nursing Live
- Nursing Careers and Jobs Fairs
- RCNi events calendar
- CPD quizzes
Preparing to Prescribe toolkit: becoming a non-medical prescriber
Lynne pearce posted 10 november 2020 - 01:00.
Reducing health inequalities by better access to hepatitis C virus testing and treatment
Type 2 diabetes: initiating non-insulin-based treatment in adults, sepsis treatment: answers to 10 questions could unlock breakthrough for outcomes, chimeric antigen receptor (car) t-cell therapy: an overview for nurses, 5 most read articles, the 10 ‘rights’ of drug administration: how do they help me practise safely, nurse pay: how do you make your band 5 salary stretch, clinical nurse educator: skills, experience and the pay for the role, record-keeping: how to avoid making serious mistakes or leaving gaps, taking on the nhs backlog: are you up for more overtime, other rcni websites.
- RCNi Learning
- RCNi Nursing Careers and Jobs Fairs
- RCNi Nursing Jobs
- RCNi Portfolio
BNF via NICE is only available in the UK
The NICE British National Formulary (BNF) site is only available to users in the UK (England, Scotland, Wales and Northern Ireland).
If you are outside the UK, you can access BNF content by subscribing to Medicines Complete .
If you believe you are seeing this page in error, please contact us .
For students
- Current Students website
- Email web access
- Make a payment
- MyExeter (student app)
- Programme and module information
- Current staff website
- Room Bookings
- Finance Helpdesk
- IT Service Desk
- Staff profile support and guidance
Popular links
Accommodation
- Job vacancies
- Temporary workers
- Future Leaders & Innovators Graduate Scheme
New and returning students
- New students website
- Returning Students Guide
Wellbeing, Inclusion and Culture
- Wellbeing services for students
- Wellbeing services for staff
- Equality, Diversity and Inclusion
Postgraduate Taught
Practice Certificate in Independent and Supplementary Prescribing
- Postgraduate Taught home
- Healthcare and Medicine
| UCAS code | 1234 |
|---|---|
| Duration | 6 months part time |
| Entry year | 2025 |
| Campus | St Luke's Campus |
| Discipline | |
| Contact |
| Typical offer
| 2.2 Honours degree (or equivalent) in a relevant discipline. |
|---|---|
|
• Designed to help you achieve accreditation for annotation as an Independent or Supplementary Prescriber on the GPhC, NMC or HCPC registers*
• Blend of online learning supported by minimal face-to-face contact days with communication and clinical skills training within our Clinical Skills Resource Centre • Problem Based Learning (PBL) scenarios allow students to tailor their learning to their own needs and develop personal learning objectives. • Expert tutors and guest lecturers will be invited from a range of clinical and research backgrounds • Can be taken as a standalone module or the credit can be used towards the MSc Clinical Pharmacy programme, MSc Advanced Clinical Practice programme or the Advanced Clinical Practice Degree Apprenticeship
• Acquiring this qualification and Independent or Supplementary prescriber status will enable you to seek extended roles in clinical practice as a non-medical prescribing practitioner * Successful completion of an accredited Independent and Supplementary Prescribing course is not a guarantee of annotation on the GPhC, NMC or HCPC registers or of future employment as an Independent or Supplementary Prescriber
View 2024 Entry
Apply for Sept 2025 entry
Fast Track (current Exeter students)
Open days and visiting us
Get a prospectus
Programme Directors: Will Farmer and Dr Rob Daniels
Web: Enquire online
Phone: +44 (0)1392 72 72 72

The programme is supported by NHS England and Health Education England through the Pharmacy Integration Fund.
Top 10 in the UK for our world-leading and internationally excellent Clinical Medicine research
Based on 4* + 3* research in REF 2021
Our Public Health research is 11th in the UK for research power
Submitted to UoA2 Public Health, Health Services and Primary Care. REF 2021
Major capital investment in new buildings and state-of-the-art facilities
Accreditations

This course was accredited by the General Pharmaceutical Council in December 2018. Please see the GPhC accreditation reports for more information. It was also accredited by The Health and Care Professionals Council (HCPC) and Nursing and Midwifery Council (NMC) in March 2021.
Entry requirements
Normally a minimum 2.2 Honours degree (or equivalent) in a relevant discipline. A personal statement, detailing your reasons for seeking to undertake this subject, will be required.
Entry requirements vary by regulator. Please check you meet the specific requirements below:
GPhC/PSNI registered pharmacist with at least two years of appropriate patient-orientated experience in a UK hospital, community or primary care setting following qualification
Registered nurse (level 1), midwife or SCPHN with at least one years’ appropriate patient-orientated experience in a UK hospital, community or primary care setting following qualification
HCPC registered physiotherapist, therapeutic/diagnostic radiographer, podiatrist or dietitian, with at least three years post-qualification experience in the area in which you will be prescribing
HCPC (Paramedics)
Registered paramedic with at least five years since qualification, practising in your area of expertise for at least 12 months
Have completed post-qualification study at level 7 (Master’s level)
All applicants must: • Have the agreement of a designated prescribing practitioner (DPP), practice assessor (PA) or Practice Educator (PE) who is willing to supervise your training • Demonstrate experience and reflective professional practice • Have identified an intended area of prescribing practice • Have support from a line manager, employer or service commissioner • Be fit to practice in accordance with the requirements of your regulator
Please visit our international equivalency pages to enable you to see if your existing academic qualifications meet our entry requirements.
Application process
Please complete the Independent and Supplementary Prescribing Course Application form and the IP SP Educational Audit Tool form before applying online.
Applicants may be invited to undertake an informal interview as part of the application process. This will take the form of an individual meeting/telephone conversation with one of our academics.
How employers can support
Ensure your staff are prepared for future prescribing roles. To undertake this programme, applicants must have support from a line manager, employer or service provider.
Undertaking the Clinical Pharmacy or Advanced Clinical Practice Programmes?
If you are already on the MSc Clinical Pharmacy or Advanced Clinical Practice programmes and want to do Independent or Supplementary Prescribing as part of this, you will not need to apply to Independent Prescribing through the online application process. Instead, please complete the Independent and Supplementary Prescribing Course Application form (ACP)
If you are applying for the MSc Clinical Pharmacy or Advanced Clinical Practice programmes and wish to take the Independent or Supplementary prescribing course as part of this, you will need to need to apply for both the MSc programme and the prescribing course at the same time.
If you are an Advanced Clinical Practice degree apprenticeship applicant and intend to choose prescribing as your year two option, you will need to complete an application form for this module in addition to your apprenticeship application. The appropriate forms will be provided as part of the DA application process
Entry requirements for international students
Please visit our entry requirements section for equivalencies from your country and further information on English language requirements .
English language requirements
International students need to show they have the required level of English language to study this course. The required test scores for this course fall under Profile B2 . Please visit our English language requirements page to view the required test scores and equivalencies from your country.
Course content
This Independent and Supplementary Prescribing course is designed to help you achieve accreditation for annotation as an Independent or Supplementary Prescriber on the GPhC, NMC or HCPC registers. We aim to produce competent non-medical prescribers who can provide safe, effective and evidence-based prescribing to address the needs of patients in their area of practice.
Features include:
- Online learning supported by face-to-face contact days
- Problem Based Learning - patient case-based activities that reflect the challenges of current clinical practice
- Communication and clinical skills training within our Clinical Skills Resource Centre
- Supportive, enthusiastic and clinically active tutors
- Increase your professional expertise and status and enhance your career prospects
- Complete the course to obtain a Practice Certificate in Independent/Supplementary Prescribing (as appropriate to your profession)
- Can be taken as a standalone module or the credit can be used towards the MSc Clinical Pharmacy programme, MSc Advanced Clinical Practice programme or the Advanced Clinical Practice Degree Apprenticeship
Our Practice Certificate in Independent and Supplementary Prescribing is a six month part-time 45 Credit programme of study at National Qualification Framework (NQF) level 7. It is taught using a blended approach to learning incorporating taught sessions, clinical skills practice and case-based discussion along with the support of online resources and moderated activities on the University of Exeter’s electronic learning platforms. Expert tutors and guest lecturers will be invited from a range of clinical and research backgrounds. Credits gained on this programme can be used towards the MSc Clinical Pharmacy programme, MSc Advanced Clinical Practice programme or the Advanced Clinical Practice Degree Apprenticeship
Contact Days
View the draft timetable of contact days for Independent Prescribing 2024/25
Please note: this timetable is a draft and may be subject to change.
The last contact day and assessment deadline for the programme will be earlier than the actual end date of your registration with the University, to allow a period of time at the end of your active studies for further support and mitigation, if needed
The modules we outline here provide examples of what you can expect to learn on this degree course based on recent academic teaching. The precise modules available to you in future years may vary depending on staff availability and research interests, new topics of study, timetabling and student demand.
Supervised practice
The GPhC, NMC and HCPC all require that a trainee non-medical prescriber be supported and supervised by a prescribing practitioner who meets a series of experiential requirements. The different accrediting bodies give this role different titles: • GPhC - Designated Prescribing Practitioner (DPP) • NMC - Practice Assessor (PA) • HCPC - Practice Educator (PE).
The NMC require a trainee to have both a Practice Assessor and a Practice Supervisor. Practice Assessors assess and confirm the student’s achievement of practice learning for a placement; they will also work with the nominated academic assessor to make a recommendation for student progression. The Practice Supervisors’ role is to support and supervise nursing and midwifery students in the practice learning environment. All students must be supervised while learning in practice environments.
For the purposes of clarity, we will refer to the Designated Prescribing Practitioner (DPP) for all roles.
The aim of the DPP role is ‘to oversee, support and assess the competence of non-medical prescribing trainees, in collaboration with academic and workplace partners, during the period of learning in practice’ (RPS, 2019). A DPP directs and supervises the trainee’s period of learning in practice – a required element of independent prescribing qualifications. They will also be responsible for assessing whether the learning outcomes have been met and whether the trainee has acquired certain competencies.
Our trainee non-medical prescribers are required to complete 12 days or 90 hours in clinical practice. This time must be planned and aligned to the trainee’s learning needs and consist of activities relevant to the development of the trainee as an autonomous practitioner. The trainee will keep detailed logs of their activities and the DPP will need to provide supervision, feedback and oversight. The Designated Prescribing Practitioner has to assess the achievement of the learning outcomes and provide confirmation by signing the student’s practice-based log. At the end of the 90 hours in practice, the DPP is required to make a declaration that the trainee is suitable for annotation as an independent or supplementary prescriber (as appropriate to your profession).
Choosing your DPP
Your DPP must meet the Royal Pharmaceutical Society’s Competency framework for Designated Prescribing Practitioners (2019) . This allows for the supervision of trainee prescribers in practice by non-medical assessors as described below.
The DPP must: • Be a registered healthcare professional in Great Britain or Northern Ireland and in good standing with their professional regulator • Be registered with their regulator as a legally independent prescriber for at least the last three years, with no significant gaps in practice which would affect this three-year requirement.
Have at least three years’ active and recent prescribing practice, patient-facing clinical and diagnostic skill within the student’s chosen therapeutic area/scope of practice, with no significant gaps in practice which would affect this three-year requirement.
• Have the support of the employing organisation(s) or learning in practice setting(s) to act as a DPP who will provide supervision, support and opportunities to develop competence in prescribing practice for the pharmacist prescriber in training.
• Have experience of teaching, supervising and assessing other health care professionals in clinical practice.
• Have adequate indemnity insurance in place for their own professional and supervisory role as a DPP and ensure that all learning in practice settings have adequate indemnity insurance in place. Further requirements for this role can be found in section 7 of the Independent Prescribing Course Application Form Finally, your DPP must be able to personally commit to the time required to provide supervised practice which must be no less than 45 hours or 50% of your time in practice.
You will need to have agreed who will be your DPP before applying for this course. Your DPP must complete and sign Section 7 of the I IP/SP Course Application Form 2022-23 before you submit your application.
Practice Placement Quality Assurance
All applicants must ensure that the University of Exeter IP SP Educational Audit Tool has been completed within the last 12 months for the organisation providing their supervised practice placement. The audit should be completed by the education lead, prescribing lead or a senior manager for the organisation, in consultation with IP/SP module leads at the university. This audit is an essential part of our processes to quality assure your practice-based learning.
A copy of the completed audit tool must be submitted with your application, if we do not already hold one for your organisation. Your NMP or Prescribing Lead will be able to advise you if this is the case. Your application cannot be approved without a current copy of the audit tool.
2025/26 entry
- UK fees: £2,650
- International fees: £2,650
Fees can normally be paid by two termly instalments and may be paid online. You will also be required to pay a tuition fee deposit to secure your offer of a place, unless you qualify for exemption. For further information about paying fees see our Student Fees pages.
Scholarships
For more information on scholarships, please visit our scholarships and bursaries page.
*Selected programmes only. Please see the Terms and Conditions for each scheme for further details.
Find out more about tuition fees and funding »
Funding and scholarships
Uk government postgraduate loan scheme.
Postgraduate loans of up to £12,167 are now available for Masters degrees. Find out more about eligibility and how to apply .
There are various funding opportunities available including Global excellence scholarships. For more information visit our Masters funding page .
Scholarships
The University of Exeter is offering scholarships to the value of over £4 million for students starting with us in September 2021. Details of scholarships, including our Global Excellence scholarships for international fee paying students, can be found on our dedicated funding page .
University of Exeter Class of 2022 Progression Scholarship
We are pleased to offer graduating University of Exeter students completing their degree in Summer 2022 and progressing direct to a standalone taught Masters degree (eg MA; MSc; MRes; MFA) or research degree (eg MPhil/PhD) with us a scholarship towards the cost of their tuition fees. These awards are worth 10% of the first year tuition fee for students enrolling on a postgraduate taught or research programme of study in 2022/23, with the exception of the PGCE programme.
Teaching and research
Our purpose is to deliver transformative education that will help tackle health challenges of national and global importance.
Workshop days:
- Interactive patient-case discussions to develop your clinical reasoning
- Small group discussions to develop your future prescribing role
- Practical communication skills sessions
- Clinical examination training in specialist facilities
- Opportunities to reflect on your Supervised practice
- Academic tutor sessions to support your progress
E-learning material:
This comprises 3 units:
- Unit 1 - Prescribing Governance
- Unit 2 - Clinical skills for Prescribing
- Unit 3 - Prescribing Partnerships
Students also have access to extensive on-line resources used on our other clinical courses and University library facilities.
Learning is backed up with individual tutor support and peer group discussions.
Multi-modal Assessment
- Assessments are varied and reflect the responsibilities of the prescribing role
- Assessments include a clinical interest essay, MCQ test, observations of your clinical skills through OSCEs and submission of your Portfolio of Practice
You will already be a registered health professional in employment in a UK healthcare setting. Acquiring this qualification and Independent/Supplementary prescriber status will enable you to seek extended roles in clinical practice as an autonomous prescribing practitioner. In addition, the ability to tailor some of the assessments to an area of practice will enable you to further your clinical interests.
Careers support
All University of Exeter students have access to Career Zone, which gives access to a wealth of business contacts, support and training as well as the opportunity to meet potential employers at our regular Careers Fairs.
Related courses
Clinical pharmacy msc.
St Luke's Campus
Advanced Clinical Practice MSc
Master of public health (mph), environment and human health msc.
Penryn Campus
Healthcare Leadership and Management MSc
Clinical education msc.
View all Healthcare and Medicine courses

Why Exeter?

Student life

Our campuses

International students

Apply for a Masters

Immigration and visas

Tuition fees and funding
Connect with us
Information for:
- Current students
- New students
- Alumni and supporters
Quick links
Streatham Campus
Truro Campus
- Using our site
- Accessibility
- Freedom of Information
- Modern Slavery Act Statement
- Data Protection
- Copyright & disclaimer
- Cookie settings
Streatham Campus in Exeter
The majority of students are based at our Streatham Campus in Exeter. The campus is one of the most beautiful in the country and offers a unique environment in which to study, with lakes, parkland, woodland and gardens as well as modern and historical buildings.
Find out more about Streatham Campus.
St Luke's Campus in Exeter
Located on the eastern edge of the city centre, St Luke's is home to Sport and Health Sciences, the Medical School, the Academy of Nursing, the Department of Allied Health Professions, and PGCE students.
Find out more about St Luke's Campus.
Penryn Campus near Falmouth, Cornwall
Our Penryn Campus is located near Falmouth in Cornwall. It is consistently ranked highly for satisfaction: students report having a highly personal experience that is intellectually stretching but great fun, providing plenty of opportunities to quickly get to know everyone.
Find out more about Penryn Campus.
Module details
Independent/ Supplementary Prescribing (PgCert)
- Duration: 24 weeks
- Mode: Part time

Find out more about studying here as a postgraduate at our next Open Day .
Why study this course
This postgraduate certificate in non-medical prescribing will provide you with the knowledge and skills to qualify as an independent prescriber.
Accredited programme
Our course is accredited by the General Pharmaceutical Council (GPhC) and Health and Care Professions Council, the (HCPC).
Learning community
You will benefit from learning alongside a diverse group who are studying at various points in their career.
Student support
You will have academic support and be assigned a designated personal tutor throughout your studies with us.
High-quality teaching
You will be taught by experienced educational and clinical staff with considerable local, national and international reputations.
The programme will develop your ability to critically analyse and to hone your personal reflection skills, preparing you for lifelong professional development. It will provide the foundation for you to develop your practice, to enable you to provide a high professional standard of care, and be accountable for that care.
The programme will introduce you to the general principles of pharmacology relevant to prescribing practice, the professional, legal, and ethical frameworks relevant to Independent and Supplementary prescribing, and clinical governance / quality assurance aspects of prescribing.
These elements will be underpinned by evaluation of your own performance, and application of the prescribing principles to your own area of practice. It will also enable you to be aware of current developments within independent and supplementary prescribing in the UK. You will study in a multi-disciplinary setting along with a range of individuals from other professions including pharmacists, facilitating shared learning as recommended by the NMC/ HCPC.
Where you'll study
School of Healthcare Sciences
Our courses are designed to provide you with the knowledge and experience you need to embark on a professional healthcare career.
- Facilities Chevron right
- Research at the School of Healthcare Sciences Chevron right
- Academic staff Chevron right
- Telephone +44(0) 29 2068 7538
- Marker University Hospital of Wales, Heath Park, Cardiff, CF14 4XN
Admissions criteria
In order to be considered for an offer for this programme you will need to meet all of the entry requirements and must comply with the Professional, Statutory and Regulatory Body (Nursing and Midwifery Council (NMC) and Health and Care Professions Council (HCPC)) specific requirements for prescribing. Your application will not be progressed if the information and evidence listed is not provided.
With your online application you will need to provide:
- A copy of your professional registration number (NMC or HCPC) in order for us to confirm your current registration status.
- currently work in an area relevant to the programme
- have a minimum of one years’ full-time equivalent patient-orientated clinical experience
- are committed to Continuing Professional Development (CPD)
- Any evidence of previous study at Masters level.
- A copy of your certificate or transcript which shows you have undertaken a clinical assessment/diagnostics and evaluation module, or evidence that demonstrates you have developed these skills in clinical practice, such as a testimonial from a senior practitioner.
- A copy of your IELTS certificate with an overall score of 6.5 with 5.5 in all subskills, or evidence of an accepted equivalent. Please include the date of your expected test if this qualification is pending. If you have alternative acceptable evidence, such as an undergraduate degree studied in the UK, please supply this in place of an IELTS.
- Why have you selected this programme?
- What interests you about this programme?
- Any relevant experience related to the programme or module content.
- How you plan to use the qualification in your career.
- How you and your profession will benefit from your studies.
- Why you feel you should be given a place on the programme.
If you are self-funding your studies (if you work outside of a health board or an NHS Trust) you must also provide two additional references that specifically comment on your clinical and academic ability to undertake the programme.
Application Deadline
We allocate places on a first-come, first-served basis, so we recommend you apply as early as possible. Applications normally close at the end of July but may close sooner if all places are filled.
Selection process
Once you have submitted your application you will be sent a Learning Agreement and Statement of Support form, which you are required to complete and return to confirm you meet the criteria set out by the NMC and HCPC before we can consider your application. Once received, we will review your application and if you meet all of the entry requirements, including an assessment of suitability through the personal statement, we will make you an offer.
Additional information
You may apply for Recognition of Prior Learning (RPL) at level 6 or level 7 of up to 60 credits, of which only 30 credits can be at level 6. RPL is considered through mapping of learning outcomes of comparable modules. This complies with the NMC (2018) and HCPC (2019) prescribing standards.
If you intend to apply for recognition for prior learning, please supply copies of your credit transcripts with your application and provide further details in your personal statement.
Please contact the PGCert Independent Prescribing/ Supplementary Prescribing Programme Manager prior to applying to discuss RPL queries: [email protected]
Find out more about English language requirements .
Criminal convictions
A DBS (Disclosure Barring Service) certificate is required to undertake the following modules:
- HCT 356 Independent/Supplementary Prescribing (core)
- HCT 357 Independent/Supplementary Prescribing (core)
If you are currently subject to any licence condition or monitoring restriction that could affect your ability to successfully complete your studies, you will be required to disclose your criminal record. Conditions include, but are not limited to:
- access to computers or devices that can store images
- use of internet and communication tools/devices
- freedom of movement
- contact with people related to Cardiff University.
Course structure
The Postgraduate Certificate in Independent/ Supplementary Prescribing consists of 2 core modules (30 credits each).
The modules shown are an example of the typical curriculum and will be reviewed prior to the 2025/26 academic year. The final modules will be published by September 2025.
You will undertake both modules in year one.
Independent/ Supplementary Prescribing.
You will need to complete a minimum of 12 days (78 hours) of learning in practice in order to develop clinical assessment and prescribing skills, supported by a designated Practice Supervisor (PS). This is a PSRB requirement.
| Module title | Module code | Credits |
|---|---|---|
| HCT356 | 30 credits | |
| HCT357 | 30 credits |
The University is committed to providing a wide range of module options where possible, but please be aware that whilst every effort is made to offer choice this may be limited in certain circumstances. This is due to the fact that some modules have limited numbers of places available, which are allocated on a first-come, first-served basis, while others have minimum student numbers required before they will run, to ensure that an appropriate quality of education can be delivered; some modules require students to have already taken particular subjects, and others are core or required on the programme you are taking. Modules may also be limited due to timetable clashes, and although the University works to minimise disruption to choice, we advise you to seek advice from the relevant School on the module choices available.
Learning and assessment
How will i be taught.
In line with Cardiff University’s Digital Learning Strategy, the programme will be delivered using a blended learning approach. The programme will aim to provide a rich and engaging online experience, including a blend of synchronous and asynchronous learning activities alongside traditional face to face teaching and learning.
We will employ a range of learning and teaching approaches, from group and individual tutorials to student led seminars, dialogue, appreciative enquiry and problem- based learning, skills workshops, self-directed study, critical discussion /debate and expert led lectures. We employ e-learning via Virtual Learning Environments (VLE) that are specifically developed for Independent/ Supplementary Prescribing programmes.
Our programme and modules will facilitate effective inter-professional learning across a wide range of professions, and the sharing of differing professional perspectives and expertise. This experience will enhance your learning and development, and enable you to widen your professional network.
We appreciate that as registered practitioners, you will enter the programme with a wide range of skills, and some of you may hold advanced practitioner roles. Your clinical and experiential experiences are highly valued and will be used to enhance the learning process in terms of independent and shared learning.
We will encourage you to take an adult approach to learning at postgraduate degree level, which involves you taking responsibility for your own learning. We aim to prepare you for professional Independent/ Supplementary Prescribing practice.
How will I be assessed?
To meet professional and statutory regulatory body requirements, you will be assessed via the following methods:
Electronic Prescribing Portfolio:
Therapeutic Framework written Assignment,
Numeracy Test: (30 minutes)
Clinical logs reflective assignment:
Structured Clinical Assessment (SCA):
Therapeutics Class test (60 minutes):
How will I be supported?
To meet professional and statutory regulatory requirements (NMC and HCPC), a number of levels of support are offered:
Personal Tutor : You will be allocated a Personal tutor at the beginning of the programme who will provide educational and pastoral support and will:
• Maintain regular contact throughout the programme;
• Advise on the academic standards;
• Provide support and guidance with respect to learning;
• Provide feedback of progress and constructive comment on any aspects of learning which will
require further development;
• Be available for personal advice and support.
Academic Assessor : You will be allocated an Academic Assessor from the programme team for the duration of their programme; in addition to the Personal Tutor who will provide educational and pastoral support. The programme manager is responsible for ensuring that the allocation and monitoring of academic assessors is compliant the NMC standards for supervision and assessment of students, and that academic assessors are prepared for the role, as per faculty standards.
Responsibilities:
- academic assessors collate and confirm student achievement of proficiencies and programme outcomes in the academic environment for each part of the programme.
- academic assessors make and record objective, evidence based decisions on conduct, proficiency and achievement, and recommendations for progression, drawing on student records and other resources.
- academic assessors maintain current knowledge and expertise relevant for the proficiencies and programme outcomes they are assessing and confirming.
- the nominated academic assessor works in partnership with a nominated practice assessor to evaluate and recommend the student for progression, in line with programme standards and local and national policies.
- academic assessors have an understanding of the student’s learning and achievement in practice.
Strategy to Support Student Learning and Development as Prescribers
It is expected by the NMC/HCPC and University that regular meetings between you and your DPP should take place to enable a valid and constructive review of your progress and agreement about any further learning experiences which are required. The Practice Assessor (PA) should also meet with you to inform assessment of the your competence. Such meetings will involve direct observation of the your practice to enable a valid assessment of competence.
Meetings also need to take place between the PA and Practice Supervisor (PS) to inform the PA’s understanding of your learning and development in practice. The PA and academic assessor are also required to meet to explore the your progress with practice and academic learning to enable a constructive assessment of the your development of appropriate proficiencies and to allow the Academic Assessor to collate student outcomes from all elements of the programme.
The programme offers you the opportunity to develop and share ideas with health professionals, enabling you to learn and benefit from the experiences of others. Opportunity is given for discussion and exchange of ideas through seminars and tutorials.
We offer you the opportunity to become a student representative and shape future educational provision and advise on key elements of your learning.
All modules within the programme make extensive use of Cardiff University’s Virtual Learning Environment (VLE) Learning Central, on which you will find course materials, links to related materials and assessment exemplars. All lectures are recorded via electronic platforms, and are available for you to view throughout your programme.
The University offers a wide range of services and activities designed to support you. These include a student counselling service, a student advisory service, day care facilities, sport and exercise facilities, as well as campus information, library and IT services.
Further information about what the University can offer you can be found in the following link:
Student life - Study - Cardiff University
Our student app also allows you to access Cardiff University services and personalised information in one place in a simple and convenient way from a smartphone via the app store.
Features include:
- Campus maps
- Student library renewals, payments and available items
- Student timetable
- Find an available PC
- Access to help and student support
- Student news
- Receive important notifications
- Links to launch other University apps such as Outlook (for email) and Blackboard (for Learning Central).
What skills will I practise and develop?
The Learning Outcomes for this Programme describe what you will be able to do as a result of your study at Cardiff University. They will help you to understand what is expected of you.
The Learning Outcomes for this Programme can be found below:
Knowledge & Understanding:
On successful completion of the Programme you will be able to:
- Critically evaluate drug actions and sources of evidence-based information, advice and decision support in prescribing practice.
- Critically explore current available clinical, pharmacological and pharmaceutical knowledge relevant to your own area of practice.
- Demonstrate a critical evaluation of legal, ethical, professional and governance issues in their prescribing role.
Intellectual Skills:
- Demonstrate the appropriate application of a critical knowledge of drug actions in prescribing practice and the effective use of evidence-based decision support tools.
- Demonstrate a critical understanding and application of legislation relevant to the practice of non-medical prescribing.
- Demonstrate a critical and independent reflective approach to practice, analysing situations resulting in a coherent and sustained argument to enable service and practice improvement and professional development.
Professional Practical Skills:
- Critically evaluate approaches to the systematic and holistic assessment of patient need and the interpretation of diagnostic indicators to achieve a differential diagnosis.
- Demonstrate a strategic approach to effective collaboration with the multidisciplinary team involved in prescribing, supplying and administration of medicines.
- Demonstrate the critical application of effective strategies in negotiation and shared decision-making with patients and carers.
- Demonstrate a strategic application in practice of the framework of professional accountability and clinical governance in non-medical prescribing.
- Effectively employ appropriate communication/ education strategies to communicate and disseminate knowledge to the patient, families and client groups.
Transferable/Key Skills:
- Engage with information systems in order to analyse and interpret data to inform prescribing practice.
- Integrate theory with professional practice.
- Synthesise information/ data from a variety of sources.
- Critically appraise, synthesise and evaluate the evidence base related to Independent/ Supplementary Prescribing.
- Take responsibility for your individual personal and professional learning and development.
- Independent project manage and demonstrate time management skills.
- Work independently.
- Problem solve and reach realistic conclusions/ recommendations.
- Communicate ideas in a clear concise manner.
- Demonstrate digital literacy.
Tuition fees for 2025 entry
Your tuition fees and how you pay them will depend on your fee status. Your fee status could be home, island or overseas.
Learn how we decide your fee status
Fees for home status
Fees will be invoiced by module. Normally, invoices will be released shortly after enrolment for each individual module. For more information please refer to our tuition fees pages .
Students from the EU, EEA and Switzerland
If you are an EU, EEA or Swiss national, your tuition fees for 2025/26 be in line with the overseas fees for international students, unless you qualify for home fee status. UKCISA have provided information about Brexit and tuition fees .
Fees for island status
Learn more about the postgraduate fees for students from the Channel Islands or the Isle of Man .
Fees for overseas status
This course does not currently accept students from outside the UK/EU.
Additional costs
Cost of Disclosure and Barring Service (DBS) certificate.
Will I need any specific equipment to study this course/programme?
We will provide any equipment required.
Living costs
We’re based in one of the UK’s most affordable cities. Find out more about living costs in Cardiff .
Postgraduate loans
If you are starting your master’s degree in September 2024 or later, you may be able to apply for a postgraduate loan to support your study at Cardiff University.
Careers and placements
The non-medical prescribing pathway will provide you with a qualification that enable you to build on your existing role; improving the patient experience and reducing waiting times.
This programme will help you develop your career by undertaking more advanced roles with greater responsibilities for managing patient care.
The PgCert is also available as a pathway through the MSc in Advanced Practice; a programme designed for health, social care and related professionals in primary, secondary and tertiary settings who wish to advance their knowledge base, clinical, leadership and management skills. Students, irrespective of their clinical specialty, will become actively involved in the advancement of practice.
You will need to be employed and practising within a clinical environment within the United Kingdom to undertake this programme. You will be required to evidence clinical hours within your own clinical environment for the following modules:
- Independent/ Supplementary Prescribing modules require 78 hours associated practice within your prescribing area (core).
Open Day visits
Make an enquiry, international, other course options, independent/ supplementary prescribing (pg cert), discover more.
Search for your courses
Related searches: Healthcare , Nursing and midwifery , Healthcare sciences
HESA Data: Copyright Higher Education Statistics Agency Limited 2021. The Higher Education Statistics Agency Limited cannot accept responsibility for any inferences or conclusions derived by third parties from its data. Data is from the latest Graduate Outcomes Survey 2019/20, published by HESA in June 2022.
Module information

Postgraduate
Progress happens when extraordinary people come together to think about what matters most. Join a community where everyone is empowered to reach their potential and make a difference.
Postgraduate prospectus 2025

Download a copy of our prospectus, school and subject brochures, and other guides.
Order or download
Get in touch if you have a question about studying with us.

V300 Independent and Supplementary Prescribing for Registered Nurses
Accredited by University College Birmingham
Apply Ask us a question
- Postgraduate
- V300 Independent and Supplementary Prescribing Programme
Choose Award
90 hours of supervised prescribing practice (protected learning time)
September, February
Course breakdown
Entry requirements
Key information
- Placements and Careers
Small teaching group sizes ensures personalised learning with excellent engagement from our teaching team
Provides the invaluable opportunity to develop professionally and advance to senior or supervisory roles
Nurse prescribing ensures that patients can promptly access necessary medicines and treatments. This is especially crucial for individuals with chronic conditions who require ongoing care.
This 40-credit V300 programme for Registered Nurses will enable you to become a safe and competent independent and supplementary (non-medical) prescriber of medicines (from the British National Formulary).
You will learn to prescribe safely, appropriately and cost-effectively in your role as an NMC registered nurse (level 1), community specialist practitioner (SPQ) or specialist community public health nurse (SCPHN). Following successful completion of the programme, you will be eligible to be recorded as an independent/supplementary prescriber (V300) on the NMC register. It is an excellent opportunity to advance to senior roles, including an advanced nurse practitioner (ANP) or an advanced clinical practitioner (ACP).
Why should I choose this course?
- INDUSTRY APPROVED – The course been developed in partnership with our employer and practice partners, industry experts and experts-by-experience (service users), so the programme meets the current health and social care priorities for prescribing practice, as well as the NMC and Royal Pharmaceutical Society requirements
- CAREER PROGRESSION – Once your annotation is active, you can prescribe within your scope of practice within the approved formulary, in your current role, or search for new roles to progress your career
- FLEXIBLE LEARNING - The programme delivery is flexible, with online as well as face-to-face teaching sessions, simulated practice learning, self-directed study, e-learning and supervised practice
Our facilities
As part of this programme, you will have access to University College Birmingham’s specialist practical and academic learning environments in Moss House and McIntyre House. These include our Health Skills and Simulation Suite , complete with a purpose-built, six-bed hospital ward with simulation manikins, Anatomage table, integrated filming and audio equipment and a community care environment for simulated scenario sessions and ‘OSCE’ practice.
Independent and Supplementary Prescribing Module
40 credit Independent and Supplementary Prescribing Module (Level 6 or Level 7):
This module will facilitate your development of the knowledge and skills required for safe and effective prescribing from a legally specified UK formulary. Successful completion of all components of the module will lead to the achievement of a recordable prescribing qualification with the NMC. The subject areas you will study include assessing the patient and considering prescribing options, pharmacology for prescribing and de-prescribing, legal and regulatory frameworks, providing information, reaching shared decisions, monitoring, and reviewing treatments, prescribing safely, professionally and as part of a team and improving prescribing practice.
Module topics:
The syllabus for the teaching reflects the Royal Pharmaceutical Society's (2021) multiprofessional, competency framework for all prescribers’ and meets current regulatory requirements to register as an independent and/or supplementary prescriber. RPS (2021) A competency framework for all prescribers .
The competencies within the framework are presented as two domains and describe the knowledge, skill, behaviour, activity or outcome that prescribers should demonstrate:
Domain one - the consultation
This domain looks at the competencies that the prescriber should demonstrate during the consultation.
Domain two - prescribing governance
This domain focuses on the competencies that the prescriber should demonstrate with respect to prescribing governance.
In addition to the above, the module content includes:
• Anatomy and physiology • Person-centred communication, information provision and shared decision making • Legal, ethical and professional issues • Clinical pharmacology, including effects of co-morbidities • Evidence-based practice and issues of quality related to prescribing practice • Professional accountability and responsibility • Concordance strategies and overcoming clinical inertia • Monitoring and reviewing strategies • Prescribing in the team context • Prescribing in the public health context including health promotion • Models of consultation and motivational interviewing • Introductions to epidemiology • Service user partnership and collaboration • Consider prescribing options. • Prescribing safety • Improving prescribing practice through reflection
The modules listed above for this course are regularly reviewed to ensure they are up to date and informed by industry as well as the latest teaching methods. On occasion, we may need to make unexpected changes to modules – if this occurs, we will contact all offer holders as soon as possible.
To be considered for a place on the V300 Independent and Supplementary prescribing programme, you must provide evidence that you meet this entry criteria:
NMC registration NMC registrants: Registered Nurse (Level 1), midwife or SCPHN, must be registered with the NMC for a minimum of one year prior to applying for entry to the programme, usually with one year’s relevant experience in the clinical field in which they are intending to prescribe
Enhanced DBS Have a satisfactory enhanced disclosure clearance (DBS), dated within three years of the programme start date.
Academic ability Have the academic ability to study at the level required for the programme (i.e. academic Level 6 (degree level) or Level 7 (master’s level). Evidence of this is required on the application form.
Experience and skills Have the ability to practise safely and effectively as a Registered Nurse at a level of proficiency appropriate to the V300 programme and your intended area of prescribing practice in all of the following areas: > clinical/health assessment > diagnostics/care management > planning/evaluating care
Evidence of this must be supported by evidence on the application form.
Governance arrangements Your workplace must have appropriate clinical governance arrangements in place for you to practise as a Registered Nurse Independent/Supplementary Prescriber, including indemnity insurance arrangements
Protected learning time You are required to attend 24 study sessions/ complete online study, so you will need protected learning time approved by your manager, plus 90 hours of supervised prescriber practice, either in your workplace, or with other prescribers across different learning environments across the programme (26 weeks). These 90 hours must be protected by your employer. Approval of this must be provided by your employer, on the manager's reference form.
Registered Nurses working in independent practice
In addition to the entry requirements above, additional information is required for nurses working in independent practice:
Non NHS and self-employed applicants: If you are a self-funding applicant, or work independently, in private practice, or external to the NHS, then you will need to assure us that you will have protected learning time to meet the programme requirements at university, study and for the 90 hours of supervised prescriber practice. You must additionally provide information relating to entry criteria that are usually signed off by an NHS manager or non-medical prescribing lead and will be requested to provide the following information:
One professional reference that addresses the points identified above. The referee must be either an NMC/HCPC/GPhC registrant. They must have recent knowledge of your practice and they must be able to provide their professional registration number. They must confirm that you have the ability to practice safely and effectively as a Registered Nurse at a level of proficiency appropriate to the V300 programme and your intended area of prescribing practice in all of the following areas: > clinical/health assessment > diagnostics/care management > planning/evaluating care
On the application form , in the personal statement, you need to provide details of your anticipated prescribing role on completion of the programme, including conditions for which you intend to prescribe.
You need to provide details of the clinical governance process that will be employed to support the safety of your prescribing, for example indemnity insurance, health and safety legislation.
The budgetary arrangement for your prescribing, e.g. will you be using an NHS prescriber code or private prescription?
Practice Assessor (PA) and Practice Supervisor (PS) commitment
Practice Assessor (PA) and Practice Supervisor (PS) commitment:
Your PA and PS must submit commitment forms as part of the application process.
This form requires a declaration of their qualifications and competence as Registered Prescribers to be able to support, supervise and assess you within their role as either Practice Supervisor or Practice Assessor.
This agreement must be provided as part of the application form and assessed by the programme lead. Enrolment will not be complete until the programme team have verified you have the required support in place, and you will not be able to start the programme until we have assurance of this.
If your application is successful, applicants will receive an invitation to enrol. If more information is required, or an applicant requests ‘Recognition for Prior Learning’, then the applicant will attend a short interview with the programme lead to discuss their application.
At this stage, the applicant chooses how to pay the programme fees - several payment options are available.
Application process
There are three components to your application:
1. Your information
2. Manager’s approval
3. Practice Supervisor and Practice Assessor commitment
As an applicant, you must complete the application form as part of the admission process to provide evidence that you meet all of the criteria for entry onto the programme.
It can take up to 6 weeks to receive a formal offer, especially if your application form is incomplete, requires information or you do not have a DBS in place. It is best to apply early to avoid disappointment.
The completed application, with manager’s commendation, must be returned to [email protected] 6 weeks before the start of the programme for assessment.
Please ensure that all elements are completed or your application may be rejected.
If you work for a Trust or an employer with a non-medical prescribing lead, they MUST approve your application.
On your application, your non-medical prescribing lead / employer will need to provide supportive evidence that you have:
- at least one year’s experience working in a role with an identified clinical need for prescribing.
- the appropriate knowledge and experience in the area in which you intend to prescribe.
- protected time for the 90 hours of supervised prescribing practice.
- protected time for the 24 days of academic study time.
- the appropriate clinical supervision, clinical governance, and indemnity insurance to cover your future prescribing practice.
- a current Disclosure and Barring Services (DBS) check.
Recognition of Prior Learning (RPL)
The programme team will consider Recognition of Prior Learning (RPL) that is capable of being mapped to the RPS Competency Framework for all prescribers. You must request a consideration for this on the application form.
RPL can be applied up to 50% of the programme learning outcomes.
Evidence of prior knowledge, experience, programmes of study (for example V100/V150), study at the same academic level (Level 6 or Level 7) will require formal evidence, for example, transcripts, certificates or manager’s reference.
Employer-sponsored applications/apprenticeships/self funding applicants
Apprentices : If the V300 programme is taken as part of the MSc Adult Social Care Nursing or Homeless and Inclusion Health Nursing Apprenticeship programmes, then the levy fee arrangement through your employer will cover the cost of the V300 as the module is included within these programmes.
Self-funded students:
If the V300 is studied as a standalone programme, at level 6 or level 7, the cost is £2000 (2024-25 cost).
If the V300 programme is taken as part of a full master’s (MSc Adult Social Care Nursing or Homeless and Inclusion Health Nursing), the cost of the MSc is £9350 (2024-25 cost), which will include the V300.
Master’s students can apply for a postgraduate loan to cover the course cost of a full MSc programme. Funding for postgraduate study can be found at Gov.uk. The maximum available loan is £12,471 for the upcoming year (courses starting from 1 August 2024)
**This programme is not available to international students.**
Teaching and assessment
The programme is designed to have a 50:50 split between theory and practice. You will be taught general principles on study days through a variety of teaching methods, then relate your learning to your own practice area with the support of your Practice Supervisor and Practice Assessor.
The induction day, two practical sessions and ALL assessments at the end of each semester are held onsite at the University's Moss House campus (OSCE and 2 x written exams).
Assessment:
- 2-part online invigilated exam – 90 minutes pharmacology (80% pass mark) and 30 minutes prescribing calculations (100% pass mark)
- Practice Assessment Document (PAD) (90 hours of supervised practice) This is to record practice-based assessment and achievement of the practice competencies for independent and supplementary prescribing
- Portfolio containing 2 x 2000-word case-based assignments or reflections
Our teaching and assessment is underpinned by our Teaching, Learning and Assessment Strategy 2021-2024 .
Teaching methods include: • Online lectures • e-learning workbooks • Group discussions • Tutorials/academic assessor meetings • Interactive sessions, including quizzes • Problem-based learning case studies and scenarios • Practical prescribing sessions • Healthcare numeracy and prescriber calculation practice • Action learning sets/small group tutorials
90 hours of supervised prescriber practice (protected learning time) You are required to meet a minimum 90 hours of supervised prescriber practice to meet the Royal Pharmaceutical Society Competency Framework for Prescribers.
In partnership with your employer, you must identify a suitable Practice Assessor (PA).
A Practice Assessor is a Registered Healthcare Professional with a prescribing qualification and a minimum of three years’ recent prescribing experience in this role, for example, a doctor, nurse, pharmacist or other professionally registered, V300 trained independent prescriber.
In conjunction with your Practice Assessor, you must identify suitable Practice Supervisor(s) (PS) to support your practice learning.
Practice Supervisors should also be registered V300 Independent/Supplementary Prescribers (or equivalent) with at least one year of experience in this role.
In exceptional circumstances (for example, where there is limited access to non-medical prescribers), nurses can request from the programme lead that the same person acts as both Practice Assessor and Practice Supervisor ( https://www.nmc.org.uk/standards/standards-for-post-registration/standards-for-prescribers) .
Further details of supervision and assessment requirements can be found in the Royal Pharmaceutical Society Designated Prescribing Practitioner Framework: RPS English Competency Framework 3.pdf (rpharms.com)
Your Practice Assessor, along with your Academic Assessor, who will be a member of the university programme team, is responsible for signing you off as a competent and safe prescriber by the end of the programme.
Self-directed study It is recommended that you complete a further 12 days of self-directed study across the year in addition to the 24 advertised university study days, or six days if studying the 40-credit module only.
Self-directed is required for research for assessments, writing assignments and preparing for exams.
Timetable and schedule
The programme is a 40-credit module, taught and assessed across one year (September to March or February to August), with supervised learning in practice running alongside theory sessions. Each module starts in either September or February.
There are 24 taught study sessions in total. This is one study session per week including online learning/self-directed study plus supervised prescriber practice in the workplace up to a total of 90 hours.
Assessments will be in March and July and any required resits in August.
All sessions are mandatory attendance.
Unibuddy Community - meet other students on your course
Starting university is an exciting time, but we understand that it can sometimes feel a little daunting. To support you, you will be invited to join our Unibuddy Community , where you can meet other students who have applied for the same course at University College Birmingham, before you start studying here.
As soon as you have been made an offer, you will be sent an invitation email to complete your registration and join the Unibuddy Community. For more information, check out our Unibuddy Community page .
of graduate employers say relevant experience is essential to getting a job with them
Who we work with
A snapshot of some of the employers we have worked with:
- Cygnet Healthcare
- Practice Plus Group (Health in Justice)
Birmingham and Solihull Integrated Care System, and the Trusts and Organisations within this:
- University Hospitals Birmingham NHS Foundation Trust
- Birmingham and Solihull Mental Health Foundation Trust
- Birmingham Women's and Children's NHS Foundation Trust
- Royal Orthopaedic Hospital NHS Foundation Trust
- Birmingham Community Healthcare NHS Foundation Trust
- Birmingham and Solihull NHS Training Hub (GP Practice)
- Sandwell and West Birmingham NHS Trust (City, Sandwell, Rowley Regis)
- Change Grow Live
- Birmingham Council
- Solihull Metropolitan Borough Council
"University College Birmingham’s prescribing team are excited to be able to offer our Independent and Supplementary Prescribing programme to Registered Nurses. T he programme will ensure you develop personally and professionally and gain new knowledge, skills and behaviours that you can use within your scope of prescribing practice in your advanced and specialist practice roles."
Neelam Faree Programme lead for the V300 programme
Career opportunities
Note : Some roles below may require further study/training. The roles and salaries below are intended as a guide only.
Community specialist practitioner
Average Salary: £36,370
Advanced clinical practitioner
Average Salary: £50,173
Advanced nurse practitioner
£35,000-£50,000
We are here to support your career goals every step of the way.
Find out more

Antony's Story
Antony worked in the NHS for 27 years before joining the team at University College Birmingham as a lecturer.

Take the next step...
Apply now Book an open day
Other courses you may like
Adult social care nursing msc.
This MSc has been specifically written for Registered Adult Nurses working across community social care environments in recognition of the specialist knowledge and skills required for nurses to lead and manage services across diverse health and social care settings. If this sounds fascinating, this could be the perfect fit for you.
Homeless and Inclusion Health Nursing MSc
This website is intended for healthcare professionals

- Product Profiles
- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Armstrong A. Staff and patient views on nurse prescribing in the urgent-care setting. Nurse Prescribing. 2015; 13:(12)614-619 https://doi.org/10.12968/npre.2015.13.12.614
Courtenay M. An overview of developments in nurse prescribing in the UK. Nurs Stand. 2018; 33:(1)40-44 https://doi.org/10.7748/ns.2018.e11078
Courtenay M, Rowbotham S, Lim R Antibiotics for acute respiratory tract infections: a mixed-methods study of patient experiences of non-medical prescriber management. BMJ Open. 2017; 7:(3) https://doi.org/10.1136/bmjopen-2016-013515
Courtenay M. Nurses can influence prescribing antibiotics. Primary Health Care. 2017a; 27:(6)14-14 https://doi.org/10.7748/phc.27.6.14.s19
Courtenay M, Khanfer R, Harries-Huntly G Overview of the uptake and implementation of non-medical prescribing in Wales: a national survey. BMJ Open. 2017b; 7:(9) https://doi.org/10.1136/bmjopen-2016-015313
Courtenay M. The benefits of nurse prescribers in primary care diabetes services. Journal of Diabetes Nursing. 2015; 19:(10)386-387
Day M. UK doctors protest at extension to nurses' prescribing powers. BMJ. 2005; 331:(7526)
Report of the advisory group on nurse prescribing.London: DH; 1989
Nurse prescribing a guide for implementation.London
Review of prescribing, supply and administration of medicine: final report (Crown Report) London. 1998;
Facilitators and barriers to non-medical prescribing - A systematic review and thematic synthesis. 2018. https://doi.org/10.1371/journal.pone.0196471
Hindi AMK, Seston EM, Bell D, Steinke D, Willis S, Schafheutle EI. Independent prescribing in primary care: A survey of patients', prescribers' and colleagues' perceptions and experiences. Health Soc Care Community. 2019; 27:(4)e459-e470 https://doi.org/10.1111/hsc.12746
Laurant M, Reeves D, Hermens R, Braspenning J, Grol R, Sibbald B. Substitution of doctors by nurses in primary care. Cochrane Database Syst Rev. 2005:(2) https://doi.org/10.1002/14651858.CD001271.pub2
Maier CB. Nurse prescribing of medicines in 13 European countries. Hum Resour Health. 2019; 17:(1) https://doi.org/10.1186/s12960-019-0429-6
NHS Health Education North West. Non-Medical Prescribing (NMP); An Economic Evaluation. 2015. http://www.i5health.com/NMP/NMPEconomicEvaluation.pdf (accessed 13 December 2022)
NHS England. Prescribing by paramedics. 2018. https://www.england.nhs.uk/ahp/medproject/paramedics/ (accessed 13 December 2022)
Skill-mix change in general practice: a qualitative comparison of three ‘new’ non-medical roles in English primary care. 2019. https://doi.org/10.3399/bjgp19X704117
Factors influencing nurse and pharmacist willingness to take or not take responsibility for non-medical prescribing. 2016. https://doi.org/10.1016/j.sapharm.2015.04.001
Task shifting between physicians and nurses in acute care hospitals: cross-sectional study in nine countries. 2018. https://doi.org/10.1186/s12960-018-0285-9
Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. 2009. https://doi.org/10.1371/journal.pmed.1000097
The long road to full prescribing powers. 2016. https://doi.org/10.7748/ns.30.33.18.s21
Identifying enablers and barriers to individually tailored prescribing: a survey of healthcare professionals in the UK. 2018. https://doi.org/10.1186/s12875-017-0705-2
Reviewing studies with diverse designs: the development and evaluation of a new tool. 2012. https://doi.org/10.1111/j.1365-2753.2011.01662.x
Nurse prescribing: An essential requirement or an expensive luxury for school nurses?. 2017. https://doi.org/10.12968/bjsn.2017.12.7.346
The Royal Pharmaceutical Society. A Competency Framework for all prescribers. 2016. http://www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Professional%20standards/Prescribing%20competency%20framework/prescribing-competencyframework.pdf (accessed 13 December 2022)
Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. 2007. https://doi.org/10.1093/intqhc/mzm042
Non-medical prescribing versus medical prescribing for acute and chronic disease management in primary and secondary care. 2016. https://doi.org/10.1002/14651858.CD011227.pub2
Medication decision making and patient outcomes in GP, nurse and pharmacist prescriber consultations. 2015. https://doi.org/10.1017/S146342361400053X
Continuing professional development needs of nursing and allied health professionals with responsibility for prescribing. 2015. https://doi.org/10.1016/j.nedt.2014.08.009
General practitioner and nurse prescriber experiences of prescribing antibiotics for respiratory tract infections in UK primary care out-of-hours services (the UNITE study). 2018. https://doi.org/10.1093/jac/dkx429
Non-medical prescribing in primary care in the UK: an overview of the current literature
Amanda Armstrong
Advanced Nurse Practitioner, Creffield Medical Center
View articles · Email Amanda

Non-medical prescribers are perceived as a complement to busy general practice in primary care.
To conduct an overview of the literature available on the role and impact of non-medical prescribers on primary care patients.
A search was conducted using multiple databases to find articles published between January 2015-January 2021. Inclusion criteria: non-medical prescribers in primary care in the UK, written in the English language. Exclusion criteria: research conducted in secondary care or outside the UK.
285 studies were identified; 15 were eligible for critical appraisal. The key themes were: non-medical prescriber's positive perceptions were autonomy, job satisfaction and colleague support. The negative perceptions included risk, lack of continuous professional development and organisational support.
By reviewing the perceptions of non-medical prescribing in primary care, organisations can ensure when employing new non-medical prescribers that adequate continued professional development and support is in place. Thereby reducing the concerns of non-medical prescribers about the ligation risk of prescribing.
The new NHS Long Term Plan (Winter, 2019) proposed an additional 20 000 non-medical prescribing (NMP) roles for primary care. Inadequacies within traditional doctor-led care systems means that to maintain patient access to prescription medicines, new approaches are urgently required. Allied health professionals, such as therapeutic radiographers, have been identified as having an integral part in the required transformational change (Chief Allied Health Professional Officers' Team, 2017). A reduction in the number of General Practitioners (GP) and the new ways of working in primary care are prompting the need for NMPs to fill these gaps (Winter, 2019).
After nurses lobbied parliament for years to be legally allowed to prescribe, nurses slowly earned more and more prescribing rights, until April 2006, when they were given the same prescribing rights as doctors ( Pearce, 2016 ). This exceeds any other non-medical prescribing rights anywhere in the world and initially caused great concern in the medical profession (Avery and Pringle, 2005; British Medical Association [BMA] 2005; Day, 2006). However, NMP is now seen to complement busy general practitioners in primary care ( Courtenay et al, 2017 ).
The primary focus of the research in NMP to date has been on its impact on patients, practitioners and organisations ( Courtenay et al, 2018 ; Carey et al, 2019). Other studies have identified motivators, such as job satisfaction and the opportunity to improve patient care, linked to increased prescribing activity ( Bailey and Taylor, 2017 ). Barriers identified to NMP included the lack of access to training and support from colleagues and the risk of litigation ( Armstrong, 2015 ; Nelson et al, 2019 ; Holden et al, 2019). There is a wide range of influences on NMP, including the trust of other members of the team (Weiss et al, 2016), the prescriber's confidence ( Courtenay et al, 2018 ), their experience ( Maddox et al, 2016 ) and the expectations of others and the organisation ( Hindi et al, 2019 ).
The present situation in the UK
Non-medical prescribing is increasingly being recognised as an essential healthcare practice, with at least 18 countries adopting NMP across Europe, the Americas and Australasia ( Courtenay et al, 2017 ). The drive behind NMP in the UK is the need to deliver high-quality healthcare to patients where and when they require it, with limited financial resources ( NHS England, 2015 ; NHS England, 2017). Innovative patient-centred care pathways have been developed using the most appropriate healthcare professionals, such as clinical pharmacists in general practice and prescribing physiotherapists streamlining musculoskeletal pathways (Carey, 2019). The reduction in the number of GPs is also causing concern regarding patients getting access to timely medical intervention (Winter, 2019).
In the UK, it is estimated that there are currently over 90 000 registered NMPs including nurses, midwives, pharmacists and allied healthcare professionals (such as optometrists, physiotherapists, podiatrists and radiographers) ( Courtenay et al, 2017 ). Since 2018, independent prescribing by advanced paramedics has been permitted, but this excluded prescribing controlled drugs ( NHS England, 2018 ).
Primary care networks
Since the NHS was created in 1948, the population has grown, and people are living longer (Winter, 2019). Many people are living with long-term conditions such as diabetes and heart disease or suffering from mental health issues and may need to access their local healthcare services more often. To meet these needs practices have begun working together with community, mental health, social care, pharmacy, hospital and voluntary services in their local area through primary care networks (Kings Fund, 2019). Around 7000 practices across England – more than 99% - have come together to form more than 1300 primary care networks (PCNs). Primary care networks are based on GP-registered lists typically serving natural communities of around 30 000 to 50 000 (The King's Fund, 2018; NHS England, 2018 ).
The key research questions are:-
- How do non-medical prescribers perceive themselves?
- How do patients perceive non-medical prescribers?
- How do other staff perceive non-medical prescribers?
A systematic process was conducted according to the PRISMA guidelines ( Figure 1 ). This utilises a transparent, structured process to review the literature and this approach is equally important when reviewing qualitative literature as it requires the identification of clear criteria to support credibility, transferability, dependability and confirmability (Bearman and Dawson, 2013). The quality of the studies was evaluated using two validated tools, COREQ ( Tong et al, 2007 ) for the interview and focus groups and the QATSDD (Sirriyeh et al, 2011) for a diverse design. All articles were scored and graded against the two checklists and then presented as percentages so they could be compared and are presented in Table 1 (Graham-Clarke et al, 2019). QSR NVivo 12 was used for the thematic analysis.
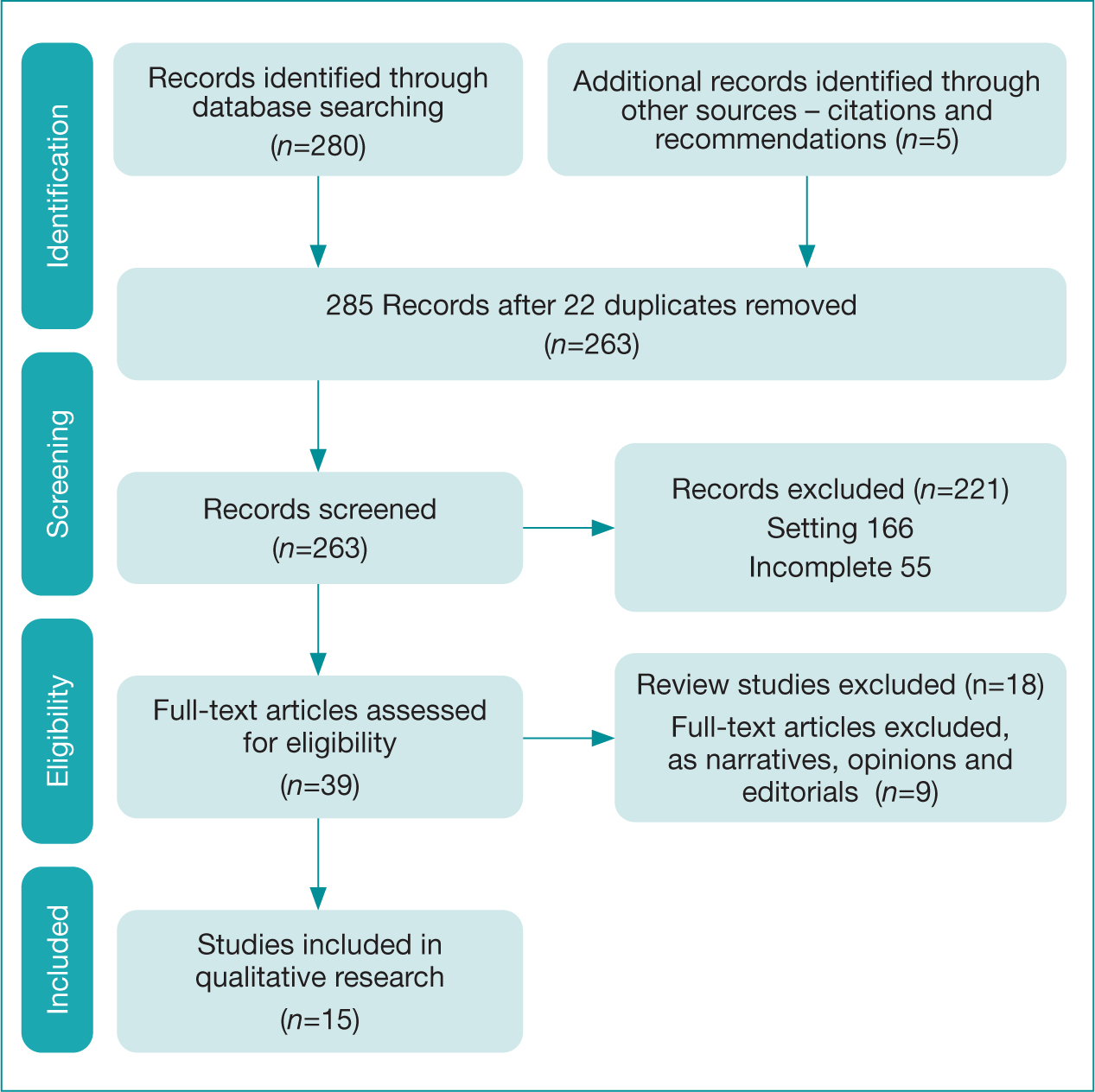
| Author(s) | Location | Study Design | Participant(s) | Findings | COREQ or QATSDD |
|---|---|---|---|---|---|
| 1. | Urgent care setting in England | SSI Questionnaire | Total number of participants: 25Senior Nurses 1Doctor 1NPs 2PP 1Patients 20 | Benefits of autonomous working identified by staff and patients.Concern over increase workload for NPs. Enhanced staff experience. Seen as a natural progression for advance nurses and continuity of care for patients. | COREQ 50% |
| 2. Carey et al (2019) | Primary Care in England | Quasi-experimental, post-test group design | Total number of participants: 3294 P. physio and 3 podiatrists compared to4 Non-P physio and 3 podiatrists315 patients. | Patients were asked for feedback on their consultations with their clinicians and then compared with prescriber and non-prescribers. Patients overall satisfied with care, professional care, ease of access to care and satisfied with information on medicines. | COREQ 31% |
| 3. | All settings in Wales | e-Delphi survey | Total number of participants: 34NP 28PP 3Physio 2Radiographer 1 | 21 statements were generated and nine factors that promoted the implementation of NMP – Positive organisational recognition, colleague support and CPD. 5actions were required for NMPs, clinical supervision, CPD, and that NMPs were valued by patients, colleagues and the organisation. | QATSDD 76.2% |
| 4. | All settings in Wales | Questionnaire | Total number of participants: 376NP 321PP 46ANP 9 | NMPs reported that they prescribed across a broad range of therapeutic areas. Infections for nurse, pain for pharmacist and MSK for physiotherapists. Lack of funding was the barrier to prescribing. | QATSDD 59.6% |
| 5. | Scotland, Wales and England | SSI And questionnaires | Total number of participants: 137Patient questionnaires and follow up 120SSI with 22 of those patientsSSI – 16 NPSSI - 1 PP | Focus on prescribing for respiratory tract infection. 96% of the patient population was satisfied or very satisfied due to a patient-centred approach. Patients reported being listened to and being taken seriously by NMPs. NMPs addressed patient expectations and concerns. | COREQ 53% |
| 6. | England | Case study | Total number of participants: 22612 case study sites in the UKIP (n=6)Nurse (n=6)Patients (n=214) | Data was compared from patients with diabetes who had been treated by a diabetic specialist nurse who could prescribe compared to diabetic nurses who could not prescribe. No statistical significant differences were found in the management of clinical outcomes such as diabetic control defined by levels of HbA1c. Increased satisfaction with all nurses but more so with nurse prescribers. | COREQ 31% |
| 7. Herklots et al (2015) | CC two PCTs in England | SSI | Total number of participants: 7NP 7 | NMPs enhancing their role and knowledge from the prescribing course was beneficial for their whole practice. Support included CPD which was variable, participants struggled to access formal CPD, however, GPs were very supportive. Being able to prescribe allowed speedier access to medicine for patients was also noted. | COREQ 50% |
| 8. | PC in England | Questionnaires | Total number of participants: 84IP 20Colleagues 26Patients 38 | Patient strongly agreed that IP improved the quality of care for the patient. Key barriers: IP's knowledge, competence and organisational factors such as workload, effective teamwork and support from colleagues. | COREQ 50% |
| 9. Holden et al (2019) | PC in England | Questionnaires and SSI | Total number of participants:1646 Physiotherapists (physios) 1637Physio Prescribers 9 | 1% of physios approaching OA were prescribers. However, they were not keen on extra responsibility despite acknowledging the GP burden. Did identify patient convenience as a benefit for prescribing. Lack of support to prescribe, burden of extensive training, and potential legal consequences. | COREQ 50% |
| 10. | PC and CC – in NW England | SSI or Focus group x3 | Total number of participants: 30PP 5NP 25 | NMPs cautious when prescribing; confidence improved with good support. NMP required improved access to CPD, clinical support and cohesive team culture. | COREQ 63% |
| 11. | PC England | SSI and focus groups | Total number of participants:38SL 9AP 8PA 4PP 6GP 5PM 6 | Themes analysis captured: purpose and place of new roles in general practice, such as physician associates as well as advanced practitioners.Findings: unclear role definitions and tension at professional boundaries. The need for training to ensure feasibility of skill mix. | COREQ 53% |
| 12. | CC England | Questionnnaire | Total number of participants: 20School Nurses 20 | Identified benefits such as improved medicine management and earlier interventions. Job satisfaction and credibility as being able to prescribe.Barriers: lack of need and lack of organisational support and CPD. | QATSDD 64.3% |
| 13. | England | SSI and focus groups | Total number of participants:15PP 1NP 11Physio 3 | Personal anxiety undermining confidence to prescribe, external barriers and other factors that exacerbate anxiety. Need for support identified through coping strategies, preferred mode or style of learning. | COREQ 56% |
| 14. Weiss et al (2016) | PC England | SSI | Total number of participants: 21GP 7NP 7PP 7 | Looked at how prescribers identify themselves ‘The doctors are king’. NP unsure who to align to, either nurses or GPs as now prescribers. PP did not feel part of the surgery as a secondary role. Organisational barriers identified. | COREQ 53% |
| 15. | Out of Hours service in PC | SSI | Total number of participants: 30GP 15NP 15 | Examined GPs and NPs prescribing antibiotics for respiratory tract infections in OOH in PC. Found that NP reported perceptions of greater accountability for their prescribing compared to GPs. Participants agreed more complex cases should be seen by GPs. | COREQ 67% |
AP: Advanced nurse practitioners
IP: Independent nurse
NP: Nurse prescriber
P.physio: Prescribing physio
PP: Prescribing practitioner
| 1992 | Legislation passed to allow limited formulary for health visitors and district nurses |
| 1999 | Health visitors and district nurses own formulary |
| 2000 | Extended independent nurse prescribers trained for walk in centre, emergency departments and primary care |
| 2002 | Extended formulary prescribing for nurses |
| 2003 | Supplementary prescribing for nurses and pharmacists |
| 2006 | Independent prescribing for nurses and pharmacistsSupplementary prescribing for therapeutic and diagnostic radiographers, physiotherapists, and podiatrists. |
| 2008 | Independent prescribing for optometrists |
| 2012 | Independent prescribing for physiotherapists and podiatrists |
| 2016 | Independent prescribing for therapeutic radiographersSupplementary prescribing for dieticians |
| 2018 | Independent prescribing for paramedics apart from controlled drugs |
Literature search
The literature search was undertaken in January 2021 using a range of databases from the University of Central Lancashire and resources were selected because of their relevance to the subject ( Table 3 ). To gather insight into the factors that could impact the NMP, the search included qualitative, quantitative and mixed-methods studies. Table 4 shows the search strategy of Nurs*, Non-medical, Primary care, and prescrib*.
| Databases and websites | Number of articles |
|---|---|
| AMED - Allied and complementary medicine database | None |
| CINAHL | 10 |
| EMBASE | 2 |
| ERIC – the Education Resource Information Centre | None |
| Google Scholar | 31 |
| HMIC – Health Management Information Consortium | None |
| MEDLINE/OVID MEDLINE Academic | 36 |
| PROQUEST HEALTH & MEDICAL | 113 |
| PUBMED | 88 |
| Search Terms | Search Terms | |
|---|---|---|
| Years 2015-2021 | Written in English | Research setting in UK |
| P (Population) | Nurse/Nurses/Non-medical prescriber/pharmacist/physiotherapist/podiatrist | Nurs* |
| Non-Medical | Primary Care | |
| I (Issue) | Prescriber/Perscribers/Prescribing | Prescrib* |
| E (Effect/Method) | Any |
Inclusion criteria
Articles published in the English language from January 2015 to January 2021 were reviewed in line with the aims. This short time frame was selected to give an overview of contemporary literature in this fast-moving field.
Exclusion criteria
Articles were ineligible for inclusion if they were published only in abstract form, opinion paper, narrative reviews, related only to secondary care or not in the UK and not published in the English language. The latter is because of a lack of resources for translation.
Ethics approval
Ethics approval was not required.
Summary of results
Of the participants, 3016 were identified in the 15 eligible studies. Most prescribers, 75%, were nurses (n=483), followed by pharmacists at 11% (n=72), physiotherapists accounting for 4% (n=21) of participants and finally four podiatrists at 1%. In Holden et al (2019), 1646 physiotherapists responded to a questionnaire regarding non-medical prescribing for osteoarthritis; however, only 1% (9) were prescribers.
All papers showed how participants were selected and the method of sampling and gave sample size. Across all papers, the details of the reflexivity of the interviewer, the relationship with the participant and whether any bias existed were covered. However, there were no details of non-participants and only three papers included interview guides ( Maddox et al, 2016 ; Williams et al, 2018 ; Nelson et al 2019 ). No-one repeated an interview and only one paper mentioned the duration of the interview and returning the interview transcription to be checked by the participant ( Maddox et al, 2016 ). Within data analysis no data coders or description of the coding tree were given as most papers did show deviations of themes and the software used.
This study highlighted the negative and positive perceptions of NMP by prescribers as well as from their colleagues and patient's perception. It gives a wider perception of the whole impact of NMP in primary care.
Positive perspective
The prescribers' perceptions of their role are mainly positive, especially about their ability to prescribe as it is generally seen as making a positive contribution to patient care including speedier access to medication ( Armstrong, 2015 ; Heklots et al 2015; Carey et al, 2019;
Heklots et al, 2015; Courtenay et al, 2019). Autonomy, increased job satisfaction and being able to make better use of skills/knowledge are also acknowledged as being positive by NMPs ( Armstrong, 2015 ; Taylor and Bailey, 2017 ; Hindi et al, 2019 ).
Negative perceptions
Negative perceptions were identified, including challenges such as non-medical prescribers having to adopt to new roles, manage extra responsibility and integrate with their practice settings in a way which supports cohesive teamwork between doctors, independent prescribers and other colleagues ( Armstrong, 2015 ; Maddox et al, 2016 ; Nelson et al, 2019 ). The risk of potential legal consequences because of the additional responsibility of prescribing was raised as a concern (Holden et al, 2019) and deterred many practitioners from training to be an NMP (Holden et al 2019; Holden et al; Carey, 2019). Lack of support from management and from colleagues was also identified as a barrier ( Maddox et al, 2016 ). The lack of CPD, lack of guidance and increased workloads were identified as well ( Armstrong. 2015 ; Courtenay et al, 2017a ; Maddox et al, 2016 ; Taylor and Bailey, 2017 ). Independent prescribing presents novel challenges to both independent prescribers and those working in a setting where they practice ( Weglicki et al, 2015 ; Weiss et al, 2016).
Patient's perception
Patient's perception on non-medical prescribing was positive, reporting positive experience and high satisfaction with accessibility and length of consultation (Carey et al, 2019; Hindi et al, 2019 ). Doctors also perceive benefits from working along-side independent prescribers such as having more time for complex cases (Herklots et al, 2015; Weiss et al, 2016).
| Paper Number | Total Participants | Nurse Prescribers | Pharmacist Prescribers | Physio Prescribers | Podiatrist Prescribers | Other NMP | Other staff | GP | Patients |
|---|---|---|---|---|---|---|---|---|---|
| 1. | 25 | 2 | 1 | 1 | 1 | 20 | |||
| 2. | 329 | 4 | 3 | 7 | 315 | ||||
| 3. | 34 | 28 | 5 | 1 | |||||
| 4. | 374 | 321 | 46 | 4 | 1 | 2 | |||
| 5. | 137 | 16 | 1 | 120 | |||||
| 6. | 226 | 6 | 6 | 214 | |||||
| 7. | 7 | 7 | |||||||
| 8. | 84 | 20 | 26 | 38 | |||||
| 9. | 1646 | 9 | 1637 | ||||||
| 10. | 30 | 25 | 5 | ||||||
| 11. | 38 | 5 | 6 | 1 | 6 | 15 | 5 | ||
| 12. | 20 | 20 | |||||||
| 13. | 15 | 11 | 1 | 3 | |||||
| 14. | 21 | 7 | 7 | 7 | |||||
| 15. | 30 | 15 | 15 | ||||||
| Total | 3,016 | 483 | 72 | 21 | 4 | 35 | 1,666 | 28 | 707 |
Organisation support
The results of this review are that the implementation of NMP is strongly influenced by organisational support (such as local policies, workload, funding and availability of medical resources and additional skills) ( Courtenay et al, 2018 ; Hindi et al, 2019 ; Taylor and Bailey, 2017 ) and for it to be successful the whole organisation has to ensure adequate preparation for not only the NMP, but the whole team, so that the NMP can be supported and reach their full potential.
Employing non-medical prescribers within healthcare services has the potential to make savings across a range of health specialities, providing more holistic patient care within an individual profession's scope of practice (Carey et al, 2019). For NMP to become more widely accepted, healthcare managers, clinical care quality and safety agencies, as well as the general public, require evidence of the overall value of NMP through the implementation of services that are patient-centred, improving the quality and safety of patient care, while simultaneously reducing costs and improving the efficiency of treatment and patient outcomes ( Courtenay et al, 2018 ).
Multiple studies have a focus on new roles and appropriate skill mix for general practice, not least because of the ongoing shortage of GPs but also because of the growing number of different issues and tasks that general practices have to tackle ( Maddox et al, 2016 ; Nelson et al, 2019 ; Carey et al, 2019).
| Perception | NMP | Patient | Organisational outcomes |
|---|---|---|---|
| Positive | Autonomy | Better outcomes for patients | Cost - effectiveness |
| Job satisfaction | Easier access to medicines | Availability of staff | |
| Support | High patient satisfaction | More multi-disciplinary team working | |
| Responsibility | |||
| Negative | Increase risk | Prefer to see GP | Lack of support |
| Lack of support | Lack of confidence in non-medical prescriber | Lack of guidance and restricted formulary | |
| Lack of continuous professional development | |||
| Lack of continuous professional development |
National policies have identified that ‘GPs will recruit multi-disciplinary teams, including pharmacists, physiotherapists, paramedics, physician associates and social prescribing support workers, freeing up family doctors to focus on the sickest patients (NHS Long Term Plan, 2019).
The studies conducted by Weglicki et al (2015) and Weiss et al (2016) highlighted the importance of organisational features, such as role collaboration and teamwork. They suggested that in the organisations they observed where different social identities were respected and supported, a positive organisational identity in terms of multi-disciplinary working may also be more likely to provide better patient care than those practices where traditional hierarchies and rigid professional boundaries predominated.
Limitations
To the best of our knowledge, there were no studies carried out in Northern Ireland and many studies included participants from secondary care and therefore were excluded from this paper. There were no studies looking particularly at the impact of NMP in primary care on minor illness. Therefore, more research needs to be carried out in this area. The literature that has been reviewed is only from the last 5 years to ensure that it is contemporary but it does not show past trends or practices in Northern Ireland.
Implications to Practice
Since 1992 with the development of NMP, patients and other practitioners have come to accept that prescribing can be safely performed by another member of staff as well as medical practitioners. To ensure that practitioners wishing to enhance their skills can undertake the appropriate training with a suitable practice mentor in place in the clinical practice. Organisational policies and procedures need to be in place to support NMPs with a clear level of responsibilities and scope of practice. Continued professional development must be in place to strengthen and support NMPs, ensuring that they are up-to-date and confident to prescribe within the scope of practice.
With the increased demand for general practice services and the decrease of medical practitioners, it will be necessary for GP surgeries to develop a multi-disciplinary approach to primary healthcare provisions. To enable the population to have adequate access to medicines, it will be key that NMPs are utilised, and that their expertise and competencies are adequately resourced. The studies identified in our search and included in the literature review have shown that outcomes and patient satisfaction are the same, if not higher than doctors. Organisations will need to develop robust continuous professional development for NMP along with clear professional and organisational guidelines on prescribing. To ensure that non-medical professionals are willing to undertake the prescribing training, they will need adequate financial incentives and career structure as well as good clinical support and supervision. GP services will have to ensure that they have systems in place to recruit, train, retain and promote non-medical prescribers to enhance primary care.
Key to making the new roles work will be to understand their place in the core general practice team or broader team and to build the relationship between professionals so that patients do not face multiple handoffs or get confused about how to access care. In choosing what additional roles to add to the team, practices must have a deep understanding of the needs of the population they serve and employ/train the right professionals with the right skills, supported by appropriate governance structure, to provide that care (Primary Care workforce commission, 2015). More research needs to be done in this area to ensure good integration of NMP into primary care.
- Non-medical prescribing in primary care is on the increase with more professions being able to prescribe.
- Positive perceptions of NMP are job autonomy, satisfaction and quicker access to medication.
- Negative perceptions of NMP are litigation risk, increase workload and lack of support.
- To successfully implement NMP the whole organsation must be ready to work with NMPs and support them.
CPD reflective questions
- What are the perceived benefits of having NMPs in primary care?
- What are the perceived challenges for NMPs in primary care?
- If you were a manager what would you do to support NMPs in primary care?
- How would you minimise the risks of NMPs in primary care?

- Pharmacist Independent Prescriber Course
- Minor Illnesses And Acute Conditions Course
- Setting Up A Private Clinic
Non-medical prescribing reflection examples
- Non-Medical Prescribing

Why do non-medical prescribers need to learn to become reflective practitioners?
During your non-medical prescribing course and clinical practice, nurse prescribers and pharmacist prescribers will be required to regularly reflect on their clinical practice to develop reflection and reflective practice skills.
Moreover, if you’re undertaking a non-medical prescribing course, you will be expected to submit as part of your coursework many reflective essays, i.e., a reflective account – so understanding what a reflection is and how to reflect is undoubtedly worth the investment.
Do medical prescribers need to reflect on their practice?
There is no one-size-fits-all answer to this question, as the need for reflection will vary depending on the individual and their clinical practice. However, medical prescribers should generally reflect on their practise to improve patient care and ensure they use evidence-based practices. Additionally, reflection can help medical prescribers identify areas where they need further education or training.
Do independent prescribers need to reflect on their practice?
Independent prescribers need to reflect on their practice to ensure that they prescribe safely and effectively. By reviewing their own practice, independent prescribers can identify areas where they may need to improve and make the necessary changes. This is important to protect patients’ safety and ensure that they are receiving the best possible care.
The above is relevant for all non-medical prescribing students, including; (1) future nurse prescribers, ; (2) allied healthcare professionals and (3) pharmacist prescribers wanting to undertake advanced practice training.
What is reflection?

Reflection is a mental process where people examine their experiences to better understand their whole profession. It allows individuals to enhance their work habits or the care they provide to patients regularly. It is an essential, continuous, and routine element of the job of healthcare and social service providers.
Teams comprised of professionals with different backgrounds, skill sets, and working experiences should be encouraged to reflect openly and honestly on what occurs when things go wrong. These practical reflective activities help develop resilience, enhance well-being, and increase professional devotion.
To be reflective during your prescribing practice, healthcare professionals must first be open to new ideas, explore them from various perspectives, be inquisitive – asking questions – and remain patient if the problem isn’t “simple.” (While this may suddenly leap out at you).
Your prescribing practice and reflective accounts need to make transparent to others and what you’re getting wrong or right. Therefore being honest with yourself is essential as a non-medical or independent prescriber.
Why do nurse prescribers, pharmacist prescribers and non-medical prescribing students need to reflect and write reflective accounts?
Reflection may help you learn a lot from your prescribing practice and prescribing decisions. There are several reasons to reflect. You can use it to:
- Learn from the experience of independent prescribing
- Improve your prescribing decision-making skills
- Help you make decisions in the future
- Identify continued professional development (CPD) needs
You can reflect on anything, but as a non-medical or independent prescriber, you should focus on your prescribing experiences. This will help you understand and develop your skills as a prescriber.
When thinking about your experiences, you should consider both the good and the bad. It’s important to reflect on what went well and what didn’t go so well. This will help you learn from your mistakes as well as your successes. Furthermore, it will ensure you identify gaps in your professional development needs.
There are many different ways to reflect. You can use written reflection, audio recordings, or even video. The important thing is that you’re taking the time to think about your experiences and what you can learn from them.
If you’re not sure how to get started, some helpful reflection templates and examples are below. You can also talk to us at MEDLRN for guidance on how to reflect on your independent prescribing experiences.
Remember, reflection is an integral part of being a successful non-medical prescriber. By reflecting on your experiences, you can improve your practice and make better decisions in the future.
Reflective practitioners and the benefits
The General Pharmaceutical Council, the General Chiropractic Council, the General Dental Council, the General Medical Council, the General Optical Council, the Health and Care Professions Council, the Nursing and Midwifery Council, and the Pharmaceutical Society of Northern Ireland’s top executives have signed a joint statement called Benefits of becoming a reflective practitioner.
https://www.pharmacyregulation.org/sites/default/files/document/benefits_of_becoming_a_reflective_practitioner_-_joint_statement_2019.pdf
This is what they say:
“We are committed to supporting our registrants in their professional development and we recognise the benefits of registrants engaging in reflective practice.
Reflective practitioners are more resilient, and adaptable and have a greater capacity to maintain their registration throughout their careers. They demonstrate professionalism by being able to reflect on their own values and behaviours, and how these might impact the people they care for.
Reflective practitioners are able to make well-informed decisions, using a range of strategies including critical thinking, problem-solving and lifelong learning. They can identify their own development needs and are committed to maintaining their registration by engaging in continuing professional development (CPD).
We would encourage all registrants to reflect on their practice and to use reflective tools and resources to support their professional development.
Reflective practice is a key part of being a healthcare professional. It helps us to learn from our experiences, both good and bad so that we can improve our practice and make better decisions in the future.
How to get started with reflective writing
Most people are unfamiliar with the concept of reflective writing. However, the following comments indicate a lack of clarity regarding reflective writing when it comes to courses and assessments: ‘I thought I wasn’t supposed to use “I” in my work.” ,,,,,,,,,, ‘I won’t say what I truly believe unless it is going to be evaluated.’
The following points will help you to understand what is meant by reflective writing and how it can be used to support your non-medical prescribing course:
- Reflective writing is a way of exploring and analyzing your own thoughts and experiences.
- It can help you learn from your own experiences and make better decisions in the future.
- Reflective writing is different from other types of academic writing as it allows you to share your own thoughts and feelings on a subject.
- When writing reflectively, you should use first-person pronouns (I, me, my) to share your own experiences.
- You should also be honest about your thoughts and feelings, as this will help you learn from your experiences.
- Reflective writing is usually informal in style and can be written in the first or third person.
- It is important to remember that reflective writing is about your own thoughts and experiences, so you should use “I” when sharing your reflections.
- When writing reflectively, it can be helpful to use a reflection template or guide. This will help you to structure your thoughts and ensure that you cover all the essential points.
- Reflective writing is an integral part of the non-medical prescribing course, as it helps you learn from your experiences. By reflecting on your prescribing experiences, you can improve your practice and make better decisions in the future.
What is a reflective essay?

A reflective essay is a type of writing in which you (the author) interact with an audience (readers, listeners, viewers) to describe an experience and how that experience has changed you.
Reflective essays are usually written after a milestone. For example, a student may write a reflective essay at the end of a course of study or after completing an internship or other practical work.
The purpose of a reflective essay is to describe the experience and examine the meaning of the experience and how it has affected you as an individual.
Reflective essays are personal pieces of writing, so they should use first-person pronouns (I, me, my, we, us) and express your own thoughts and feelings about the experience.
Reflective essays can take many different forms. Standard formats include journals, letters to the editor, blogs, and photographic essays.
When writing a reflective essay, it is essential to use descriptive language. This will help the reader to understand your experience and how it has affected you.
It is also important to use concrete details and examples in your writing. This will make your essay more attractive and easier to read.
Finally, remember to proofread your essay before you submit it. This will help ensure that there are no errors or typos in your writing.
Writing critically and reflectively during your non-medical prescribing course
Both critical and reflective may be used in a directive to ‘reflect critically’ on anything. The terms describe a writing trait in which the reader can discern that the text has been carefully considered.
To be critical, you must go beyond description and into the analysis. You evaluate ideas or methods (evaluate), apply them in your work (apply), and defend or refute them (defend). You also reflect on what you have read, thought, or experienced.
In both types of writing, the key features are similar: good, strong, and well-written essays. The major distinctions between critical and reflective writing are as follows:
1 You and your thoughts will be more apparent in your writings.
2 Your personal history – what you have done, thought about, read, and changed throughout your life – is a significant source of evidence in your writing.
3 You are more likely to use the present tense when writing reflectively.
The key features of critical and reflective writing:
Critical Writing
- More formal
- Focuses on ideas and methods
- Uses evidence from other sources
- Tends to use the past tense
Reflective Writing
- Less formal
- Focuses on you and your thoughts
- Uses your personal history as evidence
- Tends to use the present tense
Reflective writing for non-medical prescribing students and medical prescribers

Non-medical prescribing students and medical prescribers will be expected to:
- Participate in or observe an incident (such as the care of a patient)
- Discuss what went well and not so well about it
- Examine their thoughts about it by linking to relevant theory/policy/science/guidance and to the experience of others in similar circumstances
- Draw conclusions about what might be done differently next time and how this might improve patient care.
The use of frameworks to help non-medical prescribing students and medical prescribers write reflective essays or reflective accounts
A ‘framework’ is a method for structuring and analyzing an issue, scenario, or experience. It may help you extract the learning points from an event by taking a systematic approach:
- What happened?
- What was my role in it?
- What went well and not so well?
- What could I have done differently?
- What did I learn from it?
- How can I use what I learned in the future?
Reflective writing using the Gibbs Reflective Cycle
The Gibbs Reflective Cycle is a framework for reflection that helps you to think about your experiences and how they relate to your learning. The cycle is made up of six stages:
- Description
- Action Plan
These stages can be usefully applied to any reflective writing task.
An example of reflective writing using Gibbs reflective cycle
I recently observed an incident in which a patient was being discharged from the hospital. I was part of the team responsible for their care. I felt that the discharge process could have been better organized and that the patient could have been given more information about their condition and what to expect after leaving the hospital.
I evaluated the situation and identified some areas for improvement. I discussed my observations with the team, and we came up with a plan of action. I learned that it is important to be organized when discharge planning and to make sure that patients are given all the information they need to make a smooth transition from hospital to home. I will use this learning in future when discharge planning.
Example two of a reflective account using Gibbs reflective cycle
When I was first asked to do this reflective essay on weight loss, I was a little apprehensive. I wasn’t sure if I wanted to share my personal journey in this way or not. But after giving it some thought, I decided that it might be helpful for others who are either considering or currently trying to lose weight. So here goes…
I started my weight loss journey about 6 months ago. I had been feeling unhappy with my appearance for a while, and my health was also starting to suffer. I knew I needed to make a change, but I didn’t know where to start. Thankfully, a friend of mine recommended the Atkins Diet, and I decided to give it a try.
The first few weeks were tough. I had to make a lot of changes to my diet and lifestyle, and it was all very new to me. But I stuck with it, and after a few weeks, I started to see results. I felt better, both physically and mentally, and people were starting to notice the difference too.
Since then, I’ve lost a total of 30 pounds, and I’m still going strong. It hasn’t been easy, but it’s definitely been worth it. I’m now at a healthy weight, and I’m feeling the best I’ve ever felt.
The whole experience has taught me a lot about myself. I’ve learned that I’m capable of making big changes in my life, even when it’s hard. I’ve also learned that I’m stronger than I thought I was.
If you’re considering losing weight, or if you’re currently on a weight loss journey, then I encourage you to keep going. It’s not easy, but it’s so worth it. Trust me, I know from experience.
Gibbs’s Reflective Cycle (Gibbs, 1998) helps you to understand and practice your reflective skills. Use the template to reflect on a recent event in which you demonstrated a reflected ability to improve or demonstrate the need for further learning or development.
Description: what happened?
I had undertaken a supervised consultation as part of the non-medical prescribing course in the presence of my designated medical practitioner(DMP) and university tutor. Mary (pseudonym) middle-aged woman with a previous diagnosis of hypertension, was invited to attend the OSCE, which involved taking a comprehensive medical history in order to undertake a clinical assessment of the patient. Mary was invited to attend the OSCE, and prior to the OSCE, she was informed of the particulars of the assessment, e.g. the presence of my university tutor and DMP etc.
Mary was called to the consultation room, and verbal consent was gained. The consultation involved the following; undertaking a comprehensive history taking using the Cambridge and Calgary model, taking blood pressure, and an explanation of the pathology of hypertension and its management.
Upon completion of the consultation, I was informed by the DMP I had passed my assessment and feedback was given.
Feelings: what were you thinking and feeling?
As a pharmacist, this was the first time I had undertaken a structured consultation using the Cambridge and Calgary model. However, having been qualified for over 5 years, I was confident with my consultation skills, in particular, my communication skills and my knowledge of the pathophysiology and management of hypertension. In addition, I was comfortable and relaxed when taking Mary’s blood pressure as I have had considerable practice during my placement with taking blood pressure and felt confident when explaining the relevance of the readings as well as offering health advice. After the OSCE, I felt satisfied with the outcome and in agreement with the feedback of my DMP.
Evaluation: what was good and bad about the experience?
On evaluation, the event was good for a number of reasons. Firstly, Mary said she was satisfied with the advice and the explanation she was given regarding hypertension and the relevance of her blood pressure readings. In addition, feedback from my DMP included my good use of communication skills, especially eye contact and body language(NICE,2010). Furthermore, another positive of the consultation was that I was able to follow the Cambridge and Calgary model and address all the relevant assessment requirements. However, a negative of the consultation was that Mary had asked me to quantify how much of various fruits count towards your ‘5-a-day fruits requirements; however, I was a bit unsure and had to double-check the advice with my DMP even though it was correct. As such, I would have liked to have been more confident in providing that advice.
Analysis: what sense can you make of the situation?
Mary had asked me to explain to her what amount of different fruits count toward the ‘5-a-day’ requirement (NHS,2015), and I was unable to provide the answer confidently as mentioned above; this was the ‘part’ of the OSCE that did not go too well. A reason for this was that I had assumed certain health advice is ‘common knowledge and would not require much explanation. As such, It had never occurred that this was a gap in my knowledge. This negative aspect could have been avoided had I thought more deeply about the advice I offered and affirmed the understanding of patients. Conversely, a part of the consultation that did go well was that I was able to utilize the Cambridge and Calgary model to structure my consultations.
This was because I had undertaken considerable learning regarding structuring a consultation and practised the Cambridge and Calgary model on multiple occasions with my DMP and modified it slightly to address my needs. Furthermore, with regards to taking blood pressure, during my training with my DMP, I had reviewed best practice guidelines when undertaken taking blood pressure and asked for regular feedback, which ensured I was constantly improving my technique and skills.
Conclusion: what else could you have done?
As a result of the consultation, I have learned that I must confirm the understanding of the patient with regard to the health advice that is being given (Nursing Times, 2017) and ensure there is no confusion or misunderstandings. In addition, this experience (of undertaking a consultation) has highlighted the importance of ensuring there is structure to consultation and how I can use a model of consultation to suit the needs of the situation (Royal College Of General Practitioners Curriculum, 2010). Furthermore, I would have liked to have undertaken a level 3 clinical medication review (Brent CCG,2014) to determine adherence to the medication, as many hypertensives have poorly controlled blood pressure (heart Foundation,2016) with a lack of adherence to treatment cited as a major reason (Izzat,2009).
Action plan: if the situation arose again, what would you do?
In order to be better prepared to face a similar experience, I have decided I will continually practice using the Cambridge and Calgary model of consultation wherever possible and undertake self-appraisal (Royal College of General Practitioners,2013); in addition, in order to ensure I have adequate knowledge in health education, I will continue to undertake CPD and have decided to attend a training course within the next 4-8 weeks. Also, currently, I am trained to take blood pressure using an electronic machine but am not confident in measuring blood pressure manually, which would be useful if a patient had atrial fibrillation (NICE,2016). As such, I have decided to take further training under the supervision of my DMP to develop this clinical skill.
- Brent CCG ,2014. Medicines Optimisation:Clinical Medication Review [pdf]. Available at:<https://www.sps.nhs.uk/wp-content/uploads/2016/08/Brent-CCG-Medication-Review-Practice-Guide-2014.pdf> [Accessed 2nd April 2018].
- Heart Foundation,2016. Guideline for the diagnosis and management of hypertension in adults [pdf]. Available at:<https://www.heartfoundation.org.au/images/uploads/publications/PRO-167_Hypertension-guideline-2016_WEB.pdf> [Accessed 2 April 2018].
- Izzat, L.,2009. Antihypertensive concordance in elderly patients [Online] Available at <https://www.gmjournal.co.uk/media/21571/gm2april2009p28.pdf> [Accessed on 28 February 2018]
- National Institution for Health and Clinical Excellence, 2010. Principles of Good Communication [pdf].Available at:<file:///C:/Users/ProScript%20Link/Downloads/supportsheet2_1.pdf> [Accessed 1 April 2018].
- National health service, 2015. Nhs Choices 5 A Day portion sizes . [Online] Available at:<https://www.nhs.uk/Livewell/5ADAY/Pages/Portionsizes.aspx> [Accessed 1st April 2018].
- National Institute for Health and Care Excellence (2016). The clinical management of primary hypertension in adults (NICE Guideline 127). [Online] Available at: https://www.nice.org.uk/guidance/cg127 [Accessed 25 February 2018]
- Nursing Times, 2017. Communication Skills 1: benefits of effective communication for patients [online]. Available at:<https://www.nursingtimes.net/clinical-archive/assessment-skills/communication-skills-1-benefits-of-effective-communication-for-patients/7022148.article> [Accessed 1 April 2018].
- Royal College Of General Practitioners Curriculum, 2010. The GP Consultation in Practice [pdf]. Available at:<https://www.gmc-
- uk.org/2_01_The_GP_consultation_in_practice_May_2014.pdf_56884483.pdf> [Accessed 1st April 2018].
- Royal College Of General Practitioners, 2013. What are consultation models for? [pdf]/ Available at:<http://journals.sagepub.com/doi/pdf/10.1177/1755738013475436> [Accessed 2nd April 2018].
Author: Faheem Ahmed
Pharmacist Prescriber, 2x Award-Winning Pharmacist, Pharmacy and Clinic Owner, Founder of MEDLRN and loves sharing his experience with pharmacists.
Related Posts

Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Post comment
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Ther Adv Drug Saf
- v.8(6); 2017 Jun
Future perspectives on nonmedical prescribing
Derek stewart.
Robert Gordon University, Sir Ian Wood Building, Garthdee Road, Aberdeen, AB10 7GJ, UK
Tesnime Jebara
Robert Gordon University, Aberdeen, UK
Scott Cunningham
Ahmed awaisu.
Qatar University, Doha, Ad Dawhah, Qatar
Abdulrouf Pallivalapila
Hamad Medical Corporation, Qatar
Katie MacLure
Many countries have implemented nonmedical prescribing (NMP) and many others are scoping prescribing practices with a view to developing NMP. This paper provides a future perspective on NMP in light of findings of an umbrella review of aspects of NMP. This is followed by coverage of the Scottish Government strategy of pharmacist prescribing and finally, consideration of two key challenges. The review identified seven systematic reviews of influences on prescribing decision-making, processes of prescribing, and barriers and facilitators to implementation. Decision making was reported as complex with many, and often conflicting, influences. Facilitators of NMP included perceived improved patient care and professional autonomy, while barriers included lack of defined roles and resource pressures. Three systematic reviews explored patient outcomes that were noted to be equivalent or better to physician prescribing. In particular, a Cochrane review of 46 studies of clinical, patient-reported, and resource-use outcomes of NMP compared with medical prescribing showed positive intervention-group effects. Despite positive findings, authors highlighted high bias, poor definition and description of ‘prescribing’ and the ‘prescribing process’ and difficulty in separating NMP effects from the contributions of other healthcare team members. While evidence of benefit and safety is essential to inform practice, for NMP to be implemented and sustained on a large scale, there needs to be clear commitment at the highest level. The approach being taken by the Scottish Government to pharmacist prescribing implementation may inform developments in other professions and countries. The vision is that by 2023, all pharmacists providing pharmaceutical care will be pharmacist-independent prescribers. There are, however, challenges to implementing NMP into working practice; two key challenges are the need for sustainable models of care and evaluation research. These challenges could be met by considering the theoretical basis for implementation, and robust and rigorous evaluation.
Nonmedical prescribing models
The roles and responsibilities of all health professionals have undergone tremendous transformation in recent years. One key development has been the implementation of prescribing by nonmedical health professionals across many countries including Australia, Ireland, New Zealand, the United Kingdom (UK) and the United States (US). 1 Many other countries are scoping current prescribing practices with a view to developing nonmedical prescribing (NMP) models. A range of health professionals (e.g. dieticians, nurses, pharmacists, physiotherapists, radiographers) now have prescribing rights. The specific professions, their training and accreditation, and models of prescribing practice vary in different countries. Specific aims of NMP vary from country to country but are focused generally on: improving patient care outcomes without compromising patient safety; increasing patient access to medicines; and making better use of the skills of health professionals. 1 , 2
For example, in the UK, there are two models of NMP: supplementary prescribing (SP) and independent prescribing (IP). SP, introduced in 2003, is defined as a ‘voluntary partnership between an independent prescriber (doctor or dentist) and a supplementary prescriber to implement an agreed patient-specific clinical management plan (CMP) with the patient’s agreement’. 3 A later development was the introduction in 2006 of IP, defined as ‘prescribing by a practitioner (e.g. doctor, dentist, nurse, pharmacist) responsible and accountable for the assessment of patients with undiagnosed or diagnosed conditions and for decisions about the clinical management required, including prescribing’. 4 Qualification as an independent prescriber now also confers SP status. The similarities and differences between SP and IP are summarized in Table 1 .
Scope of different models of nonmedical prescribing in the UK. Adapted from Stewart et al . 1
| SP | IP | |
|---|---|---|
| Eligible health professionals | Dieticians, nurses, optometrists, pharmacists, physiotherapists, podiatrists, radiographers | Nurses, optometrists, pharmacists, physiotherapists, podiatrists, therapeutic radiographers |
| Clinical conditions managed | Any, within their clinical competence | Any, within their clinical competence |
| Diagnosis responsibilities | A doctor (or dentist) must diagnose the condition before prescribing can commence | The independent prescriber can assess and manage patients with diagnosed or undiagnosed conditions |
| Need for CMP | A written or electronic patient-specific CMP must be in place before prescribing can commence | No need for a CMP |
| Need for formal agreement | The CMP must be agreed with the doctor (or dentist) and patient before prescribing can commence | No need for any formal agreement |
| Drugs prescribed | Any, within their clinical competence | Any licensed medicines within their clinical competence. Nurse- and pharmacist-independent prescribers in particular can prescribe unlicensed medicines and controlled drugs |
SP, supplementary prescribing; IP, independent prescribing; CMP, clinical management plan.
In a recent paper in this journal, Cope and colleagues described the development of NMP, the processes required to qualify in the UK and the potential influences on NMP practice. 2 In the remainder of this paper, we consider the complexities of prescribing in general and in relation to NMP, followed by an umbrella review of all published systematic literature reviews on aspects of NMP, detailed coverage of the policy driven Scottish Government strategy relating to pharmacist prescribing and reflect on the future of NMP in light of accumulated evidence.
Complexities of prescribing
The 10 principles of good prescribing, articulated by the British Pharmacological Society, underline that prescribing is a complex and challenging task requiring considerable knowledge, skills and self-belief in capabilities ( Box 1 ).
Ten principles of good prescribing, British Pharmacological Society. 5
- Be clear about the reasons for prescribing
- Take into account the patient’s medication history before prescribing
- Take into account other factors that might alter the benefits and risks of treatment
- Take into account the patient’s ideas, concerns and expectations
- Select effective, safe, and cost-effective medicines individualized for the patient
- Adhere to national guidelines and local formularies where appropriate
- Write unambiguous legal prescriptions using the correct documentation
- Monitor the beneficial and adverse effects of medicines
- Communicate and document prescribing decisions and the reasons for them
- Prescribe within the limits of your knowledge, skills and experience
These principles apply to all prescribers, and should be borne in mind as new professional groupings are afforded prescribing rights. Point 10 is especially pertinent for newly qualified nonmedical prescribers who, despite being experienced practitioners, are inexperienced prescribers and must be prepared to seek the advice and support of their professional colleagues.
Given the evidence base demonstrating widespread suboptimal prescribing by doctors, there is great potential for nonmedical prescribers to impact positively patient care and safety. Ross and colleagues reported a systematic review of prescribing errors by junior doctors, with error prevalence rates of between 2 and 514 per 1000 items prescribed and in 4–82% of patients or charts reviewed. 6 Similarly, a systematic review by Lewis and colleagues of all prescribing errors in hospital inpatients reported median error prevalence data of 7% (interquartile range 2–14%) of medication orders, 52 (8–227) errors per 100 admissions and 24 (6–212) errors per 1000 patient days. 7 As nonmedical prescribers must have several years’ experience of interacting with patients prior to commencing their prescribing training, it could be hypothesized that this experience, together with specific prescribing training and assessment of competence, will translate into safer, more appropriate prescribing. To date, however, there has been little published research on NMP error rates. In one small study conducted in three hospitals in England, pharmacists prescribing of 1415 items revealed errors in only four items (0.3%). 8 While this appears to be positive, there is a need for further largescale research to confirm safety and appropriateness of all NMP.
One future development in the preparation of all prescribers (medical and nonmedical) may be harmonization of training, assessment, registration and regulation processes. Indeed, the National Prescribing Centre (now part of the National Institute for Health and Clinical Excellence for England and Wales) has produced a single competency framework for all prescribers. 9 The framework comprises 72 competency statements, organized into nine themed areas of knowledge, options, shared decision making, safe, professional, always improving, the healthcare system, information, self and others, in three overarching domains of the consultation, prescribing effectively and prescribing in context. It is anticipated that, if acquired and maintained, these competencies will help all prescribers become and remain effective and safe in their area of practice.
Nonmedical prescribers’ training, achieving these competencies and ongoing continuing professional development may lead to safe and effective prescribing. There remains, however, a need for robust and rigorous evidence of NMP safety and effectiveness on which to base future developments. While there are multiple published literature reviews exploring different aspects of NMP, to date there has been no comprehensive overview. Such a review would summarize the evidence from multiple-research syntheses and provide an assessment of the body of evidence to further inform developments.
Reviews of nonmedical prescribing
Umbrella reviews provide synthesis of the findings of systematic reviews. 10 Conducting such a review involves examining the quality of the included systematic review but does not require repeating the searches, assessment of study eligibility or quality assessment of the included reviews. The focus is on providing an overall picture of findings for the particular umbrella review aim. The aim of this umbrella review was to collate and summarize all the published systematic reviews on NMP in order to report aspects, including, but not limited to: models and definitions; legal frameworks; outcomes and benefits; perceptions and satisfaction of different stakeholders (e.g. general public, patients, health professionals and decision makers); and facilitators and barriers to implementing NMP. The search was conducted between March and November 2016.
Search strategy
Systematic reviews meeting the above criteria and published in English were included in the review. The following electronic bibliographic databases were searched: Medline, Cumulative Index of Nursing and Allied Health Literature, Science Direct, International Pharmaceutical Abstracts and Google Scholar. The Cochrane Library, the Centre for Reviews and Dissemination (Prospero) and Joanna Briggs Institute databases were also searched to identify any registered systematic review protocols. The reference lists of the retrieved reviews were examined to locate any further reviews.
The search strategy included only terms relating to or describing NMP, with no limits placed on the search. Alerts were created to check for further reviews for inclusion while conducting the review. An example of the search for Medline is given in Box 2 .
Medline search string.
(“non-medical prescrib*” OR “non medical prescrib*” OR NMP OR “pharmac* prescrib*” OR “nurse* prescrib*” OR “midwi* prescrib*” OR “podiatrist* prescrib*” OR “chiropodist* prescrib*” OR “optometrist* prescrib*” OR “orthoptist* prescrib*” OR “optician* prescrib*” OR “physiotherapist* prescrib*” OR “physical therapist* prescrib*” OR “dieti* prescrib*” OR “occupational therapist* prescrib*” OR “paramedic* prescrib*” OR “radiographer* prescrib*” OR “respiratory therapist* prescrib*” OR “audiologist* prescrib*”) AND (review)
Title, abstract and full text screening and assessment for inclusion was conducted by one of the reviewers (TJ), with another (DS) reviewing independently a 10% random sample to ensure sensitivity (comprehensiveness of search) and specificity (precision and relevance of reviews retrieved). Any disagreements were resolved through discussion without having to consult a third reviewer.
Quality assessment
The quality of systematic reviews that met the inclusion criteria was assessed using the Critical Appraisal Skills Programme (CASP) tool. 11 Quality assessment was conducted independently by two reviewers (TJ and DS or KM or SC or AA or ARP) and disagreements resolved through discussion without having to consult a third reviewer.
Data extraction
The characteristics of the included reviews were extracted and summarized in tables. Data extracted were: authors; year of publication; country/countries of focus; type of review; objectives; NMP definition; databases searched; number of articles; and major findings. As with the quality assessment, data extraction was undertaken independently by two reviewers.
Data synthesis
Due to heterogeneity of reviews in terms of objectives and data, a narrative synthesis was most appropriate.
Searching identified 528 studies, which was reduced to 453 after removing duplicates. A total of 405 were excluded on review of titles and abstracts (no search strategy included or not related to NMP) leaving 48, with two more identified from reference lists, making 50. Full-text screening excluded a further 26 (reasons as before). Of the remaining 24, there were 13 nonsystematic reviews, four were protocols, leaving seven systematic reviews for quality assessment, data extraction and synthesis. The PRISMA flow chart is provided in Figure 1 .

PRISMA flow chart detailing the inclusion process.
NMP, nonmedical prescribing.
The quality assessment of the seven systematic reviews is given in Table 2 . Most were deemed of high quality, although one would have benefited from searching country-specific databases and lacked quality assessment, 12 and qualitative findings could have been subjected to meta-synthesis in another. 13
Quality assessment of the seven systematic reviews. 11
| Authors | Are the results of the review valid? | What are the results? | Will the results help locally? | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Review addressed a clearly focused issue | Search relevant | Important and relevant studies included | Rigorous assessment of quality of included studies | Reasonable to combine results of review | Overall results of review | Precision of results appropriate | Applicable to local population | All important outcomes considered | |
| Van Ruth et al. | Yes | Yes | Yes | Yes | Yes, pooled if homogenous (for one review question) but noted high risk of bias in some studies | Very clear presentation of results according to aim | Yes (pooled data) | N/A | Yes |
| Kroezen et al. | Yes | Partially (peer reviewed literature less appropriate for some questions, e.g. extent of legal, educational conditions) | Partially | No explicit coverage of quality assessment | N/A as no meta-analysis or meta-synthesis | Very clear presentation of results according to aim | N/A as no pooling | N/A | Yes |
| Gielen et al. | Yes | Yes | Yes | Yes | Yes, pooled if homogenous but noted high risk of bias in some studies | Very clear presentation of results according to aim | Yes (pooled data) | N/A | Yes |
| Darvishpour et al. | Yes | Yes | Yes | Yes | Yes, qualitative meta-synthesis | Very clear presentation of results according to aim | N/A for meta-synthesis | N/A | Yes |
| McIntosh et al. | Yes | Yes | Yes | Yes | Yes, qualitative meta-synthesis | Very clear presentation of results according to aim | N/A for meta-synthesis | N/A | Yes |
| Ness et al. | Yes | Yes | Yes | Yes | No meta-synthesis of qualitative studies given | Very clear presentation of results according to aim | N/A for meta-synthesis (although not conducted) | N/A | Yes |
| Weeks et al. | Yes | Yes | Yes | Yes | Yes, pooled if homogenous but noted high risk of bias in some studies | Very clear presentation of results according to aim | Yes (pooled data) | N/A | Yes |
N/A, not applicable.
The data extraction is given in Table 3 . Five focused solely on nurse prescribing, 12 – 16 with two discussing all nonmedical prescribers. 17 , 18 While five included all studies irrespective of country or setting, 13 – 16 , 18 one included only those conducted in Western European and Anglo-Saxon countries, 12 and one was restricted to the UK. 17 The number of studies reviewed ranged from 3 to 124. Two reviews focused on aspects of influences on prescribing decision making generally 17 and prescribing behaviour related to antimicrobials. 13 One reported the extent of implementation of nurse prescribing, 12 one processes of prescribing and associated barriers and facilitators to implementation, 16 with three on various patient outcome measures. 14 , 15 , 18
Data extraction of seven systematic reviews.
| Authors | Aims/ objective(s) | Country | NMP | Databases searched and search terms used | Number of articles | Findings |
|---|---|---|---|---|---|---|
| Van Ruth et al. | Aimed to review the effects of medication being prescribed by nurses The following research questions were addressed: what are the effects of nurse prescribing compared with physician prescribing, on the quantity and types of medication being prescribed? What are the effects of nurse prescribing on patient outcomes? What are the effects of nurse prescribing on physician and nurse outcomes? What are the effects of nurse prescribing on characteristics of the health care system? | Review of all studies, irrespective of country | Nurse prescribing | Pubmed, Embase, CINAHL, Cochrane Library, Picarta, SCI, Invert, Biomed central, Virginia Henderson Library, Current Control Trials, NIVEL catalog, UK Department of Health, World Health Organization, Nurse Prescriber website, Google For PubMed, the following search terms were used: (‘Nurse prescribing’) OR (Nurs* [tiab] AND Prescri* [tiab]) OR (Nurs* AND prescriptions, drug [MeSH]) | 23 | Nurses sometimes differed from physicians in the number of patients they prescribe for and in the choice or type of medication Clinical parameters were the same or better for treatment by nurses compared with physicians across a range of conditions (diabetes and ‘various’) Perceived quality of care by nurses was similar or better The effects on professionals or on the health care system could not be described |
| Kroezen et al. | Aimed to gain insight into the scientific and professional literature describing the extent to and the ways in which nurse prescribing has been realized or is being introduced in Western European and Anglo-Saxon countries Secondly, to identify possible mechanisms underlying the introduction and organization of nurse prescribing on the basis of Abbott’s theory on the division of professional labour | Western European and Anglo-Saxon countries | Nurse prescribing | PubMed, Embase, CINAHL, Web of Science, EBSCO, NIVEL, Virginia Henderson International Nursing Library, World Health Organization website, Health professionals’ website, Google scholar. The following keywords were used: ‘nurse prescribing’, ‘independent (nurse) prescribing’, ‘autonomous prescribing’, ‘supplementary (nurse) prescribing’, ‘dependent (nurse) prescribing’, ‘collaborative prescribing’, ‘group protocols’, ‘patient group directions’, ‘time and dose prescribing’, ‘nurse formulary’ | 124 | Seven countries had implemented nurse prescribing of medicines The Netherlands and Spain were in the process of introducing nurse prescribing A diversity of external and internal forces had led to the introduction of nurse prescribing internationally The legal, educational and organizational conditions under which nurses prescribe medicines varied considerably between countries; from situations where nurses prescribed independently to situations in which prescribing by nurses was only allowed under strict conditions and supervision of physicians |
| Darvishpour et al. | Aimed to obtain new insights on nurse prescribing drugs, and to present a schematic model of nurse prescribing that could be a useful framework for its implementation The following research questions were addressed: what is the overall view on nurse prescribing? What are the positive and negative outcomes of nurse prescribing?What are the barriers and facilitators for its implementation? | Review of all studies, irrespective of country | Nurse prescribing | Integrated Digital National Library of Medicine, CINAHL, Medline, Cochrane Library, Scopus, Web of science, Elsevier, Emelard, JAMA journals, Wiley, Oxford journals, Springer and Thieme journals, World Health Organization website, Nurse prescriber website, Google scholar, Cambridge journals website The following were used: review AND nurs* prescri* | 11 | Studies revealed eight themes, namely: leading countries in prescribing, views, features, infrastructures, benefits, disadvantages, facilitators and barriers of nursing prescribing Despite the positive view on nurse prescribing, there were still issues such as legal, administrative, weak research and educational deficiencies in academic preparation of nurses |
| Gielen et al. | Aimed to identify, appraise and synthesize the evidence presented in the literature on the effectiveness of nurse prescribing compared with physician prescribing The following research questions were addressed: what are the effects of nurse prescribing on the quantity and types of medication being prescribed? What are the effects of nurse prescribing on patient outcomes? | Review of all studies, irrespective of country | Nurse prescribing | BioMed Central, CINAHL, Cochrane Database of Systematic Reviews, Current Controlled Trials, Embase, INVERT (Dutch nursing literature index), NIVEL catalogue, PiCarta (Dutch library system), PubMed, Science Citation Index and the Virginia Henderson International Nursing Library, and the website of the UK Department of Health, the website of the World Health Organization, a website for health professionals and Google Scholar For Pubmed: (‘Nurse prescribing’) OR (Nurs* [tiab] AND Prescri* [tiab]) OR (Nurs* AND prescriptions, drug [MeSH]) | 35 | Nurses prescribed in comparable ways with physicians They prescribed for equal numbers of patients and prescribe comparable types and doses of medicines Studies comparing the total amount of medication prescribed by nurses and doctors show mixed results. There appeared to be few differences between nurses and physicians in patient health outcomes: clinical parameters were the same or better for treatment by nurses, perceived quality of care was similar or better and patients treated by nurses were just as satisfied or more satisfied |
| McIntosh et al. | To critically appraise, synthesize and present evidence on the influences on prescribing decision making among supplementary and independent nonmedical prescribers in the UK | UK | All nonmedical prescribers | Medline, PsycARTICLES, CINAHL, International Pharmaceutical Abstracts, Education Resources Information Centre, Cochrane Library, Google Scholar, reference lists The following search terms were used: prescrib* and (pharmacist* or nurse* or physiotherapist* or podiatrist* or radiographer* or optometrist*) and (influenc* or decision* or decid* or judge* or factor*) | 3 | While all studies reported aspects of prescribing decision making, this was not the primary research aim for any. Studies were carried out in primary care almost exclusively among nurse prescribers ( = 67). Complex influences were evident, such as experience in the role, the use of evidence-based guidelines and peer support and encouragement from doctors; these helped participants to feel more knowledgeable and confident about their prescribing decisions. Opposing influences included prioritization of experience and concern about complications over evidence base, and peer conflict |
| Ness et al. | To present the findings of a systematic review that explored the influences on the antimicrobial prescribing behaviour of independent nurse prescribers | Review of all studies, irrespective of country | Independent nurse prescribing | Medline, CINAHL, AMED, HealthSource Nursing/Academic Edition, Proquest Health, Internurse, Cochrane Database, Web of Knowledge, Index to Thesis, ETHOS, reference lists Search terms included: Prescri* AND Antibiotic OR antimicrobial OR antibacterial AND Nurs* | 7 | Three articles expected that an antimicrobial would be given and therefore influences discussed were on the choice of the antimicrobial. Guidelines/protocols, safety, tolerability and efficacy of the antimicrobial itself, patient/parent pressure and training/experience were mentioned as influencing factors within the reported studies The other four studies explored influences on whether to prescribe. An antimicrobial or not and also found that guidelines/protocols were an influencing factor; however, the influence occurring most frequently was diagnostic uncertainty. |
| Weeks et al. | To assess clinical, patient-reported, and resource-use outcomes of NMP for managing acute and chronic health conditions in primary and secondary care settings compared with medical prescribing (usual care) | Review of all studies, irrespective of country | Healthcare providers who were not medical doctors, undertaking prescribing including, nurses, optometrist, pharmacists, physician assistants, and other allied health professionals or categories not specifically mentioned whose roles met the definition of nonmedical prescribing | Cochrane Database, DARE, HTA, Medline, Embase, PsycINFO, CINAHL, grey literature, trial registries | 46 | A meta-analysis of surrogate markers of chronic disease (systolic blood pressure, glycated haemoglobin, and low-density lipoprotein) showed positive-intervention group effects. While there appeared little difference in medication adherence across studies, a meta-analysis of continuous outcome data from four studies showed an effect favouring patient adherence in the NMP group. Patients were generally satisfied with nonmedical prescriber care. |
CMP, clinical management plan; NMP, nonmedical prescribing.
Synthesis of findings
Decision making and prescribing behaviours were reported as complex with many, and often conflicting, influences. 13 , 17 Of the three studies reviewed by McIntosh and colleagues, 17 decision making was not the primary aim for any. Acknowledging the paucity of studies and limited evidence base, key influences on decision making included nonmedical prescribers’ experience, evidence-based guidelines and treatment protocols, peer support and encouragement from medical practitioners, and patients. Ness and colleagues 13 reported similar influences on decision making in relation to antibiotic prescribing in the seven studies reviewed. Patient and parent pressure was noted as a key influence in both the decision to prescribe and which antibiotic to prescribe. These two systematic reviews have highlighted the need for further research on the decision-making processes, decisions and prescribing behaviours of nonmedical prescribers to inform NMP education, training and practice.
Facilitators of NMP included perceived improved patient care, professional autonomy and potential to apply expertise while barriers included lack of clearly defined roles of nonmedical prescribers, time for prescribing activities and other resource pressures, such as lack of funding to support prescribing roles, other competing tasks, lack of confidence of some NMPs, and the lack of acceptance of the role by other health professionals and patients. 16 This review was a meta-synthesis of 11 qualitative studies. There would be merit in updating this review to incorporate qualitative, quantitative and mixed-methodology studies but with focus on how facilitators are enabled and barriers overcome. Findings would assist greatly the development and implementation of NMP in new settings and countries.
Three systematic reviews have now been published reporting data on patient outcomes. 14 , 15 , 18 Despite the largely positive findings on a variety of outcome measures, the review authors all highlighted the absence of well-designed randomized controlled trials (RCTs) and high levels of bias associated with many of the studies included in their reviews that often resulted in the outcome findings being downgraded. In addition, the review authors noted the issue of often-poor definition and description of ‘prescribing’ and the ‘prescribing process’ within many studies, and the difficulty in separating NMP effects from the contributions of other members of the healthcare team. Review findings should therefore be interpreted with great caution. In 2007, Van Ruth and colleagues 14 reported their review of 23 studies of nurse prescribing. Of the nine studies reporting clinical outcomes, there were no differences between nurses and GPs in terms of resolution of symptoms, health status rating, clinical improvement over 2 weeks. These studies included ‘various’ patients: those presenting acutely with sore throats, need for contraception and the chronic condition of diabetes mellitus, hence limiting the opportunity for data pooling. In 2014, Gielen and colleagues 15 reported a systematic review of 35 studies of nurse prescribing. Of the 13 studies reporting clinical outcomes, there were no differences between nurse and physician prescribing in a variety of conditions including diabetes, hypertension, asthma, sore throat and contraception. The heterogeneity of patient populations and outcome measures limited the potential for any data pooling. Very recently, Weeks and colleagues 18 reported a Cochrane review of 46 studies (26 nurse and 20 pharmacist prescribers) of clinical, patient-reported, and resource-use outcomes of NMP for managing acute and chronic health conditions in primary and secondary care settings compared with medical prescribing. A meta-analysis of outcome measures of chronic disease showed positive intervention group effects. There was a moderate certainty of evidence for studies of blood pressure at 12 months (12 studies, 4229 participants) and low-density lipoprotein (7 studies, 1469 participants). Patients were generally satisfied with nonmedical prescriber care (14 studies, 7514 participants). A wide variety of resource use measures were reported across studies with little difference between groups for hospitalizations, emergency department visits, and outpatient visits. The authors concluded that there remains a need for well designed, conducted and reported randomized controlled trials of NMP compared with medical prescribing. However, as NMP is implemented increasingly into practice, there may be less desire from policy makers, healthcare leaders and funders to support such studies, preferring instead robust, rigorous evaluation of real-life practice.
Policy-driven approach to nonmedical prescribing in Scotland: pharmacist prescribing as an exemplar
While evidence of benefit and safety of NMP is essential to inform practice, for NMP to be implemented successfully and sustained on a large scale, there needs to be clear commitment at the highest level. This section provides a description of the Scottish Government strategy around the implementation of pharmacist prescribing; the approach and specific outcomes and actions described could be an exemplar for other professions and other countries. The Scottish Government strategy is to ensure that ‘all patients, regardless of their age and setting of care, will receive high quality pharmaceutical care using the clinical skills of the pharmacist to their full potential’. 19 Prescription for Excellence: a Vision and Action Plan for the right pharmaceutical care through integrated partnerships and innovation , was published by the Scottish Government in September 2013. The vision articulated within this document is that by 2023, ‘all pharmacists providing National Health Service (NHS) pharmaceutical care will be NHS accredited clinical pharmacist independent prescribers working in collaborative partnerships with medical practitioners who will continue to have overall responsibility for diagnosis’. Much of the recommendations are based on a scoping review of pharmaceutical care of patients in the community in Scotland, undertaken by Wilson and Barber. 20 There were several drivers for this landmark review including: the increasing work pressures in the NHS; the imminent lack of clinical capacity of the medical workforce; and an increasingly multimorbid older population with complex medicine-related needs. There was recognition that ‘significant changes will occur in medicine and therapeutics that will require new and innovative models of care to enable patients to obtain the maximum benefit’. 19
Enhancing and supporting the implementation of pharmacist IP to ensure patient-centred, safe, effective and efficient pharmaceutical care is fundamental to the delivery of the ambitions of Prescription for Excellence . Key specific outcomes include:
- Pharmacists in the NHS would be recognized as clinicians responsible for the provision of NHS pharmaceutical care.
- Releasing capacity of pharmacists to deliver pharmaceutical care would be facilitated by full utilization of pharmacy technicians, support staff and increased use of robotics in dispensing to improve safety and efficiency.
- All patients would have access to NHS pharmaceutical care by NHS-accredited clinical pharmacist independent prescribers in all settings.
- Patients have a close relationship with an individual pharmacist, ensuring greater continuity and consistency of care for patients, introducing the concept of the named pharmacist and patient registration with NHS Board-listed pharmacists that will underpin professional relationships with patients and local clinical governance systems.
There is an associated workplan to ensure that these outcomes (and others) are achieved within the 10-year timeframe. This includes developing approaches to:
- Embed partnership working between the patient (and possibly carer), their GP and pharmacist, therapeutic partnerships, and with other health- and social-care professionals.
- Further enhance the role of pharmacist IPs who will work with GPs to deliver medication/polypharmacy reviews, using telehealthcare and domiciliary visits, where appropriate.
- Further develop the pharmacist’s contribution to the management of common clinical conditions and develop new models of delivery of primary care services in partnership with GPs.
- Explore making better use of pharmacist prescribing post diagnosis.
There are clearly wide-ranging implications for all involved in the education, training and regulation of the pharmacy workforce, as well as all other health- and social-care professionals with whom the pharmacist IP will work and patients, their families and carers, as well as the general public. These are highlighted in terms of:
- Ensuring a workforce that is fit for purpose by implementation of NHS standards of practice for pharmaceutical care that are attained through working with the NHS, Schools of Pharmacy and Medicine, NHS Education for Scotland and the professional and regulatory bodies.
- Ensuring education and training meets the needs of patients and the NHS.
- Implementation of primary and secondary care-configured systems to allow electronic information sharing contributing to pharmaceutical care and electronic prescribing for all prescribers including pharmacist IPs.
It is, therefore, reassuring that specific reference is made to supporting ‘action research, practice research and clinical research that enables development and evaluation of pharmaceutical care’. Governance arrangements have been put in place to ensure delivery of the work programme and vision. These comprise: a Steering Board of key Scottish Government and NHS contacts to oversee and prioritise implementation; a Reference Group of a wide range of stakeholders to act as a sounding board; a Core Implementation/Management Group of the leads to oversee the working groups; and Working Groups developing a response to each action point contained in Prescription for Excellence .
There are now over 750 pharmacists in Scotland (around 20%) who are either pharmacist IPs or have commenced training with the potential to make a difference to patient care in line with the ambitions of Prescription for Excellence . A recent survey of pharmacist prescribers across Great Britain, conducted by the General Pharmaceutical Council, highlighted that almost three quarters of the respondents were active prescribers, with the three major areas of prescribing being antibiotics, pain management and cardiovascular agents. 21 Barriers to prescribing cited included lack of resources and support networks, opportunity to prescribe and recognition of the prescribing role. These issues have been demonstrated repeatedly in previous research focusing on pharmacists in Great Britain, as well as in other countries and groups of IPs in systematic reviews. 12 , 14 , 16 It is, therefore, vital that these issues of structures and processes are dealt with rigorously as Prescription for Excellence progresses in order to ensure the very best outcomes for patients. There is also a need to ensure that pharmacist IPs are truly integrated within the healthcare team and that the roles and responsibilities of all prescribers (medical and nonmedical) are understood by all.
Challenges to be overcome
There is a great opportunity for NMP to make a real difference to professional practice and patient care globally. Legislation and models of care implemented vary between countries and it is possible that this variation will widen as more countries develop their own policies, structures and processes. While there are several significant matters which must be addressed, two key issues are: the need for sustainable models of care, and robust, rigorous evaluation research.
There are many examples in healthcare of successful pilot projects not being sustained or failing once extended beyond successful pilot sites. There are also reports which indicate that a number of qualified nonmedical prescribers have not prescribed. It is, therefore, extremely important to consider the theoretical basis for implementation of any major development or change in the delivery of services. Theory is also a key consideration in the UK Medical Research Council guidance on ‘Developing and implementing complex interventions’. 22 One theory which is gaining in credibility in health-related innovation is Normalization Process Theory (NPT). NPT is a set of sociological tools developed by May and colleagues, explaining ‘…the social processes through which new or modified practices of thinking, enacting and organizing work are operationalized in healthcare and other institutionalized settings’. 23 It focuses on how work practices become routinely embedded (normalized) in everyday routines, with those practices which are normalized being much more likely to be sustained, leading to the long-term desired outcomes.
NPT offers an explanation of three obstacles: implementation, the social organization of bringing practices into action; embedding, the process through which practices become incorporated routinely; and integration, the process by which practices are sustained. 23 , 24 NPT proposes that practices are embedded routinely as the result of people working individually and collectively to implement them. Implementation is operationalized through four constructs of:
- Coherence, which relates to the sense-making work that people do individually and collectively.
- Cognitive participation, relational work that people do to build and sustain a community of practice.
- Collective action, operational work that people do to enact a set of practices.
- Reflexive monitoring, appraisal work that people do to assess and understand the ways that a new set of practices affect them and others around them.
Implementing NMP into any health system is likely to be complex when considering the number of different health professionals involved, the different processes and technological systems, the central role of the patient and influences of families, friends, carers, and many other factors which could impact negatively on the implementation and sustainability of NMP. Consider the situation where NMP is to be implemented in primary care. Patients will undoubtedly be going to interact with many health professionals and may well have more than one prescriber. For example, a medical prescriber may prescribe during a consultation for an acute condition or an acute worsening of a chronic condition. A nurse IP may manage a specific medical condition such as type 2 diabetes mellitus and the pharmacist IP may review and alter all chronic medicines. There is great potential for confusion which could lead to negative patient outcomes.
Applying the principles of NPT and considering the constructs should enable clear coherence, understanding and shared decision making of all policy makers, managers, leaders, health professionals and patients. Cognitive participation should result in organized individuals working together systematically for collective action with clearly specified roles of health professionals, prescribers, patients and pathways of care. The final construct of reflexive monitoring should ensure that there is appropriate appraisal of the structures, processes and outcomes of NMP. This would facilitate successful implementation from all the different perspectives involved and sustainability of NMP. Returning to the example of Scotland and pharmacist prescribing, much effort is being expended on the governance structures to ensure coherence at all levels, cognitive participation, collective action and reflexive monitoring. 19 This is being effected through a programme of widespread engagement, facilitated by several interlinked workstreams, an overarching reference group and a management group. Emphasis is being placed on the active involvement of stakeholders (e.g. patient groups, health professionals, managers, leader, policy makers, academics, researchers, etc.) and rapid communication of developments.
The second issue that relates directly to reflexive monitoring is concerned with the necessity for robust and rigorous evaluation. While evaluation-based research studies are considered to provide a lower level of evidence compared with findings derived from RCTs and associated systematic reviews and meta-analyses, evaluation designs are based on real-life settings and practice. Furthermore, as NMP becomes adopted into legislation and practice, it is less likely that policy makers, senior managers and research funders will support RCT designs.
The UK Health Foundation highlights three different definitions of evaluation that they consider relevant to health: the process of determining the merit, worth or value of something; using systematic, data-based inquiries about whatever is being evaluated; and a process undertaken for purposes of improvement, decision making, enlightenment and persuasion. 25 Robust and rigorous evaluation will provide valid, reliable and trustworthy data about how, why and when services are working (or not working). Better Evaluation is an ‘international collaboration to improve evaluation practice and theory by sharing and generating information about options (methods or processes) and approaches’. 26 There are seven clusters of evaluation tasks: managing an evaluation or evaluation system; defining what is to be evaluated; framing the boundaries for the evaluation; describing activities, outcomes, impacts and context; understanding causes of outcomes and impacts; synthesizing data from one or more evaluations; and reporting and supporting use of findings.
There are multiple approaches to evaluation, some examples being: case studies, focused on understanding a unit (e.g. NMP site) in its context, employing qualitative, quantitative and mixed methodologies; participatory action research, which involves practitioners in the research process from the initial design of the project through data gathering and analysis to final conclusions; and realist evaluation. In 1997, Pawson and Tilley developed the first realist-evaluation approach based on the question, ‘what works, for whom, in what respects, to what extent, in what contexts, and how?’. 27 This approach differs from others in that it is grounded in theory, is claimed to be suited to assessing (a form of theory-driven evaluation) and hence may be relevant to consider if using a theory such as NPT to facilitate implementation and sustainability. As with other evaluation approaches, the methodology may be qualitative, quantitative or mixed. However, alongside consideration of the evaluation approach, attention should be paid to who conducts the evaluation, when it should be conducted, and how to use the findings. Evaluation of NMP must consider all perspectives and while there are many examples of such evaluations, most are small scale, tend to focus on a limited number of perspectives, and often omit any theoretical underpinning to data collection, analysis or interpretation.
Paying attention to these twin issues of intervention, normalization for sustainability and producing robust and rigorous evaluation data will greatly enhance NMP realization globally.
Many countries have implemented NMP and these models of care are now being considered by others across the globe. Given that prescribing is a complex task with high potential for error, evidence of NMP outcomes is warranted. While there are a number of systematic reviews on aspects of NMP, there is a lack of evidence of prescribing safety, and clinical and cost effectiveness. The strategic approach of the Scottish Government to the implementation of pharmacist prescribing on a large scale could inform other countries as they implement and extend NMP. There are many challenges to implementing NMP into working practice; two key challenges are the need for sustainable models of care and evaluation research. These challenges could be met by considering the theoretical basis for NMP developments, and robust and rigorous evaluation to provide valid, reliable and trustworthy data about how, why and when services are working (or not working) to inform further developments.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest statement: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Contributor Information
Derek Stewart, Robert Gordon University, Sir Ian Wood Building, Garthdee Road, Aberdeen, AB10 7GJ, UK.
Tesnime Jebara, Robert Gordon University, Aberdeen, UK.
Scott Cunningham, Robert Gordon University, Aberdeen, UK.
Ahmed Awaisu, Qatar University, Doha, Ad Dawhah, Qatar.
Abdulrouf Pallivalapila, Hamad Medical Corporation, Qatar.
Katie MacLure, Robert Gordon University, Aberdeen, UK.

General Discussion
V300 personal statement.

IMAGES
VIDEO
COMMENTS
What is non-medical prescribing. Nonmedical prescribing refers to the prescribing of medications by trained professionals who are not physicians. This can include nurses, pharmacists, and other healthcare professionals. Nonmedical prescribing is becoming more common as it is recognized as a way to improve patient care.
Writing a personal statement is a crucial step in applying for a Non-Medical Prescribing (NMP) course. This guide will help you craft a compelling personal statement that highlights your qualifications, experience, and motivation for becoming a prescriber. Prerequisites for the Course. Before you begin writing your personal statement, ensure ...
The nonmedical prescribing portfolio is a collection of documents that you must submit to demonstrate that you have met the requirements for the V300 nurse prescribing course. The essay is one component of the portfolio and is mandatory. It must be submitted with the other documents.
They are qualified to prescribe only from the Nurse Prescribers Formulary (NPF) for Community Practitioners. This formulary contains appliances, dressings, pharmacy (P), general sales list (GSL) and thirteen prescription only medicines (POMs). Independent Prescribers (IP) Independent prescribers are nurses who have successfully completed an NMC ...
How to become an independent prescriber. Gaining a non-medical prescribing qualification allows pharmacists to diagnose conditions and prescribe medicines to patients. If you are innovative in your practice and think laterally, many opportunities present themselves, says independent prescriber Anja St Clair Jones. 21 November 2014.
Supplementary Prescribing: Use of Unlicensed Medicines, Reformulation of Licensed Products and Preparations made from Active Pharmaceutical Ingredients and Exipients. London: MHRA. Google Scholar. ,MHRA (2009). Revised statement on medical and non-medical prescribing and mixing medicines in clinical practice. London: MHRA.
Educating nonmedical prescribers. The last decade has seen developments in nonmedical prescribing, with the introduction of prescribing rights for healthcare professionals. In this article, we focus on the education, training and practice of nonmedical prescribers in the UK. There are around 20 000 nurse independent prescribers, 2400 pharmacist ...
Updated online resource is a step-by-step guide for nurses considering a prescribing course The toolkit guides nurses through what is involved in gaining a prescribing qualification Picture: Jim Varney Essential information Until the 1990s, only doctors and dentists were able to prescribe medicines. ... becoming a non-medical prescriber ...
6.2 Record keeping. Non-medical prescribers should ensure records are accurate, comprehensive, contemporaneous and accessible by all members of the prescribing team. The non-medical prescriber will record details of the prescribing and relevant consultation details into the patient record at the time of writing.
A range of non-medical healthcare professionals can prescribe medicines for patients as either Independent or Supplementary Prescribers. Independent prescribers are practitioners responsible and accountable for the assessment of patients with previously undiagnosed or diagnosed conditions and for decisions about the clinical management required, including prescribing.
Non-medical prescribing (NMP) was introduced into the United ... as well as prescribing within their personal competence, and support they gained from others, such as the clinical team. The theme highlighted training aspects including access to, and skills gained on, the course. ... where the top ranked statement concerned the effectiveness and ...
What are the non-medical prescribing application form sections? Most application forms are divided into the following sections; (1) personal, professional and academic qualifications; (2) personal statement; (3) suitability to apply for the course. We will explore each section in depth below.
A personal statement, detailing your reasons for seeking to undertake this subject, will be required. Entry requirements vary by regulator. Please check you meet the specific requirements below: ... support and assess the competence of non-medical prescribing trainees, in collaboration with academic and workplace partners, during the period of ...
The non-medical prescribing pathway will provide you with a qualification that enable you to build on your existing role; improving the patient experience and reducing waiting times. This programme will help you develop your career by undertaking more advanced roles with greater responsibilities for managing patient care.
On the application form, in the personal statement, you need to provide details of your anticipated prescribing role on completion of the programme, ... If you work for a Trust or an employer with a non-medical prescribing lead, they MUST approve your application.
Q: Is Non-Medical Prescribing the same as Independent Prescribing? A: Non-Medical Prescribing is the umbrella term for all the prescribing streams we offer which include: V300, V150, AHP Supplementary Prescribing, AHP Independent Prescribing and Pharmacist Independent Prescribing. For all streams you will need to make an application via the ...
NON MEDICAL PRESCRIBING ESSAY. Introduction: Independent prescribing is 'prescribing by a practitioner (e.g. doctor, dentist, nurse, physiotherapist, and pharmacist) responsible and accountable for the assessment of patients with undiagnosed or diagnosed conditions and for decisions about the clinical management required, including ...
Complete all parts of the Non medical prescribing practice document. Nonmedical prescribing clinical observation hours example. Date. 4/10/17. 3 hours. Observing a range of consultations of the patient by DMP, e.g. to discuss treatment of Hypertension, treat conjunctivitis, treat lower urinary tract symptoms in child-With DMP . LO1,LO2,LO3a ...
Non-medical prescribing is increasingly being recognised as an essential healthcare practice, with at least 18 countries adopting NMP across Europe, the Americas and Australasia (Courtenay et al, 2017). The drive behind NMP in the UK is the need to deliver high-quality healthcare to patients where and when they require it, with limited financial resources (NHS England, 2015; NHS England, 2017).
Nonmedical prescribing has been allowed in the United Kingdom (UK) since 1992. Its development over the past 24 years has been marked by changes in legislation, enabling the progression towards independent prescribing for nurses, pharmacists and a range of allied health professionals. Although the UK has led the way regarding the introduction ...
Non-medical prescribing reflection examples. Gibbs's Reflective Cycle (Gibbs, 1998) helps you to understand and practice your reflective skills. Use the template to reflect on a recent event in which you demonstrated a reflected ability to improve or demonstrate the need for further learning or development.
Conflict of interest statement: The author(s) declared no potential conflicts of interest with respect to the research, authorship, ... George J, Maclure K, et al. Non-medical prescribing versus medical prescribing for acute and chronic disease management in primary and secondary care. Cochrane Database Syst Rev 2016; 11: CD011227. [PMC free ...
v300 personal statement. Forums Alert. There was a problem loading this page.