When you choose to publish with PLOS, your research makes an impact. Make your work accessible to all, without restrictions, and accelerate scientific discovery with options like preprints and published peer review that make your work more Open.
- PLOS Biology
- PLOS Climate
- PLOS Complex Systems
- PLOS Computational Biology
- PLOS Digital Health
- PLOS Genetics
- PLOS Global Public Health
- PLOS Medicine
- PLOS Mental Health
- PLOS Neglected Tropical Diseases
- PLOS Pathogens
- PLOS Sustainability and Transformation
- PLOS Collections
- How to Write Discussions and Conclusions

The discussion section contains the results and outcomes of a study. An effective discussion informs readers what can be learned from your experiment and provides context for the results.

What makes an effective discussion?
When you’re ready to write your discussion, you’ve already introduced the purpose of your study and provided an in-depth description of the methodology. The discussion informs readers about the larger implications of your study based on the results. Highlighting these implications while not overstating the findings can be challenging, especially when you’re submitting to a journal that selects articles based on novelty or potential impact. Regardless of what journal you are submitting to, the discussion section always serves the same purpose: concluding what your study results actually mean.
A successful discussion section puts your findings in context. It should include:
- the results of your research,
- a discussion of related research, and
- a comparison between your results and initial hypothesis.
Tip: Not all journals share the same naming conventions.
You can apply the advice in this article to the conclusion, results or discussion sections of your manuscript.
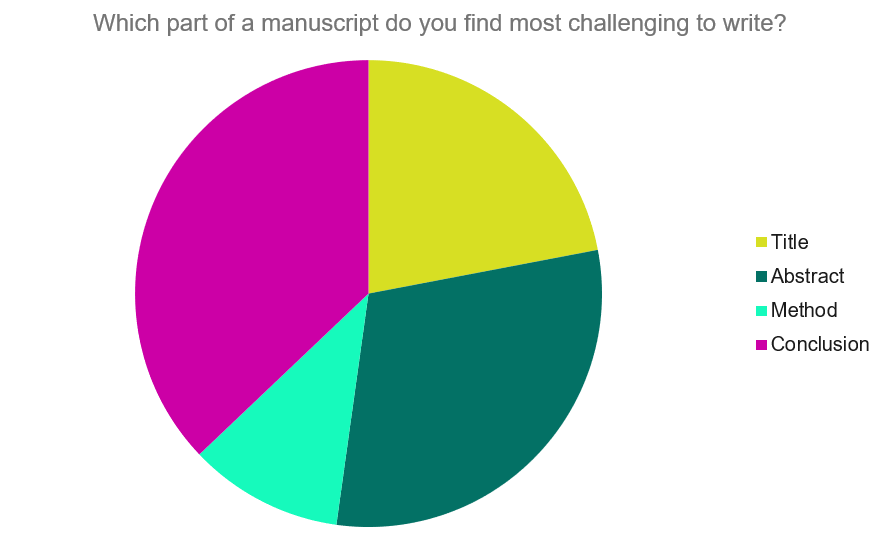
Our Early Career Researcher community tells us that the conclusion is often considered the most difficult aspect of a manuscript to write. To help, this guide provides questions to ask yourself, a basic structure to model your discussion off of and examples from published manuscripts.
Questions to ask yourself:
- Was my hypothesis correct?
- If my hypothesis is partially correct or entirely different, what can be learned from the results?
- How do the conclusions reshape or add onto the existing knowledge in the field? What does previous research say about the topic?
- Why are the results important or relevant to your audience? Do they add further evidence to a scientific consensus or disprove prior studies?
- How can future research build on these observations? What are the key experiments that must be done?
- What is the “take-home” message you want your reader to leave with?
How to structure a discussion
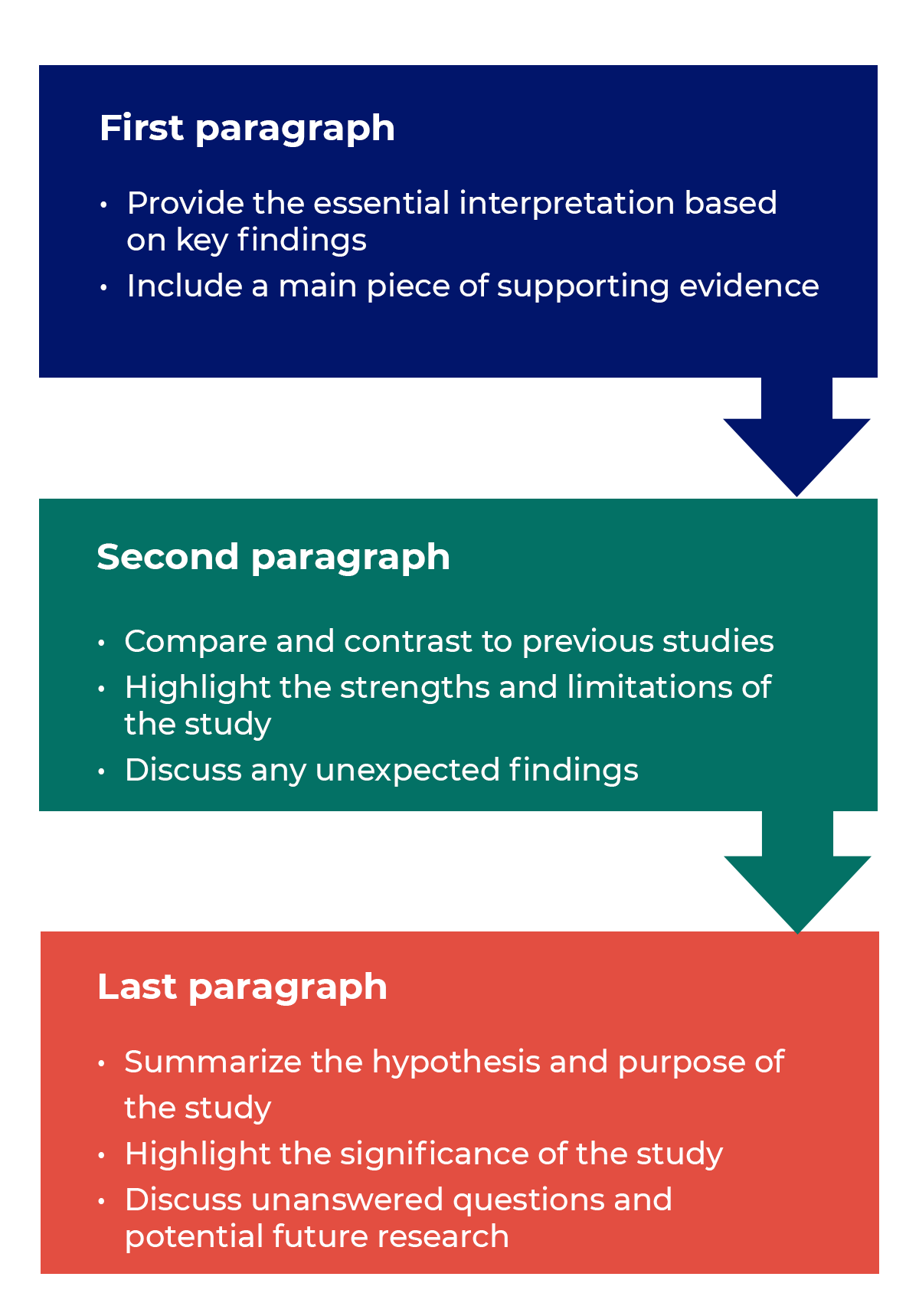
Trying to fit a complete discussion into a single paragraph can add unnecessary stress to the writing process. If possible, you’ll want to give yourself two or three paragraphs to give the reader a comprehensive understanding of your study as a whole. Here’s one way to structure an effective discussion:
Writing Tips
While the above sections can help you brainstorm and structure your discussion, there are many common mistakes that writers revert to when having difficulties with their paper. Writing a discussion can be a delicate balance between summarizing your results, providing proper context for your research and avoiding introducing new information. Remember that your paper should be both confident and honest about the results!

- Read the journal’s guidelines on the discussion and conclusion sections. If possible, learn about the guidelines before writing the discussion to ensure you’re writing to meet their expectations.
- Begin with a clear statement of the principal findings. This will reinforce the main take-away for the reader and set up the rest of the discussion.
- Explain why the outcomes of your study are important to the reader. Discuss the implications of your findings realistically based on previous literature, highlighting both the strengths and limitations of the research.
- State whether the results prove or disprove your hypothesis. If your hypothesis was disproved, what might be the reasons?
- Introduce new or expanded ways to think about the research question. Indicate what next steps can be taken to further pursue any unresolved questions.
- If dealing with a contemporary or ongoing problem, such as climate change, discuss possible consequences if the problem is avoided.
- Be concise. Adding unnecessary detail can distract from the main findings.

Don’t
- Rewrite your abstract. Statements with “we investigated” or “we studied” generally do not belong in the discussion.
- Include new arguments or evidence not previously discussed. Necessary information and evidence should be introduced in the main body of the paper.
- Apologize. Even if your research contains significant limitations, don’t undermine your authority by including statements that doubt your methodology or execution.
- Shy away from speaking on limitations or negative results. Including limitations and negative results will give readers a complete understanding of the presented research. Potential limitations include sources of potential bias, threats to internal or external validity, barriers to implementing an intervention and other issues inherent to the study design.
- Overstate the importance of your findings. Making grand statements about how a study will fully resolve large questions can lead readers to doubt the success of the research.
Snippets of Effective Discussions:
Consumer-based actions to reduce plastic pollution in rivers: A multi-criteria decision analysis approach
Identifying reliable indicators of fitness in polar bears
- How to Write a Great Title
- How to Write an Abstract
- How to Write Your Methods
- How to Report Statistics
- How to Edit Your Work
The contents of the Peer Review Center are also available as a live, interactive training session, complete with slides, talking points, and activities. …
The contents of the Writing Center are also available as a live, interactive training session, complete with slides, talking points, and activities. …
There’s a lot to consider when deciding where to submit your work. Learn how to choose a journal that will help your study reach its audience, while reflecting your values as a researcher…
- Privacy Policy

Home » Research Results Section – Writing Guide and Examples
Research Results Section – Writing Guide and Examples
Table of Contents

Research Results
Research results refer to the findings and conclusions derived from a systematic investigation or study conducted to answer a specific question or hypothesis. These results are typically presented in a written report or paper and can include various forms of data such as numerical data, qualitative data, statistics, charts, graphs, and visual aids.
Results Section in Research
The results section of the research paper presents the findings of the study. It is the part of the paper where the researcher reports the data collected during the study and analyzes it to draw conclusions.
In the results section, the researcher should describe the data that was collected, the statistical analysis performed, and the findings of the study. It is important to be objective and not interpret the data in this section. Instead, the researcher should report the data as accurately and objectively as possible.
Structure of Research Results Section
The structure of the research results section can vary depending on the type of research conducted, but in general, it should contain the following components:
- Introduction: The introduction should provide an overview of the study, its aims, and its research questions. It should also briefly explain the methodology used to conduct the study.
- Data presentation : This section presents the data collected during the study. It may include tables, graphs, or other visual aids to help readers better understand the data. The data presented should be organized in a logical and coherent way, with headings and subheadings used to help guide the reader.
- Data analysis: In this section, the data presented in the previous section are analyzed and interpreted. The statistical tests used to analyze the data should be clearly explained, and the results of the tests should be presented in a way that is easy to understand.
- Discussion of results : This section should provide an interpretation of the results of the study, including a discussion of any unexpected findings. The discussion should also address the study’s research questions and explain how the results contribute to the field of study.
- Limitations: This section should acknowledge any limitations of the study, such as sample size, data collection methods, or other factors that may have influenced the results.
- Conclusions: The conclusions should summarize the main findings of the study and provide a final interpretation of the results. The conclusions should also address the study’s research questions and explain how the results contribute to the field of study.
- Recommendations : This section may provide recommendations for future research based on the study’s findings. It may also suggest practical applications for the study’s results in real-world settings.
Outline of Research Results Section
The following is an outline of the key components typically included in the Results section:
I. Introduction
- A brief overview of the research objectives and hypotheses
- A statement of the research question
II. Descriptive statistics
- Summary statistics (e.g., mean, standard deviation) for each variable analyzed
- Frequencies and percentages for categorical variables
III. Inferential statistics
- Results of statistical analyses, including tests of hypotheses
- Tables or figures to display statistical results
IV. Effect sizes and confidence intervals
- Effect sizes (e.g., Cohen’s d, odds ratio) to quantify the strength of the relationship between variables
- Confidence intervals to estimate the range of plausible values for the effect size
V. Subgroup analyses
- Results of analyses that examined differences between subgroups (e.g., by gender, age, treatment group)
VI. Limitations and assumptions
- Discussion of any limitations of the study and potential sources of bias
- Assumptions made in the statistical analyses
VII. Conclusions
- A summary of the key findings and their implications
- A statement of whether the hypotheses were supported or not
- Suggestions for future research
Example of Research Results Section
An Example of a Research Results Section could be:
- This study sought to examine the relationship between sleep quality and academic performance in college students.
- Hypothesis : College students who report better sleep quality will have higher GPAs than those who report poor sleep quality.
- Methodology : Participants completed a survey about their sleep habits and academic performance.
II. Participants
- Participants were college students (N=200) from a mid-sized public university in the United States.
- The sample was evenly split by gender (50% female, 50% male) and predominantly white (85%).
- Participants were recruited through flyers and online advertisements.
III. Results
- Participants who reported better sleep quality had significantly higher GPAs (M=3.5, SD=0.5) than those who reported poor sleep quality (M=2.9, SD=0.6).
- See Table 1 for a summary of the results.
- Participants who reported consistent sleep schedules had higher GPAs than those with irregular sleep schedules.
IV. Discussion
- The results support the hypothesis that better sleep quality is associated with higher academic performance in college students.
- These findings have implications for college students, as prioritizing sleep could lead to better academic outcomes.
- Limitations of the study include self-reported data and the lack of control for other variables that could impact academic performance.
V. Conclusion
- College students who prioritize sleep may see a positive impact on their academic performance.
- These findings highlight the importance of sleep in academic success.
- Future research could explore interventions to improve sleep quality in college students.
Example of Research Results in Research Paper :
Our study aimed to compare the performance of three different machine learning algorithms (Random Forest, Support Vector Machine, and Neural Network) in predicting customer churn in a telecommunications company. We collected a dataset of 10,000 customer records, with 20 predictor variables and a binary churn outcome variable.
Our analysis revealed that all three algorithms performed well in predicting customer churn, with an overall accuracy of 85%. However, the Random Forest algorithm showed the highest accuracy (88%), followed by the Support Vector Machine (86%) and the Neural Network (84%).
Furthermore, we found that the most important predictor variables for customer churn were monthly charges, contract type, and tenure. Random Forest identified monthly charges as the most important variable, while Support Vector Machine and Neural Network identified contract type as the most important.
Overall, our results suggest that machine learning algorithms can be effective in predicting customer churn in a telecommunications company, and that Random Forest is the most accurate algorithm for this task.
Example 3 :
Title : The Impact of Social Media on Body Image and Self-Esteem
Abstract : This study aimed to investigate the relationship between social media use, body image, and self-esteem among young adults. A total of 200 participants were recruited from a university and completed self-report measures of social media use, body image satisfaction, and self-esteem.
Results: The results showed that social media use was significantly associated with body image dissatisfaction and lower self-esteem. Specifically, participants who reported spending more time on social media platforms had lower levels of body image satisfaction and self-esteem compared to those who reported less social media use. Moreover, the study found that comparing oneself to others on social media was a significant predictor of body image dissatisfaction and lower self-esteem.
Conclusion : These results suggest that social media use can have negative effects on body image satisfaction and self-esteem among young adults. It is important for individuals to be mindful of their social media use and to recognize the potential negative impact it can have on their mental health. Furthermore, interventions aimed at promoting positive body image and self-esteem should take into account the role of social media in shaping these attitudes and behaviors.
Importance of Research Results
Research results are important for several reasons, including:
- Advancing knowledge: Research results can contribute to the advancement of knowledge in a particular field, whether it be in science, technology, medicine, social sciences, or humanities.
- Developing theories: Research results can help to develop or modify existing theories and create new ones.
- Improving practices: Research results can inform and improve practices in various fields, such as education, healthcare, business, and public policy.
- Identifying problems and solutions: Research results can identify problems and provide solutions to complex issues in society, including issues related to health, environment, social justice, and economics.
- Validating claims : Research results can validate or refute claims made by individuals or groups in society, such as politicians, corporations, or activists.
- Providing evidence: Research results can provide evidence to support decision-making, policy-making, and resource allocation in various fields.
How to Write Results in A Research Paper
Here are some general guidelines on how to write results in a research paper:
- Organize the results section: Start by organizing the results section in a logical and coherent manner. Divide the section into subsections if necessary, based on the research questions or hypotheses.
- Present the findings: Present the findings in a clear and concise manner. Use tables, graphs, and figures to illustrate the data and make the presentation more engaging.
- Describe the data: Describe the data in detail, including the sample size, response rate, and any missing data. Provide relevant descriptive statistics such as means, standard deviations, and ranges.
- Interpret the findings: Interpret the findings in light of the research questions or hypotheses. Discuss the implications of the findings and the extent to which they support or contradict existing theories or previous research.
- Discuss the limitations : Discuss the limitations of the study, including any potential sources of bias or confounding factors that may have affected the results.
- Compare the results : Compare the results with those of previous studies or theoretical predictions. Discuss any similarities, differences, or inconsistencies.
- Avoid redundancy: Avoid repeating information that has already been presented in the introduction or methods sections. Instead, focus on presenting new and relevant information.
- Be objective: Be objective in presenting the results, avoiding any personal biases or interpretations.
When to Write Research Results
Here are situations When to Write Research Results”
- After conducting research on the chosen topic and obtaining relevant data, organize the findings in a structured format that accurately represents the information gathered.
- Once the data has been analyzed and interpreted, and conclusions have been drawn, begin the writing process.
- Before starting to write, ensure that the research results adhere to the guidelines and requirements of the intended audience, such as a scientific journal or academic conference.
- Begin by writing an abstract that briefly summarizes the research question, methodology, findings, and conclusions.
- Follow the abstract with an introduction that provides context for the research, explains its significance, and outlines the research question and objectives.
- The next section should be a literature review that provides an overview of existing research on the topic and highlights the gaps in knowledge that the current research seeks to address.
- The methodology section should provide a detailed explanation of the research design, including the sample size, data collection methods, and analytical techniques used.
- Present the research results in a clear and concise manner, using graphs, tables, and figures to illustrate the findings.
- Discuss the implications of the research results, including how they contribute to the existing body of knowledge on the topic and what further research is needed.
- Conclude the paper by summarizing the main findings, reiterating the significance of the research, and offering suggestions for future research.
Purpose of Research Results
The purposes of Research Results are as follows:
- Informing policy and practice: Research results can provide evidence-based information to inform policy decisions, such as in the fields of healthcare, education, and environmental regulation. They can also inform best practices in fields such as business, engineering, and social work.
- Addressing societal problems : Research results can be used to help address societal problems, such as reducing poverty, improving public health, and promoting social justice.
- Generating economic benefits : Research results can lead to the development of new products, services, and technologies that can create economic value and improve quality of life.
- Supporting academic and professional development : Research results can be used to support academic and professional development by providing opportunities for students, researchers, and practitioners to learn about new findings and methodologies in their field.
- Enhancing public understanding: Research results can help to educate the public about important issues and promote scientific literacy, leading to more informed decision-making and better public policy.
- Evaluating interventions: Research results can be used to evaluate the effectiveness of interventions, such as treatments, educational programs, and social policies. This can help to identify areas where improvements are needed and guide future interventions.
- Contributing to scientific progress: Research results can contribute to the advancement of science by providing new insights and discoveries that can lead to new theories, methods, and techniques.
- Informing decision-making : Research results can provide decision-makers with the information they need to make informed decisions. This can include decision-making at the individual, organizational, or governmental levels.
- Fostering collaboration : Research results can facilitate collaboration between researchers and practitioners, leading to new partnerships, interdisciplinary approaches, and innovative solutions to complex problems.
Advantages of Research Results
Some Advantages of Research Results are as follows:
- Improved decision-making: Research results can help inform decision-making in various fields, including medicine, business, and government. For example, research on the effectiveness of different treatments for a particular disease can help doctors make informed decisions about the best course of treatment for their patients.
- Innovation : Research results can lead to the development of new technologies, products, and services. For example, research on renewable energy sources can lead to the development of new and more efficient ways to harness renewable energy.
- Economic benefits: Research results can stimulate economic growth by providing new opportunities for businesses and entrepreneurs. For example, research on new materials or manufacturing techniques can lead to the development of new products and processes that can create new jobs and boost economic activity.
- Improved quality of life: Research results can contribute to improving the quality of life for individuals and society as a whole. For example, research on the causes of a particular disease can lead to the development of new treatments and cures, improving the health and well-being of millions of people.
About the author
Muhammad Hassan
Researcher, Academic Writer, Web developer
You may also like

How to Cite Research Paper – All Formats and...

Data Collection – Methods Types and Examples

Delimitations in Research – Types, Examples and...

Research Paper Format – Types, Examples and...

Research Process – Steps, Examples and Tips

Research Design – Types, Methods and Examples
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Endocrinol Metab
- v.17(2); 2019 Apr

The Principles of Biomedical Scientific Writing: Results
Zahra bahadoran.
1 Nutrition and Endocrine Research Center, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Parvin Mirmiran
2 Department of Clinical Nutrition and Diet Therapy, Faculty of Nutrition Sciences and Food Technology, National Nutrition and Food Technology Research Institute, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Azita Zadeh-Vakili
3 Cellular and Molecular Endocrine Research Center, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Farhad Hosseinpanah
4 Obesity Research Center, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Asghar Ghasemi
5 Endocrine Physiology Research Center, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran
The “results section” of a scientific paper provides the results related to all measurements and outcomes that have been posted earlier in the materials and methods section. This section consists of text, figures, and tables presenting detailed data and facts without interpretation and discussion. Results may be presented in chronological order, general to specific order, most to least important order, or may be organized according to the topic/study groups or experiment/measured parameters. The primary content of this section includes the most relevant results that correspond to the central question stated in the introduction section, whether they support the hypothesis or not. Findings related to secondary outcomes and subgroup analyses may be reported in this section. All results should be presented in a clear, concise, and sensible manner. In this review, we discuss the function, content, and organization of the “results section,” as well as the principles and the most common tips for the writing of this section.
The “results section” is the heart of the paper, around which the other sections are organized ( 1 ). Research is about results and the reader comes to the paper to discover the results ( 2 ). In this section, authors contribute to the development of scientific literature by providing novel, hitherto unknown knowledge ( 3 ). In addition to the results, this section contains data and statistical information for supporting or refuting the hypothesis proposed in the introduction ( 4 ).
“Results section” should provide an objective description of the main findings, clearly and concisely, without interpretation ( 5 , 6 ). The authors need to use an interesting combination of text, tables, and figures to answer the study questions and to tell the story without diversions ( 7 ). The systemic assessment of published articles highlights the fact that the literature frequently suffers from selective reporting of results only for certain assessed outcomes, selective reporting of statistical analyses, and confused, ambiguous, incomplete, or misleading presentation of data ( 8 , 9 ).
In this section of our series on the principles of biomedical scientific writing ( 10 , 11 ), we describe the function, content, and organization of the “results section” in a scientific paper (mostly for hypothesis-testing papers) and provide common recommendations that can help authors to write this section more effectively.
2. The Function of the Results Section
The function of the “results section” is to present the main results of experiments described in the materials and methods section ( 12 , 13 ) and to present the supporting data in the form of text, tables, and figures ( 13 ). This section should answer the basic question: “What did the authors find in research?” By providing the results, authors try to elucidate the research data, making it to the point and meaningful ( 13 ).
3. Content of the Results Section
The “results section” includes both results and data that are presented in text, tables, and figures. Results are presented in the text; data (the most important) are presented in figures and tables, with a limited amount presented in the text ( 13 ). Statistically relevant parameters including sample size, P values, and the type of statistics used are also presented in this section ( 13 ).
3.1. Difference Between Data and Results
Data and results are not the same ( 14 ); providing results but no data vs. data but no results should be avoided ( 14 , 15 ). Results are general statements in the main text that summarize or explain what the data (facts and numbers) show ( 13 , 14 ); in other words, results are text descriptions of what is important about data ( 16 ) and give meaning to the data ( 15 ). When reporting data or results, make sure that they are logical ( 2 ). See Box 1 for more differences between results and data.
a The text presented in square brackets is data and the remainder is a result.
3.2. The Appropriate Format for Presenting Data/Results
Depending on how the data best support the findings of the study, the “results section” is structured as text, tables, and figures ( 12 ) and should consist of a dynamic interplay between text and figures/tables; the most important data are usually presented in both formats ( 17 ). The reader should select the mode of presentation in a way that optimizes comprehension of the data; however, as a general rule, if you want to present three or fewer numbers, you should use a sentence; otherwise, you consider a table or a graph ( 18 ).
Selecting the best format for presenting results/data depends on the level of details (exact values or patterns) to present ( 19 ). Tables are useful to present specific information or exact values ( 19 ), and function as reference tools for readers ( 20 ) whereas figures are useful to show comparisons and patterns ( 19 ), functioning as analytic tools ( 20 ).
Tables are meant to summarize large amounts of data, to organize and display data more clearly than words, to compare groups of data, to simplify found information, and to facilitate calculations ( 19 ). A table typically has three or more interrelated columns and three or more interrelated rows; otherwise, presenting the information in the text may be more appropriate ( 19 ).
The functions of figures include: (1) showing the underlying patterns of data that are not presentable in text or tables, (2) displaying data more clearly than they can be done in text or tables, (3) more summarizing a large amount of data than they can be done in text or tables, and (4) improving the understanding and locating the specific information easily and rapidly ( 21 ).
3.3. Results
The primary content of this section includes the most relevant (but not all) results corresponding to the central question posed in the introduction section, whether they support the hypothesis or not ( 12 , 13 ). The secondary findings, e.g., results related to secondary outcomes and subgroup analyses, may also be reported in this section ( 22 ). Results must be presented for both experimental and control groups ( 13 ). Results of each item mentioned in the materials and methods should be given in the results section ( 12 , 15 ).
The text of the “results section” should state and summarize the main results and explain the data presented within tables and/or figures ( 23 ); reiteration of all numbers presented in tables and figures is not recommended ( 22 ); however, readers must be given the main messages derived from a table or figure without having to interpret the data themselves ( 7 ). It means that if there is a large amount of data in a table or figure, restating a key piece of data in the text is acceptable and helps the reader zero in on important data ( 14 ).
3.3.1. Reporting Negative Findings
Authors are highly recommended excluding irrelevant results but not ignoring valid anomalous results that contradict the research hypothesis or do not support the current scientific literature ( 22 ). The Feynman, says “if you are doing an experiment, you should report everything that you think might make it invalid-not only what you think is right about it” ( 24 ). Although reporting null or negative findings is not as straightforward as positive findings, it may lead to reexamining current scientific thinking, and guide scientists towards unabridged science ( 25 ). Reporting negative findings can also prevent the replication of the study and prevent the waste of time and resources ( 25 ). The ignorance of null or negative findings also leads to an overestimation of an effect size or treatment effect in available data ( 9 ).
3.3.2. Referring to Unpublished Results
Referring to unpublished results is not recommend unless there is a strong argument supporting their inclusion ( 14 ); therefore, authors are advised to avoid using the term “data not shown” ( 4 ).
3.3.3. Methods or Interpretation in the Results Section
Generally, the “results section” is not the place for presenting methods and experimental details or interpreting data ( 14 ). When experiments are described in this section, if a result leads to additional experiments, it is better to report the new experimental details in the “results section” ( 14 ). Sometimes authors want to refer to a specific experiment or method in results; in these cases, they should not repeat experimental details, but preferably use a transition phrase to link methods with results ( 14 ). To justify the rationale behind the experiment, using topic sentences/phrases (e.g. in order to determine whether…) provides an overview before giving details ( 12 ); however, in this case, the method statement should not be used as a topic sentence and the main verbs should describe results, not methods (e.g., “ when propranolol was administered during normal ventilation, phospholipids decreased ”; here “ method ” is subordinated in a transition clause and result is the main clause) ( 13 ). Two patterns of sentence structure are recommended for including methods in a result statement: making the method the subject of the sentence or stating the method using a transition phrase or clause and the result in the main clause ( 13 ).
The traditional view of writing the “results section” is just to report data and results without any interpretation; accordingly, the result is not expected to contain statements that need to be referenced (comparisons of findings) ( 13 , 26 ). In another view, some interpretation or brief comparisons that do not fit into the discussion may be included ( 13 , 27 ).
Data are facts and numbers, mostly presented as non-textual elements (usually in tables and figures) where they are easy to read ( 13 , 14 , 28 ). A limited amount of data may also be presented in the text, following a result statement ( 13 ) although too much data in the text make it too long ( Box 1 ) ( 28 ). Data may be in the form of raw data, summarized data, or transformed data ( 13 ); however, it is suggested that raw data (i.e. patients’ records, individual observations) not be presented in results ( 12 ). Note that numerical data are absolute while some data, e.g. microscopic data, are subjective ( 2 ).
3.4.1. Non-Textual Elements
Providing study findings visually, rather than entire textualizing, enables authors to summarize a great deal of data compactly within the text with an appropriate reference; some images convey more than words ( 29 ). The primary purpose of non-textual elements, i.e. tables, graphs, figures, and maps, is to present data such that they can be easily and quickly grasped ( 23 ) while being more informative than when appearing in the text ( 6 ). Tables and figures should be complete/comprehensible, being able to stand alone without the text ( 5 , 12 ).
Non-textual elements should be referred to in the text at the appropriate point ( 5 , 6 , 12 ). Location statements, i.e. statements referring to non-textual elements, may be presented in different patterns (e.g., A. X is shown in table/figure; B. table/figure shows; C. see table/figure; D. as shown in table/figure); pattern B is more and pattern C is less common ( 27 ).

Some general tips about using non-textual elements in the “results section” are reviewed in Box 2 . The most common rules in organizing tables and figures are given in the following. For more information about designing different types of tables/figures/graphs, please refer to additional references ( 7 , 19 , 20 , 30 , 31 ).
3.4.1.1. Tables
The use of tables is an effective way to summarize demographic information and descriptive statistics ( 23 ). Note that tables must have a purpose and be integrated into the text ( 21 ). Tables are most useful to present counts, proportions, and percentages ( 8 ), and are appropriate also for presenting details especially when exact values matter ( 32 ), being are more informative than graphs ( 29 ). However, limited information should be presented in tables; otherwise, most readers find them difficult to read and thus, may ignore them ( 5 , 23 ). Data in tables can be arranged horizontally or vertically; whenever possible, primary comparisons are preferably presented horizontally from left to right ( 19 ).
3.4.1.1.1. Basic Elements of Tables
Tables usually have at least six elements: (1) table number, (2) table title, (3) row headings (stubs), and (4) column headings (boxes), identifying information in rows and columns, (5) data in data field, and (6) horizontal lines (rules). Most also have footnotes, row subheadings, spanner headings (identifying subgroups in column headings), and expanded forms of abbreviations in the table ( 19 , 21 , 31 , 33 ).
The table title should clearly state what appears in it and provide sufficient information on the study, i.e. provide a context helping readers interpret the table information ( 19 ). Some specific details may also be provided including the type and number of subjects or the period of study ( 30 ). For developing the title of a table, one can describe the main cell entries, followed by qualification or more description ( 32 ). The table’s title is presented as a phrase not a full sentence ( 19 ). Authors need to refer to the journal’s style for rules on which words in titles are capitalized.
As a rule, comparing two (or even three) numbers should be side-by-side rather than above and below ( 30 ). Column and row headings help readers find information and they should be included group sizes and measurement units ( 19 ). Tables should be in borderless grids of rows and columns ( 5 , 32 ) with no vertical rule and limited horizontal rules ( 32 ). The first column of a table includes usually a list of variables that are presented in the table; although the first column usually does not need a header, sometimes a simple description of what appears in each row may be provided as the heading of the first column. Units for variables may be placed in parentheses immediately below the row descriptions ( 30 ).
Headings for other columns should also be informative without vague labels, e.g. group A, group B, group C, etc.; instead, a brief description summarizing group characteristics is used ( 30 ). The last column may show P values for comparison between study groups ( 34 ), except for randomized clinical trials, where P values are not needed to compare baseline characteristics of participants ( 7 ). The first letters of lines and column headings in tables should be capitalized.
The fields of tables are points at which columns and rows intersect ( 19 ). Cells of a table are the data field of the table, other than those containing row and column headings ( 21 ). Cells contain information as numerals, text, or symbols ( 19 ). Every cell must contain information; if no information is available, one can use NA in the cell and define it in the footnote as not available or not applicable; alternatively, a dash mark may be inserted ( 19 ). The content of columns need to be aligned ( 19 ); words are usually left aligned, numerals are aligned at decimals, parenthesis, and factors of 10 ( 19 , 21 ).
Table footnotes should be brief, and define abbreviations, provide statistical results, and explain discrepancies in data, e.g., “percentages do not total 100 because of rounding” ( 19 , 30 ). In addition to asterisks usually used to show statistical significance ( 33 ), the following symbols are used, in sequence, for further notes: †, ‡, §, ¶, #, ††, ‡‡ ( 30 ).
3.4.1.1.2. Different Types of Tables
Table of lists, table of baseline or clinical characteristics of subjects, table of comparisons, and table of multivariable results are various types of tables that may be used ( 30 ). The table’s format should be selected according to the purpose of the table ( 30 ). A table of lists just presents a list of items including diagnostic criteria or causes of a disease; it is critical to arrange such tables based on their contents by order (e.g., alphabetical order) or their importance (most to least) ( 30 ). Tables of study participants’ characteristics usually provide a general overview of the essential characteristics of subjects, such as age, sex, race, disease stage, and selected risk factors ( 30 ). The table of comparisons (≥ two groups) provides details for each group and differences between the groups. Tables of multivariable results elaborate results of statistical analyses assessing relationships between predictor (independent) and outcome (dependent) variables, and usually include regression coefficients, standard errors, slopes, partial correlation coefficients, and P values or odds ratio, hazard ratios, and 95% confidence intervals for regression models ( 30 ).
3.4.1.2. Figures
Graphical elements convey the important messages of research ( 20 ). A figure is “any graphical display to present information or data” ( 20 ), and it effectively presents complicated patterns ( 32 ), best used for presenting an important point at a glance or indicating trends or relationships ( 20 ). Like tables, figures should have a purpose and be integrated with the rest of the text ( 21 ).
3.4.1.2.1. Basic Elements of Figures
Most figures that present quantitative information (charts and graphs) have at least seven elements, including figure number, figure caption/legend, data field, vertical scale, horizontal scale, labels, and data (plotting symbols, lines, and so on) ( 21 ). Some figures also have reference lines in the data field to help orient readers and keys that identify data ( 21 ).
Figure caption/legend, usually given below the figure, describes the figure and must reflect the figure entirely, independent of the main text ( 21 , 31 ). For the figure to stand alone, a figure legend needs to be included four parts (a brief title, experimental or statistical information/details, definitions of symbols, line, or bar patterns, and abbreviations) ( 31 ).
Data field is a space in the figure in which data are presented; it is usually bordered on the left by the X-axis (abscissa) and on the bottom by the Y-axis (ordinate) ( 20 , 21 ). Labels identify the variables graphed and the units of measurement ( 21 ). Figure lines should be broad and the labeling text should be large enough to be legible after reduction to a single- or two-column size ( 32 ). Appropriate font size should be used to maintain legibility after fitting figures to publication size ( 31 ).
Scales on each axis should match the data range and be slightly above the highest value ( 20 ). Symbols should be uniform across the figures ( 20 ). The data point symbols should be easily distinguishable; using black and white circles (● - ∘) is the easiest way when two are needed ( 31 ); if more are needed, using up-pointing triangles (▲ - Δ) and squares (■ - □) is suggested ( 31 ). Using symbols, line types, and colors is also effective in differentiating important strata in figures ( 8 ).
3.4.1.2.2. Emphasizing Important Data on Figures
To make figures visually efficient, the subordination of all non-data elements vs. data elements is advised (gridlines should be used as thin as possible and very faint). Directly labeling objects, instead of legends, may keep readers’ attention on the most important parts of the figure ( 8 ). Using different line weights may also be helpful to emphasize the important information/data in figures ( 31 ). The use of color, shading, or 3D perspectives is not suggested unless they serve a specific explanatory function in figure ( 8 ).
3.4.1.2.3. Different Types of Figures
Two major categories of figures are statistical figures (graphs) and non-statistical figures (clinical images, photographs, diagrams, illustrations, and textual figures) ( 20 ). Graphs are suitable for presenting relationships whereas non-statistical figures are used to confirm findings or provide explanatory information ( 20 ).
In statistical figures, selecting a graphical format (bar graph, line graph, dot plot, and scatterplot) is done according to the type of relationship that authors wish to communicate ( 20 ); for example, line graphs are appropriate for showing trends and bar graphs for magnitudes ( 20 ). Using a graphing format that is easy to interpret is preferred ( 20 ); pie graphs are sparingly used because comparing different angles is complicated with them ( 20 ). Graphs should accurately represent findings; when possible, scales should start at zero, and figure axes should not be altered in order to make data more meaningful ( 20 ).
Non-statistical figures are those that visually present information that does not contain data ( 20 ). Clinical images and photographs [ultrasonograms, computed tomographic scans (CT scans), magnetic resonance images (MRI), images of patients, tissue samples, microscopic findings, and so on] provide absolute proof of findings ( 20 ). Illustrations are used for explaining structures (parts of a cell), mechanisms, and relationships ( 20 ). Diagrams (flowcharts, algorithms, pedigrees, and maps) are useful for displaying complex relations ( 20 ). Textual figures, containing only text, are mostly used for describing steps of a procedure or summarizing guidelines ( 20 ). For photographs, patient information or identifiers should be removed ( 20 ).
3.5. Statistics in the Results Section
Statistics in the “results section” must report data in a way that enables readers to assess the degree of experimental variation and to estimate the variability or precision of the findings ( 22 ). For more details, one can see SAMPL (Statistical Analysis and methods in the Published Literature) guidelines ( 35 ). To report normally distributed data, the mean and estimated variation from mean should be stated ( 13 ). Variability should be reported using standard deviation (SD), which is a descriptive statistic ( 36 ) and reflects the dispersion of individual sample observation of the sample mean ( 37 ). The standard error (SE), an inferential statistic ( 36 ) reflecting the theoretical dispersion of sample means about some population means, characterizes uncertainty about true values of population means ( 37 ). It is useful for assessing the precision of an estimator ( 36 ) and is not an appropriate estimate of the variability in observations ( 37 ). Using “mean (SD or SE)” is preferred to “mean ± SD or SE” because the “±” sign can cause confusion ( 22 ). Increasing sample size decreases SE but not SD ( 36 ). To report data with a skewed distribution, the median and the interquartile range (between 25th and 75th percentiles) should be provided ( 22 ).
To report risk, rates, and ratios, one should use a type of rate (incidence rate, survival rate), ratio (odds ratio, hazards ratio), or risk (absolute risk, relative risk, relative risk reduction) ( 35 ). The measure of precision (95% CI) for estimated risks, rates, and ratios should also be provided ( 35 ). For correlation analysis, the exact values of the correlation coefficient and 95% CI should be reported. Describing correlation using qualitative words (low, moderate, high) without providing a clear definition is not acceptable ( 35 ). Results of regression analysis should include regression coefficients (β) of each explanatory variable, corresponding 95% CI and/or P value and a measure of the “goodness-of-fit” of the model ( 35 ).
3.5.1. Significance Levels
A P value is the probability of consistency between data and the hypothesis being tested ( 38 ). Reporting the exact P values ( P = 0.34 or P = 0.02) rather than the conventional P ( P < 0.05) is recommended for all primary analyses ( 12 , 37 ) as it conveys more information ( 37 ). The use of the term “partially significant” or “marginally significant”, where the P value is almost significant (e.g. P = 0.057) is not acceptable if the significance level is defined as P = 0.05 ( 39 ). Some, however, argue that it is not always necessary to stick to P = 0.05 for the interpretation of results and it is better to report the exact P value and confidence interval for the estimator ( 40 ).
The use of the 95% confidence interval (95% CI) can provide further information compared to P values per se, and prefigures the direction of the effect size (negative or positive), its magnitude, and the degree of precision ( 17 ). A confidence interval characterizes uncertainty about the true value of population parameters ( 37 ). It is essential to provide the sample size (n) and probability values for tests of statistical significance ( 13 ).
Statements about significance must be qualified numerically ( 41 ). In the text, it is suggested that P values be reported as equalities rather than as inequalities in relation to the alpha criterion ( 41 ). In tables and figures, inequalities may be useful for groups of data ( 41 ) where asterisks *, **, and *** are usually used to show statistical significance at 0.05, 0.01, and 0.001 probability levels, respectively ( 33 ).
Although not consistent, P values < 0.001 are reported as P < 0.001; for 0.001 ≤ P values < 0.01, a three-significant digit is recommended, e.g. P = 0.003; for 0.01 ≤ P values < 0.1, a two-significant digit is sufficient (e.g. P = 0.05); for 0.1 ≤ P values ≤ 0.9, a one-significant digit is sufficient (e.g. P = 0.4); and P values > 0.9 are reported as P > 0.9 ( 42 ). For genome-wide association studies, the power of 10 is used for reporting P values, e.g. 6 × 10 -9 ( 42 ). It is generally suggested that zero be used before a decimal point when the value is below one, e.g. 0.37 ( 43 ). According to the American Psychological Association, zero before a decimal point is used for numbers that are below one, but it can also be used for values that may exceed one (e.g. 0.23 cm). Therefore, when statistics cannot be greater than one (e.g. correlations, proportions, and P values), do not use a zero before decimal fraction, e.g. P = .028 not P = 0.028 ( 18 ); this recommendation, however, is not always adopted by everyone. The international standard is P (large italic) although both ‘p’ and ‘P’ are allowed ( 40 ).
4. Organization of the Results Section
There are different ways for organizing the “results section” including ( 1 , 12 , 14 , 22 , 44 ): (1) chronological order, (2) general to specific, (3) most to least important, and (4) grouping results by topic/study groups or experiment/measured parameters. Authors decide which format is more appropriate for the presentation of their data ( 12 ); anyway, results should be presented in a logical manner ( 4 ).
4.1. Different Ways of Organizing the Results Section
4.1.1. chronological order.
The best order for organizing “results section” may be the chronological order ( 22 ). It is considered as the most straightforward approach using subheadings that parallel methods ( 14 ). This order facilitates referring to a method associated with a given result ( 14 ) such that results are presented in the same order as methods ( 15 ).
4.1.2. General to Specific
This format is mostly used in clinical studies involving multiple groups of individuals receiving different treatments ( 14 ). The “results section” usually proceeds from general to more specific findings ( 1 ). Characteristics of the overall study population (sex and age distribution and dropouts) are first given ( 14 ), followed by data and results for each group starting with the control group or the group receiving the standard treatment ( 14 ); finally, the disease group or group receiving the experimental treatment are addressed ( 14 ). As a general rule, secondary results should be given after presenting more important (primary) results, followed by any supporting information ( 22 ). A common order is stating recruitment/response, characteristics of the sample/study participants, findings from the primary analyses, findings from secondary analyses, and any additional or unexpected findings ( 17 ). In other words, the “results section” should be initiated by univariate statistics, followed by bivariate analyses to describe associations between explanatory and outcome variables; finally, it gets through by any multivariate analyses ( 7 ).
4.1.3. Most to Least Important
This format is used in case that the order of presenting results is not critical to their being comprehendible and allows the author to immediately highlight important findings ( 14 ). Results that answer the main question are presented at the beginning of the “results section,” followed by other results in next paragraphs ( 13 ).
4.1.4. Grouping by Topic or Experiment
Comparison of the diagnostic and analytical performance of a number of assays for analytes is an example of using this format ( 14 ).
4.2. Paragraphing of the Results Section
The “results section” may be initiated by two approaches: (1) by giving a general (not detailed) overview of the experiment and (2) by going directly to the results by referring to tables or figures ( 44 ). The first paragraph of this section, along with table 1, describes the characteristics of the study population (number, sex, age, and symptoms) ( 23 ). These data show the comparability of the study groups at baseline and the distribution of potential confounders between groups, as a source of bias that can affect the study findings ( 7 ). It allows the reader to decide whether or not the case and control groups are similar and represent the patient population in their private practice ( 23 ).
For clinical trials, the number of patients completing the protocol in each treatment/study group, the number of patients lost to follow-up, and the number and reasons for excluded/withdrawn subjects should be given. Commenting on whether baseline characteristics of study groups are statistically similar or different is also important ( 1 ). For further information, authors can consult reporting guidelines for the main study types available at http://www.equator-network.org.
The number of the middle paragraphs depends on the number of research questions/hypotheses and the types of statistical analyses; each hypothesis or specific analysis typically devotes at least a paragraph to itself ( 1 ). Figure legends, description of the methods and results for control groups should not be given at the beginning of paragraphs, as they do not narrate the story ( 28 ). However, sometimes, it is needed that results of the control group are presented first (e.g. for establishing the stability of baseline) ( 13 ).
5. Emphasizing Important Results
Since not all results are equally important, the reader must be able to distinguish important results and authors have to emphasize important information and de-emphasize less important information ( 13 ). There are various techniques for emphasizing important information, including condensing or omitting less important information, subordinating less important information, placing important results at the power position, and labeling, stating, and repeating important information ( 13 ).
For condensing or omitting less important information, you should be careful not to duplicate/repeat data in tables and figures or repeat them in the text ( 4 , 6 , 12 ); one or two values from tables/figures can be repeated in the text for emphasis ( 13 ).
For subordinating less important information, one should not use table titles, figure legends or methods statement as a topic sentence in the text ( 13 , 22 ). Instead, after stating the first result relevant to the table/figure, you can cite it in parenthesis ( 13 ). Since a result states a message and creates an expectation, it is a more powerful topic sentence than a figure legend or table title ( 13 ). Sometimes, control results can be subordinated by incorporating them into experimental results ( 13 ).
To highlight more important results (those that help answer questions), authors can put these results at the beginning of paragraphs, the strongest power position ( 12 , 22 , 28 ), followed by supporting details and control results ( 28 ).
Moreover, key findings may receive more attention by using a signal (e.g. we found or we observed) at the beginning of the sentence ( 13 ).
6. Other Considerations
6.1. length and paragraphing.
To see the forest for the tree, the “results section” should be as brief and uncluttered as possible ( 13 ), which can be accomplished by having a well-organized “materials and methods” section ( 3 ) and avoiding unnecessary repetition ( 13 ); for example, similar results for several variables can be reported together. The “results section” of an original manuscript usually includes 2 - 3 pages (~1000 words) with a 1.5 line spacing, font size 11 (including tables and figures) ( 45 ), and 4 - 9 paragraphs (each 130 words) on average ( 45 ); a paragraph should be devoted to one or more closely related figures ( 4 ).
Presenting additional results/data as supplementary materials is a suggestion for keeping the “results section” brief ( 17 ). In addition to save the text space, supplementary materials improve the presentation and facilitate communications among scientists ( 46 , 47 ). According to Springer, supplementary materials can be used for presenting data that are not needed to support the major conclusions but are still interesting. However, keep in mind that the unregulated use of supplementary materials is harmful to science ( 47 ). Supplementary materials should be referred to at the appropriate points in the main text.
For referring to results obtained in hypothesis testing studies, using past tenses is recommended ( 4 , 12 - 14 ); non-textual elements should be referred using present tenses, e.g. “as seen in table 1 …” or “table 1 shows …” in descriptive studies, results are reported in the present tense ( 13 ).
6.3. Word Choice
Although adverbs/adjectives are commonly used to highlight the importance of results, it is recommended altogether avoiding the use of such qualitative/emotive words in the “results section” ( 7 , 13 ). Some believe that qualitative words should not be used because they may imply an interpretation of findings ( 17 ). In biomedical publications, the terms ‘significant, significance, and significantly’ (followed by P values) are used to show statistical relationships and should not be used for other purposes for which, other terms such as substantial, considerable, or noteworthy can be used ( 14 ). See Box 3 for appropriate word choice for the “results section.”
In the “results section,” to make a comparison between the results, i.e. stating the similarity/equivalence or difference/non-equivalence, using appropriate signals is recommended ( 27 ). To show a similarity, a signal to the reader may be used such as “like”, “alike”, “similar to”, and “the same as”; to show differences, the following signals can be used: “but”, “while”, “however”, “in contrast”, “more likely than”, and “less likely than” ( 27 ).
6.4. Reporting Numbers
Numbers play an important role in scientific communication and there are some golden rules for reporting numbers in a scientific paper ( 43 , 48 ). Significant figures (significant digits) should reflect the degree of precision of the original measurement ( 12 ). The number of digits reported for a quantity should be consistent with scientific relevance ( 37 ); for example, a resolution to 0.001 units is necessary for pH but a resolution of < 1 mm Hg is unimportant for blood pressure ( 37 ). Avoid using “about” or “approximately” to qualify a measurement or calculation ( 12 ). The use of percentage for sample sizes of < 20 and decimal for sample sizes of < 100 is not recommended ( 43 ).
The numbers should be spelled out at the beginning of a sentence or when they are less than 10, e.g., twelve students improved… ( 43 ). In a sentence, the authors should be consistent where they use numbers as numerals or spelled-out ( 43 ). Before a unit of a measure, time, dates, and points, numbers should be used as numerals, e.g. 12 cm; 1 h 34 min; at 12:30 A.M., and on a 7-point scale ( 18 ).
A space between the numeral and the unit should be considered, except in the case of %. Because the terms “billion,” “trillion,” and “quadrillion” imply different numbers in Europe and the USA, they should not be used ( 48 ). To express ranges in text, the terms “to” or “through” are preferred to dashes; in tables, the use of dashes or hyphens is recommended ( 48 ).
7. Conclusions
The “results section” of a biomedical manuscript should clearly present findings of the study using an effective combination of results and data. Some dos and don’ts of writing the “results section” are provided in Box 4 . Authors should try to find the best format using a dynamic interplay between text and figures/tables. Results can be organized in different ways including chronological order or most to least important; however, results should be presented in a manner that makes sense.
Acknowledgments
The authors wish to acknowledge Ms. Niloofar Shiva for critical editing of English grammar and syntax of the manuscript.
Conflict of Interests: It is not declared by the authors.
Funding/Support: Research Institute for Endocrine Sciences supported the study.
- USC Libraries
- Research Guides
Organizing Your Social Sciences Research Paper
- 8. The Discussion
- Purpose of Guide
- Design Flaws to Avoid
- Independent and Dependent Variables
- Glossary of Research Terms
- Reading Research Effectively
- Narrowing a Topic Idea
- Broadening a Topic Idea
- Extending the Timeliness of a Topic Idea
- Academic Writing Style
- Applying Critical Thinking
- Choosing a Title
- Making an Outline
- Paragraph Development
- Research Process Video Series
- Executive Summary
- The C.A.R.S. Model
- Background Information
- The Research Problem/Question
- Theoretical Framework
- Citation Tracking
- Content Alert Services
- Evaluating Sources
- Primary Sources
- Secondary Sources
- Tiertiary Sources
- Scholarly vs. Popular Publications
- Qualitative Methods
- Quantitative Methods
- Insiderness
- Using Non-Textual Elements
- Limitations of the Study
- Common Grammar Mistakes
- Writing Concisely
- Avoiding Plagiarism
- Footnotes or Endnotes?
- Further Readings
- Generative AI and Writing
- USC Libraries Tutorials and Other Guides
- Bibliography
The purpose of the discussion section is to interpret and describe the significance of your findings in relation to what was already known about the research problem being investigated and to explain any new understanding or insights that emerged as a result of your research. The discussion will always connect to the introduction by way of the research questions or hypotheses you posed and the literature you reviewed, but the discussion does not simply repeat or rearrange the first parts of your paper; the discussion clearly explains how your study advanced the reader's understanding of the research problem from where you left them at the end of your review of prior research.
Annesley, Thomas M. “The Discussion Section: Your Closing Argument.” Clinical Chemistry 56 (November 2010): 1671-1674; Peacock, Matthew. “Communicative Moves in the Discussion Section of Research Articles.” System 30 (December 2002): 479-497.
Importance of a Good Discussion
The discussion section is often considered the most important part of your research paper because it:
- Most effectively demonstrates your ability as a researcher to think critically about an issue, to develop creative solutions to problems based upon a logical synthesis of the findings, and to formulate a deeper, more profound understanding of the research problem under investigation;
- Presents the underlying meaning of your research, notes possible implications in other areas of study, and explores possible improvements that can be made in order to further develop the concerns of your research;
- Highlights the importance of your study and how it can contribute to understanding the research problem within the field of study;
- Presents how the findings from your study revealed and helped fill gaps in the literature that had not been previously exposed or adequately described; and,
- Engages the reader in thinking critically about issues based on an evidence-based interpretation of findings; it is not governed strictly by objective reporting of information.
Annesley Thomas M. “The Discussion Section: Your Closing Argument.” Clinical Chemistry 56 (November 2010): 1671-1674; Bitchener, John and Helen Basturkmen. “Perceptions of the Difficulties of Postgraduate L2 Thesis Students Writing the Discussion Section.” Journal of English for Academic Purposes 5 (January 2006): 4-18; Kretchmer, Paul. Fourteen Steps to Writing an Effective Discussion Section. San Francisco Edit, 2003-2008.
Structure and Writing Style
I. General Rules
These are the general rules you should adopt when composing your discussion of the results :
- Do not be verbose or repetitive; be concise and make your points clearly
- Avoid the use of jargon or undefined technical language
- Follow a logical stream of thought; in general, interpret and discuss the significance of your findings in the same sequence you described them in your results section [a notable exception is to begin by highlighting an unexpected result or a finding that can grab the reader's attention]
- Use the present verb tense, especially for established facts; however, refer to specific works or prior studies in the past tense
- If needed, use subheadings to help organize your discussion or to categorize your interpretations into themes
II. The Content
The content of the discussion section of your paper most often includes :
- Explanation of results : Comment on whether or not the results were expected for each set of findings; go into greater depth to explain findings that were unexpected or especially profound. If appropriate, note any unusual or unanticipated patterns or trends that emerged from your results and explain their meaning in relation to the research problem.
- References to previous research : Either compare your results with the findings from other studies or use the studies to support a claim. This can include re-visiting key sources already cited in your literature review section, or, save them to cite later in the discussion section if they are more important to compare with your results instead of being a part of the general literature review of prior research used to provide context and background information. Note that you can make this decision to highlight specific studies after you have begun writing the discussion section.
- Deduction : A claim for how the results can be applied more generally. For example, describing lessons learned, proposing recommendations that can help improve a situation, or highlighting best practices.
- Hypothesis : A more general claim or possible conclusion arising from the results [which may be proved or disproved in subsequent research]. This can be framed as new research questions that emerged as a consequence of your analysis.
III. Organization and Structure
Keep the following sequential points in mind as you organize and write the discussion section of your paper:
- Think of your discussion as an inverted pyramid. Organize the discussion from the general to the specific, linking your findings to the literature, then to theory, then to practice [if appropriate].
- Use the same key terms, narrative style, and verb tense [present] that you used when describing the research problem in your introduction.
- Begin by briefly re-stating the research problem you were investigating and answer all of the research questions underpinning the problem that you posed in the introduction.
- Describe the patterns, principles, and relationships shown by each major findings and place them in proper perspective. The sequence of this information is important; first state the answer, then the relevant results, then cite the work of others. If appropriate, refer the reader to a figure or table to help enhance the interpretation of the data [either within the text or as an appendix].
- Regardless of where it's mentioned, a good discussion section includes analysis of any unexpected findings. This part of the discussion should begin with a description of the unanticipated finding, followed by a brief interpretation as to why you believe it appeared and, if necessary, its possible significance in relation to the overall study. If more than one unexpected finding emerged during the study, describe each of them in the order they appeared as you gathered or analyzed the data. As noted, the exception to discussing findings in the same order you described them in the results section would be to begin by highlighting the implications of a particularly unexpected or significant finding that emerged from the study, followed by a discussion of the remaining findings.
- Before concluding the discussion, identify potential limitations and weaknesses if you do not plan to do so in the conclusion of the paper. Comment on their relative importance in relation to your overall interpretation of the results and, if necessary, note how they may affect the validity of your findings. Avoid using an apologetic tone; however, be honest and self-critical [e.g., in retrospect, had you included a particular question in a survey instrument, additional data could have been revealed].
- The discussion section should end with a concise summary of the principal implications of the findings regardless of their significance. Give a brief explanation about why you believe the findings and conclusions of your study are important and how they support broader knowledge or understanding of the research problem. This can be followed by any recommendations for further research. However, do not offer recommendations which could have been easily addressed within the study. This would demonstrate to the reader that you have inadequately examined and interpreted the data.
IV. Overall Objectives
The objectives of your discussion section should include the following: I. Reiterate the Research Problem/State the Major Findings
Briefly reiterate the research problem or problems you are investigating and the methods you used to investigate them, then move quickly to describe the major findings of the study. You should write a direct, declarative, and succinct proclamation of the study results, usually in one paragraph.
II. Explain the Meaning of the Findings and Why They are Important
No one has thought as long and hard about your study as you have. Systematically explain the underlying meaning of your findings and state why you believe they are significant. After reading the discussion section, you want the reader to think critically about the results and why they are important. You don’t want to force the reader to go through the paper multiple times to figure out what it all means. If applicable, begin this part of the section by repeating what you consider to be your most significant or unanticipated finding first, then systematically review each finding. Otherwise, follow the general order you reported the findings presented in the results section.
III. Relate the Findings to Similar Studies
No study in the social sciences is so novel or possesses such a restricted focus that it has absolutely no relation to previously published research. The discussion section should relate your results to those found in other studies, particularly if questions raised from prior studies served as the motivation for your research. This is important because comparing and contrasting the findings of other studies helps to support the overall importance of your results and it highlights how and in what ways your study differs from other research about the topic. Note that any significant or unanticipated finding is often because there was no prior research to indicate the finding could occur. If there is prior research to indicate this, you need to explain why it was significant or unanticipated. IV. Consider Alternative Explanations of the Findings
It is important to remember that the purpose of research in the social sciences is to discover and not to prove . When writing the discussion section, you should carefully consider all possible explanations for the study results, rather than just those that fit your hypothesis or prior assumptions and biases. This is especially important when describing the discovery of significant or unanticipated findings.
V. Acknowledge the Study’s Limitations
It is far better for you to identify and acknowledge your study’s limitations than to have them pointed out by your professor! Note any unanswered questions or issues your study could not address and describe the generalizability of your results to other situations. If a limitation is applicable to the method chosen to gather information, then describe in detail the problems you encountered and why. VI. Make Suggestions for Further Research
You may choose to conclude the discussion section by making suggestions for further research [as opposed to offering suggestions in the conclusion of your paper]. Although your study can offer important insights about the research problem, this is where you can address other questions related to the problem that remain unanswered or highlight hidden issues that were revealed as a result of conducting your research. You should frame your suggestions by linking the need for further research to the limitations of your study [e.g., in future studies, the survey instrument should include more questions that ask..."] or linking to critical issues revealed from the data that were not considered initially in your research.
NOTE: Besides the literature review section, the preponderance of references to sources is usually found in the discussion section . A few historical references may be helpful for perspective, but most of the references should be relatively recent and included to aid in the interpretation of your results, to support the significance of a finding, and/or to place a finding within a particular context. If a study that you cited does not support your findings, don't ignore it--clearly explain why your research findings differ from theirs.
V. Problems to Avoid
- Do not waste time restating your results . Should you need to remind the reader of a finding to be discussed, use "bridge sentences" that relate the result to the interpretation. An example would be: “In the case of determining available housing to single women with children in rural areas of Texas, the findings suggest that access to good schools is important...," then move on to further explaining this finding and its implications.
- As noted, recommendations for further research can be included in either the discussion or conclusion of your paper, but do not repeat your recommendations in the both sections. Think about the overall narrative flow of your paper to determine where best to locate this information. However, if your findings raise a lot of new questions or issues, consider including suggestions for further research in the discussion section.
- Do not introduce new results in the discussion section. Be wary of mistaking the reiteration of a specific finding for an interpretation because it may confuse the reader. The description of findings [results section] and the interpretation of their significance [discussion section] should be distinct parts of your paper. If you choose to combine the results section and the discussion section into a single narrative, you must be clear in how you report the information discovered and your own interpretation of each finding. This approach is not recommended if you lack experience writing college-level research papers.
- Use of the first person pronoun is generally acceptable. Using first person singular pronouns can help emphasize a point or illustrate a contrasting finding. However, keep in mind that too much use of the first person can actually distract the reader from the main points [i.e., I know you're telling me this--just tell me!].
Analyzing vs. Summarizing. Department of English Writing Guide. George Mason University; Discussion. The Structure, Format, Content, and Style of a Journal-Style Scientific Paper. Department of Biology. Bates College; Hess, Dean R. "How to Write an Effective Discussion." Respiratory Care 49 (October 2004); Kretchmer, Paul. Fourteen Steps to Writing to Writing an Effective Discussion Section. San Francisco Edit, 2003-2008; The Lab Report. University College Writing Centre. University of Toronto; Sauaia, A. et al. "The Anatomy of an Article: The Discussion Section: "How Does the Article I Read Today Change What I Will Recommend to my Patients Tomorrow?” The Journal of Trauma and Acute Care Surgery 74 (June 2013): 1599-1602; Research Limitations & Future Research . Lund Research Ltd., 2012; Summary: Using it Wisely. The Writing Center. University of North Carolina; Schafer, Mickey S. Writing the Discussion. Writing in Psychology course syllabus. University of Florida; Yellin, Linda L. A Sociology Writer's Guide . Boston, MA: Allyn and Bacon, 2009.
Writing Tip
Don’t Over-Interpret the Results!
Interpretation is a subjective exercise. As such, you should always approach the selection and interpretation of your findings introspectively and to think critically about the possibility of judgmental biases unintentionally entering into discussions about the significance of your work. With this in mind, be careful that you do not read more into the findings than can be supported by the evidence you have gathered. Remember that the data are the data: nothing more, nothing less.
MacCoun, Robert J. "Biases in the Interpretation and Use of Research Results." Annual Review of Psychology 49 (February 1998): 259-287; Ward, Paulet al, editors. The Oxford Handbook of Expertise . Oxford, UK: Oxford University Press, 2018.
Another Writing Tip
Don't Write Two Results Sections!
One of the most common mistakes that you can make when discussing the results of your study is to present a superficial interpretation of the findings that more or less re-states the results section of your paper. Obviously, you must refer to your results when discussing them, but focus on the interpretation of those results and their significance in relation to the research problem, not the data itself.
Azar, Beth. "Discussing Your Findings." American Psychological Association gradPSYCH Magazine (January 2006).
Yet Another Writing Tip
Avoid Unwarranted Speculation!
The discussion section should remain focused on the findings of your study. For example, if the purpose of your research was to measure the impact of foreign aid on increasing access to education among disadvantaged children in Bangladesh, it would not be appropriate to speculate about how your findings might apply to populations in other countries without drawing from existing studies to support your claim or if analysis of other countries was not a part of your original research design. If you feel compelled to speculate, do so in the form of describing possible implications or explaining possible impacts. Be certain that you clearly identify your comments as speculation or as a suggestion for where further research is needed. Sometimes your professor will encourage you to expand your discussion of the results in this way, while others don’t care what your opinion is beyond your effort to interpret the data in relation to the research problem.
- << Previous: Using Non-Textual Elements
- Next: Limitations of the Study >>
- Last Updated: May 18, 2024 11:38 AM
- URL: https://libguides.usc.edu/writingguide
How to Write the Discussion Section of a Research Paper
The discussion section of a research paper analyzes and interprets the findings, provides context, compares them with previous studies, identifies limitations, and suggests future research directions.
Updated on September 15, 2023

Structure your discussion section right, and you’ll be cited more often while doing a greater service to the scientific community. So, what actually goes into the discussion section? And how do you write it?
The discussion section of your research paper is where you let the reader know how your study is positioned in the literature, what to take away from your paper, and how your work helps them. It can also include your conclusions and suggestions for future studies.
First, we’ll define all the parts of your discussion paper, and then look into how to write a strong, effective discussion section for your paper or manuscript.
Discussion section: what is it, what it does
The discussion section comes later in your paper, following the introduction, methods, and results. The discussion sets up your study’s conclusions. Its main goals are to present, interpret, and provide a context for your results.
What is it?
The discussion section provides an analysis and interpretation of the findings, compares them with previous studies, identifies limitations, and suggests future directions for research.
This section combines information from the preceding parts of your paper into a coherent story. By this point, the reader already knows why you did your study (introduction), how you did it (methods), and what happened (results). In the discussion, you’ll help the reader connect the ideas from these sections.
Why is it necessary?
The discussion provides context and interpretations for the results. It also answers the questions posed in the introduction. While the results section describes your findings, the discussion explains what they say. This is also where you can describe the impact or implications of your research.
Adds context for your results
Most research studies aim to answer a question, replicate a finding, or address limitations in the literature. These goals are first described in the introduction. However, in the discussion section, the author can refer back to them to explain how the study's objective was achieved.
Shows what your results actually mean and real-world implications
The discussion can also describe the effect of your findings on research or practice. How are your results significant for readers, other researchers, or policymakers?
What to include in your discussion (in the correct order)
A complete and effective discussion section should at least touch on the points described below.
Summary of key findings
The discussion should begin with a brief factual summary of the results. Concisely overview the main results you obtained.
Begin with key findings with supporting evidence
Your results section described a list of findings, but what message do they send when you look at them all together?
Your findings were detailed in the results section, so there’s no need to repeat them here, but do provide at least a few highlights. This will help refresh the reader’s memory and help them focus on the big picture.
Read the first paragraph of the discussion section in this article (PDF) for an example of how to start this part of your paper. Notice how the authors break down their results and follow each description sentence with an explanation of why each finding is relevant.
State clearly and concisely
Following a clear and direct writing style is especially important in the discussion section. After all, this is where you will make some of the most impactful points in your paper. While the results section often contains technical vocabulary, such as statistical terms, the discussion section lets you describe your findings more clearly.
Interpretation of results
Once you’ve given your reader an overview of your results, you need to interpret those results. In other words, what do your results mean? Discuss the findings’ implications and significance in relation to your research question or hypothesis.
Analyze and interpret your findings
Look into your findings and explore what’s behind them or what may have caused them. If your introduction cited theories or studies that could explain your findings, use these sources as a basis to discuss your results.
For example, look at the second paragraph in the discussion section of this article on waggling honey bees. Here, the authors explore their results based on information from the literature.
Unexpected or contradictory results
Sometimes, your findings are not what you expect. Here’s where you describe this and try to find a reason for it. Could it be because of the method you used? Does it have something to do with the variables analyzed? Comparing your methods with those of other similar studies can help with this task.
Context and comparison with previous work
Refer to related studies to place your research in a larger context and the literature. Compare and contrast your findings with existing literature, highlighting similarities, differences, and/or contradictions.
How your work compares or contrasts with previous work
Studies with similar findings to yours can be cited to show the strength of your findings. Information from these studies can also be used to help explain your results. Differences between your findings and others in the literature can also be discussed here.
How to divide this section into subsections
If you have more than one objective in your study or many key findings, you can dedicate a separate section to each of these. Here’s an example of this approach. You can see that the discussion section is divided into topics and even has a separate heading for each of them.
Limitations
Many journals require you to include the limitations of your study in the discussion. Even if they don’t, there are good reasons to mention these in your paper.
Why limitations don’t have a negative connotation
A study’s limitations are points to be improved upon in future research. While some of these may be flaws in your method, many may be due to factors you couldn’t predict.
Examples include time constraints or small sample sizes. Pointing this out will help future researchers avoid or address these issues. This part of the discussion can also include any attempts you have made to reduce the impact of these limitations, as in this study .
How limitations add to a researcher's credibility
Pointing out the limitations of your study demonstrates transparency. It also shows that you know your methods well and can conduct a critical assessment of them.
Implications and significance
The final paragraph of the discussion section should contain the take-home messages for your study. It can also cite the “strong points” of your study, to contrast with the limitations section.
Restate your hypothesis
Remind the reader what your hypothesis was before you conducted the study.
How was it proven or disproven?
Identify your main findings and describe how they relate to your hypothesis.
How your results contribute to the literature
Were you able to answer your research question? Or address a gap in the literature?
Future implications of your research
Describe the impact that your results may have on the topic of study. Your results may show, for instance, that there are still limitations in the literature for future studies to address. There may be a need for studies that extend your findings in a specific way. You also may need additional research to corroborate your findings.
Sample discussion section
This fictitious example covers all the aspects discussed above. Your actual discussion section will probably be much longer, but you can read this to get an idea of everything your discussion should cover.
Our results showed that the presence of cats in a household is associated with higher levels of perceived happiness by its human occupants. These findings support our hypothesis and demonstrate the association between pet ownership and well-being.
The present findings align with those of Bao and Schreer (2016) and Hardie et al. (2023), who observed greater life satisfaction in pet owners relative to non-owners. Although the present study did not directly evaluate life satisfaction, this factor may explain the association between happiness and cat ownership observed in our sample.
Our findings must be interpreted in light of some limitations, such as the focus on cat ownership only rather than pets as a whole. This may limit the generalizability of our results.
Nevertheless, this study had several strengths. These include its strict exclusion criteria and use of a standardized assessment instrument to investigate the relationships between pets and owners. These attributes bolster the accuracy of our results and reduce the influence of confounding factors, increasing the strength of our conclusions. Future studies may examine the factors that mediate the association between pet ownership and happiness to better comprehend this phenomenon.
This brief discussion begins with a quick summary of the results and hypothesis. The next paragraph cites previous research and compares its findings to those of this study. Information from previous studies is also used to help interpret the findings. After discussing the results of the study, some limitations are pointed out. The paper also explains why these limitations may influence the interpretation of results. Then, final conclusions are drawn based on the study, and directions for future research are suggested.
How to make your discussion flow naturally
If you find writing in scientific English challenging, the discussion and conclusions are often the hardest parts of the paper to write. That’s because you’re not just listing up studies, methods, and outcomes. You’re actually expressing your thoughts and interpretations in words.
- How formal should it be?
- What words should you use, or not use?
- How do you meet strict word limits, or make it longer and more informative?
Always give it your best, but sometimes a helping hand can, well, help. Getting a professional edit can help clarify your work’s importance while improving the English used to explain it. When readers know the value of your work, they’ll cite it. We’ll assign your study to an expert editor knowledgeable in your area of research. Their work will clarify your discussion, helping it to tell your story. Find out more about AJE Editing.

Adam Goulston, PsyD, MS, MBA, MISD, ELS
Science Marketing Consultant
See our "Privacy Policy"
Ensure your structure and ideas are consistent and clearly communicated
Pair your Premium Editing with our add-on service Presubmission Review for an overall assessment of your manuscript.

- LEARNING SKILLS
- Writing a Dissertation or Thesis
- Results and Discussion
Search SkillsYouNeed:
Learning Skills:
- A - Z List of Learning Skills
- What is Learning?
- Learning Approaches
- Learning Styles
- 8 Types of Learning Styles
- Understanding Your Preferences to Aid Learning
- Lifelong Learning
- Decisions to Make Before Applying to University
- Top Tips for Surviving Student Life
- Living Online: Education and Learning
- 8 Ways to Embrace Technology-Based Learning Approaches
- Critical Thinking Skills
- Critical Thinking and Fake News
- Understanding and Addressing Conspiracy Theories
- Critical Analysis
- Study Skills
- Exam Skills
- How to Write a Research Proposal
- Ethical Issues in Research
- Dissertation: The Introduction
- Researching and Writing a Literature Review
- Writing your Methodology
- Dissertation: Results and Discussion
- Dissertation: Conclusions and Extras
Writing Your Dissertation or Thesis eBook

Part of the Skills You Need Guide for Students .
- Research Methods
- Teaching, Coaching, Mentoring and Counselling
- Employability Skills for Graduates
Subscribe to our FREE newsletter and start improving your life in just 5 minutes a day.
You'll get our 5 free 'One Minute Life Skills' and our weekly newsletter.
We'll never share your email address and you can unsubscribe at any time.
Writing your Dissertation: Results and Discussion
When writing a dissertation or thesis, the results and discussion sections can be both the most interesting as well as the most challenging sections to write.
You may choose to write these sections separately, or combine them into a single chapter, depending on your university’s guidelines and your own preferences.
There are advantages to both approaches.
Writing the results and discussion as separate sections allows you to focus first on what results you obtained and set out clearly what happened in your experiments and/or investigations without worrying about their implications.This can focus your mind on what the results actually show and help you to sort them in your head.
However, many people find it easier to combine the results with their implications as the two are closely connected.
Check your university’s requirements carefully before combining the results and discussions sections as some specify that they must be kept separate.
Results Section
The Results section should set out your key experimental results, including any statistical analysis and whether or not the results of these are significant.
You should cover any literature supporting your interpretation of significance. It does not have to include everything you did, particularly for a doctorate dissertation. However, for an undergraduate or master's thesis, you will probably find that you need to include most of your work.
You should write your results section in the past tense: you are describing what you have done in the past.
Every result included MUST have a method set out in the methods section. Check back to make sure that you have included all the relevant methods.
Conversely, every method should also have some results given so, if you choose to exclude certain experiments from the results, make sure that you remove mention of the method as well.
If you are unsure whether to include certain results, go back to your research questions and decide whether the results are relevant to them. It doesn’t matter whether they are supportive or not, it’s about relevance. If they are relevant, you should include them.
Having decided what to include, next decide what order to use. You could choose chronological, which should follow the methods, or in order from most to least important in the answering of your research questions, or by research question and/or hypothesis.
You also need to consider how best to present your results: tables, figures, graphs, or text. Try to use a variety of different methods of presentation, and consider your reader: 20 pages of dense tables are hard to understand, as are five pages of graphs, but a single table and well-chosen graph that illustrate your overall findings will make things much clearer.
Make sure that each table and figure has a number and a title. Number tables and figures in separate lists, but consecutively by the order in which you mention them in the text. If you have more than about two or three, it’s often helpful to provide lists of tables and figures alongside the table of contents at the start of your dissertation.
Summarise your results in the text, drawing on the figures and tables to illustrate your points.
The text and figures should be complementary, not repeat the same information. You should refer to every table or figure in the text. Any that you don’t feel the need to refer to can safely be moved to an appendix, or even removed.
Make sure that you including information about the size and direction of any changes, including percentage change if appropriate. Statistical tests should include details of p values or confidence intervals and limits.
While you don’t need to include all your primary evidence in this section, you should as a matter of good practice make it available in an appendix, to which you should refer at the relevant point.
For example:
Details of all the interview participants can be found in Appendix A, with transcripts of each interview in Appendix B.
You will, almost inevitably, find that you need to include some slight discussion of your results during this section. This discussion should evaluate the quality of the results and their reliability, but not stray too far into discussion of how far your results support your hypothesis and/or answer your research questions, as that is for the discussion section.
See our pages: Analysing Qualitative Data and Simple Statistical Analysis for more information on analysing your results.
Discussion Section
This section has four purposes, it should:
- Interpret and explain your results
- Answer your research question
- Justify your approach
- Critically evaluate your study
The discussion section therefore needs to review your findings in the context of the literature and the existing knowledge about the subject.
You also need to demonstrate that you understand the limitations of your research and the implications of your findings for policy and practice. This section should be written in the present tense.
The Discussion section needs to follow from your results and relate back to your literature review . Make sure that everything you discuss is covered in the results section.
Some universities require a separate section on recommendations for policy and practice and/or for future research, while others allow you to include this in your discussion, so check the guidelines carefully.
Starting the Task
Most people are likely to write this section best by preparing an outline, setting out the broad thrust of the argument, and how your results support it.
You may find techniques like mind mapping are helpful in making a first outline; check out our page: Creative Thinking for some ideas about how to think through your ideas. You should start by referring back to your research questions, discuss your results, then set them into the context of the literature, and then into broader theory.
This is likely to be one of the longest sections of your dissertation, and it’s a good idea to break it down into chunks with sub-headings to help your reader to navigate through the detail.
Fleshing Out the Detail
Once you have your outline in front of you, you can start to map out how your results fit into the outline.
This will help you to see whether your results are over-focused in one area, which is why writing up your research as you go along can be a helpful process. For each theme or area, you should discuss how the results help to answer your research question, and whether the results are consistent with your expectations and the literature.
The Importance of Understanding Differences
If your results are controversial and/or unexpected, you should set them fully in context and explain why you think that you obtained them.
Your explanations may include issues such as a non-representative sample for convenience purposes, a response rate skewed towards those with a particular experience, or your own involvement as a participant for sociological research.
You do not need to be apologetic about these, because you made a choice about them, which you should have justified in the methodology section. However, you do need to evaluate your own results against others’ findings, especially if they are different. A full understanding of the limitations of your research is part of a good discussion section.
At this stage, you may want to revisit your literature review, unless you submitted it as a separate submission earlier, and revise it to draw out those studies which have proven more relevant.
Conclude by summarising the implications of your findings in brief, and explain why they are important for researchers and in practice, and provide some suggestions for further work.
You may also wish to make some recommendations for practice. As before, this may be a separate section, or included in your discussion.
The results and discussion, including conclusion and recommendations, are probably the most substantial sections of your dissertation. Once completed, you can begin to relax slightly: you are on to the last stages of writing!
Continue to: Dissertation: Conclusion and Extras Writing your Methodology
See also: Writing a Literature Review Writing a Research Proposal Academic Referencing What Is the Importance of Using a Plagiarism Checker to Check Your Thesis?

- Manuscript Preparation
How to write the results section of a research paper
- 3 minute read
- 64.5K views
Table of Contents
At its core, a research paper aims to fill a gap in the research on a given topic. As a result, the results section of the paper, which describes the key findings of the study, is often considered the core of the paper. This is the section that gets the most attention from reviewers, peers, students, and any news organization reporting on your findings. Writing a clear, concise, and logical results section is, therefore, one of the most important parts of preparing your manuscript.
Difference between results and discussion
Before delving into how to write the results section, it is important to first understand the difference between the results and discussion sections. The results section needs to detail the findings of the study. The aim of this section is not to draw connections between the different findings or to compare it to previous findings in literature—that is the purview of the discussion section. Unlike the discussion section, which can touch upon the hypothetical, the results section needs to focus on the purely factual. In some cases, it may even be preferable to club these two sections together into a single section. For example, while writing a review article, it can be worthwhile to club these two sections together, as the main results in this case are the conclusions that can be drawn from the literature.
Structure of the results section
Although the main purpose of the results section in a research paper is to report the findings, it is necessary to present an introduction and repeat the research question. This establishes a connection to the previous section of the paper and creates a smooth flow of information.
Next, the results section needs to communicate the findings of your research in a systematic manner. The section needs to be organized such that the primary research question is addressed first, then the secondary research questions. If the research addresses multiple questions, the results section must individually connect with each of the questions. This ensures clarity and minimizes confusion while reading.
Consider representing your results visually. For example, graphs, tables, and other figures can help illustrate the findings of your paper, especially if there is a large amount of data in the results.
Remember, an appealing results section can help peer reviewers better understand the merits of your research, thereby increasing your chances of publication.
Practical guidance for writing an effective results section for a research paper
- Always use simple and clear language. Avoid the use of uncertain or out-of-focus expressions.
- The findings of the study must be expressed in an objective and unbiased manner. While it is acceptable to correlate certain findings in the discussion section, it is best to avoid overinterpreting the results.
- If the research addresses more than one hypothesis, use sub-sections to describe the results. This prevents confusion and promotes understanding.
- Ensure that negative results are included in this section, even if they do not support the research hypothesis.
- Wherever possible, use illustrations like tables, figures, charts, or other visual representations to showcase the results of your research paper. Mention these illustrations in the text, but do not repeat the information that they convey.
- For statistical data, it is adequate to highlight the tests and explain their results. The initial or raw data should not be mentioned in the results section of a research paper.
The results section of a research paper is usually the most impactful section because it draws the greatest attention. Regardless of the subject of your research paper, a well-written results section is capable of generating interest in your research.
For detailed information and assistance on writing the results of a research paper, refer to Elsevier Author Services.

- Research Process
Writing a good review article


Why is data validation important in research?
You may also like.

Make Hook, Line, and Sinker: The Art of Crafting Engaging Introductions

Can Describing Study Limitations Improve the Quality of Your Paper?

A Guide to Crafting Shorter, Impactful Sentences in Academic Writing

6 Steps to Write an Excellent Discussion in Your Manuscript

How to Write Clear and Crisp Civil Engineering Papers? Here are 5 Key Tips to Consider

The Clear Path to An Impactful Paper: ②

The Essentials of Writing to Communicate Research in Medicine

Changing Lines: Sentence Patterns in Academic Writing
Input your search keywords and press Enter.
- SpringerLink shop
Discussion and Conclusions
Your Discussion and Conclusions sections should answer the question: What do your results mean?
In other words, the majority of the Discussion and Conclusions sections should be an interpretation of your results. You should:
- Discuss your conclusions in order of most to least important.
- Compare your results with those from other studies: Are they consistent? If not, discuss possible reasons for the difference.
- Mention any inconclusive results and explain them as best you can. You may suggest additional experiments needed to clarify your results.
- Briefly describe the limitations of your study to show reviewers and readers that you have considered your experiment’s weaknesses. Many researchers are hesitant to do this as they feel it highlights the weaknesses in their research to the editor and reviewer. However doing this actually makes a positive impression of your paper as it makes it clear that you have an in depth understanding of your topic and can think objectively of your research.
- Discuss what your results may mean for researchers in the same field as you, researchers in other fields, and the general public. How could your findings be applied?
- State how your results extend the findings of previous studies.
- If your findings are preliminary, suggest future studies that need to be carried out.
- At the end of your Discussion and Conclusions sections, state your main conclusions once again .
Back │ Next
Research Skills
Results, discussion, and conclusion, results/findings.
The Results (or Findings) section follows the Methods and precedes the Discussion section. This is where the authors provide the data collected during their study. That data can sometimes be difficult to understand because it is often quite technical. Do not let this intimidate you; you will discover the significance of the results next.
The Discussion section follows the Results and precedes the Conclusions and Recommendations section. It is here that the authors indicate the significance of their results. They answer the question, “Why did we get the results we did?” This section provides logical explanations for the results from the study. Those explanations are often reached by comparing and contrasting the results to prior studies’ findings, so citations to the studies discussed in the Literature Review generally reappear here. This section also usually discusses the limitations of the study and speculates on what the results say about the problem(s) identified in the research question(s). This section is very important because it is finally moving towards an argument. Since the researchers interpret their results according to theoretical underpinnings in this section, there is more room for difference of opinion. The way the authors interpret their results may be quite different from the way you would interpret them or the way another researcher would interpret them.
Note: Some articles collapse the Discussion and Conclusion sections together under a single heading (usually “Conclusion”). If you don’t see a separate Discussion section, don’t worry. Instead, look in the nearby sections for the types of information described in the paragraph above.
When you first skim an article, it may be useful to go straight to the Conclusion and see if you can figure out what the thesis is since it is usually in this final section. The research gap identified in the introduction indicates what the researchers wanted to look at; what did they claim, ultimately, when they completed their research? What did it show them—and what are they showing us—about the topic? Did they get the results they expected? Why or why not? The thesis is not a sweeping proclamation; rather, it is likely a very reasonable and conditional claim.
Nearly every research article ends by inviting other scholars to continue the work by saying that more research needs to be done on the matter. However, do not mistake this directive for the thesis; it’s a convention. Often, the authors provide specific details about future possible studies that could or should be conducted in order to make more sense of their own study’s conclusions.
- Parts of An Article. Authored by : Kerry Bowers. Provided by : University of Mississippi. Project : WRIT 250 Committee OER Project. License : CC BY-SA: Attribution-ShareAlike

Privacy Policy
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Results & Discussion
Characteristics of results & discussion.
- Results section contains data collected by scientists from experiments that they conducted.
- Data can be measurements, numbers, descriptions and/or observations.
- Scientific data is typically described using graphs, tables, figures, diagrams, maps, charts, photographs and/or equations.
- Discussion section provides an interpretation of the data, especially in context to previously published research.
The Results and Discussion sections can be written as separate sections (as shown in Fig. 2 ), but are often combined in a poster into one section called Results and Discussion. This is done in order to (1) save precious space on a poster for the many pieces of information that a scientist would like to tell their audience and (2) by combining the two sections, it becomes easier for the audience to understand the significance of the research. Combining the Results section and Discussion section in a poster is different for what is typically done for a scientific journal article. In most journal articles, the Results section is separated from the Discussion section. Journal articles are different from posters in that a scientist is not standing next to their journal article explaining it to a reader. Therefore, in a journal article, an author needs to provide more detailed information so that the reader can understand the research independently. Separating the Results section and Discussion section allows an author the space necessary to write a lengthier description of the research. Journal articles typically contain more text and more content (e.g., figures, tables) than posters.
The Results and Discussion section should contain data, typically in the form of a graph, histogram, chart, image, color-coded map or table ( Figs. 1 & 4 ). Very often data means numbers that scientists collect from making measurements. These data are typically presented to an audience in the form of graphs and charts to show a reader how these numbers change over time, space or experimental conditions ( Fig. 7 ). Numbers can increase, decrease or stay the same and a graph, or another type of figure, can be effectively used to convey this information to a reader in a visual format ( Fig. 7 ).
Figure 7. Example of a Graph
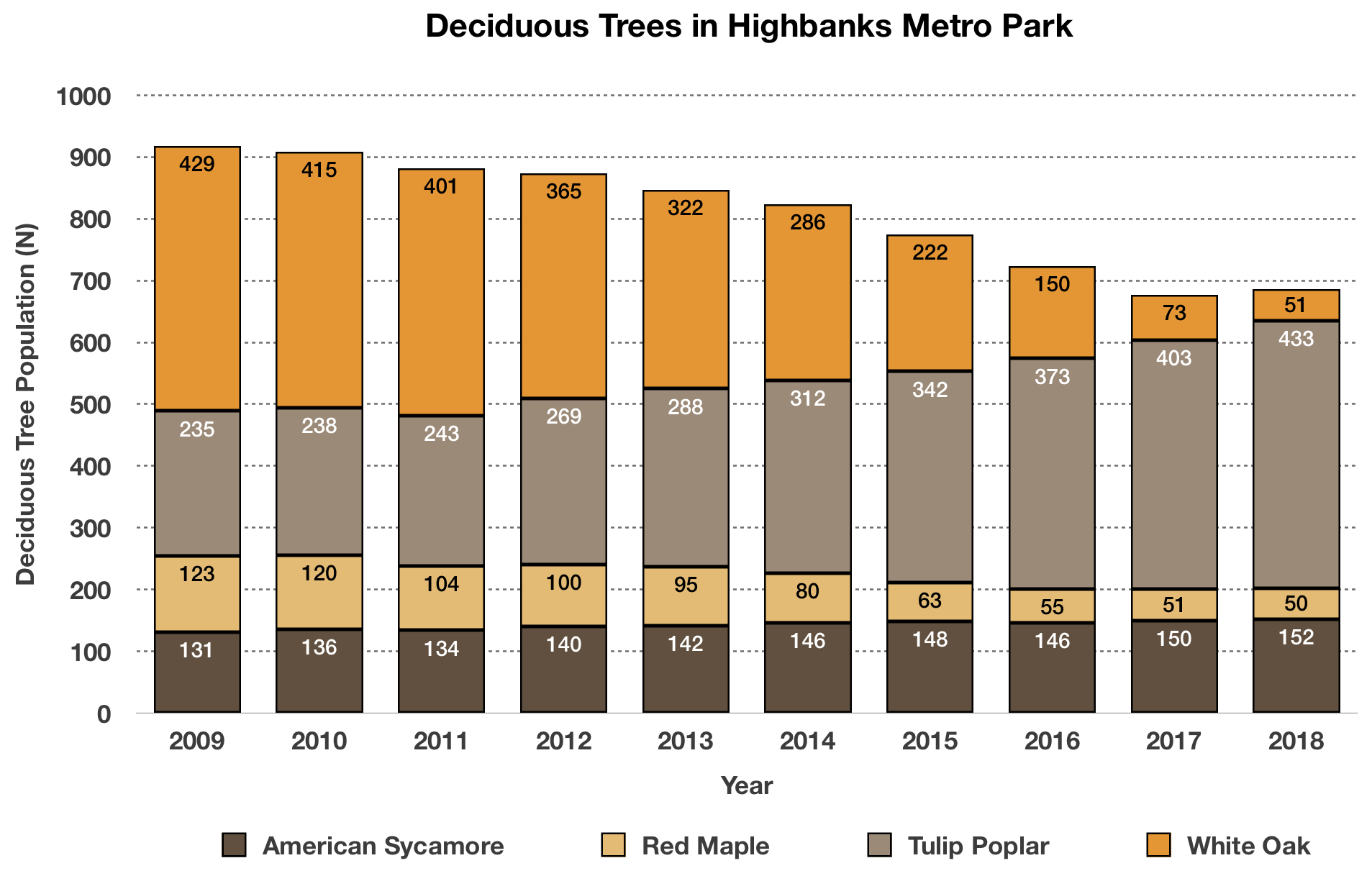
An audience will be attracted to a poster because of its figures and so it is very important for the author to pay particular attention to the creation, design and placement of the figures in a poster ( Figs. 1 & 4 ). A good figure is one that is informative, easy to comprehend and allows the reader to understand the significance of the data and experiment. Very often an author will use color to draw attention to a figure.
The Discussion section should state the importance of the research that is presented in the poster. It should provide an interpretation of the results, especially in context to previously published research. It may propose future experiments that need to be conducted as a result of the research presented in the poster. It should clearly illustrate the significance of the research with regards to new knowledge, understanding and/or discoveries that were made as part of the research.
Scientific Posters: A Learner's Guide Copyright © 2020 by Ella Weaver; Kylienne A. Shaul; Henry Griffy; and Brian H. Lower is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book
Artificial intelligence in strategy
Can machines automate strategy development? The short answer is no. However, there are numerous aspects of strategists’ work where AI and advanced analytics tools can already bring enormous value. Yuval Atsmon is a senior partner who leads the new McKinsey Center for Strategy Innovation, which studies ways new technologies can augment the timeless principles of strategy. In this episode of the Inside the Strategy Room podcast, he explains how artificial intelligence is already transforming strategy and what’s on the horizon. This is an edited transcript of the discussion. For more conversations on the strategy issues that matter, follow the series on your preferred podcast platform .
Joanna Pachner: What does artificial intelligence mean in the context of strategy?
Yuval Atsmon: When people talk about artificial intelligence, they include everything to do with analytics, automation, and data analysis. Marvin Minsky, the pioneer of artificial intelligence research in the 1960s, talked about AI as a “suitcase word”—a term into which you can stuff whatever you want—and that still seems to be the case. We are comfortable with that because we think companies should use all the capabilities of more traditional analysis while increasing automation in strategy that can free up management or analyst time and, gradually, introducing tools that can augment human thinking.
Joanna Pachner: AI has been embraced by many business functions, but strategy seems to be largely immune to its charms. Why do you think that is?
Subscribe to the Inside the Strategy Room podcast
Yuval Atsmon: You’re right about the limited adoption. Only 7 percent of respondents to our survey about the use of AI say they use it in strategy or even financial planning, whereas in areas like marketing, supply chain, and service operations, it’s 25 or 30 percent. One reason adoption is lagging is that strategy is one of the most integrative conceptual practices. When executives think about strategy automation, many are looking too far ahead—at AI capabilities that would decide, in place of the business leader, what the right strategy is. They are missing opportunities to use AI in the building blocks of strategy that could significantly improve outcomes.
I like to use the analogy to virtual assistants. Many of us use Alexa or Siri but very few people use these tools to do more than dictate a text message or shut off the lights. We don’t feel comfortable with the technology’s ability to understand the context in more sophisticated applications. AI in strategy is similar: it’s hard for AI to know everything an executive knows, but it can help executives with certain tasks.
When executives think about strategy automation, many are looking too far ahead—at AI deciding the right strategy. They are missing opportunities to use AI in the building blocks of strategy.
Joanna Pachner: What kind of tasks can AI help strategists execute today?
Yuval Atsmon: We talk about six stages of AI development. The earliest is simple analytics, which we refer to as descriptive intelligence. Companies use dashboards for competitive analysis or to study performance in different parts of the business that are automatically updated. Some have interactive capabilities for refinement and testing.
The second level is diagnostic intelligence, which is the ability to look backward at the business and understand root causes and drivers of performance. The level after that is predictive intelligence: being able to anticipate certain scenarios or options and the value of things in the future based on momentum from the past as well as signals picked in the market. Both diagnostics and prediction are areas that AI can greatly improve today. The tools can augment executives’ analysis and become areas where you develop capabilities. For example, on diagnostic intelligence, you can organize your portfolio into segments to understand granularly where performance is coming from and do it in a much more continuous way than analysts could. You can try 20 different ways in an hour versus deploying one hundred analysts to tackle the problem.
Predictive AI is both more difficult and more risky. Executives shouldn’t fully rely on predictive AI, but it provides another systematic viewpoint in the room. Because strategic decisions have significant consequences, a key consideration is to use AI transparently in the sense of understanding why it is making a certain prediction and what extrapolations it is making from which information. You can then assess if you trust the prediction or not. You can even use AI to track the evolution of the assumptions for that prediction.
Those are the levels available today. The next three levels will take time to develop. There are some early examples of AI advising actions for executives’ consideration that would be value-creating based on the analysis. From there, you go to delegating certain decision authority to AI, with constraints and supervision. Eventually, there is the point where fully autonomous AI analyzes and decides with no human interaction.
Because strategic decisions have significant consequences, you need to understand why AI is making a certain prediction and what extrapolations it’s making from which information.
Joanna Pachner: What kind of businesses or industries could gain the greatest benefits from embracing AI at its current level of sophistication?
Yuval Atsmon: Every business probably has some opportunity to use AI more than it does today. The first thing to look at is the availability of data. Do you have performance data that can be organized in a systematic way? Companies that have deep data on their portfolios down to business line, SKU, inventory, and raw ingredients have the biggest opportunities to use machines to gain granular insights that humans could not.
Companies whose strategies rely on a few big decisions with limited data would get less from AI. Likewise, those facing a lot of volatility and vulnerability to external events would benefit less than companies with controlled and systematic portfolios, although they could deploy AI to better predict those external events and identify what they can and cannot control.
Third, the velocity of decisions matters. Most companies develop strategies every three to five years, which then become annual budgets. If you think about strategy in that way, the role of AI is relatively limited other than potentially accelerating analyses that are inputs into the strategy. However, some companies regularly revisit big decisions they made based on assumptions about the world that may have since changed, affecting the projected ROI of initiatives. Such shifts would affect how you deploy talent and executive time, how you spend money and focus sales efforts, and AI can be valuable in guiding that. The value of AI is even bigger when you can make decisions close to the time of deploying resources, because AI can signal that your previous assumptions have changed from when you made your plan.
Joanna Pachner: Can you provide any examples of companies employing AI to address specific strategic challenges?
Yuval Atsmon: Some of the most innovative users of AI, not coincidentally, are AI- and digital-native companies. Some of these companies have seen massive benefits from AI and have increased its usage in other areas of the business. One mobility player adjusts its financial planning based on pricing patterns it observes in the market. Its business has relatively high flexibility to demand but less so to supply, so the company uses AI to continuously signal back when pricing dynamics are trending in a way that would affect profitability or where demand is rising. This allows the company to quickly react to create more capacity because its profitability is highly sensitive to keeping demand and supply in equilibrium.
Joanna Pachner: Given how quickly things change today, doesn’t AI seem to be more a tactical than a strategic tool, providing time-sensitive input on isolated elements of strategy?
Yuval Atsmon: It’s interesting that you make the distinction between strategic and tactical. Of course, every decision can be broken down into smaller ones, and where AI can be affordably used in strategy today is for building blocks of the strategy. It might feel tactical, but it can make a massive difference. One of the world’s leading investment firms, for example, has started to use AI to scan for certain patterns rather than scanning individual companies directly. AI looks for consumer mobile usage that suggests a company’s technology is catching on quickly, giving the firm an opportunity to invest in that company before others do. That created a significant strategic edge for them, even though the tool itself may be relatively tactical.
Joanna Pachner: McKinsey has written a lot about cognitive biases and social dynamics that can skew decision making. Can AI help with these challenges?
Yuval Atsmon: When we talk to executives about using AI in strategy development, the first reaction we get is, “Those are really big decisions; what if AI gets them wrong?” The first answer is that humans also get them wrong—a lot. [Amos] Tversky, [Daniel] Kahneman, and others have proven that some of those errors are systemic, observable, and predictable. The first thing AI can do is spot situations likely to give rise to biases. For example, imagine that AI is listening in on a strategy session where the CEO proposes something and everyone says “Aye” without debate and discussion. AI could inform the room, “We might have a sunflower bias here,” which could trigger more conversation and remind the CEO that it’s in their own interest to encourage some devil’s advocacy.
We also often see confirmation bias, where people focus their analysis on proving the wisdom of what they already want to do, as opposed to looking for a fact-based reality. Just having AI perform a default analysis that doesn’t aim to satisfy the boss is useful, and the team can then try to understand why that is different than the management hypothesis, triggering a much richer debate.
In terms of social dynamics, agency problems can create conflicts of interest. Every business unit [BU] leader thinks that their BU should get the most resources and will deliver the most value, or at least they feel they should advocate for their business. AI provides a neutral way based on systematic data to manage those debates. It’s also useful for executives with decision authority, since we all know that short-term pressures and the need to make the quarterly and annual numbers lead people to make different decisions on the 31st of December than they do on January 1st or October 1st. Like the story of Ulysses and the sirens, you can use AI to remind you that you wanted something different three months earlier. The CEO still decides; AI can just provide that extra nudge.
Joanna Pachner: It’s like you have Spock next to you, who is dispassionate and purely analytical.
Yuval Atsmon: That is not a bad analogy—for Star Trek fans anyway.
Joanna Pachner: Do you have a favorite application of AI in strategy?
Yuval Atsmon: I have worked a lot on resource allocation, and one of the challenges, which we call the hockey stick phenomenon, is that executives are always overly optimistic about what will happen. They know that resource allocation will inevitably be defined by what you believe about the future, not necessarily by past performance. AI can provide an objective prediction of performance starting from a default momentum case: based on everything that happened in the past and some indicators about the future, what is the forecast of performance if we do nothing? This is before we say, “But I will hire these people and develop this new product and improve my marketing”— things that every executive thinks will help them overdeliver relative to the past. The neutral momentum case, which AI can calculate in a cold, Spock-like manner, can change the dynamics of the resource allocation discussion. It’s a form of predictive intelligence accessible today and while it’s not meant to be definitive, it provides a basis for better decisions.
Joanna Pachner: Do you see access to technology talent as one of the obstacles to the adoption of AI in strategy, especially at large companies?
Yuval Atsmon: I would make a distinction. If you mean machine-learning and data science talent or software engineers who build the digital tools, they are definitely not easy to get. However, companies can increasingly use platforms that provide access to AI tools and require less from individual companies. Also, this domain of strategy is exciting—it’s cutting-edge, so it’s probably easier to get technology talent for that than it might be for manufacturing work.
The bigger challenge, ironically, is finding strategists or people with business expertise to contribute to the effort. You will not solve strategy problems with AI without the involvement of people who understand the customer experience and what you are trying to achieve. Those who know best, like senior executives, don’t have time to be product managers for the AI team. An even bigger constraint is that, in some cases, you are asking people to get involved in an initiative that may make their jobs less important. There could be plenty of opportunities for incorporating AI into existing jobs, but it’s something companies need to reflect on. The best approach may be to create a digital factory where a different team tests and builds AI applications, with oversight from senior stakeholders.
The big challenge is finding strategists to contribute to the AI effort. You are asking people to get involved in an initiative that may make their jobs less important.
Joanna Pachner: Do you think this worry about job security and the potential that AI will automate strategy is realistic?
Yuval Atsmon: The question of whether AI will replace human judgment and put humanity out of its job is a big one that I would leave for other experts.
The pertinent question is shorter-term automation. Because of its complexity, strategy would be one of the later domains to be affected by automation, but we are seeing it in many other domains. However, the trend for more than two hundred years has been that automation creates new jobs, although ones requiring different skills. That doesn’t take away the fear some people have of a machine exposing their mistakes or doing their job better than they do it.
Joanna Pachner: We recently published an article about strategic courage in an age of volatility that talked about three types of edge business leaders need to develop. One of them is an edge in insights. Do you think AI has a role to play in furnishing a proprietary insight edge?
Yuval Atsmon: One of the challenges most strategists face is the overwhelming complexity of the world we operate in—the number of unknowns, the information overload. At one level, it may seem that AI will provide another layer of complexity. In reality, it can be a sharp knife that cuts through some of the clutter. The question to ask is, Can AI simplify my life by giving me sharper, more timely insights more easily?
Joanna Pachner: You have been working in strategy for a long time. What sparked your interest in exploring this intersection of strategy and new technology?
Yuval Atsmon: I have always been intrigued by things at the boundaries of what seems possible. Science fiction writer Arthur C. Clarke’s second law is that to discover the limits of the possible, you have to venture a little past them into the impossible, and I find that particularly alluring in this arena.
AI in strategy is in very nascent stages but could be very consequential for companies and for the profession. For a top executive, strategic decisions are the biggest way to influence the business, other than maybe building the top team, and it is amazing how little technology is leveraged in that process today. It’s conceivable that competitive advantage will increasingly rest in having executives who know how to apply AI well. In some domains, like investment, that is already happening, and the difference in returns can be staggering. I find helping companies be part of that evolution very exciting.
Explore a career with us
Related articles.

Strategic courage in an age of volatility
Bias Busters Collection
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, automatically generate references for free.
- Knowledge Base
- Dissertation
- How to Write a Discussion Section | Tips & Examples
How to Write a Discussion Section | Tips & Examples
Published on 21 August 2022 by Shona McCombes . Revised on 25 October 2022.

The discussion section is where you delve into the meaning, importance, and relevance of your results .
It should focus on explaining and evaluating what you found, showing how it relates to your literature review , and making an argument in support of your overall conclusion . It should not be a second results section .
There are different ways to write this section, but you can focus your writing around these key elements:
- Summary: A brief recap of your key results
- Interpretations: What do your results mean?
- Implications: Why do your results matter?
- Limitations: What can’t your results tell us?
- Recommendations: Avenues for further studies or analyses
Instantly correct all language mistakes in your text
Be assured that you'll submit flawless writing. Upload your document to correct all your mistakes.

Table of contents
What not to include in your discussion section, step 1: summarise your key findings, step 2: give your interpretations, step 3: discuss the implications, step 4: acknowledge the limitations, step 5: share your recommendations, discussion section example.
There are a few common mistakes to avoid when writing the discussion section of your paper.
- Don’t introduce new results: You should only discuss the data that you have already reported in your results section .
- Don’t make inflated claims: Avoid overinterpretation and speculation that isn’t directly supported by your data.
- Don’t undermine your research: The discussion of limitations should aim to strengthen your credibility, not emphasise weaknesses or failures.
Prevent plagiarism, run a free check.
Start this section by reiterating your research problem and concisely summarising your major findings. Don’t just repeat all the data you have already reported – aim for a clear statement of the overall result that directly answers your main research question . This should be no more than one paragraph.
Many students struggle with the differences between a discussion section and a results section . The crux of the matter is that your results sections should present your results, and your discussion section should subjectively evaluate them. Try not to blend elements of these two sections, in order to keep your paper sharp.
- The results indicate that …
- The study demonstrates a correlation between …
- This analysis supports the theory that …
- The data suggest that …
The meaning of your results may seem obvious to you, but it’s important to spell out their significance for your reader, showing exactly how they answer your research question.
The form of your interpretations will depend on the type of research, but some typical approaches to interpreting the data include:
- Identifying correlations , patterns, and relationships among the data
- Discussing whether the results met your expectations or supported your hypotheses
- Contextualising your findings within previous research and theory
- Explaining unexpected results and evaluating their significance
- Considering possible alternative explanations and making an argument for your position
You can organise your discussion around key themes, hypotheses, or research questions, following the same structure as your results section. Alternatively, you can also begin by highlighting the most significant or unexpected results.
- In line with the hypothesis …
- Contrary to the hypothesised association …
- The results contradict the claims of Smith (2007) that …
- The results might suggest that x . However, based on the findings of similar studies, a more plausible explanation is x .
As well as giving your own interpretations, make sure to relate your results back to the scholarly work that you surveyed in the literature review . The discussion should show how your findings fit with existing knowledge, what new insights they contribute, and what consequences they have for theory or practice.
Ask yourself these questions:
- Do your results support or challenge existing theories? If they support existing theories, what new information do they contribute? If they challenge existing theories, why do you think that is?
- Are there any practical implications?
Your overall aim is to show the reader exactly what your research has contributed, and why they should care.
- These results build on existing evidence of …
- The results do not fit with the theory that …
- The experiment provides a new insight into the relationship between …
- These results should be taken into account when considering how to …
- The data contribute a clearer understanding of …
- While previous research has focused on x , these results demonstrate that y .
The only proofreading tool specialized in correcting academic writing
The academic proofreading tool has been trained on 1000s of academic texts and by native English editors. Making it the most accurate and reliable proofreading tool for students.

Correct my document today
Even the best research has its limitations. Acknowledging these is important to demonstrate your credibility. Limitations aren’t about listing your errors, but about providing an accurate picture of what can and cannot be concluded from your study.
Limitations might be due to your overall research design, specific methodological choices , or unanticipated obstacles that emerged during your research process.
Here are a few common possibilities:
- If your sample size was small or limited to a specific group of people, explain how generalisability is limited.
- If you encountered problems when gathering or analysing data, explain how these influenced the results.
- If there are potential confounding variables that you were unable to control, acknowledge the effect these may have had.
After noting the limitations, you can reiterate why the results are nonetheless valid for the purpose of answering your research question.
- The generalisability of the results is limited by …
- The reliability of these data is impacted by …
- Due to the lack of data on x , the results cannot confirm …
- The methodological choices were constrained by …
- It is beyond the scope of this study to …
Based on the discussion of your results, you can make recommendations for practical implementation or further research. Sometimes, the recommendations are saved for the conclusion .
Suggestions for further research can lead directly from the limitations. Don’t just state that more studies should be done – give concrete ideas for how future work can build on areas that your own research was unable to address.
- Further research is needed to establish …
- Future studies should take into account …
- Avenues for future research include …
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the ‘Cite this Scribbr article’ button to automatically add the citation to our free Reference Generator.
McCombes, S. (2022, October 25). How to Write a Discussion Section | Tips & Examples. Scribbr. Retrieved 14 May 2024, from https://www.scribbr.co.uk/thesis-dissertation/discussion/
Is this article helpful?
Shona McCombes
Other students also liked, how to write a results section | tips & examples, research paper appendix | example & templates, how to write a thesis or dissertation introduction.
- Open access
- Published: 17 May 2024
Towards inclusive learning environments in post-graduate medical education: stakeholder-driven strategies in Dutch GP-specialty training
- N.M. van Moppes ORCID: orcid.org/0000-0003-3457-7724 1 ,
- M. Nasori ORCID: orcid.org/0000-0001-8559-1791 1 ,
- J. Bont ORCID: orcid.org/0000-0002-5358-0235 1 ,
- J.M. van Es 1 ,
- M.R.M. Visser 1 &
- M.E.T.C. van den Muijsenbergh ORCID: orcid.org/0000-0002-4994-4008 2 , 3
BMC Medical Education volume 24 , Article number: 550 ( 2024 ) Cite this article
49 Accesses
Metrics details
A recent study found that ethnic minority General Practice (GP)-trainees receive more negative assessments than their majority peers. Previous qualitative research suggested that learning climate-related factors play a pivotal role in unequal opportunities for trainees in post-graduate medical settings, indicating that insufficient inclusivity had put minority students at risk of failure and dropout.
Study objectives
We aimed to develop broadly supported strategies for an inclusive learning climate in Dutch GP-specialty training.
We employed Participatory Action Research (PAR)-methods, incorporating Participatory Learning and Action (PLA)-techniques to ensure equal voices for all stakeholders in shaping Diversity, Equity, and Inclusion (DEI)-strategies for GP-specialty training. Our approach engaged stakeholders within two pilot GP-specialty training institutes across diverse roles, including management, support staff, in-faculty teachers, in-clinic supervisors, and trainees, representing ethnic minorities and the majority population. Purposeful convenience sampling formed stakeholder- and co-reader groups in two Dutch GP-specialty training institutes. Stakeholder discussion sessions were based on experiences and literature, including two relevant frameworks, and explored perspectives on the dynamics of potential ethnic minority trainees’ disadvantages and opportunities for inclusive strategies. A co-reader group commented on discussion outcomes. Consequently, a management group prioritized suggested strategies based on expected feasibility and compatibility.
Input from twelve stakeholder group sessions and thirteen co-readers led to implementation guidance for seven inclusive learning environment strategies, of which the management group prioritized three:
• Provide DEI-relevant training programs to all GP-specialty training stakeholders;
• Appoint DEI ambassadors in all layers of GP-specialty training;
• Give a significant voice to minority GP-trainees in their education.
The study’s participatory approach engaged representatives of all GP-specialty training stakeholders and identified seven inclusive learning climate strategies, of which three were prioritized for implementation in two training institutions.
Peer Review reports
Introduction
Following international migration trends [ 1 , 2 ], diversity among students and trainees is growing [ 3 , 4 ], with each of them bringing their specific cultural values, family- and migration histories [ 5 ]. However, postgraduate medical ethnic minority GP-trainees still face underrepresentation [ 3 , 4 ] and may encounter unequal opportunities for success compared to their majority peers [ 6 , 7 , 8 , 9 ]. Learning climate-related factors, notably those related to lacking inclusiveness, likely play a pivotal role in this discrepancy [ 10 , 11 , 12 ].
Educational opportunities in GP-specialty training primarily rely on in-clinic learning, encompassing formal and informal contexts. Formal learning, characterized by structured, planned, and accredited activities within educational institutions, coexists with less structured informal learning, which is self-directed and arises from in-clinic everyday experiences and interactions, often susceptible to unspoken norms. While both approaches complement each other in providing a well-rounded education, the informal context might inadvertently reflect dominant cultural values and attitudes, potentially affecting in-classroom learning [ 13 , 14 , 15 ]. Particularly for ethnic minority GP-trainees, this lacking transparency may contribute to an increased risk of facing underperformance assessments, as these unspoken norms and values may not be self-evidently familiar to them [ 10 , 11 , 12 ].
Learning environments are subject to complex dynamics. Understanding the interconnected constructs of these dynamics is crucial for implementing transformative changes [ 16 ]. Accordingly, changes for inclusive learning opportunities require input from all organizational layers [ 17 ].
With this study, we aimed to develop broadly supported recommendations for an inclusive learning climate in Dutch GP-specialty training.
We used a qualitative Participatory Action Research (PAR) approach [ 18 , 19 ], applying Participatory Learning and Action (PLA) techniques in stakeholder groups combined with insights from literature (Appendix) along with GP-trainees’ experiences related to inclusive education, to actively engage stakeholders in an inclusive dialogue [ 20 , 21 , 22 ]. This approach supported co-ownership, promoted compatibility with the organization’s actual needs, and facilitated successful implementation [ 23 ].
We employed two conceptual frameworks to shape the topic lists for stakeholder groups and guide result analysis.
The Building Equity Taxonomy (BET) framework for Diversity, Equity, and Inclusion (DEI), addressing students’ needs for equal educational opportunities, and covering the areas of physical integration, social-emotional engagement, equal learning opportunities, instructional excellence, and fostering inspired learners [ 24 , 25 ] (Fig. 1 ). This framework is relevant to various educational settings, including GP-specialty training [ 12 , 26 , 27 , 28 , 29 ].
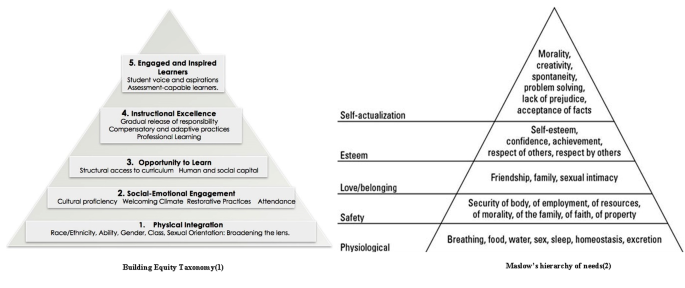
Building Equity Taxonomy [ 24 ] compared to Maslow’s hierarchy of needs [ 25 ]
The Wensing & Grol framework implementation guidance, equivalent to the internationally recognized Consolidated Framework for Implementation Research (CFIR) [ 30 ]. It provides implementation guidance for complex organizations, including clinical healthcare and educational settings [ 30 , 31 ] (Fig. 2 ). This framework underpinned our implementation guidance, which the management team used for prioritization.
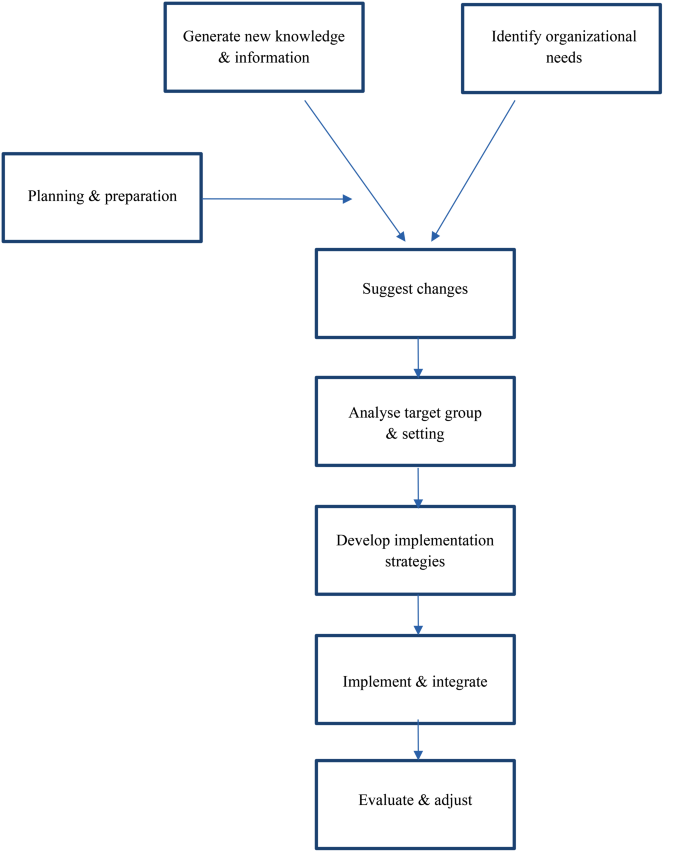
The Wensing & Groll model for implementation guidance [ 30 ]
This study took place at Amsterdam UMC’s two GP-specialty training institutes (AMC and VUmc). These institutes have demonstrated commitment to inclusiveness in their 2020–2022 annual reports, and they collaborate with the six other Dutch GP-specialty training institutes under GP-specialty Training Netherlands (HN).
One in three medical graduates in the Netherlands aims to enter GP-specialty training. In response to national medical demands, HN annually expands its acceptance of new trainees, projecting 921 in 2023 and an anticipated 1,190 in 2024, distributed across eight training institutes. About 17% of these trainees belong to ethnic minority groups, with most having completed pre-training at Dutch Medical Schools and a smaller group having graduated abroad [ 7 ]. Due to General Data Protection Regulation (GDPR) restrictions, the precise distribution of minority trainees across the eight national institutes remains undisclosed. However, a prior quantitative study indicated that by 2023, our pilot institutes showed a relatively proportional representation of Dutch GP-specialty training [ 7 ]. However, it is essential to note that qualitative research emphasizes a thorough description of the setting to enrich readers’ contextual understanding rather than strict representativeness.
The Dutch GP-specialty training program is a three-year dual-track program, supporting professional growth by combining in-clinic experience learning with one-day-a-week in-faculty education. Entry assessments aspire to guarantee the applicants’ knowledge, motivation, and Dutch proficiency. The program includes protocolled assessments, such as practical observations, systematic testing, and reviews of learning objectives.
Study population
Acknowledging the essential need of broad support for inclusive organizational changes, we engaged participants from all backgrounds represented within the organization. Our study population encompassed the ethnic majority background as well as diverse ethnic backgrounds across all organizational layers (ranging from support personnel, management, educational staff (comprising both faculty and clinical educators), and trainees themselves), divided into two stakeholder groups, one co-reader group, and a management team group (Fig. 3 ).
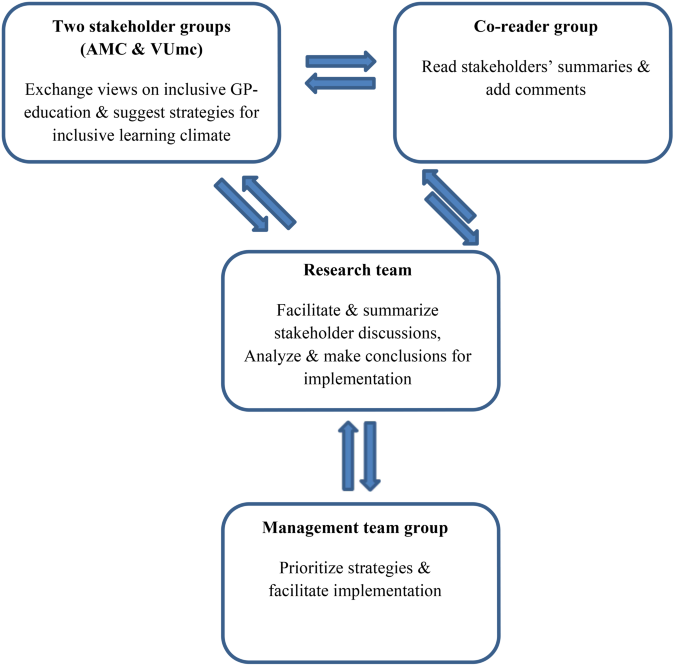
Participant groups
Aiming to prevent eligible participants from experiencing researchers’ pressure, researchers sent information letters to team leaders, requesting them to forward in-faculty teachers, in-clinic supervisors, supporting bureau and management personnel, and trainees. From those interested, we purposefully selected twelve participants (six in each stakeholder group), striving for diversity regarding the position in the institute, age, gender, and ethnicity [ 32 ]. Stakeholders ranged from supporting bureau and management personnel (further in this text referred to as ‘staff’) to trainees, in-faculty teachers, and in-clinic supervisors representing diverse minority backgrounds as well as the majority background.
Stakeholder groups, each representing one GP-specialty training institute, provided input for inclusive strategies. Additionally, a co-reader group comprising interested individuals not in the stakeholder groups provided further insights through written comments. These groups represented diverse organizational layers, cultural backgrounds, ages, and gender. Representatives from management teams then evaluated and prioritized the suggested strategies.
Data collection
Data collection and analysis took place from January 2021 to December 2022. Two researchers (MN, NvM) familiar with PLA-techniques facilitated six 90-minute PLA-based sessions for each stakeholder group. The sessions focused on inclusive learning environments and GP-specialty training’s inclusivity. In a cyclical process [ 33 ](Fig. 4 ), participants engaged in PLA techniques such as ice-breaking, flexible brainstorming, free-associating, direct ranking, mind-mapping, and visual evaluation. These methods facilitated sharing experiences and opinions and aligning these with relevant literature (Appendix, Table 1 ) to identify suitable inclusive strategies. After each stakeholder group session, the facilitator-researchers held debriefing sessions to reflect on their roles and identify areas for improvement. Independently, they summarized the key findings from each session and reached consensus through discussions. They presented these summaries in subsequent sessions for a member check and made adjustments based on participants’ feedback. To ensure a broader perspective, the co-reader group commented anonymously on these approved summaries, allowing them to contribute their personal perspectives, opinions, and experiences freely. Stakeholder groups then discussed and implemented these comments in their final session (Fig. 3 ).
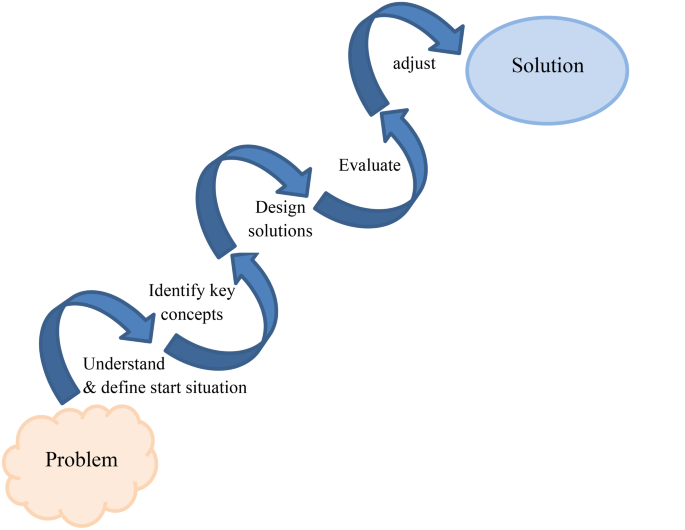
Cyclic phases until consensus of stakeholder groups’ processes [ 33 ]
The stakeholder group topic list focused on:
Exploring :
The initial educational context;
Potential learning climate-related disparities;
Out-of-the-box wishes and key elements for an inclusive learning climate;
Strategy developing and preparing for implementation:
Recommendations for inclusive GP-specialty training;
Mapping onto the BET framework’s hierarchical levels of DEI [ 24 ](Fig. 1 );
Translating recommendations into actionable strategies.
Identifying Wensing & Grol conditions and requirements for implementation [ 30 ](Fig. 2 ).
Due to the Covid-19 pandemic, we adapted the study’s in-person design to online methods for creative brainstorming. In these virtual sessions, physical distance and potential distractions of personal environments challenged trust and commitment, especially for GP-trainees who felt vulnerable sharing ideas with in-faculty teachers, in-clinic supervisors, and staff, who might also be their assessors in daily educational contexts [ 34 ]. To address this risk, we dedicated extra time, and utilized online tools: Zoom 5.13.11 for breakout rooms, Padlet 200.0.0 for visualizing PLA techniques, and concise PowerPoint presentations for member check summaries and goal-setting [ 35 ].
The facilitator-researchers (NvM, MN) collected audio recordings and written co-reader comments. An external bureau transcribed audio-recordings verbatim.
One researcher (NvM) regularly presented our findings during periodic staff meetings. These presentations not only aimed to keep the entire team informed but also played a crucial role in garnering broader support and incorporating diverse opinions for our project.
Data analysis
Within three days after each session, we (NvM, MN, and MV) analyzed the transcribed audio recordings and written co-readers’ comments, and discussed our analyses until consensus.
To provide actionable qualitative insights while responding to ongoing participant feedback, we adopted an inductive rapid qualitative data analysis approach inspired by Hamilton’s model [ 36 , 37 , 38 , 39 ]. This method prioritizes identifying key elements and mechanisms over extensive theoretical insights. Through structured data collection using topic lists and Participatory Learning and Action (PLA) techniques, along with expedited transcription, we efficiently analyzed ideas and condensed findings into concise formats like post-interview notes and matrix summaries. Although not a traditional thematic or framework analysis, we employed theme-informed and framework-informed codes to organize data, considering context and group dynamics, which allowed us to explore interactional group dynamics and communication styles in the participants’ discourse and its points of consensus or contention within specific statements [ 40 ]. We anticipated this method, aligned with the literature, to yield qualitative outcomes as consistent and rich as traditional in-depth transcription coding while facilitating the analysis of interconnected sessions [ 36 , 41 , 42 ].
We analyzed the stakeholders’ ideas, recommendations, and their identifyed Wensing & Grol conditions and requirements for implementation to create implementation guidance [ 30 ]. This guidance encompassed analyzing organizational structure, identifying change potential and barriers, defining the target population, describing tailored DEI-strategies, estimating timelines for internalization processes and implementation, and designing evaluation methods (Fig. 2 ). Subsequently, we invited management group participants for hybrid (online and in-person) meetings, where they engaged in substantive discussions to evaluate this guidance and prioritize recommended strategies, based on the expected feasibility and compatibility with their setting.
Reflexivity and ethics
Two authors, NM and MN, identify as minority females. While their unique backgrounds enhance sensitivity towards minority peers’ experiences, a potential challenge arises where these experiences resonating with them might be more salient. To mitigate this, we organized reflective debriefing sessions addressing diverse viewpoints and emphasizing the researchers’ roles as instruments in data collection and analysis. During these sessions, we engaged in candid discussions probing our experiences, expectations, preoccupations, and opinions that could have influenced our approach to data collection and analysis.
Also, the roles of participating stakeholders may have influenced views they shared in this research process. They spanned all organizational positions, ranging from department heads to trainees, in-faculty teachers, and in-clinic supervisors, representing both, majority and minority backgrounds. While deliberately seeking these varied insights, we remained mindful of potential power dynamics influenced by different positions or ethnic backgrounds. To foster a safe space and address these dynamics, facilitators employed PLA-techniques, such as ice-breakers. Also, they established clear agreements with all stakeholder group members regarding privacy, openness to differing views, and ensuring safety. Should any commitments be breached, facilitators were trained to address them promptly. In fact, stakeholders demonstrated remarkable respect and curiosity towards understanding each other’s perspectives throughout the process.
Participant characteristics
Table 1 presents participant characteristics for the stakeholder, co-reader, and management groups. In total, 31 stakeholders participated, aged 24 to 60, including eight males, 24 staff members from diverse organizational positions, seven trainees, and 12 ethnic minority participants.
The stakeholder group sessions had an attendance rate of 97%. All co-readers responded to the request for comments. During the hybrid management group session, 40% of participants attended in-person, while 60% joined online.
Stakeholder group sessions
In line with the topic list, we organized the results into two sections: [ 1 ]Exploring and [ 2 ] Strategy developing and preparing for implementation. In Sect. 2, the stakeholders aligned their results with the BET framework and structured them according to the Wensing & Grol framework.
The initial educational context
Stakeholders defined inclusiveness in the GP-specialty training as collective curiosity and support for trainees’ unique professional identities, regardless of their characteristics or backgrounds. As preconditions for in-faculty teachers, in-clinic supervisors, and staff, participants mentioned [ 1 ] willingness to encounter emotional discomfort [ 2 ], embracing failures in order to learn, and [ 3 ] acknowledgement of unconscious bias.
‘… we will not always succeed to be without prejudice, that is allowed as long as we will put the effort in gaining awareness’ (participant 2, group 1).
Participants emphasized creating a safe learning environment where all voices, including minority voices, can be heard. They suggested reflective questions starting with:
‘ Could you imagine that…’.
Participants highlighted parallel processes whereby educators foster trainees’ personal and professional development, and GPs support patients’ individual coping styles. Such an inclusive and safe learning environment would act as a flywheel, enhancing the institute’s inclusive image and attracting prospective minority trainees, teachers, and in-clinic supervisors.
Co-readers confirmed these view points and they added their concerns regarding prioritization by some staff members:
‘I have nothing to add. I think it is essential that diversity is given a priority, that we as staff all agree that this is important. The pitfall is that some of them might not see the importance’. (co-reader 2)
Potential learning climate-related disparities
Stakeholders from ethnic minority groups expressed distress experiences in a dominant white world:
‘The GP-specialty training population is predominantly white and female; trainees, in-faculty teachers, and in-clinic supervisors even seem to resemble one another. Without them saying or acting, I continuously feel the stress of having to adapt to them, which I will never be able to’ (participant 2, group 1).
Stakeholders discussed the majority’s naivety in understanding the experience of belonging to a minority and expressed concerns about some DEI programs potentially leading to paradoxical stigmatization. They noted instances where in-faculty teachers appointed minority trainees as representatives for their cultural groups, ignoring the vast diversity within these groups. Also, participants reported stereotyping case reports:
‘They always use the example of the non-Dutch speaking overweight Moroccan mother of seven children, not engaged in any sports, who favors sweet and fatty food, and suffers from diabetes’ (participant 3, group 2).
Co-readers added that this one-sided picture made minority trainees uneasy, feeling discussed rather than equal partners in GP-training. Additionally, they emphasized that presenting DEI programs as non-mandatory, implied that diversity and inclusiveness were not necessarily integral to GP-skills requirements.
‘Mandatory inclusive training for mentors, staff, and teachers holds significant importance, signifying our commitment. Participation in these courses should be integrated into evaluations and annual interviews’. (co-reader 4)
Out-of-the-box wishes and key elements for an inclusive learning climate
Upon the invitation to make a wish:
‘Wouldn’t it be wonderful if….‘ ,
stakeholders wished for diverse staff as role models, willing to learn from each other, normalizing various meaningful insights, and embracing diverse worldviews:
‘By using these differences, we keep each other awake and open-minded in exploring possibilities; thus, we allow ourselves to grow without assuming that our paved path is always the best way at the time’ (participant 3, group 1).
Stakeholders indicated the institute’s responsibility to educate GP-trainees for a diverse patient population as an essential component of an inclusive learning environment. Key elements related to such inclusiveness were:
The GP-specialty training should represent society in all its diversity:
‘It’s been a few years since I started GP-specialty training, of course, but… I’m just digging whether I had a feeling of: “I fit in there” or: “I recognize my roots there”. These are important feelings to me to feel safe at my work- and study place’ (participant 7, group 1);
A diverse GP workforce meets patients’ appreciation for GPs they can identify with:
‘Regarding this cultural background or ethnicity, I have the impression that patients from ethnic minorities often liked that I obviously am not Dutch, they said, “oh, you are not Dutch, are you?“, it led to recognition, a little laugh, and connected us. Having a doctor just like them helped my patients to share their concerns.’ (participant 2, group 2);
GP-trainees need identifiable and diverse educational role models:
‘The moment you sit down together and see that diversity, …brings different working styles, learning styles, or communication styles… that you realize we have to do it together, the greater the diversity, the more we learn from one another, the higher we rise, the more fun and creative ideas…’ (participant 4, group 2);
Diverse GP-trainee cohorts improve mutual learning processes:
‘To me, utilizing diversity means that there’s always someone in the classroom who says, “Okay, so what if we look at it from that perspective or through those glasses?’ (participant 1, group 1).
Co-readers agreed and added that GP-specialty training already utilized diversity among in-faculty teachers to some extent:
‘Great idea! Diversity among teachers is already being leveraged to some extent. Trainees can synthesize a blend of styles and insights from different teachers and mentors. Expanding on this concept could help cultivate a more inclusive learning environment’ . (co-reader 1)
Strategy developing and preparing for implementation
Recommendations for an inclusive gp-specialty training.
Participants (stakeholders in collaboration with co-readers) made six fundamental recommendations and mapped these onto the BET framework levels to ensure all aspects of inclusive education would be covered [ 24 ] (Table 2 ).
Actionable strategies
From these recommendations, participants derived seven actionable strategies for promoting inclusive GP-specialty training (Table 3 ).
Provide a clear message of inclusiveness in all internal and external communications .
Participants explored various means and media platforms for promoting the GP-specialty training’s DEI core values (websites, ads, social media, podcasts), focusing on design, content, and appeal to the target group. They recommended involving trainees with media experience rather than exclusively hiring specialized communication consultants.
Appoint DEI ambassadors in all layers of the organization .
Participants suggested involving employees as DEI ambassadors to effectively spread DEI core values in the organization. Ambassadors would undergo comprehensive training in DEI, reflective skills, leadership, and change management. They would also attend conferences, masterclasses, join knowledge networks, and contribute to think tank initiatives as part of their preparation.
Facilitate procedures for secure incident reporting .
Participants highlighting the significant impact of unintentional discriminatory behavior, often resulting in experiencing barriers to reporting such incidents. They proposed implementing low-threshold and secure reporting procedures with targeted questions on DEI and (micro)aggression. Regular team sessions would enable open discussions based on anonymous reports, fostering inclusive education, uncovering organizational trends, and providing support for trainees who faced discrimination, microaggression, or exclusion. Confidential advisors would receive training in DEI, reflective skills, and relevant legislation.
Give a significant voice to minority trainees in ongoing program development .
Participants advised inviting minority trainees to round table discussions, fostering insider perspective exchange with mutual respect, critical reflection, and empathy. Including these diverse voices would promote resilience and professional growth and attract eligible trainees and staff from diverse backgrounds.
Assign more than one in-faculty teacher per group / in-clinic training .
GP-trainees - like all individuals - naturally mirror the behavior of significant others, such as teachers, in-clinic supervisors, or peers. Participants believed that trainees with multiple role models would outperform those with single role models. They suggested introducing dual in-faculty teachers and dual in-clinic supervisors as additional role models and an extra pair of eyes during education. To ensure success, participants recommended training programs for optimum role model utilization.
Offer ‘just-in-time’ learning .
Participants agreed that effective learning is closely related to immediate learning needs. For GP-trainees, such learning needs often arise from societal encounters in the consultation room, e.g., guiding Muslims during Ramadan while simultaneously managing diabetes or comprehending increasing PTSD symptoms around Keti Koti (Afro-Surinamese Emancipation Day). Timely incorporating these contextual factors into training programs could provide directly applicable knowledge.
Provide mandatory DEI relevant training programs for professional development .
Participants emphasized the necessity of new knowledge, skills, and attitudes. They considered within-group differences valuable learning tools for diverse personal and professional development paths. Well-trained staff and trainees could drive inclusive knowledge networks, empower the organization, and positively influence external perceptions. Thus, they recommended mandatory and tailored training programs aligned with the anticipated learning needs from the suggested strategies. Where applicable, they advised considering outsourcing.
Conditions and requirements for implementation
Participants indicated the importance of in-faculty teachers, in-clinic supervisors, and staff having the courage to be vulnerable. They emphasized the essence of transparent norms and values and a welcoming learning environment, and they highlighted an attitude of:
‘… genuinely enjoying to support a diverse population in their growth towards their professional identities’ (participant 6, group 2).
‘Implementing these ideas demands courage and vulnerability, particularly as their execution could inadvertently carry stigmatizing effects’. (co-reader 6)
In this context, they mentioned the risk of unconscious bias, which could require external expert trainers at certain stages:
‘Well, you know, I had a trainee of Moroccan descent, and it shocked me that, while I always thought to be very open, diversity-minded, and curious for everything and everyone, I found it way more difficult to connect than I’d admit. I wonder what would have helped me unveil this blind spot in an earlier stage…’ (participant 5, group 1).
‘… allow and embrace the differences, see them as opportunities that actually add learning qualities, and not take them away? So, professionalism will become more colorful, and it can be viewed from different points of view, not just the traditional, established perspectives and routes’ (participant 1, group 1).
Ultimately, we provided the management group with implementation guidance for these seven strategies, along with an analysis of the target group and context, and summaries of relevant literature on DEI best practices in educational settings (Appendix). The management team agreed that enhancing DEI should have priority in Dutch GP-specialty training:
‘We should acknowledge that we are trailing behind societal advancements in diversity. Therefore, maintaining a strong focus on this topic must stay a priority’ (participant 5, management group).
Based on these comprehensive data, the management group prioritized strategies that covered the overarching recommendations and BET-levels (detailed in Table 3 ; Fig. 1 ), which aided in selecting strategies with anticipated effectiveness. To enhance alignment with the organizational requirements and feasibility, they considered implementation requirements, staff feedback from our presentations during periodic meetings, and opportunities for synergy with existing projects in other Amsterdam UMC departments.
‘We can see that literature describes these strategies as effective and we assume that stakeholders meticulously aligned them with the institute’s needs. Let us not repeat that process but rather look into strategies that can be implemented effectively in our setting’ (participant 1, management group).
‘For each suggested strategy, this guidance envisions its coverage and practical implications. Now, it is up to us to consider how far we are willing to commit. This process prompts pertinent questions on specific effective actions’ (participant 2, management group).
The management group prioritized three strategies:
Appoint DEI ambassadors in all organizational levels,
Give a significant voice to minority trainees in ongoing program development,
Provide mandatory DEI-relevant training programs for professional development to all involved in GP-specialty training.
Summary of findings
In twelve PLA-based stakeholder sessions, participants explored perspectives on potential disparities, underlying causes, and aspirations for an inclusive learning climate in the Dutch GP-specialty training. They suggested seven strategies based on six overarching recommendations, which they presented embedded in an implementation guidance to the management group:
Provide a clear message of inclusiveness in all internal and external communications.
Appoint DEI ambassadors Footnote 1 in all layers of the organization
Facilitate procedures for secure incident reporting.
Give a significant voice to minority trainees in ongoing program development.
Assign more than one in-faculty teacher per group / in-clinic supervisor per trainee.
Offer ‘just-in-time’ learning.
Provide mandatory DEI relevant training programs for professional development.
The management team selected strategies 2, 4, and 7, deeming them most effective, feasible, and aligned with the organization’s requirements.
Comparison to existing literature
Worldwide attention to inclusive learning climates in postgraduate medical education revealed the complexity and multidimensionality of educational constructs and institutes [ 29 , 43 ]. Interpretations of formal and informal learning contexts within these environments depend on the perspectives of various stakeholders [ 15 ]. Consequently, unconsciously normalized rules and codes across all layers may implicitly exclude ethnic minority professionals and -trainees in many ways throughout their careers [ 44 ].
This paper extends the literature on inclusive GP-specialty training [ 15 , 43 , 44 ], detailing the efforts to design- and create broad support for inclusive training strategies. Like most organizational changes, implementing inclusive strategies in GP-specialty training posed challenges and demanded a focus on building confidence and trust in novel approaches [ 45 ]. Hence, understanding the values and expectations of target groups and tailoring strategies to meet their needs and aspirations was crucial. Our study involved representatives from all key stakeholders, including ethnic minority trainees, aiming to address critical research gaps and enhance knowledge quality, relevance, and impact [ 46 ]. Collaborative decisions, rooted in an equal and reciprocal partnership, empowered stakeholders, raised management team awareness and inspired the research team [ 47 ]. These effects mirror findings in previous PAR studies on inclusive primary healthcare [ 48 ] and highlight PAR’s role as a catalyst for transformative change in GP-specialty training [ 33 ].
Stakeholder insights, combined with DEI-strategy literature, underscored the need for a gradual, committed cultural shift towards inclusivity in the learning environment. Based on these insights, the management group recognized that this transformation would necessitate a set of strategies addressing inclusiveness at various levels rather than relying on one single intervention [ 26 , 28 , 49 , 50 ]. They employed our Wensing and Grol-based implementation guidance to select the following feasible strategies aligned with the GP-specialty training context as a first step in an ongoing process:
Providing mandatory DEI-relevant training programs to all stakeholders supports cultural responsiveness within all strategies to be implemented. It facilitates understanding how cultural backgrounds and experiences influence teaching and learning [ 49 ]. Ultimately, it fosters engagement and motivation to create collaborative learning environments and accommodate learners’ needs based on their diverse backgrounds [ 26 ].
Appointing DEI ambassadors in all layers of the organization has in other contexts proven to enhance the effectiveness of DEI-related strategic initiatives [ 51 ]. DEI ambassadors engage change agents within their teams, foster collaboration and effective communication, facilitate diversity goals, and involve key stakeholders in sustainable, inclusive changes [ 50 ].
Giving a significant voice to minority trainees empowers and amplifies their agency. Including their experiences and perspectives in staff meetings and brainstorming sessions is a crucial first step toward an open and innovative culture. Prior research indicated that promoting minority trainees’ participation requires supportive supervision, encouraging them to share transformative ideas [ 28 ].
Strengths and limitations
Our participatory approach fostered broad support across all organizational levels. PLA-based stakeholder discussions facilitated open dialogue, refined ideas, and sparked valuable insights. Co-reader feedback prompted stakeholder group participants to reevaluate their interpretation of specific experiences. This approach allowed diverse perspectives and theoretical idea saturation, aiding participants in identifying seven actionable strategies with high potential for effective implementation. In turn, these results allowed the management group to leverage their organizational expertise and prioritize three strategies they considered feasible and compatible with the organization’s requirements.
While most post-graduate medical education settings share similarities, contextual variations, such as educational emphasis and cultural factors, may exist, leading to potential limitations in the transferability of our findings. Nonetheless, the dynamics between informal and formal in-classroom learning remain pertinent across various postgraduate medical contexts, where in-clinic learning, shaped by day-to-day experiences and supervisor-trainee dynamics, inevitably influences formal learning objectives and settings. Also, our study’s confinement to two Dutch GP-specialty training institutes and its relatively modest participant count may require caution in the transferability of our findings to other similar settings. In light of this, it is noteworthy that statistics from a previous quantitative study suggest that by 2023, our pilot institutes closely mirrored Dutch GP-specialty training in terms of minority trainee [ 7 ]. Moreover, we provided meticulous descriptions of our setting to enhance contextual understanding, aiding in assessing transferability to similar settings. Additionally, the explicit commitment to inclusiveness by the participating GP-specialty training institutions, which could be instrumental in promoting successful implementation, could pose challenges when transferring the results to less DEI-focused settings.
Still, employing multiple sources by connecting stakeholder perspectives to relevant literature and two frameworks enabled participants to structure their thoughts and opinions on the organization’s DEI strengths and limitations, along with the opportunities and challenges for implementation. For future researchers, this approach may prove valuable in identifying overarching concepts and theories that transcend specific individuals or contexts and facilitate the assessment of the transferability of our findings to similar educational settings [ 52 , 53 , 54 , 55 ].
Implications for further research and practice
Fostering a DEI-minded culture in post-graduate medical training calls for a multifaceted strategy. As training institutes diversify and curricula address nuanced topics, skills for adeptly navigating complex conversations become increasingly critical for educational staff. The ongoing process of promoting inclusive teaching, assessment, and curriculum design abilities will necessitate the inclusion of a wide range of perspectives. Consequently, we recommend involving stakeholders from the most diverse backgrounds possible. Also, the explicit commitment to inclusiveness by the participating GP-specialty training institutions may pose challenges when transferring the results to less DEI-focused settings. Therefore, we suggest further investigation in such contexts to better understand the transferability of our results.
Ensuring high-quality, inclusive learning environments in postgraduate medical education is crucial for educational opportunities and the overall quality of healthcare [ 56 ]. However, this inclusiveness is not solely shaped by the beliefs and values of teachers; it is also intricately influenced by the complex social and cultural dynamics within educational institutions [ 29 ]. Inclusiveness strategies are catalysts for enduring cultural transformation, demanding the consistent integration of multiple strategies through incremental steps over an extended period [ 43 ]. The three strategies identified in our study, which were prioritized for implementation, represent initial strides toward instigating this cultural transformation. Subsequent phases involving evaluation, adaptation, and implementation of additional strategies are imperative for sustaining engagement in a culture of inclusive postgraduate medical education. All Dutch GP-specialty training institutes closely monitor our findings and have committed to implementing mandatory DEI-relevant training programs for their staff and trainees.
Additional research on the impact of the implemented strategies and the level of stakeholder engagement throughout the implementation phase is needed. This follow-up research should encompass inclusive teaching methods, assessment strategies, curriculum design, attitudes, and the ethnic minority trainees’ experienced inclusion aligned with the BET framework.
Engaging stakeholders in PLA-based sessions at two Dutch GP-specialty training institutes proved instrumental in identifying recommendations for an inclusive learning climate. Stakeholders identified seven tangible DEI-strategies, addressing all five BET aspects:
Provide a clear message of inclusiveness in all internal and external communications: enhances inclusive accessibility and a diverse learning community;
Appoint DEI ambassadors in all layers of the organization: promotes knowledge exchange, reflection on potential biases, and active engagement in DEI networks;
Facilitate secure DEI-incident reporting procedures;
Give a significant voice to minority trainees in ongoing program development: empowers them and creates reciprocal learning;
Assign more than one teacher per group / in-clinic training: creates multiple role models and perspectives;
Offer ‘just-in-time’ learning: fosters social and educational engagement;
Provide mandatory DEI-relevant training programs for professional development: promotes DEI-expertise and awareness among all involved.
Based on anticipated feasibility and effectiveness, the management group prioritized strategy numbers 2, 4, and 7 for implementation.
Our integrative approach supported collaborative, context-specific strategy development and prioritization, effectively balancing anticipated effectiveness and compatibility. As such, this approach will prove valuable in identifying widely supported DEI strategies within varying and complex post-graduate medical educational contexts.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Ambassadors actively promote DEI values within teams by exchanging knowledge and experiences, enhancing expertise through training and literature, and addressing diversity cases through consultancy roles.
Abel GJ, Cohen JE. Bilateral international migration flow estimates for 200 countries. Sci Data. 2019;6(1):82.
Article Google Scholar
Netherlands S. How many people immigrate to the Netherlands? Web page. The Hague, the Netherlands: Statistics Netherlands; 2022. 25/03/2022.
Google Scholar
Jabbarpour Y, Westfall J. Diversity in the Family Medicine workforce. Fam Med. 2021;53(7):640–3.
Wusu MH, Tepperberg S, Weinberg JM, Saper RB. Matching our mission: a Strategic Plan to create a Diverse Family Medicine Residency. Fam Med. 2019;51(1):31–6.
Dinos S, Ascoli M, Owiti JA, Bhui K. Assessing explanatory models and health beliefs: an essential but overlooked competency for clinicians. BJPsych Adv. 2017;23(2):106–14.
Stegers-Jager K, Steyerberg E, Cohen-Schotanus J, Themmen A. Ethnic disparities in undergraduate pre-clinical and clinical performance. Med Educ. 2012;46:575–85.
van Moppes NM, Willems S, Nasori M, Bont J, Akkermans R, van Dijk N et al. Ethnic minority GP trainees at risk for underperformance assessments: a quantitative cohort study. BJGP Open. 2023;7(1).
Esmail A, Roberts C. Academic performance of ethnic minority candidates and discrimination in the MRCGP examinations between 2010 and 2012: analysis of data. BMJ (Clinical Res ed). 2013;347:f5662.
Jones AC, Nichols AC, McNicholas CM, Stanford FC. Admissions is not enough: the racial achievement gap in Medical Education. Acad Med. 2021;96(2):176–81.
Bullock JL, Lockspeiser T, Del Pino-Jones A, Richards R, Teherani A, Hauer KE. They Don’t See a Lot of People My Color: A Mixed Methods Study of Racial/Ethnic Stereotype Threat Among Medical Students on Core Clerkships. Acad Med. 2020;95(11S Association of American Medical Colleges Learn Serve Lead: Proceedings of the 59th Annual Research in Medical Education Presentations):S58-s66.
Diaz T, Navarro JR, Chen EH. An Institutional Approach to fostering inclusion and addressing racial Bias: implications for diversity in Academic Medicine. Teach Learn Med. 2020;32(1):110–6.
Roberts L, Belonging R, Inclusion, Diversity in Medical Education. Acad Medicine: J Association Am Med Colleges. 2020;95:661–4.
Karnieli-Miller O, Vu TR, Holtman MC, Clyman SG, Inui TS. Medical students’ professionalism narratives: a window on the informal and hidden curriculum. Acad Med. 2010;85(1):124–33.
Sagasser M, Kramer A, Fluit L, Weel C, Van der Vleuten C. Self-entrustment: how trainees’ self-regulated learning supports participation in the workplace. Adv Health Sci Education: Theory Pract. 2017;22.
Schönrock-Adema J, Bouwkamp-Timmer T, Hell E, Cohen-Schotanus J. Key elements in assessing the educational environment: Where is the theory? Advances in health sciences education: theory and practice. 2012;17.
Goodyear P, Carvalho L. The Analysis of Complex Learning Environments. 2019. pp. 49–65.
Kumagai AK, Lypson ML. Beyond cultural competence: critical consciousness, social justice, and multicultural education. Acad Med. 2009;84(6):782–7.
Brydon-Miller M, Maguire P. Participatory action research: contributions to the development of practitioner inquiry in education. Educational Action Res. 2009;17(1):79–93.
Chevalier J, Buckles D. Participatory Action Research: Theory and Methods for Engaged Inquiry2019.
Bozalek V, Biersteker L. Exploring power and privilege using participatory learning and action techniques. Social Work Educ. 2010;29(5):551–72.
de Brún T, Brún M, Weel-Baumgarten E, Burns N, Dowrick C, Lionis C et al. Using Participatory Learning & Action (PLA) research techniques for inter-stakeholder dialogue in primary healthcare: an analysis of stakeholders’ experiences. Res Involv Engagem. 2017;3.
Allaham S, Kumar A, Morriss F, Lakhanpaul M, Wilson E, Sikorski C, et al. Participatory learning and action (PLA) to improve health outcomes in high-income settings: a systematic review protocol. BMJ Open. 2022;12:e050784.
Ukowitz M. Who defines innovation in education? Participatory action research and organisational learning. Educational Action Res. 2023;31(2):366–83.
Smith D, Frey N, Pumpian I, Fisher D. Building equity: policies and practices to empower all learners. ASCD; 2017.
Maslow AH. Motivation and personality. Harper & Row; 1970.
Carter P, Darling-Hammond L. Teaching diverse learners. Handbook of research on teaching. 2016:593–638.
Severiens S, Wolff R. Study success of students from ethnic minority backgrounds: an overview of explanations for differences in study careers. Routledge Int Handb High Educ. 2009:61–72.
Voogt J, Taris T, van Rensen E, Schneider M, Noordegraaf M, Schaaf MF. Speaking up, support, control and work engagement of medical residents. A structural equation modelling analysis. Med Educ. 2019;53.
Gay G. Culturally responsive teaching: theory, research, and practice. teachers college; 2018.
Wensing M, Grol R. Knowledge translation in health: how implementation science could contribute more. BMC Med. 2019;17(1):88.
Fernandez ME, Ten Hoor GA, van Lieshout S, Rodriguez SA, Beidas RS, Parcel G, et al. Implementation mapping: using intervention mapping to develop implementation strategies. Front Public Health. 2019;7:158.
Mays N, Pope C. Qualitative research in health care. Assessing quality in qualitative research. BMJ. 2000;320(7226):50–2.
Cordeiro L, Rittenmeyer L, Soares CB. Action research methodology in the health care field: a scoping review protocol. JBI Database Syst Rev Implement Rep. 2015;13(8):70–8.
Akman H, Plewa C, Conduit J. Co-creating Value in Online Innovation communities. Eur J Mark. 2018;53.
Fernandez A, Shaw G. Academic Leadership in a time of Crisis: the coronavirus and COVID-19: academic leadership in a time of crisis. J Leadersh Stud. 2020;14.
Taylor B, Henshall C, Kenyon S, Litchfield I, Greenfield S. Can rapid approaches to qualitative analysis deliver timely, valid findings to clinical leaders? A mixed methods study comparing rapid and thematic analysis. BMJ Open. 2018;8:e019993.
Brown-Johnson C, Safaeinili N, Zionts D, Holdsworth LM, Shaw JG, Asch SM, et al. The Stanford Lightning Report Method: a comparison of rapid qualitative synthesis results across four implementation evaluations. Learn Health Syst. 2020;4(2):e10210.
Lewinski AA, Crowley MJ, Miller C, Bosworth HB, Jackson GL, Steinhauser K, et al. Applied Rapid Qualitative Analysis to develop a contextually appropriate intervention and increase the likelihood of Uptake. Med Care. 2021;59:S242–51.
Nevedal A, Reardon C, Opra Widerquist M, Jackson G, Cutrona S, White B, Damschroder L. Rapid versus traditional qualitative analysis using the Consolidated Framework for Implementation Research (CFIR). Implement Sci. 2021;16.
Vicsek L. A Scheme for analyzing the results of Focus Groups. Int J Qualitative Methods. 2007;6(4):20–34.
Vindrola-Padros C, Johnson G. Rapid Techniques in Qualitative Research: a critical review of the literature. Qual Health Res. 2020;30:1596–604.
Gale R, Wu J, Erhardt T, Bounthavong M, Reardon C, Damschroder L, Midboe A. Comparison of rapid vs in-depth qualitative analytic methods from a process evaluation of academic detailing in the Veterans Health Administration. Implement Sci. 2019;14.
Miles S, Ahuja A. Learning from difference: Sharing international experiences of developments in inclusive education. The SAGE handbook of special education. 2007:131 – 45.
Waldring IE. The fine art of boundary sensitivity: second-generation professionals engaging with social boundaries in the workplace. University of Antwerp; 2018.
May CR, Mair F, Finch T, MacFarlane A, Dowrick C, Treweek S, et al. Development of a theory of implementation and integration: normalization process theory. Implement Sci. 2009;4(1):29.
O’Reilly-de Brún M, de Brún T, Okonkwo E, Bonsenge-Bokanga J-S, De Almeida Silva MM, Ogbebor F, et al. Using Participatory Learning & Action research to access and engage with ‘hard to reach’ migrants in primary healthcare research. BMC Health Serv Res. 2016;16(1):25.
Weis L, Fine M. Working Method: Research and Social Justice. Working Method: Research and Social Justice. 2004:1-186.
O’Reilly-de Brún M, De Brún T. The use of Participatory Learning & Action (PLA) research in intercultural health: some examples and some questions. Engaging service-users in co-designing primary health care. 2010:27.
Lupton KL, O’Sullivan PS. How Medical Educators Can Foster Equity and Inclusion in Their Teaching: A Faculty Development Workshop Series. Acad Med. 2020;95(12S Addressing Harmful Bias and Eliminating Discrimination in Health Professions Learning Environments):S71-s6.
Kolluru S, Wanat MA, Ficzere CH, Akiyode O, Haber SL, Hayatshahi A, et al. Review of Best practices for Diversity, Equity, and inclusion committees within Colleges of Pharmacy. Am J Pharm Educ. 2023;87(4):ajpe9043.
Miguel A, Sloughter JM, Dorsey JM, Hartley R, Shih FJ, Crevier J, editors. What’s Next? From Analysis to Action. 2021 CoNECD; 2021.
Carminati L. Generalizability in qualitative research: a tale of two traditions. Qual Health Res. 2018;28(13):2094–101.
Shenton A. Strategies for ensuring trustworthiness in qualitative Research projects. Educ Inform. 2004;22:63–75.
Maxwell J. Why qualitative methods are necessary for generalization. Qualitative Psychol. 2020;8.
Polit D, Beck C. Generalization in quantitative and qualitative research: myths and strategies. Int J Nurs Stud. 2010;47:1451–8.
Brown J, Chapman T, Graham D. Becoming a new doctor: a learning or survival exercise? Med Educ. 2007;41:653–60.
Download references
Acknowledgements
We affirm that no individuals other than the listed authors provided professional writing or analysis services. Still, we thank all anonymous participants whose contributions enriched this study.
We declare that the authors have no external funding to report.
Author information
Authors and affiliations.
Amsterdam UMC location University of Amsterdam, Department of General Practice and Public Health Research Institute, Meibergdreef 9, Amsterdam, 1105 AZ, The Netherlands
N.M. van Moppes, M. Nasori, J. Bont, J.M. van Es & M.R.M. Visser
Department of General Practice, Radboud University Medical Center, Nijmegen, The Netherlands
M.E.T.C. van den Muijsenbergh
Pharos, centre of expertise on health disparities, Utrecht, The Netherlands
You can also search for this author in PubMed Google Scholar
Contributions
All authors have made substantial contributions to the conception OR design of the work; OR the acquisition, analysis, OR interpretation of data; OR have drafted the work or substantively revised it. All authors have approved the submitted version (and any substantially modified version that involves the author’s contribution to the study); and have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. Contributions per author: N.M. van Moppes: Conception, Design of the work, Acquisition, Analysis and interpretation of data, Drafted the work and integrated all revisions; M. Nasori: Conception, Design of the work, Acquisition, Analysis and interpretation of data, Substantively revised the work; J. Bont: Substantively revised the work; J.M. van Es: Substantively revised the work; M.R.M. Visser: Conception, Design of the work, Substantively revised the work; M.E.T.C. van den Muijsenbergh: Conception, Design of the work, Substantively revised the work.
Corresponding author
Correspondence to N.M. van Moppes .
Ethics declarations
Ethics approval and consent for participate.
Participation in the study was voluntary, with informed consent for participation and publication obtained from all participants. The Dutch Association for Medical Training’s Ethical Review Board approved the study (file number 2020.6.1). Data handling adhered to the General Data Protection Regulation and Amsterdam UMC Clinical Research Unit procedures, and we shared the study results with all participants.
Competing interests
We declare that the authors have no competing interests as defined by BMC Medical Education or any other interests that might be perceived to influence the results and/or discussion reported in this paper.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
van Moppes, N., Nasori, M., Bont, J. et al. Towards inclusive learning environments in post-graduate medical education: stakeholder-driven strategies in Dutch GP-specialty training. BMC Med Educ 24 , 550 (2024). https://doi.org/10.1186/s12909-024-05521-z
Download citation
Received : 12 December 2023
Accepted : 06 May 2024
Published : 17 May 2024
DOI : https://doi.org/10.1186/s12909-024-05521-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Inclusive Medical Education
- Stakeholder-driven Strategies
- GP-specialty Training
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 16 May 2024
Use of the supportive and palliative care indicators tool (SPICT™) for end-of-life discussions: a scoping review
- Melanie Mahura 1 ,
- Brigitte Karle 2 ,
- Louise Sayers 3 ,
- Felicity Dick-Smith 3 &
- Rosalind Elliott 3 , 4
BMC Palliative Care volume 23 , Article number: 119 ( 2024 ) Cite this article
82 Accesses
5 Altmetric
Metrics details
In order to mitigate the distress associated with life limiting conditions it is essential for all health professionals not just palliative care specialists to identify people with deteriorating health and unmet palliative care needs and to plan care. The SPICT™ tool was designed to assist with this.
The aim was to examine the impact of the SPICT™ on advance care planning conversations and the extent of its use in advance care planning for adults with chronic life-limiting illness.
In this scoping review records published between 2010 and 2024 reporting the use of the SPICT™, were included unless the study aim was to evaluate the tool for prognostication purposes. Databases searched were EBSCO Medline, PubMed, EBSCO CINAHL, APA Psych Info, ProQuest One Theses and Dissertations Global.
From the search results 26 records were reviewed, including two systematic review, two theses and 22 primary research studies. Much of the research was derived from primary care settings. There was evidence that the SPICT™ assists conversations about advance care planning specifically discussion and documentation of advance care directives, resuscitation plans and preferred place of death. The SPICT™ is available in at least eight languages (many versions have been validated) and used in many countries.
Conclusions
Use of the SPICT™ appears to assist advance care planning. It has yet to be widely used in acute care settings and has had limited use in countries beyond Europe. There is a need for further research to validate the tool in different languages.
Key message
What is already known on this topic?
• The SPICT ™ was developed to assist clinicians to screen patients for palliative care needs.
What this review found.
• The SPICT™ assists conversations about advance care planning and facilitates changes in documented goals of care.
• The SPICT™ is available in at least eight languages (and used in many countries.
How the findings of this review may affect practice and research.
• Evidence suggests that formalising screening for palliative care needs using the SPICT™ is advantageous for advance care planning; clinicians should consider using the SPICT™ to initiate discussions with people with life limiting conditions.
• Further research is required to validate the tool in different languages and extend its use in acute care settings and with other patient cohorts.
Peer Review reports
Introduction
The demand for palliative care services globally has outpaced service availability, particularly in low and middle-income countries [ 1 ]. This is expected to continue as the population ages and the burden of noncommunicable disease increases. Thus, non-specialist palliative care health professionals may be required to manage care. The Supportive And Palliative Care Indicators Tool (SPICT™) [ 2 ] is one instrument available for non-specialist palliative care clinicians which may assist them in assessing unmet palliative needs and care planning.
Evidence suggests that clinicians feel inadequately prepared to conduct end-of-life discussions with patients who are terminally ill [ 3 , 4 , 5 ] and are also unsure of the appropriate time to start these discussions or whether to involve a specialist palliative care team [ 5 , 6 , 7 ]. Clinicians have reported their discomfort when addressing the topic of death with seriously ill patients [ 5 ].
From the perspective of patients with advanced illness, honest information from a trusted health care professional is the preference of most [ 7 ]. A survey study conducted in Canada involving 434 patients with advanced illness found over half of patients felt it was ‘very important’ to have a sense of control over decision-making regarding their care and 56% felt it was ‘extremely important’ not to be kept alive on life support if there was little hope of recovery [ 7 ]. The default medical decision to do everything to save life may be contributing to delays in referral to a specialist palliative care team, burdensome medical treatment and poorer quality of life for many patients [ 8 ]. Thus, a standardised, reliable and validated method of assessing and planning care in collaboration with the patient is required.
The terms ‘end-of-life’ and ‘terminally ill’ have been conceptualised as synonymous and ‘apply to patients with progressive disease with months or less of expected survival.’ [ 9 ]. In the United States there is consensus that referral to specialist palliative care services is required at the time of diagnosis for patients with neurologic disease, frailty, multimorbidity, advanced cancer, organ or cognitive impairment, patients with a high symptom burden and patients with onerous family or caregiver needs [ 10 ]. However with an ageing population and increased levels of dementia and frailty non-palliative care clinicians need a tool with a common language to identify those who are nearing the end of life and to promote a palliative approach to care. According to the High Authority for Health, an independent organisation that promotes quality outcomes in the fields of health, sociology and medicine a palliative approach is, “a way of addressing end-of-life issues early on: make time to talk about ethical questions, psychological support, comfort care, the right care, and give a timely thought to the likely palliative care needs of people approaching the end-of-life.” [ 11 ], p1.
Advance care planning, “a process that supports adults at any age or stage of health in understanding and sharing their personal values, life goals, and preferences regarding future medical care” [ 12 ] is one aspect of palliative care often provided by medical professionals which may assist in ensuring people’s needs are met, and care and communication are enhanced. Early advance care planning is vital, particularly for patients with neurodegenerative conditions before they lose capacity to express their wishes [ 8 ] “to help ensure that people receive medical care that is consistent with their values, goals and preferences during serious and chronic illness.” [ 12 ] Research has revealed that patients who have had the opportunity to discuss their preferences at the end-of-life are more likely to receive care that is consistent with those preferences. Findings also include greater patient and carer satisfaction and less conflict regarding decision making when end-of-life preferences have been examined [ 13 ].
People who have life limiting conditions may benefit from the delivery of advance care planning using a systematic approach. The SPICT™, although not designed for this purpose may enhance the approach particularly when health professionals who have limited palliative care experience are required to facilitate advance care planning.
The SPICT™ [ 2 ] was designed to identify patients at risk of deteriorating or dying and to screen for unmet palliative care needs. The tool includes general indicators of deterioration and clinical indicators of life-limiting conditions. The accompanying SPICT™ guide provides prompts and tips and a suggested framework (REMAP Ready, Expect, Diagnosis, Matters, Actions and Plan) [ 14 ] for conducting future care planning conversations. The tool is reported to be simple to use and designed for use by all multidisciplinary team members in any care setting [ 13 ].
The SPICT™ was evaluated using a mixed methods participatory approach [ 2 ]. Peer review and consensus was gathered for the 15 revisions of the SPICT™ over an 18-month period. Each iteration of the tool was distributed to clinicians and policy makers internationally until consensus was reached [ 2 ]. The research team worked concurrently with clinicians in four participating units at an acute tertiary hospital in Scotland to screen all patients with advanced organ disease whose admission to hospital was unplanned ( n = 130) using a checklist that included the SPICT™ general indicators, disease specific indicators and the surprise question (SQ), “Would you be surprised if this patient were to die in the next 6 to 12 months?”. Data were gathered over an 8-week period and patients were followed up for 12 months [ 2 ]. A significantly greater number of patients who died at 12-months had two or more admissions in the previous 6 months before being screened. These patients also had increased care needs and persistent symptoms despite optimal treatment. The researchers proposed that better identification, assessment and pre-emptive care planning could reduce the risk of unplanned hospital admission and prolonged inpatient stays [ 2 ]. Of note the patients’ diagnoses were limited to advanced illness which was non-malignant and ethnicity was homogenous [ 2 ]. The SQ was removed from subsequent versions of the SPICT™ and the rationale for removing it remains unclear. The SPICT™ continues to be revised and versions are available in different languages [ 2 ].
The intention of this review was to examine the impact of the SPICT™ on advance care planning and the extent of its use. The patient cohorts, languages, and contexts in which the SPICT™ is available and used were examined.
Review questions
The following primary question was addressed:
How does use of the SPICT™ assist with conversations about advance care planning?
Secondary review questions were:
What is the extent of the use of the SPICT™ (which patient cohorts, contexts, and countries is it used)?
In which languages has the spict™ been validated.
Does use of the SPICT™ facilitate changes in documented goals of care?
Design and methods
This scoping review was performed in accordance with the Joanna Briggs Institute Manual for Evidence Synthesis Scoping Review Framework [ 15 ] and the Meta-Analyses Scoping Review extension for scoping reviews (PRISMA-ScR) checklist [ 16 ] was used to guide the reporting.
Preliminary literature search
An initial search focussed on inpatients with a chronic illness nearing the end of life however the search was expanded to include all care settings where the SPICT™ was being used for adults with a life-limiting chronic illness to evaluate its efficacy in advance care planning. Thus the search reflected the International Association for Hospice and Palliative Care definition of palliative care “the active holistic care of individuals across all ages with serious health-related suffering due to severe illness, and especially of those near the end of life.” [ 17 ]. A life-limiting illness or condition encompasses both malignant and non-malignant diseases as well as the effects of ageing.
A preliminary search of EBSCO Medline, the Cochrane database of systematic reviews, Prospero and JBI Evidence Synthesis was conducted in June 2022. No current or planned systematic or scoping reviews specifically on this topic were identified. A systematic review by Teike Luthi, et al. [ 18 ], examining instruments for the identification of patients in need of palliative care in the hospital setting was identified. The current scoping review differs from the systematic review by Teike Luthi, et al. [ 18 ] as the aim was to identify and describe all research related to how the SPICT™ is used in end-of-life discussions and what influence this has on advance care planning and goals of care.
Inclusion criteria
Participants.
The population of interest was adult patients (> 18 years) with a life-limiting chronic illness.
The concept of interest was the SPICT™. Any studies incorporating the SPICT™ were included in this review since its development in 2010. Studies evaluating the SPICT™ for prognostication purposes were excluded as this was not the intent of this review.
Published and unpublished studies in any language for which a translation could be obtained were included. Published and unpublished studies in any setting that met the eligibility criteria were included.
Evidence sources
This scoping review included both experimental and quasi-experimental study designs. In addition, analytical observational studies including prospective and retrospective cohort studies, case-control studies and analytical cross-sectional studies were considered for inclusion. Systematic reviews that met the inclusion criteria were included. Qualitative studies, theses and dissertations were also considered if they met the inclusion criteria.
Search strategy
An initial search on this topic in the EBSCO Medline and PubMed databases was reviewed for relevant abstracts and titles to determine keywords and index terms. MESH terms used in the final search strategy included: Communication; Documentation; Palliative Care; Patient Care Planning; Advance Care Plan; Decision Making and Chronic Disease. The research abstract for this scoping review was registered on the Center for Open Science website ( https://doi.org/10.17605/OSF.IO/DN27C ) in August 2022 prior to performing the definitive search in September. The search was conducted on 28th September 2022 and date limited i.e., 2010-September 2022. The database and grey literature searches were updated on 27th January 2024 to identify further studies published beyond this date.
Electronic databases searched included EBSCO Medline, PubMed, EBSCO CINAHL, APA Psych Info, ProQuest One Theses and Dissertations Global. Publications listed on the SPICT website ( www.spict.org.uk ) were cross checked with the records included from the electronic databases, duplicates were removed and further records were added to the Endnote library for screening. Reference lists of included studies were reviewed for additional studies.
All websites searched for additional records (grey literature sources) are included in supplementary file 1 . The expanded search strategy for the EBSCO Medline database is also provided in supplementary file 1 .
Study selection
All records were collated in an EndNote library. Duplicate records were removed manually by RE. The screening process involved two independent reviewers (MM and RE) reading titles and abstracts. Full text screening was conducted independently by the same two reviewers. Any discrepancies between the two reviewers at each stage of the process was resolved following review and consultation of a third reviewer (BK). Studies that did not meet the inclusion criteria were excluded with a reason recorded. Data extracted from included studies has been recorded in the standardised data extraction form (supplementary file 2 ). Critical appraisal of included studies was not performed and thus studies were not excluded based on methodological quality.
Data synthesis
Key aspects of the included studies were summarised in tables. Also consistent with the approach for a scoping review a textual narrative synthesis [ 19 ] was performed with the primary aim of addressing the review questions.
Over 2,000 records were retrieved. Five guidelines and six conference abstracts were found but these either did not relate to the review questions or did not contain sufficient information to be included. After applying the exclusion criteria 26 reports were included in this scoping review. The flow diagram (Fig. 1 ) presents the number of records retrieved, screened, excluded and included.
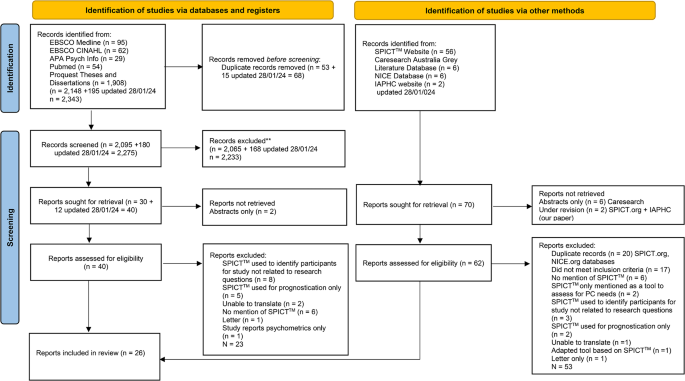
Flow diagram of number of records retrieved, screened, excluded and included **Abstract and title screening involved assessing each record for relevance to the review questions i.e., if no mention of the SPICT™ or/and advance planning conversation the record was excluded from further consideration
There were multiple study designs including validation and translation ( n = 8) studies [ 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 ] and clinical improvement projects ( n = 3) [ 28 , 29 , 30 ]. The focus of the clinical improvement projects was to increase the identification of palliative care needs and care planning through the use of the SPICT™. Two reviews (one of these included a survey study) 18 31 and two theses were included 28 29 (Table 1 ).
Research reveals that the SPICT™ appears to assist clinicians with conversations about advance care planning by providing a proforma for essential aspects of end-of-life care, a framework for end-of-life conversations and a common language to collaborate within the multidisciplinary team.
For example, in a prospective exploratory feasibility study to explore the practical use of the SPICT™ resulted in increased palliative care planning [ 32 ]. In this study general practitioners (GPs) [ n = 10] were trained in the use of the German version of the SPICT™ (SPICT-DE™) and during a two-month intervention period were asked to use the tool with any adult patients diagnosed with a life-limiting disease ( n = 79) and these patients were followed up at 6 months. The GPs’ actions as recommended by the SPICT-DE™ were considered appropriate with the most frequent actions being “Agree a current and future care plan with the person and their family; support family carers” ( n = 59 [75%)),“Review current treatment and medication to ensure the person receives optimal care; minimise polypharmacy”( n = 53 [67%]), and “Plan ahead early if loss of decision-making capacity is likely”(n = 49 [62%]). Of note “Consider referral for specialist palliative care consultation to manage complex symptoms” was considered appropriate for 25 (32%) patients. The effect of the SPICT™ was evident at the 6-month follow-up; the most frequently initiated actions were “Review current treatment and medication to ensure the person receives optimal care; minimise polypharmacy” (n = 36 [46%]) and “Plan ahead early if loss of decision-making capacity is likely” (n = 29 [37%]).
Further implementation research by Afshar et al. [ 33 ] with GPs in Germany revealed that GPs considered that the tool supported the communication and coordination of care and considered it broadened their perspectives of the meeting the needs of people especially those with non-cancer diagnoses. Of note over 50% of patients in this study had their agreed care plan initiated at the 6-month follow-up. Some GPs who had extensive experience and training claimed that the tool had no effect on their practice. However overall more than two thirds of the sample reported that they could envisage using the SPICT-DE™ in everyday practice.
In addition, three studies found that nurses who were trained to use the SPICT™ increased their self-efficacy in identifying patients who may be nearing the end of life and promoted an advance care plan discussion with these patients 28 29 34 . 21−23 In the study set in a renal ward, patients were screened on admission to identify those nearing the end of life by nurses using the SPICT™ [ 34 ]. An alert was added to the ward patient name list when a patient was identified as nearing the end of life (‘SPICT™ positive’) which prompted a review by the physician and multidisciplinary team. In this study 16% (25/152) of newly admitted patients were screened as ‘SPICT™ positive’; all of these patients received a palliative care consult and were discharged with an advance care directive including a resuscitation plan [ 34 ]. Incidentally nurses reported a significant increase in their ability to identify patients approaching end of life.
Similarly high SPICT™ screening rates and end of life conversations and referrals were revealed in a clinical improvement project designed to improve palliative care screening and consultation on admission to the cardiopulmonary unit of a long-term acute care facility using the SPICT™ [ 29 ]. In this project involving patients requiring mechanical ventilation and cardiac monitoring, 83% (59/71) of nurses working in the unit were trained in the use of the tool and screened all 50 newly admitted patients in the study period, 48 of whom were ‘SPICT™ positive’. Only 7 received a palliative care consultation within a week of admission however all 7 of these patients received a resuscitation plan and an advanced directive. Of note the use of the SPICT™ for screening resulted in a doubling of the facility’s monthly average number of palliative care referrals (from 32 to 84). In another clinical improvement project designed to increase screening and referral for palliative care among ambulatory care patients, nurse practitioners found the SPICT™ ‘. opens the door to a discussion of palliation .’ and was ‘. helpful in determining eligibility for palliative care. .’ p 22 28 . This project using both quantitative and qualitative approaches revealed an increase in palliative care referrals from 16% ( n = 8/50) to 50% ( n = 25/50) after the SPICT™ was introduced.
Two studies designed to translate and validate the SPICT-DK™ (Danish) [ 21 ] and SPICT-SE™ (Swedish) [ 24 ] involving focus groups with health care professionals revealed positive responses from doctors and nurses. The tool was described as a linguistic framework among these professionals and that use of the SPICT™ gave them a common language in which to collaborate and focus when treating and caring for patients [ 21 ]. The specificity of the tool was highlighted by nurses and medical doctors [ 24 ].
Conversely the expert committee comprising family physicians and palliative and home care specialists who provided input to the translation and cross-cultural adaptation of the SPICT™ into Japanese were more circumspect [ 27 ]. These experts were concerned that the tool might not be appropriate for framing advance planning conversations as a ‘not-telling the truth’ culture was prevalent and health care was heavily siloed into specialities so that care planning was fragmented.
The SPICT™ has been used to screen for palliative care needs in many patient cohorts, settings and countries. The cohorts in which the SPICT™ has been used include people over 65 years [ 35 ], those with advanced cancer 32 36 and with chronic diseases including cardiovascular disease [ 28 ], renal disease [ 34 ] and pulmonary disease [ 29 ].
Ten of the included studies were conducted in primary care and general practice settings 20 , 21 , 22 24 25 30 , 31 , 32 37 38 . The SPICT™ was also used in outpatient clinic settings 23 28 39 and residential aged care 29 35 . One cross sectional survey of community households in India used the SPICT™ to identify patients with palliative care needs in two rural communities [ 40 ]. The SPICT™ was originally developed for use in a hospital setting but not formally validated during its development [ 2 ]. All of the contexts in which the SPICT™ has been used are listed in Table 1 .
Of the included records ten were studies conducted in European countries 20 , 21 , 22 24 30 , 31 , 32 , 33 37 38 ; seven in Asia 23 25 27 39 , 40 , 41 , 42 ; three in the USA 28 29 36 ; two in Australia 34 35 ; one in South Africa [ 43 ] one in Chile [ 26 ] and one in Peru [ 44 ], and one paper was a review performed by authors based in Switzerland [ 18 ]. Of note the systematic review and survey of European primary care GP practice to identify patients for palliative care revealed that the United Kingdom was the only European country at the time that incorporated the SPICT™ to identify palliative care needs in primary and secondary care in clinical guidelines [ 31 ].
The SPICT ™ has been translated, cross culturally adapted and validated to identify patients with palliative care needs in Danish [ 21 ] and German [ 38 ] using the Translation, Review, Adjudication, Pre-testing and Documentation (TRAPD) model. Another study by Afshar, et al. [ 32 ] further established the validity of the SPICT-DE ™ in German in general practice with a patient cohort. In addition the SPICT ™ has been translated from English to Italian [SPICT-IT ™ ] [ 22 ], Spanish [SPICT-ES ™ ] [ 20 ], Swedish [ 24 ] and Japanese [SPICT-J ™ ] [ 23 ] using the Beaton protocol for cross cultural adaptation of health measures [ 45 ]. Farfán-Zuñiga and Zimmerman-Vildoso [ 26 ] established the reliability and validity of the SPICT-ES CHTM after culturally adapting the SPICT-ES ™ using the Beaton protocol. Nurses positively evaluated the feasibility of the tool. In addition Oishi et al. [ 27 ] also performed a translation and cross-cultural adaptation of the SPICT ™ into Japanese using a similar approach. The forward-back translated Indonesian version of the tool was found to be highly reliable and valid and greatly assisted in identifying hospital patients’ unmet palliative care needs [ 41 ].
The SPICT™ for low-income settings (LIS) was translated and cross culturally adapted for use in Thailand [ 25 ]. The interrater reliability of the final SPICT-LIS™ Thai version was high when nurses and GPs used it to ascertain palliative care needs of patients in case vignettes.
A Delphi study was used to develop the SPICT™ for the South African context [ 43 ]. Modifications to the original tool included the addition of haematological and infectious diseases and trauma however the SPICT-SA™ has yet to be validated in these patient cohorts. Although not a validated study per se in research comparing the performance of the Dutch version of the tool (SPICT-NL™) and the SQ in general practice ( n = 3,640) the SPICT™ was found to be superior to the SQ in identifying patients with palliative care needs particularly younger people [ 37 ].
Of note the SPICT4-ALL™ [ 46 ] is a simplified version of the original SPICT™ developed for family/friends and care staff to identify individual palliative care needs. It is available to download from the SPICT™ website in English, German, Danish and Spanish. Although Sudhakaran, et al. [ 40 ] successfully used it to identify palliative care needs in two communities in rural India. No studies validating or evaluating it were found in our search.
Does use of the SPICT ™ facilitate changes in documented goals of care?
There is evidence that the SPICT™ by virtue of assisting clinicians to discuss end of life care facilitates changes in documented goals of care. Specifically this was demonstrated in a pre-post intervention study in which GPs trained in palliative care and the use of the SPICT-DE™ were requested to use it in their everyday practice for 12 months with every adult patient diagnosed with a chronic, progressive disease [ 30 ]. This occurred concurrently with a public campaign focused on informing health care providers and stake holders in two counties in Germany about end-of-life care. GPs’ documentation improved after the intervention. Records of care planning increased from 33 to 51% and documentation of preferred place of death towards the end-of-life increased from 20 to 33% and patients’ wishes, and spiritual beliefs increased from 18 to 27%. Incidentally GPs’ self-reported quality of end-of-life care increased after the implementation of the SPICT-DE™ and the information campaign [ 30 ].
In a study including 187 residents in an aged care facility in Australia comparing the SPICT™ and SQ, two Directors of Nursing pre-screened residents using the SQ and if the response was ‘yes’ (SQ+) applied the SPICT™ [ 35 ]. Of the 80 (43%) residents who were SQ+, 100% of these showed signs of nearing end of life according to the SPICT™. Of these residents 39 (49%) had some form of palliative care from either GPs, a specialist palliative care physician or palliative care nurse. Nearly all 39 (97%) had a GP management plan, and 67% had an advance care directive and 67% had discussed treatment options with their care provider [ 29 ]. It is unclear whether the SPICT™ affected care planning or documentation as the study involved pre-screening with the SQ and documentation was not assessed before and after this intervention.
Death and dying are taboo in many countries and thus any discussion about end of life is challenging. However, clinicians are morally and ethically obliged to appropriately initiate discussions about advance care planning towards the end of life when patients are ready [ 47 ]. This review found that the SPICT™ may help the clinician with this conversation. Specifically, evidence suggests that the tool may be a useful proforma and a conversation ‘checklist’ to ensure that the priority areas for advance care planning are addressed. Specifically, the tool may enable an assessment of the person’s readiness to have an advance planning conversation and an exploration of their expectations, the diagnosis, what matters to them, treatment options and future plans [ 14 ]. Importantly extensive specialist training is not required to administer it; the studies in this review employed brief information interventions to prepare clinicians to use the SPICT™. Thus, the SPICT™ provides a method of ‘objectively’ assessing palliative care needs, articulating the requirement for a specialist palliative review if required and advance care planning.
This review found that the SPICT™ was used in mainly primary health care settings and predominately in European countries. Of note there were few published records of its use in countries in the Asian and African continents and North America. The tool has been translated into more than eight languages including Spanish (SPICT-ES™) [ 20 ], Italian (SPICT-IT™) [ 22 ], German (SPICT-DE™) [ 38 ] and Japanese (SPICT-J™) [ 23 ] although not all versions have been formally validated [ 25 , 26 , 27 , 33 ].
Furthermore, there is evidence to suggest that the SPICT™ may facilitate changes in the goals of care and documentation of end of life care planning and patient wishes. Incidentally the SPICT™ appears to be positively received by clinicians with some suggesting that the tool provides a common language for clinicians when collaborating to identify palliative care needs and provide palliative care.
Of note the tool did not meet the COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) criteria [ 18 ]. However arguably these criteria may not be the most appropriate criteria on which to base an assessment of the SPICT™ given that it was never meant to be used to objectively measure a parameter such as prognosis; Highet et al. [ 2 ] were clear about the remit of the tool i.e., “help clinicians working in primary and secondary care recognise when their patients might be at risk of dying and likely to benefit from supportive and palliative care in parallel with appropriate ongoing management of their advanced conditions.” [ 2 ], p11.
There is an imperative to improve recognition of palliative care needs particularly in fast paced acute care settings. Evidence suggests that a tool such as the SPICT™ is an important adjunct for initiating a conversation about end-of-life care and ensuring that key palliative care needs are identified. Importantly the SPICT™ requires little training and its brevity may be suited to settings in which there is limited opportunity to engage in lengthy conversations and in which clear unambiguous communication is key to timely referral and treatment. Formalising palliative care needs screening in an end-of-life conversation in acute care settings may reduce distress for patients and their informal care givers [ 48 ] and the SPICT™ is a relevant proforma for such a conversation. Furthermore with the increase in the numbers of people living with chronic illness globally [ 49 ] arguably the formal adoption of palliative care needs screening in all health care settings may not only reduce patient distress but may assist health care managers and policy makers to more appropriately plan services [ 50 ]. Identifying needs early in the illness trajectory may allow appropriate personalised care and services to be provided in a timely and cost effective manner thus avoiding health crises at the end of life [ 51 ].
Conversely caution should be exercised when recommending a tool to guide advance care planning and end of life conversations particularly in the setting of low health professional skill level. This was highlighted by experienced GP participants in the study by Afshar et al. [ 33 ]. The GPs did not consider that the SPICT-DE™ made any impact on their practice. A proforma or guideline cannot replace the need for exemplary health care professional communication during advance care planning and end of life conversations particularly as studies reporting the use of the SPICT™ were not specifically focused on testing its efficacy in this regard. Flexibility and sensitivity are required to assess and manage people with life limiting conditions to ensure care is individualised. Thus, a sufficiently trained and resourced workforce is vital in addition to aids such as the SPICT™.
In addition, although not the focus of this review we noticed that there was an apparent lack of attention paid to input from the family and consideration of the family context in the included studies. In practice the advance care planning conversation goes beyond using the family to identify palliative care needs and the requirement for referral. The conversation should include addressing family members’ concerns and emotions and facilitate communication between the person who is the focus of advance care planning and their family members [ 52 ].
There are translations of the English version of the SPICT™ available to download from the SPICT™ website for a number of countries including; Brazil, France, Greece, Portugal and South Africa. However, studies reporting the use of many versions of the SPICT™ indicates that formal validation has not been performed. Further validation may strengthen the efficacy and reputation of these versions of the tool. Further studies are required to establish the validity of translated versions of the SPICT™ in Swedish, Danish, Indonesian and the SPICT-LIS™ (Thai), for everyday use in other patient cohorts.
The SPICT™ has scope to be tested in other patient cohorts. Specifically more work is required to extend and test its use in acute care settings where the demand for palliative care is rising and appropriate timely referrals to specialist palliative care are vital to avoid unnecessary distress [ 51 ]. Similarly, there are research opportunities such as reliability and validity testing in relation to the SPICT-4ALL™ version which has been specifically designed to be used by family and informal carers.
Strengths and limitations
This review has strengths which warrant consideration. For example, a systematic approach based on the PRISMA-SCr methodological framework was used, and the search was extensive including 5 electronic databases and many sources of grey literature. A limitation of this review is that we were unable to access a healthcare librarian to assist with the search thus important records may have been missed. In addition, we did not have funding to arrange the translation of two studies which were identified as potentially eligible. Studies included in this scoping review were not appraised for bias thus the level of evidence for the effectiveness of the SPICT™ was not reported. Of note most studies were descriptive and thus evidence for the effectiveness in relation to review question 1 (how does the tool assist with conversations about advance care planning?) is not available.
The current scoping review aimed to assess the impact and extent of the use of the SPICT™. In summary the SPICT™ appears to enable advance care planning, review of care plans and initiation of palliative care in many settings. Previous research suggests that patients and their families greatly appreciate the opportunity to discuss end of life matters. The SPICT™ provides clinicians a proforma on which to base this conversation and a common language to collaborate for palliative care. Clinicians with advance care planning and end of life communication in all settings should consider using the SPICT™ for this purpose. Future research should focus on further validating the SPICT™ in more patient cohorts and acute care settings. Further testing of the tool beyond Europe in countries in Africa, Asia and North America is also warranted.
Data availability
Not applicable.
Worldwide Palliative Care Alliance. In: Connor S, editor. Global atlas of Palliative Care. 2nd ed. London, UK: World Health Organisation; 2020. p. 120.
Google Scholar
Highet G, Crawford D, Murray SA, et al. Development and evaluation of the supportive and Palliative Care indicators Tool (SPICT): a mixed-methods study. BMJ Supportive Palliat Care. 2014;4(3):285–90. https://doi.org/10.1136/bmjspcare-2013-000488 .
Article Google Scholar
Le B, Mileshkin L, Doan K, Saward D, Sruyt O, Yoong J, Gunawardana D, Conron M, Phillip J. Acceptability of early integration of palliative care in patients with incurable lung cancer. J Palliat Med. 2014;17(5). https://doi.org/10.1089/jpm.2013.0473 .
Perrin KO, Kazanowski M. Overcoming barriers to Palliative Care Consultation. Crit Care Nurse. 2015;35(5):44–52. https://doi.org/10.4037/ccn2015357 .
Article PubMed Google Scholar
Scholz B, Goncharov L, Emmerich N, et al. Clinicians’ accounts of communication with patients in end-of-life care contexts: a systematic review. Patient Educ Couns. 2020;103(10):1913–21. https://doi.org/10.1016/j.pec.2020.06.033 .
Aldridge MD, Hasselaar J, Garralda E, et al. Education, implementation, and policy barriers to greater integration of palliative care: a literature review. Palliat Med. 2016;30(3):224–39. https://doi.org/10.1177/0269216315606645 . [published Online First: 2015/09/26].
Heyland D, Dodek, Rocker G, Groll D, Gafni A, Pachora D, Shortt S, Tranmer J, Lazar N, Kutsogiannis A, Lam M. What matters most in end-of-life care: perceptions of seriously ill patients and their family members. CMAJ. 2006;174(5):627–33.
Article PubMed PubMed Central Google Scholar
Salins N, Ramanjulu R, Patra L, et al. Integration of early specialist palliative care in cancer care and patient related outcomes: a critical review of evidence. Indian J Palliat care. 2016;22(3). https://doi.org/10.4103/0973-1075.185028 .
Hui D, Nooruddin Z, Didwaneya N, Dev R, De La Cruz M, Kim SH, Kwon JH, Hutchins R, Liem C, Bruera E. Concepts and definitions for actively dying, end of life, terminally ill, terminal care, and transition of care: a systematic review. J Pain Symptom Manag 2014;47(1).
Kelly A, Morrison R. Palliative care for the seriously ill. N Engl J Med. 2015;373. https://doi.org/10.1056/NEJMra1404684 .
Haute autorite de sante. ORGANISATION OF PATHWAYS - essentials of the palliative approach. TOOL TO IMPROVE PROFESSIONAL PRACTICE; 2016.
Sudore RL, Lum HD, You JJ, et al. Defining Advance Care planning for adults: a Consensus Definition from a Multidisciplinary Delphi Panel. J Pain Symptom Manag. 2017;53(5):821–e321. https://doi.org/10.1016/j.jpainsymman.2016.12.331 .
Boyd K, Murray S. Recognising and managing key transitions in end-of-life care. BMJ. 2010;341. https://doi.org/10.1136/bmj.c4863 .
Group PPCR. The SPICT ™ Supportive and palliative care indicators tool Edinburgh, Scotland: University of Edinburgh; 2023. https://www.spict.org.uk/the-spict/ accessed 05 Feb 2024.
Peters MDJ, Godfrey C, McInerney P, et al. In: Munn EAZ, editor. JBI Manual for evidence synthesis. Scoping reviews: Joanna Briggs Institute; 2020. p. 45.
Tricco A, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMAScR): Checklist and explanation. Ann Intern Med. 2018;169:467–73. https://doi.org/10.7326/M18-0850 .
IAHPC. Global Consensus based palliative care definition Houston, TX, USA: The International Association for Hospice and Palliative Care. 2018. https://hospicecare.com/what-we-do/projects/consensus-based-definition-of-palliative-care/definition/ accessed 10 July 2023.
Teike Luthi F, MacDonald I, Rosselet Amoussou J, et al. Instruments for the identification of patients in need of palliative care in the hospital setting: a systematic review of measurement properties. JBI Evid Synth. 2022;20(3):761–87. https://doi.org/10.11124/JBIES-20-00555 .
Lucas PJ, Baird J, Arai L, et al. Worked examples of alternative methods for the synthesis of qualitative and quantitative research in systematic reviews. BMC Med Res Methodol. 2007;7(1):4. https://doi.org/10.1186/1471-2288-7-4 .
Fachado A, Alonso, Martínez NS, Roselló MM, et al. Spanish adaptation and validation of the supportive & palliative care indicators tool – SPICT-ES™. Rev Saúde Pública. 2018;52(0):3. https://doi.org/10.11606/S1518-8787.2018052000398 .
Bergenholtz H, Weibull A, Raunkiaer M. Supportive and palliative care indicators tool (SPICT) in a Danish healthcare context: translation, cross-cultural adaptation, and content validation. BMC Palliat Care. 2022;21(1):41. https://doi.org/10.1186/s12904-022-00931-6 . [published Online First: 2022/03/26].
Casale G, Magnani C, Fanelli R, et al. Supportive and palliative care indicators tool (SPICT): content validity, feasibility and pre-test of the Italian version. BMC Palliat Care. 2020;19(1):79. https://doi.org/10.1186/s12904-020-00584-3 . [published Online First: 2020/06/09].
Hamano J, Oishi A, Kizawa Y. Identified Palliative Care Approach needs with SPICT in Family Practice: a preliminary observational study. J Palliat Med. 2018;21(7):992–98. https://doi.org/10.1089/jpm.2017.0491 . [published Online First: 2018/02/10].
Pham L, Arnby M, Benkel I, et al. Early integration of palliative care: translation, cross-cultural adaptation and content validity of the supportive and Palliative Care indicators Tool in a Swedish healthcare context. Scand J Caring Sci. 2020;34(3):762–71. https://doi.org/10.1111/scs.12781 . [published Online First: 2019/11/02].
Sripaew S, Fumaneeshoat O, Ingviya T. Systematic adaptation of the Thai version of the supportive and palliative care indicators tool for low-income setting (SPICT-LIS). BMC Palliat Care. 2021;20(1):35. https://doi.org/10.1186/s12904-021-00729-y . [published Online First: 2021/02/21].
Farfán-Zuñiga X, Zimmermann-Vildoso M. Cultural adaptation and validation of the SPICT-ES™ instrument to identify palliative care needs in Chilean older adults. BMC Palliat Care. 2022;21(1):223. https://doi.org/10.1186/s12904-022-01111-2 . [published Online First: 2022/12/17].
Oishi A, Hamano J, Boyd K, et al. Translation and cross-cultural adaptation of the supportive and Palliative Care indicators Tool into Japanese: a preliminary Report. Palliat Med Rep. 2022;3(1):1–5. https://doi.org/10.1089/pmr.2021.0083 . [published Online First: 2022/09/06].
Clark NH. Palliative Care: improving Eligible Patient Identification to encourage early intervention [Capstone]. Northern Arizona University; 2019.
Dinega G. Improving palliative care utilization processes: An effort to enhance nurses’ contribution [D.N.P]. The College of St. Scholastica; 2016.
van Baal K, Wiese B, Muller-Mundt G, et al. Quality of end-of-life care in general practice - a pre-post comparison of a two-tiered intervention. BMC Prim Care. 2022;23(1):90. https://doi.org/10.1186/s12875-022-01689-9 . [published Online First: 2022/04/22].
Maas EA, Murray SA, Engels Y, et al. What tools are available to identify patients with palliative care needs in primary care: a systematic literature review and survey of European practice. BMJ Support Palliat Care. 2013;3(4):444–51. https://doi.org/10.1136/bmjspcare-2013-000527 . [published Online First: 2014/06/21].
Afshar K, Wiese B, Schneider N, et al. Systematic identification of critically ill and dying patients in primary care using the German version of the supportive and Palliative Care indicators Tool (SPICT-DE). Ger Med Sci. 2020;18:Doc02. https://doi.org/10.3205/000278 . [published Online First: 2020/02/13].
Afshar K, van Baal K, Wiese B, et al. Structured implementation of the supportive and Palliative Care indicators Tool in general practice – a prospective interventional study with follow-up. BMC Palliat Care. 2022;21(1):214. https://doi.org/10.1186/s12904-022-01107-y .
Lunardi L, Hill K, Crail S, et al. Supportive and Palliative Care indicators Tool (SPICT) improves renal nurses’ confidence in recognising patients approaching end of life. BMJ Support Palliat Care. 2020. https://doi.org/10.1136/bmjspcare-2020-002496 . [published Online First: 2020/11/05].
Liyanage T, Mitchell G, Senior H. Identifying palliative care needs in residential care. Aust J Prim Health. 2018;24(6):524–29. doi: 10.1071/PY17168 [published Online First: 2018/11/14].
Chan AS, Rout A, ’Adamo CRD, et al. Palliative referrals in Advanced Cancer patients: utilizing the supportive and Palliative Care indicators Tool and Rothman Index. Am J Hospice Palliat Medicine®. 2022;39(2):164–68. https://doi.org/10.1177/10499091211017873 .
van Wijmen MPS, Schweitzer BPM, Pasman HR, et al. Identifying patients who could benefit from palliative care by making use of the general practice information system: the Surprise question versus the SPICT. Fam Pract. 2020;37(5):641–47. https://doi.org/10.1093/fampra/cmaa049 . [published Online First: 2020/05/20].
Afshar K, Feichtner A, Boyd K, et al. Systematic development and adjustment of the German version of the supportive and Palliative Care indicators Tool (SPICT-DE). BMC Palliat Care. 2018;17(1):27. https://doi.org/10.1186/s12904-018-0283-7 .
Fumaneeshoat O, Ingviya T, Sripaew S. Prevalence of Cancer Patients Requiring Palliative Care in Outpatient Clinics in a Tertiary Hospital in Southern Thailand. 2021 2021;39(5):11. https://doi.org/10.31584/jhsmr.2021798 [published Online First: 2021-07-02].
Sudhakaran D, Shetty RS, Mallya SD, et al. Screening for palliative care needs in the community using SPICT. Med J Armed Forces India. 2023;79(2):213–19. [published Online First: 2023/03/28].
Effendy C, Silva JFDS, Padmawati RS. Identifying palliative care needs of patients with non-communicable diseases in Indonesia using the SPICT tool: a descriptive cross-sectional study. BMC Palliat Care. 2022;21(1):13. https://doi.org/10.1186/s12904-021-00881-5 .
Pairojkul S, Thongkhamcharoen R, Raksasataya A, et al. Integration of specialist Palliative Care into Tertiary hospitals: a Multicenter Point Prevalence Survey from Thailand. Palliat Med Rep. 2021;2(1):272–79.
Krause R, Barnard A, Burger H, et al. A Delphi study to guide the development of a clinical indicator tool for palliative care in South Africa. Afr J Prim Health Care Fam Med. 2022;14(1):e1–7. https://doi.org/10.4102/phcfm.v14i1.3351 . [published Online First: 2022/06/14].
Pinedo-Torres I, Intimayta-Escalante C, Jara-Cuadros D, et al. Association between the need for palliative care and chronic diseases in patients treated in a Peruvian hospital. Revista peruana de medicina Experimental y Salud pública. 2021;38(4):569–76. https://doi.org/10.17843/rpmesp.2021.384.9288 .
Beaton DE, Bombardier C, Guillemin F, et al. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000;25(24):3186–91. https://doi.org/10.1097/00007632-200012150-00014 . [published Online First: 2000/12/22].
Article CAS PubMed Google Scholar
University of Edinburgh. SPICT-4ALL Edinburgh, Scotland, 2023. https://www.spict.org.uk/spict-4all/ accessed 04 July 2023.
Zwakman M, Jabbarian LJ, van Delden J, et al. Advance care planning: a systematic review about experiences of patients with a life-threatening or life-limiting illness. Palliat Med. 2018;32(8):1305–21. https://doi.org/10.1177/0269216318784474 . [published Online First: 2018/06/30].
Article CAS PubMed PubMed Central Google Scholar
Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665–73. https://doi.org/10.1001/jama.300.14.1665 . [published Online First: 2008/10/09].
Hajat C, Stein E. The global burden of multiple chronic conditions: a narrative review. Prev Med Rep. 2018;12:284–93. https://doi.org/10.1016/j.pmedr.2018.10.008 . [published Online First: 2018/11/09].
Taghavi M, Johnston G, Urquhart R, et al. Workforce planning for community-based Palliative Care specialist teams using Operations Research. J Pain Symptom Manag. 2021;61(5):1012–e224. https://doi.org/10.1016/j.jpainsymman.2020.09.009 .
Hui D, Heung Y, Bruera E. Timely Palliative Care: personalizing the process of Referral. Cancers. 2022;14(4):1047.
Kishino M, Ellis-Smith C, Afolabi O, et al. Family involvement in advance care planning for people living with advanced cancer: a systematic mixed-methods review. Palliat Med. 2022;36(3):462–77. https://doi.org/10.1177/02692163211068282 . [published Online First: 2022/01/07].
Download references
Acknowledgements
The work involved in performing this review was not funded.
Author information
Authors and affiliations.
Avondale University, Wahroonga, Sydney, NSW, Australia
Melanie Mahura
Hammond Care, Greenwich, Sydney, NSW, Australia
Brigitte Karle
Royal North Shore Hospital, St. Leonards, Sydney, NSW, Australia
Louise Sayers, Felicity Dick-Smith & Rosalind Elliott
University of Technology Sydney, Ultimo, Sydney, NSW, Australia
Rosalind Elliott
You can also search for this author in PubMed Google Scholar
Contributions
We declare that this paper has not been published elsewhere and we have not submitted the paper to any other journal at the time of this submission. In addition, we Rosalind Elliott (RE), Melanie Mahura (MM), Brigitte Karle (BK), Felicity Dick-Smith (F D-S) and Louise Sayers (LS), declare that we have no known conflicts of interest in relation to the review or manuscript.All authors contributed to the research and reporting. MM lead the protocol design with input from all authors (RE, BK, FD-S and LS) and the search. MM and RE screened the search records with BK and LS acting as arbitrator. MM and BK extracted the data. Synthesis and interpretation were performed mainly by MM and BK with input from all authors. The writing was lead by MM with contributions from all authors (RE, BK, FD-S and LS). RE provided mentorship and thoroughly edited the final version. All authors (MM, RE, BK, FD-S and LS) reviewed the final version and gave their final approval for submission of the paper.
Corresponding author
Correspondence to Rosalind Elliott .
Ethics declarations
Consent for publication, ethical approval and consent to participate, ethical guidelines.
The International Medical Journal Editors’ Committee guidelines for authorship were followed.
Author’s information (optional)
Conflict of interest.
The authors know of no conflicts of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mahura, M., Karle, B., Sayers, L. et al. Use of the supportive and palliative care indicators tool (SPICT™) for end-of-life discussions: a scoping review. BMC Palliat Care 23 , 119 (2024). https://doi.org/10.1186/s12904-024-01445-z
Download citation
Received : 17 August 2023
Accepted : 25 April 2024
Published : 16 May 2024
DOI : https://doi.org/10.1186/s12904-024-01445-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Communication
- Documentation
- Palliative Care
- Patient Care Planning
- Terminal Care
BMC Palliative Care
ISSN: 1472-684X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Overexpression of sweetpotato glutamylcysteine synthetase ( IbGCS ) in Arabidopsis confers tolerance to drought and salt stresses
- Regular Paper – Physiology/Biochemistry/Molecular and Cellular Biology
- Published: 17 May 2024
Cite this article

- Zhe Yang 1 na1 ,
- Yuan Wang 2 na1 ,
- Qirui Cheng 1 ,
- Xuan Zou 1 ,
- Yanxin Yang 3 ,
- Peng Li 1 ,
- Sijie Wang 1 ,
- Dongjing Yang 4 ,
- Ho Soo Kim 5 ,
- Xiaoyun Jia 1 ,
- Lingzhi Li 2 ,
- Sang-Soo Kwak 5 &
- Wenbin Wang 1
Explore all metrics
Various environmental stresses induce the production of reactive oxygen species (ROS), which have deleterious effects on plant cells. Glutathione (GSH) is an antioxidant used to counteract reactive oxygen species. Glutathione is produced by glutamylcysteine synthetase (GCS) and glutathione synthetase (GS). However, evidence for the GCS gene in sweetpotato remains scarce. In this study, the full-length cDNA sequence of IbGCS isolated from sweetpotato cultivar Xu18 was 1566 bp in length, which encodes 521 amino acids. The qRT-PCR analysis revealed a significantly higher expression of the IbGCS in sweetpotato flowers, and the gene was induced by salinity, abscisic acid (ABA), drought, extreme temperature and heavy metal stresses. The seed germination rate, root elongation and fresh weight were promoted in T 3 Arabidopsis IbGCS -overexpressing lines (OEs) in contrast to wild type (WT) plants under mannitol and salt stresses. In addition, the soil drought and salt stress experiment results indicated that IbGCS overexpression in Arabidopsis reduced the malondialdehyde (MDA) content, enhanced the levels of GCS activity, GSH and AsA content, and antioxidant enzyme activity. In summary, overexpressing IbGCS in Arabidopsis showed improved salt and drought tolerance.
• IbGCS gene was cloned from the sweetpotato cultivar Xu18.
• The multiple abiotic stresses significantly increased the expression of IbGCS gene.
• Overexpression of IbGCS significantly improved the salt and drought stress tolerance
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
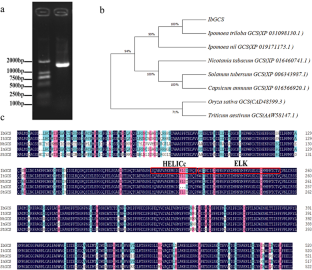
Abbreviations
Reactive oxygen species
- Glutamylcysteine synthetase
Quantitative real-time PCR
Glutathione
Ascorbic acid
Dehydroascorbic acid
Malondialdehyde
Ascorbate-glutathione cycle
Overexpression
Analysis of variance
Hydrogen peroxide
Superoxide dismutase
Ascorbate peroxidase
Aravind P, Prasad MNV (2005) Modulation of cadmium-induced oxidative stress in Ceratophyllum demersum by zinc involves ascorbate-glutathione cycle and glutathione metabolism. Plant Physiol Bioch 43:107–116. https://doi.org/10.1016/j.plaphy.2005.01.002
Article CAS Google Scholar
Areco Morales M (2014) Imaginario Espacial En La Narrativa Chilena Reciente: El Acuario Como RepresentaciÓn De La Intimidad En Relatos De Contreras, Zambra Y BolaÑo. Alpha 10:9–22. https://doi.org/10.4067/s0718-22012014000100002
Article Google Scholar
Bae MJ, Kim YS, Kim IS, Choe YH, Lee EJ, Kim YH, Park HM, Yoon HS (2013) Transgenic rice overexpressing the Brassica juncea γ -glutamylcysteine synthetase gene enhances tolerance to abiotic stress and improves grain yield under paddy field conditions. Mol Breed 31:931–945. https://doi.org/10.1007/s11032-013-9846-8
Bajguz A, Hayat S (2009) Effects of brassinosteroids on the plant responses to environmental stresses. Plant Physiol Bioch 47:1–8. https://doi.org/10.1016/j.plaphy.2008.10.002
Bashandy T, Guilleminot J, Vernoux T, Caparros-Ruiz D, Ljung K, Meyer Y, Reichheld JP (2010) Interplay between the NADP-linked thioredoxin and glutathione systems in Arabidopsis auxin signaling. Plant Cell 22:376–391. https://doi.org/10.1105/tpc.109.071225
Article CAS PubMed PubMed Central Google Scholar
Bradford MM (1976) A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72:248–254. https://doi.org/10.1016/0003-2697(76)90527-3
Article CAS PubMed Google Scholar
Caverzan A, Passaia G, Rosa SB, Ribeiro CW, Lazzarotto F, Margis-Pinheiro M (2012) Plant responses to stresses: role of ascorbate peroxidase in the antioxidant protection. Genet Mol Biol 35:1011–1019. https://doi.org/10.1590/s1415-47572012000600016
Chen SC, Liu AR, Zhang SJ, Li C, Chang R, Liu DL, Ahammed GJ, Lin XM (2013) Overexpression of mitochondrial uncoupling protein conferred resistance to heat stress and Botrytis cinerea infection in tomato. Plant Physiol Bioch 73:245–253. https://doi.org/10.1016/j.plaphy.2013.10.002
Clough SJ, Bent AF (1998) Floral dip: a simplified method for Agrobacterium-mediated transformation of Arabidopsis thaliana . Plant J 16:735–743. https://doi.org/10.1046/j.1365-313x.1998.00343.x
Cobbett CS, May MJ, Howden R, Rolls B (1998) The glutathione-deficient, cadmium-sensitive mutant, cad2-1, of Arabidopsis thaliana is deficient in γ-glutamylcysteine synthetase. Plant J 16:73–78. https://doi.org/10.1046/j.1365-313x.1998.00262.x
Cruz de Carvalho MH (2008) Drought stress and reactive oxygen species: production, scavenging and signaling. Plant Signal Behav 3:156–165. https://doi.org/10.4161/psb.3.3.5536
Article PubMed PubMed Central Google Scholar
Duvernay WH, Chinn MS, Yencho GC (2013) Hydrolysis and fermentation of sweetpotatoes for production of fermentable sugars and ethanol. Ind Crop Prod 42:527–537. https://doi.org/10.1016/j.indcrop.2012.06.028
Eltayeb AE, Yamamoto S, Habora MEE, Yin L, Tsujimoto H, Tanaka K (2011) Transgenic potato overexpressing Arabidopsis cytosolic AtDHAR1 showed higher tolerance to herbicide, drought and salt stresses. Breed Sci 61:3–10. https://doi.org/10.1270/jsbbs.61.3
Galant A, Preuss ML, Cameron JC, Jez JM (2011) Plant glutathione biosynthesis: diversity in biochemical regulation and reaction products. Front Plant Sci 2:45. https://doi.org/10.3389/fpls.2011.00045
Ghanta S, Bhattacharyya D, Sinha R, Banerjee A, Chattopadhyay S (2011) Nicotiana tabacum overexpressing γ-ECS exhibits biotic stress tolerance likely through NPR1-dependent salicylic acid-mediated pathway. Planta 233:895–910. https://doi.org/10.1007/s00425-011-1349-4
Gullner G, Komives T, Rennenberg H (2001) Enhanced tolerance of transgenic poplar plants overexpressing γ-glutamylcysteine synthetase towards chloroacetanilide herbicides. J Exp Bot 52:971–979. https://doi.org/10.1093/jexbot/52.358.971
Hell R, Bergmann L (1990) γ-Glutamylcysteine synthetase in higher plants: catalytic properties and subcellular localization. Planta 180:603–612. https://doi.org/10.1007/BF02411460
Henmi K, Tsuboi S, Demura T, Fukuda H, Iwabuchi M, Ogawa K (2001) A possible role of glutathione and glutathione disulfide in tracheary element differentiation in the cultured mesophyll cells of Zinnia elegans . Plant Cell Physiol 42:673–676. https://doi.org/10.1093/pcp/pce072
Huang M, Xu Q, Deng XX (2014) L-Ascorbic acid metabolism during fruit development in an ascorbate-rich fruit crop chestnut rose ( Rosa roxburghii Tratt). J Plant Physiol 171:1205–1216. https://doi.org/10.1016/j.jplph.2014.03.010
Ivanova LA, Ronzhina DA, Ivanov LA, Stroukova LV, Peuke AD, Rennenberg H (2011) Over-expression of gsh1 in the cytosol affects the photosynthetic apparatus and improves the performance of transgenic poplars on heavy metal-contaminated soil. Plant Biol 13:649–659. https://doi.org/10.1111/j.1438-8677.2010.00422.x
Kim KY, Kwon SY, Lee HS, Hur Y, Bang JW, Kwak SS (2003) A novel oxidative stress-inducible peroxidase promoter from sweetpotato: molecular cloning and characterization in transgenic tobacco plants and cultured cells. Plant Mol Biol 51:831–838. https://doi.org/10.1023/A:1023045218815
Kiyoshi T, Yoshiko S, Noriaki K, Kiyoshi S (1985) O 3 tolerance and the ascorbate-dependent H 2 O 2 decomposing system in chloroplasts. Plant Cell Physiol 26:1425–1431. https://doi.org/10.1016/0303-7207(85)90069-3
Kochba J, Lavee S, Spiegel-Roy P (1977) Differences in peroxidase activity and isoenzymes in embryogenic ane non-embryogenic ‘Shamouti’ orange ovular callus lines. Plant Cell Physiol 18:463–467. https://doi.org/10.1093/oxfordjournals.pcp.a075455
Li X, Zhong YL, Pang XY, Yuan YX, Liu YH, Zhang ZS (2018) Trypsin and ascorbic acid have a synergistic effect on the quality of apple processing by protecting apple cells from oxidative damage. J Food Biochem 42. https://doi.org/10.1111/jfbc.12582
Li C, Tao JQ, Wu ZX (2023) Gaseous ozone regulates reactive oxygen species metabolism and ascorbate–glutathione cycle to delay the senescence of fresh-cut red pitaya ( Selenicereus Undatus ) fruit. Sci Hortic 312:113819. https://doi.org/10.1016/j.scienta.2023.111839
Lu BY, Luo XJ, Gong CM, Bai J (2021) Overexpression of γ-glutamylcysteine synthetase gene from Caragana korshinskii decreases stomatal density and enhances drought tolerance. BMC Plant Biol 21:444. https://doi.org/10.1186/s12870-021-03226-9
Ma BH, Gao L, Zhang HX, Cui J, Shen ZG (2012) Aluminum-induced oxidative stress and changes in antioxidant defenses in the roots of rice varieties differing in Al tolerance. Plant Cell Rep 31:687–696. https://doi.org/10.1007/s00299-011-1187-7
Mittler R (2002) Oxidative stress, antioxidants and stress tolerance. Trends Plant Sci 7:405–410. https://doi.org/10.1016/s1360-1385(02)02312-9
Noctor G, Arisi ACM, Jouanin L, Kunert KJ, Rennenberg H, Foyer CH (1998) Review article. Glutathione: biosynthesis, metabolism and relationship to stress tolerance explored in transformed plants. J Exp Bot 49:623–647. https://doi.org/10.1093/jexbot/49.321.623
Noctor G, Mhamdi A, Chaouch S, Han Y, Neukermans J, Marquez-Garcia B, Queval G, Foyer CH (2012) Glutathione in plants: an integrated overview. Plant Cell Environ 35:454–484. https://doi.org/10.1111/j.1365-3040.2011.02400.x
Ogawa KI (2005) Glutathione-associated regulation of plant growth and stress responses. Antioxid Redox Sign 7:973–981. https://doi.org/10.1089/ars.2005.7.973
Ogawa KI, Hatano Iwasaki A, Yanagida M, Iwabuchi M (2004) Level of glutathione is regulated by ATP-dependent ligation of glutamate and cysteine through photosynthesis in Arabidopsis thaliana : mechanism of strong interaction of light intensity with flowering. Plant Cell Physiol 45:1–8. https://doi.org/10.1093/pcp/pch008
Potters G, De Gara L, Asard H, Horemans N (2002) Ascorbate and glutathione: guardians of the cell cycle, partners in crime? Plant Physiol Bioch 40:537–548. https://doi.org/10.1016/s0981-9428(02)01414-6
Potters G, Jansen MAK, Horemans N, Guisez Y, Pasternak T (2010) Dehydroascorbate and glutathione regulate the cellular development of Nicotiana tabacum L. SR-1 protoplasts. Vitro Cell 46:289–297. https://doi.org/10.1007/s11627-009-9266-y
Rausch T, Gromes R, Liedschulte V, Muller I, Bogs J, Galovic V, Wachter A (2007) Novel insight into the regulation of GSH biosynthesis in higher plants. Plant Biol 9:565–572. https://doi.org/10.1055/s-2007-965580
Samuilov S, Lang F, Djukic M, Djunisijevic-Bojovic D, Rennenberg H (2016) Lead uptake increases drought tolerance of wild type and transgenic poplar (Populus tremula x P. Alba) overexpressing gsh1. Environ Pollut 216:773–785. https://doi.org/10.1016/j.envpol.2016.06.047
Sengupta D, Ramesh G, Mudalkar S, Kumar KRR, Kirti PB, Reddy AR (2012) Molecular cloning and characterization of γ-Glutamyl cysteine synthetase ( VrγECS ) from roots of Vigna radiata (L.) Wilczek under progressive drought stress and recovery. Plant Mol Biol Rep 30:894–903. https://doi.org/10.1007/s11105-011-0398-y
Seth CS, Remans T, Keunen E, Jozefczak M, Gielen H, Opdenakker K, Weyens N, Vangronsveld J, Cuypers A (2012) Phytoextraction of toxic metals: a central role for glutathione. Plant Cell Environ 35:334–346. https://doi.org/10.1111/j.1365-3040.2011.02338.x
."-->Sharma P, Jha AB, Dubey RS, Pessarakli M (2012) Reactive oxygen species, oxidative damage, and antioxidative defense mechanism in plants under stressful conditions. J Bot 2012:1–26. https://doi.org/10.1155/2012/217037
Smirnoff N (1996) Botanical briefing: the function and metabolism of ascorbic acid in plants. Bot-london 78:661–669. https://doi.org/10.1006/anbo.1996.0175
Steinkamp R, Schweihofen B, Rennenberg H (2008) γ-Glutamylcyclotransferase in tobacco suspension cultures: Catalytic properties and subcellular localization. Physiol Plant 69:499–503. https://doi.org/10.1111/j.1399-3054.1987.tb09231.x
Wang YN, Liu C, Li KX, Sun FF, Hu HZ, Li X, Zhao YK, Han CY, Zhang WS, Duan YF, Liu MY, Li X (2007) Arabidopsis EIN2 modulates stress response through abscisic acid response pathway. Plant Mol Biol 64:633–644. https://doi.org/10.1007/s11103-007-9182-7
Wang WB, Kim YH, Lee HS, Kim KY, Deng XP, Kwak SS (2009) Analysis of antioxidant enzyme activity during germination of alfalfa under salt and drought stresses. Plant Physiol Bioch 47:570–577. https://doi.org/10.1016/j.plaphy.2009.02.009
Wang ZN, Xiao Y, Chen WS, Tang KX, Zhang L (2010) Increased vitamin C content accompanied by an enhanced recycling pathway confers oxidative stress tolerance in Arabidopsis . J Integr Plant Biol 52:400–409. https://doi.org/10.1111/j.1744-7909.2010.00921.x
Wang WB, Qiu XP, Kim HS, Yang YX, Hou DY, Liang X, Kwak SS (2019) Molecular cloning and functional characterization of a sweetpotato chloroplast IbDHAR3 gene in response to abiotic stress. Plant Biotechnol Rep 14:9–19. https://doi.org/10.1007/s11816-019-00576-7
Wu JM, Qu T, Chen SY, Zhao ZG, An LZ (2009) Molecular cloning and characterization of a γ-glutamylcysteine synthetase gene from Chorispora Bungeana . Protoplasma 235:27–36. https://doi.org/10.1007/s00709-008-0026-3
Xiong J, Zhang WX, Zheng D, Xiong H, Feng XJ, Zhang XM, Wang QJ, Wu FK, Xu J, Lu YL (2022) ZmLBD 5 increases drought sensitivity by suppressing ROS accumulation in Arabidopsis . Plants 11:1382. https://doi.org/10.3390/plants11101382
Yadav SK, Singla Pareek SL, Reddy MK, Sopory SK (2005) Transgenic tobacco plants overexpressing glyoxalase enzymes resist an increase in methylglyoxal and maintain higher reduced glutathione levels under salinity stress. Febs Lett 579:6265–6271. https://doi.org/10.1016/j.febslet.2005.10.006
Zechmann B, Koffler BE, Russell SD (2013) Glutathione synthesis is essential for pollen germination in vitro. BMC Plant Biol 11:54. https://doi.org/10.1186/1471-2229-11-54
Zhou FF, Zheng BW, Wang F, Cao AP, Xie SQ, Chen XF, Schick JA, Jin X, Li HB (2021) Genome-wide analysis of MDHAR gene family in four cotton species provides insights into fiber development via regulating AsA redox homeostasis. Plants 10:227. https://doi.org/10.3390/plants10020227
Zhu YL, Pilon Smits EAH, Tarun AS, Weber SU, Jouanin L, Terry N (1999) Cadmium tolerance and accumulation in Indian mustard is enhanced by overexpressing γ-glutamylcysteine synthetase. Plant Physiol 121:1169–1178. https://doi.org/10.1104/pp.121.4.1169
Download references
This work was supported by the Basic Research Program of Shanxi Province (20210302123377), Cultivate Project of National Science Foundation of Shanxi Agricultural University (2017GPY06), Science Innovation Foundation of Shanxi Agricultural University (2018yz003, 2010027), the Korea Research Institute of Bioscience and Biotechnology (KRIBB) Research Initiative Program (KGM1002311), and the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICF and Future Planning (NRF-2023R1A2C1005039).
Author information
Zhe Yang and Yuan Wang contributed equally to this work.
Authors and Affiliations
College of Life Sciences, Shanxi Agricultural University, Taigu, 030801, China
Zhe Yang, Qirui Cheng, Xuan Zou, Peng Li, Sijie Wang, Yue Su, Xiaoyun Jia & Wenbin Wang
College of Horticulture, Shanxi Agricultural University, Taigu, 030801, China
Yuan Wang & Lingzhi Li
College of Basic Sciences, Shanxi Agricultural University, Taigu, 030801, China
Yanxin Yang
Key Laboratory of Biology and Genetic Improvement of Sweetpotato, Ministry of Agriculture and Rural Affairs, Xuzhou Institute of Agricultural Sciences in Jiangsu Xuhuai District, Xuzhou, Jiangsu, 221131, China
Dongjing Yang
Plant Systems Engineering Research Center, Korea Research Institute of Bioscience and Biotechnology (KRIBB), 1 25 Gwahak-ro, Daejeon, 34141, South Korea
Ho Soo Kim & Sang-Soo Kwak
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: W.W., Z.Y., H.K.; Investigation and writing–original draft preparation: Z.Y., Y.W.; Validation: Q.C., X.Z.; Visualization: Y.Y., P.L.; Formal analysis: S.W., Y.S.; Resources: D.Y., X.J., L.L. S.K., W.W.; Writing–review and editing: W.W., H.K.; Supervision and funding acquisition: W.W., S.K.
Corresponding authors
Correspondence to Lingzhi Li , Sang-Soo Kwak or Wenbin Wang .
Ethics declarations
Competing interests.
The authors declare no conflicts of interest related to the content of this article.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Yang, Z., Wang, Y., Cheng, Q. et al. Overexpression of sweetpotato glutamylcysteine synthetase ( IbGCS ) in Arabidopsis confers tolerance to drought and salt stresses. J Plant Res (2024). https://doi.org/10.1007/s10265-024-01548-x
Download citation
Received : 24 February 2024
Accepted : 02 May 2024
Published : 17 May 2024
DOI : https://doi.org/10.1007/s10265-024-01548-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Abiotic stresses
- Functional characterization
- Gene cloning
- Sweetpotato
- Find a journal
- Publish with us
- Track your research

COMMENTS
Tips to Write the Results Section. Direct the reader to the research data and explain the meaning of the data. Avoid using a repetitive sentence structure to explain a new set of data. Write and highlight important findings in your results. Use the same order as the subheadings of the methods section.
The discussion section is where you delve into the meaning, importance, and relevance of your results.. It should focus on explaining and evaluating what you found, showing how it relates to your literature review and paper or dissertation topic, and making an argument in support of your overall conclusion.It should not be a second results section.. There are different ways to write this ...
the results of your research, a discussion of related research, and; a comparison between your results and initial hypothesis. Tip: Not all journals share the same naming conventions. You can apply the advice in this article to the conclusion, results or discussion sections of your manuscript.
Checklist: Research results 0 / 7. I have completed my data collection and analyzed the results. I have included all results that are relevant to my research questions. I have concisely and objectively reported each result, including relevant descriptive statistics and inferential statistics. I have stated whether each hypothesis was supported ...
The discussion should also address the study's research questions and explain how the results contribute to the field of study. Limitations: This section should acknowledge any limitations of the study, such as sample size, data collection methods, or other factors that may have influenced the results.
1. Context. The "results section" is the heart of the paper, around which the other sections are organized ().Research is about results and the reader comes to the paper to discover the results ().In this section, authors contribute to the development of scientific literature by providing novel, hitherto unknown knowledge ().In addition to the results, this section contains data and ...
The discussion section should relate your results to those found in other studies, particularly if questions raised from prior studies served as the motivation for your research. This is important because comparing and contrasting the findings of other studies helps to support the overall importance of your results and it highlights how and in ...
Making scientific research available to others is a key part of academic integrity and open science. Interpretation or discussion of results; This belongs in your discussion section. Your results section is where you objectively report all relevant findings and leave them open for interpretation by readers.
The discussion section provides an analysis and interpretation of the findings, compares them with previous studies, identifies limitations, and suggests future directions for research. This section combines information from the preceding parts of your paper into a coherent story. By this point, the reader already knows why you did your study ...
Writing the results and discussion as separate sections allows you to focus first on what results you obtained and set out clearly what happened in your experiments and/or investigations without ... If you are unsure whether to include certain results, go back to your research questions and decide whether the results are relevant to them. It ...
Practical guidance for writing an effective results section for a research paper. Always use simple and clear language. Avoid the use of uncertain or out-of-focus expressions. The findings of the study must be expressed in an objective and unbiased manner. While it is acceptable to correlate certain findings in the discussion section, it is ...
You should: Discuss your conclusions in order of most to least important. Compare your results with those from other studies: Are they consistent? If not, discuss possible reasons for the difference. Mention any inconclusive results and explain them as best you can. You may suggest additional experiments needed to clarify your results.
The results section of a research paper tells the reader what you found, while the discussion section tells the reader what your findings mean. The results section should present the facts in an academic and unbiased manner, avoiding any attempt at analyzing or interpreting the data. Think of the results section as setting the stage for the ...
Explaining the meaning of the results to the reader is the purpose of the discussion section of a research paper. There are elements of the discussion that should be included and other things that ...
The discussion section is one of the final parts of a research paper, in which an author describes, analyzes, and interprets their findings. They explain the significance of those results and tie everything back to the research question(s). In this handout, you will find a description of what a discussion section does, explanations of how to ...
IMRaD Results Discussion. Results and Discussion Sections in Scientific Research Reports (IMRaD) After introducing the study and describing its methodology, an IMRaD* report presents and discusses the main findings of the study. In the results section, writers systematically report their findings, and in discussion, they interpret these findings.
The Results (or Findings) section follows the Methods and precedes the Discussion section. This is where the authors provide the data collected during their study. That data can sometimes be difficult to understand because it is often quite technical. Do not let this intimidate you; you will discover the significance of the results next. Discussion
Tips for Writing the Discussion Section. Start with the big picture - WHY is your study important? o Think of yourself as telling the story of how your findings answer the question you posed and why your findings matter, how your field's status quo or understanding is changed by your results. o Clearly signal that you are answering the ...
Infographic: 5 Differences between the results and discussion sections. Most journals expect you to follow the IMRaD (Introduction, Methods, Results, and Discussion) format while writing your research paper. It is possible that you might be slightly confused about what to include in the Results and Discussions sections.
Discussion section provides an interpretation of the data, especially in context to previously published research. The Results and Discussion sections can be written as separate sections (as shown in Fig. 2 ), but are often combined in a poster into one section called Results and Discussion.
This chapter 5 presents the results of the study. First, an outline of the informants included in the study and an overview of the statistical techniques employed in the data analyses are given ...
Conservatism was also associated with less research discouragement with at least small effects for six conclusions, rs = −.11 to −.17 (significant at p < .005 for only two), but results were trending in the same direction for the other four (gender bias in STEM, racial bias in academia, political bias in social science, evolved sex ...
Marvin Minsky, the pioneer of artificial intelligence research in the 1960s, talked about AI as a "suitcase word"—a term into which you can stuff whatever you want—and that still seems to be the case. ... is listening in on a strategy session where the CEO proposes something and everyone says "Aye" without debate and discussion. AI ...
Results Vitamin D PGSs were associated with inattention in the ADHD sample and with hyperactivity when inattention symptoms were included as covariates. In the nutrigenetic sample, CYP2R1 rs10741657 and DHCR7 rs12785878 were nominally associated with impulsivity and hyperactivity, respectively, and both with vitamin D levels.
The discussion section is where you delve into the meaning, importance, and relevance of your results.. It should focus on explaining and evaluating what you found, showing how it relates to your literature review, and making an argument in support of your overall conclusion.It should not be a second results section.. There are different ways to write this section, but you can focus your ...
Regional GNSS (Global Navigation Satellite System) positioning suggests a volumetric increase of ∼1.4 × 10 7 m 3 in the first 3 months of the swarm, suggesting that fluid migration may be the cause of the Noto earthquake swarms ().Amezawa et al. assert that crustal earthquake swarms exhibit distinct spatiotemporal patterns of earthquake migration, characterized by clusters that originate at ...
A recent study found that ethnic minority General Practice (GP)-trainees receive more negative assessments than their majority peers. Previous qualitative research suggested that learning climate-related factors play a pivotal role in unequal opportunities for trainees in post-graduate medical settings, indicating that insufficient inclusivity had put minority students at risk of failure and ...
The results chapter or section simply and objectively reports what you found, without speculating on why you found these results. The discussion interprets the meaning of the results, puts them in context, and explains why they matter. In qualitative research, results and discussion are sometimes combined. But in quantitative research, it's ...
From the search results 26 records were reviewed, including two systematic review, two theses and 22 primary research studies. Much of the research was derived from primary care settings. There was evidence that the SPICT™ assists conversations about advance care planning specifically discussion and documentation of advance care directives ...
The research results will provide important evidence to unravel the molecular mechanism involved in GSH and AsA metabolism in sweetpotato and for improving stress tolerance through molecular genetics. ... Discussion. The GCS gene has been reported as a stress regulator in many plants, including Arabidopsis, tomato and rice.