How to Write About Coronavirus in a College Essay
Students can share how they navigated life during the coronavirus pandemic in a full-length essay or an optional supplement.
Writing About COVID-19 in College Essays

Getty Images
Experts say students should be honest and not limit themselves to merely their experiences with the pandemic.
The global impact of COVID-19, the disease caused by the novel coronavirus, means colleges and prospective students alike are in for an admissions cycle like no other. Both face unprecedented challenges and questions as they grapple with their respective futures amid the ongoing fallout of the pandemic.
Colleges must examine applicants without the aid of standardized test scores for many – a factor that prompted many schools to go test-optional for now . Even grades, a significant component of a college application, may be hard to interpret with some high schools adopting pass-fail classes last spring due to the pandemic. Major college admissions factors are suddenly skewed.
"I can't help but think other (admissions) factors are going to matter more," says Ethan Sawyer, founder of the College Essay Guy, a website that offers free and paid essay-writing resources.
College essays and letters of recommendation , Sawyer says, are likely to carry more weight than ever in this admissions cycle. And many essays will likely focus on how the pandemic shaped students' lives throughout an often tumultuous 2020.
But before writing a college essay focused on the coronavirus, students should explore whether it's the best topic for them.

Writing About COVID-19 for a College Application
Much of daily life has been colored by the coronavirus. Virtual learning is the norm at many colleges and high schools, many extracurriculars have vanished and social lives have stalled for students complying with measures to stop the spread of COVID-19.
"For some young people, the pandemic took away what they envisioned as their senior year," says Robert Alexander, dean of admissions, financial aid and enrollment management at the University of Rochester in New York. "Maybe that's a spot on a varsity athletic team or the lead role in the fall play. And it's OK for them to mourn what should have been and what they feel like they lost, but more important is how are they making the most of the opportunities they do have?"
That question, Alexander says, is what colleges want answered if students choose to address COVID-19 in their college essay.
But the question of whether a student should write about the coronavirus is tricky. The answer depends largely on the student.
"In general, I don't think students should write about COVID-19 in their main personal statement for their application," Robin Miller, master college admissions counselor at IvyWise, a college counseling company, wrote in an email.
"Certainly, there may be exceptions to this based on a student's individual experience, but since the personal essay is the main place in the application where the student can really allow their voice to be heard and share insight into who they are as an individual, there are likely many other topics they can choose to write about that are more distinctive and unique than COVID-19," Miller says.
Opinions among admissions experts vary on whether to write about the likely popular topic of the pandemic.
"If your essay communicates something positive, unique, and compelling about you in an interesting and eloquent way, go for it," Carolyn Pippen, principal college admissions counselor at IvyWise, wrote in an email. She adds that students shouldn't be dissuaded from writing about a topic merely because it's common, noting that "topics are bound to repeat, no matter how hard we try to avoid it."
Above all, she urges honesty.
"If your experience within the context of the pandemic has been truly unique, then write about that experience, and the standing out will take care of itself," Pippen says. "If your experience has been generally the same as most other students in your context, then trying to find a unique angle can easily cross the line into exploiting a tragedy, or at least appearing as though you have."
But focusing entirely on the pandemic can limit a student to a single story and narrow who they are in an application, Sawyer says. "There are so many wonderful possibilities for what you can say about yourself outside of your experience within the pandemic."
He notes that passions, strengths, career interests and personal identity are among the multitude of essay topic options available to applicants and encourages them to probe their values to help determine the topic that matters most to them – and write about it.
That doesn't mean the pandemic experience has to be ignored if applicants feel the need to write about it.
Writing About Coronavirus in Main and Supplemental Essays
Students can choose to write a full-length college essay on the coronavirus or summarize their experience in a shorter form.
To help students explain how the pandemic affected them, The Common App has added an optional section to address this topic. Applicants have 250 words to describe their pandemic experience and the personal and academic impact of COVID-19.
"That's not a trick question, and there's no right or wrong answer," Alexander says. Colleges want to know, he adds, how students navigated the pandemic, how they prioritized their time, what responsibilities they took on and what they learned along the way.
If students can distill all of the above information into 250 words, there's likely no need to write about it in a full-length college essay, experts say. And applicants whose lives were not heavily altered by the pandemic may even choose to skip the optional COVID-19 question.
"This space is best used to discuss hardship and/or significant challenges that the student and/or the student's family experienced as a result of COVID-19 and how they have responded to those difficulties," Miller notes. Using the section to acknowledge a lack of impact, she adds, "could be perceived as trite and lacking insight, despite the good intentions of the applicant."
To guard against this lack of awareness, Sawyer encourages students to tap someone they trust to review their writing , whether it's the 250-word Common App response or the full-length essay.
Experts tend to agree that the short-form approach to this as an essay topic works better, but there are exceptions. And if a student does have a coronavirus story that he or she feels must be told, Alexander encourages the writer to be authentic in the essay.
"My advice for an essay about COVID-19 is the same as my advice about an essay for any topic – and that is, don't write what you think we want to read or hear," Alexander says. "Write what really changed you and that story that now is yours and yours alone to tell."
Sawyer urges students to ask themselves, "What's the sentence that only I can write?" He also encourages students to remember that the pandemic is only a chapter of their lives and not the whole book.
Miller, who cautions against writing a full-length essay on the coronavirus, says that if students choose to do so they should have a conversation with their high school counselor about whether that's the right move. And if students choose to proceed with COVID-19 as a topic, she says they need to be clear, detailed and insightful about what they learned and how they adapted along the way.
"Approaching the essay in this manner will provide important balance while demonstrating personal growth and vulnerability," Miller says.
Pippen encourages students to remember that they are in an unprecedented time for college admissions.
"It is important to keep in mind with all of these (admission) factors that no colleges have ever had to consider them this way in the selection process, if at all," Pippen says. "They have had very little time to calibrate their evaluations of different application components within their offices, let alone across institutions. This means that colleges will all be handling the admissions process a little bit differently, and their approaches may even evolve over the course of the admissions cycle."
Searching for a college? Get our complete rankings of Best Colleges.
10 Ways to Discover College Essay Ideas

Tags: students , colleges , college admissions , college applications , college search , Coronavirus
2024 Best Colleges

Search for your perfect fit with the U.S. News rankings of colleges and universities.
College Admissions: Get a Step Ahead!
Sign up to receive the latest updates from U.S. News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
Ask an Alum: Making the Most Out of College
You May Also Like
Supporting low-income college applicants.
Shavar Jeffries April 16, 2024

Supporting Black Women in Higher Ed
Zainab Okolo April 15, 2024

Law Schools With the Highest LSATs
Ilana Kowarski and Cole Claybourn April 11, 2024

Today NAIA, Tomorrow Title IX?
Lauren Camera April 9, 2024

Grad School Housing Options
Anayat Durrani April 9, 2024

How to Decide if an MBA Is Worth it
Sarah Wood March 27, 2024

What to Wear to a Graduation
LaMont Jones, Jr. March 27, 2024

FAFSA Delays Alarm Families, Colleges
Sarah Wood March 25, 2024

Help Your Teen With the College Decision
Anayat Durrani March 25, 2024

Toward Semiconductor Gender Equity
Alexis McKittrick March 22, 2024

Persuasive Essay Guide
Persuasive Essay About Covid19
How to Write a Persuasive Essay About Covid19 | Examples & Tips
11 min read

People also read
A Comprehensive Guide to Writing an Effective Persuasive Essay
200+ Persuasive Essay Topics to Help You Out
Learn How to Create a Persuasive Essay Outline
30+ Free Persuasive Essay Examples To Get You Started
Read Excellent Examples of Persuasive Essay About Gun Control
Crafting a Convincing Persuasive Essay About Abortion
Learn to Write Persuasive Essay About Business With Examples and Tips
Check Out 12 Persuasive Essay About Online Education Examples
Persuasive Essay About Smoking - Making a Powerful Argument with Examples
Are you looking to write a persuasive essay about the Covid-19 pandemic?
Writing a compelling and informative essay about this global crisis can be challenging. It requires researching the latest information, understanding the facts, and presenting your argument persuasively.
But don’t worry! with some guidance from experts, you’ll be able to write an effective and persuasive essay about Covid-19.
In this blog post, we’ll outline the basics of writing a persuasive essay . We’ll provide clear examples, helpful tips, and essential information for crafting your own persuasive piece on Covid-19.
Read on to get started on your essay.
- 1. Steps to Write a Persuasive Essay About Covid-19
- 2. Examples of Persuasive Essay About Covid19
- 3. Examples of Persuasive Essay About Covid-19 Vaccine
- 4. Examples of Persuasive Essay About Covid-19 Integration
- 5. Examples of Argumentative Essay About Covid 19
- 6. Examples of Persuasive Speeches About Covid-19
- 7. Tips to Write a Persuasive Essay About Covid-19
- 8. Common Topics for a Persuasive Essay on COVID-19
Steps to Write a Persuasive Essay About Covid-19
Here are the steps to help you write a persuasive essay on this topic, along with an example essay:
Step 1: Choose a Specific Thesis Statement
Your thesis statement should clearly state your position on a specific aspect of COVID-19. It should be debatable and clear. For example:
Step 2: Research and Gather Information
Collect reliable and up-to-date information from reputable sources to support your thesis statement. This may include statistics, expert opinions, and scientific studies. For instance:
- COVID-19 vaccination effectiveness data
- Information on vaccine mandates in different countries
- Expert statements from health organizations like the WHO or CDC
Step 3: Outline Your Essay
Create a clear and organized outline to structure your essay. A persuasive essay typically follows this structure:
- Introduction
- Background Information
- Body Paragraphs (with supporting evidence)
- Counterarguments (addressing opposing views)
Step 4: Write the Introduction
In the introduction, grab your reader's attention and present your thesis statement. For example:
Step 5: Provide Background Information
Offer context and background information to help your readers understand the issue better. For instance:
Step 6: Develop Body Paragraphs
Each body paragraph should present a single point or piece of evidence that supports your thesis statement. Use clear topic sentences, evidence, and analysis. Here's an example:
Step 7: Address Counterarguments
Acknowledge opposing viewpoints and refute them with strong counterarguments. This demonstrates that you've considered different perspectives. For example:
Step 8: Write the Conclusion
Summarize your main points and restate your thesis statement in the conclusion. End with a strong call to action or thought-provoking statement. For instance:
Step 9: Revise and Proofread
Edit your essay for clarity, coherence, grammar, and spelling errors. Ensure that your argument flows logically.
Step 10: Cite Your Sources
Include proper citations and a bibliography page to give credit to your sources.
Remember to adjust your approach and arguments based on your target audience and the specific angle you want to take in your persuasive essay about COVID-19.
Paper Due? Why Suffer? That's our Job!
Examples of Persuasive Essay About Covid19
When writing a persuasive essay about the Covid-19 pandemic, it’s important to consider how you want to present your argument. To help you get started, here are some example essays for you to read:
Check out some more PDF examples below:
Persuasive Essay About Covid-19 Pandemic
Sample Of Persuasive Essay About Covid-19
Persuasive Essay About Covid-19 In The Philippines - Example
If you're in search of a compelling persuasive essay on business, don't miss out on our “ persuasive essay about business ” blog!
Examples of Persuasive Essay About Covid-19 Vaccine
Covid19 vaccines are one of the ways to prevent the spread of Covid-19, but they have been a source of controversy. Different sides argue about the benefits or dangers of the new vaccines. Whatever your point of view is, writing a persuasive essay about it is a good way of organizing your thoughts and persuading others.
A persuasive essay about the Covid-19 vaccine could consider the benefits of getting vaccinated as well as the potential side effects.
Below are some examples of persuasive essays on getting vaccinated for Covid-19.
Covid19 Vaccine Persuasive Essay
Persuasive Essay on Covid Vaccines
Interested in thought-provoking discussions on abortion? Read our persuasive essay about abortion blog to eplore arguments!
Examples of Persuasive Essay About Covid-19 Integration
Covid19 has drastically changed the way people interact in schools, markets, and workplaces. In short, it has affected all aspects of life. However, people have started to learn to live with Covid19.
Writing a persuasive essay about it shouldn't be stressful. Read the sample essay below to get idea for your own essay about Covid19 integration.
Persuasive Essay About Working From Home During Covid19
Searching for the topic of Online Education? Our persuasive essay about online education is a must-read.
Examples of Argumentative Essay About Covid 19
Covid-19 has been an ever-evolving issue, with new developments and discoveries being made on a daily basis.
Writing an argumentative essay about such an issue is both interesting and challenging. It allows you to evaluate different aspects of the pandemic, as well as consider potential solutions.
Here are some examples of argumentative essays on Covid19.
Argumentative Essay About Covid19 Sample
Argumentative Essay About Covid19 With Introduction Body and Conclusion
Looking for a persuasive take on the topic of smoking? You'll find it all related arguments in out Persuasive Essay About Smoking blog!
Examples of Persuasive Speeches About Covid-19
Do you need to prepare a speech about Covid19 and need examples? We have them for you!
Persuasive speeches about Covid-19 can provide the audience with valuable insights on how to best handle the pandemic. They can be used to advocate for specific changes in policies or simply raise awareness about the virus.
Check out some examples of persuasive speeches on Covid-19:
Persuasive Speech About Covid-19 Example
Persuasive Speech About Vaccine For Covid-19
You can also read persuasive essay examples on other topics to master your persuasive techniques!
Tips to Write a Persuasive Essay About Covid-19
Writing a persuasive essay about COVID-19 requires a thoughtful approach to present your arguments effectively.
Here are some tips to help you craft a compelling persuasive essay on this topic:
Choose a Specific Angle
Start by narrowing down your focus. COVID-19 is a broad topic, so selecting a specific aspect or issue related to it will make your essay more persuasive and manageable. For example, you could focus on vaccination, public health measures, the economic impact, or misinformation.
Provide Credible Sources
Support your arguments with credible sources such as scientific studies, government reports, and reputable news outlets. Reliable sources enhance the credibility of your essay.
Use Persuasive Language
Employ persuasive techniques, such as ethos (establishing credibility), pathos (appealing to emotions), and logos (using logic and evidence). Use vivid examples and anecdotes to make your points relatable.
Organize Your Essay
Structure your essay involves creating a persuasive essay outline and establishing a logical flow from one point to the next. Each paragraph should focus on a single point, and transitions between paragraphs should be smooth and logical.
Emphasize Benefits
Highlight the benefits of your proposed actions or viewpoints. Explain how your suggestions can improve public health, safety, or well-being. Make it clear why your audience should support your position.
Use Visuals -H3
Incorporate graphs, charts, and statistics when applicable. Visual aids can reinforce your arguments and make complex data more accessible to your readers.
Call to Action
End your essay with a strong call to action. Encourage your readers to take a specific step or consider your viewpoint. Make it clear what you want them to do or think after reading your essay.
Revise and Edit
Proofread your essay for grammar, spelling, and clarity. Make sure your arguments are well-structured and that your writing flows smoothly.
Seek Feedback
Have someone else read your essay to get feedback. They may offer valuable insights and help you identify areas where your persuasive techniques can be improved.
Tough Essay Due? Hire Tough Writers!
Common Topics for a Persuasive Essay on COVID-19
Here are some persuasive essay topics on COVID-19:
- The Importance of Vaccination Mandates for COVID-19 Control
- Balancing Public Health and Personal Freedom During a Pandemic
- The Economic Impact of Lockdowns vs. Public Health Benefits
- The Role of Misinformation in Fueling Vaccine Hesitancy
- Remote Learning vs. In-Person Education: What's Best for Students?
- The Ethics of Vaccine Distribution: Prioritizing Vulnerable Populations
- The Mental Health Crisis Amidst the COVID-19 Pandemic
- The Long-Term Effects of COVID-19 on Healthcare Systems
- Global Cooperation vs. Vaccine Nationalism in Fighting the Pandemic
- The Future of Telemedicine: Expanding Healthcare Access Post-COVID-19
In search of more inspiring topics for your next persuasive essay? Our persuasive essay topics blog has plenty of ideas!
To sum it up,
You have read good sample essays and got some helpful tips. You now have the tools you needed to write a persuasive essay about Covid-19. So don't let the doubts stop you, start writing!
If you need professional writing help, don't worry! We've got that for you as well.
MyPerfectWords.com is a professional essay writing service that can help you craft an excellent persuasive essay on Covid-19. Our experienced essay writer will create a well-structured, insightful paper in no time!
So don't hesitate and get in touch with our persuasive essay writing service today!
Frequently Asked Questions
Are there any ethical considerations when writing a persuasive essay about covid-19.
Yes, there are ethical considerations when writing a persuasive essay about COVID-19. It's essential to ensure the information is accurate, not contribute to misinformation, and be sensitive to the pandemic's impact on individuals and communities. Additionally, respecting diverse viewpoints and emphasizing public health benefits can promote ethical communication.
What impact does COVID-19 have on society?
The impact of COVID-19 on society is far-reaching. It has led to job and economic losses, an increase in stress and mental health disorders, and changes in education systems. It has also had a negative effect on social interactions, as people have been asked to limit their contact with others.

Write Essay Within 60 Seconds!

Caleb S. has been providing writing services for over five years and has a Masters degree from Oxford University. He is an expert in his craft and takes great pride in helping students achieve their academic goals. Caleb is a dedicated professional who always puts his clients first.

Paper Due? Why Suffer? That’s our Job!
Keep reading

- Newsletters
Site search
- Israel-Hamas war
- 2024 election
- Solar eclipse
- Supreme Court
- All explainers
- Future Perfect
Filed under:
Read these 12 moving essays about life during coronavirus
Artists, novelists, critics, and essayists are writing the first draft of history.
Share this story
- Share this on Facebook
- Share this on Twitter
- Share this on Reddit
- Share All sharing options
Share All sharing options for: Read these 12 moving essays about life during coronavirus
/cdn.vox-cdn.com/uploads/chorus_image/image/66606035/1207638131.jpg.0.jpg)
The world is grappling with an invisible, deadly enemy, trying to understand how to live with the threat posed by a virus . For some writers, the only way forward is to put pen to paper, trying to conceptualize and document what it feels like to continue living as countries are under lockdown and regular life seems to have ground to a halt.
So as the coronavirus pandemic has stretched around the world, it’s sparked a crop of diary entries and essays that describe how life has changed. Novelists, critics, artists, and journalists have put words to the feelings many are experiencing. The result is a first draft of how we’ll someday remember this time, filled with uncertainty and pain and fear as well as small moments of hope and humanity.
At the New York Review of Books, Ali Bhutto writes that in Karachi, Pakistan, the government-imposed curfew due to the virus is “eerily reminiscent of past military clampdowns”:
Beneath the quiet calm lies a sense that society has been unhinged and that the usual rules no longer apply. Small groups of pedestrians look on from the shadows, like an audience watching a spectacle slowly unfolding. People pause on street corners and in the shade of trees, under the watchful gaze of the paramilitary forces and the police.
His essay concludes with the sobering note that “in the minds of many, Covid-19 is just another life-threatening hazard in a city that stumbles from one crisis to another.”
Writing from Chattanooga, novelist Jamie Quatro documents the mixed ways her neighbors have been responding to the threat, and the frustration of conflicting direction, or no direction at all, from local, state, and federal leaders:
Whiplash, trying to keep up with who’s ordering what. We’re already experiencing enough chaos without this back-and-forth. Why didn’t the federal government issue a nationwide shelter-in-place at the get-go, the way other countries did? What happens when one state’s shelter-in-place ends, while others continue? Do states still under quarantine close their borders? We are still one nation, not fifty individual countries. Right?
Award-winning photojournalist Alessio Mamo, quarantined with his partner Marta in Sicily after she tested positive for the virus, accompanies his photographs in the Guardian of their confinement with a reflection on being confined :
The doctors asked me to take a second test, but again I tested negative. Perhaps I’m immune? The days dragged on in my apartment, in black and white, like my photos. Sometimes we tried to smile, imagining that I was asymptomatic, because I was the virus. Our smiles seemed to bring good news. My mother left hospital, but I won’t be able to see her for weeks. Marta started breathing well again, and so did I. I would have liked to photograph my country in the midst of this emergency, the battles that the doctors wage on the frontline, the hospitals pushed to their limits, Italy on its knees fighting an invisible enemy. That enemy, a day in March, knocked on my door instead.
In the New York Times Magazine, deputy editor Jessica Lustig writes with devastating clarity about her family’s life in Brooklyn while her husband battled the virus, weeks before most people began taking the threat seriously:
At the door of the clinic, we stand looking out at two older women chatting outside the doorway, oblivious. Do I wave them away? Call out that they should get far away, go home, wash their hands, stay inside? Instead we just stand there, awkwardly, until they move on. Only then do we step outside to begin the long three-block walk home. I point out the early magnolia, the forsythia. T says he is cold. The untrimmed hairs on his neck, under his beard, are white. The few people walking past us on the sidewalk don’t know that we are visitors from the future. A vision, a premonition, a walking visitation. This will be them: Either T, in the mask, or — if they’re lucky — me, tending to him.
Essayist Leslie Jamison writes in the New York Review of Books about being shut away alone in her New York City apartment with her 2-year-old daughter since she became sick:
The virus. Its sinewy, intimate name. What does it feel like in my body today? Shivering under blankets. A hot itch behind the eyes. Three sweatshirts in the middle of the day. My daughter trying to pull another blanket over my body with her tiny arms. An ache in the muscles that somehow makes it hard to lie still. This loss of taste has become a kind of sensory quarantine. It’s as if the quarantine keeps inching closer and closer to my insides. First I lost the touch of other bodies; then I lost the air; now I’ve lost the taste of bananas. Nothing about any of these losses is particularly unique. I’ve made a schedule so I won’t go insane with the toddler. Five days ago, I wrote Walk/Adventure! on it, next to a cut-out illustration of a tiger—as if we’d see tigers on our walks. It was good to keep possibility alive.
At Literary Hub, novelist Heidi Pitlor writes about the elastic nature of time during her family’s quarantine in Massachusetts:
During a shutdown, the things that mark our days—commuting to work, sending our kids to school, having a drink with friends—vanish and time takes on a flat, seamless quality. Without some self-imposed structure, it’s easy to feel a little untethered. A friend recently posted on Facebook: “For those who have lost track, today is Blursday the fortyteenth of Maprilay.” ... Giving shape to time is especially important now, when the future is so shapeless. We do not know whether the virus will continue to rage for weeks or months or, lord help us, on and off for years. We do not know when we will feel safe again. And so many of us, minus those who are gifted at compartmentalization or denial, remain largely captive to fear. We may stay this way if we do not create at least the illusion of movement in our lives, our long days spent with ourselves or partners or families.
Novelist Lauren Groff writes at the New York Review of Books about trying to escape the prison of her fears while sequestered at home in Gainesville, Florida:
Some people have imaginations sparked only by what they can see; I blame this blinkered empiricism for the parks overwhelmed with people, the bars, until a few nights ago, thickly thronged. My imagination is the opposite. I fear everything invisible to me. From the enclosure of my house, I am afraid of the suffering that isn’t present before me, the people running out of money and food or drowning in the fluid in their lungs, the deaths of health-care workers now growing ill while performing their duties. I fear the federal government, which the right wing has so—intentionally—weakened that not only is it insufficient to help its people, it is actively standing in help’s way. I fear we won’t sufficiently punish the right. I fear leaving the house and spreading the disease. I fear what this time of fear is doing to my children, their imaginations, and their souls.
At ArtForum , Berlin-based critic and writer Kristian Vistrup Madsen reflects on martinis, melancholia, and Finnish artist Jaakko Pallasvuo’s 2018 graphic novel Retreat , in which three young people exile themselves in the woods:
In melancholia, the shape of what is ending, and its temporality, is sprawling and incomprehensible. The ambivalence makes it hard to bear. The world of Retreat is rendered in lush pink and purple watercolors, which dissolve into wild and messy abstractions. In apocalypse, the divisions established in genesis bleed back out. My own Corona-retreat is similarly soft, color-field like, each day a blurred succession of quarantinis, YouTube–yoga, and televized press conferences. As restrictions mount, so does abstraction. For now, I’m still rooting for love to save the world.
At the Paris Review , Matt Levin writes about reading Virginia Woolf’s novel The Waves during quarantine:
A retreat, a quarantine, a sickness—they simultaneously distort and clarify, curtail and expand. It is an ideal state in which to read literature with a reputation for difficulty and inaccessibility, those hermetic books shorn of the handholds of conventional plot or characterization or description. A novel like Virginia Woolf’s The Waves is perfect for the state of interiority induced by quarantine—a story of three men and three women, meeting after the death of a mutual friend, told entirely in the overlapping internal monologues of the six, interspersed only with sections of pure, achingly beautiful descriptions of the natural world, a day’s procession and recession of light and waves. The novel is, in my mind’s eye, a perfectly spherical object. It is translucent and shimmering and infinitely fragile, prone to shatter at the slightest disturbance. It is not a book that can be read in snatches on the subway—it demands total absorption. Though it revels in a stark emotional nakedness, the book remains aloof, remote in its own deep self-absorption.
In an essay for the Financial Times, novelist Arundhati Roy writes with anger about Indian Prime Minister Narendra Modi’s anemic response to the threat, but also offers a glimmer of hope for the future:
Historically, pandemics have forced humans to break with the past and imagine their world anew. This one is no different. It is a portal, a gateway between one world and the next. We can choose to walk through it, dragging the carcasses of our prejudice and hatred, our avarice, our data banks and dead ideas, our dead rivers and smoky skies behind us. Or we can walk through lightly, with little luggage, ready to imagine another world. And ready to fight for it.
From Boston, Nora Caplan-Bricker writes in The Point about the strange contraction of space under quarantine, in which a friend in Beirut is as close as the one around the corner in the same city:
It’s a nice illusion—nice to feel like we’re in it together, even if my real world has shrunk to one person, my husband, who sits with his laptop in the other room. It’s nice in the same way as reading those essays that reframe social distancing as solidarity. “We must begin to see the negative space as clearly as the positive, to know what we don’t do is also brilliant and full of love,” the poet Anne Boyer wrote on March 10th, the day that Massachusetts declared a state of emergency. If you squint, you could almost make sense of this quarantine as an effort to flatten, along with the curve, the distinctions we make between our bonds with others. Right now, I care for my neighbor in the same way I demonstrate love for my mother: in all instances, I stay away. And in moments this month, I have loved strangers with an intensity that is new to me. On March 14th, the Saturday night after the end of life as we knew it, I went out with my dog and found the street silent: no lines for restaurants, no children on bicycles, no couples strolling with little cups of ice cream. It had taken the combined will of thousands of people to deliver such a sudden and complete emptiness. I felt so grateful, and so bereft.
And on his own website, musician and artist David Byrne writes about rediscovering the value of working for collective good , saying that “what is happening now is an opportunity to learn how to change our behavior”:
In emergencies, citizens can suddenly cooperate and collaborate. Change can happen. We’re going to need to work together as the effects of climate change ramp up. In order for capitalism to survive in any form, we will have to be a little more socialist. Here is an opportunity for us to see things differently — to see that we really are all connected — and adjust our behavior accordingly. Are we willing to do this? Is this moment an opportunity to see how truly interdependent we all are? To live in a world that is different and better than the one we live in now? We might be too far down the road to test every asymptomatic person, but a change in our mindsets, in how we view our neighbors, could lay the groundwork for the collective action we’ll need to deal with other global crises. The time to see how connected we all are is now.
The portrait these writers paint of a world under quarantine is multifaceted. Our worlds have contracted to the confines of our homes, and yet in some ways we’re more connected than ever to one another. We feel fear and boredom, anger and gratitude, frustration and strange peace. Uncertainty drives us to find metaphors and images that will let us wrap our minds around what is happening.
Yet there’s no single “what” that is happening. Everyone is contending with the pandemic and its effects from different places and in different ways. Reading others’ experiences — even the most frightening ones — can help alleviate the loneliness and dread, a little, and remind us that what we’re going through is both unique and shared by all.
Will you support Vox today?
We believe that everyone deserves to understand the world that they live in. That kind of knowledge helps create better citizens, neighbors, friends, parents, and stewards of this planet. Producing deeply researched, explanatory journalism takes resources. You can support this mission by making a financial gift to Vox today. Will you join us?
We accept credit card, Apple Pay, and Google Pay. You can also contribute via
Next Up In Culture
Sign up for the newsletter today, explained.
Understand the world with a daily explainer plus the most compelling stories of the day.
Thanks for signing up!
Check your inbox for a welcome email.
Oops. Something went wrong. Please enter a valid email and try again.

What the Supreme Court case on tent encampments could mean for homeless people

Will AI mean the end of liberal democracy?

Israel and Iran’s conflict enters a new, dangerous phase

Trump’s jury doesn’t have to like him to be fair to him

What’s behind the latest right-wing revolt against Mike Johnson

Taylor Swift seems sick of being everyone’s best friend
I Thought We’d Learned Nothing From the Pandemic. I Wasn’t Seeing the Full Picture

M y first home had a back door that opened to a concrete patio with a giant crack down the middle. When my sister and I played, I made sure to stay on the same side of the divide as her, just in case. The 1988 film The Land Before Time was one of the first movies I ever saw, and the image of the earth splintering into pieces planted its roots in my brain. I believed that, even in my own backyard, I could easily become the tiny Triceratops separated from her family, on the other side of the chasm, as everything crumbled into chaos.
Some 30 years later, I marvel at the eerie, unexpected ways that cartoonish nightmare came to life – not just for me and my family, but for all of us. The landscape was already covered in fissures well before COVID-19 made its way across the planet, but the pandemic applied pressure, and the cracks broke wide open, separating us from each other physically and ideologically. Under the weight of the crisis, we scattered and landed on such different patches of earth we could barely see each other’s faces, even when we squinted. We disagreed viciously with each other, about how to respond, but also about what was true.
Recently, someone asked me if we’ve learned anything from the pandemic, and my first thought was a flat no. Nothing. There was a time when I thought it would be the very thing to draw us together and catapult us – as a capital “S” Society – into a kinder future. It’s surreal to remember those early days when people rallied together, sewing masks for health care workers during critical shortages and gathering on balconies in cities from Dallas to New York City to clap and sing songs like “Yellow Submarine.” It felt like a giant lightning bolt shot across the sky, and for one breath, we all saw something that had been hidden in the dark – the inherent vulnerability in being human or maybe our inescapable connectedness .
More from TIME
Read More: The Family Time the Pandemic Stole
But it turns out, it was just a flash. The goodwill vanished as quickly as it appeared. A couple of years later, people feel lied to, abandoned, and all on their own. I’ve felt my own curiosity shrinking, my willingness to reach out waning , my ability to keep my hands open dwindling. I look out across the landscape and see selfishness and rage, burnt earth and so many dead bodies. Game over. We lost. And if we’ve already lost, why try?
Still, the question kept nagging me. I wondered, am I seeing the full picture? What happens when we focus not on the collective society but at one face, one story at a time? I’m not asking for a bow to minimize the suffering – a pretty flourish to put on top and make the whole thing “worth it.” Yuck. That’s not what we need. But I wondered about deep, quiet growth. The kind we feel in our bodies, relationships, homes, places of work, neighborhoods.
Like a walkie-talkie message sent to my allies on the ground, I posted a call on my Instagram. What do you see? What do you hear? What feels possible? Is there life out here? Sprouting up among the rubble? I heard human voices calling back – reports of life, personal and specific. I heard one story at a time – stories of grief and distrust, fury and disappointment. Also gratitude. Discovery. Determination.
Among the most prevalent were the stories of self-revelation. Almost as if machines were given the chance to live as humans, people described blossoming into fuller selves. They listened to their bodies’ cues, recognized their desires and comforts, tuned into their gut instincts, and honored the intuition they hadn’t realized belonged to them. Alex, a writer and fellow disabled parent, found the freedom to explore a fuller version of herself in the privacy the pandemic provided. “The way I dress, the way I love, and the way I carry myself have both shrunk and expanded,” she shared. “I don’t love myself very well with an audience.” Without the daily ritual of trying to pass as “normal” in public, Tamar, a queer mom in the Netherlands, realized she’s autistic. “I think the pandemic helped me to recognize the mask,” she wrote. “Not that unmasking is easy now. But at least I know it’s there.” In a time of widespread suffering that none of us could solve on our own, many tended to our internal wounds and misalignments, large and small, and found clarity.
Read More: A Tool for Staying Grounded in This Era of Constant Uncertainty
I wonder if this flourishing of self-awareness is at least partially responsible for the life alterations people pursued. The pandemic broke open our personal notions of work and pushed us to reevaluate things like time and money. Lucy, a disabled writer in the U.K., made the hard decision to leave her job as a journalist covering Westminster to write freelance about her beloved disability community. “This work feels important in a way nothing else has ever felt,” she wrote. “I don’t think I’d have realized this was what I should be doing without the pandemic.” And she wasn’t alone – many people changed jobs , moved, learned new skills and hobbies, became politically engaged.
Perhaps more than any other shifts, people described a significant reassessment of their relationships. They set boundaries, said no, had challenging conversations. They also reconnected, fell in love, and learned to trust. Jeanne, a quilter in Indiana, got to know relatives she wouldn’t have connected with if lockdowns hadn’t prompted weekly family Zooms. “We are all over the map as regards to our belief systems,” she emphasized, “but it is possible to love people you don’t see eye to eye with on every issue.” Anna, an anti-violence advocate in Maine, learned she could trust her new marriage: “Life was not a honeymoon. But we still chose to turn to each other with kindness and curiosity.” So many bonds forged and broken, strengthened and strained.
Instead of relying on default relationships or institutional structures, widespread recalibrations allowed for going off script and fortifying smaller communities. Mara from Idyllwild, Calif., described the tangible plan for care enacted in her town. “We started a mutual-aid group at the beginning of the pandemic,” she wrote, “and it grew so quickly before we knew it we were feeding 400 of the 4000 residents.” She didn’t pretend the conditions were ideal. In fact, she expressed immense frustration with our collective response to the pandemic. Even so, the local group rallied and continues to offer assistance to their community with help from donations and volunteers (many of whom were originally on the receiving end of support). “I’ve learned that people thrive when they feel their connection to others,” she wrote. Clare, a teacher from the U.K., voiced similar conviction as she described a giant scarf she’s woven out of ribbons, each representing a single person. The scarf is “a collection of stories, moments and wisdom we are sharing with each other,” she wrote. It now stretches well over 1,000 feet.
A few hours into reading the comments, I lay back on my bed, phone held against my chest. The room was quiet, but my internal world was lighting up with firefly flickers. What felt different? Surely part of it was receiving personal accounts of deep-rooted growth. And also, there was something to the mere act of asking and listening. Maybe it connected me to humans before battle cries. Maybe it was the chance to be in conversation with others who were also trying to understand – what is happening to us? Underneath it all, an undeniable thread remained; I saw people peering into the mess and narrating their findings onto the shared frequency. Every comment was like a flare into the sky. I’m here! And if the sky is full of flares, we aren’t alone.
I recognized my own pandemic discoveries – some minor, others massive. Like washing off thick eyeliner and mascara every night is more effort than it’s worth; I can transform the mundane into the magical with a bedsheet, a movie projector, and twinkle lights; my paralyzed body can mother an infant in ways I’d never seen modeled for me. I remembered disappointing, bewildering conversations within my own family of origin and our imperfect attempts to remain close while also seeing things so differently. I realized that every time I get the weekly invite to my virtual “Find the Mumsies” call, with a tiny group of moms living hundreds of miles apart, I’m being welcomed into a pocket of unexpected community. Even though we’ve never been in one room all together, I’ve felt an uncommon kind of solace in their now-familiar faces.
Hope is a slippery thing. I desperately want to hold onto it, but everywhere I look there are real, weighty reasons to despair. The pandemic marks a stretch on the timeline that tangles with a teetering democracy, a deteriorating planet , the loss of human rights that once felt unshakable . When the world is falling apart Land Before Time style, it can feel trite, sniffing out the beauty – useless, firing off flares to anyone looking for signs of life. But, while I’m under no delusions that if we just keep trudging forward we’ll find our own oasis of waterfalls and grassy meadows glistening in the sunshine beneath a heavenly chorus, I wonder if trivializing small acts of beauty, connection, and hope actually cuts us off from resources essential to our survival. The group of abandoned dinosaurs were keeping each other alive and making each other laugh well before they made it to their fantasy ending.
Read More: How Ice Cream Became My Own Personal Act of Resistance
After the monarch butterfly went on the endangered-species list, my friend and fellow writer Hannah Soyer sent me wildflower seeds to plant in my yard. A simple act of big hope – that I will actually plant them, that they will grow, that a monarch butterfly will receive nourishment from whatever blossoms are able to push their way through the dirt. There are so many ways that could fail. But maybe the outcome wasn’t exactly the point. Maybe hope is the dogged insistence – the stubborn defiance – to continue cultivating moments of beauty regardless. There is value in the planting apart from the harvest.
I can’t point out a single collective lesson from the pandemic. It’s hard to see any great “we.” Still, I see the faces in my moms’ group, making pancakes for their kids and popping on between strings of meetings while we try to figure out how to raise these small people in this chaotic world. I think of my friends on Instagram tending to the selves they discovered when no one was watching and the scarf of ribbons stretching the length of more than three football fields. I remember my family of three, holding hands on the way up the ramp to the library. These bits of growth and rings of support might not be loud or right on the surface, but that’s not the same thing as nothing. If we only cared about the bottom-line defeats or sweeping successes of the big picture, we’d never plant flowers at all.
More Must-Reads From TIME
- The 100 Most Influential People of 2024
- The Revolution of Yulia Navalnaya
- 6 Compliments That Land Every Time
- What's the Deal With the Bitcoin Halving?
- If You're Dating Right Now , You're Brave: Column
- The AI That Could Heal a Divided Internet
- Fallout Is a Brilliant Model for the Future of Video Game Adaptations
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]
/media/video/upload/Opener_rt.mp4)
How Science Beat the Virus
And what it lost in the process

Listen to this article
Listen to more stories on audm
This article was published online on December 14, 2020.
In fall of 2019, exactly zero scientists were studying COVID‑19, because no one knew the disease existed. The coronavirus that causes it, SARS‑CoV‑2, had only recently jumped into humans and had been neither identified nor named. But by the end of March 2020, it had spread to more than 170 countries, sickened more than 750,000 people, and triggered the biggest pivot in the history of modern science. Thousands of researchers dropped whatever intellectual puzzles had previously consumed their curiosity and began working on the pandemic instead. In mere months, science became thoroughly COVID-ized.
As of this writing, the biomedical library PubMed lists more than 74,000 COVID-related scientific papers—more than twice as many as there are about polio, measles, cholera, dengue, or other diseases that have plagued humanity for centuries. Only 9,700 Ebola-related papers have been published since its discovery in 1976; last year, at least one journal received more COVID‑19 papers than that for consideration. By September, the prestigious New England Journal of Medicine had received 30,000 submissions—16,000 more than in all of 2019. “All that difference is COVID‑19,” Eric Rubin, NEJM ’s editor in chief, says. Francis Collins, the director of the National Institutes of Health, told me, “The way this has resulted in a shift in scientific priorities has been unprecedented.”
Much like famous initiatives such as the Manhattan Project and the Apollo program, epidemics focus the energies of large groups of scientists. In the U.S., the influenza pandemic of 1918, the threat of malaria in the tropical battlegrounds of World War II, and the rise of polio in the postwar years all triggered large pivots. Recent epidemics of Ebola and Zika each prompted a temporary burst of funding and publications . But “nothing in history was even close to the level of pivoting that’s happening right now,” Madhukar Pai of McGill University told me.
That’s partly because there are just more scientists: From 1960 to 2010, the number of biological or medical researchers in the U.S. increased sevenfold , from just 30,000 to more than 220,000. But SARS-CoV-2 has also spread farther and faster than any new virus in a century. For Western scientists, it wasn’t a faraway threat like Ebola. It threatened to inflame their lungs. It shut down their labs. “It hit us at home,” Pai said.
In a survey of 2,500 researchers in the U.S., Canada, and Europe, Kyle Myers from Harvard and his team found that 32 percent had shifted their focus toward the pandemic. Neuroscientists who study the sense of smell started investigating why COVID‑19 patients tend to lose theirs. Physicists who had previously experienced infectious diseases only by contracting them found themselves creating models to inform policy makers. Michael D. L. Johnson at the University of Arizona normally studies copper’s toxic effects on bacteria. But when he learned that SARS‑CoV‑2 persists for less time on copper surfaces than on other materials, he partially pivoted to see how the virus might be vulnerable to the metal. No other disease has been scrutinized so intensely, by so much combined intellect, in so brief a time.
These efforts have already paid off. New diagnostic tests can detect the virus within minutes. Massive open data sets of viral genomes and COVID‑19 cases have produced the most detailed picture yet of a new disease’s evolution. Vaccines are being developed with record-breaking speed. SARS‑CoV‑2 will be one of the most thoroughly characterized of all pathogens, and the secrets it yields will deepen our understanding of other viruses, leaving the world better prepared to face the next pandemic.
But the COVID‑19 pivot has also revealed the all-too-human frailties of the scientific enterprise . Flawed research made the pandemic more confusing, influencing misguided policies. Clinicians wasted millions of dollars on trials that were so sloppy as to be pointless. Overconfident poseurs published misleading work on topics in which they had no expertise. Racial and gender inequalities in the scientific field widened.
Amid a long winter of sickness , it’s hard not to focus on the political failures that led us to a third surge. But when people look back on this period, decades from now, they will also tell stories, both good and bad, about this extraordinary moment for science. At its best, science is a self-correcting march toward greater knowledge for the betterment of humanity. At its worst, it is a self-interested pursuit of greater prestige at the cost of truth and rigor. The pandemic brought both aspects to the fore. Humanity will benefit from the products of the COVID‑19 pivot. Science itself will too, if it learns from the experience.
In February, Jennifer Doudna, one of America’s most prominent scientists, was still focused on CRISPR—the gene-editing tool that she’d co-discovered and that won her a Nobel Prize in October. But when her son’s high school shut down and UC Berkeley, her university, closed its campus, the severity of the impending pandemic became clear. “In three weeks, I went from thinking we’re still okay to thinking that my whole life is going to change,” she told me. On March 13, she and dozens of colleagues at the Innovative Genomics Institute, which she leads, agreed to pause most of their ongoing projects and redirect their skills to addressing COVID‑19. They worked on CRISPR-based diagnostic tests. Because existing tests were in short supply, they converted lab space into a pop-up testing facility to serve the local community. “We need to make our expertise relevant to whatever is happening right now,” she said.
Scientists who’d already been studying other emerging diseases were even quicker off the mark. Lauren Gardner, an engineering professor at Johns Hopkins University who has studied dengue and Zika, knew that new epidemics are accompanied by a dearth of real-time data. So she and one of her students created an online global dashboard to map and tally all publicly reported COVID‑19 cases and deaths. After one night of work, they released it, on January 22. The dashboard has since been accessed daily by governments, public-health agencies, news organizations, and anxious citizens.
Studying deadly viruses is challenging at the best of times, and was especially so this past year. To handle SARS‑CoV‑2, scientists must work in “biosafety level 3” labs, fitted with special airflow systems and other extreme measures; although the actual number is not known, an estimated 200 such facilities exist in the U.S. Researchers often test new drugs and vaccines on monkeys before proceeding to human trials, but the U.S. is facing a monkey shortage after China stopped exporting the animals, possibly because it needed them for research. And other biomedical research is now more difficult because of physical-distancing requirements. “Usually we had people packed in, but with COVID, we do shift work,” Akiko Iwasaki, a Yale immunologist, told me. “People are coming in at ridiculous hours” to protect themselves from the very virus they are trying to study.
Recommended Reading

What the Chaos in Hospitals Is Doing to Doctors

How the Pandemic Defeated America

The Logic of the Filing Cabinet Is Everywhere
Experts on emerging diseases are scarce: These threats go neglected by the public in the lulls between epidemics. “Just a year ago I had to explain to people why I was studying coronaviruses,” says Lisa Gralinski of the University of North Carolina at Chapel Hill. “That’s never going to be a concern again.” Stressed and stretched, she and other emerging-disease researchers were also conscripted into unfamiliar roles. They’re acting as makeshift advisers to businesses, schools, and local governments. They’re barraged by interview requests from journalists. They’re explaining the nuances of the pandemic on Twitter, to huge new follower counts. “It’s often the same person who’s helping the Namibian government to manage malaria outbreaks and is now being pulled into helping Maryland manage COVID‑19,” Gardner told me.
But the newfound global interest in viruses also means “you have a lot more people you can talk through problems with,” Pardis Sabeti, a computational geneticist at the Broad Institute of MIT and Harvard, told me. Indeed, COVID‑19 papers are more likely than typical biomedical studies to have authors who had never published together before, according to a team led by Ying Ding, who works at the University of Texas at Austin.
Fast-forming alliances could work at breakneck speed because many researchers had spent the past few decades transforming science from a plodding, cloistered endeavor into something nimbler and more transparent. Traditionally, a scientist submits her paper to a journal, which sends it to a (surprisingly small) group of peers for (several rounds of usually anonymous) comments; if the paper passes this (typically months-long) peer-review gantlet, it is published (often behind an expensive paywall). Languid and opaque, this system is ill-suited to a fast-moving outbreak. But biomedical scientists can now upload preliminary versions of their papers, or “preprints,” to freely accessible websites, allowing others to immediately dissect and build upon their results. This practice had been slowly gaining popularity before 2020, but proved so vital for sharing information about COVID‑19 that it will likely become a mainstay of modern biomedical research. Preprints accelerate science, and the pandemic accelerated the use of preprints. At the start of the year, one repository, medRxiv (pronounced “med archive”), held about 1,000 preprints. By the end of October, it had more than 12,000.
Open data sets and sophisticated new tools to manipulate them have likewise made today’s researchers more flexible. SARS‑CoV‑2’s genome was decoded and shared by Chinese scientists just 10 days after the first cases were reported. By November, more than 197,000 SARS‑CoV‑2 genomes had been sequenced. About 90 years ago, no one had even seen an individual virus; today, scientists have reconstructed the shape of SARS‑CoV‑2 down to the position of individual atoms. Researchers have begun to uncover how SARS‑CoV‑2 compares with other coronaviruses in wild bats, the likely reservoir; how it infiltrates and co-opts our cells; how the immune system overreacts to it, creating the symptoms of COVID‑19. “We’re learning about this virus faster than we’ve ever learned about any virus in history,” Sabeti said.
By March, the odds of quickly eradicating the new coronavirus looked slim. A vaccine became the likeliest endgame, and the race to create one was a resounding success. The process normally takes years, but as I write this, 54 different vaccines are being tested for safety and efficacy, and 12 have entered Phase 3 clinical trials—the final checkpoint. As of this writing, Pfizer/BioNTech and Moderna have announced that, based on preliminary results from these trials, their respective vaccines are roughly 95 percent effective at preventing COVID‑19. * “We went from a virus whose sequence was only known in January, and now in the fall, we’re finishing— finishing —a Phase 3 trial,” Anthony Fauci, the director of the National Institute of Allergy and Infectious Diseases and a member of the White House’s coronavirus task force, told me. “Holy mackerel.”
Most vaccines comprise dead, weakened, or fragmented pathogens, and must be made from scratch whenever a new threat emerges. But over the past decade, the U.S. and other countries have moved away from this slow “one bug, one drug” approach. Instead, they’ve invested in so-called platform technologies, in which a standard chassis can be easily customized with different payloads that target new viruses. For example, the Pfizer/BioNTech and Moderna vaccines both consist of nanoparticles that contain pieces of SARS‑CoV‑2’s genetic material—its mRNA. When volunteers are injected with these particles, their cells use the mRNA to reconstruct a noninfectious fragment of the virus, allowing their immune system to prepare antibodies that neutralize it. No company has ever brought an mRNA vaccine to market before, but because the basic platform had already been refined, researchers could quickly repurpose it with SARS‑CoV‑2’s mRNA. Moderna got its vaccine into Phase 1 clinical trials on March 16, just 66 days after the new virus’s genome was first uploaded—far faster than any pre-COVID vaccine.
Meanwhile, companies compressed the process of vaccine development by running what would normally be sequential steps in parallel, while still checking for safety and efficacy. The federal government’s Operation Warp Speed, an effort to accelerate vaccine distribution, funded several companies at once—an unusual move. It preordered doses and invested in manufacturing facilities before trials were complete, reducing the risk for pharmaceutical companies looking to participate. Ironically, federal ineptitude at containing SARS‑CoV‑2 helped too. In the U.S., “the fact that the virus is everywhere makes it easier to gauge the performance of a vaccine,” says Natalie Dean of the University of Florida, who studies vaccine trials. “You can’t do a [Phase 3] vaccine trial in South Korea,” because the outbreak there is under control.
Read: How the pandemic will end
Vaccines will not immediately end the pandemic . Millions of doses will have to be manufactured, allocated, and distributed ; large numbers of Americans could refuse the vaccine ; and how long vaccine-induced immunity will last is still unclear. In the rosiest scenario, the Pfizer/BioNTech and Moderna vaccines are approved and smoothly rolled out over the next 12 months. By the end of the year, the U.S. achieves herd immunity, after which the virus struggles to find susceptible hosts. It still circulates, but outbreaks are sporadic and short-lived. Schools and businesses reopen. Families hug tightly and celebrate joyously over Thanksgiving and Christmas.
And the next time a mystery pathogen emerges, scientists hope to quickly slot its genetic material into proven platforms, and move the resulting vaccines through the same speedy pipelines that were developed during this pandemic. “I don’t think the world of vaccine development will ever be the same again,” says Nicole Lurie of the Coalition for Epidemic Preparedness Innovations.
As fast as the vaccine-development process was, it could have been faster. Despite the stakes, some pharmaceutical companies with relevant expertise chose not to enter the race, perhaps dissuaded by intense competition. Instead, from February to May, the sector roughly tripled its efforts to develop drugs to treat COVID‑19, according to Kevin Bryan, an economist at the University of Toronto. The decades-old steroid dexamethasone turned out to reduce death rates among severely ill patients on ventilators by more than 12 percent. Early hints suggest that newer treatments such as the monoclonal-antibody therapy bamlanivimab, which was just approved for emergency use by the FDA, could help newly infected patients who have not yet been hospitalized. But although these wins are significant, they are scarce. Most drugs haven’t been effective. Health-care workers became better at saving hospitalized patients more through improvements in basic medical care than through pharmaceutical panaceas—a predictable outcome, because antiviral drugs tend to offer only modest benefits.
The quest for COVID‑19 treatments was slowed by a torrent of shoddy studies whose results were meaningless at best and misleading at worst. Many of the thousands of clinical trials that were launched were too small to produce statistically solid results. Some lacked a control group—a set of comparable patients who received a placebo, and who provided a baseline against which the effects of a drug could be judged. Other trials needlessly overlapped. At least 227 involved hydroxychloroquine—the antimalarial drug that Donald Trump hyped for months. A few large trials eventually confirmed that hydroxychloroquine does nothing for COVID‑19 patients, but not before hundreds of thousands of people were recruited into pointlessly small studies . More than 100,000 Americans have also received convalescent plasma—another treatment that Trump touted. But because most were not enrolled in rigorous trials, “we still don’t know if it works—and it likely doesn’t,” says Luciana Borio, the former director for medical and biodefense preparedness at the National Security Council. “What a waste of time and resources.”
Read: How we survive the winter
In the heat of a disaster, when emergency rooms are filling and patients are dying, it is hard to set up one careful study, let alone coordinate several across a country. But coordination is not impossible. During World War II , federal agencies unified private companies, universities, the military, and other entities in a carefully orchestrated effort to speed pharmaceutical development from benchtop to battlefield. The results—revolutionary malaria treatments, new ways of mass-producing antibiotics, and at least 10 new or improved vaccines for influenza and other diseases—represented “not a triumph of scientific genius but rather of organizational purpose and efficiency,” Kendall Hoyt of Dartmouth College has written.
Similar triumphs occurred last year—in other countries. In March, taking advantage of the United Kingdom’s nationalized health system, British researchers launched a nationwide study called Recovery, which has since enrolled more than 17,600 COVID‑19 patients across 176 institutions. Recovery offered conclusive answers about dexamethasone and hydroxychloroquine and is set to weigh in on several other treatments. No other study has done more to shape the treatment of COVID‑19. The U.S. is now catching up. In April, the NIH launched a partnership called ACTIV , in which academic and industry scientists prioritized the most promising drugs and coordinated trial plans across the country. Since August, several such trials have started. This model was late, but is likely to outlast the pandemic itself, allowing future researchers to rapidly sort medical wheat from pharmaceutical chaff. “I can’t imagine we’ll go back to doing clinical research in the future the way we did in the past,” the NIH’s Francis Collins said.
Even after the COVID‑19 pandemic, the fruits of the pivot will leave us better equipped for our long and intensifying war against harmful viruses. The last time a virus caused this much devastation—the flu pandemic of 1918—scientists were only just learning about viruses, and spent time looking for a bacterial culprit. This one is different. With so many scientists observing intently as a virus wreaks its horrible work upon millions of bodies, the world is learning lessons that could change the way we think about these pathogens forevermore.
Consider the long-term consequences of viral infections. Years after the original SARS virus hit Hong Kong in 2003, about a quarter of survivors still had myalgic encephalomyelitis—a chronic illness whose symptoms, such as extreme fatigue and brain fogs, can worsen dramatically after mild exertion. ME cases are thought to be linked to viral infections, and clusters sometimes follow big outbreaks. So when SARS‑CoV‑2 started spreading, people with ME were unsurprised to hear that tens of thousands of COVID‑19 “long-haulers” were experiencing incapacitating symptoms that rolled on for months . “Everyone in my community has been thinking about this since the start of the pandemic,” says Jennifer Brea, the executive director of the advocacy group #MEAction.
ME and sister illnesses such as dysautonomia, fibromyalgia, and mast cell activation syndrome have long been neglected, their symptoms dismissed as imaginary or psychiatric. Research is poorly funded, so few scientists study them. Little is known about how to prevent and treat them. This negligence has left COVID‑19 long-haulers with few answers or options, and they initially endured the same dismissal as the larger ME community. But their sheer numbers have forced a degree of recognition. They started researching, cataloging their own symptoms. They gained audiences with the NIH and the World Health Organization. Patients who are themselves experts in infectious disease or public health published their stories in top journals. “Long COVID” is being taken seriously, and Brea hopes it might drag all post-infection illnesses into the spotlight. ME never experienced a pivot. COVID‑19 might inadvertently create one.
Anthony Fauci hopes so. His career was defined by HIV, and in 2019 he said in a paper he co-wrote that “the collateral advantages of” studying HIV “have been profound.” Research into HIV/AIDS revolutionized our understanding of the immune system and how diseases subvert it. It produced techniques for developing antiviral drugs that led to treatments for hepatitis C. Inactivated versions of HIV have been used to treat cancers and genetic disorders. From one disease came a cascade of benefits. COVID‑19 will be no different. Fauci had personally seen cases of prolonged symptoms after other viral infections, but “I didn’t really have a good scientific handle on it,” he told me. Such cases are hard to study, because it’s usually impossible to identify the instigating pathogen. But COVID‑19 has created “the most unusual situation imaginable,” Fauci said—a massive cohort of people with long-haul symptoms that are almost certainly caused by one known virus. “It’s an opportunity we cannot lose,” he said.
Read: The core lesson of the COVID-19 heart debate
COVID‑19 has developed a terrifying mystique because it seems to behave in unusual ways. It causes mild symptoms in some but critical illness in others. It is a respiratory virus and yet seems to attack the heart, brain, kidneys, and other organs. It has reinfected a small number of people who had recently recovered. But many other viruses share similar abilities; they just don’t infect millions of people in a matter of months or grab the attention of the entire scientific community. Thanks to COVID‑19, more researchers are looking for these rarer sides of viral infections, and spotting them.
At least 20 known viruses, including influenza and measles, can trigger myocarditis—inflammation of the heart. Some of these cases resolve on their own, but others cause persistent scarring, and still others rapidly progress into lethal problems. No one knows what proportion of people with viral myocarditis experience the most mild fate, because doctors typically notice only those who seek medical attention. But now researchers are also intently scrutinizing the hearts of people with mild or asymptomatic COVID‑19 infections, including college athletes, given concerns about sudden cardiac arrest during strenuous workouts. The lessons from these efforts could ultimately avert deaths from other infections.
Respiratory viruses, though extremely common, are often neglected. Respiratory syncytial virus, parainfluenza viruses, rhinoviruses, adenoviruses, bocaviruses, a quartet of other human coronaviruses—they mostly cause mild coldlike illnesses, but those can be severe. How often? Why? It’s hard to say, because, influenza aside, such viruses attract little funding or interest. “There’s a perception that they’re just colds and there’s nothing much to learn,” says Emily Martin of the University of Michigan, who has long struggled to get funding to study them. Such reasoning is shortsighted folly. Respiratory viruses are the pathogens most likely to cause pandemics, and those outbreaks could potentially be far worse than COVID‑19’s.
Read: We need to talk about ventilation
Their movements through the air have been poorly studied, too. “There’s this very entrenched idea,” says Linsey Marr at Virginia Tech, that viruses mostly spread through droplets (short-range globs of snot and spit) rather than aerosols (smaller, dustlike flecks that travel farther). That idea dates back to the 1930s, when scientists were upending outdated notions that disease was caused by “bad air,” or miasma. But the evidence that SARS‑CoV‑2 can spread through aerosols “is now overwhelming,” says Marr, one of the few scientists who, before the pandemic, studied how viruses spread through air. “I’ve seen more acceptance in the last six months than over the 12 years I’ve been working on this.”
Another pandemic is inevitable, but it will find a very different community of scientists than COVID‑19 did. They will immediately work to determine whether the pathogen—most likely another respiratory virus—moves through aerosols, and whether it spreads from infected people before causing symptoms. They might call for masks and better ventilation from the earliest moments, not after months of debate. They will anticipate the possibility of an imminent wave of long-haul symptoms, and hopefully discover ways of preventing them. They might set up research groups to prioritize the most promising drugs and coordinate large clinical trials. They might take vaccine platforms that worked best against COVID‑19, slot in the genetic material of the new pathogen, and have a vaccine ready within months.
For all its benefits, the single-minded focus on COVID‑19 will also leave a slew of negative legacies. Science is mostly a zero-sum game, and when one topic monopolizes attention and money, others lose out. Last year, between physical-distancing restrictions, redirected funds, and distracted scientists, many lines of research slowed to a crawl. Long-term studies that monitored bird migrations or the changing climate will forever have holes in their data because field research had to be canceled. Conservationists who worked to protect monkeys and apes kept their distance for fear of passing COVID‑19 to already endangered species. Roughly 80 percent of non-COVID‑19 clinical trials in the U.S.—likely worth billions of dollars—were interrupted or stopped because hospitals were overwhelmed and volunteers were stuck at home. Even research on other infectious diseases was back-burnered. “All the non-COVID work that I was working on before the pandemic started is now piling up and gathering dust,” says Angela Rasmussen of Georgetown University, who normally studies Ebola and MERS. “Those are still problems.”
The COVID‑19 pandemic is a singular disaster, and it is reasonable for society—and scientists—to prioritize it. But the pivot was driven by opportunism as much as altruism. Governments, philanthropies, and universities channeled huge sums toward COVID‑19 research. The NIH alone received nearly $3.6 billion from Congress. The Bill & Melinda Gates Foundation apportioned $350 million for COVID‑19 work. “Whenever there’s a big pot of money, there’s a feeding frenzy,” Madhukar Pai told me. He works on tuberculosis, which causes 1.5 million deaths a year—comparable to COVID‑19’s toll in 2020. Yet tuberculosis research has been mostly paused. None of Pai’s colleagues pivoted when Ebola or Zika struck, but “half of us have now swung to working on COVID‑19,” he said. “It’s a black hole, sucking us all in.”
While the most qualified experts became quickly immersed in the pandemic response, others were stuck at home looking for ways to contribute. Using the same systems that made science faster, they could download data from free databases, run quick analyses with intuitive tools, publish their work on preprint servers, and publicize it on Twitter. Often, they made things worse by swerving out of their scholarly lanes and plowing into unfamiliar territory. Nathan Ballantyne, a philosopher at Fordham University, calls this “ epistemic trespassing .” It can be a good thing: Continental drift was championed by Alfred Wegener, a meteorologist; microbes were first documented by Antonie van Leeuwenhoek, a draper. But more often than not, epistemic trespassing just creates a mess, especially when inexperience couples with overconfidence.
On March 28, a preprint noted that countries that universally use a tuberculosis vaccine called BCG had lower COVID‑19 mortality rates. But such cross-country comparisons are infamously treacherous. For example, countries with higher cigarette-usage rates have longer life expectancies, not because smoking prolongs life but because it is more popular in wealthier nations. This tendency to draw faulty conclusions about individual health using data about large geographical regions is called the ecological fallacy. Epidemiologists know to avoid it. The BCG-preprint authors, who were from an osteopathic college in New York, didn’t seem to . But their paper was covered by more than 70 news outlets, and dozens of inexperienced teams offered similarly specious analyses. “People who don’t know how to spell tuberculosis have told me they can solve the link between BCG and COVID‑19,” Pai said. “Someone told me they can do it in 48 hours with a hackathon.”

Other epistemic trespassers spent their time reinventing the wheel. One new study, published in NEJM , used lasers to show that when people speak, they release aerosols. But as the authors themselves note, the same result—sans lasers—was published in 1946, Marr says. I asked her whether any papers from the 2020 batch had taught her something new. After an uncomfortably long pause, she mentioned just one.
In some cases, bad papers helped shape the public narrative of the pandemic. On March 16, two biogeographers published a preprint arguing that COVID‑19 will “marginally affect the tropics” because it fares poorly in warm, humid conditions. Disease experts quickly noted that techniques like the ones the duo used are meant for modeling the geographic ranges of animal and plant species or vector-borne pathogens, and are ill-suited to simulating the spread of viruses like SARS-CoV-2. But their claim was picked up by more than 50 news outlets and echoed by the United Nations World Food Program. COVID‑19 has since run rampant in many tropical countries, including Brazil, Indonesia, and Colombia—and the preprint’s authors have qualified their conclusions in later versions of the paper. “It takes a certain type of person to think that weeks of reading papers gives them more perspective than someone with a Ph.D. on that subject, and that type of person has gotten a lot of airtime in this pandemic,” says Colin Carlson of Georgetown.
The incentives to trespass are substantial. Academia is a pyramid scheme: Each biomedical professor trains an average of six doctoral students across her career, but only 16 percent of the students get tenure-track positions . Competition is ferocious, and success hinges on getting published—a feat made easier by dramatic results. These factors pull researchers toward speed, short-termism, and hype at the expense of rigor—and the pandemic intensified that pull. With an anxious world crying out for information, any new paper could immediately draw international press coverage—and hundreds of citations.
The tsunami of rushed but dubious work made life harder for actual experts, who struggled to sift the signal from the noise. They also felt obliged to debunk spurious research in long Twitter threads and relentless media interviews—acts of public service that are rarely rewarded in academia. And they were overwhelmed by requests to peer-review new papers. Kristian Andersen, an infectious-disease researcher at Scripps Research, told me that journals used to send him two or three such requests a month. Now “I’m getting three or five a day,” he said in September.
The pandemic’s opportunities also fell inequitably upon the scientific community. In March, Congress awarded $75 million to the National Science Foundation to fast-track studies that could quickly contribute to the pandemic response. “That money just went ,” says Cassidy Sugimoto of Indiana University, who was on rotation at the agency at the time. “It was a first-come, first-served environment. It advantaged people who were aware of the system and could act upon it quickly.” But not all scientists could pivot to COVID‑19, or pivot with equal speed.
Among scientists, as in other fields, women do more child care, domestic work, and teaching than men, and are more often asked for emotional support by their students. These burdens increased as the pandemic took hold, leaving women scientists “less able to commit their time to learning about a new area of study, and less able to start a whole new research project,” says Molly M. King, a sociologist at Santa Clara University. Women’s research hours fell by nine percentage points more than did men’s because of the pressures of COVID‑19. And when COVID‑19 created new opportunities, men grabbed them more quickly. In the spring, the proportion of papers with women as first authors fell almost 44 percent in the preprint repository medRxiv, relative to 2019. And published COVID‑19 papers had 19 percent fewer women as first authors compared with papers from the same journals in the previous year. Men led more than 80 percent of national COVID‑19 task forces in 87 countries . Male scientists were quoted four times as frequently as female scientists in American news stories about the pandemic.
American scientists of color also found it harder to pivot than their white peers, because of unique challenges that sapped their time and energy. Black, Latino, and Indigenous scientists were most likely to have lost loved ones, adding mourning to their list of duties. Many grieved, too, after the killings of Breonna Taylor, George Floyd, Ahmaud Arbery, and others. They often faced questions from relatives who were mistrustful of the medical system, or were experiencing discriminatory care. They were suddenly tasked with helping their predominantly white institutions fight racism. Neil Lewis Jr. at Cornell, who studies racial health disparities, told me that many psychologists had long deemed his work irrelevant. “All of a sudden my inbox is drowning,” he said, while some of his own relatives have become ill and one has died.
Science suffers from the so-called Matthew effect, whereby small successes snowball into ever greater advantages, irrespective of merit. Similarly, early hindrances linger. Young researchers who could not pivot because they were too busy caring or grieving for others might suffer lasting consequences from an unproductive year. COVID‑19 “has really put the clock back in terms of closing the gap for women and underrepresented minorities,” Yale’s Akiko Iwasaki says. “Once we’re over the pandemic, we’ll need to fix it all again.”
COVID-19 has already changed science immensely, but if scientists are savvy, the most profound pivot is still to come—a grand reimagining of what medicine should be. In 1848, the Prussian government sent a young physician named Rudolf Virchow to investigate a typhus epidemic in Upper Silesia. Virchow didn’t know what caused the devastating disease, but he realized its spread was possible because of malnutrition, hazardous working conditions, crowded housing, poor sanitation, and the inattention of civil servants and aristocrats—problems that require social and political reforms. “Medicine is a social science,” Virchow said, “and politics is nothing but medicine in larger scale.”
This viewpoint fell by the wayside after germ theory became mainstream in the late 19th century. When scientists discovered the microbes responsible for tuberculosis, plague, cholera, dysentery, and syphilis, most fixated on these newly identified nemeses. Societal factors were seen as overly political distractions for researchers who sought to “be as ‘objective’ as possible,” says Elaine Hernandez, a medical sociologist at Indiana University. In the U.S., medicine fractured. New departments of sociology and cultural anthropology kept their eye on the societal side of health, while the nation’s first schools of public health focused instead on fights between germs and individuals. This rift widened as improvements in hygiene, living standards, nutrition, and sanitation lengthened life spans: The more social conditions improved, the more readily they could be ignored.
The ideological pivot away from social medicine began to reverse in the second half of the 20th century. The women’s-rights and civil-rights movements, the rise of environmentalism, and anti-war protests created a generation of scholars who questioned “the legitimacy, ideology, and practice of any science … that disregards social and economic inequality,” wrote Nancy Krieger of Harvard . Beginning in the 1980s, this new wave of social epidemiologists once again studied how poverty, privilege, and living conditions affect a person’s health—to a degree even Virchow hadn’t imagined. But as COVID‑19 has shown, the reintegration is not yet complete.
Politicians initially described COVID‑19 as a “great equalizer,” but when states began releasing demographic data, it was immediately clear that the disease was disproportionately infecting and killing people of color . These disparities aren’t biological. They stem from decades of discrimination and segregation that left minority communities in poorer neighborhoods with low-paying jobs, more health problems, and less access to health care—the same kind of problems that Virchow identified more than 170 years ago.
From the September 2020 issue: How the pandemic defeated America
Simple acts like wearing a mask and staying at home, which rely on people tolerating discomfort for the collective good, became society’s main defenses against the virus in the many months without effective drugs or vaccines. These are known as nonpharmaceutical interventions—a name that betrays medicine’s biological bias. For most of 2020, these were the only interventions on offer, but they were nonetheless defined in opposition to the more highly prized drugs and vaccines.
In March, when the U.S. started shutting down, one of the biggest questions on the mind of Whitney Robinson of UNC at Chapel Hill was: Are our kids going to be out of school for two years? While biomedical scientists tend to focus on sickness and recovery, social epidemiologists like her “think about critical periods that can affect the trajectory of your life,” she told me. Disrupting a child’s schooling at the wrong time can affect their entire career, so scientists should have prioritized research to figure out whether and how schools could reopen safely. But most studies on the spread of COVID‑19 in schools were neither large in scope nor well-designed enough to be conclusive. No federal agency funded a large, nationwide study, even though the federal government had months to do so. The NIH received billions for COVID‑19 research , but the National Institute of Child Health and Human Development—one of its 27 constituent institutes and centers—got nothing.
The horrors that Rudolf Virchow saw in Upper Silesia radicalized him, pushing the future “father of modern pathology” to advocate for social reforms. The current pandemic has affected scientists in the same way. Calm researchers became incensed as potentially game-changing innovations like cheap diagnostic tests were squandered by a negligent administration and a muzzled Centers for Disease Control and Prevention. Austere publications like NEJM and Nature published explicitly political editorials castigating the Trump administration for its failures and encouraging voters to hold the president accountable. COVID‑19 could be the catalyst that fully reunifies the social and biological sides of medicine, bridging disciplines that have been separated for too long.
“To study COVID‑19 is not only to study the disease itself as a biological entity,” says Alondra Nelson, the president of the Social Science Research Council. “What looks like a single problem is actually all things, all at once. So what we’re actually studying is literally everything in society, at every scale, from supply chains to individual relationships.”
The scientific community spent the pre-pandemic years designing faster ways of doing experiments, sharing data, and developing vaccines, allowing it to mobilize quickly when COVID‑19 emerged. Its goal now should be to address its many lingering weaknesses. Warped incentives, wasteful practices, overconfidence, inequality, a biomedical bias—COVID‑19 has exposed them all. And in doing so, it offers the world of science a chance to practice one of its most important qualities: self-correction.
* The print version of this article stated that the Moderna and Pfizer/BioNTech vaccines were reported to be 95 percent effective at preventing COVID-19 infections. In fact, the vaccines prevent disease, not infection.
This article appears in the January/February 2021 print edition with the headline “The COVID-19 Manhattan Project.”

Search the United Nations
- Policy and Funding
- Recover Better
- Disability Inclusion
- Secretary-General
- Financing for Development
- ACT-Accelerator
- Member States
- Health and Wellbeing
- Policy and Guidance
- Vaccination
- COVID-19 Medevac
- i-Seek (requires login)
- Awake at Night podcast

COVID-19 photo essay: We’re all in this together
About the author, department of global communications.
The United Nations Department of Global Communications (DGC) promotes global awareness and understanding of the work of the United Nations.
23 June 2020 – The COVID-19 pandemic has demonstrated the interconnected nature of our world – and that no one is safe until everyone is safe. Only by acting in solidarity can communities save lives and overcome the devastating socio-economic impacts of the virus. In partnership with the United Nations, people around the world are showing acts of humanity, inspiring hope for a better future.
Everyone can do something

Rauf Salem, a volunteer, instructs children on the right way to wash their hands, in Sana'a, Yemen. Simple measures, such as maintaining physical distance, washing hands frequently and wearing a mask are imperative if the fight against COVID-19 is to be won. Photo: UNICEF/UNI341697
Creating hope

Venezuelan refugee Juan Batista Ramos, 69, plays guitar in front of a mural he painted at the Tancredo Neves temporary shelter in Boa Vista, Brazil to help lift COVID-19 quarantine blues. “Now, everywhere you look you will see a landscape to remind us that there is beauty in the world,” he says. Ramos is among the many artists around the world using the power of culture to inspire hope and solidarity during the pandemic. Photo: UNHCR/Allana Ferreira
Inclusive solutions

Wendy Schellemans, an education assistant at the Royal Woluwe Institute in Brussels, models a transparent face mask designed to help the hard of hearing. The United Nations and partners are working to ensure that responses to COVID-19 leave no one behind. Photo courtesy of Royal Woluwe Institute
Humanity at its best

Maryna, a community worker at the Arts Centre for Children and Youth in Chasiv Yar village, Ukraine, makes face masks on a sewing machine donated by the Office of the United Nations High Commissioner for Refugees (UNHCR) and civil society partner, Proliska. She is among the many people around the world who are voluntarily addressing the shortage of masks on the market. Photo: UNHCR/Artem Hetman
Keep future leaders learning

A mother helps her daughter Ange, 8, take classes on television at home in Man, Côte d'Ivoire. Since the COVID-19 pandemic began, caregivers and educators have responded in stride and have been instrumental in finding ways to keep children learning. In Côte d'Ivoire, the United Nations Children’s Fund (UNICEF) partnered with the Ministry of Education on a ‘school at home’ initiative, which includes taping lessons to be aired on national TV and radio. Ange says: “I like to study at home. My mum is a teacher and helps me a lot. Of course, I miss my friends, but I can sleep a bit longer in the morning. Later I want to become a lawyer or judge." Photo: UNICEF/UNI320749
Global solidarity

People in Nigeria’s Lagos State simulate sneezing into their elbows during a coronavirus prevention campaign. Many African countries do not have strong health care systems. “Global solidarity with Africa is an imperative – now and for recovering better,” said United Nations Secretary-General António Guterres. “Ending the pandemic in Africa is essential for ending it across the world.” Photo: UNICEF Nigeria/2020/Ojo
A new way of working

Henri Abued Manzano, a tour guide at the United Nations Information Service (UNIS) in Vienna, speaks from his apartment. COVID-19 upended the way people work, but they can be creative while in quarantine. “We quickly decided that if visitors can’t come to us, we will have to come to them,” says Johanna Kleinert, Chief of the UNIS Visitors Service in Vienna. Photo courtesy of Kevin Kühn
Life goes on

Hundreds of millions of babies are expected to be born during the COVID-19 pandemic. Fionn, son of Chloe O'Doherty and her husband Patrick, is among them. The couple says: “It's all over. We did it. Brought life into the world at a time when everything is so uncertain. The relief and love are palpable. Nothing else matters.” Photo: UNICEF/UNI321984/Bopape
Putting meals on the table

Sudanese refugee Halima, in Tripoli, Libya, says food assistance is making her life better. COVID-19 is exacerbating the existing hunger crisis. Globally, 6 million more people could be pushed into extreme poverty unless the international community acts now. United Nations aid agencies are appealing for more funding to reach vulnerable populations. Photo: UNHCR
Supporting the frontlines

The United Nations Air Service, run by the World Food Programme (WFP), distributes protective gear donated by the Jack Ma Foundation and Alibaba Group, in Somalia. The United Nations is using its supply chain capacity to rapidly move badly needed personal protective equipment, such as medical masks, gloves, gowns and face-shields to the frontline of the battle against COVID-19. Photo: WFP/Jama Hassan

S7-Episode 2: Bringing Health to the World
“You see, we're not doing this work to make ourselves feel better. That sort of conventional notion of what a do-gooder is. We're doing this work because we are totally convinced that it's not necessary in today's wealthy world for so many people to be experiencing discomfort, for so many people to be experiencing hardship, for so many people to have their lives and their livelihoods imperiled.”
Dr. David Nabarro has dedicated his life to global health. After a long career that’s taken him from the horrors of war torn Iraq, to the devastating aftermath of the Indian Ocean tsunami, he is still spurred to action by the tremendous inequalities in global access to medical care.
“The thing that keeps me awake most at night is the rampant inequities in our world…We see an awful lot of needless suffering.”
:: David Nabarro interviewed by Melissa Fleming

Brazilian ballet pirouettes during pandemic
Ballet Manguinhos, named for its favela in Rio de Janeiro, returns to the stage after a long absence during the COVID-19 pandemic. It counts 250 children and teenagers from the favela as its performers. The ballet group provides social support in a community where poverty, hunger and teen pregnancy are constant issues.

Radio journalist gives the facts on COVID-19 in Uzbekistan
The pandemic has put many people to the test, and journalists are no exception. Coronavirus has waged war not only against people's lives and well-being but has also spawned countless hoaxes and scientific falsehoods.
Disclaimer: This translation was last updated on August 2, 2022. For up-to-date content, please visit the English version of this page.
Disclaimer: The Spanish COVID-19 site is currently undergoing significant updates which may lead to a delay in translated content. We apologize for any inconvenience.
About COVID-19
What is covid-19.
COVID-19 (coronavirus disease 2019) is a disease caused by a virus named SARS-CoV-2. It can be very contagious and spreads quickly. Over one million people have died from COVID-19 in the United States.
COVID-19 most often causes respiratory symptoms that can feel much like a cold, the flu, or pneumonia. COVID-19 may attack more than your lungs and respiratory system. Other parts of your body may also be affected by the disease. Most people with COVID-19 have mild symptoms, but some people become severely ill.
Some people including those with minor or no symptoms will develop Post-COVID Conditions – also called “Long COVID.”
How does COVID-19 spread?
COVID-19 spreads when an infected person breathes out droplets and very small particles that contain the virus. Other people can breathe in these droplets and particles, or these droplets and particles can land on their eyes, nose, or mouth. In some circumstances, these droplets may contaminate surfaces they touch.
Anyone infected with COVID-19 can spread it, even if they do NOT have symptoms.
The risk of animals spreading the virus that causes COVID-19 to people is low. The virus can spread from people to animals during close contact. People with suspected or confirmed COVID-19 should avoid contact with animals.
What are antibodies and how do they help protect me?
Antibodies are proteins your immune system makes to help fight infection and protect you from getting sick in the future. A positive antibody test result can help identify someone who has had COVID-19 in the past or has been vaccinated against COVID-19. Studies show that people who have antibodies from an infection with the virus that causes COVID-19 can improve their level of protection by getting vaccinated.
Who is at risk of severe illness from COVID-19?
Some people are more likely than others to get very sick if they get COVID-19. This includes people who are older , are immunocompromised (have a weakened immune system), have certain disabilities , or have underlying health conditions . Understanding your COVID-19 risk and the risks that might affect others can help you make decisions to protect yourself and others .
What are ways to prevent COVID-19?
There are many actions you can take to help protect you, your household, and your community from COVID-19. CDC’s Respiratory Virus Guidance provides actions you can take to help protect yourself and others from health risks caused by respiratory viruses, including COVID-19. These actions include steps you can take to lower the risk of COVID-19 transmission (catching and spreading COVID-19) and lower the risk of severe illness if you get sick.
CDC recommends that you
- Stay up to date with COVID-19 vaccines
- Practice good hygiene (practices that improve cleanliness)
- Take steps for cleaner air
- Stay home when sick
- Seek health care promptly for testing and treatment when you are sick if you have risk factors for severe illness . Treatment may help lower your risk of severe illness.
Masks , physical distancing , and tests can provide additional layers of protection.
What are variants of COVID-19?
Viruses are constantly changing, including the virus that causes COVID-19. These changes occur over time and can lead to new strains of the virus or variants of COVID-19 . Slowing the spread of the virus, by protecting yourself and others , can help slow new variants from developing. CDC is working with state and local public health officials to monitor the spread of all variants, including Omicron.
- COVID-19 Testing
- COVID-19 Vaccines
- Preventing Respiratory Viruses
- Reinfection
- Difference Between Flu and COVID-19
- COVID Data Tracker
Search for and find historical COVID-19 pages and files. Please note the content on these pages and files is no longer being updated and may be out of date.
- Visit archive.cdc.gov for a historical snapshot of the COVID-19 website, capturing the end of the Federal Public Health Emergency on June 28, 2023.
- Visit the dynamic COVID-19 collection to search the COVID-19 website as far back as July 30, 2021.
To receive email updates about COVID-19, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

A lab technician begins semi-automated testing for COVID-19 at Northwell Health Labs on March 11, 2020, in Lake Success, New York. An emergency use authorization by the FDA allows Northwell to move from manual testing to semi-automated.
- CORONAVIRUS COVERAGE
What is the coronavirus?
COVID-19, the disease caused by the novel coronavirus, has infected tens of thousands of people worldwide. Here’s what you need to know.
Much is left to learn about the coronavirus that is changing life as we know it, but our journey has already yielded many lessons. In late December 2019, reports emerged of a novel coronavirus outbreak connected with pneumonia cases at a wildlife market in Wuhan, China. COVID-19 spread across the nation within weeks—and then stormed its way across the world. By March 11, the World Health Organization labeled COVID-19 a pandemic.
In the time since, we’ve learned some important basics about SARS-CoV-2, the novel coronavirus behind COVID-19—including how it spreads then invades the body and which parts of the world are currently facing serious outbreaks. Here are maps that illustrate its spread and answers to other key questions about COVID-19.
How many cases are there worldwide?
The coronavirus pandemic is reshaping the world. Here’s a closer look at the case counts and fatalities across the world.
Where are cases growing and declining in the U.S.?
The coronavirus is affecting U.S. regions in different ways. Here are the areas where cases and deaths are either decreasing or increasing the most, based on the last seven days compared to the previous week.
What is a coronavirus?
Coronaviruses are a large family of viruses, but only seven of its members infect humans. Four types cause minor illnesses like the common cold, while other coronaviruses have triggered far more devastating impacts such as SARS, MERS, and now COVID-19. Coronaviruses can be zoonotic, meaning they jump from animals to humans.
Like its relatives, COVID-19 is primarily a respiratory disease that starts in the lungs, causing pneumonia-like symptoms, but can also cast a storm across the entire body.
How does COVID-19 spread?
Like other respiratory diseases, COVID-19 primarily spreads through small droplets—saliva or mucus—that an infected person expels when they cough, sneeze, or talk. These droplets can travel three to six feet and remain infectious for anywhere from four to 48 hours, depending on the surface. (The virus may also spread via accidental consumption of fecal matter or aerosols, tiny particles that are mostly a concern in clinical settings.)
You can protect yourself from catching the virus by staying six feet away from others and washing your hands with soap and water for more than 20 seconds.
How long does it last on surfaces?
The virus lives longer on surfaces. Disinfectants that are at least 60 percent alcohol by volume can also kill the virus on plastic and stainless steel surfaces.
What does the coronavirus look like?
Coronaviruses get their name from their spiky structure. Like other coronaviruses , SARS-CoV-2 is spherical with spike proteins that look a bit like a corona, or crown.
How does SARS-CoV-2 invade the body?
Its spiky structure helps the coronavirus latch onto cells that it can invade. Once a virus enters the human body through the eyes, mouth, or nose, it looks for cells with its favorite doorways—proteins called receptors. If the virus finds a compatible receptor, it can invade and start replicating itself. For SARS-CoV-2, that receptor is found in lung cells and the gut.
How does age factor into the severity of the disease?
Currently, children with COVID-19 may be less likely to require intensive care and also have lower fatality rates than adults. The difference in severity is not yet fully understood.
What are the common diagnostic symptoms?
There isn’t a single diagnostic symptom, but some are more common:
What are the chronic conditions that put people at higher risk?
COVID-19 poses a particularly serious threat to people with underlying conditions such as cardiovascular disease, diabetes, chronic lung disease, high blood pressure, and cancer.
How do you diagnose the virus?
Testing is done to diagnose the presence of the virus. Swab samples taken from the nose or mouth are tested for the virus’s genetic material. Researchers are also developing protocols for tests using saliva and blood samples.
When will a vaccine be ready?
To develop immunity, vaccines may contain killed or weakened virus, viral proteins, or viral genetic material. The best strategy to use against SARS-CoV-2 is yet to be determined. It could take until January 2021 —or perhaps much longer —before a vaccine is ready for public use.
See all of National Geographic's coronavirus coverage .
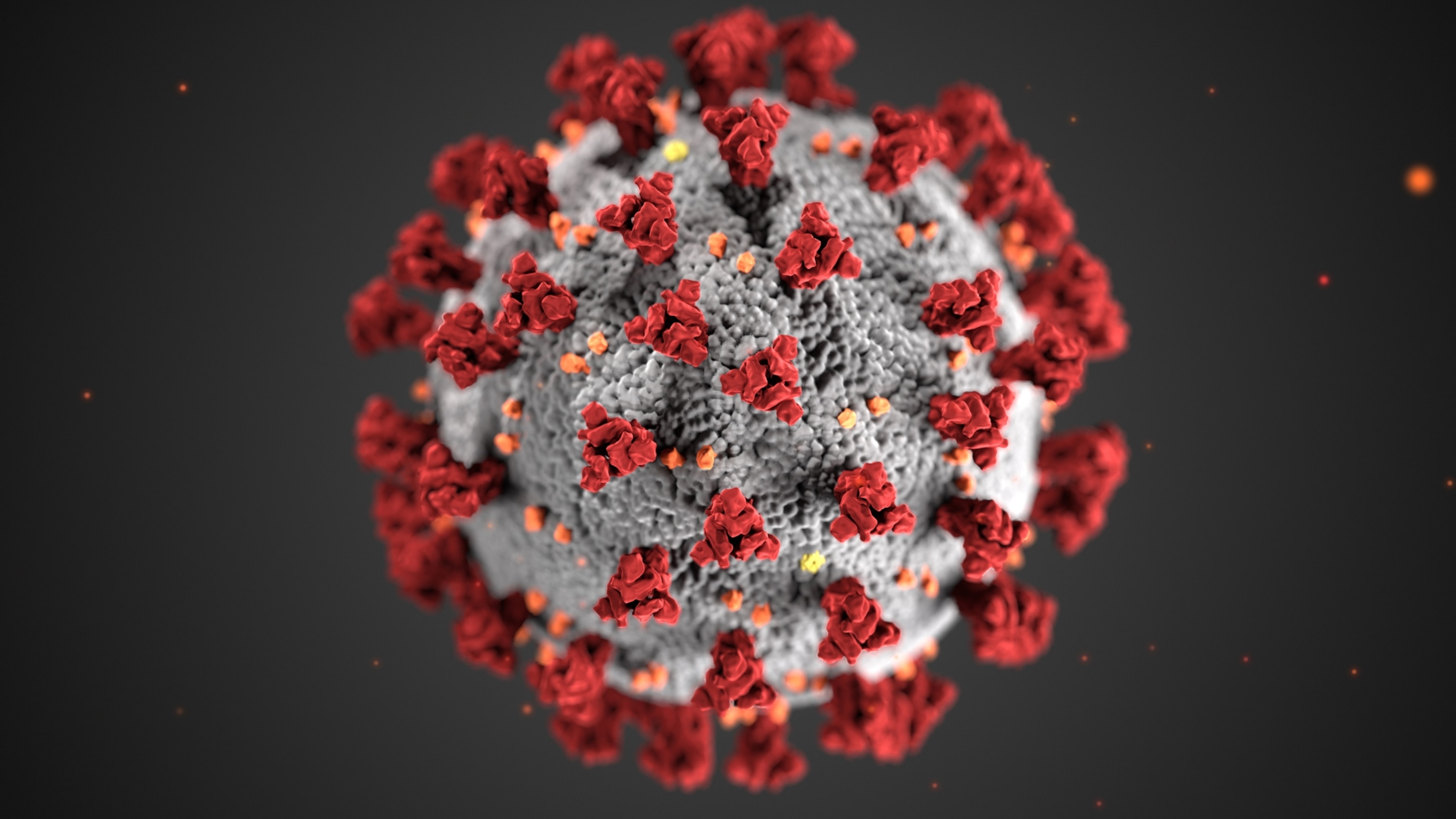
FREE BONUS ISSUE
Related topics.
- CORONAVIRUS
You May Also Like

What is 'immune amnesia?' This long-term side effect of measles is newly relevant.

A mysterious new respiratory illness is spreading in dogs. Here’s what we know.

COVID-19 has tested us. Will we be ready for the next pandemic?

Multiple COVID infections can lead to chronic health issues. Here’s what to know.

Long COVID can destroy your ability to exercise. Now we know why.
- Perpetual Planet
- Environment
- History & Culture
- Paid Content
History & Culture
- Mind, Body, Wonder
- Terms of Use
- Privacy Policy
- Your US State Privacy Rights
- Children's Online Privacy Policy
- Interest-Based Ads
- About Nielsen Measurement
- Do Not Sell or Share My Personal Information
- Nat Geo Home
- Attend a Live Event
- Book a Trip
- Inspire Your Kids
- Shop Nat Geo
- Visit the D.C. Museum
- Learn About Our Impact
- Support Our Mission
- Advertise With Us
- Customer Service
- Renew Subscription
- Manage Your Subscription
- Work at Nat Geo
- Sign Up for Our Newsletters
- Contribute to Protect the Planet
Copyright © 1996-2015 National Geographic Society Copyright © 2015-2024 National Geographic Partners, LLC. All rights reserved
- Research article
- Open access
- Published: 04 June 2021
Coronavirus disease (COVID-19) pandemic: an overview of systematic reviews
- Israel Júnior Borges do Nascimento 1 , 2 ,
- Dónal P. O’Mathúna 3 , 4 ,
- Thilo Caspar von Groote 5 ,
- Hebatullah Mohamed Abdulazeem 6 ,
- Ishanka Weerasekara 7 , 8 ,
- Ana Marusic 9 ,
- Livia Puljak ORCID: orcid.org/0000-0002-8467-6061 10 ,
- Vinicius Tassoni Civile 11 ,
- Irena Zakarija-Grkovic 9 ,
- Tina Poklepovic Pericic 9 ,
- Alvaro Nagib Atallah 11 ,
- Santino Filoso 12 ,
- Nicola Luigi Bragazzi 13 &
- Milena Soriano Marcolino 1
On behalf of the International Network of Coronavirus Disease 2019 (InterNetCOVID-19)
BMC Infectious Diseases volume 21 , Article number: 525 ( 2021 ) Cite this article
16k Accesses
28 Citations
13 Altmetric
Metrics details
Navigating the rapidly growing body of scientific literature on the SARS-CoV-2 pandemic is challenging, and ongoing critical appraisal of this output is essential. We aimed to summarize and critically appraise systematic reviews of coronavirus disease (COVID-19) in humans that were available at the beginning of the pandemic.
Nine databases (Medline, EMBASE, Cochrane Library, CINAHL, Web of Sciences, PDQ-Evidence, WHO’s Global Research, LILACS, and Epistemonikos) were searched from December 1, 2019, to March 24, 2020. Systematic reviews analyzing primary studies of COVID-19 were included. Two authors independently undertook screening, selection, extraction (data on clinical symptoms, prevalence, pharmacological and non-pharmacological interventions, diagnostic test assessment, laboratory, and radiological findings), and quality assessment (AMSTAR 2). A meta-analysis was performed of the prevalence of clinical outcomes.
Eighteen systematic reviews were included; one was empty (did not identify any relevant study). Using AMSTAR 2, confidence in the results of all 18 reviews was rated as “critically low”. Identified symptoms of COVID-19 were (range values of point estimates): fever (82–95%), cough with or without sputum (58–72%), dyspnea (26–59%), myalgia or muscle fatigue (29–51%), sore throat (10–13%), headache (8–12%) and gastrointestinal complaints (5–9%). Severe symptoms were more common in men. Elevated C-reactive protein and lactate dehydrogenase, and slightly elevated aspartate and alanine aminotransferase, were commonly described. Thrombocytopenia and elevated levels of procalcitonin and cardiac troponin I were associated with severe disease. A frequent finding on chest imaging was uni- or bilateral multilobar ground-glass opacity. A single review investigated the impact of medication (chloroquine) but found no verifiable clinical data. All-cause mortality ranged from 0.3 to 13.9%.
Conclusions
In this overview of systematic reviews, we analyzed evidence from the first 18 systematic reviews that were published after the emergence of COVID-19. However, confidence in the results of all reviews was “critically low”. Thus, systematic reviews that were published early on in the pandemic were of questionable usefulness. Even during public health emergencies, studies and systematic reviews should adhere to established methodological standards.
Peer Review reports
The spread of the “Severe Acute Respiratory Coronavirus 2” (SARS-CoV-2), the causal agent of COVID-19, was characterized as a pandemic by the World Health Organization (WHO) in March 2020 and has triggered an international public health emergency [ 1 ]. The numbers of confirmed cases and deaths due to COVID-19 are rapidly escalating, counting in millions [ 2 ], causing massive economic strain, and escalating healthcare and public health expenses [ 3 , 4 ].
The research community has responded by publishing an impressive number of scientific reports related to COVID-19. The world was alerted to the new disease at the beginning of 2020 [ 1 ], and by mid-March 2020, more than 2000 articles had been published on COVID-19 in scholarly journals, with 25% of them containing original data [ 5 ]. The living map of COVID-19 evidence, curated by the Evidence for Policy and Practice Information and Co-ordinating Centre (EPPI-Centre), contained more than 40,000 records by February 2021 [ 6 ]. More than 100,000 records on PubMed were labeled as “SARS-CoV-2 literature, sequence, and clinical content” by February 2021 [ 7 ].
Due to publication speed, the research community has voiced concerns regarding the quality and reproducibility of evidence produced during the COVID-19 pandemic, warning of the potential damaging approach of “publish first, retract later” [ 8 ]. It appears that these concerns are not unfounded, as it has been reported that COVID-19 articles were overrepresented in the pool of retracted articles in 2020 [ 9 ]. These concerns about inadequate evidence are of major importance because they can lead to poor clinical practice and inappropriate policies [ 10 ].
Systematic reviews are a cornerstone of today’s evidence-informed decision-making. By synthesizing all relevant evidence regarding a particular topic, systematic reviews reflect the current scientific knowledge. Systematic reviews are considered to be at the highest level in the hierarchy of evidence and should be used to make informed decisions. However, with high numbers of systematic reviews of different scope and methodological quality being published, overviews of multiple systematic reviews that assess their methodological quality are essential [ 11 , 12 , 13 ]. An overview of systematic reviews helps identify and organize the literature and highlights areas of priority in decision-making.
In this overview of systematic reviews, we aimed to summarize and critically appraise systematic reviews of coronavirus disease (COVID-19) in humans that were available at the beginning of the pandemic.
Methodology
Research question.
This overview’s primary objective was to summarize and critically appraise systematic reviews that assessed any type of primary clinical data from patients infected with SARS-CoV-2. Our research question was purposefully broad because we wanted to analyze as many systematic reviews as possible that were available early following the COVID-19 outbreak.
Study design
We conducted an overview of systematic reviews. The idea for this overview originated in a protocol for a systematic review submitted to PROSPERO (CRD42020170623), which indicated a plan to conduct an overview.
Overviews of systematic reviews use explicit and systematic methods for searching and identifying multiple systematic reviews addressing related research questions in the same field to extract and analyze evidence across important outcomes. Overviews of systematic reviews are in principle similar to systematic reviews of interventions, but the unit of analysis is a systematic review [ 14 , 15 , 16 ].
We used the overview methodology instead of other evidence synthesis methods to allow us to collate and appraise multiple systematic reviews on this topic, and to extract and analyze their results across relevant topics [ 17 ]. The overview and meta-analysis of systematic reviews allowed us to investigate the methodological quality of included studies, summarize results, and identify specific areas of available or limited evidence, thereby strengthening the current understanding of this novel disease and guiding future research [ 13 ].
A reporting guideline for overviews of reviews is currently under development, i.e., Preferred Reporting Items for Overviews of Reviews (PRIOR) [ 18 ]. As the PRIOR checklist is still not published, this study was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2009 statement [ 19 ]. The methodology used in this review was adapted from the Cochrane Handbook for Systematic Reviews of Interventions and also followed established methodological considerations for analyzing existing systematic reviews [ 14 ].
Approval of a research ethics committee was not necessary as the study analyzed only publicly available articles.
Eligibility criteria
Systematic reviews were included if they analyzed primary data from patients infected with SARS-CoV-2 as confirmed by RT-PCR or another pre-specified diagnostic technique. Eligible reviews covered all topics related to COVID-19 including, but not limited to, those that reported clinical symptoms, diagnostic methods, therapeutic interventions, laboratory findings, or radiological results. Both full manuscripts and abbreviated versions, such as letters, were eligible.
No restrictions were imposed on the design of the primary studies included within the systematic reviews, the last search date, whether the review included meta-analyses or language. Reviews related to SARS-CoV-2 and other coronaviruses were eligible, but from those reviews, we analyzed only data related to SARS-CoV-2.
No consensus definition exists for a systematic review [ 20 ], and debates continue about the defining characteristics of a systematic review [ 21 ]. Cochrane’s guidance for overviews of reviews recommends setting pre-established criteria for making decisions around inclusion [ 14 ]. That is supported by a recent scoping review about guidance for overviews of systematic reviews [ 22 ].
Thus, for this study, we defined a systematic review as a research report which searched for primary research studies on a specific topic using an explicit search strategy, had a detailed description of the methods with explicit inclusion criteria provided, and provided a summary of the included studies either in narrative or quantitative format (such as a meta-analysis). Cochrane and non-Cochrane systematic reviews were considered eligible for inclusion, with or without meta-analysis, and regardless of the study design, language restriction and methodology of the included primary studies. To be eligible for inclusion, reviews had to be clearly analyzing data related to SARS-CoV-2 (associated or not with other viruses). We excluded narrative reviews without those characteristics as these are less likely to be replicable and are more prone to bias.
Scoping reviews and rapid reviews were eligible for inclusion in this overview if they met our pre-defined inclusion criteria noted above. We included reviews that addressed SARS-CoV-2 and other coronaviruses if they reported separate data regarding SARS-CoV-2.
Information sources
Nine databases were searched for eligible records published between December 1, 2019, and March 24, 2020: Cochrane Database of Systematic Reviews via Cochrane Library, PubMed, EMBASE, CINAHL (Cumulative Index to Nursing and Allied Health Literature), Web of Sciences, LILACS (Latin American and Caribbean Health Sciences Literature), PDQ-Evidence, WHO’s Global Research on Coronavirus Disease (COVID-19), and Epistemonikos.
The comprehensive search strategy for each database is provided in Additional file 1 and was designed and conducted in collaboration with an information specialist. All retrieved records were primarily processed in EndNote, where duplicates were removed, and records were then imported into the Covidence platform [ 23 ]. In addition to database searches, we screened reference lists of reviews included after screening records retrieved via databases.
Study selection
All searches, screening of titles and abstracts, and record selection, were performed independently by two investigators using the Covidence platform [ 23 ]. Articles deemed potentially eligible were retrieved for full-text screening carried out independently by two investigators. Discrepancies at all stages were resolved by consensus. During the screening, records published in languages other than English were translated by a native/fluent speaker.
Data collection process
We custom designed a data extraction table for this study, which was piloted by two authors independently. Data extraction was performed independently by two authors. Conflicts were resolved by consensus or by consulting a third researcher.
We extracted the following data: article identification data (authors’ name and journal of publication), search period, number of databases searched, population or settings considered, main results and outcomes observed, and number of participants. From Web of Science (Clarivate Analytics, Philadelphia, PA, USA), we extracted journal rank (quartile) and Journal Impact Factor (JIF).
We categorized the following as primary outcomes: all-cause mortality, need for and length of mechanical ventilation, length of hospitalization (in days), admission to intensive care unit (yes/no), and length of stay in the intensive care unit.
The following outcomes were categorized as exploratory: diagnostic methods used for detection of the virus, male to female ratio, clinical symptoms, pharmacological and non-pharmacological interventions, laboratory findings (full blood count, liver enzymes, C-reactive protein, d-dimer, albumin, lipid profile, serum electrolytes, blood vitamin levels, glucose levels, and any other important biomarkers), and radiological findings (using radiography, computed tomography, magnetic resonance imaging or ultrasound).
We also collected data on reporting guidelines and requirements for the publication of systematic reviews and meta-analyses from journal websites where included reviews were published.
Quality assessment in individual reviews
Two researchers independently assessed the reviews’ quality using the “A MeaSurement Tool to Assess Systematic Reviews 2 (AMSTAR 2)”. We acknowledge that the AMSTAR 2 was created as “a critical appraisal tool for systematic reviews that include randomized or non-randomized studies of healthcare interventions, or both” [ 24 ]. However, since AMSTAR 2 was designed for systematic reviews of intervention trials, and we included additional types of systematic reviews, we adjusted some AMSTAR 2 ratings and reported these in Additional file 2 .
Adherence to each item was rated as follows: yes, partial yes, no, or not applicable (such as when a meta-analysis was not conducted). The overall confidence in the results of the review is rated as “critically low”, “low”, “moderate” or “high”, according to the AMSTAR 2 guidance based on seven critical domains, which are items 2, 4, 7, 9, 11, 13, 15 as defined by AMSTAR 2 authors [ 24 ]. We reported our adherence ratings for transparency of our decision with accompanying explanations, for each item, in each included review.
One of the included systematic reviews was conducted by some members of this author team [ 25 ]. This review was initially assessed independently by two authors who were not co-authors of that review to prevent the risk of bias in assessing this study.
Synthesis of results
For data synthesis, we prepared a table summarizing each systematic review. Graphs illustrating the mortality rate and clinical symptoms were created. We then prepared a narrative summary of the methods, findings, study strengths, and limitations.
For analysis of the prevalence of clinical outcomes, we extracted data on the number of events and the total number of patients to perform proportional meta-analysis using RStudio© software, with the “meta” package (version 4.9–6), using the “metaprop” function for reviews that did not perform a meta-analysis, excluding case studies because of the absence of variance. For reviews that did not perform a meta-analysis, we presented pooled results of proportions with their respective confidence intervals (95%) by the inverse variance method with a random-effects model, using the DerSimonian-Laird estimator for τ 2 . We adjusted data using Freeman-Tukey double arcosen transformation. Confidence intervals were calculated using the Clopper-Pearson method for individual studies. We created forest plots using the RStudio© software, with the “metafor” package (version 2.1–0) and “forest” function.
Managing overlapping systematic reviews
Some of the included systematic reviews that address the same or similar research questions may include the same primary studies in overviews. Including such overlapping reviews may introduce bias when outcome data from the same primary study are included in the analyses of an overview multiple times. Thus, in summaries of evidence, multiple-counting of the same outcome data will give data from some primary studies too much influence [ 14 ]. In this overview, we did not exclude overlapping systematic reviews because, according to Cochrane’s guidance, it may be appropriate to include all relevant reviews’ results if the purpose of the overview is to present and describe the current body of evidence on a topic [ 14 ]. To avoid any bias in summary estimates associated with overlapping reviews, we generated forest plots showing data from individual systematic reviews, but the results were not pooled because some primary studies were included in multiple reviews.
Our search retrieved 1063 publications, of which 175 were duplicates. Most publications were excluded after the title and abstract analysis ( n = 860). Among the 28 studies selected for full-text screening, 10 were excluded for the reasons described in Additional file 3 , and 18 were included in the final analysis (Fig. 1 ) [ 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ]. Reference list screening did not retrieve any additional systematic reviews.

PRISMA flow diagram
Characteristics of included reviews
Summary features of 18 systematic reviews are presented in Table 1 . They were published in 14 different journals. Only four of these journals had specific requirements for systematic reviews (with or without meta-analysis): European Journal of Internal Medicine, Journal of Clinical Medicine, Ultrasound in Obstetrics and Gynecology, and Clinical Research in Cardiology . Two journals reported that they published only invited reviews ( Journal of Medical Virology and Clinica Chimica Acta ). Three systematic reviews in our study were published as letters; one was labeled as a scoping review and another as a rapid review (Table 2 ).
All reviews were published in English, in first quartile (Q1) journals, with JIF ranging from 1.692 to 6.062. One review was empty, meaning that its search did not identify any relevant studies; i.e., no primary studies were included [ 36 ]. The remaining 17 reviews included 269 unique studies; the majority ( N = 211; 78%) were included in only a single review included in our study (range: 1 to 12). Primary studies included in the reviews were published between December 2019 and March 18, 2020, and comprised case reports, case series, cohorts, and other observational studies. We found only one review that included randomized clinical trials [ 38 ]. In the included reviews, systematic literature searches were performed from 2019 (entire year) up to March 9, 2020. Ten systematic reviews included meta-analyses. The list of primary studies found in the included systematic reviews is shown in Additional file 4 , as well as the number of reviews in which each primary study was included.
Population and study designs
Most of the reviews analyzed data from patients with COVID-19 who developed pneumonia, acute respiratory distress syndrome (ARDS), or any other correlated complication. One review aimed to evaluate the effectiveness of using surgical masks on preventing transmission of the virus [ 36 ], one review was focused on pediatric patients [ 34 ], and one review investigated COVID-19 in pregnant women [ 37 ]. Most reviews assessed clinical symptoms, laboratory findings, or radiological results.
Systematic review findings
The summary of findings from individual reviews is shown in Table 2 . Overall, all-cause mortality ranged from 0.3 to 13.9% (Fig. 2 ).

A meta-analysis of the prevalence of mortality
Clinical symptoms
Seven reviews described the main clinical manifestations of COVID-19 [ 26 , 28 , 29 , 34 , 35 , 39 , 41 ]. Three of them provided only a narrative discussion of symptoms [ 26 , 34 , 35 ]. In the reviews that performed a statistical analysis of the incidence of different clinical symptoms, symptoms in patients with COVID-19 were (range values of point estimates): fever (82–95%), cough with or without sputum (58–72%), dyspnea (26–59%), myalgia or muscle fatigue (29–51%), sore throat (10–13%), headache (8–12%), gastrointestinal disorders, such as diarrhea, nausea or vomiting (5.0–9.0%), and others (including, in one study only: dizziness 12.1%) (Figs. 3 , 4 , 5 , 6 , 7 , 8 and 9 ). Three reviews assessed cough with and without sputum together; only one review assessed sputum production itself (28.5%).

A meta-analysis of the prevalence of fever

A meta-analysis of the prevalence of cough

A meta-analysis of the prevalence of dyspnea

A meta-analysis of the prevalence of fatigue or myalgia

A meta-analysis of the prevalence of headache

A meta-analysis of the prevalence of gastrointestinal disorders

A meta-analysis of the prevalence of sore throat
Diagnostic aspects
Three reviews described methodologies, protocols, and tools used for establishing the diagnosis of COVID-19 [ 26 , 34 , 38 ]. The use of respiratory swabs (nasal or pharyngeal) or blood specimens to assess the presence of SARS-CoV-2 nucleic acid using RT-PCR assays was the most commonly used diagnostic method mentioned in the included studies. These diagnostic tests have been widely used, but their precise sensitivity and specificity remain unknown. One review included a Chinese study with clinical diagnosis with no confirmation of SARS-CoV-2 infection (patients were diagnosed with COVID-19 if they presented with at least two symptoms suggestive of COVID-19, together with laboratory and chest radiography abnormalities) [ 34 ].
Therapeutic possibilities
Pharmacological and non-pharmacological interventions (supportive therapies) used in treating patients with COVID-19 were reported in five reviews [ 25 , 27 , 34 , 35 , 38 ]. Antivirals used empirically for COVID-19 treatment were reported in seven reviews [ 25 , 27 , 34 , 35 , 37 , 38 , 41 ]; most commonly used were protease inhibitors (lopinavir, ritonavir, darunavir), nucleoside reverse transcriptase inhibitor (tenofovir), nucleotide analogs (remdesivir, galidesivir, ganciclovir), and neuraminidase inhibitors (oseltamivir). Umifenovir, a membrane fusion inhibitor, was investigated in two studies [ 25 , 35 ]. Possible supportive interventions analyzed were different types of oxygen supplementation and breathing support (invasive or non-invasive ventilation) [ 25 ]. The use of antibiotics, both empirically and to treat secondary pneumonia, was reported in six studies [ 25 , 26 , 27 , 34 , 35 , 38 ]. One review specifically assessed evidence on the efficacy and safety of the anti-malaria drug chloroquine [ 27 ]. It identified 23 ongoing trials investigating the potential of chloroquine as a therapeutic option for COVID-19, but no verifiable clinical outcomes data. The use of mesenchymal stem cells, antifungals, and glucocorticoids were described in four reviews [ 25 , 34 , 35 , 38 ].
Laboratory and radiological findings
Of the 18 reviews included in this overview, eight analyzed laboratory parameters in patients with COVID-19 [ 25 , 29 , 30 , 32 , 33 , 34 , 35 , 39 ]; elevated C-reactive protein levels, associated with lymphocytopenia, elevated lactate dehydrogenase, as well as slightly elevated aspartate and alanine aminotransferase (AST, ALT) were commonly described in those eight reviews. Lippi et al. assessed cardiac troponin I (cTnI) [ 25 ], procalcitonin [ 32 ], and platelet count [ 33 ] in COVID-19 patients. Elevated levels of procalcitonin [ 32 ] and cTnI [ 30 ] were more likely to be associated with a severe disease course (requiring intensive care unit admission and intubation). Furthermore, thrombocytopenia was frequently observed in patients with complicated COVID-19 infections [ 33 ].
Chest imaging (chest radiography and/or computed tomography) features were assessed in six reviews, all of which described a frequent pattern of local or bilateral multilobar ground-glass opacity [ 25 , 34 , 35 , 39 , 40 , 41 ]. Those six reviews showed that septal thickening, bronchiectasis, pleural and cardiac effusions, halo signs, and pneumothorax were observed in patients suffering from COVID-19.
Quality of evidence in individual systematic reviews
Table 3 shows the detailed results of the quality assessment of 18 systematic reviews, including the assessment of individual items and summary assessment. A detailed explanation for each decision in each review is available in Additional file 5 .
Using AMSTAR 2 criteria, confidence in the results of all 18 reviews was rated as “critically low” (Table 3 ). Common methodological drawbacks were: omission of prospective protocol submission or publication; use of inappropriate search strategy: lack of independent and dual literature screening and data-extraction (or methodology unclear); absence of an explanation for heterogeneity among the studies included; lack of reasons for study exclusion (or rationale unclear).
Risk of bias assessment, based on a reported methodological tool, and quality of evidence appraisal, in line with the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) method, were reported only in one review [ 25 ]. Five reviews presented a table summarizing bias, using various risk of bias tools [ 25 , 29 , 39 , 40 , 41 ]. One review analyzed “study quality” [ 37 ]. One review mentioned the risk of bias assessment in the methodology but did not provide any related analysis [ 28 ].
This overview of systematic reviews analyzed the first 18 systematic reviews published after the onset of the COVID-19 pandemic, up to March 24, 2020, with primary studies involving more than 60,000 patients. Using AMSTAR-2, we judged that our confidence in all those reviews was “critically low”. Ten reviews included meta-analyses. The reviews presented data on clinical manifestations, laboratory and radiological findings, and interventions. We found no systematic reviews on the utility of diagnostic tests.
Symptoms were reported in seven reviews; most of the patients had a fever, cough, dyspnea, myalgia or muscle fatigue, and gastrointestinal disorders such as diarrhea, nausea, or vomiting. Olfactory dysfunction (anosmia or dysosmia) has been described in patients infected with COVID-19 [ 43 ]; however, this was not reported in any of the reviews included in this overview. During the SARS outbreak in 2002, there were reports of impairment of the sense of smell associated with the disease [ 44 , 45 ].
The reported mortality rates ranged from 0.3 to 14% in the included reviews. Mortality estimates are influenced by the transmissibility rate (basic reproduction number), availability of diagnostic tools, notification policies, asymptomatic presentations of the disease, resources for disease prevention and control, and treatment facilities; variability in the mortality rate fits the pattern of emerging infectious diseases [ 46 ]. Furthermore, the reported cases did not consider asymptomatic cases, mild cases where individuals have not sought medical treatment, and the fact that many countries had limited access to diagnostic tests or have implemented testing policies later than the others. Considering the lack of reviews assessing diagnostic testing (sensitivity, specificity, and predictive values of RT-PCT or immunoglobulin tests), and the preponderance of studies that assessed only symptomatic individuals, considerable imprecision around the calculated mortality rates existed in the early stage of the COVID-19 pandemic.
Few reviews included treatment data. Those reviews described studies considered to be at a very low level of evidence: usually small, retrospective studies with very heterogeneous populations. Seven reviews analyzed laboratory parameters; those reviews could have been useful for clinicians who attend patients suspected of COVID-19 in emergency services worldwide, such as assessing which patients need to be reassessed more frequently.
All systematic reviews scored poorly on the AMSTAR 2 critical appraisal tool for systematic reviews. Most of the original studies included in the reviews were case series and case reports, impacting the quality of evidence. Such evidence has major implications for clinical practice and the use of these reviews in evidence-based practice and policy. Clinicians, patients, and policymakers can only have the highest confidence in systematic review findings if high-quality systematic review methodologies are employed. The urgent need for information during a pandemic does not justify poor quality reporting.
We acknowledge that there are numerous challenges associated with analyzing COVID-19 data during a pandemic [ 47 ]. High-quality evidence syntheses are needed for decision-making, but each type of evidence syntheses is associated with its inherent challenges.
The creation of classic systematic reviews requires considerable time and effort; with massive research output, they quickly become outdated, and preparing updated versions also requires considerable time. A recent study showed that updates of non-Cochrane systematic reviews are published a median of 5 years after the publication of the previous version [ 48 ].
Authors may register a review and then abandon it [ 49 ], but the existence of a public record that is not updated may lead other authors to believe that the review is still ongoing. A quarter of Cochrane review protocols remains unpublished as completed systematic reviews 8 years after protocol publication [ 50 ].
Rapid reviews can be used to summarize the evidence, but they involve methodological sacrifices and simplifications to produce information promptly, with inconsistent methodological approaches [ 51 ]. However, rapid reviews are justified in times of public health emergencies, and even Cochrane has resorted to publishing rapid reviews in response to the COVID-19 crisis [ 52 ]. Rapid reviews were eligible for inclusion in this overview, but only one of the 18 reviews included in this study was labeled as a rapid review.
Ideally, COVID-19 evidence would be continually summarized in a series of high-quality living systematic reviews, types of evidence synthesis defined as “ a systematic review which is continually updated, incorporating relevant new evidence as it becomes available ” [ 53 ]. However, conducting living systematic reviews requires considerable resources, calling into question the sustainability of such evidence synthesis over long periods [ 54 ].
Research reports about COVID-19 will contribute to research waste if they are poorly designed, poorly reported, or simply not necessary. In principle, systematic reviews should help reduce research waste as they usually provide recommendations for further research that is needed or may advise that sufficient evidence exists on a particular topic [ 55 ]. However, systematic reviews can also contribute to growing research waste when they are not needed, or poorly conducted and reported. Our present study clearly shows that most of the systematic reviews that were published early on in the COVID-19 pandemic could be categorized as research waste, as our confidence in their results is critically low.
Our study has some limitations. One is that for AMSTAR 2 assessment we relied on information available in publications; we did not attempt to contact study authors for clarifications or additional data. In three reviews, the methodological quality appraisal was challenging because they were published as letters, or labeled as rapid communications. As a result, various details about their review process were not included, leading to AMSTAR 2 questions being answered as “not reported”, resulting in low confidence scores. Full manuscripts might have provided additional information that could have led to higher confidence in the results. In other words, low scores could reflect incomplete reporting, not necessarily low-quality review methods. To make their review available more rapidly and more concisely, the authors may have omitted methodological details. A general issue during a crisis is that speed and completeness must be balanced. However, maintaining high standards requires proper resourcing and commitment to ensure that the users of systematic reviews can have high confidence in the results.
Furthermore, we used adjusted AMSTAR 2 scoring, as the tool was designed for critical appraisal of reviews of interventions. Some reviews may have received lower scores than actually warranted in spite of these adjustments.
Another limitation of our study may be the inclusion of multiple overlapping reviews, as some included reviews included the same primary studies. According to the Cochrane Handbook, including overlapping reviews may be appropriate when the review’s aim is “ to present and describe the current body of systematic review evidence on a topic ” [ 12 ], which was our aim. To avoid bias with summarizing evidence from overlapping reviews, we presented the forest plots without summary estimates. The forest plots serve to inform readers about the effect sizes for outcomes that were reported in each review.
Several authors from this study have contributed to one of the reviews identified [ 25 ]. To reduce the risk of any bias, two authors who did not co-author the review in question initially assessed its quality and limitations.
Finally, we note that the systematic reviews included in our overview may have had issues that our analysis did not identify because we did not analyze their primary studies to verify the accuracy of the data and information they presented. We give two examples to substantiate this possibility. Lovato et al. wrote a commentary on the review of Sun et al. [ 41 ], in which they criticized the authors’ conclusion that sore throat is rare in COVID-19 patients [ 56 ]. Lovato et al. highlighted that multiple studies included in Sun et al. did not accurately describe participants’ clinical presentations, warning that only three studies clearly reported data on sore throat [ 56 ].
In another example, Leung [ 57 ] warned about the review of Li, L.Q. et al. [ 29 ]: “ it is possible that this statistic was computed using overlapped samples, therefore some patients were double counted ”. Li et al. responded to Leung that it is uncertain whether the data overlapped, as they used data from published articles and did not have access to the original data; they also reported that they requested original data and that they plan to re-do their analyses once they receive them; they also urged readers to treat the data with caution [ 58 ]. This points to the evolving nature of evidence during a crisis.
Our study’s strength is that this overview adds to the current knowledge by providing a comprehensive summary of all the evidence synthesis about COVID-19 available early after the onset of the pandemic. This overview followed strict methodological criteria, including a comprehensive and sensitive search strategy and a standard tool for methodological appraisal of systematic reviews.
In conclusion, in this overview of systematic reviews, we analyzed evidence from the first 18 systematic reviews that were published after the emergence of COVID-19. However, confidence in the results of all the reviews was “critically low”. Thus, systematic reviews that were published early on in the pandemic could be categorized as research waste. Even during public health emergencies, studies and systematic reviews should adhere to established methodological standards to provide patients, clinicians, and decision-makers trustworthy evidence.
Availability of data and materials
All data collected and analyzed within this study are available from the corresponding author on reasonable request.
World Health Organization. Timeline - COVID-19: Available at: https://www.who.int/news/item/29-06-2020-covidtimeline . Accessed 1 June 2021.
COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Available at: https://coronavirus.jhu.edu/map.html . Accessed 1 June 2021.
Anzai A, Kobayashi T, Linton NM, Kinoshita R, Hayashi K, Suzuki A, et al. Assessing the Impact of Reduced Travel on Exportation Dynamics of Novel Coronavirus Infection (COVID-19). J Clin Med. 2020;9(2):601.
Chinazzi M, Davis JT, Ajelli M, Gioannini C, Litvinova M, Merler S, et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368(6489):395–400. https://doi.org/10.1126/science.aba9757 .
Article CAS PubMed PubMed Central Google Scholar
Fidahic M, Nujic D, Runjic R, Civljak M, Markotic F, Lovric Makaric Z, et al. Research methodology and characteristics of journal articles with original data, preprint articles and registered clinical trial protocols about COVID-19. BMC Med Res Methodol. 2020;20(1):161. https://doi.org/10.1186/s12874-020-01047-2 .
EPPI Centre . COVID-19: a living systematic map of the evidence. Available at: http://eppi.ioe.ac.uk/cms/Projects/DepartmentofHealthandSocialCare/Publishedreviews/COVID-19Livingsystematicmapoftheevidence/tabid/3765/Default.aspx . Accessed 1 June 2021.
NCBI SARS-CoV-2 Resources. Available at: https://www.ncbi.nlm.nih.gov/sars-cov-2/ . Accessed 1 June 2021.
Gustot T. Quality and reproducibility during the COVID-19 pandemic. JHEP Rep. 2020;2(4):100141. https://doi.org/10.1016/j.jhepr.2020.100141 .
Article PubMed PubMed Central Google Scholar
Kodvanj, I., et al., Publishing of COVID-19 Preprints in Peer-reviewed Journals, Preprinting Trends, Public Discussion and Quality Issues. Preprint article. bioRxiv 2020.11.23.394577; doi: https://doi.org/10.1101/2020.11.23.394577 .
Dobler CC. Poor quality research and clinical practice during COVID-19. Breathe (Sheff). 2020;16(2):200112. https://doi.org/10.1183/20734735.0112-2020 .
Article Google Scholar
Bastian H, Glasziou P, Chalmers I. Seventy-five trials and eleven systematic reviews a day: how will we ever keep up? PLoS Med. 2010;7(9):e1000326. https://doi.org/10.1371/journal.pmed.1000326 .
Lunny C, Brennan SE, McDonald S, McKenzie JE. Toward a comprehensive evidence map of overview of systematic review methods: paper 1-purpose, eligibility, search and data extraction. Syst Rev. 2017;6(1):231. https://doi.org/10.1186/s13643-017-0617-1 .
Pollock M, Fernandes RM, Becker LA, Pieper D, Hartling L. Chapter V: Overviews of Reviews. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane. 2020. Available from www.training.cochrane.org/handbook .
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions version 6.1 (updated September 2020). Cochrane. 2020; Available from www.training.cochrane.org/handbook .
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. The impact of different inclusion decisions on the comprehensiveness and complexity of overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):18. https://doi.org/10.1186/s13643-018-0914-3 .
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. A decision tool to help researchers make decisions about including systematic reviews in overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):29. https://doi.org/10.1186/s13643-018-0768-8 .
Hunt H, Pollock A, Campbell P, Estcourt L, Brunton G. An introduction to overviews of reviews: planning a relevant research question and objective for an overview. Syst Rev. 2018;7(1):39. https://doi.org/10.1186/s13643-018-0695-8 .
Pollock M, Fernandes RM, Pieper D, Tricco AC, Gates M, Gates A, et al. Preferred reporting items for overviews of reviews (PRIOR): a protocol for development of a reporting guideline for overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):335. https://doi.org/10.1186/s13643-019-1252-9 .
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Open Med. 2009;3(3):e123–30.
Krnic Martinic M, Pieper D, Glatt A, Puljak L. Definition of a systematic review used in overviews of systematic reviews, meta-epidemiological studies and textbooks. BMC Med Res Methodol. 2019;19(1):203. https://doi.org/10.1186/s12874-019-0855-0 .
Puljak L. If there is only one author or only one database was searched, a study should not be called a systematic review. J Clin Epidemiol. 2017;91:4–5. https://doi.org/10.1016/j.jclinepi.2017.08.002 .
Article PubMed Google Scholar
Gates M, Gates A, Guitard S, Pollock M, Hartling L. Guidance for overviews of reviews continues to accumulate, but important challenges remain: a scoping review. Syst Rev. 2020;9(1):254. https://doi.org/10.1186/s13643-020-01509-0 .
Covidence - systematic review software. Available at: https://www.covidence.org/ . Accessed 1 June 2021.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Borges do Nascimento IJ, et al. Novel Coronavirus Infection (COVID-19) in Humans: A Scoping Review and Meta-Analysis. J Clin Med. 2020;9(4):941.
Article PubMed Central Google Scholar
Adhikari SP, Meng S, Wu YJ, Mao YP, Ye RX, Wang QZ, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9(1):29. https://doi.org/10.1186/s40249-020-00646-x .
Cortegiani A, Ingoglia G, Ippolito M, Giarratano A, Einav S. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care. 2020;57:279–83. https://doi.org/10.1016/j.jcrc.2020.03.005 .
Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109(5):531–8. https://doi.org/10.1007/s00392-020-01626-9 .
Article CAS PubMed Google Scholar
Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(6):577–83. https://doi.org/10.1002/jmv.25757 .
Lippi G, Lavie CJ, Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): evidence from a meta-analysis. Prog Cardiovasc Dis. 2020;63(3):390–1. https://doi.org/10.1016/j.pcad.2020.03.001 .
Lippi G, Henry BM. Active smoking is not associated with severity of coronavirus disease 2019 (COVID-19). Eur J Intern Med. 2020;75:107–8. https://doi.org/10.1016/j.ejim.2020.03.014 .
Lippi G, Plebani M. Procalcitonin in patients with severe coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chim Acta. 2020;505:190–1. https://doi.org/10.1016/j.cca.2020.03.004 .
Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta. 2020;506:145–8. https://doi.org/10.1016/j.cca.2020.03.022 .
Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109(6):1088–95. https://doi.org/10.1111/apa.15270 .
Lupia T, Scabini S, Mornese Pinna S, di Perri G, de Rosa FG, Corcione S. 2019 novel coronavirus (2019-nCoV) outbreak: a new challenge. J Glob Antimicrob Resist. 2020;21:22–7. https://doi.org/10.1016/j.jgar.2020.02.021 .
Marasinghe, K.M., A systematic review investigating the effectiveness of face mask use in limiting the spread of COVID-19 among medically not diagnosed individuals: shedding light on current recommendations provided to individuals not medically diagnosed with COVID-19. Research Square. Preprint article. doi : https://doi.org/10.21203/rs.3.rs-16701/v1 . 2020 .
Mullins E, Evans D, Viner RM, O’Brien P, Morris E. Coronavirus in pregnancy and delivery: rapid review. Ultrasound Obstet Gynecol. 2020;55(5):586–92. https://doi.org/10.1002/uog.22014 .
Pang J, Wang MX, Ang IYH, Tan SHX, Lewis RF, Chen JIP, et al. Potential Rapid Diagnostics, Vaccine and Therapeutics for 2019 Novel coronavirus (2019-nCoV): a systematic review. J Clin Med. 2020;9(3):623.
Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623. https://doi.org/10.1016/j.tmaid.2020.101623 .
Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020;215(1):87–93. https://doi.org/10.2214/AJR.20.23034 .
Sun P, Qie S, Liu Z, Ren J, Li K, Xi J. Clinical characteristics of hospitalized patients with SARS-CoV-2 infection: a single arm meta-analysis. J Med Virol. 2020;92(6):612–7. https://doi.org/10.1002/jmv.25735 .
Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–5. https://doi.org/10.1016/j.ijid.2020.03.017 .
Bassetti M, Vena A, Giacobbe DR. The novel Chinese coronavirus (2019-nCoV) infections: challenges for fighting the storm. Eur J Clin Investig. 2020;50(3):e13209. https://doi.org/10.1111/eci.13209 .
Article CAS Google Scholar
Hwang CS. Olfactory neuropathy in severe acute respiratory syndrome: report of a case. Acta Neurol Taiwanica. 2006;15(1):26–8.
Google Scholar
Suzuki M, Saito K, Min WP, Vladau C, Toida K, Itoh H, et al. Identification of viruses in patients with postviral olfactory dysfunction. Laryngoscope. 2007;117(2):272–7. https://doi.org/10.1097/01.mlg.0000249922.37381.1e .
Rajgor DD, Lee MH, Archuleta S, Bagdasarian N, Quek SC. The many estimates of the COVID-19 case fatality rate. Lancet Infect Dis. 2020;20(7):776–7. https://doi.org/10.1016/S1473-3099(20)30244-9 .
Wolkewitz M, Puljak L. Methodological challenges of analysing COVID-19 data during the pandemic. BMC Med Res Methodol. 2020;20(1):81. https://doi.org/10.1186/s12874-020-00972-6 .
Rombey T, Lochner V, Puljak L, Könsgen N, Mathes T, Pieper D. Epidemiology and reporting characteristics of non-Cochrane updates of systematic reviews: a cross-sectional study. Res Synth Methods. 2020;11(3):471–83. https://doi.org/10.1002/jrsm.1409 .
Runjic E, Rombey T, Pieper D, Puljak L. Half of systematic reviews about pain registered in PROSPERO were not published and the majority had inaccurate status. J Clin Epidemiol. 2019;116:114–21. https://doi.org/10.1016/j.jclinepi.2019.08.010 .
Runjic E, Behmen D, Pieper D, Mathes T, Tricco AC, Moher D, et al. Following Cochrane review protocols to completion 10 years later: a retrospective cohort study and author survey. J Clin Epidemiol. 2019;111:41–8. https://doi.org/10.1016/j.jclinepi.2019.03.006 .
Tricco AC, Antony J, Zarin W, Strifler L, Ghassemi M, Ivory J, et al. A scoping review of rapid review methods. BMC Med. 2015;13(1):224. https://doi.org/10.1186/s12916-015-0465-6 .
COVID-19 Rapid Reviews: Cochrane’s response so far. Available at: https://training.cochrane.org/resource/covid-19-rapid-reviews-cochrane-response-so-far . Accessed 1 June 2021.
Cochrane. Living systematic reviews. Available at: https://community.cochrane.org/review-production/production-resources/living-systematic-reviews . Accessed 1 June 2021.
Millard T, Synnot A, Elliott J, Green S, McDonald S, Turner T. Feasibility and acceptability of living systematic reviews: results from a mixed-methods evaluation. Syst Rev. 2019;8(1):325. https://doi.org/10.1186/s13643-019-1248-5 .
Babic A, Poklepovic Pericic T, Pieper D, Puljak L. How to decide whether a systematic review is stable and not in need of updating: analysis of Cochrane reviews. Res Synth Methods. 2020;11(6):884–90. https://doi.org/10.1002/jrsm.1451 .
Lovato A, Rossettini G, de Filippis C. Sore throat in COVID-19: comment on “clinical characteristics of hospitalized patients with SARS-CoV-2 infection: a single arm meta-analysis”. J Med Virol. 2020;92(7):714–5. https://doi.org/10.1002/jmv.25815 .
Leung C. Comment on Li et al: COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(9):1431–2. https://doi.org/10.1002/jmv.25912 .
Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. Response to Char’s comment: comment on Li et al: COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(9):1433. https://doi.org/10.1002/jmv.25924 .
Download references
Acknowledgments
We thank Catherine Henderson DPhil from Swanscoe Communications for pro bono medical writing and editing support. We acknowledge support from the Covidence Team, specifically Anneliese Arno. We thank the whole International Network of Coronavirus Disease 2019 (InterNetCOVID-19) for their commitment and involvement. Members of the InterNetCOVID-19 are listed in Additional file 6 . We thank Pavel Cerny and Roger Crosthwaite for guiding the team supervisor (IJBN) on human resources management.
This research received no external funding.
Author information
Authors and affiliations.
University Hospital and School of Medicine, Universidade Federal de Minas Gerais, Belo Horizonte, Minas Gerais, Brazil
Israel Júnior Borges do Nascimento & Milena Soriano Marcolino
Medical College of Wisconsin, Milwaukee, WI, USA
Israel Júnior Borges do Nascimento
Helene Fuld Health Trust National Institute for Evidence-based Practice in Nursing and Healthcare, College of Nursing, The Ohio State University, Columbus, OH, USA
Dónal P. O’Mathúna
School of Nursing, Psychotherapy and Community Health, Dublin City University, Dublin, Ireland
Department of Anesthesiology, Intensive Care and Pain Medicine, University of Münster, Münster, Germany
Thilo Caspar von Groote
Department of Sport and Health Science, Technische Universität München, Munich, Germany
Hebatullah Mohamed Abdulazeem
School of Health Sciences, Faculty of Health and Medicine, The University of Newcastle, Callaghan, Australia
Ishanka Weerasekara
Department of Physiotherapy, Faculty of Allied Health Sciences, University of Peradeniya, Peradeniya, Sri Lanka
Cochrane Croatia, University of Split, School of Medicine, Split, Croatia
Ana Marusic, Irena Zakarija-Grkovic & Tina Poklepovic Pericic
Center for Evidence-Based Medicine and Health Care, Catholic University of Croatia, Ilica 242, 10000, Zagreb, Croatia
Livia Puljak
Cochrane Brazil, Evidence-Based Health Program, Universidade Federal de São Paulo, São Paulo, Brazil
Vinicius Tassoni Civile & Alvaro Nagib Atallah
Yorkville University, Fredericton, New Brunswick, Canada
Santino Filoso
Laboratory for Industrial and Applied Mathematics (LIAM), Department of Mathematics and Statistics, York University, Toronto, Ontario, Canada
Nicola Luigi Bragazzi
You can also search for this author in PubMed Google Scholar
Contributions
IJBN conceived the research idea and worked as a project coordinator. DPOM, TCVG, HMA, IW, AM, LP, VTC, IZG, TPP, ANA, SF, NLB and MSM were involved in data curation, formal analysis, investigation, methodology, and initial draft writing. All authors revised the manuscript critically for the content. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Livia Puljak .
Ethics declarations
Ethics approval and consent to participate.
Not required as data was based on published studies.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: appendix 1..
Search strategies used in the study.
Additional file 2: Appendix 2.
Adjusted scoring of AMSTAR 2 used in this study for systematic reviews of studies that did not analyze interventions.
Additional file 3: Appendix 3.
List of excluded studies, with reasons.
Additional file 4: Appendix 4.
Table of overlapping studies, containing the list of primary studies included, their visual overlap in individual systematic reviews, and the number in how many reviews each primary study was included.
Additional file 5: Appendix 5.
A detailed explanation of AMSTAR scoring for each item in each review.
Additional file 6: Appendix 6.
List of members and affiliates of International Network of Coronavirus Disease 2019 (InterNetCOVID-19).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Borges do Nascimento, I.J., O’Mathúna, D.P., von Groote, T.C. et al. Coronavirus disease (COVID-19) pandemic: an overview of systematic reviews. BMC Infect Dis 21 , 525 (2021). https://doi.org/10.1186/s12879-021-06214-4
Download citation
Received : 12 April 2020
Accepted : 19 May 2021
Published : 04 June 2021
DOI : https://doi.org/10.1186/s12879-021-06214-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Coronavirus
- Evidence-based medicine
- Infectious diseases
BMC Infectious Diseases
ISSN: 1471-2334
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Featured Clinical Reviews
- Screening for Atrial Fibrillation: US Preventive Services Task Force Recommendation Statement JAMA Recommendation Statement January 25, 2022
- Evaluating the Patient With a Pulmonary Nodule: A Review JAMA Review January 18, 2022
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
A National Strategy for the “New Normal” of Life With COVID
- 1 Perelman School of Medicine and The Wharton School, University of Pennsylvania, Philadelphia
- 2 Center for Infectious Disease Research and Policy, University of Minnesota, Minneapolis
- 3 Grossman School of Medicine, New York University, New York, New York
- Viewpoint The First 2 Years of COVID-19—Lessons to Improve Preparedness for the Next Pandemic Jennifer B. Nuzzo, DrPH, SM; Lawrence O. Gostin, JD JAMA
- Viewpoint A National Strategy for COVID-19—Testing, Surveillance, and Mitigation Strategies David Michaels, PhD, MPH; Ezekiel J. Emanuel, MD, PhD; Rick A. Bright, PhD JAMA
- Viewpoint A National Strategy for COVID-19 Medical Countermeasures Luciana L. Borio, MD; Rick A. Bright, PhD; Ezekiel J. Emanuel, MD, PhD JAMA
- Viewpoint The Pandemic Preparedness Program Eli Y. Adashi, MD, MS; I. Glenn Cohen, JD JAMA
- Medical News & Perspectives Former Biden-Harris Transition Advisors Propose a New National Strategy for COVID-19 Jennifer Abbasi JAMA
- Comment & Response Strategy for the “New Normal” of Life With COVID—Reply Ezekiel J. Emanuel, MD, PhD; Michael Osterholm, PhD, MPH; Céline R. Gounder, MD, ScM JAMA
- Comment & Response Strategy for the “New Normal” of Life With COVID Afschin Gandjour, MD, PhD, MA JAMA
- Viewpoint COVID-19 Vaccination—Becoming Part of the New Normal Peter Marks, MD, PhD; Janet Woodcock, MD; Robert Califf, MD JAMA
As the Omicron variant of SARS-CoV-2 demonstrates, COVID-19 is here to stay. In January 2021, President Biden issued the “National Strategy for the COVID-19 Response and Pandemic Preparedness.” As the US moves from crisis to control, this national strategy needs to be updated. Policy makers need to specify the goals and strategies for the “new normal” of life with COVID-19 and communicate them clearly to the public.
SARS-CoV-2 continues to persist, evolve, and surprise. In July 2021, with vaccinations apace and infection rates plummeting, Biden proclaimed that “we’ve gained the upper hand against this virus,” and the Centers for Disease Control and Prevention (CDC) relaxed its guidance for mask wearing and socializing. 1 By September 2021, the Delta variant proved these steps to be premature, and by late November, the Omicron variant created concern about a perpetual state of emergency.
In delineating a national strategy, humility is essential. The precise duration of immunity to SARS-CoV-2 from vaccination or prior infection is unknown. Also unknown is whether SARS-CoV-2 will become a seasonal infection; whether antiviral therapies will prevent long COVID; or whether even more transmissible, immune-evading, or virulent variants will arise after Omicron.
Another part of this humility is recognizing that predictions are necessary but educated guesses, not mathematical certainty. The virus, host response, and data will evolve. Biomedical and public health tools will expand, along with better understanding of their limitations. The incidence of SARS-CoV-2, vaccination rates, hospital capacity, tolerance for risk, and willingness to implement different interventions will vary geographically, and national recommendations will need to be adapted locally.
It is imperative for public health, economic, and social functioning that US leaders establish and communicate specific goals for COVID-19 management, benchmarks for the imposition or relaxation of public health restrictions, investments and reforms needed to prepare for future SARS-CoV-2 variants and other novel viruses, and clear strategies to accomplish all of this.
Redefining the Appropriate National Risk Level
The goal for the “new normal” with COVID-19 does not include eradication or elimination, eg, the “zero COVID” strategy. 2 Neither COVID-19 vaccination nor infection appear to confer lifelong immunity. Current vaccines do not offer sterilizing immunity against SARS-CoV-2 infection. Infectious diseases cannot be eradicated when there is limited long-term immunity following infection or vaccination or nonhuman reservoirs of infection. The majority of SARS-CoV-2 infections are asymptomatic or mildly symptomatic, and the SARS-CoV-2 incubation period is short, preventing the use of targeted strategies like “ring vaccination.” Even “fully” vaccinated individuals are at risk for breakthrough SARS-CoV-2 infection. Consequently, a “new normal with COVID” in January 2022 is not living without COVID-19.
The “new normal” requires recognizing that SARS-CoV-2 is but one of several circulating respiratory viruses that include influenza, respiratory syncytial virus (RSV), and more. COVID-19 must now be considered among the risks posed by all respiratory viral illnesses combined. Many of the measures to reduce transmission of SARS-CoV-2 (eg, ventilation) will also reduce transmission of other respiratory viruses. Thus, policy makers should retire previous public health categorizations, including deaths from pneumonia and influenza or pneumonia, influenza, and COVID-19, and focus on a new category: the aggregate risk of all respiratory virus infections.
What should be the peak risk level for cumulative viral respiratory illnesses for a “normal” week? Even though seasonal influenza, RSV, and other respiratory viruses circulating before SARS-CoV-2 were harmful, the US has not considered them a sufficient threat to impose emergency measures in over a century. People have lived normally with the threats of these viruses, even though more could have been done to reduce their risks.
The appropriate risk threshold should reflect peak weekly deaths, hospitalizations, and community prevalence of viral respiratory illnesses during high-severity years, such as 2017-2018. 3 That year had approximately 41 million symptomatic cases of influenza, 710 000 hospitalizations and 52 000 deaths. 4 In addition, the CDC estimates that each year RSV leads to more than 235 000 hospitalizations and 15 000 deaths in the US. 3 This would translate into a risk threshold of approximately 35 000 hospitalizations and 3000 deaths (<1 death/100 000 population) in the worst week.
Today, the US is far from these thresholds. For the week of December 13, 2021, the CDC reported the US experienced more than 900 000 COVID-19 cases, more than 50 000 new hospitalizations for COVID-19, and more than 7000 deaths. 5 , 6 The tolerance for disease, hospitalization, and death varies widely among individuals and communities. What constitutes appropriate thresholds for hospitalizations and death, at what cost, and with what trade-offs remains undetermined.
This peak week risk threshold serves at least 2 fundamental functions. This risk threshold triggers policy recommendations for emergency implementation of mitigation and other measures. In addition, health systems could rely on this threshold for planning on the bed and workforce capacity they need normally, and when to institute surge measures.
Rebuilding Public Health
To cope with pandemic, and eventually, endemic SARS-CoV-2 and to respond to future public health threats requires deploying real-time information systems, a public health implementation workforce, flexible health systems, trust in government and public health institutions, and belief in the value of collective action for public good. 7 , 8
First, the US needs a comprehensive, digital, real-time, integrated data infrastructure for public health. As Omicron has reemphasized, the US is operating with imprecise estimates of disease spread, limited genomic surveillance, projections based on select reporting sites, and data from other countries that may not be generalizable. These shortcomings are threatening lives and societal function.
The US must establish a modern data infrastructure that includes real-time electronic collection of comprehensive information on respiratory viral infections, hospitalizations, deaths, disease-specific outcomes, and immunizations merged with sociodemographic and other relevant variables. The public health data infrastructure should integrate data from local, state, and national public health units, health care systems, public and commercial laboratories, and academic and research institutions. Using modern technology and analytics, it is also essential to merge nontraditional environmental (air, wastewater) surveillance data, including genomic data, with traditional clinical and epidemiological data to track outbreaks and target containment.
Second, the US needs a permanent public health implementation workforce that has the flexibility and surge capacity to manage persistent problems while simultaneously responding to emergencies. Data collection, analysis, and technical support are necessary, but it takes people to respond to crises. This implementation workforce should include a public health agency–based community health worker system and expanded school nurse system.
A system of community public health workers could augment the health care system by testing and vaccinating for SARS-CoV-2 and other respiratory infections; ensuring adherence to ongoing treatment for tuberculosis, HIV, diabetes, and other chronic conditions; providing health screening and support to pregnant individuals and new parents and their newborns; and delivering various other public health services to vulnerable or homebound populations.
School nurses need to be empowered to address the large unmet public health needs of children and adolescents. As polio vaccination campaigns showed, school health programs are an efficient and effective way to care for children, including preventing and treating mild asthma exacerbations (often caused by viral respiratory infections), ensuring vaccination as a condition for attendance, and addressing adolescents’ mental and sexual health needs. School clinics must be adequately staffed and funded as an essential component of the nation’s public health infrastructure.
Third, because respiratory infections ebb and flow, institutionalizing telemedicine waivers, licensure to practice and enable billing across state lines, and other measures that allow the flow of medical services to severely affected regions should be a priority.
Fourth, it is essential to rebuild trust in public health institutions and a belief in collective action in service of public health. 7 Communities with higher levels of trust and reciprocity, such as Denmark, have experienced lower rates of hospitalization and death from COVID-19. 7 Improving public health data systems and delivering a diverse public health workforce that can respond in real time in communities will be important steps toward building that trust more widely.
Conclusions
After previous infectious disease threats, the US quickly forgot and failed to institute necessary reforms. That pattern must change with the COVID-19 pandemic. Without a strategic plan for the “new normal” with endemic COVID-19, more people in the US will unnecessarily experience morbidity and mortality, health inequities will widen, and trillions will be lost from the US economy. This time, the nation must learn and prepare effectively for the future.
The resources necessary to build and sustain an effective public health infrastructure will be substantial. Policy makers should weigh not only the costs but also the benefits, including fewer deaths and lost productivity from COVID-19 and all viral respiratory illnesses. Indeed, after more than 800 000 deaths from COVID-19, and a projected loss of $8 trillion in gross domestic product through 2030, 8 these interventions will be immensely valuable.
Corresponding Author: Ezekiel J. Emanuel, MD, PhD, Medical Ethics and Health Policy, Perelman School of Medicine, University of Pennsylvania, 423 Guardian Dr, Blockley Hall, Philadelphia, PA 19104 ( [email protected] ).
Published Online: January 6, 2022. doi:10.1001/jama.2021.24282
Conflict of Interest Disclosures: Dr Emanuel reported personal fees, nonfinancial support, or both from companies, organizations, and professional health care meetings and being a venture partner at Oak HC/FT; a partner at Embedded Healthcare LLC, ReCovery Partners LLC, and COVID-19 Recovery Consulting; and an unpaid board member of Village MD and Oncology Analytics. Dr Emanuel owns no stock in pharmaceutical, medical device companies, or health insurers. No other disclosures were reported.
Additional Information: Drs Emanuel, Osterholm, and Gounder were members of the Biden-Harris Transition COVID-19 Advisory Board from November 2020 to January 2021.
See More About
Emanuel EJ , Osterholm M , Gounder CR. A National Strategy for the “New Normal” of Life With COVID. JAMA. 2022;327(3):211–212. doi:10.1001/jama.2021.24282
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Virology, transmission...
Virology, transmission, and pathogenesis of SARS-CoV-2
Read our latest coverage of the coronavirus outbreak.
- Related content
- Peer review
- Muge Cevik , clinical lecturer 1 2 ,
- Krutika Kuppalli , assistant professor 3 ,
- Jason Kindrachuk , assistant professor of virology 4 ,
- Malik Peiris , professor of virology 5
- 1 Division of Infection and Global Health Research, School of Medicine, University of St Andrews, St Andrews, UK
- 2 Specialist Virology Laboratory, Royal Infirmary of Edinburgh, Edinburgh, UK and Regional Infectious Diseases Unit, Western General Hospital, Edinburgh, UK
- 3 Division of Infectious Diseases, Medical University of South Carolina, Charleston, SC, USA
- 4 Laboratory of Emerging and Re-Emerging Viruses, Department of Medical Microbiology, University of Manitoba, Winnipeg, MB, Canada
- 5 School of Public Health, LKS Faculty of Medicine, The University of Hong Kong, Hong Kong Special Administrative Region, China
- Correspondence to M Cevik mc349{at}st-andrews.ac.uk
What you need to know
SARS-CoV-2 is genetically similar to SARS-CoV-1, but characteristics of SARS-CoV-2—eg, structural differences in its surface proteins and viral load kinetics—may help explain its enhanced rate of transmission
In the respiratory tract, peak SARS-CoV-2 load is observed at the time of symptom onset or in the first week of illness, with subsequent decline thereafter, indicating the highest infectiousness potential just before or within the first five days of symptom onset
Reverse transcription polymerase chain reaction (RT-PCR) tests can detect viral SARS-CoV-2 RNA in the upper respiratory tract for a mean of 17 days; however, detection of viral RNA does not necessarily equate to infectiousness, and viral culture from PCR positive upper respiratory tract samples has been rarely positive beyond nine days of illness
Symptomatic and pre-symptomatic transmission (1-2 days before symptom onset), is likely to play a greater role in the spread of SARS-CoV-2 than asymptomatic transmission
A wide range of virus-neutralising antibodies have been reported, and emerging evidence suggests that these may correlate with severity of illness but wane over time
Since the emergence of SARS-CoV-2 in December 2019, there has been an unparalleled global effort to characterise the virus and the clinical course of disease. Coronavirus disease 2019 (covid-19), caused by SARS-CoV-2, follows a biphasic pattern of illness that likely results from the combination of an early viral response phase and an inflammatory second phase. Most clinical presentations are mild, and the typical pattern of covid-19 more resembles an influenza-like illness—which includes fever, cough, malaise, myalgia, headache, and taste and smell disturbance—rather than severe pneumonia (although emerging evidence about long term consequences is yet to be understood in detail). 1 In this review, we provide a broad update on the emerging understanding of SARS-CoV-2 pathophysiology, including virology, transmission dynamics, and the immune response to the virus. Any of the mechanisms and assumptions discussed in the article and in our understanding of covid-19 may be revised as further evidence emerges.
What we know about the virus
SARS-CoV-2 is an enveloped β-coronavirus, with a genetic sequence very similar to SARS-CoV-1 (80%) and bat coronavirus RaTG13 (96.2%). 2 The viral envelope is coated by spike (S) glycoprotein, envelope (E), and membrane (M) proteins ( fig 1 ). Host cell binding and entry are mediated by the S protein. The first step in infection is virus binding to a host cell through its target receptor. The S1 sub-unit of the S protein contains the receptor binding domain that binds to the peptidase domain of angiotensin-converting enzyme 2 (ACE 2). In SARS-CoV-2 the S2 sub-unit is highly preserved and is considered a potential antiviral target. The virus structure and replication cycle are described in figure 1 .

(1) The virus binds to ACE 2 as the host target cell receptor in synergy with the host’s transmembrane serine protease 2 (cell surface protein), which is principally expressed in the airway epithelial cells and vascular endothelial cells. This leads to membrane fusion and releases the viral genome into the host cytoplasm (2). Stages (3-7) show the remaining steps of viral replication, leading to viral assembly, maturation, and virus release
- Download figure
- Open in new tab
- Download powerpoint
Coronaviruses have the capacity for proofreading during replication, and therefore mutation rates are lower than in other RNA viruses. As SARS-CoV-2 has spread globally it has, like other viruses, accumulated some mutations in the viral genome, which contains geographic signatures. Researchers have examined these mutations to study virus characterisation and understand epidemiology and transmission patterns. In general, the mutations have not been attributed to phenotypic changes affecting viral transmissibility or pathogenicity. The G614 variant in the S protein has been postulated to increase infectivity and transmissibility of the virus. 3 Higher viral loads were reported in clinical samples with virus containing G614 than previously circulating variant D614, although no association was made with severity of illness as measured by hospitalisation outcomes. 3 These findings have yet to be confirmed with regards to natural infection.
Why is SARS-CoV-2 more infectious than SARS-CoV-1?
SARS-CoV-2 has a higher reproductive number (R 0 ) than SARS-CoV-1, indicating much more efficient spread. 1 Several characteristics of SARS-CoV-2 may help explain this enhanced transmission. While both SARS-CoV-1 and SARS-CoV-2 preferentially interact with the angiotensin-converting enzyme 2 (ACE 2) receptor, SARS-CoV-2 has structural differences in its surface proteins that enable stronger binding to the ACE 2 receptor 4 and greater efficiency at invading host cells. 1 SARS-CoV-2 also has greater affinity (or bonding) for the upper respiratory tract and conjunctiva, 5 thus can infect the upper respiratory tract and can conduct airways more easily. 6
Viral load dynamics and duration of infectiousness
Viral load kinetics could also explain some of the differences between SARS-CoV-2 and SARS-CoV-1. In the respiratory tract, peak SARS-CoV-2 load is observed at the time of symptom onset or in the first week of illness, with subsequent decline thereafter, which indicates the highest infectiousness potential just before or within the first five days of symptom onset ( fig 2 ). 7 In contrast, in SARS-CoV-1 the highest viral loads were detected in the upper respiratory tract in the second week of illness, which explains its minimal contagiousness in the first week after symptom onset, enabling early case detection in the community. 7

After the initial exposure, patients typically develop symptoms within 5-6 days (incubation period). SARS-CoV-2 generates a diverse range of clinical manifestations, ranging from mild infection to severe disease accompanied by high mortality. In patients with mild infection, initial host immune response is capable of controlling the infection. In severe disease, excessive immune response leads to organ damage, intensive care admission, or death. The viral load peaks in the first week of infection, declines thereafter gradually, while the antibody response gradually increases and is often detectable by day 14 (figure adapted with permission from https://www.sciencedirect.com/science/article/pii/S009286742030475X ; https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30230-7/fulltext )
Quantitative reverse transcription polymerase chain reaction (qRT-PCR) technology can detect viral SARS-CoV-2 RNA in the upper respiratory tract for a mean of 17 days (maximum 83 days) after symptom onset. 7 However, detection of viral RNA by qRT-PCR does not necessarily equate to infectiousness, and viral culture from PCR positive upper respiratory tract samples has been rarely positive beyond nine days of illness. 5 This corresponds to what is known about transmission based on contact tracing studies, which is that transmission capacity is maximal in the first week of illness, and that transmission after this period has not been documented. 8 Severely ill or immune-compromised patients may have relatively prolonged virus shedding, and some patients may have intermittent RNA shedding; however, low level results close to the detection limit may not constitute infectious viral particles. While asymptomatic individuals (those with no symptoms throughout the infection) can transmit the infection, their relative degree of infectiousness seems to be limited. 9 10 11 People with mild symptoms (paucisymptomatic) and those whose symptom have not yet appeared still carry large amounts of virus in the upper respiratory tract, which might contribute to the easy and rapid spread of SARS-CoV-2. 7 Symptomatic and pre-symptomatic transmission (one to two days before symptom onset) is likely to play a greater role in the spread of SARS-CoV-2. 10 12 A combination of preventive measures, such as physical distancing and testing, tracing, and self-isolation, continue to be needed.
Route of transmission and transmission dynamics
Like other coronaviruses, the primary mechanism of transmission of SARS-CoV-2 is via infected respiratory droplets, with viral infection occurring by direct or indirect contact with nasal, conjunctival, or oral mucosa, when respiratory particles are inhaled or deposited on these mucous membranes. 6 Target host receptors are found mainly in the human respiratory tract epithelium, including the oropharynx and upper airway. The conjunctiva and gastrointestinal tracts are also susceptible to infection and may serve as transmission portals. 6
Transmission risk depends on factors such as contact pattern, environment, infectiousness of the host, and socioeconomic factors, as described elsewhere. 12 Most transmission occurs through close range contact (such as 15 minutes face to face and within 2 m), 13 and spread is especially efficient within households and through gatherings of family and friends. 12 Household secondary attack rates (the proportion of susceptible individuals who become infected within a group of susceptible contacts with a primary case) ranges from 4% to 35%. 12 Sleeping in the same room as, or being a spouse of an infected individual increases the risk of infection, but isolation of the infected person away from the family is related to lower risk of infection. 12 Other activities identified as high risk include dining in close proximity with the infected person, sharing food, and taking part in group activities 12 The risk of infection substantially increases in enclosed environments compared with outdoor settings. 12 For example, a systematic review of transmission clusters found that most superspreading events occurred indoors. 11 Aerosol transmission can still factor during prolonged stay in crowded, poorly ventilated indoor settings (meaning transmission could occur at a distance >2 m). 12 14 15 16 17
The role of faecal shedding in SARS-CoV-2 transmission and the extent of fomite (through inanimate surfaces) transmission also remain to be fully understood. Both SARS-CoV-2 and SARS-CoV-1 remain viable for many days on smooth surfaces (stainless steel, plastic, glass) and at lower temperature and humidity (eg, air conditioned environments). 18 19 Thus, transferring infection from contaminated surfaces to the mucosa of eyes, nose, and mouth via unwashed hands is a possible route of transmission. This route of transmission may contribute especially in facilities with communal areas, with increased likelihood of environmental contamination. However, both SARS-CoV-1 and SARS-CoV-2 are readily inactivated by commonly used disinfectants, emphasising the potential value of surface cleaning and handwashing. SARS-CoV-2 RNA has been found in stool samples and RNA shedding often persists for longer than in respiratory samples 7 ; however, virus isolation has rarely been successful from the stool. 5 7 No published reports describe faecal-oral transmission. In SARS-CoV-1, faecal-oral transmission was not considered to occur in most circumstances; but, one explosive outbreak was attributed to aerosolisation and spread of the virus across an apartment block via a faulty sewage system. 20 It remains to be seen if similar transmission may occur with SARS-CoV-2.
Pathogenesis
Viral entry and interaction with target cells.
SARS-CoV-2 binds to ACE 2, the host target cell receptor. 1 Active replication and release of the virus in the lung cells lead to non-specific symptoms such as fever, myalgia, headache, and respiratory symptoms. 1 In an experimental hamster model, the virus causes transient damage to the cells in the olfactory epithelium, leading to olfactory dysfunction, which may explain temporary loss of taste and smell commonly seen in covid-19. 21 The distribution of ACE 2 receptors in different tissues may explain the sites of infection and patient symptoms. For example, the ACE 2 receptor is found on the epithelium of other organs such as the intestine and endothelial cells in the kidney and blood vessels, which may explain gastrointestinal symptoms and cardiovascular complications. 22 Lymphocytic endotheliitis has been observed in postmortem pathology examination of the lung, heart, kidney, and liver as well as liver cell necrosis and myocardial infarction in patients who died of covid-19. 1 23 These findings indicate that the virus directly affects many organs, as was seen in SARS-CoV-1 and influenzae.
Much remains unknown. Are the pathological changes in the respiratory tract or endothelial dysfunction the result of direct viral infection, cytokine dysregulation, coagulopathy, or are they multifactorial? And does direct viral invasion or coagulopathy directly contribute to some of the ischaemic complications such as ischaemic infarcts? These and more, will require further work to elucidate.
Immune response and disease spectrum ( figure 2 )
After viral entry, the initial inflammatory response attracts virus-specific T cells to the site of infection, where the infected cells are eliminated before the virus spreads, leading to recovery in most people. 24 In patients who develop severe disease, SARS-CoV-2 elicits an aberrant host immune response. 24 25 For example, postmortem histology of lung tissues of patients who died of covid-19 have confirmed the inflammatory nature of the injury, with features of bilateral diffuse alveolar damage, hyaline-membrane formation, interstitial mononuclear inflammatory infiltrates, and desquamation consistent with acute respiratory distress syndrome (ARDS), and is similar to the lung pathology seen in severe Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS). 26 27 A distinctive feature of covid-19 is the presence of mucus plugs with fibrinous exudate in the respiratory tract, which may explain the severity of covid-19 even in young adults. 28 This is potentially caused by the overproduction of pro-inflammatory cytokines that accumulate in the lungs, eventually damaging the lung parenchyma. 24
Some patients also experience septic shock and multi-organ dysfunction. 24 For example, the cardiovascular system is often involved early in covid-19 disease and is reflected in the release of highly sensitive troponin and natriuretic peptides. 29 Consistent with the clinical context of coagulopathy, focal intra-alveolar haemorrhage and presence of platelet-fibrin thrombi in small arterial vessels is also seen. 27 Cytokines normally mediate and regulate immunity, inflammation, and haematopoiesis; however, further exacerbation of immune reaction and accumulation of cytokines in other organs in some patients may cause extensive tissue damage, or a cytokine release syndrome (cytokine storm), resulting in capillary leak, thrombus formation, and organ dysfunction. 24 30
Mechanisms underlying the diverse clinical outcomes
Clinical outcomes are influenced by host factors such as older age, male sex, and underlying medical conditions, 1 as well as factors related to the virus (such as viral load kinetics), host-immune response, and potential cross-reactive immune memory from previous exposure to seasonal coronaviruses ( box 1 ).
Risk factors associated with the development of severe disease, admission to intensive care unit, and mortality
Underlying condition.
Hypertension
Cardiovascular disease
Chronic obstructive pulmonary disease
Presentation
Higher fever (≥39°C on admission)
Dyspnoea on admission
Higher qSOFA score
Laboratory markers
Neutrophilia/lymphopenia
Raised lactate and lactate dehydrogenase
Raised C reactive protein
Raised ferritin
Raised IL-6
Raised ACE2
D-dimer >1 μg/mL
Sex-related differences in immune response have been reported, revealing that men had higher plasma innate immune cytokines and chemokines at baseline than women. 31 In contrast, women had notably more robust T cell activation than men, and among male participants T cell activation declined with age, which was sustained among female patients. These findings suggest that adaptive immune response may be important in defining the clinical outcome as older age and male sex is associated with increased risk of severe disease and mortality.
Increased levels of pro-inflammatory cytokines correlate with severe pneumonia and increased ground glass opacities within the lungs. 30 32 In people with severe illness, increased plasma concentrations of inflammatory cytokines and biomarkers were observed compared with people with non-severe illness. 30 33 34
Emerging evidence suggests a correlation between viral dynamics, the severity of illness, and disease outcome. 7 Longitudinal characteristics of immune response show a correlation between the severity of illness, viral load, and IFN- α, IFN-γ, and TNF-α response. 34 In the same study many interferons, cytokines, and chemokines were elevated early in disease for patients who had severe disease and higher viral loads. This emphasises that viral load may drive these cytokines and the possible pathological roles associated with the host defence factors. This is in keeping with the pathogenesis of influenza, SARS, and MERS whereby prolonged viral shedding was also associated with severity of illness. 7 35
Given the substantial role of the immune response in determining clinical outcomes, several immunosuppressive therapies aimed at limiting immune-mediated damage are currently in various phases of development ( table 1 ).
Therapeutics currently under investigation
- View inline
Immune response to the virus and its role in protection
Covid-19 leads to an antibody response to a range of viral proteins, but the spike (S) protein and nucleocapsid are those most often used in serological diagnosis. Few antibodies are detectable in the first four days of illness, but patients progressively develop them, with most achieving a detectable response after four weeks. 36 A wide range of virus-neutralising antibodies have been reported, and emerging evidence suggests that these may correlate with severity but wane over time. 37 The duration and protectivity of antibody and T cell responses remain to be defined through studies with longer follow-up. CD-4 T cell responses to endemic human coronaviruses appear to manifest cross-reactivity with SARS-CoV-2, but their role in protection remains unclear. 38

Unanswered questions
Further understanding of the pathogenesis for SARS-CoV-2 will be vital in developing therapeutics, vaccines, and supportive care modalities in the treatment of covid-19. More data are needed to understand the determinants of healthy versus dysfunctional response and immune markers for protection and the severity of disease. Neutralising antibodies are potential correlates of protection, but other protective antibody mechanisms may exist. Similarly, the protective role of T cell immunity and duration of both antibody and T cell responses and the correlates of protection need to be defined. In addition, we need optimal testing systems and technologies to support and inform early detection and clinical management of infection. Greater understanding is needed regarding the long term consequences following acute illness and multisystem inflammatory disease, especially in children.
Education into practice
How would you describe SARS-CoV-2 transmission routes and ways to prevent infection?
How would you describe to a patient why cough, anosmia, and fever occur in covid-19?
Questions for future research
What is the role of the cytokine storm and how could it inform the development of therapeutics, vaccines, and supportive care modalities?
What is the window period when patients are most infectious?
Why do some patients develop severe disease while others, especially children, remain mildly symptomatic or do not develop symptoms?
What are the determinants of healthy versus dysfunctional response, and the biomarkers to define immune correlates of protection and disease severity for the effective triage of patients?
What is the protective role of T cell immunity and duration of both antibody and T cell responses, and how would you define the correlates of protection?
How patients were involved in the creation of this article
No patients were directly involved in the creation of this article.
How this article was created
We searched PubMed from 2000 to 18 September 2020, limited to publications in English. Our search strategy used a combination of key words including “COVID-19,” “SARS-CoV-2,” “SARS”, “MERS,” “Coronavirus,” “Novel Coronavirus,” “Pathogenesis,” “Transmission,” “Cytokine Release,” “immune response,” “antibody response.” These sources were supplemented with systematic reviews. We also reviewed technical documents produced by the Centers for Disease Control and Prevention and World Health Organization technical documents.
Author contributions: MC, KK, JK, MP drafted the first and subsequent versions of the manuscript and all authors provided critical feedback and contributed to the manuscript.
Competing interests The BMJ has judged that there are no disqualifying financial ties to commercial companies. The authors declare the following other interests: none.
Further details of The BMJ policy on financial interests are here: https://www.bmj.com/about-bmj/resources-authors/forms-policies-and-checklists/declaration-competing-interests
Provenance and peer review: commissioned; externally peer reviewed.
This article is made freely available for use in accordance with BMJ's website terms and conditions for the duration of the covid-19 pandemic or until otherwise determined by BMJ. You may use, download and print the article for any lawful, non-commercial purpose (including text and data mining) provided that all copyright notices and trade marks are retained.
- Bamford CGG ,
- Fischer WM ,
- Gnanakaran S ,
- Sheffield COVID-19 Genomics Group
- Corbett KS ,
- Corman VM ,
- Guggemos W ,
- Cheung MC ,
- Perera RAPM ,
- Cheng H-Y ,
- Taiwan COVID-19 Outbreak Investigation Team
- Meyerowitz E ,
- Richterman A ,
- Nergiz AI ,
- Maraolo AE ,
- Buitrago-Garcia D ,
- Egli-Gany D ,
- Counotte MJ ,
- ↵ European Centre for Disease Prevention and Control. Surveillance definitions for COVID-19. 2020. https://www.ecdc.europa.eu/en/covid-19/surveillance/surveillance-definitions .
- Klompas M ,
- ↵ Centers for Disease Control and Prevention. How COVID-19 spreads. 2020. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html
- ↵ Centers for Disease Control and Prevention. Scientific brief: SARS-CoV-2 and potential airborne transmission. 2020. https://www.cdc.gov/coronavirus/2019-ncov/more/scientific-brief-sars-cov-2.html
- Perera MRA ,
- van Doremalen N ,
- Bushmaker T ,
- Morris DH ,
- Monteil V ,
- Flammer AJ ,
- Steiger P ,
- Mangalmurti N ,
- Blanco-Melo D ,
- Nilsson-Payant BE ,
- Carsana L ,
- Sonzogni A ,
- ↵ Takahashi T, Ellingson MK, Wong P, et al. Sex differences in immune responses that underlie COVID-19 disease outcomes. Nature 2020. https://pubmed.ncbi.nlm.nih.gov/32846427/
- Yale IMPACT Team
- CAP-China Network
- Perera RA ,
- Merrick B ,
- Grifoni A ,
- Weiskopf D ,
- Ramirez SI ,
- CBSE Class 10th
- CBSE Class 12th
- UP Board 10th
- UP Board 12th
- Bihar Board 10th
- Bihar Board 12th
- Top Schools in India
- Top Schools in Delhi
- Top Schools in Mumbai
- Top Schools in Chennai
- Top Schools in Hyderabad
- Top Schools in Kolkata
- Top Schools in Pune
- Top Schools in Bangalore
Products & Resources
- JEE Main Knockout April
- Free Sample Papers
- Free Ebooks
- NCERT Notes
- NCERT Syllabus
- NCERT Books
- RD Sharma Solutions
- Navodaya Vidyalaya Admission 2024-25
- NCERT Solutions
- NCERT Solutions for Class 12
- NCERT Solutions for Class 11
- NCERT solutions for Class 10
- NCERT solutions for Class 9
- NCERT solutions for Class 8
- NCERT Solutions for Class 7
- JEE Main 2024
- MHT CET 2024
- JEE Advanced 2024
- BITSAT 2024
- View All Engineering Exams
- Colleges Accepting B.Tech Applications
- Top Engineering Colleges in India
- Engineering Colleges in India
- Engineering Colleges in Tamil Nadu
- Engineering Colleges Accepting JEE Main
- Top IITs in India
- Top NITs in India
- Top IIITs in India
- JEE Main College Predictor
- JEE Main Rank Predictor
- MHT CET College Predictor
- AP EAMCET College Predictor
- GATE College Predictor
- KCET College Predictor
- JEE Advanced College Predictor
- View All College Predictors
- JEE Main Question Paper
- JEE Main Cutoff
- JEE Main Answer Key
- JEE Main Result
- Download E-Books and Sample Papers
- Compare Colleges
- B.Tech College Applications
- JEE Advanced Registration
- MAH MBA CET Exam
- View All Management Exams
Colleges & Courses
- MBA College Admissions
- MBA Colleges in India
- Top IIMs Colleges in India
- Top Online MBA Colleges in India
- MBA Colleges Accepting XAT Score
- BBA Colleges in India
- XAT College Predictor 2024
- SNAP College Predictor
- NMAT College Predictor
- MAT College Predictor 2024
- CMAT College Predictor 2024
- CAT Percentile Predictor 2023
- CAT 2023 College Predictor
- CMAT 2024 Registration
- TS ICET 2024 Registration
- CMAT Exam Date 2024
- MAH MBA CET Cutoff 2024
- Download Helpful Ebooks
- List of Popular Branches
- QnA - Get answers to your doubts
- IIM Fees Structure
- AIIMS Nursing
- Top Medical Colleges in India
- Top Medical Colleges in India accepting NEET Score
- Medical Colleges accepting NEET
- List of Medical Colleges in India
- List of AIIMS Colleges In India
- Medical Colleges in Maharashtra
- Medical Colleges in India Accepting NEET PG
- NEET College Predictor
- NEET PG College Predictor
- NEET MDS College Predictor
- DNB CET College Predictor
- DNB PDCET College Predictor
- NEET Application Form 2024
- NEET PG Application Form 2024
- NEET Cut off
- NEET Online Preparation
- Download Helpful E-books
- LSAT India 2024
- Colleges Accepting Admissions
- Top Law Colleges in India
- Law College Accepting CLAT Score
- List of Law Colleges in India
- Top Law Colleges in Delhi
- Top Law Collages in Indore
- Top Law Colleges in Chandigarh
- Top Law Collages in Lucknow
Predictors & E-Books
- CLAT College Predictor
- MHCET Law ( 5 Year L.L.B) College Predictor
- AILET College Predictor
- Sample Papers
- Compare Law Collages
- Careers360 Youtube Channel
- CLAT Syllabus 2025
- CLAT Previous Year Question Paper
- AIBE 18 Result 2023
- NID DAT Exam
- Pearl Academy Exam
Animation Courses
- Animation Courses in India
- Animation Courses in Bangalore
- Animation Courses in Mumbai
- Animation Courses in Pune
- Animation Courses in Chennai
- Animation Courses in Hyderabad
- Design Colleges in India
- Fashion Design Colleges in Bangalore
- Fashion Design Colleges in Mumbai
- Fashion Design Colleges in Pune
- Fashion Design Colleges in Delhi
- Fashion Design Colleges in Hyderabad
- Fashion Design Colleges in India
- Top Design Colleges in India
- Free Design E-books
- List of Branches
- Careers360 Youtube channel
- NIFT College Predictor
- UCEED College Predictor
- NID DAT College Predictor
- IPU CET BJMC
- JMI Mass Communication Entrance Exam
- IIMC Entrance Exam
- Media & Journalism colleges in Delhi
- Media & Journalism colleges in Bangalore
- Media & Journalism colleges in Mumbai
- List of Media & Journalism Colleges in India
- CA Intermediate
- CA Foundation
- CS Executive
- CS Professional
- Difference between CA and CS
- Difference between CA and CMA
- CA Full form
- CMA Full form
- CS Full form
- CA Salary In India
Top Courses & Careers
- Bachelor of Commerce (B.Com)
- Master of Commerce (M.Com)
- Company Secretary
- Cost Accountant
- Charted Accountant
- Credit Manager
- Financial Advisor
- Top Commerce Colleges in India
- Top Government Commerce Colleges in India
- Top Private Commerce Colleges in India
- Top M.Com Colleges in Mumbai
- Top B.Com Colleges in India
- IT Colleges in Tamil Nadu
- IT Colleges in Uttar Pradesh
- MCA Colleges in India
- BCA Colleges in India
Quick Links
- Information Technology Courses
- Programming Courses
- Web Development Courses
- Data Analytics Courses
- Big Data Analytics Courses
- RUHS Pharmacy Admission Test
- Top Pharmacy Colleges in India
- Pharmacy Colleges in Pune
- Pharmacy Colleges in Mumbai
- Colleges Accepting GPAT Score
- Pharmacy Colleges in Lucknow
- List of Pharmacy Colleges in Nagpur
- GPAT Result
- GPAT 2024 Admit Card
- GPAT Question Papers
- NCHMCT JEE 2024
- Mah BHMCT CET
- Top Hotel Management Colleges in Delhi
- Top Hotel Management Colleges in Hyderabad
- Top Hotel Management Colleges in Mumbai
- Top Hotel Management Colleges in Tamil Nadu
- Top Hotel Management Colleges in Maharashtra
- B.Sc Hotel Management
- Hotel Management
- Diploma in Hotel Management and Catering Technology
Diploma Colleges
- Top Diploma Colleges in Maharashtra
- UPSC IAS 2024
- SSC CGL 2024
- IBPS RRB 2024
- Previous Year Sample Papers
- Free Competition E-books
- Sarkari Result
- QnA- Get your doubts answered
- UPSC Previous Year Sample Papers
- CTET Previous Year Sample Papers
- SBI Clerk Previous Year Sample Papers
- NDA Previous Year Sample Papers
Upcoming Events
- NDA Application Form 2024
- UPSC IAS Application Form 2024
- CDS Application Form 2024
- CTET Admit card 2024
- HP TET Result 2023
- SSC GD Constable Admit Card 2024
- UPTET Notification 2024
- SBI Clerk Result 2024
Other Exams
- SSC CHSL 2024
- UP PCS 2024
- UGC NET 2024
- RRB NTPC 2024
- IBPS PO 2024
- IBPS Clerk 2024
- IBPS SO 2024
- Top University in USA
- Top University in Canada
- Top University in Ireland
- Top Universities in UK
- Top Universities in Australia
- Best MBA Colleges in Abroad
- Business Management Studies Colleges
Top Countries
- Study in USA
- Study in UK
- Study in Canada
- Study in Australia
- Study in Ireland
- Study in Germany
- Study in China
- Study in Europe
Student Visas
- Student Visa Canada
- Student Visa UK
- Student Visa USA
- Student Visa Australia
- Student Visa Germany
- Student Visa New Zealand
- Student Visa Ireland
- CUET PG 2024
- IGNOU B.Ed Admission 2024
- DU Admission 2024
- UP B.Ed JEE 2024
- DDU Entrance Exam
- IIT JAM 2024
- IGNOU Online Admission 2024
- Universities in India
- Top Universities in India 2024
- Top Colleges in India
- Top Universities in Uttar Pradesh 2024
- Top Universities in Bihar
- Top Universities in Madhya Pradesh 2024
- Top Universities in Tamil Nadu 2024
- Central Universities in India
- CUET Exam City Intimation Slip 2024
- IGNOU Date Sheet
- CUET Mock Test 2024
- CUET Admit card 2024
- CUET PG Syllabus 2024
- CUET Participating Universities 2024
- CUET Previous Year Question Paper
- CUET Syllabus 2024 for Science Students
- E-Books and Sample Papers
- CUET Exam Pattern 2024
- CUET Exam Date 2024
- CUET Syllabus 2024
- IGNOU Exam Form 2024
- IGNOU Result
- CUET Courses List 2024
Engineering Preparation
- Knockout JEE Main 2024
- Test Series JEE Main 2024
- JEE Main 2024 Rank Booster
Medical Preparation
- Knockout NEET 2024
- Test Series NEET 2024
- Rank Booster NEET 2024
Online Courses
- JEE Main One Month Course
- NEET One Month Course
- IBSAT Free Mock Tests
- IIT JEE Foundation Course
- Knockout BITSAT 2024
- Career Guidance Tool
Top Streams
- IT & Software Certification Courses
- Engineering and Architecture Certification Courses
- Programming And Development Certification Courses
- Business and Management Certification Courses
- Marketing Certification Courses
- Health and Fitness Certification Courses
- Design Certification Courses
Specializations
- Digital Marketing Certification Courses
- Cyber Security Certification Courses
- Artificial Intelligence Certification Courses
- Business Analytics Certification Courses
- Data Science Certification Courses
- Cloud Computing Certification Courses
- Machine Learning Certification Courses
- View All Certification Courses
- UG Degree Courses
- PG Degree Courses
- Short Term Courses
- Free Courses
- Online Degrees and Diplomas
- Compare Courses
Top Providers
- Coursera Courses
- Udemy Courses
- Edx Courses
- Swayam Courses
- upGrad Courses
- Simplilearn Courses
- Great Learning Courses
Access premium articles, webinars, resources to make the best decisions for career, course, exams, scholarships, study abroad and much more with
Plan, Prepare & Make the Best Career Choices
Covid 19 Essay in English
Essay on Covid -19: In a very short amount of time, coronavirus has spread globally. It has had an enormous impact on people's lives, economy, and societies all around the world, affecting every country. Governments have had to take severe measures to try and contain the pandemic. The virus has altered our way of life in many ways, including its effects on our health and our economy. Here are a few sample essays on ‘CoronaVirus’.
100 Words Essay on Covid 19
200 words essay on covid 19, 500 words essay on covid 19.

COVID-19 or Corona Virus is a novel coronavirus that was first identified in 2019. It is similar to other coronaviruses, such as SARS-CoV and MERS-CoV, but it is more contagious and has caused more severe respiratory illness in people who have been infected. The novel coronavirus became a global pandemic in a very short period of time. It has affected lives, economies and societies across the world, leaving no country untouched. The virus has caused governments to take drastic measures to try and contain it. From health implications to economic and social ramifications, COVID-19 impacted every part of our lives. It has been more than 2 years since the pandemic hit and the world is still recovering from its effects.
Since the outbreak of COVID-19, the world has been impacted in a number of ways. For one, the global economy has taken a hit as businesses have been forced to close their doors. This has led to widespread job losses and an increase in poverty levels around the world. Additionally, countries have had to impose strict travel restrictions in an attempt to contain the virus, which has resulted in a decrease in tourism and international trade. Furthermore, the pandemic has put immense pressure on healthcare systems globally, as hospitals have been overwhelmed with patients suffering from the virus. Lastly, the outbreak has led to a general feeling of anxiety and uncertainty, as people are fearful of contracting the disease.
My Experience of COVID-19
I still remember how abruptly colleges and schools shut down in March 2020. I was a college student at that time and I was under the impression that everything would go back to normal in a few weeks. I could not have been more wrong. The situation only got worse every week and the government had to impose a lockdown. There were so many restrictions in place. For example, we had to wear face masks whenever we left the house, and we could only go out for essential errands. Restaurants and shops were only allowed to operate at take-out capacity, and many businesses were shut down.
In the current scenario, coronavirus is dominating all aspects of our lives. The coronavirus pandemic has wreaked havoc upon people’s lives, altering the way we live and work in a very short amount of time. It has revolutionised how we think about health care, education, and even social interaction. This virus has had long-term implications on our society, including its impact on mental health, economic stability, and global politics. But we as individuals can help to mitigate these effects by taking personal responsibility to protect themselves and those around them from infection.
Effects of CoronaVirus on Education
The outbreak of coronavirus has had a significant impact on education systems around the world. In China, where the virus originated, all schools and universities were closed for several weeks in an effort to contain the spread of the disease. Many other countries have followed suit, either closing schools altogether or suspending classes for a period of time.
This has resulted in a major disruption to the education of millions of students. Some have been able to continue their studies online, but many have not had access to the internet or have not been able to afford the costs associated with it. This has led to a widening of the digital divide between those who can afford to continue their education online and those who cannot.
The closure of schools has also had a negative impact on the mental health of many students. With no face-to-face contact with friends and teachers, some students have felt isolated and anxious. This has been compounded by the worry and uncertainty surrounding the virus itself.
The situation with coronavirus has improved and schools have been reopened but students are still catching up with the gap of 2 years that the pandemic created. In the meantime, governments and educational institutions are working together to find ways to support students and ensure that they are able to continue their education despite these difficult circumstances.
Effects of CoronaVirus on Economy
The outbreak of the coronavirus has had a significant impact on the global economy. The virus, which originated in China, has spread to over two hundred countries, resulting in widespread panic and a decrease in global trade. As a result of the outbreak, many businesses have been forced to close their doors, leading to a rise in unemployment. In addition, the stock market has taken a severe hit.
Effects of CoronaVirus on Health
The effects that coronavirus has on one's health are still being studied and researched as the virus continues to spread throughout the world. However, some of the potential effects on health that have been observed thus far include respiratory problems, fever, and coughing. In severe cases, pneumonia, kidney failure, and death can occur. It is important for people who think they may have been exposed to the virus to seek medical attention immediately so that they can be treated properly and avoid any serious complications. There is no specific cure or treatment for coronavirus at this time, but there are ways to help ease symptoms and prevent the virus from spreading.
Explore Career Options (By Industry)
- Construction
- Entertainment
- Manufacturing
- Information Technology
Data Administrator
Database professionals use software to store and organise data such as financial information, and customer shipping records. Individuals who opt for a career as data administrators ensure that data is available for users and secured from unauthorised sales. DB administrators may work in various types of industries. It may involve computer systems design, service firms, insurance companies, banks and hospitals.
Bio Medical Engineer
The field of biomedical engineering opens up a universe of expert chances. An Individual in the biomedical engineering career path work in the field of engineering as well as medicine, in order to find out solutions to common problems of the two fields. The biomedical engineering job opportunities are to collaborate with doctors and researchers to develop medical systems, equipment, or devices that can solve clinical problems. Here we will be discussing jobs after biomedical engineering, how to get a job in biomedical engineering, biomedical engineering scope, and salary.
Ethical Hacker
A career as ethical hacker involves various challenges and provides lucrative opportunities in the digital era where every giant business and startup owns its cyberspace on the world wide web. Individuals in the ethical hacker career path try to find the vulnerabilities in the cyber system to get its authority. If he or she succeeds in it then he or she gets its illegal authority. Individuals in the ethical hacker career path then steal information or delete the file that could affect the business, functioning, or services of the organization.
GIS officer work on various GIS software to conduct a study and gather spatial and non-spatial information. GIS experts update the GIS data and maintain it. The databases include aerial or satellite imagery, latitudinal and longitudinal coordinates, and manually digitized images of maps. In a career as GIS expert, one is responsible for creating online and mobile maps.
Data Analyst
The invention of the database has given fresh breath to the people involved in the data analytics career path. Analysis refers to splitting up a whole into its individual components for individual analysis. Data analysis is a method through which raw data are processed and transformed into information that would be beneficial for user strategic thinking.
Data are collected and examined to respond to questions, evaluate hypotheses or contradict theories. It is a tool for analyzing, transforming, modeling, and arranging data with useful knowledge, to assist in decision-making and methods, encompassing various strategies, and is used in different fields of business, research, and social science.
Geothermal Engineer
Individuals who opt for a career as geothermal engineers are the professionals involved in the processing of geothermal energy. The responsibilities of geothermal engineers may vary depending on the workplace location. Those who work in fields design facilities to process and distribute geothermal energy. They oversee the functioning of machinery used in the field.
Database Architect
If you are intrigued by the programming world and are interested in developing communications networks then a career as database architect may be a good option for you. Data architect roles and responsibilities include building design models for data communication networks. Wide Area Networks (WANs), local area networks (LANs), and intranets are included in the database networks. It is expected that database architects will have in-depth knowledge of a company's business to develop a network to fulfil the requirements of the organisation. Stay tuned as we look at the larger picture and give you more information on what is db architecture, why you should pursue database architecture, what to expect from such a degree and what your job opportunities will be after graduation. Here, we will be discussing how to become a data architect. Students can visit NIT Trichy , IIT Kharagpur , JMI New Delhi .
Remote Sensing Technician
Individuals who opt for a career as a remote sensing technician possess unique personalities. Remote sensing analysts seem to be rational human beings, they are strong, independent, persistent, sincere, realistic and resourceful. Some of them are analytical as well, which means they are intelligent, introspective and inquisitive.
Remote sensing scientists use remote sensing technology to support scientists in fields such as community planning, flight planning or the management of natural resources. Analysing data collected from aircraft, satellites or ground-based platforms using statistical analysis software, image analysis software or Geographic Information Systems (GIS) is a significant part of their work. Do you want to learn how to become remote sensing technician? There's no need to be concerned; we've devised a simple remote sensing technician career path for you. Scroll through the pages and read.
Budget Analyst
Budget analysis, in a nutshell, entails thoroughly analyzing the details of a financial budget. The budget analysis aims to better understand and manage revenue. Budget analysts assist in the achievement of financial targets, the preservation of profitability, and the pursuit of long-term growth for a business. Budget analysts generally have a bachelor's degree in accounting, finance, economics, or a closely related field. Knowledge of Financial Management is of prime importance in this career.
Underwriter
An underwriter is a person who assesses and evaluates the risk of insurance in his or her field like mortgage, loan, health policy, investment, and so on and so forth. The underwriter career path does involve risks as analysing the risks means finding out if there is a way for the insurance underwriter jobs to recover the money from its clients. If the risk turns out to be too much for the company then in the future it is an underwriter who will be held accountable for it. Therefore, one must carry out his or her job with a lot of attention and diligence.
Finance Executive
Product manager.
A Product Manager is a professional responsible for product planning and marketing. He or she manages the product throughout the Product Life Cycle, gathering and prioritising the product. A product manager job description includes defining the product vision and working closely with team members of other departments to deliver winning products.
Operations Manager
Individuals in the operations manager jobs are responsible for ensuring the efficiency of each department to acquire its optimal goal. They plan the use of resources and distribution of materials. The operations manager's job description includes managing budgets, negotiating contracts, and performing administrative tasks.
Stock Analyst
Individuals who opt for a career as a stock analyst examine the company's investments makes decisions and keep track of financial securities. The nature of such investments will differ from one business to the next. Individuals in the stock analyst career use data mining to forecast a company's profits and revenues, advise clients on whether to buy or sell, participate in seminars, and discussing financial matters with executives and evaluate annual reports.
A Researcher is a professional who is responsible for collecting data and information by reviewing the literature and conducting experiments and surveys. He or she uses various methodological processes to provide accurate data and information that is utilised by academicians and other industry professionals. Here, we will discuss what is a researcher, the researcher's salary, types of researchers.
Welding Engineer
Welding Engineer Job Description: A Welding Engineer work involves managing welding projects and supervising welding teams. He or she is responsible for reviewing welding procedures, processes and documentation. A career as Welding Engineer involves conducting failure analyses and causes on welding issues.
Transportation Planner
A career as Transportation Planner requires technical application of science and technology in engineering, particularly the concepts, equipment and technologies involved in the production of products and services. In fields like land use, infrastructure review, ecological standards and street design, he or she considers issues of health, environment and performance. A Transportation Planner assigns resources for implementing and designing programmes. He or she is responsible for assessing needs, preparing plans and forecasts and compliance with regulations.
Environmental Engineer
Individuals who opt for a career as an environmental engineer are construction professionals who utilise the skills and knowledge of biology, soil science, chemistry and the concept of engineering to design and develop projects that serve as solutions to various environmental problems.
Safety Manager
A Safety Manager is a professional responsible for employee’s safety at work. He or she plans, implements and oversees the company’s employee safety. A Safety Manager ensures compliance and adherence to Occupational Health and Safety (OHS) guidelines.
Conservation Architect
A Conservation Architect is a professional responsible for conserving and restoring buildings or monuments having a historic value. He or she applies techniques to document and stabilise the object’s state without any further damage. A Conservation Architect restores the monuments and heritage buildings to bring them back to their original state.
Structural Engineer
A Structural Engineer designs buildings, bridges, and other related structures. He or she analyzes the structures and makes sure the structures are strong enough to be used by the people. A career as a Structural Engineer requires working in the construction process. It comes under the civil engineering discipline. A Structure Engineer creates structural models with the help of computer-aided design software.
Highway Engineer
Highway Engineer Job Description: A Highway Engineer is a civil engineer who specialises in planning and building thousands of miles of roads that support connectivity and allow transportation across the country. He or she ensures that traffic management schemes are effectively planned concerning economic sustainability and successful implementation.
Field Surveyor
Are you searching for a Field Surveyor Job Description? A Field Surveyor is a professional responsible for conducting field surveys for various places or geographical conditions. He or she collects the required data and information as per the instructions given by senior officials.
Orthotist and Prosthetist
Orthotists and Prosthetists are professionals who provide aid to patients with disabilities. They fix them to artificial limbs (prosthetics) and help them to regain stability. There are times when people lose their limbs in an accident. In some other occasions, they are born without a limb or orthopaedic impairment. Orthotists and prosthetists play a crucial role in their lives with fixing them to assistive devices and provide mobility.
Pathologist
A career in pathology in India is filled with several responsibilities as it is a medical branch and affects human lives. The demand for pathologists has been increasing over the past few years as people are getting more aware of different diseases. Not only that, but an increase in population and lifestyle changes have also contributed to the increase in a pathologist’s demand. The pathology careers provide an extremely huge number of opportunities and if you want to be a part of the medical field you can consider being a pathologist. If you want to know more about a career in pathology in India then continue reading this article.
Veterinary Doctor
Speech therapist, gynaecologist.
Gynaecology can be defined as the study of the female body. The job outlook for gynaecology is excellent since there is evergreen demand for one because of their responsibility of dealing with not only women’s health but also fertility and pregnancy issues. Although most women prefer to have a women obstetrician gynaecologist as their doctor, men also explore a career as a gynaecologist and there are ample amounts of male doctors in the field who are gynaecologists and aid women during delivery and childbirth.
Audiologist
The audiologist career involves audiology professionals who are responsible to treat hearing loss and proactively preventing the relevant damage. Individuals who opt for a career as an audiologist use various testing strategies with the aim to determine if someone has a normal sensitivity to sounds or not. After the identification of hearing loss, a hearing doctor is required to determine which sections of the hearing are affected, to what extent they are affected, and where the wound causing the hearing loss is found. As soon as the hearing loss is identified, the patients are provided with recommendations for interventions and rehabilitation such as hearing aids, cochlear implants, and appropriate medical referrals. While audiology is a branch of science that studies and researches hearing, balance, and related disorders.
An oncologist is a specialised doctor responsible for providing medical care to patients diagnosed with cancer. He or she uses several therapies to control the cancer and its effect on the human body such as chemotherapy, immunotherapy, radiation therapy and biopsy. An oncologist designs a treatment plan based on a pathology report after diagnosing the type of cancer and where it is spreading inside the body.
Are you searching for an ‘Anatomist job description’? An Anatomist is a research professional who applies the laws of biological science to determine the ability of bodies of various living organisms including animals and humans to regenerate the damaged or destroyed organs. If you want to know what does an anatomist do, then read the entire article, where we will answer all your questions.
For an individual who opts for a career as an actor, the primary responsibility is to completely speak to the character he or she is playing and to persuade the crowd that the character is genuine by connecting with them and bringing them into the story. This applies to significant roles and littler parts, as all roles join to make an effective creation. Here in this article, we will discuss how to become an actor in India, actor exams, actor salary in India, and actor jobs.
Individuals who opt for a career as acrobats create and direct original routines for themselves, in addition to developing interpretations of existing routines. The work of circus acrobats can be seen in a variety of performance settings, including circus, reality shows, sports events like the Olympics, movies and commercials. Individuals who opt for a career as acrobats must be prepared to face rejections and intermittent periods of work. The creativity of acrobats may extend to other aspects of the performance. For example, acrobats in the circus may work with gym trainers, celebrities or collaborate with other professionals to enhance such performance elements as costume and or maybe at the teaching end of the career.
Video Game Designer
Career as a video game designer is filled with excitement as well as responsibilities. A video game designer is someone who is involved in the process of creating a game from day one. He or she is responsible for fulfilling duties like designing the character of the game, the several levels involved, plot, art and similar other elements. Individuals who opt for a career as a video game designer may also write the codes for the game using different programming languages.
Depending on the video game designer job description and experience they may also have to lead a team and do the early testing of the game in order to suggest changes and find loopholes.
Radio Jockey
Radio Jockey is an exciting, promising career and a great challenge for music lovers. If you are really interested in a career as radio jockey, then it is very important for an RJ to have an automatic, fun, and friendly personality. If you want to get a job done in this field, a strong command of the language and a good voice are always good things. Apart from this, in order to be a good radio jockey, you will also listen to good radio jockeys so that you can understand their style and later make your own by practicing.
A career as radio jockey has a lot to offer to deserving candidates. If you want to know more about a career as radio jockey, and how to become a radio jockey then continue reading the article.
Choreographer
The word “choreography" actually comes from Greek words that mean “dance writing." Individuals who opt for a career as a choreographer create and direct original dances, in addition to developing interpretations of existing dances. A Choreographer dances and utilises his or her creativity in other aspects of dance performance. For example, he or she may work with the music director to select music or collaborate with other famous choreographers to enhance such performance elements as lighting, costume and set design.
Social Media Manager
A career as social media manager involves implementing the company’s or brand’s marketing plan across all social media channels. Social media managers help in building or improving a brand’s or a company’s website traffic, build brand awareness, create and implement marketing and brand strategy. Social media managers are key to important social communication as well.
Photographer
Photography is considered both a science and an art, an artistic means of expression in which the camera replaces the pen. In a career as a photographer, an individual is hired to capture the moments of public and private events, such as press conferences or weddings, or may also work inside a studio, where people go to get their picture clicked. Photography is divided into many streams each generating numerous career opportunities in photography. With the boom in advertising, media, and the fashion industry, photography has emerged as a lucrative and thrilling career option for many Indian youths.
An individual who is pursuing a career as a producer is responsible for managing the business aspects of production. They are involved in each aspect of production from its inception to deception. Famous movie producers review the script, recommend changes and visualise the story.
They are responsible for overseeing the finance involved in the project and distributing the film for broadcasting on various platforms. A career as a producer is quite fulfilling as well as exhaustive in terms of playing different roles in order for a production to be successful. Famous movie producers are responsible for hiring creative and technical personnel on contract basis.
Copy Writer
In a career as a copywriter, one has to consult with the client and understand the brief well. A career as a copywriter has a lot to offer to deserving candidates. Several new mediums of advertising are opening therefore making it a lucrative career choice. Students can pursue various copywriter courses such as Journalism , Advertising , Marketing Management . Here, we have discussed how to become a freelance copywriter, copywriter career path, how to become a copywriter in India, and copywriting career outlook.
In a career as a vlogger, one generally works for himself or herself. However, once an individual has gained viewership there are several brands and companies that approach them for paid collaboration. It is one of those fields where an individual can earn well while following his or her passion.
Ever since internet costs got reduced the viewership for these types of content has increased on a large scale. Therefore, a career as a vlogger has a lot to offer. If you want to know more about the Vlogger eligibility, roles and responsibilities then continue reading the article.
For publishing books, newspapers, magazines and digital material, editorial and commercial strategies are set by publishers. Individuals in publishing career paths make choices about the markets their businesses will reach and the type of content that their audience will be served. Individuals in book publisher careers collaborate with editorial staff, designers, authors, and freelance contributors who develop and manage the creation of content.
Careers in journalism are filled with excitement as well as responsibilities. One cannot afford to miss out on the details. As it is the small details that provide insights into a story. Depending on those insights a journalist goes about writing a news article. A journalism career can be stressful at times but if you are someone who is passionate about it then it is the right choice for you. If you want to know more about the media field and journalist career then continue reading this article.
Individuals in the editor career path is an unsung hero of the news industry who polishes the language of the news stories provided by stringers, reporters, copywriters and content writers and also news agencies. Individuals who opt for a career as an editor make it more persuasive, concise and clear for readers. In this article, we will discuss the details of the editor's career path such as how to become an editor in India, editor salary in India and editor skills and qualities.
Individuals who opt for a career as a reporter may often be at work on national holidays and festivities. He or she pitches various story ideas and covers news stories in risky situations. Students can pursue a BMC (Bachelor of Mass Communication) , B.M.M. (Bachelor of Mass Media) , or MAJMC (MA in Journalism and Mass Communication) to become a reporter. While we sit at home reporters travel to locations to collect information that carries a news value.
Corporate Executive
Are you searching for a Corporate Executive job description? A Corporate Executive role comes with administrative duties. He or she provides support to the leadership of the organisation. A Corporate Executive fulfils the business purpose and ensures its financial stability. In this article, we are going to discuss how to become corporate executive.
Multimedia Specialist
A multimedia specialist is a media professional who creates, audio, videos, graphic image files, computer animations for multimedia applications. He or she is responsible for planning, producing, and maintaining websites and applications.
Quality Controller
A quality controller plays a crucial role in an organisation. He or she is responsible for performing quality checks on manufactured products. He or she identifies the defects in a product and rejects the product.
A quality controller records detailed information about products with defects and sends it to the supervisor or plant manager to take necessary actions to improve the production process.
Production Manager
A QA Lead is in charge of the QA Team. The role of QA Lead comes with the responsibility of assessing services and products in order to determine that he or she meets the quality standards. He or she develops, implements and manages test plans.
Process Development Engineer
The Process Development Engineers design, implement, manufacture, mine, and other production systems using technical knowledge and expertise in the industry. They use computer modeling software to test technologies and machinery. An individual who is opting career as Process Development Engineer is responsible for developing cost-effective and efficient processes. They also monitor the production process and ensure it functions smoothly and efficiently.
AWS Solution Architect
An AWS Solution Architect is someone who specializes in developing and implementing cloud computing systems. He or she has a good understanding of the various aspects of cloud computing and can confidently deploy and manage their systems. He or she troubleshoots the issues and evaluates the risk from the third party.
Azure Administrator
An Azure Administrator is a professional responsible for implementing, monitoring, and maintaining Azure Solutions. He or she manages cloud infrastructure service instances and various cloud servers as well as sets up public and private cloud systems.
Computer Programmer
Careers in computer programming primarily refer to the systematic act of writing code and moreover include wider computer science areas. The word 'programmer' or 'coder' has entered into practice with the growing number of newly self-taught tech enthusiasts. Computer programming careers involve the use of designs created by software developers and engineers and transforming them into commands that can be implemented by computers. These commands result in regular usage of social media sites, word-processing applications and browsers.
Information Security Manager
Individuals in the information security manager career path involves in overseeing and controlling all aspects of computer security. The IT security manager job description includes planning and carrying out security measures to protect the business data and information from corruption, theft, unauthorised access, and deliberate attack
ITSM Manager
Automation test engineer.
An Automation Test Engineer job involves executing automated test scripts. He or she identifies the project’s problems and troubleshoots them. The role involves documenting the defect using management tools. He or she works with the application team in order to resolve any issues arising during the testing process.
Applications for Admissions are open.

Aakash iACST Scholarship Test 2024
Get up to 90% scholarship on NEET, JEE & Foundation courses

JEE Main Important Chemistry formulas
As per latest 2024 syllabus. Chemistry formulas, equations, & laws of class 11 & 12th chapters

ALLEN NEET Coaching
Ace your NEET preparation with ALLEN Online Programs

SAT® | CollegeBoard
Registeration closing on 19th Apr for SAT® | One Test-Many Universities | 90% discount on registrations fee | Free Practice | Multiple Attempts | no penalty for guessing

TOEFL ® Registrations 2024
Thinking of Studying Abroad? Think the TOEFL® test. Register now & Save 10% on English Proficiency Tests with Gift Cards

Resonance Coaching
Enroll in Resonance Coaching for success in JEE/NEET exams
Everything about Education
Latest updates, Exclusive Content, Webinars and more.
Download Careers360 App's
Regular exam updates, QnA, Predictors, College Applications & E-books now on your Mobile
Cetifications
We Appeared in
What Is Long COVID? Understanding the Pandemic’s Mysterious Fallout
BY BROOKS LEITNER April 15, 2024
Just weeks after the first cases of COVID-19 hit U.S. shores, an op-ed appeared in The New York Times titled “We Need to Talk About What Coronavirus Recoveries Look Like: They're a lot more complicated than most people realize.” The author, Fiona Lowenstein, is a writer and yoga teacher living in New York City, who wrote about her own illness and the symptoms she was left with once she was released from the hospital. “In the weeks since I was hospitalized for the coronavirus , the same question has flooded my email inbox, texts and direct messages: Are you better yet? I don’t yet know how to answer.”
She was better, she wrote on April 13, 2020 , but she wasn’t well. And others she was in touch with were having the same issue. Unlike most diseases, Long COVID was first described not by doctors, but by the patients themselves. Even the term “Long COVID” was coined by a patient. Dr. Elisa Perego, an honorary research fellow at University College in London, came up with the hashtag #LongCOVID when tweeting about her own experience with the post-COVID syndrome. The term went viral and suddenly social media, and then the media itself, was full of these stories.
Complaints like "I can't seem to concentrate anymore" or "I'm constantly fatigued throughout the day" became increasingly common, seemingly appearing out of nowhere. With nothing abnormal turning up from their many thorough lab tests, patients and their physicians were left feeling helpless and frustrated.
The World Health Organization (WHO) has defined Long COVID as the "continuation or development of new symptoms three months after the initial SARS-CoV-2 infection, with these symptoms lasting for at least two months with no other explanation." This deliberately broad definition reflects the complex nature of this syndrome. We now understand that these symptoms are wide-ranging, including heart palpitations, cough, nausea, fatigue, cognitive impairment (commonly referred to as "brain fog"), and more. Also, many who experience Long COVID following an acute infection face an elevated risk of such medical complications as blood clots and (type 2) diabetes.
As of March 2024 , it’s estimated that about 17% of patients who get COVID-19 will go on to develop post-acute COVID-19 syndrome, the medical term for Long COVID. Data from the Centers for Disease Control and Prevention (CDC) suggest that Long COVID disproportionately affects women, and individuals between the ages of 40 and 49 have the highest reported rates of developing this post-acute infection syndrome.
Long COVID represents a new clinical challenge
Ebony Dix, MD , a Yale School of Medicine (YSM) assistant professor of psychiatry and the medical director of the geriatric psychiatry inpatient unit at Yale New Haven Hospital, said: "Unfortunately, it is not easy to say who is going to get Long COVID and who isn't." She also emphasized that "it can be overlooked and attributed to a preexisting condition. Sometimes the only thing that patients have in their history is a positive COVID test."
Dr. Dix recalled a patient she treated in the COVID psychiatry unit whose unanticipated clinical decline began with increasing fatigue during physical therapy sessions, ultimately necessitating more care over several weeks. Dr. Dix noted, "Long COVID requires time for things to settle down. It might take several months to get back to baseline." Making timely changes to a patient’s treatment plans was essential to helping her patients get back to good health, she said.
A major challenge with Long COVID is how difficult it can be to diagnose. Determining whether new-onset symptoms, such as fatigue or weakness, are related to an underlying condition or entirely attributed to a prior COVID infection is the greatest challenge for those who care for these patients. This is, in large part, due to the lack of research surrounding the topic.
Defining a basis for Long COVID with clinical research
Inderjit Singh, MBChB , a YSM assistant professor specializing in pulmonary, critical care, and sleep medicine, and director of the Pulmonary Vascular Program, is actively engaged in clinical trials aimed at uncovering the fundamental underpinnings of Long COVID. In one research study, patients suffering from unexplained fatigue and shortness of breath undergo exhaustive exercise testing. In order to be enrolled in this study, patients need to have already completed a substantial work-up, including an echocardiogram, pulmonary function testing, chest CT scans, and more, all which result in no alternative diagnosis.
Through this work, a significant revelation emerged. They observed that patients grappling with Long COVID and facing exercise difficulties were unable to efficiently extract oxygen from their bloodstream during physical exertion. This discovery identifies a specific cause underlying the biological underpinnings of Long COVID.
Recognizing the impracticality of conducting comprehensive exercise tests for every Long COVID patient, Dr. Singh, along with other researchers, is focused on the identification of blood-based markers to assess the severity of Long COVID. For example, a research group, led by Akiko Iwasaki, PhD , Sterling Professor of Immunobiology and Molecular, Cellular, and Developmental Biology, and director of the Center for Infection & Immunity at YSM, most recently created a new method to classify Long COVID severity with circulating immune markers.
Further investigations conducted by Dr. Singh's team identified distinctive protein signatures in the blood of Long COVID patients, which correlated with the degree of Long COVID severity. Researchers identified two major and distinct blood profiles among the patients. Some of them exhibited blood profiles indicating that excessive inflammation played a prominent role in their condition, while others displayed profiles indicative of impaired metabolism. Dr. Singh raises a pressing question: "Do we prioritize treating the inflammation or addressing the metabolic defects?"
Although his research findings and those of his peers are progressively unraveling the mysteries of Long COVID, he acknowledges that "significant challenges persist in defining this syndrome.”
Why does Long COVID happen?
The symptoms of Long COVID can vary significantly from one patient to another. Some individuals may be so fatigued that they find it difficult to get out of bed each morning. Others experience heart palpitations, lightheadedness, nausea, vomiting, diarrhea, or brain fog. This broad spectrum of symptoms—more than 200 documented—has led to various hypotheses about the underlying mechanisms at play.
Researchers currently believe that the impairment of a spectrum of key bodily functions may contribute to these diverse symptoms. These potential mechanisms include compromised immune system function, damage to blood vessels, and direct harm to the brain and nervous system. Importantly, it's likely that most patients experience symptoms arising from multiple underlying causes, which complicates both the diagnosis and treatment of Long COVID.
How can Long COVID be treated?
While the diagnosis and treatment of Long COVID remain challenging, the landscape of treatment options is evolving. At Yale’s Multidisciplinary Long COVID Care Center, a team, including respiratory therapists, physical therapists, and clinical social workers, along with an internist, work together to provide a comprehensive evaluation of each patient. Treatment approaches can vary widely and may encompass medications, supplements, physical therapy, or other interventions. Each regimen is designed to meet the specific presentation of Long COVID in each patient.
Dr. Singh’s apt summarization of the situation? "I don't think there's a magic bullet for it." Effective management of Long COVID necessitates a multidisciplinary approach that harnesses the expertise of a wide variety of specialists, working together to provide tailored care and support for these patients.
Brooks Leitner is an MD/PhD candidate at Yale School of Medicine.
The last word from Lisa Sanders, MD:
I’m the internist who sees patients at Yale New Haven Health’s Multidisciplinary Long COVID Care Center. In our clinic, patients are examined by a variety of specialists to determine the best next steps for these complex patients. Sometimes that entails more testing. Often patients have had extensive testing even before they arrive, and far too often—when all the tests are normal—both doctors and patients worry that their symptoms are “all in their head.”
One of our first tasks is to reassure patients that many parts of Long COVID don’t show up on tests. We don’t know enough about the cause of many of these symptoms to create a test for them. The problem is not with the patient with the symptoms, but of the science surrounding them.
If any good can be said to come out of this pandemic, it will be a better understanding of Long COVID and many of the other post-acute infection syndromes that have existed as long as the infections themselves.
If you’d like to share your experience with Long COVID for possible use in a future post (under a pseudonym), write to us at: LongCovid [email protected]
Information provided in Yale Medicine content is for general informational purposes only. It should never be used as a substitute for medical advice from your doctor or other qualified clinician. Always seek the individual advice of your health care provider for any questions you have regarding a medical condition.
More news from Yale Medicine
- Patient Care & Health Information
- Diseases & Conditions
- Coronavirus disease 2019 (COVID-19)
COVID-19, also called coronavirus disease 2019, is an illness caused by a virus. The virus is called severe acute respiratory syndrome coronavirus 2, or more commonly, SARS-CoV-2. It started spreading at the end of 2019 and became a pandemic disease in 2020.
- Coronavirus
Coronaviruses are a family of viruses. These viruses cause illnesses such as the common cold, severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS) and coronavirus disease 2019 (COVID-19).
The virus that causes COVID-19 spreads most commonly through the air in tiny droplets of fluid between people in close contact. Many people with COVID-19 have no symptoms or mild illness. But for older adults and people with certain medical conditions, COVID-19 can lead to the need for care in the hospital or death.
Staying up to date on your COVID-19 vaccine helps prevent serious illness, the need for hospital care due to COVID-19 and death from COVID-19 . Other ways that may help prevent the spread of this coronavirus includes good indoor air flow, physical distancing, wearing a mask in the right setting and good hygiene.
Medicine can limit the seriousness of the viral infection. Most people recover without long-term effects, but some people have symptoms that continue for months.
Products & Services
- A Book: Endemic - A Post-Pandemic Playbook
- A Book: Future Care
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
Typical COVID-19 symptoms often show up 2 to 14 days after contact with the virus.
Symptoms can include:
- Shortness of breath.
- Loss of taste or smell.
- Extreme tiredness, called fatigue.
- Digestive symptoms such as upset stomach, vomiting or loose stools, called diarrhea.
- Pain, such as headaches and body or muscle aches.
- Fever or chills.
- Cold-like symptoms such as congestion, runny nose or sore throat.
People may only have a few symptoms or none. People who have no symptoms but test positive for COVID-19 are called asymptomatic. For example, many children who test positive don't have symptoms of COVID-19 illness. People who go on to have symptoms are considered presymptomatic. Both groups can still spread COVID-19 to others.
Some people may have symptoms that get worse about 7 to 14 days after symptoms start.
Most people with COVID-19 have mild to moderate symptoms. But COVID-19 can cause serious medical complications and lead to death. Older adults or people who already have medical conditions are at greater risk of serious illness.
COVID-19 may be a mild, moderate, severe or critical illness.
- In broad terms, mild COVID-19 doesn't affect the ability of the lungs to get oxygen to the body.
- In moderate COVID-19 illness, the lungs also work properly but there are signs that the infection is deep in the lungs.
- Severe COVID-19 means that the lungs don't work correctly, and the person needs oxygen and other medical help in the hospital.
- Critical COVID-19 illness means the lung and breathing system, called the respiratory system, has failed and there is damage throughout the body.
Rarely, people who catch the coronavirus can develop a group of symptoms linked to inflamed organs or tissues. The illness is called multisystem inflammatory syndrome. When children have this illness, it is called multisystem inflammatory syndrome in children, shortened to MIS -C. In adults, the name is MIS -A.
When to see a doctor
Contact a healthcare professional if you test positive for COVID-19 . If you have symptoms and need to test for COVID-19 , or you've been exposed to someone with COVID-19 , a healthcare professional can help.
People who are at high risk of serious illness may get medicine to block the spread of the COVID-19 virus in the body. Or your healthcare team may plan regular checks to monitor your health.
Get emergency help right away for any of these symptoms:
- Can't catch your breath or have problems breathing.
- Skin, lips or nail beds that are pale, gray or blue.
- New confusion.
- Trouble staying awake or waking up.
- Chest pain or pressure that is constant.
This list doesn't include every emergency symptom. If you or a person you're taking care of has symptoms that worry you, get help. Let the healthcare team know about a positive test for COVID-19 or symptoms of the illness.
More Information
- COVID-19 vs. flu: Similarities and differences
- COVID-19, cold, allergies and the flu
- Unusual symptoms of coronavirus
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
COVID-19 is caused by infection with the severe acute respiratory syndrome coronavirus 2, also called SARS-CoV-2.
The coronavirus spreads mainly from person to person, even from someone who is infected but has no symptoms. When people with COVID-19 cough, sneeze, breathe, sing or talk, their breath may be infected with the COVID-19 virus.
The coronavirus carried by a person's breath can land directly on the face of a nearby person, after a sneeze or cough, for example. The droplets or particles the infected person breathes out could possibly be breathed in by other people if they are close together or in areas with low air flow. And a person may touch a surface that has respiratory droplets and then touch their face with hands that have the coronavirus on them.
It's possible to get COVID-19 more than once.
- Over time, the body's defense against the COVID-19 virus can fade.
- A person may be exposed to so much of the virus that it breaks through their immune defense.
- As a virus infects a group of people, the virus copies itself. During this process, the genetic code can randomly change in each copy. The changes are called mutations. If the coronavirus that causes COVID-19 changes in ways that make previous infections or vaccination less effective at preventing infection, people can get sick again.
The virus that causes COVID-19 can infect some pets. Cats, dogs, hamsters and ferrets have caught this coronavirus and had symptoms. It's rare for a person to get COVID-19 from a pet.
Risk factors
The main risk factors for COVID-19 are:
- If someone you live with has COVID-19 .
- If you spend time in places with poor air flow and a higher number of people when the virus is spreading.
- If you spend more than 30 minutes in close contact with someone who has COVID-19 .
Many factors affect your risk of catching the virus that causes COVID-19 . How long you are in contact, if the space has good air flow and your activities all affect the risk. Also, if you or others wear masks, if someone has COVID-19 symptoms and how close you are affects your risk. Close contact includes sitting and talking next to one another, for example, or sharing a car or bedroom.
It seems to be rare for people to catch the virus that causes COVID-19 from an infected surface. While the virus is shed in waste, called stool, COVID-19 infection from places such as a public bathroom is not common.
Serious COVID-19 illness risk factors
Some people are at a higher risk of serious COVID-19 illness than others. This includes people age 65 and older as well as babies younger than 6 months. Those age groups have the highest risk of needing hospital care for COVID-19 .
Not every risk factor for serious COVID-19 illness is known. People of all ages who have no other medical issues have needed hospital care for COVID-19 .
Known risk factors for serious illness include people who have not gotten a COVID-19 vaccine. Serious illness also is a higher risk for people who have:
- Sickle cell disease or thalassemia.
- Serious heart diseases and possibly high blood pressure.
- Chronic kidney, liver or lung diseases.
People with dementia or Alzheimer's also are at higher risk, as are people with brain and nervous system conditions such as stroke. Smoking increases the risk of serious COVID-19 illness. And people with a body mass index in the overweight category or obese category may have a higher risk as well.
Other medical conditions that may raise the risk of serious illness from COVID-19 include:
- Cancer or a history of cancer.
- Type 1 or type 2 diabetes.
- Weakened immune system from solid organ transplants or bone marrow transplants, some medicines, or HIV .
This list is not complete. Factors linked to a health issue may raise the risk of serious COVID-19 illness too. Examples are a medical condition where people live in a group home, or lack of access to medical care. Also, people with more than one health issue, or people of older age who also have health issues have a higher chance of severe illness.
Related information
- COVID-19: Who's at higher risk of serious symptoms? - Related information COVID-19: Who's at higher risk of serious symptoms?
Complications
Complications of COVID-19 include long-term loss of taste and smell, skin rashes, and sores. The illness can cause trouble breathing or pneumonia. Medical issues a person already manages may get worse.
Complications of severe COVID-19 illness can include:
- Acute respiratory distress syndrome, when the body's organs do not get enough oxygen.
- Shock caused by the infection or heart problems.
- Overreaction of the immune system, called the inflammatory response.
- Blood clots.
- Kidney injury.
Post-COVID-19 syndrome
After a COVID-19 infection, some people report that symptoms continue for months, or they develop new symptoms. This syndrome has often been called long COVID, or post- COVID-19 . You might hear it called long haul COVID-19 , post-COVID conditions or PASC. That's short for post-acute sequelae of SARS -CoV-2.
Other infections, such as the flu and polio, can lead to long-term illness. But the virus that causes COVID-19 has only been studied since it began to spread in 2019. So, research into the specific effects of long-term COVID-19 symptoms continues.
Researchers do think that post- COVID-19 syndrome can happen after an illness of any severity.
Getting a COVID-19 vaccine may help prevent post- COVID-19 syndrome.
- Long-term effects of COVID-19
The Centers for Disease Control and Prevention (CDC) recommends a COVID-19 vaccine for everyone age 6 months and older. The COVID-19 vaccine can lower the risk of death or serious illness caused by COVID-19. It lowers your risk and lowers the risk that you may spread it to people around you.
The COVID-19 vaccines available in the United States are:
2023-2024 Pfizer-BioNTech COVID-19 vaccine. This vaccine is available for people age 6 months and older.
Among people with a typical immune system:
- Children age 6 months up to age 4 years are up to date after three doses of a Pfizer-BioNTech COVID-19 vaccine.
- People age 5 and older are up to date after one Pfizer-BioNTech COVID-19 vaccine.
- For people who have not had a 2023-2024 COVID-19 vaccination, the CDC recommends getting an additional shot of that updated vaccine.
2023-2024 Moderna COVID-19 vaccine. This vaccine is available for people age 6 months and older.
- Children ages 6 months up to age 4 are up to date if they've had two doses of a Moderna COVID-19 vaccine.
- People age 5 and older are up to date with one Moderna COVID-19 vaccine.
2023-2024 Novavax COVID-19 vaccine. This vaccine is available for people age 12 years and older.
- People age 12 years and older are up to date if they've had two doses of a Novavax COVID-19 vaccine.
In general, people age 5 and older with typical immune systems can get any vaccine approved or authorized for their age. They usually don't need to get the same vaccine each time.
Some people should get all their vaccine doses from the same vaccine maker, including:
- Children ages 6 months to 4 years.
- People age 5 years and older with weakened immune systems.
- People age 12 and older who have had one shot of the Novavax vaccine should get the second Novavax shot in the two-dose series.
Talk to your healthcare professional if you have any questions about the vaccines for you or your child. Your healthcare team can help you if:
- The vaccine you or your child got earlier isn't available.
- You don't know which vaccine you or your child received.
- You or your child started a vaccine series but couldn't finish it due to side effects.
People with weakened immune systems
Your healthcare team may suggest added doses of COVID-19 vaccine if you have a moderately or seriously weakened immune system. The FDA has also authorized the monoclonal antibody pemivibart (Pemgarda) to prevent COVID-19 in some people with weakened immune systems.
Control the spread of infection
In addition to vaccination, there are other ways to stop the spread of the virus that causes COVID-19 .
If you are at a higher risk of serious illness, talk to your healthcare professional about how best to protect yourself. Know what to do if you get sick so you can quickly start treatment.
If you feel ill or have COVID-19 , stay home and away from others, including pets, if possible. Avoid sharing household items such as dishes or towels if you're sick.
In general, make it a habit to:
- Test for COVID-19 . If you have symptoms of COVID-19 test for the infection. Or test five days after you came in contact with the virus.
- Help from afar. Avoid close contact with anyone who is sick or has symptoms, if possible.
- Wash your hands. Wash your hands well and often with soap and water for at least 20 seconds. Or use an alcohol-based hand sanitizer with at least 60% alcohol.
- Cover your coughs and sneezes. Cough or sneeze into a tissue or your elbow. Then wash your hands.
- Clean and disinfect high-touch surfaces. For example, clean doorknobs, light switches, electronics and counters regularly.
Try to spread out in crowded public areas, especially in places with poor airflow. This is important if you have a higher risk of serious illness.
The CDC recommends that people wear a mask in indoor public spaces if you're in an area with a high number of people with COVID-19 in the hospital. They suggest wearing the most protective mask possible that you'll wear regularly, that fits well and is comfortable.
- COVID-19 vaccines: Get the facts - Related information COVID-19 vaccines: Get the facts
- Comparing the differences between COVID-19 vaccines - Related information Comparing the differences between COVID-19 vaccines
- Different types of COVID-19 vaccines: How they work - Related information Different types of COVID-19 vaccines: How they work
- Debunking COVID-19 myths - Related information Debunking COVID-19 myths
Travel and COVID-19
Travel brings people together from areas where illnesses may be at higher levels. Masks can help slow the spread of respiratory diseases in general, including COVID-19 . Masks help the most in places with low air flow and where you are in close contact with other people. Also, masks can help if the places you travel to or through have a high level of illness.
Masking is especially important if you or a companion have a high risk of serious illness from COVID-19 .
- COVID-19 travel advice
- COVID-19 vaccines
- COVID-19 vaccines for kids: What you need to know
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Fight coronavirus (COVID-19) transmission at home
- Herd immunity and coronavirus
- How well do face masks protect against COVID-19?
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- COVID-19 and vitamin D
- COVID-19: How can I protect myself?
- Mayo Clinic Minute: How dirty are common surfaces?
- Mayo Clinic Minute: You're washing your hands all wrong
- Goldman L, et al., eds. COVID-19: Epidemiology, clinical manifestations, diagnosis, community prevention, and prognosis. In: Goldman-Cecil Medicine. 27th ed. Elsevier; 2024. https://www.clinicalkey.com. Accessed Dec. 17, 2023.
- Coronavirus disease 2019 (COVID-19) treatment guidelines. National Institutes of Health. https://www.covid19treatmentguidelines.nih.gov/. Accessed Dec. 18, 2023.
- AskMayoExpert. COVID-19: Testing, symptoms. Mayo Clinic; Nov. 2, 2023.
- Symptoms of COVID-19. Centers for Disease Control and Preventions. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html. Accessed Dec. 20, 2023.
- AskMayoExpert. COVID-19: Outpatient management. Mayo Clinic; Oct. 10, 2023.
- Morris SB, et al. Case series of multisystem inflammatory syndrome in adults associated with SARS-CoV-2 infection — United Kingdom and United States, March-August 2020. MMWR. Morbidity and Mortality Weekly Report 2020;69:1450. DOI: http://dx.doi.org/10.15585/mmwr.mm6940e1external icon.
- COVID-19 testing: What you need to know. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/testing.html. Accessed Dec. 20, 2023.
- SARS-CoV-2 in animals. American Veterinary Medical Association. https://www.avma.org/resources-tools/one-health/covid-19/sars-cov-2-animals-including-pets. Accessed Jan. 17, 2024.
- Understanding exposure risk. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/your-health/risks-exposure.html. Accessed Jan. 10, 2024.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed Jan. 10, 2024.
- Factors that affect your risk of getting very sick from COVID-19. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/your-health/risks-getting-very-sick.html. Accessed Jan. 10, 2024.
- Regan JJ, et al. Use of Updated COVID-19 Vaccines 2023-2024 Formula for Persons Aged ≥6 Months: Recommendations of the Advisory Committee on Immunization Practices—United States, September 2023. MMWR. Morbidity and Mortality Weekly Report 2023; 72:1140–1146. DOI: http://dx.doi.org/10.15585/mmwr.mm7242e1.
- Long COVID or post-COVID conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html. Accessed Jan. 10, 2024.
- Stay up to date with your vaccines. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html. Accessed Jan. 10, 2024.
- Interim clinical considerations for use of COVID-19 vaccines currently approved or authorized in the United States. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/covid-19/clinical-considerations/covid-19-vaccines-us.html#CoV-19-vaccination. Accessed Jan. 10, 2024.
- Use and care of masks. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/about-face-coverings.html. Accessed Jan. 10, 2024.
- How to protect yourself and others. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html. Accessed Jan. 10, 2024.
- People who are immunocompromised. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-who-are-immunocompromised.html. Accessed Jan. 10, 2024.
- Masking during travel. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/page/masks. Accessed Jan. 10, 2024.
- AskMayoExpert. COVID-19: Testing. Mayo Clinic. 2023.
- COVID-19 test basics. U.S. Food and Drug Administration. https://www.fda.gov/consumers/consumer-updates/covid-19-test-basics. Accessed Jan. 11, 2024.
- At-home COVID-19 antigen tests — Take steps to reduce your risk of false negative results: FDA safety communication. U.S. Food and Drug Administration. https://www.fda.gov/medical-devices/safety-communications/home-covid-19-antigen-tests-take-steps-reduce-your-risk-false-negative-results-fda-safety. Accessed Jan. 11, 2024.
- Interim clinical considerations for COVID-19 treatment in outpatients. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/outpatient-treatment-overview.html. Accessed Jan. 11, 2024.
- Know your treatment options for COVID-19. U.S. Food and Drug Administration. https://www.fda.gov/consumers/consumer-updates/know-your-treatment-options-covid-19. Accessed Jan. 11, 2024.
- AskMayoExpert. COVID:19 Drug regimens and other treatment options. Mayo Clinic. 2023.
- Preventing spread of respiratory viruses when you're sick. Centers for Disease Control and Prevention. https://www.cdc.gov/respiratory-viruses/prevention/precautions-when-sick.html. Accessed March 5, 2024.
- AskMayoExpert. COVID-19: Quarantine and isolation. Mayo Clinic. 2023.
- COVID-19 resource and information guide. National Alliance on Mental Illness. https://www.nami.org/Support-Education/NAMI-HelpLine/COVID-19-Information-and-Resources/COVID-19-Resource-and-Information-Guide. Accessed Jan. 11, 2024.
- COVID-19 overview and infection prevention and control priorities in non-U.S. healthcare settings. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/overview/index.html. Accessed Jan. 16, 2024.
- Kim AY, et al. COVID-19: Management in hospitalized adults. https://www.uptodate.com/contents/search. Accessed Jan. 17, 2024.
- O'Horo JC, et al. Outcomes of COVID-19 with the Mayo Clinic Model of Care and Research. Mayo Clinic Proceedings. 2021; doi:10.1016/j.mayocp.2020.12.006.
- At-home OTC COVID-19 diagnostic tests. U.S. Food and Drug Administration. https://www.fda.gov/medical-devices/coronavirus-covid-19-and-medical-devices/home-otc-covid-19-diagnostic-tests. Accessed Jan. 22, 2024.
- Emergency use authorizations for drugs and non-vaccine biological products. U.S. Food and Drug Association. https://www.fda.gov/drugs/emergency-preparedness-drugs/emergency-use-authorizations-drugs-and-non-vaccine-biological-products. Accessed March 25, 2024.
- Coronavirus infection by race
- COVID-19 and pets
- COVID-19 and your mental health
- COVID-19 drugs: Are there any that work?
- COVID-19 in babies and children
- COVID-19 variant
- COVID-19: Who's at higher risk of serious symptoms?
- How do COVID-19 antibody tests differ from diagnostic tests?
- Is hydroxychloroquine a treatment for COVID-19?
- Pregnancy and COVID-19
- Sex and COVID-19
- Treating COVID-19 at home
Associated Procedures
- Convalescent plasma therapy
- COVID-19 antibody testing
- COVID-19 tests
- Extracorporeal membrane oxygenation (ECMO)
News from Mayo Clinic
- Mayo Clinic Q and A: Who should get the latest COVID-19 vaccine? Nov. 21, 2023, 01:30 p.m. CDT
- Can you get COVID-19 and the flu at the same time? A Mayo Clinic expert weighs in Oct. 16, 2023, 04:30 p.m. CDT
- At-home COVID-19 tests: A Mayo Clinic expert answers questions on expiration dates and the new variants Sept. 18, 2023, 04:00 p.m. CDT
- Mayo Clinic expert answers questions about the new COVID-19 vaccine Sept. 13, 2023, 04:15 p.m. CDT
- Study identifies risk factors for long-haul COVID disease in adults Sept. 13, 2023, 02:00 p.m. CDT
- Mayo researchers find vaccine may reduce severity of long-haul COVID symptoms Aug. 23, 2023, 04:34 p.m. CDT
- Corticosteroids lower the likelihood of in-hospital mortality from COVID-19 Aug. 04, 2023, 03:00 p.m. CDT
- COVID-19 vaccine administration simplified April 21, 2023, 07:00 p.m. CDT
- Science Saturday: COVID-19 -- the pandemic that's forever changed laboratory testing April 15, 2023, 11:00 a.m. CDT
- Mayo Clinic expert talks about the new omicron variant April 13, 2023, 02:13 p.m. CDT
- Mayo Clinic to ease universal face mask requirement April 04, 2023, 03:05 p.m. CDT
- 'Deaths of Despair' contribute to 17% rise in Minnesota's death rate during COVID-19 pandemic March 13, 2023, 12:00 p.m. CDT
- Rising cases of COVID-19 variant, XBB.1.5 Jan. 09, 2023, 05:15 p.m. CDT
- Bivalent COVID-19 booster approved for children 6 months and older Dec. 09, 2022, 09:33 p.m. CDT
- Mayo Clinic Minute: How to self-care at home when you have COVID-19 Dec. 06, 2022, 05:00 p.m. CDT
- Halloween safety tips from a Mayo Clinic infectious diseases expert Oct. 27, 2022, 02:00 p.m. CDT
- COVID-19, RSV and flu--season of respiratory infections Oct. 26, 2022, 04:30 p.m. CDT
- COVID-19 bivalent booster vaccines for kids 5-11 approved, Mayo Clinic awaits supply Oct. 13, 2022, 04:54 p.m. CDT
- Questions answered about the COVID-19 bivalent booster vaccines Oct. 12, 2022, 03:30 p.m. CDT
- Will the COVID-19 booster be like an annual flu shot? Sept. 12, 2022, 04:30 p.m. CDT
- Mayo Clinic Q and A: Who needs back-to-school COVID-19 vaccinations and boosters? Sept. 04, 2022, 11:00 a.m. CDT
- Q&A podcast: Updated COVID-19 boosters target omicron variants Sept. 02, 2022, 12:30 p.m. CDT
- Mayo Clinic Minute: Back-to-school COVID-19 vaccinations for kids Aug. 15, 2022, 03:15 p.m. CDT
- Mayo Clinic research shows bebtelovimab to be a reliable option for treating COVID-19 in era of BA.2, other subvariants Aug. 15, 2022, 02:09 p.m. CDT
- Mayo Clinic Q and A: New variants of COVID-19 Aug. 04, 2022, 12:30 p.m. CDT
- COVID-19 variant BA.5 is dominant strain; BA.2.75 is being monitored July 28, 2022, 02:30 p.m. CDT
- Mayo Clinic researchers pinpoint genetic variations that might sway course of COVID-19 July 25, 2022, 02:00 p.m. CDT
- Mayo Clinic Q&A podcast: BA.5 omicron variant fueling latest COVID-19 surge July 15, 2022, 12:00 p.m. CDT
- What you need to know about the BA.5 omicron variant July 14, 2022, 06:41 p.m. CDT
- Mayo Clinic Q&A podcast: The importance of COVID-19 vaccines for children under 5 July 06, 2022, 01:00 p.m. CDT
- COVID-19 vaccination for kids age 5 and younger starting the week of July 4 at most Mayo sites July 01, 2022, 04:00 p.m. CDT
- Patients treated with monoclonal antibodies during COVID-19 delta surge had low rates of severe disease, Mayo Clinic study finds June 27, 2022, 03:00 p.m. CDT
- Long COVID and the digestive system: Mayo Clinic expert describes common symptoms June 21, 2022, 02:43 p.m. CDT
- Mayo Clinic Q&A podcast: COVID-19 update June 17, 2022, 01:08 p.m. CDT
- Study finds few COVID-19 patients get rebound symptoms after Paxlovid treatment June 14, 2022, 10:06 a.m. CDT
- Mayo Clinic Minute: What to expect with COVID-19 vaccinations for youngest kids June 08, 2022, 04:35 p.m. CDT
- Mayo Clinic Q&A podcast: Community leaders are key to reaching people underrepresented in research May 26, 2022, 02:00 p.m. CDT
- COVID-19 booster vaccinations extended to kids 5-11 May 20, 2022, 06:10 p.m. CDT
- Mayo Clinic expert shares tips for navigating a return to work with long COVID May 19, 2022, 02:08 p.m. CDT
- Mayo Clinic Q&A podcast: COVID-19 update May 17, 2022, 01:14 p.m. CDT
- FDA limits use of J&J COVID-19 vaccine May 06, 2022, 05:06 p.m. CDT
- Mayo Clinic Q&A podcast: COVID-19 news update April 29, 2022, 12:25 p.m. CDT
- COVID-19 shines a spotlight on laboratory professionals' vital role in health care April 25, 2022, 12:30 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- COVID-19 vaccines: Get the facts
- How well do face masks protect against coronavirus?
- Post-COVID Recovery
News on coronavirus disease 2019 (COVID-19)
Learn the latest medical news about COVID-19 on Mayo Clinic News Network.
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
Essay on COVID-19 Pandemic
As a result of the COVID-19 (Coronavirus) outbreak, daily life has been negatively affected, impacting the worldwide economy. Thousands of individuals have been sickened or died as a result of the outbreak of this disease. When you have the flu or a viral infection, the most common symptoms include fever, cold, coughing up bone fragments, and difficulty breathing, which may progress to pneumonia. It’s important to take major steps like keeping a strict cleaning routine, keeping social distance, and wearing masks, among other things. This virus’s geographic spread is accelerating (Daniel Pg 93). Governments restricted public meetings during the start of the pandemic to prevent the disease from spreading and breaking the exponential distribution curve. In order to avoid the damage caused by this extremely contagious disease, several countries quarantined their citizens. However, this scenario had drastically altered with the discovery of the vaccinations. The research aims to investigate the effect of the Covid-19 epidemic and its impact on the population’s well-being.
There is growing interest in the relationship between social determinants of health and health outcomes. Still, many health care providers and academics have been hesitant to recognize racism as a contributing factor to racial health disparities. Only a few research have examined the health effects of institutional racism, with the majority focusing on interpersonal racial and ethnic prejudice Ciotti et al., Pg 370. The latter comprises historically and culturally connected institutions that are interconnected. Prejudice is being practiced in a variety of contexts as a result of the COVID-19 outbreak. In some ways, the outbreak has exposed pre-existing bias and inequity.
Thousands of businesses are in danger of failure. Around 2.3 billion of the world’s 3.3 billion employees are out of work. These workers are especially susceptible since they lack access to social security and adequate health care, and they’ve also given up ownership of productive assets, which makes them highly vulnerable. Many individuals lose their employment as a result of lockdowns, leaving them unable to support their families. People strapped for cash are often forced to reduce their caloric intake while also eating less nutritiously (Fraser et al, Pg 3). The epidemic has had an impact on the whole food chain, revealing vulnerabilities that were previously hidden. Border closures, trade restrictions, and confinement measures have limited farmer access to markets, while agricultural workers have not gathered crops. As a result, the local and global food supply chain has been disrupted, and people now have less access to healthy foods. As a consequence of the epidemic, many individuals have lost their employment, and millions more are now in danger. When breadwinners lose their jobs, become sick, or die, the food and nutrition of millions of people are endangered. Particularly severely hit are the world’s poorest small farmers and indigenous peoples.
Infectious illness outbreaks and epidemics have become worldwide threats due to globalization, urbanization, and environmental change. In developed countries like Europe and North America, surveillance and health systems monitor and manage the spread of infectious illnesses in real-time. Both low- and high-income countries need to improve their public health capacities (Omer et al., Pg 1767). These improvements should be financed using a mix of national and foreign donor money. In order to speed up research and reaction for new illnesses with pandemic potential, a global collaborative effort including governments and commercial companies has been proposed. When working on a vaccine-like COVID-19, cooperation is critical.
The epidemic has had an impact on the whole food chain, revealing vulnerabilities that were previously hidden. Border closures, trade restrictions, and confinement measures have limited farmer access to markets, while agricultural workers have been unable to gather crops. As a result, the local and global food supply chain has been disrupted, and people now have less access to healthy foods (Daniel et al.,Pg 95) . As a consequence of the epidemic, many individuals have lost their employment, and millions more are now in danger. When breadwinners lose their jobs, the food and nutrition of millions of people are endangered. Particularly severely hit are the world’s poorest small farmers and indigenous peoples.
While helping to feed the world’s population, millions of paid and unpaid agricultural laborers suffer from high levels of poverty, hunger, and bad health, as well as a lack of safety and labor safeguards, as well as other kinds of abuse at work. Poor people, who have no recourse to social assistance, must work longer and harder, sometimes in hazardous occupations, endangering their families in the process (Daniel Pg 96). When faced with a lack of income, people may turn to hazardous financial activities, including asset liquidation, predatory lending, or child labor, to make ends meet. Because of the dangers they encounter while traveling, working, and living abroad; migrant agricultural laborers are especially vulnerable. They also have a difficult time taking advantage of government assistance programs.
The pandemic also has a significant impact on education. Although many educational institutions across the globe have already made the switch to online learning, the extent to which technology is utilized to improve the quality of distance or online learning varies. This level is dependent on several variables, including the different parties engaged in the execution of this learning format and the incorporation of technology into educational institutions before the time of school closure caused by the COVID-19 pandemic. For many years, researchers from all around the globe have worked to determine what variables contribute to effective technology integration in the classroom Ciotti et al., Pg 371. The amount of technology usage and the quality of learning when moving from a classroom to a distant or online format are presumed to be influenced by the same set of variables. Findings from previous research, which sought to determine what affects educational systems ability to integrate technology into teaching, suggest understanding how teachers, students, and technology interact positively in order to achieve positive results in the integration of teaching technology (Honey et al., 2000). Teachers’ views on teaching may affect the chances of successfully incorporating technology into the classroom and making it a part of the learning process.
In conclusion, indeed, Covid 19 pandemic have affected the well being of the people in a significant manner. The economy operation across the globe have been destabilized as most of the people have been rendered jobless while the job operation has been stopped. As most of the people have been rendered jobless the living conditions of the people have also been significantly affected. Besides, the education sector has also been affected as most of the learning institutions prefer the use of online learning which is not effective as compared to the traditional method. With the invention of the vaccines, most of the developed countries have been noted to stabilize slowly, while the developing countries have not been able to vaccinate most of its citizens. However, despite the challenge caused by the pandemic, organizations have been able to adapt the new mode of online trading to be promoted.
Ciotti, Marco, et al. “The COVID-19 pandemic.” Critical reviews in clinical laboratory sciences 57.6 (2020): 365-388.
Daniel, John. “Education and the COVID-19 pandemic.” Prospects 49.1 (2020): 91-96.
Fraser, Nicholas, et al. “Preprinting the COVID-19 pandemic.” BioRxiv (2021): 2020-05.
Omer, Saad B., Preeti Malani, and Carlos Del Rio. “The COVID-19 pandemic in the US: a clinical update.” Jama 323.18 (2020): 1767-1768.
Cite this page
Similar essay samples.
- Essay on Managing Conflict at Work
- An investigation into restart errors and the effectiveness of cues pre...
- Essay on Effects of Technology
- Application of soft systems thinking in analyzing the intense internat...
- Essay on Philanthropy and Education
- Essay on Caring Love in the Gift of the Magi by O. Henry
NPR suspends senior editor Uri Berliner after essay accusing outlet of liberal bias
Npr suspended senior editor uri berliner a week after he authored an online essay accusing the outlet of allowing liberal bias in its coverage..

NPR has suspended a senior editor who authored an essay published last week on an online news site in which he argued that the network had "lost America's trust" because of a liberal bias in its coverage, the outlet reported.
Uri Berliner was suspended Friday for five days without pay, NPR reported Tuesday . The revelation came exactly a week after Berliner publicly claimed in an essay for The Free Press, an online news publication, that NPR had allowed a "liberal bent" to influence its coverage, causing the outlet to steadily lose credibility with audiences.
The essay reignited the criticism that many prominent conservatives have long leveled against NPR and prompted newsroom leadership to implement monthly internal reviews of the network's coverage, NPR reported. Berliner's essay also angered many of his colleagues and exposed NPR's new chief executive Katherine Maher to a string of attacks from conservatives over her past social media posts.
In a statement Monday to NPR, Maher refuted Berliner's claims by underscoring NPR's commitment to objective coverage of national issues.
"In America everyone is entitled to free speech as a private citizen," Maher said. "What matters is NPR's work and my commitment as its CEO: public service, editorial independence, and the mission to serve all of the American public. NPR is independent, beholden to no party, and without commercial interests."
Heat exposure law: Florida joins Texas in banning local heat protections for outdoor workers
Berliner rails against NPR's coverage of COVID-19, diversity efforts
Berliner, a senior business editor who has worked at NPR for 25 years, argued in the Free Press essay that “people at every level of NPR have comfortably coalesced around the progressive worldview.”
While he claimed that NPR has always had a "liberal bent" ever since he was hired at the outlet, he wrote that it has since lost its "open-minded spirit," and, hence, "an audience that reflects America."
The Peabody Award-winning journalist highlighted what he viewed as examples of the network's partisan coverage of several major news events, including the origins of COVID-19 and the war in Gaza . Berliner also lambasted NPR's diversity, equity and inclusion (DEI) policies – as reflected both within its newsroom and in its coverage – as making race and identity "paramount in nearly every aspect of the workplace.”
"All this reflected a broader movement in the culture of people clustering together based on ideology or a characteristic of birth," he wrote.
Uri Berliner's essay fuels conservative attacks on NPR
In response to the essay, many prominent conservatives and Republicans, including former President Donald Trump, launched renewed attacks at NPR for what they perceive as partisan coverage.
Conservative activist Christopher Rufo in particular targeted Maher for messages she posted to social media years before joining the network – her first at a news organization . Among the posts singled out were a 2020 tweet that called Trump racist .
Trump reiterated on his social media platform, Truth Social, his longstanding argument that NPR’s government funding should be rescinded.
NPR issues formal rebuke to Berliner
Berliner provided an NPR reporter with a copy of the formal rebuke for review in which the organization told the editor he had not been approved to write for other news outlets, as is required of NPR journalists.
NPR also said he publicly released confidential proprietary information about audience demographics, the outlet reported.
Leadership said the letter was a "final warning" for Berliner, who would be fired for future violations of NPR's policies, according to NPR's reporting. Berliner, who is a dues-paying member of NPR's newsroom union, told the NPR reporter that he is not appealing the punishment.
A spokeswoman for NPR said the outlet declined to comment on Berliner's essay or the news of his suspension when reached Tuesday by USA TODAY.
"NPR does not comment on individual personnel matters, including discipline," according to the statement. "We expect all of our employees to comply with NPR policies and procedures, which for our editorial staff includes the NPR Ethics Handbook ."
NPR staffer express dismay; leadership puts coverage reviews in place
According to the NPR article, Berliner's essay also invoked the ire of many of his colleagues and the reporters whose stories he would be responsible for editing.
"Newsrooms run on trust," NPR political correspondent Danielle Kurtzleben said in a post last week on social media site X, though he didn't mention Berliner by name. "If you violate everyone's trust by going to another outlet and [expletive] on your colleagues (while doing a bad job journalistically, for that matter), I don't know how you do your job now."
Amid the fallout, NPR reported that NPR's chief news executive Edith Chapin announced to the newsroom late Monday afternoon that Executive Editor Eva Rodriguez would lead monthly meetings to review coverage.
Berliner expressed no regrets about publishing the essay in an interview with NPR, adding that he tried repeatedly to make his concerns over NPR's coverage known to news leaders.
"I love NPR and feel it's a national trust," Berliner says. "We have great journalists here. If they shed their opinions and did the great journalism they're capable of, this would be a much more interesting and fulfilling organization for our listeners."
Eric Lagatta covers breaking and trending news for USA TODAY. Reach him at [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Biology of COVID-19 and related viruses: Epidemiology, signs, symptoms, diagnosis, and treatment
Alan d. kaye.
a LSU Health Shreveport, 1501 Kings Highway, Shreveport LA 71103, USA
Elyse M. Cornett
b Department of Anesthesiology, LSU Health Shreveport, 1501 Kings Highway, Shreveport LA 71103, USA
Kimberley C. Brondeel
c University of Texas Medical Branch, 301 University Blvd, Galveston TX 77555, USA
Zachary I. Lerner
d LSU Health Sciences Center New Orleans, 1901 Perdido Street, New Orleans, LA 70112, USA
Haley E. Knight
e Louisiana State University Health Sciences Center, New Orleans, LA, 70112, USA
Abigail Erwin
Karina charipova.
f Georgetown University School of Medicine, Washington, D.C., 20007, USA
Kyle L. Gress
g Department of Anesthesiology, Critical Care and Pain Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA
Richard D. Urman
h Department of Anesthesiology, Perioperative and Pain Medicine, Harvard Medical School, Brigham and Women's Hospital, 75 Francis St, Boston, MA 02115, USA
Charles J. Fox
Christopher g. kevil.
Coronaviruses belong to the family Coronaviridae order Nidovirales and are known causes of respiratory and intestinal disease in various mammalian and avian species. Species of coronaviruses known to infect humans are referred to as human coronaviruses (HCoVs). While traditionally, HCoVs have been a significant cause of the common cold, more recently, emergent viruses, including severe acute respiratory syndrome coronavirus (SARS-CoV-2) has caused a global pandemic. Here, we discuss coronavirus disease (COVID-19) biology, pathology, epidemiology, signs and symptoms, diagnosis, treatment, and recent clinical trials involving promising treatments.
Introduction
Coronaviruses are a family of positive-sense, enveloped RNA viruses that cause various illnesses in mammals and birds [ 1 ]. These viruses represent the largest group within the Nidovirales order, which comprises the families Coronaviridae , Arteriviridae , Mesoniviridae , and Roniviridae . Structurally, coronaviruses are characterized by an unusually large RNA genome and club-like glycoprotein spikes that project from the surface of its envelope [ 2 ]. These spikes result in a characteristic ultrastructure appearance resembling the solar corona, giving rise to the name “coronavirus” [ 1 , 3 ]. Although they were first identified in 1965, human coronaviruses (HCoV) have recently gained notoriety due to their role in global outbreaks [ 4 , 5 ].
The human coronaviruses HCoV-229E, HCoV-NL63, HCoV-OC43, and HCoV-HKU1 typically cause mild upper respiratory infection and are responsible for approximately 15%–30% of all cases of the common cold in adults and children [ 6 , 7 ]. Coronaviruses also cause a range of respiratory and gastrointestinal (GI) infections in animals, affecting pigs, cows, mice, bats, and chickens with varying degrees of severity [ 2 ]. Although most coronavirus strains result in mild, self-limited upper respiratory disease in humans, three global outbreaks of severe disease due to novel coronaviruses have occurred in the twenty-first century. Severe acute respiratory syndrome (SARS) was first identified in Guandong province, China, in 2002, resulting in over 8000 cases and 744 deaths worldwide before being contained in 2003. Middle East respiratory syndrome (MERS) was diagnosed in Saudi Arabia in 2012, ultimately spreading globally and leading to 2494 cases and 858 deaths [ 8 ]. Most recently, SARS-CoV-2, the novel coronavirus responsible for coronavirus disease-2019 (COVID-19), was identified in Wuhan, China, in January 2020 [ 9 ]. As of October 2020, the resulting global pandemic has caused over 33,249,000 confirmed infections and 1,000,040 deaths [ 10 ].
Early symptoms of COVID-19 infection include fatigue, fever, dry cough, and anosmia. Approximately 80% of cases are mild and self-limited, primarily affecting the upper airway with limited involvement of the lungs. Severe infection, characterized by dyspnea, tachypnea, hypoxemia, cardiovascular sequalae, and extensive lung disease, occurs in 15% of cases. Critical infection, characterized by respiratory failure, septic shock, and multisystem organ dysfunction, and often complicated by acute respiratory distress syndrome (ARDS) and disseminated intravascular coagulopathy (DIC), occurs in 5% of cases [ [11] , [12] , [13] ]. The estimated case fatality rate is 2% overall, and 49% among critically ill patients [ 14 ]. Patients with comorbid illness, including hypertension, diabetes mellitus, cardiovascular disease, lung disease, and cerebrovascular disease, have increased risk for poor outcomes due to COVID-19 [ 15 ]. Elderly patients also experience increased morbidity and mortality due to COVID-19 infection [ 11 , 16 ].
On October 22, 2020, the FDA approved the antiviral drug, remdesivir, to treat COVID-19 in patients 12 years and older who are hospitalized [ 17 , 18 ]. Furthermore, as of November 2020, two pharmaceutical companies have developed promising COVID-19 vaccines that are up to 95% effective [ 19 , 20 ]. In addition to these treatments, the management of COVID-19 is primarily supportive. Supplemental oxygen is the initial treatment for respiratory impairment, while patients with continued respiratory distress or respiratory failure may require noninvasive positive pressure ventilation and mechanical ventilation [ 21 ]. Corticosteroids have also shown promise in the management of COVID-19 [ 22 , 23 ].
In this review, we first discuss coronaviruses' molecular biology, including the viral structure and replication process. Next, we discuss the pathology of coronavirus infection and SARS-CoV-2, highlighting the role of the angiotensin-converting enzyme 2 (ACE2) receptor in viral entry to host cells. Epidemiology of the COVID-19 pandemic is examined, including a timeline of the outbreak, an account of the populations that have been affected, and a discussion of risk factors for infection and subsequent poor outcome. Signs and symptoms of COVID-19 infection are also reviewed. Finally, we outline current methodologies in diagnosing and treating COVID-19 and highlight recent clinical studies that continue to advance the body of knowledge in managing this unprecedented disease.
Biology of coronaviruses
Coronaviruses are enveloped, positive-strand RNA viruses with genomes of up to 33.5 kilobases (kb) considered the largest among all RNA viruses [ 24 , 25 ]. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), similar to other coronaviruses, is characterized by trimeric S glycoproteins located on a pleomorphic (round or oval) outer membrane [ 26 , 27 ]. The viral envelope comprises structural proteins M and E, while the genome is coupled with protein N [ 27 ]. The complex structure of the virus is thought to contribute to its ability to survive in aerosols for up to 3 h [ 27 ]. The spike-like S proteins project from the virus's surface and play an integral role in allowing the virus to bind to the ACE2 receptor, an intermembrane receptor prevalent on epithelial cells and type II pneumocytes in the lower respiratory tract (LRT) [ 25 , 26 ]. Functional studies have also demonstrated that SARS-CoV-2 S proteins utilize transmembrane serine protease 2 in addition to ACE2 for entry into the host cell [ 28 ]. Following binding through the receptor-binding domain (RBD) of the S glycoprotein, the S protein undergoes large-scale conformational changes that allow the virus to endocytose into the cell cytoplasm where it undergoes replication [ 25 , 26 ]. Like other coronaviruses, SARS-CoV-2 replicates using a mechanism of continuous RNA synthesis but conducts transcription through a discontinuous process unique in the RNA virus world and is a characterizing feature of the Nidovirales order [ 24 ]. Discontinuous transcription in the coronavirus is regulated by multiple factors, including the essential coronavirus N protein RNA chaperone, which maximizes transcription efficiency [ 24 ]. Alongside the proofreading machinery encoded by coronaviruses, the discontinuous transcription process facilitates the upkeep of the large genome [ 24 ].
Recognition of the ACE2 receptor by SARS-CoV-2 and the subsequent conformational changes in the S protein that promote viral-host cell membrane fusion are critical steps to infection [ 28 ]. Given the S protein's importance, its structure and interactions with host receptors represent a popular niche for research to develop antivirals and ultimately, a vaccine [ 28 ]. The analysis of sequenced SARS-CoV-2 genomes has demonstrated that mutations in the S protein have contributed to creating predominant virus clades in various parts of the world, such as the D614G mutation notably found in Europe [ 29 ]. Certain regions of the S protein have also enabled the differentiation of SARS-CoV-2 from SARS-CoV and improved the specificity of serologic testing [ 30 ]. Through the function of the S protein, SARS-CoV-2 is believed to replicate in the olfactory epithelium of the nasal cavity and spread along the tracts of the airway [ 31 ]. It is this initial locus of replication that is thought to explain the clinical manifestation of loss of smell experienced by some individuals [ 31 ]. In more severe cases, SARS-CoV-2 travels along the airway to the lungs to cause severe pulmonary disease with potential systemic sequelae such as neurological symptoms and multi-tissue dysfunction [ 31 , 32 ]. Wide tissue dissemination of the virus is believed to result from the presence of targets, in the form of the ACE2 receptor, on various tissue types, including the cardiovascular system, GI tract, and central nervous system [ 27 ]. Among the systemic effects of COVID-19, it has been recently suggested that CD169+ macrophages located in the spleen and lymph nodes can serve as viral carriers that can maintain viral load and facilitate tissue dissemination [ 27 ]. Some investigators have suggested that the generation of the S1 protein by the virus and release of this protein into circulation may limit the severity of infection and tissue damage to maintain adequate transmission rates [ 33 ].
Mutations in the sequences coding for S glycoprotein and other proteins in the structure of SARS-CoV-2 are believed to at least partly explain the high infectivity and pathogenesis of the virus [ 27 ]. Mutations in the spike protein's RBD have enabled the virus to bind to human, cat, and ferret ACE2 receptors with significantly higher affinity than SARS-CoV-1 [ 27 ]. Studies have yet to fully resolve whether mutations that result in lineage changes such as those that have led to different predominant clades even between the East and West Coast of the USA have impacted viral pathogenesis or overall fitness [ 27 ]. Future investigation of these mutations is also needed to discern how SARS-CoV-2 adapts to not only various climates but also fits in with endemic viruses and parasites such as malaria, tuberculosis, and HIV [ 27 ]. This kind of phylogenic analysis has the potential for not only tracing infection routes but also guiding treatment development [ 28 ]. The viral replication and livelihood of SARS-CoV-2 is promoted further by nonstructural protein 1 (nsp 1), which allows the virus to dominate the host's genomic machinery that enables it to generate progeny at the expense of the host [ 27 ]. This pathogenic factor also inhibits the host's ability to express type 1 interferons (IFN-1), leading to the subsequent decreased expression of major histocompatibility complex 1, reduced antigen presentation, and suboptimal T cell response by the host [ 27 ]. The host's antiviral resistance is further subverted by the action of viral proteins that target ubiquitin ligases and dysregulate defensive signaling [ 27 ]. The analysis of the affinity of SARS-CoV-2 products for the components of the antiviral defense of the host has demonstrated that the presence of specific HLA alleles has the potential to mediate antiviral response [ 27 ]. These studies have hypothesized that a lack of the HLA-B∗46:01 allele may predispose individuals to increased vulnerability to infection, while the presence of HLA-B∗15:03 may induce cross-protective T-cell immunity against SARS-CoV-2 and other coronaviruses [ 27 ]. Furthermore, compared to noncritically hospitalized COVID-19 patients, ICU patients with severe COVID-19 disease showed a reduced expression of mHLA-DR on circulating CD14+ monocytes at ICU admission, suggesting dysfunctions immune response in these patients [ 34 ].
While coronaviruses have long been known to cause a variety of severe illnesses in livestock and other animals, prior to the SARS-CoV outbreak in 2002, coronaviruses were thought to cause only self-limited infections in humans [ 25 ]. Historically, coronaviruses were accepted as endemic in the human population, having low virulence and causing 15%–30% of all annual respiratory tract infections [ 24 , 25 ]. The dissimilarity between the severe disease states caused by coronaviruses in nonhuman species and the mild illnesses caused by HCoVs has conventionally been thought to relate to their differential tolerance to genetic variability [ 25 ]. For instance, it has been hypothesized that the minimal sequence divergence of HCoV-229E explains its inability to cross the species barrier and infect mice [ 25 ]. The emergence of SARS-CoV not only dispelled the belief that coronaviruses could not cause life-threatening diseases in humans but also demonstrated transmission of the virus from bats to humans [ 25 ]. SARS-CoV-1, which over the span of the 2002–2003 epidemic was linked to over 8000 cases and over 700 deaths as well as billions of dollars lost in economic activity, is thought to have originated in Chinese horseshoe bats [ 25 ]. Bat SARS-related CoVs were found to be more similar to SARS-CoV than any other viruses to date and were additionally found to utilize the same ACE2 receptor known to be used by HCoVs [ 25 ]. As most HCoVs, infection with SARS-CoV resulted in more severe illness and higher mortality rates in comorbid and elderly patients [ 25 ]. Interestingly, the age-dependent increase in severity seen in humans infected with SARS-CoV has been replicated by studies analyzing the disease course in rodents infected with adapted forms of the virus [ 25 ]. Although mapping of SARS-CoV-1 showed that it spread to over 25 countries, the transmission of the virus was relatively inefficient with spread occurring only through direct contact after onset of illness [ 25 , 27 ]. The virus was largely contained through quarantining with only a small number of known cases being thought to have occurred after the outbreak was deemed controlled in June 2003 [ 25 ]. A similarly contained outbreak of coronavirus MERS-CoV took place in 2012, wherein zoonotic infection was transmitted vertically from camels to humans [ 27 ]. While the nearly 2500 infected individuals and over 868 fatalities associated with MERS are not to be discounted; to date, these infection events remain localized to the Middle East due to relatively low rates of transmission [ 27 ].
SARS-CoV-2 causes a respiratory illness now referred to as coronavirus disease-2019 (COVID-19). From its emergence in December 2019 at its epicenter in Wuhan, China, the infectious agent spread quickly to all parts of the globe and was subsequently declared a global pandemic by the World Health Organization (WHO) on March 11, 2020 [ 26 , 29 ]. The rapid spread of infection from SARS-CoV-2 quickly drew comparisons to the new strain of H1N1 influenza that emerged in 1918 and is colloquially known as the “Spanish flu” [ 27 ]. As of October 1, 2020, the virus has resulted in over 33.5 million cases and over 1 million deaths with significantly worse outcomes and higher mortality in the elderly [ 32 , 35 ]. While the mechanism by which older patients suffer more severe disease is still under investigation, it has been proposed that higher levels of cellular senescence may contribute to the development of cytokine storm, excessive inflammatory reaction, increased tissue damage, and multi-tissue dysfunction in these patients [ 32 ]. Prior to the implementation of any public health interventions, the basic reproduction number of SARS-CoV-2 was estimated to be as high as 5.7, meaning that each infected individual had the potential to transmit the disease to as many as 5 to 6 new individuals [ 27 ].
While the pathophysiology is complex and not fully understood at the time of this writing, like SARS-CoV-1, SARS-CoV-2 is thought to primarily target the lung's epithelial cells, inducing the production of proinflammatory cytokines and a concurrent reduction in T-lymphocyte response [ 25 ]. The virus has been shown to share approximately 80% of its sequence identity with its predecessor, SARS-CoV, causing significant cross-reactivity in serological testing [ 27 , 30 ]. Although the cross-reactivity of SARS-CoV-2 with SARS-CoV-1 has given rise to obstacles when it comes to testing, it also enables cross-neutralizing antibodies to SARS-CoV-1 to target SARS-CoV-2, perform opsonization, and clear the virus [ 27 ]. Recent studies have demonstrated that patients who develop only mild symptoms, the clearing of COVID-19, can occur within ten days following symptom onset through the action of alveolar macrophages that resolve inflammation within the lungs and propagate tissue remodeling following the initial inflammatory phase [ 27 ]. A recent study in New York City involving 30,000 patients reported significant viral neutralization ability, which correlated with their antibody titer levels [ 36 ]. Furthermore, long-term immunity may occur in patients who have recovered from the virus [ 37 ].
Hopefully, future studies will be able to shed light on SARS-CoV-2 transmission and the development of immunity, which helps to not only answer these questions but also to ultimately curb the spread of this deadly infection.
Epidemiology
SARS-CoV-2 first emerged in Wuhan, China, at the end of December 2019 as a cluster of atypical pneumonia cases. On January 11, 2020, China reported the first death caused by the novel coronavirus [ 38 ]. By January 21, 2020, the United States confirmed the first case of the virus with a 35-year-old previously healthy man that presented with a history of cough and subjective fever after returning from a visit to family in Wuhan, China, on January 15, 2020 [ 5 ]. On January 30, 2020, with increasing evidence of human-to-human transmission outside of China, the WHO declared the novel coronavirus a Public Health Emergency of International Concern. On March 11, 2020, the WHO officially upgraded the COVID-19 state of emergency to pandemic [ 38 ].
As of September 30, 2020, there have been 33,502,430 confirmed cases of COVID-19 worldwide, with 1,004,421 deaths reported to the WHO. At the time of writing, the United States makes up greater than 10 million of the confirmed cases, with over 250,000 deaths to date. Within the U.S., the peak of COVID-19-related deaths occurred in late April to May, with the peak of incidence occurring in late July to early August, and a third surge currently underway [ 39 ]. America is still in the leading three countries for new daily cases, with 32,688 cases reported in the last 24 h. The Region of the Americas remains the most affected WHO Region, accounting for 50% of all reported cases and 55% of deaths [ 40 ].
Diagnostic criteria and epidemiological breakdown
The WHO categorizes COVID-19 patients into mild, moderate, severe, and critical disease. Mild disease is defined by patients that meet clinical and epidemiological criteria without the evidence of viral pneumonia or hypoxia. Moderate disease is characterized by the evidence of pneumonia. Severe disease is defined by severe pneumonia with a respiratory rate >30 breaths/min or the evidence of severe respiratory distress. Critical disease is defined by severe pneumonia complicated by the onset of ARDS, sepsis, or septic shock [ 41 ]. Most people infected with COVID-19 will develop only mild-moderate symptoms (80.9%), with 13.8% of people developing severe disease and 5% developing critical disease [ 42 ].
Demographic distribution of COVID-19 in the United States
The CDC reports of demographic trends of COVID-19 in the United States are limited by reports that failed to include race/ethnicity data. Reported death data and reported incidence data contained racial/ethnicity information, only 82% and 51% of the time. Black, Non-Hispanic Americans account for 13.4% of the population but account for 18.2% of reported COVID-19 cases. Hispanic/Latino Americans account for 18.5% of the population but account for 29.1% of cases. Reported deaths follow a similar trend, but notably, Hispanic/Latino Americans trend in reported deaths is more closely matched to their representation within the population at 16.5% [ 43 , 44 ]. The CDC has reported 76.3% of cases to occur among people aged 18–64 years, with 79.2% of deaths occurring outside of this age range, in those 65 years and older. When broken down by gender, case incidence is slightly higher in female subjects though death reports are more highly reported in male subjects [ 43 ].
Epidemiological risk factors
An epidemiological study (n = 72,314) conducted early in the pandemic found that age, male gender, and the presence of comorbidities are factors of an increased risk for severe Covid-19-related disease and/or mortality [ 42 ]. When compared to non-severe COVID-19 patients, the development of severe illness or admission to ICU is more likely in patients who suffer from one or more comorbidities in the descending order of odds ratio strength: chronic obstructive pulmonary disease, diabetes, cerebrovascular disease, coronary heart disease, hypertension, and malignancy [ 45 ].
Smoking history is also a risk factor associated with severe ICU cases of COVID-19 [ 45 ]. According to the most recent analysis of smoking status in COVID-19 patients, while current smokers and those with the evidence of smoking history are more likely to develop severe or critical COVID-19 and the need for mechanical ventilation, only smoking history is significantly associated with increased in-hospital mortality [ 46 ].
Obesity in people <60 years is an independent poor prognostic epidemiological risk factor. In a study by Lighter et al. that stratified patient age and BMI, the rate of hospitalization in young patients with a BMI >30 was 2.0 times more likely. ICU admission was also found to be increased at a rate of 1.8 and 3.6 in young patients with BMIs 30–34 and ≥ 35, respectively [ 47 ]. In ICU patients who required invasive mechanical ventilation (IMV), obesity was found to be more prevalent in COVID-19-positive patients as compared to non-COVID-infected ICU controls [ 48 ]. The most recently available national data show that obesity in the United States among adults was 42.4% in 2017–2018 [ 49 ]. With poor prognostic outcomes demonstrated in obese COVID-19-positive patients, a significant portion of the United States population can be considered high risk.
Transmission and implications for PPE and quarantine guidelines
The SARS-CoV-2 virus is a member of the coronavirus family that causes respiratory disease. The virus primarily spreads through respiratory droplets but has also been shown experimentally to have sustained viability on surfaces such as plastic and stainless steel for up to 72 h, on cardboard for up to 24 h, and copper surfaces for up to 4 h [ 50 ]. Spread through aerosols has been confirmed by the CDC [ 51 ]. In a small study of confirmed COVID-19-isolated patients, viral RNA was found on environmental surfaces related to the deposition of droplets by airflow. The virus was also found in toilet bowl and sink samples suggesting viral shedding in the stool and can be measured in sewage wastewater [ 52 ].
Coughing and sneezing generate large respiratory droplets (>5 μm) where exhaling and regular talking generate small aerosols (≤5 μm) [ 53 ]. In a study of facemask efficacy in reducing spread in respiratory viruses, coronavirus was found to only be detectable in samples of respiratory droplets and aerosols collected from patients not wearing facemask coverings [ 54 ]. Because the previous SARS-CoV-1 virus could be detected in patient tears, and the current SARS-CoV-2 is transmitted through fomites and droplets that could contact the eyes, eyewear protection necessary for spread prevention [ 55 , 56 ].
The pandemic's rapid global spread is partially attributed to asymptomatic transmitters of disease that would go on to develop symptoms after creating clusters of outbreaks [ 57 ]. Early symptomatic presentation trends lead research to suggest a median incubation period of approximately five days [ 58 , 59 ]. A recent study asserts that the incubation period is longer, lasting nearly eight days with 10% of patients demonstrating the first onset of symptoms after 14 days [ 60 ]. This is a public health concern as the current quarantine guidelines suggest only a 14-day quarantine in those with suspected exposure.
Signs and symptoms
Typical and atypical signs and symptoms of covid-19 infection.
Although asymptomatic transmission of COVID-19 occurs at a high rate, an entirely asymptomatic course is unlikely, totaling up to as few as 1% of cases [ 42 ]. The asymptomatic incubation period is better thought of as a presymptomatic period. Because the WHO classification of disease starts with clinical presentation, and symptomology can take more than 14 days to present, prompt recognition of signs and symptoms is paramount to halt the spread of the disease [ 41 , 60 ]. The most reported and reliable presenting features of COVID-19 infection are fever and cough [ [61] , [62] , [63] ]. Other frequent presenting symptoms include fatigue, myalgia, and dyspnea. Atypical symptoms of infection include chills, G.I. upset, and neurological changes [ 61 ].
Fever and dyspnea
A meta-analysis compared clinical features and outcomes of COVID-19 patients between those classified as severe (ICU) and nonsevere (non-ICU). Fever and dyspnea were significantly associated with severe disease, though increased fever >39 °C was not statistically significant between groups. Other symptoms such as cough, nausea, headache, sore throat, diarrhea, myalgia, and fatigue were not statistically favored by either group [ 45 ]. Consistent with these findings, Xiang et al. found dyspnea to be the most valuable prognostic indicator of severe pathology, regardless of independent patient risk factors, high fever, headache, and diarrhea as statistically insignificant with regard to prognosis [ 64 ].
Chills are not a highly prevalent manifestation of COVID-19 infection, but when stratified against other clinical features and lab findings, they show strong positive correlations with diagnostic markers of infection. Chills demonstrate a strong negative correlation to age and lymphopenia, which are associated with worse clinical outcomes [ 61 ]. Limited data have been collected regarding chills as a feature of disease. Still, these data suggest chills to be helpful in diagnosis and as an excellent prognostic indicator of disease course.
Gastrointestinal manifestations
Gastrointestinal (GI) symptoms were overlooked in early studies due to low prevalence, but recent data show prevalence can range from 5% to 61% [ 61 , 65 ]. The ACE2 receptor is a known receptor for entry into host cells in both SARS-CoV-1 and SARS-CoV-2. High expression of this receptor has been detected in cells of the lungs and intestinal mucosa [ 66 , 67 ]. Viral shedding has been detected in fecal samples and on objects such as toilets and sinks that encounter fecal matter, lending credence to the plausibility of fecal-oral transmission [ 52 , 68 ]. Though most studies have found diarrhea and other GI symptomatology to be insignificant with regard to disease severity, one meta-analysis demonstrated the presence of GI symptoms in 17.6% of patients with a higher prevalence among severe COVID-19 patients, and a study of pediatric patients found GI symptom prevalence in 43% of severe cases [ 63 , 68 ].
Neurological manifestations
Data on neurological pathology in COVID-19 patients is not extensive because it was not initially considered a manifestation of the disease. In February, a study of hospitalized patients showed 36.4% of patients had nervous system manifestations, including CNS, PNS, and skeletal muscle injury. Patients with severe infection (41%) were more likely to develop neurological manifestations, and some of these patients presented without typical symptoms of fever, cough, anorexia, and diarrhea [ 69 ]. The expression of ACE2 is found in several places in the body, and its expression within the nervous system may lead to neurological manifestations as similarly proposed within the GI system [ 69 ]. In patients with mild disease, impaired sense of taste and smell is reported in 64%–88% [ 70 , 71 ]. See Fig. 1 .

Symptom prevalence in COVID-19 literature showing the presentation of fever, cough, dyspnea, chills, gastrointestinal symptoms, neurologic symptoms, and fatigue in recent literature.
Presentation in children
The presentation of COVID-19 in children is variable, though the disease course is generally considered mild. Available data could be influenced by cluster testing that occurs when a symptomatic parent tests positive for COVID-19. It is possible that when children are tested, they are still within the presymptomatic period of disease course [ 72 ]. A meta-analysis (n = 774) showed nearly all children who tested positive for COVID-19 only developed mild disease manifestation. An entirely asymptomatic course was reported in 19% of cases as compared to the 1% demonstrated in the adult population [ 42 , 63 ]. Severe disease was reported in only 3% of cases. The symptom prevalence is like that of the adult population, with fever and cough being the most reported symptoms. Still, they are reported to a lesser degree, with only half of the patients reporting fever or cough. Of note, while this analysis only demonstrated severe cases in 3% of patients, 43% reported the presence of G.I. symptoms [ 63 ].
Multisystem inflammatory syndrome in children (MIS-C)
In late April, clusters of children and adolescents started requiring admission to intensive care units at a rate disproportionately higher than COVID-19 trends thus far. Presenting symptoms included features that were similar to Kawasaki's disease and toxic shock syndrome [ 73 ]. Kawasaki's disease usually presents in children <5 years old, with less than 5% of cases presenting with cardiovascular shock requiring pressor management. Patients who present with Kawasaki disease-like features are of a median age of 8.3, and nearly half of patients ultimately receive vasopressor support [ 74 ]. MIS-C is proposed to be linked with SARS-CoV-2 infection, with 70% of patients testing positive for infection and 30% of patients demonstrating an epidemiological link to an infected person [ 74 ]. ACE2 expression is hypothesized to lower the risk of COVID-19 infection in children and account for the age-specific incidence of MIS-C [ 74 , 75 ].
Presentation in pregnant persons
The typical symptomatic presentation of fever and cough occurs significantly less often in pregnant patients than nonpregnant patients. Fever and cough were shown to have an incidence of 91% and 67% in the nonpregnant population as compared to only 51% and 31% in pregnant persons, respectively [ 76 ]. A diminished symptomatic presentation in pregnant patients warrants increased screening measures among this population due to demonstrated rates of increased preterm labor in COVID-19-positive pregnant patients [ 76 ]. Furthermore, when pregnant women presented symptomatically, 16.2% were admitted to an ICU and 8.5% required mechanical ventilation, with asymptomatic pregnant women who demonstrated none of these adverse outcomes [ 77 ].
Diagnosis and treatment
The WHO recommends that the decision for COVID-19 testing is based on clinical and epidemiological factors and should be linked to assessing the likelihood of infection [ 78 ]. Epidemiological factors include anyone who has had close contact with a patient with laboratory-confirmed COVID-19 within 14 days of symptom onset or a history of travel from affected geographic areas within 14 days of symptom onset [ 79 ]. To guide contact tracing, treatment options, and isolation requirements, the U.S. CDC recommends using viral tests to diagnose acute infections in both symptomatic and asymptomatic individuals [ 80 ]. Virological testing should also be performed in people who are at a high risk of repeated exposure, such as healthcare workers and first responders [ 81 ]. Healthcare workers have a higher risk of reporting positive COVID-19 tests than the general community, and this risk increases in frontline workers without adequate access to PPE [ 82 ]. As these workers are treating COVID-positive patients, their health and wellness is crucial to the successful treatment of the COVID-19 pandemic [ 83 ]. Criteria for testing symptomatic patients include the presentation of clinical manifestations, recent visits to COVID prone countries, exposure to COVID-19 patients, and to detect the resolution of the disease. Criteria for testing asymptomatic patients include a known recent exposure to COVID-19 patients, unknown exposure to COVID-19 patients, olfactory dysfunction, the loss of smell and/or taste, transplant donors, and recipients [ 84 ]. Testing for all other pathogens and upper respiratory disease sources should also be performed during the initial evaluation, but should not delay the testing for SARS-CoV-2 [ 79 , 85 ]. Comorbid infections with other respiratory infections (viral, bacterial, and fungal) have occurred in COVID-19 patients. As a result, a positive test for a non-COVID-19 pathogen does not rule out SARS-CoV-2 or vice versa. Therefore, patients who meet suspected case definitions for COVID-19 should be tested whether or not another respiratory pathogen is found [ 41 , 78 ]. Other supplemental testing includes radiographic imaging such as serology testing, hematological testing, and chest CT scanning [ 84 ].
Nucleic acid amplification testing (NAAT)
Viral testing detects the SARS-CoV-2 nucleic acid or antigen [ 80 ]. Presently, suspected patients with COVID-19 are confirmed with viral RNA detection by nucleic acid amplification tests (NAAT) [ 78 , 84 ]. PCR is the gold standard test for the molecular diagnosis of viral or bacterial infections due to its high specificity and sensitivity [ 84 ]. NAAT methods, including reverse-transcription polymerase chain reaction (RT-PCR), real-time RT-PCR (rRT-PCR), and reverse transcription loop-mediated isothermal amplification [ 86 ]. Although a diagnosis is made by the detection of SARS-CoV-2 through RT-PCR testing, a false-negative result may occur in 20%–67% of patients. This error is dependent on the quality and timing of the testing, as PCR positivity will be seen during early symptoms [ 87 ]. Upper respiratory tract (URT) viral load peaks around symptom onset, and viral shedding begins approximately 2–3 days before the onset of symptoms [ 88 ]. Because of the rate of false-negative result rates, clinical, laboratory, and imaging findings are also used to make a presumptive diagnosis [ 88 ]. PCR analysis also requires a variety of equipment and educated analysts, which can be found largely at well-established laboratories [ 89 ].
Currently, rRT-PCR is used with confirmation by nucleic acid sequencing, when necessary [ 41 ]. Thus far, the targeted viral genes include N, E, S, and RdRP [ 78 , 87 ]. Different conditions have been set and must be met, which depends on whether or not a patient is being tested in an area with or without known COVID-19 virus circulation. In areas with no known COVID-19 virus circulation, one of the following conditions must be met:
- • A positive NAAT result for at least two different targets on the COVID-19 genome – of which at least one target is preferably specific for COVID-19 virus using a validated assay OR
- • One positive NAAT result for the presence of betacoronavirus and COVID-19 virus further identified by sequencing partial or whole genome of the virus as long as the sequence target is larger or different from the amplicon probed in the NAAT assay used.
Ambiguity in results calls for resampling the patient, and if necessary, sequencing of the virus from the original specimen or of an amplicon generated from an appropriate NAAT assay. The NAAT assay must be different from the original assay used to obtain a reliable test result. For areas where the COVID-19 virus has been widely circulating, a simpler algorithm is sufficient for COVID-19 virus confirmation with NAAT. Although the use of rRT-PCR with one discriminatory target is considered sufficient for laboratory confirmation, one or more negative results do not rule out the possibility of SARS-CoV-2 active infection. The following factors may contribute to a false-negative result of a SARS-CoV-2 infected patient:
- • Poor quality of the specimen, including containing little to no patient material (as a control, might be considered a human target in the PCR testing to determine if there is a sufficient amount of human DNA).
- • Specimens were collected late or very early in the infection.
- • Specimens not handled and shipped properly (nonmaintenance of the cold chain).
- • Technical reasons that are inherent in the test (i.e., virus mutation or PCR inhibition) [ 78 , 87 ].
The WHO recommends that initial diagnostic testing be performed by collecting specimens of the URT, specifically nasopharyngeal and oropharyngeal swabs or wash in ambulatory patients [ 78 ]. If clinical suspicion remains, and URT RT-PCR is negative, LRT specimens should be collected from expectorated sputum or endotracheal aspirate/bronchoalveolar lavage in ventilated patients. Single negative URT results do not exclude a COVID diagnosis, so additional URT and LRT samples are recommended [ 41 , 78 , 87 ].
Serology testing
The U.S. CDC states that serological testing should not be used to establish the presence or absence of SARS-CoV-2 infection or reinfection, and the FDA has not authorized antibody tests to diagnose SARS-CoV-2 yet [ 80 , 90 ]. In cases where NAAT assays are negative, and there is a strong epidemiological link to COVID-19 infection, paired serum samples (in the acute and convalescent phase) could support this diagnosis once validated serology tests become available. Therefore, serum samples can be stored for these purposes [ 78 ].
Hematological testing
A meta-analysis between 3377 severe and non-severe COVID-19 patients, a significantly increased white blood cell count, and decreased lymphocytes (lymphopenia) and platelet counts (thrombocytopenia) were found in severe and fatal cases as compared to nonsevere disease and survivors. Furthermore, interleukins 6 (IL-6) and 10 (IL-10) and serum ferritin were found to be strong discriminators for severe disease [ 91 ]. Additional hematological findings are listed in the chart below. A metanalysis and systematic review of 43 studies involving 3600 patients revealed the most common hematological abnormalities as elevated C-reactive protein (68.6%), lymphopenia (57.4%), and increased lactate dehydrogenase (51.6%) [ 92 ].
An additional systematic review of 19 studies, including 2874 patients mostly from China, reported that the 88% who were hospitalized reported typical ranges of hematological abnormalities. Most of the reported characteristics are nonspecific and are common in pneumonia; therefore, hematological tests provide additional information about the progression or severity of the disease, not diagnostic [ 84 , 88 ]. Severe abnormalities have been associated with more severe infection, and D-dimer and lymphopenia (to a lesser extent) seem to have the largest prognostic associations [ 88 ]. See Fig. 2 .

Schematic of hematological abnormalities in COVID-19 patients.
Computed tomography (CT) imaging
CT imaging has been routinely performed on COVID-19 patients. Chest CT is strongly recommended in suspected COVID-19 cases for initial evaluation and follow-up due to the respiratory system being primarily affected [ 93 ]. Although imaging is not used as a primary diagnostic tool, abnormal findings have been found in infected patients and might be an important tool in monitoring disease progression. Characteristic CT imaging abnormalities of COVID-19-infected patients include diffuse, peripheral ground-glass opacities [ 88 ]. A systematic search was conducted on 5041 COVID-19-infected patients from the onset of COVID-19 outbreak to April 20, 2020. Standard CT imaging features of patients with COVID-19 pneumonia included bilateral lung infections (80%), ground-glass opacities (65%), consolidation (22%), crazy paving pattern (12%), air bronchogram signs (18%), and intralobular septal thickening (27%) [ 86 , 93 ]. Of the 20% of patients who presented with unilateral lung involvement, 62% of patients demonstrated right lung involvement, with 74% of cases involving the right lower lobe. Findings also showed that early disease revealed ground-glass opacities, followed by crazy paving development and increasing consolidation in the latter disease course [ 93 ]. CT abnormalities are nonspecific and can largely overlap with the presentation of other infections. Thus, the diagnostic value of CT imaging in SARS-CoV-2 patients is limited, as some confirmed cases show normal CT findings. In contrast, other patients show abnormal CT findings consistent with COVID-19 days before detecting SARS-CoV-2 RNA in different patients [ 88 ]. Therefore, normal chest CT imaging findings cannot exclude COVID-19, even in symptomatic patients [ 94 ].
Treatment varies depending on the severity of the disease, including mild, moderate, severe, and critical manifestations of COVID-19. The following sections outline the specific treatment management regimens for the differing clinical presentations of the SARS-CoV-19 virus. WHO has provided clinical management guidelines for each clinical manifestation, each of which is listed below in detail [ 41 ].
Mild COVID-19 patients (symptomatic treatment)
For patients with suspected or confirmed mild COVID-19, the first line of treatment is isolating the patient to contain viral transmission. This can be executed at a designated COVID-19 health facility, community facility, or at home (also known as self-isolation). The U.S. CDC recommends that for most persons with COVID-19, isolation and precautionary measures can generally be discontinued ten days after symptom onset and the resolution of fever for at least 24 h. These results were obtained without using fever-reducing medication, and other symptoms improved [ 90 , 95 ]. Decisions to isolate should be made on a case-by-case basis based on the local COVID-19 care pathway and should depend on clinical presentation, the requirement for supportive care, potential risk factors for severe disease, and conditions at home – particularly the presence of vulnerable persons in the household. Pharmacological remedies include symptomatic treatments such as antipyretics to assuage fever and pain and sufficient nutrition and rehydration. Additional counseling should be given to patients to educate them on the signs and symptoms of disease complications and progressions that require urgent care, particularly those with risk factors for severe illnesses. At-risk patients should be monitored closely, most notably for signs of rapid disease progression, including but not limited to lightheadedness, difficulty breathing, chest pain, and dehydration. Should patients develop life-threatening symptoms, they should immediately seek urgent care following the safety protocols established COVID-19 care pathways. Caregivers of children with mild COVID-19 must monitor for signs and symptoms of clinical deterioration, including but not limited to: difficulty breathing, fast or shallow breathing, blue lips or face, chest pain or pressure, new confusion, inability to awaken/not interacting when awake, inability to drink or keep down any liquids, and specifically for infants grunting or inability to breastfeed. Proper monitoring is accomplished through home-based, phone, telemedicine, or community outreach teams. Antibiotic therapy or prophylaxis for mild cases of COVID-19 are inadvisable, as they may lead to higher bacterial resistance rates that further propagate the burden of disease and deaths in a population during COVID-19 pandemic and beyond.
Moderate COVID-19 patients (pneumonia treatment)
Suspected or confirmed moderate COVID-19 cases, defined by the acquisition of pneumonia, should be isolated immediately to contain viral transmission. These patients may or may not require emergency interventions, however, they must be isolated regardless of suspicion or confirmed cases. The isolation protocol is found upon the established COVID-19 care pathways and is accomplished at a health facility, community facility, or at home. This decision should be made on a case-by-case basis and relies on clinical presentation, the requirement for potential supportive care and potentially vulnerable persons present in the household. Patients at high risk for deterioration should instead isolate at a hospital instead of isolation at home or community facilities. As with mild cases, febrile moderate COVID-19 cases should be tested and treated for other endemic infections that cause fever (i.e., malaria, dengue, etc.) per routine protocol if necessary, irrespective of the presence of respiratory signs and symptoms due to the possibility of coinfection. Patients with suspected or confirmed moderate COVID-19 should not be administered antibiotics unless under the clinical suspicion of bacterial infection. However, a recent systematic review reported only 8% of patients hospitalized with COVID-19-experienced secondary bacterial infection/fungal coinfection during hospital admission. For older patients, particularly those in long-term care facilities, and children less than five years of age, providing empiric antibiotic treatment for possible pneumonia should be considered. Given these patients are not hospitalized, access to antibiotic treatment (e.g., co-amoxicillin) is sufficient, and the preferential treatment is broad-spectrum antibiotics. Hospitalized patients should be regularly monitored for vital signs using pulse oximetry while utilizing medical early warning scores (i.e., NEWS2 and PEWS) that facilitate the early recognition and escalation of treatment for deteriorating patients. At-home patients and caregivers should receive counseling on signs and symptoms of complications (i.e., difficulty breathing, chest pain, etc.), informed to seek urgent care immediately if such complications arise [ 41 ].
Severe COVID-19 patients (severe pneumonia treatment)
The immediate administration of supplemental oxygen is paramount to any of the patients exhibiting emergency signs or to patients with a reading of SpO 2 < 90%. The most frequent emergency signs are as follows: obstructed or absent breathing, severe respiratory distress, central cyanosis, shock, convulsions, and/or coma. Device selection for the delivery of appropriate flow rates include nasal cannula for flow rates up to 5 L/min; Venturi mask for 6–10 L/min; and face mask with reservoir bag for 10–15 L/min. Adult patients with said emergency signs must receive emergency airway management and target oxygen levels of SpO 2 ≥ 94%. When patients have stabilized, oxygen target levels aim for SpO 2 > 90% in nonpregnant adults and SpO 2 ≥ 92%–95% in pregnant women. After resuscitation and stabilization of pregnant patients, fetal well-being should be monitored, with frequency of fetal heart rate observed as a function of gestational age, maternal clinical status (e.g., hypoxia), and fetal conditions. Children with emergency signs should also target oxygen levels of SpO 2 ≥ 94% during resuscitation and SpO 2 > 90% when stable; however, they should receive oxygen through nasal cannula or prongs if the patient is a particularly young child due to better tolerance of the procedure. Adults can also employ techniques such as positioning. For example, a high supported sitting posture potentially assists in optimizing oxygenation, easing breathlessness, and reducing energy expenditures. Spontaneously breathing patients may also improve oxygenation and their ventilation/perfusion ratio while in prone position when awake, but there lacks evidence to support this technique; therefore, this should be done under a clinical trial protocol to assess efficacy and safety before implementation. For adult patients who present with increased secretion production, secretion retention, and/or weak cough, airway clearance management may assist with proper secretory mechanisms and includes gravity-assisted drainage with activated cycles of breathing techniques. Mechanical insufflation-exsufflation and inspiratory positive pressure breathing should be avoided when possible, and the implementation of the aforementioned techniques must be personalized for each respective patient.
Patients should be monitored for signs of clinical deterioration (rapidly progressive respiratory failure and shock) and be immediately given supportive care interventions when circumstances dictate. Hematological and biochemical laboratory testing, ECG, and chest imaging should be performed at admission and as clinically indicated to monitor for complications. These complications include acute respiratory distress syndrome, acute liver injury, acute kidney injury, acute cardiac injury, DIC and/or shock. The application of timely, effective, and safe supportive therapies provides the cornerstone of therapy for patients who develop severe manifestations of COVID-19. Signs and symptoms suggestive of venous or arterial thromboembolism should be monitored closely – which considers the possibility of stroke, DVT, pulmonary embolism, or acute coronary syndrome. Any of these manifestations when presented would elicit the corresponding course of action in accordance with hospital protocols for these diagnoses. Fluid management in adults and children, particularly intravenous fluids, should be treated with caution in patients without tissue hypoperfusion and adequate fluid responsiveness as aggressive fluid resuscitation may worsen oxygenation in situations involving limited availability of mechanical ventilation [ 41 ].
According to the U.S. CDC, a limited number of individuals with severe illnesses may produce a replication-competent virus beyond 10 days of onset (typical isolation protocol), which may warrant the extension of the duration of isolation and precautionary measures for up to 20 days after symptom onset. With this in mind, consultation with infection control experts would be beneficial [ 90 ].
Critical COVID-19 patients (ARDS – acute respiratory distress syndrome)
Management of adult and pediatric patients with mild ards who are treated with noninvasive or high-flow nasal oxygen (hfno) systems.
Patients with COVID-19 who have mild ARDS, a trial of HFNO, noninvasive ventilation are able to use continuous positive airway pressure (CPAP) and bilevel positive airway pressure. Although HFNO may reduce the need for intubation as compared to standard oxygen therapy, patients with hypercapnia, hypoxemic respiratory failure, and hemodynamic instability, multiorgan failure, or abnormal mental status, should not receive HFNO in place of options such as invasive ventilation. NIV guidelines make no recommendations for their applicability in hypoxemic respiratory failure (apart from cardiogenic pulmonary edema, postoperative respiratory failure, and early NIV for immunocompromised patients) or in pandemic viral illness (referring to studies from SARS and pandemic influenza). Risks can include delayed intubation, large tidal volumes, and injurious transpulmonary pressure, and the limited data available suggest a high failure rate with other confounding viral infections such as MERS-CoV receiving NIV. Patients receiving a trial of HFNO or NIV should be monitored by personnel experienced in performing endotracheal intubation in case the patient acutely deteriorates or does not improve after the short trial (about 1 h), to ensure immediate intubation should these conditions present themselves. HNFO systems can deliver 60 L/min and up to 1.0 fraction of inspired oxygen (FiO2) in adults, whereas pediatric circuits can handle up to 25 L/min. Pediatric patients may still require adult circuits to deliver adequate flow. Situations where mechanical ventilation may not be available warrants the administration of bubble nasal CPAP for newborns and children with severe hypoxemia. Because of uncertainty about aerosolization , airborne precautions should be accounted for with HFNO, NIV, and bubble CPAP [ 41 ].
Recommendations for adult and pediatric patients with ARDS who need intubation and IMV
Patients may continue to have increased labored breathing or hypoxemia even with oxygen delivery through a face mask with a reservoir bag (flow rates 10–15 L/min i.e., minimum flow required to keep bag inflation, FiO2 0.60–0.95). Hypoxemic respiratory failure in ARDS commonly results from an intrapulmonary ventilation-perfusion mismatch or shunt and requires mechanical ventilation. Researchers recommend promptly recognizing progressive acute hypoxemic respiratory failure when a patient is in respiratory distress and adequately preparing to provide advanced oxygen/ventilation support when necessary. Endotracheal intubation is recommended using airborne precautions, with rapid-sequence intubation being appropriate after an airway assessment that identifies no signs of difficult intubation. Patients with ARDS, particularly young children, obese, or pregnant patients, may desaturate quickly during intubation; therefore, it is recommended to preoxygenate with 100% FiO2 for 5 min using a face mask with reservoir bag. When possible, avoid bag-valve mask ventilation to reduce exposure to aerosols [ 41 ].
Recommendations pertaining to mechanically ventilated adult and pediatric patients with ARDS
Implementation of mechanical ventilation using lower tidal volumes (4–8 mL/kg predicated body weight [PBW]) and lower inspiratory pressures (plateau pressure < 30 cmH20) is strongly recommended for adults and is also suggested for patients with sepsis-induced respiratory failure who do not meet ARDS criteria. Initial target tidal volume is 6 mL/kg PBW; tidal volume up to 8 ml/kg PBW is allowed if undesirable effects occur such as desynchrony or pH < 7.15. Permissive hypercapnia is permitted and use of deep sedation may be required to control respiratory drive and achieve tidal volume targets. Children have a lower targeted level of plateau pressure (<28 cmH2O), and a lower target of pH levels is permitted (7.15–7.30). Tidal volumes should be adapted to disease severity: 3–6 mL/kg PBW in the case of poor respiratory system compliance and 5–8 mL/kg PBW with a better conserved compliance.
Adult patients with severe ARDS (partial pressure of arterial oxygen: PaO2/FiO2 < 150) are recommended to receive prone ventilation for 12–16 h per day. Pediatric patients with severe ARDS can also be considered, but this treatment requires sufficient human resources and expertise to be safely performed. There is little evidence supporting this method for pregnant women with ARDS, although it could be considered in early pregnancy. Pregnant women in their third trimester may benefit from being placed in the lateral decubitus position. Physicians should implement conservative fluid management for ARDS patients without tissue hypoperfusion and fluid responsiveness to shorten the duration of ventilation.
In patients with moderate or severe ARDS, trials of higher-end positive-end-expiratory pressure (PEEP) are recommended over those of lower PEEP. However, they require a risk-benefit analysis—corresponding to risks of end-inspiratory distention and higher pulmonary vascular resistance versus the benefit of reducing atelectrauma and improving alveolar recruitment. It is suggested to individualize the PEEP where during titration the patient is monitored for beneficial or harmful effects and driving pressure. In younger children, maximal PEEP pressures are 15 cmHO. When disconnection is required (e.g., transferal to a transport ventilator), use in-line catheters for airway suctioning and clamp the endotracheal tube, concurrently utilizing ventilator hyperinflation as opposed to manual hyperinflation. For patients with excessive secretions or difficulty clearing secretion, consider the application of airway clearance techniques if deemed medically appropriate [ 41 ].
Recommendations pertaining to adult and pediatric patients with ARDS in whom lung protective ventilation strategy fails to achieve adequate oxygenation and ventilation
Patients who have refractory hypoxemia (i.e., including a ratio of PaO2 to the FiO2 of <50 mmHg for 3 h, a PaO2: FiO2 of <80 mmHg for > 6 h) despite having lung protective ventilation, should be referred to the treatment of COVID-19. Although ECMO was not statistically significant in primary outcomes of 60-day mortality between ECMO and standard medical management, it was associated with a reduced risk of mortality and crossover to ECMO treatment. A post-hoc Bayesian analysis of this RCT showed that ECMO has a notable probability to reduce mortality across a range of prior assumptions. In patients with MERS, ECMO vs. conventional treatment was associated with reduced mortality in a cohort study but is deemed a resource-intensive therapy that necessitates expert centers. Children with severe ARDS can be put on ECMO, but there is not much evidence supporting its therapeutic effects in this population [ 41 ].
On October 22, 2020, the FDA approved the antiviral drug, remdesivir, to treat COVID-19 [ 17 , 18 ]. Remdesivir is for use in adult and pediatric patients 12 years of age and older and weighing at least 40 kg (88 pounds) for the treatment of COVID-19 that requires hospitalization. Remdesivir can be administered in a hospital or treatment facility capable of delivering acute care equivalent to inpatient hospital care. Remdesivir is the first medication for COVID-19 to be approved by the FDA. See Table 1 .
Side effects associated with antivirals, immunomodulators, or plasma therapy.
The FDA originally issued an Emergency Use Authorization (EUA) on May 1, 2020 for the use of remdesivir for the treatment of hospitalized adult and pediatric patients with severe COVID-19 (low blood oxygen levels or needing oxygen therapy or more intensive breathing support). The EUA was reissued on August 28, 2020 to expand the treatment of all hospitalized adult and pediatric patients with suspected or laboratory-confirmed COVID-19, irrespective of their severity of disease [ 96 ]. As of October 22, 2020, remdesivir is the first treatment for COVID-19 to receive FDA approval [ 97 ]. It is indicted for the treatment of hospitalized cases of COVID-19 in adults and children 12 years or older and weighing at least 40 kg. It should only be administered in a hospital or healthcare setting capable of providing acute care comparable to hospital care. The FDA also revised the EUA for remdesivir to authorize the treatment of suspected or laboratory-confirmed COVID-19 in hospitalized pediatric patients (3.5 kg to less than 40 kg) or hospitalized pediatric patients (less than 12 years old and weighing at least 3.5 kg). Clinical trials that assess the safety and efficacy in this pediatric population continue today.
Approval of a new drug product under the Federal Food, Drug, and Cosmetic Act requires substantial evidence of effectiveness and a demonstration of safety for the drug's intended use(s), passing a rigorous scientific benefit-risk assessment to ensure that benefits outweigh its risks of intended population. See Table 2 [ 15 , 98 , 99 ].
Data from three randomized controlled clinical trials involving Veklury (remdesivir), including patients hospitalized with mild-to-severe COVID-19. ∗∗ indicates statistically significant results.
Remdesivir is an antiviral agent (a SARS-CoV-2 nucleotide analogue RNA polymerase inhibitor) that was initially designed to combat the Ebola virus disease [ 100 , 101 ].
Contraindications include hypersensitivity reactions to remdesivir or any components of the product, and lower infusions rates can be considered to potentially prevent signs and symptoms of hypersensitivity, but treatment should be discontinued should signs and symptoms of clinically significant hypersensitivity reaction persist. Before initiation and during treatment all patients should have renal and hepatic laboratory testing performed and prothrombin time assessed as clinically appropriate. The most common adverse reactions observed (calculated as incidence rates greater than or equal to 5%, all grades) include nausea, ALT increased, and AST increase. Increased risk of transaminase elevation has been reported in both healthy volunteers and patients with COVID-19 who have received remdesivir treatment [ 101 ].
The further development of future treatments for COVID-19 could use nanotechnology to address limitations of antiviral therapy. Nano-intervention is aimed at designing effective nanocarriers to counter the conventional limitations of antiviral and biological therapeutics. SARS-CoV-2 targets human cells through the characteristic viral structural spike protein (S- spike glycoprotein) that binds to ACE2 receptor [ 102 ]. The Interaction between viral S protein and ACE2 on the host cell surface is of significant interest because it initiates the infection process. Engineered nanocarriers would allow the blocking of the initial interactions of viral spike glycoproteins with host cell surface receptors; therefore, disrupting virion construction [ 103 ]. They can also be utilized in designing risk-free and effective immunization strategies for SARS-CoV-2 vaccine candidates such as protein constructs and nucleic acids.
Influenza and COVID-19: present challenge of 2020–2021 flu season
The treatment of influenza is similar in all patients, regardless of SARS-CoV-2 coinfection. The NIH reports that the Panel recommends hospitalized patients be started on empiric treatment for influenza with oseltamivir (antiviral treatment) as soon as possible, regardless if influenza testing results have been received. If URT NAAT rules out influenza for nonintubated patients and both URT and LRT specimens for intubated patients, oseltamivir can be stopped. The clinical presentation of an uncomplicated, clinically mild influenza case can overlap with mild COVID-19 presentation. While ageusia and anosmia can occur with both diseases, they are more common with COVID-19 than influenza. Fever is also not always present in patients with either disease, in particular, the elderly or immunocompromised patients. Although complications of both diseases can be similar, the onset of influenza complications and severe disease usually occurs within a week of illness onset, as opposed to severe COVID-19 that occurs in the second week of illness. This overlap in signs and symptoms requires diagnostic testing for both viruses while they are cocirculating to distinguish between the two, or to identify coinfection that has been reported with both influenza A and B viruses with SARS-CoV-2 [ 104 , 105 ]. At this time, there is no information on the frequency, severity, and risk factors for coinfection with these viruses versus either alone [ 106 ].
Recent clinical studies
Many vaccine candidates, such as mRNA-1273, are now in phase III clinical trials and vaccinations have now begun with the recent FDA approval of the vaccines produced by Pfizer and Moderna. However, it is unlikely that a vaccine against the virus will be available to the general public before the end of 2020, since it is currenlty being administed to frontline healthcare workers and residents of long-term care facilities [ 107 ]. As such, a considerable amount of research has focused on repurposing existing antivirals and immunomodulators for the treatment of this novel virus [ 108 ].
Antiviral treatment: viral protease inhibitors
Viral protease inhibitors work to hinder viral replication by interfering with the processing of viral polypeptides. Most clinical trials have concentrated on viral protease inhibitors lopinavir/ritonavir, as these have shown to be effective treatments in-vivo and in-vitro for the previous coronavirus outbreaks, MERS-CoV and SARS-CoV [ 108 , 109 ]. Despite this, lopinavir/ritonavir treatment in a randomized trial involving 199 patients with severe cases of COVID-19 showed no additional benefit to patients as compared to standard care treatment [ 110 ]. Additionally, in a randomized phase II trial involving 127 patients with mild to moderate COVID-19, treatment with lopinavir/ritonavir had effects comparable to placebo [ 111 ]. Notably, both trials reported numerous limitations, so further research on lopinavir/ritonavir's effectiveness is necessary.
Antiviral treatment: RNA polymerase inhibitors
RNA polymerase inhibitors, namely remdesivir and favipiravir, disrupt the replication of the viral genome and therefore, may be promising treatments for COVID-19 [ 108 , 112 ]. In a randomized, double-blind clinical trial, preliminary results found that IV remdesivir given over ten days significantly reduced time to recovery. Additionally, mortality decreased in those given IV remdesivir as compared to placebo, though this difference was not significant [ 17 ]. Favipiravir may also be an effective treatment as it resulted in faster viral clearance and improved chest imaging as compared to patients taking lopinavir/ritonavir in a nonrandomized trial [ 113 ].
Antiviral treatment: fusion inhibitor
Hydroxyquinoline, an immunosuppressive and anti-malarial drug that blocks viral fusion, has shown to inhibit SAR-CoV-2 in-vitro [ 114 ]. However, results from clinical trials evaluating its clinical effectiveness in COVID-19 patients are mixed. An open-label non-randomized trial with 36 positive COVID-19 patients found hydroxyquinoline and azithromycin significantly reduced viral load [ 115 ]. Conversely, in a more recent double-blind, randomized trial, hydroxyquinoline did not prevent infection when used as postexposure prophylaxis [ 116 ]. There are currently ongoing clinical trials to elucidate hydroxyquinoline's effectiveness against COVID-19 [ [117] , [118] , [119] ].
Immunomodulators
Type I IFN-I are crucial for protection against viral infections, and it has been suggested that SARS-CoV-2 can evade or inhibit their production [ 120 ]. In a randomized clinical trial consisting of 81 participants, subcutaneous administration of IFN β-1a to COVID-19 patients significantly reduced 28-day mortality as compared to the control group, particularly if given early after the onset of symptoms. Additionally, while IFN β-1a administration did not affect clinical response time, the discharge rate was significantly increased by day 14 [ 121 ]. Furthermore, the combination therapy involving IFN β-1b, ribavirin, and lopinavir/ritonavir resulted in significantly reduced viral shedding [ 111 ]. Another immunomodulator worth mentioning is tocilizumab, a monoclonal antibody that attenuates IL-6, a proinflammatory cytokine that may contribute to the fatality of COVID-19 patients [ 122 ]. Preliminary reports of an open-label randomized control trial involving 129 patients with moderate to severe COVID-19 related pneumonia have reported significantly reduced mortality or need for ventilation as compared to the control group. Note that this trial is pending peer review, and further research is warranted [ 123 ].
With over one million confirmed deaths to date, COVID-19 is the deadliest pandemic of the twenty-first century, matched only in recent history by the influenza pandemics of 1918, 1957–1958, and 1968–1970 and the ongoing HIV/AIDS pandemic [ 10 , [124] , [125] , [126] , [127] ]. This outbreak will have lasting, widespread socioeconomic effects, including disruption to education, business, and healthcare globally [ 128 ]. The need for effective diagnosis and treatment methodologies, grounded in understanding this virus's microbiology and pathophysiology, is clear.
In summary, coronaviruses are a family of enveloped RNA viruses characterized by a large genome and characteristic glycoprotein spikes. Replication of the coronavirus genome is aided by proofreading machinery, unique to coronaviruses, and necessary to maintain their relatively large genome. The process of translation in coronaviruses is unique due to the presence of ribosome frameshifting [ 1 , 2 , 129 ]. Coronaviruses utilize surface glycoproteins to bind to and enter host cells; in SARS-CoV-2, the novel coronavirus responsible for COVID-19, this glycoprotein binds host ACE2 receptors. Coronavirus infection in humans is typically mild and self-limited, confined to the upper respiratory tract, but novel strains of coronavirus can cause severe disease affecting the lungs and other organ systems. Elderly patients and those with comorbidities are particularly susceptible [ 9 ].
COVID-19 presents with fever, lethargy, and dry cough and may progress to pneumonia, respiratory failure, multisystem organ dysfunction, and death [ [11] , [12] , [13] , 21 ]. Treatment is primarily supportive, with escalation from supplemental oxygen to noninvasive positive pressure ventilation or mechanical ventilation appropriate for respiratory impairment [ 21 ]. Corticosteroids have also proven useful as an adjunctive treatment [ 22 , 23 ]. Some effective antiviral agents have been identified and are being used in particular clinical scenarios, while the search for additional treatments for this history-defining disease continues [ 21 , 130 ]. The development of a vaccine has progressed significantly; it has now been approved by the FDA on an emergency basis and is expected to be administered to the general population in the coming months.
Practice Points:
- • Coronavirus infection in humans is typically mild and self-limited, confined to the upper respiratory tract, but novel strains of coronavirus can cause severe disease that affects the lungs and other organ systems.
- • COVID-19 presents with fever, lethargy, and dry cough and may progress to pneumonia, respiratory failure, multisystem organ dysfunction, and death.
- • Treatment is primarily supportive, with escalation from supplemental oxygen to noninvasive positive pressure ventilation or mechanical ventilation appropriate for respiratory impairment.
- • Corticosteroids have also proven useful as an adjunctive treatment.
- • Several vaccines have been developed and some were recently approved by the FDA; they should be available to the general public by 2021.
Research Agenda:
- • Most effective preventative strategies to decrease the spread of COVID-19.
- • Antiviral agents that can treat existing COVID-19 infection effectively, with no significant side effects.
- • Rapid testing techniques that can be made widely available to clinicians and consumers.
- • COVID-19 vaccine development that is safe and effective.
Funding source
Declaration of competing interest.
Richard D. Urman received unrelated funding or fees from Merck, Medtronic/Covidien, AcelRx, Heron and Pfizer. Alan D. Kaye received fees from Merck. Other authors report no conflicts of interest.
Acknowledgements
Create an account
Create a free IEA account to download our reports or subcribe to a paid service.
Oil demand growing at a slower pace as post-Covid rebound runs its course

Cite commentary
IEA (2024), Oil demand growing at a slower pace as post-Covid rebound runs its course , IEA, Paris https://www.iea.org/commentaries/oil-demand-growing-at-a-slower-pace-as-post-covid-rebound-runs-its-course, Licence: CC BY 4.0
Share this commentary
- Share on Twitter Twitter
- Share on Facebook Facebook
- Share on LinkedIn LinkedIn
- Share on Email Email
- Share on Print Print
Global oil demand growth returns to historical trend
Global oil demand growth is currently in the midst of a slowdown and is expected to ease to 1.2 million barrels a day (mb/d) this year and 1.1 mb/d in 2025 – bringing a peak in consumption into view this decade. This is primarily the result of a normalisation of growth following the disruptions of 2020-2023, when oil markets were shaken by the Covid-19 pandemic and then the global energy crisis sparked by Russia’s invasion of Ukraine.
Despite the deceleration that is forecast, this level of oil demand growth remains largely in line with the pre-Covid trend, even amid muted expectations for global economic growth this year and increased deployment of clean energy technologies.
Annual oil demand growth, 2011-2025
In both 2022 and 2023, global oil consumption rose by more than 2 mb/d as economies continued their recoveries from the Covid-19 shock and saw spikes in personal mobility, along with exceptional releases of pent-up demand for travel and tourism. While there are reasonable grounds for uncertainty about how complete the global recovery is, both oil demand data and mobility indicators suggest that its pace has slowed sharply and that the period of demand growth above the historical average is coming to an end.
China’s post-Covid rebound is running out of steam
Without a steep fall in oil prices, a sudden resurgence in the post-pandemic recovery or an acceleration in economic activity, it is unlikely that global oil demand growth will approach the levels seen in 2022 and 2023. Indeed, the pace of gains slowed substantially in the second half of 2023, and the latest data shows that the trend continued at the beginning of 2024.
Oil use increased by an estimated 1.6 mb/d year-on-year in the first quarter of 2024, down from 1.9 mb/d in the fourth quarter of 2023 and more than 3 mb/d during the middle of last year. Given that China was the last major economy to lift public health restrictions related to the pandemic and saw an abrupt economic recovery in mid-2023, this easing of year-on-year demand growth is likely to continue during 2024.
Quarterly oil demand growth, 2022-2025
Indeed, because the timing of Chinese lockdowns was quite different from the rest of the world, global oil demand growth in 2023 was extremely dependent on the country. With the explosive phase of the pandemic rebound largely complete elsewhere, China contributed to more than three-quarters of the global increase in demand (1.7 mb/d out of 2.3 mb/d). The world’s second largest economy will remain the mainstay of global expansion this year. However, gains are projected to fall to 540 kb/d. In the absence of a dramatic acceleration in other countries, this will result in a wider global slowdown.
In the decade up to 2023, almost two-thirds of all oil demand growth came from China. Over this period, the nation’s GDP grew at an annual average rate of 6%. An expected slackening in economic growth, to a rate of between 4% and 5% in 2024 and 2025 – combined with the rapid domestic uptake of oil-substituting technologies such as electric vehicles (EVs) and high-speed rail – means that in 2024 and 2025, only a little over one-third of oil demand growth is expected to come from China.
Demand for aviation fuel is easing as air traffic stabilises
The other major driver of rising oil consumption in 2022 and 2023 was a steady recovery in air traffic as pandemic-era travel restrictions were relaxed. Demand for jet fuel/kerosene, primarily from the aviation sector, grew by more than 1 mb/d in both years and contributed almost half of the increase in global oil demand.
However, gains have moderated since the first half of 2023, according to Airportia data. As a result, the increase in demand for jet fuel/kerosene in 2024 is forecast to be far smaller, at 230 kb/d. In addition to a stabilisation in air traffic, there have also been large gains in the fuel efficiency of aircraft since 2019. This has meant that, despite roughly equivalent activity, fuel demand from the sector was more than 6% lower in the second half of 2023 than in the same period in 2019. This trend is set to continue as more new planes with vastly improved fuel economy enter the global fleet, helping to restrain the impact of increasing demand for air travel on oil use during the medium term.
Demand for jet fuel/kerosene lags global miles flown as aircraft fuel efficiency improves
Global consumption of oil is set to peak, but its centrality remains.
While we expect growth in oil consumption in 2024 (1.2 mb/d) and 2025 (1.1 mb/d) to remain robust by historical standards, structural factors will lead to a gradual easing of oil demand growth over the rest of this decade. Continued rapid gains in the market share of EVs, particularly in China; steady improvements in vehicle fuel economies; and, notably, efforts by Middle Eastern economies, especially Saudi Arabia, to reduce the quantity of oil used in power generation are together expected to generate an overall peak in demand by the turn of the decade.
Oil remains extremely important to the global economy, and across some of its key applications, alternatives still cannot easily be substituted. In the absence of additional energy and climate policies and an increased investment push into clean energy technologies, the decline in global oil demand following the peak will not be a steep one, leaving demand close to current levels for some time. Nevertheless, cooling Chinese demand growth and considerable progress on the deployment of clean energy transition technologies mean that the oil market is set to enter a new and consequential period of transformation.
Oil Market Report - April 2024
The IEA Oil Market Report (OMR) is one of the world's most authoritative and timely sources of data, forecasts and analysis on the global oil market – including detailed statistics and commentary on oil supply, demand, inventories, prices and refining activity, as well as oil trade for IEA and selected non-IEA countries.
Fuel report — April 2024

Subscription successful
Thank you for subscribing. You can unsubscribe at any time by clicking the link at the bottom of any IEA newsletter.
- Share full article
Advertisement
Supported by
Should Kidney Donors Be Paid?
A guest essay argued in favor of payments. Readers, including donors, offer divergent views.

To the Editor:
Re “ We Should Be Allowed to Sell Our Kidneys ,” by Dylan Walsh (Opinion guest essay, April 4):
I’ve seen firsthand how kidney transplants can transform the lives of patients living with debilitating renal disease who are often forced to spend hours each week in painful and exhausting dialysis treatments. Mr. Walsh is correct that we need to greatly boost the number of living organ donors. But before we consider paying people for their kidneys, we need to ensure that every potential donor has an equitable chance to also receive a lifesaving organ transplant.
Even though undocumented people can and do donate organs, far too many of the undocumented, Black and low-income clients we serve with severe renal disease are unable to receive treatment at transplant centers run by private hospitals, despite many of them being excellent medical candidates for a successful transplant.
It would be grossly unethical for our government to encourage them to sell their organs when they receive far less than an equitable share of needed organs.
There are many steps the federal and state governments can take to gather data on transplant equity and require tax-exempt health systems to provide fair and equitable access to transplant care, regardless of immigration or insurance status, income or race. We must create a fair system before we consider a market for organs.
Karina Albistegui Adler New York The writer is co-director of health justice for New York Lawyers for the Public Interest.
As president of the American Society of Transplantation, I know there is an extreme need for additional organs to support lifesaving organ transplantation. Dylan Walsh aptly describes the challenge.
We at the A.S.T. support the author’s intent to increase living donation. However, A.S.T. policy opposes direct remuneration for organs, as it would encourage donations for financial rather than altruistic reasons, thereby propagating disparities. Instead, we aim to remove disincentives that prevent living donors from providing a lifesaving gift.
The A.S.T. is advancing effective solutions. The Living Donor Protection Act , which ensures that life, disability and long-term care insurers cannot discriminate against living donors, has bipartisan support. Other legislation provides a one-time tax credit for living donors that would offset donors’ expenses without providing perverse incentives. The A.S.T. also encourages companies to offer paid leave for living donors through our Circle of Excellence initiative.
Living donors alone cannot meet demand. The A.S.T. is engaged in ongoing work with the Health Resources and Services Administration, patients and other stakeholders to optimize the existing system for deceased donor transplantation, maximize the use of all available organs and minimize non-use.
These activities, along with research on the best strategies to remove disincentives, will result in meaningful progress. Selling organs is not the answer we need now.
Josh Levitsky Chicago The writer is a professor of medicine, surgery and medical education at Northwestern University Feinberg School of Medicine.
Five years ago I donated my left kidney to a stranger after seeing his flyer posted in Starbucks. I was not paid money for my efforts. Yet it was one of the most rewarding endeavors in my life. Throughout the process, I learned many of the lessons that Dylan Walsh discusses.
Even though it’s too late for me to benefit financially, I strongly support the idea of paying future donors. The criticism that rich, powerful people will take advantage of the poor or vulnerable is based on the incorrect assumption that it’s not a rational decision to incur personal risks for financial and other benefits.
It is legal for women to act as paid surrogates carrying a pregnancy that poses at least as many potential medical risks as the nephrectomy. Paying people for kidneys is no different.
As a social worker who has worked with vulnerable people for decades, I believe it’s possible to create safety protocols to ensure that no one is making a decision that is coerced or lacking proper informed consent. There is no better reward than the good feeling of saving a life. Paying someone to do it is just icing on the cake.
Catherine Pearlman Laguna Niguel, Calif.
Nineteen years ago, I donated a kidney to my younger sister with the hope she would live another 10 good years. She had 12 good years, two not so good, and died at the age of 63. I am now 72 and have no regrets, but I remain strongly opposed to the concept of selling kidneys.
The organ transplant community tells only half the story, which is that donors should expect to live well with just one kidney. The other half of the story is what might be involved in recuperating from major surgery. To those involved in physical labor, I would tell them to be prepared to lose your livelihood for up to a year. Sure, there will be anecdotes like “I was mowing my lawn a week later!” But for me, even months later, my children told me that I walked funny.
With a Ph.D. in ethics, I am well aware of the ongoing debate of autonomy versus paternalism on all kinds of subjects. It’s too simplistic to say, “People should be allowed the personal freedom to sell a kidney.” We live in a society that limits our choices in all kinds of ways and for good reason.
In this case, I don’t see the transplant community ever being fully transparent about all the consequences of making this choice, just as they weren’t with me.
Thomas P. Roberts Hillsborough, N.C.
Dylan Walsh’s essay struck a chord. I have failing kidneys, brought on by being one of the millions of Americans with diabetes. Now 75, I long ago made major changes relating to diet, weight and exercise. Unfortunately, my progressive chronic kidney disease refused to get better.
So many of those thousands of Americans who are on waiting lists are young people deserving of so much more life to live. With so few donor kidneys available even for them, at my age I’ve made the decision not to seek a donor kidney, not to add my name to the waiting list. It would not be fair for those who have yet to experience a full life to miss out because I was next in line.
Would I like more time to enjoy life, love, family, etc.? Of course. If Mr. Walsh’s piece gains traction, and one day there are donor kidneys aplenty, I look forward to changing my mind.
Esteban S. Corona, Calif. The writer’s full name is not being used to protect his medical privacy.
The essay by Dylan Walsh highlights the travesty of our kidney transplant program. We are allowed to sell our blood, serum, sperm or ova but not kidneys, which are in short supply.
In addition to Mr. Walsh’s suggestion I would add another: Trade a kidney to stay out of jail. If select first offenders were given the opportunity to avoid a prison sentence by donating a kidney, they would benefit immediately by avoiding incarceration.
Society would benefit from obtaining a young healthy kidney while avoiding the cost of prison sentences. The offender/donor would avoid the many negative aspects of imprisonment. The kidney donation will save the life of someone who might otherwise die of kidney failure.
The experience of saving a life might also contribute to the rehabilitation of a first offender.
Robert W. Morgan Vero Beach, Fla. The writer is an epidemiologist.
I'm excited about Angel Reese and Caitlin Clark, but what about the pioneers of women's hoops?
Many new fans are discovering women's basketball, but i grew up around women who should have went pro, by d. watkins.
Seeing images of college sensations turning WNBA stars Angel Reese and Caitlin Clark fill my timelines and appear on all the media sites I subscribe to was heartwarming.
For the first time in my long life as a basketball fan, we are witnessing a major paradigm shift in women's sports – where the best women are treated with the love and respect they deserve from fans that hail from all walks of life. Now, there is still a huge pay disparity, that has been connected to TV contracts and ticket sales being lower for professional women basketball players in America, but with this type of attention from the media and the scores of new fans – I doubt that the days of women being paid hundreds of thousands, for what men get paid hundreds of millions, will last long. As we celebrate the surge in popularity of women's basketball, I can't help but think about those super-talented women who came up on the courts in the parks where I used to play.
When I was coming up you had to be tough as nails to play basketball in Baltimore City. Many of the best games were on concrete, and you better not call a foul or you’ll ran off the court. Of course, you may chip a tooth or bust your head or break a bone, but at the end of the day those are small prices to pay to shine amongst the best, and we had some women who used to be the brightest.
This was the early '90s, but keep in mind that the WNBA wasn't founded until 1996. . . . Most of the female players were never big stars in America.
Tanya, with big lazy eyes and sharp left hand, could cross anybody. Her step-back jump shot was lethal, and her only weakness was that she couldn't get off unless she were in a trash-talking competition. "When she starts running her mouth, you better not say anything back because she won't miss!" is what was shared amongst the dudes who battled her on the blacktop daily. You could say that Tanya’s mental game was just as good as her physical game and if you didn't pay close attention she would beat you with both. Lanky Lisa from Up Top was a fierce competitor, too, and I imagine she would have worked on her game more if she thought a future in basketball for women in America was a thing.
This was the early '90s, but keep in mind that the WNBA wasn't founded until 1996. Other professional women's basketball leagues were in different countries, but most of the female players were never big stars in America. Talented women like Tanya and Lisa didn't want to move to another country to play ball, so they figured it was just something to do, a way to earn a college scholarship and maybe major in something that paid a decent wage. Tanya went to college, but came home after her first year, and gave her life to the streets. Lisa stopped playing basketball before she finished high school, modeled for a while and then started a family. Younger than both, Neka wanted to be the first woman in the NBA.
The NBA was a pipe dream for all of us except Neka.
I only thought I was good enough to make it to the NBA because I hung with Neka. Now, obviously, I thought wrong because I never made it anywhere close to the NBA. However, Neka was so good, played so much and played so hard that you just felt like she was going to make it. You felt like she was going to will herself into a historic situation and take control of a role that had never been done by any woman before her.
"Let's get it, bro!" Neka said at 8 a.m. or 4:30 p.m. before the sun started dipping into the clouds and at 8 p.m. when the lights popped on Elmwood Park.
Let's get it, bro, meant, "D! Wake your jughead self up, and let's hit the court!"
At 12 years old, we'd pick apart the adults in our neighborhood, destroy them in games of 2 on 2 after completing our workouts and then work out again.
Hitting the court with Neka wasn't just playing basketball; it was jogging around the park, running suicides on a blacktop – a challenging exercise where you race up and down the court, stopping to touch each line before going back, starting over, and advancing to the next line. Neka also wanted t o do shooting, passing and tough layup drills, so she drove to the basket and asked me to push her out of the air when she neared the rim.
"If I'm gonna make it to the NBA, I must be better."
"You better than every girl knows and most dudes."
"Better than everyone," she’d shoot back.
At 12 years old, we'd pick apart the adults in our neighborhood, destroy them in games of 2 on 2 after completing our workouts and then work out again. Neka was more skilled than me, had a better jump shot and was more aware on the court. Physically, we were the same height, except I was stronger and faster. When we did those layup drills where she asked me to bump or push her out of the air, I remember practicing the highest level of restraint, and still, even my light touches disrupted her shot. And she would do the same to me. I would hardly feel it. We both worked out so much, that a lot of competition in the neighborhood didn't stand a chance, and any attempts at bullying her because she was a woman or me for playing against a woman rarely worked.
Rarely because there was one time where she was getting the best of a dude in a game to 21, and he started feeling her up in an inappropriate way.
“Get ya hands off me!” Neka yelled. A few guys from the game and a bunch dudes from the bench rushed the court and beat him down hard enough that I imagine he would never want to improperly touch a woman again.
By 14, my skills had increased, as hers did, too, except my physical ability continued to grow to the point where I could dunk. My dunking caused unnecessary friction, but still, together, we ran the courts — from our home turf of Ellwood to The Cage over West. And most of the dudes, especially the ones we defeated, had the same compliment about Neka's game: "She's good for a girl."
When guys said, "She's good for a girl," it was meant as a compliment. To fully understand, let's use the lens of patriarchy. In understanding the rules of patriarchy, a comment like, "She's good for a girl," is the ultimate gift that you could offer a woman. To be compared to a man should mean the world . . . or so many men who subscribe to that culture think. Neka didn't care about being compared to men or women in general; she just wanted to be great, better than anyone else on the court. And she would achieve that goal again and again.
Neka continued to work on her game, and as she reached college, I imagine that her dream of being the first woman in the pros grew further away. I was humbled, too, as I continued to travel to different courts and encountered more challenging competition. Making the NBA is impossible even if you are a man over 6 feet, practice every day and have started in high school and maybe even college. Millions of hoopers in the world with only about 300 or so odd spots. I should mention that Neka never grew past 5 foot 4.
We were now in the late '90s, and the WNBA had been off to a great start with stars like Dawn Staley, Sheryl Swoopes and Lisa Leslie. But they were at the top of the food chain, at the head of countless other professional WNBA athletes who could not earn enough off of endorsements and didn't make enough money off their basketball fame to solely live off hoops. Many talented women like Neka did not see a future and pursue basketball even after a professional league for women was created.
But this new wave of athletes is changing everything.
The top women in sports still are not getting the same contracts as men; however, they are making a ton of money off of endorsements and the many other revenue streams available to public figures. When I look at marketing sensations like Angel Reese and Caitlin Clark, I think about how my great friend Neka could be doing that if only she had been born at a different time.
Wouldn't it be great if there was a way to financially take care of the pioneers? Sadly, many of the women who paved the way for the current generation will never financially reap the benefits but deserve all of their flowers for laying the current foundation.
about this topic
- Recent Olympic rulings show dehumanization of Black women in sports
- Jill Biden owes the LSU women a full apology
- Church at the Super Bowl: Football, Jesus and fascism
D. Watkins is an Editor at Large for Salon. He is also a writer on the HBO limited series "We Own This City" and a professor at the University of Baltimore. Watkins is the author of the award-winning, New York Times best-selling memoirs “ The Beast Side: Living (and Dying) While Black in America ”, " The Cook Up: A Crack Rock Memoir ," " Where Tomorrows Aren't Promised: A Memoir of Survival and Hope " as well as " We Speak For Ourselves: How Woke Culture Prohibits Progress ." His new books, " Black Boy Smile: A Memoir in Moments ," and " The Wire: A Complete Visual History " are out now.
Related Topics ------------------------------------------
Related articles.

IMAGES
VIDEO
COMMENTS
Students can choose to write a full-length college essay on the coronavirus or summarize their experience in a shorter form. To help students explain how the pandemic affected them, The Common App ...
Writing a persuasive essay about COVID-19 requires a thoughtful approach to present your arguments effectively. Here are some tips to help you craft a compelling persuasive essay on this topic: Choose a Specific Angle. Start by narrowing down your focus. COVID-19 is a broad topic, so selecting a specific aspect or issue related to it will make ...
Coronavirus disease (COVID-19) is an infectious disease caused by the SARS-CoV-2 virus. Most people infected with the virus will experience mild to moderate respiratory illness and recover without requiring special treatment. However, some will become seriously ill and require medical attention. Older people and those with underlying medical ...
A novel coronavirus (CoV) named '2019-nCoV' or '2019 novel coronavirus' or 'COVID-19' by the World Health Organization (WHO) is in charge of the current outbreak of pneumonia that began at the beginning of December 2019 near in Wuhan City, Hubei Province, China [1-4]. COVID-19 is a pathogenic virus. From the phylogenetic analysis ...
The days dragged on in my apartment, in black and white, like my photos. Sometimes we tried to smile, imagining that I was asymptomatic, because I was the virus. Our smiles seemed to bring good ...
Yet well into the fourth year of the Covid-19 pandemic, intense political and scientific debates about its origins continue. The two major hypotheses are a natural zoonotic spillover, most likely ...
Having recognized this, the Common App added a new optional 250-word essay that will give universities a chance to understand the atypical high school experience students have had. The prompt will ...
Alex, a writer and fellow disabled parent, found the freedom to explore a fuller version of herself in the privacy the pandemic provided. "The way I dress, the way I love, and the way I carry ...
1. In fall of 2019, exactly zero scientists were studying COVID‑19, because no one knew the disease existed. The coronavirus that causes it, SARS‑CoV‑2, had only recently jumped into humans ...
Editor in Chief's Introduction to Essays on the Impact of COVID-19 on Work and Workers. On March 11, 2020, the World Health Organization declared that COVID-19 was a global pandemic, indicating significant global spread of an infectious disease ( World Health Organization, 2020 ). At that point, there were 118,000 confirmed cases of the ...
Hundreds of millions of babies are expected to be born during the COVID-19 pandemic. Fionn, son of Chloe O'Doherty and her husband Patrick, is among them. The couple says: "It's all over. We did ...
COVID-19 is a disease caused by a virus. The most common symptoms are fever, chills, and sore throat, but there are a range of others. Most people make a full recovery without needing hospital treatment. People with severe symptoms should seek medical care as soon as possible. Over 760 million cases and 6.9 million deaths have been recorded ...
COVID-19 (coronavirus disease 2019) is a disease caused by a virus named SARS-CoV-2. It can be very contagious and spreads quickly. Over one million people have died from COVID-19 in the United States. COVID-19 most often causes respiratory symptoms that can feel much like a cold, the flu, or pneumonia. COVID-19 may attack more than your lungs ...
What is a coronavirus? Coronaviruses are a large family of viruses, but only seven of its members infect humans. Four types cause minor illnesses like the common cold, while other coronaviruses ...
The spread of the "Severe Acute Respiratory Coronavirus 2" (SARS-CoV-2), the causal agent of COVID-19, was characterized as a pandemic by the World Health Organization (WHO) in March 2020 and has triggered an international public health emergency [].The numbers of confirmed cases and deaths due to COVID-19 are rapidly escalating, counting in millions [], causing massive economic strain ...
Today, the US is far from these thresholds. For the week of December 13, 2021, the CDC reported the US experienced more than 900 000 COVID-19 cases, more than 50 000 new hospitalizations for COVID-19, and more than 7000 deaths. 5,6 The tolerance for disease, hospitalization, and death varies widely among individuals and communities. What ...
It is essential to be aware of clinical manifestations of COVID-19, even though the symptoms are nonspecific. Common symptoms are fever, nonproductive cough and myalgia or fatigue, normal or decreased leukocyte counts and radiographic evidence of pneumonia. At first people may complain of diarrhea and nausea.
### What you need to know Since the emergence of SARS-CoV-2 in December 2019, there has been an unparalleled global effort to characterise the virus and the clinical course of disease. Coronavirus disease 2019 (covid-19), caused by SARS-CoV-2, follows a biphasic pattern of illness that likely results from the combination of an early viral response phase and an inflammatory second phase. Most ...
What You Need to Know COVID-19. COVID-19 is the disease caused by SARS-CoV-2, the coronavirus that emerged in December 2019. COVID-19 can be severe, and has caused millions of deaths around the world as well as lasting health problems in some who have survived the illness. The coronavirus can be spread from person to person.
100 Words Essay on Covid 19. COVID-19 or Corona Virus is a novel coronavirus that was first identified in 2019. It is similar to other coronaviruses, such as SARS-CoV and MERS-CoV, but it is more contagious and has caused more severe respiratory illness in people who have been infected. The novel coronavirus became a global pandemic in a very ...
Just weeks after the first cases of COVID-19 hit U.S. shores, an op-ed appeared in The New York Times titled "We Need to Talk About What Coronavirus Recoveries Look Like: They're a lot more complicated than most people realize."The author, Fiona Lowenstein, is a writer and yoga teacher living in New York City, who wrote about her own illness and the symptoms she was left with once she was ...
COVID-19, also called coronavirus disease 2019, is an illness caused by a virus. The virus is called severe acute respiratory syndrome coronavirus 2, or more commonly, SARS-CoV-2. It started spreading at the end of 2019 and became a pandemic disease in 2020. Coronavirus Enlarge image.
Essay on COVID-19 Pandemic. Published: 2021/11/08. Number of words: 1220. As a result of the COVID-19 (Coronavirus) outbreak, daily life has been negatively affected, impacting the worldwide economy. Thousands of individuals have been sickened or died as a result of the outbreak of this disease. When you have the flu or a viral infection, the ...
April 16, 2024. 0. Four years ago in the spring of 2020, physicians and patients coined the term "long COVID" to describe a form of the viral infection from which recovery seemed impossible. (And ...
Readers respond to First Opinion essays on nonprofit hospitals and taxes, diversity in health care, ADHD in women and girls, and more. ... With Covid-19 vaccines, initial efforts focused on ...
Berliner rails against NPR's coverage of COVID-19, diversity efforts. Berliner, a senior business editor who has worked at NPR for 25 years, argued in the Free Press essay that "people at every ...
Biology of coronaviruses. Coronaviruses are enveloped, positive-strand RNA viruses with genomes of up to 33.5 kilobases (kb) considered the largest among all RNA viruses [24,25].Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), similar to other coronaviruses, is characterized by trimeric S glycoproteins located on a pleomorphic (round or oval) outer membrane [26,27].
Indeed, the pace of gains slowed substantially in the second half of 2023, and the latest data shows that the trend continued at the beginning of 2024. Oil use increased by an estimated 1.6 mb/d year-on-year in the first quarter of 2024, down from 1.9 mb/d in the fourth quarter of 2023 and more than 3 mb/d during the middle of last year. Given ...
A guest essay argued in favor of payments. Readers, including donors, offer divergent views. To the Editor: Re " We Should Be Allowed to Sell Our Kidneys ," by Dylan Walsh (Opinion guest essay ...
Seeing images of college sensations turning WNBA stars Angel Reese and Caitlin Clark fill my timelines and appear on all the media sites I subscribe to was heartwarming.. For the first time in my ...