- Research article
- Open access
- Published: 29 January 2022

Hypertension and its related factors among patients with type 2 diabetes mellitus – a multi-hospital study in Bangladesh
- Hiba Alsaadon ORCID: orcid.org/0000-0001-8235-7481 1 ,
- Afsana Afroz 1 ,
- Afsana Karim 2 ,
- Samira Humaira Habib 2 ,
- Mohammed J. Alramadan 1 ,
- Baki Billah 1 &
- Aishwarya Narendra Shetty 1
BMC Public Health volume 22 , Article number: 198 ( 2022 ) Cite this article
7392 Accesses
9 Citations
1 Altmetric
Metrics details
Hypertension and type 2 diabetes are associated with each other, and their coexistence is linked to diabetes-related complications such as stroke, coronary artery disease, kidney disease, retinopathy and diabetic foot. This study aimed to determine the prevalence, awareness and control of hypertension and factors associated with hypertension among people with type 2 diabetes mellitus (T2DM) in Bangladesh.
A cross-sectional and retrospective study was conducted in 2017, and data from 1252 adults with T2DM were collected from six hospitals that specialise in diabetes care. These hospitals provide primary, secondary and tertiary healthcare and cover the rural and urban populations of Bangladesh. Cross-sectional data were collected from patients via face-to-face interviews, and retrospective data were collected from patients’ past medical records (medical passport), locally known as the patients’ guidebook or record book. The associations between hypertension and its related factors were examined using the bootstrapping method with multiple logistic regression to adjust for potential confounders.
The mean age of participants was 55.14 (± 12.51) years. Hypertension was found to be present among 67.2% of participants, and 95.8% were aware that they had it. Of these, 79.5% attained the blood pressure control. The mean duration of diabetes was 10.86 (± 7.73) years. The variables that were found to be related to hypertension include an age of above 60 years, physical inactivity, being overweight or obese, a longer duration of diabetes and chronic kidney disease.
The prevalence of hypertension as well as its awareness and control were very high among people with known type 2 diabetes. As there is a strong relationship between hypertension and diabetes, patients with diabetes should have their blood pressure regularly monitored to prevent major diabetes-related complications.
Peer Review reports
Hypertension is a major non-communicable disease and is identified as a global disease burden that is ranked as the third-largest cause of disability-adjusted life years [ 1 ]. Globally, there were 972 million hypertensive adults in the year 2000, and this number is on track to increase by 60% to 1.56 billion by 2025 [ 1 ]. It has been reported that people with hypertension are twice as likely to develop cardiovascular disease, four times as likely to develop congestive heart failure and seven times as likely to develop cerebrovascular disease or stroke when compared to non-hypertensive subjects [ 2 ].
Diabetes mellitus and hypertension are inter-related diseases that strongly promote the spread of atherosclerotic cardiovascular disease within populations [ 3 ]. Hypertension prevalence is doubled in the presence of diabetes and is associated with 35 to 75% of diabetic cardiovascular and renal complications [ 4 ]. In addition, it also contributes to diabetic retinopathy, which is the primary cause of newly diagnosed blindness [ 3 ]. When a patient has diabetes, there is an accelerated formation of non-enzymatic advanced glycosylation products that accumulate in the vessel wall proteins, causing vascular rigidity and resistance, which ultimately leads to hypertension. Additionally, in mild-to-moderate hyperglycaemia, there is increased retention of sodium, which leads to an increase in the total exchangeable sodium and blood pressure [ 5 ]. Another plausible explanation is that the upregulation of the renin-angiotensin-aldosterone system in diabetes has a direct effect on hypertension [ 6 ]. Thus, diabetes and hypertension have an epidemiological and pathophysiological link, and knowledge of this link will not only help with the development of early treatment strategies but will also assist with prevention.
The population of Asian, especially South Asia, is facing an increasing burden from hypertension (ranging from 50% in India [ 7 ] to 75% in Pakistan [ 8 ]) among people with type 2 diabetes mellitus (T2DM). The burden of hypertension among patients with T2DM is also high in other regions (Korea (55%) [ 9 ], Nigeria (60%) [ 10 ] and Saudi Arabia (54.2–78.1%) [ 11 , 12 ]). As of 2013, of the five South Asian countries with the highest prevalence of T2DM, Bangladesh Ranked second [ 13 ]. A report by the International Diabetes Federation stated that 7,926,300 cases of diabetes were recorded in Bangladesh [ 14 ]. A systematic review conducted in 2016 showed that the prevalence of T2DM in Bangladesh was 7.4% [ 15 ]. However, there has been a lack of studies in Bangladesh related to hypertension among people with T2DM. A study conducted in 1998 addressed hypertension among non-insulin-dependent subjects with diabetes mellitus and impaired glucose tolerance. This study reported that the proportion of people with systolic and diastolic hypertension was 32.2 and 13.6%, respectively [ 16 ]. According to the Bangladesh Demographic Health Survey 2011, the prevalence of T2DM in Bangladesh was 9.2% and among them 38.7% had hypertension [ 17 ]. Another study that was conducted in 2015, on the general population in Bangladesh, showed that 57.4% of patients with diabetes had hypertension compared to that of 15.6% of non-diabetic participants [ 18 ]. The above data shows an increasing trend in hypertension among T2DM patients in Bangladesh.
In recent years, along with the well-established pathophysiological link between T2DM and hypertension, the rapid epidemiological transition (rapid urbanisation, increased life expectancy, unhealthy diet and lifestyle changes) has led to an increase in hypertension among people with T2DM in Bangladesh. Thus, it is essential that patients and healthcare workers are aware of the co-existence of hypertension and T2DM to ensure that there is tight monitoring of blood pressure (BP) and blood sugar levels. To ensure good regulation, it is quintessential that an updated prevalence of hypertension, it’s awareness and control, and the factors associated with hypertension in patients with T2DM is available. Thus, this study aimed to determine the prevalence of hypertension and its associated factors among people with T2DM in Bangladesh.
Study design and sampling
A cross-sectional and retrospective study was conducted in 2017 in Bangladesh. Data were collected from outpatient department of six selected hospitals across the country that are under the umbrella of the Diabetic Association of Bangladesh (BADAS). All hospitals under BADAS are locally known as diabetes hospitals, as their primary focus is to treat patients with diabetes and its related complications. These hospitals are operated privately, but they provide healthcare services on a not-for-profit basis (i.e. their charged fee is lower than that of other private hospitals). These hospitals are located both outside and inside metropolitan areas across the country. The hospitals outside the metropolitan areas provide primary and secondary level healthcare services. However, within the metropolitan areas, the selected hospitals are the central hospitals that deliver primary, secondary and tertiary healthcare. The selection of the specific hospitals in this study made it possible to recruit a heterogeneous sample in terms of participants’ residential areas and socio-economic status.
BADAS has created a sustainable model of health care for people with diabetes and the general population. Most of the diabetic patients in Bangladesh prefer to visit hospitals under BADAS because of the availability of endocrinologists and diabetes-centred care and because the quality of facilities is higher than those in public hospitals. Thus, despite the fact that the participants in our study do not represent all people with T2DM in Bangladesh, they represent the majority of them. Hospitals under BADAS were purposively selected for data collection, as all patients are provided a record book or medical passport, which keeps patients’ records of laboratory test results, medications, complications and comorbidities.
It was calculated that a sample size of 1252 participants would be required to ensure accurate results. The primary outcome of this study was to determine haemoglobin A1c (HbA1c) levels and diabetes control [ 19 ], and the secondary outcome was to determine the prevalence of hypertension and its control among T2DM. Hence, to ensure that the accuracy in results was maintained for the secondary outcome of hypertension, the sample size was recalculated. This was done using a 5% significance level, 3.5% margin of error, 57.4% prevalence of hypertension among those with T2DM in Bangladesh and a design effect of 1.5 [ 20 ]. This provided a required sample size of 1150 participants. Thus, using data from 1252 participants ensured a greater level of accuracy than was required by the calculation.
During each day of data collection, around 10 patients were recruited from each hospital’s general outpatient department. The data collectors started the day by randomly selecting a patient from the first K patients attending the hospital and invited them to participate. The value of K was determined by dividing the total estimated hospital outdoor attendance each day by 10. After that, every Kth patient was approached. If this patient declined to participate in the study or did not have T2DM, the next patient was invited. The recruitment continued for 6 months, from Saturday to Thursday each week. The inclusion criteria were as follows: patients were over 18 years of age, were registered with BADAS and had had T2DM for over 1 year. The study excluded people suffering from other types of diabetes.
Data collection
A structured questionnaire was developed based on published literature and different standardised questionnaires [ 21 , 22 , 23 ]. The questionnaire was pretested using a pilot study conducted in one of the selected tertiary hospitals. After getting informed written consent, the pretested questionnaire was used to interview each patient . A PhD research student and two data collectors were recruited and trained for data collection.
Data on sociodemographic characteristics, mental health (anxiety and depression), diabetes-related medical history and lifestyle behaviours were collected. The Global Physical Activity Questionnaire (GPAQ) was used to assess physical activity level [ 24 ]. The Patient Health Questionnaire (PHQ-2) [ 21 ] and Generalised Anxiety Disorder (GAD-2) [ 25 ] scales were used to evaluate depression and anxiety respectively. Participants were measured with their shoes off and in light clothes to determine their weight and height, and waist and hip measurements were also obtained. Either a medical officer or a registered nurse measured the blood pressure (BP) of each participant twice, at a 15-min interval, using mercury sphygmomanometer and stethoscope with participants sitting in a relaxed position and their left arm at rest on a table.
The following variables were extracted from medical passports or clinical records: most recent HbA1c level, lipid profiles, most recent estimated glomerular filtration rate (GFR), diagnosis of hypertension, medications used, and history of macro-vascular (coronary artery disease (CAD), stroke and diabetic foot) and micro-vascular (nephropathy, retinopathy and neuropathy) complications. For CAD and retinopathy, patients’ past medical records, past documented diagnoses, medications or past procedures were used to extract the data. Research Electronic Data Capture (REDCap) was used to collect and manage the data [ 26 ].
Operational definition
Participants’ household income was categorised as follows: up to 20,000 Bangladeshi Taka (BDT), 21,000 to 60,000 BDT and over 60,000 BDT [ 19 ]. The monthly income was converted to USD using the mid-year currency conversion for 2017, which was 1 USD = 80 BDT [ 19 ]. At least 150 min of moderate to vigorous physical activity per week was considered as active [ 22 ]. Both PHQ-2 and GAD-2 had Likert scale questions with four options each [ 23 , 25 ]. A patient with a total score of three or more was identified as having depression or anxiety. The body mass index (BMI) was categorised as follows: < 18.50 kg/m 2 = underweight; 18.50 to 22.99 kg/m 2 = normal; 23.00 to 27.49 kg/m 2 = overweight and ≥ 27.5 = obese [ 27 , 28 , 29 ]. High waist–hip ratio was defined as > 0.90 for men and > 0.85 for woman [ 30 ]. Hypertension was defined by BP readings (either systolic ≥140 mmHg or diastolic ≥90 mmHg) or by using a documented diagnosis of hypertension for T2DM patients taking antihypertension medications [ 31 ]. Based on HbA1c level, diabetes control was categorised as a good control (HbA1c < 7.0%) or a poor control (HbA1c ≥ 7.0%). Renal impairment was determined using the most recent estimated GFR of below 60 ml/min/1.73m 2 and/or a documented diagnosis [ 32 ].
Ethical approval
This study has been approved by the Monash University Human Research Ethics Committee (ID: 1469), the Ethical Review Committee of the Bangladesh University of Health Sciences and the Ethical Review Committee of BADAS.
Data management and analysis
Stata/SE version 15.0 was used for the data analysis. Data were summarised and presented as means (± standard deviation) for numerical data and relative percentages for categorical data. Chi-square tests and univariate logistic regression analysis were used to examine associations between hypertension and its associated factors. Potential variables were then identified using a clinical assessment, literature review and the variables with a p -value of less than 0.15 from the univariate analysis [ 19 ]. Of these, three variables had missing observations: BMI (8.6%, n = 108), waist–hip ratio (19.6%, n = 245) and glycaemic control (HbA1c 20.1%, n = 252).
Missing data were imputed five times using the chained equation method, creating five imputed samples [ 33 , 34 ]. Then, the bootstrapping method [ 20 , 35 ] with replacement was carried out to select the truly independent variables for hypertension. In the bootstrapping method, 5000 random samples of the size of the original sample ( n = 1253) were drawn from each of the five imputed samples. This created 25,000 samples. A multiple logistic regression analysis was then performed for each of the 25,000 samples where all potential variables were added into the model, and the variables that appeared as significant were recorded. The percentage of the time that each variable was selected as significant (out of 25,000 samples) was calculated and variables were ranked from the highest to the lowest percentage. A multiple logistic regression model was then run using the variables that were selected in at least 40% of the bootstrap samples, which adjusted the effect of each variable with potential confounders.
A total of 1404 people with diabetes were approached, but 89 of them had type 1 or gestational diabetes, and 63 of them declined to participate (Fig. 1 ). Among the 1252 participants, 64.91% were female. The mean age was 55.14 (± 12.51) years, while the mean duration of diabetes was 10.86 (± 7.73) years.
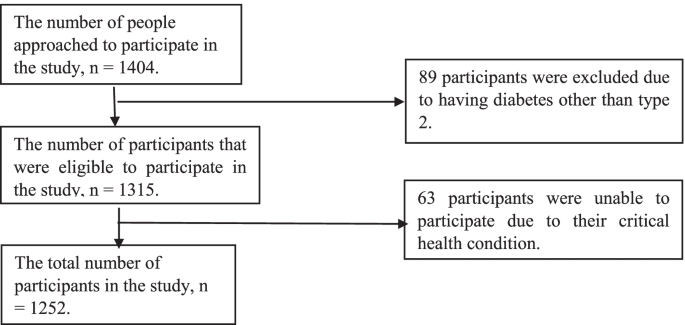
Flow-chart of selected participants
Using BP cut point of 140/90 mmHg, as recommended by most guidelines of hypertension treatment, 67.2% (842/1252) of the participants in this study had hypertension. Of those with hypertension, 95.8% (807/842) were aware that they had hypertension (informed either by a doctor or nurse on previous occasions). The remaining 4.2% ( n = 35/842) were unaware that they had it, but upon measuring their blood pressure during this present study it was found to be classified as being high. Furthermore, of those who were previously aware that they had hypertension, 79.5% ( n = 642/807) had controlled hypertension, when measured for the present study. However, using a more aggressive BP cut point of 130/80 mmHg, as recommended for patients with diabetes, hypertension prevalence, awareness and control were 72.5% ( n = 909/1252), 88.8% (807/909), and 60.2% ( n = 486/807) respectively (Fig. 2 ). There was no significant difference of hypertension control between male and female (for BP cut point of 140/90 mmHg: male 80% vs female 79.1%, p -value = 0.737; and for BP cut point of 130/80 mmHg: male 57.9% vs female 62.9%, p -value = 0.151). The prevalence of hypertension awareness for male and female was 95.3 and 96.4% ( p -value = 0.435) respectively for BP cut point of 140/90 mmHg, and that was 88.1 and 89.6% ( p -value = 0.495) for BP cut point of 130/80 mmHg respectively (Fig. 3 ).
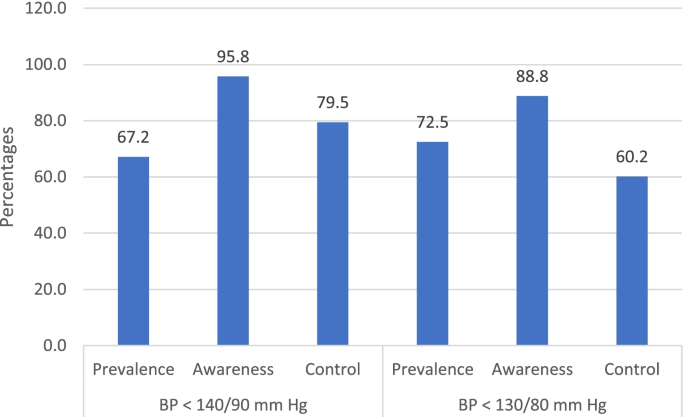
Hypertension awareness, prevalence and control among people with T2DM based on BP < 140/90 mmHg and < 130/80 mmHg. Note: Hypertension awareness: among all participants with hypertension; Hypertension control: among participants receiving hypertension treatment
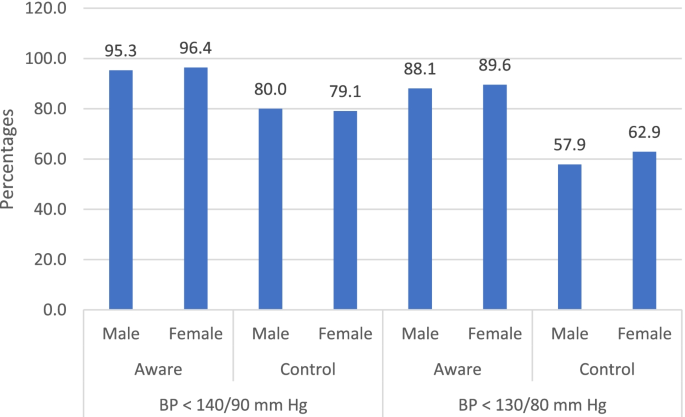
Hypertension awareness and control for male and female patients based on BP < 140/90 mmHg and < 130/80 mmHg. Note: Hypertension awareness: among all participants with hypertension; Hypertension control: among participants receiving hypertension treatment
The prevalence of hypertension was higher in those over 60 years (78%) as compared to patients 60 years and below (57.8%) ( p -value < 0.001). Hypertension prevalence was similar between male and female (male: 63.1% vs female: 64.9%, p -value = 0.308). The prevalence of hypertension was also significantly higher among people who resided in urban areas, were physically inactive, were obese or had a high waist–hip ratio ( p -value < 0.001). The presence of hypertension was also significantly higher among people who never smoked (66.1%) compared to those who smoke presently (48.9%) and did in the past (63.9%), with a p -value of 0.004 (Table 1 ).
According to the findings, people who have had diabetes for over 10 years, used insulin either solely or in combination with an oral hypoglycaemic agent (OHA) or have a history of chronic kidney diseases showed an increased prevalence of hypertension ( p < 0.001). Also, the presence of hypertension was higher among people who had depression, anxiety or micro- and macro-vascular complications ( p < 0.001) (Table 1 ).
Bootstrap method was used to find the potential variables for multiple logistic regression analysis. Being overweight or obese along with having chronic kidney disease and being older than 60 years appeared as significant in over 90% of bootstrap samples. However, a diabetes duration of over 10 years and physical inactivity appeared as significant in 41 and 49% of samples, respectively. While waist–hip ratio and depression appeared in 33 and 30% of the samples. The remaining variables appeared as significant in less than 30% of the samples. The variables that appeared in at least 40% of the bootstrap samples were added to the multiple logistic regression to adjust for potential confounders (Fig. 4 ).
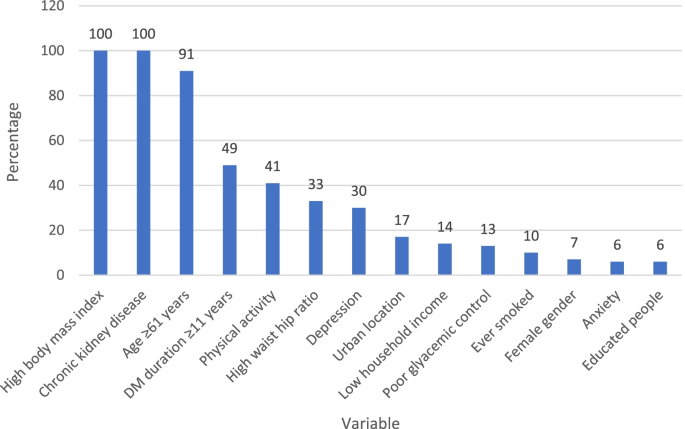
The percentage of the time that variables were significant for hypertension in bootstrap analysis
The results from multiple logistic regression analyses showed that being above 60 years (OR: 1.7, 95% CI: 1.3, 2.4), overweight (OR: 1.8, 95% CI: 1.3, 2.5), obese (OR: 3.2, 95% CI: 2.26, 4.8) or physically inactive (OR: 1.3, 95% CI: 1.0, 1.7) increased the odds of hypertension. Furthermore, higher odds were observed among patients with chronic kidney disease (OR: 3.1, 95% CI: 2.2, 4.3) and who had diabetes for over 10 years (OR: 1.4, 95% CI: 1.0, 1.8) (Table 2 ).
This study was conducted to explore hypertension prevalence, awareness and control, and factors related to hypertension among T2DM patients in diabetes hospitals in Bangladesh. The study demonstrated that 67.2% of the participants had hypertension. The prevalence of hypertension among patients with diabetes was higher in the current study than previously reported in Bangladesh (57.4%) [ 36 ] or other South Asian countries (Indian 50% [ 7 ], Bhutan 54% [ 37 ] and Nepal 36.7% [ 38 ]) except for Pakistan (75%) [ 8 ].
The prevalence of hypertension awareness among hypertensive T2DM in this study was 95.8%, and among them 79.5% had it controlled. The data on hypertension awareness and its control among T2DM patients is scarce in the South Asian countries. However, a multi-country study conducted from 2003 to 2009 on the general population in India, Pakistan and Bangladesh showed that 40.4% of the hypertensive patients were aware of it and 12.9% had it controlled [ 39 ]. In comparison with other regions, the hypertension awareness and control among T2DM in this current study was higher than that reported in China (57.5%) [ 40 ] and in the USA (53%) [ 41 ] and Malaysia (33.3%) [ 42 ] respectively. The high awareness and control of hypertension in this study might be because of the policy of the diabetes hospitals that requires blood pressure to be measured during each diabetes check-up visit and the regular onsite and camp diagnosis undertaken under BADAS to create awareness of hypertension among patients with known diabetes. Also, the free investigation and treatment the diabetes hospitals provide for the financially disadvantaged patients, making it more accessible and affordable [ 43 ]. The prevalence of hypertension awareness and control among participants with known T2DM in this study were in good levels as compared to global standards. However, a further hypertension control among hypertensive T2DM may be achieved by strengthening counselling, educating and empowering in self-monitoring. In addition, hypertension control among hypertensive T2DM may be required a more aggressive goal of BP < 130/80 mmHg as recommend for patients with diabetes mellitus.
The multivariable analysis in the current study showed that older age, physical inactivity, being overweight or obese, longer duration of diabetes and chronic kidney disease are related to hypertension among people with T2DM. As previous evidence suggests, our study demonstrated that being physically inactive was associated with an increased prevalence of hypertension [ 37 , 44 ] and insufficient physical activity was highly prevalent among T2DM in Bangladesh [ 45 ]. The findings of our study therefore amplify the need to direct efforts and resources to increase the physical activity levels of people with T2DM in Bangladesh. This study’s results further show that being overweight or obese might increase the odds of hypertension, which is supported by previous studies [ 46 , 47 ]. In recent decades, obesity among adults has been on the rise in Bangladesh and has reached a point where one in five adults is now obese [ 48 ]. Therefore, maintaining a healthy weight is essential for people with diabetes in the country. As for the duration of diabetes, this current study confirmed the previous finding that having diabetes for a long time is significantly related to hypertension [ 49 ]. The presence of chronic kidney disease was also significantly associated with hypertension in this study. Many scientific studies have clarified this relationship [ 50 ] and have established their pathophysiological link [ 51 , 52 ]. However, it is important to note that hypertension is a well-known risk factor for kidney disease, as well as the other way around.
This study has strengths and limitations. First, it used a relatively large sample that came from six diabetes hospitals that provide primary, secondary and tertiary healthcare and cover rural and urban populations. Second, in addition to a large sample size, this study used validated questionnaires, which provides a valuable repository of data that merits dissemination. Third, the investigation of various demographic, behavioural and clinical factors added strength to the study. A limitation of this study was that it was cross-sectional and retrospective in its design, which only allows for the implication of association, rather than causation. The unavailability of data on the treatment of hypertension among hypertensive T2DM patients was another limitation. Finally, a major limitation is that the findings of this study are not generalizable to diabetes patients not receiving care at BADAS hospitals.
Considering the high proportion of hypertension among patients with diabetes and the close pathophysiological association between T2DM and hypertension, patients with T2DM should have regular monitoring of blood pressure to diagnose and control hypertension. The factors related to hypertension among patients with T2DM are the same as those found in other studies, and this study highlights the need for lifestyle interventions to decrease obesity levels and increase physical activity. The BADAS hospitals’ policy of mandatory blood pressure monitoring in each diabetes check-up visit and a full or partial fee waiver for investigation and treatment for financially disadvantaged patients may be a key factor for high levels of hypertension awareness and controls among T2DM patients. This study suggests and highlights the successful policy implementation of hypertension management at hospitals in Bangladesh and other similarly positioned countries in accordance with international guidelines [ 53 ].
Availability of data and materials
The data sets generated during and/or analysed during the current study are available from the corresponding author upon reasonable request. Prior permission from the respective hospitals was obtained for collecting data such as lipid profiles, HbA1c level, and diabetes related macro- and microvascular complications from hospital records retrospectively.
Abbreviations
- Type 2 diabetes mellitus
Blood pressure
Diabetic Association of Bangladesh
Global Physical Activity Questionnaire
Patient Health Questionnaire
Generalised Anxiety Disorder
Haemoglobin A1c
Glomerular filtration rate
Coronary artery disease
Research Electronic Data Capture
Bangladeshi Taka
Unites States Dollar
Body mass index
Oral hypoglycaemic agent
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–23.
PubMed Google Scholar
Lawes CM, Vander Hoorn S, Law MR, Elliott P, MacMahon S, Rodgers A. Blood pressure and the global burden of disease 2000. Part II: estimates of attributable burden. J Hypertens. 2006;24(3):423–30.
CAS PubMed Google Scholar
Venugopal K, Mohammed M. Prevalence of hypertension in type-2 diabetes mellitus. CHRISMED J Health Res. 2014;1(4):223.
Google Scholar
Borde-Perry WC, Campbell KL, Murtaugh KH, Gidding S, Falkner B. The association between hypertension and other cardiovascular risk factors in young adult African Americans. J Clin Hypertens. 2002;4(1):17–22.
Contreras F, Rivera M, Vasquez J, De la Parte MA, Velasco M. Diabetes and hypertension physiopathology and therapeutics. J Hum Hypertens. 2000;14(Suppl 1):S26–31.
Libianto R, Batu D, MacIsaac RJ, Cooper ME, Ekinci EI. Pathophysiological links between diabetes and blood pressure. Can J Cardiol. 2018;34(5):585–94.
Singh R, Beegom R, Rastogi V, Rastogi S, Madhu V. Clinical characteristics and hypertension among known patients of non-insulin dependent diabetes mellitus in north and south Indians. J Diabet Assoc India. 1996;36:45–50.
Maheshwary N, Naveed S, Ali Z, Ahmed SM, Yousuf AM. Prevalence of hypertension in type 2 diabetics. Pak J Physiol. 2016;12(1):31–4.
Lee H, Lee S, Hwang I, Park Y, Yoon S, Han K, et al. Prevalence, awareness, treatment and control of hypertension in adults with diagnosed diabetes: the fourth Korea National Health and nutrition examination survey (KNHANES IV). J Hum Hypertens. 2013;27(6):381–7.
Unadike B, Eregie A, Ohwovoriole A. Prevalence of hypertension amongst persons with diabetes mellitus in Benin City, Nigeria. Niger J Clin Pract. 2011;14(3):300–2.
Al Harbi TJ, Tourkmani AM, Al-Khashan HI, Mishriky AM, Al Qahtani H, Bakhiet A. Adherence to the American Diabetes Association standards of care among patients with type 2 diabetes in primary care in Saudi Arabia. Saudi Med J. 2015;36(2):221.
PubMed PubMed Central Google Scholar
Alaboud AF, Tourkmani AM, Alharbi TJ, Alobikan AH, Abdelhay O, Al Batal SM, et al. Microvascular and macrovascular complications of type 2 diabetic mellitus in central, Kingdom of Saudi Arabia. Saudi Med J. 2016;37(12):1408.
Selim S, Pathan F, Saifuddin M, Latif Z, Karim N. The challenge of proper glycaemic control among patients with type 2 diabetes in Bangladesh. Sri Lanka J Diab Endocrinol Metab. 2016;6(2):16.
Cho N, et al. IDF diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81.
Biswas T, Islam A, Rawal LB, Islam SMS. Increasing prevalence of diabetes in Bangladesh: a scoping review. Public Health. 2016;138:4–11.
Sayeed MA, et al. Blood pressure and coronary heart disease in NIDDM subjects at diagnosis: prevalence and risks in a Bangladeshi population. Diabetes Res Clin Pract. 1998;39(2):147–55.
Chowdhury MAB, Uddin MJ, Haque MR, Ibrahimou B. Hypertension among adults in Bangladesh: evidence from a national cross-sectional survey. BMC Cardiovasc Disord. 2016;16:22.
Islam SMS, Rawal LB, Niessen LW. Prevalence of depression and its associated factors in patients with type 2 diabetes: a cross-sectional study in Dhaka, Bangladesh. Asian J Psychiatr. 2015;17:36–41.
Afroz A, Alam K, Ali L, Karim A, Alramadan MJ, Habib SH, et al. Type 2 diabetes mellitus in Bangladesh: a prevalence based cost-of-illness study. BMC Health Serv Res. 2019;19(1):1–12.
Afroz A, Ali L, Karim MN, Alramadan MJ, Alam K, Magliano DJ, et al. Glycaemic control for people with type 2 diabetes mellitus in Bangladesh-an urgent need for optimization of management plan. Sci Rep. 2019;9(1):1–10.
CAS Google Scholar
England CY, Thompson JL, Jago R, Cooper AR, Andrews RC. Development of a brief, reliable and valid diet assessment tool for impaired glucose tolerance and diabetes: the UK diabetes and diet questionnaire. Public Health Nutr. 2017;20(2):191–9.
Armstrong T, Bull F. Development of the world health organization global physical activity questionnaire (GPAQ). J Public Health. 2006;14(2):66–70.
Kroenke K, Spitzer RL, Williams JB. The patient health questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284–92.
Bull FC, Maslin TS, Armstrong T. Global physical activity questionnaire (GPAQ): nine country reliability and validity study. J Phys Act Health. 2009;6(6):790–804.
Skapinakis P. The 2-item generalized anxiety disorder scale had high sensitivity and specificity for detecting GAD in primary care; 2007.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Who J, Consultation FE. Diet, nutrition and the prevention of chronic diseases. World Health Organ Tech Rep Ser. 2003 Feb 27;916(i-viii):1-49.
Consultation WE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet (London, England). 2004;363(9403):157–63.
Cho J, Juon H-S. Assessing overweight and obesity risk among Korean Americans in California using World Health Organization body mass index criteria for Asians; 2006.
Organization WH. Waist circumference and waist-hip ratio: report of a WHO expert consultation, Geneva, 8-11 December 2008. 2011.
Association AD. Standards of medical care in diabetes—2017 abridged for primary care providers. Clin Diab. 2017;35(1):5.
Levey AS, Stevens LA, Schmid CH, Zhang Y, Castro AF III, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12.
Royston P. Multiple imputation of missing values. Stata J. 2004;4(3):227–41.
Rubin DB. Multiple imputation for nonresponse in surveys. Wiley; 2004. https://books.google.com.ph/books/about/Multiple_Imputation_for_Nonresponse_in_S.html?id=bQBtw6rx_mUC&redir_esc=y
Billah B, Huq MM, Smith JA, Sufi F, Tran L, Shardey GC, et al. AusSCORE II in predicting 30-day mortality after isolated coronary artery bypass grafting in Australia and New Zealand. J Thorac Cardiovasc Surg. 2014;148(5):1850–5. e2.
Islam JY, Zaman MM, Haq SA, Ahmed S, Al-Quadir Z. Epidemiology of hypertension among Bangladeshi adults using the 2017 ACC/AHA hypertension clinical practice guidelines and joint National Committee 7 guidelines. J Hum Hypertens. 2018;32(10):668–80.
CAS PubMed PubMed Central Google Scholar
Giri BR, Sharma KP, Chapagai RN, Palzom D. Diabetes and hypertension in urban bhutanese men and women. Indian J Community Med. 2013;38(3):138.
Shrestha U, Singh D, Bhattarai M. The prevalence of hypertension and diabetes defined by fasting and 2-h plasma glucose criteria in urban Nepal. Diabet Med. 2006;23(10):1130–5.
Gupta R, et al. Association of household wealth index, educational status, and social capital with hypertension awareness, treatment, and control in South Asia. Am J Hypertens. 2017;30(4):373–81.
Wang Z, Wang X, Chen Z, Zhang L, Zhu M. Prevalence, awareness, treatment, and control of hypertension in patients with type 2 diabetes: a cross-sectional survey among middle-aged people in China. Int J Noncommunicable Dis. 2016;1(1):30–6.
Chia YC, Buranakitjaroen P, Chen CH, Divinagracia R, Hoshide S, Park S, et al. Current status of home blood pressure monitoring in Asia: statement from the HOPE Asia network. J Clin Hypertens. 2017;19(11):1192–201.
Soo MJ, Chow ZY, Ching SM, Tan CH, Lee KW, Devaraj NK, et al. Prevalence, awareness and control of hypertension in Malaysia from 1980-2018: a systematic review and meta-analysis. World J MetaAnal. 2020;8(4):320–44.
Alam BB, Koziel A, Fraser-Hurt N, Shubber Z, Olabiran AF, Mamza JB. Hypertension and Type-2 Diabetes in Bangladesh: Continuum of Care Assessment and Opportunities for Action. The World Bank; 2019. https://books.google.com.au/books/about/Hypertension_and_Type_2_Diabetes_in_Bang.html?id=_4eJzgEACAAJ&redir_esc=y
Arambewela MH, Somasundaram NP, Jayasekara HBPR, Kumbukage MP. Prevalence of depression and associated factors among patients with type 2 diabetes attending the diabetic clinic at a tertiary care hospital in Sri Lanka: a descriptive study. Psychiatry J. 2019;2019:7468363.
Moniruzzaman M, Zaman MM, Islalm M, Ahasan H, Kabir H, Yasmin R. Physical activity levels in Bangladeshi adults: results from STEPS survey 2010. Public Health. 2016;137:131–8.
Salman RA, Al-Rubeaan KA. Incidence and risk factors of hypertension among Saudi type 2 diabetes adult patients: an 11-year prospective randomized study. J Diabetes Complicat. 2009;23(2):95–101.
Janghorbani M, Amini M. Hypertension in type 2 diabetes mellitus in Isfahan, Iran: incidence and risk factors. Diabetes Res Clin Pract. 2005;70(1):71–80.
University of Washington. Adult rates of overweight and obesity rise in Bangladesh. USA: IHME. https://www.icddrb.org/dmdocuments/Bangladesh%20obesity%20release.pdf
Berraho M, El Achhab Y, Benslimane A, Rhazi KE, Chikri M, Nejjari C. Hypertension and type 2 diabetes: a cross-sectional study in Morocco (EPIDIAM Study). Pan Afr Med J. 2012;11(1):52.
Hill NR, Fatoba ST, Oke JL, Hirst JA, O’Callaghan CA, Lasserson DS, et al. Global prevalence of chronic kidney disease–a systematic review and meta-analysis. PLoS One. 2016;11(7):e0158765.
Consortium CKDP. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. 2010;375(9731):2073–81.
Rashidi A, Sehgal AR, Rahman M, O’Connor AS. The case for chronic kidney disease, diabetes mellitus, and myocardial infarction being equivalent risk factors for cardiovascular mortality in patients older than 65 years. Am J Cardiol. 2008;102(12):1668–73.
Working Party of the International Diabetes Federation (European Region). Hypertension in people with type 2 diabetes: knowledge-based diabetes-specific guidelines. Diabet Med. 2003;20(12):972–87. https://doi.org/10.1046/j.1464-5491.2003.01021.x PMID: 14632698.
Article Google Scholar
Download references
Acknowledgements
Not applicable.
This study did not receive any funding .
Author information
Authors and affiliations.
Department of Epidemiology and Preventive Medicine, School of Public Health and Preventive Medicine, Faculty of Medicine, Nursing and Health Sciences, Monash University, 553 St. Kilda Rd., Level 4, Melbourne, VIC, 3004, Australia
Hiba Alsaadon, Afsana Afroz, Mohammed J. Alramadan, Baki Billah & Aishwarya Narendra Shetty
Bangladesh Institute of Research and Rehabilitation in Diabetes, Endocrine and Metabolic Disorders (BIRDEM), Dhaka, Bangladesh
Afsana Karim & Samira Humaira Habib
You can also search for this author in PubMed Google Scholar
Contributions
Concept and design (AA, BB), acquisition of data (AA, AK, SHH), data analysis and interpretation of results (HA, MA, AA, AS), drafting the manuscript, critically review to improve the content and final approval of version to be submitted has done by all authors.
Corresponding author
Correspondence to Hiba Alsaadon .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was obtained from the Monash University Human Research Ethics Committee, the Ethical Review Committee of the Bangladesh University of Health Sciences and the Ethical Review Committee of Diabetic Association of Bangladesh. Informed written consent was obtained from each participant before the interview.
Consent for publication
The manuscript does not contain any individual person’s data in any form (including any individual details, images or videos).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Alsaadon, H., Afroz, A., Karim, A. et al. Hypertension and its related factors among patients with type 2 diabetes mellitus – a multi-hospital study in Bangladesh. BMC Public Health 22 , 198 (2022). https://doi.org/10.1186/s12889-022-12509-1
Download citation
Received : 28 September 2020
Accepted : 04 January 2022
Published : 29 January 2022
DOI : https://doi.org/10.1186/s12889-022-12509-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hypertension
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]

- Previous Article
- Next Article
Current Recommendations: Blood Pressure Goals
Initial hypertension therapy in patients with diabetes, duality of interest, author contributions, hypertension management in diabetes: 2018 update.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Pasquale Passarella , Tatiana A. Kiseleva , Farida V. Valeeva , Aidar R. Gosmanov; Hypertension Management in Diabetes: 2018 Update. Diabetes Spectr 1 August 2018; 31 (3): 218–224. https://doi.org/10.2337/ds17-0085
Download citation file:
- Ris (Zotero)
- Reference Manager
IN BRIEF Several guidelines and position statements are published to help clinicians manage hypertension in patients with diabetes. Although there is an unequivocal call to treat hypertension in diabetes, professional organizations and experts have differing opinions regarding the most optimal blood pressure targets and treatments to lower vascular risks in the diabetes population. The objective of this article is to summarize the most recent hypertension management guidelines with particular attention to the origins and evidence behind these recommendations.
The importance of diabetes management in the primary care setting cannot be overstated. As of 2015, diabetes affects ∼30.3 million Americans, or about 9.4% of the population ( 1 ). Worldwide, the number is estimated to be a staggering 422 million adults, and if the incidence continues to rise at its current pace, the number of people with diabetes is projected to reach 592 million by 2035 ( 2 ).
Diabetes is a well-documented risk factor for cardiovascular disease (CVD). According to recent statistics from the American Heart Association (AHA), at least 68% of patients who are ≥65 years of age who have diabetes will die from some form of heart disease, and 16% will die from stroke. Adults with diabetes are two to four times more likely to die from heart disease than those who do not have diabetes. Diabetes can also result in microvascular complications such as retinopathy, neuropathy, and nephropathy, which are the leading causes of blindness, nontraumatic foot amputation, and end-stage renal disease, respectively.
Hypertension is a common co-morbidity in patients with type 2 diabetes. The prevalence of hypertension is higher in patients with diabetes than in the general population. Current estimates are that ∼74% of adult patients with diabetes have a systolic blood pressure (SBP) ≥140 mmHg or diastolic blood pressure (DBP) ≥90 mmHg or are on prescription medication for high blood pressure ( 1 ). The coexistence of hypertension and diabetes increases the incidences of CVD and mortality and augments the risks of nephro-pathy and retinopathy ( 3 – 5 ).
Given the frequency of the coexistence of diabetes and hypertension in patients and the significant impact both have on cardiovascular risk, management of hypertension is of utmost importance in people with diabetes. For this reason, several professional societies and groups of experts in the field in recent years have published recommendations for the management of hypertension in people with diabetes. In this article, we briefly describe the most current recommendations for blood pressure goals and initial therapy options from key organizations involved in the care of patients with diabetes.
Many, but not all, guidelines, as described in more detail below, advocate treating hypertension in people with diabetes to a blood pressure goal <130/80 mmHg. These recommendations are mostly based on data from meta-analyses, observational studies, and studies that did not set out to treat diabetic hypertension to a certain blood pressure goal. Although these data have collectively shown better CVD and mortality outcomes with blood pressure controlled to <130/80 mmHg, there have been no randomized, controlled trials (RCTs) testing this goal versus higher blood pressure targets in people with diabetes.
Thus, there is insufficient evidence to determine the blood pressure cut-point at which the benefits offered by antihypertensive therapy outweigh the related risks. There is a need for caution regarding the widespread adoption of the lower blood pressure goals supported by the Action to Control Cardiovascular Risk in Diabetes–Blood Pressure (ACCORD BP) trial. That trial, which compared the effects of SBP-lowering of 120 versus 140 mmHg, found no difference in primary outcomes between groups, whereas those in the group with the lower SBP goal had an increased incidence of adverse events ( 6 ). Until more is known about the risk-benefit ratio of achieving blood pressure goals <130/80 mmHg, and considering some limitations to the application of clinical trial data in daily practice (discussed in more detail below), we suggest following recommendations that are based on the outcomes of prospective, interventional treat-to-target RCTs.
The American Diabetes Association (ADA) defines hypertension as SBP ≥140 mmHg and DBP ≥90 mmHg that is confirmed during separate clinic visits ( 7 ). Current ADA guidelines recommend a treatment goal of SBP <140 mmHg and DBP <90 mmHg for most patients with diabetes ( Table 1 ). Those at higher cardiovascular risk may require more intensive blood pressure control to <130/80 mmHg. The 2018 ADA recommendations are based on the ACCORD BP trial that compared CVD outcomes in diabetes patients randomized to intensive versus less intensive blood pressure control ( 6 ). The ACCORD BP trial showed no benefit to the primary composite end point of nonfatal myocardial infarction, nonfatal stroke, and CVD death in the group treated to the more intensive blood pressure goal of SBP <120 mmHg compared to the standard group for whom SBP was maintained at <140 mmHg, while demonstrating an increased incidence of adverse effects (hypotension and worsening renal function) in the more intensively treated group.
Summary of Blood Pressure Goals and Initial Choice of Antihypertensive Agent for Patients With Diabetes Endorsed by Different Professional Societies or Expert Groups
May be appropriate for individuals at high risk of CVD.
Suggested for patients who can tolerate the antihypertensive medications necessary to reach this goal.
Recommended if hypertension is associated with proteinuria and suggested if hypertension is associated with microalbuminuria as the preferred first-line agent.
Recommended in the presence of known kidney disease, including microalbuminuria, or CVD.
The AHA, American College of Cardiology (ACC), and multiple other professional societies released joint guidelines for the management of hypertension in 2017 ( 8 ). These guidelines recommend initiating antihypertensive therapy for patients with diabetes at a blood pressure ≥130/80 mmHg with a goal blood pressure <130/80 mmHg. Although the ACC/AHA guidelines also use data from the ACCORD BP trial to support this recommendation, the lower blood pressure goal of <130/80 mmHg for all patients with diabetes is based on the assumption that patients with diabetes have a high cardiovascular risk and on the results of two meta-analyses that showed better cardiovascular and microvascular risk reduction if SBP is maintained at <130 mmHg ( 9 , 10 ).
The eighth Joint National Committee (JNC 8) recommendations have been a major guide to patient management in the primary care setting since they were released in 2014 ( 11 ). They recommend initiating treatment for hypertension in patients with diabetes whose blood pressure is >140/90 mmHg with a treatment goal of SBP <140 mmHg and DBP <90 mmHg. The SBP goal is based on the ACCORD BP trial similar to other current guidelines, as well as other trials that included patients with diabetes such as the Systolic Hypertension in the Elderly Program (SHEP) and Systolic Hypertension in Europe (Syst-Eur) trials ( 12 , 13 ). The choice of a DBP target <90 mmHg was based on four RCTs conducted between 1970 and 2008 that demonstrated a reduction in cerebrovascular morbidity and mortality and a decrease in heart failure incidence in patients who achieved a DBP <90 mmHg.
The U.S. Department of Veterans Affairs (VA) and Department of Defense (DoD) also released hypertension guidelines for primary care providers in 2014 ( 14 ). Based on these recommendations, the therapeutic goal for patients with diabetes of all ages is <150/85 mmHg. This guideline also suggests that some patients with diabetes who can tolerate more intensive antihypertensive therapy should be treated to a goal blood pressure of <140/85 mmHg. The standard SBP goal for patients with diabetes of <150 mmHg from the VA/DoD guidelines is based on data from the SHEP, Syst-Eur trial, and UK Prospective Diabetes Study (UKPDS) ( 12 , 13 , 15 ). The tighter SBP goal of <140 mmHg was labeled a weak recommendation compared to the strong recommendation of <150 mmHg because there have been no prospective, interventional trials in patients with diabetes testing the efficacy of targeting an SBP of <140 mmHg compared to <150 mmHg. The DBP goal of <85 mmHg is based on the outcomes of the Hypertension Optimal Treatment (HOT) trial ( 16 ) and UKPDS ( 15 ).
The Canadian Diabetes Association (CDA) released guidelines for the management of hypertension in patients with diabetes in 2013 ( 17 ). These guidelines recommend an SBP goal of <130 mmHg and a DBP goal of <80 mmHg. The major determinate for the SBP goal cited by the guidelines is the ACCORD BP trial, although the CDA also relied on data from the HOT trial and several meta-analyses.
The European Society of Hypertension (ESH) and the European Society of Cardiology (ESC) also released a joint statement on the management of hypertension in patients with diabetes ( 18 ). They recommend achieving a blood pressure goal of <140/85 mmHg in patients with diabetes. The SBP goal is based mainly on results of the ACCORD BP trial.
Although lifestyle changes, including dietary modifications, weight reduction, increased physical activity, reduction in salt intake, tobacco cessation, and appropriate sleep hygiene, are known to improve metabolic health and reduce blood pressure, pharmacological interventions are frequently required to achieve optimal blood pressure goals in patients with diabetes. According to the ADA recommendations, first-line therapy should include a drug class with demonstrated cardiovascular benefits such as a renin-angiotensin system (RAS) inhibitor (angiotensin-converting enzyme inhibitor [ACEI] or angiotensin receptor blocker [ARB]), thiazide-like diuretic, or dihydropyridine calcium channel blocker (CCB) ( 6 , 19 ) ( Table 1 ). There is no compelling evidence in favor of one drug class over another except for data supporting early use of RAS inhibitors in patients with overt proteinuria (urine albumin-to-creatinine ratio >300 mg/g). The ACC/AHA experts emphasize that blood pressure reduction is the main approach to reducing cardiovascular risk in hypertensive patients without stating a preference regarding which antihypertensive agent should be first initiated ( 8 ). Based on the recommendations of the panel members appointed to the JNC 8, non-black patients with diabetes should experience equal therapeutic benefits regardless of whether an ACEI/ARB, CCB, or thiazide-like diuretic is initiated for hypertension treatment, whereas, for black patients with diabetes, initial antihypertensive treatment should be a thiazide-like diuretic or a CCB ( 11 ).
Thiazide-like diuretics are recommended as a first-line therapy of hypertension in the general hypertensive population, including patients with diabetes, by the VA/DoD hypertension clinical practice guideline for primary care providers ( 14 ). The authors of this guideline suggest choosing chlorthalidone or indapamide over hydrochlorothiazide.
The CDA guidelines suggest that an ACEI or an ARB should be recommended as initial therapy for people with CVD or kidney disease, including those with microalbuminuria, and for those with cardiovascular risk factors ( 17 ). For individuals with diabetes and hypertension not included in the above recommendation, ACEIs/ARBs, dihydropyridine CCBs, or thiazide/thiazide-like di-uretics are deemed equally effective in blood pressure management.
Finally, the ESH/ESC recommendations emphasize that all classes of antihypertensive agents are recommended and can be used in patients with diabetes with the caveat that RAS blockers may be preferred in the presence of proteinuria or microalbuminuria ( 18 ). Figure 1 summarizes recommendations by professional societies on initiation of an optimal antihypertensive regimen in patients with diabetes.

Pathway to initial antihypertensive therapy in patients with diabetes. *Use of chlorthalidone or indapamide is preferred. **Can be suggested as first-line therapy in patients with microalbuminuria. BP, blood pressure; UACR, urine albumin-to-creatinine ratio.
Little is known regarding whether there are any additional benefits from the initial use of more intensive antihypertensive protocols in patients with diabetes. An ADA position statement recommends beginning monotherapy if a patient’s initial blood pressure is between 140/90 and 159/99 mmHg ( 19 ). For patients with a blood pressure ≥160/100 mmHg, these experts advocate an initial pharmacological regimen containing two antihypertensive medications ( 19 ). These recommendations are based on the results of two randomized studies of 3–6 months’ duration demonstrating that a greater proportion of participants with a baseline SBP >160 mmHg were able to achieve target blood pressure control when initially treated with two blood pressure–lowering medications ( 20 , 21 ). The long-term implications of these short-term studies are unknown. Hypertension is a chronic disease, and it is unclear whether rapid blood pressure reduction is of immediate benefit in patients with diabetes and particularly in those who are elderly, have multiple comorbidities including kidney disease, have polypharmacy, or are at risk for orthostatic hypotension. We suggest that providers use clinical judgment before selecting the intensity of initial antihypertensive therapy in the diabetes population.
Current professional guidelines and recommendations for the management of hypertension in patients with diabetes are based on data available from only a few RCTs in patients with type 2 diabetes. Historically, the clinical benefits of DBP control were the first tested in the diabetes population.
In this regard, the strongest evidence was provided by the UKPDS ( 22 ). Patients with a mean blood pressure of 160/94 mmHg at baseline were randomized to tight versus less tight blood pressure control (target blood pressure <150/85 vs. <180/105 mmHg). Tight control was associated with reduced risks of important outcomes, including death due to diabetes or stroke. Although this was not a direct comparison of a target DBP of ≥85 mmHg versus a lower goal, the achieved blood pressure was 144/82 mmHg in the tight control group versus an achieved blood pressure of 154/87 mmHg in the group with less tight control.
In the HOT trial, patients with a DBP between 100 and 115 mmHg were randomized to a target DBP of ≤90, ≤85, or ≤80 mmHg ( 16 ).Achieved DBPs were 85.2, 83.2, and 81.1 mmHg, respectively. Among patients with diabetes, intensive treatment was associated with significant declines in major cardiovascular events. The relatively small diabetes sub-sample and the fact that the analysis of patients with diabetes was not pre-specified limit the strength of this evidence.
Whereas these large studies recruited patients with type 2 diabetes, it is unclear how these data can be generalized to the population with type 1 diabetes. Additionally, contemporary interpretations of the clinical effects of the lower DBP goals can be somewhat limited because the UKPDS and HOT trial enrolled patients with diabetes based on fasting blood glucose levels >140 mg/dL, making application of the results less certain for patients with milder forms of diabetes using modern diagnostic criteria.
In subsequent years, clinical interest shifted toward the testing of SBP targets in patients with diabetes. So far, the ACCORD BP trial is the only prospective RCT comparing clinical outcomes of different SBP targets in a population with type 2 diabetes ( 7 ). Although it is accepted from the results of this trial that a more intensive SBP goal of <120 mmHg compared to a standard approach targeting SBP <140 mmHg did not prove beneficial with regard to the primary composite end point of nonfatal MI, nonfatal stroke, or death from cardiovascular causes, in secondary end-point analyses, the rate of cerebrovascular outcomes was significantly lower in the intensive group. On the other hand, the more intensive group was also limited by an increased rate of adverse events such as hypotension and worsening renal function. Although this study provided assurance that an SBP goal of <140 mmHg is as effective as a goal of <120 mmHg, it may have resulted in controversy about what the ideal SBP goal should be, which has been reflected in the variation in SBP goal recommendations from different professional societies. One possible reason for this is that, although the target for the less intensive arm was <140 mmHg, the average SBP actually achieved in that group was 133 mmHg. Additionally, the trial was initially intended to assess the difference between SBP goals of <120 and <130 mmHg based on the seventh JNC guidelines, but there was concern that there would not be enough of a difference between the two values to result in statistical significance, so the less intensive goal was changed to <140 mmHg. Most guidelines have accepted that an SBP of <120 mmHg would not be beneficial, but it remains unclear whether there will be any differences between an SBP goal of <130 mmHg and one of <140 mmHg. In our opinion, patients with diabetic kidney disease may benefit the most from the lower blood pressure goals if these goals can be achieved without side effects ( 23 ), whereas for the majority of patients with diabetes, a blood pressure goal of <140/90 mmHg appears to be reasonable and based on solid evidence.
The elderly comprise a growing population of patients with multiple comorbidities, including diabetes. Previous interventional studies tended to exclude older patients with diabetes, limiting generalization of their results to this group of the patients. Not surprisingly, the majority of professional recommendations do not discuss blood pressure management in the elderly. High prevalence rates of polypharmacy, renal dysfunction, cognitive impairment, and diabetes complications including neuropathy, atherosclerotic vessel disease, and other comorbid conditions in the elderly suggest that, in the absence of outcomes research, we must use caution when providing care to these patients and to do so on an individual basis. With the uncertainty surrounding blood pressure treatment goals for elderly patients with diabetes and hypertension, the VA/DoD position statement can be viewed as a compromise to address the current evidence of benefits of certain SBP and DBP targets, the lack of prospective trials targeting an SBP of <150 mmHg in the diabetes population, and the paucity of data on clinical outcomes of blood pressure regulation in the elderly ( 14 ).
Finally, with the accumulating body of evidence demonstrating the clinical benefits of hypertension control in diabetes, more questions have arisen with regard to the applicability of these research findings to routine clinical care. The ideal scenario of blood pressure measurement undertaken in the research setting consists of an average of two out of three office blood pressure measurements taken with a proper cuff size 1 minute apart after 5 minutes of rest in a quiet area with an automated or semi-automated manometer. Subjects are seated, with back supported, and bare arm placed at the level of the right atrium. No conversation occurs during blood pressure measurements. However, this ideal scenario is impossible to achieve in the busy and often-crowded clinical setting.
Recent research clearly shows that blood pressure measurements taken without the benefit of these ideal conditions are likely to overestimate the actual blood pressure. It has been suggested by several authors that clinical practice blood pressure readings will be higher by anywhere from 10/5 to 12/12 mmHg compared with blood pressure measurements in research settings ( 24 – 26 ). Therefore, non-research clinical blood pressure measurements will likely lead to overtreatment and overdiagnosis, particularly if lower blood pressure targets are accepted for therapeutic considerations, as proposed by the ACC/AHA or the CDA. Taking into account the paucity of clear research data showing additional benefits of blood pressure control to <130/80 mmHg in the general diabetes population, differences in blood pressure determinations in research settings versus clinical practice, and the growing number of patients who are old and have comorbidities, it is appealing for us to accept the ADA or VA/DoD recommendations to guide providers’ decisions regarding long-term hypertension management in the diabetes population.
Clearly, hypertension management mitigates vascular risks in diabetes. The question, however, is how low we should go with blood pressure reduction to achieve the best therapeutic benefits without significant side effects from antihypertensive therapy. Although we are witnessing a proliferation of guidelines and recommendations suggesting optimal blood pressure targets in the diabetes population, there is little scientific evidence to support aiming at lower targets such as <130/80 mmHg. Knowing the methodological differences between blood pressure measurement in the research and clinical settings that current guidelines do not take into consideration, clinicians should approach each patient individually and attempt to offer the best of available treatment options without compromising patient safety.
No potential conflicts of interest relevant to this article were reported.
A.R.G. is an employee of the U.S. Department of Veterans Affairs; opinions expressed in this article are the authors’ alone and do not necessarily represent the opinion of the Department of Veterans Affairs.
P.P. wrote the manuscript and researched data. T.A.K. and F.V.V. contributed to discussion and reviewed/edited the manuscript. A.R.G. researched data, contributed to discussion, and reviewed/edited the manuscript. A.R.G. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.

Email alerts
- Online ISSN 1944-7353
- Print ISSN 1040-9165
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account

Abstracts Medical & Health Science
Diet and exercise: behavioral management of hypertension and diabetes
This dissertation was intended to address lifestyle modifications in the context of hypertension and diabetes management and their subsequent effects on health outcomes. Specifically, we investigated how patient-level characteristics influence guideline-accordant diet, and how diet and exercise impact healthcare costs and health outcomes in patients with diabetes or hypertension.The dissertation is comprised of three studies. The first study is a cross-sectional study comparing the nutritional intake of four ethnicities against hypertension management guidelines. The second study is a longitudinal follow-up that measured the hypertension outcomes of guideline-accordant diet. The third study is a nested cohort study examining the cost and diabetes outcomes of a health club program.There are several major take-aways from findings of this dissertation. First, at the individual level, ethnicity stands out as the single most important factor that determines guideline-accordant dietary behaviors. Second, health behaviors do have impact on health outcomes, and this relationship is particularly salient when comparing people at both ends of the behavioral spectrum. Third, health behaviors and health outcomes can form a virtuous-spiral.Despite of its many limitations, this work contributes to the growing body of evidence highlighting the need for lifestyle modifications at a population level. Future research should carry forward the search on more effective behavioral interventions promoting health diet and physical activities to reduce disease and promote health.
Loading metrics
Open Access
Peer-reviewed
Research Article
Persistent high mortality rates for Diabetes Mellitus and Hypertension after excluding deaths associated with COVID-19 in Brazil, 2020–2022
Roles Writing – original draft, Writing – review & editing
Affiliation Instituto Nacional de Infectologia Evandro Chagas/Fiocruz, Rio de Janeiro, Brasil
Roles Conceptualization, Writing – original draft, Writing – review & editing
Affiliation Programa de Computação Científica, Fundação Oswaldo Cruz, Rio de Janeiro, Brasil
Affiliation Escola de Matemática Aplicada, Fundação Getulio Vargas, Rio de Janeiro, Brasil
Affiliations École de Santé Publique, Université de Montréal, Montreal, Canada, Centre de Recherche en Santé Publique, Montreal, Canada
Roles Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
- Rodrigo Moreira,
- Leonardo S. Bastos,
- Luiz Max Carvalho,
- Laís Picinini Freitas,
- Antonio G. Pacheco

- Published: May 9, 2024
- https://doi.org/10.1371/journal.pgph.0002576
- Peer Review
- Reader Comments
Introduction
The outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) posed a significant public health challenge globally, with Brazil being no exception. Excess mortality during this period reached alarming levels. Cardiovascular diseases (CVD), Systemic Hypertension (HTN), and Diabetes Mellitus (DM) were associated with increased mortality. However, the specific impact of DM and HTN on mortality during the pandemic remains poorly understood.
This study analyzed mortality data from Brazil’s mortality system, covering the period from 2015 to 2022. Data included all causes of death as listed on death certificates, categorized by International Classification of Diseases 10th edition (ICD-10) codes. Population data were obtained from the Brazilian Census. Mortality ratios (MRs) were calculated by comparing death rates in 2020, 2021, and 2022 to the average rates from 2015 to 2019. Adjusted MRs were calculated using Poisson models.
Between 2015 and 2022, Brazil recorded a total of 11,423,288 deaths. Death rates remained relatively stable until 2019 but experienced a sharp increase in 2020 and 2021. In 2022, although a decrease was observed, it did not return to pre-pandemic levels. This trend persisted even when analyzing records mentioning DM, HTN, or CVD. Excluding death certificates mentioning COVID-19 codes, the trends still showed increases from 2020 through 2022, though less pronounced.
This study highlights the persistent high mortality rates for DM and HTN in Brazil during the years 2020–2022, even after excluding deaths associated with COVID-19. These findings emphasize the need for continued attention to managing and preventing DM and HTN as part of public health strategies, both during and beyond the COVID-19 pandemic. There are complex interactions between these conditions and the pandemic’s impact on mortality rates.
Citation: Moreira R, Bastos LS, Carvalho LM, Freitas LP, Pacheco AG (2024) Persistent high mortality rates for Diabetes Mellitus and Hypertension after excluding deaths associated with COVID-19 in Brazil, 2020–2022. PLOS Glob Public Health 4(5): e0002576. https://doi.org/10.1371/journal.pgph.0002576
Editor: Jonas Wolf, Hospital Moinhos de Vento, BRAZIL
Received: October 15, 2023; Accepted: March 11, 2024; Published: May 9, 2024
Copyright: © 2024 Moreira et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The mortality data used in this study is sourced from the Brazilian mortality system (SIM - Sistema de Informação sobre Mortalidade), which is publicly available from DATASUS (Opendatasus - https://opendatasus.saude.gov.br/dataset/sim ). Additionally, population data were obtained from the Brazilian Census Bureau (IBGE – Instituto Brasileiro de Geografia e Estatística) through the SIDRA system ( http://api.sidra.ibge.gov.br/ ).
Funding: This work was supported by Fundação de Amparo a Pesquisa do Estado do Rio de Janeiro (FAPERJ) [E-26/203.172/2017 to A.G.P.] and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) [310566/2021-5 to A.G.P.]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) disease (COVID-19) has been a major public health emergency worldwide and in Brazil [ 1 ] with high burden, hitting the hardest in 2020 and 2021. Excess mortality during that period reached very high values in many countries. One study pointed to excess rates as high as 734.9 per 100,000 inhabitants in Bolivia [ 2 ] In Brazil, even though excess mortality was heterogeneous among states of residence, a rate of 186.9 per 100.000 was reported in that same study. Other studies reported excess deaths ranging from 10% to 40% in that same period in Brazil [ 3 – 5 ].
Cardiovascular diseases (CVD) and associated conditions such as Systemic Hypertension (HTN) and Diabetes Mellitus (DM) have been associated with severe COVID-19 and mortality [ 1 , 6 , 7 ]. However, the role of HTN and DM as independent risk factors are not yet clear [ 8 ]. Prior to the pandemic, CVD, DM, and HTN were already major contributors to substantial morbidity and mortality implications in the general population. However, the advent of COVID-19 has further exacerbated these challenges. People with chronic conditions such as DM, CVD and HTN are at increased risk of hospitalization and mortality in SARS-CoV [ 9 ]. At the peak of the pandemic as many as 50% of patients reported having at least one of these comorbidities upon being hospitalized with COVID-19 [ 10 ]. Several meta-analyses from observational studies have reported relative risks for death in patients with COVID-19 from 1.5 to 2.0 for DM and HTN) [ 11 – 13 ] the main contributors of CVD risk. Although the exact mechanisms underlying this increased mortality are not fully understood, insights from epidemiological studies provide some evidence. Chronic hyperglycemia and the associated chronic inflammatory state in DM can significantly compromise the body’s immune function and increase the risk of complications related to infection and inflammation [ 14 ]. Moreover, the viral invasion pathway of SARS-CoV-2 seems complex. The virus initiates human infection binding to the angiotensin-converting enzyme 2 (ACE2) receptor on the cell surface. ACE2, is a key component of the renin-angiotensin system and a target of antihypertensive medications [ 10 ]. This interaction between COVID-19 and ACE2 may potentially contribute to worse clinical outcomes in hypertensive patients.
While excess mortality and increased rates of CVD mortality have been reported worldwide and in Brazil [ 15 , 16 ], robust evidence on DM and HTN as contributing morbidities during the pandemic is scarce.
The present study aims to address this gap by analyzing public health data at the national level to investigate the contributing role of CVD, DM, and HTN on mortality impact in Brazil, both before (2015–2019) and during the COVID-19 pandemic (2020–2022) in Brazil.
In this study we compared sex, age and state of residence adjusted mortality ratios (aMR) in Brazil in 2020–2022, compared to the preceding period of 2015–2019 and in subgroups of CVD, DM and HTN whenever these conditions were mentioned on death certificates. Comparisons were made with and without COVID-19 mentioned on the death certificates.
Mortality data used in this study comes from the Brazilian mortality system (SIM— Sistema de Informação sobre Mortalidade ) and is publicly available from DATASUS (Opendatasus - https://opendatasus.saude.gov.br/dataset/sim ). Files for all-cause mortality, including multiple causes as assigned on death certificates, from January 2015 through December 2022, were downloaded and processed as described below. The 2022 database was deemed as preliminary data at the time of this analysis (accessed on Aug/30/2023).
All data from SIM consisted of variables extracted from a digital version of death certificates except information that could identify individuals and were available for analysis, including all causes of death (CoD) mentioned on death certificates and the underlying cause of death, which is a calculated variable, based on the information of immediate, contributing and concomitant causes leading to death. All causes are coded into International Classification of Diseases 10th. edition (ICD-10) codes and can thus be grouped according to what is being studied.
Population data were obtained from the Brazilian Census Bureau (IBGE– Instituto Brasileiro de Geografia e Estatística ) through the SIDRA system( http://api.sidra.ibge.gov.br/ ). We obtained population projections per age group, sex and state of residence from January 2015 to December 2022.
For this study, we worked with ICD-10 codes of interest mentioned in any field where those codes are expected to be found (i.e. section VI-49). The following groups were created:
- ICDs: B342, U071, U072
- Diabetes Mellitus (DM)
- ICDs: E10 through E14
- High blood pressure (HBP)
- ICDs: I10 through I15
- CVD: Cardiovascular diseases
- ICDs: I00 through I99, except I46 (cardiac arrest)
Mortality ratios (MRs) were calculated as the death rates in 2020, 2021 and 2022 over the average death rates from 2015 through 2019. Values above one were considered excess when compared to the non-pandemic period. The numerator of the rates included all death certificates that mentioned any ICD-10 codes described above in any field of the death certificate. To measure the impact of COVID-19, we also calculated the mortality rate excluding death certificates that mentioned COVID-19 in any field.
Adjusted MRs were calculated through Poisson models using the log of the population as an offset. All models were adjusted for state of residence, age group and sex. When controlling for state of residence, mixed-effect models with random intercepts were used.
Ethical statement
Our research uses publicly available Information and aggregated data without individual identification (DataSUS and IBGE data). Thus, an exemption from submission to the Institutional Review Board is provided by federal Brazilian resolution, CNS n.° 510, from 2016.
All analyses were performed with R 4.2.2 [ 17 ].
A total of 11,423,288 deaths were recorded in Brazil from 2015 to 2022. The observed mortality rates were fairly stable over time until 2019, after which there was a steep rise in 2020 and 2021. In 2022 there was a decrease, but not to the same level as before ( Fig 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pgph.0002576.g001
This pattern was also noticed when only records that mentioned DM, HTN or CVD were selected. When records that also mentioned COVID-19 codes were excluded, all trends still presented increases from 2020 through 2022, though much smoother ( Fig 1 ).
Overall characteristics of deaths in Brazil are depicted in S1 Table .
Overall, adjusted mortality ratios were 9% and 24% higher for 2020 and 2021, respectively, compared to 2015–2019, whereas for 2022 it was 2% lower. For all three years, when COVID-19 was removed from the numerator, total aMRs fell back to values around 0.93. A similar configuration is noted for CVD mortality rates ( Table 1 ).
https://doi.org/10.1371/journal.pgph.0002576.t001
When we look at mortality rates for DM and HTN, aMRs are higher than those for overall and CVD (ranging from 1.14 in 2022 to 1.61 in 2021 for DM and 1.14 in 2022 to 1.54 in 2021), but they did not fall below 1 when COVID-19 records are excluded, reaching a 15% increase for both conditions in 2021 ( Table 1 ).
Those figures were not homogeneous when we look within age subgroups either. As shown in Fig 2 .
A—Overall, B–DM, C–HTN, D–CVD; baseline—2015–2019.
https://doi.org/10.1371/journal.pgph.0002576.g002
Significant increased ratios were noted from 30 years and older for all groups in 2020 and 2021 but not in 2022, when looking at all causes of death (Panel A). In 2021 middle-aged adults were particularly impacted with a 48% increase in overall mortality in the 40–49-year-old group. All ratios return to less than 1 when COVID-19 is removed. A similar pattern was noted for CVD (Panel D). For DM (Panel B) and HTN (Panel C), not only does the increase in the ratios begin in younger age groups (0–19 and 20–29, respectively), but also they did not return to baseline values when death certificates that mentioned COVID-19 were removed from the analysis. Similar patterns are noted for sex ( S1 Fig ). Across states, figures were heterogeneous. In 2020 overall mortality rates increased for most states ( S2 Fig ), ranging from -2% in Rio Grande do Sul to 30% increase in Amazonas, whereas in 2021 it ranged from 12% (Alagoas and Sergipe) up to 49% in Rondônia. Of note, Amazonas, one of the states with the deadliest outcomes during the pandemic experienced a 47% increase rate in 2021 on top of that 30% in 2020. All ratios also returned to baseline values upon the removal of COVID-19. In 2022 some states did have significantly increased ratios, but all of them returned to values below 1 when COVID-19 was removed. Similar patterns were observed for CVD ( S5 Fig ). Regarding DM and HTN ( S3 and S4 Figs) it followed the same trends as the overall mortality ratios, once again with AM displaying higher aMR among all the states.
In this study, we showed increased mortality rates during the COVID-19 pandemic in Brazil among deceased individuals who had CVD, HTN and DM mentioned in their death certificates. Even though those are expected results, rates did not return to baseline values after removing cases with concomitant COVID-19 for DM and HTN, as happened with overall (total) and the CVD subgroup.
Our results are in line with the literature, in terms of the overall and CVD mortality ratios. In Brazil, overall excess mortality ranged from 10% to 40%, depending on the study and period studied [ 3 , 5 ], which is close to our mortality ratios in 2020 (9%) and 2021 (24%). If we did look at excess mortality, our data would show figures even closer to those (14% and 32.4%, respectively). CVD mortality rates were about the same level as overall rates and are also in line with the literature [ 15 ].
It is worth highlighting that Brazil faced many challenges in dealing with COVID-19, at some point having the highest number of cases and deaths in Latin America [ 18 ] Among the regions most impacted was the state of Amazonas which experienced the highest mortality rates in the country during the pandemic. Known disparities in healthcare access, overwhelming of the healthcare system and quality of care during this period, leading to delayed or inadequate treatment for COVID-19 might have contributed to such results.
We showed higher mortality rates from CVD in the presence of COVID-19 in this study. Viral infection can initiate myocardial injury and provoke inflammatory hyperactivity. Among the most prevalent cardiovascular complications observed in COVID-19 are myocardial infarction, myocarditis accompanied by reduced systolic function of the left ventricle, arrhythmias and thromboembolic complications [ 19 ].
As expected, death rates for those with HTN and DM as comorbidities also significantly increased in 2020 and 2021, but contrary to overall deaths and CVD, they did not return to baseline values after death certificates that mentioned COVID-19 were removed. Two different mechanisms may be playing a role in this pattern. The first one is the possibility of underreporting of COVID-19 among deceased individuals with those conditions in Brazil, during that period. Even though this mechanism is probably present in this case, and has been reported in Brazil [ 20 ], we do not believe this is the only factor playing a role here. First because overall and CVD death rates returned to baseline, and even to values lower than those in 2015–2019, since it is expected that mortality by causes not related to COVID-19 would decrease [ 20 ], and, because we removed all death certificates that mentioned COVID-19 and not only those with COVID-19 as the underlying cause of death, which would account for cases where misclassification occurred.
The other mechanism would be that these conditions had their prevalence increased during the pandemic, and contributed to increased death rates during this period, and even in 2022, as shown. The relationship of DM and HTN with life-style changes during the pandemic and even after it (e.g. decreased physical activity, poor glycemic control and adherence to therapy) may have had an impact on aMR in the population without COVID-19 [ 21 ]. Moreover, some studies pointed to newly diagnosed HTN and DM after acute COVID-19 diagnosis, especially in severe cases [ 22 , 23 ].
One possibility both for risk factors and increased prevalence would be the fact that most individuals with those conditions are older and would be driving this trend, as their death rates are higher than younger individuals [ 8 ]. Our results were adjusted for age, sex and state of residence, which should limit the impact of those distributions across groups. Moreover, we showed that rates in all age groups above 20–29 years have the same behavior, with a predominance among young adults ( Fig 2 ).
This study has several limitations. First, it is based on data from death certificates, which are known to suffer from misclassification, despite going through thorough revision before the information is entered into the database [ 24 ]. This problem results in both underreporting of conditions (especially when garbage ICD-10 codes are reported as an underlying cause of death) or reporting wrong diagnoses. The approach used in this study to search for all causes mentioned tends to lower this problem and has been used before to study causes of death in Brazil [ 25 ]. Moreover, census data for the year 2022 were not available at the time of this study. Therefore, population estimates for 2022 were based on official projections (IBGE) from 2015 to December 2022. These projections may introduce uncertainty into the calculation of mortality rates and ratios, particularly if population dynamics deviate significantly from the projected trends.
Another limitation is the number of variables used to adjust the rates. Even though race/ethnicity, education and other characteristics are also available on death certificates, there are difficulties with respect to missing values and population projection for those subgroups. Since in our case we wanted to control for major factors that would impact HTN and DM rates, we believe that sex, age and state of residence would cover most heterogeneities involved in those calculations.
Strong points of our study include the use of a large, representative database in Brazil, that comprises all deaths reported to the Ministry of Health and the possibility to study multiple causes of death instead of the underlying causes, as is usually done in mortality studies.
In conclusion, our study showed persistent higher mortality in individuals with a diagnosis of HTN and DM at the time of death in Brazil during the COVID-19 pandemic, even after removing those deaths related to COVID-19. This finding should point to improving the diagnosis of COVID-19 and correctly reporting it on the death certificate, and also increase surveillance for both HTN and DM in patients who recently had a COVID-19 diagnosis to better control those conditions among them.
Supporting information
Adjusted Mortality Ratios in Brazil with and without COVID-19 mentioned in the death certificate per age group–A—Overall, B–DM, C–HTN, D–CVD; baseline—2015–2019).
https://doi.org/10.1371/journal.pgph.0002576.s001
S2 Fig. State of residence.
https://doi.org/10.1371/journal.pgph.0002576.s002
S3 Fig. State of residence.
https://doi.org/10.1371/journal.pgph.0002576.s003
S4 Fig. State of residence.
https://doi.org/10.1371/journal.pgph.0002576.s004
S5 Fig. State of residence.
https://doi.org/10.1371/journal.pgph.0002576.s005
S1 Table. Characteristics of mortality data in Brazil, 2015–2022.
https://doi.org/10.1371/journal.pgph.0002576.s006
- View Article
- Google Scholar
- PubMed/NCBI
- 17. Team RDC. R: A language and environment for statistical computing. 4.2.2 ed. Vienna, Austria: R Foundation for Statistical Computing; 2023. 2023.
ORIGINAL RESEARCH article
Voices of care: unveiling patient journeys in primary care for hypertension and diabetes management in kerala, india.

- 1 Sree Chitra Tirunal Institute for Medical Sciences and Technology (SCTIMST), Thiruvananthapuram, India
- 2 Manipal Academy of Higher Education, Manipal, Karnataka, India
- 3 Amrita Institute of Medical Sciences and Research Centre, Amrita Vishwa Vidyapeetham University, Kochi, Kerala, India
The final, formatted version of the article will be published soon.

Select one of your emails
You have multiple emails registered with Frontiers:
Notify me on publication
Please enter your email address:
If you already have an account, please login
You don't have a Frontiers account ? You can register here
Background: Diabetes and hypertension are leading public health problems, particularly affecting low-and middle-income countries, with considerable variations in the care continuum between different age, socio-economic, and rural and urban groups. In this qualitative study, examining the factors affecting access to healthcare in Kerala, we aim to explore the healthcare-seeking pathways of people living with diabetes and hypertension.We conducted 20 semi-structured interviews and one focus group discussion (FGD) on a purposive sample of people living with diabetes and hypertension. Participants were recruited at four primary care facilities in Malappuram district of Kerala. Interviews were transcribed and analyzed deductively and inductively using thematic analysis underpinned by Levesque et al.'s framework.The patient journey in managing diabetes and hypertension is complex, involving multiple entry and exit points within the healthcare system. Patients did not perceive Primary Health Centres (PHCs) as their initial points of access to healthcare, despite recognizing their value for specific services. Numerous social, cultural, economic, and health system determinants underpinned access to healthcare. These included limited patient knowledge of their condition, self-medication practices, lack of trust/support, high out-of-pocket expenditure, unavailability of medicines, physical distance to health facilities, and attitude of healthcare providers.The study underscores the need to improve access to timely diagnosis, treatment, and ongoing care for diabetes and hypertension at the lower level of the healthcare system. Currently, primary healthcare services do not align with the "felt needs" of the community. Practical recommendations to address the social, cultural, economic, and health system determinants include enabling and empowering people with diabetes and hypertension and their families to engage in selfmanagement, improving existing health information systems, ensuring the availability of diagnostics and first-line drug therapy for diabetes and hypertension, and encouraging the use of single-pill combination (SPC) medications to reduce pill burden. Ensuring equitable access to drugs may improve hypertension and diabetes control in most disadvantaged groups. Furthermore, a more comprehensive approach to healthcare policy that recognizes the interconnectedness of noncommunicable diseases (NCDs) and their social determinants is essential.
Keywords: access, Primary health, health needs, Community, NCD, qualitative research, health care pathway. (Min.5-Max. 8)
Received: 23 Jan 2024; Accepted: 06 May 2024.
Copyright: © 2024 Ravindranath, Sarma, Sivasubramonian, Thankappan and Jeemon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Panniyammakal Jeemon, Sree Chitra Tirunal Institute for Medical Sciences and Technology (SCTIMST), Thiruvananthapuram, India
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- How it works

Useful Links
How much will your dissertation cost?
Have an expert academic write your dissertation paper!
Dissertation Services
Get unlimited topic ideas and a dissertation plan for just £45.00
Order topics and plan
Get 1 free topic in your area of study with aim and justification
Yes I want the free topic
45 of the Best Diabetes Dissertation Topics
Published by Owen Ingram at January 2nd, 2023 , Revised On August 16, 2023
The prevalence of diabetes among the world’s population has been increasing steadily over the last few decades, thanks to the growing consumption of fast food and an increasingly comfortable lifestyle. With the field of diabetes evolving rapidly, it is essential to base your dissertation on a trending diabetes dissertation topic that fills a gap in research.
Finding a perfect research topic is one of the most challenging aspects of dissertation writing in any discipline . Several resources are available to students on the internet to help them conduct research and brainstorm to develop their topic selection, but this can take a significant amount of time. So, we decided to provide a list of well-researched, unique and intriguing diabetes research topics and ideas to help you get started.
Other Subject Links:
- Evidence-based Practice Nursing Dissertation Topics
- Child Health Nursing Dissertation Topics
- Adult Nursing Dissertation Topics
- Critical Care Nursing Dissertation Topics
- Palliative Care Nursing Dissertation Topics
- Mental Health Nursing Dissertation Topics
- Nursing Dissertation Topics
- Coronavirus (COVID-19) Nursing Dissertation Topics
List of Diabetes Dissertation Topics
- Why do people recently diagnosed with diabetes have such difficulty accepting reality and controlling their health?
- What are the reactions of children who have recently been diagnosed with diabetes? What can be done to improve their grasp of how to treat the disease?
- In long-term research, people getting intensive therapy for the condition had a worse quality of life. What role should health professionals have in mitigating this effect?
- Why do so many individuals experience severe depression the months after their diagnosis despite displaying no other signs of deteriorating health?
- Discuss some of the advantages of a low-carbohydrate, high-fat diet for people with diabetes
- Discuss the notion of diabetes in paediatrics and why it is necessary to do this research regularly.
- Explain the current threat and difficulty of childhood obesity and diabetes, stressing some areas where parents are failing in their position as guardians to avoid the situation
- Explain some of the difficulties that persons with diabetes have, particularly when obtaining the necessary information and medical treatment
- Explain some of the most frequent problems that people with diabetes face, as well as how they affect the prevalence of the disease. Put out steps that can be implemented to help the problem.
- Discuss the diabetes problem among Asian American teens
- Even though it is a worldwide disease, particular ethnic groups are more likely to be diagnosed as a function of nutrition and culture. What can be done to improve their health literacy?
- Explain how self-management may be beneficial in coping with diabetes, particularly for people unable to get prompt treatment for their illness
- Discuss the possibility of better management for those with diabetes who are hospitalized
- What current therapies have had the most influence on reducing the number of short-term problems in patients’ bodies?
- How have various types of steroids altered the way the body responds in people with hypoglycemia more frequently than usual?
- What effects do type 1, and type 2 diabetes have on the kidneys? How do the most widely used monitoring approaches influence this?
- Is it true that people from specific ethnic groups are more likely to acquire heart disease or eye illness due to their diabetes diagnosis?
- How has the new a1c test helped to reduce the detrimental consequences of diabetes on the body by detecting the condition early?
- Explain the difficulty of uncontrolled diabetes and how it can eventually harm the kidneys and the heart
- Discuss how the diabetic genetic strain may be handed down from generation to generation
- What difficulties do diabetic people have while attempting to check their glucose levels and keep a balanced food plan?
- How have some individuals with type 1 or type 2 diabetes managed to live better lives than others with the disease?
- Is it true that eating too much sugar causes diabetes, cavities, acne, hyperactivity, and weight gain?
- What effect does insulin treatment have on type 2 diabetes?
- How does diabetes contribute to depression?
- What impact does snap participation have on diabetes rates?
- Why has the number of persons who perform blood glucose self-tests decreased? Could other variables, such as social or environmental, have contributed to this decrease?
- Why do patients in the United States struggle to obtain the treatment they require to monitor and maintain appropriate glucose levels? Is this due to increased healthcare costs?
- Nutrition is critical to a healthy lifestyle, yet many diabetic patients are unaware of what they should consume. Discuss
- Why have injuries and diabetes been designated as national health priorities?
- What factors contribute to the growing prevalence of type ii diabetes in adolescents?
- Does socioeconomic status influence the prevalence of diabetes?
- Alzheimer’s disease and type 2 diabetes: a critical assessment of the shared pathological traits
- What are the effects and consequences of diabetes on peripheral blood vessels?
- What is the link between genetic predisposition, obesity, and type 2 diabetes development?
- Diabetes modifies the activation and repression of pro- and anti-inflammatory signalling pathways in the vascular system.
- Understanding autoimmune diabetes through the tri-molecular complex prism
- Does economic status influence the regional variation of diabetes caused by malnutrition?
- What evidence is there for using traditional Chinese medicine and natural products to treat depression in people who also have diabetes?
- Why was the qualitative method used to evaluate diabetes programs?
- Investigate the most common symptoms of undiagnosed diabetes
- How can artificial intelligence help diabetes patients?
- What effect does the palaeolithic diet have on type 2 diabetes?
- What are the most common diabetes causes and treatments?
- What causes diabetes mellitus, and how does it affect the United Kingdom?
Hire an Expert Writer
Orders completed by our expert writers are
- Formally drafted in an academic style
- Free Amendments and 100% Plagiarism Free – or your money back!
- 100% Confidential and Timely Delivery!
- Free anti-plagiarism report
- Appreciated by thousands of clients. Check client reviews
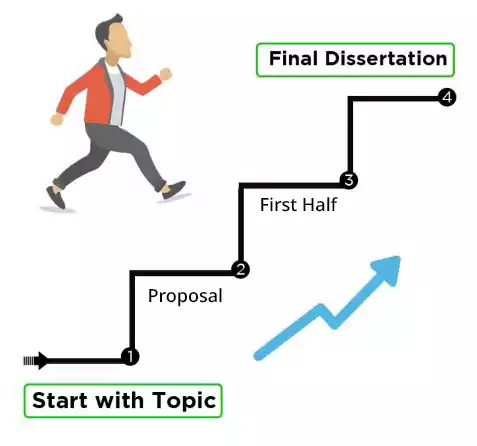
You can contact our 24/7 customer service for a bespoke list of customized diabetes dissertation topics , proposals, or essays written by our experienced writers . Each of our professionals is accredited and well-trained to provide excellent content on a wide range of topics. Getting a good grade on your dissertation course is our priority, and we make sure that happens. Find out more here .
Free Dissertation Topic
Phone Number
Academic Level Select Academic Level Undergraduate Graduate PHD
Academic Subject
Area of Research
Frequently Asked Questions
How to find diabetes dissertation topics.
To find diabetes dissertation topics:
- Study recent research in diabetes.
- Focus on emerging trends.
- Explore prevention, treatment, tech, etc.
- Consider cultural or demographic aspects.
- Consult experts or professors.
- Select a niche that resonates with you.
You May Also Like
Human civilization cannot continue to develop without environmental sustainability. A legal provision that protects the environment is called an “environmental law.” An academic study of environmental law provides a better understanding.
Need interesting and manageable sociology dissertation topics? Here are the trending sociology dissertation titles so you can choose the most suitable one.
Family law dissertation topics are included in a section of UK law. This topic is more of a minor category in terms of your broader research. Family law dissertations are challenging.
USEFUL LINKS
LEARNING RESOURCES

COMPANY DETAILS

- How It Works
- Open access
- Published: 10 May 2024
Prevalence of hypertension and diabetes mellitus in Peruvian patients with chronic kidney disease: a systematic review and meta-analysis
- Darwin A. León-Figueroa 1 ,
- Edwin Aguirre-Milachay 1 ,
- Joshuan J. Barboza 2 &
- Mario J. Valladares-Garrido 3 , 4
BMC Nephrology volume 25 , Article number: 160 ( 2024 ) Cite this article
Metrics details
Chronic Kidney Disease (CKD) represents a major challenge for public health, with hypertension and diabetes being the main causes of its occurrence. Therefore, this study aims to determine the prevalence of hypertension (HTN) and diabetes mellitus (DM) in Peruvian patients with CKD.
A systematic search for studies about CKD in Peru was carried out in PubMed, Scopus, Embase, Web of Science, ScienceDirect, Google Scholar, Virtual Health Library (VHL), and Scielo from 2011 to December 2023. The protocol of this research was registered in the international registry of systematic reviews, the Prospective International Registry of Systematic Reviews (PROSPERO), with registration number CRD42023425118. Study selection, quality assessment, and data extraction were performed independently by two authors. Study quality was assessed using the Joanna Briggs Institute Statistical Meta-Analysis Assessment and Review Instrument. A random-effects model with inverse variance weighting was used to estimate the combined prevalence of HTN and DM in Peruvian patients with CKD. To analyze data heterogeneity, the I 2 statistical test was used. Statistical analysis was performed with R version 4.2.3.
A total of 1425 studies were retrieved, of which 23 were included in the final meta-analysis. A total of 43,321 patients with CKD were evaluated, of whom 52.22% were male and 47.78% were female. The combined prevalence of HTN in Peruvian patients with CKD was 38% (95% CI: 30–46%; 41,131 participants; 21 studies, I 2 = 99%, p = 0), while the combined prevalence of DM in Peruvian patients with CKD was 33% (95% CI: 26–40%; 43,321 participants; 23 studies, I 2 = 99%, p = 0).
Approximately one-third of Peruvian patients with CKD have HTN and DM. These findings highlight the importance of implementing prevention and control measures for these chronic noncommunicable diseases in the Peruvian population, such as promoting healthy lifestyles, encouraging early detection and proper management of hypertension and diabetes, and improving access to medical care and health services.
Peer Review reports
Introduction
Chronic kidney disease (CKD) is typically defined by a glomerular filtration rate of less than 60 ml/min/1.73 m2 or the presence of other indicators of kidney damage, such as albuminuria [ 1 , 2 ]. CKD represents a global public health challenge, impacting about 10–14% of the adult population worldwide [ 3 , 4 ]. Moreover, CKD is closely linked to the increased prevalence of conditions such as diabetes mellitus (DM), hypertension (HTN), obesity, and aging, which continue to be the main causes of morbidity and premature mortality in the population affected by this disease [ 5 , 6 ].
Diabetes mellitus represents an important risk factor for the development of CKD [ 7 ], and several studies have explored its role as an independent risk factor in the incidence of CKD [ 8 , 9 ]. The prevalence of DM has been steadily increasing worldwide. Currently, about 450 million people suffer from this disease, and this figure is projected to reach 690 million by 2045 [ 10 ]. On the other hand, HTN plays a significant role in the onset and worsening of CKD [ 11 ]. The prevalence of HTN increases as renal function deteriorates, affecting approximately 60–90% of individuals with CKD [ 12 ]. HTN is the most common chronic disease in developed societies and claims about 7.1 million lives worldwide each year [ 7 ].
In Peru, the prevalence of CKD in some regions of the country can reach 16.8% [ 13 ] to 28.4% in the city of Lima [ 14 ]. In addition, it has been observed that among people with CKD, there is a prevalence of DM of 20% and HTN of 55.9% [ 14 ]. According to a 2024 press release, the Peruvian Ministry of Health reported that about 10% of adults suffer from CKD, with HTN and DM being the main causes of this condition [ 15 ]. In this context, the presence of chronic comorbidities, such as HTN and DM, in patients with CKD not only contributes to the development and progression of kidney disease but also exacerbates the risk of cardiovascular and renal complications, increasing the burden of disease and the costs associated with medical care [ 16 ].
In Peru, as in many Latin American countries, the availability of information related to the epidemiology of CKD and its association with other chronic diseases is limited [ 7 , 17 , 18 ]. This field of research is in constant development and is still being explored in depth. Due to its wide diversity in terms of socioeconomic trends, climatic and geographic zones, and social determinants of health (access to health services, economic stability, and education), Peru presents a unique opportunity to assess the burden of CKD [ 17 , 19 ].
The study aims to fill a significant gap in the understanding of renal health in the Peruvian population, focusing specifically on the prevalence of HTN and DM in patients with CKD. This research not only seeks to quantify the prevalence of these comorbid conditions but may also shed light on the risk factors and possible interactions between CKD, HTN, and DM in this specific context. By providing solid and systematized data, the study could inform more effective health policies aimed at prevention, early detection, and optimal management of these conditions in the Peruvian population, thus improving the care and quality of life of patients with CKD. In addition, it can lay the groundwork for future research and more precise and targeted intervention strategies [ 20 ].
Materials and methods
Protocol and registration.
The present research was conducted following the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [ 21 ] (Table S1 ), as well as a protocol registered in PROSPERO with the identification number CRD42023425118.
Eligibility criteria
This review included observational studies, such as cross-sectional studies and prospective and retrospective cohorts, that examined the prevalence of HTN and DM in Peruvian patients over 18 years of age diagnosed with CKD. Studies that did not meet the criteria, such as editorials, letters to the editor, randomized clinical trials, conference abstracts, and narrative or systematic reviews, were excluded.
Information sources and search strategy
Searches were conducted in various databases, including PubMed, Scopus, Embase, Web of Science, ScienceDirect, Google Scholar, Virtual Health Library (VHL), and Scielo, until December 1, 2023, with no language or development period restrictions. Studies were identified using Medical Subject Headings (MeSH) terms such as “chronic kidney disease” and “Peru”. The search strategy was independently tested by two authors and is detailed in Table S2 . In addition, other search methods were used, including a review of literature studies, consultation of article references, and review of publications in Peruvian journals specializing in chronic kidney disease. However, the potential studies identified were within the scope of the search strategy employed.
Study selection
The search strategy results were stored in the Endnote software. Subsequently, duplicate articles, titles, and abstracts were removed. Next, two investigators independently reviewed the titles and abstracts of the articles to select those that met the inclusion criteria. Then, two additional investigators conducted a thorough review of the full articles to determine if they met the inclusion criteria. Any discrepancies identified were resolved through mutual agreements.
The main outcome is to determine the prevalence of HTN and DM in Peruvian patients diagnosed with CKD.
Quality assessment
The JBI-MAStARI tool was employed to assess the quality of the articles included in the meta-analysis. The evaluation encompassed various aspects, such as the study context, outcome and explanatory variables, specific inclusion criteria, measurement standards, topic description, and precise statistical analysis. The quality of the studies was categorized as high (≥ 7 points), moderate (4 to 6 points), or low (< 4 points) based on their scores, and any discrepancies were resolved through researcher discussions (Table S3 ) [ 22 ].
Data collection process and data items
Three independent researchers were responsible for collecting relevant data from the selected articles and recording it in an Excel spreadsheet. The collected information included various details such as the author, publication year, study design, study location, sample size, and the number of participants with CKD. The prevalence of CKD, study subjects, participants’ age, and gender (both male and female), as well as the presence of HTN and DM were also recorded. Subsequently, to ensure the accuracy and quality of the extracted data, two additional researchers conducted a rigorous review and verification process.
Data analysis
The data obtained from Excel was utilized for conducting the analysis in R, specifically version 4.2.3. In order to present the research findings, tables and narrative graphs were employed. A random-effects model with inverse variance weighting was used to estimate the combined prevalence of HTN and DM in Peruvian patients with CKD. The Cochrane Q statistic was used to examine the variability among the trials. Additionally, the I2 index was used to quantify this variability. Values of 25%, 50%, and 75%, respectively, were regarded as indicating low, moderate, and high heterogeneity.
A funnel plot was employed to investigate the possibility of publication bias. Egger’s regression test was also used to investigate this matter further. When the resultant p value was less than 0.05, it was believed that there was a possibility of bias in the results.
The pooled prevalence of HTN and DM in Peruvian patients with CKD was shown graphically as a forest plot, with 95% confidence intervals included for enhanced precision in the presentation of the data.
A total of 1425 articles were found through searches in eight different databases. The selection process is detailed in the PRISMA flowchart, depicted in Fig. 1 . After eliminating duplicate articles ( n = 497), the investigators analyzed the remaining 928 articles. Subsequently, the titles and abstracts of these articles were evaluated, and 90 were selected for a comprehensive full-text review. Once this process was completed, 23 articles that met the inclusion criteria for the systematic review and meta-analysis were included [ 14 , 17 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 ].
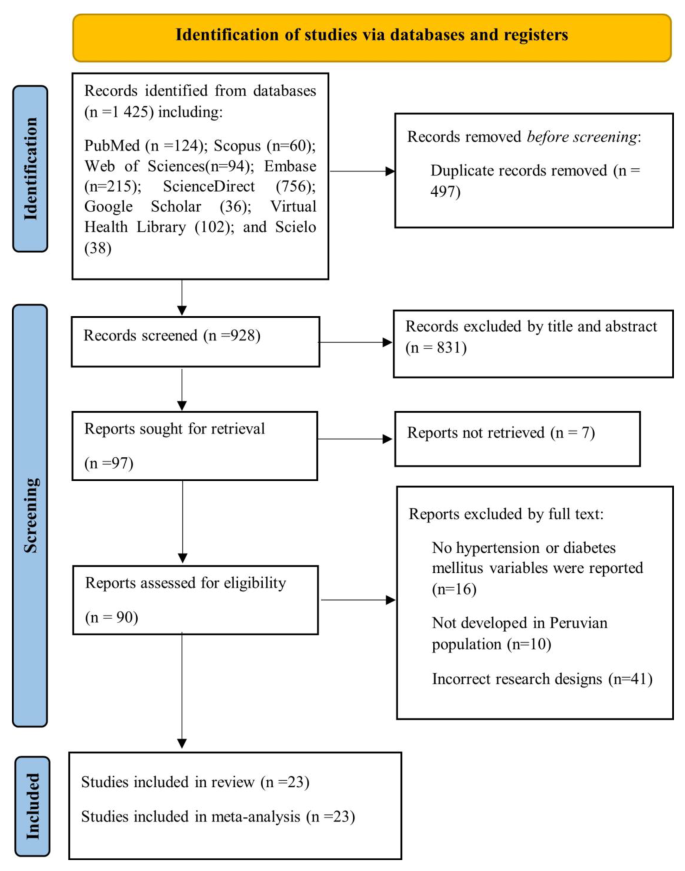
illustrates the process of study selection according to the PRISMA flowchart
Characteristics of the included studie
The analysis was based on a review of 23 observational studies published between 2011 and 2023 that examined the prevalence of HTN and DM in Peruvian patients diagnosed with CKD (Table 1 ). A total of 43,321 patients with chronic kidney disease were evaluated, of whom 52.22% (22,622) were male and 47.78% (20,699) were female [ 14 , 17 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 ]. The mean age of the participants was approximately 64 years, and most of the studies were centered in Lima, the capital of Peru (Table 1 ).
Quality of the included studies and publication bias
The quality of the studies was assessed using the JBI Critical Appraisal Tools, specifically designed for cross-sectional research. It was determined that all the studies included in the analysis demonstrated a moderate level of quality, as indicated in Table S3 [ 14 , 17 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 ]. In the analyses aimed at evaluating HTN in Peruvian patients with CKD, it was observed that when Egger’s test was applied to evaluate publication bias, a value of p = 0.5339 (t = -0.63, df = 19) was obtained. This result suggests that the null hypothesis of symmetry is accepted, indicating that there is no evidence of publication bias in the studies examined (Figure S1 ). In the analyses aimed at evaluating DM in Peruvian patients with CKD, it was evident that when Egger’s test was used to evaluate publication bias, a value of p = 0.0063 (t = 3.04, df = 21) was obtained. This result indicates an asymmetry in the data, which could explain the considerable disparities in the reported prevalence values. However, it should be noted that we were unable to conclusively demonstrate the presence of publication bias (Figure S1 ).
Joint prevalence of HTN and DM in Peruvian patients with CKD
The combined prevalence of HTN in Peruvian patients with CKD was 38% (95% CI: 30–46%; 41,131 participants; 21 studies). The I 2 test indicated significant heterogeneity among the included studies (I 2 = 99%, p = 0) (Fig. 2 ) [ 14 , 17 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 40 , 42 , 43 ]. The combined prevalence of DM in Peruvian patients with CKD was 33% (95% CI: 26–40%; 43,321 participants; 23 studies). The I 2 test indicated significant heterogeneity among the included studies (I 2 = 99%, p = 0) (Fig. 3 ) [ 14 , 17 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 ]. The combined prevalence of HTN and DM in Peruvian patients with CKD was 21% (95% CI: 19–23%; 32,860 participants; 4 studies). The I 2 test indicated significant heterogeneity among the included studies (I 2 = 89%, p = 0) (Figure S2 ) [ 14 , 29 , 34 , 36 ].

Forest plot illustrating the joint prevalence of Hypertension in Peruvian patients with chronic kidney disease

Forest plot illustrating the joint prevalence of diabetes mellitus in Peruvian patients with chronic kidney disease
Chronic kidney disease constitutes a challenge of great relevance for public health at a global level, with an ever-increasing incidence and prevalence. In addition to its considerable medical and economic burden, CKD implies a notable increase in morbidity and mortality rates among the affected population. CKD is a non-communicable disease generally caused by diabetes and hypertension [ 44 ]. Therefore, the purpose of this systematic review and meta-analysis was to determine the prevalence of HTN and DM in Peruvian patients with CKD. The most relevant results showed that the combined prevalence of HTN in this population reached 38%, while the combined prevalence of DM was 33%.
The Centers for Disease Control and Prevention’s CKD Surveillance System reported that about 14% of adults in the United States have CKD stages 1 to 4 [ 45 ]. Kovesdy CP reported that CKD affects more than 10% of the general population worldwide and is more prevalent in older people, women, racial minorities, and people who experience DM and HTN [ 3 ].
In a meta-analysis by Hill NR, et al. reported an overall prevalence of 5-stage CKD of 13.4%, and stages 3–5 was 10.6% [ 46 ]. In addition, the prevalence of individual stages of CKD was 3.5% (stage 1), 3.9% (stage 2), 7.6% (stage 3), 0.4% (stage 4), and 0.1% (stage 5) [ 47 ]. According to the National Health and Nutrition Examination Survey (NHANES), the prevalence of CKD among adults aged 70 years and older was lower in 2017–March 2020 (42.6%) than in 2001–2004 (52.1%) [ 48 ]. Hill NR, et al. reported a linearly higher prevalence for CKD stages 1–5 associated with advancing age, ranging from 13.7% in the 30–40 year age group to 27.9% in patients > 70–80 years [ 46 ].
A study by Sundström J. et al. in 2.4 million patients from 11 countries reported a CKD prevalence of 10% [ 49 ]. In Asia, the prevalence of stage 3–5 CKD in low- and middle-income countries was 11.2% [ 50 ]. Another study found that 14% of the general population and high-risk groups in South Asia had CKD [ 51 ]. In Peru, Bravo-Zúñiga J, et al. reported a prevalence of CKD of 28.4% in patients evaluated in a health network in the city of Lima [ 14 ]. Another study by Herrera-Añazco P. et al. reported a CKD prevalence of 18% [ 29 ].
The combined prevalence of HTN in Peruvian patients with CKD was 38%. In the United States, the prevalence of CKD stages 1–4 among hypertensive adults was 26.34% in 2017–2020, compared with a prevalence of 7.8% among nonhypertensive individuals [ 52 ]. Hill NR et al., in their meta-analysis, reported an association between HTN and CKD prevalence [ 46 ]. In Tanzania, Stanifer JW et al. reported that among adults with CKD, 19.3% had HTN [ 53 ]. Another study found that the prevalence of CKD was 27% in adults with HTN [ 51 ]. In Peru, Bravo-Zúñiga J. et al. evaluated a total of 20,354 participants with CKD; 38.7% had HTN [ 34 ]. These results are based on the fact that HTN is a medical condition distinguished by elevated blood pressure, which is a significant risk factor in the development and progression of CKD. This condition can cause damage to the blood vessels in the kidneys, compromising their ability to efficiently filter waste and excess fluids from the body [ 54 ].
The combined prevalence of DM in Peruvian patients with CKD was 33%. In the United States, according to NHANES (2017–2020), the prevalence of CKD stages 1–4 in diabetic adults was 38.67% [ 55 ]; in addition, the prevalence of CKD stages 3–4 (NHANES 2001–March 2020) was 10% among adults with prediabetes or undiagnosed DM and 18% among adults with diagnosed DM [ 56 ]. A study by Fernandez-Fernandez L. et al. in Spain reported a CKD prevalence of 25.3% in patients with DM [ 57 ]. Gatwood J. et al. reported that CKD was evident in 31.6% of veterans before being diagnosed with DM [ 58 ]. A meta-analysis by Hill NR et al. reported an association between DM and the prevalence of CKD [ 46 ]. In Tanzania, Stanifer JW et al. reported that among adults with CKD, 7% had DM and 14.0% had DM and HTN [ 53 ]. Another study found that the prevalence of CKD was 31% in adults with DM [ 51 ]. Sundström J. et al. reported that DM was present in 38% of patients with CKD [ 49 ]. In Peru, Bravo-Zúñiga J, et al. evaluated a total of 20,354 participants with CKD; 13.74% had DM [ 34 ]. Diabetes is positioned as one of the leading causes of CKD, triggering a number of nephropathic complications. This disorder exerts a significant influence, as elevated blood glucose levels cause progressive damage to the small blood vessels that supply blood to the kidneys. This detrimental interference compromises kidney function, creating an environment conducive to the development and aggravation of kidney disease [ 59 ].
The present study has some limitations. First, the included studies may be subject to biases and confounding factors that cannot be individually quantified. Second, it was not possible to perform a subgroup analysis by gender because the studies provided only baseline demographic data for the CKD population. Third, the prevalence of HTN and DM according to CKD stages could not be determined. Finally, the sample sizes of the included studies varied considerably, ranging from 20,354 to only 30 participants. However, among the strengths of this study, it is noteworthy that this research represents the first systematic review and meta-analysis focused on the evaluation of HTN and DM in Peruvian patients with CKD. To guarantee the quality of the included studies, the “JBI-MAStARI” tool was used as the evaluation method. In addition, a specific search strategy was designed for each database, and article selection and data extraction were carried out independently by two or more investigators. It should be noted that the studies included in this review shared the same definitions of CKD, and the recommendations established by the PRISMA guidelines were rigorously followed.
Conclusions
Data availability.
No datasets were generated or analysed during the current study.
Inker LA, Astor BC, Fox CH, Isakova T, Lash JP, Peralta CA, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis off J Natl Kidney Found. 2014;63(5):713–35. https://doi.org/10.1053/j.ajkd.2014.01.416 .
Article Google Scholar
Liyanage T, Toyama T, Hockham C, Ninomiya T, Perkovic V, Woodward M, et al. Prevalence of chronic kidney disease in Asia: a systematic review and analysis. BMJ Glob Health. 2022;7(1):e007525. https://doi.org/10.1136/bmjgh-2021-007525 .
Article PubMed PubMed Central Google Scholar
Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Suppl. 2022;12(1):7–11. https://doi.org/10.1016/j.kisu.2021.11.003 .
Samaan F, Damiani BB, Kirsztajn GM, Sesso R. A cross-sectional study on the prevalence and risk stratification of chronic kidney disease in Cardiological patients in São Paulo, Brazil. Diagn Basel Switz. 2023;13(6):1146. https://doi.org/10.3390/diagnostics13061146 .
Article CAS Google Scholar
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of Disease Study 2010. Lancet. 2012;380(9859):2095–128. https://doi.org/10.1016/S0140-6736(12)61728-0 .
Lv JC, Zhang LX. Prevalence and disease burden of chronic kidney disease. Adv Exp Med Biol. 2019;1165:3–15. https://doi.org/10.1007/978-981-13-8871-2_1 .
Article CAS PubMed Google Scholar
Erfanpoor S, Etemad K, Kazempour S, Hadaegh F, Hasani J, Azizi F, et al. Diabetes, hypertension, and incidence of chronic kidney disease: is there any Multiplicative or Additive Interaction? Int J Endocrinol Metab. 2021;19(1):e101061. https://doi.org/10.5812/ijem.101061 .
Article PubMed Google Scholar
Tohidi M, Hasheminia M, Mohebi R, Khalili D, Hosseinpanah F, Yazdani B, et al. Incidence of chronic kidney disease and its risk factors, results of over 10 year follow up in an Iranian cohort. PLoS ONE. 2012;7(9):e45304. https://doi.org/10.1371/journal.pone.0045304 .
Article CAS PubMed PubMed Central Google Scholar
Al-Rubeaan K, Youssef AM, Subhani SN, Ahmad NA, Al-Sharqawi AH, Al-Mutlaq HM, et al. Diabetic nephropathy and its risk factors in a society with a type 2 diabetes epidemic: a Saudi National Diabetes Registry-based study. PLoS ONE. 2014;9(2):e88956. https://doi.org/10.1371/journal.pone.0088956 .
Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, et al. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81. https://doi.org/10.1016/j.diabres.2018.02.023 .
Pugh D, Gallacher PJ, Dhaun N. Management of hypertension in chronic kidney disease. Drugs. 2019;79(4):365–79. https://doi.org/10.1007/s40265-019-1064-1 .
Mayne KJ, Sullivan MK, Lees JS. Sex and gender differences in the management of chronic kidney disease and hypertension. J Hum Hypertens. 2023;37(8):649–53. https://doi.org/10.1038/s41371-023-00843-9 .
Herrera-Añazco P, Benites-Zapata VA, León-Yurivilca I, Huarcaya-Cotaquispe R, Silveira-Chau M. Chronic kidney disease in Peru: a challenge for a country with an emerging economy. J Bras Nefrol. 2015;37(4):507–8. https://doi.org/10.5935/0101-2800.20150081 .
Bravo-Zúñiga J, Gálvez-Inga J, Carrillo-Onofre P, Chávez-Gómez R, Castro-Monteverde P. Early detection of chronic renal disease: coordinated work between primary and specialized care in an ambulatory renal network of Peru. J Bras Nefrol. 2019;41(2):176–84. https://doi.org/10.1590/2175-8239-JBN-2018-0101 .
Día. Mundial del Riñón: uno de cada diez adultos sufre de una enfermedad renal crónica. Available online: https://www.gob.pe/institucion/minsa/noticias/920304-dia-mundial-del-rinon-uno-de-cada-diez-adultos-sufre-de-una-enfermedad-renal-cronica (accessed on 23 March 2024).
Francis ER, Allen AK, Herrera-Añazco P, Kuo CC, Cardenas MK, Feldman HI, et al. Establishing a higher priority for chronic kidney disease in Peru. Lancet Glob Health. 2016;4(1):e17–18. https://doi.org/10.1016/S2214-109X(15)00206-5 .
Francis ER, Kuo CC, Bernabe-Ortiz A, Nessel L, Gilman RH, Checkley W, et al. Burden of chronic kidney disease in resource-limited settings from Peru: a population-based study. BMC Nephrol. 2015;16:114. https://doi.org/10.1186/s12882-015-0104-7 .
Carrillo-Larco RM, Miranda JJ, Gilman RH, Medina-Lezama J, Chirinos-Pacheco JA, Muñoz-Retamozo PV, et al. Risk score for first-screening of prevalent undiagnosed chronic kidney disease in Peru: the CRONICAS-CKD risk score. BMC Nephrol. 2017;18(1):343. https://doi.org/10.1186/s12882-017-0758-4 .
Atamari-Anahui N, Ccorahua-Rios MS, Condori-Huaraka M, Huamanvilca-Yepez Y, Amaya E, Herrera-Añazco P. Epidemiology of chronic kidney disease in Peru and its relation to social determinants of health. Int Health. 2020;12(4):264–71. https://doi.org/10.1093/inthealth/ihz071 .
Chen TK, Knicely DH, Grams ME. Chronic kidney disease diagnosis and management: a review. JAMA. 2019;322(13):1294–304. https://doi.org/10.1001/jama.2019.14745 .
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71 .
JBI Manual for Evidence Synthesis - JBI Global Wiki. Available online: https://jbi-global-wiki.refined.site/space/MANUAL (accessed on 24 October 2023).
Meneses Liendo V, León Rabanal C, Huapaya Carrera J, Cieza Zevallos J. Sobrevida en hemodiálisis según El Periodo De ingreso de pacientes entre 1982 y 2007 en Lima, Perú. Rev Med Hered. 2011;22(4):157–8.
Google Scholar
Herrera-Añazco P, Benítes-Zapata VA, Hernandez AV. Factores asociados a mortalidad intrahospitalaria de una población en hemodiálisis en el Perú. Rev Peru Med Exp Salud Pública. 2015;479 – 84. https://doi.org/10.17843/rpmesp.2015.323.1677 .
Herrera-Añazco P, Benites-Zapata V, Hernandez AV, Mezones-Holguin E, Silveira-Chau M. Mortalidade Dos pacientes com doença renal crônica em hemodiálise de manutenção em um hospital público do Peru. Braz J Nephrol. 2015;37:192–7. https://doi.org/10.5935/0101-2800.20150031 .
Huamán CL, Postigo OC, Contreras CC. Características epidemiológicas De Los pacientes que inician hemodiálisis crónica en El Hospital Alberto Sabogal Sologuren 2015. Horiz Méd Lima. 2016;16(2):6–12.
Bravo-Zúñiga J, Chávez-Gómez R, Gálvez-Inga J, Villavicencio-Carranza M, Espejo-Sotelo J, Riveros-Aguilar M. [Progression of chronic renal disease in a reference hospital of social security of Peru 2012–2015]. Rev Peru Med Exp Salud Publica. 2017;34(2):209–17. https://doi.org/10.17843/rpmesp.2017.342.2493 .
Gómez de la Torre-, del Carpio A, Bocanegra-Jesús A, Guinetti-Ortiz K, Mayta-Tristán P, Valdivia-Vega R. Mortalidad precoz en pacientes con enfermedad renal crónica que inician hemodiálisis por urgencia en una población peruana: Incidencia Y factores de riesgo. Nefrología. 2018;38(4):425–32. https://doi.org/10.1016/j.nefro.2017.11.017 .
Herrera-Añazco P, Taype-Rondan A, Lazo-Porras M, Alberto Quintanilla E, Ortiz-Soriano VM, Hernandez AV. Prevalence of chronic kidney disease in Peruvian primary care setting. BMC Nephrol. 2017;18(1):246. https://doi.org/10.1186/s12882-017-0655-x .
Pinares-Astete F, Meneses-Liendo V, Bonilla-Palacios J, Ángeles-Tacchino P, Cieza-Zevallos J. Supervivencia a largo plazo en pacientes con enfermedad renal crónica estadio 5 tratada por hemodiálisis en Lima, Perú. Acta Médica Peru. 2018;35(1):20–7.
Huauya-Leuyacc C, Palacios-Guillen AM, Benites-Zapata VA. Factores epidemiológicos asociados a la referencia temprana al nefrólogo para hemodiálisis crónica en pacientes de Un Hospital Público De Perú. Rev Nefrol Diál Traspl. 2018;126 – 33.
Herrera-Añazco P, Taype-Rondan A, Ortiz PJ, Málaga G, Del Carpio-Toia AM, Alvarez-Valdivia MG, et al. Use of medicinal plants in patients with chronic kidney disease from Peru. Complement Ther Med. 2019;47:102215. https://doi.org/10.1016/j.ctim.2019.102215 .
Loaiza-Huallpa J, Condori-Huaraka M, Quispe-Rodríguez GH, Pinares-Valderrama MP, Cruz-Huanca AI, Atamari-Anahui N, et al. Mortalidad Y factores asociados en pacientes con enfermedad renal crónica en hemodiálisis en un hospital peruano. Rev Habanera Cienc Médicas. 2019;18(1):164–75.
Bravo-Zúñiga J, Saldarriaga EM, Chávez-Gómez R, Gálvez-Inga J, Valdivia-Vega R, Villavicencio-Carranza M, et al. Effectiveness of adherence to a renal health program in a health network in Peru. Rev Saude Publica. 2020;54:80. https://doi.org/10.11606/s1518-8787.2020054002109 .
Pineda-Borja V, Andrade-Santiváñez C, Arce-Gomez G, Rabanal CL. Peritonitis en pacientes que reciben diálisis peritoneal en un hospital de Lima, Perú. Rev Peru Med Exp Salud Pública. 2020;521–6. https://doi.org/10.17843/rpmesp.2020.373.4744 .
Munive-Yachachi Y, Delgado-Pérez D, Munive-Yachachi Y, Delgado-Pérez D. Prevalencia De desnutrición en pacientes con enfermedad renal crónica terminal en un hospital nacional de Lima, Perú. Fac Med. 2021;82(1):21–6. https://doi.org/10.15381/anales.v82i1.18037 .
Valenzuela-Narváez RV, Valenzuela-Narváez DR, Valenzuela-Narváez DAO, Córdova-Noel ME, Mejía-Ruiz CL, Salcedo-Rodríguez MN, et al. Periodontal disease as a predictor of chronic kidney disease (CKD) stage in older adults. J Int Med Res. 2021;49(7):3000605211033266. https://doi.org/10.1177/03000605211033266 .
Umeres-Francia GE, Rojas-Fernández MV, Herrera-Añazco P, Benites-Zapata VA. Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio as risk factors for mortality in Peruvian adults with chronic kidney disease. Ren Replace Ther. 2022;8(1):30. https://doi.org/10.1186/s41100-022-00420-9 .
Guzman-Ventura W, Caballero-Alvarado J. Survival of patients on chronic hemodialysis versus chronic peritoneal dialysis. Rev Peru Med Exp Salud Publica. 2022;39(2):161–9. https://doi.org/10.17843/rpmesp.2022.392.10853 .
Bravo LJA, Gonzales RFL, Izarra ME, Rada APVY, Cairampoma DEM. Características epidemiológicas, de laboratorio y de tratamiento en pacientes con hemodiálisis en una población de altura. Rev Peru Cienc Salud. 2022;4(2):92–7. https://doi.org/10.37711/rpcs.2022.4.2.370 .
Venegas Justiniano JY, Hurtado Aréstegui A, Loza Muñarriz C, Venegas Justiniano JY, Hurtado Aréstegui A, Loza Muñarriz C. Características de la colocación y permanencia de catéteres venosos centrales temporales para hemodiálisis en un hospital público 2015–2019. Acta Médica Peru. 2022;39(2):128–37. https://doi.org/10.35663/amp.2022.392.2231 .
Herrera-Añazco P, Segura MA, Bravo-Zúñiga J, Vásquez JL, Taype-Rondán A. Hospitalization and mortality during the pandemic in chronic hemodialysis patients and the general population in Peru. J Bras Nefrol. 2023;S:0101–28002023005018501. https://doi.org/10.1590/2175-8239-JBN-2022-0149en .
Huaman-Carhuas L, Melo-Flores CM, Gutiérrez-Carranza MD, Huaman-Carhuas L, Melo-Flores CM, Gutiérrez-Carranza MD. Calidad Percibida Y Su relación con la satisfacción del paciente en tratamiento con hemodiálisis en un hospital público de Perú. Enferm Nefrológica. 2023;26(2):159–66. https://doi.org/10.37551/s2254-28842023016 .
Cockwell P, Fisher LA. The global burden of chronic kidney disease. Lancet. 2020;395(10225):662–4. https://doi.org/10.1016/S0140-6736(19)32977-0 .
CDC Surveillance System. CKD Among U.S. Adults, by Stage. Available online: https://nccd.cdc.gov/ckd/detail.aspx?Qnum=Q372 (accessed on 2 September 2023).
Hill NR, Fatoba ST, Oke JL, Hirst JA, O’Callaghan CA, Lasserson DS, et al. Global prevalence of chronic kidney disease – A systematic review and Meta-analysis. PLoS ONE. 2016;11(7):e0158765. https://doi.org/10.1371/journal.pone.0158765 .
Jager KJ, Kovesdy C, Langham R, Rosenberg M, Jha V, Zoccali C. A single number for advocacy and communication-worldwide more than 850 million individuals have kidney diseases. Kidney Int. 2019;96(5):1048–50. https://doi.org/10.1016/j.kint.2019.07.012 .
CDC Surveillance System: CKD Among U.S. Adults. Available online: https://nccd.cdc.gov/ckd/detail.aspx?Qnum=Q9&topic=1#refreshPosition (accessed on 2 September 2023).
Sundström J, Bodegard J, Bollmann A, Vervloet MG, Mark PB, Karasik A, et al. Prevalence, outcomes, and cost of chronic kidney disease in a contemporary population of 2·4 million patients from 11 countries: the CaReMe CKD study. Lancet Reg Health – Eur. 2022. https://doi.org/10.1016/j.lanepe.2022.100438 .
Suriyong P, Ruengorn C, Shayakul C, Anantachoti P, Kanjanarat P. Prevalence of chronic kidney disease stages 3–5 in low- and middle-income countries in Asia: a systematic review and meta-analysis. PLoS ONE. 2022;17(2):e0264393. https://doi.org/10.1371/journal.pone.0264393 .
Shrestha N, Gautam S, Mishra SR, Virani SS, Dhungana RR. Burden of chronic kidney disease in the general population and high-risk groups in South Asia: a systematic review and meta-analysis. PLoS ONE. 2021;16(10):e0258494. https://doi.org/10.1371/journal.pone.0258494 .
CDC Surveillance System: CKD Among U.S. Adults. Available online: https://nccd.cdc.gov/ckd/detail.aspx?Qnum=Q9&topic=1&Strat=Hypertension#refreshPosition (accessed on 2 September 2023).
Stanifer JW, Maro V, Egger J, Karia F, Thielman N, Turner EL, et al. The epidemiology of chronic kidney disease in Northern Tanzania: a population-based survey. PLoS ONE. 2015;10(4):e0124506. https://doi.org/10.1371/journal.pone.0124506 .
Ameer OZ. Hypertension in chronic kidney disease: what lies behind the scene. Front Pharmacol. 2022;13:949260. https://doi.org/10.3389/fphar.2022.949260 .
CDC Surveillance System: CKD Among U.S. Adults. Available online: https://nccd.cdc.gov/ckd/detail.aspx?Qnum=Q9&topic=1&Strat=Diabetes#refreshPosition (accessed on 2 September 2023).
CDC Surveillance System. CKD Stages 3–4, by Diabetes and Prediabetes. Available online: https://nccd.cdc.gov/ckd/detail.aspx?Qnum=Q702 (accessed on 2 September 2023).
Fernández-Fernández L, Barquilla-García A, Sánchez-Vega J, Risco-Solanilla JC, Suárez-González F, Buitrago F. Prevalence of chronic kidney disease in patients with diabetes in Extremadura (Spain) during the Years 2012, 2013 and 2014: an observational study. J Clin Med. 2021;10(13):2886. https://doi.org/10.3390/jcm10132886 .
Gatwood J, Chisholm-Burns M, Davis R, Thomas F, Potukuchi P, Hung A, et al. Evidence of chronic kidney disease in veterans with incident diabetes mellitus. PLoS ONE. 2018;13(2):e0192712. https://doi.org/10.1371/journal.pone.0192712 .
Pecoits-Filho R, Abensur H, Betônico CCR, Machado AD, Parente EB, Queiroz M, et al. Interactions between kidney disease and diabetes: dangerous liaisons. Diabetol Metab Syndr. 2016;8(1):50. https://doi.org/10.1186/s13098-016-0159-z .
Download references
Acknowledgements
This research received no external funding.
Author information
Authors and affiliations.
Facultad de Medicina Humana, Universidad de San Martín de Porres, Chiclayo, 15011, Peru
Darwin A. León-Figueroa & Edwin Aguirre-Milachay
Vicerrectorado de Investigación, Universidad Norbert Wiener, Lima, 15046, Peru
Joshuan J. Barboza
Universidad Continental, Lima, 15046, Peru
Mario J. Valladares-Garrido
Oficina de Epidemiología, Hospital Regional Lambayeque, Chiclayo, 14012, Peru
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization, D.A.L.F., M.J.V.G. and J.J.B.; methodology, J.J.B. and E.A.M.; software, D.A.L.F.; validation, E.A.M.; formal analysis, D.A.L.F.; investigation, M.J.V.G.; resources, A.J.R.M.; data curation, D.A.L.F.; writing—original draft prepa-ration, D.A.L.F., E.A.M. and J.J.B.; writing—review and editing, D.A.L.F., M.J.V.G., J.J.B., and E.A.M.; visualization, D.A.L.F.; supervision, J.J.B. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Correspondence to Mario J. Valladares-Garrido .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
León-Figueroa, D.A., Aguirre-Milachay, E., Barboza, J.J. et al. Prevalence of hypertension and diabetes mellitus in Peruvian patients with chronic kidney disease: a systematic review and meta-analysis. BMC Nephrol 25 , 160 (2024). https://doi.org/10.1186/s12882-024-03595-x
Download citation
Received : 02 December 2023
Accepted : 30 April 2024
Published : 10 May 2024
DOI : https://doi.org/10.1186/s12882-024-03595-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Chronic kidney disease
- Hypertension
- Diabetes mellitus
BMC Nephrology
ISSN: 1471-2369
- Submission enquiries: [email protected]
- General enquiries: [email protected]
May 9, 2024
- Introducing the 2024-2025 Magnuson Scholars
On behalf of the University of Washington, the Board of Health Sciences Deans, and the Magnuson Scholar Program, we are pleased to announce the 2024–2025 Magnuson Scholars.
The Magnuson Scholar Program is a key component of the Warren G. Magnuson Institute for Biomedical Research and Health Professions Training. The program is funded by a 1991 endowment established in the late Senator’s name. The annual income allows the University of Washington to distribute an award to one scholar from each of the six health sciences schools – Dentistry, Medicine, Nursing, Pharmacy, Public Health and Social Work – annually. As was the case in recent years, the endowment allowed a seventh scholar to receive a scholarship.
Each Health Sciences School nominates their specific scholar on the basis of outstanding academic performance and potential contributions to research in the health sciences. All Magnuson Scholars help continue the legacy of the late Senator Warren G. Magnuson and his remarkable commitment to improving the nation’s health through biomedical research, education, and responsive, sustainable healthcare discoveries. Per the endowment, at least one scholar must be engaged in research related to diabetes, it’s antecedents or treatment.
Please join us in recognizing the 2024-2025 Magnuson Scholars’ exceptional achievements while also celebrating Warren G. Magnuson’s extraordinary public service career.
The 2024-2025 Magnuson Scholars are:
Scholar Profiles

Claire Mills, School of De ntistry
Claire Mills is a dual DDS/PhD student at UW. During her dental training, she learned extensively about the challenges in both screening and treating head and neck cancer (HNSCC). This prompted her to pursue a mechanistic study of HNSCC during her PhD.
As a current PhD student, Claire also actively practices dentistry. She screens for head and neck pathologies, including cancer. Her clinical experiences underscore an increased risk of (HNSCC) in specific demographics, including patients with diabetes. She discovered that, despite regular screenings, most cases of oral cancer are not detected until tumors are significantly advanced. These challenges highlight the urgent need for more sensitive clinical screening techniques to identify early cancerous changes before they evolve into tumors.
Slobodan Beronja, PhD, highlights, “Claire adapted an approach for rapid gene targeting of human oral epithelium and cancer in the context of orthotopic transplants. She demonstrated competence, determination, and persistence that I have not seen before. I felt privileged she chose my lab for her training.”
To stop tumor formation from occurring, Claire specifically aims to identify genetic markers of pre-cancer changes in healthy tissues. These efforts will help propel her career to becoming an independent investigator and clinician-scientist, empowering her to focus on scientific pursuits in understanding oral disease, contribute to the field of oral cancer research, and build a successful career combining clinical expertise with scientific research.

Justin Lo aspires to be an academic physician scientist who conducts data-driven research focused on risk factors for diabetes and diabetes-related diseases. As an undergraduate student, Justin gained an affinity for the interconnected endocrine system, eventually becoming a teaching assistant for an endocrinology course. His undergraduate studies provided background for his research in obesity-related population health at the Institute for Health Metrics and Evaluation (IHME).
This past summer, Justin was an NIDDK Medical Student Researcher working with the Brain, Body, and Appetite Research Collaborative on a cohort analysis investigating the relationships between inflammation in body weight and glucose-regulating areas of the brain, as well as several metabolic diseases, including diabetes. He presented at the Western Medical Research Conference and was awarded the student subspecialty award in endocrinology.
Ellen A. Schur, MD, MS Professor, Medicine states, “Justin’s capacity to interpret results, compose a manuscript, and communicate findings is beyond his stage of training. He is at the level of a skilled postdoctoral scholar or above. Justin remains engaged and will continue his research with us by investigating genetic risk factors for hypothalamic gliosis. I believe he will grow into a creative and rigorous physician-investigator.”
In pursuit of a career as a physician scientist, Justin is committed to lifelong learning and professional growth. He recognizes that his analytical skillset will be valuable as medicine heads towards an era of big data. Justin’s hope is to complete a fellowship after residency, applying his skills to emerging data-driven topics such as metabolomics and diabetes. Ultimately, Justin strives for evidence-based approaches that can ameliorate the significant burden of diabetes on individuals and communities.

Elizabeth Frazier’s commitment to cardiovascular health is deeply rooted in her clinical experiences as a cardiovascular intensive care nurse. Witnessing her family navigate the burdens of living with chronic cardiac arrhythmias, particularly atrial fibrillation (AF), was the impetus for pursing a future career as a nurse scientist. Her dissertation research has the potential to advance current understanding of the links between cardiovascular disease and diabetes.
“Atrial fibrillation,” explains Elizabeth, “is the most common cardiac arrhythmia in the U.S. and is recognized as a growing epidemic. This irregular heart rhythm is often accompanied by distressing symptoms, including palpitations, fatigue, and shortness of breath. My research examines social support and the biological markers, epicardial adipose tissue and adipokines, as potential mechanisms contributing to AF symptoms differences in women and men.”
Cynthia M. Dougherty, ARNP, PhD, FAHA, FAAN Professor explains, “The link between diabetes and AF is well established, but Ms. Frazier’s focus on epicardial adipose tissue and adipokines have relevant potential to add depth to our understanding of the mechanisms connecting diabetes, AF, and sex and gender differences in diabetes and AF outcomes.”
Ms. Frazier has a long-term goal of developing biobehavioral interventions that alleviate the symptom burdens of women with cardiac arrhythmias. To achieve her goal, Elizabeth is building a program of study that expands her knowledge in advanced methodologies, statistics, and responsible, ethical research. She feels privileged to be embedded in a team of expert cardiovascular nursing researchers, led by Dr. Dougherty, and to have gained direct research experience working as a Research Assistant with Dr. Megan Streur. Through these experiences, Elizabeth is developing skills to lead her own future interdisciplinary research team and program of research.

Yue (Winnie) Wen graduated with a bachelor’s degree in Pharmaceutical Sciences and joined the Department of Pharmaceutics at UW due to her passion for scientific research. “My thesis projects,” explains Winnie, “center on liver fatty acid binding protein (FABP1) and its role in lipid and drug distribution and metabolism. Given that studies have linked FABP1 polymorphism with type 2 diabetes mellitus, I am keen to improve understanding the role of this variant in metabolic disorders, diabetes and their treatments.” By leveraging experimental, mathematical, and statistical methods, Winnie aims to improve clinical decision-making by translating in vitro and in vivo research findings into practical clinical applications.
Her involvement in diabetes and health science research has not only refined her expertise. It also deepened her commitment to the field of drug development. During a summer internship she observed the intricacies of the drug development pipeline, realizing how her contributions could translate into the clinical real-world.
Dr. Nina Isoherranen states, “During Winnie’s rotation in my lab she impressed me with her ability to analyze literature, independently develop and verify PBPK models, gain expertise in Matlab, integrate parent-metabolite kinetic models with enzyme kinetic information, and finally apply all of this into a pregnancy PBPK model that incorporates changes in kidney clearance during pregnancy. The model she developed can predict drug disposition in treatment of gestational diabetes and expand to diabetic kidney disease.” It is Winnie’s hope that by customizing therapies to individuals, she will pioneer personalized medicine in health care, reducing patient discomfort and enhancing clinical outcomes.
“I am driven to make an impact on individuals affected by prevalent conditions such as diabetes,” states Winnie. “Through my coursework in drug metabolism, pharmacokinetics, biostatistics, and applied mathematics I aspire to contribute to a future where such diseases are effectively managed and no longer pose threats to the patients.”

Amanda Brumwell’s goal as a research scientist is to help address the significant disparities witnessed first-hand in the management of diabetes. She plans to devote her dissertation research to advancing the field of diabetes care by investigating health systems and community-level approaches to managing and preventing type-II diabetes.
“I believe,” explains Amanda, “that this kind of research may help to prepare health systems to manage the burgeoning epidemic of diabetes effectively, efficiently, and equitably. It’s exciting to think that low- and middle-income settings could serve as exemplars of success.”
Her work as Managing Director at the nonprofit Advance Access & Delivery, allowed her to oversee two projects, in Durban, South Africa and Chennai, India. Both projects integrated diabetes and hypertension screening and linked to care with local tuberculosis control programs.
Amanda discovered a deep disparity between an alarming burden of diabetes and the lack of financial, structural, and political resources made available for this disease. She believes that, given the huge advances in clinical management of diabetes during recent years, there is significant opportunity for low- and middle-income settings to translate these practices to a real-world setting. Paving the way for novel strategies of treatment and preventing diabetes at a community- and population-level show great potential.
Kenneth Sherr PHD, MPH states, “Amanda is a superlative student with a strong background in implementation of health programs that address diabetes in low and middle-income countries. She is well positioned to build on this implementation experience and scientific training to move towards an independent research career that makes an impact on addressing the unmet diabetes burden globally.”

Prevention of chronic diseases like diabetes and hypertension, by improving childhood nutrition for Latinx communities via policies that promote a healthy lifestyle, is Miriana Duran’s foremost goal. Before moving to the United States, Miriana worked as a physician in Mexico, where diabetes is the second leading cause of death. “I realized,” states Miriana, “I couldn’t address some of the structural barriers or risk factors related to their illness as a physician.”
Having worked on multiple projects addressing disparities in chronic disease care and outcomes within the Latinx community, Miriana worked on a project that adapted an existing in-person program for caregivers of people with dementia (STAR-C) into a virtual program (STAR-VTF) using a cultural adaptation framework to meet the cultural and linguistic needs of Latinx caregivers. She also worked within the Latino community in rural areas in Washington state including one in which she and her team taught community health workers to identify and implement evidence-based interventions for cancer prevention.
Jessica Jones-Smith, PhD, MPH, RD, explains, “Miriana’s experience as a physician in Mexico, working with patients with obesity and diabetes, fuels her research interests and provides a valuable perspective. She is able to work collaboratively as part of a team, and also skilled enough to make great strides in this field independently.”
Her bilingual, bicultural skills help coordinate, adapt and implement culturally appropriate programs on different topics for the Latinx community. For her dissertation she intends to focus on and examine the health impacts of Seattle’s Fresh Bucks Program. Fresh Bucks is an incentive program that provides $40 per month for fruits and vegetables for lower-income Seattle residents.
Miriana draws on her interpersonal skills, life experience, background knowledge of the relevant literature, and familiarity in qualitative research methods to develop her dissertation ideas. Her intellectual ability and drive to become a leader in public health research will enable Miriana’s work to benefit communities that have been historically marginalized.

Aiming to disrupt the foster care to prison pipeline, Hannah Scheuer partners with youth, parents, and social workers, intending to interrogate a systems failure that perpetuates inequity, family instability, and poor health outcomes in Washington state. As Hannah explains, “both foster care and youth incarceration are associated with long-term negative outcomes including physical and mental health concerns and lifelong economic instability which inhibits access to quality health care. Young people in foster care or the juvenile legal system experience health problems including untreated diabetes and hypertension, sexual and reproductive conditions, respiratory and dental concerns, substance use disorders, and suicidality, at much higher rates than the general adolescent population.”
Disruption of this pipeline requires an analysis of the various points at which child welfare, juvenile legal, and legal systems intersect. Hannah’s research goal is to offer potential alternatives from the perspectives of parents and young adults who have experienced child welfare involvement and social workers who work within these systems in Washington state.
Hannah’s primary doctoral advisers, Margaret Kuklinski, PhD and Emiko Tajima, PhD believe her dissertation research and career objectives beautifully exemplify the strong potential for immediate impact as it’s a timely response to the current call for system alternatives. It emerges from the perspectives of those with lived expertise, where Hannah is conducting in partnership with a community-based coalition eager to advance evidence-informed policy and systems change.
Hannah’s research and goals will contribute to an impactful dissertation and propel a career that keeps families and communities center stage. By addressing translational research questions using mixed methods, Hannah hopes to achieve her goal of guiding tangible change.
- 2023-2024 Magnuson Scholar Winter Updates
- 2023-2024 Magnuson Scholar Recognition Luncheon
- UW Health Sciences Education Building Wins National Award
- Dr. Alice Ko, a 2023-2024 Magnuson Scholar, Featured in UW School of Dentistry News
- Magnuson Scholar Alex Wiley Featured in UW School of Pharmacy News
Be boundless
Connect with us:.
© 2024 University of Washington | Seattle, WA

IMAGES
VIDEO
COMMENTS
Type 2 diabetes (T2D) and hypertension (HTN), the two leading components of the global burden of disease, are commonly found to coexist 1 - 3. The co-existence of T2D and HTN confers a dramatically increased risk (2~4 fold) of cardiovascular disease, end-stage kidney disease, and death, compared to the normotensive and nondiabetic adults 3.
thesis aimed to study different epidemiological aspects regarding risk of mortality and cardiovascular complications among individuals with diabetes, hypertension, and hypertension with concomitant diabetes in primary care. The thesis includes four cohort studies. In Study I, people with new-onset type
Conversely, hypertension at baseline was an independent predictor of incident diabetes mellitus (in FOS, odds ratio, 3.33; 95% CI, 2.50-4.44). In >60% of the converters, progression from normotension to hypertension was characterized by a steep increase in BP values, averaging 20 mm Hg for systolic BP within 3.5 years (in MCDS).
Introduction. Hypertension (HTN) is present in more than 50% of patients with diabetes mellitus (DM) and contributes significantly to both micro and macrovascular disease in DM ( 1 - 4) ( Fig 1 ). Indeed, the risk for cardiovascular disease (CVD) is four-fold higher in patients with both DM and HTN as compared to the normotensive non-diabetic ...
Therefore, there is a chicken-egg relationship between hypertension and diabetes (Figure 1).2 To this point, hypertension occurs in 50% to 80% of patients with type 2 diabetes, who make up over 90% of the diabetic population versus ≈30% of patients with type 1 diabetes who develop hypertension.3,4 That hypertension is especially common in ...
This review focuses on basic mechanisms and environmental factors involved in promoting hypertension in diabetes, especially type 2 diabetes. It also discusses approaches for the prevention and contemporary strategies to lessen CVD and renal disease in patients with diabetes with hypertension. Figure 1. Interaction of insulin resistance ...
Type 2 diabetes mellitus (T2D) and hypertension, the 2 leading components of the global burden of disease, are commonly found to coexist. 1-3 The coexistence of T2D and hypertension confers a dramatically increased risk (2- to 4-fold) of cardiovascular disease, end-stage kidney disease, and death, compared with the normotensive and nondiabetic adults. 3 Hence, understanding the bidirectional ...
The prevalence of hypertension and diabetes as comorbidity has often been discussed however little is known regarding factors that are associated with their joint occurrence. This thesis, therefore, aims to: • Determine factors that are associated with hypertension and diabetes comorbidity (HDC)
Hypertension and type 2 diabetes are associated with each other, and their coexistence is linked to diabetes-related complications such as stroke, coronary artery disease, kidney disease, retinopathy and diabetic foot. This study aimed to determine the prevalence, awareness and control of hypertension and factors associated with hypertension among people with type 2 diabetes mellitus (T2DM) in ...
Overview of the thesis papers The Joslin Diabetes Center and Beth Israel Deaconess Medical Center diabetes and pregnancy Program is a program that offers optimal pre-conception and prenatal care for women with type 1 diabetes. Our research is based on data collected from over 700 pregnancies that occurred in this Program over the past 14 years.
The Canadian Diabetes Association (CDA) released guidelines for the management of hypertension in patients with diabetes in 2013 ( 17 ). These guidelines recommend an SBP goal of <130 mmHg and a DBP goal of <80 mmHg. The major determinate for the SBP goal cited by the guidelines is the ACCORD BP trial, although the CDA also relied on data from ...
uncontrolled hypertension worldwide (Mendis, Puska, & Norrving, 2011). In the United States, the prevalence of uncontrolled hypertension is estimated to be 53.5% of those with hypertension, affecting approximately 35.8 million persons (Centers for Disease Control and Prevention [CDC], 2012a). In a recent study in middle income countries it
The present study utilized a correlational. design to examine the relationships among diabetes distress, social support, self-efficacy, and. performance of diabetes self-care activities. A total of 33 adults with T2DM participated in the. study by completing a battery of surveys regarding performance of diabetes self-care activities.
Hypertension affects one in three American adults and is the leading modifiable risk factor of atherosclerotic cardiovascular disease deaths (Arnett et al., 2019). Medication adherence to antihypertensive medications plays an important role in controlling hypertension. Adherence is affected by multiple factors such as medication side effects,
This dissertation was intended to address lifestyle modifications in the context of hypertension and diabetes management and their subsequent effects on health outcomes. Specifically, we investigated how patient-level characteristics influence guideline-accordant diet, and how diet and exercise impact healthcare costs and health outcomes in patients with diabetes or hypertension.The ...
diabetes were 15.1 million in 2000,3 the number of people with diabetes worldwide is projected to increase to 36.6 million by 2030.4 In 2007, 23.6 million ... This dissertation research is a theory based cross-sectional study using a patient self-administered questionnaire. The exploration of the relationships
Hypertension drives the global burden of cardiovascular disease and is a leading cause of cardiovascular-related mortality worldwide, with 1.39 billion affected adults and 10.4 million deaths globally [1,2,3].The prevalence of hypertension has escalated globally with an estimated projection of a 30% increase in occurrence by the year 2025 [].Until recently, hypertension was acknowledged as a ...
Introduction The outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) posed a significant public health challenge globally, with Brazil being no exception. Excess mortality during this period reached alarming levels. Cardiovascular diseases (CVD), Systemic Hypertension (HTN), and Diabetes Mellitus (DM) were associated with increased mortality. However, the specific impact ...
Hypertension, a multifaceted cardiovascular disorder influenced by genetic, epigenetic, and environmental factors, poses a significant risk for the development of coronary artery disease (CAD) in individuals with type 2 diabetes mellitus (T2DM).
Hypertension, also known as high blood pressure, is a medical condition in which the blood pressure in the arteries is persistently elevated. Hypertension elevates the sympathetic nervous system activity leading to a decrease in the body's glucose uptake. This causes the condition of insulin resistance and eventually type 2 diabetes.
For individuals with T2DM, DSM is a fundamental aspect of diabetes care. DSM is the most widely accepted and efficacious method of promoting healthy lifestyle change for people with T2DM (American Diabetes Association, 2018). DSM is often based upon the AADE7 Self-Care Behaviors™, a product of the American Association of Diabetes Educators (AADE)
Background: Diabetes and hypertension are leading public health problems, particularly affecting low-and middle-income countries, with considerable variations in the care continuum between different age, socio-economic, and rural and urban groups. In this qualitative study, examining the factors affecting access to healthcare in Kerala, we aim ...
45 of the Best Diabetes Dissertation Topics. Published by Owen Ingram at January 2nd, 2023 , Revised On August 16, 2023. The prevalence of diabetes among the world's population has been increasing steadily over the last few decades, thanks to the growing consumption of fast food and an increasingly comfortable lifestyle.
The diagnosis of high BP (hypertension) was made according to the WHO criteria as systolic BP ≥ 140 mmHg or diastolic BP ≥ 90 mmHg. Citation 29 Participants were classified as having chronic comorbidity if they had either diabetes or hypertension, or both. When a participant was newly diagnosed with hypertension or diabetes, the participant ...
A study among 65-year-and-older hypertension patients in Asia found that the intervention group who received education on hypertension management, community-based eHealth monitoring, and monthly telephone counseling had more reduction in SBP (MD, − 10.80 mmHg; 95% CI, − 14.99 to − 6.61) compared to the control group who only received a ...
Chronic Kidney Disease (CKD) represents a major challenge for public health, with hypertension and diabetes being the main causes of its occurrence. Therefore, this study aims to determine the prevalence of hypertension (HTN) and diabetes mellitus (DM) in Peruvian patients with CKD. A systematic search for studies about CKD in Peru was carried out in PubMed, Scopus, Embase, Web of Science ...
Her dissertation research has the potential to advance current understanding of the links between cardiovascular disease and diabetes. ... Prevention of chronic diseases like diabetes and hypertension, by improving childhood nutrition for Latinx communities via policies that promote a healthy lifestyle, is Miriana Duran's foremost goal. ...
Nearly 8,000, or roughly 40 per cent, were diagnosed with prediabetes, diabetes or hypertension. "The 40 per cent rate is higher than our expectations. Originally our estimated rate, based on ...
The aim of this research was to explore perspectives and experiences of patients with hypertension while living with this disease. This is a qualitative research using content analysis approach. 27 hypertensive patients who referred to hospitals affiliated to Tehran University of Medical Sciences were selected based on purposive sampling, and ...