Open Access is an initiative that aims to make scientific research freely available to all. To date our community has made over 100 million downloads. It’s based on principles of collaboration, unobstructed discovery, and, most importantly, scientific progression. As PhD students, we found it difficult to access the research we needed, so we decided to create a new Open Access publisher that levels the playing field for scientists across the world. How? By making research easy to access, and puts the academic needs of the researchers before the business interests of publishers.
We are a community of more than 103,000 authors and editors from 3,291 institutions spanning 160 countries, including Nobel Prize winners and some of the world’s most-cited researchers. Publishing on IntechOpen allows authors to earn citations and find new collaborators, meaning more people see your work not only from your own field of study, but from other related fields too.
Brief introduction to this section that descibes Open Access especially from an IntechOpen perspective
Want to get in touch? Contact our London head office or media team here
Our team is growing all the time, so we’re always on the lookout for smart people who want to help us reshape the world of scientific publishing.
Home > Books > Genetic Disorders

Genetics and Obesity
Submitted: 25 April 2012 Published: 09 January 2013
DOI: 10.5772/52403
Cite this chapter
There are two ways to cite this chapter:
From the Edited Volume
Genetic Disorders
Edited by Maria Puiu
To purchase hard copies of this book, please contact the representative in India: CBS Publishers & Distributors Pvt. Ltd. www.cbspd.com | [email protected]
Chapter metrics overview
4,688 Chapter Downloads
Impact of this chapter
Total Chapter Downloads on intechopen.com
Total Chapter Views on intechopen.com
Overall attention for this chapters
Author Information
Maria puiu *.
- University of Medicine and Pharmacy "Victor Babes" Timisoara - Genetics Department; Emergency Hospital for Children "Louis Turcanu" Timisoara - Genetics Department, Romania
Adela Chirita Emandi
- University of Medicine and Pharmacy "Victor Babes" Timisoara - Pediatrics Department; Emergency Hospital for Children "Louis Turcanu" Timisoara - Pediatrics Department, Romania
Smaranda Arghirescu
*Address all correspondence to: [email protected]
1. Introduction
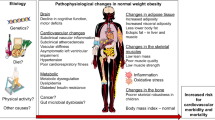
Obesity, in both children and adults, has reached epidemic proportions in multiple countries worldwide, with serious health problems and imposing a substantial economic burden on societies [ 1 – 4 ]. The increase in obesity prevalence among children is particularly alarming because obesity-related complications, including obesity-associated sleep apnea,[ 5 ] non-alcoholic fatty liver disease [ 6 ], and type 2 diabetes,[ 7 ] are increasingly diagnosed in pediatric patients. Excess weight in children may increase the likelihood of heart disease in adulthood as a result of the early establishment of risk factors [ 8 ]. Pediatric obesity has been shown to have a tremendous impact on later health [ 8 ], even independent of adult weight [ 9 ]. Additionally, childhood obesity is linked with important psychosocial consequences and poor general quality of life [ 10 ].
In order to create the best management programs and determine novel therapeutic targets, it becomes essential to understand the factors causing today’s rising epidemic of childhood obesity.
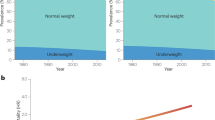
Obesity develops as a result of dietary and lifestyle factors, but studies also suggest a genetic influence on obesity [ 11 ]. Obesity is highly influenced by genetics; available data suggest that 40% to 77% of the observed variance in human body weight can be accounted for, by inherited factors [ 12 – 14 ]. Obesity, also just as clearly has environmental causes; our genetic endowments have changed minimally during the last 40 years, yet the prevalence of childhood obesity has tripled in US [ 15 ] and significantly increased worldwide [ 16 ], an observation that can only be explained by changes in external factors affecting children’s energetic balance.
This chapter provides an overview of the current knowledge on genetic factors implicated in the obesity epidemic.
Methodology
This review chapter has been developed using an evidence-based approach. Data from clinical and observational studies, review articles and twin studies were all considered when shaping this review. Literature searches for topics relating to genetic obesity were carried out in PubMed and EMBASE between 10 June and 10 August 2012, using Medical Subject Heading Terms and relevant keywords. To ensure relevance to the modern day clinical setting, literature searches were limited to articles published since 1 January 2000. Older, historically significant, articles identified by the authors were also included. Only articles from the peer-reviewed literature were included in the literature search. Articles in a non-English language were not included. Abstracts from industry-sponsored meetings were not included.
2. Hypothesis for etiology of the obesity epidemic
Currently, there are quite a few theories that intend to explain the etiology of human obesity: the thrifty gene hypothesis, the fetal programming hypothesis, the predation release hypothesis, the sedentary lifestyle hypothesis, the ethnic shift hypothesis, the increased reproductive fitness hypothesis, the assortative mating hypothesis, and the complex hypothesis [ 17 ]. However, an acceptable consensus in the field is still lacking, probably due to the fact that the development of obesity comes from highly complex interactions. The vast majority of genetic factors are presumed to affect body weight enough to cause obesity, only when specific environmental conditions pertain.
The thrifty gene hypothesis was proposed by Neel in 1962 [ 18 ] and suggests we evolved genes for efficient food collection and fat deposition, in order to survive periods of famine. Now, that food is continuously available, these genes are disadvantageous because they make us obese in preparation for a famine that never comes. In respect to this hypothesis, natural selection favored individuals carrying thrifty alleles that promote the storage of fat and energy. Polynesians likely experienced long periods of cold stress and starvation during their settlement of the Pacific and today have high rates of obesity and type 2 diabetes, possibly due to past positive selection for thrifty alleles [ 19 ].
A growing body of empirical evidence suggests the concept of fetal programming of health and disease risk. The origins of obesity and metabolic dysfunction can be traced back to the intrauterine period of life, at which time the developing fetus is influenced by suboptimal conditions during critical periods of cellular proliferation, differentiation, and maturation by producing structural and functional changes in cells, tissues and organ systems. These changes, in turn, may have long-term consequences to increase the individual's risk for developing obesity and metabolic dysfunction [ 20 – 23 ]. The major nutrition-related pathways discussed in the current literature relate to the effects of maternal nutritional insults on maternal-placental-fetal glucose/insulin physiology and their downstream effects on the developing brain and peripheral systems in the fetal compartment. Also, the potential role of intrauterine stress and stress biology is brought up for discussion in developmental programming of health and disease susceptibility [ 23 ]. In the early 1990s, Hales and Barker et al. [ 24 ], published a paper in Diabetologia postulating that not only type 2 diabetes, but also the key components of the metabolic syndrome, seemed to have at least parts of their origin in early life. Authors proved, in an unselected population sample (407 men) from Hertfordshire, UK, a direct link between low weight at birth and increased risks of developing type 2 diabetes, hypertension, elevated triglycerides and insulin resistance later in life. Thus, showing the role of fetal programming in itself and equally as important, the notion that fetal programming could represent a significant player in the origin of type 2 diabetes, the metabolic syndrome and cardiovascular disease. However, the extent to which the global diabetes epidemic may be driven by a mismatch between being born with a low birth weight and the fast propagation of overnutrition and physical inactivity, seen over recent years in developing countries, needs to be further determined [ 25 ].
The predation release hypothesis , also called the “drifty gene” hypothesis, is opposing the thrifty gene hypothesis, because famines are relatively infrequent modern phenomena that involve insufficient mortality for thrifty genes to propagate. Speakman suggests that early hominids would have been subjected to stabilizing selection for body fatness, with obesity selected against the risk of predation. Around two million years ago predation was removed as a significant factor by the development of social behavior, weapons, and fire. The absence of predation led to a change in the population distribution of body fatness due to random mutations and drift. This novel hypothesis involves random drift, rather than directed selection, thus, explaining why, even in Western society, most people are not obese [ 26 , 27 ].
The sedentary lifestyle together with excessive energy intake is the most popular etiologic hypothesis for the worldwide increasing prevalence of overweight and obesity [ 28 – 30 ].
The ethnic shift hypothesis , claims the mounting obesity rates are due to disproportionate prevalence in the fastest growing ethnicities (namely Hispanic Americans) [ 31 , 32 ].
The increased reproductive fitness hypothesis is also debated as a possible cause for obesity epidemic. Reproductive fitness can be defined as the capacity to pass on one's DNA. It is postulated that body mass index-associated reproductive fitness (natural selection) increases obesity prevalence, due to the fact that BMI has a genetic component and because individuals genetically predisposed toward higher BMIs, reproduce at a higher rate, than do individuals genetically predisposed toward lower BMIs [ 33 – 35 ].
The assortative mating hypothesis proposed by Hebebrand et al. [ 36 ] emphasizes the fact that the current obesity epidemic has a genetic component mediated by increased rates of assortative mating for body fatness. Theoretically, the genetic consequences of assortative mating for complex traits, such as obesity, are expected to become more significant as the correlation between genotype and phenotype (penetrance) increases, even if rates of assortative mating remain constant across generations [ 37 , 38 ]. Spouse concordance for obesity was associated with a 20-fold higher obesity risk for biologic offspring compared with children of concordantly non-obese parents [ 37 ].
The complex hypothesis focuses on the shared nature of common alleles in related common disorders, including obesity. This model, the common variants/multiple disease hypothesis, emphasizes that many disease genes may not be disease specific. Common deleterious alleles, found at a relatively high frequency in the population may play a cumulative role in related clinical phenotypes in the context of different genetic backgrounds and under different environmental conditions [ 39 ].
Genes can favor fat accumulation in a given environment by increased desire to overeat; the tendency to be sedentary; a diminished ability to utilize dietary fats as fuel; an enlarged, easily stimulated capacity to store body fat. The variation in how people respond to the same environmental conditions is an additional indication that genes play an important role in the development of obesity [ 40 ]. This is also consistent with the notion that obesity results from genetic variation interacting with shifting environmental conditions. The influence of genes ranges from polygenic genetic predisposition with impact on appetite, metabolism, and the deposition of fat, to rare monogenic disorders where obesity is the primary feature. Arduous efforts have been made by the scientific society to better understand the physiological basis of obesity. Crucial to this research is the inquiry of how does our body control ingestion, digestion, absorption, and metabolism and how nutrients are distributed among various tissues, organs, and systems [ 41 ]. Simultaneously, there is a growing interest regarding the role of genetics in further explaining feeding regulatory systems [ 14 ].
3. Genetic research methods used for identification of obesity susceptibility genes
The genetic contribution to common obesity has been established initially through family, twin, and adoption studies. Twin studies have shown a relatively high heritability ranging from 40%-77% [ 12 – 14 ]. However, the search for obesity susceptibility genes has been an arduous task. Gene identification for the last 15 years has been based on two broad genetic epidemiological approaches (candidate gene and genome-wide linkage methods). Recently, genome-wide association studies have brought great information on obesity related genes.
Candidate gene methods
The candidacy of a gene for obesity is based on the following resources: animal models using gene knockout and transgenic approaches; cellular model systems showing their role in metabolic pathways involved in glucose metabolism; linkage and positional cloning studies using extreme cases. This approach emphasizes on an association between a variant or mutation within or near the candidate gene and a trait of interest (such as obesity). Candidate gene approach needs to be on a large scale and well powered, in order to detect the expected small effects of genetic variants involved in common traits and disease [ 42 ].
The latest update of the Human Obesity Gene Map reported 127 candidate genes for obesity-related traits. Results of large-scale studies suggest that obesity is strongly associated with genetic variants in the melanocortin-4 receptor (MC4R) gene, leptin gene, adrenergic β 3 receptor (ADRB3) gene, prohormone convertase 1 (PCSK1) gene, brain-derived neurotrophic factor (BDNF) gene, and endocannabinoid receptor 1 (CNR1) gene [ 43 , 44 ].
Genome-wide linkage studies
Genome-wide linkage studies, through surveying the whole genome, aim to identify new, unanticipated genetic variants associated with a disease or trait of interest. Genome-wide linkage studies rely on the relatedness of study participants and test whether certain chromosomal regions cosegregate with a disease or trait across generations [ 42 ]. The latest Human Obesity Gene Map update reported 253 loci from 61 genome-wide linkage scans, of which 15 loci have been replicated in at least three studies [ 45 ]. Yet, none of these replicated loci could be narrowed down sufficiently to pinpoint the genes or variants that underline the linkage signal.
Genome-wide association studies
Genome-wide association studies are used in genetics research to look for associations between many (typically hundreds of thousands) of specific genetic variations (most commonly, single nucleotide polymorphisms -SNP) and particular diseases or traits. Similar to genome-wide linkage, the genome-wide association approach sweeps the entire genome, unrestricted by prior assumptions. Genome-wide association studies screen the whole genome at higher resolution levels than genome-wide linkage studies and are capable to narrow down the associated locus more accurately. The genome-wide association approach has effectively replaced genome-wide linkage approach for common disease [ 42 ].
Recent success of genome-wide association studies has drawn a lot of attention. High-density multistage genome-wide association analyses have so far discovered ~30 loci consistently associated with BMI and obesity-related traits. The strongest signal remains the association with variants within FTO (the fat-mass and obesity-related gene). Other signals near BDNF, SH2B1, and NEGR1 (all implicated in aspects of neuronal function),further support the idea that obesity is a disorder of hypothalamic function [ 42 ].
4. The influential role of genes in obesity
The strongest risk factor for childhood and adolescent obesity is parental obesity [ 46 ]. The risk becomes especially elevated if both parents are obese [ 47 ]. However, obesity inheritance does not usually follow classic Mendelian patterns. A combination of gene mutations, deletions and single nucleotide polymorphisms are all known to contribute to obesity. Most cases are polygenic, the result of multiple genes interacting with a shifting environment. Each “obesity gene” only makes a small contribution to phenotype, but collectively, inherited genetic variations play a major role in determining body mass and how the body maintains a balance between physical activity and nutrition. While obesity is most commonly associated with polygenic inheritance, there are other instances in which the cause is monogenic or syndromic. Monogenic obesity typically is caused by a single gene mutation with severe obesity as the main symptom. Syndromic obesity, on the other hand, has many characteristics, of which obesity is one symptom [ 48 ].
A. Monogenic obesity , that is the obesity associated with a single gene mutation. In these cases single gene variants are sufficient by themselves to cause obesity in food abundant societies. Patients with monogenic obesity usually show extremely severe phenotypes characterized by early childhood obesity onset, often associated with additional behavioral, developmental or endocrine disorders, like hyperphagia and hypogonadism. Significant developmental delays, however, are not commonly seen.
B. Syndromic obesity includes some disorders with Mendelian inheritance, in which patients are clinically obese and are additionally characterized by mental retardation, dysmorfic features, and organ-specific developmental abnormalities.
C. Polygenic obesity , the very common kind of obesity, which concerns the great majority of obese children, arises when an individual’s genetic make-up is susceptible to an environment that promotes energy consumption over energy expenditure [ 49 ].
A. Monogenic obesity
A “monogene” is by textbook definition, a gene with a strong effect on the phenotype (Mendelian traits or Mendelian - single gene conditions), giving rise to a one-on-one relationship between genotype and phenotype. A “major gene” is defined as a gene harboring, a variant which is associated with a high lifetime risk for a disease. Modifier genes and environmental factors additionally play a role in the etiology of the respective diseases [ 50 ].
The genetic causes of monogenic obesity tend to be related to the leptin-melanocortin pathway. This pathway is critical for energy balance and food intake; a disruption in this pathway will lead to severe obesity. Energy homeostasis involves the integration of afferent signals from fat (leptin) and pancreatic beta cells (insulin) and meal-related afferent signals from the gut. These inputs are integrated within the brain and regulate food intake, energy expenditure, energy partitioning and neuroendocrine status. Table 1 . summarizes the peptides proposed to affect appetite regulation (adapted from Burrage and McCandless 2007) [ 51 ].
Leptin is an adipocyte-derived hormone that is secreted proportionally to body fat content, it crosses the blood–brain barrier, and stimulates a subset of neurons in the hypothalamus to produce peptides that reduce feeding and promote increased energy expenditure (leptin–melanocortin pathway). Additionally, leptin inhibits hypothalamic neurons that produce peptides promoting feeding and decreased energy expenditure.
Attention has focused on identifying the molecular events that lie downstream of the leptin receptor in hypothalamic target neurons. In particular, neurons within the hypothalamus act as primary sensors of alterations in energy stores to control appetite and energy homeostasis. Pro-opiomelanocortin (POMC) neurons produce the anorectic peptide a-MSH (a-melanocyte stimulating hormone) together with CART (cocaine and amphetamine-related transcript), whilst a separate group expresses the orexigens: neuropeptide Y (NPY) and agouti-related protein (AGRP). AGRP is a hypothalamic neuropeptide that is a potent melanocortin-3 receptor (MC3R) and melanocortin-4 receptor (MC4R) antagonist. Activation of the NPY/AGRP neurons increases food intake and decreases energy expenditure, whereas activation of the POMC neurons decreases food intake and increases energy expenditure [ 52 ].
Peptides proposed to affect appetite regulation. adapted from Burrage and McCandless, 2007
The cumulative prevalence of monogenic obesity among children with severe obesity is about 5% [ 44 ]. Several monogenic disorders resulting from disruption of the leptin–melanocortin pathway have been identified. In these disorders, severe obesity of early onset is itself the predominant presenting feature, although often accompanied by characteristic patterns of neuroendocrine dysfunction. Mutations in the melanocortin-4 receptor gene ( MC4R ) and the leptin receptor gene ( LEPR ) have been reported in about 2.5 % and 1.5 % of children with severe obesity. An additional 0.5 % of cases can be attributed to a chromosome 16p11.2 deletion where a gene known as SH2B1 is deleted [ 48 ].
Congenital leptin deficiency
In 1997 two severely obese cousins were reported from a highly consanguineous family of Pakistani origin [ 53 ]. Despite their severe obesity, both children had undetectable levels of serum leptin and a mutation in the gene encoding leptin. Leptin deficiency is associated with hyperphagia and increased energy intake. Other phenotypic features include hypogonadotropic hypogonadism, elevated plasma insulin, T-cell abnormalities, and advanced bone age [ 54 ].
The role of leptin in some monogenic forms of obesity was further supported by the striking effect of leptin replacement in an extremely obese child with congenital leptin deficiency. In a 9-year-old boy with congenital leptin deficiency, daily subcutaneous injection of recombinant human leptin for a year, led to a complete reversal of obesity, with sustained fat-mass loss. Moreover, partial leptin deficiency in 13 Pakistani subjects, due to a heterozygous frame shift mutation in the leptin gene, was found to be associated with increased body fat [ 55 , 56 ]. However, only a handful of families with extreme forms of obesity in early infancy have mutations in these genes [ 57 ].
Mutation in the leptin receptor
Shortly after leptin deficiency was discovered, a similar phenotype, but with elevated plasma leptin levels, was identified [ 58 ]. The cause was a homozygous mutation in the leptin receptor. A later study suggested that approximately 3% of severe morbid obesity in a population including both non-consanguineous and consanguineous families could be explained by mutations in the leptin receptor [ 59 ].
Melanocortin-4 receptor deficiency (MC4R)
Mutations in another component of the leptin–melanocortin pathway melanocortin-4 receptor have also been associated with obesity. MC4R deficiency represents the most common monogenic obesity disorder that has been identified so far. It is present in about 5-6% of obese individuals from different ethnic groups, with a higher prevalence in cases with increased severity and earlier age of onset [ 60 , 61 ]. Affected subjects exhibit hyperphagia, but this is not as severe as that seen in leptin deficiency, although it often starts in the first year of life. Alongside the increase in fat mass, MC4R-deficient subjects also have an increase in lean mass, that is not seen in leptin deficiency and a marked increase in bone mineral density. The accelerated linear growth is apparently not related to a dysfunction of the GH axis and may be a consequence of the disproportionate early hyperinsulinaemia. Interestingly, both heterozygous and homozygous mutations in MC4R have been implicated in obesity, but extreme obesity is incompletely penetrant in heterozygous patients. In other words, some individuals with a single copy of the mutation are obese, whereas others are not obese [ 51 ].
Currently, there is no specific therapy for MC4R deficiency, however, it is highly likely that these subjects would respond well to pharmacotherapy that overcame the reduction in the hypothalamic melanocortinergic tone that exists in these patients [ 12 ].
Pro-opiomelanocortin (POMC) deficiency
Small numbers of patients have been described with mutations in the gene encoding pro-opiomelanocortin, which is involved in the leptin-melanocortin pathway [ 62 , 63 ]. In neonatal life, these patients present with adrenal crisis due to ACTH deficiency (POMC is a precursor of ACTH in the pituitary), also, the children have pale skin and red hair due to the lack of MSH action at melanocortin-1 receptors in the skin and hair follicles. POMC deficiency results in hyperphagia and early-onset obesity due to loss of melanocortin signaling at the melanocortin-4 receptor (MC4R) [ 12 ].
Prohormone convertase-1 (PC1) deficiency
Jackson et al described a woman with severe early-onset obesity, hypogonadotropic hypogonadism, postprandial hypoglycaemia, hypocortisolemia, and evidence of impaired processing of POMC and proinsulin who was a compound heterozygote for prohormone convertase-1 mutations [ 63 ].
Although great hope was invested in the studies of patients with early-onset severe obesity, they have revealed the identity of very few genes associated with obesity. Interestingly, the few gene mutations associated with morbid obesity appear to influence body weight primarily by altering appetite. Some of the molecules may also impact activity, but this has not yet been shown to be a significant contributor to obesity. A significant limitation of the strategy of focusing on morbid obesity is that mutations or genetic variants in these genes may not be associated with more common forms of the condition [ 51 ].
B. Syndromic obesity
Syndromic obesity is represented by at least 20 rare syndromes (shown in Table 2) , that are caused by discrete genetic defects or chromosomal abnormalities, both autosomal and X-linked, that are characterized by obesity. Most of these obesity syndromes associate mental retardation.
It was expected that the syndromic forms of obesity could help unravel novel genes relevant for idiopathic obesity. However, although the genes for several of the syndromic forms have been detected, the relevance of these genes for general obesity is still unclear [ 45 , 57 ].
Syndromes characterized by obesity.
Prader–Willi syndrome
Prader–Willi syndrome (PWS) is the most frequent of these syndromes (1 in 25,000 births). It is an autosomal-dominant disorder, characterized by obesity, hyperphagia, muscular hypotonia, mental retardation, short stature and hypogonadotropic hypogonadism. It is usually caused by a paternally inherited deletion at the chromosomal region 15q11.2–q12, and less frequently by maternal uniparental disomy (Orphanet). The cause of hyperphagia in PWS is not proven, although PWS phenotypes are consistent with a combined hypothalamic impairment, causing several endocrine abnormalities. Also, it was suggested that the elevated production of the stomach secreted peptide ghrelin seen in PWS might increase appetite by interacting with the POMC/CART and NPY hypothalamic neurons [ 57 ].
Single Minded Homologue 1 (SIM-1)
The loss of the single minded homologue 1 (SIM1) gene has also been associated with hyperphagia in syndromic obesity. This gene encodes a transcription factor that has a pivotal role in neurogenesis. In humans, deletion or disruption of the SIM1 region results in either a “Prader–Willi-like” phenotype or a form of early-onset obesity, associated with excessive food intake [ 64 ].
WAGR Syndrome
The WAGR syndrome (Wilms tumor, aniridia, genitourinary anomalies and mental retardation syndrome and obesity) is caused by heterozygous contiguous gene deletions that involve at least two genes, WT1 and PAX6 , which are present in the 11p13 region. Although persons with the WAGR syndrome typically have low-normal birth weight, marked obesity subsequently develops in a substantial subgroup [ 65 ].
Pseudohypoparathyroidism type 1A (PHP1A)
PHP1A syndrome is due to a maternally transmitted mutation in GNAS1, which encodes the α-subunit of the Gs protein. Food-intake abnormalities in patients with this syndrome might be due to the expression of the resulting variant Gs protein in the hypothalamic circuitry that controls energy balance, which involves many G-protein coupled receptors [ 66 ].
Bardet–Biedl syndrome (BBS)
Bardet–Biedl syndrome is characterized by six main features: Rod-Cone Dystrophy (the most frequent phenotype), polydactyly, learning disabilities, hypogonadism in males, renal abnormalities and obesity. In BBS patients, obesity has early onset, usually arising within the first few years of life. However, one study of post-pubertal BBS patients found that only 52% were clinically obese; therefore, this syndrome can present with a heterogeneous phenotype [ 67 ].
Albright’s hereditary osteodystrophy
Albright’s hereditary osteodystrophy describes a constellation of physical features, including short adult stature, obesity, brachydactyly, and ectopic ossifications. It is an autosomal dominant disorder due to germline mutations in GNAS1, which encodes for a-subunit of the stimulatory G protein (Gsa) [ 68 ].
Fragile X syndrome
Fragile X syndrome is characterized by moderate to severe mental retardation, macroorchidism, large ears, macrocephaly, prominent jaw (mandibular prognathism), high-pitched jocular speech and obesity. Fragile X syndrome is an X-linked, single gene disorder caused by dysfunction in the transcription of the FMR1 gene that codes for fragile X mental retardation protein (FMRP) [ 69 ].
Borjeson–Forssman–Lehmann syndrome
Borjeson, Forssman and Lehmann described a syndrome characterized by moderate to severe mental retardation, epilepsy, hypogonadism, and obesity with marked gynecomastia [ 70 ]. Mutations in a novel, widely expressed zinc-finger gene plant homeodomain (PHD)-like finger (PHF6) have been identified in affected families, although the functional properties of this protein remain unclear [ 71 ].
Alstrom syndrome
Alstrom syndrome is a homogeneous autosomal recessive disorder that is characterized by childhood obesity associated with hyperinsulinaemia, chronic hyperglycemia and neurosensory deficits. Subsets of affected individuals present with additional features such as dilated cardiomyopathy, hepatic dysfunction, hypothyroidism, male hypogonadism, short stature and mild to moderate developmental delay. Symptoms first appear in infancy and progressive development of multi-organ pathology leads to a reduced life expectancy. Variability in age of onset and severity of clinical symptoms, even within families, is likely due to genetic background. Mutations in a single gene, ALMS1, have been found to be responsible for all cases of Alstrom syndrome [ 72 ].
C. Complex polygenic obesity
Complex polygenic obesity represents the end result of behavioral, environmental, and genetic factors that may influence individual responses to diet and physical activity. Changes in our environment over the last decades, in particular the unlimited supply of cheap, highly palatable, energy-dense foods; plus a sedentary lifestyle, the so called “obesogenic” environment together with a genetic susceptibility are the culprits for today’s obesity epidemic [ 73 ].
Compared with obesity syndromes or single-gene obesity, the recent rapid increase in prevalence of childhood obesity suggests that environmental factors most likely have a larger impact on body weight in common obesity patients, although individual responses to these environmental factors are influenced by genetic factors -“susceptibility genes”.
Some traits can be due to simultaneous presence of DNA variation in multiple genes. Any of a group of alleles, at distinct gene loci that collectively control the inheritance of a quantitative phenotype or modify the expression of a qualitative character, are termed “polygenic” variants. It is generally assumed that for quantitative traits, each allele has a small effect, but the allelic effects can be additive or non-additive. Potentially, many such polygenic variants play a role in body weight regulation. It is estimated that the total number of genes with a small effect most likely exceeds 100 [ 50 ].
a Either in the GWAS or the initial sample
b Reported in the population-based cohorts EPIC, FINRISK97, BPPP and METSIM (N = 18,812)
c Reported for the Islandic sample (N = 25,344)
d Reported for children from the Northern Finland Birth Cohort (N = 5,291)
NEGR1: neuronal growth factor regulator 1; SEC16B; cerevisiae, homolog of, B; RASAL2: RAS protein activator like 2; TMEM18: transmembrane protein 18, INSIG2: insulin induced gene 2, SFRS10: splicing factor, arginine/serine-rich, 10; ETV5:etsvariant 5; DGKG diacylglycerol kinase, gamma, 90kD, GNPDA2: glucosamine-6-phosphate deaminase 2; PRL: prolactin; PTER: phosphotriesterase related; BDNF: brain derived neurotrophic factor; MTCH2: mitochondrial carrier homolog 2 (C. elegans); BCDIN3D: BCDIN3 domain containing; FAIM2: Fas apoptotic inhibitory molecule 2; SH2B1: SH2B adaptor protein 1; ATP2A1: ATPase, Ca++ transporting, cardiac muscle, fast twitch 1; FTO: fat mass and obesity associated; MAF: v-maf musculoaponeurotic fibrosarcoma oncogene homolog (avian); NPC1: Niemann-Pick disease, type C1; MC4R: melanocortin 4 receptor; CHST8: carbohydrate (N-acetylgalactosamine 4-0) sulfotransferase 8; KCTD15: potassium channel tetramerisation domain containing 15
Genetic variants with a polygenic effect on body weight in humans [ 50 ]
A large number of candidate gene association studies, of variable power, have been searched in obesity and related phenotypes. By far the most strongly replicated candidate gene from these analyses is melanocortin 4 receptor, but other replicated associations include those with adipokine and adipokine receptor genes. Further confirming the central role of behavioral stimuli in obesity, alleles of genes encoding dopamine, serotonin, and cannabinoid receptors (DRD2, HTR2C, and CBI) [ 74 – 76 ] are also reported to be associated with feeding behavior and related traits.
Genome-wide association studies have led to the identification of new candidate genes in obesity, most notably the “fat mass and obesity associated” gene (FTO). Rodent studies indicate that FTO mRNA is highly expressed in brain areas important for regulation of energy- and reward driven consumption. Food deprivation alters FTO expression in the hypothalamus in rats and mice. The contribution of the FTO variant is fairly modest, with adult homozygotes for the risk allele having only a 2- to 3-kg increase in weight [ 77 ], but the obesity high-risk allele is common in Caucasian populations and its effects begin early in life. Higher fat mass is observable from the age of 2 weeks, and carriage of the allele is associated with higher BMI and reduced satiety in children [ 11 , 50 ].
Other loci detected in genome wide association studies were identified in large study groups and via meta-analyses. Genome wide association studies (GWAS) reported novel obesity genes with small effects on human body weight. A total of more than 150,000 individuals was analyzed. Hinney et al. made a comprehensive review of these new loci in their paper published in 2010 in European Child Adolescent Psychiatry, see Table 3 -adapted from Hinney et al [ 50 ].
Alternatively, the missing heritability may be accounted for by other genetic factors like genomic copy number variation and epigenetic modifications.
5. Epigenetics
Some people have a different response of to environmental conditions and this may be the result of genetic variation alone, but there is increasing recognition that genetic expression related to disease risk may be modified by the environment during development. The “epigenetic changes” include methylation and alterations to histone proteins that alter the likelihood that specific genes are transcribed. Epigenetic changes usually occur during prenatal development or the early postnatal period. Maternal nutrition is a major factor leading to epigenetic changes. Thus, the levels of vitamins consumed in pregnancy, such as folate, methionine, and vitamin B12, which affect methylation become very important [ 78 ]. Undernutrition during prenatal development has been suggested to lead to postnatal consumption of a fatty diet. On the other hand, overnutrition of the mother is just as influential. The most convincingly shown factor is glycemic status during pregnancy. Hyperglycemia clearly affects infants’ birth weight but, beyond its effects on body weight, may increase the risk for subsequent development of insulin resistance and obesity. Nutritional signals reaching the developing hypothalamus during pregnancy may influence the sensitivity of these neurons to respond to similar signals postnatally. Infant nutrition in the neonatal period may also potentially affect future risk for obesity and its complications [ 79 ].
6. Assessment of the obese child
In order to establish the diagnosis of overweight or obese in a child, the clinician must evaluate the BMI and compare it to the standardized reference chart, appropriate for the age and sex of the child. According to World Health Organization the definition of overweight and obesity in children is established at the following cut-offs [ 80 ]:
Overweight: >+1Standard Deviations (equivalent to BMI 25 kg/m 2 at 19 years)
Obesity: >+2 Standard Deviations (equivalent to BMI 30 kg/m 2 at 19 years).
The cumulative prevalence of monogenic obesity among children with severe obesity is about 5%. There are a lot of genes implicated in obesity and too many obese patients in the world to perform molecular study for everyone. Most genetic and hormonal causes of obesity are rare. The decision to test for these abnormalities should depend upon the presence of particular phenotypes and clinical features suggesting the possibility of a diagnosable disorder [ table 4) . The presence of severe obesity in a young child (<5 yr old) associated to extreme hyperphagia, severe insulin resistance disproportionate for the degree of obesity and a positive family history of early-onset obesity may support a genetic analysis.
Assessment of the obese child.
7. Conclusions
Obesity is caused by complex interactions between environment, behavior and genetic predisposition. The increased heath risk that obesity brings is well established by now. There is growing evidence that genetic predisposition presents a cornerstone role in the development of obesity. Nevertheless, despite the enormous success of genetic studies, there are still important gaps in knowledge. Obesity-specific gene expression pattern may help in understanding the pathogenic mechanisms of obesity and its associated metabolic diseases. Recent advances in identifying genetic risk factors for obesity have contributed to understanding disease pathology, which, in term, may lead to development of new therapeutic strategies, including personalized medicine. In the everyday practice of a clinician, when facing a patient with obesity, it is important to identify particular phenotypes and clinical features that can help to recognize the children who need genetic screening.
© 2013 The Author(s). Licensee IntechOpen. This chapter is distributed under the terms of the Creative Commons Attribution 3.0 License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Continue reading from the same book
Published: 09 January 2013
By Malgorzata Mrugacz
3134 downloads
By Wen Xing, Mingjiang Xu and Feng-Chun Yang
2276 downloads
By Douglas B. Luckie and Mauri E. Krouse
2766 downloads
Genetics and Obesity
Affiliations.
- 1 Rochester General Hospital
- 2 District Endocrine/Sentara Northern Virginia Medical Center
- PMID: 34424641
- Bookshelf ID: NBK573068
The obesity epidemic around the world affects not only adults but also children. About 50% of the time, obesity in childhood is carried into adulthood in a phenomenon known as "tracking." Per the latest data from the World Health Organization, the number of overweight and obese children under five years of age is estimated to be close to 39 million. In the United States, 1 in 3 adult Americans is obese, and the Centers for Disease Control has estimated that the prevalence of obesity among children is 19.3% per data from the year 2017-2018. By 2030 some epidemiologists suggest that 20% of the world's population will be obese, i.e., having a body mass index (BMI) of more than 30 kg/m² in adults, or a BMI ≥95th percentile for age and sex in children aged 2 to 18 years. Obesity as a disease itself is multifactorial and occurs due to complex interactions occurring between genetics and the environment.
The Human Genome project was carried out between the years 1990 to 2003 to map out the human genome. Genome-Wide Association Studies (GWAS) have been ongoing since 2007 to help associate specific genetic variations with certain diseases. Around 250 genes are now associated with obesity. The FTO gene on chromosome 16 is the most important and carries the highest risk of the obesity phenotype.
The Genetic Investigation of Anthropomorphic Traits Consortium is the organization involved in furthering research in GWAS. However, genetic mutations alone cannot explain the heritability of obesity perfectly. The concept of epigenetics was introduced to help understand the heritability of obesity better. Waddington first introduced the definition of epigenetics was first introduced in the 1940s by Waddington and subsequently elaborated by Holiday in 1990. However, the modern definition of epigenetics comes from Riggs et al. in 1996. Epigenetics is defined as "the study of mitotically heritable changes in gene expression that occur without changes in the DNA sequence." Epigenetic marks on the genome alter the way each gene is read to produce a distinct phenotype. This provides a better explanation of how the environment plays a significant role in affecting how genes are expressed.
Epigenome-wide Association Studies (EWAS) began in 2013 to map the epigenome and understand the varied expressions of genes in different tissues. GWAS and EWAS have heralded a new era in the study of genetics and obesity.
Copyright © 2024, StatPearls Publishing LLC.
- Continuing Education Activity
- Introduction
- Issues of Concern
- Clinical Significance
- Other Issues
- Enhancing Healthcare Team Outcomes
- Review Questions
Publication types
- Study Guide
Weight Loss
Nutrition & Diet
Recipes & Cooking
Exercise & Fitness
Lifestyle & Mindset
The Genetics of Obesity: How Your DNA Influences Your Weight
How large a role does your DNA play when it comes to weight? Read on to understand how genes impact weight and possibly cause excess weight gain, and how to determine whether your genes might be impacting you.

Experts and researchers have determined that there is a connection between genetics and weight, with certain genes causing some people to be more predisposed to obesity than others. The link between these factors is complex and the research is still ongoing.
But even if your genes say you are at risk of obesity, does that mean your weight is set in stone, no matter how hard you try?
Here’s some good news: Not necessarily! Though genetics do play a role in our weight , experts say that maintaining consistent healthy habits over time could offset the DNA that impacts weight gain. Read on to learn what experts are discovering about this evolving area of research and how it impacts your own health.
How Genetics Can Influence Obesity Risk
Our genetics make us who we are, determining everything from our hair color to our eye color, our height, and, yes, even our weight. We are prone to a particular body type and research has confirmed that people of higher weights tend to share common genes.
A study published in 2021 found that out of the 293 genes that have been determined to impact weight, 14 of these genes can directly cause weight gain and three of these genes can help prevent it.
“These genes [that impact weight] can influence so many different things, including our hunger and the types of foods we’re drawn to, our metabolism, how our body stores fat, and even how our brain and hormones signal us to eat or to stop eating,” says Candice Seti, PsyD , a certified nutrition coach known as The Weight Loss Therapist, based in San Diego.
As an example, the food you are drawn to is influenced by a genetic trait — a concept known as “food liking,” according to a study published in 2022. The study’s researchers categorized foods into three domains: “Highly Palatable,” “Acquired,” and “Low Caloric.” Researchers confirmed the genetic correlation to “food liking” by identifying shared brain traits with the use of MRI imaging.
Those who were drawn to “Highly Palatable” foods (think deep-fried foods, cakes, and sodas) were more likely to exhibit obesity than the other two groups. The group that gravitated toward the “Low-Caloric” food domain tended to opt for vegetarian foods, such as salads and fruit. This group also reported higher physical activity than the “Highly Palatable” group.
Finally, those in the “Acquired” group preferred foods like cheese, chocolate, salty foods, coffee, and alcohol. They were associated with a lower obesity profile and had higher physical activity than the “Highly Palatable” group, but also had a higher likelihood of smoking and alcohol consumption.
According to the study, “food liking” is twice as likely to be inherited compared to other traits.
Genetics can also play a role in certain health conditions that impact our weight. Hypothyroidism, polycystic ovarian syndrome, Cushing syndrome (bruising easily), and growth hormone deficiency are a few examples of genetic diseases that could be underlying causes of weight gain, according to research published in 2019.
DNA and Weight: It’s Not Set in Stone
While DNA can be a strong factor when it comes to weight, take heart: For the vast majority of us, lifestyle bears a far greater impact on weight than genetics does. Even if you have the “food liking” gene that causes you to gravitate toward fried foods or other similar genes that can cause weight gain, lifestyle changes can counteract this, especially when it comes to our food choices and physical activity. In fact, many people who have genes that may cause them to be at a higher weight never become overweight .
“Although our genes play a part with regard to weight, our lifestyle and environmental exposures seem to influence weight in greater ways,” explains Paunel Vukasinov, MD , a board-certified internist with Medical Offices of Manhattan in New York. “While we may have certain genes that predispose us to obesity, these genes will not necessarily become active unless we engage in unhealthy lifestyles such as [too much] fried food consumption and sedentary lifestyle, which will ultimately lead to weight gain. These are examples of how our genes interact with our environment.”
Can Genetic Testing Help With Weight Loss?
If you have decided to lose weight but aren’t seeing any progress in spite of consistent nutritious eating and increased physical activity, speak with your doctor. Genetic testing is typically not done unless your specific health history is pointing toward it, but if you and your doctor determine that a genetic test could be useful, the test typically involves either a saliva sample or a blood test.
Dr. Vukasinov notes that there is a rare form of obesity called monogenic obesity, which results in spontaneous mutations of single genes and leads to early onset obesity in childhood. This is something that a genetic blood test can detect, and it may be useful information as you and your doctor navigate the best path forward for your health.
DNA testing can also point to which foods your body responds best to, adds Dr. Seti. “DNA testing can provide some useful information on how your body processes carbs, proteins, and fats. So it can provide some information on which macronutrients your body responds best to and which macronutrients might be beneficial to limit,” the expert says.

The Bottom Line
It’s not advised to approach genetic testing as a “magic formula” to weight loss. Vukasinov believes there is not yet enough research to suggest that genetic testing can determine an effective weight loss plan, and Seti echoes this. Instead, the experts say, focus your efforts on increasing your physical activity incrementally each week and incorporating more whole, unprocessed foods into your diet (such as vegetables, fruits, whole grains , beans, lean meats, and fish ).
“The idea of genetic testing being the new silver bullet to weight loss is very attractive, but this is not the answer for most people,” says Seti. “So while [genetic testing] may be beneficial for some who have been doing everything right and are not achieving any weight loss, for most of us, it really comes down to creating a healthy relationship with food and putting [nutritious] food into our bodies .”
Editorial Sources and Fact-Checking
- University of Virginia Health System. Scientists Discover 14 Genes That Cause Obesity. Science Daily . October 1, 2021.
- May-Wilson S et al. Large-Scale GWAS of Food Liking Reveals Genetic Determinants and Genetic Correlations With Distinct Neurophysiological Traits. Nature Communications . May 18, 2022.
- van der Valk ES et al. A Comprehensive Diagnostic Approach to Detect Underlying Causes of Obesity in Adults.” Obesity Reviews . March 1, 2019.

Paige Jarvie Brettingen
Paige Jarvie Brettingen is a freelance writer and educator based in Colorado. She has been published in The Atlantic, The Washington Post, DailyOM Journal, Refinery29, 5280 Magazine and Mom.com, among others. She has a passion for healthful living as well as helping moms live a more fulfilled motherhood with her coaching program and forthcoming book “The Mom-Life Reset.”
Get the latest from our newsletter!

Lose It! is mobilizing the world to achieve a healthy weight
Set Your Goals
Tell us what you want to achieve and receive personalized goals.
Track Your Food
Learn about the foods you're eating and keep your calories within your daily budget.
Lose Weight
Reach your goals and continue to set new ones for a happier, healthier you!
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 07 May 2024
Epidemiology and Population Health
Obesity: a 100 year perspective
- George A. Bray ORCID: orcid.org/0000-0001-9945-8772 1
International Journal of Obesity ( 2024 ) Cite this article
347 Accesses
23 Altmetric
Metrics details
- Biological techniques
- Health care
- Weight management
This review has examined the scientific basis for our current understanding of obesity that has developed over the past 100 plus years. Obesity was defined as an excess of body fat. Methods of establishing population and individual changes in levels of excess fat are discussed. Fat cells are important storage site for excess nutrients and their size and number affect the response to insulin and other hormones. Obesity as a reflection of a positive fat balance is influenced by a number of genetic and environmental factors and phenotypes of obesity can be developed from several perspectives, some of which have been elaborated here. Food intake is essential for maintenance of human health and for the storage of fat, both in normal amounts and in obesity in excess amounts. Treatment approaches have taken several forms. There have been numerous diets, behavioral approaches, along with the development of medications.. Bariatric/metabolic surgery provides the standard for successful weight loss and has been shown to have important effects on future health. Because so many people are classified with obesity, the problem has taken on important public health dimensions. In addition to the scientific background, obesity through publications and organizations has developed its own identity. While studying the problem of obesity this reviewer developed several aphorisms about the problem that are elaborated in the final section of this paper.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
251,40 € per year
only 20,95 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Obesity and the risk of cardiometabolic diseases

Obesity-induced and weight-loss-induced physiological factors affecting weight regain
Normal weight obesity and unaddressed cardiometabolic health risk—a narrative review
Quetelet, Adolphe Sur l’homme et le developpement de ses facultes, ou essai de physique sociale ; Paris: Bachelier, 1835 (Transl of L-A-J. A Treatise on Man and the Development of His Faculties. IN: Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 pp 423-36.
Bray GA. Quetelet: quantitative medicine. Obes Res. 1994;2:68–71.
Article CAS PubMed Google Scholar
Bray GA. Beyond BMI. Nutrients. 2023;15:2254.
Article PubMed PubMed Central Google Scholar
Flegal KM. Use and misuse of BMI categories. AMA J Ethics. 2023;25:E550–8.
Article PubMed Google Scholar
Keys A, Fidanza F, Karvonen MJ, Kimura N, Taylor HL. Indices of relative weight and obesity. J Chr Diseases. 1972;25:329–43.
Article CAS Google Scholar
Bray GA. Definition, measurement, and classification of the syndromes of obesity. Int J Obes. 1978;2:99–112.
CAS PubMed Google Scholar
Garrow JS. Treat Obesity Seriouslv-A Clinical Manual . Edinburgh: Churchill Livingstone; 1981.
Rodgers A, Woodward A, Swinburn B, Dietz WH. Prevalence trends tell us what did not precipitate the US obesity epidemic. Lancet Public Health. 2018;3:e162–3.
Bray GA. Body fat distribution and the distribution of scientific knowledge. Obes Res. 1996;4:189–92.
Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr. 2004;79:379–84.
Weeks RW. An experiment with the specialized investigation. Actuar Soc Am Trans. 1904;8:17–23.
Google Scholar
Vague J. La differenciation sexuelle facteur determinant des formes de l’obesite, Presse Medicale. 1947;55:339 340. [Translated. IN: Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 pp 693–5].
Vague J. The degree of masculine differentiation of obesities: a factor determining predisposition to diabetes, atherosclerosis, gout, and uric calculous disease. Am J Clin Nutr. 1956;4:20–34.
Larsson B, Svardsudd K, Welin L, Wihelmsen L, Bjorntorp P, Tibbllne G. Abdominal adipose tissue distribution, obesity and risk of cardiovascular disease and death: 13 year follow up of participants in the study of 792 men born in 1913. BMJ 1984;288:1401–4.
Article CAS PubMed PubMed Central Google Scholar
Bjorntorp P. Visceral obesity: a “civilization syndrome. Obes Res. 1993;1:206–22.
Behnke AR, Feen BG, Welham WC. The specific gravity of healthy men. JAMA 1942;118:495–8.
Article Google Scholar
Roentgen WC. Ueber eine neue Art von Strahlen. S.B. Phys-med Ges Wurzburg. 1895;132–41.
Wong MC, Bennett JP, Leong LT, Tian IY, Liu YE, Kelly NN, et al. Monitoring body composition change for intervention studies with advancing 3D optical imaging technology in comparison to dual-energy X-ray absorptiometry. Am J Clin Nutr. 2023:S0002-9165(23)04152-7
Church TS, Thomas DM, Tudor-Locke C, Katzmarzyk PT, Earnest CP, Rodarte RQ, et al. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS ONE. 2011;6:e19657 https://doi.org/10.1371/journal.pone.0019657 .
Schwann TH; Smith H, Trans. Microsccopical researches into the accordance in the structure and growth of animals and plants . London: Sydenham Society 1847
Hassall A. Observations on the development of the fat vesicle. Lancet. 1849;1:163–4.
Hirsch J, Knittle JL. Cellularity of human obese and nonobese adipose tissue. Fed Proc. 1970;29:1516–21.
Garvey WT. New Horizons. A new paradigm for treating to target with second-generation obesity medications. JCEM. 2022;107:e1339–47.
Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994;372:425–32.
Lavoisier AL, DeLaPlace PS. Memoir on Heat. Read to the Royal Academy of Sciences 28 June 1783 [IN: Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 pp 498–512].
Bray GA. Lavoisier and Scientific Revolution: The oxygen theory displaces air, fire, earth and water. Obes Res. 1994;2:183–8.
Helmholtz, Hermann von. Uber die Erhaltung der Kraft, ein physikalische Abhandlung, vorgetragen in der Sitzung der physicalischen Gesellschaft zu Berlin am 23sten Juli 1847. Berlin: G. Reimer, 1847.
Bray GA. Commentary on Atwater classic. Obes Res. 1993;1:223–7.
Bray GA. Energy expenditure using doubly labeled water: the unveiling of objective truth. Obes Res. 1997;5:71–7.
Lifson N, Gordon GB, McClintock R. Measurement of total carbon dioxide production by means of D 2 0 18 . J Appl Physiol. 1955;7:704–10.
Lichtman SW, Pisarska K, Berman ER, Pestone M, Dowling H, Offenbacher E, et al. Discrepancy between self-reported and actual caloric intake and exercise in obese subjects. N Engl J Med. 1992;327(Dec):1893–8.
Bray GA. Commentary on classics of obesity 4. Hypothalamic obesity. Obes Res. 1993;1:325–8.
Bruch H. The froehlich syndrome: report of the original case. Am J Dis Child. 1939;58:1281–90.
Babinski JP. Tumeur du corps pituitaire sans acromegalie et arret de development des organs genitaux. Rev Neurol. 1900;8:531–3. [Translation IN: Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 pp 740–1]
Cushing H. The Pituitary Body and Its Disorders . Philadelphia. PA: JB Lippincott; 1912.
Bray GA. Laurence, moon, Bardet Biedl: reflect a syndrome. Obes Res. 1995;3:383–6.
Laurence JZ, Moon RC. Four cases of “Retinitis Pigmentosa,” Occurring in the same family, and accompanied by general imperfections of development. Opthalmol Rev. 1866;2:32–41.
Bardet G. Sur un Syndrome d’Obesity Conginitale avec Polydactylie et Retinite Pigmentaire (Contribution a l’etude des formes clinique de 1 ’Obesite hypophysaire) . Paris: 1920. Thesis [Translation IN: Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 pp 740–1].
Biedl A. Geschwisterpaar mit adiposo-genitaler Dystrophie. Dtsch Med Woche. 1922;48:1630.
Cuenot L. Pure strains and their combinations in the mouse. Arch Zoot Exptl Gen. 1905;122:123.
Ingalls AM, Dickie MM, Snell GD. Obese, new mutation in the mouse. J Hered. 1950;41:317–8.
Coleman DL. Obesity and diabetes: two mutant genescausing obesity-obesity syndromes in mice. Diabetalogia. 1978;14:141–8.
Zucker TF, Zucker LM. Fat accretion and growth in the rat. J Nutr. 1963;80:6–20.
Schwartz MW, Seeley RJ, Zeltser LM, Drewnowski A, Ravussin E, Redman LM, et al. Obesity pathogenesis: an endocrine society scientific statement. Endocr Rev. 2017;38:267–96.
Oral EA, Simha V, Ruiz E, Andewelt A, Premkumar A, Snell P, et al. Leptin-replacement therapy for lipodystrophy. N Engl J Med. 2002;346:570–8.
Loos RJF, Yeo GSH. The genetics of obesity: from discovery to biology. Nat Rev Genet. 2022;23:120–33.
Blüher M. Metabolically healthy obesity. Endocr Rev. 2020;41:405–20.
Acosta A, Camilleri M, Abu Dayyeh B, Calderon G, Gonzalez D, McRae A, et al. Selection of antiobesity medications based on phenotypes enhances weight loss: a pragmatic trial in an obesity clinic. Obes. 2021;29:662–71.
Bray GA. Commentary on classics in obesity. 6. Science and politics of hunger. Obes Res. 1993;19:489–93.
Cannon WB, Washburn AL. An explanation of hunger. Am J Physiol. 1912;29:441–54.
Carlson AJ. Contributions to the physiology of the stomach -II. the relation between the concentrations of the empty stomach and the sensation of hunger. Am J Physiol. 1912;31:175–92.
Carlson AJ. Control of Hunger in Health and Disease . Chicago, IL: University of Chicago Press; 1916.
Flint A, Raben A, Astrup A, Holst JJ. Glucagon-like peptide 1 promotes satiety and suppresses energy intake in humans. J Clin Invest. 1998;101:515–20.
Bray GA. Eat slowly - From laboratory to clinic; behavioral control of eating. Obes Res. 1996;4:397–400.
Pavlov IP; Thompson WH, trans. The Work of the Digestive Glands . London: Charles Griffin and Co.; 1910.
Skinner BF. Contingencies of Reinforcement: A Theoretical Analysis . New York: Meredith Corporation; 1969.
Ferster CB, Nurenberger JI, Levitt EG. The Control of Eating. J. Math 1964;1:87-109.
Stuart RB. Behavioral control of overeating. Behav Res Ther. 1967;5:357–65. [Also IN: Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 pp 793–9]
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM. et a; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(Feb):393–403.
The Look AHEAD Research Group, Wadden TA, Bantle JP, Blackburn GL, Bolin P, Brancati FL, Bray GA, et al. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity. 2014;22:5–13.
Bray GA, Suminska M. From Hippocrates to the Obesity Society: A Brief History. IN Handbook of Obesity (Bray GA, Bouchard C, Katzmarzyk P, Kirwan JP, Redman LM, Schauer PL eds). Boca Raton: Taylor & Francis 2024. Vol 2, pp 3–16.
Bray GA. Commentary on Banting Letter. Obes Res. 1993;1:148–52.
Banting W. Letter on Corpulence, Addressed to the Public . London: Harrison and Sons 1863. pp 1–21.
Harvey W. On corpulence in relation to disease” With some remarks of diet . London” Henry Renshaw, 1872.
Schwartz, H. Never Satisfied. A Cultural History of Diets, Fantasies and Fat . 1977.
Foxcroft, Louise. Calories and Corsets. A history of dieting over 2000 years . London: Profile Books, 2011.
Gilman, Sander L. Obesity. The Biography . Oxford: Oxford University Press, 2010.
Linn R Stuart SL. The Last Chance Diet . A Revolutionary New Approach to Weight Loss 1977.
Magendie F. Rapport fait a l’Academie des Sciences au le nom de la Commission diet la gelatine. C.R. Academie Sci (Paris) 1841:237-83.
Bray GA. “The Science of Hunger: Revisiting Two Theories of Feeding. IN Bray GA. The Battle of the Bulge. A History of Obesity Research . Pittsburgh, Dorrance Publishing 1977 p. 238.
Sours HE, Frattalli VP, Brand CD, et al. Sudden death associated with very low calorie weight regimes. Am J Clin Nutr. 1981;34:453–61.
Bray GA. From very-low-energy diets to fasting and back. Obes Res. 1995;3:207–9.
Benedict, F.G. A Study of prolonged fasting . Washington: Carnegie Institution of Washington (Publ No 203), 1915.
Keys A, Brozek J, Henschel A, Mickelsen O,Taylor HL. The biology of human starvation . Minneapolis: University of Minnesota Press, 1950.
Cahill GF Jr, Herrera MG, Morgan AP, Soeldner JS, Steinke J, Levy PL, et al. Hormone-fuel interrelationships during fasting. J Clin Invest. 1966;45:1751–69.
Benedict FG, Miles WR, Roth P, Smith HM. Human vitality and efficiency under prolonged restricted diet. Carnegie Instit Wash, Pub. No. 280. Washington: Carnegie Institution of Washington; 1919.
Evans FA, Strang JM. The treatment of obesity with low-calorie diets. JAMA 1931;97:1063–8.
Bloom WL. Fasting as an introduction to the treatment of obesity. Metabolism 1959;8:2 14–220.
CAS Google Scholar
Bray GA, Purnell JQ. An historical review of steps and missteps in the discovery of anti-obesity drugs. IN: Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dhatariya K, Dungan K, et al. editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2022.
Lesses MF, Myerson A. Human autonomic pharmacology. NEJM 1938;218:119-24.
Cohen PA, Goday A, Swann JP. The return of rainbow diet pills. Am J Public Health. 2012;102:1676–86.
Bray GA. Nutrient intake is modulated by peripheral peptide administration. Obes Res. 1995;3:569S–572S.
Kissileff HR, Pi-Sunyer FX, Thornton J, Smith GP. C-terminal octapeptide of cholecystokinin decreases food intake in man. Am J Clin Nutr. 1981;34:154–60.
Wilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, et al. STEP 1 study group. Once-weekly semaglutide in adults with overweight or obesity. N Engl J Med. 2021;384:989–1002.
Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jódar E, Leiter LA, et al. SUSTAIN-6 investigators. semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375:1834–44.
Jastreboff AM, Aronne LJ, Ahmad NN, Wharton S, Connery L, Alves B, et al. SURMOUNT-1 investigators. tirzepatide once weekly for the treatment of obesity. N. Engl J Med. 2022;387:205–16.
Jastreboff AM, Kaplan LM, Frías JP, Wu Q, Du Y, Gurbuz S, et al. Retatrutide phase 2 obesity trial investigators. Triple-hormone-receptor agonist retatrutide for obesity - a phase 2 trial. N Engl J Med. 2023;389:514–26.
Bray GA. Obesity and surgery for a chronic disease. Obes Res. 1996;4:301–3.
Kremen AJ, Linner JH, Nelson CH. An experimental evaluation of the nutritional importance of proximal and distal small intestine. Ann Surg. 1954;140:439–48.
Payne JH, DeWind LT, Commons RR. Metabolic observations in patients with jejuno-colic shunts. Am J Surg. 1963;106:273–89.
Payne JH, DeWind LT. Surgical treatment of obesity. Am J Surg. 1969;118:141–6.
Buchwald H, Varco RL. Partial ileal bypass for hypercholesterolemia and atherosclerosis. Surg Gynecol Obstet. 1967;124:1231.
Mason EE, Ito C. Gastric bypass in obesity. Surg Clin North Am. 1967;47:1345–135.
O’Brien PE, MacDonald L, Anderson M, Brennan L, Brown WA. Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg. 2013;257:87–94.
Arterburn D, Wellman R, Emiliano A, Smith SR, Odegaard AO, Murali S, et al. PCORnet bariatric study collaborative. Comparative effectiveness and safety of bariatric procedures for weight loss: a PCORnet cohort study. Ann Intern Med. 2018;169:741–50.
Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess. 2009;13:1–190.
Christou NV, Sampalis JS, Liberman M, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg. 2004;240:416–23.
Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial - a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273:219–34.
Sjöström L. Swedish Obese Subjects, SOS: A review of results from a prospective controlled intervention trial. In: Bray GA, Bochard C, eds. Handbook of Obesity, Volume 2: Clinical Applications. New York: Informa; 2014.
Sjöström L, Narbro K, Sjöström CD, Karason K, Larsson B, Wedel H, et al. Effects of bariatric surgery on mortality in Swedish Obese Subjects. N. Engl J Med. 2007;357:741–52.
Sjöström L, Peltonen M, Jacobson P, Sjöström CD, Karason K, Wedel H, et al. Bariatric surgery and long-term cardiovascular events. JAMA 2012;307:56–65.
Carlsson LM, Peltonen M, Ahlin S, Anveden Å, Bouchard C, Carlsson B, et al. Bariatric surgery and prevention of type 2 diabetes in Swedish Obese Subjects. The New England. J Med. 2012;367:695–704.
Pories WJ, Swanson MS, MacDonald KG, Long SB, Morris PG, Brown BM, et al. Who would have thought it? an operation proves to be the most effective therapy for adult-onset. Diabetes Mellit Ann Surg. 1995;222:339–52.
Bray GA. Life insurance and overweight. Obes Res. 1995;3:97–99.
The Association of Life Insurance Medical Directors and The Actuarial Society of America. Medico- Actuarial Mortality Investigation . New York: The Association of Life Insurance Medical Directors and ‘The Actuarial Society of America; 1913.
Keys A. Seven Countries: A Multivariate Analysis of Death and Coronary Heart Disease . Cambridge, MA: Harvard University Press; 1980.
Dawber TR. The Framingham Study: The Epidemiology of Atherosclerotic Disease . Cambridge, MA: Harvard University Press; 1980.
Bray, G.A. (Ed), Obesity in Perspective . Fogarty International Center Series on Preventive Med. Vol 2, parts 1 and 2, Washington, D.C.: U.S. Govt Prtg Office, 1976, DHEW Publication #75-708.
Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960–1962 through 2017–2018. NCHS Health E-Stats. 2020.
Bray GA. Obesity: Historical development of scientific and cultural ideas. Int J Obes. 1990;14:909–26.
Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 p 30.
Short, T. A Discourse Concerning the Causes and Effects of Corpulency Together with the Method for Its Prevention and Cure , J. Robert, London, 1727.
Flemyng, M. A Discourse on the Nature, Causes and Cure of Corpulency , L Davis and C Reymers, London, 1760.
Wadd, W. Comments on corpulency lineaments of leanness mems on diet and dietetics. London: John Ebers and Co, 1829.
Chambers, TK. Corpulence, or excess fat in the human body. London: Longman, 1850.
Rony HR. Obesity and Leanness . Philadelphia: Lea and Febiger, 1940.
Rynearson EH, Gastineau CF. Obesity . Springfield, IL: Charles C. Thomas, 1949.
Bray, G.A. The Obese Patient. Major Problems in Internal Medicine , Vol 9, Philadelphia, Pa.: W.B. Saunders Company, 1976, pp. 1-450.
Bray G.A. A Guide to Obesity and the Metabolic Syndrome: Origins and Treatment . New York: CRC Press: Taylor and Francis Group. 2011.
Howard AN. The history of the association for the study of obesity. Intern J Obes. 1992;16:S1–8.
Bray GA, Greenwood MRC, Hansen BC. The obesity society is turning 40: a history of the early years. Obesity. 2021;29(Dec):1978–81.
McLean Baird I, Howard AN. Obesity: Medical and Scientific Aspects : Proceedings of the First Symposium of the Obesity Association of Great Britain held in London , October 1968. Edinburgh & London: E. S. Livingston, 1968.
Bray GA, Howard AN. Founding of the international journal of obesity: a journey in medical journalism. Int J Obes. 2015;39:75–9.
Bray G. The founding of obesity research/obesity: a brief history. Obes. 2022;30:2100–2.
Ziman J. The Force of Knowledge. The Scientific Dimension of Society . Cambridge: Cambridge University Press, 1976.
Bray GA, Kim KK, Wilding JPH. Obesity: a chronic relapsing progressive disease process: a position paper of world obesity. Obes Rev. 2017;18:715–23.
Bray GA. Obesity is a chronic, relapsing neurochemical disease. Intern J Obes. 2004;28:34–8.
Allison DB, Downey M, Atkinson RL, Billington CJ, Bray GA, Eckel RH, et al. Obesity as a disease: a white paper on evidence and arguments commissioned by the Council of the Obesity Society. Obes. 2008;16:1161–77.
Garvey WT, Garber AJ, Mechanick JI, Bray GA, Dagogo-Jack S, Einhorn D, et al. American Association of Clinical Endocrinologists and American College of Endocrinology position statement on the 2014 advanced framework for a new diagnosis of obesity as a chronic disease. Endocr Pr. 2014;20:977–89.
Bray GA, Ryan DH. Evidence-based weight loss interventions: individualized treatment options to maximize patient outcomes. Diabetes Obes Metab. 2021;23:50–62.
Ge L, Sadeghirad B, Ball GDC, da Costa BR, Hitchcock CL, Svendrovski A, et al. Comparison of dietary macronutrient patterns of 14 popular named dietary programmes for weight and cardiovascular risk factor reduction in adults: systematic review and network meta-analysis of randomised trials. BMJ 2020;369:m696.
Sjöström L, Rissanen A, Andersen T, Boldrin M, Golay A, Koppeschaar HP, et al. Randomised placebo-controlled trial of orlistat for weight loss and prevention of weight regain in obese patients. European Multicentre Orlistat Study Group. Lancet 1998;352:167–72.
Pi-Sunyer FX, Aronne LJ, Heshmati HM, Devin J, Rosenstock J. Effect of rimonabant, a cannabinoid-1 receptor blocker, on weight and cardiometabolic risk factors in overweight or obese patients: RIO-North America: a randomized controlled trial. JAMA 2006;295:761–75.
Foster GD, Wadden TA, Vogt RA, Brewer G. What is a reasonable weight loss? Patients’ expectations and evaluations of obesity treatment outcomes. J Consult Clin Psychol. 1997;65:79–85.
DiFeliceantonio AG, Coppin G, Rigoux L, Thanarajah ES, Dagher A, Tittgemeyer M, et al. Supra-additive effects of combining fat and carbohydrate on food reward. Cell Metab. 2018;28:33–44.e3.
Thanarajah SE, Backes H, DiFeliceantonio AG, Albus K, Cremer AL, Hanssen R, et al. Food intake recruits orosensory and post-ingestive dopaminergic circuits to affect eating desire in humans. Cell Metab. 2019;29:695–706.e4.
Bray GA. Is sugar addictive? Diabetes 2016;65:1797–9.
Download references
Acknowledgements
The author thanks Dr. Jennifer Lyn Baker for her helpful comments during the early stage of preparing this manuscript.
Author information
Authors and affiliations.
Pennington Biomedical Research Center/LSU, Baton Rouge, LA, 70808, USA
George A. Bray
You can also search for this author in PubMed Google Scholar
Contributions
All contributions were made by the single author.
Corresponding author
Correspondence to George A. Bray .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
MSS # 2023IJO01171.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Bray, G.A. Obesity: a 100 year perspective. Int J Obes (2024). https://doi.org/10.1038/s41366-024-01530-6
Download citation
Received : 13 November 2023
Revised : 23 April 2024
Accepted : 26 April 2024
Published : 07 May 2024
DOI : https://doi.org/10.1038/s41366-024-01530-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

COMMENTS
Polygenic (or common) obesity and rare, severe, early-onset monogenic obesity are often polarized as distinct diseases. However, gene discovery studies for both forms of obesity show that they have shared genetic and biological underpinnings, pointing to a key role for the brain in the control of body weight.
Crucially, there is a strong genetic component underlying the large interindividual variation in body weight that determines people's response to this 'obesogenic' environment. Twin, family ...
Previous research has investigated the genetic regulation of blood pressure regulatory genes using post-GWAS data , ... demonstrating a strong relationship between the brain and obesity.
In the early phase of obesity genetic research, the emphasis was on candidate genes of obesity (See Rankinen et al. for a review) (). A literature search identified 547 candidate genes derived from multiple types of studies, and the contribution of SNPs located in ±10 kb flanking sequences around these genes was investigated (). It was ...
The Biology and Genetics of Obesity — A Century of Inquiries. Author: Chin Jou, Ph.D. Author Info & Affiliations. Published May 15, 2014. N Engl J Med 2014;370: 1874 - 1877.
Genetics is now known to play a substantial role in the predisposition to obesity and may contribute up to 70% risk for the disease. Over a hundred genes and gene variants related to excess weight have been discovered. Yet, genetic obesity risk does not always translate into actual obesity development, suggesting complex interactions between ...
Some genetic and lifestyle factors affect an individual's likelihood of adult obesity; thus, the significant clusters of obesity observed in specific geographical regions and contexts also signal the impact of socioeconomic and environmental factors in "obesogenic" environments [13].Understanding the causes and determinants of obesity is a critical step toward creating effective policy and ...
The candidate gene approach was first applied in the mid-1990s and aimed to validate genes identified through human and animal models of extreme obesity for a role in common obesity (fig. 3 ...
Expanding the genetic landscape of obesity. In a recent Cell Genomics article, Kaisinger, Kentistou, Stankovic, et al. use a large-scale exome sequencing study in the UK Biobank to identify rare gene variants associated with sex-specific and life-course effects on obesity. Jian Yang discusses the authors' findings and wider context in obesity ...
Obesity prevalence among children is >30% in the Cook Islands, Nauru and Palau, with a notable increase over the past few decades. Worldwide prevalence of obesity increased at an alarming rate in ...
Obesity is a major health problem worldwide. It is more common in established countries but is on the increase in developing countries. The worldwide prevalence of obesity [body mass index (BMI) ≥ 30 kg m 2] has doubled between 1980 and 2008, with a prevalence of 13% in the adult population reported in 2014.In 2013, there were 42 million obese children below the age of five years [].
Obesity develops as a result of dietary and lifestyle factors, but studies also suggest a genetic influence on obesity [ 11 ]. Obesity is highly influenced by genetics; available data suggest that 40% to 77% of the observed variance in human body weight can be accounted for, by inherited factors [ 12 - 14 ].
In a new study in Translational Psychiatry, Morys et al. show that genetic risk for obesity in youth is linked to developmental brain changes that result in weight gain later. Obesity pandemic is ...
In this study, we reviewed a total of 97 research papers. Of these, 80 studies were population studies and 17 studies were in vivo. The relationship between T2D and obesity has been investigated and has been referred to as the role of related genes and environmental factors in the development of T2D.
Around 250 genes are now associated with obesity. The FTO gene on chromosome 16 is the most important and carries the highest risk of the obesity phenotype. The Genetic Investigation of Anthropomorphic Traits Consortium is the organization involved in furthering research in GWAS. However, genetic mutations alone cannot explain the heritability ...
Dr. Vukasinov notes that there is a rare form of obesity called monogenic obesity, which results in spontaneous mutations of single genes and leads to early onset obesity in childhood. This is something that a genetic blood test can detect, and it may be useful information as you and your doctor navigate the best path forward for your health.
Abstract. This review has examined the scientific basis for our current understanding of obesity that has developed over the past 100 plus years. Obesity was defined as an excess of body fat ...