
- Previous Article

Presentation
Clinical pearls, case study: man with type 2 diabetes and stage 1 kidney disease on atkins-like diet.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Deborah Thomas-Dobersen , Lynn Casey; Case Study: Man With Type 2 Diabetes and Stage 1 Kidney Disease on Atkins-Like Diet. Clin Diabetes 1 January 2005; 23 (1): 46–48. https://doi.org/10.2337/diaclin.23.1.46
Download citation file:
- Ris (Zotero)
- Reference Manager
C.S. is a 45-year-old Hispanic man with a 10-year history of type 2 diabetes. He has a glycated hemoglobin of 7.0% and a blood pressure of 130/80 mmHg, treated with an angiotensin-converting enzyme inhibitor for the past 2 years. He has stable background retinopathy and is a nonsmoker. His BMI has been 30 (height 5′10″, weight 210 lb) for the past year. However,lately, he has put himself on the latest high-protein diet (i.e., the Atkins diet).
His weight has dropped by 10 lb, his fasting serum triglyceride level has fallen from 185 to 130 mg/dl, and his blood pressure has decreased to 120/78 mmHg. His LDL cholesterol has remained stable at 102 mg/dl on a statin. His serum creatinine is 0.9 mg/dl, and his 24-hour urine shows a significant increase in microalbumuria from 100 mg/24 hours last year to the current 200 mg/24 hours. He has stage 1 chronic kidney disease indicating kidney damage,with a normal glomerular filtration rate (GFR) of 98 ml/min/1.73 m 2 .
Would the weight reduction, blood pressure, and lipid-lowering accomplished by this high-protein, low-carbohydrate diet be an acceptable choice for a patient who is at significant risk of cardiovascular disease?
What are the recommendations of the American Heart Association (AHA), the National Kidney Foundation (NKF), the National Academy of Sciences, and the American Diabetes Association (ADA) regarding this type of diet for diabetes and/or weight loss?
What has research revealed about appropriate levels of macronutrients for patients such as C.S.?
It is likely that microalbuminuria is the start of a continuum progressing to macroalbuminuria and proteinuria. Microalbuminuria predicts renal disease in diabetes (both type 1 and type 2) and relates to premature mortality. Microalbuminuria is also a marker for pronounced diabetic vascular disease(endothelial dysfunction and chronic low-grade inflammation). Abnormal albuminuria is a major risk factor for cardiovascular complications,predicting increased cardiovascular morbidity and mortality. 1
Twenty to thirty percent of patients with type 2 diabetes develop evidence of nephropathy. Some patients already have microalbuminuria or overt nephropathy upon diagnosis. Without intervention, 20-40% of those with microalbuminuria progress to overt nephropathy. For those on the continuum from overt nephropathy to end-stage renal disease (ESRD), the greater risk of death from coronary artery disease (CAD) may intervene. 2
The average adult protein intake in the United States is 15-20% of total calories and has remained consistent from 1909 to the present. 3 Most Americans eat 50% more protein than they need. The Recommended Dietary Allowance (RDA) is 0.8 g of good quality protein per kilogram body weight per day for men and women. The high-protein Atkins and Zone diets recommend 125 g/day (36% kcal from protein) and 127 gm/day (34% kcal from protein),respectively. 4 The initial phases of the South Beach diet are similar, but no specific nutrient intake can be found in the diet's literature. In C.S., the Atkins diet would contribute 1.3 g protein/kg body weight and 36% of total daily calories from protein. Thus, high-protein diets promote a significantly abnormally high protein intake.
There is some evidence that a sustained high-protein diet can adversely affect renal function, especially in people with diabetes with or without mild renal insufficiency. In patients without renal insufficiency, a high-protein diet may act by acutely increasing the GFR and causing intraglomerular hypertension, which may cause progressive loss of renal function. In the Nurses Health Study, 1,624 female nurses between 30 and 55 years of age were followed for a period of > 11 years. The highest quartile of total protein intake, an average of 93 g/day, was significantly associated with a decline in GFR in women with mild renal insufficiency, thus worsening renal disease. 5 Previous studies had shown mixed results of high-protein diets on renal function but had limitations such as small patient numbers, limited follow-up, and a narrow range of protein intake.
Looking at this relationship from another angle, a meta-analysis recently showed that protein restriction retards the rate of decline in GFR, thus lessening kidney damage. The resulting decrease in kidney damage was small and not impressive. However, when studies looking at people with diabetes were combined, a total of 102 patients given a mean protein restriction of 0.7 g/kg/day versus a control group given 1 g/kg/day (a narrow range), showed a more impressive improvement in renal function independent of the original renal function over 22 months. 6 A crosssectional study of > 2,600 people with type 1 diabetes found that a protein intake > 20% of calories was associated with an increased urinary albumin excretion rate. Researchers concluded that people with diabetes should not exceed a protein intake of 20% of calories. 7 Any study in type 1 diabetes is applicable to type 2 diabetes as it relates to nephropathy. Therefore, there is evidence to recommend avoidance of high protein intakes in patients at risk for renal disease, i.e. all patients with type 1 or type 2 diabetes.
Nutrient analysis of high-protein diets is a concern. With some high-protein diets, such as Atkins, come carbohydrate restrictions. Yet high-carbohydrate foods, such as fruits, vegetables, and low-fat dairy products, provide potassium, magnesium, and calcium, which modestly reduce blood pressure. 8 Normal blood pressure is critically important in preventing CAD and microalbuminuria. With high-protein diets and carbohydrate restrictions come decreased-fiber diets. High-fiber diets have many beneficial effects,including weight loss and lower cardiovascular and cancer risks. With high-protein diets come higher intakes of saturated fats, which are potentially atherogenic. 9 In addition, experimental evidence indicates that a high-protein diet and the resultant increase in saturated fat intake may accelerate the progression of renal disease. Increased LDL cholesterol can stimulate mesangial hypertrophy and stimulate cytokine formation, which may ultimately cause tissue injury. In both type 1 and type 2 diabetes, hypercholesterolemia is a predictor of deteriorating kidney function. 10
The RDA for carbohydrate is set at 130 g carbohydrate/day for adults and children based on the average minimum amount of glucose utilized by the brain to ensure optimal brain function. 11 That pretty much omits Atkins (28-33 g/day) and the early phases of the South Beach diet. Recent AHA guidelines discourage high-protein diets for weight loss,citing potential increased risk for coronary heart disease and renal disease. 12 The most recent ADA technical review on nutrition states that high-protein diets are not recommended until further research establishes their safety. 3 Concerns include renal function and cardiovascular disease. The NKF states in its Kidney Disease Outcomes Quality Initiative guidelines for chronic kidney disease that there is no benefit from a protein intake higher than the RDA of 0.8 g/kg body weight and that this is a reasonable level to recommend for patients with chronic kidney disease in stages 1-3. 13 Thus, many respected nonprofit health care organizations discourage the use of high-protein, low-carbohydrate diets.
Literature reviews of research on the effect of high-protein,low-carbohydrate diets on obesity and lipid levels are not convincing. A review of the literature describing adult outpatient recipients of low-carbohydrate, high-protein diets compared a wide variety of study designs,carbohydrate levels, durations, and calorie levels. Only five studies evaluated low-carbohydrate, high-protein diets for > 90 days, and these were nonrandomized, uncontrolled studies. The three variables that most predicted weight loss were calorie level, duration of calorie restriction, and number of very obese participants in the study. Reduced carbohydrate content was not significantly associated with weight loss. 14
Another review concluded that populations at risk for renal disease, such as patients with diabetes, should avoid high-protein diets. The authors also caution that evidence suggested that protein intakes in excess of two to three times the RDA may have harmful effects on calcium homeostasis and possibly bone mass, 15 a problem for a population already predisposed to osteoporosis. In addition, a comparison of high-protein, low-carbohydrate diets versus a low-fat diet for weight loss shows them equally effective after 1 year in duration. 16 A recent small, randomized, clinical trial comparing a low-carbohydrate (< 30 g) to a conventional low-fat diet in severely obese patients, including individuals with diabetes, showed no significant difference in weight loss after 1 year, although weight loss was minimal (11 vs. 7 lb). Of interest was that the weight loss on the low-carbohydrate diet did not appear to be sustainable and that blood urea nitrogen levels increased more in the low-carbohydrate group. 17
Reduced energy intake is an important therapeutic objective for the patient in the case described above. Reduced energy intake would reduce his blood pressure and serum lipids as well as improve his glycemic control. Weight loss was effective in lowering his blood pressure and serum triglycerides, as one would expect. However, the macronutrient content of his diet may have exacerbated the microalbuminuria. Therefore, a patient such as C.S. would be illadvised to stay on the high-protein diet because of the potential risk to his kidney function as shown by his elevated microalbuminuria.
With guidance from a registered dietitian, C.S. started a 1,500-kcal,low-fat diet with a walking program of 2 miles/day, 6 days/week. He was very tired of the restrictive nature of the high-protein diet and welcomed a change. His urine microalbumin level fell to < 50 mg/24 hours.
Two important studies show strategies that work to yield long-term weight loss. In order to determine what strategies work for long-term weight loss,the National Weight Control Registry elicited and studied information from> 800 people who have been successful in this endeavor. Only half had lost weight through weight loss programs. The remainder had lost weight without medical intervention. Keys to success were an average calorie intake of ∼1,400 kcal/day, a low-fat diet (24% of kcal), and a high energy expenditure through exercise (2,800 kcal/week). 18 The Diabetes Prevention Program also documented that a low-fat diet, increased physical activity, and educational sessions with frequent follow-up allowed participants to lose 7% of their body weight and maintain a 5% weight loss for 3 years. 19
High protein intakes cause higher workloads for kidneys, whose function is to handle amino acid fragments during protein degradation and excrete nitrogen as urea.
There is no research documenting that a high-protein diet maintains weight reduction any better than a low-fat diet, which is safer and offers long-term results.
Safety and efficacy of high-protein, low-carbohydrate diets are a concern for patients with diabetes, regardless of documented kidney disease.
Additional Information
Concerns about the low-carbohydrate diet craze of 11 leading nonprofit consumer, nutrition, and public health organizations are discussed in a format appropriate for both health professionals and patients at the Partnership for Essential Nutrition website: www.essentialnutrition.org .
Deborah Thomas-Dobersen, RD, MS, CDE, is a diabetes educator at the Center for Diabetes and Endocrinology in Arvada, Colo. Lynn Casey, RD, CSR, is a renal dietitian at Renal Care Group, Inc., in Denver, Colo.
Email alerts
- Online ISSN 1945-4953
- Print ISSN 0891-8929
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Day 1: A 62-year old, recently widowed male Hispanic patient, named Mr. Kevin Ulyses Blanco (K. U. B.) was brought in to the emergency department (ED) by his daughter for progressively worsening shortness of breath, fatigue, a lingering non-productive cough, and generalized edema. One month prior, he noticed dyspnea upon exertion, loss of appetite, nausea, vomiting and malaise, which he attributed to the flu. In the emergency department, he appeared anxious and pale, and had a dry yellow tint to the skin. He denied any chest pain, and he could not recall the last time he urinated. He has history of benign prostatic hyperplasia, diabetes mellitus type 2, hypertension, dyslipidemia, and renal insufficiency for the past two years. His ED assessment findings included: 1+ pedal edema, basilar crackles in the lungs bilaterally, and a scant amount of urine according to a bladder scan. His lab results indicated a glomerular filtration rate (GFR) of 12. Based on his subjective and objective symptoms, he was admitted with a diagnosis of progression of chronic kidney disease (CKD) to end-stage renal disease (ESRD). The plan of care was focused on managing his symptoms and consulting with his nephrologist regarding need for hemodialysis.
Day 3: Mr. K.U.B had an AV graft placed in his forearm to receive dialysis and a dual-lumen hemodialysis catheter for temporary use. His symptoms were worsening despite medical interventions and hemodialysis was needed urgently. The plan was to continue his medications to manage anemia, HTN, diabetes, and renal disease. The nurse identified psychosocial stressors of financial concern and having to live alone with his worsening health condition. With his daughter living far away, he was worried he wouldn’t have support. He stated that he was worried about the financial burden of hemodialysis and struggled with facing the reality of his diagnosis and what his quality of life would be like in the next few years of his life. A recommendation was made for a social worker and psychiatric consult.
Day 8: By the end of day 8, most of his acute symptoms had been relieved and he was stable enough to be discharged. He had been in contact with case management for his follow up appointment had been made with his primary physician and discharge teaching was given.
- What modifiable factors could Mr. K.U.B. have addressed to slow the progression of his renal disease?
- What collaborative interventions could be used to enhance his care and ensure continuity of care after discharge?
- What affect did uncontrolled hypertension and poor medication compliance have on his disease process?
Nursing Case Studies by and for Student Nurses Copyright © by jaimehannans is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book
- Open access
- Published: 02 May 2024
Establishing kidney transplantation in a low-income country: a case in Tanzania
- Francis F. Furia ORCID: orcid.org/0000-0003-2668-3041 1 , 2 , 3 ,
- Jaqueline G. Shoo 1 , 2 , 3 ,
- Paschal J. Ruggajo 1 , 2 , 3 ,
- Jonathan W. Mngumi 1 , 2 , 3 ,
- Gudila Valentine 1 , 2 , 3 ,
- Mahmoud A. Muhiddin 1 , 2 ,
- Njiku Kim 4 ,
- Isaack Mlatie 4 ,
- Moses Mulungu 5 ,
- Namala Mkopi 6 ,
- Mabula Kasubi 7 ,
- Elizabeth S. Moshi 8 ,
- Lameck Mnyanyu 8 ,
- Ramadhani Hamis 9 ,
- Deus Buma 10 ,
- Mary C. Mtolera 11 ,
- Onesmo A. Kisanga 1 , 2 ,
- Hedwiga Swai 1 &
- Lawrence Museru 12
Renal Replacement Therapy volume 10 , Article number: 29 ( 2024 ) Cite this article
337 Accesses
59 Altmetric
Metrics details
Sub-Saharan African countries, including Tanzania, have a high burden of chronic kidney diseases (CKDs) and limited capacity for the provision of services. Tanzania and other countries in the region have made significant improvements in the provision of services for patients with CKD, including hemodialysis. Few countries are offering kidney transplantation services, which is the definitive treatment for patients with CKD and kidney failure. This study was conducted to review the steps taken by Muhimbili National Hospital (MNH) to establish a kidney transplantation service in Tanzania.
This study was based on the review of the activities that were undertaken to establish kidney transplantation services at Muhimbili National Hospital in Dar es Salaam, Tanzania. It was conducted by reviewing key documents developed for kidney transplantation and interviewing key personnel who were involved in the process.
Kidney transplantation services at MNH were established in November 2017; several steps were taken in the preparatory phase including training of personnel, infrastructural modifications, and procurement of equipment and supplies. Capacity building was achieved through international collaboration with several international and local institutions, including three Hospitals in India. The transplant team, which included nephrologists, urologists, anesthesiologists, radiologists, nurses, laboratory technicians, a transplant coordinator, and a lawyer, underwent short-term training at BLK Hospital in India. Initial transplant procedures were carried out with support from visiting personnel from BLK, Sakra, and Seifee hospitals. In total, 72 transplant surgeries were conducted, of which 39 (54.2%) were performed with visiting teams and 31 (45.8%) by the local team independently. Of the initial 39 recipients, 56.4% were males and 43.5% were aged above 46 years. About half of the donors were brothers/sisters, and 43.5% had human leukocytic antigen haplomatch. Induction immunosuppression included basiliximab in the majority (64.1%) of recipients, and all recipients received prednisolone, tacrolimus, and mycophenolate mofetil/myfortic.
Conclusions
Establishing kidney transplantation in lower-income countries, such as Tanzania, is feasible; however, it requires dedicated efforts. Collaboration with local and international institutions provided an enabling environment for the transfer of skills and access to necessary supportive services.
Chronic kidney diseases (CKDs), which are estimated to affect about 12% of the global population, contribute to significant morbidity and mortality; 1.2 million deaths globally were attributed to CKD in 2017 [ 1 , 2 ]. The burden of CKD has strained health systems in most lower and middle-income countries especially in the sub-Saharan Africa (SSA) region, which has poorly developed infrastructures and human resources for the provision of services [ 3 , 4 ]. The workforce for care of CKD patients in most lower-income countries is scarce, and there is limited infrastructural capacity for renal replacement therapy, including kidney transplantation [ 4 ]. The density of nephrologists per million population is very low (< five per million) in most sub-Saharan African countries, indicating a mismatch between the workforce and the high burden of CKD in the region estimated at 13.9% [ 3 , 5 ].
Burden of chronic kidney diseases in Tanzania
Tanzania, like other countries in SSA, has a high burden of CKD with a community-based prevalence ranging between 7% and 14% [ 6 , 7 , 8 ]. A higher prevalence of CKD is reported in hospitals; Kilonzo et al. reported a prevalence of 69.5% among patients admitted to medical wards at Bugando Medical Centre (BMC) from October 2013 to March 2014 [ 9 ]. Similar findings were noted by Mubarakali et al. and Msango et al., reporting CKD prevalence rates of 83.7% and 80% for patients with diabetes mellitus and human immunodeficiency virus (HIV) infection, respectively, at BMC [ 10 , 11 ]. Diabetes mellitus, hypertension, chronic glomerulonephritis, and viral infections, including HIV, and hepatitis B and C viruses, are known risk factors for CKD in Tanzania [ 6 , 12 ].
Renal replacement therapy for patients with CKD in Tanzania
Hemodialysis is the predominant modality of renal replacement therapy in Tanzania, and in the last two decades, tremendous improvement has been made in this service. In December 2018, there were 28 hemodialysis units with 933 patients with CKD on maintenance hemodialysis [ 13 ] in Tanzania. There has been a steady increase in the number of hemodialysis units in the country operated by both public and private facilities, many regional referral hospitals are setting up facilities for hemodialysis. Despite this increase, there is limited access to these services for many patients in the country with CKD and kidney failure [ 14 , 15 ].
Acute peritoneal dialysis (PD) is also offered at some facilities in Tanzania, and with the improving coverage of hemodialysis, peritoneal dialysis has largely remained an option for the treatment of children with acute kidney injury [ 13 , 16 , 17 ]. PD is provided using improvised equipment and supplies and fluids are constituted using intravenous fluids. The type of catheters and dialysate used for PD make this modality only suitable for managing acute kidney injury (AKI), which requires short therapy.
For many decades patients with CKD and kidney failure requiring kidney transplantation were sent overseas. The first ten candidates were transplanted in the UK in the 1980s; subsequently, many patients were transplanted in India, and a few were sent to other countries, including Kenya [ 13 , 18 ]. More than 200 patients requiring kidney transplantation and their donors were supported by the government through the Ministry of Health for their treatment in India. Most of these patients received their pretransplantation workup and their posttransplantation follow-up at Muhimbili National Hospital [ 13 ]. MNH has been providing pretransplantation and posttransplantation care for many years.
The growing number of patients with CKD and kidney failure, some of whom are undergoing hemodialysis, presented the need to establish kidney transplantation services in Tanzania. The cost of a single session of hemodialysis in Tanzania is 240,000–300,000 TShs ($104–130) amounting to 35–44 million TShs ($15,000–20,000) annually; this is very expensive and is similar to other reports of cost for this service in the region [ 19 , 20 ]. Comparatively, kidney transplantation may be cheaper than hemodialysis, although the initial transplant surgery and care may be high. Establishing national kidney transplantation services is a complex process requiring enormous investments in the form of human resources, equipment as well and a legal framework to safeguard the safety of donors, recipients, and the community [ 21 ]. This study describes the initiatives undertaken by Muhimbili National Hospital in setting up a kidney transplantation service in Tanzania.
This study is a review of the actions that were undertaken by Muhimbili National Hospital (MNH) in establishing kidney transplantation. MNH is located in Dar es Salaam, Tanzania, and is the national referral hospital with a 2000 bed capacity, it has the largest hemodialysis unit with 50 hemodialysis machines and one continuous renal replacement therapy (CRRT) machine. MNH is the teaching hospital for Muhimbili University of Health and Allied Sciences (MUHAS). Multiple specialized clinics falling under nephrology unit are offered at MNH, including general nephrology, pediatric nephrology, kidney donors, and kidney recipient clinics.
This study was conducted by interviewing key personnel from departments and units that are involved in the provision of kidney transplantation services and played a part in establishing transplant services. Departments included in this study included nephrology, urology, a central pathology laboratory, anesthesiology, radiology, critical care, pharmacy, social welfare, and legal services. Key documents that were prepared for kidney transplantation were reviewed including patients’ charts for 39 transplant recipients who were transplanted with support from collaborating hospitals from India. Patient charts that were reviewed had information up to 1 month posttransplantation only. This study was approved by the ethical committee of Muhimbili National Hospital with a waiver of consent as no personal information was collected or used in the study.
The information collected in the review process included training of health personnel in kidney transplantation, and improvement of infrastructure, including procurement of equipment, creation of dedicated spaces, and preparation of necessary documents for these services.
Training of health care personnel
In August 2016, a team of doctors, nurses, and laboratory scientists traveled to BLK Hospital in India for 3 months of training, the training was aimed at exposing these practitioners to kidney transplantation services at BLK. Table 1 indicates the practitioners and the skills acquired at BLK Hospital, India.
Transplantation guideline
The team involved in transplantation at MNH developed a standard operating procedure (SOP) for kidney transplantation. This SOP guides all the procedures involved in the process of transplantation. The SOP also included the evaluation of donors and recipients and the immunosuppression protocol.
Donor and recipient evaluation
Recipients and donors are extensively evaluated before kidney transplantation, this is carried out by taking history for common risk factors and followed by laboratory tests for determining renal and liver functions, screening for medical conditions, and screening for infections and malignancies as indicated in Supplementary documents 1 and 2 . Human leukocytic antigens and CDC cross-match are also carried out as the last tests before kidney transplantation. Once all the evaluation is done and before submission of the documents to the kidney transplantation authorization committee, a joint meeting is conducted between the transplant team, including nephrologists, urologists, anesthesiologists, microbiologists, and transplant coordinators. After this meeting nephrologists and urologists discuss with the donor and recipients to inform them about the procedures and anticipated complications and also to respond to their questions. After this meeting donor and recipient files and their legal documents are submitted to the kidney transplantation authorization committee.
Immunosuppression protocol
The immunosuppression protocol included the following medications.
Induction medications;
Induction medications adopted for MNH guidelines were anti-thymocyte globulin-rabbit (ATG-rabbit) and basiliximab for high-risk and low-risk transplant pairs, respectively.
Maintenance of immunosuppression drugs;
Maintenance immunosuppressants selected included tacrolimus, mycophenolate mofetil (MMF)/myfortic acid, and prednisolone. Cyclosporine, everolimus, and azathioprine were also included as alternative drugs.
Prophylaxis;
Post kidney transplant prophylaxis was included in the SOP and prophylaxis is recommended for cytomegalovirus, pneumocystis pneumonia, and oral candida infection. Recommended drugs for prophylaxis are valganciclovir, co-trimoxazole, and clotrimazole/nystatin for cytomegalovirus (CMV), Pneumocystis carinii pneumonia (PCP), and oral candidiasis, respectively. Prophylaxis against CMV and PCP is for 6 months while candida is for 3 months.
Laboratory equipment, dedicated spaces, and provision of supplies
The hospital made a dedicated effort to establish infrastructure to support kidney transplantation, these include the procurement of allocating clinical space, and procurement of supplies and equipment. A transplant ICU was created with three beds, ventilators, monitors, and a reverse osmosis plant for hemodialysis machines. The equipment that was procured included a CRRT machine, plasmapheresis machine, arterial blood gas machine, and crossmatch machine. Other supplies that were procured included induction drugs (basiliximab and anti-thymocyte globulin -rabbit), leukodepletion tubing for blood transfusion, and spirometry.
Collaborating institutions in establishing kidney transplantation at MNH
Several local and international institutions were engaged to facilitate the establishment of the program at MNH, this collaboration offered support in the form of training, clinical support, and laboratory services as indicated in Table 2 .
Legal framework to support transplantation
There was no legal framework for organ transplantation in Tanzania, therefore to support kidney transplantation at MNH, the regulations for the legislative act, which established Muhimbili National Hospital in 2000 (Muhimbili National Hospital Act 2000), were changed and clauses for guiding kidney transplantation were included [ 22 ]. The MNH Renal Services Regulations 2017 provided the responsibility for regulating the removal, storage, and transplantation of kidneys to avoid commodification and organ trade. The regulation allows the transplantation of kidneys involving near relatives, which include a spouse, child, parent, sibling, grandparent, grandchild, cousin, nephew, niece, uncle, or aunt.
The regulations also provided for the position of transplant coordinator who should be a nurse or social worker appointed by the executive director. The establishment of a transplant authorization committee is prescribed in the regulations. The role of the transplantation authorization committee is to approve the joint application of the kidney donor and recipient for removal and transplantation; seven members of the authorization committee are appointed by the Board of Trustees of MNH. These members include:
Director of medical services–chairperson of the committee
Two medical doctors appointed by the executive director from within the hospital who are not involved in kidney transplantation
A senior officer conversant with health matters appointed by the Ministry
A senior lawyer of high integrity, social standing, and credibility (preferably a retired high court judge).
A doctor from any private hospital in Dar es Salaam
Two religious leaders, one representing Christians and the other Muslims
The secretary to the committee shall be the Head of the legal unit of MNH.
Before application to the authorization committee, a medical meeting will be convened to deliberate on the reports of the prospective donor and recipients and members of the medical meeting shall include nephrologists, urologists, transplant coordinators, social workers, the donor, and the recipient.
Process of obtaining donors at Muhimbili national hospital
The renal unit at MNH facilitates the process of identifying donors by holding family conferences in which the recipient is asked to invite his/her relatives to participate. Participants include potential donors, influential people in the family, and other key members of the family. The conference is facilitated by the transplant coordinator (who is a nurse) and social worker in the renal unit.
During the conference, information discussed with families included the transplant process, program options, risks and benefits (both live donor and deceased donor transplants), medication regimen, lifestyle adjustments, effect of transplantation on existing medical conditions, temporary relocation to Dar es Salaam (if required), and short and long term outcomes of kidney transplantation. At the conference, health information is provided to the family, and all important issues regarding kidney donation are discussed and participants are allowed to ask questions. After the conference, the family is given time to discuss and agree on potential donors who will be evaluated.
Kidney transplantation procedures performed at Muhimbili national hospital
The first kidney transplantation was carried out on 21 November 2017, and until now more than 72 patients with CKD have been transplanted. The initial 39 transplantations were carried out with support from visiting transplant teams from different institutions in India. The visiting teams were bigger in the beginning with different practitioners, their numbers were subsequently reduced with improved local capacity. Table 3 , indicates the number of personnel on the visiting team, the number of transplants carried out, and the days spent in Tanzania by the visiting teams.
Table 4 describes the clinical profile of the 39 recipients who were transplanted with the support of the collaborating teams from India; out of 39 recipients 56.4% were males, and 43.5% were aged above 46 years. Donors included brothers/sisters of recipients (46.2%) followed by sons/daughters (33.3%) and second-degree relatives (19.9%). Haplomatch was noted in 46.1% of donor-recipient pairs and the majority (64.1%) of recipients received basiliximab as induction immunosuppression. The mean creatinine at 1 month was 112 µmol/L; one recipient returned to dialysis, and one died.
Challenges experienced since the establishment of the kidney transplantation program at MNH
Several challenges were reported by interviewed participants who were involved in the program from the inception of the program. Main challenges included.
Challenges in obtaining supplies for the service include drugs that are not registered in Tanzania, particularly immunosuppressive drugs, graft preservation fluids, and cross-matching reagents. These had a short shelf life making it difficult to stock adequate supplies.
Limited financing for kidney transplantation procedures especially for patients who are not subscribed to the National Health Insurance Fund.
Limited public knowledge and misinformation on transplant procedures resulted in a decline in consent from some donors.
Tanzania, like many other countries in sub-Saharan Africa, is faced with a high CKD burden and limited capacity for the provision of services, and many countries in the region have made significant efforts to advance nephrology services. In the last decade Tanzania has made remarkable improvement in the provision of nephrology services, this is noted in the increased number of hemodialysis units [ 13 , 23 ]. This study aimed to examine steps taken by Muhimbili National Hospital to establish kidney transplantation services in Tanzania and the achievements made in 5 years.
International and local collaboration featured as one of the most important steps in establishing news services and through this collaboration, MNH was able to build capacity in human resources as well as supportive laboratory services. The international collaboration involved three hospitals from India, whereby one hospital provided short-term training for the transplant team. A similar approach was used to support the establishment of kidney transplantation in Ghana [ 24 ].
A legal framework is key for the provision of ethical organ transplantation, this was made possible through the adoption of the Istanbul declaration [ 25 ] and the amendment of regulation for the act, which established Muhimbili National Hospital. This was an important move to support services at MNH, however, this is a limiting factor for the establishment of similar services in other hospitals in Tanzania. For the sustainability and scaling of organ transplantation services in Tanzania, it is important to prepare organ transplantation legislation that will guide organ procurement, storage, and allocation and address ethical dilemmas.
The cost of transplantation is one of the main challenges for organ transplantation, and efforts to lower the costs are encouraged including using low-cost alternative drugs [ 26 ]. The first 39 transplant patients were kept on three immunosuppression drugs including prednisolone, tacrolimus, and mycophenolate mofetil/myfortic. The use of MMF/myfortic instead of azathioprine had financial implications as the price of 100 mg of azathioprine is 0.8 USD while the price of 500 mg of MMF is about 3 USD. The induction immunosuppression drugs used for the transplant recipients included ATG and basiliximab, with the majority of patients receiving basiliximab. The choice of induction drugs was driven by HLA matching, in which the majority of donor–recipient pairs had good HLA matching.
The MNH transplantation guideline was influenced by the practice in the two collaborating institutions, and the drugs included as first line are expensive. It is therefore important for emerging centers in Tanzania to consider cost-effective approaches when establishing organ transplantation and other services to ensure sustainability. To enable patients to meet the costs of medications, it may be necessary to consider switching maintenance immunosuppression drugs from MMF/myfortic to azathioprine.
The number of transplants carried out since the establishment of services at MNH is 72; an average of 14 transplants per year, which is small but encouraging, with 43 transplants being carried out by the local team. The low number of transplantations can be attributed to the difficulties of obtaining drugs, reagents, and other supplies most of which are not registered in Tanzania making their procurement from overseas challenging and time-consuming.
The availability of kidney transplantation services in Tanzania will not only improve access but also reduce the cost of sending patients overseas, which was estimated to cost US $60,000 as compared with US $10,000 with local transplantation [ 21 ]. National transplantation services will provide a regulatory and legal framework for curbing organ trade which is linked with transplantation services sought overseas [ 27 , 28 ]. The current authorization process at MNH, which makes use of an authorization committee with nonmedical members, such as religious leaders and attorneys, may be difficult to operationalize in the future with an increase in transplant procedures. The Ministry of Health in Tanzania is currently in the initial process of preparing the bill for organ donation, the experience of MNH will be useful in informing the preparation of this legislation.
The success of carrying out transplantation with a reasonable outcome in 1 month shows the potential for establishing this service in a low-resource setting, and is a good reflection of operationalization of Bamako’s resolutions of 2008, which called for emerging centers to establish kidney transplantation services through international and local collaborations [ 29 ]. This has also demonstrated feasibility for other countries in the limited resource setting to emulate, and it is high time for the African Association of Nephrology to encourage all countries in sub-Saharan Africa to establish collaborative partnerships to improve services.
Nephrology services in Tanzania have improved dramatically in the past decade with an increasing number of hemodialysis services and the establishment of kidney transplantation services in the last 5 years. International and local collaborative partnership is critical for advancing services in emerging countries, as was demonstrated in this study between MNH and three hospitals from India. Making infrastructural changes, training healthcare providers, and preparing legal framework are essential in supporting kidney transplantation services, and sustaining these services calls for concerted efforts in addressing challenges, including costs of transplantation and shortage of supplies and drugs.
Availability of data and materials
No datasets were generated or analyzed during the current study.
Abbreviations
Anti-thymocyte globulin
Chronic kidney disease
Complement-dependent cytotoxicity
Cytomegalovirus
Continuous renal replacement therapy
Diethylenetriamine pentaacetate
Human leukocytic antigen
Intensive care unit
Mycophenolate mofetil
Muhimbili National Hospital
Muhimbili University of Health and Allied Sciences
Ocean Road Cancer Institute
Pneumocystis carinii pneumonia
Standard operating procedures
Mills KT, Xu Y, Zhang W, Bundy JD, Chen C, Kelly TN, Chen J, He J. A systematic analysis of worldwide population-based data on the global burden of chronic kidney disease in 2010. Kidney Int. 2015;88:950–7.
Article PubMed PubMed Central Google Scholar
GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2020;395(10225):709–33. https://doi.org/10.1016/S0140-6736(20)30045-3 .
Article Google Scholar
Crews DC, Bello AK, Saadi G. Burden, access, and disparities in kidney disease. Nephron. 2019;141:219–26.
Article PubMed Google Scholar
Naicker S. End-stage renal disease in Sub-Saharan Africa. Kidney Int Suppl. 2013;3:161–3. https://doi.org/10.1038/kisup.2013.4 .
Stanifer JW, Jing B, Tolan S, Helmke N, Mukerjee R, Naicker S, Patel U. The epidemiology of chronic kidney disease in sub-Saharan Africa: a systematic review and meta-analysis. Lancet Glob Health. 2014;2:e174-181.
Stanifer JW, Maro V, Egger J, Karia F, Thielman N, Turner EL, et al. The epidemiology of chronic kidney disease in northern Tanzania: a population-based survey. PLoS ONE. 2015;10(4): e0124506. https://doi.org/10.1371/journal.pone.0124506 .
Article CAS PubMed PubMed Central Google Scholar
Ploth DW, Mbwambo JK, Fonner VA, Horowitz B, Zager P, Schrader R, Fredrick F, Laggis C, Sweat MD. Prevalence of CKD, diabetes, and hypertension in rural Tanzania. Kidney Int Rep. 2018;3:905–15. https://doi.org/10.1016/j.ekir.2018.04.006 .
Hodel NC, Hamad A, Praehauser C, Mwangoka G, Kasella IM, Reither K, et al. The epidemiology of chronic kidney disease and the association with non-communicable and communicable disorders in a population of sub-Saharan Africa. PLoS ONE. 2018;13(10): e0205326.
Kilonzo SB, Seiffudin AT, Bakshi FA, Gunda DW. Renal dysfunction among adult patients in Mwanza, Tanzania: prevalence, outcomes and associated factors. Tanzan J Health Res. 2016. https://doi.org/10.4314/thrb.v18i3.5 .
Msango L, Downsa JA, Kalluvya SE, Kidenya BR, Kabangila R, Johnson WD Jr, Fitzgerald DW, Peck RN. Renal dysfunction among HIV-infected patients starting antiretroviral therapy in Mwanza, Tanzania. AIDS. 2011;25(11):1421–5. https://doi.org/10.1097/QAD.0b013e328348a4b1 .
Article CAS PubMed Google Scholar
Janmohamed MN, et al. Prevalence of chronic kidney disease in diabetic adult out-patients in Tanzania. BMC Nephrol. 2013;14:183.
Meremo AJ, Masalu MB, Sabi I, Ngilangwa DP, Kapinga J, Tagalile R, et al. Prevalence and risk factors associated with chronic kidney disease among patients presenting at a haemodialysis unit in Dodoma, Tanzania. East African Health Res J. 2018;2(1):53–7. https://doi.org/10.2424/EAHRJ-D-16-00367 .
Furia FF, Shoo J, Ruggajo PJ, Kilonzo K, Basu G, Yeates K, Varughese S, Svarstad E, Kisanga O. Developing nephrology services in low-income countries: a case of Tanzania. BMC Nephrol. 2019;20:378. https://doi.org/10.1186/s12882-019-1568-7 .
Pancras G, Shayo G, Anaeli A. Non-medical facilitators and barriers towards accessing haemodialysis services: an exploration of ethical challenges. BMC Nephrol. 2018;19:342. https://doi.org/10.1186/s12882-018-1140-x .
Mohamedi S, Mosha IH. Hemodialysis therapy adherence and contributing factors among end-stage renal disease patients at Muhimbili national hospital, Dar es Salaam. Tanzania Kidney Dial. 2022;2:123–30. https://doi.org/10.3390/kidneydial2010014 .
Kilonzo KG, Ghosh S, Temu SA, Maro V, Callegari J, Carter M, Handelman G, Finkelstein FO, Levin N, Yeates K. Outcome of acute peritoneal dialysis in northern Tanzania. Perit Dial Int. 2012;32(3):261–6. https://doi.org/10.3747/pdi.2012.00083 .
Kilonzo K, Mathew A, Croome AJ. Establishment of an acute peritoneal dialysis program in Tanzania. Kidney Int Suppl. 2013;3(2):186–9.
Basinda SL, Maro EE, McLarty DG, Young AE, Wing AJ. Ten Tanzanian transplants: problems and perspectives. Postgrad Med J. 1988;64(756):778–82.
Kassa DA, Mekonnen S, Kebede A, Gebremedhin Haile TG. Cost of hemodialysis treatment and associated factors among end-stage renal disease patients at the tertiary hospitals of addis Ababa city and amhara region, Ethiopia. Clinico Econ Outcomes Res. 2020;12:399–409.
Mushi L, Krohn M, Flessa S. Cost of dialysis in Tanzania: evidence from the provider’s perspective. Heal Econ Rev. 2015;5:28. https://doi.org/10.1186/s13561-015-0064-4 .
Kobayashi S, Hidaka S. Can we still ignore renal replacement therapy in sub-Saharan Africa? All living beings are created equal. Renal Replace Ther. 2020;6:5. https://doi.org/10.1186/s41100-019-0243-6 .
Parliament of Tanzania: Muhimbili National Hospital Act of Parliament number 5 of 2000. https://www.parliament.go.tz/polis/uploads/bills/acts/1454228796-ActNo-5-2000.pdf
Fredrick F, Ruggajo P, Basu G, Svarstad E, Langeland N. Global collaboration bears fruit: Tanzania report. Kidney Int. 2015;88(6):1010–213.
Osafo C, Morton B, Ready A, Jewitt-Harris J, Adu D. Transplantation in Ghana. Transplantation. 2018;102(4):539–41.
International Summit on Transplant Tourism and Organ Trafficking. The declaration of istanbul on organ trafficking and transplant tourism. Clin J Am Soc Nephrol. 2008;3(5):1227–31. https://doi.org/10.2215/CJN.03320708 .
Arogundade FA. Kidney transplantation in a low-resource setting: Nigeria experience. Kidney Int Suppl. 2013;3:241–5. https://doi.org/10.1038/kisup.2013.23 .
Amira CO, Bello BT. Do the benefits of transplant tourism amongst Nigerian patients outweigh the risks? A single-center experience. Int J Organ Transplant Med. 2017;8(3):132–9.
CAS PubMed PubMed Central Google Scholar
Okafor UH. Transplant tourism among kidney transplant patients in Eastern Nigeria. BMC Nephrol. 2017;18:215. https://doi.org/10.1186/s12882-017-0635-1 .
Persy VP, Remuzzi G, Perico N, Benghanem Gharbi M, Adu D, Jha V, Rizvi A, Ammar MB, Fongoro S, De Broe ME. Prevention and transplantation in chronic kidney disease: what is achievable in emerging countries? Nephron Clin Pract. 2010;115(2):122–32. https://doi.org/10.1159/000312875 .
Download references
Acknowledgements
All key informants from all the departments involved in the establishment of kidney transplantation services at MNH who provided information for this study are acknowledged for their support during data collection.
No funding was obtained for this work.
Author information
Authors and affiliations.
Department of Internal Medicine, Renal Unit, Muhimbili National Hospital (MNH), Dar Es Salaam, Tanzania
Francis F. Furia, Jaqueline G. Shoo, Paschal J. Ruggajo, Jonathan W. Mngumi, Gudila Valentine, Mahmoud A. Muhiddin, Onesmo A. Kisanga & Hedwiga Swai
School of Medicine, Muhimbili University of Health and Allied Sciences (MUHAS), P. O. Box 65001, Dar Es Salaam, Tanzania
Francis F. Furia, Jaqueline G. Shoo, Paschal J. Ruggajo, Jonathan W. Mngumi, Gudila Valentine, Mahmoud A. Muhiddin & Onesmo A. Kisanga
Muhimbili Renal and Rheumatology Research Group, Muhimbili University of Health and Allied Sciences, Dar Es Salaam, Tanzania
Francis F. Furia, Jaqueline G. Shoo, Paschal J. Ruggajo, Jonathan W. Mngumi & Gudila Valentine
Department of Urology, Muhimbili National Hospital, Dar Es Salaam, Tanzania
Njiku Kim & Isaack Mlatie
Department of Anaesthesiology, Muhimbili National Hospital, Dar Es Salaam, Tanzania
Moses Mulungu
Department of Paediatrics and Child Health, Muhimbili National Hospital, Dar Es Salaam, Tanzania
Namala Mkopi
Central Pathology Laboratory, Muhimbili National Hospital, Dar Es Salaam, Tanzania
Mabula Kasubi
Departemnet of Nursing and Housekeeping, Muhimbili National Hospital, Dar Es Salaam, Tanzania
Elizabeth S. Moshi & Lameck Mnyanyu
Department of Surgery, Muhimbili University of Health and Allied Sciences, Dar Es Salaam, Tanzania
Ramadhani Hamis
Department of Pharmacy, Muhimbili National Hospital, Dar Es Salaam, Tanzania
Departemnt of Radiology, Muhimbili National Hospital, Dar Es Salaam, Tanzania
Mary C. Mtolera
Department of Surgery, Muhimbili National Hospital, Dar Es Salaam, Tanzania
Lawrence Museru
You can also search for this author in PubMed Google Scholar
Contributions
F.F. designed the study, collected data, wrote the report for this study, and drafted the manuscript. J.G.S., P.J.R., J.W.M., and G.V. participated in the study design and data collection. N.K., M.A.M., M.M., N.M., D.B., M.C.M., O.K., H.S., and L.M. critically reviewed the manuscript. All authors have read and approved the final draft of this manuscript.
Corresponding author
Correspondence to Francis F. Furia .
Ethics declarations
Ethics approval and consent to participate.
This study is based on service data and no personal data are included in the manuscript. The permission to conduct the study was granted by the Directorate of Research and Training of Muhimbili National Hospital.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: .
Donor Evaluation Form.
Additional file 2:
Recipient Evaluation Form.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Furia, F.F., Shoo, J.G., Ruggajo, P.J. et al. Establishing kidney transplantation in a low-income country: a case in Tanzania. Ren Replace Ther 10 , 29 (2024). https://doi.org/10.1186/s41100-024-00545-z
Download citation
Received : 11 December 2023
Accepted : 19 April 2024
Published : 02 May 2024
DOI : https://doi.org/10.1186/s41100-024-00545-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nephrology in Tanzania
- Nephrology training
- Nephrology in sub-Saharan Africa
Renal Replacement Therapy
ISSN: 2059-1381
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Chronic Kidney Disease (CKD) Case Study (45 min)
Watch More! Unlock the full videos with a FREE trial
Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
Mr. Stinson is a 52-year-old male with a history of HTN, DM Type II, CKD, and CHF. He presented to the Emergency Department (ED) complaining of severe itching, nausea, and vomiting. He appeared pale and is lethargic. He reported shortness of breath and the nurse notes crackles in his lungs. He has now been admitted to your unit.
What additional nursing assessments should be performed?
- Full set of vital signs
- Auscultate heart and lung sounds, as well as peripheral pulses
- Assess skin turgor and edema
- Assess the patient’s dialysis access site for functionality or bleeding
What diagnostic or lab tests would you expect the provider to order?
- Complete metabolic panel (electrolytes, renal function, etc.
- Complete blood count
- Possibly an ABG to assess for acidosis
- Possibly a BNP to assess volume overload and its effect on the heart
Upon further questioning, the patient reports he normally gets dialysis Monday, Wednesday, Friday, but that he skipped dialysis yesterday because he was “not feeling well”. He has +2 pitting edema in his legs. Vital signs are as follows:
HR 102 RR 24
BP 153/97 SpO 2 90%
The patient’s labs result and show the following:
BUN 62 mg/dL Na 134 mg/dL
Cr 3.9 mg/dL Ca 7.8 mg/dL
GFR 13 mL/min/m 2 Phos 5.0 mg/dL
K 6.3 mEq/L Mg 1.6 mg/dL
Gluc 224 mg/dL H/H 8.2 / 30%
pH 7.32 pCO 2 32 HCO 3 – 16
BNP 247 pg/mL
Interpret these lab results and explain their meaning.
- The BUN/Cr and GFR indicate the patient is definitely in kidney failure as his glomerulus is not filtering the blood like it should and the waste products are building up
- His electrolyte abnormalities (hyperkalemia, hyponatremia, hypocalcemia, hyperphosphatemia, and hypomagnesemia) are all indicative of kidney disease and acidosis. The kidneys would normally retain sodium and excrete potassium. In kidney failure, they do the opposite and potassium levels can get very high.
- He is in metabolic acidosis, likely because his kidneys are not able to retain the bicarb buffer like they normally would – this also contributes to the hyperkalemia. As the body tries to balance the H+ ions, it kicks K+ out into the bloodstream.
- His BNP is also elevated, indicating volume overload – this is probably caused both by the kidney failure and not getting dialysis and by the heart failure
- He is anemic – chronic anemia is common in chronic kidney disease patients due to the lack of erythropoietin.
What is going on with Mr. Stinson physiologically?
- Because of his CKD, Mr. Stinson requires dialysis to perform the normal functions of the kidneys, since his aren’t working. He likely felt sick because his potassium was elevated and because of the azotemia (toxins building up in his blood).
- He missed dialysis and therefore he is now even more volume overloaded and azotemic
- This will cause a risk to his heart and lungs because of the overload and the hyperkalemia
The nephrologist is consulted and determines that the patient needs hemodialysis. As soon as possible. The charge nurse of the dialysis unit is working to create a bed for him and will call back as soon as one is available, hopefully within the hour.
What do you, the nurse, need to consider and assess for Mr. Stinson PRIOR to sending him to dialysis?
- ALWAYS hold antihypertensives before HD (obtain provider order)
- Hold any medications that may be dialyzed off as they will not have their therapeutic benefit (confirm with pharmacist and obtain provider order)
- May require potassium-lowering medications before dialysis if the wait is going to be too long – hyperkalemia can be deadly
- Determine if any medications should be held prior to HD
- Assess full set of vital signs
- Obtain a weight, preferably on a standing scale
- Assess heart and lung sounds, as well as skin/edema
Mr. Stinson goes to hemodialysis, where they are able to pull of 3 L of fluid. He tolerates the procedure well and returns to his room.
What would you need to assess for Mr. Stinson AFTER he returns from Dialysis?
- Obtain a weight, preferable on a standing scale, to compare to the pre-HD weight. This helps determine how much fluid was pulled off (1 kg = 1 L)
- Obtain a full set of vital sign
- Re-draw a renal function panel as ordered to ensure electrolytes are not in a dangerous range (requires provider order)
What are some important patient education topics for Mr. Stinson before discharge?
- Importance of hemodialysis – he likely didn’t feel well because he NEEDED dialysis.
- Reasons to “skip” dialysis typically involve severe infections and fevers, in which case he should go the following day whenever possible or notify his nephrology team
- Should also reinforce teaching regarding nutrition – foods to avoid (high in potassium) and when to take medications with or without food (especially Phos-Lo and Calcium supplements)
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
Nursing Case Studies

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions
Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions
Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 12, Issue 2
- The case for a ketogenic diet in the management of kidney disease
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-5427-6748 Shaminie J Athinarayanan 1 ,
- Caroline G P Roberts 1 ,
- Chandan Vangala 2 ,
- Greeshma K Shetty 1 ,
- Amy L McKenzie 3 ,
- Thomas Weimbs 4 ,
- Jeff S Volek 5
- 1 Virta Health , Denver , Colorado , USA
- 2 BCM , Houston , Texas , USA
- 3 Abbott , Wiesbaden , Germany
- 4 Department of Molecular Cellular & Developmental Biology , University of California Santa Barbara , Santa Barbara , California , USA
- 5 Department of Human Sciences , The Ohio State University , Columbus , Ohio , USA
- Correspondence to Dr Shaminie J Athinarayanan; sarassam52{at}gmail.com
Ketogenic diets have been widely used for weight loss and are increasingly used in the management of type 2 diabetes. Despite evidence that ketones have multiple positive effects on kidney function, common misconceptions about ketogenic diets, such as high protein content and acid load, have prevented their widespread use in individuals with impaired kidney function. Clinical trial evidence focusing on major adverse kidney events is sparse. The aim of this review is to explore the effects of a ketogenic diet, with an emphasis on the pleiotropic actions of ketones, on kidney health. Given the minimal concerns in relation to the potential renoprotective effects of a ketogenic diet, future studies should evaluate the safety and efficacy of ketogenic interventions in kidney disease.
- Kidney Diseases
Data availability statement
No data are available.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjdrc-2024-004101
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Low carbohydrate eating patterns including a very low carbohydrate or ketogenic diet have been successfully used for weight loss and remitting type 2 diabetes (T2D). Among patients with T2D, the prevalence of chronic kidney disease (CKD), whether characterized as a reduced estimated glomerular filtration rate (eGFR) function or albuminuria is almost 40%. 1 Yet, a ketogenic diet is cautioned against in individuals with impaired kidney function, 2 in part, due to concerns about increased protein intake. The effect of protein intake in CKD is controversial, but high protein intake has been associated with hyperfiltration, increased acid excretion, and potentially, a decline in kidney function. 3 4 However, protein intake on a well-formulated ketogenic diet (WFKD) is moderate to effectively permit nutritional ketosis. Dietary analysis of very low carbohydrate studies usually reports daily protein intake ranging from 0.6 g/kg to 1.4 g/kg, 5–7 which is similar to that in the standard American diet and below the high protein threshold (≥2.0 g/kg) believed to be of concern. 8 The Kidney Disease Outcomes Quality Initiative clinical practice guideline for nutrition in CKD not dependent on dialysis recommends a “low-protein diet providing 0.55–0.6 g of dietary protein/kg body weight/day, or a very low-protein diet providing 0.28–0.43 g of dietary protein/kg of body weight/day with additional keto acid/amino acid analogs to meet protein requirements (0.55–0.60 g/kg/day).” 9 In contrast, Kidney Disease Improving Global Outcomes (KDIGO) 2022 CKD guideline recommended a slightly higher daily protein allowance of 0.8 g/kg/day for individuals with advanced CKD with or without T2D. 10 The Modification of Diet in Renal Disease (MDRD) study, a landmark trial examining the effect of protein restriction among 585 patients with non-diabetic CKD, did not demonstrate a significantly slower progression of disease, 11 and in fact a very low protein diet (0.28 g/kg/day) was associated with increased risk of death at a median follow-up of 3.2 years. 12 The null findings from MDRD are one of numerous inconsistent results studying protein restriction in patients with CKD. Taken altogether, systematic reviews have suggested—at best—a modest benefit for patients on a low protein diet 13 14 and given the aforementioned long-term data noting increased risk of death with very low protein diets, most nephrology experts are more comfortable with moderate protein restriction to the degree of 0.8 g/kg/day as recommended by the KDIGO 2022 guideline.
The impact of carbohydrate restriction interventions on kidney function is poorly understood. Existing studies consistently reported improvements in glycemic control, blood pressure, weight, and insulin resistance, all of which have favorable downstream implications for slowing kidney disease progression ( figure 1 ). In addition, ketone bodies themselves have a myriad of physiologic and signaling effects that could elicit renoprotective effects. For example, the renoprotective effect of sodium-glucose cotransporter 2 inhibitors (SGLT2i) has been postulated to be partially mediated by the modest medication-induced ketosis. 15–17 This low-grade ketosis induced by SGLT2i may directly or indirectly benefit the kidney by serving as an energy source during stress and kidney injury, and through its anti-inflammatory, antifibrotic, and antioxidant effects ( figure 1 ). 15 16 Given that SGLT2i-induced ketosis may be beneficial for the kidney, endogenously produced ketones resulting from a WFKD may prove to be another therapeutic option for diabetic nephropathy or kidney disease. 18 19
- Download figure
- Open in new tab
- Download powerpoint
Summary of pleiotropic renal protective effect of ketones and carbohydrate restriction. BHB, β-hydroxybutyrate; mTORC1, mammalian target of rapamycin complex 1; NLRP3, NOD-, LRR-, and pyrin domain-containing 3; PGC-1ɑ, peroxisome proliferator-activator receptor γ (PPARγ) coactivator-1-alpha; FFAR-3, free fatty acid receptor-3; HCAR, hydroxycarboxylic acid receptor-2; HDAC-3, Histone deacetylase-3; NRF2, nuclear factor erythroid 2-related factor 2; SIRT1, silent information regulator transcript-1.
In this review, we explore the pleiotropic roles and signaling effects of ketones on kidney physiology, address potential concerns of ketogenic therapy, summarize the available literature on the effect of low carbohydrate diets on kidney function, and discuss future studies that could help address the gaps in knowledge and discrepancies in the literature.
Potential roles of ketones on kidney pathophysiology and disease
Ketones as an alternative energy-efficient fuel.
The human body naturally produces ketones, mostly in the liver, at varying rates that result in circulating ketones that span more than four orders of magnitude (<0.01 to >10 mM) 20 21 depending primarily on a person’s carbohydrate intake and insulin level. Increased lipolysis and ketogenesis are upregulated in response to a low insulin-to-glucagon ratio, which occurs during calorie restriction/fasting, prolonged exercise, consumption of a ketogenic diet, or pathologic insulin deficiency. In the liver, when production of fatty acyl coenzyme A (CoA) increases during low insulin secretion and increased lipolysis, fatty acyl CoA is transported to the mitochondrial matrix, where it is then β-oxidized to produce acetyl-CoA. 22 23 Acetyl-CoA is either converted to malonyl CoA or to acetoacetyl CoA ( figure 2 ). Acetoacetyl CoA and acetyl-CoA are further condensed by a rate-limiting enzyme, 3-hydroxy 3-methylglutaryl-CoA synthase 2 (HMGCS2) to generate hydroxymethylglutaryl CoA (HMG-CoA). HMG-CoA is then converted into acetoacetate (AcAc) by hydroxymethylglutaryl coenzyme A lyase (HMGCL). 22 23 Finally, AcAc is reduced to β-hydroxybutyrate (BHB) by BHB dehydrogenase (BDH) ( figure 2 ). Both AcAc and BHB are released from the liver and transported in the blood circulation to extrahepatic tissues where they can have signaling effects and be metabolized and released or oxidized to produce energy. BHB is a vital energy source for the brain with uptake occurring in proportion to circulating levels. As such, during prolonged starvation, ketones can provide over half the brain’s energy requirements. 24 Generally, glucose is considered the most efficient fuel since it produces more ATP per oxygen consumed with a phosphate/oxygen (P/O) ratio of 2.58. 24 25 However, in a state of insulin resistance where glucose uptake and oxidation are impaired, BHB is an effective alternative dense energy molecule with a P/O ratio of 2.50. In contrast to free fatty acids (FFAs), another form of energy-dense fuel, 25 26 BHB gives better ATP yield per oxygen consumed, is water soluble, and generates fewer reactive oxygen species (ROS).
Ketogenesis pathway. AcAc, acetoacetate; BDH, BHB dehydrogenase; CoA, coenzyme A; HMGCL, hydroxymethylglutaryl coenzyme A lyase; HMG-CoA, hydroxymethylglutaryl CoA; HMGCS2, 3-hydroxy 3-methylglutaryl-CoA synthase 2; CPT1/2, carnitine palmitoyltransferase 1/2; MCT, moncarboxylate transporter.
The kidney is among the most metabolically active organs, with very high oxygen demand and the second-highest mitochondrial density after the myocardium. 27 While oxidative metabolism is the principal source of energy in the kidney, the fuel substrates for metabolism differ across regions of the kidney. In the healthy kidney, both fatty acid oxidation (FAO) in the proximal tubules and glycolysis in the distal tubules support its metabolism. The renal cortex, especially the S1/S2 tubule segments, generates energy primarily from FFAs, lactate, and glutamate versus glucose. 28 The outer medulla uses glucose, lactate, FFAs, and ketones for energy. However, in diseased kidneys, mitochondrial dysfunction has been reported as a key pathologic feature that contributes to disease initiation and progression. 29 30 For example, in diabetic nephropathy (DN), hyperglycemia-induced flux of glycolysis increases oxygen demand with the by-product of amplified ROS. 30 31 Excess glucose use in the kidney shifts the energy reliance from fatty acid metabolism to glycolysis, even in the proximal tubules. 30 31
The renoprotective effect of SGLT2i in diabetic kidney disease is driven by amelioration of the pathologic metabolic shift from FAO to glycolysis. SGLT2i decreases reabsorption of excessive glucose, reduces energy production from glucose in the kidney, and increases fatty acid utilization in the kidney. 32 Furthermore, the glycosuric effect of SGLT2i also augments the BHB level in the kidney mainly through increased production of ketones rather than reduced kidney clearance. 33 The kidney is indeed an avid consumer of ketones. 34 BHB serves as an important alternative source of energy for the kidney during metabolic imbalance. It can be effectively metabolized in all nephron regions, except the S1/S2 proximal tubule segments. 35 During starvation or fasting, the BHB level in the kidney increases 20-fold and is used as a substrate for mitochondrial energy production. 20 In the diabetic kidney disease mouse model, both SGLT2i and exogenous ketone treatment normalized the renal ATP levels by restoring its production and this intervention was also associated with kidney function improvement. 36
Anti-inflammatory effect
Inflammation is critical in both acute kidney disease and CKD, especially through activation of inflammasomes such as NOD-, LRR-, and pyrin domain-containing 3 (NLRP3). 37 Numerous studies highlight the link between DN and NLRP3 inflammasome activation, which negatively impacts podocyte function, escalates the expression of inflammatory markers like IL-1β, and is also linked with albuminuria and tubulointerstitial injury. 38 39 Consequently, targeting NLRP3 inflammasome inhibition emerges as a promising approach for kidney disease treatment, despite concerns over the safety of current experimental drugs. 40 BHB stands out for its wide-ranging anti-inflammatory actions, including its effect on inhibiting NLRP3 inflammasome activation. 41 BHB successfully suppresses NLRP3 inflammasome activation in human monocytes and murine neutrophils in vitro and in animal models of NLRP3-mediated diseases. 42 Likewise, the anti-inflammatory effect of SGLT2i in diabetic rats, characterized by subdued NLRP3 inflammasome activation and lower interleukin (IL)-1β and tumor necrosis factor (TNF)-ɑ levels, correlates with elevated BHB and reduced insulin levels in the bloodstream. 43 BHB’s primary receptor is GPR109A (HCAR2), a G protein coupled receptor (GPCR) that acts by suppressing cyclic adenosine monophosphate (cAMP). 44 Beyond NLRP3 inflammasome suppression, animal studies reveal BHB diminishes other proinflammatory cytokines, including IL-6, chemokine (C–C motif) ligand 2, and monocyte chemoattractant protein-1, through activation of GPR109A, partially influenced by BHB’s effect on nuclear factor kappa B translocation. 45–47 In humans, ketogenic diets consistently reduce inflammation indicators. Individuals with T2D on a ketogenic diet show decreased serum C reactive protein and white cell counts, 48 along with significant reductions in 15 out of 16 inflammatory/immune modulators after 1 and 2 years. 49 This anti-inflammatory benefit aligns with prior findings that observed a greater reduction in 7 out of 14 inflammation/immune modulators with a ketogenic diet compared with a low-fat diet after 12 weeks. 50
Antifibrotic effects
The antifibrotic effect of BHB is mainly mediated through the mammalian target of rapamycin complex 1 (mTORC1) pathway. In diabetic kidney disease, mTORC1 hyperactivation is associated with kidney dysfunction and increased fibrosis. 43 In a mouse model of non-proteinuric diabetic kidney disease, SGLT2i, particularly empagliflozin conferred renal protection by increasing endogenous ketones and suppressing mTORC1 activation in the kidneys. 36 The treatment with empagliflozin mirrored the effect of exogenous ketone supplementation, where both treatments reduced kidney damage as evident through lower plasma cystatin-C levels and decreased interstitial fibrosis. 36 The renoprotective mechanism of SGLT2i hinges on the ketogenesis rate-limiting enzyme HMGCS2 highlighting ketone production’s central role in its antifibrotic effects. 36 51
Antioxidative effects
Ketones, specifically BHB, act as an important signaling molecule influencing gene expression through various regulatory pathways. BHB notably inhibits class I histone deacetylase enzyme activity in kidney tissue, enhancing the expression of genes that respond to oxidative stress, including Foxo3a and Mt2 . 52 This confers protection against oxidative stress in human kidney cells and various animal models. Studies also show that a ketogenic diet or BHB treatment can activate the major detoxification and oxidative stress nuclear factor erythroid 2-related factor 2 (Nrf2) pathway. 53 In a spontaneous mouse model of T2D (db/db mice) treated with dapagliflozin, there was a noticeable reduction in the expression of genes related to oxidative stress compared with those treated with a standard vehicle or glimepiride. 54 This reduction is associated with increased levels of BHB and NRF2 protein expression. 54 Similarly, BHB treatment in human proximal tubular cells (HK-2) led to increased NRF2 expression and induced NRF2 nuclear translocation. 55 Furthermore, a ketogenic diet has been reported to increase the expression of other antioxidants such as NAD(P)H dehydrogenase quinone I (NQO1) and superoxide dismutase (SOD1/2), 56 and ameliorated paraquat (PQ)-induced elevated lipid peroxidation, toxicity, reduced antioxidant activity and decreased Nrf2 expression, 57 highlighting its potential therapeutic role in combating oxidative stress and tissue hypoxia.
Mitochondrial dysfunction
Mitochondrial dysfunction is another key feature of both acute kidney failure and CKD. 58 Ketogenic diet activates the expression of peroxisome proliferator-activator receptor γ (PPARγ) coactivator-1-alpha (PGC-1ɑ) 59 and silent information regulator transcript-1 (SIRT1). 60 61 PGC-1ɑ is the main transcription factor that controls the expression of genes involved in mitochondrial biogenesis and function, while SIRT1 activation protects organelle damage including the mitochondria and reduces oxidative stress. In a recent study on diabetic mice, a ketogenic diet improved mitochondrial function and capacity through its activation of PGC-1ɑ and SIRT1. 62 Further, administration of exogenous BHB was found to increase PGC-1ɑ and mitochondrial copy number in rat kidneys. 63 Human data on mitochondrial function are lacking, but we obtained skeletal muscle biopsies from physically active adults before and after a 12-week ketogenic diet and demonstrated that mitochondrial function and efficiency shifted towards fat oxidation while improving insulin sensitivity. 64
Traditional concerns of a ketogenic diet on kidney function
Common misconceptions about ketogenic diets related to kidney health include potential adverse effects on acid–base and electrolyte balance and risk for kidney stones. The next section briefly discusses the typical renal metabolic response to a ketogenic diet that maintains pH and electrolyte status. Most work in this space has been done in the context of normal kidney function, so we mention how the situation in CKD may differ.
Electrolyte and acid–base imbalance
Ketogenic diets promote a natriuretic and diuretic effect similar to that demonstrated during starvation. 65 66 This in part accounts for the typical rapid weight loss that occurs during the initiation of a ketogenic diet. If sodium intake is not commensurate with the additional loss of sodium, two deleterious outcomes are more likely to manifest: (1) Individuals may develop common signs and symptoms of hypovolemia, colloquially referred to as “Keto-Flu,” which include dizziness when standing, lethargy, and muscle spasms/cramps. (2) Counter-regulatory mechanisms are activated that include sympathetic and aldosterone stimulation that act to preserve plasma volume by increasing sodium reabsorption and a concomitant excretion of potassium and magnesium. These side effects can be eliminated with attention to proper electrolyte intake. For most individuals with normal kidney function consuming a ketogenic diet, it should be emphasized to ingest an additional 1–2 g sodium/day (4–5 g sodium/day total), a maintenance of 3–4 g/day potassium, and sufficient fluid intake.
In CKD, a decrease in viable nephrons and reduction in glomerular filtration rate (GFR) change the kidney’s normal physiology and sodium balance. 67 68 Even though an adaptive fractional increase in sodium excretion per individual nephron unit compensates for the reduced number of working nephrons, the kidney’s inability to excrete sufficient amounts of sodium results in sodium retention, extracellular fluid expansion, and blood pressure increase. 68 69 Likewise, the renin–angiotensin–aldosterone system is activated in CKD, further exacerbating sodium retention and causing vasoconstriction which could significantly raise blood pressure. 69 Sodium retention and its association with blood pressure in CKD are often referred to as “sodium-sensitive hypertension.” 70 Therefore, reducing salt intake is recommended to manage hypertension in patients with CKD. 68 The natriuretic and diuretic effect of the ketogenic diet may help alleviate sodium retention and improve systemic and glomerular blood pressure. Low carbohydrate and ketogenic diet studies often report a reduction in systolic and diastolic blood pressure 71 72 and blood pressure medication requirements. 73 However, the current recommendation of sodium intake in a WFKD is based on individuals with normal kidney function. 74 Recommendations for sodium and electrolyte intake for patients with CKD following a ketogenic diet should be individualized by a healthcare professional based on the patient’s renal function and electrolyte status. Future studies should assess the relationship between ketosis, sodium balance, and blood pressure.
Another misconception associated with ketogenic diets relates to promotion of acidosis owing to specific food items and the weakly acidifying effects of ketones, which could worsen kidney function, bone health, and kidney disease-associated endocrinopathies. 75 76 In healthy subjects provided a carefully prepared ketogenic diet with mean BHB levels >2 mM, serum bicarbonate was modestly reduced but well within normal ranges. 77 A ketogenic diet with mild ketosis (~1 mM) in individuals with normal kidney function has no significant impact on blood pH, serum bicarbonate level, and anion gap over 21 days 78 and 4 months. 79
When faced with an increased acid load, normal kidney function affords compensatory increases in ammonium excretion. In a somewhat mirrored perspective where the acid load is stable and the kidney function is reduced, the fewer working nephrons compensate with increased ammoniagenesis and excretion. This adaptation results in high intrarenal ammonia, which is thought to activate the alternative complement pathway eventually leading to tubulointerstitial fibrosis. Decreases in GFR to levels below 40–50 mL/min diminish the kidney’s ability to excrete more ammonium and overall acid 80 ; hence, metabolic acidosis is more commonly encountered at this level of disease. In patients with kidney disease, clinicians commonly monitor steady-state serum bicarbonate levels to assess overall acid load. However, decreases in serum bicarbonate are often reported at a later stage of the disease and it is considered inadequate to reflect the overall acid load. Eubicarbonatemic hydrogen ion retention among patients with earlier CKD is increasingly an area of focus 81 ; thus, studying ketogenic diet in all stages of CKD requires longer term study of acid excretion and the rate of kidney function decline.
Urinary acid excretion is favored as the gold standard for estimating acid load, and the prevailing wisdom was that an increased dietary acid load would burden the kidneys further and lead to more dysfunction. However, recent observations from the rich data collected in the Chronic Renal Insufficiency Cohort Study have demonstrated pitfalls to that simplistic view. 82 83 Among patients with diabetes, higher levels of net acid excretion were associated with a lower risk of CKD progression. These studies suggested that the changes in acid excretion were diet-independent and may be elicited by changes in energy metabolism and endogenous acid production from insulin resistance. 82 83 Currently, the effect of ketogenic diet on net acid excretion is unknown and this would be worthwhile exploring in patients with T2D and varying stages of CKD.
Kidney stones
Kidney stones, especially genetically driven stones, are associated with an increased risk of CKD. 84 A recent meta-analysis reported a pooled kidney stone incidence of 5.9% among patients on a ketogenic diet followed for a median of 3.7 years, 85 compared with a historical incidence rate of <0.3% per year in the general population. 86 Most studies reporting risk of kidney stones were in children receiving a ketogenic diet therapy for epilepsy 85 87–91 with higher incidence during long-term exposure (ie, 25% over 6 years, 91 which is complicated by concurrent use of antiseizure medications (eg, carbonic anhydrase inhibitors) and other risk factors in this population. In adults with obesity, who are at higher kidney stone risk based on their higher adiposity, 92 consuming a ketogenic diet over 2 years revealed no harmful effects on GFR, albuminuria, or fluid and electrolyte balance compared with a low-fat diet 93 ; and there was one possible, but not confirmed, case of kidney stones out of 153 subjects. 94
Uric acid stones are the most frequently reported by individuals on a ketogenic diet, followed by calcium oxalate stones or mixed stones with calcium and uric acid. 85 A ketogenic diet transiently increases uric acid concentration 25%–50%, which usually peaks at 2–4 weeks, and gradually returns to prediet levels by 8 weeks. 95–97 The initial rise in uric acid is concomitant with the rise in ketones, and it was postulated that the reason for this may be competition between uric acid and ketones for the same organic acid transporters, which are required for renal excretion. 98–101 After several weeks, the kidney conserves ketones, 102 presumably allowing for return of normal renal uric acid excretion and serum levels.
There may be effective strategies to mitigate the kidney stone risk in patients following a ketogenic diet. Increasing fluid intake to maintain dilute urine limits the possibility of mineral crystallization. 103 Urine alkalinization, particularly addressing hypocitraturia, may inhibit supersaturation of calcium salts and aggregation. 104 105 Moreover, studies of kidney stones have largely precluded patients with CKD where their urine parameters change alongside diminishing kidney function. A retrospective study of 811 patients with kidney stones noted that advancing kidney disease afforded reduced calcium stone formation, presumably due to reduced calciuria 106 and increased uric acid stone formation. 107 Metabolic acidosis resulting in acidic urine pH is common among individuals with CKD. 108 Low urine pH is a well-known risk factor for forming uric acid kidney stones due to the low solubility of uric acidic in acidic conditions. 109 110 At the same time, low urine pH leads to hypocitraturia which increases the risk of forming calcium oxalate kidney stones. 111 Hence, future examination of how a ketogenic diet impacts the incidence of kidney stones among patients with T2D and CKD is paramount. Being aware of and addressing the potential kidney stone risk with well-established measures—such as urine alkalization, correcting hypocitraturia, and increasing fluid intake—is prudent. Additionally, understanding that diet-imposed change in risk through modulation of ammonia excretion, uricosuria, calciuria, citraturia, and other urinary parameters will assist with future guidance.
Current evidence on very low or low carbohydrate diet intervention and its effect on kidney function
Evidence from animal studies.
Several rodent studies have specifically investigated the effects of a ketogenic diet on kidney function and disease. Two mouse studies reported benefit of ketogenic diet on DN, even reversing some of the key molecular features of DN. Poplawski et al assessed the effect of ketogenic diet on DN using both type 1 (Akita) and type 2 (db/db) murine diabetes models. In both models, the mice initially developed albuminuria on chow diet, and after transitioning to the ketogenic diet reversed and normalized urinary albumin/creatinine ratio (UACR) within 8 weeks. 112 Furthermore, the expression of several stress-induced genes involved in oxidative stress and toxicity was completely normalized by ketogenic diet in both models, with an observed effect that was more consistently robust in the type 1 mouse model. Likewise, histopathologic features of glomerular sclerosis were also partially reversed by the ketogenic diet in the T2D mouse model. 112 Jung et al examined db/db DN mice fed normal chow diet (dbNCD), high-fat diet (dbHFD), or ketogenic diet (dbKETO). dbKETO animals had lower UACR and blood urea nitrogen to creatinine ratio levels after 5 weeks compared with the dbNCD and dbHFD mice. 55 Histologic analysis of the kidney showed that dbKETO mice had less fibrotic changes than the dbNCD and dbHCD mice suggesting that the dbKETO mice delayed progression of DN histologic phenotypes. Furthermore, in the same report, treatment of the human proximal tubular cell line (HK-2) with BHB led to activated autophagy by increasing the LC3 I to LC3 II ratio, phosphorylation of adenosine 5 monophosphate-activated protein kinase (AMPK), beclin, p62 degradation, NRF2 expression, and decreased glucose-induced ROS levels. 55 Studies in a rat model of a genetic form of CKD, polycystic kidney disease, showed that a ketogenic diet not only slowed disease progression and preserved renal function in young animals but even partially reversed existing renal cystic disease in older animals. 18 The treatment resulted in improvement of renal fibrosis and inhibition of mTORC1 and epithelial proliferation. Remarkably, the effects could be replicated by administering BHB in the drinking water in a dose-dependent manner, without any food changes. 18 63 These results suggest that the actions of BHB may underlie most of the renoprotective mechanisms of nutritional ketosis, and that exogenous BHB can be effectively supplemented.

Evidence from clinical and observational studies
Clinical and observational studies that examined kidney function in response to low-carbohydrate diets ranging from <20 g/day to 30%–40% of energy expenditure are presented in online supplemental table 1 . Three of the six randomized controlled trials (RCTs) reported no significant changes in kidney function in the low carbohydrate arm compared with the comparison diet group. Two of the three studies followed the participants with normal baseline eGFR for 52 weeks 113 114 and the third study followed subjects with slightly lower baseline eGFR (<80) for 12 weeks. 115 Another two RCTs reported renal benefit in the low carbohydrate arm with improvements in serum creatinine, cystatin C, eGFR, and albumin. 93 116 The study by Tirosh et al reported greater eGFR improvement in those following a low-carbohydrate diet versus both a Mediterranean and low-fat diet. 116
Supplemental material
The use of surrogate markers, especially serum creatinine-derived estimates of kidney function, is less accurate at higher eGFRs and may be mischaracterized amidst dietary intervention, highlighting the importance of studying major adverse kidney events and assessing cystatin C-derived kidney function estimates. Thus far, only one RCT has reported hard kidney endpoints including all-cause mortality that compared a carbohydrate-restricted, low-iron, polyphenol enriched diet (CR-LIPE) with a standard protein restriction diet (SPRD). 117 The 191 participants in this study were followed for approximately 4 years. In this study, CR-LIPE significantly decreased doubling of serum creatinine (relative risk, 0.53, 95% CI 0.33 to 0.86, p<0.01), all-cause mortality (relative risk, 0.5, 95% CI 0.2 to 1.12) and also delayed end-stage renal disease and renal replacement therapy when compared with SPRD. 117 However, the CR-LIPE intervention was a multimodal dietary intervention that included carbohydrate restriction (35% of the energy intake) as one of the dietary modifications along with low-iron availability and polyphenol enrichment in the diet. Future study involving major adverse kidney endpoints is warranted to confirm if a ketogenic diet has beneficial impact on kidney disease.
Presumably because eGFR is less accurate at healthier function (eGFR >80 mL/min), some of these studies have shown that the beneficial effect of low carbohydrate diet is greater in those with lower starting baseline eGFR. For example, the study by Tirosh et al reported that the increase in eGFR was greater in those with CKD stage 3 (a 7.1-point; 10% eGFR increase from baseline) than the whole cohort (+5.3% increase from baseline) in the low carbohydrate arm. 116 While other studies included a range of baseline eGFRs, the subset of patients with more significant kidney dysfunction (eGFR <60 mL/min) exhibited a slower decline in function, and no deterioration was evident in participants with normal baseline eGFR. 118 119 Furthermore, caution is warranted when interpreting creatinine-derived eGFR measurements because any change in skeletal muscle mass during a nutritional study may affect the endogenous production of creatinine independent of actual changes in renal function. Hence, corroboration with cystatin-C measurements would strengthen these observations. The single-arm prospective 12 weeks study on individuals with relatively advanced diabetes nephropathy (eGFR <40 mL/min) reported statistically significant improvements in eGFR, serum creatinine, and cystatin C. 118 Three additional retrospective observational studies reported improvements in kidney function in individuals following a low carbohydrate diet 120–122 ( online supplemental table 1 ). One of these studies reported improvement in eGFR and decrease in UACR at an average follow-up of 30 months 119 while the other two studies reported eGFR improvement in individuals with reduced kidney function at baseline (eGFR <90 in one study and eGFR <70 in the other study). 121 122
In contrast, there were only two observational studies frequently cited when suggesting that a low carbohydrate diet is associated with adverse kidney outcomes. These studies did not focus on individuals adhering to a ketogenic diet or on those limiting their carbohydrate intake. For instance, Farhadnejad et al ’s 2018 study, which was a population-based prospective analysis, investigated the association between different tertiles of low carbohydrate high protein (LCHP) scores and the incidence of CKD. 123 Notably, none of the LCHP score tertiles in the study indicated a carbohydrate-restricted diet. Even in the tertile with the lowest LCHP score, carbohydrates contributed to 51.0% of the total energy, resembling the carbohydrate profile of a standard Western diet where 40%–60% of energy typically comes from carbohydrates. The other retrospective observational study by Li et al reported an association between elevated fasting ketone level with abnormal renal function 124 in people with T2D who were admitted to the hospital, and who were not specifically eating a ketogenic diet. The association of ketones and renal function in this study is not relevant to dietary carbohydrate restriction in an ambulatory population.
Altogether, these clinical and observational studies show no harm from low or very low carbohydrate diets for people with diabetes in the setting of normal renal function, and a possible beneficial effect in the setting of moderately reduced renal function. The kidney function improvement observed in these studies may be an ancillary outcome associated with other improvements seen in these interventions including weight loss, glycemic control, or blood pressure improvement. Interestingly, Unwin et al reported no association between observed kidney function improvement with the magnitude of weight loss, improvement in blood pressure and HbA1c, 120 while another study reported that the increase in eGFR was significantly associated with a decrease in fasting insulin and systolic blood pressure but not with the level of weight loss and protein intake in the intervention. 116 In our previous study on patients with T2D following a very low carbohydrate intervention, there was a marginally significant increase in eGFR at 1 year. 72 A post hoc analysis of these data revealed that a higher mean BHB at 1 year (β=5.04, p=0.005) was significantly associated with a greater increase in mean eGFR (unpublished data). Furthermore, in a subgroup analysis of 22 trial participants with an eGFR <60 mL/min/1.73 m 2 at baseline who remained in the study for 2 years, 72 the mean eGFR progressively increased from 51 mL/min/1.73 m 2 to 60, 63, and 68 mL/min/1.73 m 2 at 10 weeks, 1 year, and 2 years (unpublished data). Notably, the majority of the 22 participants reverted to stage 2 and no one progressed to stage 4 CKD. Evidently, a dose-dependent association exists between ketosis trajectory classes and the increase in total eGFR slope at 2 years. 125 Participants with higher endogenous ketone concentration and longer duration of ketosis maintenance exhibited the greatest rise in the 2-year eGFR slope compared with those with lower endogenous ketone concentration and unsustainable ketosis maintenance. 125 Hence, available evidence suggests that carbohydrate restriction and ketosis afford benefits to kidney function. It will be important to determine in future trials whether the improvement in kidney function translates to a sustained long-term reduction, or even reversal, in the progression of kidney disease.
Evidence from meta-analyses, systematic and narrative review
A recent review discussing the potential negative effect of purported ketogenic diets on kidney health focused on observational studies that compared low protein versus high protein diets that were not ketogenic or low carbohydrate diets, 126 and raised concern about the association of albuminuria with high animal fat but only referred to observational studies that assessed high animal fat intake in the context of a Western diet 126 negating the relevance of the studies cited for concern.
In contrast, systematic reviews and meta-analyses that assessed pooled effects of RCTs reported beneficial effects of low-carbohydrate diets. The meta-analysis by Oyabu et al evaluated nine RCTs with 861 participants in the low carbohydrate arm and 826 participants in the control group. 127 Despite a large variation in the proportion of carbohydrate intake from 4% to 45% in the low carbohydrate arm of the nine studies with a study duration ranging from 6 to 24 months, the review revealed that there was a significant increase in eGFR in the low carbohydrate group versus control group. 127 Another meta-analysis with 12 RCTs that only included patients with T2D reported no significant difference in the pooled eGFR and creatinine mean estimate between the lower carbohydrate diets (14%–45% of calories from carbohydrate) versus control diets over 5 weeks to 24 months. 128 Similarly, another meta-analysis that included five RCTs with the low carbohydrate arm had carbohydrate intake <45%, and the studies ranging from 5 weeks to 24 months reported no difference in the pooled eGFR estimate between the control and low carbohydrate diets. 129 The current evidence from systematic reviews and meta-analyses with a range of carbohydrate intake suggests that carbohydrate restriction is not associated with adverse effects on kidney function, or in some cases might be beneficial.
Evidence from genetically driven kidney disease
Individuals with autosomal dominant polycystic kidney disease (ADPKD) may benefit from calorie restriction or ketogenic diet. 19 130 131 This chronic progressive condition is characterized by hyperproliferation, inflammation, fibrosis, and cyst growth, leading to deterioration of kidney function over time. 19 132 mTOR is one of the main signaling pathways activated in ADPKD. 132 A study of various polycystic kidney disease animal models showed that time-restricted feeding, administration of a ketogenic diet, or supplementation with exogenous BHB prevented kidney cyst disease progression by inhibiting cell proliferation, fibrosis, and cyst growth. 18 63 Furthermore, the mTOR activity was inhibited in these animal models suggesting that blunting the signaling pathway inhibits cell proliferation, growth, and fibrosis in ADPKD. 18 63 133 In humans, a retrospective observational study of ADPKD patients who self-initiated ketosis either using ketogenic or time-restricted diets reported improvement in eGFR after 6 months. 134 A pilot study on 24 patients with ADPKD demonstrated the feasibility of the ketogenic diet, reporting high adherence rates and improvements in blood pressure, eGFR, and kidney pain. 130 In another exploratory RCT, 66 participants with ADPKD were randomized to ketogenic, water fasting, or control diets. The study confirmed the feasibility of the therapy in the ketogenic arm (KD) and revealed significant improvements in eGFR, including both creatinine and cystatin C-derived eGFR in the KD group but no improvements were observed in the water fasting and control diets. 131 Additionally, there were no significant differences in UACR and blood pressure among the three diets. 131
Perspectives and future direction
There is a considerable body of research suggesting that a very low carbohydrate ketogenic diet is safe in individuals with moderately diminished kidney function, even in studies that had higher protein intake than what is recommended for kidney disease and diets that are not plant-based. The diet can be safely prescribed in patients with T2D for treating and remitting diabetes even if they have underlying stage 2 or 3 CKD or reduced kidney function. Beyond safety, mechanistic plausibility, preclinical data, and even some RCT studies suggest that carbohydrate-restricted diets may be beneficial in improving moderate kidney dysfunction and in reducing progression of CKD. The preliminary proof of concept from small and short duration studies in humans and animals suggests a very low carbohydrate diet could be an effective dietary intervention for patients with CKD. Furthermore, there are predeveloped ketogenic nutritional options to consider when we plan a future trial to assess the impact of ketogenic diet on patients with CKD, such as the recently developed program for treating ADPKD known as Ren.Nu. This program is a plant-focused ketogenic medical nutrition therapy, designed to avoid renal stressors like oxalate, inorganic phosphate, and purines/uric acid. It includes a medical food formulation, KetoCitra, containing BHB with alkaline citrate which helps antagonize kidney stone formation. 129 130 Based on the findings from these different studies and currently available ketogenic medical therapy specific for kidney disease, there is a need for future larger and longer follow-up randomized controlled clinical trials on very low carbohydrate diet, including nutritional ketosis in patients with CKD with or without T2D on kidney hard endpoints including major adverse kidney events (a composite event of death, persistent renal decline >25% decline in eGFR, and a new initiation of dialysis) and other kidney-related outcomes to firmly establish the long-term effectiveness. For example, a head-to-head comparison of the safety and efficacy of ketogenic nutritional therapy versus SGLT2i pharmacologic intervention (that involves the same mechanism of raising ketone levels) could be of high interest. Weight loss from the diet can improve filtration and albuminuria. Thus, including other surrogate endpoints like eGFR slope and microalbuminuria in these studies have the potential to elucidate the degree to which weight loss and blood pressure improvement from the diet affects kidney function markers and also to explore if ketone levels independently have an impact on these markers and endpoints. Furthermore, these studies should also assess the diet’s overall safety in patients with T2D and CKD, specifically exploring its effect on net acid excretion, kidney stone formation, and maybe its beneficial effect on sodium retention hypertension. Finally, another important consideration in the clinical trial design for evaluating the efficacy of a very low carbohydrate diet in patients with CKD is understanding the diet’s additive role, especially how the diet interacts with currently available treatment drugs for patients with CKD including renin–angiotensin system blockade (angiotensin-converting enzyme inhibitor, ACEi and angiotensin receptor blockers, ARBs), SGLT2i, glucagon-like peptide-1 receptor agonists (GLP1-RA), and the non-steroidal mineralocorticoid receptor antagonists (finerenone).
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
- Dean BB , et al
- ElSayed NA ,
- Aroda VR , et al
- Park S , et al
- Esmeijer K ,
- Geleijnse JM ,
- de Fijter JW , et al
- Guyton JR , et al
- Seshadri P , et al
- Westman EC ,
- Mavropoulos JC , et al
- Cuenca-Sánchez M ,
- Navas-Carrillo D ,
- Orenes-Piñero E
- Ikizler TA ,
- Burrowes JD ,
- Byham-Gray LD , et al
- Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group
- Beck GJ , et al
- Kopple JD ,
- Wang X , et al
- Laville M ,
- Boissel JP , et al
- Wen Y , et al
- Sugahara S , et al
- Torres JA ,
- Kruger SL ,
- Broderick C , et al
- Saville J ,
- Kalantar-Zadeh K
- Balasse EO ,
- Puchalska P ,
- Crawford PA
- Röhling M , et al
- Mudaliar S ,
- Bosy-Westphal A , et al
- Baverel G ,
- Ferrier B ,
- Forbes JM ,
- Thorburn DR
- Qiao Y , et al
- Audzeyenka I ,
- Bierżyńska A ,
- Fang Y , et al
- Ferrannini E ,
- Frascerra S , et al
- Cuenoud B ,
- Hartweg M ,
- Godin J-P , et al
- McDonough AA ,
- Shahzad K ,
- Dong W , et al
- Qiu J , et al
- Liu C , et al
- Nguyen KY ,
- Grant RW , et al
- Goldberg EL ,
- Molony RD , et al
- Kim SH , et al
- Spigoni V ,
- Cinquegrani G ,
- Iannozzi NT , et al
- Gambhir D ,
- Veeranan-Karmegam R , et al
- Wang J-F , et al
- Wang JF , et al
- Bhanpuri NH ,
- Hallberg SJ ,
- Williams PT , et al
- Phinney S ,
- Athinarayanan S , et al
- Forsythe CE ,
- Phinney SD ,
- Fernandez ML , et al
- Kogot-Levin A ,
- Riahi Y , et al
- Shimazu T ,
- Hirschey MD ,
- Newman J , et al
- Milder JB ,
- Kim YJ , et al
- Hovda DA , et al
- Liu F , et al
- Pathak SJ ,
- McCarty MF ,
- DiNicolantonio JJ ,
- Scheibye-Knudsen M ,
- Mitchell SJ ,
- Fang EF , et al
- Roberts MN ,
- Wallace MA ,
- Tomilov AA , et al
- Holznecht N ,
- Asplund DA , et al
- Miller VJ ,
- LaFountain RA ,
- Barnhart E , et al
- Palmer BF ,
- Saudek CD ,
- Boulter PR ,
- Borrelli S ,
- Provenzano M ,
- Gagliardi I , et al
- Cuevas CA ,
- Zietse R , et al
- Murray SW , et al
- McKenzie AL ,
- Athinarayanan SJ ,
- McKenzie AL , et al
- Dhondup T ,
- Bistrian BR ,
- Wolfe RR , et al
- Sharma AP ,
- Ross ML , et al
- Gomez-Arbelaez D ,
- Crujeiras AB ,
- Castro AI , et al
- Pourafshar N ,
- Pourafshar S ,
- Soleimani M
- Scialla JJ ,
- Dobre M , et al
- Luciano A ,
- Pendergast J , et al
- Bergstralh EJ ,
- Melton LJ , et al
- Acharya P ,
- Acharya C ,
- Thongprayoon C , et al
- Pyzik PL , et al
- Kossoff EH ,
- Furth SL , et al
- Herzberg GZ ,
- Fivush BA ,
- Kinsman SL , et al
- Sampath A ,
- Groesbeck DK ,
- Taylor EN ,
- Stampfer MJ ,
- Friedman AN ,
- Foster GD , et al
- Foster GD ,
- Hill JO , et al
- Horton ES ,
- Sims EAH , et al
- García-Nieto VM ,
- Claverie-Martín F ,
- Moraleda-Mesa T , et al
- Goldfinger S ,
- Klinenberg E ,
- Seegmiller JE
- Lecocq FR ,
- Agarwal N ,
- Farooq O , et al
- McNally MA ,
- Rubenstein JE , et al
- Zupec-Kania BA ,
- Amark PE , et al
- Cirillo M ,
- Bilancio G ,
- Cavallo P , et al
- Simmons K ,
- Phadke M , et al
- Reaven NL , et al
- Pazos Pérez F
- Haghighatdoost F ,
- Sadeghian R ,
- Clark CCT , et al
- Poplawski MM ,
- Mastaitis JW ,
- Isoda F , et al
- Thompson CH ,
- Luscombe-Marsh ND , et al
- Brinkworth GD ,
- Buckley JD ,
- Noakes M , et al
- Zainordin NA ,
- Eddy Warman NA ,
- Mohamad AF , et al
- Harman-Boehm I , et al
- Facchini FS ,
- Chambers M ,
- Kamendulis LM , et al
- Tuccinardi D ,
- Tozzi R , et al
- Crocombe D , et al
- Mitchell NS ,
- Wilmsen N ,
- Geerlings W , et al
- Farhadnejad H ,
- Asghari G ,
- Emamat H , et al
- Shen X , et al
- Roberts CGP ,
- Adams RN , et al
- Joshi S , et al
- Hashimoto Y ,
- Fukuda T , et al
- Kingaard JJ ,
- Munits M , et al
- Cukoski S ,
- Lindemann CH ,
- Arjune S , et al
- Shillingford JM ,
- Murcia NS ,
- Larson CH , et al
- Torres JA , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Contributors SJA, JV, and CGPR conceptualized the review topic and formulated the objectives; SJA conducted the comprehensive literature search, synthesized and interpreted the data from the collected literature; SJA drafted the original manuscript; JSV, TW, CGPR, and CV provided critical revisions and edits to the manuscript; ALM and GKS reviewed and edited the manuscript; All authors have read and agreed to the final version of the manuscript.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests TW is an inventor on issued and pending patents filed by the University of California, Santa Barbara related to the topic of this article. TW is a founder and shareholder of Santa Barbara Nutrients, Inc., holds a managerial position, and has contributed to the development of the Ren.Nu ketogenic dietary program and the medical food KetoCitra. TW received speaker fees from Otsuka, was a scientific advisor of Chinook Therapeutics, and received research funding from Chinook Therapeutics. JSV is a cofounder and shareholder of Virta Health, serves as a science advisor for Simply Good Foods and Nutrishus Brands, and has authored books on ketogenic diets. SJA, CGPR, and GKS are employees and shareholders of Virta Health. ALM is a shareholder of Virta Health.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
- Open access
- Published: 10 May 2024
Prevalence of hypertension and diabetes mellitus in Peruvian patients with chronic kidney disease: a systematic review and meta-analysis
- Darwin A. León-Figueroa 1 ,
- Edwin Aguirre-Milachay 1 ,
- Joshuan J. Barboza 2 &
- Mario J. Valladares-Garrido 3 , 4
BMC Nephrology volume 25 , Article number: 160 ( 2024 ) Cite this article
1 Altmetric
Metrics details
Chronic Kidney Disease (CKD) represents a major challenge for public health, with hypertension and diabetes being the main causes of its occurrence. Therefore, this study aims to determine the prevalence of hypertension (HTN) and diabetes mellitus (DM) in Peruvian patients with CKD.
A systematic search for studies about CKD in Peru was carried out in PubMed, Scopus, Embase, Web of Science, ScienceDirect, Google Scholar, Virtual Health Library (VHL), and Scielo from 2011 to December 2023. The protocol of this research was registered in the international registry of systematic reviews, the Prospective International Registry of Systematic Reviews (PROSPERO), with registration number CRD42023425118. Study selection, quality assessment, and data extraction were performed independently by two authors. Study quality was assessed using the Joanna Briggs Institute Statistical Meta-Analysis Assessment and Review Instrument. A random-effects model with inverse variance weighting was used to estimate the combined prevalence of HTN and DM in Peruvian patients with CKD. To analyze data heterogeneity, the I 2 statistical test was used. Statistical analysis was performed with R version 4.2.3.
A total of 1425 studies were retrieved, of which 23 were included in the final meta-analysis. A total of 43,321 patients with CKD were evaluated, of whom 52.22% were male and 47.78% were female. The combined prevalence of HTN in Peruvian patients with CKD was 38% (95% CI: 30–46%; 41,131 participants; 21 studies, I 2 = 99%, p = 0), while the combined prevalence of DM in Peruvian patients with CKD was 33% (95% CI: 26–40%; 43,321 participants; 23 studies, I 2 = 99%, p = 0).
Approximately one-third of Peruvian patients with CKD have HTN and DM. These findings highlight the importance of implementing prevention and control measures for these chronic noncommunicable diseases in the Peruvian population, such as promoting healthy lifestyles, encouraging early detection and proper management of hypertension and diabetes, and improving access to medical care and health services.
Peer Review reports
Introduction
Chronic kidney disease (CKD) is typically defined by a glomerular filtration rate of less than 60 ml/min/1.73 m2 or the presence of other indicators of kidney damage, such as albuminuria [ 1 , 2 ]. CKD represents a global public health challenge, impacting about 10–14% of the adult population worldwide [ 3 , 4 ]. Moreover, CKD is closely linked to the increased prevalence of conditions such as diabetes mellitus (DM), hypertension (HTN), obesity, and aging, which continue to be the main causes of morbidity and premature mortality in the population affected by this disease [ 5 , 6 ].
Diabetes mellitus represents an important risk factor for the development of CKD [ 7 ], and several studies have explored its role as an independent risk factor in the incidence of CKD [ 8 , 9 ]. The prevalence of DM has been steadily increasing worldwide. Currently, about 450 million people suffer from this disease, and this figure is projected to reach 690 million by 2045 [ 10 ]. On the other hand, HTN plays a significant role in the onset and worsening of CKD [ 11 ]. The prevalence of HTN increases as renal function deteriorates, affecting approximately 60–90% of individuals with CKD [ 12 ]. HTN is the most common chronic disease in developed societies and claims about 7.1 million lives worldwide each year [ 7 ].
In Peru, the prevalence of CKD in some regions of the country can reach 16.8% [ 13 ] to 28.4% in the city of Lima [ 14 ]. In addition, it has been observed that among people with CKD, there is a prevalence of DM of 20% and HTN of 55.9% [ 14 ]. According to a 2024 press release, the Peruvian Ministry of Health reported that about 10% of adults suffer from CKD, with HTN and DM being the main causes of this condition [ 15 ]. In this context, the presence of chronic comorbidities, such as HTN and DM, in patients with CKD not only contributes to the development and progression of kidney disease but also exacerbates the risk of cardiovascular and renal complications, increasing the burden of disease and the costs associated with medical care [ 16 ].
In Peru, as in many Latin American countries, the availability of information related to the epidemiology of CKD and its association with other chronic diseases is limited [ 7 , 17 , 18 ]. This field of research is in constant development and is still being explored in depth. Due to its wide diversity in terms of socioeconomic trends, climatic and geographic zones, and social determinants of health (access to health services, economic stability, and education), Peru presents a unique opportunity to assess the burden of CKD [ 17 , 19 ].
The study aims to fill a significant gap in the understanding of renal health in the Peruvian population, focusing specifically on the prevalence of HTN and DM in patients with CKD. This research not only seeks to quantify the prevalence of these comorbid conditions but may also shed light on the risk factors and possible interactions between CKD, HTN, and DM in this specific context. By providing solid and systematized data, the study could inform more effective health policies aimed at prevention, early detection, and optimal management of these conditions in the Peruvian population, thus improving the care and quality of life of patients with CKD. In addition, it can lay the groundwork for future research and more precise and targeted intervention strategies [ 20 ].
Materials and methods
Protocol and registration.
The present research was conducted following the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [ 21 ] (Table S1 ), as well as a protocol registered in PROSPERO with the identification number CRD42023425118.
Eligibility criteria
This review included observational studies, such as cross-sectional studies and prospective and retrospective cohorts, that examined the prevalence of HTN and DM in Peruvian patients over 18 years of age diagnosed with CKD. Studies that did not meet the criteria, such as editorials, letters to the editor, randomized clinical trials, conference abstracts, and narrative or systematic reviews, were excluded.
Information sources and search strategy
Searches were conducted in various databases, including PubMed, Scopus, Embase, Web of Science, ScienceDirect, Google Scholar, Virtual Health Library (VHL), and Scielo, until December 1, 2023, with no language or development period restrictions. Studies were identified using Medical Subject Headings (MeSH) terms such as “chronic kidney disease” and “Peru”. The search strategy was independently tested by two authors and is detailed in Table S2 . In addition, other search methods were used, including a review of literature studies, consultation of article references, and review of publications in Peruvian journals specializing in chronic kidney disease. However, the potential studies identified were within the scope of the search strategy employed.
Study selection
The search strategy results were stored in the Endnote software. Subsequently, duplicate articles, titles, and abstracts were removed. Next, two investigators independently reviewed the titles and abstracts of the articles to select those that met the inclusion criteria. Then, two additional investigators conducted a thorough review of the full articles to determine if they met the inclusion criteria. Any discrepancies identified were resolved through mutual agreements.
The main outcome is to determine the prevalence of HTN and DM in Peruvian patients diagnosed with CKD.
Quality assessment
The JBI-MAStARI tool was employed to assess the quality of the articles included in the meta-analysis. The evaluation encompassed various aspects, such as the study context, outcome and explanatory variables, specific inclusion criteria, measurement standards, topic description, and precise statistical analysis. The quality of the studies was categorized as high (≥ 7 points), moderate (4 to 6 points), or low (< 4 points) based on their scores, and any discrepancies were resolved through researcher discussions (Table S3 ) [ 22 ].
Data collection process and data items
Three independent researchers were responsible for collecting relevant data from the selected articles and recording it in an Excel spreadsheet. The collected information included various details such as the author, publication year, study design, study location, sample size, and the number of participants with CKD. The prevalence of CKD, study subjects, participants’ age, and gender (both male and female), as well as the presence of HTN and DM were also recorded. Subsequently, to ensure the accuracy and quality of the extracted data, two additional researchers conducted a rigorous review and verification process.
Data analysis
The data obtained from Excel was utilized for conducting the analysis in R, specifically version 4.2.3. In order to present the research findings, tables and narrative graphs were employed. A random-effects model with inverse variance weighting was used to estimate the combined prevalence of HTN and DM in Peruvian patients with CKD. The Cochrane Q statistic was used to examine the variability among the trials. Additionally, the I2 index was used to quantify this variability. Values of 25%, 50%, and 75%, respectively, were regarded as indicating low, moderate, and high heterogeneity.
A funnel plot was employed to investigate the possibility of publication bias. Egger’s regression test was also used to investigate this matter further. When the resultant p value was less than 0.05, it was believed that there was a possibility of bias in the results.
The pooled prevalence of HTN and DM in Peruvian patients with CKD was shown graphically as a forest plot, with 95% confidence intervals included for enhanced precision in the presentation of the data.
A total of 1425 articles were found through searches in eight different databases. The selection process is detailed in the PRISMA flowchart, depicted in Fig. 1 . After eliminating duplicate articles ( n = 497), the investigators analyzed the remaining 928 articles. Subsequently, the titles and abstracts of these articles were evaluated, and 90 were selected for a comprehensive full-text review. Once this process was completed, 23 articles that met the inclusion criteria for the systematic review and meta-analysis were included [ 14 , 17 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 ].
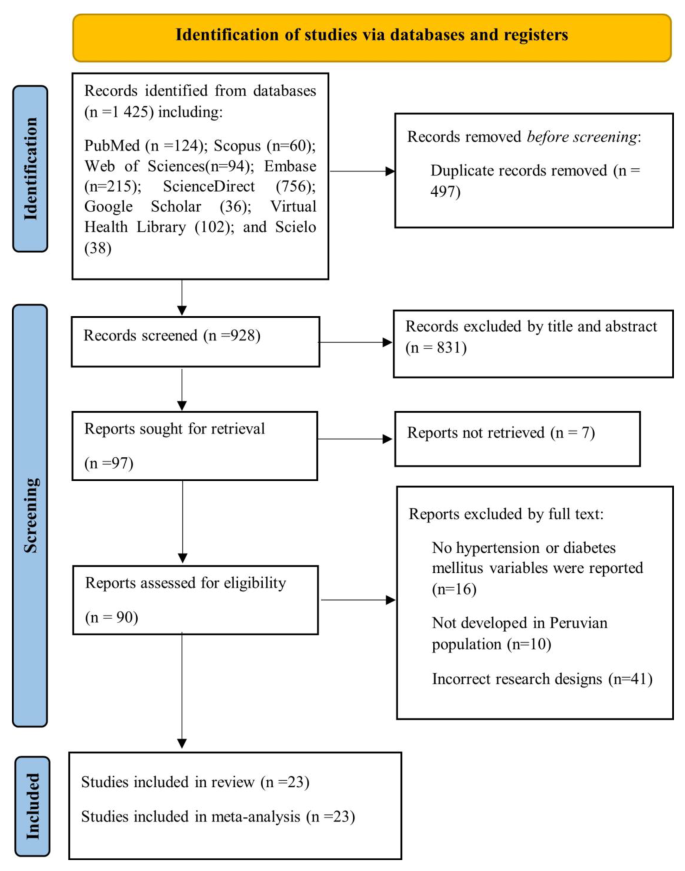
illustrates the process of study selection according to the PRISMA flowchart
Characteristics of the included studie
The analysis was based on a review of 23 observational studies published between 2011 and 2023 that examined the prevalence of HTN and DM in Peruvian patients diagnosed with CKD (Table 1 ). A total of 43,321 patients with chronic kidney disease were evaluated, of whom 52.22% (22,622) were male and 47.78% (20,699) were female [ 14 , 17 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 ]. The mean age of the participants was approximately 64 years, and most of the studies were centered in Lima, the capital of Peru (Table 1 ).
Quality of the included studies and publication bias
The quality of the studies was assessed using the JBI Critical Appraisal Tools, specifically designed for cross-sectional research. It was determined that all the studies included in the analysis demonstrated a moderate level of quality, as indicated in Table S3 [ 14 , 17 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 ]. In the analyses aimed at evaluating HTN in Peruvian patients with CKD, it was observed that when Egger’s test was applied to evaluate publication bias, a value of p = 0.5339 (t = -0.63, df = 19) was obtained. This result suggests that the null hypothesis of symmetry is accepted, indicating that there is no evidence of publication bias in the studies examined (Figure S1 ). In the analyses aimed at evaluating DM in Peruvian patients with CKD, it was evident that when Egger’s test was used to evaluate publication bias, a value of p = 0.0063 (t = 3.04, df = 21) was obtained. This result indicates an asymmetry in the data, which could explain the considerable disparities in the reported prevalence values. However, it should be noted that we were unable to conclusively demonstrate the presence of publication bias (Figure S1 ).
Joint prevalence of HTN and DM in Peruvian patients with CKD
The combined prevalence of HTN in Peruvian patients with CKD was 38% (95% CI: 30–46%; 41,131 participants; 21 studies). The I 2 test indicated significant heterogeneity among the included studies (I 2 = 99%, p = 0) (Fig. 2 ) [ 14 , 17 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 40 , 42 , 43 ]. The combined prevalence of DM in Peruvian patients with CKD was 33% (95% CI: 26–40%; 43,321 participants; 23 studies). The I 2 test indicated significant heterogeneity among the included studies (I 2 = 99%, p = 0) (Fig. 3 ) [ 14 , 17 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 ]. The combined prevalence of HTN and DM in Peruvian patients with CKD was 21% (95% CI: 19–23%; 32,860 participants; 4 studies). The I 2 test indicated significant heterogeneity among the included studies (I 2 = 89%, p = 0) (Figure S2 ) [ 14 , 29 , 34 , 36 ].

Forest plot illustrating the joint prevalence of Hypertension in Peruvian patients with chronic kidney disease

Forest plot illustrating the joint prevalence of diabetes mellitus in Peruvian patients with chronic kidney disease
Chronic kidney disease constitutes a challenge of great relevance for public health at a global level, with an ever-increasing incidence and prevalence. In addition to its considerable medical and economic burden, CKD implies a notable increase in morbidity and mortality rates among the affected population. CKD is a non-communicable disease generally caused by diabetes and hypertension [ 44 ]. Therefore, the purpose of this systematic review and meta-analysis was to determine the prevalence of HTN and DM in Peruvian patients with CKD. The most relevant results showed that the combined prevalence of HTN in this population reached 38%, while the combined prevalence of DM was 33%.
The Centers for Disease Control and Prevention’s CKD Surveillance System reported that about 14% of adults in the United States have CKD stages 1 to 4 [ 45 ]. Kovesdy CP reported that CKD affects more than 10% of the general population worldwide and is more prevalent in older people, women, racial minorities, and people who experience DM and HTN [ 3 ].
In a meta-analysis by Hill NR, et al. reported an overall prevalence of 5-stage CKD of 13.4%, and stages 3–5 was 10.6% [ 46 ]. In addition, the prevalence of individual stages of CKD was 3.5% (stage 1), 3.9% (stage 2), 7.6% (stage 3), 0.4% (stage 4), and 0.1% (stage 5) [ 47 ]. According to the National Health and Nutrition Examination Survey (NHANES), the prevalence of CKD among adults aged 70 years and older was lower in 2017–March 2020 (42.6%) than in 2001–2004 (52.1%) [ 48 ]. Hill NR, et al. reported a linearly higher prevalence for CKD stages 1–5 associated with advancing age, ranging from 13.7% in the 30–40 year age group to 27.9% in patients > 70–80 years [ 46 ].
A study by Sundström J. et al. in 2.4 million patients from 11 countries reported a CKD prevalence of 10% [ 49 ]. In Asia, the prevalence of stage 3–5 CKD in low- and middle-income countries was 11.2% [ 50 ]. Another study found that 14% of the general population and high-risk groups in South Asia had CKD [ 51 ]. In Peru, Bravo-Zúñiga J, et al. reported a prevalence of CKD of 28.4% in patients evaluated in a health network in the city of Lima [ 14 ]. Another study by Herrera-Añazco P. et al. reported a CKD prevalence of 18% [ 29 ].
The combined prevalence of HTN in Peruvian patients with CKD was 38%. In the United States, the prevalence of CKD stages 1–4 among hypertensive adults was 26.34% in 2017–2020, compared with a prevalence of 7.8% among nonhypertensive individuals [ 52 ]. Hill NR et al., in their meta-analysis, reported an association between HTN and CKD prevalence [ 46 ]. In Tanzania, Stanifer JW et al. reported that among adults with CKD, 19.3% had HTN [ 53 ]. Another study found that the prevalence of CKD was 27% in adults with HTN [ 51 ]. In Peru, Bravo-Zúñiga J. et al. evaluated a total of 20,354 participants with CKD; 38.7% had HTN [ 34 ]. These results are based on the fact that HTN is a medical condition distinguished by elevated blood pressure, which is a significant risk factor in the development and progression of CKD. This condition can cause damage to the blood vessels in the kidneys, compromising their ability to efficiently filter waste and excess fluids from the body [ 54 ].
The combined prevalence of DM in Peruvian patients with CKD was 33%. In the United States, according to NHANES (2017–2020), the prevalence of CKD stages 1–4 in diabetic adults was 38.67% [ 55 ]; in addition, the prevalence of CKD stages 3–4 (NHANES 2001–March 2020) was 10% among adults with prediabetes or undiagnosed DM and 18% among adults with diagnosed DM [ 56 ]. A study by Fernandez-Fernandez L. et al. in Spain reported a CKD prevalence of 25.3% in patients with DM [ 57 ]. Gatwood J. et al. reported that CKD was evident in 31.6% of veterans before being diagnosed with DM [ 58 ]. A meta-analysis by Hill NR et al. reported an association between DM and the prevalence of CKD [ 46 ]. In Tanzania, Stanifer JW et al. reported that among adults with CKD, 7% had DM and 14.0% had DM and HTN [ 53 ]. Another study found that the prevalence of CKD was 31% in adults with DM [ 51 ]. Sundström J. et al. reported that DM was present in 38% of patients with CKD [ 49 ]. In Peru, Bravo-Zúñiga J, et al. evaluated a total of 20,354 participants with CKD; 13.74% had DM [ 34 ]. Diabetes is positioned as one of the leading causes of CKD, triggering a number of nephropathic complications. This disorder exerts a significant influence, as elevated blood glucose levels cause progressive damage to the small blood vessels that supply blood to the kidneys. This detrimental interference compromises kidney function, creating an environment conducive to the development and aggravation of kidney disease [ 59 ].
The present study has some limitations. First, the included studies may be subject to biases and confounding factors that cannot be individually quantified. Second, it was not possible to perform a subgroup analysis by gender because the studies provided only baseline demographic data for the CKD population. Third, the prevalence of HTN and DM according to CKD stages could not be determined. Finally, the sample sizes of the included studies varied considerably, ranging from 20,354 to only 30 participants. However, among the strengths of this study, it is noteworthy that this research represents the first systematic review and meta-analysis focused on the evaluation of HTN and DM in Peruvian patients with CKD. To guarantee the quality of the included studies, the “JBI-MAStARI” tool was used as the evaluation method. In addition, a specific search strategy was designed for each database, and article selection and data extraction were carried out independently by two or more investigators. It should be noted that the studies included in this review shared the same definitions of CKD, and the recommendations established by the PRISMA guidelines were rigorously followed.
Conclusions
Data availability.
No datasets were generated or analysed during the current study.
Inker LA, Astor BC, Fox CH, Isakova T, Lash JP, Peralta CA, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis off J Natl Kidney Found. 2014;63(5):713–35. https://doi.org/10.1053/j.ajkd.2014.01.416 .
Article Google Scholar
Liyanage T, Toyama T, Hockham C, Ninomiya T, Perkovic V, Woodward M, et al. Prevalence of chronic kidney disease in Asia: a systematic review and analysis. BMJ Glob Health. 2022;7(1):e007525. https://doi.org/10.1136/bmjgh-2021-007525 .
Article PubMed PubMed Central Google Scholar
Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Suppl. 2022;12(1):7–11. https://doi.org/10.1016/j.kisu.2021.11.003 .
Samaan F, Damiani BB, Kirsztajn GM, Sesso R. A cross-sectional study on the prevalence and risk stratification of chronic kidney disease in Cardiological patients in São Paulo, Brazil. Diagn Basel Switz. 2023;13(6):1146. https://doi.org/10.3390/diagnostics13061146 .
Article CAS Google Scholar
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of Disease Study 2010. Lancet. 2012;380(9859):2095–128. https://doi.org/10.1016/S0140-6736(12)61728-0 .
Lv JC, Zhang LX. Prevalence and disease burden of chronic kidney disease. Adv Exp Med Biol. 2019;1165:3–15. https://doi.org/10.1007/978-981-13-8871-2_1 .
Article CAS PubMed Google Scholar
Erfanpoor S, Etemad K, Kazempour S, Hadaegh F, Hasani J, Azizi F, et al. Diabetes, hypertension, and incidence of chronic kidney disease: is there any Multiplicative or Additive Interaction? Int J Endocrinol Metab. 2021;19(1):e101061. https://doi.org/10.5812/ijem.101061 .
Article PubMed Google Scholar
Tohidi M, Hasheminia M, Mohebi R, Khalili D, Hosseinpanah F, Yazdani B, et al. Incidence of chronic kidney disease and its risk factors, results of over 10 year follow up in an Iranian cohort. PLoS ONE. 2012;7(9):e45304. https://doi.org/10.1371/journal.pone.0045304 .
Article CAS PubMed PubMed Central Google Scholar
Al-Rubeaan K, Youssef AM, Subhani SN, Ahmad NA, Al-Sharqawi AH, Al-Mutlaq HM, et al. Diabetic nephropathy and its risk factors in a society with a type 2 diabetes epidemic: a Saudi National Diabetes Registry-based study. PLoS ONE. 2014;9(2):e88956. https://doi.org/10.1371/journal.pone.0088956 .
Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, et al. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81. https://doi.org/10.1016/j.diabres.2018.02.023 .
Pugh D, Gallacher PJ, Dhaun N. Management of hypertension in chronic kidney disease. Drugs. 2019;79(4):365–79. https://doi.org/10.1007/s40265-019-1064-1 .
Mayne KJ, Sullivan MK, Lees JS. Sex and gender differences in the management of chronic kidney disease and hypertension. J Hum Hypertens. 2023;37(8):649–53. https://doi.org/10.1038/s41371-023-00843-9 .
Herrera-Añazco P, Benites-Zapata VA, León-Yurivilca I, Huarcaya-Cotaquispe R, Silveira-Chau M. Chronic kidney disease in Peru: a challenge for a country with an emerging economy. J Bras Nefrol. 2015;37(4):507–8. https://doi.org/10.5935/0101-2800.20150081 .
Bravo-Zúñiga J, Gálvez-Inga J, Carrillo-Onofre P, Chávez-Gómez R, Castro-Monteverde P. Early detection of chronic renal disease: coordinated work between primary and specialized care in an ambulatory renal network of Peru. J Bras Nefrol. 2019;41(2):176–84. https://doi.org/10.1590/2175-8239-JBN-2018-0101 .
Día. Mundial del Riñón: uno de cada diez adultos sufre de una enfermedad renal crónica. Available online: https://www.gob.pe/institucion/minsa/noticias/920304-dia-mundial-del-rinon-uno-de-cada-diez-adultos-sufre-de-una-enfermedad-renal-cronica (accessed on 23 March 2024).
Francis ER, Allen AK, Herrera-Añazco P, Kuo CC, Cardenas MK, Feldman HI, et al. Establishing a higher priority for chronic kidney disease in Peru. Lancet Glob Health. 2016;4(1):e17–18. https://doi.org/10.1016/S2214-109X(15)00206-5 .
Francis ER, Kuo CC, Bernabe-Ortiz A, Nessel L, Gilman RH, Checkley W, et al. Burden of chronic kidney disease in resource-limited settings from Peru: a population-based study. BMC Nephrol. 2015;16:114. https://doi.org/10.1186/s12882-015-0104-7 .
Carrillo-Larco RM, Miranda JJ, Gilman RH, Medina-Lezama J, Chirinos-Pacheco JA, Muñoz-Retamozo PV, et al. Risk score for first-screening of prevalent undiagnosed chronic kidney disease in Peru: the CRONICAS-CKD risk score. BMC Nephrol. 2017;18(1):343. https://doi.org/10.1186/s12882-017-0758-4 .
Atamari-Anahui N, Ccorahua-Rios MS, Condori-Huaraka M, Huamanvilca-Yepez Y, Amaya E, Herrera-Añazco P. Epidemiology of chronic kidney disease in Peru and its relation to social determinants of health. Int Health. 2020;12(4):264–71. https://doi.org/10.1093/inthealth/ihz071 .
Chen TK, Knicely DH, Grams ME. Chronic kidney disease diagnosis and management: a review. JAMA. 2019;322(13):1294–304. https://doi.org/10.1001/jama.2019.14745 .
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71 .
JBI Manual for Evidence Synthesis - JBI Global Wiki. Available online: https://jbi-global-wiki.refined.site/space/MANUAL (accessed on 24 October 2023).
Meneses Liendo V, León Rabanal C, Huapaya Carrera J, Cieza Zevallos J. Sobrevida en hemodiálisis según El Periodo De ingreso de pacientes entre 1982 y 2007 en Lima, Perú. Rev Med Hered. 2011;22(4):157–8.
Google Scholar
Herrera-Añazco P, Benítes-Zapata VA, Hernandez AV. Factores asociados a mortalidad intrahospitalaria de una población en hemodiálisis en el Perú. Rev Peru Med Exp Salud Pública. 2015;479 – 84. https://doi.org/10.17843/rpmesp.2015.323.1677 .
Herrera-Añazco P, Benites-Zapata V, Hernandez AV, Mezones-Holguin E, Silveira-Chau M. Mortalidade Dos pacientes com doença renal crônica em hemodiálise de manutenção em um hospital público do Peru. Braz J Nephrol. 2015;37:192–7. https://doi.org/10.5935/0101-2800.20150031 .
Huamán CL, Postigo OC, Contreras CC. Características epidemiológicas De Los pacientes que inician hemodiálisis crónica en El Hospital Alberto Sabogal Sologuren 2015. Horiz Méd Lima. 2016;16(2):6–12.
Bravo-Zúñiga J, Chávez-Gómez R, Gálvez-Inga J, Villavicencio-Carranza M, Espejo-Sotelo J, Riveros-Aguilar M. [Progression of chronic renal disease in a reference hospital of social security of Peru 2012–2015]. Rev Peru Med Exp Salud Publica. 2017;34(2):209–17. https://doi.org/10.17843/rpmesp.2017.342.2493 .
Gómez de la Torre-, del Carpio A, Bocanegra-Jesús A, Guinetti-Ortiz K, Mayta-Tristán P, Valdivia-Vega R. Mortalidad precoz en pacientes con enfermedad renal crónica que inician hemodiálisis por urgencia en una población peruana: Incidencia Y factores de riesgo. Nefrología. 2018;38(4):425–32. https://doi.org/10.1016/j.nefro.2017.11.017 .
Herrera-Añazco P, Taype-Rondan A, Lazo-Porras M, Alberto Quintanilla E, Ortiz-Soriano VM, Hernandez AV. Prevalence of chronic kidney disease in Peruvian primary care setting. BMC Nephrol. 2017;18(1):246. https://doi.org/10.1186/s12882-017-0655-x .
Pinares-Astete F, Meneses-Liendo V, Bonilla-Palacios J, Ángeles-Tacchino P, Cieza-Zevallos J. Supervivencia a largo plazo en pacientes con enfermedad renal crónica estadio 5 tratada por hemodiálisis en Lima, Perú. Acta Médica Peru. 2018;35(1):20–7.
Huauya-Leuyacc C, Palacios-Guillen AM, Benites-Zapata VA. Factores epidemiológicos asociados a la referencia temprana al nefrólogo para hemodiálisis crónica en pacientes de Un Hospital Público De Perú. Rev Nefrol Diál Traspl. 2018;126 – 33.
Herrera-Añazco P, Taype-Rondan A, Ortiz PJ, Málaga G, Del Carpio-Toia AM, Alvarez-Valdivia MG, et al. Use of medicinal plants in patients with chronic kidney disease from Peru. Complement Ther Med. 2019;47:102215. https://doi.org/10.1016/j.ctim.2019.102215 .
Loaiza-Huallpa J, Condori-Huaraka M, Quispe-Rodríguez GH, Pinares-Valderrama MP, Cruz-Huanca AI, Atamari-Anahui N, et al. Mortalidad Y factores asociados en pacientes con enfermedad renal crónica en hemodiálisis en un hospital peruano. Rev Habanera Cienc Médicas. 2019;18(1):164–75.
Bravo-Zúñiga J, Saldarriaga EM, Chávez-Gómez R, Gálvez-Inga J, Valdivia-Vega R, Villavicencio-Carranza M, et al. Effectiveness of adherence to a renal health program in a health network in Peru. Rev Saude Publica. 2020;54:80. https://doi.org/10.11606/s1518-8787.2020054002109 .
Pineda-Borja V, Andrade-Santiváñez C, Arce-Gomez G, Rabanal CL. Peritonitis en pacientes que reciben diálisis peritoneal en un hospital de Lima, Perú. Rev Peru Med Exp Salud Pública. 2020;521–6. https://doi.org/10.17843/rpmesp.2020.373.4744 .
Munive-Yachachi Y, Delgado-Pérez D, Munive-Yachachi Y, Delgado-Pérez D. Prevalencia De desnutrición en pacientes con enfermedad renal crónica terminal en un hospital nacional de Lima, Perú. Fac Med. 2021;82(1):21–6. https://doi.org/10.15381/anales.v82i1.18037 .
Valenzuela-Narváez RV, Valenzuela-Narváez DR, Valenzuela-Narváez DAO, Córdova-Noel ME, Mejía-Ruiz CL, Salcedo-Rodríguez MN, et al. Periodontal disease as a predictor of chronic kidney disease (CKD) stage in older adults. J Int Med Res. 2021;49(7):3000605211033266. https://doi.org/10.1177/03000605211033266 .
Umeres-Francia GE, Rojas-Fernández MV, Herrera-Añazco P, Benites-Zapata VA. Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio as risk factors for mortality in Peruvian adults with chronic kidney disease. Ren Replace Ther. 2022;8(1):30. https://doi.org/10.1186/s41100-022-00420-9 .
Guzman-Ventura W, Caballero-Alvarado J. Survival of patients on chronic hemodialysis versus chronic peritoneal dialysis. Rev Peru Med Exp Salud Publica. 2022;39(2):161–9. https://doi.org/10.17843/rpmesp.2022.392.10853 .
Bravo LJA, Gonzales RFL, Izarra ME, Rada APVY, Cairampoma DEM. Características epidemiológicas, de laboratorio y de tratamiento en pacientes con hemodiálisis en una población de altura. Rev Peru Cienc Salud. 2022;4(2):92–7. https://doi.org/10.37711/rpcs.2022.4.2.370 .
Venegas Justiniano JY, Hurtado Aréstegui A, Loza Muñarriz C, Venegas Justiniano JY, Hurtado Aréstegui A, Loza Muñarriz C. Características de la colocación y permanencia de catéteres venosos centrales temporales para hemodiálisis en un hospital público 2015–2019. Acta Médica Peru. 2022;39(2):128–37. https://doi.org/10.35663/amp.2022.392.2231 .
Herrera-Añazco P, Segura MA, Bravo-Zúñiga J, Vásquez JL, Taype-Rondán A. Hospitalization and mortality during the pandemic in chronic hemodialysis patients and the general population in Peru. J Bras Nefrol. 2023;S:0101–28002023005018501. https://doi.org/10.1590/2175-8239-JBN-2022-0149en .
Huaman-Carhuas L, Melo-Flores CM, Gutiérrez-Carranza MD, Huaman-Carhuas L, Melo-Flores CM, Gutiérrez-Carranza MD. Calidad Percibida Y Su relación con la satisfacción del paciente en tratamiento con hemodiálisis en un hospital público de Perú. Enferm Nefrológica. 2023;26(2):159–66. https://doi.org/10.37551/s2254-28842023016 .
Cockwell P, Fisher LA. The global burden of chronic kidney disease. Lancet. 2020;395(10225):662–4. https://doi.org/10.1016/S0140-6736(19)32977-0 .
CDC Surveillance System. CKD Among U.S. Adults, by Stage. Available online: https://nccd.cdc.gov/ckd/detail.aspx?Qnum=Q372 (accessed on 2 September 2023).
Hill NR, Fatoba ST, Oke JL, Hirst JA, O’Callaghan CA, Lasserson DS, et al. Global prevalence of chronic kidney disease – A systematic review and Meta-analysis. PLoS ONE. 2016;11(7):e0158765. https://doi.org/10.1371/journal.pone.0158765 .
Jager KJ, Kovesdy C, Langham R, Rosenberg M, Jha V, Zoccali C. A single number for advocacy and communication-worldwide more than 850 million individuals have kidney diseases. Kidney Int. 2019;96(5):1048–50. https://doi.org/10.1016/j.kint.2019.07.012 .
CDC Surveillance System: CKD Among U.S. Adults. Available online: https://nccd.cdc.gov/ckd/detail.aspx?Qnum=Q9&topic=1#refreshPosition (accessed on 2 September 2023).
Sundström J, Bodegard J, Bollmann A, Vervloet MG, Mark PB, Karasik A, et al. Prevalence, outcomes, and cost of chronic kidney disease in a contemporary population of 2·4 million patients from 11 countries: the CaReMe CKD study. Lancet Reg Health – Eur. 2022. https://doi.org/10.1016/j.lanepe.2022.100438 .
Suriyong P, Ruengorn C, Shayakul C, Anantachoti P, Kanjanarat P. Prevalence of chronic kidney disease stages 3–5 in low- and middle-income countries in Asia: a systematic review and meta-analysis. PLoS ONE. 2022;17(2):e0264393. https://doi.org/10.1371/journal.pone.0264393 .
Shrestha N, Gautam S, Mishra SR, Virani SS, Dhungana RR. Burden of chronic kidney disease in the general population and high-risk groups in South Asia: a systematic review and meta-analysis. PLoS ONE. 2021;16(10):e0258494. https://doi.org/10.1371/journal.pone.0258494 .
CDC Surveillance System: CKD Among U.S. Adults. Available online: https://nccd.cdc.gov/ckd/detail.aspx?Qnum=Q9&topic=1&Strat=Hypertension#refreshPosition (accessed on 2 September 2023).
Stanifer JW, Maro V, Egger J, Karia F, Thielman N, Turner EL, et al. The epidemiology of chronic kidney disease in Northern Tanzania: a population-based survey. PLoS ONE. 2015;10(4):e0124506. https://doi.org/10.1371/journal.pone.0124506 .
Ameer OZ. Hypertension in chronic kidney disease: what lies behind the scene. Front Pharmacol. 2022;13:949260. https://doi.org/10.3389/fphar.2022.949260 .
CDC Surveillance System: CKD Among U.S. Adults. Available online: https://nccd.cdc.gov/ckd/detail.aspx?Qnum=Q9&topic=1&Strat=Diabetes#refreshPosition (accessed on 2 September 2023).
CDC Surveillance System. CKD Stages 3–4, by Diabetes and Prediabetes. Available online: https://nccd.cdc.gov/ckd/detail.aspx?Qnum=Q702 (accessed on 2 September 2023).
Fernández-Fernández L, Barquilla-García A, Sánchez-Vega J, Risco-Solanilla JC, Suárez-González F, Buitrago F. Prevalence of chronic kidney disease in patients with diabetes in Extremadura (Spain) during the Years 2012, 2013 and 2014: an observational study. J Clin Med. 2021;10(13):2886. https://doi.org/10.3390/jcm10132886 .
Gatwood J, Chisholm-Burns M, Davis R, Thomas F, Potukuchi P, Hung A, et al. Evidence of chronic kidney disease in veterans with incident diabetes mellitus. PLoS ONE. 2018;13(2):e0192712. https://doi.org/10.1371/journal.pone.0192712 .
Pecoits-Filho R, Abensur H, Betônico CCR, Machado AD, Parente EB, Queiroz M, et al. Interactions between kidney disease and diabetes: dangerous liaisons. Diabetol Metab Syndr. 2016;8(1):50. https://doi.org/10.1186/s13098-016-0159-z .
Download references
Acknowledgements
This research received no external funding.
Author information
Authors and affiliations.
Facultad de Medicina Humana, Universidad de San Martín de Porres, Chiclayo, 15011, Peru
Darwin A. León-Figueroa & Edwin Aguirre-Milachay
Vicerrectorado de Investigación, Universidad Norbert Wiener, Lima, 15046, Peru
Joshuan J. Barboza
Universidad Continental, Lima, 15046, Peru
Mario J. Valladares-Garrido
Oficina de Epidemiología, Hospital Regional Lambayeque, Chiclayo, 14012, Peru
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization, D.A.L.F., M.J.V.G. and J.J.B.; methodology, J.J.B. and E.A.M.; software, D.A.L.F.; validation, E.A.M.; formal analysis, D.A.L.F.; investigation, M.J.V.G.; resources, A.J.R.M.; data curation, D.A.L.F.; writing—original draft prepa-ration, D.A.L.F., E.A.M. and J.J.B.; writing—review and editing, D.A.L.F., M.J.V.G., J.J.B., and E.A.M.; visualization, D.A.L.F.; supervision, J.J.B. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Correspondence to Mario J. Valladares-Garrido .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
León-Figueroa, D.A., Aguirre-Milachay, E., Barboza, J.J. et al. Prevalence of hypertension and diabetes mellitus in Peruvian patients with chronic kidney disease: a systematic review and meta-analysis. BMC Nephrol 25 , 160 (2024). https://doi.org/10.1186/s12882-024-03595-x
Download citation
Received : 02 December 2023
Accepted : 30 April 2024
Published : 10 May 2024
DOI : https://doi.org/10.1186/s12882-024-03595-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Chronic kidney disease
- Hypertension
- Diabetes mellitus
BMC Nephrology
ISSN: 1471-2369
- Submission enquiries: [email protected]
- General enquiries: [email protected]

- Government of India
Ministry of Ayush Government of India
---> Next Ministry of Ayush Government of India -->