Essential but undervalued: Millions of health care workers aren’t getting the pay or respect they deserve in the COVID-19 pandemic
Subscribe to the brookings metro update, molly kinder molly kinder fellow - brookings metro @mollykinder.
May 28, 2020
- 20 min read
This is the second post in a series on COVID-19 frontline workers. Read the stories of the workers profiled here .

Introduction
Underpaid, undervalued, and essential.
- A policy agenda for essential, low-wage health workers:
Keep all health workers safe
Introduce hazard pay, raise pay to a permanent living wage, expand paid leave, give workers the respect they deserve.
The COVID-19 pandemic has inspired an outpouring of public appreciation for the country’s frontline heroes, from television ads to firefighter salutes to essential worker toys . But while doctors and nurses deserve our praise, they are not the only ones risking their lives during the pandemic—in fact, they represent less than 20% of all essential health workers.
Too often, we overlook the heroism and dignity of millions of low-paid, undervalued, and essential health workers like Sabrina Hopps, a 46-year-old housekeeping aide in an acute nursing facility in Washington, D.C.
“If we don’t clean the rooms correctly, the pandemic will get worse,” said Hopps. She cares deeply about the patients she works with, and knows that the value of her job goes well beyond cleaning. “It’s me and the other housekeepers who sit and talk with [patients] to brighten up their day, because they can’t have family members visiting.”
Despite her contributions, she doesn’t feel recognized. “Housekeeping has never been respected,” she told me recently. “When you think about health care work, the first people you think about are the doctors and the nurses. They don’t think about housekeeping, maintenance, dietary, nursing assistants, patient care techs, and administration.”

Hopps is one of millions of low-wage essential health workers on the COVID-19 front lines. Like the higher-paid doctors and nurses they work alongside, these essential workers are risking their lives during the pandemic—but with far less prestige and recognition, very low pay, and less access to the protective equipment that could save their lives. They are nursing assistants, phlebotomists, home health aides, housekeepers, medical assistants, cooks, and more. The vast majority of these workers are women, and they are disproportionately people of color. Median pay is just $13.48 an hour.
Over the last several weeks, I interviewed nearly a dozen low-wage health workers on the front lines of COVID-19. ( You can read their stories here . ) Despite being declared “essential,” the workers I interviewed described feeling overlooked and deprioritized, even expendable. They spoke with pride about their work, but few felt respected, even as they put their lives on the line. Many expressed frustration—and sometimes anger—over their lack of life-saving protective equipment.
It is long past time that these workers are treated as truly essential. This starts with simply recognizing the value of workers like Hopps—but we can and must do more. The policy recommendations in this report aim to keep these workers safe on the job, compensate them with a living wage, support them if they fall ill, and give them the respect and appreciation they deserve.
Back to top ⇑
The underpaid but essential health care workforce in America comprises nearly 7 million people in low-paid health jobs in these three categories:
- Health care support workers assist health care providers such as doctors and nurses in providing patient care. Roles include orderlies, medical assistants, phlebotomists, and pharmacy aides.
- Direct care workers such as home health workers, nursing assistants, and personal care aides provide care to individuals with physical, cognitive, or other needs.
- Health care service workers include housekeepers, janitors, and food preparation and serving workers employed in health care settings such as hospitals and nursing homes.
More people are employed in health care support, service, and direct care jobs than in all health care practitioner and technician jobs (doctors, nurses, EMTs, lab technicians, etc.). In fact, more people work in hospitals as housekeepers and janitors—like Sabrina Hopps—than as physicians and surgeons. The size of this low-wage health workforce exceeds the size of most other occupational groups of essential workers. It employs more people than the entire transportation and warehousing industry and more than twice as many people as the grocery industry .
Median wages in health care support, service, and direct care jobs were just $13.48 an hour in 2019—well short of a living wage and far lower than the median pay of doctors (over $100 per hour) and nurses ($35.17 per hour). Home health and personal care workers earn even less, with a median hourly wage of only $11.57. The wages are so low that nearly 20% of care workers live in poverty and more than 40% rely on some form of public assistance. These fields are some of the fastest-growing of all occupations, with more than a million new jobs projected by 2028.
Table 1. Demographic profile of workers in the health care and social assistance industry, 2019
Source: Brookings analysis of U.S. Bureau of Labor Statistics’ Occupational Employment Statistics and the U.S. Census Bureau’s Current Population Survey.
Over 80% of health care support, service, and direct care workers are women. They are also disproportionately people of color. Like other low-wage jobs where women and people of color are concentrated , many of these positions are plagued by underinvestment and a lack of benefits. Now, these jobs pose an even greater risk to workers’ lives.

Despite being undervalued, low-wage health workers make essential contributions during the pandemic and beyond. “Nobody is insignificant,” said Tony Powell, a 62-year-old administrative coordinator of a hospital surgical unit in Washington, D.C. “Without environmental service, without dietary, without secretaries, without medical and surgical techs and certified nursing assistants (CNAs), it wouldn’t be a hospital.” Home health workers, for instance, provide the first line of defense against COVID-19 for millions of elderly and vulnerable people living at home. Without that, the limited capacity of hospitals today would be stretched even further.
A policy agenda for essential, low-wage health workers
Policymakers, employers, and the general public should each do their part for low-wage essential health workers during COVID-19 and beyond. The following policy recommendations are aimed at keeping these workers safe on the job, compensating them with a living wage, supporting them if they fall ill, and giving them the respect and appreciation they deserve.
A first-order priority for policymakers and employers should be keeping frontline health workers safe on the job. Dire shortages of life-saving personal protective equipment (PPE) such as surgical masks, N95 respirators, isolation gowns, gloves, and face shields are jeopardizing workers’ lives. One poll showed that two-thirds of health care workers reported insufficient face masks as recently as early May. Frustrated nurses and doctors have made urgent appeals to the federal government to activate the Defense Production Act to mobilize production of needed supplies.
While most news coverage highlights only the risks to nurses and doctors, PPE shortages are also a matter of life and death for millions of health care support, service, and direct care workers on the COVID-19 front line. These workers are at a lower priority for the already-insufficient supplies, meaning that hospitals and health care facilities sometimes overlook their safety as they ration PPE and prioritize vulnerable clinical staff who treat infectious patients.
The workers I interviewed expressed a range of emotions—from fear to frustration to anger—over their lack of access to PPE. David Saucedo, a 52-year-old cook at a Baltimore nursing home, said his supervisors initially denied his requests for PPE.
“Just because I am not a nurse or nursing assistant doesn’t mean I don’t come in contact with patients,” Saucedo told me. “Every footstep a nurse, nursing assistant, or doctor takes in that facility, I actually walk right behind them.” His Alzheimer’s patients, he noted, do not understand social distancing: “They just come up to you, grab you, and sit and talk to you.”
Saucedo had to argue his case to two supervisors before he was finally given the PPE that nurses in his facilities automatically access. “It’s like they prioritized them and forgot about everyone else,” he told me. “It makes me feel like I am secondary, not equal. You are expendable, in a way.”
Andrea (who preferred we only use her first name), a 29-year-old housekeeping aide in a hospital operating room and mother of two young children, had a similar experience. After a patient in a room she was responsible for cleaning was suspected of having the coronavirus, Andrea asked her charge nurse to be fit-tested for an N95 mask. Andrea said the nurse’s response was, “No, these are for special people.”

“One minute you are important enough,” she told me. “The next minute it is like, no you aren’t that important to get the proper equipment, but you are important enough to clean it for the next patient.”
Home care workers face additional hurdles to accessing PPE. Their employers are much lower in priority for state and federal PPE supplies than hospitals, nursing homes, and emergency services, leaving many agencies struggling to procure equipment on their own and pay for its skyrocketing costs on the private market. A recent survey found more than 75% of home care agencies face shortages of masks and sanitizer.
Like others in her field, Elizabeth Peachy, a 49-year-old home health aide in Virginia, received no PPE, COVID-19 training, or supplies from her employer. She described driving to towns across Virginia and West Virginia in search of her own equipment. Yvette Beatty, a 60-year-old home health aide in Philadelphia, said her employer was unable to access PPE despite concerted efforts.
“I would love to see us have hazard masks, instead of putting cloths over our face, or going to the Dollar Store and buying dollar masks,” Beatty told me. “We need equipment. They need to give equipment to agencies. We are running around with cloths, no protective gear. We need the exact same thing as everyone else.”
» Policy recommendations to keep workers safe:
- The federal government should fully utilize the Defense Production Act to mobilize manufacturers across the country to increase the supply of PPE. Until every health care worker has sufficient access to PPE, their lives are at risk.
- State governments should encourage companies to increase PPE supplies and help home health agencies access supplies and finance costs. They can follow the lead of Washington state, which recently added home health workers and other long-term care providers to the top tier of priority for PPE.
- Home care agencies should increase training, information, and resources to frontline workers, so home care workers do not feel like they are navigating a pandemic on their own.
The extremely low pay that health care support, service, and direct care workers earn has long been woefully inadequate. During a pandemic, it is morally reprehensible. Congress should enact hazard pay to ensure that no worker risking his or her life during this crisis is paid less than a family-sustaining wage.
For workers in health jobs, federal funding for hazard pay is especially important. Hospital finances have been hit hard by the pandemic. Home care agencies are limited in their ability to raise pay due to Medicaid reimbursement rates, a major systemic impediment to improving job quality for millions of care workers. Hazard pay for health workers has lagged behind temporary pay increases for workers in sectors such as retail and grocery.
Lawmakers on both sides of the aisle have offered proposals for federally funded hazard pay. In April, President Donald Trump signaled his support for extra compensation to doctors, nurses, and health workers. On May 15, the House of Representatives passed the HEROES Act, which included $200 billion for hazard pay for essential workers. Despite this momentum, U.S. lawmakers have not passed hazard pay into law. In Canada, however, Prime Minister Justin Trudeau announced a $4 billion commitment to increase pay for essential workers. He singled out low-paid essential workers as a priority, saying that minimum-wage workers risking their health during the pandemic deserve a raise.
The workers I interviewed expressed a strong desire for hazard pay. David Saucedo likened the hazards of his job as a nursing home cook to the risks he faced during his military service: “When I was in the Navy, when we went to war, I was getting paid hazardous duty pay. To me, it is a hazardous job right now. We should be getting paid hazardous pay.” Saucedo noted that additional compensation could be life-saving, affording his colleagues the chance to take a taxi instead of risking exposure to COVID-19 on public transit. “Everybody is contagious on buses,” he said. “The best thing you can do is limit their amount of exposure for a cook or anyone else.”

Housekeeping aide Sabrina Hopps agreed that additional compensation could be life-saving. “If pay was better, I would be able to live on my own and so could my children,” she told me. “What I make, it is not enough. So, I am forced to share an apartment with my son and daughter and my granddaughter. Going back and forth to work, I am jeopardizing their lives.” Hopps is especially concerned for her son, who has asthma and is a cancer survivor. Her employer recently introduced a new bonus for employees providing direct patient care, but excluded housekeepers and other low-paid service workers from the additional compensation.
» Policy recommendations for introducing hazard pay:
- Congress should pass federally mandated hazard pay for at-risk essential workers in the next pandemic relief bill, with a priority for lower-paid workers. Hazard pay should double the wages of low-wage workers. In the HEROES Act legislation, House Democrats included $200 billion for hazard pay through a “Heroes Fund” that would administer grants to employers of essential workers. Their proposed rate of an additional $13 per hour is roughly equivalent to the median wage of health care support, service, and direct care workers.
COVID-19 has laid bare the wide gap between the value that health care support, service, and direct care workers bring to society and the extremely low wages they earn in return. Short-term fixes such as hazard pay are urgently needed. But policymakers and employers should also make lasting changes so that these essential workers finally earn a permanent living wage .
Hospital administrative coordinator Tony Powell explained why wage increases are so critical for low-paid health workers: “They have to realize that these people, just like any other people—doctors, nurses, whoever—they have families. They have to raise their families, too. If you are working just at the poverty level, that is giving you enough to get to work, get lunch, and try to send your kids to school. But without a living wage, it’s not going to mean anything.”
Pauline Moffitt, a 50-year-old direct care worker in Philadelphia, is barely surviving on the poverty wages she earns caring for immunocompromised and elderly residents. At $9 an hour, her pay is so low that Moffitt and her recently laid-off husband cannot make ends meet, even as she commutes nearly three hours each way on five bus and train transfers. “It is a struggle,” she told me. “I have to pay a lot of bills. What am I supposed to do? I pray always: Lord, please stretch my pay. Please .”
Pennsylvania, where Moffitt works, is one of the 21 states that has not mandated a minimum wage above the federal rate of $7.25 per hour. She wants to see permanent pay increases. “I just wish they would raise it and give us a little more,” she said. “Not just for me, but all the other home health aides that are in the same situation.”

» Policy recommendations for permanently boosting pay:
- The federal government and state and local governments should raise the minimum wage to at least $15 per hour.
- State governments and the federal government should increase Medicaid funding to allow employers of home care workers to provide a living wage and offer benefits.
While workers of all incomes are vulnerable to COVID-19, low-wage workers have the least access to paid leave if they fall ill. In 2019, less than a third of workers in the bottom 10% of income earnings had access to paid sick leave, compared to nine out of 10 higher-paid workers in the top quarter of income earnings. The gaps for essential workers like home health aides are particularly large—a 2017 survey of 3,000 home care workers found that less than one in five care workers had access to paid leave.
“We don’t get any benefits,” said Elizabeth Peachy, a 49-year-old home health aide who earns $9 an hour. The funding for her work caring for geriatric patients comes through the state of Virginia, but she is not employed directly by the state. “They have us work as independent contractors,” she told me. “And that way, we get no sick leave, no overtime, no benefits at all. This is pretty standard.”
Peachy thinks policymakers should make changes: “In reality, it is a lot cheaper to pay us a little more money, give us some benefits, and allow us to take care of those patients, keep those patients from being in an ER or a nursing home, and help them have a good quality of life in their own home.”

Low-wage health workers without paid leave are in an impossible position . They face some of the highest risks of exposure to COVID-19, but have little or no ability to stay home to care for themselves or their loved ones. The public health stakes during a pandemic are high—rushing back to their jobs before they are fully recovered jeopardizes workers’ well-being and risks spreading the coronavirus to patients and colleagues. “The problem is you are going to have some workers who are still going to go to work,” said Peachy. “And they shouldn’t, because they may be sick and they may get the person sick. It would be better to have paid sick days because we need these workers to go into homes and take care of the thousands of high-risk people.”
The Families First Coronavirus Response Act took steps to temporarily address this disparity and expand paid sick leave and family and medical leave to workers during the pandemic. However, two gaps in the legislation undermine these benefits for low-wage health workers. First, the legislation only applies to employers with less than 500 employees, which could exclude upwards of half of all workers . It also stipulates that employers may exempt “health care providers,” broadly defined by the Department of Labor to include workers across health care institutions and home care settings.
» Policy recommendations for expanding paid sick leave:
- In the next pandemic relief bill, Congress should revoke exemptions for large employers and expand access to temporary paid sick leave and family and medical leave to all workers. The HEROES Act, passed on May 15, removes the employer size exemption as well as the health care provider exemptions.
- State governments and the federal government should increase Medicaid funding to allow employers of home care workers to offer benefits such as paid leave, alongside a living wage.
Long before COVID-19, 53-year-old Yolanda Ross felt her work as a home health worker outside Richmond, Va. was not respected. She told me that low-wage health workers like her are “underpaid, overlooked and forgotten about, but yet depended upon,” while others on the front line who are deemed “important” are valued differently.
Ross’s experience is reflected in the data. Brookings’s Richard V. Reeves (who is writing about the importance of respect more generally) and Hannah Van Drie recently analyzed data on the perceived social standing of essential jobs. They found a staggering gap between the high prestige of doctors and nurses and the low prestige of lesser-paid but essential hospital workers, including housekeepers.
In interviews, these workers shared stories that bring to life the lack of respect they experience. Several wondered why low-wage essential workers are never included in TV commercials that applaud doctors and nurses. ICU worker Andrea told me her charge nurse calls her “housekeeping” and still hasn’t bothered to learn Andrea’s name despite working together for seven years. Ditanya Rosebud, a 46-year-old cook and hostess at a Baltimore nursing home said her employer responds to her sacrifices by simply telling her, “This is what you signed up for.”
Rosebud and her colleagues are working extra shifts and risking their family’s lives during the pandemic. “We are just another body,” she explained. “That’s it. No more, no less.”

Workers also shared stories of life-saving PPE being reserved for “important people,” wages that do not even cover even basic expenses, hazard pay that is given only to clinical colleagues, and a lack of appreciation for workers’ sacrifices. “People are not looking at people like us on the lower end of the spectrum,” said hospital administrative coordinator Tony Powell. “We’re not even getting respect. That is the biggest thing: We are not even getting respect.”
The COVID-19 pandemic has already upended so many aspects of society, the economy, and our lives. Yolanda Ross hopes that it will also upend our long-standing notions of who deserves to be valued. “I pray there is a redirection,” she said. “That we stop doing things the same old way and listen to those who don’t have a real voice.”
» Recommendations for giving workers respect:
- Government and other civic leaders can do more to recognize the contributions of low-wage workers and give their work public visibility. A collaboration between city leaders in New York and workforce partners around the social media effort #ValueDirectCareWorkers is an example.
- The general public can do more to include lower-wage workers in their recognition of essential workers, including actions such as meal donations to hospitals, public demonstrations of thanks and support, and social media messages.
- The media should address the imbalance in coverage of workers, and publish stories, perspectives, and images of lower-wage health workers on the COVID-19 front line.
- Employers should provide low-wage health workers with respect, appreciation, more equitable pay and support, and opportunities for training, advancement, and better job quality.
It is long past time that low-wage workers who are essential to our society are treated with dignity. Employers, colleagues, policymakers, and the general public have their parts to play in finally giving these workers the respect they have always deserved. “It can change,” Yolanda Ross reminded me. “There is hope.”
Policy recommendations overview
Click here to download a shareable version of this table.
These interviews were conducted between April 1, 2020 and April 28, 2020. Participants have provided permission to Brookings to use their names, likenesses, job titles, location and transcribed words.
We are enormously grateful to Tony Powell, Andrea, Yvette Beatty, David Saucedo, Sabrina Hopps, Elizabeth Peachy, Pauline Moffitt, Ditanya Rosebud, and Yolanda Ross for sharing their stories. We thank and each and every worker on the front lines for the sacrifices they are making.
Thanks to PHI, SEIU, SEIU Local 1199, Angelina Drake, Tatia Cooper, Yvonne Slosarski, Leslie Frane, and LaNoral Thomas for their collaboration with the worker interviews. Thanks to Richard V. Reeves, Angelina Drake, Tiffany Ford, Ai-jen Poo, Greg Larson, Alan Berube, Morgan Welch, Claudia Balog, and Vicki Shabo for substantive comments and thoughtful input.
Related Content
Molly Kinder
April 10, 2020
March 25, 2020
April 9, 2020
Brookings Metro
Simon Hodson
May 8, 2024
Alan Berube, Mark Muro
May 3, 2024
Carnegie Mellon University, Pittsburgh PA
9:00 am - 11:15 am EDT
- Open access
- Published: 24 March 2022
Health care workers’ experiences during the COVID-19 pandemic: a scoping review
- Souaad Chemali 1 ,
- Almudena Mari-Sáez 1 ,
- Charbel El Bcheraoui 2 &
- Heide Weishaar ORCID: orcid.org/0000-0003-1150-0265 2
Human Resources for Health volume 20 , Article number: 27 ( 2022 ) Cite this article
24k Accesses
83 Citations
11 Altmetric
Metrics details
COVID-19 has challenged health systems worldwide, especially the health workforce, a pillar crucial for health systems resilience. Therefore, strengthening health system resilience can be informed by analyzing health care workers’ (HCWs) experiences and needs during pandemics. This review synthesizes qualitative studies published during the first year of the COVID-19 pandemic to identify factors affecting HCWs’ experiences and their support needs during the pandemic. This review was conducted using the Joanna Briggs Institute methodology for scoping reviews. A systematic search on PubMed was applied using controlled vocabularies. Only original studies presenting primary qualitative data were included.
161 papers that were published from the beginning of COVID-19 pandemic up until 28th March 2021 were included in the review. Findings were presented using the socio-ecological model as an analytical framework. At the individual level, the impact of the pandemic manifested on HCWs’ well-being, daily routine, professional and personal identity. At the interpersonal level, HCWs’ personal and professional relationships were identified as crucial. At the institutional level, decision-making processes, organizational aspects and availability of support emerged as important factors affecting HCWs’ experiences. At community level, community morale, norms, and public knowledge were of importance. Finally, at policy level, governmental support and response measures shaped HCWs’ experiences. The review identified a lack of studies which investigate other HCWs than doctors and nurses, HCWs in non-hospital settings, and HCWs in low- and lower middle income countries.
This review shows that the COVID-19 pandemic has challenged HCWs, with multiple contextual factors impacting their experiences and needs. To better understand HCWs’ experiences, comparative investigations are needed which analyze differences across as well as within countries, including differences at institutional, community, interpersonal and individual levels. Similarly, interventions aimed at supporting HCWs prior to, during and after pandemics need to consider HCWs’ circumstances.
Conclusions
Following a context-sensitive approach to empowering HCWs that accounts for the multitude of aspects which influence their experiences could contribute to building a sustainable health workforce and strengthening health systems for future pandemics.
Peer Review reports
Introduction
The COVID-19 pandemic has put health systems worldwide under pressure and tested their resilience. The World Health Organization (WHO) acknowledges health workforce as one of the six building blocks of health systems [ 1 ]. Health care workers (HCWs) are key to a health system’s ability to respond to external shocks such as outbreaks and as first responders are often the hardest hit by these shocks [ 2 ]. Therefore, interventions supporting HCWs are key to strengthening health systems resilience (ibid). To develop effective interventions to support this group, a detailed understanding of how pandemics affect HCWs is needed.
Several recent reviews [ 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 ] focus on HCWs’ experiences during COVID-19 and the impact of the pandemic on HCWs’ well-being, including their mental health [ 3 , 7 , 8 , 11 , 12 , 13 , 14 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 ]. Most of these reviews refer to psychological scales measurements to provide quantifiable information on HCWs’ well-being and mental health [ 8 , 13 , 14 , 19 , 21 , 22 , 23 , 24 , 25 , 28 ]. While useful in assessing the scale of the problem, such quantitative measures are insufficient in capturing the breadth of HCWs’ experiences and the factors that impact such experiences. The added value of qualitative studies is in understanding the complex experiences of HCWs during COVID-19 and the contextual factors that influence them [ 29 ].
This paper reviews qualitative studies published during the first year of the pandemic to investigate what is known about HCWs’ experiences during COVID-19 and the factors and support needs associated with those experiences. By presenting HCWs’ perspectives on the pandemic, the scoping review provides the much-needed evidence base for interventions that can help strengthen HCWs and alleviate the pressures they experience during pandemics.
The review follows the Joanna Briggs Institute (JBI) process and guideline on conducting scoping reviews [ 30 ]. JBI updated guidelines identify scoping reviews as the most suitable choice to explore the breadth of literature on a topic, by mapping and summarizing available evidence [ 30 ]. Scoping reviews are also suitable to address knowledge gaps and provide insightful input for decision-making [ 30 ]. The review also applies the PRISMA checklist guidance on reporting literature reviews [ 31 ].
Information sources
A systematic search was conducted on PubMed database between the 9th and 28th of March 2021.
Search strategy
Drawing on Shaw et al. [ 32 ] and WHO [ 33 ], the search strategy used a controlled vocabulary of index terms including Medical Subject Headings (Mesh) of the keywords and synonyms “COVID-19”, “HCWs”, and “qualitative”. Keywords were combined using the Boolean operator “AND” (see Additional file 1 ).
Eligibility criteria
The population of interest included all types of HCWs, independent of geography and settings. Only original studies were included in the review. Papers further had to (1) report primary qualitative data, (2) report on HCWs’ experiences and perceptions during COVID-19, and (3) be available as full texts in English, German, French, Spanish or Arabic, i.e., in a language that could be reviewed by one or several of the authors. Studies focusing solely on HCWs’ assessment of newly introduced modes of telemedicine during COVID-19 were excluded from the review as their clear emphasis on coping with technical challenges deviated from the review’s focus on HCWs’ personal and professional experiences during the pandemic.
Selection process
The initial search yielded 3976 papers. All papers were screened and assessed against the eligibility criteria by one researcher (SC) to identify relevant studies. A random 25% sample of all papers was additionally screened by a second researcher (HW). Any uncertainty or inconsistency regarding inclusion were resolved by discussing the respective articles ( n = 76) among the authors.
Data collection process
Based on the research question, an initial data extraction form was developed, independently piloted on ten papers by SC and HW and finalised to include information on: (1) author(s), (2) year of publication, (3) type of HCW, (5) study design, (6) sample size, (7) topic of investigation, (8) data collection tool(s), (9) analytical approach, (10) period of data collection, (11) country, (12) income level according to World Bank [ 34 ], (13) context, and (14) main findings related to experiences, factors and support needs. Using the final extraction form, all articles were extracted by SC, with the exception of four German articles (which were extracted by HW), one Spanish and one French article (which were extracted by AMS). As far as applicable, the quality of the included articles was appraised using the JBI critical appraisal tool for qualitative research [ 35 ].
Synthesis methods
The socio-ecological model originally developed by Brofenbrenner was adapted as a framework to analyze and present the findings [ 36 , 37 , 38 ]. The model aims to understand the interconnectedness and dynamics between personal and contextual factors in shaping human development and experiences [ 36 , 38 ]. The model was chosen, because it accounts for the multifaceted interactions between individuals and their environment and is thus suited to capture the different dimensions of HCWs’ experiences, the factors associated with those experiences as well as the sources of support identified. The five socio-ecological levels (individual, interpersonal, institutional, community and policy) of the model served as a framework for analysis and were used to categorise the main themes that were identified in the scoping review as relevant to HCWs’ experiences. The process of identifying the sub-themes was conducted by SC using an excel extraction sheet, in which the main findings were captured and mapped against the socio-ecological framework.
Study selection
The selection process and the number of papers found, screened and included are illustrated in a PRISMA flow diagram (Fig. 1 ). A total of 161 papers were included in the review (see Additional file 2 ). Table 1 lists the included studies based on study characteristics, including type of HCW, healthcare setting, income level of countries studied and data collection tools.
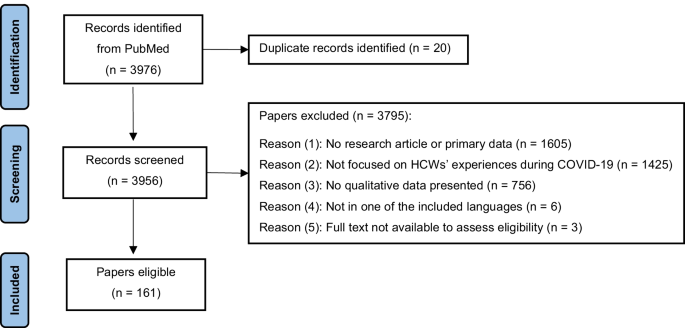
PRISMA flow diagram
Study characteristics
Included papers investigated various types of HCWs. The most investigated type were nurses, followed by doctors/physicians. Medical and nursing students were also studied frequently, while only a small number of studies focused on other professions, e.g., community health workers, therapists and managerial staff. A third of all studies studied multiple HCWs, rather than targeting single professions. The majority of papers investigated so-called “frontline staff”, i.e., HCWs who engaged directly with patients who were suspected or confirmed to be infected with COVID-19. Fewer studies focused on non-frontline staff, and some explored both frontline and non-frontline staff.
Around two-thirds of all papers studied HCWs’ experiences in high-income countries, notably the USA, followed by the UK. Many papers also focused on HCWs in upper-middle income countries, with almost half of them conducted in China. Few papers investigated HCWs in lower-middle income countries, including India, Zimbabwe, Pakistan, Nigeria, and Senegal. Finally, one paper focused on HCWs in Ethiopia, a low-income country. A couple of studies presented data from multiple countries of different income levels, and one study investigating HCWs in Palestine could not be categorised. Overall, the USA was the most studied and China the second most studied geographical location (see Additional file 3 ). Hospitals were by far the most investigated healthcare settings, whereas outpatient settings, including primary care, pharmacies, homes care, nursing homes, healthcare facilities in prisons and schools as well as clinics, were investigated to a considerably lesser extent. Several studies covered more than one setting.
All studies applied a cross-sectional study design, with 54% published in 2020, and the remainder in 2021. A range of qualitative data collection methods were applied, with interviews being by far the most prominent one, followed by open-ended questionnaires. Focus groups and a few other methods including social media, online platforms or recording systems submissions, observations and open reflections were used with rare frequencies. The sample size in studies using interviews ranged between 6 and 450 interviewees. The sample size in studies using Focus Group Discussions (FGDs) ranged between 7 and 40 participants. Further information on the composition and context of the FGDs can be found in additional file 4 . Several studies used multiple data collection tools. The majority of studies applied common analysis methods, including thematic and content analysis, with few using other specific approaches.
Results of syntheses
An overview of the findings based on the socio-ecological framework is summarised in Table 2 , which lists the main sub-themes identified under each socio-ecological level.
Individual level
At the individual level, HCWs’ experiences related to their well-being, professional and personal identity as well as daily work–life routine. In terms of well-being, HCWs reported negative impacts on their physical health (e.g., tiredness, discomfort, skin damage, sleep disorders) [ 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 ] and compromised mental health. The reported negative impact on mental health included increased levels of self-reported stress, depression, anxiety, fear, grief, guilt, anger, isolation, uncertainty and helplessness [ 39 , 41 , 43 , 44 , 45 , 46 , 47 , 49 , 50 , 51 , 52 , 53 , 54 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 ]. The reported reasons for HCWs’ reduced well-being included work-related factors, such as having to adhere to new requirements in the workplace, the lack and/or burden of using Personal Protective Equipment (PPE) [ 41 , 44 , 52 , 63 , 64 , 78 , 93 , 124 , 125 ], increased workload, lack of specialised knowledge and experience, concerns over delivering low quality of care [ 42 , 44 , 49 , 52 , 53 , 63 , 69 , 70 , 73 , 74 , 76 , 78 , 79 , 83 , 84 , 85 , 86 , 89 , 90 , 93 , 94 , 101 , 103 , 109 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 ] and being confronted with ethical dilemmas [ 43 , 72 , 76 , 78 , 136 , 141 , 142 , 143 , 144 , 145 ]. HCWs’ compromised psychological well-being was also triggered by extensive exposure to concerning information via the media and by the pressure that was experienced due to society and the media assigning HCWs hero status [ 53 , 72 , 81 , 92 , 97 , 107 , 139 , 146 ]. Factors that were reported by HCWs as helping them cope with pressure comprised diverse self-care practices and personal activities, including but not limited to psychological techniques and lifestyle adjustments [ 47 , 56 , 64 , 71 , 72 , 78 , 90 , 139 , 147 , 148 ] as well as religious practices [ 81 , 112 , 149 ].
Self-reported well-being differed across occupations, roles in the pandemic response and work settings. One study reported that HCWs working in respiratory, infection and emergency departments expressed more worries compared to HCWs who worked in other hospital wards [ 64 ]. Similarly, frontline HCWs seemed more likely to experience feelings of helplessness and guilt as they witnessed the worsening situation of COVID-19 patients, whereas non-frontline HCWs seemed to experience feelings of guilt due to not supporting their frontline colleagues [ 98 ]. HCWs with managerial responsibility reported heightened concern for their staff’s health [ 75 , 110 , 150 ]. HCWs working in nursing homes and home care reported feelings of being abandoned and not sufficiently recognised [ 75 , 123 , 144 ], while one study investigating HCWs responding to the pandemic in a slums-setting reported fear of violence [ 56 ].
HCWs reported that the pandemic impacted both positively and negatively on their professional and personal identity. While negative emotions were more dominant at the beginning of the pandemic, positive effects were reported to gradually develop after the initial pandemic phase and included an increased sense of motivation, purpose, meaningfulness, pride, resilience, problem-solving attitude, as well as professional and personal growth [ 43 , 44 , 47 , 49 , 50 , 51 , 63 , 67 , 68 , 69 , 71 , 73 , 74 , 75 , 76 , 78 , 79 , 87 , 90 , 91 , 92 , 93 , 98 , 102 , 104 , 112 , 114 , 117 , 118 , 119 , 122 , 124 , 131 , 132 , 143 , 150 , 151 , 152 , 153 , 154 , 155 , 156 , 157 , 158 , 159 , 160 , 161 ]. Frontline staff reported particularly strong positive effects related to feelings of making a difference [ 69 , 92 ]. On the other hand, some HCWs reported doubts with regard to their career choices and job dissatisfaction [ 40 , 46 , 59 , 130 ]. Junior staff, assistant doctors and students often reported feelings of exclusion and concerns about the negative effects of the pandemic on their training [ 40 , 162 , 163 ]. Challenges with regard to their professional identity and a sense of failing their colleagues on the frontline were particularly reported by HCWs who had acquired COVID-19 themselves and experienced long COVID-19 [ 121 , 160 , 164 ]. HCWs who reached out to well-being support services expressed concern at being stigmatised [ 97 ].
HCWs reported a work–life imbalance [ 57 , 97 ] as they had to adapt to the disruption of their usual work routine [ 59 , 62 , 131 ]. This disruption manifested in taking on different roles and responsibilities [ 39 , 49 , 67 , 73 , 83 , 89 , 94 , 97 , 110 , 137 , 139 , 144 , 151 ], increased or decreased workload pressure [ 85 , 128 , 130 , 133 ] and sometimes redeployment [ 57 , 155 , 165 ]. HCWs also reported negative financial effects [ 59 , 86 , 166 ].
Interpersonal level
The findings presented in this section relate to HCWs’ perceptions of their relationships in the private and professional environment during the pandemic and to the impact these relationships had on them. With regard to the home environment, HCWs’ concerns over being infected with COVID-19 and transmitting the virus to family members were identified in almost all studies [ 41 , 44 , 48 , 51 , 54 , 56 , 61 , 68 , 75 , 77 , 80 , 85 , 90 , 128 , 139 , 160 , 167 , 168 , 169 , 170 , 171 ]. HCWs living with children or elderly family members were particularly concerned [ 47 , 65 , 95 , 97 , 163 , 172 ]. In some cases, HCWs reported that they had introduced changes to their living situation to protect their loved ones, with some deciding to move out to ensure physical distance and minimise the risk of transmission [ 39 , 43 , 44 , 89 , 105 , 161 ]. Some HCWs reported sharing limited details about their COVID-19-related duties to decrease the anxiety and fear of their significant others [ 81 ]. While in several studies, interpersonal relationships were reported to cause concerns and worries, some study also identified interpersonal relationships and the subsequent emotional connectedness as a helpful resource [ 47 , 173 , 174 ] that could, for example, alleviate anxiety [ 64 ] or provide encouragement for working on the frontline [ 49 , 106 ]. However, interpersonal relationships did not always have a supportive function, with some HCWs reporting being shunned by family and friends [ 66 , 111 , 175 ].
With regard to the work environment, relationships with colleagues were mainly described as supportive and empowering, with various studies reporting the value of teamwork during the pandemic [ 47 , 51 , 52 , 67 , 71 , 77 , 83 , 91 , 97 , 98 , 108 , 134 , 148 , 151 , 161 ]. Challenges with regard to collegial relationships included social distancing (which hindered HCWs’ interaction in the work place) [ 176 ] and working with colleagues one had never worked with before (causing a lack of familiarity with the work environment and difficulties to adapt) [ 79 ]. HCWs who worked in prisons reported interpersonal conflicts due to perceived increased authoritarian behaviour by security personnel that was perceived to manifest in arrogance and non-compliance with hygiene practices [ 88 ].
In terms of HCWs’ relationships with patients, many studies reported challenges in communicating with patients [ 50 , 55 , 126 , 132 , 133 , 172 ]. This was attributed to the use of PPE during medical examinations and care and the reduction of face-to-face visits or a complete switch to telehealth [ 128 , 139 ]. The changes in the relationships with patients varied according to the nature of work. Frontline HCWs, for example, reported challenges in caring for isolated patients [ 41 , 43 , 52 , 148 ], whereas HCWs working in specific settings and occupational roles that required specific interpersonal skills faced other challenges. This was, for example, the case for HCWs working with people with intellectual disabilities, who found it challenging to explain COVID-19 measures to this group and also had to mitigate physical contact that was considered a significant part of their work [ 71 ]. For palliative care staff, the use of PPE and measures of social distancing were challenging to apply with regard to patients and family members [ 177 ]. Building relationships and providing appropriate emotional support was reported to be particularly challenging for mental health and palliative care professionals supporting vulnerable adults or children [ 117 ]. Challenges for health and social care professionals were associated with virtual consultations and more difficult conversations [ 117 ]. Physicians reported particular frustration with remote monitoring of chronic diseases when caring for low-income, rural, and/or elderly patients [ 169 ]. Having to adjust, and compromise on, the relationships with patients caused concerns about the quality of care, which in turn, was reported to impact negatively on HCWs’ professional identity and emotional well-being.
Institutional level
This section presents HCWs’ perceptions of decision-making processes in the work setting, organizational factors and availability of institutional support.
With regard to decision-making, a small number of studies reported HCWs’ trust in the institutions they worked in [ 143 , 172 ], while the majority of studies revealed discontent about institutional leadership and feelings of exclusion from decision-making processes [ 65 , 178 ]. More specifically, HCWs reported a lack of clear communication and coordination [ 41 , 70 , 144 , 148 , 179 ] and a wish to be provided with the rationales behind management decisions and to be included in recovery phase planning [ 48 ]. They perceived centralised decision-making processes as unfamiliar and restrictive [ 150 ]. Instead, HCWs endorsed de-centralised and participatory approaches to communication and decision-making [ 56 ]. Emergency and critical care physicians suggested to include bioethicists as part of the decision-making on triaging scarce critical resources [ 126 ]. Studies of both hospital and primary care settings reported perceived disconnectedness and poor collaboration between managerial, administrative and clinical staff, which was a contributing factor to burnout among HCWs [ 60 , 83 , 149 , 169 , 180 , 181 , 182 ]. Dissatisfaction with communication also related to constantly changing protocols, which were perceived as highly burdening and frustrating, creating ambiguity and negatively affecting HCWs’ work performance [ 44 , 55 , 59 , 78 , 112 , 183 ].
In terms of organizational factors, many HCWs reported a perceived lack of organizational preparedness and poor organization of care [ 60 , 65 , 120 , 179 ]. Changes in the organization of care were perceived as chaotic, especially at the beginning of the pandemic, and changes in roles and responsibilities and role allocation were perceived as unfair and unsatisfying [ 72 , 97 ]. Only in one study, changes in work organisation were perceived positively, with nurses reporting satisfaction with an improved nurse–patient ratio resulting from organisational changes [ 52 ]. Overall, frontline HCWs advocated for more stability in team structure to ensure familiarity and consistency at work [ 47 , 66 , 72 , 114 , 116 ]. HCWs appreciated multidisciplinary teams, despite challenges with regard to achieving rapid and efficient collaboration between members from different departments [ 41 , 143 , 152 ].
Regarding institutional support, in some instances, psychological, managerial, material and technical support was positively acknowledged, while the majority of studies reported HCWs’ dissatisfaction with the support provided by the institution they worked in [ 46 , 48 , 73 , 84 , 92 , 97 , 114 , 139 , 144 , 174 , 184 ]. Across studies, a lack of equipment, including the unavailability of suitable PPEs, was one of the most prominent critiques, especially in the initial phase the pandemic [ 41 , 46 , 54 , 55 , 61 , 69 , 70 , 72 , 73 , 81 , 84 , 85 , 96 , 97 , 111 , 118 , 144 , 147 , 168 ]. In one study of a rural nursing home, HCWs reported being illegally required to treat COVID-19 patients without adequate PPE [ 39 ]. Specialised physicians, such as radiologists, for example, reported that PPE were prioritised for COVID-19 ward workers [ 65 ]. In another instance, HCWs reported that they had taken care of their own mask supply [ 113 ]. Insufficient equipment and the subsequent lack of protection induced fear and anxiety regarding one’s personal safety [ 64 , 87 ]. HCWs also reported inadequate human resources, which had consequences on increased workload [ 44 , 46 , 54 , 69 , 75 , 85 ]. Dissatisfaction with limited infrastructure was reported overall and across settings, but specific limitations were particularly relevant in certain contexts [ 116 ]. HCWs in low resource settings, including Pakistan, Zimbabwe and India, reported worsening conditions regarding infrastructure, characterised by a lack of water supply and ventilation, poor conditions of isolation wards and lack of quality rest areas for staff [ 41 , 58 , 84 ]. Despite adaptive interventions aimed at shifting service delivery to outdoors, procedures such as patient registration and laboratory work took place in poorly ventilated rooms [ 56 ]. Technical support such as the accessibility to specialised knowledge and availability of training were identified by HCWs as an important resource that required strengthening. They advocated for better “tailor-made” trainings in emergency preparedness and response, crisis management, PPE use and infection control [ 41 , 52 , 61 , 68 , 73 , 127 , 144 ]. HCWs argued that the availability of such training would improve their sense of control in health emergencies, while a lack of training compromised their confidence in their ability to provide quality healthcare [ 47 , 134 ].
Structural factors such as power hierarchies and inequalities played a role in HCWs’ perceived sense of institutional support amidst the quick changes in their institutions. Such factors were particularly mentioned in studies investigating nurses who reported dissatisfaction over doctors’ dominance and discrimination in obtaining PPE [ 54 ] as well as unfairness in work allocation [ 72 , 184 ]. They also perceived ambiguity in roles and responsibilities between nurses and doctors [ 101 ]. A low sense of institutional support was also reported by other HCWs. Junior medical staff and administrative staff reported feeling exposed to unacceptable risks of infection and a lack of recognition by their institution [ 139 ]. Staff in non‐clinical roles, non-frontline staff, staff working from home, acute physicians and those on short time contracts felt less supported and less recognised compared to colleagues on the frontline [ 48 , 139 ].
Community level
This level entails how morale and norms, as well as public knowledge relate to HCWs’ experiences in the pandemic. On the positive side, societal morale and norms were perceived as enhancing supportive attitudes among the public toward HCWs and triggering community initiatives that supported HCWs in both emotional and material ways [ 47 , 78 , 92 , 108 , 140 , 147 ]. This supportive element was especially experienced by frontline HCWs, who felt valued, appreciated and empowered by their communities. HCWs’ reaction to the hero status that was assigned to them was ambivalent [ 146 , 185 ]. In response to this status attribution, HCWs reported a sense of pressure to be on the frontline and to work beyond their regular work schedule [ 51 ]. With community support being perceived as clearly focusing on hospital frontline staff, HCWs working from home, in nursing homes, home care and non-frontline facilities and wards perceived less public support [ 139 ] and appreciation [ 85 , 144 ]. One study highlighted that HCWs did not benefit from this form of public praise but preferred an appreciation in the form of tangible and financial resources instead [ 160 ].
A clear negative aspect of social norms manifested in the stigmatisation and negative judgment by community members [ 72 , 100 , 106 , 186 , 187 ], who avoided contact with HCWs based on the perceptions that they were virus carriers and spreaders [ 43 , 68 , 92 , 111 ]. Such discrimination had negative consequences with regard to HCWs’ personal lives, including lack of access to public transportation, supermarkets, childcare and other public services [ 65 , 80 , 107 ]. Chinese HCWs working abroad reported bullying due to others perceiving and labeling COVID-19 as the ‘Chinese virus’ [ 77 ]. Negative judgment was mainly reported in studies on nurses . In a study of a COVID-19-designated hospital, frontline nurses reported unusually strict social standards directed solely at them [ 122 ]. In a comparative study of nursing homes in four countries, geriatric nurses reported social stigma toward their profession, which the society perceive not worth of respect [ 75 ].
Beyond social norms, studies identified the level of public awareness, knowledge and compliance as important determinants of HCWs’ experiences and emotional well-being [ 147 ]. For example, a lack of compliance with social distancing and other preventive measures was reported to induce feelings of betrayal, anger and anxiety among HCWs [ 41 , 80 , 81 , 111 , 188 ]. The dissemination of false information and rumors and their negative influence on knowledge and compliance was also reported with anger by HCWs in general [ 58 ], an in particular by those who worked closely with local communities [ 129 ]. Online resources and voluntary groups facilitated information exchange and knowledge transfer, factors which were valued by HCWs as an important source of information and support [ 131 , 189 ].
Policy level
Findings presented here include HCWs’ perceptions of governmental responses, governmental support and the impact of governmental measures on their professional and private situation. In a small number of studies, HCWs expressed confidence in their government’s ability to respond to the pandemic and satisfaction with governmental compensation [ 45 , 47 ]. In most cases, however, HCWs expressed dissatisfactions with the governmental response, particularly with the lack of health system organisation, the lack of a coordinated, unified response and the failure to follow an evidence-based approach to policy making. HCWs also perceived governmental guidelines as chaotic, confusing and even contradicting [ 61 , 85 , 86 , 115 , 117 , 118 , 120 , 123 , 147 , 160 , 182 , 190 ]. In one study, inadequate staffing was directly attributed to inadequate governmental funding decisions [ 191 ]. Many studies reported that HCWs had a sense of being failed by their governments [ 60 , 100 , 191 ], with non-frontline staff, notably HCWs working with the disabled [ 71 , 181 ], the elderly [ 39 , 75 , 123 , 151 ] or in home-based care [ 58 ], being particularly likely to voice feelings of being forgotten, deprioritised, invisible, less recognised and less valued by their governments. Care home staff perceived governmental support to be unequally distributed across health facilities and as being focused solely on public institutions, which prevented them from receiving state benefits [ 149 ].
Measures and regulations imposed at the governmental level had a considerable impact on HCWs’ professional as well as personal experiences. In nursing homes, HCWs perceived governmental regulations such as visiting restrictions as particularly challenging and complained that rules had not been designed or implemented with consideration to individual cases [ 62 ]. The imposed rules burdened them with additional administrative tasks and forced them to compromise on the quality of care, resulting in moral distress [ 62 ]. In abortion clinics, HCWs expressed concerns about their services being classed as non-essential services during the early stages of the pandemic [ 190 ]. Governmental policies also had impacts on HCWs personally. For example, the closure of childcare negatively impacted HCWs’ ability to balance personal and private roles and commitments. National lockdowns which restricted travel made it harder for HCWs to get to work or to see their families, especially in places with low political stability [ 95 ]. The de-escalation of measures, notably the opening of airports, was perceived as betrayal by HCWs who felt they bore the burden of increased COVID-19 incidences resulting from de-escalation strategies [ 111 ].
HCWs identified clear and consistent governmental crisis communication [ 97 , 126 ], better employees’ rights and salaries, and tailored pandemic preparedness and crisis management policies that considered different healthcare settings and HCWs’ needs [ 43 , 64 , 81 , 101 , 124 , 160 , 167 , 169 , 188 , 192 , 193 ] as important areas for improvement. HCWs in primary care advocated for strengthened primary health care, improved public health education [ 45 , 130 ] and a multi-sectoral approach in pandemic management [ 129 ].
Our scoping review of HCWs’ experiences, support needs and factors that influence these experiences during COVID-19 shows that HCWs were affected at individual, interpersonal, institutional, community and policy levels. It also highlights that certain experiences can have disruptive effects on HCWs’ personal and professional lives, and thus identifies problems which need to be addressed and areas that could be strengthened to support HCWs during pandemics.
To the best of our knowledge, our review is the first to provide a comprehensive account of HCWs’ experiences during COVID-19 across contexts. By applying an exploratory angle and focusing on existing qualitative studies, the review does not only provide a rich description of the situation of HCWs but also develops an in-depth analysis of the contextual multilevel factors which impact on HCWs’ experiences.
Our scoping review shows that, while studies on HCWs’ experiences in low resource settings are scarce, the few studies that exist and the comparison with other studies point towards setting-specific experiences and challenges. We thus argue that understanding HCWs’ experiences requires comparative investigations, which not only take countries’ income levels into account but also other contextual differences. For example, in our analysis, we identify particular challenges experienced by HCWs working in urban slums and places with limited infrastructure and low political stability. Similarly, in a recent short communication in Social Science & Medicine, Smith [ 194 ] presents a case study on the particular challenges of midwives in resource-poor rural Indonesia at the start of the pandemic, highlighting increased risks and intra-country health system inequalities. Contextual intra-country differences in HCWs’ experiences also manifest at institutional level. For example, the review suggests that HCWs who work in non-hospital settings, such as primary care services, nursing homes, home based care or disability services, experienced particular challenges and felt less recognized in relation to hospital-based HCWs. In a similar vein, HCWs working in care homes felt that as state support was not equally distributed, those working in public institutions had better chances to benefit from state support.
The review highlights that occupational hierarchies play a crucial role in HCWs’ work-related experiences. Our analysis suggests that existing occupational hierarchies seem to increase or be exposed during pandemics and that occupation is a structural factor in shaping HCWs’ experiences. The review thus highlights the important role that institutions and employers play in pandemics and is in line with the growing body of evidence that associates HCWs’ well-being during COVID-19 with their occupational role [ 195 ] and the availability of institutional support [ 195 , 196 ]. The findings suggest that to address institutional differences and ensure the provision of needs-based support to all groups of HCWs, non-hierarchical and participative processes of decision-making are crucial.
Another contextual factor affecting HCWs’ experiences are their communities. While the majority of HCWs experience emotional and material support from their community, some also feel pressure by the expectations they are confronted with. The most prominent example of such perceived pressure is the ambivalence that was reported with regard to the assignment of a hero status to HCWs. On the one hand, this attribution meant that HCWs felt recognized and appreciated by their communities. On the other hand, it led to HCWs feeling pressured to work without respecting their own limits and taking care of themselves.
This scoping review points towards a number of research gaps, which, if addressed, could help to hone interventions to support HCWs and improve health system performance and resilience.
First, the majority of existing qualitative studies investigate nurses’ and doctors’ experiences during COVID-19. Given that other types of HCWs play an equally important role in pandemic responses, future research on HCWs’ experiences in pandemics should aim for more diversity and help to tease out the specific challenges and needs of different types of HCWs. Investigating different types of HCWs could inform and facilitate the development of tailored solutions and provide need-based support.
Second, the majority of studies on HCWs’ experiences focus on hospital settings. This is not surprising considering that the bulk of societal and political attention during COVID-19 has been on the provision of acute, hospital-based care. The review thus highlights a gap with regard to research on HCWs in settings which might be considered less affected and neglected but which might, in fact, be severely collaterally affected during pandemics, such as primary health centers, care homes and home-based care. It also indicates that research which compares HCWs’ experiences across levels of care can help to tease out differences and identify specific challenges and needs.
Third, the review highlights the predominance of cross-sectional studies. In fact, we were unable to identify any longitudinal studies of HCWs’ experiences during COVID-19. A possible reason for the lack of longitudinal research is the relatively short time that has passed since the start of the pandemic which might have made it difficult to complete longitudinal qualitative studies. Yet, given the dynamics and extended duration of the pandemic, and knowledge about the impact of persistent stress on an individual’s health and well-being [ 197 , 198 , 199 , 200 ], longitudinal studies on HCWs’ experiences during COVID-19 would provide added value and allow an analysis across different stages of the pandemic as well as post-pandemic times. In our review, three differences in HCWs’ experiences across the phases of the pandemic were observed. The first one is on the individual level, reflecting the dominance of the negative emotions at the initial phase of the pandemic, which was gradually followed by increased reporting of the positive impact on HCWs’ personal and professional identity. The two other differences were on the institutional level, referring to the dissatisfaction over the lack of equipment and organization of care, mainly observed at the initial pandemic phase. Further comparative analysis of changes in HCWs’ experiences over the course of a pandemic is an interesting and important topic for future research, which could also map HCWs’ experiences against hospital capacities, availability of vaccines and tests as well as changes in pandemic restrictions. Such comparative analysis can inform the development of suitable policy level interventions accounting for HCWs’ experiences at different pandemic stages, from preparedness to initial response and recovery.
Finally, the majority of studies included in the review were conducted in the Northern hemisphere, revealing a gap in understanding the reality of HCWs in low- and lower middle income countries. Ensuring diversity in geographies and including resource-poor settings in research on HCWs would help gain a better contextual understanding, contribute to strengthening pandemic preparedness in settings, where the need is greatest, and facilitate knowledge transfer between the global North and South. While further research can help to increase our understanding of HCWs’ experiences during pandemics, this scoping review establishes a first basis for the evaluation and improvement of interventions aimed at supporting HCWs prior to, during and after COVID-19. A key finding of our analysis to strengthen HCWs’ resilience are the interdependencies of factors across the five levels of the socio-ecological model. For example, institutional, community or policy level factors (such as dissatisfaction with decision-making processes, public non-compliance or failures in pandemic management) can have a negative impact on HCWs at interpersonal and individual levels by impacting on their professional relationships, mental health or work performance. Similarly, policy, community or institutional level factors (such as adequate policy measures, appreciation within the community and the provision of PPE and other equipment) can act as protective factors for HCWs’ well-being. In line with the social support literature [ 201 ], interpersonal relationships were identified as a key factor in shaping HCWs’ experiences. The identification of the inter-dependencies between factors affecting HCWs during pandemics further highlights that health systems are severely impacted by factors outside the health systems’ control. Previous scholars have recognized the embeddedness of health systems within, and their constant interaction with, their socio-economic and political environment [ 202 ]. Previous literature, however, also shows that interventions tackling distress of HCWs have largely focused on individual level factors, e.g., on interventions aimed at relieving psychological symptoms, rather than on contextual factors [ 16 ]. To strengthen HCWs and empower them to deal with pandemics, the contextual factors that affect their situation during pandemics need to be acknowledged and interventions need to follow a multi-component approach, taking the multitude of aspects and circumstances into account which impact on HCWs’ experiences.
Limitations and strengths
Our scoping review comes with a number of limitations. First, due to resource constraints, the search was conducted using only one database. The authors acknowledge that running the search strategy on other search engines could have resulted in additional interesting studies to be reviewed. To mitigate any weaknesses, extensive efforts were made to build a strong search string by reviewing previous peer-reviewed publications as well as available resources from recognized public health institutions. Considering the high numbers of studies identified, it can be, however, assumed that the search strategy and review led to valid conclusions. Second, the review excluded non-original publications. While other types of publications could have provided additional data and perspectives on HCWs’ experiences, we decided to limit our review to original, peer-reviewed research articles to ensure quality. Third, the review excluded studies on other pandemics, which could have provided further insights into HCWs’ experiences during health crises. Given the limited resources available to the research project, it was decided to focus only on COVID-19 to accommodate a larger target group of all types of HCWs and a variety of geographical locations and healthcare settings. Furthermore, it can be argued that previous pandemics did not reach the magnitude of COVID-19 and did not lead to similar responses. With the review looking at the burden of COVID-19 as a stressor, it can be assumed that the more important the stressor, the more interesting the results. Therefore, the burdens and the way in which HCWs dealt with these burdens would be particularly augmented with regard to COVID-19, making it a suitable focus example to investigate HCWs’ experiences in health crises. The authors acknowledge that during other pandemics HCWs’ experiences might differ and be less pronounced, yet this review has addressed stressors and ways of supporting HCWs that could also inform future health crises. In our view, a major strength of the review is that is does not apply any limitation in terms of the types of HCWs, the geographical locations or the healthcare settings included. This approach did not only allow us to review a wide range of literature on an expanding area of knowledge [ 30 ], but to appropriately investigate HCWs’ experiences during a public health emergency of international concern that affects countries across the globe. Providing detailed information about the contexts in which HCWs were studied, allowed us to shed light on the contextual factors affecting HCWs’ experiences.
Implications for policy and practice
Areas of future interventions that improve HCWs’ resilience at individual level could aim towards alleviating stress and responding to their specific needs during pandemics, in line with encouraging self-care activities that can foster personal psychological resilience. Beyond that, accounting for the context when designing and implementing interventions is crucial. This can be done by addressing the circumstances HCWs live and work in, referred to in German-speaking countries as “Verhältnisprävention”, i.e., prevention through tackling living and working conditions. Respective interventions should tackle all levels outlined in the socio-ecological model, applying a systems approach. At the interpersonal level, creating a positive work environment in times of crises that is supportive of uninterrupted and efficient communication among HCWs and between HCWs and patients is important. In addition, interpersonal support, e.g., by family and friends could be facilitated. At institutional level, organizational change should consider transparent and participatory decision making and responsible planning of resources availability and allocation. At community level, tracing rumors and misinformation during health emergencies is crucial, as well as advocating for accountable journalism and community initiatives that support HCWs in times of crisis. At policy level, pandemic regulations need to account for their consequences on HCWs’ work situations and personal lives. Governmental policies and guidelines should build on scientific evidence and take into account the situations and lived experiences of HCWs across all levels of care.
This scoping review of existing qualitative research on HCWs’ experiences during COVID-19 sheds light on the impact of a major pandemic on the health workforce, a key pillar of health systems. By identifying key drawbacks, strengths that can be built upon, and crucial entry-points for interventions, the review can inform strategies towards strengthening HCWs and improving their experiences. Following a systems approach which takes the five socio-ecological levels into account is crucial for the development of context-sensitive strategies to support HCWs prior to, during and after pandemics. This in turn can contribute to building a sustainable health workforce and to strengthening and better preparing health systems for future pandemics.
Availability of data and materials
All data generated during this study are included in this published article and its supplementary information files, except for a detailed extraction sheet for all studies included, which is available from the corresponding author upon request.
Abbreviations
- Health care workers
Joanna Briggs Institute
Focus Groups Discussions
Personal Protective Equipment
World Health Organization
World Health Organization. Strengthening health systems to improve health outcomes—WHO framework for action 2007. https://www.who.int/healthsystems/strategy/everybodys_business.pdf?ua=1 . Accessed 29 July 2020.
Hanefeld J, Mayhew S, Legido-Quigley H, Martineau F, Karanikolos M, Blanchet K. Towards an understanding of resilience: responding to health systems shocks. Health Policy Plan. 2018;33(3):355–67.
PubMed PubMed Central Google Scholar
Schwartz R, Sinskey JL, Anand U, Margolis RD. Addressing postpandemic clinician mental health: a narrative review and conceptual framework. Ann Intern Med. 2020;173(12):981–8.
PubMed Google Scholar
Houghton C, Meskell P, Delaney H, Smalle M, Glenton C, Booth A, et al. Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: a rapid qualitative evidence synthesis. Cochrane Database Syst Rev. 2020;4(4):CD013582.
Bhaumik S, Moola S, Tyagi J, Nambiar D, Kakoti M. Community health workers for pandemic response: a rapid evidence synthesis. BMJ Glob Health. 2020;5(6): e002769.
Chersich MF, Gray G, Fairlie L, Eichbaum Q, Mayhew S, Allwood B, et al. COVID-19 in Africa: care and protection for frontline healthcare workers. Glob Health. 2020;16(1):46.
Google Scholar
Giorgi G, Lecca LI, Alessio F, Finstad GL, Bondanini G, Lulli LG, et al. COVID-19-related mental health effects in the workplace: a narrative review. Int J Environ Res Public Health. 2020;17(21):7857.
CAS PubMed Central Google Scholar
De Brier N, Stroobants S, Vandekerckhove P, De Buck E. Factors affecting mental health of health care workers during coronavirus disease outbreaks (SARS, MERS & COVID-19): a rapid systematic review. PLoS ONE. 2020;15(12): e0244052.
Rieckert A, Schuit E, Bleijenberg N, Ten Cate D, de Lange W, de Man-van Ginkel JM, et al. How can we build and maintain the resilience of our health care professionals during COVID-19? Recommendations based on a scoping review. BMJ Open. 2021;11(1): e043718.
Kuek JTY, Ngiam LXL, Kamal NHA, Chia JL, Chan NPX, Abdurrahman A, et al. The impact of caring for dying patients in intensive care units on a physician’s personhood: a systematic scoping review. Philos Ethics Humanit Med. 2020;15(1):12.
Salazar de Pablo G, Vaquerizo-Serrano J, Catalan A, Arango C, Moreno C, Ferre F, et al. Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis. J Affect Disord. 2020;275:48–57.
CAS PubMed PubMed Central Google Scholar
Shreffler J, Petrey J, Huecker M. The impact of COVID-19 on healthcare worker wellness: a scoping review. West J Emerg Med. 2020;21(5):1059–66.
Sanghera J, Pattani N, Hashmi Y, Varley KF, Cheruvu MS, Bradley A, et al. The impact of SARS-CoV-2 on the mental health of healthcare workers in a hospital setting—a systematic review. J Occup Health. 2020;62(1): e12175.
Serrano-Ripoll MJ, Meneses-Echavez JF, Ricci-Cabello I, Fraile-Navarro D, Fiol-deRoque MA, Pastor-Moreno G, et al. Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review and meta-analysis. J Affect Disord. 2020;277:347–57.
Fernandez R, Lord H, Halcomb E, Moxham L, Middleton R, Alananzeh I, et al. Implications for COVID-19: a systematic review of nurses’ experiences of working in acute care hospital settings during a respiratory pandemic. Int J Nurs Stud. 2020;111: 103637.
Muller AE, Hafstad EV, Himmels JPW, Smedslund G, Flottorp S, Stensland S, et al. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: a rapid systematic review. Psychiatry Res. 2020;293: 113441.
Paiano M, Jaques AE, Nacamura PAB, Salci MA, Radovanovic CAT, Carreira L. Mental health of healthcare professionals in China during the new coronavirus pandemic: an integrative review. Rev Bras Enferm. 2020;73(suppl 2): e20200338.
Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic—a review. Asian J Psychiatry. 2020;51: 102119.
Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–7.
Salari N, Khazaie H, Hosseinian-Far A, Khaledi-Paveh B, Kazeminia M, Mohammadi M, et al. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health. 2020;18(1):100.
Cénat JM, Blais-Rochette C, Kokou-Kpolou CK, Noorishad PG, Mukunzi JN, McIntee SE, et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021;295: 113599.
da Silva FCT, Neto MLR. Psychiatric symptomatology associated with depression, anxiety, distress, and insomnia in health professionals working in patients affected by COVID-19: a systematic review with meta-analysis. Prog Neuro-Psychopharmacol Biol Psychiatry. 2021;104: 110057.
Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—a systematic review and meta-analysis. Psychiatry Res. 2020;291: 113190.
da Silva FCT, Neto MLR. Psychological effects caused by the COVID-19 pandemic in health professionals: a systematic review with meta-analysis. Progr Neuro-psychopharmacol Biol Psychiatry. 2021;104: 110062.
Preti E, Di Mattei V, Perego G, Ferrari F, Mazzetti M, Taranto P, et al. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: rapid review of the evidence. Curr Psychiatry Rep. 2020;22(8):43.
Carmassi C, Foghi C, Dell’Oste V, Cordone A, Bertelloni CA, Bui E, et al. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: what can we expect after the COVID-19 pandemic. Psychiatry Res. 2020;292: 113312.
Chow KM, Law BMH, Ng MSN, Chan DNS, So WKW, Wong CL, et al. A Review of psychological issues among patients and healthcare staff during two major coronavirus disease outbreaks in China: contributory factors and management strategies. Int J Environ Res Public Health. 2020;17(18):6673.
Krishnamoorthy Y, Nagarajan R, Saya GK, Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2020;293: 113382.
Xiong Y, Peng L. Focusing on health-care providers’ experiences in the COVID-19 crisis. Lancet Glob Health. 2020;8(6):e740–1.
Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18(10):2119–26.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Shaw RL, Booth A, Sutton AJ, Miller T, Smith JA, Young B, et al. Finding qualitative research: an evaluation of search strategies. BMC Med Res Methodol. 2004;4:5.
World Health Organization. Finding public health information: WHO library PubMed cochrane library 2016. https://www.gfmer.ch/SRH-Course-2019/research-methodology/pdf/WHOLibPubMedCochrane-Allen-2019.pdf . Accessed 21 Jan 2021.
World Bank. World development indicators (WDI) 2021. https://databank.worldbank.org/source/world-development-indicators . Accessed 21 July 2021.
Joanna Briggs Institute. Checklist for qualitative research critical appraisal tools for use in JBI systematic reviews 2020. https://jbi.global/sites/default/files/2020-08/Checklist_for_Qualitative_Research.pdf . Accessed 19 May 2021.
Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol. 1977;32(7):513–31.
Bronfenbrenner U. The Ecology of human development. Cambridge: Harvard University Press; 1979.
McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–77.
CAS PubMed Google Scholar
Leskovic L, Erjavec K, Leskovar R, Vukovič G. Burnout and job satisfaction of healthcare workers in Slovenian nursing homes in rural areas during the COVID-19 pandemic. Ann Agric Environ Med. 2020;27(4):664–71.
Whelehan DF, Connelly TM, Ridgway PF. COVID-19 and surgery: a thematic analysis of unintended consequences on performance, practice and surgical training. Surgeon. 2021;19(1):e20–7.
Haq W, Said F, Batool S, Awais HM. Experience of physicians during COVID-19 in a developing country: a qualitative study of Pakistan. J Infect Dev Ctries. 2021;15(2):191–7.
Okediran JO, Ilesanmi OS, Fetuga AA, Onoh I, Afolabi AA, Ogunbode O, et al. The experiences of healthcare workers during the COVID-19 crisis in Lagos, Nigeria: a qualitative study. Germs. 2020;10(4):356–66.
Muz G, Erdoğan YG. Experiences of nurses caring for patients with COVID-19 in Turkey: a phenomenological enquiry. J Nurs Manag. 2021;29(5):1026–35.
Ardebili ME, Naserbakht M, Bernstein C, Alazmani-Noodeh F, Hakimi H, Ranjbar H. Healthcare providers experience of working during the COVID-19 pandemic: a qualitative study. Am J Infect Control. 2021;49(5):547–54.
Xu Z, Ye Y, Wang Y, Qian Y, Pan J, Lu Y, et al. Primary care practitioners’ barriers to and experience of COVID-19 epidemic control in China: a qualitative study. J Gen Intern Med. 2020;35(11):3278–84.
Yıldırım N, Aydoğan A, Bulut M. A qualitative study on the experiences of the first nurses assigned to COVID-19 units in Turkey. J Nurs Manag. 2021;29(6):1366–74.
Sun N, Wei L, Shi S, Jiao D, Song R, Ma L, et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am J Infect Control. 2020;48(6):592–8.
Cubitt LJ, Im YR, Scott CJ, Jeynes LC, Molyneux PD. Beyond PPE: a mixed qualitative–quantitative study capturing the wider issues affecting doctors’ well-being during the COVID-19 pandemic. BMJ Open. 2021;11(3): e050223.
Cui S, Zhang L, Yan H, Shi Q, Jiang Y, Wang Q, et al. Experiences and psychological adjustments of nurses who voluntarily supported COVID-19 patients in Hubei Province, China. Psychol Res Behav Manag. 2020;13:1135–45.
Aksoy H, Ayhan Başer D, Fidancı İ, Arsava EY, Cankurtaran M. Family medicine research assistants’ experiences during COVID-19 pandemic: a qualitative study. Int J Clin Pract. 2020;75: e13975.
Gómez-Ibáñez R, Watson C, Leyva-Moral JM, Aguayo-González M, Granel N. Final-year nursing students called to work: experiences of a rushed labour insertion during the COVID-19 pandemic. Nurse Educ Pract. 2020;49: 102920.
Fernández-Castillo RJ, González-Caro MD, Fernández-García E, Porcel-Gálvez AM, Garnacho-Montero J. Intensive care nurses’ experiences during the COVID-19 pandemic: a qualitative study. Nurs Crit Care. 2021;26(5):397–406.
Alizadeh A, Khankeh HR, Barati M, Ahmadi Y, Hadian A, Azizi M. Psychological distress among Iranian health-care providers exposed to coronavirus disease 2019 (COVID-19): a qualitative study. BMC Psychiatry. 2020;20(1):494.
Moradi Y, Baghaei R, Hosseingholipour K, Mollazadeh F. Challenges experienced by ICU nurses throughout the provision of care for COVID-19 patients: a qualitative study. J Nurs Manag. 2021;29(5):1159–68.
Hoernke K, Djellouli N, Andrews L, Lewis-Jackson S, Manby L, Martin S, et al. Frontline healthcare workers’ experiences with personal protective equipment during the COVID-19 pandemic in the UK: a rapid qualitative appraisal. BMJ Open. 2021;11(1): e046199.
George CE, Inbaraj LR, Rajukutty S, de Witte LP. Challenges, experience and coping of health professionals in delivering healthcare in an urban slum in India during the first 40 days of COVID-19 crisis: a mixed method study. BMJ Open. 2020;10(11): e042171.
Yu JC, McIntyre M, Dow H, Robinson L, Winston P. Changes to rehabilitation service delivery and the associated physician perspectives during the COVID-19 pandemic: a mixed-methods needs assessment study. Am J Phys Med Rehabil. 2020;99(9):775–82.
Mackworth-Young CR, Chingono R, Mavodza C, McHugh G, Tembo M, Chikwari CD, et al. Community perspectives on the COVID-19 response, Zimbabwe. Bull World Health Organ. 2021;99(2):85–91.
Szabo RA, Wilson AN, Homer C, Vasilevski V, Sweet L, Wynter K, et al. Covid-19 changes to maternity care: experiences of Australian doctors. Aust N Z J Obstet Gynaecol. 2021;61(3):408–15.
Bennett P, Noble S, Johnston S, Jones D, Hunter R. COVID-19 confessions: a qualitative exploration of healthcare workers experiences of working with COVID-19. BMJ Open. 2020;10(12): e043949.
Collado-Boira EJ, Ruiz-Palomino E, Salas-Media P, Folch-Ayora A, Muriach M, Baliño P. “The COVID-19 outbreak”—an empirical phenomenological study on perceptions and psychosocial considerations surrounding the immediate incorporation of final-year Spanish nursing and medical students into the health system. Nurse Educ Today. 2020;92: 104504.
Sizoo EM, Monnier AA, Bloemen M, Hertogh C, Smalbrugge M. Dilemmas with restrictive visiting policies in dutch nursing homes during the COVID-19 pandemic: a qualitative analysis of an open-ended questionnaire with elderly care physicians. J Am Med Dir Assoc. 2020;21(12):1774-81.e2.
Chen F, Zang Y, Liu Y, Wang X, Lin X. Dispatched nurses’ experience of wearing full gear personal protective equipment to care for COVID-19 patients in China—a descriptive qualitative study. J Clin Nurs. 2021;30(13–14):2001–14.
Fang M, Xia B, Tian T, Hao Y, Wu Z. Drivers and mediators of healthcare workers’ anxiety in one of the most affected hospitals by COVID-19: a qualitative analysis. BMJ Open. 2021;11(3): e045048.
Foley SJ, O’Loughlin A, Creedon J. Early experiences of radiographers in Ireland during the COVID-19 crisis. Insights Imaging. 2020;11(1):104.
Crowe S, Howard AF, Vanderspank-Wright B, Gillis P, McLeod F, Penner C, et al. The effect of COVID-19 pandemic on the mental health of Canadian critical care nurses providing patient care during the early phase pandemic: a mixed method study. Intensive Crit Care Nurs. 2020;63: 102999.
Palacios-Ceña D, Fernández-de-Las-Peñas C, Florencio LL, de-la-Llave-Rincón AI, Palacios-Ceña M. Emotional experience and feelings during first COVID-19 outbreak perceived by physical therapists: a qualitative study in Madrid, Spain. Int J Environ Res Public Health. 2020;18(1):127.
PubMed Central Google Scholar
Urooj U, Ansari A, Siraj A, Khan S, Tariq H. Expectations, fears and perceptions of doctors during Covid-19 pandemic. Pak J Med Sci. 2020;36(Covid19-s4):S37–42.
Kaur R, Kaur A, Kumar P. An experience of otorhinolaryngologists as frontline worker with novel coronavirus: a qualitative analysis. Indian J Otolaryngol Head Neck Surg. 2021. https://doi.org/10.1007/s12070-021-02369-3 .
Article PubMed Google Scholar
González-Timoneda A, Hernández Hernández V, Pardo Moya S, Alfaro Blazquez R. Experiences and attitudes of midwives during the birth of a pregnant woman with COVID-19 infection: a qualitative study. Women Birth. 2020;34(5):465–72.
Embregts P, Tournier T, Frielink N. Experiences and needs of direct support staff working with people with intellectual disabilities during the COVID-19 pandemic: a thematic analysis. J Appl Res Intell Disabil. 2021;34(2):480–90.
Kackin O, Ciydem E, Aci OS, Kutlu FY. Experiences and psychosocial problems of nurses caring for patients diagnosed with COVID-19 in Turkey: a qualitative study. Int J Soc Psychiatry. 2020;67(2):158–67.
Tan R, Yu T, Luo K, Teng F, Liu Y, Luo J, et al. Experiences of clinical first-line nurses treating patients with COVID-19: a qualitative study. J Nurs Manag. 2020;28(6):1381–90.
Liu YE, Zhai ZC, Han YH, Liu YL, Liu FP, Hu DY. Experiences of front-line nurses combating coronavirus disease-2019 in China: a qualitative analysis. Public Health Nurs. 2020;37(5):757–63.
Sarabia-Cobo C, Pérez V, de Lorena P, Hermosilla-Grijalbo C, Sáenz-Jalón M, Fernández-Rodríguez A, et al. Experiences of geriatric nurses in nursing home settings across four countries in the face of the COVID-19 pandemic. J Adv Nurs. 2021;77(2):869–78.
Billings J, Biggs C, Ching BCF, Gkofa V, Singleton D, Bloomfield M, et al. Experiences of mental health professionals supporting front-line health and social care workers during COVID-19: qualitative study. BJPsych Open. 2021;7(2): e70.
Song J, McDonald C. Experiences of New Zealand registered nurses of Chinese ethnicity during the COVID-19 pandemic. J Clin Nurs. 2020;30(5–6):757–64.
LoGiudice JA, Bartos S. Experiences of nurses during the COVID-19 pandemic: a mixed-methods study. AACN Adv Crit Care. 2021;32(1):e1–13.
CoşkunŞimşek D, Günay U. Experiences of nurses who have children when caring for COVID-19 patients. Int Nurs Rev. 2021;68(2):219–27.
Galehdar N, Kamran A, Toulabi T, Heydari H. Exploring nurses’ experiences of psychological distress during care of patients with COVID-19: a qualitative study. BMC Psychiatry. 2020;20(1):489.
Munawar K, Choudhry FR. Exploring stress coping strategies of frontline emergency health workers dealing Covid-19 in Pakistan: a qualitative inquiry. Am J Infect Control. 2021;49(3):286–92.
Nyashanu M, Pfende F, Ekpenyong M. Exploring the challenges faced by frontline workers in health and social care amid the COVID-19 pandemic: experiences of frontline workers in the English Midlands region. UK J Interprof Care. 2020;34(5):655–61.
Gemine R, Davies GR, Tarrant S, Davies RM, James M, Lewis K. Factors associated with work-related burnout in NHS staff during COVID-19: a cross-sectional mixed methods study. BMJ Open. 2021;11(1): e042591.
Raza A, Matloob S, Abdul Rahim NF, Abdul Halim H, Khattak A, Ahmed NH, et al. Factors impeding health-care professionals to effectively treat coronavirus disease 2019 patients in Pakistan: a qualitative investigation. Front Psychol. 2020;11: 572450.
White EM, Wetle TF, Reddy A, Baier RR. Front-line nursing home staff experiences during the COVID-19 pandemic. J Am Med Dir Assoc. 2021;22(1):199–203.
Shalhub S, Mouawad NJ, Malgor RD, Johnson AP, Wohlauer MV, Coogan SM, et al. Global vascular surgeons’ experience, stressors, and coping during the coronavirus disease 2019 pandemic. J Vasc Surg. 2021;73(3):762-771.e4.
Lapum J, Nguyen M, Fredericks S, Lai S, McShane J. “Goodbye … through a glass door”: emotional experiences of working in COVID-19 acute care hospital environments. Can J Nurs Res = Revue canadienne de recherche en sciences infirmieres. 2020;53(1):5–15.
Testoni I, Francioli G, Biancalani G, Libianchi S, Orkibi H. Hardships in Italian prisons during the COVID-19 emergency: the experience of healthcare personnel. Front Psychol. 2021;12: 619687.
Ness MM, Saylor J, Di Fusco LA, Evans K. Healthcare providers’ challenges during the coronavirus disease (COVID-19) pandemic: a qualitative approach. Nurs Health Sci. 2021;23(2):389–97.
Mayfield-Johnson S, Smith DO, Crosby SA, Haywood CG, Castillo J, Bryant-Williams D, et al. Insights on COVID-19 from community health worker state leaders. J Ambul Care Manag. 2020;43(4):268–77.
He Q, Li T, Su Y, Luan Y. Instructive messages and lessons from Chinese countermarching nurses of caring for COVID-19 patients: a qualitative study. J Transcult Nurs. 2021;32(2):96–102.
DeliktasDemirci A, Oruc M, Kabukcuoglu K. ‘It was difficult, but our struggle to touch lives gave us strength’: the experience of nurses working on COVID-19 wards. J Clin Nurs. 2020;30(5–6):732–41.
Fontanini R, Visintini E, Rossettini G, Caruzzo D, Longhini J, Palese A. Italian nurses’ experiences during the COVID-19 pandemic: a qualitative analysis of internet posts. Int Nurs Rev. 2021;68(2):238–47.
Comfort AB, Krezanoski PJ, Rao L, El Ayadi A, Tsai AC, Goodman S, et al. Mental health among outpatient reproductive health care providers during the US COVID-19 epidemic. Reprod Health. 2021;18(1):49.
Maraqa B, Nazzal Z, Zink T. Mixed method study to explore ethical dilemmas and health care workers’ willingness to work amid COVID-19 pandemic in Palestine. Front Med. 2020;7: 576820.
Gesser-Edelsburg A, Cohen R, Shahbari NAE, Hijazi R. A mixed-methods sequential explanatory design comparison between COVID-19 infection control guidelines’ applicability and their protective value as perceived by Israeli healthcare workers, and healthcare executives’ response. Antimicrob Resist Infect Control. 2020;9(1):148.
Feeley T, Ffrench-O’Carroll R, Tan MH, Magner C, L’Estrange K, O’Rathallaigh E, et al. A model for occupational stress amongst paediatric and adult critical care staff during COVID-19 pandemic. Int Arch Occup Environ Health. 2021;94(7):1–17.
Shaw C, Gallagher K, Petty J, Mancini A, Boyle B. Neonatal nursing during the COVID-19 global pandemic: a thematic analysis of personal reflections. J Neonatal Nurs. 2021;27(3):165–71.
García-Martín M, Roman P, Rodriguez-Arrastia M, Diaz-Cortes MDM, Soriano-Martin PJ, Ropero-Padilla C. Novice nurse”s transitioning to emergency nurse during COVID-19 pandemic: a qualitative study. J Nurs Manag. 2021;29(2):258–67.
Arnetz JE, Goetz CM, Arnetz BB, Arble E. Nurse reports of stressful situations during the COVID-19 pandemic: qualitative analysis of survey responses. Int J Environ Res Public Health. 2020;17(21):8126.
Jia Y, Chen O, Xiao Z, Xiao J, Bian J, Jia H. Nurses’ ethical challenges caring for people with COVID-19: a qualitative study. Nurs Ethics. 2021;28(1):33–45.
Danielis M, Peressoni L, Piani T, Colaetta T, Mesaglio M, Mattiussi E, et al. Nurses’ experiences of being recruited and transferred to a new sub-intensive care unit devoted to COVID-19 patients. J Nurs Manag. 2021;29(5):1149–58.
Gao X, Jiang L, Hu Y, Li L, Hou L. Nurses’ experiences regarding shift patterns in isolation wards during the COVID-19 pandemic in China: a qualitative study. J Clin Nurs. 2020;29(21–22):4270–80.
Zhang MM, Niu N, Zhi XX, Zhu P, Wu B, Wu BN, et al. Nurses’ psychological changes and coping strategies during home isolation for the 2019 novel coronavirus in China: a qualitative study. J Adv Nurs. 2021;77(1):308–17.
Arcadi P, Simonetti V, Ambrosca R, Cicolini G, Simeone S, Pucciarelli G, et al. Nursing during the COVID-19 outbreak: a phenomenological study. J Nurs Manag. 2021;29(5):1111–9.
KalatehSadati A, Zarei L, Shahabi S, Heydari ST, Taheri V, Jiriaei R, et al. Nursing experiences of COVID-19 outbreak in Iran: a qualitative study. Nurs Open. 2020;8(1):72–9.
Ohta R, Matsuzaki Y, Itamochi S. Overcoming the challenge of COVID-19: a grounded theory approach to rural nurses’ experiences. J Gen Fam Med. 2020;22(3):134–40.
Vindrola-Padros C, Andrews L, Dowrick A, Djellouli N, Fillmore H, Bautista Gonzalez E, et al. Perceptions and experiences of healthcare workers during the COVID-19 pandemic in the UK. BMJ Open. 2020;10(11): e040503.
Banerjee D, Vajawat B, Varshney P, Rao TS. Perceptions, experiences, and challenges of physicians involved in dementia care during the COVID-19 lockdown in India: a qualitative study. Front Psychiatry. 2020;11: 615758.
White JH. A phenomenological study of nurse managers’ and assistant nurse managers’ experiences during the COVID-19 pandemic in the United States. J Nurs Manag. 2021;29(6):1525–34.
Gunawan J, Aungsuroch Y, Marzilli C, Fisher ML, Nazliansyah, Sukarna A. A phenomenological study of the lived experience of nurses in the battle of COVID-19. Nurs Outlook. 2021;69(4):652–9.
Norful AA, Rosenfeld A, Schroeder K, Travers JL, Aliyu S. Primary drivers and psychological manifestations of stress in frontline healthcare workforce during the initial COVID-19 outbreak in the United States. Gen Hosp Psychiatry. 2021;69:20–6.
Moradi Y, Baghaei R, Hosseingholipour K, Mollazadeh F. Protective reactions of ICU nurses providing care for patients with COVID-19: a qualitative study. BMC Nurs. 2021;20(1):45.
Zhang Y, Wei L, Li H, Pan Y, Wang J, Li Q, et al. The psychological change process of frontline nurses caring for patients with COVID-19 during its outbreak. Issues Ment Health Nurs. 2020;41(6):525–30.
Fawaz M, Itani M. The psychological experiences of Lebanese ground zero front-line nurses during the most recent COVID-19 outbreak post Beirut blast: a qualitative study. Int J Soc Psychiatry. 2021. https://doi.org/10.1177/00207640211004989 .
Zerbini G, Ebigbo A, Reicherts P, Kunz M, Messman H. Psychosocial burden of healthcare professionals in times of COVID-19—a survey conducted at the University Hospital Augsburg. German Med Sci. 2020;18:Doc05.
Aughterson H, McKinlay AR, Fancourt D, Burton A. Psychosocial impact on frontline health and social care professionals in the UK during the COVID-19 pandemic: a qualitative interview study. BMJ Open. 2021;11(2): e047353.
Lee RLT, West S, Tang ACY, Cheng HY, Chong CYY, Chien WT, et al. A qualitative exploration of the experiences of school nurses during COVID-19 pandemic as the frontline primary health care professionals. Nurs Outlook. 2020;69(3):399–408.
Paula ACR, Carletto AGD, Lopes D, Ferreira JC, Tonini NS, Trecossi SPC. Reactions and feelings of health professionals in the care of hospitalized patients with suspected covid-19. Revista gaucha de enfermagem. 2021;42(spe): e20200160.
Iheduru-Anderson K. Reflections on the lived experience of working with limited personal protective equipment during the COVID-19 crisis. Nurs Inquiry. 2021;28(1): e12382.
Taylor AK, Kingstone T, Briggs TA, O’Donnell CA, Atherton H, Blane DN, et al. ‘Reluctant pioneer’: a qualitative study of doctors’ experiences as patients with long COVID. Health Expect. 2021;24(3):833–42.
Lee N, Lee HJ. South Korean nurses’ experiences with patient care at a COVID-19-designated hospital: growth after the frontline battle against an infectious disease pandemic. Int J Environ Res Public Health. 2020;17(23):9015.
Nyashanu M, Pfende F, Ekpenyong MS. Triggers of mental health problems among frontline healthcare workers during the COVID-19 pandemic in private care homes and domiciliary care agencies: lived experiences of care workers in the Midlands region, UK. Health Soc Care Community. 2020;30(2):e370–6.
Galehdar N, Toulabi T, Kamran A, Heydari H. Exploring nurses’ perception of taking care of patients with coronavirus disease (COVID-19): a qualitative study. Nurs Open. 2021;8(1):171–9.
Arasli H, Furunes T, Jafari K, Saydam MB, Degirmencioglu Z. Hearing the voices of wingless angels: a critical content analysis of nurses’ COVID-19 experiences. Int J Environ Res Public Health. 2020;17(22):8484.
Mulla A, Bigham BL, Frolic A, Christian MD. Canadian emergency medicine and critical care physician perspectives on pandemic triage in COVID-19. J Emerg Manag. 2020;18(7):31–5.
Ortiz Z, Antonietti L, Capriati A, Ramos S, Romero M, Mariani J, et al. Concerns and demands regarding COVID-19. Survey of health personnel. Medicina. 2020;80(Suppl 3):16–24.
Monzani A, Ragazzoni L, Della Corte F, Rabbone I, Franc JM. COVID-19 pandemic: perspective from italian pediatric emergency physicians. Disaster Med Public Health Prep. 2020;14(5):648–51.
Al Ghafri T, Al Ajmi F, Anwar H, Al Balushi L, Al Balushi Z, Al Fahdi F, et al. The experiences and perceptions of health-care workers during the COVID-19 pandemic in Muscat, Oman: a qualitative study. J Prim Care Community Health. 2020;11:2150132720967514.
Yin Y, Chu X, Han X, Cao Y, Di H, Zhang Y, et al. General practitioner trainees’ career perspectives after COVID-19: a qualitative study in China. BMC Fam Pract. 2021;22(1):18.
Foye U, Dalton-Locke C, Harju-Seppänen J, Lane R, Beames L, Vera San Juan N, et al. How has Covid-19 affected mental health nurses and the delivery of mental health nursing care in the UK? Results of a mixed methods study. J Psychiatr Ment Health Nurs. 2021;28(2):126–37.
Goh YS, Ow Yong QYJ, Chen TH, Ho SHC, Chee YIC, Chee TT. The impact of COVID-19 on nurses working in a University Health System in Singapore: a qualitative descriptive study. Int J Ment Health Nurs. 2020;30(3):643–52.
Verhoeven V, Tsakitzidis G, Philips H, Van Royen P. Impact of the COVID-19 pandemic on the core functions of primary care: will the cure be worse than the disease? A qualitative interview study in Flemish GPs. BMJ Open. 2020;10(6): e039674.
Travers JL, Schroeder K, Norful AA, Aliyu S. The influence of empowered work environments on the psychological experiences of nursing assistants during COVID-19: a qualitative study. BMC Nurs. 2020;19:98.
Semaan A, Audet C, Huysmans E, Afolabi B, Assarag B, Banke-Thomas A, et al. Voices from the frontline: findings from a thematic analysis of a rapid online global survey of maternal and newborn health professionals facing the COVID-19 pandemic. BMJ Glob Health. 2020;5(6): e002967.
Begerow A, Michaelis U, Gaidys U. Wahrnehmungen von Pflegenden im Bereich der Intensivpflege während der COVID-19-Pandemie. Pflege. 2020;33(4):229–36.
Santos J, Balsanelli AP, Freitas EO, Menegon FHA, Carneiro IA, Lazzari DD, et al. Work environment of hospital nurses during the COVID-19 pandemic in Brazil. Int Nurs Rev. 2021;68(2):228–37.
Fan J, Jiang Y, Hu K, Chen X, Xu Q, Qi Y, et al. Barriers to using personal protective equipment by healthcare staff during the COVID-19 outbreak in China. Medicine. 2020;99(48): e23310.
Digby R, Winton-Brown T, Finlayson F, Dobson H, Bucknall T. Hospital staff well-being during the first wave of COVID-19: staff perspectives. Int J Ment Health Nurs. 2020;30(2):440–50.
Nelson H, Hubbard Murdoch N, Norman K. The role of uncertainty in the experiences of nurses during the Covid-19 pandemic: a phenomenological study. Can J Nurs Res = Revue canadienne de recherche en sciences infirmieres. 2021;53(2):124–33.
Patterson JE, Edwards TM, Griffith JL, Wright S. Moral distress of medical family therapists and their physician colleagues during the transition to COVID-19. J Marital Fam Ther. 2021;47(2):289–303.
Palinkas LA, Whiteside L, Nehra D, Engstrom A, Taylor M, Moloney K, et al. Rapid ethnographic assessment of the COVID-19 pandemic April 2020 ‘surge’ and its impact on service delivery in an Acute Care Medical Emergency Department and Trauma Center. BMJ Open. 2020;10(10): e041772.
Hou Y, Zhou Q, Li D, Guo Y, Fan J, Wang J. Preparedness of our emergency department during the coronavirus disease outbreak from the nurses’ perspectives: a qualitative research study. J Emerg Nurs. 2020;46(6):848-861.e1.
Sterling MR, Tseng E, Poon A, Cho J, Avgar AC, Kern LM, et al. Experiences of home health care workers in New York City during the coronavirus disease 2019 pandemic: a qualitative analysis. JAMA Intern Med. 2020;180(11):1453–9.
Butler CR, Wong SPY, Wightman AG, O’Hare AM. US clinicians’ experiences and perspectives on resource limitation and patient care during the COVID-19 pandemic. JAMA Netw Open. 2020;3(11): e2027315.
Halberg N, Jensen PS, Larsen TS. We are not heroes—the flipside of the hero narrative amidst the COVID19-pandemic: a Danish hospital ethnography. J Adv Nurs. 2021;77(5):2429–36.
Hennein R, Lowe S. A hybrid inductive-abductive analysis of health workers’ experiences and wellbeing during the COVID-19 pandemic in the United States. PLoS ONE. 2020;15(10): e0240646.
Casafont C, Fabrellas N, Rivera P, Olivé-Ferrer MC, Querol E, Venturas M, et al. Experiences of nursing students as healthcare aid during the COVID-19 pandemic in Spain: a phemonenological research study. Nurse Educ Today. 2021;97: 104711.
Bilal A, Saeed MA, Yousafzai T. Elderly care in the time of coronavirus: perceptions and experiences of care home staff in Pakistan. Int J Geriatr Psychiatry. 2020;35(12):1442–8.
Butler CR, Wong SPY, Vig EK, Neely CS, O’Hare AM. Professional roles and relationships during the COVID-19 pandemic: a qualitative study among US clinicians. BMJ Open. 2021;11(3): e047782.
Williams CM, Couch A, Haines T, Menz HB. Experiences of Australian podiatrists working through the 2020 coronavirus (COVID-19) pandemic: an online survey. J Foot Ankle Res. 2021;14(1):11.
Liu Q, Luo D, Haase JE, Guo Q, Wang XQ, Liu S, et al. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. Lancet Glob Health. 2020;8(6):e790–8.
Härter M, Bremer D, Scherer M, von dem Knesebeck O, Koch-Gromus U. Impact of COVID-19-pandemic on clinical care, work flows and staff at a University Hospital: results of an interview-study at the UKE. Gesundheitswesen (Bundesverband der Arzte des Offentlichen Gesundheitsdienstes (Germany)). 2020;82(8–09):676–81.
Sheng Q, Zhang X, Wang X, Cai C. The influence of experiences of involvement in the COVID-19 rescue task on the professional identity among Chinese nurses: a qualitative study. J Nurs Manag. 2020;28(7):1662–9.
Donnelly C, Ashcroft R, Bobbette N, Mills C, Mofina A, Tran T, et al. Interprofessional primary care during COVID-19: a survey of the provider perspective. BMC Fam Pract. 2021;22(1):31.
Losty LS, Bailey KD. Leading through chaos: perspectives from nurse executives. Nurs Adm Q. 2021;45(2):118–25.
Catania G, Zanini M, Hayter M, Timmins F, Dasso N, Ottonello G, et al. Lessons from Italian front-line nurses’ experiences during the COVID-19 pandemic: a qualitative descriptive study. J Nurs Manag. 2020;29(3):404–11.
Daphna-Tekoah S, MegadasiBrikman T, Scheier E, Balla U. Listening to hospital personnel’s narratives during the COVID-19 outbreak. Int J Environ Res Public Health. 2020;17(17):6413.
Fan J, Hu K, Li X, Jiang Y, Zhou X, Gou X, et al. A qualitative study of the vocational and psychological perceptions and issues of transdisciplinary nurses during the COVID-19 outbreak. Aging. 2020;12(13):12479–92.
Missel M, Bernild C, Dagyaran I, Christensen SW, Berg SK. A stoic and altruistic orientation towards their work: a qualitative study of healthcare professionals’ experiences of awaiting a COVID-19 test result. BMC Health Serv Res. 2020;20(1):1031.
Pravder HD, Langdon-Embry L, Hernandez RJ, Berbari N, Shelov SP, Kinzler WL. Experiences of early graduate medical students working in New York hospitals during the COVID-19 pandemic: a mixed methods study. BMC Med Educ. 2021;21(1):118.
de Wit K, Mercuri M, Wallner C, Clayton N, Archambault P, Ritchie K, et al. Canadian emergency physician psychological distress and burnout during the first 10 weeks of COVID-19: a mixed-methods study. J Am College Emerg Physicians Open. 2020;1(5):1030–8.
Kuliukas L, Hauck Y, Sweet L, Vasilevski V, Homer C, Wynter K, et al. A cross sectional study of midwifery students’ experiences of COVID-19: uncertainty and expendability. Nurse Educ Pract. 2021;51: 102988.
Ladds E, Rushforth A, Wieringa S, Taylor S, Rayner C, Husain L, et al. Developing services for long COVID: lessons from a study of wounded healers. Clin Med. 2021;21(1):59–65.
Searby A, Burr D. The impact of COVID-19 on alcohol and other drug nurses’ provision of care: a qualitative descriptive study. J Clin Nurs. 2021;30(11–12):1730–41.
Hower KI, Pfaff H, Pförtner TK. Pflege in Zeiten von COVID-19: onlinebefragung von Leitungskräften zu Herausforderungen. Belastungen und Bewältigungsstrategien Pflege. 2020;33(4):207–18.
He K, Stolarski A, Whang E, Kristo G. Addressing general surgery residents’ concerns in the early phase of the COVID-19 pandemic. J Surg Educ. 2020;77(4):735–8.
Góes FGB, Silva A, Santos A, Pereira-Ávila FMV, Silva LJD, Silva LFD, et al. Challenges faced by pediatric nursing workers in the face of the COVID-19 pandemic. Rev Lat Am Enfermagem. 2020;28: e3367.
Halley MC, Mathews KS, Diamond LC, Linos E, Sarkar U, Mangurian C, et al. The intersection of work and home challenges faced by physician mothers during the coronavirus disease 2019 pandemic: a mixed-methods analysis. J Women’s Health. 2021;30(4):514–24.
Algunmeeyn A, El-Dahiyat F, Altakhineh MM, Azab M, Babar ZU. Understanding the factors influencing healthcare providers’ burnout during the outbreak of COVID-19 in Jordanian hospitals. J Pharm Policy Pract. 2020;13:53.
Sougou NM, Diouf JB, Diallo AA, Seck I. Risk perception of COVID-19 pandemic among health care providers: qualitative study conducted at the King Baudoin Hospital in Guédiawaye, the first hospital faced with managing a community-acquired COVID-19 case in Senegal. Pan Afr Med J. 2020;37(Suppl 1):23.
Conlon C, McDonnell T, Barrett M, Cummins F, Deasy C, Hensey C, et al. The impact of the COVID-19 pandemic on child health and the provision of care in paediatric emergency departments: a qualitative study of frontline emergency care staff. BMC Health Serv Res. 2021;21(1):279.
Bender AE, Berg KA, Miller EK, Evans KE, Holmes MR. “Making sure we are all okay”: healthcare workers’ strategies for emotional connectedness during the COVID-19 pandemic. Clin Soc Work J. 2021;49(4):1–11.
Yin X, Zeng L. A study on the psychological needs of nurses caring for patients with coronavirus disease 2019 from the perspective of the existence, relatedness, and growth theory. Int J Nurs Sci. 2020;7(2):157–60.
Creese J, Byrne JP, Conway E, Barrett E, Prihodova L, Humphries N. “We all really need to just take a breath”: composite narratives of hospital doctors’ well-being during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(4):2051.
Silies K, Schley A, Sill J, Fleischer S, Müller M, Balzer K. Die COVID-19-Pandemie im akutstationären Setting aus Sicht von Führungspersonen und Hygienefachkräften in der Pflege - Eine qualitative Studie. Pflege. 2020;33(5):289–98.
Tremblay-Huet S, McMorrow T, Wiebe E, Kelly M, Hennawy M, Sum B. The impact of the COVID-19 pandemic on medical assistance in dying in Canada and the relationship of public health laws to private understandings of the legal order. J Law Biosci. 2020;7(1): lsaa087.
Geremia DS, Vendruscolo C, Celuppi IC, Adamy EK, Toso B, Souza JB. 200 years of Florence and the challenges of nursing practices management in the COVID-19 pandemic. Rev Lat Am Enfermagem. 2020;28: e3358.
Kurotschka PK, Serafini A, Demontis M, Serafini A, Mereu A, Moro MF, et al. General practitioners’ experiences during the first phase of the COVID-19 pandemic in Italy: a critical incident technique study. Front Public Health. 2021;9: 623904.
Renaa T, Brekke M. Restructuring in a GP practice during the COVID-19 pandemic—a focus-group study. Tidsskrift for den Norske laegeforening: tidsskrift for praktisk medicin, ny raekke. 2021. https://doi.org/10.4045/tidsskr.20.0713 .
Article Google Scholar
Desroches ML, Ailey S, Fisher K, Stych J. Impact of COVID-19: nursing challenges to meeting the care needs of people with developmental disabilities. Disabil Health J. 2021;14(1): 101015.
Damian AJ, Gonzalez M, Oo M, Anderson D. A national study of community health centers’ readiness to address COVID-19. J Am Board Fam Med. 2021;34(Suppl):S85–94.
Schroeder K, Norful AA, Travers J, Aliyu S. Nursing perspectives on care delivery during the early stages of the covid-19 pandemic: a qualitative study. Int J Nurs Stud Adv. 2020;2: 100006.
Cho H, Sagherian K, Steege LM. Hospital nursing staff perceptions of resources provided by their organizations during the COVID-19 pandemic. Workplace Health Saf. 2021;69(4):174–81.
Hennekam S, Ladge J, Shymko Y. From zero to hero: an exploratory study examining sudden hero status among nonphysician health care workers during the COVID-19 pandemic. J Appl Psychol. 2020;105(10):1088–100.
He J, Liu L, Chen X, Qi B, Liu Y, Zhang Y, et al. The experiences of nurses infected with COVID-19 in Wuhan, China: a qualitative study. J Nurs Manag. 2021;29(5):1180–8.
Fawaz M, Samaha A. The psychosocial effects of being quarantined following exposure to COVID-19: a qualitative study of Lebanese health care workers. Int J Soc Psychiatry. 2020;66(6):560–5.
Mersha A, Shibiru S, Girma M, Ayele G, Bante A, Kassa M, et al. Perceived barriers to the practice of preventive measures for COVID-19 pandemic among health professionals in public health facilities of the Gamo zone, southern Ethiopia: a phenomenological study. BMC Public Health. 2021;21(1):199.
Austin Z, Gregory P. Resilience in the time of pandemic: the experience of community pharmacists during COVID-19. Res Soc Adm Pharm. 2021;17(1):1867–75.
Roberts SCM, Schroeder R, Joffe C. COVID-19 and independent abortion providers: findings from a rapid-response survey. Perspect Sex Reprod Health. 2020;52(4):217–25.
Brophy JT, Keith MM, Hurley M, McArthur JE. Sacrificed: Ontario healthcare workers in the time of COVID-19. New Solut. 2021;30(4):267–81.
Ilesanmi OS, Afolabi AA, Akande A, Raji T, Mohammed A. Infection prevention and control during COVID-19 pandemic: realities from health care workers in a north central state in Nigeria. Epidemiol Infect. 2021;149: e15.
Halcomb E, Williams A, Ashley C, McInnes S, Stephen C, Calma K, et al. The support needs of Australian primary health care nurses during the COVID-19 pandemic. J Nurs Manag. 2020;28(7):1553–60.
Smith C. The structural vulnerability of healthcare workers during COVID-19: observations on the social context of risk and the equitable distribution of resources. Soc Sci Med. 2020;258: 113119.
Khanal P, Devkota N, Dahal M, Paudel K, Joshi D. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Glob Health. 2020;16(1):89.
Labrague LJ, De Los Santos JAA. COVID-19 anxiety among front-line nurses: predictive role of organisational support, personal resilience and social support. J Nurs Manag. 2020;28(7):1653–61.
Abdallah CG, Geha P. Chronic pain and chronic stress: two sides of the same coin? Chronic Stress. 2017. https://doi.org/10.1177/2470547017704763 .
Article PubMed PubMed Central Google Scholar
Vachon-Presseau E. Effects of stress on the corticolimbic system: implications for chronic pain. Prog Neuropsychopharmacol Biol Psychiatry. 2018;87(Pt B):216–23.
Salvagioni DAJ, Melanda FN, Mesas AE, González AD, Gabani FL, Andrade SM. Physical, psychological and occupational consequences of job burnout: a systematic review of prospective studies. PLoS ONE. 2017;12(10): e0185781.
Hapke U, Maske UE, Scheidt-Nave C, Bode L, Schlack R, Busch MA. Chronic stress among adults in Germany: results of the German health interview and examination survey for adults (DEGS1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56(5–6):749–54.
Killgore WDS, Taylor EC, Cloonan SA, Dailey NS. Psychological resilience during the COVID-19 lockdown. Psychiatry Res. 2020;291: 113216.
Karl B, Sara LN, Ben R, Francisco P-M. Governance and capacity to manage resilience of health systems: towards a new conceptual framework. Int J Health Policy Manag. 2017;6(8):431–5.
Download references
Acknowledgements
Not applicable.
Open Access funding enabled and organized by Projekt DEAL. The study was funded by the German Federal Ministry of Health (Bundesministerium für Gesundheit, BMG).
Author information
Authors and affiliations.
Centre for International Health Protection, Robert Koch Institute, Nordufer 20, 13353, Berlin, Germany
Souaad Chemali & Almudena Mari-Sáez
Evidence-Based Public Health, Centre for International Health Protection, Robert Koch Institute, Nordufer 20, 13353, Berlin, Germany
Charbel El Bcheraoui & Heide Weishaar
You can also search for this author in PubMed Google Scholar
Contributions
HW and AMS conceived and designed the scoping review. SC extracted, analyzed and conceptualized the data as well as drafted the initial version of this manuscript. HW and AMS provided quality checks for the methodology and analysis. HW, AMS and CEB substantively revised each version of the manuscript and provided substantial inputs. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Heide Weishaar .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
: Table S1. Search strategy. The document includes the search strings for the review.
Additional file 2
: Table S2. List of included papers. The file lists the 161 included papers, detailing the title, authors, publication year and DOI link.
Additional file 3
: Table S3. List of countries studied. The file includes a table listing the countries in which the included studies were conducted according to frequency.
Additional file 4
: Table S4. Detailed information on FGDs. This document provides information extracted from studies that used FGDs as a qualitative data collection tool. The table lists the overall number of focus group discussion’s participants in each of those studies, the number of FGDs per study, whether FGDs were conducted online or offline, the type of study participants, and any other information on the methods that could be extracted.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Chemali, S., Mari-Sáez, A., El Bcheraoui, C. et al. Health care workers’ experiences during the COVID-19 pandemic: a scoping review. Hum Resour Health 20 , 27 (2022). https://doi.org/10.1186/s12960-022-00724-1
Download citation
Received : 23 September 2021
Accepted : 09 March 2022
Published : 24 March 2022
DOI : https://doi.org/10.1186/s12960-022-00724-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Experiences
- Health systems
Human Resources for Health
ISSN: 1478-4491
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Don't have an account? Sign up to download reports and comment on narrative perspectives.
Why are community health workers important?
At least half of the world's population does not have access to the essential health services it needs. A combination of economic, social, and geographic barriers - compounded by a global shortage of health care workers - prevent people from accessing primary health care (PHC). 1 The shortage of health care workers, estimated at 7.2 million health workers today, is expected to widen to 18 million by 2030, according to the World Health Organization.
Community health workers (CHWs), as part of primary health care teams, can help fill this critical gap. CHWs can be trained much more quickly than doctors, nurses and other frontline health workers, allowing governments to ramp up services relatively quickly, to meet critical needs. Despite their narrower skill set, CHWs can provide PHC services that address some of the most important causes of maternal, child and neonatal mortality, improve sexual and reproductive health, and prevent and treat other communicable and non-communicable diseases. Critically, CHWs deliver care on the doorsteps and in the communities of those who need it most. By providing these services in otherwise overlooked or underserved communities, CHWs expand access to PHC services, improve health, and save lives, particularly in rural, remote, and vulnerable communities, and where there are cultural barriers to health care.
Even in geographies with a robust health workforce, CHWs can improve health outcomes by serving as effective health educators, increasing demand for health care and promoting healthy behaviors, such as exclusive breastfeeding, support for immunization, proper complementary feeding, and proper sanitation.
The power of CHWs
Investing in CHWs is a powerful way to increase access to PHC services, increase health-seeking behavior, and improve clinical outcomes because CHWs of the following:
Geographic proximity
CHWs reduce the travel time and cost needed to access medical care, making it more accessible and timely. Rural-focused programs have higher costs than programs that include urban CHWs. In general, cost per person served decreases as the scale of the program increases. Rural programs, however, are typically more effective because they reach populations with poor access to health care.
Trust from the community
As trusted members of the community they serve, CHWs can improve demand for services and accelerate behavior change. CHWs can sensitively address traditional customs and norms that undermine health. Their fluency with culturally appropriate language, and mechanisms for communicating health and hygiene best practices can ensure better competence with health instructions.
Frequency of contacts
Too often, remote communities' only contract with health systems is via intermittent campaigns. CHWs shift this paradigm by providing regular services that meaningfully extend the continuum of care. By virtue of living and working the community, they can monitor chronic health conditions or continually reinforce key health messages - such as the importance of exclusive breastfeeding or proper complementary feeding for infants - and readily identify unmet health needs.
Bridging community and health and welfare services
CHWs can serve as a bridge between the formal health system and vulnerable communities, helping their colleagues, such as nurses and doctors, better understand the patients they serve and prioritize their time addressing more complex medical problems. CHWs also help patients, who may have no previous experience with preventive care, better appreciate the benefits of and follow the unfamiliar protocols of preventive care. Likewise, they can link communities to other government social services that may impact health. Furthermore, CHWs can help patients navigate complex health systems and ensure they comply with recommended treatment and follow-up visits.
- 1 Tracking universal health coverage: 2017 global monitoring report. World Health Organization and International Bank for Reconstruction and Development / The World Bank; 2017. Licence: CC BY-NC-SA 3.0 IGO. https://apps.who.int/iris/bitstream/handle/10665/259817/9789241513555-eng.pdf?sequence=1.
What impact can CHWs have?
Success! Your password has been reset. Please login.
Forgot Password
Connect directly with topic and country experts in global health..
Please be specific and include necessary contextual and background information for us to connect you to the right person and ensure we provide the most helpful response.
Sign up for an Exemplars in Global Health account to download reports, post annotations, and comment on narrative perspectives.
Already have an account? Login
By signing up you agree to our Terms of Use and Privacy Policy
Ask An Expert
Exemplars staff are available to answer questions that clarify our research, insights, methodology, and conclusions.
Need something else? Learn More .
Sign up for our newsletter
Stay up-to-date with Exemplars in Global Health (EGH) by receiving updates, newsletters, and other communications from the Exemplars Program.
Please select your area of interest.
Already have an account? Log In & Download
Log in to Download
Your download will begin immediately after logging in.
Content Type
Topic Categories
- Data Visualization
- Research Briefs
- Email Signup
- Careers & Internships
- Terms & Conditions
- Privacy Policy
Home > Topics > Community Health Workers: Their Important Role in Public Health
Infographics
Community Health Workers: Their Important Role in Public Health
Coronavirus / Health Care Coverage
Published on: April 07, 2021. Updated on: April 13, 2021.
This infographic shows how Community Health Workers (CHWs) promote health equity and improve public health. The CHW workforce is diverse, growing, and drawing attention to its ability to address determinants of poor health. As trusted advocates, educators and counselors embedded in their communities, CHWs facilitate culturally competent service delivery. Tapping into this workforce can strengthen the response to COVID-19 and address longstanding inequities.
This infographic was reviewed by Denise Octavia Smith, MBA, CHW, PN, Founding Executive Director of the National Association of Community Health Workers .
Community health workers definitions : “Community Health Workers.” American Public Health Association.
CHWs’ many titles : “CDC - Community Health Worker Resources - STLT Gateway.” Centers for Disease Control and Prevention, 18 Aug. 2016.
Not defined by training : Opinion by Kangovi, Shreya, et al. “Opinion: This Group of Workers Could Help Turnaround Quality of Life -- and the Economy.” CNN, 10 Feb. 2021.
Advance health equity, improve health outcomes, and reduce health care costs : “Community Health Workers: Evidence of Their Effectiveness.” Association of State and Territorial Health Officials and the National Association of Community Health Workers.
Addressing social determinants of health : Peretz, Patricia J., et al. “Community Health Workers and Covid-19 - Addressing Social Determinants of Health in Times of Crisis and Beyond: NEJM.” New England Journal of Medicine, 10 Mar. 2021.
Root causes of poor health: Opinion by Kangovi, Shreya, et al. “Opinion: This Group of Workers Could Help Turnaround Quality of Life -- and the Economy.” CNN, 10 Feb. 2021.
Examples of services CHWs provide:
- Outreach, community education, informal counseling, social support and advocacy : “Support for Community Health Workers to Increase Health Access and to Reduce Health Inequities.” American Public Health Association. 10 Nov. 2009
- Translation/interpreting, health care navigation, and tracking progress : “Rural Health Information Hub.” Community Health Workers in Rural Settings Introduction.
86,000 CHWs : "Community Health Worker National Workforce Study." U.S. Department of Health and Human Services Health Resources and Services Administration Bureau of Health Professions. March 2007.
Expected increase : “Health Educators and Community Health Workers: Occupational Outlook Handbook.” U.S. Bureau of Labor Statistics, U.S. Bureau of Labor Statistics, 1 Sept. 2020.
Call for rapid increase: NACHW National Policy Platform: Policy Recommendations to Respect, Protect and Partner with Community Health Workers During the Pandemic and Beyond.
President Biden’s proposal : “President Biden Announces American Rescue Plan.” The White House, The United States Government, 20 Jan. 2021.
American Rescue Plan : Yarmuth, John A. “H.R.1319 - 117th Congress (2021-2022): American Rescue Plan Act of 2021.” Congress.gov, 11 Mar. 2021,
Partners in Health : “Public Health Job Corps: Responding to COVID-19, rebuilding the community health workforce.” Partners in Health United States. Updated 22 Jan. 2021.
CHWs sharing characteristics with community members : “Role of Community Health Workers.” National Heart Lung and Blood Institute, U.S. Department of Health and Human Services.
CHW race and ethnicity : National Community Health Worker Advocacy Survey: 2014 Preliminary Data Report for the United States and Territories. Tucson, Arizona: Arizona Prevention Research Center, Zuckerman College of Public Health, University of Arizona; 2014.
Bilingual : “Community Health Workers in the Midwest: Understanding and developing the workforce” Wilder Research, June 2012.
CHW Employers : “Health Educators and Community Health Workers: Occupational Outlook Handbook.” U.S. Bureau of Labor Statistics, U.S. Bureau of Labor Statistics, 1 Sept. 2020.
Shift CHW employment : Malcarney MB, Pittman P, Quigley L, Horton K, Seiler N. The Changing Roles of Community Health Workers. Health Serv Res. 2017;52 Suppl 1(Suppl 1):360-382. doi:10.1111/1475-6773.12657
Evidence of CHWs Effectiveness : “Community Health Workers: Evidence of Their Effectiveness.” Association of State and Territorial Health Officials and the National Association of Community Health Workers.
- $2.47:1 return on investment : Kangovi, Shreya, et al. “Evidence-Based Community Health Worker Program Addresses Unmet Social Needs And Generates Positive Return On Investment: Health Affairs Journal.” Health Affairs, 1 Feb. 2020.
- 34% decrease in days in hospitals: Vasan, A, Morgan, JW, Mitra, N, et al. Effects of a standardized community health worker intervention on hospitalization among disadvantaged patients with multiple chronic conditions: A pooled analysis of three clinical trials. Health Serv Res. 2020; 55: 894– 901.
- Improve Glycemic Control : Palmas W, March D, Darakjy S, Findley SE, Teresi J, Carrasquillo O, Luchsinger JA. Community Health Worker Interventions to Improve Glycemic Control in People with Diabetes: A Systematic Review and Meta-Analysis. J Gen Intern Med. 2015 Jul;30(7):1004-12.
- Mental Health : Weaver A, Lapidos A. Mental Health Interventions with Community Health Workers in the United States: A Systematic Review. J Health Care Poor Underserved.
Role of CHWs in COVID-19 response:
- Advocate for vaccinations : “Joint Statement on Ensuring Racial Equity in the Development and Distribution of a COVID-19 Vaccine.” Health Leads, 26 Jan. 2021.
- Trusted messengers : “To Strengthen The Public Health Response To COVID-19, We Need Community Health Workers, " Health Affairs Blog, May 6, 2020.
- Build Capacity : Advancing Equity & Public Health: The Community-Based Workforce Alliance.
- Address social needs and ensure care : Peretz, Patricia J., et al. “Community Health Workers and Covid-19 - Addressing Social Determinants of Health in Times of Crisis and Beyond: NEJM.” New England Journal of Medicine, 10 Mar. 2021.
Recommendations and strategies for supporting this workforce:
- Funding, training, integrate, and promote : “Advancing the Profession of Community Health Workers: CHRT.” Center for Health & Research Transformation, 19 Feb. 2021.
- Combat compassion fatigue : “Battling Burnout: Self-Care and Organizational Tools to Increase Community Health Worker Retention and Satisfaction.” Health Leads, 23 Jan. 2020.
- More research is needed : Peretz, Patricia J., et al. “Community Health Workers and Covid-19 - Addressing Social Determinants of Health in Times of Crisis and Beyond: NEJM.” New England Journal of Medicine, 10 Mar. 2021.
The National Association of Community Health Workers :
An Environmental Scan to Inform Community Health Worker Strategies within the Morehouse National COVID-19 Resiliency Network : Jane Berry, Aurora GrantWingate, and Denise Octavia Smith. The National Association of Community Health Workers, the Morehouse School of Medicine, and the National COVID-19 Resiliency Network. December 2020.
NACHW National Policy Platform : Policy Recommendations to Respect, Protect and Partner with Community Health Workers During the Pandemic and Beyond.
The Penn Center for Community Health Workers
Rural Community Health Workers Toolkit : Rural Health Information Hub
Robert Wood Johnson Foundation’s Culture of Health Blog : Proctor, Dwayne. “Community Health Workers: Walking In The Shoes of Those They Serve.” RWJF , 2 Feb. 2021.
Marill, Michele Cohen. “Community Health Workers, Often Overlooked, Bring Trust to the Pandemic Fight.” Kaiser Health News , 10 Feb. 2021 .
Waters, Rob, et al. “Community Workers Lend Human Connection To COVID-19 Response: Health Affairs Journal.” Health Affairs , 1 July 2020,
Shreya Kangovi, Uché Blackstock. “Opinion | Community Health Workers Are Essential in This Crisis. We Need More of Them.” The Washington Post , WP Company, 3 July 2020.
We think you'll also like
March 25, 2021
Community Health Workers & Pharmacists: Their Frontline Role in the Response to COVID-19
Get nihcm updates
Updates on timely topics and webinars delivered to your inbox
More Related Content
May 01, 2024
Telehealth: A Vital Piece of the Care Access Puzzle
Cost & Quality / Affordability / Health Care Coverage / Health Care Reform
Mini-Infographics
Published on: January 11, 2024.
Respiratory Illnesses are Elevated Across the Country
Coronavirus
Research Insights
Published on: November 08, 2023. Updated on: November 08, 2023.
The Health & Economic Consequences of Firearm Injuries in Children on Survivors & Families
Cost & Quality / Behavioral Health / Health Care Coverage / Social Determinants of Health
See More on: Coronavirus | Health Care Coverage
- Research article
- Open access
- Published: 06 September 2021
Experiences of frontline healthcare workers and their views about support during COVID-19 and previous pandemics: a systematic review and qualitative meta-synthesis
- Jo Billings ORCID: orcid.org/0000-0003-1238-2440 1 ,
- Brian Chi Fung Ching 1 ,
- Vasiliki Gkofa 1 ,
- Talya Greene 1 , 2 &
- Michael Bloomfield 1 , 3 , 4 , 5
BMC Health Services Research volume 21 , Article number: 923 ( 2021 ) Cite this article
88k Accesses
205 Citations
32 Altmetric
Metrics details
Healthcare workers across the world have risen to the demands of treating COVID-19 patients, potentially at significant cost to their own health and wellbeing. There has been increasing recognition of the potential mental health impact of COVID-19 on frontline workers and calls to provide psychosocial support for them. However, little attention has so far been paid to understanding the impact of working on a pandemic from healthcare workers’ own perspectives or what their views are about support.
We searched key healthcare databases (Medline, PsychINFO and PubMed) from inception to September 28, 2020. We also reviewed relevant grey literature, screened pre-print servers and hand searched reference lists of key texts for all published accounts of healthcare workers’ experiences of working on the frontline and views about support during COVID-19 and previous pandemics/epidemics. We conducted a meta-synthesis of all qualitative results to synthesise findings and develop an overarching set of themes and sub-themes which captured the experiences and views of frontline healthcare workers across the studies.
This review identified 46 qualitative studies which explored healthcare workers’ experiences and views from pandemics or epidemics including and prior to COVID-19. Meta-synthesis derived eight key themes which largely transcended temporal and geographical boundaries. Participants across all the studies were deeply concerned about their own and/or others’ physical safety. This was greatest in the early phases of pandemics and exacerbated by inadequate Personal Protective Equipment (PPE), insufficient resources, and inconsistent information. Workers struggled with high workloads and long shifts and desired adequate rest and recovery. Many experienced stigma. Healthcare workers’ relationships with families, colleagues, organisations, media and the wider public were complicated and could be experienced concomitantly as sources of support but also sources of stress.
Conclusions
The experiences of healthcare workers during the COVID-19 pandemic are not unprecedented; the themes that arose from previous pandemics and epidemics were remarkably resonant with what we are hearing about the impact of COVID-19 globally today. We have an opportunity to learn from the lessons of previous crises, mitigate the negative mental health impact of COVID-19 and support the longer-term wellbeing of the healthcare workforce worldwide.
Peer Review reports
COVID-19 has placed extreme demands on healthcare workers. They have faced genuine threats to their own physical safety and indirectly to that of their families. They have had to manage higher numbers of patients with high mortality rates in a high-pressure environment. They have dealt with challenges in delivering care with strict infection control measures in place and not always with adequate personal protective equipment (PPE). Many have been redeployed into new roles, teams or newly purposed wards so have been working in unfamiliar settings and without established social support from colleagues.
As COVID-19 has progressed around the world, we have heard repeatedly about the mental health burden faced by frontline healthcare workers globally as they have worked to treat patients affected by the virus. Media representations have described frontline healthcare workers “on their knees” in response to the crisis, leading to forewarning of an ensuing mental health epidemic amongst the healthcare workforce [ 1 , 2 ].
Healthcare workers are, for the most part, psychologically resilient professionals, trained and experienced in dealing with illness and death [ 3 ]. However, the mental health and psychological wellbeing of this group prior to the current COVID-19 pandemic was already being identified as a major healthcare issue, evidenced by the growing incidence of stress, burnout, depression, drug and alcohol dependence and suicide across all groups of health professionals, in many countries [ 4 ]. High stress roles coupled with the unique demands of the COVID-19 crisis have undoubtedly placed frontline healthcare workers at additional risk for mental health problems, with early reports from around the world indicating elevated rates of depression, anxiety, post-traumatic stress disorder (PTSD) and suicidality [ 5 , 6 , 7 , 8 ].
In response to such emerging data and many a military metaphor of healthcare workers “waging war on the front line” against COVID-19, there have been growing calls to mobilise mental health support for healthcare workers. However, there is also currently a lack of evidence about what interventions are most helpful for staff working in such high-risk occupational roles, with what evidence there is about effectiveness being mixed, and often demonstrating that well intentioned interventions (i.e. debriefing) can actually increase the likelihood of developing mental health problems such as PTSD [ 9 , 10 ]. Emerging literature from around the world has also demonstrated that staff may not prioritise psychological interventions in the peak phase of the crisis and may even be reluctant to engage with services offered to them [ 11 ].
Early research on COVID-19 has been mostly quantitative in nature, reporting on a proliferation of surveys, and mostly measuring rates of distress in specific samples. Whilst important, this research does not help us to understand the complexities and nuances of healthcare workers’ experiences of working on the frontline nor their views about what support is most helpful to them and when. Better understanding this will enable us to develop and provide support for frontline workers in ways which are acceptable and timely, in line with healthcare workers’ own stated views and preferences.
So, what is it like to work on the frontline and what support do frontline healthcare workers want during a pandemic such as COVID-19? We set out to answer this question by conducting a systematic review and meta-synthesis of qualitative literature describing healthcare workers’ experiences of working on the frontline and their views about psychosocial support, during COVID-19 or previous pandemics and epidemics, such as Severe Acute Respiratory Syndrome (SARS), Middle East Respiratory Syndrome (MERS) or Ebola. Understanding healthcare workers’ views, experiences and needs is critical now more than ever, as countries around the world continue to battle with ongoing waves of COVID-19, but will also be essential in the future, as we face further inevitable healthcare crises.
We have adhered to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [ 12 ] guidance throughout this review.
Search strategy and selection criteria
We identified eligible papers through searches on Medline, PsychINFO and PubMed. All searches took place from inception, with final searches taking place on September 28, 2020. Key search terms were related to the population (i.e. healthcare worker*, health professional* nurse*, doctor*, hospital staff), the intervention (i.e. psychosocial, psychological or emotional and experiences, support, intervention or help) and a number of disease specific key terms (i.e. COVID-19, SARS, MERS, H1N1, Ebola). (See supplementary material for our full list of search terms). We also hand searched reference lists of included papers, grey literature and pre-print servers to identify other potentially relevant studies.
We included papers that reported original, published, qualitative research describing frontline healthcare workers’ experiences of working during a pandemic or epidemic, and/or views of psychosocial support offered to them. This included mixed-methods studies where data on the qualitative component of the study was available. We included studies on all healthcare professionals, including students and trainees and qualified professionals working in a voluntary capacity. We excluded studies where less than 50% of the participants were frontline healthcare workers or where we could not extract data for healthcare workers alone. Due to the rapidity required for this review, only papers published in English were included.
Data screening and extraction
We removed duplicate articles then two reviewers independently screened titles and abstracts of retrieved papers for relevance. The texts of selected articles were then read in full by the two independent reviewers. We resolved any discrepancies about papers to be included at any stage through discussion between the two reviewers and the first author. Data from the selected papers were extracted onto a pre-designed data extraction template by the two reviewers (see Table 1 ). We included all papers in the qualitative meta-synthesis.
Quality appraisal
We assessed the quality of the studies included in the meta-synthesis using the Critical Appraisal Skills Programme (CASP) [ 13 ] qualitative research checklist (see Table 2 ). The quality appraisal was carried out by the two independent reviewers and discrepancies were resolved through discussion. The CASP checklists are designed to be used as educational pedagogic tools and therefore are not intended to derive a quantitative rating for quality. In this review, we have followed CASP guidance and the methods described by Lachal et al. [ 14 ] to describe whether studies met, partially met, or did not meet the CASP criteria. This information is provided to enable the reader to judge study quality for themselves (see supplementary materials ). Of note, these ratings reflect what is included in the available report of the study and may not necessarily reflect detail that was attended to in the research process but not necessarily written up in the presented paper.
We did not exclude any studies from the meta-synthesis based on their quality or sample size. This is a new and emerging topic of concern and we did not want to exclude smaller scale studies from less well-established settings given the insight they could potentially offer to this review question.
- Meta-synthesis
We followed guidance provided by Lachal et al. [ 14 ] on synthesising qualitative literature in psychiatry. We extracted data from the results sections of papers (or general text in the case of published commentaries or reflective accounts) where information was given about healthcare workers’ experiences and/or views of any form of psychosocial support provided during their work in response to a pandemic. This information was exported into NVivo Pro version 12 and analysed thematically [ 15 ].
In keeping with traditional thematic analysis, we sought initial immersion in the data by reading and re-reading all the papers. We developed an initial coding frame from ten of the most immediately relevant and current papers. The coding frame was further developed and refined through coding of the full 46 papers, looking for shared themes, but also nuances and exceptions within the themes. Adhering to the principles of inductive methodology, we sought to derive our themes from the data, in this case the themes and examples given in the original papers, but then to synthesise these findings and develop an overarching set of themes and sub-themes which captured the experiences and views of frontline healthcare workers across the studies. Examples and illustrative quotes are provided throughout to evidence our analyses.
Reflexivity
Reflexivity is important in all qualitative research and enables the reader to consider the validity of any qualitative analysis by better understanding the composition and position of the research team who have produced it. This research team is made up of a diverse group, representing different clinical specialities, career stages and cultural backgrounds. JB is a Consultant Clinical Psychologist and Associate Clinical Professor, specialising in trauma, PTSD and the mental health and wellbeing of high-risk occupational groups. BCFC and VG are MSc graduates in Clinical Mental Health. TG is a Senior Lecturer specialising in PTSD and responses to mass traumatic events. MB is a Principal Clinical Research Fellow and Consultant Psychiatrist. As such we brought a mix of different perspectives and experience to this topic.
A total of 1019 records were initially returned. 37 articles were identified through other sources (hand searching of reference lists, grey literature, and pre-print servers). After de-duplication, the titles and abstracts of 808 articles were screened by the two reviewers. Of these, 665 were agreed to be irrelevant, resulting in 143 studies which were read in full by the two reviewers. At this stage, 97 studies were excluded as either the wrong study design ( n = 86) or not having relevant outcomes ( n = 11). This resulted in 46 papers which we included in the review and meta-synthesis (see Fig. 1).
Characteristics of the 46 studies included in the meta-synthesis are shown in Table 1 .
Out of the 46 studies included in the meta-synthesis, 21 studies were based on participants in Asia, 12 in Africa, seven in North America, four in Australasia and two in Europe. Fifteen studies looked at experiences of Ebola, 14 at SARS, five at COVID-19, four at unspecified influenza pandemics, three at MERS, three at H1N1, one at Avian flu, one at swine flu and one at general public health emergencies (one study looked at both SARS and H1N1). Most participants were described as healthcare workers, nurses or medical staff. All studies were published between 1999 and 2020. In most studies data were collected through individual interviews or focus groups, although one study was a personal reflective account and one paper a commentary citing interviews which had been conducted. A variety of analytic methods were used including thematic analysis, content analysis, framework analysis and phenomenological analysis, although many papers did not state the specific method used to analyse their data.
The quality of studies varied, although most were of moderate quality. Many studies included in this synthesis were rated as only partially meeting criteria due to issues of clarity regarding recruitment strategies, data collection and methods of analysis, ethical issues and consideration of the relationship between participants and researchers. The results of the quality assessment of included studies using CASP [ 13 ] criteria are shown in Table 2 (please see supplementary materials for individual study quality ratings).
Themes derived from the meta-synthesis are shown in Table 3 .
1. Physical health, safety and security
Themes related to physical health, safety and security pervaded nearly all included papers.
1.1 Concerns for self
The predominant concern across most staff groups, across all pandemics, was becoming infected with the virus themselves. For example, Gershon et al. [ 16 ] writing about healthcare volunteers’ experiences of treating Ebola in Emergency Treatment Units (ETUs) in West Africa describe:
Thoughts of getting infected were the uppermost concern for most, especially during the beginning of the deployment when they were still becoming acclimated to the ETU and whenever there was a breach in infection control protocol and practice. For some, fear was constant. One participant recalled constantly thinking, “Don’t let me get Ebola, don’t let me get Ebola.” (pp. 9–10)
Fears of contamination were exacerbated by experiences of inadequate PPE which was a recurrent theme across many papers, transcending different countries and pandemics. Shih et al. [ 17 ] explored nurses’ experiences of treating SARS in Taiwan in the early 2000s and noted:
In this beginning stage, the factors contributing to the nurses’ fear about fatal infection by SARS were based on a lack of defensive protection against the disease (p. 173)
Thirteen years later, Yin & Zeng [ 18 ] document nurses’ experiences of treating COVID-19 in China and quote one of their participants:
“I hope that personal protective equipment is available every day so that I don’t have to worry as much about myself or my colleagues getting infected.” (p. 2)
1.2 Concerns for others
A few studies provided exceptions where frontline workers reported less concern over their own immediate health, but nevertheless still expressed significant concerns for others [ 11 ]. Workers were preoccupied about their families becoming ill and were particularly concerned that they themselves might transmit the illness to their loved ones. For example, talking about nurses’ experiences of SARS in Singapore, Koh et al. [ 19 ] reported that:
Some participants were not concerned about themselves, rather they were concerned that they would, because of their exposure to infected patients, colleagues or visitors to the organization, inadvertently infect their family. (p. 199)
Many made sacrifices and sought to protect their loved ones by staying away from them. For example, Yin and Zeng [ 18 ] quote a nurse in China in the early stages of COVID-19:
“I stay at a hotel every day and am afraid of getting my family sick. I’m afraid to go home and haven’t seen my mom and dad for a long time.” (p. 3)
Fellow healthcare workers falling ill with the virus was a significant cause for preoccupation and distress amongst participants [ 20 ]. Chung et al. [ 21 ] describe nurses’ experiences of treating colleagues affected by SARS in Hong Kong:
All of the participants described being particularly vulnerable when caring for patients who were healthcare workers, whether doctors, nurses or support staff who had contracted the disease at work. That the patients were colleagues in a similar situation in life gave a more personally emotive dimension of the experience (p. 513)
1.3 Practical and environmental issues
Healthcare workers were also impacted by practical and environmental issues in the settings in which they worked. Whilst, for the most part, healthcare workers’ fears were allayed by adequate PPE, it was also noted in several papers how the PPE caused discomfort and impacted on communication. For example, Broom et al. [ 22 ] describe the experience of doctors and nurses in an Australian hospital:
The equipment was described as cumbersome and hot, and staff reported finding it difficult to communicate with others who were wearing the PPE. Basic clinical procedures were deemed impossible by participants while wearing the recommended PPE . (p. 106)
Some studies commented on the pay off between staff safety and patient care. For example, Moore et al. [ 23 ] describing the treatment of SARS in Canada quote one participant:
“What we’ve been told is...that [in] triage, you change your goggles, gloves, mask and gown between every patient and its 100% not feasible. It can’t be done. Patients would be dying waiting at the triage desk.” (p. 265)
Many studies also commented on the settings in which healthcare workers treated those affected by the pandemic being unfit for purpose and lacking in essential resources. Talking about nurses’ experiences of the Ebola crisis in West Africa, Gershon et al. [ 16 ] state:
By any measure and at multiple levels, the early humanitarian response to the Ebola epidemic was extraordinarily challenging. Health care facilities and systems, already severely under-resourced in the affected areas, were strained to the limit. (p. 8)
This was not unique to developing countries, with similar challenges reported in Canada [ 23 ] and Australia [ 22 ].
2. Workload
Healthcare workers commonly reported elevated workloads, which impacted on their psychosocial wellbeing. They cited increased hours and weekend shifts, additional time taken to manage PPE and increased paperwork as frequent sources of stress [ 24 ]. This was compounded by staff shortages (due to inadequate staffing or staff absences because of ill health or caring responsibilities) resulting in requirements for staff to work overtime. This led to the workers feeling fatigued and risking mistakes. A nurse from Toronto in the study by Moore et al. [ 23 ] described her experiences:
“I work 12-hour shifts in emergency, rarely got a break, we were not permitted to have fluids at the desk. None. None in the care area. So we were going for five or six hours with nothing to drink. We were so exhausted. So at the end of your 12 hour shift by 6 or 7 hours you’re so exhausted that you’re crazy. That is now leading to sloppy practice.” (p. 265)
However, because of staff shortages, some participants were noted to describe feeling guilty for taking time off to rest [ 16 , 25 ]. Even when able to take a break, this was not always possible. Several studies described staff being unable to leave the hospital or hotel environment, feeling isolated outside of work or having little access to other activities [ 25 , 26 ].
Financial consequences of working, or not working, during the pandemic were also discussed. For some, sickness entitlements were considerably less than usual salaries and some staff were not paid at all if unable to work. This led to significant financial hardship and a motivation for some to work even when unwell [ 27 ]. Some were offered a ‘risk allowance’ for the work that they undertook, which was a source of motivation for some, although professional duty of care usually outweighed financial incentives for most. Nevertheless, when financial remuneration was offered but delayed or not provided, workers felt abandoned and betrayed. Such betrayals of trust exacerbated pre-existing disaffection amongst healthcare workers. For example, Bergeron et al. [ 24 ] quote one participant in their sample of community nurses working on SARS:
“The SARS epidemic changed my view of nursing in Ontario. I finally realized that nurses were undervalued, underappreciated and undercompensated for the risks they take on daily to provide adequate healthcare to their clients.” (p. 49)
Participants in many of the studies talked about experiencing stigma as a result of working on the pandemic. This was greatest in the earlier phases of the outbreaks or in contexts where less was understood about transmission of the virus.
In addition to their own fear of becoming infected with Ebola, the midwives also had to deal with the public fear of the contagious disease. Ebola was an unknown disease in Sierra Leone prior to the outbreak, and lack of knowledge resulted in rumours and misunderstandings among the general population [ 28 ] (p. 25)
Stigma also appeared in the studies of COVID-19. Fawaz and Samaha [ 29 ] quoted one of the nurses in their sample from Lebanon:
“My aunt was standing way far from me when I saw her in the street…she felt like I was infected…treated me as if I am the virus.” (p. 563)
This stigma extended to the families of healthcare workers with some reporting their children being discriminated against [ 30 ]. Other studies pointed to the hypocrisy that some healthcare workers experienced when they were publicly commended for their work but privately discriminated against [ 26 ].
4. Ethical, moral and professional dilemmas
One of the greatest sources of tension was the competing obligation healthcare workers felt between providing good patient care and protecting their own physical safety. Strict infection control procedures meant that staff were not always able to intervene in the way they wanted, resulting in them feeling like they fell short of their usual standards of care. For example, Lamb [ 31 ] quotes a healthcare worker in West African during the Ebola outbreak:
“The biggest conflict within me, was the lack of ability…to put your hand on a shoulder…or hold their hand.” (p. 132)
Further constraints due to lacking resources exacerbated healthcare workers distress and led to a sense of futility. Comments such as “I couldn’t do anything to stop it” [ 32 ] p. 107 and “we could not do enough” [ 33 ] (p. 2884) pervaded many narratives. Several studies discussed the undignified manner of patient deaths and healthcare workers’ lack of ability to provide access to adequate pain medication due to limited resources or give them any measure of comfort due to PPE and safety measures as a great source of distress. For example, Liu and Liehr [ 33 ] in their study of nurses caring for SARS patients in China describe:
Another source of pressure for the nurse was the demise of patients and the coexisting feeling that they could not do enough. Wards to isolate and care for SARS patients were often created from available space, such as outpatient centres, which lacked optimal equipment to manage the complexity of SARS patient care. The feeling of not being able to do enough occurred partly because of the limited resources of the environment. “Things we did for patients, such as cleaning patients, were not enough…the thought that I didn’t try my best for patients could not disappear.” (p. 2884)
Staff shortages and the associated lack of support meant workers were left to make difficult, often life and death, decisions on their own, which were noted to cause serious ethical dilemmas. Inequalities and decisions about who should get access to resources; beds, medication and vaccines also caused staff significant upset. The impact of these dilemmas appeared to continue after the crisis had passed. Gershon et al. [ 16 ] describe the experiences of US healthcare volunteers after returning from the Ebola crisis in West Africa:
Participants reported feelings of grief, mourning, sadness, depression, remorse, and regret upon their return. As one participant said, “Oh, we could have done much, much more.” (p. 15)
Nevertheless, for the most part, workers felt inherently motivated to undertake this work and held a strong conviction that not doing so would be unethical. The idea of not treating patients affected by the virus was seen as “cowardly” [ 34 ] (p. 244) and “morally unacceptable” [ 35 ] (p. 6) and staff who avoided this work were viewed with scepticism.
5. Personal and professional growth
Concurrent to the pressures noted above, many healthcare workers described aspects of the work as enjoyable and rewarding and appeared to derive job satisfaction from work that they felt was “important” and “meaningful” [ 36 ] p. 648.
These sentiments seemed more pronounced when workers saw patients improve and leave the ward, and over time as the number of infections and deaths declined [ 36 ]. The gratitude of others; patients, their families and wider society was noted to increase their sense of fulfilment [ 25 ].
Even in some of the most challenging moments, many healthcare workers found meaning in their work, for example, Erland and Dahl [ 28 ] describe midwives caring from pregnant women dying from Ebola in Sierra Leone who “found it meaningful to be there and care for the women in their last moment of life.” (p. 25).
Overcoming such immense challenges tested the participants and imbued some with a sense of greater professional confidence and competency [ 37 ]. Several studies described staff gaining new knowledge and skills which they felt would equip them in their future work, especially if they ever worked in a pandemic situation again. Some also reported personal growth and developing confidence in their own resilience [ 38 ].
Nevertheless, deriving meaning and taking pride in their achievements did not render healthcare workers immune from the longer lasting impact of the work.
“I’ve just lost my way. When I got back, the problems were still there…Reforming a new life has been tough. I guess you could call it PTSD. I’m proud of what I did…. but in my personal life, I’ve paid a heavy price.” [ 16 ]. (pp. 16–17)
6. Support to and from others
Sources of support were discussed in many of the papers, although healthcare workers’ experiences demonstrated that many potential sources of support could also be additional sources of stress.
6.1 Family and friends
Families and friends were important sources of support but could place pressure on the healthcare workers. Some tried to dissuade them from working on the pandemic, leading the workers, in some cases, to withhold from their families what they were doing [ 16 ].
For the most part, healthcare workers appreciated the opportunity to stay in touch with friends and family, usually over the phone. This was reported to bring them comfort as well as allay the worries of their loved ones. However, this could still place an emotional burden on the workers:
“Sometimes, I was too tired to talk over the phone but I still wanted to switch on the mobile because I was concerned about my family’s condition…I found I could not control my temper during that period. After two sentences of talk with my family, I felt short of breath and became very frustrated. I understood that my family would like to listen to my voice, but I just could not talk.” [ 39 ] (p. 157)
The competing demands of managing work and family life during a pandemic was also a source of stress. As described by Bergeron et al. [ 24 ] during SARS in Canada:
The juggling of work/family demands often had personal costs: “I rarely saw my husband and when I did I had little energy left for him. The strain almost cost me my marriage.” (p. 50)
Reintegrating into normal family life after their work on the pandemic was over was also problematic for some. Several studies described workers missing colleagues and struggling to re-engage with previous work. For example, Gershon et al. [ 16 ] describe US healthcare workers struggling to readjust on returning from volunteering in West Africa:
Others mentioned feeling isolated because the only people that they felt they could really talk to and who understood what they were feeling were the people who had deployed with them. “You breathe, you eat, you sleep it, for 24 hours of every day. It’s not like you can come back home and relax with your family. Your heart is just not into it.” . (p. 16)
6.2 Colleagues and peers
For the most part, working with colleagues during the pandemic was noted to provide an important source of mutual support, opportunities to learn from each other and facilitate camaraderie.
Buddying systems, whereby more experienced staff supported newer staff, seemed appreciated, as were opportunities for informal group reflection. This seemed to enable staff groups to normalise difficult responses and provide appropriate reassurance. As described, in Lamb’s [ 31 ] study of Ebola:
Participants described how they would simply sit down together at the end of a shift, share a cup of tea and discuss the events of the day: “quite a few of them [juniors] had never seen a dead body before, certainly never dealt with dying patients. .. but we would just sort of just sit down and chat about it and about how they were feeling…it was ok to feel upset, it’s just a perfectly normal reaction.” (p. 133)
Some healthcare workers also spoke about the value of social media platforms for keeping in touch with colleagues, such as WhatsApp groups. Some did nevertheless lament the loss of previous opportunities to socialise with colleagues face to face and outside of work [ 18 ].
Colleague and peer relationships could also be the source of some stress. Unfair distribution of work and the refusal of some colleagues to treat patients affected by the virus caused notable tensions.
“There was real division created amongst staff. We’d all be working in the ICU and there was a long list of people who said they’re not going in because of so and so…And this created resentment, hostility because there were a core group of us who went in there more often than we would have had to otherwise had all of us been sharing that responsibility. We carried a burden that wasn’t equally shared.” [ 40 ] (p. 2570)
This was exacerbated by inequities in pay and conditions for what healthcare professionals perceived to be equivalent work with the same risks.
6.3 Organisations
Healthcare workers valued support from their organisations but gave many examples of not feeling adequately supported. Some workers reported feeling coerced into working with infected patients or in inappropriate conditions [ 40 ]. Participants across most studies felt that their organisations had an institutional duty to provide staff with sufficient protection to work safely.
Workers reported feeling supported by their organisations when there was clear alignment and shared decision making between senior managers and frontline healthcare workers but less supported when staff safety was not a clear priority. Workers also valued their organisations supporting them to take time off from their roles.
Workers’ perceptions of their organisation’s preparedness varied with workers in several studies reporting a lack of established protocols. Staff in some studies commented on hoping that their organisations would learn from these experiences and be better prepared in the future.
Workers wanted their hard work and sacrifices to be recognised by their organisations, although the degree to which they expected to be additionally rewarded varied. Nevertheless, they expected a degree of support in return for the sacrifices they made that not all felt was met. For example, Guimard et al. [ 41 ] commenting on a focus group discussion amongst nurses write:
It was revealed during discussions that most of the nurses who volunteered to care for Ebola patients were very disappointed about the recognition they received for their actions. Most of them felt abandoned by the managers of the hospital and felt they received insufficient financial and psychologic support during the epidemic (p. 272)
6.4 Media and the public
The media’s portrayal of the pandemic had both positive and negative impacts. Some studies described the role of the media in perpetuating stigma. Al Knawy et al. [ 42 ] writing about MERS in Saudi Arabia commented:
All participants referred to consistent and pervasive negative media commentary on the MERS-CoV outbreak…These negative commentaries were evident across local mass media (television, radio and newspapers) and social media - particularly Twitter. The negative media reporting was cited as negatively impacting staff morale and affecting workers socially and psychologically. (p. 7)
Many healthcare workers felt that catastrophic portrayals of the pandemic on the news compounded families’ concerns [ 31 ]. Such representations were also argued to be partly responsible for discouraging people to attend hospitals for other health concerns, to the detriment of public health and with financial repercussions for hospital departments [ 43 ].
The media, however, was often a source of information which healthcare workers found helpful, especially when they felt they were not party to information from their organisations. The media was also noted to be helpful in advocating for healthcare workers and mobilising resources, such as exerting pressure to provide more PPE.
The support of the wider public was considered vital and where the public did not comply with related directives this caused the healthcare workers anxiety and frustration. Bergeron et al. [ 24 ] quoted one nurse from their study of SARS in Canada:
“My experience in the workplace regarding lack of compliance from clients in quarantine orders also makes me angry and afraid. I feel that even after all the work of ALL health care professionals, this issue may be impossible to be contained without support of the public.” (p. 47)
Healthcare workers also sought recognition and validation from the public.
They wanted the public to know what they had been through and how they had put their own lives at risk to help protect others [ 16 ] (p. 14)
Knowledge and information
A pervasive narrative amongst the healthcare workers across all the pandemics was that of uncertainty, which precipitated and perpetuated fear and anxiety. Knowledge was key in decreasing uncertainty and many participants sought information, clarity and consensus with the purpose of achieving greater certainty.
Communication
Communication was vital to the healthcare workers, however, not always experienced as helpful. Many reported inconsistent and ineffective messaging and a lack consensus between sources of information. Ives et al. [ 35 ], for example, report a lack of communication in their study of healthcare workers in the UK:
The majority of participants said they had been given neither information about pandemic influenza, nor been made aware of what would be expected of them during such a crisis, and this gave many the impression that their employing Trust did not care about them or take their needs seriously. (p. 9)
Equally prevalent were comments about there being too much information. Rapidly changing and inconsistent information “increased frustration and uncertainty” [ 21 ] (p. 514). This resulted in “confusion and lack of trust in the information received” and subsequently “dismissal of the information as clinicians were unable to assimilate the information in the limited time they had” [ 22 ] (p. 104).
Communication was valued when it was centralised and co-ordinated and came from reliable authorities. Participants also valued leaders who were available and visible during the crisis.
How information was shared was also an important point, with healthcare workers pointing out that many staff did not have the time or access to be repeatedly checking emails. Clearly visible posters and information cascaded through team leaders at shift handovers were cited as helpful.
Healthcare workers also believed that communication is a two-way process and that their feedback and knowledge should be recognised and acted upon. They felt they should be consulted and involved in decision making and that their learning from doing this work on the frontline was vital for responding to the current as well as future pandemics.
Healthcare workers’ experiences of training were variable. For many, training imparted important information, allayed anxiety and facilitated greater confidence. Participants in the studies valued training in infection control procedures and safe use of PPE as well as more general training about the virus.
Participants in several studies, however, felt that they had not received adequate training. As one healthcare worker in Gershon et al.’s [ 16 ] study of Ebola in West Africa described:
“They (the sponsoring agency) handed me a viral haemorrhagic fever guide. I read it on the plane, showed up, but I had no real idea of what I was doing.” (p. 7)
Even though some participants described feeling unprepared, there was a sense in some studies of limited or superficial engagement with training. Training seemed better received when it was deemed as relevant, realistic and timely. Practical simulations increased workers’ confidence. Workers also highlighted the importance of learning through experience and commented on competence and confidence increasing over time.
Formal support
The psychological impact on healthcare workers was acknowledged in many papers, however, few studies reported on workers’ experiences of any formal psychological interventions. The idea that mental health support would be available seemed to be important and helped to alleviate workers’ anxiety. For example, Yin and Zeng [ 18 ] quoted one nurse in the early phase of the COVID-19 outbreak in China:
“I hope that the hospital sets up a psychological support task force to ease our tension and fears.” (p. 3)
When psychological support services were mentioned, they seemed to be of most value when available on site, were flexible and informal, and were offered individually or in small groups which fitted around the workers’ shifts. Workshops on coping and emotional support were also described positively in some studies. Some participants appreciated the availability of helplines, although others described these as too impersonal.
Even when formal support was available, some staff were ambivalent about engaging. Chen et al. [ 11 ] in their commentary on medical staff in China in the early stages COVID-19 described:
The implementation of psychological intervention services encountered obstacles, as medical staff were reluctant to participate in the group or individual psychology interventions provided to them. Moreover, individual nurses showed excitability, irritability, unwillingness to rest, and signs of psychological distress, but refused any psychological help and stated that they did not have any problems (p. 15)
After the peak of the pandemic, the emotional impact of the work appeared to be acknowledged more. Workers in several papers were noted to report difficulties sleeping, experiencing invasive memories and ongoing hyper-arousal as well as struggling to adjust to being back at home and their normal work. Few described access to any kind of formal follow up, although when this was offered, this appeared to be appreciated. Even amongst those who described coping well and who did not want to engage with formal services, informal follow ups and check ins from their organisations and colleagues were valued.
After deployment, they stressed the need for mental health and psychosocial support, and they requested deeper knowledge about coping strategies. The respondents reported being focused on their duties and safety during deployment, and only allowing emotional reactions afterwards [ 44 ]. (p. 6)
In this review we sought to better understand healthcare workers’ experiences of working on the frontline and their views about support during COVID-19 and previous epidemics. We found 46 qualitative papers which met our inclusion criteria, and which covered a number of different pandemics and epidemics over the past 20 years. Studies were heterogenous in their sample sizes, locations and samples. However, meta-synthesis revealed eight key themes which largely transcended temporal and geographical boundaries. Participants across all the studies were deeply concerned about their own and/or others’ physical safety. This was greatest in the early phases of pandemics and exacerbated by inadequate PPE, insufficient resources, and inconsistent information. Workers struggled with high workloads and long shifts and desired adequate rest and recovery. Many experienced stigma. Healthcare workers’ relationships with families, colleagues, organisations, the media and the wider public were complicated and nuanced and could be experienced concomitantly as sources of support but also sources of stress.
The results of this review show that the current experiences of frontline healthcare workers are not without precedent. The themes identified in this review from previous pandemics and epidemics are remarkably resonant with what we are hearing about the impact of COVID-19 on healthcare workers across the world at the current time. This points to a potential mental health impact on staff that is comparable to that experienced in previous pandemics. A recently published review and meta-analysis of the mental health impact of working on pandemics including SARS, MERS, Ebola and COVID-19 [ 45 ] suggested that healthcare workers exposed to virus-related work are 1.7 times more likely to develop psychological distress and PTSD compared to non-exposed workers. Our review sheds light on potential risk factors and their mechanisms of effect including fear associated with threat to life, uncertainty due to inconsistent or rapidly changing information, and threat to integrity due to discrimination.
This review also shows that accessing social support, a previously well-established protective factor against mental health difficulties such as PTSD [ 46 ], was complex. Workers often self-isolated to protect their loved ones, did not disclose details of their work to them, struggled to manage the competing demands of work and family life and felt like the people in their usual support systems could not relate to what they had been through. This compromised healthcare workers use of social support, which may potentially have a longer-term adverse impact on their mental wellbeing.
The ethical, moral and professional dilemmas that healthcare workers faced also increases their risk of ‘moral injury’. Moral injury has been defined as the psychological distress caused by actions, or inactions, which violate an individual’s moral code, or a sense of betrayal by others, and has been highlighted as a potentially significant concern for healthcare workers during COVID-19 [ 47 ]. The healthcare workers in this review were often unable to deliver the level of care they felt professionally and morally obliged to provide and many felt betrayed by their colleagues, organisations and society. Moral injury is not in itself a mental health disorder but is a risk factor for further mental health problems and may be particularly pernicious in the context of a pandemic.
The results of this review also highlight potential protective factors. Healthcare workers valued clear, consistent, and compassionate communication. They engaged well with training when it was practical and specific. The felt valued by their organisations when they prioritised their safety and supported them with manageable workloads and time out from work. The wanted to be consulted and included in decision-making. Staff appreciated peer support and tended to seek emotional guidance from their colleagues. This draws attention to potential opportunities to further develop peer support systems and increase mental health awareness in the workplace. However, colleagues could also be a source of tension, so peer support interventions in this workforce warrant careful evaluation. We also need to carefully consider how peer-based interventions may work in such a crisis so as not to place an additional burden on the healthcare workers providing them when, by definition, they are going through the same stressors.
This review also demonstrates that psychological growth was possible. Most healthcare workers were inherently motivated to undertake this work due to a sense of professional duty. Many derived meaning and satisfaction from their work and reported learning and professional development. They also frequently reported strong team cohesiveness and camaraderie. As suggested by Gerada [ 48 ] in a recent editorial comment, “some good must come out of COVID-19” (p. 1) and there is potential for greater recognition and appreciation of healthcare work.
Public attitudes and the media had both positive and negative impacts on the healthcare workers in these studies but have the potential to provide support and validation of their work. Nonetheless, gestures of solidarity, such as applause for healthcare workers which have been taking place around the world during COVID-19, have the potential to feel meaningless and hypocritical if support for healthcare workers from the public and government is not sustained after the pandemic. Similarly, calls for adequate pay and conditions for healthcare staff continue to be echoed in the current crisis, as they were with previous epidemics and pandemics.
One potential difference between previous pandemics and COVID-19 is that there is now greater acknowledgement of the mental health impact on healthcare workers and increasing recognition of the need to support their wellbeing [ 49 ]. However, there is yet little evidence about what is effective and what healthcare workers themselves want. The studies included in this review focused little on formal psychological interventions. It is therefore difficult to establish whether this was not of primary importance to the healthcare workers, whether they were not aware of sources of mental health support, or whether these interventions were simply not available to them. When mental health support was mentioned, participants tended to speak of it as desirable. However, some studies suggested a reluctance to engage. This is perhaps indicative of potentially enduring stigma amongst healthcare workers, exacerbated by militaristic metaphors and heroic narratives in the media, which make it harder for them to admit when they are struggling. This is an additional area that warrants exploration in order to better understand workers’ ambivalence and to ensure that they feel able to engage with appropriate mental health support when needed.
The results of this review also suggest that healthcare workers’ mental health needs may change over time. In the early stages of these crises, workers prioritised more basic human needs, such as physical safety and rest. At the peak, workers seemed to focus on the work at hand and rely on colleagues for support. After the crisis had passed, there seemed to be greater recognition of the impact of working on the pandemic on mental health and an associated recognition of the need for more support. At the current time, whilst attention is being paid to the impact on frontline healthcare workers’ mental health, there is still a paucity of research into psychosocial interventions specifically for frontline healthcare workers. Future research with this population can helpfully focus on what works for whom and when.
We also know that the global healthcare workforce was experiencing high levels of distress and disaffection prior to COVID-19 [ 4 ], so we need to consider what should be set up as standard support for healthcare workers in the longer term. This will be particularly important as we deal with further waves of COVID-19, but also in the face of other, inevitable, future healthcare crises. We need to ensure that we maintain a psychologically healthy workforce, not just for the wellbeing of the workers, but also for the sustainability of healthcare services globally.
Implications
The findings of this review highlight a number of important implications which are relevant globally.
Provision of adequate safety equipment is a priority to enable safe and effective working but also to mitigate negative mental health outcomes.
Workloads need to be manageable, and sufficient periods of rest and recovery mandated to mitigate fatigue and burnout.
Training should be relevant, practical, and timely. Learning on the job is valued alongside formal training.
Communication needs to be clear and consistent and decision making shared. Leaders should be accessible and visible.
Mechanisms to facilitate staff peer support should be put in place, including ringfenced time and mental health awareness training.
Competing demands between work and family life should be acknowledged and staff supported in maintaining family roles as much as possible. Staff should be supported in taking time off from work.
Anxiety, guilt, and moral injury may be mitigated by reducing lone working, encouraging buddying systems, facilitating ethical forums which allow workers to discuss difficult decisions and focusing on the meaningfulness of the work.
Mental health follow-up will be imperative for the early detection and treatment of emerging mental health problems and to ensure staff feel supported by their organisations. Ongoing peer support is likely to be important.
Strengths and limitations
This review should be considered within the context of its strengths and limitations. This paper offers a rapid but systematic review of a comprehensive body of literature, for the purposes of providing urgent feedback and guidance for those planning the support of frontline healthcare workers during the current COVID-19 crisis. We conducted our search across three major databases and hand searched reference lists of key papers, grey literature and pre-print servers. We used two independent reviewers for searching, screening, data extraction and quality appraisal. We conducted a meta-synthesis for the reader to highlight overarching themes in relation to healthcare workers’ experiences of working on the frontline during a pandemic and their views about support.
There are a number of limitations inherent in the papers included. This review has highlighted a dearth of research exploring healthcare workers own views, needs and preferences. What research there is has focused predominantly on doctors and nurses with little or no identified research on other key frontline healthcare groups including physiotherapists, pharmacists, receptionists, porters or cleaners. Nearly all of the studies were of moderate-quality, with particular limitations regarding clarity of data collection and methods of analyses, therefore caution must be observed when considering the transferability of the findings.
There are also some limitations of the current review. Due to the rapidity required we did not pre-register a study protocol on Prospero. We also only searched a limited number of databases; therefore, some papers could possibly have been missed, which may have provided more detail or contradicted the findings summarised here. While research from across the world was included in this review, we were only able to include studies published in English. This review may therefore be subject to some publication bias. Ongoing attention is warranted as papers reporting on this phenomenon continue to be published, which may reveal experiences more unique to COVID-19.
The experiences of healthcare workers during COVID-19 are not unprecedented. We have an opportunity to learn from the lessons of previous pandemics and provide better support for frontline healthcare workers. More high-quality qualitative research is urgently needed in order to better understand the experiences, needs and preferences of the healthcare workforce, particularly those frontline healthcare workers whose voices have not yet been adequately represented. We need to develop clinical guidance specific to supporting this workforce. This guidance should be developed in consultation and collaboration with the healthcare workers themselves. Interventions to prevent and treat mental health distress in healthcare workers need to be developed and their timing, effectiveness and acceptability carefully evaluated. We have an opportunity to mitigate the negative mental health impact of COVID-19 and support the longer-term wellbeing of the healthcare workforce across the world.
Availability of data and materials
Data included in this review is already available in the public domain.

Abbreviations
Critical Appraisal Skills Programme
Personal Protective Equipment
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Post Traumatic Stress Disorder
Severe Acute Respiratory Syndrome
Middle East Respiratory Syndrome
Ghebreyesus TA. Addressing mental health needs: an integral part of COVID-19 response. World Psychiatry. 2020;19(2):129–30. https://doi.org/10.1002/wps.20768 .
Article Google Scholar
Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–60. https://doi.org/10.1016/S2215-0366(20)30168-1 .
Article PubMed PubMed Central Google Scholar
Brooks S, Amlôt R, Rubin GJ, Greenberg N. Psychological resilience and post-traumatic growth in disaster-exposed organisations: overview of the literature. BMJ Military Health. 2020;166(1):52–6. https://doi.org/10.1136/jramc-2017-000876 .
Article PubMed Google Scholar
Carrieri D, Briscoe S, Jackson M, Mattick K, Papoutsi C, Pearson M, et al. ‘Care Under Pressure’: a realist review of interventions to tackle doctors’ mental ill-health and its impacts on the clinical workforce and patient care. BMJ Open. 2018;8(2):e021273.
Greene T, Harju-Seppänen J, Adeniji M, Steel C, Grey N, Brewin CR et al. Predictors of PTSD, depression and anxiety in UK frontline health and social care workers during COVID-19. medRxiv 2020. Available from: https://doi.org/10.1101/2020.10.21.20216804 . [Accessed 25 Oct 2020].
Gunnell D, Appleby L, Arensman E, Hawton K, John A, Kapur N, et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7(6):468–71. https://doi.org/10.1016/S2215-0366(20)30171-1 .
Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976 .
Rossi R, Socci V, Pacitti F, Di Lorenzo G, Di Marco A, Siracusano A, et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw Open. 2020;3(5):e2010185. https://doi.org/10.1001/jamanetworkopen.2020.10185 .
National Institute for Health and Care Excellence. Post-traumatic stress disorder: Evidence reviews for psychological, psychosocial and other non-pharmacological interventions for the prevention of PTSD in adults (NICE Guideline No. 116) 2018. Retrieved from https://www.nice.org.uk/guidance/ng116/evidence/ . Accessed 6 June 2020.
Rose SC, Bisson J, Churchill R, Wessely S. Psychological debriefing for preventing post traumatic stress disorder (PTSD). Cochrane Database Syst Rev. 2002;2.
Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e15–6. https://doi.org/10.1016/S2215-0366(20)30078-X .
Moher D, Liberati A, Tetzlaff J, Altman DG. Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS med. 2009;6(7):e1000097.
CASP UK. Critical appraisal skills programme (CASP). Qualitative Research Checklist. 2017;31(13):449.
Google Scholar
Lachal J, Revah-Levy A, Orri M, Moro MR. Meta-synthesis: an original method to synthesize qualitative literature in psychiatry. Front Psychiatry. 2017;8:269. https://doi.org/10.3389/fpsyt.2017.00269 .
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. https://doi.org/10.1191/1478088706qp063oa .
Gershon R, Dernehl LA, Nwankwo E, Zhi Q, Qureshi K. Experiences and psychosocial impact of West Africa Ebola deployment on US health care volunteers. PLoS Currents. 2016;8. https://doi.org/10.1371/currents.outbreaks.c7afaae124e35d2da39ee7e07291b6b5 .
Shih FJ, Gau ML, Kao CC, Yang CY, Lin YS, Liao YC, et al. Dying and caring on the edge: Taiwan's surviving nurses' reflections on taking care of patients with severe acute respiratory syndrome. Appl Nurs Res. 2007;20(4):171–80. https://doi.org/10.1016/j.apnr.2006.08.007 .
Yin X, Zeng L. A study on the psychological needs of nurses caring for patients with coronavirus disease 2019 from the perspective of the existence, relatedness, and growth theory. Int J Nurs Sci. 2020;7(2):157–60. https://doi.org/10.1016/j.ijnss.2020.04.002 .
Koh Y, Hegney D, Drury V. Nurses' perceptions of risk from emerging respiratory infectious diseases: a Singapore study. Int J Nurs Pract. 2012;18(2):195–204. https://doi.org/10.1111/j.1440-172X.2012.02018.x .
Raven J, Baral S, Wurie H, Witter S, Samai M, Paudel P, et al. What adaptation to research is needed following crises: a comparative, qualitative study of the health workforce in Sierra Leone and Nepal. Health Res Policy Syst. 2018;16(1):6. https://doi.org/10.1186/s12961-018-0285-1 .
Chung BPM, Wong TKS, Suen ESB, Chung JWY. SARS: caring for patients in Hong Kong. J Clin Nurs. 2005;14(4):510–7. https://doi.org/10.1111/j.1365-2702.2004.01072.x .
Broom J, Broom A, Bowden V. Ebola outbreak preparedness planning: a qualitative study of clinicians' experiences. Public Health. 2017;143:103–8. https://doi.org/10.1016/j.puhe.2016.11.008 .
Article CAS PubMed Google Scholar
Moore DM, Gilbert M, Saunders S, Bryce E, Yassi A. Occupational health and infection control practices related to severe acute respiratory syndrome: health care worker perceptions. AAOHN J. 2005;53(6):257–66. https://doi.org/10.1177/216507990505300606 .
Bergeron SM, Cameron S, Armstrong-Stassen M, Pare K. Diverse implications of a national health crisis: A qualitative exploration of community nurses' SARS experiences. Can J Nurs Res Archive. 2006;38(2):42–54.
Rubin GJ, Harper S, Williams PD, Öström S, Bredbere S, Amlôt R, et al. How to support staff deploying on overseas humanitarian work: a qualitative analysis of responder views about the 2014/15 west African Ebola outbreak. Eur J Psychotraumatol. 2016;7(1):30933. https://doi.org/10.3402/ejpt.v7.30933 .
Im SB, Baumann SL, Ahn M, Kim H, Youn BH, Park MK, et al. The experience of Korean nurses during the Middle East respiratory syndrome outbreak. Nurs Sci Q. 2018;31(1):72–6. https://doi.org/10.1177/0894318417741119 .
Aghaizu A, Elam G, Ncube F, Thomson G, Szilágyi E, Eckmanns T, et al. Preventing the next 'SARS' - European healthcare workers' attitudes towards monitoring their health for the surveillance of newly emerging infections: qualitative study. BMC Public Health. 2011;11(1):541. https://doi.org/10.1186/1471-2458-11-541 .
Erland E, Dahl B. Midwives’ experiences of caring for pregnant women admitted to Ebola centres in Sierra Leone. Midwifery. 2017;55:23–8. https://doi.org/10.1016/j.midw.2017.08.005 .
Fawaz M, Samaha A. The psychosocial effects of being quarantined following exposure to COVID-19: A qualitative study of Lebanese health care workers. Int J Soc Psychiatry. 2020;66(6);560–5. https://doi.org/10.1177/0020764020932202 .
Kim Y. Nurses' experiences of care for patients with Middle East respiratory syndrome-coronavirus in South Korea. Am J Infect Control. 2018;46(7):781–7. https://doi.org/10.1016/j.ajic.2018.01.012 .
Lamb D. Factors affecting the delivery of healthcare on a humanitarian operation in West Africa: a qualitative study. Appl Nurs Res. 2018;40:129–36. https://doi.org/10.1016/j.apnr.2018.01.009 .
Smith MW, Smith PW, Kratochvil CJ, Schwedhelm S. The psychosocial challenges of caring for patients with Ebola virus disease. Health Security. 2017;15(1):104–9. https://doi.org/10.1089/hs.2016.0068 .
Liu H, Liehr P. Instructive messages from Chinese nurses’ stories of caring for SARS patients. J Clin Nurs. 2009;18(20):2880–7. https://doi.org/10.1111/j.1365-2702.2009.02857.x .
Lam KK, Hung SYM. Perceptions of emergency nurses during the human swine influenza outbreak: a qualitative study. Int Emerg Nurs. 2013;21(4):240–6. https://doi.org/10.1016/j.ienj.2012.08.008 .
Ives J, Greenfield S, Parry JM, Draper H, Gratus C, Petts JI, et al. Healthcare workers' attitudes to working during pandemic influenza: a qualitative study. BMC Public Health. 2009;9(1):56. https://doi.org/10.1186/1471-2458-9-56 .
Andertun S, Hornsten A, Hajdarevic S. Ebola virus disease: caring for patients in Sierra Leone – a qualitative study. J Adv Nurs. 2017;73(3):643–52.
Sun N, Wei L, Shi S, Jiao D, Son R et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am J Infect Control. 2020;1;48(6):592–8.
Chiang HH, Chen MB, Sue IL. Self-state of nurses in caring for SARS survivors. Nurs Ethics. 2007;14(1):18–26. https://doi.org/10.1177/0969733007071353 .
Mok E, Chung BP, Chung JW, Wong TK. An exploratory study of nurses suffering from severe acute respiratory syndrome (SARS). Int J Nurs Pract. 2005;11(4):150–60. https://doi.org/10.1111/j.1440-172X.2005.00520.x .
Bensimon CM, Tracy CS, Bernstein M, Shaul RZ, Upshur RE. A qualitative study of the duty to care in communicable disease outbreaks. Soc Sci Med. 2007;65(12):2566–75. https://doi.org/10.1016/j.socscimed.2007.07.017 .
Guimard Y, Bwaka MA, Colebunders R, Calain P, Massamba M et al. Organization of patient care during the Ebola hemorrhagic fever epidemic in Kikwit, Democratic Republic of the Congo, 1995. J Infect Dis 1999; 179(Supplement_1), S268-73.
Al Knawy BA, Al-Kadri HM, Elbarbary M, Arabi Y, Balkhy HH, Clark A. Perceptions of post outbreak management by management and healthcare workers of a Middle East respiratory syndrome outbreak in a tertiary care hospital: a qualitative study. BMJ Open. 2019;9(5):e017476. https://doi.org/10.1136/bmjopen-2017-017476 .
Shih FJ, Turale S, Lin YS, Gau ML, Kao CC, et al. Surviving a life-threatening crisis: Taiwan’s nurse leaders’ reflections and difficulties fighting the SARS epidemic. J Clin Nurs. 2008;18(24):3391–400.
von Strauss E, Paillard-Borg S, Holmgren J, Saaristo P. Global nursing in an Ebola viral haemorrhagic fever outbreak: before, during and after deployment. Glob Health Action. 2017;10(1):1371427. https://doi.org/10.1080/16549716.2017.1371427 .
Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642.
Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68(5):748–66. https://doi.org/10.1037/0022-006X.68.5.748 .
Greenberg N, Tracy D. What healthcare leaders need to do to protect the psychological well-being of frontline staff in the COVID-19 pandemic. BMJ Leader. 2020;4:3.
Gerada C. Some good must come out of covid-19. BMJ. 2020;369.
Billings J, Greene T, Kember T, Grey N, El-Leithy S, et al. Supporting hospital staff during COVID-19: early interventions. Occup Med. 2020;70(5):327–9.
Hewlett BL, Hewlett BS. Providing care and facing death: nursing during Ebola outbreaks in Central Africa. J Transcult Nurs. 2005;16(4):289–97. https://doi.org/10.1177/1043659605278935 .
Honey M, Wang WY. New Zealand nurses perceptions of caring for patients with influenza a (H1N1). Nurs Critical Care. 2013;18(2):63–9. https://doi.org/10.1111/j.1478-5153.2012.00520.x .
Lau PY, Chan CW. SARS (severe acute respiratory syndrome): reflective practice of a nurse manager. J Clin Nurs. 2005;14(1):28–34. https://doi.org/10.1111/j.1365-2702.2004.00995.x .
Lee SH, Juang YY, Su,YJ, Lee HL, Lin YH, Chao CC. Facing SARS: psychological impacts on SARS team nurses and psychiatric services in a Taiwan general hospital. Gen Hosp Psychiatry. 2005;27(5):352–8. https://doi.org/10.1016/j.genhosppsych.2005.04.007 .
Liu C, Wang H, Zhou L, Xie H, Yang H et al. Sources and symptoms of stress among nurses in the first Chinese anti-Ebola medical team during the Sierra Leone aid mission: A qualitative study. Int J Nurs Sci. 2019;10;6(2):187–91.
Liu YE, Zhai ZC, Han YH, Liu YL, Liu FP, Hu DY. Experiences of front-line nurses combating coronavirus disease-2019 in China: A qualitative analysis. Public Health Nursing 2020; Published online September 2020.
Locsin RC, Kongsuwan W, Nambozi G. Ugandan nurses’ experience of caring for persons dying from Ebola hemorrhagic fever. Int J Hum Caring. 2009;13(4):26–32. https://doi.org/10.20467/1091-5710.13.4.26 .
McMahon SA, Ho LS, Scott K, Brown H, Miller L et al. “We and the nurses are now working with one voice”: How community leaders and health committee members describe their role in Sierra Leone’s Ebola response. BMC Health Serv Res. 2017;17(1):495.
O'Boyle C, Robertson C, Secor-Turner M. Nurses' beliefs about public health emergencies: fear of abandonment. Am J Infect Control. 2006;1;34(6):351–7.
O'Sullivan TL, Amaratunga C, Phillips KP, Corneil W, O'Connor E, Lemyre L, Dow D If schools are closed, who will watch our kids? Family caregiving and other sources of role conflict among nurses during large-scale outbreaks. Prehospital Disaster Med. 2009;24(4):321–5. https://doi.org/10.1017/S1049023X00007044 .
Pearce C, Shearer M, Phillips C, Hall S, Kljakovic M, Glasgow NJ, et al. Views of GPs and practice nurses on support needed to respond to pandemic influenza: a qualitative study. Aust Health Rev. 2011;35(1):111–5. https://doi.org/10.1071/AH09788 .
Raven J, Wurie H, Witter S. Health workers’ experiences of coping with the Ebola epidemic in Sierra Leone’s health system: a qualitative study. BMC Health Serv Res. 2018;18(1):251. https://doi.org/10.1186/s12913-018-3072-3 .
Sarikaya O, Erbaydar T. Avian influenza outbreak in Turkey through health personnel's views: a qualitative study. BMC Public Health. 2007;7(1):330. https://doi.org/10.1186/1471-2458-7-330 .
Shaw KA, Chilcott A, Hansen E, Winzenberg T. The GP's response to pandemic influenza: a qualitative study. Fam Pract. 2006;23(3):267–72. https://doi.org/10.1093/fampra/cml014 .
Taylor HA, Rutkow L, Barnett DJ. Local preparedness for infectious disease outbreaks: a qualitative exploration of willingness and ability to respond. Health Security. 2018;16(5):311–9. https://doi.org/10.1089/hs.2018.0046 .
Wong EL, Wong SY, Lee N, Cheung A, Griffiths S. Healthcare workers’ duty concerns of working in the isolation ward during the novel H1N1 pandemic. J Clin Nurs. 2012;21(9–10):1466–75. https://doi.org/10.1111/j.1365-2702.2011.03783.x .
Download references
Acknowledgements
Not applicable.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Division of Psychiatry, University College London, 6th Floor, Maple House, 149 Tottenham Court Road, London, W1T 7NF, UK
Jo Billings, Brian Chi Fung Ching, Vasiliki Gkofa, Talya Greene & Michael Bloomfield
Department of Community Mental Health, University of Haifa, Haifa, Israel
Talya Greene
Traumatic Stress Clinic, Camden & Islington NHS Foundation Trust, London, UK
Michael Bloomfield
National Institute for Health Research University College London Hospitals Biomedical Research Centre, London, UK
University College London Hospitals NHS Foundation Trust, London, UK
You can also search for this author in PubMed Google Scholar
Contributions
JB conceived of the idea for this review, conducted the meta-synthesis, wrote the draft of the manuscript and incorporated contributions from all the other authors. BCFC and VG completed the literature searches, screening, data extraction and quality appraisal under supervision of JB. TG and MB provided peer consultation on the design of the review. All contributed to validity checks on the meta-synthesis of the data. All authors commented on drafts of the paper and approved the final manuscript.
Corresponding author
Correspondence to Jo Billings .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Billings, J., Ching, B.C.F., Gkofa, V. et al. Experiences of frontline healthcare workers and their views about support during COVID-19 and previous pandemics: a systematic review and qualitative meta-synthesis. BMC Health Serv Res 21 , 923 (2021). https://doi.org/10.1186/s12913-021-06917-z
Download citation
Received : 16 December 2020
Accepted : 19 August 2021
Published : 06 September 2021
DOI : https://doi.org/10.1186/s12913-021-06917-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Systematic review
- Qualitative
- Frontline healthcare workers
- Psychosocial support
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Fresh Perspectives
Why I Love Working in a Community Health Center
I was first introduced to the concept of a community health center (CHC) during residency. There were certain things about the experience that stood out to me: The waiting room was always full, patients had to take numbers like customers at a deli and the door that led from the waiting room to the exam rooms only opened if a staff member pushed a button to buzz someone in.

But beyond the seemingly cold atmosphere of the waiting room, the overall ambiance of the clinic was warm, and patients and those I worked with were joyful.
It was at that CHC that I witnessed firsthand the barriers to health that many Americans face every day. Although I didn’t know the phrase at the time, I was learning how the social determinants of health impacted the work we do. I became determined to dedicate my medical career to tackling these barriers head-on, so I joined a CHC after I graduated from residency.
I love the work I do. In fact, while many of my peers working in other settings struggle with burnout, I find great professional and personal joy in my own career. My hope is that more medical students, residents and family doctors already in practice will be drawn to this satisfying work.
CHCs come in different shapes and sizes, ranging from rural practices with only a handful of physicians to multispecialty offices with multiple sites in urban areas, but they are all rooted in the 1960s civil rights movement and War on Poverty, and they share a common aim: to serve the underserved populations of our country. Many aspiring medical students express a desire to serve the underserved in admission essays and interviews, yet that honorable goal is often lost in the mix of training and medical school debt.
Health centers are an ideal place to serve the underserved, but research shows that almost 70 percent of all CHCs are in need of more family doctors. This is unfortunate not just for the health centers but for patients who arguably have some of the greatest needs in health care.
There are many reasons why some family doctors might not be interested in working in a CHC, but I find they can be distilled down to two: The pay might not be as lucrative as other settings, and the patients can be challenging.
I recently spoke with some of my colleagues who also work in CHCs and also contribute to this blog, and I would like to share with you the main reasons we love working in CHCs and why the pay and the challenge shouldn't deter you from working in this model.
We Love Our Mission and Those We Work With
My organization's primary mission is "providing quality, compassionate primary medical and dental care and social services to those who need it most."
My co-workers fully embrace this mission, and in doing so, we are united behind a singular purpose of improving the health of our community.
Lalita Abhyankar, M.D., M.H.S., who helps teach medical students at a CHC in Brooklyn, N.Y., told me, "The medical assistants, social workers, mental health clinicians, care navigators, diabetes educators and nurses that we have at our practice are exceptionally competent, often going out of their way to ensure patients get the care they need. We value working with the underserved and find our particular site to be a place for continued learning."
Kimberly Becher, M.D., who practices in a CHC in Clay, W.V., said, "We don't just provide health care, we work to make achieving health possible. My office is filled with people who go out of their way to help patients get the care they need, whether that means physical help getting through the front door or emotional support with difficult family dynamics or contributing their own time and money for incentive programs for colon and breast cancer screening."
We See Many Types of Patients and Medical Conditions
I never know what is going to walk through my door, but isn't that part of the excitement of medicine? I recently saw a 26-year-old woman who has never had a period. She had never undergone a full workup for reasons that can be summed up in one word: poverty. Another patient had several months of abdominal pain that was unexplained -- that is, until a CT scan showed multiple hepatic abscesses consistent with amoebiasis. He had traveled to his home country in South America several months earlier and brought back a few "friends." Patients with Marfan, Prader-Willi and Kleinfelter syndromes have all presented in our office after being misdiagnosed elsewhere. Needless to say, I have been challenged in a good way, and my differential steps outside what may be seen in a typical family medicine office.
Chris Baumert, M.D., who works in a CHC in Billings, Mont., told me, "I never get stuck in a boring routine or mental rut at my job. I get to provide prenatal care, including first trimester ultrasounds, do well-child care, perform procedures and counsel on end-of-life decision-making -- a real broad scope of practice."
Dr. Becher said she doesn't see much racial or ethnic diversity in rural West Virginia, but she has a huge variability in patient complexity and health literacy.
"It is common for me to see a patient who has either never seen a doctor or not seen one in decades," she said. "I see people who can't read, while in the next room I may see someone who has an iPad with an app trending their blood sugars who is reading primary literature."
CHCs Are Centers of Innovation
Because we're motivated by our mission to improve the health of a population that faces many challenges, we've had to think outside the box to deliver the best care we can. Every CHC innovates differently based on patient needs.
Many CHCs, including mine, provide services that include medication-assisted therapy for drug and alcohol abuse, in-house behavioral health and psychiatry, and even nutritionists to guide our patients. My practice has been screening all adolescents and adult patients for substance use disorders using the Screening, Brief Intervention and Referral to Treatment tool, which has revealed many cases that would have otherwise gone undiagnosed. Additionally, when a patient is struggling to get food or transportation to a subspecialist appointment, we have care navigators who can facilitate access to these resources.
Dr. Becher has integrated home visits into her practice.
"Through my home visits, I often provide complex acute care when patients refuse ER or hospital care," she said. "I manage IV antibiotics at home and have even done biopsies and sutures in patients' living rooms."
Dr. Baumert's office recently started screening patients for social determinants of health. In being able to identify and assist with those factors, they have seen a decrease in A1c levels in patients who received targeted case management.
We Are Making a Difference
Perhaps most rewarding in our type of work is the positive change we can make in our communities. Every year, my organization has challenged clinicians and staff to help improve a handful of patient-specific quality measures, and every year, we've succeeded in increasing the rates of our cancer screenings and appropriate therapies.
Dr. Abhyankar told me, "I can't begin to describe how happy I am when I see blood pressure controlled or A1cs improving."
For Dr. Baumert, even more than the measurable clinical impacts, it's the gratitude he receives.
"Our patients are beyond grateful for our help; thank you cards for helping patients quit smoking or for caring for their mother at the end of life dot my wall and remind me what an important role I play in their lives," he said. "Identifying the reason behind poor health of the CHC patients is like an intriguing puzzle, and finding and addressing the missing piece -- chronic financial stress, poor health literacy, history of sexual or emotional trauma -- can be a rewarding process."
Challenges Keep Us Sharp
The broad scope of CHC practice, the variety of patients we see and their socioeconomic barriers to good health are certainly challenging. All the same, I believe that if we're not challenged in our practice, our work can become stale and we can lose our skills as physicians. The variety is exciting and helps us enjoy learning from our patients; in doing so, we can also build strong relationships with them.
Making "achieving health possible" is really the primary mission of CHCs. Those of us who have taken this mission to heart have found a great purpose in our lives. Since we are driven by a mission that focuses on patients who are most in need, this creates a sense of unity and family.
Finally, CHCs are centers of innovation that also recognize that every individual patient has a story. They are well positioned to give patients the tools they need to write new chapters of greater health and well-being and to make a difference in both the lives of patients and in the delivery of health care in our country.
We are passionate about the work we do and find it incredibly fulfilling. We are leaders in primary care delivery, and we want you to be a part of it. Visit the Health Resources and Services Administration to find a CHC near you.
Luis Garcia, M.D., is a family physician in York, Pa., working at Family First Health, a federally qualified health center. He focuses on caring for the Spanish-speaking community and spending time with his wife and two daughters. His hobbies include gardening and photography.
The opinions and views expressed here are those of the authors and do not necessarily represent or reflect the opinions and views of the American Academy of Family Physicians. This blog is not intended to provide medical, financial, or legal advice. All comments are moderated and will be removed if they violate our Terms of Use .
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
We use cookies to enhance our website for you. Proceed if you agree to this policy or learn more about it.
- Essay Database >
- Essay Examples >
- Essays Topics >
- Essay on Obesity
Health Care Workers Essay Examples
Type of paper: Essay
Topic: Obesity , Health , Workplace , Psychology , Human Resource Management , Nursing , Health Care , Habits
Published: 02/10/2020
ORDER PAPER LIKE THIS
How realistic is it to expect health care workers to model mental, physical, and spiritual health?
Health care workers are expected to embody all the characteristics and traits which manifest living a healthy life. This is crucial so that they become the perfect models of physical, mental, and spiritual health. As emphasized in a study reported by MacReady (2012), there could be potential problems when healthcare workers seem to have problems of practicing what they preach. As health care practitioners, they are expected to have gained greater in-depth understanding of health issues, including maintaining a health disposition through holistic observance of balanced diet, exercise, and regular check-ups through theoretical frameworks and work experience.
If Americans tend to be overweight, underactive workaholics who experience burnout, why should health care workers be any different?
Health care workers should exhibit standards of excellence in embodying good health so that they could be reliable in their field of endeavor. It was explicitly indicated that “healthcare professionals play a central role in health promotion and lifestyle information towards patients as well as towards the general population, and it has been shown that own lifestyle habits can influence attitudes and counselling practice towards patients” . Due to the highly influential nature of health care professionals’ roles in patient care, there is extreme significance in observing good habits and behavioral patterns that are consistent with healthy habits. It is part of the responsibilities of health care practitioners to address various health dilemmas, including overweight (physical chronic illnesses), burnout due to mental stress, and even assisting in fast recovery through spiritual healing. Therefore, it is just appropriate that these healthcare practitioners should be in the best of health for them to be believable, credible, and viable in their profession.
Ingibjörg H Jonsdottir, I., Börjesson, M., & Ahlborg Jr., G. (2011). Healthcare workers’ participation in a healthy lifestyle-promotion project in western Sweden. BMC Public Health, 11: 448, 1-9. MacReady, N. (2012, December 19). Healthcare Workers Often Fail to Practice What They Preach. Retrieved from Medscape Today: http://www.medscape.com/viewarticle/776474

Cite this page
Share with friends using:
Removal Request

Finished papers: 2531
This paper is created by writer with
ID 284214811
If you want your paper to be:
Well-researched, fact-checked, and accurate
Original, fresh, based on current data
Eloquently written and immaculately formatted
275 words = 1 page double-spaced

Get your papers done by pros!
Other Pages
Gender differences term papers, corn term papers, memories theses, immune response essays, illegality essays, stock exchange essays, stock split essays, indulging essays, stressor essays, neuropathy essays, hands essays, stagnation essays, irritability essays, prime ministers essays, legal documents essays, seldon essays, algor essays, downdraft essays, fevers essays, etiologies essays, papilloma essays, space research essays, dichroism essays, denaturation essays, denatured essays, rotatory essays, counterclockwise essays, amyloidosis essays, mortgage loan essays, hewitt associates essays, why transform this gives the learner an opportunity to know the reasons of transforming essay sample, report on the marketing mix components that are also called 4ps are place price promotion, feedback reinforcement article review example, organization movie review examples, essay on recommendation 4, good capstone project about capstone, kants moral theory essay samples, good example of thematic analysis of the orphan masters son novel book review, good essay on los angeles county natural history museum, good example of term paper on nameprofessor, free paper assignment 1 essay sample, artist and personal statement thesis statement example, good human resource management report example 2.
Password recovery email has been sent to [email protected]
Use your new password to log in
You are not register!
By clicking Register, you agree to our Terms of Service and that you have read our Privacy Policy .
Now you can download documents directly to your device!
Check your email! An email with your password has already been sent to you! Now you can download documents directly to your device.
or Use the QR code to Save this Paper to Your Phone
The sample is NOT original!
Short on a deadline?
Don't waste time. Get help with 11% off using code - GETWOWED
No, thanks! I'm fine with missing my deadline
- Recommended

Health care workers during the COVID-19 crisis: superheroes or human-heroes?
This essay is for my colleagues. When I say “colleagues,” I am referring to all health care workers who are currently working on the frontlines of the COVID-19 crisis or are engaging in patient care at any level. This might be an unconventional essay coming from a doctor, but I wanted to send out my thoughts and heartfelt wishes for the well-being of health care workers during this time. Health care workers are being hailed as “heroes” at this time – and indeed, they are heroes. What worries me is that “heroes” are typically viewed as superhuman – beyond human. And that puts doctors, nurses, technicians, respiratory therapists, medical assistants, etc. into a category-leading to disownment of their human nature to function and take care of patients. This has been a reality for health care workers even before the COVID-19 pandemic.
As a doctor, I felt there was this unspoken rule that I must be above emotions, above pain, above breakdown – until difficult times came that challenged these notions. We all have difficult times, but doctors and health care providers may believe they should be able to get over feeling overwhelmed, sad, scared, or in pain rapidly in order to be there for their patients and their suffering. Theirs is the stance of having answers and solutions. If the time comes when no further solutions or treatments are possible, health care workers must be a source of comfort and stability for patients and their families. This is a noble calling, one that I cherish deeply. However, now more than ever, health care workers on the frontlines will feel the pain of their patients who are suffering from COVID-19, the sadness of the families who cannot visit their loved ones, their own fear of contracting COVID-19, and the terror of their families potentially also becoming infected with COVID-19. All of these fears can become overwhelming as this pandemic goes on. Yet we must keep in mind that health care workers must function and endure these pains and trials – not as “superheroes” but as “human heroes” – with emotions that are valid, must be owned, and may need to be addressed.
Self-honesty and communication with trusted people in our lives regarding anxiety, fear, or uncertainty that may be arising is a vital necessity at this time. These trusted people may be family members, friends, or fellow colleagues, where honesty, non-judgment, and compassion can begin to heal the pain. The sooner that health care workers get honest and talk about their fears, the earlier their anxiety (sometimes terror) might reduce. This situation is not each person’s burden to bear in isolation; sharing fears really does deflate anxiety that might otherwise lead to a paralyzing fear that ultimately could compromise patient care. And what is the point of that? Honesty about challenges and struggles is key to achieving emotional balance, feeling connected, and seeking perhaps needed help so that health care workers can show up for their patients, families, and in their own lives.
Nature is another source of healing. Outdoor time is very rejuvenating. Time spent in the hospital or clinic detracts from the awareness that the flowers are blooming, the birds are singing, and the days are lengthening. Babies are being born. Nature has inherent restorative power. Take it in whenever possible, even if it is a light walk, a vigorous run, or just a long, lingering gaze at the blooming trees. Let Mother Nature take some of the pain, uncertainty, and fear and demonstrate how resilient we actually are and how life blooms again.
Finally, self-compassion is also critical at this time. As I said before, health care workers are human too. Feeling sadness, rage at the disease, frustration, fear, or terror is to be expected at this time. Health care workers are not immune to human feelings, and there is no shame in experiencing human emotions. As such, be gentle with yourselves and try to let go, little by little, of this myth that you are supposed to be superhuman. Get necessary rest, seek help as needed, and talk about the struggles and triumphs with each other and our loved ones for a shared human experience. These emotions may creep up later or linger much longer than expected and may even lead to post-traumatic stress. Again, self-compassion, honesty, and seeking professional help may be useful and needed.
There are many other techniques and tools that may be helpful to ease anxiety in this stressful time. To be sure, we cannot be in denial. These are extremely difficult times. And health care workers are indeed heroes – heroes in human flesh with human emotions that must be acknowledged. These are just thoughts from one doctor who has been observing many of her colleagues demonstrate true heroism and also struggle with being a hero. If this unconventional essay helps even one health care worker give themselves inner permission to get honest about how they are feeling and not suffer in silence, then I think it was worth it. We do not have to go through this alone; in fact, the world needs more heroes who show up in their full humanity to heal each other as we overcome this crisis together.
Veda N. Giri is a hematology-oncology physician.
Image credit: Shutterstock.com

You're just the anesthesiology resident

How a physician finds laughter during this dark time

Tagged as: COVID , Infectious Disease , Psychiatry
Related Posts

Major medical groups back mandatory COVID vaccine for health care workers

COVID-19 proved that diverse voices make health care better

How social media can help or hurt your health care career

COVID-19 adds a new health care gap: internet disparity

The COVID-19 pandemic is a catalyst for reimagining future health care delivery

Health care workers need policy changes, not just applause
More in conditions.

The dichotomy of patient health literacy

Growing up with diabetes
Health care in turmoil: costs, shortages, and pandemic strains.

Mental health treatment plan goals: Setting providers and patients up for success
Virtual rehabilitation of central sensitization syndromes.

Science supports it and patients want it: Bringing whole-person care to cancer treatment
Most popular.

Bridging care and culture: a Filipino doctor’s journey in direct primary care

Honoring humanity: lessons from a medical encounter

An internal medicine doctor’s appreciation of a patient’s name

Gender bias is pervasive within state medical board official documents and websites
Past 6 months.

We are all concierge doctors now

Your A+ in anatomy and physiology won’t improve the American health care system

Medicine’s struggle for inclusivity

Venture-backed telemental health care companies are creating a new opioid epidemic

Elite access vs. public scrutiny: Medication disparities exposed
Recent posts.
![Psychological safety: a physician’s journey [PODCAST] essay about health workers](https://www.kevinmd.com/wp-content/uploads/Psychological-safety-a-physicians-journey-190x100.jpg)
Psychological safety: a physician’s journey [PODCAST]

Artificial intelligence: Revolutionizing patient education in primary care

Uncovering health care’s true challenges: beyond doctor-patient dynamics

Healing together: patient and physician well-being [PODCAST]
Subscribe to kevinmd and never miss a story.
Get free updates delivered free to your inbox.
Find jobs at Careers by KevinMD.com
Search thousands of physician, PA, NP, and CRNA jobs now.
CME Spotlights
Leave a Comment
Comments are moderated before they are published. Please read the comment policy .
Health Workers’ Migration Essay
Shortages of health workers in developing countries are the result of a global trend known as ‘brain drain’. Many young health workers from developing countries choose to stay in foreign countries after completing their studies in order to receive well-paid jobs. As a result, the health care in many communities in developing countries does not respond to standards because of the significant paucity of doctors and nurses.
‘Brain drain’ can be discussed as a global trend that is caused by social and economic factors, and its potential impact on the global health is negative because of significant reductions in the quality of health care in many world regions.
Thus, ‘brain drain’ is a notion used to describe the global trend of the health workers’ migration. It is possible to speak about ‘brain drain’ when competent health workers from developing countries move to the developed countries in search of a better life. The obvious result of such migrations is the disproportionate distribution of health workers in developing and developed countries ( Kill or Cure: Doctors and Nurses , 2010).
The current impact of this trend on the global health is the acute shortage of the workforce in heath care facilities in many Asian, Middle Eastern, and African countries.
The potential negative impact on the global population’s health is more dramatic because of the impossibility of doctors in developing countries to control epidemics (Kasper & Bajunirwe, 2012, p. 974). Furthermore, ‘brain drain’ affects the health status of developing nations during decades, and it is a significant barrier to the development of global health goals and to the implementation of relevant health care policies.
While referring to the factors that can contribute to the progress of ‘brain drain’, it is necessary to focus on such economic factors as low wages and economic statuses in developing countries and such social factors as the lack of educational opportunities, the stable growth of population in developing countries, and the limited access to health care services.
African countries suffer from the crisis in the health care industry because physicians and nurses affected by problematic economic and social situations choose to study and work in Europe ( Kill or Cure: Doctors and Nurses , 2010).
As a result, trying to escape difficult economic conditions, health workers from developing countries support the development of the ‘brain drain’ tendency and the worsening on the social situation in their native countries while referring to the health care provision.
In order to address the crisis in the global health and respond to the problem of health workers’ migration, it is necessary to recommend an effective strategy to follow in such developing countries as Malawi and India. The active ‘brain drain’ results in reducing the number of health workers for every 10,000 people in developing countries (Kasper & Bajunirwe, 2012, p. 974).
To address the problem, it is necessary to propose the combination of economic and social strategies. Thus, in order to attract health workers to developing regions, it is necessary to improve funding and support in health care industries of developing countries. The effective strategy should respond to the health workers’ expectations regarding their wages and working conditions.
Investments into health care, additional funding, support of the research, and increases in health workers’ salaries are important to attract nurses and doctors (Kasper & Bajunirwe, 2012, p. 976).
The next step is the improvement of the occupational safety, working conditions, and competence with the help of international workforce policies and training programs provided by the world health organizations and other global public organizations.
It is possible to state that the lack of the competent health personnel is a problem typical for developing countries that is caused by ‘brain drain’ effects.
Inadequate working conditions make health workers migrate to developed countries in search of a better life in spite of the fact that their skills and knowledge are necessary in developing countries of Africa and Asia. The results of this trend are workforce shortages and unequal distribution of health services in regions.
‘Brain drain’ is a complex process which should be discussed from two perspectives. On the one hand, ‘brain drain’ can be described as a loss of health workers in developing countries because of the active migration. On the other hand, ‘brain drain’ is a lack of the access to the research results observed in developing countries.
Following the statistical data, it is possible to state that high-income countries provide jobs for more than 30% of all international medical graduates (Muula, 2005, p. 24). From this perspective, only 10% of health care workers return to their native developing countries because low-income countries cannot provide them with all the necessary conditions for the effective work (Muula, 2005, p. 25).
Health care workers seek for respect and prestige while working in developed countries. Moreover, contributing to the research in the health care sphere, medical professionals have no adequate opportunities to influence the development of health care in their native countries.
As a result, ‘brain drain’ as a global tendency can be discussed as having a negative effect on the distribution of the human capital in the health care industry and on the reduction of health care issues in low-income countries. The potential impact of ‘brain drain’ on the health in developing countries can be considered as dramatic because of the necessity to overcome workforce shortages.
Responding to the question about factors which influence ‘brain drain’, it is important to refer to such aspects as poor resources and significant income differences between developed and developing countries. Being provided with superior job opportunities in high-income countries, health workers intend to improve the socioeconomic conditions.
Thus, the social and political instability observed in developing countries is one more contributing factor to the development of the ‘brain drain’ tendency. The problem is in the fact that medical students undertaking feel safe protected while studying and working in developed countries.
Returning to their native countries, the medical workers focus on the poor availability of resources and facilities (Blacklock, Ward, & Heneghan, 2014, p. 100). Thus, a lack of resources and adequate health care facilities is a leading cause of death in developing countries. In this regard, health workers prefer working in countries where research is funded and health care reforms are effectively implemented.
The factor of comfortable working environments and opportunities for the career growth and development also influence health workers’ decisions.
The structure of the health care industry in developing countries is one more factor that contributes to ‘brain drain’ because of the extreme workflow and inadequate investment in the healthcare service delivery (Blacklock et al., 2014, p. 100). Having no job satisfaction and prospects for further education, health workers choose to migrate in order to receive effective training and opportunities for the career progress.
Blacklock, C., Ward, A., & Heneghan, C. (2014). Exploring the migration decisions of health workers and trainees from Africa: a meta-ethnographic synthesis. Social Science & Medicine, 100 (2), 99-106.
Kasper, J., & Bajunirwe, F. (2012). Brain drain in sub-Saharan Africa: contributing factors, potential remedies and the role of academic medical centres. Archives of Disease in Childhood, 97 (11), 973-979.
Kill or Cure: Doctors and Nurses . (2010). Retrieved from https://www.youtube.com/watch?v=HPaMwIkx2PA
Muula, A. (2005). Is there any solution to the “brain drain” of health professionals and knowledge from Africa? Croatian Medical Journal, 46 (1), 21-29.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2023, December 16). Health Workers’ Migration. https://ivypanda.com/essays/health-workers-migration/
"Health Workers’ Migration." IvyPanda , 16 Dec. 2023, ivypanda.com/essays/health-workers-migration/.
IvyPanda . (2023) 'Health Workers’ Migration'. 16 December.
IvyPanda . 2023. "Health Workers’ Migration." December 16, 2023. https://ivypanda.com/essays/health-workers-migration/.
1. IvyPanda . "Health Workers’ Migration." December 16, 2023. https://ivypanda.com/essays/health-workers-migration/.
Bibliography
IvyPanda . "Health Workers’ Migration." December 16, 2023. https://ivypanda.com/essays/health-workers-migration/.
- Illegal Immigrants to Demonstrate or Strike
- Global Labor Mobility Reasons and Challenges
- Treatment of Severe Otitis Externa
- The Global Health Policy Issues
- Implementation of Effective Training in Health Care Facilities
- The Global Definition of Health
- Quality Management in Healthcare
- Policies and Regulations for the Twenty-First Century Healthcare Organizations
Health care workers are burned out and overwhelmed. AI can streamline operations and help them do their real job: treating patients

At its best, the health care system is a finely-tuned machine. Seasoned doctors, thoughtful nurses, and diligent administrative staff work together smoothly, prioritizing patient outcomes and operational efficiency, keeping safety and wellness as their highest goal.
Yet despite the hard work each of these professionals puts into their jobs, the demands of modern health care too often outpace the tools that medical workers have been given. When combined with persistent workforce shortages that are particularly pronounced in remote and underserved areas, it becomes increasingly clear that the best efforts of medical workers nationwide cannot balance out the rising administrative and operational complexities health care workers confront every day.
The latest symplr State of Healthcare Supply Chain Survey, conducted in February, confirms this. Respondents sounded the alarm on two critical fronts: margin pressures and the perennial struggle with staffing and resource allocation. Among the nearly 100 supply chain leaders surveyed, 63% earmarked cost savings as their organization’s top priority for this year, highlighting the urgent need for streamlined operations amidst tightening budgets. Meanwhile, 32% said that their supply chain teams have yet to rebound to pre-pandemic staffing levels, underscoring the persistent battle to adequately equip health care systems for the challenges ahead.
Other studies back up the concerns voiced in the survey, making it clear that it’s not just one part of the health care system that faces such challenges. For example, the 2023 NSI National Health Care Retention & RN Staffing Report paints a stark picture of the workforce crisis gripping the industry, with over three-quarters of hospitals facing nurse vacancy rates exceeding 10%. These shortages not only strain existing staff but also imperil patient care, compounding organizational hurdles.
These challenges do not have to be permanently debilitating to the health care industry. The expanded use of artificial intelligence in the workplace is one way that we can work to improve patient outcomes and avoid health care worker burnout. Companies that integrate AI into their software will be able to ensure that health care systems can deploy talent wisely, allowing them to focus on patient care first and foremost.
How can AI be helpful to health care workers?
If you ask the average person about what artificial intelligence means to them, they will immediately jump to generative AI programs like ChatGPT. In reality, AI is a far broader category of software that simulates intuition to handle complex tasks. Through machine learning and AI that is deployed smartly, intentionally, and safely, we can streamline processes and create efficiencies that empower health care workers to focus their time where it is most needed—caring for patients.
This potential is reflected in the areas of optimism that health care supply chain leaders have for the future of their industry. In February, they indicated that “leveraging technology to transform manual processes and accelerate supply chain workflows” is among the biggest opportunities to improve supply chain ops. In addition, 84% of health care leaders said in 2023 that consolidating software at their organization would help clinicians redirect a substantial amount of time to patient care, and 80% said working with disparate systems complicates their job. Properly developed AI software solutions will help health care organizations consolidate and simplify paperwork and help workers reach more patients in less time.
The opportunity for AI to improve health care workers’ lives is not without risk. Entrusting such important work to automated systems will, of course, need to be done in a thoughtful manner. It’s important that health care leaders ask the right questions and follow a thoughtful process as they integrate AI into their operations.
There’s no one-size-fits-all AI solution to health care
As a longtime software executive, I’ve learned that customers know their organizations better than you do. It’s important to start by understanding the gaps that a customer needs to fill and the inefficiencies they hope to address before prescribing an AI-powered solution. Above all else, changing a software system for an organization as large as even one hospital must be a methodical process.
Deploying powerful technology without a strategy for how it will function in a broader health care system can make it ineffective or even detrimental. For health care systems integrating AI into their operations, it’s important to find a partner that is experienced with this work. The good news is that while many people think of AI as a completely new technology, many great companies have been working with earlier iterations of AI for decades. In my 20 years in the tech sector, I’ve seen it integrated into operations at many different companies to great success.
Industry leaders have been developing machine learning for years and are familiar with its capabilities and nuances. Many of our customers aren’t even aware that it’s part of the software powering their operations. The next generation of health care solutions that incorporate machine learning will be more client-facing—but that doesn’t mean it will disrupt health care workers’ understanding of their jobs. Instead, work will simply become easier and more streamlined, saving man-hours while making staff more efficient and sustainable.
This is the kind of subtle yet transformative change that can happen when AI is deployed correctly in our health care systems. It’s important to be incredibly thoughtful with such changes in the health care space. That’s because the health care system depends on patient trust. Patients and their loved ones must trust doctors to deliver high-quality care and protect their well-being. The bond between patient and caregiver needs to be treasured.
I’m confident that AI technology can improve care and strengthen this sacred bond. Deploying it is a meaningful responsibility and a delicate task. Health care leaders must work with technologists to ensure that AI is used to address real problems with as little disruption as possible. Together, we can ensure that our hospitals continue to work for patients, today and tomorrow.
BJ Schaknowski is the CEO of symplr, a health care technology company that provides software solutions for 9 of 10 hospitals in the U.S.
More must-read commentary:
- My 2-year-old daughter needed a pacemaker. That spurred me to engineer a virtual heart, and now customized 3D simulations are saving lives
- $122 Thai delivery and $26 to-go coffees: New wage laws meant to help gig workers are backfiring big-time
- Never complain, but do explain: How to handle job tasks in the hiring process , whether Gen Z is involved or not
- Outdated laws prevent gig economy workers from getting benefits. This pilot program shows the path forward
The opinions expressed in Fortune.com commentary pieces are solely the views of their authors and do not necessarily reflect the opinions and beliefs of Fortune .
Latest in Commentary

Birthing mothers’ near-death experience rates are 100 times higher than maternal mortality—and we don’t even know exactly why

Should you give job applicants an assignment during the interview process? Be thoughtful about the ask

Shark Tank entrepreneur: E-commerce giants are eating my sister’s lunch—and destroying the American Dream

Congress could soon spell the end of employment arbitration—but it’s not all good news for American workers

I’m the CTO of Canada’s biggest airport. AI isn’t destroying jobs in aviation—it’s giving us superpowers to improve air travel

Ask Andy: I’m a founder struggling with mental-health issues. How can I step away from my startup?
Most popular.

Meet the boomers who’d rather spend $100k to renovate their homes than risk the frozen housing market: ‘It would be too hard to purchase anything else’

Hedge fund billionaire Ken Griffin says college protests are the result of a ‘cultural revolution’ and Harvard should ’embrace our Western values’

‘Housing has hit rock bottom’: Top real estate CEO says high home prices are shutting people out of the market

Apple cofounder Steve Wozniak was expelled from the school where he just delivered his commencement speech—’be leaders, not followers’

Bumble’s Whitney Wolfe Herd says your dating ‘AI concierge’ will soon date hundreds of other people’s ‘concierges’ for you

China’s economy is headed for a ‘dead-end,’ and Beijing won’t do anything to stop it, scholar says

- Arts & Entertainment
- Crime & Security
- International
- 4 minutes 4 change
- Chronicles of a Chronic Guyana Chronicler
- Frederick Kissoon
- Its in Our Nature
- LCDS in perspective
- Oil, Gas & You
- Talking Culture
- The Science of COVID-19
- Beyond the Runway
- Big Little Voice
- Consumer Concern
- Dentist Advises
- Lead Stories
- Fables of a Wondering Mind
- Focus On The Village
- Psychologist
- The Write Mind
- Youth Perspective

- | May 12, 2024
- By Pat Dyal
- - May 12, 2024
IN April, Health and Safety in the Workplace Month was designated worldwide by the International Labour Organisation (ILO) to prevent accidents and disease, and promote general well-being at the workplace. This year’s commemoration theme was, “We are running out of time: Ensuring Safe and Healthy Work now in a Changing Climate”, and highlights the roles of workers, employers and the State in the workplace. Climate Change is now beginning to have severe effects on the world of work, and this is experienced by those who work outdoors in physically demanding industries such as Construction and Mining.
Indoor workers who are in hot and poorly ventilated premises are equally at risk. Although our focus will be on the workplace, Health and Safety in the Home Environment are equally important, especially for children and women. Before the Industrial Revolution, when Agriculture was the main employer, far fewer deaths occurred on the farms than in the new industrial factories with their machines with large numbers of workers congregating under one roof. Workers would die or be injured from unprotected saws, falling debris, heat of the unventilated factories, and inhalation of dangerous dust or chemicals. In industries such as mining, construction, logging, security, transportation by large vehicles, vulcanization, and even aeronautics, workers would lose their lives or be injured. Eventually, after World War II, Society became more aware of the necessity of protecting the health and safety of workers. The injury or death of a worker on the job ceased to be regarded as a risk that the worker themself took, and that the responsibility, therefore, rested with the worker. It came to be realised that the employer and the employer organisations, the Trade Unions and the State were the stakeholders, and owed a duty to protect the worker.
In Guyana, it is estimated that 20 to 30 workers per year lose their lives in various industries, the majority being in the mining and construction industries with the expansion of the Guyana economy. And with the advent of the oil-and-gas industries, it is feared that the death toll will be higher, unless urgent measures are taken to establish a regime of protection. Accordingly, it is widely expected that the State, mainly through the Ministry of Labour, the employers’ organisations and the Trade Unions, as stakeholders, would strengthen their collaboration in this regard.
The Ministry of Labour has strengthened its Occupational Safety and Health Department, and more inspectors have been appointed. The Minister of Labour has recently called for Occupational Safety and Health to be deemed a Profession, thus giving greater status and authority to the officers charged with enforcing the safety and health regulations.
Adequate training in ensuring safety and health in the various industries would be intensified, resulting in employers having proper equipment and properly maintaining them. For example, in the construction industry, proper scaffolding should provide areas for resting without the threat of falling, and in the mining industry, measures must be taken to prevent the “cave-ins” that could bury miners. Other personal safety equipment would include safety boots, safety helmets, appropriate gloves, cell phone safety vests for appropriate industries, masks and respirators for those working in chemical industries or with cement and luminous vests for those involved in the aeronautics industry. With such training of inspectors and workers being trained appropriately and the acquisition of appropriate equipment by companies, death and injury rates should almost disappear.
Finally, workplaces, as some actually do at present, should institute regular medical check-ups of their workers, especially those engaged in dangerous activities such as dealing with chemicals or cement packing. Homeowners tend to develop their own menus of safety precautions, but these should include having a medicine kit, a list of important telephone numbers, including those of the police and doctor and nearest neighbour, ensuring that one telephone in the home is always functional and that burglar alarm and security cameras are in working order if the homeowner has such. Keep dogs penned so that would-be criminals may not feed them any poisonous food.


More from this author
- | 2024-05-12

Mailing Address
Lama Avenue, Bel Air Park, Georgetown, Guyana.
General Numbers
(592) 226-3243-9
[email protected] (Editorial) (Advertising Department) [email protected] or [email protected]
E-Papers Daily
Business supplement.

- Share full article
Advertisement
Supported by
Citing Safety, New York Moves Mentally Ill People Out of the Subway
Medical workers and police officers are removing people suffering from psychiatric distress. The most troubled are forced to the hospital.

Inside a subway station in Lower Manhattan, a group of police officers slowly followed a disheveled man in a soiled gray sweatshirt who was stammering and thrashing his arms wildly.
“Please, leave me alone,” he shouted. He thumped his chest with an open palm and then, growing exasperated, sat down on a staircase. “What did I do wrong?”
Mucus had crusted in his beard. A pair of stained pants hung off his slender frame.
“Come on,” one officer, Heather Cicinnati, said as the man stumbled forward, disoriented and agitated. “We’ve got to leave the station.”
The police officers were part of a team led by a medical worker whose job is to move — by force, if needed — mentally ill people, who are often homeless, out of New York City’s transit system. On that brisk March morning, the team handcuffed him and dragged him out of the subway station. Then, they placed a white spit hood over his head.
The intervention teams are part of an expansive effort to make the subway safer after a string of shocking crimes. Part of the plan involves finding solutions to one of the transit system’s most frustrating problems: people experiencing mental health issues and homelessness living on trains and in stations.
Officials with the Metropolitan Transportation Authority, which operates the subway, said they were doing what was necessary to help troubled people while keeping them away from passengers. In survey after survey , riders have said they would use mass transit more often if they saw fewer people behaving erratically and more police officers.
But some advocates for mentally ill people believe the teams use heavy-handed tactics that do more harm than good. Ruth Lowenkron, director of the disability justice program for New York Lawyers for the Public Interest, expressed dismay over the team’s use of a spit hood and called it “an anachronistic tool.”
“This is not who we want to be as a society,” Ms. Lowenkron said. “There’s no reason to do this. And it is not going to make people safer.”
In defense of the method, M.T.A. officials said that the agency’s police officers must sometimes restrain people who are suffering from severe psychiatric distress in order to provide them with critical medical care.
Launched last fall, the program, called Subway Co-Response Outreach, or SCOUT , has removed at least 113 people from the subway. Most go willingly to shelters, or to hospitals for medical treatment, according to transit officials.
Among the people removed from the subway, 16 have been sent to the hospital against their will for psychiatric assessments. Most involuntary detainees were admitted as patients.
“This is the governor and the city and the M.T.A. coming together to do something about it,” Tim Minton, a spokesman for the authority, said as the officers detained the distraught man in March. “To try to help people who need treatment, who need assistance, and not just walk away from it.”
Violent attacks by homeless, mentally ill people are relatively rare, and mentally ill people are more likely to be the victim of a violent crime than to commit one. But some New Yorkers were put on edge by a series of high-profile attacks carried out by mentally ill homeless people in recent months. Crime rates also surged in the transit system early this year before easing.
The SCOUT program is growing — in March, Gov. Kathy Hochul said the state would provide $20 million to expand it from two teams to as many as a dozen by the end of 2025. City and state officials have also flooded the transit system with thousands of police officers and surveillance cameras. In March, Ms. Hochul deployed the National Guard in the system, building up to a force of roughly 3,000 law enforcement officers dedicated to patrolling mass transit. In late 2022, she told the M.T.A. to put cameras in every train car, and today there are about 16,000 systemwide.
Every weekday, the two SCOUT teams, each made up of one medical worker and two to three M.T.A. police officers , roam some of the subway’s busiest stations in search of people who appear to be sheltering there.
Just before the encounter in March at the Fulton Street station in Lower Manhattan, the team’s medical worker, Ameed Ademolu, 41, had already ejected several people from the subway that morning without any resistance.
Mr. Ademolu was carrying a clipboard and wearing an orange vest and face mask when he walked up to the man in the gray sweatshirt. The officers, standing a few yards away as they awaited Mr. Ademolu’s orders, watched in case the man or any onlookers lashed out.
Mr. Ademolu quickly made the call: The officers would need to take the man to a hospital against his will. He resisted for about 20 minutes, ranting and fumbling through his pockets.
State laws allow both the police and medical workers to take people to a hospital by force when their behavior poses a threat of “serious harm” to themselves or others.
Once outside, the officers pressed the handcuffed man against a wall and put the spit hood over his head because, they said, he was spraying mucus onto the officers as he shouted. Then, they strapped him to a gurney for transport to Bellevue Hospital.
Nancy Juarez, 25, from Brooklyn, was walking by the scene with a friend when she stopped and urged the officers to let the man go.
“This is harm,” said Ms. Juarez, who said that she works mostly remotely as a policy analyst at the Center on Juvenile and Criminal Justice, a San Francisco-based nonprofit organization that opposes incarceration. “This causes more trauma.”
But officials said that some people who have been removed from the system have behaved in ways that put themselves and others at risk. One person was known to light fires inside a station. Another was reported to have pushed a rider toward the tracks, and a third said he believed that he was in Iraq and that the outreach team was a group of hostile soldiers.
Sergeant Steven Simmons, 26, who serves on a SCOUT team, said he was frustrated by the reactions of some observers who seemed to misunderstand the team’s intent. He said he believed that the work he was doing was helping people who would otherwise languish on the street.
“We just have to know in our own hearts that we’re getting him the help he needs,” he said. “Sometimes, you can’t please everyone, unfortunately.”
Ana Ley is a Times reporter covering New York City’s mass transit system and the millions of passengers who use it. More about Ana Ley
- Skip to main content
- Keyboard shortcuts for audio player
Goats and Soda
- Infectious Disease
- Development
- Women & Girls
- Coronavirus FAQ
The invisible lives — and deaths — of the children of sex workers
Gabrielle Emanuel

Havilah Uloma doesn't have any pictures of her son, Kamsi.
"I had to destroy the pictures," she says.
Uloma – who lives in Rivers State, Nigeria, and works in a brothel – says it's too painful to remember her son, who died in November. He was 1 year old.
"I didn't go to the hospital. There was no money," says Uloma, who is 40 and doesn't have any other children. "I was buying roadside [medications] to give him. That was when he gave up. He left. He died."
She doesn't know exactly what killed her son; she thinks it might have been an infection or maybe the roadside medications were counterfeit. What Uloma does know is that as painful as her experience is, it is "common," she says. Many of her fellow sex workers have lost children.
While countries routinely collect child mortality data, very little is known about the lives — and premature deaths — of sex workers' children. Sometimes there are no records of these kids' births or deaths.
"They could be born in a brothel and their birth is not registered. So for many of these children, on paper, they may not exist," says Dr. Wendy Macias-Konstantopoulos , an associate professor at Harvard Medical School and a specialist in health equity.
Researchers have also ignored this population. "Although there are studies on HIV among female sex workers, these children are not making the radar," she says.
Now there are efforts to shed light: A study published in March provides some of the first figures on the possible causes of death for these youngsters. In addition, a program for pregnant sex workers and their children at a small Nigerian hospital has revealed dire health problems. This push is spearheaded by the nonprofit Global Health Promise , which is based in Oregon and works in nine countries, focusing on the health of mothers who are sex workers and their children.
"The issues are overwhelming. I think I'd actually call it a state of emergency," says Dr. Patrick Ezie , medical director of Silver Cross Hospital in Abuja, Nigeria, which houses the new program for pregnant sex workers and their children. "It is shocking — and we don't get shocked easily."
'These babies are born struggling'
Ezie has been a doctor in Nigeria for 15 years. In that time, he's seen a lot of suffering, he says. But still, he was taken aback by the severity of the health problems he saw when his hospital began the program for pregnant sex workers in November 2023.
For starters, he says, many of the sex workers he's met have received no prenatal care. He cites both financial constraints and logistical constraints, since many work at night and sleep during the day. The lack of prenatal care is a particular problem for the mothers who learn at the time of delivery that they are HIV positive or have syphilis, he says. Without preventive medication during pregnancy, it is hard to avoid transmission to the baby.
For those women who are brought into the program early enough for prenatal care, Ezie's clinical staff have noticed a number of issues. He says the women often don't have enough food during pregnancy and many face harsh situations. "They have to work even though they're pregnant and the male partner that they meet every night may not be gentle," he explains.
Ezie's found that when sex workers deliver their babies, the newborns are more likely to be born small, weak or in need of resuscitation.
"These babies are born struggling," he says, adding that their struggle often continues into childhood. Many infants are weaned off breast milk and given solid foods far too young, sometimes at just one month old, because their mothers have to work. Not only do those kids lose the protective benefits of breast milk but they could be at risk of choking. A too-early diet of solids is also associated with long-term health complications such as obesity and diabetes.
And Ezie sees children with stunted growth. For example, many of the 5-year-olds who come to his hospital's program are the size of an average 3-year-old because they're malnourished.
Ezie's program currently serves about 40 sex workers and their families. Global Health Promise also supports maternal and child health programs for sex workers in five other Nigerian cities as well as in Uganda and Kenya.
"What we're doing is very insignificant compared to the volume of the women who are out there who are doing sex work and need help," Ezie says.
'Let me give this child this drug'
Brian Willis – who is the founder and director of Global Health Promise – argues that there's not more help because the population is often invisible. The lack of information, he says, means there are "no policies, no funding, no awareness." He's trying to change that.
In 2019, the researchers for the study interviewed sex workers in Angola, Brazil, the Democratic Republic of the Congo, India, Indonesia, Kenya, Nigeria and South Africa. They gathered detailed information on the deaths of nearly 600 children of sex workers. The findings were published in March in The Journal of Global Health, a peer-reviewed journal.
The study used an approach called "community knowledge" – interviewing sex workers about the children of fellow sex workers who had died.
In research circles, t his methodology is employed in hard to reach populations and when it is challenging to get information directly from the source. Willis says his team found that mothers are sometimes reluctant to talk about their own child's death, likely because it's emotionally hard and shameful or because parents fear consequences if neglect is involved.
"Most of us would know if the child of a friend died or a neighbor died. And they do too. It is no different than that," says Willis, who explains that the researchers combed the data to ensure duplicate deaths were removed.
"What we found was that there are a large number of deaths among the children of female sex workers across these countries," says Macias-Konstantopoulos, of Harvard Medical School, who is the lead author of the study and an adviser to Global Health Promise.
The researchers got as many details as they could about why each child might have died and found that malnutrition was common as were accidents – like house fires – and communicable diseases – like malaria and HIV. Another cause of death frequently cited by the mothers was a reaction to medication.
This doesn't surprise Uloma, the sex worker from Nigeria whose 1-year-old son died.
She says one of her fellow sex workers, who had to work at night and didn't have anyone to watch her 2-year-old daughter, gave her child Tramadol, a strong pain killer known to make people drowsy. The goal was for the toddler to sleep through the night.
"She was like: 'Let me give this child this drug. She will sleep. Nobody will know I am not around,' " recounts Uloma. "But unfortunately to her, before she came back, the child died."
Outside experts have praised the research for beginning to fill a major gap in information. "It's commendable that they were able to engage in this work and collect this data so that we even have a starting point," says Jennifer Seager , an associate professor in the department of global health at George Washington University.
However, people in the field say there are many unanswered questions about the study. Seager wondered why the study was not able to draw conclusions about how much more or less likely it is for sex workers' children to die compared to children in a similar economic setting. The researchers say they looked at just a small subset of the population of sex workers and nobody knows the total numbers.
Seager also wonders whether there are different rates and causes of child mortality among sex workers who work on the street compared to those in a brothel or those who do sex work as a second job.
For her part, Uloma is eager to see action to improve the situation. And she has an idea of what might help: "The community, the society need more awareness," she says. "Most times people don't really know that sex workers, they even have children."
One thing she does is try to let people in her community know that sex workers have children – and those children "have their own lives to live."
- sex workers
- child mortality
Bosses mandated them back to the office. They took legal action instead.
As employers take a hard-line stance, workers are fighting back against office mandates with legal action.
After more than two years of protesting and fighting return-to-office mandates, workers are fed up with their bosses’ inflexible policies and are taking their battle to court.
Zacchery Belval, a designer from Connecticut who has congenital heart disease and severe anxiety, was fired after he refused to return to the office. Despite submitting several doctor’s notices about his medical need to work from home, his employer denied his request, citing in-person job duties. Now, he’s suing the company in U.S. District Court in Connecticut.
“They just said either you come back … or you’re fired,” Belval said. “It was literally screaming matches with management every day saying, ‘Hey, this is about health,’ and management going, ‘We don’t care.’”
As companies across the United States increasingly take a hard-line stance on back-to-office mandates , an increasing number of workers are elevating their complaints to court and federal labor agencies, including the National Labor Relations Board and the Equal Employment Opportunity Commission. Workers argue that the mandates can be unjust, discriminate against people with disabilities and are retaliatory actions against unionization efforts. Employers that have backtracked from flexible work policies argue that being in the office is necessary, as it improves company culture, collaboration and productivity. The outcomes of these cases could be critical and force employers to reevaluate their policies, some lawyers say.
“They can have a significant impact if there’s an agency or court ruling,” said Andrew Melzer, partner at civil rights law firm Sanford Heisler Sharp. It could determine “what’s considered permissible.”
Despite the corporate push, the percentage of workers who have returned to the office in the United States hasn’t risen. In March, nearly 23 percent of workers did their jobs remotely, at least part time, compared with 19.5 percent a year prior, according to the U.S. Bureau of Labor Statistics.
We want to hear from you

Return to office “is the issue that just doesn’t seem to go away,” said Dan Kaplan, a senior client partner with Korn Ferry’s chief human resource officer practice. The landscape remains in flux, Kaplan said, in part because some companies have struggled to configure office policies that account for the burden on parents, caregivers, the immunocompromised and others who may be taxed by mandates.
Since the mandates began, employees have raised a fuss through public outcry, petitions calling for policy changes and other internal pushback. Now, “litigation seems to be their last resort,” Kaplan said.
Escalating legal action
Workers who have resorted to filing legal action over remote work say their employers’ rejections have been shocking and unfortunate.
For Belval, 31, the issue dragged on for years, ending with his dismissal in August. Now he’s seeking to recover lost wages, be reimbursed for attorney’s fees, and compensated for his pain and suffering. His employer, Electric Boat, a unit of General Dynamics, declined to comment on the lawsuit.
Belval’s attorney, Peter Goselin, said he’s seeing a rise in workers filing lawsuits against their employers to work remotely. Belval’s lawsuit boils down to whether working from the office is considered essential to his job and whether remote work is a “reasonable” accommodation, he said.
Two circuit courts have ruled that remote work could be considered reasonable, Goselin said. A federal appeals court made that ruling in a case in which Dionne Montague, a public relations worker who has a nerve condition, requested that the U.S. Postal Service allow her to work some mornings from home and go to the office in the afternoon. And another federal appeals court came to a similar conclusion after Joseph Mobley, a customer service worker diagnosed with multiple sclerosis, asked St. Luke’s Health System to work from home when during flare-ups.
“That [remote work] has huge significance for people with disabilities and health issues,” Goselin said.
Since the pandemic, the EEOC has received at least a handful of remote-work cases. One in Baltimore resulted in a $25,000 settlement to the employee.
Lina Lucifero filed a lawsuit with the EEOC after Design & Integration refused to allow her to work remotely one day a week for a few weeks because of her anxiety and depression, much of which spiked because of job stress, she said. Instead, she alleges, the company fired her, suggesting that it would not have hired her had it known about her mental health issues.
“Right away, I said, ‘This is discrimination,” Lucifero said. “I felt dehumanized and labeled … I am someone with a mental illness and was kicked out because of it.”
In addition to the payout, Design & Integration was required to develop and distribute an American Disabilities Act policy to employees, provide training and post a notice of the settlement. The company did not respond to a request for comment.
Collective power
Not all complaints center on health and disabilities. Unfair labor practice charges have been filed with the NLRB by workers at the New York Times, Google, Cognizant, X, Grindr and The Washington Post. Concerns include alleged retaliation for unionization efforts, unlawful dismissal for publicly criticizing an office mandate, and failure to bargain over the issue.
The Times, The Post and X did not respond to requests for comment.
Last year, LGBTQ+ dating app Grindr lost about 45 percent of its employees after it required people to move across the country and work from assigned offices two days a week. So workers filed a charge with the NLRB.
Quinn McGee, a New York resident and former Grindr product manager who uses they/them pronouns, said they would have had to move to either Los Angeles or the Bay Area, where Grindr had not yet set up an office, despite living close to the Brooklyn office. But the engineers with whom McGee worked daily were assigned to the Chicago office, so McGee would be restricted to working with colleagues on Zoom.
Management delivered the mandate two weeks after employees filed to form a union, McGee said, and it refused to take questions.
“This was absolutely heartbreaking,” they said. “My partner is a medical provider, and I’m a trans person who has local health-care professionals I trust. We can’t just up and leave with no notice.”
Drew Brunning, a former Grinder engineer who lives in Middleton, Wis., said he wouldn’t have been able to move his family and enroll his daughter at a school in Chicago within the required two-week time frame.
“They’re firing us for trying to form a union,” he remembers thinking. “It was a nuclear option that’s supposed to be illegal, and no company would try it. But they did it.”
Grindr said it implemented its policy to improve collaboration and productivity. In a statement emailed to The Post, Sarah Bauer, a spokesperson for Grindr, said the company’s decision to implement the mandate “preceded the union election petition.” Grindr also said workers were given two weeks to decide whether to relocate and two months to move.
“It was only after staff knew that the transition to in-office work was underway that employees began signing union cards,” Bauer said, adding that the company supports employees’ right to unionize.
Meanwhile, a group of Austin-based YouTube Music workers say they experienced something similar and filed an NLRB charge.
Cognizant, which Google hired to subcontract the work, announced a return-to-office mandate in December 2022, two months after employees filed for a union election. The mandate required employees to return starting two days a week and eventually five days a week. The employer also revoked its policy on unpaid time off, said Katie-Marie Marschner, forcing her and others to give up other jobs needed to make ends meet.
“Everybody assumes we’re just spoiled tech workers,” Marschner said, adding that Google pays its employees 10 times as much as what those working through such subcontractors as Cognizant make. “It’s not a living wage, and adding the commute would force us further into poverty.”
Workers went on strike before getting laid off while appealing to the Austin City Council for help . Employers then asked workers to train contractors overseas to do their jobs, Marschner said. They were sent to work from an unfinished office, told they couldn’t have anything — including cellphones — at their desks and weren’t given much work, she added.
Google, which is fighting its designation as a joint employer, and Cognizant said the layoffs came after the normal end of a business contract. Cognizant said that hybrid work is “the way of the future” and that the Austin workers’ contracts required them to work from the office.
An uphill battle
Melissa Atkins, a labor and employment lawyer at Obermayer, said her clients, who are employers, are not considering the potential for legal action as a major factor in shaping their return-to-office policies.
“It’s a management right to change a policy,” Atkins said. Absent a collective bargaining agreement that hinges on the ability to work from home, or employers breaking contracts guaranteeing flexible work, “I can’t really see any real legal basis to challenge these policies.”
Workers who try to challenge their employers over office mandates in court will face an uphill battle, Atkins said.
Despite the difficulty, Marschner, the former YouTube Music worker who is now motivated to get a job as an organizer, said the fight is worth it.
“It’s really all about power,” she said. “So you have to organize to flex your collective power. That’s the only way out of this mess.”
Help Desk: Making tech work for you
Help Desk is a destination built for readers looking to better understand and take control of the technology used in everyday life.
Take control: Sign up for The Tech Friend newsletter to get straight talk and advice on how to make your tech a force for good.
Tech tips to make your life easier: 10 tips and tricks to customize iOS 16 | 5 tips to make your gadget batteries last longer | How to get back control of a hacked social media account | How to avoid falling for and spreading misinformation online
Data and Privacy: A guide to every privacy setting you should change now . We have gone through the settings for the most popular (and problematic) services to give you recommendations. Google | Amazon | Facebook | Venmo | Apple | Android
Ask a question: Send the Help Desk your personal technology questions .


IMAGES
VIDEO
COMMENTS
The World Health Organization (WHO) is calling on governments and health care leaders to address persistent threats to the health and safety of health workers and patients. "The COVID-19 pandemic has reminded all of us of the vital role health workers play to relieve suffering and save lives," said Dr Tedros Adhanom Ghebreyesus, WHO Director-General. "No country, hospital or clinic can ...
Health workers are the backbone of the global Covid-19 response and will continue to be frontline defenders of people's lives and health. As workers, they deserve equal protection of their rights.
The gaps for essential workers like home health aides are particularly large—a 2017 survey of 3,000 home care workers found that less than one in five care workers had access to paid leave.
Health worker burnout is a serious threat to the nation's health and economic security. The time for incremental change has passed. We need bold, fundamental change that gets at the roots of the ...
Various health labour market frameworks have been developed to analyse supply and demand for health workers (for example, Vujicic and Zurn7 and Witter et al7, 8). These typically view the demand of health workers for training as a function of the number of applicants, tuition costs, and expected wages.
The COVID-19 pandemic has challenged and, in many cases, exceeded the capacity of hospitals and intensive care units (ICUs) worldwide. Health-care workers have continued to provide care for patients despite exhaustion, personal risk of infection, fear of transmission to family members, illness or death of friends and colleagues, and the loss of many patients.
To the Editor: Re "Give Health Workers Hazard Pay," by Sandeep Jauhar (Opinion guest essay, Jan. 10): As a fellow physician at Northwell, I appreciate Dr. Jauhar's sentiment regarding hazard ...
COVID-19 has challenged health systems worldwide, especially the health workforce, a pillar crucial for health systems resilience. Therefore, strengthening health system resilience can be informed by analyzing health care workers' (HCWs) experiences and needs during pandemics. This review synthesizes qualitative studies published during the first year of the COVID-19 pandemic to identify ...
A healthcare worker is one who delivers care and services to the sick and ailing either directly as doctors and nurses or indirectly as aides, helpers, laboratory technicians, or even medical waste handlers. There are approximately 59 million healthcare workers worldwide. Recognizing the vital role played by health care workers as "the most ...
Ms. Brown is a nurse and the author of "Healing: When a Nurse Becomes a Patient.". America was in a health care crisis before Covid, and the stresses of the pandemic have made it worse. Since ...
INTRODUCTION. The COVID-19 pandemic has resulted in significant burdens globally. Detrimental effects include high rates of infection and death, financial hardships faced by individuals, stress related to known and particularly unknown information, and fear of the uncertainty regarding continued impact. Healthcare workers (HCWs), at the heart ...
At least half of the world's population does not have access to the essential health services it needs. A combination of economic, social, and geographic barriers - compounded by a global shortage of health care workers - prevent people from accessing primary health care (PHC). 1 The shortage of health care workers, estimated at 7.2 million health workers today, is expected to widen to 18 ...
Exhibit 1 National Workforce Programs Of The Robert Wood Johnson Foundation, As Of 31 December 1995. Program title Start End Dollars a; Medical Student Aid Program: 1972: 1978: $ 12,600,000 ...
Updated on: April 13, 2021. This infographic shows how Community Health Workers (CHWs) promote health equity and improve public health. The CHW workforce is diverse, growing, and drawing attention to its ability to address determinants of poor health. As trusted advocates, educators and counselors embedded in their communities, CHWs facilitate ...
Healthcare workers across the world have risen to the demands of treating COVID-19 patients, potentially at significant cost to their own health and wellbeing. There has been increasing recognition of the potential mental health impact of COVID-19 on frontline workers and calls to provide psychosocial support for them. However, little attention has so far been paid to understanding the impact ...
View our collection of healthcare essays. Find inspiration for topics, titles, outlines, & craft impactful healthcare papers. Read our healthcare papers today! ... which can enable data entry, storage and the use of health care and administrative data about the patients, health care workers, health institution and other institutions connected ...
I became determined to dedicate my medical career to tackling these barriers head-on, so I joined a CHC after I graduated from residency. I love the work I do. In fact, while many of my peers ...
Health care workers are expected to embody all the characteristics and traits which manifest living a healthy life. This is crucial so that they become the perfect models of physical, mental, and spiritual health. As emphasized in a study reported by MacReady (2012), there could be potential problems when healthcare workers seem to have ...
This essay is for my colleagues. When I say "colleagues," I am referring to all health care workers who are currently working on the frontlines of the COVID-19 crisis or are engaging in patient care at any level. This might be an unconventional essay coming from a doctor, but I wanted to send out my thoughts and heartfelt wishes for the ...
In this essay, a family doctor considers why that is and why it matters. ... the health care system ... Most workers who have been at a job for a year or more get between 10 and 14 days ...
The COVID-19 pandemic is a healthcare crisis, leading to unprecedented impact on healthcare services, notable morbidity and mortality of the public and healthcare workers (HCWs), economic repercussions, and significant psychological effects. To reduce the risk of viral transmission from person to person during the pandemic, the Indian ...
Health Workers' Migration Essay. Shortages of health workers in developing countries are the result of a global trend known as 'brain drain'. Many young health workers from developing countries choose to stay in foreign countries after completing their studies in order to receive well-paid jobs. As a result, the health care in many ...
Health care workers are burned out and overwhelmed. AI can streamline operations and help them do their real job: treating patients. BY BJ Schaknowski. May 6, 2024, 1:43 PM PDT. Health care ...
Beyond mere compliance, occupational health services, and workplace injury prevention, having an onsite health clinic fosters a culture of care that boosts employee health and business bottom lines alike. Join the ranks of forward-thinking companies that prioritize cost-effective onsite healthcare and employee well-being to discover how an ...
E - Papers. E - Papers . Health and safety in the workplace and the home. By Pat Dyal ... Society became more aware of the necessity of protecting the health and safety of workers. The injury or death of a worker on the job ceased to be regarded as a risk that the worker themself took, and that the responsibility, therefore, rested with the ...
The U.S. may be missing human cases of bird flu, scientists say. The U.S. Department of Agriculture is ordering dairy producers to test cows that produce milk for infections from highly pathogenic ...
Since last fall, New York City has sent teams of medical workers and police officers to remove mentally ill people from the subway system, sometimes forcibly. Some advocates say the tactics do ...
Children of sex workers are a neglected population facing serious health issues and at risk for premature death. A new effort sheds light on a group that's often missing from official data.
Updated May 6, 2024 at 2:19 p.m. EDT | Published May 6, 2024 at 7:00 a.m. EDT. (Illustration by Elena Lacey/The Washington Post; iStock) 9 min. After more than two years of protesting and fighting ...
Rothschild SK, Martin MA, Swider SM, Lynas CMT, Janssen I, Avery EF, et al. Mexican American trial of community health workers: a randomized controlled trial of a community health worker intervention for Mexican Americans with type 2 diabetes mellitus. Am J Public Health. 2014; 104 (8):1540-8. doi: 10.2105/AJPH.2013.301439.