

List of 500 Plus Nursing Capstone Project Ideas to Consider as a nursing Student

In most nursing schools, you might be required to work on a capstone project, often known as a senior capstone. It is usually a prerequisite for your final course in a degree program that requires its completion. Most nursing students prefer undertaking a capstone nursing course.
A capstone project is an individualized research project on a specific nursing topic of your professional or personal interest. It is usually completed within between 4 to 12 weeks, depending on the nursing school and the program you are pursuing. It is usually part of a project-based nursing capstone course that runs within a selected duration and is led by a capstone instructor. The first step of writing a capstone is choosing a topic that focuses on the quality improvement process, procedure, or policy and creating a nursing capstone project proposal/nursing project proposal or presentation.
A standard nursing capstone project is between 20 to 100 pages, but that depends on the institutional requirements and the preference of your capstone instructor. It is a chance to show what you have learned, enhance your professional development, specialize in your nursing career, and investigate/solve community-related health issues. The capstone project paper is based on evidence-based practice (EBP) project , which makes it necessary to follow the PICO format . Therefore, the first step is choosing the topic when doing the capstone at BSN, MSN, or DNP level.
This guide is about the first step, specifically to help you choose a good and manageable topic for your nursing capstone project. Cognizant that selecting a topic depends on the area of specialization that you are interested in (Family nursing, forensic nursing, informatics, pediatrics, nursing administration and management, nursing education, or public health, etc.), we have categorized the ideas and topics into nursing specialties to make it easier for you to brainstorm and choose a good topic for your nursing capstone paper.
General Nursing Capstone Ideas
- Patient-controlled fluid restriction monitoring
- The effects of tai chi on cardiovascular risk factors of hypertension, BMI, anxiety, depression, quality of life, and its safety and feasibility
- Exercise to improve cancer-related fatigue
- CPM machine protocol for knee replacements
- Managing hypertension with lifestyle modifications
- Self-engagement to decrease blood pressure readings and reduce non-compliance
- The application of the ABCDE bundle in ICU
- Controlled donation after circulatory death
- Effectiveness of using virtual reality in oncology settings
- Impacts of the clinically aligned pain assessment tool (CAPA) on pain management
- The influence of "deliberate practice" on skill competency
- Consequences of massage therapy for agitation in dementia
- Impact of virtual simulation on knowledge transfer
- Increased discharge compliance through mental health follow-up
- Impacts of early mobilization
- Impacts of bedside shift reports on patient safety
- Effects of physical activity and patient education on rheumatoid arthritis
- Benefits of non-physician-led hypertension management
- Reducing the rates of use of emergency departments by homeless and at-risk homeless through screening
- Improving discharge timeliness and patient outcomes
- Role of Nurses in policymaking
- Video education on fever to empower and educate caregivers
- Protecting the health and safety of nurses working with at-risk populations
Forensic Nursing Capstone Project Ideas
Forensic nursing is a very lucrative area of specialization in nursing. If you consider specializing in forensic nursing to become a Nurse Death Investigator (NDI), sexual assault nurse examiner (SANE), legal nurse consultant, forensic psychiatry nurse, correctional nurse consultant, forensic nurse educator, or forensic nurse examiner, consider these topics and ideas for your capstone. It is not exhaustive but gives you an upper hand when selecting a suitable topic for your forensic nursing capstone project. If you are looking for nursing ebp project ideas related to forensic nursing, check out these:
- Impacts of forensic nurses in preventing intimate partner violence
- Role of forensic nurses in developing community interventions to prevent elderly abuse and neglect
- Coordinated community response as a strategy to address elderly abuse
- Role of forensic nurses in identifying and preventing sexual abuse in pediatric emergency departments
- Does Sexual Assault Nurse Examiner (SANE) training affect the attitudes of Emergency Department nurses toward sexual assault survivors?
- How sexual assault nurse examiners practice trauma-informed care
- Roles of forensic outpatient nurses
- Use of simulation in training forensic nurses
- Attitudes of forensic nurses working at psychiatric facilities
- Benefits of incorporating forensic nurses as part of the multidisciplinary teams in psychiatric health facilities
- Importance of forensic nurse research
- Collaboration between forensic nurses and law enforcement agencies
- Implementation of sexual assault services in a clinic setting
- Effects of an emotional education program on prisoners
- Occupational injuries and workplace violence among forensic nurses
- Stress and burnout among forensic nurses working in mental health facilities
- Role of forensic nurses in examining medical error
- Role of forensic nurse examiner in patient education for victims of sexual assault
- The rhetoric of therapy in forensic psychiatric nursing
- Evaluation of a Standardized Patient Simulation on Undergraduate Nursing Students' Knowledge and Confidence On Intimate Partner Violence
- Evidence-based practice in forensic mental health nursing
- Standards of practice for forensic mental health nurses
- Innovative assessments for retention of sexual assault nurse examiners
- Collection and preservation of evidence by forensic nurses
- Compassion fatigue among pediatric forensic nurse examiners
- Investigating chronic traumatic encephalopathy among national football league players
- Nurses and Medicolegal Death Investigation
- Strategies for documenting evidence used by forensic nurses
- Forensic nurses as expert witnesses in courts of law
- Role of forensic nurses in research in correctional facilities
- Causes and consequences of forensic nurse shortage
- Ethical issues encountered by forensic nurses in correctional facilities
- De-escalation and limit-setting in forensic mental health units
- How forensic nurses can prevent human and organ trafficking
- Risk factors for domestic minor sex trafficking in the United States
- Mental illness as a vulnerability for sexual assault
- Cardiovascular risk factors among prisoners
- Establishing the therapeutic relationship between a forensic nurse and a patient
- Benefits of a holistic approach to training forensic nurse examiners
- Impacts of trauma-informed care training on the competency and confidence of forensic nurses
- Forensic nursing interventions with patients with personality disorder
- A forensic nurse's perspective of trauma-informed care approaches to medico legal death investigation
- How forensic nurses handle families and loved ones of those who succumb in emergency departments
- Forensic nurses and human rights abuse
- Responsibilities of forensic nurses
- SANE vs. non-SANE forensic nurses
- Required skills for forensic psychiatric nurse
- Veracity for children in pediatric forensics
- Strategies for screening children for abuse and neglect
- Trauma-Informed Care Education in Baccalaureate Nursing Curricula in the United States
- Understanding nonfatal strangulation
- Role of forensic nurses in advocating for pregnant women in correctional facilities
- The professional identity of prison nurses
- Role of education and continuous professional development in strengthening the science of forensic nursing
- Stress and burnout in forensic health nursing
- Using telehealth for sexual assault forensic examinations
- Promoting professional quality of life and resiliency in sexual assault nurse examiners
- Child labor trafficking essentials for forensic nurses
- Sexual assault nurse examiner forensic examinations for immigrant victims
You can find more topics concerning forensic nursing from Topics by Science.gov
Critical Care Nursing Capstone Project Ideas
Critical care nursing, also called intensive care nursing , is a domain of nursing practice that deals with seriously ill patients. If you are interested in pursuing critical care/ICU nursing, you can focus your capstone project on a related topic. Here are some ideas for critical nursing or ICU nursing capstone project.
- Impacts of critical incident stress debriefing for nurses in acute care departments
- Strategies to address stress and burnout among critical care nursing staff
- Role of critical care nurses in palliative care
- Nursing interventions to prevent central line bloodstream infection (CLABSI) in the ICU settings
- Benefits of SNF infection prevention online training on CLABSI prevention
- The role of law and policy in addressing healthcare-associated infections in critical care
- Impact of needleless connector change frequency on central line-associated bloodstream infection rate
- Effects of surveillance of hospital-acquired CLABSI in pediatric NICU
- Impacts of CLABSI on length of stay and readmission in ICU
- Using Nurse-Driven Protocols to Eliminate Routine Gastric Residual Volume Measurements
- Implementing a standardized communication tool in an intensive care unit
- Decreasing 30-day readmission rates in patients with heart failure
- Strategies for assessing discomfort in critically ill patients
- Increasing nurses' knowledge of and self-confidence with family presence during pediatric resuscitation
- The link between perceived and actual risk assessment by ICU nurses and the use of catheters
- How critical care nurses can prevent blood contamination during transfusion
- Risk factors and preventive measures for pressure ulcers among patients in critical care units
- Factors Leading to critical nurses shortage in the USA
- Compassion fatigue among ICU nurses and strategies to prevent it
- Pain assessment by critical care nurses through physical and physiological monitoring
- The use of CDSS in decision-making within the ICU
- Critical Nurses' education and Competencies in the USA
- Impacts of nurse-patient Ratio on patient safety and Outcomes in critical care units
- Prevalence of nurse burnout syndrome among ICU nurses
- Strategies to help critical nurses achieve excellence
- Collaborative decision-making between ICU nurses and patients in end-of-life care
- Attitudes of critical care nurses on terminally ill patients
- Hand hygiene adherence among critical care nurses
- How critical care nurses can leverage big data and AI to improve safety and outcomes
- Strategies to optimize intubation in the ICU
- The link between ICU staffing and patient outcomes
- Quality improvement strategies for neonatal ICU
- The application of telemedicine in ICU settings
- Strategies to optimize mechanical ventilation in the neonatal ICU
- Patient education strategies for children with adult patients in the ICU
- ICU nurses assist patients in making the DNR orders
- Payment Structure and morale among ICU nurses
- Challenges experienced by ICU nurses during the COVID-19 pandemic
- Intensive care nurses' knowledge and practice on endotracheal suctioning of the intubated patient
- Benefits of promoting shared decision-making in the ICU
- Intensive care nurses' experiences and perceptions of delirium and delirium care.
- Reasons why nurses should have empathy with newborn families in neonatal ICU
- Nurses' Perceptions of Telemedicine Adoption in the Intensive Care Unit
- Importance of allowing ICU nurses to grieve when patients die
- The perceptions and attitudes of ICU nurses on the use of ICU diaries
- The experiences of new nurses in ICU units
- Strategies ICU nurses use to screen delirium among ICU patients
- Impacts of brownout on ICU nurses
- Attitudes of ICU nurses on caring for patients with mental illness
- Impacts of hemodynamic monitoring training for ICU nurses on patient safety and outcomes
- Readiness of novice nurses to practice in ICU
- Nurses' experiences of caring for patients during a prolonged critical illness
- Oral practices for ICU nurses
- Caring for non-sedated mechanically ventilated patients: Attitudes of ICU nurses
- Knowledge and practice of physical restraints in ICU
Nursing Education Topics and Ideas
Nursing education is a vast area. You can never run out of ideas to explore in your nursing education capstone. Here are some potential rn to bsn capstone project ideas to consider:
- The impacts of the Nurse Residency Program
- Undergraduate pediatric nursing education: Issues, challenges, and recommendations
- How mentorship post-residency affects the experiences of new graduates transitioning from novice to competent
- Benefits of mindful meditation for nursing students
- A new leadership development model for nursing education
- Evidence-based practice and quality improvement in nursing education
- Role of stakeholder engagement in nursing education
- Strategies to improve nurse to patient ratio through nursing education
- Use of simulation in nursing education
- Effectiveness of a venous thromboembolism course using flipped classroom with nursing students
- Perceptions of the use of reflective learning journals in online graduate nursing education
- Effects of nursing education on students' pain management knowledge
- Cultural competencies for graduate nursing education
- Implications of virtual reality and augmented reality in nursing education
- The use of gamification in education with digital badges
- Strategies to dismantle racism and disparities in nursing education
- Importance of teaching reflective practice among nursing students
- Arts-based inquiry in nursing education
- Supporting the integrative health care curriculum in schools of nursing
- Educational pathways to becoming a registered nurse
- Strategies to make nursing education lucrative for the millennial generation
- How educators can influence the success of nursing students
- Philosophical perspectives of nursing education
- Use of social media and technology in nursing education
- Should nurses stay longer in college?
- Faculty shortage in nursing schools
- Impacts of the scarcity of clinical experiences on the competency of new nurses
- The gap between education and practice and the nursing staff shortage
- Benefits of integrating climate change topics in nursing curricula
- Impacts of problem-based learning models in nursing schools
- Benefits of promoting multicultural nursing education
- Integrating diversity, equity, and inclusion topics into an undergraduate nursing research course
- Benefits of nurses having a personal philosophy in nursing school
- Using active simulation to enhance the learning of nursing ethics
You can also consider topics related to mental health issues or mentally ill patients. The goal is to find the best topic to stand out among the nursing capstone projects submitted to your professor.
Health Promotion Ideas for Capstone Projects
- Implementing community cooking courses to prevent nutritional knowledge deficit
- Promoting the use of honey in diabetes foot ulcer management
- Application of the health belief model in tailoring nursing interventions to prevent adolescent smoking
- Using an educational program based on the health belief model to improve the preventive behaviors of nurses against cardiovascular diseases
- Factors affecting health promotion activities by nurses
- Attitudes of registered nurses and midwives toward health promotion targeting obese patients
- Attitudes of Nurses towards health Promotion
- Role of Nurses in health promotion and Disease prevention
- Health promotion strategies to reduce smoking among nurse practitioners
- Roles of Nurses in preventive care
- Impacts of nursing advocacy on health promotion
- Role of advanced practice nurse in health promotion
- Healthy lifestyle behaviors and health promotion attitudes in preregistered nurses
- Practical approaches to health promotion in nursing
- Translating social ecological theory into guidelines for community health promotion
- Health promotion strategies that work best with indigenous populations
- Ethical dilemmas in health promotion by nurses
- Strategies to promote mental health promotion in psychiatric facilities
Nursing Shortage and Burnout Topics and Ideas for Capstone
- Benefits of having an official mentoring program on nursing retention and job satisfaction
- Impacts of burnout and fatigue on patient outcomes
- Results of implementing patient acuity tool on nurse satisfaction
- Effects of meaningful recognition on med-surgical unit's staff satisfaction and retention
- Benefits of compassion fatigue education on oncology nurses
Women's Health Topics and Ideas for Capstone
- Benefits of early screening for postpartum depression
- Impacts of patient education on reducing postpartum depression
- Breastfeeding and consumption of sweetened foods
- Challenges facing women with disabilities in exclusive breastfeeding
- Relationship between the mental health of the mother and the outcomes of a pregnancy
- Promoting physical activity and healthy lifestyles among women
- Helping women address the challenges that come with menopause: perspectives of a nurse
- Long-term effects of preeclampsia on mother and neonate
- Strategies to prevent preeclampsia
- Preeclampsia screening within healthcare facilities
- Diagnosis and management of atypical preeclampsia-eclampsia
- Cardiovascular Sequels During and After Preeclampsia
- Impacts of superimposed preeclampsia on women
- Preeclampsia and maternal risk of breast cancer
- Nursing care approach for women with preeclampsia and eclampsia
- Administration of NSAIDs during pregnancy and the initiation of lactation
- Diagnosis and management of fetal alcohol syndrome
- Educating women on the dangers of consuming alcohol when pregnant
- Sexual dysfunction in women with alcohol dependence syndrome
- Impacts of female genital mutilation on the reproductive health of women
- Assessment and prevention of postpartum depression among pregnant women
- Etiology and consequences of postpartum depression
- Use of oxytocin in the management of postpartum depression
- Postpartum depression and breastfeeding efficacy
- Diagnosis and treatment of cytomegalovirus during pregnancy
- Relaxation techniques for pain management during labor
- Benefits of multiple-micronutrient supplementation for women during pregnancy
- Methods of milk expression for lactating women
- Effects of disorder eating on the fertility of women
- Hypertension disorders of pregnancy
- Implementation of the maternal-fetal triage index to improve obstetric triage
- Strategies to prevent obstetric hemorrhage
- Childbirth experiences of women with an autism spectrum disorder in acute care settings
Pediatrics Topics and Ideas for Capstone
- Efficacy of using music therapy in NICU
- Pain and Sedation Scales in the Pediatric Intensive Care Unit
- Impacts of skin-to-skin contact as a method for body warmth for infants with low birth weight
- How to maintain normothermia among newly born infants
- Effects of very early skin-to-skin contact on the success of breastfeeding
- Chest-to-back skin-to-skin contact in regulating body temperature for preterm babies
- Early intervention to achieve thermal balance in term neonates
- Benefits of infant massage for infants and parents in the NICU
Patient Falls Topics and Ideas for Capstone
Patient falls management is another excellent area to consider for your capstone. You should inquire into some of the best strategies to solve patient falls associated with mortality and morbidity. Reducing falls is an indicator of quality improvement in healthcare settings. Here are some ideas and topics to get you started:
- Impact of Hourly Rounding on Fall Rates
- Evidence-based fall management strategies for patients aging in place
- Nursing-led interventions to prevent falls in clinical settings
- A multifactorial approach to fall management in healthcare settings
- Impacts of patient education on fall rates
- Multi-professional team approach in fall management
- Use of telehealth to assess and address fall risk among elderly patients
- Fall risk assessment and patient safety
- Evaluation and management of fall risk in primary care settings
- The link between polypharmacy and fall rates among older adults
- Rates of falls and hospital readmissions among the older adults
- Utilizing technology to prevent falls in healthcare settings
- Benefits of patient-centered fall prevention toolkit in reducing falls and injuries among patients
- Fall Prevention Decision-Making of Acute Care Registered Nurses
- Occupational therapy falls prevention interventions for community-dwelling older adults
- Multifactorial falls prevention programs for older adults presenting to the emergency department with a fall
- Fall prevention strategies for Emergency departments
- The effectiveness of exercise for fall prevention in nursing home residents
- Role of physical therapists and aromatherapy for fall prevention in older people
- Use of radar and sensor technology to prevent falls in primary care settings
- Use of alarms to prevent falls on medical-surgical floors
- Applying bed exit alarms to prevent falls
- Using bathroom safety constructions to prevent elderly falls
- Application of intelligent socks system to reduce falls in clinical settings
- Addressing the nutritional needs of elderly patients to prevent falls
- Using smartphones to detect and prevent falls in homes and hospitals
- Use of robots in fall management
Patient Education Capstone Project Ideas
- Impacts of polypharmacy teaching in reducing adverse effects at an acute setting
- Benefits of patient education in promoting healthy lifestyles
- Patient education and reduced falls within home settings
- Impacts of using social media to facilitate patient education
- Role of patient-centered education in improving adherence and outcomes of patients in long-term care facilities
- Patient education in wound management and outcomes
- Impact of patient education on utilization of nonpharmacological modalities for persistent pain management
- Patient education and self-care management practices
- Benefits of patient education in medical rehabilitation
- Therapeutic patient education and outcomes in heart failure patients
- Benefits of multi-professional approach in diabetes patient education
- The benefits and challenges of providing patient education digitally
- Factors affecting patient education in healthcare settings
- Using healthcare information infrastructure to deliver education to patients with chronic conditions
- Impacts of using electronic health records to facilitate education for patients in rural areas
- The Effects of Tailored Diabetic Education in the Patient with Type 2 Diabetes Mellitus
Emergency Nursing Topics and Ideas for Capstone
If you are struggling to develop a perfect topic for your capstone project and are interested in emergency nursing, you can consider these capstone ideas and topics. Emergency nurse practitioners often face many challenges, including workplace incivility, lateral violence, bullying, brownout, stress, and high workload, which is a great place to start. You can also address their roles in emergency preparedness and management. Here are some ideas:
- Solutions and strategies to address Emergency Department overcrowding
- Causes and consequences of emergency room overcrowding
- Nurse-led strategies to prevent emergency room overcrowding
- Evidence-based approaches to address ED overcrowding
- Challenges for patient onboarding in the ED
- Use of technology and data modeling to address ED overcrowding
- Use of RFID technology to reduce ED overcrowding
- Application of telemedicine in addressing ER overcrowding
- Innovations to reduce demand and crowding in emergency care
- The use of wearable tech to address overcrowding in the ER
- Strategies to improve access to ER in rural areas
- Role of ER nurses in disaster management
- Factors affecting emergency nurses' perceptions of the triage systems
- Attitudes and skills of ER nurses in triage decision-making
- Perceptions of ER nurses in the assessment of the risk of emerging infectious disease in ED
- Role of ER nurses in disease surveillance
- Role of ER Nurses in disease outbreaks
- Strategies to prevent ER nurses from burnout and stress
- Addressing compassion satisfaction and fatigue among ER nurses
- Benefits of cultural competence training for ER nurses
- Feelings and emotions of ER nurses related to dying and death of patients
- Factors causing high turnover among emergency room nurses
- Pediatric pain management strategies that ER nurses managing pediatric patients use
- Strategies to address work fatigue and musculoskeletal disorders among ER nurses
- Strategies to improve communication skills among ER nurses and other healthcare practitioners in the ED
- Enhancing systems thinking for undergraduate nursing students using Friday night at the ER
- How ER nurses can apply nursing theories when caring for patients
- The impact of reflective journaling and diaries for ER nurses
- Perceptions and attitudes of ER nurses on teamwork in ED
- Causes of occupational stress among ER nurses
- Factors affecting radiation protection behaviors among ER nurses
- How ER nurses provide care to patients with self-harm
- Impacts of incivility, bullying, and workplace violence on effectiveness and performance of ER nurses
- Strategies to foster collegiality and civility
- Impacts of educational intervention through online training on incivility among ER nurses
- Lateral violence among ER nurses
- Interventions to reduce the risk of violence toward emergency department staff
- The emergency nurse's perception of incivility in the workplace
- Impacts of cognitive rehearsal training for ER nurses on confronting bullying and lateral violence
- Importance of implementing a psychiatric triage algorithm
- Use of simulation-based emergency to train ER nurses on responding to emergency situations
- Benefits of using emergency nursing competency scale for school nurses
- The lived experiences of ER nurses encountering patients with mental illness in prehospital emergency care
- Knowledge and practice of nursing students regarding bioterrorism and emergency preparedness
- Impacts of continuous competency assessment and education for ER nurses
- Emergency nurses' knowledge, attitude, and perceived barriers regarding pain Management in Resource-Limited Settings
- Effect of problem-based learning on severity classification agreement by triage nurses
- Effects of a standardized patient-based simulation in anaphylactic shock management for new graduate ER nurses
- Emergency Room nurses' perceptions of leadership, teamwork, turnover intention and patient safety
- Attitudes of ER nurses towards patient safety
- Factors affecting patient satisfaction in nurse-led triage in ED
- ER Nurses' experience with emergency room psychiatry services
- Impacts of CPR training for ER nurses on patient outcomes
- Nurses' attitudes to supporting people who are suicidal in emergency departments
Telemetry Capstone Ideas and Topics
- Improving cardiac telemetry use
- Improving Quiet-at-Night on a telemetry unit
- Reducing Cardiac Telemetry Alarm Fatigue
- Impacts of alarm fatigues on patient safety
- Evaluation of Telemetry Utilization in Medical-Surgical Unit
- Customizing Physiologic Alarms in the Emergency Department
- Impacts of default order set settings on telemetry ordering
- Strategies for transitioning Novice Nurses to Expert Nurses in Progressive Telemetry Care
- Preventing stress and burnout among nurses in the telemetry unit
- Strategies to optimize the use of telemetry in nursing training
- Is simulation efficient for telemetry nurse trainees?
- An Evidence-Based Approach to Reducing Cardiac Telemetry Alarm Fatigue.
- Physiologic monitoring alarm load on medical/surgical floors of a community hospital.
- Impacts of alarm management program on alarm fatigue among telemetry and ICU RNs
- Benefits of customizing physiologic alarms in ED
- Effect of a Nurse-Managed Telemetry Discontinuation Protocol on Monitoring Duration, Alarm Frequency, and Adverse Patient Events
- Impacts of introducing patient-customized monitoring bundle in decreasing alarm fatigue in ICU
- Alternative strategies for cardiac alarm management on telemetry units
- Role of monitor watchers in decreasing alarm burden of nurses
- Stress and burnout among telemetry nurses
Geriatrics/Gerontology Topics and Ideas for Capstone
- Perspectives of nursing students undertaking a practicum at a gerontology facility on their experience
- Geriatric assessment in daily oncology practice for nurses and allied health care professionals
- Hospital nurses' perception of the geriatric nurse practice environment
- Use of a screening tool and primary health care gerontology nurse specialist for high-needs older people
- Competency and skills of nurses practicing in elderly homes
- Assessing the perceptions and attitudes among geriatric resource nurses
- Attitudes of nurses on physical restraint for hospitalized elderly people
- Role of geriatric nurses in addressing falls among elderly patients
- Strategies to reduce restraint use for older adults in acute care
- Strategies to care for elderly patients with schizophrenia and dementia
- Addressing the nutritional needs of elderly adults who are homeless through a community nursing center
- Strategies to promote physical activity among the elderly patients
- How to improve the quality of life of elderly adults who are veterans
- Caring for elderly adults with cerebrovascular accidents
- Burnout and stress among registered nurses working in nursing homes
- Addressing social isolation and loneliness among elderly patients
- The application of robots in dementia care
- Benefits of administering vitamin C supplements to elderly adults
- Impacts of tai chi and yoga on improving the health of elderly patients
- Nonpharmacological interventions to improve sleep patterns among elderly patients
- Effectiveness of geriatric nurses getting trained in dementia care
- Use of social media to reduce depression among elderly adults
- Role of community health nurses in addressing osteoporosis among the elderly populations
To find more topics you can search for nursing capstone project examples pdf online and peer-reviewed nursing journals. You can be inspired to choose a unique, memorable, and manageable topic.
Final Remarks!
For topics on nursing informatics, check out our exclusive blog article, where we share a list of nursing informatics topics that you can choose for your capstone project.
Related Reading:
- Critical nursing research topics for nursing papers
- Writing an outstanding personal nursing philosophy paper.
- Is WGU BSN worth it?
- Tips and tricks for shadow health assessments
The main goal of a capstone project is for the nursing student to demonstrate their ability to identify specific health issues, conduct community assessments, and develop evidence-based strategies, interventions, or plans to address these critical health problems in the healthcare environment.
It is also a chance for students to demonstrate their awareness of the importance of nursing research and the nursing profession/practice in addressing societal challenges. It also helps students disseminate knowledge on pertinent issues that face the rapidly changing healthcare industry from the nursing perspective within a scholarly environment. A nursing student who completes a nursing capstone is ready to undertake leadership, administration, management, and educational functions, which promotes career growth and development.
We understand that the senior nursing capstone is an intensive and demanding project, so we have writers who can help you at every stage. As you work with your nursing capstone instructor, preceptor, or supervisor (visiting nurse), our nursing capstone project writers will work with you to produce relevant papers.
After choosing your topic from the list above or developing one of your own, you can get help from our website. As a leading nursing writing website , we guarantee 100% confidential, private, reliable, and available service. You will also get 100% original paper written from scratch using nursing lingo, format, and peer-reviewed sources published in the last 5 years.
Struggling with
Related Articles

How to Write a Nursing Essay for a Nursing Class | Student's Guide
Applying Carper’s Ways of Knowing in Essays & Practice

Writing an Engaging Disusion Post/Response in Nursing School
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.
Capstone Projects for Nursing Programs

NurseJournal.org is committed to delivering content that is objective and actionable. To that end, we have built a network of industry professionals across higher education to review our content and ensure we are providing the most helpful information to our readers.
Drawing on their firsthand industry expertise, our Integrity Network members serve as an additional step in our editing process, helping us confirm our content is accurate and up to date. These contributors:
- Suggest changes to inaccurate or misleading information.
- Provide specific, corrective feedback.
- Identify critical information that writers may have missed.
Integrity Network members typically work full time in their industry profession and review content for NurseJournal.org as a side project. All Integrity Network members are paid members of the Red Ventures Education Integrity Network.
Explore our full list of Integrity Network members.
Are you ready to earn your online nursing degree?
Capstone courses function as a bridge between the end of school and the beginning of a career, allowing nursing students to put what they’ve learned into practice. As the name suggests, students complete capstones toward the end of their nursing training. Not every nursing program requires a capstone, but those that do generally culminate in a bachelor of science in nursing (BSN) or doctor of nursing practice (DNP) degree.
Each nursing program sets their own requirements. While capstone formats differ between programs, they typically consist of an evidence-based practice formal paper or presentation. Students might complete their capstone projects as team leaders, and BSN candidates may present their papers to a faculty panel. Projects could include case studies, program evaluations, and policy analyses.
The focus on evidence-based practice allows students to apply research and experiential evidence toward solving a healthcare problem. For example, candidates may develop intervention strategies that promote health, improve outcomes, enhance quality of life, and foster safe practices for patients.
Capstone goals center on the application of knowledge gained during nursing training programs, including topics related to leadership , management, research, theories, and evidence-based practice, along with the strategies needed to transition from students to baccalaureate-level nurses.
Choosing Your Nursing Capstone Topic
When selecting a capstone topic, students should evaluate their interests, strengths, and weaknesses, along with their chosen nursing specialty area. Luther College recommends that students with lower GPAs and weaker nursing skills consider a basic medical-surgical topic. Those with strong clinical skills and high GPAs might choose emergency or intensive care medicine, although some students might prefer outpatient topics, such as clinical services, long-term care, or public health. However, this is simply an example of one school’s approach, and readers should keep in mind that each school sets its own policies and recommendations.
Asking for guidance from faculty, supervisors, preceptors, and fellow students also helps narrow down capstone topics. Advisors can also provide assistance in choosing an appropriate capstone site, helping with questions of geographical location, facility size, patient population, and care delivery model.
Students develop and learn the skills needed to complete their capstones throughout their training. These include organization and time management, knowledge of evidence-based practice, writing, and critical thinking. They also learn to conduct literature searches, identify research designs, and evaluate evidence.
Completing Your Nursing Capstone
Capstone formats and completion times widely vary between programs. Students at Luther College and Purdue University Northwest complete their capstones in 4-5 weeks, while Ferris State University specifies a timeframe of 30 hours of online classes and 90 hours of applied project work. Case Western Reserve University’s capstone spans 10 weeks.
Regardless of the program, most students follow a PICO format for project proposal questions of inquiry: population, intervention, comparison or condition, and outcome.
Some universities allow capstone projects to be completed in teams, in which students develop and implement the project. Capstone components may include defining the project and the team leader’s role, selecting team members, and formulating the project plan.
In addition to the skills previously referenced, such as knowledge of evidence-based care, critical thinking, and effective writing, capstone courses hone leadership and management abilities These include mastering therapeutic communication, applying leadership and management concepts, and developing collaborative relationships and working on multidisciplinary teams.
Presenting Your Nursing Capstone
The capstone process culminates in a paper or presentation that measures students’ skills in communication, information dissemination, and application of evidence-based practice skills. Members of the public may attend.
Utilizing the poster format, students commonly use three panels to illustrate: (1) the background, problem, and purpose; (2) methodology; and (3) 2-3 key findings and implications. Students who present using PowerPoint on a laptop or other device should pay attention to time limits, planning for one slide per minute, and verify that equipment and internet connectivity are available.
Visuals like graphs, figures, and bullet points are more effective than large blocks of text . Students should practice presenting in front of others to ensure that they thoroughly know their content and can answer questions. Backing up a copy of a PowerPoint presentation and printing out copies or transparencies guards against last-minute glitches.
How is a Nursing Capstone Graded?
Capstone grading methods differ between programs, with some issuing letter grades and others using a pass/no pass system. Grades typically hinge on a percentage basis of the project’s written sections, the final proposal, and the presentation. Faculty evaluate how students execute the capstone course objectives, which may include the following:
Students’ presentation skill evaluation criteria include exhibiting thorough preparation and knowledge of the subject matter, clear and concise communication, adherence to any time limits, ability to answer questions and cite references, and persuasiveness.
What is the Difference Between a Nursing Capstone and a Thesis?
Students complete capstones individually or in groups, while thesis projects must be done alone. Capstone project time lengths span between four and 12 weeks, while graduate students work on their thesis projects throughout their 2- to 3-year programs. Graduate thesis courses generally take place over 1-2 semesters to keep students on track.
Finally, capstone topics evaluate current issues and theories; thesis students incorporate existing case studies and literature while exploring and arguing for their own original research. Some schools require students to publish their thesis papers in a healthcare journal.
Reviewed By:

Theresa Granger
Theresa Granger, Ph.D., MN, NP-C With over two decades of teaching and clinical practice as a family nurse practitioner, Dr. Granger is an expert in nursing education and clinical practice at all levels of education (associate, baccalaureate, and graduate). She has published and lectured extensively on nursing education and clinical practice-related content. Her expertise ranges from student advising and mentoring to curricular and content design (both on ground and online) to teaching and formal course delivery. Dr. Granger is one of the founding faculty members of the University of Southern California’s first ever fully online graduate family nurse practitioner program .
Whether you’re looking to get your pre-licensure degree or taking the next step in your career, the education you need could be more affordable than you think. Find the right nursing program for you.
You might be interested in

Best Online Nursing Programs and Degrees
Overwhelmed by the abundance of online nursing programs? This guide can help you navigate the possibilities and narrow down the options.

Nurse Practitioner Career Overview

Certified Nursing Assistant (CNA) Career Overview
Form Is Invalid!
Michael James - Feb 21, 2024 - 7 min read - 1k Likes
The Ultimate Guide To Nursing Capstone Projects

If you’re a nursing student looking to excel in your capstone project, you’ve come to the right place. In this guide, we will provide you with essential information, tips, and examples to help you navigate the challenging world of nursing capstone projects and achieve outstanding results.
Nursing capstone projects are a crucial part of your educational journey, providing an opportunity to apply the knowledge and skills you’ve gained throughout your studies. By undertaking a nursing capstone project, you’ll have the chance to tackle real-world healthcare issues, conduct research, and make a meaningful impact on patient care.
Throughout this guide, we will explore best practices for nursing capstone projects and offer practical advice to help you succeed. Whether you’re just starting or amid your capstone project, we’ve got you covered.
Table of Contents
Understanding Nursing Capstone Projects
In this section, we will explore the basics of nursing capstone projects, including their purpose, goals, and requirements. Nursing capstone projects provide an opportunity for students to apply their knowledge and skills acquired throughout their nursing education in a real-world setting. These projects are usually undertaken as a requirement for graduation in nursing programs.
A nursing capstone project proposal is an essential first step in the process. It outlines the scope of the project, identifies the research question or problem to be addressed, and proposes a methodology to carry out the project. The proposal should align with the guidelines set by your institution and demonstrate a clear understanding of the project’s objectives and expected outcomes.
When developing your nursing capstone project proposal,
It is crucial to consider the following requirements:
- Clear identification of the problem or research question.
- A strong rationale for the project, highlighting its relevance and potential impact on nursing practice.
- A well-defined methodology that outlines the approach, data collection methods, and analysis techniques.
- Consideration of ethical considerations and the protection of human subjects, if applicable.
- A realistic timeline for project completion.
- Approval from your institution’s capstone project committee.
By carefully addressing these requirements and crafting a compelling nursing capstone project proposal, you lay the foundation for a successful project and ensure that it meets the necessary academic standards.
Developing a Successful Nursing Capstone Project
When it comes to writing a nursing capstone project, choosing the right topic is crucial. It should be something that resonates with your passion and interests. To help you get started, here are some capstone project ideas for nursing students:
- Exploring the impact of technology in nursing practice
- Evaluating the effectiveness of nurse-led interventions in managing chronic illnesses
- Analyzing the ethical dilemmas faced by nurses in end-of-life care
- Investigating the role of cultural competence in delivering patient-centered care
Once you have chosen a topic, the next step is to outline your project. This will serve as a roadmap for your research and writing process. Consider using the following structure:
- Introduction: Clearly state your research question or objective and provide background information on the topic.
- Literature Review: Review relevant literature and studies related to your topic. Identify key theories, concepts, and gaps in knowledge.
- Methods: Describe the research design, sample size, data collection methods, and ethical considerations.
- Results and Analysis: Present your findings and analyze the data using appropriate statistical methods or qualitative analysis techniques.
- Discussion: Interpret your results, discuss their implications, and relate them to your research question.
- Conclusion: Summarize the main findings of your project and offer recommendations for future research or practice.
Now you are ready to write the best nursing blog or research topics but, remember to consult your advisor or professor for specific guidelines and requirements for your nursing capstone project. They can provide valuable feedback and help ensure that your project meets the necessary standards.
Throughout this article, we have explored the essential aspects of nursing capstone projects, from understanding the basics to developing successful projects.
By now, you have gained a solid understanding of the purpose and requirements of nursing capstone projects, as well as valuable insights into how to plan, research, and write your project effectively.
To excel in your nursing capstone project, keep in mind the best practices we have discussed. Start by carefully selecting a relevant and meaningful topic that aligns with your interests and career goals. Conduct thorough research and utilize evidence-based practices to support your project.
Develop a well-structured and organized project proposal that adheres to your institution’s guidelines. And finally, confidently present your findings and recommendations, demonstrating your expertise in nursing.
FAQ’s
What are the best practices for nursing capstone projects.
Some best practices for nursing capstone projects include selecting a topic of interest and relevance, conducting thorough research, planning and organizing project milestones, seeking feedback from faculty and mentors, and dedicating sufficient time for revisions and improvements.
Can You Provide Some Examples Of Nursing Capstone Projects?
Examples of nursing capstone projects can include developing a new nursing intervention, creating a community education program, conducting a research study to address a nursing issue, or implementing quality improvement initiatives in a healthcare setting.
How Do I Write A Nursing Capstone Project?
To write a nursing capstone project, you need to start with a well-defined research question or problem statement. Then, conduct a comprehensive literature review, collect and analyze data if required, and present your findings and recommendations in a clear and organized manner.
What Are The Requirements For A Nursing Capstone Project?
The requirements for a nursing capstone project may vary depending on your institution. Generally, it involves extensive research, critical analysis, and the presentation of findings in a written report. Some programs may also require an oral presentation or a practical component.
How Can I Choose A Suitable Topic Or Idea For My Nursing Capstone Project?
Choosing a suitable topic for your nursing capstone project requires considering your area of interest, identifying current nursing issues or problems, and brainstorming potential research ideas.
Consult with your faculty or mentor to ensure the topic aligns with the learning outcomes of the program and is feasible within the given timeframe.
I am Michael James, a dedicated Spinal Surgeon committed to the comprehensive care of patients with spinal disorders. With a focus on precision and a deep understanding of spinal conditions, I bring 17 of experience in performing intricate spinal surgeries and interventions.
Fitness starts with what you eat
Balancing regular fitness activities with a nutritious diet is the key to cultivating a healthy and vibrant lifestyle.
most popular posts


- Understanding the Basics of a DNP Project
- How to Develop a DNP Project Using an Evidence-Based Approach
- Stages and Components of a DNP Project
- DNP Project Ideas
Sponsored School(s)
The Doctor of Nursing Practice DNP project represents the culmination of your doctoral studies and an opportunity for you to translate your acquired knowledge into practice. It is also the epitome of the practice-focused DNP and an essential part of the integrative practice experience. Preparing your DNP project is an exciting time, as it allows you to lay the groundwork for future scholarship while at the same time giving you a chance to make a potentially meaningful contribution to improving nursing practice and patient outcomes.
In a whitepaper published in August 2015 entitled The Doctor of Nursing Practice: Current Issues and Clarifying Recommendations , the AACN recommended that the DNP Project be referred to simply as the “DNP Project” as a way to distinguish it from final projects in other types of graduate programs. While the term DNP Project is still commonly used, it’s worth noting that schools and professional organizations are in the process of uniformly adopting the term “DNP Project.”

Here’s what you’ll want to know:
What is a DNP Project?
A DNP project is the umbrella term used to describe a scholarly project with the express purpose of translating evidence into practice. You may also hear it referred to as a final or research DNP project. Your DNP project will reflect your specialization/area of interest, allowing you to delve deep and create a project focused on clinical practice . You will use your DNP project to demonstrate mastery of your advanced nursing specialty.
Fortunately, given the wide breadth of clinical nursing practice, your choices for a DNP project are nearly limitless.
For example, your DNP project may be a practice portfolio that explores the impact or outcomes of nursing practice, or it may be a practice change initiative represented by a program evaluation. It may be a quality improvement project, a consulting project, or the evaluation of a new practice model. It may be a practice topic dissemination, a systemic review, or a manuscript submitted for publication—and that’s just to start.
Although DNP projects may take on various forms, depending on your college/university’s requirements and your area of advanced nursing practice, all DNP projects have three things in common: They all include planning, implementation, and evaluation components.
These components reflect the American Association of Colleges of Nursing’s (AACN) DNP Essentials, which states that a DNP project should be able to successfully integrate some or all of the following into practice:
- Focus on a change that impacts healthcare outcomes through either direct or indirect care
- Have a systems (micro-, meso-, or macro-level) or population/aggregate focus
- Implement the appropriate area of practice
- Include a plan for sustainability (e.g., financial, systems, or political realities)
- Include an evaluation of processes and/or outcomes
All projects should be designed so that processes/outcomes can be evaluated to guide practice and policy, and all should provide a foundation for future practice scholarship.
What is the Purpose of the DNP Project?
The goal of the DNP project is to inform the methods you will use to deliver care and educate others in your chosen population/community. You will use the DNP project to demonstrate your ability to lead and practice at the highest level of clinical nursing practice.
You will be asked to integrate a number of skills into your final project:
- Expertise in reflective practice
- Expertise in your area of interest
- Independent practice inquiry (identifying existing problems/needs in nursing practice and/or healthcare systems)
- The ability to evaluate, translate, and use research and evidence to improve health and quality of care outcomes
- Organizational and systems leadership skills (developing, implementing, and evaluating interventions to improve outcomes for diverse populations and/or communities)
- Knowledge of advanced healthcare policy, ethics, and law to develop a population-based program based on the best available and current evidence
Back to Top
This is your time to shine, so don’t let the task of choosing a DNP project stress you out.
Using your area of clinical expertise as a springboard, develop your project using an evidence-based process:
- Formulate a well-developed question: Describe an innovation or clinical inquiry; identify a problem/issue
- Review the literature to identify evidence-based resources that answer your question: Apply the best evidence from literature
- Assess the validity of your resources using evidence: Collect data using standard and acceptable methods/tools
- Apply that evidence: Define outcomes to be measured upon implementation
- Implement outcomes and/or analyze results: Re-evaluate the application and identify areas for improvement
An example of how one DNP student followed this 5-step evidence-based process to develop a change project with the goal of increasing vaccination among healthcare personnel working in a college:
Step 1. A change project was initiated to increase influenza vaccination among healthcare personnel at a college
Step 2. Barriers to vaccination as well as factors that would help facilitate vaccination were identified using a pre-intervention questionnaire survey
Step 3. Interventions were planned based on the findings of the pre-intervention questionnaire survey
Step 4. Interventions were implemented
Step 5. The effectiveness of the interventions was assessed through a post-intervention survey
An example of how one DNP student followed this 5-step evidence-based process to develop a quality improvement project with the goal of reducing delays in treatment for patients with hand trauma:
Step 1. A quality improvement project was initiated to avoid delays in care for patients with hand trauma
Step 2. Over 2,000 consultations and notes from emergency room and urgent care departments were reviewed to assess adherence to guidelines for treating hand trauma
Step 3. Factors associated with a lack of adherence to treatment guidelines were identified
Step 5. Outcomes were assessed
Questions to Ask
One of the best ways to ensure your DNP project accomplishes your objectives is to ask yourself questions to make sure the project meets the required standards:
- Does my project focus on individuals, communities, populations, and/or systems?
- What problems/issues will my project address?
- Is my DNP project grounded in clinical practice? Will it solve problems or directly inform my practice?
- Will my project demonstrate mastery of DNP competencies achieved through my doctoral education?
- Is my project supported by evidence provided through existing literature?
- Does my project address outcomes associated with patients and healthcare?
- Does my project provide a foundation for future scholarship in nursing?
- Executive summary of the project
- Introduction to the project
- Description of the problem, how it is defined, and the clinical setting/environment and target environment
- Data supporting the existence of the problem
- Description of the creative approach to resolving the problem
The steps required to complete a DNP project will also vary somewhat from one program to the next. Generally speaking, DNP projects include the following stages:
- Student identifies a focus area for the DNP project.
- A Capstone Chairperson is selected based on mutual agreement of the student and faculty member and the clinical/scholarly interests and area of expertise of the faculty member. Note: Careful selection of a capstone chairperson is important, as the student and chairperson will develop a plan of study and work closely throughout the process .
- Student selects a Capstone Committee (usually includes at least three faculty members, one of whom is the Capstone Chairperson).
- Student earns eligibility to defend the capstone proposal (the proposal must be formally approved by all Committee members).
- Student works with Capstone Chairperson to develop the proposal, using the Committee in an advisory capacity, as needed.
- Student prepares and distributes the proposal defense to the Committee members.
- Student arranges a meeting of the Committee to discuss the proposal and to rule on its acceptability (Committee members ensure the proposal’s feasibility, clinical relevance, and quality.).
- Upon acceptance of the proposal, the student begins the process of implementing the DNP project (must receive administrative approval for all steps of the project).
- Student schedules the final defense of the DNP project upon completing the written project and upon getting approval from the Capstone Chairperson.
- Student distributes the final copy to the Committee members and prepares for the oral defense of the DNP project.
- Committee members critique the project, identify any changes or additional work to be done, and determine the outcome of the DNP project defense.
- Smoking Cessation Program for Patients with Coronary Artery Disease
- Safe Foot Care in African American Type 2 Diabetes
- A Community Based Approach to Promoting Nutritional Awareness and Improving Dietary Habits
- Standardized Procedure for Assessment and Documentation of Pain in Long-Term Care
- Evidence-Based Practice Update for Nurse Practitioners in Urgent Care
- Strategies to Improve Patient Flow in an Urgent Care Facility
- Empowering Community Health: A Faith-Based Approach
- A Medication Safety Education Program to Reduce the Risk of Harm Caused by Medication Errors
- Integrated Model of Dementia Care in a Nursing Home
- An Evaluation of a School-Based Asthma Protocol
- A Strategy to Reduce Distress Among Isolated Blood and Marrow Transplant Patients Post-Transplantation
- An Evidence-Based Toolkit to Prevent Meningococcal Meningitis in College Students
- An Evidence-Based Ovarian Cancer Education Toolkit: A Pilot Study
- Consequences, Prevention, and Treatment of Childhood Overweight and Obesity
- Prevalence of Symptoms in Multiple Sclerosis Patients
- Obesity Prevention in Young Children
- Predictors of the First-Year Nursing Student at Risk for Early Departure
- The Predictive Value of Second Trimester Blood Pressures on the Development of Preeclampsia
- Nursing Informatics Certification and Competencies: A Report on the Current State and Recommendations for the Future
- Development of a Web-Based Health Information Database and Call Center
- Translation of Autism Screening Research into Practice
- Effectiveness of Chronic Disease Self-Management Programs for Mentally Ill Inmates with Diabetes
- Optimizing Inpatient Heart Failure Education to Support Self-Care After Discharge
- Strategic Plan for a Patient-Centered Medical Home Adaptation
- Development of a Virtual Nursing Learning Lounge to Bridge the Practice Gap
- Leadership, Advocacy, and Policy: Development of a Professional Organization for Doctors of Nursing Practice
- Media Influence on Nutritional Choices in School-Age Children
- Interdisciplinary Simulation Training for Evidence-Based Obstetric Crisis Management
- A Web-Based Group Intervention for Patients with Recurrent or Metastatic Pancreatic Cancer
- Evaluation of Pain Management Practices Among Laboring Women
- A Multi-Method Approach to Evaluating Online Distance Learning in Nursing Education
- Effects of Health Education on Nutrition and Physical Activity of School Children
- Clinical-Academic Partnership Education and Socialization into the Nursing Role
- Development of a Strategic Plan for a Dedicated Education Unit and Clinical Teaching Associate Role
- A Strategic Plan for Promoting Health in the Hispanic/Latino Population through Internet-Based Social Networks
- A Criterion-Based Job Description and Performance Assessment for the Advanced Practice Nurse
- A Strategic Plan for the Development of an Inpatient Hospice Program
- Deploying a Geriatric Nurse Practitioner in an Emergency Department to Improve Outcomes for Geriatric Patients
- Implementing Evidence-Based Practice in an Acute-Care Hospital
- A Strategic Plan for the Development of a Model of Care for HIV Co-Infected Diabetics in an Inner-City Clinic
- Implementation of Routine HIV Testing for the Hospitalized Patient
- Development of an Evidence-Based, In-Patient Alcohol Detoxification Guideline for Culturally Diverse Adults
- Conducting a Randomized Household Survey in an Underserved Urban Community
- Fall Prevention in the Medical Surgical Setting
- A Comprehensive Systematic Review of the Influence of Transformational Leadership Style on Nursing Staff in Acute Care Hospitals
University of Notre Dame
College of sceince, hillebrand center for compassionate care in medicine.
- Undergraduate Students >
2021 Capstone Projects
Andrew alexander - the widespread, multilevel impact of compassionate care on healthcare organization success .
In the first decade of the 2000s, the number of elderly men and women in American prisons increased by over 80%. Moreover, as the result of three-strike laws, life sentencing, and mandatory minimum sentences, spending the remainder of one's life in the confines of a correctional facility has become commonplace for incarcerated individuals. When combined with the poor health outcomes and the high prevalence of physical and mental disabilities among prisoners, these determinate sentencing practices result in an elevated risk for dying in captivity and in such a way that violates what is both professionally and morally acceptable. Fortunately, over the past few decades, many prisons and correctional facilities have adopted in-facility hospice programs in an attempt to restore compassion to the dying process. For individuals serving time in facilities that have yet to adopt such programs, however, early release programs, commonly referred to as compassionate release, offer a preferable alternative to dying in prison for many patients. Nonetheless, numerous obstacles ranging from the attitudes of correctional healthcare providers to inefficient and underdeveloped protocols oftentimes render these paths to ‘dying well’ ineffective at accomplishing their aim. Thus, this study seeks to summarize both what it means to ‘die well’ as well as the major approaches and barriers to providing compassionate and high-quality end-of-life care to the American prison population. Additionally, this study will examine existing end-of-life care programs and practices with the hopes of informing the future of a more compassionate model of end-of-life care for the incarcerated.
Hope Baldwin - Applying the Science of Compassion to the Future of Artificial Intelligence in the Medical Field

Recent advances in artificial intelligence with clinical applications has led many to consider how the implementation of such technologies into medicine will affect the healthcare system. And, extensive research has demonstrated the scientific basis of compassion and its positive impacts on patient, provider, and system outcomes. Although many think these ideas of technology and compassionate or humanistic healthcare are competing, the integration of AI into medical practice can ultimately serve to make healthcare more compassionate. Deep learning algorithms offer the potential to increase accuracy and efficiency in diagnosis and treatment strategies, while natural language processing can limit clerical duties of physicians to improve patient-physician encounters and decrease clinician burnout. Additionally, a shift from information overload towards increased integration of important skills like communication and emotional regulation in medical school curriculums, as well as the use of new learning technologies, can help to create more competent and compassionate physicians. If physicians truly desire to provide the best possible care for their patients, they will learn how to properly integrate AI into their practice as this shift in the medical field occurs, as such technology can enable increased physician competency and better patient-physician relationships by serving a model of healthcare that places compassion at the center.
Mary Benz - Poverty in Medicine: Pathways Forward - examining the factors that lead to physician fatigue, burnout, and shortages in poor and underserved communities: the role of the compassion mindset in restoring and sustaining physicians in their practice with the underserved

There are more than 640 counties in the United States that are considered “healthcare deserts” due to their limited access to healthcare resources, especially primary care physicians. Despite the great need for physicians and other healthcare professionals in these regions, many clinicians face significant challenges when practicing medicine in underserved communities, such as financial burden, lack of proper training, emotional distress, and role strain. These obstacles can make it exceedingly difficult for doctors to sustain careers for an extended period of time in these underserved communities, which is why there continues to be such an extreme shortage of healthcare workers in poor communities throughout the country. Although this is a complex, multifaceted problem, this analysis addresses the factors which can motivate or dissuade physicians from practicing in underserved communities, and promising strategies to sustain them in such work. Such strategies for improving a physician’s ability to thrive while caring for those of lower socioeconomic status include: incorporating proper training and exposure early on in medical training, improving federal loan repayment programs, building networks of support in local communities, teaching the compassion mindset, and encouraging physicians to engage with their spirituality. While these efforts are complex and require a great number of resources and engagement, they, nevertheless, provide realistic pathways forward in the effort to empower physicians and other healthcare workers to not only survive in their medical practice with the underserved but to thrive and find deep fulfillment as they care for the most vulnerable populations.
Kate Bockholt - Coping with Cancer: The Necessity of Prioritizing Compassion in Oncology
The burden of cancer on patients, caregivers and health care teams, and oncologists is extensive, and mental illness is identified as a comorbidity for many. Depression, anxiety, and post-traumatic stress disorder are especially common for cancer patients and survivors, leading to worsened cancer outcomes and continued psychological distress even after the completion of cancer treatment. These psychological disorders are also frequently observed in oncologists, who experience heightened risk of mental illness and burnout relative to many medical specialties. Through an extensive review of the available data and literature on the topic of cancer and mental illness, this paper discusses the burden of cancer, the association of mental illness with cancer and its continued impact through the lifetime of the patient, and the factors that contribute to the magnitude of this occurrence. Given the pervasiveness of mental illness in cancer patients and survivors, the need for compassionate care in medicine – specifically oncology – is established with evidence from the new science of compassion. The obligation to prioritize compassion in oncology is explained through a patient lens as well as a clinician lens, both of which exhibit an empirically grounded need for compassionate caring and evidenced benefits of this practice. The foundation for these practices is defined through an analysis of the mechanism by which compassionate caring (termed C 2 ) is established, with a particular focus on the importance of emotional intelligence in clinicians. The feasibility of implementing compassionate caring practices in cancer care is analyzed with consideration of potential challenges and common hesitations, namely time and cost associated with training health care staff and administering these changes to current medical practices. Despite uncertainty and hesitancy from many, financial- and time-related costs of compassionate caring practices have not been found to be significant. The necessity of compassion in oncology is thus inarguable. Its immediate and longitudinal benefits and the marked improvement of mental and physical health outcomes provide hope for the future of cancer care – for patients and clinicians alike.
Leah Bode - The Neuroscientific Benefits of Hobbies and Leisure Activities for Healthcare Providers: How Self-care Improves Patient Care

The job of caring for others in their most critical and vulnerable states takes a toll on healthcare providers. One study found that 60.7% of doctors experience exhaustion or stress three or more days of the week and that ‘having no coping mechanisms’ was a predictive factor for mental health problems in physicians (Chambers & Belcher, 1994). Periods of rest and recovery from the hard work of healthcare are vital to ensuring that providers remain both effective and compassionate caregivers. The brain undergoes important changes during periods of awake leisure, including processing the events of the day, building resiliency, improving mood, and boosting creativity. Hobbies have the ability to help providers recover from compassion fatigue and take proactive measures towards self-care. The chemical effect of neurotransmitters, the broaden and build theory of positive emotions, acts of self-compassion, and changes in creativity and memory all provide supportive evidence for how self-care is hugely beneficial to clinicians and their patients. Physical exercise, creating music, art/handcrafts, cooking/baking, and yoga/physical meditation are discussed in this paper as hobbies with particularly compelling evidence for healthcare providers. The culture of medical training is changing to embrace the emotional needs of trainees along with their educational responsibilities. The compelling evidence for hobbies’ neuroscientific benefits is presented as a way for clinicians to protect themselves against stress and burnout while sustaining skillful, compassionate care towards patients.
Aidan Crowley - Mental Performance of Physicians in High-Stress Clinical Specialties During COVID-19: A Qualitative Interview Study
The science of compassion is a novel field of inquiry within the study of psychological and behavioral aspects of the patient-physician encounter. More than simply being “kind” or having “bedside manners,” compassion is a four-step biological and psychological process that activates neurological pathways distinct from empathy (Vachon, 2020). Operating in a zone of balanced compassionate caring can mitigate physician burnout as well as improve accuracy of diagnosis, appropriateness of treatment, and patient health outcomes (Trzeciak & Mazzarelli, 2019). However, little is known about mental and emotional strategies and techniques physicians use to actively foster a compassion mindset in their daily work. This is especially true in high-stress clinical specialties such as surgery, emergency medicine, and critical care, and this stress is compounded in the context of a global pandemic. This qualitative interview study seeks to identify the practices and techniques by which physicians in high-stress clinical specialties remain mentally and emotionally present with their patients during the novel coronavirus pandemic. Semi-structured interviews were conducted using an appreciative inquiry approach with twelve physicians from specialties including surgery, emergency medicine, and critical care. Interview transcripts were independently analyzed using the qualitative methodology of grounded theory in NVivo software and discussed to majority consensus by a five-member research team. Results uncovered a broad range of techniques for actively maintaining mental performance before, during, and after work, as well as clear dichotomies between emotional processing and emotional “detachment.” Participants primarily acquired these techniques through trial-and-error over years of gradual professional development. These findings are relevant for physicians to share, disseminate, and train best practices for mitigating burnout and bolstering fulfillment in the emotionally demanding profession of medicine. They also suggest a need to promote increased discussion around such techniques longitudinally throughout physician formation, and they highlight a largely untapped resource in the psychology of the clinician mind.
Vanessa Davis - Compassionate Trauma-Informed Treatment of Patients in the Clinical Setting

Adverse childhood experiences (ACEs) and trauma have significant detrimental impacts on patient emotional, physical, and cognitive health. Early traumatic experiences negatively affect neurological and physiological development, often resulting in a hindered or altered trajectory of development for brain regions involved in emotional regulation, such as the amygdala, prefrontal cortex, and hippocampus, as well as the hypothalamic-pituitary-adrenal (HPA) axis, contributing to decreased regulation of the cortisol stress-response and overall emotional regulation (Anda et al., 2006). These maladaptive alterations in development, combined with socio-economic factors, contribute to the increased health risk seen in victims. An ACE score of four or greater is correlated with increased risk for alcoholism, drug abuse, depression, suicide attempt, smoking, and obesity, among many others (Felitti et al., 1998). Trauma also affects the way victims interact with society, especially within the healthcare system. Victims often struggle forming healthy, positive interpersonal relationships and exhibiting a secure attachment style (Poole et al., 2018). This affects the way physicians must interact with them in the clinical setting to optimize the effects of treatment and increase positive outcomes. Despite high demand, few physicians are adequately trained to provide trauma-sensitive treatment, limiting the efficiency and consistency needed to provide optimal care (Kappel et al., 2020). Standardizing trauma-informed training within the medical curriculum and treatment in the clinical setting could help reduce some of the barriers that patients with trauma histories face within the healthcare system.
Irving Delgado-Arellanes - Compassionate Insights on the Treatment of Addiction

Addiction is not a new problem that the United States and the world has faced, yet the attention and treatment of addiction has lagged behind the rest of modern medicine. Addiction is a complex problem that has been obscured by its reputation and the perspectives from the public and the clinical world continue to differ. Historically, patients recovering from addiction have been dehumanized and disregarded because of the nature of the condition. Here, I present a perspective that recovering addict patients are indeed deserving of standard quality of care, and that their condition should be viewed as a disease since there are profound physiological changes to the brain and other systems when a person has developed an addiction. Addiction has been studied in detail in the neurosciences, and its investigations reflect these profound changes in brain circuitry. Along with this perspective, I provide several dimensions of the problem of addiction including its differential development, perspective from society and perspective from clinicians. Addiction itself holds various implications beyond the health of the addict, such as aversive experiences in their social and emotional lives. It is important to consider these facets of patients since their condition is not only physiological in nature. The current state of treatment of addiction does not reflect the standard levels of other conditions despite there being several avenues of remedy. Rehabilitation centers struggle with funding and access to them is not consistent across communities. Novel treatments of addiction are currently being investigated and show great promise, such as psychedelic-assisted treatments. These treatments have had more success than their conventional alternatives because of their brain-restructuring mechanisms. Along psychedelic-assisted treatment are Mindfulness-Based-Interventions (MIBs) which employ a non-invasive and introspective approach to addiction treatment. They too have shown great promise without the risks and side effects of purely pharmacological interventions. Integrating these views, the way forward with the treatment of addiction lies in the effort to maintain a compassionate mindset with these patients and acknowledging the road to recovery is strenuous. In the end, addicts are humans too, and they deserve the same care and concern that any other condition calls for – hopefully medicine will reflect this in the future.
Giuliana Di Bono - Causes, Consequences and Coping Methods for Burnout in Clinicians that Serve in Underserved Hospitals in Honduras

In 2018 more than 78% of physicians reported they had burnout, 54.3% reported fatigue and 6.5% reported recent suicidal ideation. Physician burnout is a global crisis that has been faced by all in the field and keeps increasing. Physician burnout keeps increasing due to a sense of powerlessness, lack of autonomy, asymmetric rewards and personal characteristics. Personal characteristics that negatively affect clinicians are perfectionism, self-criticism, sleep deprivation, over commitment, work life imbalances and a lack of social support. Physician burnout leads to negative consequences for themselves, the organization they work in and the patients they treat. Moreover, when clinicians serve in underserved hospitals and treat low income patients the burn out can be even more common. Due to the highly negative consequences of burnout there needs to be individual and systematic changes that aid in protecting/buffering physicians from burnout. This study focuses on an in depth of analysis of burn out factors and consequences and the accelerating factors for clinicians that serve in under serve hospitals. Additionally, this study will explore individual coping methods for clinicians that serve in under serve populations and propose ways that these health care organizations can protect their clinicians from burnout even with limited financial resources.
Mariana Ferre - Applying the Science of Compassion to Improve the Caregiving Relationships of Dementia Patients and their Loved Ones

Dementia is a progressive disease characterized by an observable decline in cognitive abilities such as memory, thinking, behavior, and the performance of daily activities. This disease poses one of the greatest global challenges for health and social care in the 21 st century with approximately 50 million people currently affected and nearly 10 million new cases every year. In addition to debilitating the cognitive and psychological health of diagnosed individuals, the disability and dependency characteristics of dementia have been shown to negatively impact the health of patients’ loved ones, especially if they play a role of caregiver. The purpose of this paper is to help familial caregivers learn about the challenges both patients and caregivers will face in light of this diagnosis and provide resources to help them navigate the difficulties of caring for a loved one with dementia. More specifically, I will be discussing how compassionate skills, such as communication skills and emotion-based coping mechanisms, can be used to improve the livelihood and overall health of patients with dementia and their family members respectively. While there is still no cure for dementia, learning about the science of compassion and how it can be employed in the treatment of this disease can help improve the lives of both those who suffer from this disease and their loved one.
Mary Freedlund - Addressing Barriers to Healthcare: Applying the Science of Compassion at Free Clinics for Uninsured and Low-Income Patients

Approaching the healthcare system can be an especially complicated process for uninsured and low-income patient populations in the United States. High costs of care, a lack of sufficient healthcare coverage, and limited available resources at medical facilities essentially exclude the underserved from receiving medical care. Thus, free charitable clinics as well as residency-run free clinics function to make health resources more accessible to patients. While the mission of free clinics embodies the core attributes of compassionate caring in medicine, the act of providing compassionate care effectively to patients at free clinics requires further attention. Although physicians have no control over systemic practices that bar the underserved from medical care, they play an integral role in the health outcomes of uninsured and low-income patients at free clinics. How they choose to approach systemic challenges and utilize compassionate caring techniques affects their patient outcomes. This paper analyzes the perspectives and experiences of both patients receiving care and physicians providing care at free clinics. Utilizing the clinician compassion mindset and self-reflection techniques in free clinics has the potential to improve the experiences and health outcomes of physicians and their patients.
Michelle Grady - Compassionate Solutions to Conserve Dignity During End-of-Life Care

End-of-life care includes a variety of patient aspects such as physical needs, emotional support, spiritual support, and practical comforts. Far too often, the emotional needs of the patient and their family are unknowingly neglected by the healthcare provider in favor of attending to the physical suffering of the patient. Several barriers have been identified by patients, providers, and their families that block access to adequate end-of-life care. These barriers are namely fear and uncertainty revolving around prognosis and treatment options on behalf of both the patient and provider, which result in inadequate communication. These barriers then lead to a significant delay in conversations surround end-of-life care, contributing to a loss of dignity and quality of life for the patient. Compassion offers a way to overcome such barriers by using a holistic approach to care, one that incorporates the continuous interaction of psychological and physiological influences on patient well-being. Compassion centered communication enables providers to communicate with patients and families both in a timely and effective manner while addressing needs beyond physiological symptoms. Additionally, compassion acts as a safeguard for providers, offering protection from emotional exhaustion and depersonalization through the practice of self-compassion and mindfulness. End-of-life care can be better achieved through a compassionate approach to communication that promotes early and thorough discussion of possible paths, leading to the best possible outcome for all involved.
Meghan Greene - Pervasive Discrepancy in Quality Healthcare for Individuals with Intellectual Disabilities

A significant disparity exists in quality healthcare for individuals with intellectual disabilities, particularly in current mainstream healthcare services. Equal access to and quality of these services are lacking. Numerous explicit objectives exist to promote equal rights to high quality healthcare for individuals with intellectual disabilities, including from the United Nation’s Convention on the Rights of Persons with Disabilities. However, despite these professed efforts to increase inclusion of individuals with intellectual disabilities in mainstream healthcare services, this pervasive discrepancy persists due to systemic negative attitudes and perceptions towards the entire population of these individuals. In the current western world, stigma surrounds individuals with intellectual disabilities which creates implicit biases in physicians towards the entire population. In my opinion, this stigma is rooted in the uncertainty of treating those different from us, often due to lack of experience with doing so. Additional variability elicits negative attitudes of healthcare professionals that often detrimentally impact their medical decisions for individuals with intellectual disabilities. Furthermore, perceived lack of self-reliance of individuals with intellectual disabilities significantly contributes to the discrepancy in mainstream healthcare services. Preventing these individuals from contributing to their own medical decisions forcefully removes their autonomy, depriving them of basic human rights and further contributing to inconsistencies in healthcare for this population. Unfortunately, dehumanization of patients, particularly those with intellectual disabilities, is very prevalent in physicians and other healthcare staff. Because compassion prioritizes seeing each patient as a person, compassionate care in medicine is especially important for remediating the disparity. All healthcare professionals have an obligation to provide unbiased treatment, and this is especially true for those that treat individuals with disabilities. Compassionate care is characterized by a genuine desire for what is best for the patient regardless of preexisting attitudes or perceptions that often exist for patients with disabilities. Further research and efforts to combat this discrepancy should primarily focus on education. Educational efforts should aim to increase confidence in healthcare professionals to treat patients with intellectual disabilities, implement anti-stigma interventions and promote positive attitudes towards these individuals in future healthcare professionals.
Rebecca Hammond - Moral Injury: The Roots, Causes, and Manifestations in Physicians

Physicians commit suicide at rates higher than the general population and report increasingly worse mental health and well-being. Previously, poor physician mental health has been attributed to burnout. However, researchers and physicians alike are beginning to suggest that what was previously thought of as burnout is actually moral injury. Moral injury was first characterized in combat veterans and was suggested as an alternative diagnosis to PTSD. While practicing medicine is not synonymous to going to war, physicians on the front lines of healthcare face human suffering every day and may feel they are fighting a battle of allegiances between patients, hospital systems, insurance companies, and their own personal values. The COVID-19 pandemic has further highlighted this struggle. Moral injury is the psychological suffering that results from engaging in, failing to prevent, or witnessing an act or situation that violates one’s beliefs and values. It is related to concepts such as moral distress and disorders like PTSD and depression; however, it is unique. Moral injury is even identified by the US Department of Veterans Affairs as a distinct phenomenon that occurs in both military populations and healthcare professionals. There are a multitude of risk factors including younger age, shorter time spent practicing, low religiosity as well as a changing healthcare system that prioritizes the business side of healthcare. Scales are now being developed, such as the Moral Injury Symptom Scale-HP, to identify moral injury in healthcare professionals specifically. Further, studies are currently investigating its neural correlates via brain imaging. This paper reviews the roots, causes, and manifestations of moral injury in healthcare professionals, specifically physicians, and applies the research on moral injury in military populations to physicians. Included in this discussion is a review of possible therapeutic interventions to relieve symptoms of moral injury and long-term institutional changes to reduce the occurrence of potentially morally injurious events.
Sarah Hatfield - Additions to Standard Patient-Centered Care for Individuals with Severe or Profound Intellectual and Developmental Disabilities

The cultivation of a patient-centered care approach to medicine has become increasingly prevalent in recent years. Patient-centered care recognizes the role of patients in their own healthcare decisions and focuses on collaboration between the physician, with their vast medical knowledge, and the patient’s autonomy. People with intellectual and developmental disabilities make up a large portion of our population and are deserving of the same high-quality care that is emerging. Despite this fact, many physicians do not receive adequate training to feel comfortable and confident in providing high-quality care to the specific needs of these patients. People with serve or profound intellectual and developmental disabilities add a unique component to the patient-physician relationship with the addition of a caregiver, forming a non-conventional, triadic relationship. Navigating this triadic relationship and building it in trust may look different for people with severe or profound IDD. Additions to standard patient-centered care can be made to ensure people in this population are receiving the same high-quality care as others. Particular factors to focus on are figuring out effective modes of communication with the patient, having a recognition of common humanity towards the patient, and acceptance of physician’s role to enter into the patient-caregiver relationship forming a triad. These additions to standard patient-centered care, as well as others, will provide physicians with the proper knowledge and training to maintain a high standard of care for patients with severe or profound intellectual and developmental disabilities.
Nick Iovino - End-of-Life Care Behind Bars: Compassion for the Incarcerated and Dying
Olivia Jazbutis - Cognition and Emotion: The Role of Emotional Intelligence in Patient-Centered Care

Our lives are infused with emotions, which play an integral role in the cognitive processing of information, decision-making, and memory formation. Neuroscience demonstrates that cognition and emotion are inherently intertwined, and clinical work requires both cognitive and emotional components. Patient-centered care is enacted when a clinician self-monitors how he or she is both relating to patients and adjusting to patient needs. To adequately practice patient-centered care, clinicians must learn to strike a balance between being emotionally underinvested and overinvested with patients. Training clinicians to be aware of their own emotions, to regulate their emotions, to recognize patient emotions, and to pick up on cues from patients has the potential to change how emotions are understood and utilized in healthcare. Emotional intelligence may ultimately act as a vehicle for guiding a clinician’s competency to the patient’s best interests. Emotionally intelligent care is not only correlated with better patient outcomes, but it also fosters protective features for the clinician. It should therefore actively be promoted and cultivated on both an individual and an organizational level when implementing a compassion-centric paradigm of healthcare. Individual ways to cultivate emotional intelligence include journaling, daily meditation, positive visualization, appreciative inquiry, thought before action, and empathic listening. Emotionally intelligent care is already used on an individual level by some clinicians, but little formal training exists in terms of learning effective emotional regulation techniques for dealing with the emotional aspects of working in healthcare. With a tendency to focus on objectivity and developing expertise with technical procedures, there is still much work left to be done with training emotional intelligence to achieve and sustain a compassion mindset. RULER, which stands for recognizing, understanding, labeling, expressing, and regulating, is an evidence-based approach to social-emotional learning developed by the Yale Center for Emotional Intelligence that embeds emotional intelligence into norms, routines, policies, instruction, and relationships in K-12 schools. Given that the RULER approach mirrors the competencies of emotionally intelligent care in the healthcare field, and its efficacious implementation in schools, it may potentially be modified to cater to the social, emotional, and cognitive aspects of clinicians. Further, active implementation of the CERB framework, which is comprised of cognitive, emotional, relational, and behavioral emotionally intelligent strategies, along with additional personal feedback is an alternative approach for the healthcare field to implement emotionally intelligent care. Ultimately, training clinicians’ emotional intelligence may function as a realistic long-lasting solution that addresses the neuroscience of compassion as well as the increasing pressures clinicians continue to face in healthcare.
Kelly Kolleck - Challenges to Physician Compassion During COVID-19

The science of compassion is an emerging field, and thus unlikely to be a high priority of physicians facing challenging conditions during the COVID-19 pandemic. However, compassion offers tools which can help the physician to better connect with and care for their patients, ultimately improving patient satisfaction and physician fulfillment. The clinician compassion mindset is an invaluable tool used to ensure compassion is the organizing factor in all patient interactions. Clinicians that were most strongly affected by pandemic stressors might have relied upon a compassionate mindset to better care for patients in the face of adversity. But the pandemic did present myriad challenges which might have overwhelmed these mindsets. Direct tolls, such as cognitive uncertainty, fear of transmission, and overwhelming work hours, in addition to indirect tolls, including moral injury, compassion fatigue, and increased burnout, all contributed to grueling work conditions. Polyvagal theory and empathic distress fatigue help to explain why employing a compassion mindset at certain times was nearly impossible. These pandemic were imposed upon a backdrop of high national physician burnout rates and betrayal by the public. Thus, physicians had countless challenges stacked against them. This paper seeks to determine which stressors unique to the pandemic have affected clinician compassion and offers a forward-looking perspective to compassion recovery as the pandemic continues. Time dedicated to compassion recovery and reconnecting with families will be crucial to help physicians heal post-pandemic.
Kathryn Kostolansky - Compassion-etics: The Necessity for Compassion in Genetic Counseling
The field of genetic counseling is expected to grow over 20% from 2019 to 2029 (U.S. Bureau of Labor Statistics, 2020). With an extreme increase in number of genetic counseling professionals to come in the next decade, it is of the utmost importance that compassionate care in medicine is understood and practiced. Compassion is not only a concept, but a hard science and should be taught to genetic counseling students in order to provide them with necessary skills for their career. Compassion, which involves a combination of neural bottom-up processing with mirror neurons and top-down processing, is based on evolutionary biology and serves as a protective mechanism against compassion fatigue and burnout. Furthermore, the use of compassion in the practice of genetic counseling aids the genetic counselor in efficiency, patient interactions, and job satisfaction, which in an ever fast paced and technological age, allows for better patient experience due to increased trust between a counselor and client due to compassionate care.
Joseph Lazzara - The Neuroscience of Exercise and its Role in Combating Burnout and Cultivating Compassionate Physicians

Burnout is characterized by “emotional exhaustion, depersonalization, and a decreased sense of personal accomplishment caused by work-related stress” (Dimou, 2016, p.1). It occurs to some extent in every profession but is even more prevalent among those in the medical field. Physicians are at an increased risk for burnout due to long work hours, difficulty maintaining work-life balance, and challenges associated with constantly caring for others who are ill. Burnout has been linked to depression, and many theorize clinicians experiencing burnout are predisposed to declining mental health. Further, burnout can lead to changes in appetite, disengagement, insomnia, and anxiety (Moalem, 2017). The consequences of such factors can be quite severe and include divorce, strained personal relationships, and in some cases suicide. Burnout poses a serious threat for all physicians, and a variety of methods have been developed to combat its effects. Many of these solutions are centered around reducing stress, improving work-life balance, and developing better relationships with colleagues. However, the literature often oversimplifies methods like physical activity, placing them into one of these categories. Exercise is frequently viewed as a method of stress reduction that works for some people, but not others. The literature suggests a negative correlation between physical activity and burnout but calls for further analysis regarding its method of action. This capstone project seeks to develop a deeper understanding of the benefits of exercise in the context of burnout and demonstrate its ability to cultivate compassionate and caring physicians.
Monique Le Tran - Compassion in the NICU: The Importance of Responding to the Psychosocial Needs of Parents of Very Preterm Infants
The purpose of this study is to explore the different psychosocial and logistical issues that parents reported having with nurses and other staff members while their child was in the neonatal intensive care unit (NICU), ways that nurses can provide the compassionate support that parents need, and how burnout in the NICU/ICU can interfere with this caregiving. It is crucial that nurses are educated on how to respond empathetically to the needs of parents and to help them cope with the hospitalization of their child. Some common themes of psychosocial needs that parents have reported include emotional support, trust in the healthcare provider, and privacy. To respond to these needs, nurses and other healthcare professionals should receive specific training in communication skills and family-centered care, as it will allow them to empathetically support both parent and child during their stay at the hospital. However, as the NICU is a high stress environment, burnout and compassion fatigue is especially prevalent, which can interfere with the quality of care infants receive. In addition to this, interacting with worried and upset parents can also be emotionally taxing for nurses, especially when they are not trained to handle situations like this. When nurses are not able to provide compassionate care, parents are less satisfied with their NICU experience and are less confident in their roles as parents. Therefore, responding to parents with understanding and empathy will encourage parents to cope with their situation
Maura Lee - Organizational Methods of Compassionate Care: Caring for Doctors So That They Can Care for Patients

The Physician Foundation discovered in their “2016 Physician Survey” that 78% of clinicians are experiencing sensations of burnout and that 50% of doctors are completely burnt out (2016, p. 7). Burnout, or experiencing emotional exhaustion, depersonalization, and a lack of personal accomplishment (i.e. the feeling that your efforts achieve nothing), is expensive for physicians, patients, and health systems (Maslach & Leiter, 1997). Johns Hopkins estimates that burnout costs the United States billions of dollars and hundreds of thousands of lives each year (Johns Hopkins Medicine, 2016, p. 1). A new movement in the scientific literature proposes compassion – not simply a sentiment but rather a body of science based on neuroscience, biology, and evolution – as a solution to sensations of burnout. During every encounter with a suffering patient, the physician automatically undergoes the “Clinician Compassion Mindset Process” (CCMP), which determines how emotions of empathy and mirror neuron firing will impact the physiology of the doctors’ brain as they continue to practice medicine (Vachon, 2020, p. 102). Unhealthy processing of these intense emotions is an accurate predictor of sensations of burnout. Doctors cannot give of themselves to care for their patients if the healthcare systems in which they work do not care for them. Organizations must show compassion for doctors first, taking responsibility for the overall health and well-being of their physicians by cultivating a culture of compassionate care. Included in this capstone project are literature-reviewed methods through which healthcare administrations can work to reduce burnout by showing compassion for their clinicians: employing emotionally intelligent and supportive immediate superiors, taking physician feedback into consideration when making new policies, implementing a professional practice model, re-introducing community into the workplace, re-inspiring clinicians’ internal motivations, and giving doctors some freedom in treating their patients. This paper also seeks to explain how organizations intentionally taking steps to build a culture of compassion can prevent and protect against burnout at the point of care, allowing physicians to more successfully engage with their CCMP. Although many healthcare organizations are taking steps to combat the prevalence of burnout in their workforce, a fundamental paradigm shift is necessary to ensure a culture of compassion in medicine is the norm, not an added benefit for those who can afford it.
Allison LeHanka - The Shift to the Shared Decision-Making Model in Medicine

In the 1970s, American healthcare systems began to move away from a paternalistic approach in the patient-physician relationship towards the shared decision-making model. While the paternalistic approach focuses on a physician’s expertise and authority in making medical decisions, the shared decision-making model grants new power to the patient in their own care. The shared decision-making model is characterized by clinician and patient collaboration on medical decision-making, where the doctor supplies their medical training, clinical experience, and knowledge of current treatments and research and the patient expresses their values and personal preferences relevant to the decision at hand. This model can be broken down into a five-step process in which partnership is built, a choice is explicitly identified, options with their corresponding risks and benefits are discussed, and a decision is ultimately made. The shared decision-making model not only satisfies patient demands for autonomy in care, but also can improve patient outcomes, especially in the affective-cognitive realm. Further benefits of the shared decision-making model remain to be seen as correct implementation of the model continues to increase across the US.
Chelsea Logo - Applying the Science of Compassion to the Delivery of Bad News: Can Teaching Unemotional Physicians to Be More Emotionally Regulated Facilitate This Process?

Though physicians are responsible for breaking bad news, a majority of practicing physicians have reported receiving no formal training in effectively communicating bad news. Since bad news in and of itself can cause suffering, the way bad news is delivered can have a significant impact on patients’ perspectives of their illness and their relationship with their healthcare provider. For patients, bad news can threaten their identity and challenge their sense of meaning, and patients can become more distressed when physicians deliver bad news in an inappropriate manner. Thus, teaching physicians how to deliver bad news well is an important area of study. Currently, medical schools are using strategies like the SPIKES protocol and the ABCDE mnemonic to teach physicians how to deliver bad news well. While these strategies are effective, I propose the application of the science of compassion to the delivery of bad news with three types of physicians in mind: physicians who are emotionally detached, physicians who are emotionally over-involved, and physicians who are emotionally inexpressive. Emotional regulation plays a very important role in the delivery of bad news, particularly because bad news often elicits a profound emotional response from the patient and triggers an equal emotional response in the physician who has to deliver the news. By understanding the role of emotions and empathy in healthcare, I highlight the possibility that teaching physicians to be emotionally regulated is a means by which the science of compassion can be used to assuage the burden of delivering bad news.
Emma Mazurek - Narrative Medicine: Bridging the Gap Between the Biomedical and Biopsychosocial Models of Medical Practice
The medical field is experiencing a paradigm shift from the biomedical to the biopsychosocial model of health. Narrative-based medicine (NBM) is a key factor in completing the transition from a detached stance to a more holistic and interdisciplinary practice of medicine. Focusing on the narrative and illness experience of the patient returns autonomy and agency to the sufferer, augments the physician-patient relationship, and allows healing to continue. Ultimately, NBM improves health outcomes in patients with chronic illnesses and is a useful tool to enhance trust between physician and patient in other specialties. While more extensive research is needed, especially in specialties outside primary care, medical curricula should include medical humanities and holistic caring models in their education in order to train competent future physicians. By implementing a narrative approach, medicine will remain in touch with the demands of the public and will see higher efficacy among its patients. Narrative medicine is necessary to transition fully to the biopsychosocial model of health, and it provides a means to practice the art of medicine.
Megan McCabe - Addressing the Barriers that Pediatric Rare Disease Patients and their Families Face when Receiving Medical Care, and Application of the SPIKES Protocol for Healthcare Professionals to Reduce these Barriers

“Rare disease” is an umbrella term for a variety of rare and neglected disorders. For a pediatric patient with a rare disease, a main part of their life will be receiving medical care from physicians, nurses, therapists, or other healthcare professionals. Due to a lack of awareness and compassion for pediatric patients with rare diseases and their family members, they often face many barriers when trying to receive medical care. The goal of this capstone project is to first outline the many barriers that pediatric rare disease patients and their families face in the medical field. Some of these barriers and difficulties that they face include the diagnostic process, a lack of healthcare provider competence, psychosocial needs, or the doctor-patient relationship itself. Next, a common technique used in the medical community called the SPIKES protocol will be used to suggest a framework that healthcare professionals can use to approach pediatric rare disease patient visits. The SPIKES protocol stands for setting up the interview, assessing the patient’s perceptions, obtaining the patient’s invitation, addressing patient emotions with empathetic responses, and strategy and summary. The rationale for using SPIKES is to use a protocol that is already well-known in the medical community for the pediatric rare disease patient and family member population who is much less well-known. After a detailed analysis of how the SPIKES protocol can be used for pediatric rare disease medical visits, a set of resources will be presented that both healthcare professionals and the rare disease community can use to increase education, awareness, and advocacy for rare diseases. Some of these resources include the National Organization for Rare Disorders, the Boler-Parseghian Center for Rare and Neglected Diseases, Young Adult Representatives of RDLA, Developmental-Behavioral Pediatrics, Medical Genetics, and support groups. Through discussing barriers, the SPIKES model, and these resources, this capstone paper will express the needs of the pediatric rare disease community in the medical field, and make specific suggestions to address these needs
Monica Mesecar - Compassionate Care in Neurology: The Importance of Practicing Primary Neuropalliative Care

This paper will first define what neurology is, followed by a discussion of what neurologists treat. Then after emphasizing the global importance of neurological disorders, the most significant problem facing neurology will be revealed as the “diagnose and adios” mentality. This phrase refers to the approach of simply diagnosing the patient and following-up with treatment with little to no emphasis on helping the patient live well with their condition. After exploring the significance of this problem, the solution of implementing the science of compassionate care will be generally proposed. Following this section, this paper will argue that in neurology, using this approach means practicing primary neuropalliative care. Primary neuropalliative care refers to utilizing the principles and practices of palliative care in routine, daily practice in a way that is specific to patients living with long-term neurological conditions. Next, after defining neuropalliative care, this paper will discuss the unique challenges to practice posed by patients with long-term neurological conditions, followed by a practical approach to implementation. This paper will then conclude with a discussion of why practicing neuropalliative care is beneficial with an emphasis on the improvement of patient outcomes, as well as its potential to buffer against the ever-growing problem of neurologist burnout.
Christian Oakley - Systemic, Institutional, and Individual-level Factors Influencing the Adoption and Efficacy of Mindfulness-based Stress Reduction Interventions in Surgical Residents
Surgical residents experience significant emotional and logistical stressors that can increase their susceptibility to burnout and compassion fatigue. The numerous systemic, institutional, and individual-level factors influencing the adoption and the efficacy of mindfulness-based stress reduction (MBSR) interventions are unclear. Moreover, the effects of MBSR interventions on surgical residents remain uncertain. To better understand these factors and the effects of MBSR on surgical residents, a comprehensive literature search strategy was performed on PubMed and Google Scholar to find studies that 1) discussed the factors influencing the adoption and efficacy and MBSR interventions or 2) evaluated the effect of MBSR interventions on resident and physician burnout, empathy, mindfulness, stress, executive functioning, mood, or surgical performance. Multiple studies examining the factors influencing the adoption and efficacy of MBSR interventions were identified. Surgeon stoicism, expectations of emotional resilience by attendings, long work hours, and a lack of understanding of MBSR interventions were identified as systemic factors, while hospital profitability and residency administrative structures were identified as institutional factors. Leadership attitudes and individual-resident qualities were discussed as individual-level factors. The search also returned four randomized clinical trials and one single-arm cohort study examining the effects of MBSR interventions on physicians or surgical residents. Findings from these studies suggest that MBSR interventions are associated with decreased burnout and perceived stress and increased mindfulness, empathy, and mood regulation in the short and long-term. From these findings, it is clear that there are numerous systemic, institutional, and individual factors affecting MBSR intervention use and success. While studies suggest that MBSR interventions are efficacious, larger randomized controlled trials with increased statistical power are needed to better discern the effects of MBSR interventions on surgical residents.
Mairead Pfaff - Diagnosis of Chronic Illness in Pediatric Patients: Distinctions in Clinical Practices and Importance of Quality Communication from Physicians

Pediatric patients have distinct needs from adults in a clinical setting; children often require simpler explanations of medical jargon, with more analogies being used. The job of the physician is more difficult since they must cater to the patient as well as the parents or guardians present. The parents will have different types of questions from their child, and each party may expect a different style of communication from the physician. Parents of children with a chronic illness often experience a major change in lifestyle after the diagnosis of their child. The memory of the physician delivering news of the illness to the parent and child often remains clear for years following the diagnosis. These moments can be categorized as “flashbulb memories”; the parent and child’s predisposition to remember details of the diagnosis conversation makes this moment highly important for quality communication by the physician. Most research shows that parents want to be shown “empathy” or “compassion”, but few studies outline what that means for the physician in practice. Furthermore, the diagnosis of chronic illness in pediatric patients has the potential to affect the child for the rest of their life. In cases of chronic illness, as the child grows older, they will assume more responsibility for their own health. The way a pediatric patient is treated at the beginning of their journey with chronic illness can impact the way the child progresses towards taking an active role in their own care. It is important to recognize the perspectives of the child, parents, and physician during these conversations. Focusing on the diagnosis is important for the remainder of the child’s relationship with their illness. To minimize the parent and child’s trauma from the experience, the physician must be compassionate towards both parties and recognize their individual and mutual needs. Best practices to act in a compassionate manner during difficult diagnoses are not clearly outlined for pediatric physicians, and current published guidelines on communication do not delve into the complexities of distinctive disease scenarios. This research describes the importance of the specific moment of diagnosis for a pediatric patient with a chronic illness. The perspectives of the parents, the child, and the physician are explored; each party’s specific needs are outlined as they have been currently described in the literature. Recommendations are made to standardize these practices for clinicians in clinical practice. The purpose of this research is to demonstrate a need for physicians to focus on compassionate communication during the diagnosis of a child with any chronic illness.
Keegan Riggs - Burnout Disproportionately Affects the Emergency Department: Is Compassion a Solution?

Physicians experience higher rates of burnout than any other profession with a 48.5% prevalence nationwide. In the emergency department specifically, the prevalence is 68%, the highest out of any specialty (Shanafelt et al. 2012). The disproportionately high level of burnout in the ED has historically been attributed to the long hours and inconsistent schedules. However, recent data shows that despite having a higher percentage of burnout than other specialties, emergency medicine has above average satisfaction with work-life balance. So, why does burnout continue to plague emergency departments nationwide? There are factors specific to the ED beyond the tough schedule that result in the high percentage of burnout. Many specialties encounter suffering, but none in as fast-paced of an environment as the emergency department. Emergency physicians rarely have time cope with the tragedies they witness. Much of health care has become business-oriented, but no specialty has been affected by a profit-driven workplace more than the ED. Physicians are rewarded for seeing as many patients as fast as possible, frequently at the expense of establishing a strong patient-clinician relationship. These key factors, along with many others, can be detrimental to the clinician compassion mindset. There is a positive correlation between burnout and depersonalization, workplace fragmentation, and other aspects of non-compassionate health care culture. Decreasing hours, offering stress workshops, and requiring mandatory wellness training have been unsuccessful at decreasing burnout in emergency departments nationwide. Just as a band-aid cannot patch a gunshot wound, these “simple fixes” cannot rid the emergency department of the issues deeply rooted in the workplace culture. To solve the burnout crisis in the ED, health care organizations need to strive for widespread shifts towards a compassionate culture. Compassion has been studied to improve both physician well-being and patient satisfaction, but a compassionate mindset is only sustainable if shared amongst the whole organization. Hospitals will have to reorganize their departments for better collaboration, encourage development of compassionate relationships amongst colleagues, and remove the pressure to provide quick and profitable treatment. The ED can never be ridden of suffering, tragedy, and hard work, but changing the approach towards these hardships can improve outcomes for physicians, patients, and medicine as a whole.
Justin Roy - iCare: Maintaining Compassionate Care Practices in the Throes of the Digital Age
The dawn of the digital age has sparked rapid innovation throughout all sectors of society. These improvements have afforded many improvements in convenience, including in healthcare – electronic health records, faster system organization, telehealth. Yet, there are still discrepancies that present issues in maintaining compassionate care in medicine in conjunction with technological advancement. Digitalization has taken away personal and humanistic aspects of healthcare, leading patients to feel as though they are talking to a computer as opposed to interacting with their clinician, both in person and through telehealth. As a result, websites like WebMD have created a resource for patients to self-diagnose, which has formed nuances in care in which the patients try to diagnose themselves, resulting in potential differing views with experienced, knowledgeable clinicians. In addition, pushback from healthcare workers on the lack of user-friendly technology – or lack of willingness to learn – creates a further rift which hampers the efficacy of compassionate, caring attitudes and interactions that should be seen between clinicians and their patients. Medicine cannot be made convenient in ways that online shopping and streaming services are. Rather, with the ushering in of a digital age to the healthcare sphere, there becomes a glaring necessity for clinicians to evolve and adapt simultaneously as opposed to feel hindered by new technological options. Examining the scope of healthcare technology and its flaws in compassionate care allows clinicians to enhance their compassion techniques in order to mitigate the rift between patients and clinicians. First and foremost, expanding digital literacy among clinicians presents a strong foothold in bridging the gap of compassionate care through educational sessions, digital workshops, and also EMR improvements. In addition, research notes that clinicians – and patients, alike – must continue to build empathic awareness in technological media to enhance correspondence, appointment efficiency, and caring, communicative mindsets. Healthcare can facilitate these efforts by emphasizing education of the youth, who are not only the future of medicine, but also future patients and administrators as well. Roadblocks to the zone of compassionate care in medicine are perpetuated by a stagnancy in efforts and education. Thus, further research toward methods in which clinicians can create a duality of compassionate care with the evolution of technology will pilot medicine into more effective health outcomes and a healthier future.
Michael Shannon - Investigating the Role of Burnout and Compassion in Organ Donation and Transplantation

Pioneered in the mid-twentieth century by the work of Dr. Thomas Starzl and bolstered by advances in surgical technology, organ donation and transplantation have seen drastic evolution over the years. The medicine of this field is a highly integrated process and involves coordination between providers serving in several specialized roles. Working in the realm of transplantation is rife with exposure to psychological challenges. These may include caring for terminally ill patients, difficulty in procuring organs for needy recipients, and facing the ethical challenges associated with organ allocation. Broadly, the healthcare field is currently burdened by an epidemic of clinician burnout. This phenomenon is characterized by symptoms of emotional exhaustion, reduced personal accomplishment, and depersonalization. Given their unique selection of stressors, the nurses, doctors, and transplant coordinators working in organ transplantation may be at an elevated risk to succumb to burnout. To date, research on burnout in these professions suggests tangible levels of burnout and compassion fatigue. Factors that influence the prevalence of this malady include a surplus of roles and responsibilities, missed opportunities as a result of career choice, and feelings of inadequate compensation. However, research into clinical burnout has also managed to elucidate several strategies that may assist in buffering against its manifestation. Namely, the nascent science of compassion may hold many important implications for enabling clinicians to stave off burnout, maintain a healthy and balanced lifestyle, and preserve their ability to deliver optimal patient care. Methods to continually reinvigorate a compassionate mindset include mind-training techniques, meditation, and adequate leisure time for decompression. Additionally, incorporating these considerations into training for clinicians may help prepare them to retain a compassionate mindset throughout their experiences with mental and emotional taxation. Overall, more research is needed in order to determine the exact nature of burnout in this field, as well as the effectiveness of different strategies in preventing its occurrence. However, the importance of compassion is prominent, and should remain a subject of discussion in seeking to improve clinician well-being, patient outcomes, and the healthcare system as a whole.
Kelly Straub - A Case Study on Compassionate Care Manifestation in Organ Transplantation and How Treatment is Perceived by the Patient and Loved Ones

Compassion shown in health care is an emerging concept that is gaining momentum in the field. It was once thought that providers should “cut straight and care less,” but now it is apparent that caring is an important part of the healing process. Organ transplantation illustrates the significance of compassion and empathy’s impact on clinicians, patients, and loved ones. The fundamentals of organ transplantation, including ethics and biases, display how compassionate care is necessary in health care. Using the case study of a double organ transplant patient, compassion and empathy were shown to have a major impact on the patient, clinicians, and loved ones. Assessors determining who gets on the transplant list, surgeons, nurses, and PAs all uniquely demonstrate compassion to both the patient and loved ones; in return, this rejuvenates the clinician, buffers against burnout, and creates a helpful relationship with the patient. Additionally, the patient perceives the clinicians’ efforts toward him or her as either compassionate or uncompassionate. Patients also exemplify compassion towards physicians using techniques to build relationships, thus helping the clinician treat the patient more holistically. Finally, loved ones also perceive a clinician’s responses to the patient’s pain as well as employ their own techniques to show compassion towards their sick loved one. As compassionate care continues to permeate into the health care culture, it is important for clinicians to learn and become aware of compassion’s influence in order to use its benefits both to optimally treat a patient and maintain a patient-centered mindset.
Tanner Tarkelson - Managerial Changes in Emergency Medicine to Improve the Patient and Clinician Experiences
The science of compassion is a new and rapidly expanding field of study. Within a healthcare setting, implementing the suggestions that come from this research can have implications for health outcomes, administrative organization, finances, etc. While the science of compassion is often seen as a “soft subject”, there exists plentiful hard evidence for the benefits that empathetic resonance followed by action to relieve suffering (a shortened definition of compassion) can have. Emergency medicine is one of the most difficult sectors of healthcare to manage. This struggle arises from the division’s fast-paced nature, variety in patient conditions, and consistent need to be prepared for crisis. With these facets in mind, the patient and clinician experiences are an aspect of emergency medicine that is oftentimes overlooked. However, the specific administrative changes within the emergency department needed to create an environment of compassion and improve the patient and clinician experiences have not yet been succinctly organized. Here, suggestions are made to emergency department administrations in order to improve their patient and clinician experiences. Namely, the suggestions made to improve the patient experience (the first part of this thesis) include (1) creating a more compassionate environment for healthcare professionals and patients, (2) improving upon teaching styles and techniques, and (3) reducing the language barriers that are so common in the emergency department. Suggestions made to improve the clinician experience (the second part of this thesis) include (1) molding the facility’s mission around compassion, (2) encouraging emotion regulation techniques, and (3) utilizing team-based care. The results demonstrate the practicality of implementing the suggestions generated from a study of the science of compassion. It is anticipated that this thesis will provide a groundwork for emergency department administrations to use in terms of improving the experience, and consequently health and financial outcomes, of everyone within their facility. This thesis is additionally one of the first to analyze the tri-layer network between patients, clinicians, and administrators within the emergency department. Further work is necessary to fully examine the intricacies of such relationships and to create solutions to reduce the friction between them.
Olivia Venvertloh - Presence Amidst Emotional, Physical, and Structural Problems: A Case Study in the Compassionate Mindset of Elderly Caregiving

As the baby boomer generation ages and the fertility rate declines, the number of people dependent on caregivers will only continue to rise in the coming years. The United Nations reports that one in six people will be over the age of 65 by 2050. The healthcare system, already strained by a global pandemic, a shortage of healthcare workers and clinician burnout, will continue to be impacted as more elderly need assistance in long-term care facilities. The only way out of this predicament is training healthcare workers in the compassion mindset, which applies compassion to all stages of patient interactions. By maintaining an inner motivation to care for others and mitigating organizational challenges faced at work, resilient elderly caregivers who utilize the compassion mindset will become an example for other caregivers. This paper will explore the compassion mindset through a series of interviews conducted with an elderly healthcare professional as a part of an IRB-approved study investigating mental performance in high stress specialties. Dedication to providing top quality care through physical, emotional, and spiritual presence while implementing the compassion mindset is a powerful example for future caregivers navigating systemic difficulties.

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
1. Pre-Planning for Your Capstone Project
Learning Objectives
By the end of this chapter, you will be able to:
- Explain the capstone experience.
- Identify soft skills that can be developed/refined throughout the capstone experience.
- Describe the importance of capstone projects for academic and professional career development.
- Identify at least two steps you can take to pre-plan/prepare for your capstone project.
This chapter will guide you through the pre-planning phase of your capstone experience. Examples of capstone formats utilized by various schools and universities are included in this chapter. General educational goals of capstone projects are reviewed and the importance of a capstone experience for academic and professional career advancement is discussed. Strategies that can help you prepare for your capstone experience are explained.
Introduction
The amount of stress that accumulates over the course of one’s college experience can be overwhelming. Understanding what a capstone project entails and using strategies and skills that have been acquired throughout your academic career, will help you pre-plan for relevant and meaningful capstone experiences, while reducing stress.
What Exactly Is a Capstone Project?
A capstone project is a multifaceted assignment for professional students that serves as a culminating academic and intellectual experience. Therefore, capstone projects can also be referred to as capstone
experiences, culminating projects, or senior exhibitions. Capstone projects usually occur in the final year of professional academic programs and they may or may not be research based. Constructed by your school, your professional program within your school or university, and learning experience, capstone projects can take a variety of forms (Refer to Table 1-1: Examples of Capstone Project Formats). While capstone projects are in some ways like a college thesis, capstone projects are typically long-term investigative projects that culminate into a final product, presentation, and/or performance (Sabbot, 2016).
Table 1-1: Examples of Capstone Project Formats
Source: Moore, J. L. (2021, December 2). Capstone experiences . Center for Engaged Learning. Retrieved July 15, 2022, from https://www.centerforengagedlearning.org/resources/capstone-experiences/
Within health professions, the clinical doctorate has been traditionally driven by innovation in practice and the advancement and evolution of the health profession’s field. Furthermore, clinical doctorate degrees are meant to provide graduates with the skills necessary to engage in direct clinical practice and leadership endeavors, which may influence healthcare program development and policy changes. Simply, doctoral capstones provide accomplished students with an opportunity for in-depth professional practice within an area of focus (Kemp, Domina, Delbert, Rivera & Navarro-Walker, 2020).
Capstone projects have long been a hallmark of professional education. Capstone projects aim to help you recognize your own growth and development during your scholarly pursuits. Capstone projects are also an effective method of showcasing attained and refined skills and competencies (Moore, 2021). Furthermore, capstone projects are designed to encourage you to think critically, solve challenging problems, and showcase hard and unique soft skills. (Refer to Table 1-2: Examples of Hard Skills and Soft Skills for Clinical Professionals and Professional Students)
Table 1-2 : Examples of Hard Skills and Soft Skills for Clinical Professionals and Professional Students
Sources: Benz, C., Johns, S., & Team, the R. G. (2022, February 18). What are hard skills? definition & 51 hard skills examples. Resume Genius. Retrieved July 16, 2022, from https://resumegenius.com/blog/resume-help/hard-skills; Coombe, T. (2021, February 25). Soft & Hard Skills for occupational therapy students: How to get them. EduMed. Retrieved July 16, 2022, from https://www.edumed.org/online-schools/occupational-therapy programs/studentskills/; and Kohler, C. (2021, December 17). What are soft skills? here’s how to showcase them on your resume . TopResume. Retrieved July 16, 2022, from https://www.topresume.com/career-advice/soft-skills-and-how-to-showcase-them-on-resume.
Educational Goals for Capstone Projects
Capstone experiences within some schools and universities are designed to provide students with opportunities to become engaged in some aspect of clinical practice. Consequently, educational institutions will typically have their own capstone-specific goals. Even within a single school or university, the range of capstone-related goals and expectations can differ from program to program. For these reasons, it is important to review your specific program’s capstone project requirements and capstone syllabi. By recognizing the general educational goals of capstone projects, you will acquire a better understanding of the capstone process and how it can be used for professional development not only throughout but beyond your academic career (Sabbot, 2016). (Refer to Table 1-3: General Educational Goals of Capstone Projects).
Table 1-3: General Educational Goals of Capstone Projects
Source: Moore, J. L. (2021, December 2). Capstone experiences . Center for Engaged Learning. Retrieved July 15, 2022, from https://www.centerforengagedlearning.org/resources/capstone-experiences/.
Importance of Capstone Projects
Clinical doctoral programs are rigorous and demanding practice-focused programs that are designed to prepare students to become experts in clinical practice settings. In this vein, capstone projects are heavily focused on innovative and evidence-based practices that not only reflect your ability to transfer didactic knowledge and research findings into a practice setting but to also evaluate and disseminate new knowledge to advance evidence-based care (Anderson, Knestrick & Barroso, 2015). For example, in a school or university students are continually working on theoretical assignments, which allows them to acquire basic knowledge that supports their career path. However, the capstone project extends beyond textbooks and classrooms as you begin to become immersed in real-world cases in real-life environments. Capstone projects can help you to become familiar with some of the issues professionals in your chosen area of study and/or interest may commonly face in the field. Consequently, the experiential learning you will gain from your capstone experience is invaluable in relation to your entry into, and advancement in, your respective profession (Russel, 2022).
Capstone projects are considered scholarly pieces of work. The intent of capstone projects is to create an effective and comprehensive product that will provide you with an opportunity to showcase your academic abilities, skills, and competencies. In this fashion, capstone projects can be viewed as a springboard for career advancement or an entrepreneurial venture. By taking a few steps to understand and prepare for your capstone experience, you will be able to effectively integrate learned knowledge into a real-world issue in a manner that is purposeful, meaningful, and marketable (Refer to Table 1.4: Preplanning Strategies Students Can Use for Meaningful Capstone Experiences).
Table 1.4: Preplanning Strategies Students Can Use for Meaningful Capstone Experiences
Understanding what a capstone project is and why it is an important component of academic and professional development will help you appreciate your capstone experience and maybe even enjoy it. This chapter provided you with tips and strategies that will help you preplan for your capstone project. The development of a meaningful and robust capstone experience requires a demonstration of need coupled with a professional area of interest (Bednarski, Bell & DeAngelis, 2020). Preplanning can help ensure that your capstone project is relevant and impactful.
Case Study: Examples
Glynn is an occupational therapist, who currently works in a physical disability rehabilitation setting. Glynn is currently participating in a post-professional occupational therapy doctorate (OTD) program in an urban university setting. According to Glynn’s OTD program, she will begin her capstone courses next semester. In order for Glynn to prepare for their upcoming capstone experience, they will do the following:
- Review their resume and update it, as necessary
- Update their biographical information
- Review the educational goals of capstone projects within their program of study (OTD)
- Review the format of capstone projects within their program of study (OTD)
- Self-reflect on their professional career and consider topics of interest that could be potential capstone projects
- Glynn is taking an OTD course, which addresses health literacy initiatives for low-health literate patients. Glynn is very intrigued with this topic and is considering this topic for their capstone project.
Optimizing Your Capstone Experience: A Guidebook for Allied Health Professionals Copyright © 2023 by Virginia E. Koenig is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book
MMHC Capstone Strategy Project
The Capstone Project engages teams of students on projects of significant importance to their organizations. The student team is responsible for diagnosing the critical problem, defining an appropriate scope of work, managing institutional expectations, and producing a suitable recommendation in both written and presentation form.
Your Capstone Team
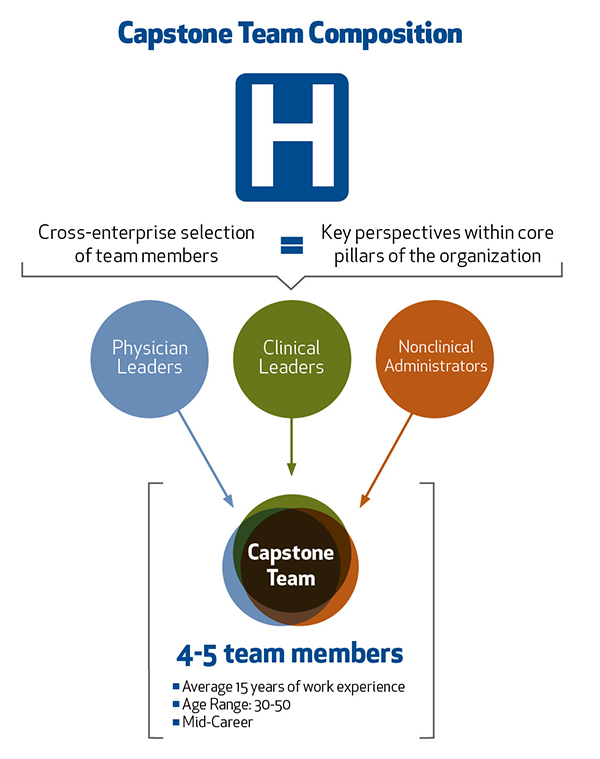
It takes many managers, healthcare practitioners and other executives to care for a patient and to manage a healthcare organization. Having the skills to manage a team, evaluate critical problems, and execute solutions is required to be an effective business leader. This is why your Capstone Team will be comprised of a cross-functional group of 4-5 executives, each with a diverse set of backgrounds and industry experiences, giving you an experience that emulates the work environment of a healthcare delivery organization. Support includes coaching on team dynamics and the progress of your work together, checkpoints to ensure you’re on track, and guidance for projects that serve as a real-world learning lab.
The Project
The Capstone Strategy Project complements the classroom instruction and is defined as learning by construction. It is a total immersion experience in which students are challenged to use all of the tools and concepts learned to date to tackle a current business problem for a healthcare organization.
With faculty oversight, you demonstrate rigorous application of business concepts and disciplines. Leading a project of utmost importance for your organization provides immediate impact that benefits the student and the sponsoring organization.
Your team will kick off the Capstone Strategy Project in Mod 3 by meeting with the client sponsor to outline and discuss the initiative at hand. Your team will spend the next six months working on all aspects of the project, including:

As the class makeup represents a very diverse talent pool within a healthcare organization, it promotes working outside of our comfort zones and valuing the skills and experiences of others. There is no doubt that the biggest thing I will miss after graduation is the weekly (and often several times weekly depending on team project deadlines) camaraderie experienced by the class. Gaelyn Garrett MMHC 2015
The Benefits For You
For the students, the Capstone Strategy Projects are opportunities to exhibit the healthcare business management knowledge you’ve acquired. You will demonstrate, to yourself and your organization, your ability to problem-solve creatively, make strategic decisions, and manage as part of a high-level executive team. Learn More .
The Benefits for Your Organization
For an organization, the Capstone Strategy Projects is an opportunity to have a team of experienced mid-level health care professionals conduct an intense engagement to address a current business need. Learn More .
See how MMHC students' capstone helped improve Emergency Department wait times and efficiency at VUMC.
How MMHC benefits your organization
A closer look at the program through the eyes of students, faculty and sponsoring organizations
Critical Challenge Project
- Master's in Healthcare Leadership
Take the Next Step
Address real-time challenges with applied learning that draws upon your interests and experience..
The Critical Challenge Project (CCP) is central to the learning experience and will become the focus of an independent study. You will identify a challenge related to your field and interests, drawing from your own experience and vision for the future. Each student works collaboratively with their peers, professional colleagues, course faculty, and advisors, integrating various perspectives across healthcare sectors into the project.
The CCP allows you to address problems in real-time and apply the knowledge and skills learned throughout the program, with emphasis on integrating healthcare, business and policy factors, and collaborating across healthcare sectors. Projects should consider ethical implications and have practical applicability to the field of healthcare — taking into account multiple stakeholders and cross-sector perspectives as you develop innovative and viable solutions.
Key principles students use to define their CCPs include:
- Relevant: Meaningful to the student in terms of background, interests, current job, future aspirations, and/or organization
- Consequential: Project is broad enough scope to have an impact on stakeholders across the healthcare industry, including patients, providers, and payers
- Realistic: Feasible and viable set of steps and expectations within the 12-month program (the overarching challenge does not need to be resolved within the program, but measurable progress toward the defined CCP must be reasonable and appropriate)
- Measurable: Contains measurable outcomes of success
Soof Solutions Inc: Giving a Voice to the Speechless
Through the Critical Challenge Project, Dr. Maheen Mausoof Adamson turned her medical technology idea into a healthcare company devoted to providing a happier life to older adults, like her father, by giving them a voice.
Recent Capstone Projects
Sample Project Titles
- The Use of Telemedicine to Increase Access to Healthcare for the Residents of the Bahamas Out-Islands
- Utilizing Critical Access Hospital Infrastructure to Provide Opioid Use Disorder Services to Rural Communities
- A Proposed Alternative Care Model to Reduce Unnecessary Emergency Department Utilization in an Elderly Medicare Advantage Population
- Homelessness and Stabilization Unit Stays: Analyzing Current Discharge Planning Processes
View Critical Challenge Project Examples Download More Information
Thesis and Capstone Requirements for Public Health Programs
Most graduate programs in public health include a thesis or capstone project, which students usually undertake after completing other coursework. While completing these projects, students must apply knowledge and skills gained throughout the program. The thesis or capstone tests the student’s ability to make a unique contribution to their field while demonstrating mastery of the subject.
These culminating projects reflect the kind of work students will do during the course of their careers.
These culminating projects reflect the kind of work students will do during the course of their careers. Public health students may complete an academic article or a detailed plan for dealing with the outbreak of a disease. Some projects involve working alongside professionals in the field, while others require significant research in archives and libraries. The completed thesis or capstone project demonstrates the student’s ability to perform duties within the public health field.
What’s the Difference Between a Capstone and a Thesis in Public Health Programs?
A thesis is an academic article that presents an argument or research findings. Common in graduate programs, thesis projects are often by an adviser or other faculty member. Capstone projects take various forms and, although more common in undergraduate studies, may be a requirement of master’s programs. Capstones are often research projects presented in a non-article format and involve hands-on experience.
What Is a Capstone Like in Public Health Programs?
Public health capstone format.
Capstones are typically independent projects, which students undertake toward the end of their program.
Capstones can take a variety of forms, but they generally consist of written and oral portions. The written portion could be a short article or a summary of findings, while the oral portion may involve a presentation at a conference. Capstones are typically independent projects, which students undertake toward the end of their program. A capstone may last one or two terms. Some programs allow students to choose project topics and begin research early.
Choosing Your Public Health Capstone Topic
Typically, students choose a capstone topic relevant to their specializations and career interests, which one or more faculty members must approve. Capstone projects are an opportunity to build connections with public health professionals. Capstone topics often address contemporary problems in the field, and individual programs or faculty may provide a selection of topics from which students must choose. Some programs pair students with faculty advisers.
Completing Your Public Health Capstone
Regardless of the capstone format, a few aspects are generally the same. Students first choose a topic or research question on which to base the project. Learners may conduct research to determine the limits of the project or may simply complete an outline. Before beginning on a capstone project, one or more faculty members must approve the student’s topic; the faculty member may be the student’s adviser or the professor of the capstone course. After receiving approval, the student can begin further research, project development, and execution of the capstone. Methods and resources vary based on the student’s field, subfield, and specialization.
Presenting Your Public Health Capstone
Presentation circumstances vary by program, but students generally present their capstone to a panel of three to five faculty members. These presentations are often open to the public and may include an opportunity for audience members to ask the student questions. Though visual aids such as slideshows and videos are common, the project’s subject and format guides presentation methods.
How Is a Public Health Capstone Graded?
While students may receive a rubric, master’s-level capstone projects rarely receive letter grades. These projects are typically pass or fail, though some students may pass with distinction. While it is possible to fail a capstone, students rarely fail a capstone they have completed and presented; advisers ensure the project is of passing quality.

What Is a Thesis Like in Public Health Programs?
Public health thesis format.
A thesis is an individual project, typically a piece of academic writing based on research, sometimes involving experimentation.
A thesis is an individual project, typically a piece of academic writing based on research, sometimes involving experimentation. A faculty adviser generally oversees the student’s completion of their thesis project. Some programs require students to present their thesis. The amount of time allotted to complete a thesis project varies by program and depends largely on how early the student may submit a topic for approval. Many programs require students to enroll in a thesis course, or courses, which allows the program to award credit for the project and provides a specific time for students to meet with advisers and complete thesis work.
Choosing Your Public Health Thesis Topic
While completing their thesis project, students typically work with a faculty member who approves their topic, suggests sources or methods, and helps guide the student through the research and writing processes. Though some programs specify certain topics or stipulate that students address a current issue, students generally have the final say regarding their thesis topic. The main requirement of thesis topics in public health is that they contribute to the field.
Completing Your Public Health Thesis
The first step to writing a master’s of public health thesis is choosing an approved topic. Students must then research and write about that topic. Students must typically obtain approval early in the process and must usually check in with advisers regularly as they progress. The format of the thesis project varies by field and school. Learners typically submit their thesis to advisers, who suggest changes and additions before the student submits the thesis to the school for digital or physical publication and inclusion in the school’s library or archives.
Presenting Your Public Health Thesis
A thesis presentation often involves questions from a panel of advisers and other faculty. These questions should help clarify and further define aspects of the thesis. While a presentation may include a slideshow or other aids, the focus of the presentation should be on replying to the panel’s concerns, rather than presenting new information. Most thesis presentations are open to the public, and audience members are usually allowed or encouraged to ask questions, though they may not have read the thesis itself. Students typically present after submitting their thesis to advisers but before finalizing the project and submitting it to the school.
How Is a Public Health Thesis Graded?
Most programs grade thesis papers pass or fail. A thesis is the culmination of a student’s education and is designed to be a challenging but ultimately successful process. A good adviser works directly with the student to ensure the final version of the student’s thesis is passing quality.
Take the next step toward your future with online learning.
Discover schools with the programs and courses you’re interested in, and start learning today.

Program Capstone for the Master's in Health Informatics, Northwestern University School of Professional Studies - Northwestern School of Professional Studies
- Post-baccalaureate
- Undergraduate
- Professional Development
- Pre-College
- Center for Public Safety
- Get Information

Health Informatics Capstone
Health Informatics
What is the Capstone project?
As a culminating experience , each student will independently put into practice the knowledge and skills they learned during their coursework through a Capstone Project.
Students will have the opportunity to develop and implement a Health Informatics project in their workplace or other academic / industry organizations . The project will challenge each student to conduct research and apply knowledge, skills and competencies built through coursework completed in the MHI program.
If students are unable to find a real-world project, they can alternatively develop a culminating, two-part project, that will leverage health informatics to provide a solution to a need or problem arising as part of a case study. Note: Finding a real-world project would be preferred over working on a case study.
Each student will work with the course instructor to identify a “Knowledge Expert” for their capstone project along with a faculty advisor from the Northwestern University Health Informatics program.
What can students expect during the MHI Capstone course?
A challenging but rewarding experience that would prepare or enhance their professional skills in the field of Health Informatics. There will be a focus on more career and real-world experiences than the other courses in the MHI program. The Capstone course is more about the hands-on (or applied experiences) in the world of Health Informatics. Depending on the complexity of your project, you can expect to spend 5 to 10 hours a week, or 50 to 100 hours during the quarter working on your project.
With whom can you do a capstone project ?
Your Employer / Workplace: You may work on a discrete project from your workplace for your capstone project. This will need to be above and beyond your day-to-day job responsibilities. You will need to identify a Knowledge Expert / Mentor at your organization to support you during the project.
“Sponsor” organization projects : You may partner with an external organization in the industry who may be interested in sponsoring a capstone project. There may be opportunities available through Northwestern University or you will need to find one on your own.
Academic Partners: You may work with a MHI Faculty member, or with other academic partners at Northwestern University (such as Feinberg School of Medicine or Northwestern Memorial Hospital), or other academic institutions to work on an informatics or research based capstone project.
Capstone Project Cases : Alternatively, if you are unable to find a real-world project, you may choose to work on one of the capstone project cases made available through the course.
What is the Capstone Course timeline?
The MHI Capstone Course can only be done in the last quarter of the MHI program prior to your graduation. Like the other courses in the program, you will have 10 weeks to complete your capstone project. Due to this aggressive timeline in the quarter, we will divide your capstone project in the following phases:
- Capstone Identification and Proposal: 1-2 weeks
- Capstone Implementation: 5-7 weeks
- Capstone Paper and Presentation: 1-2 weeks
How to Prepare for the Capstone
Capstone pre-work: complete prior to starting the capstone course.
- Reflect on your career goals. What do you want to do after you graduate from the MHI program? There is no right or wrong answer to this. If you have not yet thought about it, this exercise should help you get started.
- Prepare your CV / Resume that includes your most up to date professional and academic experiences (including the MHI program) prior to the start of the MHI Capstone Course.
- Start thinking about capstone project ideas that ideally align with your career goals.
- Do you already have a “sponsor” or organization in mind to do your capstone with?
- If you are currently working in the healthcare industry, explore possible capstone project opportunities with your employer that would be above and beyond your day-to-day job responsibilities. I would also encourage you to reach out to any relevant contacts in your professional network to find a capstone project opportunity, if needed.
- Some “sponsors” or organizations will work with you in a virtual environment, while others may prefer an in-person or hybrid model.
- If you have already selected a project for your capstone, then complete any onboarding work such as contracting, drug tests, training, IRB approvals, etc. as soon as possible so that you can start working on your project implementation during the capstone course.
Capstone Advising Sessions
This Capstone course has been overwhelmingly successful with respect to the student experience based on feedback. The only critique of Capstone is the timeframe – students feel that one quarter to complete the project limits the potential for projects.
In order to address the time constraint of a single quarter, students will be given the opportunity to meet with their capstone instructor during pre-capstone advising sessions in the quarter prior to their capstone. This will allow students to navigate the pre-work with the support of their instructor, allowing for more time to connect with potential partners for their proposed project leading to a more time fulfilling project experience.
Students approaching their final quarter will be contacted to set up an appointment with the capstone instructor during the quarter prior to the capstone.
The MHI Capstone Experience
Student reflections.
MHI faculty member Imran Khan interviewed two of his graduating students, Regina Schwind and Angela Mazzari, to discuss their experiences in the MHI program and their respective Capstone projects.
Recent Capstone Project Topics
- Reducing Infant and Maternal Mortality Rates in the Black Populations of Athens, GA
- Population Health Provider and Patient Engagement Strategy
- Scalable Monitoring System to Address Emergency Care Usage among Patients with Multiple Chronic Conditions
- Improving Anticoagulation Safety & Drug Compliance (of cardiac patients) through a Remote Monitoring System
- WordGlass: Technology to Provide Live Closed Captioning for the Hearing- Impaired in the Health Care Setting
- Hand Hygiene Audit Tool
- Adoption of an Electronic Lab Notebook in a WSU Research Lab
- Digital Health Solutions for a Rural Healthcare System
- A Comprehensive Solution to Improving Diabetic Outcomes and Improved Shared- Savings Returns by Achieving the Together to Goal Program Metrics
- Hierarchical Condition Category Risk Adjustment Documentation in Epic
- Clinical Decision Support System for the Prenatal Care of Obese Patients at a Family Practice Residency Clinic
- Engaging High-Need Patients to Produce Scalable High-Value Health Care
- A Care Management Dashboard for Population Stratification using Johns Hopkins ACG System in the Enterprise Data Warehouse

Biomedical Graduate Education
Capstone Projects
2022-2023 graduates, nelson moore.
Data Scientist at Essential Software Inc
Capstone Project: Modeling and code implementation to support data search and filter through the NCI Cancer Data Aggregator Industry Mentor: Frederick National Lab for Cancer Research: FNLCR
Joelle Fitzgerald
Business Analyst at Ascension Health Care
Capstone Project: Analysis of patient safety event reports data. Industry Mentor: MedStar Health. National Center for Human Factors in Healthcare
Kader (Abdelkader) Bouregag
Healthcare Xplorer | Medical Informatics at Genentech (internship)
Capstone Project: Transforming the Immuno-Oncology data to the OMOP CDM Industry Mentor: MSKCC/ MedStar/ Georgetown University/ Hackensack
Junaid Imam
Data Scientist at Medstar Institute
Capstone Project: Create an [trans-] eQTL visualization tool
Industry Mentor: Pfizer Inc / Harvard
Abbie Gillen
Staff Data Analyst at Nice Healthcare
Capstone Project: Nice Healthcare: Predicting Nice healthcare utilization
Industry Mentor: Nice Healthcare
Capstone Project: Next Generation Data Commons
Industry Mentor: ICF International
2021-2022 Graduates
Ahson saiyed.
NLP Engineer/Data Scientist at TrinetX
Capstone Project : Research Data Platform Pipelines Industry Mentor: Invitae
Walid Nashashibi
Data Scientist at FEMA
Capstone Project: Xenopus RNA-Seq Analysis to Understand Tissue Regeneration Mechanisms Industry Mentor: FDA
Tony Albini
Data Analyst at ClearView Healthcare Partners
Capstone project: Data Mining to understand the patient landscape of Chronic Kidney Disease Population Industry Mentor: AstraZeneca
Anvitha Gooty Agraharam
Business Account Manager at GeneData
Capstone Project: Computational estimation of Pleiotropy in Genome-Phenome Associations for target discovery Industry Mentor: AstraZeneca
Natalie Cortopassi
Researcher at the Institute for Health Metrics and Evaluation
Capstone project: Analysis of Clinical Trial Attrition in Neuropsychiatric Clinical Trials using Machine Learning Industry Mentor: AstraZeneca
Christle Iroezi
Business System Analyst at Centene Corporation
Capstone project: Visualize Digital HealthCare ROI Industry Mentor: MedStar Health
R & D Analyst II at GEICO
Capstone project: Heat Waves and Health Outcomes Industry Mentor: ICF
Research Specialist at Georgetown University
Capstone project: Mental Health Data Commons Industry Mentor: ICF
2020-2021 Graduates
Technology Transformation Analyst, Grant Thornton LLP
Capstone Project: Research Data Platform Pipelines Industry Mentor: Invitae
Research Technician at Georgetown University
Capstone Project: Using a configurable, open-source framework to create a fully functional data commons with the REMBRANDT dataset Industry Mentor: Frederick National Lab for Cancer Research – FNLCR
Consultant at Deloitte
Capstone Project: Building a patient centric data warehouse Industry Mentor: Invitae
Marcio Rosas
Project Manager of Technology and Informatics at Georgetown University
Capstone Project: Knowledge-Based Predictive Modeling of Clinical Trials Enrollment Rates Industry Mentor : AstraZeneca
Yuezheng (Kerry) He
Data Product Associate at YipitData
Capstone Project: ClinicalTrials2Vec – Accelerating trial-level computing using a vectorized model of clinical trial summaries and results Industry Mentor: AstraZeneca
Data Programmer at Chemonics International
Capstone Project: Multi-scale modeling to enable data-driven biomarker and target discovery Industry Mentor: AstraZeneca
2019-2020 Graduates
Pratyush tandale.
Informatics Specialist I at Mayo Clinic
Capstone Project: Improving clinical mapping process for lab data using LOINC Industry Mentor: Flatiron Roche
Shabeeb Kannattikuni
Senior Statistical Programmer at PRA Health Sciences (ICON Pl)
Capstone Project: NGS Data Analysis for the QA of viral vaccines Industry Mentor: Argentys Informatics
Fuyuan Wang (Bruce)
Software Engineer at Essential Software Inc , Frederick National Labs
Capstone Project: Cancer Data Model Visualization framework Industry Mentor: Frederick National Laboratory for Cancer Research
Ayah Elshikh
Capstone Project: NGS Data Analysis for the QA of viral vaccines
Industry Mentor: Argentys Informatics
Yue (Lilian) Li
Biostatistician and Statistical Programmer , Baim Institute for Clinical Research
Capstone Project: Analysis of COVID-19 Serological test data to improve the COVID-19 Detection capabalities Industry Mentor: Argentys Informatics
Algorithm Performance Engineer at Optovue
Capstone Project: Socioeconomic factors to readmissions after major cancer surgery Industry Mentor: Medstar Health
Jiazhong Zhang
Management Trainee at China Bohai Bank
Jianyi Zhang

Top 27+ Most Interesting Nursing Capstone Project Ideas
Nursing capstone project ideas are a culmination of your academic field. It allows you to showcase your knowledge, skills, and passion in the field of nursing. These nursing capstone projects provide students with an opportunity to address real-world healthcare issues, make a positive impact, and demonstrate their readiness for the profession.
In this blog, we will explore 27+ intriguing nursing capstone project ideas , covering various fields within the nursing profession.
What Is the Nursing Capstone Project
Table of Contents
A nursing capstone project is a comprehensive, culminating academic assignment or project that serves as a capstone to a nursing student’s education. It is typically undertaken in the final year of a nursing program, such as a Bachelor of Science in Nursing (BSN) or a Master of Science in Nursing (MSN), and is designed to demonstrate the student’s knowledge, skills, and readiness for professional nursing practice.
Basic Characteristics Nursing Capstone Project
These are the major characteristics of nursing capstone project ideas.

- Integration of Knowledge: The project brings together the knowledge and skills acquired throughout the nursing program. It often involves the application of nursing theory, clinical experiences, research, etc.
- Real-World Relevance: Capstone projects are usually grounded in real-world healthcare settings. Students work on problems or topics.
- Interdisciplinary Collaboration: Depending on the project’s scope, students may collaborate with other healthcare professionals, such as physicians, social workers, or pharmacists.
- Research Component: Many nursing capstone projects involve research, data collection, analysis, and evidence-based practice. Students may conduct literature reviews, and design and implement studies.
- Innovative Solutions: Nursing capstone projects often require students to propose innovative solutions, interventions, or improvements to address healthcare issues.
27+ Most Interesting Nursing Capstone Project Ideas
Following are the good nursing capstone project ideas for students. it is such as;
Medical-Surgical Nursing Capstone Projects
- Pressure Ulcer Prevention : Develop strategies and protocols to reduce pressure ulcers in hospitalized patients.
- Medication Error Reduction : Investigate methods to minimize medication errors in healthcare settings.
- Postoperative Pain Management : Analyze and improve postoperative pain management protocols for better patient outcomes.
Pediatric Nursing Capstone Project Ideas
- Childhood Obesity Intervention : Design programs to combat childhood obesity and promote healthier lifestyles.
- Immunization Campaigns : Develop strategies to increase childhood immunization rates in underprivileged communities.
- Pediatric Palliative Care : Enhance palliative care services for pediatric patients with life-limiting illnesses.
Maternal Health Nursing
- Teenage Pregnancy Prevention : Create educational programs aimed at reducing teenage pregnancy rates.
- Maternal Mental Health : Explore ways to improve screening and support for maternal mental health.
- Postpartum Hemorrhage Management : Develop protocols for the early detection and management of postpartum hemorrhage.
Nursing Capstone Project Ideas For Mental Health
- Mental Health Stigma Reduction : Design campaigns to reduce stigma associated with mental health conditions.
- Telepsychiatry Implementation : Investigate the effectiveness of telepsychiatry in providing mental health services.
- Therapeutic Art and Music : Assess the impact of art and music therapy on mental health patients.
- Health Education for Underserved Communities : Create programs to educate and empower underserved populations.
- Community-Based Diabetes Management : Develop strategies for managing diabetes in community settings.
- Homelessness and Healthcare : Explore ways to improve healthcare access for homeless individuals.
Geriatric Nursing Capstone Project Ideas
- Fall Prevention in Elderly : Implement fall prevention programs in nursing homes and assisted living facilities.
- Cognitive Impairment Care : Develop care plans for patients with Alzheimer’s and other cognitive impairments.
- End-of-Life Care in Geriatrics : Improve end-of-life care for elderly patients in long-term care facilities.
Good Pediatric Intensive Care Nursing Projects
- Neonatal Intensive Care Unit (NICU) Protocols : Create protocols for neonatal care in the NICU.
- Pediatric Trauma Care : Analyze and improve trauma care for pediatric patients.
- Pediatric Cardiac Care : Enhance care for children with congenital heart conditions.
Good Public Health Nursing Capstone projects
- Pandemic Preparedness : Develop strategies for better preparedness in response to future pandemics.
- Tobacco Cessation Programs : Implement smoking cessation programs in the community.
- School Health Promotion : Improve health promotion in schools, focusing on nutrition and physical activity.
Emergency Nursing Capstone Project Ideas
- Emergency Response Protocols : Evaluate and update emergency response protocols in hospitals.
- Disaster Preparedness : Develop disaster preparedness plans for healthcare facilities.
- Trauma Triage Guidelines : Improve triage guidelines for trauma patients in the emergency department.
Nursing Informatics
- Electronic Health Record Optimization : Optimize EHR systems for better patient care and data management.
- Telemedicine Integration : Explore the integration of telemedicine technologies into healthcare settings.
- Big Data in Nursing : Analyze the potential of big data in nursing research and practice.
Nursing Capstone Project Ideas In Education
- Simulation-Based Training : Evaluate the effectiveness of simulation-based training for nursing students.
- Curriculum Development : Design a nursing curriculum that aligns with current healthcare trends.
- Mentorship Programs : Create mentorship programs for nursing students to enhance their clinical skills.
Nursing Leadership
- Nursing Leadership Development : Develop leadership training programs for aspiring nurse leaders.
- Patient-Centered Care Initiatives : Implement initiatives to promote patient-centered care in healthcare organizations.
- Nurse Staffing Models : Analyze and improve nurse staffing models for better patient care.
Holistic Nursing
- Yoga and Meditation in Nursing : Study the benefits of yoga and meditation in promoting holistic nursing care.
- Complementary Therapies : Explore the integration of complementary therapies into nursing practice.
- Mindfulness-Based Stress Reduction : Assess the impact of mindfulness-based stress reduction programs for nurses.
Ethical Nursing Capstone Project Ideas
- Ethical Dilemmas in Nursing : Analyze and propose solutions for common ethical dilemmas in nursing.
- Cultural Competence Training : Develop cultural competence training for nurses to provide culturally sensitive care.
- End-of-Life Decision-Making : Explore end-of-life decision-making and advance care planning in nursing.
Nursing Capstone Project Ideas In Research
- Evidence-Based Practice Implementation : Promote evidence-based practice in healthcare settings.
- Nursing Research on Quality Improvement : Conduct research on quality improvement in nursing care.
- Patient Outcomes Research : Investigate the impact of nursing interventions on patient outcomes.
How To Choose A Good Nursing Capstone Project Ideas
Here are some steps and considerations to help you select a strong and meaningful nursing capstone project idea:
1. Identify Your Interests and Passions
Start by reflecting on your personal interests within the field of nursing. What topics or areas of nursing do you find most engaging and motivating? Passion for your project can drive your commitment and enthusiasm throughout the process.
2. Consider Clinical Experience
Reflect on your clinical experiences and rotations during your nursing program. Is there a particular patient population, healthcare issue, or clinical setting that left a lasting impression on you? These experiences can provide valuable inspiration for your capstone project.
3. Assess Current Healthcare Needs
Look at the healthcare landscape in your region or the world. Are there pressing healthcare issues, challenges, or gaps in care that you’re passionate about addressing? A capstone project that aligns with current healthcare needs can be impactful and relevant.
4. Review the Literature
Conduct a literature review to explore existing research and knowledge gaps in nursing. This can help you identify areas where additional research or intervention is needed. Look for recent studies and emerging trends.
5. Consult with Faculty and Preceptors
Seek guidance from your nursing faculty members or preceptors. They can offer insights into potential project ideas, recommend relevant literature, and provide valuable feedback on the feasibility of your proposed project.
6. Brainstorm and Narrow Down Ideas
Generate a list of potential project ideas and concepts based on your interests and research. Brainstorm a variety of possibilities before narrowing down your choices. Consider the scope, complexity, and feasibility of each idea.
7. Consider Resources and Access
Assess the availability of resources, data, and access to the population or setting relevant to your project. Ensure that you have the necessary support and infrastructure to carry out your project successfully.
8. Set Clear Goals and Objectives
Define clear and specific goals and objectives for your capstone project. What do you aim to achieve with your project, and what outcomes do you expect? Having well-defined objectives will guide your project’s development.
9. Think About Impact and Sustainability
Consider the potential impact of your project on patient care, nursing practice, or healthcare systems. Additionally, think about the sustainability of your project beyond the capstone course. Can your work continue to benefit patients or the healthcare community?
10. Seek Feedback and Validation
Share your project ideas with peers, mentors, and healthcare professionals for feedback and validation. Their input can help refine your concept and ensure it aligns with nursing best practices.
Conclusion – Nursing Capstone Project Ideas
These 27+ nursing capstone project ideas encompass a wide range of fields within the nursing profession. They offer students the opportunity to delve into critical healthcare issues, contribute to patient care, and demonstrate their readiness for the nursing profession. Simply choose a project that aligns with your interests and goals, and make a meaningful impact in the world of healthcare. Your dedication and passion will shine through in your capstone project, leaving a lasting impression on your academic journey and future nursing career.
What is a capstone project for RNs?
The Capstone is an individualized research project on a nursing topic of your professional or personal interest.
What is an example of a capstone project in healthcare?
Examples of capstone projects: Create a marketing campaign for a healthcare facility. Work with management to revise existing policies and procedures and maximize operational efficiency.
Similar Articles
How To Do Homework Fast – 11 Tips To Do Homework Fast
Homework is one of the most important parts that have to be done by students. It has been around for…

How to Write an Assignment Introduction – 6 Best Tips
In essence, the writing tasks in academic tenure students are an integral part of any curriculum. Whether in high school,…
Leave a Comment Cancel Reply
Your email address will not be published. Required fields are marked *
This site uses Akismet to reduce spam. Learn how your comment data is processed .

Home > Public Health > IPH_CAPSTONE
Public Health Capstone Projects
Capstone projects from 2024 2024.
Can’t Help You Here; Barriers to Access and Necessary Measures for Improving Health Inequities for Transgender Sex Workers , Andrew E. Colvin
PrEP Inequities Among Black and Latino MSM in the United States: Identifying Barriers and Opportunities Using a Social Ecological Model (SEM) Framework , Ryan Fisher
Tracking Childhood Vaccination Trends by Race: Analyzing MMR-Only, DTaP-Only, and Varicella-Only Vaccine Coverage Rates from 2016-2022 , Victoria Gallagher
Payment Assessment of Giving Birth in America Among Insurance Types for Years 2017 through 2021 , Jacy D. Harrell
The Association between Oral Contraceptives and Cardiovascular Disease: A Biomarker Analysis using Total Cholesterol, Low-Density Lipoprotein, and High-Sensitivity C-Reactive Protein , Maryam Z. Kenning
The Relationship between Mental and Environmental Health in Urban Salvador Brazil: Development of a Research Protocol , Rashad Parmer
Long COVID Among US Women: Racial Disparities and the Mediating Role of Severe COVID Infection , Amelia Phan
Analyzing the Associations between Pre- and Post-COVID-19 Pandemic Childhood ADHD Prevalence, Demographics and Environmental Factors in the United States , Reisha Rhodenbaugh
The Most Diverse Square Mile in America: Sociodemographic, Health Profiles, and Access to Healthcare among the Refugee, Immigrant, and Migrant Population in Clarkston, Georgia , Win Min Thein
Assessment of a Multidisciplinary Feeding Program's Caregiver Education Material through the Application of Health Literacy Principles , Mary Thomas
Capstone Projects from 2023 2023
Positive Behavior Support Parent Academy Curriculum - An Additional Approach , Lupe Arteaga
Association between Socio economic Factors and Contraceptive Use among Married Women in Guinea and Mali: An Examination of the Demographic and Health Survey Data 2018 , Mamadou Abdoulaye R Diallo
Fall Risk Assessment of Elderly Community-Dwelling Individuals , Jha'Meisheia Griffin
Reducing Health Disparities for U.S. Hispanics by Increasing the Cultural Literacy of Nutrition Professionals , Norma Esther Guardado López
The Associations between Selected Demographic, Socioeconomic, and Health Factors for Depression in Elderly Americans , Pema Lhewa
Epigenetic Changes and Health Disparities: An Evaluation Plan for Mamatoto Village Programming , Diamond T. Robinson
Adapting the International Protocol for Sexual Violence within the Department of Defense: Sexual Assault Prevention & Response Office , Tehnyat Sohail
Stigma, Social Norms, and Culture as Mediators of HIV and AIDS Incidence in South Africa , Skyeisha Swain
Capstone Projects from 2022 2022
Survival of Anthrax Patients with Fluid Collections by Treatment Status , Sophie Binney
A Review of Economic Policies to Reduce and Prevent Child Maltreatment and Other Adverse Childhood Experiences , Kaila Farmer
Behavioral and Epidemiological factors behind Vaccine Hesitancy in The United States , Maggie Hanusek
The Evaluation Plan for the LGBTQ+ Runaway & Homelessness Youth (LRHY) Outreach Program , Jade Matthews
Analysis of the Association between Physical and Mental Health in Adults: Understanding the Literature and Developing a Plan for Future Research , Max Moskowitz
Health Insurance Status and Severe Maternal Morbidity Outcomes in the United States - A Policy Review , Adejumobi Otekunrin
The Associations Between Overweight/Obesity Among Children and Select Social and Economic Predictors , Lauren A. Powell
“We Really are Seeing Racism in the Hospitals”: Racism and Doula Care , Ayeesha Sayyad
Concepts for Antiracist Policy Formulation , Sophia Steinberg
“a Doula Is Not a Visitor...a Birth Doula Is an Essential Part of the Birth Team”: Interprofessional Dynamics among Doulas, Doctors, and Nurses , Kaniya Williamson
Capstone Projects from 2021 2021
Challenges and Prospects of Implementing Mobile Health in Angola: Lessons Learned from Kenya and Denmark. , Maria da Graca Ambrosio
Evaluating Funding Structures of Federally Qualified Health Centers (FQHCs) in Metropolitan Atlanta: A Basis for Public Policy , Mamta Sanam Chaudhary
Levels of Engagement in a Comprehensive Parenting Intervention to Reduce Child Neglect Among Mothers without a High School Diploma: A Profile Examination , De Gao
The Need for Speed: Broadband Access as a Social Determinant of Health , Mwoddah Habib
An Evaluation Plan for Georgia's Injury Prevention Program , Joy Ngene
Examining United States Drug Policy from 2010-2021: A Qualitative Summation Using PEST Framework Model , Izadora A. Nunes
U.S. Rural Healthcare Shortage: A Review of Strategies in the U.S., Canada, and Colombia. , Carlos Perez
Comparing Water Quality Data of Atlanta's Sewage Overflows and Spills , Bonnie M. Pirlot
Policy Recommendations to Address Disproportionate Health Outcomes Caused by Healthy Food Access in Relation to Housing Districts Segregated by Class and Race , Roselyn Quarcoo
Characterization of Hand Hygiene Techniques Among Intensive Care Nurses: A Descriptive Study , Ashley L. Reyes
Analysis of Loss of Work during the COVID-19 Pandemic in the United States , Mira Shah
Research Proposal: COVID-19 Pandemic and Birth Experiences: Describing the Relationship Between Policies and the Birth Experiences of Georgia Mothers , Katherine Thornburgh
Georgia Commercial Sexual Exploitation of Children (CSEC) Resource and Protocol Guide , Sanon Williams
Developing and Disseminating the Children’s Environmental Health Index with Web GIS , Allegra Yeley
Branched Chain Amino Acids and Risk of Type 2 Diabetes Mellitus: A Literature Review , Alina Yemelyanov
Capstone Projects from 2020 2020
The Role of Policy in Preventing Adverse Childhood Experiences (ACEs) and Childhood Trauma in Georgia , Hallie Andrews
StayNeighbor: Community Platform for Essential Supplies and Services During the COVID-19 Pandemic , Samuel Archbold
Strategies in Maintaining Financial Sustainability of National Health Insurance Under A Single-payer System in Indonesia, Taiwan, and Canada: A Comparative Study , Arif Budiman
Aligning the Georgia Child Abuse & Neglect Prevention Plan with Governor Kemp's Priorities and Initiatives , Taylor Jennings
Healthcare for All: Achieving Universal Health Coverage (UHC) through the Strengthening of Health Systems , Diene Kaba
Youth Vaping: An Analysis of an Epidemic , Tina Kilpatrick
Georgia’s Child Sexual Abuse and Exploitation Prevention Technical Assistance Resource Guide (TARG) Evaluation Report , Maureen Oginga
U.S. Opioid Epidemic: Challenges and Opportunities for Evidence-based Policies , Imoh S. Okon
The Association between Mental Illness and Incarceration Among the African American/Black Population in the United States , Brittany Oladipupo
Capstone Projects from 2019 2019
A Cross-Sectional Study to Identify Factors Associated with Extrapulmonary Tuberculosis Among Foreign-Born In DeKalb County Georgia During 2008-2018 , Chinedu F. Egbuonu
WHO Drinking Water Guidelines , Aja Jagne
Evaluating Strategies for Community-sourced Photography for Mapping Alcohol Adverts in the Urban Slums in Kampala, Uganda , Joseph Madden
Community Organizing as a Vehicle to Promote Public Health in Clarkston, GA: A Literature Review & Case Study of Georgia Refugee Health and Mental Health , Maylott Mulugeta
The Use of Art to Increase Awareness about Mental Well-being and Promotion of Mental Health among the African American Community , Andromada Murden
Hepatitis C Virus (HCV) and Human Immunodeficiency Virus (HIV) Opt-out Testing in a Southern Federally Qualified Health Center (FQHC) , Leah Pinholster
A Resource Guide on the Epidemiology, Prevention, and Treatment of Opioid and Other Substance Use. , Anthony F. Rotoloni
Promoting an Urban Utopia: The Role of Community Gardens on Community Vitality , Kayla Danielle Staley
Augmenting Coastal Georgia’s Fresh-Water Supply while Reducing Local Salt-Water Intrusion into Groundwater Reservoirs , Forrest A. Strickland
Capstone Projects from 2018 2018
A Resource Guide To Empower Older Adults to Make Informed Health Decisions About Prescription Opioids And The Potential For Misuse , Kandia S. Al-Haddad
Program Evaluation Aspects of Atlanta Streets Alive , Rebecca A. Ament
A Systematic Analysis of Hepatitis C Virus Screening Trends and Linkage to Care Program in the United States , Ijeoma Azih
Understanding Educational Vulnerability in the Context of Disasters Using Visualizations , Cherish Caldwell
Tobacco-free Campus Post-implementation Program , Ashley Campbell
Examining the Relationship between Drought and Mental Health Outcomes of Depression and Anxiety in the U.S. , Robyn J. Cathey
Urban Water Planning in Lagos, Nigeria: An Analysis of Current Infrastructure Developments and Future Water Management Solutions , Adaure Chiori
A Review of Childhood Obesity Prevention Efforts among Evidence-Based Home Visiting Programs , Olga Costa
Prevention Messages to Reduce the Risk of Shigellosis among Men who have Sex with Men , Steve Evener
A Baseline Comparison of PATSCH and Parent as Teachers , Irasema Garcia-Rosales
A Mobile Initiative for Waste Disposal in Bringing Awareness to the Damage Littering Behavior Has on Storm Drains , Kimberly Hung
Examining the Community Outreach Efforts of Local African American Religious Organizations in Relation to Drug Use and HIV Transmission , Alyshia Jackson
A Qualitative Analysis of the Environmental and Personal Factors which Influence the Help-Seeking Behaviors of Men who have Sex with Men in Light of the Emerging Threat of Antimicrobial Resistance to Shigella Bacteria , Kathleen Jacobson
Alcohol Use among Orphans in Sub-saharan Africa: a Literature Review , Megan M. Mallett
Community- Based Walking Programs to Reduce Chronic Illness Among Racial/Ethnic Minorities in Limited Resource Neighborhoods: A Literature Review and Program Materials for Walk the Line , Alanti McGill
Consolidating Resources for the Aged-Out Human Trafficking Population Using a Mobile Application , Soumya Nalli
Mobile Application for Survivors of Domestic Violence , Varsha Neelam
A Historical Review of the Influenza Outbreaks Within Military Settings and Understanding the Viral Spread of the 1918 Influenza Pandemic , Naomi Ngadiman
How Social and Lifestyle Factors of African American Women Influence Behavior and Prevalence of Obesity: Literature Review , Briana E. Oliver
The Epidemiology of Wasting in Nigeria , Oluwatoyin Victoria Omotosho
Understanding Open Access Data Using Visualizations in R , Hazel Shah
An Evaluation of A National Sexual Violence Prevention Program: The Rape Prevention and Education Program , Arielle Shiver
Protecting College Students with Good Samaritan Policies: A Call to Action! , Nia Sutton
Assessment of Policies and Programs That Apply Adverse Childhood Experiences (ACE) Study Research , Rohjan Tajik
Capstone Projects from 2017 2017
Policy Recommendations for Addressing Health Insurance Network Adequacy and Provider Network Standards in the Georgia Insurance Market , Oluwatoyin Adedapo-Jimoh
A Grant Proposal to Evaluate the Effect Antibiotic TB Treatment has on the Gut Microbiota and on Metabolic Functions of Pediatric TB Patients in Dekalb County , Oluwatobiloba Adeola Akingbade
An Evaluation of a School-based Behavioral Health Initiative in Three Rural Counties , Bianca Anderson
Relationships Between Physical Activity and Neighborhood Walking Characteristics: Analysis of the 2015 National Health Interview Survey , Colby Brown
Epidemiology of Type 2 Diabetes in populations of African Descent , Kenyatta Bruce
Physical Injury as a Result of Intimate Partner Violence: An Individual, County, and State Level Analysis , Sharon Caslin
Factors That Contribute to The Disproportionate Rates of HIV among Black Men Who Have Sex with Men (MSM): A Systematic Review , Santanna S. Comer
Exploring Mental Health Services for Women Post Incarceration , Jalisa Cruver
An Examination of Metabolic Syndrome in Asthmatic Subjects: A Study Using the 2013-2014 National Health and Nutrition Examination Survey , Jasmine N. Cunningham
Health Interventions to Promote the Polio Vaccine within the Global Polio Eradication Initiative: A Systematic Review From 2000-2014. , Aime Serge Dali
Evidence of Injury Following Sexual Assault: A Research Proposal , Brea Echard
Street Medicine: A Program Evaluation , Ariel L. Edwards
Exploring Strategies to Increase Fruit and Vegetable Consumption Among Students in a School Cafeteria , Abigail Furtner
Branched Chain Amino Acids: Causal or Predictive of Type 2 Diabetes , Jency George
A Systematic Review on the Association Between Hormonal Contraception and Antiretroviral Therapy in HIV-Positive Women , Evan Graham
Advanced Search
- Notify me via email or RSS
- Collections
- Disciplines
- Submit Project
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
Passion Drives Medical Students' Scholarly Projects
- Education at Baystate
- Community & Public Health
Capstone Projects: The Culmination of 4 Years of Scholarly Work
Medical students in the Population-based Urban and Rural Community Health (PURCH) pathway at Baystate Health gathered with their peers at the UMass Chan Medical School main campus to present their Capstone projects.
In the Capstone Scholarship and Discovery (CSD) course students choose project topics based upon their interests and their project advisor mentors them throughout their four years of medical school.
2023 Capstone Awards
Capstone merit award.
This award recognizes students who exemplify the spirit of the CSD course—they not only accomplish an advanced level of scholarship, they also exhibit tenacity and maintain high levels of professionalism.
Kendall Burdick | What 9-1-1 gets you: Who has access to a pediatric trauma center? Project Advisor - Eric Fleegler, MD, MPH | Learning Community Mentor - Jacqueline Wu, MD
Sarah Calove | An Investigation Into Medical Practices Contributing to Sexual and Gender Minority Disparities Project Advisor - Carey Candrian, PhD | Learning Community Mentor - Jacqueline Wu, MD
Eve Manghis | Perceptions of the Prescription Drug Monitoring Program Among Massachusetts Emergency Department Leaders: A Qualitative Inquiry Project Advisor - William Soares, MD, MS | Learning Community Mentor - Eric Churchill, MD, MPH
Victoria Powell | Assessing and Reducing Barriers to Treatment for Hepatitis C on Tapestry Health’s Mobile Health Van: Survey and Pilot Program Development Project Advisor - Anne Jenney, MS, PA-C | Learning Community Mentor - Eric Churchill, MD, MPH
Capstone Project Advisor Award
This award recognizes project advisors for their continued support and dynamic involvement in the Capstone Scholarship and Discovery Course. (Photo-right: Dr. Jesse Casaubon)
Jesse Casaubon, MD | Assistant Professor, Department of Surgery, UMass Chan - Baystate Advisees - Zilin Cui and Emily Vicks
Mitchell Cahan, MD, MBA, MLS, FACS | Adjunct Professor, Department of Surgery, UMass Chan Medical School Advisees - Jennifer Sullivan and Chloe Young
2023 PURCH Capstone Projects
Annabelle Batten | Assessing the Utility of Telehealth in Franklin County Project Advisor - Cheryl Pascucci, NP | Learning Community Mentor - Eric Churchill, MD
Hannah Caringal | Creating a Resource Directory for those Utilizing the Worcester Asylum Clinic Project Advisor - Payal Modi, MD, MPH, MSc | Learning Community Mentor - Eric Churchill MD, MPH
Zilin Cui | Mental Health Attitudes and Help-Seeking Behaviors of Chinese Americans during the COVID-19 Pandemic Project Advisor - Xiaoduo Fan MD, MPH | Learning Community Mentor - Sam Borden, MD
Joe Douglass | Assessment of the Impacts of Climate Change on Human Health in the Undergraduate Medical Curriculum Project Advisor - Christopher Sassetti, PhD | Learning Community Mentor - Elizabeth Eagleson, MD
Colin Hart | Improving Deaf Patient Interactions through Curriculum Development Project Advisor - Tim Moriarty, MPA | Learning Community Mentor - Eric Churchill, MD, MPH
Kristina Jakobson & Taylor Dickinson | Assessing the need for a clinical terminology curriculum during the preclinical years: Survey of UMass Chan Medical School Students Project Advisor - Alexandra Wink, MD | Learning Community Mentor - Sam Borden, MD
Rachel Lister | Knitted Connections: A Quality Improvement Project for a Knitting Group Project Advisor - Bonnie O'Donnell | Learning Community Mentor - Elizabeth Eagleson, MD
Mary Marchese | Wellness on Wheels: Proposing a Mobile Health Intervention to Improve Adolescent Sexual Health Education and Screening Services in Western Massachusetts Project Advisor - Kelly Lamas, MPH | Learning Community Mentor - Jacqueline Wu, MD
Paige Mastalerz | MELAS: A Case Report and a Psychiatric Perspective to a Neuropsychiatric Condition Project Advisor - Deepika Sundararaj, MD | Learning Community Mentor - Sam Borden, MD
Saranya Ramandurai | Assessing Barriers and Motivators to Voter Mobilization in Springfield Massachusetts Project Advisor - Kathryn Jobbins, DO | Learning Community Mentor - Sam Borden, MD
Calvin Schaffer | Patient Assessment of Resident Care (PARC): Evaluating the care and communication of resident physicians Project Advisor - Reva Kleppel, MSW, MPH | Learning Community Mentor - Sam Borden, MD
Diana Sibai | Identifying Barriers to a Healthy Diet in Pregnant Patients with a History or Risk of Hypertension: A Focus on Food Insecurity and Access Project Advisor - Lara Kovell, MD | Learning Community Mentor - Eric Churchill, MD, MPH
Jennifer Sullivan | Influence of Insurance Status on Subdural Hematoma Management- An NTDB Analysis Project Advisor - Mitchell Cahan, MD, MBA, MLS, FACS | Learning Community Mentor - Elizabeth Eagleson, MD
Nathan Taber | Medical Spanish: One Student's Approach to Combatting Language Barriers Project Advisor - Nathan Macedo, MD, MPH | Learning Community Mentor - Jacqueline Wu, MD
Emily Vicks | Association between multiple breast lesions of uncertain malignant potential discovered by core needle biopsy on upstage to malignancy in surgical excision Project Advisor - Jesse Casaubon, DO | Learning Community Mentor - Jacqueline Wu, MD
Paula Whitmire | Intimate Partner Violence: Experiences of Rural Healthcare Workers in the UMass Chan – Baystate Network Project Advisor - Emma Wood, DO | Learning Community Mentor - Sam Borden, MD
Jaclyn Wong | Evaluating and Improving an Annual Community Health Fair Project Advisor - Jacqueline Wu, MD | Learning Community Mentor - Jacqueline Wu, MD
Chloe Young | Hispanic Farmers Experience Shorter EMS Response Times But Longer Emergency Department Length of Stay Following Occupational Injuries Project Advisor - Mitchell Cahan, MD, MBA, MLS, FACS | Learning Community Mentor - Jacqueline Wu, MD

Health & Wellness Tips
Related news.

Making Magic Thanks to Maddie

Endowment Ensures Hope for Breast Cancer Research and Care

Harold Grinspoon Advances Future of Mental Health Through Donation

President & CEO Mark Keroack Named “Health System CEO Influencer”

Awake Left Atrial Appendage Occlusion Surgery Gives Patients More Freedom

PURCH Class of 2023 Honored at Graduation Celebration

Baystate Health Awarded $5 Million Grant Towards Digital Equity

Celebrating Our Brother, Our Uncle, Our Friend, Our Storyteller

Kevin and Sue Lawson Transform Patient Experience with Legacy Gift

The New Valley Springs Behavioral Health Hospital Scheduled to Open in Holyoke in a Few Months is Designed to Provide a Sanctuary for Healing in Western Massachusetts
Back to Top
Data Science Master’s Students Tackle Diverse, Real-World Challenges in Capstone Projects

Human trafficking, illegal fishing, small business contracts — these are all issues that, at first glance, seemingly have little in common.
Yet, for students in the University of Virginia’s data science residential master’s program , these disparate subjects have one critical common denominator: they could all be better understood through the application of data science methods.
Fifteen groups of graduate students at the School of Data Science recently presented the findings of their capstone projects before a sizable crowd of faculty, staff, and fellow students at the Graduate hotel in Charlottesville.
Capstone projects have long been a cornerstone of the data science master’s program. In them, students work in groups with a faculty mentor as well as an outside sponsor to tackle a real-world problem.
It’s an opportunity for students to collaborate with their classmates and apply what they are learning from faculty toward addressing a real issue that their sponsor is dealing with — experiences that often leave lasting impressions.
“When we talk to alumni years later, they all say that the two things that they remember most about the program are the capstone experience and also a cohort experience,” said Phil Bourne , founding dean of the School of Data Science, in opening remarks.
The projects offered students the chance to learn about new subjects and methods as well as develop skills that could prove vital as they begin their careers.
“While you’ve done many projects, this is the first time that it was a very large project that you had to break it up and project manage it,” Adam Tashman , an associate professor of data science and capstone program director, told the students.
He added that perhaps the most important lesson students will take from the experience is “how to deliver for a customer.”
For more than four hours, with a break for lunch, groups of students laid out their findings in brief presentations followed by questions from the audience.
In one, which focused on predicting which federal agencies small businesses could match with to secure contracts, David Diaz , whose father owns a small business in California, described the personal nature of the group’s work.
“I’ve seen this firsthand; I still see it with my dad now. There are a lot of long hours. It isn’t really a 9 to 5 job — it’s a 24/7 job,” Diaz said, describing the continual process that small business owners face in gathering information to try to secure bids while ensuring business operations run efficiently.
“So, the goal of this project is to hopefully reduce that research time in reaching the federal contracting market and, hopefully, allow businesses to have a finer scope into what they’re looking for,” he added.

Another group laid out their work on illegal fishing, discussing the complexity of this global issue and the vast problems it creates. They also highlighted a key point that any data scientist must confront: how to classify the data they had.
“Kind of like an indie album, our data set is unlabeled,” joked Samuel Brown, who explained how he and his group created labels to differentiate between illegal and illegal fishing.
The group discussed how their project demonstrated how machine learning could be used to help predict illegal fishing, information that could, potentially, reduce its prevalence.
Like any complex challenge, completing a capstone project can be stressful. And in those difficult times, sources of wisdom are sometimes found in unexpected places.
Sunidhi Goyal , who works as a tennis instructor for UVA Recreation, recounted how one of her six-year-old students asked her one day what was bothering her.
Goyal, part of a group that worked with LMI on empowering their enterprise architecture team, said she wasn’t sure how she could explain the complexities of their project to a young child.
But she tried, describing, in simple terms, how she and her collaborators needed to find a way to allow enterprise architects to sort through a large number of documents and keep just the relevant ones — the “good” documents, she called them.
“She was like, ‘Oh, what if the good could be a magnet, and you could keep it together and let go of the bad,” Goyal said the student responded.
“This is exactly what we ended up doing,” Goyal said, explaining how her team used a method called principal component analysis to retain only the most relevant documents, an approach that helped lead them to their solution.

As the day wound down, audience members voted on awards, and Tashman praised the students for the effort, passion, and purpose they exhibited in taking on the challenges presented by their sponsors.
“These are all important things that our sponsors need help with, and you all took ownership of that. I think you took it to heart and really put your heart and soul into it,” he said.
And while the completion of their capstone projects signaled an end to their time as master’s students at the School of Data Science, it also marked the beginning of a much longer journey to come.
“Let this be the first of many real-world problems that you face and that you tackle,” Tashman said.
Awards, as voted on by the audience
Most Innovative Analytical Solution : “Optimizing the ALMA Research Proposal Process with Machine Learning”
Group members: Brendan Puglisi, Arnav Boppudi, Kaleigh O’Hara, Noah McIntire, Ryan Lipps
Most Compelling Data Visualization : “Detecting Illegal Fishing with Automatic Identification Systems and Machine Learning”
Group members: Samuel Brown, Danielle Katz, Dana Korotovskikh, Stephen Kullman
Most Engaging Data Story : “Predicting Winter California Precipitation with Convolutional Neural Networks”
Group members: Anthony Chiado, Kristian Olsson, Luke Rohlwing, Michael Vaden
Most Impactful Ethical Engagement : “Detecting Human Trafficking
Group members: Jacqui Unciano, Grace Zhang, Tatev Gomtsyan, Serene Lu

‘A Big Moment’: Online Data Science Master’s Students Present Captone Projects
Professor Promotes Data Literacy With New Book

News Roundup: School of Data Science Celebrates Grand Opening of New Home
Get the latest news.
Subscribe to receive updates from the School of Data Science.
- Prospective Student
- School of Data Science Alumnus
- UVA Affiliate
- Industry Member
Hypothesized Surface: Sample Return from Hypothesized Surfaces – RIT – A
“18977 – nasa psyche sample containment”, institution.
Rochester Institute of Technology (RIT)
Tungsten Class (2023 – 2024)
STUDENT TEAM
Raina Barboza – Mechanical Engineering Ilker Bilgen – Mechanical Engineering Anthony Caropreso – Mechanical Engineering Erin Gillette – Mechanical Engineering Emily Lawton – Mechanical Engineering Aubrey Tarmu – Computer Engineering Chelsea Taylor – Industrial Engineering
SCIENTIFIC AND TECHNICAL GUIDANCE
Academic guidance.
Dr. Carlos Barrios – Academic Guide (RIT) Dr. Cassie Bowman – Client & NASA Guide
PROJECT DESCRIPTION
We are designing and creating, with guidance from the NASA Psyche Program, a sample return containment device that has the ability to preserve a sample from the metallic asteroid Psyche, either from the surface or underneath. The container will open and close, rotate to accept samples, seal to preserve the sample in the appropriate conditions, and be functional with minimal human interaction. This mechanism must function on all ranges of hypothesized surfaces that may be found on Psyche, including a mostly flat metallic surface, rocky terrain, high-relief metallic craters, and rocky or metallic debris. Our project will require extensive testing to validate the device, as it will experience pressures and temperatures on both asteroid Psyche and reentry to Earth, as well as gravity in the environment of space.
This work was created in partial fulfillment of the Rochester Institute of Technology Capstone Course “MECE 497”. The work is a result of the Psyche Student Collaborations component of NASA’s Psyche Mission (https://psyche.asu.edu). “Psyche: A Journey to a Metal World” [Contract number NNM16AA09C] is part of the NASA Discovery Program mission to solar system targets. Trade names and trademarks of ASU and NASA are used in this work for identification only. Their usage does not constitute an official endorsement, either expressed or implied, by Arizona State University or National Aeronautics and Space Administration. The content is solely the responsibility of the authors and does not necessarily represent the official views of ASU or NASA.

IMAGES
VIDEO
COMMENTS
Most nursing students prefer undertaking a capstone nursing course. A capstone project is an individualized research project on a specific nursing topic of your professional or personal interest. It is usually completed within between 4 to 12 weeks, depending on the nursing school and the program you are pursuing.
A capstone project or capstone experience involves the identification of an existing problem in a real-world setting and the application of learned skills and methods to develop a solution that addresses the problem directly. In some cases, a capstone project will be geared toward research, while others are more oriented toward problem-solving.
Capstone grading methods differ between programs, with some issuing letter grades and others using a pass/no pass system. Grades typically hinge on a percentage basis of the project's written sections, the final proposal, and the presentation. Faculty evaluate how students execute the capstone course objectives, which may include the following:
Nursing capstone projects provide an opportunity for students to apply their knowledge and skills acquired throughout their nursing education in a real-world setting. These projects are usually undertaken as a requirement for graduation in nursing programs. A nursing capstone project proposal is an essential first step in the process.
An example of how one DNP student followed this 5-step evidence-based process to develop a change project with the goal of increasing vaccination among healthcare personnel working in a college: Step 1. A change project was initiated to increase influenza vaccination among healthcare personnel at a college. Step 2.
The goal of this capstone project is to first outline the many barriers that pediatric rare disease patients and their families face in the medical field. Some of these barriers and difficulties that they face include the diagnostic process, a lack of healthcare provider competence, psychosocial needs, or the doctor-patient relationship itself.
Through the Capstone one is asked to demonstrate that he/she can conduct a research project largely independently, yet in consultation with one's Capstone Advisor. The Capstone is to have the qualities of being conducted independently; is original in nature; is a rigorous study; and has the potential to advance the profession of healthcare ...
The Capstone experience is your final graduate scholarly project. Your work will focus on performing a literature review, working on the project, and interacting with your mentor/organization to progress through your project. The other activities will be completing and putting the portfolio together.
Table 1-1: Examples of Capstone Project Formats Designing or building a product, intervention , or program to address a n identified need or problem Researching an industry or market, and creating a viable business plan for a proposed company that is the n introduced to stakeholders
The Capstone Strategy Project complements the classroom instruction and is defined as learning by construction. It is a total immersion experience in which students are challenged to use all of the tools and concepts learned to date to tackle a current business problem for a healthcare organization. With faculty oversight, you demonstrate ...
Welcome to the Capstone Project: Evidence-Based Health Care (EBHC). This is an exciting project, which will increase your proficiency in reviewing research literature, principles and theory; and refine your skills in applying evidence-based practice to your profession. The purpose of the capstone project is to assist you in learning the skills ...
The capstone project and accompanying research paper serve as the culminating assessment in the MHA program. Examples of capstone projects: Create a marketing campaign for a healthcare facility. Work with management to revise existing policies and procedures and maximize operational efficiency. Plan and manage a fundraiser for a healthcare ...
The capstone project ideas on healthcare quality improvement, PICOT questions examples, evidence-based practice project ideas, research paper topics, and research questions in this article are a valuable starting point for nurses and healthcare professionals seeking to make a meaningful impact on the quality of care delivered to patients. FAQs. 1.
The Critical Challenge Project (CCP) is central to the learning experience and will become the focus of an independent study. You will identify a challenge related to your field and interests, drawing from your own experience and vision for the future. Each student works collaboratively with their peers, professional colleagues, course faculty ...
A thesis is an academic article that presents an argument or research findings. Common in graduate programs, thesis projects are often by an adviser or other faculty member. Capstone projects take various forms and, although more common in undergraduate studies, may be a requirement of master's programs. Capstones are often research projects ...
What is the Capstone project? As a culminating experience, each student will independently put into practice the knowledge and skills they learned during their coursework through a Capstone Project.. Students will have the opportunity to develop and implement a Health Informatics project in their workplace or other academic / industry organizations.The project will challenge each student to ...
Design your project built around applying evidence-based knowledge to enhance your place of practice. Work with your faculty mentor and stakeholders. Collaborate with colleagues and co-workers in larger group projects! Develop, execute, evaluate and present findings to peers, faculty and professionals. This includes a written defense.
Capstone Project: Nice Healthcare: Predicting Nice healthcare utilization. Industry Mentor: Nice Healthcare. Yuan Lian. Capstone Project: Next Generation Data Commons. Industry Mentor: ICF International. 2021-2022 Graduates. Ahson Saiyed. NLP Engineer/Data Scientist at TrinetX.
Nursing capstone project ideas are a culmination of your academic field. It allows you to showcase your knowledge, skills, and passion in the field of nursing. These nursing capstone projects provide students with an opportunity to address real-world healthcare issues, make a positive impact, and demonstrate their readiness for the profession.
A capstone project is a multifaceted academic experience typically required for students during the final year of an academic program. It is a comprehensive and interdisciplinary project that often requires students to apply the knowledge and skills acquired throughout their academic careers to solve real-world problems or issues.
A successful capstone project depends on the student's ability to evaluate critical problems, effectively lead a team, and execute appropriate solutions. Here are five capstone ideas for healthcare management degree programs. You may also like: Top 20 Master's in Healthcare Management Degree Programs. Better Health Services for Veterans
A 20-minute presentation might ideally have between 15-20 slides. Don't have too much text on slides. Keep slides to a minimum of five or six lines of text on them. Stick to one font size for bullet text. Don't resize text to fit it on one slide: insert a new slide!
Capstone Projects from 2023. Positive Behavior Support Parent Academy Curriculum - An Additional Approach, Lupe Arteaga. Association between Socio economic Factors and Contraceptive Use among Married Women in Guinea and Mali: An Examination of the Demographic and Health Survey Data 2018, Mamadou Abdoulaye R Diallo.
Capstone projects represent students' work over 4 years. Medical students in the Population-based Urban and Rural Community Health (PURCH) pathway at Baystate Health gathered with their peers at the UMass Chan Medical School main campus to present their Capstone projects.. In the Capstone Scholarship and Discovery (CSD) course students choose project topics based upon their interests and their ...
Capstone vs. Research Capstone (SC476) Research (SC495/496) •1 semester "research" + 2 chem electives = 9 total credits (6 lec + 3 lab) •work with a lab partner on a project selected from a list or
The group discussed how their project demonstrated how machine learning could be used to help predict illegal fishing, information that could, potentially, reduce its prevalence. Like any complex challenge, completing a capstone project can be stressful. And in those difficult times, sources of wisdom are sometimes found in unexpected places.
Our project will require extensive testing to validate the device, as it will experience pressures and temperatures on both asteroid Psyche and reentry to Earth, as well as gravity in the environment of space. This work was created in partial fulfillment of the Rochester Institute of Technology Capstone Course "MECE 497".