Causes and Effects of Obesity Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment

Introduction
Laziness as the main cause of obesity, social effects of obesity, effects of obesity: health complications.
Bibliography
Maintaining good body weight is highly recommended by medical doctors as a way of promoting a healthy status of the body. This is to say that there is allowed body weight, which a person is supposed to maintain. Extreme deviations from this weight expose a person to several health complications.
While being underweight is not encouraged, cases of people who are overweight and increasing effects of this condition have raised concerns over the need of addressing the issue of obesity in the society today, where statistics are rising day and night. What is obesity? This refers to a medical condition in which a person’s body has high accumulation of body fat to the level of being fatal or a cause of serious health complications. Additionally, obesity is highly associated with one’s body mass index, abbreviated as BMI.
This denotes the value obtained when a person’s weight in kilograms is divided by the square of their height in meters (Burniat 3). According to medical experts, obesity occurs when the BMI exceeds 30kg/m 2 . While this is the case, people who have a BMI of between 25 and 29 and considered to be overweight. Obesity has a wide-range of negative effects, which may be a threat to the life of a person.
The fist effect of obesity is that it encourages laziness in the society. It is doubtless that obese people find it hard and strenuous to move from one point to the other because of accumulated fats. As a result, most of these people lead a sedentary lifestyle, which is usually characterized by minimal or no movement. In such scenarios, victims prefer being helped doing basic activities, including moving from one point to another.
Moreover, laziness makes one to be inactive and unproductive. For example, a student who is obese may find it hard to attend to his or her homework and class assignments, thus affecting performance. With regard to physical exercises, obese people perceive exercises as punishment, which is not meant for them (Korbonits 265). As a result, they do not accept simple activities like jogging because of their inability to move.
In line with this, obese people cannot participate in games like soccer, athletics, and rugby among others. Based on this sedentary lifestyle, obese people spend a lot of their time watching television, movies, and playing video games, which worsen the situation.
The main effect of obesity is health complications. Research indicates that most of the killer diseases like diabetes, heart diseases, and high blood pressure are largely associated with obesity. In the United States, obesity-related complications cost the nation approximately 150 billion USD and result into 0.3 million premature deaths annually.
When there is increase in body fat, it means that the body requires more nutrients and oxygen to support body tissues (Burniat 223). Since these elements can only be transported by the blood to various parts of the body, the workload of the heart is increased.
This increase in the workload of the heart exerts pressure on blood vessels, leading to high blood pressure. An increase in the heart rate may also be dangerous due to the inability of the body to supply required blood to various parts. Moreover, obesity causes diabetes, especially among adults as the body may become resistant to insulin. This resistance may lead to a high level of blood sugar, which is fatal.
Besides health complications, obesity causes an array of psychological effects, including inferiority complex among victims. Obese people suffer from depression, emanating from negative self-esteem and societal rejection. In some cases, people who become obese lose their friends and may get disapproval from teachers and other personalities (Korbonits 265). This is mainly based on the assumption that people become obese due to lack of self-discipline. In extreme cases, obese people may not be considered for promotion at workplaces, because of the negative perception held against them.
Due to inferiority complex, obese people avoid being in public and prefer being alone. This is because they imagine how the world sees them and may also find it hard being involved in public activities because of their sizes.
This further makes them to consider themselves unattractive based on their deviation from what is considered as the normal body size and shape. Regardless of how obese people are treated, they always believe that they are being undermined because of their body size.
In summary, obesity is a major cause of premature deaths in the United States and around the world. This health condition occurs when there is excess accumulation of body fat, caused by unhealthy lifestyles. Obesity is largely associated with several killer diseases like high blood pressure, diabetes, and diseases of the heart.
These diseases drain world economies since most of them are fatal and expensive to manage. Additionally, obesity promotes sedentary life where victims minimize movement by adopting an inactive lifestyle. Moreover, obese victims suffer psychologically because of societal rejection. In general, obesity has a wide-range of negative effects, which may be a threat to the life of a person.
Burniat, Walter. Child and Adolescent Obesity: Causes and Consequences, Prevention and Management . United Kingdom: Cambridge University Press, 2002. Print.
Korbonits, Márta. Obesity and Metabolism . Switzerland: Karger Publishers, 2008. Print.
- Screening for Obesity
- Parental Education on Overweight and Obese Children
- Blood Pressure and Obesity Solution
- Eating Disorders: Assessment & Misconceptions
- Human Digestion
- Definitions of Obesity and Criteria for Diagnosing It
- Obesity Could Be Catching
- White Wines vs. Red Wines
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2018, December 11). Causes and Effects of Obesity Essay. https://ivypanda.com/essays/effects-of-obesity/
"Causes and Effects of Obesity Essay." IvyPanda , 11 Dec. 2018, ivypanda.com/essays/effects-of-obesity/.
IvyPanda . (2018) 'Causes and Effects of Obesity Essay'. 11 December.
IvyPanda . 2018. "Causes and Effects of Obesity Essay." December 11, 2018. https://ivypanda.com/essays/effects-of-obesity/.
1. IvyPanda . "Causes and Effects of Obesity Essay." December 11, 2018. https://ivypanda.com/essays/effects-of-obesity/.
IvyPanda . "Causes and Effects of Obesity Essay." December 11, 2018. https://ivypanda.com/essays/effects-of-obesity/.
Obesity in America: Cause and Effect Essay Sample
It is clear that the American lifestyle has contributed to the increasing prevalence of obesity. With estimates from the Washington-based Centers for Disease Prevention in the Department of Health and Human Services indicating that one in three American adults is overweight, it is evident that the country is facing an obesity epidemic. To better understand the causes and effects of obesity, research is needed to further explore the issue. For those struggling with obesity, coursework assistance may be available to help them make the necessary lifestyle changes in order to live a healthier life.
Writing a thesis paper on the topic of obesity can be extremely challenging. It requires extensive research and time to adequately cover the subject. However, there are services available that can provide assistance with the writing process. Pay for a thesis allows for the benefit of having an experienced professional provide guidance and support throughout the entire process.
Causes of Obesity
Every phenomenon must have a reason. In order to write a cause and effect essay , you need to analyze the topic carefully to cover all aspects. Obesity is considered to be a complex illness, with a number of factors contributing to its development. These can be:
- hereditary;
As you may have guessed, it is the latter category of causes and effects that we are interested in. At this point, we care about the five ones that have made the biggest contribution.
Product Range
The main cause of obesity is junk food and an unbalanced diet rich in simple carbohydrates, fats, and sugars, plus a bunch of additives. Manufactured, processed, refined, and packaged meals are the most popular. Thanks to advances in technology, Americans have come to mass-produce meals that keep fresh longer and taste better. It takes less time to prepare unhealthy, processed foods in the microwave than it does to cook them yourself.
Lack of a work-life balance, high-stress levels, insufficient sleeping hours contribute to body weight gain. Not only do these factors contribute to this, but failing to take the time to do your homework can also have a negative impact on your physical health. Without a healthy, balanced approach to work, rest, and play, you may find yourself increasingly dependent on a sedentary lifestyle that can lead to overweight consequences. Many Americans work 50, 60, or more hours a week and suffer from a deficit of leisure hours. Cooking processed foods saves them hours and money, even though they end up costing them a lot more – by causing cardiovascular disease. In addition, obese people feel stressed on a regular basis in the United States metropolitan areas. Many of them are simply binge eating under the influence of negative emotions. Chronic overeating leads to a disturbance in the appetite center in the brain, and the normal amount of food eaten can no longer suppress hunger as much as necessary, affecting the body mass.
Food Deserts
The term ‘ food desert ‘ refers to poor areas (urban, suburban and rural) with limited access to fresh fruit, grains, and vegetables – places where it is much easier to access junk food. A grocery shop in a food desert that sells healthy foods may be 10-15 miles away, while a mini-market or cheap shop that sells harmful snacks is close to the house. In such a world, it takes much more effort to eat healthier, form eating habits, and stay slim.
Everyone’s Passion for Sweets
Consuming sweets in large quantities is addictive: the more and easier we give the body energy, the more the brain uses serotonin and dopamine to encourage it – it will make obese people want sweets again and again during the day. Cakes and pastries are fast carbohydrates that easily satisfy hunger and increase body mass. Despite the harm of sweets, obese people experience the need for them to satiate. Sweetened carbonated drinks are one of the main sources of sugar in the American diet. Moreover, some individuals may be more adversely affected by such diets than others: patients with a genetic predisposition to obesity gain body mass faster from sugary drinks than those without it. This leads to childhood obesity.
The Harm of Tolerance
Every year, the body positive movement is becoming more and more popular all over the world. It would seem that this major trend should have freed us from the problems associated with the cult of thinness and society’s notorious standards. In many ways, a positive attitude towards the body has proved fruitful. For example, the notion of beauty has clearly broadened. Now on fashion shows and magazine covers, you can see not only a girl with perfectly retouched skin and without a single hint of body fat but also an ordinary person with its inherent features: overweight, wrinkles, hair, and individual skin features. In general, all the things that we are all so familiar with in real life.
Does it really make that much sense? Is this a positive thing in terms of the cause and effect topic regarding obesity? In short, opinions are divided. Extremes aren’t easy to overcome. Not everyone manages to do it. Researchers have concluded that due to plus size having become positioned as a variant of the norm, more persons have become obese. Many obese Americans have formed the opinion that it is really quite normal, and they have become oblivious to the damage it does to their health. This is what we are going to focus on next.
Effects of Obesity
We all know that obesity is dangerous to health. However, medical studies show that most adults are unaware of the number of complications and diseases that obesity in America entails. So they are fairly comfortable with becoming gradually fatter. But indifference is replaced by concern when obesity related diseases begin to occur.
For interesting examples of students writing that also reveal the causes and effects of other phenomena, consult the custom essay service offering essays by professionals. In this way, you will realize the importance of highlighting the effects right after the causes.
Is obesity an aesthetic disadvantage, an inconvenience, a limitation in physical activity or is it an illness after all? How does it affect health, and what are the consequences? The visible signs of obesity are by no means the only complication associated with this condition. Obesity creates a high risk of life-threatening diseases such as atherosclerosis, hypertension, heart attack, myocardial infarction, and kidney and liver problems. Moreover, it can also lead to disability.
Cardiovascular Disease
This is the most serious and damaging impact on the body and blood vessels in particular. Every extra kilo is a huge additional load on the heart. Obesity increases the risk of heart attacks. Experts from the American Heart Association have developed a paper on the relationship between obesity and cardiovascular disease, which discusses the impact of obesity on the diagnosis and outcomes of patients with atherosclerotic cardiovascular disease, heart failure, and arrhythmias. Childhood obesity aggravates the course of cardiovascular disease from a very early age. The fact that even kids and adolescents are obese is associated with high blood pressure, dyslipidemia, and hyperglycemia.
The result is excessive insulin production in the body. This, in turn, leads to an overabundance of insulin in the blood, which makes the peripheral tissues more resistant to it. As a consequence of the above, sodium metabolism is disturbed, and blood pressure rises. It is important to remember that excessive carbohydrate food intake leads to increased production of insulin by the pancreas. Excess insulin in the human body easily converts glucose into fat. And obesity reduces tissue sensitivity to insulin itself. This kind of vicious circle leads to type 2 diabetes.
Effects on Joints
Obesity increases the load on joints to a great extent, especially if one undergoes little or no physical activity. For instance, if one lives in a megalopolis, where all physical activity consists of getting off the sofa, walking to the car, and plumping up in an office chair at work. All this leads to a reduction in muscle mass, which is already weak, and all the load falls on the joints and ligaments.
The result is arthritis, arthrosis, and osteochondrosis. Consequently, a seemingly illogical situation is formed – there is practically no exercise, but joints are worn out harder than in the case of powerlifters. In turn, according to a study by the University of California, reducing body weight reduces the risk of osteoarthritis.
Infertility
In most cases, being obese leads to endocrine infertility, as it causes an irregular menstrual cycle. Women experience thyroid disease, polycystic ovarian syndrome, problems with conception, and decreased progesterone hormone. Obese men are faced with erectile dysfunction, reduced testosterone levels, and infertility. It should be noted that the mother’s obesity affects not only her health but also the one of her unborn child. These children are at higher risk of congenital malformations.
Corresponding Inconveniences
Public consciousness is still far from the notion that obese people are sick individuals. The social significance of the issue is that people who are severely obese find it difficult to get a job. They experience discriminatory restrictions on promotion, daily living disadvantages, restrictions on mobility, clothing choices, discomfort with adequate hygiene, and sexual dysfunction. Some of these individuals not only suffer from illness and limited mobility but also have low self-esteem, depression, and other psychological problems due to involuntary isolation by watching television or playing video games. Therefore, the public has to recognize the need to establish and implement national and childhood obesity epidemic prevention programs.
Society today provokes unintentional adult and childhood obesity among its members by encouraging the consumption of high-fat, high-calorie foods and, at the same time, by technological advances, promoting sedentary lifestyles like spending time watching television or playing video games. These social and technological factors have contributed to the rise in obesity in recent decades. Developing a responsible attitude towards health will only have a full impact if people are given the opportunity to enjoy a healthy lifestyle. At the level of the community as a whole, it is therefore important to support people in adhering to dieting recommendations through the continued implementation of evidence-based and demographic-based policies to make regular physical activity and good nutrition both affordable and feasible for all. It is recommended to cut down on the food consumed.

Related posts:
- The Great Gatsby (Analyze this Essay Online)
- Pollution Cause and Effect Essay Sample
- Essay Sample on How Can I Be a Good American
- The Power of Imaging: Why I am Passionate about Becoming a Sonographer
Improve your writing with our guides

Youth Culture Essay Prompt and Discussion

Why Should College Athletes Be Paid, Essay Sample

Reasons Why Minimum Wage Should Be Raised Essay: Benefits for Workers, Society, and The Economy
Get 15% off your first order with edusson.
Connect with a professional writer within minutes by placing your first order. No matter the subject, difficulty, academic level or document type, our writers have the skills to complete it.
100% privacy. No spam ever.

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 27 February 2019
Obesity: global epidemiology and pathogenesis
- Matthias Blüher 1
Nature Reviews Endocrinology volume 15 , pages 288–298 ( 2019 ) Cite this article
56k Accesses
2560 Citations
981 Altmetric
Metrics details
- Epidemiology
- Health policy
- Pathogenesis
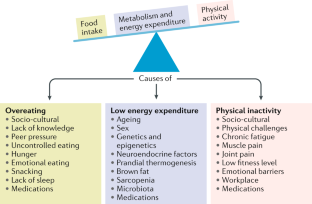
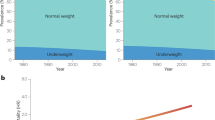
The prevalence of obesity has increased worldwide in the past ~50 years, reaching pandemic levels. Obesity represents a major health challenge because it substantially increases the risk of diseases such as type 2 diabetes mellitus, fatty liver disease, hypertension, myocardial infarction, stroke, dementia, osteoarthritis, obstructive sleep apnoea and several cancers, thereby contributing to a decline in both quality of life and life expectancy. Obesity is also associated with unemployment, social disadvantages and reduced socio-economic productivity, thus increasingly creating an economic burden. Thus far, obesity prevention and treatment strategies — both at the individual and population level — have not been successful in the long term. Lifestyle and behavioural interventions aimed at reducing calorie intake and increasing energy expenditure have limited effectiveness because complex and persistent hormonal, metabolic and neurochemical adaptations defend against weight loss and promote weight regain. Reducing the obesity burden requires approaches that combine individual interventions with changes in the environment and society. Therefore, a better understanding of the remarkable regional differences in obesity prevalence and trends might help to identify societal causes of obesity and provide guidance on which are the most promising intervention strategies.
Obesity prevalence has increased in pandemic dimensions over the past 50 years.
Obesity is a disease that can cause premature disability and death by increasing the risk of cardiometabolic diseases, osteoarthritis, dementia, depression and some types of cancers.
Obesity prevention and treatments frequently fail in the long term (for example, behavioural interventions aiming at reducing energy intake and increasing energy expenditure) or are not available or suitable (bariatric surgery) for the majority of people affected.
Although obesity prevalence increased in every single country in the world, regional differences exist in both obesity prevalence and trends; understanding the drivers of these regional differences might help to provide guidance for the most promising intervention strategies.
Changes in the global food system together with increased sedentary behaviour seem to be the main drivers of the obesity pandemic.
The major challenge is to translate our knowledge of the main causes of increased obesity prevalence into effective actions; such actions might include policy changes that facilitate individual choices for foods that have reduced fat, sugar and salt content.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Obesity and the risk of cardiometabolic diseases

Obesity: a 100 year perspective

Obesity-induced and weight-loss-induced physiological factors affecting weight regain
World Health Organization. Noncommunicable diseases progress monitor, 2017. WHO https://www.who.int/nmh/publications/ncd-progress-monitor-2017/en/ (2017).
Fontaine, K. R., Redden, D. T., Wang, C., Westfall, A. O. & Allison, D. B. Years of life lost due to obesity. JAMA 289 , 187–193 (2003).
PubMed Google Scholar
Berrington de Gonzalez, A. et al. Body-mass index and mortality among 1.46 million white adults. N. Engl. J. Med. 363 , 2211–2219 (2010).
CAS PubMed Google Scholar
Prospective Studies Collaboration. Body-mass index and cause-specific mortality in 900000 adults: collaborative analyses of 57 prospective studies. Lancet 373 , 1083–1096 (2009).
PubMed Central Google Scholar
Woolf, A. D. & Pfleger, B. Burden of major musculoskeletal conditions. Bull. World Health Organ. 81 , 646–656 (2003).
PubMed PubMed Central Google Scholar
Bray, G. A. et al. Obesity: a chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes. Rev. 18 , 715–723 (2017).
World Health Organization. Obesity and overweight. WHO https://www.who.int/mediacentre/factsheets/fs311/en/ (2016).
World Health Organization. Political declaration of the high-level meeting of the general assembly on the prevention and control of non-communicable diseases. WHO https://www.who.int/nmh/events/un_ncd_summit2011/political_declaration_en.pdf (2012).
Franco, M. et al. Population-wide weight loss and regain in relation to diabetes burden and cardiovascular mortality in Cuba 1980-2010: repeated cross sectional surveys and ecological comparison of secular trends. BMJ 346 , f1515 (2013).
Swinburn, B. A. et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet 378 , 804–814 (2011).
Yanovski, J. A. Obesity: Trends in underweight and obesity — scale of the problem. Nat. Rev. Endocrinol. 14 , 5–6 (2018).
Heymsfield, S. B. & Wadden, T. A. Mechanisms, pathophysiology, and management of obesity. N. Engl. J. Med. 376 , 254–266 (2017).
Murray, S., Tulloch, A., Gold, M. S. & Avena, N. M. Hormonal and neural mechanisms of food reward, eating behaviour and obesity. Nat. Rev. Endocrinol. 10 , 540–552 (2014).
Farooqi, I. S. Defining the neural basis of appetite and obesity: from genes to behaviour. Clin. Med. 14 , 286–289 (2014).
Google Scholar
Anand, B. K. & Brobeck, J. R. Hypothalamic control of food intake in rats and cats. Yale J. Biol. Med. 24 , 123–140 (1951).
CAS PubMed PubMed Central Google Scholar
Zhang, Y. et al. Positional cloning of the mouse obese gene and its human homologue. Nature 372 , 425–432 (1994).
Coleman, D. L. & Hummel, K. P. Effects of parabiosis of normal with genetically diabetic mice. Am. J. Physiol. 217 , 1298–1304 (1969).
Farooqi, I. S. & O’Rahilly, S. 20 years of leptin: human disorders of leptin action. J. Endocrinol. 223 , T63–T70 (2014).
Börjeson, M. The aetiology of obesity in children. A study of 101 twin pairs. Acta Paediatr. Scand. 65 , 279–287 (1976).
Stunkard, A. J., Harris, J. R., Pedersen, N. L. & McClearn, G. E. The body-mass index of twins who have been reared apart. N. Engl. J. Med. 322 , 1483–1487 (1990).
Montague, C. T. et al. Congenital leptin deficiency is associated with severe early-onset obesity in humans. Nature 387 , 903–908 (1997).
Farooqi, I. S. et al. Effects of recombinant leptin therapy in a child with congenital leptin deficiency. N. Engl. J. Med. 341 , 879–884 (1999).
Clément, K. et al. A mutation in the human leptin receptor gene causes obesity and pituitary dysfunction. Nature 392 , 398–401 (1998).
Farooqi, I. S. et al. Dominant and recessive inheritance of morbid obesity associated with melanocortin 4 receptor deficiency. J. Clin. Invest. 106 , 271–279 (2000).
Krude, H. et al. Severe early-onset obesity, adrenal insufficiency and red hair pigmentation caused by POMC mutations in humans. Nat. Genet. 19 , 155–157 (1998).
Hebebrand, J., Volckmar, A. L., Knoll, N. & Hinney, A. Chipping away the ‘missing heritability’: GIANT steps forward in the molecular elucidation of obesity - but still lots to go. Obes. Facts 3 , 294–303 (2010).
Speliotes, E. K. et al. Association analyses of 249,796 individuals reveal 18 new loci associated with body mass index. Nat. Genet. 42 , 937–948 (2010).
Sharma, A. M. & Padwal, R. Obesity is a sign - over-eating is a symptom: an aetiological framework for the assessment and management of obesity. Obes. Rev. 11 , 362–370 (2010).
Berthoud, H. R., Münzberg, H. & Morrison, C. D. Blaming the brain for obesity: integration of hedonic and homeostatic mechanisms. Gastroenterology 152 , 1728–1738 (2017).
Government Office for Science. Foresight. Tackling obesities: future choices – project report. GOV.UK https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/287937/07-1184x-tackling-obesities-future-choices-report.pdf (2007).
World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th revision. WHO http://apps.who.int/classifications/icd10/browse/2010/en (2010).
Hebebrand, J. et al. A proposal of the European Association for the Study of Obesity to improve the ICD-11 diagnostic criteria for obesity based on the three dimensions. Obes. Facts 10 , 284–307 (2017).
Ramos Salas, X. et al. Addressing weight bias and discrimination: moving beyond raising awareness to creating change. Obes. Rev. 18 , 1323–1335 (2017).
Sharma, A. M. et al. Conceptualizing obesity as a chronic disease: an interview with Dr. Arya Sharma. Adapt. Phys. Activ Q. 35 , 285–292 (2018).
Hebebrand, J. et al. “Eating addiction”, rather than “food addiction”, better captures addictive-like eating behavior. Neurosci. Biobehav. Rev. 47 , 295–306 (2014).
Phelan, S. M. et al. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes. Rev. 16 , 319–326 (2015).
Kushner, R. F. et al. Obesity coverage on medical licensing examinations in the United States. What is being tested? Teach Learn. Med. 29 , 123–128 (2017).
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 390 , 2627–2642 (2017).
NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 387 , 1377–1396 (2016).
Organisation for Economic Co-operation and Development. Obesity update 2017. OECD https://www.oecd.org/els/health-systems/Obesity-Update-2017.pdf (2017).
Geserick, M. et al. BMI acceleration in early childhood and risk of sustained obesity. N. Engl. J. Med. 379 , 1303–1312 (2018).
Ezzati, M. & Riboli, E. Behavioral and dietary risk factors for noncommunicable diseases. N. Engl. J. Med. 369 , 954–964 (2013).
Kleinert, S. & Horton, R. Rethinking and reframing obesity. Lancet 385 , 2326–2328 (2015).
Roberto, C. A. et al. Patchy progress on obesity prevention: emerging examples, entrenched barriers, and new thinking. Lancet 385 , 2400–2409 (2015).
Lundborg, P., Nystedt, P. & Lindgren, B. Getting ready for the marriage market? The association between divorce risks and investments in attractive body mass among married Europeans. J. Biosoc. Sci. 39 , 531–544 (2007).
McCabe, M. P. et al. Socio-cultural agents and their impact on body image and body change strategies among adolescents in Fiji, Tonga, Tongans in New Zealand and Australia. Obes. Rev. 12 , 61–67 (2011).
Hayashi, F., Takimoto, H., Yoshita, K. & Yoshiike, N. Perceived body size and desire for thinness of young Japanese women: a population-based survey. Br. J. Nutr. 96 , 1154–1162 (2006).
Hardin, J., McLennan, A. K. & Brewis, A. Body size, body norms and some unintended consequences of obesity intervention in the Pacific islands. Ann. Hum. Biol. 45 , 285–294 (2018).
Monteiro, C. A., Conde, W. L. & Popkin, B. M. Income-specific trends in obesity in Brazil: 1975–2003. Am. J. Public Health 97 , 1808–1812 (2007).
Mariapun, J., Ng, C. W. & Hairi, N. N. The gradual shift of overweight, obesity, and abdominal obesity towards the poor in a multi-ethnic developing country: findings from the Malaysian National Health and Morbidity Surveys. J. Epidemiol. 28 , 279–286 (2018).
Gebrie, A., Alebel, A., Zegeye, A., Tesfaye, B. & Ferede, A. Prevalence and associated factors of overweight/ obesity among children and adolescents in Ethiopia: a systematic review and meta-analysis. BMC Obes. 5 , 19 (2018).
Rokholm, B., Baker, J. L. & Sørensen, T. I. The levelling off of the obesity epidemic since the year 1999 — a review of evidence and perspectives. Obes. Rev. 11 , 835–846 (2010).
Hauner, H. et al. Overweight, obesity and high waist circumference: regional differences in prevalence in primary medical care. Dtsch. Arztebl. Int. 105 , 827–833 (2008).
Myers, C. A. et al. Regional disparities in obesity prevalence in the United States: a spatial regime analysis. Obesity 23 , 481–487 (2015).
Wilkinson, R. G. & Pickett, K. The Spirit Level: Why More Equal Societies Almost Always Do Better 89–102 (Bloomsbury Press London, 2009).
Sarget, M. Why inequality is fatal. Nature 458 , 1109–1110 (2009).
Plachta-Danielzik, S. et al. Determinants of the prevalence and incidence of overweight in children and adolescents. Public Health Nutr. 13 , 1870–1881 (2010).
Bell, A. C., Ge, K. & Popkin, B. M. The road to obesity or the path to prevention: motorized transportation and obesity in China. Obes. Res. 10 , 277–283 (2002).
Ludwig, J. et al. Neighborhoods, obesity, and diabetes — a randomized social experiment. N. Engl. J. Med. 365 , 1509–1519 (2011).
Beyerlein, A., Kusian, D., Ziegler, A. G., Schaffrath-Rosario, A. & von Kries, R. Classification tree analyses reveal limited potential for early targeted prevention against childhood overweight. Obesity 22 , 512–517 (2014).
Reilly, J. J. et al. Early life risk factors for obesity in childhood: cohort study. BMJ 330 , 1357 (2005).
Kopelman, P. G. Obesity as a medical problem. Nature 404 , 635–643 (2000).
CAS Google Scholar
Bouchard, C. et al. The response to long-term overfeeding in identical twins. N. Engl. J. Med. 322 , 1477–1482 (1990).
Sadeghirad, B., Duhaney, T., Motaghipisheh, S., Campbell, N. R. & Johnston, B. C. Influence of unhealthy food and beverage marketing on children’s dietary intake and preference: a systematic review and meta-analysis of randomized trials. Obes. Rev. 17 , 945–959 (2016).
Gilbert-Diamond, D. et al. Television food advertisement exposure and FTO rs9939609 genotype in relation to excess consumption in children. Int. J. Obes. 41 , 23–29 (2017).
Frayling, T. M. et al. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science 316 , 889–894 (2007).
Loos, R. J. F. & Yeo, G. S. H. The bigger picture of FTO-the first GWAS-identified obesity gene. Nat. Rev. Endocrinol. 10 , 51–61 (2014).
Wardle, J. et al. Obesity associated genetic variation in FTO is associated with diminished satiety. J. Clin. Endocrinol. Metab. 93 , 3640–3643 (2008).
Tanofsky-Kraff, M. et al. The FTO gene rs9939609 obesity-risk allele and loss of control over eating. Am. J. Clin. Nutr. 90 , 1483–1488 (2009).
Hess, M. E. et al. The fat mass and obesity associated gene (Fto) regulates activity of the dopaminergic midbrain circuitry. Nat. Neurosci. 16 , 1042–1048 (2013).
Fredriksson, R. et al. The obesity gene, FTO, is of ancient origin, up-regulated during food deprivation and expressed in neurons of feeding-related nuclei of the brain. Endocrinology 149 , 2062–2071 (2008).
Cohen, D. A. Neurophysiological pathways to obesity: below awareness and beyond individual control. Diabetes 57 , 1768–1773 (2008).
Richard, D. Cognitive and autonomic determinants of energy homeostasis in obesity. Nat. Rev. Endocrinol. 11 , 489–501 (2015).
Clemmensen, C. et al. Gut-brain cross-talk in metabolic control. Cell 168 , 758–774 (2017).
Timper, K. & Brüning, J. C. Hypothalamic circuits regulating appetite and energy homeostasis: pathways to obesity. Dis. Model. Mech. 10 , 679–689 (2017).
Kim, K. S., Seeley, R. J. & Sandoval, D. A. Signalling from the periphery to the brain that regulates energy homeostasis. Nat. Rev. Neurosci. 19 , 185–196 (2018).
Cutler, D. M., Glaeser, E. L. & Shapiro, J. M. Why have Americans become more obese? J. Econ. Perspect. 17 , 93–118 (2003).
Löffler, A. et al. Effects of psychological eating behaviour domains on the association between socio-economic status and BMI. Public Health Nutr. 20 , 2706–2712 (2017).
Chan, R. S. & Woo, J. Prevention of overweight and obesity: how effective is the current public health approach. Int. J. Environ. Res. Public Health 7 , 765–783 (2010).
Hsueh, W. C. et al. Analysis of type 2 diabetes and obesity genetic variants in Mexican Pima Indians: marked allelic differentiation among Amerindians at HLA. Ann. Hum. Genet. 82 , 287–299 (2018).
Schulz, L. O. et al. Effects of traditional and western environments on prevalence of type 2 diabetes in Pima Indians in Mexico and the US. Diabetes Care 29 , 1866–1871 (2006).
Rotimi, C. N. et al. Distribution of anthropometric variables and the prevalence of obesity in populations of west African origin: the International Collaborative Study on Hypertension in Blacks (ICSHIB). Obes. Res. 3 , 95–105 (1995).
Durazo-Arvizu, R. A. et al. Rapid increases in obesity in Jamaica, compared to Nigeria and the United States. BMC Public Health 8 , 133 (2008).
Hu, F. B., Li, T. Y., Colditz, G. A., Willett, W. C. & Manson, J. E. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA 289 , 1785–1791 (2003).
Rissanen, A. M., Heliövaara, M., Knekt, P., Reunanen, A. & Aromaa, A. Determinants of weight gain and overweight in adult Finns. Eur. J. Clin. Nutr. 45 , 419–430 (1991).
Zimmet, P. Z., Arblaster, M. & Thoma, K. The effect of westernization on native populations. Studies on a Micronesian community with a high diabetes prevalence. Aust. NZ J. Med. 8 , 141–146 (1978).
Ulijaszek, S. J. Increasing body size among adult Cook Islanders between 1966 and 1996. Ann. Hum. Biol. 28 , 363–373 (2001).
Snowdon, W. & Thow, A. M. Trade policy and obesity prevention: challenges and innovation in the Pacific Islands. Obes. Rev. 14 , 150–158 (2013).
McLennan, A. K. & Ulijaszek, S. J. Obesity emergence in the Pacific islands: why understanding colonial history and social change is important. Public Health Nutr. 18 , 1499–1505 (2015).
Becker, A. E., Gilman, S. E. & Burwell, R. A. Changes in prevalence of overweight and in body image among Fijian women between 1989 and 1998. Obes. Res. 13 , 110–117 (2005).
Swinburn, B., Sacks, G. & Ravussin, E. Increased food energy supply is more than sufficient to explain the US epidemic of obesity. Am. J. Clin. Nutr. 90 , 1453–1456 (2009).
Swinburn, B. A. et al. Estimating the changes in energy flux that characterize the rise in obesity prevalence. Am. J. Clin. Nutr. 89 , 1723–1728 (2009).
US Department of Agriculture. Food availability (per capita) data system. USDA https://www.ers.usda.gov/data-products/food-availability-per-capita-data-system/ (updated 29 Oct 2018).
Carden, T. J. & Carr, T. P. Food availability of glucose and fat, but not fructose, increased in the U.S. between 1970 and 2009: analysis of the USDA food availability data system. Nutr. J. 12 , 130 (2013).
Hall, K. D., Guo, J., Dore, M. & Chow, C. C. The progressive increase of food waste in America and its environmental impact. PLOS ONE 4 , e7940 (2009).
Scarborough, P. et al. Increased energy intake entirely accounts for increase in body weight in women but not in men in the UK between 1986 and 2000. Br. J. Nutr. 105 , 1399–1404 (2011).
McGinnis, J. M. & Nestle, M. The Surgeon General’s report on nutrition and health: policy implications and implementation strategies. Am. J. Clin. Nutr. 49 , 23–28 (1989).
Krebs-Smith, S. M., Reedy, J. & Bosire, C. Healthfulness of the U.S. food supply: little improvement despite decades of dietary guidance. Am. J. Prev. Med. 38 , 472–477 (2010).
Malik, V. S., Popkin, B. M., Bray, G. A., Després, J. P. & Hu, F. B. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation 121 , 1356–1364 (2010).
Schulze, M. B. et al. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA 292 , 927–934 (2004).
Mozaffarian, D., Hao, T., Rimm, E. B., Willett, W. C. & Hu, F. B. Changes in diet and lifestyle and long-term weight gain in women and men. N. Engl. J. Med. 364 , 2392–2404 (2011).
Malik, V. S. & Hu, F. B. Sugar-sweetened beverages and health: where does the evidence stand? Am. J. Clin. Nutr. 94 , 1161–1162 (2011).
Qi, Q. et al. Sugar-sweetened beverages and genetic risk of obesity. N. Engl. J. Med. 367 , 1387–1396 (2012).
Heiker, J. T. et al. Identification of genetic loci associated with different responses to high-fat diet-induced obesity in C57BL/6N and C57BL/6J substrains. Physiol. Genomics 46 , 377–384 (2014).
Wahlqvist, M. L. et al. Early-life influences on obesity: from preconception to adolescence. Ann. NY Acad. Sci. 1347 , 1–28 (2015).
Rohde, K. et al. Genetics and epigenetics in obesity. Metabolism . https://doi.org/10.1016/j.metabol.2018.10.007 (2018).
Article PubMed Google Scholar
Panzeri, I. & Pospisilik, J. A. Epigenetic control of variation and stochasticity in metabolic disease. Mol. Metab. 14 , 26–38 (2018).
Ruiz-Hernandez, A. et al. Environmental chemicals and DNA methylation in adults: a systematic review of the epidemiologic evidence. Clin. Epigenet. 7 , 55 (2015).
Quarta, C., Schneider, R. & Tschöp, M. H. Epigenetic ON/OFF switches for obesity. Cell 164 , 341–342 (2016).
Dalgaard, K. et al. Trim28 haploinsufficiency triggers bi-stable epigenetic obesity. Cell 164 , 353–364 (2015).
Michaelides, M. et al. Striatal Rgs4 regulates feeding and susceptibility to diet-induced obesity. Mol. Psychiatry . https://doi.org/10.1038/s41380-018-0120-7 (2018).
Article PubMed PubMed Central Google Scholar
Weihrauch-Blüher, S. et al. Current guidelines for obesity prevention in childhood and adolescence. Obes. Facts 11 , 263–276 (2018).
Nakamura, R. et al. Evaluating the 2014 sugar-sweetened beverage tax in Chile: An observational study in urban areas. PLOS Med. 15 , e1002596 (2018).
Colchero, M. A., Molina, M. & Guerrero-López, C. M. After Mexico implemented a tax, purchases of sugar-sweetened beverages decreased and water increased: difference by place of residence, household composition, and income level. J. Nutr. 147 , 1552–1557 (2017).
Brownell, K. D. & Warner, K. E. The perils of ignoring history: Big Tobacco played dirty and millions died. How similar is Big Food? Milbank Q. 87 , 259–294 (2009).
Mialon, M., Swinburn, B., Allender, S. & Sacks, G. ‘Maximising shareholder value’: a detailed insight into the corporate political activity of the Australian food industry. Aust. NZ J. Public Health 41 , 165–171 (2017).
Peeters, A. Obesity and the future of food policies that promote healthy diets. Nat. Rev. Endocrinol. 14 , 430–437 (2018).
Hawkes, C., Jewell, J. & Allen, K. A food policy package for healthy diets and the prevention of obesity and diet-related non-communicable diseases: the NOURISHING framework. Obes. Rev. 14 (Suppl. 2), 159–168 (2013).
World Health Organisation. Global database on the Implementation of Nutrition Action (GINA). WHO https://www.who.int/nutrition/gina/en/ (2012).
Popkin, B., Monteiro, C. & Swinburn, B. Overview: Bellagio Conference on program and policy options for preventing obesity in the low- and middle-income countries. Obes. Rev. 14 (Suppl. 2), 1–8 (2013).
Download references
Reviewer information
Nature Reviews Endocrinology thanks G. Bray, A. Sharma and H. Toplak for their contribution to the peer review of this work.
Author information
Authors and affiliations.
Department of Medicine, University of Leipzig, Leipzig, Germany
Matthias Blüher
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Matthias Blüher .
Ethics declarations
Competing interests.
The author declares no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Blüher, M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol 15 , 288–298 (2019). https://doi.org/10.1038/s41574-019-0176-8
Download citation
Published : 27 February 2019
Issue Date : May 2019
DOI : https://doi.org/10.1038/s41574-019-0176-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Body composition, lifestyle, and depression: a prospective study in the uk biobank.
BMC Public Health (2024)
Physical activity, gestational weight gain in obese patients with early gestational diabetes and the perinatal outcome – a randomised–controlled trial
- Lukasz Adamczak
- Urszula Mantaj
- Ewa Wender-Ozegowska
BMC Pregnancy and Childbirth (2024)
Effects of N-acetylcysteine on the expressions of UCP1 and factors related to thyroid function in visceral adipose tissue of obese adults: a randomized, double-blind clinical trial
- Mohammad Hassan Sohouli
- Ghazaleh Eslamian
Genes & Nutrition (2024)
Effect of COVID-19 Pandemic Lockdowns on Body Mass Index of Primary School Children from Different Socioeconomic Backgrounds
- Ludwig Piesch
- Robert Stojan
- Till Utesch
Sports Medicine - Open (2024)

Prevalence and risk factors of obesity among undergraduate student population in Ghana: an evaluation study of body composition indices
- Christian Obirikorang
- Evans Asamoah Adu
- Lois Balmer
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Epidemiology
The causes of obesity: an in-depth review
- 10(4):90-94

- Northampton General Hospital NHS Trust
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Dent Update

- Ali Alqarni

- Zulika Arshad

- Sherzad Abdulahad Shabu Shabu
- Mohammad F. Hashim
- Fatima S. Sabah

- INT J OBESITY

- Unurjargal Galindev

- Galindev Batnasan

- Nadya Shinta Nandra
- Steven Tandiono

- Kristin J Serodio

- Chaoyang Li

- M. P. H. James
- SEMIN REPROD MED

- Forum Health Econ Pol

- Albert J. Stunkard
- Thorkild I. A. Sørensen

- Fini Schulsinger
- Andrew M Prentice
- Susan A Jebb
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
10.8 Cause and Effect
Learning objectives.
- Determine the purpose and structure of cause and effect in writing.
- Understand how to write a cause-and-effect essay.
The Purpose of Cause and Effect in Writing
It is often considered human nature to ask, “why?” and “how?” We want to know how our child got sick so we can better prevent it from happening in the future, or why our colleague a pay raise because we want one as well. We want to know how much money we will save over the long term if we buy a hybrid car. These examples identify only a few of the relationships we think about in our lives, but each shows the importance of understanding cause and effect.
A cause is something that produces an event or condition; an effect is what results from an event or condition. The purpose of the cause-and-effect essay is to determine how various phenomena relate in terms of origins and results. Sometimes the connection between cause and effect is clear, but often determining the exact relationship between the two is very difficult. For example, the following effects of a cold may be easily identifiable: a sore throat, runny nose, and a cough. But determining the cause of the sickness can be far more difficult. A number of causes are possible, and to complicate matters, these possible causes could have combined to cause the sickness. That is, more than one cause may be responsible for any given effect. Therefore, cause-and-effect discussions are often complicated and frequently lead to debates and arguments.
Use the complex nature of cause and effect to your advantage. Often it is not necessary, or even possible, to find the exact cause of an event or to name the exact effect. So, when formulating a thesis, you can claim one of a number of causes or effects to be the primary, or main, cause or effect. As soon as you claim that one cause or one effect is more crucial than the others, you have developed a thesis.
Consider the causes and effects in the following thesis statements. List a cause and effect for each one on your own sheet of paper.
- The growing childhood obesity epidemic is a result of technology.
- Much of the wildlife is dying because of the oil spill.
- The town continued programs that it could no longer afford, so it went bankrupt.
- More young people became politically active as use of the Internet spread throughout society.
- While many experts believed the rise in violence was due to the poor economy, it was really due to the summer-long heat wave.
Write three cause-and-effect thesis statements of your own for each of the following five broad topics.
- Health and nutrition
The Structure of a Cause-and-Effect Essay
The cause-and-effect essay opens with a general introduction to the topic, which then leads to a thesis that states the main cause, main effect, or various causes and effects of a condition or event.
The cause-and-effect essay can be organized in one of the following two primary ways:
- Start with the cause and then talk about the effects.
- Start with the effect and then talk about the causes.
For example, if your essay were on childhood obesity, you could start by talking about the effect of childhood obesity and then discuss the cause or you could start the same essay by talking about the cause of childhood obesity and then move to the effect.
Regardless of which structure you choose, be sure to explain each element of the essay fully and completely. Explaining complex relationships requires the full use of evidence, such as scientific studies, expert testimony, statistics, and anecdotes.
Because cause-and-effect essays determine how phenomena are linked, they make frequent use of certain words and phrases that denote such linkage. See Table 10.4 “Phrases of Causation” for examples of such terms.
Table 10.4 Phrases of Causation
| as a result | consequently |
| because | due to |
| hence | since |
| thus | therefore |
The conclusion should wrap up the discussion and reinforce the thesis, leaving the reader with a clear understanding of the relationship that was analyzed.
Be careful of resorting to empty speculation. In writing, speculation amounts to unsubstantiated guessing. Writers are particularly prone to such trappings in cause-and-effect arguments due to the complex nature of finding links between phenomena. Be sure to have clear evidence to support the claims that you make.
Look at some of the cause-and-effect relationships from Note 10.83 “Exercise 2” . Outline the links you listed. Outline one using a cause-then-effect structure. Outline the other using the effect-then-cause structure.
Writing a Cause-and-Effect Essay
Choose an event or condition that you think has an interesting cause-and-effect relationship. Introduce your topic in an engaging way. End your introduction with a thesis that states the main cause, the main effect, or both.
Organize your essay by starting with either the cause-then-effect structure or the effect-then-cause structure. Within each section, you should clearly explain and support the causes and effects using a full range of evidence. If you are writing about multiple causes or multiple effects, you may choose to sequence either in terms of order of importance. In other words, order the causes from least to most important (or vice versa), or order the effects from least important to most important (or vice versa).
Use the phrases of causation when trying to forge connections between various events or conditions. This will help organize your ideas and orient the reader. End your essay with a conclusion that summarizes your main points and reinforces your thesis. See Chapter 15 “Readings: Examples of Essays” to read a sample cause-and-effect essay.
Choose one of the ideas you outlined in Note 10.85 “Exercise 3” and write a full cause-and-effect essay. Be sure to include an engaging introduction, a clear thesis, strong evidence and examples, and a thoughtful conclusion.
Key Takeaways
- The purpose of the cause-and-effect essay is to determine how various phenomena are related.
- The thesis states what the writer sees as the main cause, main effect, or various causes and effects of a condition or event.
The cause-and-effect essay can be organized in one of these two primary ways:
- Start with the cause and then talk about the effect.
- Start with the effect and then talk about the cause.
- Strong evidence is particularly important in the cause-and-effect essay due to the complexity of determining connections between phenomena.
- Phrases of causation are helpful in signaling links between various elements in the essay.
Writing for Success Copyright © 2015 by University of Minnesota is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License , except where otherwise noted.

Band 8 Sample | Causes of Obesity
Essay topic
In some countries the average weight of people is increasing and their levels of health and fitness are decreasing. What do you think are the causes of these problems and what measures could be taken to solve them?
Band 8 essay sample
It is a fact that in some countries, the average weight of the citizens is shooting up while their fitness and health conditions are worsening. In my view this is mainly because of the food habits and modern lifestyle they follow. In this essay, I will examine these two factors and then propose a viable solution.
One of the foremost reasons for obesity is the consumption of unhealthy foods. Many people started to follow western food habits and eventually ended up eating high fat content foods like pizza and burger. Regular consumption of these fat rich foods will increase a person’s weight in a short span of time.
In addition to that, now-a-days, more and more people are living a sedentary lifestyle. They do not dedicate any time to do any kind of physical activity. As a result, they lose their resistance power. If this lifestyle continues then people will fall ill more frequently and lose their health permanently.
It is necessary that the government takes steps to open many sports complexes and fitness studios near residential communities. Most of the people who do not want to travel far to go to a sports center will be ready to use one if it is available nearby. In a study conducted by a popular newspaper 90% of the respondents said that they are willing to use the gym or any physical activity centers if they are within 3 kilometer radius.
To conclude, encouraging people to do more physical activities will not only improve their fitness and overall health but also help people to shed their weight.
(265 words)
Share with friends
Scan below qr code to share with your friends, related ielts tips.

Essay Writing Evaluation with model answer for band 8
Here’s a recently asked Essay Writing Question- Most countries...

Self-employment is better than a job in a company
Some people say that self-employment is better than a job in a company...

Essay Writing Evaluation for Band 8 with model answer
here’s one more Essay Writing Evaluation question.The question...

The following is an essay submitted by one of our students. In some countries,...
Band 8 Sample About The Advantages And Disadvantages Of English As A Global Language
The advantages provided by English as a global language will continue to...
Thank you for contacting us!
We have received your message.
We will get back within 48 hours.
You have subscribed successfully.
Thank you for your feedback, we will investigate and resolve the issue within 48 hours.
Your answers has been saved successfully.
Add Credits
You do not have enough iot credits.
Your account does not have enough IOT Credits to complete the order. Please purchase IOT Credits to continue.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Gastroenterol Hepatol (N Y)
- v.6(12); 2010 Dec
The Obesity Epidemic: Challenges, Health Initiatives, and Implications for Gastroenterologists
Ryan t. hurt.
Dr. Hurt serves as an Assistant Professor of Medicine in the Division of General Internal Medicine at the Mayo Clinic in Rochester, Minnesota, and as Assistant Clinical Professor in the Department of Medicine at the University of Louisville School of Medicine in Louisville, Kentucky.
Christopher Kulisek
Dr. Kulisek is a Gastroenterology Fellow in the Department of Medicine at the University of Louisville School of Medicine in Louisville, Kentucky.
Laura A. Buchanan
Dr. Buchanan serves as a Resident in the Department of Medicine at the University of Louisville School of Medicine in Louisville, Kentucky.
Stephen A. McClave
Dr. McClave is a Professor of Medicine in the Division of Gastroenterology, Hepatology, and Nutrition at the University of Louisville School of Medicine in Louisville, Kentucky.
Obesity is the next major epidemiologic challenge facing today's doctors, with the annual allocation of healthcare resources for the disease and related comorbidities projected to exceed $150 billion in the United States. The incidence of obesity has risen in the United States over the past 30 years; 60% of adults are currently either obese or overweight. Obesity is associated with a higher incidence of a number of diseases, including diabetes, cardiovascular disease, and cancer. Consumption of fast food, trans fatty acids (TFAs), and fructose—combined with increasing portion sizes and decreased physical activity—has been implicated as a potential contributing factor in the obesity crisis. The use of body mass index (BMI) alone is of limited utility for predicting adverse cardiovascular outcomes, but the utility of this measure may be strengthened when combined with waist circumference and other anthropomorphic measurements. Certain public health initiatives have helped to identify and reduce some of the factors contributing to obesity. In New York City and Denmark, for example, such initiatives have succeeded in passing legislation to reduce or remove TFAs from residents' diets. The obesity epidemic will likely change practice for gastroenterologists, as shifts will be seen in the incidence of obesity-related gastrointestinal disorders, disease severity, and the nature of comorbidities. The experience gained with previous epidemiologic problems such as smoking should help involved parties to expand needed health initiatives and increase the likelihood of preventing future generations from suffering the consequences of obesity.
Obesity has been defined as a body mass index (BMI) greater than 30 kg/m 2 , with extreme obesity defined as a BMI greater than 40 kg/m 2 . Obesity is rapidly becoming the leading cause of preventable death in the United States, with obesity-related deaths projected to soon surpass deaths related to tobacco abuse. The incidence of obesity has doubled in the United States since 1960, with one third of the adult population currently obese. 1 , 2 Perhaps more alarming is the increase in overweight children; over the past 25 years, this rate has risen from 6% to 19%. 3 , 4
Numerous comorbid conditions have been associated with obesity, including type 2 diabetes, hypertension, hypercholesterolemia, hypertriglyceridemia, and nonalcoholic fatty liver disease. As a result of these comorbidities, the medical costs directly related to obesity are difficult to determine, but a conservative estimate would place the healthcare burden for obesity at approximately $150 billion per year in the United States. 4 – 6 The increase in mortality among obese individuals is likely related to comorbid conditions, rather than obesity per se; because of their various obesity-associated conditions, obese patients present challenging and complex issues in medical and surgical intensive care units. In the current debate over healthcare reform in the United States, no proposed solution can reasonably ignore or minimize the role that obesity plays with regard to economic and health consequences.
This article will give an overview of the epidemiology of obesity, provide measures of defining obesity, and discuss the impact of public health and environmental factors associated with the marked increase in obesity. Potential health initiatives that might be successful in preventing obesity and its associated consequences in future generations will also be discussed. Finally, this article will address the implications that obesity has for gastroenterologists.
Obesity Epidemiology
In 2001, the US Surgeon General released a report raising concerns about the growing obesity epidemic; this report was the first to note that obesity and obesity-related diseases might soon overtake smoking as the leading cause of preventable death in the United States. The number of overweight (BMI >25 kg/m 2 ) and obese (BMI >30 kg/m 2 ) adults has increased dramatically in recent years. 4 , 7 , 8 The rate of adults between the ages of 20 and 74 years who were classified as either obese or overweight has risen from 44.9% in 1960–1962 to 66.2% in 2003–2004, with similar trends for both men and women. 4 , 7 , 8 The rate of individuals who were overweight but not obese ranged between 31.5% and 33.4% over the same time period. 4 The major shift in the prevalence of obesity occurred between 1980 and 2004, effectively doubling in just 25 years (from 15.0% in 1980 to 32.9% in 2004). The number of people who were classified as extremely obese (BMI >40 kg/m 2 ) increased from 0.9% in 1960 to 5.1% in 2004. 4 , 7
More concerning than the rise in obesity among adults is the increased prevalence of obesity among chil-dren. 3 , 4 , 8 In the United States, the prevalence of obesity in children has tripled in just 30 years; not surprisingly, rates of dyslipidemia and type 2 diabetes among children have shown a corresponding increase over the same time period. 9 In children, obesity is defined based on growth charts from the Centers for Disease Control and Prevention. For children aged 19 years or younger, obesity is defined as a weight at or above the 95th percentile for age; overweight children are those whose weight is between the 85th and 95th percentiles for age. In 1974, 5.1% of children were considered obese and 10.4% were considered overweight by these definitions. In 2008, 14.6% of children were considered obese. 4 , 8 , 10 , 11
The prevalence of obesity shows striking disparities with regard to race and ethnicity in both adults and children. 2 , 3 , 7 , 8 , 12 Between 1999 and 2004, the prevalence of obesity in non-Hispanic white adult women was 30.5%, compared to 39.8% in Mexican American women and 50.6% in non-Hispanic African American women. 4 Obesity rates in adult men showed no significant differences between ethnic groups. 4 The distribution of obesity among children aged 2–19 years with regard to race showed trends similar to those seen in adults. The prevalence of obesity was lower among non-Hispanic white children (13.9%) compared to non-Hispanic African American children (18.8%) and Mexican American children (19.7%). When gender and race were considered, significantly higher rates of obesity were seen in Mexican American boys (22.7%) than in non-Hispanic white boys (14.8%) or non-Hispanic African American boys (16.1%). Non-Hispanic African American girls had significantly higher rates of obesity (21.6%) than non-Hispanic white girls (13.0%).
While obesity is clearly a major public health issue in the United States, the increased prevalence of obesity is not limited to this country; indeed, obesity is now a global epidemic. Over the past 10 years, the World Health Organization (WHO) has recognized the increasing number of people who are overweight or obese, and attention is now being given to the global implications associated with this trend. In an analysis of the leading causes of global mortality and burden of disease, obesity and being overweight were among the top 10 causes for each. 13 The presence of a worldwide epidemic is suggested by the fact that in various regions of the world—North America, Central America, South America, most of Western Europe, the Middle East, and Eastern Europe—the majority of countries report that at least 40% of their population between the ages of 45 and 59 years are overweight or obese. 14 East Asian countries such as China, Japan, Vietnam, and India report lower rates of obesity, but the use of BMI alone may be problematic due to cultural and ethnic variability in adipose proportion and distribution. 15 In the latter geographic areas, rates of diabetes and cardiovascular disease (CVD) are increased at BMIs below the WHO cutoff for being overweight (25 kg/m 2 ), a phenomenon most likely linked to proportionate increases in body fat in these populations. 16 , 17
Body Mass Index as an Estimate of Obesity and Mortality
Using BMI alone to define obesity has been problematic in some settings, given differences in genetics, fat distribution, and percentage of body adiposity among various countries. Because Asian populations have a higher proportion of body fat, for example, lower BMIs have been proposed to identify individuals in these populations who are overweight or obese. 14 , 15 , 18 A cross-sectional study looking at 3 different ethnic groups in Singapore (Chinese, Malays, and Indians) demonstrated the limitations of using BMI alone to estimate body fat percentage. Compared to white subjects, BMI underestimated body fat percentage in Chinese, Malay, and Indian subjects, with the error ranging from 2.7% to 5.6%. Furthermore, Asians had a higher risk of developing diabetes and CVD and had increased mortality at normal BMIs compared to other ethnic groups. 15 , 19
Further problems occur when epidemiologic studies use self-reported data to calculate BMI. Many of the larger international studies used to estimate the number of overweight and obese individuals in foreign countries have used surveys involving self-reported heights and weights. 4 However, the use of self-reported data often results in inaccurate estimations of weight and height and, subsequently, inaccurate BMI values. 4 A study of 16,000 individuals examined the validity of self-reported data for BMI calculation. 20 In this study, subjects were asked to report their weight and height, after which these estimates were compared to measured values. On average, BMIs in older individuals were 1 unit lower when calculated using self-reported values compared to BMIs calculated using measured values. Furthermore, this self-reporting bias worsened as true BMI values increased. In a subsequent study of 6,000 individuals in the National Health and Nutrition Examination Epidemiological Study (NHANES), researchers found that every 1-unit increase in BMI correlated with a 2-lb underestimation of weight. 21 When gender was considered, men were found to overestimate their weight by 5.0 lbs, and women underestimated their weight by 1.8 lbs, on average. In an earlier French study of 7,250 individuals, values for both self-reported weight and height were inaccurate. 22 Weight was significantly underestimated (by a mean of 0.54 kg among men and 0.85 kg among women). In contrast, height was significantly overestimated (by a mean of 0.54 cm among men and 0.40 cm among women). This combination of errors led to an underestimation of BMI— by 0.29 kg/m 2 in men and 0.44 kg/m 2 in women—and an underestimation of the rate of individuals who were overweight, by 13% in men and 17% in women. 22
Large cohort studies have shown that elevated BMI has been associated with an increased risk of future cardiovascular events. 23 , 24 In the largest of these studies, over 1 million adults were prospectively followed for 14 years, and the cause of mortality was evaluated. When other risk factors such as smoking were removed from the analysis, higher BMIs were associated with an increased risk of mor-tality. 23 Among white men and women with a BMI above 40 kg/m 2 , the relative risk (RR) for mortality was 2.58 and 2.0, respectively, compared to individuals with a BMI in the normal range (22.9–24.9 kg/m 2 ). In a similar group of African American subjects with BMIs above 40 kg/m 2 , no increase in mortality was seen compared to normal-weight controls. When death from cardiovascular causes was evaluated, men with BMIs greater than 40 kg/m 2 had an increased risk of mortality compared to their lean counterparts (RR=2.90; 95% confidence interval [CI] 2.37–3.56).
In a subsequent large prospective cohort study of 527,265 US men and women between the ages of 50 and 71 years, researchers evaluated the association between BMI and death from any cause over a 10-year period (1996–2005). 24 Obesity was associated with an increase in mortality across all races and both genders. When individuals without preexisting cardiovascular conditions (including smoking) were isolated, overweight individuals still showed an increase in mortality. In a subcohort analysis of 50-year-old individuals who had never smoked, those who were morbidly obese (BMI >40 kg/m 2 ) had an increased risk of mortality (RR=3.82; 95% CI 2.87–5.08) compared to individuals with a BMI in the normal range (23–24.9 kg/m 2 ). While BMI is thus a useful predictor in some settings, how BMI compares to other anthropo-metric measurements in terms of accurately determining obesity, associated comorbid diseases, and respective mortality has been a topic of recent debate.
Central Adiposity
While the WHO still uses BMI to identify individuals who are overweight or obese, mounting evidence suggests that a pattern of central adiposity is more accurate in predicting obesity-related cardiovascular consequences. 25 – 33 In a large case-control study of 27,000 people in 52 countries, the correlation between myocardial infarction (MI) and either waist-to-hip ratio (WHR) or BMI was evaluated. WHR, waist circumference (WC), and hip circumference were individually associated with an increased risk of subsequent MI independent of other risk factors, including BMI. 27 When other cardiovascular risk factors and WHR were taken into account, there was no significant association between MI and BMI (odds ratio 0.98; 95% CI 0.88–1.09). The attributable risk for MI in the top 2 quintiles for WHR was 24.3% (95% CI 22.5–26.2%), compared to 7.7% in similar quintiles for BMI (95% CI 6.0–10%).
A recent cohort study examined the possibility of using WC, WHR, and BMI in conjunction with Framing-ham risk scores to predict coronary heart disease (CHD) and CVD mortality. A total of 4,175 Australian men who were free of CVD, CHD, diabetes, and stroke at baseline were followed for 15 years. 34 Baseline Framingham risk scores were calculated, and WC, WHR, and BMI measurements were taken. Initial Framingham scores were strong predictors of CVD and CHD deaths 15 years later. WHR was found to be an independent predictor of CVD and CHD deaths, and WC predicted CVD deaths. BMI did not predict mortality due to either CVD or CHD.
Two different meta-analyses evaluated measures of abdominal adiposity and their relationship to cardiac events, as well as their ability to predict the development of associated cardiac risk factors. In the first of these meta-analyses, BMI was compared to measures of central adiposity—including WHR, WC, and waist-to-height ratio (WHtR)—to determine the best predictor for development of hypertension, type 2 diabetes, and hyperlip-idemia. A total of 10 studies met the inclusion criteria, and a total of 88,514 adult subjects (54% female) in 9 countries were included in the meta-analysis. 35 WHtR was found to be the best discriminator for development of all 3 cardiovascular risk factors, while BMI was the worst. The majority of the patients included in this study were from Asia and the Middle East.
The second meta-analysis, which examined the association between WC or WHR and the incidence of CVD, included 258,114 patients from 15 randomized controlled trials (RCTs) or prospective cohort studies. For every 1-cm increase in WC, the RR of a cardiovascular event increased by 2% (95% CI 1–3%). WHR and WC were both associated with an increased risk of future cardiovascular events (WHR RR=1.95, 95% CI 1.55–2.44; WC RR=1.63, 95% CI 1.31–2.04).
In comparing these different measures of central adiposity, it is important to note that technical limitations can make it difficult to measure WHtR consistently. Although visceral adipose stores can be directly measured by computerized axial tomography, magnetic resonance imaging, or dual energy x-ray absorptiometry, the high cost of these tests limits their applicability in large epidemiologic studies. 36 , 37 In contrast, WC and WHR can be measured easily in the clinical setting and are not limited by cost or technical issues.
Health Burden and Obesity-associated Diseases
Several studies have shown a relationship between elevated BMI and chronic medical conditions such as diabetes mellitus, hypertension, hyperlipidemia, and obesity-related cancers. 38 – 40 Epidemiologic studies have also shown an association between adult obesity and premature death from all-cause mortality. 23 , 41 One study found that obesity was associated with a 7-year decrease in life expectancy for women and a 6-year decrease for men, which is similar to findings from past studies on smoking. 41 Furthermore, pediatric obesity is associated with many of the same cardiovascular risk factors as adult obesity, including hypertension, diabetes, metabolic syndrome, and hyperlipidemia. 42
Conversely, other studies have shown reduced mortality due to cardiovascular causes in obese patients compared to lean controls. These latter studies appear to reflect an increase in the diagnosis and early treatment of cardiovascular risk factors in this high-risk group more so than a decreased incidence of obesity-related comorbid conditions such as diabetes, hypertension, and hyperlipidemia. 43 These clinically significant outcomes are not restricted to medical fields, but also complicate surgical outcomes. Postoperative complications occur more frequently in obese patients than lean controls, with an increased incidence of MI, peripheral nerve injury, wound infection, and cardiac arrest. 44
In addition to the potential impact on mortality, the overall morbidity seen in this growing patient population remains a key issue contributing to decreased quality of life in overweight and obese individuals. Impairment in activities of daily living—such as eating, dressing, and transferring to and from a bed or wheelchair—occur at a younger age in obese patients compared to nonobese controls. 45 If overall mortality decreases but the diagnosis and treatment of obesity-related conditions continue to increase, the cost of managing the obese patient population could be overwhelming.
While the hazards of obesity have long been known, the benefits of weight loss and exercise have only recently become more apparent. One study investigated 3,234 nondiabetic patients with elevated fasting glucose levels and randomly assigned them to treatment with placebo, metformin, or lifestyle modification (including weight loss and exercise). Metformin reduced the likelihood of developing diabetes by 31%, whereas lifestyle modification reduced the chance of developing diabetes by 58% (with weight loss >7%). 46 A subsequent meta-analysis examining the effect of weight loss on blood pressure showed that for every 1 kg of weight lost, blood pressure dropped by 1.1 mmHg systolic/0.9 mmHg diastolic. 47 Additional meta-analyses have also demonstrated improvements in cardiovascular risk factors related to weight loss. 48 Loss of only 1 kg was shown to be associated with improvement in serum cholesterol (–1.0%), low-density lipoprotein cholesterol (–0.68%), triglycer-ides (–1.9%), and high-density lipoprotein cholesterol (+0.2%). Furthermore, loss of 5 kg was associated with a decrease in fasting plasma glucose levels of 18 mg/dL, an improvement similar to that achieved from treatment with current oral hypoglycemic agents. 48
Fast Food and Trans Fat
The parallel between the national and international expansion of fast food companies over the past 50 years and the growth of the obesity epidemic is no coincidence. The United States now has approximately 250,000 fast food restaurants, and total fast food consumption has risen from 2% to 10% of total energy intake per person over a 20-year period. 49 , 50 Surveys have revealed that the top 3 reasons US consumers choose fast food over healthier alternatives are: fast food is quick (92% of respondents), restaurants are easy to visit (80%), and the food tastes good (69%). 51 There remains debate about the degree to which fast food companies, with their provision of high trans-fat foods, are responsible for the obesity epidemic. 52 – 54 In a large, multicenter, prospective cohort study, 3,031 adults between the ages of 18 and 30 years were followed for 15 years to evaluate their fast food habits, development of insulin resistance, and changes in body weight. 50 Participants were drawn from 4 major US cities, included an equal number of African Americans and whites, and had variable levels of education. This study found a strong positive correlation between visits to fast food restaurants and weight gain with development of insulin resistance. 50 The average frequency of fast food intake was 1.3 times per week among white women and 2.0 times per week among other ethnic/gender groups. Higher baseline consumption of fast food was associated with increased weight gain after 15 years. Increased fast food consumption was also associated with significantly increased insulin resistance in all ethnic/gender groups. Other cross-sectional studies have shown similar associations between fast food intake and increased body weight. 55 , 56
The specific aspect of fast food consumption that contributes most to obesity and insulin resistance is currently the subject of much debate. One possibility is that the high caloric density of fast food is the sole culprit, but there may also be a specific component in fast food that contributes to the increased risk for obesity and diabetes. Fast food is indeed characterized by a high caloric density (energy content/food weight ratio), and the total caloric content of a typical fast food meal exceeds that of the average meal by 65%. 53 In addition to high caloric density, fast food has historically had higher amounts of industrially produced trans fatty acids (TFAs). Compared to other fats, TFAs have higher melting points, better taste, and longer shelf lives. 52 , 53 , 57 , 58 The lower rates of CVD in countries such as France, where use of TFAs is limited but total fat consumption remains high, has led to observational studies evaluating the link between TFAs and heart disease. 52 , 57 In the United States, an average daily intake of 5 g of TFAs has been estimated to increase an individual's risk of heart disease by 25%. 59 – 61 The Nurses Health Study found that intake of TFAs was directly related to risk of CHD, and a subsequent observational study of 21,930 Finnish men who were followed for 6 years found a positive correlation between TFA intake and risk of death from CHD. 62 , 63 Individuals in the top quintile of TFA intake (6.2 g/day) had a multivariate RR of 1.39 (95% CI 1.09–1.78) for death from CHD, compared to those in the lowest quintile of TFA intake (1.3 g/day).
The Expert Committee of the American Medical Association recently concluded that there is strong evidence that eating away from home, specifically consumption of fast food, is a risk factor for childhood obesity. 64 , 65 Fast food children's meals were first introduced in the late 1970s and have been very popular with toddlers and adolescents. 66 In terms of nutrient composition, fast food children's meals are high in total fat and TFAs, have high caloric density, and offer very little nutritional value. 66 A recent study examined the nutrient quality of fast food meals marketed to young children. 66 Criteria from the National School Lunch Program (NSLP) were used to analyze these meals in terms of their percentage of energy from fat and carbohydrates, overall energy density, and vitamin composition. Only 3% of the fast food children's meals met the NSLP criteria for healthy meals; those meals were offered with milk and fruit, and the majority were deli sandwich–based meals. 66 Children's meals are often offered with toys, which promotes brand recognition and repeated visits to the restaurant. 66 , 67 Given the nutritional composition of children's fast food meals, it is not surprising that obese and overweight children consume more meals away from home than normal-weight children. 68
In addition to children's fast food meals and the early brand recognition they build, children are bombarded with television advertising from fast food companies. Branding involves developing recognition and positive associations with a product. Studies have found that children aged 3–6 years view, understand, and remember advertising when cartoon characters are used. 67 , 69 One study examined the content of advertising contained in children's television programs on 3 popular networks (Public Broadcasting Service, Disney, and Nickelodeon) using randomly selected 4-hour blocks from 9 am to 1 pm. 67 In 96 half-hour blocks, there were 130 food-related advertisements (1.4 per half hour). Half of these advertisements were specifically aimed at children, with most from fast food companies. The fast food advertisements seemed to focus on building brand recognition and positive associations through the use of logos and cartoon characters. 67
In addition to fast food advertising directed at children, some evidence suggests that a disproportionate number of fast food restaurants are located in close proximity to schools. 70 Using the California Healthy Kids Survey of over 500,000 children, data were analyzed for specific questions about high-risk behaviors such as fast food consumption and proximity of fast food restaurants to home. The primary outcome in this study was BMI. 70 Students with fast food restaurants within 0.5 miles of their home were more likely to be overweight or obese. These children also consumed more soda and ate less fruits and vegetables. 70 Other studies have shown similar findings, demonstrating a link between increased rates of obesity in urban areas with a predominately poor, African American population and a high density of fast food restaurants, versus lower rates of obesity in white neighborhoods with large chain grocery stores. 71 , 72
Portion Distortion, Soft Drinks, and Fructose
The high caloric density and trans-fat content of fast food are only some of the factors contributing to the obesity epidemic. In the past 30 years, the portion sizes of many foods have increased, leading to increased energy intake. 73 – 76 Fast food companies have increased portion sizes 2- to 5-fold since the items were originally introduced over 50 years ago. 77 In response to the 2004 documentary Super Size Me, McDonald's announced plans to phase out their “Super Size” items. Despite this action, items on McDonald's current menu still dwarf the portion sizes introduced in 1955. These items include French fries (increased by 250%), soda (increased by 457%), and hamburgers (precooked weight increased by 500%). 77 Despite dropping the “Super Size” name, a large order of French fries in 2006 (6.0 oz) was only slightly smaller than the “Super Size” French fries served in 1998 (6.3 oz). Wendy's followed suit and dropped the “Biggie” label from its largest-portioned items, but this change was only in name. The “Great Biggie” French fries served in 2002 (6.7 oz) became large French fries in 2006 (6.7 oz), and the 2002 “Biggie Soda” (32 oz) increased in size to become the 2006 large soda (42 oz). The largest increase in portion sizes has come with the ever expanding size of hamburger options. 77 In 2003, Hardee's introduced the “Monster Thickburger,” with 1,420 calories, and Burger King's “Angry Triple Whopper” is the highest-calorie item on the restaurant's menu, with 1,360 calories.
Consumption of soft drinks has been linked with metabolic syndrome and cardiovascular risk based on the Framingham study. 78 The number of calories consumed in sodas and fruit juices has increased significantly over the past 30 years. 79 The largest study to show this trend examined beverage consumption in the United States among 73,335 individuals over the age of 2 years. 79 Overall energy intake from sweetened beverages increased by 135% from 1977 until 2001, increasing average daily caloric intake by 278 calories. During the same time period, milk consumption decreased by 38%. These trends coincided with the expansion of the obesity epidemic. Prospective studies have linked increased intake of sweetened beverages directly with increased weight gain. 80 , 81 The first of these studies enrolled 548 ethnically diverse students (average age of 11.7 years) from public schools in 4 Massachusetts communities and followed their consumption of sugar-sweetened beverages over 19 months. 81 For each additional serving of sweetened beverage consumed on a daily basis, BMI and the incidence of obesity were significantly increased. A second prospective study examined the effect of sucrose and artificial sweeteners on weight gain in a population of overweight adults. 80 Subjects were randomized to receive sucrose supplements (152 g sucrose/day) or artificial sweeteners (0 g sucrose/day) for 10 weeks. The change in weight differed significantly between groups, with the sucrose-supplement group gaining a mean of 1.6 kg, while the artificial-sweetener group lost a mean of 1.0 kg. A recent systematic review of prospective studies reached similar conclusions, finding that increased sugar-sweetened beverage consumption was associated with weight gain and obesity and proposing that strategies to reduce consumption of these beverages would likely help reverse the obesity epidemic. 82
The consumption of high fructose corn syrup (HFCS) has also been evaluated as a possible independent risk factor for the development of obesity. 83 Fructose typically comes from 3 main sources: sucrose, HFCS, and fruit. 84 The amount of fructose in fruit, which is relatively small compared to that in soft drinks, seems to serve the function of enticing individuals to consume other nutrients. In contrast, the HFCS added to soft drinks contains much higher concentrations of fructose and has no other nutritional benefits. Beyond adding excess calories to an individual's diet, fructose has also been linked to central adiposity, gout, and hyperlipidemia. 85 , 86 In 1 study, high fructose intake for 6 weeks was found to increase postprandial serum triglycerides by 32% compared to a similar diet of isocaloric high glucose intake. 87 These findings have been confirmed by other studies. 85 , 88 , 89
The amount of fructose consumed in the United States has increased over the past 30 years. An analysis of the NHANES database showed that in 1977 the average estimated daily intake of fructose was 37 g/day (8% of total daily calories). 90 Approximately 15 years later, the average daily intake of fructose had increased to 54.7 g/day (10.4% of total daily calories). Not surprisingly, adolescents have the highest daily consumption of fructose (72.8 g/day; 12.1% of total daily calories), and 25% of adolescents receive more than 15% of their total daily calories from fructose. 90 The correlation between obesity and soft drink consumption alone warrants limiting the amount of HFCS in an individual's diet.
Physical Inactivity
Physical activity (PA) has been suggested as an essential requirement for decreasing the incidence of obesity and reducing the number of overweight individuals. 91 Certainly, PA in any form helps to tip the balance of energy consumption versus energy expenditure in a favorable direction. A study using the NHANES database found that adults who reported low levels of PA were more likely to have gained significant weight over the previous 10-year period. Self-reported levels of PA (low, medium, or high) were compared to change in weight after 10 years. Individuals who reported low PA at the follow-up visit were more likely to have experienced major weight gain (greater than 13 kg). The study found no significant correlation between baseline PA and subsequent weight gain. 91 Looking at this relationship prospectively, another study measured 24-hour energy expenditure and future weight gain in 95 people. 92 Individuals with low 24-hour energy expenditure (200 kcal below predicted values) were 4 times more likely to gain at least 7.5 kg over a 2-year period compared to individuals with high 24-hour energy expenditure (200 kcal above predicted values). 92
The role that PA has played in the rise in adolescent obesity over the past 20 years has been the subject of considerable debate. A recent analysis of PA showed no clear decline in PA among adolescents over the past 20 years. 93 This analysis examined 7 large studies from the Youth Risk Behavior Surveillance Surveys from 1991 to 2007. Vigorous PA was defined as any activity that caused increased sweating and a sensation of breathing hard for more than 20 minutes during 3 of the previous 7 days. The amount of vigorous PA reported by adolescents did not differ significantly between 1993 (65.8%) and 2005 (64.1%). Furthermore, the adolescent attendance rate for physical education class and the amount of exercising for over 20 minutes during class has significantly increased in recent years, and the amount of television viewing has significantly decreased. 93 These data call into question the role that PA has played in the increase in obesity among adolescents.
One of the factors thought to be responsible for decreased PA is the increase in time spent watching television. A recent study examined the role of increased television viewing on all-cause and cardiovascular mortality. 94 A total of 8,800 adults followed for a median of 6.6 years were evaluated for numerous cardiovascular risk factors. This study found a significant positive linear relationship with both BMI and WC as hours of television increased, when adjusted for age and sex. 94 Even after adjusting for age, sex, WC, and exercise, an increase in television viewing was still associated with a significant increase in all-cause and cardiovascular mortality. 94
Probably the most important role for exercise and increased PA in individuals with obesity is the prevention of recidivism after successful weight loss from dieting and the maintenance of lean body mass as body fat mass is reduced. A meta-analysis examined the effect of exercise, exercise plus diet, and diet alone on weight gain. 95 Over the course of 15 weeks, weight loss in the exercise-only group was 2.9±0.4 kg, compared to 10.7±0.5 kg in the diet-only group. The weight loss that occurred by combining diet with exercise was not significantly different from that seen with diet alone. At the 1-year follow-up visit, however, the diet-plus-exercise group had maintained the weight loss better than the diet-only group (mean 8.6±0.8 kg total weight lost compared to 6.6±0.5 kg, respectively). Other studies have confirmed that exercise alone usually incurs only a small amount of weight loss and that the more important role of exercise is maintaining weight loss after a successful diet program. 96 , 97
Health Initiatives to Prevent Obesity
Obesity is the next major epidemiologic battle for physicians, public health experts, government officials, and the general population. By many estimates, obesity has already surpassed smoking as the most pressing public health threat. In much the same way that antismoking campaigns were developed, health initiatives must now be developed to effectively prevent obesity and its associated diseases. While smoking and obesity share many similarities from a public health perspective, obesity is potentially more problematic since adequate nutrition is essential to survival; therefore, abstinence from food is not an option. Also, what constitutes good nutrition as opposed to harmful food choices is often not clearly understood by the general public. As changes to the healthcare system in the United States are discussed, plans should be offered that directly and aggressively target obesity through health initiatives and prevention programs.
Food Labeling
Labeling the nutritional content of food products and fast food has been proposed as a way to allow consumers to make informed choices about the types of foods they consume. Beginning in the 1960s, the government required tobacco products to have labels from the US Surgeon General stating that smoking may be hazardous to one's health. These labeling requirements have since progressed to more specific statements, ie, that smoking causes lung cancer and emphysema and that quitting smoking may reduce the risk for serious health concerns. 98 The problem with these labels is that they appear in small print and people often do not read them. Indeed, there are little data to suggest that this labeling has been effective in preventing smoking. Ironically, these labels have been used by tobacco manufacturers in litigation against patients with smoking-related diseases to claim that patients were properly warned about the dangers of smoking. 99 – 101
In a similar fashion, little data exist to show that labeling food products has improved eating habits. In a recent RCT from Germany, a variety of food labeling strategies were compared, including no labeling, food labels with daily recommended levels for specific nutrients, labels with healthy choice designations, and traffic light labels indicating the level of healthiness. 102 No significant differences were found in consumption habits between the different labeling strategies. 102 In a study evaluating a similar “stop light” labeling technique, adolescents at 3 different high school cafeterias were found to purchase more items deemed to be high calorie (red) compared to lower calorie options (green and yellow), despite being given a higher percentage of healthier options. 103
One of the main problems with the current strategy for labeling nutritional content is that this information is very difficult for consumers to comprehend. Most consumers are unaware of the dietary content of restaurant foods. A recent RCT was conducted to evaluate whether providing calorie information influenced the types of foods purchased at fast food restaurants. 104 After randomization, half of the 594 participants were provided with menus containing calorie information, while the other half were given menus without this information. 104 The number of calories consumed was not statistically different between the 2 groups. 104 However, some data suggest that providing calorie information does influence consumption patterns, at least for females. 105
The Nutrition and Education Labeling Act of 1994 specifically exempted restaurants from providing nutritional labeling of their products. 106 Recently, however, New York City mandated that fast food companies provide nutritional labeling for all of their products. 107 Initial data suggested that 1,156 customers had perceived a change in consumption because of the labeling, but comparison to a similar population in New Jersey (where labeling is not mandated) showed that there was no difference in actual calories consumed. 107 Nonetheless, having nutritional labeling on restaurant food should lead to more informed decisions about consumption. Overall, there may be a role for nutritional labeling, but use of this technique without other strategies or regulation of nutritional content should not be expected to significantly alter eating habits or prevent obesity-related consequences.
Eliminating Trans Fat in New York City, Denmark, and Beyond
The average daily per capita intake of TFAs in the United States has been shown to increase heart disease risk by 25%, and most leading health organizations have advocated the complete removal of TFAs from foods. 108 – 110 To achieve this objective, however, consumers would need to read labels and become educated about the TFA content of food, and healthcare providers would need to provide counsel on TFA-free options. In 2003, the US Food and Drug Administration required all packaged goods to reveal the amount of TFA if it exceeded 0.5 g. 108 , 111 However, the food industry has circumvented these labeling requirements. For example, fast food companies have reduced serving sizes to keep the amount of TFA below 0.5 g, allowing them to continue using TFA without having to report it on labels. 109 Furthermore, restaurants are not required to report the amount of TFA in the food they serve. In addition to such roadblocks, educating patients about healthy food options is often frustrating and time-consuming for healthcare providers. Therefore, the best option is to eliminate the use of industrially produced TFAs and shift toward the use of safer fats in both packaged goods and restaurant food.
In 2006, the New York City Department of Health and Mental Hygiene put forth a bold proposal to eliminate all artificial TFAs from restaurant food. The response from the restaurant and food industry was not surprising, with critics calling the ban a threat to the flavor of food and saying that the increased cost of converting to TFA-free food would be an economic burden. 108 The first phase of the ban involved restricting TFAs in cooking oils and spreads only, as this goal was more easily obtainable than the complete elimination of TFAs. By the summer of 2008, 99% of restaurants had successfully changed to oils and spreads low in TFAs. 108 The second phase of the ban involved the complete elimination of artificial TFAs from other foods and ingredients. Approximately 6 months after the second phase was initiated, the use of artificial TFAs had been reduced from 50% to 1.6%. 108 By using healthier replacement oils, the amount of saturated fats was also reduced. Outcome data regarding the impact of this measure will not be available for several years, but previous studies suggest that the elimination of TFAs should reduce the risk of heart disease and hyperlipidemia among residents of New York City.
Denmark has been monitoring artificial TFAs in the diets of its residents for over 30 years. 112 – 114 Authorities there determined that labeling was not an effective way to reduce the consumption of foods high in TFAs, such as fast food (especially children's meals), and in March 2003, Denmark became the first country to restrict the use of TFAs in food products. 112 The consumption of food potentially high in TFAs was analyzed before and after this ban, and researchers found that the amount of TFA in the same representative food (such as a large order of French fries and chicken nuggets) was reduced from 30 g to less than 1 g. Over the same period, the same meal in countries without a ban (such as Hungary, Poland, and the United States) still contained 36–42 g of TFAs.
As a result of the successful efforts in New York City and Denmark, legislation to ban artificial TFAs from restaurants has been passed by 1 state legislature, 10 local city governments, and Puerto Rico, and 17 more states are considering similar legislation. 109 , 115 While these programs are encouraging, a complete ban on TFAs in all states may be necessary to optimize the health of the US population.
Taxation of High Calorie Beverages
Large portion sizes and increased consumption of soft drinks and fruit juices are partially responsible for the obesity epidemic. These beverages are prevalent in schools, which may place children at an increased risk of diabetes. The current debate is how to limit the consumption of these beverages in the US school system. Two ideas that have been proposed are to increase taxation on high calorie beverages and to restrict their availability in vending machines in schools. 116 , 117 While the volume of soft drinks consumed by adolescents that comes from vending machines in schools is much smaller than the volume purchased in commercial stores or restaurants, much of the legislative effort has focused only on restricting vending machine sales. 118
The current level of taxation on high calorie beverages is probably insufficient to decrease consumption. 119 A recent study used multivariate linear regression analysis to determine how state taxes on soft drinks affect adolescent obesity. 119 Self-reported BMI data were obtained from students in the 8th, 10th, and 12th grades between 1996 and 2007. The BMI data were compared to differences in taxation for vending machine products from various states. No significant correlation was found between the rate of adolescent obesity and the level of taxation in the various states involved in the study. 119 The most obvious explanation for this finding was that these taxes were all very small and thus were unlikely to have an effect on consumption or long-term consequences such as weight gain. The average state tax on a $1.00 bottle of soda sold in a store is approximately $0.04. 119
Newly proposed legislative strategies have suggested raising the tax on nondiet soda, fruit drinks, and flavored milk. 119 – 121 The governor of New York recently included an 18% tax on nondiet sodas in his proposed budget. 120 Others have suggested placing a per-ounce excise tax of $0.01 on non-diet sodas. 120 Such a strategy would add a tax of $0.20 to a 20-oz bottle of soda (normally sold for approximately $1.00), thus increasing the total cost by 20%. When offered options of diet sodas or other healthier beverages costing 20% less than the nondiet beverages, consumers may be more likely to choose the lower calorie alternatives. Such behavior has been seen when tobacco products have been taxed at higher rates. 122 – 124 Adolescents aged 12–18 years in states with a cigarette tax in the highest quartile ($0.60–$1.00 per pack) were less likely to experiment with tobacco and become established smokers than adolescents in states with a tax in the lowest quartile. 123
Implications for Gastroenterologists
In addition to the many consequences already mentioned, the growing obesity epidemic is also expected to impact the morbidity and mortality associated with certain gastroen-terologic disease processes, the performance of endoscopic procedures, and the complexity of patient management. When evaluating patients in a clinic setting, therefore, gastroenterologists should calculate BMIs and determine whether patients are overweight or obese, as well as determine their WCs and make a determination regarding central versus peripheral adiposity. Determining the degree of obesity (normal weight, overweight, obese, and so on) and the distribution of adiposity will help to identify patients at increased risk for complications from certain gastrointestinal disorders.
The incidence of cholecystitis and choledocho-lithiasis will likely increase as the obesity epidemic continues to affect more individuals. A recent prospective observational study found that obese patients with acute cholecystitis were more likely to be admitted to the hospital and spent more days in the hospital than nonobese patients. 125 The incidence of gastroesophageal reflux disease (GERD) is also increased in overweight and obese individuals. 126 , 127 Increased WC (>80 cm), but not greater BMI, has been shown to correlate with an increased incidence of Barrett esophagus. 126 , 128 Obesity alone is associated with increased severity in acute pancreatitis. 129 Similar to the data for GERD, umbilical WC was shown to be better than BMI for predicting the development of severe acute pancreatitis in obese patients. 130 Additionally, central adiposity is a driving factor in nonalcoholic steatohepatitis (NASH). 131 , 132 Increases in the incidence of NASH and cirrhosis will likely occur as a result of this obesity epidemic. Eventually, NASH cirrhosis may become the most common indication for liver transplantation. 131
Obesity increases morbidity for critically ill patients compared to their lean counterparts. 133 , 134 In trauma patients in a surgical intensive care unit, obesity may also increase mortality. 135 , 136 Potentially, the observed increase in mortality among obese trauma patients could be explained by obesity-associated decreases in hepatic blood flow. 137 In these critically ill obese patients, gastroenter-ologists may increasingly be called upon to achieve enteral access and manage enteral feeding. Optimal nutritional therapy in this situation is controversial and involves high protein, hypocaloric “permissive” underfeeding. 138 – 141 In the near future, nutritional formulas may involve phar-maconutrition with specific formulas for obese patients that are designed to reduce oxidative stress, remove fat from the liver, and promote microvascular perfusion. 142 – 145
Gastroenterologists will also increasingly be called upon to manage complications in patients who have undergone bariatric surgery. The anatomic alterations from these surgical procedures can result in myriad micronutrient deficiencies that require the skills of a clinical nutritionist for long-term management. 146 – 148 Severe nutritional deficits can be avoided with aggressive supplementation following bariatric surgery. 147 Endoscopy is often required in the evaluation of such patients when nausea, vomiting, gastrointestinal bleeding, or anastomotic ulceration complicates the postoperative course. Obesity may increase the complexity of such endoscopic procedures. Obese patients are also at risk for restrictive lung disease as well as central or obstructive sleep apnea. 149 Thus, clinicians may have greater difficulty when performing conscious sedation, as obese patients may have a greater likelihood for oxygen desaturation. As a result, a larger number of endoscopic procedures may need to be performed under medical anesthesia care.
Finally, endoscopic therapies to promote weight loss in obese patients are already on the horizon. Gastric inflat-able balloons, one of the earliest endoluminal concepts to treat obesity by promoting early satiety, are being reevalu-ated as a weight loss technique and potential bridge to later bariatric surgery. 150 , 151 Two new strategies to achieve gastric restriction using endoscopic suturing or stapling devices are also being investigated. Endoluminal vertical gastroplasty utilizes the EndoCinch Suturing System (C. R. Bard), which was previously used for the treatment of GERD, to apply a running suture line from the fundus to the antrum, effectively reducing gastric luminal capacity. 152 Similarly, transoral gastroplasty utilizes an endoluminal stapling device to achieve a full-thickness tissue plication and pleating of the gastric folds from opposing stomach walls to create a similar restriction of the gastric lumen. 153 Finally, the duodenojejunal bypass sleeve is a temporary, removable stenting device that is anchored in the duodenal bulb and extends beyond the ligament of Treitz; this sleeve is designed to promote a variable degree of malabsorption. 154
Obesity is the next major public health challenge facing the United States. Currently, over 60% of the US population is overweight or obese. The health consequences of obesity include increased rates of diabetes, hyperlipidemia, heart disease, and cancer. BMI is a useful epidemiologic tool that can approximate body adiposity for large groups of people, but clinicians may need to combine BMI with WC in the office setting in order to more accurately identify patients at risk for CVD. Currently, health initiatives to address obesity need to be developed and promoted. Based on previous experience with the smoking epidemic, allowing the food industry to control the rate and direction of such measures will result in inadequate or suboptimal programs. Instead, artificial TFAs should be completely banned, as was done in Denmark and New York City, and the number of high calorie beverages consumed on a daily basis should be limited; increased taxation and restricted access to vending machines in schools may help decrease the number of calories consumed from soda and other high calorie beverages. Finally, a renewed emphasis on PA in the school curriculum may help to prevent children from becoming overweight or obese. The obesity epidemic will undoubtedly affect gastroenterologists, whether through obesity-related gastrointestinal disorders, the emerging need for endoscopic therapies to treat obesity, or the greater complexity of patient management in this population. The obesity epidemic must be fought using a wide range of strategies, as initiatives that address only certain portions of the problem at any given time have been shown to be ineffective.
Contributor Information
Ryan T. Hurt, Dr. Hurt serves as an Assistant Professor of Medicine in the Division of General Internal Medicine at the Mayo Clinic in Rochester, Minnesota, and as Assistant Clinical Professor in the Department of Medicine at the University of Louisville School of Medicine in Louisville, Kentucky.
Christopher Kulisek, Dr. Kulisek is a Gastroenterology Fellow in the Department of Medicine at the University of Louisville School of Medicine in Louisville, Kentucky.
Laura A. Buchanan, Dr. Buchanan serves as a Resident in the Department of Medicine at the University of Louisville School of Medicine in Louisville, Kentucky.
Stephen A. McClave, Dr. McClave is a Professor of Medicine in the Division of Gastroenterology, Hepatology, and Nutrition at the University of Louisville School of Medicine in Louisville, Kentucky.
- Share full article
Advertisement
Supported by
Guest Essay
A Year on Ozempic Taught Me We’re Thinking About Obesity All Wrong

By Johann Hari
Mr. Hari is a British journalist and the author of “Magic Pill: The Extraordinary Benefits — and Disturbing Risks — of the New Weight Loss Drugs.”
Ever since I was a teenager, I have dreamed of shedding a lot of weight. So when I shrank from 203 pounds to 161 in a year, I was baffled by my feelings. I was taking Ozempic, and I was haunted by the sense that I was cheating and doing something immoral.
I’m not the only one. In the United States (where I now split my time), over 70 percent of people are overweight or obese, and according to one poll, 47 percent of respondents said they were willing to pay to take the new weight-loss drugs. It’s not hard to see why. They cause users to lose an average of 10 to 20 percent of their body weight, and clinical trials suggest that the next generation of drugs (probably available soon) leads to a 24 percent loss, on average. Yet as more and more people take drugs like Ozempic, Wegovy and Mounjaro, we get more confused as a culture, bombarding anyone in the public eye who takes them with brutal shaming.
This is happening because we are trapped in a set of old stories about what obesity is and the morally acceptable ways to overcome it. But the fact that so many of us are turning to the new weight-loss drugs can be an opportunity to find a way out of that trap of shame and stigma — and to a more truthful story.
In my lifetime, obesity has exploded, from being rare to almost being the norm. I was born in 1979, and by the time I was 21, obesity rates in the United States had more than doubled . They have skyrocketed since. The obvious question is, why? And how do these new weight-loss drugs work? The answer to both lies in one word: satiety. It’s a concept that we don’t use much in everyday life but that we’ve all experienced at some point. It describes the sensation of having had enough and not wanting any more.
The primary reason we have gained weight at a pace unprecedented in human history is that our diets have radically changed in ways that have deeply undermined our ability to feel sated. My father grew up in a village in the Swiss mountains, where he ate fresh, whole foods that had been cooked from scratch and prepared on the day they were eaten. But in the 30 years between his childhood and mine, in the suburbs of London, the nature of food transformed across the Western world. He was horrified to see that almost everything I ate was reheated and heavily processed. The evidence is clear that the kind of food my father grew up eating quickly makes you feel full. But the kind of food I grew up eating, much of which is made in factories, often with artificial chemicals, left me feeling empty and as if I had a hole in my stomach. In a recent study of what American children eat, ultraprocessed food was found to make up 67 percent of their daily diet. This kind of food makes you want to eat more and more. Satiety comes late, if at all.
One scientific experiment — which I have nicknamed Cheesecake Park — seemed to me to crystallize this effect. Paul Kenny, a neuroscientist at Mount Sinai Hospital in New York, grew up in Ireland. After he moved in 2000 to the United States, when he was in his 20s, he gained 30 pounds in two years. He began to wonder if the American diet has some kind of strange effect on our brains and our cravings, so he designed an experiment to test it. He and his colleague Paul Johnson raised a group of rats in a cage and gave them an abundant supply of healthy, balanced rat chow made out of the kind of food rats had been eating for a very long time. The rats would eat it when they were hungry, and then they seemed to feel sated and stopped. They did not become fat.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
- Entertainment
- Newsletters
Obesity drug used in Mounjaro and Zepbound may help treat dangerous sleep apnea
Jonel Aleccia
Associated Press
A popular obesity drug may help treat a dangerous disorder in which people struggle to breathe while they sleep, a new study finds.
Tirzepatide, the medication in the weight-loss drug Zepbound and also the diabetes treatment Mounjaro, appeared to reduce the severity of sleep apnea along with reducing weight and improving blood pressure and other health measures in patients with obesity who took the drug for a year.
Recommended Videos
Eli Lilly and Co., the drug's maker who paid for the research, has asked the Food and Drug Administration to expand use of the drug to treat moderate to severe sleep apnea, in which people stop and start breathing during sleep, a spokesperson said Friday. A decision is expected by the end of the year.
But an outside expert cautioned in an editorial that more research will be needed to tell if the drug can be used as “a sole treatment” for obstructive sleep apnea, which occurs when tissue in the throat relaxes and collapses during sleep, fully or partially blocking the airway. It affects an estimated 20 million Americans and can cause short-term issues such as snoring, brain fog and daytime sleepiness but also severe long-term issues such as heart disease, dementia and early death.
The research, published Friday in the New England Journal of Medicine and presented at a medical meeting, included nearly 500 people diagnosed with obesity and sleep apnea. Half of them used what's typically known as a CPAP machine that feeds oxygen through a mask to keep airways open during sleep. The other group included people for whom a CPAP machine had failed or wasn't tolerated.
The study found that patients in both groups who got weekly injections of tirzepatide reduced the number of episodes per hour in which their breathing slowed or stopped completely during sleep by about half to nearly 60%, compared to about 10% in people who got a dummy drug. Up to half of the patients taking tirzepatide reduced the apnea episodes enough to potentially resolve the disorder, compared with up to 16% of those using the placebo medication, according to the research.
On average, patients who took tirzepatide also lost between 18% and 20% of their body weight and showed improvements in blood pressure and a condition in which blood oxygen drops during sleep. Patients also reported better sleep and fewer sleep disturbances, the study found.
The new research shows that tirzepatide is “a more effective knife in the drawer,” for treating sleep apnea, said lead author Dr. Atul Malhotra, a sleep medicine specialist at the University of California, San Diego.
In an accompanying editorial, Dr. Sanjay Patel, a sleep medicine specialist at the University of Pittsburgh, cautioned that whether tirzepatide can treat sleep apnea in real-world patients “remains unclear” because of the way improvement is measured. He also noted that cost and access remain obstacles to using tirzepatide and that the addition of the drug as a treatment could exacerbate racial and other disparities in addressing sleep apnea.
Dr. Paul Peppard, a sleep medicine researcher at the University of Wisconsin who was not involved in the study, said losing weight has long been recommended as a way to reduce the severity of sleep apnea by expanding lung capacity, reducing fat in the airways and improving oxygen usage. While diet and exercise can spur weight loss and reduce the consequences of the disorder, the ongoing obesity epidemic in the U.S. proves that shedding pounds is difficult for many people, he said. In such cases, medications such as tirzepatide can help.
“I expect that these drugs could be used as a tool to treat many of the established outcomes of obesity,” Peppard said.
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.
Copyright 2024 The Associated Press. All rights reserved. This material may not be published, broadcast, rewritten or redistributed without permission.

IMAGES
VIDEO
COMMENTS
This essay will explore the various causes of obesity and their effects on individuals and society as a whole. One of the primary causes of obesity is dietary habits and nutritional intake. The consumption of high-calorie, low-nutrient foods, such as fast food, sugary beverages, and processed snacks, has become increasingly prevalent in modern ...
Obesity has become a global epidemic and is one of today's most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer (Bluher, 2019).Obesity is mainly caused by imbalanced energy intake and expenditure due to a ...
Besides health complications, obesity causes an array of psychological effects, including inferiority complex among victims. Obese people suffer from depression, emanating from negative self-esteem and societal rejection. In some cases, people who become obese lose their friends and may get disapproval from teachers and other personalities ...
Causes of Obesity. Every phenomenon must have a reason. In order to write a cause and effect essay, you need to analyze the topic carefully to cover all aspects. Obesity is considered to be a complex illness, with a number of factors contributing to its development. These can be: external; internal; hereditary; hormonal; social. As you may have ...
Conclusion. In conclusion, obesity is a complex issue with multiple causes and significant effects on individuals and society. Poor dietary habits, sedentary lifestyles, and genetic factors contribute to its prevalence. The health consequences, economic costs, and social and psychological effects of obesity are profound and demand attention.
Conclusion. In conclusion, obesity is a growing problem worldwide, with numerous causes and effects. Encouraging healthy eating habits, physical activity, and increasing access to healthy food options are potential solutions to this issue. However, resistance to change, cost, and cultural differences may be potential obstacles.
Abstract. The epidemic of overweight and obesity presents a major challenge to chronic disease prevention and health across the life course around the world. Fueled by economic growth, industrialization, mechanized transport, urbanization, an increasingly sedentary lifestyle, and a nutritional transition to processed foods and high calorie ...
This paper provides a comprehensive overview of the obesity epidemic, examining its causes, consequences, and potential solutions. It explores the complex interplay of genetic, environmental, and ...
Some genetic and lifestyle factors affect an individual's likelihood of adult obesity; thus, the significant clusters of obesity observed in specific geographical regions and contexts also signal the impact of socioeconomic and environmental factors in "obesogenic" environments [13].Understanding the causes and determinants of obesity is a critical step toward creating effective policy and ...
Obesity prevalence among children is >30% in the Cook Islands, Nauru and Palau, with a notable increase over the past few decades. Worldwide prevalence of obesity increased at an alarming rate in ...
A sedentary lifestyle, poor food choices, and genetic susceptibility are the. main causes of obesity. These elements play a part in the body's excessiv e fat buildup, which. can result in a number ...
In the United States, overweight and obesity are chronic diseases that contribute to excess morbidity and mortality. Despite public health efforts, these disorders are on the rise, and their consequences are burgeoning. 1 The Centers for Disease Control and Prevention report that during 2017 to 2018, the prevalence of obesity in the United States was 42.4%, which was increased from the ...
In today's society, obesity has dramatically increased to epidemic proportions and has become the leading cause of ill health [1]. Obesity, usually defined as an individual's body mass index (BMI ...
The obesity epidemic. The World Health Organization (WHO) defines overweight and obesity as abnormal or excessive fat accumulation that presents a risk to health (WHO, 2016a).A body mass index (BMI) ≥25 kg/m 2 is generally considered overweight, while obesity is considered to be a BMI ≥ 30 kg/m 2.It is well known that obesity and overweight are a growing problem globally with high rates in ...
Causes and Effects of Obesity in Children and Adults Essay- 700 Word Long Essay. Most Significant Causes of Obesity. Bad Diet. Lack of Physical Activity and Exercise. Stress Anxiety and Social Problems. Medical Conditions. The Age Factor. Most Significant Effects of Obesity. Hight Blood Pressure Strokes and Heart Diseases.
The growing childhood obesity epidemic is a result of technology. Much of the wildlife is dying because of the oil spill. ... The cause-and-effect essay opens with a general introduction to the topic, which then leads to a thesis that states the main cause, main effect, or various causes and effects of a condition or event. ...
The Causes and Effects of Obesity Essay. So much of what occurs in this world is a result of cause and effect. For instance, if a match is struck; a flame ignites, if water is put on the flame; the flame is extinguished, if more fuel is added to the fire; the fire gets bigger. A major problem in our society today, the problem of obesity ...
answer this question along the lines of our population being overweight. Obesity is one of the leading causes of death in the US with at least 30,000 people dying from this disease each year (Obesity Epidemic). Obesity symptoms often arise at an early age and can lead to an array of issues well beyond excessive weight gain, but who is to blame?
In this essay, I will examine these two factors and then propose a viable solution. One of the foremost reasons for obesity is the consumption of unhealthy foods. Many people started to follow western food habits and eventually ended up eating high fat content foods like pizza and burger. Regular consumption of these fat rich foods will ...
Abstract. Obesity is the next major epidemiologic challenge facing today's doctors, with the annual allocation of healthcare resources for the disease and related comorbidities projected to exceed $150 billion in the United States. The incidence of obesity has risen in the United States over the past 30 years; 60% of adults are currently either ...
2 Obesity Cause and Effect Essay The epidemic of obesity is a significant threat to public health, affecting millions of people all over the globe. It may devastate one's physical, mental, and social well-being. Adolescents and younger children are particularly vulnerable to the long-term health effects and stunted growth that might result from this condition.
Argumentative Essay on Obesity. Obesity is a growing epidemic that has plagued societies around the world. With the rise of fast food chains, sedentary lifestyles, and a lack of education on proper nutrition, obesity rates have skyrocketed in recent years. While some argue that obesity is a personal choice and should not be seen as a public ...
According to Dr. Viana, there isn't one #1 cause. "Obesity medicine specialists wish there was a number one cause, as this would make treatment a lot easier," he reveals. But the NIH is a little ...
Activists argued that the drug entrenched old norms about body image — people still seemed to want to be thin. Ozempic was weight loss; weight loss was Ozempic. It's like Kleenex or Scotch ...
Reducing or reversing obesity hugely boosts health, on average: We know from years of studying bariatric surgery that it slashes the risks of cancer, heart disease and diabetes-related death.
Obesity can also cause respiratory problems, sleep apnea, and osteoarthritis. Obesity is linked to various psychological problems such as depression, anxiety, and low self-esteem. The stigma associated with obesity can lead to social rejection, discrimination, and negative body image. These psychological problems can reduce the quality of life ...
A popular obesity drug may help treat a dangerous disorder in which people struggle to breathe while they sleep, a new study finds. Tirzepatide, the medication in the weight-loss drug Zepbound and ...
Among non-users, the kidney-specific outcome was recorded in 12.5% of semaglutide subjects and 15.6% of placebo recipients. MACEs were less frequent in the semaglutide group regardless of baseline ...
Stay Hydrated. Pay attention to how you feel. If you start to feel dizzy, nauseous, or overly fatigued, stop exercising immediately and find a cool place to rest. High humidity can make it harder ...