Effects of Sleep Deprivation

Staff Writer
Rob writes about the intersection of sleep and mental health and previously worked at the National Cancer Institute.
Want to read more about all our experts in the field?

Dr. Abhinav Singh
Sleep Medicine Physician
Dr. Singh is the Medical Director of the Indiana Sleep Center. His research and clinical practice focuses on the entire myriad of sleep disorders.
Sleep Foundation
Fact-Checking: Our Process
The Sleep Foundation editorial team is dedicated to providing content that meets the highest standards for accuracy and objectivity. Our editors and medical experts rigorously evaluate every article and guide to ensure the information is factual, up-to-date, and free of bias.
The Sleep Foundation fact-checking guidelines are as follows:
- We only cite reputable sources when researching our guides and articles. These include peer-reviewed journals, government reports, academic and medical associations, and interviews with credentialed medical experts and practitioners.
- All scientific data and information must be backed up by at least one reputable source. Each guide and article includes a comprehensive bibliography with full citations and links to the original sources.
- Some guides and articles feature links to other relevant Sleep Foundation pages. These internal links are intended to improve ease of navigation across the site, and are never used as original sources for scientific data or information.
- A member of our medical expert team provides a final review of the content and sources cited for every guide, article, and product review concerning medical- and health-related topics. Inaccurate or unverifiable information will be removed prior to publication.
- Plagiarism is never tolerated. Writers and editors caught stealing content or improperly citing sources are immediately terminated, and we will work to rectify the situation with the original publisher(s)
- Although Sleep Foundation maintains affiliate partnerships with brands and e-commerce portals, these relationships never have any bearing on our product reviews or recommendations. Read our full Advertising Disclosure for more information.
Table of Contents

What Are the Effects of Sleep Deprivation?
How much sleep is enough, symptoms of sleep deprivation, causes of sleep deprivation, treatment for sleep deprivation, preventing sleep issues.
Sleep deprivation happens when a person does not get the sleep they need to sustain their health and well-being. It is common for people to sacrifice sleep for work, school, or fun, but even one night of inadequate sleep can leave people feeling tired, less productive, and more prone to mistakes the next day.
Nearly half of people in the U.S. have trouble sleeping, and around one-third of adults sleep less than seven hours each night. Without enough sleep, the body begins to accumulate sleep debt.
As sleep debt grows over time, it begins to take a toll on mental and physical health . Long-term sleep deprivation can reduce quality of life and may increase the risk of health issues including obesity, diabetes, and cardiovascular disease.
Learn more about the impacts of sleep deprivation, including its causes, and how prioritizing sleep hygiene can help people get the rest they need.
Research has found that sleep deprivation affects systems throughout the body, leading to a wide range of negative effects.
- Daytime sleepiness: Not getting enough sleep is a common cause of people feeling tired during the day Trusted Source UpToDate More than 2 million healthcare providers around the world choose UpToDate to help make appropriate care decisions and drive better health outcomes. UpToDate delivers evidence-based clinical decision support that is clear, actionable, and rich with real-world insights. View Source . Daytime sleepiness can leave a person without the energy to do the things they enjoy and cause problems at work, school, and in relationships.
- Impaired mental function: One of the most noticeable effects of sleep loss is cognitive impairment. As sleep debt grows Trusted Source Centers for Disease Control and Prevention (CDC) As the nation’s health protection agency, CDC saves lives and protects people from health threats. View Source , a person becomes less alert and may have difficulty multitasking. Reductions in attention make a sleep-deprived person more prone to mistakes, increasing the risk of a workplace or motor vehicle accident.
- Mood changes: Sleep loss can lead to mood changes and make a person feel more anxious or depressed. Without enough sleep, people may feel irritable, frustrated, and unmotivated. They may also struggle to deal with change and to regulate their emotions.
- Reduced immune function: Sleep is important for maintaining a healthy immune system, so sleep deprivation can weaken immune function. In fact, research suggests that people who are sleep deprived are less responsive to the flu vaccine and are more likely to get infections like the common cold.
- Weight gain: Sleep is important for maintaining a healthy weight Trusted Source National Heart, Lung, and Blood Institute (NHLBI) The NHLBI is the nation's leader in the prevention and treatment of heart, lung, blood and sleep disorders. View Source . Not getting enough sleep can affect appetite and metabolism in ways that can lead to weight gain. Insufficient sleep has been associated with an increased risk of obesity.
Sleep deprivation can have a drastic effect on the ability to safely drive a car. Not only does sleep loss reduce a person’s ability to pay attention Trusted Source National Heart, Lung, and Blood Institute (NHLBI) The NHLBI is the nation's leader in the prevention and treatment of heart, lung, blood and sleep disorders. View Source and react quickly , it can also lead to microsleeps, which involve unknowingly falling asleep for a brief moment. Drowsy driving is linked to tens of thousands of injuries Trusted Source National Highway Traffic Safety Administration (NHTSA) Through enforcing vehicle performance standards and partnerships with state and local governments, NHTSA reduces deaths, injuries and economic losses from motor vehicle crashes. View Source and hundreds of deaths in the U.S. each year.
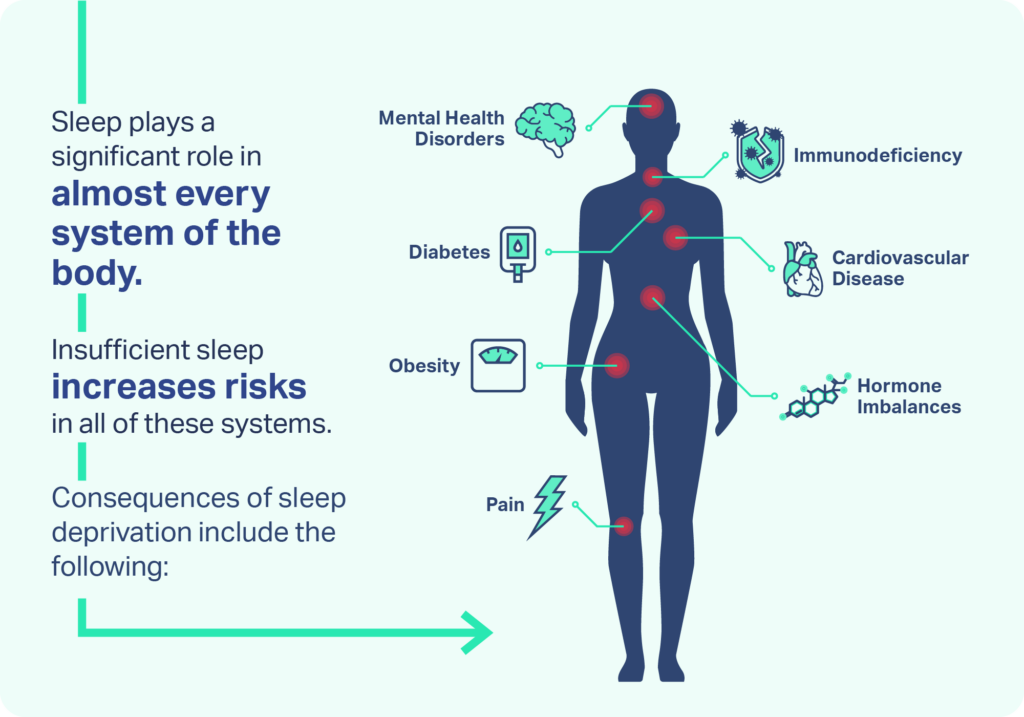
When sleep loss becomes a regular occurrence, chronic sleep deprivation can lead to changes in the nervous system, contribute to long-term health complications, and exacerbate chronic medical conditions.
- Diabetes: A lack of sleep can make it more difficult for the body to process sugar, contributing to glucose intolerance Trusted Source National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) NIDDK research creates knowledge about and treatments for diseases that are among the most chronic, costly, and consequential for patients, their families, and the Nation. View Source and increasing the risk of type 2 diabetes.
- Heart disease: During normal sleep, blood pressure drops in ways that are believed to support heart health. Sleep deprivation prevents this drop in blood pressure and triggers inflammation, heightening the risk of cardiovascular diseases , such as heart disease and stroke.
- Mental health conditions: Sleep deprivation is closely linked to mental health Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source . Sleep loss may increase the risk of mental health issues, and those issues can make it harder to get enough sleep.
Experts have created guidelines Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source for the amount of sleep needed to maintain optimal mental health, physical health, and emotional well-being. Without this amount of sleep, people begin to accumulate sleep debt and experience the consequences of sleep deprivation.
| Age Group | Age Range | |
|---|---|---|
| Infant | 4-12 months | 12-16 hours (including naps) |
| Toddler | 1-2 years | 11-14 hours (including naps) |
| Preschool | 3-5 years | 10-13 hours (including naps) |
| School-age | 6-12 years | 9-12 hours |
| Teen | 13-18 years | 8-10 hours |
| Adult | 18 years and older | 7 hours or more |
Sleep needs vary across the lifespan but also from person to person. This means that how much sleep an individual needs depends on more than just their age. For example, some people may be naturally long or naturally short sleepers who require more or less than the recommended number of hours to wake up feeling rested.
How much sleep a person needs also depends on their health and typical daily activities. In the short-term, the need for sleep is temporarily increased after demanding activities, when a person is sick, or when recovering from a period of sleep deprivation.
Additionally, avoiding sleep deprivation is about more than just spending enough hours in bed. Healthy and restorative rest also depends on the quality of sleep. So even if a person gets the right amount of hours of sleep, they may still be sleep deprived if their sleep quality is reduced from waking up too often at night.
The symptoms of sleep deprivation may be obvious or subtle depending on how much sleep is missed and how accustomed a person is to sleep deprivation. Signs to watch out for include:
- Waking up feeling unrefreshed
- Daytime sleepiness
- Falling asleep unexpectedly during the day
- Difficulty functioning at home, work, or school
- Trouble concentrating and slow reaction times
- Mood changes and problems controlling emotions
- Spending more than 30 minutes trying to fall asleep
- Feeling tiredness in the morning despite a full night of sleep
- Waking up frequently during the night
- Snoring loudly or gasping for air while sleeping
Some symptoms of sleep deprivation may look different in children than in adults. In addition to dozing off during the day, children with sleep deprivation may exhibit an increase in energy or hyperactivity. Children may also have frequent changes in mood, difficulty controlling their behavior, or poor academic achievement.
There are many potential causes of sleep deprivation, ranging from natural changes in the body as people age to an undiagnosed medical condition or sleep disorder.
In teens, sleep deprivation can develop because of changes during puberty that lead adolescents to prefer later bedtimes. This natural preference for late nights often conflicts with early morning school schedules, making it difficult for teens to get the sleep they need.
In women and people assigned female at birth, sleep loss can occur at certain times during their menstrual cycle. People commonly have fragmented sleep in the week before their period begins Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source . Sleep loss is also common during and after pregnancy and during menopause.
Other causes of sleep deprivation include poor sleep habits, busy schedules, and health issues that interfere with getting enough quality rest.
- Poor sleep habits: Daytime habits can either help or hinder nighttime sleep. Sleep deprivation can be caused by poor sleep habits, such as using a cell phone, TV, or other electronics in bed, drinking caffeine too close to bedtime, or having an inconsistent sleep schedule.
- Full schedules: A common reason for losing sleep is a busy schedule that involves activities in the late evening. People who work late or overbook themselves in the evening may sacrifice sleep in hopes of sleeping in on the weekend. Unfortunately, extra sleep on the weekend is not able to fully compensate for lost sleep during the week.
- Stress: Stress is a natural reaction to challenging situations, but if left unchecked it can make it more difficult to fall asleep Trusted Source Medline Plus MedlinePlus is an online health information resource for patients and their families and friends. View Source at night. Excess stress causes the body to release hormones that trigger alertness, which can interfere with normal sleep.
- Issues in the sleep environment: A person’s sleep environment can have a significant impact on their sleep. People who live in noisy areas may find it difficult to get quality sleep. Sleep can also be interrupted by too much ambient light and temperatures that are too hot or too cold.
- Medical conditions: Many medical problems can interfere with sleep, including pain, heart failure, and asthma. Some medical conditions may flare up Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source or get worse at night, like acid reflux or chronic obstructive pulmonary disease (COPD).
- Medications and substances: A wide variety of medications can interrupt sleep or make it more challenging to doze off. These include certain steroids, decongestants, pain medications, and drugs used to treat anxiety and depression.
- Mental health conditions: Several mental health conditions are linked to sleep challenges, including depression, anxiety, and bipolar disorder, as well as attention deficit hyperactivity disorder (ADHD) Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source , and autism spectrum disorder.
Another potential cause of sleep deprivation is an undiagnosed or untreated sleep disorder . In fact, as many as 70 million people in the U.S. live with a chronic sleep disorder. Sleep disorders that can make it difficult to get enough sleep include insomnia, obstructive sleep apnea, and restless legs syndrome.
Treatment for sleep deprivation involves finding ways to get more hours of high-quality sleep. The best approach to achieving this depends on the cause of an individual’s sleep problems. In people with persistent sleep deprivation, it may take several weeks or longer Trusted Source Merck Manual|MSD Manuals View Source to resolve the symptoms of sleep loss.
When symptoms of sleep loss continue despite an improvement in sleep habits, working with a doctor is an important step in addressing the causes of sleep problems. To help determine the cause of sleep deprivation, a doctor may ask questions related to routines and sleep habits, such as:
- What time do you go to bed and wake up each day, including on the weekends?
- What is your work schedule?
- Is sleep refreshing or is it difficult to get up in the morning?
- Do you wake up often during the night?
- How often do you take daytime naps?
- Does daytime sleepiness ever interfere with your life?
Using this information, a doctor may recommend additional tests to find the source of sleep issues. A doctor may suggest starting a sleep diary to keep track of symptoms and habits that may be causing sleep deprivation.
To reduce the risk of sleep deprivation, it is important to take steps to improve sleep hygiene .
- Make sleep a priority: Prioritize sleep health by creating a comfortable sleep environment and keeping a consistent sleep schedule. This means going to sleep and waking up at around the same time each day and avoiding the temptation to stay up later or sleep in on the weekends.
- Combat stress: To combat bedtime stress, give yourself plenty of time to wind down from the day. Use this time to listen to calming music, stretch, or write in a journal. Boost your ability to relieve stress by trying out new relaxation techniques and seeing what helps the most.
- Time your light exposure: Ambient light can signal to the body whether it is time to be awake or prepare for sleep, so be intentional about light exposure. Try to get at least 30 minutes of sunlight exposure during the day and then dim or turn off lights in the evening. Shut off phones, TVs, and computers at least an hour before bed.
- Watch your caffeine intake: Caffeine can linger in the body for eight or more hours, so consuming caffeine in the afternoon may affect how long it takes to doze off at bedtime.
- Nap wisely: Although they cannot replace quality nighttime rest, naps can be a helpful tool to improve daytime alertness. If naps are too long or poorly timed, though, they can make it more difficult to fall asleep in the evening. Adults should aim for naps that are no longer than 20 minutes and should avoid napping in the late afternoon.
- Stay active: Regular exercise can make it easier to get to sleep at bedtime. Try to get at least 30 minutes of physical activity every day, but it is best to avoid highly strenuous exercise too close to bedtime.
Medical Disclaimer: The content on this page should not be taken as medical advice or used as a recommendation for any specific treatment or medication. Always consult your doctor before taking a new medication or changing your current treatment.
References 13 Sources
Cirelli, C. (2022, October 10). Insufficient sleep: Definition, epidemiology, and adverse outcomes. In R. Benca (Ed.). UpToDate., Retrieved December 18, 2022, from
National Institute for Occupational Safety and Health. (2020, April 1). Sleep debt. Centers for Disease Control and Prevention., Retrieved December 18, 2022, from
National Heart, Lung, and Blood Institute. (2011, August). Your guide to healthy sleep., Retrieved December 18, 2022, from
National Heart, Lung, and Blood Institute. (n.d.). Sleep deprivation and deficiency., Retrieved December 18, 2022, from
National Highway Traffic Safety Administration. (n.d.). Drowsy Driving., Retrieved December 18, 2022, from
National Institute of Diabetes and Digestive and Kidney Diseases. (2021, March 17). The impact of poor sleep on type 2 diabetes., Retrieved December 18, 2022, from
Scott, A. J., Webb, T. L., & Rowse, G. (2017). Does improving sleep lead to better mental health? A protocol for a meta-analytic review of randomized controlled trials. BMJ open, 7(9), e016873.
Consensus Conference Panel, Watson, N. F., Badr, M. S., Belenky, G., Bliwise, D. L., Buxton, O. M., Buysse, D., Dinges, D. F., Gangwisch, J., Grandner, M. A., Kushida, C., Malhotra, R. K., Martin, J. L., Patel, S. R., Quan, S. F., Tasali, E., Non-Participating Observers, Twery, M., Croft, J. B., Maher, E., … Heald, J. L. (2015). Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Journal of Clinical Sleep Medicine, 11(6), 591–592.
Rajagopal, A., & Sigua, N. L. (2018). Women and sleep. American Journal of Respiratory and Critical Care Medicine, 197(11), P19–P20.
A.D.A.M. Medical Encyclopedia. (2022, April 30). Stress and your health. MedlinePlus., Retrieved December 18, 2022, from
Shah, P., & Krishnan, V. (2019). Hospitalization and sleep. American Journal of Respiratory and Critical Care Medicine, 199(10), P19–P20.
Bandyopadhyay, A., & Sigua, N. L. (2019). What is sleep deprivation? American Journal of Respiratory and Critical Care Medicine, 199(6), P11–P12.
Schwab, R. J. (2022, May). Insomnia and excessive daytime sleepiness (EDS). Merck Manual Professional Version., Retrieved December 18, 2022, from
Learn More About Sleep Deprivation

Can a Lack of Sleep Cause Headaches?

How Sleep Deprivation Affects Your Heart

Interrupted Sleep: Causes & Helpful Tips

Sleep Deprivation: Symptoms, Treatment, & Effects

Lack of Sleep May Increase Calorie Consumption

Sleepless Nights: How to Function on No Sleep

What All-Nighters Do To Your Cognition

Sleep Deprivation and Reaction Time

Understanding Sleep Deprivation and New Parenthood
Other articles of interest, sleep solutions, sleep hygiene, sleep apnea.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases & Disorders Education Program
- Publications and Resources
- Clinical Trials
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Ask a Scientist
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- < Back To Sleep Deprivation and Deficiency
- How Sleep Affects Your Health
- What Are Sleep Deprivation and Deficiency?
- What Makes You Sleep?
- How Much Sleep Is Enough
- Healthy Sleep Habits
MORE INFORMATION
Sleep Deprivation and Deficiency How Sleep Affects Your Health
Language switcher.
Getting enough quality sleep at the right times can help protect your mental health, physical health, quality of life, and safety.
How do I know if I’m not getting enough sleep?
Sleep deficiency can cause you to feel very tired during the day. You may not feel refreshed and alert when you wake up. Sleep deficiency also can interfere with work, school, driving, and social functioning.
How sleepy you feel during the day can help you figure out whether you're having symptoms of problem sleepiness.
You might be sleep deficient if you often feel like you could doze off while:
- Sitting and reading or watching TV
- Sitting still in a public place, such as a movie theater, meeting, or classroom
- Riding in a car for an hour without stopping
- Sitting and talking to someone
- Sitting quietly after lunch
- Sitting in traffic for a few minutes
Sleep deficiency can cause problems with learning, focusing, and reacting. You may have trouble making decisions, solving problems, remembering things, managing your emotions and behavior, and coping with change. You may take longer to finish tasks, have a slower reaction time, and make more mistakes.
Symptoms in children
The symptoms of sleep deficiency may differ between children and adults. Children who are sleep deficient might be overly active and have problems paying attention. They also might misbehave, and their school performance can suffer.
Sleep-deficient children may feel angry and impulsive, have mood swings, feel sad or depressed, or lack motivation.
Sleep and your health
The way you feel while you're awake depends in part on what happens while you're sleeping. During sleep, your body is working to support healthy brain function and support your physical health. In children and teens, sleep also helps support growth and development.
The damage from sleep deficiency can happen in an instant (such as a car crash), or it can harm you over time. For example, ongoing sleep deficiency can raise your risk of some chronic health problems. It also can affect how well you think, react, work, learn, and get along with others.
Mental health benefits
Sleep helps your brain work properly. While you're sleeping, your brain is getting ready for the next day. It's forming new pathways to help you learn and remember information.
Studies show that a good night's sleep improves learning and problem-solving skills. Sleep also helps you pay attention, make decisions, and be creative.
Studies also show that sleep deficiency changes activity in some parts of the brain. If you're sleep deficient, you may have trouble making decisions, solving problems, controlling your emotions and behavior, and coping with change. Sleep deficiency has also been linked to depression, suicide, and risk-taking behavior.
Children and teens who are sleep deficient may have problems getting along with others. They may feel angry and impulsive, have mood swings, feel sad or depressed, or lack motivation. They also may have problems paying attention, and they may get lower grades and feel stressed.
Physical health benefits
Sleep plays an important role in your physical health.
Good-quality sleep:
- Heals and repairs your heart and blood vessels.
- Helps support a healthy balance of the hormones that make you feel hungry (ghrelin) or full (leptin): When you don't get enough sleep, your level of ghrelin goes up and your level of leptin goes down. This makes you feel hungrier than when you're well-rested.
- Affects how your body reacts to insulin: Insulin is the hormone that controls your blood glucose (sugar) level. Sleep deficiency results in a higher-than-normal blood sugar level, which may raise your risk of diabetes.
- Supports healthy growth and development: Deep sleep triggers the body to release the hormone that promotes normal growth in children and teens. This hormone also boosts muscle mass and helps repair cells and tissues in children, teens, and adults. Sleep also plays a role in puberty and fertility.
- Affects your body’s ability to fight germs and sickness: Ongoing sleep deficiency can change the way your body’s natural defense against germs and sickness responds. For example, if you're sleep deficient, you may have trouble fighting common infections.
- Decreases your risk of health problems, including heart disease, high blood pressure, obesity, and stroke.
Research for Your Health
NHLBI-funded research found that adults who regularly get 7-8 hours of sleep a night have a lower risk of obesity and high blood pressure. Other NHLBI-funded research found that untreated sleep disorders rase the risk for heart problems and problems during pregnancy, including high blood pressure and diabetes.
Daytime performance and safety
Getting enough quality sleep at the right times helps you function well throughout the day. People who are sleep deficient are less productive at work and school. They take longer to finish tasks, have a slower reaction time, and make more mistakes.
After several nights of losing sleep — even a loss of just 1 to 2 hours per night — your ability to function suffers as if you haven't slept at all for a day or two.
Lack of sleep also may lead to microsleep. Microsleep refers to brief moments of sleep that happen when you're normally awake.
You can't control microsleep, and you might not be aware of it. For example, have you ever driven somewhere and then not remembered part of the trip? If so, you may have experienced microsleep.
Even if you're not driving, microsleep can affect how you function. If you're listening to a lecture, for example, you might miss some of the information or feel like you don't understand the point. You may have slept through part of the lecture and not realized it.
Some people aren't aware of the risks of sleep deficiency. In fact, they may not even realize that they're sleep deficient. Even with limited or poor-quality sleep, they may still think they can function well.
For example, sleepy drivers may feel able to drive. Yet studies show that sleep deficiency harms your driving ability as much or more than being drunk. It's estimated that driver sleepiness is a factor in about 100,000 car accidents each year, resulting in about 1,500 deaths.
Drivers aren't the only ones affected by sleep deficiency. It can affect people in all lines of work, including healthcare workers, pilots, students, lawyers, mechanics, and assembly line workers.

Lung Health Basics: Sleep
People with lung disease often have trouble sleeping. Sleep is critical to overall health, so take the first step to sleeping better: learn these sleep terms, and find out about treatments that can help with sleep apnea.
- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram
Among teens, sleep deprivation an epidemic
Sleep deprivation increases the likelihood teens will suffer myriad negative consequences, including an inability to concentrate, poor grades, drowsy-driving incidents, anxiety, depression, thoughts of suicide and even suicide attempts.
October 8, 2015 - By Ruthann Richter

The most recent national poll shows that more than 87 percent of U.S. high school students get far less than the recommended eight to 10 hours of sleep each night. Christopher Silas Neal
Carolyn Walworth, 17, often reaches a breaking point around 11 p.m., when she collapses in tears. For 10 minutes or so, she just sits at her desk and cries, overwhelmed by unrelenting school demands. She is desperately tired and longs for sleep. But she knows she must move through it, because more assignments in physics, calculus or French await her. She finally crawls into bed around midnight or 12:30 a.m.
The next morning, she fights to stay awake in her first-period U.S. history class, which begins at 8:15. She is unable to focus on what’s being taught, and her mind drifts. “You feel tired and exhausted, but you think you just need to get through the day so you can go home and sleep,” said the Palo Alto, California, teen. But that night, she will have to try to catch up on what she missed in class. And the cycle begins again.
“It’s an insane system. … The whole essence of learning is lost,” she said.
Walworth is among a generation of teens growing up chronically sleep-deprived. According to a 2006 National Sleep Foundation poll, the organization’s most recent survey of teen sleep, more than 87 percent of high school students in the United States get far less than the recommended eight to 10 hours, and the amount of time they sleep is decreasing — a serious threat to their health, safety and academic success. Sleep deprivation increases the likelihood teens will suffer myriad negative consequences, including an inability to concentrate, poor grades, drowsy-driving incidents, anxiety, depression, thoughts of suicide and even suicide attempts. It’s a problem that knows no economic boundaries.
While studies show that both adults and teens in industrialized nations are becoming more sleep deprived, the problem is most acute among teens, said Nanci Yuan , MD, director of the Stanford Children’s Health Sleep Center . In a detailed 2014 report, the American Academy of Pediatrics called the problem of tired teens a public health epidemic.
“I think high school is the real danger spot in terms of sleep deprivation,” said William Dement , MD, PhD, founder of the Stanford Sleep Disorders Clinic , the first of its kind in the world. “It’s a huge problem. What it means is that nobody performs at the level they could perform,” whether it’s in school, on the roadways, on the sports field or in terms of physical and emotional health.
Social and cultural factors, as well as the advent of technology, all have collided with the biology of the adolescent to prevent teens from getting enough rest. Since the early 1990s, it’s been established that teens have a biologic tendency to go to sleep later — as much as two hours later — than their younger counterparts.
Yet when they enter their high school years, they find themselves at schools that typically start the day at a relatively early hour. So their time for sleep is compressed, and many are jolted out of bed before they are physically or mentally ready. In the process, they not only lose precious hours of rest, but their natural rhythm is disrupted, as they are being robbed of the dream-rich, rapid-eye-movement stage of sleep, some of the deepest, most productive sleep time, said pediatric sleep specialist Rafael Pelayo , MD, with the Stanford Sleep Disorders Clinic.
“When teens wake up earlier, it cuts off their dreams,” said Pelayo, a clinical professor of psychiatry and behavioral sciences. “We’re not giving them a chance to dream.”

Teens have a biologic tendency to go to sleep later, yet many high schools start the day at a relatively early hour, disrupting their natural rhythym. Monkey Business/Fotolia
Understanding teen sleep
On a sunny June afternoon, Dement maneuvered his golf cart, nicknamed the Sleep and Dreams Shuttle, through the Stanford University campus to Jerry House, a sprawling, Mediterranean-style dormitory where he and his colleagues conducted some of the early, seminal work on sleep, including teen sleep.
Beginning in 1975, the researchers recruited a few dozen local youngsters between the ages of 10 and 12 who were willing to participate in a unique sleep camp. During the day, the young volunteers would play volleyball in the backyard, which faces a now-barren Lake Lagunita, all the while sporting a nest of electrodes on their heads.
At night, they dozed in a dorm while researchers in a nearby room monitored their brain waves on 6-foot electroencephalogram machines, old-fashioned polygraphs that spit out wave patterns of their sleep.
One of Dement’s colleagues at the time was Mary Carskadon, PhD, then a graduate student at Stanford. They studied the youngsters over the course of several summers, observing their sleep habits as they entered puberty and beyond.
Dement and Carskadon had expected to find that as the participants grew older, they would need less sleep. But to their surprise, their sleep needs remained the same — roughly nine hours a night — through their teen years. “We thought, ‘Oh, wow, this is interesting,’” said Carskadon, now a professor of psychiatry and human behavior at Brown University and a nationally recognized expert on teen sleep.
Moreover, the researchers made a number of other key observations that would plant the seed for what is now accepted dogma in the sleep field. For one, they noticed that when older adolescents were restricted to just five hours of sleep a night, they would become progressively sleepier during the course of the week. The loss was cumulative, accounting for what is now commonly known as sleep debt.
“The concept of sleep debt had yet to be developed,” said Dement, the Lowell W. and Josephine Q. Berry Professor in the Department of Psychiatry and Behavioral Sciences. It’s since become the basis for his ongoing campaign against drowsy driving among adults and teens. “That’s why you have these terrible accidents on the road,” he said. “People carry a large sleep debt, which they don’t understand and cannot evaluate.”
The researchers also noticed that as the kids got older, they were naturally inclined to go to bed later. By the early 1990s, Carskadon established what has become a widely recognized phenomenon — that teens experience a so-called sleep-phase delay. Their circadian rhythm — their internal biological clock — shifts to a later time, making it more difficult for them to fall asleep before 11 p.m.
Teens are also biologically disposed to a later sleep time because of a shift in the system that governs the natural sleep-wake cycle. Among older teens, the push to fall asleep builds more slowly during the day, signaling them to be more alert in the evening.
“It’s as if the brain is giving them permission, or making it easier, to stay awake longer,” Carskadon said. “So you add that to the phase delay, and it’s hard to fight against it.”
Pressures not to sleep
After an evening with four or five hours of homework, Walworth turns to her cellphone for relief. She texts or talks to friends and surfs the Web. “It’s nice to stay up and talk to your friends or watch a funny YouTube video,” she said. “There are plenty of online distractions.”
While teens are biologically programmed to stay up late, many social and cultural forces further limit their time for sleep. For one, the pressure on teens to succeed is intense, and they must compete with a growing number of peers for college slots that have largely remained constant. In high-achieving communities like Palo Alto, that translates into students who are overwhelmed by additional homework for Advanced Placement classes, outside activities such as sports or social service projects, and in some cases, part-time jobs, as well as peer, parental and community pressures to excel.

William Dement
At the same time, today’s teens are maturing in an era of ubiquitous electronic media, and they are fervent participants. Some 92 percent of U.S. teens have smartphones, and 24 percent report being online “constantly,” according to a 2015 report by the Pew Research Center. Teens have access to multiple electronic devices they use simultaneously, often at night. Some 72 percent bring cellphones into their bedrooms and use them when they are trying to go to sleep, and 28 percent leave their phones on while sleeping, only to be awakened at night by texts, calls or emails, according to a 2011 National Sleep Foundation poll on electronic use. In addition, some 64 percent use electronic music devices, 60 percent use laptops and 23 percent play video games in the hour before they went to sleep, the poll found. More than half reported texting in the hour before they went to sleep, and these media fans were less likely to report getting a good night’s sleep and feeling refreshed in the morning. They were also more likely to drive when drowsy, the poll found.
The problem of sleep-phase delay is exacerbated when teens are exposed late at night to lit screens, which send a message via the retina to the portion of the brain that controls the body’s circadian clock. The message: It’s not nighttime yet.
Yuan, a clinical associate professor of pediatrics, said she routinely sees young patients in her clinic who fall asleep at night with cellphones in hand.
“With academic demands and extracurricular activities, the kids are going nonstop until they fall asleep exhausted at night. There is not an emphasis on the importance of sleep, as there is with nutrition and exercise,” she said. “They say they are tired, but they don’t realize they are actually sleep-deprived. And if you ask kids to remove an activity, they would rather not. They would rather give up sleep than an activity.”
The role of parents
Adolescents are also entering a period in which they are striving for autonomy and want to make their own decisions, including when to go to sleep. But studies suggest adolescents do better in terms of mood and fatigue levels if parents set the bedtime — and choose a time that is realistic for the child’s needs. According to a 2010 study published in the journal Sleep , children are more likely to be depressed and to entertain thoughts of suicide if a parent sets a late bedtime of midnight or beyond.
In families where parents set the time for sleep, the teens’ happier, better-rested state “may be a sign of an organized family life, not simply a matter of bedtime,” Carskadon said. “On the other hand, the growing child and growing teens still benefit from someone who will help set the structure for their lives. And they aren’t good at making good decisions.”
They say they are tired, but they don’t realize they are actually sleep-deprived. And if you ask kids to remove an activity, they would rather not. They would rather give up sleep than an activity.
According to the 2011 sleep poll, by the time U.S. students reach their senior year in high school, they are sleeping an average of 6.9 hours a night, down from an average of 8.4 hours in the sixth grade. The poll included teens from across the country from diverse ethnic backgrounds.
American teens aren’t the worst off when it comes to sleep, however; South Korean adolescents have that distinction, sleeping on average 4.9 hours a night, according to a 2012 study in Sleep by South Korean researchers. These Asian teens routinely begin school between 7 and 8:30 a.m., and most sign up for additional evening classes that may keep them up as late as midnight. South Korean adolescents also have relatively high suicide rates (10.7 per 100,000 a year), and the researchers speculate that chronic sleep deprivation is a contributor to this disturbing phenomenon.
By contrast, Australian teens are among those who do particularly well when it comes to sleep time, averaging about nine hours a night, possibly because schools there usually start later.
Regardless of where they live, most teens follow a pattern of sleeping less during the week and sleeping in on the weekends to compensate. But many accumulate such a backlog of sleep debt that they don’t sufficiently recover on the weekend and still wake up fatigued when Monday comes around.
Moreover, the shifting sleep patterns on the weekend — late nights with friends, followed by late mornings in bed — are out of sync with their weekday rhythm. Carskadon refers to this as “social jet lag.”
“Every day we teach our internal circadian timing system what time it is — is it day or night? — and if that message is substantially different every day, then the clock isn’t able to set things appropriately in motion,” she said. “In the last few years, we have learned there is a master clock in the brain, but there are other clocks in other organs, like liver or kidneys or lungs, so the master clock is the coxswain, trying to get everybody to work together to improve efficiency and health. So if the coxswain is changing the pace, all the crew become disorganized and don’t function well.”
This disrupted rhythm, as well as the shortage of sleep, can have far-reaching effects on adolescent health and well-being, she said.
“It certainly plays into learning and memory. It plays into appetite and metabolism and weight gain. It plays into mood and emotion, which are already heightened at that age. It also plays into risk behaviors — taking risks while driving, taking risks with substances, taking risks maybe with sexual activity. So the more we look outside, the more we’re learning about the core role that sleep plays,” Carskadon said.
Many studies show students who sleep less suffer academically, as chronic sleep loss impairs the ability to remember, concentrate, think abstractly and solve problems. In one of many studies on sleep and academic performance, Carskadon and her colleagues surveyed 3,000 high school students and found that those with higher grades reported sleeping more, going to bed earlier on school nights and sleeping in less on weekends than students who had lower grades.
Sleep is believed to reinforce learning and memory, with studies showing that people perform better on mental tasks when they are well-rested. “We hypothesize that when teens sleep, the brain is going through processes of consolidation — learning of experiences or making memories,” Yuan said. “It’s like your brain is filtering itself — consolidating the important things and filtering out those unimportant things.” When the brain is deprived of that opportunity, cognitive function suffers, along with the capacity to learn.
“It impacts academic performance. It’s harder to take tests and answer questions if you are sleep-deprived,” she said.
That’s why cramming, at the expense of sleep, is counterproductive, said Pelayo, who advises students: Don’t lose sleep to study, or you’ll lose out in the end.
The panic attack
Chloe Mauvais, 16, hit her breaking point at the end of a very challenging sophomore year when she reached “the depths of frustration and anxiety.” After months of late nights spent studying to keep up with academic demands, she suffered a panic attack one evening at home.
“I sat in the living room in our house on the ground, crying and having horrible breathing problems,” said the senior at Menlo-Atherton High School. “It was so scary. I think it was from the accumulated stress, the fear over my grades, the lack of sleep and the crushing sense of responsibility. High school is a very hard place to be.”
We hypothesize that when teens sleep, the brain is going through processes of consolidation — learning of experiences or making memories. It’s like your brain is filtering itself.
Where she once had good sleep habits, she had drifted into an unhealthy pattern of staying up late, sometimes until 3 a.m., researching and writing papers for her AP European history class and prepping for tests.
“I have difficulty remembering events of that year, and I think it’s because I didn’t get enough sleep,” she said. “The lack of sleep rendered me emotionally useless. I couldn’t address the stress because I had no coherent thoughts. I couldn’t step back and have perspective. … You could probably talk to any teen and find they reach their breaking point. You’ve pushed yourself so much and not slept enough and you just lose it.”
The experience was a kind of wake-up call, as she recognized the need to return to a more balanced life and a better sleep pattern, she said. But for some teens, this toxic mix of sleep deprivation, stress and anxiety, together with other external pressures, can tip their thinking toward dire solutions.
Research has shown that sleep problems among adolescents are a major risk factor for suicidal thoughts and death by suicide, which ranks as the third-leading cause of fatalities among 15- to 24-year-olds. And this link between sleep and suicidal thoughts remains strong, independent of whether the teen is depressed or has drug and alcohol issues, according to some studies.
“Sleep, especially deep sleep, is like a balm for the brain,” said Shashank Joshi, MD, associate professor of psychiatry and behavioral sciences at Stanford. “The better your sleep, the more clearly you can think while awake, and it may enable you to seek help when a problem arises. You have your faculties with you. You may think, ‘I have 16 things to do, but I know where to start.’ Sleep deprivation can make it hard to remember what you need to do for your busy teen life. It takes away the support, the infrastructure.”
Sleep is believed to help regulate emotions, and its deprivation is an underlying component of many mood disorders, such as anxiety, depression and bipolar disorder. For students who are prone to these disorders, better sleep can help serve as a buffer and help prevent a downhill slide, Joshi said.
Rebecca Bernert, PhD, who directs the Suicide Prevention Research Lab at Stanford, said sleep may affect the way in which teens process emotions. Her work with civilians and military veterans indicates that lack of sleep can make people more receptive to negative emotional information, which they might shrug off if they were fully rested, she said.
“Based on prior research, we have theorized that sleep disturbances may result in difficulty regulating emotional information, and this may lower the threshold for suicidal behaviors among at-risk individuals,” said Bernert, an instructor of psychiatry and behavioral sciences. Now she’s studying whether a brief nondrug treatment for insomnia reduces depression and risk for suicide.
Sleep deprivation also has been shown to lower inhibitions among both adults and teens. In the teen brain, the frontal lobe, which helps restrain impulsivity, isn’t fully developed, so teens are naturally prone to impulsive behavior. “When you throw into the mix sleep deprivation, which can also be disinhibiting, mood problems and the normal impulsivity of adolescence, then you have a potentially dangerous situation,” Joshi said.
Some schools shift
Given the health risks associated with sleep problems, school districts around the country have been looking at one issue over which they have some control: when school starts in the morning. The trend was set by the town of Edina, Minnesota, a well-to-do suburb of Minneapolis, which conducted a landmark experiment in student sleep in the late 1990s. It shifted the high school’s start time from 7:20 a.m. to 8:30 a.m. and then asked University of Minnesota researchers to look at the impact of the change. The researchers found some surprising results: Students reported feeling less depressed and less sleepy during the day and more empowered to succeed. There was no comparable improvement in student well-being in surrounding school districts where start times remained the same.
With these findings in hand, the entire Minneapolis Public School District shifted start times for 57,000 students at all of its schools in 1997 and found similarly positive results. Attendance rates rose, and students reported getting an hour’s more sleep each school night — or a total of five more hours of sleep a week — countering skeptics who argued that the students would respond by just going to bed later.
For the health and well-being of the nation, we should all be taking better care of our sleep, and we certainly should be taking better care of the sleep of our youth.
Other studies have reinforced the link between later start times and positive health benefits. One 2010 study at an independent high school in Rhode Island found that after delaying the start time by just 30 minutes, students slept more and showed significant improvements in alertness and mood. And a 2014 study in two counties in Virginia found that teens were much less likely to be involved in car crashes in a county where start times were later, compared with a county with an earlier start time.
Bolstered by the evidence, the American Academy of Pediatrics in 2014 issued a strong policy statement encouraging middle and high school districts across the country to start school no earlier than 8:30 a.m. to help preserve the health of the nation’s youth. Some districts have heeded the call, though the decisions have been hugely contentious, as many consider school schedules sacrosanct and cite practical issues, such as bus schedules, as obstacles.
In Fairfax County, Virginia, it took a decade of debate before the school board voted in 2014 to push back the opening school bell for its 57,000 students. And in Palo Alto, where a recent cluster of suicides has caused much communitywide soul-searching, the district superintendent issued a decision in the spring, over the strenuous objections of some teachers, students and administrators, to eliminate “zero period” for academic classes — an optional period that begins at 7:20 a.m. and is generally offered for advanced studies.
Certainly, changing school start times is only part of the solution, experts say. More widespread education about sleep and more resources for students are needed. Parents and teachers need to trim back their expectations and minimize pressures that interfere with teen sleep. And there needs to be a cultural shift, including a move to discourage late-night use of electronic devices, to help youngsters gain much-needed rest.
“At some point, we are going to have to confront this as a society,” Carskadon said. “For the health and well-being of the nation, we should all be taking better care of our sleep, and we certainly should be taking better care of the sleep of our youth.”

About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
Hope amid crisis
Psychiatry’s new frontiers

- Previous Article
- Next Article
To Study or to Sleep: How Seeing the Effect of Sleep Deprivation Changed Students’ Choices
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Reprints and Permissions
- Cite Icon Cite
- Search Site
Vincent P. Coletta; To Study or to Sleep: How Seeing the Effect of Sleep Deprivation Changed Students’ Choices. Phys. Teach. 1 April 2020; 58 (4): 244–246. https://doi.org/10.1119/1.5145469
Download citation file:
- Ris (Zotero)
- Reference Manager
Adequate sleep is essential for students to be able to solve challenging problems effectively. After many years of advising students to get enough sleep the night before their final exam, two studies were conducted with students in introductory physics classes to investigate their sleep habits. In the first previously published study, few students got adequate sleep and there was a significant positive correlation between hours of sleep and final exam score. In the second study the following semester, students were shown the results of the first study. Showing students the negative effect that sleep deprivation the night before a final exam had on exam scores in a prior class appears to have changed students’ sleep choices the night before their own final exam, based on students’ self-reports of sleep. Once students saw evidence that staying up all night studying for a final exam would likely hurt their score on the exam, class average hours of reported sleep significantly increased.
Citing articles via
- Online ISSN 1943-4928
- Print ISSN 0031-921X
- For Researchers
- For Librarians
- For Advertisers
- Our Publishing Partners
- Physics Today
- Conference Proceedings
- Special Topics
pubs.aip.org
- Privacy Policy
- Terms of Use
Connect with AIP Publishing
This feature is available to subscribers only.
Sign In or Create an Account
Theses on Sleep
Summary: In this essay, I question some of the consensus beliefs about sleep, such as the need for at least 7 hours of sleep for adults, harmfulness of acute sleep deprivation, and harmfulness of long-term sleep deprivation and our inability to adapt to it.
It appears that the evidence for all of these beliefs is much weaker than sleep scientists and public health experts want us to believe. In particular, I conclude that it’s plausible that at least acute sleep deprivation is not only not harmful but beneficial in some contexts and that it’s that we are able to adapt to long-term sleep deprivation.
I also discuss the bidirectional relationship of sleep and mania/depression and the costs of unnecessary sleep, noting that sleeping 1.5 hours per day less results in gaining more than a month of wakefulness per year, every year.
Note: I sleep the normal 7-9 hours if I don’t restrict my sleep. However, stimulants like coffee, modafinil, and adderall seem to have much smaller effect on my cognition than on cognition of most people I know. My brain in general, as you might guess from reading this site , is not very normal. So, be cautious before trying anything with your sleep on the basis of the arguments I lay out below. Specifically do not make any drastic changes to your sleep schedule on the basis of reading this essay and, if you want to experiment with sleep, do it gradually (i.e. varying the average amount of sleep by no more than 30 minutes at a time) and carefully.
Also see Natália Coelho Mendonça Counter-theses on Sleep .
Comfortable modern sleep is an unnatural superstimulus. Sleepiness, just like hunger, is normal.
The default argument for sleeping 7-9 hours a night is that this is the amount of sleep most of us get “naturally” when we sleep without using alarms. In this section, I argue against this line of reasoning, using the following analogy:
- Experiencing hunger is normal and does not necessarily imply that you are not eating enough. Never being hungry means you are probably eating too much.
- Experiencing sleepiness is normal and does not necessarily imply that you are undersleeping. Never being sleepy means you are probably sleeping too much.
Most of us (myself included) eat a lot of junk food and candy if we don’t restrict ourselves. Does this mean that lots of junk food and candy is the “natural” or the “optimal” amount for health?
Obviously, no. Modern junk food and candy are unnatural superstimuli, much tastier and much more abundant than any natural food, so they end up overwhelming our brains with pleasure, especially given that we are bored at work, college, or in high school so much of the day.
What if the only food available to you was junk food and candy?
- If you don’t eat any, you starve.
- If you eat just enough to be lean, you’ll keep salivating at the sight of pizzas and ice cream and feel distracted and hungry all the time. Importantly, in this situation, the feeling of hunger does not mean that you should eat more – it’s your brain being overpowered by a superstimulus while being bored.
- And if you eat way too much candy or pizza at once, you’ll be feeling terrible afterwards, however tasty the food was.
Most of us (myself included) sleep 7-9 hours if we don’t have any alarms in the morning and if we get out of bed when we feel like it. Does this mean that 7-9 hours of sleep is the “natural” or the “optimal” amount?
My thesis is: obviously, no. Modern sleep, in its infinite comfort, is an unnatural superstimulus that overwhelms our brains with pleasure and comfort (note: I’m not saying that it’s bad, simply that being in bed today is much more pleasurable than being in “bed” in the past.)
Think about sleep 10,000 years ago. You sleep in a cave, in a hut, or under the sky, with predators and enemy tribes roaming around. You are on a wooden floor, on an animal’s skin, or on the ground. The temperature will probably drop 5-10°C overnight, meaning that if you were comfortable when you were falling asleep, you are going to be freezing when you wake up. Finally, there’s moon shining right at you and all kinds of sounds coming from the forest around you.
In contrast, today: you sleep on your super-comfortable machine-crafted foam of the exact right firmness for you. You are completely safe in your home, protected by thick walls and doors. Your room’s temperature stays roughly constant, ensuring that you stay warm and comfy throughout the night. Finally, you are in a light and sound-insulated environment of your house. And if there’s any kind of disturbance you have eye masks and earplugs.
Does this sound “natural”?
Now, what if the only sleep available to you was modern sleep?
- If you don’t sleep at all, you go crazy, because some amount of sleep is necessary.
- If you sleep just enough to be awake during the day, you’ll be dreaming of getting a nap at the sight of a bed and will be distracted and sleepy all the time. Importantly, I claim, in this situation, the feeling of sleepiness does not mean that you should sleep more – it’s your brain being overpowered by a superstimulus while being bored.
- And if you sleep way too much at once, you’ll be feeling terrible afterwards, however pleasant the sleep was.
Even if I convinced you about the “sleeping too much” part, you are still probably wondering: but what does depression have to do with anything? Isn’t sleeping a lot good for mental health? Well…
Depression <-> oversleeping. Mania <-> acute sleep deprivation
In this section, I argue that depression triggers/amplifies oversleeping while oversleeping triggers/amplifies depression. Similarly, mania triggers/amplifies acute sleep deprivation while acute sleep deprivation triggers/amplifies mania.
One of the most notable facts about sleep is just how interlinked excessive sleep is with depression and how interlinked sleep deprivation is with mania in bipolar people.
Someone in r/BipolarReddit asked: How many hours do you sleep when stable vs (hypo)manic? Depressed?
Here are all 8 answers that compare hours for manic and depressed states, I excluded answers that describe hypomania but do not describe mania or that only describe mania or only describe depression. note the consistency:
- “Manic/hypomanic: 0-6 hours Stable: 7-9 hours Depressed: 10-19 hours”
- “Manic, 2-3, hypo, 5-6, stable 8-9, depressed 10-12. 8 is the number I try to hit.”
- “Severely depressed w/o mixed features - 12 to 15 hours Low to Moderate depressed w/o mixed - 10 hours, if no alarm. With alarm less, but super hangover Stable -Usually 7-9 hours Hypomanic taking sedating evening meds - 5 to 7 hours Hypomanic with no sedating evening meds - 3 to 5 hours Manic out of hand - 0 to 3 hours Manic in hospital put on maximum sedating meds or injections - 4 to 6 hours Mixed episodes = same as hypo(manic)”
- “I try to get at least 8 hours but when I’m depressed I nap a lot. When I’m hypo I sleep pretty much the same but when I’m manic I’m lucky to get 3 hours. Huhs”
- “Just got out of a manic episode. A few all-nighters, a lot of 3 hour nights, and a good night of sleep was 6 hours. Now I’m depressed and I’ve been sleeping from 9pm to noon and staying in bed for much longer after I’m awake.”
- “Manic 2-4, stable 6-7, depressed 10-12”
- “Around 15 hours of sleep per night while depressed, and between 0-4 hours per night while manic.”
Lack of sleep is such a potent trigger for mania that acute sleep deprivation is literally used to treat depression. Aside from ketamine, not sleeping for a night is the only medicine we have to quickly – literally overnight – and reliably (in ~50% of patients) improve mood in depressed patients (until they go to bed, unless you keep advancing their sleep phase Riemann, D., König, A., Hohagen, F., Kiemen, A., Voderholzer, U., Backhaus, J., Bunz, J., Wesiack, B., Hermle, L. and Berger, M., 1999. How to preserve the antidepressive effect of sleep deprivation: A comparison of sleep phase advance and sleep phase delay. European archives of psychiatry and clinical neuroscience, 249(5), pp.231-237. ). NOTE: DO NOT TRY THIS IF YOU ARE BIPOLAR, YOU MIGHT GET A MANIC EPISODE.
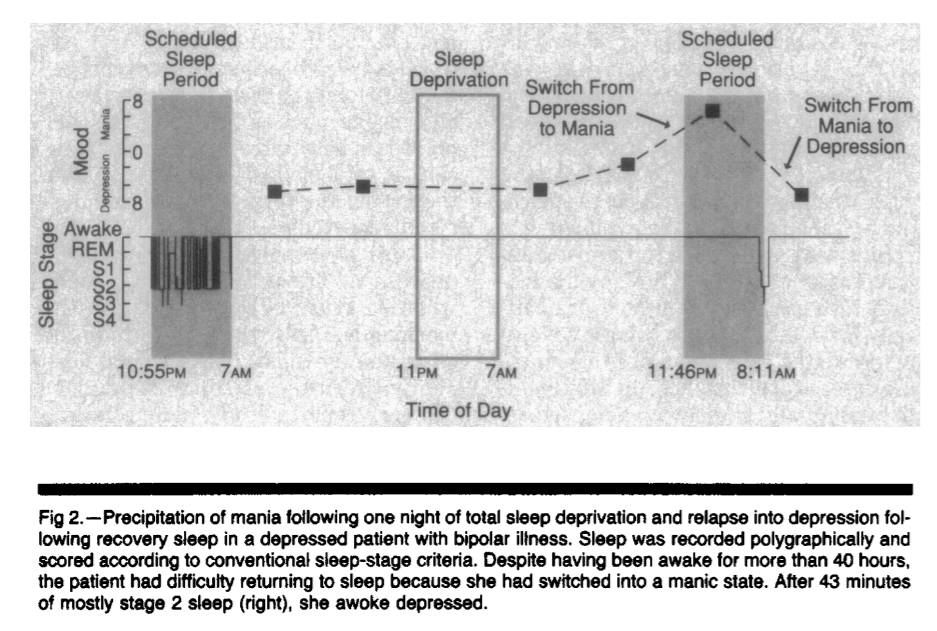
Figure 1. Copied from Wehr TA. Improvement of depression and triggering of mania by sleep deprivation. JAMA. 1992 Jan 22;267(4):548-51.
Why does the lack of sleep promote manic states while long sleep promotes depression? I don’t know. But here are a couple of pointers to interesting papers relevant to the question: Can non-REM sleep be depressogenic? Beersma DG, Van den Hoofdakker RH. Can non-REM sleep be depressogenic?. Journal of affective disorders. 1992 Feb 1;24(2):101-8. Brain-derived neurotrophic factor (BDNF) is associated with synapse growth. Sleep deprivation appears to increase BDNF [and therefore neurogenesis?]. Papers that showed up when I googled “sleep deprivation bdnf”: The Brain-Derived Neurotrophic Factor: Missing Link Between Sleep Deprivation, Insomnia, and Depression . Rahmani M, Rahmani F, Rezaei N. The brain-derived neurotrophic factor: missing link between sleep deprivation, insomnia, and depression. Neurochemical research. 2020 Feb;45(2):221-31. The link between sleep, stress and BDNF . Eckert A, Karen S, Beck J, Brand S, Hemmeter U, Hatzinger M, Holsboer-Trachsler E. The link between sleep, stress and BDNF. European Psychiatry. 2017 Apr;41(S1):S282-. BDNF: an indicator of insomnia? . Giese M, Unternährer E, Hüttig H, Beck J, Brand S, Calabrese P, Holsboer-Trachsler E, Eckert A. BDNF: an indicator of insomnia?. Molecular psychiatry. 2014 Feb;19(2):151-2. Recovery Sleep Significantly Decreases BDNF In Major Depression Following Therapeutic Sleep Deprivation . Goldschmied JR, Rao H, Dinges D, Goel N, Detre JA, Basner M, Sheline YI, Thase ME, Gehrman PR. 0886 Recovery Sleep Significantly Decreases BDNF In Major Depression Following Therapeutic Sleep Deprivation. Sleep. 2019 Apr;42(Supplement_1):A356-.
Jeremy Hadfield writes:
My (summarized/simplified) hypothesis based on what I’ve read: depression involves rigid, non-flexible brain states that correspond to rigid depressive world models. Depression also involves a non-updating of models or inability to draw new connections (brain is even literally slightly lighter in depressed patients). Sleep involves revising/simplifying world models based on connections learned during the day, involves pruning unneeded or irrelevant synaptic connections. Thus, excessive sleep + depression = even less world model updating, even more rigid brain, even fewer new connections. Sleep deprivation can resolve this problem at least temporarily by ensuring that you stay awake for longer and keep adding connections, thus compensating for the decreased connection-building caused by depression and “forcing” a brain update (perhaps through neural annealing - see QRI article).
Occasional acute sleep deprivation is good for health and promotes more efficient sleep
One other argument for sleeping the “natural” (7-9) number of hours is that we feel bad on days when we sleep less. In this section, I argue against this line of reasoning by asking: if fasting and exercising are good, shouldn’t acute sleep deprivation also be good? And I conclude that it is probably good.
Let’s continue our analogy of sleep to eating and add exercise to the mix.
It seems to me that most common arguments against acute sleep deprivation equally “demonstrate” that fasting and exercise are bad.
For example, I ran 7 kilometers 2 days ago and my legs still hurt like hell and I can’t run at all. Does this mean that running is “bad”?
Well, consensus seems to be that dizziness, muscle damage (and thus pain) and decreased physical performance after the run, are not just not bad, but are in fact necessary for the organism to train to run faster or to run longer distances by increasing muscle mass, muscle efficiency, and lung capacity.
What about fasting? When I fast, I am more anxious, I think about food a lot, meaning that focus is more difficult, and I feel cold. And if I decided to fast too much, I would pass out and then die. Does this mean that fasting is “bad”? Well, consensus seems to be that occasional fasting actually activates some “good” kind of stress, promotes healthy autophagy, (obviously) helps to lose weight, etc. and is in fact good.
Now, what happens when I sleep for 2 hours instead of 7 one night? I feel somewhat tingly in my hands, my mood is heightened a little bit, and, if I start watching a movie with my wife at 6pm, I’ll fall asleep. Does this mean that sleeping 2 hours one night is bad for my health?
Obviously no. The only thing we observe is that my organism was subjected to acute stress. However, the reaction to acute stress does not tell us anything about the long-term effects of this kind of stress. As we know, both in running and in fasting, short-term acute stress response results in adaptation and in long-term increase in performance and in benefit to the organism.
I combed through a lot of sleep literature and I haven’t seen a single study that made a parallel to either fasting or exercise and I haven’t seen a single pre-registered RCT that tried to see what happens to someone if you subject them to 1-3 nights per week of acute sleep deprivation and allow to recover the rest of the nights. Do they perform better or worse in the long-term on cognitive tests? Do they have more or less inflammation? Do they need less recovery sleep over time?
I think that the answers are:
- Acute sleep deprivation combined with caffeine or some other stimulant that cancels out sleep pressure does not result in decreased cognitive ability at least until 30-40 hours of wakefulness (if this is true, then sleepiness , rather absence of sleep per se is responsible for decreased cognitive performance during acute sleep deprivation).
- Occasional acute sleep deprivation has no impact on long-term cognitive ability or health.
- Sleep does become more efficient over time and, in complete analogy to exercise, you withstand both acute sleep deprivation better and can function at baseline with a lower amount of sleep in the long-term.
(The only parallel to fasting I’m aware of anyone making is by Nassim Taleb… when he was quote-tweeting me.)
Appendix: anecdotes about acute sleep deprivation
Appendix: philipp streicher on homeostasis, its relationship to mania/depression, and on other points i make, our priors about sleep research should be weak.
In this section, I note that most sleep research is extremely unreliable and we shouldn’t conclude much on the basis of it.
Do you believe in power-posing? In ego depletion? In hungry judges and brain training?
If the answer is no, then your priors for our knowledge about sleep should be weak because “sleep science” is mostly just rebranded cognitive psychology, with the vast majority of it being small-n, not pre-registered, p-hacked experiments.
I have been able to find exactly one pre-registered experiment of the impact of prolonged sleep deprivation on cognition. It was published by economists from Harvard and MIT in 2021 and its pre-registered analysis found null or negative effects of sleep on all primary outcomes Bessone P, Rao G, Schilbach F, Schofield H, Toma M. The economic consequences of increasing sleep among the urban poor. The Quarterly Journal of Economics. 2021 Aug;136(3):1887-941. (note that both the abstract and the main body of this paper report results without the multiple-hypothesis correction, in contradiction to the pre-registration plan of the study. The paper does not mention this change anywhere. See comments for the details. ).
So why has sleep research not been facing a severe replication crisis, similar to psychology?
First, compared to psychology, where you just have people fill out questionnaires, sleep research is slow, relatively expensive, and requires specialized equipment (e.g. EEG, actigraphs). So skeptical outsiders go for easier targets (like social psychology) while the insiders keep doing the same shoddy experiments because they need to keep their careers going somehow .
Second, imagine if sleep researchers had conclusively shown that sleep is not important for memory, health, etc. – would they get any funding? No. Their jobs are literally predicated on convincing the NIH and other grantmakers that sleep is important. As Patrick McKenzie notes , “If you want a problem solved make it someone’s project. If you want it managed make it someone’s job.”
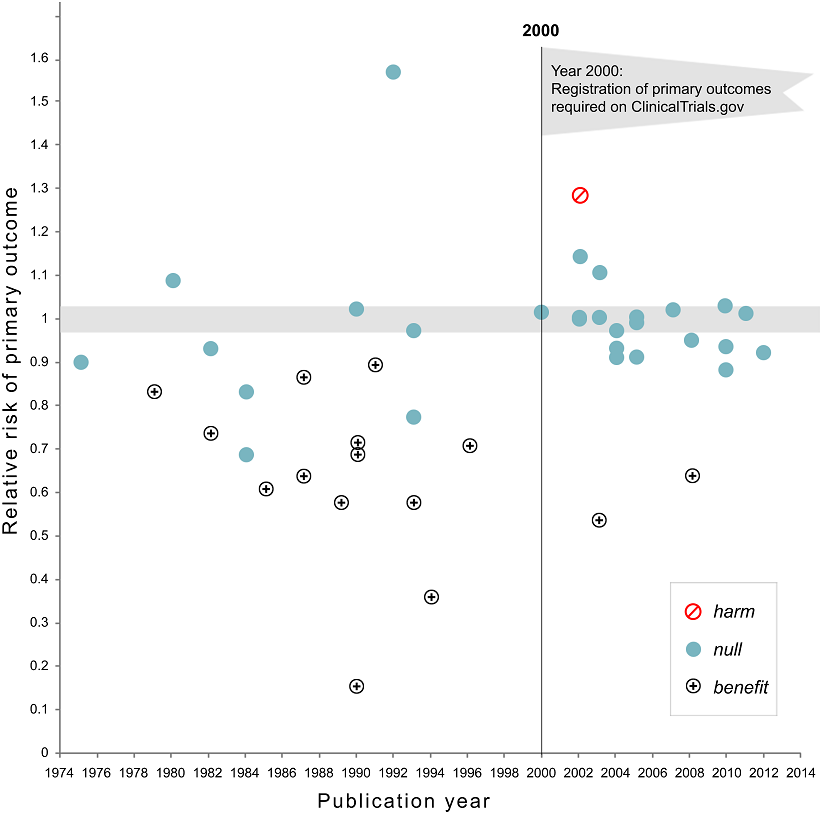
Figure 2. Relative risk of showing benefit or harm of treatment by year of publication for large NHLBI trials on pharmaceutical and dietary supplement interventions. Copied from Kaplan RM, Irvin VL. Likelihood of null effects of large NHLBI clinical trials has increased over time. PloS one. 2015 Aug 5;10(8):e0132382.
Figure 3. Eric Turner on Twitter: “Negative depression trials…Now you see ‘em, now you don’t. Published literature vs FDA, from [ Turner EH, Matthews AM, Linardatos E, Tell RA, Rosenthal R. Selective publication of antidepressant trials and its influence on apparent efficacy. New England Journal of Medicine. 2008 Jan 17;358(3):252-60. ]"
Even in medicine, without pre-registered RCTs truth is extremely difficult to come by, with more than one half Kaiser J. More than half of high-impact cancer lab studies could not be replicated in controversial analysis. AAAS Articles DO Group. 2021; of high-impact cancer papers failing to be replicated, and with one half of RCTs without pre-registration of positive outcomes being spun Kaplan RM, Irvin VL. Likelihood of null effects of large NHLBI clinical trials has increased over time. PloS one. 2015 Aug 5;10(8):e0132382. by researchers as providing benefit when there’s none. And this is in medicine, which is infinitely more consequential and rigorous than psychology.
Also see: Appendix: I have no trust in sleep scientists .
Decreasing sleep by 1-2 hours a night in the long-term has no negative health effects
In this section, I outline several lines of evidence that bring me to the conclusion that decreasing sleep by 1-2 hours a night in the long-term has no negative health effects. To summarize:
- A sleep researcher who trains sailors to sleep efficiently in order to maximize their race performance believes that 4.5-5.5 hours of sleep is fine.
- 70% of 84 hunter-gatherers studied in 2013 slept less than 7 hours per day, with 46% sleeping less than 6 hours.
- A single-point mutation can decrease the amount of required sleep by 2 hours, with no negative side-effects.
- A brain surgery can decrease the amount of sleep required by 3 hours, with no negative-side effects.
- Sleep is not required for memory consolidation.
- Claudio Stampi is a Newton, Massachusetts based sleep researcher. But he is not your normal sleep researcher whose career is built on observational studies or p-hacked n=20 experiments that always show “significant” results. He is one of the only sleep researchers with skin in the game: the goal of his research is to maximize performance of sailors by tinkering with their sleep cycles, and he believes that 4.5-5.5 hours of sleep is fine, The article uses the phrase “get by” and does not state that there’s no decrease in performance. However, it does state that the decrease in performance at 3 hours of sleep with lots of naps is 12-25%, so increasing sleep by 50-83% from this, seems unlikely to result in any decrease in performance, compared to 8 hours of sleep (“he had them shift to their three-hour routines. After more than a month, the monophasic group showed a 30 percent loss in cognitive performance. The group that divided its sleep between nighttime and short naps showed a 25 percent drop. But the polyphasic group, which slept exclusively in short naps, showed only a 12 percent drop."). as long as it’s broken down into core sleep and a series of short (usually 20-minute) naps. Here’s Outside :
“Solo sailing is one of the best models of 24/7 activity, and brains and muscles are required,” Stampi said one day at his home, from which he runs the institute. “If you sleep too much, you don’t win. If you don’t sleep enough, you break.” …
“For those sailors who are seriously competing, Stampi is a necessity,” says Brad Van Liew, a 37-year-old Californian who began working with Stampi in 1998 and went on to become America’s most accomplished solo racer and the winner in his class of the 2002-2003 Around Alone, a 28,000-mile global solo race. “You have to sleep efficiently, or it’s like having a bad set of sails or a boat bottom that isn’t prepared properly.” …
both Golding and MacArthur sleep about the same amount while racing, between 4.5 and 5.5 hours on average in every 24—the minimum amount, Stampi believes, on which humans can get by.
In 2013, scientists tracked the sleep of 84 hunter-gatherers from 3 different tribes Yetish G, Kaplan H, Gurven M, Wood B, Pontzer H, Manger PR, Wilson C, McGregor R, Siegel JM. Natural sleep and its seasonal variations in three pre-industrial societies. Current Biology. 2015 Nov 2;25(21):2862-8. (each person’s sleep was measured for about a week but measurements for different groups were taken in different parts of the year). The average amount of sleep among these 84 people was 6.5 hours. Judging by CDC’s “7 hours or more” recommendation , Consensus Conference Panel:, Watson, N.F., Badr, M.S., Belenky, G., Bliwise, D.L., Buxton, O.M., Buysse, D., Dinges, D.F., Gangwisch, J., Grandner, M.A. and Kushida, C., 2015. Joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society on the recommended amount of sleep for a healthy adult: methodology and discussion. Journal of Clinical Sleep Medicine, 11(8), pp.931-952. 70% out of these 84 undersleep:
- 6 people slept between 4 and 5 hours
- 19 people slept between 5 and 6 hours
- 34 people slept between 6 and 7 hours
- 21 people slept between 7 and 8 hours
- 4 people slept between 8 and 9 hours
One group of hunter-gatherers (10 people from Tsimane tribe studied in November/December of 2013) slept just 5.6 hours on average.
The authors of this study also note that “None of these groups began sleep near sunset, onset occurring, on average, 3.3 hr after sunset” (they are probably getting too much artificial light… or something).
What I’m getting from all of this is: there’s nothing “natural” about sleeping 7-9 hours. If you think that the amount of sleep hunter-gatherers are getting is the amount of sleep humans have evolved to get, then you should not worry at all about getting 4, 5, or 6 hours of sleep a night.
The CDC and the professional sleep researchers pull the numbers out of their asses without any kind of rigorous scientific evidence for their “consensus recommendations”. There’s no causal evidence that sleeping 7-9 hours is healthier than sleeping 6 hours or less. Correlational evidence suggests Shen X, Wu Y, Zhang D. Nighttime sleep duration, 24-hour sleep duration and risk of all-cause mortality among adults: a meta-analysis of prospective cohort studies. Scientific Reports. 2016 Feb 22;6:21480. that people who sleep 4 hours have the same if not lower mortality as those who sleep 8 hours and that people who sleep 6-7 hours have the lowest mortality.

Also see: Appendix: Jerome Siegel and Robert Vertes vs the sleep establishment
It appears that there is a distinct single-point mutation that allows some people to sleep several hours less than typical on average. A Rare Mutation of β1-Adrenergic Receptor Affects Sleep/Wake Behaviors : Shi G, Xing L, Wu D, Bhattacharyya BJ, Jones CR, McMahon T, Chong SC, Chen JA, Coppola G, Geschwind D, Krystal A. A rare mutation of β1-adrenergic receptor affects sleep/wake behaviors. Neuron. 2019 Sep 25;103(6):1044-55.
We have identified a mutation in the β1-adrenergic receptor gene in humans who require fewer hours of sleep than most. In vitro, this mutation leads to decreased protein stability and dampened signaling in response to agonist treatment. In vivo, the mice carrying the same mutation demonstrated short sleep behavior. We found that this receptor is highly expressed in the dorsal pons and that these ADRB1+ neurons are active during rapid eye movement (REM) sleep and wakefulness. Activating these neurons can lead to wakefulness, and the activity of these neurons is affected by the mutation. These results highlight the important role of β1-adrenergic receptors in sleep/wake regulation.
The study compares carriers of the mutation in one family to non-carriers in the same family and finds that carriers sleep about 2 hours per day less. Given the complexity of sleep and the multitude of its functions, it seems extremely implausible that just one mutation in the β1-adrenergic receptor gene was able to increase its efficiency by about 25%. It seems that it just made carriers sleep less (due to more stimulation of a group of neurons in the brain responsible for sleep/wakefulness) without anything else obviously changing when compared to non-carriers.
A similar example of a drop in the amount of sleep required without negative side effects and driven by a single factor was described in Development of a Short Sleeper Phenotype after Third Ventriculostomy in a Patient with Ependymal Cysts . Seystahl K, Könnecke H, Sürücü O, Baumann CR, Poryazova R. Development of a short sleeper phenotype after third ventriculostomy in a patient with ependymal cysts. Journal of Clinical Sleep Medicine. 2014 Feb 15;10(2):211-3. To sum up: a 59-year-old patient had chronic hydrocephalus. An endoscopic third ventriculostomy was performed on him. His sleep dropped from 7-8 hours a night to 4-5 hours a night without him becoming sleepy, he stopped being depressed, and his physical or cognitive performance stayed normal, as measured by the doctors.
Sleep is not required for memory consolidation. Jerome Siegel (the author of the hunter-gatherers study mentioned above) writes in Memory Consolidation Is Similar in Waking and Sleep : Siegel JM. Memory Consolidation Is Similar in Waking and Sleep. Current Sleep Medicine Reports. 2021 Mar;7(1):15-8.
Under interference conditions, such as exist during sleep deprivation, subjects, by staying awake, necessarily interacting with the experimenter keeping them awake and experiencing the laboratory environment, will remember more than just the items that are presented. But they may be less able to recall the particular items the experimenter is measuring. This can lead to the mistaken conclusion that sleep is required for memory consolidation [7].
Recent work has, for the first time, dealt with this issue. It was shown that a quiet waking period or a meditative waking state in which the environment is being ignored, produces a gain in recall similar to that seen in sleep, relative to an active waking state or a sleep-deprived state [8–16]. …
REM sleep has been hypothesized to have a key role in memory consolidation [20]. But it has been reported that near total REM sleep deprivation for a period of 14 to 40 days by administration of the monoamine oxidase inhibitor phenelzine has no apparent effect on cognitive function in humans [21]. A systematic study using serotonin or norepinephrine re-uptake inhibitors to suppress REM sleep in humans had no deleterious effects on a variety of learning tasks [22, 23]. Humans rarely survive the damage to the pontine region which when discretely lesioned in animals greatly reduces or eliminates REM sleep [20, 23–25]. However, one such subject with pontine damage that severely reduced REM sleep has been thoroughly studied. The studies show normal or above normal cognitive performance and no deficit in memory formation or recall [26•]. It has been claimed that learning results in greater total amounts of sleep, or greater amounts of REM sleep [27], or greater amounts of sleep spindles, or slow wave activity. However, a systematic test of this hypothesis in 929 human subjects with night-long EEG recording found no such correlation with retention [28•].
The entire Scientific Consensus™ about sleep being essential for memory consolidation appears to be heavily flawed, driven by people like Matthew Walker, and making me lose the last remnants of trust in sleep science that I had .
Appendix: how I wake up after 6 or less hours of sleep
Appendix: anecdotes about long-term sleep deprivation.
- Appendix: the idea that sleep’s purpose is metabolite clearance, if not total bs, is massively overhyped
Chadwick worked for several nights straight without sleep on the seminal discovery [of the neutron, for which he was awarded the 1935 Nobel in physics]. When he was done he went to a meeting of the Kapitza Club at Cambridge and gave a talk about it, ending with the words, “Now I wish to be chloroformed and put to sleep”.
I’m not what they call a “natural short sleeper”. If I don’t restrict my sleep, I often sleep more than 8 hours and I still struggle with getting out of bed. I used to be really scared of not sleeping enough and almost never set the alarm for less than 7.5 hours after going to bed.
My sleep statistics tells me that I slept an average of 5:25 hours over the last 7 days, 5:49 hours over the last 30 days, and 5:57 over the last 180 days hours, meaning that I’m awake for 18 hours per day instead of 16.5 hours. I usually sleep 5.5-6 hours during the night and take a nap a few times a week when sleepy during the day.
This means that I’m gaining 33 days of life every year. 1 more year of life every 11 years. 5 more years of life every 55 years.
Why are people not all over this? Why is everyone in love with charlatans who say that sleeping 5 hours a night will double your risk of cancer, make you pre-diabetic, and cause Alzheimer’s, despite studies showing that people who sleep 5 hours have the same, if not lower, mortality than those who sleep 8 hours? Convincing a million 20-year-olds to sleep an unnecessary hour a day is equivalent, in terms of their hours of wakefulness, to killing 62,500 of them.
I wrote large chunks of this essay having slept less than 1.5 hours over a period of 38 hours. I came up with and developed the biggest arguments of it when I slept an average of 5 hours 39 minutes per day over the preceding 14 days. At this point, I’m pretty sure that the entire “not sleeping ‘enough’ makes you stupid” is a 100% psyop. It makes you somewhat more sleepy, yes. More stupid, no. I literally did an experiment in which I tried to find changes in my cognitive ability after sleeping 4 hours a day for 12-14 days , I couldn’t find any. My friends who I was talking to a lot during the experiment simply didn’t notice anything.
What do I lose due to sleeping 1.5 hours a day less? I’m somewhat more sleepy every day and staying awake during boring calls is even more difficult now. On the other hand, just a prospect of playing an exciting video game, makes me 100% alert even after sleeping for 2-3 hours. Related: Horne JA, Pettitt AN. High incentive effects on vigilance performance during 72 hours of total sleep deprivation. Acta psychologica. 1985 Feb 1;58(2):123-39. There’s no guarantee that what I’m doing is healthy after all, although, as I explained above, I think that it’s extremely unlikely due to likely adaptation, and likely beneficial effects of sleep deprivation (e.g. increased BDNF, less susceptibility to depression), and since I take a 20-minute nap under my wife’s watch whenever I don’t feel good.
Subscribe to the updates here – I usually send them every 1-2 months (example: last update ):
Acknowledgements
I would like to thank (in reverse alphabetic order): Misha Yagudin , Guy Wilson , Bart Sturm, Ulysse Sabbag , Stephen Malina , Gavin Leech , Anastasia Kuptsova , Jake Koenig , Aleksandr Kotyurgin, Alexander Kim , Basil Halperin , Jeremy Hadfield , Steve Gadd , and Willy Chertman for reading drafts of this essay and for disagreeing with many parts of it vehemently. All errors mine.
Guzey, Alexey. Theses on Sleep. Guzey.com. 2022 February. Available from https://guzey.com/theses-on-sleep/ .
Or download a BibTeX file here .
- One popular sleep tip I’ve come to wholeheartedly believe is the importance of waking up at the same time: from my experience, it does really seem that the organism adjusts the time it is ready to wake up if you keep a consistent schedule.
- observation: I find staying awake during boring lectures impossible and reliably fall asleep during them, regardless of the amount of sleep I’m getting
- observation: I can play video games with little sleep for several days and feel 100% alert (a superstimulus of its own, but still a valuable observation)
- observation: I become sleepy when I’m working on something boring and difficult
Common objections
Objection: “When I’m underslept I notice that I’m less productive.”
Yes, this is expected as per the analogy to exercise I make above . After exercise you are tired but over time you become stronger.
It might be that undersleeping itself causes you to be less productive. However, it might also be the case that there’s an upstream cause that results in both undersleeping and lack of productivity. I think either could be the case depending on the person but understanding what exactly happens is much harder than people typically appreciate when they notice such co-occurrences.

As Nick Wignall notes on Twitter:
People are also not great at distinguishing true sleepiness from tiredness.
Analogy would be: of all the times when you feel hungry, how much of that is true hunger vs a craving?
Also related: when people say that e.g. they have a small child, are doing medical residency, etc. and feel terrible due to undersleep, note that there’s a big difference between being randomly forced to not sleep when you want to sleep and managing one’s sleep consciously. The analogy would be to saying that fasting is bad because if you are forbidden by someone from eating randomly throughout the day.
Objection: “Driving when you are sleepy is dangerous, therefore you are wrong.”
Answer: Yep, I agree that driving while being sleepy is dangerous and I don’t want anyone to drive, to operate heavy machinery, etc. when they are sleepy. This, however, bears no relationship on any of the arguments I make.
Objection: “The graph that shows more sleep being associated with higher doesn’t tell us anything because sick people tend to sleep more.”
Answer: It is true that some diseases lead to prolonged sleep. However, some diseases also lead to shortened sleep. For example, many stroke patients suffer from insomnia Sterr A, Kuhn M, Nissen C, Ettine D, Funk S, Feige B, Umarova R, Urbach H, Weiller C, Riemann D. Post-stroke insomnia in community-dwelling patients with chronic motor stroke: physiological evidence and implications for stroke care. Scientific Reports. 2018 May 30;8(1):8409. and people with fatal familial insomnia struggle with insomnia. Therefore, if you want to make the argument that the association between longer sleep and higher mortality is not indicative of the effect of sleep, you have to accept that the same is true about shorter sleep and higher mortality.
Appendix: I have no trust in sleep scientists
Why do I bother with all of this theorizing? Why do I think I can discover something about sleep that thousands of them couldn’t discover over many decades?
The reason is that I have approximately 0 trust in the integrity of the field of sleep science.
As you might be aware, 2 years ago I wrote a detailed criticism of the book Why We Sleep written by a Professor of Neuroscience at psychology at UC Berkeley, the world’s leading sleep researcher and the most famous expert on sleep, and the founder and director of the Center for Human Sleep Science at UC Berkeley, Matthew Walker.
Here are just a few of biggest issues (there were many more) with the book.
Walker wrote: “Routinely sleeping less than six or seven hours a night demolishes your immune system, more than doubling your risk of cancer”, despite there being no evidence that cancer in general and sleep are related. There are obviously no RCTs on this, and, in fact, there’s not even a correlation between general cancer risk and sleep duration.
Walker falsified a graph from an academic study in the book.
Walker outright fakes data to support his “sleep epidemic” argument. The data on sleep duration Walker presents on the graph below simply does not exist :

Here’s some actual data on sleep duration over time:

By the time my review was published, the book had sold hundreds of thousands if not millions of copies and was praised by the New York Times , The Guardian , and many other highly-respected papers. It was named one of NPR’s favorite books of 2017 while Walker went on a full-blown podcast tour.
Did any sleep scientists voice the concerns they with the book or with Walker? No. They were too busy listening to his keynote at the Cognitive Neuroscience Society 2019 meeting.
Did any sleep scientists voice their concerns after I published my essay detailing its errors and fabrications? No (unless you count people replying to me on Twitter as “voicing a concern”).
Did Walker lose his status in the community, his NIH grants, or any of his appointments? No, no, and no.
I don’t believe that a community of scientists that refuses to police fraud and of which Walker is a foremost representative (recall that he is the director of the Center for Human Sleep Science at UC Berkeley) could be a community of scientists that would produce a trustworthy and dependable body of scientific work.
Appendix: the idea that sleep’s purpose is metabolite clearance, if not total bs, is massively overhyped
Specifically, the original 2013 paper Xie L, Kang H, Xu Q, Chen MJ, Liao Y, Thiyagarajan M, O’Donnell J, Christensen DJ, Nicholson C, Iliff JJ, Takano T. Sleep drives metabolite clearance from the adult brain. science. 2013 Oct 18;342(6156):373-7. accumulated more than 3,000 (!) citations in less than 10 years and is highly misleading.
The paper is called “Sleep Drives Metabolite Clearance from the Adult Brain”. The abstract says:
The conservation of sleep across all animal species suggests that sleep serves a vital function. We here report that sleep has a critical function in ensuring metabolic homeostasis. Using real-time assessments of tetramethylammonium diffusion and two-photon imaging in live mice, we show that natural sleep or anesthesia are associated with a 60% increase in the interstitial space, resulting in a striking increase in convective exchange of cerebrospinal fluid with interstitial fluid. In turn, convective fluxes of interstitial fluid increased the rate of β-amyloid clearance during sleep. Thus, the restorative function of sleep may be a consequence of the enhanced removal of potentially neurotoxic waste products that accumulate in the awake central nervous system.
At the same time, the paper found that anesthesia without sleep results in the same clearance (paper: “Aβ clearance did not differ between sleeping and anesthetized mice”), meaning that clearance is not caused by sleep per se, but instead only co-occurrs with it. Authors did not mention this in the abstract and mistitled the paper, thus misleading the readers. As far as I can tell, literally nobody pointed this out previously.
And on top of all of this “125I-Aβ1-40 was injected intracortically”, meaning that they did not actually find any brain waste products that would be cleared out. This is an exogenous compound that was injected god knows where disrupting god knows what in the brain.
Max Levchin in Founders at Work :
The product wasn’t really finished, and about a week before the beaming at Buck’s I realized that we weren’t going to be able to do it, because the code wasn’t done. Obviously it was really simple to mock it up—to sort of go, “Beep! Money is received.” But I was so disgusted with the idea. We have this security company; how could I possibly use a mock-up for something worth $4.5 million? What if it crashes? What if it shows something? I’ll have to go and commit ritual suicide to avoid any sort of embarrassment. So instead of just getting the mock-up done and getting reasonable rest, my two coders and I coded nonstop for 5 days. I think some people slept; I know I didn’t sleep at all. It was just this insane marathon where we were like, “We have to get this thing working.” It actually wound up working perfectly. The beaming was at 10:00 a.m.; we were done at 9:00 a.m.
/u/CPlusPlusDeveloper on Gwern’s Writing in the Morning :
We know that acute sleep deprivation seems to have a manic and euphoric effect on at least some percent of the population some percent of the time. For example staying up all night is one of the most effective ways to temporarily aleve depression. Of course the problem is that chronic sleep deprivation has the opposite effect, and the temporary mania and euphoria is not sustainable.
My speculative take is that whatever this mechanism, it was the main reason you experienced a productivity boost. By waking up early you intentionally were fighting against your chronobiology, hence adding an element of acute sleep deprivation regardless of how many hours you got the night before. That mania fuels an amphetamine like focus.
The upshot, if my hypothesis is true, is that waking up early would not produce similar gains if you did it everyday. Like the depressive who stays up all night, it may feels like you’ve discovered an intervention that will pay lasting gains. But if you were to actually make it part of your recurring lifestyle, the benefits would stop, and eventually the impact would work in reverse.
Along those lines that’s probably why you naturally tend to stop conforming to that pattern after a few days. As acute sleep deprivation becomes chronic, you’re most likely intuitively recognizing that the pattern has crossed over to the point of being counter-productive.
Lots of writers and software engineers note that their creative juices start flowing by evening extending late into the night - I think this phenomenon is closely related to the one described in the comment above.
Brian Timar :
sleep anecdote- In undergrad I had zero sleep before several major tests; also before quals in grad school. Basically wouldn’t sleep before things I really considered important (this included morning meetings I didn’t want to miss!). On such occasions I would feel:
miserable, then absurd and in a good humor, weirdly elated, then Super PumpedTM, and
really sharp when the test (or whatever) actually started.
Appendix: a well-documented case-study of a person living without sleep for 4 months
Total Wake: Natural, Pathological, and Experimental Limits to Sleep Reduction , Panchin Y, Kovalzon VM. Total Wake: Natural, Pathological, and Experimental Limits to Sleep Reduction. Frontiers in neuroscience. 2021 Apr 7;15:288. quoting Le sommeil, la conscience et l’éveil : Jouvet M. Le sommeil, la conscience et l’éveil. Odile Jacob; 2016 Mar 9.
There is such pathology as Morvan’s disease, in which quasi-wakefulness, which lasted 3,000 h (more precisely, 2,880), or 4 months, was not accompanied by sleep rebound, since the sleep generation system itself was disturbed.” Throughout this period the patient was under continuous polysomnographic control, so his agrypnia was confirmed objectively. Jouvet conclude that “… slow wave (NREM) and paradoxical (REM) sleep are not necessary for life (at least for 4–5 months for the first and about 8 months for the second), and we cannot consider their suppression to be the cause of any serious disorders in the body. A person who had lack of sleep and dreams for 4 months, of which there are only a few minutes of nightly hallucinations, can turn out to read newspapers during the day, make plans, play cards and win, and at the same time lie on the bed in the dark all night without sleep! In conclusion, we admit: this observation makes most theories about the functions of sleep and paradoxical (REM) sleep obsolete at once, but offers nothing else
I once tried to cheat sleep, and for a year I succeeded (strong peak-performance-sailing vibes):
In the summer of 2009, I was finishing the first—and toughest—year of my doctorate. …
To keep up this crazy sleep schedule, I always needed a good reason to wake up the next morning after my 3.5-hour nighttime sleep. So before I went to bed, I reviewed the day gone past and planned what I would do the next day. I’ve carried on with this habit, and it serves me well even today.
But the Everyman schedule was reasonably flexible. Some days when I missed a nap, I simply slept a little more at night. There were also days when I couldn’t manage a single nap, but it didn’t seem to affect me very much the next day.
To the surprise of many, and even myself, I had managed to be on the polyphasic schedule for more than a year. But then came a conference where for a week I could not get a single nap. It was unsettling but I was sure I would be able to get back to sleeping polyphasic without too much trouble.
I was wrong. When I tried to get back into the schedule, I couldn’t find the motivation to do it; I didn’t have the same urgent goals that I had had a year ago. So I returned to sleeping like an average human.
James Gleck in Chaos on Mitch Feigenbaum:
In the spring of 1976 he entered a mode of existence more intense than any he had lived through. He would concentrate as if in a trance, programming furiously, scribbling with his pencil, programming again. He could not call C division for help, because that would mean signing off the computer to use the telephone, and reconnection was chancy. He could not stop for more than five minutes’ thought, because the computer would automatically disconnect his line. Every so often the computer would go down anyway, leaving him shaking with adrenaline. He worked for two months without pause. His functional day was twenty-two hours. He would try to go to sleep in a kind of buzz, and awaken two hours later with his thoughts exactly where he had left them. His diet was strictly coffee. (Even when healthy and at peace, Feigenbaum subsisted exclusively on the reddest possible meat, coffee, and red wine. His friends speculated that he must be getting his vitamins from cigarettes.)
In the end, a doctor called it off. He prescribed a modest regimen of Valium and an enforced vacation. But by then Feigenbaum had created a universal theory.
Ryan Kulp’s experience with decreasing the amount of sleep by several hours :
i began learning to code in 2015. since i was working full-time i needed to maximize after-hours to learn quickly. i experimented for 10 days straight… go to sleep at 4am, wake up at 8am for work. felt fine.
actually, the first 5-10 minutes of “getting up” after 3-4 hours of sleep sucks more than if i sleep ~8 hours. but after 15 mins of moving around, a shower, etc, i feel as if i slept 8 hours.
since then i’ve routinely slept 4-6 hours /day and definitely been more productive. i think if more people experimented for themselves and had the same “aha” moment i did (that you feel fine after the initial gut-wrenching “i slept too little” reaction), they’d get more done too.
This is a very good point that shows that: there’s (1) how sleepy we feel when waking up and (2) how sleepy we feel during the day. (2) is probably more important but most people are focused on (1) and the implicit assumption is that poor (1) leads to (2) – which is unwarranted.
Also: https://twitter.com/BroodVx/status/1492227577896787969,
Nabeel Qureshi writes:
you’re combining two things here: (1) your brain is overpowered by the comfy soft temp-controlled bed (2) you’re bored. they might both be right but i think you conflate them, and they’re separate arguments. this is important bc i think the strongest counterargument to what you’re saying is the classic experience of: you force yourself to wake up early (say 6), you have a project you’re genuinely excited about (hence #2 is false), but when you sit down to work, you’re tired and can’t quite focus. in this scenario, i think your theory would say that i’m not really that excited about what i’m doing, because if i were (see video game argument) then i’d be awake. i’d disagree and say that the researcher should just go take a nap, and they’ll probably be able to make more progress per hour than the extra hours they gain… trying to force yourself to do something while underslept, subjectively, feels hellish. i’m sure you’ve had this experience - did you figure out a workaround?
It is completely true that if you are excited by a project but it’s not super stimulating, it’s still very easy to wake up after less than usual number of hours of sleep and feel sleepy and terrible. This is true for me as well. I found a solution to this: instead of heading straight to the computer, I first unload the clean plates from the dishwasher and load it with dirty plates. This activity is quite special in that it is:
- Why this matters: moving around wakes up the body much better than just sitting.
- Why this matters: moving around in automatic pre-defined movements eventually results in the brain just performing these movements on autopilot without waking up.
- Why this matters: I and people I know tend to find intense physical activities right after waking up really unpleasant and somewhat nauseating.
In about 90% of the cases, 10 minutes later when I’m done with the dishwasher, I find that I’m fully awake and don’t actually want to sleep anymore. In the remaining 10% of the cases, I stay awake and work until my wife wakes up and then go take a 20-minute nap under her watch (and take as many 20-minute naps as I need during the day, although I only end up taking a few naps a week and rarely more than one per day, unless I’m sick).
Appendix: Elon Musk on working 120 hours a week and sleep
On Tesla’s first-quarter earnings conference call in May, Musk referred to inquiries from Wall Street analysts as “boring, bonehead questions” and as “so dry. They’re killing me.” On the next earnings conference call in August, Musk said he was sorry for “being impolite” on the previous call.
“Obviously I think there’s really no excuse for bad manners and I was violating my own rule in that regard. There are reasons for it, I got no sleep, 120 hour weeks, but nonetheless, there is still no excuse, so my apologies for not being polite on the prior call,” Musk said.
Later in August, in conversation with the New York Times, Musk reported using prescription sleep medication Ambien to sleep.
“Yeah. It’s not like for fun or something,” Musk told Swisher Wednesday. “If you’re super stressed, you can’t go to sleep. You either have a choice of, like, okay, I’ll have zero sleep and then my brain won’t work tomorrow, or you’re gonna take some kind of sleep medication to fall asleep.”
Musk said he was working such insane hours to get Tesla through the ramp up in production for its Model 3 vehicle. ”[A]s a startup, a car company, it is far more difficult to be successful than if you’re an established, entrenched brand. It is absurd that Tesla is alive. Absurd! Absurd.”
Philipp ( @Cautes ):
First, I wanted to share a way of thinking about some of your findings that builds on the idea of a homeostatic control system (brought to you from engineering via cybernetics). The classic example is a thermostat, which keeps temperature of a room close to a set point. Biology is quite a bit more messy than this, of course, but the body makes use of a plenty of feedback mechanisms to stay close to set points as well. You’re right in pointing out that these set points don’t need to be healthy though. For example, measured via EEG, PTSD patients have alpha power (which primarily modulates neural inhibition in frontal, parietal and occipital areas of the brain) set points far below that of healthy control groups. One way to deal with these suboptimal set points is to simply disrupt the system. Here’s a model that makes this point nicely: imagine all possible brain state dynamics as a two-dimensional plane and place a ball on it which represents the current brain state space. As the ball moves, the brain dynamics change as well (in frequency, phase, amplitude - you name it). On the plane, you have basins that give stability to the brain state, and repellers in the form of hills, as well as random noise and outside interference which drives the ball into various directions. Sometimes the ball will get stuck in basins which are highly suboptimal, but they are deep enough that exploration of other set points is not possible. If the system is disrupted, the ball might get jolted out of its basin though, and be again able to fall into a more optimal position.
With that said, there’s plenty of evidence that stability in itself (even within better basins) is suboptimal for perfect health, because contexts change. For example, people who are very physically healthy (athletes, for example), tend to have far greater variance in the time interval between individual heart beats (heart rate variability) than even the average person, and as the average person gets healthier, their heart rate variability increases as well. Basically, the body becomes more resilient by introducing a noise signal that produces chaotic fluctuations to homeostatic control mechanisms (controlled allostasis) and there are good reasons to think that this is true of psychological health as well.
Because of this, I think that you’re right in suggesting that varying the amount of time you sleep is a good thing - especially if you’re currently struggling with depression or mania. Not even necessarily because sleep per se is the culprit, but because it might dislodge a ball stuck in a suboptimal basin, so to speak. Depressed people tend to oversleep, people with mania tend to sleep too little, so steering in the opposite direction is only logical. For perfectly healthy people, sleep cycling is probably the best way to go - kind of a mirroring the logic of heart rate variability: introduce some noise to keep your body on your toes. It’s just like fasting, working out, cold exposure, saunas, etc. - it’s al about producing stressors on the body which stir up repair processes which keep you healthy (and biologically younger). I have done plenty of self-experiments with polyphasic 5-6 hour sleeping (similar to the the approach studied by Stampi, who you mentioned), with no negative consequences. The main thing that makes it impractical is that intermittent napping is sometimes hard to combine with professional responsibilities and a social life.
As a side note, because you ask the question about why depressed people sleep longer, and people with mania sleep less, the answer to this is very likely highly multi-causal. With that said, I wanted to point out that depressed people generally exhibit excessive alpha activity in eyes-open waking states, which normally becomes more pronounced in people as they drift off to sleep (because of the neural inhibition function). We also have reason to believe that it mediates between BDNF and subclinical depressed mood, so that’s a link to something else you talk about in your article. As for mania, I haven’t looked at this myself, but I remember hearing that it’s almost a mirror image, with generally decreased synchronisation of slower oscillations and heightened faster rhythms, generally associated with greater arousal and wakefulness.
One last thing: as you point out, sleep is likely not required for memory retention. Any claim that sleep is about any specific cognitive function should be suspect on the principle that the phenomenon of sleep predates the development of organisms with brains - it can’t have evolved specifically for something as high-level as memory retention. It’s more likely about something more basic like general metabolic health.
Appendix: Jerome Siegel and Robert Vertes vs the sleep establishment
Time for the Sleep Community to Take a Critical Look at the Purported Role of Sleep in Memory Processing Vertes RP, Siegel JM. Time for the sleep community to take a critical look at the purported role of sleep in memory processing. Sleep. 2005 Oct 1;28(10):1228-9. by Robert Vertes and Jerome Siegel (a reply to Walker claiming that the debate on memory processing in sleep is essentially settled):
The present ‘debate’ was sparked by an editorial by Robert Stickgold in SLEEP on an article in that issue by Schabus et a on paired associate learning and sleep spindles in humans
Regarding Stickgold’s editorial, I was particularly troubled by his opening statement, as follows: “The study of sleep-dependent memory consolidation has moved beyond the question of whether it exists to questions of its extent and of the mechanisms supporting it”. He then proceeded to cite evidence justifying this statement. Surprisingly, there was no mention of opposing views or a discussion of data inconsistent with the sleep-memory consolidation (S-MC) hypothesis. It seemed that the controversial nature of this issue should have at least been acknowledged, but apparently to do so would have undermined Stickgold’s position that the door is closed on this debate and only the fine points need be resolved. …
By all accounts, sleep does not serve a role in declarative memory. As reviewed by Smith, with few exceptions, reports have shown that depriving subjects of REM sleep does not disrupt learning/memory, or exposure to intense learning situations does not produce subsequent increases in REM sleep. Smith concluded: “REM sleep is not involved with consolidation of declarative material.” The study by Schabus et al (see above) is another example that the learning of declarative material is unaffected by sleep. They reported that subjects showed no significant difference in the percentage of word-pairs correctly recalled before and after 8 hours of sleep. Or as Stickgold stated in his editorial [the editorial Vertes and Siegel are replying to], “Performance in the morning was essentially unchanged from the night before”. It would seem important for Stickgold/Walker to acknowledge that the debate on sleep and memory has been reduced to a consideration of procedural memory – to the exclusion of declarative memory. If there are exceptions, they should note. Several lines of evidence indicate that REM sleep is not involved in memory processing/consolidation – or at least not in humans. Perhaps the strongest argument for this is the demonstration that the marked suppression or elimination of REM sleep in individuals with brainstem lesions or on antidepressant drugs has no detrimental effect on cognition. A classic case is that of an Israeli man who at the age of 19 suffered damage to the brainstem from shrapnel from a gunshot wound, and when examined at the age of 33 he showed no REM sleep. The man, now 55, is a lawyer, a painter and interestingly the editor of a puzzle column for an Israeli magazine. Recently commenting on his ‘famous’ patient, Peretz Lavie stated that “he is probably the most normal person I know and one of the most successful ones”. There are several other well documented cases of individuals with greatly reduced or absent REM sleep that exhibit no apparent cognitive deficits. It would seem that these individuals would be a valuable resource for examining the role of sleep in memory. …
In Memory Consolidation Is Similar in Waking and Sleep cited above, Siegel notes: Siegel JM. Memory Consolidation Is Similar in Waking and Sleep. Current Sleep Medicine Reports. 2021 Mar;7(1):15-8.
To critically evaluate this hypothesis [that sleep has a critical role in memory consolidation], we must take “interference” effects into account. If you learn something before or after the experimenter induced learning that is being measured in the typical sleep-memory study, it degrades recall of the tested information. For example if you tell a subject that the capital of Australia is Canberra and then allow the subject to have a normal night’s sleep, there is a high probability that the subject will remember this upon awakening. If on the other hand you tell the subject that the capital of Australia is Canberra, the capital of Brazil is Brasilia, the capital of Canada is Ottawa, the capital of Iceland is Reykjavik, the capital of Libya is Tripoli, the capital of Pakistan is Islamabad, etc., it is much less likely the subject will remember the capital of Australia. The effect of proactive and retroactive interference is dependent on the temporal juxtaposition, complexity, and similarity of the encountered material to the associations being tested. Interference is a well-established concept in the learning literature [1–6]. Under interference conditions, such as exist during sleep deprivation, subjects, by staying awake, necessarily interacting with the experimenter keeping them awake and experiencing the laboratory environment, will remember more than just the items that are presented. But they may be less able to recall the particular items the experimenter is measuring. This can lead to the mistaken conclusion that sleep is required for memory consolidation [7].
Fur Seals Suppress REM Sleep for Very Long Periods without Subsequent Rebound : Lyamin OI, Kosenko PO, Korneva SM, Vyssotski AL, Mukhametov LM, Siegel JM. Fur seals suppress REM sleep for very long periods without subsequent rebound. Current Biology. 2018 Jun 18;28(12):2000-5.
Virtually all land mammals and birds have two sleep states: slow-wave sleep (SWS) and rapid eye movement (REM) sleep [1, 2]. After deprivation of REM sleep by repeated awakenings, mammals increase REM sleep time [3], supporting the idea that REM sleep is homeostatically regulated. * Some evidence suggests that periods of REM sleep deprivation for a week or more cause physiological dysfunction and eventual death [4, 5]. However, separating the effects of REM sleep loss from the stress of repeated awakening is difficult [2, 6]. The northern fur seal (Callorhinus ursinus) is a semiaquatic mammal [7]. It can sleep on land and in seawater. The fur seal is unique in showing both the bilateral SWS seen in most mammals and the asymmetric sleep previously reported in cetaceans [8]. Here we show that when the fur seal stays in seawater, where it spends most of its life [7], it goes without or greatly reduces REM sleep for days or weeks. After this nearly complete elimination of REM, it displays minimal or no REM rebound upon returning to baseline conditions. Our data are consistent with the hypothesis that REM sleep may serve to reverse the reduced brain temperature and metabolism effects of bilateral nonREM sleep, a state that is greatly reduced when the fur seal is in the seawater, rather than REM sleep being directly homeostatically regulated. This can explain the absence of REM sleep in the dolphin and other cetaceans and its increasing proportion as the end of the sleep period approaches in humans and other mammals.
Appendix: more papers I found interesting
The end of sleep: ‘Sleep debt’ versus biological adaptation of human sleep to waking needs : Horne J. The end of sleep:‘sleep debt’versus biological adaptation of human sleep to waking needs. Biological psychology. 2011 Apr 1;87(1):1-4.
It is argued that the latter part of usual human sleep is phenotypically adaptable (without ‘sleep debt’) to habitual shortening or lengthening, according to environmental influences of light, safety, food availability and socio-economic factors, but without increasing daytime sleepiness. Pluripotent brain mechanisms linking sleep, hunger, foraging, locomotion and alertness, facilitate this time management, with REM acting as a ‘buffer’ between wakefulness and nonREM (‘true’) sleep. The adaptive sleep range is approximately 6–9 h, although, a timely short (<20 min) nap can equate to 1 h ‘extra’ nighttime sleep. Appraisal of recent epidemiological findings linking habitual sleep duration to mortality and morbidity points to nominal causal effects of sleep within this range. Statistical significance, here, may not equate to real clinical significance. Sleep durations outside 6–9 h are usually surrogates of common underlying causes, with sleep associations taking years to develop. Manipulation of sleep, alone, is unlikely to overcome these health effects, and there are effective, rapid, non-sleep, behavioural countermeasures. Sleep can be taken for pleasure, with minimal sleepiness; such ‘sleepability’ is ‘unmasked’ by sleep-conducive situations. Sleep is not the only anodyne to sleepiness, but so is wakefulness, inasmuch that some sleepiness disappears when wakefulness becomes more challenging and eventful. A more ecological approach to sleep and sleepiness is advocated.
Long-term moderate elevation of corticosterone facilitates avian food-caching behaviour and enhances spatial memory Pravosudov VV. Long-term moderate elevation of corticosterone facilitates avian food-caching behaviour and enhances spatial memory. Proceedings of the Royal Society of London. Series B: Biological Sciences. 2003 Dec 22;270(1533):2599-604.
It is widely assumed that chronic stress and corresponding chronic elevations of glucocorticoid levels have deleterious effects on animals' brain functions such as learning and memory. Some animals, however, appear to maintain moderately elevated levels of glucocorticoids over long periods of time under natural energetically demanding conditions, and it is not clear whether such chronic but moderate elevations may be adaptive. I implanted wild–caught food–caching mountain chickadees (Poecile gambeli), which rely at least in part on spatial memory to find their caches, with 90–day continuous time–release corticosterone pellets designed to approximately double the baseline corticosterone levels. Corticosterone–implanted birds cached and consumed significantly more food and showed more efficient cache recovery and superior spatial memory performance compared with placebo–implanted birds. Thus, contrary to prevailing assumptions, long–term moderate elevations of corticosterone appear to enhance spatial memory in food–caching mountain chickadees. These results suggest that moderate chronic elevation of corticosterone may serve as an adaptation to unpredictable environments by facilitating feeding and food–caching behaviour and by improving cache–retrieval efficiency in food–caching birds.
Racemic Ketamine as an Alternative to Electroconvulsive Therapy for Unipolar Depression: A Randomized, Open-Label, Non-Inferiority Trial (KetECT) (via Tomas Roos ): Ekstrand J, Fattah C, Persson M, Cheng T, Nordanskog P, Åkeson J, Tingström A, Lindström M, Nordenskjöld A, Movahed RP. Racemic Ketamine as an Alternative to Electroconvulsive Therapy for Unipolar Depression:: A Randomized, Open-Label, Non-Inferiority Trial (KetECT). International Journal of Neuropsychopharmacology. 2021.
Background Ketamine has emerged as a fast-acting and powerful antidepressant, but no head to head trial has been performed, Here, ketamine is compared with electroconvulsive therapy (ECT), the most effective therapy for depression.
Methods Hospitalized patients with unipolar depression were randomized (1:1) to thrice-weekly racemic ketamine (0.5 mg/kg) infusions or ECT in a parallel, open-label, non-inferiority study. The primary outcome was remission (Montgomery Åsberg Depression Rating Scale score ≤10). Secondary outcomes included adverse events (AEs), time to remission, and relapse. Treatment sessions (maximum of 12) were administered until remission or maximal effect was achieved. Remitters were followed for 12 months after the final treatment session.
Results In total 186 inpatients were included and received treatment. Among patients receiving ECT, 63% remitted compared with 46% receiving ketamine infusions (P = .026; difference 95% CI 2%, 30%). Both ketamine and ECT required a median of 6 treatment sessions to induce remission. Distinct AEs were associated with each treatment. Serious and long-lasting AEs, including cases of persisting amnesia, were more common with ECT, while treatment-emergent AEs led to more dropouts in the ketamine group. Among remitters, 70% and 63%, with 57 and 61 median days in remission, relapsed within 12 months in the ketamine and ECT groups, respectively (P = .52).
Conclusion Remission and cumulative symptom reduction following multiple racemic ketamine infusions in severely ill patients (age 18–85 years) in an authentic clinical setting suggest that ketamine, despite being inferior to ECT, can be a safe and valuable tool in treating unipolar depression.
Beersma DG, Van den Hoofdakker RH. Can non-REM sleep be depressogenic?. Journal of affective disorders. 1992 Feb 1;24(2):101-8.
Bessone P, Rao G, Schilbach F, Schofield H, Toma M. The economic consequences of increasing sleep among the urban poor. The Quarterly Journal of Economics. 2021 Aug;136(3):1887-941.
Consensus Conference Panel:, Watson, N.F., Badr, M.S., Belenky, G., Bliwise, D.L., Buxton, O.M., Buysse, D., Dinges, D.F., Gangwisch, J., Grandner, M.A. and Kushida, C., 2015. Joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society on the recommended amount of sleep for a healthy adult: methodology and discussion. Journal of Clinical Sleep Medicine, 11(8), pp.931-952.
Eckert A, Karen S, Beck J, Brand S, Hemmeter U, Hatzinger M, Holsboer-Trachsler E. The link between sleep, stress and BDNF. European Psychiatry. 2017 Apr;41(S1):S282-.
Ekstrand J, Fattah C, Persson M, Cheng T, Nordanskog P, Åkeson J, Tingström A, Lindström M, Nordenskjöld A, Movahed RP. Racemic Ketamine as an Alternative to Electroconvulsive Therapy for Unipolar Depression:: A Randomized, Open-Label, Non-Inferiority Trial (KetECT). International Journal of Neuropsychopharmacology. 2021.
Giese M, Unternährer E, Hüttig H, Beck J, Brand S, Calabrese P, Holsboer-Trachsler E, Eckert A. BDNF: an indicator of insomnia?. Molecular psychiatry. 2014 Feb;19(2):151-2.
Goldschmied JR, Rao H, Dinges D, Goel N, Detre JA, Basner M, Sheline YI, Thase ME, Gehrman PR. 0886 Recovery Sleep Significantly Decreases BDNF In Major Depression Following Therapeutic Sleep Deprivation. Sleep. 2019 Apr;42(Supplement_1):A356-.
Horne J. The end of sleep:‘sleep debt’versus biological adaptation of human sleep to waking needs. Biological psychology. 2011 Apr 1;87(1):1-4.
Horne JA, Pettitt AN. High incentive effects on vigilance performance during 72 hours of total sleep deprivation. Acta psychologica. 1985 Feb 1;58(2):123-39.
Kaiser J. More than half of high-impact cancer lab studies could not be replicated in controversial analysis. AAAS Articles DO Group. 2021;
Kaplan RM, Irvin VL. Likelihood of null effects of large NHLBI clinical trials has increased over time. PloS one. 2015 Aug 5;10(8):e0132382.
Lyamin OI, Kosenko PO, Korneva SM, Vyssotski AL, Mukhametov LM, Siegel JM. Fur seals suppress REM sleep for very long periods without subsequent rebound. Current Biology. 2018 Jun 18;28(12):2000-5.
Pravosudov VV. Long-term moderate elevation of corticosterone facilitates avian food-caching behaviour and enhances spatial memory. Proceedings of the Royal Society of London. Series B: Biological Sciences. 2003 Dec 22;270(1533):2599-604.
Turner EH, Matthews AM, Linardatos E, Tell RA, Rosenthal R. Selective publication of antidepressant trials and its influence on apparent efficacy. New England Journal of Medicine. 2008 Jan 17;358(3):252-60.
Rahmani M, Rahmani F, Rezaei N. The brain-derived neurotrophic factor: missing link between sleep deprivation, insomnia, and depression. Neurochemical research. 2020 Feb;45(2):221-31.
Riemann, D., König, A., Hohagen, F., Kiemen, A., Voderholzer, U., Backhaus, J., Bunz, J., Wesiack, B., Hermle, L. and Berger, M., 1999. How to preserve the antidepressive effect of sleep deprivation: A comparison of sleep phase advance and sleep phase delay. European archives of psychiatry and clinical neuroscience, 249(5), pp.231-237.
Seystahl K, Könnecke H, Sürücü O, Baumann CR, Poryazova R. Development of a short sleeper phenotype after third ventriculostomy in a patient with ependymal cysts. Journal of Clinical Sleep Medicine. 2014 Feb 15;10(2):211-3.
Shen X, Wu Y, Zhang D. Nighttime sleep duration, 24-hour sleep duration and risk of all-cause mortality among adults: a meta-analysis of prospective cohort studies. Scientific Reports. 2016 Feb 22;6:21480.
Shi G, Xing L, Wu D, Bhattacharyya BJ, Jones CR, McMahon T, Chong SC, Chen JA, Coppola G, Geschwind D, Krystal A. A rare mutation of β1-adrenergic receptor affects sleep/wake behaviors. Neuron. 2019 Sep 25;103(6):1044-55.
Siegel JM. Memory Consolidation Is Similar in Waking and Sleep. Current Sleep Medicine Reports. 2021 Mar;7(1):15-8.
Sterr A, Kuhn M, Nissen C, Ettine D, Funk S, Feige B, Umarova R, Urbach H, Weiller C, Riemann D. Post-stroke insomnia in community-dwelling patients with chronic motor stroke: physiological evidence and implications for stroke care. Scientific Reports. 2018 May 30;8(1):8409.
Vertes RP, Siegel JM. Time for the sleep community to take a critical look at the purported role of sleep in memory processing. Sleep. 2005 Oct 1;28(10):1228-9.
Xie L, Kang H, Xu Q, Chen MJ, Liao Y, Thiyagarajan M, O’Donnell J, Christensen DJ, Nicholson C, Iliff JJ, Takano T. Sleep drives metabolite clearance from the adult brain. science. 2013 Oct 18;342(6156):373-7.
Yetish G, Kaplan H, Gurven M, Wood B, Pontzer H, Manger PR, Wilson C, McGregor R, Siegel JM. Natural sleep and its seasonal variations in three pre-industrial societies. Current Biology. 2015 Nov 2;25(21):2862-8.
Youngstedt SD, Goff EE, Reynolds AM, Kripke DF, Irwin MR, Bootzin RR, Khan N, Jean-Louis G. Has adult sleep duration declined over the last 50+ years?. Sleep medicine reviews. 2016 Aug 1;28:69-85.
Subscribe to receive updates ( archive ):
The Role of Sleep in Humans’ Well-Being Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment

Introduction
Brief summaries of videos, the valuable information obtained from videos.
Sleep is considered one of the most important parts of any individual’s life. Some researchers emphasize the usefulness of sleep for productivity, while others focus on its impact on people’s health. The present paper will offer several different opinions on the role that sleep plays in the satisfaction of humans’ well-being. A brief overview of four videos will be followed by a discussion of the lessons that should be taken from the speeches.
Each of the speakers in the videos focuses on a different characteristic of sleep, but all of them agree that without enough sleep, one does not perform to the fullest potential. Arianna Huffington (2010) analyzes sleep as a crucial constituent of happiness. In her speech, Huffington (2010) mentions that sleep deprivation can lead to detrimental outcomes and describes her own negative example of not receiving enough rest. The speaker remarks that women are more likely to arrange the revolution of sleep because, for men, sleep deprivation has become “a virility symbol” (Huffington, 2010). Thus, this speech stresses the importance of sleep and considers women as the most probable change agents in the sleep revolution.
Another speech given by a woman is not focused on feminism. Jessa Gamble (2010) considers sleep as a vital element of humans’ body clocks. In her presentation, Gamble (2010) offers several examples of how people’s sleep habits are correspondent with animals’ chemical clocks. Sleep is thus associated with culture, and the role of sleep in the establishment of a healthy lifestyle is underlined in the speech.
The other two videos present researchers’ talks on sleep and its functions. Russel Foster (2013), a neuroscientist, explains why people need sleep and what can happen when they disregard this vital behavioral experience. In his speech, Foster (2013) provides numerous examples of how people treated sleep at different times and notes that individuals’ ignorance about sleep is too big. Therefore, from the neuroscientist’s point of view, not only the duration of sleep but also its quality is highly important.
The last speech is focused on unique functions of the brain that can only be performed while one is asleep. Jeff Iliff (2014) remarks that during sleep, brain vessels “clear away waste,” which is impossible to do while being awake. Thus, it is crucial for people to have enough sleep for their brain to receive time for restoration. Appropriate brain rest helps to avoid serious disease and enables individuals to discover the full potential of their brain.
Although all speakers analyze sleep from different points of view, they all agree that it is highly significant for people to have a sufficient amount of rest. The videos give information on the value of sleep for health, safety, happiness, academic achievement, and other aspects without which it would be impossible for individuals to live successfully. The most crucial data is given by Iliff (2014) and Foster (2013). These two speakers provide a detailed account of neurological processes taking place in the brain and explain a variety of functions that sleep deprivation can obstruct or eliminate. In particular, scholars remark that the brain does not sleep when the organism is resting. A variety of genes work only during sleep (Foster, 2013; Iliff, 2014). Therefore, sleep is needed not only for restoration but also for the productive work of the organism on the next day. Both Iliff (2014) and Foster (2013) compare the need to clear the brain at night to the need to clean one’s house. Neither of the two kinds of “chores” can be put off for a long time since postponing them would cause inconvenience and discomfort. Thus, from the scientific point of view, sleep is highly important for the brain.
Irrespective of their profession and connection with science, all four speakers emphasize the positive effect of sleep on the well-being of any person. Huffington (2010) mentions that having enough sleep makes individuals more inspired and productive. Gamble (2010) remarks that a body clock is crucial for organizing one’s life successfully. Iliff (2014) notes that the clarity of the mind helps to sustain one’s body in harmony. Foster (2013) explains that at every age, people’s sleep needs are different, but these requirements are frequently higher than people allow themselves to spend sleeping. Particular attention is paid to the negative impact of shift work on one’s sleep pattern (Foster, 2013; Gambler, 2010). Therefore, all speakers urge the audience to review their attitude to sleep and start having enough rest to become healthier and happier.
Sleep is a rather significant component of any individual’s existence. The videos give insight into the most intricate aspects of neural processes and explain why it is not acceptable to sleep too little. All speakers focus on the importance of sleep for people’s health, productivity, and happiness. Watching these videos helps to realize how thoughtless people sometimes are and how necessary it is for them to alter some of their habits in order to be strong both physically and morally.
Foster, R. (2013). Why do we sleep? [Video file]. Web.
Gamble, J. (2010). Our natural sleep cycle is nothing like what we do now . [Video file]. Web.
Huffington, A. (2010). How to succeed? Get more sleep [Video file]. Web.
Iliff, J. (2014). One more reason to get a good night’s sleep [Video file]. Web.
- Sleep Helps to Repair Damaged DNA in Neurons
- Elderly Dementia: Holistic Approaches to Memory Care
- Problem of Sleep Deprivation
- Evolution of the Clock
- Harris’s “Can We Build AI…?” Talk: Rhetorical Analysis
- Neurological Disorders and Differential Diagnoses
- The Concept of Asymmetrical Tonic Neck Reflex
- Dancing and Risk of Alzheimer’s Disease
- Parkinson’s Disease: Neurotransmitter Chart
- Alcohol and It Effects on Brain Functioning
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2021, June 19). The Role of Sleep in Humans' Well-Being. https://ivypanda.com/essays/the-role-of-sleep-in-humans-well-being/
"The Role of Sleep in Humans' Well-Being." IvyPanda , 19 June 2021, ivypanda.com/essays/the-role-of-sleep-in-humans-well-being/.
IvyPanda . (2021) 'The Role of Sleep in Humans' Well-Being'. 19 June.
IvyPanda . 2021. "The Role of Sleep in Humans' Well-Being." June 19, 2021. https://ivypanda.com/essays/the-role-of-sleep-in-humans-well-being/.
1. IvyPanda . "The Role of Sleep in Humans' Well-Being." June 19, 2021. https://ivypanda.com/essays/the-role-of-sleep-in-humans-well-being/.
Bibliography
IvyPanda . "The Role of Sleep in Humans' Well-Being." June 19, 2021. https://ivypanda.com/essays/the-role-of-sleep-in-humans-well-being/.
- Undergraduate
- High School
- Architecture
- American History
- Asian History
- Antique Literature
- American Literature
- Asian Literature
- Classic English Literature
- World Literature
- Creative Writing
- Linguistics
- Criminal Justice
- Legal Issues
- Anthropology
- Archaeology
- Political Science
- World Affairs
- African-American Studies
- East European Studies
- Latin-American Studies
- Native-American Studies
- West European Studies
- Family and Consumer Science
- Social Issues
- Women and Gender Studies
- Social Work
- Natural Sciences
- Pharmacology
- Earth science
- Agriculture
- Agricultural Studies
- Computer Science
- IT Management
- Mathematics
- Investments
- Engineering and Technology
- Engineering
- Aeronautics
- Medicine and Health
- Alternative Medicine
- Communications and Media
- Advertising
- Communication Strategies
- Public Relations
- Educational Theories
- Teacher's Career
- Chicago/Turabian
- Company Analysis
- Education Theories
- Shakespeare
- Canadian Studies
- Food Safety
- Relation of Global Warming and Extreme Weather Condition
- Movie Review
- Admission Essay
- Annotated Bibliography
- Application Essay
- Article Critique
Article Review
- Article Writing
- Book Review
- Business Plan
- Business Proposal
- Capstone Project
- Cover Letter
- Creative Essay
- Dissertation
- Dissertation - Abstract
- Dissertation - Conclusion
- Dissertation - Discussion
- Dissertation - Hypothesis
- Dissertation - Introduction
- Dissertation - Literature
- Dissertation - Methodology
- Dissertation - Results
- GCSE Coursework
- Grant Proposal
- Marketing Plan
- Multiple Choice Quiz
- Personal Statement
- Power Point Presentation
- Power Point Presentation With Speaker Notes
- Questionnaire
- Reaction Paper
Research Paper
- Research Proposal
- SWOT analysis
- Thesis Paper
- Online Quiz
- Literature Review
- Movie Analysis
- Statistics problem
- Math Problem
- All papers examples
- How It Works
- Money Back Policy
- Terms of Use
- Privacy Policy
- We Are Hiring
Sleep Deprivation, Essay Example
Pages: 2
Words: 652
Hire a Writer for Custom Essay
Use 10% Off Discount: "custom10" in 1 Click 👇
You are free to use it as an inspiration or a source for your own work.
Introduction
In this discussion some important aspects of sleep deprivation will be highlighted. They include explorations into the effects of sleep deprivation; when someone becomes tired what are the consequences, how it will affect one’s sleeping pattern, some causes of sleep disturbances and how to improve the quality of sleep.
Development
Lack of sleep affects the body in many ways yet people allow themselves to be deprived of it. Ten serious consequences of sleep deprivation include the potential of getting into accidents, which could cause loss of life along with those of others. Studies show where people who work in factories tend to become injured due to sleep loss. With respect to danger on the body lack of sleep first manifests as thinking difficulties, which contribute to accidents. Essentially, people are less alert because energy levels fall. The body needs sleep to build red blood cells. This is responsible for many effects of sleep deprivation on the body. Sleep cycles are important for replenishing mental energy. Besides, concentrating and learning is impaired (Smith, Robinson, & Segal, 2011).
Among other adverse effects on the body are the risks for heart disease, hypertension, diabetes, irregular heart rhythm along with loss of sexual appetite. Studies show that 90% of persons with sleep deprivation ultimately suffer from insomnia, which leads to depression and an aging skin tone. Later the reaction could lead to either weight loss or excessive weight gain. More importantly, studies reveal that lack of sleep hastens death through cardio vascular disease (Pilcher & Huffcutt, 2015).
Tiredness severely affects the desire to sleep. Scientists have defined perpetual tiredness as chronic fatigue syndrome. Researchers are aware that fatigue and tiredness do affect sleep desire, but distinct characteristic relating the two variables have not been clearly understood. The body’s sleep mechanism requires some measure of relaxation of body and mind. When someone is tired the body and mind are tense and the mechanism required to activate sleep is inhibited. This is why doctors prescribe tranquilizers to initiate sleep in cases when tiredness overtakes the individual (Pilcher & Huffcutt, 2015).
One cause of sleep deprivation is alcohol consumption. Scientists contend that the glass of wine some people think that they need before going to bed can be very dangerous. The initial effect of alcohol might be the desire to sleep, but after that feeling subsides the sleep difficulty emerges. Scientists contend that the body breaks down alcohol as any substance it receives. As this happens the initial stimulating effect rebounds preventing deeper stages of sleep to occur. Bedtime snack is another reason for preventing sleep. When the stomach is supposed to rest a bed time snack causes it to work producing tiredness and withholding sleep (Pilcher & Huffcutt, 2015).
The question is now asked what can be done to improve sleep qualities. They range from therapies to medication depending on the underlying cause of sleep loss. Some peope just feel compelled not to sleep thinking that either they are disturbed. Others have trained themselves into a routine of taking less than the required amount needed for their bodies. These persons would require therapeutic interventions (Graci & Hardie, 2007). Others who are deprived due to pain or depression would need medication in resolving the problem. Besides, it is advised to avoid caffeine, nicotine and alcohol, which inhibit sleep or limit your exposure to toxic chemicals (Ramakrishnan & Scheid, 2007).
Graci, G., & Hardie, J. (2007). Evidenced-Based Hypnotherapy for the Management of Sleep Disorders. International Journal of Clinical and Experimental Hypnosis 55 (3): 288–302
Ramakrishnan, K., & Scheid, D. (2007). Treatment options for insomnia. American family physician 76 (4): 517–526
Smith, M. Robinson, L., & Segal, R. (2011). Sleep Disorders and Sleeping Problems. NINDS Narcolepsy .
Pilcher, J., & Huffcutt, A (2015). Effects Of Sleep Deprivation On Performance: A Meta-Analysis. Sleep , 19(4); 12 -22.
Stuck with your Essay?
Get in touch with one of our experts for instant help!
Issues Discussed in Republican Debates, Research Paper Example
Effect of Therapist Colour-Blindness on Empathy, Article Review Example
Time is precious
don’t waste it!
Plagiarism-free guarantee
Privacy guarantee
Secure checkout
Money back guarantee

Related Essay Samples & Examples
Voting as a civic responsibility, essay example.
Pages: 1
Words: 287
Utilitarianism and Its Applications, Essay Example
Words: 356
The Age-Related Changes of the Older Person, Essay Example
Words: 448
The Problems ESOL Teachers Face, Essay Example
Pages: 8
Words: 2293
Should English Be the Primary Language? Essay Example
Pages: 4
Words: 999
The Term “Social Construction of Reality”, Essay Example
Words: 371

Improving writing skills since 2002
(855) 4-ESSAYS
Type a new keyword(s) and press Enter to search
Teenage sleep deprivation.
- Word Count: 1052
- Approx Pages: 4
- View my Saved Essays
- Downloads: 29
- Grade level: High School
- Problems? Flag this paper!
Sleep is one of the most important things a person does each day. It allows the body to rest and to replenish itself so that it is better able to serve its function of living. Yet, many people who don't have enough hours in the day to do everything have to cut out sleep before any other activity. This is especially true for teenagers, who are frantically trying to grasp onto the edge of their childhood, while at the same time reaching for adulthood. Many things that lead to teenage sleep loss; the effects of this loss are devastating. . School is one of the most important aspects of a young person's life, whether or not the teenager is willing to admit it. The teenager spends most of his time either in school or doing homework to further his education. The pressures of school are enormous. Stress is brought on with every project, experiment, and essay assigned to the student. He is forced to muddle through loads of work, continuously trying to catch up to where they must be, all in order to receive good grades. On many occasions, these students will be up late studying, typing, reading, basically doing everything but sleeping. Sleep is put off so that more schoolwork can be fit into the day. . Along with the educational system's pressure for good grades comes the pressure to participate in extra curricular activities such as plays, band, student government, clubs, and sports. Not only do teens have to keep up their grades, but they must also balance a calendar of school events. This can be difficult for many with heavy academic schedules. They will spend the afternoon in school, and then come home to eat dinner and begin their homework. Many will be up until three in the morning diligently typing into their computers, only to go to sleep exhausted, and wake up three to four hours later to begin the day again. Compounding this already minuscule amount of sleep, many adolescents also feel the basic need for money and a steady income during their teen years because of pressure from parents and a sudden lack of allowance.
- Page 1 of 3
Essays Related to Teenage Sleep Deprivation
1. sleep deprivation and it's effects on teenagers.

This all too common problem of sleep deprivation in teenage students can be diminished as soon as we take action against it. ... A small 15% of teenage students get at least 8.5 hours of sleep on weekdays, and over 25% of teenage students get less than 7 hours of sleep on weekdays ("Sleepy Teen Troubles"). ... This situation is the main cause of sleep deprivation (Link, Ancolisrael). The effects of sleep deprivation are damaging to the human body, physically and mentally. ... One account of how severe sleep deprivation can be extremely dangerous is a doctor's experience with a ment...
- Word Count: 1657
- Approx Pages: 7
- Grade Level: High School
2. Sleep Deprivation

Students who have been educated when they were younger about sleep deprivation, and have learned to have good sleeping habits will be better prepared when they older to get the necessary amount of sleep. ... The target group for this study are teenage students that are entering, or in puberty. Teenage students are the most suspectable to sleep deprivation. ... The teenage students need at least 8 ½ hours of sleep. ... The researcher will rather observe how well just the subject group learns and applies good sleeping habits from a pre-pubescent age to teenage years. ...
- Word Count: 1407
- Approx Pages: 6
3. Sleep is the Best Medication

Sleep in the night.... As sleep deprivation serves as a leading catalyst threatening the health, safety, and academic performance of teens across the country, pushing for a later starting time provides for a logical solution to fix these troubling factors. ... Rising early in the morning interrupts sleep that is crucial for maintaining the natural sleep-cycle engineered into teenagers' biological makeup. ... This mishap was credited directly to the teenage driver's lack of sleep. ... Sleep deprivation affects the body's capability of managing normal functions, such as coping wi...
- Word Count: 801
- Approx Pages: 3
4. Sleep Disorders and How to Treat Them
Conditions that keep people from sleeping, and causes daytime tiredness are known as sleep disorders. ... When a person's breathing is interrupted during sleep it is said to be called, Sleep Apnea. ... The next type of sleep order is known as Central sleep apnea, which isn't so popular. ... Most kids outgrow the disorder in their teenage years. ... Many things can contribute to sleep terrors such as: sleep deprivation and extreme tiredness, stress, fever (in children), sleeping in unfamiliar surroundings, lights or noise, or an overfull bladder. ...
- Word Count: 1945
- Approx Pages: 8
5. The Problem of Teenage Depression

Teenage depression is frequently illustrated as an invisible illness that has symptoms that easily mask one's negative emotions. ... A majority of high schools aren't intended to diagnose and manage emotions or mental illness, but high school teenage depression is widespread. ... Sad moods, sleep disturbances, and lack of energy become more frequent (NIMH, "Teen Depression"). ... Their sleep habits change; they may oversleep or sleep for fewer hours. ... The constant amount of homework and projects assigned can cause sleep deprivation, which consists of unhealthy sleeping...
- Word Count: 1193
- Approx Pages: 5
- Has Bibliography
- Grade Level: Undergraduate
6. Transition to parenthood
Sleep deprivation, postpartum depression, interrupted schedules, dirty diapers, are just some of the many stresses that new parents face. ... The pressure of becoming a parent is especially hard on women, teenage mothers in particular. ...
- Word Count: 254
- Approx Pages: 1
7. Distorted Sexual Values

The findings of the behavioral science demonstrates that deprivation of physical pleasure, particularly during the formative periods of development, often resulting family breakdown, child abuse, adolescent runaways crime, violence, alcoholism, and other forms of dehumanizing behavior, we assert that physical pleasure within the context of meaningful human relationships is essential both as a moral value and for its contribution to wholesome social relationships (Leone 18). ... The teenage years are very delicate years in a person's life. Many things that happen or are taught during the t...
- Word Count: 2178
- Approx Pages: 9
8. Taming of the Shrew and 10 Things I Hate About You

After marrying Petruchio, she is deprived of food, clothing, and sleep. Petruchio uses this deprivation as a mechanism for taming her, or forcing her into submission. ... In other words, he is the film's token jock, probably added to attract teenage girls to come see the film. ... Patrick has to work hard to earn Kat's love, affection, and trust, unlike Petruchio, who simply deprived Katherine of food, water, and sleep until she submitted to him. ...
- Word Count: 1517
9. Taming of the Shrew

- Word Count: 1575
Home — Essay Samples — Sociology — Effects of Social Media — Impact Social Media on Sleep Deprivation
Sleeping Habits and Social Media Usage
- Categories: Effects of Social Media Social Media
About this sample

Words: 1546 |
Published: Mar 19, 2020
Words: 1546 | Pages: 4 | 8 min read
Table of contents
Introduction.
- Tandon, A., Kaur, P., Dhir, A., & Mäntymäki, M. (2020). Sleepless due to social media? Investigating problematic sleep due to social media and social media sleep hygiene. https://www.sciencedirect.com/science/article/pii/S0747563220302399 Computers in human behavior, 113, 106487.
- Alonzo, R., Hussain, J., Stranges, S., & Anderson, K. K. (2021). Interplay between social media use, sleep quality, and mental health in youth: A systematic review. Sleep medicine reviews, 56, 101414. (https://www.sciencedirect.com/science/article/abs/pii/S108707922030157X)
- Kolhar, M., Kazi, R. N. A., & Alameen, A. (2021). Effect of social media use on learning, social interactions , and sleep duration among university students. https://pubmed.ncbi.nlm.nih.gov/33911938/ Saudi Journal of Biological Sciences, 28(4), 2216-2222.
- Shimoga, S. V., Erlyana, E., & Rebello, V. (2019). Associations of social media use with physical activity and sleep adequacy among adolescents: Cross-sectional survey. Journal of medical Internet research, 21(6), e14290. (https://www.jmir.org/2019/6/e14290/)
- Abi-Jaoude, E., Naylor, K. T., & Pignatiello, A. (2020). Smartphones, social media use and youth mental health. Cmaj, 192(6), E136-E141. (https://www.cmaj.ca/content/192/6/E136.short)
Should follow an “upside down” triangle format, meaning, the writer should start off broad and introduce the text and author or topic being discussed, and then get more specific to the thesis statement.
Provides a foundational overview, outlining the historical context and introducing key information that will be further explored in the essay, setting the stage for the argument to follow.
Cornerstone of the essay, presenting the central argument that will be elaborated upon and supported with evidence and analysis throughout the rest of the paper.
The topic sentence serves as the main point or focus of a paragraph in an essay, summarizing the key idea that will be discussed in that paragraph.
The body of each paragraph builds an argument in support of the topic sentence, citing information from sources as evidence.
After each piece of evidence is provided, the author should explain HOW and WHY the evidence supports the claim.
Should follow a right side up triangle format, meaning, specifics should be mentioned first such as restating the thesis, and then get more broad about the topic at hand. Lastly, leave the reader with something to think about and ponder once they are done reading.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr. Heisenberg
Verified writer
- Expert in: Sociology

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 917 words
3 pages / 1166 words
2 pages / 983 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Effects of Social Media
There are many ways in which humans can choose to live healthier. Two key behaviors of a healthy lifestyle are getting enough sleep and adequately exercising (Voelker, 2016). Our bodies need rest to rejuvenate and if an [...]
The prevalence of technology and social media in modern society The potential harm of social media on mental health Statistics on social media usage among young adults Operant conditioning theory and its [...]
Social media life right now has incredible effect on how information is acquired and traded. Therefore, organizations need to grow new methodologies in hierarchical correspondence, while social media life can wind up noteworthy [...]
“A profound and heart-rending study of personality, class and culture” To what extent do you agree with this assessment of the novel? Throughout “The Remains of the Day”, Mr Stevens, the protagonist, not only explores the [...]
Wole Soyinka once said, “History teaches us to beware of the excitation of the liberated and the injustices that often accompany their righteous thirst for justice”.A Nigerian playwright, Soyinka, was born into a Yoruba [...]
A key to any revolution, in any time period, is spreading the keypoints within the ideology of the revolution in an efficient and effective manner. The Protestant Reformation, which is accredited chiefly to the efforts of the [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- PMC10948475

The Impact of Social Media Use on Sleep and Mental Health in Youth: a Scoping Review
Danny j. yu.
Li Chiu Kong Family Sleep Assessment Unit, Department of Psychiatry, Faculty of Medicine, The Chinese University of Hong Kong, Shatin, Hong Kong SAR, China
Yun Kwok Wing
Tim m. h. li, ngan yin chan, associated data.
Since this review article solely relies on published articles and does not include individual participant data, therefore no data sharing is available.
Purpose of Review
Social media use (SMU) and other internet-based technologies are ubiquitous in today’s interconnected society, with young people being among the commonest users. Previous literature tends to support that SMU is associated with poor sleep and mental health issues in youth, despite some conflicting findings. In this scoping review, we summarized relevant studies published within the past 3 years, highlighted the impacts of SMU on sleep and mental health in youth, while also examined the possible underlying mechanisms involved. Future direction and intervention on rational use of SMU was discussed.
Recent Findings
Both cross-sectional and longitudinal cohort studies demonstrated the negative impacts of SMU on sleep and mental health, with preliminary evidence indicating potential benefits especially during the COVID period at which social restriction was common. However, the limited longitudinal research has hindered the establishment of directionality and causality in the association among SMU, sleep, and mental health.
Recent studies have made advances with a more comprehensive understanding of the impact of SMU on sleep and mental health in youth, which is of public health importance and will contribute to improving sleep and mental health outcomes while promoting rational and beneficial SMU. Future research should include the implementation of cohort studies with representative samples to investigate the directionality and causality of the complex relationships among SMU, sleep, and mental health; the use of validated questionnaires and objective measurements; and the design of randomized controlled interventional trials to reduce overall and problematic SMU that will ultimately enhance sleep and mental health outcomes in youth.
Introduction
Youth population, which typically refers to individuals between the ages of 15 and 24, experience substantial changes in their neurobiology, physical development, behavior, and emotions, making it a vulnerable stage for the development of both sleep and mental health problems [ 1 – 3 ]. In Hong Kong, approximately 64.5% of adolescents sleep less than 8 h during weekdays [ 4 ] and 29.2% have reported insomnia symptoms [ 5 ]. Both cross-sectional and longitudinal studies have demonstrated that sleep loss and disturbances in youth lead to significant personal distress, increase risk of psychiatric illnesses, and risky behaviors such as drug abuse and dangerous driving [ 5 , 6 ]. In addition to sleep disturbances, mental health problems are highly prevalent among the youth population. Evidence suggested that nearly 75% of psychiatric illnesses have their age onset during adolescence [ 7 , 8 ].
There are multiple risk factors that commonly contribute to sleep and mental health problems, including being female, heavy school workload, physical inactivity, and worse general health [ 9 ]. Recently, a growing number of studies indicate that social media use (SMU) is associated with both sleep and mental health problems in youth [ 10 •]. In particular, identity development and peer acceptance during adolescence are important developmental needs, at which social media may apparently serve as a convenient means to meet these needs. A previous study reported that over 80% of adolescents (16–19 years) use electronic devices near bedtime [ 11 ]. On the other hand, excessive SMU can have detrimental health effects [ 12 , 13 ], and contribute to various negative repercussions such as cyberbullying [ 14 ], gender stereotypes [ 15 ], self-objectification [ 16 ], and exposure to inappropriate content, such as unsolicited violent and sexual contents [ 17 ]. The effect becomes more prominent in young people who are considered as digital native [ 18 ]. Nevertheless, SMU also comes with some potential benefits [ 19 ] such as increased self-esteem [ 20 ], increased social capital [ 21 ], identity presentation and sexual exploration [ 22 ], and social support [ 23 ].
Despite the emerging evidence supporting the link among SMU, sleep, and mental health, the relationship and directionality are complex and inconsistent. For example, two recent studies did not find significant associations among SMU, sleep, and mental health [ 24 , 25 •]. Nonetheless, a US study reported that greater SMU was significantly associated with sleep disturbances [ 26 ], and some also reported bidirectional relationship at which poor sleepers tend to use electronic devices as a sleep aid [ 27 ]. In general, it is believed that youth are at a higher risk of experiencing the negative impacts of SMU as they are more susceptible to peer pressure and fear of missing out (FOMO). FOMO refers to the perception of missing out on enjoyable experiences, followed up with a compulsive behavior to maintain these social connections with others to avoid being excluded from those experiences [ 28 – 30 ]. Hence, understanding the association and directionality among SMU, sleep, and mental health is crucial for developing public health strategies on how to cultivate healthy SMU habits and develop effective interventions targeting inappropriate and excessive SMU.
This scoping review summarized recent studies on SMU, sleep, and mental health in youth (Fig. 1 ) and explored the potential underlying mechanisms of how SMU affects sleep and mental health in youth (Fig. 2 ). Finally, we have put forward several potential avenues for future research and recommendations in this area. Search terms including #adolescent, #social media, #sleep, and #mental health were used to search for relevant studies that were published between January 2020 and July 2023 in MEDLINE. A summary of the study attributes, such as the authors, the country/region where the study was conducted, study design, the number of participants, sample age range, characteristics, as well as the measures used to assess SMU, sleep, and mental health are listed in Table 1 .

Structure of the scoping review

Potential pathways of social media use on sleep and mental health
Table 1
Summary of studies on social media use (SMU), sleep, and mental health
| Age | Female % | |||||||
|---|---|---|---|---|---|---|---|---|
| Barthorpe et al. | UK | Cross-sectional | 4032 | 13–15 | 55.2 | SMU (time use diary) | Self-harm (single question) Depressive symptoms (short mood and feelings questionnaire, SMFQ) Self-esteem (5-item shortened Rosenberg scale) | A greater amount of time spent on social media was associated with increased risk of self-harm and depression and lower levels of self-esteem in females |
| Bailey et al. | Australia | Cross-sectional | 371 | 16–25 | 70.4 | SMU (self-report questionnaire) | Mental health (Depression Anxiety Stress Scales (DASS-21)) Diagnosis of mental health problem (single question) Impact of COVID-19 on mental health (single question) | High levels of daily SMU were associated with poorer mental health Young people use social media to seek support for suicidal thoughts and self-harm |
| Berfeld and Bulck | US | Cross-sectional | 410 | 12–18 | 54.3 | Affordances of social media (self-report questionnaire) Nighttime SMU (self-report questionnaire) Problematic SMU (the Bergen Facebook Addiction Scale) Adverse SMU (self-report questionnaire) | Sleep displacement (sleep diary) Pre-sleep arousal (the Pre-Sleep Arousal Scale) Sleep quality (the Pittsburgh Sleep Quality Index, PSQI) | Use of Snapchat but not Instagram predicted a later bedtime Social media affordances were associated with at least one sleep parameter Being the second most viewed content, viewing post of celebrities had no relationship with sleep |
| Brailovskaia et al. | Russia | Cross-sectional | 1123 | 18–29 | 100 | SMU (time tracked by specific applications, and self-report questionnaire) Problematic SMU (the brief version of the Bergen Social Media Addiction Scale, BSMAS) | Daily stress (the Brief Daily Stressors Screening Tool, BDSS-Tool) Depression and anxiety symptoms (the Depression Anxiety Stress Scales 21 (DASS-21)) Positive mental health (the unidimensional Positive Mental Health Scale, PMH-Scale) Lifetime suicide-related outcomes (the Suicidal Behaviors Questionnaire-Revised, SBQ-R) | SMU was associated with low mental health, and increased suicide-related outcomes |
| Buda et al. | Lithuania | Cross-sectional (representative sample) | 4191 | 13.9 | 49.1 | Problematic SMU (the nine-item Social Media Disorder Scale) | Sleep problems (difficulties in getting to sleep, and tiredness in the morning) (self-report questionnaire) | Increased SMU is associated with worse sleep quality |
| Burnell et al. | US | Cross-sectional | 388 | 13.37 | 50 | Daily digital technology use (total amount of messages sent and duration spent online and on phone) | Subjective sleep parameters (sleep duration, sleep quality) (sleep diary) Objective sleep parameters (Jawbone wearable device) | Greater non-academic digital technology use was associated with shorter subjective and objective sleep duration, and later bedtime |
| Chao et al. | China | Cross-sectional | 1346 | 14.97 | 51.8 | Short video platform use (self-report questionnaire) Short video addiction (the short version of smartphone addiction scale, SAS-SV) | Sleep quality and duration (self-report questionnaire) Social anxiety (the social interaction anxiety scale, SIAS-6) Psychological distress (the 21-item Depression Anxiety Stress Scale, DASS-21) Loneliness (the UCLA loneliness scale, ULS-4) | Significant association between short video use, sleep quality, and mental health conditions was observed |
| Charmaraman et al. | US | Cross-sectional | 772 | 11–15 | N/A | SMU (self-report questionnaire) | Sleep (sleep duration and bedtime) (self-report questionnaire) | Self-report SMU behaviours were associated with negative sleep outcomes |
| Fardouly et al. | Australia | Cross-sectional | 528 | 10–12 | 49.1 | SMU (self-report questionnaire) | Body satisfaction (the Body Esteem Scale for Adolescents and Adults) Eating pathology (the Children’s Eating Attitude Test) Depressive symptoms (the Short Mood and Feelings Questionnaire) Social anxiety (the Spence Children’s Anxiety Scale) | Users of YouTube, Instagram, and Snapchat reported more body image concerns and eating pathology than non‐users Social media appearance comparisons are associated with negative mental health among preadolescents |
| Friebel et al. | UK | Cross-sectional | 101 | 19.7 | N/A | Emotional investment in social media (the Social Media Use Integration Scale) SMU in the last hour before sleep | Sleep quality (the Pittsburgh Sleep Quality Index, PSQI) Objective sleep parameters (actigraphy) Depressive symptoms (the 10-item Centre for the Epidemiologic Studies of Depression Short Form, CESD-10) | Bedtime SMU may not be detrimental to sleep in youth Youth with increased levels of depressive symptoms are at higher risk of experiencing negative impacts of bedtime SMU |
| Gaya et al. | Spain | Cross-sectional | 1101 | 12–17 | 54.2 | SMU (self-report questionnaire, and ecological momentary assessment) | Sleep duration and sleep-related problems (self-report questionnaire, the BEARS scale | A relationship between cell phones, playing video games, and use of social networks and sleep problems |
| Gumport et al. | US | Cross-sectional | 176 | 10–18 | 58 | SMU (self-report questionnaire and ecological momentary assessment | Objective sleep parameters (total sleep time, bedtime, and sleep onset latency) (actigraphy) Emotional health (Ecological Momentary Assessment) | Technology use was associated with increased sleep onset latency, but better emotional health |
| Hamilton et al. | US | Cross-sectional | 93 | 12–17 | 100 | SMU (self-report questionnaire) | Perceived sleep (sleep quality and sleep duration) (self-report questionnaire) Depressive symptoms (6-item Patient Health Questionnaire) Anxiety symptoms (Generalized Anxiety Disorder-7, GAD-7) | During COVID-19 pandemic, higher levels of SMU and lower levels of physical activity are associated with later sleep timing |
| Hasan Beyari | Saudi Arabia | Cross-sectional | 385 | 18–24 | 44.7 | SMU (self-report questionnaire) | Mental health (self-report questionnaire) | Social media has a significant negative impact on the mental health of Saudi Arabian youth |
| Henzel and Håkansson | Sweden | Cross-sectional | 182 | 16–24 | N/A | Social media addiction (the Bergen Social Media Addiction Scale, BSMAS; the Problematic and Risky Internet Use Screening Scale-3, PRIUSS) SMU over the past 12 months (self-report questionnaire) | Mental health (the Kessler Psychological Distress Scale, Kessler-6) Addictive disorder (the Gaming Addiction Scale, GAS; The Problem Gambling Severity Index, PGSI) | Bidirectional relationship was observed between problematic SMU and psychological distress, as well as alcohol abuse |
| Khan et al. | Europe and North America | Cross-sectional (representative sample) | 195,668 | 13.6 | 51 | Self-report discretional time spent watching TV, electronic gaming, and computer use | Difficulty in falling sleep (self-report questionnaire) | Higher levels of recreational screen use were associated with sleep-onset difficulties |
| Kortesoja et al. | Finland | Cross-sectional | 1084 | 15–20 | 45.7 | Evening and late-night SMU (self-report questionnaire) SMU after lights out (self-report questionnaire) | Sleep quality (the Pittsburgh Sleep Quality Index, PSQI) Chronotype (the Morningness-Eveningness Questionnaire) Bedtime, wake-up time, and sleep duration (self-report questionnaire) Insufficient sleep (self-report questionnaire) | Youth with evening chronotype are at greater risks of late-night media use, which negatively affect sleep |
| Li et al. | Hong Kong | Cross-sectional | 3455 | 14.9 | 55.7 | Electronic media use (self-report questionnaire) | Sleep (the Insomnia Severity Index, ISI) Chronotype preference (the reduced Horne and Östberg Morningness and Eveningness Questionnaire, rMEQ) Sleep deprivation Social jetlag Emotional difficulties (the Strengths and Difficulties Questionnaire, SDQ) | Bedtime electronic media use of computers, electronic game consoles, and phones contributed to increased risks of sleep, circadian problems and mental health issues in adolescents |
| Liu et al. | China | Cross-sectional | 4852 | 13.8 | 51.5 | Problematic internet use (the 26-item Chinese Internet Addiction Scale-Revised) | Sleep quality (the Chinese version of the 8-item Athens Insomnia Scale) | Problematic internet use was associated with higher level of insomnia severity |
| Michelle O’Reilly | UK | Cross-sectional | 54 | 11–18 | 44.4 | N/A | Mental health (focus group discussion) | SMU confers negative impacts on mental health of adolescents, although there was acknowledgement of potential benefits |
| Nagata et al. | US | Cross-sectional (Representative sample) | 11,878 | 12.0 | 48.8 | Bedtime screen usage (self-report questionnaire) Overall screen usage (self-report questionnaire) | Sleep disturbance (self-report questionnaire) Presence of sleep disorders (26-item parent-report questionnaire) | Engaging in electronic devices use was associated with overall sleep disturbance, sleep onset and daytime sleepiness |
| Nissim et al. | Europe and North America | Cross-sectional (Representative sample) | 86,542 | 13–15 | 50.9 | Intense SMU (EU Kids Online Survey) Problematic SMU (the Social Media Disorder Scale) | Sleep duration (self-report questionnaire) | Across 18 countries, both intense and problematic SMU were associated with shorter sleep duration, later bedtimes and greater social jetlag |
| Tao and Fisher | US | Cross-sectional | 407 | 15–18 | 82.3 | Hours of SMU (self-report questionnaire) Social media intergroup contact (the Developmental Intergroup Contact Measure, DICM) Social media racial justice civic engagement (the Online Civic Engagement Behaviour Construct) Social media racial discrimination (the Online Victimization Scale) | Depressive symptoms (the 20-item Center for Epidemiologic Studies Depression Scale, CES-D) Anxiety symptoms (the 7-item Generalized Anxiety Disorder, GAD-7) Alcohol use disorder (Alcohol Use Disorders Identification Test (AUDIT)) Illicit drug use and problems (self-report questionnaire) | SMU and racial discrimination are associated with poor mental health and drug use problem |
| Valero et al. | UK | Cross-sectional | 2232 | 18.0 | 51.1 | Problematic digital technology use (the Compulsive Internet Use Scale) | Sleep quality (the Pittsburgh Sleep Quality Index, PSQI) Loneliness (the UCLA Loneliness Scale, version 3) Depression and anxiety symptoms (structured clinical interview) | Problematic use of technology was associated with poor sleep quality, after controlling for loneliness, depressive and anxiety symptoms, neighbourhood disorder, sex, and maternal insomnia |
| Woods and Scoot | UK | Cross-sectional | 467 | 11–17 | N/A | Overall and night-time-specific SMU (self-report questionnaire) | Anxiety and depression (the Hospital Anxiety and Depression Scale (HADS)) Self-esteem (the Rosenberg Self-Esteem Scale, RSES) Emotional investment in social media (the Social Media Use Integration Scale) Sleep quality (the Pittsburgh Sleep Quality Index (PSQI)) | Overall and night-time-specific SMU were associated with lower self-esteem and increased anxiety and depression |
| Xie et al. | Macau | Cross-sectional | 212 | 15–24 | 51.9 | Screen-based electronic media device usage (self-report questionnaire) | Sleep quality (the Pittsburgh Sleep Quality Index (PSQI)) | A J-shape relationship was observed between TV, computer, mobile phone use and sleep quality |
| Beeres et al. | Sweden | Cohort | 3501 | 14–15 | 51.5 | SMU (self-report questionnaire) | Mental health (Strength and Difficulties Questionnaire (SDQ)) | Higher use of social media was associated with more symptoms of mental health problems. No longitudinal association was found |
| Eijnden et al. | Netherlands | Cohort | 2021 | 13.9 | 45.4 | Frequency of SMU (self-report questionnaire) Problematic SMU (the Social Media Disorder (SMD)) | Sleep quality (the 5-item Groningen Sleep Quality Scale (GSKS)) Bedtime (self-report questionnaire) | The intensity of SMU and problematic SMU delay bedtime of adolescents |
| Lee et al. | US | Cohort | 5114 | 12–14 | 48.7 | SMU (self-report questionnaire) | Mental health (the Global Appraisal of Individual Needs-Short Screener (GAIN-)SS) | Frequent SMU negatively affects mental health in this recent representative sample of US adolescents |
| Maksniemi et al. | Finland | Cohort | 426 | 13–19 | 65.7 | Active SMU (the Socio-Digital Participation Inventory) | Bedtime on schooldays (self-report questionnaire) Emotional exhaustion (the School Burnout Inventory) | No clear pattern between active SMU and bedtime across adolescence Active SMU was associated with emotional exhaustion |
| Plackett et al. | UK | Cohort (representative sample) | 3228 | 10–15 | 51.4 | SMU (self-report questionnaire) | Mental health (the Strengths and Difficulties Questionnaire (SDQ)) | SMU was not longitudinally associated with poorer mental health 2 years later |
| Richardson et al. | Australia | Cohort | 528 | 10–12 | 49 | Time spent using technology (self-report questionnaire) Parental control of technology (self-report questionnaire) | Chronotype preference (the 10-item Children’s Morningness-Eveningness Scale (MESC)) School night sleep duration (self-report questionnaire) Daytime sleepiness (the 8 item Paediatric Daytime Sleepiness Scale (PDSS)) | This current study suggested a bidirectional relationship between technology use and sleep in adolescents Parental restriction of technology use may not predict prospective changes in adolescent technology use, nor sleep, over time |
| Zhou, et al. | China | Cohort | 2329 | 18.4 | 63.1 | SMU (self-report questionnaire) | Mental health (self-report questionnaire) | Problematic internet use was reciprocally associated with mental health issues |
Overview of SMU
SMU refers to the act of engaging with online platforms specifically designed for social interaction, whereas electronic media use (or digital use, digital media, internet use, screen time) is a broader term that encompasses various forms of media delivered electronically, including but not limited to social media. In this scoping review, we focus on SMU.
Over the past decade, subjective measures have been the primary tool to investigate individual perceptions, opinions, or personal experiences of SMU. For example, a self-report scale was developed to assess compulsive use of social media and its severity [ 31 ]. Besides, there are several platform-specific scales for social media addiction features such as salience, mood modification, tolerance, withdrawal, conflict, and relapse. The Bergen Facebook Addiction Scale, for instance, focuses specifically on addiction to Facebook [ 32 •], while the Bergen Social Media Addiction Scale has emerged to examine a broader scope, including social media platforms beyond Facebook [ 33 •, 34 ]. Indeed, more researchers used general metrics to measure SMU across multiple platforms collectively such as the Social Media Disorder Scale which measures aspects of social media addiction features, such as preoccupation with social media, excessive time spent, withdrawal symptoms, and negative consequences [ 35 – 37 ]. Other SMU experiences are also captured including social comparison on social media and negative experiences such as bullying, FOMO, and extensive negative feedback [ 32 •].
In addition, the duration and timing of SMU also have significant implications for sleep and mental health, as excessive or inappropriate use of social media at certain timing, for example at bedtime, can potentially contribute to negative biopsychosocial effects. The Socio-Digital Participation Inventory includes four items to measure the frequency of SMU on a seven-point frequency scale (1 = never, 2 = a couple of times a year, 3 = monthly, 4 = weekly, 5 = daily, 6 = multiple times a day, 7 = all the time) [ 25 •]. The total time spent on SMU (in daytime and night-time) are usually captured by questionnaires and social media time use diary [ 38 •]. In view of the limitation of self-reported measures, there has been a shift towards incorporating more objective measures in addition to subjective self-report scales. Increasing number of studies used time tracker via specific apps (installed on participants’ devices used for online activity) to reduce recall bias [ 33 •]. Other objective features, such as the number of followers, likes, comments, shares, bookmarks, and total interactions, which can be retrieved from various social media platforms [ 39 •] were also used to reflect social medica engagement. In addition, the content (e.g., educational vs non-educational) posted, read, and shared on social media platforms plays a significant role in shaping user experiences, engagement levels, and the overall impact of SMU. It is worth to note that no included studies attempted to measure multi-device SMU as it can be challenging due to the wide range of devices that people use to access social media platforms. Traditional research methods often rely on self-reporting, surveys, or tracking software installed on specific devices, which may not capture the full extent of multi-device usage. Some individuals may switch between multiple devices throughout the day, making it challenging to track their overall social media engagement accurately.
Overview of Recent Studies
Study characteristics.
A total of 33 studies were included in this scoping review, with 26 of them were cross-sectional in nature, indicating a snapshot overview of the relationship between SMU, sleep, and mental health. Moreover, only a few studies utilized representative samples [ 35 , 36 , 40 , 41 ], as outlined in Table 1 . It is also worth noting that the sample sizes varied significantly across studies, ranging from 54 to 195,668 participants.
Measurement of SMU
In terms of the measurement of SMU, all studies used either self-developed questionnaires (e.g., “in a typical school week, how often do you check social media?” and “on a normal weekday, how many hours you spend on social medias, write blogs/read each people blogs, or chat online?”) or validated self-report questionnaires (e.g., the 26-item Chinese Internet Addiction Scale-Revised and the Online Civic Engagement Behavior Construct). Different dimensions of SMU were measured such as overall and night-time SMU, problematic SMU, emotional investment in social media, racial discrimination, and racial justice civic engagement on social media. Only a limited number of studies incorporated more reliable measurements such as ecological momentary assessment [ 42 ] and total message count [ 43 ].
Measurement of Sleep and Mental Health
In terms of sleep outcome assessment, most of these studies employed subjective instruments such as sleep diary [ 32 •], self-developed self-report questionnaires (e.g., “How many hours did you sleep over the past week?”) [ 43 ], and validated self-report questionnaires (e.g., the Pittsburgh Sleep Quality Index and the Insomnia Severity Index) [ 44 , 45 •] to measure different sleep outcomes including sleep quality, sleep duration, sleep displacement, bedtime, and sleep-onset latency. In addition to these subjective instruments, 3 studies have utilized objective devices such as actigraphy and other wearable devices to capture objective sleep data [ 43 , 46 , 47 ]. While for mental health aspects, depression and anxiety are the main outcomes. Most of the recent studies utilized standardized questionnaires such as the Short Mood and Feelings Questionnaire, the Depression Anxiety Stress Scales 21, and the Suicidal Behaviors Questionnaire-Revised to measure the symptoms of depression and anxiety.
Synthesis of Recent Findings
Smu and sleep.
Both longitudinal and cross-sectional studies tend to support the association between SMU and sleep disturbances (Table 1 ). A total of 17 cross-sectional studies observed an association between SMU and various sleep parameters in youth. Of these studies, a total of 16 reported a significant association between different dimensions of SMU (internet addition, duration of screen use, inappropriate time use (near bedtime), with one additionally measure parent control of technology) and poor sleep outcomes (both subjectively and objectively measured sleep parameters, such as bedtime, sleep-onset latency, sleep duration, and sleep quality) [ 31 , 32 •, 35 , 36 , 40 , 42 – 44 , 45 •, 47 – 53 ]. Nevertheless, a study of 101 undergraduate students did not find that bedtime SMU was detrimental to sleep [ 46 ]. However, in the subgroup analysis, the authors found that youth with increased levels of depressive symptoms are at higher risk of experiencing negative impacts of bedtime SMU on sleep [ 46 ].
Among the three cohort studies, two indicated that higher levels of SMU predicted later bedtime and shorter sleep duration in youth after 1–2 years of follow-up [ 37 , 54 ]. These studies revealed that both frequent and problematic use of SMU could result in later bedtime [ 37 , 54 ]. In addition, Richardson and colleagues further found that SMU predicted greater daytime sleepiness in adolescence [ 54 ]. In addition, adolescents with evening chronotype preference and shorter sleep duration were found to have longer usage of social media, suggesting a potential bidirectional relationship between SMU and sleep duration [ 54 ]. Another cohort study conducted by Maksniemi and colleagues did not find a significant association between SMU and bedtime among 426 youth aged between 13 and 19 [ 25 •]. Interestingly, subgroup analyses indicated that significant associations were only observed in early adolescence (at age 13 and 14), but not in middle (at age 14 and 15) nor late adolescence (at age 17 and 18) [ 25 •]. This finding highlights the importance of considering the developmental stages of youth in order to unravel the complex relationship between SMU and sleep [ 55 ].
SMU and Mental Health
A total of 9 cross-sectional studies examined the relationship between SMU and mental health [ 33 •, 34 , 38 •, 39 •, 56 •, 57 – 60 ]. A greater amount of time spent on social media was associated with an increased risk of depression, self-harm, and lower self-esteem. On the other hand, adolescents who exhibited mental health issues tended to spend more time on social media platforms, suggesting a potential bidirectional relationship between SMU and mental health. However, it is important to point out that despite appealing hypotheses, actual effect size estimates of SMU on various mental health outcomes (e.g., self-esteem, life satisfaction, depression, and loneliness) were of small-to-medium magnitude as reported in previous meta-analytic studies, ranging from − 0.11 to − 0.32 [ 61 •, 62 ].
Four longitudinal cohort studies reported mixed findings between SMU and mental health [ 41 , 63 , 64 •, 65 ]. Two cohort studies conducted in the USA and China reported that frequent and problematic SMU were significantly associated subsequent mental health issues [ 64 •, 65 ]. Interestingly, the authors identified substantial sex differences in the mental health trajectories, with only girls showing a deteriorating linear trend ( β = 0.23, p < 0.05) [ 64 •]. On the contrary, the other two longitudinal studies conducted in Sweden and UK reported that although frequent SMU was associated with increased levels of mental problems at a single timepoint, there was no longitudinal association [ 41 , 63 ], which suggests that SMU may be only an indicator for mental health instead of a risk factor.
SMU, Sleep, and Mental Health
A total of 7 studies measured both sleep and mental health outcomes [ 31 , 45 •, 46 – 48 , 50 , 59 ]. Five of these studies reported significant associations among SMU, sleep, and mental health outcome [ 31 , 45 •, 46 , 50 , 59 ]. It was reported that SMU was significantly associated with poor sleep quality and increased mental health issues [ 31 , 45 •, 46 , 50 , 59 ], and sleep was found to mediate the negative impacts of SMU on mental health and emotional symptoms in adolescents [ 45 •]. Poor sleep was also shown to be significantly associated with mental health outcomes [ 31 , 50 , 59 ]. Furthermore, adolescents with higher level of depressive symptoms were at higher risk of experiencing negative impacts of bedtime SMU on sleep outcomes [ 46 ]. Indeed, these findings preliminarily unveiled the complex interplay among SMU, sleep, and mental health.
Nevertheless, it is essential to highlight that recent research has also recognized the positive impacts of SMU on mental health, particularly in the context of the COVID-19 pandemic, at which physical social interactions were significantly disrupted [ 56 •, 58 ]. Adolescents in Australia and UK were found to use social media as an active coping strategy to relieve external stressors (e.g., exam pressure), to seek support for suicidal ideation or self-harm behavior, and to support others via social media [ 56 •, 58 ].
This scoping review synthesized recent publications from the past 3 years that investigated the impact of SMU on sleep and/or mental health outcomes in youth. The majority of the studies provide supporting evidence for an association between SMU, poor sleep quality, and adverse mental health outcomes. Problematic SMU or addiction, as well as the duration of SMU, were identified as the most prevalent aspects of social media examined in the included studies. Sleep duration, bedtime, and insomnia emerged as the most commonly assessed sleep problems, while depression and anxiety were the most frequently measured mental health outcomes. However, it is important to note that despite the significant associations identified among these variables, the directionality of the relationship remains unclear in view of inconsistent findings across studies.
Underlying Mechanism Between SMU and Sleep
Numerous mechanisms have been proposed to elucidate the relationship between social/digital media usage and sleep quantity and quality [ 66 ]. Hyperarousal, a core mechanism in explaining insomnia [ 67 ], plays a role in explaining how night-time SMU disrupts sleep. Active engagement in media activities can directly induce physiological and psychological arousal, leading to longer sleep onset latency [ 68 ]. This effect is particularly noticeable when individuals actively engage in interactive digital media, such as social messaging and social media, as opposed to passive media consumption like television viewing [ 69 •], likely due to the heightened arousal associated with interactive activities [ 70 ]. Interestingly, a study found that engaging in phone conversations near bedtime was associated with longer sleep duration, while the use of social media and texting displayed a negative association [ 71 ]. It has been hypothesized that conversing with a friend may positively influence emotional well-being, thereby promoting sleep [ 72 ]. However, social networking, despite its potential for fostering friendships, may also trigger FOMO and social media stress. In addition to the psychological arousal induced by electronic media usage, the light emitted from device screens is another hypothesis explaining the detrimental effects of digital media on sleep. Specifically, the light emitted by electronic devices, especially blue light (at a wavelength of 480 nm), has a significant impact on the suppression of melatonin, a hormone that promotes sleep [ 73 ]. Moreover, a recent study indicated that high-risk adolescents whose parents with bipolar affective disorder have lower level of nocturnal melatonin secretion. It might be possible that adolescents with certain risk factors (even without psychopathologies) may be particularly hypersensitive and vulnerable to light suppression of melatonin secretion [ 74 ], which are considered as high-risk group that require early intervention. Furthermore, it is plausible that an interaction or interplay might exist between arousal and light exposure, and the combination of these conditions could potentially heighten the risk of sleep disturbances. Additionally, the direct displacement of sleep resulting from engagement in social media activities may also lead to shorter sleep duration. Although initial evidence suggests a negative impact of both content and light emitted by electronic devices on sleep, the precise underlying mechanism remains poorly established. Last but not least, some preliminary studies have also investigated other sleep- and circadian-related factors such as chronotype preference and daytime sleepiness in mediating and/or moderating the relationship between SMU and sleep [ 32 •, 44 , 54 ], albeit the findings have been inconclusive. Future studies are warranted to thoroughly explore the role of these factors in the interplay between SMU and sleep.
Underlying Mechanism Between SMU and Mental Health
It has been suggested both behavioral and cognitive factors mediate the impact of SMU on mental health. Among the behavioral factors, sleep has been identified as one of the notable mediators of the association [ 31 , 44 , 45 •, 46 , 50 , 59 , 75 ]. Physiologically, prolonged SMU before bedtime delays sleep onset, reduces sleep duration, and mediates the association between eveningness and sleep as well as daytime sleepiness [ 44 ], which have been identified as risk factors for mental illness [ 76 – 78 ]. This complex interplay between sleep and mental health has also been documented in interventional studies. Our previous clinical trial demonstrated that a brief insomnia prevention program, adapted from cognitive-behavioral therapy for insomnia, significantly decreased the severity of depressive symptoms in adolescents at 12-month follow-up [ 79 ], suggesting the potential mediating role of sleep in mental health. While for the cognitive factors, FOMO has been recognized as a possible mediator. In particular, Elhai et al. reported that FOMO mediated relationship between anxiety and smartphone use frequency, as well as problematic SMU [ 80 ]. Besides FOMO, recent literatures have also identified several other cognitive factors that mediate the relationship between SMU and mental health, such as self-esteem [ 38 •], body satisfaction [ 57 ], and emotional investment [ 59 ].
In addition to these behavioral and cognitive factors, cyberbullying is also one of the important mediators of SMU and mental health in youth [ 81 ]. Cyberbullying has become a prevalent phenomenon worldwide, with victimization rates in children and adolescents ranging from 14 to 57.5%, and lifetime perpetration rates ranging from 6.0 to 46.3% [ 82 , 83 ]. Previous meta-analytical study demonstrated that cyberbullying significantly increased the risks of developing depression, self-harm, suicidal attempts, and ideation [ 84 ]. Moreover, over the COVID-19 pandemic, stressors associated with disasters have also been reported to potentially exacerbate the negative effects of SMU on mental health, thereby increasing the risk for mental health issues [ 85 , 86 ].
In summary, there have been significant developments in recent years in understanding the magnitude and mechanisms that underlie the association between SMU and mental health. However, most of the studies employed a cross-sectional design, which prevented from a thorough understanding of the causality. Experimental and interventional studies are warranted to better comprehend the underlying mechanisms, establish causality, and improve the negative outcomes.
Future Direction
There are several potential avenues for future investigation. Firstly, prospective cohort studies using representative samples are needed to elucidate the magnitude and directionality of relationships among SMU, sleep, and mental health, which is of clinical practice implication for precision intervention. To capture the varying dynamics among SMU, sleep, and mental health across different age groups of adolescents (early and late adolescents), it is recommended that prospective studies may need to have a follow-up period that will better cover the entirety of adolescence period [ 41 ]. Secondly, the lack of consistency in the methodologies employed by different studies measuring SMU has been a major contributing factor to the conflicting findings found in the current literature. It is imperative to use validated questionnaires to measure the SMU. More importantly, objective measurements (e.g., screen time monitors on smartphones [ 87 ], ecological momentary assessments [ 88 ], and wearable devices [ 89 ]) should also be incorporated. Apart from timing, it is equally important to capture the content, and number of devices that subjects engage with. Thirdly, future research should consider conducting randomized controlled trials at different levels (e.g., individual, school, and family) to reduce overall and problematic SMU and to ultimately improve sleep and mental health outcomes in youth. The design of the intervention may benchmark to existing guidelines such as the American Academy of Paediatrics recommendations 2016 on media use [ 90 ], and the WHO guidelines on physical activity and sedentary behavior [ 91 ], in which both guidelines recommend limiting the amount of recreational screen time, and avoiding SMU 1 h before bedtime. Intervention formats may consider psychoeducation, cognitive and behavioral techniques, and motivational interviewing. Finally, priority may be given to conduct observational and interventional studies on SMU in vulnerable populations, such as youth experiencing mood or sleep problems, as well as those who are high-risk offspring of parents with sleep and mood disorders, as these populations are more susceptible to experience significant negative impacts from inappropriate and excessive SMU [ 92 ].
Despite the heterogeneity observed in the recent studies, both cross-sectional and cohort studies highlight the impact of SMU on poor sleep and mental health, albeit there are some inconsistent findings. Research has progressed from focusing solely on “screen time” to exploring the social, emotional, and cognitive dimensions of SMU. When measuring sleep outcomes, researchers have investigated the sleep duration and quality and also consider factors such as chronotype and pre-sleep arousal, which will enable a better understanding of how social media impacts sleep in a broader context. Similar advancements have also been made in the field of SMU-related mental health research. Recognizing the interconnections among SMU, sleep, and mental health is crucial for public health and will contribute to improving sleep and mental health outcomes while promoting rational SMU. Future studies should evaluate the effectiveness of interventions on reducing SMU, with ultimate goal to improve sleep and mental health.
Acknowledgements
We would like to thank Mr. Lin, Colin Qin Li, and Mr. Sin, Calvin Chun Hei for their help during the literature review.
Author Contribution
All authors conceived the study and formulated the research question. Drs. Yu, Li, and Chan drafted the initial version of the manuscript. All authors revised the manuscript for important intellectual content and approved the final version of the manuscript.
Data Availability
Declarations.
This review article does not require medical ethical approval.
The authors declare no competing interests.
This review article does not require medical ethical approval or human informed consent.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Tim M. H. Li, Email: kh.ude.khuc@ilohnam .
Ngan Yin Chan, Email: [email protected] .
Papers of particular interest, published recently, have been highlighted as: • Of importance

COMMENTS
This sleep deprivation essay explores how the functioning of the human body is influenced by various factors, primarily determined by an individual's health status. While most people do not understand the implications of sleep, human effectiveness solely depends on the amount of time dedicated to sleeping. However, for various reasons, people ...
As sleep debt grows over time, it begins to take a toll on mental and physical health.Long-term sleep deprivation can reduce quality of life and may increase the risk of health issues including obesity, diabetes, and cardiovascular disease.. Learn more about the impacts of sleep deprivation, including its causes, and how prioritizing sleep hygiene can help people get the rest they need.
Problem of Sleep Deprivation. This is due to disruption of the sleep cycle. Based on the negative effects of sleep deprivation, there is need to manage this disorder among Americans. The Issue of Chronic Sleep Deprivation. The quality of sleep significantly impacts the health and performance of the human body.
INTRODUCTION. Sleep is vital for health and well-being in children, adolescents, and adults. 1-3 Healthy sleep is important for cognitive functioning, mood, mental health, and cardiovascular, cerebrovascular, and metabolic health. 4 Adequate quantity and quality of sleep also play a role in reducing the risk of accidents and injuries caused by sleepiness and fatigue, including workplace ...
1. Introduction. Sleep loss has a negative effect on multiple neurobehavioral functions, such as psychomotor vigilance performance (cognitive), daytime sleepiness, and affect (Franzen et al., 2011; Van Dongen et al., 2003).Degradation of vigilance following sleep deprivation is one of the most robust alterations in healthy young adults aged 18-30 years (Lim & Dinges, 2010).
Sitting in traffic for a few minutes. Sleep deficiency can cause problems with learning, focusing, and reacting. You may have trouble making decisions, solving problems, remembering things, managing your emotions and behavior, and coping with change. You may take longer to finish tasks, have a slower reaction time, and make more mistakes.
In a detailed 2014 report, the American Academy of Pediatrics called the problem of tired teens a public health epidemic. "I think high school is the real danger spot in terms of sleep deprivation," said William Dement, MD, PhD, founder of the Stanford Sleep Disorders Clinic, the first of its kind in the world. "It's a huge problem.
Sleep deprivation leads to poor performance in the workplace and in schools. Children need 10-12 hours of sleep per day, while adults need 7-8 hours minimum (Blass et al. 28). Lack of sleep among school-going children can result in bad grades, while adults may underperform at work. The body needs sleep to enhance thinking and learning, and a ...
Sleep deprivation is a significant issue that affects millions of people worldwide. It can have profound effects on physical health, mental well-being, and overall quality of life.Understanding the causes, effects, and potential solutions to sleep deprivation is crucial for individuals' well-being and society as a whole. This essay will explore the various factors leading to sleep deprivation ...
Sleep Deprivation And The Sleep. Sleep is a basic necessity of everyday life. According to the National Foundation of sleep, a person is required to sleep at least seven to nine hours a day. (citation) As mentioned by Matt T. Bianchi in the book Sleep Deprivation and Disease, " The normal quantity of sleep depends on the individual and a ...
Showing students the negative effect that sleep deprivation the night before a final exam had on exam scores in a prior class appears to have changed students' sleep choices the night before their own final exam, based on students' self-reports of sleep. Once students saw evidence that staying up all night studying for a final exam would ...
People who are exposed to sleep loss usually experience a decline in cognitive performance and changes in mood (for meta-analyses, see Pilcher and Huffcutt 1996; Philibert 2005 ). Sleep deprivation is a study design to assess the effects of sleep loss. In acute total SD protocols, the subjects are kept awake continuously, generally for 24-72 ...
Summary: In this essay, I question some of the consensus beliefs about sleep, such as the need for at least 7 hours of sleep for adults, harmfulness of acute sleep deprivation, and harmfulness of long-term sleep deprivation and our inability to adapt to it. It appears that the evidence for all of these beliefs is much weaker than sleep scientists and public health experts want us to believe ...
It is clear that sleep deprivation has a significant effect on academic performance. The American Academy of Sleep Medicine says that a lack of sleep impacts performance by reducing concentration, creating attention deficits, slowing reaction times, increasing distractibility, impairing decision-making skills and causing forgetfulness.
Jessa Gamble (2010) considers sleep as a vital element of humans' body clocks. In her presentation, Gamble (2010) offers several examples of how people's sleep habits are correspondent with animals' chemical clocks. Sleep is thus associated with culture, and the role of sleep in the establishment of a healthy lifestyle is underlined in ...
A. Sleep is crucial for cognitive function, which includes learning, memory consolidation, and problem-solving. You may be more productive and effective during the day by getting a decent night's sleep. Sleep also helps the body repair and regenerate and it boosts the immune system. B.
Sleep deprivation makes it difficult for brain cells to communicate effectively which can in turn cause mental lapses that affect memory and visual perception (Samantha 2017). Nerve-signaling chemicals called neurotransmitters control when we are asleep or awake by acting on different groups of neurons in the brain.
The body needs sleep to build red blood cells. This is responsible for many effects of sleep deprivation on the body. Sleep cycles are important for replenishing mental energy. Besides, concentrating and learning is impaired (Smith, Robinson, & Segal, 2011). Among other adverse effects on the body are the risks for heart disease, hypertension ...
For sleep deprivation after learning, mean statistical power to find the meta-analytic effect size was just 14%; for sleep deprivation before learning, it was higher though still far less than optimal at 55%. Given that power is a function of the effect size, sample size, and the statistical test being employed, the difference in obtained power ...
Sleep deprivation also impairs cognitive performance by affecting certain parts of the brain that control higher functions like language and creativity [1]. A lack of sleep can also greatly impact certain parts of the brain, particularly the prefrontal cortex, which is associated with executive functions and one's personality [1].
A small 15% of teenage students get at least 8.5 hours of sleep on weekdays, and over 25% of teenage students get less than 7 hours of sleep on weekdays ("Sleepy Teen Troubles"). ... This situation is the main cause of sleep deprivation (Link, Ancolisrael). The effects of sleep deprivation are damaging to the human body, physically and mentally
Evidence & citing: First, the time young people spend on social media may actually encroach on the time that is available to sleep, this is the time displacement hyphothesis. Second, social media use is known to increase arousal. Third, when adolescents engage in social media use they are exposed to bright screen lights, which can disrupt the ...
Social media use (SMU) and other internet-based technologies are ubiquitous in today's interconnected society, with young people being among the commonest users. Previous literature tends to support that SMU is associated with poor sleep and mental health issues in youth, despite some conflicting findings. In this scoping review, we ...