An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List


Biological, Psychological, and Social Determinants of Depression: A Review of Recent Literature
Olivia remes.
1 Institute for Manufacturing, University of Cambridge, Cambridge CB3 0FS, UK
João Francisco Mendes
2 NOVA Medical School, Universidade NOVA de Lisboa, 1099-085 Lisbon, Portugal; ku.ca.mac@94cfj
Peter Templeton
3 IfM Engage Limited, Institute for Manufacturing, University of Cambridge, Cambridge CB3 0FS, UK; ku.ca.mac@32twp
4 The William Templeton Foundation for Young People’s Mental Health (YPMH), Cambridge CB2 0AH, UK
Associated Data
Depression is one of the leading causes of disability, and, if left unmanaged, it can increase the risk for suicide. The evidence base on the determinants of depression is fragmented, which makes the interpretation of the results across studies difficult. The objective of this study is to conduct a thorough synthesis of the literature assessing the biological, psychological, and social determinants of depression in order to piece together the puzzle of the key factors that are related to this condition. Titles and abstracts published between 2017 and 2020 were identified in PubMed, as well as Medline, Scopus, and PsycInfo. Key words relating to biological, social, and psychological determinants as well as depression were applied to the databases, and the screening and data charting of the documents took place. We included 470 documents in this literature review. The findings showed that there are a plethora of risk and protective factors (relating to biological, psychological, and social determinants) that are related to depression; these determinants are interlinked and influence depression outcomes through a web of causation. In this paper, we describe and present the vast, fragmented, and complex literature related to this topic. This review may be used to guide practice, public health efforts, policy, and research related to mental health and, specifically, depression.
1. Introduction
Depression is one of the most common mental health issues, with an estimated prevalence of 5% among adults [ 1 , 2 ]. Symptoms may include anhedonia, feelings of worthlessness, concentration and sleep difficulties, and suicidal ideation. According to the World Health Organization, depression is a leading cause of disability; research shows that it is a burdensome condition with a negative impact on educational trajectories, work performance, and other areas of life [ 1 , 3 ]. Depression can start early in the lifecourse and, if it remains unmanaged, may increase the risk for substance abuse, chronic conditions, such as cardiovascular disease, and premature mortality [ 4 , 5 , 6 , 7 , 8 ].
Treatment for depression exists, such as pharmacotherapy, cognitive behavioural therapy, and other modalities. A meta-analysis of randomized, placebo-controlled trials of patients shows that 56–60% of people respond well to active treatment with antidepressants (selective serotonin reuptake inhibitors, tricyclic antidepressants) [ 9 ]. However, pharmacotherapy may be associated with problems, such as side-effects, relapse issues, a potential duration of weeks until the medication starts working, and possible limited efficacy in mild cases [ 10 , 11 , 12 , 13 , 14 ]. Psychotherapy is also available, but access barriers can make it difficult for a number of people to get the necessary help.
Studies on depression have increased significantly over the past few decades. However, the literature remains fragmented and the interpretation of heterogeneous findings across studies and between fields is difficult. The cross-pollination of ideas between disciplines, such as genetics, neurology, immunology, and psychology, is limited. Reviews on the determinants of depression have been conducted, but they either focus exclusively on a particular set of determinants (ex. genetic risk factors [ 15 ]) or population sub-group (ex. children and adolescents [ 16 ]) or focus on characteristics measured predominantly at the individual level (ex. focus on social support, history of depression [ 17 ]) without taking the wider context (ex. area-level variables) into account. An integrated approach paying attention to key determinants from the biological, psychological, and social spheres, as well as key themes, such as the lifecourse perspective, enables clinicians and public health authorities to develop tailored, person-centred approaches.
The primary aim of this literature review: to address the aforementioned challenges, we have synthesized recent research on the biological, psychological, and social determinants of depression and we have reviewed research from fields including genetics, immunology, neurology, psychology, public health, and epidemiology, among others.
The subsidiary aim: we have paid special attention to important themes, including the lifecourse perspective and interactions between determinants, to guide further efforts by public health and medical professionals.
This literature review can be used as an evidence base by those in public health and the clinical setting and can be used to inform targeted interventions.
2. Materials and Methods
We conducted a review of the literature on the biological, psychological, and social determinants of depression in the last 4 years. We decided to focus on these determinants after discussions with academics (from the Manchester Metropolitan University, University of Cardiff, University of Colorado, Boulder, University of Cork, University of Leuven, University of Texas), charity representatives, and people with lived experience at workshops held by the University of Cambridge in 2020. In several aspects, we attempted to conduct this review according to PRISMA guidelines [ 18 ].
The inclusion and exclusion criteria are the following:
- - We included documents, such as primary studies, literature reviews, systematic reviews, meta-analyses, reports, and commentaries on the determinants of depression. The determinants refer to variables that appear to be linked to the development of depression, such as physiological factors (e.g., the nervous system, genetics), but also factors that are further away or more distal to the condition. Determinants may be risk or protective factors, and individual- or wider-area-level variables.
- - We focused on major depressive disorder, treatment-resistant depression, dysthymia, depressive symptoms, poststroke depression, perinatal depression, as well as depressive-like behaviour (common in animal studies), among others.
- - We included papers regardless of the measurement methods of depression.
- - We included papers that focused on human and/or rodent research.
- - This review focused on articles written in the English language.
- - Documents published between 2017–2020 were captured to provide an understanding of the latest research on this topic.
- - Studies that assessed depression as a comorbidity or secondary to another disorder.
- - Studies that did not focus on rodent and/or human research.
- - Studies that focused on the treatment of depression. We made this decision, because this is an in-depth topic that would warrant a separate stand-alone review.
- Next, we searched PubMed (2017–2020) using keywords related to depression and determinants. Appendix A contains the search strategy used. We also conducted focused searches in Medline, Scopus, and PsycInfo (2017–2020).
- Once the documents were identified through the databases, the inclusion and exclusion criteria were applied to the titles and abstracts. Screening of documents was conducted by O.R., and a subsample was screened by J.M.; any discrepancies were resolved through a communication process.
- The full texts of documents were retrieved, and the inclusion and exclusion criteria were again applied. A subsample of documents underwent double screening by two authors (O.R., J.M.); again, any discrepancies were resolved through communication.
- a. A data charting form was created to capture the data elements of interest, including the authors, titles, determinants (biological, psychological, social), and the type of depression assessed by the research (e.g., major depression, depressive symptoms, depressive behaviour).
- b. The data charting form was piloted on a subset of documents, and refinements to it were made. The data charting form was created with the data elements described above and tested in 20 studies to determine whether refinements in the wording or language were needed.
- c. Data charting was conducted on the documents.
- d. Narrative analysis was conducted on the data charting table to identify key themes. When a particular finding was noted more than once, it was logged as a potential theme, with a review of these notes yielding key themes that appeared on multiple occasions. When key themes were identified, one researcher (O.R.) reviewed each document pertaining to that theme and derived concepts (key determinants and related outcomes). This process (a subsample) was verified by a second author (J.M.), and the two authors resolved any discrepancies through communication. Key themes were also checked as to whether they were of major significance to public mental health and at the forefront of public health discourse according to consultations we held with stakeholders from the Manchester Metropolitan University, University of Cardiff, University of Colorado, Boulder, University of Cork, University of Leuven, University of Texas, charity representatives, and people with lived experience at workshops held by the University of Cambridge in 2020.
We condensed the extensive information gleaned through our review into short summaries (with key points boxes for ease of understanding and interpretation of the data).
Through the searches, 6335 documents, such as primary studies, literature reviews, systematic reviews, meta-analyses, reports, and commentaries, were identified. After applying the inclusion and exclusion criteria, 470 papers were included in this review ( Supplementary Table S1 ). We focused on aspects related to biological, psychological, and social determinants of depression (examples of determinants and related outcomes are provided under each of the following sections.
3.1. Biological Factors
The following aspects will be discussed in this section: physical health conditions; then specific biological factors, including genetics; the microbiome; inflammatory factors; stress and hypothalamic–pituitary–adrenal (HPA) axis dysfunction, and the kynurenine pathway. Finally, aspects related to cognition will also be discussed in the context of depression.
3.1.1. Physical Health Conditions
Studies on physical health conditions—key points:
- The presence of a physical health condition can increase the risk for depression
- Psychological evaluation in physically sick populations is needed
- There is large heterogeneity in study design and measurement; this makes the comparison of findings between and across studies difficult
A number of studies examined the links between the outcome of depression and physical health-related factors, such as bladder outlet obstruction, cerebral atrophy, cataract, stroke, epilepsy, body mass index and obesity, diabetes, urinary tract infection, forms of cancer, inflammatory bowel disorder, glaucoma, acne, urea accumulation, cerebral small vessel disease, traumatic brain injury, and disability in multiple sclerosis [ 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 ]. For example, bladder outlet obstruction has been linked to inflammation and depressive behaviour in rodent research [ 24 ]. The presence of head and neck cancer also seemed to be related to an increased risk for depressive disorder [ 45 ]. Gestational diabetes mellitus has been linked to depressive symptoms in the postpartum period (but no association has been found with depression in the third pregnancy trimester) [ 50 ], and a plethora of other such examples of relationships between depression and physical conditions exist. As such, the assessment of psychopathology and the provision of support are necessary in individuals of ill health [ 45 ]. Despite the large evidence base on physical health-related factors, differences in study methodology and design, the lack of standardization when it comes to the measurement of various physical health conditions and depression, and heterogeneity in the study populations makes it difficult to compare studies [ 50 ].
The next subsections discuss specific biological factors, including genetics; the microbiome; inflammatory factors; stress and hypothalamic–pituitary–adrenal (HPA) axis dysfunction, and the kynurenine pathway; and aspects related to cognition.
3.1.2. Genetics
Studies on genetics—key points:
There were associations between genetic factors and depression; for example:
- The brain-derived neurotrophic factor (BDNF) plays an important role in depression
- Links exist between major histocompatibility complex region genes, as well as various gene polymorphisms and depression
- Single nucleotide polymorphisms (SNPs) of genes involved in the tryptophan catabolites pathway are of interest in relation to depression
A number of genetic-related factors, genomic regions, polymorphisms, and other related aspects have been examined with respect to depression [ 61 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 ]. The influence of BDNF in relation to depression has been amply studied [ 117 , 118 , 141 , 142 , 143 ]. Research has shown associations between depression and BDNF (as well as candidate SNPs of the BDNF gene, polymorphisms of the BDNF gene, and the interaction of these polymorphisms with other determinants, such as stress) [ 129 , 144 , 145 ]. Specific findings have been reported: for example, a study reported a link between the BDNF rs6265 allele (A) and major depressive disorder [ 117 ].
Other research focused on major histocompatibility complex region genes, endocannabinoid receptor gene polymorphisms, as well as tissue-specific genes and gene co-expression networks and their links to depression [ 99 , 110 , 112 ]. The SNPs of genes involved in the tryptophan catabolites pathway have also been of interest when studying the pathogenesis of depression.
The results from genetics studies are compelling; however, the findings remain mixed. One study indicated no support for depression candidate gene findings [ 122 ]. Another study found no association between specific polymorphisms and major depressive disorder [ 132 ]. As such, further research using larger samples is needed to corroborate the statistically significant associations reported in the literature.
3.1.3. Microbiome
Studies on the microbiome—key points:
- The gut bacteria and the brain communicate via both direct and indirect pathways called the gut-microbiota-brain axis (the bidirectional communication networks between the central nervous system and the gastrointestinal tract; this axis plays an important role in maintaining homeostasis).
- A disordered microbiome can lead to inflammation, which can then lead to depression
- There are possible links between the gut microbiome, host liver metabolism, brain inflammation, and depression
The common themes of this review have focused on the microbiome/microbiota or gut metabolome [ 146 , 147 , 148 , 149 , 150 , 151 , 152 , 153 , 154 , 155 , 156 , 157 , 158 , 159 , 160 , 161 ], the microbiota-gut-brain axis, and related factors [ 152 , 162 , 163 , 164 , 165 , 166 , 167 ]. When there is an imbalance in the intestinal bacteria, this can interfere with emotional regulation and contribute to harmful inflammatory processes and mood disorders [ 148 , 151 , 153 , 155 , 157 ]. Rodent research has shown that there may be a bidirectional association between the gut microbiota and depression: a disordered gut microbiota can play a role in the onset of this mental health problem, but, at the same time, the existence of stress and depression may also lead to a lower level of richness and diversity in the microbiome [ 158 ].
Research has also attempted to disentangle the links between the gut microbiome, host liver metabolism, brain inflammation, and depression, as well as the role of the ratio of lactobacillus to clostridium [ 152 ]. The literature has also examined the links between medication, such as antibiotics, and mood and behaviour, with the findings showing that antibiotics may be related to depression [ 159 , 168 ]. The links between the microbiome and depression are complex, and further studies are needed to determine the underpinning causal mechanisms.
3.1.4. Inflammation
Studies on inflammation—key points:
- Pro-inflammatory cytokines are linked to depression
- Pro-inflammatory cytokines, such as the tumour necrosis factor (TNF)-alpha, may play an important role
- Different methods of measurement are used, making the comparison of findings across studies difficult
Inflammation has been a theme in this literature review [ 60 , 161 , 164 , 169 , 170 , 171 , 172 , 173 , 174 , 175 , 176 , 177 , 178 , 179 , 180 , 181 , 182 , 183 , 184 ]. The findings show that raised levels of inflammation (because of factors such as pro-inflammatory cytokines) have been associated with depression [ 60 , 161 , 174 , 175 , 178 ]. For example, pro-inflammatory cytokines, such as tumour necrosis factor (TNF)-alpha, have been linked to depression [ 185 ]. Various determinants, such as early life stress, have also been linked to systemic inflammation, and this can increase the risk for depression [ 186 ].
Nevertheless, not everyone with elevated inflammation develops depression; therefore, this is just one route out of many linked to pathogenesis. Despite the compelling evidence reported with respect to inflammation, it is difficult to compare the findings across studies because of different methods used to assess depression and its risk factors.
3.1.5. Stress and HPA Axis Dysfunction
Studies on stress and HPA axis dysfunction—key points:
- Stress is linked to the release of proinflammatory factors
- The dysregulation of the HPA axis is linked to depression
- Determinants are interlinked in a complex web of causation
Stress was studied in various forms in rodent populations and humans [ 144 , 145 , 155 , 174 , 176 , 180 , 185 , 186 , 187 , 188 , 189 , 190 , 191 , 192 , 193 , 194 , 195 , 196 , 197 , 198 , 199 , 200 , 201 , 202 , 203 , 204 , 205 , 206 , 207 , 208 , 209 , 210 , 211 ].
Although this section has some overlap with others (as is to be expected because all of these determinants and body systems are interlinked), a number of studies have focused on the impact of stress on mental health. Stress has been mentioned in the literature as a risk factor of poor mental health and has emerged as an important determinant of depression. The effects of this variable are wide-ranging, and a short discussion is warranted.
Stress has been linked to the release of inflammatory factors, as well as the development of depression [ 204 ]. When the stress is high or lasts for a long period of time, this may negatively impact the brain. Chronic stress can impact the dendrites and synapses of various neurons, and may be implicated in the pathway leading to major depressive disorder [ 114 ]. As a review by Uchida et al. indicates, stress may be associated with the “dysregulation of neuronal and synaptic plasticity” [ 114 ]. Even in rodent studies, stress has a negative impact: chronic and unpredictable stress (and other forms of tension or stress) have been linked to unusual behaviour and depression symptoms [ 114 ].
The depression process and related brain changes, however, have also been linked to the hyperactivity or dysregulation of the HPA axis [ 127 , 130 , 131 , 182 , 212 ]. One review indicates that a potential underpinning mechanism of depression relates to “HPA axis abnormalities involved in chronic stress” [ 213 ]. There is a complex relationship between the HPA axis, glucocorticoid receptors, epigenetic mechanisms, and psychiatric sequelae [ 130 , 212 ].
In terms of the relationship between the HPA axis and stress and their influence on depression, the diathesis–stress model offers an explanation: it could be that early stress plays a role in the hyperactivation of the HPA axis, thus creating a predisposition “towards a maladaptive reaction to stress”. When this predisposition then meets an acute stressor, depression may ensue; thus, in line with the diathesis–stress model, a pre-existing vulnerability and stressor can create fertile ground for a mood disorder [ 213 ]. An integrated review by Dean and Keshavan [ 213 ] suggests that HPA axis hyperactivity is, in turn, related to other determinants, such as early deprivation and insecure early attachment; this again shows the complex web of causation between the different determinants.
3.1.6. Kynurenine Pathway
Studies on the kynurenine pathway—key points:
- The kynurenine pathway is linked to depression
- Indolamine 2,3-dioxegenase (IDO) polymorphisms are linked to postpartum depression
The kynurenine pathway was another theme that emerged in this review [ 120 , 178 , 181 , 184 , 214 , 215 , 216 , 217 , 218 , 219 , 220 , 221 ]. The kynurenine pathway has been implicated not only in general depressed mood (inflammation-induced depression) [ 184 , 214 , 219 ] but also postpartum depression [ 120 ]. When the kynurenine metabolism pathway is activated, this results in metabolites, which are neurotoxic.
A review by Jeon et al. notes a link between the impairment of the kynurenine pathway and inflammation-induced depression (triggered by treatment for various physical diseases, such as malignancy). The authors note that this could represent an important opportunity for immunopharmacology [ 214 ]. Another review by Danzer et al. suggests links between the inflammation-induced activation of indolamine 2,3-dioxegenase (the enzyme that converts tryptophan to kynurenine), the kynurenine metabolism pathway, and depression, and also remarks about the “opportunities for treatment of inflammation-induced depression” [ 184 ].
3.1.7. Cognition
Studies on cognition and the brain—key points:
- Cognitive decline and cognitive deficits are linked to increased depression risk
- Cognitive reserve is important in the disability/depression relationship
- Family history of cognitive impairment is linked to depression
A number of studies have focused on the theme of cognition and the brain. The results show that factors, such as low cognitive ability/function, cognitive vulnerability, cognitive impairment or deficits, subjective cognitive decline, regression of dendritic branching and hippocampal atrophy/death of hippocampal cells, impaired neuroplasticity, and neurogenesis-related aspects, have been linked to depression [ 131 , 212 , 222 , 223 , 224 , 225 , 226 , 227 , 228 , 229 , 230 , 231 , 232 , 233 , 234 , 235 , 236 , 237 , 238 , 239 ]. The cognitive reserve appears to act as a moderator and can magnify the impact of certain determinants on poor mental health. For example, in a study in which participants with multiple sclerosis also had low cognitive reserve, disability was shown to increase the risk for depression [ 63 ]. Cognitive deficits can be both causal and resultant in depression. A study on individuals attending outpatient stroke clinics showed that lower scores in cognition were related to depression; thus, cognitive impairment appears to be associated with depressive symptomatology [ 226 ]. Further, Halahakoon et al. [ 222 ] note a meta-analysis [ 240 ] that shows that a family history of cognitive impairment (in first degree relatives) is also linked to depression.
In addition to cognitive deficits, low-level cognitive ability [ 231 ] and cognitive vulnerability [ 232 ] have also been linked to depression. While cognitive impairment may be implicated in the pathogenesis of depressive symptoms [ 222 ], negative information processing biases are also important; according to the ‘cognitive neuropsychological’ model of depression, negative affective biases play a central part in the development of depression [ 222 , 241 ]. Nevertheless, the evidence on this topic is mixed and further work is needed to determine the underpinning mechanisms between these states.
3.2. Psychological Factors
Studies on psychological factors—key points:
- There are many affective risk factors linked to depression
- Determinants of depression include negative self-concept, sensitivity to rejection, neuroticism, rumination, negative emotionality, and others
A number of studies have been undertaken on the psychological factors linked to depression (including mastery, self-esteem, optimism, negative self-image, current or past mental health conditions, and various other aspects, including neuroticism, brooding, conflict, negative thinking, insight, cognitive fusion, emotional clarity, rumination, dysfunctional attitudes, interpretation bias, and attachment style) [ 66 , 128 , 140 , 205 , 210 , 228 , 235 , 242 , 243 , 244 , 245 , 246 , 247 , 248 , 249 , 250 , 251 , 252 , 253 , 254 , 255 , 256 , 257 , 258 , 259 , 260 , 261 , 262 , 263 , 264 , 265 , 266 , 267 , 268 , 269 , 270 , 271 , 272 , 273 , 274 , 275 , 276 , 277 , 278 , 279 , 280 , 281 , 282 , 283 , 284 , 285 , 286 , 287 , 288 , 289 , 290 ]. Determinants related to this condition include low self-esteem and shame, among other factors [ 269 , 270 , 275 , 278 ]. Several emotional states and traits, such as neuroticism [ 235 , 260 , 271 , 278 ], negative self-concept (with self-perceptions of worthlessness and uselessness), and negative interpretation or attention biases have been linked to depression [ 261 , 271 , 282 , 283 , 286 ]. Moreover, low emotional clarity has been associated with depression [ 267 ]. When it comes to the severity of the disorder, it appears that meta-emotions (“emotions that occur in response to other emotions (e.g., guilt about anger)” [ 268 ]) have a role to play in depression [ 268 ].
A determinant that has received much attention in mental health research concerns rumination. Rumination has been presented as a mediator but also as a risk factor for depression [ 57 , 210 , 259 ]. When studied as a risk factor, it appears that the relationship of rumination with depression is mediated by variables that include limited problem-solving ability and insufficient social support [ 259 ]. However, rumination also appears to act as a mediator: for example, this variable (particularly brooding rumination) lies on the causal pathway between poor attention control and depression [ 265 ]. This shows that determinants may present in several forms: as moderators or mediators, risk factors or outcomes, and this is why disentangling the relationships between the various factors linked to depression is a complex task.
The psychological determinants are commonly researched variables in the mental health literature. A wide range of factors have been linked to depression, such as the aforementioned determinants, but also: (low) optimism levels, maladaptive coping (such as avoidance), body image issues, and maladaptive perfectionism, among others [ 269 , 270 , 272 , 273 , 275 , 276 , 279 , 285 , 286 ]. Various mechanisms have been proposed to explain the way these determinants increase the risk for depression. One of the underpinning mechanisms linking the determinants and depression concerns coping. For example, positive fantasy engagement, cognitive biases, or personality dispositions may lead to emotion-focused coping, such as brooding, and subsequently increase the risk for depression [ 272 , 284 , 287 ]. Knowing the causal mechanisms linking the determinants to outcomes provides insight for the development of targeted interventions.
3.3. Social Determinants
Studies on social determinants—key points:
- Social determinants are the conditions in the environments where people are born, live, learn, work, play, etc.; these influence (mental) health [ 291 ]
- There are many social determinants linked to depression, such as sociodemographics, social support, adverse childhood experiences
- Determinants can be at the individual, social network, community, and societal levels
Studies also focused on the social determinants of (mental) health; these are the conditions in which people are born, live, learn, work, play, and age, and have a significant influence on wellbeing [ 291 ]. Factors such as age, social or socioeconomic status, social support, financial strain and deprivation, food insecurity, education, employment status, living arrangements, marital status, race, childhood conflict and bullying, violent crime exposure, abuse, discrimination, (self)-stigma, ethnicity and migrant status, working conditions, adverse or significant life events, illiteracy or health literacy, environmental events, job strain, and the built environment have been linked to depression, among others [ 52 , 133 , 235 , 236 , 239 , 252 , 269 , 280 , 292 , 293 , 294 , 295 , 296 , 297 , 298 , 299 , 300 , 301 , 302 , 303 , 304 , 305 , 306 , 307 , 308 , 309 , 310 , 311 , 312 , 313 , 314 , 315 , 316 , 317 , 318 , 319 , 320 , 321 , 322 , 323 , 324 , 325 , 326 , 327 , 328 , 329 , 330 , 331 , 332 , 333 , 334 , 335 , 336 , 337 , 338 , 339 , 340 , 341 , 342 , 343 , 344 , 345 , 346 , 347 , 348 , 349 , 350 , 351 , 352 , 353 , 354 , 355 , 356 , 357 , 358 , 359 , 360 , 361 , 362 , 363 , 364 , 365 , 366 , 367 , 368 , 369 , 370 , 371 ]. Social support and cohesion, as well as structural social capital, have also been identified as determinants [ 140 , 228 , 239 , 269 , 293 , 372 , 373 , 374 , 375 , 376 , 377 , 378 , 379 ]. In a study, part of the findings showed that low levels of education have been shown to be linked to post-stroke depression (but not severe or clinical depression outcomes) [ 299 ]. A study within a systematic review indicated that having only primary education was associated with a higher risk of depression compared to having secondary or higher education (although another study contrasted this finding) [ 296 ]. Various studies on socioeconomic status-related factors have been undertaken [ 239 , 297 ]; the research has shown that a low level of education is linked to depression [ 297 ]. Low income is also related to depressive disorders [ 312 ]. By contrast, high levels of education and income are protective [ 335 ].
A group of determinants touched upon by several studies included adverse childhood or early life experiences: ex. conflict with parents, early exposure to traumatic life events, bullying and childhood trauma were found to increase the risk of depression (ex. through pathways, such as inflammation, interaction effects, or cognitive biases) [ 161 , 182 , 258 , 358 , 362 , 380 ].
Gender-related factors were also found to play an important role with respect to mental health [ 235 , 381 , 382 , 383 , 384 , 385 ]. Gender inequalities can start early on in the lifecourse, and women were found to be twice as likely to have depression as men. Gender-related factors were linked to cognitive biases, resilience and vulnerabilities [ 362 , 384 ].
Determinants can impact mental health outcomes through underpinning mechanisms. For example, harmful determinants can influence the uptake of risk behaviours. Risk behaviours, such as sedentary behaviour, substance abuse and smoking/nicotine exposure, have been linked to depression [ 226 , 335 , 355 , 385 , 386 , 387 , 388 , 389 , 390 , 391 , 392 , 393 , 394 , 395 , 396 , 397 , 398 , 399 , 400 , 401 ]. Harmful determinants can also have an impact on diet. Indeed, dietary aspects and diet components (ex. vitamin D, folate, selenium intake, iron, vitamin B12, vitamin K, fiber intake, zinc) as well as diet-related inflammatory potential have been linked to depression outcomes [ 161 , 208 , 236 , 312 , 396 , 402 , 403 , 404 , 405 , 406 , 407 , 408 , 409 , 410 , 411 , 412 , 413 , 414 , 415 , 416 , 417 , 418 , 419 , 420 , 421 , 422 , 423 , 424 , 425 , 426 , 427 , 428 ]. A poor diet has been linked to depression through mechanisms such as inflammation [ 428 ].
Again, it is difficult to constrict diet to the ‘social determinants of health’ category as it also relates to inflammation (biological determinants) and could even stand alone as its own category. Nevertheless, all of these factors are interlinked and influence one another in a complex web of causation, as mentioned elsewhere in the paper.
Supplementary Figure S1 contains a representation of key determinants acting at various levels: the individual, social network, community, and societal levels. The determinants have an influence on risk behaviours, and this, in turn, can affect the mood (i.e., depression), body processes (ex. can increase inflammation), and may negatively influence brain structure and function.
3.4. Others
Studies on ‘other’ determinants—key points:
- A number of factors are related to depression
- These may not be as easily categorized as the other determinants in this paper
A number of factors arose in this review that were related to depression; it was difficult to place these under a specific heading above, so this ‘other’ category was created. A number of these could be sorted under the ‘social determinants of depression’ category. For example, being exposed to deprivation, hardship, or adversity may increase the risk for air pollution exposure and nighttime shift work, among others, and the latter determinants have been found to increase the risk for depression. Air pollution could also be regarded as an ecologic-level (environmental) determinant of mental health.
Nevertheless, we have decided to leave these factors in a separate category (because their categorization may not be as immediately clear-cut as others), and these factors include: low-level light [ 429 ], weight cycling [ 430 ], water contaminants [ 431 ], trade [ 432 ], air pollution [ 433 , 434 ], program-level variables (ex. feedback and learning experience) [ 435 ], TV viewing [ 436 ], falls [ 437 ], various other biological factors [ 116 , 136 , 141 , 151 , 164 , 182 , 363 , 364 , 438 , 439 , 440 , 441 , 442 , 443 , 444 , 445 , 446 , 447 , 448 , 449 , 450 , 451 , 452 , 453 , 454 , 455 , 456 , 457 , 458 , 459 , 460 , 461 , 462 , 463 , 464 , 465 , 466 , 467 , 468 , 469 ], mobile phone use [ 470 ], ultrasound chronic exposure [ 471 ], nighttime shift work [ 472 ], work accidents [ 473 ], therapy enrollment [ 226 ], and exposure to light at night [ 474 ].
4. Cross-Cutting Themes
4.1. lifecourse perspective.
Studies on the lifecourse perspective—key points:
- Early life has an importance on mental health
- Stress has been linked to depression
- In old age, the decline in social capital is important
Trajectories and life events are important when it comes to the lifecourse perspective. Research has touched on the influence of prenatal or early life stress on an individual’s mental health trajectory [ 164 , 199 , 475 ]. Severe stress that occurs in the form of early-life trauma has also been associated with depressive symptoms [ 362 , 380 ]. It may be that some individuals exposed to trauma develop thoughts of personal failure, which then serve as a catalyst of depression [ 380 ].
At the other end of the life trajectory—old age—specific determinants have been linked to an increased risk for depression. Older people are at a heightened risk of losing their social networks, and structural social capital has been identified as important in relation to depression in old age [ 293 ].
4.2. Gene–Environment Interactions
Studies on gene–environment interactions—key points:
- The environment and genetics interact to increase the risk of depression
- The etiology of depression is multifactorial
- Adolescence is a time of vulnerability
A number of studies have touched on gene–environment interactions [ 72 , 77 , 82 , 119 , 381 , 476 , 477 , 478 , 479 , 480 , 481 ]. The interactions between genetic factors and determinants, such as negative life events (ex. relationship and social difficulties, serious illness, unemployment and financial crises) and stressors (ex. death of spouse, minor violations of law, neighbourhood socioeconomic status) have been studied in relation to depression [ 82 , 135 , 298 , 449 , 481 ]. A study reported an interaction of significant life events with functional variation in the serotonin-transporter-linked polymorphic region (5-HTTLPR) allele type (in the context of multiple sclerosis) and linked this to depression [ 361 ], while another reported an interaction between stress and 5-HTTLPR in relation to depression [ 480 ]. Other research reported that the genetic variation of HPA-axis genes has moderating effects on the relationship between stressors and depression [ 198 ]. Another study showed that early-life stress interacts with gene variants to increase the risk for depression [ 77 ].
Adolescence is a time of vulnerability [ 111 , 480 ]. Perceived parental support has been found to interact with genes (GABRR1, GABRR2), and this appears to be associated with depressive symptoms in adolescence [ 480 ]. It is important to pay special attention to critical periods in the lifecourse so that adequate support is provided to those who are most vulnerable.
The etiology of depression is multifactorial, and it is worthwhile to examine the interaction between multiple factors, such as epigenetic, genetic, and environmental factors, in order to truly understand this mental health condition. Finally, taking into account critical periods of life when assessing gene–environment interactions is important for developing targeted interventions.
5. Discussion
Depression is one of the most common mental health conditions, and, if left untreated, it can increase the risk for substance abuse, anxiety disorders, and suicide. In the past 20 years, a large number of studies on the risk and protective factors of depression have been undertaken in various fields, such as genetics, neurology, immunology, and epidemiology. However, there are limitations associated with the extant evidence base. The previous syntheses on depression are limited in scope and focus exclusively on social or biological factors, population sub-groups, or examine depression as a comorbidity (rather than an independent disorder). The research on the determinants and causal pathways of depression is fragmentated and heterogeneous, and this has not helped to stimulate progress when it comes to the prevention and intervention of this condition—specifically unravelling the complexity of the determinants related to this condition and thus refining the prevention and intervention methods.
The scope of this paper was to bring together the heterogeneous, vast, and fragmented literature on depression and paint a picture of the key factors that contribute to this condition. The findings from this review show that there are important themes when it comes to the determinants of depression, such as: the microbiome, dysregulation of the HPA axis, inflammatory reactions, the kynurenine pathway, as well as psychological and social factors. It may be that physical factors are proximal determinants of depression, which, in turn, are acted on by more distal social factors, such as deprivation, environmental events, and social capital.
The Marmot Report [ 291 ], the World Health Organization [ 482 ], and Compton et al. [ 483 ] highlight that the most disadvantaged segments of society are suffering (the socioeconomic context is important), and this inequality in resources has translated to inequality in mental health outcomes [ 483 ]. To tackle the issue of egalitarianism and restore equality in the health between the groups, the social determinants need to be addressed [ 483 ]. A wide range of determinants of mental health have been identified in the literature: age, gender, ethnicity, family upbringing and early attachment patterns, social support, access to food, water and proper nutrition, and community factors. People spiral downwards because of individual- and societal-level circumstances; therefore, these circumstances along with the interactions between the determinants need to be considered.
Another important theme in the mental health literature is the lifecourse perspective. This shows that the timing of events has significance when it comes to mental health. Early life is a critical period during the lifespan at which cognitive processes develop. Exposure to harmful determinants, such as stress, during this period can place an individual on a trajectory of depression in adulthood or later life. When an individual is exposed to harmful determinants during critical periods and is also genetically predisposed to depression, the risk for the disorder can be compounded. This is why aspects such as the lifecourse perspective and gene–environment interactions need to be taken into account. Insight into this can also help to refine targeted interventions.
A number of interventions for depression have been developed or recommended, addressing, for example, the physical factors described here and lifestyle modifications. Interventions targeting various factors, such as education and socioeconomic status, are needed to help prevent and reduce the burden of depression. Further research on the efficacy of various interventions is needed. Additional studies are also needed on each of the themes described in this paper, for example: the biological factors related to postpartum depression [ 134 ], and further work is needed on depression outcomes, such as chronic, recurrent depression [ 452 ]. Previous literature has shown that chronic stress (associated with depression) is also linked to glucocorticoid receptor resistance, as well as problems with the regulation of the inflammatory response [ 484 ]. Further work is needed on this and the underpinning mechanisms between the determinants and outcomes. This review highlighted the myriad ways of measuring depression and its determinants [ 66 , 85 , 281 , 298 , 451 , 485 ]. Thus, the standardization of the measurements of the outcomes (ex. a gold standard for measuring depression) and determinants is essential; this can facilitate comparisons of findings across studies.
5.1. Strengths
This paper has important strengths. It brings together the wide literature on depression and helps to bridge disciplines in relation to one of the most common mental health problems. We identified, selected, and extracted data from studies, and provided concise summaries.
5.2. Limitations
The limitations of the review include missing potentially important studies; however, this is a weakness that cannot be avoided by literature reviews. Nevertheless, the aim of the review was not to identify each study that has been conducted on the risk and protective factors of depression (which a single review is unable to capture) but rather to gain insight into the breadth of literature on this topic, highlight key biological, psychological, and social determinants, and shed light on important themes, such as the lifecourse perspective and gene–environment interactions.
6. Conclusions
We have reviewed the determinants of depression and recognize that there are a multitude of risk and protective factors at the individual and wider ecologic levels. These determinants are interlinked and influence one another. We have attempted to describe the wide literature on this topic, and we have brought to light major factors that are of public mental health significance. This review may be used as an evidence base by those in public health, clinical practice, and research.
This paper discusses key areas in depression research; however, an exhaustive discussion of all the risk factors and determinants linked to depression and their mechanisms is not possible in one journal article—which, by its very nature, a single paper cannot do. We have brought to light overarching factors linked to depression and a workable conceptual framework that may guide clinical and public health practice; however, we encourage other researchers to continue to expand on this timely and relevant work—particularly as depression is a top priority on the policy agenda now.
Acknowledgments
Thank you to Isla Kuhn for the help with the Medline, Scopus, and PsycInfo database searches.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/brainsci11121633/s1 , Figure S1: Conceptual framework: Determinants of depression, Table S1: Data charting—A selection of determinants from the literature.
Appendix A.1. Search Strategy
Search: ((((((((((((((((“Gene-Environment Interaction”[Majr]) OR (“Genetics”[Mesh])) OR (“Genome-Wide Association Study”[Majr])) OR (“Microbiota”[Mesh] OR “Gastrointestinal Microbiome”[Mesh])) OR (“Neurogenic Inflammation”[Mesh])) OR (“genetic determinant”)) OR (“gut-brain-axis”)) OR (“Kynurenine”[Majr])) OR (“Cognition”[Mesh])) OR (“Neuronal Plasticity”[Majr])) OR (“Neurogenesis”[Mesh])) OR (“Genes”[Mesh])) OR (“Neurology”[Majr])) OR (“Social Determinants of Health”[Majr])) OR (“Glucocorticoids”[Mesh])) OR (“Tryptophan”[Mesh])) AND (“Depression”[Mesh] OR “Depressive Disorder”[Mesh]) Filters: from 2017—2020.
Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations, Daily and Versions(R)
- exp *Depression/
- exp *Depressive Disorder/
- exp *”Social Determinants of Health”/
- exp *Tryptophan/
- exp *Glucocorticoids/
- exp *Neurology/
- exp *Genes/
- exp *Neurogenesis/
- exp *Neuronal Plasticity/
- exp *Kynurenine/
- exp *Genetics/
- exp *Neurogenic Inflammation/
- exp *Gastrointestinal Microbiome/
- exp *Genome-Wide Association Study/
- exp *Gene-Environment Interaction/
- exp *Depression/et [Etiology]
- exp *Depressive Disorder/et
- or/4-16 637368
- limit 22 to yr = “2017–Current”
- “cause* of depression”.mp.
- “cause* of depression”.ti.
- (cause adj3 (depression or depressive)).ti.
- (caus* adj3 (depression or depressive)).ti.
Appendix A.2. PsycInfo
(TITLE ( depression OR “ Depressive Disorder ”) AND TITLE (“ Social Determinants of Health ” OR tryptophan OR glucocorticoids OR neurology OR genes OR neurogenesis OR “ Neuronal Plasticity ” OR kynurenine OR genetics OR “ Neurogenic Inflammation ” OR “ Gastrointestinal Microbiome ” OR “ Genome-Wide Association Study ” OR “ Gene-Environment Interaction ” OR aetiology OR etiology )) OR TITLE ( cause* W/3 ( depression OR depressive )).
Author Contributions
O.R. was responsible for the design of the study and methodology undertaken. Despite P.T.’s involvement in YPMH, he had no role in the design of the study; P.T. was responsible for the conceptualization of the study. Validation was conducted by O.R. and J.F.M. Formal analysis (data charting) was undertaken by O.R. O.R. and P.T. were involved in the investigation, resource acquisition, and data presentation. The original draft preparation was undertaken by O.R. The writing was conducted by O.R., with review and editing by P.T. and J.F.M. Funding acquisition was undertaken by O.R. and P.T. All authors have read and agreed to the published version of the manuscript.
This research was funded by The William Templeton Foundation for Young People’s Mental Health, Cambridge Philosophical Society, and the Aviva Foundation.
Conflicts of Interest
The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
- Living With
- In Children
Causes and Risk Factors of Depression
Nancy Schimelpfening, MS is the administrator for the non-profit depression support group Depression Sanctuary. Nancy has a lifetime of experience with depression, experiencing firsthand how devastating this illness can be.
Carly Snyder, MD is a reproductive and perinatal psychiatrist who combines traditional psychiatry with integrative medicine-based treatments.
:max_bytes(150000):strip_icc():format(webp)/carly-935717a415724b9b9c849c26fd0450ea.jpg)
Verywell / Joshua Seong
Common Causes of Depression
- Family History & Genetics
- Brain & Body Causes
- Lifestyle Causes
- Next in Depression Guide How Depression Is Diagnosed According to the DSM-5
If you or a loved one are struggling with depression, contact the Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline at 1-800-662-4357 for information on support and treatment facilities in your area.
For more mental health resources, see our National Helpline Database .
Depression is one of the most common mental disorders in the United States. It can affect anyone at almost any age, but what causes depression in some people is not always known . Potential depression causes can include genetics, brain chemistry, life events, medical conditions, and lifestyle factors.
The Centers for Disease Control and Prevention reported that approximately 1 in 5 U.S. adults have received a depression diagnosis in their lifetime. The World Health Organization estimates that 5% of men and 9% of women experience depressive disorders in any given year.
This article discusses common causes of depression. It covers the genetic, biological, and environmental factors that can play a role in the condition.
Researchers suspect there are actually many different causes of depression and that it is not always preventable. Factors that can contribute to depression include:
- Brain chemistry
- Certain medical conditions
- Substance use
- Poor nutrition
Depression does not have a single cause. There are many factors that play a role in increasing the risk that a person will develop the condition. Women experience depression at higher rates than men (10.5% of women vs. 6.2% of men), which experts suggest may be due to hormonal factors.
Family History and Genetics
A family history of depression may increase your risk of developing the condition. You are more likely to experience symptoms of depression if others in your family also have depression or another type of mood disorder . Estimates suggest that depression is approximately 40% determined by genetics.
Twin, adoption, and family studies have linked depression to genetics. While studies suggest that there is a strong genetic component, researchers are not yet certain about all the genetic risk factors for depression.
Studies show that having a parent and grandparent with depression doubles the risk of having the condition.
It is still unclear exactly which genes play a role in depression, but researchers do know that there are many different genes that can play a role. By better understanding how they function, gene researchers hope to be able to create more effective treatments.
It is important to remember that no single cause of depression acts in isolation. Genetics may increase your risk and environmental influences may then determine how likely you are to develop depression.
Brain and Body Causes of Depression
Some causes of depression are related to the brain and body. These can raise your risk for depression.
Brain Chemistry Imbalances
One potential biological cause of depression is an imbalance in the neurotransmitters which are involved in mood regulation. Certain neurotransmitters, including dopamine, serotonin , and norepinephrine, play an important role in mood.
Neurotransmitters are chemical substances that help different areas of the brain communicate with each other. When certain neurotransmitters are in short supply, it may lead to the symptoms we recognize as clinical depression.
This theory of depression suggests that having too much or too little of certain neurotransmitters causes, or at least contributes to, depression.
While this explanation is often cited as a major cause of depression, it remains unproven and many experts believe that it doesn't paint a complete picture of the complex factors that contribute to the condition.
Medications to treat depression often focus on altering the levels of certain chemicals in the brain. Some of these treatments include selective serotonin reuptake inhibitors (SSRIs) , serotonin-norepinephrine reuptake inhibitors (SNRIs), monoamine oxidase inhibitors (MAOIs), and tricyclic antidepressants (TCAs).
Physical Health and Certain Medical Conditions
You may be more likely to experience symptoms of depression if you have a chronic illness, sleep disorder, or thyroid condition. Depression rates also tend to be higher among people who have chronic pain, diabetes, multiple sclerosis, and cancer.
The mind and the body are linked. If you are experiencing a physical health problem, you may discover changes in your mental health as well.
Illness is related to depression in two ways. The stress of having a chronic illness may trigger an episode of major depression. In addition, certain illnesses, such as thyroid disorders, Addison's disease, and liver disease, can cause depression symptoms.
Female Sex Hormones
It has been widely documented that women experience major depression about twice as often as men. Because of the incidence of depressive disorders peaks during women's reproductive years, it is believed that hormonal risk factors may be at play.
Women are especially prone to depressive disorders during times when their hormones are in flux, such as around the time of their menstrual period , pregnancy, childbirth, and perimenopause. The risk of depression declines after menopause.
Hormone fluctuations caused by childbirth and thyroid conditions can also contribute to depression. Postpartum depression may occur after childbirth and is believed to result from the rapid hormonal changes that take place immediately after giving birth.
Some Common Causes of Depression
Lifestyle causes of depression.
There are also a number of lifestyle factors that can play a role in causing depression. While many of the risk factors for depression, such as sex or family history, cannot be changed, people have much more control over lifestyle factors.
Circadian Rhythm Disturbances
One type of depression, called seasonal affective disorder (officially known as major depressive disorder with seasonal pattern) is believed to be caused by a disturbance in the normal circadian rhythm of the body.
Light entering the eye influences this rhythm. During the shorter days of winter, when people may spend limited time outdoors, this rhythm may become disrupted.
People who reside in colder climates where there are short, dark days may be at the highest risk.
In addition to disruptions in circadian rhythm, reduced sunlight can also lead to a drop in serotonin levels in the brain, which may influence mood. Seasonal changes can also alter melatonin levels in the body, which can disrupt sleep and contribute to mood changes.
While you cannot control seasonal shifts, there are steps you can take to minimize the effect these changes have on your mental health. Light therapy, spending more time outdoors, eating a healthy diet, and exercising regularly may help combat seasonal depression.
Poor Nutrition
A poor diet can contribute to depression in several ways. A variety of vitamin and mineral deficiencies are known to cause symptoms of depression. In addition, diets high in sugar have been associated with depression.
Some studies have found that diets either low in omega-3 fatty acids or with an imbalanced ratio of omega-6 to omega-3 fats are associated with increased rates of depression.
Stressful life events, which overwhelm a person's ability to cope, can also be a cause of depression. Researchers suspect high levels of the hormone cortisol, which are secreted during periods of stress , may affect the neurotransmitter serotonin and contribute to depression.
Grief and Loss
Following the loss of a loved one, people who are grieving experience many of the same symptoms of depression. Trouble sleeping, poor appetite, and a loss of pleasure or interest in activities are a normal response to loss.
The symptoms of grief are expected to subside over time. But when symptoms get worse, grief may turn into depression.
Substance Use
Drug and alcohol use can contribute to depressive disorders. But even some prescription drugs have been linked to depression.
Some drugs that have been found to be associated with depression include anticonvulsants, statins, stimulants, benzodiazepines, corticosteroids, and beta-blockers. It's important to review any medications that you've been prescribed and to speak with your physician if you are feeling depressed.
Centers for Disease Control and Prevention. National, State-Level, and County-Level Prevalence Estimates of Adults Aged ≥18 Years Self-Reporting a Lifetime Diagnosis of Depression — United States, 2020 .
National Institute of Mental Health. Major depression .
Lohoff FW. Overview of the genetics of major depressive disorder . Curr Psychiatry Rep . 2010;12(6):539-546. doi:10.1007/s11920-010-0150-6
National Institute of Mental Health. Chronic illness & mental health .
Weissman MM, Berry OO, Warner V. A 30-year study of 3 generations at high risk and low risk for depression . JAMA Psychiatry . 2016;73(9):970-977. doi:10.1001/jamapsychiatry.2016.1586
Ng E, Browne CJ, Samsom JN, Wong AHC. Depression and substance use comorbidity: What we have learned from animal studies . Am J Drug Alcohol Abuse . 2017;43(4):456-474. doi:10.1080/00952990.2016.1183020
Yang L, Zhao Y, Wang Y, et al. The effects of psychological stress on depression . Curr Neuropharmacol . 2015;13(4):494-504. doi:10.2174/1570159x1304150831150507
Knüppel A, Shipley MJ, Llewellyn CH, Brunner EJ. Sugar intake from sweet food and beverages, common mental disorder and depression: Prospective findings from the Whitehall II study . Sci Rep . 2017;7(1):6287. doi:10.1038/s41598-017-05649-7
Larrieu T, Layé S. Food for mood: Relevance of nutritional omega-3 fatty acids for depression and anxiety . Front Physiol . 2018;9:1047. doi:10.3389/fphys.2018.01047
Zisook S, Shear K. Grief and bereavement: What psychiatrists need to know . World Psychiatry . 2009;8(2):67-74. doi:10.1002/j.2051-5545.2009.tb00217.x
Qato, DM, Ozenberger, K, Olfson, M. Prevalence of prescription medications with depression as a potential adverse effect among adults in the United States . JAMA. 2018;319(22):2289-2298. doi:10.1001/jama.2018.6741
Aziz R, Steffens D. What are the causes of late-life depression? . Psychiatr Clin North Am . 2013;36(4):497-516. doi:10.1016/j.psc.2013.08.001
Wigner P, Czarny P, Galecki P, Su KP, Sliwinski T. The molecular aspects of oxidative & nitrosative stress and the tryptophan catabolites pathway (TRYCATs) as potential causes of depression . Psychiatr Res . 2018;262:566-574. doi:10.1016/j.psychres.2017.09.045
By Nancy Schimelpfening Nancy Schimelpfening, MS is the administrator for the non-profit depression support group Depression Sanctuary. Nancy has a lifetime of experience with depression, experiencing firsthand how devastating this illness can be.
- Patient Care & Health Information
- Diseases & Conditions
- Depression (major depressive disorder)
- What is depression? A Mayo Clinic expert explains.
Learn more about depression from Craig Sawchuk, Ph.D., L.P., clinical psychologist at Mayo Clinic.
Hi, I'm Dr. Craig Sawchuk, a clinical psychologist at Mayo Clinic. And I'm here to talk with you about depression. Whether you're looking for answers for yourself, a friend, or loved one, understanding the basics of depression can help you take the next step.
Depression is a mood disorder that causes feelings of sadness that won't go away. Unfortunately, there's a lot of stigma around depression. Depression isn't a weakness or a character flaw. It's not about being in a bad mood, and people who experience depression can't just snap out of it. Depression is a common, serious, and treatable condition. If you're experiencing depression, you're not alone. It honestly affects people of all ages and races and biological sexes, income levels and educational backgrounds. Approximately one in six people will experience a major depressive episode at some point in their lifetime, while up to 16 million adults each year suffer from clinical depression. There are many types of symptoms that make up depression. Emotionally, you may feel sad or down or irritable or even apathetic. Physically, the body really slows down. You feel tired. Your sleep is often disrupted. It's really hard to get yourself motivated. Your thinking also changes. It can just be hard to concentrate. Your thoughts tend to be much more negative. You can be really hard on yourself, feel hopeless and helpless about things. And even in some cases, have thoughts of not wanting to live. Behaviorally, you just want to pull back and withdraw from others, activities, and day-to-day responsibilities. These symptoms all work together to keep you trapped in a cycle of depression. Symptoms of depression are different for everyone. Some symptoms may be a sign of another disorder or medical condition. That's why it's important to get an accurate diagnosis.
While there's no single cause of depression, most experts believe there's a combination of biological, social, and psychological factors that contribute to depression risk. Biologically, we think about genetics or a family history of depression, health conditions such as diabetes, heart disease or thyroid disorders, and even hormonal changes that happen over the lifespan, such as pregnancy and menopause. Changes in brain chemistry, especially disruptions in neurotransmitters like serotonin, that play an important role in regulating many bodily functions, including mood, sleep, and appetite, are thought to play a particularly important role in depression. Socially stressful and traumatic life events, limited access to resources such as food, housing, and health care, and a lack of social support all contribute to depression risk. Psychologically, we think of how negative thoughts and problematic coping behaviors, such as avoidance and substance use, increase our vulnerability to depression.
The good news is that treatment helps. Effective treatments for depression exist and you do have options to see what works best for you. Lifestyle changes that improve sleep habits, exercise, and address underlying health conditions can be an important first step. Medications such as antidepressants can be helpful in alleviating depressive symptoms. Therapy, especially cognitive behavioral therapy, teaches skills to better manage negative thoughts and improve coping behaviors to help break you out of cycles of depression. Whatever the cause, remember that depression is not your fault and it can be treated.
To help diagnose depression, your health care provider may use a physical exam, lab tests, or a mental health evaluation. These results will help identify various treatment options that best fit your situation.
Help is available. You don't have to deal with depression by yourself. Take the next step and reach out. If you're hesitant to talk to a health care provider, talk to a friend or loved one about how to get help. Living with depression isn't easy and you're not alone in your struggles. Always remember that effective treatments and supports are available to help you start feeling better. Want to learn more about depression? Visit mayoclinic.org. Do take care.
Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest. Also called major depressive disorder or clinical depression, it affects how you feel, think and behave and can lead to a variety of emotional and physical problems. You may have trouble doing normal day-to-day activities, and sometimes you may feel as if life isn't worth living.
More than just a bout of the blues, depression isn't a weakness and you can't simply "snap out" of it. Depression may require long-term treatment. But don't get discouraged. Most people with depression feel better with medication, psychotherapy or both.
Depression care at Mayo Clinic
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Although depression may occur only once during your life, people typically have multiple episodes. During these episodes, symptoms occur most of the day, nearly every day and may include:
- Feelings of sadness, tearfulness, emptiness or hopelessness
- Angry outbursts, irritability or frustration, even over small matters
- Loss of interest or pleasure in most or all normal activities, such as sex, hobbies or sports
- Sleep disturbances, including insomnia or sleeping too much
- Tiredness and lack of energy, so even small tasks take extra effort
- Reduced appetite and weight loss or increased cravings for food and weight gain
- Anxiety, agitation or restlessness
- Slowed thinking, speaking or body movements
- Feelings of worthlessness or guilt, fixating on past failures or self-blame
- Trouble thinking, concentrating, making decisions and remembering things
- Frequent or recurrent thoughts of death, suicidal thoughts, suicide attempts or suicide
- Unexplained physical problems, such as back pain or headaches
For many people with depression, symptoms usually are severe enough to cause noticeable problems in day-to-day activities, such as work, school, social activities or relationships with others. Some people may feel generally miserable or unhappy without really knowing why.
Depression symptoms in children and teens
Common signs and symptoms of depression in children and teenagers are similar to those of adults, but there can be some differences.
- In younger children, symptoms of depression may include sadness, irritability, clinginess, worry, aches and pains, refusing to go to school, or being underweight.
- In teens, symptoms may include sadness, irritability, feeling negative and worthless, anger, poor performance or poor attendance at school, feeling misunderstood and extremely sensitive, using recreational drugs or alcohol, eating or sleeping too much, self-harm, loss of interest in normal activities, and avoidance of social interaction.
Depression symptoms in older adults
Depression is not a normal part of growing older, and it should never be taken lightly. Unfortunately, depression often goes undiagnosed and untreated in older adults, and they may feel reluctant to seek help. Symptoms of depression may be different or less obvious in older adults, such as:
- Memory difficulties or personality changes
- Physical aches or pain
- Fatigue, loss of appetite, sleep problems or loss of interest in sex — not caused by a medical condition or medication
- Often wanting to stay at home, rather than going out to socialize or doing new things
- Suicidal thinking or feelings, especially in older men
When to see a doctor
If you feel depressed, make an appointment to see your doctor or mental health professional as soon as you can. If you're reluctant to seek treatment, talk to a friend or loved one, any health care professional, a faith leader, or someone else you trust.
When to get emergency help
If you think you may hurt yourself or attempt suicide, call 911 in the U.S. or your local emergency number immediately.
Also consider these options if you're having suicidal thoughts:
- Call your doctor or mental health professional.
- Contact a suicide hotline.
- In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline, available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential.
- U.S. veterans or service members who are in crisis can call 988 and then press “1” for the Veterans Crisis Line . Or text 838255. Or chat online .
- The Suicide & Crisis Lifeline in the U.S. has a Spanish language phone line at 1-888-628-9454 (toll-free).
- Reach out to a close friend or loved one.
- Contact a minister, spiritual leader or someone else in your faith community.
If you have a loved one who is in danger of suicide or has made a suicide attempt, make sure someone stays with that person. Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
More Information
Depression (major depressive disorder) care at Mayo Clinic
- Male depression: Understanding the issues
- Nervous breakdown: What does it mean?
- Pain and depression: Is there a link?
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
It's not known exactly what causes depression. As with many mental disorders, a variety of factors may be involved, such as:
- Biological differences. People with depression appear to have physical changes in their brains. The significance of these changes is still uncertain, but may eventually help pinpoint causes.
- Brain chemistry. Neurotransmitters are naturally occurring brain chemicals that likely play a role in depression. Recent research indicates that changes in the function and effect of these neurotransmitters and how they interact with neurocircuits involved in maintaining mood stability may play a significant role in depression and its treatment.
- Hormones. Changes in the body's balance of hormones may be involved in causing or triggering depression. Hormone changes can result with pregnancy and during the weeks or months after delivery (postpartum) and from thyroid problems, menopause or a number of other conditions.
- Inherited traits. Depression is more common in people whose blood relatives also have this condition. Researchers are trying to find genes that may be involved in causing depression.
- Marijuana and depression
- Vitamin B-12 and depression
Risk factors
Depression often begins in the teens, 20s or 30s, but it can happen at any age. More women than men are diagnosed with depression, but this may be due in part because women are more likely to seek treatment.
Factors that seem to increase the risk of developing or triggering depression include:
- Certain personality traits, such as low self-esteem and being too dependent, self-critical or pessimistic
- Traumatic or stressful events, such as physical or sexual abuse, the death or loss of a loved one, a difficult relationship, or financial problems
- Blood relatives with a history of depression, bipolar disorder, alcoholism or suicide
- Being lesbian, gay, bisexual or transgender, or having variations in the development of genital organs that aren't clearly male or female (intersex) in an unsupportive situation
- History of other mental health disorders, such as anxiety disorder, eating disorders or post-traumatic stress disorder
- Abuse of alcohol or recreational drugs
- Serious or chronic illness, including cancer, stroke, chronic pain or heart disease
- Certain medications, such as some high blood pressure medications or sleeping pills (talk to your doctor before stopping any medication)
Complications
Depression is a serious disorder that can take a terrible toll on you and your family. Depression often gets worse if it isn't treated, resulting in emotional, behavioral and health problems that affect every area of your life.
Examples of complications associated with depression include:
- Excess weight or obesity, which can lead to heart disease and diabetes
- Pain or physical illness
- Alcohol or drug misuse
- Anxiety, panic disorder or social phobia
- Family conflicts, relationship difficulties, and work or school problems
- Social isolation
- Suicidal feelings, suicide attempts or suicide
- Self-mutilation, such as cutting
- Premature death from medical conditions
- Depression and anxiety: Can I have both?
There's no sure way to prevent depression. However, these strategies may help.
- Take steps to control stress, to increase your resilience and boost your self-esteem.
- Reach out to family and friends, especially in times of crisis, to help you weather rough spells.
- Get treatment at the earliest sign of a problem to help prevent depression from worsening.
- Consider getting long-term maintenance treatment to help prevent a relapse of symptoms.
- Brown AY. Allscripts EPSi. Mayo Clinic, Rochester, Minn. Nov. 17, 2016.
- Research report: Psychiatry and psychology, 2016-2017. Mayo Clinic. http://www.mayo.edu/research/departments-divisions/department-psychiatry-psychology/overview?_ga=1.199925222.939187614.1464371889. Accessed Jan. 23, 2017.
- Depressive disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. Arlington, Va.: American Psychiatric Association; 2013. http://www.psychiatryonline.org. Accessed Jan. 23, 2017.
- Depression. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/depression/index.shtml. Accessed Jan. 23, 2017.
- Depression. National Alliance on Mental Illness. http://www.nami.org/Learn-More/Mental-Health-Conditions/Depression/Overview. Accessed Jan. 23, 2017.
- Depression: What you need to know. National Institute of Mental Health. https://www.nimh.nih.gov/health/publications/depression-what-you-need-to-know/index.shtml. Accessed Jan. 23, 2017.
- What is depression? American Psychiatric Association. https://www.psychiatry.org/patients-families/depression/what-is-depression. Accessed Jan. 23, 2017.
- Depression. NIH Senior Health. https://nihseniorhealth.gov/depression/aboutdepression/01.html. Accessed Jan. 23, 2017.
- Children’s mental health: Anxiety and depression. Centers for Disease Control and Prevention. https://www.cdc.gov/childrensmentalhealth/depression.html#depression. Accessed. Jan. 23, 2017.
- Depression and complementary health approaches: What the science says. National Center for Complementary and Integrative Health. https://nccih.nih.gov/health/providers/digest/depression-science. Accessed Jan. 23, 2017.
- Depression. Natural Medicines. https://naturalmedicines.therapeuticresearch.com/databases/medical-conditions/d/depression.aspx. Accessed Jan. 23, 2017.
- Natural medicines in the clinical management of depression. Natural Medicines. http://naturaldatabase.therapeuticresearch.com/ce/CECourse.aspx?cs=naturalstandard&s=ND&pm=5&pc=15-111. Accessed Jan. 23, 2017.
- The road to resilience. American Psychological Association. http://www.apa.org/helpcenter/road-resilience.aspx. Accessed Jan. 23, 2017.
- Simon G, et al. Unipolar depression in adults: Choosing initial treatment. http://www.uptodate.com/home. Accessed Jan. 23, 2017.
- Stewart D, et al. Risks of antidepressants during pregnancy: Selective serotonin reuptake inhibitors (SSRIs). http://www.uptodate.com/home. Accessed Jan. 23, 2017.
- Kimmel MC, et al. Safety of infant exposure to antidepressants and benzodiazepines through breastfeeding. http://www.uptodate.com/home. Accessed Jan. 23, 2017.
- Bipolar and related disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. Arlington, Va.: American Psychiatric Association; 2013. http://www.psychiatryonline.org. Accessed Jan. 23, 2017.
- Hirsch M, et al. Monoamine oxidase inhibitors (MAOIs) for treating depressed adults. http://www.uptodate.com/home. Accessed Jan. 24, 2017.
- Hall-Flavin DK (expert opinion). Mayo Clinic, Rochester, Minn. Jan. 31, 2017.
- Krieger CA (expert opinion). Mayo Clinic, Rochester, Minn. Feb. 2, 2017.
- Antidepressant withdrawal: Is there such a thing?
- Antidepressants and alcohol: What's the concern?
- Antidepressants and weight gain: What causes it?
- Antidepressants: Can they stop working?
- Antidepressants: Selecting one that's right for you
- Antidepressants: Side effects
- Antidepressants: Which cause the fewest sexual side effects?
- Atypical antidepressants
- Clinical depression: What does that mean?
- Depression in women: Understanding the gender gap
- Depression, anxiety and exercise
- Depression: Supporting a family member or friend
- MAOIs and diet: Is it necessary to restrict tyramine?
- Monoamine oxidase inhibitors (MAOIs)
- Natural remedies for depression: Are they effective?
- Selective serotonin reuptake inhibitors (SSRIs)
- Serotonin and norepinephrine reuptake inhibitors (SNRIs)
- Treatment-resistant depression
- Tricyclic antidepressants and tetracyclic antidepressants
Associated Procedures
- Complete blood count (CBC)
- Electroconvulsive therapy (ECT)
- Psychotherapy
- Transcranial magnetic stimulation
- Vagus nerve stimulation
News from Mayo Clinic
- Mayo Clinic Q and A: How to support a loved one with depression Oct. 23, 2022, 11:00 a.m. CDT
- Mayo study lays foundation to predict antidepressant response in people with suicide attempts Oct. 03, 2022, 03:30 p.m. CDT
- Science Saturday: Researchers validate threshold for determining effectiveness of antidepressant treatment Aug. 27, 2022, 11:00 a.m. CDT
- Mayo Clinic expert explains differences between adult and teen depression May 24, 2022, 12:19 p.m. CDT
Mayo Clinic in Rochester, Minnesota, has been recognized as one of the top Psychiatry hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.
Calculate for all schools
Your chance of acceptance, your chancing factors, extracurriculars, college essay on depression.
I've been dealing with depression for a while and I feel like it's played a big part in shaping who I am today. Is it a good idea to write my college essay about it? Will admissions officers view it negatively? Any insights would be appreciated.
Writing about depression in your college essay can be a powerful and meaningful way to share your personal experiences and reflect on your growth. However, it's essential to approach the topic thoughtfully and carefully, as mental health is a sensitive subject.
1. Focus on growth and resilience: Instead of primarily describing your struggles with depression, emphasize how you've navigated those challenges and grown as a result. Discuss coping strategies, support systems, and other positive changes you've made that have helped you move forward.
2. Show self-awareness: Demonstrate an understanding of your situation and acknowledge your progress, while still recognizing that recovering from depression is an ongoing journey. This can give college admissions officers a sense of maturity and emotional intelligence on your part.
3. Keep it relevant to your college goals: Connect your experiences with depression to your educational and career aspirations. Perhaps overcoming depression has influenced your choice of major, or it has motivated you to engage in volunteer work or other extracurricular activities.
4. Seek feedback from trusted individuals: Ask someone you trust, like a teacher or counselor, to review your essay and provide input. Their perspectives can ensure that you're discussing depression sensitively and that your essay is appropriate for college admissions officers.
5. Be cautious of oversharing: While it's important to be genuine and authentic, avoid revealing deeply personal or disturbing details about your mental health struggles. Some admissions officers may not be comfortable with this level of disclosure, and it could overshadow your accomplishments and other positive aspects of your application.
In summary, writing about depression in your college essay is a personal choice. If you can present your experiences in a thoughtful, growth-focused manner, and connect your journey to your future goals, then it may be a powerful and effective essay topic. However, always consider seeking feedback from trusted individuals to ensure you are addressing the topic appropriately.
About CollegeVine’s Expert FAQ
CollegeVine’s Q&A seeks to offer informed perspectives on commonly asked admissions questions. Every answer is refined and validated by our team of admissions experts to ensure it resonates with trusted knowledge in the field.
Home — Essay Samples — Nursing & Health — Depression — Depression And Its Main Causes
Depression and Its Main Causes
- Categories: Cognitive Behavioral Therapy Depression Mental Health
About this sample

Words: 1373 |
Published: Jan 28, 2021
Words: 1373 | Pages: 3 | 7 min read
- Beyondblue. (n.d.). Retrieved from https://www.beyondblue.org.au/the-facts/depression/treatments-for-depression/psychological-treatments-for-depression
- Hannibal, J. (2012). Psychology for the IB diploma. Oxford: Oxford University Press, 149-61.
- Harvard Health Publishing. (n.d.). What causes depression? Retrieved from https://www.health.harvard.edu/mind-and-mood/what-causes-depression
- Lyness, D. (Ed.). (2016, August). Why Do People Get Depressed? (for Teens). Retrieved from https://kidshealth.org/en/teens/why-depressed.html
- Morin, A., & Lcsw. (n.d.). How Many People Are Actually Affected by Depression Every Year? Retrieved from https://www.verywellmind.com/depression-statistics-everyone-should-know-4159056
- Schimelpfening, N., & Gans, S. (n.d.). Why Some People Are More Prone to Depression Than Others. Retrieved from https://www.verywellmind.com/why-are-some-people-more-prone-to-depression-1067622

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Psychology Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 1087 words
1 pages / 605 words
1 pages / 618 words
2 pages / 834 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Depression
Pessimism and depression are two psychological phenomena that often go hand in hand, creating a complex and challenging experience for those who grapple with them. While pessimism is a general outlook characterized by a negative [...]
Nurse burnout has become a pressing issue in the healthcare industry, with detrimental effects on both nurses and patient care. Understanding the causes and effects of burnout, as well as implementing strategies for prevention, [...]
Depression is a prevalent mental health condition that affects millions of people worldwide. According to the World Health Organization (WHO), depression is the leading cause of disability globally, and it is a major contributor [...]
Depression is a common mental health disorder that affects millions of people worldwide. It can have a significant impact on an individual's quality of life and overall well-being. Understanding the causes, symptoms, and [...]
In the world of psychology, the case study of Ileana Chivescu stands out as a compelling and complex examination of the human mind. This tale of a young woman's struggle with anxiety, depression, and self-doubt offers a poignant [...]
Obesity and Depression today are one of the biggest issues that our societies are facing. These two problems are looked differently upon by the masses however they both share common links and connections between in which both [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!

Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free

A Story of Depression as a Disease
How we think about depression impacts clinical treatment..
Updated January 3, 2024 | Reviewed by Monica Vilhauer
- What Is Depression?
- Find counselling to overcome depression
- A model of depression as a disease is incomplete and misleading. It leads to suboptimal treatment choices.
- The "separation distress hypothesis" is an alternative model. It is an integrated, causal model of depression.
- This alternative model leads to psychologically meaningful treatments with higher efficacy than SSRIs.
Is there a difference between these statements: “I have depression ” and "I am depressed?" The first sentence describes something lasting, possibly chronic. The second one describes the state of the person's brain and mind.
As Jonathan Shedler pointed out, the first description provides an illusion of an explanation of why the person is distressed : “Why do I feel this way? Because I have an illness called “depression.”
Can we pause here for a moment? This is not an accident that we talk about depression as a disease. We have been taught to do so. How?
Programming by language happens all the time in our culture. For example, we speak Starbucks: “I’d like a grande-soy-latte, please.”
In Chapter 4 of Ethan Watters’ book [1], McGill University professor Laurence Kirmayer and Keio University Professor Junko Kitanaka shared a remarkable account of how one of the stories of depression was written in Japan [1]. Before the 1990s, there was no word in Japanese for mild-to-moderate depression; and the sales of selective serotonin reuptake inhibitors (SSRIs) were zero, while the sales were approximately 13 billion dollars per year in other countries combined. Then, GlaxoSmithKline, the manufacturer of Paxil, started a massive marketing campaign. Two of their campaign's key messages were that depression was a common disease caused by a chemical imbalance in the brain and that “antidepressants” restored the balance. As a result, the sales of Paxil in Japan reached the level of a billion dollars per year by 2008.
One of the components of this story was the term “antidepressant,” which has been used in the USA since the 1950s. This term is attributed to Max Lurie, a psychiatrist in Cincinnati [2]. He referred to isoniazid , a monoamine oxidase inhibitor (MAOI) as an “antidepressant.” Thereafter, all pills prescribed for depression have been called “antidepressants,” including selective serotonin reuptake inhibitors (SSRIs). In labeling isoniazid as an “antidepressant,” Dr. Lurie did something quite customary in medicine (consider anti-inflammatory or antinausea medications). However, he was influenced by the story that depression was a disease, which led him to use medical terminology.
The prefix “anti” creates an impression of a dichotomous system, where the disease drives the pathological process forward, while an “anti-depressant” drives it back to health.
Here is what I think happens when people hear the term antidepressant : “There is a clear-cut thing, called depression. Depression is a disease, caused by a chemical imbalance in the brain. A cure from this disease is an “antidepressant” – it restores the chemical balance.”
Then, there is a twist:
“When your antidepressant didn’t work, we will consider your depression to be ' treatment-resistant .' Why? Because the anti-depressant was supposed to work. The very name suggests so. The only reason why it didn’t work was that your unruly depression was 'resistant.' Then what? Electro-convulsive therapy (ECT). Still resistant? Ketamine . Resistant still? Surgery.”
Please note that “treatment-resistant depression” was defined in the 1970s as a person’s lack of symptomatic improvement in response to two different courses of “antidepressants” [3]. Therefore, the term “treatment-resistant depression” assumes that anti-depressants are supposed to work. Such a definition is an example of circular logic – you define a drug based on the disease, and then you redefine the disease based on the patient's reaction to the drug.
Now we know that there is no causal theory of serotonin imbalance leading to depressive symptoms [9], and the evidence of the efficacy of SSRIs for depression is weak – it is three times lower than that of psychodynamic psychotherapy [4].
If the tale of depression as a disease is misleading, what are the alternatives? Jonathan Shedler suggested a useful metaphor – a fever. Fever is a non-specific state – it is common in various conditions. Flu, on the other hand, is a disease and we know its etiology (a set of causes) – it is a viral infection. Shedler suggested that depression, like fever, is a non-specific state, not a disease.
We know that Tylenol treats the symptom (fever) but does not cure the flu. Treating symptoms is important [5], as we could die from hyperthermia, but we need to know that the immune system cures the flu, not the Tylenol. Therefore, it would be misleading to describe a lasting flu as “treatment resistant” based on it not responding to Tylenol.
In addition to Shedler’s metaphor of a fever, an integrated, causal model of depression as a state was proposed in 2009 [10], and then further elaborated and refined [6, 9]. This model comes from Affective Neuroscience by the late Jaak Panksepp and his colleague Douglas Watt, as well as Mark Solms, Maggie Zellner, and others [6, 9]. It is called the "separation distress hypothesis." Some of the ideas in this model go back to Sigmund Freud and John Bowlby , but Pansepp and Watt made critical multidisciplinary contributions.

Summarizing the separation distress hypothesis here would not do it justice, as it is reasonably complex (so is the phenomenon it represents). You can find the latest update and systematic review of this model here [9]. The separation distress hypothesis combines innate, developmental, biological, psychological, and environmental factors. It does not reduce the macro phenomenon of depression to a molecular level of serotonin while ignoring all the levels in between. By now we have accumulated considerable evidence from multiple perspectives in support of the separation distress hypothesis [see 9 for a comprehensive review, as well as 6 and 8].
Repeated experiences of neglect, abuse, or abandonment in childhood , maladaptive habits, sleep disturbance, acute traumas at any age, complex trauma, and other factors can all lead to the patient suffering from repeated episodes (states) of depression. As you can see, depression, like fever, is non-specific and there are many possible pathways to it. It is biological and psychological at the same time.
What might the shift to the separation distress hypothesis result in? First, the dominant chemical imbalance story would have to be de-prioritized. An alternative understanding described by Mark Solms and his colleagues is that the feeling of depression means something [6,7]. Solms reminds us that this is not a new idea in medicine. A sensation of acute pain in the leg means that there is possibly a laceration there. Nausea means a possibly upset stomach. These “messages” guide us to what the problem is and where.
One of the meanings of depression, according to Mark Solms, is that our normal need to feel cared for is unmet [6, 7]. We feel painfully alone, unattached, or abandoned. This message is something we can notice, acknowledge, and work with in psychotherapy. Further, there are meaningful psychological reasons why the patient feels depressed, episodically or chronically. There is a way to discover in psychotherapy how this state came about and then work together with the patient to get to a stable resolution of this problem.
Using an etiological approach to depression would allow us to focus on the causal treatment that has shown significantly higher efficacy than SSRIs [4].
It is worthwhile saying that the separation distress hypothesis, like any other theory, has some limitations. For example, it lacks cultural sensitivity. However, I believe that this etiology-based, integrated model is more beneficial in guiding treatment choices for depression than the "chemical imbalance" model.
[1] Watters, E. (2010). Crazy like us: The globalization of the American psyche. Simon and Schuster.
[2] Pereira, V. S., & Hiroaki-Sato, V. A. (2018). A brief history of antidepressant drug development: from tricyclics to beyond ketamine. Acta neuropsychiatrica, 30(6), 307-322.
[3] Murphy JA, Sarris J, Byrne GJ. A review of the conceptualisation and risk factors associated with treatment-resistant depression. Depress Res Treat. 2017;2017:4176825. doi:10.1155/2017/4176825
[4] Shedler, J. (2010). The efficacy of psychodynamic psychotherapy. American psychologist, 65(2), 98.
[5] Solms, M. (2018). The scientific standing of psychoanalysis. BJPsych International, 15(1), 5-8.
[6] Zellner, M. R., Watt, D. F., Solms, M., & Panksepp, J. (2011). Affective neuroscientific and neuropsychoanalytic approaches to two intractable psychiatric problems: why depression feels so bad and what addicts really want. Neuroscience & Biobehavioral Reviews, 35(9), 2000-2008.
[7] Solms, M. L. (2018). The neurobiological underpinnings of psychoanalytic theory and therapy. Frontiers in Behavioral Neuroscience, 12, 402180.
[8] Blomstedt, P., Hariz, M. I., Lees, A., Silberstein, P., Limousin, P., Yelnik, J., & Agid, Y. (2008). Acute severe depression induced by intraoperative stimulation of the substantia nigra: a case report. Parkinsonism & related disorders, 14(3), 253-256.
[9] Watt, D. F. (2023). The separation distress hypothesis of depression–an update and systematic review. Neuropsychoanalysis, 1-57.
[10] Watt, D. F., & Panksepp, J. (2009). Depression: An evolutionarily conserved mechanism to terminate protracted separation distress. A review of aminergic, peptidergic and neural network perspectives. (Target article with invited commentaries). Neuropsychoanalysis, 11(1), 7–51. https://doi.org/10.1080/15294145.2009.10773593

Alexey Tolchinsky, Psy.D. , is a clinical psychologist in private practice in Maryland and a Clinical Fellow of the Neuropsychoanalysis Association.
- Find a Therapist
- Find a Treatment Center
- Find a Support Group
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
Essay On Depression: Causes, Symptoms And Effects
Our life is full of emotional ups and downs, but when the time of down lasts too long or influences our ability to function, in this case, probably, you suffer from common serious illness, which is called depression. Clinical depression affects your mood, thinking process, your body and behaviour. According to the researches, in the United States about 19 million people, i.e. one in ten adults, annually suffer from depression, and about 2/3 of them do not get necessary help. An appropriate treatment can alleviate symptoms of depression in more than 80% of such cases. However, since depression is usually not recognized, it continues to cause unnecessary suffering.
Depression is a disease that dominates you and weakens your body, it influences men as well as women, but women experience depression about two times more often than men.
Since this issue is very urgent nowadays, we decided to write this cause and effect essay on depression to attract the public attention one more time to this problem. I hope it will be informative and instructive for you. If you are interested in reading essays on similar or any other topic, you should visit our website . There you will find not only various essays, but also you can get help in essay writing . All you need is to contact our team, and everything else we will do for you.
Depression is a strong psychological disorder, from which usually suffers not only a patients, but also his / hers family, relatives, friends etc.
General information
More often depression develops on the basis of stress or prolonged traumatic situation. Frequently depressive disorders hide under the guise of a bad mood or temper features. In order to prevent severe consequences it is important to figure out how and why depression begins.
Symptoms and causes of depression
As a rule, depression develops slowly and insensibly for a person and for his close ones. At the initial stage most of people are not aware about their illness, because they think that many symptoms are just the features of their personality. Experiencing inner discomfort, which can be difficult to express in words, people do not ask for professional help, as a rule. They usually go to doctor at the moment, when the disease is already firmly holds the patient causing unbearable suffering.
Risk factors for depression:
- being female;
- the presence of depression in family anamnesis;
- early depression in anamnesis;
- early loss of parents;
- the experience of violence in anamnesis;
- personal features;
- stressors (parting, guilt);
- alcohol / drug addiction;
- neurological diseases (Parkinson's disease, apoplexy).
Signs of depression
Depression influences negatively all the aspects of human life. Inadequate psychological defense mechanisms, in their turn, affect destructively not only psychological, but also biological processes.
The first signs of depression are apathy, not depending on the circumstances, indifference to everything what is going on, weakening of motor activity; these are the main clinical symptoms of depression . If their combination is observed for more than two weeks, urgent professional help is required.
Psychological symptoms:
- depressed mood, unhappiness;
- loss of interest, reduced motivation, loss of energy;
- self-doubt, guilt, inner emptiness;
- decrease in speed of thinking, inability to make decisions;
- anxiety, fear and pessimism about the future;
- daily fluctuations;
- possible delirium;
- suicidal thoughts.
Somatic symptoms:
- vital disorders;
- disturbed sleep (early waking, oversleeping);
- eating disorders;
- constipation;
- feeling of tightness of the skull, dizziness, feeling of compression;
- vegetative symptoms.
Causes of depression
It is accepted to think in modern psychiatry that the development of depression, as well as most of other mental disorders, requires the combined effect of three factors: psychological, biological and social.
Psychological factor (“Personality structure”)
There are three types of personality especially prone to depression:
1) “Statothymic personality” that is characterized by exaggerated conscientiousness, diligence, accuracy;
2) Melancholic personality type with its desire for order, constancy, pedantry, exessive demands on itself;
3) Hyperthymic type of personality that is characterized by self-doubt, frequent worries, with obviously low self-esteem.
People, whose organism biologically tends to depression development, due to education and other social environmental factors form such personality features, which in adverse social situations, especially while chronic stress, cause failure of psychological adaptation mechanisms, skills to deal with stress or lack of coping strategies.
Such people are characterized by:
- lack of confidence in their own abilities;
- excessive secrecy and isolation;
- excessive self-critical attitude towards yourself;
- waiting for the support of the close ones;
- developed pessimism;
- inability to resist stress situations;
- emotional expressiveness.
Biological factor:
- the presence of unfavorable heredity;
- somatic and neurological head injury that violated brain activity;
- changes in the hormonal system;
- chronobiological factors: seasonal depressive disorders, daily fluctuations, shortening of REM sleep;
- side effects of some medications.
- Heredity and family tendency to depression play significant role in predisposition to this disease. It is noticed that relatives of those who suffer from depression usually have different psychosomatic disorders.
Social factor:
- the presence of frequent stress situations, chronic stress;
- adverse family relationships;
- adverse childhood experience, the absence of tenderness from parents, ill-treatment and sexual harassment, interpersonal loss, severe methods of education, negative childhood memories;
- urbanization;
- significant changes in the life;
- population migration;
- increased lifetime.
People in a state of chronic stress suffer from depression more often. If some acute stress situation happens during the period of chronic stress, the probability of depression symptoms development increases.
If you decide to fight the depression, remember that you are not alone! Every fifth person in the world at least once in the life experienced depression. If you notice the signs of depression that disturb you for more than two weeks, you should go to the specialist.
Do not delay visit, in this case time does not heal. The professionalism of the doctors and a complex program of treatment will help to get rid of any kind of depression.
Where to go for help
If you do not where to go for help, ask your family physician, obstetrician, gynecologist or the clinic. In an emergency situation, the emergency doctor can provide temporary help for patients with emotional problems and give them an advice where and how they can ask for the further help.
Here is the list of people and organizations that can diagnose and suggest a course of treatment, or can give a direction to the examination and treatment.
- Family doctors.
- Such specialists as psychiatrists, psychologists, social workers and consultants on mental health.
- Health maintenance organizations.
- Local centers for the treatment of mental illness.
- The Department of Psychiatry in hospitals and outpatient clinics.
- Programs at universities and medical schools.
- Family assistance services and social services departments.
- Private clinics and institutions.
- Care centers in the workplace.
- Local health and (or) mental health communities.
It is very important in depressive episode treatment to understand that this is depression of a certain person, do not make attempts to excessive generalization of symptoms and factors of disease development. It requires personal approach to each patient.
So, as you can see, depression is a serious disease that requires professional treatment. If you manage to recognize the signs of depression at its early stage and ask for professional help, you can successfully overcome this problem. I hope this essay about depression was useful for you, and you got what you were looking for.
Calculate Your Price
- Free Samples
- Popular topics
Recent posts
- Best Dissertation Writer: Stop Being Helpless
- Essay On Empathy: How Not to Lose Yourself
- Competent and Experienced Online Assignment Writing Service
- Papers Editing Services Help to Find Your Calling
- It Is Time to Order Best Dissertation Writing Services
Tired of endless home tasks on quarantine? No more worries!
Use your limited chance to get a special 22% OFF!
Apply the code "stayhome" while placing your order and enjoy the outstanding results!
- Open access
- Published: 26 March 2024
Depression during pregnancy and associated factors among women in Ethiopia: a systematic review and meta-analysis
- Solomon Shitu Ayen 1 ,
- Abebaw Wasie Kasahun 2 &
- Amare Zewdie 2
BMC Pregnancy and Childbirth volume 24 , Article number: 220 ( 2024 ) Cite this article
113 Accesses
Metrics details
Pregnancy is one of the most remarkable experiences in a woman’s life. Prenatal depression, characterized by stress and worry associated with pregnancy, can reach severe levels. On a global scale, mental and addictive disorders affect more than one billion people, causing 19% of years lived with disability. It is estimated that 25–35% of pregnant women experience depressive symptoms, with 20% meeting the diagnostic criteria for major depression.
A systematic review and meta-analysis were conducted to examine depression during pregnancy in Ethiopia. The search was conducted from March 1–31, 2023. Data extraction used Microsoft Excel, and analysis was performed using STATA version 17. The New Castle-Ottawa Scale quality assessment tool was employed to evaluate the methodological quality of included studies. The Cochrane Q test and I2 statistics were used to assess heterogeneity. A weighted inverse variance random-effects model estimated the pooled level of antenatal depression (APD). Publication bias was detected using a funnel plot and Begg’s and Egger’s tests.
Out of 350 studies searched, 18 were included in the analysis. The overall pooled prevalence of depression in Ethiopia was 27.85% (95% CI: 23.75–31.96). Harari region reported the highest prevalence (37.44%), while Amhara region had the lowest (23.10%). Factors significantly associated with depression included unplanned pregnancies, low social support, low income, previous history of depression, intimate partner violence, and history of abortion.
This systematic review and meta-analysis demonstrate that approximately one-quarter of pregnant women in Ethiopia experience depression during pregnancy. Unplanned pregnancy, low social support, low income, previous history of depression, history of abortion, and intimate partner violence are determinants of depression. To address this high prevalence, the Ethiopian government and stakeholders should develop policies that incorporate counseling during pregnancy follow-ups. Improving the quality of life for pregnant women is crucial for the well-being of families, communities, and the nation as a whole.
Peer Review reports
Introduction
Pregnancy is a significant life event for women, involving numerous physical, emotional, and social changes. This period can heighten the susceptibility of women and their fetuses to mental, physical, and psychological health issues. Among various mental health problems that occur during pregnancy, depression is the most prevalent psychiatric disorder affecting pregnant women. Depression during pregnancy, also known as antenatal depression (APD), is caused by anxiety and stress related to pregnancy and can stem from hormonal fluctuations, psychological disturbances, relationship issues, family or personal history of depression, life stress, low family support, unintended or unplanned pregnancies, and violence. If left untreated, APD can lead to adverse pregnancy outcomes, such as hypertension, low birth weight babies, preterm birth, and postnatal depression.
Depression is characterized by symptoms like excessive sleeping or insomnia, difficulty concentrating, forgetfulness, emotional instability, extreme irritability, fatigue, overeating or appetite loss, decreased interest in sex, feelings of guilt, sadness, suicidal thoughts, or death ideation. Globally, over one billion people suffer from mental or addictive disorders, accounting for 19% of all years lived with disability. Depression affects more than 350 million people across all age groups, with women being more vulnerable than men. Studies suggest that 25–35% of pregnant women experience depressive symptoms, and 20% of them meet the diagnostic criteria for major depression. The prevalence of APD varies in different countries, ranging from 20% in the United States to 30% in Finland and 35–50% in some lower and middle-income countries (LMICs).
In Africa, mental health issues among pregnant women and mothers have been extensively reported. APD is a critical public health concern in developing nations due to its intergenerational impact on mothers, infants, and children. In Ethiopia, the prevalence of APD and its associated factors differ across regions and time. Factors like older age, less education, being single, unemployment, low income, intimate partner violence, lack of social support, unplanned pregnancies, previous pregnancy loss, history of abortion, obstetric complications, and substance abuse contribute to APD.
Previous studies have provided inconsistent findings regarding APD prevalence and predictors at the national level, leaving policymakers with inconclusive information. This systematic review and meta-analysis aim to estimate the pooled prevalence of depression during pregnancy and its predictors among pregnant women in Ethiopia. By including recent studies and a larger sample of research articles (18 in total), this study offers a more comprehensive understanding of APD in Ethiopia.
Study design and setting
To ensure the originality and avoid redundancy of the research, the International Prospective Register of Systematic Reviews (PROSPERO) database was consulted. Upon checking the database ( http://www.library.ucsf.edu/ ), no published or ongoing research related to antenatal depression (APD) in Ethiopia was found. To proceed with the research, the protocol of the systematic review and meta-analysis was registered in the PROSPERO database with the ID CRD42023423700. The study adheres to the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines to maintain the highest standards of research transparency and quality [ 1 ].
Data sources and search strategy
Articles included in the review were searched from the following databases: MEDLINE, Scopus, PubMed, Science Direct, Google Scholar, African Journals Online, and Web of Sciences to retrieve related articles. Search terms were formulated using PICO guidelines through online databases. Medical Subject Headings (MeSH) and key terms had been developed using different Boolean operators ‘AND’ and ‘OR’. Each database was searched from its start date to March 2023 by using the following words: Depression (Mesh), depress ∗ (all fields), “antepartum depression” (Mesh), “antepartum depression” (Mesh), “antenatal depression” (Mesh), Ethiopia(Mesh), “prenatal depression” (Mesh), “pregnancy and depression” (Mesh), mental health (all fields). Furthermore, librarians were consulted to find unpublished research works on our area of interest for this review. The literature search was conducted by two separate researchers (SSA and AWK) to avoid missing articles.
Eligibility criteria
In this systematic review and meta-analysis, the scope was to include all community and facility-based studies that reported the prevalence of antepartum depression (APD) and its determinants. This comprehensive approach aimed to ensure the study captured as much relevant information as possible. Both published and unpublished studies were considered to minimize potential publication bias. If multiple reports of the same study existed, the most recent and comprehensive study was chosen to ensure the analysis was based on the latest and most accurate data available.
The language restriction for the included articles was limited to English to facilitate the understanding and analysis of the data. This decision was made considering the limitations of the research team’s language capabilities and the widespread use of English in academic and scientific publications.
The timeframe for the search and inclusion of studies was set until March 30, 2023. This date allowed for a relatively recent and up-to-date analysis of the prevalence of APD and its associated factors in Ethiopia. As new research continues to emerge, future updates to the review may consider extending the search period or re-evaluating the study to incorporate more recent findings.
Exclusion criteria
To maintain the focus and accuracy of the systematic review and meta-analysis, several exclusion criteria were applied. Articles that did not report the outcome variables of interest, such as the prevalence of antepartum depression (APD) or its determinants were excluded. This ensured that only relevant data was considered in the analysis.
Additionally, certain study types were excluded to maintain the quality and reliability of the review. Systematic reviews, case series, commentaries, conference abstracts, letters to editors, technical reports, qualitative studies, and other opinion publications were not included, as they might not provide sufficient quantitative data or meet the required methodological standards.
To avoid double-counting studies, potential duplicates were also excluded. This involved removing studies conducted in the same area with similar findings during the same study period. This step ensured that the final analysis included a diverse and representative sample of studies, reducing the risk of overrepresentation or redundancy in the data.
Measurement of the outcome of interest
In this systematic review and meta-analysis, the primary focus was on determining the prevalence of antepartum depression (APD) in Ethiopia. The pooled prevalence was calculated as the primary outcome variable to provide an overall estimate of the proportion of affected individuals within the studied population.
The secondary outcome variable was to identify the factors associated with APD. To achieve this, a pooled Adjusted Odds Ratio (AOR) with 95% Confidence Intervals (CIs) was employed. This statistical measure allowed for the estimation of the strength and significance of the relationship between various determinants and the occurrence of APD.
To assess depressive symptoms in the studies, participants were typically asked specific questions. If they responded affirmatively (“Yes”) to these questions, they were considered to be experiencing depression. On the other hand, if they responded negatively (“NO”), they were not classified as depressed. This approach enabled the identification and analysis of individuals with potential APD within the studied population.
Data extraction strategy
To ensure a comprehensive and organized review process, several steps were taken to manage and analyze the collected data. Initially, duplicate articles were identified and removed using EndNote X8, citation management software. This helped to avoid any overlapping data or double-counting of studies in the analysis.
Data extraction was carried out using a Microsoft Excel spreadsheet, which was designed with a pre-settled and piloted format. The format was adapted from the Joanna Briggs Institute (JBI) data extraction format to ensure a standardized and thorough approach to data collection. The extracted information included:
The primary author’s name, publication year, study year, study design, study area, study setup, sample size, response rate, data collection technique, The proportion of APD, adjusted Odds Ratio (AOR) with their 95% confidence interval. To facilitate the data extraction process, multiple researchers (SS, AW, and AZ) worked separately, ensuring a more accurate and reliable data collection. They used 2 by-2 tables for the second objective of the review, which focused on identifying factors associated with APD.
Finally, the data analysis was performed using STATA software version 17. This statistical software allowed for the appropriate handling and interpretation of the collected data, contributing to a more robust and reliable systematic review and meta-analysis.
Quality assessment
The Newcastle-Ottawa Scale (NOS) was employed to assess the quality of the included studies in this systematic review. The NOS is a widely recognized and validated tool that evaluates the quality of non-randomized studies, such as cohort and case-control studies, in a structured manner. It focuses on three main components. The principal component, which evaluates the methodological quality of each primary study and is graded with five stars. The comparability of each study, which is graded from two stars and assesses the similarity of study participants and other factors that may influence the results. The outcomes and statistical analysis of each original study, graded from three stars and examining the adequacy of the reported results and statistical methods. The NOS uses a scoring system with a maximum score of 9 points. The quality of each study was rated based on the following scoring algorithms. A score of 7 points or more was considered “good” quality. A score between 2 and 6 points was considered “fair” quality. A score of 1 point indicated a “poor” quality study [ 2 ].
To ensure the validity and reliability of the systematic review results, only primary studies with fair to good quality were included in the analysis. The quality assessment was conducted by two authors (AW and SS), who evaluated the methodological quality, sample selection, sample size, comparability, and the outcome and statistical analysis of each original study.
Data processing and analysis
After importing the selected articles into a Microsoft Excel spreadsheet, the data was exported to STATA version 17 for statistical analysis. The choice of statistical methods depended on the nature of the data and the presence of heterogeneity between studies.
To estimate the pooled prevalence of APD, a weighted inverse variance random-effects model was used. This model takes into account the variability between studies and provides a more conservative estimate when heterogeneity is present. The presence of statistical heterogeneity across the included studies was determined using Higgins I2 statistics and the Cochran-Q test. The interpretation of I2 values was based on the following criteria. 75–100%: considerable heterogeneity, 50–90%: substantial heterogeneity, 30–60%: moderate heterogeneity, 0–40%: mild heterogeneity [ 3 ].
When studies showed significant heterogeneity, a random-effects model was used. In cases of homogeneous studies, a fixed-effects model was applied. To assess the possibility of publication bias, a Funnel plot and Eggers test were conducted. Publication bias was considered justified if the p -value was greater than 0.05. The results were presented in a forest plot format, which displays the pooled prevalence of APD with its 95% confidence interval (CI).
For the analysis of the adjusted odds ratio (AOR) from eligible studies, along with their 95% confidence intervals, the pooled AORs were computed using either a random or fixed-effect model, depending on the presence of heterogeneity. Finally, forest plots were used to visually represent the pooled estimates for APD and its determinants, along with their respective 95% confidence intervals, allowing for a comprehensive understanding of the relationship between these factors and APD.
Characteristics of included studies
In total, 350 studies were initially identified from various search engines, including 341 from the specified data sets and 9 from other sources. After removing duplicates, 63 studies were excluded, leaving 287 studies. Among these, 201 studies were further excluded based on their titles and abstracts, not meeting the inclusion criteria.
Subsequently, 68 studies were excluded after reviewing their full texts due to insufficient data or not satisfying the predefined criteria. Finally, 18 studies were deemed eligible for inclusion in the analysis (Fig. 1 ). These studies were conducted across different regions of Ethiopia, with four studies each in the South Nations, Nationalities, and Peoples’ Region (SNNPR) and Oromia, three studies each in Amhara and Addis Ababa, two studies in Tigray, and one study in each of Somali and Harari (Table 1 ). The population exposure and outcome (PEO) of the study participants are demonstrated in Table 2 , providing a clear overview of the study population and the outcomes assessed in the included studies.
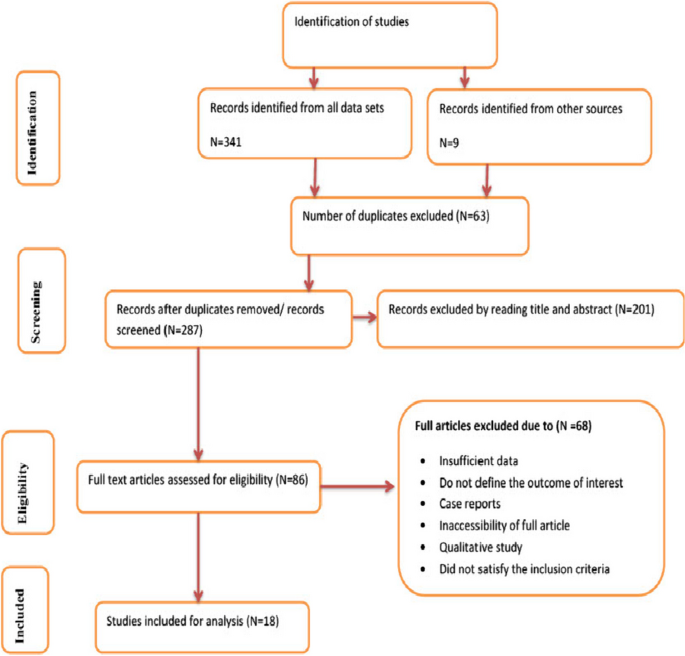
Flow chart of selection for systematic review and meta-analysis on DDP and associated factors in Ethiopia, 2023
Sensitivity analysis
The sensitivity analysis, performed using the random-effects model, aimed to assess the influence of individual studies on the overall estimate of atrial fibrillation and flutter (APF) prevalence in Ethiopia. The results of this sensitivity analysis, presented in Fig. 2 , indicate that no single study significantly impacted or unduly influenced the overall estimate of APD prevalence in Ethiopia. This finding suggests that the results are robust and stable, as the overall prevalence estimate remains consistent even when specific studies are removed from the analysis.
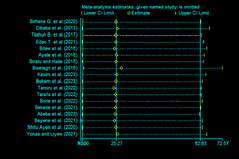
Sensitivity test of studies included in systematic review and meta-analysis on DDP and associated factors in Ethiopia, 2023
Publication bias
To further evaluate the possibility of publication bias, funnel plots were employed to visually inspect the asymmetry of the distribution of study effect sizes against their standard errors. An inverted funnel shape that appears symmetrical suggests a low likelihood of publication bias. In this case, the funnel plot displayed a large, symmetrical inverted funnel shape (Fig. 3 ), indicating that the chance of publication bias is minimal.
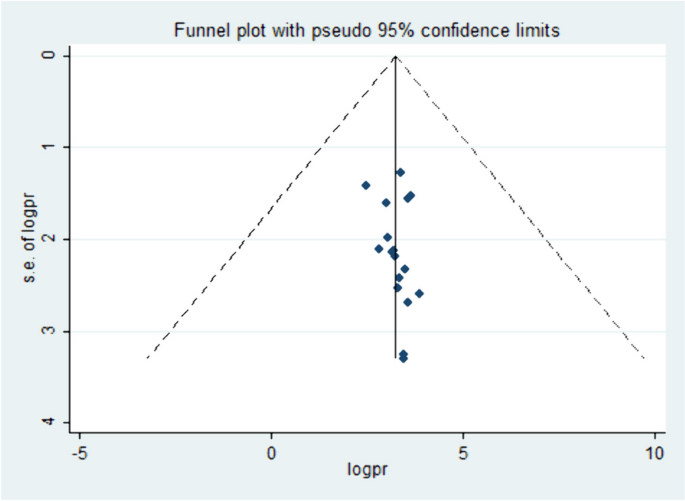
Funnel plot showing the symmetric distribution of articles on DDP in Ethiopia, 2023
In addition to the visual assessment, statistical methods such as Egger’s and Begg’s tests were used to provide supplementary evidence. A p -value less than 0.05 are generally considered statistically significant, and in this context, it suggests that there is no significant publication bias present in the included studies, supporting the visual assessment findings.
The pooled prevalence of APD in Ethiopia
The prevalence of atrial fibrillation and flutter (APF) in Ethiopia varied across the studies, demonstrating significant heterogeneity. The heterogeneity was quite high, with an I2 value of 95.0% and a statistically significant P -value less than 0.000. This high level of heterogeneity indicates that there are substantial differences in the study results that cannot be explained by chance alone. Despite this heterogeneity, the overall pooled prevalence of APF in Ethiopia was estimated to be 27.85% (95% confidence interval: 23.75–31.96). This combined prevalence figure is summarized using a forest plot (Fig. 4 ), which visually represents the individual study results and their contribution to the overall prevalence estimate.
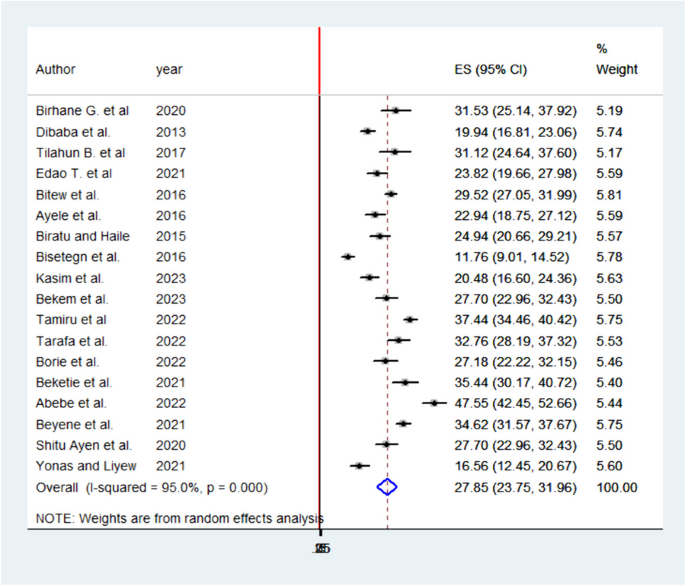
Pooled prevalence systematic review and meta-analysis on DDP and associated factors in Ethiopia, 2023
The high heterogeneity among studies highlights the importance of considering the context and methodology of each individual study when interpreting the overall prevalence estimate. Further research and investigation may be required to understand the factors contributing to this variability and to develop targeted strategies for managing and preventing APF in Ethiopia.
Subgroup analyses of APD in Ethiopia
Subgroup analyses were conducted by the study region. Accordingly, the highest prevalence of APD was reported in Harari and lowest in Amhara regions with prevalence and I 2 of 37.44% (95% CI: 34.46–40.42) I 2 95% P = 0.000 and 23.10 (95% CI: 8.56–37.64) I 2 98.3% P = 0.000 respectively (Fig. 5 ).
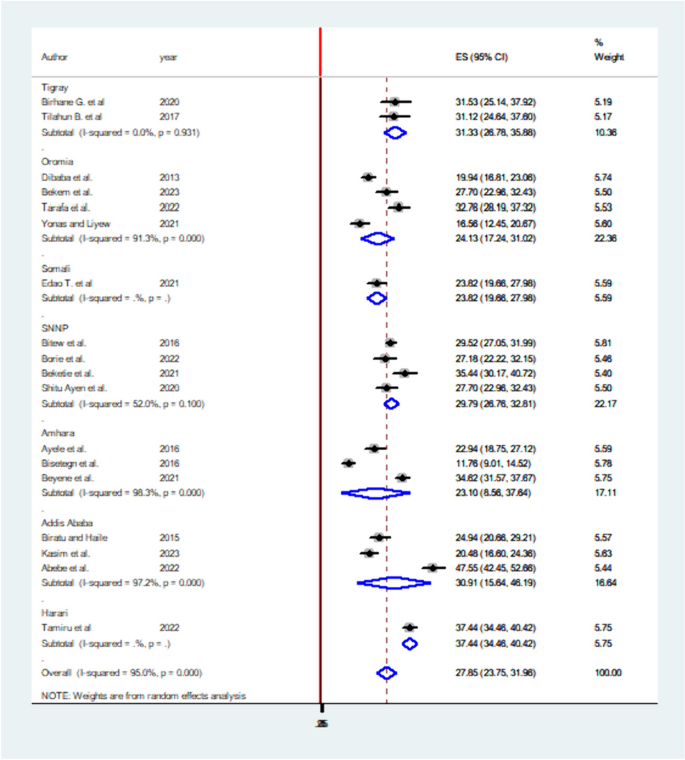
Subgroup analysis of systematic review and meta-analysis on DDP and associated factors in Ethiopia, 2023
Factors associated with APD in Ethiopia
Six significant factors have been identified in this systematic review and meta-analysis to be associated with atrial premature depolarization (APD) in Ethiopia. These factors are unplanned pregnancy, social support, history of abortion, intimate partner violence, low income, and previous history of depression. Each factor’s association with APD is quantified using adjusted odds ratios (AOR) and their respective confidence intervals.
Unplanned pregnancy: Women experiencing unplanned pregnancies have a 2.47 times higher likelihood of developing APD compared to those with planned pregnancies (AOR: 2.47, 95% CI: 1.92–3.19). Low social support and income: Pregnant mothers with low social support and income are 2 times more likely to develop APD than their counterparts (AOR: 2.06, 95% CI: 1.44–2.94 for low social support; AOR: 2.13, 95% CI: 1.54–2.91 for low income). Previous history of depression: Women with a history of depression have a 3 times higher likelihood of developing APD (AOR: 3.49, 95% CI: 2.40–5.08). History of intimate partner violence: Women with a history of intimate partner violence are 2.7 times more likely to develop APD than those without such history (AOR: 2.71, 95% CI: 2.07–3.55). History of abortion: Women with a history of abortion have a 2 times higher likelihood of developing APD compared to those without (AOR: 2.12, 95% CI: 1.392–3.25).
These findings, summarized in Table 3 , provide valuable insights into the potential risk factors associated with APD in Ethiopia. Addressing these factors and implementing targeted interventions could help reduce the prevalence and impact of APD on affected women in the country.
This systemic review and meta-analysis provide valuable insights into the prevalence and associated factors of antepartum depression (APD) in Ethiopia. The pooled prevalence of APD in Ethiopia is 27.85% (95% CI: 23.75–31.96), which is in line with studies conducted in Nigeria, Ghana, and Africa as a whole [ 14 , 15 , 16 ], but higher than studies in Brazil, Nepal, South Africa, and rural Ghana [ 17 , 18 , 19 , 20 , 21 , 22 , 23 ]. The prevalence in Ethiopia might be higher due to differences in study periods, populations, and areas. However, the prevalence of this systemic review and meta-analysis was lower than in studies done in Tanzania, Côte d’Ivoire, Kenya [ 15 , 24 , 25 ] the reason might be due to most of the studies are single area findings which may not be strong too as compared to this systemic review which is pooled prevalence. Also, it may be due to the study period, study population, and study area differences.
Sub-group analysis reveals the highest prevalence in the Harari region (37.44%) and the lowest in the Amhara region (23.1%). Factors significantly associated with APD include unplanned pregnancy, social support, history of abortion, intimate partner violence, low income, and previous history of depression. These associations are quantified using adjusted odds ratios (AOR) and their respective confidence intervals.
Low social support and low income are associated with a twofold increased likelihood of developing APD. This finding is consistent with studies conducted in Nepal, Tanzania, Nigeria, South Africa, and systemic reviews in Africa. Women with unplanned pregnancies have a 2.47 times higher likelihood of developing APD, possibly due to economic stress and concerns related to unplanned pregnancies in developing countries [ 18 , 19 , 20 , 21 , 22 , 24 ].
In this systemic review and meta-analysis, women with low income were two times more likely to develop APD than women with good income AOR 2.13; 95% CI; 1.54–2.91. The finding was in line with studies conducted in Tanzania, Nigeria, and systemic reviews in Africa [ 16 , 21 , 24 ]. This may be due to a family with poor income may be related to the economic problem and she became stressed thinking of how can she give care for the newborn and the family.
Women with a history of unplanned pregnancy were 2.47 times more likely to develop APD than women with planned pregnancy AOR 2.47; 95% CI; 1.92–3.19. The reason may be in developing countries planning to get pregnant will be associated with the economy of the household so women with unplanned pregnancies may be stressed by thinking of economic problems after birth which may lead to depressive conditions [ 21 ].
A previous history of depression has been associated with APD in this review. Women with a previous history of depression had 3.5 times more likely to develop APD than their counterparts AOR 3.49; 95% CI; 2.40–5.08. The finding was consistent with studies done in Brazil and South Africa [ 17 , 20 ]. A possible explanation might be scientifically the reoccurrence of APD is most likely in consecutive pregnancies unless possible risk factors are avoided [ 20 ].
The probability of the women developing APD was 2.71 times more likely with intimate partner violence as compared to their counterparts AOR 2.71; 95% CI; 2.07–3.55. The finding was supported by studies in Kenya, Nigeria, and South Africa. The possible explanation might be as the name indicates violence is violating the rights of the person physically, sexually, or emotionally. Thus, women with violence might be more likely to develop depression. It may also be a partner who violates the rights of the woman may have poor educational conditions and can’t respect others [ 14 , 19 , 25 ].
Women with a history of abortion were two times more likely to develop depression during pregnancy than their counterparts AOR 2.12; 95% CI; 1.39–3.25. The possible reason might be women who experience abortion may be stressed due to fear of repeated abortion and loss of their baby. The finding was supported by a study done in Nigeria [ 21 ].
These findings can help guide interventions and policies to address the factors associated with APD in Ethiopia, ultimately reducing its prevalence and impact on affected women.
Strengths and limitations of the study
The study presents several strengths and limitations. One of the main strengths lies in the comprehensive search strategy employed to retrieve related articles. By searching different databases and following the PRISMA flow charts strictly, the study ensures a systematic and thorough approach to identifying relevant studies. Additionally, including studies published over different years allows for an analysis of potential trends in antepartum depression (APD) during pregnancy in Ethiopia.
However, there are some limitations to consider. Firstly, the study is limited to English-language articles, which might have resulted in excluding relevant studies published in other languages. This could potentially affect the generalizability and comprehensiveness of the findings. Secondly, the absence of studies from some regions of Ethiopia might raise questions about the generalizability of the results across the entire country. This could be due to various factors, such as regional differences in access to healthcare, cultural practices, or research focus. To address these limitations, future studies could consider expanding their search to include non-English articles and aim to include studies from all regions of Ethiopia to enhance the generalizability of their findings.
The findings of this systemic review and meta-analysis highlight the significant prevalence of antepartum depression (APD) in Ethiopia, affecting one-quarter of pregnant women. Addressing the determinant factors of depression, such as unplanned pregnancies, low social support, low income, previous history of depression, history of abortion, and intimate partner violence, is crucial for reducing the prevalence of APD.
To address this issue, the government of Ethiopia and other stakeholders should consider incorporating depression counseling during antenatal care (ANC) follow-ups. By providing information and support to pregnant women, they can better understand and cope with potential risk factors and seek appropriate help when needed. This approach not only improves the well-being of individual women but also contributes to the overall well-being of their families, communities, and the nation.
Incorporating depression awareness and prevention measures into ANC services can help create a supportive environment for pregnant women, empowering them to make informed decisions and seek assistance when facing challenges. This holistic approach to maternal health can lead to better mental health outcomes for pregnant women, ultimately benefiting the entire society.
Availability of data and materials
The result of this systematic review and meta-analysis was extracted from the data gathered and analyzed based on the stated methods and materials. All the relevant data are within the paper.
Abbreviations
Adjusted Odds Ratio
Ante Partum Depression
Depression during Pregnancy
Joanna Briggs Institute
Lower and Middle-Income Countries
Newcastle-Ottawa Scale
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
South Nations, Nationalities, and People Region
World Health Organization
Prisma transparent reporting of systematic reviews and meta-analyses. http://www.prisma-statement.org/PRISMAStatement/Checklist.aspx . Cited 2021 Nov 18.
ells GA, O’Connell BSD, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp .
The Cochrane Collaboration and John Wiley & Sons Ltd, Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews. England: Wiley; 2008.
Google Scholar
Dibaba Y, Fantahun M, Hindin MJ. The association of unwanted pregnancy and social support with depressive symptoms in pregnancy: evidence from rural Southwestern Ethiopia. BMC Pregn Childb. 2013;13(1):1–8.
Article Google Scholar
Bitew T, Hanlon C, Kebede E, Medhin G, Fekadu A. Antenatal depressive symptoms and maternal health care utilization: a population-based study of pregnant women in Ethiopia. BMC Pregn Childb. 2016;16(1):1–1.
Ayele TA, Azale T, Alemu K, Abdissa Z, Mulat H, Fekadu A. Prevalence and associated factors of antenatal depression among women attending antenatal care service at Gondar University Hospital, Northwest Ethiopia. Plos One. 2016;11(5):e0155125. https://doi.org/10.1371/journal.pone.0155125 .
Article CAS PubMed PubMed Central Google Scholar
Biratu A, Haile D. Prevalence of antenatal depression and associated factors among pregnant women in Addis Ababa, Ethiopia: a cross-sectional study. Reprod Health. 2015;12(1):1–8.
Bisetegn TA, Mihretie G, Muche T. Prevalence and predictors of depression among pregnantwomen in Debretabor Town, Northwest Ethiopia. Plos One. 2016;11(9):e0161108. https://doi.org/10.1371/journal.pone.0161108 .
Tamiru D, Misgana T, Tariku M, Tesfaye D, Alemu D, Weldesenbet AB, Gebremichael B, Theresa M. Prevalence and associated factors of common mental disorders among pregnant mothers in rural eastern Ethiopia. Front Psychiatry. 2022;13:843984.
Article PubMed PubMed Central Google Scholar
Tarafa H, Alemayehu Y, Nigussie M. Factors associated with pregnancy-related anxiety among pregnant women attending antenatal care follow-up at Bedelle General Hospital and Metu Karl comprehensive specialized hospital Southwest Ethiopia. Front Psychiatry. 2022;2133:938277.
Beketie ED, Kahsay HB, Nigussie FG, Tafese WT. Magnitude and associated factors of antenatal depression among mothers attending antenatal care in Arba Minch town, Ethiopia, 2018. Plos One. 2021;16(12):e0260691. https://doi.org/10.1371/journal.pone.0260691 .
Abebe W, Gebremariam M, Molla M, Teferra S, Wissow L, Ruff A. Prevalence of depression among HIV-positive pregnant women and its association with adherence to antiretroviral therapy in Addis Ababa, Ethiopia. Plos One. 2022;17(1):e0262638. https://doi.org/10.1371/journal.pone.0262638 .
Beyene GM, Azale T, Gelaye KA, Ayele TA. The effect of antenatal depression on birth weight among newborns in South Gondar Zone, Northwest Ethiopia: a population-based prospective cohort study. Arch Public Health. 2021;79(1):1–2.
Thompson O, Ajayi I. Prevalence of antenatal depression and associated risk factors among pregnant women attending antenatal clinics in Abeokuta North Local Government Area. Nigeria Depress Res Treat. 2016;2016:4518979. https://doi.org/10.1155/2016/4518979 . (Epub 2016 Aug 18. PMID: 27635258; PMCID: PMC5007324).
Article PubMed Google Scholar
Bindt C, Appiah-Poku J, Te Bonle M, Schoppen S, Feldt T, Barkmann C, Koffi M, Baum J, Nguah SB, Tagbor H, Guo N, N’Goran E, Ehrhardt S, International CDS Study Group. Antepartum depression and anxiety associated with disability in African women: cross-sectional results from the CDS study in Ghana and Côte d’Ivoire. PLoS One. 2012;7(10):e48396. https://doi.org/10.1371/journal.pone.0048396 . (PMID: 23110236; PMCID: PMC3482210).
Dadi AF, Wolde HF, Baraki AG, Akalu TY. Epidemiology of antenatal depression in Africa: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2020;20(1):251. https://doi.org/10.1186/s12884-020-02929-5 . (PMID: 32345263; PMCID: PMC7189721).
Coll CVN, da Silveira MF, Bassani DG, Netsi E, Wehrmeister FC, Barros FC, Stein A. Antenatal depressive symptoms among pregnant women: evidence from a Southern Brazilian population-based cohort study. J Affect Disord. 2017;209:140–6 (Epub 2016 Nov 26. PMID: 27914247; PMCID: PMC5282400).
Joshi D, Shrestha S, Shrestha N. Understanding the antepartum depressive symptoms and its risk factors among the pregnant women visiting public health facilities of Nepal. PLoS ONE. 2019;14(4):e0214992 PMID: 30947251; PMCID: PMC6448918. https://doi.org/10.1371/journal.pone.0214992 .
Govender D, Naidoo S, Taylor M. Antenatal and postpartum depression: prevalence and associated risk factors among adolescents’ in KwaZulu-Natal, South Africa. Depress Res Treat. 2020;2020:5364521. https://doi.org/10.1155/2020/5364521 . (PMID: 32411457; PMCID: PMC7204344).
Sulyman D, Aminu MB, Ayanda KA, Dattijo LM. Antepartum depression among women attending antenatal clinic in a Nigerian teaching hospital. Niger J Med. 2021;30:556–60.
Redinger S, Pearson RM, Houle B, Norris SA, Rochat TJ. Antenatal depression and anxiety across pregnancy in urban South Africa. J Affect Disord. 2020;277:296–305. https://doi.org/10.1016/j.jad.2020.08.010 . (Epub 2020 Aug 13. PMID: 32858310).
Adeoye IA, Sogbesan A, Esan O. Prevalence, associated factors and perinatal outcomes of antepartum depression in Ibadan Nigeria. BMC Pregnancy Childbirth. 2022;22(1):219. https://doi.org/10.1186/s12884-022-04549-7 . (PMID: 35303804; PMCID: PMC8933907).
Weobong B, ten Asbroek AHA, Soremekun S, Manu AA, Owusu-Agyei S, et al. Association of antenatal depression with adverse consequences for the mother and newborn in Rural Ghana: findings from the DON population-based cohort study. PLoS ONE. 2014;9(12): e116333. https://doi.org/10.1371/journal.pone.0116333 .
Rwakarema M, Premji SS, Nyanza EC, Riziki P, Palacios-Derflingher L. Antenatal depression is associated with pregnancy-related anxiety, partner relations, and wealth in women in Northern Tanzania: a cross-sectional study. BMC Womens Health. 2015;15:68. https://doi.org/10.1186/s12905-015-0225-y . (PMID: 26329331; PMCID: PMC4557331).
Tele A, Kathono J, Mwaniga S, Nyongesa V, Yator O, Gachuno O, Wamalwa D, Amugune B, Cuijpers P, Saxena S, McKay M, Carvajal L, Lai J, Huang KY, Merali Z, Kumar M. Prevalence and risk factors associated with depression in pregnant adolescents in Nairobi, Kenya. J Affect Disord Rep. 2022;10:100424 (Epub 2022 Sep 19. PMID: 36970124; PMCID: PMC10038142).
Download references
Acknowledgements
We would like to thank all authors of the primary studies which are included in this systematic review and meta-analysis.
Institutional review board statement
Not applicable.
This systematic review and meta-analysis used and analyzed information obtained from pre-existing studies.
There is no funder for this systematic meta-analysis.
Author information
Authors and affiliations.
Department of Midwifery, College of Medicine and Health Science, Wolkite University, Wolkite, 07, Ethiopia
Solomon Shitu Ayen
Department of Public Health, College of Medicine and Health Science, Wolkite University, Wolkite, Ethiopia
Abebaw Wasie Kasahun & Amare Zewdie
You can also search for this author in PubMed Google Scholar
Contributions
As per the guidelines for authorship, all authors of this study have made significant contributions to the work reported and have fulfilled the following criteria. Conception and design, data extraction and analysis, study design and execution, acquisition of data, interpretation of results, drafting, revising, and critically reviewing the article, final approval of the version to be published, agreement to be accountable for all aspects of the work, taking responsibility for the integrity and accuracy of the research and its presentation. By fulfilling these criteria, all authors have demonstrated their active involvement in various aspects of the research and manuscript preparation, ensuring the quality and reliability of the study's findings.
Corresponding author
Correspondence to Solomon Shitu Ayen .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
All authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ayen, S.S., Kasahun, A.W. & Zewdie, A. Depression during pregnancy and associated factors among women in Ethiopia: a systematic review and meta-analysis. BMC Pregnancy Childbirth 24 , 220 (2024). https://doi.org/10.1186/s12884-024-06409-y
Download citation
Received : 23 October 2023
Accepted : 11 March 2024
Published : 26 March 2024
DOI : https://doi.org/10.1186/s12884-024-06409-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Depression during pregnancy
- Pregnant women
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 25 March 2024
Influencing factors of sleep quality in pregnant: a structural equation model approach
- Mailiman Bahani 1 na1 ,
- Yuxia Zhang 2 na1 ,
- Yufeng Guo 1 na1 ,
- Salawati Haretebieke 1 ,
- Di Wu 1 &
- Liping Zhang 3
BMC Psychology volume 12 , Article number: 171 ( 2024 ) Cite this article
138 Accesses
Metrics details
To describe the changes in the level of sleep quality during pregnancy among pregnant women in Urumqi; also to construct a structural equation model of the factors influencing the sleep quality of pregnant women, to analyze the path relationship between the influencing factors, and to take reasonable interventions to prevent and reduce the occurrence of sleep disorders among pregnant women.
986 pregnant women who gave birth in Urumqi Maternal and Child Health Hospital and Urumqi Youai Hospital between August 2021 and May 2023 were selected. The Pittsburgh Sleep Quality Index (PSQI), Self-Rating Anxiety Scale (SAS), and Edinburgh Postpartum Depression Scale (EPDS) were used to assess the sleep, anxiety, and depression of pregnant women, Building a structural equation model based on AMOS 23.0 Tools.
The results of structural equation modeling showed that: basic characteristics, obstetrical characteristics, tocolysis, lifestyle, psychological had a direct effect on the PSQI, with path coefficients of 0.243, 0.106, 0.140, 0.174, 0.658, the corresponding T-values for each path are 4.585, 2.677, 2.578, 2.297, and 9.036. The indirect effect of basic characteristics, obstetric characteristics and lifestyle on PSQI was 0.123, 0.020, 0.027.
Conclusions
The high incidence of sleep disorders in pregnant women and their close association with psychological symptoms in pregnant women should focus on screening and counseling regarding psychological disorders in pregnant women, thus improving the quality of sleep in pregnant women.
Peer Review reports
Introduction
Sleep is an indispensable life activity for human beings and an important protective mechanism, occupying almost one-third of life. Adequate and good sleep can satisfy both physical and psychological needs of human beings, as well as allow people to recover physical and mental strength and enhance work efficiency. Pregnancy is a short and unique process, due to the hormone levels during pregnancy affecting pregnant women in physical, physiological, social and psychological changes, making pregnant women more prone to insomnia, urinary frequency, frequent waking up at night and sleep deprivation, which can lead to sleep disorders and adverse pregnancy outcome [ 1 ]. In addition, socio-demographic characteristics (age, education level, economic income and BMI), mood disorders have been reported to affect the quality of sleep in pregnant women, with higher depression and anxiety scores associated with poorer sleep quality [ 2 , 3 ].
Most pregnant mothers report altered sleep during pregnancy, and results from previous studies have shown a wide range in the prevalence of poor sleep quality in women during pregnancy, ranging from 29–84% [ 4 , 5 ],with a mean PSQI score of 6.07 [5.30, 6.85] during pregnancy [ 4 ],Sleep quality is characterized by poorer subjective sleep quality, reduced habitual sleep efficiency, and sleep disturbances increase, and longer time to fall asleep. Chronic low-quality sleep exacerbates the risk of multiple negative perinatal pregnancy outcomes, including mood disorders [ 5 , 6 ], cesarean section rate, prolonged labor and delivery, gestational diabetes mellitus [ 7 ], preeclampsia, preterm labor, and low birth weight of neonates [ 1 , 8 , 9 ]. It is thus clear that sleep disorders pose a serious threat to the health of both the pregnant woman and the fetus.
Given the complex interplay of these factors, a comprehensive analysis was deemed necessary to understand the current status and influences on sleep quality in pregnant women. Structural equation modeling (SEM) provides a valuable statistical method to synthesize path-reflective relationships between variables and identify the direct and indirect effects of multiple factors on sleep quality. In this study, a theoretical model was initially constructed using sleep quality as an endogenous latent variable and basic characteristics, obstetrical characteristics, tocolysis, lifestyle, and psychological status as exogenous latent variables, and the fit of the theoretical model was verified to explain and predict the factors affecting sleep quality in pregnant women to ensure that the model proposed by the investigators was supported by data under real conditions. In turn, the key factors leading to poor sleep quality were identified, healthcare professionals can implement targeted interventions and develop strategies to promote better sleep during pregnancy in order to improve the overall health of pregnant women during gestation, optimize their pregnancy experience, while promoting healthy fetal development in the womb.
Participants
The present study was a cross-sectional study in which pregnant women in pregnancy who underwent labor checkups at the obstetrics outpatient clinics of Urumqi Maternal and Child Health Hospital and Urumqi You’ai Hospital during the period of August 2021 ∼ May 2023 were selected by simple random sampling, and pregnant women who met the inclusion criteria were surveyed face-to-face with an electronic questionnaire. Firstly, the purpose, procedure and filling requirements of this survey were explained to pregnant women, and after fully understanding this study, they signed the informed consent form. At the beginning of the survey, pregnant women could choose to fill out the questionnaire independently in the hospital public number with their cell phones, and professionally trained investigators were beside them to explain the entries that were not understood by the research subjects in time; for pregnant women who were not able to answer the questionnaire independently on their cell phones, they could also choose to fill out the paper questionnaire, and fill out the questionnaire in the form of a one-question-one-answer format between the investigators and the pregnant women.
Inclusion criteria
Pregnant women aged ≥ 18 years;
Volunteered to participate in this research study and was able to complete the electronic questionnaire independently;
Local permanent residents (≥ 1 year of residence).
Exclusion criteria
Suffering from a serious mental illness;
Planned early termination of pregnancy;
Incomplete information on the questionnaire.
Data collection tools
Basic information questionnaire.
The Basic Information Questionnaire collects basic information on pregnant women’s gestation period, age, height, weight, ethnicity, literacy, place of residence, occupation, husband’s information, per capita monthly household income, past medical history, maternal history, exercise, health behaviors, husband-wife relationship, in-laws’ relationship, and whether they are sociable or not.
Pittsburgh sleep quality index scale
The Pittsburgh Sleep Quality Index (PSQI) was used to evaluate the sleep of pregnant women [ 4 ]. The scale is a questionnaire containing 18 entries to measure habitual sleep quality over a recent month [ 10 ]; it consists of seven subscales assessing sleep duration, nocturnal sleep disturbances, sleep latency, sleep quality, daytime dysfunction, sleep medication use and sleep efficiency. Scores for each subscale ranged from 0 to 3, and overall scores ranged from 0 to 21. Higher scores indicate poorer sleep quality in women during pregnancy. In this study PSQI score greater than 7 indicates poor quality of sleep and less than or equal to 7 is good quality of sleep [ 11 ].The Cronbach’s α was 0.721.
Self-rating anxiety scale
The Self-Rating Anxiety Scale (SAS) was used to assess anxiety symptoms in pregnant women [ 12 ]. The scale consists of 20 items, and the scores of each item are summed to obtain a crude score, which is multiplied and rounded to 1.25 to obtain a standardized total score (SAS). In this study, a SAS greater than or equal to 50 was defined as the presence of anxiety symptoms, with higher scores indicating a more pronounced anxiety condition [ 13 ]. The Cronbach’s α was 0.733.
Edinburgh postnatal depression scale
The Edinburgh Postpartum Depression Scale (EPDS) was applied to assess depression during pregnancy [ 14 ], the scale score is obtained by summing the 10 entries included, with a total score ranging from 0 to 30, and a total EPDS score of greater than or equal to 10 was used in the study as the threshold for screening for depressive symptoms [ 15 ]. The Cronbach’s α was 0.808.
Statistical analysis
Survey data were entered using the Epidata 3.1 database, and statistical analyses were performed using IBM SPSS Statistics 27.0 (IBM Corporation, Armonk, NY, USA) and AMOS 23.0 (IBM, New York, NY, USA). For measurement information, expressed as mean ± standard deviation, t-test was used for comparison between two groups and analysis of variance (ANOVA) was used between multiple groups if normal distribution and chi-square were met; rank-sum test was used when normal distribution was not met. For the count data, expressed as frequency and percentage, the \( \chi^{2} \) test was used for comparison between groups. to describe the current epidemiologic status of sleep quality among pregnant women in Urumqi and the prevalence trends on different demographic characteristics. Spearman correlation was applied to analyze the correlation between variables. The main influences on sleep quality of pregnant women and the path relationships between them were explored through structural equation modeling, and the following goodness-of-fit indices were used to evaluate the model: λ²/df < 5, CFI > 0.90,GFI > 0.90, AGFI > 0.90, IFI > 0.90, and RMSEA < 0.05.
Moral statement
Participation in the study was voluntary and anonymous, and participants were given the option to opt out at any time while undergoing the survey to ensure that personal privacy was respected and protected. Prior to the start of the survey, all subjects signed a written informed consent to participate in the program. The study involving human subjects in this protocol was reviewed and approved by the Nutrition and Health Ethics Committee of the Chinese Center for Disease Control and Prevention (No. 2021-008), in accordance with the Declaration of Helsinki.
Basic characteristic
Table 1 describes the basic characteristics of the included study population, which included 986 pregnant women, of whom 217, 471, and 298 were in the early, middle, and late stages of pregnancy, respectively. The age ranged from 20 to 47 years, with a mean age of 31.28 ± 4.25 years, 620 (62.9%) were Han, and 312 (31.6%) were predominantly educated to undergraduate level. There were 39.0% of pregnant women who had their first pregnancy and 232 (23.5%) who were on birth control. The PSQI score of pregnant women was 4.84 ± 3.12, 179 (18.2%) pregnant women had sleep disorders, 111 (11.3%) and 297 (30.1%) had symptoms of anxiety and depression, 48 (43.2%) pregnant women had both anxiety and sleep disorders, 104 (18.2%) pregnant women had both depression and sleep disorders, and there was a significant difference between both and the non-sleep disordered group. disorder group were significantly different.
Table 2 shows the overall score, component scores and depression and anxiety scores of sleep quality in women in early, mid and late pregnancy. As the course of pregnancy increased, both sleep quality scores and depression and anxiety scores showed an increasing trend, with significant differences in overall sleep quality scores across trimesters of 4.22 (3.13), 4.81 (2.97), and 5.34 (3.25), and depression scores of: 6.25 (4.90), 7.56 (4.56), and 7.56 (4.92). There were significant differences in all the indicators except Anxiety, Sleep latency, Use Hypnotic drug, Daytime dysfunction.
Correlation analysis
Table 3 shows Spearman’s correlation between socio-demographic factors, depression and anxiety and sleep quality among all participating pregnant women ( n = 986). Sleep quality was correlated with education level ( r = 0.129, p < 0.001), parity ( r = 0.080, p < 0.05), gravidity, primiparity, vaginal bleeding, tocolysis ( r = 0.099, p < 0.001), husband drinking alcohol, anxiety ( r = 0.232, p < 0.001), depressed ( r = 0.287, p < 0.001) were correlated. The higher the level of education, the greater the correlation between the emergence of sleep quality problems in pregnant women. Similarly, the more pronounced the expression of depression and anxiety, the increase in sleep disorders in women during pregnancy is associated. The strength of the correlation between these variables was between weak and moderate, and there was no correlation between the quality of sleep of pregnant women and their occupation and monthly income.
- Structural equation model
In order to reasonably and comprehensively study the changes in the level of sleep quality during pregnancy among pregnant women in Urumqi; and to explore the influencing factors of sleep quality among women during pregnancy, an initial structural equation model was established based on the results of previous studies in the relevant literature. Inclusion of study variables in exploratory factorial molecules. KMO test and Bartlet’s Sphericity test, the KMO value was 0.649 and the Bartlet ‘s sphericity test had a difference (P < 0.001) and the results showed that the data satisfied the factor analysis. The principal component analysis method was used to extract factors, in order to make the difference between the attributes of the factors is obvious, using the maximum variance rotation method to rotate the factors, the cumulative explanation of 61.62% of the variance, to get the rotated factor loadings as in Table 4, factor 1 is named obstetric characteristics (Primiparity, Parity, Gravidity), factor 2 is named basic characteristics (Monthly income, Occupation, Educatin level), factor 3 is named as tocolysis (Vaginal Bleeding, Tocolytic), factor 4 is named as psychological (Anxious, Depressed), factor 5 is named as Lifestyle (Smoke, Alcohol, Husband drinking alcohol). The initial structural equation modeling of the five variables of basic characteristics, obstetric characteristics, tocolysis, lifestyle, and psychological with sleep quality was established. As shown in Fig. 1 .
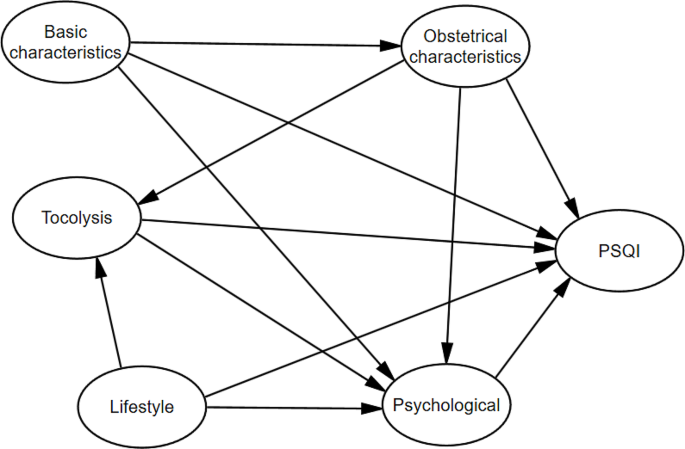
Theoretical model of sleep quality in women during pregnancy
The initial model is tested and corrected, and the maximum likelihood method is chosen for parameter estimation. Comprehensive consideration of the correction index, deletion of meaningless paths and other measures after repeated modifications, the SEM model with a better fit is shown in Fig. 2 . The results of the main fitting indexes show that: Chi/df = 3.038,GFI = 0.951,AGFI = 0.935,IFI = 0.926,TLI = 0.910,RMSEA = 0.046.The specific results are shown in Table 5 .
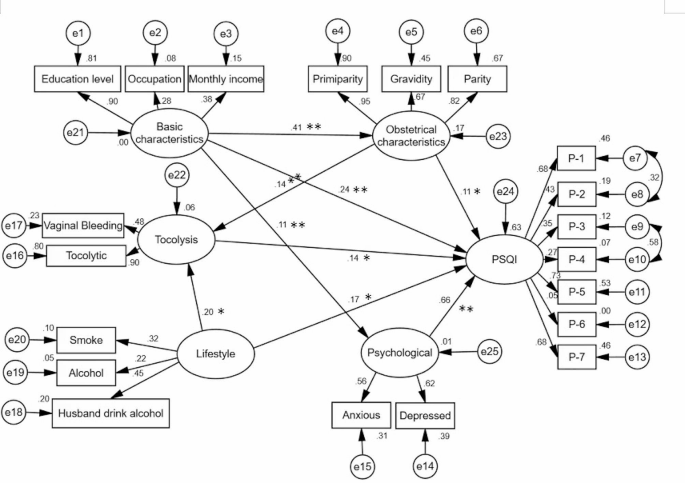
Structure equation model of sleep quality in pregnant women AMOS pathway diagram
Note: P-1: Subjective sleep quality, P-2: Sleep latency, P-3:Sleep duration,P-4:Sleep duration, P-5: Sleep disturbance, P-6: Use Hypnotic drug,P-7: Daytime dysfunction
Notes:** P < 0.001;* P < 0.05.
The summary table of path coefficients shows that there is a direct effect of obstetric characteristics → PSQI with a path coefficient of 0.106 and a t-value of 2.677 ( P < 0.001), a positive and direct effect of obstetric characteristics → tocolysis with a path coefficient of 0.142 and a t-value of 3.876 ( P < 0.001), and a direct and positive effect of tocolysis → PSQI with a path coefficient of 0.140 and a t-value of 2.578 ( P < 0.05). The standardized path coefficient of basic characteristics on PSQI through tocolysis was 0.020 (0.14*0.14), the indirect effect was 0.020, the direct effect was 0.106, and the total effect was 0.126. The direct and indirect effects accounted for 84.1% and 15.9% of the total effect, respectively. Thus, 15.9% of the effect of obstetrical characteristics on PSQI was through tocolysis. The direct effect of basic characteristics → PSQI was 0.243 with a t-value of 4.548 ( P < 0.001) and the indirect effect was 0.123; psychological → PSQI had a direct effect with a path coefficient of 0.658 and a t-value of 9.036. lifestyle → PSQI had a path coefficient of 0.174 and a t-value of 2.297 ( P < 0.05). The indirect effect of lifestyle on pregnant women’s sleep quality through birth control was 0.027,accounting for 13.43% of the total effect. See Table 6 .
Sleep disorders are common throughout pregnancy. Previous national and international studies have shown that pregnant women have varying degrees of sleep quality problems during all trimesters [ 16 ]. In this study, the mean PSQI score of all subjects was 4.84 ± 3.12, and 18.2% of pregnant women had sleep disorders. It was lower than the findings of Li [ 17 ]. who had a sleep disorder rate of 54.3%, and this difference may come from the difference in the threshold value of PSQI (PSQI > 5). Where the scores were 4.22 ± 3.13, 4.81 ± 2.97, and 5.34 ± 3.25 in early, middle, and late pregnancy, respectively, we found that PSQI scores increased with the progression of pregnancy, and that pregnant women’s sleep quality was most susceptible to disturbances in late pregnancy. Similar to the findings of Kızılırmak’s study [ 18 ]. This increasing trend may be related to poor sleep quality due to hormone levels, fetal movement, physical discomfort, and frequent nighttime bathroom visits during pregnancy [ 19 , 20 ].
In this study, we found that the quality of sleep in pregnant women was also associated with age, education, whether they were primiparous, pregnancy history, and birth control. The prevalence of sleep disorders in pregnant women of higher gestational age (age ≥ 35) was 24.1%, which was higher than that of lower age, which was 17.1%. That is, the higher the maternal age, the higher the prevalence of sleep disorders during pregnancy [ 16 , 21 ]. It may also be related to the fact that older women are themselves more susceptible to workplace pressures, caring for their families and children, and the concern about the higher risk of adverse pregnancy outcomes associated with advanced age, which makes their psychological burden heavier and affects their sleep [ 22 ]. We found that there is also a close relationship between the level of education of pregnant women and sleep status, undergraduate and postgraduate there is a sleep retardation rate of 49.9%, high educational level but affect the quality of sleep, to consider that it may be related to the probability of this group of people to engage in mental labor is relatively large, the pressure of the work is high, so they are more susceptible to the impactt. There is a discrepancy with the findings of Cai[5], who concluded that the higher the level of education, the more knowledge and access pregnant women acquire to regulate their sleep, leading to better sleep improvement.
The present study further explored the direct and indirect effects of sleep quality in pregnant women based on structural equation modeling with the aim of providing better interventions for better improvement of sleep quality during pregnancy. The results of the study showed that basic characteristics, obstetric characteristics,tocolysis, lifestyle, psychological had a direct effect on PSQI. tocolysis had a mediating effect between obstetric characteristics and PSQI, indicating that obstetric characteristics not only directly affect PSQI, but also indirectly affect sleep quality through tocolysis. The mediating effect was 15.9%. Parity and pregnancy history were risk factors for sleep quality. Compared to primiparous women, transient women reported poorer sleep quality, which may be related to the physical and psychological stress that exists during pregnancy itself, the fact that women also have to take care of their first child and the expectation of the gender of the second child in some families, which makes the pregnant women anxious, thus leading to poorer quality of sleep [ 23 , 24 , 25 ]. Van [ 26 ]compared the effect of comparing the presence or absence of a history of miscarriage on the quality of sleep in the later part of pregnancy in pregnant women who were pregnant during the late stage of pregnancy. showed that sleep duration (7.1 ± 1.1 h) and sleep efficiency (83.7 ± 7.9%) were similar in both groups, however, the PSQI score of the miscarriage group (7.8 ± 2.6) was significantly lower than that of the control group (6.7 ± 3.1), suggesting that having a history of miscarriage is an influencing factor in the low quality of sleep in women with a late pregnancy. At the same time, when pregnant women with vaginal bleeding and their own low back and abdominal pain receive tocolysis treatment, anxiety, anxiety and other adverse psychological emotions due to the fear of their own and fetal health, leading to poor treatment compliance and affecting the effect of sleep quality. Therefore, it is necessary to pay attention to the pregnancy history of pregnant women, and adopt the treatment of Tocolytic for pregnant women with threatened abortion, along with certain psychological guidance, to prevent the occurrence of adverse pregnancy outcomes [ 27 ].
Lifestyle has a direct effect on sleep quality (0.174), can also indirectly affect the quality of pregnant women’s sleep from tocolysis(0.027), the total effect is( 0.201). Alcohol not only harms the drinker, in the case of alcohol consumption, alcohol fluctuates moods domestic violence will rise, resulting in harm to family members and the atmosphere, foreign scholars have shown that if the husband is drinking, the woman is more likely to be subjected to domestic violence, more susceptible to physical and psychological stress, which further affects sleep [ 28 , 29 , 30 ].
In addition, pregnancy sleep quality during pregnancy is strongly associated with pregncancy’s psychological, and we found that psychological had a direct and significant effect on the quality of sleep of pregnant women with a path coefficient of 0.658. Based on previous studies, it was found that pregnant women experience high mood swings throughout pregnancy, which are accompanied by varying degrees of anxiety and stress as well as depression, and the higher the level of depression in pregnant women, the worse the quality of sleep [ 31 , 32 ]. Polo-Kantola [ 33 ] confirmed a correlation between sleep quality and depression and anxiety during pregnancy. LI found a direct effect of anxiety on depression, suggesting that pregnant women with symptoms of anxiety during pregnancy have a higher risk of developing depressive symptoms [ 34 ], and therefore anxiety is one of the strongest factors that have been strongly associated with prenatal depression one of the strongest associations with prenatal depression [ 35 ]. Another study shows that depression and anxiety scores in pregnant women are important hubs for regulating the relationship between objective and subjective sleep [ 36 ]. Many pregnant women after pregnancy will have concerns about their competence as a mother, worry about their inability to complete the role transition, worry about their delivery and infant feeding methods and the hopes of relatives for pregnant women can produce pregnancy-related anxiety and anxiety, which [ 37 ], if appropriate interventions are not taken, will potentially lead to adverse consequences of postpartum depression.
The results of this study indicate that sleep quality problems are prevalent among pregnant women in Urumqi and increase with the trimester of pregnancy. Considering the path relationships between the variables, basic characteristics, obstetric characteristics, tocolysis, lifestyle、psychological were found to be influential factors for sleep quality, especially the impact of psychology on the sleep quality of pregnant women is particularly significant. Therefore, healthcare organizations should pay attention to screening pregnant women for sleep disorders and psychological disorders, and develop reasonable and effective interventions to reduce the incidence of adverse pregnancy outcomes caused by sleep disorders.
Limitations
Our research also has certain limitations. Firstly, due to cross-sectional design, it is limited to comprehensively explore the influencing factors of sleep quality in pregnant women; Secondly, our research did not consider social support factors, which may have a certain impact on our results; Finally, the scale for evaluating sleep quality, depression and anxiety in this study was objectively filled out by pregnant women, and there may be some recall bias.
Data availability
The authors will supply the relevant data in response to reasonable requests.
Lu Q, Zhang X, Wang Y, et al. Sleep disturbances during pregnancy and adverse maternal and fetal outcomes: a systematic review and meta-analysis. Sleep Med Rev. 2021;58:101436.
Article PubMed Google Scholar
Wang Y, Liu H, Zhang C, et al. Antepartum sleep quality, mental status, and postpartum depressive symptoms: a mediation analysis. BMC Psychiatry. 2022;22(1):521.
Article PubMed PubMed Central Google Scholar
Tomfohr LM, Buliga E, Letourneau NL, et al. Trajectories of Sleep Quality and associations with Mood during the Perinatal Period. Sleep. 2015;38(8):1237–45.
Buysse DJ, Reynolds CF 3rd, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213.
Cai S, Tan S, Gluckman PD et al. Sleep Quality and Nocturnal Sleep Duration in Pregnancy and Risk of Gestational Diabetes Mellitus. Sleep. 2017; 40(2)
Pauley AM, Moore GA, Mama SK, et al. Associations between prenatal sleep and psychological health: a systematic review. J Clin Sleep Medicine: JCSM: Official Publication Am Acad Sleep Med. 2020;16(4):619–30.
Google Scholar
Reutrakul S, Anothaisintawee T, Herring SJ, et al. Short sleep duration and hyperglycemia in pregnancy: aggregate and individual patient data meta-analysis. Sleep Med Rev. 2018;40:31–42.
Warland J, Dorrian J, Morrison JL, et al. Maternal sleep during pregnancy and poor fetal outcomes: a scoping review of the literature with meta-analysis. Sleep Med Rev. 2018;41:197–219.
Xu T, Feng Y, Peng H, et al. Obstructive sleep apnea and the risk of perinatal outcomes: a meta-analysis of cohort studies. Sci Rep. 2014;4:6982.
Okun ML, Mancuso RA, Hobel CJ, et al. Poor sleep quality increases symptoms of depression and anxiety in postpartum women. J Behav Med. 2018;41(5):703–10.
Mao XF, Shao L, Zhao X, et al. Sleep quality and influencing factors of perimenopausal women in Ningbo region. J Zhejiang Univ Med Sci. 2011;40(1):85–9.
Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–9.
Roberson EK, Hurwitz EL, Li D, et al. Depression, anxiety, and Pharmacotherapy around the time of pregnancy in Hawaii. Int J Behav Med. 2016;23(4):515–26.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry: J Mental Sci. 1987;150:782–6.
Article Google Scholar
Lee DT, Yip SK, Chiu HF, et al. Detecting postnatal depression in Chinese women. Validation of the Chinese version of the Edinburgh postnatal depression scale. Br J Psychiatry: J Mental Sci. 1998;172:433–7.
Sedov ID, Cameron EE, Madigan S, et al. Sleep quality during pregnancy: a meta-analysis. Sleep Med Rev. 2018;38:168–76.
Li P, Wang H, Chen G, et al. Association between Nausea and vomiting during pregnancy and Sleep Quality: Mediating Effect of depressive symptoms. Int J Gen Med. 2021;14:41–9.
Kızılırmak A, Timur S, Kartal B. Insomnia in pregnancy and factors related to insomnia. TheScientificWorldJournal. 2012; 2012:197093.
Hutchison BL, Stone PR, McCowan LM, et al. A postal survey of maternal sleep in late pregnancy. BMC Pregnancy Childbirth. 2012;12:144.
Tan L, Zou J, Zhang Y, et al. A longitudinal study of physical activity to improve Sleep Quality during pregnancy. Nat Sci Sleep. 2020;12:431–42.
Jemere T, Getahun B, Tadele F, et al. Poor sleep quality and its associated factors among pregnant women in Northern Ethiopia, 2020: a cross sectional study. PLoS ONE. 2021;16(5):e0250985.
Signal TL, Paine SJ, Sweeney B, et al. Prevalence of abnormal sleep duration and excessive daytime sleepiness in pregnancy and the role of socio-demographic factors: comparing pregnant women with women in the general population. Sleep Med. 2014;15(12):1477–83.
Cai Y, Shen Z, Zhou B, et al. Psychological Status during the second pregnancy and its influencing factors. Patient Prefer Adherence. 2022;16:2355–63.
Christian LM, Carroll JE, Porter K, et al. Sleep quality across pregnancy and postpartum: effects of parity and race. Sleep Health. 2019;5(4):327–34.
Du M, Liu J, Han N, et al. Maternal sleep quality during early pregnancy, risk factors and its impact on pregnancy outcomes: a prospective cohort study. Sleep Med. 2021;79:11–8.
Van P, Gay CL, Lee KA. Prior pregnancy loss and sleep experience during subsequent pregnancy. Sleep Health. 2023;9(1):33–9.
Ota H, Hasegawa J, Sekizawa A. Effect of sleep disorders on threatened premature delivery. J Perinat Med. 2017;45(1):57–61.
Bhatta N, Assanangkornchai S, Rajbhandari I. Does husband’s alcohol consumption increase the risk of domestic violence during the pregnancy and postpartum periods in Nepalese women? BMC Public Health. 2021;21(1):5.
Gebrezgi BH, Badi MB, Cherkose EA, et al. Factors associated with intimate partner physical violence among women attending antenatal care in Shire Endaselassie town, Tigray, northern Ethiopia: a cross-sectional study, July 2015. Reproductive Health. 2017;14(1):76.
Viellas EF, Gama SG, Carvalho ML, et al. Factors associated with physical aggression in pregnant women and adverse outcomes for the newborn. Jornal De Pediatria. 2013;89(1):83–90.
Yang Y, Mao J, Ye Z, et al. Determinants of sleep quality among pregnant women in China: a cross-sectional survey. J maternal-fetal Neonatal Medicine: Official J Eur Association Perinat Med Federation Asia Ocean Perinat Soc Int Soc Perinat Obstet. 2018;31(22):2980–5.
Yu Y, Li M, Pu L, et al. Sleep was associated with depression and anxiety status during pregnancy: a prospective longitudinal study. Arch Women Ment Health. 2017;20(5):695–701.
Polo-Kantola P, Aukia L, Karlsson H, et al. Sleep quality during pregnancy: associations with depressive and anxiety symptoms. Acta Obstet Gynecol Scand. 2017;96(2):198–206.
Li Y, Zeng Y, Zhu W, et al. Path model of antenatal stress and depressive symptoms among Chinese primipara in late pregnancy. BMC Pregnancy Childbirth. 2016;16(1):180.
Lancaster CA, Gold KJ, Flynn HA, et al. Risk factors for depressive symptoms during pregnancy: a systematic review. Am J Obstet Gynecol. 2010;202(1):5–14.
Volkovich E, Tikotzky L, Manber RJA. Objective and subjective sleep during pregnancy: links with depressive and anxiety symptoms. 2016; 19:173–81.
Bao C, Jin D, Sun S, et al. Trajectories and depressive symptoms during the Perinatal period: a Longitudinal Population-based study in China. Front Psychiatry. 2022;13:762719.
Download references
Acknowledgements
We sincerely thank all the pregnant women and staff who participated in this study.
This work has been funded by the National Natural Science Foundation of China funded projects (72163033).
Author information
Mailiman Bahani, Yuxia Zhang and Yufeng Guo contributed equally to this work.
Authors and Affiliations
College of Public Health, Xinjiang Medical University, Urumqi, China
Mailiman Bahani, Yufeng Guo, Salawati Haretebieke & Di Wu
Department of Clinical Nutrition, Urumqi Maternal and Child Health Institute, Urumqi, China
Yuxia Zhang
College of Medical Engineering and Technology, Xinjiang Medical University, Urumqi, China
Liping Zhang
You can also search for this author in PubMed Google Scholar
Contributions
MB: conceptualization, writing– original draft, writing– review & editing. YZ and YG: Collect the data. MB, SH and DW: statistical analysis, editing the manuscript. LZ: editing and review the manuscript.
Corresponding author
Correspondence to Liping Zhang .
Ethics declarations
Ethics approval and consent to participate.
The Ethics Committee of the Nutrition and Health Ethics Committee of the Chinese Center for Disease Control and Prevention (CDC) reviewed and approved the protocol, No. 2021-008.Informed consent signed by all participants prior to the survey.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bahani, M., Zhang, Y., Guo, Y. et al. Influencing factors of sleep quality in pregnant: a structural equation model approach. BMC Psychol 12 , 171 (2024). https://doi.org/10.1186/s40359-024-01657-1
Download citation
Received : 23 November 2023
Accepted : 11 March 2024
Published : 25 March 2024
DOI : https://doi.org/10.1186/s40359-024-01657-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sleep quality
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
We included papers that focused on human and/or rodent research.- ... In the past 20 years, a large number of studies on the risk and protective factors of depression have been undertaken in various fields, such as genetics, neurology, immunology, and epidemiology. However, there are limitations associated with the extant evidence base. The ...
Depression manifests differently in various age groups and mediums of expression. This essay embarks on a journey to compare and contrast the symptoms and risk factors of depression in adolescents and adults, shedding light on the unique challenges faced by each demographic. Example Conclusion Paragraph for a Compare and Contrast Essay:
Second, the continuation of the search for aetiological and pathophysiological factors implicated in the development of depression, especially outside the immediate boundaries of the brain. And third, a stronger focus on translational efforts that use established basic neuroscientific insights to improve clinical practice and research.
Common Causes of Depression. Researchers suspect there are actually many different causes of depression and that it is not always preventable. Factors that can contribute to depression include: Genetics. Brain chemistry. Certain medical conditions. Substance use. Stress. Poor nutrition.
Several factors can make depression more likely. These may include: family history and genetics. chronic stress. history of trauma. gender. poor nutrition. unresolved grief or loss. personality ...
The baseline risk of depression in the population is 10 percent; having a first-degree relative (parent or sibling) with depression doubles or triples an individual's risk, to 20 to 30 percent ...
Depression is more than just sadness; it is the most common mental disorder. People with depression may also experience physical, cognitive, and social changes, including altered eating or sleeping habits, lack of energy or motivation, difficulty concentrating or making decisions, and withdrawal from social activities.
2. Environmental Triggers. Trauma and Adverse Life Events: Traumatic experiences, such as abuse, neglect, or significant life stressors like loss, divorce, or financial difficulties, can trigger depression. The impact of trauma may be cumulative, influencing mental health over time.
Studies show that one factor consistently associated with depression is the number and degree of major stresses experienced in life. Poverty, for example, is a significant, enduring stressor, not ...
a persistent feeling of loneliness or sadness. lack of energy. feelings of hopelessness. getting too much or too little sleep. eating too much or too little. difficulties with concentration or ...
Factors that seem to increase the risk of developing or triggering depression include: Certain personality traits, such as low self-esteem and being too dependent, self-critical or pessimistic Traumatic or stressful events, such as physical or sexual abuse, the death or loss of a loved one, a difficult relationship, or financial problems
Depression can cause a range of psychological and physical symptoms, including: persistent depressed mood. loss of interest or pleasure in hobbies and activities. changes in appetite and body ...
Writing about depression in your college essay can be a powerful and meaningful way to share your personal experiences and reflect on your growth. However, it's essential to approach the topic thoughtfully and carefully, as mental health is a sensitive subject. 1. Focus on growth and resilience: Instead of primarily describing your struggles with depression, emphasize how you've navigated ...
The essay provides a comprehensive overview of depression and its main causes. The organization of the essay is clear and logical, with a well-defined introduction, body, and conclusion. The author successfully focuses on the key factors that contribute to depression, including biological, psychological, and environmental factors.
250 Words Essay on Depression Understanding Depression. Depression, a common yet serious mental health disorder, is characterized by persistent feelings of sadness, hopelessness, and a lack of interest or pleasure in activities. It affects individuals differently, leading to a variety of physical and emotional problems. Causes and Risk Factors
A model of depression as a disease is incomplete and misleading. It leads to suboptimal treatment choices. The "separation distress hypothesis" is an alternative model. It is an integrated, causal ...
This depression essay is devoted to mental disorder called depression, its symptoms, signs of development, causes and effects of the disease. Toggle navigation. Home ... Risk factors for depression: being female; the presence of depression in family anamnesis; early depression in anamnesis; early loss of parents;
Depression rates in young people have risen sharply in the past decade, especially in females, which is of concern because adolescence is a period of rapid social, emotional, and cognitive development and key life transitions. Adverse outcomes associated with depression in young people include depression recurrence; the onset of other psychiatric disorders; and wider, protracted impairments in ...
Topic: Depression, Mental Illness, Suicide. Pages: 1 (658 words) Views: 669. Grade: 4.8. Download. You've lost connections with friends and family, you can't bring yourself to go outside, it feels like the world is against you. This is the life of having depression, a horrible cycle of low moods, sadness and an overall feeling of dejectedness.
Pregnancy is one of the most remarkable experiences in a woman's life. Prenatal depression, characterized by stress and worry associated with pregnancy, can reach severe levels. On a global scale, mental and addictive disorders affect more than one billion people, causing 19% of years lived with disability. It is estimated that 25-35% of pregnant women experience depressive symptoms, with ...
Table 2 shows the overall score, component scores and depression and anxiety scores of sleep quality in women in early, mid and late pregnancy. As the course of pregnancy increased, both sleep quality scores and depression and anxiety scores showed an increasing trend, with significant differences in overall sleep quality scores across trimesters of 4.22 (3.13), 4.81 (2.97), and 5.34 (3.25 ...