- Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- HIV and AIDS
- Hypertension
- Mental disorders
- Top 10 causes of death
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases

Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- Data collection tools
- Global Health Observatory
- Insights and visualizations
- COVID excess deaths
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment case
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Health topics /
Brain health
Brain health is the state of brain functioning across cognitive, sensory, social-emotional, behavioural and motor domains, allowing a person to realize their full potential over the life course, irrespective of the presence or absence of disorders.
Different determinants related to physical health, healthy environments, safety and security, life-long learning and social connection as well as access to quality services influence the way our brains develop, adapt and respond to stress and adversity. These give way to strategies for promotion and prevention across the life course. Optimizing brain health by addressing these determinants not only improves mental and physical health but also creates positive social and economic impacts that contribute to greater well-being and help advance society.
However, conditions affecting the brain and nervous system in general emerge throughout the life course and are characterized by disruptions in brain growth, damage to brain structure and/or impaired brain functioning. These include for example congenital and neurodevelopmental conditions as well as neurological disorders across the life. Health and social care for these conditions require multisectoral and interdisciplinary collaborations with a holistic person-centred approach focused on promotion, prevention, treatment, care and rehabilitation and the active engagement of persons with lived experience, their families and carers.
The global burden of neurological and neurodevelopmental conditions is high, with approximately 70% of the burden in low- and middle-income countries. Neurological conditions are the leading cause of disability adjusted life years (DALYs) and account for about 9 million deaths per year.
The largest contributors of neurological DALYs in 2016 were stroke (42.2%), migraine (16.3%), dementia (10.4%), meningitis (7.9%) and epilepsy (5%). Parkinson disease, propelled by an increasingly ageing population, is the fastest growing neurological disorder. Premature birth, neonatal encephalopathy and neuroinfections contribute substantially to high disease burden in South-East Asia and Africa. In 2016, developmental disabilities accounted for 13.3% of the 29.3 million years lived with disability for all health conditions among children younger than 5 years.
Despite the large burden, only 28% of low-income countries have a dedicated policy for neurological diseases in comparison with 64% of high-income countries. Available resources for these conditions are insufficient in most countries, with unacceptably high treatment gaps for many neurological and neurodevelopmental conditions. For example, in low- and middle-income countries, there are only three adult neurologists per 10 million people while high-income countries have approximately 160 times more. Resources for the assessment and care of children with neurological and neurodevelopmental conditions are even more scarce.
In May 2022, WHO Member States adopted the Intersectoral global action plan on epilepsy and other neurological disorders 2022–2031 . This action plan aims to improve care, recovery, well-being and participation of people living with neurological disorders across the life-course, while reducing associated mortality, morbidity and disability associated with neurological conditions.
In the context of Universal Health Coverage and the UN Sustainable Development Goals and in line with WHO’s existing mandates for conditions affecting the brain such as autism spectrum disorder , epilepsy and dementia , WHO’s brain health work is focused on promoting optimal brain development, cognitive health and well-being across the life course. The main activities involve:
- strengthening policies, service delivery, health information systems, technology (including but not limited to artificial intelligence, e-health and big data), research and innovation, especially in low- and middle-income countries;
- providing technical assistance on how to formulate an integrated approach to brain health conditions focused on promotion, prevention, treatment, care and rehabilitation, focusing on low- and middle-income countries; and
- fostering increased investment and inter-agency collaboration globally as well as the involvement of different specialties and sectors.
- Cardiovascular diseases (CVDs)
- Guillain–Barré syndrome
- Migraine and other headache disorders
- Japanese encephalitis
- Parkinson disease
- Spinal cord injury
- ATLAS Country Resources for Neurological Disorders
- Global Dementia Observatory
- WHA75.11: decision to adopt the Intersectoral global action plan on epilepsy and other neurological disorders 2022–2031
- WHA67.8: Comprehensive and coordinated efforts for the management of autism spectrum disorders
- WHA68.20: Global burden of epilepsy and the need for coordinated action at the country level to address its health, social and public knowledge implications
- WHA66.8: Comprehensive mental health action plan 2013–2020
- WHA70/28: Draft global action plan on the public health response to dementia: report by the Director-General
- WHA66/8: Draft comprehensive global monitoring framework and targets for the prevention and control of noncommunicable diseases: report by the Director-General
- Department of Mental Health and Substance Use
- Maternal, newborn, child and adolescent health
Over 1 in 3 people affected by neurological conditions, the leading cause of illness and disability worldwide
WHO issues new and updated recommendations on treatment of mental, neurological and substance use conditions
New report highlights neglected health needs of children with developmental disabilities
New global action plan on epilepsy and other neurological disorders published
Latest publications

Clinical descriptions and diagnostic requirements for ICD-11 mental, behavioural and neurodevelopmental...
The Clinical descriptions and diagnostic requirements for ICD-11 mental, behavioural and neurodevelopmental disorders (CDDR) is a comprehensive diagnostic...

Measures of early-life brain health at population level
Brain health is increasingly attracting attention thanks to scientific and technological advances. Investing in brain health across the life course through...

Mental Health Gap Action Programme (mhGAP) guideline for mental, neurological and substance use disorders
The mhGAP guideline supports countries to strengthen capacity to deal with the growing burden of mental, neurological and substance use (MNS) conditions...

Why encephalitis matters? Report of the virtual meeting, 28-29 June 2022
Encephalitis is an inflammation of the brain caused by an infection or by host immune responses. Many different causative organisms have been recognized,...
Scaling up epilepsy care in Myanmar
The Fight against epilepsy in Ghana
Pilot studies help close the epilepsy treatment gap
Zika response accelerates as WHO Director-General visits Brazil

mhGAP: training videos

mhGAP: mental health care in low resource settings - video showing that millions can be treated at low cost

WHO: Introduction to mental health
Episode #103 - Brain health
How can you keep your brain healthy and who is at risk of poor brain health? Dr Tarun Dua explains all you need to know about brain health in Science in 5.
Related health topics
Mental health

How COVID-19 Affects the Brain
Share this article
An online risk calculator could help doctors predict, and hopefully prevent, brain-related complications in COVID-19 patients.
What you need to know
An NIH-funded study is developing an online risk calculator to help doctors predict which COVID-19 patients will develop brain-related complications. The study will also look at how COVID-19 causes these complications.
What is this research about?
Scientists and doctors do not fully understand how COVID-19 causes problems with the brain or why these problems occur in some patients and not others. In this new study, researchers from the Cleveland Clinic will use tools that they developed from earlier NIH-supported projects to study how COVID-19 affects the brain. They will focus on fatigue, headaches, loss of smell or taste, and memory loss, or “brain fog.” They will also look at more serious but less common complications, such as epilepsy and stroke.
What are the researchers doing?
The researchers are analyzing data from the hospital records of thousands of patients who tested positive for COVID-19 and were enrolled in the Cleveland Clinic COVID-19 Registry and Biobank. These records have information on a patient’s age, race and ethnicity, and social determinants of health, which are the conditions in a person’s environment that can affect health and wellbeing. The hospital records also include a patient’s COVID-19 symptoms and how seriously ill the patient was, and whether the patient smokes or has serious health conditions such as cancer, diabetes, heart disease, and high blood pressure.
The researchers will first find out how many of these patients developed problems with the brain while they had COVID-19 or after they recovered. They will then use computer programs to compare patient information and find out whether problems with the brain are more common in any specific group of patients . They will also find out whether any combination of factors increased the risk of problems with the brain. The researchers will use this information to develop a new computer program that predicts whether new patients are more likely to have problems with the brain based on their own demographic and health information.
The researchers plan to expand the study to include health information from large datasets at the Mayo Clinic and the University of Campinas in Brazil. This will help ensure that the risk calculator is accurate for diverse groups and can be used globally.
Why is this research important?
An effective online risk calculator and information on how COVID-19 affects the brain could help doctors predict and possibly prevent neurological complications in people who have COVID-19. The researchers plan to develop risk calculators for other short- and long-term complications of COVID-19 to help improve medical care for this disease.
Where can I go to learn more?
Neurological Complications of COVID-19 Are Focus of New NIH Grant Supplement to Cleveland Clinic Researchers .
- Learn more about this project from Cleveland Clinic.
Taking a Closer Look at COVID-19’s Effects on the Brain .
- In this blog post, NIH Director Francis Collins, M.D., Ph.D., discusses research by NIH scientists to better understand how COVID-19 affects brain function.
Neurological Complications of COVID-19 and NINDS Clinical Research .
- In this video, Avindra Nath, M.D., of the National Institute of Neurological Disorders and Stroke (NINDS) discusses how COVID-19 affects the brain.
NIH Launches Database to Track Neurological Symptoms Associated with COVID-19 .
- Read about NIH’s database for tracking how COVID-19 affects the brain, spinal cord, and nerves.
NIH Study Uncovers Blood Vessel Damage and Inflammation in COVID-19 Patients’ Brains but No Infection .
- Read about research by NIH scientists designed to better understand how COVID-19 affects the brain.
CombatCOVID.HHS.Gov .
- Find out more about COVID-19 and opportunities to participate in clinical trials.
Jehi, L. (2020). A nomogram to predict seizure outcomes after resective epilepsy surgery. NIH RePORTER. Retrieved February 8, 2021, from https://reporter.nih.gov/project-details/10181321#description
Cleveland Clinic. (2020). Neurological complications of COVID-19 are focus of new NIH grant supplement to Cleveland Clinic researchers . Retrieved February 8, 2021, from https://consultqd.clevelandclinic.org/neurological-complications-of-covid-19-are-focus-of-new-nih-grant-supplement-to-cleveland-clinic-researchers/

News and Stories
Read stories about the efforts underway to prevent, detect, and treat COVID-19 and its effects on our health.
NIH COVID-19 Resources by Topic
COVID-19 research information and resources by topic from NIH institutes and centers
- High Contrast
- Increase Font
- Decrease Font
- Default Font
- Turn Off Animations

Home » Press Releases & Statements » Survey Finds Americans Curious and Optimistic About Brain Health Research
Survey Finds Americans Curious and Optimistic About Brain Health Research

Also Finds Concerns, a Knowledge Gap, and Desire for Patients to Have More Input in Setting Research Priorities
January 2023 Update — read our Executive Overview of the Brain Health Survey .
Brain health issues directly impact more than 8 in 10 Americans, according to a new survey released today; 82% of respondents said they know someone or have themselves experienced at least one brain disorder or mental health condition. Commissioned by Research!America in partnership with the Dana Foundation, the August 2022 national survey captures Americans views on brain health and brain health research. ( View slide deck of survey results. )
Despite the widespread personal impact of brain health issues, 66% of respondents reported having little or no knowledge about brain health research. Of interest is that the same percentage of respondents, 66%, indicated strong curiosity to learn more. Respondents also displayed striking optimism about the promise of brain health research:
- 91% of respondents, across all demographics (including political affiliation), agree brain data is a valuable tool to understand and improve their health.
- 89% agree brain health research might develop a way to correct brain damage.
- 89% agree brain health research might deliver better treatments for brain diseases and mental illnesses.
While Americans feel positive about the possible outcomes of brain health research, concerns include: possible misuse of data (64%), unwanted brain manipulation (61%), risk of injury (58%), and potential social stigma for participants (56%). Nearly two-thirds (62%) of Americans want patients to have more of a voice in setting research priorities.
These concerns don’t appear to significantly dampen enthusiasm:
- 2 in 3 respondents say that despite potential risks, brain health research will have an overall benefit to society (68%). African Americans are more likely to say that there are too many risks involved (28% as compared with 16% of total respondents).
- Americans across party lines are strongly in favor of increased federal funding for brain health research (78%) and favor having the federal government incentivize private sector investment to find treatments and cures for diseases (80%).
“This survey reinforces longstanding, American support for advancing research for health and reveals the desire of the public to better understand and engage with brain health research,” said Research!America President and CEO Mary Woolley. “By studying public opinion on brain health research, the Dana Foundation can assist the research community in its efforts to be more aware of concerns and meet Americans’ interests for greater understanding and engagement.”
Additional highlights from the Dana Foundation/Research!America survey include:
- 56% say advances in brain health should inform policy decisions and legislation.
- 84% say brain data should have the same privacy protections as other health information.
- 59% of respondents chose the word “hopeful” to reflect their attitude toward brain health research; 39% chose the word “cautious”.
- Respondents are split on whether adequate safeguards are in place to ensure brain health research is ethically conducted: 45% said there are adequate safeguards, 29% said there are not, and 26% were unsure.
- In comparison to another survey conducted in 2019, nearly double the respondents report having participated in any kind of research (reported participation in clinical trials increased from 7% to 13%).
- Respondents ranked the opportunity to improve individual health (68%) and the possibility of curing serious diseases (58%) as the top motivators for participating in brain health research.
“The Dana Foundation partnered with Research!America to gain a deeper sense of public understanding and perceptions of neuroscience. The survey results support the need for increased education on brain health, and for the inclusion of public voices — especially those of patients — in research,” said Dana Foundation President and CEO Caroline Montojo, PhD. “We also recognize that Americans are hopeful and optimistic about brain health research, but it is critical to address ethical and societal considerations that accompany these scientific advances to strengthen public trust and support for research.”
Survey Methodology: The nationwide online survey was conducted by Zogby Analytics on behalf of Research!America in August 2022 among 1,023 adults, plus 1,218 additional adults for minority population oversampling. The survey has a theoretical sampling error of +/- 3.1 percent. The theoretical sampling error was higher for subgroups.
For questions about the survey, or to set up an interview with Mary Woolley, contact Tim Haynes, Senior Director of Communications for Research!America, at 571-482-2737 or [email protected] with press inquiries; to set up an interview with Caroline Montojo, PhD, contact Ann Whitman, Director of Communications for the Dana Foundation, at [email protected] .
About the Dana Foundation
The Dana Foundation is a private philanthropic organization dedicated to advancing neuroscience and society by supporting cross-disciplinary intersections such as neuroscience and ethics, law, policy, humanities, and arts. The Foundation explores the connections between neuroscience and society’s challenges and opportunities, working to maximize the potential of the field to do good. Visit www.dana.org .
About Research!America
Research!America is a non-profit medical and health research advocacy alliance which advocates for science, discovery, and innovation to achieve better health for all. For 30 years, Research!America has been commissioning surveys to help understand public support for medical, health, and scientific research, among other state, national, and global issues related to public health and research and innovation. Visit www.researchamerica.org .
- Take Action
- Testimony & Letters
- Advocacy Tools
- Science & Technology Action Committee (STAC)
- Research Ecosystem
- Federal Research Agencies
- COVID-19 and Pandemic Preparedness
- Global Health
- Public Health
- Civic Science
- Other Topics
- Events Calendar
- Advocacy Awards
- Alliance Discussions
- Early Career Summit
- Discovery | Innovation | Health Prize
- National Health Research Forum
- Additional Programming
- Mary Woolley’s Weekly Letter
- Press Releases & Statements
- In the News
- Stay Informed
- Fact Sheets And Graphics
- Become a Member
- More Ways to Get Involved
- Member Organizations
- Mission, Vision, & Values
- History & Key Milestones
- Board Of Directors & Officers
- Leadership & Staff
- Annual Reports
- Financial & Governance

The Safety and Quality of Abortion Care in the United States (2018)
Chapter: 5 conclusions, 5 conclusions.
This report provides a comprehensive review of the state of the science on the safety and quality of abortion services in the United States. The committee was charged with answering eight specific research questions. This chapter presents the committee’s conclusions by responding individually to each question. The research findings that are the basis for these conclusions are presented in the previous chapters. The committee was also asked to offer recommendations regarding the eight questions. However, the committee decided that its conclusions regarding the safety and quality of U.S. abortion care responded comprehensively to the scope of this study. Therefore, the committee does not offer recommendations for specific actions to be taken by policy makers, health care providers, and others.
1. What types of legal abortion services are available in the United States? What is the evidence regarding which services are appropriate under different clinical circumstances (e.g., based on patient medical conditions such as previous cesarean section, obesity, gestational age)?
Four legal abortion methods—medication, 1 aspiration, dilation and evacuation (D&E), and induction—are used in the United States. Length of gestation—measured as the amount of time since the first day of the last
___________________
1 The terms “medication abortion” and “medical abortion” are used interchangeably in the literature. This report uses “medication abortion” to describe the U.S. Food and Drug Administration (FDA)-approved prescription drug regimen used up to 10 weeks’ gestation.
menstrual period—is the primary factor in deciding what abortion procedure is the most appropriate. Both medication and aspiration abortions are used up to 10 weeks’ gestation. Aspiration procedures may be used up to 14 to 16 weeks’ gestation.
Mifepristone, sold under the brand name Mifeprex, is the only medication specifically approved by the FDA for use in medication abortion. The drug’s distribution has been restricted under the requirements of the FDA Risk Evaluation and Mitigation Strategy program since 2011—it may be dispensed only to patients in clinics, hospitals, or medical offices under the supervision of a certified prescriber. To become a certified prescriber, eligible clinicians must register with the drug’s distributor, Danco Laboratories, and meet certain requirements. Retail pharmacies are prohibited from distributing the drug.
When abortion by aspiration is no longer feasible, D&E and induction methods are used. D&E is the superior method; in comparison, inductions are more painful for women, take significantly more time, and are more costly. However, D&Es are not always available to women. The procedure is illegal in Mississippi 2 and West Virginia 3 (both states allow exceptions in cases of life endangerment or severe physical health risk to the woman). Elsewhere, access to the procedure is limited because many obstetrician/gynecologists (OB/GYNs) and other physicians lack the requisite training to perform D&Es. Physicians’ access to D&E training is very limited or nonexistent in many areas of the country.
Few women are medically ineligible for abortion. There are, however, specific contraindications to using mifepristone for a medication abortion or induction. The drug should not be used for women with confirmed or suspected ectopic pregnancy or undiagnosed adnexal mass; an intrauterine device in place; chronic adrenal failure; concurrent long-term systemic corticosteroid therapy; hemorrhagic disorders or concurrent anticoagulant therapy; allergy to mifepristone, misoprostol, or other prostaglandins; or inherited porphyrias.
Obesity is not a risk factor for women who undergo medication or aspiration abortions (including with the use of moderate intravenous sedation). Research on the association between obesity and complications during a D&E abortion is less certain—particularly for women with Class III obesity (body mass index ≥40) after 14 weeks’ gestation.
A history of a prior cesarean delivery is not a risk factor for women undergoing medication or aspiration abortions, but it may be associated
2 Mississippi Unborn Child Protection from Dismemberment Abortion Act, Mississippi HB 519, Reg. Sess. 2015–2016 (2016).
3 Unborn Child Protection from Dismemberment Abortion Act, West Virginia SB 10, Reg. Sess. 2015–2016 (2016).
with an increased risk of complications during D&E abortions, particularly for women with multiple cesarean deliveries. Because induction abortions are so rare, it is difficult to determine definitively whether a prior cesarean delivery increases the risk of complications. The available research suggests no association.
2. What is the evidence on the physical and mental health risks of these different abortion interventions?
Abortion has been investigated for its potential long-term effects on future childbearing and pregnancy outcomes, risk of breast cancer, mental health disorders, and premature death. The committee found that much of the published literature on these topics does not meet scientific standards for rigorous, unbiased research. Reliable research uses documented records of a prior abortion, analyzes comparable study and control groups, and controls for confounding variables shown to affect the outcome of interest.
Physical health effects The committee identified high-quality research on numerous outcomes of interest and concludes that having an abortion does not increase a woman’s risk of secondary infertility, pregnancy-related hypertensive disorders, abnormal placentation (after a D&E abortion), preterm birth, or breast cancer. Although rare, the risk of very preterm birth (<28 weeks’ gestation) in a woman’s first birth was found to be associated with having two or more prior aspiration abortions compared with first births among women with no abortion history; the risk appears to be associated with the number of prior abortions. Preterm birth is associated with pregnancy spacing after an abortion: it is more likely if the interval between abortion and conception is less than 6 months (this is also true of pregnancy spacing in general). The committee did not find well-designed research on abortion’s association with future ectopic pregnancy, miscarriage or stillbirth, or long-term mortality. Findings on hemorrhage during a subsequent pregnancy are inconclusive.
Mental health effects The committee identified a wide array of research on whether abortion increases women’s risk of depression, anxiety, and/or posttraumatic stress disorder and concludes that having an abortion does not increase a woman’s risk of these mental health disorders.
3. What is the evidence on the safety and quality of medical and surgical abortion care?
Safety The clinical evidence clearly shows that legal abortions in the United States—whether by medication, aspiration, D&E, or induction—are
safe and effective. Serious complications are rare. But the risk of a serious complication increases with weeks’ gestation. As the number of weeks increases, the invasiveness of the required procedure and the need for deeper levels of sedation also increase.
Quality Health care quality is a multidimensional concept. Six attributes of health care quality—safety, effectiveness, patient-centeredness, timeliness, efficiency, and equity—were central to the committee’s review of the quality of abortion care. Table 5-1 details the committee’s conclusions regarding each of these quality attributes. Overall, the committee concludes that the quality of abortion care depends to a great extent on where women live. In many parts of the country, state regulations have created barriers to optimizing each dimension of quality care. The quality of care is optimal when the care is based on current evidence and when trained clinicians are available to provide abortion services.
4. What is the evidence on the minimum characteristics of clinical facilities necessary to effectively and safely provide the different types of abortion interventions?
Most abortions can be provided safely in office-based settings. No special equipment or emergency arrangements are required for medication abortions. For other abortion methods, the minimum facility characteristics depend on the level of sedation that is used. Aspiration abortions are performed safely in office and clinic settings. If moderate sedation is used, the facility should have emergency resuscitation equipment and an emergency transfer plan, as well as equipment to monitor oxygen saturation, heart rate, and blood pressure. For D&Es that involve deep sedation or general anesthesia, the facility should be similarly equipped and also have equipment to provide general anesthesia and monitor ventilation.
Women with severe systemic disease require special measures if they desire or need deep sedation or general anesthesia. These women require further clinical assessment and should have their abortion in an accredited ambulatory surgery center or hospital.
5. What is the evidence on what clinical skills are necessary for health care providers to safely perform the various components of abortion care, including pregnancy determination, counseling, gestational age assessment, medication dispensing, procedure performance, patient monitoring, and follow-up assessment and care?
Required skills All abortion procedures require competent providers skilled in patient preparation (education, counseling, and informed consent);
TABLE 5-1 Does Abortion Care in the United States Meet the Six Attributes of Quality Health Care?
| Quality Attribute | Definition | Committee’s Conclusions |
|---|---|---|
| Safety | Avoiding injuries to patients from the care that is intended to help them. | Legal abortions—whether by medication, aspiration, D&E, or induction—are safe. Serious complications are rare and occur far less frequently than during childbirth. Safety is enhanced when the abortion is performed as early in pregnancy as possible. |
| Effectiveness | Providing services based on scientific knowledge to all who could benefit and refraining from providing services to those not likely to benefit (avoiding underuse and overuse, respectively). | Legal abortions—whether by medication, aspiration, D&E, or induction—are effective. The likelihood that women will receive the type of abortion services that best meets their needs varies considerably depending on where they live. In many parts of the country, abortion-specific regulations on the site and nature of care, provider type, provider training, and public funding diminish this dimension of quality care. The regulations may limit the number of available providers, misinform women of the risks of the procedures they are considering, overrule women’s and clinician’s medical decision making, or require medically unnecessary services and delays in care. These include policies that |
| Quality Attribute | Definition | Committee’s Conclusions |
|---|---|---|
| Patient-Centeredness | Providing care that is respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions. | Patients’ personal circumstances and individual preferences (including preferred abortion method), needs, and values may be disregarded depending on where they live (as noted above). The high state-to-state variability regarding the specifics of abortion care may be difficult for patients to understand and navigate. Patients’ ability to be adequately informed in order to make sound medical decisions is impeded when state regulations require that |
| Timeliness | Reducing waits and sometimes harmful delays for both those who receive and those who give care. | The timeliness of an abortion depends on a variety of local factors, such as the availability of care, affordability, distance from the provider, and state requirements for an in-person counseling appointment and waiting periods (18 to 72 hours) between counseling and the abortion. |
| Efficiency | Avoiding waste, including waste of equipment, supplies, ideas, and energy. | An extensive body of clinical research has led to important refinements and improvements in the procedures, techniques, and methods for performing abortions. The extent to which abortion care is delivered efficiently depends, in part, on the alignment of state regulations with current evidence on best practices. Regulations that require medically unnecessary equipment, services, and/or additional patient visits increase cost, and thus decrease efficiency. |
| Quality Attribute | Definition | Committee’s Conclusions |
|---|---|---|
| Equity | Providing care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status. | State-level abortion regulations are likely to affect women differently based on their geographic location and socioeconomic status. Barriers (lack of insurance coverage, waiting periods, limits on qualified providers, and requirements for multiple appointments) are more burdensome for women who reside far from providers and/or have limited resources. |
a These attributes of quality health care were first proposed by the Institute of Medicine’s Committee on Quality of Health Care in America in the 2001 report Crossing the Quality Chasm: A New Health System for the 21st Century.
b Elsewhere in this report, effectiveness refers to the successful completion of the abortion without the need for a follow-up aspiration.
clinical assessment (confirming intrauterine pregnancy, determining gestation, taking a relevant medical history, and physical examination); pain management; identification and management of expected side effects and serious complications; and contraceptive counseling and provision. To provide medication abortions, the clinician should be skilled in all these areas. To provide aspiration abortions, the clinician should also be skilled in the technical aspects of an aspiration procedure. To provide D&E abortions, the clinician needs the relevant surgical expertise and sufficient caseload to maintain the requisite surgical skills. To provide induction abortions, the clinician requires the skills needed for managing labor and delivery.
Clinicians that have the necessary competencies Both trained physicians (OB/GYNs, family medicine physicians, and other physicians) and advanced practice clinicians (APCs) (physician assistants, certified nurse-midwives, and nurse practitioners) can provide medication and aspiration abortions safely and effectively. OB/GYNs, family medicine physicians, and other physicians with appropriate training and experience can perform D&E abortions. Induction abortions can be provided by clinicians (OB/GYNs,
family medicine physicians, and certified nurse-midwives) with training in managing labor and delivery.
The extensive body of research documenting the safety of abortion care in the United States reflects the outcomes of abortions provided by thousands of individual clinicians. The use of sedation and anesthesia may require special expertise. If moderate sedation is used, it is essential to have a nurse or other qualified clinical staff—in addition to the person performing the abortion—available to monitor the patient, as is the case for any other medical procedure. Deep sedation and general anesthesia require the expertise of an anesthesiologist or certified registered nurse anesthetist to ensure patient safety.
6. What safeguards are necessary to manage medical emergencies arising from abortion interventions?
The key safeguards—for abortions and all outpatient procedures—are whether the facility has the appropriate equipment, personnel, and emergency transfer plan to address any complications that might occur. No special equipment or emergency arrangements are required for medication abortions; however, clinics should provide a 24-hour clinician-staffed telephone line and have a plan to provide emergency care to patients after hours. If moderate sedation is used during an aspiration abortion, the facility should have emergency resuscitation equipment and an emergency transfer plan, as well as equipment to monitor oxygen saturation, heart rate, and blood pressure. D&Es that involve deep sedation or general anesthesia should be provided in similarly equipped facilities that also have equipment to monitor ventilation.
The committee found no evidence indicating that clinicians that perform abortions require hospital privileges to ensure a safe outcome for the patient. Providers should, however, be able to provide or arrange for patient access or transfer to medical facilities equipped to provide blood transfusions, surgical intervention, and resuscitation, if necessary.
7. What is the evidence on the safe provision of pain management for abortion care?
Nonsteroidal anti-inflammatory drugs (NSAIDs) are recommended to reduce the discomfort of pain and cramping during a medication abortion. Some women still report high levels of pain, and researchers are exploring new ways to provide prophylactic pain management for medication abortion. The pharmaceutical options for pain management during aspiration, D&E, and induction abortions range from local anesthesia, to minimal sedation/anxiolysis, to moderate sedation/analgesia, to deep sedation/
analgesia, to general anesthesia. Along this continuum, the physiological effects of sedation have increasing clinical implications and, depending on the depth of sedation, may require special equipment and personnel to ensure the patient’s safety. The greatest risk of using sedative agents is respiratory depression. The vast majority of abortion patients are healthy and medically eligible for all levels of sedation in office-based settings. As noted above (see Questions 4 and 6), if sedation is used, the facility should be appropriately equipped and staffed.
8. What are the research gaps associated with the provision of safe, high-quality care from pre- to postabortion?
The committee’s overarching task was to assess the safety and quality of abortion care in the United States. As noted in the introduction to this chapter, the committee decided that its findings and conclusions fully respond to this charge. The committee concludes that legal abortions are safe and effective. Safety and quality are optimized when the abortion is performed as early in pregnancy as possible. Quality requires that care be respectful of individual patient preferences, needs, and values so that patient values guide all clinical decisions.
The committee did not identify gaps in research that raise concerns about these conclusions and does not offer recommendations for specific actions to be taken by policy makers, health care providers, and others.
The following are the committee’s observations about questions that merit further investigation.
Limitation of Mifepristone distribution As noted above, mifepristone, sold under the brand name Mifeprex, is the only medication approved by the FDA for use in medication abortion. Extensive clinical research has demonstrated its safety and effectiveness using the FDA-recommended regimen. Furthermore, few women have contraindications to medication abortion. Nevertheless, as noted earlier, the FDA REMS restricts the distribution of mifepristone. Research is needed on how the limited distribution of mifepristone under the REMS process impacts dimensions of quality, including timeliness, patient-centeredness, and equity. In addition, little is known about pharmacist and patient perspectives on pharmacy dispensing of mifepristone and the potential for direct-to-patient models through telemedicine.
Pain management There is insufficient evidence to identify the optimal approach to minimizing the pain women experience during an aspiration procedure without sedation. Paracervical blocks are effective in decreasing procedural pain, but the administration of the block itself is painful, and
even with the block, women report experiencing moderate to significant pain. More research is needed to learn how best to reduce the pain women experience during abortion procedures.
Research on prophylactic pain management for women undergoing medication abortions is also needed. Although NSAIDs reduce the pain of cramping, women still report high levels of pain.
Availability of providers APCs can provide medication and aspiration abortions safely and effectively, but the committee did not find research assessing whether APCs can also be trained to perform D&Es.
Addressing the needs of women of lower income Women who have abortions are disproportionately poor and at risk for interpersonal and other types of violence. Yet little is known about the extent to which they receive needed social and psychological supports when seeking abortion care or how best to meet those needs. More research is needed to assess the need for support services and to define best clinical practice for providing those services.
Abortion is a legal medical procedure that has been provided to millions of American women. Since the Institute of Medicine first reviewed the health implications of national legalized abortion in 1975, there has been a plethora of related scientific research, including well-designed randomized clinical trials, systematic reviews, and epidemiological studies examining abortion care. This research has focused on examining the relative safety of abortion methods and the appropriateness of methods for different clinical circumstances. With this growing body of research, earlier abortion methods have been refined, discontinued, and new approaches have been developed.
The Safety and Quality of Abortion Care in the United States offers a comprehensive review of the current state of the science related to the provision of safe, high-quality abortion services in the United States. This report considers 8 research questions and presents conclusions, including gaps in research.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
- Skip to main content
- Skip to primary sidebar
- Skip to footer
- QuestionPro

- Solutions Industries Gaming Automotive Sports and events Education Government Travel & Hospitality Financial Services Healthcare Cannabis Technology Use Case NPS+ Communities Audience Contactless surveys Mobile LivePolls Member Experience GDPR Positive People Science 360 Feedback Surveys
- Resources Blog eBooks Survey Templates Case Studies Training Help center
Home Market Research
Research Reports: Definition and How to Write Them

Reports are usually spread across a vast horizon of topics but are focused on communicating information about a particular topic and a niche target market. The primary motive of research reports is to convey integral details about a study for marketers to consider while designing new strategies.
Certain events, facts, and other information based on incidents need to be relayed to the people in charge, and creating research reports is the most effective communication tool. Ideal research reports are extremely accurate in the offered information with a clear objective and conclusion. These reports should have a clean and structured format to relay information effectively.
What are Research Reports?
Research reports are recorded data prepared by researchers or statisticians after analyzing the information gathered by conducting organized research, typically in the form of surveys or qualitative methods .
A research report is a reliable source to recount details about a conducted research. It is most often considered to be a true testimony of all the work done to garner specificities of research.
The various sections of a research report are:
- Background/Introduction
- Implemented Methods
- Results based on Analysis
- Deliberation
Learn more: Quantitative Research
Components of Research Reports
Research is imperative for launching a new product/service or a new feature. The markets today are extremely volatile and competitive due to new entrants every day who may or may not provide effective products. An organization needs to make the right decisions at the right time to be relevant in such a market with updated products that suffice customer demands.
The details of a research report may change with the purpose of research but the main components of a report will remain constant. The research approach of the market researcher also influences the style of writing reports. Here are seven main components of a productive research report:
- Research Report Summary: The entire objective along with the overview of research are to be included in a summary which is a couple of paragraphs in length. All the multiple components of the research are explained in brief under the report summary. It should be interesting enough to capture all the key elements of the report.
- Research Introduction: There always is a primary goal that the researcher is trying to achieve through a report. In the introduction section, he/she can cover answers related to this goal and establish a thesis which will be included to strive and answer it in detail. This section should answer an integral question: “What is the current situation of the goal?”. After the research design was conducted, did the organization conclude the goal successfully or they are still a work in progress – provide such details in the introduction part of the research report.
- Research Methodology: This is the most important section of the report where all the important information lies. The readers can gain data for the topic along with analyzing the quality of provided content and the research can also be approved by other market researchers . Thus, this section needs to be highly informative with each aspect of research discussed in detail. Information needs to be expressed in chronological order according to its priority and importance. Researchers should include references in case they gained information from existing techniques.
- Research Results: A short description of the results along with calculations conducted to achieve the goal will form this section of results. Usually, the exposition after data analysis is carried out in the discussion part of the report.
Learn more: Quantitative Data
- Research Discussion: The results are discussed in extreme detail in this section along with a comparative analysis of reports that could probably exist in the same domain. Any abnormality uncovered during research will be deliberated in the discussion section. While writing research reports, the researcher will have to connect the dots on how the results will be applicable in the real world.
- Research References and Conclusion: Conclude all the research findings along with mentioning each and every author, article or any content piece from where references were taken.
Learn more: Qualitative Observation
15 Tips for Writing Research Reports
Writing research reports in the manner can lead to all the efforts going down the drain. Here are 15 tips for writing impactful research reports:
- Prepare the context before starting to write and start from the basics: This was always taught to us in school – be well-prepared before taking a plunge into new topics. The order of survey questions might not be the ideal or most effective order for writing research reports. The idea is to start with a broader topic and work towards a more specific one and focus on a conclusion or support, which a research should support with the facts. The most difficult thing to do in reporting, without a doubt is to start. Start with the title, the introduction, then document the first discoveries and continue from that. Once the marketers have the information well documented, they can write a general conclusion.
- Keep the target audience in mind while selecting a format that is clear, logical and obvious to them: Will the research reports be presented to decision makers or other researchers? What are the general perceptions around that topic? This requires more care and diligence. A researcher will need a significant amount of information to start writing the research report. Be consistent with the wording, the numbering of the annexes and so on. Follow the approved format of the company for the delivery of research reports and demonstrate the integrity of the project with the objectives of the company.
- Have a clear research objective: A researcher should read the entire proposal again, and make sure that the data they provide contributes to the objectives that were raised from the beginning. Remember that speculations are for conversations, not for research reports, if a researcher speculates, they directly question their own research.
- Establish a working model: Each study must have an internal logic, which will have to be established in the report and in the evidence. The researchers’ worst nightmare is to be required to write research reports and realize that key questions were not included.
Learn more: Quantitative Observation
- Gather all the information about the research topic. Who are the competitors of our customers? Talk to other researchers who have studied the subject of research, know the language of the industry. Misuse of the terms can discourage the readers of research reports from reading further.
- Read aloud while writing. While reading the report, if the researcher hears something inappropriate, for example, if they stumble over the words when reading them, surely the reader will too. If the researcher can’t put an idea in a single sentence, then it is very long and they must change it so that the idea is clear to everyone.
- Check grammar and spelling. Without a doubt, good practices help to understand the report. Use verbs in the present tense. Consider using the present tense, which makes the results sound more immediate. Find new words and other ways of saying things. Have fun with the language whenever possible.
- Discuss only the discoveries that are significant. If some data are not really significant, do not mention them. Remember that not everything is truly important or essential within research reports.
Learn more: Qualitative Data
- Try and stick to the survey questions. For example, do not say that the people surveyed “were worried” about an research issue , when there are different degrees of concern.
- The graphs must be clear enough so that they understand themselves. Do not let graphs lead the reader to make mistakes: give them a title, include the indications, the size of the sample, and the correct wording of the question.
- Be clear with messages. A researcher should always write every section of the report with an accuracy of details and language.
- Be creative with titles – Particularly in segmentation studies choose names “that give life to research”. Such names can survive for a long time after the initial investigation.
- Create an effective conclusion: The conclusion in the research reports is the most difficult to write, but it is an incredible opportunity to excel. Make a precise summary. Sometimes it helps to start the conclusion with something specific, then it describes the most important part of the study, and finally, it provides the implications of the conclusions.
- Get a couple more pair of eyes to read the report. Writers have trouble detecting their own mistakes. But they are responsible for what is presented. Ensure it has been approved by colleagues or friends before sending the find draft out.
Learn more: Market Research and Analysis
MORE LIKE THIS
Exploring Types of Correlation for Patterns and Relationship
Jun 10, 2024

Life@QuestionPro: The Journey of Kristie Lawrence
Jun 7, 2024

How Can I Help You? — Tuesday CX Thoughts
Jun 5, 2024
Why Multilingual 360 Feedback Surveys Provide Better Insights
Jun 3, 2024
Other categories
- Academic Research
- Artificial Intelligence
- Assessments
- Brand Awareness
- Case Studies
- Communities
- Consumer Insights
- Customer effort score
- Customer Engagement
- Customer Experience
- Customer Loyalty
- Customer Research
- Customer Satisfaction
- Employee Benefits
- Employee Engagement
- Employee Retention
- Friday Five
- General Data Protection Regulation
- Insights Hub
- Life@QuestionPro
- Market Research
- Mobile diaries
- Mobile Surveys
- New Features
- Online Communities
- Question Types
- Questionnaire
- QuestionPro Products
- Release Notes
- Research Tools and Apps
- Revenue at Risk
- Survey Templates
- Training Tips
- Uncategorized
- Video Learning Series
- What’s Coming Up
- Workforce Intelligence
- USC Libraries
- Research Guides
Organizing Your Social Sciences Research Paper
- Choosing a Title
- Purpose of Guide
- Design Flaws to Avoid
- Independent and Dependent Variables
- Glossary of Research Terms
- Reading Research Effectively
- Narrowing a Topic Idea
- Broadening a Topic Idea
- Extending the Timeliness of a Topic Idea
- Academic Writing Style
- Applying Critical Thinking
- Making an Outline
- Paragraph Development
- Research Process Video Series
- Executive Summary
- The C.A.R.S. Model
- Background Information
- The Research Problem/Question
- Theoretical Framework
- Citation Tracking
- Content Alert Services
- Evaluating Sources
- Primary Sources
- Secondary Sources
- Tiertiary Sources
- Scholarly vs. Popular Publications
- Qualitative Methods
- Quantitative Methods
- Insiderness
- Using Non-Textual Elements
- Limitations of the Study
- Common Grammar Mistakes
- Writing Concisely
- Avoiding Plagiarism
- Footnotes or Endnotes?
- Further Readings
- Generative AI and Writing
- USC Libraries Tutorials and Other Guides
- Bibliography
The title summarizes the main idea or ideas of your study. A good title contains the fewest possible words needed to adequately describe the content and/or purpose of your research paper.
Importance of Choosing a Good Title
The title is the part of a paper that is read the most, and it is usually read first . It is, therefore, the most important element that defines the research study. With this in mind, avoid the following when creating a title:
- If the title is too long, this usually indicates there are too many unnecessary words. Avoid language, such as, "A Study to Investigate the...," or "An Examination of the...." These phrases are obvious and generally superfluous unless they are necessary to covey the scope, intent, or type of a study.
- On the other hand, a title which is too short often uses words which are too broad and, thus, does not tell the reader what is being studied. For example, a paper with the title, "African Politics" is so non-specific the title could be the title of a book and so ambiguous that it could refer to anything associated with politics in Africa. A good title should provide information about the focus and/or scope of your research study.
- In academic writing, catchy phrases or non-specific language may be used, but only if it's within the context of the study [e.g., "Fair and Impartial Jury--Catch as Catch Can"]. However, in most cases, you should avoid including words or phrases that do not help the reader understand the purpose of your paper.
- Academic writing is a serious and deliberate endeavor. Avoid using humorous or clever journalistic styles of phrasing when creating the title to your paper. Journalistic headlines often use emotional adjectives [e.g., incredible, amazing, effortless] to highlight a problem experienced by the reader or use "trigger words" or interrogative words like how, what, when, or why to persuade people to read the article or click on a link. These approaches are viewed as counter-productive in academic writing. A reader does not need clever or humorous titles to catch their attention because the act of reading research is assumed to be deliberate based on a desire to learn and improve understanding of the problem. In addition, a humorous title can merely detract from the seriousness and authority of your research.
- Unlike everywhere else in a college-level social sciences research paper [except when using direct quotes in the text], titles do not have to adhere to rigid grammatical or stylistic standards. For example, it could be appropriate to begin a title with a coordinating conjunction [i.e., and, but, or, nor, for, so, yet] if it makes sense to do so and does not detract from the purpose of the study [e.g., "Yet Another Look at Mutual Fund Tournaments"] or beginning the title with an inflected form of a verb such as those ending in -ing [e.g., "Assessing the Political Landscape: Structure, Cognition, and Power in Organizations"].
Appiah, Kingsley Richard et al. “Structural Organisation of Research Article Titles: A Comparative Study of Titles of Business, Gynaecology and Law.” Advances in Language and Literary Studies 10 (2019); Hartley James. “To Attract or to Inform: What are Titles for?” Journal of Technical Writing and Communication 35 (2005): 203-213; Jaakkola, Maarit. “Journalistic Writing and Style.” In Oxford Research Encyclopedia of Communication . Jon F. Nussbaum, editor. (New York: Oxford University Press, 2018): https://oxfordre.com/communication.
Structure and Writing Style
The following parameters can be used to help you formulate a suitable research paper title:
- The purpose of the research
- The scope of the research
- The narrative tone of the paper [typically defined by the type of the research]
- The methods used to study the problem
The initial aim of a title is to capture the reader’s attention and to highlight the research problem under investigation.
Create a Working Title Typically, the final title you submit to your professor is created after the research is complete so that the title accurately captures what has been done . The working title should be developed early in the research process because it can help anchor the focus of the study in much the same way the research problem does. Referring back to the working title can help you reorient yourself back to the main purpose of the study if you find yourself drifting off on a tangent while writing. The Final Title Effective titles in research papers have several characteristics that reflect general principles of academic writing.
- Indicate accurately the subject and scope of the study,
- Rarely use abbreviations or acronyms unless they are commonly known,
- Use words that create a positive impression and stimulate reader interest,
- Use current nomenclature from the field of study,
- Identify key variables, both dependent and independent,
- Reveal how the paper will be organized,
- Suggest a relationship between variables which supports the major hypothesis,
- Is limited to 5 to 15 substantive words,
- Does not include redundant phrasing, such as, "A Study of," "An Analysis of" or similar constructions,
- Takes the form of a question or declarative statement,
- If you use a quote as part of the title, the source of the quote is cited [usually using an asterisk and footnote],
- Use correct grammar and capitalization with all first words and last words capitalized, including the first word of a subtitle. All nouns, pronouns, verbs, adjectives, and adverbs that appear between the first and last words of the title are also capitalized, and
- Rarely uses an exclamation mark at the end of the title.
The Subtitle Subtitles are frequently used in social sciences research papers because it helps the reader understand the scope of the study in relation to how it was designed to address the research problem. Think about what type of subtitle listed below reflects the overall approach to your study and whether you believe a subtitle is needed to emphasize the investigative parameters of your research.
1. Explains or provides additional context , e.g., "Linguistic Ethnography and the Study of Welfare Institutions as a Flow of Social Practices: The Case of Residential Child Care Institutions as Paradoxical Institutions." [Palomares, Manuel and David Poveda. Text & Talk: An Interdisciplinary Journal of Language, Discourse and Communication Studies 30 (January 2010): 193-212]
2. Adds substance to a literary, provocative, or imaginative title or quote , e.g., "Listen to What I Say, Not How I Vote": Congressional Support for the President in Washington and at Home." [Grose, Christian R. and Keesha M. Middlemass. Social Science Quarterly 91 (March 2010): 143-167]
3. Qualifies the geographic scope of the research , e.g., "The Geopolitics of the Eastern Border of the European Union: The Case of Romania-Moldova-Ukraine." [Marcu, Silvia. Geopolitics 14 (August 2009): 409-432]
4. Qualifies the temporal scope of the research , e.g., "A Comparison of the Progressive Era and the Depression Years: Societal Influences on Predictions of the Future of the Library, 1895-1940." [Grossman, Hal B. Libraries & the Cultural Record 46 (2011): 102-128]
5. Focuses on investigating the ideas, theories, or work of a particular individual , e.g., "A Deliberative Conception of Politics: How Francesco Saverio Merlino Related Anarchy and Democracy." [La Torre, Massimo. Sociologia del Diritto 28 (January 2001): 75 - 98]
6. Identifies the methodology used , e.g. "Student Activism of the 1960s Revisited: A Multivariate Analysis Research Note." [Aron, William S. Social Forces 52 (March 1974): 408-414]
7. Defines the overarching technique for analyzing the research problem , e.g., "Explaining Territorial Change in Federal Democracies: A Comparative Historical Institutionalist Approach." [ Tillin, Louise. Political Studies 63 (August 2015): 626-641.
With these examples in mind, think about what type of subtitle reflects the overall approach to your study. This will help the reader understand the scope of the study in relation to how it was designed to address the research problem.
Anstey, A. “Writing Style: What's in a Title?” British Journal of Dermatology 170 (May 2014): 1003-1004; Balch, Tucker. How to Compose a Title for Your Research Paper. Augmented Trader blog. School of Interactive Computing, Georgia Tech University; Bavdekar, Sandeep B. “Formulating the Right Title for a Research Article.” Journal of Association of Physicians of India 64 (February 2016); Choosing the Proper Research Paper Titles. AplusReports.com, 2007-2012; Eva, Kevin W. “Titles, Abstracts, and Authors.” In How to Write a Paper . George M. Hall, editor. 5th edition. (Oxford: John Wiley and Sons, 2013), pp. 33-41; Hartley James. “To Attract or to Inform: What are Titles for?” Journal of Technical Writing and Communication 35 (2005): 203-213; General Format. The Writing Lab and The OWL. Purdue University; Kerkut G.A. “Choosing a Title for a Paper.” Comparative Biochemistry and Physiology Part A: Physiology 74 (1983): 1; “Tempting Titles.” In Stylish Academic Writing . Helen Sword, editor. (Cambridge, MA: Harvard University Press, 2012), pp. 63-75; Nundy, Samiran, et al. “How to Choose a Title?” In How to Practice Academic Medicine and Publish from Developing Countries? A Practical Guide . Edited by Samiran Nundy, Atul Kakar, and Zulfiqar A. Bhutta. (Springer Singapore, 2022), pp. 185-192.
- << Previous: Applying Critical Thinking
- Next: Making an Outline >>
- Last Updated: May 30, 2024 9:38 AM
- URL: https://libguides.usc.edu/writingguide
Center for Gun Violence Solutions
- Make a Gift
- Stay Up-To-Date
- Research & Reports
- Firearm Violence in the United States
- National Survey of Gun Policy
The Public Health Approach to Prevent Gun Violence
A public health approach to prevent gun violence brings together a range of experts across sectors—including researchers, advocates, legislators, community-based organizations, and others—in a common effort to develop, evaluate, and implement equitable, evidence-based solutions.
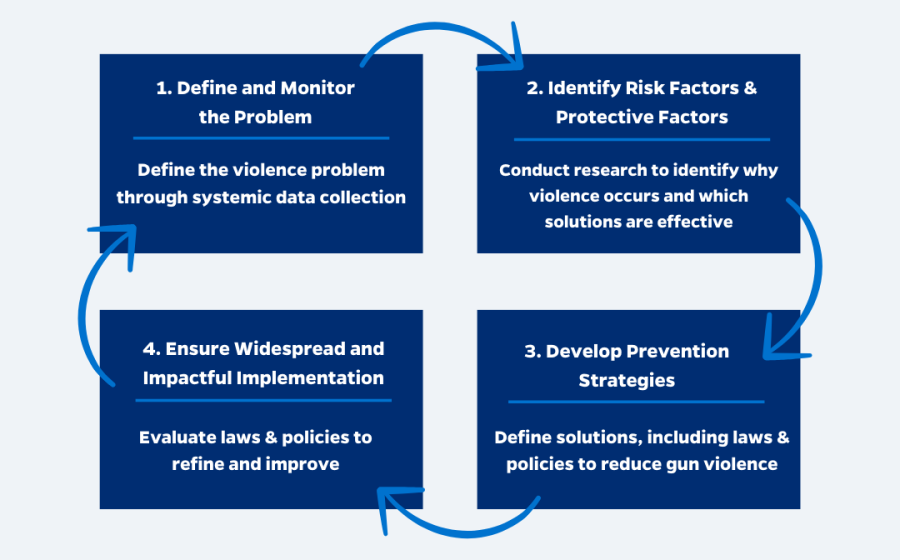
Public health is the science of reducing and preventing injury, disease, and death and promoting the health and well-being of populations through the use of data, research, and effective policies and practices. A public health approach to prevent gun violence is a population level approach that addresses both firearm access and the factors that contribute to and protect from gun violence. This approach brings together institutions and experts across disciplines in a common effort to: 1) define and monitor the problem, 2) identify risk and protective factors, 3) develop and test prevention strategies, and 4) ensure widespread adoption of effective strategies. By using a public health approach we can prevent gun violence in all its forms and strive towards health equity, where everyone can live free from gun violence.
Quick Facts About the Public Health Approach to Prevent Gun Violence:
Gun violence is a public health epidemic,.
resulting in nearly 45,000 deaths annually in recent years (2019-2021) and an estimated 76,000 nonfatal injuries. 1,2
The public health approach
addresses the many forms of gun violence by focusing both on firearm access and underlying risk factors that contribute to gun violence.
The public health approach is divided into four steps:
(1) define and monitor the problem,
(2) identify risk and protective factors,
(3) develop prevention strategies, and
(4) ensure widespread adoption of effective strategies.
The public health epidemic of gun violence is preventable
The Center recommends evidence-based solutions to prevent gun death and injury in all of its forms. These solutions include Firearm Purchaser Licensing; Extreme Risk Protection Orders and Domestic Violence Protection Orders; safe and secure firearm storage practices; strong laws limiting public carry, and Community Violence Intervention programs.
Each day more than 120 Americans die by firearms. 3 These deaths are preventable.
A comprehensive public health approach is needed to address the gun violence epidemic. This approach brings together a wide range of experts to determine the problem, identify key risk factors, develop evidence-based policies and programs, and ensure effective implementation and evaluation. Through a public health approach to gun violence, we can cure this epidemic, save thousands of lives, and make gun violence in America rare and abnormal.
MAKE A GIFT
What is Public Health?
Public health is the science of reducing and preventing injury, disease, and death and promoting the health and well-being of populations through the use of data, research, and effective policies and practices. Public health works to address the underlying causes of a disease or injury before they occur, promote healthy behaviors, and control the spread of outbreaks. Public health researchers and practitioners then work with communities and populations to implement and evaluate programs and policies that are based on research. Policymakers, researchers, and advocates have successfully used the public health approach in the United States to drastically decrease premature death rates, reduce injury, and improve the health and well-being of the population, including by eradicating diseases like polio, promoting widespread usage of vaccines, reducing smoking-related deaths, addressing environmental toxins, and decreasing motor vehicle crashes.
Why is Gun Violence a Public Health Epidemic?
Gun violence is a public health epidemic that affects the well-being and public safety of all Americans. In 2021, nearly 49,000 Americans were killed by gun violence, more than the number of Americans killed in car crashes. 4 An additional 76,000 Americans suffer nonfatal firearm injuries, and millions of Americans face the trauma of losing a loved one or living in fear of being shot. 5 The impacts of gun violence, both direct and indirect, inflict an enormous burden on American society. When a child is shot and killed, they lose decades of potential: the potential to grow up, have a family, contribute to society, and pursue their passions in life. When compared to other communicable and infectious diseases, gun violence often poses a larger burden on society in terms of potential years of life lost. In 2020, firearm deaths accounted for 1,131,105 years of potential life lost before the age of 65—more than diabetes, stroke, and liver disease combined. 6
Scope of Gun Violence
Americans are impacted by various forms of gun violence – including suicide, homicide, and unintentional deaths, as well as nonfatal gunshot injuries, threats, and exposure to gun violence in communities and society.
Firearm Suicide:
Each year, nearly 25,000 Americans die by firearm suicide. 7
Half of all suicide deaths are by firearm. 8
Suicide attempts by firearm are almost always deadly — 9 out of 10 firearm suicide attempts result in death. 9
Access to a firearm in the home increases the odds of suicide more than three-fold. 10
Firearm Homicide:
Each year 18,000 Americans die by firearm homicide. 11
Eight out of ten (79%) of homicides are committed with a firearm. 12
Access to firearms — such as the presence of a gun in the home — doubles the risk for homicide victimization. 13,14
The firearm homicide rate in the United States is 25.2 times higher than other industrialized countries. 15
Domestic Violence:
More than half of female intimate partner homicides are committed with a gun. 16
There are about 4.5 million women in America who have been threatened with a gun and nearly 1 million women who have been shot or shot at by an intimate partner. 17
A woman is five times more likely to be murdered when her abuser has access to a gun. 18
Police-Involved Shootings:
1,000 Americans are shot and killed by police every year. 19
Black Americans are disproportionately impacted by police-involved shootings and are killed at more than twice the rate as White Americans. 20
An estimated 800 of people are wounded by police shootings each year. 21
Unintentional Shootings:
Each year, more than 520 people die from unintentional firearm injuries — an average of one death every 17 hours. 22
More than 140 children and teens (0-19) die each year due to unintentional gun injuries. 23
Americans are four times more likely to die from an unintentional gun injury than people living in other high-income countries. 24
Mass Shootings:
Each year, there are an estimated 600 mass shootings with four or more people shot and/or killed in a single event — more than 500 people are killed and 2,000 are injured. 25
From 2019 to 2021, there were an average of 27 incidents annually where four or more people were killed at a single event —in total more than 130 people were killed. 26
From 2013 to 2022, the number of mass shootings (shootings where four or more people were shot and/or killed) have doubled; so too has the number of people killed and injured from the shootings. 27
States with more permissive gun laws and greater gun ownership had higher rates of mass shootings. 28
Nonfatal Firearm Injuries:
For every person in the United States who dies by firearm, two people are treated at hospitals for nonfatal gunshot wounds. 29
Each year there are over 76,000 nonfatal gunshot injuries, costing hospitals an estimated $2.8 billion annually. 30,31
Gun assaults and unintentional injuries make up the vast majority of nonfatal gun injuries; gun suicide attempts accounted for aproximetaly 5% of nonfatal gun injuries. 32
Exposure to Gun Violence:
More than half of all adults in the U.S. report that they, or a family member have been involved in a gun violence-related incident. 33
One in five adults say they have had a family member killed by a gun.
One in five adults report being personally threated or intimated with a gun. 34
One-third of US adults report that fear of a mass shooting has prevented them from attending certain places or events. 35
How Public Health Differs from Healthcare
People often assume that public health is the same as healthcare. While both strive to improve health and well-being, they approach this goal differently. In healthcare, the focus is on improving the health of the individual. In contrast, public health focuses on improving the health of an entire population through large-scale interventions and prevention programs.
Public health works to address the many factors that determine the health and well-being of populations. These factors are often referred to as risk and protective factors. They are characteristics or behaviors in individuals, families, communities, and the larger society that increase or decrease the likelihood of premature death, injury, or poor health.

What is the Public Health Approach?
The Centers for Disease Control and Prevention and World Health Organization outline a public health approach to violence prevention based on four steps: (1) define and monitor the problem, (2) identify risk and protective factors, (3) develop and test prevention strategies, (4) ensure widespread adoption of effective strategies. 36,37
Researchers and policymakers need reliable data to understand the scope and complexity of gun violence. There are many different types of gun violence, and each type often requires different prevention strategies. Collecting and distributing reliable firearm data is essential to combating gun violence through a public health approach. Gun violence prevention researchers need reliable and timely data around the number of firearm fatalities and nonfatal injuries that occur in the United States each year. This data should include the demographics of the victim and shooter (if applicable), the location and time of the shooting, and the type of gun violence that occurred. Databases should classify the types of gun violence (suicides, intimate partner violence, mass shootings, interpersonal violence, police shootings, unintentional injuries) based on clearly defined and standardized definitions. This data should be made widely available and easily accessible to the general public free of charge.
The public health approach focuses on prevention and addresses population level risk factors that lead to gun violence and protective factors that reduce gun violence. A thorough body of research has identified specific risk factors, both at the individual level and at the community and societal level, which increase the likelihood of engaging in gun violence. At an individual level, having access to guns is a risk factor for violence, increasing the likelihood that a dangerous situation will become fatal. Simply having a gun in one's home doubles the chance of dying by homicide and increases the likelihood of suicide death by over three-fold. 38 Other individual risk factors closely linked to gun violence include: a history of violent behavior, exposure to violence, and risky alcohol and drug use. 39,40 Community level factors also increase the likelihood of gun violence. Under-resourced neighborhoods with high concentrations of poverty, lack of economic opportunity, and social mobility are more likely to experience high rates of violence. These community level factors are often the result of deep structural inequities rooted in racism. 41,42 Policies and programs should mitigate risk factors and promote protective factors at the individual and community levels.
Policymakers and practitioners must craft interventions which address the risk factors for gun violence. These interventions should be routinely tested to ensure they are effective and equitable; rigorous evaluations should be conducted on a routine basis. The foundation for effective gun violence prevention policy is a universal background check law, ensuring that each person who seeks to purchase or transfer a firearm undergoes a background check prior to purchase. Universal background checks should be supplemented by a firearm purchaser licensing system, which regulates and tracks the flow of firearms, to ensure that firearms do not make it into the hands of prohibited individuals. Building upon this, policymakers can create interventions which target behavioral risk-factors for gun violence (e.g. extreme risk laws, DVPO) and they can push for policies which address community risk factors that lead to violence (e.g. investing in community based violence prevention programs). In addition to these gun violence prevention policies, there are a number of evidence-based strategies that can reduce gun violence within communities. For example, community based violence intervention programs work to de-escalate conflicts, interrupt cycles of retaliatory violence, and support those at elevated risk for violence.
While it is essential to pass strong laws, it is equally important to enforce and implement these laws and to scale up evidence-based programs. Strong gun violence prevention policies are only effective if they are properly implemented and enforced in an equitable manner. A key focus of the public health approach is ensuring that these strategies are not only effective but that they also promote equity. Historically disenfranchised groups should be involved in the implementation process to ensure that public health strategies do not have unintended consequences. For example, gun violence prevention policies should be consistently evaluated to ensure that they do not stigmatize individuals living with mental illness or perpetuate the discriminatory and racist practices embedded in the criminal justice system. The public health approach includes a focus on allocating funds for implementation and evaluation of these gun violence prevention strategies at the federal, state, and local level. Funds should be allocated to train the proper stakeholders to ensure that new policies and programs are properly adopted and achieve measurable and equitable outcomes.
Health Impact Pyramid
The goal of public health is to maximize the overall health and well-being of populations. Public health practitioners do this by developing a wide-range of interventions. These interventions address risk and protective factors ranging from factors at the individual level to the societal level. The public health pyramid helps researchers conceptualize the many different levels of intervention needed to address a public health problem like gun violence. 43
At the top of the pyramid are narrowly tailored interventions that work with individuals at risk for gun violence. These interventions, like lethal means safety counseling and violence intervention programs, can have tremendous impact in reducing gun violence. Yet, they also require individual action. These programs provide the tools and support to change behavior, but the individuals themselves must be willing to take action and change behavior.
The middle of the pyramid includes interventions that require less individual action. They are often laws and policies that change the environments within communities to mitigate risk factors. One such policy is universal background checks and firearm purchaser licensing. Research shows that when individuals are required to undergo a background check and obtain a license to purchase a firearm, far fewer firearms are diverted into illegal markets and used to perpetrate violence.
At the bottom of the public health pyramid are the conditions within society that lead to poor health outcomes like gun violence. These factors are often referred to as the root causes or social determinants of health. Socioeconomic factors, such as racial disparities, inequality, poverty, inadequate housing and education, are all risk factors for interpersonal gun violence. Policies that address these root causes have enormous potential to reduce gun violence and improve health. These policies, while requiring a broad collective effort to achieve, require minimal individual effort to be effective at reducing gun violence.
How Do We Address Gun Violence Through the Public Health Approach?
The public health approach is multifaceted and comprehensive and brings together institutions and experts across disciplines in a common effort to develop a variety of evidence-based interventions. 45 This comprehensive approach to tackling public health crises in America has been used over the last century to eradicate diseases like polio, reduce smoking deaths, and make cars safer. This public health approach has saved millions of lives. We can learn from the public health successes -- like car safety -- and apply these lessons to preventing gun violence.
Applying the public health successes of car safety to prevent gun violence
One of the greatest American public health successes is our nation’s work to make cars safer.
By using a comprehensive public health approach to car safety, the United States reduced per-mile driving deaths by nearly 80% from 1967 to 2017. 46 This public health approach to car safety prevented more than 3.5 million deaths over these fifty years. 47 In the years since 2017 car crashes have begun to increase. This recent increase illustrates how threats to public health constantly evolve, and the work of public health practitioners is never complete. They must continue to monitor the problem, identify emerging risks, and develop new solutions. While the work in U.S. auto safety is far from complete, the comparisons illustrates the steps needed to address the epidemic of gun violence. To reduce gun violence, we should apply this same time-tested public health approach.
Sources: National Traffic Highway Safety Administration (NTHSA). Motor Vehicle Traffic Fatalities and Fatality Rates, 1899-2017; Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System, Mortality 1968-2017 on CDC WONDER Online Database.
Applying the Public Health Successes of Auto Safety to Gun Violence Prevention
|
|
|
|
|
| Allocate funds to study the epidemic of motor vehicle crashes. | Allocate funds to the CDC and the NIH to research gun violence. |
|
| Federal agencies regulate car manufacturers and ensure car safety. | Allow federal agencies to regulate firearm manufacturers and ensure gun safety. |
|
| Drivers must submit an application and pass a test to obtain a driver’s license. | Require firearm purchasers to submit an application, undergo a background check, and take safety education to obtain a license to own a firearm. |
|
| Car registration is required at each point of sale. | Pass firearm registration laws to ensure that firearms are registered at each point of sale. |
|
| Reckless and drunk driving laws ensure that risky individuals do not endanger others on the road. | Expand firearm prohibitions to include individuals who are at elevated risk for violence. |
|
| Manufacturers are required to make safer cars by installing seat belts and airbags. | Require manufacturers to make fireams safer, including requiring that guns be outfitted with microstamping technology. |
|
| Age requirements for obtaining a driver’s license, including a graduated licensing system (driver’s permit) for young drivers. | Enact stronger age requirements for owning or possessing all types of firearms. |
|
| Drivers are required to renew their license periodically. | Require gun owners to renew their license on a routine basis. |
|
| New models of cars are monitored and regulated, and recalls are issued for unsafe models. | Allow Consumer Product Safety Commission to regulate safety of firearms and ensure industry accountability. |
|
| Manufacturers are held liable if they sell a dangerous vehicle. | Repeal the Protection of Lawful Commerce in Arms Act (PLCAA) to hold firearm manufacturers accountable for dangerous and reckless distribution of firearms. |
Recommendations
Apply the public health approach for effective gun violence prevention.
Public health is the science of reducing and preventing injury, disease, and death and promoting the health and well-being of populations through the use of data, research, and effective policies and practices. The public health approach has been successfully applied to tackle a wide variety of complex health problems at the population level. Gun violence is a public health epidemic that requires a public health solution. We recommend the following:
Better Data Collection
Federal, state, and local governments should collect more comprehensive gun violence data for fatal and non-fatal firearm injuries, shootings that may not involve physical injuries, and firearm-involved crimes where no shots were fired, including domestic violence-related threats. Federal, state, and local governments should make data publicly available where possible and particularly to researchers studying gun violence and its prevention.
Research Funding
Enhanced research funding is key for advancing knowledge and improving public health interventions and outcomes. Federal, state, and local governments, in addition to foundations and universities, should dedicate funding to research gun violence prevention.
Evidence-based Policies and Practices
Gun violence is a muliticated problem that takes many forms and requires a multitude of data-driven solutions. Gun violence prevention policies and practices should be evidence-based.
- Firearm Purchaser Licensing or permit-to-purchase laws require all prospective gun purchasers to obtain license prior to buying a gun from a dealer or a private seller. These laws enhance universal background checks by establishing a licensing application process as well as considering additional components such as fingerpinting, a more through vetting process, and a built-in waiting period to prevent individuals with a history of violence, those at risk for future interpersonal violence or suicide, and gun traffickers from obtaining firearms.
- Extreme Risk Protection Order (ERPO) is a civil process allowing law enforcement, family members, and, in some states, medical professionals and other parties to petition a court to temporarily restrict access to guns from individuals determined to be at elevated risk of harming themselves or others. ERPO laws are associated with lower rates of firearm suicide and have been successfully used in mass shooting threats. 48
- Community Violence Intervention (CVI) programs aim to identify and support the small number of people at risk for violence by providing them with wraparound mental health and social supports. Investing in CVI programs provides a public health approach to gun violence prevention, interrupting cycles of violence, and addressing the unique needs of the community where systemic racism, disinvestment, and trauma occur.
- Safe and secure gun storage practices, such as Child Access Prevention (CAP) laws, require households with a child or teen to keep firearms unloaded and locked when unattended. These practices promote responsible firearm storage practices protecting children and teenagers from various forms of gun violence, including unintentional shootings and gun suicides. CAP laws are linked to sizable reductions in child and teen gun deaths, including reductions in youth suicide, accidental shootings, and homicides. 49,50
- Public carry of firearms poses a serious threat to safety. Permissive public carry and “stand your ground” laws increase violence by allowing people with violent histories to carry their firearms in public, providing more opportunities for armed intimidation and shootings in response to hostile interactions, and increasing criminals’ access to guns. States should regulate the carrying of guns in public by prohibiting open carry of firearms particularly in sensitive places, passing strong concealed carry permitting laws, and repealing “stand your ground” laws.
Implementation and Evaluation
It is essential to pass evidence-based policies that address gun violence, but that is not enough. Gun violence takes many forms and impacts a variety of groups, requiring ongoing surveillance and evaluation to ensure effective implementation of policies and practices. Federal, state, and local governments should dedicate resources to ensure proper implementation, education and ongoing evaluation of gun violence prevention policies.
1 Three - y e a r average, 2019-2021. Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death . Available: https://wonder.cdc.gov/ucd-icd10-expanded.html .
2 Song Z, Zubizarreta JR, & Giuriato M. (2022). Changes in health care spending, use, and clinical outcomes after nonfatal firearm injuries among survivors and family members . Annals of Internal Medicine . https://doi.org/10.7326/M21-2812
3 Three-year average, 2019-2021. Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death. Available: https://wonder.cdc.gov/ucd-icd10-expanded.html.
4 Three-year average, 2019-2021. Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death. Available: https://wonder.cdc.gov/ucd-icd10-expanded.html.
5 Schnippel K, Burd-Sharps S, Miller T, Lawrence B, Swedler DL. (2021). Nonfatal firearm injuries by intent in the United States: 2016-2018 Hospital Discharge Records from the Healthcare Cost and Utilization Project. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health . https://doi.org/10.5811/westjem.2021.3.51925
6 National Center for Injury Prevention and Control, CDC. WISQARS Years of Potential Life Lost (YPLL) Report . Available: https://www.cdc.gov/injury/wisqars/index.html
7 Three-year average, 2019-2021. Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death. Available: https://wonder.cdc.gov/ucd-icd10-expanded.html.
8 Three-year average, 2019-2021. Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death. Available: https://wonder.cdc.gov/ucd-icd10-expanded.html.
9 Conner A, Azrael D, & Miller M. (2019). Suicide case-fatality rates in the United States, 2007 to 2014: A nationwide population-based study. Annals of Internal Medicine .
10 Anglemyer A, Horvath T, & Rutherford G. (2014). The accessibility of firearms and risk for suicide and homicide victimization among household members: a systematic review and meta-analysis. Annals of Internal Medicine .
11 Three-year average, 2019-2021. Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death. Available: https://wonder.cdc.gov/ucd-icd10-expanded.html.
12 Three-year average, 2019-2021. Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death. Available: https://wonder.cdc.gov/ucd-icd10-expanded.html.
13 Anglemyer A, Horvath T, & Rutherford G. (2014). The accessibility of firearms and risk for suicide and homicide victimization among household members: a systematic review and meta-analysis . Annals of Internal Medicine .
14 Dahlberg LL, Ikeda RM, & Kresnow MJ. (2004). Guns in the home and risk of a violent death in the home: findings from a national study . American Journal of Epidemiology .
15 Choron R, Spitzer S, & Sakran JV. (2019). Firearm violence in America: is there a solution? Advances in Surgery.
16 Zeoli AM, Malinski R, & Turchan B. (2016). Risks and targeted interventions: Firearms in intimate partner violence . Epidemiologic Reviews .
17 Sorenson SB, & Schut RA. (2018). Nonfatal Gun Use in Intimate Partner Violence: A Systematic Review of the Literature . Trauma, Violence, & Abuse .
18 Campbell JC, Webster D, Koziol -McLain J, Block C, Campbell D, Curry MA… & Laughon K. (2003). Risk factors for femicide in abusive relationships: results from a multisite case control study . American Journal of Public Health.
19 Fatal Force database . (2020). Washington Post .
20 Fatal Force database . (2020). Washington Post .
21 Average annual nonfatal shootings by police, 2018-2020. Ward, J. A. (2023). Beyond Urban Fatalities: An Analysis of Shootings by Police in the United States (Doctoral dissertation, Johns Hopkins University).
22 Three-year average, 2019-2021. Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death. Available: https://wonder.cdc.gov/ucd-icd10-expanded.html.
23 Three-year average, 2019-2021. Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death. Available: https://wonder.cdc.gov/ucd-icd10-expanded.html.
24 Solnick SJ, & Hemenway D. (2019). Unintentional firearm deaths in the United States 2005–2015 . Injury Epidemiology.
25 Three-year average, 2019-2021. Gun Violence Archive. (2023). Available: https://www.gunviolencearchive.org/ .
26 Three-year average, 2019-2021. Gun Violence Archive. (2023). Available: https://www.gunviolencearchive.org/ .
27 Gun Violence Archive. (2023). Available: https://www.gunviolencearchive.org/ .
28 Reeping PM, Cerda M, Kalesan B, Wiebe DJ, Galea S, & Branas CC. (2019). State gun laws, gun ownership, and mass shootings in the US: Cross sectional time series. BMJ Journal . https://doi.org/10.1136/bmj.l542
29 Schnippel K, Burd-Sharps S, Miller T, Lawrence B, Swedler DL. (2021). Nonfatal firearm injuries by intent in the United States: 2016-2018 Hospital Discharge Records from the Healthcare Cost and Utilization Project. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health . https://doi.org/10.5811/westjem.2021.3.51925
30 Schnippel K, Burd-Sharps S, Miller T, Lawrence B, Swedler DL. (2021). Nonfatal firearm injuries by intent in the United States: 2016-2018 Hospital Discharge Records from the Healthcare Cost and Utilization Project. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health . https://doi.org/10.5811/westjem.2021.3.51925
31 Avraham JB, Frangos SG, & DiMaggio CJ. (2018). The epidemiology of firearm injuries managed in US emergency departments . Injury Epidemiology.
32 Schnippel K, Burd-Sharps S, Miller T, Lawrence B, Swedler DL. (2021). Nonfatal firearm injuries by intent in the United States: 2016-2018 Hospital Discharge Records from the Healthcare Cost and Utilization Project. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health . https://doi.org/10.5811/westjem.2021.3.51925
33 One in Five Adults Say They’ve Had a Family Member Killed by a Gun, Including Suicide, and One in Six Have Witnessed a Shooting; Among Black Adults, a Third Have Experienced Each. (2023). KFF. Available: https://www.kff.org/other/press-release/one-in-five-adults-say-theyve-had-a-family-member-killed-by-a-gun-including-suicide-and-one-in-six-have-witnessed-a-shooting-among-black-adults-a-third-have-experienced-each/
34 One in Five Adults Say They’ve Had a Family Member Killed by a Gun, Including Suicide, and One in Six Have Witnessed a Shooting; Among Black Adults, a Third Have Experienced Each. (2023). KFF. Available: https://www.kff.org/other/press-release/one-in-five-adults-say-theyve-had-a-family-member-killed-by-a-gun-including-suicide-and-one-in-six-have-witnessed-a-shooting-among-black-adults-a-third-have-experienced-each/
35 One-third of US Adults say fear of mass shootings prevents them from going to certain places or events. (2019) American Psychological Association. Press Release. https://www.apa.org/news/press/releases/2019/08/fear-mass-shooting
36 Centers for Disease Control and Prevention. The National Center for Injury Prevention and Control, Division of Violence Prevention. The Public Health Approach to Violence Prevention .
37 World Health Organization. Violence Prevention Alliance. The Public Health Approach .
38 Anglemyer A, Horvath T, & Rutherford G. (2014). The accessibility of firearms and risk for suicide and homicide victimization among household members: a systematic review and meta-analysis . Annals of Internal Medicine .
39 Consortium for Risk‐Based Firearm Policy. (2013). Guns, public health, and mental illness: An evidence-based approach for state policy .
40 Consortium for Risk‐Based Firearm Policy. (20 2 3). Alcohol Misuse and Gun Violence: An Evidence-Based Approach for State Policy. Available: https://riskbasedfirearmpolicy.org/reports/alcohol-misuse-and-gun-violence-an-evidence-based-approach-for-state-policy/
41 Centers for Disease Control and Prevention. (2019). Risk and Protective Factors .
42 Sampson RJ. (2012). Great American city: Chicago and the enduring neighborhood effect . University of Chicago Press.
43 Frieden TR. (2010). A framework for public health action: the health impact pyramid. American journal of public health.
44 Frieden, TR. (2010). A framework for public health action: The health impact pyramid. American Journal of Public Health . https://doi.org/10.2105/AJPH.2009.185652
45 Hemenway D, & Miller M. (2013). Public health approach to the prevention of gun violence . New England Journal of Medicine.
46 Traffic Safety Facts: A Compilation of Motor Vehicle Crash Data. (2020). Annual Report Tables . National Highway Traffic Safety Administration. Available:
47 On 50th anniversary of ralph nader’s ‘unsafe at any speed,’ safety group reports auto safety regulation has saved 3.5 million lives. (2015). The Nation.
48 Research on Extreme Risk Protection Orders: An Evidence-Based Policy That Saves Lives. (2023). Johns Hopkins Center for Gun Violence Solutions. Available: https://publichealth.jhu.edu/sites/default/files/2023-02/research-on-extreme-risk-protection-orders.pdf
49 Azad HA, Monuteaux MC, Rees CA, Siegel M, Mannix R, Lee LK, Sheehan KM, & Fleegler EW. (2020). Child Access Prevention firearm laws and firearm fatalities among children aged 0 to 14 Years, 1991-2016. JAMA Pediatrics. https://jamanetwork.com/journals/jamapediatrics/fullarticle/2761305
50 Webster DW, Vernick JS, Zeoli AM, & Manganello JA. (2004). Association between youth-focused firearm laws and youth suicides. Jama Network. h ttps://jamanetwork.com/journals/jama/fullarticle/199194
The independent source for health policy research, polling, and news.

Policy Tracker: Youth Access to Gender Affirming Care and State Policy Restrictions
Lindsey Dawson and Jennifer Kates
Last updated on May 22, 2024
states have enacted laws /policies limiting youth access to GAC
of trans youth (ages 13-17) live in a state with a laws/policies limiting their access to GAC
states are facing lawsuits challenging their laws/policies limiting youth access to GAC
states impose professional or legal penalties on health care practitioners providing minors with GAC
State laws and policies prohibiting or restricting minor access to gender affirming care have proliferated in recent years. The first state to pass such a law was Arkansas in 2021. By January 2024, that number increased more than five-fold, with states having passed such laws/policies. Most are being challenged in court, though the majority remain in effect.
This tracker provides an overview of these laws/policies and any associated litigation by state, identifying which groups of people are impacted in addition to minors (e.g. providers, parents, etc.), the types of penalties providers face (i.e. professional or felony), the status of legal challenges, and other key information.
Learn more in this short analysis assessing the policy landscape as of January 24, 2024: The Proliferation of State Actions Limiting Youth Access to Gender Affirming Care
What is Gender Affirming Care (GAC)?
Gender-affirming care is a model of care which includes a spectrum of “medical, surgical, mental health, and non-medical services for transgender and nonbinary people” aimed at affirming and supporting an individual’s gender identity. Gender-affirming care is a model of care which includes a spectrum of “medical, surgical, mental health, and non-medical services for transgender and nonbinary people” aimed at affirming and supporting an individual’s gender identity. Gender affirmation is highly individualized . Not all trans people seek the same types of gender affirming care or services and some people choose not to use medical services as a part of their transition.
Work Trend Index
Research and data on the trends reshaping the world of work
AI at Work Is Here. Now Comes the Hard Part
Employees want AI, leaders are looking for a path forward.
About Work Trend Index
31,000 people. 31 countries. Trillions of productivity signals.
The Work Trend Index conducts global, industry-spanning surveys as well as observational studies to offer unique insights on the trends reshaping work for every employee and leader.

Special Report · November 15, 2023
What Can Copilot’s Earliest Users Teach Us About Generative AI at Work?
Annual Report · May 9, 2023
Will AI Fix Work?
The pace of work is outpacing our ability to keep up. AI is poised to create a whole new way of working.

Special Report · April 20, 2023
The New Performance Equation in the Age of AI
New research shows that employee engagement matters to the bottom line—especially amid economic uncertainty
Special Report · September 22, 2022
Hybrid Work Is Just Work. Are We Doing It Wrong?
In choppy economic waters, new data points to three urgent pivots for leaders to help employees and organizations thrive

Annual Report · March 16, 2022
Great Expectations: Making Hybrid Work Work
From when to go to the office to why work in the first place, employees have a new “worth it” equation. And there’s no going back.

Special Report · January 12, 2022
Technology Can Help Unlock a New Future for Frontline Workers
New data shows that now is the time to empower the frontline with the right digital tools
Special Report · September 9, 2021
To Thrive in Hybrid Work, Build a Culture of Trust and Flexibility
Microsoft employee survey data shows the importance of embracing different work styles—and the power of simple conversations

Special Report · April 20, 2021
Research Proves Your Brain Needs Breaks
New options help you carve out downtime between meetings

Special Report · March 30, 2021
In Hybrid Work, Managers Keep Teams Connected
Researchers found that feelings of connection among Microsoft’s teams diminished during the pandemic. They also discovered the remedy.

Annual Report · March 22, 2021
The Next Great Disruption Is Hybrid Work—Are We Ready?
Exclusive research and expert insights into a year of work like no other reveal urgent trends leaders should consider as hybrid work unfolds.

Special Report · September 22, 2020
A Checkup on Employee Wellbeing
Explore how the pandemic is impacting wellbeing at work around the world.

Special Report · July 8, 2020
The Knowns and Unknowns of the Future of Work
Learn how a sudden shift to remote work may have lasting effects around the world.

Special Report · April 9, 2020
Remote Work Trend Report: Meetings
See how global meeting habits changed during the world’s largest work-from-home mandate.

The WorkLab Newsletter: Science-based insights on the future of work, direct to your inbox
Discover more from WorkLab

Additional research on the future of work
Privacy Approach
Microsoft takes privacy seriously. We remove all personal and organization-identifying information, such as company name, from the data before analyzing it and creating reports. We never use customer content—such as information within an email, chat, document, or meeting—to produce reports. Our goal is to discover and share broad workplace trends that are anonymized by aggregating the data broadly from those trillions of signals that make up the Microsoft Graph.
The state of AI in early 2024: Gen AI adoption spikes and starts to generate value
If 2023 was the year the world discovered generative AI (gen AI) , 2024 is the year organizations truly began using—and deriving business value from—this new technology. In the latest McKinsey Global Survey on AI, 65 percent of respondents report that their organizations are regularly using gen AI, nearly double the percentage from our previous survey just ten months ago. Respondents’ expectations for gen AI’s impact remain as high as they were last year , with three-quarters predicting that gen AI will lead to significant or disruptive change in their industries in the years ahead.
About the authors
This article is a collaborative effort by Alex Singla , Alexander Sukharevsky , Lareina Yee , and Michael Chui , with Bryce Hall , representing views from QuantumBlack, AI by McKinsey, and McKinsey Digital.
Organizations are already seeing material benefits from gen AI use, reporting both cost decreases and revenue jumps in the business units deploying the technology. The survey also provides insights into the kinds of risks presented by gen AI—most notably, inaccuracy—as well as the emerging practices of top performers to mitigate those challenges and capture value.
AI adoption surges
Interest in generative AI has also brightened the spotlight on a broader set of AI capabilities. For the past six years, AI adoption by respondents’ organizations has hovered at about 50 percent. This year, the survey finds that adoption has jumped to 72 percent (Exhibit 1). And the interest is truly global in scope. Our 2023 survey found that AI adoption did not reach 66 percent in any region; however, this year more than two-thirds of respondents in nearly every region say their organizations are using AI. 1 Organizations based in Central and South America are the exception, with 58 percent of respondents working for organizations based in Central and South America reporting AI adoption. Looking by industry, the biggest increase in adoption can be found in professional services. 2 Includes respondents working for organizations focused on human resources, legal services, management consulting, market research, R&D, tax preparation, and training.
Also, responses suggest that companies are now using AI in more parts of the business. Half of respondents say their organizations have adopted AI in two or more business functions, up from less than a third of respondents in 2023 (Exhibit 2).
Gen AI adoption is most common in the functions where it can create the most value
Most respondents now report that their organizations—and they as individuals—are using gen AI. Sixty-five percent of respondents say their organizations are regularly using gen AI in at least one business function, up from one-third last year. The average organization using gen AI is doing so in two functions, most often in marketing and sales and in product and service development—two functions in which previous research determined that gen AI adoption could generate the most value 3 “ The economic potential of generative AI: The next productivity frontier ,” McKinsey, June 14, 2023. —as well as in IT (Exhibit 3). The biggest increase from 2023 is found in marketing and sales, where reported adoption has more than doubled. Yet across functions, only two use cases, both within marketing and sales, are reported by 15 percent or more of respondents.
Gen AI also is weaving its way into respondents’ personal lives. Compared with 2023, respondents are much more likely to be using gen AI at work and even more likely to be using gen AI both at work and in their personal lives (Exhibit 4). The survey finds upticks in gen AI use across all regions, with the largest increases in Asia–Pacific and Greater China. Respondents at the highest seniority levels, meanwhile, show larger jumps in the use of gen Al tools for work and outside of work compared with their midlevel-management peers. Looking at specific industries, respondents working in energy and materials and in professional services report the largest increase in gen AI use.
Investments in gen AI and analytical AI are beginning to create value
The latest survey also shows how different industries are budgeting for gen AI. Responses suggest that, in many industries, organizations are about equally as likely to be investing more than 5 percent of their digital budgets in gen AI as they are in nongenerative, analytical-AI solutions (Exhibit 5). Yet in most industries, larger shares of respondents report that their organizations spend more than 20 percent on analytical AI than on gen AI. Looking ahead, most respondents—67 percent—expect their organizations to invest more in AI over the next three years.
Where are those investments paying off? For the first time, our latest survey explored the value created by gen AI use by business function. The function in which the largest share of respondents report seeing cost decreases is human resources. Respondents most commonly report meaningful revenue increases (of more than 5 percent) in supply chain and inventory management (Exhibit 6). For analytical AI, respondents most often report seeing cost benefits in service operations—in line with what we found last year —as well as meaningful revenue increases from AI use in marketing and sales.
Inaccuracy: The most recognized and experienced risk of gen AI use
As businesses begin to see the benefits of gen AI, they’re also recognizing the diverse risks associated with the technology. These can range from data management risks such as data privacy, bias, or intellectual property (IP) infringement to model management risks, which tend to focus on inaccurate output or lack of explainability. A third big risk category is security and incorrect use.
Respondents to the latest survey are more likely than they were last year to say their organizations consider inaccuracy and IP infringement to be relevant to their use of gen AI, and about half continue to view cybersecurity as a risk (Exhibit 7).
Conversely, respondents are less likely than they were last year to say their organizations consider workforce and labor displacement to be relevant risks and are not increasing efforts to mitigate them.
In fact, inaccuracy— which can affect use cases across the gen AI value chain , ranging from customer journeys and summarization to coding and creative content—is the only risk that respondents are significantly more likely than last year to say their organizations are actively working to mitigate.
Some organizations have already experienced negative consequences from the use of gen AI, with 44 percent of respondents saying their organizations have experienced at least one consequence (Exhibit 8). Respondents most often report inaccuracy as a risk that has affected their organizations, followed by cybersecurity and explainability.
Our previous research has found that there are several elements of governance that can help in scaling gen AI use responsibly, yet few respondents report having these risk-related practices in place. 4 “ Implementing generative AI with speed and safety ,” McKinsey Quarterly , March 13, 2024. For example, just 18 percent say their organizations have an enterprise-wide council or board with the authority to make decisions involving responsible AI governance, and only one-third say gen AI risk awareness and risk mitigation controls are required skill sets for technical talent.
Bringing gen AI capabilities to bear
The latest survey also sought to understand how, and how quickly, organizations are deploying these new gen AI tools. We have found three archetypes for implementing gen AI solutions : takers use off-the-shelf, publicly available solutions; shapers customize those tools with proprietary data and systems; and makers develop their own foundation models from scratch. 5 “ Technology’s generational moment with generative AI: A CIO and CTO guide ,” McKinsey, July 11, 2023. Across most industries, the survey results suggest that organizations are finding off-the-shelf offerings applicable to their business needs—though many are pursuing opportunities to customize models or even develop their own (Exhibit 9). About half of reported gen AI uses within respondents’ business functions are utilizing off-the-shelf, publicly available models or tools, with little or no customization. Respondents in energy and materials, technology, and media and telecommunications are more likely to report significant customization or tuning of publicly available models or developing their own proprietary models to address specific business needs.
Respondents most often report that their organizations required one to four months from the start of a project to put gen AI into production, though the time it takes varies by business function (Exhibit 10). It also depends upon the approach for acquiring those capabilities. Not surprisingly, reported uses of highly customized or proprietary models are 1.5 times more likely than off-the-shelf, publicly available models to take five months or more to implement.
Gen AI high performers are excelling despite facing challenges
Gen AI is a new technology, and organizations are still early in the journey of pursuing its opportunities and scaling it across functions. So it’s little surprise that only a small subset of respondents (46 out of 876) report that a meaningful share of their organizations’ EBIT can be attributed to their deployment of gen AI. Still, these gen AI leaders are worth examining closely. These, after all, are the early movers, who already attribute more than 10 percent of their organizations’ EBIT to their use of gen AI. Forty-two percent of these high performers say more than 20 percent of their EBIT is attributable to their use of nongenerative, analytical AI, and they span industries and regions—though most are at organizations with less than $1 billion in annual revenue. The AI-related practices at these organizations can offer guidance to those looking to create value from gen AI adoption at their own organizations.
To start, gen AI high performers are using gen AI in more business functions—an average of three functions, while others average two. They, like other organizations, are most likely to use gen AI in marketing and sales and product or service development, but they’re much more likely than others to use gen AI solutions in risk, legal, and compliance; in strategy and corporate finance; and in supply chain and inventory management. They’re more than three times as likely as others to be using gen AI in activities ranging from processing of accounting documents and risk assessment to R&D testing and pricing and promotions. While, overall, about half of reported gen AI applications within business functions are utilizing publicly available models or tools, gen AI high performers are less likely to use those off-the-shelf options than to either implement significantly customized versions of those tools or to develop their own proprietary foundation models.
What else are these high performers doing differently? For one thing, they are paying more attention to gen-AI-related risks. Perhaps because they are further along on their journeys, they are more likely than others to say their organizations have experienced every negative consequence from gen AI we asked about, from cybersecurity and personal privacy to explainability and IP infringement. Given that, they are more likely than others to report that their organizations consider those risks, as well as regulatory compliance, environmental impacts, and political stability, to be relevant to their gen AI use, and they say they take steps to mitigate more risks than others do.
Gen AI high performers are also much more likely to say their organizations follow a set of risk-related best practices (Exhibit 11). For example, they are nearly twice as likely as others to involve the legal function and embed risk reviews early on in the development of gen AI solutions—that is, to “ shift left .” They’re also much more likely than others to employ a wide range of other best practices, from strategy-related practices to those related to scaling.
In addition to experiencing the risks of gen AI adoption, high performers have encountered other challenges that can serve as warnings to others (Exhibit 12). Seventy percent say they have experienced difficulties with data, including defining processes for data governance, developing the ability to quickly integrate data into AI models, and an insufficient amount of training data, highlighting the essential role that data play in capturing value. High performers are also more likely than others to report experiencing challenges with their operating models, such as implementing agile ways of working and effective sprint performance management.
About the research
The online survey was in the field from February 22 to March 5, 2024, and garnered responses from 1,363 participants representing the full range of regions, industries, company sizes, functional specialties, and tenures. Of those respondents, 981 said their organizations had adopted AI in at least one business function, and 878 said their organizations were regularly using gen AI in at least one function. To adjust for differences in response rates, the data are weighted by the contribution of each respondent’s nation to global GDP.
Alex Singla and Alexander Sukharevsky are global coleaders of QuantumBlack, AI by McKinsey, and senior partners in McKinsey’s Chicago and London offices, respectively; Lareina Yee is a senior partner in the Bay Area office, where Michael Chui , a McKinsey Global Institute partner, is a partner; and Bryce Hall is an associate partner in the Washington, DC, office.
They wish to thank Kaitlin Noe, Larry Kanter, Mallika Jhamb, and Shinjini Srivastava for their contributions to this work.
This article was edited by Heather Hanselman, a senior editor in McKinsey’s Atlanta office.
Explore a career with us
Related articles.

Moving past gen AI’s honeymoon phase: Seven hard truths for CIOs to get from pilot to scale

A generative AI reset: Rewiring to turn potential into value in 2024
Implementing generative AI with speed and safety
New Select Subcommittee Report Recommends EcoHealth Alliance President Debarred and Criminally Investigated, Exposes Failures in NIH Grant Procedures
WASHINGTON — Today, Select Subcommittee on the Coronavirus Pandemic Chairman Brad Wenstrup (R-Ohio) issued an interim staff report titled “ An Evaluation of the Evidence Surrounding EcoHealth Alliance, Inc.’s Research Activities ”. This report details the Select Subcommittee’s comprehensive investigation into the U.S. government’s funding and lack of oversight of gain-of-function research, EcoHealth Alliance (EcoHealth), and the Wuhan Institute of Virology (WIV). The report reveals serious, systemic weaknesses in the National Institute of Allergy and Infectious Diseases (NIAID) and National Institutes of Health’s (NIH) grant procedures and examines how these failures enabled EcoHealth President Dr. Peter Daszak to fund dangerous gain-of-function research in Wuhan, China without sufficient oversight.
Overwhelming primary source documents and credible firsthand testimony gathered throughout the Select Subcommittee’s investigation provide significant evidence that Dr. Daszak repeatedly violated the terms of the NIH grant awarded to EcoHealth. Given Dr. Daszak’s apparent contempt for the American people and disregard for legal reporting requirements the Select Subcommittee recommends the formal debarment of and a criminal investigation into EcoHealth and its President. In addition, as a result of NIH’s inadequate oversight of American taxpayer funds, the Select Subcommittee is also recommending immediate Congressional action to improve grant procedures at NIH and NIAID.
“ EcoHealth Alliance President Dr. Peter Daszak is not a good steward of U.S. taxpayer dollars and should never again receive funding from the U.S. taxpayer. Dr. Daszak and his organization conducted dangerous gain-of-function research at the WIV, willfully violated the terms of a multi-million-dollar NIH grant, and placed U.S. national security at risk. This blatant contempt for the American people is reprehensible. It is imperative to establish higher standards of oversight at the NIH. The Select Subcommittee’s detailed and comprehensive report today holds Dr. Daszak and EcoHealth Alliance accountable and sheds light on severe shortcomings in our public health systems ,” said Chairman Wenstrup .
Key Report Recommendations
- The Select Subcommittee on the Coronavirus Pandemic recommends that EcoHealth Alliance and Dr. Peter Daszak are formally debarred and cut off from receiving any future U.S. taxpayer funding.
- The Select Subcommittee also recommends that the U.S. Department of Justice conduct a formal investigation into Dr. Daszak.
- Further, the Select Subcommittee recommends eight improvements to NIAID and NIH procedures that will improve grant compliance, increase biosafety and biosecurity of high-risk research, and advance transparency and accountability in America’s federal health agencies.
- Evidence obtained by the Select Subcommittee through document requests and transcribed interviews — including with former NIH Director Lawrence Tabak — confirms that EcoHealth facilitated gain-of-function research at the WIV during the fifth year it received funding from the NIH.
- Dr. Daszak, Dr. Fauci, and other health leaders have repeatedly played semantics with the long standing, widely understood definition of “gain-of-function” in order to avoid accountability for funding and facilitating this dangerous research.
- Notably, the NIH removed the longstanding definition of “gain-of-function” from its website on the same day that former NIH Director Tabak reported EcoHealth’s dangerous experiments to Congress.
- EcoHealth Alliance was required to immediately report any gain-of-function experiment that exhibited greater than “one log growth” — meaning a virus was modified to be 10 times more infectious.
- Evidence shows that Dr. Daszak was aware of an experiment conducted with EcoHealth Alliance funding at the Wuhan Institute of Virology that exhibited this potentially dangerous “one log growth” characteristic, yet he failed to report the experiment to NIH.
- EcoHealth was awarded five years of funding by the NIH to conduct research aimed at preventing pandemics. In the fifth year of receiving these funds — which concerningly coincides with the time period immediately preceding the COVID-19 pandemic — EcoHealth failed to submit its annual research update report to NIH before the required deadline.
- NIH finally received the report from EcoHealth in August 2021, nearly two years after the September 2019 deadline.
- Dr. Fauci and former NIH Director Lawrence Tabak testified that Mark Meadows — Chief of Staff to then President Donald Trump — instructed the NIH to terminate EcoHealth’s grant after the Trump Administration discovered significant malfeasance.
- The NIH official in charge of grant compliance testified he was unaware of any problems with either EcoHealth or its grant to the WIV prior to the Trump Administration’s intervention.
- Despite suggestions of political persecution against EcoHealth, NIH leadership supported every compliance action recommended by the Trump Administration after the malfeasance was discovered.
- NIH reinstated EcoHealth’s problematic grant in 2023 — in part because Dr. Daszak claimed to be in possession of virus sequences and samples that had not yet been tested and were previously paid for by the federal government.
- When Dr. Daszak applied for grant reinstatement, he omitted the material fact that the unanalyzed samples and sequences were not in his custody, but instead, are in the custody and control of the WIV.
- The terms of the WIV’s debarment not only prohibit EcoHealth from funding the lab but also prohibit the lab from influencing any activity that is funded by the U.S. taxpayer.
- Since the untested samples remain at the WIV and are used to influence EcoHealth’s research, NIH’s funding of EcoHealth subsequently violates the WIV’s formal debarment.
Read the final report here , excerpts from select transcribed interviews here , and supporting materials here .
Transcribed interviews with Dr. Daszak and other individuals influential to the findings of the report can be found below:
- Dr. Lawrence Tabak
- Dr. Michael Lauer
- Dr. David Morens (Part 1)
- Dr. David Morens (Part 2)
- Dr. Emily Erbelding
- Dr. Erik Stemmy
- Dr. Peter Daszak
- Dr. Ralph Baric
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Institutes of Health (US); Biological Sciences Curriculum Study. NIH Curriculum Supplement Series [Internet]. Bethesda (MD): National Institutes of Health (US); 2007.

NIH Curriculum Supplement Series [Internet].
Information about mental illness and the brain, defining mental illness 1.
We can all be "sad" or "blue" at times in our lives. We have all seen movies about the madman and his crime spree, with the underlying cause of mental illness. We sometimes even make jokes about people being crazy or nuts, even though we know that we shouldn't. We have all had some exposure to mental illness, but do we really understand it or know what it is? Many of our preconceptions are incorrect. A mental illness can be defined as a health condition that changes a person's thinking, feelings, or behavior (or all three) and that causes the person distress and difficulty in functioning. As with many diseases, mental illness is severe in some cases and mild in others. Individuals who have a mental illness don't necessarily look like they are sick, especially if their illness is mild. Other individuals may show more explicit symptoms such as confusion, agitation, or withdrawal. There are many different mental illnesses, including depression , schizophrenia , attention deficit hyperactivity disorder (ADHD), autism , and obsessive-compulsive disorder . Each illness alters a person's thoughts, feelings, and/or behaviors in distinct ways. In this module, we will at times discuss mental illness in general terms and at other times, discuss specific mental illnesses. Depression, schizophrenia, and ADHD will be presented in greater detail than other mental illnesses.
Not all brain diseases are categorized as mental illnesses. Disorders such as epilepsy, Parkinson's disease, and multiple sclerosis are brain disorders, but they are considered neurological diseases rather than mental illnesses. Interestingly, the lines between mental illnesses and these other brain or neurological disorders is blurring somewhat. As scientists continue to investigate the brains of people who have mental illnesses, they are learning that mental illness is associated with changes in the brain's structure, chemistry, and function and that mental illness does indeed have a biological basis. This ongoing research is, in some ways, causing scientists to minimize the distinctions between mental illnesses and these other brain disorders. In this curriculum supplement, we will restrict our discussion of mental illness to those illnesses that are traditionally classified as mental illnesses, as listed in the previous paragraph.
Mental Illness in the Population 2
Many people feel that mental illness is rare, something that only happens to people with life situations very different from their own, and that it will never affect them. Studies of the epidemiology of mental illness indicate that this belief is far from accurate. In fact, the surgeon general reports that mental illnesses are so common that few U.S. families are untouched by them. 44
Few U.S. families are untouched by mental illness.
Mental Illness in Adults
Scientists estimate that one of every four people is affected by mental illness either directly or indirectly.
Even if you or a family member has not experienced mental illness directly, it is very likely that you have known someone who has. Estimates are that at least one in four people is affected by mental illness either directly or indirectly. Consider the following statistics to get an idea of just how widespread the effects of mental illness are in society: 4 , 25 , 44
- According to recent estimates, approximately 20 percent of Americans, or about one in five people over the age of 18, suffer from a diagnosable mental disorder in a given year.
- Four of the 10 leading causes of disability—major depression, bipolar disorder , schizophrenia, and obsessive-compulsive disorder—are mental illnesses.
- About 3 percent of the population have more than one mental illness at a time.
- About 5 percent of adults are affected so seriously by mental illness that it interferes with their ability to function in society. These severe and persistent mental illnesses include schizophrenia, bipolar disorder, other severe forms of depression, panic disorder , and obsessive-compulsive disorder.
- Approximately 20 percent of doctor's appointments are related to anxiety disorders such as panic attacks.
- Eight million people have depression each year.
- Two million Americans have schizophrenia disorders, and 300,000 new cases are diagnosed each year.
Mental Illness in Children and Adolescents
Mental illness is not uncommon among children and adolescents. Approximately 12 million children under the age of 18 have mental disorders. 4 The National Mental Health Association 33 has compiled some statistics about mental illness in children and adolescents:
- Mental health problems affect one in every five young people at any given time.
- An estimated two-thirds of all young people with mental health problems are not receiving the help they need.
- Less than one-third of the children under age 18 who have a serious mental health problem receive any mental health services.
- As many as 1 in every 33 children may be depressed. Depression in adolescents may be as high as 1 in 8.
- Suicide is the third leading cause of death for 15- to 24-years-olds and the sixth leading cause of death for 5- to 15-year-olds.
- Schizophrenia is rare in children under age 12, but it occurs in about 3 of every 1,000 adolescents.
- Between 118,700 and 186,600 youths in the juvenile justice system have at least one mental illness.
- Of the 100,000 teenagers in juvenile detention, an estimated 60 percent have behavioral, cognitive, or emotional problems.
Warning Signs for Mental Illness 3
Each mental illness has its own characteristic symptoms. (See Section 10 for information about some specific illnesses.) However, there are some general warning signs that might alert you that someone needs professional help. 4 Some of these signs include
- marked personality change,
- inability to cope with problems and daily activities,
- strange or grandiose ideas,
- excessive anxieties ,
- prolonged depression and apathy,
- marked changes in eating or sleeping patterns,
- thinking or talking about suicide or harming oneself,
- extreme mood swings—high or low,
- abuse of alcohol or drugs, and
- excessive anger, hostility, or violent behavior.
A person who shows any of these signs should seek help from a qualified health professional.
Diagnosing Mental Illness 3
Mental health professionals.
To be diagnosed with a mental illness, a person must be evaluated by a qualified professional who has expertise in mental health. Mental health professionals include psychiatrists , psychologists , psychiatric nurses, social workers, and mental health counselors. Family doctors, internists, and pediatricians are usually qualified to diagnose common mental disorders such as depression, anxiety disorders, and ADHD. In many cases, depending on the individual and his or her symptoms , a mental health professional who is not a psychiatrist will refer the patient to a psychiatrist. A psychiatrist is a medical doctor (M.D.) who has received additional training in the field of mental health and mental illnesses. Psychiatrists evaluate the person's mental condition in coordination with his or her physical condition and can prescribe medication. Only psychiatrists and other M.D.s can prescribe medications to treat mental illness.
Mental Illnesses are Diagnosed by Symptoms
Unlike some disease diagnoses, doctors can't do a blood test or culture some microorganisms to determine whether a person has a mental illness. Maybe scientists will develop discrete physiological tests for mental illnesses in the future; until then, however, mental health professionals will have to diagnose mental illnesses based on the symptoms that a person has. Basing a diagnosis on symptoms and not on a quantitative medical test, such as a blood chemistry test, a throat swab, X-rays, or urinalysis, is not unusual. Physicians diagnose many diseases, including migraines, Alzheimer's disease, and Parkinson's disease based on their symptoms alone. For other diseases, such as asthma or mononucleosis, doctors rely on analyzing symptoms to get a good idea of what the problem is and then use a physiological test to provide additional information or to confirm their diagnosis.
When a mental health professional works with a person who might have a mental illness, he or she will, along with the individual, determine what symptoms the individual has, how long the symptoms have persisted, and how his or her life is being affected. Mental health professionals often gather information through an interview during which they ask the patient about his or her symptoms, the length of time that the symptoms have occurred, and the severity of the symptoms. In many cases, the professional will also get information about the patient from family members to obtain a more comprehensive picture. A physician likely will conduct a physical exam and consult the patient's history to rule out other health problems.
Mental health professionals evaluate symptoms to make a diagnosis of mental illness. They rely on the criteria specified in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; currently, the fourth edition), published by the American Psychiatric Association, to diagnose a specific mental illness. 5 For each mental illness, the DSM-IV gives a general description of the disorder and a list of typical symptoms. Mental health professionals refer to the DSM-IV to confirm that the symptoms a patient exhibits match those of a specific mental illness. Although the DSM-IV provides valuable information that helps mental health professionals diagnose mental illness, these professionals realize that it is important to observe patients over a period of time to understand the individual's mental illness and its effects on his or her life. We present the DSM-IV criteria for the specific diseases discussed in this module in Section 10, Information about Specific Mental Illnesses .
Mental health professionals evaluate symptoms to make a diagnosis of mental illness.
Mental Illness and the Brain 4
The term mental illness clearly indicates that there is a problem with the mind. But is it just the mind in an abstract sense, or is there a physical basis to mental illness? As scientists continue to investigate mental illnesses and their causes, they learn more and more about how the biological processes that make the brain work are changed when a person has a mental illness.
The Basics of Brain Function
Before thinking about the problems that occur in the brain when someone has a mental illness, it is helpful to think about how the brain functions normally. The brain is an incredibly complex organ. It makes up only 2 percent of our body weight, but it consumes 20 percent of the oxygen we breathe and 20 percent of the energy we take in. It controls virtually everything we as humans experience, including movement, sensing our environment, regulating our involuntary body processes such as breathing, and controlling our emotions. Hundreds of thousands of chemical reactions occur every second in the brain; those reactions underlie the thoughts, actions, and behaviors with which we respond to environmental stimuli. In short, the brain dictates the internal processes and behaviors that allow us to survive.
The neuron, or nerve cell, is the functional unit of the nervous system. The neuron has processes called dendrites that receive signals and an axon that transmits signals to another neuron.
How does the brain take in all this information, process it, and cause a response? The basic functional unit of the brain is the neuron. A neuron is a specialized cell that can produce different actions because of its precise connections with other neurons, sensory receptors, and muscle cells. A typical neuron has four structurally and functionally defined regions: the cell body, dendrites, axons, and the axon terminals.
The cell body is the metabolic center of the neuron. The nucleus is located in the cell body and most of the cell's protein synthesis occurs here.
A neuron usually has multiple fibers called dendrites that extend from the cell body. These processes usually branch out somewhat like tree branches and serve as the main apparatus for receiving input from other nerve cells.
The cell body also gives rise to the axon. The axon is usually much longer than the dendrites; in some cases, an axon can be up to 1 meter long. The axon is the part of the neuron that is specialized to carry messages away from the cell body and to relay messages to other cells. Some large axons are surrounded by a fatty insulating material called myelin, which enables the electrical signals to travel down the axon at higher speeds.
Near its end, the axon divides into many fine branches that have specialized swellings called axon terminals or presynaptic terminals. The axon terminals end near the dendrites of another neuron. The dendrites of one neuron receive the message sent from the axon terminals of another neuron.
Diagram of a synapse.
The site where an axon terminal ends near a receiving dendrite is called the synapse. The cell that sends out information is called the presynaptic neuron , and the cell that receives the information is called the postsynaptic neuron . It is important to note that the synapse is not a physical connection between the two neurons; there is no cytoplasmic connection between the two neurons. The intercellular space between the presynaptic and postsynaptic neurons is called the synaptic space or synaptic cleft. An average neuron forms approximately 1,000 synapses with other neurons. It has been estimated that there are more synapses in the human brain than there are stars in our galaxy. Furthermore, synaptic connections are not static. Neurons form new synapses or strengthen synaptic connections in response to life experiences. This dynamic change in neuronal connections is the basis of learning.
Neurons relay their information using both electrical signals and chemical messages in a process called neurotransmission.
Neurons communicate using both electrical signals and chemical messages. Information in the form of an electrical impulse is carried away from the neuron's cell body along the axon of the presynaptic neuron toward the axon terminals. When the electrical signal reaches the presynaptic axon terminal, it cannot cross the synaptic space, or synaptic cleft. Instead, the electrical signal triggers chemical changes that can cross the synapse to affect the postsynaptic cell. When the electrical impulse reaches the presynaptic axon terminal, membranous sacs called vesicles move toward the membrane of the axon terminal. When the vesicles reach the membrane, they fuse with the membrane and release their contents into the synaptic space. The molecules contained in the vesicles are chemical compounds called neurotransmitters . Each vesicle contains many molecules of a neurotransmitter. The released neurotransmitter molecules drift across the synaptic cleft and then bind to special proteins, called receptors , on the postsynaptic neuron. A neurotransmitter molecule will bind only to a specific kind of receptor.
The binding of neurotransmitters to their receptors causes that neuron to generate an electrical impulse. The electrical impulse then moves away from the dendrite ending toward the cell body. After the neurotransmitter stimulates an electrical impulse in the postsynaptic neuron, it releases from the receptor back into the synaptic space. Specific proteins called transporters or reuptake pumps carry the neurotransmitter back into the presynaptic neuron. When the neurotransmitter molecules are back in the presynaptic axon terminal, they can be repackaged into vesicles for release the next time an electrical impulse reaches the axon terminal. Enzymes present in the synaptic space degrade neurotransmitter molecules that are not taken back up into the presynaptic neuron.
The nervous system uses a variety of neurotransmitter molecules, but each neuron specializes in the synthesis and secretion of a single type of neurotransmitter. Some of the predominant neurotransmitters in the brain include glutamate, GABA, serotonin , dopamine, and norepinephrine. Each of these neurotransmitters has a specific distribution and function in the brain; the specifics of each are beyond the scope of this module, but a few of the names will arise in reference to particular mental illnesses.
Investigating Brain Function
Mental health professionals base their diagnosis and treatment of mental illness on the symptoms that a person exhibits. The goal for these professionals in treating a patient is to relieve the symptoms that are interfering with the person's life so that the person can function well. Research scientists, on the other hand, have a different goal. They want to learn about the chemical or structural changes that occur in the brain when someone has a mental illness. If scientists can determine what happens in the brain, they can use that knowledge to develop better treatments or find a cure.
Scientists use a variety of imaging techniques to investigate brain structure and function.
The techniques that scientists use to investigate the brain depend on the questions they are asking. For some questions, scientists use molecular or biochemical methods to investigate specific genes or proteins in the neurons. For other questions, scientists want to visualize changes in the brain so that they can learn more about how the activity or structure of the brain changes. Historically, scientists could examine brains only after death, but new imaging procedures enable scientists to study the brain in living animals, including humans. It is important to realize that these brain imaging techniques are not used for diagnosing mental illness. Mental illnesses are diagnosed by the set of symptoms that an individual exhibits. The imaging techniques described in the following paragraphs would not enable the mental health professional to diagnose or treat the patient more effectively. Some of the techniques are also invasive and expose patients to small amounts of radiation. Research studies using these tests are generally not conducted with children or adolescents.
One extensively used technique to study brain activity and how mental illness changes the brain is positron emission tomography (PET). PET measures the spatial distribution and movement of a radioactive chemical injected into the tissues of living subjects. Because the patient is awake, the technique can be used to investigate the relationship between behavioral and physiological effects and changes in brain activity. PET scans can detect very small (nanomolar) concentrations of tracer molecules and achieve spatial resolution of about 4 millimeters. In addition, computers can reconstruct images obtained from a PET scan in two or three dimensions.
PET requires the use of compounds that are labeled with positron-emitting isotopes. A positron has the same mass and spin as an electron but the opposite charge; an electron has a negative charge and a positron has a positive charge. A cyclotron accelerates protons into the nucleus of nitrogen, carbon, oxygen, or fluorine to generate these isotopes. The additional proton makes the isotope unstable. To become stable again, the proton must break down into a neutron and a positron. The unstable positron travels away from the site of generation and dissipates energy along the way. Eventually, the positron collides with an electron, leading to the emission of two gamma rays at 180 degrees from one another. The gamma rays reach a pair of detectors that record the event. Because the detectors respond only to simultaneous emissions, scientists can precisely map the location where the gamma rays were generated. The radioactive chemicals used for PET are very short lived. The half-life (the time for half of the radioactive label to disintegrate) of the commonly used radioisotopes ranges from approximately two minutes to less than two hours, depending on the specific compound. Because a PET scan requires only small amounts (a few micrograms) of short-lived radioisotopes, this technique can be used safely in humans.
PET scans can answer a variety of questions about brain function, including where the neurons are most active. Scientists use different radiolabeled compounds to investigate different biological questions. For example, radiolabeled glucose can identify parts of the brain that become more active in response to a specific stimulus. Active neurons metabolize more glucose than inactive neurons. Active neurons emit more positrons, and this shows as red or yellow on PET scans compared with blue or purple in areas where the neurons are not highly active. (Different computer enhancement techniques may use a different color scheme, but the use of a spectrum with red indicating high activity and blue indicating low activity is common.) Scientists can use PET to measure changes in the activity of specific brain areas in a person who has a mental illness. Scientists can also investigate how the mentally ill brain changes after a person receives treatment.
PET imaging is not the only technique that researchers use to investigate how mental illness changes the brain. Different techniques provide different information to scientists. Another important technique is magnetic resonance imaging (MRI). Unlike PET, which reveals changes in activity level, MRI is used to look at structural changes in the brain. For example, MRI studies reveal that the ventricles , or spaces within the brain, are larger in individuals who have schizophrenia compared with those of healthy individuals. Other techniques that scientists use to investigate function in the living brain include single photon emission computed tomography (SPECT), functional magnetic resonance imaging (fMRI), and electroencephalography (EEG). Each technique has its own advantages, and each provides different information about brain structure and function. Scientists often use more than one technique when conducting their research.
Scientists believe that mental illnesses result from problems with the communication system in the brain.
The Causes of Mental Illnesses 5
At this time, scientists do not have a complete understanding of what causes mental illnesses. If you think about the structural and organizational complexity of the brain together with the complexity of effects that mental illnesses have on thoughts, feelings, and behaviors, it is hardly surprising that figuring out the causes of mental illnesses is a daunting task. The fields of neuroscience, psychiatry, and psychology address different aspects of the relationship between the biology of the brain and individuals' behaviors, thoughts, and feelings, and how their actions sometimes get out of control. Through this multidisciplinary research, scientists are trying to find the causes of mental illnesses. Once scientists can determine the causes of a mental illness, they can use that knowledge to develop new treatments or to find a cure.
The Biology of Mental Illnesses
Scientists understand that mental illnesses are associated with changes in neurochemicals. For example, in people who have depression, less of the neurotransmitter serotonin (small circles) is released into the synaptic space than in people who do not (more...)
Most scientists believe that mental illnesses result from problems with the communication between neurons in the brain ( neurotransmission ). For example, the level of the neurotransmitter serotonin is lower in individuals who have depression. This finding led to the development of certain medications for the illness. Selective serotonin reuptake inhibitors (SSRIs) work by reducing the amount of serotonin that is taken back into the presynaptic neuron. This leads to an increase in the amount of serotonin available in the synaptic space for binding to the receptor on the postsynaptic neuron. Changes in other neurotransmitters (in addition to serotonin) may occur in depression, thus adding to the complexity of the cause underlying the disease.
Scientists believe that there may be disruptions in the neurotransmitters dopamine, glutamate, and norepinephrine in individuals who have schizophrenia. One indication that dopamine might be an important neurotransmitter in schizophrenia comes from the observation that cocaine addicts sometimes show symptoms similar to schizophrenia. Cocaine acts on dopamine-containing neurons in the brain to increase the amount of dopamine in the synapse.
Risk Factors for Mental Illnesses
Although scientists at this time do not know the causes of mental illnesses, they have identified factors that put individuals at risk. Some of these factors are environmental, some are genetic, and some are social. In fact, all these factors most likely combine to influence whether someone becomes mentally ill.
Genetic, environmental, and social factors interact to influence whether someone becomes mentally ill.
Environmental factors such as head injury, poor nutrition, and exposure to toxins (including lead and tobacco smoke) can increase the likelihood of developing a mental illness.
Genes also play a role in determining whether someone develops a mental illness. The illnesses that are most likely to have a genetic component include autism, bipolar disorder, schizophrenia, and ADHD. For example, the observation that children with ADHD are much more likely to have a sibling or parent with ADHD supports a role for genetics in determining whether someone is at risk for ADHD. In studies of twins, ADHD is significantly more likely to be present in an identical twin than a fraternal twin. The same can be said for schizophrenia and depression. Mental illnesses are not triggered by a change in a single gene; scientists believe that the interaction of several genes may trigger mental illness. Furthermore, the combination of genetic, environmental, and social factors might determine whether a case of mental illness is mild or severe.
Social factors also present risks and can harm an individual's, especially a child's, mental health. Social factors include
- severe parental discord,
- death of a family member or close friend,
- parent's mental illness,
- parent's criminality,
- overcrowding,
- economic hardship,
- neglect, and
- exposure to violence.
Treating Mental Illnesses 6
At this time, most mental illnesses cannot be cured, but they can usually be treated effectively to minimize the symptoms and allow the individual to function in work, school, or social environments. To begin treatment, an individual needs to see a qualified mental health professional. The first thing that the doctor or other mental health professional will do is speak with the individual to find out more about his or her symptoms, how long the symptoms have lasted, and how the person's life is being affected. The physician will also do a physical examination to determine whether there are other health problems. For example, some symptoms (such as emotional swings) can be caused by neurological or hormonal problems associated with chronic illnesses such as heart disease, or they can be a side effect of certain medications. After the individual's overall health is evaluated and the condition diagnosed, the doctor will develop a treatment plan. Treatment can involve both medications and psychotherapy, depending on the disease and its severity.
At this time, most mental illnesses cannot be cured, but they can usually be treated effectively to minimize the symptoms and allow the individual to function in work, school, or social environments.
Medications
Medicines are one part of an effective treatment plan for mental illnesses.
Medications are often used to treat mental illnesses. Through television commercials and magazine advertisements, we are becoming more aware of those medications. To become fully effective, medications for treating mental illness must be taken for a few days or a few weeks. When a patient begins taking medication, it is important for a doctor to monitor the patient's health. If the medication causes undesirable side effects, the doctor may change the dose or switch to a different medication that produces fewer side effects. If the medication does not relieve the symptoms, the doctor may prescribe a different medication. 2
Sometimes, individuals who have a mental illness do not want to take their medications because of the side effects. It is important to remember that all medications have both positive and negative effects. For example, antibiotics have revolutionized treatment for some bacterial diseases. However, antibiotics often affect beneficial bacteria in the human body, leading to side effects such as nausea and diarrhea. Psychiatric drugs, like other medications, can alleviate symptoms of mental illness but can also produce unwanted side effects. People who take a medication to treat an illness, whether it is a mental illness or another disease, should work with their doctors to understand what medication they are taking, why they are taking it, how to take it, and what side effects to watch for.
Occasionally, the media reports stories in which the side effects of a psychiatric medication are tied to a potentially serious consequence, such as suicide. In these cases, it is usually very difficult to determine how much suicidal behavior was due to the mental disorder and what the role of the medication might have been. Medications for treating mental illness can, like other medications, have side effects. The psychiatrist or physician can usually adjust the dose or change the medication to alleviate side effects.
Psychotherapy
Psychotherapy is a treatment method in which a mental health professional (psychiatrist, psychologist, or other mental health professional) and the patient discuss problems and feelings. This discussion helps patients understand the basis of their problems and find solutions. Psychotherapy may take different forms. The therapy can help patients
- change thought or behavior patterns,
- understand how past experiences influence current behaviors,
- solve other problems in specific ways, or
- learn illness self-management skills.
Psychotherapy may occur between a therapist and an individual; a therapist and an individual and his or her family members; or a therapist and a group. Often, treatment for mental illness is most successful when psychotherapy is used in combination with medications. For severe mental illnesses, medication relieves the symptoms and psychotherapy helps individuals cope with their illness. 3
Just as there are no medications that can instantly cure mental illnesses, psychotherapy is not a one-time event. The amount of time a person spends in psychotherapy can range from a few visits to a few years, depending on the nature of the illness or problem. In general, the more severe the problem, the more lengthy the psychotherapy should be. 3
The Stigma of Mental Illness 7
"The last great stigma of the twentieth century is the stigma of mental illness." —Tipper Gore, wife of the former U.S. Vice President 37
Words can hurt. Many derogatory words and phrases are used in relation to mental illness. However, these words maintain the stereotyped image and not the reality about mental illness. Try not to use these words, and encourage students not to use them. (more...)
"Mentally ill people are nuts, crazy, wacko." "Mentally ill people are morally bad." "Mentally ill people are dangerous and should be locked in an asylum forever." "Mentally ill people need somebody to take care of them." How often have we heard comments like these or seen these types of portrayals in movies, television shows, or books? We may even be guilty of making comments like them ourselves. Is there any truth behind these portrayals, or is that negative view based on our ignorance and fear?
Stigmas are negative stereotypes about groups of people. Common stigmas about people who are mentally ill are
- Individuals who have a mental illness are dangerous.
- Individuals who have a mental illness are irresponsible and can't make life decisions for themselves.
- People who have a mental illness are childlike and must be taken care of by parents or guardians.
- People who have a mental illness should just get over it. 11
Each of those preconceptions about people who have a mental illness is based on false information. Very few people who have a mental illness are dangerous to society. Most can hold jobs, attend school, and live independently. A person who has a mental illness cannot simply decide to get over it any more than someone who has a different chronic disease such as diabetes, asthma, or heart disease can. A mental illness, like those other diseases, is caused by a physical problem in the body.
Stigmas against individuals who have a mental illness lead to injustices, including discriminatory decisions regarding housing, employment, and education. Overcoming the stigmas commonly associated with mental illness is yet one more challenge that people who have a mental illness must face. Indeed, many people who successfully manage their mental illness report that the stigma they face is in many ways more disabling than the illness itself. The stigmatizing attitudes toward mental illness held by both the public and those who have a mental illness lead to feelings of shame and guilt, loss of self-esteem, social dependence, and a sense of isolation and hopelessness. 11 , 44 One of the worst consequences of stigma is that people who are struggling with a mental illness may be reluctant to seek treatment that, in most cases, would significantly relieve their symptoms.
Providing accurate information is one way to reduce stigmas about mental illness. Advocacy groups protest stereotypes imposed upon those who are mentally ill. They demand that the media stop presenting inaccurate views of mental illness and that the public stops believing these negative views. A powerful way of countering stereotypes about mental illness occurs when members of the public meet people who are effectively managing a serious mental illness: holding jobs, providing for themselves, and living as good neighbors in a community. Interaction with people who have mental illnesses challenges a person's assumptions and changes a person's attitudes about mental illness.
Providing accurate information is one way to reduce stigmas about mental illness.
Attitudes about mental illness are changing, although there is a long way to go before people accept that mental illness is a disease with a biological basis. A survey by the National Mental Health Association found that 55 percent of people who have never been diagnosed with depression recognize that depression is a disease and not something people should "snap out of." 34 This is a substantial increase over the 38 percent of survey respondents in 1991 who recognized depression as a disease.
The Consequences of Not Treating Mental Illness 8
Most people don't think twice before going to a doctor if they have an illness such as bronchitis, asthma, diabetes, or heart disease. However, many people who have a mental illness don't get the treatment that would alleviate their suffering. Studies estimate that two-thirds of all young people with mental health problems are not receiving the help they need and that less than one-third of the children under age 18 who have a serious mental health problem receive any mental health services. Mental illness in adults often goes untreated, too. What are the consequences of letting mental illness go untreated?
In September 2000, the U.S. surgeon general held a conference on children's mental health. The former surgeon general, Dr. David Satcher, emphasized the importance of mental health in children by stating, "Children and families are suffering because of missed opportunities for prevention and early identification, fragmented services, and low priorities for resources. Overriding all of this is the issue of stigma, which continues to surround mental illness." 45
The consequences of mental illness in children and adolescents can be substantial. Many mental health professionals speak of accrued deficits that occur when mental illness in children is not treated. To begin with, mental illness can impair a student's ability to learn. Adolescents whose mental illness is not treated rapidly and aggressively tend to fall further and further behind in school. They are more likely to drop out of school and are less likely to be fully functional members of society when they reach adulthood. 45 We also now know that depressive disorders in young people confer a higher risk for illness and interpersonal and psychosocial difficulties that persist after the depressive episode is over. Furthermore, many adults who suffer from mental disorders have problems that originated in childhood. 44 Depression in youth may predict more severe illness in adult life. 27 Attention deficit hyperactivity disorder, once thought to affect children and adolescents only, may persist into adulthood and may be associated with social, legal, and occupational problems. 14
Mental illness impairs a student's ability to learn. Adolescents whose mental illness is not treated rapidly and aggressively tend to fall further and further behind in school.
The high incidence of mental illness has a great impact on society. Depression alone causes employers to lose over $23 billion each year due to decreased productivity and absenteeism of employees. 46 The Global Burden of Disease Study, conducted by the World Health Organization, assessed the burden of all diseases in units that measure lost years of healthy life due to premature death or disability (disability-adjusted life years, or DALYs). Over 15 percent of the total DALYs were due to mental illness. 26 In 1996, the United States spent more than $69 billion for the direct treatment of mental illnesses. Indirect costs of mental illness due to lost productivity in the workplace, schools, or homes represented a $79 billion loss for the U.S. economy in 1990. 44
Treatment, including psychotherapy and medication management, is cost-effective for patients, their families, and society. The benefits include fewer visits to other doctors' offices, diagnostic laboratories, and hospitals for physical ailments that are based in psychological distress; reduced need for psychiatric hospitalization; fewer sick days and disability claims; and increased job stability. Conversely, the costs of not treating mental disorders can be seen in ruined relationships, job loss or poor job performance, personal anguish, substance abuse, unnecessary medical procedures, psychiatric hospitalization, and suicide. 3
Information about Specific Mental Illnesses 9
A diagnosis of mental illness is rarely simple and straightforward. There are no infallible physiological tests that determine whether a person has a mental illness. Diagnosis requires that qualified healthcare professionals identify several specific symptoms that the person exhibits. Each mental illness has characteristic signs and symptoms that are related to the underlying biological dysfunction. The following sections describe the symptoms and outcomes of three mental illnesses that are highlighted in this curriculum supplement: depression, attention deficit hyperactivity disorder, and schizophrenia.
Depression, or depressive disorders, is a leading cause of disability in the United States as well as worldwide. It affects an estimated 9.5 percent of American adults in a given year. 28 Nearly twice as many women as men have depression. 25 Epidemiological studies have reported that up to 2.5 percent of children and 8.3 percent of adolescents in the United States suffer from depression. 22
The symptoms of depression
Depression is more than just being in a bad mood or feeling sad. Everyone experiences these feelings on occasion, but that does not constitute depression. Depression is actually not a single disease; there are three main types of depressive disorders. 23 , 27 They are
- major depressive disorder , 10
- dysthymia , and
- bipolar disorder (manic-depression).
While some of the symptoms of depression are common during a passing "blue mood," major depressive disorder is diagnosed when a person has five or more of the symptoms nearly every day during a two-week period. 27 Symptoms of depression include
- a sad mood,
- a loss of interest in activities that one used to enjoy,
- a change in appetite or weight,
- oversleeping or difficulty sleeping,
- physical slowing or agitation,
- energy loss,
- feelings of worthlessness or inappropriate guilt,
- difficulty concentrating, and
- recurrent thoughts of death or suicide.
When people have depression, their lives are affected severely: they have trouble performing at work or school, and they aren't interested in normal family and social activities. In adults, an untreated major depressive episode lasts an average of nine months. At least half of the people who experience an episode of major depression will have another episode of depression at some point. 44
In children, depression lasts an average of seven to nine months with symptoms similar to those in adults. 44 Symptoms in children may include
- loss of interest in activities they used to enjoy,
- self-criticism,
- feelings that they are unloved,
- hopelessness about the future,
- thoughts of suicide,
- irritability,
- indecisiveness,
- trouble concentrating, and
- lack of energy.
Children and adolescents with depression are more likely than adults to have anxiety symptoms and general aches and pains, stomachaches, and headaches. The majority of children and adolescents who have a major depressive disorder also have another mental illness such as an anxiety disorder, disruptive or antisocial behavior, or a substance-abuse disorder. Children and adolescents who suffer from depression are more likely to commit suicide than are other youths. As in adults, episodes of depression are likely to recur. 44
Dysthymia is less severe than major depressive disorder, but it is more chronic. In dysthymia, a depressed mood along with at least two other symptoms of depression persist for at least two years in adults, or one year in children or adolescents. 22 These symptoms may not be as disabling, but they do keep affected people from functioning well or feeling good. Dysthymia often begins in childhood, adolescence, or early adulthood. 25 On average, untreated dysthymia lasts four years in children and adolescents. 44
A third type of depressive disorder is bipolar disorder, also called manic-depression. A person who has bipolar disorder alternates between episodes of major depression and mania (periods of abnormally and persistently elevated mood or irritability). During manic periods, the person will also have three or more of the following symptoms:
- overly inflated self-esteem,
- decreased need for sleep,
- increased talkativeness,
- racing thoughts,
- distractibility,
- increased goal-directed activity or physical agitation, and
- excessive involvement in pleasurable activities that have a high potential for painful consequences. 27
While in a manic phase, adolescents may engage in risky or reckless behaviors such as fast driving and unsafe sex.
Bipolar disorder frequently begins during adolescence or young adulthood. Adults with bipolar disorder often have clearly defined episodes of mania and depression, with periods of mania every two to four years. Children and adolescents with bipolar disorder, however, may cycle rapidly between depression and mania many times within a day. 29 Bipolar disorder in youths may be difficult to distinguish from other mental illnesses because the symptoms often overlap with those of other mental illnesses such as ADHD, conduct disorder, or oppositional defiant disorder.
The causes of depression (depressive disorders)
Depression, like other mental illnesses, is probably caused by a combination of biological, environmental, and social factors, but the exact causes are not yet known. For years, scientists thought that low levels of certain neurotransmitters (such as serotonin, dopamine, or norepinephrine) in the brain caused depression. However, scientists now believe that the interplay of factors leading to depression is much more complex. Genetic causes have been suggested from family studies that have shown that between 20 and 50 percent of children and adolescents with depression have a family history of depression and that children of depressed parents are more than three times as likely as children with nondepressed parents to experience a depressive disorder. 44 Abnormal endocrine function, specifically of the hypothalamus or pituitary , may play a role in causing depression. Other risk factors for depressive disorders in youths include
- cigarette smoking,
- loss of a parent,
- the breakup of a romantic relationship,
- attention disorders,
- learning disorders,
- other trauma including experiencing a natural disaster. 22
Depression, like other mental illnesses, is probably caused by a combination of biological, environmental, and social factors, but the exact causes are not yet known.
Scientists have studied changes in the brain associated with depressive disorders. Imaging studies using PET have shown that brain activity in certain areas is substantially decreased in a depressed individual whereas activity in other brain regions is increased compared with the same individual after successful treatment. 13 PET imaging has also shown that depressed patients have lower neurotransmitter receptor binding potential in some areas of the brain. 48 Scientists looking at changes in the brains of bipolar patients found decreases in the size of the cerebellum (the part of the brain that regulates balance and controlled movements), changes in the metabolism of some chemical compounds, and a decrease in the activity of specific brain regions (prefrontal cortex) during the depression phase. 42
Treating depression
A variety of antidepressant medications and psychotherapies are used to treat depression. The most effective treatment for most people is a combination of medication and psychotherapy. 23
Many of us are aware that medications are available to treat depressive disorders—we see the ads on television and in magazines. Up to 70 percent of people with depression can be treated effectively with medication. 44 Medications used to treat depressive disorders usually act on the neurotransmission pathway. For example, some medications affect the activity of certain neurotransmitters, such as serotonin or norepinephrine. Different depressive disorders require different medication therapies. For example, individuals who have bipolar disorder are often treated with a mood-stabilizing drug, such as lithium, during their manic phase and a combination of mood-stabilizer and antidepressant medications during their depressive phase.
Medications usually lead to relief from the symptoms of depression within six to eight weeks. If one drug doesn't relieve symptoms, doctors can prescribe a different antidepressant drug. As with drugs to treat other mental illnesses, patients are monitored closely by their doctor for symptoms of depression and for side effects. Patients who continue to take their medication for at least six months after recovery from major depression are 70 percent less likely to experience a relapse. 1
Psychotherapy helps patients learn more effective ways to deal with the problems in their lives. These therapies usually involve 6 to 20 weekly meetings. These treatment plans should be revised if there is no improvement of symptoms within three or four months. 44
The combination of medications and psychotherapy is effective in the majority of cases and represents the standard care; however, doctors can employ other methods. One therapy that is highly effective when antidepressants and psychotherapy are not effective is electroconvulsive therapy (ECT), or electroshock therapy . 23 ECT is not commonly used in children and adolescents. When ECT is performed, the individual is anesthetized and receives an electrical shock in specific parts of the brain. The patient does not consciously experience the shock. ECT can provide dramatic and rapid relief, but the effects usually last a fairly short time. After ECT, individuals usually take antidepressant medications.
The combination of medications and psychotherapy is effective in the majority of cases.
A few years ago, the herbal supplement St. John's wort received great attention in the media as an over-the-counter treatment for mild to moderate depression. However, many of the claims did not have good scientific evidence to back them up. The effectiveness and safety of St. John's wort remain uncertain, and its use is generally not recommended. 31
Coping with depression
People who have depression (or another depressive disorder) feel exhausted, worthless, helpless, and hopeless. These negative thoughts and feelings that are part of depression make some people feel like giving up. As treatment takes effect, these thoughts begin to go away. Some strategies that can help a person waiting for treatment to take effect include
- setting realistic goals in light of the depression and assuming a reasonable amount of responsibility;
- breaking large tasks into small ones, setting some priorities, and doing what one can as one can;
- trying to be with other people and to confide in someone—it is usually better than being alone and secretive;
- participating in activities that may make one feel better;
- getting some mild exercise, going to a movie or a ball game, or participating in religious, social, or other activities;
- expecting one's mood to improve gradually, not immediately (feeling better takes time);
- postponing important decisions until the depression has lifted and discussing big decisions with family or friends who have a more objective view of the situation;
- remembering that positive thinking will replace the negative thinking that is part of the depression as one's depression responds to treatment; and
- letting one's family and friends help. 23
A potential, tragic consequence of untreated depression is suicide. In 1997, over 30,000 people in the United States died from suicide, and suicide was the third leading cause of death among 10- to 24-year-olds. 22 , 25 Over 90 percent of these people had a mental illness, typically either a depressive disorder or a substance-abuse disorder. 25 Research from the National Institute of Mental Health estimates that as many as seven percent of adolescents who develop a major depressive disorder become victims of suicide. 22
Danger signs that a teen may be considering suicide include
- undergoing dramatic personality change;
- giving away prized possessions;
- writing notes or poems about death;
- talking about suicide, even jokingly;
- making comments such as, "I can't take it anymore" or "I won't be a problem for you much longer";
- previously attempting suicide;
- running away from home; and
- having other symptoms or risk factors for depression, such as difficulty getting along with parents and friends, difficulty in school, or acting bored or withdrawn.
Children and adolescents who are suicidal report feelings of depression, anger, anxiety, hopelessness, and worthlessness. They feel helpless to change frustrating circumstances or to find a solution for their problems. In addition to depression, family conflicts and suicidal death of a relative, friend, or acquaintance are risk factors for suicide among children and adolescents. 44 In the case of another person's suicide, children or teens may need intervention to prevent feelings of guilt, trauma, or social isolation. Programs offered by school professionals that address these concerns can be extremely helpful for identifying grieving youths who may need help.
Public health approaches to preventing suicide include establishing telephone crisis hot lines, restricting access to suicide methods (for example, firearms), counseling media to reduce "copycat" suicides, screening teens for risk factors of suicide, and training professionals to improve recognition and treatment of mood disorders. Research about the effectiveness of these methods indicates that the screening and training strategies are more helpful for preventing suicides among young people than the other methods are. 44
Attention Deficit Hyperactivity Disorder (ADHD)
Attention deficit hyperactivity disorder (ADHD) is the most commonly diagnosed behavioral disorder of childhood. In any six-month period, ADHD affects an estimated 4.1 percent of youths ages 9 to 17. Boys are two to three times more likely than girls to develop ADHD. 25 Although ADHD is usually associated with children, the disorder can persist into adulthood. 19 One researcher 6 estimated that as many as two-thirds of the children he evaluated with ADHD continued to have the disorder in their twenties, and that many of those who no longer fit the clinical description of ADHD nonetheless had significant problems at work or in other social settings.
The symptoms of ADHD
The three predominant symptoms of ADHD are impaired ability to regulate activity level (hyperactivity), to attend to tasks (inattention), and to inhibit behavior (impulsivity). 19 Individuals who have ADHD may display predominantly hyperactive/ impulsive behavior, predominately inattentive behavior, or a combination of both. Children and adolescents with ADHD
- are often unpopular among their peers,
- have trouble in school,
- have higher injury rates than their peers,
- have difficulty paying attention to details,
- are easily distracted,
- find it difficult and unpleasant to finish their schoolwork,
- put off things that require continued mental effort,
- make careless mistakes,
- are disorganized,
- appear not to listen when spoken to, and
- fail to follow through on tasks. 18 , 30 , 44
The DSM-IV 5 specifies several conditions in addition to the symptoms listed above before making a diagnosis of ADHD. For a diagnosis of ADHD, the behaviors must
- appear before age seven,
- continue for at least six months,
- be more frequent or severe than in other children of the same age, and
- cause dysfunction in at least two areas of life, such as school, home, work, or social settings. 19
The diagnosis of ADHD can be made reliably using well-tested diagnostic interview methods. However, as of yet, there is no independent valid test for ADHD.
Among children, ADHD frequently occurs along with other learning, behavior, or mood problems such as learning disabilities, oppositional defiant disorder , anxiety disorders, and depression.
The causes of ADHD
The exact causes of ADHD are unknown; however, research has demonstrated that factors that many people associate with the development of ADHD do not cause the disorder. For example, ADHD is not caused by minor head injuries, damage to the brain from complications during birth, food allergies, excess sugar intake, too much television, poor schools, or poor parenting. 7 , 19 No single cause of ADHD has been discovered. Rather, a number of significant risk factors affecting neurodevelopment and behavior expression have been implicated. Events such as maternal alcohol and tobacco use that affect the development of the fetal brain can increase the risk for ADHD. Injuries to the brain from environmental toxins such as lack of iron have also been implicated.
Scientists have investigated the role of the neurotransmitter dopamine in the development of ADHD because this neurotransmitter plays a key role in regulating movement, increasing motivation and alertness, and inducing insomnia. The observation that ADHD tends to run in families strongly suggests that the disease has a genetic component. Children who have ADHD usually have at least one close relative who also has the disorder. 24 One group of researchers found that a child whose identical twin has ADHD is 11 to 18 times more likely to develop the disorder than a nontwin sibling.
Investigations of particular genes involved in ADHD have focused on a dopamine receptor gene (DRD) on chromosome 11 and the dopamine transporter gene (DAT1) on chromosome 5. 44 Ongoing studies continue to examine these genes and others as factors in ADHD. Most likely, a combination of several genes and environmental factors determines whether a person has ADHD.
Imaging studies have shown differences in the brains of boys with ADHD compared with boys who do not have ADHD. Researchers found that certain parts of the brain are, on average, smaller in boys with ADHD. 8 Other studies found that the total brain volume is smaller in girls who have ADHD than in control subjects; these results match similar findings about the brains of boys with ADHD. 9 Scientists have speculated that the changes in the particular brain regions may be involved in the inability to inhibit thoughts, which is a symptom of ADHD.
Treating ADHD
A variety of medications and behavioral interventions are used to treat ADHD. The most widely used medications are methylphenidate (Ritalin), d -amphetamine, and other amphetamines. These drugs are stimulants that affect the level of the neurotransmitter dopamine at the synapse. 40 Nine out of 10 children improve while taking one of these drugs. 19
When used as prescribed by qualified physicians, these drugs are considered quite safe. Side effects associated with moderate doses are decreased appetite and insomnia. These side effects generally occur early in treatment and often decrease with time. Some studies have shown that the stimulants used to treat ADHD decrease growth rate, but ultimate height is not affected.
Interventions used to treat ADHD include several forms of psychotherapy, such as cognitive-behavioral therapy, social skills training, support groups, and parent and educator skills training. A combination of medication and psychotherapy is more effective than either treatment alone in improving social skills, parent-child relations, reading achievement, and aggressive symptoms. 24
Treating ADHD with a combination of medication and psychotherapy is more effective than either treatment alone in improving social skills, parent-child relations, reading achievement, and aggressive symptoms.
In addition to the well-established treatments described above, some parents and therapists have tried a variety of nutritional interventions to treat ADHD. A few studies have found that some children benefit from such treatments. Nevertheless, no well-established nutritional interventions have consistently been shown to be effective for treating ADHD. 24
Coping with ADHD
As the symptoms indicate, ADHD interferes with a person's daily life. Treatment is available to help individuals and relieve the symptoms, but some simple strategies — including those listed below —can also help.
- Asking the teacher or boss to repeat instructions (rather than guessing what they were).
- Breaking large assignments or job tasks into small, simple tasks. Set a deadline for each task and give a reward as each one is completed.
- Making a list of what needs to be done each day. Plan the best order for doing each task. Then make a schedule for doing them. Use a calendar or daily planner to keep on track.
- Working in a quiet area. Do one thing at a time. Take short breaks.
- Writing things that need to be remembered in a notebook with dividers. Carry the book at all times.
- Posting notes as reminders of things to do.
- Storing similar things together.
- Creating a routine. Get ready for school or work at the same time, in the same way, every day.
- Exercising, eating a balanced diet, and getting enough sleep.
Schizophrenia
Schizophrenia affects approximately 1 percent of the population, or 2.2 million U.S. adults. Men and women are equally affected. 25 , 32 The illness usually emerges in young people in their teens or twenties. Although children over the age of five can develop schizophrenia, it is rare before adolescence. 21 In children, the disease usually develops gradually and is often preceded by developmental delays in motor or speech development. Childhood-onset schizophrenia tends to be harder to treat and has a less favorable prognosis than does the adult-onset form.
The symptoms of schizophrenia
There are many myths and misconceptions about schizophrenia. Schizophrenia is not a multiple or split personality, nor are individuals who have this illness constantly incoherent or psychotic. Although the media often portray individuals with schizophrenia as violent, in reality, very few affected people are dangerous to others. 32 In fact, individuals with schizophrenia are more likely to be victims of violence than violent themselves.
Schizophrenia has severe symptoms. A diagnosis of schizophrenia requires that at least two of the symptoms below be present during a significant portion of a one-month period:
- delusions (false beliefs such as conspiracies, mind control, or persecution);
- hallucinations (usually voices criticizing or commenting on the person's behavior);
- disorganized speech (incomprehensible or difficult to understand);
- grossly disorganized or catatonic behavior; and
- negative symptoms such as flat emotions, lack of facial expressions, and inattention to basic self-care needs such as bathing and eating. 5
However, the presence of either one of the first two symptoms is sufficient to diagnose schizophrenia if the delusions are especially bizarre or if the hallucinations consist of one or more voices that keep a running commentary on the person's behavior or thoughts. 5
The DSM-IV specifies additional criteria for a diagnosis of schizophrenia:
- social or occupational dysfunction,
- persistence of the disturbance for at least six months,
- exclusion of a mood disorder,
- exclusion of a substance-abuse or medical condition that causes similar symptoms, and
- consideration of a possible pervasive developmental disorder. 44
The course of schizophrenia varies considerably from one individual to the next. Most people who have schizophrenia experience at least one, and usually more, relapses after their first psychotic episode. 32 Relapses are periods of more intense symptoms of illness (hallucinations and delusions). During remissions, the negative symptoms related to emotion or personal care are usually still present. About 10 percent of patients remain severely ill for long periods of time and do not return to their previous state of mental functioning. Several long-term studies found that as many as one-third to one-half of people with schizophrenia improve significantly or even recover completely from their illness. 44
The causes of schizophrenia
Like the other mental illnesses discussed here, scientists are still working to determine what causes schizophrenia. Also like the other mental illnesses, genetic and environmental factors most likely interact to cause the disease. Several studies suggest that an imbalance of chemical neurotransmitter systems of the brain, including the dopamine, GABA, glutamate, and norepinephrine neurotransmitter systems, are involved in the development of schizophrenia. 20 , 36
Family, twin, and adoption studies support the idea that genetics plays an important role in the illness. For example, children of people with schizophrenia are 13 times more likely, and identical twins are 48 times more likely, to develop the illness than are people in the general population. 44 Scientists continue to look at genes that may play a role in causing schizophrenia. One gene of interest to scientists who study schizophrenia codes for an enzyme that breaks down dopamine in the synapse. 12 Investigations to confirm the role of this and other genes are ongoing.
Imaging studies have revealed differences in brain structure and function in individuals with schizophrenia compared with control individuals. Brain imaging studies show that young people who have schizophrenia have structural differences in their brains compared with individuals who do not have schizophrenia. These changes include a reduced total volume of the cerebrum (the upper portion of the brain, which is divided into halves), a reduced amount of gray matter (the tissue that makes up a majority of the brain and consists mainly of neuron cell bodies and dendrites), enlarged brain ventricles (the cavities, or spaces, in the brain that are filled with cerebrospinal fluid), and other abnormalities. 38 , 39 , 41 PET scans of identical twins have revealed that the twin with schizophrenia has lower brain activity in the frontal lobes (the front section of the cerebral lobes) than does the twin who does not have schizophrenia. 47 One group of researchers used MRI to periodically scan the brains of teens with childhood-onset schizophrenia and an age-matched control group over a five-year period. They found that teens with schizophrenia lose four times the amount of neurons in a specific region of the brain that teens in the control group lose. 43
Treating schizophrenia
There is no cure for schizophrenia; however, effective treatments that make the illness manageable for most affected people are available. The optimal treatment includes antipsychotic medication combined with a variety of psychotherapeutic interventions. 44
Since the 1950s, doctors have used antipsychotic drugs, such as chlorpromazine and haloperidol, to relieve the hallucinations and delusions typical of schizophrenia. Recently, newer (also called atypical) antipsychotic drugs such as risperidone and clozapine have proven to be more effective. Early and sustained treatment that includes antipsychotic medication is important for long-term improvement of the course of the disease. Patients who discontinue medication are likely to experience a relapse of their illness. 32
People who manage schizophrenia best combine medication with psychosocial rehabilitation (life-skills training). 17 Therapies that combine family and community support, education, and behavioral and cognitive skills to address specific challenges help schizophrenic patients improve their functioning and the quality of their lives.
The optimal treatment for schizophrenia includes antipsychotic medication and psychotherapy.
Finding Help for Someone with Mental Illness 11
As a teacher, you may occasionally have students who show symptoms of or who have significant risk factors for a mental illness. A first step for helping these students is to contact the school nurse or guidance counselor. These individuals should know the appropriate next steps to take, including directing the student's parents or guardians to contact their physician or their city or county mental health services.
If you think a friend or colleague might have a mental illness, encourage him or her to see a physician. Physicians can make referrals to mental health specialists in the community. In addition, your state or county health departments may offer services for people struggling with a mental illness. The National Mental Health Association has an affiliate network throughout the country. The programs offered by the NMHA affiliates include support groups, public education and advocacy campaigns, rehabilitation, and housing services. You can access the NMHA's affiliate network through its Web site: http://www.nmha.org/nav/section/affiliate.cfm .
The Additional Resources for Teachers section describes other online resources about mental illnesses (page 53).
The delays or lack of development in emotional, social, academic, or behavioral skills that a child or adolescent experiences because of untreated mental illness. The mental illness keeps the individual from developing these life skills at the usual stage of life. An individual may never fully make up for these deficiencies.
Refers to a disease or condition that has a rapid onset, marked intensity, and short duration.
A medication used to treat depression.
An abnormal sense of fear, nervousness, and apprehension about something that might happen in the future.
Any of a group of illnesses that fill people's lives with overwhelming anxieties and fears that are chronic and unremitting. Anxiety disorders include panic disorder, obsessive-compulsive disorder, post-traumatic stress disorder, phobias, and generalized anxiety disorder.
See attention deficit hyperactivity disorder.
A mental illness characterized by an impaired ability to regulate activity level (hyperactivity), attend to tasks (inattention), and inhibit behavior (impulsivity). For a diagnosis of ADHD, the behaviors must appear before an individual reaches age seven, continue for at least six months, be more frequent than in other children of the same age, and cause impairment in at least two areas of life (school, home, work, or social function).
A mental illness that typically affects a person's ability to communicate, form relationships with others, and respond appropriately to the environment. Some people with autism have few problems with speech and intelligence and are able to function relatively well in society. Others are mentally retarded or mute or have serious language delays. Autism makes some people seem closed off and shut down; others seem locked into repetitive behaviors and rigid patterns of thinking.
The long, fiberlike part of a neuron by which the cell carries information to target cells.
A depressive disorder in which a person alternates between episodes of major depression and mania (periods of abnormally and persistently elevated mood). Also referred to as manic-depression.
The upper part of the brain that consists of the left and right hemispheres.
Refers to a disease or condition that persists over a long period of time.
Conscious mental activity that informs a person about his or her environment. Cognitive actions include perceiving, thinking, reasoning, judging, problem solving, and remembering.
A personality disorder of children and adolescents involving persistent antisocial behavior. Individuals with conduct disorder frequently participate in activities such as stealing, lying, truancy, vandalism, and substance abuse.
A false belief that persists even when a person has evidence that the belief is not true.
The specialized fibers that extend from a neuron's cell body and receive messages from other neurons.
A group of diseases including major depressive disorder (commonly referred to as depression), dysthymia, and bipolar disorder (manic-depression). See bipolar disorder, dysthymia, and major depressive disorder.
A book published by the American Psychiatric Association that gives general descriptions and characteristic symptoms of different mental illnesses. Physicians and other mental health professionals use the DSM-IV to confirm diagnoses for mental illnesses.
A synonym for illness. See illness.
An abnormality in mental or physical health. In this module, disorder is used as a synonym for illness.
A depressive disorder that is less severe than major depressive disorder but is more persistent. In children and adolescents, dysthymia lasts for an average of four years.
A treatment for severe depression that is usually used only when people do not respond to medications and psychotherapy. ECT involves passing a low-voltage electric current through the brain. The person is under anesthesia at the time of treatment. ECT is not commonly used in children and adolescents.
A method of recording the electrical activity in the brain through electrodes attached to the scalp.
See electroconvulsive therapy.
One of the four divisions of each cerebral hemisphere. The frontal lobe is important for controlling movement and associating the functions of other cortical areas.
The portion of brain tissue that is dark in color. The gray matter consists primarily of nerve cell bodies, dendrites, and axon endings.
The perception of something, such as a sound or visual image, that is not actually present other than in the mind.
The part of the brain that controls several body functions, including feeding, breathing, drinking, temperature, and the release of many hormones.
A problem in which some part or parts of the body do not function normally, in a way that interferes with a person's life. For the purpose of this module, other terms considered to be synonyms for illness include disease, disorder, condition, and syndrome.
An imaging technique that uses magnetic fields to take pictures of the structure of the brain.
A depressive disorder commonly referred to as depression. Depression is more than simply being sad; to be diagnosed with depression, a person must have five or more characteristic symptoms nearly every day for a two-week period.
Feelings of intense mental and physical hyperactivity, elevated mood, and agitation.
See bipolar disorder.
A health condition that changes a person's thinking, feelings, or behavior (or all three) and that causes the person distress and difficulty in functioning.
A condition in which a person has an IQ that is below average and that affects an individual's learning, behavior, and development. This condition is present from birth.
A fatty material that surrounds and insulates the axons of some neurons.
A unique type of cell found in the brain and body that processes and transmits information.
A term no longer used medically as a diagnosis for a relatively mild mental or emotional disorder that may involve anxiety or phobias but does not involve losing touch with reality.
The process that occurs when a neuron releases neurotransmitters that relay a signal to another neuron across the synapse.
A chemical produced by neurons that carries messages to other neurons.
An anxiety disorder in which a person experiences recurrent unwanted thoughts or rituals that the individual cannot control. A person who has OCD may be plagued by persistent, unwelcome thoughts or images or by the urgent need to engage in certain rituals, such as hand washing or checking.
A disruptive pattern of behavior of children and adolescents that is characterized by defiant, disobedient, and hostile behaviors directed toward adults in positions of authority. The behavior pattern must persist for at least six months.
An anxiety disorder in which people have feelings of terror, rapid heart beat, and rapid breathing that strike suddenly and repeatedly with no warning. A person who has panic disorder cannot predict when an attack will occur and may develop intense anxiety between episodes, worrying when and where the next one will strike.
An intense fear of something that poses little or no actual danger. Examples of phobias include fear of closed-in places, heights, escalators, tunnels, highway driving, water, flying, dogs, and injuries involving blood.
An endocrine organ closely linked with the hypothalamus. The pituitary secretes a number of hormones that regulate the activity of other endocrine organs in the human body.
A positively charged particle that has the same mass and spin as—but the opposite charge of—an electron.
An imaging technique for measuring brain function in living subjects by detecting the location and concentration of small amounts of radioactive chemicals.
The neuron that receives messages from other neurons.
The neuron that sends messages to other neurons by releasing neurotransmitters into the synapse.
A medical doctor (M.D.) who specializes in treating mental diseases. A psychiatrist evaluates a person's mental health along with his or her physical health and can prescribe medications.
The branch of medicine that deals with identifying, studying, and treating mental, emotional, and behavioral disorders.
A mental health professional who has received specialized training in the study of the mind and emotions. A psychologist usually has an advanced degree such as a Ph.D.
A serious mental disorder in which a person loses contact with reality and experiences hallucinations or delusions.
A treatment method for mental illness in which a mental health professional (psychiatrist, psychologist, counselor) and a patient discuss problems and feelings to find solutions. Psychotherapy can help individuals change their thought or behavior patterns or understand how past experiences affect current behaviors.
A molecule that recognizes specific chemicals, including neurotransmitters and hormones, and transmits the message into the cell on which the receptor resides.
The reoccurrence of symptoms of a disease.
The large molecule that carries neurotransmitter molecules back into the presynaptic neuron from which they were released. Also referred to as a transporter.
The chance or possibility of experiencing harm or loss.
Something that increases a person's risk or susceptibility to harm.
A chronic, severe, and disabling brain disease. People with schizophrenia often suffer terrifying symptoms such as hearing internal voices or believing that other people are reading their minds, controlling their thoughts, or plotting to harm them. These symptoms may leave them fearful and withdrawn. Their speech and behavior can be so disorganized that they may be incomprehensible or frightening to others.
A group of medications used to treat depression. These medications cause an increase in the amount of the neurotransmitter serotonin in the brain.
A neurotransmitter that regulates many functions, including mood, appetite, and sensory perception.
A brain imaging process that measures the emission of single photons of a given energy from radioactive tracers in the human body.
A negative stereotype about a group of people.
An herb sometimes used to treat mild cases of depression. Although the popular media have reported successes using St. John's wort, it is not a recommended treatment. The scientific evidence for its effectiveness and safety is not conclusive.
Something that indicates the presence of a disease.
The site where presynaptic and postsynaptic neurons communicate with each other.
The intercellular space between a presynaptic and postsynaptic neuron. Also referred to as the synaptic cleft.
A group of symptoms or signs that are characteristic of a disease. In this module, the word syndrome is used as a synonym for illness.
A large protein on the cell membrane of axon terminals. It removes neurotransmitter molecules from the synaptic space by carrying them back into the axon terminal that released them. Also referred to as the reuptake pump.
One of the cavities or spaces in the brain that are filled with cerebrospinal fluid.
A membranous sac within an axon terminal that stores and releases neurotransmitters.
Relevant to Lessons 1, 2, and 5
Relevant to Lesson 3.
Relevant to Lessons 2, 3, 4, and 5.
Relevant to Lessons 1, 2, and 4.
Relevant to Lessons 2, and 3.
Relevant to Lessons 4 and 5.
Relevant to Lessons 1, 2, 3, 4, and 5.
Relevant to Lessons 2, 3, 4, 5, and 6.
In this module, the term depression refers to major depressive disorder. We will use the terms dysthymia and bipolar disorder specifically when we are referring to those types of depressive disorders.
Relevant to Lessons 1, 2, 3, 4, 5, and 6.
- Cite this Page National Institutes of Health (US); Biological Sciences Curriculum Study. NIH Curriculum Supplement Series [Internet]. Bethesda (MD): National Institutes of Health (US); 2007. Information about Mental Illness and the Brain.
In this Page
- Defining Mental Illness
- Mental Illness in the Population
- Warning Signs for Mental Illness
- Diagnosing Mental Illness
- Mental Illness and the Brain
- The Causes of Mental Illnesses
- Treating Mental Illnesses
- The Stigma of Mental Illness
- The Consequences of Not Treating Mental Illness
- Information about Specific Mental Illnesses
- Finding Help for Someone with Mental Illness
Related Items in Bookshelf
- All Textbooks
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Information about Mental Illness and the Brain - NIH Curriculum Supplement Serie... Information about Mental Illness and the Brain - NIH Curriculum Supplement Series
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
2. Definitions of Physical Activity, Exercise, Training, Sport, and Health. Definitions and terms are based on "Physical activity in the prevention and treatment of disease" (FYSS, www.fyss.se [Swedish] []), World Health Organization (WHO) [] and the US Department of Human Services [].The definition of physical activity in FYSS is: "Physical activity is defined purely physiologically, as ...
For topic A, you can investigate public health strategies that have been developed to combat potential pandemics such as Covid-19, SARS, C.difficile, Avian Flu, or H1N1. Provide examples of effective strategies that have been implemented and their impact on public health. For topic B, you should locate a media report on a public health issue such as the handling of Covid-19, SARS, or the ...
Implementation of Healthy People 2030 will by strengthened by engaging users from many sectors and ensuring the effective use and alignment of resources. Promoting the nation's health and well-being is a shared responsibility—at the national, state, territorial, tribal, and community levels. It requires involving the public, private, and not ...
Consequently, in 2022, the Social Security Administration requested that the National Academies convene a committee of relevant experts to investigate and provide an overview of the current status of diagnosis, treatment, and prognosis of long-term health effects related to Long COVID. This report presents the committee conclusions.
Patient Safety: Patients should not be harmed by health care services that are intended to help them. The IOM report, To Err Is Human, 26 found that between 46,000 and 98,000 Americans were dying in hospitals each year due to medical errors. Subsequent research has found medical errors common across all health care settings. The problem is not due to the lack of dedication to quality care by ...
WHO COVID-19 Research Database. The WHO COVID-19 Research Database was a resource created in response to the Public Health Emergency of International Concern (PHEIC). It contained citations with abstracts to scientific articles, reports, books, preprints, and clinical trials on COVID-19 and related literature.
Mental health is a lot more than the absence of illness: it is an intrinsic part of our individual and collective health and well-being. As this "World Mental Health Report" shows, to achieve the global objectives set out in the WHO "Comprehensive mental health action plan 2013-2030" and the Sustainable Development Goals, we need to transform our attitudes, actions and approaches to ...
Brain health. Brain health is the state of brain functioning across cognitive, sensory, social-emotional, behavioural and motor domains, allowing a person to realize their full potential over the life course, irrespective of the presence or absence of disorders. Different determinants related to physical health, healthy environments, safety and ...
In this new study, researchers from the Cleveland Clinic will use tools that they developed from earlier NIH-supported projects to study how COVID-19 affects the brain. They will focus on fatigue, headaches, loss of smell or taste, and memory loss, or "brain fog.". They will also look at more serious but less common complications, such as ...
Brain health issues directly impact more than 8 in 10 Americans, according to a new survey released today; 82% of respondents said they know someone or have themselves experienced at least one brain disorder or mental health condition. Commissioned by Research!America in partnership with the Dana Foundation, the August 2022 national survey captures Americans views on brain health and brain ...
The committee was charged with answering eight specific research questions. This chapter presents the committee's conclusions by responding individually to each question. ... a These attributes of quality health care were first proposed by the Institute of Medicine's Committee on Quality of Health Care in America in the 2001 report Crossing ...
The given task is to write a research report of at least 900 words on a topic of your choice. A research report is a formal piece of writing that includes documenting sources properly, using MLA format, using well-developed paragraphs, and effective transitions, and free of conventional and grammatical errors.
Introduction. In recent years, there has been an increased interest in the relationship between diet and health. Numerous studies have shown that diet can have a significant impact on our health and well-being. Eating a balanced and nutritious diet can lead to lower risks of chronic diseases, improved brain function, and enhanced physical and ...
Research reports are recorded data prepared by researchers or statisticians after analyzing the information gathered by conducting organized research, typically in the form of surveys or qualitative methods. A research report is a reliable source to recount details about a conducted research. It is most often considered to be a true testimony ...
Brainly is the knowledge-sharing community where hundreds of millions of students and experts put their heads together to crack their toughest homework questions. Brainly - Learning, Your Way. - Homework Help, AI Tutor & Test Prep
Abstract. In addition to the apparent physical health benefits, physical activity also affects mental health positively. Physically inactive individuals have been reported to have higher rates of morbidity and healthcare expenditures. Commonly, exercise therapy is recommended to combat these challenges and preserve mental wellness.
The study was funded by National Institutes of Health (NIH) research grants UM1 CA186107, P01 CA87969, R01 HL034594, U01 CA176726, U01 CA167552, R01 HL035464, R01 DK120870, and R01 DK126698.
The Subtitle Subtitles are frequently used in social sciences research papers because it helps the reader understand the scope of the study in relation to how it was designed to address the research problem. Think about what type of subtitle listed below reflects the overall approach to your study and whether you believe a subtitle is needed to emphasize the investigative parameters of your ...
Burnout can have a major impact on a person's well-being. It is typified by four core symptoms: exhaustion, mental distancing, cognitive impairment, and emotional impairment. But the problems don't usually stop there: burnout is also associated with negative brain health symptoms such as anxiety or depression—which in turn can be ...
A public health approach to prevent gun violence brings together a range of experts across sectors—including researchers, advocates, legislators, community-based organizations, and others—in a common effort to develop, evaluate, and implement equitable, evidence-based solutions. Public health is the science of reducing and preventing injury ...
This website would contain relevant data, statistics, and other information about the health care system in Canada that would be helpful for Kenyi's research paper.An encyclopedia entry about the history of health care in Canada may provide historical background information but may not necessarily provide current information about the quality ...
Currently, the right to contraception is protected by two landmark Supreme Court decisions, Griswold v. Connecticut (1965) and Eisenstadt v. Baird (1972). In Griswold, the Court recognized that ...
Background: Brain health is a multi-faceted concept used to describe brain physiology, cognitive function, mental health and well-being. Diseases of the brain account for one third of the global burden of disease and are becoming more prevalent as populations age. Diet, social interaction as well as physical and cognitive activity are lifestyle factors that can potentially influence facets of ...
KFF Headquarters: 185 Berry St., Suite 2000, San Francisco, CA 94107 | Phone 650-854-9400 Washington Offices and Barbara Jordan Conference Center: 1330 G Street, NW, Washington, DC 20005 | Phone ...
Research and data on the trends reshaping the world of work. Annual Report · May 8, 2024. AI at Work Is Here. Now Comes the Hard Part ... Special Report · April 20, 2021. Research Proves Your Brain Needs Breaks. New options help you carve out downtime between meetings. Read the report > Special Report · March 30, 2021.
If 2023 was the year the world discovered generative AI (gen AI), 2024 is the year organizations truly began using—and deriving business value from—this new technology.In the latest McKinsey Global Survey on AI, 65 percent of respondents report that their organizations are regularly using gen AI, nearly double the percentage from our previous survey just ten months ago.
Introduction. Brain health can be defined as the preservation of optimal brain integrity and mental and cognitive function at a given age in the absence of overt brain diseases that affect normal brain function. 1 The ageing population in the world is increasing and the number of people aged over 60 years is expected to grow to 2 billion in 2050. 2 The Global Burden of Disease Study 2013 ...
The paper should be structured with an introduction, body paragraphs, and conclusion, and should include a thesis statement and works cited. SEO keywords include research paper, outline, summary, original thinking, and thesis statement. Explanation: How to write a research paper: Writing a research paper involves several steps:
The report reveals serious, systemic weaknesses in the National Institute of Allergy and Infectious Diseases (NIAID) and National Institutes of Health's (NIH) grant procedures and examines how these failures enabled EcoHealth President Dr. Peter Daszak to fund dangerous gain-of-function research in Wuhan, China without sufficient oversight.
In 1997, over 30,000 people in the United States died from suicide, and suicide was the third leading cause of death among 10- to 24-year-olds. 22, 25 Over 90 percent of these people had a mental illness, typically either a depressive disorder or a substance-abuse disorder. 25 Research from the National Institute of Mental Health estimates that ...