Health Care Reform
- First Online: 26 February 2022

Cite this chapter

- Jonathan Oberlander 5
1051 Accesses
1 Altmetric
This chapter analyzes the Affordable Care Act’s (ACA) turbulent political journey and the current state of health care reform in the United States, with particular focus on developments in health politics and policy during the Obama and Trump administrations. Reforming American health care is perennially a politically treacherous task due to a combination of interest group pressures, fragmented political institutions, and a prominent anti-government strain in US political ideology. The adoption of piecemeal, incremental reforms during the twentieth century makes it difficult to enact more comprehensive solutions to the formidable problems in American health care today. Recent developments in US health politics show that it is possible to move past the inertia of the status quo—but progress is both fragile and limited. The sustained battles over the ACA’s implementation and repeal are shaped by growing ideological and political divisions between Democrats and Republicans, and partisan polarization has altered the normal political trajectory that follows the enactment of a major new social policy program like the ACA. The chapter explains why the ACA proved much more politically vulnerable than initially anticipated, but also resilient despite sustained efforts to roll it back. The chapter also considers the impact of Covid-19 and how the (dis)organization of American health care and health policy has complicated the challenge of responding to the pandemic in the United States.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Banthin, J., and J. Holahan. 2020. Making Sense of Competing Estimates: The Covid-19 Recession’s Effect on Health Coverage . Available from: https://www.urban.org/sites/default/files/publication/102777/making-sense-of-competing-estimates_1.pdf .
Béland, D., P. Rocco, and A. Waddan. 2016. Obamacare Wars: Federalism, State Politics, and the Affordable Care Act . Lawrence: University Press of Kansas.
Google Scholar
Brown, L.D. 2011. The Elements of Surprise: How Health Reform Happened. Journal of Health Politics, Policy and Law 36 (3): 419–427.
Article Google Scholar
Hacker, J.S., and P. Pierson. 2018. The Dog That Almost Barked: What the ACA Repeal Fight Says About the Resilience of the American Welfare State. Journal of Health Politics, Policy and Law 43 (4): 551–577.
Jost, T.S., and K. Keith. 2020. ACA Litigation: Politics Pursued Through Other Means. Journal of Health Politics, Policy and Law 45 (4): 485–499.
Levitt, L. 2020. The Affordable Care Act’s Enduring Resilience. Journal of Health Politics, Policy and Law 45 (4): 609–616.
McCarty, N. 2019. Polarization: What Everyone Needs to Know . New York: Oxford University Press.
Book Google Scholar
Morone, J.A. 1992. Bias of American Politics: Rationing Health Care in a Weak State. University of Pennsylvania Law Review 140: 1923–1938.
Nather, D., and L. Gamio. 2017. The Most Unpopular Bill in Three Decades. Available from: https://www.axios.com/unpopular-health-care-bill-2454397857.html .
Oberlander, J. 2003. The Politics of Health Reform: Why Do Bad Things Happen to Good Health Plans? Health Affairs 22 (Suppl.), W3: 391–404.
———. 2010. Long Time Coming: Why Health Reform Finally Passed. Health Affairs 9 (6): 1112–1116.
———. 2016. Implementing the ACA: The Promise and Limits of Health Care Reform. Journal of Health Politics, Policy and Law 41 (4): 803–826.
———. 2017. Replace, Repeal, Repair, Retreat—Republicans’ Health Care Quagmire. New England Journal of Medicine 377 (11): 1001–1003.
———. 2019. Lessons from the Long and Winding Road to Medicare for All. American Journal of Public Health 109 (11): 1497–1500.
———. 2020. The Ten Years’ War: Politics, Partisanship, and the ACA. Health Affairs 39 (3): 471–478.
Peterson, M.A. 2005. The Congressional Graveyard for Health Care Reform. In Healthy, Wealthy and Fair: Health Care for a Good Society , ed. L.D. Brown, L.R. Jacobs, and J.A. Morone, 205–234. New York: Oxford University Press.
Chapter Google Scholar
Schwartz, K., K. Pollitz, J. Tolbert, and M. Musumeci. 2020. Gaps in Cost Sharing Protections for Covid-19 Testing and Treatment Could Spark Public Concerns about Covid-19 Vaccine Costs . Available from: https://www.kff.org/health-costs/issue-brief/gaps-in-cost-sharing-protections-for-covid-19-testing-and-treatment-could-spark-public-concerns-about-covid-19-vaccine-costs/ . Accessed 11 Apr 2021.
Starr, P. 2011. Remedy and Reaction: The Peculiar American Struggle Over Health Care Reform . New Haven: Yale University Press.
Steinmo, S., and J. Watts. 1995. It’s the Institutions, Stupid! Why Comprehensive National Health Insurance Always Fails in America. Journal of Health Politics, Policy and Law 20 (2): 329–372.
Tolbert, J., K. Orgera, and A. Damico. 2020. Key Facts About the Uninsured Population . Available from: https://www.kff.org/uninsured/issue-brief/key-facts-about-the-uninsured-population/ . Accessed 8 Apr 2021.
White, J. 2013. The 2010 U.S. Health Care Reform: Approaching and Avoiding How Other Countries Finance Health Care. Health Economics, Policy and Law 8 (3): 289–315.
Further Reading
The involvement of presidents from Franklin Delano Roosevelt to Barack Obama in health care reform is vividly explored in David Blumenthal and James Morone’s (2009) The Heart of Power (Berkeley: University of California Press). Other excellent accounts of the history and politics of US health policy during the twentieth century include Paul Starr’s (2nd edition, 2017) The Social Transformation of American Medicine (New York: Basic Books), Theodore Marmor’s (2nd edition, 2000) The Politics of Medicare (London: Routledge), and Jacob Hacker’s (1996) The Road to Nowhere (Princeton: Princeton University Press).
There is a large and growing literature on the politics of the Affordable Care Act (ACA). John McDonough’s (2011) Inside National Health Reform (Berkeley: University of California Press) and Paul Starr’s (2011) Remedy and Reaction (2011) (New Haven: Yale University Press) explore the remarkable constellation of political forces and choices that led to the law’s enactment as well as the promise and limits of the ACA’s design. The post-enactment conflicts over the ACA at the state level and in the context of federalism are skillfully analyzed by Daniel Béland, Philip Rocco, and Alex Waddan’s (2016) Obamacare Wars and David Jones’ (2017) Exchange Politics (New York: Oxford University Press). Jamila Michener’s excellent (2018) Fragmented Democracy (Cambridge: Cambridge University Press) goes beyond the ACA to show how federalism reproduces inequalities in state Medicaid programs and how enrollment in such programs impact political participation by low-income beneficiaries.
Recent scholarship in American health politics has also examined the formidable barriers to controlling health care costs. Miriam Laugesen’s (2016) Fixing Medical Prices (Cambridge: Harvard University Press) and Eric Patashnik, Alan Gerber, and Conor Dowling’s (2017) Unhealthy Politics (Princeton: Princeton University Press) are exceptional accounts of the political forces that shape US health care spending. Beyond the scholarly literature, the Kaiser Family Foundation ( https://www.kff.org/ ) and Commonwealth Fund ( https://www.commonwealthfund.org/ ) are essential sources of news, data, and analysis of current issues in U.S. health care policy.
Download references
Author information
Authors and affiliations.
Department of Health Policy and Management, University of North Carolina, Chapel Hill, NC, USA
Jonathan Oberlander
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Jonathan Oberlander .
Editor information
Editors and affiliations.
Lady Margaret Hall, University of Oxford, Oxford, UK
Gillian Peele
Department of Political Science, Stanford University, Stanford, CA, USA
Bruce E. Cain
School of Social, Political and Global Studies, Keele University, Staffordshire, UK
Jon Herbert
School of Politics and International Relations, University of Kent, Canterbury, Kent, UK
Andrew Wroe
Rights and permissions
Reprints and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Oberlander, J. (2022). Health Care Reform. In: Peele, G., Cain, B.E., Herbert, J., Wroe, A. (eds) Developments in American Politics 9. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-030-89740-6_15
Download citation
DOI : https://doi.org/10.1007/978-3-030-89740-6_15
Published : 26 February 2022
Publisher Name : Palgrave Macmillan, Cham
Print ISBN : 978-3-030-89739-0
Online ISBN : 978-3-030-89740-6
eBook Packages : Political Science and International Studies Political Science and International Studies (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Search Menu
- Advance articles
- Editor's Choice
- Cover Archive
- Research from China
- Highly Cited Collection
- Review Series Index
- Supplements
- Author Guidelines
- Submission Site
- Open Access
- About The Association of Physicians
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
The american health care system, american perceptions of other health care systems, comparisons of health care systems, acknowledgements.
- < Previous
Health care reforms in America: perspectives, comparisons and realities *
*Based on a Lecture given at the John Radcliffe Hospital, University of Oxford on 6 October 2009.
- Article contents
- Figures & tables
- Supplementary Data
R.J. Glassock, Health care reforms in America: perspectives, comparisons and realities , QJM: An International Journal of Medicine , Volume 103, Issue 9, September 2010, Pages 709–714, https://doi.org/10.1093/qjmed/hcq072
- Permissions Icon Permissions
Health care reforms are now a reality in America after a long and tortuous debate. President Obama has achieved a 'victory' unlike anything seen since the term of President Lyndon Johnson, over 40 years ago. The new law brings America closer to universal coverage and access to affordable health care for its citizens, but the cost of the program and its impact on individuals, physicians, hospitals, the pharmaceutical and device industry and insurance companies is not yet fully known. The debate preceding the enactment of health care reform brought up numerous comparisons (often invidious and falsified) between the American system of health care and other systems throughout the world, including the National Health Service in the United Kingdom and Medicare in Canada. This overview examines the issues raised in the debate, perceptions of health care systems on a global basis, provides some perspectives on the reform of health care systems and examines some of the realities underlying these changes for the future of health care in America.
The great generational debate on how to reform the health care system in America came to a dramatic conclusion late in the evening of 21 March 2010 when the House of Representatives approved (by a vote of 219 to 212) a previously approved Senate version of health reform legislation. 1 Two days later, President Obama signed the landmark legislation into law and became the first President since Lyndon Johnson in 1965 to accomplish such a major change in the American health care. 2 Clarion calls for repeal and lawsuits over its constitutionality appeared quickly after the passage of this historic reform effort. As of this writing it appears that the law may become a significant factor in the mid-term elections of 2010. Issues such as payment for abortion, mandates on individuals and companies to purchase or provide insurance with penalties (‘play or pay’), new regulatory requirements on insurance companies, costs of the new programs and how to pay for them, and the impact of reform on a burgeoning federal budget, including deficits continue to be discussed. Underlying this post-passage debate is the very real and pervasive effect of a slowly reversing recession and continued high unemployment rates. The nature of the debate that preceded passage has had a polarizing effect on American political discourse that will be a challenge, perhaps the greatest one, facing the young administration of President Obama. This grand debate on health care reform proved to be tortuous, partisan and often rancorous; full of accusations and counter-accusations, distortions and invidious comparisons; and burdened by the enormous complexity of the American health care system itself and the environment (a generational economic recession) in which an attempt at change was initiated.
The stakes in health care reform are enormous. Health care in America in 2009 consumed about one in every six dollars ($2.3-Trillion total) of the gross domestic product (GDP) and the costs are rising at a pace that greatly exceeds general inflation, although the rate of rise has attenuated somewhat since 2006. The venerated Medicare program, a government-funded but privately administered (though fiscal intermediaries) health insurance program for 15-million elderly (over 65 years of age) and disabled citizens (including over 500 000 Americans with end-stage renal disease), is predicted to be insolvent by 2017 or earlier. Medicare spending varies widely in America depending on health status, income level and other regional factors. 3 A promise to slow the projected growth of the Medicare program may delay insolvency, but will be difficult to actually accomplish. The Medicaid program, funded jointly by the Federal and State governments, provides care for ∼13-million individuals below a designated ‘poverty level’ of income, is severely strained by the economic crisis and is already greatly underfunded. Payment rates currently in Medicaid are so low than many doctors and hospitals eschew participation, as is their right. The new law will greatly increase the number of Medicaid recipients and thus will require an even greater transfer of federal funds to the states. Premium payments for private (non-governmental) insurance are skyrocketing, and many employers who pay a large portion of the premium costs, are balking at payment increases since these additional costs reduce their competitiveness on the world economic stage. The impact of the new law, and its provisions of new regulations governing private insurance, on the rate of rise in private insurance premiums is not yet known, but many believe that these rates will continue to escalate. Overall expenditures for health care in America have been rising steadily and dramatically, from 6% of GDP in 1965 to almost 17% in 2009 and projected to increase to over 20% of GDP by 2015. The escalating costs are fueled in large part by over abundant use of expensive high-technology, new and costly brand-name pharmaceuticals (including drugs that basically replicate the effects of already available drugs), limits on the availability of generic drugs and the accelerating aging of the society at large. Litigation costs of medical negligence claims and the practice of ‘defensive medicine’ have made a relatively minor impact on rising expenditures, despite the claims of organized medicine to the contrary. 4 The fundamental ‘fee-for-service’ model thrives on volume not on quality or efficiency of medical case. All of this has occurred while the uninsured (or underinsured) class has burgeoned to over 47-million individuals, including ∼13-million undocumented (non-citizen) persons (‘illegal aliens’). The new law will provide coverage by making subsidies available to purchase health insurance at affordable rates to ∼32-million of these previously uninsured or under-insured individuals, leaving only the undocumented aliens without some form of either public or private insurance.
The picture of the ‘health care system’ in America that emerged as the debate proceeded was not a pretty one, and the new law seems on the surface to be a step in the direction of correcting many of its most glaring deficiencies, but the fine details of the new law will only become apparent as its provisions are ‘rolled-out’ over the next 5–10 years. The desire to introduce reform into the health care system is not new to American politics. Indeed, for the last 80 years every President has half-heatedly or enthusiastically supported reform beginning with Franklin Delano Roosevelt who attempted, unsuccessfully, to include ‘universal health care’ as a part of his social security program enacted during the ‘great depression’ of the 1930’s.
The ‘dysfunctional’ American health care system that exists in 2010 and is about to undergo its most dramatic change in over 45 years can best be described as a unique hybrid of: (i) privately owned (for-profit) health insurance entities (largely employment driven); (ii) government funded but privately administered insurance plans for the elderly and disabled (Medicare); (iii) a State–Federal insurance program for a portion of the poor (Medicaid); (iv) a mixture of Federal government owned and operated systems (veterans administration, military and Indian health service hospitals and clinics); (v) a scattering of not-for-profit entitles owning hospitals and staffed by salaried physicians (e.g. the Kaiser Permanente System); and (vi) a conglomeration of locally supported (through taxation of the citizens) public hospitals and clinics, largely serving the poor and the uninsured (including non-citizens). Employment-based health insurance (self-insured or purchased via employer from an insurance company) currently accounts for over 60% of the health insurance coverage in America USA (see also Figure 1 ). 5
Health care coverage in America. 5
This ‘patchwork system’ has evolved over many decades. Its individual components are not well integrated. Its ‘fee-for-service’ approaches to payment encourages the dominance of high-technology oriented specialty practice and threatens the viability of primary care practice, by economically dis-incentivizing new entrants into this vital part of an integrated system of care. Control of burgeoning costs in the overall system has resisted mostly half-hearted efforts. Only a few sub-systems have been successful in melding specialty with primary care practice in ways that both control costs and provide tangible benefits of integrated care to subscribers. One of the great anachronisms of the American system was that unlike nearly all other health care systems in the industrialized world, it continued to adhere to the notion that access to affordable health care is a privilege and not a fundamental right for its citizenry. The enactment of the new law partly corrects this persistent anomaly in arguably one of the richest and most developed countries in the world.
Thus, reform of the ‘dysfunctional’ and ‘economically unsustainable’ American health care and health insurance systems has focused on changing the insurance rules, attempting to curtail the ever-escalating costs, and extending coverage to as many citizens as possible—all without fundamentally altering the ‘hybrid’ system of organization, dominated by ‘fee-for-service’ payment methods. Consideration of a single payer system of universal coverage (like Medicare in Canada) and a Federally owned and operated system of universal coverage [like the National Health Service (NHS) in the UK] were quickly rejected as not fitting the American model of ‘free-enterprise’ and were vigorously opposed by political conservatives who believe in limiting government intervention into fundamentally private matters, such as access to and choice of health care providers. Throughout the debate leading to enactment of the new law intense lobbying efforts by stakeholders (organized medicine, hospital associations, insurance entities, pharmaceutical companies, state and local government leaders, constituency groups, labour unions and the like) shaped the structure and complexity of the final legislation. In the end, each gave some and received some (or more than they gave), and the new law remedies some inequities but it creates others. Whether any reform will be successful in restraining the rising and unsustainable costs of health care remains be seen, although promises have been made. Keeping these promises will be another matter for another time.
One of the most striking aspects of the long and rancorous debate over health care reform in America was how the health systems in other countries were characterized and in many instances defamed in the media and in ‘town-hall’ style gatherings. For example, the single-payer, universal coverage Medicare system in Canada, managed at a provincial level in a prospective budgeting process, was widely characterized as ‘rationing by the queue’. Citizens of Canada sacrificed immediate access to a provider of their choice for the assurances that everyone would be covered but not necessarily at their beck and call. Canadians were described as ‘unhappy’ with their system and ‘flocking in droves’ to America for needed care. At the same time many American citizens were sending their prescriptions to Canada to avoid the high costs of drugs prevalent in the American system.
The NHS in England was also characterized, unfairly in my view, as understaffed, underfunded, operated by an inefficient and impersonal bureaucracy, within antiquated facilities having few amenities, with long-waiting times for elective procedures, limiting care for the elderly, lacking in freedom of choice of providers, and practicing covert ‘rationing by the queue’ as well as overtly, via the National Institute for Clinical Excellence program of comparative effectiveness evaluation linked to funding for drugs and procedures. At the same time, in America, comparative effectiveness research was being strongly encouraged by both federal and private funds. 6 In addition, clinical practice guidelines promulgated by professional societies and organizations were growing industries in the USA and elsewhere, but in general these were divorced from cost considerations.
In a fascinating, recently published and sometimes poignant book 7 (also called ‘naive’ by one reviewer 8 ), Washington Post correspondent. T.R. Reid provides unique insights and a wealth of historical information on how the ‘systems’ of health care coverage evolved in the various countries of world. 7 Reid notes that the beginning of health care systems can be traced to the ‘Iron Chancellor’ Otto von Bismarck’s pioneering social system inaugurated in Germany in 1883. The Bismarck model, as it is now known, uses a private but not-for-profit system of tightly regulated insurers jointly financed by employer and employee (or subsidized by the Federal government for the unemployed). Both doctors and hospitals are private entities and patients are given free-choice of plans and providers in a tightly regulated system of fees and re-imbursement. The creation of the NHS by Aneurin ‘Nye’ Bevan and Clement Atlee in the UK in 1948 brought forth a new system, known as the Beveridge model after Lord William Beveridge who virtually single-handedly wrote the landmark report in 1942 upon which the NHS was built. Unlike the Bismarck system, most facilities are owned and operated by the government and many providers (except General Practioners; GP) are employees of the NHS. Universal coverage is provided through taxation and a tightly regulated (and highly politicized) budgetary system. ‘Free at the point of delivery’ is a frequently repeated mantra. General practioners contract with the government for global care of panels of patients and access to specialists is controlled. A parallel private system of insurance has evolved but is used by only a minority of citizens. A third model also arose in the post-WW-II period in Canada, created first by Thomas ‘Tommie’ Douglas in the province of Saskatchewan in 1945 and Canada-wide in 1961 called Medicare . It is a universal coverage program in which the central government provides (via the Provinces) a national ‘single-payer’ health insurance in a tightly regulated budgetary system. ‘Out of plan’ care is allowed, as in the NHS. Doctors and hospitals are mostly private. A final ‘model’ system is also described by Reid; the ‘Out-of-Pocket’ model in which the care is provided on a cash basis—those without cash generally go un-served or depend on intermittent and episodic acute care in emergency rooms or charity clinics and hospitals. Outside of America the Bismark plan, or one of its variants, has been the most popular.
In America, all of these models can be found in some form. For the employed, under age 65 years it is like Germany (or France and Japan) except most insurance plans are for-profit (The new law puts a ‘cap’ on administraive cost); for the over 65 year age group, it is like Canada (or South Korea or Taiwan); for the Native Americans, Military or Veterans it is like the UK (and Cuba); and for the unemployed and uninsured it is like many countries that do not have an organized system of public health insurance, such as India, most parts of China and in equatorial Africa. In America, there are also a few models that resemble the NHS—the Kaiser-Permanente System and the Puget Sound Health Care system. These systems adopt an employed staff-model of managed care within a not-for-profit ownership system of hospitals and clinics linked to a premium-based insurance plans. Care is provided in a highly integrated system of primary care physicians and specialists. A full-range of services is available either within the system or on contract to other providers.
Of all of these, the Bismarck model provides the greatest choice of providers except when insurance and care is provided under one corporate umbrellas as is the case in some parts of Japan. The Bismarck model as applied in France is very highly regarded for ease of access, extent of coverage, overall cost, integration of health information systems (‘Carte Vitale’) and outcomes. The health care systems in the Netherlands and in Northern European countries are also highly esteemed and emulated. 9
However, regardless of the model system employed, there is general agreement, and much angst, that pressures of escalating cost (largely due to high use of advanced technology) are straining budgets and that rationing of care (either covert or overt) is increasing. Cost-containment remains as an over-riding issue in all systems of care, despite incremental reforms, including the new law in America. No effective plans for controlling ever-spiraling upward costs have yet been put in place—the new law in America is no exception. Government-sponsored universal health care systems, such as those in Canada, are reconsidering a role for private health care and have been largely unsuccessful in reducing costs.
The American hybrid system is viewed by many as fragmented, chaotic, difficult and complex to navigate, and harboring some disturbingly unfair insurance practices. Some of these may eventually be corrected by implementation of the new law, aptly called the Patient Protection and Affordable Care Act (PPAC). Despite its shortcomings, 60–70% of Americans are ‘satisfied’ with their health care, according to polling results. The American system remains as specialty and fee-for-service dominated, expensive (over $7600 per capita per year), and high-technology oriented. Primary care is poorly integrated and electronic information systems are crude and underutilized. Prevention often takes a distant third place behind diagnosis and treatment in priorities for care. It is litigious, profit-driven and rife with ‘defensive-medicine’ and entrepreneurial practices. 10 Extra-ordinarily wide geographic variation in costs are well documented, 3 and not directly related to quality of care, which is mediocre in too many and excellent in too few sites. Until enactment of PPAC access to affordable care was not guaranteed to everyone leading to de facto rationing based on ability-to-pay. The main governmental support systems for health care are bordering on insolvency and without dramatic changes will be ‘bankrupt’ in the next decade. The bright spots are that America continues as a center of innovation and experimentation in new ways to deliver excellent care efficiently and inexpensively, is a training ground for some of the best doctors in the world and is a major site for research and development of new drugs and procedures. Non-Americans view the American system as wasteful of precious resources, full of redundant capacity, woefully insufficient in terms of access to primary care, only average in overall quality compared to cost (poor in value) and unconscionably out of step with the industrialized nations of the world by denial of the fundamental right to affordable health care for all of its inhabitants. The last of these justifiable criticisms has been, at least in part, corrected by the enactment of the new law.
The reforms signed into law by President Obama charts a new and uncertain path for the unique hybrid American health care system, and may inadvertently create a panoply of new issues. The overall costs of care and the efficiency of the system in which care is delivered will come under increasingly harsh scrutiny, particularly as the unsustainable costs of health care become more evident in each succeeding year. Crossing the moral divide and providing access to basic and affordable health care to nearly all its citizens is perhaps the most significant step taken by America in 2010, even though 13-million persons, mainly undocumented aliens, will likely remain outside the system. Improved emphasis on preventative care, comparative cost effectiveness and electronic medical records might help stem the oncoming financial tidal wave but the long-term economic benefits of these steps is far from clear. Universal health care provided by a single governmental organization seems quite unattainable at present. Fear of uncontrollable budget deficits, added tax burdens and a ‘government’ takeover of one-sixth of the nation’s economy have provided major, and perhaps crucial, resistance to change. Maintenance of free choice of providers, preservation of physician autonomy and reform of the litigation system of injury from sub-standard care is also high on the agenda.
The future of the American health care system, as reformatted by the new law, can only be seen dimly as the implementation phase shifts into gear. 11 Retention of the antiquated fee-for-service reimbursement system seems destined to fuel further cost inflation. The effect of mandates (‘play or pay’) on employees, individuals and employers to purchase or provide health insurance and the eventual costs to business is hard to estimate but early data suggests that health care insurance premiums will rise. Opening the flood-gates for issuance of millions of new insurance policies, heavily subsidized by federal and state governments, will only intensify the precarious state of the governmental systems, already strapped for cash. What the broadened access to medical care will do to the insurance industry, the public and private hospital systems and to a medical establishment already bereft of primary care providers can only be guessed. A serious shortage of primary care providers already exists in America, and the effect of new incentives for newly minted doctors to enter primary care instead of specialty careers is largely unknown. Trillions of dollars will have to be extracted from current programs over the next decade or so in order to pay for the newly insured without promoting unsustainable new budget deficits. Will future Congresses and Administrations have the courage to make these cuts and deal with the pain they will create in their constituencies? Only time will tell. It does appear likely that health care reform in America will have to be revisited soon and repeatedly to resolve the issue of costs in a way that promotes value and rational use of limited resources. Stay tuned.
The author is indebted to Dr Alan Hull, Dr Christopher O’Callaghan and Dr Christopher Winearls and to Mr Charles Baird for their review of an earlier version of this manuscript and their many helpful suggestions.
Google Scholar
Google Preview
Author notes
- health care reform
- universal health insurance
- statutes and laws
- pharmacy (field)
- health care systems
- medical devices
- national health service (uk)
- barack obama
Email alerts
More on this topic, related articles in pubmed, citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1460-2393
- Print ISSN 1460-2725
- Copyright © 2024 Association of Physicians of Great Britain and Ireland
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Featured Clinical Reviews
- Screening for Atrial Fibrillation: US Preventive Services Task Force Recommendation Statement JAMA Recommendation Statement January 25, 2022
- Evaluating the Patient With a Pulmonary Nodule: A Review JAMA Review January 18, 2022
- Download PDF
- CME & MOC
- Share X Facebook Email LinkedIn
- Permissions
The US Medicaid Program : Coverage, Financing, Reforms, and Implications for Health Equity
- 1 Department of Health Policy and Management, University of Pittsburgh School of Public Health, Pittsburgh, Pennsylvania
- 2 Grantmakers In Health, Washington, DC
- 3 Department of Government and School of Public Policy, Cornell University, Ithaca, New York
- Editorial Medicaid as a Driver of Health Equity Alice Hm Chen, MD, MPH; Mark A. Ghaly, MD, MPH JAMA
- Viewpoint Assessing Health Outcomes Attributable to Medicaid Expansion At 5 Years Heidi Allen, PhD, MSW; Benjamin D. Sommers, MD, PhD JAMA
- Viewpoint A Blueprint for Comprehensive Medicaid Reform Rebekah E. Gee, MD, MPH; David Shulkin, MD; Iyah Romm, BS JAMA
- Viewpoint Value-Based Care in the Center for Medicare and Medicaid Innovation John E. McDonough, DrPH, MPA; Eli Y. Adashi, MD, MS JAMA
- Viewpoint Medicaid’s Moment for Protecting and Promoting Women’s Health Mohammad Hussain Dar, MD; Charissa Fotinos, MD, MS; Christopher R. Cogle, MD JAMA
Question Who does Medicaid insure, how is the program financed and delivered, how have policies evolved, and how could reforms address racial and ethnic health equity?
Findings In 2022, Medicaid insured approximately 80.6 million individuals (56.4% from racial and ethnic minority groups in 2019). In 2020, estimated Medicaid spending was $671.2 billion (16.3% of total US health spending). The proportion of beneficiaries enrolled in Medicaid managed care was 69.5% in 2019, 45 states have pursued 139 Medicaid delivery system reforms from 2003 to 2019, and 38 states and Washington, DC, have expanded Medicaid under the Affordable Care Act. Racial and ethnic health disparities are common within Medicaid, and evidence on the association of Medicaid policies and reforms with achieving racial health equity remains limited.
Meaning Medicaid is an important source of insurance and accounts for substantial health care spending. Medicaid reforms have expanded coverage and provide further opportunities to reduce disparities and address health inequities.
Importance Medicaid is the largest health insurance program by enrollment in the US and has an important role in financing care for eligible low-income adults, children, pregnant persons, older adults, people with disabilities, and people from racial and ethnic minority groups. Medicaid has evolved with policy reform and expansion under the Affordable Care Act and is at a crossroads in balancing its role in addressing health disparities and health inequities against fiscal and political pressures to limit spending.
Objective To describe Medicaid eligibility, enrollment, and spending and to examine areas of Medicaid policy, including managed care, payment, and delivery system reforms; Medicaid expansion; racial and ethnic health disparities; and the potential to achieve health equity.
Evidence Review Analyses of publicly available data reported from 2010 to 2022 on Medicaid enrollment and program expenditures were performed to describe the structure and financing of Medicaid and characteristics of Medicaid enrollees. A search of PubMed for peer-reviewed literature and online reports from nonprofit and government organizations was conducted between August 1, 2021, and February 1, 2022, to review evidence on Medicaid managed care, delivery system reforms, expansion, and health disparities. Peer-reviewed articles and reports published between January 2003 and February 2022 were included.
Findings Medicaid covered approximately 80.6 million people (mean per month) in 2022 (24.2% of the US population) and accounted for an estimated $671.2 billion in health spending in 2020, representing 16.3% of US health spending. Medicaid accounted for an estimated 27.2% of total state spending and 7.6% of total federal expenditures in 2021. States enrolled 69.5% of Medicaid beneficiaries in managed care plans in 2019 and adopted 139 delivery system reforms from 2003 to 2019. The 38 states (and Washington, DC) that expanded Medicaid under the Affordable Care Act experienced gains in coverage, increased federal revenues, and improvements in health care access and some health outcomes. Approximately 56.4% of Medicaid beneficiaries were from racial and ethnic minority groups in 2019, and disparities in access, quality, and outcomes are common among these groups within Medicaid. Expanding Medicaid, addressing disparities within Medicaid, and having an explicit focus on equity in managed care and delivery system reforms may represent opportunities for Medicaid to advance health equity.
Conclusions and Relevance Medicaid insures a substantial portion of the US population, accounts for a significant amount of total health spending and state expenditures, and has evolved with delivery system reforms, increased managed care enrollment, and state expansions. Additional Medicaid policy reforms are needed to reduce health disparities by race and ethnicity and to help achieve equity in access, quality, and outcomes.
- Editorial Medicaid as a Driver of Health Equity JAMA
Read More About
Donohue JM , Cole ES , James CV , Jarlenski M , Michener JD , Roberts ET. The US Medicaid Program : Coverage, Financing, Reforms, and Implications for Health Equity . JAMA. 2022;328(11):1085–1099. doi:10.1001/jama.2022.14791
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Open access
- Published: 04 August 2022
What next for the polyclinic? New models of primary health care are required in many former Soviet Union countries
- Nigel Edwards 1 &
- Igor Sheiman ORCID: orcid.org/0000-0002-5238-4187 2
BMC Primary Care volume 23 , Article number: 194 ( 2022 ) Cite this article
2511 Accesses
Metrics details
There is unfinished reform in primary care in Russia and other former Soviet Union (FSU) countries. The traditional ‘Semashko’ multi-specialty polyclinic model has been retained, while its major characteristics are increasingly questioned. The search for a new model is on a health policy agenda. It is relevant for many other countries.
In this paper, we explore the strengths and weaknesses of the multi-specialty polyclinic model currently found in Russia and other FSU countries, as well as the features of the emerging multi-disciplinary and large-scale primary care models internationally. The comparison of the two is a major research question. Health policy implications are discussed.
We use data from two physicians’ surveys and recent literature to identify the characteristics of multi-specialty polyclinics, indicators of their performance and the evaluation in the specific country context. The review of the literature is used to describe new primary care models internationally.
The Semashko polyclinic model has lost some of its original strengths due to the excessive specialization of service delivery. We demonstrate the strengths of extended practices in Western countries and conclude that FSU countries should “leapfrog” the phase of developing solo practices and build a multi-disciplinary model similar to the extended practices model in Europe. The latter may act as a ‘golden mean’ between the administrative dominance of the polyclinic model and the limited capacity of solo practices. The new model requires a separation of primary care and outpatient specialty care, with the transformation of polyclinics into centers of outpatient diagnostic and specialty services that become part of hospital services while working closely with primary care.
The comprehensiveness of care in a big setting and potential economies of scale, which are major strengths of the polyclinic model, should be retained in the provision of specialty care rather than primary care. Internationally, there are lessons about the risks associated with models based on narrow specialization in caring for patients who increasingly have multiple conditions.
• The Semashko polyclinic model has lost strengths due to excessive specialization.
• Solo and group PHC practices are no longer suitable to manage multimorbidity.
• A new ‘extended general practice’ reorients the health system towards PHC.
• Restructuring polyclinics is possible by transforming them into outpatient specialty units of hospital structures.
Peer Review reports
In the former Soviet Union (FSU) and some Central and Eastern European (CEE) countries, the traditional ‘Semashko’ Soviet multi-specialty polyclinic model, originally developed in the 1930s, has been retained [ 1 ]. However, in many rural and some urban areas of FSU countries, the traditional polyclinic model shifted towards solo and group primary care practices in the 1990s in response to policymakers’ demands for stronger primary health care (PHC). This shift towards solo and group practices continues today in many countries of this region [ 2 ].
The existing PHC models are currently facing a number of challenges. The professionals running standalone practices are struggling to respond to a growing proportion of people with multi-morbidity and complex healthcare needs, in a context of underdeveloped and underfunded supportive services, such as social care, rehabilitation, long-term care and palliative care [ 3 ]. While in theory, the mostly urban polyclinic-based generalists could be delivering more comprehensive care, in practice, patients seek out ‘narrow’ specialists based in polyclinics (cardiologists, neurologists, etc., further referred as specialists) instead for the management of relatively common conditions that would be in the scope of PHC providers in other countries [ 1 ]. Neither the polyclinic approach taken in urban areas nor the rural solo/group practice are functioning well and new approaches are needed.
In this paper, we focus on the Russian Federation and consider a number of questions that policy makers, payers and medical leaders could discuss when planning changes to their services. Firstly, what are the current strengths and weaknesses of the polyclinic model currently found in Russia and other FSU countries and does this mean that there are some aspects that should be preserved. Secondly, what are the features of the emerging multi-disciplinary and large-scale primary care models internationally. Thirdly, which elements of the new models of primary care could be adapted to the Russian and other similar settings. We argue the case that polyclinics should be transformed – not into the model of standalone or small group practices that is common – but instead into the ‘extended general practice’ model seen across Europe that re-orients the health system towards comprehensive PHC delivered by multi-disciplinary teams.
The evidence on the strengths and weaknesses of the polyclinic model set out in this paper is based on a review of the literature and two physician surveys. The review is focused on: a) determining characteristics of multi-specialty polyclinics in Russia, indicators of their performance and the evaluation in the specific country context; b) description of the emerging extended PHC practices internationally; c) comparison of the two models. We searched MEDLINE using the query: (Ambulatory Care Facilities[mh] OR polyclinic) AND (model OR type OR semashko) AND (USSR OR russia OR europe OR european union) AND 1990:2022[dp]. 1614 findings were checked manually and 36 were relevant. We also used sources snowballed from these reports and the grey literature related to Russian health care, including those in limited circulation, unpublished documents, memorandums, and presentations from our personal collections covering more than twenty years.
The surveys of Russian physicians are designed to explore the managerial environment for their performance of the staff in polyclinics. Firstly, the managerial control is evaluated via questions like: Is the number of patient visits planned by the polyclinics’ administrators? Does the failure to implement plans can cause a reduction in physicians’ remuneration? Who determines the average length of a patient visit and what happens if it is regularly violated? Are physicians involved in managerial actions to improve the performance of polyclinics?
Secondly, we assess the level of physicians’ clinical autonomy. The examples of questions: Do you select patients for check-ups and screening or rely on administrative decisions? Do your referrals to hospital admissions and CT/MRI tests require the authorization of polyclinics administrators? Which indicators of performance are used for your reporting to the administration?
Thirdly, teamwork and coordination of providers in polyclinics is evaluated. We ask questions about their joint planning of curative activities, inter-discipline consultations and training sessions, as well as the leading role of district physicians in the team—in joint planning and managing chronic cases.
International comparisons of primary care performance are based on the national and OECD databases.
A small-scale survey of polyclinics’ physicians was conducted in January 2020 in three urban polyclinics in Moscow city and Moscow oblast (the region near Moscow). They represent a big multi-specialty urban polyclinic with an average number of staff of around 80–90 health workers. In Moscow city, these polyclinics have been consolidated into bigger outpatient centers with three to five polyclinics each. But this new level of administration was not taken into account, to reflect the usual pattern of administration of polyclinics in Russian big cities. The questions relate only to the staff of individual polyclinics (not their amalgamation). The special area of interest is the attitude of generalists and specialists. A list of 13 questions (appendix 1 ) was sent to all three polyclinics’ physicians through the Russian social network “Vkontakte”. This survey was anonymous, respondents were not compensated and were reassured that any negative feedback would not affect them. The postgraduate students of the National Research University Higher School of Economics (Moscow) dispersed the survey. It was sent to 129 physicians, 103 physicians (80%) responded, including 67 district physicians and 37 specialists. The questionnaire had the same questions to all respondents, and the latter were required to answer all questions by the design of the survey. Therefore, the response rate was the same for all questions. Similarly, the fraction of participants and respondents was the same for each question. Ten physicians on the list were randomly selected and approached directly for face-to-face interviews.
This small-scale survey doesn’t represent all physicians in the country, but it can provide additional evidence to our observations on the limitations of professional autonomy in polyclinics. Some questions from this survey were also used in our recent study of the national preventive program [ 4 ].
This survey was designed to receive more detailed evidence of the level of interaction between professionals in polyclinics, including the exchange of information about patients’ emergency calls, the level of awareness of patients’ hospital admissions, the involvement of polyclinics' physicians in the rehabilitation activities after hospital admissions of stroke and heart attack cases. A special area of interest is the referral pattern of district physicians: what is the share of first visits that is referred to specialists?
The second survey was conducted online in October 2020 in the middle of the COVID-19 pandemic through the mobile ap “Handbook of Physician” (available in Google Play and AppStore) with 540 thousand registered users. 2316 physicians responded to the survey. They represented 81 of 85 regions of the country. 1118 respondents worked in polyclinics (48%), 1068 – in hospitals (46%), the rest – in other settings. Since the survey was designed to look at broader issues of service integration (between polyclinics, hospitals, emergency care centers, etc.), we selected respondents that worked in polyclinics and studied their responses to the questions about the level of integration within polyclinics. All questions were asked with the note “in regular conditions of work before March 2020”. This part of the questionnaire is provided in appendix 2 .
Survey 2 covers generalists and specialists in the staff of polyclinics in practically all types of primary care settings in Russia which vary in size. A high popularity of the ap in all Russian regions and a substantial number of respondents that represent various medical organizations and physician specialties make the survey a reliable instrument of the study.
The polyclinic model
The polyclinic model was established in the USSR in the early 1930s and inherited by FSU and some CEE countries. The polyclinic is a multi-specialty entity providing both primary care and most outpatient specialty care. Typically, there are separate clinics for adults and children and each has a catchment area and a patient list managed mostly by district therapists, district pediatricians and general practitioners (GPs) – all of which are collectively referred to as ‘district physicians’ (DPs). Mental health care is not provided by this service – this is the area of specialty organizations. GPs with a broad task profile are only emerging and account for only 15% of DPs. The catchment population of polyclinics in big urban areas ranges from 30,000 to 120,000 people [ 5 ].
People can choose a polyclinic, and most choose the provider closest to their place of residence. Patients enrolled in a polyclinic form the patient list. According to federal regulations, DPs and GPs act as gatekeepers and refer patients to specialists and hospitals. But many regions loosen the requirements of gatekeeping: patients increasingly see specialists directly without a referral from primary-care physicians.
There has been a trend towards specialization within PHC since the 1990s. The Semashko model of a district unit with mainly a district physician has given way to multi-specialist polyclinics, which currently employ 15–20 categories of specialists in big urban areas (including for example, cardiology, gynecology, surgery, etc.), and three to five categories in small cities. Rural and small city areas are served mostly by small solo practices. Outpatient specialists account for around two-thirds of polyclinic staff and service activity [ 5 ]. It is important to note that the increased professional diversity of the polyclinic staff has been based on a growing number of medical specialists rather than nurses and other allied health professionals. The role of nurses is limited to non-clinical functions. The nurses to physicians ratio is only 2.1, as against 3.0 in Germany, 3.8 in Canada and 4.3 in the US ([ 6 ], p.179).
Legislation defines the polyclinic as a PHC model, which consists of ‘primary physician service’ (care provided by DPs) and ‘specialty primary care’. The latter includes some care equivalent to that provided by outpatient specialists in Western countries, but also care that is effectively managed by family doctors elsewhere, for example, angina and type 2 diabetes.
The governance of polyclinics is highly centralized. The regional health authority appoints directors of polyclinics and manages their performance, most of the rules and patterns of care provision are set by the federal Ministry of Health. The administration of polyclinics is a multilayered structure: a director, a medical director, a few deputies, the head of the district unit, and heads of specialty and diagnostic units. Most polyclinics are state owned and staffed with salaried medical personnel. The growing private sector is also based on this model.
The majority of a polyclinic’s financial revenue is derived from a regional mandatory health insurance (MHI) fund on a capitation basis. But the revenue of a polyclinic can be reduced if it has not reached a minimum number of visits. This target is set and controlled by the regional health authority and MHI fund (which jointly act as a purchaser of care). When there is a risk of not reaching a planned number of visits, the administration of polyclinics has to encourage multiple referrals of patients. Polyclinics’ preventive services are paid for on a fee-for-service basis. The rates of payment are set for a fixed package of services under a so called “program of dispensarization” (a nation-wide vertical program of check-ups and screenings). The control of the actual number of preventive services is conducted by MHI funds and administration of polyclinics. While this method of payment motivates physicians to implement the program, it limits their professional autonomy on the choice of preventive services for an individual. They have to provide the entire bundle of services to be reimbursed, irrespective of the actual need of a patient [ 4 ].
The salary of medical personnel has fixed and variable parts. The latter is based on some pay-for-performance indicators, including the number of visits managed by the individual physician, number of patient complaints and some preventive services. The variable part is determined individually by administration.
Evaluation of the model
There is an unfavourable context for the operation of the urban polyclinic model in modern Russia. There are low levels of health funding (currently, public funding is around 3.5% of GDP), there is a 30% shortage of district therapists, structural distortions in the workforce which are explored below, a hospital-centred model and little focus on chronic disease management [ 7 ].
A major strength of the model is its capacity to provide an easy access to primary and specialist care, at least in theory. Patients can see a DP, receive diagnostic services and have consultations with specialists ‘under one roof’. Specialists may or may not be located in the same premises. But even if they are, this does not mean that patients can have tests and see specialists the same day. This process usually takes weeks because of the shortage of specialists [ 7 ].
Polyclinics have a number of potential advantages due to the consolidation of service delivery. These include additional leverage to implement care pathways and shared use of capital investment resources. Polyclinics can also centralize administrative and support services, with potential economies of scale. Furthermore, large settings can redistribute resources across geographic areas through setting up small branches in remote areas and polyclinic workers can stand in for each other in case of illness or holidays. There is evidence that these strengths are not fully realized in Russia and managerial action is needed to deal with this [ 8 ].
Another potential strength of the polyclinic model is better financial sustainability relative to solo and group practices. The model has enabled the introduction of a fundholding scheme in some regions of Russia, with polyclinics as major financial risk-bearers. Within a short period of its implementation (four to five years in most regions), this has allowed strong economic incentives to be used to increase the role of PHC in the health system [ 5 ].
The larger scale of polyclinics also allows them to respond to national health programs more effectively. For example, larger scale has allowed the implementation of the recent federal program called “Resource-saving polyclinics” that covers most big polyclinics in the country. The objective is to improve the efficiency of internal processes through new appointment systems, separation of patient flows across individual providers, improve electronic communication and develop better organization of the working space, etc. These innovations are more cost effective in big settings. The response to COVID-19 is also facilitated by large-scale facilities.
There are, however, a number of major weaknesses of the polyclinic model.
First, strong administrative pressure on physicians in polyclinics and their limited professional autonomy . Physicians are poorly involved in the management of polyclinics. They work according to the rules determined by polyclinics’ administrators, who in turn follow the commands of the federal and regional health authorities. Administrators set DPs’ catchment areas, plan the number of patient visits, develop the norms for the average length of a patient visit, determine the scope of preventive services and their coverage, ration expensive diagnostic resources for each physician and approve referrals to hospital.
The first survey provided evidence of managerial control and limited professional autonomy:
66% of physicians reported that plans for the number of patient visits are developed by the polyclinics’ administrators. Only 34% plan this activity themselves.
59% indicated that the failure to implement plans on the number of visits can cause a reduction in their remuneration.
66% reported ‘administrative action’ if the norms for the average length of a patient visit are regularly violated.
Only 25% of physicians select patients for check-ups and screening programmes themselves after assessing their risk factors. The rest rely on administrative decisions on the targeted populations. The share of those who select patients for chronic disease management themselves is higher though – 69%.
Just under 50% reported that their referral of patients to hospital requires the authorization of heads of specialty units, 15% – the deputy director, 12% – medical commissioners and 6% – other actors. There is a similar distribution of responses for the authorization of CT and MRI referrals.
28% of respondents reported administrators’ ‘excessive administrative regulation’ of clinical decisions.
Second, the loss of the primary care providers’ leading curative and coordination roles . In Russia, DPs are traditionally seen as gatekeepers for access to specialty services. Theoretically, they are supposed to act as a patient’s guide through the health system and ensure continuity of treatment. However, a high level of polyclinic care specialization distorts the coordination role of primary care providers. In a big multi-specialist entity with a growing division of labour and many specialists working together, many traditional curative functions of DPs are delegated to specialists. It is hard for DP to resist the temptation to refer a patient to a specialist next door. Clinical recommendations, pathways and quality control actors tend to incentivise specialist consultation. Polyclinics’ administrators often encourage referrals to specialists to meet the specified minimum number of visits. The task profile of DPs’ curative work therefore gradually narrows. They deal with a few simple diseases, and the majority of patient care (even gastritis, ulcer, bronchitis) is managed by specialists [ 5 ]. Contrary to GPs, district physicians are allowed to practice without postgraduate training. As a result, a DP’s coordination role also narrows.
The first survey provides the following evidence of a lack of cooperation and coordination in the urban polyclinic:
35.5% of DPs said that the development of plans for the joint management of cases by DPs and specialists did not occur, 45.2% said it ‘rarely’ occurred, 9.7% said it ‘sometimes’ occurred and only 1.6% said it ‘always’ happened. This is contrary to the expectation that a big entity facilitates joint working.
Training sessions for DPs with the involvement of specialists were reported as a regular event by only 4% of polyclinics’ physicians, as a rare event by 35%, while the rest of the respondents indicated their absence.
Only 3.2% of respondents reported medical case conferences as a regular event.
This survey allows us to determine a task profile of DPs and their role in a multi-specialty team:
Only 29,7% of DPs reported that they referred to specialists less than 10% of patients, that is had referral patterns similar to European GPs who referred from 5 to 15% of patients to specialists [ 2 ]. The bulk of Russian physicians referred every second patient to specialists, indicating an excessive specialization of primary care and a limited task profile of generalists. Unsurprisingly, only 26% of DPs reported themselves as “captains of the team” in joint planning of curative activities.
The second survey provides a more detailed evidence of a level of integration in Russian polyclinics. Its results were compared with similar estimates made in 2012 [ 9 ].
An important indicator of the interaction of polyclinics and hospitals is the level of information exchange between them. Only 19.6% of respondents said that their polyclinics received the information about all hospital admissions of patients in their catchment area in 2020; 18.5%—didn’t receive it at all; 23.9% could not answer this question, which was close to the negative answer. The level of physicians’ awareness of hospital admissions in 2020 was even less than in 2012 (Fig. 1 ). This in turn complicates the continuity of care after hospitals admissions. The survey indicates that even for “catastrophic” cases of a stroke or a myocardial infarction the practice of visiting patients within the first days of their hospital admission is not common: it is reported only by 45.5% of respondents (Fig. 2 ).
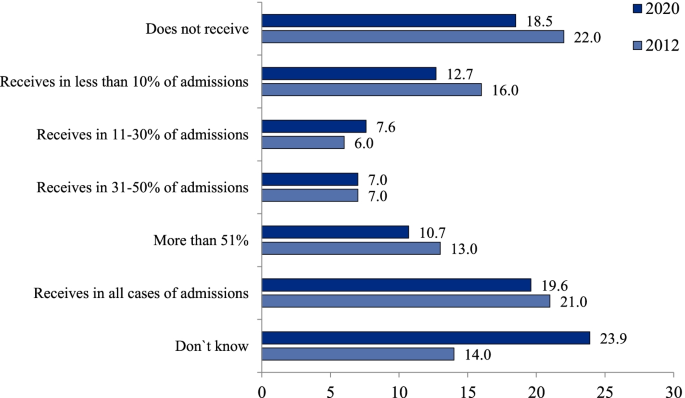
Distribution of polyclinic physicians’ responses to the question `How often does your polyclinic receive information about hospital admissions of patients in the catchment area`, % (survey 2)
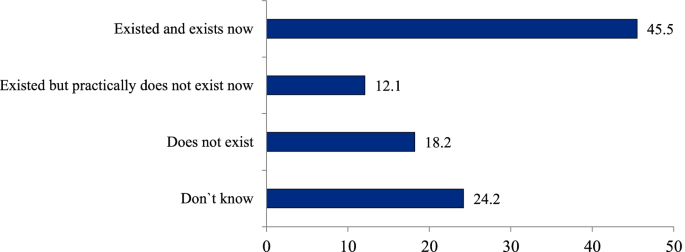
Distribution of polyclinic physicians’ responses to the question `Does your polyclinic have a regular practice of visiting patients within first days after their hospital admission with a stroke or a myocardial infarction`, % (survey 2)
Substantial efforts have been undertaken recently in introducing modern IT in medical facilities, but a national electronic medical record system has not been built yet. Only a few big cities have a system that covers both outpatient and inpatient facilities. The majority of outpatient physicians don’t know much about care utilization on other stages of service delivery.
Third, the limitation of outpatient specialists’ task profile and curative competences. For the reasons mentioned above, a multi-specialist polyclinic generates demand for specialty care . This demand is served by two specific types of specialist who provide only outpatient care: those who work in polyclinics dealing only with simple cases as first-contact providers; and those who provide only inpatient care for complex cases. The former face the problem of professional isolation from their counterparts in hospitals and have limited clinical competences, for example, they do not carry out operations or manage difficult cases. The latter have very limited responsibilities for outpatient consultations. Thus, a multi-specialist polyclinic not only generates demand but also requires a growing supply of specialists. Only 13% of physicians in Russia are generalists [ 5 ], compared with 27% in the UK, 29% in France and 48% in Canada, with 23% being the average for the OECD countries [ 6 ].
Fourth, the lack of economic incentives in a multi-specialty polyclinic . A salaried status and the principle of a ‘common pot’ inherent in a big entity decrease the economic motivation of polyclinics’ health workers relative to their self-employed counterparts in solo and group practices. The first survey of physicians indicates that their income is poorly linked to the financial revenue of the polyclinic: 49% of respondents reported that they did not see this link, 37% saw the link, while the rest did not answer.
Fifth, a low potential for patient choice of PHC providers and their competition . Russian citizens have a strong interest in provider choice but the majority cannot choose due to the prevalence of big entities. Also, there is a growing interest in physician practices that are smaller and therefore closer to patients’ homes.
Some indicators of polyclinics’ performance
Large-scale provision of primary care in polyclinics might be expected to reduce the burden on hospitals, but this has not been the case. In spite of a relatively high number of outpatient physician consultations (9.9 per person), the hospital admission rate in Russia is 52% higher than the OECD average and even higher than in European countries, including Estonia, which had similar high levels of admission in the first post-Soviet period and then had rejected a multi-specialty polyclinic model. A poor-performing primary care system in Russia increases the probability of acute deterioration in people living with asthma, chronic obstructive pulmonary disease, congestive heart failure and some other illnesses, therefore requires hospital admissions that are avoided internationally. Together with a high average length of hospital stay, a significant frequency of admissions produce a very high total utilization of inpatient care: bed-days per capita in Russia is more than two times higher than the OECD average (Table 1 ). Similarly, the utilization of emergency care per capita in Russia is nearly three times higher than the average for OECD countries [ 5 ].
This can be attributed to a number of factors. Firstly, inpatient care remains a major priority of health policy, with a major proportion of funding going to this sector. Secondly, the curative capacity of outpatient specialists in polyclinics is lower than that of their counterparts in hospitals because they deal only with relatively simple cases. Thirdly, patients prefer to be admitted to a hospital due to a traditional mistrust of polyclinic physicians. Administrative pressure – a major characteristic of the model – does not allow patients’ trust to increase.
A theoretically important feature of the polyclinic model is its focus on preventive activities but this does not happen in practice. Physicians and other professionals have no discretion over their patients’ involvement in large-scale health programs and cannot adapt them to the specific environment of their work. An example is the current federal program of ‘dispensarization’, which covers all adults with check-ups and screenings and is implemented according to standard rules. Polyclinics’ physicians are not involved in the design of the program and cannot choose the scope of preventive activities, the targeted populations or the forms of follow-up activities for identified cases of chronic disease. This has caused a number of serious problems: an overburden on DPs, distortions in reporting, poor communication between providers of preventive and curative services, excessive prescribing of diagnostic tests and a lack of follow-up activities for identified cases. The survey of physicians conducted online in April 2019 (randomly selected 1103 physicians) demonstrated that only 7.7% of respondents indicated that a set of actual curative activities met the requirements of a pattern of dispensary surveillance issued by the Federal Ministry of Health. The analysis of medical records of 7043 patients after their hospital admissions with a stroke or a myocardial infarction indicates that nearly half of these patients have not seen a doctor during the year prior to admission [ 11 ].
Heart attacks and other cardiac ischemia mortality rate in Russia is 310 per 100 000 population (in 2019) – nearly three time higher than the average OECD (110). There is a similar gap is for stroke mortality (180 vs 60) ([ 10 ] p. 91).
Polyclinics’ responses to challenges resulting from the COVID-19 pandemic demonstrate both the strengths and weaknesses of the model. There is some evidence of its potential for the mobilization of resources, which has allowed polyclinics to allocate resources to the most vulnerable areas of service delivery and organize flexible testing and tracing of patients and their contacts. This has been facilitated by polyclinics being instructed to implement government policy through decrees and commands. On the other hand, physicians in polyclinics do not have the competences required to take on a major role in triaging or managing new cases. Hospitals have become overburdened as they have taken on this role. The excessive specialization of primary care has also prevented continuity of outpatient care for people with coronavirus.
Discussion: where next for primary care in FSU countries?
Developing a new approach – learning from elsewhere.
FSU and some CEE countries are seeking a new model of PHC that combines the strengths of solo, close-to-home practices and large multi-specialist polyclinics while addressing their weaknesses. A shift to the model of small independent primary care practices, that have been common in Western Europe, may not be a reasonable alternative to the polyclinic model. Firstly, because patients in Russia do not favour this model and its historic legacy means they will try to bypass it. Secondly, the scale of change in the workforce required would be very large and potentially impractical. Thirdly, and most significantly, it would potentially mean losing the opportunity to adopt a more modern and appropriate approach to primary care rather than copying an old model that is starting to exhibit difficulties.
In a number of countries there has been growing interest in the development of larger multidisciplinary primary care practices or networks in response to the growing complexity of patients, the desire to provide more care locally, demand for extended hours and pressures on the workforce. In Spain [ 12 ], France [ 13 ] and the UK [ 14 ] it is increasingly common for primary care services to cover in excess of 20,000 population and these are very different from the existing polyclinics as they rely on a much wider spectrum of primary care expertise including pharmacists, a number of different therapy disciplines, mental health professionals, dentists, opticians, hearing aid technicians and dieticians. They also have an extensive role for nurses. They may also provide a base for social work and staff who can assist patients with non-medical problems and who can direct people to services that can help them. Larger units may have administrative staff to reduce the time taken on non-clinical tasks by health professionals.
The main points of difference to the current multi-specialty polyclinic model in Russia are the following:
The level of narrow specialization of care is much higher in the polyclinic model than in an ‘extended general practice’ model. Groenengen et al. (2015) [ 15 ] found that the median number of additional professionals in extended general practice is five to six in Australia, England, Iceland, New Zealand, Poland, Slovenia, Spain and Sweden, while in Russia it may reach 20 categories [ 5 ]. This excessive specialization has destroyed the polyclinic’s original design as a centre of PHC based on teamwork, coordination and continuity of care and resulted in a fragmented provision of services with the duplication of specialists in outpatient and inpatient settings.
The curative and coordination role of generalists remains central in the extended practices in Western Europe, while it tends to be small in the polyclinic model: specialists replace rather than supplement generalists.
Polyclinics have extended their scope through the introduction of new categories of outpatient specialists. In contrast, while some new primary care models may include some specialists, they rely on GPs with a wide range of skills, including the ability to manage many conditions.
Paediatric and adult care are generally provided under the same roof in the new extended primary care models, rather than in separate clinics as is often the case in urban areas in FSU countries.
Clinicians in the new extended primary care practices are expected to follow guidelines and are subject to quality audit, but generally have more autonomy in decision-making than doctors in polyclinics.
Developing multi-disciplinary group practices
With some considerable work, the existing polyclinics could be transformed into the type of multidisciplinary group practices described above. These would be linked to smaller satellite primary care centres to enable easy access for patients. These networks should take responsibility for the primary care of the whole population – including children – and where they are in separate facilities they should be brought together. A minimum population of 20–30,000 people will provide a critical mass to allow a wide range of primary care services, as around 10–15 GPs working together would justify hiring other professionals, including nurses and pharmacists. Larger networks, which are easier to create in urban areas, could allow even more services to be developed, including diagnostic imaging and a base for visiting specialists.
At the core of the ‘extended general practice’ model are GPs. District therapists and some of the narrow specialists would need extensive retraining to undertake the role of GP. In those systems that have retained paediatricians, it may be better to improve their capability as clinicians for children through enhanced training and to integrate them into the primary care centres, working alongside family doctors. Such a change may be easier than trying to retrain doctors who have had a purely paediatric training to work in family medicine (and vice versa) – not least because in many FSU countries, sub-specialisation in paediatrics takes place very early in training. This is also likely to be more acceptable to the population, who are used to taking children to see paediatricians, and there is some evidence that specialist primary care for children produces better outcomes [ 16 , 17 ]. Locating GPs and paediatricians in the same practice would also allow issues relating to the whole family context to be understood.
Nurses in the multidisciplinary group practices would need to deliver many more services than the quasi-administrative roles that many currently undertake. There would need to be a significant programme of training for them and the wider range of primary care professionals that the model requires (mental health workers, social workers, physiotherapists etc.). Changes in regulatory rules will be required in a number of countries to allow for this, in particular to permit nurse prescribing.
The existing model, in which a lot of activity has been generated by annual screening, pre-employment checks, the issuing of sick certificates and referral to other providers, would need to be replaced. A more proactive approach based on risk assessment and the selection of preventive services for each individual patient would also be required. The new model would also necessitate a significant change in the mindset of staff and patients.
The long-term goal for the extended general practice model is that it will encompass the broad range of primary care services including rapid access for immediate problems and the management of many long-term conditions. Elements of women’s health and less serious mental health conditions would be part of this. For long-term conditions the role of specialists would be to provide assistance with diagnosis, develop management plans, provide advice where changes in these plans are needed, support or take over the management of very complex or refractory cases and, where required, periodically review the care plans and the patient’s progress. To do this means that specialists will see fewer patients and these will be more complex. They will also need to be available by phone or email to provide advice and there will be more emphasis on support, education and training provided to primary care clinicians. The reimbursement system will need to recognise this and, in those countries where it is an issue, also consider the income lost to doctors from informal payments.
The goal of integrated care would take a long time to realize, which requires a set of integrative activities in both multidisciplinary group practices and hospitals. These include:
expanding capacity for direct information exchange
joint planning of care through the chain of providers
establishing process and outcome indicators for chronic disease management
increasing people’s economic motivation for integration
restoring GPs’ gatekeeping function and coordination role
Most importantly, regulation is needed to promote a greater interaction of GPs with specialists and hospitals beyond a simple referral system. This could include the provision of email and telephone advice, education and training, clinical supervision and other joint activities.
Specialists who currently work in polyclinics would need to be retrained either to work in primary care or to bring their skills up to a level that is appropriate for hospital outpatient/ inpatient services.
The preferable option for outpatient centres is to employ specialists who work in both inpatient and outpatient settings. To facilitate this process, the centres should become structural units of hospitals. This would avoid specialists’ professional isolation and may decrease demand for the number of specialists in the entire health system.
In most cases, access to specialist opinion would be provided by hospital outpatients departments and would be by referral from a primary care doctor (and over time by other clinicians). This would need to be supported by the development of guidelines and pathways. To be most effective, primary care would need to have access to a range of laboratory and imaging tests to help improve the appropriateness of referrals.
One area where more rapid progress could be made is in the development of primary care and outpatient consultations by digital means. Health systems have been rapidly adopting such approaches in response to the COVID-19 pandemic, although there were already a number of examples before the crisis where substantial amounts of care were delivered through these means. In common with many other countries, rural areas have great difficulty recruiting medical and nursing staff but access to smartphones with internet capability is growing rapidly and, subject to there being reasonable mobile phone coverage, a combination of digital and mobile services could help to fill this gap.
FSU countries should ‘leapfrog over’ the phase of developing solo practices and build a multidisciplinary model similar to the extended general practice model seen across much of Europe. The latter may act as a ‘golden middle point’ between the excessive specialization and administrative dominance of the polyclinic model and the limited capacity of solo practices. The new model requires a separation of primary care and outpatient specialty care, with the transformation of polyclinics into centres of outpatient diagnostic and specialty services that become structural units of hospitals. A transition to this model requires retraining specialists, extending the task profile of traditional district physicians, therapists and paediatricians, consolidation of adult and child primary care, and increasing the role of nurses and other professionals. The comprehensiveness of care in a big setting and potential economies of scale, which are major strengths of the polyclinic model, would be retained in the provision of specialty care in hospitals rather than primary care.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Kuhlbrandt C. Primary care reforms in countries of the former Soviet Union: success and challenges. In: Rechel B, Richardson E, McKee M, editors. Trends in health systems in the former Soviet countries. Copenhagen: World Health Organization; 2014.
Google Scholar
Kringos D, Boerma W, Hutchinson A, Saltman R. Building primary care in a changing Europe. Vol. 1, No. 38. Copenhagen: The European Observatory on Health Systems and Health Policies; 2015.
Jakab M, Farrington J, Borgermans L, Mantingh F. Health systems respond to noncommunicable diseases: time for ambition. Copenhagen: WHO Regional Office for Europe; 2018. p. 137 ( http://www.euro.who.int/__data/assets/pdf_file/0009/380997/Book-NCD-HS.pdf?ua=1 [Accessed 10 03 21]).
Sheiman I, Shishkin S, Sazhina SV. Vertical program of screenings and check-ups in the Russian Federation: design, implementation and lessons learnt. Arch Public Health. 2022;80:123 (Article 123).
Article Google Scholar
Sheiman I, Shevsky V, Shishkin S. The evolving Semashko model of primary health care: the case of the Russian Federation. Risk Manage Healthc Policy. 2018;11:209–20.
OECD (2019) Health at a Glance 2019: OECD indicators. OECD Publishing, Paris,p. 179. https://doi.org/10.1787/98e2d5de-en [Accessed 10 03 21].
Sheiman I, Gerry C. Too many and too few: the paradoxical case of physicians in the Russian Federation. Int J Health Plann Manage. 2018;33(1):391–402.
Sheiman I, Shevsky V. Concentration of health care providers: does it contribute to integration of service delivery? Risk Manage Healthc Policy. 2019;12:153–66.
Article CAS Google Scholar
Sheiman I, Shevski V. Evaluation of health care delivery integration: the case of the Russian Federation. Health Policy. 2014;115(2–3):128–37.
OECD. Health at a Glance 2021: OECD indicators. Paris: OECD Publishing; p. 135–9. https://doi.org/10.1787/4dd50c09-en .
Sheiman I, Shishkin S, Shevsky V, Sazhina S, Ponkratova O. Dispanserization of the population: expectation and reality. Mir Rossii// Mir Rossii. 2021;4:6–29. https://doi.org/10.17323/1811-038X-2021-30-4-6-29 ([in Russian]).
Dedeu T, Marti T. Multiprofile primary health care teams in Catalonia, Spain: a population-based effective model of service delivery. Copenhagen: World Health Organization; 2018. ( https://www.euro.who.int/en/health-topics/Health-systems/health-systems-response-to-ncds/publications/2018/multiprofile-primary-health-care-teams-in-catalonia,-spain-a-population-based-effective-model-of-services-delivery-2018 [Accessed 10 03 21]).
Ministère des Solidarités et de la Santé. Les maisons de santé. Paris: Ministère des Solidarités et de la Santé; 2020. ( https://solidarites-sante.gouv.fr/systeme-de-sante-et-medico-social/structures-de-soins/article/les-maisons-de-sante-300889 [Accessed 10 03 21]).
Kumpunen S, Natasha Curry, Maddy Farnworth, Rebecca Rosen. Collaboration in general practice: Surveys of GP practice and clinical commissioning groups. Nuffield Trust, Royal College of General Practitioners; 2017. https://www.nuffieldtrust.org.uk/research/collaboration-in-general-practice-surveys-of-gp-practice-and-clinical-commissioning-groups
Groenewegen P, Heinemann S, Greb S, Scharfer W. Primary care practice composition in 34 countries. Health Policy. 2015;119:1576–83.
Wolfe I, Thompson M, Gill P, Tamburlini G, Blair M, van den Bruel A, et al. Health services for children in western Europe. Lancet. 2013;381(9873):1224–34 ( https://pubmed.ncbi.nlm.nih.gov/23541056/ [Accessed 10 03 21]).
Wolfe I, Cass H, Thompon MJ, Craft A, Peile E, Wiegersma PA, et al. Improving child health services in the UK: insights from Europe and their implications for the NHS reforms. BMJ. 2011;342:d1277 ( https://www.bmj.com/content/342/bmj.d1277.full [Accessed 10 03 21]).
Download references
Acknowledgements
This paper is an output of the research project implemented as a part of the Basic Research Program at the National Research University Higher School of Economics in Moscow, Russian Federation. The authors are grateful to Rowan Dennison and Svetlana Sazhina for their kind assistance.
No funding for the paper.
Author information
Authors and affiliations.
Nuffield Trust, 59 New Cavendish St, London, W1G 7LP, UK
Nigel Edwards
National Research University Higher School of Economics, 0 Myasnitskaya str., 101000, Moscow, Russian Federation
Igor Sheiman
You can also search for this author in PubMed Google Scholar
Contributions
Nigel Edwards (NE) participated in the design of the study, collection of literature, writing and reviewing the text. Igor Sheiman (IS) participated in conducting physicians’ surveys and face-to-face interviews, writing and reviewing the text. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Igor Sheiman .
Ethics declarations
Ethics approval and consent to participate.
Two surveys of physicians were taken in the study. Methods of surveys were carried out in accordance with relevant guidelines and regulations. These methods were approved by the “Commission on the intra university surveys and ethical reviews of empirical research projects” of the National Research University High School of Economics https://www.hse.ru/org/hse/irb/ . Informed consent was obtained from all subjects.
Consent for publication
Nigel Edwards and Igor Sheiman agree to publish the paper”What next of the polyclinic? New models of primary health care are required in many Former Soviet countries”.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., additional file 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Edwards, N., Sheiman, I. What next for the polyclinic? New models of primary health care are required in many former Soviet Union countries. BMC Prim. Care 23 , 194 (2022). https://doi.org/10.1186/s12875-022-01812-w
Download citation
Received : 16 November 2021
Accepted : 12 July 2022
Published : 04 August 2022
DOI : https://doi.org/10.1186/s12875-022-01812-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Primary health care
- Multi-specialty model

BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]
- Open access
- Published: 15 April 2022
Vertical program of screenings and check-ups in the Russian Federation: design, implementation and lessons learnt
- Igor Sheiman ORCID: orcid.org/0000-0002-5238-4187 1 ,
- Sergey Shishkin ORCID: orcid.org/0000-0002-0807-3277 2 &
- Svetlana Sazhina ORCID: orcid.org/0000-0002-2023-3384 2
Archives of Public Health volume 80 , Article number: 123 ( 2022 ) Cite this article
1648 Accesses
2 Citations
Metrics details
The Russian Federation has introduced a vertical large-scale program of ‘dispensarization’ (Program) that includes health check-ups and screenings for the entire adult population. It is expected to improve the results of medical interventions and ensure health gains at a relatively low cost. The major research question: Does the design and implementation of the program meet the expectations?
We analyze regulatory acts and the literature on the design and the outcomes of the Program. Physicians’ surveys and interviews are conducted to understand the capacity of primary care providers to meet the requirements of the Program, as well as the link between the early identification of new illnesses and their follow-up management, administration of the program, the barriers to its successful implementation.
There is a substantial progress in the coverage of the population and increase in the number of identified illnesses. Some specific instruments of the Program implementation work well, others require more careful design and additional integrative and managerial activities. The capacity of primary care providers does not allow to provide high quality preventive services, as well as to ensure a continuum of preventive and curative work. The pattern of the Program administration facilitates its nation-wide implementation according to the unified rules, but makes it more difficult to account for the local conditions and limits the autonomy of professionals to choose specific population risk groups and a list of services. The interaction of providers in preventive activities is inadequate.
The expectations of the Program are too high due to the inconsistencies in its design and implementation. The major lesson learnt is that the program like this should meet the capacity of primary care and be designed as a complex of interrelated activities to identify illnesses and provide their follow-up management.
Peer Review reports
The majority of European countries have implemented comprehensive approaches to public health. Population-based check-ups and screenings have become an important instrument of the early identification of illnesses and their follow-up management. These activities are usually viewed as the way to improve the chances of survival for people living with cancer and other illnesses by ensuring that health services can focus on diagnosing and treating the disease earlier [ 1 ]. The population coverage by screenings is high and growing in many OECD countries [ 2 ].
The impact of these activities on health outcomes is not as easy as it might seem. It depends on the selection of preventive services, as well as on the implementation practices in the specific national context. There is a substantial body of literature on the justification of screening programs. Wilson and Jungner [ 3 ] set out ten principles of the choice of screenings, which remain the cornerstone of the literature on this issue, particularly the principle that the ratio of cost/utility should not be lower for screenings than for the curative activities. Numerous studies evaluate the expected impact of these programs on mortality and other health indicators, as well as the expected cost effectiveness of the alternative programs [ 4 , 5 , 6 ]. There is a growing consensus on the principle of selecting the program: ‘Screening may bring benefits but also harm; just because it can be done does not mean that it should be done’ [ 7 ].
Another body of literature addresses the design and organization of screening programs. WHO Regional Office for Europe [ 8 ] suggests core steps of screening pathway from identifying target populations to monitoring and evaluation. The major research areas include the ways individuals in the target population are identified, forms of their involvement, the appropriate management of screen positive and negative results, actors of service provision and their interaction [ 9 ].
Practically all these studies address the developments in Western countries. Much less attention is paid to the post-Soviet countries. Some of them have deeply rooted traditions of the population-based preventive campaigns. Modern Russia inherited the Semashko model, which had declared the priority of preventive activities. But their implementation after the dissolution of the USSR has been limited by chronic underfunding of health system. Public funding has not exceeded 3.5% GDP over the last three decades [ 10 ]. In the early 2010s, the priority of prevention campaigns has been re-vitalized in the form of a nation-wide vertical program of ‘dispensarization’ (further Program), that is a set of preventive activities, including health check-ups and screenings. This is a term from the original Semashko model, practically unknown in the international literature.
The expectations of the Program are very high in Russia. The official attitude is that the early detection of ill health will allow to improve the results of medical interventions and ensure health gains at a relatively low cost. The Federal Ministry of Health (MoH) estimates the contribution of the prevention campaign to ‘keeping people healthy’ at the level of 60% [ 11 ]. Also, the Program is viewed as a tool that will decrease the need for curative work of primary care providers. The MoH predictes a fall of curative visits share from 60 to 40% of all primary care physicians visits with a corresponding increase in the share of preventive visits [ 12 ]. Such optimistic expectations explain a substantial involvement of the government in the implementation of the Program.
The Program design provides for the specific instruments of its implementation – highly centralized administration, a universal set of services to identify illnesses among centrally determined target groups, methods of planning, reporting, monitoring, etc. Some of these instruments, for example, provision of preventive services in multi-specialty primary care settings, a large-scale promotion campaign, the establishment of special units responsible for this work, are not common internationally.
The recently implemented policies to strengthen health prevention in Russia have prompted a number of questions: Does the design and implementation of the Program meet the capacity of the current health system? Do specific Russian instruments really work? Does a highly centralized pattern of the Program administration facilitate or complicate its successful implementation? Which lessons can be learnt from this Program for other the countries? Addressing these questions may be of interest to health policy makers in other countries seeking the ways to improve public health. We explore these questions by reviewing the design of the Program, studying its implementation practices and discussing the results. The selection of specific check-ups and screenings is not discussed in the paper, since it is country-specific and is beyond our research questions.
The motivation to produce this paper is to encourage a more careful study of population-based prevention programs, particularly in countries with limited financial resources for health care. Their policy makers often seek ways to solve health care problems through the early identification of new illnesses. The major message is that this activity does not automatically yield health gain. The population-based programs of check-ups and screenings should meet the capacity of primary health care. They should be designed as a complex of interrelated activities to identify illnesses and provide a follow-up management of chronic cases. Physicians should have a discretion regarding the choice of prevention patterns, including the coverage of specific population risk groups and a list of check-ups and screenings. A close interaction of providers in the course of new diseases identification is also needed.
Thus, the aim of the paper is to analyze the design, implementation and outcomes of the Program in the context of domestic and international developments in public health.
We analyze design, implementation and outcomes of the Program using as research tools the review of regulatory acts and the literature, statistical analysis, physician surveys, face-to-face interviews with physicians and health managers. A framework of the analysis is presented in Fig. 1 .
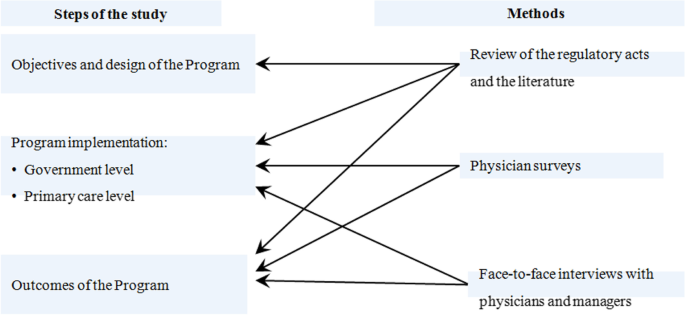
Study design and methods
Study design
We follow a three-step methodological framework. The first step involves the analysis of objectives and design of the Program. The regulation is explored to determine the preventive activities requirements and their matching standard pathways recommended by WHO. We explore the patterns of check-ups and screenings provision, planning preventive activities, reporting outcomes, monitoring, payment methods. The limitations of the design are highlighted.
The second step addresses the issues of the Program implementation. It consists of two stages. The first is to highlight the administration of the program at the governmental level. The second is to explore the implementation of the Program at the level of primary health care (PHC) settings. The focus is on the following characteristics of their performance: a) the adequacy of primary care capacity to implement the Program; b) the interactions between providers in terms of the flow of information on the early identification of new illnesses; c) the prevalence of the follow-up management of these illnesses, d) the modes how providers of preventive services choose target groups for screening, plan their activity, report the outcomes. These parameters of implementation are studied with the use of physician surveys and face-to-face interviews.
The third step involves the analysis of outcomes of the Program as they are defined in the regulatory acts. The official estimates of the population coverage and the identification of new illnesses are compared with the estimates of physicians obtained through the survey. The collected evidence allows us to come up with concluding points about the potential of the Program to meet the public expectations.
Data sources and instruments
To explore the objectives and the design of the Program, we analyze the regulatory acts of the government and the domestic literature on the subject, including the reports in limited circulation, unpublished documents, memorandums, and presentations from our personal collections. The literature on the similar programs in other countries was searched in the MEDLINE data base using the query “screening”, “health check-up”, “public health programs”. All findings were checked manually and around 30% were relevant.
The practices of the Program implementation were explored using a physician survey. It was conducted online in April–May 2019 through the mobile ap “Handbook of Physician” (available in Google Play and AppStore) with 540 thousand of registered users. We randomly selected 1100 physicians and feldshers (paramedics) who were directly involved in provision of preventive services in primary care settings under the Program, including district therapists (63.2% of respondents), outpatient specialists (18.7%), general practitioners (9.9%), paramedical personnel (8%). They represent most of regions (81 out of 85 regions of the country) and the structure of population residence (658 physicians from regional centers, 172 – other urban areas, 273 – from rural areas). A questionnaire with 25 questions on the above mentioned dimensions of implementation practices was sent to the selected group of respondents (appendix 1 ). Only part of the survey results is presented in the paper due to its limited space.
To understand the degree of professional autonomy on the choice of target population groups and specific preventive services, we conducted a small-scale survey of 103 primary care physicians and outpatient specialists in three big multi-specialty urban polyclinics in Moscow city and Moscow oblast (the region around the capital) in January 2020 when Covid-19 pandemic had not affected the work of primary care yet. We explored the ways preventive activities were administered in polyclinics with 13 questions (appendix 2 ). Ten physicians on the list were approached directly for face-to-face interviews.
We also conducted face-to-face interviews with two high-level managers of private medical companies that were involved in the realization of the Program. The main interview topics were: What is the estimate of the actual coverage by the program?” “Can primary care physicians select population groups and their own ways to conduct health check-ups|?” “Does centralized administration of the Program facilitate or complicate its successful implementation?” “What is needed to ensure a follow-up management of patients with the early identified diseases?” The interview data were compared with the results of public opinion surveys conducted by polling companies.
The analysis of the Program implementation and outcomes is based on the statistical data and reports of the federal MoH and the estimates of physicians.
Objectives and design of the program
The regulatory document of the Federal Ministry of Health [ 13 ] defines the dispensarization as ‘a complex of activities that includes health check-ups and additional methods of investigations conducted with the aim of evaluating health status … of targeted groups of population’. The Program pathway is similar to the one recommended by WHO for screening programs: identification of the population eligible for screening, invitation and information, testing, referrals to specialists, diagnosis, follow-up management of identified cases, reporting the outcomes [ 7 ]. Most of these steps are in place in the Program, except for the follow-up management. The latter is mentioned in the regulatory act as a so called ‘dispensary surveillance’. This term of the original Semashko model means that every identified case of a serious disease is subject to a certain set of clinical protocols (which is close to the modern programs of chronic disease management). However, the follow-up management of the case does not constitute a component of the Program. One of its objective is formulated as ‘establishing the group of dispensary surveillance of patients with chronic diseases and high risks of circulatory system diseases”, that is determining the need for such a surveillance rather than its actual provision. The regulation also sets the requirement of distributing participants into three health groups according to the severity of identified illnesses.
Thus, the Program is viewed as the way to ensure the early identification of illnesses and prevention of their complication. The dispensarization process for an individual is finalized with a documentation of medical examination results, assigning to a health group and some awareness of health problems.
Patterns of health check-up and screening provision
A set of preventive activities is based on the evidence of their outcomes collected by research institutions. A universal set of these activities are determined for the entire country. The process of dispensarization for an individual patient consists of two stages. The first stage is aimed to detect risk factors and deviations in a patient’s health. The second stage is to confirm or reject the first stage findings. Patients are referred to specialists for consultation and/or additional tests. These services are provided to the target age and sex groups of population. People older than 40 years in all regions of the country are supposed to go through a required set of check-ups and screenings once a year. The group of 18–39 years old – once in three years. Most of children go through only the stage of check-ups.
The design of the Program is based on the assumption that most preventive activities are provided in the same outpatient setting – a multi-specialty polyclinic with 10–15 categories of outpatient specialists in big urban areas, 3–5 categories in small cities and the number of people served ranging from 30 to 300 thousand people. The major providers of the first stage activities for adults are district therapists and GPs, for children – district pediatricians (together they are further referred to as district physicians – DPs). In big polyclinics, they are reinforced by the staff of a preventive unit – physicians and nurses responsible only for preventive activities. Such units exist in practically all urban polyclinics [ 14 ]. Specialists deal with the second stage of the Program. Rural and small town areas are served mostly by solo practices (physician ambulatories). They take on preventive activities of the first stage and refer patients to urban polyclinics for the second stage activities. Feldshers do this work in the smallest rural areas.
Planning and reporting the outcomes
The administration Program is highly centralized and implemented by the federal Ministry of Health. The requirements of planning and reporting are based on the federal regulation. The major indicator is the coverage of the eligible citizens. It is planned vertically – for the entire country, regions, communities, medical organizations, district units served by DPs. Also, the Federal Program of state guarantees of free medical care – the major health planning and funding document – sets the targets for the number of physician visits with the “preventive aim” and their unit cost. Using these targets, regions plan their own volumes of preventive care and their funding with the following distribution of these volumes across communities and polyclinics.
In addition to the population coverage, the prevalence of detected cases of illnesses is reported through a vertical chain of governmental agencies and medical settings. This reporting focuses on the cases of circulatory system diseases and cancer. In the latter case, it includes the indicators of cancer identification at first and second stages. Some regions of the country plan the number of new cases identified in the course of the Program implementation and even set targets for this indicator.
Monitoring the program
It follows the lines of planning and reporting. The major indicators of success are a high and growing population coverage, a high share of the early identified cases, and a high share of the identified cases that is subject to dispensary surveillance has been added. However, monitoring the actual follow-up curative activities is not required by the regulation, let alone monitoring the outcomes of dispensary surveillance. The actual health gains of the Program are beyond the scope of monitoring.
In addition to the aggregate information, detailed data is collected: the number of specific services, detected illnesses, prevalence of risk factors, the number of patients who need a dispensary surveillance, health groups and their structure. Theoretically, this data allows to analyze the outcomes of preventive activities across stages of the Program, specific screenings, groups of population, geographic areas. But the regulation does not require such a detailed monitoring. Moreover, this information is not open for the public.
Payment method
Preventive services under the Program are reimbursed by regional mandatory health insurance (MHI) funds. The rates of payment are set for a so called ‘finished case of dispensarization’, that is a fixed package of services determined by the regulation for the first stage of the Program. A ‘luft’ of 15% of the number of services is allowed, while all screenings are obligatory. A bundled payment for the first stage is supplemented with a fee-for-service reimbursement of additional consultations and tests at the second stage. The control of the actual number of ‘finished cases’ is conducted by health insurers – mostly private entities that are involved in MHI. In addition to this amount, polyclinics receive a small bonus (around 13–15 USD) for each identified new oncological case [ 15 ]. The revenue of polyclinics under the Program is linked to the planned volume of preventive activities. If the actual volume is lower, then the amount of funding is lower than planned.
The idea behind this pattern of payment is to motivate providers to supply preventive services. The opposite side of the coin is that this instrument limits the professional autonomy of physicians on the choice of preventive services for an individual. They have to provide the entire bundle of services to be reimbursed, irrespective of the actual need of a patient. Inversely, a necessary test that is not included in the list of the ‘finished case’ will not be paid. Also, the regulation does not provide for additional payment for managing identified chronic cases. Dispensary surveillance is not incentivized by payment methods. This is another limitation of the Program design.
Implementation of the program
The role of the government.
The role of a highly centralized administration of the Program is controversial. On the one hand, the federal government has initiated it, provided regions with additional funding, involved providers in preventive activities, made the Program implementation a priority of health policy. The opportunities and benefits of preventive activities are widely presented in the state media and official websites with the focus on the information how and where to pass medical examination. Private employers are legally required to promote the involvement of their employees and to offer them a day-off once a year to undergo the dispensarization. In some regions, temporal offices for check-ups have been established in popular trade and recreation zones, as well as in big educational institutions and industrial centers. In addition to the support activities, administrative pressure is used wherever possible. Public servants, teachers, medical workers, students and some other groups of population are strongly recommended to participate in the campaign. There are voices to introduce financial sanctions for those who ignore the Program. All these strategies contribute to the population coverage.
On the other hand, a highly centralized administration has a number of drawbacks. Uniform target population groups and a set of preventive activities limit the flexibility of regions in responding to local needs and special conditions – variation in the disease incidence, the capacity of PHC, the most vulnerable population groups. Centrally established indicators of the population coverage, volumes of preventive care and the number of identified illnesses make regional health authorities and PHC providers look for the ways to reach the targets irrespective of the local capacity to treat new cases. Monitoring the Program outcomes follows the logic of the centralized administration and politically loaded campaigns. The federal MoH makes an emphasis on easily attainable indicators and targets so that to show the progress.
Health managers in their face-to-face interviews indicate that the centralized administration of the Program complicates the actual preventive work. Plans of the population coverage don’t take into account the age structure of eligible groups. If the share of elderly people is high, then the planned targets can’t be reached, because elderly people usually know enough about their illnesses and prefer to see a doctor for curative purpose rather than to have check-ups. If the targets can’t be reached, physicians have to look for the ways how to distort reporting about the coverage of the program. Also, the requirements of the federal MOH often change, which in turn requires changes in electronic forms for medical examinations, procedures of reporting and billing, etc. The citations of interviews:
“Rigid plans for medical examinations turn dispensarization into a competition of numbers and indicators that are not related to the reality”.
“Permanently changing federal rules of dispensarization divert physicians from the actual preventive work and overburden them with routine reporting work”.
“Tough federal requirements and plans force providers to distort reports of the coverage and identification of illnesses”.
The performance of primary care providers
A low capacity of primary care.
The Program has been implemented in the health system where DPs are overburdened with a curative work. The survey of 1100 physicians (appendix 1 ) indicates that 63.9% of district therapists serve more adults than a normative workload of physician established by the MoH – 1700 adults per district therapist. 21.7% of respondents report that they exceed this target nearly by two times.
Our statistical estimate indicates that the average size of the catchment area per district therapist in the country is 2900 adults, while in some regions – 3–4 thousand [ 16 ]. The estimate of the deficit of district therapists to meet the normative workload is 33%, district pediatricians – 19% [ 17 ]. Their task profile has increased substantially due to the introduction of the Program. In many medical settings, they have to substitute a usual curative work for check-ups and screenings which are mandatory and closely controlled by administrators of all levels.
The interaction of providers
The implementation of the Program in urban areas is based on the model of a big multi-specialty polyclinic. The major strength of this model is its capacity to provide comprehensive preventive and curative care. Patients can undergo check-ups and screenings, see DPs and specialists ‘under one roof”. Also, a polyclinic model is expected to demonstrate the additional leverage to implement integrated care pathways. But to make this happen, specific integrative activities are needed. Our previous studies indicate that they are lacking in the curative work [ 18 ]. They are equally lacking in the area of preventive services.
The major problem is a poor flow of information about identified illnesses between professionals involved in the implementation of the Program. According to the survey, nearly two thirds of respondents (63.8%) report that health check-ups are conducted by DPs, 13% – by physicians of preventive units, 22.4% – jointly. Only half of DPs always (32.2%) or often (18.2%) receive information about check-up results when they are conducted by preventive units. The rest seldom or never receives it (Fig. 2 ). This is a sign of a blurring responsibility for check-ups between DPs and preventive units, as well as a poor interaction between them.
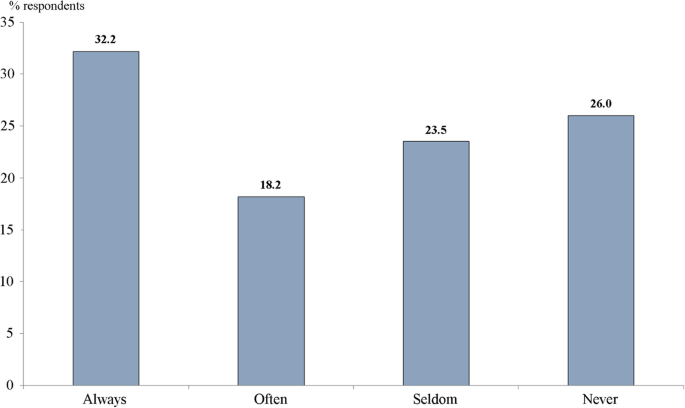
Distribution of responses to the question ‘Do you receive information about results of medical examinations of your patients under the program of dispensarization when they are conducted by preventive units?’ % of all respondents
As indicated above, the Program provides for the distribution of the eligible population across health groups. This is an important information for district physicians who are responsible for their patient list. However, the survey indicates that more than half of DPs (53%) are unaware of the distribution of their patients across health groups. Check-ups and screenings are conducted, patients with health problems are identified, but many physicians responsible for their follow-up management don’t know about results of preventive activities.
Another area of providers’ interaction is between DPs and specialists. Every third DP (34.2%) seldom receives information about the results of the second stage dispensarization, every fourth (24.3%) doesn’t receive it at all. Thus, more than a half of DPs don’t report coordination with specialists involved in the Program.
The patterns of the follow-up management of identified illnesses
Only 7.7% of respondents indicate that a set of actual curative activities meets the requirements of a pattern of dispensary surveillance issued by the Federal MoH. The majority reports that these requirements are met only for some patients or are not met at all (Fig. 3 ).
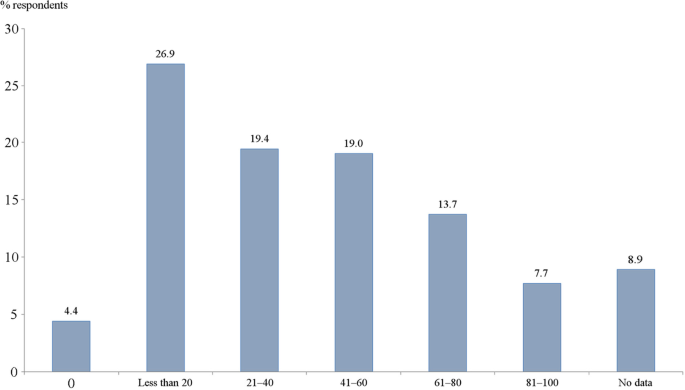
Distribution of responses to the question ‘What is an approximate share of patients (who are assigned to a DP) is managed according to the requirements of the pattern of dispensary surveillance issued by the Ministry of Health?’ % of all respondents
The usual practice to evaluate the outcomes of chronic disease management is to look at the number of disability days, emergency care visits, hospital admissions, disease-specific mortality rates [ 19 ]. In this research, we tried to explore a trend of these indicators according to the estimates of the respondents. A decrease in the number of disability days of chronic patients is reported by only 14% of physicians. More than a half of respondents are unaware of the number of emergency care visits and hospital admissions of their chronic patients.
These findings are similar to a clinical expertize conducted by the private health insurer ‘Rosgosstrah-Medicina’. The analysis of medical records of 7043 patients after their hospital admissions with a stroke or a myocardial infarction indicates that nearly half of these patients have not seen a doctor during the year prior to admission [ 20 ]. The nation-wide survey of physicians in late 2018 demonstrate that 72% of respondents agree with the point that the Program has not contributed to the management of the identified new diseases [ 21 ].
The revealed interaction of preventive and curative activities does not meet internationally recognized assumption that a screening program pathway should include a stage of the follow-up management of the detected illnesses: ‘ … there is no point in offering a screening program if there are insufficient facilities or health personnel to provide treatment for those who need it’. For example, a mass screening program for thyroid cancer in South Korea in 1999 led to the number of cases being detected increasing 15-fold and yet no reduction in mortality from thyroid cancer [ 7 ]. In Russia, the Program is focused on the identification of new illnesses. It is supposed that a follow-up treatment will be organized in the course of usual performance of health providers. But as indicated above, the principle of continuum of preventive and curative activities is observed only for a part of identified cases.
The patterns of the program administration in primary care settings
A centralized Program administration sets a chain of vertically determined rules. Physicians involved in the implementation of the Program work according to the rules determined by their polyclinics’ administrators, who in turn follow the commands of the federal and regional health authorities. The following evidence of physicians’ limited professional autonomy is collected in the survey of 103 physicians of multi-specialty polyclinics in Moscow city and Moscow region:
66% of physicians report that they have individual plans of the number of preventive and curative visits, developed by polyclinics administrators. Only 34% plan their activity themselves;
59% indicate that the failure to implement individual plans on the number of visits may cause reduction in their remuneration;
only 25% of physicians select patients themselves for check-ups and screenings after assessing their risk factors, that is invite those with the highest risks. The majority relies on the centrally determined target population groups.
Administrators of multi-specialty polyclinics plan the number of visits and the Program coverage in the catchment areas, control the activity of physicians. The professional autonomy of physicians to select their own patterns of preventive work is limited. The face-to-face interviews with physicians confirmed this conclusion.
The outcomes of the program
As stated above, the major outcome indicator in the official reporting is the coverage of the eligible population. The Federal Fund of MHI reports that in 2018 92% of eligible population has actually undergone dispensarization, in 2019–110% [ 22 ], while the latter estimate probably accounts for those who passed medical examinations more than once. However, physicians are less optimistic. According to the survey of physicians, more than half (51.4%) report that this share is less than 60%, while 17.4% think that the coverage is less than 20%.
We also asked a question ‘Why do you think there is a common opinion in the society that the number of people that have actually undergone dispensarization is lower than official estimates?’ Nearly two thirds of physicians (62.6%) report that the major reason for this opinion is that people are reluctant to undergo dispensarization, therefore physicians have to report an upward distortion of the coverage.
The estimates of the number of identified illnesses are based on the reports of the federal MoH for individual years, the reliability of which cannot be verified due to the unavailability of the original accounting information. Particularly impressive are reports of an increase in the number of diagnosed oncological diseases - from 21.3 thousand in 2013 to 55 thousand in 2019, or by 2.6 times. The frequency of newly diagnosed breast cancer in the period 2013–2018 increased from 39.2 per 100 thousand in 2013 to 73.3 per 100 thousand in 2018 or by 1.9 times. For other cancer localizations, the data for individual years are incomparable. In 2018, the MoH gave estimates of the proportion of cancer detected at stages 1–2: cervical cancer - 67.9%, breast cancer - 68.7%, colorectal cancer - 57.1% [ 17 ]. Comparable data for other years are not available.
According to the same source, the number of diagnosed cardiovascular diseases increased from 1.6 million in 2014 to 8.5 million in 2018, or 5.3 times. Particularly impressive is the dynamics of the diabetes mellitus detection: in 2015, more than 300 thousand cases were detected, in 2016 - already 531 thousand cases, or 1.8 times more. Approximately the same picture is emerging for respiratory diseases: there was an increase in the number of detected cases from 500 thousand to 710 thousand, or by 40% in one year [ 17 ].
Health groups characterize the distribution of the population according to the prevalence of pathologies of varying complexity. The share of the third group with the lowest health status increased from 44% in 2013 to 54% in 2018 [ 23 ].
Thus, the available official data indicate a significant increase in the coverage of medical examinations, a high rate of disease identification, an increase in the proportion of the population with serious diseases. As indicated above, the official estimates of the coverage are disputed by physicians.
The Program of dispensarization in Russia has raised the priority of the population-based preventive activities. The early identification of illnesses is currently viewed as one of the major areas of health policy. Primary care providers are increasingly focused on delivering check-ups and screenings to identify new cases. This work is supported by the government. There is a substantial progress in the coverage of the population and the number of identified illnesses. However, the collected evidence demonstrates major issues that don’t allow to expect substantial health gains – a low capacity of primary providers, the weakness of the follow-up management of identified illnesses.
The major barriers to successful outcomes of the Program reflect the characteristics of the current health system governance in Russia. It is highly centralized. Democratic institutions are very weak. The role of regional governments in choosing the priorities of health policy is marginal. Local communities and professional organizations are rarely involved in decision-making on health issues. Patient empowerment practically does not exist. The input of civil society bodies is largely imitative. Therefore, the design of the Program has not been publicly discussed and it has not been adjusted to the low capacity of PHC, as well as to the requirements of holistic provision of preventive and curative services. In the pandemic of COVID-19, the Program has been suspended but will most likely be re-started in the unchanged form.
The study has a number of limitations. First, the section on the Program outcomes is based mostly on the official estimates that overestimate the positive input of dispensarization. The reports of the federal MoH claim that check-ups and screenings are the major contributors to the early detection of diseases [ 11 , 12 ], but this seems to be a strong exaggeration. The estimates of Russian oncologists indicate that the input of the Program to the total number of newly diagnosed cases of oncological diseases is relatively low and growing only slightly: in 2013 it was 25%, and in 2018–36%. The major part of these cases can be accounted to the regular curative work [ 24 ]. The insufficiency and unreliability of the data make our survey-based estimates preliminary. Second, our research was not designed to assess: a) the impact of specific tests and screenings on the identification of new cases, b) the actual coverage, specific activities and health outcomes of the follow-up dispensary surveillance, c) the cost of specific preventive services. Third, the cost effectiveness of the entire Program and its elements is beyond the scope of the research. These are the areas of future research.
The design of two physician surveys, as it is seen in questionnaires (appendixes 1 , 2 ), has allowed to receive interesting results on a wide range of the Program characteristics. Some of them are not presented in this paper due to its limited space. For the same reason, some qualitative assessments are not supported by figures and tables with distribution of responses.
Report bias of the nation-wide physician survey relates to the question about the common opinion that the official estimates of the Program coverage are too high. Most respondents agree with this opinion but attribute it to the reluctance of eligible population to participate in the Program. A logical link between the two is dubious. Physicians tend to distort reporting under the pressure of administrators who are keen about reaching targets. This is a major reason for the overestimate of the coverage.
There is some bias in the design of the survey of 103 primary care physicians in two regions of the country. They definitely don’t represent all physicians in the country. The only justification for this small-scale survey is that it is related to a narrow and more or less clear area of professional autonomy limitations. We wanted to receive an additional evidence without conducting a large-scale survey.
No single aspect of the research would be sufficiently robust on its own, but the combination of literature and regulatory acts analysis, physician survey, face-to-face interviews, national public opinion surveys and statistical data create a rich picture of how the Program is designed and implemented, what are the barriers to achieving positive outcomes. There are grounds to believe that the generalizability of findings is high.
The Program of dispensarization has increased the coverage of the population with check-ups and screenings. The Program aims at increasing the number of identified illnesses with a low priority of the follow-up management of new cases. The empirical evidence indicates that the capacity of primary health care does not allow to provide check-ups and screenings, as well as to ensure a continuum of preventive and curative work. A highly centralized pattern of the Program administration facilitates its nation-wide introduction and implementation according to the unified rules, but makes it more difficult to account for local conditions. The balance between centralized governance and the right of regions to adjust the Program to the local conditions has not been reached yet. This is an important task for any large-scale prevention campaign. Some specific instruments work well, particularly the establishment of preventive units in primary care settings, forming health groups of the eligible population, large-scale support and promotion of preventive campaign by the government. Others require more careful design and additional integrative and managerial activities.
The major lesson learnt from this bold experiment is the understanding of insufficiency of a simplistic approach to health care problems by increasing the priority of the early identification of illnesses with the expectation that this may become a ‘magic tool’ of health improvement. The expectations of the program are too high, but there is a lack of consistency in its design and implementation. The population-based programs of check-ups and screenings should meet the capacity of the health care and be designed as a complex of interrelated activities to identify illnesses and provide their management with the focus on chronic cases.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgements
This paper is an output of the research project implemented as a part of the Basic Research Program at the National Research University Higher School of Economics in Moscow, Russian Federation.
No funding for the paper.
Author information
Authors and affiliations.
The National Research University Higher School of Economics, Faculty of Social Sciences, 20, Myasnitskaya St, Moscow, 101000, Russian Federation
Igor Sheiman
The National Research University Higher School of Economics, Centre for Health Policy, 4 Slavyanskaya Ploshchad, Building 2, Moscow, 109074, Russia
Sergey Shishkin & Svetlana Sazhina
You can also search for this author in PubMed Google Scholar
Contributions
Igor Sheiman participated in conducting physicians surveys and face-to-face interviews, writing and reviewing the text. Sergey Shishkin participated in the design of the study, writing and reviewing the text. Svetlana Sazhina participated in conducting physicians surveys and face-to-face interviews, writing and reviewing the text. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Igor Sheiman .
Ethics declarations
Ethics approval and consent to participate.
National Research University High School of Economics has a “Commission on the intra university surveys and ethical reviews of empirical research projects” https://www.hse.ru/org/hse/irb/ . Projects under the Basic research program do not require an ethics approval statement from this commission. The authors are ready to participate.
Consent for publication
Igor Sheiman, Sergey Shishkin, Svetlana Sazhina agree to publish this paper.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., additional file 2., additional file 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Sheiman, I., Shishkin, S. & Sazhina, S. Vertical program of screenings and check-ups in the Russian Federation: design, implementation and lessons learnt. Arch Public Health 80 , 123 (2022). https://doi.org/10.1186/s13690-022-00878-3
Download citation
Received : 17 December 2021
Accepted : 01 April 2022
Published : 15 April 2022
DOI : https://doi.org/10.1186/s13690-022-00878-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Vertical health program
- Public health
- Russian Federation
Archives of Public Health
ISSN: 2049-3258
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Risk Manag Healthc Policy
The evolving Semashko model of primary health care: the case of the Russian Federation
Igor sheiman.
Center for Health Policy, National Research University Higher School of Economics, Moscow, Russia, [email protected]
Sergey Shishkin
Vladimir shevsky.
This paper addresses the major developments in primary care in the Russian Federation under the evolving Semashko model. The overview of the original model and its current version indicates some positive characteristics, including the financial accessibility of care, focus on prevention, patient lists, and gatekeeping by primary-care providers. However, in practice these characteristics do not work according to expectations. The current primary-care system is inefficient and has low quality of care by international standards. The major reasons for the gap between the positive characteristics of the model and the actual developments are discussed, including the excessive specialization of primary care, weak health-workforce policy, the delay in the shift to a general practitioner model, and the dominance of the multispecialty polyclinic, which does not prove advantageous over alternative models. Government attempts to strengthen primary care cover a wide range of activities, but they are not enough to improve the system and cannot do this without more a systematic and consistent approach. The major lesson learnt is that the lack of generalists and coordination cannot be compensated for by the growing number of specialists in the staff of primary-care facilities. Big multispecialty settings (polyclinics in the Russian context) have the potential for more integrated service delivery, but to make it happen, action is needed. Simple decisions, like merging polyclinics, do not help much.
Introduction
Primary health care (PHC) is the first point of contact with health care where most preventive and curative health care needs are satisfied. This generalist care is focused on the person as a whole, instead of only one specific organ or health problem. 1 , 2 There is evidence that countries with strong PHC systems have relatively higher indicators of health outcomes. 3 Strengthening this sector is an important strategy for improving service delivery, including decreasing avoidable hospital admissions and emergency visits, 4 and enhancing patient satisfaction. This is an important element of health policy throughout the world. 5
Russia and most other postcommunist countries have inherited the Semashko model of primary care (named after the first Minister of Health in the USSR – Nikolai Semashko), dominated by publicly owned medical facilities, salaried health workers, large providers of PHC, and an exceptionally high degree of governmental administration. This system provides universal access to care, and thus has substantially improved the health status of the population relative to the starting point of its implementation in the late 1920s. 6 , 7 However, in the USSR, health care was heavily underfunded and had a number of noticeable problems with the dominance of inpatient care, inefficient service provision, and weak incentives for providers. 8 , 9 These problems have promoted the search for a new health-finance and -provision model.
After the collapse of the USSR in 1991, Russia introduced a social health-insurance system and started service-delivery restructuring with a focus on downsizing hospital capacity and moving patients to outpatient settings. Strengthening PHC was declared a priority in all the strategic documents of the transition period. However, the actual development of this sector has been slow and inconsistent. Contrary to postcommunist Central and Eastern European (CEE) countries, Russia developed its own system of primary-care development, emphasizing highly consolidated service provision in big multispecialty facilities and the dominance of public ownership. General practice is still in its infancy, while an attempt has been made to compensate for this with a growing number of specialists in primary-care settings. Currently, PHC is a complex mix of inherited and new institutions, which together make a model that is an alternative to the prevailing European model of self-employed GPs or group practices. 2
International literature on PHC in Russia is limited. The papers available state that the country has a strategy of incremental reforms. 10 , 11 Some papers have explored the priority of PHC in the overall health care system, and concluded that actual monetary support has lagged behind political declarations. Specialty care still prevails in Russia and other former Soviet countries. 12 Most authors conclude that the Semashko model has remained practically untouched, 10 – 12 although this is not entirely true. This model has evolved significantly, but not always positively.
Another body of literature has compared PHC internationally. The Primary Health Care Activity Monitor in Europe (PHAMEU), which includes nine CEE countries, concludes that the traditional division between “East and West” is disappearing. Estonia, Lithuania, and Slovenia are among the countries with the strongest PHC systems in Europe. 2 A number of papers address the specific characteristics of PHC transformation, including GP task profiles 13 – 15 and the growing variety of primary-care practices. 16
This analysis does not cover Russia or other former Soviet Union countries with similar health systems, such as Belarus, Ukraine, Kazakhstan, and Armenia. This is a serious gap in the literature, since these countries have a specific model of PHC. This paper fills this gap. Our objectives are twofold: first, to highlight the characteristics and developments of the Russian PHC model, and second, to look at the outcomes of this model from an international perspective and discuss their strengths and weaknesses. An overview of key primary-care characteristics is provided, followed by a presentation of the major problems of the sector and recent efforts to ameliorate them, and then a comparison of the efficiency and quality of primary care internationally. We conclude with a discussion of this model and lessons learnt.
The analysis is based on a review of the literature on PHC developments, as well as the materials from the Russian federal and regional ministries of health. Recent plans to strengthen this sector are also evaluated. Statistical analysis is based on national data. World Health Organization and Organization for Economic Cooperation and Development (OECD) databases are used to compare economic conditions, workforce developments, and efficiency. The comparison of the comprehensiveness of PHC is based on the methodology of the PHAMEU 2 and a survey of 171 primary-care physicians from 14 Russian regions. A list of questions from the European report was distributed through the Russian social network Vkontakte in May 2016 and then supplemented with face-to-face interviews with 20 physicians in Moscow polyclinics. The sample of respondents was developed with specific selection criteria. As such, a descriptive analysis was supplemented with a survey and interviews.
The authors are deeply involved in developing the national health care strategy in the capacity of independent experts. This paper summarizes the current approaches to strengthen PHC. Our major motivation to produce this paper is to share information on recent developments in Russia with policy makers in countries that have delayed major reforms of primary care and are now looking for the ways to catch up with the European mainstream. Another motivation is to revisit the Semashko model (which is usually criticized in the literature) and to compare its original design with the actual implementation.
Major characteristics of the Russian primary-care system
The major principle of the Semashko model is the financial accessibility of care. This has not been questioned in modern Russia. All citizens are entitled to free health care. However, the health system is heavily underfunded. Public health funding is currently only 3.5% of GDP, while in European countries it is 6%–10%. 17 , 18 Limited financial resources undermine the principle of financial accessibility. People often have to pay formally and informally. The share of private funding is 39% of total health care expenditure against an average 24% for Europe. 17 , 18 The share of outpatient care is much lower than for inpatient care. Most visits to the doctor and diagnostic tests are free.
The governance of PHC is centralized at the level of regional governments. This is seen as a way to consolidate resources and mitigate imbalances across communities in the region (There are 85 regions in the country with the population ranging from 500,000 to 12 million. Each region has 10-20 local communities [municipalities]). The downside is that the role of communities is insignificant: most decisions are made by regional health authorities and territorial social health-insurance funds that act as major purchasers of care. Attempts to decentralize governance in the 1990s were not successful, given serious underfunding and the geographic inequity of economic capacity. 19
A major provider of PHC is the multispecialty, publicly owned polyclinic. This is usually much bigger than traditional general practices in Western countries. The capacity of polyclinics varies from 100 to 120,000 people served in big cities to fewer than 15,000 in small towns and rural areas. PHC for adults and children is separated, with separate adult and child polyclinics operating in urban areas. District therapists serve adults and district pediatricians serve children (together they are further referred to as district physicians [DPs]). GPs or family doctors are relatively rare.
Polyclinics provide primary and specialty care for uninfectious diseases and preventive services. The “district service” is a structural unit of polyclinics with a staff of DPs, GPs, and nurses. In the original Semashko model, DPs were the sole providers of primary care, but currently specialists provide a greater volume of care in polyclinics. Depending on the size of the policlinic, there are five to 20 categories of specialists providing most of the polyclinic’s services: 60%–65% of visits. 20 Most polyclinics have diagnostic units (eg, laboratories, endoscopy) and units that are responsible for preventive services and health promotion. Patients of polyclinics have access to a wide range of services under the same roof.
People can choose a polyclinic, and most choose the provider closest to their place of residence. Patients enrolled in a polyclinic form the patient list. DPs and GPs have smaller catchment areas, while specialists serve all the enrollees of the polyclinic. The patient list is an important characteristic of the system. It existed in the original Semashko model, and has not been questioned since. Polyclinics are responsible for their enrollees’ health care on a long-term basis, which is usually regarded as the indicator of strong primary care. 2 , 10 , 15
According to federal regulations, DPs and GPs act as “gatekeepers” and refer patients to specialists and hospitals. This is also a characteristic of a strong PHC system, since it ensures the coordination and continuity of care provided at various levels of service delivery. 2 , 10 , 15 The gatekeeping function was in the design of the original Semashko model, but currently it is not strictly followed in many regions. As the following section shows, patients can see some specialists directly without a referral from primary-care physicians.
The Semashko model considers prevention, a major area of primary care and the scope of preventive activities, has been increasing. A recent innovation is a large-scale federal program of “dispensarization” (a term from the original Semashko model), which includes a wide range of checkups and screenings and covers around a third of the population. Each polyclinic enrollee is supposed to have them once every 3 years. Program monitoring is based on the number of detected cases of disease, including those at an early stage. 21
A special characteristic of the Semashko model is the “method of dynamic dispensary surveillance”. This method presumes that every detected case of a serious disease is subject to a certain set of protocols, including planning curative activities, documenting them, ensuring the required number of contacts with DPs and specialists, a monitoring process, and outcome indicators. The design of these protocols (they were developed in the late 1960s) has some resemblance to the modern programs of chronic-disease management that are common in many Western countries, 22 , 23 although they do not include some elements of these programs, such as multi-specialty groups of providers, distant monitoring of patients’ status, and bundled payment. This method was relatively well developed in the USSR, but in the decades since it has given way to the large-scale detection of new cases under the program of “dispensarization” without clear follow-up targets.
The original Semashko model was based on total public ownership of medical facilities and on medical workers as employees. The situation has changed over the last two decades. The number of private providers has increased substantially, mostly in the area of outpatient specialty care. But their share of the total number of physician visits remains low – 6.4%. Most physicians in private facilities are employees, similarly to public facilities. The bulk of services provided by private facilities is for out-of-pocket payment. The involvement of private providers in the provision of publicly funded care is limited to around 4%. 24 The principles of patient lists and gatekeeping do not extend to private settings: they operate without catchment areas, do not have any commitments for the constant management of cases, and most contacts do not require primary-care referrals. GPs are equally uncommon in private settings.
PHC in Russia is much broader than was presumed by the original concept (as mostly generalist care). It is also broader than in most Western countries. The concept of “extended primary-care composition” advocated by some international scholars 10 in Russia has reached the form of multispecialty polyclinics. The federal law “On the basics of health protection in the Russian Federation” (2011) conceptualized extended primary care by introducing the concepts of primary physician care and specialized primary medical care. The former is provided by DPs and GPs, the latter by polyclinic specialists.
These concepts mean that the borders of PHC and outpatient care practically coincide, while in Western countries a distinction between outpatient and primary care remains even in extended PHC systems: outpatient care is significantly wider in scope and totally different in function and clinical areas. Specialists do neither act as gatekeepers and coordinators of care, nor do they provide comprehensive care focused on the patient as a whole. Most importantly, specialists are not responsible for the ongoing surveillance of patients; rather, they provide episodic care. Even when specialists are first-contact physicians, all other characteristics of PHC are absent or limited.
The extended composition of PHC is the major distinction of its organization in Russia. The other basic features of the system – financial accessibility, patient list, gatekeeping, preventive-care orientation, ongoing surveillance of serious cases – can be regarded as indicators of a strong PHC system. Contrary to many criticisms of the Semashko model of primary care, it was originally well designed by modern standards. However, Russia currently faces a lot of problems with the implementation of this design.
Current activities to strengthen primary care
The government is attempting to solve PHC problems in the following directions:
- overcoming the shortage of DPs and improving their competence;
- improving polyclinic performance;
- strengthening preventive activities;
- closing the gap between urban and rural PHC;
- increasing the remuneration of primary-care physicians.
Overcoming the shortage of primary-care physicians and improving their competence
The worldwide tendency of specialization of the health workforce and a decrease in the share of generalists 25 , 26 is particularly strong in Russia. This tendency started in the USSR in the 1970s and continues today. Most clinical functions of DPs have been delegated to specialists, and the number of the latter has increased to a level where specialists outnumber other doctors in such polyclinics as PHC facilities. DPs have turned into the internal medicine specialists dealing with the simplest cases and losing their core position in PHC. 27
A shift to a GP model was declared in the 1990s, but then gave way to reservations about this model. It is seen as appropriate mostly for rural areas and small urban neighborhoods. The actual implementation of this shift has been very inconsistent, contrary to most CEE countries, which have trained enough GPs to replace DPs during the 8–10 years of transition. 13 The number of GPs in Russia in 2014 was only 0.7 per 10,000 residents compared to an average of 8.7 in the pre-2004 EU and 5.7 in the post-2004 EU. 17 The total number of primary-care physicians (DPs and GPs) per resident has been decreasing. This decrease over the last 10 years has not been compensated for by the insignificant increase in the number of GPs. The latter still have a marginal role in PHC. They account for only 13% of the total number of primary-care physicians ( Figure 1 ).

Number of primary-care physicians per 100,000 population between 2006–2015 in Russia.
Notes: Data from The Russian Federation Ministry of Health. 39
Regulation of the supply of health workers in Russia is poorly focused on primary care. Medical universities have substantial discretion in setting the structure of undergraduate and postgraduate training. A study of medical university capacity indicated that in 2016, only 20% of universities had general practice as a subject in undergraduate medical training and only 70% had postgraduate positions in general practice, while in European countries all medical schools have this subject for undergraduates and postgraduates. 2 The proportion of students that choose to become GPs in Russia is <5%, while the average figure for 31 European countries is 17% and in some countries (eg, France) is 35%–45%. 28 Our estimate of the shortage of DPs is 33%, and for district pediatricians 12%. The estimate is based on the standards of the enrolled population – 1,700 for district therapist and 800 for district pediatrician. To meet these standards, the country needs 90,600 DPs, but the current number is only 60,600. The physicians available have to hold more than one position and are thus overburdened. The average number of residents served by district therapists is 2,630 patients, which is about 50% higher than the target (1,700 residents) established by the Russian federal Ministry of Health (MoH).
Apart from the inadequate number of DPs, their task profile is limited by Western standards. To measure the comprehensiveness of care (ie, competence to treat a set of diseases), we rely on the indicators that were used by the PHAMEU in 31 European countries 2 and the aforementioned survey of Russian DPs. A major indicator of PHC comprehensiveness is the percentage of total contacts with patients handled solely by primary-care physicians without referral to specialists. Russian DPs were asked to make this estimate for their own practices. The average share for all respondents was 70%. This is a very optimistic estimate. However, it is substantially lower than in most European countries, where 85%–95% of contacts are handled by general practitioners without the involvement of specialists. 2 Other indicators of comprehensiveness are also relatively low in Russia. 29 This can be interpreted as a result of the excessive specialization of PHC and the inadequate training and professional development of DPs.
The government is looking for ways to overcome the shortage of DPs and strengthen their clinical capacity. The strategy of health-workforce development includes a shift to 2–5 years’ postgraduate training, continuous postgraduate training to replace periodic training, the development of a new system of accreditation, and strengthening the role of medical associations in accreditation. 30 These are the activities planned for the medium term. The immediate action (which started in 2017) is loosening the requirements to work as a DP. Most medical graduates are accredited for practicing as DPs without postgraduate training. The new approach may mitigate the shortage of DPs in the short run, but at the expense of the quality of primary care. No other country fills vacancies of primary-care physicians through loosening the requirements for practice. The most important alternative approaches are economic incentives and the regulation of postgraduate training by promoting postgraduate training of general practitioners. 25 , 31
Improving polyclinic performance
As major PHC providers, polyclinics are underfunded. While having a low share of public health expenditure in GDP, Russia spends more on inpatient care than outpatient care: 50.3% and 33.2% respectively. 32 The financial priority of this sector is relatively low. Underfunding is the major reason for the inadequate infrastructure of primary care, the lack of diagnostic capacity and modern IT, with the resultant long waiting times, and rationing and underprovision of services. There are problems with inadequate patient-flow logistics, the appointment system, and the division of labor between physicians and nurses and between individual units of polyclinics.
Contrary to expectations, polyclinics do not integrate the coordination or continuity of care. Based on a survey of physicians in 2012, 33 there was service-delivery fragmentation:
- the joint development of patient management plans by DPs and specialists was very rare, ie, they did not work cooperatively;
- the frequency of direct patient visits to specialists bypassing DPs was high, which can be interpreted as the result of lack of coordination of the latter;
- the frequency of timely feedback of specialists to a referring physician on the results of treatment was very low, which indicated a low level of teamwork and continuity of care;
- the level of awareness of polyclinic physicians of their patients’ hospital admissions and emergency visits was low, which limits the scope for integrative care.
The government is currently dealing with the most obvious areas of polyclinic inefficiency. There are two major directions for these activities. The first is the consolidation of service delivery through merging polyclinics into big local complexes. The reason for this consolidation is to concentrate expensive diagnostic equipment and specialists (that are in short supply) in big facilities, thereby increasing their accessibility. The second direction is to improve the organization of service delivery in the polyclinics themselves.
The first strategy is particularly strong in Moscow. Since 2011, 452 polyclinics have been merged into 46 outpatient centers for adult care, with a catchment area of 250–300,000 enrollees each. A total of 40 child-outpatient centers have been established, with 30,000–50,000 enrollees each. 34 The enrollees of these centers now have better access to a wider range of polyclinics, including those where major diagnostic equipment is concentrated. The number of computed tomography tests doubled from 2010 to 2014, while magnetic resonance imaging tests tripled. The waiting time has become much shorter ( Table 1 ).
Number of diagnostic tests and waiting time in 2010 and 2014 in Moscow city outpatient centers 34
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging.
Access to polyclinic specialists has improved. The waiting time for consultations reduced by 2–3 times in 2010–2014, while their number remained constant. Improved access can be accounted for by organizational changes rather than additional financial input. 34 Merging polyclinics in Moscow has allowed three levels of service delivery to be developed: DPs plus some categories of specialists – cardiologists, ophthalmologists, surgeons, and urologists – who are accessible to patients without referral, most other outpatient specialists who work in designated units of outpatient centers, and outpatient departments of hospitals where the best specialists are concentrated. These are linked to each other by a referral system. The Moscow health department regulates the “routes” of patients and establishes referral patterns according to the availability and workload of PHC physicians. When they are too busy, direct access to some specialists is allowed. A new information system has been introduced to support this organizational scheme.
Following the restructuring of the polyclinics, patients have to travel further to reach the outpatient center where diagnostic and specialty services are provided. However, shorter waiting times are probably a more important indicator of better access to these services. In addition to these activities, the following innovations have been introduced: 34
- Visits to patients’ homes previously made by DPs have been shifted to a special home-visit service, which is a separate unit. This service is staffed with physicians and nurses who specialize in this service. There are two objectives of this innovation: to reduce the burden on DPs and allow them to spend more time with patients in their offices, and to redistribute emergency calls from the centralized city emergency service to the polyclinics, which are closer to the patients and less costly.
- Patients can make an appointment with any DP, rather than to a regular doctor. The objective is to encourage patient choice and facilitate access to care.
- The position of duty physician has been introduced in polyclinics. This physician is responsible for the provision of care to those who need health care, but do not have an appointment.
- Nurses’ posts have been established for concentrating routine activities.
- IT has been introduced to facilitate appointments, medical records, prescriptions, and communication among providers within polyclinics. Completion of this process is planned for 2018.
- A separate unit for managing chronic multimorbidity cases is being piloted in a few polyclinics.
These innovations have reorganized polyclinics through the specialization of some curative and organizational functions. The positive part of this process is the possibility to increase physicians’ productivity and allow them to spend more time with their patients. This is particularly important for DPs, who are heavily overburdened.
The negative side is the risk of further decreasing the role of DPs as core providers of PHC. With a narrowing area of gatekeeping, they are losing their responsibility for patient lists. Patients increasingly have to deal with physicians who do not know them, which makes health care even more fragmented. Reservations about this process were made public by a group of Moscow district therapists. They urged that the fundamental principle of a patient list and gatekeeping are undermined by delegation of DP functions to other personnel. 50
The second direction of PHC reform is represented by “Resource-saving polyclinics”. The objective is to make PHC more patient-oriented and increase the efficiency of internal processes in polyclinics. Currently, the project is being piloted in three regions (Yaroslavl and Kaliningrad oblasts and Sebastopol city), and is planned for the entire country. It includes the following activities: 35
- delegation of some physicians’ functions to nurses;
- improving logistics in polyclinics, including more careful separation of patient flows across individual providers;
- improving the appointment system;
- introducing electronic communication and reducing the amount of paperwork;
- new structural units for preventive activities.
The 2 years of this project (2015–2016) gave promising results. According to the MoH, the average time of physicians’ contact with patients doubled in these regions, appointments with physicians were easier to make, and patient waiting time reduced by a factor of 12. 35
Strengthening prevention and health promotion
Although prevention has traditionally been an important characteristic of primary care, a new wave of preventive activities started in the current decade, focusing on the detection of new cases under the “dispensarization” program. The substantial coverage of the program increased the number of detected new cases more than sevenfold in 2015 relative to the start of the program in 2012. Identification of the first and second stages of cancer was 60%–80% of the total number of new cancer cases. 36
Substantial results have been achieved in the area of health education. Polyclinics are increasingly involved in promoting healthy lifestyles. Together with some regulatory initiatives (decreasing smoking and alcohol abuse, encouraging healthy diets, and building new sport grounds in residential areas), the new policy reduced the sales of alcohol from 10.7 L per capita in 2011 to 8.7 in 2015. The share of smokers reduced from 35% of the adult population in 2014 to 31% in 2016. Over the last 15 years, the share of people who are regularly involved in physical exercise has tripled, and is now close to 30%. 37
The unsolved problem is the lack of consistency in the implementation of the principle of dynamic dispensary surveillance of detected cases. No more than half the cases with indication of a serious disease detected under the program are covered by constant management by primary-care providers, 21 ie, follow-up activities are still limited. Moreover, these activities are not even planned or monitored by the program. In spite of large-scale preventive measures, a substantial number of acute cases become chronic without appropriate management. Chronic-disease management covers only 10.6% of myocardial infarctions, 23% of unstable cardiac angina, and 43.6% of ischemic heart disease. The target outcomes of these measures are not specified, and there is a lack of teamwork among specialists. 38 Therefore, the program’s positive effect is partly devalued.
Improving primary care in rural and remote areas
An attempt has been made to mitigate the gap between the supply of health workers in urban and rural areas. Physicians are encouraged to work in rural areas through lump-sum compensation for housing costs under the “Rural physicians” program. The number of rural physicians increased from 44,758 in 2011 to 55,812 in 2016. 35 However, these attempts have so far had limited effect. The number of physicians willing to participate in the program decreased from 7,413 to 4,922 in 2016. A substantial gap in physician-population ratio in urban and rural areas still remains: 45.2 vs 14.5 per 10,000 residents. 39 It is clear that the economic incentives are not strong enough to compensate for the low basic salary of rural physicians and lack of possibilities for professional development.
PHC in remote areas where a substantial number of people live is also to be strengthened. The MoH has issued a regulatory act on requirements for the location of medical facilities with specific targets of PHC accessibility in terms of the maximum distance between residential areas and medical facilities. Each region of the country has developed a road map to reach these targets in the next 3–4 years. Mobile health units are being organized. Each residential area will be equipped with emergency communication. The first steps have been made to establish health telecommunication. 40 , 41
New policy of health-worker remuneration
Russia inherited the low Soviet remuneration of health workers. Until recently, the salary of physicians was only 25% higher than the national average (compared to two to five times higher in Western countries). 18 Nurses’ salaries are 27% lower, and medical assistants 52% lower. The average salary of primary care physicians is traditionally much lower than their counterparts in hospitals. A deeply rooted perception of physicians as a “cheap” health care resource has traditionally limited the motivation to work in primary care. 42
In 2012, a presidential decree initiated an ambitious project to increase the average salaries of physicians to 200% of the average wage in the economy of the region where they work by 2018, and salaries of nurses and medical assistants to 100%. Targets were successfully reached in the first years of this project (2012–2015), but then progress slowed, due to the economic crisis. The original targets are most likely to be reached in 2018, a presidential election year.
Another innovation is the “effective contract”, a Russian version of pay for performance. Health authorities and polyclinic managers developed a set of performance indicators for each category of health workers and pay them for reaching these indicators. The major indicators for primary care include the number of physician visits, rate of hospital admissions and emergency calls across polyclinic catchment areas, and number of cancer and TB cases detected at early stages. The results of patient surveys are also taken into account. The range of these indicators varies across regions and individual polyclinics. According to the MoH, 83% of employees are currently covered by an effective contract. 35
The actual outcome of this policy remains unclear. Many polyclinics use pay-for-performance schemes that are designed to create collective incentives for better performance, rather than incentives for individual employees. In the first years of the program (2012–2015), additional funding for increasing salaries was poorly linked to performance, and thus most of the increase in average salary was not related to the target indicators. Currently, there is a search for new incentives. 37
In contrast to Western countries, where the basic salary makes up the bulk of remuneration, with concerns about too much focus on pay for performance in some countries, 43 in Russia the basic salary is low. For example, polyclinic physicians in small cities often have an average basic salary of US$200–300 per month. Bonuses added to a low basic salary will not radically change the motivation of physicians. A national survey of physicians in 2013 indicated that only 20% of them were ready to work more effectively with the available bonuses and that most were seeking a higher level of basic salary. 44 This perception has been taken into account in the recent recommendations of the MoH to increase the share of basic salary to 85%–90% (including payment for special conditions). Even with all these inconsistencies and contradictions, the effective contract is viewed positively by most health workers. This innovation, together with the centralized policy of remuneration, may encourage better performance by primary-care providers.
Efficiency and quality of primary care
The OECD report 4 uses the following indicators of PHC efficiency: hospital-admission rates, volumes of inpatient care, and frequency of emergency care because of the unavailability of primary care. The presumption is that stronger PHC systems are more likely to reduce demand for inpatient and emergency care. The major indicator of quality is patient satisfaction with regular primary-care physicians. We use a similar approach to evaluate the performance of primary care in Russia.
The major long-term positive outcome is a decrease in inpatient care. This trend is even stronger than it is internationally ( Figure 2 ). However, the dominance of hospitals in the Russian health care system remains. There is a strong public perception that quality care is provided only in inpatient facilities. The competence of primary-care physicians is often questioned by patients. The capacity of polyclinics is not always enough to take on cases that are no longer treated in hospitals after their capacity was reduced. Therefore, in spite of the hospital restructuring, the number of bed-days per capita remains 70%–75% higher than in the EU and nearly three times higher than in the US. Russia uses more inpatient care relative to most CEE countries, which had similar indicators at the start of transition to a new model of service delivery. Only Belarus has even higher indicators. Both Russia and Belarus used a very conservative strategy of primary-care development during the transition period. 11 , 12

Number of bed days per capita in all inpatient-care facilities in Russia and selected countries in 1995–2014.
Notes: Data from Rosstat 17 and World Health Organization. 18
The number of emergency visits per 1,000 residents in Russia was stable during 2000–2013 and then went down sharply ( Figure 3 ). This decrease was the result of shifting a substantial portion of emergency visits from the general medical emergency service (a separate institution) to polyclinics where special emergency units had been established. In 2015, these units provided 279 emergency visits per 1,000 residents, in addition to 326 emergency visits made by the general emergency service. This makes a total of 605 emergency visits per 1,000 residents. Therefore, the total frequency of emergency visits has increased.

Emergency care visits rate per 1,000 population of Russia in 2000–2015.
Notes: Data from The Russian Federation Ministry of Health. 40
This indicator can be approximately compared with the “proportion of residents who visited an emergency department because primary care was not available” from the OECD report for Europe as an indicator of primary-care strength. The average of this proportion is 23% for 26 EU countries, with most countries ranging between 8% and 30%. 18 We tentatively conclude that in Russia, the frequency of emergency visits is nearly three times higher than the average for OECD countries.
The Levada Center (one of the biggest sociological organizations in Russia) survey indicated that in mid-2016, 44% of respondents were dissatisfied with the length of visits to polyclinics and 63% with the qualifications and number of polyclinic physicians. 45 Similar estimates for European countries indicate that 80%–90% of respondents are satisfied with their GPs. 2 Over the last decade, Russia has achieved substantial improvements in health indicators – total and specific disease mortality – and life expectancy. This is the result of the economic growth in the early 2010s and additional health funding; however, these indicators are still substantially lower than in Western countries. 37
Primary care in Russia was originally well designed under the Semashko model. Financial accessibility, a focus on prevention, including the dynamic dispensary surveillance method, patient lists, and gatekeeping made the system potentially strong. However, in practice, this potential is not fulfilled. The gap between expectations regarding the prevailing model of service delivery and its actual implementation has increased over the last few decades. The model does not ensure the efficiency or quality of care. There is substantial evidence of the low priority of PHC, a shortage of DPs, low economic incentives for medical workers, and a gap between urban and rural areas. The detection of new cases under a large-scale prevention program is not followed by their management, contrary to the original design of the system. The gatekeeping function of primary-care providers is weakening.
The current problems of PHC have nothing to do with the original design of the Semashko model; rather, they are deeply rooted in the long-term developments that started in the USSR and continued in modern Russia. First, specialization in PHC, common in many countries, has gone too far in Russia. Specialists have replaced a substantial number of DPs, rather than supplementing them. This process has resulted in a decline in DPs’ clinical areas and their coordination function. They are no longer in the driver’s seat 10 in big multispecialty polyclinics. Importantly, the new division of labor in primary care does not compensate for the shortage of DPs, because specialists usually deal with episodic demand and have limited commitment to the constant surveillance of patients’ health needs and comorbidity cases. The need for strong generalists has not diminished.
Second, the government has lost the leverage to regulate the supply of physicians. Postgraduate training is skewed toward specialists, particularly those who provide private services (eg, dentists, urologists), while the number of generalists in training is falling. The structural imbalances in supply have become a characteristic of the current health system, 42 which reflects the lack of strategic vision in the governance of the system.
Third, the country has missed the shift to the GP model, which has allowed CEE countries to extend the comprehensiveness of primary care. 29 In Russia, the presumption was that generalists can be strengthened by a growing number of specialists in the model of multispecialty polyclinics. But this has not happened. The narrow clinical area of DPs, together with their shortage, generates demand for the growing number of specialists and eventually leads to a shortage of specialists as well, creating the vicious circle of shortages. The current attempt to fill the vacancies of DPs with graduates of medical universities without postgraduate training is a manifestation of this process. The alternative to this approach is to train the required number of qualified GPs with an extended clinical area and make them major providers of primary care. This will take a few years, but cannot be avoided.
Finally, the model of the multispecialty polyclinic as the major provider of PHC has not changed in the transition period and is not questioned now. Although this model is promising for the integration of care, its potential is dependent on the coordination of care, its continuity, and the joint work of individual providers. There is a substantial body of international evidence on this point. 46 – 48 Recent attempts to consolidate polyclinics into bigger entities is not a panacea for inefficient service delivery. The first evidence of its impact is contradictory: better access to expensive diagnostic resources is coupled with a growing demand for specialty care and a loosening of the coordination of primary-care providers. The same holds true for organizational restructuring. The positive part of this process is the possibility to increase physicians’ productivity and the amount of time spent with their patients. The negative side is the risk of further dismantling the role of DPs as core providers of primary care. They are losing their patients, who are increasingly having to deal with physicians who do not know them well, which fragments health care even more. This is a corollary of the excessive specialization of primary care.
The comparison of primary care models in Russia and CEE countries 29 does not demonstrate the strength of polyclinics relative to the smaller settings of solo- and group-GP practices, which dominate most CEE countries. Apart from the lack of evidence of higher integration, there is the problem of weak economic incentives in polyclinics. The recent innovations of pay for performance are not related to the comprehensiveness of care, and thus do not provide incentives for professional development. The salary of GPs is only 10%–15% higher than that of DPs. The economic “signal” for an entire facility does not reach individual physicians and nurses in a big setting. 49
The polyclinic model has created a new category of specialists that provide only outpatient care and thus have limited professional competence (eg, nonoperating urologists in polyclinics). In the absence of GPs with a wide clinical area, specialists work with simple cases and most specialists are not affiliated with hospitals; therefore, their incentives for professional development are limited. A polyclinic is an administrative body, rather than a voluntary cooperative of physicians in group practices. They are headed by administrators who make decisions on patient lists for individual DPs, determine the scope of preventive services, ration diagnostic resources for each physician, and set salaries. This administrative pressure does not fit with the work of PHC providers: the sole responsibility for the health of patients on the list, a wide variety of activities that are not easy to predict (eg, interaction with families, community, specialists), and the high level of creativity that is needed to ensure the successful management of cases. Not surprisingly, newly trained GPs usually feel uncomfortable in polyclinics. Some of them prefer the position of DP.
Russian primary care has evolved from the Semashko model to a model that has lost some of the positive characteristics of the original and does not ensure efficient and quality care. This can be attributed to the excessive specialization of primary care, weak health-workforce policy, delays in the shift to a GP model, and the dominance of the multispecialty polyclinic, which has not proved better than alternative models. Some of the attempts to strengthen PHC are promising, but they are not enough to compensate for the lack of strategic vision in previous decades. More systematic and consistent reforms are needed. Major lessons learnt are:
- The low priority of primary care generates demand for specialty care and eventually results in structural imbalances in the entire health system.
- The lack of generalists and coordination cannot be compensated for by the growing number of specialists on the staff of primary-care facilities.
- Big multispecialty settings (polyclinics in the Russian context) have the potential for better service-delivery integration, but to make this happen, action is needed. Simple decisions, like merging polyclinics, do not help much.
- Delegating some functions of primary-care physicians to other categories of medical personnel may or may not contribute to higher performance of primary-care facilities, depending on how this delegation is managed.
Acknowledgments
This paper is an output of a research project implemented as part of the Basic Research Program at the National Research University Higher School of Economics (HSE) in Moscow, Russia.
The authors report no conflicts of interest in this work.

IMAGES
COMMENTS
The flaws of the U.S. health care system have been exposed and exacerbated by the coronavirus pandemic. This paper posits three underlying causes of our persistent poor performance: flawed assumptions; inadequate information; and fragmented delivery, payment, and insurance systems that make it easier to profit by shifting risk or costs to others than by improving value.
1. INTRODUCTION. In the United States (U.S.) between 1960 and 2019, healthcare spending as a percentage of U.S. Gross Domestic Product (GDP) grew from 5% to 17.7%, reaching $3.8 trillion dollars in 2019 (Figure 1). 1 Payment reform models have emerged to both control this growing expense and realign how quality, as a return on investment of the healthcare dollar spent, is measured.
Search for more papers by this author. ... we launched the 1% Steps for Health Care Reform Project in February 2021. 1 Our goal was to harness the power of academic research by generating a series of briefs for policy makers that describe tangible, evidence-based interventions that could each lower health care costs in the United States by a ...
The mission of the American Heart Association is to be a relentless force for a world of longer, healthier lives. The American Heart Association has consistently prioritized the needs and perspective of the patient in taking positions on healthcare reform while recognizing the importance of biomedical research, providers, and healthcare delivery systems in advancing the care of patients and ...
The Affordable Care Act has made significant progress toward solving long-standing challenges facing the US health care system related to access, affordability, and quality of care. Since the Affordable Care Act became law, the uninsured rate has declined by 43%, from 16.0% in 2010 to 9.1% in 2015, primarily because of the law's reforms.
A shift in federal research funding priorities is necessary, however, to fully enable a national strategy to improve health care quality and reduce disparities. 50 In 2007, the United States spent 4.5% of total health care expenditures on biomedical research, but only 0.1% on health services research. 51 The National Institute of Health (NIH ...
Central to achieving increased coverage and access, high quality, and cost control is change in reimbursement arrangements, increased accountability for both costs and outcomes, and criteria for rationing based on the evidence and accepted as legitimate by all stakeholders. Consensus about health reform requires trust.
Abstract. This chapter analyzes the Affordable Care Act's (ACA) turbulent political journey and the current state of health care reform in the United States, with particular focus on developments in health politics and policy during the Obama and Trump administrations. Reforming American health care is perennially a politically treacherous ...
The great generational debate on how to reform the health care system in America came to a dramatic conclusion late in the evening of 21 March 2010 when the House of Representatives approved (by a vote of 219 to 212) a previously approved Senate version of health reform legislation. 1 Two days later, President Obama signed the landmark legislation into law and became the first President since ...
In 2008, the United States devoted 16% of the economy to health care, an increase of almost one-quarter since 1998 (when 13% of the economy was spent on health care), yet much of that spending did not translate into better outcomes for patients. 1-4 The health care system also fell short on quality of care, too often failing to keep patients ...
2.6 Lessons learned from Medicare and Medicaid for Future Healthcare Reform 27 Chapter 3: The Creation of the Affordable Care Act 29 3.1 The Patient Protection and Affordable Care Act (ACA) 29 3.2 Healthcare Climate Leading up to the ACA 33 3.3 Post-Implementation Changes to the ACA 35 3.4 Lessons learned from the ACA for Future Healthcare ...
CMMI has increased federal spending without producing meaningful reforms of federal health care entitlement programs. This paper will review CMMI's statutory authorities and track record and show how faulty fiscal assumptions made by the Congressional Budget Office can impede congressional efforts to reform CMMI.
An important goal of health care reform should be to replace the current byzantine system of premiums, taxes, tax exemptions, deductions, subsidies, and out-of-pocket payments with a much simpler system of financing health care. ... High-income individuals also prefer US health care research that emphasizes product improvement and ignores cost ...
Introduction. Health equity is a basic value assumed in the health policies of many countries worldwide 1.In April 2009, the Chinese government issued a new healthcare reform plan 2 meant to provide equity, safe, effective, medical services for residents. An additional 850 billion yuan (approximately US $125 billion) was planned for 2009-2011, with the aim of providing basic healthcare that ...
After nearly 6 decades, Medicaid has become the largest health insurance program by enrollment in the US and accounts for a substantial amount of health care expenditures. Medicaid has improved access to care and health among low-income populations and disproportionately insures people from racial and ethnic minority groups.
Background There is unfinished reform in primary care in Russia and other former Soviet Union (FSU) countries. The traditional 'Semashko' multi-specialty polyclinic model has been retained, while its major characteristics are increasingly questioned. The search for a new model is on a health policy agenda. It is relevant for many other countries. Objectives In this paper, we explore the ...
Purpose: This paper explores the impact of health provider concentration on service delivery integration through the indicators of teamwork, coordination and continuity of care in outpatient and ...
Cluster 8 provides some insights on the state of art in the healthcare research field. Beyond case studies, the topic becomes relevant only relative to the spreading of digital services in the care system. Other studies (eg, 62), retrieved in the previous step, describe a potential stream of organizational change issues in the healthcare ...
Shishkin S. Russia's health care system: difficult path of reform. In: Weber S, Alexeev MV, editors. The Oxford handbook of the Russian economy. Oxford: Oxford University Press; 2013. ... This paper is an output of the research project implemented as a part of the Basic Research Program at the National Research University Higher School of ...
Abstract. This paper addresses the major developments in primary care in the Russian Federation under the evolving Semashko model. The overview of the original model and its current version indicates some positive characteristics, including the financial accessibility of care, focus on prevention, patient lists, and gatekeeping by primary-care ...