
An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel

The Role of Community Pharmacists in Patient Safety
What is a community pharmacy.
Community pharmacies are sometimes equated to retail pharmacies, operating out of both large and small chains or grocery stores. However, what constitutes a community-based pharmacy is much broader than the traditional retail setting. Community-based pharmacies also include outpatient pharmacies found within health systems, Federally Qualified Health Centers, primary care clinics, compounding pharmacies that prepare medications for patients who require unique dosing or modified formulations, 1 and specialty pharmacies where patients receive outpatient care for complex medication therapies. 2 Pharmacists may pursue community-based residencies or fellowships to enhance their clinical and leadership skills, preparing them for a role in community pharmacy. 3
What roles does a community pharmacist play in patient safety?
Historically, the concept of the “five rights” has been used to describe the steps that lead to safe medication use: the right dose of the right medication taken by the right patient at the right time and by the right route. However, this concept is oversimplified, as there are additional steps of safe medication use that should also be considered; steps that are dependent on the context in which the medication-related process is occurring. Each part of the medication use process may contain different numbers and types of “rights”. For example, in the community pharmacy setting, outcomes like the right education, right monitoring, right documentation, and right drug formulation may also be considered.
The modern concept of medication safety is much broader in scope than the “five rights” and the focus has subsequently shifted with an increased emphasis placed on the contribution of systems factors to medication safety. Factors not directly related to medications are considered, including how the workflow, technologies, policies and procedures, and other systems factors support the outcomes of the various rights, rather than focusing solely on completion of an oversimplified checklist.
Pharmacists in the community ensure medication safety similarly to how they would in any healthcare environment: throughout the medication-use process, including the ordering of medications to their storage, transcription, preparation, dispensing, counseling, and more. Prior to the dispensing process, the community pharmacist provides a clinical review of prescribed medications to ensure the therapies are appropriate. This review includes dosing appropriateness, interactions with other prescribed medications, contraindications, and more, while also considering that medications may have been ordered by multiple prescribers. 4,5 The pharmacist also provides critical monitoring in the dispensing of controlled substances, such as consulting prescription drug monitoring programs to look for patterns that might indicate abuse or diversion and to screen for potentially fatal interactions between medications that may come from multiple prescribers. 6,7 Pharmacists must identify patients at risk for fatal overdose and facilitate access to the emergency opioid reversal drug Narcan® (naloxone) as well as substance abuse treatment services when appropriate.
A clinical review is essential for all prescriptions and can help ensure that any errors occurring as a result of the care transition process are caught and corrected before the medication is dispensed. 8 For example, in the discharge process, the inpatient providers may have an incomplete history of the patient’s existing prescriptions when formulating the treatment plan. In addition, medications that may have been appropriate during the inpatient stay, but inappropriate for home use, may inadvertently be carried over into the patient’s outpatient treatment plan.
In addition to the dispensing process, the community pharmacist plays a critical patient safety role when it comes to ensuring that patients appropriately understand their medications. 4 Community pharmacists are equipped to provide education and counseling to patients to address questions they may have regarding factors such as dosing, administration, storage, potential side effects, and how to taper medications for acute events. Similarly, community pharmacists are an invaluable resource for supporting public health initiatives. One study found that patients visited a community-based pharmacy 35 times per year, as compared to a primary care physician, which occurs, on average, 4 times per year. 2 This frequent contact with patients makes community pharmacists optimally positioned to support public health initiatives and triage concerns. Numerous studies have proven the positive impact of pharmacists on preventative care such as health screenings and immunizations, opioid management, smoking cessation efforts, and management of chronic diseases such as diabetes. 9
What supports community pharmacies in providing patient safety?
Patient safety is best achieved in organizations that have a strong culture of safety . Organizations with a strong culture of safety are not only better positioned to ensure patient safety from the outset, but also more likely to recognize the importance of dedicating the time and resources to tracking, understanding, and appropriately addressing patient safety events or near-misses. Surveys such as the Agency for Healthcare Research and Quality Community Pharmacy Survey on Patient Safety can help pharmacies assess the current state of their safety culture and identify any areas for improvement.
In addition to a strong culture of safety, open communication with, and ease of access to, prescribers can support community pharmacists in the prevention of errors. 10,11 Interoperability between data systems, notably electronic health records and state-based health information exchanges, facilitates this open communication by ensuring consistency of information and seamless sharing of patient data between the pharmacist and the prescriber. Ease of access to providers enables the pharmacist to efficiently address potential concerns discovered upon clinical review of the patient’s treatment plan.
Finally, fostering relationships between patients and pharmacists can support safe continuity of care by helping patients develop trust in their pharmacists, increasing their likelihood to seek counseling, address concerns regarding their medication therapy, and provide a more comprehensive medical history.
Georgia Galanou Luchen, Pharm. D. Director, Member Relations Section of Community Pharmacy Practitioners and Section of Pharmacy Educators American Society of Health-System Pharmacists Bethesda, MD
Kendall K. Hall, MD, MS Managing Director, IMPAQ Health IMPAQ International Columbia, MD
Kate R. Hough, MA Editor, IMPAQ Health IMPAQ International Columbia, MD
- Compounding. National Community Pharmacists Association. Accessed June 25, 2021. https://ncpa.org/compounding
- Moose J, Branham A. Pharmacists as influencers of patient adherence. Pharmacy Times. August 21, 2014. Accessed June 25, 2021. https://www.pharmacytimes.com/view/pharmacists-as-influencers-of-patient-adherence-
- American Society of Health-System Pharmacists, American Pharmacists Association. Guidance document for the accreditation standard for postgraduate year one (PGY1) community-based pharmacy residency program. Updated March 2021. Accessed June 28, 2021. https://www.ashp.org/-/media/assets/professional-development/residencies/docs/ashp-apha-pgy1-community-based-standard-guidance.ashx
- Goode JV, Owen J, Page A, Gatewood S. Community-based pharmacy practice innovation and the role of the community-based pharmacist practitioner in the United States. Pharmacy (Basel) . 2019;7(3):106. doi:10.3390/pharmacy7030106
- Messerli M, Blozik E, Vriends N, Hersberger KE. Impact of a community pharmacist-led medication review on medicines use in patients on polypharmacy--a prospective randomised controlled trial. BMC Health Serv Res . 2016;16:145. doi:10.1186/s12913-016-1384-8
- Doong KS, Gaccione DM, Brown TA. Community pharmacist involvement in prescription drug monitoring programs. Pharmacy Times . December 13, 2016. Accessed June 25, 2021. https://www.pharmacytimes.com/view/community-pharmacist-involvement-in-prescription-drug-monitoring-programs
- Upton C, Gernant SA, Rickles NM. Prescription drug monitoring programs in community pharmacy: an exploration of pharmacist time requirements and labor cost. J Am Pharm Assoc (2003). 2020;60(6):943-950. doi:10.1016/j.japh.2020.07.002
- Tetuan CE, Guthrie KD, Stoner SC, May JR, Hartwig DM, Liu Y. Impact of community pharmacist-performed post-discharge medication reviews in transitions of care. J Am Pharm Assoc (2003). 2018;58(6):659-666. doi:10.1016/j.japh.2018.06.017
- Strand MA, DiPietro Mager NA, Hall L, Martin SL, Sarpong DF. Pharmacy contributions to improved population health: expanding the public health roundtable. Prev Chronic Dis. 2020;17:E113. Published 2020 Sep 24. doi:10.5888/pcd17.200350
- Botross A, Botross E, Ho C. Communication is key to medication safety. Hospital News. Accessed June 25, 2021. https://hospitalnews.com/communication-is-key-to-medication-safety
- National Healthcareer Association. Effective communication in vital for pharmacy technicians. Pharmacy Times. May 7, 2021. Accessed June 25, 2021. https://www.pharmacytimes.com/view/effective-communication-is-vital-for-pharmacy-technicians
In Conversation With... Georgia Galanou Luchen, Pharm. D.
Editor’s Note: Georgia Galanou Luchen, Pharm. D., is the Director of Member Relations at the American Society of Health-System Pharmacists (ASHP). In this role, she leads initiatives related to community pharmacy practitioners and their impact throughout the care continuum. We spoke with her about different types of community pharmacists and the role they play in ensuring patient safety.
Kendall Hall: So, Gina, can you just introduce yourself and describe your current role?
Gina Luchen: My name is Gina Galanou Luchen, and I am a pharmacist by training. I completed my undergraduate and Doctor of Pharmacy degrees at the University of Kansas School of Pharmacy. I then completed a postgraduate community-based pharmacy residency, followed by the ASHP [American Society of Health-System Pharmacists] Executive Fellowship in Association Leadership and Management. I am currently serving as the ASHP Director of Member Relations for the Section of Community Pharmacy Practitioners and Section of Pharmacy Educators. A little bit about my organization: the American Society of Health-System Pharmacists (ASHP) represents pharmacists serving as patient care providers both in acute and ambulatory care settings. We have nearly 58,000 members that work in pharmacy across the continuum of care with a goal to improve medication use, enhance patient safety, and advance pharmacy practice. In my role, I focus on community-based practitioners who are practicing within health systems or other community pharmacy settings. I am also highly involved with pharmacy education, supporting our members who educate student pharmacists and pharmacy residents and train the pharmacy workforce.
KH: Let’s talk about the training. Are there differences between how you train for working in an acute care facility versus in a community setting?
GL: That's a great question. When you graduate from a college or school of pharmacy, there are many postgraduate training opportunities. There are first- and second-year residency training programs. First-year pharmacy residencies are broken down into three major categories. One is what we consider the traditional pharmacy practice residency in an acute care setting. Residents usually train in a hospital or health-system environment, providing inpatient and outpatient pharmacy services within that institution. Second are community-based residencies, focusing on training within community pharmacies and ambulatory care clinics. Third are managed care residencies, and that's more specialized and looks at using clinical evidence and economics to optimize population health outcomes and medication benefits. There are also fellowship programs in research, policy, academia, nonprofit, industry, or other specialty practice areas.
KH: Thank you—that's very helpful for some context. To provide some clarity for individuals who may not be as familiar, what does it mean to be a community pharmacy, and what are the various operational types?
GL: When you think about a community pharmacy, most people bring to their mind their neighborhood pharmacy. But in the broad sense, community pharmacy is any healthcare setting that provides medication-related services to a patient within their community. The practice encompasses a large number of services and settings. You have the retail setting that can be found as stand-alone stores, both in smaller or larger chains, within grocery stores, or other retail settings. Then you have hospital or health-system outpatient pharmacies, which may serve patients of that particular institution or serve the larger public. And then you have clinic-based pharmacies that might be part of an ambulatory practice. For example, think of a specialized psychiatry clinic, or a primary care and multi-specialty physicians’ office, or assisted living facilities that may have community pharmacies embedded within them. Then you might have pharmacies that serve individuals who are homebound or provide home infusion therapy. Some pharmacies are designated as specialty pharmacies, and they provide specialized medications that treat complex conditions. There are also mail order pharmacies. And, if a patient requires nontraditional dosage forms or strengths of the medication, there are compounding pharmacies that handle custom compounded medications. In a nutshell, there are many settings in which community pharmacists practice and where community pharmacies can be found, but whenever you think of a patient condition that requires any type of medication therapy or any type of intervention within the community, you will likely find a pharmacy that helps to serve that patient and meet those needs.
KH: Wonderful. Thank you. I don't think we realized just how broad that term is and what it covers. With all of these different settings, what are the common and overarching goals of these community-based pharmacies?
GL: I think the goal of community-based practice is to support patients on an individual level not just in managing their medications, but also in managing their health, and to support public health in general. Outside of the traditional dispensing of medications, pharmacies in the community setting offer a variety of other services like medication counseling or disease state education. They assist patients in managing their entire medication therapy. Most community pharmacies today also provide immunizations, they provide point-of-care testing, and they provide consultations and other services needed within that population. There was a study that looked at accessibility for community pharmacies and found that nearly 90% of Americans live within 5 miles of a pharmacy. 1 This represents the tremendous opportunity that community pharmacists have to impact patient care, and that's why all these services that go beyond medication dispensing are so crucial to patients. When you think about the pharmacy’s responsibility, it's really to protect patients and to ensure that their therapy is optimal, safe, and effective. The pharmacist role within the community, and really across the continuum of care, is to increase medication optimization and safety, and ultimately to practice at the top of their license to help patients be healthier.
KH: Well, I think that's a great transition point to start talking about patient safety. What are some of the common patient safety events that can occur across these different settings? And what are some of the considerations that the pharmacist manages in order to protect the public?
GL: Pharmacists in the community manage safety similarly to how they would in any healthcare environment where patients are treated, and medications are handled. To start with, every pharmacist ensures that the services they provide encompass what we refer to as the “Five Rights,” and those are that the right drug makes it to the right patient, at the right dose, in the right route, and at the right time. Although these Five Rights are fundamental in establishing medication handling and dispensing, it's not always simple to ensure because, as we mentioned earlier, community-based pharmacists are part of a larger care continuum, and they provide services that are well beyond the dispensing process. So, when we're thinking about the safety considerations for a community pharmacy, we have to look at every single step, from the medication order to dispensing, the patient’s receipt of the medication, and the patient’s home.
The Institute for Safe Medication Practices (ISMP) released a report 2 about the key elements of a medication review system for community pharmacies, and they described a number of different elements within that process. But in summary, it starts with the procurement of the medication, so that's purchasing the medication, which includes navigating through drug shortages, verifying that the medication comes from reputable sources, accounting for the shelf life and the storage of the medication, and even keeping a quantity on hand of key medications that are needed in the community for immediate access. That’s all what we call part of the medication supply chain safety and integrity, and those are things that community pharmacists look at on a daily basis.
You then have the therapeutic considerations of safety—that is, ensuring that the medication prescribed is intended to treat or manage the patient’s disease appropriately. This can take into account pharmacists screening for medication duplications, omissions, allergy screenings that could interfere with the prescribed therapy, a new diagnosis that may have been added and needs to be accounted for, ensuring that the dose is appropriate, looking at drug interaction, etc. So there’s a whole therapeutic profile review that occurs in every medication that's dispensed in the community, and it requires a full understanding of the patient's medication profile and their health status. Sometimes verification requires picking up the phone and calling the prescriber or patient.
Then you move into the dispensing process. We mentioned those Five Rights, verifying that the interpretation of the prescription you're getting is appropriately entered and accurately dispensed and that you're filling the correct medication. Other factors would be operational workflow, staffing, technology, and the environment.
Two more things that people don't necessarily think about within the pharmacist’s realm of what we do to secure patient safety include the patient education component. This is ensuring that the patient understands the treatment provided to them. An example can be a pharmacist who is completing a medication review to ensure that the patient is comfortable with what they're taking, that they understand why they're taking their therapy, or counseling on controlled substance utilization or even opioid storage and safety. Lastly, care transitions. It's important to remember that community pharmacists are part of the overall healthcare team for a patient. Their role is crucial in reinforcing education after discharge, coordinating with the prescriber or multiple specialists, to ensure that everybody is on the same page as far as the medication profile for the patient, and preventing any duplications or omissions. The pharmacist is the last line of defense between the patient and that medication, and it's the last opportunity to protect the health of patients.
KH: Listening to you makes me realize that there's such an opportunity for the pharmacist in these settings to serve as a safety net or a double check to some of the things that go on both in the physician's office and at home. How do you take advantage of that? Is it the education piece with the patients?
GL: The community pharmacy, and pharmacy as a profession in general, has a really strong culture of safety. We realize how important our role is in protecting the public. If you look at the oath of the pharmacist, it starts by saying, “I'll consider the welfare of humanity and relief of suffering as my primary concerns” and then goes on to mention that assuring optimal outcomes for patients is really a top priority. You carry a lot of that responsibility as part of the overall culture of being a pharmacist. But the responsibility is with everyone. It starts with the pharmacy technician who takes the medication at the drop-off, to the pharmacist that provides the review, through to the collaboration between the pharmacist and the nurse or the physician to discuss any questions that may arise. From a culture standpoint, there are protocols in place for continuous evaluation and quality improvement within the pharmacy. Each institution has their own methods for ensuring that the staff is well-trained and comfortable performing their duties, that there's appropriate automation and technology, and the environment is distraction-free. And then, of course, there are tools that community pharmacies use to continue enhancing that safety culture. AHRQ [the Agency for Healthcare Research and Quality] has a community pharmacy survey, Community Pharmacy Survey on Patient Safety Culture , that's intended for pharmacy sites to evaluate their approach to safety. It is a self-critique of sorts and asks, “How can I learn from my staff? How can I learn from my patients?” For improving that safety process, ISMP has a self-assessment for community pharmacies as well, outlining different elements of the medication use system to help improve and prevent errors. Then there are even voluntary accreditations for pharmacies. ASHP has an accreditation standard for community and outpatient pharmacy practices with an entire section dedicated to medication safety, patient safety, and supporting continuous quality improvement. So, I think it's an ongoing process, regardless of your setting, establishing that culture to ensure that anyone who touches any aspect of care regards the patient’s safety as a top priority.
KH: So, what would you say are the biggest challenges to safety in the community pharmacy space?
GL: Every community pharmacy operates a little differently and the patient populations and services they offer also vary, but I think if you're speaking generally about common challenges we see in the community-based setting, I would say time available for conducting patient-related services. Again, ISMP has looked at errors that relate to the time the pharmacist has available to review and dispense the medication. and it's clear that pushing for higher volumes and faster dispensing and introducing multiple interruptions creates a risk. Another big challenge for community-based practitioners is that reimbursement is tied to the dispensing, not the clinical services that are so crucial to the safety. This means that the time the pharmacist spends conducting the therapeutic review, clarifying questions with the provider, and talking to the patient are not covered by reimbursement. This limits the availability that you have as a pharmacist.
Then you have interoperability concerns. Having access to patient information is extremely important for ensuring that community pharmacies are able to appropriately conduct a profile review, screen for allergies, do that therapeutic screening that we discussed earlier. If you're tied to a clinic or hospital, you might have access to the patient's direct chart or patient records, which allows you to do a more comprehensive review. However, unfortunately, that's not the case for most of our community pharmacies, who may have to piece it together and spend the extra time calling the nurse line and trying to get a hold of the physician, which I think brings us to a third challenge, which is access to the providers. This again affects the timing and safety of working with patients. In a clinic or health system, you might have a direct line of communication with providers when issues arise. That becomes more challenging in community settings where a pharmacist has to spend a significant amount of time trying to access the prescriber and there's no standard way to communicate with every provider. But overall, when you think about patient safety, it's important to remember it’s not just about the dispensing, it’s about the service provided, and it's about assessing the overall care and the overall system to ensure that safety is in place. Community pharmacies are great at continuous quality improvement as a gold standard. They keep looking at the issues and they keep evaluating what's going right and what's going wrong, in order to continue improving.
KH: You know, it seems that having continuity is something that I keep hearing in what you're saying in terms of having good communication with providers, with the patients. With transitions of care, could we talk a bit about those pharmacies that are part of health systems and their role in care transitions?
GL: I think every pharmacy has an extremely important role in care transitions. Ultimately, we talked about community pharmacies being the final safety net for that patient before they go home with a medication. But going back to the issues that we mentioned, interoperability is a huge component of being able to perform safe transitions. In an ideal world, what we would like to see is all community pharmacists having access to patient records and being able to review medication profiles, have access to providers, and document their interventions. Think about care as a feedback loop versus silos of care. Community pharmacies have a tremendous role to play because they often have the most touch points with the patient. At times they see patients on a weekly basis. So that's an opportunity for education, an opportunity for further clarification, an opportunity to look at the patient and evaluate, how's your adherence? Are you comfortable with your therapy? Can you afford your medication? These are all factors that play into patient safety. We could do everything right and then that patient goes home and doesn’t understand their therapy and doesn’t adhere to the therapy and then we're back to non-optimized use, not because anything went wrong with the diagnosis or anything went wrong with the actual care of the patient, but because they just didn't understand how to appropriately utilize their treatment. So, care transitions are critical in ensuring patient safety, and community pharmacies are really important in helping establish those relationships with providers and with patients and avoiding those mistakes.
KH: Are there any tools available for pharmacies that are not part of the system where the patient usually gets care? Or is it a reliance on the use of interoperable computer systems?
GL: There are definitely ways to ensure patient safety, no matter if you're part of an integrated system or a part of a stand-alone pharmacy. For a pharmacy provider who works in a community setting that may not have access to the electronic health record, or may not have direct access to the provider, there's still the responsibility of taking care of the patient. Professional education in these instances is so important, ensuring that you're up to speed with the latest treatment guidelines and understanding the appropriateness of therapy from your clinical expertise. The pharmacy team has the responsibility to serve as a patient advocate and communicate on behalf of the patient. The team also participates in quality reviews, looking at where errors happened, and collecting data that can be presented both to their institution, but also to collaborative organizations or collaborative practitioners and say, “Hey, we're seeing that these are the errors that are occurring, how can we work together to improve them? How can we collaborate better?” Most errors are related to system gaps, not individual providers, so constant reassessment of the processes is key.
Engaging patients in their own care is really important because ultimately, the patient can give you more information than anybody else. Maybe they can connect you directly to their provider, or maybe they can provide you more information about where the confusion arises. From the patient’s standpoint, they, or their caregivers, need to ensure they are actively involved in their own care and advocate for their own needs. Ensure that they understand why a medication change was made to their treatment. Sometimes patients are afraid to ask, but it's really important to talk with their pharmacist, talk with their provider, and understand why changes are being made so an error can be prevented, and medication use can be optimized. It also allows the development of trusting relationships with providers. We often hear the term “pharmacy hopping.” But it is important to establish long-term relationships with one pharmacist, one primary provider, and consistent specialists. This brings continuity to your care and goes a long way in preventing errors.
KH: Are there formal mechanisms by which pharmacists and clinicians whose patients are coming to them can communicate about patterns or trends?
GL: It goes back to the ongoing patient safety monitoring and the error reports that pharmacists review. A really strong, ongoing safety program is documenting errors or near-misses. There are many different documentation forms out there- one is called Assess-ERR™, and it guides you through how to document the error or near-miss to understand what type of error was it? What kind of medication did it involve? What were the circumstances around it? So, when the pharmacist or administrator reviews these documents, they can look at trends and determine if something is a one-off mistake or a pattern. Sometimes there could be a systems issue that requires staff education or updating a policy or process. Or it could be we're seeing a recurring misunderstanding from a provider warranting a call or clarification. So that's why that continuous quality improvement process is so important, because it looks at errors not only in an isolated incident, but trends over time, and identifies internal and external opportunities in a more formalized way.
KH: How is that feedback provided? Is it provided directly to those involved? Is it provided back to the safety group at the hospital? How do you to make sure that you get the information to the right people?
GL: It depends on the circumstances. If it's a prescribing or dispensing trend like we talked about earlier, then that would be a communication with the specific provider’s office or mak[ing] an internal change to the system or process. But if it is a transitions-of-care concern that you find, such as a medication missed at discharge, the pharmacist would call the discharge facility to confirm whether there was, in fact, an error or if it was intentional, and then make the changes with the provider. So, it's all on a case-by-case basis, depending on what type of error you're seeing. Overall, the complete medication review is that key component that happens before the patient goes home to ensure that all medications are correct.
KH: Is there anything that you think we should cover that we've missed or anything additional around patient safety in this setting?
GL: I think talking about some of the changes that are on the horizon that are helpful in planning for patient safety would be good to cover. From an operational standpoint, there's an effort to provide broader access to key providers and ensure that community pharmacists everywhere have access to the health information data that they need. CMS [the Centers for Medicare & Medicaid Services] is working to build out a roadmap for electronic exchange of data and e-prescribing to avoid errors and help with more communication and integration. There are also groups like the Pharmacy HIT [Health Information Technology] Collaborative that advocate for integrated networks of care. And then similarly, CPESN [Community Pharmacy Enhanced Services Network] is working to encourage community pharmacies’ involvement in providing enhanced patient care services. So, from an interoperability standpoint, there's a lot of action because we realize it's so important to communicate with one another. We're also seeing consistent use of technology to avoid errors, like barcode scanning and clinical decision support tools. These [technologies] catch errors that maybe the provider might not. We're also seeing innovative partnerships between settings to promote safety. For example, we're seeing partnerships between health systems and community-based pharmacies, creating collaborations for care transitions. Lastly, we mentioned some barriers with the time available for dispensing and clinical services, such as patient education. There is a push for regulatory change right now in recognizing pharmacists as providers and reimbursement for both dispensing and for other clinical responsibilities, such as counseling. The important thing to recognize is that community pharmacists do so much more than dispense medication.
1. National Association of Chain Drug Stores Foundation. Face-to-face with community pharmacies. Accessed July 12, 2021. https://www.nacds.org/pdfs/about/rximpact-leavebehind.pdf
2. Institute for Safe Medication Practices. Improving medication safety in community pharmacy: Assessing risk and opportunities for change. 2009. Accessed July 12, 2021. https://www.ismp.org/sites/default/files/attachments/2018-02/ISMP_AROC_whole_document.pdf
This project was funded under contract number 75Q80119C00004 from the Agency for Healthcare Research and Quality (AHRQ), U.S. Department of Health and Human Services. The authors are solely responsible for this report’s contents, findings, and conclusions, which do not necessarily represent the views of AHRQ. Readers should not interpret any statement in this report as an official position of AHRQ or of the U.S. Department of Health and Human Services. None of the authors has any affiliation or financial involvement that conflicts with the material presented in this report. View AHRQ Disclaimers
Perspectives on Safety
Perspective
WebM&M Cases
Annual Perspective
Ensuring medication reconciliation. December 19, 2007
After his wife died, he joined nurses to push for new staffing rules in hospitals. March 6, 2024
Rx for a better prescription. Hospital bans doctors from using confusing medical abbreviations. October 5, 2005
The First Annual HealthGrades Pediatric Patient Safety in American Hospitals Study. August 25, 2010
HealthGrades Eighth Annual Patient Safety in American Hospitals Study. March 23, 2011
Patient Safety: Research into Practice. September 13, 2006
Insurers' Medical Loss Ratios and Quality Improvement Spending in 2011. April 10, 2013
Safety in Numbers: Evidence-based Development of a Medicine Management Learning Tool. May 22, 2013
Sustaining Improvement. July 20, 2016
Achieving the Promise of Health Information Technology: Improving Care Through Patient Access to Their Records. October 7, 2015
Internal Bleeding: The Truth Behind America's Terrifying Epidemic of Medical Mistakes. Updated edition. March 27, 2005
Improving the Reliability of Health Care. February 8, 2006
Adult Hospital Stays with Infections Due to Medical Care, 2007. September 15, 2010
You can't understand something you hide: transparency as a path to improve patient safety. July 8, 2015
Silence Kills: The Seven Crucial Conversations for Healthcare. March 6, 2005
Hospital Survey on Patient Safety Culture: 2018 User Database Report. April 4, 2018
Quality and Safety Education. August 12, 2009
Quality and Safety Education for Nurses. June 13, 2007
To ask or not to ask?: the results of a formative assessment of a video empowering patients to ask their health care providers to perform hand hygiene. February 10, 2010
Health Information Technology in the United States: The Information Base for Progress. October 25, 2006
Impact of the Care Quality Commission on Provider Performance: Room for Improvement? November 21, 2018
Improving Diagnosis. November 28, 2018
AHRQ Nursing Home Survey on Patient Safety Culture: 2016 User Comparative Database Report. November 23, 2016
Patient Safety in Ambulatory Settings. November 2, 2016
Obstetric Care Consensus No. 5: Severe Maternal Morbidity: Screening and Review. May 9, 2018
With Safety in Mind: Mental Health Services and Patient Safety. September 6, 2006
Magnet in Support of Patient Safety. November 26, 2014
The English Patient Safety Programme. February 10, 2010
Leadership Guide to Patient Safety: Resources and Tools for Establishing and Maintaining Patient Safety. September 28, 2005
Advancing Patient Safety: Reviews From the Agency for Healthcare Research and Quality's Making Healthcare Safer III Report. September 2, 2020
A simple surgery with harrowing complications. August 8, 2012
The 2019 John M. Eisenberg Patient Safety and Quality Awards. July 8, 2020
The 2014 John M. Eisenberg Patient Safety and Quality Awards. May 6, 2015
Characteristics of Weekday and Weekend Hospital Admissions, 2007. March 17, 2010
Guide for Developing a Community-Based Patient Safety Advisory Council. October 3, 2007
Whistle-blowing nurse is acquitted in Texas. February 24, 2010
Risky business: James Bagian—NASA astronaut turned patient safety expert—on being wrong. July 14, 2010
Getting Your Best Health Care: Real-World Stories for Patient Empowerment. April 27, 2011
Latex: a lingering and lurking safety risk. April 4, 2018
Surviving a bad diagnosis. September 28, 2016
Prevention of perioperative medication errors. March 17, 2023
The star of the diagnostic journey: assessing patient perspectives. November 28, 2018
Hospitals may be the worst place to stay when you're sick. March 14, 2012
For second opinion, consult a computer? December 12, 2012
Drug shortages persist in US, harming care. November 28, 2012
The hidden dangers of outsourcing radiology. November 30, 2011
Speaking up for safety—it’s not simple. October 3, 2018
Why are so many women being misdiagnosed? August 30, 2017
Is the future of medical diagnosis in computer algorithms? May 29, 2019
Mother says ER misdiagnosis leads to son's death. December 4, 2013
Healthcare 411: medication safety toolkit. March 18, 2009
Kaiser learns from tragic medical errors. June 4, 2008
Do no harm: promoting patient safety. September 28, 2005
What pilots can teach hospitals about patient safety. November 8, 2006
Doctors say 'I'm sorry' before 'See you in court.' May 28, 2008
Your hospital's deadly secret. March 12, 2008
Hospitals put emphasis on collection of medication data. August 30, 2006
Hospital design plays important role in patient outcomes. April 27, 2005
Measuring shared mental models in healthcare. November 7, 2018
2018 John M. Eisenberg Patient Safety and Quality Awards. July 17, 2019
Contributions from Ergonomics and Human Factors. November 17, 2010
Patient Safety Papers. November 22, 2006
The fading art of the physical exam. September 29, 2010
US drug shortages threatening those whose lives depend on crucial remedies. May 18, 2011
Doctors could learn something about medical handoffs from the Navy. May 4, 2011
Leading High-Reliability Organizations in Healthcare. May 4, 2016
Freedom to Speak Up: A Review of Whistleblowing in the NHS. May 27, 2015
Medical errors in dentistry. November 4, 2015
Report of the Mid Staffordshire NHS Foundation Trust: Public Inquiry. February 20, 2013
The best medicine for fixing the modern hospital. December 12, 2012
The drawbacks of data-driven medicine. June 26, 2013
New system for patients to report medical mistakes. October 3, 2012
ISMP Targeted Medication Safety Best Practices for Community Pharmacy. April 19, 2023
Defining and enhancing collaboration between community pharmacists and primary care providers to improve medication safety. February 22, 2023
ASHP Guidelines on Preventing Diversion of Controlled Substances. December 14, 2022
Concerns regarding tablet splitting: a systematic review. December 7, 2022
Medication adverse events in the ambulatory setting: a mixed-methods analysis. October 26, 2022
Community Pharmacy Survey on Patient Safety Culture. October 24, 2022
Disrespectful behavior in your workplace. April 13, 2022
Pharmacy Education and Practice. January 26, 2022
Medication safety issues with newly authorized PAXLOVID. January 12, 2022
Mix-ups between the influenza (Flu) vaccine and COVID-19 vaccines. October 20, 2021
Important Actions Community Pharmacists Need to Take Now to Reduce Potentially Harmful Dispensing Errors. October 26, 2021 - October 26, 2021
Medicine self-administration errors in the older adult population: a systematic review. June 9, 2021
Medication incident recovery and prevention utilising an Australian community pharmacy incident reporting system: the QUMwatch study. May 5, 2021
Drug shortages amid the COVID-19 pandemic. February 24, 2021
Pharmacist counseling when dispensing naloxone by standing order: a secret shopper study of 4 chain pharmacies. December 9, 2020
Wrong drug and wrong dose dispensing errors identified in pharmacist professional liability claims. November 4, 2020
Fighting against COVID-19: innovative strategies for clinical pharmacists. May 6, 2020
Pharmacist linkage in care transitions: from academic medical center to community. October 30, 2019
Special Issue on Prescription Drug Misuse. September 25, 2019
Community pharmacy medication review, death and re-admission after hospital discharge: a propensity score-matched cohort study. September 4, 2019
Ten ways to improve medication safety in community pharmacies. August 7, 2019
Impact of medication reviews delivered by community pharmacist to elderly patients on polypharmacy: a meta-analysis of randomized controlled trials. June 26, 2019
Effect of a central call center on employee perceptions of safety culture within community pharmacies in an academic health system. June 5, 2019
Patient Safety. May 22, 2019

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.

The Future of Community Pharmacy: Direct Patient Care

Community-based pharmacy is evolving from a place of product distribution into a healthcare destination.
By Athena Ponushis and Nidhi Gandhi, Pharm.D.
Many pharmacists who spend time filling prescriptions keep hearing of a future where their role will be more focused on the patient, not the product. It’s anticipated that their attention will shift from dispensing to providing convenient clinical care. Some forward-thinking pharmacies are already enabling pharmacists to live in this awaited world, helping patients manage their medication experience and documenting interventions. These pharmacies are sharing their innovative models and schools are studying the impact, providing a window into the future of community-based pharmacy practice.
Picture pharmacists having routine interactions with patients to review, optimize and synchronize medications rather than just episodic or transactional meetings at the counter. Pharmacists will collaborate with primary care practices as part of an integrated healthcare team, making recommendations on one shared medical record, reinforcing patient care plans. Patients who want care on demand go to their pharmacists for point-of-care testing, immunizations and travel consults, or prescriptions for contraception, smoking cessation and HIV prevention. Imagine pharmacogenomic screenings being commonplace, as pharmacists look at genetics to predict drug response and tailor treatments. So goes the perceived evolution of community-based pharmacists, from performing clinical interventions to becoming initial clinicians, ushering in a time when community pharmacies are considered essential to the healthcare landscape.
“We are training our student pharmacists for the future and this is the future we see,” said Linda Garrelts MacLean, interim dean, clinical professor of pharmacotherapy at Washington State University College of Pharmacy and Pharmaceutical Sciences. “I believe that community pharmacies are going to be the place where care is delivered, that access to the learned intermediary, someone who can assess, evaluate, prescribe when appropriate and even more importantly, refer when necessary.”
Washington state has been progressive on a number of pharmacy fronts since the 1970s. MacLean and Dr. Julie Akers, clinical associate professor of pharmacotherapy at WSU, are finalizing a study on the effectiveness of pharmacy treatments, comparing the care pharmacists provide for minor illnesses and self-limiting conditions to what is offered at more traditional settings, such as physician offices, urgent care centers or hospital emergency departments. The study will inherently set a baseline to measure how enhanced pharmacy services are influencing quality of care and access to care.
Once analyzed, MacLean believes the study will provide evidence that community pharmacists can contribute to caring for patients, compelling other states and pharmacies to replicate services and treat common ailments such as strep throat, urinary tract infections and severe headaches, including migraines. Akers has found, through surveys and anecdotally, that patients are confident in receiving care from pharmacists. It may take a little education (patients don’t always know what training pharmacists have had or what services are being offered) but once they know, Akers has not seen any hesitation in a patient’s willingness to be seen by a pharmacist.
“More involved direct patient care is the future of pharmacy practice, and schools need to ensure that they are graduating practice-ready pharmacists who are prepared to move into that role. Schools should take the time to fully assess their curriculum, making sure it is robust enough to where they are going to have pharmacists who are confident and ready to go start these services,” Akers said. “Also ensuring that they are building strong advocacy with their students so that as students want to move toward this future, they understand the legislative and regulatory framework of what they are allowed to do within their state and how to overcome any barriers.”
At WSU, student pharmacists take an intensive, weeklong, point-of-care and clinical services course at the beginning of their second year. Rather than re-create the material the state pharmacy association had created for continuing education for practicing pharmacists, faculty collaborated with the association, giving students access to online modules that they complete over the summer before school begins. Students spend the entire first day of class going condition by condition, reviewing key guidelines through patient cases, deciding whether to use prescriptive authority, refer to a more advanced care setting or recognize that over-the-counter self-care products are appropriate for that case.
“What I find interesting is that prior to this course, our students have completed their over-the-counter self-care pharmacotherapy course, and in that course it’s over-the-counter or refer because the patient needs a prescription. So it’s always comical when we’re doing these patient cases that the students’ automatic response is, ‘We have to refer because that’s what we’ve learned before.’ It’s changing that mindset for them, realizing that as an advanced care practitioner pharmacist, you can handle some of these minor illnesses and conditions with prescriptive authority,” Akers said.
Other days are dedicated to immunizations. Students are certified in immunization administration and receive specialty training on pediatric immunization. Students learn how to screen for HIV, strep and influenza, practicing throat and nasal swabs on themselves or a team member before going through a rubric-graded assessment, ensuring they can collect the sample without it being contaminated. They have open practice laboratory sessions and breakout sessions where they learn how to run a travel consultation, interact with a patient and do the paperwork.
“We began this course after getting approval from our full faculty to move it forward as required curriculum for all of our graduates. That’s what was most important: getting all of our faculty to recognize that we truly believe as a program that this is the future of pharmacy,” Akers noted. “We really believe that this is the base knowledge that’s required for an entry-level pharmacist.”
The Path Forward
In its 2018 report, “The Next Transition in Community-Based Pharmacy Practice,” the American Pharmacists Association found that pharmacists are trained to perform certain tasks but often experience work settings that are not conducive to such practice. The study found that new roles abound for community pharmacists in this “new patient-centered, medication experience era,” but stressed the difference between professional identity and commercial identity. To change perceptions of community pharmacy, the APhA encouraged pharmacists to see transformation “through the patient’s eyes.” From the patient’s vantage point, a medication experience is not clinical, it’s personal.
The Council of Deans formed a task force to find opportunities to improve community-based practice and give viable recommendations to AACP and member institutions to pursue such possibilities and make them realities. The task force chair, Dr. Jennifer Adams, associate dean for academic affairs, director of interprofessional education, clinical associate professor at Idaho State University College of Pharmacy, said the task force will structure recommendations in three separate areas.
First, advancing pharmacy technician practice. Pharmacists must have good support staff if they are going to take on new roles, so elevating pharmacy technicians is crucial. “What are the types of tasks pharmacy technicians can do? What can we train them to do if they don’t already have that level of training, and what’s appropriate there, in terms of scope? What needs to be reserved for pharmacists?” Adams asked. “The way Idaho has tackled this is really from the perspective of delegating, allowing pharmacists to delegate tasks to technicians as long as those tasks are appropriate for their education, training and experience.” An example would be immunization administration. Determining if it’s the right immunization for that patient at that time would be the responsibility of the pharmacist, but the actual administration could be done by a technician. Same with point-of-care testing: the pharmacist would decide to do the test but the technician could administer it. Some pharmacies are delegating the accuracy checking of the dispensing process to technicians. “Data show that when they are delegated that task and given that authority, pharmacy technicians are actually more accurate than pharmacists because they tend to have fewer distractions,” Adams added.
Second, advancing the scope of pharmacy practice. “Our university has been closely involved with our board of pharmacy and our state association and we have navigated relationships with legislators to advance scope of practice,” Adams said. The Idaho board looked at other boards of pharmacy, but also looked at medicine and nursing, examining how their licensees were regulated and found they regulate based on this concept of standard of care.
“What our board of pharmacy learned from our healthcare colleagues was, pardon the pun, but pharmacists tend to be really prescriptive in their regulations. We write out the exact details of how hot the water in the pharmacy needs to be, the amount of counter space that needs to be provided, we get way into the weeds, rather than saying the facility needs to be appropriate so that the practitioners in the facility can provide the appropriate standard of care,” Adams said. “So there is nuance, and sometimes it’s unnerving for pharmacists to begin to think that way, but our board of pharmacy in Idaho has shifted all of our regulation to a standard of care model, which allows pharmacists to practice at the top of their education and training and not be restricted by their license.”.
More involved direct patient care is the future of pharmacy practice, and schools need to ensure that they are graduating practice-ready pharmacists who are prepared to move into that role.
Idaho has been the trailblazer for independent prescriptive authority. Pharmacists in Idaho can prescribe based on four parameters: when no new diagnosis is required, when a CLIA-waived test can guide diagnosis, when a condition is minor and self-limiting or in an emergency. At first, the board of pharmacy made a list of medications pharmacists could prescribe for those categories, each year adding new medications to the list for legislators to approve. Legislators saw the same scenario playing out—they would hear opposition from the medical community, give pharmacists a chance and then see the positive outcomes. At the end of the 2019 legislative session, legislators eliminated the list. It’s now up to a pharmacist or pharmacy to determine what fits into those categories.
“One advantage to that is that during a public health emergency like COVID-19, a pharmacy can say, ‘You know what, we are going to do our best to take care of everyone who we want to keep out of urgent care centers and hospital emergency rooms because we want to relieve the burden on the healthcare system, so now we are going to treat acute sinusitis and uncomplicated urinary tract infections,’” Adams said. Several states have passed emergency regulations during this crisis, allowing pharmacists to do more, like extend refills. “My thought is, how better to be prepared for an emergency situation than to have that be what your daily practice is?” Adams pointed out. “If I am already doing these things and I am already taking care of patients at this level, it’s not such a stressful shift for me in an emergency.”
Third, the task force will provide recommendations to advance payment reimbursement for services. Idaho was successful in adding pharmacists to the list of nonphysician providers in its Medicaid basic plan this year, enabling pharmacists to bill for services based on scope of practice, with no restricted services. Adams believes a groundswell from state Medicaid programs will lead the effort of reimbursement, showing that when you pay pharmacists for services, outcomes improve and costs go down. “The other component the task force has talked about is not trying to create a new or different way for pharmacists to get reimbursed,” Adams said, “but that we fit ourselves in with the way the rest of the healthcare system bills for services.”
My thought is, how better to be prepared for an emergency situation than to have that be what your daily practice is? If I am already doing these things and I am already taking care of patients at this level, it’s not such a stressful shift for me in an emergency.
AACP President Todd Sorensen’s Bold Aim for the profession, that by 2025, 50 percent of primary care physicians in the U.S. will have a formal relationship with a pharmacist, prompted the 2020 Professional Affairs Committee to present a policy recommendation that will be considered by the 2020 AACP House of Delegates. The committee is also developing a survey tool, a database of successful models to serve as a resource for schools and pharmacies. “We want to take a comprehensive approach of looking at how pharmacists can collaborate with primary care practices, from models that we know about and models that maybe we are less familiar with, but helping to disseminate that information to schools, identifying the needs for these collaborations and ways to build sustainable models,” said Dr. Gina Moore, assistant dean for clinical and professional affairs, associate professor, University of Colorado Skaggs School of Pharmacy, and chair of the committee.
Schools are the thread running through all the recommendations, bringing people together, doing the research and engaging in advocacy to advance community-based practice. “We must share our success stories, not just within pharmacy, but with other audiences, including physicians, professional organizations and the public,” Moore said. “We must share the benefits of collaborating with community pharmacists.”
A Model to Unite, Mobilize and Amplify
Americans have access to more than 62,000 community pharmacy locations for medication therapy management, immunizations and walk-in patient consultations. To adapt to the rapidly evolving value-based healthcare system, the community pharmacy practice model must be transformed into a place for patients to receive comprehensive medication-related care from pharmacists and the pharmacy team.
In July 2019, the Academia-CPESN Transformation (ACT) Pharmacy Collaborative was formed as a nationwide forum where community pharmacy leaders and schools of pharmacy could come together to make the patient-centered vision of community pharmacy a reality. The goal of this collaborative is to support the transformation of community-based pharmacy practice from a product-based care model to a community-based pharmacy care delivery model, focusing on the enhanced services that support people who are taking medications to help them reach their health goals. Some examples of enhanced services include clinical medication synchronization, medication reconciliation, comprehensive medication management, durable medical equipment evaluation and support, point-of-care testing, travel immunizations and travel medication consultations.
The establishment of the ACT Pharmacy Collaborative came as a result of a grant from the Community Pharmacy Foundation to the University of Pittsburgh School of Pharmacy in partnership with CPESN USA. The Collaborative, with support from AACP, has three main drivers: to unite, mobilize and amplify community pharmacy practice transformation with colleges/schools and community pharmacy partners nationwide. A full description of the Collaborative and how colleges/schools can be involved can be found in the “Blueprint for Building a National Partnership Collaborative” on the ACT Pharmacy Collaborative’s centralized website (www.actforpharmacy.com).
Dr. Sophia (Cothrel) Herbert is a Community Pharmacy Practice Development Fellow within the Community Leadership and Innovation in Practice Center at the University of Pittsburgh School of Pharmacy and works to support the transformation of community pharmacy practice. She serves as the Pennsylvania Flip the Pharmacy Team Project Manager, also funded by the Community Pharmacy Foundation, and is a member of the leadership team for the ACT Pharmacy Collaborative under the mentorship of professors Kim Coley and Melissa McGivney. Within her research initiatives with community partners, she mentors student pharmacists for research and quality improvement projects.
The University of Pittsburgh School of Pharmacy recently created a community pharmacy practice-based research network to support ongoing practice transformation in Pennsylvania. Herbert noted, “The idea behind the network is to engage community pharmacists who are willing and able to perform practice-based research in collaboration with patients and research partners. There will continue to be a focus on stakeholder engagement in all network activities.”
For Herbert, community pharmacy means “patient access to care within their own communities. There is a successful future for community pharmacies that strive to meet the medication and other health needs of their patients, within their own communities where they live, work and play,” she said. “The combined efforts of the ACT Pharmacy Collaborative, Flip the Pharmacy and CPESN are driving community pharmacy practice toward a patient-centered care model, and the combination of these forces and efforts will bring us closer to that vision of community pharmacies providing optimal patient care.”
During her fellowship, Herbert has worked on several projects involving student pharmacist participation through the ACT Pharmacy Collaborative such as the National Day of Service, Patient Case Challenge, CPESN/ACT Student Scholar program and CPESN/ACT Student Match program, which facilitates student experiences at community pharmacies across the country in light of the COVID-19 pandemic. “I have been most excited about facilitating student connections and experiences through these initiatives, especially the CPESN/ACT Student Scholar program that will allow selected students to interact with and learn from community leaders and CPESN practices in an impactful way,” she said.
Athena Ponushis is a freelance writer based in Ft. Lauderdale, Florida. Nidhi Gandhi is the Academic Leadership and Education Fellow at AACP
- Research article
- Open access
- Published: 21 July 2011
Public health in community pharmacy: A systematic review of pharmacist and consumer views
- Claire E Eades 1 ,
- Jill S Ferguson 2 &
- Ronan E O'Carroll 1
BMC Public Health volume 11 , Article number: 582 ( 2011 ) Cite this article
57k Accesses
315 Citations
15 Altmetric
Metrics details
The increasing involvement of pharmacists in public health will require changes in the behaviour of both pharmacists and the general public. A great deal of research has shown that attitudes and beliefs are important determinants of behaviour. This review aims to examine the beliefs and attitudes of pharmacists and consumers towards pharmaceutical public health in order to inform how best to support and improve this service.
Five electronic databases were searched for articles published in English between 2001 and 2010. Titles and abstracts were screened by one researcher according to the inclusion criteria. Papers were included if they assessed pharmacy staff or consumer attitudes towards pharmaceutical public health. Full papers identified for inclusion were assessed by a second researcher and data were extracted by one researcher.
From the 5628 papers identified, 63 studies in 67 papers were included. Pharmacy staff: Most pharmacists viewed public health services as important and part of their role but secondary to medicine related roles. Pharmacists' confidence in providing public health services was on the whole average to low. Time was consistently identified as a barrier to providing public health services. Lack of an adequate counselling space, lack of demand and expectation of a negative reaction from customers were also reported by some pharmacists as barriers. A need for further training was identified in relation to a number of public health services. Consumers: Most pharmacy users had never been offered public health services by their pharmacist and did not expect to be offered. Consumers viewed pharmacists as appropriate providers of public health advice but had mixed views on the pharmacists' ability to do this. Satisfaction was found to be high in those that had experienced pharmaceutical public health
Conclusions
There has been little change in customer and pharmacist attitudes since reviews conducted nearly 10 years previously. In order to improve the public health services provided in community pharmacy, training must aim to increase pharmacists' confidence in providing these services. Confident, well trained pharmacists should be able to offer public health service more proactively which is likely to have a positive impact on customer attitudes and health.
Peer Review reports
Promotion of healthy lifestyles is one of the five core roles of a pharmacist, as defined by the Royal Pharmaceutical Society of Great Britain, (RPSGB) [ 1 ]. Although pharmacists have always had some involvement in health improvement, the focus on this aspect has greatly increased over recent years [ 2 ]. This changing role was formalised by the introduction of the new pharmacy contract in 2005 in England and Wales and 2006 in Scotland which outlined the public health service pharmacists would be required to provide. These services include provision of advice on healthy living and self care and involvement in health promotion campaigns in Scotland, England and Wales with the additional requirement to provide a smoking cessation and sexual health service in Scotland [ 3 , 4 ].
Community pharmacy holds a number of benefits as a setting for public health activities. With extended opening hours and no appointment needed for advice, community pharmacy can be more accessible than other settings. An estimated 600,000 people visit community pharmacies in Scotland every day and approximately 94% of the Scottish population visit a community pharmacy at least once in a year [ 5 ]. This gives community pharmacies access to a range of individuals in both good and poor health, and to those that may not have contact with any other health professionals. Reviews of evidence assessing public health initiatives in community pharmacy have confirmed the potential of pharmacy in this area and suggest that pharmacists can indeed make a positive contribution to public health [ 6 , 7 ].
Although there is clear potential for pharmacy to contribute in a unique way to public health, changes in the behaviour of both pharmacists and pharmacy customers are likely to be required for the service to be successful. Pharmacists must accept their role in public health and make the necessary changes in behaviour to carry out the service. Similarly, the general public must accept pharmacists as providers of public health services and be willing to seek advice on some health issues from pharmacists rather than other sources.
The factors that affect and predict behaviour have been the subject of a great deal of research. The theory of planned behaviour (TPB) is a model that has been widely used to predict and change behaviour across a range of settings [ 8 ]. The model states that voluntary behaviours are largely predicted by our intentions regarding the behaviour. Intentions are in turn determined by our attitude towards the behaviour (our judgement of whether the behaviour is a good thing to do), subjective norms (our judgement of what important others think of the behaviour), and perceived behavioural control (our expectation of how successful we will be in carrying out the behaviour). A review by Sutton found that on average the TPB predicted between 40 and 50% of the variance in intention and between 19 and 38% of the variance in behaviour [ 9 ]. While theories such as the TPB cannot entirely predict behaviour, these findings demonstrate the important role of beliefs in understanding behaviour.
Therefore, in order to understand and assist the behaviour changes associated with providing a public health service in community pharmacy, it is important to establish the beliefs of the general public and pharmacists regarding this role. Three systematic reviews have previously been carried out in this area. One assessed pharmacist views and another general public views towards various public health services [ 10 , 11 ]. The third reviewed papers on the provision of emergency hormonal contraception (EHC) in pharmacy and included public and pharmacist views [ 12 ]. The review of pharmacists' perceptions of public health covered literature published up to 2001 and found that although pharmacists valued the health improvement role they were more comfortable with medicine related health improvement work [ 10 ]. The review also found that pharmacists had concerns about being intrusive and believed they needed more support to provide public health services. Training was found to positively affect pharmacists' attitudes and behaviours in relation to health promotion [ 10 ].
The review on consumer views covered literature up to 2002 and found that pharmacists were perceived as 'drug experts' rather than experts on health and illness. Although consumers were generally satisfied with health advice given by pharmacists, they primarily used pharmacies for dispensing prescriptions and buying over the counter medication [ 11 ]. The final review summarised literature on the provision of EHC in pharmacy up to the end of 2004. The review reported that the service was largely viewed positively by both pharmacists and service users but that some concerns were raised by consumers regarding privacy [ 12 ].
Since these reviews were conducted, the introduction of the new pharmacy contract has brought about a great deal of change in community pharmacies. In order to continue to improve the public health service provided in community pharmacies, up to date information is needed regarding the beliefs and attitudes of pharmacists and consumers towards pharmaceutical public health. Beliefs about the public health role may or may not be similar to those found in the previous review. Establishing current views would allow potential barriers to the public health service to be established and appropriately tackled. The objective of this review is to summarise and evaluate quantitative and qualitative evidence published since the previous reviews were conducted on the beliefs and attitudes of pharmacists and consumers towards pharmaceutical public health.
The electronic databases MEDLINE, EMBASE, PsycINFO, CINAHL and Dissertation Abstracts International were searched for articles published in English from February 2001 to February 2010. The following combination of search terms was used with each database: (pharm* or pharmacy staff or community pharmacy or consumer or public or customer) and (attitud* or belie* or perce* or knowledge or view or opinion) and (public health or health improvement or health promotion or self care or self management or smoking cessation or sexual health or prevent* or diet or healthy diet or healthy eating or exercise or physical activity or weight or health education or chlamydia testing or emergency contraception or alcohol or needle exchange or methadone or injecting equipment or drug misuse).
Titles and abstracts were screened against the inclusion criteria outlined in table 1 . Full text papers were retrieved for studies considered relevant and for those with titles and abstracts that contained insufficient information to allow judgement of relevance. The full text papers were assessed against the inclusion criteria by one researcher and those identified as relevant were checked again by a second researcher. Data were extracted from included studies using a data extraction form based on the example provided by the Centre for Reviews and Dissemination [ 13 ]. In order to assess methodological quality, studies were assessed against the checklist outlined by Crombie which is suitable for use with descriptive surveys [ 14 ]. The methodological quality of qualitative studies was assessed against the Critical Appraisal Skills Programme checklist for qualitative studies [ 15 ].
Literature Search
A total of 5628 abstracts were reviewed and 122 full text papers were assessed against the inclusion criteria outlined in Table 1 . A second researcher assessed the 71 papers shortlisted for inclusion and 63 studies published in 67 papers were included for review. Figure 1 shows the flow of studies identified by the searches.
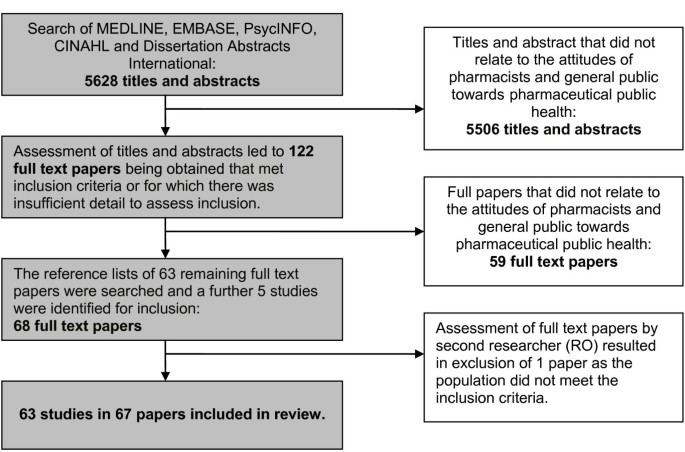
Flow diagram of searches and inclusion assessment of studies .
Description of Included Studies
The characteristics of the studies included in the review are presented in additional file 1 . The majority of studies assessed the views of pharmacists (n = 29), support staff (n = 3) or both (n = 1). Three studies investigated both pharmacist and general public views and the remaining studies assessed the views of the general public or pharmacy customers (n = 27). The most common topics investigated were sexual health services (n = 17), smoking cessation (n = 14), general health promotion/screening (n = 12), and services for drug misusers (n = 10). The majority of studies were carried out in Europe (n = 31) and North America (n = 23). The most commonly employed methodology was surveys (n = 50). Eight studies used structured or semi-structured interviews, two used focus groups and two studies used both focus group and survey methods. Table 2 outlines the country of publication of papers included in the review sorted by topic area. It shows the proportion of UK and non-UK papers published after the introduction of the new pharmacy contract in the UK (2006 to 2010).
Quality of Included Studies
Quality varied across the studies included. The quality of reporting was often poor with 16 studies not reporting any information on the age of participants [ 16 – 35 ], 8 not reporting age or gender [ 36 – 43 ] and 2 not reporting gender [ 44 , 45 ]. Fifteen studies did not report response rates [ 17 , 25 , 29 , 43 , 46 – 56 ] and two only reported the response rates for part of the sample [ 57 , 58 ]. Only three studies followed up a sample of non-responders [ 59 – 61 ]. Response rates where reported were generally average to good with the majority (71%) achieving response rates of 50% and over. The way participants were recruited was not clearly reported in one study [ 50 ] and the results were not adequately explained in another [ 62 ]. In the latter case, the names of themes arising from the analysis of interviews were stated with little explanation of the direction of opinion of pharmacists in relation to these themes. The majority of studies included in the review employed convenience sampling (n = 29), 5 used purposive sampling [ 41 , 56 , 62 – 64 ] and only 13 used random sampling methods [ 16 , 18 , 32 – 38 , 47 , 50 , 58 , 65 – 68 ]. Of the 12 studies included that used qualitative methodologies only one employed respondent validation [ 62 ] or made a statement of how the personal characteristics of the researchers may have influenced analysis [ 69 ]. Methods and analysis were not adequately described in one study [ 43 ], data was not transcribed verbatim in another study [ 70 ] and multiple coding was not used in two further studies [ 41 , 51 ].
- Pharmacy Staff
The attitudes and beliefs of pharmacists and pharmacy staff investigated in the papers included in this review related to four main topics: perceptions of role, competence/confidence, barriers and training.
Perceptions of Role
The majority of participants in a survey in Scotland agreed (63%) or strongly agreed (16%) that public health is important to their practice and a little over half agreed (48%) or strongly agreed (8%) that they were public health practitioners [ 21 ]. A survey in Nigeria also reported that the majority of participants (94%) thought it was acceptable for pharmacists to be involved in health promotion activities [ 71 ]. Pharmacists and support staff taking part in focus groups in Sweden on the whole welcomed their role as a health promoter [ 56 ]. However, it was noted that not all participants felt this way and preferred to develop activities in areas in which they received their basic training. Consistent with this, a study in Moldova found that participants rated public health activities significantly lower in importance than all other aspects of professional practice assessed (e.g. dispensing activities) [ 65 ]. Furthermore, a survey in Scotland offering participants a choice of hypothetical jobs found that participants would rather provide a minor illness service than health promotion advice and would forgo £2798 of income to do this [ 72 ].
Perceptions regarding the pharmacists' role in smoking cessation counselling were generally favourable. Nearly all pharmacists surveyed in Thailand, Finland and the USA agreed that they should play a role in smoking cessation [ 45 , 37 , 16 ]. The majority of participants (83%) in another survey in the USA believed that pharmacists should be more active in assisting with smoking cessation [ 55 ]. However, in a survey in Turkey only 57% of participants thought that pharmacists should warn patients about the harmful effects of smoking [ 50 ]. A study in Canada found that pharmacists rated medicine related aspects (e.g. advising on the use of NRT) of their smoking cessation role as more important than other aspects (e.g. assessing patients' dependence on nicotine) [ 34 ]. Another paper based on the same sample found that participants were significantly more likely to carry out smoking cessation interventions with customers if they scored above the median in ratings of importance of various smoking cessation roles [ 32 ].
Perceptions about the pharmacist's role in sexual health services were generally positive. The majority of pharmacists (98%) surveyed in a study in Scotland agreed that they would be willing to offer free Chlamydia postal testing kits [ 26 ]. In a survey in the USA 55% of pharmacists were interested in providing emergency hormonal contraception (EHC) [ 68 ]. Pharmacists interviewed in a study in the UK [ 69 ] were found to hold largely positive views about providing EHC. However, around one quarter of pharmacists in another study in the USA were opposed to providing EHC largely due to religious and moral beliefs [ 67 ]. Pharmacists in the latter two studies also reported concerns that the service may be overused and lead to increases in unprotected sex and sexually transmitted diseases [ 67 , 69 ]. The benefits of providing this service that were highlighted by pharmacists in these two studies included increasing access to EHC, confidentiality, reducing unwanted pregnancies and improving status of the pharmacy profession [ 67 , 69 ].
Attitudes towards providing services for drug misusers have become more favourable over recent years. Surveys in England and Scotland in 2007 reported that attitudes were significantly more positive since assessed in a similar survey in 1995 [ 38 , 60 ]. Similarly, a study in the USA reported an increase in the number of pharmacists who agreed that sterile needles should be made available through community pharmacy [ 39 ].
Despite a shift in attitudes, views towards providing services for drug misusers are still mixed. Pharmacists taking part in focus groups in Estonia and a survey in the USA highlighted a number of concerns about the effect of selling sterile needles on customers and business [ 58 , 41 ]. Support staff in a survey in Scotland also reported similar concerns [ 30 ]. Only half of support staff (52.6%) in this study thought that their pharmacy should provide services to drug misusers [ 31 ]. The possibility of providing free injecting equipment to drug misusers was met with strong resistance in the study in Estonia. The majority of pharmacists in a survey in Scotland disagreed or neither agreed or disagreed that HIV/hepatitis prevention is an important role for pharmacists [ 73 ].
However pharmacists supplying sterile needles for purchase in the USA and UK reported few problems providing this service and little detrimental effect on customers or their business [ 41 , 42 ]. Pharmacists selling sterile injecting equipment in Vietnam reported that they felt a responsibility to prevent blood borne infection and were willing to provide health education to customers that were drug misusers [ 43 ]. More positive views were also reported in a study in the USA with nearly all pharmacists (98%) reporting that they felt they should play a part in helping prevent the spread of blood borne infections such as HIV and over two thirds supporting the availability of sterile needles for purchase in community pharmacies [ 41 ].
Competence/Confidence
Findings regarding confidence and competence in providing health promotion services were mixed. A survey of pharmacists in Scotland found that around one third of participants did not feel that they were competent in promoting and protecting the populations' health or encouraging behavioural change [ 21 ]. Around two thirds felt they lacked the underpinning knowledge and one third felt they could not apply their knowledge. Pharmacists taking part in a survey in Moldova rated their competence in health promotion activities at between 2.9 and 3.6 (0 = low competence and 5 = high competence) which was lower than competence scores for all other aspects of professional practice [ 65 ]. In contrast, the majority of pharmacists (95%) in a survey in Nigeria felt confident in advising patients on health promotion [ 71 ].
Pharmacists in Australia were reasonably confident in providing a smoking cessation service, with a mean confidence score of 3.7 (1 = not confident and 5 = extremely confident), and did not report confidence as a major barrier to smoking cessation activity [ 19 ]. Nearly all participants (92%) in a study in Canada [ 33 ] agreed that pharmacists can be effective in promoting smoking cessation with most customers. In another study in the USA around two thirds of pharmacists thought that the effectiveness of pharmacist counselling was average or good [ 55 ]. In two of these studies confidence was found to be the greatest predictor of the amount of smoking cessation activity reported and in one perceived effectiveness was also a significant predictor [ 19 , 55 ].
Confidence in advising on the prevention HIV/hepatitis was fairly low in pharmacists in a survey in Scotland [ 73 ]. Around half of pharmacists felt confident in advising customers on prevention of HIV and around a third on Hepatitis B/C. Confidence in advising on safer sex was higher with the majority of pharmacists reporting that they would be able to give advice on this to any customer or a drug misuser (78% and 72% respectively). However, only around one third were confident in advising a gay man on safer sex (35%) [ 73 ]. Support staff in a similar survey in Scotland reported lower confidence for advising on safer sex than pharmacists [ 74 ]. Only half of support staff felt able to give accurate advice to any customer (51%) and one third a drug misuser (34%) or a gay man.
Pharmacists' confidence in achieving positive outcomes in weight management counselling was low in one study. Pharmacists in a study in the USA reported mean confidence (1 = not at all confident and 5 = extremely confident) scores of only 3.0 for achieving weight loss in patients as a result of pharmacist counselling and 2.8 for achieving consumption of a calorie controlled diet in patients [ 18 ]. Mean confidence scores for medicine related aspects of obesity counselling (e.g. minimisation of adverse effects of anti-obesity medication) were higher at between 3.3 and 3.4. Self reported frequency of obesity counselling was found to be positively correlated with confidence in achieving positive outcomes. Confidence in providing brief alcohol screening and interventions was also low with over half of pharmacists in a study in New Zealand feeling neutral or disagreeing that they could appropriately advise patients about drinking [ 61 ].
A number of common barriers to public health practice were highlighted across the different services. These included availability of a private counselling area, time, customer demand/reaction and reimbursement for public health services.
The findings regarding a lack of private counselling area were mixed. This was identified as a main barrier to providing advice on health promotion in focus groups in Sweden and advice on prevention of HIV/hepatitis in pharmacists and support staff in Scotland [ 56 , 73 , 74 ]. Nearly two thirds of pharmacists in a survey in Canada felt that having a designated space in pharmacy was very or somewhat important in facilitating smoking cessation practice and nearly half of participants in a study in Thailand (43%) thought the pharmacy setting was barrier to smoking cessation counselling [ 35 , 45 ]. Pharmacists' perception of having adequate facilities was found to be a significant predictor of frequency of smoking cessation counselling in one study [ 55 ]. Although a predictor of service provision, the majority of pharmacists (71.7%) in this study did not view the pharmacy setting was an important barrier to smoking cessation counselling. Similarly, pharmacists in Nigeria (93.1%) did not think facilities were a barrier to patient interaction in relation to health promotion generally [ 71 ]. Pharmacists interviewed in England also felt they had adequate facilities to provide a Chlamydia testing and treatment service [ 22 ].
Lack of time was identified as a main barrier to providing advice on prevention of HIV/hepatitis by pharmacists and support staff in Scotland and for health promotion activities by the majority (75%) of pharmacists in a study in Malaysia [ 73 – 75 ]. Between 50 and 70% of participants in two studies in the USA and one in Thailand agreed that time was a barrier to providing smoking cessation counselling and over half in one of the USA studies felt that they were not adequately staffed for providing smoking cessation services [ 15 , 55 , 45 ]. Similarly, around 70% of participants in a study in New Zealand thought that being too busy was a barrier to carrying out brief alcohol screening [ 61 ]. Time was reported as a barrier to providing EHC by 67% of pharmacists surveyed in a study in the USA [ 67 ]. However, a study on health promotion in Nigeria and another on Chlamydia testing in England reported that time was not an issue in providing these services [ 71 , 22 ].
Views on patient demand for public health services in community pharmacy and patient reactions to being offered these services were mixed. Around 60% of pharmacists in a survey in Thailand reported that lack of patient demand was a barrier to providing smoking cessation services [ 45 ]. Focus group participants in Sweden also perceived that patients had low expectations of receiving health promotion advice from pharmacists [ 56 ]. Furthermore, over half of pharmacy assistants in a survey in Scotland felt that client embarrassment was a barrier to offering advice on HIV/hepatitis prevention and a similar proportion of pharmacists in a study in New Zealand felt that patients would resent being asked about their alcohol consumption [ 74 , 61 ]. Pharmacists interviewed in the USA reported that they viewed this as a sensitive topic and were hesitant to initiate conversations about smoking as they expected to receive a negative response from customers [ 62 ].
In contrast, the majority of participants in surveys on health promotion and smoking cessation in Nigeria, the USA and Finland did not think that lack of demand was a barrier and thought that patients were motivated to seek health advice from pharmacists, welcomed and valued this advice and were not discouraged from returning to the pharmacy as a result of being offered advice [ 71 , 33 , 55 , 37 ]. Pharmacists in a survey carried out in the USA agreed that customers are becoming more willing to discuss health problems and more accepting of counselling provided by pharmacists, but did not agree as strongly that customers were more accepting of pharmacists managing chronic disease [ 76 ]. Finally, pharmacists involved in offering a Chlamydia testing service reported that client reactions were to being offered the service were mixed but that they were predominantly satisfied as long as discretion was used [ 22 ].
Reimbursement for providing public health services does not seem to be a barrier for most pharmacists. The majority of participants (63.7%) in a study in Malaysia felt neutral or disagreed that a lack of reimbursement was a barrier to their involvement in health promotion and most pharmacists (87.6%) in a survey in Nigeria agreed that it is alright to be involved in health promotion whether there is reimbursement or not [ 75 , 71 ]. Studies in the USA, Thailand, and Canada also reported similar findings in relation to smoking cessation [ 55 , 45 , 33 , 34 ].
A need for training was identified in a number of surveys on different public health services. Over half of pharmacists in a study in Scotland reported that attaining additional pharmaceutical public health knowledge was a priority for their practice now and two thirds thought it would be a priority in the future [ 21 ]. Between one third and one half of pharmacists in three studies felt that lack of training or lack of knowledge and skills was a barrier to their smoking cessation practice [ 15 , 50 , 55 ]. Pharmacists and support staff in Scotland also felt that lack of training was a main difficulty in providing advice on prevention of HIV/hepatitis and over 80% of pharmacists in a study in New Zealand felt it was a barrier to providing alcohol screening and brief interventions [ 73 , 74 , 61 ]. Over 70% of pharmacists in a survey in Scotland reported that they would like further training on drug misuse [ 59 ]. The majority of pharmacists in Nigeria felt that they had good knowledge on health promotion (86.9%) but also agreed that they would be willing to retrain on health promotion (93.2%) [ 71 ].
Pharmacists taking part in a smoking cessation training needs assessment in Canada reported that training would be helpful on all aspects of smoking cessation practice but rated training on behavioural techniques for quitting smoking and motivating patients as most helpful [ 34 ]. Pharmacists in Scotland taking part in a survey on training needs for working with drug misusers most often cited motivational and counselling skills as areas they would like more training on [ 77 ]. No clear area for future training was identified in a survey in Scotland with the majority of pharmacists agreeing (79.3%) that training should focus on generic knowledge and skills but also with the statement that training should focus on priority health issues such as chronic heart disease (77.2%) [ 21 ]. Training for pharmacy technicians on smoking cessation was found to significantly increase knowledge, confidence and perceptions of the effectiveness of smoking cessation counselling in a study in the USA [ 24 ].
The attitudes and beliefs of the general public and pharmacy customers towards pharmaceutical public health investigated in the papers in this review related to four topics: use of community pharmacies, appropriateness of pharmacists' involvement in public health, satisfaction with pharmaceutical public health and perceptions of pharmacists' ability.
Use of community pharmacies
A survey of pharmacy customers in Australia found that the majority had never received advice on diet and exercise (88.2%) or on preventing health problems (65.1%) from a pharmacist [ 47 ]. The majority of smokers (57.8%) in the sample also reported having never received advice on smoking from a pharmacist.
Most pharmacy customers in a survey in Sweden expected to receive information from pharmacists on drugs (80.5%), while only around a third (36%) expected information on general health issues and less than a quarter expected advice on diet (24%), smoking cessation (21%) or disease/illness (20.5%) [ 78 ]. Users of nicotine replacement therapy in a survey in the USA found it most useful and were most likely to discuss medicine related smoking cessation topics (e.g. side effects of smoking cessation medication) with a pharmacist and were least likely and found it least useful to discuss behavioural topics (e.g. how to cope with difficulties encountered) [ 52 ]. A survey of pharmacy customers in Nigeria found that satisfaction was lower for the availability of public health services than other medicine related services [ 20 ].
Appropriateness of pharmacists' involvement in public health
The majority of participants in studies on smoking cessation (83%), health screening and promotion (71% and 74% respectively), EHC (65%), services for drug misusers and Chlamydia testing (75%) thought that pharmacists were appropriate providers of these services [ 17 , 56 , 49 , 64 , 70 ]. Users of nicotine replacement therapy in a study in the USA on average rated the appropriateness of pharmacists taking an active role in smoking cessation as 6.9 out of 10 (1 = not at all appropriate and 10 = extremely appropriate) [ 52 ]. However, less than one quarter (22%) of participants surveyed at a medical centre thought that pharmacists should monitor long term conditions such as asthma [ 59 ].
Satisfaction with pharmaceutical public health
Although it seems that customers often do not expect or receive advice from pharmacists on public health topics, satisfaction in those that have experienced pharmacy public health services is high. A survey in Australia found significantly more positive attitudes in those that had experience of pharmacy health screening or promotion than those that did not [ 57 ]. Attitudes in those with no experience of public health services were also found to be significantly more positive compared to a similar survey carried out around seven years previously.
Nearly all individuals receiving community pharmacy osteoporosis screening and education in two surveys in the USA reported that the information provided increased awareness (98%), that they were satisfied with the interaction (92%) and found the advice valuable or highly valuable [ 79 , 53 ]. The majority of participants receiving self management interventions from community pharmacists for asthma (89%) and diabetes (97.5%) were also satisfied with the care they received from the pharmacist [ 54 , 80 ]. Only 71% and 61% of those receiving the asthma self management interventions were satisfied by the education and counselling provided by physicians and nurses respectively [ 54 ].
Participants in a survey in the USA reported very positive experiences of community pharmacy based smoking cessation services [ 40 ]. Patients' agreement with ten statements about their satisfaction with the service (1 = lowest satisfaction and 10 = highest satisfaction) was high with mean scores between 8.5 and 9.9 for all of the statements. Intravenous drug users taking part in focus groups in Estonia reported that pharmacies were more convenient and easier to access than other needle exchange services, but that they experienced discomfort and embarrassment as a result of perceived negative attitude of the pharmacist and other customers towards them [ 58 ].
Women who received EHC from community pharmacy reported largely positive experiences of this service. The majority of women participating in surveys, interviews and focus groups in the USA, Canada and England reported that they were satisfied with their consultation with the pharmacist [ 81 , 82 , 27 , 48 , 69 ]. Over 80% of women in the survey conducted in the USA and another in Canada were satisfied with the amount of privacy in the pharmacy [ 81 , 27 ]. The flexibility and convenience of the pharmacy setting were viewed as benefits to this setting and were the primary reason for attending pharmacy over than other settings such as family planning clinics [ 63 , 82 , 69 ]. Indeed the majority of women (65%) sampled for a study in Sweden reported that they would prefer to purchase EHC from a pharmacy over visiting a clinic with availability selected as the motive for this choice by most women (64%) [ 66 ].
Despite largely positive views towards the service, concerns were reported by women in some studies. Some participants in focus groups in Europe, interviews in England and interviews in the UK felt that there were issues with privacy in the community pharmacy setting [ 51 , 48 , 63 ]. Significantly more women who obtained EHC from other services (e.g. family planning clinics) in the survey in England reported that they felt comfortable, had adequate privacy, adequate advice, and had discussed future contraception than those attending pharmacy [ 48 ]. Participants in the focus groups in Europe and Sweden also expressed mixed views on their interaction with the pharmacists [ 51 , 25 ]. Some participants perceived that the pharmacist was judgemental towards them in the consultation [ 51 , 25 ].
The majority of women surveyed after taking a postal Chlamydia testing kit from a pharmacy in Amsterdam reported that it was a good method of screening (68%) [ 23 ]. In a similar study in England, the majority of customers taking a Chlamydia testing kit were very satisfied with the service (80%), found the consultation sufficiently private (95%) and were comfortable discussing sexual health with the pharmacist (100%) [ 70 ]. In telephone interviews participants commented on the excellent communication skills of the pharmacist and the short waiting times and anonymity at the pharmacy. However, the interviews also revealed that while customers were satisfied with the confidentiality of the consultation, there were concerns regarding confidentiality at the counter [ 70 ].
Perceptions of pharmacists' ability
Around one third of pharmacy customers in a survey in the UK were unsure if the pharmacist was qualified to issue advice on sexual health issues or had enough experience or knowledge to deal with sexual health related issues [ 44 ]. Approximately three quarters of patients surveyed at a medical centre in the USA were undecided, disagreed or strongly disagreed with the statement that pharmacists are trained to provide smoking cessation services [ 17 ]. Those that reported a greater frequency of discussing medications with their pharmacists were more likely to agree or strongly agree with the statement. In a sample of the general public in the USA, 82% and 94.2% of participants respectively thought that pharmacists and physicians would be a very good or somewhat good source of advice on quitting smoking [ 36 ]. Nicotine replacement therapy users in a survey in the USA rated pharmacists' smoking cessation knowledge as highest in relation to prescription medicines at an average of 8.1 out of a maximum score of 10 and lowest in relation to knowledge of non-drug strategies to help tobacco users to quit at an average of 4.0 [ 52 ].
Patients with type 2 diabetes in a study in the United Arab Emirates showed a significant increase in their perceptions of pharmacists' ability to help them to reduce their blood sugar after receiving a pharmacist led self management intervention [ 46 ]. At baseline 32% of participants agreed or strongly agreed that their pharmacist can help decrease their blood sugar and 92% agreed or strongly agreed with the same statement for their doctor. Over half of participants (56%) agreed or strongly agreed that the pharmacist could help after receiving the intervention. A survey in Sweden found that around three quarters of pharmacy customers thought that pharmacy could influence people's willingness to improve their health [ 78 ].
Pharmacy staff
The majority of pharmacists in the review were positive about providing public health services and felt that this was an important role. This suggests that the changing role of community pharmacy from traditional dispensing activities to greater involvement in health improvement is largely accepted, and the importance of providing these services is understood. However, the review indicates that the public health role is still considered secondary to medicine related roles. Pharmacists viewed public health activities as less important than traditional roles and were less confident in providing these. Less positive views were also held by some pharmacists in relation to certain public health services, particularly services for drug misusers. These findings are consistent with those of the previous systematic reviews on this topic [ 6 , 7 , 12 ].
Reported levels of confidence in providing public health services varied from service to service in the current review, but on the whole were average to low. Confidence in our ability to perform a behaviour (known as self efficacy) has been found to be crucial in predicting whether we engage in the behaviour [ 83 ]. A review found that self efficacy can predict as much as 35% of the variance in behaviour [ 84 ]. This link between confidence and behaviour was supported in the current review with two studies reporting that confidence was the greatest predictor of self reported smoking cessation activity in pharmacists [ 19 , 55 ].
This review and the previous review identified a need for further training for a number of different public health services. Encouragingly, training was found to have a positive effect on pharmacists' attitudes in the previous reviews [ 6 , 7 , 10 ]. Although very few studies in the current review assessed specific areas for future training, the findings of the review do suggest how training may be best targeted. A study on drug misuse and another on smoking cessation indicated that training on motivating patients and behavioural techniques would be most useful [ 77 , 34 ]. Training for health professionals often devotes time to explaining the importance of the health issue in question and what part the professional can play in tackling this. However, the findings of this review suggest that pharmacists understand this and that tackling pharmacists' self efficacy may have a much greater impact on practice. Although self efficacy is an important determinant of behaviour, there is limited evidence on interventions to increase self efficacy [ 85 ]. Therefore, further research is needed to investigate interventions to increase pharmacists' self efficacy for providing public health services.
Although most studies found that a lack of patient demand and negative customer reactions were not a barrier to public health practice, some pharmacists did perceive these to be a problem. Similarly, the previous review found that pharmacists were concerned about being intrusive when offering public health services. These beliefs could be addressed during training by outlining the results of research on customer experiences of pharmaceutical public health.
Time was fairly consistently identified in the current review as a barrier to a number of public health services. Similarly, the previous review reported that dispensing duties were a barrier to public health activities. Findings in the current review were more mixed regarding availability of an adequate counselling space as a barrier to public health practice, which may reflect differences in availability of counselling areas rather than differences in perceptions of their importance. Remuneration for providing public health services was not reported to be a barrier in the current review suggesting that current levels of remuneration are perceived to be adequate.
Only three studies in the current review reported the attitudes of support staff separately from those of pharmacists [ 22 , 56 , 30 ]. Fewer support staff reported that they were confident in providing accurate advice on prevention of HIV and hepatitis [ 22 ] than pharmacists in another similar survey [ 18 ]. Support staff are often the first point of contact for pharmacy customers and can play a vital role in alleviating the time pressures on pharmacists by offering public health services and carrying out initial screening. Research is needed to establish the attitudes of support staff to allow support and training to be appropriately targeted for this group.
Customer attitudes towards pharmaceutical public health were on the whole quite positive. Customers found the pharmacy a convenient setting and felt that pharmacists should provide public health services. Those that had experienced public health services in community pharmacy, such as self management interventions, emergency hormonal contraception and Chlamydia screening, were largely satisfied with their experience of these. However, two studies revealed that most customers did not expect, and had never been offered, public health advice from a pharmacist [ 47 , 78 ]. This suggests that pharmacists' perceptions of low demand for public health services are accurate. However, the expectation of a negative customer reaction to pharmaceutical public health services held by some pharmacists seems to be unfounded. These findings are also consistent with those of the previous systematic reviews in the area [ 6 , 7 , 12 ]. Customers in the previous review valued the pharmacists input in public health services, but perceived pharmacists as drug experts and did not often use pharmacies for general health advice.
Customers' perceptions of pharmacists' ability to provide public health services were mixed in the current review, with some perceiving pharmacists as good sources of advice on health and other not. One study found a significant increase in customers' perceptions of pharmacists' ability after receiving a diabetes self management intervention from pharmacist. Similarly another study reported significantly more positive attitudes in members of the public who had experienced pharmacy health screening or promotion than those that had not.
Issues with privacy were raised in four studies investigating sexual health services in community pharmacy and were also highlighted in the previous review on customer attitudes [ 48 , 51 , 63 , 70 , 11 ]. Although private counselling areas are becoming more common in pharmacy, these studies highlight that there are still issues with privacy, particularly at the pharmacy counter. The nature of the pharmacy setting can make complete privacy difficult to achieve, but future projects involving sensitive topics such as sexual health must make attempts to remedy this issue.
Pharmaceutical public health services are clearly well received by those that experience them and result in high levels of satisfaction. Considering the findings of this review, it seems likely that the more these services are offered and experienced by the general public, the more positive attitudes will become. Successfully changing the public's perception of pharmacist in this way will require pharmacists to be proactive in offering public health services. As discussed, pharmacists may need additional support and training in order to feel confident about doing this.
Limitations of the review
Heterogeneity in the included studies reduced the ability of the review to summarise trends and may have accounted for some of the inconsistencies in findings. Studies were conducted in a variety of countries across the world with differing health care systems and it is not known how these different cultures and systems may affect customer and pharmacy staff attitudes. A number of factors increased the risk of bias within the included studies. Response rates were generally average, with the majority of studies achieving rates of 50% and over. One quarter of studies did not report response rates and only three studies followed up and assessed non-respondents. Convenience sampling was used in the majority of studies included in the review. These factors may mean that the views of those sampled were not representative of the population as a whole and therefore limit the generalisability of the findings.
The consistency of the findings of the current review with the previous reviews is striking. Despite the introduction of public health services to the pharmacy contract in the UK, current attitudes of pharmacists and the public appear to be largely similar to before these changes. Although this is discouraging it is perhaps not surprising considering the magnitude of the changes pharmacists have experienced in their role. Around half of non-UK papers and one third of UK papers in the present review were published prior to the introduction of the new pharmacy contract in the UK (See table 2 ). This fact considered with the possible lag between research being conducted and published may also partly explain why there was little difference found in attitudes between the current and previous systematic reviews.
It is important that the positive attitudes of pharmaceutical public health users and pharmacists found in both reviews are extended and built upon. Appropriate training and support is needed in order increasing pharmacists' confidence in providing public health services. Future research needs to investigate the effectiveness of strategies for increasing pharmacists' confidence and changing their public health practice. If pharmacists can be supported to offer public health services more proactively, it is likely that increased exposure to public health services will have a positive effect of the attitudes and health of the general public.
Royal Pharmaceutical Society of Great Britain: Pharmacy in a new age: Building the future. 1996, London: RPSPG
Google Scholar
Scottish Executive: The right medicine: A strategy for pharmaceutical care in Scotland. 2002, Edinburgh, Accessed 10 th December 2009, [ http://www.scotland.gov.uk/Publications/2002/02/10633/File-1 ]
Scottish Executive: New community pharmacy contract update, HDL, 36. 2004, Edinburgh, Accessed 1 st December 2009, [ http://www.sehd.scot.nhs.uk/mels/HDL2004_36.pdf ]
Department of Health: Framework for a new community pharmacy contract. 2003, London, Accessed 31 st March 2010, [ http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4068357.pdf ]
Royal Pharmaceutical Society of Great Britain: Community pharmacy: the choice is yours. 1996, London: RPSPG
Anderson C, Blenkinsopp A, Armstrong M: The contribution of community pharmacy to improving the public's health: Report 1 Evidence from the peer reviewed literature 1990-2001. 2003, London: Pharmacy Health Link
Blenkinsopp A, Anderson C, Armstrong M: The contribution of community pharmacy to improving the public's health: Report 2 Evidence from the UK non peer-reviewed literature 1990-2002. 2003, London: Pharmacy Health Link
Ajzen I: The theory of planned behaviour. Organizational Behavior and Human Decision Processes. 1991, 50: 179-211. 10.1016/0749-5978(91)90020-T.
Article Google Scholar
Sutton S: Predicting and explaining intentions and behaviors: How well are we doing?. Journal of Applied Social Psychology. 1998, 28: 1317-1338. 10.1111/j.1559-1816.1998.tb01679.x.
Anderson C, Blenkinsopp A, Armstrong M: Pharmacists' perceptions regarding their contribution to improving the public's health: a systematic review of the United Kingdom and international literature 1990-2001. International Journal of Pharmacy Practice. 2003, 11: 111-120. 10.1211/0022357021297.
Anderson C, Blenkinsopp A, Armstrong M: Feedback from community pharmacy users on the contribution of community pharmacy to improving public's health: a systematic review of the peer reviewed and non-peer reviewed literature 1990-2002. Health Expectations. 2004, 7: 191-202. 10.1111/j.1369-7625.2004.00274.x.
Article PubMed Google Scholar
Anderson C, Blenkinsopp A: Community pharmacy supply of emergency hormonal contraception: a structured literature review of international evidence. Human Reproduction. 2006, 21: 272-284.
Article CAS PubMed Google Scholar
Centre for Reviews and Dissemination: Systematic Reviews. CRD's guidance for undertaking reviews in healthcare. 2008, York
Crombie IK: The pocket guide to critical appraisal. 1996, London: BMJ publishing group
Public Health Resource Unit: Critical appraisal skills programme: 10 questions to help you make sense of qualitative research. 2006, England, Accessed 12 th October 2010, [ http://www.sph.nhs.uk/sph-files/Qualitative%20Appraisal%20Tool.pdf ]
Aquilino M, Farris K, Zillich A, Lowe J: Smoking cessation services in Iowa community pharmacies. Pharmacotherapy. 2003, 23: 666-673. 10.1592/phco.23.5.666.32192.
Couchenour R, Carson D, Segal A: Patients' views of pharmacists as providers of smoking cessation services. Journal of the American Pharmaceutical.
Dastani H, Brown C, O'Donnell D: Combating the obesity epidemic: community pharmacists counselling on obesity management. Annals of Pharmacotherapy. 2004, 38: 1800-1804. 10.1345/aph.1E205.
Edwards D, Freeman T, Gilbert A: Pharmacists' role in smoking cessation: an examination of current practice and barriers to service provision. International Journal of Pharmacy Practice. 2006, 14: 315-317. 10.1211/ijpp.14.4.0013.
Oparah A, Kikanme L: Consumer satisfaction with community pharmacies in Warri, Nigeria. Research in Social and Administrative Pharmacy. 2006, 2: 499-511. 10.1016/j.sapharm.2006.02.004.
Pfleger D, McHattie L, Diack H, McCaig D, Stewart D: Views, attitudes and self assessed training needs of Scottish community pharmacists to public health practice and competence. Pharmacy World and Science. 2008, 30: 801-809. 10.1007/s11096-008-9228-1.
Thomas G, Humphris G, Ozakinci G, O'Brien K, Roberts S, Hopkins M, Brabin L: A qualitative study of pharmacists' views on offering Chlamydia screening to women requesting emergency hormonal contraception. British Journal of Obstetrics and Gynaecology. 2010, 117: 109-113. 10.1111/j.1471-0528.2009.02362.x.
Van Bergen J, Postma M, Peerbooms P, Spanbergen A, Tjwn-A-Tak J, Bindels P: Effectiveness and cost-effectiveness of a pharmacy based screening programme for Chlamydia trachomatis in a high risk health centre population in Amsterdam using home collected urine samples. International Journal of STD and AIDS. 15: 797-802.
Zillich A, Aqulino M, Farris K: Knowledge and attitudes about smoking cessation among pharmacy technicians. Journal of the American Pharmacists Association. 2004, 44: 578-582. 10.1331/1544-3191.44.5.578.Zillich.
Aneblom G, Larsson M, von Essen L, Tyden T: Women's voices about emergency contraceptive pills "over the counter": a Swedish perspective. Contraception. 2002, 66: 339-343. 10.1016/S0010-7824(02)00367-0.
Cameron S, Melvin L, Glaiser A, Scott G, Johnstone A, Young H: Willingness of gynaecologists, doctors in family planning, GPs, practice nurses and pharmacists to adopt novel interventions for treating sexual partners of women with chlamydia. British Journal of Obstetrics and Gynaecology. 2007, 114: 1516-1521. 10.1111/j.1471-0528.2007.01506.x.
Dunn S, Brown T, Cohen M, Cockerill R, Wichman K, Weir N, Pancham A: Pharmacy provision of emergency contraception: the Ontario emergency contraception pilot project. Journal of Obstetrics and Gynaecology Canada. 2003, 25: 923-930.
Gray M, Rajaei-Dehkordi Z, Ewan M, Wysocki R: Investigating the potential contribution of pharmacists in identifying, understanding and meeting the bone health needs of patients in collaboration with GPs. International Journal of Pharmacy Practice. 2002, 10 (suppl): R34-
Krska J, Lovelady C, Connolly D, Parmar S, Davies M: Community pharmacy contribution to weight management: identifying opportunities. International Journal of Pharmacy Practice. 2010, 18: 7-12.
PubMed Google Scholar
MacKridge A, Scott J: Experiences, attitudes and training needs of pharmacy support staff providing services to drug users in Great Britain: A qualitative study. Journal of Substance Use. 2009, 14: 375-384. 10.3109/14659890802695840.
Scott J, MacKridge A: Pharmacy support staff involvement in, and attitudes towards pharmacy-based services for drug misusers. International Journal of Pharmacy Practice. 2009, 17: 325-332. 10.1211/ijpp.17.06.0002.
Ashley M, Brewster J, Victor J: Pharmacists smoking cessation practices: relationship to their knowledge and skills, attitudes and perceptions of roles. Journal of the American Pharmacists Association. 2006, 46: 729-737.
Ashley M, Victor J, Brewster J: Pharmacists' attitudes, role perceptions and interventions regarding smoking cessation: Findings from four Canadian provinces. Chronic Diseases in Canada. 2007, 28: 20-28.
Brewster J, Ashley M, Laurier C, Dioso R, Victor J, Ferrence R, Cohen J: On the front line of smoking cessation: Education needs of community pharmacists. Canadian Pharmaceutical Journal. 2005, 138: 26-31.
Brewster J, Ashley M, Laurier C, Dioso R, Victor C, Ferrence R, Cohen J: On the front line of smoking cessation: Pharmacists' practices and self perception. Canadian Pharmaceutical Journal. 2007, 138: 32-38.
Brewster J, Victor J, Ashley M: Views of Ontarians about health professionals' smoking cessation advice. Canadian Journal of Public Health. 2007, 98: 395-399.
Kurko T, Linden K, Vasama M, Pietila K, Airaksinen M: Nicotine replacement therapy practices in Finland one year after deregulation of the product sale - has anything changed from the community pharmacy perspective?. Health Policy. 2009, 91: 277-285. 10.1016/j.healthpol.2008.12.013.
Sheridan J, Manning V, Ridge G, Strang J: Community pharmacies and the provision of opioid substitution services for drug misusers: changes in activity and attitudes of community pharmacists across England 1995-2005. Addiction. 2007, 102: 1824-1830. 10.1111/j.1360-0443.2007.02016.x.
Deibert R, Goldbaum G, Parker T, Hagan H, Marks R, Hanrahan M, Thiede H: Increased access to unrestricted pharmacy sales of syringes in Seattle - King County, Washington: Structural and individual level changes, 1996 versus 2003. American Journal of Public Health. 2006, 96: 1347-1353. 10.2105/AJPH.2003.032698.
Article PubMed PubMed Central Google Scholar
Kennedy D, Giles J, Chang Z, Small R, Edwards J: Results of a smoking cessation clinic in community pharmacy practice. Journal of the American Pharmaceutical Association. 2002, 42: 51-56. 10.1331/108658002763538071.
Lewis B, Koester S, Bush T: Pharmacists' attitudes and concerns regarding syringe sales to injection drug users in Denver, Colorado. Journal of the American Pharmaceutical Association. 2002, 42 (s2): s46-s51.
Tesoriero J, Battles H, Klein S, Kaufman E, Birkhead G: Expanding access to sterile syringes through pharmacies: assessment of New York's expanded syringe access program. Journal of the American Pharmacists Association. 2009, 49: 407-416. 10.1331/JAPhA.2009.07127.
Pankonin C, Higgs P, Reid G, Aitken C: Selling syringes to injecting drug users: a study of five pharmacies in Hanoi, Vietnam. Journal of Infection in Developing Countries. 2008, 2: 51-58.
Wood N, James D: Young people's views about chlamydia testing in community pharmacy. International Journal of Pharmacy Practice. 2010, s2: 49-
Thananithisak C, Nimpitakpong P, Chaiyakunapruk N: Activities and perceptions of pharmacists providing tobacco control services in community pharmacy in Thailand. Nicotine Tob Res. 2008, 10: 921-925. 10.1080/14622200802027115.
Abduelkarem A, Sackville M: Changes of some health indicators in patients with type 2 diabetes: A prospective study in three community pharmacies in Sharjah, United Arab Emirates. Libyan Journal of Medicine. 4: 29-38.
Sunderland B, Burrows S, Joyce A, McManus A, Maycock B: Rural pharmacy not delivering on its health promotion potential. Australian Journal of Rural Health. 2006, 14: 116-119. 10.1111/j.1440-1584.2006.00774.x.
Black K, Mercer C, Kubba A, Wellings K: Provision of emergency contraception: A pilot study comparing access through pharmacies and clinical setting. Contraception. 2008, 77: 181-185. 10.1016/j.contraception.2007.12.001.
Calabretto H: Emergency contraception - knowledge and attitudes in a group of Australian university students. Australian and New Zealand Journal of Public Health. 2009, 33: 234-239. 10.1111/j.1753-6405.2009.00381.x.
Calgan Z, Tahir E, Yegenoglu S, Bilir N: Community pharmacists' attitude, habits and actual activities regarding smoking and health promotion in the 1. Region of Ankara chamber of pharmacists. Turkish Journal of Pharmaceutical Science. 2007, 4: 125-138.
Gainer E, Blum J, Toveru E, Portugal N, Tyden T, Nesheim B, Larsson M, et al: Bringing emergency contraception over the counter: experiences of non-prescription users in France, Norway, Sweden and Portugal. Contraception. 2003, 68: 117-124. 10.1016/S0010-7824(03)00114-8.
Hudmon K, Hemberger K, Corelli R, Kroon L, Prokhorov A: Smoking cessation counselling: perceptions of users of non-prescription nicotine replacement therapy. Journal of American Pharmacists Association. 2003, 43: 573-582. 10.1331/154434503322452201.
MacLaughlin E, MacLaughlin A, Snella K, Winston T, Fike D, Raehl C: Osteoporosis screening and education in community pharmacists using a team approach. Pharmacotherapy. 2005, 25: 379-386. 10.1592/phco.25.3.379.61604.
Nahri U, Airaksinen M, Enlund H: Pharmacists solving problems in asthma management - experiences from a one year intervention programme in Finland. The International Journal of Pharmacy Practice. 2002, 10: 55-59. 10.1111/j.2042-7174.2002.tb00588.x.
Hudmon K, Prokhorov A, Corelli R: Tobacco cessation counselling: Pharmacists' opinions and practices. Patient Education and Counselling. 2006, 61: 152-160. 10.1016/j.pec.2005.03.009.
Bjorkman I, Viberg N, Rydberg L, Stalsby Lundborg C: Health promotion at Swedish pharmacies - views of the staff. Pharmacy Practice. 2008, 6: 211-218.
Teh R, Chen T, Krass I: Consumer perceptions of pharmacist delivered health information and screening services. International Journal of Pharmacy Practice. 2001, 9: 261-267. 10.1111/j.2042-7174.2001.tb01057.x.
Vorobjov S, Uuskula A, Abel-Ollo K, Talu A, Jarlais D: Should pharmcists have a role in harm reduction services for IDUs? A qualitative study in Tallinn Estonia. Journal of Urban Health. 2009, 86: 918-928. 10.1007/s11524-009-9400-5.
Iversen L, Mollison J, MacLeod T: Attitudes of the general public to the expanding role of community pharmacists: A pilot study. Family Practice. 2001, 18: 534-536. 10.1093/fampra/18.5.534.
Matheson C, Bond C, Tinelli M: Community pharmacy harm reduction services for drug misusers: national service delivery and professional attitude development over a decade in Scotland. Journal of Public Health. 2007, 29: 350-357. 10.1093/pubmed/fdm064.
Sheridan J, Wheeler A, Chen L, Huang A, Leung I, Tien K: Screening and brief interventions for alcohol: attitudes, knowledge and experience of community pharmacists in Auckland, New Zealand. Drug and Alcohol Review. 2008, 27: 380-387. 10.1080/09595230802093760.
Patwardhan P, Chewning B: Ask, advise and refer: Hypothesis generation to promote a brief tobacco-cessation intervention in community pharmacies. International Journal of Pharmacy Practice. 2009, 17: 221-229. 10.1211/ijpp.17.04.0005.
Folkes L, Graham A, Weiss M: A qualitative study of the views of women aged 18-29 on over the counter availability of hormonal emergency contraception. Journal of family planning ad reproductive health care. 2001, 27: 189-192. 10.1783/147118901101195731.
Article CAS Google Scholar
Lawrie T, Matheson C, Bond C, Roberts K: Pharmacy customers' views and experiences of using pharmacies which provide drug misuse services. Drug and Alcohol Review. 2004, 23: 195-202. 10.1080/09595230410001704181.
Cordina M, Safta V, Ciobanu A, Sautenkova N: An assessment of community pharmacists' attitudes towards of professional practice in the Republic of Moldova. Pharmacy Practice. 2008, 6: 1-8.
Larsson M, Eurenius K, Westerling R, Tyden T: Emergency contraceptive pills over the counter: a population based survey of young Swedish women. Contraception. 2004, 69: 309-315. 10.1016/j.contraception.2003.11.013.
Griggs S, Brown C: Texas community pharmacists'' willingness to participate in pharmacist initiated emergency contraception. Journal of American Pharmacists Association. 2007, 47: 48-57. 10.1331/1544-3191.47.1.48.Griggs.
Landau S, Besinque K, Chung F, Dries-Daffner I, Monastersky Maderes N, Taylor McGhee B, Greene Foster D: Pharmacists interest in and attitudes toward direct pharmacy access to hormonal contraception in the United States. Journal of the American Pharmacists Association. 2009, 49: 43-50. 10.1331/JAPhA.2009.07154.
Bissell P, Anderson C: Supplying emergency contraception via community pharmacies in the UK: reflections on the experiences of users and providers. Social science and medicine. 2003, 57: 2367-2378. 10.1016/S0277-9536(03)00129-1.
Baraitser P, Pearce V, Holmes J, Horne N, Boynton P: Chlamydia testing in community pharmacies: Evaluation of a feasibility pilot in south east London. Quality and Safety in Health Care. 2007, 16: 303-307. 10.1136/qshc.2006.020883.
Article CAS PubMed PubMed Central Google Scholar
Oparah A, Okojie O: Health promotion perceptions among community pharmacists in Nigeria. International Journal of Pharmacy Practice. 2005, 13: 213-221. 10.1211/ijpp.13.3.0007.
Scott A, Bond C, Inch J, Grant A: Preferences of community pharmacists for extended roles in primary care. Pharmacoeconomics. 2007, 25: 783-792. 10.2165/00019053-200725090-00006.
Watson L, Bond C, Gault C: A survey of community pharmacists on prevention of HIV and hepatitis B and C: current practice and attitudes in Grampian. Journal of Public Health Medicine. 2003, 25: 13-18. 10.1093/pubmed/fdg004.
Watson L, Bond C, Gault C: A survey of pharmacy assistants in Grampian on prevention of HIV and hepatitis B and C. International Journal of Pharmacy Practice. 2006, 14: 129-134. 10.1211/ijpp.14.2.0007.
Hassali M, Subish P, Shafie A, Ibrahim M: Perceptions and barriers towards provision of health promotion activities among community pharmacists in the State of Penang, Malaysia. Journal of Clinical and Diagnostic Research. 2009, 3: 1562-1568.
Suh DC, Greenberg M, Schneider D, Colaizzi J: Pharmacists' perceptions of healthy people goals in economically stressed cities. Journal of Community Health. 2002, 27: 133-150. 10.1023/A:1014513301260.
Cameron I, Matheson C, Bond C: A survey of community pharmacists training needs in the management of opioid dependent clients in Grampian, Scotland. The Pharmaceutical Journal. 2006, 275: 601-603.
Larsson E, Viberg N, Vernby A, Nordmark J, Stalsby-Lundborg C: Health information, an area of competition for Swedish pharmacies. Pharmacy Practice. 2008, 6: 74-78.
Law A, Shapiro K: Impact of a community pharmacist directed clinic in improving screening and awareness of osteoporosis. Journal of Evaluation in Clinical Practice. 2005, 11: 247-255. 10.1111/j.1365-2753.2005.00531.x.
Fera T, Bluml B, Ellis W, Schaller C, Garrett D: The diabetes ten city challenge: Interim clinical and humanistic outcomes of a multisite community pharmacy diabetes care program. Journal of the American Pharmacists Association. 2008, 48: 181-190. 10.1331/JAPhA.2008.07166.
Sucato G, Gardner J, Koepsell T: Adolescents use of emergency contraception provided by Washington State Pharmacists. Journal of Paediatric and Adolescent Gynaecology. 2001, 14: 163-169. 10.1016/S1083-3188(01)00124-3.
Foster D, Landau S, Monastersky N, Chung F, Kim N: Pharmacy access to emergency contraception in California. Perspectives on Sexual and Reproductive Health. 2006, 38: 46-52. 10.1363/3804606.
Bandura A: Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977, 84: 191-215.
Armitage CJ, Conner M: Efficacy of the theory of planned behaviour: A meta-analytic review. British Journal of Social Psychology. 2001, 40: 471-499. 10.1348/014466601164939.
Ashford S, Edmunds J, French D: What is the best way to change self efficacy to promote lifestyle and recreational physical activity? A systematic review with meta-analysis. British Journal of Health Psychology. 2010, 15: 265-288. 10.1348/135910709X461752.
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-2458/11/582/prepub
Download references
Acknowledgements
Funding to undertake this review was provided by Pharmacy Services, NHS Forth Valley and NHS Education for Scotland.
Author information
Authors and affiliations.
Department of Psychology, University of Stirling, Stirling, FK9 4LA, Scotland, UK
Claire E Eades & Ronan E O'Carroll
NHS Forth Valley Pharmacy Services, Eurohouse, Wellgreen Place, Stirling, FK8 2DJ, Scotland, UK
Jill S Ferguson
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Claire E Eades .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
CE conducted the design, screening, data abstraction, data analysis, and drafted the manuscript. JF assisted in the design of the study and helped draft the manuscript. RO assisted in the design of the study, assessing papers for inclusion and drafting the manuscript. All authors read and approved the final manuscript.
Electronic supplementary material
12889_2010_3320_moesm1_esm.xls.
Additional file 1: Characteristics of included studies. Excel table showing characteristics of studies included in the review. (XLS 100 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Eades, C.E., Ferguson, J.S. & O'Carroll, R.E. Public health in community pharmacy: A systematic review of pharmacist and consumer views. BMC Public Health 11 , 582 (2011). https://doi.org/10.1186/1471-2458-11-582
Download citation
Received : 23 December 2010
Accepted : 21 July 2011
Published : 21 July 2011
DOI : https://doi.org/10.1186/1471-2458-11-582
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Smoking Cessation
- Nicotine Replacement Therapy
- Community Pharmacy
- Public Health Service
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Integr Pharm Res Pract

Defining pharmacy and its practice: a conceptual model for an international audience
1 School of Management, Massey Business School, Massey University, Albany, Auckland, New Zealand
2 Pharmacy School, The Islamia University of Bahawalpur, Bahawalpur, Pakistan
3 School of Pharmacy, University of Huddersfield, Huddersfield, England, UK
4 School of Pharmacy, Faculty of Medical and Health Sciences, University of Auckland, Auckland, New Zealand
There is much fragmentation and little consensus in the use of descriptors for the different disciplines that make up the pharmacy sector. Globalization, reprofessionalization and the influx of other disciplines means there is a requirement for a greater degree of standardization. This has not been well addressed in the pharmacy practice research and education literature.
To identify and define the various subdisciplines of the pharmacy sector and integrate them into an internationally relevant conceptual model based on narrative synthesis of the literature.
A literature review was undertaken to understand the fragmentation in dialogue surrounding definitions relating to concepts and practices in the context of the pharmacy sector. From a synthesis of this literature, the need for this model was justified. Key assumptions of the model were identified, and an organic process of development took place with the three authors engaging in a process of sense-making to theorize the model.
The model is “fit for purpose” across multiple countries and includes two components making up the umbrella term “pharmaceutical practice”. The first component is the four conceptual dimensions, which outline the disciplines including social and administrative sciences, community pharmacy, clinical pharmacy and pharmaceutical sciences. The second component of the model describes the “acts of practice”: teaching, research and professional advocacy; service and academic enterprise.
Conclusions
This model aims to expose issues relating to defining pharmacy and its practice and to create dialogue. No model is perfect, but there are implications for what is posited in the areas of policy, education and practice and future research. The main point is the need for increased clarity, or at least beginning the discussion to increase the clarity of definition and consistency of meaning in-and-across the pharmacy sector locally, nationally and internationally.
Introduction
The aim of this article is to identify and define the various subdisciplines of the pharmacy sector and integrate them into an internationally relevant conceptual model based on narrative synthesis of the literature. It is expected that significant dialogue will be derived from this article, and it is expected that it will provide a platform for moving forward in international pharmacy education. This is important because there is much fragmentation and little consensus in the use of descriptors for the different disciplines that make up the pharmaceutical sector. Globalization, reprofessionalization and the influx of other disciplines means there is a requirement for a greater degree of standardization. This has not been well addressed in the pharmacy practice research and education literature.
Pharmacy education can be broadly divided into four areas: 1) pharmaceutics (sometimes labeled as pharmaceutical technology) and pharmacokinetics, 2) pharmaceutical chemistry, 3) pharmacology and 4) pharmacy practice includes clinical pharmacy, pharmacotherapy, social and administrative sciences, and pharmaceutical care. These subparts of the fourth category are often aggregated in a disparate manner. The first three categories are closely aligned with the basic sciences; the fourth category is inclusive of the human sciences. This fourth category has greater ambiguity, at least from the stance of definitions. 1 Internationally, social and administrative pharmacy, clinical pharmacy, pharmaceutical care and pharmacy practice are terms used to describe different aspects of pharmacy practice. 1 – 7 However, these terms have a level of subjectivity and mean different things to different people.
There is an emergent literature on the field of social pharmacy 8 – 15 and particularly in terms of education. 16 – 22 There is a literature that defines pharmaceutical care 5 , 23 – 26 with some focus on community pharmacy. 27 – 30 Similarly, there is a dialogue on what constitutes clinical pharmacy and how this relates to pharmaceutical care, 31 – 33 but there is no model which defines these concepts and draws them together as a whole. 34 – 36 Even between the proponents of the closely related concepts of social pharmacy and pharmacy practice, there is a lack of consensus on the research agendas for each subdiscipline and a call for a systematic analysis of this and further dialog. 1 – 4 , 6 , 7 , 32 33 , 37 , 38 Equally, translational sresearch – that is taking bench to bedside (and the reverse) – is increasingly blurring the lines between what is considered “hard science” and what is deemed to be “soft practice”. In fact, “the sciences” fit under the umbrella of pharmaceutical practice, and we argue that these basic sciences should be part of a conceptual model of what it is to be “pharmacy”.
This article posits a model of pharmaceutical practice, which includes the professional practice activities of pharmacist clinicians. The term is distinct and has less controversial connotations than many others used interchangeably. The model also considers the broader roles undertaken by pharmacists, such as involvement in the development of health policy. The model incorporates the influx of significant others (sociologists, psychologists, etc.) into the academic discipline of pharmacy, and the roles that these groupings have and the contribution of their work to pharmaceutical practice. 37 These roles are seen as a series of distinct disciplines within the conceptual model, but are at times blurred and have the potential to influence each other. The model outlines a conceptual approach to redefining the labels attached to these various disciplines, but also the practices of pharmacy within each of these. Absolute consensus of a model like this is near impossible, with the overlap and conflation of the different disciplines being difficult to unpack. What is possible though is an increased level of international dialogue and a drive toward a greater level of consistency than is currently seen. This is a theoretical framework, a beginning!
Alignment between real-world practice and academic pharmacy is thought about and melded into the model. It is expected that this will be an evolving conceptual model informed by the history of research and international commentary surrounding this topic.
The need for a global model
The need for a global conceptual model stems from the series of issues given below:
Reason 1 – different things to different people: multiple definitions
It is generally accepted that the disciplines of pharmaceutical science are founded on the basic sciences. Pharmaceutics, pharmaceutical chemistry, pharmacology and pharmacokinetics are well-established subdisciplines of the pharmaceutical sciences. The same cannot be said for new evolving clinically oriented disciplines. Even in these relatively circumscribed areas of pharmacy theory and practice, there is a significant divergence in opinion of what constitutes each and how, where and why these terms overlap. 1 , 3 , 4 , 32 , 33 , 39 , 40 Clinical pharmacy, pharmacy practice, community pharmacy, retail pharmacy, social pharmacy and translational research are all likely to mean different things to different people.
In the area of hospital pharmacy, the terms pharmacy practice, clinical pharmacy, pharmacotherapy and public sector pharmacy have all been used interchangeably. Descriptions for community pharmacy have included pharmacy practice, retail pharmacy, community pharmacy, private sector pharmacy, private sector hospital pharmacy and clinical pharmacy practice in community pharmacies. 1
Social and administrative pharmacy is used loosely to describe a collection of different interests, which outline the social aspects of pharmacy, sometimes labeled social pharmacy, other times administrative pharmacy but also pharmacy management. The broad discipline is founded on the principles of social science and organizational theory and has as a central interest in the beliefs, values and behaviors that people display in relation to medicine use and society at the individual and organizational levels. 1 – 3 , 36 , 38 , 41 – 43 In some Commonwealth countries such as the UK, New Zealand and Australia, pharmacy practice seems to identify with community pharmacy with social pharmacy being considered a part of this. However, in the USA, social and administrative sciences has developed as a completely separate discipline and this also seems to be the case in parts of Asia.
Different from, but linked to, definitional difference is the idea that laws affecting practice will be different around the globe, and this means that it is more difficult to develop a consistent approach to interpreting practice-based definitions. Although the model may be limited by this, there is an expectation that the context will determine how the model is applied in different countries and the overall assumptions and basic reasoning for the model apply globally – the need for further dialogue in this area certainly applies on an international scale! Furthermore, people can take from the model what they wish and apply it locally!
Reason 2 – the trend of clinical pharmacy and the Pharm D “tag”
Clinical pharmacy is an important discipline in the practice of pharmacy – it has a lot to offer and has played an important role in transformation of the pharmacy profession over the past two decades. Clinical pharmacy has been part of the “re-professionalization” agenda both within the hospital and community sectors. 16 , 44 – 47 However, there are many definitions of clinical pharmacy, and the term “clinical pharmacy” has been understood differently across the globe. Some relate it to “patient care”, whereas others associate it more with the “managing appropriate use of medicines”. 32
Amid these discussions in the developed world, the change has also greatly affected the pharmacy sector in developing countries, where establishing “clinical pharmacy” programs is considered a novel phenomenon. Under this influence, pharmaceutical care is popular jargon with the basic undergraduate pharmacy degrees having been changed to Doctor of Pharmacy (Pharm D) and the number of years of study simply extended in expectation of that. 48 It would appear that pharmacy schools across Asia and within the Middle East are joining the “bandwagon” to promote clinical pharmacy. 1 These countries are re-adjusting their degree programs by introducing Pharm D degrees as entry level qualifications into pharmacy. In some countries, in particular, “clinical pharmacy” is evolving in a very interesting manner. For example, in Pakistan, there was no separate discipline of clinical pharmacy, which is being taught under the umbrella of pharmaceutics in some universities. However, recently a new pharmacy practice discipline has been established. Anecdotal evidence also suggests that tensions and rifts between pharmacy and pharmacology colleagues have occurred. Pharmacologists believe that they should teach clinical pharmacy programs. The pharmacologists’ rationale is that clinical pharmacy is close to their domain, pharmacology being the study drug action on the body.
In Western countries, clinical pharmacy is established only when a stable medicine system is in place in the hospitals and drug regulatory authorities are mandated and efficient. Most developing countries do not have this luxury and are struggling with the issues of quality, safety, efficacy and distribution of medicines. 49 In this context, clinical pharmacy is promoted as an isolated concept of practice and the underpinning philosophies are poorly understood and little has changed in terms of patient care. 2

Reason 3 – passionate and motivated by our individual subdisciplines
Academics and practitioners see their discipline as central; yet, the literature is scarce when considering the pharmacy profession as a whole. Ahmed et al recognize these differences and suggest that a strong need exists to definitions relating to clinical pharmacy and pharmaceutical care. 31 These standard definitions must be agreed upon and disseminated globally so that they are understood clearly (ie, clinical pharmacy and pharmaceutical care). This needs to be the case not only for pharmacists but also for other healthcare professionals and the wider disciplines, such as sociology and psychology. And, in this article, we take the work of Ahmed et al one step further and expand the need to develop a much broader model for pharmacists, other healthcare workers, government policy-makers and educators to take a sector-wide approach. 31
Reason 4 – what it is to be “pharmacy”
In our experience and through anecdote, a question that is commonly fielded from key stakeholders (patients, public and other health professionals) is “what is pharmacy about?”; “what is it you do as a pharmacy profession – do you just count pills?” How then do we explain to colleagues and external stakeholders what we actually do, what our potential is as a profession and what our teaching encapsulates and what our research is all about? How in the broadest sense do we explain what pharmacy aims to contribute to health outcomes and further, how it might do so? We have a lot of different terminologies to describe ourselves as the pharmacy profession. We might say we work in the area of pharmacy practice, clinical pharmacy or social and administrative sciences. Importantly, medicines are not singularly the domain of pharmacists, and there is a need to help other nonpharmacy disciplines to understand what constitutes the pharmacy sector by standardizing terminology. In this way, it will also be easier to fit with policy, or at least integrate with and be understood by policy-makers and clinician stakeholders.
Part of the confusion and fragmentation surrounding the pharmacy profession comes from the overlap in “what we do” and “how we do it” but also how we label “who we are” and “what we do”. For example, translational research is where basic and clinical sciences collide, cutting through boundaries between the research bench and patient bedside, empiric knowledge and soft practices. This creates an inherent blurring in what is deemed to be pharmaceutical science and what is deemed to be “clinical practice”; at least, this is the case from an academic viewpoint. Pharmacy practice and social pharmacy are also loose and slippery concepts to define, less so pharmaceutical care. Again the boundaries are blurred, but there is a need to put a stake in the ground and define these concepts so that things are more concrete.
The pharmacy sector is evolving and with the influx of significant others (such as sociologists, psychologists, anthropologists, historians, health economists, organizational and political scientists) into pharmacy academia and practice, the boundaries of the sector as a whole seem to have been extended and strengthened. For example, sociologists can conceptualize and operationalize research and practice that contribute significantly to introducing various behavioral models to the understanding of medicines use, thereby improving health outcomes. Research around pharmaceutical policy development and implementation, access to medicines and their use and pharmacoepidemiology are good examples of this type of work.
Summary of the need for a conceptual model
The definition of what constitutes “the pharmacy sector” and disciplines and practices thereof can be defined as broadly or as narrowly as one wishes. A narrow approach would feature the traditional elements of pharmacy, namely source and supply within a professional and regulated distribution model. 44 – 47 Conversely, a broad conceptual stance would adopt elements from social and basic sciences as well. 45 Either way a model is required, which redefines the pharmacy sector and the practices involved within the sector, both academic and professional. The model cuts through the current loose and interchangeable use of terminology and is founded on robust theoretical grounds. The authors’ own insights and experiences are also infused into the model, which has developed in an organic fashion. 50
This conceptual model is founded on the notion of consistency in definitions with respect to both the dimensions of the model and the model as a whole. The literature is scarce in describing the pharmacy sector “as a whole” and there are no “think piece” frameworks in this way. The main implication of the proposed model for theory is the call for clarity about the various parts of the pharmacy sector and how as a profession these dimensions may fit together.
Pharmaceutical practice: a conceptual model
Underpinned by the context previously outlined and with the need firmly established, we posit the term “pharmaceutical practice” and the associated conceptual model, which underpins this notion ( Figure 1 ). The idea is that pharmaceutical practice encompasses everything, which is related to availability of medicines, access and use at the individual and the population levels. This term encapsulates the research, development, formulation, distribution, access and clinical use of medicines. It incorporates the human capital required to deliver pharmacy services and the impact on end users of pharmaceutical products and services.

A conceptual model for pharmaceutical practice.
The dimensions: the glue making the whole
Dimensions of disciplines.
Social and administrative sciences, community pharmacy, clinical pharmacy and pharmaceutical sciences are the dimensions of our conceptual model, and a description of each of the dimensions is outlined below.
Social and administrative sciences
The field of social pharmacy developed initially within high-income countries, including Scandinavia, Finland, the UK and the USA. 45 More recently, there has been interest from academics in low- to middle-income countries and these groups have made significant contributions to this field. 1 , 3 , 31 The International Social Pharmacy Workshop (ISPW) has been a foundation platform for the development of the research and practice networks within the discipline of social and administrative sciences. There are subtle differences between each workshop; however, the focus has been on research directed toward pharmaceutical policy, access to medicines, medicine use and pharmacoepidemiology, pharmacoeconomics, organizational behavior and individual pharmacist practice.
There are pockets of academics particularly passionate about the field of social pharmacy. Norris highlighted the challenges that the discipline of social pharmacy faces. 37 Hassali et al have suggested social pharmacy as a field of study with a particular focus on the needs and challenges in global pharmacy education. 3 However, we believe that social pharmacy is an important part of the broader construct of pharmaceutical practice but is not the central umbrella concept – it is one of the four main dimensions. What are the other three?
Community pharmacy
Found within primary care, the practice of community pharmacy is reasonably clear cut at least with respect to its dual nature, as retailer and as primary healthcare provider and its separation from the rest of the profession. 51 There seems to be a number of “labels” applied to this aspect of pharmacy, including community pharmacy, retail pharmacy, private sector pharmacy and corporate pharmacy. Despite significant differences in service delivery models, we see community pharmacy as a collective form of practice centered on an organization embedded within a community. Although much activity is undertaken in community pharmacy, there is a scarcity of research at the organizational level. 42
Clinical pharmacy
Clinical pharmacy is the term that is most commonly used in the context of hospital pharmacy, where the focus is on pharmacotherapy and advanced subspecialties within this sector. The development of the clinical discipline is best reflected through the professionalization of hospital pharmacy in the USA. 44 Although clinical pharmacy could be deemed to be carried out in the setting of community pharmacy, in the proposed model, there is a clear distinction between advanced clinical practice in the primary (clinical advisory pharmacists), secondary and tertiary care sectors (hospital clinical pharmacists), and clinical activities that are undertaken within the four walls of a community pharmacy. Pharmaceutical care involves a defined process and warrants consideration as it crosses boundaries by being able to be implemented in hospital pharmacy and also in the context of advanced clinical practice in the community pharmacy setting. Essentially, this is a clinical pharmacy service. The term “pharmacotherapy” also introduces a level of ambiguity as the label describes a process that could be owned by any health professional who is considered to have training in the area; nurse practitioners and clinical pharmacists are two examples.
Pharmaceutical sciences
As with the label of community pharmacy, pharmaceutical science is a relatively clear cut and well-defined aspect of the model. Ambiguity in this aspect of practice emerges only when one thinks about the potential of pharmaceutical sciences as a platform for translational research; bench research to bedside clinical use and bedside clinical issues influencing research activities at the bench! This is where crossover at multiple levels creates an inherent “blurriness”, which we believe the proposed model will help to manage. It is also an area where universities are attempting to develop expertise and differentiate themselves from competitors, such as contract research organizations.
The act of practice
The act of practice can be thought of as those normative practices, the activities that are underpinned by what the culture of the specific discipline suggests is “normal”. 52 Regardless of whether the practice is considered clinical pharmacy or community pharmacy, it will be underpinned by values and beliefs that drive normative behavior. 52 , 53 These values and behaviors are expected to align with the concept of what it is to be “pharmacy” within the individual subdisciplines outlined in our model.
Teaching will vary dependent on the models of pharmacy that are practiced in any one country. However, the “labels” for each of the subdimensions of our model should be used in the same manner to describe the normative practices undertaken and the manner in which these practices are taught, regardless of country. That is, despite there being different needs in individual countries, the nomenclature/terminology being used should be broadly the same. The meaning of a definition in one country should be the same as in the next, despite slight variations in practice. The context may change but the meaning should not.
Research underpins practice, and practice can also inform research questions. There is a potential research agenda that could be developed based on questions and issues raised by this model. This agenda is outlined as part of the implications of our model, found later in this modeling paper.
Service – advocacy, professional sector development and academic enterprise
Service and advocacy is an act of practice that does not appear as part of other models in the literature or dialogue about what constitutes a particular discipline. Essential to the model, this act of practice describes professional leadership. The absence of this is a possible contributor to the lack of voice and recognition of pharmacy’s global role and the reason that pharmacy may be marginalized. 54 , 55 As such, we believe this is an important and integral aspect of any pharmaceutical practice model as is the leadership, which underpins the model. 55
The importance of local context in an international world
The individual dimensions of the pharmacy sector and their associated practices are influenced by local context. The proposed model takes this into consideration. There is a potential for tension between the viewpoints of those who call for curriculum development based wholly on local need analysis, alongside those who take the stance that “off-the-shelf ” standardized degree programs from universities located in high-income countries is the optimal approach. 56 The proposed model allows for both, however, but under the proviso that there is standardization in the use of terminology.
International consistency: implications for policy, practice and research
The proposed conceptual model calls for a contemporary “rethink” about what constitutes the pharmacy sector in today’s terms. 45 Historical review suggests that the pharmacy profession has changed over the past 100 years and considerably over the past few decades. This has occurred mostly in the context of high-income countries. 45 However, through migration and technology, the world is becoming an increasingly small place. In general, there has been a lag in pharmacy education and practice change within low- to middle-income countries, which are now playing “catch up”, and there are significant implications of the proposed model, which takes a global perspective. 57 This is not the case for all developing countries and there are examples such as Thailand with a long and strong tradition of social pharmacy and advocacy around medicines regulation, which many in high-income countries could learn from.
Implications for policy
The proposed model has implications for educational policy and practice. The first implication is that this model provides a level of consistency with respect to the different dimensions within the pharmacy sector and the associated practices that relate to these. Therefore, it should be clear to educational and medicine-related policy-makers what the different aspects of the pharmacy sector represent, regardless of country context. In this way, resultant policy is able to be more uniform and ideally could be shared within and across countries. At least this is a starting point, a platform by which to develop locally relevant policy. Furthermore, intercountry comparisons of policy interventions could be undertaken; there is a dearth of information in this area.
Implications for education and practice
There is a level of globalization occurring within pharmacy education and in pharmacy practice circles, with the drift of pharmacists from low- to high-income countries on the increase. 56 For countries that contribute to the “export market” of pharmacists from low- to high-income countries, there will be a need for terminology and definitions that have the same broad meaning within and across these countries. This will also be necessary in those countries that are not contributing to the pharmacist export market, but are publishing practice policy, guidelines or research.
The word “practice” is conceptualized as the “act of doing” 52 and each of the four dimensions that constitute the pharmacy sector have an associated practice. With a conceptual model such as this, the act of practice can be better defined within each of the aspects that make up the pharmacy sector, they being community pharmacy, clinical pharmacy, social and administrative sciences and pharmaceutical science.
Implications for a future research agenda
The proposed model of what constitutes the pharmacy sector provides a platform for standardization of pharmacy concepts and ideologies and defines these in a clear manner. The aim is to significantly reduce the ambiguity associated with the labeling what we do in pharmacy; however, it is simply a starting point. There is a need to conduct an international survey (as part of a justification process) among a large number of pharmacy leaders around the globe and others concerned, and then to present any amendments to this model. Facilitation of the survey could occur through the use of established international networks, such as ISPW, Pharmaceutical Care Network Europe or International Pharmaceutical Federation. The finalized model could then provide guidance for action with respect to policy development and implementation, practice and future research.
The proposed model was developed because of a perceived need to reduce the fragmentation and confusion that lies within the various subdisciplines of the pharmacy sector and to provide a starting point for discussion, which might help to unify the sector. A significant and well-informed research agenda is able to be developed by thinking about the different aspects of the proposed model. The model could be used to explore gaps in policy, practice and research across the four aspects of the pharmacy sector within and across high-, low- and middle-income countries.
Through this article, we bring up a very relevant issue and suggest a solution by presenting a conceptual model, which is quite a challenge. There is a definite need for clarifications and international standardizations of different aspects of pharmacy because of the various interpretations both within and between countries. To what extent practicing pharmacists, university professors, researchers and policy-makers agree with our interpretations and our division of conceptual disciplines and facets is less relevant than the thought provoked and the dialogue generated.
The article addresses the high level of fragmentation associated with labels applied to the various disciplines within the pharmacy sector. This model takes due care in outlining high-level reasons for why this model is required, which include the following: discipline labels meaning different things to different people, the upward trend of clinical pharmacy, passionate and motivated drivers for subdisciplines and what it means to be part of the pharmacy sector. The model itself is fit for purpose across multiple countries and includes two components of an umbrella term labeled “pharmaceutical practice”. The first component is the four conceptual dimensions, which outline the disciplines including social and administrative sciences, community pharmacy, clinical pharmacy and pharmaceutical sciences. The second component of the model describes the facets of the “act of practice”: teaching, research and professional advocacy. This overarching model is expected to provide a platform for further dialogue in the move toward consistency and rationalization of terminologies, which describe the global pharmacy sector. There are implications of this work for policy, education and practice, the main point being increased clarity, or at least beginning the discussion to increase the clarity of definition and consistency of meaning in and across the pharmacy sector locally, nationally and internationally. Finally, a think piece of this nature throws up as many questions as it attempts to answer and it is expected that multicountry comparisons could be made based on such a model.
The authors report no conflicts of interest in this work.

Walmart Essay Winner: A Community Pharmacist's Impact Can Go a Long Way
"The total time that I spent with this man was less than 20 minutes, but the impact that I had on his life when he thought he was all alone will last a lifetime."
A discharge from a hospital stay can be an overwhelming experience for a patient—especially when the hospital stay was due to an unexpected event like a stroke. A patient presented to my pharmacy on a Wednesday evening just prior to closing with a bag full of prescription bottles. He had slurred speech, an unsteady gait and a pale appearance. He revealed that he had had a stroke the previous weekend while playing with his grandchildren who were visiting from out-of-state, and his daughter rushed him to the emergency department. Unfortunately, she had to return to her job, so this left him alone to navigate this post-stroke life while caring for his elderly mother who had severe dementia.
I sat down with him, went over each medication, both new and old, and we made a schedule that he could follow, since he admitted to having trouble remembering things all of a sudden. In this 15-minute interaction, I expressed that I was genuinely concerned about his safety and needs and asked about his follow-up care. He admitted that he assumed he was supposed to already have scheduled an appointment with a neurologist, but he kept forgetting to call. I offered to call him the following morning to remind him, tears welled up in his eyes as he said that he didn’t expect that from me. The next morning, I gave him a call. He said he still wasn’t feeling well, but he had remembered to make an appointment for the following day. He expressed sincere gratitude for taking the time to follow up with him. Turns out, that at his appointment, he was sent back into the hospital for a few days. Upon discharge, he stopped by the pharmacy and once again, looking much better, thanked us for taking the time to help him. The total time that I spent with this man was less than 20 minutes, but the impact that I had on his life when he thought he was all alone will last a lifetime.
This is why I went into community pharmacy, and this is why I am still happy to help.
Mischa Pesicek, PharmD, is a graduate of the University of Pittsburgh, and has been a pharmacist with Walmart for 3 years. She is currently a staff RPh at Walmart Supercenter #4564 in Goldsboro, North Carolina.
Continuing Education Programming Focuses on Specialty Pharmacy Skills

Pharmacy Policy Updates, March 2024

Condition Watch: Dry Eye Relief

Fun Fact: What Are Sirtfoods, and Are They Good for You?

Inventory Specialist Can Be a Challenging but Rewarding Role for Pharmacy Technicians

Community Pharmacy Can Help Solve Health Equity Challenges in Clinical Research
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

Reflective account example: a community pharmacist reflects on his communication skills

Shutterstock.com
As the General Pharmaceutical Council’s (GPhC’s) revalidation deadline (31 October 2019) approaches, many pharmacists will be recording their learning and considering how to complete their reflective account.
The following example reflective account is intended to act as a guide to better enable you to complete your own learning record for submission to the myGPhC site. You should not replicate or copy and paste this material, rather create your own entry based on your experience. You should reflect on your own practice and consider how your patients or service users have benefited from your learning.
In your first year of completing a reflective account, you need to reflect on one or more of the following standards:
- Standard 3 – pharmacy professionals must communicate effectively;
- Standard 6 – pharmacy professionals must behave professionally;
- Standard 9 – pharmacy professionals must demonstrate leadership.
The following example is based on standard 3.
Improving my communication technique
What’s your area of work/ who are your service users?
Provide us with a reflective account of how you met one or more of the standards for pharmacy professionals. Give a real example(s) taken from your practice to illustrate how you meet the standards we have selected.
I am a community pharmacist manager working in a small pharmacy chain based in Scotland. I work alongside a pharmacy technician, two dispensers and several pharmacy counter assistants.
My service users vary, but are generally made up of patients, parents/carers, pharmacy staff members and other healthcare professionals (e.g. those from nearby general practices).
It is necessary as a community pharmacist to communicate effectively on a daily basis, whether this is with patients, staff or other healthcare professionals. However, after several years of practice, I realised I had not considered the effectiveness of my communication skills.
When considering the third standard ‘Pharmacy professionals must communicate effectively’, I thought about how I could improve my communication to ensure I am delivering person-centred care. I was conscious that communication encompasses not simply the words I use, but also body language and tone of voice. I wanted to ensure that I was being as effective as possible and where I could make improvements for my patients.
To better understand my current communication style, I asked a pharmacy colleague to observe me while I spoke to a patient about a minor ailment and make notes based on what she thought went well and what did not go well. Prior to the patient consultation I informed the patient that a colleague would be observing, but that the consultation would continue as normal and no details of the patient were going to be recorded. The patient was happy to continue with the consultation with an observer.
After the consultation my colleague collected her thoughts and made a list of points. We discussed these and I was able to find aspects of my professional practice that required improvement, such as consciously changing my body language and trying to ask fewer closed questions. In order to do this, I practiced body positioning in front of the mirror and created a list of open questions that would aid me in future consultations. I shared my learning with the team and encouraged them to let me know if they observed further communication issues.
The colleague who conducted the initial observation has since observed my general consultation and communication skills and provided me with feedback indicating that I have addressed the issues discussed. This has experience has helped me ensure patients are getting the best possible experience from me during consultations.
Before creating your own reflective account, see ‘ Revalidation: how to complete your reflective account ’, which provides a step-by-step guide for pharmacists and pharmacy technicians writing and submitting this vital part of revalidation.
You may also find the following articles on effective communication useful:
- ‘ Dispensing errors: where does responsibility lie? ’
- ‘ A day caring for vulnerable people with learning disabilities ’
- ‘ WhatsApp groups improve communication within pharmacy teams, finds study ’
How the Royal Pharmaceutical Society is supporting members with revalidation
A dedicated revalidation support hub, which also provides more information on the various support services offered is available on the Royal Pharmaceutical Society (RPS) website and includes:
- RPS MyCPD app – An app supported by The Pharmaceutical Journal. Available for iOS devices via the App Store and Android devices via Google Play . For information on how to use the app, see ‘ How to use the new ‘RPS MyCPD’ app for pharmacy revalidation ’.
- Revalidation support service – Members can contact this service by phone (0333 733 2570 Monday to Friday 9:00 to 17:00) or email [email protected] .
- Revalidation events – Information on the latest events can be found on the website.
- MyCPD Portfolio – members can create a portfolio allowing you to make records of any CPD you have engaged with and retain these records throughout your career.
You may also be interested in

Entrustable professional activities: a new approach to supervising trainee pharmacists on clinical placements

Amira Guirguis: ‘We want to use our expertise to prepare for future threats’
The privilege of becoming an rps fellow.

We would love to connect with you.
Click the button for a list of our upcoming events.
Join Our Talent Community
Sign up, stay connected and get opportunities that match your skills sent right to your inbox
Email Address
Phone Number
Upload Resume/CV (Must be under 1MB) Remove
Job Category* Select One Advanced Practice Providers Business Education Engineering Executive Facilities Support Global Security Housekeeping Information Technology Internship Laboratory Nursing Office Support Patient Care - Other Pharmacy Phlebotomy Physician Post Doctoral Radiology Imaging Research Scientist Surgical Services Therapy
Location Select Location Albert Lea, Minnesota Austin, Minnesota Barron, Wisconsin Bloomer, Wisconsin Caledonia, Minnesota Cannon Falls, Minnesota Decorah, Iowa Duluth, Minnesota Eau Claire, Wisconsin Fairmont, Minnesota Faribault, Minnesota Holmen, Wisconsin Jacksonville, Florida Kasson, Minnesota La Crosse, Wisconsin Lake City, Minnesota London, England Mankato, Minnesota Menomonie, Wisconsin Minneapolis-St. Paul-Bloomington, Minnesota New Prague, Minnesota Onalaska, Wisconsin Osseo, Wisconsin Owatonna, Minnesota Phoenix, Arizona Prairie du Chien, Wisconsin Red Wing, Minnesota Rice Lake, Wisconsin Rochester, Minnesota Saint Cloud, Minnesota Saint James, Minnesota Scottsdale, Arizona Sparta, Wisconsin Waseca, Minnesota
Area of Interest Select One Nursing Research Laboratory Medicine & Pathology Radiology Surgery Pharmacy Facilities Psychiatry & Psychology Physical Medicine & Rehabilitation General Services Surgical Technician Cardiovascular Medicine Finance Licensed Practical Nurse (LPN) Respiratory Therapy Emergency Medicine Neurology Environmental Services Mayo Collaborative Services Social Work Ambulance Services Radiation Oncology Anesthesiology & Perioperative Medicine Family Medicine Information Technology Orthopedics Gastroenterology & Hepatology Global Security Medical Oncology Surgical Assistant Urology Administration Cardiovascular Surgery Critical Care Healthcare Technology Management International Transplant Pediatrics Hospital Internal Medicine Mayo Clinic Laboratories Obstetrics & Gynecology Office Support Desk Operations Hematology Ophthalmology Community Internal Medicine Education Oncology Otolaryngology (ENT) Patient Scheduling Biochemistry & Molecular Biology Dermatology Pulmonary/Sleep Medicine Senior Care Engineering Hospice & Palliative Care Digital General Internal Medicine Artificial Intelligence & Informatics Clinical Genomics Clinical Nutrition Endocrinology Infectious Diseases Linen & Central Services Molecular Medicine Neurologic Surgery Physiology & Biomedical Engineering Sports Medicine Cancer Center Development/Philanthropy Epidemiology Immunology Neurosciences Primary Care Business Development Cancer Biology Communications Comparative Medicine Mayo Clinic Platform Nephrology & Hypertension Quality Regenerative Biotherapeutics Rheumatology Addiction Services Center for Individualized Medicine Clinical Trials & Biostatistics Dental Specialities Executive Office Health Care Delivery Research Marketing Media Support Services Molecular Pharmacology & Experimental Therapeutics Spiritual Care Travel Computational Biology Geriatric Medicine & Gerontology Health Information Management Services Human Resources Information Security Legal Occupational/Preventative Medicine Pain Medicine Risk Management Spine Center Volunteer Services
- Pharmacy, Eau Claire, Wisconsin, United States Remove
Confirm Email
By submitting your information, you consent to receive email communication from Mayo Clinic.
Join our talent community.
Join our global talent community to receive alerts when new life-changing opportunities become available.

If you want to know what it's really like at Mayo Clinic, just ask. You'll find that our pride–in where we work, and in what we do–is a common trait. You will also find a lot of inspiring stories about lives changed for the better.

Nurse Residency Program
The Nurse Residency Program (NRP) is for all nurses with less that 12 months of experience, to be completed within the first year. NRP provides a framework for a successful transition to a professional nurse by promoting educational and personal advancement.

As your career evolves, our compensation and benefits packages are designed to change with you — meeting needs now, and anticipating what comes next. We know that when Mayo Clinic takes care of you, you can take better care of our patients.
Equal opportunity
All qualified applicants will receive consideration for employment without regard to race, color, religion, sex, gender identity, sexual orientation, national origin, protected veteran status, or disability status. Learn more about "EEO is the Law." Mayo Clinic participates in E-Verify and may provide the Social Security Administration and, if necessary, the Department of Homeland Security with information from each new employee's Form I-9 to confirm work authorization.
Reasonable accommodations
Mayo Clinic provides reasonable accommodations to individuals with disabilities to increase opportunities and eliminate barriers to employment. If you need a reasonable accommodation in the application process; to access job postings, to apply for a job, for a job interview, for pre-employment testing, or with the onboarding process, please contact HR Connect at 507-266-0440 or 888-266-0440.
Job offers are contingent upon successful completion of a post offer placement assessment including a urine drug screen, immunization review and tuberculin (TB) skin testing, if applicable.
Advertising
Mayo Clinic is a not-for-profit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
Advertising and sponsorship policy | Advertising and sponsorship opportunities
Reprint permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
Any use of this site constitutes your agreement to the Terms and Conditions and Privacy Policy linked below.
Terms and Conditions | Privacy Policy | Notice of Privacy Practices | Notice of Nondiscrimination
© 1998-2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.

- Bahasa Indonesia
- Eastern Europe
- Moscow Oblast
Elektrostal
Elektrostal Localisation : Country Russia , Oblast Moscow Oblast . Available Information : Geographical coordinates , Population, Area, Altitude, Weather and Hotel . Nearby cities and villages : Noginsk , Pavlovsky Posad and Staraya Kupavna .
Information
Find all the information of Elektrostal or click on the section of your choice in the left menu.
- Update data
Elektrostal Demography
Information on the people and the population of Elektrostal.
Elektrostal Geography
Geographic Information regarding City of Elektrostal .
Elektrostal Distance
Distance (in kilometers) between Elektrostal and the biggest cities of Russia.
Elektrostal Map
Locate simply the city of Elektrostal through the card, map and satellite image of the city.
Elektrostal Nearby cities and villages
Elektrostal weather.
Weather forecast for the next coming days and current time of Elektrostal.
Elektrostal Sunrise and sunset
Find below the times of sunrise and sunset calculated 7 days to Elektrostal.
Elektrostal Hotel
Our team has selected for you a list of hotel in Elektrostal classified by value for money. Book your hotel room at the best price.
Elektrostal Nearby
Below is a list of activities and point of interest in Elektrostal and its surroundings.
Elektrostal Page

- Information /Russian-Federation--Moscow-Oblast--Elektrostal#info
- Demography /Russian-Federation--Moscow-Oblast--Elektrostal#demo
- Geography /Russian-Federation--Moscow-Oblast--Elektrostal#geo
- Distance /Russian-Federation--Moscow-Oblast--Elektrostal#dist1
- Map /Russian-Federation--Moscow-Oblast--Elektrostal#map
- Nearby cities and villages /Russian-Federation--Moscow-Oblast--Elektrostal#dist2
- Weather /Russian-Federation--Moscow-Oblast--Elektrostal#weather
- Sunrise and sunset /Russian-Federation--Moscow-Oblast--Elektrostal#sun
- Hotel /Russian-Federation--Moscow-Oblast--Elektrostal#hotel
- Nearby /Russian-Federation--Moscow-Oblast--Elektrostal#around
- Page /Russian-Federation--Moscow-Oblast--Elektrostal#page
- Terms of Use
- Copyright © 2024 DB-City - All rights reserved
- Change Ad Consent Do not sell my data
Why Easter brings me back to church
Even though i don’t practice in earnest anymore, memories and community give me a reason to return every spring, by gabriella ferrigine.
“Please — come join us in the cafeteria after Mass has concluded!”
Father Ariel’s jaunty voice echoed from where he was standing at the slabbed marble pulpit, as he smiled out at the congregation. His family, who had arrived from the Philippines in droves to celebrate his 50th birthday, beamed from the first several rows of glossy, varnished pews.
I’m not an atheist per se, but trying to find an equilibrium with faith has undoubtedly become a game of mental Tetris.
Mid-morning light filtered through stained glass depicting saints and the Stations of the Cross, casting soft pinks and blues and greens across the church: our local parish, St. James. Sun illuminated the top of Father Ariel’s head, and behind him, a domed mural of the stages of Jesus’ life — his birth in a manger, his crucifixion atop Calvary, and his resurrection after emerging from a stone sepulchre — seemed to swell higher with every slow, measured note of music from the raftered choir.
It was a Sunday morning in April, not exactly Easter but right around the time. The smell of incense — a combination of frankincense and myrrh — leached from every corner of the space, creating a somewhat soporific effect. I pictured my family, friends and neighbors gently falling asleep to its bitter, powdery aroma, like Dorothy did in the poppy field. Everything felt buoyant and peaceful.
My family and many other parishioners — mainly gentle, geriatric hordes — joined Father Ariel with his multitude of relatives in my middle-school cafeteria for an authentic Filipino feast. Side dishes of pearly quail eggs, roasted fish and meats, bright salads and an array of desserts adorned every inch of table space, the very same where I ate many peanut butter and jelly sandwiches in my youth. At the center of it all was a huge roast pig, or lechón, with delicate, crisped skin. I looked at the pig’s face, then at the people ambling around the dingy, linoleum floors, and immediately felt love.
This was nearly 10 years ago, back during a time when I went to Church every Sunday and consistently prayed to God. I don’t consider myself a particularly religious person anymore. I’m not an atheist per se, but trying to find an equilibrium with faith has undoubtedly become a game of mental Tetris. Sure, Jesus seemed like a pretty cool guy — to me, his message has always unequivocally been "love,” in a broader sense. I’m on board with that.
But I still remain immensely put off by how Catholicism’s sordid underbelly has blended into sociopolitical life, underpinning the dismantling of women’s reproductive rights and enabling sexual abusers. I find myself still clinging to it largely because it’s woven tightly into many people I love. It’s a perturbing relationship; I feel as though my continued shunning of organized religion has in a sense estranged me from the memory of some very important people.
And yet, Easter and springtime always bring me back to church. I find myself craving, not exactly the scriptures and the teachings embedded in them, but how the space evokes the memories of people I love — chiefly my maternal grandmother and my mom — and an inclusive sense of community.
A deeply spiritual person, my grandma — born in a small Bolivian jungle village called Riberalta — spent her teenage years living in a convent with a U.S.-based congregation of nuns performing foreign missionary work. She was readying to enter the sisterhood when she met my grandfather, a Sicilian and civil engineer volunteering with a Catholic mission group to help build new infrastructure in Riberalta. They returned to America together and settled in Bayonne, New Jersey, joined in a union forged out of a shared devotion to God and each other.
Though my mom didn’t pray a daily rosary or make pilgrimages to Lourdes like my grandma, she was deeply affected by her religious upbringing, a heritage she inculcated her five children with through weekly mass, and offering up nightly intentions along with prayers before dinner: family and friends who were sick or had died, poverty and homelessness, wartime conflict, our cat Sweet Pea’s hypothyroidism.
In my grandmother’s house and my own, the iconography of Jesus and other religious figures was everywhere, peppering walls and mantelpieces alongside family photos and wedding albums. Each time one of my more than 25 cousins or I received a sacrament — Baptism, First Holy Eucharist, Confirmation — a sprawling, family-wide party followed, usually at an Italian restaurant with a generically benevolent, pot-bellied owner who would toddle around and ask, “How yous all likin’ the food?” And of course, there was always a large white sheet cake, piped in bubbled fonts: “God Bless ____!”
Seeing as my mom’s eight siblings were spread out across central New Jersey, I essentially ran the gauntlet of various Catholic parishes in our area for different holidays and events. I had my favorite churches. St. James retained the top position. Then came St. Michael’s, a red-bricked church that was famous for its live-animal manger display during the Christmas season. Holy Cross — located in one of the more affluent towns in my county — had a stunning interior, but its reputation had always been somewhat sullied in my mind from a 2006 embezzlement incident .
While I was able to evade formal liturgical participation, my three younger sisters were all urged to be altar servers, helping St. James’ priests — mostly middle-aged men from the Phillippines and India — prepare and proceed with weekly Sunday mass. One sister recalled a time when she and another altar server accidentally spilled open a bag of already-consecrated Eucharist wafers as they were preparing for mass in the wood-paneled sacristy.
“Oh! Uh, don’t worry girls — I’ll consume these later,” the priest said when he walked in and saw them scooping the body of Christ off the floor and into Ziploc bags.
Another time several years ago, my family was running late for Easter Sunday mass, half of us with our hair still wet. “Overflow,” an usher posted outside the church doors said as we approached, jerking his thumb toward the rear parking lot where the grammar school was located. Given that creasters (Catholics who only attend church on Christmas and Easter) come out of the woodwork every winter and spring, tardy worshippers are forced to attend the secondary service, held in the gymnasium or auditorium.
From my seat in a metal folding chair, nostalgia washed over me as the priest carried a gold crucifix across the same floor where I’d once played dodgeball, toward the makeshift altar where I’d watched classmates act out a rendition of “The Little Mermaid.”
I feel as though my continued shunning of organized religion has in a sense estranged me from the memory of some very important people.
I spent last Easter in Newport, Rhode Island with my family for a short holiday vacation. The weekend was oceanic cliffs and Gilded Age mansions and a kaleidoscopic assortment of saltwater taffy. On Easter Sunday, we walked from our quaint bed and breakfast to St. Mary’s, Our Lady of the Isle, where JFK and Jackie O wed in September of 1953. We took turns waiting outside with our two Great Pyrenees, who had reaped the benefits of Newport’s reputation for being dog-friendly.
Ahead of the homily, the part of the service when the priest explains the Gospel reading in further detail, I elected to relieve my mom of dog duty, knowing she wouldn’t want to miss the crux of the mass.
As I turned toward the door to trade off with her, the sharp New England morning air — and an emotional pang — made me bristle. I didn’t want to leave. Mashed tightly in hard-backed pews alongside other Catholics, loyalists and creasters alike, I felt a distinct sense of calm. The very same that came to me years ago as I gazed at a pig’s snout.
This Easter, we’ll be going back to St. James. Father Ariel is no longer at the parish — I don’t know many of the priests there anymore, my connection to the parish steadily eroded by distance, time and sheer obstinance on my part. It’s an elegiac relationship, compounded by the recent passing of my grandmother, who embodied holiness and unadulterated love in every sense.
And while I may not take the time to philosophize about my salvation on Sunday, I’m certain I’ll think of her and what my being there would mean to her. For me, that’s enough to return every spring.
about this topic
- Do Christians believe Jesus was resurrected from the dead? Well, it's complicated
- The history of the Easter butter lamb, an enduring Polish tradition in the states
- Best Easter pageant ever? Half a century of "Jesus Christ Superstar"
Gabriella Ferrigine is a staff writer at Salon. Originally from the Jersey Shore, she moved to New York City in 2016 to attend Columbia University, where she received her B.A. in English and M.A. in American Studies. Formerly a staff writer at NowThis News, she has an M.A. in Magazine Journalism from NYU and was previously a news fellow at Salon.
Related Topics ------------------------------------------
Related articles.
- Share full article

Opinion Guest Essay
An Idyll on the Shores of a Toxic Lake
Supported by
Text by Jaime Lowe
Photographs by Nicholas Albrecht
Ms. Lowe is the author of, most recently, “Breathing Fire: Female Inmate Firefighters on the Front Lines of California’s Wildfires.” Mr. Albrecht is a photographer based in Oakland, Calif.
- March 29, 2024
There are two ways to experience the town of Bombay Beach, Calif., as a visitor: gawk at the spectacle or fall into the vortex. Thousands of tourists cruise through each year, often without getting out of their cars to see decaying art installations left over from an annual mid-March gathering of artists, photographers and documentarians known jokingly as the Bombay Beach Biennale. When I went to the town for the first time in 2021, I was looking for salvation in this weird desert town on the Salton Sea south of Palm Springs and Joshua Tree National Park. I dropped in, felt vibes and left with stories. I stared at the eccentric large-scale art, posted photos on Instagram of ruin porn and a hot pink sign on the beach that said, “If you’re stuck, call Kim.” I posed in front of a mountain of painted televisions, swung on a swing over the edge of the lake’s retreating shoreline and explored the half-buried, rusted-out cars that make up an abandoned ersatz drive-in movie theater. On that trip, it felt as if I were inside a “Mad Max” simulation, but I was only scratching the surface of the town.
I returned in December to try to understand why Bombay Beach remains so compelling, especially as extreme weather — heat, hurricanes and drought — and pollution wreak ever more intense havoc on it. Summer temperatures can reach 120 degrees Fahrenheit, tremors from the San Andreas Fault strike regularly, bomb testing from nearby military facilities can be heard and felt, and the air is so toxic from pesticide use, exhaust fumes, factory emissions and dust rising from the retreating Salton Sea that one study showed asthma rates among children in the region are three times the national average. By the end of the decade, the Salton Sea, California’s largest inland body of water, at about 325 square miles, may lose three-quarters of its volume; in the past 20 years, the sea’s surface area has shrunk about 38 square miles .
But people who live in Bombay Beach stay because the town offers a tight-knit community in the midst of catastrophe. Though its residents contend with environmental adversity on a daily basis, they’re also demonstrating how to navigate the uncertain future we all face — neglect, the fight for scarce resources, destruction of home, the feeling of having no place to go. They are an example of how people can survive wild climate frontiers together.
The 250 or so town residents live in the low desert on the east shore of the Salton Sea, which formed in 1905 when the then-flush Colorado River spilled into a depression, creating a freshwater lake that became increasingly saline. There used to be fish — mullet and carp, then tilapia. In the 1950s and ’60s, the area was marketed as a tourist destination and was advertised as Palm Springs by the Sea. More tourists visited Bombay Beach than Yosemite. There were yacht clubs, boat races and water skiing. It became a celebrity magnet: Frank Sinatra hung out there; so did the Beach Boys and Sonny and Cher.
Eventually, as agricultural runoff kept accumulating in a body of water with no drainage, it became toxic and created a lake with salinity that is now 50 percent greater than that of the ocean. In the 1980s, dead fish washed up on the sand, car ruins rusted in the sun, tires rotted on the shore. Tourism vanished. But some in the community hung on. One way to define Bombay Beach is through environmental disaster, but another way is as an example of how to live through disaster and how to live in general.

Candace Youngberg, a town council member and a bartender at the Ski Inn, remembers a very different Bombay Beach. When she was growing up in the 1980s, she’d ride bikes with neighborhood children and run from yard to yard in a pack because there were no fences. But over time, the town changed. With each passing year, she watched necessities disappear. Now there’s no gas station, no laundromat, no hardware store. Fresh produce is hard to come by. A trailer that was devoted to medical care shut down. In 2021, 60.9 percent of Bombay Beach residents lived below the poverty line, compared with the national average of 12.6 percent.
As painful as it was to witness the town of her youth disappear and as deep as the problems there go, Ms. Youngberg admits that adversity bonded those who stayed. She wanted to return Bombay Beach to the version of the town she remembered, to recreate a beautiful place to live year-round, not just in winter, not just during the art season, not just for the tourists posing in front of wreckage. She wanted people to see the homes, the town, the community that once thrived thrive again. With the art came attention and the potential for more resources. She got on the Bombay Beach Community Services District, a town council, and started to work toward improvements like fixing the roads and planting trees to improve air quality.
It might just be that Bombay Beach is a small town, but when I visited last winter, there was something that felt more collaborative, as though everybody’s lives and business and projects overlapped. I’m not sure the community that’s there now started out as intentional, but when fragmented groups of people come together as custodians of an enigmatic space, responsible for protecting it and one another, community is inevitable. Plus, there’s only one place to socialize, one place to gossip, one place to dance out anxiety and only about two-thirds of a square mile to wander. Whether you like it or not, your neighbors are your people — a town in its purest form.
When I was there, I walked the streets with Denia Nealy, an artist who goes by Czar, and my friend Brenda Ann Kenneally, a photographer and writer, who would shout names, and people would instantly emerge. A stranger offered a handful of Tater Tots to Czar and me in a gesture that felt emblematic: Of course a complete stranger on an electric unicycle would cruise by and share nourishment. I was given a butterfly on a stick, which I carried around like a magic wand because that seemed appropriate and necessary. I was told that if I saw a screaming woman walking down the street with a shiv in her hand, not to worry and not to make eye contact and she’d leave me alone; it was just Stabby. There was talk of the Alcoholics Anonymous meeting on the beach, the weekly church sermon led by Jack the preacher (who is also a plumber), a potluck lasagna gathering.
Last year Ms. Kenneally created a trash fashion show/photo series for the Biennale in which she created couture designs out of trash collected from the beach, enlisted regulars in town to model the outfits, then photographed them. (She exhibited a similar series at this year’s festival as well.) The work was a way to showcase the people and the place. Jonathan Hart, a fireworks specialist who slept on the beach, posed like a gladiator; a woman who normally rode through town with a stuffed Kermit the Frog toy strapped to her bike was wrapped in a clear tarp and crown, looking like royalty emerging from the Salton Sea. The environment was harsh, the poses striking. Each frame straddled the line between glamour and destruction but also showcased a community’s pride in survival. Residents were undaunted by the armor of refuse; in fact, it made them stronger. The detritus, what outsiders might think of as garbage, became gorgeous. The landscape that is often described as apocalyptic became ethereal and magical. And that’s because it is.
On my second day, we went down to the docks at noon, and I found myself sitting on a floral mustard couch watching half a dozen or so people taking turns riding Jet Skis into the sun. The sun was hot, even though it was the cool season. Time felt elastic. Mr. Hart told me that he and some friends had fixed up the water scooters to give everyone in town the chance to blow off some steam, to smile a little. It had been a rough couple of months in the region. In preparation for Hurricane Hilary, which hit Mexico and the southwestern United States last August, 26 volunteers made 200 sandbags and delivered them door to door. Neighbors helped secure as many structures as possible.
Most media outlets reported that the hurricane was downgraded to a tropical storm because that’s the weather system that hit Los Angeles, but it was close to a hurricane in Bombay Beach, with winds hitting 60 miles per hour, and most properties were surrounded by water. Roofs collapsed or blew away entirely. “When faced with something like that, they were like, ‘Boom, we’re on it,’” Ms. Youngberg told me. They were together in disaster and in celebrating survival.
It reminded me of the writer Rebecca Solnit’s book “A Paradise Built in Hell,” which considers the upside to catastrophe. She finds that people rise to the occasion and oftentimes do it with joy because disaster and survival leave a wake of purposefulness, consequential work and community. Disasters require radical acts of imagination and interaction. It seemed that because Bombay Beach lived hard, surviving climate catastrophes like extreme weather on top of everyday extremes, it celebrated even harder. It seemed that in Bombay Beach there’s enough to celebrate if you just get through the day, gaze at the night sky and do it all again in the morning.
A lot of the residents who live there now arrived with trauma. Living there is its own trauma. But somehow the combination creates a place of care and physical and emotional presence. People experience life intensely, as one. It’s a town that is isolated, but in spite of a loneliness epidemic, it doesn’t seem so lonely to be there. I felt unexpected joy in what, from everything I’d read from afar, was a place that might as well have been sinking into the earth. I felt so safe and so happy that if we had sunk into the earth together, it wouldn’t have felt like such a bad way to go.
On my last night in Bombay Beach, I went to the Ski Inn, a bar that serves as the center of all social activity. I’d been in town for only two days, and yet it felt as if I’d been to the Ski Inn a million times, as if I already knew everyone and they knew me. A band was playing, we danced and drank, and I forgot about the 8 p.m. kitchen cutoff. The chef apologized, but he’d been working since 11:45 a.m. and had already cleaned the grill and fryer. He’d saved one mac and cheese for the bartender, and when she heard I hadn’t eaten, she offered to split it with me, not wanting me to go hungry or leave without having tried the mac and cheese.
Bombay Beach is a weird place. And this was an especially weird feeling. I had been instantly welcomed into the fold of community and cared for, even though I was a stranger in a very strange land.
I realized I didn’t want to leave. There were lessons there — how to live with joy and purpose in the face of certain catastrophe, how to exist in the present without the ever presence of doom. Next time, I thought, I’d stay longer, maybe forever, and actually ride a Jet Ski.
Jaime Lowe is a Knight-Wallace journalism fellow at the University of Michigan and the author of, most recently, “Breathing Fire: Female Inmate Firefighters on the Front Lines of California’s Wildfires.” Nicholas Albrecht is a photographer based in Oakland, Calif. His first monograph, “One, No One and One Hundred Thousand,” was the culmination of a multiyear project made while living on the shores of the Salton Sea.
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
Advertisement
ELECTROSTAL HISTORY AND ART MUSEUM: All You Need to Know BEFORE You Go (with Photos)
- (0.19 mi) Elektrostal Hotel
- (1.21 mi) Yakor Hotel
- (1.27 mi) Mini Hotel Banifatsiy
- (1.18 mi) Elemash
- (1.36 mi) Hotel Djaz
- (0.07 mi) Prima Bolshogo
- (0.13 mi) Makecoffee
- (0.25 mi) Amsterdam Moments
- (0.25 mi) Pechka
- (0.26 mi) Mazhor

IMAGES
VIDEO
COMMENTS
Essay On Community Pharmacy. 1227 Words5 Pages. Exploring Community Pharmacies and Their Role in Health Promotion. A community pharmacy is vital part within the healthcare system when it comes to health promotion. Pharmacists are an excellent resource when it comes to educating patients with medication knowledge, and directing patients towards ...
Conclusion. Health inequalities are unfair and create avoidable differences in health and access to healthcare. Community pharmacy teams can play an important role in reducing health inequalities and improving access to good quality healthcare in the community through the provision of clinical services. However, success will require pharmacy ...
Pharmacists in the community ensure medication safety similarly to how they would in any healthcare environment: throughout the medication-use process, including the ordering of medications to their storage, transcription, preparation, dispensing, counseling, and more. Prior to the dispensing process, the community pharmacist provides a ...
The Path Forward. In its 2018 report, "The Next Transition in Community-Based Pharmacy Practice," the American Pharmacists Association found that pharmacists are trained to perform certain tasks but often experience work settings that are not conducive to such practice. The study found that new roles abound for community pharmacists in this ...
Please use one of the following formats to cite this article in your essay, paper or report: APA. Smith, Yolanda. (2023, July 22). Community Pharmacy.
Community pharmacists have a very important role in the society, as they are usually the first ones whom patients come in contact with regarding healthcare. The role of community pharmacists has been greatly expanded since the past decade. The main roles of pharmacists in community pharmacy are supplying safe and suitable medicines, dispensing ...
In line with our study, the study of Iranmanesh et al. shows different ethical challenges in community pharmacy including privacy and confidentiality, pharmacists' awareness of their own professional commitment, considering patient's interests, responsibility, quality of medication, and rational drug use (Iranmanesh et al., 2020).
Anderson C, Blenkinsopp A, Armstrong M: Feedback from community pharmacy users on the contribution of community pharmacy to improving public's health: a systematic review of the peer reviewed and non-peer reviewed literature 1990-2002. Health Expectations. 2004, 7: 191-202. 10.1111/j.1369-7625.2004.00274.x.
There is an emergent literature on the field of social pharmacy 8 - 15 and particularly in terms of education. 16 - 22 There is a literature that defines pharmaceutical care 5, 23 - 26 with some focus on community pharmacy. 27 - 30 Similarly, there is a dialogue on what constitutes clinical pharmacy and how this relates to ...
This is why I went into community pharmacy, and this is why I am still happy to help. Mischa Pesicek, PharmD, is a graduate of the University of Pittsburgh, and has been a pharmacist with Walmart for 3 years. She is currently a staff RPh at Walmart Supercenter #4564 in Goldsboro, North Carolina.
Standard 9 - pharmacy professionals must demonstrate leadership. The following example is based on standard 3. Title. Improving my communication technique. ... I am a community pharmacist manager working in a small pharmacy chain based in Scotland. I work alongside a pharmacy technician, two dispensers and several pharmacy counter assistants. ...
The Pharmacists Mutual Community Pharmacy Scholarship is a scholarship program sponsored by Pharmacists Mutual Insurance Company. Recipients selected for the Pharmacists Mutual Community Pharmacy Scholarship will each be awarded $3,000. Up to $60,000 in scholarships may be awarded annually. This program acknowledges students interested in ...
Decent Essays. 1120 Words. 5 Pages. Open Document. As I reflect on my experience of a pharmacy practice, I realize how much of my personality has changed in only few months. The experiences I gained during my first rotation at Walgreens were particularly rewarding, especially those gained while working as a team to achieve a common goal of a ...
In the essay "Community Pharmacy Practice and Experience" the author analyzes the Rite Pharmacy, which is a community-based pharmacy. It services vary to accommodate the needs of its customers from walk-in, drive-thru, to delivery. It has created a system that is very organized and efficient…
Community Pharmacy Essay. 1199 Words3 Pages. Community pharmacist (CP) is highly competent and the most accessible health care profession to the public in the UK. It is estimated more than 550 million visits to community pharmacy take place in the UK annually. There are roughly 32000 qualified CP serving in 13000 community pharmacies in England.
IPPE Midpoint Reflection My second year rotation site was at HEB pharmacy, located on the corner of 4444 Kostory Road and Gollihar in Corpus Christy, TX. This community pharmacy is well managed under my preceptor, Jaime Lee. During the first morning of site on August 26th, 2016, I had the opportunity to observed my preceptor performance full ...
Short Application Essay for Law School. My first personal introduction to the profusion of environmental laws in our country came while working for my father. I worked for over eleven years at my father's business, an Exxon Service Center. While there, I performed every job, task, and duty associated with the operation of a service station.
Community Pharmacy Internship Reflection Paper - Free download as Word Doc (.doc / .docx), PDF File (.pdf), Text File (.txt) or read online for free. Pharmacy Intern Reflection
Responsibilities. Pharmacy Tech levels 1 - 5: Assists the pharmacist in providing optimal pharmaceutical care to the patient. Gathers, labels and distributes medications accurately and efficiently. Packages, prepares and safely compounds medications including hazardous substances accurately and efficiently.
At least 37 people have been killed by two explosions which hit the Moscow Metro system at the peak of the morning rush hour, Russian officials have said. The first blast went off in the central Lubyanka station at 0756 (0356 GMT). Police said the dead included 14 people inside a train and 11 on...
The journey from Moscow to Elektrostal by train is 32.44 mi and takes 2 hr 7 min. There are 71 connections per day, with the first departure at 12:15 AM and the last at 11:46 PM. It is possible to travel from Moscow to Elektrostal by train for as little as or as much as . The best price for this journey is .
Elektrostal Geography. Geographic Information regarding City of Elektrostal. Elektrostal Geographical coordinates. Latitude: 55.8, Longitude: 38.45. 55° 48′ 0″ North, 38° 27′ 0″ East. Elektrostal Area. 4,951 hectares. 49.51 km² (19.12 sq mi) Elektrostal Altitude.
And yet, Easter and springtime always bring me back to church. I find myself craving, not exactly the scriptures and the teachings embedded in them, but how the space evokes the memories of people ...
An Idyll on the Shores of a Toxic Lake. Ms. Lowe is the author of, most recently, "Breathing Fire: Female Inmate Firefighters on the Front Lines of California's Wildfires.". Mr. Albrecht is ...
If the system detects something that potentially contradicts our community guidelines, the review is not published. When the system detects a problem, a review may be automatically rejected, sent to the reviewer for validation, or manually reviewed by our team of content specialists, who work 24/7 to maintain the quality of the reviews on our site.